User login
Official Newspaper of the American College of Surgeons
Paradigm shift: Prophylactic salpingectomy for ovarian cancer risk reduction
LAS VEGAS – Removing the fallopian tubes at the time of pelvic surgeries as a potential means of reducing ovarian cancer risk appears to be a movement that’s picking up steam in clinical practice.
A recent survey of 234 U.S. gynecologists showed prophylactic bilateral salpingectomy is catching on when performed in conjunction with hysterectomy, but far less so for tubal sterilization, Dr. Austin Findley observed at the annual Minimally Invasive Surgery Week.
A total of 54% of respondents indicated they routinely perform salpingectomy at the time of hysterectomy in an effort to reduce the risk of ovarian cancer as well as to avoid the need for reoperations. However, only 7% of the gynecologic surgeons said they perform salpingectomy for tubal sterilization, even though 58% of respondents stated they believe the procedure is the most effective form of tubal sterilization (J. Minim. Invasive Gynecol. 2013;20:517-21).
“In my experience at various hospitals, I think these numbers are a pretty accurate reflection of what folks are doing,” commented Dr. Findley of Wright State University in Dayton, Ohio.
The prophylactic salpingectomy movement is an outgrowth of the tubal hypothesis of ovarian cancer.
“There is now increasing and dramatic evidence to suggest that most ovarian cancers actually originate in the distal fallopian tubes. I think this is a concept most people are unaware of or are just becoming accustomed to. The tubal hypothesis represents a major paradigm shift in the way we think about ovarian cancers. The previous belief that excessive ovulation is a cause of ovarian cancer is no longer regarded as accurate,” he explained at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
Ovarian cancer is the No. 1 cause of mortality from gynecologic malignancy, accounting for more than 14,000 deaths per year, according to National Cancer Institute data. The lifetime risk of the malignancy is 1.3%, with the average age at diagnosis being 63 years.
Only 10%-15% of ovarian cancers occur in women at high risk for the malignancy because they carry a BRCA mutation or other predisposing gene. The vast majority of ovarian cancer deaths are caused by high-grade serous tumors that have been shown to be strongly associated with precursor lesions in the distal fallopian tubes of women at low risk for the malignancy.
There is no proven-effective screening program or risk-reduction method for these low-risk women. However, with 600,000 hysterectomies and 700,000 tubal sterilizations being performed annually in the United States, prophylactic salpingectomy has been advocated as an attractive opportunity to potentially reduce ovarian cancer risk. Other common pelvic surgeries in which it might be used for this purpose include excision of endometriosis and laparoscopy for pelvic pain. It also has recently been shown to be feasible and safe post partum at cesarean or vaginal delivery (Obstet. Gynecol. 2014 [doi: 10.1097/01.AOG.0000447427.80479.ae]).
But the key word here is “potentially.” It must be emphasized that at present the ovarian cancer prevention benefit of prophylactic salpingectomy remains hypothetical; in theory, the procedure should reduce ovarian cancer risk, but there is not yet persuasive evidence that it actually does, Dr. Findley emphasized at the meeting, presented by the Society of Laparoendoscopic Surgeons and affiliated societies.
In contrast, one well-established ancillary benefit of prophylactic salpingectomy is that it eliminates the need for future reoperation for salpingectomy. This was demonstrated in a large Danish cohort study including close to 10,000 women undergoing hysterectomy and a similar number undergoing sterilization procedures. Among the nearly two-thirds of hysterectomy patients who had both fallopian tubes retained, there was a 2.13-fold increased likelihood of subsequent salpingectomy, compared with nonhysterectomized women.
Similarly, Danish women who underwent a sterilization procedure with retention of the fallopian tubes – typically tubal ligation with clips – were 2.42 times more likely to undergo subsequent salpingectomy, most often because of the development of hydrosalpinx, infection, ectopic pregnancy, or other complications (BMJ Open 2013;3 [doi:10.1136/bmjopen-2013-002845]).
The most commonly cited potential risk of prophylactic salpingectomy – decreased ovarian function – now appears to be a nonissue. This was demonstrated in a recent retrospective Italian study (Gynecol. Oncol. 2013;129:448-51) as well as in a pilot randomized controlled trial conducted by Dr. Findley and his coworkers (Fertil. Steril. 2013;100:1704-8), which appears to have answered many skeptics’ concerns. Indeed, Dr. Findley’s coinvestigator Dr. Matthew Siedhoff said he has recently been approached by researchers interested in collaborating in a larger confirmatory randomized trial, but all parties eventually agreed it was a no-go.
“It’s a little hard to demonstrate equipoise for a larger randomized controlled trial. We’re beyond that now, given that prophylactic salpingectomy really doesn’t seem to make a difference as far as ovarian function,” according to Dr. Siedhoff, director of the division of advanced laparoscopy and pelvic pain at the University of North Carolina, Chapel Hill.
Another oft-expressed reservation about salpingectomy as a means of reducing ovarian cancer risk in women seeking sterilization is that salpingectomy’s irreversibility may lead to “tubal regret” on the part of patients who later change their mind about further pregnancies. However, Dr. Findley cited a recent editorial whose authors criticized colleagues who made that claim. The editorialists argued that the tubal regret concern indicates surgeons weren’t really listening to their patients’ true desires during the informed consent conversation.
“We should not have started thinking about salpingectomy for female sterilization only once a decrease in ovarian cancer risk became part of the equation,” they declared (Obstet. Gynecol. 2014;124:596-9).
Dr. Findley noted that Canadian gynecologists are leading the way forward regarding prophylactic salpingectomy as a potential method of ovarian cancer prevention. The Society of Gynecologic Oncology of Canada in a 2011 policy statement recommended patient/physician discussion of the risks and benefits of bilateral salpingectomy for patients undergoing hysterectomy or requesting permanent sterilization. The Society of Gynecologic Oncology followed suit with a similar clinical practice statement in late 2013.
Additionally, the Canadian group declared that a national ovarian cancer prevention study focused on fallopian tube removal should be a top priority.
Gynecologic oncologists in British Columbia recently reported the eye-catching results of a province-wide educational initiative targeting gynecologists and their patients. In 2010, all British Columbia gynecologists had to attend a course on the role of the fallopian tubes in the development of ovarian cancer, during which they were advised to consider performing bilateral salpingectomy for ovarian cancer risk reduction.
Surgical practice changed dramatically in British Columbia in response. In 2009 – the year prior to the physician education initiative – salpingectomy was utilized in just 0.3% of permanent sterilization procedures. In 2010, it was 11.4%. By 2011, it was 33.3%.
Similarly, only 7% of hysterectomies performed in British Columbia in 2009 were accompanied by bilateral salpingectomy. This figure climbed to 23% in 2010 and jumped further to 35% in 2011. Meanwhile the rate of hysterectomy with bilateral salpingo-oophorectomy remained steady over time at 44% (Am. J. Obstet. Gynecol. 2014;210:471.e1-11).
This project was conducted in collaboration with the B.C. Cancer Agency, which maintains comprehensive province-wide registries. Over time, it will be possible to demonstrate whether prophylactic salpingectomy is indeed associated with a reduction in the incidence of ovarian cancer. “I think this study demonstrated that there’s a lack of awareness on this issue, but also [that there’s] potential effectiveness of introducing an educational initiative like this in changing our practice patterns. As we start talking more about this issue amongst our colleagues and our patients, we’re more likely to see a practice pattern shift in the United States as well,” Dr. Findley commented.
He reported having no financial conflicts with regard to his presentation.
The practice of salpingectomy for ovarian cancer risk reduction has quietly gained momentum in the gynecology world, however, it has not been well advertised in the patient community, despite steadily increasing amounts of data to support its plausibility as a risk-reducing strategy. Recent surveys reveal that physicians are slowly changing practices and including “prophylactic” salpingectomy during benign gynecologic surgeries, including at the time of hysterectomy, tubal sterilization (including at the time of cesarean section), and at the time of surgery for other benign gynecologic conditions, such as laparoscopy for endometriosis.
While the change in practice is encouraging, the supporting hypothesis is still in its infancy. The historical theory of the etiology of ovarian cancer states that ovulation events led to an increased risk of ovarian cancer. The theory of “incessant ovulation” suggested that the epithelium of the ovary is sensitive to the number of events of ovulation, which may in turn act as a promoting factor in the carcinogenic process (Clinical Gynecologic Oncology, 8th ed.; Epithelial Ovarian Cancer (Chapter 11) [Maryland Heights, Mo.: Mosby, 2012]). This was supported by epidemiologic data that noted that women who used oral contraceptives, had multiple pregnancies, breastfed, and underwent late menarche and early menopause were at decreased risk of developing ovarian cancer (Cancer Causes Control 2007;18:517 ; Am. J. Epidemiol. 1992;136:1184-203; Int. J. Epidemiol. 2000;29:799-802). The hypothesis was adopted, as the epidemiology of ovulation was supportive.
The weakness of the incessant ovulation theory has been our inability to identify precursor lesions. In almost all other gynecologic malignancies, a precursor lesion has been identified and supports a theory of carcinogenesis. In patients with ovarian cancer, over 80% are diagnosed with advanced stage, and this is where the new theory of the pathogenesis of ovarian cancer originating in the fimbriated end of the fallopian tube begins to have credibility. Serous tubal intraepithelial carcinoma (STIC) lesions are the proposed precursor lesions to high-grade serous carcinomas. STIC lesions exhibit histologic features of morphologic atypia (increased nuclear/cytoplasmic ratio, prominent nucleoli, increased proliferation with an intact basement membrane, variably stratified fallopian tube epithelium with nuclear pleomorphism) and have evidence of TP53 mutations (J. Pathol. 2012;226:421-6 ). STIC lesions were first described as a potential precursor to fallopian tube serous carcinoma in the 1950s, however, it was not proposed as a precursor to extra-fallopian tube serous pelvic cancers until the 2000s (Am. J. Obstet. Gynecol. 1950;59:58-67). One of the suggested pathogeneses of this evolving hypothesis stipulates that TP53 mutations are associated with telomere shortening, one of the main genetic manifestations in cancer development, leading to chromosomal instability, gene expression reprogramming, and tumor progression (Am. J. Surg. Pathol. 2010;34:829-3). The finding of TP-53 mutations in STIC further supports the STIC precursor hypothesis, as identical mutations have been reported in concurrent high-grade serous carcinomas, providing evidence that supports the clonal relationship of the two lesions (J. Pathol. 2012;226:421-6 ). The theory further stipulates that STIC cells can exfoliate and disseminate to the ovary and peritoneal surfaces prior to becoming invasive, and subsequently demonstrating invasion at the distant sites. In addition, this theory can explain the development of primary peritoneal high-grade serous cancer, a disease essentially identical to high-grade serous ovarian cancer, although the etiology of this disease is largely unknown.
Interest in the STIC to extra–fallopian tube serous cancers hypothesis was enhanced by the histopathologic evaluation of the ovaries and fallopian tubes of BRCA-positive women undergoing prophylactic bilateral salpingo-oophorectomy. In this population, women were diagnosed with a serous cancer (up to 17%), and roughly 80% occurred in the fallopian tube (Gynecol. Oncol. 2002;87:52-6 ). STIC was subsequently described to occur not only in BRCA-positive women, but in sporadic cases of serous cancer as well (Am. J. Surg. Pathol. 2007;31:161-9).Additionally, up to 60%-70% of sporadic high-grade serous cancers (ovarian, primary peritoneal) have been reported to have STIC lesions on final pathology (Int. J. Gynecol. Cancer 2009;19:58-64 ). The finding of a STIC lesion is not routinely noted in pathology reports however, possibly due to the lack of serial sectioning of tubes and ovaries in the general population, when no germline mutation is present.
While the majority of the data supporting STIC as a potential precursor lesion to ovarian cancer is from the BRCA literature, the application of the theory can be and has been extrapolated to women at baseline ovarian cancer risk. As described in the article presented, there appears to be a paradigm shift in benign gynecology practice towards prophylactic salpingectomy for ovarian cancer risk reduction. The appropriate application of the prophylactic salpingectomy should be as described – at the time of benign hysterectomies, tubal sterilizations, and can be performed at the time of surgeries for other benign conditions (endometriosis, pelvic masses, diagnostic laparoscopies).
The data from this paradigm shift in practice will contribute significantly to answering some of the many questions surrounding this hypothesis, including the incidence of STIC in the baseline risk population, as well as answer the question of whether this practice will actually reduce the ovarian cancer incidence in the years to come. Additionally, investigation into the efficacy of ovarian cancer risk reduction of prophylactic salpingectomy in the high-risk patients (those with germline mutations) who undergo ovarian conservation at the time of salpingectomy is imperative. These women are currently counseled to undergo prophylactic bilateral salpingo-oophorectomy at the age of 35 or at the time of childbearing completion. As data support that oophorectomy for benign disease in women under the age of 50 increases all-cause mortality (Obstet. Gynecol. 2009;113:1027-37), the impact that prophylactic salpingectomy with ovarian conservation has in this population could be monumental, as this represents a group of women subjected to the sequelae of early surgical menopause. Furthermore, given the current economic climate of modern medicine, additional investigation into the cost-effectiveness of salpingectomy as a risk-reducing option in both women with increased risk (germline mutation) and in the general population, is indicated.
In conclusion, the practice of prophylactic salpingectomy is still in its infancy. The early paradigm shift will certainly contribute to the existing literature and potentially improve our ability to reduce risk of ovarian cancer, without compromising the overall health of our patients through surgical castration. The current hypothesis of STIC as the primary site for ovarian cancer carcinogenesis is certainly plausible and may allow for improved screening modalities and targeted therapies, which may lead to improved outcomes for our patients.
Caroline C. Billingsley, M.D., and Larry J. Copeland, M.D., who are gynecologic oncologists at Ohio State University, Columbus, wrote this commentary.
The practice of salpingectomy for ovarian cancer risk reduction has quietly gained momentum in the gynecology world, however, it has not been well advertised in the patient community, despite steadily increasing amounts of data to support its plausibility as a risk-reducing strategy. Recent surveys reveal that physicians are slowly changing practices and including “prophylactic” salpingectomy during benign gynecologic surgeries, including at the time of hysterectomy, tubal sterilization (including at the time of cesarean section), and at the time of surgery for other benign gynecologic conditions, such as laparoscopy for endometriosis.
While the change in practice is encouraging, the supporting hypothesis is still in its infancy. The historical theory of the etiology of ovarian cancer states that ovulation events led to an increased risk of ovarian cancer. The theory of “incessant ovulation” suggested that the epithelium of the ovary is sensitive to the number of events of ovulation, which may in turn act as a promoting factor in the carcinogenic process (Clinical Gynecologic Oncology, 8th ed.; Epithelial Ovarian Cancer (Chapter 11) [Maryland Heights, Mo.: Mosby, 2012]). This was supported by epidemiologic data that noted that women who used oral contraceptives, had multiple pregnancies, breastfed, and underwent late menarche and early menopause were at decreased risk of developing ovarian cancer (Cancer Causes Control 2007;18:517 ; Am. J. Epidemiol. 1992;136:1184-203; Int. J. Epidemiol. 2000;29:799-802). The hypothesis was adopted, as the epidemiology of ovulation was supportive.
The weakness of the incessant ovulation theory has been our inability to identify precursor lesions. In almost all other gynecologic malignancies, a precursor lesion has been identified and supports a theory of carcinogenesis. In patients with ovarian cancer, over 80% are diagnosed with advanced stage, and this is where the new theory of the pathogenesis of ovarian cancer originating in the fimbriated end of the fallopian tube begins to have credibility. Serous tubal intraepithelial carcinoma (STIC) lesions are the proposed precursor lesions to high-grade serous carcinomas. STIC lesions exhibit histologic features of morphologic atypia (increased nuclear/cytoplasmic ratio, prominent nucleoli, increased proliferation with an intact basement membrane, variably stratified fallopian tube epithelium with nuclear pleomorphism) and have evidence of TP53 mutations (J. Pathol. 2012;226:421-6 ). STIC lesions were first described as a potential precursor to fallopian tube serous carcinoma in the 1950s, however, it was not proposed as a precursor to extra-fallopian tube serous pelvic cancers until the 2000s (Am. J. Obstet. Gynecol. 1950;59:58-67). One of the suggested pathogeneses of this evolving hypothesis stipulates that TP53 mutations are associated with telomere shortening, one of the main genetic manifestations in cancer development, leading to chromosomal instability, gene expression reprogramming, and tumor progression (Am. J. Surg. Pathol. 2010;34:829-3). The finding of TP-53 mutations in STIC further supports the STIC precursor hypothesis, as identical mutations have been reported in concurrent high-grade serous carcinomas, providing evidence that supports the clonal relationship of the two lesions (J. Pathol. 2012;226:421-6 ). The theory further stipulates that STIC cells can exfoliate and disseminate to the ovary and peritoneal surfaces prior to becoming invasive, and subsequently demonstrating invasion at the distant sites. In addition, this theory can explain the development of primary peritoneal high-grade serous cancer, a disease essentially identical to high-grade serous ovarian cancer, although the etiology of this disease is largely unknown.
Interest in the STIC to extra–fallopian tube serous cancers hypothesis was enhanced by the histopathologic evaluation of the ovaries and fallopian tubes of BRCA-positive women undergoing prophylactic bilateral salpingo-oophorectomy. In this population, women were diagnosed with a serous cancer (up to 17%), and roughly 80% occurred in the fallopian tube (Gynecol. Oncol. 2002;87:52-6 ). STIC was subsequently described to occur not only in BRCA-positive women, but in sporadic cases of serous cancer as well (Am. J. Surg. Pathol. 2007;31:161-9).Additionally, up to 60%-70% of sporadic high-grade serous cancers (ovarian, primary peritoneal) have been reported to have STIC lesions on final pathology (Int. J. Gynecol. Cancer 2009;19:58-64 ). The finding of a STIC lesion is not routinely noted in pathology reports however, possibly due to the lack of serial sectioning of tubes and ovaries in the general population, when no germline mutation is present.
While the majority of the data supporting STIC as a potential precursor lesion to ovarian cancer is from the BRCA literature, the application of the theory can be and has been extrapolated to women at baseline ovarian cancer risk. As described in the article presented, there appears to be a paradigm shift in benign gynecology practice towards prophylactic salpingectomy for ovarian cancer risk reduction. The appropriate application of the prophylactic salpingectomy should be as described – at the time of benign hysterectomies, tubal sterilizations, and can be performed at the time of surgeries for other benign conditions (endometriosis, pelvic masses, diagnostic laparoscopies).
The data from this paradigm shift in practice will contribute significantly to answering some of the many questions surrounding this hypothesis, including the incidence of STIC in the baseline risk population, as well as answer the question of whether this practice will actually reduce the ovarian cancer incidence in the years to come. Additionally, investigation into the efficacy of ovarian cancer risk reduction of prophylactic salpingectomy in the high-risk patients (those with germline mutations) who undergo ovarian conservation at the time of salpingectomy is imperative. These women are currently counseled to undergo prophylactic bilateral salpingo-oophorectomy at the age of 35 or at the time of childbearing completion. As data support that oophorectomy for benign disease in women under the age of 50 increases all-cause mortality (Obstet. Gynecol. 2009;113:1027-37), the impact that prophylactic salpingectomy with ovarian conservation has in this population could be monumental, as this represents a group of women subjected to the sequelae of early surgical menopause. Furthermore, given the current economic climate of modern medicine, additional investigation into the cost-effectiveness of salpingectomy as a risk-reducing option in both women with increased risk (germline mutation) and in the general population, is indicated.
In conclusion, the practice of prophylactic salpingectomy is still in its infancy. The early paradigm shift will certainly contribute to the existing literature and potentially improve our ability to reduce risk of ovarian cancer, without compromising the overall health of our patients through surgical castration. The current hypothesis of STIC as the primary site for ovarian cancer carcinogenesis is certainly plausible and may allow for improved screening modalities and targeted therapies, which may lead to improved outcomes for our patients.
Caroline C. Billingsley, M.D., and Larry J. Copeland, M.D., who are gynecologic oncologists at Ohio State University, Columbus, wrote this commentary.
The practice of salpingectomy for ovarian cancer risk reduction has quietly gained momentum in the gynecology world, however, it has not been well advertised in the patient community, despite steadily increasing amounts of data to support its plausibility as a risk-reducing strategy. Recent surveys reveal that physicians are slowly changing practices and including “prophylactic” salpingectomy during benign gynecologic surgeries, including at the time of hysterectomy, tubal sterilization (including at the time of cesarean section), and at the time of surgery for other benign gynecologic conditions, such as laparoscopy for endometriosis.
While the change in practice is encouraging, the supporting hypothesis is still in its infancy. The historical theory of the etiology of ovarian cancer states that ovulation events led to an increased risk of ovarian cancer. The theory of “incessant ovulation” suggested that the epithelium of the ovary is sensitive to the number of events of ovulation, which may in turn act as a promoting factor in the carcinogenic process (Clinical Gynecologic Oncology, 8th ed.; Epithelial Ovarian Cancer (Chapter 11) [Maryland Heights, Mo.: Mosby, 2012]). This was supported by epidemiologic data that noted that women who used oral contraceptives, had multiple pregnancies, breastfed, and underwent late menarche and early menopause were at decreased risk of developing ovarian cancer (Cancer Causes Control 2007;18:517 ; Am. J. Epidemiol. 1992;136:1184-203; Int. J. Epidemiol. 2000;29:799-802). The hypothesis was adopted, as the epidemiology of ovulation was supportive.
The weakness of the incessant ovulation theory has been our inability to identify precursor lesions. In almost all other gynecologic malignancies, a precursor lesion has been identified and supports a theory of carcinogenesis. In patients with ovarian cancer, over 80% are diagnosed with advanced stage, and this is where the new theory of the pathogenesis of ovarian cancer originating in the fimbriated end of the fallopian tube begins to have credibility. Serous tubal intraepithelial carcinoma (STIC) lesions are the proposed precursor lesions to high-grade serous carcinomas. STIC lesions exhibit histologic features of morphologic atypia (increased nuclear/cytoplasmic ratio, prominent nucleoli, increased proliferation with an intact basement membrane, variably stratified fallopian tube epithelium with nuclear pleomorphism) and have evidence of TP53 mutations (J. Pathol. 2012;226:421-6 ). STIC lesions were first described as a potential precursor to fallopian tube serous carcinoma in the 1950s, however, it was not proposed as a precursor to extra-fallopian tube serous pelvic cancers until the 2000s (Am. J. Obstet. Gynecol. 1950;59:58-67). One of the suggested pathogeneses of this evolving hypothesis stipulates that TP53 mutations are associated with telomere shortening, one of the main genetic manifestations in cancer development, leading to chromosomal instability, gene expression reprogramming, and tumor progression (Am. J. Surg. Pathol. 2010;34:829-3). The finding of TP-53 mutations in STIC further supports the STIC precursor hypothesis, as identical mutations have been reported in concurrent high-grade serous carcinomas, providing evidence that supports the clonal relationship of the two lesions (J. Pathol. 2012;226:421-6 ). The theory further stipulates that STIC cells can exfoliate and disseminate to the ovary and peritoneal surfaces prior to becoming invasive, and subsequently demonstrating invasion at the distant sites. In addition, this theory can explain the development of primary peritoneal high-grade serous cancer, a disease essentially identical to high-grade serous ovarian cancer, although the etiology of this disease is largely unknown.
Interest in the STIC to extra–fallopian tube serous cancers hypothesis was enhanced by the histopathologic evaluation of the ovaries and fallopian tubes of BRCA-positive women undergoing prophylactic bilateral salpingo-oophorectomy. In this population, women were diagnosed with a serous cancer (up to 17%), and roughly 80% occurred in the fallopian tube (Gynecol. Oncol. 2002;87:52-6 ). STIC was subsequently described to occur not only in BRCA-positive women, but in sporadic cases of serous cancer as well (Am. J. Surg. Pathol. 2007;31:161-9).Additionally, up to 60%-70% of sporadic high-grade serous cancers (ovarian, primary peritoneal) have been reported to have STIC lesions on final pathology (Int. J. Gynecol. Cancer 2009;19:58-64 ). The finding of a STIC lesion is not routinely noted in pathology reports however, possibly due to the lack of serial sectioning of tubes and ovaries in the general population, when no germline mutation is present.
While the majority of the data supporting STIC as a potential precursor lesion to ovarian cancer is from the BRCA literature, the application of the theory can be and has been extrapolated to women at baseline ovarian cancer risk. As described in the article presented, there appears to be a paradigm shift in benign gynecology practice towards prophylactic salpingectomy for ovarian cancer risk reduction. The appropriate application of the prophylactic salpingectomy should be as described – at the time of benign hysterectomies, tubal sterilizations, and can be performed at the time of surgeries for other benign conditions (endometriosis, pelvic masses, diagnostic laparoscopies).
The data from this paradigm shift in practice will contribute significantly to answering some of the many questions surrounding this hypothesis, including the incidence of STIC in the baseline risk population, as well as answer the question of whether this practice will actually reduce the ovarian cancer incidence in the years to come. Additionally, investigation into the efficacy of ovarian cancer risk reduction of prophylactic salpingectomy in the high-risk patients (those with germline mutations) who undergo ovarian conservation at the time of salpingectomy is imperative. These women are currently counseled to undergo prophylactic bilateral salpingo-oophorectomy at the age of 35 or at the time of childbearing completion. As data support that oophorectomy for benign disease in women under the age of 50 increases all-cause mortality (Obstet. Gynecol. 2009;113:1027-37), the impact that prophylactic salpingectomy with ovarian conservation has in this population could be monumental, as this represents a group of women subjected to the sequelae of early surgical menopause. Furthermore, given the current economic climate of modern medicine, additional investigation into the cost-effectiveness of salpingectomy as a risk-reducing option in both women with increased risk (germline mutation) and in the general population, is indicated.
In conclusion, the practice of prophylactic salpingectomy is still in its infancy. The early paradigm shift will certainly contribute to the existing literature and potentially improve our ability to reduce risk of ovarian cancer, without compromising the overall health of our patients through surgical castration. The current hypothesis of STIC as the primary site for ovarian cancer carcinogenesis is certainly plausible and may allow for improved screening modalities and targeted therapies, which may lead to improved outcomes for our patients.
Caroline C. Billingsley, M.D., and Larry J. Copeland, M.D., who are gynecologic oncologists at Ohio State University, Columbus, wrote this commentary.
LAS VEGAS – Removing the fallopian tubes at the time of pelvic surgeries as a potential means of reducing ovarian cancer risk appears to be a movement that’s picking up steam in clinical practice.
A recent survey of 234 U.S. gynecologists showed prophylactic bilateral salpingectomy is catching on when performed in conjunction with hysterectomy, but far less so for tubal sterilization, Dr. Austin Findley observed at the annual Minimally Invasive Surgery Week.
A total of 54% of respondents indicated they routinely perform salpingectomy at the time of hysterectomy in an effort to reduce the risk of ovarian cancer as well as to avoid the need for reoperations. However, only 7% of the gynecologic surgeons said they perform salpingectomy for tubal sterilization, even though 58% of respondents stated they believe the procedure is the most effective form of tubal sterilization (J. Minim. Invasive Gynecol. 2013;20:517-21).
“In my experience at various hospitals, I think these numbers are a pretty accurate reflection of what folks are doing,” commented Dr. Findley of Wright State University in Dayton, Ohio.
The prophylactic salpingectomy movement is an outgrowth of the tubal hypothesis of ovarian cancer.
“There is now increasing and dramatic evidence to suggest that most ovarian cancers actually originate in the distal fallopian tubes. I think this is a concept most people are unaware of or are just becoming accustomed to. The tubal hypothesis represents a major paradigm shift in the way we think about ovarian cancers. The previous belief that excessive ovulation is a cause of ovarian cancer is no longer regarded as accurate,” he explained at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
Ovarian cancer is the No. 1 cause of mortality from gynecologic malignancy, accounting for more than 14,000 deaths per year, according to National Cancer Institute data. The lifetime risk of the malignancy is 1.3%, with the average age at diagnosis being 63 years.
Only 10%-15% of ovarian cancers occur in women at high risk for the malignancy because they carry a BRCA mutation or other predisposing gene. The vast majority of ovarian cancer deaths are caused by high-grade serous tumors that have been shown to be strongly associated with precursor lesions in the distal fallopian tubes of women at low risk for the malignancy.
There is no proven-effective screening program or risk-reduction method for these low-risk women. However, with 600,000 hysterectomies and 700,000 tubal sterilizations being performed annually in the United States, prophylactic salpingectomy has been advocated as an attractive opportunity to potentially reduce ovarian cancer risk. Other common pelvic surgeries in which it might be used for this purpose include excision of endometriosis and laparoscopy for pelvic pain. It also has recently been shown to be feasible and safe post partum at cesarean or vaginal delivery (Obstet. Gynecol. 2014 [doi: 10.1097/01.AOG.0000447427.80479.ae]).
But the key word here is “potentially.” It must be emphasized that at present the ovarian cancer prevention benefit of prophylactic salpingectomy remains hypothetical; in theory, the procedure should reduce ovarian cancer risk, but there is not yet persuasive evidence that it actually does, Dr. Findley emphasized at the meeting, presented by the Society of Laparoendoscopic Surgeons and affiliated societies.
In contrast, one well-established ancillary benefit of prophylactic salpingectomy is that it eliminates the need for future reoperation for salpingectomy. This was demonstrated in a large Danish cohort study including close to 10,000 women undergoing hysterectomy and a similar number undergoing sterilization procedures. Among the nearly two-thirds of hysterectomy patients who had both fallopian tubes retained, there was a 2.13-fold increased likelihood of subsequent salpingectomy, compared with nonhysterectomized women.
Similarly, Danish women who underwent a sterilization procedure with retention of the fallopian tubes – typically tubal ligation with clips – were 2.42 times more likely to undergo subsequent salpingectomy, most often because of the development of hydrosalpinx, infection, ectopic pregnancy, or other complications (BMJ Open 2013;3 [doi:10.1136/bmjopen-2013-002845]).
The most commonly cited potential risk of prophylactic salpingectomy – decreased ovarian function – now appears to be a nonissue. This was demonstrated in a recent retrospective Italian study (Gynecol. Oncol. 2013;129:448-51) as well as in a pilot randomized controlled trial conducted by Dr. Findley and his coworkers (Fertil. Steril. 2013;100:1704-8), which appears to have answered many skeptics’ concerns. Indeed, Dr. Findley’s coinvestigator Dr. Matthew Siedhoff said he has recently been approached by researchers interested in collaborating in a larger confirmatory randomized trial, but all parties eventually agreed it was a no-go.
“It’s a little hard to demonstrate equipoise for a larger randomized controlled trial. We’re beyond that now, given that prophylactic salpingectomy really doesn’t seem to make a difference as far as ovarian function,” according to Dr. Siedhoff, director of the division of advanced laparoscopy and pelvic pain at the University of North Carolina, Chapel Hill.
Another oft-expressed reservation about salpingectomy as a means of reducing ovarian cancer risk in women seeking sterilization is that salpingectomy’s irreversibility may lead to “tubal regret” on the part of patients who later change their mind about further pregnancies. However, Dr. Findley cited a recent editorial whose authors criticized colleagues who made that claim. The editorialists argued that the tubal regret concern indicates surgeons weren’t really listening to their patients’ true desires during the informed consent conversation.
“We should not have started thinking about salpingectomy for female sterilization only once a decrease in ovarian cancer risk became part of the equation,” they declared (Obstet. Gynecol. 2014;124:596-9).
Dr. Findley noted that Canadian gynecologists are leading the way forward regarding prophylactic salpingectomy as a potential method of ovarian cancer prevention. The Society of Gynecologic Oncology of Canada in a 2011 policy statement recommended patient/physician discussion of the risks and benefits of bilateral salpingectomy for patients undergoing hysterectomy or requesting permanent sterilization. The Society of Gynecologic Oncology followed suit with a similar clinical practice statement in late 2013.
Additionally, the Canadian group declared that a national ovarian cancer prevention study focused on fallopian tube removal should be a top priority.
Gynecologic oncologists in British Columbia recently reported the eye-catching results of a province-wide educational initiative targeting gynecologists and their patients. In 2010, all British Columbia gynecologists had to attend a course on the role of the fallopian tubes in the development of ovarian cancer, during which they were advised to consider performing bilateral salpingectomy for ovarian cancer risk reduction.
Surgical practice changed dramatically in British Columbia in response. In 2009 – the year prior to the physician education initiative – salpingectomy was utilized in just 0.3% of permanent sterilization procedures. In 2010, it was 11.4%. By 2011, it was 33.3%.
Similarly, only 7% of hysterectomies performed in British Columbia in 2009 were accompanied by bilateral salpingectomy. This figure climbed to 23% in 2010 and jumped further to 35% in 2011. Meanwhile the rate of hysterectomy with bilateral salpingo-oophorectomy remained steady over time at 44% (Am. J. Obstet. Gynecol. 2014;210:471.e1-11).
This project was conducted in collaboration with the B.C. Cancer Agency, which maintains comprehensive province-wide registries. Over time, it will be possible to demonstrate whether prophylactic salpingectomy is indeed associated with a reduction in the incidence of ovarian cancer. “I think this study demonstrated that there’s a lack of awareness on this issue, but also [that there’s] potential effectiveness of introducing an educational initiative like this in changing our practice patterns. As we start talking more about this issue amongst our colleagues and our patients, we’re more likely to see a practice pattern shift in the United States as well,” Dr. Findley commented.
He reported having no financial conflicts with regard to his presentation.
LAS VEGAS – Removing the fallopian tubes at the time of pelvic surgeries as a potential means of reducing ovarian cancer risk appears to be a movement that’s picking up steam in clinical practice.
A recent survey of 234 U.S. gynecologists showed prophylactic bilateral salpingectomy is catching on when performed in conjunction with hysterectomy, but far less so for tubal sterilization, Dr. Austin Findley observed at the annual Minimally Invasive Surgery Week.
A total of 54% of respondents indicated they routinely perform salpingectomy at the time of hysterectomy in an effort to reduce the risk of ovarian cancer as well as to avoid the need for reoperations. However, only 7% of the gynecologic surgeons said they perform salpingectomy for tubal sterilization, even though 58% of respondents stated they believe the procedure is the most effective form of tubal sterilization (J. Minim. Invasive Gynecol. 2013;20:517-21).
“In my experience at various hospitals, I think these numbers are a pretty accurate reflection of what folks are doing,” commented Dr. Findley of Wright State University in Dayton, Ohio.
The prophylactic salpingectomy movement is an outgrowth of the tubal hypothesis of ovarian cancer.
“There is now increasing and dramatic evidence to suggest that most ovarian cancers actually originate in the distal fallopian tubes. I think this is a concept most people are unaware of or are just becoming accustomed to. The tubal hypothesis represents a major paradigm shift in the way we think about ovarian cancers. The previous belief that excessive ovulation is a cause of ovarian cancer is no longer regarded as accurate,” he explained at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
Ovarian cancer is the No. 1 cause of mortality from gynecologic malignancy, accounting for more than 14,000 deaths per year, according to National Cancer Institute data. The lifetime risk of the malignancy is 1.3%, with the average age at diagnosis being 63 years.
Only 10%-15% of ovarian cancers occur in women at high risk for the malignancy because they carry a BRCA mutation or other predisposing gene. The vast majority of ovarian cancer deaths are caused by high-grade serous tumors that have been shown to be strongly associated with precursor lesions in the distal fallopian tubes of women at low risk for the malignancy.
There is no proven-effective screening program or risk-reduction method for these low-risk women. However, with 600,000 hysterectomies and 700,000 tubal sterilizations being performed annually in the United States, prophylactic salpingectomy has been advocated as an attractive opportunity to potentially reduce ovarian cancer risk. Other common pelvic surgeries in which it might be used for this purpose include excision of endometriosis and laparoscopy for pelvic pain. It also has recently been shown to be feasible and safe post partum at cesarean or vaginal delivery (Obstet. Gynecol. 2014 [doi: 10.1097/01.AOG.0000447427.80479.ae]).
But the key word here is “potentially.” It must be emphasized that at present the ovarian cancer prevention benefit of prophylactic salpingectomy remains hypothetical; in theory, the procedure should reduce ovarian cancer risk, but there is not yet persuasive evidence that it actually does, Dr. Findley emphasized at the meeting, presented by the Society of Laparoendoscopic Surgeons and affiliated societies.
In contrast, one well-established ancillary benefit of prophylactic salpingectomy is that it eliminates the need for future reoperation for salpingectomy. This was demonstrated in a large Danish cohort study including close to 10,000 women undergoing hysterectomy and a similar number undergoing sterilization procedures. Among the nearly two-thirds of hysterectomy patients who had both fallopian tubes retained, there was a 2.13-fold increased likelihood of subsequent salpingectomy, compared with nonhysterectomized women.
Similarly, Danish women who underwent a sterilization procedure with retention of the fallopian tubes – typically tubal ligation with clips – were 2.42 times more likely to undergo subsequent salpingectomy, most often because of the development of hydrosalpinx, infection, ectopic pregnancy, or other complications (BMJ Open 2013;3 [doi:10.1136/bmjopen-2013-002845]).
The most commonly cited potential risk of prophylactic salpingectomy – decreased ovarian function – now appears to be a nonissue. This was demonstrated in a recent retrospective Italian study (Gynecol. Oncol. 2013;129:448-51) as well as in a pilot randomized controlled trial conducted by Dr. Findley and his coworkers (Fertil. Steril. 2013;100:1704-8), which appears to have answered many skeptics’ concerns. Indeed, Dr. Findley’s coinvestigator Dr. Matthew Siedhoff said he has recently been approached by researchers interested in collaborating in a larger confirmatory randomized trial, but all parties eventually agreed it was a no-go.
“It’s a little hard to demonstrate equipoise for a larger randomized controlled trial. We’re beyond that now, given that prophylactic salpingectomy really doesn’t seem to make a difference as far as ovarian function,” according to Dr. Siedhoff, director of the division of advanced laparoscopy and pelvic pain at the University of North Carolina, Chapel Hill.
Another oft-expressed reservation about salpingectomy as a means of reducing ovarian cancer risk in women seeking sterilization is that salpingectomy’s irreversibility may lead to “tubal regret” on the part of patients who later change their mind about further pregnancies. However, Dr. Findley cited a recent editorial whose authors criticized colleagues who made that claim. The editorialists argued that the tubal regret concern indicates surgeons weren’t really listening to their patients’ true desires during the informed consent conversation.
“We should not have started thinking about salpingectomy for female sterilization only once a decrease in ovarian cancer risk became part of the equation,” they declared (Obstet. Gynecol. 2014;124:596-9).
Dr. Findley noted that Canadian gynecologists are leading the way forward regarding prophylactic salpingectomy as a potential method of ovarian cancer prevention. The Society of Gynecologic Oncology of Canada in a 2011 policy statement recommended patient/physician discussion of the risks and benefits of bilateral salpingectomy for patients undergoing hysterectomy or requesting permanent sterilization. The Society of Gynecologic Oncology followed suit with a similar clinical practice statement in late 2013.
Additionally, the Canadian group declared that a national ovarian cancer prevention study focused on fallopian tube removal should be a top priority.
Gynecologic oncologists in British Columbia recently reported the eye-catching results of a province-wide educational initiative targeting gynecologists and their patients. In 2010, all British Columbia gynecologists had to attend a course on the role of the fallopian tubes in the development of ovarian cancer, during which they were advised to consider performing bilateral salpingectomy for ovarian cancer risk reduction.
Surgical practice changed dramatically in British Columbia in response. In 2009 – the year prior to the physician education initiative – salpingectomy was utilized in just 0.3% of permanent sterilization procedures. In 2010, it was 11.4%. By 2011, it was 33.3%.
Similarly, only 7% of hysterectomies performed in British Columbia in 2009 were accompanied by bilateral salpingectomy. This figure climbed to 23% in 2010 and jumped further to 35% in 2011. Meanwhile the rate of hysterectomy with bilateral salpingo-oophorectomy remained steady over time at 44% (Am. J. Obstet. Gynecol. 2014;210:471.e1-11).
This project was conducted in collaboration with the B.C. Cancer Agency, which maintains comprehensive province-wide registries. Over time, it will be possible to demonstrate whether prophylactic salpingectomy is indeed associated with a reduction in the incidence of ovarian cancer. “I think this study demonstrated that there’s a lack of awareness on this issue, but also [that there’s] potential effectiveness of introducing an educational initiative like this in changing our practice patterns. As we start talking more about this issue amongst our colleagues and our patients, we’re more likely to see a practice pattern shift in the United States as well,” Dr. Findley commented.
He reported having no financial conflicts with regard to his presentation.
EXPERT ANALYSIS FROM MINIMALLY INVASIVE SURGERY WEEK
Laparoscopic resection improved short-term outcomes in patients with cirrhotic liver cancer
Patients with liver cancer and cirrhosis who underwent laparoscopic hepatic resection had fewer complications, shorter hospital stays, no port site recurrences, and no significant difference in survival, compared with patients who had open resections, according to a single-center, 10-year study published online in the Journal of the American College of Surgeons.
The study is the first to report long-term favorable results of laparoscopic hepatic resection for liver cancer in patients with cirrhosis, said Dr. Yo-ichi Yamashita and associates at Kyushu University, Fukuoka, Japan. Based on the data, laparoscopic instead of open resection should be considered for patients with cirrhosis whose hepatocellular carcinomas fall within the Milan criteria, the investigators said (J. Am. Coll. Surg. 2014 Sept. 9 [doi: 10.1016/j.jamcollsurg.2014.09.003]).
The retrospective study included 162 patients with cirrhosis and hepatocellular carcinoma within the Milan criteria. In all, 99 patients had open hepatic resections, while 63 underwent laparoscopic resections, the investigators said. Only 10% of laparoscopy patients had complications of grade 2 or higher, compared with 26% of open surgery cases (P = .0459), they reported. And while 7% of the open surgery patients developed ascites after surgery, none of the laparoscopy patients did (P = .0077), possibly because they experienced less tissue damage and because the deliberate induction of carbon dioxide pneumoperitoneum during laparoscopy can reduce local inflammatory responses, the researchers said. Laparoscopy patients also averaged 6 fewer days in the hospital after their procedures, Dr. Yamashita and associates reported (median length of stay, 10 vs. 16 days; P = .0008).
The laparoscopy group had no port site recurrences or peritoneal seeding of hepatocellular carcinoma, the investigators noted. Rates of disease-free and overall survival were similar between the two groups (P = .5196 and P = .6791, respectively), they added. Five-year and 10-year overall survival rates were 78% and 69% for laparoscopy patients, and were 77% and 57% for open resection patients, they said.
The authors disclosed no funding sources and reported having no conflicts of interest.
Patients with liver cancer and cirrhosis who underwent laparoscopic hepatic resection had fewer complications, shorter hospital stays, no port site recurrences, and no significant difference in survival, compared with patients who had open resections, according to a single-center, 10-year study published online in the Journal of the American College of Surgeons.
The study is the first to report long-term favorable results of laparoscopic hepatic resection for liver cancer in patients with cirrhosis, said Dr. Yo-ichi Yamashita and associates at Kyushu University, Fukuoka, Japan. Based on the data, laparoscopic instead of open resection should be considered for patients with cirrhosis whose hepatocellular carcinomas fall within the Milan criteria, the investigators said (J. Am. Coll. Surg. 2014 Sept. 9 [doi: 10.1016/j.jamcollsurg.2014.09.003]).
The retrospective study included 162 patients with cirrhosis and hepatocellular carcinoma within the Milan criteria. In all, 99 patients had open hepatic resections, while 63 underwent laparoscopic resections, the investigators said. Only 10% of laparoscopy patients had complications of grade 2 or higher, compared with 26% of open surgery cases (P = .0459), they reported. And while 7% of the open surgery patients developed ascites after surgery, none of the laparoscopy patients did (P = .0077), possibly because they experienced less tissue damage and because the deliberate induction of carbon dioxide pneumoperitoneum during laparoscopy can reduce local inflammatory responses, the researchers said. Laparoscopy patients also averaged 6 fewer days in the hospital after their procedures, Dr. Yamashita and associates reported (median length of stay, 10 vs. 16 days; P = .0008).
The laparoscopy group had no port site recurrences or peritoneal seeding of hepatocellular carcinoma, the investigators noted. Rates of disease-free and overall survival were similar between the two groups (P = .5196 and P = .6791, respectively), they added. Five-year and 10-year overall survival rates were 78% and 69% for laparoscopy patients, and were 77% and 57% for open resection patients, they said.
The authors disclosed no funding sources and reported having no conflicts of interest.
Patients with liver cancer and cirrhosis who underwent laparoscopic hepatic resection had fewer complications, shorter hospital stays, no port site recurrences, and no significant difference in survival, compared with patients who had open resections, according to a single-center, 10-year study published online in the Journal of the American College of Surgeons.
The study is the first to report long-term favorable results of laparoscopic hepatic resection for liver cancer in patients with cirrhosis, said Dr. Yo-ichi Yamashita and associates at Kyushu University, Fukuoka, Japan. Based on the data, laparoscopic instead of open resection should be considered for patients with cirrhosis whose hepatocellular carcinomas fall within the Milan criteria, the investigators said (J. Am. Coll. Surg. 2014 Sept. 9 [doi: 10.1016/j.jamcollsurg.2014.09.003]).
The retrospective study included 162 patients with cirrhosis and hepatocellular carcinoma within the Milan criteria. In all, 99 patients had open hepatic resections, while 63 underwent laparoscopic resections, the investigators said. Only 10% of laparoscopy patients had complications of grade 2 or higher, compared with 26% of open surgery cases (P = .0459), they reported. And while 7% of the open surgery patients developed ascites after surgery, none of the laparoscopy patients did (P = .0077), possibly because they experienced less tissue damage and because the deliberate induction of carbon dioxide pneumoperitoneum during laparoscopy can reduce local inflammatory responses, the researchers said. Laparoscopy patients also averaged 6 fewer days in the hospital after their procedures, Dr. Yamashita and associates reported (median length of stay, 10 vs. 16 days; P = .0008).
The laparoscopy group had no port site recurrences or peritoneal seeding of hepatocellular carcinoma, the investigators noted. Rates of disease-free and overall survival were similar between the two groups (P = .5196 and P = .6791, respectively), they added. Five-year and 10-year overall survival rates were 78% and 69% for laparoscopy patients, and were 77% and 57% for open resection patients, they said.
The authors disclosed no funding sources and reported having no conflicts of interest.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
Key clinical point: Patients with liver cancer and cirrhosis who underwent laparoscopic hepatic resections had lower postoperative morbidity and shorter hospital stays than patients who had open resections.
Major finding: Laparoscopy patients had significantly less postoperative morbidity (10% vs. 26%; P = .0459) and shorter hospital stays (10 vs. 16 days; P = .0008), compared with patients who underwent open resection, with no port site recurrences and no significant differences in long-term survival.
Data source:Retrospective, single-center study of 162 patients with cirrhosis and primary hepatocellular carcinoma who underwent curative hepatic resections, of whom 99 underwent open procedures and 63 underwent laparoscopies.
Disclosures: The authors disclosed no funding sources and reported having no conflicts of interest.
Health experts push flu vaccination for patients and providers
WASHINGTON – The best way to fight the flu is to “get a flu shot this year and every year,” said Dr. Thomas Frieden.
Last year was a bad year, especially for adults aged 18-64 years, who had their highest rate of flu-related hospitalizations since the 2009 pandemic, Dr. Frieden, director of the Centers for Disease Control and Prevention, Atlanta, said at a recent press conference sponsored by the National Foundation for Infectious Diseases.
Approximately 150 million doses of flu vaccine are expected to be available this season, and there should be plenty to go around, he emphasized.
The CDC has a three-pronged message for patients and health care providers: Get vaccinated, stay home if you are sick, and take medications if they are prescribed.
Overall vaccination coverage of the U.S. population aged 6 months and older was 46% in 2013-2014, which was a slight increase from the previous year. The upward trend is encouraging, Dr. Frieden said, especially the 65% of adults aged 65 and older and 70% of children aged 6 months to 5 years who received flu vaccination last year, but there is certainly room for improvement.
Fortunately, there are more flu vaccine options, and places to get them, than ever before, said Dr. William Schaffner, professor and chairman of the department of preventive medicine at Vanderbilt University, Nashville, past president of the NFID. Choices include the traditional intramuscular shot, an intradermal version with a smaller needle, nasal spray, an egg-free vaccine, and a high-dose vaccine especially for adults aged 65 and older, he said.
This year, for the first time, the CDC recommends the nasal spray as the preferred flu vaccination method for children aged 2-8 years if they have no contraindications, said Dr. Paul A. Offit, chief of the division of infectious diseases and director of the vaccine education center of the Children’s Hospital of Philadelphia. Parents, however, should not postpone vaccinating their children with a different vaccine if the spray is not available, since all are effective, he said.
Although flu vaccination rates in children are up, coverage of pregnant women held steady, said Dr. Laura E. Riley, medical director of labor and delivery in the obstetrics service of Massachusetts General Hospital, Boston.
Vaccination coverage among pregnant women during the 2013-2014 flu season was 52%, only a slight increase from 51% the previous year. Coverage rates varied by age: 46% for pregnant women aged 18-24 years, 57% for those aged 24-34 years, and 53% for those aged 35-49 years.
Numerous studies have shown that the flu shot is safe during all trimesters, although the nasal spray is not recommended for pregnant women, Dr. Riley noted. Employ each doctor visit as an opportunity to offer and recommend flu vaccination. “A strong recommendation” from a health care provider has been significantly associated with increased vaccination across all demographic groups of pregnant women, she said.
Health care personnel seem to be getting the message about flu vaccination, said Dr. Schaffner. Overall, 75% of health care personnel received a flu vaccine last year, including 92% of physicians and 90% of nurses.
He exhorted health care workers to keep the trend going and to get vaccinated for their patients’ health, as well as their own.
“Immunization of health care personnel is, first and foremost, a patient safety issue,” he said.
Complete data on vaccination coverage in health care workers and patient populations were published in the CDC’s Morbidity and Mortality Weekly Report on Sept. 19 (MMWR 2014;63:805-11). Data on flu vaccine coverage in the U.S. population are available online.
WASHINGTON – The best way to fight the flu is to “get a flu shot this year and every year,” said Dr. Thomas Frieden.
Last year was a bad year, especially for adults aged 18-64 years, who had their highest rate of flu-related hospitalizations since the 2009 pandemic, Dr. Frieden, director of the Centers for Disease Control and Prevention, Atlanta, said at a recent press conference sponsored by the National Foundation for Infectious Diseases.
Approximately 150 million doses of flu vaccine are expected to be available this season, and there should be plenty to go around, he emphasized.
The CDC has a three-pronged message for patients and health care providers: Get vaccinated, stay home if you are sick, and take medications if they are prescribed.
Overall vaccination coverage of the U.S. population aged 6 months and older was 46% in 2013-2014, which was a slight increase from the previous year. The upward trend is encouraging, Dr. Frieden said, especially the 65% of adults aged 65 and older and 70% of children aged 6 months to 5 years who received flu vaccination last year, but there is certainly room for improvement.
Fortunately, there are more flu vaccine options, and places to get them, than ever before, said Dr. William Schaffner, professor and chairman of the department of preventive medicine at Vanderbilt University, Nashville, past president of the NFID. Choices include the traditional intramuscular shot, an intradermal version with a smaller needle, nasal spray, an egg-free vaccine, and a high-dose vaccine especially for adults aged 65 and older, he said.
This year, for the first time, the CDC recommends the nasal spray as the preferred flu vaccination method for children aged 2-8 years if they have no contraindications, said Dr. Paul A. Offit, chief of the division of infectious diseases and director of the vaccine education center of the Children’s Hospital of Philadelphia. Parents, however, should not postpone vaccinating their children with a different vaccine if the spray is not available, since all are effective, he said.
Although flu vaccination rates in children are up, coverage of pregnant women held steady, said Dr. Laura E. Riley, medical director of labor and delivery in the obstetrics service of Massachusetts General Hospital, Boston.
Vaccination coverage among pregnant women during the 2013-2014 flu season was 52%, only a slight increase from 51% the previous year. Coverage rates varied by age: 46% for pregnant women aged 18-24 years, 57% for those aged 24-34 years, and 53% for those aged 35-49 years.
Numerous studies have shown that the flu shot is safe during all trimesters, although the nasal spray is not recommended for pregnant women, Dr. Riley noted. Employ each doctor visit as an opportunity to offer and recommend flu vaccination. “A strong recommendation” from a health care provider has been significantly associated with increased vaccination across all demographic groups of pregnant women, she said.
Health care personnel seem to be getting the message about flu vaccination, said Dr. Schaffner. Overall, 75% of health care personnel received a flu vaccine last year, including 92% of physicians and 90% of nurses.
He exhorted health care workers to keep the trend going and to get vaccinated for their patients’ health, as well as their own.
“Immunization of health care personnel is, first and foremost, a patient safety issue,” he said.
Complete data on vaccination coverage in health care workers and patient populations were published in the CDC’s Morbidity and Mortality Weekly Report on Sept. 19 (MMWR 2014;63:805-11). Data on flu vaccine coverage in the U.S. population are available online.
WASHINGTON – The best way to fight the flu is to “get a flu shot this year and every year,” said Dr. Thomas Frieden.
Last year was a bad year, especially for adults aged 18-64 years, who had their highest rate of flu-related hospitalizations since the 2009 pandemic, Dr. Frieden, director of the Centers for Disease Control and Prevention, Atlanta, said at a recent press conference sponsored by the National Foundation for Infectious Diseases.
Approximately 150 million doses of flu vaccine are expected to be available this season, and there should be plenty to go around, he emphasized.
The CDC has a three-pronged message for patients and health care providers: Get vaccinated, stay home if you are sick, and take medications if they are prescribed.
Overall vaccination coverage of the U.S. population aged 6 months and older was 46% in 2013-2014, which was a slight increase from the previous year. The upward trend is encouraging, Dr. Frieden said, especially the 65% of adults aged 65 and older and 70% of children aged 6 months to 5 years who received flu vaccination last year, but there is certainly room for improvement.
Fortunately, there are more flu vaccine options, and places to get them, than ever before, said Dr. William Schaffner, professor and chairman of the department of preventive medicine at Vanderbilt University, Nashville, past president of the NFID. Choices include the traditional intramuscular shot, an intradermal version with a smaller needle, nasal spray, an egg-free vaccine, and a high-dose vaccine especially for adults aged 65 and older, he said.
This year, for the first time, the CDC recommends the nasal spray as the preferred flu vaccination method for children aged 2-8 years if they have no contraindications, said Dr. Paul A. Offit, chief of the division of infectious diseases and director of the vaccine education center of the Children’s Hospital of Philadelphia. Parents, however, should not postpone vaccinating their children with a different vaccine if the spray is not available, since all are effective, he said.
Although flu vaccination rates in children are up, coverage of pregnant women held steady, said Dr. Laura E. Riley, medical director of labor and delivery in the obstetrics service of Massachusetts General Hospital, Boston.
Vaccination coverage among pregnant women during the 2013-2014 flu season was 52%, only a slight increase from 51% the previous year. Coverage rates varied by age: 46% for pregnant women aged 18-24 years, 57% for those aged 24-34 years, and 53% for those aged 35-49 years.
Numerous studies have shown that the flu shot is safe during all trimesters, although the nasal spray is not recommended for pregnant women, Dr. Riley noted. Employ each doctor visit as an opportunity to offer and recommend flu vaccination. “A strong recommendation” from a health care provider has been significantly associated with increased vaccination across all demographic groups of pregnant women, she said.
Health care personnel seem to be getting the message about flu vaccination, said Dr. Schaffner. Overall, 75% of health care personnel received a flu vaccine last year, including 92% of physicians and 90% of nurses.
He exhorted health care workers to keep the trend going and to get vaccinated for their patients’ health, as well as their own.
“Immunization of health care personnel is, first and foremost, a patient safety issue,” he said.
Complete data on vaccination coverage in health care workers and patient populations were published in the CDC’s Morbidity and Mortality Weekly Report on Sept. 19 (MMWR 2014;63:805-11). Data on flu vaccine coverage in the U.S. population are available online.
Closing large dermal defects much like a Victorian corset
EDINBURGH – Barbed absorbable sutures are a useful new tool to facilitate dermal closure of facial and nonfacial defects following tumor resection.
“These are not the bad old sutures that you might of heard about before, that were nonabsorbable sutures and attempted for use in cosmetic procedures,” Dr. John Strasswimmer said at the 15th World Congress on Cancers of the Skin.
Last year, Dr. Strasswimmer, medical director of melanoma and cutaneous oncology at the Lynn Cancer Institute in Boca Raton, Fla., reported his initial experience using a procedure he calls “Corseta” to close a large Mohs defect on the trunk of an 83-year-old man (JAMA Dermatol. 2013;149:853-4).
The procedure employs a barbed, bioabsorbable suture (Ethicon’s Stratafix and Covidien’s V-Loc) that is run in a continuous vertical looping manner in the subcutaneous layer, with minimal to no undermining of the wound. Undermining is typically used in cutaneous surgery to relieve tension or provide structure around anatomical landmarks, but it can increase the risk of bleeding, swelling, and patient discomfort, he said.
Instead, the first suture pass is placed in the deepest portion of the subcutaneous tissue and brought out within the more superficial subcutaneous layer. Each bite of the barbed suture extends peripherally at least 2.0 cm from the edge of the wound, so the point of tension is lateral to the wound margins. At every two passes, tension is placed evenly across the sutures to close the deepest layer of tissue and to engage the barbs, much like closing of a Victorian corset, Dr. Strasswimmer said.
The second arm of the suture is passed in a similar manner in the subcutaneous plane, superficial to the first pass.
“This is a lacing, not a suturing technique,” he said. “You get tissue approximation, but more importantly, because we’re bringing in all that deep tissue, you automatically get beautiful wound-edge eversion and very nice cosmetic results.”
Because the sutures have barbs cut into them, however, a 0-0 weight polydioxane or other absorbable material suture can have a breaking strength of a #2-0 suture. “You have to look very carefully at the manufacturer’s sizing and strength requirements,” Dr. Strasswimmer cautioned.
Since their initial case report, Dr. Strasswimmer and his colleagues have expanded use of the Corseta technique to more than 600 facial and nonfacial reconstructions. The Corseta procedure is not as helpful for curved topography such as the central face or scalp, he said in an interview. Still, of the 600 or so cases, none required conversion to another closure technique.
“The traditional closure technique would not have worked in those challenging cases,” Dr. Strasswimmer said. “In the most difficult situations, such as older patients with severely atrophic skin, even the best suturing won’t work. In that case, the Corseta at least produces a partial closure, thereby reducing the wound and accelerating healing.” The Corseta procedure is often coupled with tumescent anesthesia to decrease the risk of bleeding, particularly in patients on anticoagulation, he noted.
The conference was sponsored by the Skin Cancer Foundation.
EDINBURGH – Barbed absorbable sutures are a useful new tool to facilitate dermal closure of facial and nonfacial defects following tumor resection.
“These are not the bad old sutures that you might of heard about before, that were nonabsorbable sutures and attempted for use in cosmetic procedures,” Dr. John Strasswimmer said at the 15th World Congress on Cancers of the Skin.
Last year, Dr. Strasswimmer, medical director of melanoma and cutaneous oncology at the Lynn Cancer Institute in Boca Raton, Fla., reported his initial experience using a procedure he calls “Corseta” to close a large Mohs defect on the trunk of an 83-year-old man (JAMA Dermatol. 2013;149:853-4).
The procedure employs a barbed, bioabsorbable suture (Ethicon’s Stratafix and Covidien’s V-Loc) that is run in a continuous vertical looping manner in the subcutaneous layer, with minimal to no undermining of the wound. Undermining is typically used in cutaneous surgery to relieve tension or provide structure around anatomical landmarks, but it can increase the risk of bleeding, swelling, and patient discomfort, he said.
Instead, the first suture pass is placed in the deepest portion of the subcutaneous tissue and brought out within the more superficial subcutaneous layer. Each bite of the barbed suture extends peripherally at least 2.0 cm from the edge of the wound, so the point of tension is lateral to the wound margins. At every two passes, tension is placed evenly across the sutures to close the deepest layer of tissue and to engage the barbs, much like closing of a Victorian corset, Dr. Strasswimmer said.
The second arm of the suture is passed in a similar manner in the subcutaneous plane, superficial to the first pass.
“This is a lacing, not a suturing technique,” he said. “You get tissue approximation, but more importantly, because we’re bringing in all that deep tissue, you automatically get beautiful wound-edge eversion and very nice cosmetic results.”
Because the sutures have barbs cut into them, however, a 0-0 weight polydioxane or other absorbable material suture can have a breaking strength of a #2-0 suture. “You have to look very carefully at the manufacturer’s sizing and strength requirements,” Dr. Strasswimmer cautioned.
Since their initial case report, Dr. Strasswimmer and his colleagues have expanded use of the Corseta technique to more than 600 facial and nonfacial reconstructions. The Corseta procedure is not as helpful for curved topography such as the central face or scalp, he said in an interview. Still, of the 600 or so cases, none required conversion to another closure technique.
“The traditional closure technique would not have worked in those challenging cases,” Dr. Strasswimmer said. “In the most difficult situations, such as older patients with severely atrophic skin, even the best suturing won’t work. In that case, the Corseta at least produces a partial closure, thereby reducing the wound and accelerating healing.” The Corseta procedure is often coupled with tumescent anesthesia to decrease the risk of bleeding, particularly in patients on anticoagulation, he noted.
The conference was sponsored by the Skin Cancer Foundation.
EDINBURGH – Barbed absorbable sutures are a useful new tool to facilitate dermal closure of facial and nonfacial defects following tumor resection.
“These are not the bad old sutures that you might of heard about before, that were nonabsorbable sutures and attempted for use in cosmetic procedures,” Dr. John Strasswimmer said at the 15th World Congress on Cancers of the Skin.
Last year, Dr. Strasswimmer, medical director of melanoma and cutaneous oncology at the Lynn Cancer Institute in Boca Raton, Fla., reported his initial experience using a procedure he calls “Corseta” to close a large Mohs defect on the trunk of an 83-year-old man (JAMA Dermatol. 2013;149:853-4).
The procedure employs a barbed, bioabsorbable suture (Ethicon’s Stratafix and Covidien’s V-Loc) that is run in a continuous vertical looping manner in the subcutaneous layer, with minimal to no undermining of the wound. Undermining is typically used in cutaneous surgery to relieve tension or provide structure around anatomical landmarks, but it can increase the risk of bleeding, swelling, and patient discomfort, he said.
Instead, the first suture pass is placed in the deepest portion of the subcutaneous tissue and brought out within the more superficial subcutaneous layer. Each bite of the barbed suture extends peripherally at least 2.0 cm from the edge of the wound, so the point of tension is lateral to the wound margins. At every two passes, tension is placed evenly across the sutures to close the deepest layer of tissue and to engage the barbs, much like closing of a Victorian corset, Dr. Strasswimmer said.
The second arm of the suture is passed in a similar manner in the subcutaneous plane, superficial to the first pass.
“This is a lacing, not a suturing technique,” he said. “You get tissue approximation, but more importantly, because we’re bringing in all that deep tissue, you automatically get beautiful wound-edge eversion and very nice cosmetic results.”
Because the sutures have barbs cut into them, however, a 0-0 weight polydioxane or other absorbable material suture can have a breaking strength of a #2-0 suture. “You have to look very carefully at the manufacturer’s sizing and strength requirements,” Dr. Strasswimmer cautioned.
Since their initial case report, Dr. Strasswimmer and his colleagues have expanded use of the Corseta technique to more than 600 facial and nonfacial reconstructions. The Corseta procedure is not as helpful for curved topography such as the central face or scalp, he said in an interview. Still, of the 600 or so cases, none required conversion to another closure technique.
“The traditional closure technique would not have worked in those challenging cases,” Dr. Strasswimmer said. “In the most difficult situations, such as older patients with severely atrophic skin, even the best suturing won’t work. In that case, the Corseta at least produces a partial closure, thereby reducing the wound and accelerating healing.” The Corseta procedure is often coupled with tumescent anesthesia to decrease the risk of bleeding, particularly in patients on anticoagulation, he noted.
The conference was sponsored by the Skin Cancer Foundation.
EXPERT ANALYSIS FROM WCCS 2014
Splenectomy rare after first 24 hours in trauma, early trial results show
PHILADELPHIA – Delayed splenectomy for delayed splenic rupture is a feared complication of forgoing surgery on a blunt spleen injury, but early results of the Splenic Injury Outcomes Trial show that the vast majority of trauma patients rarely need splenectomy after the first 24 hours, and the use of angiography and CT to monitor healing of the spleen in asymptomatic patients may not be necessary in most cases.
Dr. Ben Zarzaur of Indiana University, Indianapolis, reported on early results from the Splenic Injury Outcomes Trial study of 383 patients from 11 level 1 trauma centers. The aim of the study is to provide a snapshot of how trauma surgeons manage critically injured patients with a spleen injury. He presented the findings at the annual meeting of the American Association for the Surgery of Trauma, which sponsored the trial.
“Out of that cohort, the in-hospital risk of splenectomy after the first 24 hours was about 3.6%, and after discharge the risk out to 6 months was 0.27%,” Dr. Zarzaur reported. In all, 12 patients had their spleens removed within 10 days of injury, and 4 patients died of causes not spleen related. The trial followed 87% of enrolled patients for up to 6 months after treatment.
One goal of the trial was to determine if the use of angiography and follow-up CT were necessary in monitoring the spleen in critically injured patients. The findings may help clarify management of patients with grade 1 injuries, Dr. Zarzaur said. “These patients likely don’t need any further interventions, because no [individuals with] grade 1 injuries had a splenectomy after the first 24 hours,” he said.
“Patients probably need close observation for 10-14 days after blunt spleen injury, and that can occur as an inpatient or can be done as an outpatient with very explicit instructions to return to the hospital if they have signs or symptoms of bleeding,” he said.
The trial also evaluated whether embolization made a difference in salvaging spleens. “There was no statistical difference in splenectomy rates in patients who were embolized versus those who were not,” Dr. Zarzaur said. He noted, however, that in more patients with grade 3 injuries or greater, the incidence of splenectomy was lower after embolization, but it was not statistically significant. “With regard to angiography embolization, it’s likely helpful. There are probably some high-risk patient populations, and we should concentrate on those in order to maximize the benefit and minimize the risk of patients with blunt splenic injury,” he said.
“There are about 39,000 spleen injuries a year, about 35,000 of which will be managed nonoperatively successfully over 24 hours,” Dr. Zarzaur said after his presentation. “So if we do the calculations for all injury grades, if we do angiography in these patients at the rates we saw in the study, we would save 84 additional spleens. If we concentrate on just higher-grade injuries – just grades 3 to 5 – we might save an additional 274 spleens a year. I think we have to ask ourselves, is that worth all the effort and cost and radiation exposure of angiography?”
That’s not a question the trial authors can answer at this point, Dr. Zarzaur said. A larger randomized clinical trial would be in order to get there, so he said the next step for him and the Splenic Injury Outcomes Trial coauthors is to put together a protocol for that.
Dr. Zarzaur reported having no relevant financial disclosures.
PHILADELPHIA – Delayed splenectomy for delayed splenic rupture is a feared complication of forgoing surgery on a blunt spleen injury, but early results of the Splenic Injury Outcomes Trial show that the vast majority of trauma patients rarely need splenectomy after the first 24 hours, and the use of angiography and CT to monitor healing of the spleen in asymptomatic patients may not be necessary in most cases.
Dr. Ben Zarzaur of Indiana University, Indianapolis, reported on early results from the Splenic Injury Outcomes Trial study of 383 patients from 11 level 1 trauma centers. The aim of the study is to provide a snapshot of how trauma surgeons manage critically injured patients with a spleen injury. He presented the findings at the annual meeting of the American Association for the Surgery of Trauma, which sponsored the trial.
“Out of that cohort, the in-hospital risk of splenectomy after the first 24 hours was about 3.6%, and after discharge the risk out to 6 months was 0.27%,” Dr. Zarzaur reported. In all, 12 patients had their spleens removed within 10 days of injury, and 4 patients died of causes not spleen related. The trial followed 87% of enrolled patients for up to 6 months after treatment.
One goal of the trial was to determine if the use of angiography and follow-up CT were necessary in monitoring the spleen in critically injured patients. The findings may help clarify management of patients with grade 1 injuries, Dr. Zarzaur said. “These patients likely don’t need any further interventions, because no [individuals with] grade 1 injuries had a splenectomy after the first 24 hours,” he said.
“Patients probably need close observation for 10-14 days after blunt spleen injury, and that can occur as an inpatient or can be done as an outpatient with very explicit instructions to return to the hospital if they have signs or symptoms of bleeding,” he said.
The trial also evaluated whether embolization made a difference in salvaging spleens. “There was no statistical difference in splenectomy rates in patients who were embolized versus those who were not,” Dr. Zarzaur said. He noted, however, that in more patients with grade 3 injuries or greater, the incidence of splenectomy was lower after embolization, but it was not statistically significant. “With regard to angiography embolization, it’s likely helpful. There are probably some high-risk patient populations, and we should concentrate on those in order to maximize the benefit and minimize the risk of patients with blunt splenic injury,” he said.
“There are about 39,000 spleen injuries a year, about 35,000 of which will be managed nonoperatively successfully over 24 hours,” Dr. Zarzaur said after his presentation. “So if we do the calculations for all injury grades, if we do angiography in these patients at the rates we saw in the study, we would save 84 additional spleens. If we concentrate on just higher-grade injuries – just grades 3 to 5 – we might save an additional 274 spleens a year. I think we have to ask ourselves, is that worth all the effort and cost and radiation exposure of angiography?”
That’s not a question the trial authors can answer at this point, Dr. Zarzaur said. A larger randomized clinical trial would be in order to get there, so he said the next step for him and the Splenic Injury Outcomes Trial coauthors is to put together a protocol for that.
Dr. Zarzaur reported having no relevant financial disclosures.
PHILADELPHIA – Delayed splenectomy for delayed splenic rupture is a feared complication of forgoing surgery on a blunt spleen injury, but early results of the Splenic Injury Outcomes Trial show that the vast majority of trauma patients rarely need splenectomy after the first 24 hours, and the use of angiography and CT to monitor healing of the spleen in asymptomatic patients may not be necessary in most cases.
Dr. Ben Zarzaur of Indiana University, Indianapolis, reported on early results from the Splenic Injury Outcomes Trial study of 383 patients from 11 level 1 trauma centers. The aim of the study is to provide a snapshot of how trauma surgeons manage critically injured patients with a spleen injury. He presented the findings at the annual meeting of the American Association for the Surgery of Trauma, which sponsored the trial.
“Out of that cohort, the in-hospital risk of splenectomy after the first 24 hours was about 3.6%, and after discharge the risk out to 6 months was 0.27%,” Dr. Zarzaur reported. In all, 12 patients had their spleens removed within 10 days of injury, and 4 patients died of causes not spleen related. The trial followed 87% of enrolled patients for up to 6 months after treatment.
One goal of the trial was to determine if the use of angiography and follow-up CT were necessary in monitoring the spleen in critically injured patients. The findings may help clarify management of patients with grade 1 injuries, Dr. Zarzaur said. “These patients likely don’t need any further interventions, because no [individuals with] grade 1 injuries had a splenectomy after the first 24 hours,” he said.
“Patients probably need close observation for 10-14 days after blunt spleen injury, and that can occur as an inpatient or can be done as an outpatient with very explicit instructions to return to the hospital if they have signs or symptoms of bleeding,” he said.
The trial also evaluated whether embolization made a difference in salvaging spleens. “There was no statistical difference in splenectomy rates in patients who were embolized versus those who were not,” Dr. Zarzaur said. He noted, however, that in more patients with grade 3 injuries or greater, the incidence of splenectomy was lower after embolization, but it was not statistically significant. “With regard to angiography embolization, it’s likely helpful. There are probably some high-risk patient populations, and we should concentrate on those in order to maximize the benefit and minimize the risk of patients with blunt splenic injury,” he said.
“There are about 39,000 spleen injuries a year, about 35,000 of which will be managed nonoperatively successfully over 24 hours,” Dr. Zarzaur said after his presentation. “So if we do the calculations for all injury grades, if we do angiography in these patients at the rates we saw in the study, we would save 84 additional spleens. If we concentrate on just higher-grade injuries – just grades 3 to 5 – we might save an additional 274 spleens a year. I think we have to ask ourselves, is that worth all the effort and cost and radiation exposure of angiography?”
That’s not a question the trial authors can answer at this point, Dr. Zarzaur said. A larger randomized clinical trial would be in order to get there, so he said the next step for him and the Splenic Injury Outcomes Trial coauthors is to put together a protocol for that.
Dr. Zarzaur reported having no relevant financial disclosures.
AT THE AAST ANNUAL MEETING
Key clinical point: Follow-up angiography and CT may not be necessary for trauma patients with blunt spleen injury because of the low rates of splenectomy after 24 hours.
Major finding: Only 3.6% of trauma patients required in-hospital splenectomy between 24 hours and 9 days after surgery; the vast majority were discharged with spleen intact.
Data source: Splenic Injury Outcomes Trial, a prospective study involving 383 patients at 11 level 1 trauma centers.
Disclosures: Dr. Zarzaur reported having no relevant financial disclosures.
PROOVIT registry results make case for expansion
PHILADELPHIA – About 7 in 10 patients who enter the trauma bay with vascular injuries are male, and about one-third have an Injury Severity Score of 15 or higher. Penetrating injuries account for more than a third of these cases, and prehospital tourniquet for extremity injuries is used in one in five patients.
These are some of the data from the first year of a registry that is gathering previously uncollected information on management of trauma-related vascular injuries, such as rates of arterial injuries, nonoperative management and amputations. Study coordinator Dr. Joseph DuBose of the University of Texas Health Science Center, Houston, reported on the PROOVIT registry – for Prospective Observational Vascular Injury Treatment – at the annual meeting of the American Association for the Surgery of Trauma (AAST).
PROOVIT grew out of an effort of the AAST leaders, Dr. DuBose said. “We discussed this with the senior leadership of the AAST as well as the AAST Multicenter Committee, recognizing there really is no registry presently that absolutely links the key variables specific to the management of vascular injury and subsequent outcome,” Dr. DuBose said.
While a number of registries exist, including the National Trauma Databank of the American College of Surgeons and the Society for Vascular Surgery Vascular Quality Initiative, along with a number of military registries, they lack key details or are not readily applicable to vascular injury in trauma, he said.
“We desire to establish an aggregate database of information on presentation, diagnosis, management, but to be acutely definitive on surveillance and outcomes in vascular trauma,” Dr. DuBose said.
First-year registry data also looked at secondary outcomes to help establish links between treatments and outcomes specific to vascular trauma, he said. PROOVIT collected data on 542 injuries from 14 trauma centers, 13 of them Level 1 centers, since February 2013. The study population included 484 arterial injuries and 79 major venous injuries (a cohort of patients had both). The most common injury cause was motor vehicle crash, accounting for 28% of all injuries, and the most common types of injuries were blunt trauma (47%) and penetrating trauma (36.5%).
PROOVIT also did a deep dive on the condition of trauma victims. Average Injury Severity Score was 20.7, and was greater than 15 in about a third of patients. A total of 121% of patients were hypotensive with systolic BP of 90 mm Hg or less, and nearly 30% of patients had some sort of vascular injury. The most common method for identifying vascular trauma injuries was CT angiography, used in nearly 40% of cases. “This database provides us an opportunity to look very closely at specific types of injury patterns,” Dr. DuBose said.
“We believe the PROOVIT registry is a viable tool based upon our first year of experience for establishing a much needed link between vascular injury management and subsequent outcome and evolving vascular injury care,” he said. The goal is to develop data out to 7 years of follow-up and beyond. “It would be my hope that we could plan that for 10- to 20-year data to collect much-needed information on long-term outcomes,” he said.
Dr. DuBose acknowledged that securing funding and enrolling more Level 2 trauma centers are goals, and that the registry is integral to quality improvement initiatives. “We can look at individual centers that have better outcomes,” he said. “What practice are they doing better than other people?”
Dr. DuBose said the registry continues to accrue patient data and the PROOVIT investigators invite all trauma centers caring for these patient populations to participate in enrollment. Information is available at the AAST multicenter studies webpage (www.aast.org/Research/MultiInstitutionalStudies.aspx), or by contacting the PROOVIT team at [email protected].
Dr. DuBose reported having no relevant financial disclosures.
This is a splendid initiative and enterprise. One might quibble with this early delivery of results to this audience. It is perhaps a bit premature, but it is clearly post-natal, and the results should engender comments that might increase its influence.
The PROOVIT finding that tourniquets were used in 20% of vascular injuries is heartwarming. This would not have occurred 2 decades ago, and it’s a testament to the influence of tactical combat casualty care, However, cost is a determinant for the future of the registry. The cost must be estimated and it must be borne by some body of support.
Dr. Howard Champion is a trauma surgeon in Annapolis, Md. He was the discussant of the presentation at the meeting.
This is a splendid initiative and enterprise. One might quibble with this early delivery of results to this audience. It is perhaps a bit premature, but it is clearly post-natal, and the results should engender comments that might increase its influence.
The PROOVIT finding that tourniquets were used in 20% of vascular injuries is heartwarming. This would not have occurred 2 decades ago, and it’s a testament to the influence of tactical combat casualty care, However, cost is a determinant for the future of the registry. The cost must be estimated and it must be borne by some body of support.
Dr. Howard Champion is a trauma surgeon in Annapolis, Md. He was the discussant of the presentation at the meeting.
This is a splendid initiative and enterprise. One might quibble with this early delivery of results to this audience. It is perhaps a bit premature, but it is clearly post-natal, and the results should engender comments that might increase its influence.
The PROOVIT finding that tourniquets were used in 20% of vascular injuries is heartwarming. This would not have occurred 2 decades ago, and it’s a testament to the influence of tactical combat casualty care, However, cost is a determinant for the future of the registry. The cost must be estimated and it must be borne by some body of support.
Dr. Howard Champion is a trauma surgeon in Annapolis, Md. He was the discussant of the presentation at the meeting.
PHILADELPHIA – About 7 in 10 patients who enter the trauma bay with vascular injuries are male, and about one-third have an Injury Severity Score of 15 or higher. Penetrating injuries account for more than a third of these cases, and prehospital tourniquet for extremity injuries is used in one in five patients.
These are some of the data from the first year of a registry that is gathering previously uncollected information on management of trauma-related vascular injuries, such as rates of arterial injuries, nonoperative management and amputations. Study coordinator Dr. Joseph DuBose of the University of Texas Health Science Center, Houston, reported on the PROOVIT registry – for Prospective Observational Vascular Injury Treatment – at the annual meeting of the American Association for the Surgery of Trauma (AAST).
PROOVIT grew out of an effort of the AAST leaders, Dr. DuBose said. “We discussed this with the senior leadership of the AAST as well as the AAST Multicenter Committee, recognizing there really is no registry presently that absolutely links the key variables specific to the management of vascular injury and subsequent outcome,” Dr. DuBose said.
While a number of registries exist, including the National Trauma Databank of the American College of Surgeons and the Society for Vascular Surgery Vascular Quality Initiative, along with a number of military registries, they lack key details or are not readily applicable to vascular injury in trauma, he said.
“We desire to establish an aggregate database of information on presentation, diagnosis, management, but to be acutely definitive on surveillance and outcomes in vascular trauma,” Dr. DuBose said.
First-year registry data also looked at secondary outcomes to help establish links between treatments and outcomes specific to vascular trauma, he said. PROOVIT collected data on 542 injuries from 14 trauma centers, 13 of them Level 1 centers, since February 2013. The study population included 484 arterial injuries and 79 major venous injuries (a cohort of patients had both). The most common injury cause was motor vehicle crash, accounting for 28% of all injuries, and the most common types of injuries were blunt trauma (47%) and penetrating trauma (36.5%).
PROOVIT also did a deep dive on the condition of trauma victims. Average Injury Severity Score was 20.7, and was greater than 15 in about a third of patients. A total of 121% of patients were hypotensive with systolic BP of 90 mm Hg or less, and nearly 30% of patients had some sort of vascular injury. The most common method for identifying vascular trauma injuries was CT angiography, used in nearly 40% of cases. “This database provides us an opportunity to look very closely at specific types of injury patterns,” Dr. DuBose said.
“We believe the PROOVIT registry is a viable tool based upon our first year of experience for establishing a much needed link between vascular injury management and subsequent outcome and evolving vascular injury care,” he said. The goal is to develop data out to 7 years of follow-up and beyond. “It would be my hope that we could plan that for 10- to 20-year data to collect much-needed information on long-term outcomes,” he said.
Dr. DuBose acknowledged that securing funding and enrolling more Level 2 trauma centers are goals, and that the registry is integral to quality improvement initiatives. “We can look at individual centers that have better outcomes,” he said. “What practice are they doing better than other people?”
Dr. DuBose said the registry continues to accrue patient data and the PROOVIT investigators invite all trauma centers caring for these patient populations to participate in enrollment. Information is available at the AAST multicenter studies webpage (www.aast.org/Research/MultiInstitutionalStudies.aspx), or by contacting the PROOVIT team at [email protected].
Dr. DuBose reported having no relevant financial disclosures.
PHILADELPHIA – About 7 in 10 patients who enter the trauma bay with vascular injuries are male, and about one-third have an Injury Severity Score of 15 or higher. Penetrating injuries account for more than a third of these cases, and prehospital tourniquet for extremity injuries is used in one in five patients.
These are some of the data from the first year of a registry that is gathering previously uncollected information on management of trauma-related vascular injuries, such as rates of arterial injuries, nonoperative management and amputations. Study coordinator Dr. Joseph DuBose of the University of Texas Health Science Center, Houston, reported on the PROOVIT registry – for Prospective Observational Vascular Injury Treatment – at the annual meeting of the American Association for the Surgery of Trauma (AAST).
PROOVIT grew out of an effort of the AAST leaders, Dr. DuBose said. “We discussed this with the senior leadership of the AAST as well as the AAST Multicenter Committee, recognizing there really is no registry presently that absolutely links the key variables specific to the management of vascular injury and subsequent outcome,” Dr. DuBose said.
While a number of registries exist, including the National Trauma Databank of the American College of Surgeons and the Society for Vascular Surgery Vascular Quality Initiative, along with a number of military registries, they lack key details or are not readily applicable to vascular injury in trauma, he said.
“We desire to establish an aggregate database of information on presentation, diagnosis, management, but to be acutely definitive on surveillance and outcomes in vascular trauma,” Dr. DuBose said.
First-year registry data also looked at secondary outcomes to help establish links between treatments and outcomes specific to vascular trauma, he said. PROOVIT collected data on 542 injuries from 14 trauma centers, 13 of them Level 1 centers, since February 2013. The study population included 484 arterial injuries and 79 major venous injuries (a cohort of patients had both). The most common injury cause was motor vehicle crash, accounting for 28% of all injuries, and the most common types of injuries were blunt trauma (47%) and penetrating trauma (36.5%).
PROOVIT also did a deep dive on the condition of trauma victims. Average Injury Severity Score was 20.7, and was greater than 15 in about a third of patients. A total of 121% of patients were hypotensive with systolic BP of 90 mm Hg or less, and nearly 30% of patients had some sort of vascular injury. The most common method for identifying vascular trauma injuries was CT angiography, used in nearly 40% of cases. “This database provides us an opportunity to look very closely at specific types of injury patterns,” Dr. DuBose said.
“We believe the PROOVIT registry is a viable tool based upon our first year of experience for establishing a much needed link between vascular injury management and subsequent outcome and evolving vascular injury care,” he said. The goal is to develop data out to 7 years of follow-up and beyond. “It would be my hope that we could plan that for 10- to 20-year data to collect much-needed information on long-term outcomes,” he said.
Dr. DuBose acknowledged that securing funding and enrolling more Level 2 trauma centers are goals, and that the registry is integral to quality improvement initiatives. “We can look at individual centers that have better outcomes,” he said. “What practice are they doing better than other people?”
Dr. DuBose said the registry continues to accrue patient data and the PROOVIT investigators invite all trauma centers caring for these patient populations to participate in enrollment. Information is available at the AAST multicenter studies webpage (www.aast.org/Research/MultiInstitutionalStudies.aspx), or by contacting the PROOVIT team at [email protected].
Dr. DuBose reported having no relevant financial disclosures.
AT THE AAST ANNUAL MEETING
Key clinical point: Gathering previously uncollected information on management of trauma-related vascular injuries can inform treatment and may improve outcomes.
Major finding: The most common injury cause was motor vehicle crash, accounting for 28% of all injuries, and the most common types of injuries were blunt trauma (47%) and penetrating trauma (36.5%).
Data source: The AAST PROOVIT registry involving 13 Level 1 and 1 Level 2 trauma centers with data on 542 injuries.
Disclosures: Dr. DuBose reported having no relevant financial disclosures.
Morcellation shows favorable risk/benefit ratio in decision analysis
LAS VEGAS – Morcellation during laparoscopic hysterectomy or myomectomy for presumed large fibroids provides slightly better 5-year overall survival and higher quality of life scores than abdominal hysterectomy, according to a new study.
The strength of this soon-to-be-published decision analysis lies in its balance and comprehensive nature. It utilized the best-available published literature to estimate the mortality risk stemming from tissue dissemination of occult leiomyosarcoma through power morcellation – an issue of hot controversy – but it also incorporated the increased risks of procedure-related morbidity and mortality associated with the alternative to morcellation in patients with large fibroids: that is, abdominal hysterectomy, Dr. Matthew Siedhoff explained at the annual Minimally Invasive Surgery Week.
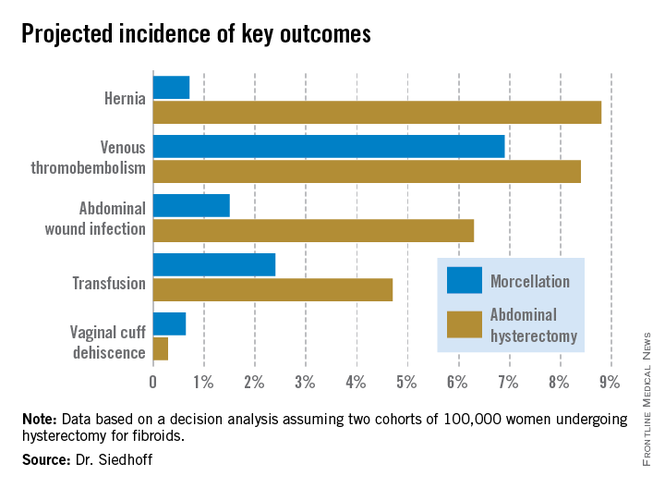
The decision analysis was undertaken in the wake of the Food and Drug Administration’s April 2014 safety warning citing a 1 in 350 risk of occult malignancy in women undergoing hysterectomies or myomectomies for removal of presumed fibroids and that laparoscopic surgeries involving power morcellation performed in women with unsuspected uterine sarcomas may spread cancerous tissue, potentially shortening survival. The attendant publicity has caused considerable alarm and confusion among patients and the general public. The FDA is currently deliberating possible actions ranging from a black box warning to outright banning of power morcellation.
Meanwhile, several prominent medical centers, including Brigham and Women’s Hospital, Massachusetts General Hospital, both in Boston, and the Cleveland Clinic, have banned the use of power morcellation – precipitously, in Dr. Siedhoff’s view.
Also since the FDA safety statement, Johnson & Johnson has taken its power morcellator off the market and several large insurance companies have announced plans to halt reimbursement when power morcellation is used in gynecologic surgery. However, exactly how that would happen is unclear because there is no billing code associated with power morcellation, and it would be arduous for insurers to actually read through all operative reports.
“This decision analysis is a tool for surgeons and patients to help make informed decisions. It balances the FDA analysis, which pretty much just emphasizes morcellation risk to the exclusion of all the known benefits of laparoscopy. The analysis argues that reducing the risk associated with morcellation – perhaps through the use of specimen containment or preoperative leiomyosarcoma diagnosis – is a better approach than abandoning minimally invasive gynecologic surgery for fibroids. That would be throwing the baby out with the bathwater,” declared Dr. Siedhoff, an ob.gyn. and director of the division of advanced laparoscopy and pelvic pain at the University of North Carolina, Chapel Hill.
A decision analysis entails probability modeling of outcomes based upon consensus event rates obtained from studies in the published literature.
“It’s helpful to do a decision analysis when you can’t do a randomized controlled trial, which you certainly can’t for this issue,” he observed at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
The decision analysis was carried out by Dr. Siedhoff and coinvestigators at the University of North Carolina at Chapel Hill, with department of obstetrics and gynecology chair Dr. Daniel Clarke-Peterson as senior author. The researchers assumed two hypothetical cohorts of 100,000 women undergoing hysterectomy for fibroids large enough that surgical options were limited to laparoscopic hysterectomy with morcellation or abdominal hysterectomy. The primary outcomes were 5-year overall mortality and quality of life as measured in quality-adjusted life-years (QALYs).
The analysis assumed that among the 100,000 women in each group there would be 120 FIGO Stage I or II occult leiomyosarcomas, with an associated 59% 5-year mortality from cancer. It was further assumed that intraperitoneal dissemination of tumor via morcellation would in effect boost those cancers to FIGO Stage III, with 72% mortality at 5 years. This would result in 86 deaths from leiomyosarcoma over 5 years in the morcellation group, compared with 71 in women who underwent abdominal hysterectomy. However, this was counterbalanced by more hysterectomy-related deaths in the abdominal hysterectomy group: 32, compared with 12 in women undergoing morcellation. The final 5-year tally: 98 deaths overall in the morcellation group and 103 in the abdominal hysterectomy group.
QALYs are calculated by estimating how much a given adverse event – for example, venous thromboembolism, along with its attendant treatment and potential further complications – would diminish a theoretical year of otherwise perfect health. The total QALYs in the group of 100,000 women undergoing morcellation was estimated at 499,171, compared with 490,711 over 5 years in the abdominal hysterectomy group. That’s because with the exception of vaginal cuff dehiscence, all of the other complications assessed in the decision analysis, including wound infections, transfusions, hernias, and venous thromboembolisms, were more frequent in the abdominal hysterectomy group. The forthcoming final publication will include the citations on which all of the event probabilities were based.
An alternative and perhaps more readily grasped way of expressing the QALY results is that patients undergoing laparoscopic hysterectomy enjoyed an additional 0.85 QALY, or roughly 1 extra month of life in perfect health over a 5-year time period, Dr. Siedhoff explained.
The decision analysis didn’t include the well-established facts that laparoscopic hysterectomy entails less postoperative pain, a shorter average hospital length of stay, and faster return to daily activities.
Dr. Siedhoff was quick to assert that the true incidence of occult leiomyosarcoma in women undergoing surgery for presumed fibroids is unknown. An American College of Obstetricians and Gynecologist’s position statement issued earlier this year quoted an estimate of 1 in 500. The FDA cited a figure of 1 in 350. But when the North Carolina researchers examined the 10 studies published during 1990-2013, upon which the FDA based its estimate, the investigators felt compelled to reject 6 of them because of poor quality. For example, several studies included morcellation in patients with preoperative known or suspected sarcoma, even though morcellation should absolutely never be done in that situation. Based upon a weighted analysis of the remaining four highest-quality studies, the investigators came up with an estimate of 12 cases/10,000 women.
Noting that the largest of the studies in the FDA analysis included just 1,584 women with 2 cases of leiomyosarcoma, Dr. Siedhoff said, “I think it’s important to point out that really important decisions are being made on awfully small numerators and denominators. The truth of the matter is we have no idea what the true number is. It could be twice as high as our estimate or half as low.”
He admitted that he has been personally affected by the rancorous tone of recent public debate regarding morcellation safety, in which the procedure’s defenders often are demonized.
“It’s been confusing to me why in the Wall Street Journal they talk about these evil doctors who want to use this technique, as if it somehow benefits us. It’s not easier to do laparoscopic surgery, and it’s certainly not easier to morcellate tissue. The only reason that we’re talking about this is because we care about the outcomes for our patients,” the gynecologic surgeon said at the meeting presented by the Society of Laparoendoscopic Surgeons and affiliated societies. “One of the things that has been most difficult about all this,” he continued, “is the way that the information has moved from some very vocal people who feel strongly about this issue to the level of the lay person that you see in the elevator, or worse yet, your own patient. I think it’s almost like a game of telephone, so that by the time it gets down to a person who’s not a surgeon, the message is ‘morcellation causes cancer.’”Not only is the true prevalence of occult malignancy in women undergoing laparoscopic surgery for removal of fibroids unclear, but the data on the adverse impact of morcellation in this situation is sketchy as well. To date, it consists of two single-center retrospective studies. The more recent report, from Brigham and Women’s Hospital, involved 19 patients who underwent morcellation and 39 who had a total abdominal hysterectomy, all found to have leiomyosarcoma. The cancer recurrence rate was significantly higher in women who had morcellation, by a margin of 74% to 51%. However, there was no significant difference in overall survival (Cancer 2014 [doi:10.1002/cncr.28844]).
In contrast, an earlier Korean study involving a consecutive series comprised of 25 patients with occult leiomyosarcoma who underwent morcellation and 31 with total abdominal hysterectomy found a significant difference in 5-year overall survival: 46% in the morcellation group, and what Dr. Siedhoff deemed an unusually favorable 73% in the total abdominal hysterectomy patients (Gynecol. Oncol. 2011;122:255-9).
There is a great unmet need for a reliable preoperative method to distinguish leiomyosarcomas from benign fibroids. Imaging is of limited value. Endometrial biopsy is rarely positive. No biomarkers have been identified. Clinical factors that increase the likelihood of leiomyosarcoma include rapid growth, African American ethnicity, older age, a history of pelvic radiation, and the presence of the retinoblastoma gene.
In his own practice, Dr. Siedhoff sometimes uses specimen retrieval bags when performing morcellation, but finds the currently available versions to be cumbersome and a challenge to work with. Besides, he noted, there is to date no evidence that they are actually effective in reducing leiomyosarcoma recurrence risk. He was a member of an AAGL task force which in May issued a position statement on morcellation, which noted, “Use of morcellation within specimen retrieval pouches for containment of benign or malignant uterine tissue requires significant skill and experience, and use of specimen retrieval pouches should be further investigated for safety and outcomes in a controlled setting.”
Dr. Siedhoff reported having no financial conflicts regarding the decision analysis, conducted with university funds.
LAS VEGAS – Morcellation during laparoscopic hysterectomy or myomectomy for presumed large fibroids provides slightly better 5-year overall survival and higher quality of life scores than abdominal hysterectomy, according to a new study.
The strength of this soon-to-be-published decision analysis lies in its balance and comprehensive nature. It utilized the best-available published literature to estimate the mortality risk stemming from tissue dissemination of occult leiomyosarcoma through power morcellation – an issue of hot controversy – but it also incorporated the increased risks of procedure-related morbidity and mortality associated with the alternative to morcellation in patients with large fibroids: that is, abdominal hysterectomy, Dr. Matthew Siedhoff explained at the annual Minimally Invasive Surgery Week.
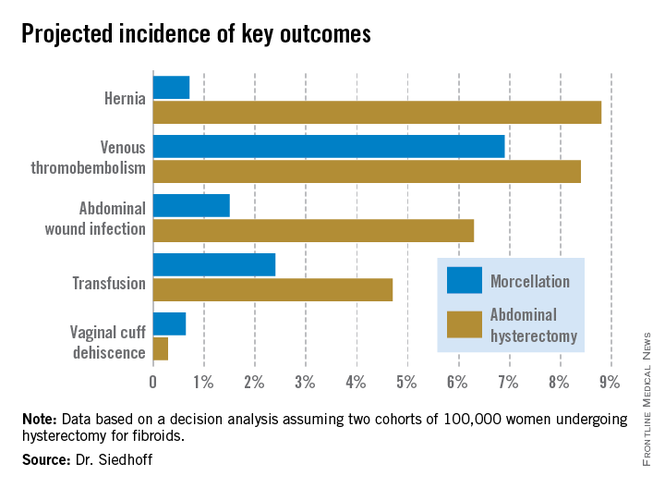
The decision analysis was undertaken in the wake of the Food and Drug Administration’s April 2014 safety warning citing a 1 in 350 risk of occult malignancy in women undergoing hysterectomies or myomectomies for removal of presumed fibroids and that laparoscopic surgeries involving power morcellation performed in women with unsuspected uterine sarcomas may spread cancerous tissue, potentially shortening survival. The attendant publicity has caused considerable alarm and confusion among patients and the general public. The FDA is currently deliberating possible actions ranging from a black box warning to outright banning of power morcellation.
Meanwhile, several prominent medical centers, including Brigham and Women’s Hospital, Massachusetts General Hospital, both in Boston, and the Cleveland Clinic, have banned the use of power morcellation – precipitously, in Dr. Siedhoff’s view.
Also since the FDA safety statement, Johnson & Johnson has taken its power morcellator off the market and several large insurance companies have announced plans to halt reimbursement when power morcellation is used in gynecologic surgery. However, exactly how that would happen is unclear because there is no billing code associated with power morcellation, and it would be arduous for insurers to actually read through all operative reports.
“This decision analysis is a tool for surgeons and patients to help make informed decisions. It balances the FDA analysis, which pretty much just emphasizes morcellation risk to the exclusion of all the known benefits of laparoscopy. The analysis argues that reducing the risk associated with morcellation – perhaps through the use of specimen containment or preoperative leiomyosarcoma diagnosis – is a better approach than abandoning minimally invasive gynecologic surgery for fibroids. That would be throwing the baby out with the bathwater,” declared Dr. Siedhoff, an ob.gyn. and director of the division of advanced laparoscopy and pelvic pain at the University of North Carolina, Chapel Hill.
A decision analysis entails probability modeling of outcomes based upon consensus event rates obtained from studies in the published literature.
“It’s helpful to do a decision analysis when you can’t do a randomized controlled trial, which you certainly can’t for this issue,” he observed at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
The decision analysis was carried out by Dr. Siedhoff and coinvestigators at the University of North Carolina at Chapel Hill, with department of obstetrics and gynecology chair Dr. Daniel Clarke-Peterson as senior author. The researchers assumed two hypothetical cohorts of 100,000 women undergoing hysterectomy for fibroids large enough that surgical options were limited to laparoscopic hysterectomy with morcellation or abdominal hysterectomy. The primary outcomes were 5-year overall mortality and quality of life as measured in quality-adjusted life-years (QALYs).
The analysis assumed that among the 100,000 women in each group there would be 120 FIGO Stage I or II occult leiomyosarcomas, with an associated 59% 5-year mortality from cancer. It was further assumed that intraperitoneal dissemination of tumor via morcellation would in effect boost those cancers to FIGO Stage III, with 72% mortality at 5 years. This would result in 86 deaths from leiomyosarcoma over 5 years in the morcellation group, compared with 71 in women who underwent abdominal hysterectomy. However, this was counterbalanced by more hysterectomy-related deaths in the abdominal hysterectomy group: 32, compared with 12 in women undergoing morcellation. The final 5-year tally: 98 deaths overall in the morcellation group and 103 in the abdominal hysterectomy group.
QALYs are calculated by estimating how much a given adverse event – for example, venous thromboembolism, along with its attendant treatment and potential further complications – would diminish a theoretical year of otherwise perfect health. The total QALYs in the group of 100,000 women undergoing morcellation was estimated at 499,171, compared with 490,711 over 5 years in the abdominal hysterectomy group. That’s because with the exception of vaginal cuff dehiscence, all of the other complications assessed in the decision analysis, including wound infections, transfusions, hernias, and venous thromboembolisms, were more frequent in the abdominal hysterectomy group. The forthcoming final publication will include the citations on which all of the event probabilities were based.
An alternative and perhaps more readily grasped way of expressing the QALY results is that patients undergoing laparoscopic hysterectomy enjoyed an additional 0.85 QALY, or roughly 1 extra month of life in perfect health over a 5-year time period, Dr. Siedhoff explained.
The decision analysis didn’t include the well-established facts that laparoscopic hysterectomy entails less postoperative pain, a shorter average hospital length of stay, and faster return to daily activities.
Dr. Siedhoff was quick to assert that the true incidence of occult leiomyosarcoma in women undergoing surgery for presumed fibroids is unknown. An American College of Obstetricians and Gynecologist’s position statement issued earlier this year quoted an estimate of 1 in 500. The FDA cited a figure of 1 in 350. But when the North Carolina researchers examined the 10 studies published during 1990-2013, upon which the FDA based its estimate, the investigators felt compelled to reject 6 of them because of poor quality. For example, several studies included morcellation in patients with preoperative known or suspected sarcoma, even though morcellation should absolutely never be done in that situation. Based upon a weighted analysis of the remaining four highest-quality studies, the investigators came up with an estimate of 12 cases/10,000 women.
Noting that the largest of the studies in the FDA analysis included just 1,584 women with 2 cases of leiomyosarcoma, Dr. Siedhoff said, “I think it’s important to point out that really important decisions are being made on awfully small numerators and denominators. The truth of the matter is we have no idea what the true number is. It could be twice as high as our estimate or half as low.”
He admitted that he has been personally affected by the rancorous tone of recent public debate regarding morcellation safety, in which the procedure’s defenders often are demonized.
“It’s been confusing to me why in the Wall Street Journal they talk about these evil doctors who want to use this technique, as if it somehow benefits us. It’s not easier to do laparoscopic surgery, and it’s certainly not easier to morcellate tissue. The only reason that we’re talking about this is because we care about the outcomes for our patients,” the gynecologic surgeon said at the meeting presented by the Society of Laparoendoscopic Surgeons and affiliated societies. “One of the things that has been most difficult about all this,” he continued, “is the way that the information has moved from some very vocal people who feel strongly about this issue to the level of the lay person that you see in the elevator, or worse yet, your own patient. I think it’s almost like a game of telephone, so that by the time it gets down to a person who’s not a surgeon, the message is ‘morcellation causes cancer.’”Not only is the true prevalence of occult malignancy in women undergoing laparoscopic surgery for removal of fibroids unclear, but the data on the adverse impact of morcellation in this situation is sketchy as well. To date, it consists of two single-center retrospective studies. The more recent report, from Brigham and Women’s Hospital, involved 19 patients who underwent morcellation and 39 who had a total abdominal hysterectomy, all found to have leiomyosarcoma. The cancer recurrence rate was significantly higher in women who had morcellation, by a margin of 74% to 51%. However, there was no significant difference in overall survival (Cancer 2014 [doi:10.1002/cncr.28844]).
In contrast, an earlier Korean study involving a consecutive series comprised of 25 patients with occult leiomyosarcoma who underwent morcellation and 31 with total abdominal hysterectomy found a significant difference in 5-year overall survival: 46% in the morcellation group, and what Dr. Siedhoff deemed an unusually favorable 73% in the total abdominal hysterectomy patients (Gynecol. Oncol. 2011;122:255-9).
There is a great unmet need for a reliable preoperative method to distinguish leiomyosarcomas from benign fibroids. Imaging is of limited value. Endometrial biopsy is rarely positive. No biomarkers have been identified. Clinical factors that increase the likelihood of leiomyosarcoma include rapid growth, African American ethnicity, older age, a history of pelvic radiation, and the presence of the retinoblastoma gene.
In his own practice, Dr. Siedhoff sometimes uses specimen retrieval bags when performing morcellation, but finds the currently available versions to be cumbersome and a challenge to work with. Besides, he noted, there is to date no evidence that they are actually effective in reducing leiomyosarcoma recurrence risk. He was a member of an AAGL task force which in May issued a position statement on morcellation, which noted, “Use of morcellation within specimen retrieval pouches for containment of benign or malignant uterine tissue requires significant skill and experience, and use of specimen retrieval pouches should be further investigated for safety and outcomes in a controlled setting.”
Dr. Siedhoff reported having no financial conflicts regarding the decision analysis, conducted with university funds.
LAS VEGAS – Morcellation during laparoscopic hysterectomy or myomectomy for presumed large fibroids provides slightly better 5-year overall survival and higher quality of life scores than abdominal hysterectomy, according to a new study.
The strength of this soon-to-be-published decision analysis lies in its balance and comprehensive nature. It utilized the best-available published literature to estimate the mortality risk stemming from tissue dissemination of occult leiomyosarcoma through power morcellation – an issue of hot controversy – but it also incorporated the increased risks of procedure-related morbidity and mortality associated with the alternative to morcellation in patients with large fibroids: that is, abdominal hysterectomy, Dr. Matthew Siedhoff explained at the annual Minimally Invasive Surgery Week.
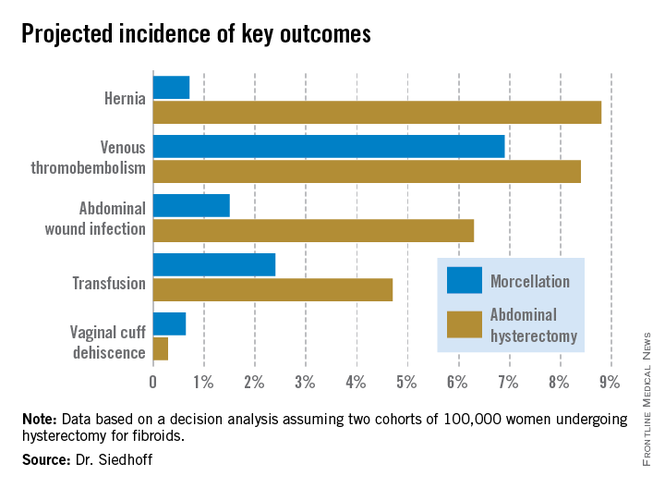
The decision analysis was undertaken in the wake of the Food and Drug Administration’s April 2014 safety warning citing a 1 in 350 risk of occult malignancy in women undergoing hysterectomies or myomectomies for removal of presumed fibroids and that laparoscopic surgeries involving power morcellation performed in women with unsuspected uterine sarcomas may spread cancerous tissue, potentially shortening survival. The attendant publicity has caused considerable alarm and confusion among patients and the general public. The FDA is currently deliberating possible actions ranging from a black box warning to outright banning of power morcellation.
Meanwhile, several prominent medical centers, including Brigham and Women’s Hospital, Massachusetts General Hospital, both in Boston, and the Cleveland Clinic, have banned the use of power morcellation – precipitously, in Dr. Siedhoff’s view.
Also since the FDA safety statement, Johnson & Johnson has taken its power morcellator off the market and several large insurance companies have announced plans to halt reimbursement when power morcellation is used in gynecologic surgery. However, exactly how that would happen is unclear because there is no billing code associated with power morcellation, and it would be arduous for insurers to actually read through all operative reports.
“This decision analysis is a tool for surgeons and patients to help make informed decisions. It balances the FDA analysis, which pretty much just emphasizes morcellation risk to the exclusion of all the known benefits of laparoscopy. The analysis argues that reducing the risk associated with morcellation – perhaps through the use of specimen containment or preoperative leiomyosarcoma diagnosis – is a better approach than abandoning minimally invasive gynecologic surgery for fibroids. That would be throwing the baby out with the bathwater,” declared Dr. Siedhoff, an ob.gyn. and director of the division of advanced laparoscopy and pelvic pain at the University of North Carolina, Chapel Hill.
A decision analysis entails probability modeling of outcomes based upon consensus event rates obtained from studies in the published literature.
“It’s helpful to do a decision analysis when you can’t do a randomized controlled trial, which you certainly can’t for this issue,” he observed at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
The decision analysis was carried out by Dr. Siedhoff and coinvestigators at the University of North Carolina at Chapel Hill, with department of obstetrics and gynecology chair Dr. Daniel Clarke-Peterson as senior author. The researchers assumed two hypothetical cohorts of 100,000 women undergoing hysterectomy for fibroids large enough that surgical options were limited to laparoscopic hysterectomy with morcellation or abdominal hysterectomy. The primary outcomes were 5-year overall mortality and quality of life as measured in quality-adjusted life-years (QALYs).
The analysis assumed that among the 100,000 women in each group there would be 120 FIGO Stage I or II occult leiomyosarcomas, with an associated 59% 5-year mortality from cancer. It was further assumed that intraperitoneal dissemination of tumor via morcellation would in effect boost those cancers to FIGO Stage III, with 72% mortality at 5 years. This would result in 86 deaths from leiomyosarcoma over 5 years in the morcellation group, compared with 71 in women who underwent abdominal hysterectomy. However, this was counterbalanced by more hysterectomy-related deaths in the abdominal hysterectomy group: 32, compared with 12 in women undergoing morcellation. The final 5-year tally: 98 deaths overall in the morcellation group and 103 in the abdominal hysterectomy group.
QALYs are calculated by estimating how much a given adverse event – for example, venous thromboembolism, along with its attendant treatment and potential further complications – would diminish a theoretical year of otherwise perfect health. The total QALYs in the group of 100,000 women undergoing morcellation was estimated at 499,171, compared with 490,711 over 5 years in the abdominal hysterectomy group. That’s because with the exception of vaginal cuff dehiscence, all of the other complications assessed in the decision analysis, including wound infections, transfusions, hernias, and venous thromboembolisms, were more frequent in the abdominal hysterectomy group. The forthcoming final publication will include the citations on which all of the event probabilities were based.
An alternative and perhaps more readily grasped way of expressing the QALY results is that patients undergoing laparoscopic hysterectomy enjoyed an additional 0.85 QALY, or roughly 1 extra month of life in perfect health over a 5-year time period, Dr. Siedhoff explained.
The decision analysis didn’t include the well-established facts that laparoscopic hysterectomy entails less postoperative pain, a shorter average hospital length of stay, and faster return to daily activities.
Dr. Siedhoff was quick to assert that the true incidence of occult leiomyosarcoma in women undergoing surgery for presumed fibroids is unknown. An American College of Obstetricians and Gynecologist’s position statement issued earlier this year quoted an estimate of 1 in 500. The FDA cited a figure of 1 in 350. But when the North Carolina researchers examined the 10 studies published during 1990-2013, upon which the FDA based its estimate, the investigators felt compelled to reject 6 of them because of poor quality. For example, several studies included morcellation in patients with preoperative known or suspected sarcoma, even though morcellation should absolutely never be done in that situation. Based upon a weighted analysis of the remaining four highest-quality studies, the investigators came up with an estimate of 12 cases/10,000 women.
Noting that the largest of the studies in the FDA analysis included just 1,584 women with 2 cases of leiomyosarcoma, Dr. Siedhoff said, “I think it’s important to point out that really important decisions are being made on awfully small numerators and denominators. The truth of the matter is we have no idea what the true number is. It could be twice as high as our estimate or half as low.”
He admitted that he has been personally affected by the rancorous tone of recent public debate regarding morcellation safety, in which the procedure’s defenders often are demonized.
“It’s been confusing to me why in the Wall Street Journal they talk about these evil doctors who want to use this technique, as if it somehow benefits us. It’s not easier to do laparoscopic surgery, and it’s certainly not easier to morcellate tissue. The only reason that we’re talking about this is because we care about the outcomes for our patients,” the gynecologic surgeon said at the meeting presented by the Society of Laparoendoscopic Surgeons and affiliated societies. “One of the things that has been most difficult about all this,” he continued, “is the way that the information has moved from some very vocal people who feel strongly about this issue to the level of the lay person that you see in the elevator, or worse yet, your own patient. I think it’s almost like a game of telephone, so that by the time it gets down to a person who’s not a surgeon, the message is ‘morcellation causes cancer.’”Not only is the true prevalence of occult malignancy in women undergoing laparoscopic surgery for removal of fibroids unclear, but the data on the adverse impact of morcellation in this situation is sketchy as well. To date, it consists of two single-center retrospective studies. The more recent report, from Brigham and Women’s Hospital, involved 19 patients who underwent morcellation and 39 who had a total abdominal hysterectomy, all found to have leiomyosarcoma. The cancer recurrence rate was significantly higher in women who had morcellation, by a margin of 74% to 51%. However, there was no significant difference in overall survival (Cancer 2014 [doi:10.1002/cncr.28844]).
In contrast, an earlier Korean study involving a consecutive series comprised of 25 patients with occult leiomyosarcoma who underwent morcellation and 31 with total abdominal hysterectomy found a significant difference in 5-year overall survival: 46% in the morcellation group, and what Dr. Siedhoff deemed an unusually favorable 73% in the total abdominal hysterectomy patients (Gynecol. Oncol. 2011;122:255-9).
There is a great unmet need for a reliable preoperative method to distinguish leiomyosarcomas from benign fibroids. Imaging is of limited value. Endometrial biopsy is rarely positive. No biomarkers have been identified. Clinical factors that increase the likelihood of leiomyosarcoma include rapid growth, African American ethnicity, older age, a history of pelvic radiation, and the presence of the retinoblastoma gene.
In his own practice, Dr. Siedhoff sometimes uses specimen retrieval bags when performing morcellation, but finds the currently available versions to be cumbersome and a challenge to work with. Besides, he noted, there is to date no evidence that they are actually effective in reducing leiomyosarcoma recurrence risk. He was a member of an AAGL task force which in May issued a position statement on morcellation, which noted, “Use of morcellation within specimen retrieval pouches for containment of benign or malignant uterine tissue requires significant skill and experience, and use of specimen retrieval pouches should be further investigated for safety and outcomes in a controlled setting.”
Dr. Siedhoff reported having no financial conflicts regarding the decision analysis, conducted with university funds.
AT MINIMALLY INVASIVE SURGERY WEEK
Key clinical point: Despite the much-publicized risk of intraperitoneal dissemination of tumor during morcellation in women undergoing laparoscopic hysterectomy for fibroids, the projected 5-year overall survival is better than with abdominal hysterectomy.
Major finding: In a hypothetical population of 200,000 women undergoing hysterectomy for presumed fibroids, laparoscopic surgery with morcellation would result in a projected 98 deaths from all causes during 5 years of follow-up and abdominal hysterectomy would result in 103 deaths.
Data source: This was a decision analysis in which the probabilities of various surgical outcomes based upon studies in the published literature were applied to a hypothetical cohort of 200,000 women undergoing hysterectomy for removal of fibroids, half laparoscopically with morcellation and half via abdominal hysterectomy.
Disclosures: The presenter reported having no financial conflicts of interest regarding the decision analysis study.
CMS website snafu could lead to penalties for meaningful users
First-time meaningful use participants who are using older technology, but who did not get a hardship exemption by July 1, will see their Medicare pay reduced 1% in 2015.
Because of a confluence of factors, a certain subset of physicians who engaged in meaningful use for the first time this year will not be able to attest to their participation by the Oct. 1 deadline set by the Centers for Medicare & Medicaid Services – and thus, will be penalized.
“Physicians are not only frustrated, but perhaps reaching despondency on the topic,” Dr. Steven J. Stack, president-elect of the American Medical Association, said in an interview.
Overall, about half of physicians had not participated in meaningful use as of the beginning of this year. Theoretically, all of them could face the 1% reduction in Medicare pay, though it’s likely that a smaller subset will, Dr. Stack said.
Those who did not meet meaningful use criteria in 2013 and who anticipated that they would not do so again in 2014 could have applied for a hardship exemption by July 1 to avoid a penalty in 2015. Physicians who were starting on the meaningful use process for the first time in 2014 also had until July 1 to apply for that exemption.
After determining that many vendors did not have 2014 software ready for physicians, CMS proposed in late May to give all meaningful users more flexibility. Physicians were told they could use either a 2011 version, a 2014 version, or some combination, and not be penalized in 2015. That proposal was made final in late August.
Applying for that flexibility will be done via the CMS website, which is slated to be ready a few weeks after Oct. 1.
But first-time meaningful use participants must make their attestation to the CMS by Oct. 1.
The bottom line is that first-time participants who are using older technology and did not get the exemption will be penalized.
A CMS spokesman said that they could still receive an incentive payment for 2014 – if they go online in mid-October and apply for the flexibility option.
But Dr. Stack called that little consolation. It is as if the CMS took away $100 of a $1,000 pot and said that there was still $900 left, he said.
“It doesn’t seem reasonable and certainly undermines the premise that they offered any kind of relief,” said Dr. Stack.
Thom Kuhn, a staff member at the American College of Physicians, also said that the CMS explanation was not good enough.
“Failure to have a system ready by the time a final rule is issued is a management failure,” said Mr. Kuhn, in an interview.
Meanwhile, two members of Congress - Rep. Renee Ellmers (R-N.C.) and Rep. Jim Matheson (D-Utah) - have called on the CMS to extend that Oct. 1 deadline. In a letter to the agency, they requested "an administrative delay" for those attempting to attest to meaningful use for the first time in 2014.*
On Twitter @aliciaault
*Correction, 9/24/2014: An earlier version of this article implied that the administrative delay was requested in legislation. It was requested in a letter.
First-time meaningful use participants who are using older technology, but who did not get a hardship exemption by July 1, will see their Medicare pay reduced 1% in 2015.
Because of a confluence of factors, a certain subset of physicians who engaged in meaningful use for the first time this year will not be able to attest to their participation by the Oct. 1 deadline set by the Centers for Medicare & Medicaid Services – and thus, will be penalized.
“Physicians are not only frustrated, but perhaps reaching despondency on the topic,” Dr. Steven J. Stack, president-elect of the American Medical Association, said in an interview.
Overall, about half of physicians had not participated in meaningful use as of the beginning of this year. Theoretically, all of them could face the 1% reduction in Medicare pay, though it’s likely that a smaller subset will, Dr. Stack said.
Those who did not meet meaningful use criteria in 2013 and who anticipated that they would not do so again in 2014 could have applied for a hardship exemption by July 1 to avoid a penalty in 2015. Physicians who were starting on the meaningful use process for the first time in 2014 also had until July 1 to apply for that exemption.
After determining that many vendors did not have 2014 software ready for physicians, CMS proposed in late May to give all meaningful users more flexibility. Physicians were told they could use either a 2011 version, a 2014 version, or some combination, and not be penalized in 2015. That proposal was made final in late August.
Applying for that flexibility will be done via the CMS website, which is slated to be ready a few weeks after Oct. 1.
But first-time meaningful use participants must make their attestation to the CMS by Oct. 1.
The bottom line is that first-time participants who are using older technology and did not get the exemption will be penalized.
A CMS spokesman said that they could still receive an incentive payment for 2014 – if they go online in mid-October and apply for the flexibility option.
But Dr. Stack called that little consolation. It is as if the CMS took away $100 of a $1,000 pot and said that there was still $900 left, he said.
“It doesn’t seem reasonable and certainly undermines the premise that they offered any kind of relief,” said Dr. Stack.
Thom Kuhn, a staff member at the American College of Physicians, also said that the CMS explanation was not good enough.
“Failure to have a system ready by the time a final rule is issued is a management failure,” said Mr. Kuhn, in an interview.
Meanwhile, two members of Congress - Rep. Renee Ellmers (R-N.C.) and Rep. Jim Matheson (D-Utah) - have called on the CMS to extend that Oct. 1 deadline. In a letter to the agency, they requested "an administrative delay" for those attempting to attest to meaningful use for the first time in 2014.*
On Twitter @aliciaault
*Correction, 9/24/2014: An earlier version of this article implied that the administrative delay was requested in legislation. It was requested in a letter.
First-time meaningful use participants who are using older technology, but who did not get a hardship exemption by July 1, will see their Medicare pay reduced 1% in 2015.
Because of a confluence of factors, a certain subset of physicians who engaged in meaningful use for the first time this year will not be able to attest to their participation by the Oct. 1 deadline set by the Centers for Medicare & Medicaid Services – and thus, will be penalized.
“Physicians are not only frustrated, but perhaps reaching despondency on the topic,” Dr. Steven J. Stack, president-elect of the American Medical Association, said in an interview.
Overall, about half of physicians had not participated in meaningful use as of the beginning of this year. Theoretically, all of them could face the 1% reduction in Medicare pay, though it’s likely that a smaller subset will, Dr. Stack said.
Those who did not meet meaningful use criteria in 2013 and who anticipated that they would not do so again in 2014 could have applied for a hardship exemption by July 1 to avoid a penalty in 2015. Physicians who were starting on the meaningful use process for the first time in 2014 also had until July 1 to apply for that exemption.
After determining that many vendors did not have 2014 software ready for physicians, CMS proposed in late May to give all meaningful users more flexibility. Physicians were told they could use either a 2011 version, a 2014 version, or some combination, and not be penalized in 2015. That proposal was made final in late August.
Applying for that flexibility will be done via the CMS website, which is slated to be ready a few weeks after Oct. 1.
But first-time meaningful use participants must make their attestation to the CMS by Oct. 1.
The bottom line is that first-time participants who are using older technology and did not get the exemption will be penalized.
A CMS spokesman said that they could still receive an incentive payment for 2014 – if they go online in mid-October and apply for the flexibility option.
But Dr. Stack called that little consolation. It is as if the CMS took away $100 of a $1,000 pot and said that there was still $900 left, he said.
“It doesn’t seem reasonable and certainly undermines the premise that they offered any kind of relief,” said Dr. Stack.
Thom Kuhn, a staff member at the American College of Physicians, also said that the CMS explanation was not good enough.
“Failure to have a system ready by the time a final rule is issued is a management failure,” said Mr. Kuhn, in an interview.
Meanwhile, two members of Congress - Rep. Renee Ellmers (R-N.C.) and Rep. Jim Matheson (D-Utah) - have called on the CMS to extend that Oct. 1 deadline. In a letter to the agency, they requested "an administrative delay" for those attempting to attest to meaningful use for the first time in 2014.*
On Twitter @aliciaault
*Correction, 9/24/2014: An earlier version of this article implied that the administrative delay was requested in legislation. It was requested in a letter.
Surgeons’ earnings lowest in nonmetropolitan areas
General surgeons from group practices in nonmetropolitan areas earn less than their counterparts in more urban areas, the Medical Group Management Association reported.
The median compensation for general surgeons from nonmetropolitan (population of 49,999 or fewer) areas was $352,000 in 2013, compared with $388,000 for the smallest (50,000-250,000 pop.) metropolitan areas, $412,000 for metro areas between 250,001 and 1 million population, and $385,000 for metro areas with more than 1 million population, according to the MGMA’s “Physician Compensation and Production Survey: 2014 Report Based on 2013 Data.”
Compared with general surgeons, the median income for all specialists was lower in nonmetro and medium-size metro areas and higher in small and large metropolitan areas.
The survey involved 4,197 groups representing 66,299 providers (including nurse practitioners and physician assistants). The MGMA received responses from 223 practices representing 978 general surgeons.
General surgeons from group practices in nonmetropolitan areas earn less than their counterparts in more urban areas, the Medical Group Management Association reported.
The median compensation for general surgeons from nonmetropolitan (population of 49,999 or fewer) areas was $352,000 in 2013, compared with $388,000 for the smallest (50,000-250,000 pop.) metropolitan areas, $412,000 for metro areas between 250,001 and 1 million population, and $385,000 for metro areas with more than 1 million population, according to the MGMA’s “Physician Compensation and Production Survey: 2014 Report Based on 2013 Data.”
Compared with general surgeons, the median income for all specialists was lower in nonmetro and medium-size metro areas and higher in small and large metropolitan areas.
The survey involved 4,197 groups representing 66,299 providers (including nurse practitioners and physician assistants). The MGMA received responses from 223 practices representing 978 general surgeons.
General surgeons from group practices in nonmetropolitan areas earn less than their counterparts in more urban areas, the Medical Group Management Association reported.
The median compensation for general surgeons from nonmetropolitan (population of 49,999 or fewer) areas was $352,000 in 2013, compared with $388,000 for the smallest (50,000-250,000 pop.) metropolitan areas, $412,000 for metro areas between 250,001 and 1 million population, and $385,000 for metro areas with more than 1 million population, according to the MGMA’s “Physician Compensation and Production Survey: 2014 Report Based on 2013 Data.”
Compared with general surgeons, the median income for all specialists was lower in nonmetro and medium-size metro areas and higher in small and large metropolitan areas.
The survey involved 4,197 groups representing 66,299 providers (including nurse practitioners and physician assistants). The MGMA received responses from 223 practices representing 978 general surgeons.
Antihypertension drugs may have clotting protection in obese trauma patients
PHILADELPHIA – Antihypertension drugs may have a protective effect in obese trauma victims, while a better understanding of how obesity influences blood clotting may help trauma surgeons target treatment more effectively, according to early results from two trials involving obese patients.
“With the growing incidence of obesity, coupled with the increased incidence of trauma injury worldwide, elucidating the intimate associations between these two disease states is critical,” Dr. Lucy Kornblith of the University of California, San Francisco, said, reporting on a prospective analysis that determined that obese trauma victims have clotting properties superior to normal patients.
In another paper, investigators at the Washington University, St. Louis evaluated obese trauma victims who took ACE inhibitors or angiotensin receptor blocker (ARB) drugs before injury. “Obese patients who were not on ACE inhibitors or ARB drugs did develop organ failure, while those obese patients who took those medications did not,” Dr. Robert D. Winfield reported at the annual meeting of the American Association for the Surgery of Trauma.
The Washington University trial involved 1,932 patients, 94 of whom took the hypertension drugs and had body mass index (BMI) data available, a group that included 55 obese individuals. Obese subjects on the drugs had Marshall Multiple Organ Dysfunction and Denver-2 Postinjury Multiple Organ Failure trauma scores similar to nonobese patients either taking or not taking the drugs, 5.83 and 2.45, respectively, Dr. Winfield said.
He explained the drugs may enable cells in obese individuals to express more CD47, a cell surface marker that plays a role in monocyte maturation. “What we see in those obese patients taking ACE-I or ARB preinjury is not a perfect response, but it is better,” he said. “We see more cells expressing CD47, and as a result, we see improved cell maturation and tracking and the ability to battle, in particular, secondary insults.”
The next step involves animal research to see if ACE-I and ARB use before and after injury can modulate the immune response, which Washington University and the American College of Surgeons are funding, according to Dr. Winfield.
The UCSF study did not draw any definitive conclusion of the overall benefits or drawbacks of hypercoagulability in the obese after injury, Dr. Kornblith said, although it did suggest one significant deleterious effect in multivariate analysis. “We found that for every 5 kg/m2 increase in BMI, there was an 85% increase in the odds of developing a clinically significant thromboembolic complication,” she said.
The study, using data from “Inflammation and the Host Response to Injury” database, evaluated 377 patients with an average BMI of 25.8 kg/m2, about a quarter of whom were obese (average BMI 33 kg/m2). Obese patients had higher admission platelet counts (302.69 x 103mcL vs. 268.58 x 103mcL) and factor IX (134% vs. 119% activity), and lower D-dimer counts (1.88 vs. 4.00 mc/mL) than did normal weight patients. Thromboelastography measured stronger clot and higher levels of functional fibrinogen on admission in obese patients. These findings of hypercoagulability in the obese patients existed out to 24-120 hours after injury.
Dr. Kornblith acknowledged several limitations to the study. “We do not do a screening duplex ultrasound for DVTs [deep vein thromboses] at our institution,” she said. “There may also be a much higher incidence of nonclinically significant clots in this population; however, based on this, if anything, our numbers are really an underestimate reflecting only those that were clinically significant.”
More work needs to be done, Dr. Kornblith noted. “It is known that excess adipose tissue is far from inert, and it plays a cardinal role in the biology and physiology of obesity,” she said. “Untangling the complex interaction of inflammation, coagulation, and injury will really help contribute to a better understanding of the clinical outcome differences seen in obese patients after injury and may help with targeted treatment of this at-risk group.”
Dr. Kornblith and Dr. Winfield reported having no financial disclosures.
PHILADELPHIA – Antihypertension drugs may have a protective effect in obese trauma victims, while a better understanding of how obesity influences blood clotting may help trauma surgeons target treatment more effectively, according to early results from two trials involving obese patients.
“With the growing incidence of obesity, coupled with the increased incidence of trauma injury worldwide, elucidating the intimate associations between these two disease states is critical,” Dr. Lucy Kornblith of the University of California, San Francisco, said, reporting on a prospective analysis that determined that obese trauma victims have clotting properties superior to normal patients.
In another paper, investigators at the Washington University, St. Louis evaluated obese trauma victims who took ACE inhibitors or angiotensin receptor blocker (ARB) drugs before injury. “Obese patients who were not on ACE inhibitors or ARB drugs did develop organ failure, while those obese patients who took those medications did not,” Dr. Robert D. Winfield reported at the annual meeting of the American Association for the Surgery of Trauma.
The Washington University trial involved 1,932 patients, 94 of whom took the hypertension drugs and had body mass index (BMI) data available, a group that included 55 obese individuals. Obese subjects on the drugs had Marshall Multiple Organ Dysfunction and Denver-2 Postinjury Multiple Organ Failure trauma scores similar to nonobese patients either taking or not taking the drugs, 5.83 and 2.45, respectively, Dr. Winfield said.
He explained the drugs may enable cells in obese individuals to express more CD47, a cell surface marker that plays a role in monocyte maturation. “What we see in those obese patients taking ACE-I or ARB preinjury is not a perfect response, but it is better,” he said. “We see more cells expressing CD47, and as a result, we see improved cell maturation and tracking and the ability to battle, in particular, secondary insults.”
The next step involves animal research to see if ACE-I and ARB use before and after injury can modulate the immune response, which Washington University and the American College of Surgeons are funding, according to Dr. Winfield.
The UCSF study did not draw any definitive conclusion of the overall benefits or drawbacks of hypercoagulability in the obese after injury, Dr. Kornblith said, although it did suggest one significant deleterious effect in multivariate analysis. “We found that for every 5 kg/m2 increase in BMI, there was an 85% increase in the odds of developing a clinically significant thromboembolic complication,” she said.
The study, using data from “Inflammation and the Host Response to Injury” database, evaluated 377 patients with an average BMI of 25.8 kg/m2, about a quarter of whom were obese (average BMI 33 kg/m2). Obese patients had higher admission platelet counts (302.69 x 103mcL vs. 268.58 x 103mcL) and factor IX (134% vs. 119% activity), and lower D-dimer counts (1.88 vs. 4.00 mc/mL) than did normal weight patients. Thromboelastography measured stronger clot and higher levels of functional fibrinogen on admission in obese patients. These findings of hypercoagulability in the obese patients existed out to 24-120 hours after injury.
Dr. Kornblith acknowledged several limitations to the study. “We do not do a screening duplex ultrasound for DVTs [deep vein thromboses] at our institution,” she said. “There may also be a much higher incidence of nonclinically significant clots in this population; however, based on this, if anything, our numbers are really an underestimate reflecting only those that were clinically significant.”
More work needs to be done, Dr. Kornblith noted. “It is known that excess adipose tissue is far from inert, and it plays a cardinal role in the biology and physiology of obesity,” she said. “Untangling the complex interaction of inflammation, coagulation, and injury will really help contribute to a better understanding of the clinical outcome differences seen in obese patients after injury and may help with targeted treatment of this at-risk group.”
Dr. Kornblith and Dr. Winfield reported having no financial disclosures.
PHILADELPHIA – Antihypertension drugs may have a protective effect in obese trauma victims, while a better understanding of how obesity influences blood clotting may help trauma surgeons target treatment more effectively, according to early results from two trials involving obese patients.
“With the growing incidence of obesity, coupled with the increased incidence of trauma injury worldwide, elucidating the intimate associations between these two disease states is critical,” Dr. Lucy Kornblith of the University of California, San Francisco, said, reporting on a prospective analysis that determined that obese trauma victims have clotting properties superior to normal patients.
In another paper, investigators at the Washington University, St. Louis evaluated obese trauma victims who took ACE inhibitors or angiotensin receptor blocker (ARB) drugs before injury. “Obese patients who were not on ACE inhibitors or ARB drugs did develop organ failure, while those obese patients who took those medications did not,” Dr. Robert D. Winfield reported at the annual meeting of the American Association for the Surgery of Trauma.
The Washington University trial involved 1,932 patients, 94 of whom took the hypertension drugs and had body mass index (BMI) data available, a group that included 55 obese individuals. Obese subjects on the drugs had Marshall Multiple Organ Dysfunction and Denver-2 Postinjury Multiple Organ Failure trauma scores similar to nonobese patients either taking or not taking the drugs, 5.83 and 2.45, respectively, Dr. Winfield said.
He explained the drugs may enable cells in obese individuals to express more CD47, a cell surface marker that plays a role in monocyte maturation. “What we see in those obese patients taking ACE-I or ARB preinjury is not a perfect response, but it is better,” he said. “We see more cells expressing CD47, and as a result, we see improved cell maturation and tracking and the ability to battle, in particular, secondary insults.”
The next step involves animal research to see if ACE-I and ARB use before and after injury can modulate the immune response, which Washington University and the American College of Surgeons are funding, according to Dr. Winfield.
The UCSF study did not draw any definitive conclusion of the overall benefits or drawbacks of hypercoagulability in the obese after injury, Dr. Kornblith said, although it did suggest one significant deleterious effect in multivariate analysis. “We found that for every 5 kg/m2 increase in BMI, there was an 85% increase in the odds of developing a clinically significant thromboembolic complication,” she said.
The study, using data from “Inflammation and the Host Response to Injury” database, evaluated 377 patients with an average BMI of 25.8 kg/m2, about a quarter of whom were obese (average BMI 33 kg/m2). Obese patients had higher admission platelet counts (302.69 x 103mcL vs. 268.58 x 103mcL) and factor IX (134% vs. 119% activity), and lower D-dimer counts (1.88 vs. 4.00 mc/mL) than did normal weight patients. Thromboelastography measured stronger clot and higher levels of functional fibrinogen on admission in obese patients. These findings of hypercoagulability in the obese patients existed out to 24-120 hours after injury.
Dr. Kornblith acknowledged several limitations to the study. “We do not do a screening duplex ultrasound for DVTs [deep vein thromboses] at our institution,” she said. “There may also be a much higher incidence of nonclinically significant clots in this population; however, based on this, if anything, our numbers are really an underestimate reflecting only those that were clinically significant.”
More work needs to be done, Dr. Kornblith noted. “It is known that excess adipose tissue is far from inert, and it plays a cardinal role in the biology and physiology of obesity,” she said. “Untangling the complex interaction of inflammation, coagulation, and injury will really help contribute to a better understanding of the clinical outcome differences seen in obese patients after injury and may help with targeted treatment of this at-risk group.”
Dr. Kornblith and Dr. Winfield reported having no financial disclosures.
FROM AATS ANNUAL MEETING
Key clinical point: ACE-I and ARB medications may help obese trauma patients maintain trauma scores similar to nonobese patients.
Major finding: Obese patients who took ACE inhibitors or ARB drugs before their injuries had trauma scores similar to nonobese trauma patients, while obese patients in a prospective study displayed hypercoagulability, compared with that of normal weight patients.
Data source: Analysis of data from Inflammation and the Host Response to Injury database, and prospective analysis of demographic, outcomes and laboratory measures of 377 patients of varying BMI.
Disclosures: Dr. Kornblith and Dr. Winfield reported having no financial disclosures.