User login
Official Newspaper of the American College of Surgeons
Robotics: General surgery goes its own way
HOUSTON – Subspecialties such as urology and gynecology have seen a steady increase in robot-assisted surgery and an offsetting decline in open procedures, but in general surgery, robot-assisted procedures seem to be making gains at the expense of laparoscopy, according to researchers from the University of Nebraska.
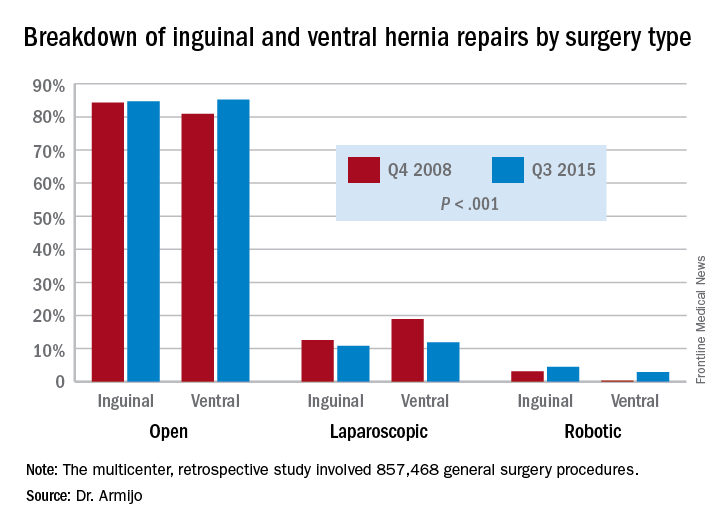
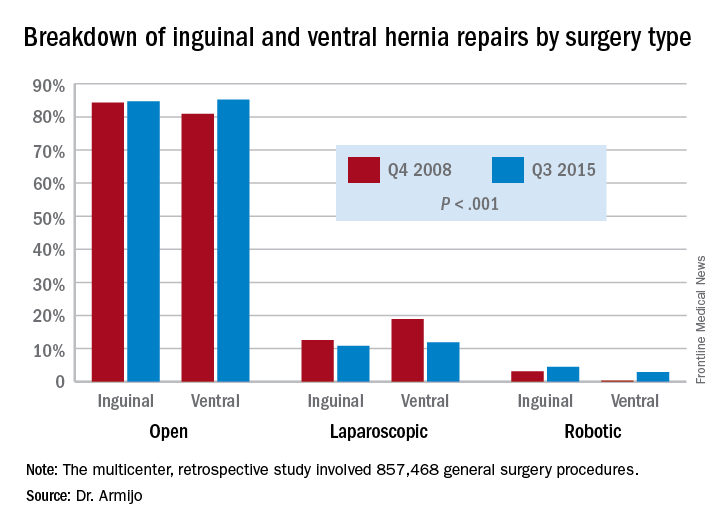
In two specific operations, ventral and inguinal hernia repairs (VHR and IHR), the percentage of open procedures has increased or held steady over the 7-year study period while the share of laparoscopic operations declined and robot-assisted surgeries (RAS) increased, Priscila Rodrigues Armijo, MD, reported at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
This shift to RAS rather than laparoscopy could have significant implications because RAS is significantly more costly than laparoscopy, Dr. Armijo said. “In our study, the open procedures were the most expensive, followed by the robot-assisted surgeries and then laparoscopy,” she said. Median direct costs were $14,364 for open procedures, $11,376 for RAS and $7,945 for laparoscopy.
The Nebraska study retrospectively analyzed five different general surgery procedures: colectomy, cholecystectomy, and bariatric procedures in addition to VHR and IHR. The researchers analyzed 857,468 operations entered into the University HealthSystem Consortium Clinical Database Resource Manager from October 2008 to September 2015.
Dr. Armijo explained that the goal was to study trends in general surgery because while several studies have examined trends in urologic and gynecologic surgery, few studies have done so in general surgery.
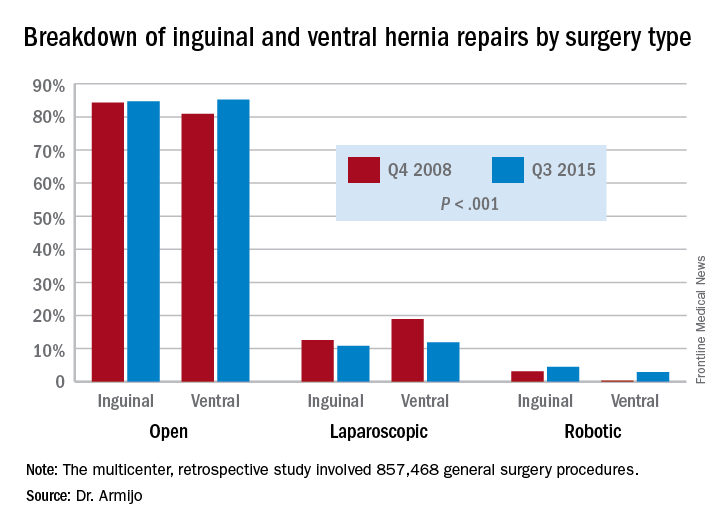
“There was a significant increase in minimally invasive utilizations over time, and robotic surgery increased disproportionately compared to the laparoscope counterpart,” Dr. Armijo said. “And although we cannot prove where those patients are coming from, we believe that, especially for inguinal and ventral hernia repairs, they are coming from laparoscopic surgeons who now are adopting robotic techniques and not from open surgeons switching to the robotic approach.”
In 7 years, the study showed a significant decrease in the share of open procedures in colectomy (from 71.8% to 61.9%), cholecystectomy (35.7% to 27.1%), and bariatric surgery (20.1% to 10.1%), but an increase in both laparoscopic and RAS approaches in these surgeries.
However, in IHR, open procedures held steady at around 84% through the study period, while laparoscopic procedures declined from 12.6% to 10.8% and RAS jumped 3.1% to 4.5%. For VHR, the share of open procedures actually jumped from 80.9% to 85.2%, while the proportion of laparoscopic procedures fell from 18.9% to 11.9% and RAS operations jumped more than tenfold, from 0.2% to 2.9%.
“For ventral hernia repair there was a significant decrease in the laparoscopic approach with a significant increase in both open and robotic procedures, which may be due to new open techniques, including component separation, that have been shown to be more durable as a repair,” Dr. Armijo said. “In addition, those repair techniques are more easily performed with the robotic approach. Laparoscopic surgeons are finding that robotic technology is enabling them to execute surgical tasks, such as suturing mesh.”
Coauthor Dmitry Oleynikov, MD, FACS, disclosed he is a stockholder in Virtual Incision Corp. Dr. Armijo and other coauthors had no financial relationships to disclose.
HOUSTON – Subspecialties such as urology and gynecology have seen a steady increase in robot-assisted surgery and an offsetting decline in open procedures, but in general surgery, robot-assisted procedures seem to be making gains at the expense of laparoscopy, according to researchers from the University of Nebraska.
In two specific operations, ventral and inguinal hernia repairs (VHR and IHR), the percentage of open procedures has increased or held steady over the 7-year study period while the share of laparoscopic operations declined and robot-assisted surgeries (RAS) increased, Priscila Rodrigues Armijo, MD, reported at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
This shift to RAS rather than laparoscopy could have significant implications because RAS is significantly more costly than laparoscopy, Dr. Armijo said. “In our study, the open procedures were the most expensive, followed by the robot-assisted surgeries and then laparoscopy,” she said. Median direct costs were $14,364 for open procedures, $11,376 for RAS and $7,945 for laparoscopy.
The Nebraska study retrospectively analyzed five different general surgery procedures: colectomy, cholecystectomy, and bariatric procedures in addition to VHR and IHR. The researchers analyzed 857,468 operations entered into the University HealthSystem Consortium Clinical Database Resource Manager from October 2008 to September 2015.
Dr. Armijo explained that the goal was to study trends in general surgery because while several studies have examined trends in urologic and gynecologic surgery, few studies have done so in general surgery.
“There was a significant increase in minimally invasive utilizations over time, and robotic surgery increased disproportionately compared to the laparoscope counterpart,” Dr. Armijo said. “And although we cannot prove where those patients are coming from, we believe that, especially for inguinal and ventral hernia repairs, they are coming from laparoscopic surgeons who now are adopting robotic techniques and not from open surgeons switching to the robotic approach.”
In 7 years, the study showed a significant decrease in the share of open procedures in colectomy (from 71.8% to 61.9%), cholecystectomy (35.7% to 27.1%), and bariatric surgery (20.1% to 10.1%), but an increase in both laparoscopic and RAS approaches in these surgeries.
However, in IHR, open procedures held steady at around 84% through the study period, while laparoscopic procedures declined from 12.6% to 10.8% and RAS jumped 3.1% to 4.5%. For VHR, the share of open procedures actually jumped from 80.9% to 85.2%, while the proportion of laparoscopic procedures fell from 18.9% to 11.9% and RAS operations jumped more than tenfold, from 0.2% to 2.9%.
“For ventral hernia repair there was a significant decrease in the laparoscopic approach with a significant increase in both open and robotic procedures, which may be due to new open techniques, including component separation, that have been shown to be more durable as a repair,” Dr. Armijo said. “In addition, those repair techniques are more easily performed with the robotic approach. Laparoscopic surgeons are finding that robotic technology is enabling them to execute surgical tasks, such as suturing mesh.”
Coauthor Dmitry Oleynikov, MD, FACS, disclosed he is a stockholder in Virtual Incision Corp. Dr. Armijo and other coauthors had no financial relationships to disclose.
HOUSTON – Subspecialties such as urology and gynecology have seen a steady increase in robot-assisted surgery and an offsetting decline in open procedures, but in general surgery, robot-assisted procedures seem to be making gains at the expense of laparoscopy, according to researchers from the University of Nebraska.
In two specific operations, ventral and inguinal hernia repairs (VHR and IHR), the percentage of open procedures has increased or held steady over the 7-year study period while the share of laparoscopic operations declined and robot-assisted surgeries (RAS) increased, Priscila Rodrigues Armijo, MD, reported at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
This shift to RAS rather than laparoscopy could have significant implications because RAS is significantly more costly than laparoscopy, Dr. Armijo said. “In our study, the open procedures were the most expensive, followed by the robot-assisted surgeries and then laparoscopy,” she said. Median direct costs were $14,364 for open procedures, $11,376 for RAS and $7,945 for laparoscopy.
The Nebraska study retrospectively analyzed five different general surgery procedures: colectomy, cholecystectomy, and bariatric procedures in addition to VHR and IHR. The researchers analyzed 857,468 operations entered into the University HealthSystem Consortium Clinical Database Resource Manager from October 2008 to September 2015.
Dr. Armijo explained that the goal was to study trends in general surgery because while several studies have examined trends in urologic and gynecologic surgery, few studies have done so in general surgery.
“There was a significant increase in minimally invasive utilizations over time, and robotic surgery increased disproportionately compared to the laparoscope counterpart,” Dr. Armijo said. “And although we cannot prove where those patients are coming from, we believe that, especially for inguinal and ventral hernia repairs, they are coming from laparoscopic surgeons who now are adopting robotic techniques and not from open surgeons switching to the robotic approach.”
In 7 years, the study showed a significant decrease in the share of open procedures in colectomy (from 71.8% to 61.9%), cholecystectomy (35.7% to 27.1%), and bariatric surgery (20.1% to 10.1%), but an increase in both laparoscopic and RAS approaches in these surgeries.
However, in IHR, open procedures held steady at around 84% through the study period, while laparoscopic procedures declined from 12.6% to 10.8% and RAS jumped 3.1% to 4.5%. For VHR, the share of open procedures actually jumped from 80.9% to 85.2%, while the proportion of laparoscopic procedures fell from 18.9% to 11.9% and RAS operations jumped more than tenfold, from 0.2% to 2.9%.
“For ventral hernia repair there was a significant decrease in the laparoscopic approach with a significant increase in both open and robotic procedures, which may be due to new open techniques, including component separation, that have been shown to be more durable as a repair,” Dr. Armijo said. “In addition, those repair techniques are more easily performed with the robotic approach. Laparoscopic surgeons are finding that robotic technology is enabling them to execute surgical tasks, such as suturing mesh.”
Coauthor Dmitry Oleynikov, MD, FACS, disclosed he is a stockholder in Virtual Incision Corp. Dr. Armijo and other coauthors had no financial relationships to disclose.
AT SAGES 2017
Key clinical point: In inguinal and ventral hernia repair, laparoscopic surgeons are more likely than are open surgery counterparts to move to surgical robot.
Major finding: Over the 7-year study period, the share of open ventral hernia repair procedures increased from 80.9% to 85.2%, while the proportion of laparoscopic procedures fell from 18.9% to 11.9% and RAS operations increased from 0.2% to 2.9%.
Data source: Multicenter, retrospective study of 857,468 general surgery procedures from 2008 to 2015 in the University HealthSystem Consortium Clinical Database Resource Manager.
Disclosures: Dr. Armijo reported having no financial disclosures. Coauthor Dmitry Oleynikov, MD, disclosed stock holding in Virtual Incision Corp.
Observation works for most smaller splanchnic artery aneurysms
CHICAGO – Guidelines for the management of splanchnic artery aneurysms have been hard to come by because of their rarity, but investigators at Massachusetts General Hospital and Harvard Medical School, both in Boston, have surveyed their 20-year experience to conclude that surveillance is appropriate for most cases of aneurysms smaller than 25 mm, and selective open or endovascular repair is indicated for larger lesions, depending on their location.
“Most of the small splanchnic artery aneurysms (SAAs) of less than 25 mm did not grow or rupture over time and can be observed with axial imaging every 3 years,” Mark F. Conrad, MD, reported at a symposium on vascular surgery sponsored by Northwestern University.
The predominant sites of aneurysm were the splenic artery (95, 36%) and the celiac artery (78, 30%), followed by the hepatic artery (34, 13%), pancreaticoduodenal artery (PDA; 25, 9.6%), superior mesenteric artery (SMA; 17, 6%), gastroduodenal artery (GDA; 11, 4%), jejunal artery (3, 1%) and inferior mesenteric artery (1, 0.4%).
Surveillance consisted of imaging every 3 years. Of the surveillance cohort, 138 patients had longer-term follow-up. The average aneurysm size was 16.3 mm, “so they’re small,” Dr. Conrad said. Of that whole group, only 12 (9%), of SAAs grew in size, and of those, 8 were 25 mm or smaller when they were identified; 8 of the 12 required repair. “The average time to repair was 2 years,” Dr. Conrad said. “There were no ruptures in the surveillance cohort.”
Among the early repair group, 13 (14.7%) had rupture upon presentation, 3 of which (23%) were pseudoaneurysms. The majority of aneurysms in this group were in either the splenic artery, PDA, or GDA. “Their average size was 31 mm – much larger than the patients that we watched,” he said. A total of 70% of all repairs were endovascular in nature, the remainder open, but endovascular comprised a higher percentage of rupture repairs: 10 (77%) vs. 3 (23%) that underwent open procedures.
The outcomes for endovascular and open repair were similar based on the small number of subjects, Dr. Conrad said: 30-day morbidity of 17% for endovascular repair and 22.2% for open; and 30-day mortality of 3.5% and 4.5%, respectively. However, for ruptured lesions, the outcomes were starkly significant: 54% morbidity and 8% mortality at 30 days.
The researchers performed a univariate analysis of predictors for aneurysm. They were aneurysm size with an odds ratio of 1.04 for every 1 mm of growth; PDA or GDA lesions with an OR of 11.2; and Ehlers-Danlos type IV syndrome with an OR of 32.5. The latter included all the three study patients with Ehlers-Danlos syndrome.
Among patients who had splenic SAAs, 99 (93%) were asymptomatic and 5 (5.3%) had pseudoaneurysm, and almost half (47) went into surveillance. Over a mean observation period of 35 months, six (12.8%) grew in size, comprising half of the growing SAAs in the observation group. Thirty-two had endovascular repair and four open repair, with a 30-day morbidity of 22% and 30-day mortality of 2.7%.
Celiac SAAs proved most problematic in terms of symptomatology; all 78 patients with this variant were asymptomatic, and 12 (15%) had dissection. Sixty patients went into surveillance with a mean time of 43 months, and three (5) had aneurysms that grew in size. Five had intervention, four with open repair, with 30-day morbidity of 20% and no 30-day mortality.
Hepatic SAAs affected 34 study subjects, 29 (85%) of whom were asymptomatic, 4 (15%) who had dissection, and 7 (21%) with pseudoaneurysm. Eleven entered surveillance for an average of 28 months, but none showed any aneurysmal growth. The 16 who had intervention were evenly split between open and endovascular repair with 30-day morbidity of 25% and 30-day morality of 12.5%.
The PDA and GDA aneurysms “are really interesting,” Dr. Conrad said. “I think they’re different in nature than the other aneurysms,” he said, noting that 12 (33%) of these aneurysms were symptomatic and 6 (17%) were pseudoaneurysms. Because of the high rate of rupture of PDA/GDA aneurysms, Dr. Conrad advised repair at diagnosis: “97% of these patients had a celiac stenosis, and of those, two-thirds were atherosclerosis related and one-third related to the median arcuate ligament compression.” The rupture rate was comparatively high – 20%. Twenty cases underwent endovascular repair with a 90% success rate while four cases had open repair. Thirty-day morbidity for intact lesions was 11% with no deaths, and 50% with 14% mortality rate for ruptured lesions.
Of the SMA aneurysms in the study population, only 17% were mycotic with the remainder asymptomatic, Dr. Conrad said. Nine underwent surveillance, with one growing in size over a mean observation period of 28 months, four had open repair, and two endovascular repair. Morbidity was 17% at 30 days with no deaths.
The guidelines Dr. Conrad and his group developed recommend treatment for symptomatic patients and a more nuanced approach for asymptomatic patients, depending on the location and size of SAA. All lesions 25 mm or smaller, except those of the PDA/GDA, can be observed with axial imaging every 3 years, he said; intervention is indicated for all larger lesions. Endovascular repair is in order for all splenic SAAs in pregnancy, liver transplantation, and pseudoaneurysm. For hepatic SAAs, open or endovascular repair is indicated for pseudoaneurysm, but open repair only is indicated for asymptomatic celiac SAAs with pseudoaneurysm. Endovascular intervention can address most SAA aneurysms of the PDA and GDA.
Dr. Conrad disclosed he is a consultant to Medtronic and Volcano and is a member of Bard’s clinical events committee.
CHICAGO – Guidelines for the management of splanchnic artery aneurysms have been hard to come by because of their rarity, but investigators at Massachusetts General Hospital and Harvard Medical School, both in Boston, have surveyed their 20-year experience to conclude that surveillance is appropriate for most cases of aneurysms smaller than 25 mm, and selective open or endovascular repair is indicated for larger lesions, depending on their location.
“Most of the small splanchnic artery aneurysms (SAAs) of less than 25 mm did not grow or rupture over time and can be observed with axial imaging every 3 years,” Mark F. Conrad, MD, reported at a symposium on vascular surgery sponsored by Northwestern University.
The predominant sites of aneurysm were the splenic artery (95, 36%) and the celiac artery (78, 30%), followed by the hepatic artery (34, 13%), pancreaticoduodenal artery (PDA; 25, 9.6%), superior mesenteric artery (SMA; 17, 6%), gastroduodenal artery (GDA; 11, 4%), jejunal artery (3, 1%) and inferior mesenteric artery (1, 0.4%).
Surveillance consisted of imaging every 3 years. Of the surveillance cohort, 138 patients had longer-term follow-up. The average aneurysm size was 16.3 mm, “so they’re small,” Dr. Conrad said. Of that whole group, only 12 (9%), of SAAs grew in size, and of those, 8 were 25 mm or smaller when they were identified; 8 of the 12 required repair. “The average time to repair was 2 years,” Dr. Conrad said. “There were no ruptures in the surveillance cohort.”
Among the early repair group, 13 (14.7%) had rupture upon presentation, 3 of which (23%) were pseudoaneurysms. The majority of aneurysms in this group were in either the splenic artery, PDA, or GDA. “Their average size was 31 mm – much larger than the patients that we watched,” he said. A total of 70% of all repairs were endovascular in nature, the remainder open, but endovascular comprised a higher percentage of rupture repairs: 10 (77%) vs. 3 (23%) that underwent open procedures.
The outcomes for endovascular and open repair were similar based on the small number of subjects, Dr. Conrad said: 30-day morbidity of 17% for endovascular repair and 22.2% for open; and 30-day mortality of 3.5% and 4.5%, respectively. However, for ruptured lesions, the outcomes were starkly significant: 54% morbidity and 8% mortality at 30 days.
The researchers performed a univariate analysis of predictors for aneurysm. They were aneurysm size with an odds ratio of 1.04 for every 1 mm of growth; PDA or GDA lesions with an OR of 11.2; and Ehlers-Danlos type IV syndrome with an OR of 32.5. The latter included all the three study patients with Ehlers-Danlos syndrome.
Among patients who had splenic SAAs, 99 (93%) were asymptomatic and 5 (5.3%) had pseudoaneurysm, and almost half (47) went into surveillance. Over a mean observation period of 35 months, six (12.8%) grew in size, comprising half of the growing SAAs in the observation group. Thirty-two had endovascular repair and four open repair, with a 30-day morbidity of 22% and 30-day mortality of 2.7%.
Celiac SAAs proved most problematic in terms of symptomatology; all 78 patients with this variant were asymptomatic, and 12 (15%) had dissection. Sixty patients went into surveillance with a mean time of 43 months, and three (5) had aneurysms that grew in size. Five had intervention, four with open repair, with 30-day morbidity of 20% and no 30-day mortality.
Hepatic SAAs affected 34 study subjects, 29 (85%) of whom were asymptomatic, 4 (15%) who had dissection, and 7 (21%) with pseudoaneurysm. Eleven entered surveillance for an average of 28 months, but none showed any aneurysmal growth. The 16 who had intervention were evenly split between open and endovascular repair with 30-day morbidity of 25% and 30-day morality of 12.5%.
The PDA and GDA aneurysms “are really interesting,” Dr. Conrad said. “I think they’re different in nature than the other aneurysms,” he said, noting that 12 (33%) of these aneurysms were symptomatic and 6 (17%) were pseudoaneurysms. Because of the high rate of rupture of PDA/GDA aneurysms, Dr. Conrad advised repair at diagnosis: “97% of these patients had a celiac stenosis, and of those, two-thirds were atherosclerosis related and one-third related to the median arcuate ligament compression.” The rupture rate was comparatively high – 20%. Twenty cases underwent endovascular repair with a 90% success rate while four cases had open repair. Thirty-day morbidity for intact lesions was 11% with no deaths, and 50% with 14% mortality rate for ruptured lesions.
Of the SMA aneurysms in the study population, only 17% were mycotic with the remainder asymptomatic, Dr. Conrad said. Nine underwent surveillance, with one growing in size over a mean observation period of 28 months, four had open repair, and two endovascular repair. Morbidity was 17% at 30 days with no deaths.
The guidelines Dr. Conrad and his group developed recommend treatment for symptomatic patients and a more nuanced approach for asymptomatic patients, depending on the location and size of SAA. All lesions 25 mm or smaller, except those of the PDA/GDA, can be observed with axial imaging every 3 years, he said; intervention is indicated for all larger lesions. Endovascular repair is in order for all splenic SAAs in pregnancy, liver transplantation, and pseudoaneurysm. For hepatic SAAs, open or endovascular repair is indicated for pseudoaneurysm, but open repair only is indicated for asymptomatic celiac SAAs with pseudoaneurysm. Endovascular intervention can address most SAA aneurysms of the PDA and GDA.
Dr. Conrad disclosed he is a consultant to Medtronic and Volcano and is a member of Bard’s clinical events committee.
CHICAGO – Guidelines for the management of splanchnic artery aneurysms have been hard to come by because of their rarity, but investigators at Massachusetts General Hospital and Harvard Medical School, both in Boston, have surveyed their 20-year experience to conclude that surveillance is appropriate for most cases of aneurysms smaller than 25 mm, and selective open or endovascular repair is indicated for larger lesions, depending on their location.
“Most of the small splanchnic artery aneurysms (SAAs) of less than 25 mm did not grow or rupture over time and can be observed with axial imaging every 3 years,” Mark F. Conrad, MD, reported at a symposium on vascular surgery sponsored by Northwestern University.
The predominant sites of aneurysm were the splenic artery (95, 36%) and the celiac artery (78, 30%), followed by the hepatic artery (34, 13%), pancreaticoduodenal artery (PDA; 25, 9.6%), superior mesenteric artery (SMA; 17, 6%), gastroduodenal artery (GDA; 11, 4%), jejunal artery (3, 1%) and inferior mesenteric artery (1, 0.4%).
Surveillance consisted of imaging every 3 years. Of the surveillance cohort, 138 patients had longer-term follow-up. The average aneurysm size was 16.3 mm, “so they’re small,” Dr. Conrad said. Of that whole group, only 12 (9%), of SAAs grew in size, and of those, 8 were 25 mm or smaller when they were identified; 8 of the 12 required repair. “The average time to repair was 2 years,” Dr. Conrad said. “There were no ruptures in the surveillance cohort.”
Among the early repair group, 13 (14.7%) had rupture upon presentation, 3 of which (23%) were pseudoaneurysms. The majority of aneurysms in this group were in either the splenic artery, PDA, or GDA. “Their average size was 31 mm – much larger than the patients that we watched,” he said. A total of 70% of all repairs were endovascular in nature, the remainder open, but endovascular comprised a higher percentage of rupture repairs: 10 (77%) vs. 3 (23%) that underwent open procedures.
The outcomes for endovascular and open repair were similar based on the small number of subjects, Dr. Conrad said: 30-day morbidity of 17% for endovascular repair and 22.2% for open; and 30-day mortality of 3.5% and 4.5%, respectively. However, for ruptured lesions, the outcomes were starkly significant: 54% morbidity and 8% mortality at 30 days.
The researchers performed a univariate analysis of predictors for aneurysm. They were aneurysm size with an odds ratio of 1.04 for every 1 mm of growth; PDA or GDA lesions with an OR of 11.2; and Ehlers-Danlos type IV syndrome with an OR of 32.5. The latter included all the three study patients with Ehlers-Danlos syndrome.
Among patients who had splenic SAAs, 99 (93%) were asymptomatic and 5 (5.3%) had pseudoaneurysm, and almost half (47) went into surveillance. Over a mean observation period of 35 months, six (12.8%) grew in size, comprising half of the growing SAAs in the observation group. Thirty-two had endovascular repair and four open repair, with a 30-day morbidity of 22% and 30-day mortality of 2.7%.
Celiac SAAs proved most problematic in terms of symptomatology; all 78 patients with this variant were asymptomatic, and 12 (15%) had dissection. Sixty patients went into surveillance with a mean time of 43 months, and three (5) had aneurysms that grew in size. Five had intervention, four with open repair, with 30-day morbidity of 20% and no 30-day mortality.
Hepatic SAAs affected 34 study subjects, 29 (85%) of whom were asymptomatic, 4 (15%) who had dissection, and 7 (21%) with pseudoaneurysm. Eleven entered surveillance for an average of 28 months, but none showed any aneurysmal growth. The 16 who had intervention were evenly split between open and endovascular repair with 30-day morbidity of 25% and 30-day morality of 12.5%.
The PDA and GDA aneurysms “are really interesting,” Dr. Conrad said. “I think they’re different in nature than the other aneurysms,” he said, noting that 12 (33%) of these aneurysms were symptomatic and 6 (17%) were pseudoaneurysms. Because of the high rate of rupture of PDA/GDA aneurysms, Dr. Conrad advised repair at diagnosis: “97% of these patients had a celiac stenosis, and of those, two-thirds were atherosclerosis related and one-third related to the median arcuate ligament compression.” The rupture rate was comparatively high – 20%. Twenty cases underwent endovascular repair with a 90% success rate while four cases had open repair. Thirty-day morbidity for intact lesions was 11% with no deaths, and 50% with 14% mortality rate for ruptured lesions.
Of the SMA aneurysms in the study population, only 17% were mycotic with the remainder asymptomatic, Dr. Conrad said. Nine underwent surveillance, with one growing in size over a mean observation period of 28 months, four had open repair, and two endovascular repair. Morbidity was 17% at 30 days with no deaths.
The guidelines Dr. Conrad and his group developed recommend treatment for symptomatic patients and a more nuanced approach for asymptomatic patients, depending on the location and size of SAA. All lesions 25 mm or smaller, except those of the PDA/GDA, can be observed with axial imaging every 3 years, he said; intervention is indicated for all larger lesions. Endovascular repair is in order for all splenic SAAs in pregnancy, liver transplantation, and pseudoaneurysm. For hepatic SAAs, open or endovascular repair is indicated for pseudoaneurysm, but open repair only is indicated for asymptomatic celiac SAAs with pseudoaneurysm. Endovascular intervention can address most SAA aneurysms of the PDA and GDA.
Dr. Conrad disclosed he is a consultant to Medtronic and Volcano and is a member of Bard’s clinical events committee.
AT THE NORTHWESTERN VASCULAR SYMPOSIUM
Key clinical point: Surveillance imaging every three years may be adequate to manage splanchnic artery aneurysms (SAA) smaller than 25 mm, because they rarely expand significantly.
Major finding: In the surveillance group that had long-term follow-up, 9% had SAAs that grew in size.
Data source: Analysis of 250 patients with 264 SAAs during 1994-2014 in the Research Patient Data Registry at Massachusetts General Hospital.
Disclosures: Dr. Conrad disclosed he is a consultant to Medtronic and Volcano and is a member of Bard’s clinical events committee.
Study supports NCCN recommendations on risk-reducing salpingo-oophorectomy
NATIONAL HARBOR, MD – A large hereditary cancer study supports National Comprehensive Cancer Network guidance to consider risk-reducing salpingo-oophorectomy (RRSO) between ages 45 and 50 years for women with BRIP1, RAD51C, or RAD51D mutations, Lydia Usha, MD, said at the annual meeting of the Society of Gynecologic Oncology.
The average ages for an ovarian cancer diagnosis were 56 years for women with RAD51D mutations, 61 years for RAD51C mutations, and 64 years for BRIP1 mutations, said Dr. Usha of Rush Medical College, Chicago. When appropriate, delaying RRSO “avoids the psychosocial and medical complications of premature menopause,” she said.
Among all women, mutation prevalence was 0.3% for BRIP1, 0.1% for RAD51C and RAD51D, 1.2% for BRCA1, and 1.3% for BRCA2 mutations, Dr. Usha reported. Among 18,719 women who had a personal history of ovarian cancer, the most common mutation was BRCA1 (3.5%), followed by BRCA2 (2.7%). In contrast, the combined prevalence of BRIP1, RAD51C, and RAD51D mutations among cancer patients was only 1.6%.
Cancer prevalence was highest among women who had mutations of RAD51C (22%), followed by RAD51D (19%), BRCA1 and BRIP1 (16% in each case), and BRCA2 (11%). Thus, while BRIP1 and RAD51D mutations were uncommon, their presence signified an ovarian cancer risk that was similar to that with BRCA1 mutations, and a greater risk than with BRCA2, Dr. Usha said.
The average ages for ovarian cancer diagnosis were 64 years for BRIP1, 61 years for RAD51C, 60 years for BRCA2, 56 years for RAD51C, and 54 years for BRCA1. “More than 80% of women with ovarian cancer who had a mutation in BRIP1, RAD51C, or BRCA2 were diagnosed after age 50,” Dr. Usha noted. These findings support considering RRSO closer to age 45 years for RAD51D mutation carriers and closer to age 50 years for women with pathogenic variants of BRIP1, added discussant Kari Ring, MD, of the University of Virginia, Charlottesville.
Mutation type did not significantly correlate with ethnicity or type of ovarian cancer, Dr. Usha noted. “Collectively, these findings may aid clinical decisions about the medical management of women with mutations in these genes,” she said. “Our data may also assist with reproductive decisions, such as age of childbearing.”
Dr. Usha did not report external funding sources, but disclosed travel expenses from Myriad Genetics.
NATIONAL HARBOR, MD – A large hereditary cancer study supports National Comprehensive Cancer Network guidance to consider risk-reducing salpingo-oophorectomy (RRSO) between ages 45 and 50 years for women with BRIP1, RAD51C, or RAD51D mutations, Lydia Usha, MD, said at the annual meeting of the Society of Gynecologic Oncology.
The average ages for an ovarian cancer diagnosis were 56 years for women with RAD51D mutations, 61 years for RAD51C mutations, and 64 years for BRIP1 mutations, said Dr. Usha of Rush Medical College, Chicago. When appropriate, delaying RRSO “avoids the psychosocial and medical complications of premature menopause,” she said.
Among all women, mutation prevalence was 0.3% for BRIP1, 0.1% for RAD51C and RAD51D, 1.2% for BRCA1, and 1.3% for BRCA2 mutations, Dr. Usha reported. Among 18,719 women who had a personal history of ovarian cancer, the most common mutation was BRCA1 (3.5%), followed by BRCA2 (2.7%). In contrast, the combined prevalence of BRIP1, RAD51C, and RAD51D mutations among cancer patients was only 1.6%.
Cancer prevalence was highest among women who had mutations of RAD51C (22%), followed by RAD51D (19%), BRCA1 and BRIP1 (16% in each case), and BRCA2 (11%). Thus, while BRIP1 and RAD51D mutations were uncommon, their presence signified an ovarian cancer risk that was similar to that with BRCA1 mutations, and a greater risk than with BRCA2, Dr. Usha said.
The average ages for ovarian cancer diagnosis were 64 years for BRIP1, 61 years for RAD51C, 60 years for BRCA2, 56 years for RAD51C, and 54 years for BRCA1. “More than 80% of women with ovarian cancer who had a mutation in BRIP1, RAD51C, or BRCA2 were diagnosed after age 50,” Dr. Usha noted. These findings support considering RRSO closer to age 45 years for RAD51D mutation carriers and closer to age 50 years for women with pathogenic variants of BRIP1, added discussant Kari Ring, MD, of the University of Virginia, Charlottesville.
Mutation type did not significantly correlate with ethnicity or type of ovarian cancer, Dr. Usha noted. “Collectively, these findings may aid clinical decisions about the medical management of women with mutations in these genes,” she said. “Our data may also assist with reproductive decisions, such as age of childbearing.”
Dr. Usha did not report external funding sources, but disclosed travel expenses from Myriad Genetics.
NATIONAL HARBOR, MD – A large hereditary cancer study supports National Comprehensive Cancer Network guidance to consider risk-reducing salpingo-oophorectomy (RRSO) between ages 45 and 50 years for women with BRIP1, RAD51C, or RAD51D mutations, Lydia Usha, MD, said at the annual meeting of the Society of Gynecologic Oncology.
The average ages for an ovarian cancer diagnosis were 56 years for women with RAD51D mutations, 61 years for RAD51C mutations, and 64 years for BRIP1 mutations, said Dr. Usha of Rush Medical College, Chicago. When appropriate, delaying RRSO “avoids the psychosocial and medical complications of premature menopause,” she said.
Among all women, mutation prevalence was 0.3% for BRIP1, 0.1% for RAD51C and RAD51D, 1.2% for BRCA1, and 1.3% for BRCA2 mutations, Dr. Usha reported. Among 18,719 women who had a personal history of ovarian cancer, the most common mutation was BRCA1 (3.5%), followed by BRCA2 (2.7%). In contrast, the combined prevalence of BRIP1, RAD51C, and RAD51D mutations among cancer patients was only 1.6%.
Cancer prevalence was highest among women who had mutations of RAD51C (22%), followed by RAD51D (19%), BRCA1 and BRIP1 (16% in each case), and BRCA2 (11%). Thus, while BRIP1 and RAD51D mutations were uncommon, their presence signified an ovarian cancer risk that was similar to that with BRCA1 mutations, and a greater risk than with BRCA2, Dr. Usha said.
The average ages for ovarian cancer diagnosis were 64 years for BRIP1, 61 years for RAD51C, 60 years for BRCA2, 56 years for RAD51C, and 54 years for BRCA1. “More than 80% of women with ovarian cancer who had a mutation in BRIP1, RAD51C, or BRCA2 were diagnosed after age 50,” Dr. Usha noted. These findings support considering RRSO closer to age 45 years for RAD51D mutation carriers and closer to age 50 years for women with pathogenic variants of BRIP1, added discussant Kari Ring, MD, of the University of Virginia, Charlottesville.
Mutation type did not significantly correlate with ethnicity or type of ovarian cancer, Dr. Usha noted. “Collectively, these findings may aid clinical decisions about the medical management of women with mutations in these genes,” she said. “Our data may also assist with reproductive decisions, such as age of childbearing.”
Dr. Usha did not report external funding sources, but disclosed travel expenses from Myriad Genetics.
AT THE ANNUAL MEETING ON WOMEN'S CANCER
Key clinical point: A large hereditary cancer study supports National Comprehensive Cancer Network guidance to consider risk-reducing salpingo-oophorectomy between age 45 and 50 years for women with BRIP1, RAD51C, or RAD51D mutations.
Major finding: Average ages for an ovarian cancer diagnosis were 56 years for women with RAD51D mutations, 61 years for RAD51C mutations, and 64 years for BRIP1 mutations.
Data source: Analyses of a 25-gene hereditary panel performed in 345,667 women.
Disclosures: Dr. Usha did not report external funding sources, but disclosed travel expenses from Myriad Genetics.
Liver disease likely to become increasing indication for bariatric surgery
PHILADELPHIA – There is a long list of benefits from bariatric surgery in the morbidly obese, but prevention of end-stage liver disease and the need for a first or second liver transplant is likely to grow as an indication, according to an overview of weight loss surgery at Digestive Diseases: New Advances, held by Rutgers, the State University of New Jersey, and Global Academy for Medical Education.
“Bariatric surgery is associated with significant improvement not just in diabetes, dyslipidemia, hypertension, and other complications of metabolic disorders but for me more interestingly, it is effective for treating fatty liver disease where you can see a 90% improvement in steatosis,” reported Subhashini Ayloo, MD, chief of minimally invasive robotic hepato-pancreato-biliary surgery and liver transplantation at New Jersey Medical School, Newark.
Trained in both bariatric surgery and liver transplant, Dr. Ayloo predicts that these fields will become increasingly connected because of the obesity epidemic and the related rise in nonalcoholic fatty liver disease (NAFLD). Dr. Ayloo reported that bariatric surgery is already being used in her center to avoid a second liver transplant in obese patients who are unable to lose sufficient weight to prevent progressive NAFLD after a first transplant.
The emphasis Dr. Ayloo placed on the role of bariatric surgery in preventing progression of NAFLD to nonalcoholic steatohepatitis and the inflammatory process that leads to fibrosis, cirrhosis, and liver decompensation, was drawn from her interest in these two fields. However, she did not ignore the potential of protection from obesity control for other diseases.
“Obesity adversely affects every organ in the body,” Dr. Ayloo pointed out. As a result of weight loss achieved with bariatric surgery, there is now a large body of evidence supporting broad benefits, not just those related to fat deposited in hepatocytes.
“We have a couple of decades of experience that has been published [with bariatric surgery], and this has shown that it maintains weight loss long term, it improves all the obesity-associated comorbidities, and it is cost effective,” Dr. Ayloo said. Now with long-term follow-up, “all of the studies are showing that bariatric surgery improves survival.”
Although most of the survival data have been generated by retrospective cohort studies, Dr. Ayloo cited nine sets of data showing odds ratios associating bariatric surgery with up to a 90% reduction in death over periods of up to 10 years of follow-up. In a summary slide presented by Dr. Ayloo, the estimated mortality benefit over 5 years was listed as 85%. The same summary slide listed large improvements in relevant measures of morbidity for more than 10 organ systems, such as improvement or resolution of dyslipidemia and hypertension in the circulatory system, improvement or resolution of asthma and other diseases affecting the respiratory system, and resolution or improvement of gastroesophageal reflux disease and other diseases affecting the gastrointestinal system.
Specific to the liver, these benefits included a nearly 40% reduction in liver inflammation and 20% reduction in fibrosis. According to Dr. Ayloo, who noted that NAFLD is expected to overtake hepatitis C virus as the No. 1 cause of liver transplant within the next 5 years, these data are important for drawing attention to bariatric surgery as a strategy to control liver disease. She suggested that there is a need to create a tighter link between efforts to treat morbid obesity and advanced liver disease.
“There is an established literature showing that if somebody is morbidly obese, the rate of liver transplant is lower than when compared to patients with normal weight,” Dr. Ayloo said. “There is a call out in the transplant community that we need to address this and we cannot just be throwing this under the table.”
Because of the strong relationship between obesity and NAFLD, a systematic approach is needed to consider liver disease in obese patients and obesity in patients with liver disease, she said. The close relationship is relevant when planning interventions for either. Liver disease should be assessed prior to bariatric surgery regardless of the indication and then monitored closely as part of postoperative care, she said.
Dr. Ayloo identified weight control as an essential part of posttransplant care to prevent hepatic fat deposition that threatens transplant-free survival.
Global Academy and this news organization are owned by the same company. Dr. Ayloo reports no relevant financial relationships.
PHILADELPHIA – There is a long list of benefits from bariatric surgery in the morbidly obese, but prevention of end-stage liver disease and the need for a first or second liver transplant is likely to grow as an indication, according to an overview of weight loss surgery at Digestive Diseases: New Advances, held by Rutgers, the State University of New Jersey, and Global Academy for Medical Education.
“Bariatric surgery is associated with significant improvement not just in diabetes, dyslipidemia, hypertension, and other complications of metabolic disorders but for me more interestingly, it is effective for treating fatty liver disease where you can see a 90% improvement in steatosis,” reported Subhashini Ayloo, MD, chief of minimally invasive robotic hepato-pancreato-biliary surgery and liver transplantation at New Jersey Medical School, Newark.
Trained in both bariatric surgery and liver transplant, Dr. Ayloo predicts that these fields will become increasingly connected because of the obesity epidemic and the related rise in nonalcoholic fatty liver disease (NAFLD). Dr. Ayloo reported that bariatric surgery is already being used in her center to avoid a second liver transplant in obese patients who are unable to lose sufficient weight to prevent progressive NAFLD after a first transplant.
The emphasis Dr. Ayloo placed on the role of bariatric surgery in preventing progression of NAFLD to nonalcoholic steatohepatitis and the inflammatory process that leads to fibrosis, cirrhosis, and liver decompensation, was drawn from her interest in these two fields. However, she did not ignore the potential of protection from obesity control for other diseases.
“Obesity adversely affects every organ in the body,” Dr. Ayloo pointed out. As a result of weight loss achieved with bariatric surgery, there is now a large body of evidence supporting broad benefits, not just those related to fat deposited in hepatocytes.
“We have a couple of decades of experience that has been published [with bariatric surgery], and this has shown that it maintains weight loss long term, it improves all the obesity-associated comorbidities, and it is cost effective,” Dr. Ayloo said. Now with long-term follow-up, “all of the studies are showing that bariatric surgery improves survival.”
Although most of the survival data have been generated by retrospective cohort studies, Dr. Ayloo cited nine sets of data showing odds ratios associating bariatric surgery with up to a 90% reduction in death over periods of up to 10 years of follow-up. In a summary slide presented by Dr. Ayloo, the estimated mortality benefit over 5 years was listed as 85%. The same summary slide listed large improvements in relevant measures of morbidity for more than 10 organ systems, such as improvement or resolution of dyslipidemia and hypertension in the circulatory system, improvement or resolution of asthma and other diseases affecting the respiratory system, and resolution or improvement of gastroesophageal reflux disease and other diseases affecting the gastrointestinal system.
Specific to the liver, these benefits included a nearly 40% reduction in liver inflammation and 20% reduction in fibrosis. According to Dr. Ayloo, who noted that NAFLD is expected to overtake hepatitis C virus as the No. 1 cause of liver transplant within the next 5 years, these data are important for drawing attention to bariatric surgery as a strategy to control liver disease. She suggested that there is a need to create a tighter link between efforts to treat morbid obesity and advanced liver disease.
“There is an established literature showing that if somebody is morbidly obese, the rate of liver transplant is lower than when compared to patients with normal weight,” Dr. Ayloo said. “There is a call out in the transplant community that we need to address this and we cannot just be throwing this under the table.”
Because of the strong relationship between obesity and NAFLD, a systematic approach is needed to consider liver disease in obese patients and obesity in patients with liver disease, she said. The close relationship is relevant when planning interventions for either. Liver disease should be assessed prior to bariatric surgery regardless of the indication and then monitored closely as part of postoperative care, she said.
Dr. Ayloo identified weight control as an essential part of posttransplant care to prevent hepatic fat deposition that threatens transplant-free survival.
Global Academy and this news organization are owned by the same company. Dr. Ayloo reports no relevant financial relationships.
PHILADELPHIA – There is a long list of benefits from bariatric surgery in the morbidly obese, but prevention of end-stage liver disease and the need for a first or second liver transplant is likely to grow as an indication, according to an overview of weight loss surgery at Digestive Diseases: New Advances, held by Rutgers, the State University of New Jersey, and Global Academy for Medical Education.
“Bariatric surgery is associated with significant improvement not just in diabetes, dyslipidemia, hypertension, and other complications of metabolic disorders but for me more interestingly, it is effective for treating fatty liver disease where you can see a 90% improvement in steatosis,” reported Subhashini Ayloo, MD, chief of minimally invasive robotic hepato-pancreato-biliary surgery and liver transplantation at New Jersey Medical School, Newark.
Trained in both bariatric surgery and liver transplant, Dr. Ayloo predicts that these fields will become increasingly connected because of the obesity epidemic and the related rise in nonalcoholic fatty liver disease (NAFLD). Dr. Ayloo reported that bariatric surgery is already being used in her center to avoid a second liver transplant in obese patients who are unable to lose sufficient weight to prevent progressive NAFLD after a first transplant.
The emphasis Dr. Ayloo placed on the role of bariatric surgery in preventing progression of NAFLD to nonalcoholic steatohepatitis and the inflammatory process that leads to fibrosis, cirrhosis, and liver decompensation, was drawn from her interest in these two fields. However, she did not ignore the potential of protection from obesity control for other diseases.
“Obesity adversely affects every organ in the body,” Dr. Ayloo pointed out. As a result of weight loss achieved with bariatric surgery, there is now a large body of evidence supporting broad benefits, not just those related to fat deposited in hepatocytes.
“We have a couple of decades of experience that has been published [with bariatric surgery], and this has shown that it maintains weight loss long term, it improves all the obesity-associated comorbidities, and it is cost effective,” Dr. Ayloo said. Now with long-term follow-up, “all of the studies are showing that bariatric surgery improves survival.”
Although most of the survival data have been generated by retrospective cohort studies, Dr. Ayloo cited nine sets of data showing odds ratios associating bariatric surgery with up to a 90% reduction in death over periods of up to 10 years of follow-up. In a summary slide presented by Dr. Ayloo, the estimated mortality benefit over 5 years was listed as 85%. The same summary slide listed large improvements in relevant measures of morbidity for more than 10 organ systems, such as improvement or resolution of dyslipidemia and hypertension in the circulatory system, improvement or resolution of asthma and other diseases affecting the respiratory system, and resolution or improvement of gastroesophageal reflux disease and other diseases affecting the gastrointestinal system.
Specific to the liver, these benefits included a nearly 40% reduction in liver inflammation and 20% reduction in fibrosis. According to Dr. Ayloo, who noted that NAFLD is expected to overtake hepatitis C virus as the No. 1 cause of liver transplant within the next 5 years, these data are important for drawing attention to bariatric surgery as a strategy to control liver disease. She suggested that there is a need to create a tighter link between efforts to treat morbid obesity and advanced liver disease.
“There is an established literature showing that if somebody is morbidly obese, the rate of liver transplant is lower than when compared to patients with normal weight,” Dr. Ayloo said. “There is a call out in the transplant community that we need to address this and we cannot just be throwing this under the table.”
Because of the strong relationship between obesity and NAFLD, a systematic approach is needed to consider liver disease in obese patients and obesity in patients with liver disease, she said. The close relationship is relevant when planning interventions for either. Liver disease should be assessed prior to bariatric surgery regardless of the indication and then monitored closely as part of postoperative care, she said.
Dr. Ayloo identified weight control as an essential part of posttransplant care to prevent hepatic fat deposition that threatens transplant-free survival.
Global Academy and this news organization are owned by the same company. Dr. Ayloo reports no relevant financial relationships.
Hot Threads in ACS Communities
Your colleagues have a lot to say! Here are the top discussion threads in ACS Communities in March (all of these threads are from the General Surgery community):
1. Sully
3. Time has changed
4. Who fires your EEA staplers?
5. Neurosurgeon Sentenced to Life in Prison
6. Close the current VA health system as it is …
7. Surgery resident hours
8. Diagnostic laparotomy/laparoscopy
9. High jejunal resection in critically ill
10. Consults: Phone call or Text
To join communities, log in to ACS Communities at http://acscommunities.facs.org/home, go to “Browse All Communities” near the top of any page, and click the blue “Join” button next to the community you’d like to join. If you have any questions, please send them to [email protected].
Your colleagues have a lot to say! Here are the top discussion threads in ACS Communities in March (all of these threads are from the General Surgery community):
1. Sully
3. Time has changed
4. Who fires your EEA staplers?
5. Neurosurgeon Sentenced to Life in Prison
6. Close the current VA health system as it is …
7. Surgery resident hours
8. Diagnostic laparotomy/laparoscopy
9. High jejunal resection in critically ill
10. Consults: Phone call or Text
To join communities, log in to ACS Communities at http://acscommunities.facs.org/home, go to “Browse All Communities” near the top of any page, and click the blue “Join” button next to the community you’d like to join. If you have any questions, please send them to [email protected].
Your colleagues have a lot to say! Here are the top discussion threads in ACS Communities in March (all of these threads are from the General Surgery community):
1. Sully
3. Time has changed
4. Who fires your EEA staplers?
5. Neurosurgeon Sentenced to Life in Prison
6. Close the current VA health system as it is …
7. Surgery resident hours
8. Diagnostic laparotomy/laparoscopy
9. High jejunal resection in critically ill
10. Consults: Phone call or Text
To join communities, log in to ACS Communities at http://acscommunities.facs.org/home, go to “Browse All Communities” near the top of any page, and click the blue “Join” button next to the community you’d like to join. If you have any questions, please send them to [email protected].
Laparoscopic and abdominal hysterectomy yield equivalent survival
Laparoscopic hysterectomy yields equivalent disease-free and overall survival at 4.5 years, compared with abdominal hysterectomy in stage I endometrial cancer, according to a report published online March 28 in JAMA.
Several short-term advantages with the laparoscopic approach have been well documented, including less pain, less morbidity, better quality of life, decreased risk of surgery-related adverse events, and cost savings. But until now, no large international trial has demonstrated that longer-term survival outcomes are at least as good with laparoscopic as with open abdominal hysterectomy in this patient population, reported Monika Janda, PhD, of Queensland University of Technology, Brisbane (Australia) and her colleagues.
They conducted the Laparoscopic Approach to Cancer of the Endometrium (LACE) trial, a randomized equivalence study involving 760 women treated at 20 medical centers in Australia, New Zealand, and Hong Kong during 2005-2010. The women were followed for a median of 4.5 years.
All of the women had histologically confirmed stage I adenocarcinoma of the endometrium. A total of 407 patients were randomly assigned to undergo total laparoscopic hysterectomy and 353 patients to undergo total abdominal hysterectomy. Medical comorbidities were equally distributed between the two study groups, and there were no significant between-group differences in tumor type, histologic grade, number of involved lymph nodes, or adjuvant treatments.
Disease-free survival at 4.5 years was 81.6% with laparoscopic hysterectomy and 81.3% with abdominal hysterectomy, meeting the criteria for equivalence. Overall survival at 4.5 years was 92.0% and 92.4%, respectively. Cancer recurred near the operative site in 3% of each group and at a regional or distant site in 2% or less of each group. Causes of death also were similar between the two study groups, with 56% of all deaths attributed to endometrial cancer (JAMA. 2017;317[12]:1224-33).
Of note, two patients who underwent laparoscopic surgery developed port-site metastases and two patients who underwent abdominal surgery developed metastases at the site of the abdominal wound.
The study was funded by Cancer Councils in Australia, the National Health and Medical Research Council, Cancer Australia, QLD Health, and numerous others. Dr. Janda reported having no relevant financial disclosures; one of her coauthors reported ties to the O.R. Company, SurgicalPerformance Pty, and Covidien.
This study adds to a growing body of literature that suggests laparoscopic hysterectomy is not only safe, but also the preferred modality of hysterectomy for women with endometrial cancer.
Despite the clear benefits of laparoscopic hysterectomy, the findings from the LACE trial should be interpreted in the context of the study design. Importantly, patients randomized to the study represent a highly select group of women with endometrial cancer. The study entry criteria involved a low-risk population of women with stage I tumors of endometrioid histology with a uterine size of less than 10 weeks’ gestation. In practice, laparoscopic hysterectomy is now routinely used for women with nonendometrioid histologies and in those with more advanced disease.
The LACE trial reported by Janda et al. provides confirmation that laparoscopic hysterectomy is a safe and effective treatment modality for women with early-stage endometrial cancer. The favorable short-term outcomes along with equivalent oncological outcomes make laparoscopic hysterectomy the preferred surgical modality in this setting. Even though the road to defining the benefits of laparoscopic hysterectomy has been long, efforts to promote the procedure for women with endometrial cancer should now be a priority.
Jason D. Wright, MD, is at the Herbert Irving Comprehensive Cancer Center and the department of ob.gyn. at Columbia University, New York. He reported having no relevant financial disclosures. These comments are excerpted from an accompanying editorial (JAMA 2017;317[12]:1215-6).
This study adds to a growing body of literature that suggests laparoscopic hysterectomy is not only safe, but also the preferred modality of hysterectomy for women with endometrial cancer.
Despite the clear benefits of laparoscopic hysterectomy, the findings from the LACE trial should be interpreted in the context of the study design. Importantly, patients randomized to the study represent a highly select group of women with endometrial cancer. The study entry criteria involved a low-risk population of women with stage I tumors of endometrioid histology with a uterine size of less than 10 weeks’ gestation. In practice, laparoscopic hysterectomy is now routinely used for women with nonendometrioid histologies and in those with more advanced disease.
The LACE trial reported by Janda et al. provides confirmation that laparoscopic hysterectomy is a safe and effective treatment modality for women with early-stage endometrial cancer. The favorable short-term outcomes along with equivalent oncological outcomes make laparoscopic hysterectomy the preferred surgical modality in this setting. Even though the road to defining the benefits of laparoscopic hysterectomy has been long, efforts to promote the procedure for women with endometrial cancer should now be a priority.
Jason D. Wright, MD, is at the Herbert Irving Comprehensive Cancer Center and the department of ob.gyn. at Columbia University, New York. He reported having no relevant financial disclosures. These comments are excerpted from an accompanying editorial (JAMA 2017;317[12]:1215-6).
This study adds to a growing body of literature that suggests laparoscopic hysterectomy is not only safe, but also the preferred modality of hysterectomy for women with endometrial cancer.
Despite the clear benefits of laparoscopic hysterectomy, the findings from the LACE trial should be interpreted in the context of the study design. Importantly, patients randomized to the study represent a highly select group of women with endometrial cancer. The study entry criteria involved a low-risk population of women with stage I tumors of endometrioid histology with a uterine size of less than 10 weeks’ gestation. In practice, laparoscopic hysterectomy is now routinely used for women with nonendometrioid histologies and in those with more advanced disease.
The LACE trial reported by Janda et al. provides confirmation that laparoscopic hysterectomy is a safe and effective treatment modality for women with early-stage endometrial cancer. The favorable short-term outcomes along with equivalent oncological outcomes make laparoscopic hysterectomy the preferred surgical modality in this setting. Even though the road to defining the benefits of laparoscopic hysterectomy has been long, efforts to promote the procedure for women with endometrial cancer should now be a priority.
Jason D. Wright, MD, is at the Herbert Irving Comprehensive Cancer Center and the department of ob.gyn. at Columbia University, New York. He reported having no relevant financial disclosures. These comments are excerpted from an accompanying editorial (JAMA 2017;317[12]:1215-6).
Laparoscopic hysterectomy yields equivalent disease-free and overall survival at 4.5 years, compared with abdominal hysterectomy in stage I endometrial cancer, according to a report published online March 28 in JAMA.
Several short-term advantages with the laparoscopic approach have been well documented, including less pain, less morbidity, better quality of life, decreased risk of surgery-related adverse events, and cost savings. But until now, no large international trial has demonstrated that longer-term survival outcomes are at least as good with laparoscopic as with open abdominal hysterectomy in this patient population, reported Monika Janda, PhD, of Queensland University of Technology, Brisbane (Australia) and her colleagues.
They conducted the Laparoscopic Approach to Cancer of the Endometrium (LACE) trial, a randomized equivalence study involving 760 women treated at 20 medical centers in Australia, New Zealand, and Hong Kong during 2005-2010. The women were followed for a median of 4.5 years.
All of the women had histologically confirmed stage I adenocarcinoma of the endometrium. A total of 407 patients were randomly assigned to undergo total laparoscopic hysterectomy and 353 patients to undergo total abdominal hysterectomy. Medical comorbidities were equally distributed between the two study groups, and there were no significant between-group differences in tumor type, histologic grade, number of involved lymph nodes, or adjuvant treatments.
Disease-free survival at 4.5 years was 81.6% with laparoscopic hysterectomy and 81.3% with abdominal hysterectomy, meeting the criteria for equivalence. Overall survival at 4.5 years was 92.0% and 92.4%, respectively. Cancer recurred near the operative site in 3% of each group and at a regional or distant site in 2% or less of each group. Causes of death also were similar between the two study groups, with 56% of all deaths attributed to endometrial cancer (JAMA. 2017;317[12]:1224-33).
Of note, two patients who underwent laparoscopic surgery developed port-site metastases and two patients who underwent abdominal surgery developed metastases at the site of the abdominal wound.
The study was funded by Cancer Councils in Australia, the National Health and Medical Research Council, Cancer Australia, QLD Health, and numerous others. Dr. Janda reported having no relevant financial disclosures; one of her coauthors reported ties to the O.R. Company, SurgicalPerformance Pty, and Covidien.
Laparoscopic hysterectomy yields equivalent disease-free and overall survival at 4.5 years, compared with abdominal hysterectomy in stage I endometrial cancer, according to a report published online March 28 in JAMA.
Several short-term advantages with the laparoscopic approach have been well documented, including less pain, less morbidity, better quality of life, decreased risk of surgery-related adverse events, and cost savings. But until now, no large international trial has demonstrated that longer-term survival outcomes are at least as good with laparoscopic as with open abdominal hysterectomy in this patient population, reported Monika Janda, PhD, of Queensland University of Technology, Brisbane (Australia) and her colleagues.
They conducted the Laparoscopic Approach to Cancer of the Endometrium (LACE) trial, a randomized equivalence study involving 760 women treated at 20 medical centers in Australia, New Zealand, and Hong Kong during 2005-2010. The women were followed for a median of 4.5 years.
All of the women had histologically confirmed stage I adenocarcinoma of the endometrium. A total of 407 patients were randomly assigned to undergo total laparoscopic hysterectomy and 353 patients to undergo total abdominal hysterectomy. Medical comorbidities were equally distributed between the two study groups, and there were no significant between-group differences in tumor type, histologic grade, number of involved lymph nodes, or adjuvant treatments.
Disease-free survival at 4.5 years was 81.6% with laparoscopic hysterectomy and 81.3% with abdominal hysterectomy, meeting the criteria for equivalence. Overall survival at 4.5 years was 92.0% and 92.4%, respectively. Cancer recurred near the operative site in 3% of each group and at a regional or distant site in 2% or less of each group. Causes of death also were similar between the two study groups, with 56% of all deaths attributed to endometrial cancer (JAMA. 2017;317[12]:1224-33).
Of note, two patients who underwent laparoscopic surgery developed port-site metastases and two patients who underwent abdominal surgery developed metastases at the site of the abdominal wound.
The study was funded by Cancer Councils in Australia, the National Health and Medical Research Council, Cancer Australia, QLD Health, and numerous others. Dr. Janda reported having no relevant financial disclosures; one of her coauthors reported ties to the O.R. Company, SurgicalPerformance Pty, and Covidien.
FROM JAMA
Key clinical point:
Major finding: Disease-free survival at 4.5 years was 81.6% with laparoscopic hysterectomy and 81.3% with abdominal hysterectomy.
Data source: An international, randomized, phase III equivalence trial involving 760 women treated with total abdominal or total laparoscopic hysterectomy.
Disclosures: The study was funded by Cancer Councils in Australia, the National Health and Medical Research Council, Cancer Australia, QLD Health, and others. Dr. Janda reported having no relevant financial disclosures; one of her coauthors reported ties to the O.R. Company, SurgicalPerformance Pty, and Covidien.
ACP: Substance use disorder is a chronic medical condition
Substance use disorder should be approached as a chronic medical condition, with treatment programs in place of incarceration and improved training programs with which physicians can treat patients with substance abuse.
Such programs are among the eight major recommendations the American College of Physicians has made to improve the nation’s approach to preventing and treating substance abuse in a position paper released March 27 (Ann Intern Med. 2017. doi: 10.7326/M16-2953).
The ACP’s recommendations address the growing rates of opioid addiction, as well as the financial burden of substance abuse on the medical system.
“In 2014, 22.5 million people in the United States needed treatment for an illicit drug or alcohol use problem, but only 18% received any treatment,” according to the paper’s authors. “The medical complications of untreated substance use disorder also drive up health care system costs. Hospitalizations for opioid use disorder rose from nearly 302,000 to more than 520,000 from 2002 to 2012, and costs for such care quadrupled to $15 billion in 2012.”
The complete list of the ACP’s recommendations are:
1) Substance abuse should be approached as a chronic medical disorder. Substance abuse can be treated through evidence-based health programs, according to the ACP. Effort should be put into developing research initiatives, as well as combating the social stigmas associated with substance use disorders.
2) The ACP encourages the establishment of substance abuse programs as a replacement for incarceration. Treatment for substance abuse is a time-sensitive matter, which should be given to patients as soon as possible, including those found guilty of the sale or possession of illegal substances.
3) Policy makers should consider reducing the punishments for drug-related crimes committed by nonviolent offenders. Officials should consider decriminalization, legalization, or treatment alternatives for crimes regarding certain drugs based on the potential risk associated with that drug, the accessibility of treatment in criminal facilities, any disproportionate affects on different sections of the population, and the potential decrease in rates of abuses.
4) There should be multiple stakeholders involved in the creation of programs to eliminate substance abuse. Physicians, policymakers, advocacy groups, and health care professionals are encouraged to work together to create strategies to combat and prevent substance abuse, including programs that expand naloxone access for opioid users or the establishment of a national prescription drug monitoring program. Extensive education programs on proper pain reduction methods should also be made available to physicians to help prevent future dependencies.
5) Coverage of substance use and mental disorder treatments should be mandatory for health insurance companies. Evidence-based treatments for mental health conditions and substance abuse, including counseling, medications, legal services, and education, should be covered by patients’ health insurance. The ACP asserts strict oversight would be essential; however, it is also essential that patients receive nonpharmacologic treatments, which are usually not covered by insurance.
6) There should be an increase in professionals trained to treat substance abuse. There are 4,500 health care professionals in the United States who have mental health and/or substance abuse training, according to the Health Resources and Services Administration. This number shows a high demand for those qualified to treat mental health conditions and substance abuse. Efforts should also be focused on creating a more ethnically diverse group among trained professionals to further increase access to these services.
7) Substance abuse treatment methods should be added to professionals’ continuing medical education. In 2000, 17% of primary care physicians felt very prepared to identify illegal drug use, and 30% could identify drug misuse, according to a study conducted by the National Center on Addiction and Substance Abuse. In response, education for physicians “should be rigorously evaluated to ensure effectiveness and continued access to care and should be designed to prevent onerous burdens on patients and physicians,” according to the paper’s authors.
8) Further study should be conducted on effectiveness of substance abuse programs. Current substance abuse intervention methods should be evaluated to see how effective they are. Among those, safe injection sites should especially be encouraged, as these initiatives have proven effective in reducing unsafe needle sharing in Canada, Australia, and Denmark.
The researchers had no relevant financial disclosures.
[email protected] On Twitter @EAZTweets
Substance use disorder should be approached as a chronic medical condition, with treatment programs in place of incarceration and improved training programs with which physicians can treat patients with substance abuse.
Such programs are among the eight major recommendations the American College of Physicians has made to improve the nation’s approach to preventing and treating substance abuse in a position paper released March 27 (Ann Intern Med. 2017. doi: 10.7326/M16-2953).
The ACP’s recommendations address the growing rates of opioid addiction, as well as the financial burden of substance abuse on the medical system.
“In 2014, 22.5 million people in the United States needed treatment for an illicit drug or alcohol use problem, but only 18% received any treatment,” according to the paper’s authors. “The medical complications of untreated substance use disorder also drive up health care system costs. Hospitalizations for opioid use disorder rose from nearly 302,000 to more than 520,000 from 2002 to 2012, and costs for such care quadrupled to $15 billion in 2012.”
The complete list of the ACP’s recommendations are:
1) Substance abuse should be approached as a chronic medical disorder. Substance abuse can be treated through evidence-based health programs, according to the ACP. Effort should be put into developing research initiatives, as well as combating the social stigmas associated with substance use disorders.
2) The ACP encourages the establishment of substance abuse programs as a replacement for incarceration. Treatment for substance abuse is a time-sensitive matter, which should be given to patients as soon as possible, including those found guilty of the sale or possession of illegal substances.
3) Policy makers should consider reducing the punishments for drug-related crimes committed by nonviolent offenders. Officials should consider decriminalization, legalization, or treatment alternatives for crimes regarding certain drugs based on the potential risk associated with that drug, the accessibility of treatment in criminal facilities, any disproportionate affects on different sections of the population, and the potential decrease in rates of abuses.
4) There should be multiple stakeholders involved in the creation of programs to eliminate substance abuse. Physicians, policymakers, advocacy groups, and health care professionals are encouraged to work together to create strategies to combat and prevent substance abuse, including programs that expand naloxone access for opioid users or the establishment of a national prescription drug monitoring program. Extensive education programs on proper pain reduction methods should also be made available to physicians to help prevent future dependencies.
5) Coverage of substance use and mental disorder treatments should be mandatory for health insurance companies. Evidence-based treatments for mental health conditions and substance abuse, including counseling, medications, legal services, and education, should be covered by patients’ health insurance. The ACP asserts strict oversight would be essential; however, it is also essential that patients receive nonpharmacologic treatments, which are usually not covered by insurance.
6) There should be an increase in professionals trained to treat substance abuse. There are 4,500 health care professionals in the United States who have mental health and/or substance abuse training, according to the Health Resources and Services Administration. This number shows a high demand for those qualified to treat mental health conditions and substance abuse. Efforts should also be focused on creating a more ethnically diverse group among trained professionals to further increase access to these services.
7) Substance abuse treatment methods should be added to professionals’ continuing medical education. In 2000, 17% of primary care physicians felt very prepared to identify illegal drug use, and 30% could identify drug misuse, according to a study conducted by the National Center on Addiction and Substance Abuse. In response, education for physicians “should be rigorously evaluated to ensure effectiveness and continued access to care and should be designed to prevent onerous burdens on patients and physicians,” according to the paper’s authors.
8) Further study should be conducted on effectiveness of substance abuse programs. Current substance abuse intervention methods should be evaluated to see how effective they are. Among those, safe injection sites should especially be encouraged, as these initiatives have proven effective in reducing unsafe needle sharing in Canada, Australia, and Denmark.
The researchers had no relevant financial disclosures.
[email protected] On Twitter @EAZTweets
Substance use disorder should be approached as a chronic medical condition, with treatment programs in place of incarceration and improved training programs with which physicians can treat patients with substance abuse.
Such programs are among the eight major recommendations the American College of Physicians has made to improve the nation’s approach to preventing and treating substance abuse in a position paper released March 27 (Ann Intern Med. 2017. doi: 10.7326/M16-2953).
The ACP’s recommendations address the growing rates of opioid addiction, as well as the financial burden of substance abuse on the medical system.
“In 2014, 22.5 million people in the United States needed treatment for an illicit drug or alcohol use problem, but only 18% received any treatment,” according to the paper’s authors. “The medical complications of untreated substance use disorder also drive up health care system costs. Hospitalizations for opioid use disorder rose from nearly 302,000 to more than 520,000 from 2002 to 2012, and costs for such care quadrupled to $15 billion in 2012.”
The complete list of the ACP’s recommendations are:
1) Substance abuse should be approached as a chronic medical disorder. Substance abuse can be treated through evidence-based health programs, according to the ACP. Effort should be put into developing research initiatives, as well as combating the social stigmas associated with substance use disorders.
2) The ACP encourages the establishment of substance abuse programs as a replacement for incarceration. Treatment for substance abuse is a time-sensitive matter, which should be given to patients as soon as possible, including those found guilty of the sale or possession of illegal substances.
3) Policy makers should consider reducing the punishments for drug-related crimes committed by nonviolent offenders. Officials should consider decriminalization, legalization, or treatment alternatives for crimes regarding certain drugs based on the potential risk associated with that drug, the accessibility of treatment in criminal facilities, any disproportionate affects on different sections of the population, and the potential decrease in rates of abuses.
4) There should be multiple stakeholders involved in the creation of programs to eliminate substance abuse. Physicians, policymakers, advocacy groups, and health care professionals are encouraged to work together to create strategies to combat and prevent substance abuse, including programs that expand naloxone access for opioid users or the establishment of a national prescription drug monitoring program. Extensive education programs on proper pain reduction methods should also be made available to physicians to help prevent future dependencies.
5) Coverage of substance use and mental disorder treatments should be mandatory for health insurance companies. Evidence-based treatments for mental health conditions and substance abuse, including counseling, medications, legal services, and education, should be covered by patients’ health insurance. The ACP asserts strict oversight would be essential; however, it is also essential that patients receive nonpharmacologic treatments, which are usually not covered by insurance.
6) There should be an increase in professionals trained to treat substance abuse. There are 4,500 health care professionals in the United States who have mental health and/or substance abuse training, according to the Health Resources and Services Administration. This number shows a high demand for those qualified to treat mental health conditions and substance abuse. Efforts should also be focused on creating a more ethnically diverse group among trained professionals to further increase access to these services.
7) Substance abuse treatment methods should be added to professionals’ continuing medical education. In 2000, 17% of primary care physicians felt very prepared to identify illegal drug use, and 30% could identify drug misuse, according to a study conducted by the National Center on Addiction and Substance Abuse. In response, education for physicians “should be rigorously evaluated to ensure effectiveness and continued access to care and should be designed to prevent onerous burdens on patients and physicians,” according to the paper’s authors.
8) Further study should be conducted on effectiveness of substance abuse programs. Current substance abuse intervention methods should be evaluated to see how effective they are. Among those, safe injection sites should especially be encouraged, as these initiatives have proven effective in reducing unsafe needle sharing in Canada, Australia, and Denmark.
The researchers had no relevant financial disclosures.
[email protected] On Twitter @EAZTweets
House leaders ‘came up short’ in effort to kill Obamacare
Despite days of intense negotiations and last-minute concessions to win over wavering GOP conservatives and moderates, House Republican leaders Friday failed to secure enough support to pass their plan to repeal and replace the Affordable Care Act.
House Speaker Paul Ryan pulled the bill from consideration after he rushed to the White House to tell President Donald Trump that there weren’t the 216 votes necessary for passage.
“We came really close today, but we came up short,” he told reporters at a hastily called news conference.
When pressed about what happens to the federal health law, he added, “Obamacare is the law of the land. … We’re going to be living with Obamacare for the foreseeable future.”
President Trump laid the blame at the feet of Democrats, complaining that not one was willing to help Republicans on the measure, and he warned again that the Obamacare insurance markets are in serious danger. “Bad things are going to happen to Obamacare,” he told reporters at the White House. “There’s not much you can do to help it. I’ve been saying that for a year and a half. I said, look, eventually, it’s not sustainable. The insurance companies are leaving.”
But he said the collapse of the bill might allow Republicans and Democrats to work on a replacement. “I honestly believe the Democrats will come to us and say, ‘Look, let’s get together and get a great health care bill or plan that’s really great for the people of our country,’” he said.
Mr. Ryan originally had hoped to hold a floor vote on the measure Thursday – timed to coincide with the 7th anniversary of the ACA – but decided to delay that effort because GOP leaders didn’t have enough “yes” votes. The House was in session Friday, before his announcement, while members debated the bill.
House Democratic leader Nancy Pelosi (Calif.) said the speaker’s decision to pull the bill “is pretty exciting for us … a victory for the Affordable Care Act, more importantly for the American people.”
The legislation was damaged by a variety of issues raised by competing factions of the party. Many members were nervous about reports by the Congressional Budget Office showing that the bill would lead eventually to 24 million people losing insurance, while some moderate Republicans worried that ending the ACA’s Medicaid expansion would hurt low-income Americans.
At the same time, conservatives, especially the hard-right House Freedom Caucus that often has needled party leaders, complained that the bill kept too much of the ACA structure in place. They wanted a straight repeal of Obamacare, but party leaders said that couldn’t pass the Senate, where Republicans don’t have enough votes to stop a filibuster. They were hoping to use a complicated legislative strategy called budget reconciliation that would allow them to repeal parts of the ACA that only affect federal spending.
The decision came after a chaotic week of negotiations, as party leaders sought to woo more conservatives. The president lobbied 120 members through personal meetings or phone calls, according to a count provided Friday by his spokesman, Sean Spicer. “The president and the team here have left everything on the field,” Mr. Spicer said.
On Thursday evening, Mr. Trump dispatched Office of Management and Budget Director Mick Mulvaney to tell his former House GOP colleagues that the president wanted a vote on Friday. It was time to move on to other priorities, including tax reform, he told House Republicans.
“He said the president needs this, the president has said he wants a vote tomorrow, up or down. If for any reason it goes down, we’re just going to move forward with additional parts of his agenda. This is our moment in time,” Rep. Chris Collins (R-N.Y.), a loyal Trump ally, told reporters late Thursday. “If it doesn’t pass, we’re moving beyond health care. … We are done negotiating.”
Trump’s edict clearly irked some lawmakers, including the Freedom Caucus chairman, Rep. Mark Meadows (R-N.C), whose group of more than two dozen members represented the strongest bloc against the measure.
“Anytime you don’t have 216 votes, negotiations are not totally over,” he told reporters who had surrounded him in a Capitol basement hallway as he headed in to the party’s caucus meeting.
President Trump, Speaker Ryan, and other GOP lawmakers tweaked their initial package in a variety of ways to win over both conservatives and moderates. But every time one change was made to win votes in one camp, it repelled support in another.
The White House on Thursday accepted conservatives’ demands that the legislation strip federal guarantees of essential health benefits from insurance policies. But that was another problem for moderates, and Democrats suggested the provision would not survive in the Senate.
Republican moderates in the House – as well as the Senate – objected to the bill’s provisions that would shift Medicaid from an open-ended entitlement to a set amount of funding for states that also would give governors and state lawmakers more flexibility over the program. Moderates also were concerned that the package’s tax credits would not be generous enough to help older Americans – who could be charged five times more for coverage than would their younger counterparts – afford coverage.
The House package also lost the support of key GOP allies, including the Club for Growth and Heritage Action. Physician, patient and hospital groups also opposed it.
But Mr. Ryan’s comments made clear how difficult this decision was. “This is a disappointing day for us,” he said. “Doing big things is hard. All of us. All of us – myself included – we will need time to reflect on how we got to this moment, what we could have done to do it better.”
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Despite days of intense negotiations and last-minute concessions to win over wavering GOP conservatives and moderates, House Republican leaders Friday failed to secure enough support to pass their plan to repeal and replace the Affordable Care Act.
House Speaker Paul Ryan pulled the bill from consideration after he rushed to the White House to tell President Donald Trump that there weren’t the 216 votes necessary for passage.
“We came really close today, but we came up short,” he told reporters at a hastily called news conference.
When pressed about what happens to the federal health law, he added, “Obamacare is the law of the land. … We’re going to be living with Obamacare for the foreseeable future.”
President Trump laid the blame at the feet of Democrats, complaining that not one was willing to help Republicans on the measure, and he warned again that the Obamacare insurance markets are in serious danger. “Bad things are going to happen to Obamacare,” he told reporters at the White House. “There’s not much you can do to help it. I’ve been saying that for a year and a half. I said, look, eventually, it’s not sustainable. The insurance companies are leaving.”
But he said the collapse of the bill might allow Republicans and Democrats to work on a replacement. “I honestly believe the Democrats will come to us and say, ‘Look, let’s get together and get a great health care bill or plan that’s really great for the people of our country,’” he said.
Mr. Ryan originally had hoped to hold a floor vote on the measure Thursday – timed to coincide with the 7th anniversary of the ACA – but decided to delay that effort because GOP leaders didn’t have enough “yes” votes. The House was in session Friday, before his announcement, while members debated the bill.
House Democratic leader Nancy Pelosi (Calif.) said the speaker’s decision to pull the bill “is pretty exciting for us … a victory for the Affordable Care Act, more importantly for the American people.”
The legislation was damaged by a variety of issues raised by competing factions of the party. Many members were nervous about reports by the Congressional Budget Office showing that the bill would lead eventually to 24 million people losing insurance, while some moderate Republicans worried that ending the ACA’s Medicaid expansion would hurt low-income Americans.
At the same time, conservatives, especially the hard-right House Freedom Caucus that often has needled party leaders, complained that the bill kept too much of the ACA structure in place. They wanted a straight repeal of Obamacare, but party leaders said that couldn’t pass the Senate, where Republicans don’t have enough votes to stop a filibuster. They were hoping to use a complicated legislative strategy called budget reconciliation that would allow them to repeal parts of the ACA that only affect federal spending.
The decision came after a chaotic week of negotiations, as party leaders sought to woo more conservatives. The president lobbied 120 members through personal meetings or phone calls, according to a count provided Friday by his spokesman, Sean Spicer. “The president and the team here have left everything on the field,” Mr. Spicer said.
On Thursday evening, Mr. Trump dispatched Office of Management and Budget Director Mick Mulvaney to tell his former House GOP colleagues that the president wanted a vote on Friday. It was time to move on to other priorities, including tax reform, he told House Republicans.
“He said the president needs this, the president has said he wants a vote tomorrow, up or down. If for any reason it goes down, we’re just going to move forward with additional parts of his agenda. This is our moment in time,” Rep. Chris Collins (R-N.Y.), a loyal Trump ally, told reporters late Thursday. “If it doesn’t pass, we’re moving beyond health care. … We are done negotiating.”
Trump’s edict clearly irked some lawmakers, including the Freedom Caucus chairman, Rep. Mark Meadows (R-N.C), whose group of more than two dozen members represented the strongest bloc against the measure.
“Anytime you don’t have 216 votes, negotiations are not totally over,” he told reporters who had surrounded him in a Capitol basement hallway as he headed in to the party’s caucus meeting.
President Trump, Speaker Ryan, and other GOP lawmakers tweaked their initial package in a variety of ways to win over both conservatives and moderates. But every time one change was made to win votes in one camp, it repelled support in another.
The White House on Thursday accepted conservatives’ demands that the legislation strip federal guarantees of essential health benefits from insurance policies. But that was another problem for moderates, and Democrats suggested the provision would not survive in the Senate.
Republican moderates in the House – as well as the Senate – objected to the bill’s provisions that would shift Medicaid from an open-ended entitlement to a set amount of funding for states that also would give governors and state lawmakers more flexibility over the program. Moderates also were concerned that the package’s tax credits would not be generous enough to help older Americans – who could be charged five times more for coverage than would their younger counterparts – afford coverage.
The House package also lost the support of key GOP allies, including the Club for Growth and Heritage Action. Physician, patient and hospital groups also opposed it.
But Mr. Ryan’s comments made clear how difficult this decision was. “This is a disappointing day for us,” he said. “Doing big things is hard. All of us. All of us – myself included – we will need time to reflect on how we got to this moment, what we could have done to do it better.”
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Despite days of intense negotiations and last-minute concessions to win over wavering GOP conservatives and moderates, House Republican leaders Friday failed to secure enough support to pass their plan to repeal and replace the Affordable Care Act.
House Speaker Paul Ryan pulled the bill from consideration after he rushed to the White House to tell President Donald Trump that there weren’t the 216 votes necessary for passage.
“We came really close today, but we came up short,” he told reporters at a hastily called news conference.
When pressed about what happens to the federal health law, he added, “Obamacare is the law of the land. … We’re going to be living with Obamacare for the foreseeable future.”
President Trump laid the blame at the feet of Democrats, complaining that not one was willing to help Republicans on the measure, and he warned again that the Obamacare insurance markets are in serious danger. “Bad things are going to happen to Obamacare,” he told reporters at the White House. “There’s not much you can do to help it. I’ve been saying that for a year and a half. I said, look, eventually, it’s not sustainable. The insurance companies are leaving.”
But he said the collapse of the bill might allow Republicans and Democrats to work on a replacement. “I honestly believe the Democrats will come to us and say, ‘Look, let’s get together and get a great health care bill or plan that’s really great for the people of our country,’” he said.
Mr. Ryan originally had hoped to hold a floor vote on the measure Thursday – timed to coincide with the 7th anniversary of the ACA – but decided to delay that effort because GOP leaders didn’t have enough “yes” votes. The House was in session Friday, before his announcement, while members debated the bill.
House Democratic leader Nancy Pelosi (Calif.) said the speaker’s decision to pull the bill “is pretty exciting for us … a victory for the Affordable Care Act, more importantly for the American people.”
The legislation was damaged by a variety of issues raised by competing factions of the party. Many members were nervous about reports by the Congressional Budget Office showing that the bill would lead eventually to 24 million people losing insurance, while some moderate Republicans worried that ending the ACA’s Medicaid expansion would hurt low-income Americans.
At the same time, conservatives, especially the hard-right House Freedom Caucus that often has needled party leaders, complained that the bill kept too much of the ACA structure in place. They wanted a straight repeal of Obamacare, but party leaders said that couldn’t pass the Senate, where Republicans don’t have enough votes to stop a filibuster. They were hoping to use a complicated legislative strategy called budget reconciliation that would allow them to repeal parts of the ACA that only affect federal spending.
The decision came after a chaotic week of negotiations, as party leaders sought to woo more conservatives. The president lobbied 120 members through personal meetings or phone calls, according to a count provided Friday by his spokesman, Sean Spicer. “The president and the team here have left everything on the field,” Mr. Spicer said.
On Thursday evening, Mr. Trump dispatched Office of Management and Budget Director Mick Mulvaney to tell his former House GOP colleagues that the president wanted a vote on Friday. It was time to move on to other priorities, including tax reform, he told House Republicans.
“He said the president needs this, the president has said he wants a vote tomorrow, up or down. If for any reason it goes down, we’re just going to move forward with additional parts of his agenda. This is our moment in time,” Rep. Chris Collins (R-N.Y.), a loyal Trump ally, told reporters late Thursday. “If it doesn’t pass, we’re moving beyond health care. … We are done negotiating.”
Trump’s edict clearly irked some lawmakers, including the Freedom Caucus chairman, Rep. Mark Meadows (R-N.C), whose group of more than two dozen members represented the strongest bloc against the measure.
“Anytime you don’t have 216 votes, negotiations are not totally over,” he told reporters who had surrounded him in a Capitol basement hallway as he headed in to the party’s caucus meeting.
President Trump, Speaker Ryan, and other GOP lawmakers tweaked their initial package in a variety of ways to win over both conservatives and moderates. But every time one change was made to win votes in one camp, it repelled support in another.
The White House on Thursday accepted conservatives’ demands that the legislation strip federal guarantees of essential health benefits from insurance policies. But that was another problem for moderates, and Democrats suggested the provision would not survive in the Senate.
Republican moderates in the House – as well as the Senate – objected to the bill’s provisions that would shift Medicaid from an open-ended entitlement to a set amount of funding for states that also would give governors and state lawmakers more flexibility over the program. Moderates also were concerned that the package’s tax credits would not be generous enough to help older Americans – who could be charged five times more for coverage than would their younger counterparts – afford coverage.
The House package also lost the support of key GOP allies, including the Club for Growth and Heritage Action. Physician, patient and hospital groups also opposed it.
But Mr. Ryan’s comments made clear how difficult this decision was. “This is a disappointing day for us,” he said. “Doing big things is hard. All of us. All of us – myself included – we will need time to reflect on how we got to this moment, what we could have done to do it better.”
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Nonoperative management of pediatric appendicitis appears feasible
Nonoperative management of uncomplicated acute appendicitis in the pediatric population appeared feasible and didn’t raise the risk of complications in the first metaanalysis to examine this approach, investigators reported March 27 in JAMA Pediatrics.
Nonoperative management, based on antibiotic treatment and close monitoring of the patient, is accepted as safe and effective in adults but has not been well studied in children and adolescents. “Owing to specific anatomical and pathophysiologic features of children, the clinical scenario of acute appendicitis in pediatric patients is different from that in adults, and treatment decisions for children are more difficult,” said Libin Huang, MD, of West China Hospital and Sichuan University, Chengdu, and his associates.
The few clinical trials that have been performed in children have had small sample sizes, so the investigators performed a meta-analysis to pool the results for 404 patients aged 5-18 years. They analyzed data from four single-center prospective but nonrandomized controlled trials and one single-center randomized controlled trial to compare outcomes between 168 patients initially treated with antibiotics and 236 who underwent immediate appendectomy.
Sixteen patients in the nonoperative group (9.5%) had treatment failure, defined as appendectomy within 48 hours (11 patients) or within 1 month of follow-up (5 patients). Three of these patients developed a complication (perforated appendicitis). In comparison, none of the surgery group had treatment failure, and one developed a complication requiring reoperation. Thus, the rate of success in the nonoperative group was 152 of 168 patients, or 90.5%, and the rate of complications was not significantly different between the two study groups, Dr. Huang and his associates said (JAMA Ped. 2017 Mar 27. doi: 10.1001/jamapediatrics.2017.0057).
During the following year, 27 patients in the nonoperative group had a histopathologically confirmed recurrence of appendicitis and underwent appendectomy; another 8 had the surgery because of parents’ requests. Nonoperative management was significantly more likely to fail in patients who had an appendicolith, so this approach should be considered inappropriate for this subgroup of patients, the investigators said.
Larger clinical trials with a randomized design, standardized criteria for antibiotic therapy, and longer follow-up are needed to confirm these preliminary findings, they added.
No sponsor was cited for this study. Dr. Huang and his associates reported having no relevant financial disclosures.
This is the first data synthesis on the effectiveness of nonoperative management compared with appendectomy in children, and it shows that the evidence at this time is simply insufficient to warrant a change in clinical practice. Appendectomy remains the standard of care for this disease.
Despite the high early “success rate” for nonoperative treatment, patients in this group were nearly nine times more likely to have “treatment failure” than those who underwent immediate appendectomy.
The nonoperative approach remains an experimental proposition and should be offered only under protocol in a clinical trial setting. It clearly merits ongoing consideration, but much more data from high-quality clinical trials are needed.
Monica E. Lopez, MD, and David E. Wesson, MD, are both with the division of pediatric surgery at Baylor College of Medicine and the department of surgery at Texas Children’s Hospital, both in Houston. They reported having no relevant financial disclosures. Dr. Lopez and Dr. Wesson made these remarks in an editorial accompanying Dr. Huang’s report (JAMA Ped. 2017 Mar 27. doi: 10.1001/jamapediatrics.2017.0056).
This is the first data synthesis on the effectiveness of nonoperative management compared with appendectomy in children, and it shows that the evidence at this time is simply insufficient to warrant a change in clinical practice. Appendectomy remains the standard of care for this disease.
Despite the high early “success rate” for nonoperative treatment, patients in this group were nearly nine times more likely to have “treatment failure” than those who underwent immediate appendectomy.
The nonoperative approach remains an experimental proposition and should be offered only under protocol in a clinical trial setting. It clearly merits ongoing consideration, but much more data from high-quality clinical trials are needed.
Monica E. Lopez, MD, and David E. Wesson, MD, are both with the division of pediatric surgery at Baylor College of Medicine and the department of surgery at Texas Children’s Hospital, both in Houston. They reported having no relevant financial disclosures. Dr. Lopez and Dr. Wesson made these remarks in an editorial accompanying Dr. Huang’s report (JAMA Ped. 2017 Mar 27. doi: 10.1001/jamapediatrics.2017.0056).
This is the first data synthesis on the effectiveness of nonoperative management compared with appendectomy in children, and it shows that the evidence at this time is simply insufficient to warrant a change in clinical practice. Appendectomy remains the standard of care for this disease.
Despite the high early “success rate” for nonoperative treatment, patients in this group were nearly nine times more likely to have “treatment failure” than those who underwent immediate appendectomy.
The nonoperative approach remains an experimental proposition and should be offered only under protocol in a clinical trial setting. It clearly merits ongoing consideration, but much more data from high-quality clinical trials are needed.
Monica E. Lopez, MD, and David E. Wesson, MD, are both with the division of pediatric surgery at Baylor College of Medicine and the department of surgery at Texas Children’s Hospital, both in Houston. They reported having no relevant financial disclosures. Dr. Lopez and Dr. Wesson made these remarks in an editorial accompanying Dr. Huang’s report (JAMA Ped. 2017 Mar 27. doi: 10.1001/jamapediatrics.2017.0056).
Nonoperative management of uncomplicated acute appendicitis in the pediatric population appeared feasible and didn’t raise the risk of complications in the first metaanalysis to examine this approach, investigators reported March 27 in JAMA Pediatrics.
Nonoperative management, based on antibiotic treatment and close monitoring of the patient, is accepted as safe and effective in adults but has not been well studied in children and adolescents. “Owing to specific anatomical and pathophysiologic features of children, the clinical scenario of acute appendicitis in pediatric patients is different from that in adults, and treatment decisions for children are more difficult,” said Libin Huang, MD, of West China Hospital and Sichuan University, Chengdu, and his associates.
The few clinical trials that have been performed in children have had small sample sizes, so the investigators performed a meta-analysis to pool the results for 404 patients aged 5-18 years. They analyzed data from four single-center prospective but nonrandomized controlled trials and one single-center randomized controlled trial to compare outcomes between 168 patients initially treated with antibiotics and 236 who underwent immediate appendectomy.
Sixteen patients in the nonoperative group (9.5%) had treatment failure, defined as appendectomy within 48 hours (11 patients) or within 1 month of follow-up (5 patients). Three of these patients developed a complication (perforated appendicitis). In comparison, none of the surgery group had treatment failure, and one developed a complication requiring reoperation. Thus, the rate of success in the nonoperative group was 152 of 168 patients, or 90.5%, and the rate of complications was not significantly different between the two study groups, Dr. Huang and his associates said (JAMA Ped. 2017 Mar 27. doi: 10.1001/jamapediatrics.2017.0057).
During the following year, 27 patients in the nonoperative group had a histopathologically confirmed recurrence of appendicitis and underwent appendectomy; another 8 had the surgery because of parents’ requests. Nonoperative management was significantly more likely to fail in patients who had an appendicolith, so this approach should be considered inappropriate for this subgroup of patients, the investigators said.
Larger clinical trials with a randomized design, standardized criteria for antibiotic therapy, and longer follow-up are needed to confirm these preliminary findings, they added.
No sponsor was cited for this study. Dr. Huang and his associates reported having no relevant financial disclosures.
Nonoperative management of uncomplicated acute appendicitis in the pediatric population appeared feasible and didn’t raise the risk of complications in the first metaanalysis to examine this approach, investigators reported March 27 in JAMA Pediatrics.
Nonoperative management, based on antibiotic treatment and close monitoring of the patient, is accepted as safe and effective in adults but has not been well studied in children and adolescents. “Owing to specific anatomical and pathophysiologic features of children, the clinical scenario of acute appendicitis in pediatric patients is different from that in adults, and treatment decisions for children are more difficult,” said Libin Huang, MD, of West China Hospital and Sichuan University, Chengdu, and his associates.
The few clinical trials that have been performed in children have had small sample sizes, so the investigators performed a meta-analysis to pool the results for 404 patients aged 5-18 years. They analyzed data from four single-center prospective but nonrandomized controlled trials and one single-center randomized controlled trial to compare outcomes between 168 patients initially treated with antibiotics and 236 who underwent immediate appendectomy.
Sixteen patients in the nonoperative group (9.5%) had treatment failure, defined as appendectomy within 48 hours (11 patients) or within 1 month of follow-up (5 patients). Three of these patients developed a complication (perforated appendicitis). In comparison, none of the surgery group had treatment failure, and one developed a complication requiring reoperation. Thus, the rate of success in the nonoperative group was 152 of 168 patients, or 90.5%, and the rate of complications was not significantly different between the two study groups, Dr. Huang and his associates said (JAMA Ped. 2017 Mar 27. doi: 10.1001/jamapediatrics.2017.0057).
During the following year, 27 patients in the nonoperative group had a histopathologically confirmed recurrence of appendicitis and underwent appendectomy; another 8 had the surgery because of parents’ requests. Nonoperative management was significantly more likely to fail in patients who had an appendicolith, so this approach should be considered inappropriate for this subgroup of patients, the investigators said.
Larger clinical trials with a randomized design, standardized criteria for antibiotic therapy, and longer follow-up are needed to confirm these preliminary findings, they added.
No sponsor was cited for this study. Dr. Huang and his associates reported having no relevant financial disclosures.
FROM JAMA PEDIATRICS
Key clinical point: Nonoperative management of uncomplicated appendicitis in the pediatric population appeared feasible and didn’t raise the risk of complications in the first metaanalysis to examine this approach.
Major finding: The rate of treatment success in the nonoperative group was 90.5% (152 of 168 patients).
Data source: A metaanalysis of five single-center clinical trials involving 404 patients aged 5-18 years.
Disclosures: No sponsor was cited for this study. Dr. Huang and his associates reported having no relevant financial disclosures.
ACGME finalizes return of trainees’ 24-hour max shift
First-year residents will once again be permitted to work up to 24 consecutive hours following a reversal of a rule implemented in 2011 that restricted them to 16 hours, the Accreditation Council for Graduate Medical Education (ACGME) announced.
According to a memo issued by the ACGME March 10, 2017, the change reverting back to the 24-hour ceiling was evidence based.
“The preponderance of the evidence from a number of studies conducted after the current 16-hour cap was implemented in 2011 suggests that it may not have had an incremental benefit in patient safety, and that there might be significant negative impacts to the quality of physician education and professional development,” the memo states. The work week is still capped at 80 hours worked per week, with 1 day free from clinical experience or education in 7, and in-house call no more frequent than every third night.
An ACGME task force determined “that the hypothesized benefits associated with the changes made to first-year resident scheduled hours in 2011 have not been realized, and the disruption of team-based care and supervisory systems has had a significant negative impact on the professional education of the first-year resident, and the effectiveness of care delivery of the team as a whole.”
Sharmila Dissanaike, MD, FACS, chair and professor of surgery at Texas Tech University, Lubbock, said in an interview that the change back to a 24-hour ceiling provides “an increased flexibility for all residents in order to allow completion of immediate patient care responsibilities, such as finishing an operation, and ensure smooth handoffs. Both of these should improve work flow for both trainees and supervisors.”
Mark A. Malangoni, MD, FACS, associate executive director of the American Board of Surgery, said he believes the change back to 24 hours is a positive thing.
“The 16-hour requirement posed a lot of scheduling problems,” he said in an interview. “In essence, what it meant was you had residents that either couldn’t take call or they did take call, it was very limited in what they could do.”
Complicating the issue of time is the nature of what needs to be taught to residents.
“What has definitely changed is the breadth of knowledge and repertoire of technical skills that must be learned by today’s residents,” Dr. Dissanaike said. “As scientific knowledge and technical capabilities expand, there is ever more to learn and increasingly less time in which to learn it.”
Dr. Malangoni added that the time restraints didn’t allow for residents to see the natural progression of the patient’s condition. “You don’t have the chance to continue to assess that over a longer period of time,” he said. “That is really important in learning when to operate on someone, but also when not to operate on someone because they will get better without an operation.”
Compounding that is a greater need for reporting to meet regulatory requirements.
“Concurrently, we have increased requirements for documentation and clerical tasks, and reduced time available to do it,” Dr. Dissanaike continued. “All of this has led to a severe ‘work-compression’ for the modern resident, and I suspect the high rates of burnout and depression that are being reported in many specialties are at least partly a result of this phenomenon.”
That being said, Dr. Dissanaike was quick to add that this latest change should not be considered a “final solution” and that there are “many ongoing issues around resident fatigue, as well as adequacy of educational experience that still need to be addressed.”
Dr. Malangoni added that residents need to be more mindful and take more responsibility for their own health and well-being.
“I think what residents need to understand is they are really in charge of their own well-being. Making that point is really a key,” he said. “So it’s not only what you do while you are in the hospital, but you are also responsible for what you do when you are not in the hospital. ACGME cannot regulate what people do in their free time. If you work a 24-hour shift and you decide you are not going to sleep the next day for whatever reason, your well-being is likely not going to be what you want it to be and what, I think, your patients want it to be.”
First-year residents will once again be permitted to work up to 24 consecutive hours following a reversal of a rule implemented in 2011 that restricted them to 16 hours, the Accreditation Council for Graduate Medical Education (ACGME) announced.
According to a memo issued by the ACGME March 10, 2017, the change reverting back to the 24-hour ceiling was evidence based.
“The preponderance of the evidence from a number of studies conducted after the current 16-hour cap was implemented in 2011 suggests that it may not have had an incremental benefit in patient safety, and that there might be significant negative impacts to the quality of physician education and professional development,” the memo states. The work week is still capped at 80 hours worked per week, with 1 day free from clinical experience or education in 7, and in-house call no more frequent than every third night.
An ACGME task force determined “that the hypothesized benefits associated with the changes made to first-year resident scheduled hours in 2011 have not been realized, and the disruption of team-based care and supervisory systems has had a significant negative impact on the professional education of the first-year resident, and the effectiveness of care delivery of the team as a whole.”
Sharmila Dissanaike, MD, FACS, chair and professor of surgery at Texas Tech University, Lubbock, said in an interview that the change back to a 24-hour ceiling provides “an increased flexibility for all residents in order to allow completion of immediate patient care responsibilities, such as finishing an operation, and ensure smooth handoffs. Both of these should improve work flow for both trainees and supervisors.”
Mark A. Malangoni, MD, FACS, associate executive director of the American Board of Surgery, said he believes the change back to 24 hours is a positive thing.
“The 16-hour requirement posed a lot of scheduling problems,” he said in an interview. “In essence, what it meant was you had residents that either couldn’t take call or they did take call, it was very limited in what they could do.”
Complicating the issue of time is the nature of what needs to be taught to residents.
“What has definitely changed is the breadth of knowledge and repertoire of technical skills that must be learned by today’s residents,” Dr. Dissanaike said. “As scientific knowledge and technical capabilities expand, there is ever more to learn and increasingly less time in which to learn it.”
Dr. Malangoni added that the time restraints didn’t allow for residents to see the natural progression of the patient’s condition. “You don’t have the chance to continue to assess that over a longer period of time,” he said. “That is really important in learning when to operate on someone, but also when not to operate on someone because they will get better without an operation.”
Compounding that is a greater need for reporting to meet regulatory requirements.
“Concurrently, we have increased requirements for documentation and clerical tasks, and reduced time available to do it,” Dr. Dissanaike continued. “All of this has led to a severe ‘work-compression’ for the modern resident, and I suspect the high rates of burnout and depression that are being reported in many specialties are at least partly a result of this phenomenon.”
That being said, Dr. Dissanaike was quick to add that this latest change should not be considered a “final solution” and that there are “many ongoing issues around resident fatigue, as well as adequacy of educational experience that still need to be addressed.”
Dr. Malangoni added that residents need to be more mindful and take more responsibility for their own health and well-being.
“I think what residents need to understand is they are really in charge of their own well-being. Making that point is really a key,” he said. “So it’s not only what you do while you are in the hospital, but you are also responsible for what you do when you are not in the hospital. ACGME cannot regulate what people do in their free time. If you work a 24-hour shift and you decide you are not going to sleep the next day for whatever reason, your well-being is likely not going to be what you want it to be and what, I think, your patients want it to be.”
First-year residents will once again be permitted to work up to 24 consecutive hours following a reversal of a rule implemented in 2011 that restricted them to 16 hours, the Accreditation Council for Graduate Medical Education (ACGME) announced.
According to a memo issued by the ACGME March 10, 2017, the change reverting back to the 24-hour ceiling was evidence based.
“The preponderance of the evidence from a number of studies conducted after the current 16-hour cap was implemented in 2011 suggests that it may not have had an incremental benefit in patient safety, and that there might be significant negative impacts to the quality of physician education and professional development,” the memo states. The work week is still capped at 80 hours worked per week, with 1 day free from clinical experience or education in 7, and in-house call no more frequent than every third night.
An ACGME task force determined “that the hypothesized benefits associated with the changes made to first-year resident scheduled hours in 2011 have not been realized, and the disruption of team-based care and supervisory systems has had a significant negative impact on the professional education of the first-year resident, and the effectiveness of care delivery of the team as a whole.”
Sharmila Dissanaike, MD, FACS, chair and professor of surgery at Texas Tech University, Lubbock, said in an interview that the change back to a 24-hour ceiling provides “an increased flexibility for all residents in order to allow completion of immediate patient care responsibilities, such as finishing an operation, and ensure smooth handoffs. Both of these should improve work flow for both trainees and supervisors.”
Mark A. Malangoni, MD, FACS, associate executive director of the American Board of Surgery, said he believes the change back to 24 hours is a positive thing.
“The 16-hour requirement posed a lot of scheduling problems,” he said in an interview. “In essence, what it meant was you had residents that either couldn’t take call or they did take call, it was very limited in what they could do.”
Complicating the issue of time is the nature of what needs to be taught to residents.
“What has definitely changed is the breadth of knowledge and repertoire of technical skills that must be learned by today’s residents,” Dr. Dissanaike said. “As scientific knowledge and technical capabilities expand, there is ever more to learn and increasingly less time in which to learn it.”
Dr. Malangoni added that the time restraints didn’t allow for residents to see the natural progression of the patient’s condition. “You don’t have the chance to continue to assess that over a longer period of time,” he said. “That is really important in learning when to operate on someone, but also when not to operate on someone because they will get better without an operation.”
Compounding that is a greater need for reporting to meet regulatory requirements.
“Concurrently, we have increased requirements for documentation and clerical tasks, and reduced time available to do it,” Dr. Dissanaike continued. “All of this has led to a severe ‘work-compression’ for the modern resident, and I suspect the high rates of burnout and depression that are being reported in many specialties are at least partly a result of this phenomenon.”
That being said, Dr. Dissanaike was quick to add that this latest change should not be considered a “final solution” and that there are “many ongoing issues around resident fatigue, as well as adequacy of educational experience that still need to be addressed.”
Dr. Malangoni added that residents need to be more mindful and take more responsibility for their own health and well-being.
“I think what residents need to understand is they are really in charge of their own well-being. Making that point is really a key,” he said. “So it’s not only what you do while you are in the hospital, but you are also responsible for what you do when you are not in the hospital. ACGME cannot regulate what people do in their free time. If you work a 24-hour shift and you decide you are not going to sleep the next day for whatever reason, your well-being is likely not going to be what you want it to be and what, I think, your patients want it to be.”