User login
Official Newspaper of the American College of Surgeons
Senate committee moves Gorsuch nomination forward
Judge Neil Gorsuch has moved one step closer to becoming the next U.S. Supreme Court Justice.
The U.S. Senate Committee on the Judiciary approved Judge Gorsuch’s nomination by a 11-9 vote on April 3. The vote was a strict party line vote with 11 Republicans voting in favor of Judge Gorsuch and 9 Democrats voting against him.
“He’s a mainstream judge who’s earned the universal respect of his colleagues on the bench and in the bar,” Sen. Grassley said. “He applies the law as we in Congress write it – as the judicial oath says, ‘Without respect to persons.’ And he refuses to compromise his independence. This nominee ... is a judge’s judge. He’s a picture of the kind of justice we should have on the Supreme Court.”
Conversely, Sen. Dianne Feinstein (D-Calif.) expressed opposition to Judge Gorsuch, criticizing his past rulings and calling his answers during his nomination hearing vague and ambiguous.
“As I’ve said, our job is to assess whether the nominee will protect the legal and constitutional rights of all Americans and whether the nominee will recognize the humanity and justice required when evaluating the cases before him,” Sen. Feinstein said before the vote. “Unfortunately, based on the judge’s record at the Department of Justice, his tenure on the bench, his appearance before the Senate, and his written questions for the record, I cannot support his nomination.”
The full Senate is expected to vote on Judge Gorsuch’s nomination on April 7.
[email protected]
On Twitter @legal_med
Judge Neil Gorsuch has moved one step closer to becoming the next U.S. Supreme Court Justice.
The U.S. Senate Committee on the Judiciary approved Judge Gorsuch’s nomination by a 11-9 vote on April 3. The vote was a strict party line vote with 11 Republicans voting in favor of Judge Gorsuch and 9 Democrats voting against him.
“He’s a mainstream judge who’s earned the universal respect of his colleagues on the bench and in the bar,” Sen. Grassley said. “He applies the law as we in Congress write it – as the judicial oath says, ‘Without respect to persons.’ And he refuses to compromise his independence. This nominee ... is a judge’s judge. He’s a picture of the kind of justice we should have on the Supreme Court.”
Conversely, Sen. Dianne Feinstein (D-Calif.) expressed opposition to Judge Gorsuch, criticizing his past rulings and calling his answers during his nomination hearing vague and ambiguous.
“As I’ve said, our job is to assess whether the nominee will protect the legal and constitutional rights of all Americans and whether the nominee will recognize the humanity and justice required when evaluating the cases before him,” Sen. Feinstein said before the vote. “Unfortunately, based on the judge’s record at the Department of Justice, his tenure on the bench, his appearance before the Senate, and his written questions for the record, I cannot support his nomination.”
The full Senate is expected to vote on Judge Gorsuch’s nomination on April 7.
[email protected]
On Twitter @legal_med
Judge Neil Gorsuch has moved one step closer to becoming the next U.S. Supreme Court Justice.
The U.S. Senate Committee on the Judiciary approved Judge Gorsuch’s nomination by a 11-9 vote on April 3. The vote was a strict party line vote with 11 Republicans voting in favor of Judge Gorsuch and 9 Democrats voting against him.
“He’s a mainstream judge who’s earned the universal respect of his colleagues on the bench and in the bar,” Sen. Grassley said. “He applies the law as we in Congress write it – as the judicial oath says, ‘Without respect to persons.’ And he refuses to compromise his independence. This nominee ... is a judge’s judge. He’s a picture of the kind of justice we should have on the Supreme Court.”
Conversely, Sen. Dianne Feinstein (D-Calif.) expressed opposition to Judge Gorsuch, criticizing his past rulings and calling his answers during his nomination hearing vague and ambiguous.
“As I’ve said, our job is to assess whether the nominee will protect the legal and constitutional rights of all Americans and whether the nominee will recognize the humanity and justice required when evaluating the cases before him,” Sen. Feinstein said before the vote. “Unfortunately, based on the judge’s record at the Department of Justice, his tenure on the bench, his appearance before the Senate, and his written questions for the record, I cannot support his nomination.”
The full Senate is expected to vote on Judge Gorsuch’s nomination on April 7.
[email protected]
On Twitter @legal_med
Long-term durability low for nonmesh vaginal prolapse repair
SAN ANTONIO – At 5-year follow-up, outcomes were slightly better on most measures for transvaginal uterosacral ligament suspension versus transvaginal sacrospinous ligament fixation for apical prolapse, but the differences were not statistically significant, according to the first randomized trial to compare the two techniques.
Quality of life improvements were durable, but the overall 5-year success rate – defined as the absence of descent of the vaginal apex more than one-third into the vagina; anterior or posterior vaginal wall descent beyond the hymen; bothersome vaginal bulge symptoms; and further treatment for prolapse – was 39% in the 109 women randomized to bilateral uterosacral ligament suspension (ULS) and 30% in the 109 women randomized to unilateral sacrospinous ligament fixation (SSLF).
But there was a notable finding in the study. If women failed to meet all the requirements for success at any one visit, they were classified as surgical failures. However, many who missed the mark at one visit met all the requirements for success on other visits, including their last follow-up.
“We don’t think as surgeons that a bulge comes and goes on a yearly basis, but people actually moved in and out of success and failure over time, and that’s new,” Dr. Jelovsek said. “We just don’t understand the dynamic variables of anatomic prolapse, because no one’s looked at it. The assumption of ‘once a failure, always a failure’ may underestimate success rates.”
Nonetheless, using that approach in the study, the investigators found that the anatomic success was 54% in the ULS and 38% in the SSLF groups at 5 years, and 37% of women in the ULS group reported bothersome vaginal bulge symptoms, versus 42% of women with SSLF. A total of 12% of women with ULS and 8% of women with SSLF had undergone POP retreatment at 5 years, either by pessary or secondary surgery but, again, the differences were not statistically significant.
Of the 145 anatomic failures in the study, 41% were stage 3 or 4.
Quality of life improvements, assessed annually by phone, “were maintained over 5 years despite progressive increases in surgical failure rates over time,” with about a 70-point improvement in the Pelvic Organ Prolapse Distress Inventory and similar gains in other measures in both groups, Dr. Jelovsek reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
There were no between-group differences in suture exposure (about 25% in both groups) or sling erosion (about 3%) at 5 years.
There was a difference in granulation tissue: 28.9% with ULS and 18.8% with SSLF (odds ratio with ULS, 1.9; 95% confidence interval 1-3.7). The majority of adverse events occurred within 2 years of surgery.
Early pelvic floor muscle training made no difference in outcomes for the women randomized to it.
The women in the study had stage 2-4 prolapse at baseline. In addition to vaginal suspension surgery, they had vaginal hysterectomies if there was uterine prolapse, and all the women had concomitant retropubic midurethral sling surgery for stress incontinence.
At 2 years, composite success rates were about 60% in both groups (JAMA. 2014 Mar 12;311[10]:1023-34).
The study didn’t identify risk factors for failure, but they would be helpful to know, Dr. Jelovsek said. High-risk women might benefit from a more durable mesh repair. For now at least, “most women say the risk” of pain and other serious mesh complications “completely outweighs the bulge symptoms,” he said.
The trial, an extension of OPTIMAL (Operations and Pelvic Muscle Training in the Management of Apical Support Loss), was conducted at nine U.S. centers in the Pelvic Floor Disorders Network, which is funded by the National Institutes of Health. Dr. Jelovsek reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – At 5-year follow-up, outcomes were slightly better on most measures for transvaginal uterosacral ligament suspension versus transvaginal sacrospinous ligament fixation for apical prolapse, but the differences were not statistically significant, according to the first randomized trial to compare the two techniques.
Quality of life improvements were durable, but the overall 5-year success rate – defined as the absence of descent of the vaginal apex more than one-third into the vagina; anterior or posterior vaginal wall descent beyond the hymen; bothersome vaginal bulge symptoms; and further treatment for prolapse – was 39% in the 109 women randomized to bilateral uterosacral ligament suspension (ULS) and 30% in the 109 women randomized to unilateral sacrospinous ligament fixation (SSLF).
But there was a notable finding in the study. If women failed to meet all the requirements for success at any one visit, they were classified as surgical failures. However, many who missed the mark at one visit met all the requirements for success on other visits, including their last follow-up.
“We don’t think as surgeons that a bulge comes and goes on a yearly basis, but people actually moved in and out of success and failure over time, and that’s new,” Dr. Jelovsek said. “We just don’t understand the dynamic variables of anatomic prolapse, because no one’s looked at it. The assumption of ‘once a failure, always a failure’ may underestimate success rates.”
Nonetheless, using that approach in the study, the investigators found that the anatomic success was 54% in the ULS and 38% in the SSLF groups at 5 years, and 37% of women in the ULS group reported bothersome vaginal bulge symptoms, versus 42% of women with SSLF. A total of 12% of women with ULS and 8% of women with SSLF had undergone POP retreatment at 5 years, either by pessary or secondary surgery but, again, the differences were not statistically significant.
Of the 145 anatomic failures in the study, 41% were stage 3 or 4.
Quality of life improvements, assessed annually by phone, “were maintained over 5 years despite progressive increases in surgical failure rates over time,” with about a 70-point improvement in the Pelvic Organ Prolapse Distress Inventory and similar gains in other measures in both groups, Dr. Jelovsek reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
There were no between-group differences in suture exposure (about 25% in both groups) or sling erosion (about 3%) at 5 years.
There was a difference in granulation tissue: 28.9% with ULS and 18.8% with SSLF (odds ratio with ULS, 1.9; 95% confidence interval 1-3.7). The majority of adverse events occurred within 2 years of surgery.
Early pelvic floor muscle training made no difference in outcomes for the women randomized to it.
The women in the study had stage 2-4 prolapse at baseline. In addition to vaginal suspension surgery, they had vaginal hysterectomies if there was uterine prolapse, and all the women had concomitant retropubic midurethral sling surgery for stress incontinence.
At 2 years, composite success rates were about 60% in both groups (JAMA. 2014 Mar 12;311[10]:1023-34).
The study didn’t identify risk factors for failure, but they would be helpful to know, Dr. Jelovsek said. High-risk women might benefit from a more durable mesh repair. For now at least, “most women say the risk” of pain and other serious mesh complications “completely outweighs the bulge symptoms,” he said.
The trial, an extension of OPTIMAL (Operations and Pelvic Muscle Training in the Management of Apical Support Loss), was conducted at nine U.S. centers in the Pelvic Floor Disorders Network, which is funded by the National Institutes of Health. Dr. Jelovsek reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – At 5-year follow-up, outcomes were slightly better on most measures for transvaginal uterosacral ligament suspension versus transvaginal sacrospinous ligament fixation for apical prolapse, but the differences were not statistically significant, according to the first randomized trial to compare the two techniques.
Quality of life improvements were durable, but the overall 5-year success rate – defined as the absence of descent of the vaginal apex more than one-third into the vagina; anterior or posterior vaginal wall descent beyond the hymen; bothersome vaginal bulge symptoms; and further treatment for prolapse – was 39% in the 109 women randomized to bilateral uterosacral ligament suspension (ULS) and 30% in the 109 women randomized to unilateral sacrospinous ligament fixation (SSLF).
But there was a notable finding in the study. If women failed to meet all the requirements for success at any one visit, they were classified as surgical failures. However, many who missed the mark at one visit met all the requirements for success on other visits, including their last follow-up.
“We don’t think as surgeons that a bulge comes and goes on a yearly basis, but people actually moved in and out of success and failure over time, and that’s new,” Dr. Jelovsek said. “We just don’t understand the dynamic variables of anatomic prolapse, because no one’s looked at it. The assumption of ‘once a failure, always a failure’ may underestimate success rates.”
Nonetheless, using that approach in the study, the investigators found that the anatomic success was 54% in the ULS and 38% in the SSLF groups at 5 years, and 37% of women in the ULS group reported bothersome vaginal bulge symptoms, versus 42% of women with SSLF. A total of 12% of women with ULS and 8% of women with SSLF had undergone POP retreatment at 5 years, either by pessary or secondary surgery but, again, the differences were not statistically significant.
Of the 145 anatomic failures in the study, 41% were stage 3 or 4.
Quality of life improvements, assessed annually by phone, “were maintained over 5 years despite progressive increases in surgical failure rates over time,” with about a 70-point improvement in the Pelvic Organ Prolapse Distress Inventory and similar gains in other measures in both groups, Dr. Jelovsek reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
There were no between-group differences in suture exposure (about 25% in both groups) or sling erosion (about 3%) at 5 years.
There was a difference in granulation tissue: 28.9% with ULS and 18.8% with SSLF (odds ratio with ULS, 1.9; 95% confidence interval 1-3.7). The majority of adverse events occurred within 2 years of surgery.
Early pelvic floor muscle training made no difference in outcomes for the women randomized to it.
The women in the study had stage 2-4 prolapse at baseline. In addition to vaginal suspension surgery, they had vaginal hysterectomies if there was uterine prolapse, and all the women had concomitant retropubic midurethral sling surgery for stress incontinence.
At 2 years, composite success rates were about 60% in both groups (JAMA. 2014 Mar 12;311[10]:1023-34).
The study didn’t identify risk factors for failure, but they would be helpful to know, Dr. Jelovsek said. High-risk women might benefit from a more durable mesh repair. For now at least, “most women say the risk” of pain and other serious mesh complications “completely outweighs the bulge symptoms,” he said.
The trial, an extension of OPTIMAL (Operations and Pelvic Muscle Training in the Management of Apical Support Loss), was conducted at nine U.S. centers in the Pelvic Floor Disorders Network, which is funded by the National Institutes of Health. Dr. Jelovsek reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
Key clinical point:
Major finding: The overall 5-year success rate was 39% in women randomized to bilateral uterosacral ligament suspension and 30% in women randomized to unilateral sacrospinous ligament fixation.
Data source: The first randomized trial to compare the two commonly used techniques was conducted among 218 women at nine U.S. centers in the Pelvic Floor Disorders Network.
Disclosures: The Pelvic Floor Disorders Network is funded by the National Institutes of Health. The lead investigator reported having no relevant financial disclosures.
Coming soon!
Watch for our on-site coverage of the 18th annual meeting of the American Society of Breast Surgeons, which will take place in Las Vegas April 26-30.
Watch for our on-site coverage of the 18th annual meeting of the American Society of Breast Surgeons, which will take place in Las Vegas April 26-30.
Watch for our on-site coverage of the 18th annual meeting of the American Society of Breast Surgeons, which will take place in Las Vegas April 26-30.
U.S. thyroid cancer incidence, mortality on the upswing
ORLANDO – with incidence-based mortality increasing by 1.1% annually from 1994 to 2013, according to a study conducted by the National Cancer Institute.
In a study of 77,726 patients diagnosed with thyroid cancer between 1974 and 2013, incidence rates increased from 4.56 per 100,000 person-years during 1974-1977 to 14.42 per 100,000 person-years during 2010-2013, according to Hyeyeun Lim, PhD, a postdoctoral fellow at National Cancer Institute, and colleagues (JAMA. 2017;317[13]:1338-48).
A majority of patients in the sample were female (75%) and white (82%); average age was 48 years.
A notable trend was the increase in papillary thyroid cancer (PTC). PTC was the most common thyroid cancer at 83.6% of diagnoses, followed by follicular, medullary, anaplastic, and other at 10.8%, 2.2%, 1.3%, and 2.1%, respectively. PTC was associated with the highest annual percent change (4.4%) and the only positive incidence-based mortality annual percent change (1.7%) among all histologic types, according to the researchers.
Regional and distant tumors accounted for 53.2% and 29% of deaths, respectively, compared to 13.5% for local tumors.
Dr. Lim and colleagues interpret the increase in incidence to contradict a common idea among researchers that attributes rising rates to new methods of detection such as ultrasound imaging and fine-needle aspiration biopsies.
“Such changes could account for the rapid increases in the incidence rates for localized and small PTCs that have been previously observed,” the researchers reported. “However, the significant, albeit less-rapid increase in advanced-stage and larger PTC incidence rates and increasing thyroid cancer mortality rates among patients diagnosed with advanced-stage PTC is not consistent with the notion that over-diagnosis is solely responsible for the changing trends in PTC incidence.”
While the researchers reported increased mortality rates among all PTC demographics, statistical significance was found solely in patients with distant disease (annual percentage changes, 2.9% [95% confidence interval, 1.1%-4.7%]), stage IV disease (APC, 12.9%[95%CI, 7.2%-19.0%]), or both, according to researchers.
Researchers speculate increased rates of obesity, childhood ionizing radiation exposure, and increased exposure to pesticides may be possible sources for increased rates of PTC, however Dr. Lim and peers assert further research must be conducted.
Based on these findings, researchers suggest “renewed focus on aggressive transdisciplinary management that includes surgery, adjuvant radioactive iodine, and, when indicated for the 5%-10% of patients who develop progressive disease, systemic therapy,” for patients with advanced-stage PTC.
Due to the nature of the study, researchers were limited to speculating potential reasons for increase in thyroid cancer incidence. Information of tumor size and stage was limited to the years when this information began to be recorded, after the initial years included in the study.
[email protected]
On Twitter @EAZTweets
ORLANDO – with incidence-based mortality increasing by 1.1% annually from 1994 to 2013, according to a study conducted by the National Cancer Institute.
In a study of 77,726 patients diagnosed with thyroid cancer between 1974 and 2013, incidence rates increased from 4.56 per 100,000 person-years during 1974-1977 to 14.42 per 100,000 person-years during 2010-2013, according to Hyeyeun Lim, PhD, a postdoctoral fellow at National Cancer Institute, and colleagues (JAMA. 2017;317[13]:1338-48).
A majority of patients in the sample were female (75%) and white (82%); average age was 48 years.
A notable trend was the increase in papillary thyroid cancer (PTC). PTC was the most common thyroid cancer at 83.6% of diagnoses, followed by follicular, medullary, anaplastic, and other at 10.8%, 2.2%, 1.3%, and 2.1%, respectively. PTC was associated with the highest annual percent change (4.4%) and the only positive incidence-based mortality annual percent change (1.7%) among all histologic types, according to the researchers.
Regional and distant tumors accounted for 53.2% and 29% of deaths, respectively, compared to 13.5% for local tumors.
Dr. Lim and colleagues interpret the increase in incidence to contradict a common idea among researchers that attributes rising rates to new methods of detection such as ultrasound imaging and fine-needle aspiration biopsies.
“Such changes could account for the rapid increases in the incidence rates for localized and small PTCs that have been previously observed,” the researchers reported. “However, the significant, albeit less-rapid increase in advanced-stage and larger PTC incidence rates and increasing thyroid cancer mortality rates among patients diagnosed with advanced-stage PTC is not consistent with the notion that over-diagnosis is solely responsible for the changing trends in PTC incidence.”
While the researchers reported increased mortality rates among all PTC demographics, statistical significance was found solely in patients with distant disease (annual percentage changes, 2.9% [95% confidence interval, 1.1%-4.7%]), stage IV disease (APC, 12.9%[95%CI, 7.2%-19.0%]), or both, according to researchers.
Researchers speculate increased rates of obesity, childhood ionizing radiation exposure, and increased exposure to pesticides may be possible sources for increased rates of PTC, however Dr. Lim and peers assert further research must be conducted.
Based on these findings, researchers suggest “renewed focus on aggressive transdisciplinary management that includes surgery, adjuvant radioactive iodine, and, when indicated for the 5%-10% of patients who develop progressive disease, systemic therapy,” for patients with advanced-stage PTC.
Due to the nature of the study, researchers were limited to speculating potential reasons for increase in thyroid cancer incidence. Information of tumor size and stage was limited to the years when this information began to be recorded, after the initial years included in the study.
[email protected]
On Twitter @EAZTweets
ORLANDO – with incidence-based mortality increasing by 1.1% annually from 1994 to 2013, according to a study conducted by the National Cancer Institute.
In a study of 77,726 patients diagnosed with thyroid cancer between 1974 and 2013, incidence rates increased from 4.56 per 100,000 person-years during 1974-1977 to 14.42 per 100,000 person-years during 2010-2013, according to Hyeyeun Lim, PhD, a postdoctoral fellow at National Cancer Institute, and colleagues (JAMA. 2017;317[13]:1338-48).
A majority of patients in the sample were female (75%) and white (82%); average age was 48 years.
A notable trend was the increase in papillary thyroid cancer (PTC). PTC was the most common thyroid cancer at 83.6% of diagnoses, followed by follicular, medullary, anaplastic, and other at 10.8%, 2.2%, 1.3%, and 2.1%, respectively. PTC was associated with the highest annual percent change (4.4%) and the only positive incidence-based mortality annual percent change (1.7%) among all histologic types, according to the researchers.
Regional and distant tumors accounted for 53.2% and 29% of deaths, respectively, compared to 13.5% for local tumors.
Dr. Lim and colleagues interpret the increase in incidence to contradict a common idea among researchers that attributes rising rates to new methods of detection such as ultrasound imaging and fine-needle aspiration biopsies.
“Such changes could account for the rapid increases in the incidence rates for localized and small PTCs that have been previously observed,” the researchers reported. “However, the significant, albeit less-rapid increase in advanced-stage and larger PTC incidence rates and increasing thyroid cancer mortality rates among patients diagnosed with advanced-stage PTC is not consistent with the notion that over-diagnosis is solely responsible for the changing trends in PTC incidence.”
While the researchers reported increased mortality rates among all PTC demographics, statistical significance was found solely in patients with distant disease (annual percentage changes, 2.9% [95% confidence interval, 1.1%-4.7%]), stage IV disease (APC, 12.9%[95%CI, 7.2%-19.0%]), or both, according to researchers.
Researchers speculate increased rates of obesity, childhood ionizing radiation exposure, and increased exposure to pesticides may be possible sources for increased rates of PTC, however Dr. Lim and peers assert further research must be conducted.
Based on these findings, researchers suggest “renewed focus on aggressive transdisciplinary management that includes surgery, adjuvant radioactive iodine, and, when indicated for the 5%-10% of patients who develop progressive disease, systemic therapy,” for patients with advanced-stage PTC.
Due to the nature of the study, researchers were limited to speculating potential reasons for increase in thyroid cancer incidence. Information of tumor size and stage was limited to the years when this information began to be recorded, after the initial years included in the study.
[email protected]
On Twitter @EAZTweets
AT ENDO 2017
Key clinical point:
Major finding: Thyroid cancer incidence increased 3.6% from 1974 to 2013 and incidence-based mortality increased by 1.1% per year from 1994 to 2013.
Data source: A retrospective study of 77,726 patient records attained from Surveillance, Epidemiology, and End Results–9 cancer registry database, analyzed via log-linear regression.
Disclosures: Dr. Julie Sosa reported being on the Data Monitoring Committee of the Medullary Thyroid Cancer Consortium Registry, which is sponsored by AstraZeneca, Eli Lilly, GlaxoSmithKline, and Novo Nordisk.
What do doctors want from health reform?
With the demise of Republican repeal and replace legislation, analysts say the landscape is ripe for repairs to the Affordable Care Act or for additional legislation that both political parties could support. So what do physicians want from health reform?
The first step should be stabilizing the health insurance marketplaces by strengthening and perhaps extending risk mitigation measures such as the risk adjustment, risk corridors, and reinsurance provisions of the law, said Patricia Salber, MD, an internist and health care consultant who blogs at TheDoctorWeighsIn.com. Those three ACA provisions were intended to promote insurer competition on the basis of quality and value and promote insurance market stability.
Keeping premiums at manageable levels for patients should also be addressed, said William J. Burke, DO, dean of Ohio University Heritage College of Osteopathic Medicine.
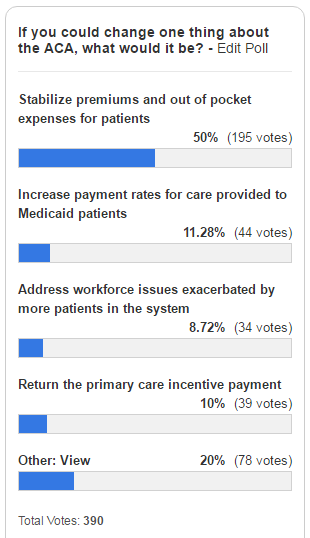
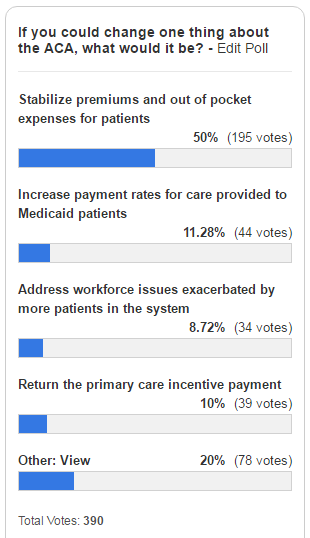
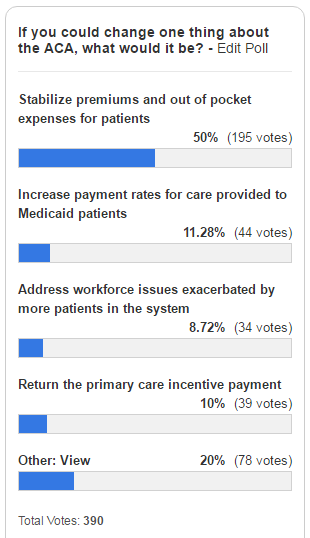
That was echoed in a poll taken by this news organization. Of 390 respondents, fully half (50%) said they would repair the ACA by stabilizing premiums and out-of-pocket costs for patients as of April 2. About 11% stated they would increase payment rates for care provided to Medicaid patients, and 10% said they would return the primary care incentive payment. About 9% of those surveyed would address workforce issues exacerbated by more patients in the system.
Improving reimbursement for Medicaid services is a necessary health reform change, agreed Diane J. Horvath-Cosper MD, an obstetrician-gynecologist and reproductive health advocacy fellow for Physicians for Reproductive Health, a reproductive rights advocacy organization.
“Reimbursement rates are so low that sometimes [physicians] have to limit the number of Medicaid patients to be able to pay staff,” Dr. Horvath said in an interview. “That’s a terrible position to put physicians in because we want to be able to see as many people who want to see us.”
Speaking of Medicaid, Dr. Salber adds that governors should be encouraged to continue expanding Medicaid to eliminate the coverage gap for the “near poor” that exists in states that did not participate in the expansion.
“Now that the [American Health Care Act] has failed, I think we will see some expansion take place organically even in states that were deeply opposed before,” she said.
“The volume of prior authorizations that all physicians face, but especially primary care physicians, is huge,” Dr. Munger said in an interview. “In many cases, we’re having to hire extra staff just to handle all of the prior authorizations. Every patient may not just have one prior authorization, but they may require two or three or four prior authorizations each month or quarterly. It really detracts from meaningful time you can spend with the patient.”
For starters, doctors should provide care to patients based on mutually agreed terms and without the interference of insurers, Dr. Orient said in an interview. In such a private medicine system, patients would pay doctors for services, and patients would then file claims with their insurer for reimbursement. Similarly, physicians should not be at the mercy of Medicare for payment, Dr. Orient said.
“Doctors can sign away their rights if they want in a Medicare participation agreement,” she said. “Doctors who do not sign the agreement to take assignment in all cases doctors should be freed of price controls and coding demands. Their patients should be allowed to file their own simple claims to Medicare with an itemized bill as they did before the 1990s law that requires physicians to submit the claims. Non-participating doctors should be exempted from MACRA [the Medicare Access and CHIP Reauthorization Act], and without the price controls, there is no need for [Recovery Audit Contractors] and other auditors.”
While contraceptive care was strengthened by the ACA, Dr. Horvath said further efforts should be made to improve coverage and level the playing field for reproductive medicine. In addition, she said that abortion should be treated a valid medical procedure, rather than parsed out, and both public and private insurers should be required to pay for the procedure, she said.
“I would love to see strengthened provisions for contraception coverage,” Dr. Horvath said. “[We need to] make sure that doesn’t get bargained away. The other thing is to expand coverage and make sure every method is covered, not just one method in each category.”
However, Robert Doherty, ACP senior vice president of governmental affairs and public policy, said the college is concerned that the current administration may fail to maintain the ACA now that its proposed repeal law has fallen through.
Without aggressively pushing ACA enrollment for younger patients and continued support for the individual mandate, more insurers may pull out of the marketplaces, and the ACA could implode, Mr. Doherty said.
“There are a number of ways that Republicans could either make things better or worse with action or inaction,” Mr. Doherty said during the press conference. “The insurance [companies] have gone to this administration with a wish list of things that will help keep them in the market. What remains to be seen is whether this administration is going to be receptive. If they don’t aggressively enforce the requirement that people buy coverage, more younger people will opt out and stay out until they get sick. That would make the problem of adverse selection even worse and could create the death cycle for insurance.”
Dr. Price consistently answered that Americans should be able to select the kinds of coverage they want. What “we believe is that individuals ought to be able to have access to the kind of coverage that they select for themselves and for their families and not what the government forces them to buy,” Dr. Price testified, echoing the message from his confirmation hearings.
He was also pressed on issues such as the individual mandate, and while noting that it is his duty to uphold the law of the land, he also remained noncommittal in answering questions about whether he would direct the agency to enforce the individual mandate. The first executive order from President Trump beginning his administration gave the agency discretion to not enforce mandates if they caused harm.
[email protected]
On Twitter @legal_med
Gregory Twachtman contributed to this report.
With the demise of Republican repeal and replace legislation, analysts say the landscape is ripe for repairs to the Affordable Care Act or for additional legislation that both political parties could support. So what do physicians want from health reform?
The first step should be stabilizing the health insurance marketplaces by strengthening and perhaps extending risk mitigation measures such as the risk adjustment, risk corridors, and reinsurance provisions of the law, said Patricia Salber, MD, an internist and health care consultant who blogs at TheDoctorWeighsIn.com. Those three ACA provisions were intended to promote insurer competition on the basis of quality and value and promote insurance market stability.
Keeping premiums at manageable levels for patients should also be addressed, said William J. Burke, DO, dean of Ohio University Heritage College of Osteopathic Medicine.
That was echoed in a poll taken by this news organization. Of 390 respondents, fully half (50%) said they would repair the ACA by stabilizing premiums and out-of-pocket costs for patients as of April 2. About 11% stated they would increase payment rates for care provided to Medicaid patients, and 10% said they would return the primary care incentive payment. About 9% of those surveyed would address workforce issues exacerbated by more patients in the system.
Improving reimbursement for Medicaid services is a necessary health reform change, agreed Diane J. Horvath-Cosper MD, an obstetrician-gynecologist and reproductive health advocacy fellow for Physicians for Reproductive Health, a reproductive rights advocacy organization.
“Reimbursement rates are so low that sometimes [physicians] have to limit the number of Medicaid patients to be able to pay staff,” Dr. Horvath said in an interview. “That’s a terrible position to put physicians in because we want to be able to see as many people who want to see us.”
Speaking of Medicaid, Dr. Salber adds that governors should be encouraged to continue expanding Medicaid to eliminate the coverage gap for the “near poor” that exists in states that did not participate in the expansion.
“Now that the [American Health Care Act] has failed, I think we will see some expansion take place organically even in states that were deeply opposed before,” she said.
“The volume of prior authorizations that all physicians face, but especially primary care physicians, is huge,” Dr. Munger said in an interview. “In many cases, we’re having to hire extra staff just to handle all of the prior authorizations. Every patient may not just have one prior authorization, but they may require two or three or four prior authorizations each month or quarterly. It really detracts from meaningful time you can spend with the patient.”
For starters, doctors should provide care to patients based on mutually agreed terms and without the interference of insurers, Dr. Orient said in an interview. In such a private medicine system, patients would pay doctors for services, and patients would then file claims with their insurer for reimbursement. Similarly, physicians should not be at the mercy of Medicare for payment, Dr. Orient said.
“Doctors can sign away their rights if they want in a Medicare participation agreement,” she said. “Doctors who do not sign the agreement to take assignment in all cases doctors should be freed of price controls and coding demands. Their patients should be allowed to file their own simple claims to Medicare with an itemized bill as they did before the 1990s law that requires physicians to submit the claims. Non-participating doctors should be exempted from MACRA [the Medicare Access and CHIP Reauthorization Act], and without the price controls, there is no need for [Recovery Audit Contractors] and other auditors.”
While contraceptive care was strengthened by the ACA, Dr. Horvath said further efforts should be made to improve coverage and level the playing field for reproductive medicine. In addition, she said that abortion should be treated a valid medical procedure, rather than parsed out, and both public and private insurers should be required to pay for the procedure, she said.
“I would love to see strengthened provisions for contraception coverage,” Dr. Horvath said. “[We need to] make sure that doesn’t get bargained away. The other thing is to expand coverage and make sure every method is covered, not just one method in each category.”
However, Robert Doherty, ACP senior vice president of governmental affairs and public policy, said the college is concerned that the current administration may fail to maintain the ACA now that its proposed repeal law has fallen through.
Without aggressively pushing ACA enrollment for younger patients and continued support for the individual mandate, more insurers may pull out of the marketplaces, and the ACA could implode, Mr. Doherty said.
“There are a number of ways that Republicans could either make things better or worse with action or inaction,” Mr. Doherty said during the press conference. “The insurance [companies] have gone to this administration with a wish list of things that will help keep them in the market. What remains to be seen is whether this administration is going to be receptive. If they don’t aggressively enforce the requirement that people buy coverage, more younger people will opt out and stay out until they get sick. That would make the problem of adverse selection even worse and could create the death cycle for insurance.”
Dr. Price consistently answered that Americans should be able to select the kinds of coverage they want. What “we believe is that individuals ought to be able to have access to the kind of coverage that they select for themselves and for their families and not what the government forces them to buy,” Dr. Price testified, echoing the message from his confirmation hearings.
He was also pressed on issues such as the individual mandate, and while noting that it is his duty to uphold the law of the land, he also remained noncommittal in answering questions about whether he would direct the agency to enforce the individual mandate. The first executive order from President Trump beginning his administration gave the agency discretion to not enforce mandates if they caused harm.
[email protected]
On Twitter @legal_med
Gregory Twachtman contributed to this report.
With the demise of Republican repeal and replace legislation, analysts say the landscape is ripe for repairs to the Affordable Care Act or for additional legislation that both political parties could support. So what do physicians want from health reform?
The first step should be stabilizing the health insurance marketplaces by strengthening and perhaps extending risk mitigation measures such as the risk adjustment, risk corridors, and reinsurance provisions of the law, said Patricia Salber, MD, an internist and health care consultant who blogs at TheDoctorWeighsIn.com. Those three ACA provisions were intended to promote insurer competition on the basis of quality and value and promote insurance market stability.
Keeping premiums at manageable levels for patients should also be addressed, said William J. Burke, DO, dean of Ohio University Heritage College of Osteopathic Medicine.
That was echoed in a poll taken by this news organization. Of 390 respondents, fully half (50%) said they would repair the ACA by stabilizing premiums and out-of-pocket costs for patients as of April 2. About 11% stated they would increase payment rates for care provided to Medicaid patients, and 10% said they would return the primary care incentive payment. About 9% of those surveyed would address workforce issues exacerbated by more patients in the system.
Improving reimbursement for Medicaid services is a necessary health reform change, agreed Diane J. Horvath-Cosper MD, an obstetrician-gynecologist and reproductive health advocacy fellow for Physicians for Reproductive Health, a reproductive rights advocacy organization.
“Reimbursement rates are so low that sometimes [physicians] have to limit the number of Medicaid patients to be able to pay staff,” Dr. Horvath said in an interview. “That’s a terrible position to put physicians in because we want to be able to see as many people who want to see us.”
Speaking of Medicaid, Dr. Salber adds that governors should be encouraged to continue expanding Medicaid to eliminate the coverage gap for the “near poor” that exists in states that did not participate in the expansion.
“Now that the [American Health Care Act] has failed, I think we will see some expansion take place organically even in states that were deeply opposed before,” she said.
“The volume of prior authorizations that all physicians face, but especially primary care physicians, is huge,” Dr. Munger said in an interview. “In many cases, we’re having to hire extra staff just to handle all of the prior authorizations. Every patient may not just have one prior authorization, but they may require two or three or four prior authorizations each month or quarterly. It really detracts from meaningful time you can spend with the patient.”
For starters, doctors should provide care to patients based on mutually agreed terms and without the interference of insurers, Dr. Orient said in an interview. In such a private medicine system, patients would pay doctors for services, and patients would then file claims with their insurer for reimbursement. Similarly, physicians should not be at the mercy of Medicare for payment, Dr. Orient said.
“Doctors can sign away their rights if they want in a Medicare participation agreement,” she said. “Doctors who do not sign the agreement to take assignment in all cases doctors should be freed of price controls and coding demands. Their patients should be allowed to file their own simple claims to Medicare with an itemized bill as they did before the 1990s law that requires physicians to submit the claims. Non-participating doctors should be exempted from MACRA [the Medicare Access and CHIP Reauthorization Act], and without the price controls, there is no need for [Recovery Audit Contractors] and other auditors.”
While contraceptive care was strengthened by the ACA, Dr. Horvath said further efforts should be made to improve coverage and level the playing field for reproductive medicine. In addition, she said that abortion should be treated a valid medical procedure, rather than parsed out, and both public and private insurers should be required to pay for the procedure, she said.
“I would love to see strengthened provisions for contraception coverage,” Dr. Horvath said. “[We need to] make sure that doesn’t get bargained away. The other thing is to expand coverage and make sure every method is covered, not just one method in each category.”
However, Robert Doherty, ACP senior vice president of governmental affairs and public policy, said the college is concerned that the current administration may fail to maintain the ACA now that its proposed repeal law has fallen through.
Without aggressively pushing ACA enrollment for younger patients and continued support for the individual mandate, more insurers may pull out of the marketplaces, and the ACA could implode, Mr. Doherty said.
“There are a number of ways that Republicans could either make things better or worse with action or inaction,” Mr. Doherty said during the press conference. “The insurance [companies] have gone to this administration with a wish list of things that will help keep them in the market. What remains to be seen is whether this administration is going to be receptive. If they don’t aggressively enforce the requirement that people buy coverage, more younger people will opt out and stay out until they get sick. That would make the problem of adverse selection even worse and could create the death cycle for insurance.”
Dr. Price consistently answered that Americans should be able to select the kinds of coverage they want. What “we believe is that individuals ought to be able to have access to the kind of coverage that they select for themselves and for their families and not what the government forces them to buy,” Dr. Price testified, echoing the message from his confirmation hearings.
He was also pressed on issues such as the individual mandate, and while noting that it is his duty to uphold the law of the land, he also remained noncommittal in answering questions about whether he would direct the agency to enforce the individual mandate. The first executive order from President Trump beginning his administration gave the agency discretion to not enforce mandates if they caused harm.
[email protected]
On Twitter @legal_med
Gregory Twachtman contributed to this report.
Don’t shy away from vaginal salpingectomy
SAN ANTONIO – Surgeons at Houston Methodist Hospital reported a 75% success rate in removing both fallopian tubes during vaginal hysterectomy in a study presented at the annual scientific meeting of the Society of Gynecologic Surgeons.
Serous ovarian carcinoma is now thought to arise from the distal fallopian tube, and it’s estimated that salpingectomy prevents diagnosis of ovarian cancer in 1 in 225 women and death from ovarian cancer in 1 in 450 women. The American Congress of Obstetricians and Gynecologists recommends that surgeons and patients “discuss the potential benefits of the removal of the fallopian tubes” during hysterectomy in women not having an oophorectomy.
The findings from the Houston team show that “it’s feasible in most cases, with very little risk,” said Danielle Antosh, MD, lead investigator and director of the Center for Restorative Pelvic Medicine at Houston Methodist Urogynecology Associates.
“People are doing laparoscopic hysterectomies or robotic hysterectomies” to get at the fallopian tubes, “but they shouldn’t be deterred from trying to remove the fallopian tubes vaginally,” Dr. Antosh said at the SGS 2017 meeting. When women are having a vaginal hysterectomy, “why not try to remove the fallopian tubes? It’s something I would definitely consider counseling your patients about.”
Dr. Antosh said that residents should be taught how to perform salpingectomy during vaginal hysterectomy. “I think it is definitely feasible for residents to do.” Technically, “it’s a lot easier than removing the ovaries” vaginally, she said.
The 70 women in the study were undergoing vaginal hysterectomies by attending physicians for benign reasons, mostly uterine prolapse, followed by heavy menstrual flow and fibroids. In total, 52 (75%) had successful concomitant bilateral vaginal salpingectomies, and 7 additional women had one tube removed. Success was more likely with increasing parity and a history of prolapse. Most of the failures were because the tubes were too high in the pelvis or there were adhesions from prior adnexal surgery. Even with prior adnexal surgery, however, the success rate was 50%.
Vaginal salpingectomy added a mean of 11 minutes to surgery and a mean of 5 mL blood loss. There were no complications reported from including salpingectomy with vaginal hysterectomy. The study wasn’t powered to detect an impact on menopause symptoms, but there was a decrease in menopause symptoms at 16 week follow-up in the salpingectomy group, perhaps related to less sexual dysfunction and urinary incontinence.
The mean age in the study was 51 years, and mean body mass index was 27 kg/m2. There were no malignancies found on tubal pathology.
Five women were transferred to an abdominal approach because of a large uterus or discovery of ovarian pathology. None were transferred for the purpose of salpingectomy.
There was no external funding for the study, and the investigators reported no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – Surgeons at Houston Methodist Hospital reported a 75% success rate in removing both fallopian tubes during vaginal hysterectomy in a study presented at the annual scientific meeting of the Society of Gynecologic Surgeons.
Serous ovarian carcinoma is now thought to arise from the distal fallopian tube, and it’s estimated that salpingectomy prevents diagnosis of ovarian cancer in 1 in 225 women and death from ovarian cancer in 1 in 450 women. The American Congress of Obstetricians and Gynecologists recommends that surgeons and patients “discuss the potential benefits of the removal of the fallopian tubes” during hysterectomy in women not having an oophorectomy.
The findings from the Houston team show that “it’s feasible in most cases, with very little risk,” said Danielle Antosh, MD, lead investigator and director of the Center for Restorative Pelvic Medicine at Houston Methodist Urogynecology Associates.
“People are doing laparoscopic hysterectomies or robotic hysterectomies” to get at the fallopian tubes, “but they shouldn’t be deterred from trying to remove the fallopian tubes vaginally,” Dr. Antosh said at the SGS 2017 meeting. When women are having a vaginal hysterectomy, “why not try to remove the fallopian tubes? It’s something I would definitely consider counseling your patients about.”
Dr. Antosh said that residents should be taught how to perform salpingectomy during vaginal hysterectomy. “I think it is definitely feasible for residents to do.” Technically, “it’s a lot easier than removing the ovaries” vaginally, she said.
The 70 women in the study were undergoing vaginal hysterectomies by attending physicians for benign reasons, mostly uterine prolapse, followed by heavy menstrual flow and fibroids. In total, 52 (75%) had successful concomitant bilateral vaginal salpingectomies, and 7 additional women had one tube removed. Success was more likely with increasing parity and a history of prolapse. Most of the failures were because the tubes were too high in the pelvis or there were adhesions from prior adnexal surgery. Even with prior adnexal surgery, however, the success rate was 50%.
Vaginal salpingectomy added a mean of 11 minutes to surgery and a mean of 5 mL blood loss. There were no complications reported from including salpingectomy with vaginal hysterectomy. The study wasn’t powered to detect an impact on menopause symptoms, but there was a decrease in menopause symptoms at 16 week follow-up in the salpingectomy group, perhaps related to less sexual dysfunction and urinary incontinence.
The mean age in the study was 51 years, and mean body mass index was 27 kg/m2. There were no malignancies found on tubal pathology.
Five women were transferred to an abdominal approach because of a large uterus or discovery of ovarian pathology. None were transferred for the purpose of salpingectomy.
There was no external funding for the study, and the investigators reported no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – Surgeons at Houston Methodist Hospital reported a 75% success rate in removing both fallopian tubes during vaginal hysterectomy in a study presented at the annual scientific meeting of the Society of Gynecologic Surgeons.
Serous ovarian carcinoma is now thought to arise from the distal fallopian tube, and it’s estimated that salpingectomy prevents diagnosis of ovarian cancer in 1 in 225 women and death from ovarian cancer in 1 in 450 women. The American Congress of Obstetricians and Gynecologists recommends that surgeons and patients “discuss the potential benefits of the removal of the fallopian tubes” during hysterectomy in women not having an oophorectomy.
The findings from the Houston team show that “it’s feasible in most cases, with very little risk,” said Danielle Antosh, MD, lead investigator and director of the Center for Restorative Pelvic Medicine at Houston Methodist Urogynecology Associates.
“People are doing laparoscopic hysterectomies or robotic hysterectomies” to get at the fallopian tubes, “but they shouldn’t be deterred from trying to remove the fallopian tubes vaginally,” Dr. Antosh said at the SGS 2017 meeting. When women are having a vaginal hysterectomy, “why not try to remove the fallopian tubes? It’s something I would definitely consider counseling your patients about.”
Dr. Antosh said that residents should be taught how to perform salpingectomy during vaginal hysterectomy. “I think it is definitely feasible for residents to do.” Technically, “it’s a lot easier than removing the ovaries” vaginally, she said.
The 70 women in the study were undergoing vaginal hysterectomies by attending physicians for benign reasons, mostly uterine prolapse, followed by heavy menstrual flow and fibroids. In total, 52 (75%) had successful concomitant bilateral vaginal salpingectomies, and 7 additional women had one tube removed. Success was more likely with increasing parity and a history of prolapse. Most of the failures were because the tubes were too high in the pelvis or there were adhesions from prior adnexal surgery. Even with prior adnexal surgery, however, the success rate was 50%.
Vaginal salpingectomy added a mean of 11 minutes to surgery and a mean of 5 mL blood loss. There were no complications reported from including salpingectomy with vaginal hysterectomy. The study wasn’t powered to detect an impact on menopause symptoms, but there was a decrease in menopause symptoms at 16 week follow-up in the salpingectomy group, perhaps related to less sexual dysfunction and urinary incontinence.
The mean age in the study was 51 years, and mean body mass index was 27 kg/m2. There were no malignancies found on tubal pathology.
Five women were transferred to an abdominal approach because of a large uterus or discovery of ovarian pathology. None were transferred for the purpose of salpingectomy.
There was no external funding for the study, and the investigators reported no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
AT SGS 2017
Key clinical point:
Major finding: Three-quarters of women undergoing vaginal hysterectomy for benign reasons had successful concomitant bilateral vaginal salpingectomy.
Data source: A single-center, observational study among 70 women undergoing vaginal hysterectomy for benign reasons.
Disclosures: There was no external funding and the investigators reported no relevant financial disclosures.
ACS New SSR Offers Webinar Training Sessions
The American College of Surgeons (ACS) has announced the launch of the new Surgeon Specific Registry (SSR), hosted by QuintilesIMS. The new SSR is set to go live in this spring. The latest version of the registry will have several enhanced features, including improved reporting capabilities, delegate-level access to enter data, and the ability to add custom fields for additional relevant variables.
To help you prepare for this transition, the SSR team will host several educational webinars to demonstrate the new system’s capabilities and features. The ACS encourages both current and potential users to participate. To view the available times and register for one of the upcoming webinars, visit the SSR News and Updates web page at facs.org/quality-programs/ssr/news.
Contact [email protected] if you have any questions.
The American College of Surgeons (ACS) has announced the launch of the new Surgeon Specific Registry (SSR), hosted by QuintilesIMS. The new SSR is set to go live in this spring. The latest version of the registry will have several enhanced features, including improved reporting capabilities, delegate-level access to enter data, and the ability to add custom fields for additional relevant variables.
To help you prepare for this transition, the SSR team will host several educational webinars to demonstrate the new system’s capabilities and features. The ACS encourages both current and potential users to participate. To view the available times and register for one of the upcoming webinars, visit the SSR News and Updates web page at facs.org/quality-programs/ssr/news.
Contact [email protected] if you have any questions.
The American College of Surgeons (ACS) has announced the launch of the new Surgeon Specific Registry (SSR), hosted by QuintilesIMS. The new SSR is set to go live in this spring. The latest version of the registry will have several enhanced features, including improved reporting capabilities, delegate-level access to enter data, and the ability to add custom fields for additional relevant variables.
To help you prepare for this transition, the SSR team will host several educational webinars to demonstrate the new system’s capabilities and features. The ACS encourages both current and potential users to participate. To view the available times and register for one of the upcoming webinars, visit the SSR News and Updates web page at facs.org/quality-programs/ssr/news.
Contact [email protected] if you have any questions.
Applications for 2018 Alliance Scholar Awards Accepted through June 30
Applications for 2018 Alliance Scholar Awards Accepted through June 30
The Alliance for Clinical Trials in Oncology Foundation is accepting applications for the 2018 Alliance Scholar Awards. Applications must be submitted by 12:00 midnight (CST) on June 30.
Alliance Scholar Award applicants must be oncology junior faculty at Alliance institutions within five years of training (rank below associate professor) and have completed training in an oncology clinical specialty (medical, surgical, radiation, gynecologic, and so on). Additionally, proposals must include a letter of support from the appropriate Alliance Scientific Committee Chair to ensure the proposal is closely tied to the Alliance’s research agenda of the Alliance.
Alliance Scholar Award recipients will receive a two-year, non-renewable cancer research grant of $40,000 in direct costs per year, plus 10 percent in indirect costs for each of the two years. Successful applicants will be announced at the plenary session at the 2017 Alliance Fall Group Meeting held in Chicago, IL, November 2–4. Funding will begin approximately January 1, 2018. For application requirements and the link to the online submission portal, visit the Alliance Scholar Awards page on the Alliance website at http://bit.ly/1JMXkwS.
The Alliance/American College of Surgeons Clinical Research Program offers opportunities for surgeons to become involved in the research and development of evidence-based practices in surgical oncology. If you would like to participate in oncology clinical research or oncology-related projects, contact [email protected].
Applications for 2018 Alliance Scholar Awards Accepted through June 30
The Alliance for Clinical Trials in Oncology Foundation is accepting applications for the 2018 Alliance Scholar Awards. Applications must be submitted by 12:00 midnight (CST) on June 30.
Alliance Scholar Award applicants must be oncology junior faculty at Alliance institutions within five years of training (rank below associate professor) and have completed training in an oncology clinical specialty (medical, surgical, radiation, gynecologic, and so on). Additionally, proposals must include a letter of support from the appropriate Alliance Scientific Committee Chair to ensure the proposal is closely tied to the Alliance’s research agenda of the Alliance.
Alliance Scholar Award recipients will receive a two-year, non-renewable cancer research grant of $40,000 in direct costs per year, plus 10 percent in indirect costs for each of the two years. Successful applicants will be announced at the plenary session at the 2017 Alliance Fall Group Meeting held in Chicago, IL, November 2–4. Funding will begin approximately January 1, 2018. For application requirements and the link to the online submission portal, visit the Alliance Scholar Awards page on the Alliance website at http://bit.ly/1JMXkwS.
The Alliance/American College of Surgeons Clinical Research Program offers opportunities for surgeons to become involved in the research and development of evidence-based practices in surgical oncology. If you would like to participate in oncology clinical research or oncology-related projects, contact [email protected].
Applications for 2018 Alliance Scholar Awards Accepted through June 30
The Alliance for Clinical Trials in Oncology Foundation is accepting applications for the 2018 Alliance Scholar Awards. Applications must be submitted by 12:00 midnight (CST) on June 30.
Alliance Scholar Award applicants must be oncology junior faculty at Alliance institutions within five years of training (rank below associate professor) and have completed training in an oncology clinical specialty (medical, surgical, radiation, gynecologic, and so on). Additionally, proposals must include a letter of support from the appropriate Alliance Scientific Committee Chair to ensure the proposal is closely tied to the Alliance’s research agenda of the Alliance.
Alliance Scholar Award recipients will receive a two-year, non-renewable cancer research grant of $40,000 in direct costs per year, plus 10 percent in indirect costs for each of the two years. Successful applicants will be announced at the plenary session at the 2017 Alliance Fall Group Meeting held in Chicago, IL, November 2–4. Funding will begin approximately January 1, 2018. For application requirements and the link to the online submission portal, visit the Alliance Scholar Awards page on the Alliance website at http://bit.ly/1JMXkwS.
The Alliance/American College of Surgeons Clinical Research Program offers opportunities for surgeons to become involved in the research and development of evidence-based practices in surgical oncology. If you would like to participate in oncology clinical research or oncology-related projects, contact [email protected].
Nominate an Inspiring Woman for WiSC Award
The American College of Surgeons (ACS) Women in Surgery Committee (WiSC) is accepting nominations for the second annual Dr. Mary Edwards Walker Inspiring Women in Surgery Award, which will be presented at Clinical Congress 2017 in San Diego, CA. The award will be accorded in recognition of an individual’s significant contributions to the advancement of women in the field of surgery. Nominations are due April 30.
The award honors Dr. Mary Edwards Walker for the example she set for future generations as the first woman surgeon to serve as a U.S. Army physician and the only woman to ever receive the U.S. Armed Forces Medal of Honor for bravery.
All nominations must be accompanied by the following documents:
• A letter of nomination outlining how the candidate has contributed to the advancement of women in the field of surgery
• An up-to-date curriculum vitae
Self-nominations are acceptable and should include a letter of reference. Nominations and questions should be submitted to Connie Bura at [email protected].
The American College of Surgeons (ACS) Women in Surgery Committee (WiSC) is accepting nominations for the second annual Dr. Mary Edwards Walker Inspiring Women in Surgery Award, which will be presented at Clinical Congress 2017 in San Diego, CA. The award will be accorded in recognition of an individual’s significant contributions to the advancement of women in the field of surgery. Nominations are due April 30.
The award honors Dr. Mary Edwards Walker for the example she set for future generations as the first woman surgeon to serve as a U.S. Army physician and the only woman to ever receive the U.S. Armed Forces Medal of Honor for bravery.
All nominations must be accompanied by the following documents:
• A letter of nomination outlining how the candidate has contributed to the advancement of women in the field of surgery
• An up-to-date curriculum vitae
Self-nominations are acceptable and should include a letter of reference. Nominations and questions should be submitted to Connie Bura at [email protected].
The American College of Surgeons (ACS) Women in Surgery Committee (WiSC) is accepting nominations for the second annual Dr. Mary Edwards Walker Inspiring Women in Surgery Award, which will be presented at Clinical Congress 2017 in San Diego, CA. The award will be accorded in recognition of an individual’s significant contributions to the advancement of women in the field of surgery. Nominations are due April 30.
The award honors Dr. Mary Edwards Walker for the example she set for future generations as the first woman surgeon to serve as a U.S. Army physician and the only woman to ever receive the U.S. Armed Forces Medal of Honor for bravery.
All nominations must be accompanied by the following documents:
• A letter of nomination outlining how the candidate has contributed to the advancement of women in the field of surgery
• An up-to-date curriculum vitae
Self-nominations are acceptable and should include a letter of reference. Nominations and questions should be submitted to Connie Bura at [email protected].
Celebrating our accomplishments
I recently had the good fortune to read a commentary written by Dr. Peter Angelos in ACS Surgery News entitled, The Right Choice? Surgeons, confidence, and humility (2017, February, p. 11). The essay touches on the philosophy, psychology, and attitudes that surgeons adopt and express in their daily interactions with the public.
The article refers to “the balance between lack of confidence and overconfidence, and between thoughtful introspection and paralyzing fear of future complications.” This is a critically important struggle in the mind of the surgeon. I would like to propose an exercise to bolster self-esteem in the psyche of the surgeon, particularly in the formative stages of one’s career, without fostering false or pathological bravado.
I certainly see the benefit in this tradition of analyzing and reviewing surgical misadventures and discussing the proper management of uninvited complications. It is a process rooted in the concepts of honesty, transparency, introspection, reflection, collaboration, and trust.
What I would like to propose is not the cessation of the M & M conference, but the addition of a complementary conference, which I refer to as Success and Survival conference. This meeting would showcase clinical scenarios in which a given patient should have succumbed to his illness but, instead, thrived as a result of the exemplary care provided by the surgical team involved. This would shine a bright spotlight on what it is that we do, and why our profession is so extraordinary. It would serve as a wonderful reminder for surgeons at all stages of their careers as to why we chose such a rigorous, challenging, and difficult vocation as our life’s work.
Such a venue would provide young surgeons an opportunity – not to flaunt – but to share and take well-deserved pride in their victories. I believe this conference would be as effective in terms of its educational value as the M & M, but it would not be associated with negative emotions of guilt, shame, and fear. The S & S would be a setting in which the young surgeon could shine in front of his or her peers as well as the attending staff and faculty.
The academic culture that prides itself on adages such as, “Whatever doesn’t kill you makes you stronger,” “The only problem with being on call every other night is that you miss half the pathology,” and “Eat when you can, sleep when you can, and don’t mess with the pancreas,” is long overdue in celebrating the accomplishments of surgeons publicly and on a regular basis
In the end, we should want to promote future generations of surgeons who are technically sound, demonstrate excellent judgment under the most difficult circumstances, and who are able to achieve, ideally, their full surgical potential by arriving at a true harmony between self-assurance and uncertainty.
Dr. Chuback is a vascular surgeon in private practice in Paramus, N.J.
I recently had the good fortune to read a commentary written by Dr. Peter Angelos in ACS Surgery News entitled, The Right Choice? Surgeons, confidence, and humility (2017, February, p. 11). The essay touches on the philosophy, psychology, and attitudes that surgeons adopt and express in their daily interactions with the public.
The article refers to “the balance between lack of confidence and overconfidence, and between thoughtful introspection and paralyzing fear of future complications.” This is a critically important struggle in the mind of the surgeon. I would like to propose an exercise to bolster self-esteem in the psyche of the surgeon, particularly in the formative stages of one’s career, without fostering false or pathological bravado.
I certainly see the benefit in this tradition of analyzing and reviewing surgical misadventures and discussing the proper management of uninvited complications. It is a process rooted in the concepts of honesty, transparency, introspection, reflection, collaboration, and trust.
What I would like to propose is not the cessation of the M & M conference, but the addition of a complementary conference, which I refer to as Success and Survival conference. This meeting would showcase clinical scenarios in which a given patient should have succumbed to his illness but, instead, thrived as a result of the exemplary care provided by the surgical team involved. This would shine a bright spotlight on what it is that we do, and why our profession is so extraordinary. It would serve as a wonderful reminder for surgeons at all stages of their careers as to why we chose such a rigorous, challenging, and difficult vocation as our life’s work.
Such a venue would provide young surgeons an opportunity – not to flaunt – but to share and take well-deserved pride in their victories. I believe this conference would be as effective in terms of its educational value as the M & M, but it would not be associated with negative emotions of guilt, shame, and fear. The S & S would be a setting in which the young surgeon could shine in front of his or her peers as well as the attending staff and faculty.
The academic culture that prides itself on adages such as, “Whatever doesn’t kill you makes you stronger,” “The only problem with being on call every other night is that you miss half the pathology,” and “Eat when you can, sleep when you can, and don’t mess with the pancreas,” is long overdue in celebrating the accomplishments of surgeons publicly and on a regular basis
In the end, we should want to promote future generations of surgeons who are technically sound, demonstrate excellent judgment under the most difficult circumstances, and who are able to achieve, ideally, their full surgical potential by arriving at a true harmony between self-assurance and uncertainty.
Dr. Chuback is a vascular surgeon in private practice in Paramus, N.J.
I recently had the good fortune to read a commentary written by Dr. Peter Angelos in ACS Surgery News entitled, The Right Choice? Surgeons, confidence, and humility (2017, February, p. 11). The essay touches on the philosophy, psychology, and attitudes that surgeons adopt and express in their daily interactions with the public.
The article refers to “the balance between lack of confidence and overconfidence, and between thoughtful introspection and paralyzing fear of future complications.” This is a critically important struggle in the mind of the surgeon. I would like to propose an exercise to bolster self-esteem in the psyche of the surgeon, particularly in the formative stages of one’s career, without fostering false or pathological bravado.
I certainly see the benefit in this tradition of analyzing and reviewing surgical misadventures and discussing the proper management of uninvited complications. It is a process rooted in the concepts of honesty, transparency, introspection, reflection, collaboration, and trust.
What I would like to propose is not the cessation of the M & M conference, but the addition of a complementary conference, which I refer to as Success and Survival conference. This meeting would showcase clinical scenarios in which a given patient should have succumbed to his illness but, instead, thrived as a result of the exemplary care provided by the surgical team involved. This would shine a bright spotlight on what it is that we do, and why our profession is so extraordinary. It would serve as a wonderful reminder for surgeons at all stages of their careers as to why we chose such a rigorous, challenging, and difficult vocation as our life’s work.
Such a venue would provide young surgeons an opportunity – not to flaunt – but to share and take well-deserved pride in their victories. I believe this conference would be as effective in terms of its educational value as the M & M, but it would not be associated with negative emotions of guilt, shame, and fear. The S & S would be a setting in which the young surgeon could shine in front of his or her peers as well as the attending staff and faculty.
The academic culture that prides itself on adages such as, “Whatever doesn’t kill you makes you stronger,” “The only problem with being on call every other night is that you miss half the pathology,” and “Eat when you can, sleep when you can, and don’t mess with the pancreas,” is long overdue in celebrating the accomplishments of surgeons publicly and on a regular basis
In the end, we should want to promote future generations of surgeons who are technically sound, demonstrate excellent judgment under the most difficult circumstances, and who are able to achieve, ideally, their full surgical potential by arriving at a true harmony between self-assurance and uncertainty.
Dr. Chuback is a vascular surgeon in private practice in Paramus, N.J.

















