User login
ADA releases guidelines for type 2 diabetes in children, youth
The American Diabetes Association’s guidelines for the evaluation and management of pediatric patients with type 2 diabetes differ from those for adults.
“Puberty-related physiologic insulin resistance, particularly in obese youth, may play a role” in the fact that youth are more insulin resistant than adults. Also, type 2 diabetes apparently is “more aggressive in youth than adults, with a faster rate of deterioration of beta-cell function and poorer response to glucose-lowering medications,” wrote Silva Arslanian, MD, from the division of pediatric endocrinology, metabolism, and diabetes mellitus at the University of Pittsburgh, and her colleagues. “Even though our knowledge of youth-onset type 2 diabetes has increased tremendously over the last 2 decades, robust and evidence-based data are still limited regarding diagnostic and therapeutic approaches and prevention of complications.”
The ADA position statement by Dr. Arslanian and her colleagues outlines management of type 2 diabetes in children and youth.
Diagnosis
and repeat testing should occur at least every 3 years for these patients. Pancreatic autoantibody tests should also be considered in this patient population to rule out autoimmune type 1 diabetes, and genetic evaluation should be performed to test for monogenic diabetes, “based on clinical characteristics and presentation,” they wrote.
Use fasting plasma glucose, 2-hour fasting plasma glucose after a 75-g oral glucose tolerance test, or glycosylated hemoglobin (HbA1C) to test for diabetes or prediabetes. Also consider factors like medication adherence and treatment effects when prescribing glucose-lowering or other medications for overweight or obese children and adolescents with type 2 diabetes.
Lifestyle management
With regard to lifestyle management programs, the intervention should be introduced as a part of diabetes care – aimed at reducing between 7% and 10% of body weight – and be based on a chronic care model. The intervention should include 30-60 minutes of moderate to intense physical activity for 5 days each week, strength training 3 days per week, and incorporate healthy eating plans. Dr. Arslanian and her associates noted there was limited evidence for pharmacotherapy for weight reduction in children and adolescents with type 2 diabetes.
Pharmacologic therapy
Pharmacologic therapy should be started together with lifestyle therapy once a diagnosis is made, according to the recommendations.
Metformin is the preferred initial pharmacologic treatment for patients with normal renal function who are asymptomatic and with HbA1C levels of less than 8.5%.
Patients with blood glucose greater than or equal to 250 mg/dL and HbA1C greater than or equal to 8.5% with symptoms such as weight loss, polydipsia, polyuria, or nocturia should receive basal insulin during initiation and titration of metformin.
Patients with ketosis or ketoacidosis should receive intravenous insulin to address hyperglycemia. Once the acidosis is corrected, initiate metformin with subcutaneous insulin therapy. For patients who are reaching home-based glucose monitoring targets, consider tapering the dose over 2-6 weeks with a 10%-30% reduction in insulin every few days.
In patients where metformin alone is not meeting the glycemic target, consider basal insulin therapy and, if that fails to help achieve glycemic targets, more intensive approaches should be considered, such as metabolic surgery.
Jay Cohen, MD, FACE, medical director at the Endocrine Clinic in Memphis, said in an interview that he agreed with the ADA position statement except for the pharmacologic therapy recommendations.
“The pharmacology therapy is 4 years outdated,” he said. “We routinely use all of the medications that are not Food and Drug Administration [approved] for kids, but are FDA approved for adults.”
He also questioned the ADA’s recommendation to give basal insulin to patients who are insulin resistant.
“Why give insulin if these people are insulin resistant?” said Dr. Cohen, who also is a Clinical Endocrinology News editorial board member. “The oral and injectable noninsulins work fabulously with less weight gain – already a problem for these patients – and less hypoglycemia, less side effects, and better compliance.”
Treatment goals
The HbA1C goal for children and adolescents with type 2 diabetes is less than 7% when treated with oral agents alone. HbA1C should be tested every 3 months and should be individualized, according to the ADA recommendations. In some patients, such as those with a shorter diabetes duration, lesser degrees of beta-cell dysfunction, and those who achieve significant weight improvement through lifestyle changes or taking metformin, consider lowering the HbA1C goal to less than 6.5%.
Give individualized care with regard to home self-monitoring of blood glucose. Also provide patients and their families with “culturally competent” diabetes self-management tools and lifestyle programs. Consider social factors such as housing stability, food insecurity, and financial barriers when making treatment decisions.
Screening for complications
To screen for nephropathy, take BP measurements at every visit and promote lifestyle management to reduce risk of diabetic kidney disease and improve weight loss. After 6 months, if a patient’s BP remains greater than the 95th percentile for their age, gender, and height, ACE inhibitors, or angiotensin receptor blockers are initial therapeutic options, according to the position statement. Other BP-lowering treatments may be added as necessary.
Also monitor protein intake (0.8 g/kg per day) as well as urine albumin/creatinine ratio (UACR) and estimated glomerular filtration rate (eGFR) annually. Patients with diabetes and hypertension who are not pregnant should receive an ACE inhibitor or angiotensin receptor blocker if their UACR is modestly elevated (30-299 mg/g creatinine). Such a regimen is strongly recommended if their UACR is above 300 mg/g creatinine and/or if their eGFR is less than 60 mL/min per 1.73 m2.
Screening issues
When considering diabetes distress and mental or behavioral health in children and adolescents with type 2 diabetes, use standardized and validated tools to assess symptoms such as depression and disordered eating behaviors. Regularly screen for smoking and alcohol use and provide preconception counseling for female patients of child-bearing age.
Screen for neuropathy, retinopathy, and nonalcoholic fatty liver disease annually and for obstructive sleep apnea at each visit. Lipid testing should be performed annually once patients have achieved glycemic control. Polycystic ovary syndrome should be considered in female patients with type 2 diabetes and treated with metformin together with lifestyle changes to address menstrual cyclicity and hyperandrogenism, the authors recommended.
Dr. Arslanian is on a data monitoring committee for AstraZeneca; data safety monitoring board for Boehringer Ingelheim; and advisory boards for Eli Lilly, Novo Nordisk, and Sanofi-Aventis; and has received research grants from Eli Lilly and Novo Nordisk. Other authors reported various relationships with a number of pharmaceutical companies.
SOURCE: Arslanian S et al. Diabetes Care. 2018 Nov 13. doi: 10.2337/dci18-0052.
The American Diabetes Association’s guidelines for the evaluation and management of pediatric patients with type 2 diabetes differ from those for adults.
“Puberty-related physiologic insulin resistance, particularly in obese youth, may play a role” in the fact that youth are more insulin resistant than adults. Also, type 2 diabetes apparently is “more aggressive in youth than adults, with a faster rate of deterioration of beta-cell function and poorer response to glucose-lowering medications,” wrote Silva Arslanian, MD, from the division of pediatric endocrinology, metabolism, and diabetes mellitus at the University of Pittsburgh, and her colleagues. “Even though our knowledge of youth-onset type 2 diabetes has increased tremendously over the last 2 decades, robust and evidence-based data are still limited regarding diagnostic and therapeutic approaches and prevention of complications.”
The ADA position statement by Dr. Arslanian and her colleagues outlines management of type 2 diabetes in children and youth.
Diagnosis
and repeat testing should occur at least every 3 years for these patients. Pancreatic autoantibody tests should also be considered in this patient population to rule out autoimmune type 1 diabetes, and genetic evaluation should be performed to test for monogenic diabetes, “based on clinical characteristics and presentation,” they wrote.
Use fasting plasma glucose, 2-hour fasting plasma glucose after a 75-g oral glucose tolerance test, or glycosylated hemoglobin (HbA1C) to test for diabetes or prediabetes. Also consider factors like medication adherence and treatment effects when prescribing glucose-lowering or other medications for overweight or obese children and adolescents with type 2 diabetes.
Lifestyle management
With regard to lifestyle management programs, the intervention should be introduced as a part of diabetes care – aimed at reducing between 7% and 10% of body weight – and be based on a chronic care model. The intervention should include 30-60 minutes of moderate to intense physical activity for 5 days each week, strength training 3 days per week, and incorporate healthy eating plans. Dr. Arslanian and her associates noted there was limited evidence for pharmacotherapy for weight reduction in children and adolescents with type 2 diabetes.
Pharmacologic therapy
Pharmacologic therapy should be started together with lifestyle therapy once a diagnosis is made, according to the recommendations.
Metformin is the preferred initial pharmacologic treatment for patients with normal renal function who are asymptomatic and with HbA1C levels of less than 8.5%.
Patients with blood glucose greater than or equal to 250 mg/dL and HbA1C greater than or equal to 8.5% with symptoms such as weight loss, polydipsia, polyuria, or nocturia should receive basal insulin during initiation and titration of metformin.
Patients with ketosis or ketoacidosis should receive intravenous insulin to address hyperglycemia. Once the acidosis is corrected, initiate metformin with subcutaneous insulin therapy. For patients who are reaching home-based glucose monitoring targets, consider tapering the dose over 2-6 weeks with a 10%-30% reduction in insulin every few days.
In patients where metformin alone is not meeting the glycemic target, consider basal insulin therapy and, if that fails to help achieve glycemic targets, more intensive approaches should be considered, such as metabolic surgery.
Jay Cohen, MD, FACE, medical director at the Endocrine Clinic in Memphis, said in an interview that he agreed with the ADA position statement except for the pharmacologic therapy recommendations.
“The pharmacology therapy is 4 years outdated,” he said. “We routinely use all of the medications that are not Food and Drug Administration [approved] for kids, but are FDA approved for adults.”
He also questioned the ADA’s recommendation to give basal insulin to patients who are insulin resistant.
“Why give insulin if these people are insulin resistant?” said Dr. Cohen, who also is a Clinical Endocrinology News editorial board member. “The oral and injectable noninsulins work fabulously with less weight gain – already a problem for these patients – and less hypoglycemia, less side effects, and better compliance.”
Treatment goals
The HbA1C goal for children and adolescents with type 2 diabetes is less than 7% when treated with oral agents alone. HbA1C should be tested every 3 months and should be individualized, according to the ADA recommendations. In some patients, such as those with a shorter diabetes duration, lesser degrees of beta-cell dysfunction, and those who achieve significant weight improvement through lifestyle changes or taking metformin, consider lowering the HbA1C goal to less than 6.5%.
Give individualized care with regard to home self-monitoring of blood glucose. Also provide patients and their families with “culturally competent” diabetes self-management tools and lifestyle programs. Consider social factors such as housing stability, food insecurity, and financial barriers when making treatment decisions.
Screening for complications
To screen for nephropathy, take BP measurements at every visit and promote lifestyle management to reduce risk of diabetic kidney disease and improve weight loss. After 6 months, if a patient’s BP remains greater than the 95th percentile for their age, gender, and height, ACE inhibitors, or angiotensin receptor blockers are initial therapeutic options, according to the position statement. Other BP-lowering treatments may be added as necessary.
Also monitor protein intake (0.8 g/kg per day) as well as urine albumin/creatinine ratio (UACR) and estimated glomerular filtration rate (eGFR) annually. Patients with diabetes and hypertension who are not pregnant should receive an ACE inhibitor or angiotensin receptor blocker if their UACR is modestly elevated (30-299 mg/g creatinine). Such a regimen is strongly recommended if their UACR is above 300 mg/g creatinine and/or if their eGFR is less than 60 mL/min per 1.73 m2.
Screening issues
When considering diabetes distress and mental or behavioral health in children and adolescents with type 2 diabetes, use standardized and validated tools to assess symptoms such as depression and disordered eating behaviors. Regularly screen for smoking and alcohol use and provide preconception counseling for female patients of child-bearing age.
Screen for neuropathy, retinopathy, and nonalcoholic fatty liver disease annually and for obstructive sleep apnea at each visit. Lipid testing should be performed annually once patients have achieved glycemic control. Polycystic ovary syndrome should be considered in female patients with type 2 diabetes and treated with metformin together with lifestyle changes to address menstrual cyclicity and hyperandrogenism, the authors recommended.
Dr. Arslanian is on a data monitoring committee for AstraZeneca; data safety monitoring board for Boehringer Ingelheim; and advisory boards for Eli Lilly, Novo Nordisk, and Sanofi-Aventis; and has received research grants from Eli Lilly and Novo Nordisk. Other authors reported various relationships with a number of pharmaceutical companies.
SOURCE: Arslanian S et al. Diabetes Care. 2018 Nov 13. doi: 10.2337/dci18-0052.
The American Diabetes Association’s guidelines for the evaluation and management of pediatric patients with type 2 diabetes differ from those for adults.
“Puberty-related physiologic insulin resistance, particularly in obese youth, may play a role” in the fact that youth are more insulin resistant than adults. Also, type 2 diabetes apparently is “more aggressive in youth than adults, with a faster rate of deterioration of beta-cell function and poorer response to glucose-lowering medications,” wrote Silva Arslanian, MD, from the division of pediatric endocrinology, metabolism, and diabetes mellitus at the University of Pittsburgh, and her colleagues. “Even though our knowledge of youth-onset type 2 diabetes has increased tremendously over the last 2 decades, robust and evidence-based data are still limited regarding diagnostic and therapeutic approaches and prevention of complications.”
The ADA position statement by Dr. Arslanian and her colleagues outlines management of type 2 diabetes in children and youth.
Diagnosis
and repeat testing should occur at least every 3 years for these patients. Pancreatic autoantibody tests should also be considered in this patient population to rule out autoimmune type 1 diabetes, and genetic evaluation should be performed to test for monogenic diabetes, “based on clinical characteristics and presentation,” they wrote.
Use fasting plasma glucose, 2-hour fasting plasma glucose after a 75-g oral glucose tolerance test, or glycosylated hemoglobin (HbA1C) to test for diabetes or prediabetes. Also consider factors like medication adherence and treatment effects when prescribing glucose-lowering or other medications for overweight or obese children and adolescents with type 2 diabetes.
Lifestyle management
With regard to lifestyle management programs, the intervention should be introduced as a part of diabetes care – aimed at reducing between 7% and 10% of body weight – and be based on a chronic care model. The intervention should include 30-60 minutes of moderate to intense physical activity for 5 days each week, strength training 3 days per week, and incorporate healthy eating plans. Dr. Arslanian and her associates noted there was limited evidence for pharmacotherapy for weight reduction in children and adolescents with type 2 diabetes.
Pharmacologic therapy
Pharmacologic therapy should be started together with lifestyle therapy once a diagnosis is made, according to the recommendations.
Metformin is the preferred initial pharmacologic treatment for patients with normal renal function who are asymptomatic and with HbA1C levels of less than 8.5%.
Patients with blood glucose greater than or equal to 250 mg/dL and HbA1C greater than or equal to 8.5% with symptoms such as weight loss, polydipsia, polyuria, or nocturia should receive basal insulin during initiation and titration of metformin.
Patients with ketosis or ketoacidosis should receive intravenous insulin to address hyperglycemia. Once the acidosis is corrected, initiate metformin with subcutaneous insulin therapy. For patients who are reaching home-based glucose monitoring targets, consider tapering the dose over 2-6 weeks with a 10%-30% reduction in insulin every few days.
In patients where metformin alone is not meeting the glycemic target, consider basal insulin therapy and, if that fails to help achieve glycemic targets, more intensive approaches should be considered, such as metabolic surgery.
Jay Cohen, MD, FACE, medical director at the Endocrine Clinic in Memphis, said in an interview that he agreed with the ADA position statement except for the pharmacologic therapy recommendations.
“The pharmacology therapy is 4 years outdated,” he said. “We routinely use all of the medications that are not Food and Drug Administration [approved] for kids, but are FDA approved for adults.”
He also questioned the ADA’s recommendation to give basal insulin to patients who are insulin resistant.
“Why give insulin if these people are insulin resistant?” said Dr. Cohen, who also is a Clinical Endocrinology News editorial board member. “The oral and injectable noninsulins work fabulously with less weight gain – already a problem for these patients – and less hypoglycemia, less side effects, and better compliance.”
Treatment goals
The HbA1C goal for children and adolescents with type 2 diabetes is less than 7% when treated with oral agents alone. HbA1C should be tested every 3 months and should be individualized, according to the ADA recommendations. In some patients, such as those with a shorter diabetes duration, lesser degrees of beta-cell dysfunction, and those who achieve significant weight improvement through lifestyle changes or taking metformin, consider lowering the HbA1C goal to less than 6.5%.
Give individualized care with regard to home self-monitoring of blood glucose. Also provide patients and their families with “culturally competent” diabetes self-management tools and lifestyle programs. Consider social factors such as housing stability, food insecurity, and financial barriers when making treatment decisions.
Screening for complications
To screen for nephropathy, take BP measurements at every visit and promote lifestyle management to reduce risk of diabetic kidney disease and improve weight loss. After 6 months, if a patient’s BP remains greater than the 95th percentile for their age, gender, and height, ACE inhibitors, or angiotensin receptor blockers are initial therapeutic options, according to the position statement. Other BP-lowering treatments may be added as necessary.
Also monitor protein intake (0.8 g/kg per day) as well as urine albumin/creatinine ratio (UACR) and estimated glomerular filtration rate (eGFR) annually. Patients with diabetes and hypertension who are not pregnant should receive an ACE inhibitor or angiotensin receptor blocker if their UACR is modestly elevated (30-299 mg/g creatinine). Such a regimen is strongly recommended if their UACR is above 300 mg/g creatinine and/or if their eGFR is less than 60 mL/min per 1.73 m2.
Screening issues
When considering diabetes distress and mental or behavioral health in children and adolescents with type 2 diabetes, use standardized and validated tools to assess symptoms such as depression and disordered eating behaviors. Regularly screen for smoking and alcohol use and provide preconception counseling for female patients of child-bearing age.
Screen for neuropathy, retinopathy, and nonalcoholic fatty liver disease annually and for obstructive sleep apnea at each visit. Lipid testing should be performed annually once patients have achieved glycemic control. Polycystic ovary syndrome should be considered in female patients with type 2 diabetes and treated with metformin together with lifestyle changes to address menstrual cyclicity and hyperandrogenism, the authors recommended.
Dr. Arslanian is on a data monitoring committee for AstraZeneca; data safety monitoring board for Boehringer Ingelheim; and advisory boards for Eli Lilly, Novo Nordisk, and Sanofi-Aventis; and has received research grants from Eli Lilly and Novo Nordisk. Other authors reported various relationships with a number of pharmaceutical companies.
SOURCE: Arslanian S et al. Diabetes Care. 2018 Nov 13. doi: 10.2337/dci18-0052.
FROM DIABETES CARE
CAC scores in type 1 diabetes no higher than general population
CHICAGO – Roughly 70% of some 1,200 adult patients with type 1 diabetes screened for coronary artery calcium had a score of zero, about the same prevalence as in the general, U.S. adult population, suggesting the unexpected conclusion that a majority of middle-aged patients with type 1 diabetes do not have an elevated risk for coronary artery disease, in contrast to patients with type 2 diabetes.
Among 1,205 asymptomatic people with type 1 diabetes who underwent coronary artery calcium (CAC) measurement and were followed for an average of about 11 years, 71% had a CAC score of zero at baseline followed by a cardiovascular disease event rate of 5.6 events/1,000 patient years of follow-up, a “very low” event rate that made these patients no more likely to have an event than any adult of similar age and sex in the general U.S. population, Matthew J. Budoff, MD, said at the American Heart Association scientific sessions.
In prior reports, about half of patients with type 2 diabetes had a CAC score of zero, noted Dr. Budoff, professor of medicine and a specialist in cardiac CT imaging and preventive cardiology at the University of California, Los Angeles. In a general adult population that’s about 45 years old roughly three-quarters would have a CAC score of zero, he noted.
Until now, little has been known about CAC scores in asymptomatic, middle-aged adults with type 1 diabetes. The findings reported by Dr. Budoff raise questions about the 2018 revision of the cholesterol guideline from the American College of Cardiology and American Heart Association, released during the meeting (J Am Coll Cardiol. 2018. doi: 10.1016/j.jacc.2018.11.003), which lumps type 1 and type 2 diabetes together as a special high-risk category for cholesterol management.
The guideline should instead “advocate for more therapy with a CAC score of more than 100 and less therapy with a CAC score of zero in patients with type 1 diabetes,” Dr. Budoff suggested. “A statin for someone with a CAC score of zero probably won’t result in event reduction. The 70% of patients with type 1 diabetes who have a CAC score of zero potentially may not benefit from a statin,” he said in a video interview.
Dr. Budoff and his associates used CAC scores and outcomes data collected on 1,205 asymptomatic people with type 1 diabetes enrolled in the EDIC (Epidemiology of Diabetes Interventions and Complications) trial who underwent CAC scoring as part of the study protocol when they averaged 43 years of age. Follow-up tracked the incidence of cardiovascular disease events in 1,156 of these patients for an average of about 11 years. During follow-up, 105 patients had a cardiovascular disease event, an overall rate of 8.5 events/1,000 patient years of follow-up.
The results also confirmed the prognostic power of the CAC score in these patients. Compared with the very low event rate among those with a zero score, patients with a score of 1-100 had 71% more events, patients with a CAC score of 101-300 had a 5.4-fold higher event rate as those with no coronary calcium, and patients with a CAC score of greater than 300 had a 6.9-fold higher event rate than those with no coronary calcium, Dr. Budoff reported.
Coronary calcium deposits, a direct reflection of atheroma load, can change over time, but somewhat slowly. A CAC score of zero is very reliable for predicting a very low rate of cardiovascular disease events over the subsequent 5 years, and in many people it can reliably predict for as long as 10 years, Dr. Budoff said. Beyond that, follow-up CAC scoring is necessary to check for changes in coronary status, “especially in patients with type 1 diabetes,”
SOURCE: Budoff M et al. Abstract 13133.
CHICAGO – Roughly 70% of some 1,200 adult patients with type 1 diabetes screened for coronary artery calcium had a score of zero, about the same prevalence as in the general, U.S. adult population, suggesting the unexpected conclusion that a majority of middle-aged patients with type 1 diabetes do not have an elevated risk for coronary artery disease, in contrast to patients with type 2 diabetes.
Among 1,205 asymptomatic people with type 1 diabetes who underwent coronary artery calcium (CAC) measurement and were followed for an average of about 11 years, 71% had a CAC score of zero at baseline followed by a cardiovascular disease event rate of 5.6 events/1,000 patient years of follow-up, a “very low” event rate that made these patients no more likely to have an event than any adult of similar age and sex in the general U.S. population, Matthew J. Budoff, MD, said at the American Heart Association scientific sessions.
In prior reports, about half of patients with type 2 diabetes had a CAC score of zero, noted Dr. Budoff, professor of medicine and a specialist in cardiac CT imaging and preventive cardiology at the University of California, Los Angeles. In a general adult population that’s about 45 years old roughly three-quarters would have a CAC score of zero, he noted.
Until now, little has been known about CAC scores in asymptomatic, middle-aged adults with type 1 diabetes. The findings reported by Dr. Budoff raise questions about the 2018 revision of the cholesterol guideline from the American College of Cardiology and American Heart Association, released during the meeting (J Am Coll Cardiol. 2018. doi: 10.1016/j.jacc.2018.11.003), which lumps type 1 and type 2 diabetes together as a special high-risk category for cholesterol management.
The guideline should instead “advocate for more therapy with a CAC score of more than 100 and less therapy with a CAC score of zero in patients with type 1 diabetes,” Dr. Budoff suggested. “A statin for someone with a CAC score of zero probably won’t result in event reduction. The 70% of patients with type 1 diabetes who have a CAC score of zero potentially may not benefit from a statin,” he said in a video interview.
Dr. Budoff and his associates used CAC scores and outcomes data collected on 1,205 asymptomatic people with type 1 diabetes enrolled in the EDIC (Epidemiology of Diabetes Interventions and Complications) trial who underwent CAC scoring as part of the study protocol when they averaged 43 years of age. Follow-up tracked the incidence of cardiovascular disease events in 1,156 of these patients for an average of about 11 years. During follow-up, 105 patients had a cardiovascular disease event, an overall rate of 8.5 events/1,000 patient years of follow-up.
The results also confirmed the prognostic power of the CAC score in these patients. Compared with the very low event rate among those with a zero score, patients with a score of 1-100 had 71% more events, patients with a CAC score of 101-300 had a 5.4-fold higher event rate as those with no coronary calcium, and patients with a CAC score of greater than 300 had a 6.9-fold higher event rate than those with no coronary calcium, Dr. Budoff reported.
Coronary calcium deposits, a direct reflection of atheroma load, can change over time, but somewhat slowly. A CAC score of zero is very reliable for predicting a very low rate of cardiovascular disease events over the subsequent 5 years, and in many people it can reliably predict for as long as 10 years, Dr. Budoff said. Beyond that, follow-up CAC scoring is necessary to check for changes in coronary status, “especially in patients with type 1 diabetes,”
SOURCE: Budoff M et al. Abstract 13133.
CHICAGO – Roughly 70% of some 1,200 adult patients with type 1 diabetes screened for coronary artery calcium had a score of zero, about the same prevalence as in the general, U.S. adult population, suggesting the unexpected conclusion that a majority of middle-aged patients with type 1 diabetes do not have an elevated risk for coronary artery disease, in contrast to patients with type 2 diabetes.
Among 1,205 asymptomatic people with type 1 diabetes who underwent coronary artery calcium (CAC) measurement and were followed for an average of about 11 years, 71% had a CAC score of zero at baseline followed by a cardiovascular disease event rate of 5.6 events/1,000 patient years of follow-up, a “very low” event rate that made these patients no more likely to have an event than any adult of similar age and sex in the general U.S. population, Matthew J. Budoff, MD, said at the American Heart Association scientific sessions.
In prior reports, about half of patients with type 2 diabetes had a CAC score of zero, noted Dr. Budoff, professor of medicine and a specialist in cardiac CT imaging and preventive cardiology at the University of California, Los Angeles. In a general adult population that’s about 45 years old roughly three-quarters would have a CAC score of zero, he noted.
Until now, little has been known about CAC scores in asymptomatic, middle-aged adults with type 1 diabetes. The findings reported by Dr. Budoff raise questions about the 2018 revision of the cholesterol guideline from the American College of Cardiology and American Heart Association, released during the meeting (J Am Coll Cardiol. 2018. doi: 10.1016/j.jacc.2018.11.003), which lumps type 1 and type 2 diabetes together as a special high-risk category for cholesterol management.
The guideline should instead “advocate for more therapy with a CAC score of more than 100 and less therapy with a CAC score of zero in patients with type 1 diabetes,” Dr. Budoff suggested. “A statin for someone with a CAC score of zero probably won’t result in event reduction. The 70% of patients with type 1 diabetes who have a CAC score of zero potentially may not benefit from a statin,” he said in a video interview.
Dr. Budoff and his associates used CAC scores and outcomes data collected on 1,205 asymptomatic people with type 1 diabetes enrolled in the EDIC (Epidemiology of Diabetes Interventions and Complications) trial who underwent CAC scoring as part of the study protocol when they averaged 43 years of age. Follow-up tracked the incidence of cardiovascular disease events in 1,156 of these patients for an average of about 11 years. During follow-up, 105 patients had a cardiovascular disease event, an overall rate of 8.5 events/1,000 patient years of follow-up.
The results also confirmed the prognostic power of the CAC score in these patients. Compared with the very low event rate among those with a zero score, patients with a score of 1-100 had 71% more events, patients with a CAC score of 101-300 had a 5.4-fold higher event rate as those with no coronary calcium, and patients with a CAC score of greater than 300 had a 6.9-fold higher event rate than those with no coronary calcium, Dr. Budoff reported.
Coronary calcium deposits, a direct reflection of atheroma load, can change over time, but somewhat slowly. A CAC score of zero is very reliable for predicting a very low rate of cardiovascular disease events over the subsequent 5 years, and in many people it can reliably predict for as long as 10 years, Dr. Budoff said. Beyond that, follow-up CAC scoring is necessary to check for changes in coronary status, “especially in patients with type 1 diabetes,”
SOURCE: Budoff M et al. Abstract 13133.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Key clinical point: .
Major finding: Seventy-one percent of patients with type 1 diabetes had a coronary artery calcium score of zero.
Study details: Review of data collected from 1,205 patients in the EDIC trial.
Disclosures: The EDIC trial had no commercial funding. Dr. Budoff has received research funding from General Electric.
Source: Budoff M et al. AHA 2018, Abstract 13133.
Advancements in the Delivery of Biologics for the Treatment of Diabetes
Diabetes medication administration often forces patients into uncomfortable situations. Those with complicated treatment or with a fear of needles might hesitate to adhere to their suggested regimen, placing themselves at risk. Over the years, several mechanisms have evolved to help make insulin delivery, and so, betting patient adherence.
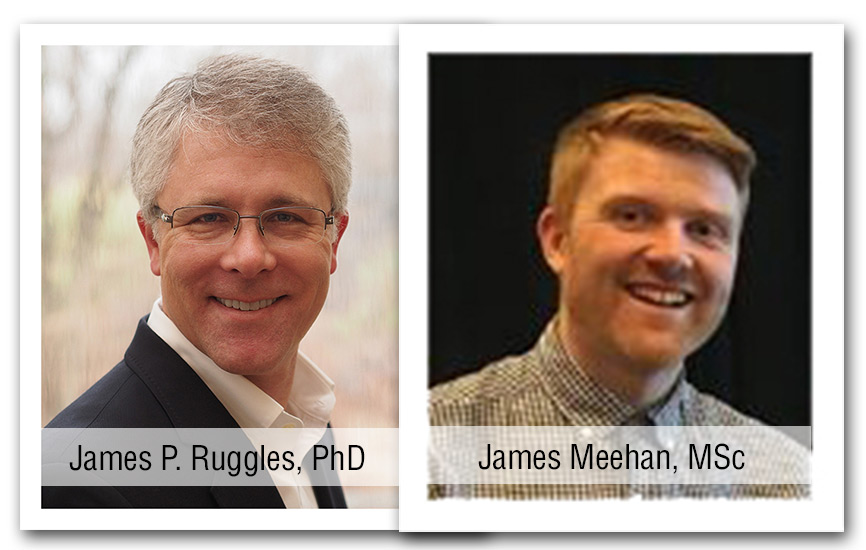
This fifth eNewsletter in the series, entitled Advancements in the Delivery of Biologics for the Treatment of Diabetes was written by James Ruggles, PhD, and James Meehan, MSc. It covers the history of insulin delivery methods starting from 1922 and through present day.
Click here to read the supplement
About the Authors:

James Ruggles, PhD
AstraZeneca
Wilmington, DE, USA

James Meehan, MSc
AstraZeneca
Macclesfield, Cheshire, UK
Diabetes medication administration often forces patients into uncomfortable situations. Those with complicated treatment or with a fear of needles might hesitate to adhere to their suggested regimen, placing themselves at risk. Over the years, several mechanisms have evolved to help make insulin delivery, and so, betting patient adherence.
This fifth eNewsletter in the series, entitled Advancements in the Delivery of Biologics for the Treatment of Diabetes was written by James Ruggles, PhD, and James Meehan, MSc. It covers the history of insulin delivery methods starting from 1922 and through present day.
Click here to read the supplement
About the Authors:

James Ruggles, PhD
AstraZeneca
Wilmington, DE, USA

James Meehan, MSc
AstraZeneca
Macclesfield, Cheshire, UK
Diabetes medication administration often forces patients into uncomfortable situations. Those with complicated treatment or with a fear of needles might hesitate to adhere to their suggested regimen, placing themselves at risk. Over the years, several mechanisms have evolved to help make insulin delivery, and so, betting patient adherence.
This fifth eNewsletter in the series, entitled Advancements in the Delivery of Biologics for the Treatment of Diabetes was written by James Ruggles, PhD, and James Meehan, MSc. It covers the history of insulin delivery methods starting from 1922 and through present day.
Click here to read the supplement
About the Authors:

James Ruggles, PhD
AstraZeneca
Wilmington, DE, USA

James Meehan, MSc
AstraZeneca
Macclesfield, Cheshire, UK
Empagliflozin reduces left ventricular mass
CHICAGO – Empagliflozin significantly reduced left ventricular mass compared with placebo over the course of 6 months in patients with type 2 diabetes and stable coronary artery disease in the randomized EMPA-HEART CardioLink-6 trial.
Use of empagliflozin (Jardiance), a sodium-glucose cotransporter 2 inhibitor (SGLT2i), also was associated with a clinically meaningful reduction in ambulatory systolic blood pressure and a boost in hematocrit in this population of normotensive patients with preserved left ventricular ejection fraction and high utilization of background guideline-directed medical therapy, Subodh Verma, MD, reported at the American Heart Association scientific sessions.
“Taken together, these data suggest that empagliflozin promotes early statistically and clinically significant reverse remodeling, which may contribute to the cardiovascular and heart failure benefits observed in the EMPA-REG OUTCOME trial and other SGLT2i studies,” added Dr. Verma, professor of surgery, pharmacology, and toxicology at the University of Toronto.
EMPA-REG OUTCOME was a landmark randomized trial that included 7,020 patients with type 2 diabetes and established ischemic cardiovascular disease in which the SGLT2i reduced all-cause mortality by 32%, compared with placebo over a median 3.1 years of follow-up, cardiovascular mortality by 38%, and hospitalizations for heart failure by 35% (N Engl J Med. 2015 Nov 26;373[22]:2117-28).
The mechanism responsible for these impressive clinical benefits has been unclear. The EMPA-HEART CardioLink-6 trial was a small study – 97 randomized patients – designed to shed light on this issue. The hypothesis was that SGLT2i therapy facilitates cardiac reverse remodeling. This indeed turned out to be the case when cardiac MRI findings at baseline and after 6 months were compared by blinded evaluators.
From a baseline mean left ventricular mass indexed to body surface area of 60 g/m2, which is within normal range, left ventricular mass decreased by a mean of 4.71 g in the empagliflozin group, compared with a mere 0.39-g reduction in placebo-treated controls.
Dr. Verma underscored the importance of this result: “Left ventricular mass is a strong and independent predictor of major cardiovascular events, including cardiovascular and all-cause mortality, myocardial infarction, and heart failure. Furthermore, the magnitude of left ventricular mass regression correlates with the extent of clinical outcome benefit seen with pharmacological and device therapies.”
In a prespecified subgroup analysis stratified by baseline LV mass index, patients with a baseline value greater than 60 g/m2 experienced a much greater benefit from empagliflozin, with a mean between-group difference in LV mass index reduction of 7.26 g/m2, compared with a 0.46-g/m2 difference between the SGLT2i and placebo among those with a baseline LV mass index of 60 g/m2 or less.
Ambulatory systolic blood pressure fell from a baseline of 139 mm Hg by a mean of 7.9 mm Hg in the empagliflozin group and 0.7 mm Hg with placebo. From a baseline hematocrit of 42%, hematocrit improved by an absolute 1.91% more with empagliflozin than placebo. However, there were no significant between-group differences in the secondary cardiac MRI outcomes of change in LV end-systolic volume index, LV end-diastolic volume index, or LV ejection fraction.
Discussant Elliott M. Antman, MD, hailed EMPA-HEART CardioLink-6 as “a very important mechanistic study.”
“As I leave Chicago for home, I plan to further increase the use of SGLT2 inhibitors in my patients with type 2 diabetes, especially if they have a history of heart failure, and especially if they have coronary artery disease. I would encourage you to think about doing the same, and I would also recommend that we urge our colleagues in general medicine, endocrinology, and nephrology to consider this information as well,” said Dr. Antman, professor of medicine and associate dean for clinical and translational research at Harvard Medical School, Boston, as well as an AHA past president.
He noted that EMPA-HEART CardioLink-6 provides “biologically plausible data” to explain the mechanism for the major clinical benefits of empagliflozin earlier documented in EMPA-REG OUTCOME. The likely driver of the reduction in left ventricular mass seen in EMPA-HEART CardioLink-6 was the combination of lower systolic blood pressure and higher hematocrit.
“These surrogates suggest that our traditional concepts of afterload and preload appear to be favorably affected by SGLT2 inhibition,” according to the cardiologist.
The EMPA-HEART CardioLink-6 study was funded by Boehringer Ingelheim. Dr. Verma reported receiving research support and/or speaker payments from that pharmaceutical company and roughly a dozen others. Dr. Antman had no disclosures.
SOURCE: Verma S. AHA 2018, Abstract 19332.
CHICAGO – Empagliflozin significantly reduced left ventricular mass compared with placebo over the course of 6 months in patients with type 2 diabetes and stable coronary artery disease in the randomized EMPA-HEART CardioLink-6 trial.
Use of empagliflozin (Jardiance), a sodium-glucose cotransporter 2 inhibitor (SGLT2i), also was associated with a clinically meaningful reduction in ambulatory systolic blood pressure and a boost in hematocrit in this population of normotensive patients with preserved left ventricular ejection fraction and high utilization of background guideline-directed medical therapy, Subodh Verma, MD, reported at the American Heart Association scientific sessions.
“Taken together, these data suggest that empagliflozin promotes early statistically and clinically significant reverse remodeling, which may contribute to the cardiovascular and heart failure benefits observed in the EMPA-REG OUTCOME trial and other SGLT2i studies,” added Dr. Verma, professor of surgery, pharmacology, and toxicology at the University of Toronto.
EMPA-REG OUTCOME was a landmark randomized trial that included 7,020 patients with type 2 diabetes and established ischemic cardiovascular disease in which the SGLT2i reduced all-cause mortality by 32%, compared with placebo over a median 3.1 years of follow-up, cardiovascular mortality by 38%, and hospitalizations for heart failure by 35% (N Engl J Med. 2015 Nov 26;373[22]:2117-28).
The mechanism responsible for these impressive clinical benefits has been unclear. The EMPA-HEART CardioLink-6 trial was a small study – 97 randomized patients – designed to shed light on this issue. The hypothesis was that SGLT2i therapy facilitates cardiac reverse remodeling. This indeed turned out to be the case when cardiac MRI findings at baseline and after 6 months were compared by blinded evaluators.
From a baseline mean left ventricular mass indexed to body surface area of 60 g/m2, which is within normal range, left ventricular mass decreased by a mean of 4.71 g in the empagliflozin group, compared with a mere 0.39-g reduction in placebo-treated controls.
Dr. Verma underscored the importance of this result: “Left ventricular mass is a strong and independent predictor of major cardiovascular events, including cardiovascular and all-cause mortality, myocardial infarction, and heart failure. Furthermore, the magnitude of left ventricular mass regression correlates with the extent of clinical outcome benefit seen with pharmacological and device therapies.”
In a prespecified subgroup analysis stratified by baseline LV mass index, patients with a baseline value greater than 60 g/m2 experienced a much greater benefit from empagliflozin, with a mean between-group difference in LV mass index reduction of 7.26 g/m2, compared with a 0.46-g/m2 difference between the SGLT2i and placebo among those with a baseline LV mass index of 60 g/m2 or less.
Ambulatory systolic blood pressure fell from a baseline of 139 mm Hg by a mean of 7.9 mm Hg in the empagliflozin group and 0.7 mm Hg with placebo. From a baseline hematocrit of 42%, hematocrit improved by an absolute 1.91% more with empagliflozin than placebo. However, there were no significant between-group differences in the secondary cardiac MRI outcomes of change in LV end-systolic volume index, LV end-diastolic volume index, or LV ejection fraction.
Discussant Elliott M. Antman, MD, hailed EMPA-HEART CardioLink-6 as “a very important mechanistic study.”
“As I leave Chicago for home, I plan to further increase the use of SGLT2 inhibitors in my patients with type 2 diabetes, especially if they have a history of heart failure, and especially if they have coronary artery disease. I would encourage you to think about doing the same, and I would also recommend that we urge our colleagues in general medicine, endocrinology, and nephrology to consider this information as well,” said Dr. Antman, professor of medicine and associate dean for clinical and translational research at Harvard Medical School, Boston, as well as an AHA past president.
He noted that EMPA-HEART CardioLink-6 provides “biologically plausible data” to explain the mechanism for the major clinical benefits of empagliflozin earlier documented in EMPA-REG OUTCOME. The likely driver of the reduction in left ventricular mass seen in EMPA-HEART CardioLink-6 was the combination of lower systolic blood pressure and higher hematocrit.
“These surrogates suggest that our traditional concepts of afterload and preload appear to be favorably affected by SGLT2 inhibition,” according to the cardiologist.
The EMPA-HEART CardioLink-6 study was funded by Boehringer Ingelheim. Dr. Verma reported receiving research support and/or speaker payments from that pharmaceutical company and roughly a dozen others. Dr. Antman had no disclosures.
SOURCE: Verma S. AHA 2018, Abstract 19332.
CHICAGO – Empagliflozin significantly reduced left ventricular mass compared with placebo over the course of 6 months in patients with type 2 diabetes and stable coronary artery disease in the randomized EMPA-HEART CardioLink-6 trial.
Use of empagliflozin (Jardiance), a sodium-glucose cotransporter 2 inhibitor (SGLT2i), also was associated with a clinically meaningful reduction in ambulatory systolic blood pressure and a boost in hematocrit in this population of normotensive patients with preserved left ventricular ejection fraction and high utilization of background guideline-directed medical therapy, Subodh Verma, MD, reported at the American Heart Association scientific sessions.
“Taken together, these data suggest that empagliflozin promotes early statistically and clinically significant reverse remodeling, which may contribute to the cardiovascular and heart failure benefits observed in the EMPA-REG OUTCOME trial and other SGLT2i studies,” added Dr. Verma, professor of surgery, pharmacology, and toxicology at the University of Toronto.
EMPA-REG OUTCOME was a landmark randomized trial that included 7,020 patients with type 2 diabetes and established ischemic cardiovascular disease in which the SGLT2i reduced all-cause mortality by 32%, compared with placebo over a median 3.1 years of follow-up, cardiovascular mortality by 38%, and hospitalizations for heart failure by 35% (N Engl J Med. 2015 Nov 26;373[22]:2117-28).
The mechanism responsible for these impressive clinical benefits has been unclear. The EMPA-HEART CardioLink-6 trial was a small study – 97 randomized patients – designed to shed light on this issue. The hypothesis was that SGLT2i therapy facilitates cardiac reverse remodeling. This indeed turned out to be the case when cardiac MRI findings at baseline and after 6 months were compared by blinded evaluators.
From a baseline mean left ventricular mass indexed to body surface area of 60 g/m2, which is within normal range, left ventricular mass decreased by a mean of 4.71 g in the empagliflozin group, compared with a mere 0.39-g reduction in placebo-treated controls.
Dr. Verma underscored the importance of this result: “Left ventricular mass is a strong and independent predictor of major cardiovascular events, including cardiovascular and all-cause mortality, myocardial infarction, and heart failure. Furthermore, the magnitude of left ventricular mass regression correlates with the extent of clinical outcome benefit seen with pharmacological and device therapies.”
In a prespecified subgroup analysis stratified by baseline LV mass index, patients with a baseline value greater than 60 g/m2 experienced a much greater benefit from empagliflozin, with a mean between-group difference in LV mass index reduction of 7.26 g/m2, compared with a 0.46-g/m2 difference between the SGLT2i and placebo among those with a baseline LV mass index of 60 g/m2 or less.
Ambulatory systolic blood pressure fell from a baseline of 139 mm Hg by a mean of 7.9 mm Hg in the empagliflozin group and 0.7 mm Hg with placebo. From a baseline hematocrit of 42%, hematocrit improved by an absolute 1.91% more with empagliflozin than placebo. However, there were no significant between-group differences in the secondary cardiac MRI outcomes of change in LV end-systolic volume index, LV end-diastolic volume index, or LV ejection fraction.
Discussant Elliott M. Antman, MD, hailed EMPA-HEART CardioLink-6 as “a very important mechanistic study.”
“As I leave Chicago for home, I plan to further increase the use of SGLT2 inhibitors in my patients with type 2 diabetes, especially if they have a history of heart failure, and especially if they have coronary artery disease. I would encourage you to think about doing the same, and I would also recommend that we urge our colleagues in general medicine, endocrinology, and nephrology to consider this information as well,” said Dr. Antman, professor of medicine and associate dean for clinical and translational research at Harvard Medical School, Boston, as well as an AHA past president.
He noted that EMPA-HEART CardioLink-6 provides “biologically plausible data” to explain the mechanism for the major clinical benefits of empagliflozin earlier documented in EMPA-REG OUTCOME. The likely driver of the reduction in left ventricular mass seen in EMPA-HEART CardioLink-6 was the combination of lower systolic blood pressure and higher hematocrit.
“These surrogates suggest that our traditional concepts of afterload and preload appear to be favorably affected by SGLT2 inhibition,” according to the cardiologist.
The EMPA-HEART CardioLink-6 study was funded by Boehringer Ingelheim. Dr. Verma reported receiving research support and/or speaker payments from that pharmaceutical company and roughly a dozen others. Dr. Antman had no disclosures.
SOURCE: Verma S. AHA 2018, Abstract 19332.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Key clinical point: .
Major finding: Six months of empagliflozin reduced left ventricular mass by a mean of 4.71 g, vs. 0.39 g with placebo.
Study details: This 97-patient, 6-month, randomized trial evaluated the impact of SGLT2 inhibition with empagliflozin on left ventricular remodeling.
Disclosures: The EMPA-HEART CardioLink-6 study was funded by Boehringer Ingelheim. The presenter reported receiving research support and/or speaker payments from that pharmaceutical company and roughly a dozen others. Source: Verma S. AHA 2018, Abstract 19332.
Children with poor cardiorespiratory fitness have a higher risk of type 2 diabetes and cardiovascular disease
according to the analysis of an ongoing Finnish study of physical activity and dietary intervention in school children.
“Our results are in agreement with previous findings that cardiorespiratory fitness measured in exercise test laboratories or using field tests and scaled by body mass (BM) using the ratio standard method had a strong inverse association with cardiometabolic risk in children,” lead author Andrew O. Agbaje, MD, MPH, and his coauthors wrote in the Scandinavian Journal of Medicine & Science in Sports.
The coauthors assessed the cardiorespiratory fitness of 352 primary school children – 186 boys and 166 girls – from Kuopio, Finland, all of whom were already participating in the ongoing PANIC (Physical Activity and Nutrition in Children) Study. The children were asked to perform a maximal exercise test, upon which fitness was assessed by measuring peak oxygen uptake (VO2 peak), noted Dr. Agbaje, a PhD student at the University of Eastern Finland’s Institute of Biomedicine in Kuopio, and his colleagues.
Body mass and lean mass were also measured by bioelectrical impedance and used to scale VO2 peak, while variables such as waist circumference, insulin, glucose, HDL cholesterol, and triglycerides were used to calculate a continuous cardiometabolic risk score. Upon analysis, VO2 peak less than 45.8 mL/kg BM-1 min-1 in boys and less than 44.1 mL/kg BM-1 min-1 in girls was associated with increased cardiometabolic risk.
The coauthors noted that cardiorespiratory fitness can be influenced by genetics and that adjustments for puberty had “no effect on the relationships between VO2 peak and cardiometabolic risk.” As such, they recommended that “longitudinal studies are needed to clarify the role of CRF in cardiometabolic health during growth and maturation.”
That said, despite advocating caution in regard to determining proper CRF thresholds, the coauthors suggested that CRF scaled by BM could be used to screen children and improve prevention efforts. “Cardiometabolic risk tracks from childhood into adulthood and the early identification of individuals at increased risk is essential in developing public health actions targeted at preventing cardiometabolic diseases,” they wrote.
The study was funded by grants from the Ministry of Education and Culture of Finland, Ministry of Social Affairs and Health of Finland, Research Committee of the Kuopio University Hospital Catchment Area (State Research Funding), Finnish Innovation Fund Sitra, Social Insurance Institution of Finland, Finnish Cultural Foundation, Foundation for Paediatric Research, Diabetes Research Foundation in Finland, Finnish Foundation for Cardiovascular Research, Juho Vainio Foundation, Paavo Nurmi Foundation, and the Yrjö Jahnsson Foundation. Dr. Agbaje reported grant support from the Olvi Foundation and the Urho Känkanen Foundation.
SOURCE: Agbaje AO et al. Scand J Med Sci Sports. 2018 Sep 19. doi: 10.1111/sms.13307.
according to the analysis of an ongoing Finnish study of physical activity and dietary intervention in school children.
“Our results are in agreement with previous findings that cardiorespiratory fitness measured in exercise test laboratories or using field tests and scaled by body mass (BM) using the ratio standard method had a strong inverse association with cardiometabolic risk in children,” lead author Andrew O. Agbaje, MD, MPH, and his coauthors wrote in the Scandinavian Journal of Medicine & Science in Sports.
The coauthors assessed the cardiorespiratory fitness of 352 primary school children – 186 boys and 166 girls – from Kuopio, Finland, all of whom were already participating in the ongoing PANIC (Physical Activity and Nutrition in Children) Study. The children were asked to perform a maximal exercise test, upon which fitness was assessed by measuring peak oxygen uptake (VO2 peak), noted Dr. Agbaje, a PhD student at the University of Eastern Finland’s Institute of Biomedicine in Kuopio, and his colleagues.
Body mass and lean mass were also measured by bioelectrical impedance and used to scale VO2 peak, while variables such as waist circumference, insulin, glucose, HDL cholesterol, and triglycerides were used to calculate a continuous cardiometabolic risk score. Upon analysis, VO2 peak less than 45.8 mL/kg BM-1 min-1 in boys and less than 44.1 mL/kg BM-1 min-1 in girls was associated with increased cardiometabolic risk.
The coauthors noted that cardiorespiratory fitness can be influenced by genetics and that adjustments for puberty had “no effect on the relationships between VO2 peak and cardiometabolic risk.” As such, they recommended that “longitudinal studies are needed to clarify the role of CRF in cardiometabolic health during growth and maturation.”
That said, despite advocating caution in regard to determining proper CRF thresholds, the coauthors suggested that CRF scaled by BM could be used to screen children and improve prevention efforts. “Cardiometabolic risk tracks from childhood into adulthood and the early identification of individuals at increased risk is essential in developing public health actions targeted at preventing cardiometabolic diseases,” they wrote.
The study was funded by grants from the Ministry of Education and Culture of Finland, Ministry of Social Affairs and Health of Finland, Research Committee of the Kuopio University Hospital Catchment Area (State Research Funding), Finnish Innovation Fund Sitra, Social Insurance Institution of Finland, Finnish Cultural Foundation, Foundation for Paediatric Research, Diabetes Research Foundation in Finland, Finnish Foundation for Cardiovascular Research, Juho Vainio Foundation, Paavo Nurmi Foundation, and the Yrjö Jahnsson Foundation. Dr. Agbaje reported grant support from the Olvi Foundation and the Urho Känkanen Foundation.
SOURCE: Agbaje AO et al. Scand J Med Sci Sports. 2018 Sep 19. doi: 10.1111/sms.13307.
according to the analysis of an ongoing Finnish study of physical activity and dietary intervention in school children.
“Our results are in agreement with previous findings that cardiorespiratory fitness measured in exercise test laboratories or using field tests and scaled by body mass (BM) using the ratio standard method had a strong inverse association with cardiometabolic risk in children,” lead author Andrew O. Agbaje, MD, MPH, and his coauthors wrote in the Scandinavian Journal of Medicine & Science in Sports.
The coauthors assessed the cardiorespiratory fitness of 352 primary school children – 186 boys and 166 girls – from Kuopio, Finland, all of whom were already participating in the ongoing PANIC (Physical Activity and Nutrition in Children) Study. The children were asked to perform a maximal exercise test, upon which fitness was assessed by measuring peak oxygen uptake (VO2 peak), noted Dr. Agbaje, a PhD student at the University of Eastern Finland’s Institute of Biomedicine in Kuopio, and his colleagues.
Body mass and lean mass were also measured by bioelectrical impedance and used to scale VO2 peak, while variables such as waist circumference, insulin, glucose, HDL cholesterol, and triglycerides were used to calculate a continuous cardiometabolic risk score. Upon analysis, VO2 peak less than 45.8 mL/kg BM-1 min-1 in boys and less than 44.1 mL/kg BM-1 min-1 in girls was associated with increased cardiometabolic risk.
The coauthors noted that cardiorespiratory fitness can be influenced by genetics and that adjustments for puberty had “no effect on the relationships between VO2 peak and cardiometabolic risk.” As such, they recommended that “longitudinal studies are needed to clarify the role of CRF in cardiometabolic health during growth and maturation.”
That said, despite advocating caution in regard to determining proper CRF thresholds, the coauthors suggested that CRF scaled by BM could be used to screen children and improve prevention efforts. “Cardiometabolic risk tracks from childhood into adulthood and the early identification of individuals at increased risk is essential in developing public health actions targeted at preventing cardiometabolic diseases,” they wrote.
The study was funded by grants from the Ministry of Education and Culture of Finland, Ministry of Social Affairs and Health of Finland, Research Committee of the Kuopio University Hospital Catchment Area (State Research Funding), Finnish Innovation Fund Sitra, Social Insurance Institution of Finland, Finnish Cultural Foundation, Foundation for Paediatric Research, Diabetes Research Foundation in Finland, Finnish Foundation for Cardiovascular Research, Juho Vainio Foundation, Paavo Nurmi Foundation, and the Yrjö Jahnsson Foundation. Dr. Agbaje reported grant support from the Olvi Foundation and the Urho Känkanen Foundation.
SOURCE: Agbaje AO et al. Scand J Med Sci Sports. 2018 Sep 19. doi: 10.1111/sms.13307.
FROM THE SCANDINAVIAN JOURNAL OF MEDICINE & SCIENCE IN SPORTS
Key clinical point: Peak oxygen uptake less than 45.8 mL/kg BM-1 min-1 in boys and less than 44.1 mL/kg BM-1 min-1 in girls was associated with increased cardiometabolic risk.
Major finding: Cardiorespiratory fitness scaled by body mass could be used to screen for cardiometabolic risk in children.
Study details: An analysis of 352 Finnish children, all aged 9-11 years, who took a maximal exercise test as part of an ongoing physical activity and dietary intervention study.
Disclosures: The study was funded by grants from the Ministry of Education and Culture of Finland, Ministry of Social Affairs and Health of Finland, Research Committee of the Kuopio University Hospital Catchment Area, Finnish Innovation Fund Sitra, Social Insurance Institution of Finland, Finnish Cultural Foundation, Foundation for Paediatric Research, Diabetes Research Foundation in Finland, Finnish Foundation for Cardiovascular Research, Juho Vainio Foundation, Paavo Nurmi Foundation, and the Yrjö Jahnsson Foundation. Dr. Agbaje reported grant support from the Olvi Foundation and the Urho Känkanen Foundation.
Source: Agbaje AO et al. Scand J Med Sci Sports. 2018 Sep 19. doi: 10.1111/sms.13307.
Cardiologist: Obesity has basically stopped progress on cardiovascular disease
NASHVILLE – It’s all hands on deck to fight the obesity epidemic, according to a cardiologist who made a plea for collaboration at the opening session at a meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery. said Steven Nissen, MD, because when significant weight loss is achieved, “we can have an amazing effect on cardiovascular death, stroke, myocardial infarction, and these feared complications of obesity.”
From Dr. Nissen’s perspective, though, rates of death from cardiovascular disease have plateaued and are creeping up after decades of marked improvement.
“I am sorry to tell you that these rates are beginning to go up again – because of the obesity epidemic. That’s why we need to work together on this problem,” said Dr. Nissen, chair of the department of cardiovascular medicine at the Cleveland Clinic. “It has basically stopped progress on cardiovascular disease.”
Dr. Nissen drew from the broad literature intertwining obesity and cardiometabolic health to tell a story that went beyond weight loss to focus on outcomes.
For bariatric surgery, the evidence of reduction in cardiovascular risk is looking very good, said Dr. Nissen. “There are just huge changes in the metabolic risk factors. … Clearly we have evidence that if we get people to lose substantial weight, you can get people to normalize major metabolic risk factors.”
Recent data from a multisite, retrospective, matched cohort study of patients with diabetes and severe obesity show the promise of substantial weight loss in reducing risk. The study tracked 5,301 bariatric surgery patients and compared them with 14,934 “well-matched” control participants who did not have bariatric surgery but received usual care for diabetes, said Dr. Nissen.
During 7 years of follow-up, the bariatric surgery group had a hazard ratio for coronary events of 0.64 (95% confidence interval, 0.42-0.99; P less than .001). A post hoc analysis showed an HR of 0.34 for all-cause mortality among the bariatric surgery patients (95% CI, 0.15-0.74; P less than .001; JAMA. 2018;320[15]:1570-82).
“I’ve been practicing in this field for about 40 years,” said Dr. Nissen. “With statins, we get about 25% risk reduction … a 34% risk reduction is just a whopping big reduction.” Background risk was high among this population with diabetes, and this was a cohort study, not a randomized, controlled trial (RCT).
“We need RCTs,” he said. “I hope we can come together – all of us – and do a large, multicenter, global RCT on the effects of bariatric surgery on cardiovascular outcomes. But barring that, these are the best data we are going to have.”
But can these changes be achieved and sustained without surgery?
“Can diet or drug therapy favorably affect atherosclerotic cardiovascular outcomes? To me, this is the holy grail,” Dr. Nissen said.
A major cautionary note was sounded by a European Medicines Agency–mandated cardiovascular outcomes study of sibutramine, said Dr. Nissen. In clinical trials, patients taking sibutramine had seen modest weight loss, with increased HDL cholesterol and decreased triglycerides. However, blood pressure rose by 1-3 mm Hg, and heart rates also climbed by 4-5 beats per minute, changes consistent with sibutramine’s sympathomimetic effects, said Dr. Nissen. The EMA-mandated trial included over 10,000 patients and looked at a composite endpoint of major cardiovascular events, including death, MI, stroke, and resuscitated arrest. Patients were included if they were aged older than 55 years, had a body mass index of greater than 27 kg/m2, and had a history of cardiovascular disease or diabetes with an additional risk factor. Patients who had significant heart rate or blood pressure increases during the study run-in period were excluded.
In the end, patients taking sibutramine had an increased risk for the composite endpoint (11.4% vs. 10.0%; P = .02). The risk for nonfatal stroke and nonfatal MI was also significantly elevated for the sibutramine group (N Engl J Med. 2010; 363:905-17).
Phentermine is a pharmacologic relative of sibutramine, with similar effects on blood pressure and heart rate. Since it was approved prior to the current increased focus on real-world clinical outcomes in drug approvals, phentermine’s cardiovascular outcomes have never been studied by means of a RCT. “Nobody’s going to do this study unless we push for it, but it has to be done,” he said. “Although this drug reduces weight, there is considerable uncertainty whether it increases cardiovascular outcomes.”
Even looking at weight loss alone, pharmacologic treatments show marginal benefit over time, said Dr. Nissen, citing, as an example, recently published outcome data on lorcaserin. Over 40 months of treatment, there was a “complete absence of any benefit for lorcaserin,” compared with placebo, and participants saw an average weight loss of just 1.9 kg by the end of the study period, with no change in cardiovascular outcomes (N Engl J Med. 2018;379:1107-17).
To drive home the point, Dr. Nissen shared a slide entitled “Established Benefits of Weight Loss Drugs on Clinically Important Outcomes.” The slide’s text read, “This slide intentionally left blank.”
“It’s very hard for me to argue in favor of giving any of these drugs,” said Dr. Nissen. “In the absence of established outcome benefits, there are only risks and costs. I know this is not going to be popular with everyone in this audience, but I have to tell you what I really believe here: We have to do better.”
More broadly, “I think we have to demand outcome trials for obesity drugs,” said Dr. Nissen. He noted that such trials are underway for some glucagonlike peptide–1 agonists, “and I applaud them. ... I hope you will participate in those studies, because they are going to give us some answers.”
Calling for renewed efforts to improve the efficacy of lifestyle interventions, Dr. Nissen said, “What we have to do is try. .... You know as well as I that there are some outliers” who will achieve profound weight loss without surgery, and those patients are likely to reap big benefits in risk reduction.
“We’ve got a problem that affects tens of millions of people, and we’ve got to find a societal approach to this. But we share these patients; let’s work together on trying to make them better.”
Dr. Nissen did not report any relevant financial disclosures.
NASHVILLE – It’s all hands on deck to fight the obesity epidemic, according to a cardiologist who made a plea for collaboration at the opening session at a meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery. said Steven Nissen, MD, because when significant weight loss is achieved, “we can have an amazing effect on cardiovascular death, stroke, myocardial infarction, and these feared complications of obesity.”
From Dr. Nissen’s perspective, though, rates of death from cardiovascular disease have plateaued and are creeping up after decades of marked improvement.
“I am sorry to tell you that these rates are beginning to go up again – because of the obesity epidemic. That’s why we need to work together on this problem,” said Dr. Nissen, chair of the department of cardiovascular medicine at the Cleveland Clinic. “It has basically stopped progress on cardiovascular disease.”
Dr. Nissen drew from the broad literature intertwining obesity and cardiometabolic health to tell a story that went beyond weight loss to focus on outcomes.
For bariatric surgery, the evidence of reduction in cardiovascular risk is looking very good, said Dr. Nissen. “There are just huge changes in the metabolic risk factors. … Clearly we have evidence that if we get people to lose substantial weight, you can get people to normalize major metabolic risk factors.”
Recent data from a multisite, retrospective, matched cohort study of patients with diabetes and severe obesity show the promise of substantial weight loss in reducing risk. The study tracked 5,301 bariatric surgery patients and compared them with 14,934 “well-matched” control participants who did not have bariatric surgery but received usual care for diabetes, said Dr. Nissen.
During 7 years of follow-up, the bariatric surgery group had a hazard ratio for coronary events of 0.64 (95% confidence interval, 0.42-0.99; P less than .001). A post hoc analysis showed an HR of 0.34 for all-cause mortality among the bariatric surgery patients (95% CI, 0.15-0.74; P less than .001; JAMA. 2018;320[15]:1570-82).
“I’ve been practicing in this field for about 40 years,” said Dr. Nissen. “With statins, we get about 25% risk reduction … a 34% risk reduction is just a whopping big reduction.” Background risk was high among this population with diabetes, and this was a cohort study, not a randomized, controlled trial (RCT).
“We need RCTs,” he said. “I hope we can come together – all of us – and do a large, multicenter, global RCT on the effects of bariatric surgery on cardiovascular outcomes. But barring that, these are the best data we are going to have.”
But can these changes be achieved and sustained without surgery?
“Can diet or drug therapy favorably affect atherosclerotic cardiovascular outcomes? To me, this is the holy grail,” Dr. Nissen said.
A major cautionary note was sounded by a European Medicines Agency–mandated cardiovascular outcomes study of sibutramine, said Dr. Nissen. In clinical trials, patients taking sibutramine had seen modest weight loss, with increased HDL cholesterol and decreased triglycerides. However, blood pressure rose by 1-3 mm Hg, and heart rates also climbed by 4-5 beats per minute, changes consistent with sibutramine’s sympathomimetic effects, said Dr. Nissen. The EMA-mandated trial included over 10,000 patients and looked at a composite endpoint of major cardiovascular events, including death, MI, stroke, and resuscitated arrest. Patients were included if they were aged older than 55 years, had a body mass index of greater than 27 kg/m2, and had a history of cardiovascular disease or diabetes with an additional risk factor. Patients who had significant heart rate or blood pressure increases during the study run-in period were excluded.
In the end, patients taking sibutramine had an increased risk for the composite endpoint (11.4% vs. 10.0%; P = .02). The risk for nonfatal stroke and nonfatal MI was also significantly elevated for the sibutramine group (N Engl J Med. 2010; 363:905-17).
Phentermine is a pharmacologic relative of sibutramine, with similar effects on blood pressure and heart rate. Since it was approved prior to the current increased focus on real-world clinical outcomes in drug approvals, phentermine’s cardiovascular outcomes have never been studied by means of a RCT. “Nobody’s going to do this study unless we push for it, but it has to be done,” he said. “Although this drug reduces weight, there is considerable uncertainty whether it increases cardiovascular outcomes.”
Even looking at weight loss alone, pharmacologic treatments show marginal benefit over time, said Dr. Nissen, citing, as an example, recently published outcome data on lorcaserin. Over 40 months of treatment, there was a “complete absence of any benefit for lorcaserin,” compared with placebo, and participants saw an average weight loss of just 1.9 kg by the end of the study period, with no change in cardiovascular outcomes (N Engl J Med. 2018;379:1107-17).
To drive home the point, Dr. Nissen shared a slide entitled “Established Benefits of Weight Loss Drugs on Clinically Important Outcomes.” The slide’s text read, “This slide intentionally left blank.”
“It’s very hard for me to argue in favor of giving any of these drugs,” said Dr. Nissen. “In the absence of established outcome benefits, there are only risks and costs. I know this is not going to be popular with everyone in this audience, but I have to tell you what I really believe here: We have to do better.”
More broadly, “I think we have to demand outcome trials for obesity drugs,” said Dr. Nissen. He noted that such trials are underway for some glucagonlike peptide–1 agonists, “and I applaud them. ... I hope you will participate in those studies, because they are going to give us some answers.”
Calling for renewed efforts to improve the efficacy of lifestyle interventions, Dr. Nissen said, “What we have to do is try. .... You know as well as I that there are some outliers” who will achieve profound weight loss without surgery, and those patients are likely to reap big benefits in risk reduction.
“We’ve got a problem that affects tens of millions of people, and we’ve got to find a societal approach to this. But we share these patients; let’s work together on trying to make them better.”
Dr. Nissen did not report any relevant financial disclosures.
NASHVILLE – It’s all hands on deck to fight the obesity epidemic, according to a cardiologist who made a plea for collaboration at the opening session at a meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery. said Steven Nissen, MD, because when significant weight loss is achieved, “we can have an amazing effect on cardiovascular death, stroke, myocardial infarction, and these feared complications of obesity.”
From Dr. Nissen’s perspective, though, rates of death from cardiovascular disease have plateaued and are creeping up after decades of marked improvement.
“I am sorry to tell you that these rates are beginning to go up again – because of the obesity epidemic. That’s why we need to work together on this problem,” said Dr. Nissen, chair of the department of cardiovascular medicine at the Cleveland Clinic. “It has basically stopped progress on cardiovascular disease.”
Dr. Nissen drew from the broad literature intertwining obesity and cardiometabolic health to tell a story that went beyond weight loss to focus on outcomes.
For bariatric surgery, the evidence of reduction in cardiovascular risk is looking very good, said Dr. Nissen. “There are just huge changes in the metabolic risk factors. … Clearly we have evidence that if we get people to lose substantial weight, you can get people to normalize major metabolic risk factors.”
Recent data from a multisite, retrospective, matched cohort study of patients with diabetes and severe obesity show the promise of substantial weight loss in reducing risk. The study tracked 5,301 bariatric surgery patients and compared them with 14,934 “well-matched” control participants who did not have bariatric surgery but received usual care for diabetes, said Dr. Nissen.
During 7 years of follow-up, the bariatric surgery group had a hazard ratio for coronary events of 0.64 (95% confidence interval, 0.42-0.99; P less than .001). A post hoc analysis showed an HR of 0.34 for all-cause mortality among the bariatric surgery patients (95% CI, 0.15-0.74; P less than .001; JAMA. 2018;320[15]:1570-82).
“I’ve been practicing in this field for about 40 years,” said Dr. Nissen. “With statins, we get about 25% risk reduction … a 34% risk reduction is just a whopping big reduction.” Background risk was high among this population with diabetes, and this was a cohort study, not a randomized, controlled trial (RCT).
“We need RCTs,” he said. “I hope we can come together – all of us – and do a large, multicenter, global RCT on the effects of bariatric surgery on cardiovascular outcomes. But barring that, these are the best data we are going to have.”
But can these changes be achieved and sustained without surgery?
“Can diet or drug therapy favorably affect atherosclerotic cardiovascular outcomes? To me, this is the holy grail,” Dr. Nissen said.
A major cautionary note was sounded by a European Medicines Agency–mandated cardiovascular outcomes study of sibutramine, said Dr. Nissen. In clinical trials, patients taking sibutramine had seen modest weight loss, with increased HDL cholesterol and decreased triglycerides. However, blood pressure rose by 1-3 mm Hg, and heart rates also climbed by 4-5 beats per minute, changes consistent with sibutramine’s sympathomimetic effects, said Dr. Nissen. The EMA-mandated trial included over 10,000 patients and looked at a composite endpoint of major cardiovascular events, including death, MI, stroke, and resuscitated arrest. Patients were included if they were aged older than 55 years, had a body mass index of greater than 27 kg/m2, and had a history of cardiovascular disease or diabetes with an additional risk factor. Patients who had significant heart rate or blood pressure increases during the study run-in period were excluded.
In the end, patients taking sibutramine had an increased risk for the composite endpoint (11.4% vs. 10.0%; P = .02). The risk for nonfatal stroke and nonfatal MI was also significantly elevated for the sibutramine group (N Engl J Med. 2010; 363:905-17).
Phentermine is a pharmacologic relative of sibutramine, with similar effects on blood pressure and heart rate. Since it was approved prior to the current increased focus on real-world clinical outcomes in drug approvals, phentermine’s cardiovascular outcomes have never been studied by means of a RCT. “Nobody’s going to do this study unless we push for it, but it has to be done,” he said. “Although this drug reduces weight, there is considerable uncertainty whether it increases cardiovascular outcomes.”
Even looking at weight loss alone, pharmacologic treatments show marginal benefit over time, said Dr. Nissen, citing, as an example, recently published outcome data on lorcaserin. Over 40 months of treatment, there was a “complete absence of any benefit for lorcaserin,” compared with placebo, and participants saw an average weight loss of just 1.9 kg by the end of the study period, with no change in cardiovascular outcomes (N Engl J Med. 2018;379:1107-17).
To drive home the point, Dr. Nissen shared a slide entitled “Established Benefits of Weight Loss Drugs on Clinically Important Outcomes.” The slide’s text read, “This slide intentionally left blank.”
“It’s very hard for me to argue in favor of giving any of these drugs,” said Dr. Nissen. “In the absence of established outcome benefits, there are only risks and costs. I know this is not going to be popular with everyone in this audience, but I have to tell you what I really believe here: We have to do better.”
More broadly, “I think we have to demand outcome trials for obesity drugs,” said Dr. Nissen. He noted that such trials are underway for some glucagonlike peptide–1 agonists, “and I applaud them. ... I hope you will participate in those studies, because they are going to give us some answers.”
Calling for renewed efforts to improve the efficacy of lifestyle interventions, Dr. Nissen said, “What we have to do is try. .... You know as well as I that there are some outliers” who will achieve profound weight loss without surgery, and those patients are likely to reap big benefits in risk reduction.
“We’ve got a problem that affects tens of millions of people, and we’ve got to find a societal approach to this. But we share these patients; let’s work together on trying to make them better.”
Dr. Nissen did not report any relevant financial disclosures.
EXPERT ANALYSIS FROM OBESITY WEEK 2018
DECLARE: Dapagliflozin improves some cardiovascular, renal outcomes
For patients with type 2 diabetes who have or are at risk for atherosclerotic cardiovascular disease, do, according to investigators.
A composite measure of major adverse cardiovascular events (MACE), including cardiovascular death, ischemic stroke, or myocardial infarction, was comparable between dapagliflozin and placebo; in contrast, diabetic ketoacidosis occurred more frequently with dapagliflozin, reported lead author Stephen D. Wiviott, MD at the American Heart Association scientific sessions.
“As a result of [the] intersection of diabetes, atherosclerotic cardiovascular disease, and heart failure, the importance of determining diabetes therapies that are not only safe but also effective in reducing cardiovascular risk is paramount,” Dr. Wiviott and colleagues wrote in an article published simultaneously in the New England Journal of Medicine.
“Dapagliflozin is a selective inhibitor of sodium–glucose cotransporter (SGLT2) that blocks glucose resorption in the proximal tubule of the kidney and promotes glucosuria,” the investigators wrote. “Other SGLT2 inhibitors have shown favorable cardiovascular effects, including a reduction in the risk of hospitalization for heart failure, predominantly in patients with type 2 diabetes and established cardiovascular disease; they have also been shown to delay the progression of kidney disease.”
The goal of the Dapagliflozin Effect on Cardiovascular Events–Thrombolysis in Myocardial Infarction 58 (DECLARE–TIMI 58) trial was to determine what impact, if any, dapagliflozin has on renal and cardiovascular outcomes in a diverse array of patients with or at risk for atherosclerotic cardiovascular disease. The phase III, double-blind, placebo-controlled, randomized study involved 17,160 adults with type 2 diabetes from 33 countries. Of these, nearly 7,000 patients had atherosclerotic cardiovascular disease and the remaining 10,000 or so patients had multiple risk factors for atherosclerotic cardiovascular disease. Patients were at least 40 years of age, had a creatinine clearance of at least 60 mL/minute, and a HbA1c level between 6.5% and 12.0%. They were randomly assigned to receive either dapagliflozin 10 mg daily or placebo. Every 6 months, patients had laboratory testing with in-person follow-up for safety, clinical response, and adherence; patients were contacted via telephone at the halfway point between appointments (3 months).
The primary safety outcome of the study was major adverse cardiovascular outcomes (MACE: ischemic stroke, myocardial infarction, or cardiovascular death). The trial began with MACE as the sole primary safety outcome, as guided by the Food and Drug Administration, but this changed before completion. “During the trial,” the investigators explained, “compelling external scientific information from the EMPA-REG OUTCOME trial, which evaluated another SGLT2 inhibitor, showed greater benefit with respect to cardiovascular death and hospitalization for heart failure than with respect to MACE.” Therefore, before data were known, the investigators added a second primary outcome: a composite of cardiovascular death or hospitalization for heart failure. The two secondary outcomes were a renal composite (new end-stage renal disease, estimated glomerular filtration rate decrease by at least 40% to less than 60 m/min per 1.73 m2 of body-surface area, or death from renal or cardiovascular disease), and death from any cause.
The primary safety outcome (MACE rate) showed that dapagliflozin was noninferior to placebo (upper boundary of the 95% confidence interval, less than 1.3; P less than .001 for noninferiority). Although the MACE rate was similar between treatment groups (8.8% for dapagliflozin vs 9.4% for placebo; P = .017), the composite rate of cardiovascular death or hospitalization for heart failure was 17% lower for patients receiving dapagliflozin, compared with those who received placebo (4.9% vs 5.8%); this latter finding was attributable mostly to a 27% lower risk of hospitalization, instead of the 2% reduction in cardiovascular death. Seven percent fewer deaths of any kind were observed in the dapagliflozin group (6.2%) than in the placebo group (6.6%). Renal events saw a bigger difference, of 23% (4.3% vs 5.6%).
Statistically significant adverse events seen in more dapagliflozin than placebo patients included diabetic ketoacidosis and genital infection. Dr. Wiviott noted that adverse events favoring hypoglycemia included major hypoglycemia and bladder cancer..
“We did not find that SGLT2 inhibition with dapagliflozin resulted in a lower rate of cardiovascular death or death from any cause than placebo, a finding that contrasts with that in the EMPA-REG OUTCOME trial,” the investigators noted. Apart from possible differences in drugs within the same class, the investigators pointed to more restrictive renal criteria in the DECLARE trial and possible inherent differences between patient populations, among other possible factors.
“…in a broad population of patients with type 2 diabetes [dapagliflozin] did result in a significantly lower rate of cardiovascular death or hospitalization for heart failure than placebo, with additional findings supporting a possible lower rate of adverse renal outcomes,” the investigators concluded.
The DECLARE-TIMI 58 trial was sponsored by AstraZeneca and Bristol-Myers Squibb. Authors reported various financial affiliations with Eisai, Medtronic, Sanofi Aventis, Abbott, Regeneron, and others.
SOURCE: Wiviott et al. N Engl J Med. 2018 Nov 10. doi: 10.1056/NEJMoa1812389
For patients with type 2 diabetes who have or are at risk for atherosclerotic cardiovascular disease, do, according to investigators.
A composite measure of major adverse cardiovascular events (MACE), including cardiovascular death, ischemic stroke, or myocardial infarction, was comparable between dapagliflozin and placebo; in contrast, diabetic ketoacidosis occurred more frequently with dapagliflozin, reported lead author Stephen D. Wiviott, MD at the American Heart Association scientific sessions.
“As a result of [the] intersection of diabetes, atherosclerotic cardiovascular disease, and heart failure, the importance of determining diabetes therapies that are not only safe but also effective in reducing cardiovascular risk is paramount,” Dr. Wiviott and colleagues wrote in an article published simultaneously in the New England Journal of Medicine.
“Dapagliflozin is a selective inhibitor of sodium–glucose cotransporter (SGLT2) that blocks glucose resorption in the proximal tubule of the kidney and promotes glucosuria,” the investigators wrote. “Other SGLT2 inhibitors have shown favorable cardiovascular effects, including a reduction in the risk of hospitalization for heart failure, predominantly in patients with type 2 diabetes and established cardiovascular disease; they have also been shown to delay the progression of kidney disease.”
The goal of the Dapagliflozin Effect on Cardiovascular Events–Thrombolysis in Myocardial Infarction 58 (DECLARE–TIMI 58) trial was to determine what impact, if any, dapagliflozin has on renal and cardiovascular outcomes in a diverse array of patients with or at risk for atherosclerotic cardiovascular disease. The phase III, double-blind, placebo-controlled, randomized study involved 17,160 adults with type 2 diabetes from 33 countries. Of these, nearly 7,000 patients had atherosclerotic cardiovascular disease and the remaining 10,000 or so patients had multiple risk factors for atherosclerotic cardiovascular disease. Patients were at least 40 years of age, had a creatinine clearance of at least 60 mL/minute, and a HbA1c level between 6.5% and 12.0%. They were randomly assigned to receive either dapagliflozin 10 mg daily or placebo. Every 6 months, patients had laboratory testing with in-person follow-up for safety, clinical response, and adherence; patients were contacted via telephone at the halfway point between appointments (3 months).
The primary safety outcome of the study was major adverse cardiovascular outcomes (MACE: ischemic stroke, myocardial infarction, or cardiovascular death). The trial began with MACE as the sole primary safety outcome, as guided by the Food and Drug Administration, but this changed before completion. “During the trial,” the investigators explained, “compelling external scientific information from the EMPA-REG OUTCOME trial, which evaluated another SGLT2 inhibitor, showed greater benefit with respect to cardiovascular death and hospitalization for heart failure than with respect to MACE.” Therefore, before data were known, the investigators added a second primary outcome: a composite of cardiovascular death or hospitalization for heart failure. The two secondary outcomes were a renal composite (new end-stage renal disease, estimated glomerular filtration rate decrease by at least 40% to less than 60 m/min per 1.73 m2 of body-surface area, or death from renal or cardiovascular disease), and death from any cause.
The primary safety outcome (MACE rate) showed that dapagliflozin was noninferior to placebo (upper boundary of the 95% confidence interval, less than 1.3; P less than .001 for noninferiority). Although the MACE rate was similar between treatment groups (8.8% for dapagliflozin vs 9.4% for placebo; P = .017), the composite rate of cardiovascular death or hospitalization for heart failure was 17% lower for patients receiving dapagliflozin, compared with those who received placebo (4.9% vs 5.8%); this latter finding was attributable mostly to a 27% lower risk of hospitalization, instead of the 2% reduction in cardiovascular death. Seven percent fewer deaths of any kind were observed in the dapagliflozin group (6.2%) than in the placebo group (6.6%). Renal events saw a bigger difference, of 23% (4.3% vs 5.6%).
Statistically significant adverse events seen in more dapagliflozin than placebo patients included diabetic ketoacidosis and genital infection. Dr. Wiviott noted that adverse events favoring hypoglycemia included major hypoglycemia and bladder cancer..
“We did not find that SGLT2 inhibition with dapagliflozin resulted in a lower rate of cardiovascular death or death from any cause than placebo, a finding that contrasts with that in the EMPA-REG OUTCOME trial,” the investigators noted. Apart from possible differences in drugs within the same class, the investigators pointed to more restrictive renal criteria in the DECLARE trial and possible inherent differences between patient populations, among other possible factors.
“…in a broad population of patients with type 2 diabetes [dapagliflozin] did result in a significantly lower rate of cardiovascular death or hospitalization for heart failure than placebo, with additional findings supporting a possible lower rate of adverse renal outcomes,” the investigators concluded.
The DECLARE-TIMI 58 trial was sponsored by AstraZeneca and Bristol-Myers Squibb. Authors reported various financial affiliations with Eisai, Medtronic, Sanofi Aventis, Abbott, Regeneron, and others.
SOURCE: Wiviott et al. N Engl J Med. 2018 Nov 10. doi: 10.1056/NEJMoa1812389
For patients with type 2 diabetes who have or are at risk for atherosclerotic cardiovascular disease, do, according to investigators.
A composite measure of major adverse cardiovascular events (MACE), including cardiovascular death, ischemic stroke, or myocardial infarction, was comparable between dapagliflozin and placebo; in contrast, diabetic ketoacidosis occurred more frequently with dapagliflozin, reported lead author Stephen D. Wiviott, MD at the American Heart Association scientific sessions.
“As a result of [the] intersection of diabetes, atherosclerotic cardiovascular disease, and heart failure, the importance of determining diabetes therapies that are not only safe but also effective in reducing cardiovascular risk is paramount,” Dr. Wiviott and colleagues wrote in an article published simultaneously in the New England Journal of Medicine.
“Dapagliflozin is a selective inhibitor of sodium–glucose cotransporter (SGLT2) that blocks glucose resorption in the proximal tubule of the kidney and promotes glucosuria,” the investigators wrote. “Other SGLT2 inhibitors have shown favorable cardiovascular effects, including a reduction in the risk of hospitalization for heart failure, predominantly in patients with type 2 diabetes and established cardiovascular disease; they have also been shown to delay the progression of kidney disease.”
The goal of the Dapagliflozin Effect on Cardiovascular Events–Thrombolysis in Myocardial Infarction 58 (DECLARE–TIMI 58) trial was to determine what impact, if any, dapagliflozin has on renal and cardiovascular outcomes in a diverse array of patients with or at risk for atherosclerotic cardiovascular disease. The phase III, double-blind, placebo-controlled, randomized study involved 17,160 adults with type 2 diabetes from 33 countries. Of these, nearly 7,000 patients had atherosclerotic cardiovascular disease and the remaining 10,000 or so patients had multiple risk factors for atherosclerotic cardiovascular disease. Patients were at least 40 years of age, had a creatinine clearance of at least 60 mL/minute, and a HbA1c level between 6.5% and 12.0%. They were randomly assigned to receive either dapagliflozin 10 mg daily or placebo. Every 6 months, patients had laboratory testing with in-person follow-up for safety, clinical response, and adherence; patients were contacted via telephone at the halfway point between appointments (3 months).
The primary safety outcome of the study was major adverse cardiovascular outcomes (MACE: ischemic stroke, myocardial infarction, or cardiovascular death). The trial began with MACE as the sole primary safety outcome, as guided by the Food and Drug Administration, but this changed before completion. “During the trial,” the investigators explained, “compelling external scientific information from the EMPA-REG OUTCOME trial, which evaluated another SGLT2 inhibitor, showed greater benefit with respect to cardiovascular death and hospitalization for heart failure than with respect to MACE.” Therefore, before data were known, the investigators added a second primary outcome: a composite of cardiovascular death or hospitalization for heart failure. The two secondary outcomes were a renal composite (new end-stage renal disease, estimated glomerular filtration rate decrease by at least 40% to less than 60 m/min per 1.73 m2 of body-surface area, or death from renal or cardiovascular disease), and death from any cause.
The primary safety outcome (MACE rate) showed that dapagliflozin was noninferior to placebo (upper boundary of the 95% confidence interval, less than 1.3; P less than .001 for noninferiority). Although the MACE rate was similar between treatment groups (8.8% for dapagliflozin vs 9.4% for placebo; P = .017), the composite rate of cardiovascular death or hospitalization for heart failure was 17% lower for patients receiving dapagliflozin, compared with those who received placebo (4.9% vs 5.8%); this latter finding was attributable mostly to a 27% lower risk of hospitalization, instead of the 2% reduction in cardiovascular death. Seven percent fewer deaths of any kind were observed in the dapagliflozin group (6.2%) than in the placebo group (6.6%). Renal events saw a bigger difference, of 23% (4.3% vs 5.6%).
Statistically significant adverse events seen in more dapagliflozin than placebo patients included diabetic ketoacidosis and genital infection. Dr. Wiviott noted that adverse events favoring hypoglycemia included major hypoglycemia and bladder cancer..
“We did not find that SGLT2 inhibition with dapagliflozin resulted in a lower rate of cardiovascular death or death from any cause than placebo, a finding that contrasts with that in the EMPA-REG OUTCOME trial,” the investigators noted. Apart from possible differences in drugs within the same class, the investigators pointed to more restrictive renal criteria in the DECLARE trial and possible inherent differences between patient populations, among other possible factors.
“…in a broad population of patients with type 2 diabetes [dapagliflozin] did result in a significantly lower rate of cardiovascular death or hospitalization for heart failure than placebo, with additional findings supporting a possible lower rate of adverse renal outcomes,” the investigators concluded.
The DECLARE-TIMI 58 trial was sponsored by AstraZeneca and Bristol-Myers Squibb. Authors reported various financial affiliations with Eisai, Medtronic, Sanofi Aventis, Abbott, Regeneron, and others.
SOURCE: Wiviott et al. N Engl J Med. 2018 Nov 10. doi: 10.1056/NEJMoa1812389
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Key clinical point: For patients with type 2 diabetes who have or are at risk for atherosclerotic cardiovascular disease, dapagliflozin is associated with a lower composite rate of cardiovascular death or hospitalization for heart failure, compared with placebo.
Major finding: Of patients taking dapagliflozin, 4.9% died of cardiovascular disease or were hospitalized for heart failure, compared with 5.8% of patients receiving placebo (P = .005).
Study details: The phase III DECLARE–TIMI 58 trial was a double-blind, placebo-controlled, randomized study that involved 17,160 patients with type 2 diabetes who had or were at risk for atherosclerotic cardiovascular disease.
Disclosures: DECLARE–TIMI 58 was sponsored by AstraZeneca and Bristol-Myers Squibb. Authors reported various financial affiliations with Eisai, Medtronic, Sanofi Aventis, Abbott, Regeneron, and others.
Source: Wiviott et al. N Engl J Med. 2018 Nov 10. doi: ___________
Lower glucose targets show improved mortality in cardiac patients
Tighter glucose control while minimizing the risk of severe hypoglycemia is associated with lower mortality among critically ill cardiac patents, new research suggests.
Researchers reported in CHEST on the outcomes of a multicenter retrospective cohort study in 1,809 adults in cardiac ICUs. Patients were treated either to a blood glucose target of 80-110 mg/dL or 90-140 mg/dL, based on the clinician’s preference, but using a computerized ICU insulin infusion protocol that the authors said had resulted in low rates of severe hypoglycemia.
The study found patients treated to the 80-110 mg/dL blood glucose target had a significantly lower unadjusted 30-day mortality compared to patients treated to the 90-140 mg/dL target (4.3% vs. 9.2%; P less than .001). The lower mortality in the lower target group was evident among both diabetic (4.7% vs. 12.9%; P less than .001) and nondiabetic patients (4.1% vs. 7.4%; P = .02).
Researchers also saw that unadjusted 30-day mortality increased with increasing median glucose levels; 5.5% in patients with a blood glucose of 70-110 mg/dL, 8.3% mortality in those with blood glucose levels of 141-180 mg/dL, and 25% in those with a blood glucose level higher than 180 mg/dL.
Patients treated to the 80-110 mg/dL blood glucose target were more likely to experience an episode of moderate hypoglycemia, compared with those in the higher target group (18.6% vs. 8.3%; P less than .001). However, the rates of severe hypoglycemia were low in both groups, and the difference between the low and high target groups did not reach statistical significance (1.16% vs. 0.35%; P = .051).
The authors did note that patients whose blood glucose dropped below 60 mg/dL showed increased mortality, regardless of what target they was set for them. The 30-day unadjusted mortality in these patients was 15%, compared with 5.2% for patients in either group who did not experience a blood glucose level below 60 mg/dL.
“Our results further the discussion about the appropriate BG [blood glucose] target in the critically ill because they suggest that the BG target and severe hypoglycemia effects can be separated,” wrote Andrew M. Hersh, MD, of the division of pulmonary and critical care at San Antonio Military Medical Center, and his coauthors.
But they said the large differences in mortality seen between the two treatment targets should be interpreted with caution, as it was difficult to attribute that difference solely to an 18 mg/dL difference in blood glucose treatment targets.
“While we attempted to capture factors that influenced clinician choice, and while our model successfully achieved balance, suggesting that residual confounding was minimized, we suspect that some of the mortality signal may be attributable to residual confounding,” they wrote.
Another explanation could be that hypoglycemia was an ‘epiphenomenon’ of multiorgan failure, as some studies have found that both spontaneous and iatrogenic hypoglycemia were independently associated with mortality. “However, given the very-low rates of severe hypoglycemia found in both groups it is unlikely that this was a main driver of the mortality difference found,” the investigators wrote.
The majority of patients in the study had been admitted to the hospital for chest pain or acute coronary syndrome (43.3%), while 31.9% were admitted for cardiothoracic surgery, 6.8% for heart failure including cardiogenic shock, and 6% for vascular surgery.
The authors commented that a safe and reliable protocol for intensive insulin therapy, with high clinician compliance, could be the key to realizing its benefits, and could be aided by recent advances such as closed-loop insulin delivery systems.
They also stressed that their results did not support a rejection of current guidelines and instead called for large randomized, clinical trials to find a balance between benefits and harms of intensive insulin therapy.
“Instead our analysis suggests that trials such as NICE-SUGAR, and the conclusion they drew, may have been accurate only in the setting of technologies, which led to high rates of severe hypoglycemia.”
No conflicts of interest were declared.
After the multicenter NICE-SUGAR trial showed higher 90-day mortality in patients treated with intensive insulin therapy to lower blood glucose targets, compared with more moderate targets, enthusiasm has waned for tighter blood glucose control, James S. Krinsley, MD, argued in an editorial accompanying the study (CHEST 2018; 154[5]:1004-5). But the assumption of a “one-size-fits-all” approach to glucose control in the critically ill is a potential flaw of randomized clinical trials, he noted, and some patients may be better suited to tighter control than others. This study has shown that standardized protocols, including frequent measurement of blood glucose, can safely achieve tight blood glucose control in the ICU with low rates of hypoglycemia. If these findings are confirmed in larger multicenter clinical trials, it should prompt a rethink of blood glucose targets in the critically ill, he concluded.
Dr. Krinsley is director of critical care at Stamford (Conn.) Hospital and clinical professor of medicine at the Columbia University College of Physicians and Surgeons, New York. He declared consultancies or advisory board positions with Edwards Life Sciences, Medtronic, OptiScan Biomedical, and Roche Diagnostics.
After the multicenter NICE-SUGAR trial showed higher 90-day mortality in patients treated with intensive insulin therapy to lower blood glucose targets, compared with more moderate targets, enthusiasm has waned for tighter blood glucose control, James S. Krinsley, MD, argued in an editorial accompanying the study (CHEST 2018; 154[5]:1004-5). But the assumption of a “one-size-fits-all” approach to glucose control in the critically ill is a potential flaw of randomized clinical trials, he noted, and some patients may be better suited to tighter control than others. This study has shown that standardized protocols, including frequent measurement of blood glucose, can safely achieve tight blood glucose control in the ICU with low rates of hypoglycemia. If these findings are confirmed in larger multicenter clinical trials, it should prompt a rethink of blood glucose targets in the critically ill, he concluded.
Dr. Krinsley is director of critical care at Stamford (Conn.) Hospital and clinical professor of medicine at the Columbia University College of Physicians and Surgeons, New York. He declared consultancies or advisory board positions with Edwards Life Sciences, Medtronic, OptiScan Biomedical, and Roche Diagnostics.
After the multicenter NICE-SUGAR trial showed higher 90-day mortality in patients treated with intensive insulin therapy to lower blood glucose targets, compared with more moderate targets, enthusiasm has waned for tighter blood glucose control, James S. Krinsley, MD, argued in an editorial accompanying the study (CHEST 2018; 154[5]:1004-5). But the assumption of a “one-size-fits-all” approach to glucose control in the critically ill is a potential flaw of randomized clinical trials, he noted, and some patients may be better suited to tighter control than others. This study has shown that standardized protocols, including frequent measurement of blood glucose, can safely achieve tight blood glucose control in the ICU with low rates of hypoglycemia. If these findings are confirmed in larger multicenter clinical trials, it should prompt a rethink of blood glucose targets in the critically ill, he concluded.
Dr. Krinsley is director of critical care at Stamford (Conn.) Hospital and clinical professor of medicine at the Columbia University College of Physicians and Surgeons, New York. He declared consultancies or advisory board positions with Edwards Life Sciences, Medtronic, OptiScan Biomedical, and Roche Diagnostics.
Tighter glucose control while minimizing the risk of severe hypoglycemia is associated with lower mortality among critically ill cardiac patents, new research suggests.
Researchers reported in CHEST on the outcomes of a multicenter retrospective cohort study in 1,809 adults in cardiac ICUs. Patients were treated either to a blood glucose target of 80-110 mg/dL or 90-140 mg/dL, based on the clinician’s preference, but using a computerized ICU insulin infusion protocol that the authors said had resulted in low rates of severe hypoglycemia.
The study found patients treated to the 80-110 mg/dL blood glucose target had a significantly lower unadjusted 30-day mortality compared to patients treated to the 90-140 mg/dL target (4.3% vs. 9.2%; P less than .001). The lower mortality in the lower target group was evident among both diabetic (4.7% vs. 12.9%; P less than .001) and nondiabetic patients (4.1% vs. 7.4%; P = .02).
Researchers also saw that unadjusted 30-day mortality increased with increasing median glucose levels; 5.5% in patients with a blood glucose of 70-110 mg/dL, 8.3% mortality in those with blood glucose levels of 141-180 mg/dL, and 25% in those with a blood glucose level higher than 180 mg/dL.
Patients treated to the 80-110 mg/dL blood glucose target were more likely to experience an episode of moderate hypoglycemia, compared with those in the higher target group (18.6% vs. 8.3%; P less than .001). However, the rates of severe hypoglycemia were low in both groups, and the difference between the low and high target groups did not reach statistical significance (1.16% vs. 0.35%; P = .051).
The authors did note that patients whose blood glucose dropped below 60 mg/dL showed increased mortality, regardless of what target they was set for them. The 30-day unadjusted mortality in these patients was 15%, compared with 5.2% for patients in either group who did not experience a blood glucose level below 60 mg/dL.
“Our results further the discussion about the appropriate BG [blood glucose] target in the critically ill because they suggest that the BG target and severe hypoglycemia effects can be separated,” wrote Andrew M. Hersh, MD, of the division of pulmonary and critical care at San Antonio Military Medical Center, and his coauthors.
But they said the large differences in mortality seen between the two treatment targets should be interpreted with caution, as it was difficult to attribute that difference solely to an 18 mg/dL difference in blood glucose treatment targets.
“While we attempted to capture factors that influenced clinician choice, and while our model successfully achieved balance, suggesting that residual confounding was minimized, we suspect that some of the mortality signal may be attributable to residual confounding,” they wrote.
Another explanation could be that hypoglycemia was an ‘epiphenomenon’ of multiorgan failure, as some studies have found that both spontaneous and iatrogenic hypoglycemia were independently associated with mortality. “However, given the very-low rates of severe hypoglycemia found in both groups it is unlikely that this was a main driver of the mortality difference found,” the investigators wrote.
The majority of patients in the study had been admitted to the hospital for chest pain or acute coronary syndrome (43.3%), while 31.9% were admitted for cardiothoracic surgery, 6.8% for heart failure including cardiogenic shock, and 6% for vascular surgery.
The authors commented that a safe and reliable protocol for intensive insulin therapy, with high clinician compliance, could be the key to realizing its benefits, and could be aided by recent advances such as closed-loop insulin delivery systems.
They also stressed that their results did not support a rejection of current guidelines and instead called for large randomized, clinical trials to find a balance between benefits and harms of intensive insulin therapy.
“Instead our analysis suggests that trials such as NICE-SUGAR, and the conclusion they drew, may have been accurate only in the setting of technologies, which led to high rates of severe hypoglycemia.”
No conflicts of interest were declared.
Tighter glucose control while minimizing the risk of severe hypoglycemia is associated with lower mortality among critically ill cardiac patents, new research suggests.
Researchers reported in CHEST on the outcomes of a multicenter retrospective cohort study in 1,809 adults in cardiac ICUs. Patients were treated either to a blood glucose target of 80-110 mg/dL or 90-140 mg/dL, based on the clinician’s preference, but using a computerized ICU insulin infusion protocol that the authors said had resulted in low rates of severe hypoglycemia.
The study found patients treated to the 80-110 mg/dL blood glucose target had a significantly lower unadjusted 30-day mortality compared to patients treated to the 90-140 mg/dL target (4.3% vs. 9.2%; P less than .001). The lower mortality in the lower target group was evident among both diabetic (4.7% vs. 12.9%; P less than .001) and nondiabetic patients (4.1% vs. 7.4%; P = .02).
Researchers also saw that unadjusted 30-day mortality increased with increasing median glucose levels; 5.5% in patients with a blood glucose of 70-110 mg/dL, 8.3% mortality in those with blood glucose levels of 141-180 mg/dL, and 25% in those with a blood glucose level higher than 180 mg/dL.
Patients treated to the 80-110 mg/dL blood glucose target were more likely to experience an episode of moderate hypoglycemia, compared with those in the higher target group (18.6% vs. 8.3%; P less than .001). However, the rates of severe hypoglycemia were low in both groups, and the difference between the low and high target groups did not reach statistical significance (1.16% vs. 0.35%; P = .051).
The authors did note that patients whose blood glucose dropped below 60 mg/dL showed increased mortality, regardless of what target they was set for them. The 30-day unadjusted mortality in these patients was 15%, compared with 5.2% for patients in either group who did not experience a blood glucose level below 60 mg/dL.
“Our results further the discussion about the appropriate BG [blood glucose] target in the critically ill because they suggest that the BG target and severe hypoglycemia effects can be separated,” wrote Andrew M. Hersh, MD, of the division of pulmonary and critical care at San Antonio Military Medical Center, and his coauthors.
But they said the large differences in mortality seen between the two treatment targets should be interpreted with caution, as it was difficult to attribute that difference solely to an 18 mg/dL difference in blood glucose treatment targets.
“While we attempted to capture factors that influenced clinician choice, and while our model successfully achieved balance, suggesting that residual confounding was minimized, we suspect that some of the mortality signal may be attributable to residual confounding,” they wrote.
Another explanation could be that hypoglycemia was an ‘epiphenomenon’ of multiorgan failure, as some studies have found that both spontaneous and iatrogenic hypoglycemia were independently associated with mortality. “However, given the very-low rates of severe hypoglycemia found in both groups it is unlikely that this was a main driver of the mortality difference found,” the investigators wrote.
The majority of patients in the study had been admitted to the hospital for chest pain or acute coronary syndrome (43.3%), while 31.9% were admitted for cardiothoracic surgery, 6.8% for heart failure including cardiogenic shock, and 6% for vascular surgery.
The authors commented that a safe and reliable protocol for intensive insulin therapy, with high clinician compliance, could be the key to realizing its benefits, and could be aided by recent advances such as closed-loop insulin delivery systems.
They also stressed that their results did not support a rejection of current guidelines and instead called for large randomized, clinical trials to find a balance between benefits and harms of intensive insulin therapy.
“Instead our analysis suggests that trials such as NICE-SUGAR, and the conclusion they drew, may have been accurate only in the setting of technologies, which led to high rates of severe hypoglycemia.”
No conflicts of interest were declared.
FROM CHEST
Key clinical point: Tighter blood glucose control may reduce 30-day mortality in critically ill cardiac patients.
Major finding: Unadjusted 30-day mortality increased with increasing median glucose levels; 5.5% in patients with a blood glucose between 70 and 110 mg/dL, and 25% in those above 180 mg/dL.
Study details: A retrospective cohort study in 1,809 adults in cardiac intensive care units.
Disclosures: No conflicts of interest were declared.
Source: Hersh AM et al. Chest. 2018 Nov;154(5):1044-51.
Closed-loop basal insulin delivery improves suboptimal T1DM control
BERLIN – Adults, adolescents, and children with type 1 diabetes mellitus (T1DM) achieved better glycemic control and spent less time in a hypoglycemic state with an investigational closed-loop basal insulin delivery system than with a sensor-augmented insulin pump.
The primary trial endpoint of the proportion of time spent in a target glucose range of 3.9-10 mmol/L at 12 weeks was achieved by 65% of closed-loop users versus 54% of sensor-augmented insulin-pump users (P less than .0001).
In addition, fewer patients had periods of blood glucose less than 3.9 mmol/L at 12 weeks, potentially reducing their risk for hypoglycemic episodes (2.6% vs. 3.9%, P = .0130). The percentages of patients with blood glucose concentrations higher than the target range were also significantly reduced with the closed-loop system.
Glycated hemoglobin (HbA1c) improved in both groups, from a baseline of 8% to 7.4% at 12 weeks in the closed-loop users and from 7.8% to 7.7% in the sensor-augmented insulin-pump users (mean difference –0.036%, P less than .0001). Mean glucose levels also significantly improved, with a mean between-group difference of –0.45 mmol/L (P less than .0001).
“Most of the improvements are overnight,” with a striking difference between the control and closed-loop groups of time in range, said senior study investigator Roman Hovorka, PhD, during a press briefing at the annual meeting of the European Association for the Study of Diabetes.
“Usually what people need to do is titrate insulin based on blood sugar tests, but in our system those tests are done by a monitoring system and the insulin is titrated by a computer algorithm,” study investigator Martin Tauschmann, MD, explained in an interview after the press briefing.
The prototype system consists of a modified insulin pump (Medtronic 640G) and a continuous glucose sensor (Enlite 3) that are linked by the proprietary “Cambridge control” algorithm via an Android phone. The latter calculates the optimum insulin dose, which is then relayed to the insulin pump every 10 minutes to determine how many insulin units are needed.
“The algorithm is based on mathematical modeling that is trying to predict what the glucose levels will be in the future and trying to work out the optimum insulin dose to bring the predicted glucose levels down,” noted Dr. Tauschmann, who is a pediatrician at Cambridge University (England).
It’s not a fully closed-loop system, he added, it’s a hybrid, so users still need to calculate their carbohydrate intake around mealtimes and input that into the algorithm and use bolus insulin.
“A problem with using currently available insulin formulations is that you are always behind, because we are delivering insulin in the subcutaneous tissue and it just takes some time for the insulin to be absorbed, and, in the meantime, the blood sugar levels go up,” Dr. Tauschmann observed. Studies with fully closed–loop systems, so far, have shown glucose peaking after meals. Perhaps when faster-acting insulins are tested in this setting it could work, he suggested, but perhaps simplifying how the users announce their meals is a future development for the hybrid systems.
Closed-loop insulin delivery is not a new concept. There is already one system available in the United States produced by Medtronic (670G), which was approved by the Food and Drug Administration in September 2016. However, there are no systems available in Europe and there are limited trial data on their use in an outpatient setting.
The aim of the current study, which was an open-label, multicenter, multinational, parallel-group, randomized, controlled trial, was to compare closed-loop basal insulin delivery and sensor augmented insulin pump therapy in helping a mixed adult and pediatric population of patients T1DM achieve good glucose control.
In all, 86 adults, adolescents, and children (age 6 years or older) were randomized: 46 to the closed-loop system and 40 to the control arm of sensor-augmented insulin pump therapy. The mean age of participants was 22 years in the closed-loop group and 21 years in the sensor group, with a respective 24% and 30% aged 6-12 years, 24% and 20% aged 13-21 years, 39% and 35% aged 22-40 years, and 13% and 15% aged 41 years or older. The mean duration of diabetes was 13 and 10 years, in each group, respectively.
The study data “provide more evidence that closed-loop insulin delivery, compared with standard pump and sensor, really improves HbA1c, time spent in range, and mean glucose, and it also reduces hypoglycemia,” Dr. Tauschmann said.
“We didn’t have any real safety issues,” noted Dr. Hovorka, who is professor and director of research in the department of pediatrics at the University of Cambridge. There was one episode of diabetic ketoacidosis caused by infusion set failure in the closed-loop group; 16 other adverse events were noted (13 in the closed-loop group, three in the control group) that were not related to treatment.
“We have a number of studies in the pipeline,” Dr. Hovorka said. “Two exciting studies are in development. In one we are recruiting 70 subjects with newly diagnosed type 1 diabetes mellitus who will be treated with a closed-loop system. There is also a study in children aged between 1 and 7 years that is projected to start next year.”
Work is also underway to create a platform that will work with all insulin pumps and create a commercial product.
The study was funded by the Juvenile Diabetes Research Foundation with additional support from the National Institute for Health Research (England) and the Wellcome Trust. Dr. Tauschmann reported receiving speaker honoraria from Medtronic and Novo Nordisk. Dr. Hovorka reported receiving speaker honoraria from Eli Lilly and Novo Nordisk, serving on an advisory panel for Eli Lilly, receiving license fees from B. Braun Medical and Medtronic, and having patents and patent applications.
SOURCES: Tauschmann M et al. EASD 2018, Oral Presentation 19.
BERLIN – Adults, adolescents, and children with type 1 diabetes mellitus (T1DM) achieved better glycemic control and spent less time in a hypoglycemic state with an investigational closed-loop basal insulin delivery system than with a sensor-augmented insulin pump.
The primary trial endpoint of the proportion of time spent in a target glucose range of 3.9-10 mmol/L at 12 weeks was achieved by 65% of closed-loop users versus 54% of sensor-augmented insulin-pump users (P less than .0001).
In addition, fewer patients had periods of blood glucose less than 3.9 mmol/L at 12 weeks, potentially reducing their risk for hypoglycemic episodes (2.6% vs. 3.9%, P = .0130). The percentages of patients with blood glucose concentrations higher than the target range were also significantly reduced with the closed-loop system.
Glycated hemoglobin (HbA1c) improved in both groups, from a baseline of 8% to 7.4% at 12 weeks in the closed-loop users and from 7.8% to 7.7% in the sensor-augmented insulin-pump users (mean difference –0.036%, P less than .0001). Mean glucose levels also significantly improved, with a mean between-group difference of –0.45 mmol/L (P less than .0001).
“Most of the improvements are overnight,” with a striking difference between the control and closed-loop groups of time in range, said senior study investigator Roman Hovorka, PhD, during a press briefing at the annual meeting of the European Association for the Study of Diabetes.
“Usually what people need to do is titrate insulin based on blood sugar tests, but in our system those tests are done by a monitoring system and the insulin is titrated by a computer algorithm,” study investigator Martin Tauschmann, MD, explained in an interview after the press briefing.
The prototype system consists of a modified insulin pump (Medtronic 640G) and a continuous glucose sensor (Enlite 3) that are linked by the proprietary “Cambridge control” algorithm via an Android phone. The latter calculates the optimum insulin dose, which is then relayed to the insulin pump every 10 minutes to determine how many insulin units are needed.
“The algorithm is based on mathematical modeling that is trying to predict what the glucose levels will be in the future and trying to work out the optimum insulin dose to bring the predicted glucose levels down,” noted Dr. Tauschmann, who is a pediatrician at Cambridge University (England).
It’s not a fully closed-loop system, he added, it’s a hybrid, so users still need to calculate their carbohydrate intake around mealtimes and input that into the algorithm and use bolus insulin.
“A problem with using currently available insulin formulations is that you are always behind, because we are delivering insulin in the subcutaneous tissue and it just takes some time for the insulin to be absorbed, and, in the meantime, the blood sugar levels go up,” Dr. Tauschmann observed. Studies with fully closed–loop systems, so far, have shown glucose peaking after meals. Perhaps when faster-acting insulins are tested in this setting it could work, he suggested, but perhaps simplifying how the users announce their meals is a future development for the hybrid systems.
Closed-loop insulin delivery is not a new concept. There is already one system available in the United States produced by Medtronic (670G), which was approved by the Food and Drug Administration in September 2016. However, there are no systems available in Europe and there are limited trial data on their use in an outpatient setting.
The aim of the current study, which was an open-label, multicenter, multinational, parallel-group, randomized, controlled trial, was to compare closed-loop basal insulin delivery and sensor augmented insulin pump therapy in helping a mixed adult and pediatric population of patients T1DM achieve good glucose control.
In all, 86 adults, adolescents, and children (age 6 years or older) were randomized: 46 to the closed-loop system and 40 to the control arm of sensor-augmented insulin pump therapy. The mean age of participants was 22 years in the closed-loop group and 21 years in the sensor group, with a respective 24% and 30% aged 6-12 years, 24% and 20% aged 13-21 years, 39% and 35% aged 22-40 years, and 13% and 15% aged 41 years or older. The mean duration of diabetes was 13 and 10 years, in each group, respectively.
The study data “provide more evidence that closed-loop insulin delivery, compared with standard pump and sensor, really improves HbA1c, time spent in range, and mean glucose, and it also reduces hypoglycemia,” Dr. Tauschmann said.
“We didn’t have any real safety issues,” noted Dr. Hovorka, who is professor and director of research in the department of pediatrics at the University of Cambridge. There was one episode of diabetic ketoacidosis caused by infusion set failure in the closed-loop group; 16 other adverse events were noted (13 in the closed-loop group, three in the control group) that were not related to treatment.
“We have a number of studies in the pipeline,” Dr. Hovorka said. “Two exciting studies are in development. In one we are recruiting 70 subjects with newly diagnosed type 1 diabetes mellitus who will be treated with a closed-loop system. There is also a study in children aged between 1 and 7 years that is projected to start next year.”
Work is also underway to create a platform that will work with all insulin pumps and create a commercial product.
The study was funded by the Juvenile Diabetes Research Foundation with additional support from the National Institute for Health Research (England) and the Wellcome Trust. Dr. Tauschmann reported receiving speaker honoraria from Medtronic and Novo Nordisk. Dr. Hovorka reported receiving speaker honoraria from Eli Lilly and Novo Nordisk, serving on an advisory panel for Eli Lilly, receiving license fees from B. Braun Medical and Medtronic, and having patents and patent applications.
SOURCES: Tauschmann M et al. EASD 2018, Oral Presentation 19.
BERLIN – Adults, adolescents, and children with type 1 diabetes mellitus (T1DM) achieved better glycemic control and spent less time in a hypoglycemic state with an investigational closed-loop basal insulin delivery system than with a sensor-augmented insulin pump.
The primary trial endpoint of the proportion of time spent in a target glucose range of 3.9-10 mmol/L at 12 weeks was achieved by 65% of closed-loop users versus 54% of sensor-augmented insulin-pump users (P less than .0001).
In addition, fewer patients had periods of blood glucose less than 3.9 mmol/L at 12 weeks, potentially reducing their risk for hypoglycemic episodes (2.6% vs. 3.9%, P = .0130). The percentages of patients with blood glucose concentrations higher than the target range were also significantly reduced with the closed-loop system.
Glycated hemoglobin (HbA1c) improved in both groups, from a baseline of 8% to 7.4% at 12 weeks in the closed-loop users and from 7.8% to 7.7% in the sensor-augmented insulin-pump users (mean difference –0.036%, P less than .0001). Mean glucose levels also significantly improved, with a mean between-group difference of –0.45 mmol/L (P less than .0001).
“Most of the improvements are overnight,” with a striking difference between the control and closed-loop groups of time in range, said senior study investigator Roman Hovorka, PhD, during a press briefing at the annual meeting of the European Association for the Study of Diabetes.
“Usually what people need to do is titrate insulin based on blood sugar tests, but in our system those tests are done by a monitoring system and the insulin is titrated by a computer algorithm,” study investigator Martin Tauschmann, MD, explained in an interview after the press briefing.
The prototype system consists of a modified insulin pump (Medtronic 640G) and a continuous glucose sensor (Enlite 3) that are linked by the proprietary “Cambridge control” algorithm via an Android phone. The latter calculates the optimum insulin dose, which is then relayed to the insulin pump every 10 minutes to determine how many insulin units are needed.
“The algorithm is based on mathematical modeling that is trying to predict what the glucose levels will be in the future and trying to work out the optimum insulin dose to bring the predicted glucose levels down,” noted Dr. Tauschmann, who is a pediatrician at Cambridge University (England).
It’s not a fully closed-loop system, he added, it’s a hybrid, so users still need to calculate their carbohydrate intake around mealtimes and input that into the algorithm and use bolus insulin.
“A problem with using currently available insulin formulations is that you are always behind, because we are delivering insulin in the subcutaneous tissue and it just takes some time for the insulin to be absorbed, and, in the meantime, the blood sugar levels go up,” Dr. Tauschmann observed. Studies with fully closed–loop systems, so far, have shown glucose peaking after meals. Perhaps when faster-acting insulins are tested in this setting it could work, he suggested, but perhaps simplifying how the users announce their meals is a future development for the hybrid systems.
Closed-loop insulin delivery is not a new concept. There is already one system available in the United States produced by Medtronic (670G), which was approved by the Food and Drug Administration in September 2016. However, there are no systems available in Europe and there are limited trial data on their use in an outpatient setting.
The aim of the current study, which was an open-label, multicenter, multinational, parallel-group, randomized, controlled trial, was to compare closed-loop basal insulin delivery and sensor augmented insulin pump therapy in helping a mixed adult and pediatric population of patients T1DM achieve good glucose control.
In all, 86 adults, adolescents, and children (age 6 years or older) were randomized: 46 to the closed-loop system and 40 to the control arm of sensor-augmented insulin pump therapy. The mean age of participants was 22 years in the closed-loop group and 21 years in the sensor group, with a respective 24% and 30% aged 6-12 years, 24% and 20% aged 13-21 years, 39% and 35% aged 22-40 years, and 13% and 15% aged 41 years or older. The mean duration of diabetes was 13 and 10 years, in each group, respectively.
The study data “provide more evidence that closed-loop insulin delivery, compared with standard pump and sensor, really improves HbA1c, time spent in range, and mean glucose, and it also reduces hypoglycemia,” Dr. Tauschmann said.
“We didn’t have any real safety issues,” noted Dr. Hovorka, who is professor and director of research in the department of pediatrics at the University of Cambridge. There was one episode of diabetic ketoacidosis caused by infusion set failure in the closed-loop group; 16 other adverse events were noted (13 in the closed-loop group, three in the control group) that were not related to treatment.
“We have a number of studies in the pipeline,” Dr. Hovorka said. “Two exciting studies are in development. In one we are recruiting 70 subjects with newly diagnosed type 1 diabetes mellitus who will be treated with a closed-loop system. There is also a study in children aged between 1 and 7 years that is projected to start next year.”
Work is also underway to create a platform that will work with all insulin pumps and create a commercial product.
The study was funded by the Juvenile Diabetes Research Foundation with additional support from the National Institute for Health Research (England) and the Wellcome Trust. Dr. Tauschmann reported receiving speaker honoraria from Medtronic and Novo Nordisk. Dr. Hovorka reported receiving speaker honoraria from Eli Lilly and Novo Nordisk, serving on an advisory panel for Eli Lilly, receiving license fees from B. Braun Medical and Medtronic, and having patents and patent applications.
SOURCES: Tauschmann M et al. EASD 2018, Oral Presentation 19.
REPORTING FROM EASD 2018
Key clinical point: Improved glycemic control and reduced risk of hypoglycemia was seen across a wide age range.
Major finding: Blood glucose was within the target range of 3.9-10.0 mmol/L at 12 weeks (P less than .0001) in 65% of closed-loop versus 54% of sensor-augmented insulin-pump users.
Study details: An open-label, multicenter, parallel-group, randomized, controlled trial comparing closed-loop basal insulin delivery and sensor-augmented insulin pump therapy in 86 children (age 6 years or older) and adults with suboptimally controlled T1DM.
Disclosures: The study was funded by the Juvenile Diabetes Research Foundation with additional support from the National Institute for Health Research (England) and the Wellcome Trust. Dr. Tauschmann reported receiving speaker honoraria from Medtronic and Novo Nordisk. Dr. Hovorka reported receiving speaker honoraria from Eli Lilly and Novo Nordisk, serving on an advisory panel for Eli Lilly, receiving license fees from B. Braun Medical and Medtronic, and having patents and patent applications.
Sources: Tauschmann M et al. EASD 2018, Oral Presentation 19.
U.S. death rates from chronic liver disease continue to rise
SAN FRANCISCO –
“I believe it’s all related to a big increase in obesity and type 2 diabetes in this country,” lead study author Zobair M. Younossi, MD, MPH, said in an interview in advance of the annual meeting of the American Association for the Study of Liver Diseases. “Those two risk factors drive NAFLD and its progressive type, nonalcoholic steatohepatitis (NASH). That accounts for at least part of the increase in mortality related to liver disease.”
In an effort to evaluate recent mortality trends in chronic liver disease in the United States, Dr. Younossi and his colleagues drew from National Vital Statistics Data during 2007-2016. They used ICD-10 codes to select mortality data for alcoholic liver disease, chronic hepatitis B and C, iron overload, NAFLD, cirrhosis, and hepatocellular carcinoma. NAFLD cases were defined as those having an ICD-10 code for NAFLD/NASH or an ICD-10 code for “cirrhosis of unknown etiology.” Next, the researchers adjusted age-standardized death rates to the 2000 U.S. Census population and used logistic regression and propensity scores to estimate predictors of chronic liver disease-related deaths.
Dr. Younossi, who chairs the department of medicine at Inova Fairfax Medical Campus, in Falls Church, Va., and his colleagues reported findings from 838,809 chronic liver disease–related deaths during the study period. They found that the age-standardized death rate for chronic liver disease increased from 21.9/100,000 population in 2007 to 24.9/100,000 population in 2016, which translated into an annual percentage change of 1.3% for males and 2.5% for females. Chronic liver disease–related deaths increased with age and were highest among those aged 55-64 years, followed by those aged 65-74 years – an average annual percentage change of 3.4% and 3.1% in each group.
Among chronic liver disease–related deaths, the most common diagnostic etiology was NAFLD (34.7%), followed by alcoholic liver disease (28.8%) and chronic hepatitis C (21.1%). Between 2007 and 2016, death rates increased from 7.6 to 9.0 per 100,000 population for NAFLD (an average annual percentage change of 2.1%) and from 6.1 to 7.9 per 100,000 population for alcoholic liver disease (an average annual percentage change of 3.1%). “What surprised me was that, despite highly effective treatment for HCV, we still have a burden of hepatitis C in this country,” Dr. Younossi said. “It’s still the most common cause of liver disease in the U.S. But it seems like hepatitis C–related liver disease is being replaced quickly by liver disease from nonalcoholic steatohepatitis. This transition between hepatitis C as the most important cause of liver disease and liver mortality to NASH or obesity-related NASH is becoming more rapid than I expected.”
On multivariate analysis, three factors were independently associated with an increased risk of death in NAFLD: the presence of type 2 diabetes (odds ratio, 1.78), cardiovascular disease (OR, 1.07), and renal failure (OR, 1.08).
“One important message from this study is that NASH is very common in the U.S. population,” said Dr. Younossi, who is also a professor of medicine at Virginia Commonwealth University, Richmond. “These patients are underrecognized and underdiagnosed because they are asymptomatic. The second message is that there is a subtype of patients with fatty liver disease – even a subtype of NASH – that can progress to cirrhosis and its complications. We have to pay attention to this silent disease to identify patients who are at risk for progressive liver disease and try to address some of the risk issues, such as tight control of diabetes, obesity, and control of hypertension and hyperlipidemia. Short of that, right now we have very few medical treatments such as vitamin E and pioglitazone recommended for a very selected group. In contrast, there are plenty of new medications that are being developed. The first step in tackling this disease is to identify who the patients are with fatty liver disease who are at risk for bad outcomes and make sure they’re linked to care by a knowledgeable caregiver [who] understands the importance of NASH.”
Dr. Younossi acknowledged certain limitations of the study, including the fact that liver disease diagnoses were based on ICD-10 coding. He disclosed that he is a consultant for Gilead, Intercept, Novo Nordisk, BMS, AbbVie, Viking, Term Quest Diagnostics, Echosens,and Shionogi. He has also received grant/research support from Gilead, Intercept, and BMS.
Source: Hepatol. 2018;68[S1], Abstract 763.
SAN FRANCISCO –
“I believe it’s all related to a big increase in obesity and type 2 diabetes in this country,” lead study author Zobair M. Younossi, MD, MPH, said in an interview in advance of the annual meeting of the American Association for the Study of Liver Diseases. “Those two risk factors drive NAFLD and its progressive type, nonalcoholic steatohepatitis (NASH). That accounts for at least part of the increase in mortality related to liver disease.”
In an effort to evaluate recent mortality trends in chronic liver disease in the United States, Dr. Younossi and his colleagues drew from National Vital Statistics Data during 2007-2016. They used ICD-10 codes to select mortality data for alcoholic liver disease, chronic hepatitis B and C, iron overload, NAFLD, cirrhosis, and hepatocellular carcinoma. NAFLD cases were defined as those having an ICD-10 code for NAFLD/NASH or an ICD-10 code for “cirrhosis of unknown etiology.” Next, the researchers adjusted age-standardized death rates to the 2000 U.S. Census population and used logistic regression and propensity scores to estimate predictors of chronic liver disease-related deaths.
Dr. Younossi, who chairs the department of medicine at Inova Fairfax Medical Campus, in Falls Church, Va., and his colleagues reported findings from 838,809 chronic liver disease–related deaths during the study period. They found that the age-standardized death rate for chronic liver disease increased from 21.9/100,000 population in 2007 to 24.9/100,000 population in 2016, which translated into an annual percentage change of 1.3% for males and 2.5% for females. Chronic liver disease–related deaths increased with age and were highest among those aged 55-64 years, followed by those aged 65-74 years – an average annual percentage change of 3.4% and 3.1% in each group.
Among chronic liver disease–related deaths, the most common diagnostic etiology was NAFLD (34.7%), followed by alcoholic liver disease (28.8%) and chronic hepatitis C (21.1%). Between 2007 and 2016, death rates increased from 7.6 to 9.0 per 100,000 population for NAFLD (an average annual percentage change of 2.1%) and from 6.1 to 7.9 per 100,000 population for alcoholic liver disease (an average annual percentage change of 3.1%). “What surprised me was that, despite highly effective treatment for HCV, we still have a burden of hepatitis C in this country,” Dr. Younossi said. “It’s still the most common cause of liver disease in the U.S. But it seems like hepatitis C–related liver disease is being replaced quickly by liver disease from nonalcoholic steatohepatitis. This transition between hepatitis C as the most important cause of liver disease and liver mortality to NASH or obesity-related NASH is becoming more rapid than I expected.”
On multivariate analysis, three factors were independently associated with an increased risk of death in NAFLD: the presence of type 2 diabetes (odds ratio, 1.78), cardiovascular disease (OR, 1.07), and renal failure (OR, 1.08).
“One important message from this study is that NASH is very common in the U.S. population,” said Dr. Younossi, who is also a professor of medicine at Virginia Commonwealth University, Richmond. “These patients are underrecognized and underdiagnosed because they are asymptomatic. The second message is that there is a subtype of patients with fatty liver disease – even a subtype of NASH – that can progress to cirrhosis and its complications. We have to pay attention to this silent disease to identify patients who are at risk for progressive liver disease and try to address some of the risk issues, such as tight control of diabetes, obesity, and control of hypertension and hyperlipidemia. Short of that, right now we have very few medical treatments such as vitamin E and pioglitazone recommended for a very selected group. In contrast, there are plenty of new medications that are being developed. The first step in tackling this disease is to identify who the patients are with fatty liver disease who are at risk for bad outcomes and make sure they’re linked to care by a knowledgeable caregiver [who] understands the importance of NASH.”
Dr. Younossi acknowledged certain limitations of the study, including the fact that liver disease diagnoses were based on ICD-10 coding. He disclosed that he is a consultant for Gilead, Intercept, Novo Nordisk, BMS, AbbVie, Viking, Term Quest Diagnostics, Echosens,and Shionogi. He has also received grant/research support from Gilead, Intercept, and BMS.
Source: Hepatol. 2018;68[S1], Abstract 763.
SAN FRANCISCO –
“I believe it’s all related to a big increase in obesity and type 2 diabetes in this country,” lead study author Zobair M. Younossi, MD, MPH, said in an interview in advance of the annual meeting of the American Association for the Study of Liver Diseases. “Those two risk factors drive NAFLD and its progressive type, nonalcoholic steatohepatitis (NASH). That accounts for at least part of the increase in mortality related to liver disease.”
In an effort to evaluate recent mortality trends in chronic liver disease in the United States, Dr. Younossi and his colleagues drew from National Vital Statistics Data during 2007-2016. They used ICD-10 codes to select mortality data for alcoholic liver disease, chronic hepatitis B and C, iron overload, NAFLD, cirrhosis, and hepatocellular carcinoma. NAFLD cases were defined as those having an ICD-10 code for NAFLD/NASH or an ICD-10 code for “cirrhosis of unknown etiology.” Next, the researchers adjusted age-standardized death rates to the 2000 U.S. Census population and used logistic regression and propensity scores to estimate predictors of chronic liver disease-related deaths.
Dr. Younossi, who chairs the department of medicine at Inova Fairfax Medical Campus, in Falls Church, Va., and his colleagues reported findings from 838,809 chronic liver disease–related deaths during the study period. They found that the age-standardized death rate for chronic liver disease increased from 21.9/100,000 population in 2007 to 24.9/100,000 population in 2016, which translated into an annual percentage change of 1.3% for males and 2.5% for females. Chronic liver disease–related deaths increased with age and were highest among those aged 55-64 years, followed by those aged 65-74 years – an average annual percentage change of 3.4% and 3.1% in each group.
Among chronic liver disease–related deaths, the most common diagnostic etiology was NAFLD (34.7%), followed by alcoholic liver disease (28.8%) and chronic hepatitis C (21.1%). Between 2007 and 2016, death rates increased from 7.6 to 9.0 per 100,000 population for NAFLD (an average annual percentage change of 2.1%) and from 6.1 to 7.9 per 100,000 population for alcoholic liver disease (an average annual percentage change of 3.1%). “What surprised me was that, despite highly effective treatment for HCV, we still have a burden of hepatitis C in this country,” Dr. Younossi said. “It’s still the most common cause of liver disease in the U.S. But it seems like hepatitis C–related liver disease is being replaced quickly by liver disease from nonalcoholic steatohepatitis. This transition between hepatitis C as the most important cause of liver disease and liver mortality to NASH or obesity-related NASH is becoming more rapid than I expected.”
On multivariate analysis, three factors were independently associated with an increased risk of death in NAFLD: the presence of type 2 diabetes (odds ratio, 1.78), cardiovascular disease (OR, 1.07), and renal failure (OR, 1.08).
“One important message from this study is that NASH is very common in the U.S. population,” said Dr. Younossi, who is also a professor of medicine at Virginia Commonwealth University, Richmond. “These patients are underrecognized and underdiagnosed because they are asymptomatic. The second message is that there is a subtype of patients with fatty liver disease – even a subtype of NASH – that can progress to cirrhosis and its complications. We have to pay attention to this silent disease to identify patients who are at risk for progressive liver disease and try to address some of the risk issues, such as tight control of diabetes, obesity, and control of hypertension and hyperlipidemia. Short of that, right now we have very few medical treatments such as vitamin E and pioglitazone recommended for a very selected group. In contrast, there are plenty of new medications that are being developed. The first step in tackling this disease is to identify who the patients are with fatty liver disease who are at risk for bad outcomes and make sure they’re linked to care by a knowledgeable caregiver [who] understands the importance of NASH.”
Dr. Younossi acknowledged certain limitations of the study, including the fact that liver disease diagnoses were based on ICD-10 coding. He disclosed that he is a consultant for Gilead, Intercept, Novo Nordisk, BMS, AbbVie, Viking, Term Quest Diagnostics, Echosens,and Shionogi. He has also received grant/research support from Gilead, Intercept, and BMS.
Source: Hepatol. 2018;68[S1], Abstract 763.
AT THE LIVER MEETING 2018
Key clinical point: Nonalcoholic steatohepatitis is very common in the U.S. population.
Major finding: Between 2007 and 2016, the age-standardized death rate for chronic liver disease increased from 21.9/100,000 population to 24.9/100,000 population.
Study details: An analysis of 838,809 chronic liver disease–related deaths from 2007 to 2016.
Disclosures: Dr. Younossi disclosed that he is a consultant for Gilead, Intercept, Novo Nordisk, Bristol-Myers Squibb, AbbVie, Viking, Term Quest Diagnostics, Echosens, and Shionogi. He has also received grant/research support from Gilead, Intercept, and Bristol-Myers Squibb.
Source: Hepatol. 2018;68[S1], Abstract 763.