User login
Microbleeds After Brain Injury Predict Worse Disability
Traumatic microbleeds (TMBs) may indicate vascular injury and predict worse outcomes after even minor brain injury, according to a study at the National Institute of Neurological Disorders and Stroke.
The study involved 439 adults with head injuries treated in the emergency department. The participants had magnetic resonance imaging (MRI) scans within 48 hours of the injury and again during 4 subsequent visits. They also completed behavioral and outcome questionnaires.
Microbleeds appear as small dark lesions on MRI scans but are usually too small to be seen on computer tomography (CT) scans. Sometimes they appear as dots (punctate), sometimes they are linear. In previous studies, researchers examined TMBs in the acute phase of traumatic brain injury (TBI) and stroke and found linear-appearing TMBs only in patients with TBI, suggesting that at least linear TMBs are consistent with trauma and might be the result of injured vessels. They conjectured that TMBs seen on MRI might be a form of traumatic vascular injury distinct from primary injury to the axons.
In this study, one-third of the patients had TMBs. More than half (58%) of the participants with severe head injury showed microbleeds, as did 27% of patients with mild injuries. In most patients with microbleeds, they appeared as linear streaks or dotted lesions. The study also revealed that the frontal lobes were the region most likely to show microbleeds.
The researchers controlled for variables known to predict poor outcome, such as trauma level and trauma-related injury on CT. Even so, microbleeds significantly predicted worse outcome. Patients with both punctate and linear TMBs were twice as likely to have disability (Glasgow Outcome Scale-Extended ≤6) on follow-up.
One participant’s family donated his brain for further analysis after he died. Imaging with a more powerful MRI scanner and a detailed histologic analysis allowed the researchers to better understand the pathology.
The researchers found that what appeared as a punctate TMB on MRI corresponded to iron-laden macrophages in the perivascular space surrounding a vascular tree that extended over centimeters. That was surprising, the researchers say. They expected to see iron within the parenchyma, but they also found iron inside macrophages outside of the parenchyma between the vessel and neuropil, tracking alongside vessels.
The researchers say that finding signified that the extent of injury was more extensive than indicated on MRI and had consequences to cellular function over a larger area of brain. In fact, they suggest, punctate and linear TMBs may not be distinct entities: The difference in shape may be “an issue of resolution.”
The researchers conclude that TMBs could be biomarkers for vascular injury. They also note that the leakage of blood from damaged blood vessels can trigger an inflammatory response. The damage to vessels, the disruption of normal pathways of blood flow, and the influx of inflammatory cells could result in secondary injury to the brain tissue due to ischemia.
Thus, TMBs may also be useful biomarkers for identifying which patients are candidates for treatments that reduce ischemic damage or improve microvascular cerebral blood flow.
Traumatic microbleeds (TMBs) may indicate vascular injury and predict worse outcomes after even minor brain injury, according to a study at the National Institute of Neurological Disorders and Stroke.
The study involved 439 adults with head injuries treated in the emergency department. The participants had magnetic resonance imaging (MRI) scans within 48 hours of the injury and again during 4 subsequent visits. They also completed behavioral and outcome questionnaires.
Microbleeds appear as small dark lesions on MRI scans but are usually too small to be seen on computer tomography (CT) scans. Sometimes they appear as dots (punctate), sometimes they are linear. In previous studies, researchers examined TMBs in the acute phase of traumatic brain injury (TBI) and stroke and found linear-appearing TMBs only in patients with TBI, suggesting that at least linear TMBs are consistent with trauma and might be the result of injured vessels. They conjectured that TMBs seen on MRI might be a form of traumatic vascular injury distinct from primary injury to the axons.
In this study, one-third of the patients had TMBs. More than half (58%) of the participants with severe head injury showed microbleeds, as did 27% of patients with mild injuries. In most patients with microbleeds, they appeared as linear streaks or dotted lesions. The study also revealed that the frontal lobes were the region most likely to show microbleeds.
The researchers controlled for variables known to predict poor outcome, such as trauma level and trauma-related injury on CT. Even so, microbleeds significantly predicted worse outcome. Patients with both punctate and linear TMBs were twice as likely to have disability (Glasgow Outcome Scale-Extended ≤6) on follow-up.
One participant’s family donated his brain for further analysis after he died. Imaging with a more powerful MRI scanner and a detailed histologic analysis allowed the researchers to better understand the pathology.
The researchers found that what appeared as a punctate TMB on MRI corresponded to iron-laden macrophages in the perivascular space surrounding a vascular tree that extended over centimeters. That was surprising, the researchers say. They expected to see iron within the parenchyma, but they also found iron inside macrophages outside of the parenchyma between the vessel and neuropil, tracking alongside vessels.
The researchers say that finding signified that the extent of injury was more extensive than indicated on MRI and had consequences to cellular function over a larger area of brain. In fact, they suggest, punctate and linear TMBs may not be distinct entities: The difference in shape may be “an issue of resolution.”
The researchers conclude that TMBs could be biomarkers for vascular injury. They also note that the leakage of blood from damaged blood vessels can trigger an inflammatory response. The damage to vessels, the disruption of normal pathways of blood flow, and the influx of inflammatory cells could result in secondary injury to the brain tissue due to ischemia.
Thus, TMBs may also be useful biomarkers for identifying which patients are candidates for treatments that reduce ischemic damage or improve microvascular cerebral blood flow.
Traumatic microbleeds (TMBs) may indicate vascular injury and predict worse outcomes after even minor brain injury, according to a study at the National Institute of Neurological Disorders and Stroke.
The study involved 439 adults with head injuries treated in the emergency department. The participants had magnetic resonance imaging (MRI) scans within 48 hours of the injury and again during 4 subsequent visits. They also completed behavioral and outcome questionnaires.
Microbleeds appear as small dark lesions on MRI scans but are usually too small to be seen on computer tomography (CT) scans. Sometimes they appear as dots (punctate), sometimes they are linear. In previous studies, researchers examined TMBs in the acute phase of traumatic brain injury (TBI) and stroke and found linear-appearing TMBs only in patients with TBI, suggesting that at least linear TMBs are consistent with trauma and might be the result of injured vessels. They conjectured that TMBs seen on MRI might be a form of traumatic vascular injury distinct from primary injury to the axons.
In this study, one-third of the patients had TMBs. More than half (58%) of the participants with severe head injury showed microbleeds, as did 27% of patients with mild injuries. In most patients with microbleeds, they appeared as linear streaks or dotted lesions. The study also revealed that the frontal lobes were the region most likely to show microbleeds.
The researchers controlled for variables known to predict poor outcome, such as trauma level and trauma-related injury on CT. Even so, microbleeds significantly predicted worse outcome. Patients with both punctate and linear TMBs were twice as likely to have disability (Glasgow Outcome Scale-Extended ≤6) on follow-up.
One participant’s family donated his brain for further analysis after he died. Imaging with a more powerful MRI scanner and a detailed histologic analysis allowed the researchers to better understand the pathology.
The researchers found that what appeared as a punctate TMB on MRI corresponded to iron-laden macrophages in the perivascular space surrounding a vascular tree that extended over centimeters. That was surprising, the researchers say. They expected to see iron within the parenchyma, but they also found iron inside macrophages outside of the parenchyma between the vessel and neuropil, tracking alongside vessels.
The researchers say that finding signified that the extent of injury was more extensive than indicated on MRI and had consequences to cellular function over a larger area of brain. In fact, they suggest, punctate and linear TMBs may not be distinct entities: The difference in shape may be “an issue of resolution.”
The researchers conclude that TMBs could be biomarkers for vascular injury. They also note that the leakage of blood from damaged blood vessels can trigger an inflammatory response. The damage to vessels, the disruption of normal pathways of blood flow, and the influx of inflammatory cells could result in secondary injury to the brain tissue due to ischemia.
Thus, TMBs may also be useful biomarkers for identifying which patients are candidates for treatments that reduce ischemic damage or improve microvascular cerebral blood flow.
Soccer pros may face increased risk of death from neurodegenerative disease
, findings from a retrospective epidemiologic analysis suggest.
Former professional soccer players included in the analysis also received more dementia-related medication prescriptions than did controls, Daniel F. Mackay, PhD, of the Institute of Health and Wellbeing at the University of Glasgow (Scotland) and his colleagues reported online Oct. 21 in The New England Journal of Medicine.
Overall mortality during a median follow-up of 18 years from study entry at the age of 40 years was 15.4% among 7,676 former players, and 16.5% among 23,028 controls matched based on age, sex, and degree of social deprivation. All-cause mortality was lower among players versus controls before age 70 years, and was higher thereafter, and the mortality rates associated with ischemic heart disease and lung cancer were lower among the players (hazard ratios, 0.80 and 0.53, respectively), the investigators found.
Mortality rates from stroke or cerebrovascular disease were similar in the players and controls (HR, 0.88), they noted.
However, mortality with neurodegenerative disease listed as the primary cause was 1.7% in players versus 0.5% in controls (HR adjusted for competing risks of death, 3.45), they said. The estimated risk of death with neurodegenerative disease was highest among those with Alzheimer’s disease and lowest for those with Parkinson’s disease (HRs, 5.07 and 2.15, respectively).
Dementia-related medications also were prescribed more frequently for players vs. controls (odds ratio, 4.90).
A subgroup analysis showed no significant difference between goalkeepers and outfielders with respect to mortality with neurodegenerative disease listed as a factor (HR, 0.73), but dementia-related medications were prescribed less often to goalkeepers (OR, 0.41).
Concerns about the risk of neurodegenerative diseases among participants in contact sports have been raised, in part because of the recognition of pathologic changes of chronic traumatic encephalopathy among participants across a range of such sports, the investigators explained, noting that data regarding the risk of neurodegenerative disease among former professional soccer players are limited.
The findings of the current study, in terms of lower all-cause mortality up to the age of 70 years, are similar to those in previous studies involving elite athletes across a range of sports, and “may reflect higher levels of physical activity and lower levels of obesity and smoking in elite athletes than in the general population,” they noted.
“In contrast, mortality from neurodegenerative disease was higher among former soccer players, a finding consistent with studies involving former players in the U.S. National Football League,” they added, concluding that the findings, which “may be valuable to inform the management of risks in the sport,” require confirmation in prospective studies.
This study was supported by the Football Association and Professional Footballers’ Association, and by an NHS Research Scotland Career Researcher Fellowship. Dr. Mackay reported having no relevant financial disclosures.
SOURCE: Mackay D et al. N Engl J Med. 2019 Oct 21. doi: 10.1056/NEJMoa1908483.
The good news from the study by Mackay et al. is that mortality from common nonneurologic diseases is lower among former elite soccer players vs. controls; the bad news is that mortality from neurodegenerative diseases is higher and prescriptions for dementia-related medications more common, Robert A. Stern, PhD, wrote in an editorial.
The findings add to existing evidence that repetitive head impact in contact sports may increase the risk of neurodegenerative disease and dementia, but “should not engender undue fear and panic among soccer players, parents, and coaches,” as the findings cannot be generalized to recreational, amateur, or collegiate-level soccer, Dr. Stern said.
The findings should, however, lead to research and awareness of potential consequences of heading the ball in amateur soccer, he argued, noting that “perhaps ... there is already adequate evidence that repeated blows to the brain from heading in professional soccer is an occupational risk that needs to be addressed.”
Dr. Stern is with the Boston University Chronic Traumatic Encephalopathy Center, Boston University. He disclosed financial relationships (receipt of grants, personal fees, and/or other relationships outside the submitted work) with the National Institute of Neurological Disorders and Stroke, the National Institute on Aging, the Concussion Legacy Foundation, Biogen, Eli Lilly, Psychological Assessment Resources, and King Devick Technologies.
The good news from the study by Mackay et al. is that mortality from common nonneurologic diseases is lower among former elite soccer players vs. controls; the bad news is that mortality from neurodegenerative diseases is higher and prescriptions for dementia-related medications more common, Robert A. Stern, PhD, wrote in an editorial.
The findings add to existing evidence that repetitive head impact in contact sports may increase the risk of neurodegenerative disease and dementia, but “should not engender undue fear and panic among soccer players, parents, and coaches,” as the findings cannot be generalized to recreational, amateur, or collegiate-level soccer, Dr. Stern said.
The findings should, however, lead to research and awareness of potential consequences of heading the ball in amateur soccer, he argued, noting that “perhaps ... there is already adequate evidence that repeated blows to the brain from heading in professional soccer is an occupational risk that needs to be addressed.”
Dr. Stern is with the Boston University Chronic Traumatic Encephalopathy Center, Boston University. He disclosed financial relationships (receipt of grants, personal fees, and/or other relationships outside the submitted work) with the National Institute of Neurological Disorders and Stroke, the National Institute on Aging, the Concussion Legacy Foundation, Biogen, Eli Lilly, Psychological Assessment Resources, and King Devick Technologies.
The good news from the study by Mackay et al. is that mortality from common nonneurologic diseases is lower among former elite soccer players vs. controls; the bad news is that mortality from neurodegenerative diseases is higher and prescriptions for dementia-related medications more common, Robert A. Stern, PhD, wrote in an editorial.
The findings add to existing evidence that repetitive head impact in contact sports may increase the risk of neurodegenerative disease and dementia, but “should not engender undue fear and panic among soccer players, parents, and coaches,” as the findings cannot be generalized to recreational, amateur, or collegiate-level soccer, Dr. Stern said.
The findings should, however, lead to research and awareness of potential consequences of heading the ball in amateur soccer, he argued, noting that “perhaps ... there is already adequate evidence that repeated blows to the brain from heading in professional soccer is an occupational risk that needs to be addressed.”
Dr. Stern is with the Boston University Chronic Traumatic Encephalopathy Center, Boston University. He disclosed financial relationships (receipt of grants, personal fees, and/or other relationships outside the submitted work) with the National Institute of Neurological Disorders and Stroke, the National Institute on Aging, the Concussion Legacy Foundation, Biogen, Eli Lilly, Psychological Assessment Resources, and King Devick Technologies.
, findings from a retrospective epidemiologic analysis suggest.
Former professional soccer players included in the analysis also received more dementia-related medication prescriptions than did controls, Daniel F. Mackay, PhD, of the Institute of Health and Wellbeing at the University of Glasgow (Scotland) and his colleagues reported online Oct. 21 in The New England Journal of Medicine.
Overall mortality during a median follow-up of 18 years from study entry at the age of 40 years was 15.4% among 7,676 former players, and 16.5% among 23,028 controls matched based on age, sex, and degree of social deprivation. All-cause mortality was lower among players versus controls before age 70 years, and was higher thereafter, and the mortality rates associated with ischemic heart disease and lung cancer were lower among the players (hazard ratios, 0.80 and 0.53, respectively), the investigators found.
Mortality rates from stroke or cerebrovascular disease were similar in the players and controls (HR, 0.88), they noted.
However, mortality with neurodegenerative disease listed as the primary cause was 1.7% in players versus 0.5% in controls (HR adjusted for competing risks of death, 3.45), they said. The estimated risk of death with neurodegenerative disease was highest among those with Alzheimer’s disease and lowest for those with Parkinson’s disease (HRs, 5.07 and 2.15, respectively).
Dementia-related medications also were prescribed more frequently for players vs. controls (odds ratio, 4.90).
A subgroup analysis showed no significant difference between goalkeepers and outfielders with respect to mortality with neurodegenerative disease listed as a factor (HR, 0.73), but dementia-related medications were prescribed less often to goalkeepers (OR, 0.41).
Concerns about the risk of neurodegenerative diseases among participants in contact sports have been raised, in part because of the recognition of pathologic changes of chronic traumatic encephalopathy among participants across a range of such sports, the investigators explained, noting that data regarding the risk of neurodegenerative disease among former professional soccer players are limited.
The findings of the current study, in terms of lower all-cause mortality up to the age of 70 years, are similar to those in previous studies involving elite athletes across a range of sports, and “may reflect higher levels of physical activity and lower levels of obesity and smoking in elite athletes than in the general population,” they noted.
“In contrast, mortality from neurodegenerative disease was higher among former soccer players, a finding consistent with studies involving former players in the U.S. National Football League,” they added, concluding that the findings, which “may be valuable to inform the management of risks in the sport,” require confirmation in prospective studies.
This study was supported by the Football Association and Professional Footballers’ Association, and by an NHS Research Scotland Career Researcher Fellowship. Dr. Mackay reported having no relevant financial disclosures.
SOURCE: Mackay D et al. N Engl J Med. 2019 Oct 21. doi: 10.1056/NEJMoa1908483.
, findings from a retrospective epidemiologic analysis suggest.
Former professional soccer players included in the analysis also received more dementia-related medication prescriptions than did controls, Daniel F. Mackay, PhD, of the Institute of Health and Wellbeing at the University of Glasgow (Scotland) and his colleagues reported online Oct. 21 in The New England Journal of Medicine.
Overall mortality during a median follow-up of 18 years from study entry at the age of 40 years was 15.4% among 7,676 former players, and 16.5% among 23,028 controls matched based on age, sex, and degree of social deprivation. All-cause mortality was lower among players versus controls before age 70 years, and was higher thereafter, and the mortality rates associated with ischemic heart disease and lung cancer were lower among the players (hazard ratios, 0.80 and 0.53, respectively), the investigators found.
Mortality rates from stroke or cerebrovascular disease were similar in the players and controls (HR, 0.88), they noted.
However, mortality with neurodegenerative disease listed as the primary cause was 1.7% in players versus 0.5% in controls (HR adjusted for competing risks of death, 3.45), they said. The estimated risk of death with neurodegenerative disease was highest among those with Alzheimer’s disease and lowest for those with Parkinson’s disease (HRs, 5.07 and 2.15, respectively).
Dementia-related medications also were prescribed more frequently for players vs. controls (odds ratio, 4.90).
A subgroup analysis showed no significant difference between goalkeepers and outfielders with respect to mortality with neurodegenerative disease listed as a factor (HR, 0.73), but dementia-related medications were prescribed less often to goalkeepers (OR, 0.41).
Concerns about the risk of neurodegenerative diseases among participants in contact sports have been raised, in part because of the recognition of pathologic changes of chronic traumatic encephalopathy among participants across a range of such sports, the investigators explained, noting that data regarding the risk of neurodegenerative disease among former professional soccer players are limited.
The findings of the current study, in terms of lower all-cause mortality up to the age of 70 years, are similar to those in previous studies involving elite athletes across a range of sports, and “may reflect higher levels of physical activity and lower levels of obesity and smoking in elite athletes than in the general population,” they noted.
“In contrast, mortality from neurodegenerative disease was higher among former soccer players, a finding consistent with studies involving former players in the U.S. National Football League,” they added, concluding that the findings, which “may be valuable to inform the management of risks in the sport,” require confirmation in prospective studies.
This study was supported by the Football Association and Professional Footballers’ Association, and by an NHS Research Scotland Career Researcher Fellowship. Dr. Mackay reported having no relevant financial disclosures.
SOURCE: Mackay D et al. N Engl J Med. 2019 Oct 21. doi: 10.1056/NEJMoa1908483.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Concussion effects may linger on MRI 1 year after athletes resume play
Among athletes with concussion, the effects of the injury on brain physiology may persist when they return to play and 1 year later.
MRI measures from 24 athletes with concussion significantly differed from those of controls at various time points and changed over time, according to a study published in Neurology. “Different aspects of brain physiology have different patterns of long-term recovery,” the researchers wrote.
While guidelines for safe return to play mainly rely on the resolution of symptoms, “the findings in this study indicate that more research is needed ... to better understand optimal recovery time from a biological standpoint,” wrote first author Nathan W. Churchill, PhD, a researcher at St. Michael’s Hospital in Toronto, and colleagues.
The study provides “evidence of incomplete or ongoing recovery” when athletes return to play, which could entail “a potential risk for long-term sequelae, given the evidence of worse outcomes if a second concussion occurs before recovery is complete,” according to the investigators. In addition,
To examine whether concussion-related brain changes dissipate by 1 year after athletes receive medical clearance to return to play, Dr. Churchill and colleagues analyzed MRI data from 24 college athletes with concussion and 122 control athletes without concussion.
Athletes with concussion were scanned within 1 week of the injury, at return to play a median of 27 days after the concussion, and 1 year after return to play. Control athletes were scanned before the start of the season. Participants’ sports included volleyball, hockey, soccer, football, rugby, basketball, lacrosse, and water polo. The participants had a mean age of about 20 years, and about half were women.
Athletes with concussion had elevated mean diffusivity within 1 week of injury, at return to play, and 1 year later, compared with controls. In athletes with concussion, cerebral blood flow was elevated soon after concussion, normal at return to play, and decreased 1 year later, relative to controls. Global functional connectivity increased and white matter fractional anisotropy decreased near the time of injury and at return to play, but these measures did not significantly differ from those of controls at 1 year.
The study did not capture MRI changes between return to play and 1 year later. In addition, MRI changes might be influenced by a lack of training before resuming play, as well as by exertion and subconcussive impacts after returning to play, the authors noted.
The Canadian Institutes of Health Research, the Canadian Institute for Military and Veterans Health Research, and Siemens Healthineers Canada supported the study. Siemens makes the MRI equipment used in the study. Dr. Churchill and colleagues had no relevant disclosures.
SOURCE: Churchill NW et al. Neurology. 2019 Oct 16. doi: 10.1212/WNL.0000000000008523.
Among athletes with concussion, the effects of the injury on brain physiology may persist when they return to play and 1 year later.
MRI measures from 24 athletes with concussion significantly differed from those of controls at various time points and changed over time, according to a study published in Neurology. “Different aspects of brain physiology have different patterns of long-term recovery,” the researchers wrote.
While guidelines for safe return to play mainly rely on the resolution of symptoms, “the findings in this study indicate that more research is needed ... to better understand optimal recovery time from a biological standpoint,” wrote first author Nathan W. Churchill, PhD, a researcher at St. Michael’s Hospital in Toronto, and colleagues.
The study provides “evidence of incomplete or ongoing recovery” when athletes return to play, which could entail “a potential risk for long-term sequelae, given the evidence of worse outcomes if a second concussion occurs before recovery is complete,” according to the investigators. In addition,
To examine whether concussion-related brain changes dissipate by 1 year after athletes receive medical clearance to return to play, Dr. Churchill and colleagues analyzed MRI data from 24 college athletes with concussion and 122 control athletes without concussion.
Athletes with concussion were scanned within 1 week of the injury, at return to play a median of 27 days after the concussion, and 1 year after return to play. Control athletes were scanned before the start of the season. Participants’ sports included volleyball, hockey, soccer, football, rugby, basketball, lacrosse, and water polo. The participants had a mean age of about 20 years, and about half were women.
Athletes with concussion had elevated mean diffusivity within 1 week of injury, at return to play, and 1 year later, compared with controls. In athletes with concussion, cerebral blood flow was elevated soon after concussion, normal at return to play, and decreased 1 year later, relative to controls. Global functional connectivity increased and white matter fractional anisotropy decreased near the time of injury and at return to play, but these measures did not significantly differ from those of controls at 1 year.
The study did not capture MRI changes between return to play and 1 year later. In addition, MRI changes might be influenced by a lack of training before resuming play, as well as by exertion and subconcussive impacts after returning to play, the authors noted.
The Canadian Institutes of Health Research, the Canadian Institute for Military and Veterans Health Research, and Siemens Healthineers Canada supported the study. Siemens makes the MRI equipment used in the study. Dr. Churchill and colleagues had no relevant disclosures.
SOURCE: Churchill NW et al. Neurology. 2019 Oct 16. doi: 10.1212/WNL.0000000000008523.
Among athletes with concussion, the effects of the injury on brain physiology may persist when they return to play and 1 year later.
MRI measures from 24 athletes with concussion significantly differed from those of controls at various time points and changed over time, according to a study published in Neurology. “Different aspects of brain physiology have different patterns of long-term recovery,” the researchers wrote.
While guidelines for safe return to play mainly rely on the resolution of symptoms, “the findings in this study indicate that more research is needed ... to better understand optimal recovery time from a biological standpoint,” wrote first author Nathan W. Churchill, PhD, a researcher at St. Michael’s Hospital in Toronto, and colleagues.
The study provides “evidence of incomplete or ongoing recovery” when athletes return to play, which could entail “a potential risk for long-term sequelae, given the evidence of worse outcomes if a second concussion occurs before recovery is complete,” according to the investigators. In addition,
To examine whether concussion-related brain changes dissipate by 1 year after athletes receive medical clearance to return to play, Dr. Churchill and colleagues analyzed MRI data from 24 college athletes with concussion and 122 control athletes without concussion.
Athletes with concussion were scanned within 1 week of the injury, at return to play a median of 27 days after the concussion, and 1 year after return to play. Control athletes were scanned before the start of the season. Participants’ sports included volleyball, hockey, soccer, football, rugby, basketball, lacrosse, and water polo. The participants had a mean age of about 20 years, and about half were women.
Athletes with concussion had elevated mean diffusivity within 1 week of injury, at return to play, and 1 year later, compared with controls. In athletes with concussion, cerebral blood flow was elevated soon after concussion, normal at return to play, and decreased 1 year later, relative to controls. Global functional connectivity increased and white matter fractional anisotropy decreased near the time of injury and at return to play, but these measures did not significantly differ from those of controls at 1 year.
The study did not capture MRI changes between return to play and 1 year later. In addition, MRI changes might be influenced by a lack of training before resuming play, as well as by exertion and subconcussive impacts after returning to play, the authors noted.
The Canadian Institutes of Health Research, the Canadian Institute for Military and Veterans Health Research, and Siemens Healthineers Canada supported the study. Siemens makes the MRI equipment used in the study. Dr. Churchill and colleagues had no relevant disclosures.
SOURCE: Churchill NW et al. Neurology. 2019 Oct 16. doi: 10.1212/WNL.0000000000008523.
FROM NEUROLOGY
Key clinical point: Among athletes with concussion, the effects of the injury on brain physiology may persist when they return to play and 1 year later.
Major finding: Athletes with concussion had elevated mean diffusivity within 1 week of injury, at return to play, and 1 year later, compared with controls. In athletes with concussion, cerebral blood flow was elevated soon after concussion, normal at return to play, and decreased 1 year later. Global functional connectivity increased and white matter fractional anisotropy decreased near the time of injury and at return to play, but these measures did not significantly differ from those of controls at 1 year.
Study details: An observational study of 24 college athletes with concussion.
Disclosures: The study was supported by the Canadian Institutes of Health Research, the Canadian Institute for Military and Veterans Health Research, and Siemens Healthineers Canada. Siemens makes the MRI equipment used in the study. The researchers had no relevant disclosures.
Source: Churchill NW et al. Neurology. 2019 Oct 16. doi: 10.1212/WNL.0000000000008523.
Urine Reveals Biomarker for Potential TBI
Even a mild blast to the brain can cause long-term, life-changing health problems, says Riyi Shi, professor of neuroscience and biomedical engineering at Purdue University in Lafayette, Indiana. However, the effects can be subtle: “The individual appears to be fine, and it’s difficult to tell if you just look at a person. But the fact is that these types of hits are multiplied over years and often ignored until someone reaches an age when other factors come into play.”
Treating the incidents sooner can help mitigate later-life issues, such as Parkinson disease (PD). Shi led a study that found checking the urine within 7 days following a blast incident—even a mild one—provides faster diagnosis when brain injury is suspected.
A simple urine analysis reveals elevations in the neurotoxin acrolein, Shi says, which is a biomarker for brain injury. In the study, the researchers evaluated the changes of α-synuclein and tyrosine hydroxylase, hallmarks of PD, and acrolein, a marker of oxidative stress. The researchers say in animal models of PD and traumatic brain injury (TBI), acrolein is “likely a point of pathogenic convergence.”
They found that after a single mild blast TBI, acrolein was elevated for up to a week, systemically in urine, and in whole brain tissue, specifically the substantia nigra and striatum. The elevation was accompanied by heightened α-synuclein oligomerization, dopaminergic dysregulation, and acrolein/α-synuclein interaction in the same brain regions. Taken together, the researchers say, the data suggest that acrolein likely plays a key role in inducing PD following blast TBI.
The presence of the biomarker “alerts us to the injury, creating an opportunity for intervention,” Shi says. “This early detection and subsequent treatment window could offer tremendous benefits for long-term patient neurologic health.”
Even a mild blast to the brain can cause long-term, life-changing health problems, says Riyi Shi, professor of neuroscience and biomedical engineering at Purdue University in Lafayette, Indiana. However, the effects can be subtle: “The individual appears to be fine, and it’s difficult to tell if you just look at a person. But the fact is that these types of hits are multiplied over years and often ignored until someone reaches an age when other factors come into play.”
Treating the incidents sooner can help mitigate later-life issues, such as Parkinson disease (PD). Shi led a study that found checking the urine within 7 days following a blast incident—even a mild one—provides faster diagnosis when brain injury is suspected.
A simple urine analysis reveals elevations in the neurotoxin acrolein, Shi says, which is a biomarker for brain injury. In the study, the researchers evaluated the changes of α-synuclein and tyrosine hydroxylase, hallmarks of PD, and acrolein, a marker of oxidative stress. The researchers say in animal models of PD and traumatic brain injury (TBI), acrolein is “likely a point of pathogenic convergence.”
They found that after a single mild blast TBI, acrolein was elevated for up to a week, systemically in urine, and in whole brain tissue, specifically the substantia nigra and striatum. The elevation was accompanied by heightened α-synuclein oligomerization, dopaminergic dysregulation, and acrolein/α-synuclein interaction in the same brain regions. Taken together, the researchers say, the data suggest that acrolein likely plays a key role in inducing PD following blast TBI.
The presence of the biomarker “alerts us to the injury, creating an opportunity for intervention,” Shi says. “This early detection and subsequent treatment window could offer tremendous benefits for long-term patient neurologic health.”
Even a mild blast to the brain can cause long-term, life-changing health problems, says Riyi Shi, professor of neuroscience and biomedical engineering at Purdue University in Lafayette, Indiana. However, the effects can be subtle: “The individual appears to be fine, and it’s difficult to tell if you just look at a person. But the fact is that these types of hits are multiplied over years and often ignored until someone reaches an age when other factors come into play.”
Treating the incidents sooner can help mitigate later-life issues, such as Parkinson disease (PD). Shi led a study that found checking the urine within 7 days following a blast incident—even a mild one—provides faster diagnosis when brain injury is suspected.
A simple urine analysis reveals elevations in the neurotoxin acrolein, Shi says, which is a biomarker for brain injury. In the study, the researchers evaluated the changes of α-synuclein and tyrosine hydroxylase, hallmarks of PD, and acrolein, a marker of oxidative stress. The researchers say in animal models of PD and traumatic brain injury (TBI), acrolein is “likely a point of pathogenic convergence.”
They found that after a single mild blast TBI, acrolein was elevated for up to a week, systemically in urine, and in whole brain tissue, specifically the substantia nigra and striatum. The elevation was accompanied by heightened α-synuclein oligomerization, dopaminergic dysregulation, and acrolein/α-synuclein interaction in the same brain regions. Taken together, the researchers say, the data suggest that acrolein likely plays a key role in inducing PD following blast TBI.
The presence of the biomarker “alerts us to the injury, creating an opportunity for intervention,” Shi says. “This early detection and subsequent treatment window could offer tremendous benefits for long-term patient neurologic health.”
‘Fast MRI’ may be option in TBI screening for children
“Fast MRI,” which allows scans to be taken quickly without sedation, is a “reasonable alternative” to screen certain younger children for traumatic brain injury, a new study found.
The fast MRI option has “the potential to eliminate ionizing radiation exposure for thousands of children each year,” the study authors wrote in Pediatrics. “The ability to complete imaging in about 6 minutes, without the need for anesthesia or sedation, suggests that fast MRI is appropriate even in acute settings, where patient throughput is a priority.”
Daniel M. Lindberg, MD, of the University of Colorado at Denver, Aurora, and associates wrote that children make between 600,000 and 1.6 million ED visits in the United States each year for evaluation of possible traumatic brain injury (TBI). While the incidence of clinically significant injury from TBI is low, 20%-70% of these children are exposed to potentially dangerous radiation as they undergo CT.
The new study focuses on fast MRI. Unlike traditional MRI, it doesn’t require children to remain motionless – typically with the help of sedation – to be scanned.
The researchers performed fast MRI in 223 children aged younger than 6 years (median age, 12.6 months; interquartile range, 4.7-32.6) who sought emergency care at a level 1 pediatric trauma center from 2015 to 2018. They had all had CT scans performed.
CT identified TBI in 111 (50%) of the subjects, while fast MRI identified it in 103 (sensitivity, 92.8%; 95% confidence interval, 86.3-96.8). Fast MRI missed six participants with isolated skull fractures and two with subarachnoid hemorrhage; CT missed five participants with subdural hematomas, parenchymal contusions, and subarachnoid hemorrhage.
While the researchers hoped for a higher sensitivity level, they wrote that “we feel that the benefit of avoiding radiation exposure outweighs the concern for missed injury.”
In a commentary, Brett Burstein, MDCM, PhD, MPH, and Christine Saint-Martin, MDCM, MSc, of Montreal Children’s Hospital and McGill University Health Center, also in Montreal, wrote that the study is “well conducted.”
However, they noted that “the reported feasibility reflects a highly selected cohort of stable patients in whom fast MRI is already likely to succeed. Feasibility results in a more generalizable population of head-injured children cannot be extrapolated.”
And, they added, “fast MRI was unavailable for 65 of 299 consenting, eligible patients because of lack of overnight staffing. Although not included among the outcome definitions of imaging time, this would be an important ‘feasibility’ consideration in most centers.”
Dr. Burstein and Dr. Saint-Martin wrote that “centers migrating toward this modality for neuroimaging children with head injuries should still use clinical judgment and highly sensitive, validated clinical decision rules when determining the need for any neuroimaging for head-injured children.”
The study was funded by the Colorado Traumatic Brain Injury Trust Fund (MindSource) and the Colorado Clinical and Translational Sciences Institute. The study and commentary authors reported no relevant financial disclosures.
SOURCES: Lindberg DM et al. Pediatrics. 2019 Sep 18. doi: 10.1542/peds.2019-0419; Burstein B, Saint-Martin C. Pediatrics. 2019 Sep 18. doi: 10.1542/peds.2019-2387.
“Fast MRI,” which allows scans to be taken quickly without sedation, is a “reasonable alternative” to screen certain younger children for traumatic brain injury, a new study found.
The fast MRI option has “the potential to eliminate ionizing radiation exposure for thousands of children each year,” the study authors wrote in Pediatrics. “The ability to complete imaging in about 6 minutes, without the need for anesthesia or sedation, suggests that fast MRI is appropriate even in acute settings, where patient throughput is a priority.”
Daniel M. Lindberg, MD, of the University of Colorado at Denver, Aurora, and associates wrote that children make between 600,000 and 1.6 million ED visits in the United States each year for evaluation of possible traumatic brain injury (TBI). While the incidence of clinically significant injury from TBI is low, 20%-70% of these children are exposed to potentially dangerous radiation as they undergo CT.
The new study focuses on fast MRI. Unlike traditional MRI, it doesn’t require children to remain motionless – typically with the help of sedation – to be scanned.
The researchers performed fast MRI in 223 children aged younger than 6 years (median age, 12.6 months; interquartile range, 4.7-32.6) who sought emergency care at a level 1 pediatric trauma center from 2015 to 2018. They had all had CT scans performed.
CT identified TBI in 111 (50%) of the subjects, while fast MRI identified it in 103 (sensitivity, 92.8%; 95% confidence interval, 86.3-96.8). Fast MRI missed six participants with isolated skull fractures and two with subarachnoid hemorrhage; CT missed five participants with subdural hematomas, parenchymal contusions, and subarachnoid hemorrhage.
While the researchers hoped for a higher sensitivity level, they wrote that “we feel that the benefit of avoiding radiation exposure outweighs the concern for missed injury.”
In a commentary, Brett Burstein, MDCM, PhD, MPH, and Christine Saint-Martin, MDCM, MSc, of Montreal Children’s Hospital and McGill University Health Center, also in Montreal, wrote that the study is “well conducted.”
However, they noted that “the reported feasibility reflects a highly selected cohort of stable patients in whom fast MRI is already likely to succeed. Feasibility results in a more generalizable population of head-injured children cannot be extrapolated.”
And, they added, “fast MRI was unavailable for 65 of 299 consenting, eligible patients because of lack of overnight staffing. Although not included among the outcome definitions of imaging time, this would be an important ‘feasibility’ consideration in most centers.”
Dr. Burstein and Dr. Saint-Martin wrote that “centers migrating toward this modality for neuroimaging children with head injuries should still use clinical judgment and highly sensitive, validated clinical decision rules when determining the need for any neuroimaging for head-injured children.”
The study was funded by the Colorado Traumatic Brain Injury Trust Fund (MindSource) and the Colorado Clinical and Translational Sciences Institute. The study and commentary authors reported no relevant financial disclosures.
SOURCES: Lindberg DM et al. Pediatrics. 2019 Sep 18. doi: 10.1542/peds.2019-0419; Burstein B, Saint-Martin C. Pediatrics. 2019 Sep 18. doi: 10.1542/peds.2019-2387.
“Fast MRI,” which allows scans to be taken quickly without sedation, is a “reasonable alternative” to screen certain younger children for traumatic brain injury, a new study found.
The fast MRI option has “the potential to eliminate ionizing radiation exposure for thousands of children each year,” the study authors wrote in Pediatrics. “The ability to complete imaging in about 6 minutes, without the need for anesthesia or sedation, suggests that fast MRI is appropriate even in acute settings, where patient throughput is a priority.”
Daniel M. Lindberg, MD, of the University of Colorado at Denver, Aurora, and associates wrote that children make between 600,000 and 1.6 million ED visits in the United States each year for evaluation of possible traumatic brain injury (TBI). While the incidence of clinically significant injury from TBI is low, 20%-70% of these children are exposed to potentially dangerous radiation as they undergo CT.
The new study focuses on fast MRI. Unlike traditional MRI, it doesn’t require children to remain motionless – typically with the help of sedation – to be scanned.
The researchers performed fast MRI in 223 children aged younger than 6 years (median age, 12.6 months; interquartile range, 4.7-32.6) who sought emergency care at a level 1 pediatric trauma center from 2015 to 2018. They had all had CT scans performed.
CT identified TBI in 111 (50%) of the subjects, while fast MRI identified it in 103 (sensitivity, 92.8%; 95% confidence interval, 86.3-96.8). Fast MRI missed six participants with isolated skull fractures and two with subarachnoid hemorrhage; CT missed five participants with subdural hematomas, parenchymal contusions, and subarachnoid hemorrhage.
While the researchers hoped for a higher sensitivity level, they wrote that “we feel that the benefit of avoiding radiation exposure outweighs the concern for missed injury.”
In a commentary, Brett Burstein, MDCM, PhD, MPH, and Christine Saint-Martin, MDCM, MSc, of Montreal Children’s Hospital and McGill University Health Center, also in Montreal, wrote that the study is “well conducted.”
However, they noted that “the reported feasibility reflects a highly selected cohort of stable patients in whom fast MRI is already likely to succeed. Feasibility results in a more generalizable population of head-injured children cannot be extrapolated.”
And, they added, “fast MRI was unavailable for 65 of 299 consenting, eligible patients because of lack of overnight staffing. Although not included among the outcome definitions of imaging time, this would be an important ‘feasibility’ consideration in most centers.”
Dr. Burstein and Dr. Saint-Martin wrote that “centers migrating toward this modality for neuroimaging children with head injuries should still use clinical judgment and highly sensitive, validated clinical decision rules when determining the need for any neuroimaging for head-injured children.”
The study was funded by the Colorado Traumatic Brain Injury Trust Fund (MindSource) and the Colorado Clinical and Translational Sciences Institute. The study and commentary authors reported no relevant financial disclosures.
SOURCES: Lindberg DM et al. Pediatrics. 2019 Sep 18. doi: 10.1542/peds.2019-0419; Burstein B, Saint-Martin C. Pediatrics. 2019 Sep 18. doi: 10.1542/peds.2019-2387.
FROM PEDIATRICS
Hyperphosphorylated tau visible in TBI survivors decades after brain injury
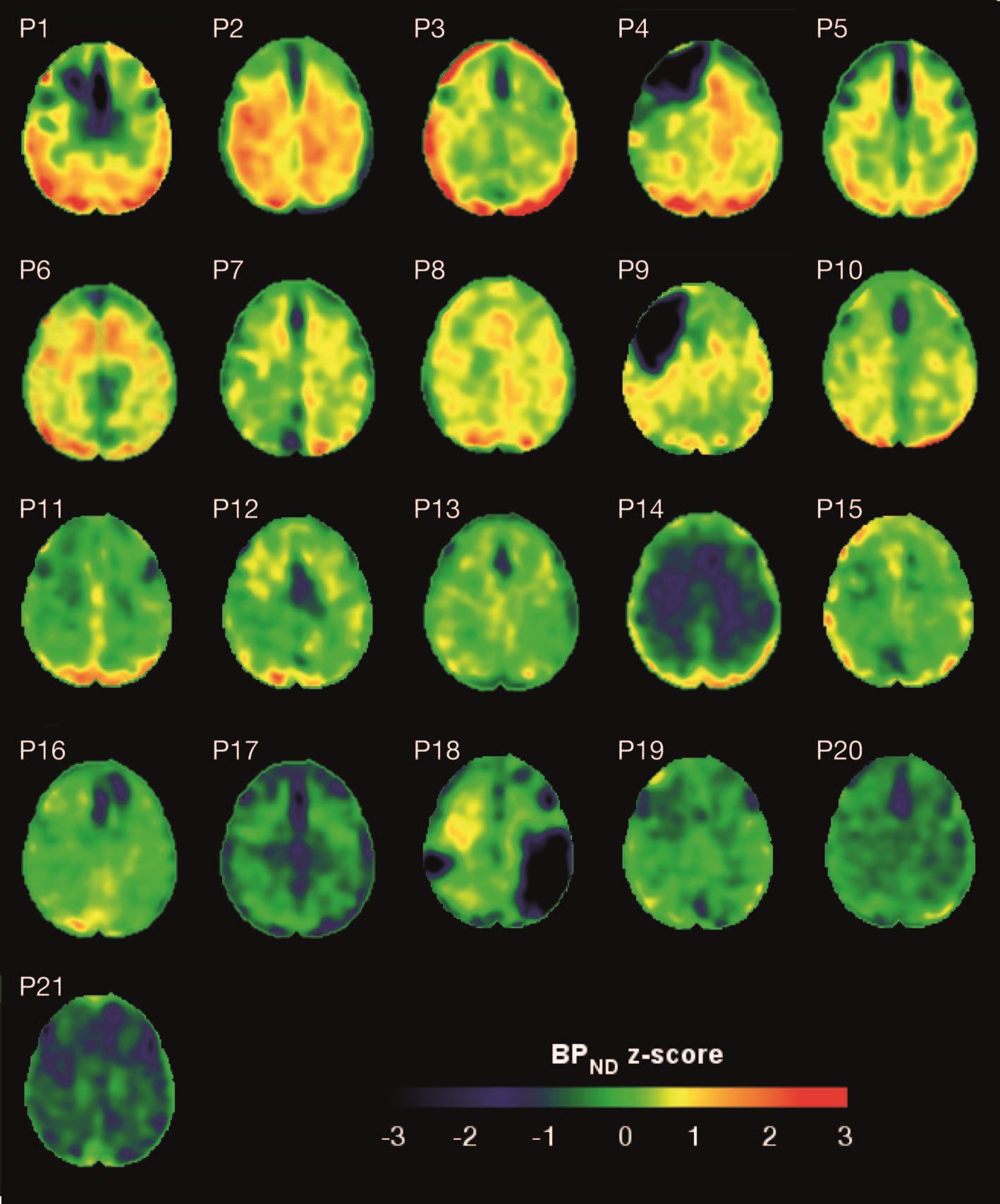
Brain deposits of hyperphosphorylated tau are detectable in traumatic brain injury (TBI) patients 18-51 years after a single moderate to severe incident occurred, researchers reported Sept. 4 in Science Translational Medicine.
Imaging with the tau-specific PET radioligand flortaucipir showed that the protein was most apparent in the right occipital cortex, and was associated with changes in cognitive scores, tau and beta amyloid in cerebrospinal fluid (CSF), and white matter density, Nikos Gorgoraptis, PhD, of Imperial College London and his colleagues wrote.
“The ability to detect tau pathology in vivo after TBI has major potential implications for diagnosis and prognostication of clinical outcomes after TBI,” the researchers explained. “It is also likely to assist in patient selection and stratification for future treatment trials targeting tau.”
The cohort study comprised 21 subjects (median age, 49 years) who had experienced a single moderate to severe TBI a median of 32 years (range, 18-51 years) before enrollment. A control group comprised 11 noninjured adults who were matched for age and other demographic factors. Everyone underwent a PET scan with flortaucipir, brain MRI, CSF sampling, apolipoprotein E genotyping, and neuropsychological testing.
TBI subjects were grouped according to recovery status: good and disabled. Overall, they showed impairments on multiple cognitive domains (processing speed, executive function, motivation, inhibition, and verbal and visual memory), compared with controls. These findings were largely driven by the disabled group.
Eight TBI subjects had elevated tau binding greater than 2,000 voxels above the threshold of detection (equivalent to 16 cm3 of brain volume), and seven had an increase of 249-1,999 voxels above threshold. Tau binding in the remainder was similar to that in controls. Recovery status didn’t correlate with the tau-binding strength.
Overall, the tau-binding signal appeared most strongly in the right lateral occipital cortex, regardless of functional recovery status.
In TBI subjects, CSF total tau correlated significantly with flortaucipir uptake in cortical gray matter, but not white matter. CSF phosphorylated tau correlated with uptake in white matter, but not gray matter.
The investigators also examined fractional anisotropy, a measure of fiber density, axonal diameter, and myelination in white matter. In TBI subjects, there was more flortaucipir uptake in areas of decreased fractional anisotropy, including association, commissural, and projection tracts.
“Correlations were observed in the genu and body of the corpus callosum, as well as in several association tracts within the ipsilateral (right) hemisphere, including the cingulum bundle, inferior longitudinal fasciculus, uncinate fasciculus, and anterior thalamic radiation, but not in the contralateral hemisphere. Higher cortical flortaucipir [signal] was associated with reduced tissue density in remote white matter regions including the corpus callosum and right prefrontal white matter. The same analysis for gray matter density did not show an association.”
The increased tau signal in TBI subjects “is in keeping with a causative role for traumatic axonal injury in the pathophysiology of posttraumatic tau pathology,” the authors said. “Mechanical forces exerted at the time of head injury are thought to disrupt axonal organization, producing damage to microtubule structure and associated axonal tau. This damage may lead to hyperphosphorylation of tau, misfolding, and neurofibrillary tangle formation, which eventually causes neurodegeneration. Mechanical forces are maximal in points of geometric inflection such as the base of cortical sulci, where tau pathology is seen in chronic traumatic encephalopathy.”
These patterns suggest that tau imaging could provide valuable diagnostic information about the type of posttraumatic neurodegeneration, they said.
The work was supported by the Medical Research Council and UK Dementia Research Institute. None of the authors declared having any competing interests related to the current study. Some authors reported financial ties to pharmaceutical companies.
SOURCE: Gorgoraptis N et al. Sci Transl Med. 2019;11:eaaw1993. doi: 10.1126/scitranslmed.aaw1993.
Brain deposits of hyperphosphorylated tau are detectable in traumatic brain injury (TBI) patients 18-51 years after a single moderate to severe incident occurred, researchers reported Sept. 4 in Science Translational Medicine.
Imaging with the tau-specific PET radioligand flortaucipir showed that the protein was most apparent in the right occipital cortex, and was associated with changes in cognitive scores, tau and beta amyloid in cerebrospinal fluid (CSF), and white matter density, Nikos Gorgoraptis, PhD, of Imperial College London and his colleagues wrote.
“The ability to detect tau pathology in vivo after TBI has major potential implications for diagnosis and prognostication of clinical outcomes after TBI,” the researchers explained. “It is also likely to assist in patient selection and stratification for future treatment trials targeting tau.”
The cohort study comprised 21 subjects (median age, 49 years) who had experienced a single moderate to severe TBI a median of 32 years (range, 18-51 years) before enrollment. A control group comprised 11 noninjured adults who were matched for age and other demographic factors. Everyone underwent a PET scan with flortaucipir, brain MRI, CSF sampling, apolipoprotein E genotyping, and neuropsychological testing.
TBI subjects were grouped according to recovery status: good and disabled. Overall, they showed impairments on multiple cognitive domains (processing speed, executive function, motivation, inhibition, and verbal and visual memory), compared with controls. These findings were largely driven by the disabled group.
Eight TBI subjects had elevated tau binding greater than 2,000 voxels above the threshold of detection (equivalent to 16 cm3 of brain volume), and seven had an increase of 249-1,999 voxels above threshold. Tau binding in the remainder was similar to that in controls. Recovery status didn’t correlate with the tau-binding strength.
Overall, the tau-binding signal appeared most strongly in the right lateral occipital cortex, regardless of functional recovery status.
In TBI subjects, CSF total tau correlated significantly with flortaucipir uptake in cortical gray matter, but not white matter. CSF phosphorylated tau correlated with uptake in white matter, but not gray matter.
The investigators also examined fractional anisotropy, a measure of fiber density, axonal diameter, and myelination in white matter. In TBI subjects, there was more flortaucipir uptake in areas of decreased fractional anisotropy, including association, commissural, and projection tracts.
“Correlations were observed in the genu and body of the corpus callosum, as well as in several association tracts within the ipsilateral (right) hemisphere, including the cingulum bundle, inferior longitudinal fasciculus, uncinate fasciculus, and anterior thalamic radiation, but not in the contralateral hemisphere. Higher cortical flortaucipir [signal] was associated with reduced tissue density in remote white matter regions including the corpus callosum and right prefrontal white matter. The same analysis for gray matter density did not show an association.”
The increased tau signal in TBI subjects “is in keeping with a causative role for traumatic axonal injury in the pathophysiology of posttraumatic tau pathology,” the authors said. “Mechanical forces exerted at the time of head injury are thought to disrupt axonal organization, producing damage to microtubule structure and associated axonal tau. This damage may lead to hyperphosphorylation of tau, misfolding, and neurofibrillary tangle formation, which eventually causes neurodegeneration. Mechanical forces are maximal in points of geometric inflection such as the base of cortical sulci, where tau pathology is seen in chronic traumatic encephalopathy.”
These patterns suggest that tau imaging could provide valuable diagnostic information about the type of posttraumatic neurodegeneration, they said.
The work was supported by the Medical Research Council and UK Dementia Research Institute. None of the authors declared having any competing interests related to the current study. Some authors reported financial ties to pharmaceutical companies.
SOURCE: Gorgoraptis N et al. Sci Transl Med. 2019;11:eaaw1993. doi: 10.1126/scitranslmed.aaw1993.
Brain deposits of hyperphosphorylated tau are detectable in traumatic brain injury (TBI) patients 18-51 years after a single moderate to severe incident occurred, researchers reported Sept. 4 in Science Translational Medicine.
Imaging with the tau-specific PET radioligand flortaucipir showed that the protein was most apparent in the right occipital cortex, and was associated with changes in cognitive scores, tau and beta amyloid in cerebrospinal fluid (CSF), and white matter density, Nikos Gorgoraptis, PhD, of Imperial College London and his colleagues wrote.
“The ability to detect tau pathology in vivo after TBI has major potential implications for diagnosis and prognostication of clinical outcomes after TBI,” the researchers explained. “It is also likely to assist in patient selection and stratification for future treatment trials targeting tau.”
The cohort study comprised 21 subjects (median age, 49 years) who had experienced a single moderate to severe TBI a median of 32 years (range, 18-51 years) before enrollment. A control group comprised 11 noninjured adults who were matched for age and other demographic factors. Everyone underwent a PET scan with flortaucipir, brain MRI, CSF sampling, apolipoprotein E genotyping, and neuropsychological testing.
TBI subjects were grouped according to recovery status: good and disabled. Overall, they showed impairments on multiple cognitive domains (processing speed, executive function, motivation, inhibition, and verbal and visual memory), compared with controls. These findings were largely driven by the disabled group.
Eight TBI subjects had elevated tau binding greater than 2,000 voxels above the threshold of detection (equivalent to 16 cm3 of brain volume), and seven had an increase of 249-1,999 voxels above threshold. Tau binding in the remainder was similar to that in controls. Recovery status didn’t correlate with the tau-binding strength.
Overall, the tau-binding signal appeared most strongly in the right lateral occipital cortex, regardless of functional recovery status.
In TBI subjects, CSF total tau correlated significantly with flortaucipir uptake in cortical gray matter, but not white matter. CSF phosphorylated tau correlated with uptake in white matter, but not gray matter.
The investigators also examined fractional anisotropy, a measure of fiber density, axonal diameter, and myelination in white matter. In TBI subjects, there was more flortaucipir uptake in areas of decreased fractional anisotropy, including association, commissural, and projection tracts.
“Correlations were observed in the genu and body of the corpus callosum, as well as in several association tracts within the ipsilateral (right) hemisphere, including the cingulum bundle, inferior longitudinal fasciculus, uncinate fasciculus, and anterior thalamic radiation, but not in the contralateral hemisphere. Higher cortical flortaucipir [signal] was associated with reduced tissue density in remote white matter regions including the corpus callosum and right prefrontal white matter. The same analysis for gray matter density did not show an association.”
The increased tau signal in TBI subjects “is in keeping with a causative role for traumatic axonal injury in the pathophysiology of posttraumatic tau pathology,” the authors said. “Mechanical forces exerted at the time of head injury are thought to disrupt axonal organization, producing damage to microtubule structure and associated axonal tau. This damage may lead to hyperphosphorylation of tau, misfolding, and neurofibrillary tangle formation, which eventually causes neurodegeneration. Mechanical forces are maximal in points of geometric inflection such as the base of cortical sulci, where tau pathology is seen in chronic traumatic encephalopathy.”
These patterns suggest that tau imaging could provide valuable diagnostic information about the type of posttraumatic neurodegeneration, they said.
The work was supported by the Medical Research Council and UK Dementia Research Institute. None of the authors declared having any competing interests related to the current study. Some authors reported financial ties to pharmaceutical companies.
SOURCE: Gorgoraptis N et al. Sci Transl Med. 2019;11:eaaw1993. doi: 10.1126/scitranslmed.aaw1993.
FROM SCIENCE TRANSLATIONAL MEDICINE
Blood test may reveal brain injury
researchers reported Aug. 26 in BMJ Paediatrics Open.
“GFAP outperformed UCH-L1 in detecting concussion in both children and adults within 4 hours of injury,” reported lead author Linda Papa, MD, and collaborators. Dr. Papa is an emergency medicine doctor at Orlando Health. “UCH-L1 was expressed at much higher levels than GFAP in those with nonconcussive trauma, particularly in children. Elevations of these biomarkers in nonconcussive head trauma suggest possible subconcussive brain injury. GFAP could be potentially useful to detect concussion for up to a week post injury.”
In 2018 the Food and Drug Administration approved the use of these biomarkers to guide CT scan ordering in adults with mild to moderate traumatic brain injury, but investigators have not established their ability to detect concussion in children or adults. Clinicians lack an objective measure to diagnose concussion acutely.
To assess the ability of GFAP and UCH-L1 to detect concussion, Dr. Papa and colleagues conducted a prospective cohort study. The researchers enrolled trauma patients of all ages at three level I trauma centers in the United States. They included patients with and without head trauma who had a Glasgow Coma Scale score of 15 and who presented within 4 hours of injury. Investigators screened for concussion symptoms, obtained biomarker data from 712 trauma patients, and conducted repeated blood sampling in adults.
They grouped patients by those with concussion (n = 371), those with head trauma without overt signs of concussion (n = 149), and those with peripheral trauma without head trauma or concussion (n = 192). The study included 175 children. Injury mechanisms included car crashes, falls, bicycle accidents, and sports injuries.
Patients with concussion had significantly higher GFAP concentrations, compared with patients with body trauma and patients with nonconcussive head trauma. UCH-L1 levels did not significantly differ between patients with concussion and head trauma controls, however.
“Based on these results, the potential utility of GFAP to distinguish concussion from body trauma controls over 7 days postinjury was fair to excellent,” with area under the receiver operating characteristics curves (AUCs) of 0.75-0.89, the researchers said. “UCH-L1’s ability was guarded and variable with AUCs from poor to good depending on timing of samples.” UCH-L1 demonstrated AUCs that ranged from 0.54 to 0.78; earlier samples performed better.
GFAP elevations in head trauma controls “may represent milder forms of concussion that do not elicit typical signs or symptoms associated with concussion,” the authors wrote. “These injuries may be irrelevant, or they may represent important trauma that is just below the level of clinical detection and referred to as subconcussive trauma. ... Biomarkers (such as GFAP and UCH-L1) could provide a more objective measure of injury and potentially identify those at risk for neurocognitive problems.”
The study was supported by the National Institute of Neurological Disorders and Stroke. Dr. Papa is an unpaid scientific consultant for Banyan Biomarkers, which developed kits to measure the biomarkers, and coauthors receive contract research funding from Banyan Biomarkers.
SOURCE: Papa L et al. BMJ Paediatr Open. 2019 Aug 26. doi: 10.1136/bmjpo-2019-000473.
researchers reported Aug. 26 in BMJ Paediatrics Open.
“GFAP outperformed UCH-L1 in detecting concussion in both children and adults within 4 hours of injury,” reported lead author Linda Papa, MD, and collaborators. Dr. Papa is an emergency medicine doctor at Orlando Health. “UCH-L1 was expressed at much higher levels than GFAP in those with nonconcussive trauma, particularly in children. Elevations of these biomarkers in nonconcussive head trauma suggest possible subconcussive brain injury. GFAP could be potentially useful to detect concussion for up to a week post injury.”
In 2018 the Food and Drug Administration approved the use of these biomarkers to guide CT scan ordering in adults with mild to moderate traumatic brain injury, but investigators have not established their ability to detect concussion in children or adults. Clinicians lack an objective measure to diagnose concussion acutely.
To assess the ability of GFAP and UCH-L1 to detect concussion, Dr. Papa and colleagues conducted a prospective cohort study. The researchers enrolled trauma patients of all ages at three level I trauma centers in the United States. They included patients with and without head trauma who had a Glasgow Coma Scale score of 15 and who presented within 4 hours of injury. Investigators screened for concussion symptoms, obtained biomarker data from 712 trauma patients, and conducted repeated blood sampling in adults.
They grouped patients by those with concussion (n = 371), those with head trauma without overt signs of concussion (n = 149), and those with peripheral trauma without head trauma or concussion (n = 192). The study included 175 children. Injury mechanisms included car crashes, falls, bicycle accidents, and sports injuries.
Patients with concussion had significantly higher GFAP concentrations, compared with patients with body trauma and patients with nonconcussive head trauma. UCH-L1 levels did not significantly differ between patients with concussion and head trauma controls, however.
“Based on these results, the potential utility of GFAP to distinguish concussion from body trauma controls over 7 days postinjury was fair to excellent,” with area under the receiver operating characteristics curves (AUCs) of 0.75-0.89, the researchers said. “UCH-L1’s ability was guarded and variable with AUCs from poor to good depending on timing of samples.” UCH-L1 demonstrated AUCs that ranged from 0.54 to 0.78; earlier samples performed better.
GFAP elevations in head trauma controls “may represent milder forms of concussion that do not elicit typical signs or symptoms associated with concussion,” the authors wrote. “These injuries may be irrelevant, or they may represent important trauma that is just below the level of clinical detection and referred to as subconcussive trauma. ... Biomarkers (such as GFAP and UCH-L1) could provide a more objective measure of injury and potentially identify those at risk for neurocognitive problems.”
The study was supported by the National Institute of Neurological Disorders and Stroke. Dr. Papa is an unpaid scientific consultant for Banyan Biomarkers, which developed kits to measure the biomarkers, and coauthors receive contract research funding from Banyan Biomarkers.
SOURCE: Papa L et al. BMJ Paediatr Open. 2019 Aug 26. doi: 10.1136/bmjpo-2019-000473.
researchers reported Aug. 26 in BMJ Paediatrics Open.
“GFAP outperformed UCH-L1 in detecting concussion in both children and adults within 4 hours of injury,” reported lead author Linda Papa, MD, and collaborators. Dr. Papa is an emergency medicine doctor at Orlando Health. “UCH-L1 was expressed at much higher levels than GFAP in those with nonconcussive trauma, particularly in children. Elevations of these biomarkers in nonconcussive head trauma suggest possible subconcussive brain injury. GFAP could be potentially useful to detect concussion for up to a week post injury.”
In 2018 the Food and Drug Administration approved the use of these biomarkers to guide CT scan ordering in adults with mild to moderate traumatic brain injury, but investigators have not established their ability to detect concussion in children or adults. Clinicians lack an objective measure to diagnose concussion acutely.
To assess the ability of GFAP and UCH-L1 to detect concussion, Dr. Papa and colleagues conducted a prospective cohort study. The researchers enrolled trauma patients of all ages at three level I trauma centers in the United States. They included patients with and without head trauma who had a Glasgow Coma Scale score of 15 and who presented within 4 hours of injury. Investigators screened for concussion symptoms, obtained biomarker data from 712 trauma patients, and conducted repeated blood sampling in adults.
They grouped patients by those with concussion (n = 371), those with head trauma without overt signs of concussion (n = 149), and those with peripheral trauma without head trauma or concussion (n = 192). The study included 175 children. Injury mechanisms included car crashes, falls, bicycle accidents, and sports injuries.
Patients with concussion had significantly higher GFAP concentrations, compared with patients with body trauma and patients with nonconcussive head trauma. UCH-L1 levels did not significantly differ between patients with concussion and head trauma controls, however.
“Based on these results, the potential utility of GFAP to distinguish concussion from body trauma controls over 7 days postinjury was fair to excellent,” with area under the receiver operating characteristics curves (AUCs) of 0.75-0.89, the researchers said. “UCH-L1’s ability was guarded and variable with AUCs from poor to good depending on timing of samples.” UCH-L1 demonstrated AUCs that ranged from 0.54 to 0.78; earlier samples performed better.
GFAP elevations in head trauma controls “may represent milder forms of concussion that do not elicit typical signs or symptoms associated with concussion,” the authors wrote. “These injuries may be irrelevant, or they may represent important trauma that is just below the level of clinical detection and referred to as subconcussive trauma. ... Biomarkers (such as GFAP and UCH-L1) could provide a more objective measure of injury and potentially identify those at risk for neurocognitive problems.”
The study was supported by the National Institute of Neurological Disorders and Stroke. Dr. Papa is an unpaid scientific consultant for Banyan Biomarkers, which developed kits to measure the biomarkers, and coauthors receive contract research funding from Banyan Biomarkers.
SOURCE: Papa L et al. BMJ Paediatr Open. 2019 Aug 26. doi: 10.1136/bmjpo-2019-000473.
FROM BMJ PAEDIATRICS OPEN
Key clinical point: Levels of glial fibrillary acidic protein (GFAP) and ubiquitin C-terminal hydrolase L1 (UCH-L1) are lowest in patients with nonconcussive body trauma, higher in patients with nonconcussive head trauma, and highest in patients with concussion.
Major finding: GFAP was fair to excellent at distinguishing concussion from body trauma, with area under the receiver operating characteristics curves of 0.75-0.89.
Study details: A prospective cohort study of 712 trauma patients of all ages at three level I trauma centers in the United States. The study included patients with and without head trauma who had a Glasgow Coma Scale score of 15 and presented within 4 hours of injury.
Disclosures: The study was supported by the National Institute of Neurological Disorders and Stroke. Dr. Papa is an unpaid scientific consultant for Banyan Biomarkers, which developed kits to measure the biomarkers. Coauthors receive contract research funding from Banyan Biomarkers.
Source: Papa L et al. BMJ Paediatr Open. 2019 Aug 26. doi: 10.1136/bmjpo-2019-000473.
Researchers examine potential causes of dementia in CTE
, according to a cross-sectional study published online Aug. 5 in JAMA Neurology.
The study of older, deceased former American football players with CTE showed that more years of play were associated with more severe white matter rarefaction and greater burden of neurofibrillary tau tangles in the dorsolateral frontal cortex, wrote Michael L. Alosco, PhD, assistant professor of neurology at Boston University’s CTE Center, and colleagues.
An analysis of donated brains
Repetitive head impacts are associated with CTE. The clinical presentation of CTE includes cognitive, behavioral, and mood changes that can progress to dementia. The contributions of pathologic changes in phosphorylated tau, white matter degeneration, and cerebrovascular disease to dementia in the context of CTE are poorly understood. Dr. Alosco and colleagues examined arteriosclerosis, infarcts, microinfarcts, microbleeds, and white matter rarefaction in donated brains to illuminate these contributions.
The researchers examined data from the Understanding Neurologic Injury and Traumatic Encephalopathy (UNITE) Study and Veterans Affairs–Boston University–Concussion Legacy Foundation brain bank. The population included deceased men who had played football and had received a neuropathologic diagnosis of CTE. Eligible participants had a history of repetitive head impacts. Brains that had been donated after a prolonged time postmortem and those with poor tissue quality were excluded.
Neuropathologists blinded to clinical data analyzed patients’ CTE stage and severity of neurofibrillary tangle burden in the dorsolateral frontal cortex as semiquantitative scales of phosphorylated tau severity. Neurofibrillary tangle burden was dichotomized as none or mild versus moderate or severe. The neuropathologists also rated white matter rarefaction and arteriolosclerosis severity using a scale of 0 points (i.e., none) to 3 points (i.e., severe changes). The investigators obtained clinical data through online surveys and retrospective telephone interviews with informants. They adjudicated consensus diagnoses of dementia based on modified criteria from DSM-IV.
White matter rarefaction was common
Dr. Alosco and colleagues included 180 individuals in their analysis, excluding those aged younger than 40 years because of low pathologic burden and minimal presence of dementia. Mean age at death was nearly 68 years. Fifty patients had no or mild neurofibrillary tangle burden, and 130 had moderate to severe burden. Thirty-five patients had CTE at stage I or II, and 145 had CTE at stage III or IV. In all, 120 patients were determined to have had dementia. About 47% of the sample had moderate to severe white matter rarefaction, and about 47% had arteriolosclerosis. Infarcts, microinfarcts, and microbleeds were uncommon.
When the investigators created a simultaneous equations regression model and controlled for age and race, they found that more years of play was associated with more severe white matter rarefaction, greater phosphorylated tau accumulation, and high CTE stage. Furthermore, white matter rarefaction and dorsolateral frontal cortex neurofibrillary tangles were associated with dementia. The association of years of play with dementia was mediated by white matter rarefaction and neurofibrillary tangle burden. Arteriolosclerosis was not associated with years of play, but arteriolosclerosis was independently associated with dementia.
The odds ratio for dementia was 1.69 among participants with more severe white matter rarefaction and 1.81 among patients with arteriolosclerosis. After the researchers controlled for age and race, the odds ratio of dementia was 2.65 among participants with a high neurofibrillary tangle burden, compared with participants with a low burden.
“Studies that include direct cardiovascular disease and repetitive head impacts metrics and refined measures of white matter integrity are needed to improve understanding of the pathogenesis of white matter rarefaction and cerebral small vessel changes in CTE,” Dr. Alosco and colleagues wrote.
The study was funded by grants from the National Institute on Aging, National Institute of Neurological Disorders and Stroke, the Department of Veterans Affairs, the Nick and Lynn Buoniconti Foundation, and the National Center for Advancing Translational Sciences. Some of the authors reported financial ties to the pharmaceutical industry and serving on professional sports committees.
SOURCE: Alosco ML et al. JAMA Neurol. 2019 Aug 5. doi: 10.1001/jamaneurol.2019.2244.
The study by Alosco et al. provides new insights into the pathogenesis of dementia in deceased former football players with chronic traumatic encephalopathy (CTE), Julie A. Schneider, MD, professor of neuropathology at Rush University, Chicago, wrote in an accompanying editorial (JAMA Neurol. 2019 Aug 5. doi: 10.1001/jamaneurol.2019.1089).
Significant and widespread white matter injury is an established result of head trauma resulting from acceleration-deceleration injuries. In addition, studies of single and repetitive traumatic brain injury have shown disruption of axons and white matter. The findings of Alosco et al. “underscore the importance of studying the risk factors and mechanisms for the white matter rarefaction, in addition to the tauopathy, in individuals who have played U.S. football and have CTE,” Dr. Schneider wrote.
The comprehensive neuropathologic examinations, advanced statistical techniques, and multiple sensitivity analyses that the investigators performed are among the study’s strengths. An important limitation, however, is selection bias. “The frequency of pathologic characteristics in this group should not be generalized to estimate the prevalence of neuropathologic conditions in living individuals who have played or are playing U.S. football,” Dr. Schneider wrote. “Moreover, individuals who played football who were selected for autopsy and found to have CTE may differ in other important ways from those who did not undergo autopsy or did not have CTE.” Recall bias could alter associations between years of play and dementia diagnosis, and the study’s semiquantitative assessments could result in decreased power to observe relevant associations, she said.
“In spite of these limitations, the authors should be applauded for elegant work and compelling support for multiple pathologic pathways to dementia in football players with CTE,” Dr. Schneider concluded.
Dr. Schneider is with the Rush Alzheimer’s Disease Center at Rush University, Chicago. She has been an expert consultant for the National Football League and the National Hockey League.
The study by Alosco et al. provides new insights into the pathogenesis of dementia in deceased former football players with chronic traumatic encephalopathy (CTE), Julie A. Schneider, MD, professor of neuropathology at Rush University, Chicago, wrote in an accompanying editorial (JAMA Neurol. 2019 Aug 5. doi: 10.1001/jamaneurol.2019.1089).
Significant and widespread white matter injury is an established result of head trauma resulting from acceleration-deceleration injuries. In addition, studies of single and repetitive traumatic brain injury have shown disruption of axons and white matter. The findings of Alosco et al. “underscore the importance of studying the risk factors and mechanisms for the white matter rarefaction, in addition to the tauopathy, in individuals who have played U.S. football and have CTE,” Dr. Schneider wrote.
The comprehensive neuropathologic examinations, advanced statistical techniques, and multiple sensitivity analyses that the investigators performed are among the study’s strengths. An important limitation, however, is selection bias. “The frequency of pathologic characteristics in this group should not be generalized to estimate the prevalence of neuropathologic conditions in living individuals who have played or are playing U.S. football,” Dr. Schneider wrote. “Moreover, individuals who played football who were selected for autopsy and found to have CTE may differ in other important ways from those who did not undergo autopsy or did not have CTE.” Recall bias could alter associations between years of play and dementia diagnosis, and the study’s semiquantitative assessments could result in decreased power to observe relevant associations, she said.
“In spite of these limitations, the authors should be applauded for elegant work and compelling support for multiple pathologic pathways to dementia in football players with CTE,” Dr. Schneider concluded.
Dr. Schneider is with the Rush Alzheimer’s Disease Center at Rush University, Chicago. She has been an expert consultant for the National Football League and the National Hockey League.
The study by Alosco et al. provides new insights into the pathogenesis of dementia in deceased former football players with chronic traumatic encephalopathy (CTE), Julie A. Schneider, MD, professor of neuropathology at Rush University, Chicago, wrote in an accompanying editorial (JAMA Neurol. 2019 Aug 5. doi: 10.1001/jamaneurol.2019.1089).
Significant and widespread white matter injury is an established result of head trauma resulting from acceleration-deceleration injuries. In addition, studies of single and repetitive traumatic brain injury have shown disruption of axons and white matter. The findings of Alosco et al. “underscore the importance of studying the risk factors and mechanisms for the white matter rarefaction, in addition to the tauopathy, in individuals who have played U.S. football and have CTE,” Dr. Schneider wrote.
The comprehensive neuropathologic examinations, advanced statistical techniques, and multiple sensitivity analyses that the investigators performed are among the study’s strengths. An important limitation, however, is selection bias. “The frequency of pathologic characteristics in this group should not be generalized to estimate the prevalence of neuropathologic conditions in living individuals who have played or are playing U.S. football,” Dr. Schneider wrote. “Moreover, individuals who played football who were selected for autopsy and found to have CTE may differ in other important ways from those who did not undergo autopsy or did not have CTE.” Recall bias could alter associations between years of play and dementia diagnosis, and the study’s semiquantitative assessments could result in decreased power to observe relevant associations, she said.
“In spite of these limitations, the authors should be applauded for elegant work and compelling support for multiple pathologic pathways to dementia in football players with CTE,” Dr. Schneider concluded.
Dr. Schneider is with the Rush Alzheimer’s Disease Center at Rush University, Chicago. She has been an expert consultant for the National Football League and the National Hockey League.
, according to a cross-sectional study published online Aug. 5 in JAMA Neurology.
The study of older, deceased former American football players with CTE showed that more years of play were associated with more severe white matter rarefaction and greater burden of neurofibrillary tau tangles in the dorsolateral frontal cortex, wrote Michael L. Alosco, PhD, assistant professor of neurology at Boston University’s CTE Center, and colleagues.
An analysis of donated brains
Repetitive head impacts are associated with CTE. The clinical presentation of CTE includes cognitive, behavioral, and mood changes that can progress to dementia. The contributions of pathologic changes in phosphorylated tau, white matter degeneration, and cerebrovascular disease to dementia in the context of CTE are poorly understood. Dr. Alosco and colleagues examined arteriosclerosis, infarcts, microinfarcts, microbleeds, and white matter rarefaction in donated brains to illuminate these contributions.
The researchers examined data from the Understanding Neurologic Injury and Traumatic Encephalopathy (UNITE) Study and Veterans Affairs–Boston University–Concussion Legacy Foundation brain bank. The population included deceased men who had played football and had received a neuropathologic diagnosis of CTE. Eligible participants had a history of repetitive head impacts. Brains that had been donated after a prolonged time postmortem and those with poor tissue quality were excluded.
Neuropathologists blinded to clinical data analyzed patients’ CTE stage and severity of neurofibrillary tangle burden in the dorsolateral frontal cortex as semiquantitative scales of phosphorylated tau severity. Neurofibrillary tangle burden was dichotomized as none or mild versus moderate or severe. The neuropathologists also rated white matter rarefaction and arteriolosclerosis severity using a scale of 0 points (i.e., none) to 3 points (i.e., severe changes). The investigators obtained clinical data through online surveys and retrospective telephone interviews with informants. They adjudicated consensus diagnoses of dementia based on modified criteria from DSM-IV.
White matter rarefaction was common
Dr. Alosco and colleagues included 180 individuals in their analysis, excluding those aged younger than 40 years because of low pathologic burden and minimal presence of dementia. Mean age at death was nearly 68 years. Fifty patients had no or mild neurofibrillary tangle burden, and 130 had moderate to severe burden. Thirty-five patients had CTE at stage I or II, and 145 had CTE at stage III or IV. In all, 120 patients were determined to have had dementia. About 47% of the sample had moderate to severe white matter rarefaction, and about 47% had arteriolosclerosis. Infarcts, microinfarcts, and microbleeds were uncommon.
When the investigators created a simultaneous equations regression model and controlled for age and race, they found that more years of play was associated with more severe white matter rarefaction, greater phosphorylated tau accumulation, and high CTE stage. Furthermore, white matter rarefaction and dorsolateral frontal cortex neurofibrillary tangles were associated with dementia. The association of years of play with dementia was mediated by white matter rarefaction and neurofibrillary tangle burden. Arteriolosclerosis was not associated with years of play, but arteriolosclerosis was independently associated with dementia.
The odds ratio for dementia was 1.69 among participants with more severe white matter rarefaction and 1.81 among patients with arteriolosclerosis. After the researchers controlled for age and race, the odds ratio of dementia was 2.65 among participants with a high neurofibrillary tangle burden, compared with participants with a low burden.
“Studies that include direct cardiovascular disease and repetitive head impacts metrics and refined measures of white matter integrity are needed to improve understanding of the pathogenesis of white matter rarefaction and cerebral small vessel changes in CTE,” Dr. Alosco and colleagues wrote.
The study was funded by grants from the National Institute on Aging, National Institute of Neurological Disorders and Stroke, the Department of Veterans Affairs, the Nick and Lynn Buoniconti Foundation, and the National Center for Advancing Translational Sciences. Some of the authors reported financial ties to the pharmaceutical industry and serving on professional sports committees.
SOURCE: Alosco ML et al. JAMA Neurol. 2019 Aug 5. doi: 10.1001/jamaneurol.2019.2244.
, according to a cross-sectional study published online Aug. 5 in JAMA Neurology.
The study of older, deceased former American football players with CTE showed that more years of play were associated with more severe white matter rarefaction and greater burden of neurofibrillary tau tangles in the dorsolateral frontal cortex, wrote Michael L. Alosco, PhD, assistant professor of neurology at Boston University’s CTE Center, and colleagues.
An analysis of donated brains
Repetitive head impacts are associated with CTE. The clinical presentation of CTE includes cognitive, behavioral, and mood changes that can progress to dementia. The contributions of pathologic changes in phosphorylated tau, white matter degeneration, and cerebrovascular disease to dementia in the context of CTE are poorly understood. Dr. Alosco and colleagues examined arteriosclerosis, infarcts, microinfarcts, microbleeds, and white matter rarefaction in donated brains to illuminate these contributions.
The researchers examined data from the Understanding Neurologic Injury and Traumatic Encephalopathy (UNITE) Study and Veterans Affairs–Boston University–Concussion Legacy Foundation brain bank. The population included deceased men who had played football and had received a neuropathologic diagnosis of CTE. Eligible participants had a history of repetitive head impacts. Brains that had been donated after a prolonged time postmortem and those with poor tissue quality were excluded.
Neuropathologists blinded to clinical data analyzed patients’ CTE stage and severity of neurofibrillary tangle burden in the dorsolateral frontal cortex as semiquantitative scales of phosphorylated tau severity. Neurofibrillary tangle burden was dichotomized as none or mild versus moderate or severe. The neuropathologists also rated white matter rarefaction and arteriolosclerosis severity using a scale of 0 points (i.e., none) to 3 points (i.e., severe changes). The investigators obtained clinical data through online surveys and retrospective telephone interviews with informants. They adjudicated consensus diagnoses of dementia based on modified criteria from DSM-IV.
White matter rarefaction was common
Dr. Alosco and colleagues included 180 individuals in their analysis, excluding those aged younger than 40 years because of low pathologic burden and minimal presence of dementia. Mean age at death was nearly 68 years. Fifty patients had no or mild neurofibrillary tangle burden, and 130 had moderate to severe burden. Thirty-five patients had CTE at stage I or II, and 145 had CTE at stage III or IV. In all, 120 patients were determined to have had dementia. About 47% of the sample had moderate to severe white matter rarefaction, and about 47% had arteriolosclerosis. Infarcts, microinfarcts, and microbleeds were uncommon.
When the investigators created a simultaneous equations regression model and controlled for age and race, they found that more years of play was associated with more severe white matter rarefaction, greater phosphorylated tau accumulation, and high CTE stage. Furthermore, white matter rarefaction and dorsolateral frontal cortex neurofibrillary tangles were associated with dementia. The association of years of play with dementia was mediated by white matter rarefaction and neurofibrillary tangle burden. Arteriolosclerosis was not associated with years of play, but arteriolosclerosis was independently associated with dementia.
The odds ratio for dementia was 1.69 among participants with more severe white matter rarefaction and 1.81 among patients with arteriolosclerosis. After the researchers controlled for age and race, the odds ratio of dementia was 2.65 among participants with a high neurofibrillary tangle burden, compared with participants with a low burden.
“Studies that include direct cardiovascular disease and repetitive head impacts metrics and refined measures of white matter integrity are needed to improve understanding of the pathogenesis of white matter rarefaction and cerebral small vessel changes in CTE,” Dr. Alosco and colleagues wrote.
The study was funded by grants from the National Institute on Aging, National Institute of Neurological Disorders and Stroke, the Department of Veterans Affairs, the Nick and Lynn Buoniconti Foundation, and the National Center for Advancing Translational Sciences. Some of the authors reported financial ties to the pharmaceutical industry and serving on professional sports committees.
SOURCE: Alosco ML et al. JAMA Neurol. 2019 Aug 5. doi: 10.1001/jamaneurol.2019.2244.
FROM JAMA NEUROLOGY
Tranexamic acid may not improve neurologic outcomes in patients with TBI
PHILADELPHIA – according to an investigation presented at the annual meeting of the American Academy of Neurology. For patients with TBI and intracranial hemorrhage (ICH), however, treatment with a 2-gram bolus of tranexamic acid within 42 minutes of injury significantly improves the rate of 28-day survival. Tranexamic acid therefore “is the first therapeutic with evidence for benefit in acute TBI,” said Susan Rowell, MD, trauma medical director at Duke University in Durham, North Carolina.
No effective treatment is available for TBI, which is a major cause of death after trauma. In 2010, the CRASH-2 trial (Lancet. 2010 Jul 03;376[9734]:23-32), suggested that tranexamic acid, a lysine analogue that decreases the breakdown of clots, safely reduced the rate of death from hemorrhage in patients with trauma and bleeding. Patients treated within 1 hour of injury were significantly more likely to survive than those treated at 1 hour or more after injury.
Two small, prospective trials failed to show that tranexamic acid reduced in-hospital mortality, improved neurologic function at discharge, or reduced the progression of ICH. A meta-analysis of both trials, however, showed a trend toward a benefit of treatment with this therapy.
A multicenter, prehospital trial
Dr. Rowell and colleagues hypothesized that prehospital administration of tranexamic acid to patients with moderate to severe TBI early after injury would increase the likelihood of a favorable neurologic outcome. Between March 2015 and March 2017, they enrolled 1,280 participants in a multicenter, prehospital trial. Eligible participants had moderate to severe TBI, were not in shock (as evidenced by a systolic blood pressure greater than 90 mm Hg before randomization), and were enrolled within 2 hours of injury.
Patients were randomized to one of three treatment arms and followed for 6 months. The first treatment arm received a 1-gram bolus of tranexamic acid before hospital admission and an 8-hour, 1-gram infusion of tranexamic acid in the hospital. The second arm received a 2-gram bolus of tranexamic acid before hospital admission and a placebo infusion in the hospital. The third arm received a placebo bolus and placebo infusion. Paramedics and participants were blinded to treatment assignment. The trial was conducted at 20 hospitals and 39 emergency medical services agencies in the United States and Canada.
The study’s primary outcome was functional neurologic outcome at 6 months, as measured by the Glasgow Outcomes Scale – Extended (GOSE). The investigators dichotomized results into favorable and poor categories. Other prespecified outcomes included early and late mortality, the disability rating scale (DRS), and progression of ICH.
Treatment was administered early
The researchers identified 1,280 eligible patients, of whom 1,063 were randomized. The modified intention-to-treat analysis included 309 participants in the placebo group, 312 in the bolus-maintenance group (the 1-gram group), and 345 in the bolus-only group (the 2-gram group). The population’s average age was approximately 42 years, and 75% of the sample was male. About half of the patients had a Glasgow Coma Scale score between 3 and 8. Injury severity and prehospital care were similar among the groups.
The researchers provided the drug infusion at an average of 0.7 hours (42 minutes) after injury, “which is actually quite early,” said Dr. Rowell. They observed few infusion-related deviations, and the entire bolus was infused in about 95% of patients. Approximately 70% of patients received the full 8-hour infusion. This result was influenced partly by stopping rules and by providers who requested unblinding to give open-label tranexamic acid. Overall, 57% of patients in the trial had an ICH on head CT, which was approximately the proportion that the researchers had anticipated.
Dr. Rowell and colleagues completed the 6-month follow-up for 85% of patients. They saw no difference in the 6-month neurologic outcome between the group of all patients who received tranexamic acid and those who received placebo. The investigators also saw no differences between groups in early and late mortality and the DRS.
About half of patients with ICH were evaluated for progression. Progression occurred in 20% of the placebo arm, 17% of the bolus-maintenance arm, and 15% of the bolus-only arm. The differences between groups were not statistically significant. Participants in the bolus-only group, however, were significantly less likely to die, compared with the placebo and the bolus-maintenance groups. The odds ratio of death for the bolus-only group, compared with the others, was about 0.5. The absolute mortality rate for the placebo and bolus-maintenance groups was 17%, compared with 12% for the bolus-only group. Most deaths were attributable to TBI, and few patients died of exsanguination.
In addition, the bolus-only group also had improved long-term neurologic outcome, as assessed by the 6-month DRS and the 6-month GOSE, compared with the bolus maintenance group.
Among patients with ICH, survival increased by approximately 12% at 10 hours after injury in the bolus-only group, compared with the bolus-maintenance and placebo groups. This difference persisted throughout the follow-up period, said Dr. Rowell.
Among predefined major adverse events, seizure-like activity occurred in 5% of the bolus-only group, compared with 2% of the placebo and bolus-maintenance groups. The researchers found no significant differences in any thrombotic event between the bolus-only group and the placebo group.
The study was sponsored by University of Washington, Seattle. Collaborators included the National Heart, Lung, and Blood Institute; the U.S. Army Medical Research and Development Command; and the American Heart Association. Dr. Rowell had no relevant disclosures.
SOURCE: Rowell S et al. AAN 2019, Abstract.
PHILADELPHIA – according to an investigation presented at the annual meeting of the American Academy of Neurology. For patients with TBI and intracranial hemorrhage (ICH), however, treatment with a 2-gram bolus of tranexamic acid within 42 minutes of injury significantly improves the rate of 28-day survival. Tranexamic acid therefore “is the first therapeutic with evidence for benefit in acute TBI,” said Susan Rowell, MD, trauma medical director at Duke University in Durham, North Carolina.
No effective treatment is available for TBI, which is a major cause of death after trauma. In 2010, the CRASH-2 trial (Lancet. 2010 Jul 03;376[9734]:23-32), suggested that tranexamic acid, a lysine analogue that decreases the breakdown of clots, safely reduced the rate of death from hemorrhage in patients with trauma and bleeding. Patients treated within 1 hour of injury were significantly more likely to survive than those treated at 1 hour or more after injury.
Two small, prospective trials failed to show that tranexamic acid reduced in-hospital mortality, improved neurologic function at discharge, or reduced the progression of ICH. A meta-analysis of both trials, however, showed a trend toward a benefit of treatment with this therapy.
A multicenter, prehospital trial
Dr. Rowell and colleagues hypothesized that prehospital administration of tranexamic acid to patients with moderate to severe TBI early after injury would increase the likelihood of a favorable neurologic outcome. Between March 2015 and March 2017, they enrolled 1,280 participants in a multicenter, prehospital trial. Eligible participants had moderate to severe TBI, were not in shock (as evidenced by a systolic blood pressure greater than 90 mm Hg before randomization), and were enrolled within 2 hours of injury.
Patients were randomized to one of three treatment arms and followed for 6 months. The first treatment arm received a 1-gram bolus of tranexamic acid before hospital admission and an 8-hour, 1-gram infusion of tranexamic acid in the hospital. The second arm received a 2-gram bolus of tranexamic acid before hospital admission and a placebo infusion in the hospital. The third arm received a placebo bolus and placebo infusion. Paramedics and participants were blinded to treatment assignment. The trial was conducted at 20 hospitals and 39 emergency medical services agencies in the United States and Canada.
The study’s primary outcome was functional neurologic outcome at 6 months, as measured by the Glasgow Outcomes Scale – Extended (GOSE). The investigators dichotomized results into favorable and poor categories. Other prespecified outcomes included early and late mortality, the disability rating scale (DRS), and progression of ICH.
Treatment was administered early
The researchers identified 1,280 eligible patients, of whom 1,063 were randomized. The modified intention-to-treat analysis included 309 participants in the placebo group, 312 in the bolus-maintenance group (the 1-gram group), and 345 in the bolus-only group (the 2-gram group). The population’s average age was approximately 42 years, and 75% of the sample was male. About half of the patients had a Glasgow Coma Scale score between 3 and 8. Injury severity and prehospital care were similar among the groups.
The researchers provided the drug infusion at an average of 0.7 hours (42 minutes) after injury, “which is actually quite early,” said Dr. Rowell. They observed few infusion-related deviations, and the entire bolus was infused in about 95% of patients. Approximately 70% of patients received the full 8-hour infusion. This result was influenced partly by stopping rules and by providers who requested unblinding to give open-label tranexamic acid. Overall, 57% of patients in the trial had an ICH on head CT, which was approximately the proportion that the researchers had anticipated.
Dr. Rowell and colleagues completed the 6-month follow-up for 85% of patients. They saw no difference in the 6-month neurologic outcome between the group of all patients who received tranexamic acid and those who received placebo. The investigators also saw no differences between groups in early and late mortality and the DRS.
About half of patients with ICH were evaluated for progression. Progression occurred in 20% of the placebo arm, 17% of the bolus-maintenance arm, and 15% of the bolus-only arm. The differences between groups were not statistically significant. Participants in the bolus-only group, however, were significantly less likely to die, compared with the placebo and the bolus-maintenance groups. The odds ratio of death for the bolus-only group, compared with the others, was about 0.5. The absolute mortality rate for the placebo and bolus-maintenance groups was 17%, compared with 12% for the bolus-only group. Most deaths were attributable to TBI, and few patients died of exsanguination.
In addition, the bolus-only group also had improved long-term neurologic outcome, as assessed by the 6-month DRS and the 6-month GOSE, compared with the bolus maintenance group.
Among patients with ICH, survival increased by approximately 12% at 10 hours after injury in the bolus-only group, compared with the bolus-maintenance and placebo groups. This difference persisted throughout the follow-up period, said Dr. Rowell.
Among predefined major adverse events, seizure-like activity occurred in 5% of the bolus-only group, compared with 2% of the placebo and bolus-maintenance groups. The researchers found no significant differences in any thrombotic event between the bolus-only group and the placebo group.
The study was sponsored by University of Washington, Seattle. Collaborators included the National Heart, Lung, and Blood Institute; the U.S. Army Medical Research and Development Command; and the American Heart Association. Dr. Rowell had no relevant disclosures.
SOURCE: Rowell S et al. AAN 2019, Abstract.
PHILADELPHIA – according to an investigation presented at the annual meeting of the American Academy of Neurology. For patients with TBI and intracranial hemorrhage (ICH), however, treatment with a 2-gram bolus of tranexamic acid within 42 minutes of injury significantly improves the rate of 28-day survival. Tranexamic acid therefore “is the first therapeutic with evidence for benefit in acute TBI,” said Susan Rowell, MD, trauma medical director at Duke University in Durham, North Carolina.
No effective treatment is available for TBI, which is a major cause of death after trauma. In 2010, the CRASH-2 trial (Lancet. 2010 Jul 03;376[9734]:23-32), suggested that tranexamic acid, a lysine analogue that decreases the breakdown of clots, safely reduced the rate of death from hemorrhage in patients with trauma and bleeding. Patients treated within 1 hour of injury were significantly more likely to survive than those treated at 1 hour or more after injury.
Two small, prospective trials failed to show that tranexamic acid reduced in-hospital mortality, improved neurologic function at discharge, or reduced the progression of ICH. A meta-analysis of both trials, however, showed a trend toward a benefit of treatment with this therapy.
A multicenter, prehospital trial
Dr. Rowell and colleagues hypothesized that prehospital administration of tranexamic acid to patients with moderate to severe TBI early after injury would increase the likelihood of a favorable neurologic outcome. Between March 2015 and March 2017, they enrolled 1,280 participants in a multicenter, prehospital trial. Eligible participants had moderate to severe TBI, were not in shock (as evidenced by a systolic blood pressure greater than 90 mm Hg before randomization), and were enrolled within 2 hours of injury.
Patients were randomized to one of three treatment arms and followed for 6 months. The first treatment arm received a 1-gram bolus of tranexamic acid before hospital admission and an 8-hour, 1-gram infusion of tranexamic acid in the hospital. The second arm received a 2-gram bolus of tranexamic acid before hospital admission and a placebo infusion in the hospital. The third arm received a placebo bolus and placebo infusion. Paramedics and participants were blinded to treatment assignment. The trial was conducted at 20 hospitals and 39 emergency medical services agencies in the United States and Canada.
The study’s primary outcome was functional neurologic outcome at 6 months, as measured by the Glasgow Outcomes Scale – Extended (GOSE). The investigators dichotomized results into favorable and poor categories. Other prespecified outcomes included early and late mortality, the disability rating scale (DRS), and progression of ICH.
Treatment was administered early
The researchers identified 1,280 eligible patients, of whom 1,063 were randomized. The modified intention-to-treat analysis included 309 participants in the placebo group, 312 in the bolus-maintenance group (the 1-gram group), and 345 in the bolus-only group (the 2-gram group). The population’s average age was approximately 42 years, and 75% of the sample was male. About half of the patients had a Glasgow Coma Scale score between 3 and 8. Injury severity and prehospital care were similar among the groups.
The researchers provided the drug infusion at an average of 0.7 hours (42 minutes) after injury, “which is actually quite early,” said Dr. Rowell. They observed few infusion-related deviations, and the entire bolus was infused in about 95% of patients. Approximately 70% of patients received the full 8-hour infusion. This result was influenced partly by stopping rules and by providers who requested unblinding to give open-label tranexamic acid. Overall, 57% of patients in the trial had an ICH on head CT, which was approximately the proportion that the researchers had anticipated.
Dr. Rowell and colleagues completed the 6-month follow-up for 85% of patients. They saw no difference in the 6-month neurologic outcome between the group of all patients who received tranexamic acid and those who received placebo. The investigators also saw no differences between groups in early and late mortality and the DRS.
About half of patients with ICH were evaluated for progression. Progression occurred in 20% of the placebo arm, 17% of the bolus-maintenance arm, and 15% of the bolus-only arm. The differences between groups were not statistically significant. Participants in the bolus-only group, however, were significantly less likely to die, compared with the placebo and the bolus-maintenance groups. The odds ratio of death for the bolus-only group, compared with the others, was about 0.5. The absolute mortality rate for the placebo and bolus-maintenance groups was 17%, compared with 12% for the bolus-only group. Most deaths were attributable to TBI, and few patients died of exsanguination.
In addition, the bolus-only group also had improved long-term neurologic outcome, as assessed by the 6-month DRS and the 6-month GOSE, compared with the bolus maintenance group.
Among patients with ICH, survival increased by approximately 12% at 10 hours after injury in the bolus-only group, compared with the bolus-maintenance and placebo groups. This difference persisted throughout the follow-up period, said Dr. Rowell.
Among predefined major adverse events, seizure-like activity occurred in 5% of the bolus-only group, compared with 2% of the placebo and bolus-maintenance groups. The researchers found no significant differences in any thrombotic event between the bolus-only group and the placebo group.
The study was sponsored by University of Washington, Seattle. Collaborators included the National Heart, Lung, and Blood Institute; the U.S. Army Medical Research and Development Command; and the American Heart Association. Dr. Rowell had no relevant disclosures.
SOURCE: Rowell S et al. AAN 2019, Abstract.
REPORTING FROM AAN 2019
Key clinical point: Early administration of tranexamic acid after TBI does not improve neurologic outcome at 6 months.
Major finding: Patients with TBI and ICH who received a 2-g bolus of tranexamic acid had a 50% lower rate of mortality.
Study details: A multicenter, prehospital trial that enrolled 1,063 patients with moderate to severe TBI.
Disclosures: The study was sponsored by University of Washington, Seattle. Collaborators included the National Heart, Lung, and Blood Institute; the U.S. Army Medical Research and Development Command; and the American Heart Association. Dr. Rowell had no relevant disclosures.
Source: Rowell S et al. AAN 2019, Abstract.
Can serum inflammatory markers predict concussion recovery?
Levels of interleukin-6 (IL-6) and IL-1 receptor antagonist (IL-1RA) are significantly elevated 6 hours after concussion, and higher IL-6 levels are associated with slower recovery, according to a study of 41 high school and college football players with concussion. The findings were published online ahead of print July 3 in Neurology.
“With so many people sustaining concussions and a sizeable number of them having prolonged symptoms and recovery, any tools we can develop to help determine who would be at greater risk of problems would be very beneficial,” said study author Timothy B. Meier, PhD, assistant professor of neurosurgery at the Medical College of Wisconsin in Milwaukee, in a news release. “These results are a crucial first step.”
Symptoms of sport-related concussion typically resolve within 1-2 weeks but may last longer. Although prior studies have focused on biomarkers that are specific to brain injury, nonspecific inflammatory markers also may hold promise in predicting recovery after a mild traumatic brain injury, the authors said.
To examine whether acute elevations in serum inflammatory markers predict symptom recovery following sport-related concussion, Dr. Meier and his research colleagues enrolled 857 high school and college football players into a prospective cohort study. They included in their analyses 41 concussed athletes and 43 matched control athletes with an average age of 18 years. None of the concussed athletes lost consciousness, two had posttraumatic amnesia, and one had retrograde amnesia. The concussed athletes had a mean symptom duration of 8.86 days.
The researchers measured serum levels of IL-6, IL-1RA, IL-1 beta, IL-10, tumor necrosis factor, C-reactive protein, and interferon-gamma and recorded Sport Concussion Assessment Tool, 3rd edition, symptom severity scores.
Participants with concussion underwent testing at the start of the season, within 6 hours of injury, 24-48 hours after injury, and at 8, 15, and 45 days after injury. Control athletes underwent testing at similar times.
Among athletes with concussion, IL-1RA and IL-6 were elevated at 6 hours, compared with all other postinjury visits and with controls. IL-6 and IL-1RA significantly discriminated concussed from control athletes at 6 hours postconcussion with an area under the receiver operating characteristic curve of 0.79 for IL-6 and 0.79 for IL-1RA. Furthermore, IL-6 levels at 6 hours significantly correlated with symptom duration, “with a 1-unit increase in natural log-transformed IL-6 associated with 39% lower hazard of symptom recovery,” the researchers reported.
The extent to which these results generalize to females, youth athletes, or athletes who develop postconcussion syndrome is unclear, and larger studies may be needed to adequately assess inflammatory markers as clinical biomarkers of sport-related concussion, the authors noted.
“Eventually, these results may help us better understand the relationship between injury and inflammation and potentially lead to new treatments,” Dr. Meier said.
The research was supported by the U.S. Department of Defense, National Institute of Neurological Disorders and Stroke, National Institute of General Medical Sciences, National Institute of Mental Health, and the National Center for Advancing Translational Sciences. The authors had no relevant disclosures.
SOURCE: Nitta ME et al. Neurology. 2019 Jul 3. doi: 10.1212/WNL.0000000000007864.
Levels of interleukin-6 (IL-6) and IL-1 receptor antagonist (IL-1RA) are significantly elevated 6 hours after concussion, and higher IL-6 levels are associated with slower recovery, according to a study of 41 high school and college football players with concussion. The findings were published online ahead of print July 3 in Neurology.
“With so many people sustaining concussions and a sizeable number of them having prolonged symptoms and recovery, any tools we can develop to help determine who would be at greater risk of problems would be very beneficial,” said study author Timothy B. Meier, PhD, assistant professor of neurosurgery at the Medical College of Wisconsin in Milwaukee, in a news release. “These results are a crucial first step.”
Symptoms of sport-related concussion typically resolve within 1-2 weeks but may last longer. Although prior studies have focused on biomarkers that are specific to brain injury, nonspecific inflammatory markers also may hold promise in predicting recovery after a mild traumatic brain injury, the authors said.
To examine whether acute elevations in serum inflammatory markers predict symptom recovery following sport-related concussion, Dr. Meier and his research colleagues enrolled 857 high school and college football players into a prospective cohort study. They included in their analyses 41 concussed athletes and 43 matched control athletes with an average age of 18 years. None of the concussed athletes lost consciousness, two had posttraumatic amnesia, and one had retrograde amnesia. The concussed athletes had a mean symptom duration of 8.86 days.
The researchers measured serum levels of IL-6, IL-1RA, IL-1 beta, IL-10, tumor necrosis factor, C-reactive protein, and interferon-gamma and recorded Sport Concussion Assessment Tool, 3rd edition, symptom severity scores.
Participants with concussion underwent testing at the start of the season, within 6 hours of injury, 24-48 hours after injury, and at 8, 15, and 45 days after injury. Control athletes underwent testing at similar times.
Among athletes with concussion, IL-1RA and IL-6 were elevated at 6 hours, compared with all other postinjury visits and with controls. IL-6 and IL-1RA significantly discriminated concussed from control athletes at 6 hours postconcussion with an area under the receiver operating characteristic curve of 0.79 for IL-6 and 0.79 for IL-1RA. Furthermore, IL-6 levels at 6 hours significantly correlated with symptom duration, “with a 1-unit increase in natural log-transformed IL-6 associated with 39% lower hazard of symptom recovery,” the researchers reported.
The extent to which these results generalize to females, youth athletes, or athletes who develop postconcussion syndrome is unclear, and larger studies may be needed to adequately assess inflammatory markers as clinical biomarkers of sport-related concussion, the authors noted.
“Eventually, these results may help us better understand the relationship between injury and inflammation and potentially lead to new treatments,” Dr. Meier said.
The research was supported by the U.S. Department of Defense, National Institute of Neurological Disorders and Stroke, National Institute of General Medical Sciences, National Institute of Mental Health, and the National Center for Advancing Translational Sciences. The authors had no relevant disclosures.
SOURCE: Nitta ME et al. Neurology. 2019 Jul 3. doi: 10.1212/WNL.0000000000007864.
Levels of interleukin-6 (IL-6) and IL-1 receptor antagonist (IL-1RA) are significantly elevated 6 hours after concussion, and higher IL-6 levels are associated with slower recovery, according to a study of 41 high school and college football players with concussion. The findings were published online ahead of print July 3 in Neurology.
“With so many people sustaining concussions and a sizeable number of them having prolonged symptoms and recovery, any tools we can develop to help determine who would be at greater risk of problems would be very beneficial,” said study author Timothy B. Meier, PhD, assistant professor of neurosurgery at the Medical College of Wisconsin in Milwaukee, in a news release. “These results are a crucial first step.”
Symptoms of sport-related concussion typically resolve within 1-2 weeks but may last longer. Although prior studies have focused on biomarkers that are specific to brain injury, nonspecific inflammatory markers also may hold promise in predicting recovery after a mild traumatic brain injury, the authors said.
To examine whether acute elevations in serum inflammatory markers predict symptom recovery following sport-related concussion, Dr. Meier and his research colleagues enrolled 857 high school and college football players into a prospective cohort study. They included in their analyses 41 concussed athletes and 43 matched control athletes with an average age of 18 years. None of the concussed athletes lost consciousness, two had posttraumatic amnesia, and one had retrograde amnesia. The concussed athletes had a mean symptom duration of 8.86 days.
The researchers measured serum levels of IL-6, IL-1RA, IL-1 beta, IL-10, tumor necrosis factor, C-reactive protein, and interferon-gamma and recorded Sport Concussion Assessment Tool, 3rd edition, symptom severity scores.
Participants with concussion underwent testing at the start of the season, within 6 hours of injury, 24-48 hours after injury, and at 8, 15, and 45 days after injury. Control athletes underwent testing at similar times.
Among athletes with concussion, IL-1RA and IL-6 were elevated at 6 hours, compared with all other postinjury visits and with controls. IL-6 and IL-1RA significantly discriminated concussed from control athletes at 6 hours postconcussion with an area under the receiver operating characteristic curve of 0.79 for IL-6 and 0.79 for IL-1RA. Furthermore, IL-6 levels at 6 hours significantly correlated with symptom duration, “with a 1-unit increase in natural log-transformed IL-6 associated with 39% lower hazard of symptom recovery,” the researchers reported.
The extent to which these results generalize to females, youth athletes, or athletes who develop postconcussion syndrome is unclear, and larger studies may be needed to adequately assess inflammatory markers as clinical biomarkers of sport-related concussion, the authors noted.
“Eventually, these results may help us better understand the relationship between injury and inflammation and potentially lead to new treatments,” Dr. Meier said.
The research was supported by the U.S. Department of Defense, National Institute of Neurological Disorders and Stroke, National Institute of General Medical Sciences, National Institute of Mental Health, and the National Center for Advancing Translational Sciences. The authors had no relevant disclosures.
SOURCE: Nitta ME et al. Neurology. 2019 Jul 3. doi: 10.1212/WNL.0000000000007864.
FROM NEUROLOGY
Key clinical point: Serum biomarkers of inflammation may help identify which athletes will take longer to recover after a sport-related concussion.
Major finding: IL-6 and IL-1RA significantly discriminated concussed from control athletes at 6 hours postconcussion with an area under the receiver operating characteristic curve of 0.79 for IL-6 and 0.79 for IL-1RA. Furthermore, IL-6 levels at 6 hours significantly correlated with symptom duration.
Study details: A prospective cohort study of high school and college football players. The analyses included 41 concussed athletes and 43 matched control athletes with an average age of about 18 years.
Disclosures: The research was supported by the U.S. Department of Defense, National Institute of Neurological Disorders and Stroke, National Institute of General Medical Sciences, National Institute of Mental Health, and the National Center for Advancing Translational Sciences. The authors had no relevant disclosures.
Source: Nitta ME et al. Neurology. 2019 Jul 3. doi: 10.1212/WNL.0000000000007864.