User login
Molecule accelerates recovery after BMT

Photo by Chad McNeeley
A small molecule may be able to accelerate cell recovery in bone marrow transplant (BMT) recipients and patients with liver or colon disease, researchers believe.
The molecule, SW033291, inhibits 15-PGDH, a prostaglandin-degrading enzyme that regulates tissue regeneration in multiple organs.
SW033291 accelerated hematopoietic recovery in mice that received BMTs and promoted tissue regeneration in mice with liver or colon injuries.
“We propose that SW033291 will be useful in accelerating recovery of bone marrow cells following a bone marrow transplant and may also be a treatment for colitis,” said James Willson, MD, of the University of Texas Southwestern Medical Center in Dallas.
He and his colleagues described their work with SW033291 in Science.
To examine the effects of inhibiting 15-PGDH on the bone marrow, the researchers conducted experiments with 15-PGDH-knockout mice and SW033291-treated mice, comparing them to control mice.
The team saw a 43% increase in neutrophil counts and a 39% increase in bone marrow Sca-1+ C-kit+ Lin– (SKL) cells in 15-PGDH knockout compared to wild-type mice. There were no significant differences in counts of other peripheral blood cells, bone marrow cellularity, or counts of bone marrow Sca-1+ C-kit+ Lin– CD48– CD150+ (SLAM) cells.
SW033291-treated mice had double the peripheral neutrophil counts of controls, a 65% increase in marrow SKL cells, and a 71% increase in marrow SLAM cells.
Results of additional experiments indicated that SW033291 works by increasing PGE2 levels in the bone marrow, and PGE2 functions through the EP2 and EP4 receptors to induce expression of CXCL12 and SCF.
The researchers also tested whether SW033291 could increase the bone marrow’s ability to attract and support new hematopoietic stem cells after BMT in mice. They found that BMT recipients treated with SW033291 had a 2- to 3-fold increase in the number of donor cells that homed to their bone marrow, compared to vehicle-treated BMT recipients.
The researchers said this SW033291-induced homing of transplanted bone marrow cells was driven, at least in part, by the induction of CXCL12 expression in CD45– nonmyeloid cells that were already resident in the bone marrow of recipient mice.
These results suggest 15-PGDH inhibition causes an increase in bone marrow PGE2, which induces the expression of bone marrow CXCL12 and SCF, and these cytokines alter the bone marrow microenvironment to better support the homing of transplanted cells.
The researchers also evaluated whether 15-PGDH inhibition promotes hematopoietic recovery after BMT. They studied lethally irradiated mice that received 200,000 strain-matched donor bone marrow cells, which were insufficient to reconstitute hematopoiesis in the mice.
When the mice were treated with SW033291, they survived for more than 30 days. All control mice, on the other hand, died between days 6 and 14.
For the last of their BMT experiments, the researchers examined the effect of SW033291 on mice transplanted with 500,000 bone marrow cells.
All SW033291-treated mice and 63% of control mice survived for 30 days, which allowed the team to compare hematopoietic recovery between the two groups. They found that SW033291 significantly accelerated the recovery of neutrophils, platelets, and red blood cells.
Experiments in mice with liver or colon injuries suggested that SW033291 can aid recovery in these models as well. ![]()

Photo by Chad McNeeley
A small molecule may be able to accelerate cell recovery in bone marrow transplant (BMT) recipients and patients with liver or colon disease, researchers believe.
The molecule, SW033291, inhibits 15-PGDH, a prostaglandin-degrading enzyme that regulates tissue regeneration in multiple organs.
SW033291 accelerated hematopoietic recovery in mice that received BMTs and promoted tissue regeneration in mice with liver or colon injuries.
“We propose that SW033291 will be useful in accelerating recovery of bone marrow cells following a bone marrow transplant and may also be a treatment for colitis,” said James Willson, MD, of the University of Texas Southwestern Medical Center in Dallas.
He and his colleagues described their work with SW033291 in Science.
To examine the effects of inhibiting 15-PGDH on the bone marrow, the researchers conducted experiments with 15-PGDH-knockout mice and SW033291-treated mice, comparing them to control mice.
The team saw a 43% increase in neutrophil counts and a 39% increase in bone marrow Sca-1+ C-kit+ Lin– (SKL) cells in 15-PGDH knockout compared to wild-type mice. There were no significant differences in counts of other peripheral blood cells, bone marrow cellularity, or counts of bone marrow Sca-1+ C-kit+ Lin– CD48– CD150+ (SLAM) cells.
SW033291-treated mice had double the peripheral neutrophil counts of controls, a 65% increase in marrow SKL cells, and a 71% increase in marrow SLAM cells.
Results of additional experiments indicated that SW033291 works by increasing PGE2 levels in the bone marrow, and PGE2 functions through the EP2 and EP4 receptors to induce expression of CXCL12 and SCF.
The researchers also tested whether SW033291 could increase the bone marrow’s ability to attract and support new hematopoietic stem cells after BMT in mice. They found that BMT recipients treated with SW033291 had a 2- to 3-fold increase in the number of donor cells that homed to their bone marrow, compared to vehicle-treated BMT recipients.
The researchers said this SW033291-induced homing of transplanted bone marrow cells was driven, at least in part, by the induction of CXCL12 expression in CD45– nonmyeloid cells that were already resident in the bone marrow of recipient mice.
These results suggest 15-PGDH inhibition causes an increase in bone marrow PGE2, which induces the expression of bone marrow CXCL12 and SCF, and these cytokines alter the bone marrow microenvironment to better support the homing of transplanted cells.
The researchers also evaluated whether 15-PGDH inhibition promotes hematopoietic recovery after BMT. They studied lethally irradiated mice that received 200,000 strain-matched donor bone marrow cells, which were insufficient to reconstitute hematopoiesis in the mice.
When the mice were treated with SW033291, they survived for more than 30 days. All control mice, on the other hand, died between days 6 and 14.
For the last of their BMT experiments, the researchers examined the effect of SW033291 on mice transplanted with 500,000 bone marrow cells.
All SW033291-treated mice and 63% of control mice survived for 30 days, which allowed the team to compare hematopoietic recovery between the two groups. They found that SW033291 significantly accelerated the recovery of neutrophils, platelets, and red blood cells.
Experiments in mice with liver or colon injuries suggested that SW033291 can aid recovery in these models as well. ![]()

Photo by Chad McNeeley
A small molecule may be able to accelerate cell recovery in bone marrow transplant (BMT) recipients and patients with liver or colon disease, researchers believe.
The molecule, SW033291, inhibits 15-PGDH, a prostaglandin-degrading enzyme that regulates tissue regeneration in multiple organs.
SW033291 accelerated hematopoietic recovery in mice that received BMTs and promoted tissue regeneration in mice with liver or colon injuries.
“We propose that SW033291 will be useful in accelerating recovery of bone marrow cells following a bone marrow transplant and may also be a treatment for colitis,” said James Willson, MD, of the University of Texas Southwestern Medical Center in Dallas.
He and his colleagues described their work with SW033291 in Science.
To examine the effects of inhibiting 15-PGDH on the bone marrow, the researchers conducted experiments with 15-PGDH-knockout mice and SW033291-treated mice, comparing them to control mice.
The team saw a 43% increase in neutrophil counts and a 39% increase in bone marrow Sca-1+ C-kit+ Lin– (SKL) cells in 15-PGDH knockout compared to wild-type mice. There were no significant differences in counts of other peripheral blood cells, bone marrow cellularity, or counts of bone marrow Sca-1+ C-kit+ Lin– CD48– CD150+ (SLAM) cells.
SW033291-treated mice had double the peripheral neutrophil counts of controls, a 65% increase in marrow SKL cells, and a 71% increase in marrow SLAM cells.
Results of additional experiments indicated that SW033291 works by increasing PGE2 levels in the bone marrow, and PGE2 functions through the EP2 and EP4 receptors to induce expression of CXCL12 and SCF.
The researchers also tested whether SW033291 could increase the bone marrow’s ability to attract and support new hematopoietic stem cells after BMT in mice. They found that BMT recipients treated with SW033291 had a 2- to 3-fold increase in the number of donor cells that homed to their bone marrow, compared to vehicle-treated BMT recipients.
The researchers said this SW033291-induced homing of transplanted bone marrow cells was driven, at least in part, by the induction of CXCL12 expression in CD45– nonmyeloid cells that were already resident in the bone marrow of recipient mice.
These results suggest 15-PGDH inhibition causes an increase in bone marrow PGE2, which induces the expression of bone marrow CXCL12 and SCF, and these cytokines alter the bone marrow microenvironment to better support the homing of transplanted cells.
The researchers also evaluated whether 15-PGDH inhibition promotes hematopoietic recovery after BMT. They studied lethally irradiated mice that received 200,000 strain-matched donor bone marrow cells, which were insufficient to reconstitute hematopoiesis in the mice.
When the mice were treated with SW033291, they survived for more than 30 days. All control mice, on the other hand, died between days 6 and 14.
For the last of their BMT experiments, the researchers examined the effect of SW033291 on mice transplanted with 500,000 bone marrow cells.
All SW033291-treated mice and 63% of control mice survived for 30 days, which allowed the team to compare hematopoietic recovery between the two groups. They found that SW033291 significantly accelerated the recovery of neutrophils, platelets, and red blood cells.
Experiments in mice with liver or colon injuries suggested that SW033291 can aid recovery in these models as well. ![]()
Establishing cause of death in HSCT recipients

With a new study, researchers hope to establish definitions for specific causes of death in patients who undergo allogeneic hematopoietic stem cell transplant (HSCT).
The group noted that scientists conducting clinical trials commonly use committees to review and define endpoints.
However, investigators conducting genome-wide association studies rarely do, relying instead on center-reported outcomes, which are variable.
“It is important that we accurately define outcomes in these types of genomic studies as precisely as possible,” said Lara Sucheston-Campbell, PhD, of Roswell Park Cancer Institute in Buffalo, New York.
To that end, she and her colleagues convened a consensus panel to review specific causes of death in HSCT recipients. The panel evaluated outcome data for 1484 patients who had been treated for acute leukemia or myelodysplasia at 1 of 11 US transplant centers and died within a year of undergoing HSCT.
Dr Sucheston-Campbell and her colleagues reported the results of this evaluation in Biology of Blood and Marrow Transplantation.
In the cases where the transplant center reported disease-related mortality, the researchers found almost perfect agreement between the consensus panel and the transplant center, in terms of how those deaths were classified. The panel agreed with more than 99% of deaths that were reported as disease-related.
There was less agreement for transplant-related mortality, however. The panel agreed with about 80% of deaths reported to be transplant-related.
And the level of agreement/discordance varied depending on the specific cause of death. For example, the panel agreed with transplant centers on most of the deaths that were reportedly caused by graft-vs-host disease.
But the panel reclassified many of the deaths that reportedly resulted from organ failure, saying these deaths should be considered disease-related, a result of graft-vs-host disease, infection-related, or due to “other” causes.
These results indicate that transplant-related mortality needs to be better defined, the researchers said. They believe this study provides a mechanism for prioritizing those HSCT cases that should be reviewed.
“We need to make sure that patients who experienced similar clinical events after a transplant were consistently defined regardless of where they were treated,” said study author Theresa Hahn, PhD, also of Roswell Park Cancer Center.
“This is a difficult topic to consider, but we can’t make progress to improve transplant outcomes without these discussions.” ![]()

With a new study, researchers hope to establish definitions for specific causes of death in patients who undergo allogeneic hematopoietic stem cell transplant (HSCT).
The group noted that scientists conducting clinical trials commonly use committees to review and define endpoints.
However, investigators conducting genome-wide association studies rarely do, relying instead on center-reported outcomes, which are variable.
“It is important that we accurately define outcomes in these types of genomic studies as precisely as possible,” said Lara Sucheston-Campbell, PhD, of Roswell Park Cancer Institute in Buffalo, New York.
To that end, she and her colleagues convened a consensus panel to review specific causes of death in HSCT recipients. The panel evaluated outcome data for 1484 patients who had been treated for acute leukemia or myelodysplasia at 1 of 11 US transplant centers and died within a year of undergoing HSCT.
Dr Sucheston-Campbell and her colleagues reported the results of this evaluation in Biology of Blood and Marrow Transplantation.
In the cases where the transplant center reported disease-related mortality, the researchers found almost perfect agreement between the consensus panel and the transplant center, in terms of how those deaths were classified. The panel agreed with more than 99% of deaths that were reported as disease-related.
There was less agreement for transplant-related mortality, however. The panel agreed with about 80% of deaths reported to be transplant-related.
And the level of agreement/discordance varied depending on the specific cause of death. For example, the panel agreed with transplant centers on most of the deaths that were reportedly caused by graft-vs-host disease.
But the panel reclassified many of the deaths that reportedly resulted from organ failure, saying these deaths should be considered disease-related, a result of graft-vs-host disease, infection-related, or due to “other” causes.
These results indicate that transplant-related mortality needs to be better defined, the researchers said. They believe this study provides a mechanism for prioritizing those HSCT cases that should be reviewed.
“We need to make sure that patients who experienced similar clinical events after a transplant were consistently defined regardless of where they were treated,” said study author Theresa Hahn, PhD, also of Roswell Park Cancer Center.
“This is a difficult topic to consider, but we can’t make progress to improve transplant outcomes without these discussions.” ![]()

With a new study, researchers hope to establish definitions for specific causes of death in patients who undergo allogeneic hematopoietic stem cell transplant (HSCT).
The group noted that scientists conducting clinical trials commonly use committees to review and define endpoints.
However, investigators conducting genome-wide association studies rarely do, relying instead on center-reported outcomes, which are variable.
“It is important that we accurately define outcomes in these types of genomic studies as precisely as possible,” said Lara Sucheston-Campbell, PhD, of Roswell Park Cancer Institute in Buffalo, New York.
To that end, she and her colleagues convened a consensus panel to review specific causes of death in HSCT recipients. The panel evaluated outcome data for 1484 patients who had been treated for acute leukemia or myelodysplasia at 1 of 11 US transplant centers and died within a year of undergoing HSCT.
Dr Sucheston-Campbell and her colleagues reported the results of this evaluation in Biology of Blood and Marrow Transplantation.
In the cases where the transplant center reported disease-related mortality, the researchers found almost perfect agreement between the consensus panel and the transplant center, in terms of how those deaths were classified. The panel agreed with more than 99% of deaths that were reported as disease-related.
There was less agreement for transplant-related mortality, however. The panel agreed with about 80% of deaths reported to be transplant-related.
And the level of agreement/discordance varied depending on the specific cause of death. For example, the panel agreed with transplant centers on most of the deaths that were reportedly caused by graft-vs-host disease.
But the panel reclassified many of the deaths that reportedly resulted from organ failure, saying these deaths should be considered disease-related, a result of graft-vs-host disease, infection-related, or due to “other” causes.
These results indicate that transplant-related mortality needs to be better defined, the researchers said. They believe this study provides a mechanism for prioritizing those HSCT cases that should be reviewed.
“We need to make sure that patients who experienced similar clinical events after a transplant were consistently defined regardless of where they were treated,” said study author Theresa Hahn, PhD, also of Roswell Park Cancer Center.
“This is a difficult topic to consider, but we can’t make progress to improve transplant outcomes without these discussions.” ![]()
Harnessing immune defense to treat Candida infection
An upset in the body’s natural balance of gut bacteria that may lead to life-threatening bloodstream infections can be reversed by enhancing an
immune response, according to research published in Nature Medicine.
Researchers found that a transcription factor known as HIF-1α works with LL-37, a naturally occurring antibiotic, to kill the infection-causing fungi Candida albicans.
And this response can be enhanced with a drug called L-mimosine.
The researchers noted that Candida albicans can be lethal if it invades the bloodstream from the gut. And stem cell transplant recipients and immunosuppressed cancer patients have a high risk for this type of infection.
“For a cancer patient with a Candida bloodstream infection, the fatality rate is about 30%, [and] Candida is the number 1 fungal pathogen,” said study author Andrew Koh, MD, of the University of Texas Southwestern Medical Center in Dallas.
With that in mind, he and his colleagues set out to determine how the body’s natural immune defense system might be enhanced to fight a Candida infection. By studying how mice infected with Candida responded in different scenarios, the team found their answer.
“The commensal bacteria stimulate gut tissue to make a transcription factor and a natural antibiotic, which then kills the Candida fungus,” Dr Koh explained.
“When we gave the mice a pharmacologic agent called L-mimosine that stimulates the transcription factor, the agent knocked down Candida 100-fold, which translated into a 50% reduction in mortality from invasive Candida infection.”
Specifically, the researchers found that enhancing the transcription factor HIF-1α with L-mimosine led to increased production of the natural antibiotic peptide LL-37, which, in turn, killed the fungi. L-mimosine is a natural product derived from seeds of the koa haole tree that is known to boost HIF-1α activity.
The study also suggested that certain gut bacteria—Clostridial Firmicutes and Bacteroidetes—may be important in producing short-chain fatty acids that help fight infection.
The researchers said more work is needed to pinpoint the optimal method of inducing the body’s gut defense system, whether through use of an agent like L-mimosine or by administering short-chain fatty acids such as vinegar.
“Can we modulate the gut system to maintain balance so that it never gets to the point of pathogens invading the bloodstream?” Dr Koh asked. “Boosting [gastrointestinal] mucosal immune effectors to reduce fungal burden may be the key to tipping the balance back toward normal and preventing invasive fungal disease.” ![]()
An upset in the body’s natural balance of gut bacteria that may lead to life-threatening bloodstream infections can be reversed by enhancing an
immune response, according to research published in Nature Medicine.
Researchers found that a transcription factor known as HIF-1α works with LL-37, a naturally occurring antibiotic, to kill the infection-causing fungi Candida albicans.
And this response can be enhanced with a drug called L-mimosine.
The researchers noted that Candida albicans can be lethal if it invades the bloodstream from the gut. And stem cell transplant recipients and immunosuppressed cancer patients have a high risk for this type of infection.
“For a cancer patient with a Candida bloodstream infection, the fatality rate is about 30%, [and] Candida is the number 1 fungal pathogen,” said study author Andrew Koh, MD, of the University of Texas Southwestern Medical Center in Dallas.
With that in mind, he and his colleagues set out to determine how the body’s natural immune defense system might be enhanced to fight a Candida infection. By studying how mice infected with Candida responded in different scenarios, the team found their answer.
“The commensal bacteria stimulate gut tissue to make a transcription factor and a natural antibiotic, which then kills the Candida fungus,” Dr Koh explained.
“When we gave the mice a pharmacologic agent called L-mimosine that stimulates the transcription factor, the agent knocked down Candida 100-fold, which translated into a 50% reduction in mortality from invasive Candida infection.”
Specifically, the researchers found that enhancing the transcription factor HIF-1α with L-mimosine led to increased production of the natural antibiotic peptide LL-37, which, in turn, killed the fungi. L-mimosine is a natural product derived from seeds of the koa haole tree that is known to boost HIF-1α activity.
The study also suggested that certain gut bacteria—Clostridial Firmicutes and Bacteroidetes—may be important in producing short-chain fatty acids that help fight infection.
The researchers said more work is needed to pinpoint the optimal method of inducing the body’s gut defense system, whether through use of an agent like L-mimosine or by administering short-chain fatty acids such as vinegar.
“Can we modulate the gut system to maintain balance so that it never gets to the point of pathogens invading the bloodstream?” Dr Koh asked. “Boosting [gastrointestinal] mucosal immune effectors to reduce fungal burden may be the key to tipping the balance back toward normal and preventing invasive fungal disease.” ![]()
An upset in the body’s natural balance of gut bacteria that may lead to life-threatening bloodstream infections can be reversed by enhancing an
immune response, according to research published in Nature Medicine.
Researchers found that a transcription factor known as HIF-1α works with LL-37, a naturally occurring antibiotic, to kill the infection-causing fungi Candida albicans.
And this response can be enhanced with a drug called L-mimosine.
The researchers noted that Candida albicans can be lethal if it invades the bloodstream from the gut. And stem cell transplant recipients and immunosuppressed cancer patients have a high risk for this type of infection.
“For a cancer patient with a Candida bloodstream infection, the fatality rate is about 30%, [and] Candida is the number 1 fungal pathogen,” said study author Andrew Koh, MD, of the University of Texas Southwestern Medical Center in Dallas.
With that in mind, he and his colleagues set out to determine how the body’s natural immune defense system might be enhanced to fight a Candida infection. By studying how mice infected with Candida responded in different scenarios, the team found their answer.
“The commensal bacteria stimulate gut tissue to make a transcription factor and a natural antibiotic, which then kills the Candida fungus,” Dr Koh explained.
“When we gave the mice a pharmacologic agent called L-mimosine that stimulates the transcription factor, the agent knocked down Candida 100-fold, which translated into a 50% reduction in mortality from invasive Candida infection.”
Specifically, the researchers found that enhancing the transcription factor HIF-1α with L-mimosine led to increased production of the natural antibiotic peptide LL-37, which, in turn, killed the fungi. L-mimosine is a natural product derived from seeds of the koa haole tree that is known to boost HIF-1α activity.
The study also suggested that certain gut bacteria—Clostridial Firmicutes and Bacteroidetes—may be important in producing short-chain fatty acids that help fight infection.
The researchers said more work is needed to pinpoint the optimal method of inducing the body’s gut defense system, whether through use of an agent like L-mimosine or by administering short-chain fatty acids such as vinegar.
“Can we modulate the gut system to maintain balance so that it never gets to the point of pathogens invading the bloodstream?” Dr Koh asked. “Boosting [gastrointestinal] mucosal immune effectors to reduce fungal burden may be the key to tipping the balance back toward normal and preventing invasive fungal disease.” ![]()
Study suggests need for change in matching criteria

Photo by Chad McNeeley
A donor’s CD8 cell count can affect the outcome of hematopoietic stem cell transplant (HSCT) in older patients, according to a study published in the Journal of Clinical Oncology.
Older patients who received stem cells from unrelated donors with higher CD8 counts had a significantly lower risk of relapse and higher rate of
survival than patients who received grafts with lower CD8 counts, even if those grafts were from matched sibling donors.
This suggests that screening for donor T-cell characteristics could optimize donor selection and ultimately lead to more successful transplants in an older population, study investigators said.
“Developing better tools to identify ideal donors is an exciting prospect and fundamental to improving transplant outcomes,” said Ran Reshef, MD, of the Abramson Cancer Center at the University of Pennsylvania in Philadelphia.
“There may be suitable donors out there who are overlooked because they are considered a poorer match by today’s donor selection algorithms. Refining the screening method could greatly increase the chances of finding the most appropriate donor, one that will induce the most potent graft-vs-tumor response.”
For this study, Dr Reshef and his colleagues retrospectively evaluated associations between a graft’s T-cell dose and outcomes in 200 patients undergoing HSCT to treat acute myeloid leukemia, myelodysplastic syndrome, non-Hodgkin lymphoma, and other hematologic disorders.
The investigators looked specifically at CD4 and CD8 counts and found the number of CD8 cells in the graft had an impact on survival. They also found that high CD8 cell counts were much more common among young donors.
The 4-year overall survival rates were 59% for patients who received grafts from younger (<50 years), unrelated donors with high CD8 counts; 18% for those who received grafts from younger, unrelated donors with low CD8 counts; and 33% for patients who received grafts from older (>50 years), HLA-matched sibling donors.
In multivariable analysis, CD8 count was an independent predictor of relapse (adjusted hazard ratio [aHR]=0.43; P=0.009), relapse-free survival (aHR=0.50; P=0.006), and overall survival (aHR=0.57; P=0.04).
The investigators also assessed the effect of CD8 count on survival using a cutoff of 0.72 x 108 CD8 cells/kg. They found that patients with CD8 doses above this cutoff had significantly better relapse-free survival (P=0.005) and overall survival (P=0.007) rates than patients with CD8 doses below this cutoff.
These results suggest it would be better to use a younger, unrelated donor graft with a high CD8 cell count rather than an older sibling donor, the investigators said. However, this strategy should be tested in a prospective trial.
“This is a method deserving additional investigation,” Dr Reshef said, “which could refine the standardized matching system used by registries, such as Be the Match and others, and ultimately optimize the donor pool for older patients undergoing these transplants.” ![]()

Photo by Chad McNeeley
A donor’s CD8 cell count can affect the outcome of hematopoietic stem cell transplant (HSCT) in older patients, according to a study published in the Journal of Clinical Oncology.
Older patients who received stem cells from unrelated donors with higher CD8 counts had a significantly lower risk of relapse and higher rate of
survival than patients who received grafts with lower CD8 counts, even if those grafts were from matched sibling donors.
This suggests that screening for donor T-cell characteristics could optimize donor selection and ultimately lead to more successful transplants in an older population, study investigators said.
“Developing better tools to identify ideal donors is an exciting prospect and fundamental to improving transplant outcomes,” said Ran Reshef, MD, of the Abramson Cancer Center at the University of Pennsylvania in Philadelphia.
“There may be suitable donors out there who are overlooked because they are considered a poorer match by today’s donor selection algorithms. Refining the screening method could greatly increase the chances of finding the most appropriate donor, one that will induce the most potent graft-vs-tumor response.”
For this study, Dr Reshef and his colleagues retrospectively evaluated associations between a graft’s T-cell dose and outcomes in 200 patients undergoing HSCT to treat acute myeloid leukemia, myelodysplastic syndrome, non-Hodgkin lymphoma, and other hematologic disorders.
The investigators looked specifically at CD4 and CD8 counts and found the number of CD8 cells in the graft had an impact on survival. They also found that high CD8 cell counts were much more common among young donors.
The 4-year overall survival rates were 59% for patients who received grafts from younger (<50 years), unrelated donors with high CD8 counts; 18% for those who received grafts from younger, unrelated donors with low CD8 counts; and 33% for patients who received grafts from older (>50 years), HLA-matched sibling donors.
In multivariable analysis, CD8 count was an independent predictor of relapse (adjusted hazard ratio [aHR]=0.43; P=0.009), relapse-free survival (aHR=0.50; P=0.006), and overall survival (aHR=0.57; P=0.04).
The investigators also assessed the effect of CD8 count on survival using a cutoff of 0.72 x 108 CD8 cells/kg. They found that patients with CD8 doses above this cutoff had significantly better relapse-free survival (P=0.005) and overall survival (P=0.007) rates than patients with CD8 doses below this cutoff.
These results suggest it would be better to use a younger, unrelated donor graft with a high CD8 cell count rather than an older sibling donor, the investigators said. However, this strategy should be tested in a prospective trial.
“This is a method deserving additional investigation,” Dr Reshef said, “which could refine the standardized matching system used by registries, such as Be the Match and others, and ultimately optimize the donor pool for older patients undergoing these transplants.” ![]()

Photo by Chad McNeeley
A donor’s CD8 cell count can affect the outcome of hematopoietic stem cell transplant (HSCT) in older patients, according to a study published in the Journal of Clinical Oncology.
Older patients who received stem cells from unrelated donors with higher CD8 counts had a significantly lower risk of relapse and higher rate of
survival than patients who received grafts with lower CD8 counts, even if those grafts were from matched sibling donors.
This suggests that screening for donor T-cell characteristics could optimize donor selection and ultimately lead to more successful transplants in an older population, study investigators said.
“Developing better tools to identify ideal donors is an exciting prospect and fundamental to improving transplant outcomes,” said Ran Reshef, MD, of the Abramson Cancer Center at the University of Pennsylvania in Philadelphia.
“There may be suitable donors out there who are overlooked because they are considered a poorer match by today’s donor selection algorithms. Refining the screening method could greatly increase the chances of finding the most appropriate donor, one that will induce the most potent graft-vs-tumor response.”
For this study, Dr Reshef and his colleagues retrospectively evaluated associations between a graft’s T-cell dose and outcomes in 200 patients undergoing HSCT to treat acute myeloid leukemia, myelodysplastic syndrome, non-Hodgkin lymphoma, and other hematologic disorders.
The investigators looked specifically at CD4 and CD8 counts and found the number of CD8 cells in the graft had an impact on survival. They also found that high CD8 cell counts were much more common among young donors.
The 4-year overall survival rates were 59% for patients who received grafts from younger (<50 years), unrelated donors with high CD8 counts; 18% for those who received grafts from younger, unrelated donors with low CD8 counts; and 33% for patients who received grafts from older (>50 years), HLA-matched sibling donors.
In multivariable analysis, CD8 count was an independent predictor of relapse (adjusted hazard ratio [aHR]=0.43; P=0.009), relapse-free survival (aHR=0.50; P=0.006), and overall survival (aHR=0.57; P=0.04).
The investigators also assessed the effect of CD8 count on survival using a cutoff of 0.72 x 108 CD8 cells/kg. They found that patients with CD8 doses above this cutoff had significantly better relapse-free survival (P=0.005) and overall survival (P=0.007) rates than patients with CD8 doses below this cutoff.
These results suggest it would be better to use a younger, unrelated donor graft with a high CD8 cell count rather than an older sibling donor, the investigators said. However, this strategy should be tested in a prospective trial.
“This is a method deserving additional investigation,” Dr Reshef said, “which could refine the standardized matching system used by registries, such as Be the Match and others, and ultimately optimize the donor pool for older patients undergoing these transplants.” ![]()
Lymphocyte recovery linked to outcome of HSCT

Photo courtesy of VCU
Massey Cancer Center
Results of a retrospective study suggest lymphocyte recovery is associated with outcomes after allogeneic hematopoietic stem cell transplant (HSCT).
Researchers found that, after transplant, lymphocyte recovery occurred in 1 of 3 general patterns.
And these patterns were associated with the rate of survival, relapse, and graft-vs-host disease (GVHD), as well as the need for further donor immune cell infusions to treat the patients’ disease.
Amir Toor, MD, of VCU Massey Cancer Center in Richmond, Virginia, and his colleagues reported these findings in Biology of Blood & Marrow Transplantation.
The team had examined lymphocyte recovery and clinical outcome data from a phase 2 trial (NCT00709592) of 41 patients who received an HSCT from a related or unrelated donor.
As part of the trial protocol, the patients underwent low-dose radiation therapy and received 1 of 2 different doses of anti-thymocyte globulin as GVHD prophylaxis.
The researchers found that, after transplant, lymphocyte recovery followed 1 of 3 general patterns that correlated with patient outcomes.
“We began considering lymphocyte reconstitution following stem cell transplantation as similar to population growth models,” Dr Toor explained. “So we graphed the lymphocyte counts of our patients at various times following their transplant as a logistic function and observed distinct patterns that correlated with clinical outcomes.”
Patients in group A experienced fast, early lymphoid expansion, culminating in a high absolute lymphoid count (ALC) within 2 months of HSCT. Group B experienced a slower, but steady, lymphoid expansion that peaked much later than group A with a lower ALC. Group C experienced very poor lymphocyte recovery that demonstrated an early, but brief, lymphoid expansion with a very low ALC.
Group B had the best survival rate—86%—compared to 67% in group A and 30% in group C. Relapse rates between groups A and B were similar, at 33% and 29%, respectively, while group C experienced a 90% relapse rate.
GVHD occurred in 67% of patients in group A, 43% in group B, and 10% in group C. And adoptive immunotherapy with donor cell infusions was required for 13% of patients in group A, 21% in group B, and 70% in group C.
“Our goal is to use this data to develop models that can predict complications from stem cell transplantation,” Dr Toor said. “Then, we may be able to intervene at key points in time with appropriate clinical treatments that will make the most positive impact on patients’ outcomes.” ![]()

Photo courtesy of VCU
Massey Cancer Center
Results of a retrospective study suggest lymphocyte recovery is associated with outcomes after allogeneic hematopoietic stem cell transplant (HSCT).
Researchers found that, after transplant, lymphocyte recovery occurred in 1 of 3 general patterns.
And these patterns were associated with the rate of survival, relapse, and graft-vs-host disease (GVHD), as well as the need for further donor immune cell infusions to treat the patients’ disease.
Amir Toor, MD, of VCU Massey Cancer Center in Richmond, Virginia, and his colleagues reported these findings in Biology of Blood & Marrow Transplantation.
The team had examined lymphocyte recovery and clinical outcome data from a phase 2 trial (NCT00709592) of 41 patients who received an HSCT from a related or unrelated donor.
As part of the trial protocol, the patients underwent low-dose radiation therapy and received 1 of 2 different doses of anti-thymocyte globulin as GVHD prophylaxis.
The researchers found that, after transplant, lymphocyte recovery followed 1 of 3 general patterns that correlated with patient outcomes.
“We began considering lymphocyte reconstitution following stem cell transplantation as similar to population growth models,” Dr Toor explained. “So we graphed the lymphocyte counts of our patients at various times following their transplant as a logistic function and observed distinct patterns that correlated with clinical outcomes.”
Patients in group A experienced fast, early lymphoid expansion, culminating in a high absolute lymphoid count (ALC) within 2 months of HSCT. Group B experienced a slower, but steady, lymphoid expansion that peaked much later than group A with a lower ALC. Group C experienced very poor lymphocyte recovery that demonstrated an early, but brief, lymphoid expansion with a very low ALC.
Group B had the best survival rate—86%—compared to 67% in group A and 30% in group C. Relapse rates between groups A and B were similar, at 33% and 29%, respectively, while group C experienced a 90% relapse rate.
GVHD occurred in 67% of patients in group A, 43% in group B, and 10% in group C. And adoptive immunotherapy with donor cell infusions was required for 13% of patients in group A, 21% in group B, and 70% in group C.
“Our goal is to use this data to develop models that can predict complications from stem cell transplantation,” Dr Toor said. “Then, we may be able to intervene at key points in time with appropriate clinical treatments that will make the most positive impact on patients’ outcomes.” ![]()

Photo courtesy of VCU
Massey Cancer Center
Results of a retrospective study suggest lymphocyte recovery is associated with outcomes after allogeneic hematopoietic stem cell transplant (HSCT).
Researchers found that, after transplant, lymphocyte recovery occurred in 1 of 3 general patterns.
And these patterns were associated with the rate of survival, relapse, and graft-vs-host disease (GVHD), as well as the need for further donor immune cell infusions to treat the patients’ disease.
Amir Toor, MD, of VCU Massey Cancer Center in Richmond, Virginia, and his colleagues reported these findings in Biology of Blood & Marrow Transplantation.
The team had examined lymphocyte recovery and clinical outcome data from a phase 2 trial (NCT00709592) of 41 patients who received an HSCT from a related or unrelated donor.
As part of the trial protocol, the patients underwent low-dose radiation therapy and received 1 of 2 different doses of anti-thymocyte globulin as GVHD prophylaxis.
The researchers found that, after transplant, lymphocyte recovery followed 1 of 3 general patterns that correlated with patient outcomes.
“We began considering lymphocyte reconstitution following stem cell transplantation as similar to population growth models,” Dr Toor explained. “So we graphed the lymphocyte counts of our patients at various times following their transplant as a logistic function and observed distinct patterns that correlated with clinical outcomes.”
Patients in group A experienced fast, early lymphoid expansion, culminating in a high absolute lymphoid count (ALC) within 2 months of HSCT. Group B experienced a slower, but steady, lymphoid expansion that peaked much later than group A with a lower ALC. Group C experienced very poor lymphocyte recovery that demonstrated an early, but brief, lymphoid expansion with a very low ALC.
Group B had the best survival rate—86%—compared to 67% in group A and 30% in group C. Relapse rates between groups A and B were similar, at 33% and 29%, respectively, while group C experienced a 90% relapse rate.
GVHD occurred in 67% of patients in group A, 43% in group B, and 10% in group C. And adoptive immunotherapy with donor cell infusions was required for 13% of patients in group A, 21% in group B, and 70% in group C.
“Our goal is to use this data to develop models that can predict complications from stem cell transplantation,” Dr Toor said. “Then, we may be able to intervene at key points in time with appropriate clinical treatments that will make the most positive impact on patients’ outcomes.” ![]()
No survival difference with allo- or auto-SCT in PTCL

© ASCO/Max Gersh
CHICAGO—Allogeneic and autologous transplants produce similar survival rates when used as first-line therapy in younger patients with peripheral
T-cell lymphoma (PTCL), according to interim results of the AATT trial.
The study also showed that deaths among patients who received autologous stem cell transplants (auto-SCTs) were a result of relapse and salvage treatment, while deaths among allogeneic SCT (allo-SCT) recipients were transplant-related.
Norbert Schmitz, MD, PhD, of Asklepios Hospital St. Georg in Hamburg, Germany, presented these findings at the 2015 ASCO Annual Meeting (abstract 8507*).
Dr Schmitz noted that only previous study comparing auto-SCT with allo-SCT as first-line therapy in PTCL was not designed or powered to evaluate the differences between the transplant types.
So he and his colleagues conducted the AATT trial to determine the differences. The team hypothesized that allo-SCT would improve 3-year event-free survival from 35% to 60%, given an α of 5% and a power of 80%. They needed 140 patients to prove or disprove this theory.
Ultimately, the investigators enrolled 104 patients and performed an interim analysis when 58 patients were evaluable for response.
Of the 58 patients, 30 were randomized to the auto-SCT arm and 28 to the allo-SCT arm. Baseline characteristics were similar between the arms, including patients’ median ages (49 and 50, respectively), the proportion of patients with stage III/IV disease (87% and 93%), and the proportion with ECOG status greater than 1 (23% and 18%).
Most patients in both arms had PTCL not otherwise specified (36% in the auto-SCT arm and 50% in the allo-SCT arm). Other subtypes included angioimmunoblastic T-cell lymphoma (23% and 32%, respectively), ALK-negative anaplastic large-cell lymphoma (20% and 4%), and “other” PTCLs (20% and 8%). The other PTCLs were NK/T-cell lymphoma, intestinal T/NK-cell lymphoma, hepatosplenic γδ lymphoma, and subcutaneous panniculitis-like PTCL.
Treatment characteristics
Before undergoing transplant, patients in both arms received treatment with CHOEP (cyclophosphamide, doxorubicin, etoposide, vincristine, and prednisone) on days 1, 15, 29, and 43. If they experienced a complete response (CR), partial response, or no change, patients received DHAP (dexamethasone, cytarabine, and cisplatin) on day 64.
Patients in the auto-SCT arm received BEAM (carmustine, etoposide, cytarabine, and melphalan) prior to transplant. And patients in the allo-SCT arm received FBC (fludarabine, busulfan, and cyclophosphamide).
Overall, 36 patients (62%) completed treatment per protocol, 19 in the auto-SCT arm and 17 in the allo-SCT arm. Thirty-eight percent of all patients could not proceed to transplant per protocol, mostly because of early lymphoma progression.
Response and survival
The researchers observed CRs/unconfirmed CRs (CRus) in 33% (n=10) of patients in the auto-SCT arm and 39% (n=11) in the allo-SCT arm. CR/CRus and progressive disease within 2 months occurred in 3% (n=1) and 4% (n=1) of patients, respectively.
Partial responses were seen in 17% (n=5) of patients in the auto-SCT arm and 7% (n=2) in the allo-SCT arm. There was no change in 7% (n=2) and 0% of patients, respectively. And responses were unknown in 7% (n=2) of patients in the auto-SCT arm.
Progressive disease occurred in 33% (n=10) of patients in the auto-SCT arm and 36% (n=10) in the allo-SCT arm. And treatment-related death occurred in 0% (n=0) and 14% (n=4), respectively.
At the interim analysis, there was no significant difference between the treatment arms with regard to event-free survival (P=0.963) or overall survival (P=0.174).
“At that time, the decision was made to stop the study,” Dr Schmitz said.
He explained that a conditional power analysis showed a low probability that the primary endpoint—a 25% improvement in event-free survival with allo-SCT—could still be met. So the data safety monitoring board decided to stop enrollment.
An updated analysis, performed at a median observation time of 26 months, showed there was still no significant difference in overall survival between the treatment arms (P=0.362).
Cause of death
In the intent-to-treat population—30 patients in the auto-SCT arm and 28 in the allo-SCT arm—there were 16 lymphoma-related deaths, 10 in the auto-SCT arm and 6 in the allo-SCT arm.
There were 6 deaths related to study treatment (4 early and 2 late), all in the allo-SCT arm. One patient in the allo-SCT arm died of post-transplant lymphoproliferative disorder, and 1 patient in the same arm died of hemorrhage after salvage. One patient in each arm died as a result of salvage treatment.
Dr Schmitz and his colleagues also looked at the cause of death among patients who received a transplant—19 in the auto-SCT arm and 17 in the allo-SCT arm.
After SCT, there were 7 deaths in each arm. In the auto-SCT arm, there were 6 lymphoma-related deaths and 1 death related to salvage treatment. In the allo-SCT arm, there were 7 cases of non-relapse-related mortality, including 1 patient with post-transplant lymphoproliferative disorder.
“There certainly seems to be a [graft-vs-lymphoma] effect of allo-transplant in T-cell lymphoma that is, unfortunately, in some way, counterbalanced by high transplant-related mortality,” Dr Schmitz said.
He added that results of a final analysis of the 104 patients enrolled on this study should be available in 2017. ![]()
*Information in the abstract differs from that presented at the meeting.

© ASCO/Max Gersh
CHICAGO—Allogeneic and autologous transplants produce similar survival rates when used as first-line therapy in younger patients with peripheral
T-cell lymphoma (PTCL), according to interim results of the AATT trial.
The study also showed that deaths among patients who received autologous stem cell transplants (auto-SCTs) were a result of relapse and salvage treatment, while deaths among allogeneic SCT (allo-SCT) recipients were transplant-related.
Norbert Schmitz, MD, PhD, of Asklepios Hospital St. Georg in Hamburg, Germany, presented these findings at the 2015 ASCO Annual Meeting (abstract 8507*).
Dr Schmitz noted that only previous study comparing auto-SCT with allo-SCT as first-line therapy in PTCL was not designed or powered to evaluate the differences between the transplant types.
So he and his colleagues conducted the AATT trial to determine the differences. The team hypothesized that allo-SCT would improve 3-year event-free survival from 35% to 60%, given an α of 5% and a power of 80%. They needed 140 patients to prove or disprove this theory.
Ultimately, the investigators enrolled 104 patients and performed an interim analysis when 58 patients were evaluable for response.
Of the 58 patients, 30 were randomized to the auto-SCT arm and 28 to the allo-SCT arm. Baseline characteristics were similar between the arms, including patients’ median ages (49 and 50, respectively), the proportion of patients with stage III/IV disease (87% and 93%), and the proportion with ECOG status greater than 1 (23% and 18%).
Most patients in both arms had PTCL not otherwise specified (36% in the auto-SCT arm and 50% in the allo-SCT arm). Other subtypes included angioimmunoblastic T-cell lymphoma (23% and 32%, respectively), ALK-negative anaplastic large-cell lymphoma (20% and 4%), and “other” PTCLs (20% and 8%). The other PTCLs were NK/T-cell lymphoma, intestinal T/NK-cell lymphoma, hepatosplenic γδ lymphoma, and subcutaneous panniculitis-like PTCL.
Treatment characteristics
Before undergoing transplant, patients in both arms received treatment with CHOEP (cyclophosphamide, doxorubicin, etoposide, vincristine, and prednisone) on days 1, 15, 29, and 43. If they experienced a complete response (CR), partial response, or no change, patients received DHAP (dexamethasone, cytarabine, and cisplatin) on day 64.
Patients in the auto-SCT arm received BEAM (carmustine, etoposide, cytarabine, and melphalan) prior to transplant. And patients in the allo-SCT arm received FBC (fludarabine, busulfan, and cyclophosphamide).
Overall, 36 patients (62%) completed treatment per protocol, 19 in the auto-SCT arm and 17 in the allo-SCT arm. Thirty-eight percent of all patients could not proceed to transplant per protocol, mostly because of early lymphoma progression.
Response and survival
The researchers observed CRs/unconfirmed CRs (CRus) in 33% (n=10) of patients in the auto-SCT arm and 39% (n=11) in the allo-SCT arm. CR/CRus and progressive disease within 2 months occurred in 3% (n=1) and 4% (n=1) of patients, respectively.
Partial responses were seen in 17% (n=5) of patients in the auto-SCT arm and 7% (n=2) in the allo-SCT arm. There was no change in 7% (n=2) and 0% of patients, respectively. And responses were unknown in 7% (n=2) of patients in the auto-SCT arm.
Progressive disease occurred in 33% (n=10) of patients in the auto-SCT arm and 36% (n=10) in the allo-SCT arm. And treatment-related death occurred in 0% (n=0) and 14% (n=4), respectively.
At the interim analysis, there was no significant difference between the treatment arms with regard to event-free survival (P=0.963) or overall survival (P=0.174).
“At that time, the decision was made to stop the study,” Dr Schmitz said.
He explained that a conditional power analysis showed a low probability that the primary endpoint—a 25% improvement in event-free survival with allo-SCT—could still be met. So the data safety monitoring board decided to stop enrollment.
An updated analysis, performed at a median observation time of 26 months, showed there was still no significant difference in overall survival between the treatment arms (P=0.362).
Cause of death
In the intent-to-treat population—30 patients in the auto-SCT arm and 28 in the allo-SCT arm—there were 16 lymphoma-related deaths, 10 in the auto-SCT arm and 6 in the allo-SCT arm.
There were 6 deaths related to study treatment (4 early and 2 late), all in the allo-SCT arm. One patient in the allo-SCT arm died of post-transplant lymphoproliferative disorder, and 1 patient in the same arm died of hemorrhage after salvage. One patient in each arm died as a result of salvage treatment.
Dr Schmitz and his colleagues also looked at the cause of death among patients who received a transplant—19 in the auto-SCT arm and 17 in the allo-SCT arm.
After SCT, there were 7 deaths in each arm. In the auto-SCT arm, there were 6 lymphoma-related deaths and 1 death related to salvage treatment. In the allo-SCT arm, there were 7 cases of non-relapse-related mortality, including 1 patient with post-transplant lymphoproliferative disorder.
“There certainly seems to be a [graft-vs-lymphoma] effect of allo-transplant in T-cell lymphoma that is, unfortunately, in some way, counterbalanced by high transplant-related mortality,” Dr Schmitz said.
He added that results of a final analysis of the 104 patients enrolled on this study should be available in 2017. ![]()
*Information in the abstract differs from that presented at the meeting.

© ASCO/Max Gersh
CHICAGO—Allogeneic and autologous transplants produce similar survival rates when used as first-line therapy in younger patients with peripheral
T-cell lymphoma (PTCL), according to interim results of the AATT trial.
The study also showed that deaths among patients who received autologous stem cell transplants (auto-SCTs) were a result of relapse and salvage treatment, while deaths among allogeneic SCT (allo-SCT) recipients were transplant-related.
Norbert Schmitz, MD, PhD, of Asklepios Hospital St. Georg in Hamburg, Germany, presented these findings at the 2015 ASCO Annual Meeting (abstract 8507*).
Dr Schmitz noted that only previous study comparing auto-SCT with allo-SCT as first-line therapy in PTCL was not designed or powered to evaluate the differences between the transplant types.
So he and his colleagues conducted the AATT trial to determine the differences. The team hypothesized that allo-SCT would improve 3-year event-free survival from 35% to 60%, given an α of 5% and a power of 80%. They needed 140 patients to prove or disprove this theory.
Ultimately, the investigators enrolled 104 patients and performed an interim analysis when 58 patients were evaluable for response.
Of the 58 patients, 30 were randomized to the auto-SCT arm and 28 to the allo-SCT arm. Baseline characteristics were similar between the arms, including patients’ median ages (49 and 50, respectively), the proportion of patients with stage III/IV disease (87% and 93%), and the proportion with ECOG status greater than 1 (23% and 18%).
Most patients in both arms had PTCL not otherwise specified (36% in the auto-SCT arm and 50% in the allo-SCT arm). Other subtypes included angioimmunoblastic T-cell lymphoma (23% and 32%, respectively), ALK-negative anaplastic large-cell lymphoma (20% and 4%), and “other” PTCLs (20% and 8%). The other PTCLs were NK/T-cell lymphoma, intestinal T/NK-cell lymphoma, hepatosplenic γδ lymphoma, and subcutaneous panniculitis-like PTCL.
Treatment characteristics
Before undergoing transplant, patients in both arms received treatment with CHOEP (cyclophosphamide, doxorubicin, etoposide, vincristine, and prednisone) on days 1, 15, 29, and 43. If they experienced a complete response (CR), partial response, or no change, patients received DHAP (dexamethasone, cytarabine, and cisplatin) on day 64.
Patients in the auto-SCT arm received BEAM (carmustine, etoposide, cytarabine, and melphalan) prior to transplant. And patients in the allo-SCT arm received FBC (fludarabine, busulfan, and cyclophosphamide).
Overall, 36 patients (62%) completed treatment per protocol, 19 in the auto-SCT arm and 17 in the allo-SCT arm. Thirty-eight percent of all patients could not proceed to transplant per protocol, mostly because of early lymphoma progression.
Response and survival
The researchers observed CRs/unconfirmed CRs (CRus) in 33% (n=10) of patients in the auto-SCT arm and 39% (n=11) in the allo-SCT arm. CR/CRus and progressive disease within 2 months occurred in 3% (n=1) and 4% (n=1) of patients, respectively.
Partial responses were seen in 17% (n=5) of patients in the auto-SCT arm and 7% (n=2) in the allo-SCT arm. There was no change in 7% (n=2) and 0% of patients, respectively. And responses were unknown in 7% (n=2) of patients in the auto-SCT arm.
Progressive disease occurred in 33% (n=10) of patients in the auto-SCT arm and 36% (n=10) in the allo-SCT arm. And treatment-related death occurred in 0% (n=0) and 14% (n=4), respectively.
At the interim analysis, there was no significant difference between the treatment arms with regard to event-free survival (P=0.963) or overall survival (P=0.174).
“At that time, the decision was made to stop the study,” Dr Schmitz said.
He explained that a conditional power analysis showed a low probability that the primary endpoint—a 25% improvement in event-free survival with allo-SCT—could still be met. So the data safety monitoring board decided to stop enrollment.
An updated analysis, performed at a median observation time of 26 months, showed there was still no significant difference in overall survival between the treatment arms (P=0.362).
Cause of death
In the intent-to-treat population—30 patients in the auto-SCT arm and 28 in the allo-SCT arm—there were 16 lymphoma-related deaths, 10 in the auto-SCT arm and 6 in the allo-SCT arm.
There were 6 deaths related to study treatment (4 early and 2 late), all in the allo-SCT arm. One patient in the allo-SCT arm died of post-transplant lymphoproliferative disorder, and 1 patient in the same arm died of hemorrhage after salvage. One patient in each arm died as a result of salvage treatment.
Dr Schmitz and his colleagues also looked at the cause of death among patients who received a transplant—19 in the auto-SCT arm and 17 in the allo-SCT arm.
After SCT, there were 7 deaths in each arm. In the auto-SCT arm, there were 6 lymphoma-related deaths and 1 death related to salvage treatment. In the allo-SCT arm, there were 7 cases of non-relapse-related mortality, including 1 patient with post-transplant lymphoproliferative disorder.
“There certainly seems to be a [graft-vs-lymphoma] effect of allo-transplant in T-cell lymphoma that is, unfortunately, in some way, counterbalanced by high transplant-related mortality,” Dr Schmitz said.
He added that results of a final analysis of the 104 patients enrolled on this study should be available in 2017. ![]()
*Information in the abstract differs from that presented at the meeting.
Reducing distress in caregivers of HSCT recipients

Photo by Chad McNeeley
Research has shown that caring for cancer patients after hematopoietic stem cell transplant (HSCT) can have negative psychological effects on the caregiver, but results of a new study suggest a psychosocial intervention could change that.
The trial showed that counseling sessions focused on stress management could significantly reduce stress, anxiety, depression, and mood disturbance among these caregivers.
“The first 100 days after a stem cell transplant is a critical period for patients, in which caregivers are called upon to deliver around-the-clock care, providing support for patients’ everyday needs and also patients’ emotional health, but who takes care of the caregivers?” asked Mark Laudenslager, PhD, of the University of Colorado Denver.
To address this problem, Dr Laudenslager and his colleagues studied 148 caregivers of patients who underwent allogeneic HSCT. The team described this research in Bone Marrow Transplantation.
The caregivers were randomized to a group that was offered a psychosocial intervention (n=74) and a group that received standard treatment, in which mental health support services were available but not required (n=74).
In the experimental group, caregivers attended 8 sessions on stress management. These one-on-one sessions focused on understanding stress and its physical consequences, changing roles as caregivers, cognitive behavioral stress management, pacing respiration, and identifying social support. The researchers call this intervention PsychoEducation, Paced Respiration and Relaxation (PEPRR).
After a patient underwent HSCT, Dr Laudenslager and his colleagues used several questionnaires to follow the trajectory of caregiver distress over time. The questionnaires were used to measure stress, depression, anxiety, mood disturbance, sleep quality, and other mental health outcomes.
There was no significant difference in stress or other mental health measures between the 2 treatment groups at baseline.
However, at 3 months after transplant, caregivers in the PEPRR group saw some significant improvements over caregivers in the standard treatment group.
The PEPRR group had less stress according to the Perceived Stress Scale (P=0.039), less depression according to the Center for Epidemiologic Studies Depression test (P=0.016), less anxiety according to the State-Trait Anxiety Inventory-State questionnaire (P=0.0009), and less mood disturbance according to the Profile of Mood States-Total Mood Disturbance test (P=0.039).
Overall caregiver distress (composite scores from the questionnaires) was significantly lower in the PEPRR group than the standard treatment group (P=0.019).
However, there was no significant difference in caregiver well-being (composite scores) or scores on the Caregiver Reaction Assessment, Pittsburgh Sleep Quality Index, Short Form 36 Health Survey, or Impact of Events scale.
Still, the other improvements caregivers experienced suggest PEPRR is a promising intervention, Dr Laudenslager said.
He and his colleagues are now recruiting subjects for a follow-up study (NCT02037568) focused on evaluating quality of life in allogeneic HSCT recipients whose caregivers participate in programs similar to the PEPRR intervention. ![]()

Photo by Chad McNeeley
Research has shown that caring for cancer patients after hematopoietic stem cell transplant (HSCT) can have negative psychological effects on the caregiver, but results of a new study suggest a psychosocial intervention could change that.
The trial showed that counseling sessions focused on stress management could significantly reduce stress, anxiety, depression, and mood disturbance among these caregivers.
“The first 100 days after a stem cell transplant is a critical period for patients, in which caregivers are called upon to deliver around-the-clock care, providing support for patients’ everyday needs and also patients’ emotional health, but who takes care of the caregivers?” asked Mark Laudenslager, PhD, of the University of Colorado Denver.
To address this problem, Dr Laudenslager and his colleagues studied 148 caregivers of patients who underwent allogeneic HSCT. The team described this research in Bone Marrow Transplantation.
The caregivers were randomized to a group that was offered a psychosocial intervention (n=74) and a group that received standard treatment, in which mental health support services were available but not required (n=74).
In the experimental group, caregivers attended 8 sessions on stress management. These one-on-one sessions focused on understanding stress and its physical consequences, changing roles as caregivers, cognitive behavioral stress management, pacing respiration, and identifying social support. The researchers call this intervention PsychoEducation, Paced Respiration and Relaxation (PEPRR).
After a patient underwent HSCT, Dr Laudenslager and his colleagues used several questionnaires to follow the trajectory of caregiver distress over time. The questionnaires were used to measure stress, depression, anxiety, mood disturbance, sleep quality, and other mental health outcomes.
There was no significant difference in stress or other mental health measures between the 2 treatment groups at baseline.
However, at 3 months after transplant, caregivers in the PEPRR group saw some significant improvements over caregivers in the standard treatment group.
The PEPRR group had less stress according to the Perceived Stress Scale (P=0.039), less depression according to the Center for Epidemiologic Studies Depression test (P=0.016), less anxiety according to the State-Trait Anxiety Inventory-State questionnaire (P=0.0009), and less mood disturbance according to the Profile of Mood States-Total Mood Disturbance test (P=0.039).
Overall caregiver distress (composite scores from the questionnaires) was significantly lower in the PEPRR group than the standard treatment group (P=0.019).
However, there was no significant difference in caregiver well-being (composite scores) or scores on the Caregiver Reaction Assessment, Pittsburgh Sleep Quality Index, Short Form 36 Health Survey, or Impact of Events scale.
Still, the other improvements caregivers experienced suggest PEPRR is a promising intervention, Dr Laudenslager said.
He and his colleagues are now recruiting subjects for a follow-up study (NCT02037568) focused on evaluating quality of life in allogeneic HSCT recipients whose caregivers participate in programs similar to the PEPRR intervention. ![]()

Photo by Chad McNeeley
Research has shown that caring for cancer patients after hematopoietic stem cell transplant (HSCT) can have negative psychological effects on the caregiver, but results of a new study suggest a psychosocial intervention could change that.
The trial showed that counseling sessions focused on stress management could significantly reduce stress, anxiety, depression, and mood disturbance among these caregivers.
“The first 100 days after a stem cell transplant is a critical period for patients, in which caregivers are called upon to deliver around-the-clock care, providing support for patients’ everyday needs and also patients’ emotional health, but who takes care of the caregivers?” asked Mark Laudenslager, PhD, of the University of Colorado Denver.
To address this problem, Dr Laudenslager and his colleagues studied 148 caregivers of patients who underwent allogeneic HSCT. The team described this research in Bone Marrow Transplantation.
The caregivers were randomized to a group that was offered a psychosocial intervention (n=74) and a group that received standard treatment, in which mental health support services were available but not required (n=74).
In the experimental group, caregivers attended 8 sessions on stress management. These one-on-one sessions focused on understanding stress and its physical consequences, changing roles as caregivers, cognitive behavioral stress management, pacing respiration, and identifying social support. The researchers call this intervention PsychoEducation, Paced Respiration and Relaxation (PEPRR).
After a patient underwent HSCT, Dr Laudenslager and his colleagues used several questionnaires to follow the trajectory of caregiver distress over time. The questionnaires were used to measure stress, depression, anxiety, mood disturbance, sleep quality, and other mental health outcomes.
There was no significant difference in stress or other mental health measures between the 2 treatment groups at baseline.
However, at 3 months after transplant, caregivers in the PEPRR group saw some significant improvements over caregivers in the standard treatment group.
The PEPRR group had less stress according to the Perceived Stress Scale (P=0.039), less depression according to the Center for Epidemiologic Studies Depression test (P=0.016), less anxiety according to the State-Trait Anxiety Inventory-State questionnaire (P=0.0009), and less mood disturbance according to the Profile of Mood States-Total Mood Disturbance test (P=0.039).
Overall caregiver distress (composite scores from the questionnaires) was significantly lower in the PEPRR group than the standard treatment group (P=0.019).
However, there was no significant difference in caregiver well-being (composite scores) or scores on the Caregiver Reaction Assessment, Pittsburgh Sleep Quality Index, Short Form 36 Health Survey, or Impact of Events scale.
Still, the other improvements caregivers experienced suggest PEPRR is a promising intervention, Dr Laudenslager said.
He and his colleagues are now recruiting subjects for a follow-up study (NCT02037568) focused on evaluating quality of life in allogeneic HSCT recipients whose caregivers participate in programs similar to the PEPRR intervention.
IL-2 variant proves active against ATL, GVHD

Photo by Rhoda Baer
Researchers say they have created interleukin-2 (IL-2) variants that function as IL-2-receptor signaling “clamps” and allow for “fine tuning” of the signaling amplitude.
One variant, known as H9-RETR, was able to inhibit the actions of endogenous IL-2 and IL-15, prolong survival in a mouse model of graft-vs-host disease (GVHD), and inhibit the proliferation of cells derived from a patient with smoldering adult T-cell
leukemia (ATL).
The researchers reported these results in Immunity.
Warren J. Leonard, MD, of the National Heart, Lung, and Blood Institute in Bethesda, Maryland, and his colleagues developed IL-2 variants in which activity can be tuned to either boost or block immune responses, depending on the desired therapeutic application.
The researchers said these variants had high affinity for IL-2Rβ and inhibited binding of endogenous IL-2, but their interaction with γc was weakened, thereby weakening IL-2Rβ-γc heterodimerization.
The team found that IL-2 signaling strength was inversely correlated with the degree of mutation at the γc interface. And differential effects on cell proliferation were dependent upon the cells’ state of activation.
One of the IL-2 variants, H9-RETR, inhibited IL-2- and IL-15-mediated proliferation and cytotoxicity. H9-RETR inhibited cytokine signaling and natural killer cell activity as well or better than blocking antibodies to IL-2Rα and IL-2Rβ.
In experiments with cells isolated from a patient with smoldering ATL, H9-RETR blocked IL-2 signaling and inhibited the spontaneous proliferation of ATL cells. In this regard, H9-RETR was at least as effective as the anti-IL-2Rα antibody daclizumab and much more effective than the anti-IL-2Rβ antibody Mikβ1.
In a mouse model of GVHD, animals that received a stabilized, Fc-fusion version of H9-RETR (H9-RETR-Fc4) had significantly longer survival than control mice (which received only Fc4 protein).
All of the control mice had died by 40 days post-injection, but it took 60 days for all of the H9-RETR-Fc4-treated mice to die (P=0.0001).
The researchers believe their receptor-clamping approach could potentially be used to engineer other immune-system cytokines with therapeutic potential.

Photo by Rhoda Baer
Researchers say they have created interleukin-2 (IL-2) variants that function as IL-2-receptor signaling “clamps” and allow for “fine tuning” of the signaling amplitude.
One variant, known as H9-RETR, was able to inhibit the actions of endogenous IL-2 and IL-15, prolong survival in a mouse model of graft-vs-host disease (GVHD), and inhibit the proliferation of cells derived from a patient with smoldering adult T-cell
leukemia (ATL).
The researchers reported these results in Immunity.
Warren J. Leonard, MD, of the National Heart, Lung, and Blood Institute in Bethesda, Maryland, and his colleagues developed IL-2 variants in which activity can be tuned to either boost or block immune responses, depending on the desired therapeutic application.
The researchers said these variants had high affinity for IL-2Rβ and inhibited binding of endogenous IL-2, but their interaction with γc was weakened, thereby weakening IL-2Rβ-γc heterodimerization.
The team found that IL-2 signaling strength was inversely correlated with the degree of mutation at the γc interface. And differential effects on cell proliferation were dependent upon the cells’ state of activation.
One of the IL-2 variants, H9-RETR, inhibited IL-2- and IL-15-mediated proliferation and cytotoxicity. H9-RETR inhibited cytokine signaling and natural killer cell activity as well or better than blocking antibodies to IL-2Rα and IL-2Rβ.
In experiments with cells isolated from a patient with smoldering ATL, H9-RETR blocked IL-2 signaling and inhibited the spontaneous proliferation of ATL cells. In this regard, H9-RETR was at least as effective as the anti-IL-2Rα antibody daclizumab and much more effective than the anti-IL-2Rβ antibody Mikβ1.
In a mouse model of GVHD, animals that received a stabilized, Fc-fusion version of H9-RETR (H9-RETR-Fc4) had significantly longer survival than control mice (which received only Fc4 protein).
All of the control mice had died by 40 days post-injection, but it took 60 days for all of the H9-RETR-Fc4-treated mice to die (P=0.0001).
The researchers believe their receptor-clamping approach could potentially be used to engineer other immune-system cytokines with therapeutic potential.

Photo by Rhoda Baer
Researchers say they have created interleukin-2 (IL-2) variants that function as IL-2-receptor signaling “clamps” and allow for “fine tuning” of the signaling amplitude.
One variant, known as H9-RETR, was able to inhibit the actions of endogenous IL-2 and IL-15, prolong survival in a mouse model of graft-vs-host disease (GVHD), and inhibit the proliferation of cells derived from a patient with smoldering adult T-cell
leukemia (ATL).
The researchers reported these results in Immunity.
Warren J. Leonard, MD, of the National Heart, Lung, and Blood Institute in Bethesda, Maryland, and his colleagues developed IL-2 variants in which activity can be tuned to either boost or block immune responses, depending on the desired therapeutic application.
The researchers said these variants had high affinity for IL-2Rβ and inhibited binding of endogenous IL-2, but their interaction with γc was weakened, thereby weakening IL-2Rβ-γc heterodimerization.
The team found that IL-2 signaling strength was inversely correlated with the degree of mutation at the γc interface. And differential effects on cell proliferation were dependent upon the cells’ state of activation.
One of the IL-2 variants, H9-RETR, inhibited IL-2- and IL-15-mediated proliferation and cytotoxicity. H9-RETR inhibited cytokine signaling and natural killer cell activity as well or better than blocking antibodies to IL-2Rα and IL-2Rβ.
In experiments with cells isolated from a patient with smoldering ATL, H9-RETR blocked IL-2 signaling and inhibited the spontaneous proliferation of ATL cells. In this regard, H9-RETR was at least as effective as the anti-IL-2Rα antibody daclizumab and much more effective than the anti-IL-2Rβ antibody Mikβ1.
In a mouse model of GVHD, animals that received a stabilized, Fc-fusion version of H9-RETR (H9-RETR-Fc4) had significantly longer survival than control mice (which received only Fc4 protein).
All of the control mice had died by 40 days post-injection, but it took 60 days for all of the H9-RETR-Fc4-treated mice to die (P=0.0001).
The researchers believe their receptor-clamping approach could potentially be used to engineer other immune-system cytokines with therapeutic potential.
Combo can fight infection, GVHD

Image courtesy of NIAID
NEW ORLEANS—Results of a phase 1 trial suggest that modified T cells can fight infection in patients who have undergone haploidentical hematopoietic
stem cell transplant (haplo-HSCT), and subsequent administration of a bio-inert drug can ameliorate graft-vs-host disease (GVHD) in these patients.
Researchers introduced the suicide gene inducible caspase 9 (iC9) into T cells and infused them into transplant recipients to promote immune reconstitution.
For patients who went on to develop GVHD, the researchers activated the suicide gene by administering a dose of the drug rimiducid (AP1903).
This cleared the patients of GVHD symptoms without jeopardizing the remaining T cells’ ability to fight infection.
The researchers presented these results at the American Society of Gene and Cell Therapy Annual Meeting and reported them in Blood.
The trial was sponsored by Baylor College of Medicine, but Bellicum Pharmaceuticals is the company developing rimiducid and the so-called iC9 “safety switch,” also known as CaspaCIDe.
“We’ve shown that the therapy works, fighting viruses that threaten immune-compromised patients,” said Xiaoou Zhou, PhD, of Baylor College of Medicine in Houston, Texas.
“We have also shown that the switch can turn off the T cells that reproduce out of control, attacking the patient’s graft-vs-host disease. This study was the first to look at any potential effect on the ability of the T cells to fight infection. We found there was no compromise.”
The study included 12 patients with a median age of 10 (range, 2-50) who had undergone haplo-HSCT. They received donor-derived T cells engineered with CaspaCIDe using a dose escalation schedule from 1×104 to 5×106 cells/kg, at a median of 42 days after transplant (range, 31-82 days).
All 12 patients had more rapid immune reconstitution and fewer infections after the infusions, when compared with previously reported results in T-cell-depleted, haplo-HSCT procedures. The CaspaCIDe T cells successfully provided protection from EBV, CMV, VZV, HHV6, and BKV viruses.
The researchers said there were no immediate toxicities related to the T-cell infusions, but 4 patients went on to develop GVHD.
Treatment with rimiducid resolved the patients’ GVHD symptoms within 6 to 48 hours. The researchers found that rimiducid could eliminate the uncontrolled T cells in the central nervous system as well as the peripheral blood.
Even after the problematic T cells were killed, the remaining T cells were able to fight infection without causing further GVHD.
One patient experienced a decrease in cell counts after receiving rimiducid, but counts had normalized by 48 hours. The researchers said there were no other immediate or delayed adverse effects associated with the drug.
One patient developed cytokine release syndrome, but this was resolved in 2 hours with a single dose of rimiducid.
“This study shows that infusing larger numbers of haploidentical donor T cells engineered with CaspaCIDe leads to better infection control,” Dr Zhou said. “We also showed that, if GVHD occurs, it can be rapidly controlled and eliminated by removing alloreactive cells with rimiducid in vivo, and that the productive, antiviral and anticancer cells remain, repopulate, and maintain immunity.”
“This is a significant finding that can lead to broader adoption of curative haploidentical transplants for cancers and genetic blood disorders. It also suggests that CaspaCIDe has great potential with CAR T and TCR therapies, where rapid control of dangerous T-cell-mitigated toxicities, such as cytokine release syndrome, is needed to achieve wide adoption.”

Image courtesy of NIAID
NEW ORLEANS—Results of a phase 1 trial suggest that modified T cells can fight infection in patients who have undergone haploidentical hematopoietic
stem cell transplant (haplo-HSCT), and subsequent administration of a bio-inert drug can ameliorate graft-vs-host disease (GVHD) in these patients.
Researchers introduced the suicide gene inducible caspase 9 (iC9) into T cells and infused them into transplant recipients to promote immune reconstitution.
For patients who went on to develop GVHD, the researchers activated the suicide gene by administering a dose of the drug rimiducid (AP1903).
This cleared the patients of GVHD symptoms without jeopardizing the remaining T cells’ ability to fight infection.
The researchers presented these results at the American Society of Gene and Cell Therapy Annual Meeting and reported them in Blood.
The trial was sponsored by Baylor College of Medicine, but Bellicum Pharmaceuticals is the company developing rimiducid and the so-called iC9 “safety switch,” also known as CaspaCIDe.
“We’ve shown that the therapy works, fighting viruses that threaten immune-compromised patients,” said Xiaoou Zhou, PhD, of Baylor College of Medicine in Houston, Texas.
“We have also shown that the switch can turn off the T cells that reproduce out of control, attacking the patient’s graft-vs-host disease. This study was the first to look at any potential effect on the ability of the T cells to fight infection. We found there was no compromise.”
The study included 12 patients with a median age of 10 (range, 2-50) who had undergone haplo-HSCT. They received donor-derived T cells engineered with CaspaCIDe using a dose escalation schedule from 1×104 to 5×106 cells/kg, at a median of 42 days after transplant (range, 31-82 days).
All 12 patients had more rapid immune reconstitution and fewer infections after the infusions, when compared with previously reported results in T-cell-depleted, haplo-HSCT procedures. The CaspaCIDe T cells successfully provided protection from EBV, CMV, VZV, HHV6, and BKV viruses.
The researchers said there were no immediate toxicities related to the T-cell infusions, but 4 patients went on to develop GVHD.
Treatment with rimiducid resolved the patients’ GVHD symptoms within 6 to 48 hours. The researchers found that rimiducid could eliminate the uncontrolled T cells in the central nervous system as well as the peripheral blood.
Even after the problematic T cells were killed, the remaining T cells were able to fight infection without causing further GVHD.
One patient experienced a decrease in cell counts after receiving rimiducid, but counts had normalized by 48 hours. The researchers said there were no other immediate or delayed adverse effects associated with the drug.
One patient developed cytokine release syndrome, but this was resolved in 2 hours with a single dose of rimiducid.
“This study shows that infusing larger numbers of haploidentical donor T cells engineered with CaspaCIDe leads to better infection control,” Dr Zhou said. “We also showed that, if GVHD occurs, it can be rapidly controlled and eliminated by removing alloreactive cells with rimiducid in vivo, and that the productive, antiviral and anticancer cells remain, repopulate, and maintain immunity.”
“This is a significant finding that can lead to broader adoption of curative haploidentical transplants for cancers and genetic blood disorders. It also suggests that CaspaCIDe has great potential with CAR T and TCR therapies, where rapid control of dangerous T-cell-mitigated toxicities, such as cytokine release syndrome, is needed to achieve wide adoption.”

Image courtesy of NIAID
NEW ORLEANS—Results of a phase 1 trial suggest that modified T cells can fight infection in patients who have undergone haploidentical hematopoietic
stem cell transplant (haplo-HSCT), and subsequent administration of a bio-inert drug can ameliorate graft-vs-host disease (GVHD) in these patients.
Researchers introduced the suicide gene inducible caspase 9 (iC9) into T cells and infused them into transplant recipients to promote immune reconstitution.
For patients who went on to develop GVHD, the researchers activated the suicide gene by administering a dose of the drug rimiducid (AP1903).
This cleared the patients of GVHD symptoms without jeopardizing the remaining T cells’ ability to fight infection.
The researchers presented these results at the American Society of Gene and Cell Therapy Annual Meeting and reported them in Blood.
The trial was sponsored by Baylor College of Medicine, but Bellicum Pharmaceuticals is the company developing rimiducid and the so-called iC9 “safety switch,” also known as CaspaCIDe.
“We’ve shown that the therapy works, fighting viruses that threaten immune-compromised patients,” said Xiaoou Zhou, PhD, of Baylor College of Medicine in Houston, Texas.
“We have also shown that the switch can turn off the T cells that reproduce out of control, attacking the patient’s graft-vs-host disease. This study was the first to look at any potential effect on the ability of the T cells to fight infection. We found there was no compromise.”
The study included 12 patients with a median age of 10 (range, 2-50) who had undergone haplo-HSCT. They received donor-derived T cells engineered with CaspaCIDe using a dose escalation schedule from 1×104 to 5×106 cells/kg, at a median of 42 days after transplant (range, 31-82 days).
All 12 patients had more rapid immune reconstitution and fewer infections after the infusions, when compared with previously reported results in T-cell-depleted, haplo-HSCT procedures. The CaspaCIDe T cells successfully provided protection from EBV, CMV, VZV, HHV6, and BKV viruses.
The researchers said there were no immediate toxicities related to the T-cell infusions, but 4 patients went on to develop GVHD.
Treatment with rimiducid resolved the patients’ GVHD symptoms within 6 to 48 hours. The researchers found that rimiducid could eliminate the uncontrolled T cells in the central nervous system as well as the peripheral blood.
Even after the problematic T cells were killed, the remaining T cells were able to fight infection without causing further GVHD.
One patient experienced a decrease in cell counts after receiving rimiducid, but counts had normalized by 48 hours. The researchers said there were no other immediate or delayed adverse effects associated with the drug.
One patient developed cytokine release syndrome, but this was resolved in 2 hours with a single dose of rimiducid.
“This study shows that infusing larger numbers of haploidentical donor T cells engineered with CaspaCIDe leads to better infection control,” Dr Zhou said. “We also showed that, if GVHD occurs, it can be rapidly controlled and eliminated by removing alloreactive cells with rimiducid in vivo, and that the productive, antiviral and anticancer cells remain, repopulate, and maintain immunity.”
“This is a significant finding that can lead to broader adoption of curative haploidentical transplants for cancers and genetic blood disorders. It also suggests that CaspaCIDe has great potential with CAR T and TCR therapies, where rapid control of dangerous T-cell-mitigated toxicities, such as cytokine release syndrome, is needed to achieve wide adoption.”
Modified T cells may treat GVHD
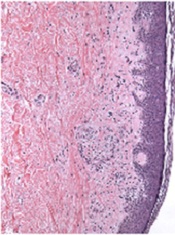
Image from PLOS ONE
A T-cell therapy designed to mitigate graft-vs-host disease (GVHD) is both feasible and safe, according to results of a pilot study published in Molecular Therapy.
To create this therapy, researchers transduced donor T cells with γ-retroviruses carrying a CD34-TK75 fusion gene.
The team said this allows them to track the cells via PET/CT and induce apoptosis by administering the antiviral drug ganciclovir if patients begin showing signs of GVHD.
“If donor T cells expand and cause severe graft-vs-host disease, we can give the patient ganciclovir, and it should kill the T cells and stop the process,” said study author John F. DiPersio, MD, PhD, of the Washington University School of Medicine in St Louis, Missouri.
Dr DiPersio and his colleagues tested the CD34-TK75-enriched T cells in 8 patients—4 with acute myeloid leukemia and 4 with myelodysplastic syndromes—who relapsed after allogeneic transplant. Six patients underwent [18F]FHBG PET/CT to track the T cells at several time points after infusion.
Patients received T-cell infusions ranging from 0.1 × 106 cells/kg to 1.3 × 106 cells/kg. Seven of the 8 patients received chemotherapy before T-cell infusion.
Four patients achieved a complete remission, 1 had progressive disease, and 3 patients died before the researchers could evaluate them for response.
Two patients developed GVHD—1 before T-cell infusion and 1 after. The patient who developed GVHD before infusion had grade 2 liver GVHD that resolved after an increased dose of steroids. The patient ultimately died of relapsed leukemia.
The patient who developed GVHD after T-cell infusion did not respond to chemotherapy or T-cell infusion. At 64 days after infusion, he exhibited symptoms consistent with grade 4 liver GVHD. He was treated with high-dose steroids and ganciclovir but did not respond. His primary cause of death was relapsed/progressive disease.
The mean overall survival after T-cell infusion was 165 days, 4 patients were still alive at 6 months, and 1 patient lived 408 days. All of the patients ultimately died.
The researchers said they did not detect any replication competent retrovirus or any antibodies against CD34-TK in any of the patients. The team also said there were no toxicities related to the CD34-TK75-enriched T cells.
Among patients who underwent imaging, there was no clear distinction between the [18F]FHBG biodistribution at baseline and later time points. And there was no difference between images in the patient who developed GVHD after infusion and patients who did not.
Past work from Dr DiPersio’s lab showed that leukemic mice that receive donor T cells and go on to develop GVHD show a characteristic migration pattern of the T cells through the body. When the cells gather early in the thymus, the mice develop GVHD. When T cells don’t migrate to the thymus, GVHD doesn’t occur.
In the current study, the patients received a relatively small number of CD34-TK75-enriched T cells, so the researchers were not able to show whether the migration patterns in mice were similar in humans.
However, based on the results of this study, Dr DiPersio and his colleagues are participating in a larger trial in partnership with a company based in Italy. The researchers are planning to include patients from multiple medical centers, and each participant should receive about 50 times more of the CD34-TK75-enriched T cells than were administered in this trial.
Washington University is the only center in the new trial that will be able to perform the imaging studies examining migration patterns of the T cells.
Image from PLOS ONE
A T-cell therapy designed to mitigate graft-vs-host disease (GVHD) is both feasible and safe, according to results of a pilot study published in Molecular Therapy.
To create this therapy, researchers transduced donor T cells with γ-retroviruses carrying a CD34-TK75 fusion gene.
The team said this allows them to track the cells via PET/CT and induce apoptosis by administering the antiviral drug ganciclovir if patients begin showing signs of GVHD.
“If donor T cells expand and cause severe graft-vs-host disease, we can give the patient ganciclovir, and it should kill the T cells and stop the process,” said study author John F. DiPersio, MD, PhD, of the Washington University School of Medicine in St Louis, Missouri.
Dr DiPersio and his colleagues tested the CD34-TK75-enriched T cells in 8 patients—4 with acute myeloid leukemia and 4 with myelodysplastic syndromes—who relapsed after allogeneic transplant. Six patients underwent [18F]FHBG PET/CT to track the T cells at several time points after infusion.
Patients received T-cell infusions ranging from 0.1 × 106 cells/kg to 1.3 × 106 cells/kg. Seven of the 8 patients received chemotherapy before T-cell infusion.
Four patients achieved a complete remission, 1 had progressive disease, and 3 patients died before the researchers could evaluate them for response.
Two patients developed GVHD—1 before T-cell infusion and 1 after. The patient who developed GVHD before infusion had grade 2 liver GVHD that resolved after an increased dose of steroids. The patient ultimately died of relapsed leukemia.
The patient who developed GVHD after T-cell infusion did not respond to chemotherapy or T-cell infusion. At 64 days after infusion, he exhibited symptoms consistent with grade 4 liver GVHD. He was treated with high-dose steroids and ganciclovir but did not respond. His primary cause of death was relapsed/progressive disease.
The mean overall survival after T-cell infusion was 165 days, 4 patients were still alive at 6 months, and 1 patient lived 408 days. All of the patients ultimately died.
The researchers said they did not detect any replication competent retrovirus or any antibodies against CD34-TK in any of the patients. The team also said there were no toxicities related to the CD34-TK75-enriched T cells.
Among patients who underwent imaging, there was no clear distinction between the [18F]FHBG biodistribution at baseline and later time points. And there was no difference between images in the patient who developed GVHD after infusion and patients who did not.
Past work from Dr DiPersio’s lab showed that leukemic mice that receive donor T cells and go on to develop GVHD show a characteristic migration pattern of the T cells through the body. When the cells gather early in the thymus, the mice develop GVHD. When T cells don’t migrate to the thymus, GVHD doesn’t occur.
In the current study, the patients received a relatively small number of CD34-TK75-enriched T cells, so the researchers were not able to show whether the migration patterns in mice were similar in humans.
However, based on the results of this study, Dr DiPersio and his colleagues are participating in a larger trial in partnership with a company based in Italy. The researchers are planning to include patients from multiple medical centers, and each participant should receive about 50 times more of the CD34-TK75-enriched T cells than were administered in this trial.
Washington University is the only center in the new trial that will be able to perform the imaging studies examining migration patterns of the T cells.
Image from PLOS ONE
A T-cell therapy designed to mitigate graft-vs-host disease (GVHD) is both feasible and safe, according to results of a pilot study published in Molecular Therapy.
To create this therapy, researchers transduced donor T cells with γ-retroviruses carrying a CD34-TK75 fusion gene.
The team said this allows them to track the cells via PET/CT and induce apoptosis by administering the antiviral drug ganciclovir if patients begin showing signs of GVHD.
“If donor T cells expand and cause severe graft-vs-host disease, we can give the patient ganciclovir, and it should kill the T cells and stop the process,” said study author John F. DiPersio, MD, PhD, of the Washington University School of Medicine in St Louis, Missouri.
Dr DiPersio and his colleagues tested the CD34-TK75-enriched T cells in 8 patients—4 with acute myeloid leukemia and 4 with myelodysplastic syndromes—who relapsed after allogeneic transplant. Six patients underwent [18F]FHBG PET/CT to track the T cells at several time points after infusion.
Patients received T-cell infusions ranging from 0.1 × 106 cells/kg to 1.3 × 106 cells/kg. Seven of the 8 patients received chemotherapy before T-cell infusion.
Four patients achieved a complete remission, 1 had progressive disease, and 3 patients died before the researchers could evaluate them for response.
Two patients developed GVHD—1 before T-cell infusion and 1 after. The patient who developed GVHD before infusion had grade 2 liver GVHD that resolved after an increased dose of steroids. The patient ultimately died of relapsed leukemia.
The patient who developed GVHD after T-cell infusion did not respond to chemotherapy or T-cell infusion. At 64 days after infusion, he exhibited symptoms consistent with grade 4 liver GVHD. He was treated with high-dose steroids and ganciclovir but did not respond. His primary cause of death was relapsed/progressive disease.
The mean overall survival after T-cell infusion was 165 days, 4 patients were still alive at 6 months, and 1 patient lived 408 days. All of the patients ultimately died.
The researchers said they did not detect any replication competent retrovirus or any antibodies against CD34-TK in any of the patients. The team also said there were no toxicities related to the CD34-TK75-enriched T cells.
Among patients who underwent imaging, there was no clear distinction between the [18F]FHBG biodistribution at baseline and later time points. And there was no difference between images in the patient who developed GVHD after infusion and patients who did not.
Past work from Dr DiPersio’s lab showed that leukemic mice that receive donor T cells and go on to develop GVHD show a characteristic migration pattern of the T cells through the body. When the cells gather early in the thymus, the mice develop GVHD. When T cells don’t migrate to the thymus, GVHD doesn’t occur.
In the current study, the patients received a relatively small number of CD34-TK75-enriched T cells, so the researchers were not able to show whether the migration patterns in mice were similar in humans.
However, based on the results of this study, Dr DiPersio and his colleagues are participating in a larger trial in partnership with a company based in Italy. The researchers are planning to include patients from multiple medical centers, and each participant should receive about 50 times more of the CD34-TK75-enriched T cells than were administered in this trial.
Washington University is the only center in the new trial that will be able to perform the imaging studies examining migration patterns of the T cells.