User login
Protein may be biomarker of cGVHD

Image courtesy of PLOS ONE
A study published in Blood has revealed a protein that could be used to diagnose chronic graft-versus-host disease (cGVHD).
Investigators found elevated levels of the protein, CXCL10, in the blood of transplant recipients around the time they developed cGVHD.
The team therefore believes that testing a transplant patient for this protein could potentially enable early diagnosis of cGVHD.
“Diagnostic tests are desperately needed to make blood and marrow transplants safer,” said study author Kirk Schultz, of BC Children’s Hospital in Vancouver, British Columbia, Canada.
“At this time, there are no good tests to diagnose cGVHD, and the disease can only be identified too late—when it is already established. If we can diagnose it earlier and better, then treatments can be used to stop it before it becomes a chronic, disabling disease.”
For this study, Dr Schultz and his colleagues searched for cGVHD biomarkers in blood samples from 2 groups of adult patients—36 cGVHD patients who were at least 1 month from diagnosis and 31 time-matched control subjects without cGVHD.
This revealed 11 potential biomarkers. The investigators went on to test the validity of these biomarkers in 2 replication cohorts, which included a total of 134 patients with cGVHD and 154 control subjects.
Results showed that the inflammatory protein CXCL10 was consistently elevated in patients with cGVHD. This protein appears to impact a patient’s normal immune cells, preventing the body from fighting cGVHD.
The investigators also found evidence to suggest that another protein, sBAFF, is a biomarker of cGVHD.
Although these results may bring us one step closer to a diagnostic test for cGVHD, the team said further study is needed in larger patient groups. ![]()

Image courtesy of PLOS ONE
A study published in Blood has revealed a protein that could be used to diagnose chronic graft-versus-host disease (cGVHD).
Investigators found elevated levels of the protein, CXCL10, in the blood of transplant recipients around the time they developed cGVHD.
The team therefore believes that testing a transplant patient for this protein could potentially enable early diagnosis of cGVHD.
“Diagnostic tests are desperately needed to make blood and marrow transplants safer,” said study author Kirk Schultz, of BC Children’s Hospital in Vancouver, British Columbia, Canada.
“At this time, there are no good tests to diagnose cGVHD, and the disease can only be identified too late—when it is already established. If we can diagnose it earlier and better, then treatments can be used to stop it before it becomes a chronic, disabling disease.”
For this study, Dr Schultz and his colleagues searched for cGVHD biomarkers in blood samples from 2 groups of adult patients—36 cGVHD patients who were at least 1 month from diagnosis and 31 time-matched control subjects without cGVHD.
This revealed 11 potential biomarkers. The investigators went on to test the validity of these biomarkers in 2 replication cohorts, which included a total of 134 patients with cGVHD and 154 control subjects.
Results showed that the inflammatory protein CXCL10 was consistently elevated in patients with cGVHD. This protein appears to impact a patient’s normal immune cells, preventing the body from fighting cGVHD.
The investigators also found evidence to suggest that another protein, sBAFF, is a biomarker of cGVHD.
Although these results may bring us one step closer to a diagnostic test for cGVHD, the team said further study is needed in larger patient groups. ![]()

Image courtesy of PLOS ONE
A study published in Blood has revealed a protein that could be used to diagnose chronic graft-versus-host disease (cGVHD).
Investigators found elevated levels of the protein, CXCL10, in the blood of transplant recipients around the time they developed cGVHD.
The team therefore believes that testing a transplant patient for this protein could potentially enable early diagnosis of cGVHD.
“Diagnostic tests are desperately needed to make blood and marrow transplants safer,” said study author Kirk Schultz, of BC Children’s Hospital in Vancouver, British Columbia, Canada.
“At this time, there are no good tests to diagnose cGVHD, and the disease can only be identified too late—when it is already established. If we can diagnose it earlier and better, then treatments can be used to stop it before it becomes a chronic, disabling disease.”
For this study, Dr Schultz and his colleagues searched for cGVHD biomarkers in blood samples from 2 groups of adult patients—36 cGVHD patients who were at least 1 month from diagnosis and 31 time-matched control subjects without cGVHD.
This revealed 11 potential biomarkers. The investigators went on to test the validity of these biomarkers in 2 replication cohorts, which included a total of 134 patients with cGVHD and 154 control subjects.
Results showed that the inflammatory protein CXCL10 was consistently elevated in patients with cGVHD. This protein appears to impact a patient’s normal immune cells, preventing the body from fighting cGVHD.
The investigators also found evidence to suggest that another protein, sBAFF, is a biomarker of cGVHD.
Although these results may bring us one step closer to a diagnostic test for cGVHD, the team said further study is needed in larger patient groups. ![]()
Lenalidomide maintenance after transplant improves OS in MM

the ASCO Annual Meeting
© ASCO/Todd Buchanan
CHICAGO—Lenalidomide maintenance after high-dose melphalan and autologous stem cell transplant (ASCT) should be considered the standard of care in
newly diagnosed multiple myeloma (MM) patients, according to a meta-analysis presented at the 2016 ASCO Annual Meeting.
Lenalidomide maintenance increased overall survival (OS), with a 26% reduction in the risk of death, representing an estimated 2.5-year increase in median survival.
Several studies have demonstrated that lenalidomide maintenance post-ASCT reduces the risk of disease progression or death in patients with MM by about 50%.
However, these studies were not powered for OS, said Philip McCarthy, MD, of Roswell Park Cancer Institute in Buffalo, New York.
With this in mind, Dr McCarthy and his colleagues conducted a meta-analysis to assess the effect of post-ASCT lenalidomide maintenance on OS using a pooled analysis of primary source patient data. A search revealed 17 randomized, controlled trials using lenalidomide post-ASCT.
Three trials met pre-specified inclusion criteria and had sufficient OS events to test a treatment effect. The studies intended for lenalidomide maintenance to be given until progression.
In these trials, 1209 MM patients, with a median age of 58, were randomized from 2005 to 2009 to receive lenalidomide (605 patients) at 10 mg/day on days 1-21/28 or days 1-28/28. The remaining 604 patients served as controls. Baseline characteristics were generally balanced between the 2 groups.
With a median follow-up of 6.6 years, 491 patients (41%) had died.
After induction and single (82%) or tandem (18%) ASCT, 55% of patients achieved a complete response (CR) or very good partial response.
The median OS has not been reached in the lenalidomide arm but was 86 months for the control arm.
“There is a 26% reduction in the risk of death, representing an estimated 2.5-year increase in median survival,” Dr McCarthy said.
The OS benefit favoring lenalidomide was generally consistent across the majority of subgroup analyses, including age, sex, ISS stage, response after ASCT, and prior induction therapy.
All studies contributed to the positive results of the meta-analysis. Heterogeneity tests showed significant differences across trials, mainly because of a difference in the magnitude of treatment effect, Dr McCarthy said.
The mean treatment duration of maintenance was 25 to 30 months in the lenalidomide group and 13 to 20 months in controls. About one-third to more than half of the patients received therapy for 3 or more years, Dr McCarthy said.
Lenalidomide led to an increased risk in the cumulative incidence of hematologic and solid tumor second primary malignancies. However, Dr McCarthy said the OS benefit of lenalidomide maintenance outweighs the risk of developing second primary malignancy.
“This large meta-analysis demonstrates that lenalidomide maintenance significantly prolonged OS post-ASCT, including in patients who achieved CR, demonstrating benefit in patients in all response categories,” Dr McCarthy said.
“Lenalidomide maintenance after ASCT can be considered a standard of care for newly diagnosed multiple myeloma patients. However, we have more to learn. Understanding the role of minimal residual disease detection and immune reconstitution after transplant should allow us to further improve OS. Critically, developing early endpoints as surrogates for long-term outcome and OS is important for the future. Otherwise, trials may continue for 10 years or longer.”
Dr McCarthy presented these findings as abstract 8001. ![]()

the ASCO Annual Meeting
© ASCO/Todd Buchanan
CHICAGO—Lenalidomide maintenance after high-dose melphalan and autologous stem cell transplant (ASCT) should be considered the standard of care in
newly diagnosed multiple myeloma (MM) patients, according to a meta-analysis presented at the 2016 ASCO Annual Meeting.
Lenalidomide maintenance increased overall survival (OS), with a 26% reduction in the risk of death, representing an estimated 2.5-year increase in median survival.
Several studies have demonstrated that lenalidomide maintenance post-ASCT reduces the risk of disease progression or death in patients with MM by about 50%.
However, these studies were not powered for OS, said Philip McCarthy, MD, of Roswell Park Cancer Institute in Buffalo, New York.
With this in mind, Dr McCarthy and his colleagues conducted a meta-analysis to assess the effect of post-ASCT lenalidomide maintenance on OS using a pooled analysis of primary source patient data. A search revealed 17 randomized, controlled trials using lenalidomide post-ASCT.
Three trials met pre-specified inclusion criteria and had sufficient OS events to test a treatment effect. The studies intended for lenalidomide maintenance to be given until progression.
In these trials, 1209 MM patients, with a median age of 58, were randomized from 2005 to 2009 to receive lenalidomide (605 patients) at 10 mg/day on days 1-21/28 or days 1-28/28. The remaining 604 patients served as controls. Baseline characteristics were generally balanced between the 2 groups.
With a median follow-up of 6.6 years, 491 patients (41%) had died.
After induction and single (82%) or tandem (18%) ASCT, 55% of patients achieved a complete response (CR) or very good partial response.
The median OS has not been reached in the lenalidomide arm but was 86 months for the control arm.
“There is a 26% reduction in the risk of death, representing an estimated 2.5-year increase in median survival,” Dr McCarthy said.
The OS benefit favoring lenalidomide was generally consistent across the majority of subgroup analyses, including age, sex, ISS stage, response after ASCT, and prior induction therapy.
All studies contributed to the positive results of the meta-analysis. Heterogeneity tests showed significant differences across trials, mainly because of a difference in the magnitude of treatment effect, Dr McCarthy said.
The mean treatment duration of maintenance was 25 to 30 months in the lenalidomide group and 13 to 20 months in controls. About one-third to more than half of the patients received therapy for 3 or more years, Dr McCarthy said.
Lenalidomide led to an increased risk in the cumulative incidence of hematologic and solid tumor second primary malignancies. However, Dr McCarthy said the OS benefit of lenalidomide maintenance outweighs the risk of developing second primary malignancy.
“This large meta-analysis demonstrates that lenalidomide maintenance significantly prolonged OS post-ASCT, including in patients who achieved CR, demonstrating benefit in patients in all response categories,” Dr McCarthy said.
“Lenalidomide maintenance after ASCT can be considered a standard of care for newly diagnosed multiple myeloma patients. However, we have more to learn. Understanding the role of minimal residual disease detection and immune reconstitution after transplant should allow us to further improve OS. Critically, developing early endpoints as surrogates for long-term outcome and OS is important for the future. Otherwise, trials may continue for 10 years or longer.”
Dr McCarthy presented these findings as abstract 8001. ![]()

the ASCO Annual Meeting
© ASCO/Todd Buchanan
CHICAGO—Lenalidomide maintenance after high-dose melphalan and autologous stem cell transplant (ASCT) should be considered the standard of care in
newly diagnosed multiple myeloma (MM) patients, according to a meta-analysis presented at the 2016 ASCO Annual Meeting.
Lenalidomide maintenance increased overall survival (OS), with a 26% reduction in the risk of death, representing an estimated 2.5-year increase in median survival.
Several studies have demonstrated that lenalidomide maintenance post-ASCT reduces the risk of disease progression or death in patients with MM by about 50%.
However, these studies were not powered for OS, said Philip McCarthy, MD, of Roswell Park Cancer Institute in Buffalo, New York.
With this in mind, Dr McCarthy and his colleagues conducted a meta-analysis to assess the effect of post-ASCT lenalidomide maintenance on OS using a pooled analysis of primary source patient data. A search revealed 17 randomized, controlled trials using lenalidomide post-ASCT.
Three trials met pre-specified inclusion criteria and had sufficient OS events to test a treatment effect. The studies intended for lenalidomide maintenance to be given until progression.
In these trials, 1209 MM patients, with a median age of 58, were randomized from 2005 to 2009 to receive lenalidomide (605 patients) at 10 mg/day on days 1-21/28 or days 1-28/28. The remaining 604 patients served as controls. Baseline characteristics were generally balanced between the 2 groups.
With a median follow-up of 6.6 years, 491 patients (41%) had died.
After induction and single (82%) or tandem (18%) ASCT, 55% of patients achieved a complete response (CR) or very good partial response.
The median OS has not been reached in the lenalidomide arm but was 86 months for the control arm.
“There is a 26% reduction in the risk of death, representing an estimated 2.5-year increase in median survival,” Dr McCarthy said.
The OS benefit favoring lenalidomide was generally consistent across the majority of subgroup analyses, including age, sex, ISS stage, response after ASCT, and prior induction therapy.
All studies contributed to the positive results of the meta-analysis. Heterogeneity tests showed significant differences across trials, mainly because of a difference in the magnitude of treatment effect, Dr McCarthy said.
The mean treatment duration of maintenance was 25 to 30 months in the lenalidomide group and 13 to 20 months in controls. About one-third to more than half of the patients received therapy for 3 or more years, Dr McCarthy said.
Lenalidomide led to an increased risk in the cumulative incidence of hematologic and solid tumor second primary malignancies. However, Dr McCarthy said the OS benefit of lenalidomide maintenance outweighs the risk of developing second primary malignancy.
“This large meta-analysis demonstrates that lenalidomide maintenance significantly prolonged OS post-ASCT, including in patients who achieved CR, demonstrating benefit in patients in all response categories,” Dr McCarthy said.
“Lenalidomide maintenance after ASCT can be considered a standard of care for newly diagnosed multiple myeloma patients. However, we have more to learn. Understanding the role of minimal residual disease detection and immune reconstitution after transplant should allow us to further improve OS. Critically, developing early endpoints as surrogates for long-term outcome and OS is important for the future. Otherwise, trials may continue for 10 years or longer.”
Dr McCarthy presented these findings as abstract 8001. ![]()
HIV not a contraindication for transplant in lymphoma

cultured lymphocyte
Image courtesy of CDC
With the advent of effective anti-retroviral therapy, patients with HIV-related lymphoma receive standard therapeutic regimens and achieve outcomes comparable to those of non-HIV-infected individuals.
Based on results of a multicenter phase 2 study, this now extends to treatment with autologous stem cell transplant (ASCT).
Researchers found that outcomes were not significantly different between HIV-infected patients who received ASCT and matched controls.
“These findings are remarkably important for a group of patients who, up until now, have been inconsistently treated,” said lead study author Joseph C. Alvarnas, MD, of City of Hope National Medical Center in Duarte, California.
“Based on our data, autologous stem cell transplant should be considered the standard of care for patients with HIV-related lymphomas for the same indications and under the same circumstances that we would use it in patients without HIV infection.”
To arrive at this recommendation, investigators enrolled 43 HIV-infected patients with relapsed or persistent non-Hodgkin lymphoma (NHL) or classical Hodgkin lymphoma (HL) onto the Blood and Marrow Transplant Clinical Trials Network (BMT CTN) 0803/AIDS Malignancy Consortium (AMC) 071 study.
They reported their findings in Blood.
Eligibility
Patients had to be 15 years or older, have documented evidence of HIV infection, and have a Karnofsky performance status of greater than 70%.
They had to have persistent or recurrent diffuse large B-cell lymphoma, immunoblastic lymphoma, plasmablastic lymphoma, Burkitt lymphoma, Burkitt-like NHL, or classic HL.
Patients could have had no more than 3 prior treatment regimens or 2 or fewer salvage regimens.
They had to have adequate organ function, fewer than 10% blasts in their marrow, no prior autologous or allogeneic transplant, and adequate hematopoietic progenitor cell mobilization of more than 1.5 x 106 CD34+ cells/kg to be eligible.
Transplant regimen
Patients received the BEAM (carmustine, etoposide, cytarabine, and melphalan) transplant regimen on day 0. They did not receive antiretroviral therapy from the time of the start of BEAM until 7 days after completion of the preparative regimen.
Efavirenz was held for 2 weeks prior to BEAM initiation, and an alternative agent was substituted during this time period. Zidovudine was prohibited following transplant because of its myelosuppressive effects.
Patients received growth factor, transfusion, and antimicrobial supportive care according to institutional standards of the transplant center.
Patient characteristics
Of the original 43 patients enrolled, 3 patients experienced disease progression prior to the conditioning regimen and did not undergo transplant. Therefore, investigators did not include them in the study analysis.
Forty patients received ASCT at 16 different transplant centers. They were a median age of 46.9 (range, 22.5–62.2), and 35 were male.
All patients received peripheral blood stem cell grafts at a median dose of 3.9 x 106 CD34+ cells/kg (range, 1.6–11.0). And all patients were able to mobilize hematopoietic progenitor cells in a median of 2 apheresis collections (range, 1–5).
Most patients (n=32; 80%) had a pre-transplant HIV viral load that was undetectable. The median viral load for those 8 patients with detectable disease was 80 copies/mL (range, 50–17,455).
Patients had a median pre-transplant CD4+ T-cell count of 249.0 CD4+/μL (range, 39–797).
Investigators followed the patients for a median of 24.8 months (range, 2.8–27.2).
Response
Seven patients died during the follow-up period, 5 within 1 year of transplant. Four of the deaths within 1 year of transplant were due to relapse or disease progression.
One-year transplant-related mortality (TRM) was 5.2%.
The 1-year overall survival (OS) probability was 87.3%, and, at 2 years, it was 82%. The 2-year progression-free survival (PFS) was 79.8%, and the cumulative incidence of relapse/progression at 2 years was 12.5%.
The probabilities for OS and PFS at 2 years were comparable for both NHL and HL patients.
The median time to post-transplant neutrophil recovery was 11 days, and 97.5% of patients recovered their neutrophil counts by day 28.
The median time to platelet recovery was 18 days, and 92.5% of patients recovered their platelet counts by day 100.
At 100 days post-transplant, 28.9% of the evaluable patients (11/38) had recovered hematologic function. And at 1 year, 74.2% (23/31) had recovered hematologic function.
Adverse events
A little more than half (55%) the patients had at least 1 infectious event within a year of transplant, including 11 who had a severe infection.
Of the 57 infections that occurred post-transplant, 25 were due to bacteria, 22 to viruses, 6 to fungal organisms, 2 to protozoa, and 2 to other organisms. No patient developed Pneumocystis jiroveci pneumonia after transplant.
Nine patients experienced a total of 13 grade 3–5 adverse events. This included infection/sepsis (5 events), venous thromboembolism (2 events), and 1 event each for esophageal candidiasis, enteritis, hyperglycemia, hypernatremia, acute appendicitis, and acute coronary syndrome.
Sixteen patients had to be re-admitted to the hospital after the transplant, for a total of 34 readmissions. Infection (18) and fever (6) were the most common reasons for readmission.
Data comparison
The investigators compared the OS and PFS results to a control group identified through the Center for International Bone Marrow Transplant Research (CIBMTR).
One hundred fifty-one controls matched for age, performance status, primary disease, and disease status at transplant were identified for the 40 HIV-lymphoma cases.
The 1-year OS for the control group was 87.7%, and the 2-year PFS was 69.5%. This compared with the 87.3% and 79.8% for OS and PFS, respectively, for the HIV-lymphoma patients.
These results, the investigators wrote, were not significantly different from outcomes of CIBMTR controls, with a hazard ratio for overall mortality in the HIV-lymphoma patients of 0.67 (95% CI: 0.30–1.50, P=0.33) compared to controls.
And the hazard ratio for treatment failure in the HIV-lymphoma patients was 0.52 (95% CI: 0.2927–1.03, P=0.06) compared to controls.
The investigators concluded that HIV infection alone should not be considered a contraindication to ASCT for patients who otherwise meet transplant inclusion criteria. And ASCT should be considered the standard of care for patients with HIV-related lymphoma, provided that the HIV infection is treatment-responsive.
The team added that these patients should also be considered “appropriate potential participants” for future ASCT clinical trials. ![]()

cultured lymphocyte
Image courtesy of CDC
With the advent of effective anti-retroviral therapy, patients with HIV-related lymphoma receive standard therapeutic regimens and achieve outcomes comparable to those of non-HIV-infected individuals.
Based on results of a multicenter phase 2 study, this now extends to treatment with autologous stem cell transplant (ASCT).
Researchers found that outcomes were not significantly different between HIV-infected patients who received ASCT and matched controls.
“These findings are remarkably important for a group of patients who, up until now, have been inconsistently treated,” said lead study author Joseph C. Alvarnas, MD, of City of Hope National Medical Center in Duarte, California.
“Based on our data, autologous stem cell transplant should be considered the standard of care for patients with HIV-related lymphomas for the same indications and under the same circumstances that we would use it in patients without HIV infection.”
To arrive at this recommendation, investigators enrolled 43 HIV-infected patients with relapsed or persistent non-Hodgkin lymphoma (NHL) or classical Hodgkin lymphoma (HL) onto the Blood and Marrow Transplant Clinical Trials Network (BMT CTN) 0803/AIDS Malignancy Consortium (AMC) 071 study.
They reported their findings in Blood.
Eligibility
Patients had to be 15 years or older, have documented evidence of HIV infection, and have a Karnofsky performance status of greater than 70%.
They had to have persistent or recurrent diffuse large B-cell lymphoma, immunoblastic lymphoma, plasmablastic lymphoma, Burkitt lymphoma, Burkitt-like NHL, or classic HL.
Patients could have had no more than 3 prior treatment regimens or 2 or fewer salvage regimens.
They had to have adequate organ function, fewer than 10% blasts in their marrow, no prior autologous or allogeneic transplant, and adequate hematopoietic progenitor cell mobilization of more than 1.5 x 106 CD34+ cells/kg to be eligible.
Transplant regimen
Patients received the BEAM (carmustine, etoposide, cytarabine, and melphalan) transplant regimen on day 0. They did not receive antiretroviral therapy from the time of the start of BEAM until 7 days after completion of the preparative regimen.
Efavirenz was held for 2 weeks prior to BEAM initiation, and an alternative agent was substituted during this time period. Zidovudine was prohibited following transplant because of its myelosuppressive effects.
Patients received growth factor, transfusion, and antimicrobial supportive care according to institutional standards of the transplant center.
Patient characteristics
Of the original 43 patients enrolled, 3 patients experienced disease progression prior to the conditioning regimen and did not undergo transplant. Therefore, investigators did not include them in the study analysis.
Forty patients received ASCT at 16 different transplant centers. They were a median age of 46.9 (range, 22.5–62.2), and 35 were male.
All patients received peripheral blood stem cell grafts at a median dose of 3.9 x 106 CD34+ cells/kg (range, 1.6–11.0). And all patients were able to mobilize hematopoietic progenitor cells in a median of 2 apheresis collections (range, 1–5).
Most patients (n=32; 80%) had a pre-transplant HIV viral load that was undetectable. The median viral load for those 8 patients with detectable disease was 80 copies/mL (range, 50–17,455).
Patients had a median pre-transplant CD4+ T-cell count of 249.0 CD4+/μL (range, 39–797).
Investigators followed the patients for a median of 24.8 months (range, 2.8–27.2).
Response
Seven patients died during the follow-up period, 5 within 1 year of transplant. Four of the deaths within 1 year of transplant were due to relapse or disease progression.
One-year transplant-related mortality (TRM) was 5.2%.
The 1-year overall survival (OS) probability was 87.3%, and, at 2 years, it was 82%. The 2-year progression-free survival (PFS) was 79.8%, and the cumulative incidence of relapse/progression at 2 years was 12.5%.
The probabilities for OS and PFS at 2 years were comparable for both NHL and HL patients.
The median time to post-transplant neutrophil recovery was 11 days, and 97.5% of patients recovered their neutrophil counts by day 28.
The median time to platelet recovery was 18 days, and 92.5% of patients recovered their platelet counts by day 100.
At 100 days post-transplant, 28.9% of the evaluable patients (11/38) had recovered hematologic function. And at 1 year, 74.2% (23/31) had recovered hematologic function.
Adverse events
A little more than half (55%) the patients had at least 1 infectious event within a year of transplant, including 11 who had a severe infection.
Of the 57 infections that occurred post-transplant, 25 were due to bacteria, 22 to viruses, 6 to fungal organisms, 2 to protozoa, and 2 to other organisms. No patient developed Pneumocystis jiroveci pneumonia after transplant.
Nine patients experienced a total of 13 grade 3–5 adverse events. This included infection/sepsis (5 events), venous thromboembolism (2 events), and 1 event each for esophageal candidiasis, enteritis, hyperglycemia, hypernatremia, acute appendicitis, and acute coronary syndrome.
Sixteen patients had to be re-admitted to the hospital after the transplant, for a total of 34 readmissions. Infection (18) and fever (6) were the most common reasons for readmission.
Data comparison
The investigators compared the OS and PFS results to a control group identified through the Center for International Bone Marrow Transplant Research (CIBMTR).
One hundred fifty-one controls matched for age, performance status, primary disease, and disease status at transplant were identified for the 40 HIV-lymphoma cases.
The 1-year OS for the control group was 87.7%, and the 2-year PFS was 69.5%. This compared with the 87.3% and 79.8% for OS and PFS, respectively, for the HIV-lymphoma patients.
These results, the investigators wrote, were not significantly different from outcomes of CIBMTR controls, with a hazard ratio for overall mortality in the HIV-lymphoma patients of 0.67 (95% CI: 0.30–1.50, P=0.33) compared to controls.
And the hazard ratio for treatment failure in the HIV-lymphoma patients was 0.52 (95% CI: 0.2927–1.03, P=0.06) compared to controls.
The investigators concluded that HIV infection alone should not be considered a contraindication to ASCT for patients who otherwise meet transplant inclusion criteria. And ASCT should be considered the standard of care for patients with HIV-related lymphoma, provided that the HIV infection is treatment-responsive.
The team added that these patients should also be considered “appropriate potential participants” for future ASCT clinical trials. ![]()

cultured lymphocyte
Image courtesy of CDC
With the advent of effective anti-retroviral therapy, patients with HIV-related lymphoma receive standard therapeutic regimens and achieve outcomes comparable to those of non-HIV-infected individuals.
Based on results of a multicenter phase 2 study, this now extends to treatment with autologous stem cell transplant (ASCT).
Researchers found that outcomes were not significantly different between HIV-infected patients who received ASCT and matched controls.
“These findings are remarkably important for a group of patients who, up until now, have been inconsistently treated,” said lead study author Joseph C. Alvarnas, MD, of City of Hope National Medical Center in Duarte, California.
“Based on our data, autologous stem cell transplant should be considered the standard of care for patients with HIV-related lymphomas for the same indications and under the same circumstances that we would use it in patients without HIV infection.”
To arrive at this recommendation, investigators enrolled 43 HIV-infected patients with relapsed or persistent non-Hodgkin lymphoma (NHL) or classical Hodgkin lymphoma (HL) onto the Blood and Marrow Transplant Clinical Trials Network (BMT CTN) 0803/AIDS Malignancy Consortium (AMC) 071 study.
They reported their findings in Blood.
Eligibility
Patients had to be 15 years or older, have documented evidence of HIV infection, and have a Karnofsky performance status of greater than 70%.
They had to have persistent or recurrent diffuse large B-cell lymphoma, immunoblastic lymphoma, plasmablastic lymphoma, Burkitt lymphoma, Burkitt-like NHL, or classic HL.
Patients could have had no more than 3 prior treatment regimens or 2 or fewer salvage regimens.
They had to have adequate organ function, fewer than 10% blasts in their marrow, no prior autologous or allogeneic transplant, and adequate hematopoietic progenitor cell mobilization of more than 1.5 x 106 CD34+ cells/kg to be eligible.
Transplant regimen
Patients received the BEAM (carmustine, etoposide, cytarabine, and melphalan) transplant regimen on day 0. They did not receive antiretroviral therapy from the time of the start of BEAM until 7 days after completion of the preparative regimen.
Efavirenz was held for 2 weeks prior to BEAM initiation, and an alternative agent was substituted during this time period. Zidovudine was prohibited following transplant because of its myelosuppressive effects.
Patients received growth factor, transfusion, and antimicrobial supportive care according to institutional standards of the transplant center.
Patient characteristics
Of the original 43 patients enrolled, 3 patients experienced disease progression prior to the conditioning regimen and did not undergo transplant. Therefore, investigators did not include them in the study analysis.
Forty patients received ASCT at 16 different transplant centers. They were a median age of 46.9 (range, 22.5–62.2), and 35 were male.
All patients received peripheral blood stem cell grafts at a median dose of 3.9 x 106 CD34+ cells/kg (range, 1.6–11.0). And all patients were able to mobilize hematopoietic progenitor cells in a median of 2 apheresis collections (range, 1–5).
Most patients (n=32; 80%) had a pre-transplant HIV viral load that was undetectable. The median viral load for those 8 patients with detectable disease was 80 copies/mL (range, 50–17,455).
Patients had a median pre-transplant CD4+ T-cell count of 249.0 CD4+/μL (range, 39–797).
Investigators followed the patients for a median of 24.8 months (range, 2.8–27.2).
Response
Seven patients died during the follow-up period, 5 within 1 year of transplant. Four of the deaths within 1 year of transplant were due to relapse or disease progression.
One-year transplant-related mortality (TRM) was 5.2%.
The 1-year overall survival (OS) probability was 87.3%, and, at 2 years, it was 82%. The 2-year progression-free survival (PFS) was 79.8%, and the cumulative incidence of relapse/progression at 2 years was 12.5%.
The probabilities for OS and PFS at 2 years were comparable for both NHL and HL patients.
The median time to post-transplant neutrophil recovery was 11 days, and 97.5% of patients recovered their neutrophil counts by day 28.
The median time to platelet recovery was 18 days, and 92.5% of patients recovered their platelet counts by day 100.
At 100 days post-transplant, 28.9% of the evaluable patients (11/38) had recovered hematologic function. And at 1 year, 74.2% (23/31) had recovered hematologic function.
Adverse events
A little more than half (55%) the patients had at least 1 infectious event within a year of transplant, including 11 who had a severe infection.
Of the 57 infections that occurred post-transplant, 25 were due to bacteria, 22 to viruses, 6 to fungal organisms, 2 to protozoa, and 2 to other organisms. No patient developed Pneumocystis jiroveci pneumonia after transplant.
Nine patients experienced a total of 13 grade 3–5 adverse events. This included infection/sepsis (5 events), venous thromboembolism (2 events), and 1 event each for esophageal candidiasis, enteritis, hyperglycemia, hypernatremia, acute appendicitis, and acute coronary syndrome.
Sixteen patients had to be re-admitted to the hospital after the transplant, for a total of 34 readmissions. Infection (18) and fever (6) were the most common reasons for readmission.
Data comparison
The investigators compared the OS and PFS results to a control group identified through the Center for International Bone Marrow Transplant Research (CIBMTR).
One hundred fifty-one controls matched for age, performance status, primary disease, and disease status at transplant were identified for the 40 HIV-lymphoma cases.
The 1-year OS for the control group was 87.7%, and the 2-year PFS was 69.5%. This compared with the 87.3% and 79.8% for OS and PFS, respectively, for the HIV-lymphoma patients.
These results, the investigators wrote, were not significantly different from outcomes of CIBMTR controls, with a hazard ratio for overall mortality in the HIV-lymphoma patients of 0.67 (95% CI: 0.30–1.50, P=0.33) compared to controls.
And the hazard ratio for treatment failure in the HIV-lymphoma patients was 0.52 (95% CI: 0.2927–1.03, P=0.06) compared to controls.
The investigators concluded that HIV infection alone should not be considered a contraindication to ASCT for patients who otherwise meet transplant inclusion criteria. And ASCT should be considered the standard of care for patients with HIV-related lymphoma, provided that the HIV infection is treatment-responsive.
The team added that these patients should also be considered “appropriate potential participants” for future ASCT clinical trials. ![]()
Corticosteroid prophylaxis reduces GVHD in high-risk patients

Image courtesy of PLOS ONE
A team of researchers has found that risk-stratified, low-dose corticosteroid prophylaxis can significantly reduce the incidence of acute graft-versus-host disease (GVHD), accelerate platelet recovery, and reduce adverse events without increasing infections in patients who undergo haploidentical transplantation.
They believe this is the first test of a novel risk stratification–directed prophylaxis strategy. The strategy effectively prevented acute GVHD among patients who were at high risk for GVHD, without unnecessarily exposing patients who were at low risk to excessive toxicity from additional immunosuppressive agents.
To evaluate the prophylaxis strategy, the team enrolled 228 patients who underwent haploidentical transplant onto this controlled, open-label, randomized trial.
Corresponding author Xiao-Jun Huang, MD, of Peking University in Beijing, China, and colleagues reported the results in JCO.
The team stratified patients as high risk or low risk for developing GVHD based on biomarkers.
They categorized patients as high risk if they had CD4:CD8 ratios of 1.15 or greater in bone marrow grafts or more than 1.9 x 106/kg CD56bright NK cells in allogeneic grafts.
Patients who did not qualify for the high-risk group were considered to be low risk.
The team randomly assigned the high-risk patients to either receive or not receive the investigational intervention of methylprednisolone (MP).
All patients received cyclosporine, mycophenolate mofetil, and methotrexate for GVHD prevention.
Patients in any arm who developed acute GVHD higher than grade II received MP. If they did not respond, they received basiliximab.
Study population
Of the 228 patients enrolled, 83 were in the low-risk group, 72 in the high-risk experimental prophylaxis group, and 73 in the high-risk control group.
Patient characteristics were similar across all cohorts, including the conditioning regimens, except for their biomarker status.
Patients were a median age of about 30 years, (range 14 – 58), about half were male, and most had a diagnosis of acute myeloid leukemia or acute lymphoblastic leukemia.
GVHD incidence
The cumulative, 100-day incidence of acute GVHD grades II to IV was 21% in the high-risk prophylaxis arm.
This was similar to the incidence of 26% in the low-risk arm, P=0.43.
Both cohorts were significantly lower than the incidence of 48% in the high-risk control group, P<0.001.
Multivariate analysis showed that risk-stratified prophylaxis with low-dose corticosteroid significantly reduced the incidence of acute GVHD compared with no low-dose corticosteroid, with a hazard ratio of 0.66, P=0.007.
However, investigators found no differences between cohorts in the incidence of grades III to IV GVHD.
Corticosteroid-refractory acute GVHD developed in 14% of high-risk patients in the experimental arm, 18% in the control arm, and 23% in the low-risk group. Basiliximab, an anti-CD25 antibody, was used to treat it.
Hematopoietic and immune recovery
The median times to myeloid and platelet recovery were significantly shorter in the high-risk prophylaxis group (P<0.05 for both) and the low-risk group (P<0.05) than in the high-risk control group.
And immune reconstitution was comparable among all 3 cohorts.
Safety
Cumulative incidences among the low-risk, high-risk prophylaxis, and high-risk control groups, respectively, of cytomegalovirus reactivation (80%, 82%, 81%), Epstein-Barr virus reactivation (7%, 14%, 14%), post-transplantation lymphoproliferative disorder (0%, 1%, 4%), hemorrhagic cystitis (56%, 45%, 47%), bacteremia (13%, 10%, 11%), and invasive fungal infection (11%, 8%, 8%) were similar across the cohorts.
Osteonecrosis of the femoral head (P=0.034) and secondary hypertension (P=0.015) were significantly lower in the high-risk prophylaxis group than in the high-risk control group.
Transplant outcomes
Transplant outcomes, both relapse and non-relapse mortality at 100 days and 1 year, were similar among the 3 cohorts.
After a median follow-up of 505 days, the cumulative incidence of chronic GVHD was 44% in the high-risk prophylaxis group, 64% in the low-risk group, and 59% in the high-risk control group.
However, moderate to severe chronic GVHD was lower in the high-risk prophylaxis group, at 21%, compared to 50% in the low-risk group and 36% in the high-risk control group.
Thirty-two patients died of non-relapse causes, and the 3-year probabilities of leukemia-free survival and overall survival were similar among the 3 groups. ![]()

Image courtesy of PLOS ONE
A team of researchers has found that risk-stratified, low-dose corticosteroid prophylaxis can significantly reduce the incidence of acute graft-versus-host disease (GVHD), accelerate platelet recovery, and reduce adverse events without increasing infections in patients who undergo haploidentical transplantation.
They believe this is the first test of a novel risk stratification–directed prophylaxis strategy. The strategy effectively prevented acute GVHD among patients who were at high risk for GVHD, without unnecessarily exposing patients who were at low risk to excessive toxicity from additional immunosuppressive agents.
To evaluate the prophylaxis strategy, the team enrolled 228 patients who underwent haploidentical transplant onto this controlled, open-label, randomized trial.
Corresponding author Xiao-Jun Huang, MD, of Peking University in Beijing, China, and colleagues reported the results in JCO.
The team stratified patients as high risk or low risk for developing GVHD based on biomarkers.
They categorized patients as high risk if they had CD4:CD8 ratios of 1.15 or greater in bone marrow grafts or more than 1.9 x 106/kg CD56bright NK cells in allogeneic grafts.
Patients who did not qualify for the high-risk group were considered to be low risk.
The team randomly assigned the high-risk patients to either receive or not receive the investigational intervention of methylprednisolone (MP).
All patients received cyclosporine, mycophenolate mofetil, and methotrexate for GVHD prevention.
Patients in any arm who developed acute GVHD higher than grade II received MP. If they did not respond, they received basiliximab.
Study population
Of the 228 patients enrolled, 83 were in the low-risk group, 72 in the high-risk experimental prophylaxis group, and 73 in the high-risk control group.
Patient characteristics were similar across all cohorts, including the conditioning regimens, except for their biomarker status.
Patients were a median age of about 30 years, (range 14 – 58), about half were male, and most had a diagnosis of acute myeloid leukemia or acute lymphoblastic leukemia.
GVHD incidence
The cumulative, 100-day incidence of acute GVHD grades II to IV was 21% in the high-risk prophylaxis arm.
This was similar to the incidence of 26% in the low-risk arm, P=0.43.
Both cohorts were significantly lower than the incidence of 48% in the high-risk control group, P<0.001.
Multivariate analysis showed that risk-stratified prophylaxis with low-dose corticosteroid significantly reduced the incidence of acute GVHD compared with no low-dose corticosteroid, with a hazard ratio of 0.66, P=0.007.
However, investigators found no differences between cohorts in the incidence of grades III to IV GVHD.
Corticosteroid-refractory acute GVHD developed in 14% of high-risk patients in the experimental arm, 18% in the control arm, and 23% in the low-risk group. Basiliximab, an anti-CD25 antibody, was used to treat it.
Hematopoietic and immune recovery
The median times to myeloid and platelet recovery were significantly shorter in the high-risk prophylaxis group (P<0.05 for both) and the low-risk group (P<0.05) than in the high-risk control group.
And immune reconstitution was comparable among all 3 cohorts.
Safety
Cumulative incidences among the low-risk, high-risk prophylaxis, and high-risk control groups, respectively, of cytomegalovirus reactivation (80%, 82%, 81%), Epstein-Barr virus reactivation (7%, 14%, 14%), post-transplantation lymphoproliferative disorder (0%, 1%, 4%), hemorrhagic cystitis (56%, 45%, 47%), bacteremia (13%, 10%, 11%), and invasive fungal infection (11%, 8%, 8%) were similar across the cohorts.
Osteonecrosis of the femoral head (P=0.034) and secondary hypertension (P=0.015) were significantly lower in the high-risk prophylaxis group than in the high-risk control group.
Transplant outcomes
Transplant outcomes, both relapse and non-relapse mortality at 100 days and 1 year, were similar among the 3 cohorts.
After a median follow-up of 505 days, the cumulative incidence of chronic GVHD was 44% in the high-risk prophylaxis group, 64% in the low-risk group, and 59% in the high-risk control group.
However, moderate to severe chronic GVHD was lower in the high-risk prophylaxis group, at 21%, compared to 50% in the low-risk group and 36% in the high-risk control group.
Thirty-two patients died of non-relapse causes, and the 3-year probabilities of leukemia-free survival and overall survival were similar among the 3 groups. ![]()

Image courtesy of PLOS ONE
A team of researchers has found that risk-stratified, low-dose corticosteroid prophylaxis can significantly reduce the incidence of acute graft-versus-host disease (GVHD), accelerate platelet recovery, and reduce adverse events without increasing infections in patients who undergo haploidentical transplantation.
They believe this is the first test of a novel risk stratification–directed prophylaxis strategy. The strategy effectively prevented acute GVHD among patients who were at high risk for GVHD, without unnecessarily exposing patients who were at low risk to excessive toxicity from additional immunosuppressive agents.
To evaluate the prophylaxis strategy, the team enrolled 228 patients who underwent haploidentical transplant onto this controlled, open-label, randomized trial.
Corresponding author Xiao-Jun Huang, MD, of Peking University in Beijing, China, and colleagues reported the results in JCO.
The team stratified patients as high risk or low risk for developing GVHD based on biomarkers.
They categorized patients as high risk if they had CD4:CD8 ratios of 1.15 or greater in bone marrow grafts or more than 1.9 x 106/kg CD56bright NK cells in allogeneic grafts.
Patients who did not qualify for the high-risk group were considered to be low risk.
The team randomly assigned the high-risk patients to either receive or not receive the investigational intervention of methylprednisolone (MP).
All patients received cyclosporine, mycophenolate mofetil, and methotrexate for GVHD prevention.
Patients in any arm who developed acute GVHD higher than grade II received MP. If they did not respond, they received basiliximab.
Study population
Of the 228 patients enrolled, 83 were in the low-risk group, 72 in the high-risk experimental prophylaxis group, and 73 in the high-risk control group.
Patient characteristics were similar across all cohorts, including the conditioning regimens, except for their biomarker status.
Patients were a median age of about 30 years, (range 14 – 58), about half were male, and most had a diagnosis of acute myeloid leukemia or acute lymphoblastic leukemia.
GVHD incidence
The cumulative, 100-day incidence of acute GVHD grades II to IV was 21% in the high-risk prophylaxis arm.
This was similar to the incidence of 26% in the low-risk arm, P=0.43.
Both cohorts were significantly lower than the incidence of 48% in the high-risk control group, P<0.001.
Multivariate analysis showed that risk-stratified prophylaxis with low-dose corticosteroid significantly reduced the incidence of acute GVHD compared with no low-dose corticosteroid, with a hazard ratio of 0.66, P=0.007.
However, investigators found no differences between cohorts in the incidence of grades III to IV GVHD.
Corticosteroid-refractory acute GVHD developed in 14% of high-risk patients in the experimental arm, 18% in the control arm, and 23% in the low-risk group. Basiliximab, an anti-CD25 antibody, was used to treat it.
Hematopoietic and immune recovery
The median times to myeloid and platelet recovery were significantly shorter in the high-risk prophylaxis group (P<0.05 for both) and the low-risk group (P<0.05) than in the high-risk control group.
And immune reconstitution was comparable among all 3 cohorts.
Safety
Cumulative incidences among the low-risk, high-risk prophylaxis, and high-risk control groups, respectively, of cytomegalovirus reactivation (80%, 82%, 81%), Epstein-Barr virus reactivation (7%, 14%, 14%), post-transplantation lymphoproliferative disorder (0%, 1%, 4%), hemorrhagic cystitis (56%, 45%, 47%), bacteremia (13%, 10%, 11%), and invasive fungal infection (11%, 8%, 8%) were similar across the cohorts.
Osteonecrosis of the femoral head (P=0.034) and secondary hypertension (P=0.015) were significantly lower in the high-risk prophylaxis group than in the high-risk control group.
Transplant outcomes
Transplant outcomes, both relapse and non-relapse mortality at 100 days and 1 year, were similar among the 3 cohorts.
After a median follow-up of 505 days, the cumulative incidence of chronic GVHD was 44% in the high-risk prophylaxis group, 64% in the low-risk group, and 59% in the high-risk control group.
However, moderate to severe chronic GVHD was lower in the high-risk prophylaxis group, at 21%, compared to 50% in the low-risk group and 36% in the high-risk control group.
Thirty-two patients died of non-relapse causes, and the 3-year probabilities of leukemia-free survival and overall survival were similar among the 3 groups. ![]()
Tandem ASCT for neuroblastoma comes with caveat

Photo by Chad McNeeley
CHICAGO—A phase 3 study of tandem autologous stem cell transplant (ASCT) for children with high-risk neuroblastoma has shown that tandem transplant as consolidation significantly improved event-free survival (EFS).
Nevertheless, the improvement comes “with an important caveat,” according to Julie R. Park, MD, “that this is in children who survive induction without disease progression after induction or severe induction-related toxicity.”
Of note, the tandem transplant did not increase toxicity or regimen-related mortality.
Dr Park, of the Seattle Children’s Hospital and University of Washington, presented the study data on behalf of the Children’s Oncology Group and the COG ANBL0532 Study Committee during the plenary session at the 2016 ASCO Annual Meeting (LBA3*).
Neuroblastoma, Dr Park explained, is a disease that occurs in young children and is the most common extracranial tumor of childhood. Patients with high-risk neuroblastoma account for 50% of all children diagnosed with the disease, and neuroblastoma accounts for more than 10% of all childhood cancer mortality.
The outcome for high-risk neuroblastoma patients is dismal: fewer than 50% survive following current multi-agent, aggressive therapy, she said.
Randomized clinical trials performed over the last 25 years “have taught us that dose intensification of therapy is important,” Dr Park said, “and the treatment of minimal residual disease with non-cross resistant therapies is equally important.”
Pilot studies of tandem ASCT demonstrated tolerable toxicity and suggested efficacy, and clinical trials demonstrated that collecting peripheral blood stem cells in small children with neuroblastoma was feasible.
So the investigators undertook the current study to improve 3-year EFS of high-risk neuroblastoma patients using a strategy of tandem transplant consolidation.
Eligibility
Patients with newly diagnosed high-risk neuroblastoma were eligible. They had to have metastatic disease (INSS stage 4) and be older than 18 months to be eligible for the trial.
They could be any age if they had INSS stage 2, 3, or 4 with MYCN amplification.
“Our prior studies had identified that the group with regional disease and toddlers with MYCN non-amplified metastatic disease had a better outcome compared to other children with high-risk neuroblastoma,” Dr Park commented.
“Therefore, these children were non-randomly assigned to single transplant and are not included in the randomization results provided today,” she explained.
All children had to have normal cardiac, liver, and renal function.
Trial design: Induction
Induction therapy consisted of 6 cycles of chemotherapy—2 cycles of cyclophosphamide/topotecan, followed by 4 alternating cycles of cisplatin/etoposide and cyclophosphamide/vincristine/doxorubicin.
Peripheral blood stem cells (PBSCs) were harvested after the first 2 cycles of dose intensive cyclophosphamide and topotecan.
Patients had surgery on the primary tumor after 5 cycles of induction.
Trial design: Consolidation
Following completion of induction therapy, patients were assessed for eligibility for consolidation. These criteria included sufficient PBSC harvest, adequate organ function, no evidence of disease progression, and consent for post induction therapy.
Children eligible for consolidation were randomized to either the standard transplant with carboplatin, etoposide, melphalan or tandem transplant with cyclophosphamide and thiotepa followed 6 – 8 weeks later by the second transplant with carboplatin, etoposide, and melphalan.
Patients in both arms received radiotherapy to their primary tumor site.
Trial Design: Post-consolidation
Patients then went on for post consolidation chemotherapy with isotretinoin.
“During the conduct of ANBL0532,” Dr Park pointed out, “there was an additional trial running within the Children’s Oncology Group for which patients were eligible to enroll.”
So from 2007 – 2009, the additional trial (ANBL0032) randomized patients to their then standard of isotretinoin or isotretinoin plus the anti-GD2 antibody dinutuximab and cytokines.
“In 2009, results of that study were released and the dinutuximab arm was superior,” she noted, so patients were no longer randomized to isotretinoin only.
Prior studies indicated that 40% of patients went off trial at the end of induction therapy, so the investigators enrolled 665 patients to ensure a randomization of at least 332 patients.
Data cut-off for the presentation was March 31, 2016.
Patient demographics
Of the 665 patients accrued, 13 were ineligible. Twenty-seven patients with favorable prognosis were non-randomly assigned to single ASCT.
Forty percent (229 patients) went off protocol therapy prior to randomization. The main reasons for this were death (8 patients), progressive disease (48 patients), and physician and patient discretion (206 patients).
Investigators randomized 355 patients, 179 to single ASCT and 176 to tandem ASCT.
Patients were a median age of 37.2 months, 38.2% had MYCN amplification, and 88% were INSS stage 4.
The randomized cohorts of patients were similar to the overall patient cohort in terms of age, MYCN amplification, and stage 4 disease.
The randomizations were also well balanced in terms of MYCN amplifications, stage 4 disease, and response to induction chemotherapy.
The investigators retrospectively reviewed the patient characteristics, including age at diagnosis, early response to induction, and assignment to receive immunotherapy, “and there was no statistically significant difference between the randomized cohorts for these characteristics,” Dr Park said.
Safety
The most commonly observed grade 3 or greater non-hematologic toxicities in the single and tandem arms included infection (18.3% and 17.9%, respectively), mucosal toxicities (17.2% and 13.6%, respectively), and hepatic toxicities, including sinusoidal obstructive disorder (6.5% and 6.2%, respectively).
The investigators observed no significant differences between the arms in regard to the rate of these toxicities. In addition, they observed no difference between the arms in the rate of regimen-related mortality, 4.1% in the single arm, and 1.2% in the tandem arm.
Efficacy
For all patients (n=652) from time of enrollment, the 3-year EFS was 51.0% and the 3-year OS was 68.3%.
In randomized patients (n=355), from the time of randomization, the 3-year EFS was 54.8% and the 3-year OS, 71.5%, with a median survival time of 4.6 years.
There was a statistically significant improvement in EFS for those patients assigned to tandem transplant, with a 3-year EFS of 61.4% as compared to those assigned to single transplant, who had a 3-year EFS of 48.4% (P=0.0081).
There was not a statistically significant difference in OS. However, Dr Park pointed out that the trial was not powered to detect a difference in overall survival.
When looking at the cohort of stage 4 patients who were older than 18 months, investigators again saw a statistically significant improvement in EFS. The 3-year EFS was 59%.1 for tandem transplants vs 45.5% for single transplants, P=0.0083.
Again, there was no difference in OS in the INSS stage 4 patients older than 18 months.
“And finally, when we analyzed the outcome for children who were assigned to receive immunotherapy,” Dr Park pointed out, “from the time of start of immunotherapy, there was a statistically significant improvement in both event-free survival and overall survival for those children who received tandem transplants.”
The 3-year EFS for patients who received a tandem transplant and immunotherapy was 73.7% compared to the 3-year EFS of 56.0% for patients who received a single transplant and immunotherapy (P=0.0033).
The 3-year overall survival was also significantly improved for patients who received tandem transplants and immunotherapy (83.7%) compared to those who received a single transplant and immunotherapy (74.4%) (P=0.0322).
Conclusions
“Tandem transplant consolidation improves outcome in patients with high-risk neuroblastoma,” Dr Park said, with the important caveat mentioned earlier.
The tandem transplant does not increase toxicity or regimen-related mortality, and the benefit of tandem ASCT remains following anti-GD2-directed immunotherapy. ![]()
*Data in the presentation differ slightly from the abstract

Photo by Chad McNeeley
CHICAGO—A phase 3 study of tandem autologous stem cell transplant (ASCT) for children with high-risk neuroblastoma has shown that tandem transplant as consolidation significantly improved event-free survival (EFS).
Nevertheless, the improvement comes “with an important caveat,” according to Julie R. Park, MD, “that this is in children who survive induction without disease progression after induction or severe induction-related toxicity.”
Of note, the tandem transplant did not increase toxicity or regimen-related mortality.
Dr Park, of the Seattle Children’s Hospital and University of Washington, presented the study data on behalf of the Children’s Oncology Group and the COG ANBL0532 Study Committee during the plenary session at the 2016 ASCO Annual Meeting (LBA3*).
Neuroblastoma, Dr Park explained, is a disease that occurs in young children and is the most common extracranial tumor of childhood. Patients with high-risk neuroblastoma account for 50% of all children diagnosed with the disease, and neuroblastoma accounts for more than 10% of all childhood cancer mortality.
The outcome for high-risk neuroblastoma patients is dismal: fewer than 50% survive following current multi-agent, aggressive therapy, she said.
Randomized clinical trials performed over the last 25 years “have taught us that dose intensification of therapy is important,” Dr Park said, “and the treatment of minimal residual disease with non-cross resistant therapies is equally important.”
Pilot studies of tandem ASCT demonstrated tolerable toxicity and suggested efficacy, and clinical trials demonstrated that collecting peripheral blood stem cells in small children with neuroblastoma was feasible.
So the investigators undertook the current study to improve 3-year EFS of high-risk neuroblastoma patients using a strategy of tandem transplant consolidation.
Eligibility
Patients with newly diagnosed high-risk neuroblastoma were eligible. They had to have metastatic disease (INSS stage 4) and be older than 18 months to be eligible for the trial.
They could be any age if they had INSS stage 2, 3, or 4 with MYCN amplification.
“Our prior studies had identified that the group with regional disease and toddlers with MYCN non-amplified metastatic disease had a better outcome compared to other children with high-risk neuroblastoma,” Dr Park commented.
“Therefore, these children were non-randomly assigned to single transplant and are not included in the randomization results provided today,” she explained.
All children had to have normal cardiac, liver, and renal function.
Trial design: Induction
Induction therapy consisted of 6 cycles of chemotherapy—2 cycles of cyclophosphamide/topotecan, followed by 4 alternating cycles of cisplatin/etoposide and cyclophosphamide/vincristine/doxorubicin.
Peripheral blood stem cells (PBSCs) were harvested after the first 2 cycles of dose intensive cyclophosphamide and topotecan.
Patients had surgery on the primary tumor after 5 cycles of induction.
Trial design: Consolidation
Following completion of induction therapy, patients were assessed for eligibility for consolidation. These criteria included sufficient PBSC harvest, adequate organ function, no evidence of disease progression, and consent for post induction therapy.
Children eligible for consolidation were randomized to either the standard transplant with carboplatin, etoposide, melphalan or tandem transplant with cyclophosphamide and thiotepa followed 6 – 8 weeks later by the second transplant with carboplatin, etoposide, and melphalan.
Patients in both arms received radiotherapy to their primary tumor site.
Trial Design: Post-consolidation
Patients then went on for post consolidation chemotherapy with isotretinoin.
“During the conduct of ANBL0532,” Dr Park pointed out, “there was an additional trial running within the Children’s Oncology Group for which patients were eligible to enroll.”
So from 2007 – 2009, the additional trial (ANBL0032) randomized patients to their then standard of isotretinoin or isotretinoin plus the anti-GD2 antibody dinutuximab and cytokines.
“In 2009, results of that study were released and the dinutuximab arm was superior,” she noted, so patients were no longer randomized to isotretinoin only.
Prior studies indicated that 40% of patients went off trial at the end of induction therapy, so the investigators enrolled 665 patients to ensure a randomization of at least 332 patients.
Data cut-off for the presentation was March 31, 2016.
Patient demographics
Of the 665 patients accrued, 13 were ineligible. Twenty-seven patients with favorable prognosis were non-randomly assigned to single ASCT.
Forty percent (229 patients) went off protocol therapy prior to randomization. The main reasons for this were death (8 patients), progressive disease (48 patients), and physician and patient discretion (206 patients).
Investigators randomized 355 patients, 179 to single ASCT and 176 to tandem ASCT.
Patients were a median age of 37.2 months, 38.2% had MYCN amplification, and 88% were INSS stage 4.
The randomized cohorts of patients were similar to the overall patient cohort in terms of age, MYCN amplification, and stage 4 disease.
The randomizations were also well balanced in terms of MYCN amplifications, stage 4 disease, and response to induction chemotherapy.
The investigators retrospectively reviewed the patient characteristics, including age at diagnosis, early response to induction, and assignment to receive immunotherapy, “and there was no statistically significant difference between the randomized cohorts for these characteristics,” Dr Park said.
Safety
The most commonly observed grade 3 or greater non-hematologic toxicities in the single and tandem arms included infection (18.3% and 17.9%, respectively), mucosal toxicities (17.2% and 13.6%, respectively), and hepatic toxicities, including sinusoidal obstructive disorder (6.5% and 6.2%, respectively).
The investigators observed no significant differences between the arms in regard to the rate of these toxicities. In addition, they observed no difference between the arms in the rate of regimen-related mortality, 4.1% in the single arm, and 1.2% in the tandem arm.
Efficacy
For all patients (n=652) from time of enrollment, the 3-year EFS was 51.0% and the 3-year OS was 68.3%.
In randomized patients (n=355), from the time of randomization, the 3-year EFS was 54.8% and the 3-year OS, 71.5%, with a median survival time of 4.6 years.
There was a statistically significant improvement in EFS for those patients assigned to tandem transplant, with a 3-year EFS of 61.4% as compared to those assigned to single transplant, who had a 3-year EFS of 48.4% (P=0.0081).
There was not a statistically significant difference in OS. However, Dr Park pointed out that the trial was not powered to detect a difference in overall survival.
When looking at the cohort of stage 4 patients who were older than 18 months, investigators again saw a statistically significant improvement in EFS. The 3-year EFS was 59%.1 for tandem transplants vs 45.5% for single transplants, P=0.0083.
Again, there was no difference in OS in the INSS stage 4 patients older than 18 months.
“And finally, when we analyzed the outcome for children who were assigned to receive immunotherapy,” Dr Park pointed out, “from the time of start of immunotherapy, there was a statistically significant improvement in both event-free survival and overall survival for those children who received tandem transplants.”
The 3-year EFS for patients who received a tandem transplant and immunotherapy was 73.7% compared to the 3-year EFS of 56.0% for patients who received a single transplant and immunotherapy (P=0.0033).
The 3-year overall survival was also significantly improved for patients who received tandem transplants and immunotherapy (83.7%) compared to those who received a single transplant and immunotherapy (74.4%) (P=0.0322).
Conclusions
“Tandem transplant consolidation improves outcome in patients with high-risk neuroblastoma,” Dr Park said, with the important caveat mentioned earlier.
The tandem transplant does not increase toxicity or regimen-related mortality, and the benefit of tandem ASCT remains following anti-GD2-directed immunotherapy. ![]()
*Data in the presentation differ slightly from the abstract

Photo by Chad McNeeley
CHICAGO—A phase 3 study of tandem autologous stem cell transplant (ASCT) for children with high-risk neuroblastoma has shown that tandem transplant as consolidation significantly improved event-free survival (EFS).
Nevertheless, the improvement comes “with an important caveat,” according to Julie R. Park, MD, “that this is in children who survive induction without disease progression after induction or severe induction-related toxicity.”
Of note, the tandem transplant did not increase toxicity or regimen-related mortality.
Dr Park, of the Seattle Children’s Hospital and University of Washington, presented the study data on behalf of the Children’s Oncology Group and the COG ANBL0532 Study Committee during the plenary session at the 2016 ASCO Annual Meeting (LBA3*).
Neuroblastoma, Dr Park explained, is a disease that occurs in young children and is the most common extracranial tumor of childhood. Patients with high-risk neuroblastoma account for 50% of all children diagnosed with the disease, and neuroblastoma accounts for more than 10% of all childhood cancer mortality.
The outcome for high-risk neuroblastoma patients is dismal: fewer than 50% survive following current multi-agent, aggressive therapy, she said.
Randomized clinical trials performed over the last 25 years “have taught us that dose intensification of therapy is important,” Dr Park said, “and the treatment of minimal residual disease with non-cross resistant therapies is equally important.”
Pilot studies of tandem ASCT demonstrated tolerable toxicity and suggested efficacy, and clinical trials demonstrated that collecting peripheral blood stem cells in small children with neuroblastoma was feasible.
So the investigators undertook the current study to improve 3-year EFS of high-risk neuroblastoma patients using a strategy of tandem transplant consolidation.
Eligibility
Patients with newly diagnosed high-risk neuroblastoma were eligible. They had to have metastatic disease (INSS stage 4) and be older than 18 months to be eligible for the trial.
They could be any age if they had INSS stage 2, 3, or 4 with MYCN amplification.
“Our prior studies had identified that the group with regional disease and toddlers with MYCN non-amplified metastatic disease had a better outcome compared to other children with high-risk neuroblastoma,” Dr Park commented.
“Therefore, these children were non-randomly assigned to single transplant and are not included in the randomization results provided today,” she explained.
All children had to have normal cardiac, liver, and renal function.
Trial design: Induction
Induction therapy consisted of 6 cycles of chemotherapy—2 cycles of cyclophosphamide/topotecan, followed by 4 alternating cycles of cisplatin/etoposide and cyclophosphamide/vincristine/doxorubicin.
Peripheral blood stem cells (PBSCs) were harvested after the first 2 cycles of dose intensive cyclophosphamide and topotecan.
Patients had surgery on the primary tumor after 5 cycles of induction.
Trial design: Consolidation
Following completion of induction therapy, patients were assessed for eligibility for consolidation. These criteria included sufficient PBSC harvest, adequate organ function, no evidence of disease progression, and consent for post induction therapy.
Children eligible for consolidation were randomized to either the standard transplant with carboplatin, etoposide, melphalan or tandem transplant with cyclophosphamide and thiotepa followed 6 – 8 weeks later by the second transplant with carboplatin, etoposide, and melphalan.
Patients in both arms received radiotherapy to their primary tumor site.
Trial Design: Post-consolidation
Patients then went on for post consolidation chemotherapy with isotretinoin.
“During the conduct of ANBL0532,” Dr Park pointed out, “there was an additional trial running within the Children’s Oncology Group for which patients were eligible to enroll.”
So from 2007 – 2009, the additional trial (ANBL0032) randomized patients to their then standard of isotretinoin or isotretinoin plus the anti-GD2 antibody dinutuximab and cytokines.
“In 2009, results of that study were released and the dinutuximab arm was superior,” she noted, so patients were no longer randomized to isotretinoin only.
Prior studies indicated that 40% of patients went off trial at the end of induction therapy, so the investigators enrolled 665 patients to ensure a randomization of at least 332 patients.
Data cut-off for the presentation was March 31, 2016.
Patient demographics
Of the 665 patients accrued, 13 were ineligible. Twenty-seven patients with favorable prognosis were non-randomly assigned to single ASCT.
Forty percent (229 patients) went off protocol therapy prior to randomization. The main reasons for this were death (8 patients), progressive disease (48 patients), and physician and patient discretion (206 patients).
Investigators randomized 355 patients, 179 to single ASCT and 176 to tandem ASCT.
Patients were a median age of 37.2 months, 38.2% had MYCN amplification, and 88% were INSS stage 4.
The randomized cohorts of patients were similar to the overall patient cohort in terms of age, MYCN amplification, and stage 4 disease.
The randomizations were also well balanced in terms of MYCN amplifications, stage 4 disease, and response to induction chemotherapy.
The investigators retrospectively reviewed the patient characteristics, including age at diagnosis, early response to induction, and assignment to receive immunotherapy, “and there was no statistically significant difference between the randomized cohorts for these characteristics,” Dr Park said.
Safety
The most commonly observed grade 3 or greater non-hematologic toxicities in the single and tandem arms included infection (18.3% and 17.9%, respectively), mucosal toxicities (17.2% and 13.6%, respectively), and hepatic toxicities, including sinusoidal obstructive disorder (6.5% and 6.2%, respectively).
The investigators observed no significant differences between the arms in regard to the rate of these toxicities. In addition, they observed no difference between the arms in the rate of regimen-related mortality, 4.1% in the single arm, and 1.2% in the tandem arm.
Efficacy
For all patients (n=652) from time of enrollment, the 3-year EFS was 51.0% and the 3-year OS was 68.3%.
In randomized patients (n=355), from the time of randomization, the 3-year EFS was 54.8% and the 3-year OS, 71.5%, with a median survival time of 4.6 years.
There was a statistically significant improvement in EFS for those patients assigned to tandem transplant, with a 3-year EFS of 61.4% as compared to those assigned to single transplant, who had a 3-year EFS of 48.4% (P=0.0081).
There was not a statistically significant difference in OS. However, Dr Park pointed out that the trial was not powered to detect a difference in overall survival.
When looking at the cohort of stage 4 patients who were older than 18 months, investigators again saw a statistically significant improvement in EFS. The 3-year EFS was 59%.1 for tandem transplants vs 45.5% for single transplants, P=0.0083.
Again, there was no difference in OS in the INSS stage 4 patients older than 18 months.
“And finally, when we analyzed the outcome for children who were assigned to receive immunotherapy,” Dr Park pointed out, “from the time of start of immunotherapy, there was a statistically significant improvement in both event-free survival and overall survival for those children who received tandem transplants.”
The 3-year EFS for patients who received a tandem transplant and immunotherapy was 73.7% compared to the 3-year EFS of 56.0% for patients who received a single transplant and immunotherapy (P=0.0033).
The 3-year overall survival was also significantly improved for patients who received tandem transplants and immunotherapy (83.7%) compared to those who received a single transplant and immunotherapy (74.4%) (P=0.0322).
Conclusions
“Tandem transplant consolidation improves outcome in patients with high-risk neuroblastoma,” Dr Park said, with the important caveat mentioned earlier.
The tandem transplant does not increase toxicity or regimen-related mortality, and the benefit of tandem ASCT remains following anti-GD2-directed immunotherapy. ![]()
*Data in the presentation differ slightly from the abstract
Team develops new approach to programming T cells
Using mouse models, researchers have developed a new cellular programming approach to create alloreactive T cells they say eliminate leukemic cells without causing graft-versus-host disease (GVHD).
They created the T cells using the donor key immune cell. When used in allogeneic hematopoietic stem cell transplantation and anti-leukemia therapy, the new approach reduced the toxicities that cause GVHD while preserving the anti-leukemia activity of the immune cell.
“This approach will be useful in the future when developing novel methods for immunotherapy,” said Yi Zhang, MD, PhD, of Temple University in Philadelphia, Pennsylvania.
Dr Zhang and colleagues took murine bone marrow using Flt3 ligand and Toll-like receptor agonists to produce δ-like ligand 4-positive dendritic cells (Dll4hiDCs). When the dendritic cells were stimulated, CD4+ naïve T cells underwent effector differentiation and produced high levels of IFN-γ and IL-17 in vitro.
The team then transferred the allogeneic Dll4hiDC-induced T cells into the mice. The cells did not induce severe GVHD and preserved anti-leukemic activity, “significantly improving the survival of leukemic mice undergoing allogeneic HSCT,” they said.
They noted that the IFN-γ was important for Dll4hiDC programming in reducing the GVHD toxicities of alloreactive T cells. When the researchers transferred unstimulated T cells into mice, 5 of 8 mice died from GVHD and 3 of 8 died with tumor. Those that received Dll4hiDC-induced T cells did not develop GVHD.
They also emphasized that this platform does not require transfection with viral vectors, which has limitations of safety and efficiency.
“This system will not only be useful for reducing GvHD,” Dr Zhang said, “but can also be used in the identification of T cells for the improvement of other types of immunotherapy for advanced cancer.”
The team published this research in Blood. ![]()
Using mouse models, researchers have developed a new cellular programming approach to create alloreactive T cells they say eliminate leukemic cells without causing graft-versus-host disease (GVHD).
They created the T cells using the donor key immune cell. When used in allogeneic hematopoietic stem cell transplantation and anti-leukemia therapy, the new approach reduced the toxicities that cause GVHD while preserving the anti-leukemia activity of the immune cell.
“This approach will be useful in the future when developing novel methods for immunotherapy,” said Yi Zhang, MD, PhD, of Temple University in Philadelphia, Pennsylvania.
Dr Zhang and colleagues took murine bone marrow using Flt3 ligand and Toll-like receptor agonists to produce δ-like ligand 4-positive dendritic cells (Dll4hiDCs). When the dendritic cells were stimulated, CD4+ naïve T cells underwent effector differentiation and produced high levels of IFN-γ and IL-17 in vitro.
The team then transferred the allogeneic Dll4hiDC-induced T cells into the mice. The cells did not induce severe GVHD and preserved anti-leukemic activity, “significantly improving the survival of leukemic mice undergoing allogeneic HSCT,” they said.
They noted that the IFN-γ was important for Dll4hiDC programming in reducing the GVHD toxicities of alloreactive T cells. When the researchers transferred unstimulated T cells into mice, 5 of 8 mice died from GVHD and 3 of 8 died with tumor. Those that received Dll4hiDC-induced T cells did not develop GVHD.
They also emphasized that this platform does not require transfection with viral vectors, which has limitations of safety and efficiency.
“This system will not only be useful for reducing GvHD,” Dr Zhang said, “but can also be used in the identification of T cells for the improvement of other types of immunotherapy for advanced cancer.”
The team published this research in Blood. ![]()
Using mouse models, researchers have developed a new cellular programming approach to create alloreactive T cells they say eliminate leukemic cells without causing graft-versus-host disease (GVHD).
They created the T cells using the donor key immune cell. When used in allogeneic hematopoietic stem cell transplantation and anti-leukemia therapy, the new approach reduced the toxicities that cause GVHD while preserving the anti-leukemia activity of the immune cell.
“This approach will be useful in the future when developing novel methods for immunotherapy,” said Yi Zhang, MD, PhD, of Temple University in Philadelphia, Pennsylvania.
Dr Zhang and colleagues took murine bone marrow using Flt3 ligand and Toll-like receptor agonists to produce δ-like ligand 4-positive dendritic cells (Dll4hiDCs). When the dendritic cells were stimulated, CD4+ naïve T cells underwent effector differentiation and produced high levels of IFN-γ and IL-17 in vitro.
The team then transferred the allogeneic Dll4hiDC-induced T cells into the mice. The cells did not induce severe GVHD and preserved anti-leukemic activity, “significantly improving the survival of leukemic mice undergoing allogeneic HSCT,” they said.
They noted that the IFN-γ was important for Dll4hiDC programming in reducing the GVHD toxicities of alloreactive T cells. When the researchers transferred unstimulated T cells into mice, 5 of 8 mice died from GVHD and 3 of 8 died with tumor. Those that received Dll4hiDC-induced T cells did not develop GVHD.
They also emphasized that this platform does not require transfection with viral vectors, which has limitations of safety and efficiency.
“This system will not only be useful for reducing GvHD,” Dr Zhang said, “but can also be used in the identification of T cells for the improvement of other types of immunotherapy for advanced cancer.”
The team published this research in Blood. ![]()
Young HCT survivors have increased risk for frailty

for transplant
Photo credit: Chad McNeeley
Frailty among young adult hematopoietic cell transplant (HCT) survivors is high and approaches that of a community-based elderly population, according to results of the Bone Marrow Transplant Survivor Study.
Of the 998 HCT participants, frailty exceeded 8%, and they were 8.4 times more likely to be frail than their siblings.
Investigators defined frailty as exhibiting 3 or more of the following traits: clinically underweight, exhaustion, low energy expenditure, slow walking speed, and muscle weakness.
Because HCT recipients are exposed to high-intensity chemotherapy, radiation, and immunosuppression at points before, during, and after transplant, the investigators set out to determine whether non-elderly HCT recipients who have survived 2 years or more after transplant were at a higher risk of frailty compared with a sibling comparator group.
Smita Bhatia, MD, of the University of Alabama at Birmingham, and colleagues conducted the study of HCT survivors between the ages of 18 and 64 and compared the results to a sibling control group. The authors also looked at the subsequent mortality of HCT survivors.
They reported their findings in JAMA Oncology.
The 998 HCT survivors who participated in the study received their transplants at City of Hope in Duarte, California, or at the University of Minnesota in Minneapolis, between 1974 and 1998. The survivors and the 297 siblings completed questionnaires between February 1999 and June 2005.
Demographics
The HCT survivors were a mean age of 42.5 years, and 911 (93%) had health insurance coverage.
This was comparable to the sibling controls, who were a mean age of 43.8 years (P=0.09) and 279 (95%) had health insurance coverage.
However, more siblings were female (64%), non-Hispanic white (88%), college graduates (56%), and 92% had annual household incomes of $20,000 or more.
In the HCT survivor group, 46% were female (P<0.001), 81% non-Hispanic white (P=0.004), 49% college graduates (P<0.001), and 80% had annual incomes of $20,000 or more (P<0.001).
HCT survivors were a mean age of 33.8 years when they had their transplants and the interval between HCT and participation in the study was 8.7 years.
Hematologic malignancies were the major diagnoses leading to HCT. Twenty-three percent had a primary diagnosis of chronic myeloid leukemia, 24% had acute myeloid leukemia, 19% had non-Hodgkin lymphoma, 10% had acute lymphoblastic leukemia, and 9% had Hodgkin lymphoma.
Seventy-seven percent of the HCT survivors had total body irradiation, and 300 of the 562 who received allogeneic transplants had chronic GVHD, with 24% of them reporting active GVHD at the time they participated in the study.
Frailty
Only 2 siblings (0.7%) considered themselves frail compared to 84 (8.4%) HCT survivors.
More survivors were underweight and reported low energy expenditure compared to the sibling group, but the differences were not statistically significant, P=0.26 and P=0.14, respectively.
However, significantly more survivors reported exhaustion (P<0.001), slowness (P<0.001), and weakness (P<0.001) compared to the sibling group,
The investigators then adjusted the data for age at study participation, sex, race/ethnicity, education, household income, health insurance, presence of grades 3 or 4 chronic health conditions, and transplant institution. They then found the HCT survivors to be 8.35 times more likely to be frail than their siblings (P=0.003).
HCT survivors with low annual incomes (P=0.03), less than a college education (P=0.002), with grades 3 or 4 chronic health conditions (P=0.02), with multiple myeloma (P=0.05), or with resolved chronic (P=0.04) or active chronic GVHD (P<0.001) were more likely to be frail compared to the other HCT survivors.
Mortality
The investigators followed the patients for a median of 10.3 years from the time participants completed the survey. At that time, 182 (18%) patients had died.
The 10-year cumulative all-cause mortality was 39.3% for patients with frailty and 14.7% for patients without frailty (P<0.001).
The 10-year cumulative relapse-related mortality was 15.5% among frail HCT patients and 4.5% for non-frail HCT patients.
And the 10-year cumulative non-relapse mortality was also higher among frail HCT recipients, 23.9% compared to 10.2% of the non-frail HCT recipients (P<0.001).
Multivariate analysis revealed that frailty was associated with a 2.76-fold increase in death. The variables included age at study participation, sex, presence of grades 3 to 4 chronic health conditions, primary diagnosis, annual household income, and risk of relapse at transplant.
The investigators concluded that the therapies transplant patients undergo and post-transplant complications constitute a substantial stressor, placing HCT survivors at risk for frailty and premature aging.
“These findings demonstrate the need for interventions,” they added, “including personalized assessments and multidisciplinary efforts targeting both pre-frail and frail individuals to improve outcomes.” ![]()

for transplant
Photo credit: Chad McNeeley
Frailty among young adult hematopoietic cell transplant (HCT) survivors is high and approaches that of a community-based elderly population, according to results of the Bone Marrow Transplant Survivor Study.
Of the 998 HCT participants, frailty exceeded 8%, and they were 8.4 times more likely to be frail than their siblings.
Investigators defined frailty as exhibiting 3 or more of the following traits: clinically underweight, exhaustion, low energy expenditure, slow walking speed, and muscle weakness.
Because HCT recipients are exposed to high-intensity chemotherapy, radiation, and immunosuppression at points before, during, and after transplant, the investigators set out to determine whether non-elderly HCT recipients who have survived 2 years or more after transplant were at a higher risk of frailty compared with a sibling comparator group.
Smita Bhatia, MD, of the University of Alabama at Birmingham, and colleagues conducted the study of HCT survivors between the ages of 18 and 64 and compared the results to a sibling control group. The authors also looked at the subsequent mortality of HCT survivors.
They reported their findings in JAMA Oncology.
The 998 HCT survivors who participated in the study received their transplants at City of Hope in Duarte, California, or at the University of Minnesota in Minneapolis, between 1974 and 1998. The survivors and the 297 siblings completed questionnaires between February 1999 and June 2005.
Demographics
The HCT survivors were a mean age of 42.5 years, and 911 (93%) had health insurance coverage.
This was comparable to the sibling controls, who were a mean age of 43.8 years (P=0.09) and 279 (95%) had health insurance coverage.
However, more siblings were female (64%), non-Hispanic white (88%), college graduates (56%), and 92% had annual household incomes of $20,000 or more.
In the HCT survivor group, 46% were female (P<0.001), 81% non-Hispanic white (P=0.004), 49% college graduates (P<0.001), and 80% had annual incomes of $20,000 or more (P<0.001).
HCT survivors were a mean age of 33.8 years when they had their transplants and the interval between HCT and participation in the study was 8.7 years.
Hematologic malignancies were the major diagnoses leading to HCT. Twenty-three percent had a primary diagnosis of chronic myeloid leukemia, 24% had acute myeloid leukemia, 19% had non-Hodgkin lymphoma, 10% had acute lymphoblastic leukemia, and 9% had Hodgkin lymphoma.
Seventy-seven percent of the HCT survivors had total body irradiation, and 300 of the 562 who received allogeneic transplants had chronic GVHD, with 24% of them reporting active GVHD at the time they participated in the study.
Frailty
Only 2 siblings (0.7%) considered themselves frail compared to 84 (8.4%) HCT survivors.
More survivors were underweight and reported low energy expenditure compared to the sibling group, but the differences were not statistically significant, P=0.26 and P=0.14, respectively.
However, significantly more survivors reported exhaustion (P<0.001), slowness (P<0.001), and weakness (P<0.001) compared to the sibling group,
The investigators then adjusted the data for age at study participation, sex, race/ethnicity, education, household income, health insurance, presence of grades 3 or 4 chronic health conditions, and transplant institution. They then found the HCT survivors to be 8.35 times more likely to be frail than their siblings (P=0.003).
HCT survivors with low annual incomes (P=0.03), less than a college education (P=0.002), with grades 3 or 4 chronic health conditions (P=0.02), with multiple myeloma (P=0.05), or with resolved chronic (P=0.04) or active chronic GVHD (P<0.001) were more likely to be frail compared to the other HCT survivors.
Mortality
The investigators followed the patients for a median of 10.3 years from the time participants completed the survey. At that time, 182 (18%) patients had died.
The 10-year cumulative all-cause mortality was 39.3% for patients with frailty and 14.7% for patients without frailty (P<0.001).
The 10-year cumulative relapse-related mortality was 15.5% among frail HCT patients and 4.5% for non-frail HCT patients.
And the 10-year cumulative non-relapse mortality was also higher among frail HCT recipients, 23.9% compared to 10.2% of the non-frail HCT recipients (P<0.001).
Multivariate analysis revealed that frailty was associated with a 2.76-fold increase in death. The variables included age at study participation, sex, presence of grades 3 to 4 chronic health conditions, primary diagnosis, annual household income, and risk of relapse at transplant.
The investigators concluded that the therapies transplant patients undergo and post-transplant complications constitute a substantial stressor, placing HCT survivors at risk for frailty and premature aging.
“These findings demonstrate the need for interventions,” they added, “including personalized assessments and multidisciplinary efforts targeting both pre-frail and frail individuals to improve outcomes.” ![]()

for transplant
Photo credit: Chad McNeeley
Frailty among young adult hematopoietic cell transplant (HCT) survivors is high and approaches that of a community-based elderly population, according to results of the Bone Marrow Transplant Survivor Study.
Of the 998 HCT participants, frailty exceeded 8%, and they were 8.4 times more likely to be frail than their siblings.
Investigators defined frailty as exhibiting 3 or more of the following traits: clinically underweight, exhaustion, low energy expenditure, slow walking speed, and muscle weakness.
Because HCT recipients are exposed to high-intensity chemotherapy, radiation, and immunosuppression at points before, during, and after transplant, the investigators set out to determine whether non-elderly HCT recipients who have survived 2 years or more after transplant were at a higher risk of frailty compared with a sibling comparator group.
Smita Bhatia, MD, of the University of Alabama at Birmingham, and colleagues conducted the study of HCT survivors between the ages of 18 and 64 and compared the results to a sibling control group. The authors also looked at the subsequent mortality of HCT survivors.
They reported their findings in JAMA Oncology.
The 998 HCT survivors who participated in the study received their transplants at City of Hope in Duarte, California, or at the University of Minnesota in Minneapolis, between 1974 and 1998. The survivors and the 297 siblings completed questionnaires between February 1999 and June 2005.
Demographics
The HCT survivors were a mean age of 42.5 years, and 911 (93%) had health insurance coverage.
This was comparable to the sibling controls, who were a mean age of 43.8 years (P=0.09) and 279 (95%) had health insurance coverage.
However, more siblings were female (64%), non-Hispanic white (88%), college graduates (56%), and 92% had annual household incomes of $20,000 or more.
In the HCT survivor group, 46% were female (P<0.001), 81% non-Hispanic white (P=0.004), 49% college graduates (P<0.001), and 80% had annual incomes of $20,000 or more (P<0.001).
HCT survivors were a mean age of 33.8 years when they had their transplants and the interval between HCT and participation in the study was 8.7 years.
Hematologic malignancies were the major diagnoses leading to HCT. Twenty-three percent had a primary diagnosis of chronic myeloid leukemia, 24% had acute myeloid leukemia, 19% had non-Hodgkin lymphoma, 10% had acute lymphoblastic leukemia, and 9% had Hodgkin lymphoma.
Seventy-seven percent of the HCT survivors had total body irradiation, and 300 of the 562 who received allogeneic transplants had chronic GVHD, with 24% of them reporting active GVHD at the time they participated in the study.
Frailty
Only 2 siblings (0.7%) considered themselves frail compared to 84 (8.4%) HCT survivors.
More survivors were underweight and reported low energy expenditure compared to the sibling group, but the differences were not statistically significant, P=0.26 and P=0.14, respectively.
However, significantly more survivors reported exhaustion (P<0.001), slowness (P<0.001), and weakness (P<0.001) compared to the sibling group,
The investigators then adjusted the data for age at study participation, sex, race/ethnicity, education, household income, health insurance, presence of grades 3 or 4 chronic health conditions, and transplant institution. They then found the HCT survivors to be 8.35 times more likely to be frail than their siblings (P=0.003).
HCT survivors with low annual incomes (P=0.03), less than a college education (P=0.002), with grades 3 or 4 chronic health conditions (P=0.02), with multiple myeloma (P=0.05), or with resolved chronic (P=0.04) or active chronic GVHD (P<0.001) were more likely to be frail compared to the other HCT survivors.
Mortality
The investigators followed the patients for a median of 10.3 years from the time participants completed the survey. At that time, 182 (18%) patients had died.
The 10-year cumulative all-cause mortality was 39.3% for patients with frailty and 14.7% for patients without frailty (P<0.001).
The 10-year cumulative relapse-related mortality was 15.5% among frail HCT patients and 4.5% for non-frail HCT patients.
And the 10-year cumulative non-relapse mortality was also higher among frail HCT recipients, 23.9% compared to 10.2% of the non-frail HCT recipients (P<0.001).
Multivariate analysis revealed that frailty was associated with a 2.76-fold increase in death. The variables included age at study participation, sex, presence of grades 3 to 4 chronic health conditions, primary diagnosis, annual household income, and risk of relapse at transplant.
The investigators concluded that the therapies transplant patients undergo and post-transplant complications constitute a substantial stressor, placing HCT survivors at risk for frailty and premature aging.
“These findings demonstrate the need for interventions,” they added, “including personalized assessments and multidisciplinary efforts targeting both pre-frail and frail individuals to improve outcomes.”
Dose of transplanted HSCs affects their behavior

in the bone marrow
The dose of hematopoietic stem cells (HSCs) given in a transplant affects how those cells behave in the body, according to research published in Cell Reports.
To track the behavior of transplanted HSCs, researchers “barcoded” individual mouse HSCs with a genetic marker and observed their contributions to hematopoiesis.
The team found that only 20% to 30% of HSCs differentiated into all types of blood cells.
This relatively small group of HSCs produced a disproportionately large amount of blood.
The remaining 70% to 80% of HSCs were more strategic, and their behavior was dependent on the dose of HSCs transplanted.
At higher HSC doses, the “strategic majority” of HSCs opted to differentiate early, producing a balanced array of T cells and B cells. But at low HSC doses, the strategic HSCs prioritized T-cell production.
“The dose of transplanted bone marrow has strong and lasting effects on how HSCs specialize and coordinate their behavior,” said study author Rong Lu, PhD, of the University of Southern California in Los Angeles.
“This suggests that altering transplantation dose could be a tool for improving outcomes for patients—promoting bone marrow engraftment, reducing the risk of infection, and, ultimately, saving lives.”

in the bone marrow
The dose of hematopoietic stem cells (HSCs) given in a transplant affects how those cells behave in the body, according to research published in Cell Reports.
To track the behavior of transplanted HSCs, researchers “barcoded” individual mouse HSCs with a genetic marker and observed their contributions to hematopoiesis.
The team found that only 20% to 30% of HSCs differentiated into all types of blood cells.
This relatively small group of HSCs produced a disproportionately large amount of blood.
The remaining 70% to 80% of HSCs were more strategic, and their behavior was dependent on the dose of HSCs transplanted.
At higher HSC doses, the “strategic majority” of HSCs opted to differentiate early, producing a balanced array of T cells and B cells. But at low HSC doses, the strategic HSCs prioritized T-cell production.
“The dose of transplanted bone marrow has strong and lasting effects on how HSCs specialize and coordinate their behavior,” said study author Rong Lu, PhD, of the University of Southern California in Los Angeles.
“This suggests that altering transplantation dose could be a tool for improving outcomes for patients—promoting bone marrow engraftment, reducing the risk of infection, and, ultimately, saving lives.”

in the bone marrow
The dose of hematopoietic stem cells (HSCs) given in a transplant affects how those cells behave in the body, according to research published in Cell Reports.
To track the behavior of transplanted HSCs, researchers “barcoded” individual mouse HSCs with a genetic marker and observed their contributions to hematopoiesis.
The team found that only 20% to 30% of HSCs differentiated into all types of blood cells.
This relatively small group of HSCs produced a disproportionately large amount of blood.
The remaining 70% to 80% of HSCs were more strategic, and their behavior was dependent on the dose of HSCs transplanted.
At higher HSC doses, the “strategic majority” of HSCs opted to differentiate early, producing a balanced array of T cells and B cells. But at low HSC doses, the strategic HSCs prioritized T-cell production.
“The dose of transplanted bone marrow has strong and lasting effects on how HSCs specialize and coordinate their behavior,” said study author Rong Lu, PhD, of the University of Southern California in Los Angeles.
“This suggests that altering transplantation dose could be a tool for improving outcomes for patients—promoting bone marrow engraftment, reducing the risk of infection, and, ultimately, saving lives.”
FDA approves CMV test for use in HSCT recipients
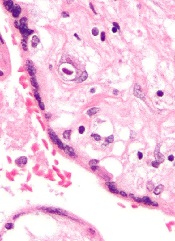
The US Food and Drug Administration (FDA) has approved the first cytomegalovirus (CMV) test for use in hematopoietic stem cell transplant (HSCT) recipients.
With this approval, the COBAS® AmpliPrep/COBAS® TaqMan® CMV Test is available for monitoring CMV treatment in all types of transplant patients in the US.
The test, which was developed by Roche, is an in vitro nucleic acid amplification test that quantitates CMV DNA in human plasma.
It is intended to aid the management of HSCT recipients and solid-organ transplant recipients who are undergoing anti-CMV therapy.
In this population, serial DNA measurements can be used to assess virological response to antiviral treatment. The results from the test must be interpreted within the context of all relevant clinical and laboratory findings.
The COBAS® AmpliPrep/COBAS® TaqMan® CMV Test is not intended for use as a screening test for the presence of CMV DNA in blood or blood products.
The test is designed for use on the automated COBAS® AmpliPrep/COBAS® TaqMan® System, an established platform for viral load monitoring of multiple infectious diseases.
The system combines the COBAS® AmpliPrep Instrument for automated sample preparation and the COBAS® TaqMan® Analyzer or the smaller COBAS® TaqMan® 48 Analyzer for automated real-time PCR amplification and detection.
The COBAS® AmpliPrep/COBAS® TaqMan® System has parallel processing with other molecular diagnostics assays targeting other diseases. Roche’s AmpErase enzyme is also included in each test and is designed to prevent cross-contamination of samples and labs.
The US Food and Drug Administration (FDA) has approved the first cytomegalovirus (CMV) test for use in hematopoietic stem cell transplant (HSCT) recipients.
With this approval, the COBAS® AmpliPrep/COBAS® TaqMan® CMV Test is available for monitoring CMV treatment in all types of transplant patients in the US.
The test, which was developed by Roche, is an in vitro nucleic acid amplification test that quantitates CMV DNA in human plasma.
It is intended to aid the management of HSCT recipients and solid-organ transplant recipients who are undergoing anti-CMV therapy.
In this population, serial DNA measurements can be used to assess virological response to antiviral treatment. The results from the test must be interpreted within the context of all relevant clinical and laboratory findings.
The COBAS® AmpliPrep/COBAS® TaqMan® CMV Test is not intended for use as a screening test for the presence of CMV DNA in blood or blood products.
The test is designed for use on the automated COBAS® AmpliPrep/COBAS® TaqMan® System, an established platform for viral load monitoring of multiple infectious diseases.
The system combines the COBAS® AmpliPrep Instrument for automated sample preparation and the COBAS® TaqMan® Analyzer or the smaller COBAS® TaqMan® 48 Analyzer for automated real-time PCR amplification and detection.
The COBAS® AmpliPrep/COBAS® TaqMan® System has parallel processing with other molecular diagnostics assays targeting other diseases. Roche’s AmpErase enzyme is also included in each test and is designed to prevent cross-contamination of samples and labs.
The US Food and Drug Administration (FDA) has approved the first cytomegalovirus (CMV) test for use in hematopoietic stem cell transplant (HSCT) recipients.
With this approval, the COBAS® AmpliPrep/COBAS® TaqMan® CMV Test is available for monitoring CMV treatment in all types of transplant patients in the US.
The test, which was developed by Roche, is an in vitro nucleic acid amplification test that quantitates CMV DNA in human plasma.
It is intended to aid the management of HSCT recipients and solid-organ transplant recipients who are undergoing anti-CMV therapy.
In this population, serial DNA measurements can be used to assess virological response to antiviral treatment. The results from the test must be interpreted within the context of all relevant clinical and laboratory findings.
The COBAS® AmpliPrep/COBAS® TaqMan® CMV Test is not intended for use as a screening test for the presence of CMV DNA in blood or blood products.
The test is designed for use on the automated COBAS® AmpliPrep/COBAS® TaqMan® System, an established platform for viral load monitoring of multiple infectious diseases.
The system combines the COBAS® AmpliPrep Instrument for automated sample preparation and the COBAS® TaqMan® Analyzer or the smaller COBAS® TaqMan® 48 Analyzer for automated real-time PCR amplification and detection.
The COBAS® AmpliPrep/COBAS® TaqMan® System has parallel processing with other molecular diagnostics assays targeting other diseases. Roche’s AmpErase enzyme is also included in each test and is designed to prevent cross-contamination of samples and labs.
Broad-spectrum antibiotics may worsen GVHD

Broad-spectrum antibiotics may increase the severity of graft-versus-host disease (GVHD), according to research published in Science Translational Medicine.
Researchers evaluated the relationship between antibiotics and GVHD using data from more than 850 transplant patients and by conducting experiments in mice.
Their results suggested that selecting antibiotics that spare “good” bacteria may help protect patients from GVHD.
Results in patients
Yusuke Shono, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York, New York, and his colleagues conducted this study, first mining the clinical records of 857 patients who underwent allogeneic hematopoietic stem cell transplant
(HSCT).
The team found that patients who received imipenem-cilastatin and piperacillin-tazobactam antibiotics to treat neutropenic fever had a higher incidence of GVHD-related mortality at 5 years than patients who did not receive these drugs.
The incidence of GVHD-related death was 21.5% in patients who received imipenem-cilastatin and 13.1% in those who did not (P=0.025). The incidence was 19.8% in patients who received piperacillin-tazobactam and 11.9% in those who did not (P=0.007).
Two other antibiotics used to treat neutropenic fever, aztreonam and cefepime, were not associated with an increased risk of GVHD-related mortality.
The incidence of GVHD-related death was 13.8% in patients who received cefepime and 14.6% in those who did not (P=0.98). The incidence was 17.5% in patients who received aztreonam and 14.2% in those who did not (P=0.78).
The researchers also found that piperacillin-tazobactam and imipenem-cilastatin were both associated with an increased incidence of grade 2-4 GVHD (P=0.0167 and P=0.0165, respectively), upper gastrointestinal GVHD (P=0.002 and P=0.045, respectively), and lower gastrointestinal GVHD (P=0.019 and P=0.036, respectively).
When the team analyzed patients’ stool samples, they found that piperacillin-tazobactam perturbed the gut microbiome, killing off protective bacteria. The therapy was associated with a greater loss of Bacteroidetes and Lactobacillus, when compared to treatment with aztreonam or cefepime.
The change in abundance of Enterococcus, Akkermansia, and Erysipelotrichia was similar with the 3 therapies. But there was a trend toward a decrease in Clostridia and Actinobacteria with piperacillin-tazobactam.
The researchers said they could not assess the effects of imipenem-cilastatin on bacterial populations because, at their center, imipenem-cilastatin is almost always given to HSCT patients as second-line therapy for neutropenic fever.
Results in mice
In mice treated with various antibiotic regimens following HSCT, those given broad-spectrum antibiotics developed more severe GVHD.
Specifically, the researchers observed aggravated GVHD mortality with imipenem-cilastatin or piperacillin-tazobactam compared to aztreonam (P<0.01 and P<0.05, respectively).
They also found evidence of increased GVHD pathology localized in the colon of mice that received imipenem-cilastatin (P<0.05). Mice with GVHD that received imipenem-cilastatin experienced loss of the protective mucus lining of the colon (P<0.01) and compromised intestinal barrier function (P<0.05).
When the researchers sequenced stool samples from mice with GVHD that received imipenem-cilastatin, they saw an increase in Akkermansia muciniphila (P<0.001), a commensal bacterium with mucus-degrading capabilities. They said this raises the possibility that mucus degradation may contribute to murine GVHD.
The researchers noted that these findings must be confirmed in clinical trials, but they caution against the use of broad-spectrum antibiotics in HSCT patients at risk of GVHD.

Broad-spectrum antibiotics may increase the severity of graft-versus-host disease (GVHD), according to research published in Science Translational Medicine.
Researchers evaluated the relationship between antibiotics and GVHD using data from more than 850 transplant patients and by conducting experiments in mice.
Their results suggested that selecting antibiotics that spare “good” bacteria may help protect patients from GVHD.
Results in patients
Yusuke Shono, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York, New York, and his colleagues conducted this study, first mining the clinical records of 857 patients who underwent allogeneic hematopoietic stem cell transplant
(HSCT).
The team found that patients who received imipenem-cilastatin and piperacillin-tazobactam antibiotics to treat neutropenic fever had a higher incidence of GVHD-related mortality at 5 years than patients who did not receive these drugs.
The incidence of GVHD-related death was 21.5% in patients who received imipenem-cilastatin and 13.1% in those who did not (P=0.025). The incidence was 19.8% in patients who received piperacillin-tazobactam and 11.9% in those who did not (P=0.007).
Two other antibiotics used to treat neutropenic fever, aztreonam and cefepime, were not associated with an increased risk of GVHD-related mortality.
The incidence of GVHD-related death was 13.8% in patients who received cefepime and 14.6% in those who did not (P=0.98). The incidence was 17.5% in patients who received aztreonam and 14.2% in those who did not (P=0.78).
The researchers also found that piperacillin-tazobactam and imipenem-cilastatin were both associated with an increased incidence of grade 2-4 GVHD (P=0.0167 and P=0.0165, respectively), upper gastrointestinal GVHD (P=0.002 and P=0.045, respectively), and lower gastrointestinal GVHD (P=0.019 and P=0.036, respectively).
When the team analyzed patients’ stool samples, they found that piperacillin-tazobactam perturbed the gut microbiome, killing off protective bacteria. The therapy was associated with a greater loss of Bacteroidetes and Lactobacillus, when compared to treatment with aztreonam or cefepime.
The change in abundance of Enterococcus, Akkermansia, and Erysipelotrichia was similar with the 3 therapies. But there was a trend toward a decrease in Clostridia and Actinobacteria with piperacillin-tazobactam.
The researchers said they could not assess the effects of imipenem-cilastatin on bacterial populations because, at their center, imipenem-cilastatin is almost always given to HSCT patients as second-line therapy for neutropenic fever.
Results in mice
In mice treated with various antibiotic regimens following HSCT, those given broad-spectrum antibiotics developed more severe GVHD.
Specifically, the researchers observed aggravated GVHD mortality with imipenem-cilastatin or piperacillin-tazobactam compared to aztreonam (P<0.01 and P<0.05, respectively).
They also found evidence of increased GVHD pathology localized in the colon of mice that received imipenem-cilastatin (P<0.05). Mice with GVHD that received imipenem-cilastatin experienced loss of the protective mucus lining of the colon (P<0.01) and compromised intestinal barrier function (P<0.05).
When the researchers sequenced stool samples from mice with GVHD that received imipenem-cilastatin, they saw an increase in Akkermansia muciniphila (P<0.001), a commensal bacterium with mucus-degrading capabilities. They said this raises the possibility that mucus degradation may contribute to murine GVHD.
The researchers noted that these findings must be confirmed in clinical trials, but they caution against the use of broad-spectrum antibiotics in HSCT patients at risk of GVHD.

Broad-spectrum antibiotics may increase the severity of graft-versus-host disease (GVHD), according to research published in Science Translational Medicine.
Researchers evaluated the relationship between antibiotics and GVHD using data from more than 850 transplant patients and by conducting experiments in mice.
Their results suggested that selecting antibiotics that spare “good” bacteria may help protect patients from GVHD.
Results in patients
Yusuke Shono, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York, New York, and his colleagues conducted this study, first mining the clinical records of 857 patients who underwent allogeneic hematopoietic stem cell transplant
(HSCT).
The team found that patients who received imipenem-cilastatin and piperacillin-tazobactam antibiotics to treat neutropenic fever had a higher incidence of GVHD-related mortality at 5 years than patients who did not receive these drugs.
The incidence of GVHD-related death was 21.5% in patients who received imipenem-cilastatin and 13.1% in those who did not (P=0.025). The incidence was 19.8% in patients who received piperacillin-tazobactam and 11.9% in those who did not (P=0.007).
Two other antibiotics used to treat neutropenic fever, aztreonam and cefepime, were not associated with an increased risk of GVHD-related mortality.
The incidence of GVHD-related death was 13.8% in patients who received cefepime and 14.6% in those who did not (P=0.98). The incidence was 17.5% in patients who received aztreonam and 14.2% in those who did not (P=0.78).
The researchers also found that piperacillin-tazobactam and imipenem-cilastatin were both associated with an increased incidence of grade 2-4 GVHD (P=0.0167 and P=0.0165, respectively), upper gastrointestinal GVHD (P=0.002 and P=0.045, respectively), and lower gastrointestinal GVHD (P=0.019 and P=0.036, respectively).
When the team analyzed patients’ stool samples, they found that piperacillin-tazobactam perturbed the gut microbiome, killing off protective bacteria. The therapy was associated with a greater loss of Bacteroidetes and Lactobacillus, when compared to treatment with aztreonam or cefepime.
The change in abundance of Enterococcus, Akkermansia, and Erysipelotrichia was similar with the 3 therapies. But there was a trend toward a decrease in Clostridia and Actinobacteria with piperacillin-tazobactam.
The researchers said they could not assess the effects of imipenem-cilastatin on bacterial populations because, at their center, imipenem-cilastatin is almost always given to HSCT patients as second-line therapy for neutropenic fever.
Results in mice
In mice treated with various antibiotic regimens following HSCT, those given broad-spectrum antibiotics developed more severe GVHD.
Specifically, the researchers observed aggravated GVHD mortality with imipenem-cilastatin or piperacillin-tazobactam compared to aztreonam (P<0.01 and P<0.05, respectively).
They also found evidence of increased GVHD pathology localized in the colon of mice that received imipenem-cilastatin (P<0.05). Mice with GVHD that received imipenem-cilastatin experienced loss of the protective mucus lining of the colon (P<0.01) and compromised intestinal barrier function (P<0.05).
When the researchers sequenced stool samples from mice with GVHD that received imipenem-cilastatin, they saw an increase in Akkermansia muciniphila (P<0.001), a commensal bacterium with mucus-degrading capabilities. They said this raises the possibility that mucus degradation may contribute to murine GVHD.
The researchers noted that these findings must be confirmed in clinical trials, but they caution against the use of broad-spectrum antibiotics in HSCT patients at risk of GVHD.