User login
NetWorks: Mass shootings, MACRA, asthma in pregnancy Disaster Response Practice Operations Transplant Women’s Health
Mass shootings
There are multiple definitions for a mass shooting. Some definitions require a certain number of people be killed. Some definitions require a certain number of people be shot. Some definitions do not include gang violence. Regardless of the definition used, the number of mass shootings in the United States is increasing.
There are also multiple definitions of what qualifies as a medical disaster. These definitions can be summarized with the statement that a medical disaster is an event that produces a number of casualties that overwhelms the local health system.
Most mass shootings fit the definition of a medical disaster. When a mass shooting occurs, medical resources are diverted from current patients to those injured in the shooting. Patients with acute medical problems unrelated to the shooting must endure a prolonged wait for medical care.
The CHEST Disaster Response NetWork feels that it is necessary to take action to reduce the number of mass shootings. Unlike natural disasters, mass shootings are man-made. As such, we should proactively work to prevent them. Prevention is a large part of medicine. Working together with community leaders, law enforcement, and government officials, we can and should work to eliminate mass shootings so that we can minimize gun-related injury and death.
MACRA: Reincarnation of Medicare physician reimbursement model
In April 2015, President Obama signed the Medicare Access and CHIP Reauthorization Act (MACRA) eradicating the detested sustainable growth rate (SGR) formula. If this is your first dive into MACRA as an eligible professional (EP), it may be a bit baffling trying to understand its impact on your practice.
Under MIPS, rules are divided into four categories. During the first year, each category will make up a certain percentage to the physician’s overall score, which will result in a penalty or payment as a lump sum in 2019. If you are an Advanced APM in 2017 and receive 25% of Medicare payments or see 20% of your Medicare patients through this model, you can earn up to a 5% incentive payment in 2019.
The performance period started on January 1, 2017. Submission of performance data is due by March 31, 2018. MACRA is complicated and here to stay. Learn and educate yourself to avoid downward payment adjustment. For full details, please visit https://qpp.cms.gov/docs/QPP_Executive_Summary_of_Final_Rule.pdf.
References
1. CMS MACRA Proposed Rule. http://1.usa.gov/1PpBpMt
2. CMS MACRA Executive Summary. https://qpp.cms.gov/docs/QPP_Executive_Summary_of_Final_Rule.pdf
3. American Medical Association. http://bit.ly/1miEtBD
4. Policy and Medicine. MACRA http://bit.ly/1PTLkKa. MIPS http://bit.ly/20RoMzZ. APMs http://bit.ly/1OlxoxH
Frailty in lung transplantation
Two of the greatest challenges in lung transplantation are to identify optimal transplant candidates and to help those transplant recipients thrive in the years following surgery. Frailty is emerging as a marker of increased posttransplant morbidity and may represent an area where both the recipient selection process and posttransplant outcomes can be optimized. Described by some as “biologic age” rather than “chronologic age,” frailty is a syndrome of functional impairment and weakness that predisposes to adverse health outcomes. The adverse effects of frailty have been described in multiple clinical scenarios, including the ICU, chronic lung diseases, heart failure, liver transplant, kidney transplant, geriatrics, and others.
Remaining challenges include determining which clinical assessments best define frailty in the lung transplant population, documenting the adverse effects of frailty in well-designed multicenter prospective studies, and developing interventions to mitigate the adverse effects of frailty.
Asthma treatment during pregnancy
Asthma is common in pregnancy, occurring in 3% to 8% of pregnant women. While the course of asthma during pregnancy is variable, the objectives of asthma treatment do not change and aim to prevent acute exacerbations and optimize management. Uncontrolled asthma is associated with an increased risk of perinatal morbidity. Published guidelines on pharmacologic therapies during pregnancy recommend the same step-wise approach as in nonpregnant women.
The diagnosis of asthma, the use of other concurrent medications, and medication compliance may all be potential confounders. ICS use in pregnancy was associated with endocrine and metabolic disturbances in the offspring in a national cohort (Tegethoff M et al. Am J Respir Crit Care Med. 2012;185[5]:557-63). However, this study did not report on systemic steroid use, asthma severity, or details of these disturbances.
Mass shootings
There are multiple definitions for a mass shooting. Some definitions require a certain number of people be killed. Some definitions require a certain number of people be shot. Some definitions do not include gang violence. Regardless of the definition used, the number of mass shootings in the United States is increasing.
There are also multiple definitions of what qualifies as a medical disaster. These definitions can be summarized with the statement that a medical disaster is an event that produces a number of casualties that overwhelms the local health system.
Most mass shootings fit the definition of a medical disaster. When a mass shooting occurs, medical resources are diverted from current patients to those injured in the shooting. Patients with acute medical problems unrelated to the shooting must endure a prolonged wait for medical care.
The CHEST Disaster Response NetWork feels that it is necessary to take action to reduce the number of mass shootings. Unlike natural disasters, mass shootings are man-made. As such, we should proactively work to prevent them. Prevention is a large part of medicine. Working together with community leaders, law enforcement, and government officials, we can and should work to eliminate mass shootings so that we can minimize gun-related injury and death.
MACRA: Reincarnation of Medicare physician reimbursement model
In April 2015, President Obama signed the Medicare Access and CHIP Reauthorization Act (MACRA) eradicating the detested sustainable growth rate (SGR) formula. If this is your first dive into MACRA as an eligible professional (EP), it may be a bit baffling trying to understand its impact on your practice.
Under MIPS, rules are divided into four categories. During the first year, each category will make up a certain percentage to the physician’s overall score, which will result in a penalty or payment as a lump sum in 2019. If you are an Advanced APM in 2017 and receive 25% of Medicare payments or see 20% of your Medicare patients through this model, you can earn up to a 5% incentive payment in 2019.
The performance period started on January 1, 2017. Submission of performance data is due by March 31, 2018. MACRA is complicated and here to stay. Learn and educate yourself to avoid downward payment adjustment. For full details, please visit https://qpp.cms.gov/docs/QPP_Executive_Summary_of_Final_Rule.pdf.
References
1. CMS MACRA Proposed Rule. http://1.usa.gov/1PpBpMt
2. CMS MACRA Executive Summary. https://qpp.cms.gov/docs/QPP_Executive_Summary_of_Final_Rule.pdf
3. American Medical Association. http://bit.ly/1miEtBD
4. Policy and Medicine. MACRA http://bit.ly/1PTLkKa. MIPS http://bit.ly/20RoMzZ. APMs http://bit.ly/1OlxoxH
Frailty in lung transplantation
Two of the greatest challenges in lung transplantation are to identify optimal transplant candidates and to help those transplant recipients thrive in the years following surgery. Frailty is emerging as a marker of increased posttransplant morbidity and may represent an area where both the recipient selection process and posttransplant outcomes can be optimized. Described by some as “biologic age” rather than “chronologic age,” frailty is a syndrome of functional impairment and weakness that predisposes to adverse health outcomes. The adverse effects of frailty have been described in multiple clinical scenarios, including the ICU, chronic lung diseases, heart failure, liver transplant, kidney transplant, geriatrics, and others.
Remaining challenges include determining which clinical assessments best define frailty in the lung transplant population, documenting the adverse effects of frailty in well-designed multicenter prospective studies, and developing interventions to mitigate the adverse effects of frailty.
Asthma treatment during pregnancy
Asthma is common in pregnancy, occurring in 3% to 8% of pregnant women. While the course of asthma during pregnancy is variable, the objectives of asthma treatment do not change and aim to prevent acute exacerbations and optimize management. Uncontrolled asthma is associated with an increased risk of perinatal morbidity. Published guidelines on pharmacologic therapies during pregnancy recommend the same step-wise approach as in nonpregnant women.
The diagnosis of asthma, the use of other concurrent medications, and medication compliance may all be potential confounders. ICS use in pregnancy was associated with endocrine and metabolic disturbances in the offspring in a national cohort (Tegethoff M et al. Am J Respir Crit Care Med. 2012;185[5]:557-63). However, this study did not report on systemic steroid use, asthma severity, or details of these disturbances.
Mass shootings
There are multiple definitions for a mass shooting. Some definitions require a certain number of people be killed. Some definitions require a certain number of people be shot. Some definitions do not include gang violence. Regardless of the definition used, the number of mass shootings in the United States is increasing.
There are also multiple definitions of what qualifies as a medical disaster. These definitions can be summarized with the statement that a medical disaster is an event that produces a number of casualties that overwhelms the local health system.
Most mass shootings fit the definition of a medical disaster. When a mass shooting occurs, medical resources are diverted from current patients to those injured in the shooting. Patients with acute medical problems unrelated to the shooting must endure a prolonged wait for medical care.
The CHEST Disaster Response NetWork feels that it is necessary to take action to reduce the number of mass shootings. Unlike natural disasters, mass shootings are man-made. As such, we should proactively work to prevent them. Prevention is a large part of medicine. Working together with community leaders, law enforcement, and government officials, we can and should work to eliminate mass shootings so that we can minimize gun-related injury and death.
MACRA: Reincarnation of Medicare physician reimbursement model
In April 2015, President Obama signed the Medicare Access and CHIP Reauthorization Act (MACRA) eradicating the detested sustainable growth rate (SGR) formula. If this is your first dive into MACRA as an eligible professional (EP), it may be a bit baffling trying to understand its impact on your practice.
Under MIPS, rules are divided into four categories. During the first year, each category will make up a certain percentage to the physician’s overall score, which will result in a penalty or payment as a lump sum in 2019. If you are an Advanced APM in 2017 and receive 25% of Medicare payments or see 20% of your Medicare patients through this model, you can earn up to a 5% incentive payment in 2019.
The performance period started on January 1, 2017. Submission of performance data is due by March 31, 2018. MACRA is complicated and here to stay. Learn and educate yourself to avoid downward payment adjustment. For full details, please visit https://qpp.cms.gov/docs/QPP_Executive_Summary_of_Final_Rule.pdf.
References
1. CMS MACRA Proposed Rule. http://1.usa.gov/1PpBpMt
2. CMS MACRA Executive Summary. https://qpp.cms.gov/docs/QPP_Executive_Summary_of_Final_Rule.pdf
3. American Medical Association. http://bit.ly/1miEtBD
4. Policy and Medicine. MACRA http://bit.ly/1PTLkKa. MIPS http://bit.ly/20RoMzZ. APMs http://bit.ly/1OlxoxH
Frailty in lung transplantation
Two of the greatest challenges in lung transplantation are to identify optimal transplant candidates and to help those transplant recipients thrive in the years following surgery. Frailty is emerging as a marker of increased posttransplant morbidity and may represent an area where both the recipient selection process and posttransplant outcomes can be optimized. Described by some as “biologic age” rather than “chronologic age,” frailty is a syndrome of functional impairment and weakness that predisposes to adverse health outcomes. The adverse effects of frailty have been described in multiple clinical scenarios, including the ICU, chronic lung diseases, heart failure, liver transplant, kidney transplant, geriatrics, and others.
Remaining challenges include determining which clinical assessments best define frailty in the lung transplant population, documenting the adverse effects of frailty in well-designed multicenter prospective studies, and developing interventions to mitigate the adverse effects of frailty.
Asthma treatment during pregnancy
Asthma is common in pregnancy, occurring in 3% to 8% of pregnant women. While the course of asthma during pregnancy is variable, the objectives of asthma treatment do not change and aim to prevent acute exacerbations and optimize management. Uncontrolled asthma is associated with an increased risk of perinatal morbidity. Published guidelines on pharmacologic therapies during pregnancy recommend the same step-wise approach as in nonpregnant women.
The diagnosis of asthma, the use of other concurrent medications, and medication compliance may all be potential confounders. ICS use in pregnancy was associated with endocrine and metabolic disturbances in the offspring in a national cohort (Tegethoff M et al. Am J Respir Crit Care Med. 2012;185[5]:557-63). However, this study did not report on systemic steroid use, asthma severity, or details of these disturbances.
Connect to CHEST members and leaders
Build your network and access the CHEST Member and Leader Directory. Use the directory to search for members and leaders. Easily search by name, specialty, location, or CHEST committee name to find others in the CHEST community. All members current in their dues are included in the directory.
Access to the directory is an exclusive CHEST member benefit. To view the directory, visit the following address: https://www.chestnet.org/Get-Involved/Membership/Member-Directory.
Build your network and access the CHEST Member and Leader Directory. Use the directory to search for members and leaders. Easily search by name, specialty, location, or CHEST committee name to find others in the CHEST community. All members current in their dues are included in the directory.
Access to the directory is an exclusive CHEST member benefit. To view the directory, visit the following address: https://www.chestnet.org/Get-Involved/Membership/Member-Directory.
Build your network and access the CHEST Member and Leader Directory. Use the directory to search for members and leaders. Easily search by name, specialty, location, or CHEST committee name to find others in the CHEST community. All members current in their dues are included in the directory.
Access to the directory is an exclusive CHEST member benefit. To view the directory, visit the following address: https://www.chestnet.org/Get-Involved/Membership/Member-Directory.
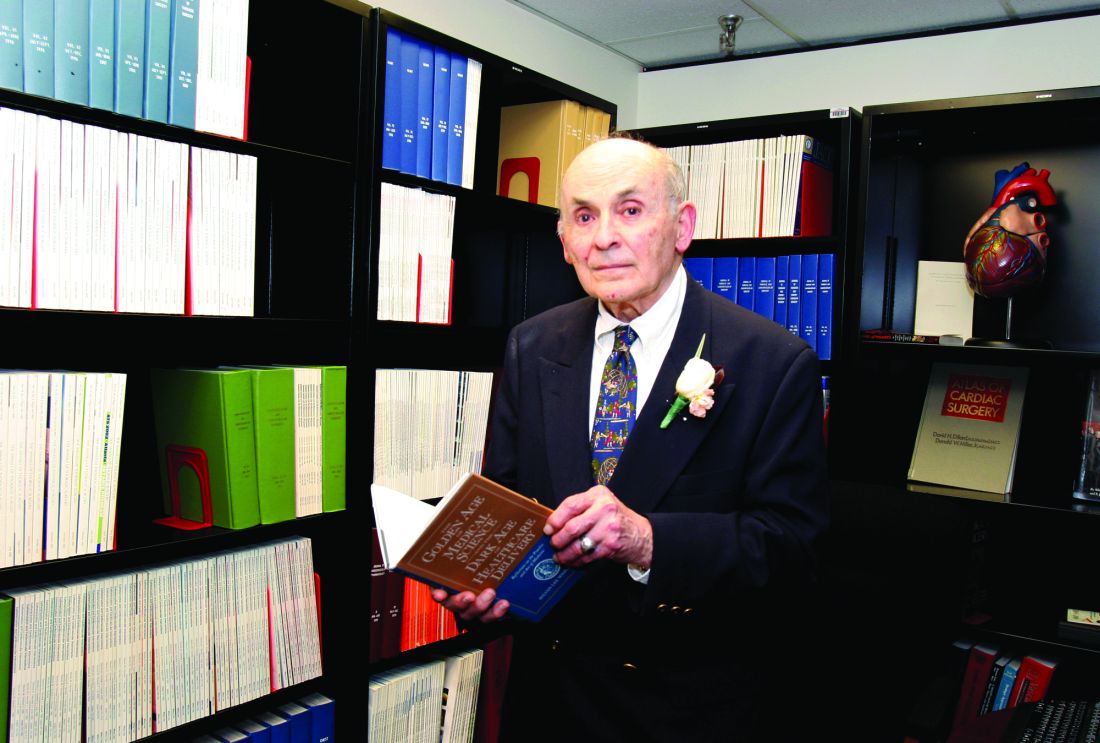
In memoriam
Sylvan Lee Weinberg, MD, FCCP, MACC, a Past President of the American College of Chest Physicians (1983-1984), died Jan 17, 2017, in Dayton, Ohio. Dr. Weinberg was born in Nashville, TN, and received both his bachelor of science and doctor of medicine degrees from Northwestern University in Evanston, IL. He spent his time as an intern, medical resident, and fellow in cardiology at the Michael Reese Hospital in Chicago and went on to serve as a physician at Good Samaritan Hospital in Dayton, Ohio, for more than 40 years, ultimately becoming chief of cardiology and founder of the first coronary care unit in Ohio. Dr. Weinberg was also a clinical professor of medicine at the Wright State University School of Medicine in Dayton, and led a group cardiology practice until his retirement in 2000.
CHEST extends its heartfelt condolences to Dr. Weinberg’s family and friends.
Sylvan Lee Weinberg, MD, FCCP, MACC, a Past President of the American College of Chest Physicians (1983-1984), died Jan 17, 2017, in Dayton, Ohio. Dr. Weinberg was born in Nashville, TN, and received both his bachelor of science and doctor of medicine degrees from Northwestern University in Evanston, IL. He spent his time as an intern, medical resident, and fellow in cardiology at the Michael Reese Hospital in Chicago and went on to serve as a physician at Good Samaritan Hospital in Dayton, Ohio, for more than 40 years, ultimately becoming chief of cardiology and founder of the first coronary care unit in Ohio. Dr. Weinberg was also a clinical professor of medicine at the Wright State University School of Medicine in Dayton, and led a group cardiology practice until his retirement in 2000.
CHEST extends its heartfelt condolences to Dr. Weinberg’s family and friends.
Sylvan Lee Weinberg, MD, FCCP, MACC, a Past President of the American College of Chest Physicians (1983-1984), died Jan 17, 2017, in Dayton, Ohio. Dr. Weinberg was born in Nashville, TN, and received both his bachelor of science and doctor of medicine degrees from Northwestern University in Evanston, IL. He spent his time as an intern, medical resident, and fellow in cardiology at the Michael Reese Hospital in Chicago and went on to serve as a physician at Good Samaritan Hospital in Dayton, Ohio, for more than 40 years, ultimately becoming chief of cardiology and founder of the first coronary care unit in Ohio. Dr. Weinberg was also a clinical professor of medicine at the Wright State University School of Medicine in Dayton, and led a group cardiology practice until his retirement in 2000.
CHEST extends its heartfelt condolences to Dr. Weinberg’s family and friends.
Calls for faculty participation in the CHEST PREP program
About PREP
The CHEST PREP Clinical Immersion program is an unbranded, disease-state program that educates industry members and partners to advance their knowledge into understanding that builds their confidence for engagement in clinical
conversations with health-care teams. We are seeking faculty for the following initiatives:
1. The CHEST PREP program is embarking on a curriculum and content development initiative and is seeking interested faculty members to consider participating in the development of content in the areas of CTEPH, Alpha-1 Antitrypsin, and Bronchiectasis.
2. The CHEST PREP program is seeking interested CHEST members in Chicago-based institutions to consider participating as faculty presenters in the following disease areas: COPD, Asthma, PAH, CTEPH, IPF, SCLC, and NSCLC.
Requirements for participation
1. PREP welcomes faculty who would be interested in creating two or more presentations and/or cases on an assigned topic using a flipped classroom, interactive design. A minimum of four faculty experts will be needed per disease state indicated previously. Honorarium provided.
2. PREP welcomes faculty from Chicago-based institutions who would be interested in participating as faculty presenters in the disease states indicated previously. Honorarium provided.
Selection criteria
To be considered, please indicate the disease area in which you are interested in participating as content developer or faculty presenter, as well as providing the best way to contact you. For the asthma curriculum, we have a specific need for expertise/interest in moderate to severe asthma and the use of biologics in treatment.
If you are interested in participating in this initiative, please contact Jasmine Turner ([email protected]). Thank you.
About PREP
The CHEST PREP Clinical Immersion program is an unbranded, disease-state program that educates industry members and partners to advance their knowledge into understanding that builds their confidence for engagement in clinical
conversations with health-care teams. We are seeking faculty for the following initiatives:
1. The CHEST PREP program is embarking on a curriculum and content development initiative and is seeking interested faculty members to consider participating in the development of content in the areas of CTEPH, Alpha-1 Antitrypsin, and Bronchiectasis.
2. The CHEST PREP program is seeking interested CHEST members in Chicago-based institutions to consider participating as faculty presenters in the following disease areas: COPD, Asthma, PAH, CTEPH, IPF, SCLC, and NSCLC.
Requirements for participation
1. PREP welcomes faculty who would be interested in creating two or more presentations and/or cases on an assigned topic using a flipped classroom, interactive design. A minimum of four faculty experts will be needed per disease state indicated previously. Honorarium provided.
2. PREP welcomes faculty from Chicago-based institutions who would be interested in participating as faculty presenters in the disease states indicated previously. Honorarium provided.
Selection criteria
To be considered, please indicate the disease area in which you are interested in participating as content developer or faculty presenter, as well as providing the best way to contact you. For the asthma curriculum, we have a specific need for expertise/interest in moderate to severe asthma and the use of biologics in treatment.
If you are interested in participating in this initiative, please contact Jasmine Turner ([email protected]). Thank you.
About PREP
The CHEST PREP Clinical Immersion program is an unbranded, disease-state program that educates industry members and partners to advance their knowledge into understanding that builds their confidence for engagement in clinical
conversations with health-care teams. We are seeking faculty for the following initiatives:
1. The CHEST PREP program is embarking on a curriculum and content development initiative and is seeking interested faculty members to consider participating in the development of content in the areas of CTEPH, Alpha-1 Antitrypsin, and Bronchiectasis.
2. The CHEST PREP program is seeking interested CHEST members in Chicago-based institutions to consider participating as faculty presenters in the following disease areas: COPD, Asthma, PAH, CTEPH, IPF, SCLC, and NSCLC.
Requirements for participation
1. PREP welcomes faculty who would be interested in creating two or more presentations and/or cases on an assigned topic using a flipped classroom, interactive design. A minimum of four faculty experts will be needed per disease state indicated previously. Honorarium provided.
2. PREP welcomes faculty from Chicago-based institutions who would be interested in participating as faculty presenters in the disease states indicated previously. Honorarium provided.
Selection criteria
To be considered, please indicate the disease area in which you are interested in participating as content developer or faculty presenter, as well as providing the best way to contact you. For the asthma curriculum, we have a specific need for expertise/interest in moderate to severe asthma and the use of biologics in treatment.
If you are interested in participating in this initiative, please contact Jasmine Turner ([email protected]). Thank you.
Pulmonary Hypertension Care Center initiative moves forward
The Pulmonary Hypertension Association (PHA) launched its Pulmonary Hypertension Care Center (PHCC) initiative 2 years ago. This initiative was designed to raise the quality of care, as well as long-term outcomes for this disease that is often misdiagnosed and progressive. The PHCC program has designated 41 adult and 6 pediatric sites as Comprehensive Care Centers with ongoing accreditation of new sites. As part of this program, the PHA Registry was established to provide input to improve the care of PH patients. The PHA Registry (PHAR) is a multicenter, prospective observational registry of newly evaluated patients with pulmonary arterial hypertension (PAH) and has enrolled 200 patients to date. PHAR participation is open to any PHCC-accredited center.
PHCC accreditation has two pathways: Comprehensive Care Centers and Regional Care Centers. Accreditation is based on adherence “to consensus guidelines for the diagnosis and treatment of PH, the scope of PH-related services provided at the center, and the expertise of the center’s PH Care Team members.” PHCC accreditation is potentially available to all PH centers that meet the established criteria that can be found at the PHCC website.
Additional information may be found at the PHCC website (https://phassociation.org/PHCareCenters).
The Pulmonary Hypertension Association (PHA) launched its Pulmonary Hypertension Care Center (PHCC) initiative 2 years ago. This initiative was designed to raise the quality of care, as well as long-term outcomes for this disease that is often misdiagnosed and progressive. The PHCC program has designated 41 adult and 6 pediatric sites as Comprehensive Care Centers with ongoing accreditation of new sites. As part of this program, the PHA Registry was established to provide input to improve the care of PH patients. The PHA Registry (PHAR) is a multicenter, prospective observational registry of newly evaluated patients with pulmonary arterial hypertension (PAH) and has enrolled 200 patients to date. PHAR participation is open to any PHCC-accredited center.
PHCC accreditation has two pathways: Comprehensive Care Centers and Regional Care Centers. Accreditation is based on adherence “to consensus guidelines for the diagnosis and treatment of PH, the scope of PH-related services provided at the center, and the expertise of the center’s PH Care Team members.” PHCC accreditation is potentially available to all PH centers that meet the established criteria that can be found at the PHCC website.
Additional information may be found at the PHCC website (https://phassociation.org/PHCareCenters).
The Pulmonary Hypertension Association (PHA) launched its Pulmonary Hypertension Care Center (PHCC) initiative 2 years ago. This initiative was designed to raise the quality of care, as well as long-term outcomes for this disease that is often misdiagnosed and progressive. The PHCC program has designated 41 adult and 6 pediatric sites as Comprehensive Care Centers with ongoing accreditation of new sites. As part of this program, the PHA Registry was established to provide input to improve the care of PH patients. The PHA Registry (PHAR) is a multicenter, prospective observational registry of newly evaluated patients with pulmonary arterial hypertension (PAH) and has enrolled 200 patients to date. PHAR participation is open to any PHCC-accredited center.
PHCC accreditation has two pathways: Comprehensive Care Centers and Regional Care Centers. Accreditation is based on adherence “to consensus guidelines for the diagnosis and treatment of PH, the scope of PH-related services provided at the center, and the expertise of the center’s PH Care Team members.” PHCC accreditation is potentially available to all PH centers that meet the established criteria that can be found at the PHCC website.
Additional information may be found at the PHCC website (https://phassociation.org/PHCareCenters).
Alternative to 10-year ABIM exam starts 2018
On December 14, the American Board of Internal Medicine (ABIM) announced an alternative to the 10-year Internal Medicine recertification exam, effective 2018. Currently, ABIM board–certified physicians can participate in Maintenance of Certification (MOC) by earning 100 MOC points every 5 years and passing a maintenance of certification exam every 10 years.
Beginning in 2018, physicians who are certified by the ABIM in Internal Medicine will have the option to take a lower-stakes exam every 2 years, rather than taking the current high-stakes exam every 10 years. The low-stakes exam option provides greater flexibility to the diplomate by allowing one to complete the examination at a convenient time set by the physician at home or in the office. While this new option will initially be available only to Internal Medicine diplomates, the ABIM intends to extend this alternative recertification model to subspecialties in the future.
CHEST is exploring how our education will evolve to address these key changes. For additional information, please visit ABIM’s website.
On December 14, the American Board of Internal Medicine (ABIM) announced an alternative to the 10-year Internal Medicine recertification exam, effective 2018. Currently, ABIM board–certified physicians can participate in Maintenance of Certification (MOC) by earning 100 MOC points every 5 years and passing a maintenance of certification exam every 10 years.
Beginning in 2018, physicians who are certified by the ABIM in Internal Medicine will have the option to take a lower-stakes exam every 2 years, rather than taking the current high-stakes exam every 10 years. The low-stakes exam option provides greater flexibility to the diplomate by allowing one to complete the examination at a convenient time set by the physician at home or in the office. While this new option will initially be available only to Internal Medicine diplomates, the ABIM intends to extend this alternative recertification model to subspecialties in the future.
CHEST is exploring how our education will evolve to address these key changes. For additional information, please visit ABIM’s website.
On December 14, the American Board of Internal Medicine (ABIM) announced an alternative to the 10-year Internal Medicine recertification exam, effective 2018. Currently, ABIM board–certified physicians can participate in Maintenance of Certification (MOC) by earning 100 MOC points every 5 years and passing a maintenance of certification exam every 10 years.
Beginning in 2018, physicians who are certified by the ABIM in Internal Medicine will have the option to take a lower-stakes exam every 2 years, rather than taking the current high-stakes exam every 10 years. The low-stakes exam option provides greater flexibility to the diplomate by allowing one to complete the examination at a convenient time set by the physician at home or in the office. While this new option will initially be available only to Internal Medicine diplomates, the ABIM intends to extend this alternative recertification model to subspecialties in the future.
CHEST is exploring how our education will evolve to address these key changes. For additional information, please visit ABIM’s website.
VAM Registration, Housing Now Open
Registration and housing for the 2017 Vascular Annual Meeting are now open. VAM will be held May 31-June 3 in San Diego, with plenaries and exhibits open June 1-3. Register here and make housing reservations here. Already, more than 150 people have registered; look who’s coming here.
Registration and housing for the 2017 Vascular Annual Meeting are now open. VAM will be held May 31-June 3 in San Diego, with plenaries and exhibits open June 1-3. Register here and make housing reservations here. Already, more than 150 people have registered; look who’s coming here.
Registration and housing for the 2017 Vascular Annual Meeting are now open. VAM will be held May 31-June 3 in San Diego, with plenaries and exhibits open June 1-3. Register here and make housing reservations here. Already, more than 150 people have registered; look who’s coming here.
Plan to attend CHEST 2017 in Toronto
Oct 28 – Nov 1
Toronto, Ontario, Canada
Join us in wonderful Toronto for CHEST 2017, where we’ll connect a global community in clinical chest medicine. Our program will deliver current pulmonary, critical care, and sleep medicine topics presented by world-renowned faculty in a variety of innovative instruction formats. Take advantage of these opportunities to get involved now:
Submit Abstracts and Case Reports
Submission deadline: March 31
- Fellow Case Reports.
- Medical Student/Resident Case Reports.
- Global Case Reports.
- Clinical Case Puzzlers.
Learn more and submit at chest2017.abstractcentral.com.
Apply for 2017 CHEST Foundation Grants
Application deadline: March 31
The CHEST Foundation has started accepting applications for its clinical research, distinguished scholar, and community service grants. Every year, the CHEST Foundation awards more than a half-million dollars to the next generation of lung health champions.
The grants available are:
- GlaxoSmithKline Distinguished Scholar Research Grant in Respiratory Health: $150,000 over 3 years
- CHEST Foundation Research Grant in Lung Cancer: $50,000-$100,000* over 2 years
- CHEST Foundation Research Grant in Pulmonary Arterial Hypertension: $25,000 1-year grant
- CHEST Foundation and Alpha-1 Foundation Research Grant in Alpha-1 Antitrypsin Deficiency: $25,000 1-year grant
- CHEST Foundation Research Grant in Nontuberculous Mycobacteria: $10,000-$30,000* 1-year grant
- CHEST Foundation Research Grant in Venous Thromboembolism: $30,000 1-year grant
- CHEST Foundation Research Grant in Pulmonary Fibrosis: $30,000 1-year grant
- CHEST Foundation Research Grant in Chronic Obstructive Pulmonary Disease: $50,000 1-year grant
- CHEST Foundation Research Grant in Women’s Lung Health: $10,000 1-year grant
- CHEST Foundation Research Grant in Asthma: $15,000 - $30,000* 1-year grant
- CHEST Foundation Research Grant in Cystic Fibrosis: $30,000 1-year grant
- Community Service Grant Honoring D. Robert McCaffree, MD, Master FCCP: multiple awards up to $15,000 per 1-year grant
*Amount contingent on funding.Apply for grants at chestfoundation.org/grants.
Oct 28 – Nov 1
Toronto, Ontario, Canada
Join us in wonderful Toronto for CHEST 2017, where we’ll connect a global community in clinical chest medicine. Our program will deliver current pulmonary, critical care, and sleep medicine topics presented by world-renowned faculty in a variety of innovative instruction formats. Take advantage of these opportunities to get involved now:
Submit Abstracts and Case Reports
Submission deadline: March 31
- Fellow Case Reports.
- Medical Student/Resident Case Reports.
- Global Case Reports.
- Clinical Case Puzzlers.
Learn more and submit at chest2017.abstractcentral.com.
Apply for 2017 CHEST Foundation Grants
Application deadline: March 31
The CHEST Foundation has started accepting applications for its clinical research, distinguished scholar, and community service grants. Every year, the CHEST Foundation awards more than a half-million dollars to the next generation of lung health champions.
The grants available are:
- GlaxoSmithKline Distinguished Scholar Research Grant in Respiratory Health: $150,000 over 3 years
- CHEST Foundation Research Grant in Lung Cancer: $50,000-$100,000* over 2 years
- CHEST Foundation Research Grant in Pulmonary Arterial Hypertension: $25,000 1-year grant
- CHEST Foundation and Alpha-1 Foundation Research Grant in Alpha-1 Antitrypsin Deficiency: $25,000 1-year grant
- CHEST Foundation Research Grant in Nontuberculous Mycobacteria: $10,000-$30,000* 1-year grant
- CHEST Foundation Research Grant in Venous Thromboembolism: $30,000 1-year grant
- CHEST Foundation Research Grant in Pulmonary Fibrosis: $30,000 1-year grant
- CHEST Foundation Research Grant in Chronic Obstructive Pulmonary Disease: $50,000 1-year grant
- CHEST Foundation Research Grant in Women’s Lung Health: $10,000 1-year grant
- CHEST Foundation Research Grant in Asthma: $15,000 - $30,000* 1-year grant
- CHEST Foundation Research Grant in Cystic Fibrosis: $30,000 1-year grant
- Community Service Grant Honoring D. Robert McCaffree, MD, Master FCCP: multiple awards up to $15,000 per 1-year grant
*Amount contingent on funding.Apply for grants at chestfoundation.org/grants.
Oct 28 – Nov 1
Toronto, Ontario, Canada
Join us in wonderful Toronto for CHEST 2017, where we’ll connect a global community in clinical chest medicine. Our program will deliver current pulmonary, critical care, and sleep medicine topics presented by world-renowned faculty in a variety of innovative instruction formats. Take advantage of these opportunities to get involved now:
Submit Abstracts and Case Reports
Submission deadline: March 31
- Fellow Case Reports.
- Medical Student/Resident Case Reports.
- Global Case Reports.
- Clinical Case Puzzlers.
Learn more and submit at chest2017.abstractcentral.com.
Apply for 2017 CHEST Foundation Grants
Application deadline: March 31
The CHEST Foundation has started accepting applications for its clinical research, distinguished scholar, and community service grants. Every year, the CHEST Foundation awards more than a half-million dollars to the next generation of lung health champions.
The grants available are:
- GlaxoSmithKline Distinguished Scholar Research Grant in Respiratory Health: $150,000 over 3 years
- CHEST Foundation Research Grant in Lung Cancer: $50,000-$100,000* over 2 years
- CHEST Foundation Research Grant in Pulmonary Arterial Hypertension: $25,000 1-year grant
- CHEST Foundation and Alpha-1 Foundation Research Grant in Alpha-1 Antitrypsin Deficiency: $25,000 1-year grant
- CHEST Foundation Research Grant in Nontuberculous Mycobacteria: $10,000-$30,000* 1-year grant
- CHEST Foundation Research Grant in Venous Thromboembolism: $30,000 1-year grant
- CHEST Foundation Research Grant in Pulmonary Fibrosis: $30,000 1-year grant
- CHEST Foundation Research Grant in Chronic Obstructive Pulmonary Disease: $50,000 1-year grant
- CHEST Foundation Research Grant in Women’s Lung Health: $10,000 1-year grant
- CHEST Foundation Research Grant in Asthma: $15,000 - $30,000* 1-year grant
- CHEST Foundation Research Grant in Cystic Fibrosis: $30,000 1-year grant
- Community Service Grant Honoring D. Robert McCaffree, MD, Master FCCP: multiple awards up to $15,000 per 1-year grant
*Amount contingent on funding.Apply for grants at chestfoundation.org/grants.
Household air pollution: Foundation grantee champions lung health
In 2016, Catherine Oberg, MD, was awarded the CHEST Foundation Research Grant in Women’s Lung Health for her project on household air pollution in Ghana. In this recent interview with Dr. Oberg, she describes how she is championing lung health.
How I got involved
In medical school, I was very interested in international medicine and took a trip to Tanzania to do primary care work when I was in my fourth year. I saw firsthand how the people, women especially, sleep, cook, eat, and take care of their children and animals all in one house. I saw how direct smoke exposure from cooking caused symptoms of cough, phlegm, and shortness of breath. I knew this was an area where I could make an impact.
Fortunately, I learned about CHEST Foundation grants through my mentor, Alison Lee, MD, who was a CHEST Foundation grant recipient early in her career. With the help of the grant, I was able to furnish my own supplies, get everything to Ghana, train native health-care providers, and start doing assessments. I received the CHEST Foundation grant at the perfect time. I am so appreciative and honored to be a CHEST Foundation grant recipient. It’s such a humbling experience to be able to act on these things that I’ve been looking into for so many months. I’m just excited and thankful, and can’t wait to see what we’re able to show.
Tackling a leading cause of lung disease
In rural areas around the world, people cook with ineffective fuels, such as animal dung, that cause damaging household air pollution. This is a leading cause of asthma, COPD, and lung cancer worldwide, and it preferentially affects women and children because of their roles in the household. My project focuses on household air pollution with a goal to measure the effectiveness of utilizing a clean burning stove as an intervention.
We have a cohort of women in Ghana and have had randomized clusters using either a liquefied petroleum gas (LPG) clean burning stove or a traditional cook stove for 18 months now. We’re going to look at their lung function, inflammatory markers, and respiratory symptoms and compare the groups to see if the intervention has made a difference.
The impact
Being able to breathe is a function many of us take for granted. The ability to impact something this vital to everyday life is a really exciting and important challenge. It’s an area where I think we can make a big impact.
The future
This project could bring about further research and hopefully provide evidence supporting these types of interventions. The impact could affect millions of people around the world. The CHEST Foundation grant is providing materials that are the foundation of our project. This grant allows us to design better studies in the future, to educate patients in a more effective manner, and to prevent these life-threatening diseases.
The next CHEST Foundation grants cycle is open from February 1 to March 31, 2017. How will you champion lung health? Learn more about foundation grants and how you can apply at https://chest.realmagnet.land/chest-foundation-grants.
In 2016, Catherine Oberg, MD, was awarded the CHEST Foundation Research Grant in Women’s Lung Health for her project on household air pollution in Ghana. In this recent interview with Dr. Oberg, she describes how she is championing lung health.
How I got involved
In medical school, I was very interested in international medicine and took a trip to Tanzania to do primary care work when I was in my fourth year. I saw firsthand how the people, women especially, sleep, cook, eat, and take care of their children and animals all in one house. I saw how direct smoke exposure from cooking caused symptoms of cough, phlegm, and shortness of breath. I knew this was an area where I could make an impact.
Fortunately, I learned about CHEST Foundation grants through my mentor, Alison Lee, MD, who was a CHEST Foundation grant recipient early in her career. With the help of the grant, I was able to furnish my own supplies, get everything to Ghana, train native health-care providers, and start doing assessments. I received the CHEST Foundation grant at the perfect time. I am so appreciative and honored to be a CHEST Foundation grant recipient. It’s such a humbling experience to be able to act on these things that I’ve been looking into for so many months. I’m just excited and thankful, and can’t wait to see what we’re able to show.
Tackling a leading cause of lung disease
In rural areas around the world, people cook with ineffective fuels, such as animal dung, that cause damaging household air pollution. This is a leading cause of asthma, COPD, and lung cancer worldwide, and it preferentially affects women and children because of their roles in the household. My project focuses on household air pollution with a goal to measure the effectiveness of utilizing a clean burning stove as an intervention.
We have a cohort of women in Ghana and have had randomized clusters using either a liquefied petroleum gas (LPG) clean burning stove or a traditional cook stove for 18 months now. We’re going to look at their lung function, inflammatory markers, and respiratory symptoms and compare the groups to see if the intervention has made a difference.
The impact
Being able to breathe is a function many of us take for granted. The ability to impact something this vital to everyday life is a really exciting and important challenge. It’s an area where I think we can make a big impact.
The future
This project could bring about further research and hopefully provide evidence supporting these types of interventions. The impact could affect millions of people around the world. The CHEST Foundation grant is providing materials that are the foundation of our project. This grant allows us to design better studies in the future, to educate patients in a more effective manner, and to prevent these life-threatening diseases.
The next CHEST Foundation grants cycle is open from February 1 to March 31, 2017. How will you champion lung health? Learn more about foundation grants and how you can apply at https://chest.realmagnet.land/chest-foundation-grants.
In 2016, Catherine Oberg, MD, was awarded the CHEST Foundation Research Grant in Women’s Lung Health for her project on household air pollution in Ghana. In this recent interview with Dr. Oberg, she describes how she is championing lung health.
How I got involved
In medical school, I was very interested in international medicine and took a trip to Tanzania to do primary care work when I was in my fourth year. I saw firsthand how the people, women especially, sleep, cook, eat, and take care of their children and animals all in one house. I saw how direct smoke exposure from cooking caused symptoms of cough, phlegm, and shortness of breath. I knew this was an area where I could make an impact.
Fortunately, I learned about CHEST Foundation grants through my mentor, Alison Lee, MD, who was a CHEST Foundation grant recipient early in her career. With the help of the grant, I was able to furnish my own supplies, get everything to Ghana, train native health-care providers, and start doing assessments. I received the CHEST Foundation grant at the perfect time. I am so appreciative and honored to be a CHEST Foundation grant recipient. It’s such a humbling experience to be able to act on these things that I’ve been looking into for so many months. I’m just excited and thankful, and can’t wait to see what we’re able to show.
Tackling a leading cause of lung disease
In rural areas around the world, people cook with ineffective fuels, such as animal dung, that cause damaging household air pollution. This is a leading cause of asthma, COPD, and lung cancer worldwide, and it preferentially affects women and children because of their roles in the household. My project focuses on household air pollution with a goal to measure the effectiveness of utilizing a clean burning stove as an intervention.
We have a cohort of women in Ghana and have had randomized clusters using either a liquefied petroleum gas (LPG) clean burning stove or a traditional cook stove for 18 months now. We’re going to look at their lung function, inflammatory markers, and respiratory symptoms and compare the groups to see if the intervention has made a difference.
The impact
Being able to breathe is a function many of us take for granted. The ability to impact something this vital to everyday life is a really exciting and important challenge. It’s an area where I think we can make a big impact.
The future
This project could bring about further research and hopefully provide evidence supporting these types of interventions. The impact could affect millions of people around the world. The CHEST Foundation grant is providing materials that are the foundation of our project. This grant allows us to design better studies in the future, to educate patients in a more effective manner, and to prevent these life-threatening diseases.
The next CHEST Foundation grants cycle is open from February 1 to March 31, 2017. How will you champion lung health? Learn more about foundation grants and how you can apply at https://chest.realmagnet.land/chest-foundation-grants.
Catching up with our CHEST Past Presidents
Where are they now? What have they been up to? CHEST’s Past Presidents each forged the way for the many successes of the American College of Chest Physicians, leading to enhanced patient care around the globe. Their outstanding leadership and vision are evidenced today in many of CHEST’s strategic initiatives. Let’s check in with Dr. Mathers.
President 2008-2009
It was a great honor to be inaugurated as President of the American College of Chest Physicians at the 2008 Annual Meeting in Philadelphia. My chosen vocation was community-based private practice, and from my early years in practice, I found the opportunity to interact with the clinically oriented scholars of CHEST invaluable. My wife Susan and I fondly remember activities with staff, others in leadership, and their families. My immediate goals for my presidential year were to ensure the financial security of the College, in light of the evolving restrictions on industry funding, and to raise the profile of telemedicine for the care of patients with chronic conditions and the critically ill. However, that year is probably most remembered for the unanticipated need to formulate a step-down agreement with then-CEO Alvin Lever, who had served the College for the preceding 17 years.
Early in my practice, I became interested in addressing federal policies that interfered with the ability to provide state-of-the-art care to my patient population. My first committee appointment with CHEST was the Government Relations Committee. Our activities were closely coordinated with the National Association for Medical Direction of Respiratory Care (NAMDRC) and the American Thoracic Society. During my year as Immediate Past President of the College, I was approached by NAMDRC and invited to write their monthly publication, The Washington Watchline. I have continued to enjoy that opportunity, as well as interacting with their membership. When called upon by NAMDRC, I travel to Washington, DC, to meet with Medicare staff to discuss policy issues important in the care of pulmonary patients.
Where are they now? What have they been up to? CHEST’s Past Presidents each forged the way for the many successes of the American College of Chest Physicians, leading to enhanced patient care around the globe. Their outstanding leadership and vision are evidenced today in many of CHEST’s strategic initiatives. Let’s check in with Dr. Mathers.
President 2008-2009
It was a great honor to be inaugurated as President of the American College of Chest Physicians at the 2008 Annual Meeting in Philadelphia. My chosen vocation was community-based private practice, and from my early years in practice, I found the opportunity to interact with the clinically oriented scholars of CHEST invaluable. My wife Susan and I fondly remember activities with staff, others in leadership, and their families. My immediate goals for my presidential year were to ensure the financial security of the College, in light of the evolving restrictions on industry funding, and to raise the profile of telemedicine for the care of patients with chronic conditions and the critically ill. However, that year is probably most remembered for the unanticipated need to formulate a step-down agreement with then-CEO Alvin Lever, who had served the College for the preceding 17 years.
Early in my practice, I became interested in addressing federal policies that interfered with the ability to provide state-of-the-art care to my patient population. My first committee appointment with CHEST was the Government Relations Committee. Our activities were closely coordinated with the National Association for Medical Direction of Respiratory Care (NAMDRC) and the American Thoracic Society. During my year as Immediate Past President of the College, I was approached by NAMDRC and invited to write their monthly publication, The Washington Watchline. I have continued to enjoy that opportunity, as well as interacting with their membership. When called upon by NAMDRC, I travel to Washington, DC, to meet with Medicare staff to discuss policy issues important in the care of pulmonary patients.
Where are they now? What have they been up to? CHEST’s Past Presidents each forged the way for the many successes of the American College of Chest Physicians, leading to enhanced patient care around the globe. Their outstanding leadership and vision are evidenced today in many of CHEST’s strategic initiatives. Let’s check in with Dr. Mathers.
President 2008-2009
It was a great honor to be inaugurated as President of the American College of Chest Physicians at the 2008 Annual Meeting in Philadelphia. My chosen vocation was community-based private practice, and from my early years in practice, I found the opportunity to interact with the clinically oriented scholars of CHEST invaluable. My wife Susan and I fondly remember activities with staff, others in leadership, and their families. My immediate goals for my presidential year were to ensure the financial security of the College, in light of the evolving restrictions on industry funding, and to raise the profile of telemedicine for the care of patients with chronic conditions and the critically ill. However, that year is probably most remembered for the unanticipated need to formulate a step-down agreement with then-CEO Alvin Lever, who had served the College for the preceding 17 years.
Early in my practice, I became interested in addressing federal policies that interfered with the ability to provide state-of-the-art care to my patient population. My first committee appointment with CHEST was the Government Relations Committee. Our activities were closely coordinated with the National Association for Medical Direction of Respiratory Care (NAMDRC) and the American Thoracic Society. During my year as Immediate Past President of the College, I was approached by NAMDRC and invited to write their monthly publication, The Washington Watchline. I have continued to enjoy that opportunity, as well as interacting with their membership. When called upon by NAMDRC, I travel to Washington, DC, to meet with Medicare staff to discuss policy issues important in the care of pulmonary patients.