User login
From the Vascular Community
In memoriam: Edward B. Diethrich
Edward B. Diethrich, MD, the world-renowned cardiovascular/endovascular surgeon, inventor, and philanthropist, succumbed after a brave fight with a brain tumor on February 23, 2017, at the age of 81.
Dr. Diethrich was a pioneer in noninvasive cardiovascular and vascular disease diagnosis and innovative in surgical and endovascular therapy. He obtained his undergraduate and medical degrees at the University of Michigan and completed his surgical residency at St. Joseph’s Mercy Hospital in Ann Arbor and the Henry Ford Hospital in Detroit. He went on to complete his cardiovascular surgery training under Michael DeBakey at the Baylor College of Medicine in Houston, where he played an important role in the development of human heart transplantation.
One of his first accomplishments was the invention of the sternal saw in 1962, which is still used today for open-chest surgery. He also contributed to the development of a preservation chamber for heart transplantation and established one of the first ultrasound companies. Dr. Diethrich spent a lifetime developing new technologies, from a bubble oxygenator for open-heart surgery to developing and manufacturing stent grafts for aortic aneurysms. He remained actively involved in advancing the practice of vascular surgery and keeping it up-to-date with the changing times: He founded a company that develops and manufactures endoluminal grafts, established a Translational Research Center that is dedicated to clinical research and developing new technologies, and started a company devoted to the prevention and management of cardiovascular disease. His contributions to surgical education are also legendary. He organized an annual meeting that attracted physicians from all over the world and show-cased state-of-the-art techniques and innovations. He authored over 400 scientific articles, several textbooks, and lay publications and produced hundreds of educational videos and films. In fact, he organized the first live international telecast of open-heart surgery. Above all, Dr. Diethrich trained several hundred surgeons and other specialists in cardiovascular surgery and endovascular techniques, and traveled the world to demonstrate his techniques and teach local physicians. He recently endowed the Edward B. Diethrich Research Professorship in Biomedical Engineering and Vascular Surgery at the University of Michigan to recognize the collaboration that is required between surgeons and engineers.
Dr. Diethrich has received several honors, such as the Frederick A. Coller Award; Presidency of the Denton A. Cooley Cardiovascular Surgical Society; the Medal for Innovation in Vascular Surgery from the Society for Vascular Surgery; the Medal of Independence from King Hussein of Jordan; and an honorary fellowship from the Royal College of Surgeons, Glasgow. The Edward B. Diethrich Vascular Surgical Society was established by several hundred of his trainees. I was honored to serve as the first President of that society.
It’s ironic that Dr. Diethrich was an early supporter of ceiling-mounted radiographic equipment, which is essential to endovascular interventions. Even with the most advanced radiation protection, Dr. Diethrich paid the ultimate price for his nearly daily exposure to radiation, which led to his 4-year battle with glioma, and, ultimately, his death. But true to form, he even used this unfortunate illness to educate others by working with the Organization for Occupational Radiation Safety in Interventional Fluoroscopy to produce a documentary on the ill effects of radiation.
Dr. Diethrich recently completed his memoirs (SLED: The Serendipitous Life of Edward Diethrich), which recounts his extraordinary 50-year career, from his early days of working and training with the world’s most renowned surgeons to his legendary international success as a cardiovascular surgeon and innovator.
In summary, Dr. Diethrich was a multifaceted, passionate, and charismatic man: a sportsman, musician, scientist, inventor, author, film producer, media personality, along with many others. His confidence, dexterity, and technical expertise were evident in both the operating room and the endovascular suite. Dr. Diethrich was a world-renowned leader and pioneer in Vascular Surgery. He was an eloquent speaker, prolific innovative scholar, and dedicated teacher. His energy was endless, and his manners were impeccable. He will be sorely missed, but his legendary contributions to medicine/vascular surgery, his trainees, and the many people he influenced will live on.
Dr. Diethrich is survived by his wife of 61 years, Gloria; daughter Lynne; son Tad; son-in-law Joe Jackson; daughter-in-law Terri Diethrich, and grandchildren Danielle Diethrich-Vargas, Courtney, Reese, and Trey Diethrich; Mackenzie, Tatum, Peyton, and Zack Jackson.
A celebration of his life will be planned in the near future. Details will be posted at drteddiethrich.com.
In memoriam: Edward B. Diethrich
Edward B. Diethrich, MD, the world-renowned cardiovascular/endovascular surgeon, inventor, and philanthropist, succumbed after a brave fight with a brain tumor on February 23, 2017, at the age of 81.
Dr. Diethrich was a pioneer in noninvasive cardiovascular and vascular disease diagnosis and innovative in surgical and endovascular therapy. He obtained his undergraduate and medical degrees at the University of Michigan and completed his surgical residency at St. Joseph’s Mercy Hospital in Ann Arbor and the Henry Ford Hospital in Detroit. He went on to complete his cardiovascular surgery training under Michael DeBakey at the Baylor College of Medicine in Houston, where he played an important role in the development of human heart transplantation.
One of his first accomplishments was the invention of the sternal saw in 1962, which is still used today for open-chest surgery. He also contributed to the development of a preservation chamber for heart transplantation and established one of the first ultrasound companies. Dr. Diethrich spent a lifetime developing new technologies, from a bubble oxygenator for open-heart surgery to developing and manufacturing stent grafts for aortic aneurysms. He remained actively involved in advancing the practice of vascular surgery and keeping it up-to-date with the changing times: He founded a company that develops and manufactures endoluminal grafts, established a Translational Research Center that is dedicated to clinical research and developing new technologies, and started a company devoted to the prevention and management of cardiovascular disease. His contributions to surgical education are also legendary. He organized an annual meeting that attracted physicians from all over the world and show-cased state-of-the-art techniques and innovations. He authored over 400 scientific articles, several textbooks, and lay publications and produced hundreds of educational videos and films. In fact, he organized the first live international telecast of open-heart surgery. Above all, Dr. Diethrich trained several hundred surgeons and other specialists in cardiovascular surgery and endovascular techniques, and traveled the world to demonstrate his techniques and teach local physicians. He recently endowed the Edward B. Diethrich Research Professorship in Biomedical Engineering and Vascular Surgery at the University of Michigan to recognize the collaboration that is required between surgeons and engineers.
Dr. Diethrich has received several honors, such as the Frederick A. Coller Award; Presidency of the Denton A. Cooley Cardiovascular Surgical Society; the Medal for Innovation in Vascular Surgery from the Society for Vascular Surgery; the Medal of Independence from King Hussein of Jordan; and an honorary fellowship from the Royal College of Surgeons, Glasgow. The Edward B. Diethrich Vascular Surgical Society was established by several hundred of his trainees. I was honored to serve as the first President of that society.
It’s ironic that Dr. Diethrich was an early supporter of ceiling-mounted radiographic equipment, which is essential to endovascular interventions. Even with the most advanced radiation protection, Dr. Diethrich paid the ultimate price for his nearly daily exposure to radiation, which led to his 4-year battle with glioma, and, ultimately, his death. But true to form, he even used this unfortunate illness to educate others by working with the Organization for Occupational Radiation Safety in Interventional Fluoroscopy to produce a documentary on the ill effects of radiation.
Dr. Diethrich recently completed his memoirs (SLED: The Serendipitous Life of Edward Diethrich), which recounts his extraordinary 50-year career, from his early days of working and training with the world’s most renowned surgeons to his legendary international success as a cardiovascular surgeon and innovator.
In summary, Dr. Diethrich was a multifaceted, passionate, and charismatic man: a sportsman, musician, scientist, inventor, author, film producer, media personality, along with many others. His confidence, dexterity, and technical expertise were evident in both the operating room and the endovascular suite. Dr. Diethrich was a world-renowned leader and pioneer in Vascular Surgery. He was an eloquent speaker, prolific innovative scholar, and dedicated teacher. His energy was endless, and his manners were impeccable. He will be sorely missed, but his legendary contributions to medicine/vascular surgery, his trainees, and the many people he influenced will live on.
Dr. Diethrich is survived by his wife of 61 years, Gloria; daughter Lynne; son Tad; son-in-law Joe Jackson; daughter-in-law Terri Diethrich, and grandchildren Danielle Diethrich-Vargas, Courtney, Reese, and Trey Diethrich; Mackenzie, Tatum, Peyton, and Zack Jackson.
A celebration of his life will be planned in the near future. Details will be posted at drteddiethrich.com.
In memoriam: Edward B. Diethrich
Edward B. Diethrich, MD, the world-renowned cardiovascular/endovascular surgeon, inventor, and philanthropist, succumbed after a brave fight with a brain tumor on February 23, 2017, at the age of 81.
Dr. Diethrich was a pioneer in noninvasive cardiovascular and vascular disease diagnosis and innovative in surgical and endovascular therapy. He obtained his undergraduate and medical degrees at the University of Michigan and completed his surgical residency at St. Joseph’s Mercy Hospital in Ann Arbor and the Henry Ford Hospital in Detroit. He went on to complete his cardiovascular surgery training under Michael DeBakey at the Baylor College of Medicine in Houston, where he played an important role in the development of human heart transplantation.
One of his first accomplishments was the invention of the sternal saw in 1962, which is still used today for open-chest surgery. He also contributed to the development of a preservation chamber for heart transplantation and established one of the first ultrasound companies. Dr. Diethrich spent a lifetime developing new technologies, from a bubble oxygenator for open-heart surgery to developing and manufacturing stent grafts for aortic aneurysms. He remained actively involved in advancing the practice of vascular surgery and keeping it up-to-date with the changing times: He founded a company that develops and manufactures endoluminal grafts, established a Translational Research Center that is dedicated to clinical research and developing new technologies, and started a company devoted to the prevention and management of cardiovascular disease. His contributions to surgical education are also legendary. He organized an annual meeting that attracted physicians from all over the world and show-cased state-of-the-art techniques and innovations. He authored over 400 scientific articles, several textbooks, and lay publications and produced hundreds of educational videos and films. In fact, he organized the first live international telecast of open-heart surgery. Above all, Dr. Diethrich trained several hundred surgeons and other specialists in cardiovascular surgery and endovascular techniques, and traveled the world to demonstrate his techniques and teach local physicians. He recently endowed the Edward B. Diethrich Research Professorship in Biomedical Engineering and Vascular Surgery at the University of Michigan to recognize the collaboration that is required between surgeons and engineers.
Dr. Diethrich has received several honors, such as the Frederick A. Coller Award; Presidency of the Denton A. Cooley Cardiovascular Surgical Society; the Medal for Innovation in Vascular Surgery from the Society for Vascular Surgery; the Medal of Independence from King Hussein of Jordan; and an honorary fellowship from the Royal College of Surgeons, Glasgow. The Edward B. Diethrich Vascular Surgical Society was established by several hundred of his trainees. I was honored to serve as the first President of that society.
It’s ironic that Dr. Diethrich was an early supporter of ceiling-mounted radiographic equipment, which is essential to endovascular interventions. Even with the most advanced radiation protection, Dr. Diethrich paid the ultimate price for his nearly daily exposure to radiation, which led to his 4-year battle with glioma, and, ultimately, his death. But true to form, he even used this unfortunate illness to educate others by working with the Organization for Occupational Radiation Safety in Interventional Fluoroscopy to produce a documentary on the ill effects of radiation.
Dr. Diethrich recently completed his memoirs (SLED: The Serendipitous Life of Edward Diethrich), which recounts his extraordinary 50-year career, from his early days of working and training with the world’s most renowned surgeons to his legendary international success as a cardiovascular surgeon and innovator.
In summary, Dr. Diethrich was a multifaceted, passionate, and charismatic man: a sportsman, musician, scientist, inventor, author, film producer, media personality, along with many others. His confidence, dexterity, and technical expertise were evident in both the operating room and the endovascular suite. Dr. Diethrich was a world-renowned leader and pioneer in Vascular Surgery. He was an eloquent speaker, prolific innovative scholar, and dedicated teacher. His energy was endless, and his manners were impeccable. He will be sorely missed, but his legendary contributions to medicine/vascular surgery, his trainees, and the many people he influenced will live on.
Dr. Diethrich is survived by his wife of 61 years, Gloria; daughter Lynne; son Tad; son-in-law Joe Jackson; daughter-in-law Terri Diethrich, and grandchildren Danielle Diethrich-Vargas, Courtney, Reese, and Trey Diethrich; Mackenzie, Tatum, Peyton, and Zack Jackson.
A celebration of his life will be planned in the near future. Details will be posted at drteddiethrich.com.
Purchase On-Demand Library at VAM Registration
Don't forget you can take VAM home with you! You can pre-purchase all VAM PowerPoint slides, audio and a limited selection of assorted videotaped sessions in the On-Demand Library.
This valuable resource of almost 400 individual presentations will be available shortly following the meeting’s conclusion, with access continued for up to one year.
Cost is just $99. For those who have already registered and now want to add the On-Demand Library, simply return to the registration page and add the library separately.
Register here for VAM and make housing reservations here.
Don't forget you can take VAM home with you! You can pre-purchase all VAM PowerPoint slides, audio and a limited selection of assorted videotaped sessions in the On-Demand Library.
This valuable resource of almost 400 individual presentations will be available shortly following the meeting’s conclusion, with access continued for up to one year.
Cost is just $99. For those who have already registered and now want to add the On-Demand Library, simply return to the registration page and add the library separately.
Register here for VAM and make housing reservations here.
Don't forget you can take VAM home with you! You can pre-purchase all VAM PowerPoint slides, audio and a limited selection of assorted videotaped sessions in the On-Demand Library.
This valuable resource of almost 400 individual presentations will be available shortly following the meeting’s conclusion, with access continued for up to one year.
Cost is just $99. For those who have already registered and now want to add the On-Demand Library, simply return to the registration page and add the library separately.
Register here for VAM and make housing reservations here.
AGA offers free patient education tools on IBS
Approximately 35 million Americans are affected by irritable bowel syndrome (IBS). April is IBS Awareness Month, which is a perfect time to ensure you have the resources to care for your IBS patients.
To help your IBS patients, AGA provides credible, accessible education information on the following topics in English and Spanish.
- • What is irritable bowel syndrome?
- • Symptoms
- • Getting tested
- • Newly diagnosed
- • Treatment
- • Complications
Visit www.gastro.org/IBS to access our patient materials.
Approximately 35 million Americans are affected by irritable bowel syndrome (IBS). April is IBS Awareness Month, which is a perfect time to ensure you have the resources to care for your IBS patients.
To help your IBS patients, AGA provides credible, accessible education information on the following topics in English and Spanish.
- • What is irritable bowel syndrome?
- • Symptoms
- • Getting tested
- • Newly diagnosed
- • Treatment
- • Complications
Visit www.gastro.org/IBS to access our patient materials.
Approximately 35 million Americans are affected by irritable bowel syndrome (IBS). April is IBS Awareness Month, which is a perfect time to ensure you have the resources to care for your IBS patients.
To help your IBS patients, AGA provides credible, accessible education information on the following topics in English and Spanish.
- • What is irritable bowel syndrome?
- • Symptoms
- • Getting tested
- • Newly diagnosed
- • Treatment
- • Complications
Visit www.gastro.org/IBS to access our patient materials.
A gift in your will: Getting started
A simple, flexible and versatile way to ensure The AGA Research Foundation can continue our work for years to come is a gift in your will or living trust, known as a charitable bequest. To make a charitable bequest, you need a current will or living trust.
Your gift can be made as a percentage of your estate. Or you can make a specific bequest by giving a certain amount of cash, securities, or property. After your lifetime, the AGA Research Foundation receives your gift.
We hope you’ll consider including a gift to the AGA Research Foundation in your will or living trust. It’s simple – just a few sentences in your will or trust are all that is needed. The official bequest language for the AGA Research Foundation is: “I, [name], of [city, state, ZIP], give, devise, and bequeath to the AGA Research Foundation [written amount or percentage of the estate or description of property] for its unrestricted use and purpose.”
When planning a future gift, it’s sometimes difficult to determine what size donation will make sense. Emergencies happen, and you need to make sure your family is financially taken care of first. Including a bequest of a percentage of your estate ensures that your gift will remain proportionate no matter how your estate’s value fluctuates over the years.
Whether you would like to put your donation to work today or benefit us after your lifetime, you can find a charitable plan that lets you provide for your family and support the AGA Research Foundation.
Please contact us for more information at [email protected] or visit http://gastro.planmylegacy.org/.
A simple, flexible and versatile way to ensure The AGA Research Foundation can continue our work for years to come is a gift in your will or living trust, known as a charitable bequest. To make a charitable bequest, you need a current will or living trust.
Your gift can be made as a percentage of your estate. Or you can make a specific bequest by giving a certain amount of cash, securities, or property. After your lifetime, the AGA Research Foundation receives your gift.
We hope you’ll consider including a gift to the AGA Research Foundation in your will or living trust. It’s simple – just a few sentences in your will or trust are all that is needed. The official bequest language for the AGA Research Foundation is: “I, [name], of [city, state, ZIP], give, devise, and bequeath to the AGA Research Foundation [written amount or percentage of the estate or description of property] for its unrestricted use and purpose.”
When planning a future gift, it’s sometimes difficult to determine what size donation will make sense. Emergencies happen, and you need to make sure your family is financially taken care of first. Including a bequest of a percentage of your estate ensures that your gift will remain proportionate no matter how your estate’s value fluctuates over the years.
Whether you would like to put your donation to work today or benefit us after your lifetime, you can find a charitable plan that lets you provide for your family and support the AGA Research Foundation.
Please contact us for more information at [email protected] or visit http://gastro.planmylegacy.org/.
A simple, flexible and versatile way to ensure The AGA Research Foundation can continue our work for years to come is a gift in your will or living trust, known as a charitable bequest. To make a charitable bequest, you need a current will or living trust.
Your gift can be made as a percentage of your estate. Or you can make a specific bequest by giving a certain amount of cash, securities, or property. After your lifetime, the AGA Research Foundation receives your gift.
We hope you’ll consider including a gift to the AGA Research Foundation in your will or living trust. It’s simple – just a few sentences in your will or trust are all that is needed. The official bequest language for the AGA Research Foundation is: “I, [name], of [city, state, ZIP], give, devise, and bequeath to the AGA Research Foundation [written amount or percentage of the estate or description of property] for its unrestricted use and purpose.”
When planning a future gift, it’s sometimes difficult to determine what size donation will make sense. Emergencies happen, and you need to make sure your family is financially taken care of first. Including a bequest of a percentage of your estate ensures that your gift will remain proportionate no matter how your estate’s value fluctuates over the years.
Whether you would like to put your donation to work today or benefit us after your lifetime, you can find a charitable plan that lets you provide for your family and support the AGA Research Foundation.
Please contact us for more information at [email protected] or visit http://gastro.planmylegacy.org/.
See you at DDW and the AGA Postgraduate course
AGA looks forward to seeing our members at Digestive Disease Week® (DDW) 2017, May 6-9 in Chicago. If you’re not yet registered for the meeting, visit www.ddw.org to reserve your spot.
Please also join us for the 2017 AGA Postgraduate Course. The 2017 course is set for May 6 and 7, 2017, in conjunction with DDW. This 1.5-day course is designed to help you step beyond basic learning and get the full scope of GI advances. You will measure, learn, and apply the newest advances that will help you make confident decisions for your patients.
The course will feature six general sessions:
- • Hot Topics (abdominal pain and opioid therapy, microbiome and obesity, viral hepatitis, and fecal microbiota transplantation)
- • IBD: It’s a Beautiful Day (IBD) to discuss Inflammatory Bowel Disease (IBD)
- • The Biliary Tree and Pancreas
- • Love the Liver
- • All Guts and Glory: Esophagus, Stomach and Small Intestine
- • Bringing Up the Rear: Disorders of the Colon and Rectum
The course will also include 29 breakout sessions. These focused, small-group sessions allow you to delve deeper into specific clinical topics and provide direct access to internationally renowned faculty.
To learn more about the AGA Postgraduate course, visit pgcourse.gastro.org.
AGA looks forward to seeing our members at Digestive Disease Week® (DDW) 2017, May 6-9 in Chicago. If you’re not yet registered for the meeting, visit www.ddw.org to reserve your spot.
Please also join us for the 2017 AGA Postgraduate Course. The 2017 course is set for May 6 and 7, 2017, in conjunction with DDW. This 1.5-day course is designed to help you step beyond basic learning and get the full scope of GI advances. You will measure, learn, and apply the newest advances that will help you make confident decisions for your patients.
The course will feature six general sessions:
- • Hot Topics (abdominal pain and opioid therapy, microbiome and obesity, viral hepatitis, and fecal microbiota transplantation)
- • IBD: It’s a Beautiful Day (IBD) to discuss Inflammatory Bowel Disease (IBD)
- • The Biliary Tree and Pancreas
- • Love the Liver
- • All Guts and Glory: Esophagus, Stomach and Small Intestine
- • Bringing Up the Rear: Disorders of the Colon and Rectum
The course will also include 29 breakout sessions. These focused, small-group sessions allow you to delve deeper into specific clinical topics and provide direct access to internationally renowned faculty.
To learn more about the AGA Postgraduate course, visit pgcourse.gastro.org.
AGA looks forward to seeing our members at Digestive Disease Week® (DDW) 2017, May 6-9 in Chicago. If you’re not yet registered for the meeting, visit www.ddw.org to reserve your spot.
Please also join us for the 2017 AGA Postgraduate Course. The 2017 course is set for May 6 and 7, 2017, in conjunction with DDW. This 1.5-day course is designed to help you step beyond basic learning and get the full scope of GI advances. You will measure, learn, and apply the newest advances that will help you make confident decisions for your patients.
The course will feature six general sessions:
- • Hot Topics (abdominal pain and opioid therapy, microbiome and obesity, viral hepatitis, and fecal microbiota transplantation)
- • IBD: It’s a Beautiful Day (IBD) to discuss Inflammatory Bowel Disease (IBD)
- • The Biliary Tree and Pancreas
- • Love the Liver
- • All Guts and Glory: Esophagus, Stomach and Small Intestine
- • Bringing Up the Rear: Disorders of the Colon and Rectum
The course will also include 29 breakout sessions. These focused, small-group sessions allow you to delve deeper into specific clinical topics and provide direct access to internationally renowned faculty.
To learn more about the AGA Postgraduate course, visit pgcourse.gastro.org.
AGA announces appointment of new Governing Board members
AGA is pleased to announce new AGA Institute Governing Board designate-elects for 2017-2018.
Hashem B. El-Serag, MD, MPH, AGAF, is the vice president-elect designate. Dr. El-Serag is professor and chair of medicine, Baylor College of Medicine, Houston, TX. He is the editor of Clinical Gastroenterology and Hepatology until July 2017, and serves on the AGA Institute Leadership and Publications Committee.
Lawrence S. Kim, MD, AGAF, is the secretary/treasurer-elect designate. Dr. Kim is a partner at South Denver Gastroenterology, P.C., Littleton, CO. He currently serves on the AGA Institute Clinical Practice Updates, Audit, and Finance and Operations Committees. Dr. Kim has previously served as an AGA Institute Private Practice Councillor.
Dr. El-Serag and Dr. Kim begin their terms immediately following Digestive Disease Week® (DDW) 2017.
AGA is pleased to announce new AGA Institute Governing Board designate-elects for 2017-2018.
Hashem B. El-Serag, MD, MPH, AGAF, is the vice president-elect designate. Dr. El-Serag is professor and chair of medicine, Baylor College of Medicine, Houston, TX. He is the editor of Clinical Gastroenterology and Hepatology until July 2017, and serves on the AGA Institute Leadership and Publications Committee.
Lawrence S. Kim, MD, AGAF, is the secretary/treasurer-elect designate. Dr. Kim is a partner at South Denver Gastroenterology, P.C., Littleton, CO. He currently serves on the AGA Institute Clinical Practice Updates, Audit, and Finance and Operations Committees. Dr. Kim has previously served as an AGA Institute Private Practice Councillor.
Dr. El-Serag and Dr. Kim begin their terms immediately following Digestive Disease Week® (DDW) 2017.
AGA is pleased to announce new AGA Institute Governing Board designate-elects for 2017-2018.
Hashem B. El-Serag, MD, MPH, AGAF, is the vice president-elect designate. Dr. El-Serag is professor and chair of medicine, Baylor College of Medicine, Houston, TX. He is the editor of Clinical Gastroenterology and Hepatology until July 2017, and serves on the AGA Institute Leadership and Publications Committee.
Lawrence S. Kim, MD, AGAF, is the secretary/treasurer-elect designate. Dr. Kim is a partner at South Denver Gastroenterology, P.C., Littleton, CO. He currently serves on the AGA Institute Clinical Practice Updates, Audit, and Finance and Operations Committees. Dr. Kim has previously served as an AGA Institute Private Practice Councillor.
Dr. El-Serag and Dr. Kim begin their terms immediately following Digestive Disease Week® (DDW) 2017.
Announcing new Crohn’s & colitis congress
AGA and the Crohn’s & Colitis Foundation are partnering to cosponsor a new annual conference for health care professionals and researchers. By joining the nation’s leading IBD patient organization with the premier GI professional organization, this will be the must-attend IBD conference, bringing state-of-the-art comprehensive care together with the latest research to advance prevention, treatment, and cures for IBD patients.
Save the date – Jan. 18-20, 2018, in Las Vegas. Get ready to expand your knowledge, network with other leaders, and be inspired! Stay tuned for our website launch and more details coming this spring.
AGA and the Crohn’s & Colitis Foundation are partnering to cosponsor a new annual conference for health care professionals and researchers. By joining the nation’s leading IBD patient organization with the premier GI professional organization, this will be the must-attend IBD conference, bringing state-of-the-art comprehensive care together with the latest research to advance prevention, treatment, and cures for IBD patients.
Save the date – Jan. 18-20, 2018, in Las Vegas. Get ready to expand your knowledge, network with other leaders, and be inspired! Stay tuned for our website launch and more details coming this spring.
AGA and the Crohn’s & Colitis Foundation are partnering to cosponsor a new annual conference for health care professionals and researchers. By joining the nation’s leading IBD patient organization with the premier GI professional organization, this will be the must-attend IBD conference, bringing state-of-the-art comprehensive care together with the latest research to advance prevention, treatment, and cures for IBD patients.
Save the date – Jan. 18-20, 2018, in Las Vegas. Get ready to expand your knowledge, network with other leaders, and be inspired! Stay tuned for our website launch and more details coming this spring.
Education: Register Now for the 2017 VAM
The topic is vascular care. The subjects to be covered are nearly too numerous to count. And the clock is ticking for signing up.
Registration and housing will open in early March for the 2017 Vascular Annual Meeting, set for May 31 to June 3 in San Diego, Calif., with plenaries and exhibits from June 1 to 3. This premier meeting of vascular specialists will be held at the San Diego Convention Center. The headquarters hotel, the Marriott Marquis San Diego Marina Hotel, adjoins the center.
There is plenty going on.
Additional programming: Expanded programming begins Wednesday and continues through Saturday. Be sure to plan your travel to attend these informative sessions. This year’s meeting includes more concurrent sessions, and the number of joint society programs has doubled from last year.
Free postgraduate courses for SVS members: Once again, all SVS member-registrants receive free admittance to the six Wednesday postgraduate courses, a savings of $300. Non-members plus anyone registering only for the postgraduate courses must pay the appropriate registration fee. Self-assessment credit is available to all physician attendees.
SVS/STS Aortic Summit: New this year, and a highlight for Saturday, is the SVS/STS Summit: Advances and Controversies in the Management of Complex Thoracoabdominal Aneurysmal Diseases and Type B Aortic Dissection. This program will take place from 1 to 5 p.m. and is co-sponsored by the Society of Thoracic Surgeons. An additional fee is required. 
Revamped workshops: Wednesday’s workshops will feature a new format, with four separate two-hour timeslots, and the opportunity to rotate between sessions in each time period. Cost is $100 for each timeslot and registration is required. Attendance is limited to 25 registrants per workshop; register early for the best selection.
Expanded international programming: A new session has been added to Wednesday’s International program: “International Consortium of Vascular Registries: Quality Improvement in Vascular Surgery Goes Global.” This presentation will be held from 8 to 10 a.m. and kicks off a full day of international events.
VQI @ VAM – VQI’s Second Annual Meeting: Vascular Quality Initiative’s second Annual Meeting has expanded to 1 ½ days, beginning Tuesday afternoon, May 30, and continuing all day Wednesday. Also new this year are a poster session and networking reception. Registration and a separate $200 fee are required.
Exhibit Hall: Learn first-hand from our industry partners about the latest devices, products and services. The Exhibit Hall also hosts the Opening Reception, box lunches and coffee breaks Thursday through Saturday. Industry participation in the exhibits underwrites a signification portion of VAM – allowing us to keep registration fees at lower rates than other industry meetings – so please support our industry partners.
And more: VAM also will include: breakfast sessions; a discount for the On-Demand Library; texting of questions; Interactive Poster Session, programming for fellows, residents and students; the Physician Vascular Interpretation Examination Review course; SVS Member Business Luncheon, with the election of officers plus the presentation of SVS and SVS Foundation awards; Vascular Live sessions highlighting the latest products and developments; plus socializing, with alumni receptions and other events.
For information and to register, visit vsweb.org/VAM17.
The topic is vascular care. The subjects to be covered are nearly too numerous to count. And the clock is ticking for signing up.
Registration and housing will open in early March for the 2017 Vascular Annual Meeting, set for May 31 to June 3 in San Diego, Calif., with plenaries and exhibits from June 1 to 3. This premier meeting of vascular specialists will be held at the San Diego Convention Center. The headquarters hotel, the Marriott Marquis San Diego Marina Hotel, adjoins the center.
There is plenty going on.
Additional programming: Expanded programming begins Wednesday and continues through Saturday. Be sure to plan your travel to attend these informative sessions. This year’s meeting includes more concurrent sessions, and the number of joint society programs has doubled from last year.
Free postgraduate courses for SVS members: Once again, all SVS member-registrants receive free admittance to the six Wednesday postgraduate courses, a savings of $300. Non-members plus anyone registering only for the postgraduate courses must pay the appropriate registration fee. Self-assessment credit is available to all physician attendees.
SVS/STS Aortic Summit: New this year, and a highlight for Saturday, is the SVS/STS Summit: Advances and Controversies in the Management of Complex Thoracoabdominal Aneurysmal Diseases and Type B Aortic Dissection. This program will take place from 1 to 5 p.m. and is co-sponsored by the Society of Thoracic Surgeons. An additional fee is required. 
Revamped workshops: Wednesday’s workshops will feature a new format, with four separate two-hour timeslots, and the opportunity to rotate between sessions in each time period. Cost is $100 for each timeslot and registration is required. Attendance is limited to 25 registrants per workshop; register early for the best selection.
Expanded international programming: A new session has been added to Wednesday’s International program: “International Consortium of Vascular Registries: Quality Improvement in Vascular Surgery Goes Global.” This presentation will be held from 8 to 10 a.m. and kicks off a full day of international events.
VQI @ VAM – VQI’s Second Annual Meeting: Vascular Quality Initiative’s second Annual Meeting has expanded to 1 ½ days, beginning Tuesday afternoon, May 30, and continuing all day Wednesday. Also new this year are a poster session and networking reception. Registration and a separate $200 fee are required.
Exhibit Hall: Learn first-hand from our industry partners about the latest devices, products and services. The Exhibit Hall also hosts the Opening Reception, box lunches and coffee breaks Thursday through Saturday. Industry participation in the exhibits underwrites a signification portion of VAM – allowing us to keep registration fees at lower rates than other industry meetings – so please support our industry partners.
And more: VAM also will include: breakfast sessions; a discount for the On-Demand Library; texting of questions; Interactive Poster Session, programming for fellows, residents and students; the Physician Vascular Interpretation Examination Review course; SVS Member Business Luncheon, with the election of officers plus the presentation of SVS and SVS Foundation awards; Vascular Live sessions highlighting the latest products and developments; plus socializing, with alumni receptions and other events.
For information and to register, visit vsweb.org/VAM17.
The topic is vascular care. The subjects to be covered are nearly too numerous to count. And the clock is ticking for signing up.
Registration and housing will open in early March for the 2017 Vascular Annual Meeting, set for May 31 to June 3 in San Diego, Calif., with plenaries and exhibits from June 1 to 3. This premier meeting of vascular specialists will be held at the San Diego Convention Center. The headquarters hotel, the Marriott Marquis San Diego Marina Hotel, adjoins the center.
There is plenty going on.
Additional programming: Expanded programming begins Wednesday and continues through Saturday. Be sure to plan your travel to attend these informative sessions. This year’s meeting includes more concurrent sessions, and the number of joint society programs has doubled from last year.
Free postgraduate courses for SVS members: Once again, all SVS member-registrants receive free admittance to the six Wednesday postgraduate courses, a savings of $300. Non-members plus anyone registering only for the postgraduate courses must pay the appropriate registration fee. Self-assessment credit is available to all physician attendees.
SVS/STS Aortic Summit: New this year, and a highlight for Saturday, is the SVS/STS Summit: Advances and Controversies in the Management of Complex Thoracoabdominal Aneurysmal Diseases and Type B Aortic Dissection. This program will take place from 1 to 5 p.m. and is co-sponsored by the Society of Thoracic Surgeons. An additional fee is required. 
Revamped workshops: Wednesday’s workshops will feature a new format, with four separate two-hour timeslots, and the opportunity to rotate between sessions in each time period. Cost is $100 for each timeslot and registration is required. Attendance is limited to 25 registrants per workshop; register early for the best selection.
Expanded international programming: A new session has been added to Wednesday’s International program: “International Consortium of Vascular Registries: Quality Improvement in Vascular Surgery Goes Global.” This presentation will be held from 8 to 10 a.m. and kicks off a full day of international events.
VQI @ VAM – VQI’s Second Annual Meeting: Vascular Quality Initiative’s second Annual Meeting has expanded to 1 ½ days, beginning Tuesday afternoon, May 30, and continuing all day Wednesday. Also new this year are a poster session and networking reception. Registration and a separate $200 fee are required.
Exhibit Hall: Learn first-hand from our industry partners about the latest devices, products and services. The Exhibit Hall also hosts the Opening Reception, box lunches and coffee breaks Thursday through Saturday. Industry participation in the exhibits underwrites a signification portion of VAM – allowing us to keep registration fees at lower rates than other industry meetings – so please support our industry partners.
And more: VAM also will include: breakfast sessions; a discount for the On-Demand Library; texting of questions; Interactive Poster Session, programming for fellows, residents and students; the Physician Vascular Interpretation Examination Review course; SVS Member Business Luncheon, with the election of officers plus the presentation of SVS and SVS Foundation awards; Vascular Live sessions highlighting the latest products and developments; plus socializing, with alumni receptions and other events.
For information and to register, visit vsweb.org/VAM17.
Bipartisan Budget Act (BBA) of 2015 threatens growth of pulmonary rehab
In late 2015, Congress passed the Bipartisan Budget Act (BBA) to address numerous wide-ranging budget concerns, including issues related to agriculture, pensions, the strategic petroleum reserve, along with some Medicare issues. Section 603 of BBA is now coming back to haunt pulmonary rehabilitation services.
The intent of Section 603 is reasonable – to address the phenomenon of hospitals purchasing physician practices to take advantage of payment differentials between identical or virtually identical services when comparing the hospital outpatient prospective payment system (HOPPS) and the physician fee schedule (PFS). For example, an orthopedic practice might own its own MRI and related support services. It will bill for those services under the PFS. However, if the practice sells that segment of the revenue stream (the MRI assets, etc) to a hospital, the hospital can bill Medicare for those same services under the hospital outpatient prospective payment system at an amount notably higher than the PFS payment.
To address this payment aberration, Congress instructed the Centers for Medicare & Medicaid Services to craft a system to preclude a hospital from such behavior. If a hospital offers new or expanded outpatient services, it could NOT bill Medicare under the hospital outpatient services methodology and would be required to bill under the PFS payment methodology. Importantly, a few exemptions exist. If the new or expanded service is within 250 yards of the main hospital campus, the outpatient billing methodology is permitted. Likewise, if expansion of a current off-campus service occurs at the same location of the current off-site service, the hospital may continue to bill under the outpatient rules. Several other technical exceptions are permitted, for example construction planned prior to passage of BBA.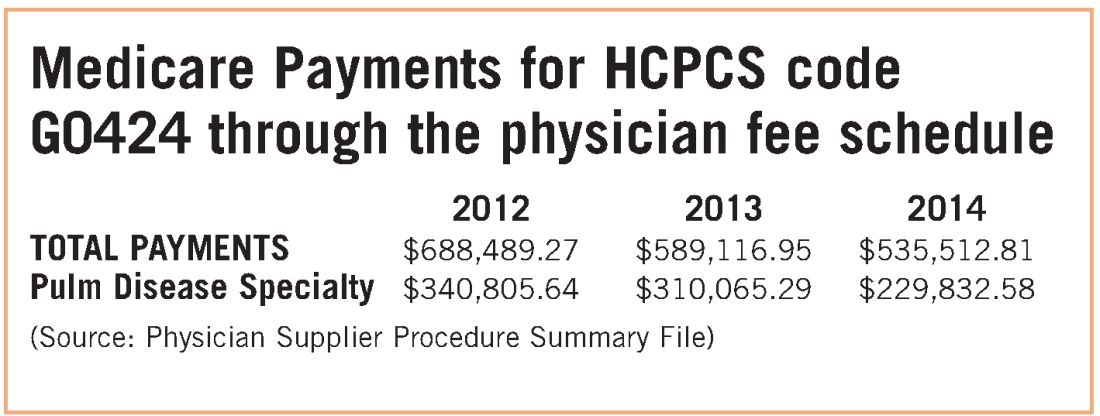
The implications for pulmonary rehabilitation are critical to its growth. A hospital that wishes to expand its current program and bill under the hospital outpatient methodology MUST do so by expanding at its current location. An expansion at a new location that is not within 250 yards of the main hospital campus triggers Section 603 provisions, and the hospital will bill at the physician fee schedule rate. Because the PFS payment rate is just over half of the payment rate for HOPPS payment, it is unlikely that a hospital would expand an existing program or establish a new one if it would be forced to bill under the lower rate.
While congressional logic may be relatively understandable, for pulmonary medicine, it is based on the premise that a hospital would purchase a pulmonary practice because that practice had a lucrative pulmonary rehabilitation services cash flow. NAMDRC and other societies were able to document major flaws in the basic premise, resulting in very problematic unintended consequences. A detailed review of Medicare claims data provides strong evidence that pulmonary practices simply do not provide pulmonary rehab services.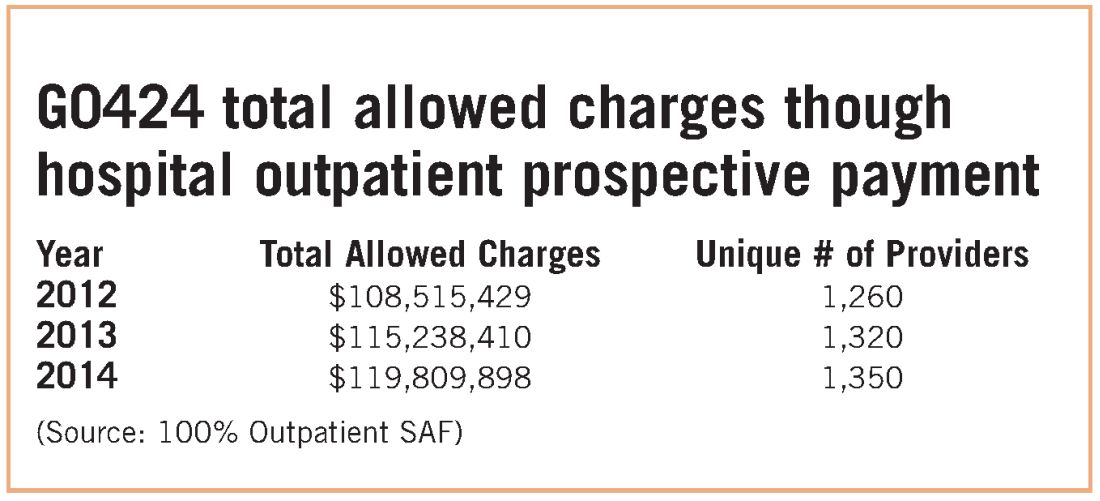
These data strongly indicate that G0424 pulmonary practice physician office billing for the most recent year data are available ($230K), compared with hospital outpatient allowed charges ($119M), is less than two-tenths of 1% of billing through the hospital setting. To argue that hospitals are purchasing pulmonary practices for financial gain tied to pulmonary rehab services defies Medicare data, as well as financial logic. If the CMS premise was valid, one would expect the aggregate physician office billing to be much greater than $535K. In discussions with CMS, the Agency did agree that there are likely to be unintended consequences related to Section 603 implementation. The Agency also emphasizes that it does not have the statutory authority for a “carve out” exemption. CMS stated that even if it agreed with us, it simply lacked the authority to exempt pulmonary rehab services. CMS also agreed that there is growing evidence that pulmonary rehab is a underutilized service that may very well save the program money through reduced hospitalizations and rehospitalizations, but it has little choice to implement the statute as Congress so mandated.
Therefore, the only solution is a legislative one. NAMDRC and other societies are seriously considering approaching Congress for such resolution.
In late 2015, Congress passed the Bipartisan Budget Act (BBA) to address numerous wide-ranging budget concerns, including issues related to agriculture, pensions, the strategic petroleum reserve, along with some Medicare issues. Section 603 of BBA is now coming back to haunt pulmonary rehabilitation services.
The intent of Section 603 is reasonable – to address the phenomenon of hospitals purchasing physician practices to take advantage of payment differentials between identical or virtually identical services when comparing the hospital outpatient prospective payment system (HOPPS) and the physician fee schedule (PFS). For example, an orthopedic practice might own its own MRI and related support services. It will bill for those services under the PFS. However, if the practice sells that segment of the revenue stream (the MRI assets, etc) to a hospital, the hospital can bill Medicare for those same services under the hospital outpatient prospective payment system at an amount notably higher than the PFS payment.
To address this payment aberration, Congress instructed the Centers for Medicare & Medicaid Services to craft a system to preclude a hospital from such behavior. If a hospital offers new or expanded outpatient services, it could NOT bill Medicare under the hospital outpatient services methodology and would be required to bill under the PFS payment methodology. Importantly, a few exemptions exist. If the new or expanded service is within 250 yards of the main hospital campus, the outpatient billing methodology is permitted. Likewise, if expansion of a current off-campus service occurs at the same location of the current off-site service, the hospital may continue to bill under the outpatient rules. Several other technical exceptions are permitted, for example construction planned prior to passage of BBA.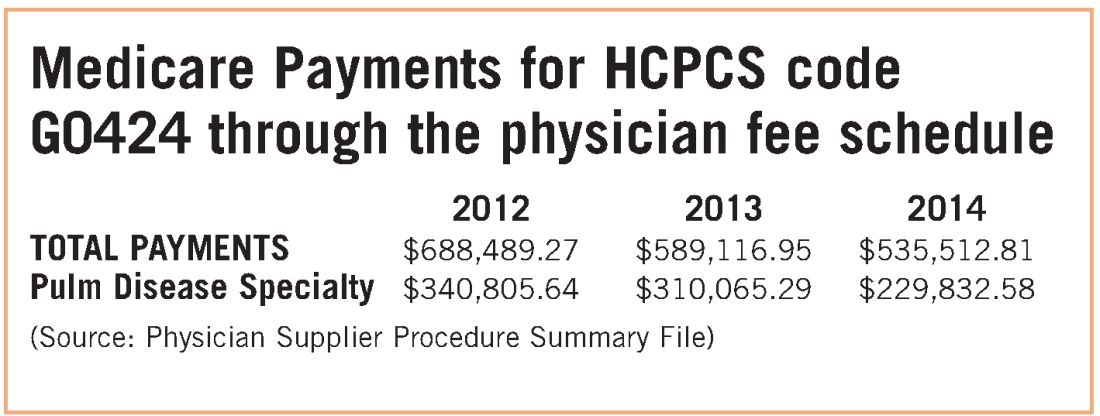
The implications for pulmonary rehabilitation are critical to its growth. A hospital that wishes to expand its current program and bill under the hospital outpatient methodology MUST do so by expanding at its current location. An expansion at a new location that is not within 250 yards of the main hospital campus triggers Section 603 provisions, and the hospital will bill at the physician fee schedule rate. Because the PFS payment rate is just over half of the payment rate for HOPPS payment, it is unlikely that a hospital would expand an existing program or establish a new one if it would be forced to bill under the lower rate.
While congressional logic may be relatively understandable, for pulmonary medicine, it is based on the premise that a hospital would purchase a pulmonary practice because that practice had a lucrative pulmonary rehabilitation services cash flow. NAMDRC and other societies were able to document major flaws in the basic premise, resulting in very problematic unintended consequences. A detailed review of Medicare claims data provides strong evidence that pulmonary practices simply do not provide pulmonary rehab services.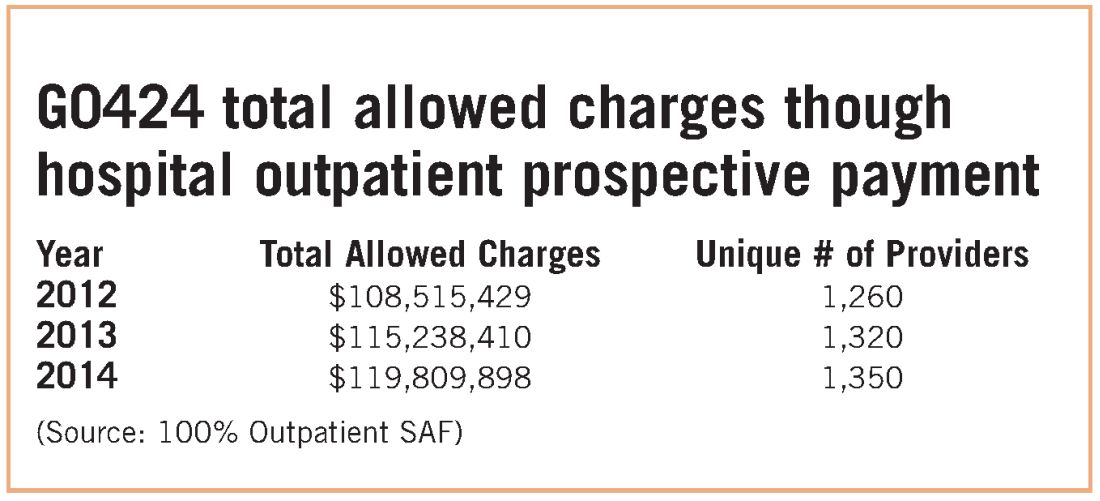
These data strongly indicate that G0424 pulmonary practice physician office billing for the most recent year data are available ($230K), compared with hospital outpatient allowed charges ($119M), is less than two-tenths of 1% of billing through the hospital setting. To argue that hospitals are purchasing pulmonary practices for financial gain tied to pulmonary rehab services defies Medicare data, as well as financial logic. If the CMS premise was valid, one would expect the aggregate physician office billing to be much greater than $535K. In discussions with CMS, the Agency did agree that there are likely to be unintended consequences related to Section 603 implementation. The Agency also emphasizes that it does not have the statutory authority for a “carve out” exemption. CMS stated that even if it agreed with us, it simply lacked the authority to exempt pulmonary rehab services. CMS also agreed that there is growing evidence that pulmonary rehab is a underutilized service that may very well save the program money through reduced hospitalizations and rehospitalizations, but it has little choice to implement the statute as Congress so mandated.
Therefore, the only solution is a legislative one. NAMDRC and other societies are seriously considering approaching Congress for such resolution.
In late 2015, Congress passed the Bipartisan Budget Act (BBA) to address numerous wide-ranging budget concerns, including issues related to agriculture, pensions, the strategic petroleum reserve, along with some Medicare issues. Section 603 of BBA is now coming back to haunt pulmonary rehabilitation services.
The intent of Section 603 is reasonable – to address the phenomenon of hospitals purchasing physician practices to take advantage of payment differentials between identical or virtually identical services when comparing the hospital outpatient prospective payment system (HOPPS) and the physician fee schedule (PFS). For example, an orthopedic practice might own its own MRI and related support services. It will bill for those services under the PFS. However, if the practice sells that segment of the revenue stream (the MRI assets, etc) to a hospital, the hospital can bill Medicare for those same services under the hospital outpatient prospective payment system at an amount notably higher than the PFS payment.
To address this payment aberration, Congress instructed the Centers for Medicare & Medicaid Services to craft a system to preclude a hospital from such behavior. If a hospital offers new or expanded outpatient services, it could NOT bill Medicare under the hospital outpatient services methodology and would be required to bill under the PFS payment methodology. Importantly, a few exemptions exist. If the new or expanded service is within 250 yards of the main hospital campus, the outpatient billing methodology is permitted. Likewise, if expansion of a current off-campus service occurs at the same location of the current off-site service, the hospital may continue to bill under the outpatient rules. Several other technical exceptions are permitted, for example construction planned prior to passage of BBA.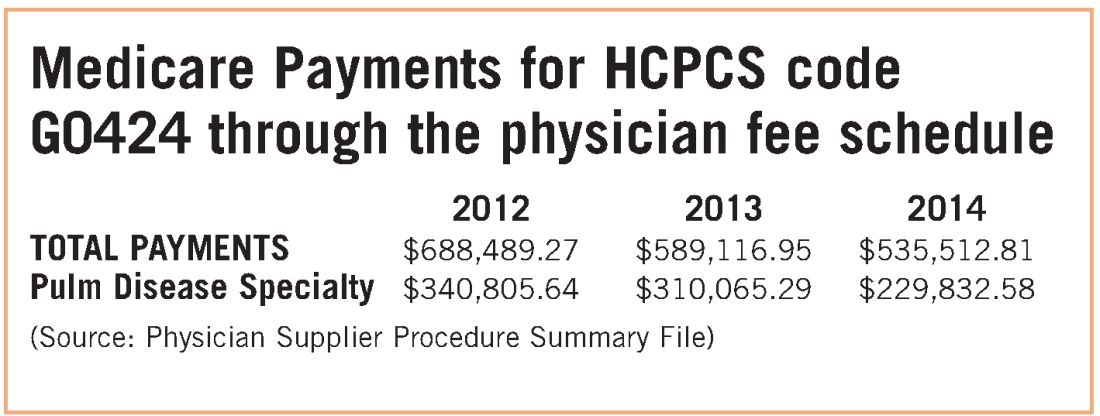
The implications for pulmonary rehabilitation are critical to its growth. A hospital that wishes to expand its current program and bill under the hospital outpatient methodology MUST do so by expanding at its current location. An expansion at a new location that is not within 250 yards of the main hospital campus triggers Section 603 provisions, and the hospital will bill at the physician fee schedule rate. Because the PFS payment rate is just over half of the payment rate for HOPPS payment, it is unlikely that a hospital would expand an existing program or establish a new one if it would be forced to bill under the lower rate.
While congressional logic may be relatively understandable, for pulmonary medicine, it is based on the premise that a hospital would purchase a pulmonary practice because that practice had a lucrative pulmonary rehabilitation services cash flow. NAMDRC and other societies were able to document major flaws in the basic premise, resulting in very problematic unintended consequences. A detailed review of Medicare claims data provides strong evidence that pulmonary practices simply do not provide pulmonary rehab services.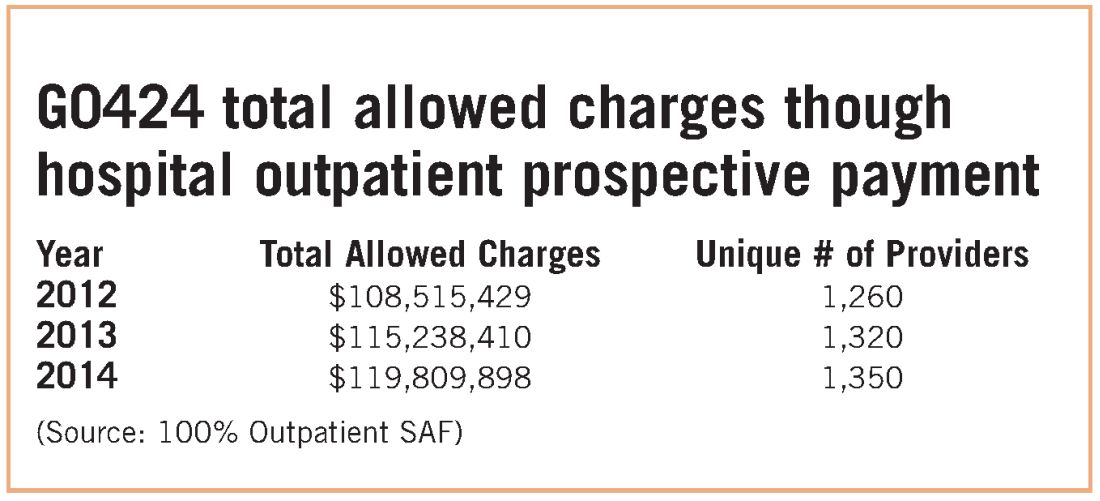
These data strongly indicate that G0424 pulmonary practice physician office billing for the most recent year data are available ($230K), compared with hospital outpatient allowed charges ($119M), is less than two-tenths of 1% of billing through the hospital setting. To argue that hospitals are purchasing pulmonary practices for financial gain tied to pulmonary rehab services defies Medicare data, as well as financial logic. If the CMS premise was valid, one would expect the aggregate physician office billing to be much greater than $535K. In discussions with CMS, the Agency did agree that there are likely to be unintended consequences related to Section 603 implementation. The Agency also emphasizes that it does not have the statutory authority for a “carve out” exemption. CMS stated that even if it agreed with us, it simply lacked the authority to exempt pulmonary rehab services. CMS also agreed that there is growing evidence that pulmonary rehab is a underutilized service that may very well save the program money through reduced hospitalizations and rehospitalizations, but it has little choice to implement the statute as Congress so mandated.
Therefore, the only solution is a legislative one. NAMDRC and other societies are seriously considering approaching Congress for such resolution.
Registration is now open for CHEST Board Review 2017
Looking for in-person board review prep? Join us in Orlando, August 18 to 27, for the best live review of pulmonary, critical care, and sleep medicine.
Register by March 31 and save $100. Registration can be done at http://boardreview.chestnet.org.
Looking for in-person board review prep? Join us in Orlando, August 18 to 27, for the best live review of pulmonary, critical care, and sleep medicine.
Register by March 31 and save $100. Registration can be done at http://boardreview.chestnet.org.
Looking for in-person board review prep? Join us in Orlando, August 18 to 27, for the best live review of pulmonary, critical care, and sleep medicine.
Register by March 31 and save $100. Registration can be done at http://boardreview.chestnet.org.