User login
Time is of the essence: DST up for debate again
Seasonal time change is now up for consideration in the U.S. Congress, prompting sleep medicine specialists to weigh in on the health impact of a major policy change.
As lawmakers in Washington propose an end to seasonal time changes by permanently establishing daylight saving time (DST), the American Academy of Sleep Medicine (AASM) is pushing for a Congressional hearing so scientists can present evidence in favor of converse legislation – to make standard time the new norm.
According to the AASM, ; however, the switch from standard time to DST incurs more risk.
“Current evidence best supports the adoption of year-round standard time, which aligns best with human circadian biology and provides distinct benefits for public health and safety,” the AASM noted in a 2020 position statement on DST.
The statement cites a number of studies that have reported associations between the switch to DST and acute, negative health outcomes, including higher rates of hospital admission, cardiovascular morbidity, atrial fibrillation, and stroke. The time shift has been associated with a spectrum of cellular, metabolic, and circadian derangements, from increased production of inflammatory markers, to higher blood pressure, and loss of sleep. These biological effects may have far-reaching consequences, including increased rates of fatal motor accidents in the days following the time change, and even increased volatility in the stock market, which may stem from cognitive deficits.
U.S. Senator Marco Rubio (R-Fla.) and others in the U.S. Congress have reintroduced the 2019 Sunshine Protection Act, legislation that would make DST permanent across the country. According to a statement on Sen. Rubio’s website, “The bill reflects the Florida legislature’s 2018 enactment of year-round DST; however, for Florida’s change to apply, a change in the federal statute is required. Fifteen other states – Arkansas, Alabama, California, Delaware, Georgia, Idaho, Louisiana, Maine, Ohio, Oregon, South Carolina, Tennessee, Utah, Washington, and Wyoming – have passed similar laws, resolutions, or voter initiatives, and dozens more are looking. The legislation, if enacted, would apply to those states [that] currently participate in DST, which most states observe for eight months out of the year.”
A stitch in time
“The sudden change in clock time disrupts sleep/wake patterns, decreasing total sleep time and sleep quality, leading to decrements in daytime cognition,” said Kannan Ramar, MBBS, MD, president of the AASM and a sleep medicine specialist at Mayo Clinic, Rochester, Minn.
Emphasizing this point, Dr. Ramar noted a recent study that reported an 18% increase in “patient safety-related incidents associated with human error” among health care workers within a week of the spring time change.
“Irregular bedtimes and wake times disrupt the timing of our circadian rhythms, which can lead to symptoms of insomnia or long-term, excessive daytime sleepiness. Lack of sleep can lead to numerous adverse effects on our minds, including decreased cognitive function, trouble concentrating, and general moodiness,” Dr. Ramar said.
He noted that these impacts may be more significant among certain individuals.
“The daylight saving time changes can be especially problematic for any populations that already experience chronic insufficient sleep or other sleep difficulties,” Dr. Ramar said. “Populations at greatest risk include teenagers, who tend to experience chronic sleep restriction during the school week, and night shift workers, who often struggle to sleep well during daytime hours.”
While fewer studies have evaluated the long-term effects of seasonal time changes, the AASM position statement cited evidence that “the body clock does not adjust to daylight saving time after several months,” possibly because “daylight saving time is less well-aligned with intrinsic human circadian physiology, and it disrupts the natural seasonal adjustment of the human clock due to the effect of late-evening light on the circadian rhythm.”
According to the AASM, permanent DST, as proposed by Sen. Rubio and colleagues, could “result in permanent phase delay, a condition that can also lead to a perpetual discrepancy between the innate biological clock and the extrinsic environmental clock, as well as chronic sleep loss due to early morning social demands that truncate the opportunity to sleep.” This mismatch between sleep/wake cycles and social demands, known as “social jet lag,” has been associated with chronic health risks, including metabolic syndrome, obesity, depression, and cardiovascular disease.
Cardiac impacts of seasonal time change
Muhammad Adeel Rishi, MD, a sleep specialist at Mayo Clinic, Eau Claire, Wis., and lead author of the AASM position statement, highlighted cardiovascular risks in a written statement for this article, noting increased rates of heart attack following the spring time change, and a higher risk of atrial fibrillation.
“Mayo Clinic has not taken a position on this issue,” Dr. Rishi noted. Still, he advocated for permanent standard time as the author of the AASM position statement and vice chair of the AASM public safety committee.
Jay Chudow, MD, and Andrew K. Krumerman, MD, of Montefiore Medical Center, New York, lead author and principal author, respectively, of a recent study that reported increased rates of atrial fibrillation admissions after DST transitions, had the same stance.
“We support elimination of seasonal time changes from a health perspective,” they wrote in a joint comment. “There is mounting evidence of a negative health impact with these seasonal time changes related to effects on sleep and circadian rhythm. Our work found the spring change was associated with more admissions for atrial fibrillation. This added to prior evidence of increased cardiovascular events related to these time changes. If physicians counsel patients on reducing risk factors for disease, shouldn’t we do the same as a society?”
Pros and cons
Not all sleep experts are convinced. Mary Jo Farmer, MD, PhD, FCCP, a sleep specialist and director of pulmonary hypertension services at Baystate Medical Center, and assistant professor of medicine at the University of Massachusetts, Springfield, considers perspectives from both sides of the issue.
“Daylight saving time promotes active lifestyles as people engage in more outdoor activities after work and school, [and] daylight saving time produces economic and safety benefits to society as retail revenues are higher and crimes are lower,” Dr. Farmer said. “Alternatively, moving the clocks forward is a cost burden to the U.S. economy when health issues, decreased productivity, and workplace injuries are considered.”
If one time system is permanently established, Dr. Farmer anticipates divided opinions from patients with sleep issues, regardless of which system is chosen.
“I can tell you, I have a cohort of sleep patients who prefer more evening light and look forward to the spring time change to daylight saving time,” she said. “However, they would not want the sun coming up at 9:00 a.m. in the winter months if we stayed on daylight saving time year-round. Similarly, patients would not want the sun coming up at 4:00 a.m. on the longest day of the year if we stayed on standard time all year round.”
Dr. Farmer called for more research before a decision is made.
“I suggest we need more information about the dangers of staying on daylight saving or standard time year-round because perhaps the current strategy of keeping morning light consistent is not so bad,” she said.
Time for a Congressional hearing?
According to Dr. Ramar, the time is now for a Congressional hearing, as lawmakers and the public need to be adequately informed when considering new legislation.
“There are public misconceptions about daylight saving time and standard time,” Dr. Ramar said. “People often like the idea of daylight saving time because they think it provides more light, and they dislike the concept of standard time because they think it provides more darkness. The reality is that neither time system provides more light or darkness than the other; it is only the timing that changes.”
Until new legislation is introduced, Dr. Ramar offered some practical advice for navigating seasonal time shifts.
“Beginning 2-3 days before the time change, it can be helpful to gradually adjust sleep and wake times, as well as other daily routines such as meal times,” he said. “After the time change, going outside for some morning light can help adjust the timing of your internal body clock.”
The investigators reported no conflicts of interest.
Seasonal time change is now up for consideration in the U.S. Congress, prompting sleep medicine specialists to weigh in on the health impact of a major policy change.
As lawmakers in Washington propose an end to seasonal time changes by permanently establishing daylight saving time (DST), the American Academy of Sleep Medicine (AASM) is pushing for a Congressional hearing so scientists can present evidence in favor of converse legislation – to make standard time the new norm.
According to the AASM, ; however, the switch from standard time to DST incurs more risk.
“Current evidence best supports the adoption of year-round standard time, which aligns best with human circadian biology and provides distinct benefits for public health and safety,” the AASM noted in a 2020 position statement on DST.
The statement cites a number of studies that have reported associations between the switch to DST and acute, negative health outcomes, including higher rates of hospital admission, cardiovascular morbidity, atrial fibrillation, and stroke. The time shift has been associated with a spectrum of cellular, metabolic, and circadian derangements, from increased production of inflammatory markers, to higher blood pressure, and loss of sleep. These biological effects may have far-reaching consequences, including increased rates of fatal motor accidents in the days following the time change, and even increased volatility in the stock market, which may stem from cognitive deficits.
U.S. Senator Marco Rubio (R-Fla.) and others in the U.S. Congress have reintroduced the 2019 Sunshine Protection Act, legislation that would make DST permanent across the country. According to a statement on Sen. Rubio’s website, “The bill reflects the Florida legislature’s 2018 enactment of year-round DST; however, for Florida’s change to apply, a change in the federal statute is required. Fifteen other states – Arkansas, Alabama, California, Delaware, Georgia, Idaho, Louisiana, Maine, Ohio, Oregon, South Carolina, Tennessee, Utah, Washington, and Wyoming – have passed similar laws, resolutions, or voter initiatives, and dozens more are looking. The legislation, if enacted, would apply to those states [that] currently participate in DST, which most states observe for eight months out of the year.”
A stitch in time
“The sudden change in clock time disrupts sleep/wake patterns, decreasing total sleep time and sleep quality, leading to decrements in daytime cognition,” said Kannan Ramar, MBBS, MD, president of the AASM and a sleep medicine specialist at Mayo Clinic, Rochester, Minn.
Emphasizing this point, Dr. Ramar noted a recent study that reported an 18% increase in “patient safety-related incidents associated with human error” among health care workers within a week of the spring time change.
“Irregular bedtimes and wake times disrupt the timing of our circadian rhythms, which can lead to symptoms of insomnia or long-term, excessive daytime sleepiness. Lack of sleep can lead to numerous adverse effects on our minds, including decreased cognitive function, trouble concentrating, and general moodiness,” Dr. Ramar said.
He noted that these impacts may be more significant among certain individuals.
“The daylight saving time changes can be especially problematic for any populations that already experience chronic insufficient sleep or other sleep difficulties,” Dr. Ramar said. “Populations at greatest risk include teenagers, who tend to experience chronic sleep restriction during the school week, and night shift workers, who often struggle to sleep well during daytime hours.”
While fewer studies have evaluated the long-term effects of seasonal time changes, the AASM position statement cited evidence that “the body clock does not adjust to daylight saving time after several months,” possibly because “daylight saving time is less well-aligned with intrinsic human circadian physiology, and it disrupts the natural seasonal adjustment of the human clock due to the effect of late-evening light on the circadian rhythm.”
According to the AASM, permanent DST, as proposed by Sen. Rubio and colleagues, could “result in permanent phase delay, a condition that can also lead to a perpetual discrepancy between the innate biological clock and the extrinsic environmental clock, as well as chronic sleep loss due to early morning social demands that truncate the opportunity to sleep.” This mismatch between sleep/wake cycles and social demands, known as “social jet lag,” has been associated with chronic health risks, including metabolic syndrome, obesity, depression, and cardiovascular disease.
Cardiac impacts of seasonal time change
Muhammad Adeel Rishi, MD, a sleep specialist at Mayo Clinic, Eau Claire, Wis., and lead author of the AASM position statement, highlighted cardiovascular risks in a written statement for this article, noting increased rates of heart attack following the spring time change, and a higher risk of atrial fibrillation.
“Mayo Clinic has not taken a position on this issue,” Dr. Rishi noted. Still, he advocated for permanent standard time as the author of the AASM position statement and vice chair of the AASM public safety committee.
Jay Chudow, MD, and Andrew K. Krumerman, MD, of Montefiore Medical Center, New York, lead author and principal author, respectively, of a recent study that reported increased rates of atrial fibrillation admissions after DST transitions, had the same stance.
“We support elimination of seasonal time changes from a health perspective,” they wrote in a joint comment. “There is mounting evidence of a negative health impact with these seasonal time changes related to effects on sleep and circadian rhythm. Our work found the spring change was associated with more admissions for atrial fibrillation. This added to prior evidence of increased cardiovascular events related to these time changes. If physicians counsel patients on reducing risk factors for disease, shouldn’t we do the same as a society?”
Pros and cons
Not all sleep experts are convinced. Mary Jo Farmer, MD, PhD, FCCP, a sleep specialist and director of pulmonary hypertension services at Baystate Medical Center, and assistant professor of medicine at the University of Massachusetts, Springfield, considers perspectives from both sides of the issue.
“Daylight saving time promotes active lifestyles as people engage in more outdoor activities after work and school, [and] daylight saving time produces economic and safety benefits to society as retail revenues are higher and crimes are lower,” Dr. Farmer said. “Alternatively, moving the clocks forward is a cost burden to the U.S. economy when health issues, decreased productivity, and workplace injuries are considered.”
If one time system is permanently established, Dr. Farmer anticipates divided opinions from patients with sleep issues, regardless of which system is chosen.
“I can tell you, I have a cohort of sleep patients who prefer more evening light and look forward to the spring time change to daylight saving time,” she said. “However, they would not want the sun coming up at 9:00 a.m. in the winter months if we stayed on daylight saving time year-round. Similarly, patients would not want the sun coming up at 4:00 a.m. on the longest day of the year if we stayed on standard time all year round.”
Dr. Farmer called for more research before a decision is made.
“I suggest we need more information about the dangers of staying on daylight saving or standard time year-round because perhaps the current strategy of keeping morning light consistent is not so bad,” she said.
Time for a Congressional hearing?
According to Dr. Ramar, the time is now for a Congressional hearing, as lawmakers and the public need to be adequately informed when considering new legislation.
“There are public misconceptions about daylight saving time and standard time,” Dr. Ramar said. “People often like the idea of daylight saving time because they think it provides more light, and they dislike the concept of standard time because they think it provides more darkness. The reality is that neither time system provides more light or darkness than the other; it is only the timing that changes.”
Until new legislation is introduced, Dr. Ramar offered some practical advice for navigating seasonal time shifts.
“Beginning 2-3 days before the time change, it can be helpful to gradually adjust sleep and wake times, as well as other daily routines such as meal times,” he said. “After the time change, going outside for some morning light can help adjust the timing of your internal body clock.”
The investigators reported no conflicts of interest.
Seasonal time change is now up for consideration in the U.S. Congress, prompting sleep medicine specialists to weigh in on the health impact of a major policy change.
As lawmakers in Washington propose an end to seasonal time changes by permanently establishing daylight saving time (DST), the American Academy of Sleep Medicine (AASM) is pushing for a Congressional hearing so scientists can present evidence in favor of converse legislation – to make standard time the new norm.
According to the AASM, ; however, the switch from standard time to DST incurs more risk.
“Current evidence best supports the adoption of year-round standard time, which aligns best with human circadian biology and provides distinct benefits for public health and safety,” the AASM noted in a 2020 position statement on DST.
The statement cites a number of studies that have reported associations between the switch to DST and acute, negative health outcomes, including higher rates of hospital admission, cardiovascular morbidity, atrial fibrillation, and stroke. The time shift has been associated with a spectrum of cellular, metabolic, and circadian derangements, from increased production of inflammatory markers, to higher blood pressure, and loss of sleep. These biological effects may have far-reaching consequences, including increased rates of fatal motor accidents in the days following the time change, and even increased volatility in the stock market, which may stem from cognitive deficits.
U.S. Senator Marco Rubio (R-Fla.) and others in the U.S. Congress have reintroduced the 2019 Sunshine Protection Act, legislation that would make DST permanent across the country. According to a statement on Sen. Rubio’s website, “The bill reflects the Florida legislature’s 2018 enactment of year-round DST; however, for Florida’s change to apply, a change in the federal statute is required. Fifteen other states – Arkansas, Alabama, California, Delaware, Georgia, Idaho, Louisiana, Maine, Ohio, Oregon, South Carolina, Tennessee, Utah, Washington, and Wyoming – have passed similar laws, resolutions, or voter initiatives, and dozens more are looking. The legislation, if enacted, would apply to those states [that] currently participate in DST, which most states observe for eight months out of the year.”
A stitch in time
“The sudden change in clock time disrupts sleep/wake patterns, decreasing total sleep time and sleep quality, leading to decrements in daytime cognition,” said Kannan Ramar, MBBS, MD, president of the AASM and a sleep medicine specialist at Mayo Clinic, Rochester, Minn.
Emphasizing this point, Dr. Ramar noted a recent study that reported an 18% increase in “patient safety-related incidents associated with human error” among health care workers within a week of the spring time change.
“Irregular bedtimes and wake times disrupt the timing of our circadian rhythms, which can lead to symptoms of insomnia or long-term, excessive daytime sleepiness. Lack of sleep can lead to numerous adverse effects on our minds, including decreased cognitive function, trouble concentrating, and general moodiness,” Dr. Ramar said.
He noted that these impacts may be more significant among certain individuals.
“The daylight saving time changes can be especially problematic for any populations that already experience chronic insufficient sleep or other sleep difficulties,” Dr. Ramar said. “Populations at greatest risk include teenagers, who tend to experience chronic sleep restriction during the school week, and night shift workers, who often struggle to sleep well during daytime hours.”
While fewer studies have evaluated the long-term effects of seasonal time changes, the AASM position statement cited evidence that “the body clock does not adjust to daylight saving time after several months,” possibly because “daylight saving time is less well-aligned with intrinsic human circadian physiology, and it disrupts the natural seasonal adjustment of the human clock due to the effect of late-evening light on the circadian rhythm.”
According to the AASM, permanent DST, as proposed by Sen. Rubio and colleagues, could “result in permanent phase delay, a condition that can also lead to a perpetual discrepancy between the innate biological clock and the extrinsic environmental clock, as well as chronic sleep loss due to early morning social demands that truncate the opportunity to sleep.” This mismatch between sleep/wake cycles and social demands, known as “social jet lag,” has been associated with chronic health risks, including metabolic syndrome, obesity, depression, and cardiovascular disease.
Cardiac impacts of seasonal time change
Muhammad Adeel Rishi, MD, a sleep specialist at Mayo Clinic, Eau Claire, Wis., and lead author of the AASM position statement, highlighted cardiovascular risks in a written statement for this article, noting increased rates of heart attack following the spring time change, and a higher risk of atrial fibrillation.
“Mayo Clinic has not taken a position on this issue,” Dr. Rishi noted. Still, he advocated for permanent standard time as the author of the AASM position statement and vice chair of the AASM public safety committee.
Jay Chudow, MD, and Andrew K. Krumerman, MD, of Montefiore Medical Center, New York, lead author and principal author, respectively, of a recent study that reported increased rates of atrial fibrillation admissions after DST transitions, had the same stance.
“We support elimination of seasonal time changes from a health perspective,” they wrote in a joint comment. “There is mounting evidence of a negative health impact with these seasonal time changes related to effects on sleep and circadian rhythm. Our work found the spring change was associated with more admissions for atrial fibrillation. This added to prior evidence of increased cardiovascular events related to these time changes. If physicians counsel patients on reducing risk factors for disease, shouldn’t we do the same as a society?”
Pros and cons
Not all sleep experts are convinced. Mary Jo Farmer, MD, PhD, FCCP, a sleep specialist and director of pulmonary hypertension services at Baystate Medical Center, and assistant professor of medicine at the University of Massachusetts, Springfield, considers perspectives from both sides of the issue.
“Daylight saving time promotes active lifestyles as people engage in more outdoor activities after work and school, [and] daylight saving time produces economic and safety benefits to society as retail revenues are higher and crimes are lower,” Dr. Farmer said. “Alternatively, moving the clocks forward is a cost burden to the U.S. economy when health issues, decreased productivity, and workplace injuries are considered.”
If one time system is permanently established, Dr. Farmer anticipates divided opinions from patients with sleep issues, regardless of which system is chosen.
“I can tell you, I have a cohort of sleep patients who prefer more evening light and look forward to the spring time change to daylight saving time,” she said. “However, they would not want the sun coming up at 9:00 a.m. in the winter months if we stayed on daylight saving time year-round. Similarly, patients would not want the sun coming up at 4:00 a.m. on the longest day of the year if we stayed on standard time all year round.”
Dr. Farmer called for more research before a decision is made.
“I suggest we need more information about the dangers of staying on daylight saving or standard time year-round because perhaps the current strategy of keeping morning light consistent is not so bad,” she said.
Time for a Congressional hearing?
According to Dr. Ramar, the time is now for a Congressional hearing, as lawmakers and the public need to be adequately informed when considering new legislation.
“There are public misconceptions about daylight saving time and standard time,” Dr. Ramar said. “People often like the idea of daylight saving time because they think it provides more light, and they dislike the concept of standard time because they think it provides more darkness. The reality is that neither time system provides more light or darkness than the other; it is only the timing that changes.”
Until new legislation is introduced, Dr. Ramar offered some practical advice for navigating seasonal time shifts.
“Beginning 2-3 days before the time change, it can be helpful to gradually adjust sleep and wake times, as well as other daily routines such as meal times,” he said. “After the time change, going outside for some morning light can help adjust the timing of your internal body clock.”
The investigators reported no conflicts of interest.
Less sleep, more burnout linked to higher COVID-19 risk, study shows
among health care workers considered to be at high risk for exposure to patients with COVID-19, new evidence reveals.
For each additional hour of sleep at night, for example, risk for COVID-19 dropped by 12% in a study of 2844 frontline health care workers.
Furthermore, those who reported experiencing work-related burnout every day were 2.6 times more likely to report having COVID-19, to report having COVID-19 for a longer time, and to experience COVID-19 of more severity.
“This study underscores the importance of non–hygiene-related risk factors for COVID-19 and supports a holistic approach to health – including optimal sleep and job stress reduction to protect our health care workers from this and future pandemics,” senior author Sara B. Seidelmann, MD, said in an interview.
“Our findings add to the literature that sleep duration at night, sleep problems, and burnout may be risk factors for viral illnesses like COVID-19,” wrote Dr. Seidelmann and colleagues.
This is the first study to link COVID-19 risk to sleep habits – including number of hours of sleep at night, daytime napping hours, and severe sleep problems – among health care workers across multiple countries.
The study was published online March 22 in BMJ Nutrition, Prevention, and Health.
The researchers surveyed health care professionals in specialties considered to place personnel at high risk for exposure to SARS-CoV-2: critical care, emergency care, and internal medicine.
The association between sleep and burnout risk factors and COVID-19 did not vary significantly by specialty. “We didn’t detect any significant interactions between age, sex, specialty, or country,” said Dr. Seidelmann, assistant professor of clinical medicine at Columbia University College of Physicians and Surgeons, New York, and an internist at Stamford (Conn.) Hospital.
In addition to the 12% lower risk associated with each additional hour of sleep at night, each 1 additional hour of daytime napping was linked with a 6% increased risk for COVID-19 in an adjusted analysis (odds ratio [OR], 1.06; 95% confidence interval [CI], 1.01-1.12).
Daytime napping slightly increased risk for COVID-19 in five of the six countries included in the study: France, Germany, Italy, the United Kingdom, and the United States. In contrast, in Spain, napping had a nonsignificant protective effect.
The survey asked health care workers to recall nighttime sleep duration, sleep disorders, and burnout in the year prior to onset of the COVID-19 pandemic.
‘Significant, close contact’ with COVID-19?
Lead author Hyunju Kim, NP, Dr. Seidelmann, and colleagues conducted the population-based, case-control study from July 17 to Sept. 25, 2020. They identified health care workers from the SurveyHealthcareGlobus (SHG) network.
Of the respondents, 72% were men. The mean age of the participants was 48 years, and the study population was 77% White, 12% Asian, 6% mixed background, 2% Black, and 1% other. (The remainder preferred not to say).
The 568 health care workers considered to have COVID-19 were classified on the basis of self-reported symptoms. Control participants had no symptoms associated with COVID-19.
All 2,844 participants answered yes to a question about having “significant close contact” with COVID-19 patients in their workplace.
Compared to reporting no sleep problems, having three such problems – difficulty sleeping at night, poor sleep continuity, and frequent use of sleeping pills – was associated with 88% greater odds of COVID-19 (OR, 1.88; 95% CI, 1.17–3.01).
Having one sleep problem was not associated with COVID-19.
More burnout, greater risk
The health care workers reported the severity of any work-related burnout. “There was a significant dose-response relationship between frequency of burnout and COVID-19,” the researchers noted.
Those who reported having burnout rarely or weekly had a 1.3-1.4 greater chance of reporting COVID-19 compared to those who reported having no burnout, for example.
In addition, reporting a high level of burnout was linked to about three times the risk for having COVID-19 of longer duration and of greater severity.
What drives the association between sleep problems, burnout, and higher risk for COVID-19 and severe COVID-19 remains unknown.
“The mechanism underlying these associations isn’t clear, but suboptimal sleep, sleep disorders, and stress may result in immune system dysregulation, increased inflammation, and alterations in hormones such as cortisol and melatonin that may increase vulnerability to viral infections,” Dr. Seidelmann said.
Strengths and limitations
Using a large network of health care workers in the early phase of the pandemic is a strength of the study. How generalizable the findings are outside the SHG database of 1.5 million health care workers remains unknown.
Another limitation was reliance on self-reporting of COVID-19 patient exposure, outcomes, and covariates, which could have introduced bias.
“However,” the researchers noted, “health care workers are likely a reliable source of information.”
Insomnia a common challenge
A 2020 meta-analysis examined the effect of insomnia and psychological factors on COVID-19 risk among health care workers. Lead author Kavita Batra, PhD, of the University of Nevada, Las Vegas (UNLV), and colleagues found that the pooled prevalence of insomnia was almost 28%.
“The recent six-country study by Kim and colleagues also underscores this relationship between lack of sleep and having higher odds of COVID-19 infection,” Manoj Sharma, MBBS, PhD, professor of social and behavioral health in the UNLV department of environmental and occupational health, and one of the study authors, said in an interview.
More research is warranted to learn the direction of the association, he said. Does reduced sleep lower immunity and make a health care worker more susceptible to SARS-CoV-2 infection, or does the anxiety associated with COVID-19 contribute to insomnia?
“Practicing sleep hygiene is a must not only for health workers but also for everyone,” Dr. Sharma added. Recommendations include having fixed hours of going to bed, fixed hours of waking up, not overdoing naps, having at least 30 minutes of winding down before sleeping, having a dark bedroom devoid of all electronics and other disturbances, avoiding smoking, alcohol, and stimulants (such as caffeine) before sleeping, and practicing relaxation right before sleeping, he said.
“It is hard for some health care workers, especially those who work night shifts, but it must be a priority to follow as many sleep hygiene measures as possible,” Dr. Sharma said. “After all, if you do not take care of yourself how can you take care of others?”
Dr. Seidelmann, Dr. Batra, and Dr. Sharma have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
among health care workers considered to be at high risk for exposure to patients with COVID-19, new evidence reveals.
For each additional hour of sleep at night, for example, risk for COVID-19 dropped by 12% in a study of 2844 frontline health care workers.
Furthermore, those who reported experiencing work-related burnout every day were 2.6 times more likely to report having COVID-19, to report having COVID-19 for a longer time, and to experience COVID-19 of more severity.
“This study underscores the importance of non–hygiene-related risk factors for COVID-19 and supports a holistic approach to health – including optimal sleep and job stress reduction to protect our health care workers from this and future pandemics,” senior author Sara B. Seidelmann, MD, said in an interview.
“Our findings add to the literature that sleep duration at night, sleep problems, and burnout may be risk factors for viral illnesses like COVID-19,” wrote Dr. Seidelmann and colleagues.
This is the first study to link COVID-19 risk to sleep habits – including number of hours of sleep at night, daytime napping hours, and severe sleep problems – among health care workers across multiple countries.
The study was published online March 22 in BMJ Nutrition, Prevention, and Health.
The researchers surveyed health care professionals in specialties considered to place personnel at high risk for exposure to SARS-CoV-2: critical care, emergency care, and internal medicine.
The association between sleep and burnout risk factors and COVID-19 did not vary significantly by specialty. “We didn’t detect any significant interactions between age, sex, specialty, or country,” said Dr. Seidelmann, assistant professor of clinical medicine at Columbia University College of Physicians and Surgeons, New York, and an internist at Stamford (Conn.) Hospital.
In addition to the 12% lower risk associated with each additional hour of sleep at night, each 1 additional hour of daytime napping was linked with a 6% increased risk for COVID-19 in an adjusted analysis (odds ratio [OR], 1.06; 95% confidence interval [CI], 1.01-1.12).
Daytime napping slightly increased risk for COVID-19 in five of the six countries included in the study: France, Germany, Italy, the United Kingdom, and the United States. In contrast, in Spain, napping had a nonsignificant protective effect.
The survey asked health care workers to recall nighttime sleep duration, sleep disorders, and burnout in the year prior to onset of the COVID-19 pandemic.
‘Significant, close contact’ with COVID-19?
Lead author Hyunju Kim, NP, Dr. Seidelmann, and colleagues conducted the population-based, case-control study from July 17 to Sept. 25, 2020. They identified health care workers from the SurveyHealthcareGlobus (SHG) network.
Of the respondents, 72% were men. The mean age of the participants was 48 years, and the study population was 77% White, 12% Asian, 6% mixed background, 2% Black, and 1% other. (The remainder preferred not to say).
The 568 health care workers considered to have COVID-19 were classified on the basis of self-reported symptoms. Control participants had no symptoms associated with COVID-19.
All 2,844 participants answered yes to a question about having “significant close contact” with COVID-19 patients in their workplace.
Compared to reporting no sleep problems, having three such problems – difficulty sleeping at night, poor sleep continuity, and frequent use of sleeping pills – was associated with 88% greater odds of COVID-19 (OR, 1.88; 95% CI, 1.17–3.01).
Having one sleep problem was not associated with COVID-19.
More burnout, greater risk
The health care workers reported the severity of any work-related burnout. “There was a significant dose-response relationship between frequency of burnout and COVID-19,” the researchers noted.
Those who reported having burnout rarely or weekly had a 1.3-1.4 greater chance of reporting COVID-19 compared to those who reported having no burnout, for example.
In addition, reporting a high level of burnout was linked to about three times the risk for having COVID-19 of longer duration and of greater severity.
What drives the association between sleep problems, burnout, and higher risk for COVID-19 and severe COVID-19 remains unknown.
“The mechanism underlying these associations isn’t clear, but suboptimal sleep, sleep disorders, and stress may result in immune system dysregulation, increased inflammation, and alterations in hormones such as cortisol and melatonin that may increase vulnerability to viral infections,” Dr. Seidelmann said.
Strengths and limitations
Using a large network of health care workers in the early phase of the pandemic is a strength of the study. How generalizable the findings are outside the SHG database of 1.5 million health care workers remains unknown.
Another limitation was reliance on self-reporting of COVID-19 patient exposure, outcomes, and covariates, which could have introduced bias.
“However,” the researchers noted, “health care workers are likely a reliable source of information.”
Insomnia a common challenge
A 2020 meta-analysis examined the effect of insomnia and psychological factors on COVID-19 risk among health care workers. Lead author Kavita Batra, PhD, of the University of Nevada, Las Vegas (UNLV), and colleagues found that the pooled prevalence of insomnia was almost 28%.
“The recent six-country study by Kim and colleagues also underscores this relationship between lack of sleep and having higher odds of COVID-19 infection,” Manoj Sharma, MBBS, PhD, professor of social and behavioral health in the UNLV department of environmental and occupational health, and one of the study authors, said in an interview.
More research is warranted to learn the direction of the association, he said. Does reduced sleep lower immunity and make a health care worker more susceptible to SARS-CoV-2 infection, or does the anxiety associated with COVID-19 contribute to insomnia?
“Practicing sleep hygiene is a must not only for health workers but also for everyone,” Dr. Sharma added. Recommendations include having fixed hours of going to bed, fixed hours of waking up, not overdoing naps, having at least 30 minutes of winding down before sleeping, having a dark bedroom devoid of all electronics and other disturbances, avoiding smoking, alcohol, and stimulants (such as caffeine) before sleeping, and practicing relaxation right before sleeping, he said.
“It is hard for some health care workers, especially those who work night shifts, but it must be a priority to follow as many sleep hygiene measures as possible,” Dr. Sharma said. “After all, if you do not take care of yourself how can you take care of others?”
Dr. Seidelmann, Dr. Batra, and Dr. Sharma have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
among health care workers considered to be at high risk for exposure to patients with COVID-19, new evidence reveals.
For each additional hour of sleep at night, for example, risk for COVID-19 dropped by 12% in a study of 2844 frontline health care workers.
Furthermore, those who reported experiencing work-related burnout every day were 2.6 times more likely to report having COVID-19, to report having COVID-19 for a longer time, and to experience COVID-19 of more severity.
“This study underscores the importance of non–hygiene-related risk factors for COVID-19 and supports a holistic approach to health – including optimal sleep and job stress reduction to protect our health care workers from this and future pandemics,” senior author Sara B. Seidelmann, MD, said in an interview.
“Our findings add to the literature that sleep duration at night, sleep problems, and burnout may be risk factors for viral illnesses like COVID-19,” wrote Dr. Seidelmann and colleagues.
This is the first study to link COVID-19 risk to sleep habits – including number of hours of sleep at night, daytime napping hours, and severe sleep problems – among health care workers across multiple countries.
The study was published online March 22 in BMJ Nutrition, Prevention, and Health.
The researchers surveyed health care professionals in specialties considered to place personnel at high risk for exposure to SARS-CoV-2: critical care, emergency care, and internal medicine.
The association between sleep and burnout risk factors and COVID-19 did not vary significantly by specialty. “We didn’t detect any significant interactions between age, sex, specialty, or country,” said Dr. Seidelmann, assistant professor of clinical medicine at Columbia University College of Physicians and Surgeons, New York, and an internist at Stamford (Conn.) Hospital.
In addition to the 12% lower risk associated with each additional hour of sleep at night, each 1 additional hour of daytime napping was linked with a 6% increased risk for COVID-19 in an adjusted analysis (odds ratio [OR], 1.06; 95% confidence interval [CI], 1.01-1.12).
Daytime napping slightly increased risk for COVID-19 in five of the six countries included in the study: France, Germany, Italy, the United Kingdom, and the United States. In contrast, in Spain, napping had a nonsignificant protective effect.
The survey asked health care workers to recall nighttime sleep duration, sleep disorders, and burnout in the year prior to onset of the COVID-19 pandemic.
‘Significant, close contact’ with COVID-19?
Lead author Hyunju Kim, NP, Dr. Seidelmann, and colleagues conducted the population-based, case-control study from July 17 to Sept. 25, 2020. They identified health care workers from the SurveyHealthcareGlobus (SHG) network.
Of the respondents, 72% were men. The mean age of the participants was 48 years, and the study population was 77% White, 12% Asian, 6% mixed background, 2% Black, and 1% other. (The remainder preferred not to say).
The 568 health care workers considered to have COVID-19 were classified on the basis of self-reported symptoms. Control participants had no symptoms associated with COVID-19.
All 2,844 participants answered yes to a question about having “significant close contact” with COVID-19 patients in their workplace.
Compared to reporting no sleep problems, having three such problems – difficulty sleeping at night, poor sleep continuity, and frequent use of sleeping pills – was associated with 88% greater odds of COVID-19 (OR, 1.88; 95% CI, 1.17–3.01).
Having one sleep problem was not associated with COVID-19.
More burnout, greater risk
The health care workers reported the severity of any work-related burnout. “There was a significant dose-response relationship between frequency of burnout and COVID-19,” the researchers noted.
Those who reported having burnout rarely or weekly had a 1.3-1.4 greater chance of reporting COVID-19 compared to those who reported having no burnout, for example.
In addition, reporting a high level of burnout was linked to about three times the risk for having COVID-19 of longer duration and of greater severity.
What drives the association between sleep problems, burnout, and higher risk for COVID-19 and severe COVID-19 remains unknown.
“The mechanism underlying these associations isn’t clear, but suboptimal sleep, sleep disorders, and stress may result in immune system dysregulation, increased inflammation, and alterations in hormones such as cortisol and melatonin that may increase vulnerability to viral infections,” Dr. Seidelmann said.
Strengths and limitations
Using a large network of health care workers in the early phase of the pandemic is a strength of the study. How generalizable the findings are outside the SHG database of 1.5 million health care workers remains unknown.
Another limitation was reliance on self-reporting of COVID-19 patient exposure, outcomes, and covariates, which could have introduced bias.
“However,” the researchers noted, “health care workers are likely a reliable source of information.”
Insomnia a common challenge
A 2020 meta-analysis examined the effect of insomnia and psychological factors on COVID-19 risk among health care workers. Lead author Kavita Batra, PhD, of the University of Nevada, Las Vegas (UNLV), and colleagues found that the pooled prevalence of insomnia was almost 28%.
“The recent six-country study by Kim and colleagues also underscores this relationship between lack of sleep and having higher odds of COVID-19 infection,” Manoj Sharma, MBBS, PhD, professor of social and behavioral health in the UNLV department of environmental and occupational health, and one of the study authors, said in an interview.
More research is warranted to learn the direction of the association, he said. Does reduced sleep lower immunity and make a health care worker more susceptible to SARS-CoV-2 infection, or does the anxiety associated with COVID-19 contribute to insomnia?
“Practicing sleep hygiene is a must not only for health workers but also for everyone,” Dr. Sharma added. Recommendations include having fixed hours of going to bed, fixed hours of waking up, not overdoing naps, having at least 30 minutes of winding down before sleeping, having a dark bedroom devoid of all electronics and other disturbances, avoiding smoking, alcohol, and stimulants (such as caffeine) before sleeping, and practicing relaxation right before sleeping, he said.
“It is hard for some health care workers, especially those who work night shifts, but it must be a priority to follow as many sleep hygiene measures as possible,” Dr. Sharma said. “After all, if you do not take care of yourself how can you take care of others?”
Dr. Seidelmann, Dr. Batra, and Dr. Sharma have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
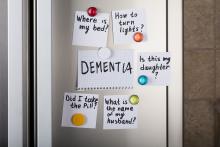
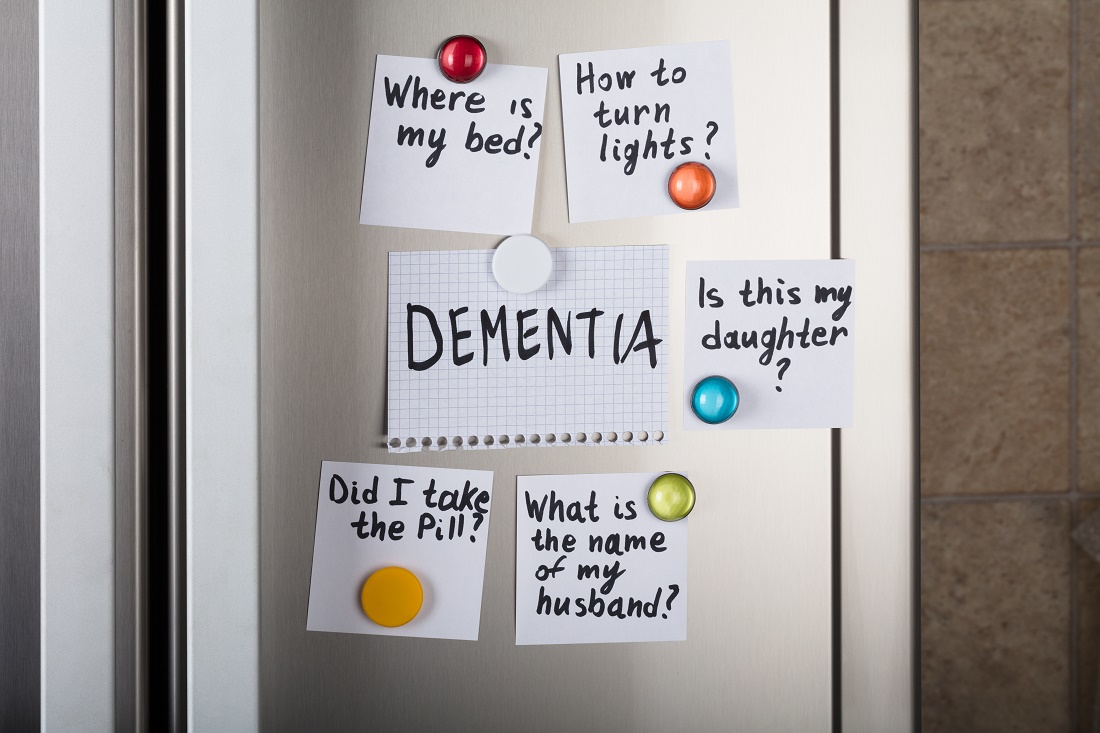
Cannabinoids promising for improving appetite, behavior in dementia
For patients with dementia, cannabinoids may be a promising intervention for treating neuropsychiatric symptoms (NPS) and the refusing of food, new research suggests.
Results of a systematic literature review, presented at the 2021 meeting of the American Association for Geriatric Psychiatry, showed that cannabinoids were associated with reduced agitation, longer sleep, and lower NPS. They were also linked to increased meal consumption and weight gain.
Refusing food is a common problem for patients with dementia, often resulting in worsening sleep, agitation, and mood, study investigator Niraj Asthana, MD, a second-year resident in the department of psychiatry, University of California, San Diego, said in an interview. Dr. Asthana noted that certain cannabinoid analogues are now used to stimulate appetite for patients undergoing chemotherapy.
Filling a treatment gap
After years of legal and other problems affecting cannabinoid research, there is renewed interest in investigating its use for patients with dementia. Early evidence suggests that cannabinoids may also be beneficial for pain, sleep, and aggression.
The researchers noted that cannabinoids may be especially valuable in areas where there are currently limited therapies, including food refusal and NPS.
“Unfortunately, there are limited treatments available for food refusal, so we’re left with appetite stimulants and electroconvulsive therapy, and although atypical antipsychotics are commonly used to treat NPS, they’re associated with an increased risk of serious adverse events and mortality in older patients,” said Dr. Asthana.
Dr. Asthana and colleague Dan Sewell, MD, carried out a systematic literature review of relevant studies of the use of cannabinoids for dementia patients.
“We found there are lot of studies, but they’re small scale; I’d say the largest was probably about 50 patients, with most studies having 10-50 patients,” said Dr. Asthana. In part, this may be because, until very recently, research on cannabinoids was controversial.
To review the current literature on the potential applications of cannabinoids in the treatment of food refusal and NPS in dementia patients, the researchers conducted a literature review.
They identified 23 relevant studies of the use of synthetic cannabinoids, including dronabinol and nabilone, for dementia patients. These products contain tetrahydrocannabinol (THC), the main psychoactive compound in cannabis.
More research coming
Several studies showed that cannabinoid use was associated with reduced nighttime motor activity, improved sleep duration, reduced agitation, and lower Neuropsychiatric Inventory scores.
One crossover placebo-controlled trial showed an overall increase in body weight among dementia patients who took dronabinol.
This suggests there might be something to the “colloquial cultural association between cannabinoids and the munchies,” said Dr. Asthana.
Possible mechanisms for the effects on appetite may be that cannabinoids increase levels of the hormone ghrelin, which is also known as the “hunger hormone,” and decrease leptin levels, a hormone that inhibits hunger. Dr. Asthana noted that, in these studies, the dose of THC was low and that overall, cannabinoids appeared to be safe.
“We found that, at least in these small-scale studies, cannabinoid analogues are well tolerated,” possibly because of the relatively low doses of THC, said Dr. Asthana. “They generally don’t seem to have a ton of side effects; they may make people a little sleepy, which is actually good, because these patents also have a lot of trouble sleeping.”
He noted that more recent research suggests cannabidiol oil may reduce agitation by up to 40%.
“Now that cannabis is losing a lot of its stigma, both culturally and in the scientific community, you’re seeing a lot of grant applications for clinical trials,” said Dr. Asthana. “I’m excited to see what we find in the next 5-10 years.”
In a comment, Kirsten Wilkins, MD, associate professor of psychiatry, Yale University, New Haven, Conn., who is also a geriatric psychiatrist at the Veterans Affairs Connecticut Health Care System, welcomed the new research in this area.
“With limited safe and effective treatments for food refusal and neuropsychiatric symptoms of dementia, Dr. Asthana and Dr. Sewell highlight the growing body of literature suggesting cannabinoids may be a novel treatment option,” she said.
A version of this article first appeared on Medscape.com.
For patients with dementia, cannabinoids may be a promising intervention for treating neuropsychiatric symptoms (NPS) and the refusing of food, new research suggests.
Results of a systematic literature review, presented at the 2021 meeting of the American Association for Geriatric Psychiatry, showed that cannabinoids were associated with reduced agitation, longer sleep, and lower NPS. They were also linked to increased meal consumption and weight gain.
Refusing food is a common problem for patients with dementia, often resulting in worsening sleep, agitation, and mood, study investigator Niraj Asthana, MD, a second-year resident in the department of psychiatry, University of California, San Diego, said in an interview. Dr. Asthana noted that certain cannabinoid analogues are now used to stimulate appetite for patients undergoing chemotherapy.
Filling a treatment gap
After years of legal and other problems affecting cannabinoid research, there is renewed interest in investigating its use for patients with dementia. Early evidence suggests that cannabinoids may also be beneficial for pain, sleep, and aggression.
The researchers noted that cannabinoids may be especially valuable in areas where there are currently limited therapies, including food refusal and NPS.
“Unfortunately, there are limited treatments available for food refusal, so we’re left with appetite stimulants and electroconvulsive therapy, and although atypical antipsychotics are commonly used to treat NPS, they’re associated with an increased risk of serious adverse events and mortality in older patients,” said Dr. Asthana.
Dr. Asthana and colleague Dan Sewell, MD, carried out a systematic literature review of relevant studies of the use of cannabinoids for dementia patients.
“We found there are lot of studies, but they’re small scale; I’d say the largest was probably about 50 patients, with most studies having 10-50 patients,” said Dr. Asthana. In part, this may be because, until very recently, research on cannabinoids was controversial.
To review the current literature on the potential applications of cannabinoids in the treatment of food refusal and NPS in dementia patients, the researchers conducted a literature review.
They identified 23 relevant studies of the use of synthetic cannabinoids, including dronabinol and nabilone, for dementia patients. These products contain tetrahydrocannabinol (THC), the main psychoactive compound in cannabis.
More research coming
Several studies showed that cannabinoid use was associated with reduced nighttime motor activity, improved sleep duration, reduced agitation, and lower Neuropsychiatric Inventory scores.
One crossover placebo-controlled trial showed an overall increase in body weight among dementia patients who took dronabinol.
This suggests there might be something to the “colloquial cultural association between cannabinoids and the munchies,” said Dr. Asthana.
Possible mechanisms for the effects on appetite may be that cannabinoids increase levels of the hormone ghrelin, which is also known as the “hunger hormone,” and decrease leptin levels, a hormone that inhibits hunger. Dr. Asthana noted that, in these studies, the dose of THC was low and that overall, cannabinoids appeared to be safe.
“We found that, at least in these small-scale studies, cannabinoid analogues are well tolerated,” possibly because of the relatively low doses of THC, said Dr. Asthana. “They generally don’t seem to have a ton of side effects; they may make people a little sleepy, which is actually good, because these patents also have a lot of trouble sleeping.”
He noted that more recent research suggests cannabidiol oil may reduce agitation by up to 40%.
“Now that cannabis is losing a lot of its stigma, both culturally and in the scientific community, you’re seeing a lot of grant applications for clinical trials,” said Dr. Asthana. “I’m excited to see what we find in the next 5-10 years.”
In a comment, Kirsten Wilkins, MD, associate professor of psychiatry, Yale University, New Haven, Conn., who is also a geriatric psychiatrist at the Veterans Affairs Connecticut Health Care System, welcomed the new research in this area.
“With limited safe and effective treatments for food refusal and neuropsychiatric symptoms of dementia, Dr. Asthana and Dr. Sewell highlight the growing body of literature suggesting cannabinoids may be a novel treatment option,” she said.
A version of this article first appeared on Medscape.com.
For patients with dementia, cannabinoids may be a promising intervention for treating neuropsychiatric symptoms (NPS) and the refusing of food, new research suggests.
Results of a systematic literature review, presented at the 2021 meeting of the American Association for Geriatric Psychiatry, showed that cannabinoids were associated with reduced agitation, longer sleep, and lower NPS. They were also linked to increased meal consumption and weight gain.
Refusing food is a common problem for patients with dementia, often resulting in worsening sleep, agitation, and mood, study investigator Niraj Asthana, MD, a second-year resident in the department of psychiatry, University of California, San Diego, said in an interview. Dr. Asthana noted that certain cannabinoid analogues are now used to stimulate appetite for patients undergoing chemotherapy.
Filling a treatment gap
After years of legal and other problems affecting cannabinoid research, there is renewed interest in investigating its use for patients with dementia. Early evidence suggests that cannabinoids may also be beneficial for pain, sleep, and aggression.
The researchers noted that cannabinoids may be especially valuable in areas where there are currently limited therapies, including food refusal and NPS.
“Unfortunately, there are limited treatments available for food refusal, so we’re left with appetite stimulants and electroconvulsive therapy, and although atypical antipsychotics are commonly used to treat NPS, they’re associated with an increased risk of serious adverse events and mortality in older patients,” said Dr. Asthana.
Dr. Asthana and colleague Dan Sewell, MD, carried out a systematic literature review of relevant studies of the use of cannabinoids for dementia patients.
“We found there are lot of studies, but they’re small scale; I’d say the largest was probably about 50 patients, with most studies having 10-50 patients,” said Dr. Asthana. In part, this may be because, until very recently, research on cannabinoids was controversial.
To review the current literature on the potential applications of cannabinoids in the treatment of food refusal and NPS in dementia patients, the researchers conducted a literature review.
They identified 23 relevant studies of the use of synthetic cannabinoids, including dronabinol and nabilone, for dementia patients. These products contain tetrahydrocannabinol (THC), the main psychoactive compound in cannabis.
More research coming
Several studies showed that cannabinoid use was associated with reduced nighttime motor activity, improved sleep duration, reduced agitation, and lower Neuropsychiatric Inventory scores.
One crossover placebo-controlled trial showed an overall increase in body weight among dementia patients who took dronabinol.
This suggests there might be something to the “colloquial cultural association between cannabinoids and the munchies,” said Dr. Asthana.
Possible mechanisms for the effects on appetite may be that cannabinoids increase levels of the hormone ghrelin, which is also known as the “hunger hormone,” and decrease leptin levels, a hormone that inhibits hunger. Dr. Asthana noted that, in these studies, the dose of THC was low and that overall, cannabinoids appeared to be safe.
“We found that, at least in these small-scale studies, cannabinoid analogues are well tolerated,” possibly because of the relatively low doses of THC, said Dr. Asthana. “They generally don’t seem to have a ton of side effects; they may make people a little sleepy, which is actually good, because these patents also have a lot of trouble sleeping.”
He noted that more recent research suggests cannabidiol oil may reduce agitation by up to 40%.
“Now that cannabis is losing a lot of its stigma, both culturally and in the scientific community, you’re seeing a lot of grant applications for clinical trials,” said Dr. Asthana. “I’m excited to see what we find in the next 5-10 years.”
In a comment, Kirsten Wilkins, MD, associate professor of psychiatry, Yale University, New Haven, Conn., who is also a geriatric psychiatrist at the Veterans Affairs Connecticut Health Care System, welcomed the new research in this area.
“With limited safe and effective treatments for food refusal and neuropsychiatric symptoms of dementia, Dr. Asthana and Dr. Sewell highlight the growing body of literature suggesting cannabinoids may be a novel treatment option,” she said.
A version of this article first appeared on Medscape.com.
Melatonin not recommended for early-stage NSCLC
There was a hint of benefit with melatonin among patients with stage III/IV NSCLC. These patients had a hazard reduction of 25% in 5-year DFS. However, the median DFS for patients with advanced disease was the same whether they received melatonin or placebo – 18 months.
In the overall study population, melatonin had no beneficial effects on quality of life, sleep, anxiety, depression, pain, or fatigue, and it did not reduce adverse events from chemotherapy or radiation.
These results were reported in EClinicalMedicine.
“In light of the results, we do not recommend the inclusion of adjuvant melatonin for patients with early-stage NSCLC. Evidence suggests there may be a benefit for those with late-stage disease,” the authors wrote. “However, because of the mixed findings observed, we recommend a follow-up randomized, controlled trial involving a larger population focusing on later-stage resected lung cancer to clarify these results.”
“I would very much like to pursue another controlled study of melatonin specifically in a group of late-stage lung cancer and possibly in other more advanced cancer types,” said lead author Dugald Seely, ND, of the Canadian College of Naturopathic Medicine in Toronto.
Study rationale and design
Melatonin has shown promise for treating patients with lung cancer, Dr. Seely and colleagues noted. Melatonin is often recommended by naturopathic doctors following lung cancer surgery, but until now there was no high-level evidence regarding the practice.
For their study, Dr. Seely and colleagues evaluated 709 patients who had undergone NSCLC resection. The patients were randomized to receive placebo (n = 353) or melatonin (n = 356) 1 hour before bedtime for 1 year. A 20-mg melatonin dose was used, which is common in clinical practice and research.
The study arms were well matched, with no “clinically meaningful” differences in demographics, surgery type, cancer type, stage of cancer, or preoperative comorbidities, according to the researchers.
The mean age in both treatment arms was 67 years. Overall, 134 participants received adjuvant chemotherapy (66 melatonin, 68 placebo), and 43 had adjuvant radiation (22 melatonin, 21 placebo).
Results
For 2-year DFS, melatonin showed an adjusted relative risk of 1.01 (95% confidence interval, 0.83-1.22; P = .94) versus placebo. The adjusted relative risk in the per-protocol analysis was 1.12 (95% CI, 0.96-1.32; P = .14.)
At 5 years, the median DFS was not reached in either treatment arm. Melatonin showed a hazard ratio of 0.97 (95% CI, 0.86-1.09; P = .84) for 5-year DFS.
Among patients with stage I-II NSCLC, the median DFS was not reached at 5 years in either treatment arm. Among patients with stage III-IV NSCLC, the median DFS was 18 months in both arms.
Melatonin showed a hazard ratio of 0.97 (95% CI, 0.85-1.11; P = .66) in patients with early-stage NSCLC and a hazard reduction of 25% (HR, 0.75; 95% CI, 0.61-0.92; P = .005) in patients with late-stage NSCLC.
For the entire cohort, there were no significant differences between treatment arms in the number, severity, or seriousness of adverse events. Likewise, there were no significant differences between the treatment arms with regard to fatigue, quality of life, or sleep at 1 or 2 years.
Dr. Seely said the most surprising thing about this study was that melatonin didn’t help with sleep.
“Since initiation of the trial, my thinking on the right dose of melatonin to support sleep has changed. Clinically, I see extended-release and, indeed, lower doses to be more effective than 20 mg nightly,” he noted.
Dr. Seely and colleagues also assessed proposed mechanisms for melatonin’s possible benefit in NSCLC but found no effect on natural killer cell cytotoxicity or phenotype and no effect on blood levels of inflammatory cytokines in a substudy of 92 patients.
This research was funded by the Lotte and John Hecht Memorial Foundation and the Gateway for Cancer Research Foundation. The researchers had no relevant disclosures.
There was a hint of benefit with melatonin among patients with stage III/IV NSCLC. These patients had a hazard reduction of 25% in 5-year DFS. However, the median DFS for patients with advanced disease was the same whether they received melatonin or placebo – 18 months.
In the overall study population, melatonin had no beneficial effects on quality of life, sleep, anxiety, depression, pain, or fatigue, and it did not reduce adverse events from chemotherapy or radiation.
These results were reported in EClinicalMedicine.
“In light of the results, we do not recommend the inclusion of adjuvant melatonin for patients with early-stage NSCLC. Evidence suggests there may be a benefit for those with late-stage disease,” the authors wrote. “However, because of the mixed findings observed, we recommend a follow-up randomized, controlled trial involving a larger population focusing on later-stage resected lung cancer to clarify these results.”
“I would very much like to pursue another controlled study of melatonin specifically in a group of late-stage lung cancer and possibly in other more advanced cancer types,” said lead author Dugald Seely, ND, of the Canadian College of Naturopathic Medicine in Toronto.
Study rationale and design
Melatonin has shown promise for treating patients with lung cancer, Dr. Seely and colleagues noted. Melatonin is often recommended by naturopathic doctors following lung cancer surgery, but until now there was no high-level evidence regarding the practice.
For their study, Dr. Seely and colleagues evaluated 709 patients who had undergone NSCLC resection. The patients were randomized to receive placebo (n = 353) or melatonin (n = 356) 1 hour before bedtime for 1 year. A 20-mg melatonin dose was used, which is common in clinical practice and research.
The study arms were well matched, with no “clinically meaningful” differences in demographics, surgery type, cancer type, stage of cancer, or preoperative comorbidities, according to the researchers.
The mean age in both treatment arms was 67 years. Overall, 134 participants received adjuvant chemotherapy (66 melatonin, 68 placebo), and 43 had adjuvant radiation (22 melatonin, 21 placebo).
Results
For 2-year DFS, melatonin showed an adjusted relative risk of 1.01 (95% confidence interval, 0.83-1.22; P = .94) versus placebo. The adjusted relative risk in the per-protocol analysis was 1.12 (95% CI, 0.96-1.32; P = .14.)
At 5 years, the median DFS was not reached in either treatment arm. Melatonin showed a hazard ratio of 0.97 (95% CI, 0.86-1.09; P = .84) for 5-year DFS.
Among patients with stage I-II NSCLC, the median DFS was not reached at 5 years in either treatment arm. Among patients with stage III-IV NSCLC, the median DFS was 18 months in both arms.
Melatonin showed a hazard ratio of 0.97 (95% CI, 0.85-1.11; P = .66) in patients with early-stage NSCLC and a hazard reduction of 25% (HR, 0.75; 95% CI, 0.61-0.92; P = .005) in patients with late-stage NSCLC.
For the entire cohort, there were no significant differences between treatment arms in the number, severity, or seriousness of adverse events. Likewise, there were no significant differences between the treatment arms with regard to fatigue, quality of life, or sleep at 1 or 2 years.
Dr. Seely said the most surprising thing about this study was that melatonin didn’t help with sleep.
“Since initiation of the trial, my thinking on the right dose of melatonin to support sleep has changed. Clinically, I see extended-release and, indeed, lower doses to be more effective than 20 mg nightly,” he noted.
Dr. Seely and colleagues also assessed proposed mechanisms for melatonin’s possible benefit in NSCLC but found no effect on natural killer cell cytotoxicity or phenotype and no effect on blood levels of inflammatory cytokines in a substudy of 92 patients.
This research was funded by the Lotte and John Hecht Memorial Foundation and the Gateway for Cancer Research Foundation. The researchers had no relevant disclosures.
There was a hint of benefit with melatonin among patients with stage III/IV NSCLC. These patients had a hazard reduction of 25% in 5-year DFS. However, the median DFS for patients with advanced disease was the same whether they received melatonin or placebo – 18 months.
In the overall study population, melatonin had no beneficial effects on quality of life, sleep, anxiety, depression, pain, or fatigue, and it did not reduce adverse events from chemotherapy or radiation.
These results were reported in EClinicalMedicine.
“In light of the results, we do not recommend the inclusion of adjuvant melatonin for patients with early-stage NSCLC. Evidence suggests there may be a benefit for those with late-stage disease,” the authors wrote. “However, because of the mixed findings observed, we recommend a follow-up randomized, controlled trial involving a larger population focusing on later-stage resected lung cancer to clarify these results.”
“I would very much like to pursue another controlled study of melatonin specifically in a group of late-stage lung cancer and possibly in other more advanced cancer types,” said lead author Dugald Seely, ND, of the Canadian College of Naturopathic Medicine in Toronto.
Study rationale and design
Melatonin has shown promise for treating patients with lung cancer, Dr. Seely and colleagues noted. Melatonin is often recommended by naturopathic doctors following lung cancer surgery, but until now there was no high-level evidence regarding the practice.
For their study, Dr. Seely and colleagues evaluated 709 patients who had undergone NSCLC resection. The patients were randomized to receive placebo (n = 353) or melatonin (n = 356) 1 hour before bedtime for 1 year. A 20-mg melatonin dose was used, which is common in clinical practice and research.
The study arms were well matched, with no “clinically meaningful” differences in demographics, surgery type, cancer type, stage of cancer, or preoperative comorbidities, according to the researchers.
The mean age in both treatment arms was 67 years. Overall, 134 participants received adjuvant chemotherapy (66 melatonin, 68 placebo), and 43 had adjuvant radiation (22 melatonin, 21 placebo).
Results
For 2-year DFS, melatonin showed an adjusted relative risk of 1.01 (95% confidence interval, 0.83-1.22; P = .94) versus placebo. The adjusted relative risk in the per-protocol analysis was 1.12 (95% CI, 0.96-1.32; P = .14.)
At 5 years, the median DFS was not reached in either treatment arm. Melatonin showed a hazard ratio of 0.97 (95% CI, 0.86-1.09; P = .84) for 5-year DFS.
Among patients with stage I-II NSCLC, the median DFS was not reached at 5 years in either treatment arm. Among patients with stage III-IV NSCLC, the median DFS was 18 months in both arms.
Melatonin showed a hazard ratio of 0.97 (95% CI, 0.85-1.11; P = .66) in patients with early-stage NSCLC and a hazard reduction of 25% (HR, 0.75; 95% CI, 0.61-0.92; P = .005) in patients with late-stage NSCLC.
For the entire cohort, there were no significant differences between treatment arms in the number, severity, or seriousness of adverse events. Likewise, there were no significant differences between the treatment arms with regard to fatigue, quality of life, or sleep at 1 or 2 years.
Dr. Seely said the most surprising thing about this study was that melatonin didn’t help with sleep.
“Since initiation of the trial, my thinking on the right dose of melatonin to support sleep has changed. Clinically, I see extended-release and, indeed, lower doses to be more effective than 20 mg nightly,” he noted.
Dr. Seely and colleagues also assessed proposed mechanisms for melatonin’s possible benefit in NSCLC but found no effect on natural killer cell cytotoxicity or phenotype and no effect on blood levels of inflammatory cytokines in a substudy of 92 patients.
This research was funded by the Lotte and John Hecht Memorial Foundation and the Gateway for Cancer Research Foundation. The researchers had no relevant disclosures.
FROM ECLINICALMEDICINE
Buprenorphine for OUD may also mitigate risk with concomitant benzo, Z-drug use
Buprenorphine for the treatment of opioid-use disorder (OUD) may also mitigate the risk associated with concomitant benzodiazepine and Z-drug use, which is frequent in this patient population, new research suggests.
A case-crossover study of more than 20,000 participants with OUD showed that drug treatment days in which benzodiazepines and Z-drugs were taken were associated with an 88% increase in nonfatal overdose; buprenorphine appeared to reduce this risk by almost 40%.
“One of our two primary findings is that patients with opioid use disorder can still benefit substantially from buprenorphine treatment, even if they have benzodiazepines on board,” lead author Kevin Xu, MD, a resident at the Washington University, St. Louis, told this news organization.
The other key finding was that “not all benzodiazepines are equal” and that some are associated with higher risk than others, Dr. Xu added.
“If anything, patients who are on buprenorphine and benzodiazepines do not necessarily need to be abruptly tapered off their benzodiazepines. Our data actually demonstrate that there are safe avenues for them,” he added.
The findings were published online March 3 in the American Journal of Psychiatry.
Cloudy relationship
Buprenorphine is commonly used to treat patients with OUD because of its ability to decrease all-cause mortality. However,
In addition, recent research shows that benzodiazepine/Z-drug use is associated with a variety of potential adverse effects, including respiratory depression, overdose, and addiction risk.
The relationship between benzodiazepine use and buprenorphine treatment outcomes is poorly characterized in individuals with OUD. Although some studies suggest benzodiazepines may enhance retention in buprenorphine maintenance treatment, others suggest a link to increased adverse events, including all-cause mortality, drug-related poisonings, and accidental injury–related emergency department visits.
In addition, there has been little research on the potential adverse effects associated with use of selective benzodiazepine receptor modulators in patients with OUD. These so-called Z-drugs include zolpidem, zaleplon, and eszopiclone.
Nevertheless, previous research in the general population shows that these medications have a range of adverse effects similar to those of benzodiazepines, with comparable dose-response effects on all-cause mortality.
“The challenge for any clinician is that many patients who are addicted to opioids are also polysubstance users,” said Dr. Xu. “There are so many hopeful articles regarding the benefits of buprenorphine treatment in opioid use disorder patients, but it seems like the individuals with polysubstance use are largely ignored in the setting of the opioid epidemic.”
“And this is really the back story that got me inspired to study this particular topic,” he added.
Improve, nullify, or reverse?
Given these questions, the researchers set out to quantify the odds of nonfatal drug-related poisoning, including overdoses, associated with benzodiazepine or Z-drug use by patients with OUD who were also taking buprenorphine.
“While the drug-related poisoning variable encompasses opioid overdoses, we used a broad definition per CDC guidelines to also include other types of drug overdoses – including poisoning events involving stimulants, overdoses involving sedatives, and overdoses involving psychotropic prescription drugs” that are commonly used by patients with OUD, said Dr. Xu.
They also wanted to determine whether the use of benzodiazepines or Z-drugs would improve, nullify, or reverse the protective effect of buprenorphine. The researchers also evaluated whether different sedative and hypnotic subtypes of these drugs were associated with different poisoning risks.
The researchers analyzed pharmaceutical claims data from 304,676 individuals (aged 12-64 years) in the IBM MarketScan Commercial and Multi-State Medicaid Databases. All had received buprenorphine treatment for OUD between Jan. 1, 2006, and Dec. 31, 2016.
Buprenorphine use was converted to a daily milligram dose and was classified as either greater than 12 mg or less than or equal to 12 mg, because previous research suggests there may be differences in treatment retention associated with this dose. Given the case-control nature of the investigation, patients who did not experience a drug-related poisoning were excluded from the analysis.
The study’s primary unit of observation was person-days, which were those days during which patients were enrolled in a health insurance plan. Participants were evaluated for 1 year before their first drug-related poisoning and 1 year after their first such poisoning. The primary outcome was nonfatal drug-related poisonings, including overdoses. The primary exposure was determined on the basis of benzodiazepine or Z-drug prescriptions.
The daily dose of benzodiazepines or Z-drugs was standardized as a function of diazepam-equivalent milligrams. Doses were classified as either high dose (diazepam-equivalent mg dose >30 mg) or low dose (≤30 mg). The drugs were also distinguished on the basis of their pharmacologic properties, such as whether they were short-acting or long-acting.
37% risk reduction
Of the original cohort of 304,676 patients with OUD, the study’s final analytic sample included 23,036 patients (mean age, 30 years; 51% men), representing 14,213,075 person-days of insurance coverage. Of these, 2,210,927 person-days (15.6%) entailed claims for buprenorphine (mean daily dose, 15.4 mg; SD, 7.31 mg).
A total of 474,181 person-days included claims for benzodiazepines or Z-drugs with concurrent buprenorphine treatment. The mean daily dose of any benzodiazepine or Z-drug was 23.4 diazepam-milligram equivalents. The mean daily dose of short-acting benzodiazepines, long-acting benzodiazepines, and Z-drugs was 25.3, 31.3, and 4.9 diazepam-milligram equivalents, respectively.
Buprenorphine treatment days were associated with a 37% lower chance of drug-related poisoning (95% confidence interval, 0.60-0.66) in comparison with nontreatment days. On the other hand, the odds of poisoning increased by 81% on days on which patients were treated with Z-drugs or benzodiazepines (95% CI, 1.73-1.91).
Interestingly, individual analyses showed that benzodiazepine and Z-drug treatment days were associated with increased odds of poisoning events (odds ratio, 1.29; 95% CI, 1.19-1.39). Odds of poisoning events on benzodiazepine-only treatment days, on the other hand, were markedly lower (OR, 1.88; 95% CI, 1.78-1.98).
Subgroup analyses revealed that both short-acting and long-acting benzodiazepine treatment days were associated with comparably elevated odds of drug-related poisoning (OR, 1.86 and 1.68, respectively). High-dose benzodiazepine treatment days were associated with higher increased odds of a poisoning event (122%) in comparison with low-dose treatment days (78%).
High-dose, but not low-dose, benzodiazepine or Z-drug treatment was linked to increased poisonings when the drug was taken concurrently with buprenorphine (OR, 1.64; 95% CI, 1.39-1.93). However, the risk was still lower than the risk associated with taking the agents without concurrent treatment with buprenorphine (low-dose OR, 1.69; high-dose OR, 2.23).
‘Not all benzodiazepines are bad’
Dr. Xu noted that the findings have potentially important implications for clinical practice, beginning with the dose-dependent relationship between benzodiazepine/Z-drug use and drug-related poisonings among individuals with OUD. This indicates that lowering doses or shortening treatment duration may reduce risk, he said.
Similarly, the lower risk associated with long-acting benzodiazepines relative to short-acting beonzodiazepines – as well as the substantially lower risk associated with Z-drugs, compared with either short- or long-acting benzodiazepines – suggests that switching from benzodiazepines to long-acting agents or Z-drugs may lower the risk for overdose, he added.
“Clinicians are often challenged by patients with opioid use disorder who are also on benzodiazepines or Z-drugs. There’s an inclination to say no to them, because they’re too high risk to start buprenorphine maintenance, or abruptly taper the benzodiazepines, which can be very destabilizing,” he noted.
“Our data show that people on benzodiazepines can absolutely receive buprenorphine and still get some benefit,” Dr. Xu said. “In addition, not all benzodiazepines are bad for these individuals. There are safer formulations and safer doses, too.”
However, he added, he would not initiate benzodiazepine treatment if he didn’t have to, especially long-term treatment.
“One of the messages from our data is that this clearly contributes to higher overdose risk. But we often inherit patients who already have benzodiazepines on board, so we need to figure out what to do. That is the question that nobody had really clearly addressed prior to this study,” Dr. Xu concluded.
Vigilance needed
Commenting on the findings for this news organization, Jerrold F. Rosenbaum, MD, Stanley Cobb Professor of Psychiatry, Harvard Medical School, Boston, urged caution when combining benzodiazepines with opioids.
“There are situations where you need to be circumspect about the use of benzodiazepines, and that’s clearly when people are being prescribed them in combination with other drugs that could be either sedating or respiratory depressant,” said Dr. Rosenbaum, who was not involved with the research.
“This paper reminds us that physicians need to be particularly vigilant about situations where patients might be combining the two agents,” he added.
Dr. Rosenbaum noted that patients who are using more medication than prescribed are at risk “for not appreciating the synergy” between the two treatments in terms of adverse events such as respiratory depression.
In addition, “if they’re intending to do themselves harm, the lethality of an overdose will be certainly far more than the benzodiazepines or opiates alone,” he said.
Another potential challenge for clinicians are situations in which patients are taking benzodiazepines for preexisting conditions that also require opiates. “Then you have to use special vigilance and try to use lowest doses to reduce the total burden of medication to minimize the potential risk,” said Dr. Rosenbaum.
The study was funded by the National Institutes of Health. Dr. Xu has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Buprenorphine for the treatment of opioid-use disorder (OUD) may also mitigate the risk associated with concomitant benzodiazepine and Z-drug use, which is frequent in this patient population, new research suggests.
A case-crossover study of more than 20,000 participants with OUD showed that drug treatment days in which benzodiazepines and Z-drugs were taken were associated with an 88% increase in nonfatal overdose; buprenorphine appeared to reduce this risk by almost 40%.
“One of our two primary findings is that patients with opioid use disorder can still benefit substantially from buprenorphine treatment, even if they have benzodiazepines on board,” lead author Kevin Xu, MD, a resident at the Washington University, St. Louis, told this news organization.
The other key finding was that “not all benzodiazepines are equal” and that some are associated with higher risk than others, Dr. Xu added.
“If anything, patients who are on buprenorphine and benzodiazepines do not necessarily need to be abruptly tapered off their benzodiazepines. Our data actually demonstrate that there are safe avenues for them,” he added.
The findings were published online March 3 in the American Journal of Psychiatry.
Cloudy relationship
Buprenorphine is commonly used to treat patients with OUD because of its ability to decrease all-cause mortality. However,
In addition, recent research shows that benzodiazepine/Z-drug use is associated with a variety of potential adverse effects, including respiratory depression, overdose, and addiction risk.
The relationship between benzodiazepine use and buprenorphine treatment outcomes is poorly characterized in individuals with OUD. Although some studies suggest benzodiazepines may enhance retention in buprenorphine maintenance treatment, others suggest a link to increased adverse events, including all-cause mortality, drug-related poisonings, and accidental injury–related emergency department visits.
In addition, there has been little research on the potential adverse effects associated with use of selective benzodiazepine receptor modulators in patients with OUD. These so-called Z-drugs include zolpidem, zaleplon, and eszopiclone.
Nevertheless, previous research in the general population shows that these medications have a range of adverse effects similar to those of benzodiazepines, with comparable dose-response effects on all-cause mortality.
“The challenge for any clinician is that many patients who are addicted to opioids are also polysubstance users,” said Dr. Xu. “There are so many hopeful articles regarding the benefits of buprenorphine treatment in opioid use disorder patients, but it seems like the individuals with polysubstance use are largely ignored in the setting of the opioid epidemic.”
“And this is really the back story that got me inspired to study this particular topic,” he added.
Improve, nullify, or reverse?
Given these questions, the researchers set out to quantify the odds of nonfatal drug-related poisoning, including overdoses, associated with benzodiazepine or Z-drug use by patients with OUD who were also taking buprenorphine.
“While the drug-related poisoning variable encompasses opioid overdoses, we used a broad definition per CDC guidelines to also include other types of drug overdoses – including poisoning events involving stimulants, overdoses involving sedatives, and overdoses involving psychotropic prescription drugs” that are commonly used by patients with OUD, said Dr. Xu.
They also wanted to determine whether the use of benzodiazepines or Z-drugs would improve, nullify, or reverse the protective effect of buprenorphine. The researchers also evaluated whether different sedative and hypnotic subtypes of these drugs were associated with different poisoning risks.
The researchers analyzed pharmaceutical claims data from 304,676 individuals (aged 12-64 years) in the IBM MarketScan Commercial and Multi-State Medicaid Databases. All had received buprenorphine treatment for OUD between Jan. 1, 2006, and Dec. 31, 2016.
Buprenorphine use was converted to a daily milligram dose and was classified as either greater than 12 mg or less than or equal to 12 mg, because previous research suggests there may be differences in treatment retention associated with this dose. Given the case-control nature of the investigation, patients who did not experience a drug-related poisoning were excluded from the analysis.
The study’s primary unit of observation was person-days, which were those days during which patients were enrolled in a health insurance plan. Participants were evaluated for 1 year before their first drug-related poisoning and 1 year after their first such poisoning. The primary outcome was nonfatal drug-related poisonings, including overdoses. The primary exposure was determined on the basis of benzodiazepine or Z-drug prescriptions.
The daily dose of benzodiazepines or Z-drugs was standardized as a function of diazepam-equivalent milligrams. Doses were classified as either high dose (diazepam-equivalent mg dose >30 mg) or low dose (≤30 mg). The drugs were also distinguished on the basis of their pharmacologic properties, such as whether they were short-acting or long-acting.
37% risk reduction
Of the original cohort of 304,676 patients with OUD, the study’s final analytic sample included 23,036 patients (mean age, 30 years; 51% men), representing 14,213,075 person-days of insurance coverage. Of these, 2,210,927 person-days (15.6%) entailed claims for buprenorphine (mean daily dose, 15.4 mg; SD, 7.31 mg).
A total of 474,181 person-days included claims for benzodiazepines or Z-drugs with concurrent buprenorphine treatment. The mean daily dose of any benzodiazepine or Z-drug was 23.4 diazepam-milligram equivalents. The mean daily dose of short-acting benzodiazepines, long-acting benzodiazepines, and Z-drugs was 25.3, 31.3, and 4.9 diazepam-milligram equivalents, respectively.
Buprenorphine treatment days were associated with a 37% lower chance of drug-related poisoning (95% confidence interval, 0.60-0.66) in comparison with nontreatment days. On the other hand, the odds of poisoning increased by 81% on days on which patients were treated with Z-drugs or benzodiazepines (95% CI, 1.73-1.91).
Interestingly, individual analyses showed that benzodiazepine and Z-drug treatment days were associated with increased odds of poisoning events (odds ratio, 1.29; 95% CI, 1.19-1.39). Odds of poisoning events on benzodiazepine-only treatment days, on the other hand, were markedly lower (OR, 1.88; 95% CI, 1.78-1.98).
Subgroup analyses revealed that both short-acting and long-acting benzodiazepine treatment days were associated with comparably elevated odds of drug-related poisoning (OR, 1.86 and 1.68, respectively). High-dose benzodiazepine treatment days were associated with higher increased odds of a poisoning event (122%) in comparison with low-dose treatment days (78%).
High-dose, but not low-dose, benzodiazepine or Z-drug treatment was linked to increased poisonings when the drug was taken concurrently with buprenorphine (OR, 1.64; 95% CI, 1.39-1.93). However, the risk was still lower than the risk associated with taking the agents without concurrent treatment with buprenorphine (low-dose OR, 1.69; high-dose OR, 2.23).
‘Not all benzodiazepines are bad’
Dr. Xu noted that the findings have potentially important implications for clinical practice, beginning with the dose-dependent relationship between benzodiazepine/Z-drug use and drug-related poisonings among individuals with OUD. This indicates that lowering doses or shortening treatment duration may reduce risk, he said.
Similarly, the lower risk associated with long-acting benzodiazepines relative to short-acting beonzodiazepines – as well as the substantially lower risk associated with Z-drugs, compared with either short- or long-acting benzodiazepines – suggests that switching from benzodiazepines to long-acting agents or Z-drugs may lower the risk for overdose, he added.
“Clinicians are often challenged by patients with opioid use disorder who are also on benzodiazepines or Z-drugs. There’s an inclination to say no to them, because they’re too high risk to start buprenorphine maintenance, or abruptly taper the benzodiazepines, which can be very destabilizing,” he noted.
“Our data show that people on benzodiazepines can absolutely receive buprenorphine and still get some benefit,” Dr. Xu said. “In addition, not all benzodiazepines are bad for these individuals. There are safer formulations and safer doses, too.”
However, he added, he would not initiate benzodiazepine treatment if he didn’t have to, especially long-term treatment.
“One of the messages from our data is that this clearly contributes to higher overdose risk. But we often inherit patients who already have benzodiazepines on board, so we need to figure out what to do. That is the question that nobody had really clearly addressed prior to this study,” Dr. Xu concluded.
Vigilance needed
Commenting on the findings for this news organization, Jerrold F. Rosenbaum, MD, Stanley Cobb Professor of Psychiatry, Harvard Medical School, Boston, urged caution when combining benzodiazepines with opioids.
“There are situations where you need to be circumspect about the use of benzodiazepines, and that’s clearly when people are being prescribed them in combination with other drugs that could be either sedating or respiratory depressant,” said Dr. Rosenbaum, who was not involved with the research.
“This paper reminds us that physicians need to be particularly vigilant about situations where patients might be combining the two agents,” he added.
Dr. Rosenbaum noted that patients who are using more medication than prescribed are at risk “for not appreciating the synergy” between the two treatments in terms of adverse events such as respiratory depression.
In addition, “if they’re intending to do themselves harm, the lethality of an overdose will be certainly far more than the benzodiazepines or opiates alone,” he said.
Another potential challenge for clinicians are situations in which patients are taking benzodiazepines for preexisting conditions that also require opiates. “Then you have to use special vigilance and try to use lowest doses to reduce the total burden of medication to minimize the potential risk,” said Dr. Rosenbaum.
The study was funded by the National Institutes of Health. Dr. Xu has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Buprenorphine for the treatment of opioid-use disorder (OUD) may also mitigate the risk associated with concomitant benzodiazepine and Z-drug use, which is frequent in this patient population, new research suggests.
A case-crossover study of more than 20,000 participants with OUD showed that drug treatment days in which benzodiazepines and Z-drugs were taken were associated with an 88% increase in nonfatal overdose; buprenorphine appeared to reduce this risk by almost 40%.
“One of our two primary findings is that patients with opioid use disorder can still benefit substantially from buprenorphine treatment, even if they have benzodiazepines on board,” lead author Kevin Xu, MD, a resident at the Washington University, St. Louis, told this news organization.
The other key finding was that “not all benzodiazepines are equal” and that some are associated with higher risk than others, Dr. Xu added.
“If anything, patients who are on buprenorphine and benzodiazepines do not necessarily need to be abruptly tapered off their benzodiazepines. Our data actually demonstrate that there are safe avenues for them,” he added.
The findings were published online March 3 in the American Journal of Psychiatry.
Cloudy relationship
Buprenorphine is commonly used to treat patients with OUD because of its ability to decrease all-cause mortality. However,
In addition, recent research shows that benzodiazepine/Z-drug use is associated with a variety of potential adverse effects, including respiratory depression, overdose, and addiction risk.
The relationship between benzodiazepine use and buprenorphine treatment outcomes is poorly characterized in individuals with OUD. Although some studies suggest benzodiazepines may enhance retention in buprenorphine maintenance treatment, others suggest a link to increased adverse events, including all-cause mortality, drug-related poisonings, and accidental injury–related emergency department visits.
In addition, there has been little research on the potential adverse effects associated with use of selective benzodiazepine receptor modulators in patients with OUD. These so-called Z-drugs include zolpidem, zaleplon, and eszopiclone.
Nevertheless, previous research in the general population shows that these medications have a range of adverse effects similar to those of benzodiazepines, with comparable dose-response effects on all-cause mortality.
“The challenge for any clinician is that many patients who are addicted to opioids are also polysubstance users,” said Dr. Xu. “There are so many hopeful articles regarding the benefits of buprenorphine treatment in opioid use disorder patients, but it seems like the individuals with polysubstance use are largely ignored in the setting of the opioid epidemic.”
“And this is really the back story that got me inspired to study this particular topic,” he added.
Improve, nullify, or reverse?
Given these questions, the researchers set out to quantify the odds of nonfatal drug-related poisoning, including overdoses, associated with benzodiazepine or Z-drug use by patients with OUD who were also taking buprenorphine.
“While the drug-related poisoning variable encompasses opioid overdoses, we used a broad definition per CDC guidelines to also include other types of drug overdoses – including poisoning events involving stimulants, overdoses involving sedatives, and overdoses involving psychotropic prescription drugs” that are commonly used by patients with OUD, said Dr. Xu.
They also wanted to determine whether the use of benzodiazepines or Z-drugs would improve, nullify, or reverse the protective effect of buprenorphine. The researchers also evaluated whether different sedative and hypnotic subtypes of these drugs were associated with different poisoning risks.
The researchers analyzed pharmaceutical claims data from 304,676 individuals (aged 12-64 years) in the IBM MarketScan Commercial and Multi-State Medicaid Databases. All had received buprenorphine treatment for OUD between Jan. 1, 2006, and Dec. 31, 2016.
Buprenorphine use was converted to a daily milligram dose and was classified as either greater than 12 mg or less than or equal to 12 mg, because previous research suggests there may be differences in treatment retention associated with this dose. Given the case-control nature of the investigation, patients who did not experience a drug-related poisoning were excluded from the analysis.
The study’s primary unit of observation was person-days, which were those days during which patients were enrolled in a health insurance plan. Participants were evaluated for 1 year before their first drug-related poisoning and 1 year after their first such poisoning. The primary outcome was nonfatal drug-related poisonings, including overdoses. The primary exposure was determined on the basis of benzodiazepine or Z-drug prescriptions.
The daily dose of benzodiazepines or Z-drugs was standardized as a function of diazepam-equivalent milligrams. Doses were classified as either high dose (diazepam-equivalent mg dose >30 mg) or low dose (≤30 mg). The drugs were also distinguished on the basis of their pharmacologic properties, such as whether they were short-acting or long-acting.
37% risk reduction
Of the original cohort of 304,676 patients with OUD, the study’s final analytic sample included 23,036 patients (mean age, 30 years; 51% men), representing 14,213,075 person-days of insurance coverage. Of these, 2,210,927 person-days (15.6%) entailed claims for buprenorphine (mean daily dose, 15.4 mg; SD, 7.31 mg).
A total of 474,181 person-days included claims for benzodiazepines or Z-drugs with concurrent buprenorphine treatment. The mean daily dose of any benzodiazepine or Z-drug was 23.4 diazepam-milligram equivalents. The mean daily dose of short-acting benzodiazepines, long-acting benzodiazepines, and Z-drugs was 25.3, 31.3, and 4.9 diazepam-milligram equivalents, respectively.
Buprenorphine treatment days were associated with a 37% lower chance of drug-related poisoning (95% confidence interval, 0.60-0.66) in comparison with nontreatment days. On the other hand, the odds of poisoning increased by 81% on days on which patients were treated with Z-drugs or benzodiazepines (95% CI, 1.73-1.91).
Interestingly, individual analyses showed that benzodiazepine and Z-drug treatment days were associated with increased odds of poisoning events (odds ratio, 1.29; 95% CI, 1.19-1.39). Odds of poisoning events on benzodiazepine-only treatment days, on the other hand, were markedly lower (OR, 1.88; 95% CI, 1.78-1.98).
Subgroup analyses revealed that both short-acting and long-acting benzodiazepine treatment days were associated with comparably elevated odds of drug-related poisoning (OR, 1.86 and 1.68, respectively). High-dose benzodiazepine treatment days were associated with higher increased odds of a poisoning event (122%) in comparison with low-dose treatment days (78%).
High-dose, but not low-dose, benzodiazepine or Z-drug treatment was linked to increased poisonings when the drug was taken concurrently with buprenorphine (OR, 1.64; 95% CI, 1.39-1.93). However, the risk was still lower than the risk associated with taking the agents without concurrent treatment with buprenorphine (low-dose OR, 1.69; high-dose OR, 2.23).
‘Not all benzodiazepines are bad’
Dr. Xu noted that the findings have potentially important implications for clinical practice, beginning with the dose-dependent relationship between benzodiazepine/Z-drug use and drug-related poisonings among individuals with OUD. This indicates that lowering doses or shortening treatment duration may reduce risk, he said.
Similarly, the lower risk associated with long-acting benzodiazepines relative to short-acting beonzodiazepines – as well as the substantially lower risk associated with Z-drugs, compared with either short- or long-acting benzodiazepines – suggests that switching from benzodiazepines to long-acting agents or Z-drugs may lower the risk for overdose, he added.
“Clinicians are often challenged by patients with opioid use disorder who are also on benzodiazepines or Z-drugs. There’s an inclination to say no to them, because they’re too high risk to start buprenorphine maintenance, or abruptly taper the benzodiazepines, which can be very destabilizing,” he noted.
“Our data show that people on benzodiazepines can absolutely receive buprenorphine and still get some benefit,” Dr. Xu said. “In addition, not all benzodiazepines are bad for these individuals. There are safer formulations and safer doses, too.”
However, he added, he would not initiate benzodiazepine treatment if he didn’t have to, especially long-term treatment.
“One of the messages from our data is that this clearly contributes to higher overdose risk. But we often inherit patients who already have benzodiazepines on board, so we need to figure out what to do. That is the question that nobody had really clearly addressed prior to this study,” Dr. Xu concluded.
Vigilance needed
Commenting on the findings for this news organization, Jerrold F. Rosenbaum, MD, Stanley Cobb Professor of Psychiatry, Harvard Medical School, Boston, urged caution when combining benzodiazepines with opioids.
“There are situations where you need to be circumspect about the use of benzodiazepines, and that’s clearly when people are being prescribed them in combination with other drugs that could be either sedating or respiratory depressant,” said Dr. Rosenbaum, who was not involved with the research.
“This paper reminds us that physicians need to be particularly vigilant about situations where patients might be combining the two agents,” he added.
Dr. Rosenbaum noted that patients who are using more medication than prescribed are at risk “for not appreciating the synergy” between the two treatments in terms of adverse events such as respiratory depression.
In addition, “if they’re intending to do themselves harm, the lethality of an overdose will be certainly far more than the benzodiazepines or opiates alone,” he said.
Another potential challenge for clinicians are situations in which patients are taking benzodiazepines for preexisting conditions that also require opiates. “Then you have to use special vigilance and try to use lowest doses to reduce the total burden of medication to minimize the potential risk,” said Dr. Rosenbaum.
The study was funded by the National Institutes of Health. Dr. Xu has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Fauci worries about possible post–COVID-19 ‘mental health pandemic’
Anthony Fauci, MD, says he’s concerned about how Americans will react once the coronavirus pandemic is brought under control, CBS News reports.
Noting that an American Psychological Association survey showed people reporting high stress levels because of the pandemic, CBS’s Norah O’Donnell asked if Dr. Fauci was concerned about a possible “mental health pandemic.”
“Very much so,” Dr. Fauci, director of the National Institute of Allergy and Infectious Diseases and a top White House coronavirus adviser, replied.
“That’s the reason why I want to get the virological aspect of this pandemic behind us as quickly as we possibly can because the long-term ravages of this are so multifaceted,” Dr. Fauci said.
, he said.
“And then the other things: Not only the mental health effects, but many people have put off routine types of medical examinations that they normally would have done,” Dr. Fauci said.
“I hope we don’t see an increase in some preventable situations that would not have happened if people had the normal access to medical care, which clearly was interrupted by the shutdown associated with COVID-19,” he added.
The American Psychological Association released the survey results March 11 in what many people consider the 1-year anniversary of the start of the coronavirus pandemic.
“The prolonged stress experienced by adults, especially the high levels of stress reported by Americans directly linked to the pandemic, is seriously affecting mental and physical health, including changes to weight, sleep and alcohol use,” the APA said in a news release.
Some of the key findings of the survey include:
- 61% of respondents reported experiencing undesired weight changes since the start of the pandemic.
- 67% said their sleep habits changed, with 35% saying they slept more and 31% less.
- 23% reported drinking more alcohol to cope with stress.
- 47% said they delayed or canceled health care services because of the pandemic.
- 48% said their stress levels had increased.
A version of this article first appeared on Medscape.com.
Anthony Fauci, MD, says he’s concerned about how Americans will react once the coronavirus pandemic is brought under control, CBS News reports.
Noting that an American Psychological Association survey showed people reporting high stress levels because of the pandemic, CBS’s Norah O’Donnell asked if Dr. Fauci was concerned about a possible “mental health pandemic.”
“Very much so,” Dr. Fauci, director of the National Institute of Allergy and Infectious Diseases and a top White House coronavirus adviser, replied.
“That’s the reason why I want to get the virological aspect of this pandemic behind us as quickly as we possibly can because the long-term ravages of this are so multifaceted,” Dr. Fauci said.
, he said.
“And then the other things: Not only the mental health effects, but many people have put off routine types of medical examinations that they normally would have done,” Dr. Fauci said.
“I hope we don’t see an increase in some preventable situations that would not have happened if people had the normal access to medical care, which clearly was interrupted by the shutdown associated with COVID-19,” he added.
The American Psychological Association released the survey results March 11 in what many people consider the 1-year anniversary of the start of the coronavirus pandemic.
“The prolonged stress experienced by adults, especially the high levels of stress reported by Americans directly linked to the pandemic, is seriously affecting mental and physical health, including changes to weight, sleep and alcohol use,” the APA said in a news release.
Some of the key findings of the survey include:
- 61% of respondents reported experiencing undesired weight changes since the start of the pandemic.
- 67% said their sleep habits changed, with 35% saying they slept more and 31% less.
- 23% reported drinking more alcohol to cope with stress.
- 47% said they delayed or canceled health care services because of the pandemic.
- 48% said their stress levels had increased.
A version of this article first appeared on Medscape.com.
Anthony Fauci, MD, says he’s concerned about how Americans will react once the coronavirus pandemic is brought under control, CBS News reports.
Noting that an American Psychological Association survey showed people reporting high stress levels because of the pandemic, CBS’s Norah O’Donnell asked if Dr. Fauci was concerned about a possible “mental health pandemic.”
“Very much so,” Dr. Fauci, director of the National Institute of Allergy and Infectious Diseases and a top White House coronavirus adviser, replied.
“That’s the reason why I want to get the virological aspect of this pandemic behind us as quickly as we possibly can because the long-term ravages of this are so multifaceted,” Dr. Fauci said.
, he said.
“And then the other things: Not only the mental health effects, but many people have put off routine types of medical examinations that they normally would have done,” Dr. Fauci said.
“I hope we don’t see an increase in some preventable situations that would not have happened if people had the normal access to medical care, which clearly was interrupted by the shutdown associated with COVID-19,” he added.
The American Psychological Association released the survey results March 11 in what many people consider the 1-year anniversary of the start of the coronavirus pandemic.
“The prolonged stress experienced by adults, especially the high levels of stress reported by Americans directly linked to the pandemic, is seriously affecting mental and physical health, including changes to weight, sleep and alcohol use,” the APA said in a news release.
Some of the key findings of the survey include:
- 61% of respondents reported experiencing undesired weight changes since the start of the pandemic.
- 67% said their sleep habits changed, with 35% saying they slept more and 31% less.
- 23% reported drinking more alcohol to cope with stress.
- 47% said they delayed or canceled health care services because of the pandemic.
- 48% said their stress levels had increased.
A version of this article first appeared on Medscape.com.
The siesta solution
Are you a napper? Unless you’re retired that may sound like a ridiculous question. When could you possibly fit in the time to doze off for even 20 minutes? I suspect there may be one or two of you who, although you are still working, have found a way to schedule a nap into your schedules. The rest of us must wait until we no longer have clinical responsibilities.
In my experience, you regular nappers seem to be the lucky few who have discovered the art of nodding off after lunch and waking up refreshed and ready to take on a full afternoon of patients. We in the unlucky majority may have tried taking a nap but run the risk of its flowing into a deep slumber the length of which we can’t control. Or, more likely, we find that we wake feeling groggy and disoriented and, even worse, the daytime nod off has messed up our nighttime schedule.
Well, it turns out the ability to take daytime naps and reap their cardiometabolic benefits is not just luck but has a significant genetic component. Investigators at Massachusetts General Hospital in Boston have recently published a study in which they report finding more than a score of gene regions that determine a person’s propensity to take daytime naps.. The researchers have also unearthed preliminary evidence supporting a link between daytime napping and cardiometabolic health. My mother began napping when my sister and I were infants and never gave it up. Unfortunately, I seem to have ended up on the wrong side of the genomic shuffle.
Although this new research is interesting, I don’t think the investigators have enough information to answer one of the questions that every pediatrician fields multiple times each week. “When should my toddler grow out of his afternoon nap?” Although it looks like we may be getting closer to a gene-based answer, I have always couched my reply in terms of behavior modification and the fostering of habit-forming associations.
As a child begins to transition from multiple short naps interspersed with feedings to a pattern of two distinct naps, I suggest to parents that they begin to think of the afternoon nap as a siesta. In other words, the nap is something that always comes immediately after lunch with no intervening shenanigans. No playtime, no Teletubbies videos, no quick trips to the grocery store, nothing, nada, zip.
At least for me, lunch has always been soporific. And I suspect we will learn eventually that association cuts across the entire genetic landscape to one degree or another. It makes sense to take advantage of that association and remove all other distractions. For some parents, that means creating the illusion that they too are taking a siesta: No TV, no phone calls. Imagine that the whole household has suddenly moved to Spain for the next hour or two. If you’ve ever been a tourist in rural Spain and tried to do anything, buy anything, or visit a museum between 2 and 4 p.m. you’ve got the idea.
When the child is young he or she will probably fall asleep as long as his parents have been reasonably successful at maintaining sleep hygiene practices. As the child is gaining more stamina and gives up the morning nap, the siesta will remain as a quiet time because that’s the way it’s always been in the household. The child may sleep or play quietly, or be read a sleep-inducing story because no other options will be available until some predetermined time. An hour is usually reasonable. If sleep hasn’t overtaken them, an earlier bedtime will probably be in order. The child will outgrow the napping part of the siesta when his or her sleep need is gone. But, the siesta/quiet time can remain as an option until all-day school intervenes. This scheme works if you can get parents to appropriately prioritize their child’s sleep needs. That’s not always an easy sell.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Are you a napper? Unless you’re retired that may sound like a ridiculous question. When could you possibly fit in the time to doze off for even 20 minutes? I suspect there may be one or two of you who, although you are still working, have found a way to schedule a nap into your schedules. The rest of us must wait until we no longer have clinical responsibilities.
In my experience, you regular nappers seem to be the lucky few who have discovered the art of nodding off after lunch and waking up refreshed and ready to take on a full afternoon of patients. We in the unlucky majority may have tried taking a nap but run the risk of its flowing into a deep slumber the length of which we can’t control. Or, more likely, we find that we wake feeling groggy and disoriented and, even worse, the daytime nod off has messed up our nighttime schedule.
Well, it turns out the ability to take daytime naps and reap their cardiometabolic benefits is not just luck but has a significant genetic component. Investigators at Massachusetts General Hospital in Boston have recently published a study in which they report finding more than a score of gene regions that determine a person’s propensity to take daytime naps.. The researchers have also unearthed preliminary evidence supporting a link between daytime napping and cardiometabolic health. My mother began napping when my sister and I were infants and never gave it up. Unfortunately, I seem to have ended up on the wrong side of the genomic shuffle.
Although this new research is interesting, I don’t think the investigators have enough information to answer one of the questions that every pediatrician fields multiple times each week. “When should my toddler grow out of his afternoon nap?” Although it looks like we may be getting closer to a gene-based answer, I have always couched my reply in terms of behavior modification and the fostering of habit-forming associations.
As a child begins to transition from multiple short naps interspersed with feedings to a pattern of two distinct naps, I suggest to parents that they begin to think of the afternoon nap as a siesta. In other words, the nap is something that always comes immediately after lunch with no intervening shenanigans. No playtime, no Teletubbies videos, no quick trips to the grocery store, nothing, nada, zip.
At least for me, lunch has always been soporific. And I suspect we will learn eventually that association cuts across the entire genetic landscape to one degree or another. It makes sense to take advantage of that association and remove all other distractions. For some parents, that means creating the illusion that they too are taking a siesta: No TV, no phone calls. Imagine that the whole household has suddenly moved to Spain for the next hour or two. If you’ve ever been a tourist in rural Spain and tried to do anything, buy anything, or visit a museum between 2 and 4 p.m. you’ve got the idea.
When the child is young he or she will probably fall asleep as long as his parents have been reasonably successful at maintaining sleep hygiene practices. As the child is gaining more stamina and gives up the morning nap, the siesta will remain as a quiet time because that’s the way it’s always been in the household. The child may sleep or play quietly, or be read a sleep-inducing story because no other options will be available until some predetermined time. An hour is usually reasonable. If sleep hasn’t overtaken them, an earlier bedtime will probably be in order. The child will outgrow the napping part of the siesta when his or her sleep need is gone. But, the siesta/quiet time can remain as an option until all-day school intervenes. This scheme works if you can get parents to appropriately prioritize their child’s sleep needs. That’s not always an easy sell.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Are you a napper? Unless you’re retired that may sound like a ridiculous question. When could you possibly fit in the time to doze off for even 20 minutes? I suspect there may be one or two of you who, although you are still working, have found a way to schedule a nap into your schedules. The rest of us must wait until we no longer have clinical responsibilities.
In my experience, you regular nappers seem to be the lucky few who have discovered the art of nodding off after lunch and waking up refreshed and ready to take on a full afternoon of patients. We in the unlucky majority may have tried taking a nap but run the risk of its flowing into a deep slumber the length of which we can’t control. Or, more likely, we find that we wake feeling groggy and disoriented and, even worse, the daytime nod off has messed up our nighttime schedule.
Well, it turns out the ability to take daytime naps and reap their cardiometabolic benefits is not just luck but has a significant genetic component. Investigators at Massachusetts General Hospital in Boston have recently published a study in which they report finding more than a score of gene regions that determine a person’s propensity to take daytime naps.. The researchers have also unearthed preliminary evidence supporting a link between daytime napping and cardiometabolic health. My mother began napping when my sister and I were infants and never gave it up. Unfortunately, I seem to have ended up on the wrong side of the genomic shuffle.
Although this new research is interesting, I don’t think the investigators have enough information to answer one of the questions that every pediatrician fields multiple times each week. “When should my toddler grow out of his afternoon nap?” Although it looks like we may be getting closer to a gene-based answer, I have always couched my reply in terms of behavior modification and the fostering of habit-forming associations.
As a child begins to transition from multiple short naps interspersed with feedings to a pattern of two distinct naps, I suggest to parents that they begin to think of the afternoon nap as a siesta. In other words, the nap is something that always comes immediately after lunch with no intervening shenanigans. No playtime, no Teletubbies videos, no quick trips to the grocery store, nothing, nada, zip.
At least for me, lunch has always been soporific. And I suspect we will learn eventually that association cuts across the entire genetic landscape to one degree or another. It makes sense to take advantage of that association and remove all other distractions. For some parents, that means creating the illusion that they too are taking a siesta: No TV, no phone calls. Imagine that the whole household has suddenly moved to Spain for the next hour or two. If you’ve ever been a tourist in rural Spain and tried to do anything, buy anything, or visit a museum between 2 and 4 p.m. you’ve got the idea.
When the child is young he or she will probably fall asleep as long as his parents have been reasonably successful at maintaining sleep hygiene practices. As the child is gaining more stamina and gives up the morning nap, the siesta will remain as a quiet time because that’s the way it’s always been in the household. The child may sleep or play quietly, or be read a sleep-inducing story because no other options will be available until some predetermined time. An hour is usually reasonable. If sleep hasn’t overtaken them, an earlier bedtime will probably be in order. The child will outgrow the napping part of the siesta when his or her sleep need is gone. But, the siesta/quiet time can remain as an option until all-day school intervenes. This scheme works if you can get parents to appropriately prioritize their child’s sleep needs. That’s not always an easy sell.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Traumatic brain injury tied to long-term sleep problems
Veterans who have suffered a traumatic brain injury (TBI) are significantly more likely to develop insomnia and other sleep problems years later compared to their counterparts who have not suffered a brain injury, a new study shows.
Results of a large longitudinal study show that those with TBI were about 40% more likely to develop insomnia, sleep apnea, excessive daytime sleepiness, or another sleep disorder in later years, after adjusting for demographics and medical and psychiatric conditions.
Interestingly, the association with sleep disorders was strongest among those with mild TBI versus a more severe brain injury.
The study showed that the risk for sleep disorders increased up to 14 years after a brain injury, an indicator that “clinicians should really pay attention to sleep disorders in TBI patients both in the short term and the long term,” study investigator Yue Leng, MD, PhD, assistant professor, department of psychiatry and behavioral sciences, University of California, San Francisco, told this news organization.
The study was published online March 3 in Neurology.
First long-term look
TBI is common among veterans, who may have sleep complaints or psychiatric symptoms, but previous studies into the consequences of TBI have examined the short- vs. long-term impact, said Dr. Leng.
To examine the longitudinal association between TBI and sleep disorders, the investigators examined data on 98,709 Veterans Health Administration patients diagnosed with TBI and an age-matched group of the same number of veterans who had not received such a diagnosis. The mean age of the participants was 49 years at baseline, and 11.7% were women. Of the TBI cases, 49.6% were mild.
Researchers used an exposure survey and diagnostic codes to establish TBI and its severity.
Patients with TBI were more likely to be male and were much more likely to have a psychiatric condition, such as a mood disorder (22.4% vs. 9.3%), anxiety (10.5% vs. 4.4%), posttraumatic stress disorder (19.5% vs. 4.4%), or substance abuse (11.4% vs. 5.2%). They were also more likely to smoke or use tobacco (13.5% vs. 8.7%).
Researchers assessed a number of sleep disorders, including insomnia, hypersomnia disorders, narcolepsy, sleep-related breathing disorders, and sleep-related movement disorders.
During a follow-up period that averaged 5 years but ranged up to 14 years, 23.4% of veterans with TBI and 15.8% of those without TBI developed a sleep disorder.
After adjusting for age, sex, race, education, and income, those who had suffered a TBI were 50% more likely to develop any sleep disorder, compared with those who had not had a TBI (hazard ratio, 1.50; 95% confidence interval, 1.47-1.53.)
After controlling for medical conditions that included diabetes, hypertension, myocardial infarction, and cerebrovascular disease, as well as psychiatric disorders such as mood disorders, anxiety, PTSD, substance use disorder, and tobacco use, the HR for developing a sleep disorder was 1.41 (95% CI, 1.37-1.44).
The association with TBI was stronger for some sleep disorders. Adjusted HRs were 1.50 (95% CI, 1.45-1.55) for insomnia, 1.50 (95% CI, 1.39-1.61) for hypersomnia, 1.33 (95% CI, 1.16-1.52) for sleep-related movement disorders, and 1.28 (95% CI, 1.24-1.32) for sleep apnea.
It’s unclear what causes postinjury sleep problems, but it could be that TBI induces structural brain damage, or it could affect melatonin secretion or wake-promoting neurons.
Damage to arousal-promoting neurons could help explain the reason the link between TBI and sleep disorders was strongest for insomnia and hypersomnia, although the exact mechanism is unclear, said Dr. Leng.
Greater risk with mild TBI
Overall, the association was stronger for mild TBI than for moderate to severe TBI. This, said Dr. Leng, might be because of differences in the brain injury mechanism.
Mild TBI often involves repetitive concussive or subconcussive injuries, such as sports injuries or blast injury among active-duty military personnel. This type of injury is more likely to cause diffuse axonal injury and inflammation, whereas moderate or severe TBI is often attributable to a direct blow with more focal but severe damage, explained Dr. Leng.
She noted that veterans with mild TBI were more likely to have a psychiatric condition, but because the study controlled for such conditions, this doesn’t fully explain the stronger association between mild TBI and sleep disorders.
Further studies are needed to sort out the exact mechanisms, she said.
The association between TBI and risk for sleep disorders was reduced somewhat but was still moderate in an analysis that excluded patients who developed a sleep disorder within 2 years of a brain injury.
This analysis, said Dr. Leng, helped ensure that the sleep disorder developed after the brain injury.
The researchers could not examine the trajectory of sleep problems, so it’s not clear whether sleep problems worsen or get better over time, said Dr. Leng.
Because PTSD also leads to sleep problems, the researchers thought that having both PTSD and TBI might increase the risk for sleep problems. “But actually we found the association was pretty similar in those with, and without, PTSD, so that was kind of contrary to our hypothesis,” she said.
The new results underline the need for more screening for sleep disorders among patients with TBI, both in the short term and the long term, said Dr. Leng. “Clinicians should ask TBI patients about their sleep, and they should follow that up,” she said.
She added that long-term sleep disorders can affect a patient’s health and can lead to psychiatric problems and neurodegenerative diseases.
Depending on the type of sleep disorder, there are a number of possible treatments. For example, for patients with sleep apnea, continuous positive airway pressure treatment may be considered.
‘Outstanding’ research
Commenting for this news organization, Frank Conidi, MD, director, Florida Center for Headache and Sports Neurology; CEO, Brainsport, Team Neurologist, the Florida Panthers of the National Hockey League; and past president, Florida Society of Neurology, said the study is “by far” the largest to investigate the correlation between sleep disorders and head trauma.
The design and outcome measures “were well thought out,” and the researchers “did an outstanding job in sorting through and analyzing the data,” said Dr. Conidi.
He added that he was particularly impressed with how the researchers addressed PTSD, which is highly prevalent among veterans with head trauma and is known to affect sleep.
The new results “solidify what those of us who see individuals with TBI have observed over the years: that there is a higher incidence of all types of sleep disorders” in individuals with a TBI, said Dr. Conidi.
However, he questioned the study’s use of guidelines to classify the various types of head trauma. These guidelines, he said, “are based on loss of consciousness, which we have started to move away from when classifying TBI.”
In addition, Dr. Conidi said he “would have loved to have seen” some correlation with neuroimaging studies, such as those used to assess subdural hematoma, epidural hematoma, subarachnoid hemorrhage, and diffuse axonal injury, but that this “could be an impetus for future studies.”
In “a perfect world,” all patients with a TBI would undergo a polysomnography study in a sleep laboratory, but insurance companies now rarely cover such studies and have attempted to have clinicians shift to home sleep studies, said Dr. Conidi. “These are marginal at best for screening for sleep disorders,” he noted.
At his centers, every TBI patient is screened for sleep disorders and, whenever possible, undergoes formal evaluation in the sleep lab, he added.
The study was supported by the U.S. Army Medical Research and Material Command and the U.S. Department of Veterans Affairs. Dr. Leng and Dr. Conidi have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Veterans who have suffered a traumatic brain injury (TBI) are significantly more likely to develop insomnia and other sleep problems years later compared to their counterparts who have not suffered a brain injury, a new study shows.
Results of a large longitudinal study show that those with TBI were about 40% more likely to develop insomnia, sleep apnea, excessive daytime sleepiness, or another sleep disorder in later years, after adjusting for demographics and medical and psychiatric conditions.
Interestingly, the association with sleep disorders was strongest among those with mild TBI versus a more severe brain injury.
The study showed that the risk for sleep disorders increased up to 14 years after a brain injury, an indicator that “clinicians should really pay attention to sleep disorders in TBI patients both in the short term and the long term,” study investigator Yue Leng, MD, PhD, assistant professor, department of psychiatry and behavioral sciences, University of California, San Francisco, told this news organization.
The study was published online March 3 in Neurology.
First long-term look
TBI is common among veterans, who may have sleep complaints or psychiatric symptoms, but previous studies into the consequences of TBI have examined the short- vs. long-term impact, said Dr. Leng.
To examine the longitudinal association between TBI and sleep disorders, the investigators examined data on 98,709 Veterans Health Administration patients diagnosed with TBI and an age-matched group of the same number of veterans who had not received such a diagnosis. The mean age of the participants was 49 years at baseline, and 11.7% were women. Of the TBI cases, 49.6% were mild.
Researchers used an exposure survey and diagnostic codes to establish TBI and its severity.
Patients with TBI were more likely to be male and were much more likely to have a psychiatric condition, such as a mood disorder (22.4% vs. 9.3%), anxiety (10.5% vs. 4.4%), posttraumatic stress disorder (19.5% vs. 4.4%), or substance abuse (11.4% vs. 5.2%). They were also more likely to smoke or use tobacco (13.5% vs. 8.7%).
Researchers assessed a number of sleep disorders, including insomnia, hypersomnia disorders, narcolepsy, sleep-related breathing disorders, and sleep-related movement disorders.
During a follow-up period that averaged 5 years but ranged up to 14 years, 23.4% of veterans with TBI and 15.8% of those without TBI developed a sleep disorder.
After adjusting for age, sex, race, education, and income, those who had suffered a TBI were 50% more likely to develop any sleep disorder, compared with those who had not had a TBI (hazard ratio, 1.50; 95% confidence interval, 1.47-1.53.)
After controlling for medical conditions that included diabetes, hypertension, myocardial infarction, and cerebrovascular disease, as well as psychiatric disorders such as mood disorders, anxiety, PTSD, substance use disorder, and tobacco use, the HR for developing a sleep disorder was 1.41 (95% CI, 1.37-1.44).
The association with TBI was stronger for some sleep disorders. Adjusted HRs were 1.50 (95% CI, 1.45-1.55) for insomnia, 1.50 (95% CI, 1.39-1.61) for hypersomnia, 1.33 (95% CI, 1.16-1.52) for sleep-related movement disorders, and 1.28 (95% CI, 1.24-1.32) for sleep apnea.
It’s unclear what causes postinjury sleep problems, but it could be that TBI induces structural brain damage, or it could affect melatonin secretion or wake-promoting neurons.
Damage to arousal-promoting neurons could help explain the reason the link between TBI and sleep disorders was strongest for insomnia and hypersomnia, although the exact mechanism is unclear, said Dr. Leng.
Greater risk with mild TBI
Overall, the association was stronger for mild TBI than for moderate to severe TBI. This, said Dr. Leng, might be because of differences in the brain injury mechanism.
Mild TBI often involves repetitive concussive or subconcussive injuries, such as sports injuries or blast injury among active-duty military personnel. This type of injury is more likely to cause diffuse axonal injury and inflammation, whereas moderate or severe TBI is often attributable to a direct blow with more focal but severe damage, explained Dr. Leng.
She noted that veterans with mild TBI were more likely to have a psychiatric condition, but because the study controlled for such conditions, this doesn’t fully explain the stronger association between mild TBI and sleep disorders.
Further studies are needed to sort out the exact mechanisms, she said.
The association between TBI and risk for sleep disorders was reduced somewhat but was still moderate in an analysis that excluded patients who developed a sleep disorder within 2 years of a brain injury.
This analysis, said Dr. Leng, helped ensure that the sleep disorder developed after the brain injury.
The researchers could not examine the trajectory of sleep problems, so it’s not clear whether sleep problems worsen or get better over time, said Dr. Leng.
Because PTSD also leads to sleep problems, the researchers thought that having both PTSD and TBI might increase the risk for sleep problems. “But actually we found the association was pretty similar in those with, and without, PTSD, so that was kind of contrary to our hypothesis,” she said.
The new results underline the need for more screening for sleep disorders among patients with TBI, both in the short term and the long term, said Dr. Leng. “Clinicians should ask TBI patients about their sleep, and they should follow that up,” she said.
She added that long-term sleep disorders can affect a patient’s health and can lead to psychiatric problems and neurodegenerative diseases.
Depending on the type of sleep disorder, there are a number of possible treatments. For example, for patients with sleep apnea, continuous positive airway pressure treatment may be considered.
‘Outstanding’ research
Commenting for this news organization, Frank Conidi, MD, director, Florida Center for Headache and Sports Neurology; CEO, Brainsport, Team Neurologist, the Florida Panthers of the National Hockey League; and past president, Florida Society of Neurology, said the study is “by far” the largest to investigate the correlation between sleep disorders and head trauma.
The design and outcome measures “were well thought out,” and the researchers “did an outstanding job in sorting through and analyzing the data,” said Dr. Conidi.
He added that he was particularly impressed with how the researchers addressed PTSD, which is highly prevalent among veterans with head trauma and is known to affect sleep.
The new results “solidify what those of us who see individuals with TBI have observed over the years: that there is a higher incidence of all types of sleep disorders” in individuals with a TBI, said Dr. Conidi.
However, he questioned the study’s use of guidelines to classify the various types of head trauma. These guidelines, he said, “are based on loss of consciousness, which we have started to move away from when classifying TBI.”
In addition, Dr. Conidi said he “would have loved to have seen” some correlation with neuroimaging studies, such as those used to assess subdural hematoma, epidural hematoma, subarachnoid hemorrhage, and diffuse axonal injury, but that this “could be an impetus for future studies.”
In “a perfect world,” all patients with a TBI would undergo a polysomnography study in a sleep laboratory, but insurance companies now rarely cover such studies and have attempted to have clinicians shift to home sleep studies, said Dr. Conidi. “These are marginal at best for screening for sleep disorders,” he noted.
At his centers, every TBI patient is screened for sleep disorders and, whenever possible, undergoes formal evaluation in the sleep lab, he added.
The study was supported by the U.S. Army Medical Research and Material Command and the U.S. Department of Veterans Affairs. Dr. Leng and Dr. Conidi have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Veterans who have suffered a traumatic brain injury (TBI) are significantly more likely to develop insomnia and other sleep problems years later compared to their counterparts who have not suffered a brain injury, a new study shows.
Results of a large longitudinal study show that those with TBI were about 40% more likely to develop insomnia, sleep apnea, excessive daytime sleepiness, or another sleep disorder in later years, after adjusting for demographics and medical and psychiatric conditions.
Interestingly, the association with sleep disorders was strongest among those with mild TBI versus a more severe brain injury.
The study showed that the risk for sleep disorders increased up to 14 years after a brain injury, an indicator that “clinicians should really pay attention to sleep disorders in TBI patients both in the short term and the long term,” study investigator Yue Leng, MD, PhD, assistant professor, department of psychiatry and behavioral sciences, University of California, San Francisco, told this news organization.
The study was published online March 3 in Neurology.
First long-term look
TBI is common among veterans, who may have sleep complaints or psychiatric symptoms, but previous studies into the consequences of TBI have examined the short- vs. long-term impact, said Dr. Leng.
To examine the longitudinal association between TBI and sleep disorders, the investigators examined data on 98,709 Veterans Health Administration patients diagnosed with TBI and an age-matched group of the same number of veterans who had not received such a diagnosis. The mean age of the participants was 49 years at baseline, and 11.7% were women. Of the TBI cases, 49.6% were mild.
Researchers used an exposure survey and diagnostic codes to establish TBI and its severity.
Patients with TBI were more likely to be male and were much more likely to have a psychiatric condition, such as a mood disorder (22.4% vs. 9.3%), anxiety (10.5% vs. 4.4%), posttraumatic stress disorder (19.5% vs. 4.4%), or substance abuse (11.4% vs. 5.2%). They were also more likely to smoke or use tobacco (13.5% vs. 8.7%).
Researchers assessed a number of sleep disorders, including insomnia, hypersomnia disorders, narcolepsy, sleep-related breathing disorders, and sleep-related movement disorders.
During a follow-up period that averaged 5 years but ranged up to 14 years, 23.4% of veterans with TBI and 15.8% of those without TBI developed a sleep disorder.
After adjusting for age, sex, race, education, and income, those who had suffered a TBI were 50% more likely to develop any sleep disorder, compared with those who had not had a TBI (hazard ratio, 1.50; 95% confidence interval, 1.47-1.53.)
After controlling for medical conditions that included diabetes, hypertension, myocardial infarction, and cerebrovascular disease, as well as psychiatric disorders such as mood disorders, anxiety, PTSD, substance use disorder, and tobacco use, the HR for developing a sleep disorder was 1.41 (95% CI, 1.37-1.44).
The association with TBI was stronger for some sleep disorders. Adjusted HRs were 1.50 (95% CI, 1.45-1.55) for insomnia, 1.50 (95% CI, 1.39-1.61) for hypersomnia, 1.33 (95% CI, 1.16-1.52) for sleep-related movement disorders, and 1.28 (95% CI, 1.24-1.32) for sleep apnea.
It’s unclear what causes postinjury sleep problems, but it could be that TBI induces structural brain damage, or it could affect melatonin secretion or wake-promoting neurons.
Damage to arousal-promoting neurons could help explain the reason the link between TBI and sleep disorders was strongest for insomnia and hypersomnia, although the exact mechanism is unclear, said Dr. Leng.
Greater risk with mild TBI
Overall, the association was stronger for mild TBI than for moderate to severe TBI. This, said Dr. Leng, might be because of differences in the brain injury mechanism.
Mild TBI often involves repetitive concussive or subconcussive injuries, such as sports injuries or blast injury among active-duty military personnel. This type of injury is more likely to cause diffuse axonal injury and inflammation, whereas moderate or severe TBI is often attributable to a direct blow with more focal but severe damage, explained Dr. Leng.
She noted that veterans with mild TBI were more likely to have a psychiatric condition, but because the study controlled for such conditions, this doesn’t fully explain the stronger association between mild TBI and sleep disorders.
Further studies are needed to sort out the exact mechanisms, she said.
The association between TBI and risk for sleep disorders was reduced somewhat but was still moderate in an analysis that excluded patients who developed a sleep disorder within 2 years of a brain injury.
This analysis, said Dr. Leng, helped ensure that the sleep disorder developed after the brain injury.
The researchers could not examine the trajectory of sleep problems, so it’s not clear whether sleep problems worsen or get better over time, said Dr. Leng.
Because PTSD also leads to sleep problems, the researchers thought that having both PTSD and TBI might increase the risk for sleep problems. “But actually we found the association was pretty similar in those with, and without, PTSD, so that was kind of contrary to our hypothesis,” she said.
The new results underline the need for more screening for sleep disorders among patients with TBI, both in the short term and the long term, said Dr. Leng. “Clinicians should ask TBI patients about their sleep, and they should follow that up,” she said.
She added that long-term sleep disorders can affect a patient’s health and can lead to psychiatric problems and neurodegenerative diseases.
Depending on the type of sleep disorder, there are a number of possible treatments. For example, for patients with sleep apnea, continuous positive airway pressure treatment may be considered.
‘Outstanding’ research
Commenting for this news organization, Frank Conidi, MD, director, Florida Center for Headache and Sports Neurology; CEO, Brainsport, Team Neurologist, the Florida Panthers of the National Hockey League; and past president, Florida Society of Neurology, said the study is “by far” the largest to investigate the correlation between sleep disorders and head trauma.
The design and outcome measures “were well thought out,” and the researchers “did an outstanding job in sorting through and analyzing the data,” said Dr. Conidi.
He added that he was particularly impressed with how the researchers addressed PTSD, which is highly prevalent among veterans with head trauma and is known to affect sleep.
The new results “solidify what those of us who see individuals with TBI have observed over the years: that there is a higher incidence of all types of sleep disorders” in individuals with a TBI, said Dr. Conidi.
However, he questioned the study’s use of guidelines to classify the various types of head trauma. These guidelines, he said, “are based on loss of consciousness, which we have started to move away from when classifying TBI.”
In addition, Dr. Conidi said he “would have loved to have seen” some correlation with neuroimaging studies, such as those used to assess subdural hematoma, epidural hematoma, subarachnoid hemorrhage, and diffuse axonal injury, but that this “could be an impetus for future studies.”
In “a perfect world,” all patients with a TBI would undergo a polysomnography study in a sleep laboratory, but insurance companies now rarely cover such studies and have attempted to have clinicians shift to home sleep studies, said Dr. Conidi. “These are marginal at best for screening for sleep disorders,” he noted.
At his centers, every TBI patient is screened for sleep disorders and, whenever possible, undergoes formal evaluation in the sleep lab, he added.
The study was supported by the U.S. Army Medical Research and Material Command and the U.S. Department of Veterans Affairs. Dr. Leng and Dr. Conidi have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Smartphone ‘addiction’ tied to poor sleep in young adults
Smartphone “addiction” may explain poor sleep quality in a significant proportion of young adults, new research suggests.
Investigators found that almost 40% of adults aged 18-30 years who self-reported excessive smartphone use also reported poor sleep.
“Our study provides further support to the growing body of evidence that smartphone addiction has a deleterious impact on sleep,” wrote the researchers.
The study was published online March 2 in Frontiers of Psychiatry.
Not a clinical diagnosis
Smartphone addiction is not formally recognized as a clinical diagnosis, but it’s an “active” area of research, lead investigator Ben Carter, PhD, King’s College London, noted in the report.
In a cross-sectional survey, 1,043 college students (aged 18-30 years, 73% women) completed the 10-question validated Smartphone Addiction Scale Short Version (SAS-SV) and the adapted Pittsburgh Sleep Quality Score Index.
On the SAS-SV, 406 students (38.9%) reported “addiction” to their smartphones. This estimated prevalence is consistent with other reported studies in young adult populations globally, which is in the range of 30%-45%, the researchers noted.
Overall, 61.6% of participants surveyed reported poor sleep; among those who reported smartphone addiction, 68.7% had poor sleep quality, vs. 57.1% of those who did not report smartphone addiction.
In multivariable analysis that adjusted for a variety of relevant factors, among those for whom there was evidence of smartphone addiction, the odds of poor sleep were increased by 41% (adjusted odds ratio [aOR] = 1.41; 95% confidence interval, 1.06-1.87, P = .018).
The findings also suggest that a greater amount of time spent using the phone and greater use late at night can raise the risk for smartphone addiction.
“Should smartphone addiction become firmly established as a focus of clinical concern, those using their phones after midnight or using their phones for four or more hours per day are likely to be at high risk, and should guide administration of the SAS-SV,” the researchers wrote.
Caveats, cautions, and concerns
Reached for comment, Paul Weigle, MD, psychiatrist with Hartford HealthCare and Hartford (Conn.) Hospital, and member of the American Academy of Child and Adolescent Psychiatry, said the finding of a relationship between addictive smartphone usage and poor sleep quality is not surprising.
“Great increases in adolescent screen media habits in recent decades have seen a concurrent increase in rates of insomnia among this population,” he said in an interview.
Dr. Weigle also noted that young people who use the phone excessively often do so in bed, “which decreases sleep onset by disrupting conditioning (the tendency for our bodies to relate bed with sleep) and by increasing physiological arousal, which makes it more difficult to fall asleep. The blue light from smartphones used at night disrupts our body’s natural circadian rhythms, confusing our brains regarding whether it is night or day, and further worsens sleep.”
Dr. Weigle said in an interview that some of his patients come to him seeking sleep medications, although the best treatment is to perform a “smartphone-ectomy” every evening.
Teenage patients will “beg, borrow, or steal” to be allowed to keep their phones by the bed with the promise not to use them overnight. Three-quarters of the time, when the parents are able to charge the phone in another room, “the sleep problem resolves,” Dr. Weigle said.
One caveat, he said, is that it’s “somewhat unclear whether this is best classified as an addiction or simply a seriously problematic habit. Either way, this type of habit causes a great deal of distress and dysfunction in the lives of those it affects, so it is important to understand,” he said.
In a statement, Bob Patton, PhD, lecturer in clinical psychology, University of Surrey, Guildford, England, noted that this is a cross-sectional study “and as such cannot lead to any firm conclusions about phone usage as the cause of reduced sleep quality.
“It does, however, provide some compelling evidence,” Dr. Patton said, “that the nature of smartphone usage and its related consequences are important considerations in addressing the emerging phenomenon of ‘smartphone addiction.’ ”
Also weighing in, Andrew Przybylski, PhD, director of research, Oxford (England) Internet Institute, University of Oxford, said by any global health body and is not a psychiatric disorder.
“The study is a correlational analysis of a sample of participants recruited on university campuses and therefore only reflects the experiences of those who had the purpose of the study explained to them. It can say nothing about behaviors in the general population,” Dr. Przybylski said in a statement.
“Readers should be cautious of making any firm conclusions about the impact of smartphone use in the general population, or the idea that they’re addictive in any objective sense, on the basis of this work,” he added. The study had no specific funding. Dr. Carter, Dr. Weigle, Dr. Patton, and Dr. Przybylski have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Smartphone “addiction” may explain poor sleep quality in a significant proportion of young adults, new research suggests.
Investigators found that almost 40% of adults aged 18-30 years who self-reported excessive smartphone use also reported poor sleep.
“Our study provides further support to the growing body of evidence that smartphone addiction has a deleterious impact on sleep,” wrote the researchers.
The study was published online March 2 in Frontiers of Psychiatry.
Not a clinical diagnosis
Smartphone addiction is not formally recognized as a clinical diagnosis, but it’s an “active” area of research, lead investigator Ben Carter, PhD, King’s College London, noted in the report.
In a cross-sectional survey, 1,043 college students (aged 18-30 years, 73% women) completed the 10-question validated Smartphone Addiction Scale Short Version (SAS-SV) and the adapted Pittsburgh Sleep Quality Score Index.
On the SAS-SV, 406 students (38.9%) reported “addiction” to their smartphones. This estimated prevalence is consistent with other reported studies in young adult populations globally, which is in the range of 30%-45%, the researchers noted.
Overall, 61.6% of participants surveyed reported poor sleep; among those who reported smartphone addiction, 68.7% had poor sleep quality, vs. 57.1% of those who did not report smartphone addiction.
In multivariable analysis that adjusted for a variety of relevant factors, among those for whom there was evidence of smartphone addiction, the odds of poor sleep were increased by 41% (adjusted odds ratio [aOR] = 1.41; 95% confidence interval, 1.06-1.87, P = .018).
The findings also suggest that a greater amount of time spent using the phone and greater use late at night can raise the risk for smartphone addiction.
“Should smartphone addiction become firmly established as a focus of clinical concern, those using their phones after midnight or using their phones for four or more hours per day are likely to be at high risk, and should guide administration of the SAS-SV,” the researchers wrote.
Caveats, cautions, and concerns
Reached for comment, Paul Weigle, MD, psychiatrist with Hartford HealthCare and Hartford (Conn.) Hospital, and member of the American Academy of Child and Adolescent Psychiatry, said the finding of a relationship between addictive smartphone usage and poor sleep quality is not surprising.
“Great increases in adolescent screen media habits in recent decades have seen a concurrent increase in rates of insomnia among this population,” he said in an interview.
Dr. Weigle also noted that young people who use the phone excessively often do so in bed, “which decreases sleep onset by disrupting conditioning (the tendency for our bodies to relate bed with sleep) and by increasing physiological arousal, which makes it more difficult to fall asleep. The blue light from smartphones used at night disrupts our body’s natural circadian rhythms, confusing our brains regarding whether it is night or day, and further worsens sleep.”
Dr. Weigle said in an interview that some of his patients come to him seeking sleep medications, although the best treatment is to perform a “smartphone-ectomy” every evening.
Teenage patients will “beg, borrow, or steal” to be allowed to keep their phones by the bed with the promise not to use them overnight. Three-quarters of the time, when the parents are able to charge the phone in another room, “the sleep problem resolves,” Dr. Weigle said.
One caveat, he said, is that it’s “somewhat unclear whether this is best classified as an addiction or simply a seriously problematic habit. Either way, this type of habit causes a great deal of distress and dysfunction in the lives of those it affects, so it is important to understand,” he said.
In a statement, Bob Patton, PhD, lecturer in clinical psychology, University of Surrey, Guildford, England, noted that this is a cross-sectional study “and as such cannot lead to any firm conclusions about phone usage as the cause of reduced sleep quality.
“It does, however, provide some compelling evidence,” Dr. Patton said, “that the nature of smartphone usage and its related consequences are important considerations in addressing the emerging phenomenon of ‘smartphone addiction.’ ”
Also weighing in, Andrew Przybylski, PhD, director of research, Oxford (England) Internet Institute, University of Oxford, said by any global health body and is not a psychiatric disorder.
“The study is a correlational analysis of a sample of participants recruited on university campuses and therefore only reflects the experiences of those who had the purpose of the study explained to them. It can say nothing about behaviors in the general population,” Dr. Przybylski said in a statement.
“Readers should be cautious of making any firm conclusions about the impact of smartphone use in the general population, or the idea that they’re addictive in any objective sense, on the basis of this work,” he added. The study had no specific funding. Dr. Carter, Dr. Weigle, Dr. Patton, and Dr. Przybylski have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Smartphone “addiction” may explain poor sleep quality in a significant proportion of young adults, new research suggests.
Investigators found that almost 40% of adults aged 18-30 years who self-reported excessive smartphone use also reported poor sleep.
“Our study provides further support to the growing body of evidence that smartphone addiction has a deleterious impact on sleep,” wrote the researchers.
The study was published online March 2 in Frontiers of Psychiatry.
Not a clinical diagnosis
Smartphone addiction is not formally recognized as a clinical diagnosis, but it’s an “active” area of research, lead investigator Ben Carter, PhD, King’s College London, noted in the report.
In a cross-sectional survey, 1,043 college students (aged 18-30 years, 73% women) completed the 10-question validated Smartphone Addiction Scale Short Version (SAS-SV) and the adapted Pittsburgh Sleep Quality Score Index.
On the SAS-SV, 406 students (38.9%) reported “addiction” to their smartphones. This estimated prevalence is consistent with other reported studies in young adult populations globally, which is in the range of 30%-45%, the researchers noted.
Overall, 61.6% of participants surveyed reported poor sleep; among those who reported smartphone addiction, 68.7% had poor sleep quality, vs. 57.1% of those who did not report smartphone addiction.
In multivariable analysis that adjusted for a variety of relevant factors, among those for whom there was evidence of smartphone addiction, the odds of poor sleep were increased by 41% (adjusted odds ratio [aOR] = 1.41; 95% confidence interval, 1.06-1.87, P = .018).
The findings also suggest that a greater amount of time spent using the phone and greater use late at night can raise the risk for smartphone addiction.
“Should smartphone addiction become firmly established as a focus of clinical concern, those using their phones after midnight or using their phones for four or more hours per day are likely to be at high risk, and should guide administration of the SAS-SV,” the researchers wrote.
Caveats, cautions, and concerns
Reached for comment, Paul Weigle, MD, psychiatrist with Hartford HealthCare and Hartford (Conn.) Hospital, and member of the American Academy of Child and Adolescent Psychiatry, said the finding of a relationship between addictive smartphone usage and poor sleep quality is not surprising.
“Great increases in adolescent screen media habits in recent decades have seen a concurrent increase in rates of insomnia among this population,” he said in an interview.
Dr. Weigle also noted that young people who use the phone excessively often do so in bed, “which decreases sleep onset by disrupting conditioning (the tendency for our bodies to relate bed with sleep) and by increasing physiological arousal, which makes it more difficult to fall asleep. The blue light from smartphones used at night disrupts our body’s natural circadian rhythms, confusing our brains regarding whether it is night or day, and further worsens sleep.”
Dr. Weigle said in an interview that some of his patients come to him seeking sleep medications, although the best treatment is to perform a “smartphone-ectomy” every evening.
Teenage patients will “beg, borrow, or steal” to be allowed to keep their phones by the bed with the promise not to use them overnight. Three-quarters of the time, when the parents are able to charge the phone in another room, “the sleep problem resolves,” Dr. Weigle said.
One caveat, he said, is that it’s “somewhat unclear whether this is best classified as an addiction or simply a seriously problematic habit. Either way, this type of habit causes a great deal of distress and dysfunction in the lives of those it affects, so it is important to understand,” he said.
In a statement, Bob Patton, PhD, lecturer in clinical psychology, University of Surrey, Guildford, England, noted that this is a cross-sectional study “and as such cannot lead to any firm conclusions about phone usage as the cause of reduced sleep quality.
“It does, however, provide some compelling evidence,” Dr. Patton said, “that the nature of smartphone usage and its related consequences are important considerations in addressing the emerging phenomenon of ‘smartphone addiction.’ ”
Also weighing in, Andrew Przybylski, PhD, director of research, Oxford (England) Internet Institute, University of Oxford, said by any global health body and is not a psychiatric disorder.
“The study is a correlational analysis of a sample of participants recruited on university campuses and therefore only reflects the experiences of those who had the purpose of the study explained to them. It can say nothing about behaviors in the general population,” Dr. Przybylski said in a statement.
“Readers should be cautious of making any firm conclusions about the impact of smartphone use in the general population, or the idea that they’re addictive in any objective sense, on the basis of this work,” he added. The study had no specific funding. Dr. Carter, Dr. Weigle, Dr. Patton, and Dr. Przybylski have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Home noninvasive ventilation in hypercapnic COPD: Progress but important unanswered questions
Patients with COPD may develop sustained hypercapnia, often defined as an awake arterial PCO2 of >45 mm Hg. Other synonymous terms include alveolar hypoventilation or chronic hypercapnic respiratory failure, noting that the specific terminology used may reflect local practice, an assessment of patient severity, or specific insurance requirements. Regardless, available data suggest that hypercapnic COPD patients are at high risk for adverse health outcomes (Yang H, et al. BMJ Open. 2015;5[12]:e008909). Moreover, there appears to have been a growing interest in this population driven by a focus on reducing COPD hospitalizations, increasing recognition of sleep disordered breathing, and progress in potential therapeutic strategies.
There are a number of factors that might drive COPD patients to develop hypercapnia. Lower airway obstruction, expiratory flow limitation and air trapping cause mechanical load on breathing, as well as a trade-off between time spent in inspiration vs prolonged expiration. The function of the diaphragm is impacted by hyperinflation leading to mal-positioning, as well as possibly by local and/or systemic myopathy. The net result is often decreased overall minute ventilation. In terms of gas exchange, increased dead space and ventilation-perfusion mismatching leads to reduced efficiency of ventilation towards CO2 removal. Breathing changes during sleep play an important role, as evidenced by worsened hypercapnia during sleep that can drive chronic CO2 retention (O’Donoghue FJ, et al. Eur Respir J. 2003;21[6]:977). The pathogenesis includes reduced central respiratory drive, increased upper airway resistance and/or obstructive hypopneas and apneas, and respiratory muscle atonia, particularly during REM sleep. The extent to which each of these factors contributes to hypercapnia varies across individual patients, in accordance with the known substantial heterogeneity of COPD. Regardless of underlying traits, patients with COPD who develop hypercapnia have sufficiently severe perturbations to disrupt the normally tight control over CO2 homeostasis.
Nocturnal home noninvasive ventilation (NIV) has been examined as a potential therapeutic strategy for patients with hypercapnic COPD. While older studies have not shown consistent benefits, more recent evidence suggests that NIV can reduce hospitalizations, improve quality of life, and potentially reduce mortality among those with hypercapnic COPD. Accordingly, the American Thoracic Society recently released a clinical practice guideline regarding the use of NIV in patients with chronic stable hypercapnic COPD (Macrea M, et al. Am J Respir Crit Care Med. 2020;202[4]:e74-e87). Recommendations from the guideline included:
1) The use of nocturnal NIV for patients with chronic stable hypercapnic COPD
2) Screening for OSA before initiation of long-term NIV
3) Not using in-hospital initiation of long-term NIV after an episode of acute or chronic hypercapnic respiratory failure, favoring instead reassessment for NIV at 2–4 weeks after resolution
4) Not using an in-laboratory overnight PSG to initially titrate NIV
5) Targeting normalization of PaCO2.
Although it now seems clear that efforts should be made to use NIV in COPD to decrease chronic hypercapnia, there are a number of important questions that remain, particularly surrounding the topic of concurrent OSA, titration, and devices:
• What is the appropriate approach towards patients with suspected concurrent OSA? Most studies of NIV have excluded patients with OSA, or otherwise at higher risk of OSA. Nonetheless, such patients may be common, both based on continued high prevalence of obesity, as well as the potential role that upper airway obstructive events may play towards elevations in CO2 (Resta O., et al. Sleep Breath. 2002;6[1]:11-8). COPD epidemiological studies indicate obesity as a risk factor for several poor outcomes, including severe COPD exacerbation (Lambert AA, et al. Chest. 2017;151[1]:68-77), while studies of COPD and OSA suggest that the presence of hypercapnia defines a high-risk group Jaoude P., Lung. 2014;192:215). Recognizing the potential importance of OSA in this group, ATS guidelines recommend that a general questionnaire-based screening be performed. If screening is positive, the implication would be to perform diagnostic polysomnography to confirm the diagnosis of OSA. However, this may be a challenge for chronically ill patients, and likely would result in delays in NIV initiation. Of note, emerging evidence suggests that home sleep apnea testing (HSAT) might have reasonable accuracy in this group, which may facilitate formal diagnosis. Other concerns in this area include the lack of questionnaire validation in COPD patients.
• Should patients with OSA be managed differently than those without OSA? A diagnosis of OSA might impact several subsequent management decisions related to appropriate NIV therapy and titration. Patients with OSA have increased upper airway collapsibility, which might necessitate higher EPAP support than the minimal EPAP used in NIV trials with non-OSA patients (often fixed at 4 cm water). Potential strategies for optimizing EPAP include use of an NIV device with auto-titrating EPAP, titration in the sleep laboratory (discussed below), or outpatient titration based on clinical parameters and subsequent device download follow-up. On the other hand, one might consider all patients to be at risk for upper airway obstruction and need for additional EPAP titration, which would obviate the need for OSA diagnostic testing.
• What is the role of the sleep laboratory towards successful titration? The inpatient hospital setting has been the traditional site to initiate home NIV in some institutions but is highly resource intensive and increasingly impractical in many health systems. On the other hand, advances in home remote device monitoring now provide the clinician with the ability to examine daily usage, estimated leak, tidal volumes, respiratory rate, and other parameters – often reported as recently as the prior night. In addition, setting changes can be made via these remote monitoring tools (for nonventilator devices), allowing titration to be performed over time on outpatients. Several studies support the effectiveness of this approach over hospital titration in neuromuscular disease and now in COPD (Duiverman ML, et al. Thorax. 2020;75[3]:244-52). Similarly, data suggest that titration under polysomnographic guidance might not be necessary (Patout M, Arbane G, Cuvelier A, Muir JF, Hart N, Murphy PB. Polysomnography versus limited respiratory monitoring and nurse-led titration to optimize non-invasive ventilation set-up: a pilot randomised clinical trial. Thorax. 2019;74:83-86).
Limitations towards the sleep lab as the site of initial titration include waiting time, cost and insurance coverage, and the need to accommodate issues such as impaired mobility or reliance on a caretaker. In addition, titration goals must be clearly outlined in protocols and via staff training specific to NIV. The sleep laboratory may be most appropriately utilized in the minority of patients in whom outpatient titration is unsuccessful. Relatively common issues that might be best addressed in the lab setting include excessive mask leaks, residual apneas and hypopneas, failure to control CO2, or other sleep complaints. In general, studies should probably be focused primarily on titrating EPAP to alleviate upper airway obstructive events. The goals in terms of IPAP titration (or ventilation titration, in the case of “VAPS” modes) are less clear, and overly aggressive increases may complicate the picture with excessive leaks or airway obstruction due to glottic closure. Attempting to accomplish “too much” often leads to a study with limited utility. In contrast, simply performing the study in the patient’s home settings can provide useful diagnostic information regarding the problem one is trying to solve.
• When and where should one initiate NIV following a severe COPD exacerbation? In contrast to the ATS guidelines, the European Respiratory Society guidelines suggest that patients recovering from severe COPD exacerbations be initiated on NIV during that hospitalization, noting that this is a group at high risk for early rehospitalization and mortality (Ergan B, et al. Eur Respir J. 2019;54[3]:1901003). ATS guidelines had the concern of unnecessary start of NIV in those who might normalize their CO2 after recovery, and the possibility of prolonging hospitalizations for titration. For the clinician, the decision will probably be individualized based on risk and available resources. For patients with frequent ICU admissions and/or difficulty with close outpatient follow-up, earlier NIV initiation is certainly a reasonable approach, but adherence and effectiveness remains a concern and, thus, more data are needed.
• Which patients should receive a bedside respiratory assist device (RAD, i.e., BIPAP machine) vs. a noninvasive ventilator? Two classes of devices can be used for home NIV. While both can provide similar positive pressure ventilation, ventilators are designed as life support with alarms and batteries, and may have modes not otherwise available (e.g., auto-titrating EPAP). On the other hand, RAD devices are more convenient for patients and less expensive, but difficult qualification requirements (particularly for devices capable of Bilevel ST or VAPS) have likely resulted in their underutilization. CHEST is spearheading an effort to reconsider Medicare coverage determinations (current rules are from 1998), which will hopefully better align device qualification requirements with emerging evidence regarding patient needs and preferences.
Home non-invasive ventilation can improve outcomes in these high-risk patients with hypercapnic COPD, and the new clinical practice guidelines are an important step in outlining appropriate management. Further progress is needed to delineate an individualized approach based on underlying patient pathophysiology, COPD manifestations/phenotypes, and systems-based practice considerations.
Dr. Orr is Assistant Professor, Division of Pulmonary, Critical Care, and Sleep Medicine, UC San Diego.
Patients with COPD may develop sustained hypercapnia, often defined as an awake arterial PCO2 of >45 mm Hg. Other synonymous terms include alveolar hypoventilation or chronic hypercapnic respiratory failure, noting that the specific terminology used may reflect local practice, an assessment of patient severity, or specific insurance requirements. Regardless, available data suggest that hypercapnic COPD patients are at high risk for adverse health outcomes (Yang H, et al. BMJ Open. 2015;5[12]:e008909). Moreover, there appears to have been a growing interest in this population driven by a focus on reducing COPD hospitalizations, increasing recognition of sleep disordered breathing, and progress in potential therapeutic strategies.
There are a number of factors that might drive COPD patients to develop hypercapnia. Lower airway obstruction, expiratory flow limitation and air trapping cause mechanical load on breathing, as well as a trade-off between time spent in inspiration vs prolonged expiration. The function of the diaphragm is impacted by hyperinflation leading to mal-positioning, as well as possibly by local and/or systemic myopathy. The net result is often decreased overall minute ventilation. In terms of gas exchange, increased dead space and ventilation-perfusion mismatching leads to reduced efficiency of ventilation towards CO2 removal. Breathing changes during sleep play an important role, as evidenced by worsened hypercapnia during sleep that can drive chronic CO2 retention (O’Donoghue FJ, et al. Eur Respir J. 2003;21[6]:977). The pathogenesis includes reduced central respiratory drive, increased upper airway resistance and/or obstructive hypopneas and apneas, and respiratory muscle atonia, particularly during REM sleep. The extent to which each of these factors contributes to hypercapnia varies across individual patients, in accordance with the known substantial heterogeneity of COPD. Regardless of underlying traits, patients with COPD who develop hypercapnia have sufficiently severe perturbations to disrupt the normally tight control over CO2 homeostasis.
Nocturnal home noninvasive ventilation (NIV) has been examined as a potential therapeutic strategy for patients with hypercapnic COPD. While older studies have not shown consistent benefits, more recent evidence suggests that NIV can reduce hospitalizations, improve quality of life, and potentially reduce mortality among those with hypercapnic COPD. Accordingly, the American Thoracic Society recently released a clinical practice guideline regarding the use of NIV in patients with chronic stable hypercapnic COPD (Macrea M, et al. Am J Respir Crit Care Med. 2020;202[4]:e74-e87). Recommendations from the guideline included:
1) The use of nocturnal NIV for patients with chronic stable hypercapnic COPD
2) Screening for OSA before initiation of long-term NIV
3) Not using in-hospital initiation of long-term NIV after an episode of acute or chronic hypercapnic respiratory failure, favoring instead reassessment for NIV at 2–4 weeks after resolution
4) Not using an in-laboratory overnight PSG to initially titrate NIV
5) Targeting normalization of PaCO2.
Although it now seems clear that efforts should be made to use NIV in COPD to decrease chronic hypercapnia, there are a number of important questions that remain, particularly surrounding the topic of concurrent OSA, titration, and devices:
• What is the appropriate approach towards patients with suspected concurrent OSA? Most studies of NIV have excluded patients with OSA, or otherwise at higher risk of OSA. Nonetheless, such patients may be common, both based on continued high prevalence of obesity, as well as the potential role that upper airway obstructive events may play towards elevations in CO2 (Resta O., et al. Sleep Breath. 2002;6[1]:11-8). COPD epidemiological studies indicate obesity as a risk factor for several poor outcomes, including severe COPD exacerbation (Lambert AA, et al. Chest. 2017;151[1]:68-77), while studies of COPD and OSA suggest that the presence of hypercapnia defines a high-risk group Jaoude P., Lung. 2014;192:215). Recognizing the potential importance of OSA in this group, ATS guidelines recommend that a general questionnaire-based screening be performed. If screening is positive, the implication would be to perform diagnostic polysomnography to confirm the diagnosis of OSA. However, this may be a challenge for chronically ill patients, and likely would result in delays in NIV initiation. Of note, emerging evidence suggests that home sleep apnea testing (HSAT) might have reasonable accuracy in this group, which may facilitate formal diagnosis. Other concerns in this area include the lack of questionnaire validation in COPD patients.
• Should patients with OSA be managed differently than those without OSA? A diagnosis of OSA might impact several subsequent management decisions related to appropriate NIV therapy and titration. Patients with OSA have increased upper airway collapsibility, which might necessitate higher EPAP support than the minimal EPAP used in NIV trials with non-OSA patients (often fixed at 4 cm water). Potential strategies for optimizing EPAP include use of an NIV device with auto-titrating EPAP, titration in the sleep laboratory (discussed below), or outpatient titration based on clinical parameters and subsequent device download follow-up. On the other hand, one might consider all patients to be at risk for upper airway obstruction and need for additional EPAP titration, which would obviate the need for OSA diagnostic testing.
• What is the role of the sleep laboratory towards successful titration? The inpatient hospital setting has been the traditional site to initiate home NIV in some institutions but is highly resource intensive and increasingly impractical in many health systems. On the other hand, advances in home remote device monitoring now provide the clinician with the ability to examine daily usage, estimated leak, tidal volumes, respiratory rate, and other parameters – often reported as recently as the prior night. In addition, setting changes can be made via these remote monitoring tools (for nonventilator devices), allowing titration to be performed over time on outpatients. Several studies support the effectiveness of this approach over hospital titration in neuromuscular disease and now in COPD (Duiverman ML, et al. Thorax. 2020;75[3]:244-52). Similarly, data suggest that titration under polysomnographic guidance might not be necessary (Patout M, Arbane G, Cuvelier A, Muir JF, Hart N, Murphy PB. Polysomnography versus limited respiratory monitoring and nurse-led titration to optimize non-invasive ventilation set-up: a pilot randomised clinical trial. Thorax. 2019;74:83-86).
Limitations towards the sleep lab as the site of initial titration include waiting time, cost and insurance coverage, and the need to accommodate issues such as impaired mobility or reliance on a caretaker. In addition, titration goals must be clearly outlined in protocols and via staff training specific to NIV. The sleep laboratory may be most appropriately utilized in the minority of patients in whom outpatient titration is unsuccessful. Relatively common issues that might be best addressed in the lab setting include excessive mask leaks, residual apneas and hypopneas, failure to control CO2, or other sleep complaints. In general, studies should probably be focused primarily on titrating EPAP to alleviate upper airway obstructive events. The goals in terms of IPAP titration (or ventilation titration, in the case of “VAPS” modes) are less clear, and overly aggressive increases may complicate the picture with excessive leaks or airway obstruction due to glottic closure. Attempting to accomplish “too much” often leads to a study with limited utility. In contrast, simply performing the study in the patient’s home settings can provide useful diagnostic information regarding the problem one is trying to solve.
• When and where should one initiate NIV following a severe COPD exacerbation? In contrast to the ATS guidelines, the European Respiratory Society guidelines suggest that patients recovering from severe COPD exacerbations be initiated on NIV during that hospitalization, noting that this is a group at high risk for early rehospitalization and mortality (Ergan B, et al. Eur Respir J. 2019;54[3]:1901003). ATS guidelines had the concern of unnecessary start of NIV in those who might normalize their CO2 after recovery, and the possibility of prolonging hospitalizations for titration. For the clinician, the decision will probably be individualized based on risk and available resources. For patients with frequent ICU admissions and/or difficulty with close outpatient follow-up, earlier NIV initiation is certainly a reasonable approach, but adherence and effectiveness remains a concern and, thus, more data are needed.
• Which patients should receive a bedside respiratory assist device (RAD, i.e., BIPAP machine) vs. a noninvasive ventilator? Two classes of devices can be used for home NIV. While both can provide similar positive pressure ventilation, ventilators are designed as life support with alarms and batteries, and may have modes not otherwise available (e.g., auto-titrating EPAP). On the other hand, RAD devices are more convenient for patients and less expensive, but difficult qualification requirements (particularly for devices capable of Bilevel ST or VAPS) have likely resulted in their underutilization. CHEST is spearheading an effort to reconsider Medicare coverage determinations (current rules are from 1998), which will hopefully better align device qualification requirements with emerging evidence regarding patient needs and preferences.
Home non-invasive ventilation can improve outcomes in these high-risk patients with hypercapnic COPD, and the new clinical practice guidelines are an important step in outlining appropriate management. Further progress is needed to delineate an individualized approach based on underlying patient pathophysiology, COPD manifestations/phenotypes, and systems-based practice considerations.
Dr. Orr is Assistant Professor, Division of Pulmonary, Critical Care, and Sleep Medicine, UC San Diego.
Patients with COPD may develop sustained hypercapnia, often defined as an awake arterial PCO2 of >45 mm Hg. Other synonymous terms include alveolar hypoventilation or chronic hypercapnic respiratory failure, noting that the specific terminology used may reflect local practice, an assessment of patient severity, or specific insurance requirements. Regardless, available data suggest that hypercapnic COPD patients are at high risk for adverse health outcomes (Yang H, et al. BMJ Open. 2015;5[12]:e008909). Moreover, there appears to have been a growing interest in this population driven by a focus on reducing COPD hospitalizations, increasing recognition of sleep disordered breathing, and progress in potential therapeutic strategies.
There are a number of factors that might drive COPD patients to develop hypercapnia. Lower airway obstruction, expiratory flow limitation and air trapping cause mechanical load on breathing, as well as a trade-off between time spent in inspiration vs prolonged expiration. The function of the diaphragm is impacted by hyperinflation leading to mal-positioning, as well as possibly by local and/or systemic myopathy. The net result is often decreased overall minute ventilation. In terms of gas exchange, increased dead space and ventilation-perfusion mismatching leads to reduced efficiency of ventilation towards CO2 removal. Breathing changes during sleep play an important role, as evidenced by worsened hypercapnia during sleep that can drive chronic CO2 retention (O’Donoghue FJ, et al. Eur Respir J. 2003;21[6]:977). The pathogenesis includes reduced central respiratory drive, increased upper airway resistance and/or obstructive hypopneas and apneas, and respiratory muscle atonia, particularly during REM sleep. The extent to which each of these factors contributes to hypercapnia varies across individual patients, in accordance with the known substantial heterogeneity of COPD. Regardless of underlying traits, patients with COPD who develop hypercapnia have sufficiently severe perturbations to disrupt the normally tight control over CO2 homeostasis.
Nocturnal home noninvasive ventilation (NIV) has been examined as a potential therapeutic strategy for patients with hypercapnic COPD. While older studies have not shown consistent benefits, more recent evidence suggests that NIV can reduce hospitalizations, improve quality of life, and potentially reduce mortality among those with hypercapnic COPD. Accordingly, the American Thoracic Society recently released a clinical practice guideline regarding the use of NIV in patients with chronic stable hypercapnic COPD (Macrea M, et al. Am J Respir Crit Care Med. 2020;202[4]:e74-e87). Recommendations from the guideline included:
1) The use of nocturnal NIV for patients with chronic stable hypercapnic COPD
2) Screening for OSA before initiation of long-term NIV
3) Not using in-hospital initiation of long-term NIV after an episode of acute or chronic hypercapnic respiratory failure, favoring instead reassessment for NIV at 2–4 weeks after resolution
4) Not using an in-laboratory overnight PSG to initially titrate NIV
5) Targeting normalization of PaCO2.
Although it now seems clear that efforts should be made to use NIV in COPD to decrease chronic hypercapnia, there are a number of important questions that remain, particularly surrounding the topic of concurrent OSA, titration, and devices:
• What is the appropriate approach towards patients with suspected concurrent OSA? Most studies of NIV have excluded patients with OSA, or otherwise at higher risk of OSA. Nonetheless, such patients may be common, both based on continued high prevalence of obesity, as well as the potential role that upper airway obstructive events may play towards elevations in CO2 (Resta O., et al. Sleep Breath. 2002;6[1]:11-8). COPD epidemiological studies indicate obesity as a risk factor for several poor outcomes, including severe COPD exacerbation (Lambert AA, et al. Chest. 2017;151[1]:68-77), while studies of COPD and OSA suggest that the presence of hypercapnia defines a high-risk group Jaoude P., Lung. 2014;192:215). Recognizing the potential importance of OSA in this group, ATS guidelines recommend that a general questionnaire-based screening be performed. If screening is positive, the implication would be to perform diagnostic polysomnography to confirm the diagnosis of OSA. However, this may be a challenge for chronically ill patients, and likely would result in delays in NIV initiation. Of note, emerging evidence suggests that home sleep apnea testing (HSAT) might have reasonable accuracy in this group, which may facilitate formal diagnosis. Other concerns in this area include the lack of questionnaire validation in COPD patients.
• Should patients with OSA be managed differently than those without OSA? A diagnosis of OSA might impact several subsequent management decisions related to appropriate NIV therapy and titration. Patients with OSA have increased upper airway collapsibility, which might necessitate higher EPAP support than the minimal EPAP used in NIV trials with non-OSA patients (often fixed at 4 cm water). Potential strategies for optimizing EPAP include use of an NIV device with auto-titrating EPAP, titration in the sleep laboratory (discussed below), or outpatient titration based on clinical parameters and subsequent device download follow-up. On the other hand, one might consider all patients to be at risk for upper airway obstruction and need for additional EPAP titration, which would obviate the need for OSA diagnostic testing.
• What is the role of the sleep laboratory towards successful titration? The inpatient hospital setting has been the traditional site to initiate home NIV in some institutions but is highly resource intensive and increasingly impractical in many health systems. On the other hand, advances in home remote device monitoring now provide the clinician with the ability to examine daily usage, estimated leak, tidal volumes, respiratory rate, and other parameters – often reported as recently as the prior night. In addition, setting changes can be made via these remote monitoring tools (for nonventilator devices), allowing titration to be performed over time on outpatients. Several studies support the effectiveness of this approach over hospital titration in neuromuscular disease and now in COPD (Duiverman ML, et al. Thorax. 2020;75[3]:244-52). Similarly, data suggest that titration under polysomnographic guidance might not be necessary (Patout M, Arbane G, Cuvelier A, Muir JF, Hart N, Murphy PB. Polysomnography versus limited respiratory monitoring and nurse-led titration to optimize non-invasive ventilation set-up: a pilot randomised clinical trial. Thorax. 2019;74:83-86).
Limitations towards the sleep lab as the site of initial titration include waiting time, cost and insurance coverage, and the need to accommodate issues such as impaired mobility or reliance on a caretaker. In addition, titration goals must be clearly outlined in protocols and via staff training specific to NIV. The sleep laboratory may be most appropriately utilized in the minority of patients in whom outpatient titration is unsuccessful. Relatively common issues that might be best addressed in the lab setting include excessive mask leaks, residual apneas and hypopneas, failure to control CO2, or other sleep complaints. In general, studies should probably be focused primarily on titrating EPAP to alleviate upper airway obstructive events. The goals in terms of IPAP titration (or ventilation titration, in the case of “VAPS” modes) are less clear, and overly aggressive increases may complicate the picture with excessive leaks or airway obstruction due to glottic closure. Attempting to accomplish “too much” often leads to a study with limited utility. In contrast, simply performing the study in the patient’s home settings can provide useful diagnostic information regarding the problem one is trying to solve.
• When and where should one initiate NIV following a severe COPD exacerbation? In contrast to the ATS guidelines, the European Respiratory Society guidelines suggest that patients recovering from severe COPD exacerbations be initiated on NIV during that hospitalization, noting that this is a group at high risk for early rehospitalization and mortality (Ergan B, et al. Eur Respir J. 2019;54[3]:1901003). ATS guidelines had the concern of unnecessary start of NIV in those who might normalize their CO2 after recovery, and the possibility of prolonging hospitalizations for titration. For the clinician, the decision will probably be individualized based on risk and available resources. For patients with frequent ICU admissions and/or difficulty with close outpatient follow-up, earlier NIV initiation is certainly a reasonable approach, but adherence and effectiveness remains a concern and, thus, more data are needed.
• Which patients should receive a bedside respiratory assist device (RAD, i.e., BIPAP machine) vs. a noninvasive ventilator? Two classes of devices can be used for home NIV. While both can provide similar positive pressure ventilation, ventilators are designed as life support with alarms and batteries, and may have modes not otherwise available (e.g., auto-titrating EPAP). On the other hand, RAD devices are more convenient for patients and less expensive, but difficult qualification requirements (particularly for devices capable of Bilevel ST or VAPS) have likely resulted in their underutilization. CHEST is spearheading an effort to reconsider Medicare coverage determinations (current rules are from 1998), which will hopefully better align device qualification requirements with emerging evidence regarding patient needs and preferences.
Home non-invasive ventilation can improve outcomes in these high-risk patients with hypercapnic COPD, and the new clinical practice guidelines are an important step in outlining appropriate management. Further progress is needed to delineate an individualized approach based on underlying patient pathophysiology, COPD manifestations/phenotypes, and systems-based practice considerations.
Dr. Orr is Assistant Professor, Division of Pulmonary, Critical Care, and Sleep Medicine, UC San Diego.