User login
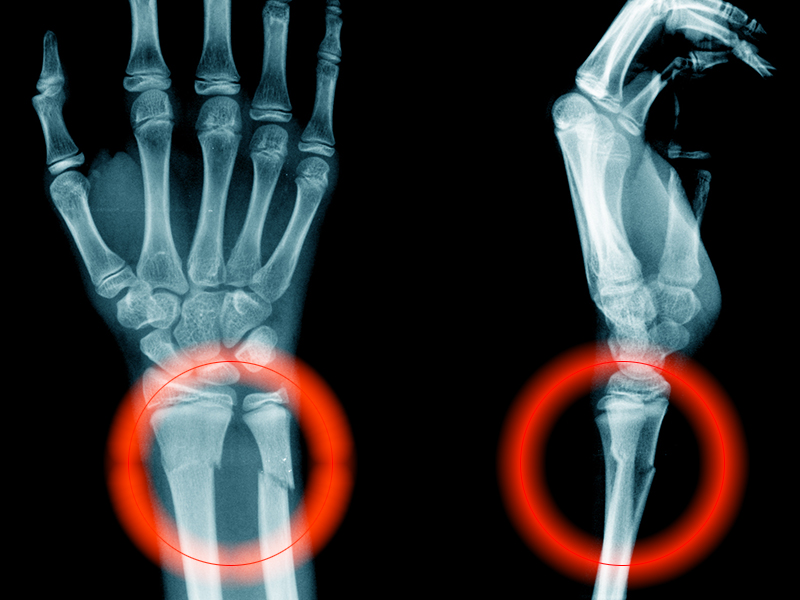
Frailty, diabetes increase fragility fracture risk
increasing their risk of fragility fracture, according to findings from a prospective cohort study.
A total of 3,149 participants (70% women) were included in the study, 138 (60% women) of whom had type 2 diabetes. The mean age was 65 years and mean follow-up was 9.2 years. Over the study period, 611 fragility fractures were reported, of which 35 were in patients with diabetes and 576 in patients without diabetes. Overall, 25.4% of patients with diabetes experienced a fragility fracture, compared with 19.1% of control patients. Diabetes was associated with a significantly increased risk of all fragility fractures (hazard ratio, 1.54). It was also significantly associated with risk of hip fracture (HR, 2.60) but not clinical spine fracture.
In a Cox model incorporating the interaction between frailty index (FI) scores and diabetes, there was a significant association between FI and overall fracture risk per 0.01-point FI increase (HR, 1.02; 95% confidence interval, 1.01-1.03) and per 0.10-point FI increase (HR, 1.19; 95% CI, 1.10-1.33). However, no interaction between frailty and diabetes was observed for hip or clinical spine fractures.
“Frailty status may aid in the understanding of the paradox and thus enhance the quality of assessment and care for diabetes,” wrote Guowei Li, MBBS, PhD, of McMaster University, Hamilton, Ont., and his colleagues, adding that “particular attention should be paid to diabetes as a risk factor for fragility fractures in those who are frail.”
Four study authors reported conflicts of interest with some pharmaceutical companies that manufacture therapies for osteoporosis.
SOURCE: Li G et al. Diabetes Care. 2019 Jan 28. doi: 10.2337/dc18-1965.
increasing their risk of fragility fracture, according to findings from a prospective cohort study.
A total of 3,149 participants (70% women) were included in the study, 138 (60% women) of whom had type 2 diabetes. The mean age was 65 years and mean follow-up was 9.2 years. Over the study period, 611 fragility fractures were reported, of which 35 were in patients with diabetes and 576 in patients without diabetes. Overall, 25.4% of patients with diabetes experienced a fragility fracture, compared with 19.1% of control patients. Diabetes was associated with a significantly increased risk of all fragility fractures (hazard ratio, 1.54). It was also significantly associated with risk of hip fracture (HR, 2.60) but not clinical spine fracture.
In a Cox model incorporating the interaction between frailty index (FI) scores and diabetes, there was a significant association between FI and overall fracture risk per 0.01-point FI increase (HR, 1.02; 95% confidence interval, 1.01-1.03) and per 0.10-point FI increase (HR, 1.19; 95% CI, 1.10-1.33). However, no interaction between frailty and diabetes was observed for hip or clinical spine fractures.
“Frailty status may aid in the understanding of the paradox and thus enhance the quality of assessment and care for diabetes,” wrote Guowei Li, MBBS, PhD, of McMaster University, Hamilton, Ont., and his colleagues, adding that “particular attention should be paid to diabetes as a risk factor for fragility fractures in those who are frail.”
Four study authors reported conflicts of interest with some pharmaceutical companies that manufacture therapies for osteoporosis.
SOURCE: Li G et al. Diabetes Care. 2019 Jan 28. doi: 10.2337/dc18-1965.
increasing their risk of fragility fracture, according to findings from a prospective cohort study.
A total of 3,149 participants (70% women) were included in the study, 138 (60% women) of whom had type 2 diabetes. The mean age was 65 years and mean follow-up was 9.2 years. Over the study period, 611 fragility fractures were reported, of which 35 were in patients with diabetes and 576 in patients without diabetes. Overall, 25.4% of patients with diabetes experienced a fragility fracture, compared with 19.1% of control patients. Diabetes was associated with a significantly increased risk of all fragility fractures (hazard ratio, 1.54). It was also significantly associated with risk of hip fracture (HR, 2.60) but not clinical spine fracture.
In a Cox model incorporating the interaction between frailty index (FI) scores and diabetes, there was a significant association between FI and overall fracture risk per 0.01-point FI increase (HR, 1.02; 95% confidence interval, 1.01-1.03) and per 0.10-point FI increase (HR, 1.19; 95% CI, 1.10-1.33). However, no interaction between frailty and diabetes was observed for hip or clinical spine fractures.
“Frailty status may aid in the understanding of the paradox and thus enhance the quality of assessment and care for diabetes,” wrote Guowei Li, MBBS, PhD, of McMaster University, Hamilton, Ont., and his colleagues, adding that “particular attention should be paid to diabetes as a risk factor for fragility fractures in those who are frail.”
Four study authors reported conflicts of interest with some pharmaceutical companies that manufacture therapies for osteoporosis.
SOURCE: Li G et al. Diabetes Care. 2019 Jan 28. doi: 10.2337/dc18-1965.
FROM DIABETES CARE
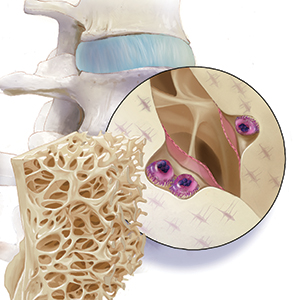
FDA committee votes yes on romosozumab for osteoporosis
In an 18-1 vote, the FDA’s Bone, Reproductive, and Urologic Drugs Advisory Committee agreed that the risk-benefit profile of romosozumab, to be marketed by Amgen as Evenity, was favorable enough to support approval. Relative risk reductions of up to 75%, compared with placebo, and 36%, compared with alendronate, were seen in pivotal clinical trials.
A signal for increased major adverse cardiovascular events (MACE) among those receiving romosozumab had been seen in just one of the clinical trials, with a hazard ratio for MACE of 1.87 for those taking romosozumab, compared with those taking alendronate (95% confidence interval, 1.11-3.14).
Committee members were enthusiastic about the efficacy of the monoclonal antibody, which binds to sclerostin and prevents its inhibiting effect, allowing robust new bone formation. “I want to emphasize the remarkable skeletal efficacy of this drug; truly, it’s better than anything we’ve seen before,” said committee member Sundeep Khosla, MD, professor of medicine and physiology at the Mayo Clinic, Rochester, Minn.
In its application, the sponsor relied on two clinical trials. In the first, 7,180 women with osteoporosis aged 55-90 years were randomized 1:1 to receive romosozumab or placebo for 12 months in a double-blind trial. After this time, participants in each arm received follow-on treatment with denosumab (Prolia) for another 12 months. This study, dubbed Trial 337, followed morphometric vertebral fractures at 12 and 24 months. Morphometric fractures included both symptomatic and asymptomatic fractures.
Those treated with romosozumab had relative risk reductions of new vertebral fractures of 73% and 75%, compared with those given placebo at 12 and 24 months. Absolute risk reductions for vertebral fractures were 1.30% and 1.89% at 1 and 2 years (P less than .001 for both).
The second study, Trial 142, was a double-blind, active-controlled study that included 4,093 women aged 55-90 years with osteoporosis and a history of prior fragility fracture. Participants were randomized 1:1 to receive either romosozumab or alendronate for 12 months, with an additional variable period of alendronate follow-on of at least 12 months for both arms.
For Trial 142, one primary endpoint was morphometric vertebral fractures at month 24. An additional endpoint, clinical fracture, was a composite of symptomatic vertebral fractures and nonvertebral fractures. This second endpoint was assessed at the time of primary analysis, an event-driven cut point that occurred when at least 330 participants experienced a clinical fracture and all participants had completed the 24-month visit.
Hip fractures were less common among those given romosozumab, and bone mineral density increased significantly as well.
Vertebral fractures were reduced by 36% in the romosozumab group relative to the alendronate group, and clinical fractures by 27% (P less than .001 for both).
Overall, the number of adverse events for the more than 7,500 patients in the safety population was similar between those receiving romosozumab and either placebo or alendronate, said Scott Wasserman, MD, vice president of global development for Amgen.
However, in Trial 142, which included patients who were slightly older and on more cardiovascular medications at baseline than in Trial 337, MACE – defined as cardiovascular death, MI, and stroke – occurred more frequently among those taking romosozumab, driven primarily by increased cardiac and cerebral ischemic events occurring within the first 12 months of beginning the study drug. At 12 months, the romosozumab arm saw 41 instances of MACE, compared with 22 in the alendronate arm to produce the HR of 1.87 (2.0% vs. 1.1%).
With regard to the imbalance in MACE seen in Trial 142, both the FDA and presenters for the sponsor entertained the notion that alendronate may have been somewhat protective for cardiovascular events. Although there is some biologic plausibility for a cardioprotective event for bisphosphonates, alendronate is highly specific for bone activity and the preponderance of previous studies have not shown such cardioprotection, the FDA, sponsors, and committee members all agreed.
Marc Sabatine, MD, the Lewis Dexter, MD Distinguished Chair in Cardiovascular Medicine at Harvard Medical School, Boston, was available to answer questions on behalf of the study’s sponsor. He noted at several points during the meeting just how few total cardiovascular events were seen overall in the romosozumab trial. The overall small numbers, he said, made it very difficult to distinguish whether the smaller number of MACE seen in the alendronate arm of Trial 142 were a true safety signal or just “a play of chance.”
Almost all the committee’s questioning and discussion centered on this potential increased cardiovascular risk. Amgen, in discussion with the FDA, had agreed to a black box warning designed to wave off prescribing romosozumab to those at increased risk for cardiovascular disease, focusing on those with a history of MI or stroke.
Additionally, the sponsor proposed a postmarketing real-world observational study to track incidence of MACE in those receiving romosozumab, comparing them with those receiving standard of care for osteoporosis.
Several committee members pointed out a problem with the proposed safety mitigation scheme: By conducting a postmarketing observational study for a drug that has a black-box warning to exclude those at high risk for MACE, the chance of detecting an actual cardiovascular safety problem plummets. “This is the textbook example of when observational studies struggle or are virtually guaranteed to fail,” noted Tobias Gerhard, PhD, a pharmacoepidemiologist at Rutgers University, New Brunswick, N.J.
On the other hand, noted several committee members, pausing to conduct a premarketing randomized, controlled trial would keep a beneficial drug away from a population in need. A postmarketing randomized, controlled trial, even a simple trial, still presents challenges, some of the committee acknowledged. Dr. Khosla voiced the opinion that “A randomized, controlled trial is virtually impossible.”
The committee, which was charged with discussing, but not voting on, what additional data should be obtained – and when – to sort out the cardiovascular safety question, was approximately evenly divided in the matter of whether an observational or registry-based trial, or a controlled trial, would be the best path forward.
Committee member Robert A. Adler, MD, put a realistic frame around the debate. “As an endocrinologist, I deal with nuances every day. I really think the kind of clinician who is going to be using this drug is used to dealing with benefits and risks and trying to tailor treatment to a given patient,” said Dr. Adler, professor of internal medicine and epidemiology at Virginia Commonwealth University, Richmond.
In its proposed indication, Amgen defined the population of menopausal women at high risk of fracture as those with a history of osteoporotic fracture, multiple risk factors for fracture, or patients who have failed or are intolerant to other available osteoporosis therapy. Romosozumab would be given as a once-monthly subcutaneous injection of 210 mg for a period of 12 months, to be followed by antiresorptive therapy.
Most of the participants in the clinical trials resided outside the United States, primarily because of the difficulty of recruiting clinical trial participants in the United States, Amgen officials said during their presentation. However, neither the time to the first positively adjudicated MACE nor bone mineral density responses at month 12 differed significantly across the various geographic regions where clinical trial sites were located, said Rachel Wagman, MD, the executive medical director of global clinical development for Amgen. Still, several committee members called for postmarketing data to focus on U.S. patients.
Romosozumab was approved for marketing in Japan on Jan. 8, 2019; approval is also being sought in Europe .
The FDA usually follows the recommendations of its advisory panels.
In an 18-1 vote, the FDA’s Bone, Reproductive, and Urologic Drugs Advisory Committee agreed that the risk-benefit profile of romosozumab, to be marketed by Amgen as Evenity, was favorable enough to support approval. Relative risk reductions of up to 75%, compared with placebo, and 36%, compared with alendronate, were seen in pivotal clinical trials.
A signal for increased major adverse cardiovascular events (MACE) among those receiving romosozumab had been seen in just one of the clinical trials, with a hazard ratio for MACE of 1.87 for those taking romosozumab, compared with those taking alendronate (95% confidence interval, 1.11-3.14).
Committee members were enthusiastic about the efficacy of the monoclonal antibody, which binds to sclerostin and prevents its inhibiting effect, allowing robust new bone formation. “I want to emphasize the remarkable skeletal efficacy of this drug; truly, it’s better than anything we’ve seen before,” said committee member Sundeep Khosla, MD, professor of medicine and physiology at the Mayo Clinic, Rochester, Minn.
In its application, the sponsor relied on two clinical trials. In the first, 7,180 women with osteoporosis aged 55-90 years were randomized 1:1 to receive romosozumab or placebo for 12 months in a double-blind trial. After this time, participants in each arm received follow-on treatment with denosumab (Prolia) for another 12 months. This study, dubbed Trial 337, followed morphometric vertebral fractures at 12 and 24 months. Morphometric fractures included both symptomatic and asymptomatic fractures.
Those treated with romosozumab had relative risk reductions of new vertebral fractures of 73% and 75%, compared with those given placebo at 12 and 24 months. Absolute risk reductions for vertebral fractures were 1.30% and 1.89% at 1 and 2 years (P less than .001 for both).
The second study, Trial 142, was a double-blind, active-controlled study that included 4,093 women aged 55-90 years with osteoporosis and a history of prior fragility fracture. Participants were randomized 1:1 to receive either romosozumab or alendronate for 12 months, with an additional variable period of alendronate follow-on of at least 12 months for both arms.
For Trial 142, one primary endpoint was morphometric vertebral fractures at month 24. An additional endpoint, clinical fracture, was a composite of symptomatic vertebral fractures and nonvertebral fractures. This second endpoint was assessed at the time of primary analysis, an event-driven cut point that occurred when at least 330 participants experienced a clinical fracture and all participants had completed the 24-month visit.
Hip fractures were less common among those given romosozumab, and bone mineral density increased significantly as well.
Vertebral fractures were reduced by 36% in the romosozumab group relative to the alendronate group, and clinical fractures by 27% (P less than .001 for both).
Overall, the number of adverse events for the more than 7,500 patients in the safety population was similar between those receiving romosozumab and either placebo or alendronate, said Scott Wasserman, MD, vice president of global development for Amgen.
However, in Trial 142, which included patients who were slightly older and on more cardiovascular medications at baseline than in Trial 337, MACE – defined as cardiovascular death, MI, and stroke – occurred more frequently among those taking romosozumab, driven primarily by increased cardiac and cerebral ischemic events occurring within the first 12 months of beginning the study drug. At 12 months, the romosozumab arm saw 41 instances of MACE, compared with 22 in the alendronate arm to produce the HR of 1.87 (2.0% vs. 1.1%).
With regard to the imbalance in MACE seen in Trial 142, both the FDA and presenters for the sponsor entertained the notion that alendronate may have been somewhat protective for cardiovascular events. Although there is some biologic plausibility for a cardioprotective event for bisphosphonates, alendronate is highly specific for bone activity and the preponderance of previous studies have not shown such cardioprotection, the FDA, sponsors, and committee members all agreed.
Marc Sabatine, MD, the Lewis Dexter, MD Distinguished Chair in Cardiovascular Medicine at Harvard Medical School, Boston, was available to answer questions on behalf of the study’s sponsor. He noted at several points during the meeting just how few total cardiovascular events were seen overall in the romosozumab trial. The overall small numbers, he said, made it very difficult to distinguish whether the smaller number of MACE seen in the alendronate arm of Trial 142 were a true safety signal or just “a play of chance.”
Almost all the committee’s questioning and discussion centered on this potential increased cardiovascular risk. Amgen, in discussion with the FDA, had agreed to a black box warning designed to wave off prescribing romosozumab to those at increased risk for cardiovascular disease, focusing on those with a history of MI or stroke.
Additionally, the sponsor proposed a postmarketing real-world observational study to track incidence of MACE in those receiving romosozumab, comparing them with those receiving standard of care for osteoporosis.
Several committee members pointed out a problem with the proposed safety mitigation scheme: By conducting a postmarketing observational study for a drug that has a black-box warning to exclude those at high risk for MACE, the chance of detecting an actual cardiovascular safety problem plummets. “This is the textbook example of when observational studies struggle or are virtually guaranteed to fail,” noted Tobias Gerhard, PhD, a pharmacoepidemiologist at Rutgers University, New Brunswick, N.J.
On the other hand, noted several committee members, pausing to conduct a premarketing randomized, controlled trial would keep a beneficial drug away from a population in need. A postmarketing randomized, controlled trial, even a simple trial, still presents challenges, some of the committee acknowledged. Dr. Khosla voiced the opinion that “A randomized, controlled trial is virtually impossible.”
The committee, which was charged with discussing, but not voting on, what additional data should be obtained – and when – to sort out the cardiovascular safety question, was approximately evenly divided in the matter of whether an observational or registry-based trial, or a controlled trial, would be the best path forward.
Committee member Robert A. Adler, MD, put a realistic frame around the debate. “As an endocrinologist, I deal with nuances every day. I really think the kind of clinician who is going to be using this drug is used to dealing with benefits and risks and trying to tailor treatment to a given patient,” said Dr. Adler, professor of internal medicine and epidemiology at Virginia Commonwealth University, Richmond.
In its proposed indication, Amgen defined the population of menopausal women at high risk of fracture as those with a history of osteoporotic fracture, multiple risk factors for fracture, or patients who have failed or are intolerant to other available osteoporosis therapy. Romosozumab would be given as a once-monthly subcutaneous injection of 210 mg for a period of 12 months, to be followed by antiresorptive therapy.
Most of the participants in the clinical trials resided outside the United States, primarily because of the difficulty of recruiting clinical trial participants in the United States, Amgen officials said during their presentation. However, neither the time to the first positively adjudicated MACE nor bone mineral density responses at month 12 differed significantly across the various geographic regions where clinical trial sites were located, said Rachel Wagman, MD, the executive medical director of global clinical development for Amgen. Still, several committee members called for postmarketing data to focus on U.S. patients.
Romosozumab was approved for marketing in Japan on Jan. 8, 2019; approval is also being sought in Europe .
The FDA usually follows the recommendations of its advisory panels.
In an 18-1 vote, the FDA’s Bone, Reproductive, and Urologic Drugs Advisory Committee agreed that the risk-benefit profile of romosozumab, to be marketed by Amgen as Evenity, was favorable enough to support approval. Relative risk reductions of up to 75%, compared with placebo, and 36%, compared with alendronate, were seen in pivotal clinical trials.
A signal for increased major adverse cardiovascular events (MACE) among those receiving romosozumab had been seen in just one of the clinical trials, with a hazard ratio for MACE of 1.87 for those taking romosozumab, compared with those taking alendronate (95% confidence interval, 1.11-3.14).
Committee members were enthusiastic about the efficacy of the monoclonal antibody, which binds to sclerostin and prevents its inhibiting effect, allowing robust new bone formation. “I want to emphasize the remarkable skeletal efficacy of this drug; truly, it’s better than anything we’ve seen before,” said committee member Sundeep Khosla, MD, professor of medicine and physiology at the Mayo Clinic, Rochester, Minn.
In its application, the sponsor relied on two clinical trials. In the first, 7,180 women with osteoporosis aged 55-90 years were randomized 1:1 to receive romosozumab or placebo for 12 months in a double-blind trial. After this time, participants in each arm received follow-on treatment with denosumab (Prolia) for another 12 months. This study, dubbed Trial 337, followed morphometric vertebral fractures at 12 and 24 months. Morphometric fractures included both symptomatic and asymptomatic fractures.
Those treated with romosozumab had relative risk reductions of new vertebral fractures of 73% and 75%, compared with those given placebo at 12 and 24 months. Absolute risk reductions for vertebral fractures were 1.30% and 1.89% at 1 and 2 years (P less than .001 for both).
The second study, Trial 142, was a double-blind, active-controlled study that included 4,093 women aged 55-90 years with osteoporosis and a history of prior fragility fracture. Participants were randomized 1:1 to receive either romosozumab or alendronate for 12 months, with an additional variable period of alendronate follow-on of at least 12 months for both arms.
For Trial 142, one primary endpoint was morphometric vertebral fractures at month 24. An additional endpoint, clinical fracture, was a composite of symptomatic vertebral fractures and nonvertebral fractures. This second endpoint was assessed at the time of primary analysis, an event-driven cut point that occurred when at least 330 participants experienced a clinical fracture and all participants had completed the 24-month visit.
Hip fractures were less common among those given romosozumab, and bone mineral density increased significantly as well.
Vertebral fractures were reduced by 36% in the romosozumab group relative to the alendronate group, and clinical fractures by 27% (P less than .001 for both).
Overall, the number of adverse events for the more than 7,500 patients in the safety population was similar between those receiving romosozumab and either placebo or alendronate, said Scott Wasserman, MD, vice president of global development for Amgen.
However, in Trial 142, which included patients who were slightly older and on more cardiovascular medications at baseline than in Trial 337, MACE – defined as cardiovascular death, MI, and stroke – occurred more frequently among those taking romosozumab, driven primarily by increased cardiac and cerebral ischemic events occurring within the first 12 months of beginning the study drug. At 12 months, the romosozumab arm saw 41 instances of MACE, compared with 22 in the alendronate arm to produce the HR of 1.87 (2.0% vs. 1.1%).
With regard to the imbalance in MACE seen in Trial 142, both the FDA and presenters for the sponsor entertained the notion that alendronate may have been somewhat protective for cardiovascular events. Although there is some biologic plausibility for a cardioprotective event for bisphosphonates, alendronate is highly specific for bone activity and the preponderance of previous studies have not shown such cardioprotection, the FDA, sponsors, and committee members all agreed.
Marc Sabatine, MD, the Lewis Dexter, MD Distinguished Chair in Cardiovascular Medicine at Harvard Medical School, Boston, was available to answer questions on behalf of the study’s sponsor. He noted at several points during the meeting just how few total cardiovascular events were seen overall in the romosozumab trial. The overall small numbers, he said, made it very difficult to distinguish whether the smaller number of MACE seen in the alendronate arm of Trial 142 were a true safety signal or just “a play of chance.”
Almost all the committee’s questioning and discussion centered on this potential increased cardiovascular risk. Amgen, in discussion with the FDA, had agreed to a black box warning designed to wave off prescribing romosozumab to those at increased risk for cardiovascular disease, focusing on those with a history of MI or stroke.
Additionally, the sponsor proposed a postmarketing real-world observational study to track incidence of MACE in those receiving romosozumab, comparing them with those receiving standard of care for osteoporosis.
Several committee members pointed out a problem with the proposed safety mitigation scheme: By conducting a postmarketing observational study for a drug that has a black-box warning to exclude those at high risk for MACE, the chance of detecting an actual cardiovascular safety problem plummets. “This is the textbook example of when observational studies struggle or are virtually guaranteed to fail,” noted Tobias Gerhard, PhD, a pharmacoepidemiologist at Rutgers University, New Brunswick, N.J.
On the other hand, noted several committee members, pausing to conduct a premarketing randomized, controlled trial would keep a beneficial drug away from a population in need. A postmarketing randomized, controlled trial, even a simple trial, still presents challenges, some of the committee acknowledged. Dr. Khosla voiced the opinion that “A randomized, controlled trial is virtually impossible.”
The committee, which was charged with discussing, but not voting on, what additional data should be obtained – and when – to sort out the cardiovascular safety question, was approximately evenly divided in the matter of whether an observational or registry-based trial, or a controlled trial, would be the best path forward.
Committee member Robert A. Adler, MD, put a realistic frame around the debate. “As an endocrinologist, I deal with nuances every day. I really think the kind of clinician who is going to be using this drug is used to dealing with benefits and risks and trying to tailor treatment to a given patient,” said Dr. Adler, professor of internal medicine and epidemiology at Virginia Commonwealth University, Richmond.
In its proposed indication, Amgen defined the population of menopausal women at high risk of fracture as those with a history of osteoporotic fracture, multiple risk factors for fracture, or patients who have failed or are intolerant to other available osteoporosis therapy. Romosozumab would be given as a once-monthly subcutaneous injection of 210 mg for a period of 12 months, to be followed by antiresorptive therapy.
Most of the participants in the clinical trials resided outside the United States, primarily because of the difficulty of recruiting clinical trial participants in the United States, Amgen officials said during their presentation. However, neither the time to the first positively adjudicated MACE nor bone mineral density responses at month 12 differed significantly across the various geographic regions where clinical trial sites were located, said Rachel Wagman, MD, the executive medical director of global clinical development for Amgen. Still, several committee members called for postmarketing data to focus on U.S. patients.
Romosozumab was approved for marketing in Japan on Jan. 8, 2019; approval is also being sought in Europe .
The FDA usually follows the recommendations of its advisory panels.
Spending on medical marketing increased by $12.2 billion over the last 2 decades
Total spending on medical marketing in the United States increased from $17.7 billion in 1997 to $29.9 billion in 2016, according to an analysis of direct-to-consumer (DTC) and professional marketing for prescription drugs, disease awareness campaigns, health services, and laboratory tests.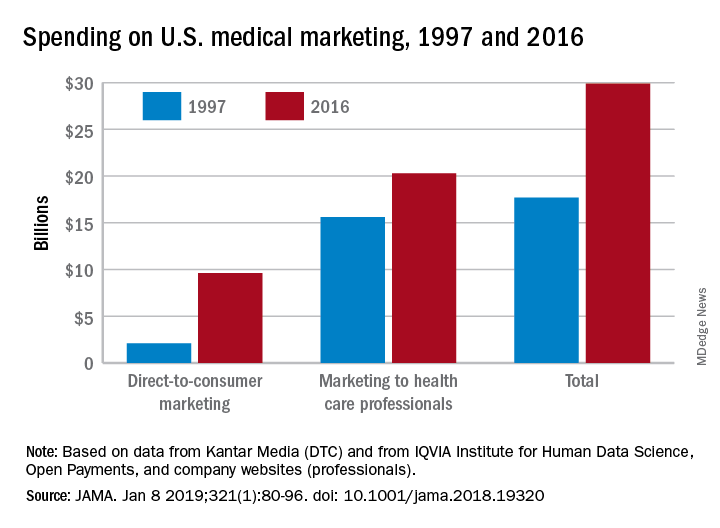
“Increased medical marketing reflects a convergence of scientific, economic, legal, and social forces,” wrote Lisa M. Schwartz, MD, and her coauthor, adding that “although marketing expanded over 20 years, regulatory oversight remains relatively limited.” Dr. Schwartz, then codirector of the Center for Medicine and Media at The Dartmouth Institute in Lebanon, N.H., died in November of 2018, after her work was accepted for publication in JAMA.
Dr. Schwartz and her coauthor, David Woloshin, MD, also of Dartmouth, reviewed consumer advertising and professional marketing data, along with searches of medical literature and business journals, to ascertain the quantity and impact of spending. The most money was spent on marketing to medical professionals, which increased from $15.6 billion in 1997 to $20.3 billion in 2016. In terms of percentages, the biggest increase was seen in DTC advertising: $2.1 billion in 1997 (11.9% of total spending) ballooned to $9.6 billion (32.1% of total spending).
These increases were not accompanied by corresponding regulatory efforts to limit influence or protect patients and consumers. In 2016, the Food and Drug Administration’s Office of Prescription Drug Promotion received 97,252 promotional materials that drug companies submitted for review, compared with 34,182 in 1997, but violation letters for prescription drug advertising decreased from 156 to 11. In the same year, the FDA reviewed 41% of core materials – such as risk disclosures and key messages – for new drugs or indications prior to launch, a performance measure the coauthors called “critically important.”
In regard to disease awareness campaigns, 2004 guidance from the FDA on awareness advertising – including standards for unbranded campaigns and recommendations to avoid encouraging self-diagnosis and self-treatment – was withdrawn in 2015 and never replaced. The Federal Trade Commission, which has jurisdiction over unbranded advertising, has not taken regulatory action of its own; any FDA requests for investigation are unknown. In addition, these 2 decades have not seen state attorneys general initiate any action against deceptive consumer advertising, nor has the FTC acted against misleading laboratory test promotion.
“The FDA and FTC should establish and enforce standards for responsible disease awareness campaigns,” the coauthors wrote, “including criteria to validate symptom quizzes (or banning them) and evidence-based strategies to minimize misconceptions that a drug can treat all symptoms of disease.”
Overall, spending on medical marketing actually increased faster than did spending on health services overall. Marketing saw a remarkable 430% increase ($542 million to $2.9 billion) over the 2 decades, while health services spending increased by 90% ($1.2 trillion to $2.2 trillion).
One of the rare similarities from 1997 to 2016 was spending on marketing prescription drugs to physicians, typically through face-to-face meetings and hospital visits; this held steady at approximately $5 billion. However, spending on drug samples increased from $8.9 billion to $13.5 billion, while medical journal advertising declined drastically from $744 million to $119 million.
Spending on DTC marketing of prescription drugs increased across all therapeutic categories but three: cholesterol, allergy, and osteoporosis, each of which saw top-selling drugs either become over-the-counter or lose patent protection. Spending on drugs for diabetes/endocrine disease went from $27 million in 1997 to a whopping $725 million in 2016, followed by dermatology drugs ($67 million to $605 million) and pain/central nervous system drugs ($56 million to $542 million).
The coauthors shared potential limitations of their study, including the likelihood that they underestimated how much is actually spent on medical marketing. “Data on professional marketing (e.g., detailing) of laboratory tests, health services or devices, and pharmaceutical company spending on coupons or rebates, online promotion, and meetings and events could not be obtained,” they noted. In addition, company marketing budgets often do not include additional expenses that should count toward this total, and any published literature on medical marketing’s return on investment is largely based on observational data and cannot be fully relied upon.
The two coauthors previously served as medical experts in testosterone litigation and were cofounders of a company that provided data about the benefits and harms of prescription drugs, which ceased operations in December 2016. No other conflicts of interest were reported.
SOURCE: Schwartz LM et al. JAMA. 2019 Jan 8. doi: 10.1001/jama.2018.19320.
Total spending on medical marketing in the United States increased from $17.7 billion in 1997 to $29.9 billion in 2016, according to an analysis of direct-to-consumer (DTC) and professional marketing for prescription drugs, disease awareness campaigns, health services, and laboratory tests.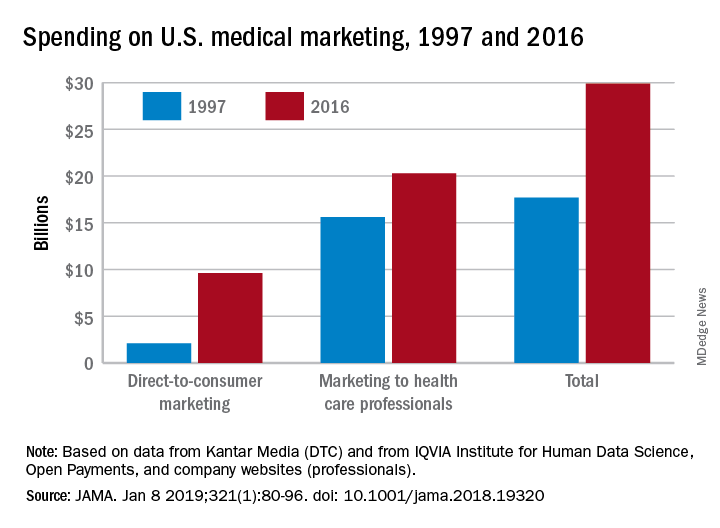
“Increased medical marketing reflects a convergence of scientific, economic, legal, and social forces,” wrote Lisa M. Schwartz, MD, and her coauthor, adding that “although marketing expanded over 20 years, regulatory oversight remains relatively limited.” Dr. Schwartz, then codirector of the Center for Medicine and Media at The Dartmouth Institute in Lebanon, N.H., died in November of 2018, after her work was accepted for publication in JAMA.
Dr. Schwartz and her coauthor, David Woloshin, MD, also of Dartmouth, reviewed consumer advertising and professional marketing data, along with searches of medical literature and business journals, to ascertain the quantity and impact of spending. The most money was spent on marketing to medical professionals, which increased from $15.6 billion in 1997 to $20.3 billion in 2016. In terms of percentages, the biggest increase was seen in DTC advertising: $2.1 billion in 1997 (11.9% of total spending) ballooned to $9.6 billion (32.1% of total spending).
These increases were not accompanied by corresponding regulatory efforts to limit influence or protect patients and consumers. In 2016, the Food and Drug Administration’s Office of Prescription Drug Promotion received 97,252 promotional materials that drug companies submitted for review, compared with 34,182 in 1997, but violation letters for prescription drug advertising decreased from 156 to 11. In the same year, the FDA reviewed 41% of core materials – such as risk disclosures and key messages – for new drugs or indications prior to launch, a performance measure the coauthors called “critically important.”
In regard to disease awareness campaigns, 2004 guidance from the FDA on awareness advertising – including standards for unbranded campaigns and recommendations to avoid encouraging self-diagnosis and self-treatment – was withdrawn in 2015 and never replaced. The Federal Trade Commission, which has jurisdiction over unbranded advertising, has not taken regulatory action of its own; any FDA requests for investigation are unknown. In addition, these 2 decades have not seen state attorneys general initiate any action against deceptive consumer advertising, nor has the FTC acted against misleading laboratory test promotion.
“The FDA and FTC should establish and enforce standards for responsible disease awareness campaigns,” the coauthors wrote, “including criteria to validate symptom quizzes (or banning them) and evidence-based strategies to minimize misconceptions that a drug can treat all symptoms of disease.”
Overall, spending on medical marketing actually increased faster than did spending on health services overall. Marketing saw a remarkable 430% increase ($542 million to $2.9 billion) over the 2 decades, while health services spending increased by 90% ($1.2 trillion to $2.2 trillion).
One of the rare similarities from 1997 to 2016 was spending on marketing prescription drugs to physicians, typically through face-to-face meetings and hospital visits; this held steady at approximately $5 billion. However, spending on drug samples increased from $8.9 billion to $13.5 billion, while medical journal advertising declined drastically from $744 million to $119 million.
Spending on DTC marketing of prescription drugs increased across all therapeutic categories but three: cholesterol, allergy, and osteoporosis, each of which saw top-selling drugs either become over-the-counter or lose patent protection. Spending on drugs for diabetes/endocrine disease went from $27 million in 1997 to a whopping $725 million in 2016, followed by dermatology drugs ($67 million to $605 million) and pain/central nervous system drugs ($56 million to $542 million).
The coauthors shared potential limitations of their study, including the likelihood that they underestimated how much is actually spent on medical marketing. “Data on professional marketing (e.g., detailing) of laboratory tests, health services or devices, and pharmaceutical company spending on coupons or rebates, online promotion, and meetings and events could not be obtained,” they noted. In addition, company marketing budgets often do not include additional expenses that should count toward this total, and any published literature on medical marketing’s return on investment is largely based on observational data and cannot be fully relied upon.
The two coauthors previously served as medical experts in testosterone litigation and were cofounders of a company that provided data about the benefits and harms of prescription drugs, which ceased operations in December 2016. No other conflicts of interest were reported.
SOURCE: Schwartz LM et al. JAMA. 2019 Jan 8. doi: 10.1001/jama.2018.19320.
Total spending on medical marketing in the United States increased from $17.7 billion in 1997 to $29.9 billion in 2016, according to an analysis of direct-to-consumer (DTC) and professional marketing for prescription drugs, disease awareness campaigns, health services, and laboratory tests.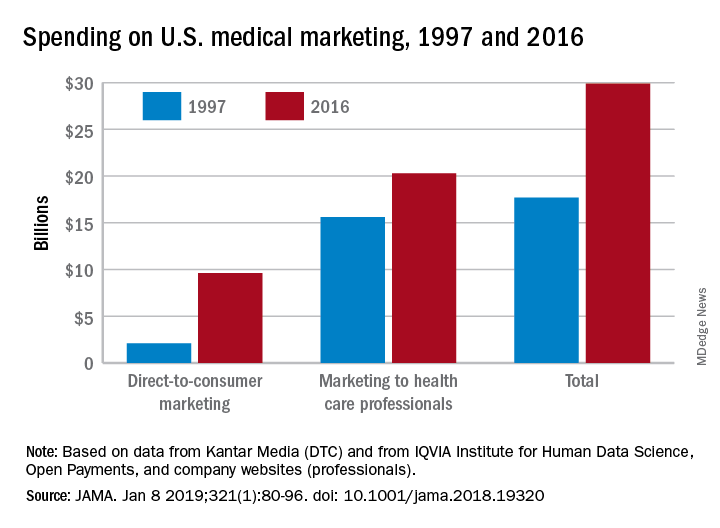
“Increased medical marketing reflects a convergence of scientific, economic, legal, and social forces,” wrote Lisa M. Schwartz, MD, and her coauthor, adding that “although marketing expanded over 20 years, regulatory oversight remains relatively limited.” Dr. Schwartz, then codirector of the Center for Medicine and Media at The Dartmouth Institute in Lebanon, N.H., died in November of 2018, after her work was accepted for publication in JAMA.
Dr. Schwartz and her coauthor, David Woloshin, MD, also of Dartmouth, reviewed consumer advertising and professional marketing data, along with searches of medical literature and business journals, to ascertain the quantity and impact of spending. The most money was spent on marketing to medical professionals, which increased from $15.6 billion in 1997 to $20.3 billion in 2016. In terms of percentages, the biggest increase was seen in DTC advertising: $2.1 billion in 1997 (11.9% of total spending) ballooned to $9.6 billion (32.1% of total spending).
These increases were not accompanied by corresponding regulatory efforts to limit influence or protect patients and consumers. In 2016, the Food and Drug Administration’s Office of Prescription Drug Promotion received 97,252 promotional materials that drug companies submitted for review, compared with 34,182 in 1997, but violation letters for prescription drug advertising decreased from 156 to 11. In the same year, the FDA reviewed 41% of core materials – such as risk disclosures and key messages – for new drugs or indications prior to launch, a performance measure the coauthors called “critically important.”
In regard to disease awareness campaigns, 2004 guidance from the FDA on awareness advertising – including standards for unbranded campaigns and recommendations to avoid encouraging self-diagnosis and self-treatment – was withdrawn in 2015 and never replaced. The Federal Trade Commission, which has jurisdiction over unbranded advertising, has not taken regulatory action of its own; any FDA requests for investigation are unknown. In addition, these 2 decades have not seen state attorneys general initiate any action against deceptive consumer advertising, nor has the FTC acted against misleading laboratory test promotion.
“The FDA and FTC should establish and enforce standards for responsible disease awareness campaigns,” the coauthors wrote, “including criteria to validate symptom quizzes (or banning them) and evidence-based strategies to minimize misconceptions that a drug can treat all symptoms of disease.”
Overall, spending on medical marketing actually increased faster than did spending on health services overall. Marketing saw a remarkable 430% increase ($542 million to $2.9 billion) over the 2 decades, while health services spending increased by 90% ($1.2 trillion to $2.2 trillion).
One of the rare similarities from 1997 to 2016 was spending on marketing prescription drugs to physicians, typically through face-to-face meetings and hospital visits; this held steady at approximately $5 billion. However, spending on drug samples increased from $8.9 billion to $13.5 billion, while medical journal advertising declined drastically from $744 million to $119 million.
Spending on DTC marketing of prescription drugs increased across all therapeutic categories but three: cholesterol, allergy, and osteoporosis, each of which saw top-selling drugs either become over-the-counter or lose patent protection. Spending on drugs for diabetes/endocrine disease went from $27 million in 1997 to a whopping $725 million in 2016, followed by dermatology drugs ($67 million to $605 million) and pain/central nervous system drugs ($56 million to $542 million).
The coauthors shared potential limitations of their study, including the likelihood that they underestimated how much is actually spent on medical marketing. “Data on professional marketing (e.g., detailing) of laboratory tests, health services or devices, and pharmaceutical company spending on coupons or rebates, online promotion, and meetings and events could not be obtained,” they noted. In addition, company marketing budgets often do not include additional expenses that should count toward this total, and any published literature on medical marketing’s return on investment is largely based on observational data and cannot be fully relied upon.
The two coauthors previously served as medical experts in testosterone litigation and were cofounders of a company that provided data about the benefits and harms of prescription drugs, which ceased operations in December 2016. No other conflicts of interest were reported.
SOURCE: Schwartz LM et al. JAMA. 2019 Jan 8. doi: 10.1001/jama.2018.19320.
FROM JAMA
Key clinical point: Medical marketing spending – especially on direct-to-consumer advertising for drugs and health services – increased exponentially over the last 2 decades.
Major finding: From 1997 through 2016, spending on medical marketing of drugs, disease awareness campaigns, health services, and laboratory testing increased from $17.7 to $29.9 billion.
Study details: An analysis of consumer advertising and professional marketing data, along with a review of regulations and legal actions undertaken by U.S. federal agencies.
Disclosures: The two coauthors previously served as medical experts in testosterone litigation and were cofounders of a company that provided data about the benefits and harms of prescription drugs, which ceased operations in December 2016. No other conflicts of interest were reported.
Source: Schwartz LM et al. JAMA. 2019 Jan 8. doi: 10.1001/jama.2018.19320.
Antidepressants tied to greater hip fracture incidence in older adults
Older patients in a Swedish registry who took antidepressants had a greater incidence of hip fracture the year before beginning antidepressant therapy and the year after starting therapy, compared with individuals in a matched control group.
The use of antidepressants is associated with adverse events such as a higher risk of falls, wrote Jon Brännström, MD, and his colleagues in JAMA Psychiatry. Some evidence also suggests that antidepressants “might affect bone metabolism, thereby increasing the risk of hip fracture.”
To examine the relationship between antidepressants and hip fracture, Dr. Brännström and his colleagues performed a nationwide cohort study of 204,072 individuals in the Prescribed Drug Register of Sweden’s National Board of Health and Welfare. All of the individuals were aged at least 65 years (mean age, 80.1 years; 63.1% women) and filled a prescription for an antidepressant between July 2006 and December 2011. Selective serotonin reuptake inhibitors made up 62.6% of the antidepressants used.
Patients who filled an antidepressant prescription during that time period were matched with a control group of individuals by birth year and gender and were studied the year before and after beginning antidepressant therapy.
In the year after initiating antidepressant therapy, there was a 3.5% incidence rate for hip fractures, compared with 1.3% in the control group.
After adjusting the results using a conditional logistic regression model, the highest rate of hip fracture among antidepressant users occurred between 16 days and 30 days prior to filling the prescription (odds ratio, 5.76; 95% confidence interval, 4.73-7.01); this association persisted in further subgroup analyses based on age, reported Dr. Brännström, who is affiliated with the department of community medicine and rehabilitation and geriatric medicine at Umeå University (Sweden), and his colleagues.
They noted that, although the study included all Swedish individuals who filled prescriptions for antidepressants during the study period, there is an absence of primary care comorbidity data and indications for antidepressant use. In addition, the definition of high- and low-medication doses does not always match what is considered high and low therapeutically and the information that can be gleaned from merging data from several different registries was limited.
“These findings raise questions about associations between antidepressant use and hip fracture seen in previous observational studies,” Dr. Brännström and his colleagues wrote. “Further analysis of this association in treatment studies and examination of the incidence of hip fracture before and after the discontinuation of treatment is required and may shed further light on the possible residual risk associated with treatment.”
This study was funded by the Swedish Research Council. The authors reported no relevant conflicts of interest.
SOURCE: Brännström J et al. JAMA Psychiatry. 2019 Jan 2. doi: 10.1001/jamapsychiatry.2018.3679.
In many cases where an adverse event is linked to a medication, such as in the case of gastrointestinal bleeds and blood thinners, the adverse event is not linked to the medication. However, this is not the case with antidepressants and hip fracture, Andrea Iaboni, MD, DPhil, and Donovan T. Maust, MD, wrote in a related editorial (JAMA Psychiatry. 2019 Jan 2. doi: 10.1001/jamapsychiatry.2018.3632).
“Patients are routinely prescribed antidepressants following a fracture,” the authors wrote, noting that depression can occur for patients who do not have a history of depression and can last as long as 1 year after hip fracture. The reasons for depression after hip fracture are possibly caused by the consequences of the event or a comorbid condition, such as cerebrovascular disease burden, cognitive impairment, frailty, and impaired functional status. In addition, new antidepressant prescriptions are 10 times the normal rate for older adults in the months after a hip fracture.
Many older users of antidepressants have a hip fracture event in their past, which could be caused by an untreated case of depression and an elevated risk of elevated fall or fracture, as suggested by Brännström et al., while other reasons could include off-label indications such as insomnia, poor motivation during rehabilitation therapy, pain, or hyperactive delirium.
“If individuals with untreated depression are at risk of falls and fractures, it follows that there would be an elevated rate of fractures before antidepressant use,” the authors wrote. “However, as discussed earlier, it is also important to recognize that, during the postfracture period, rightly or wrongly, antidepressants are prescribed at a high rate.”
Clinicians who treat these patients should not stop all antidepressant prescribing to this population. Instead, “a pragmatic preventive approach is warranted, starting with selecting the antidepressant, a cautious initial dose and dose-escalation schedule, a review of potentially interacting therapies ... and referral to fall prevention programs for patients with other risk factors for falls,” they wrote.
“For most older adults, the toll of untreated depression will likely outweigh the potential risks associated with antidepressant use.”
Dr. Iabroni is with the Toronto Rehabilitation Institute and the University of Toronto. He reported receiving fees from serving as a scientific adviser for Winterlight Labs. Dr. Maust is with the department of psychiatry at the University of Michigan, Ann Arbor. He reported no relevant conflicts of interest.
In many cases where an adverse event is linked to a medication, such as in the case of gastrointestinal bleeds and blood thinners, the adverse event is not linked to the medication. However, this is not the case with antidepressants and hip fracture, Andrea Iaboni, MD, DPhil, and Donovan T. Maust, MD, wrote in a related editorial (JAMA Psychiatry. 2019 Jan 2. doi: 10.1001/jamapsychiatry.2018.3632).
“Patients are routinely prescribed antidepressants following a fracture,” the authors wrote, noting that depression can occur for patients who do not have a history of depression and can last as long as 1 year after hip fracture. The reasons for depression after hip fracture are possibly caused by the consequences of the event or a comorbid condition, such as cerebrovascular disease burden, cognitive impairment, frailty, and impaired functional status. In addition, new antidepressant prescriptions are 10 times the normal rate for older adults in the months after a hip fracture.
Many older users of antidepressants have a hip fracture event in their past, which could be caused by an untreated case of depression and an elevated risk of elevated fall or fracture, as suggested by Brännström et al., while other reasons could include off-label indications such as insomnia, poor motivation during rehabilitation therapy, pain, or hyperactive delirium.
“If individuals with untreated depression are at risk of falls and fractures, it follows that there would be an elevated rate of fractures before antidepressant use,” the authors wrote. “However, as discussed earlier, it is also important to recognize that, during the postfracture period, rightly or wrongly, antidepressants are prescribed at a high rate.”
Clinicians who treat these patients should not stop all antidepressant prescribing to this population. Instead, “a pragmatic preventive approach is warranted, starting with selecting the antidepressant, a cautious initial dose and dose-escalation schedule, a review of potentially interacting therapies ... and referral to fall prevention programs for patients with other risk factors for falls,” they wrote.
“For most older adults, the toll of untreated depression will likely outweigh the potential risks associated with antidepressant use.”
Dr. Iabroni is with the Toronto Rehabilitation Institute and the University of Toronto. He reported receiving fees from serving as a scientific adviser for Winterlight Labs. Dr. Maust is with the department of psychiatry at the University of Michigan, Ann Arbor. He reported no relevant conflicts of interest.
In many cases where an adverse event is linked to a medication, such as in the case of gastrointestinal bleeds and blood thinners, the adverse event is not linked to the medication. However, this is not the case with antidepressants and hip fracture, Andrea Iaboni, MD, DPhil, and Donovan T. Maust, MD, wrote in a related editorial (JAMA Psychiatry. 2019 Jan 2. doi: 10.1001/jamapsychiatry.2018.3632).
“Patients are routinely prescribed antidepressants following a fracture,” the authors wrote, noting that depression can occur for patients who do not have a history of depression and can last as long as 1 year after hip fracture. The reasons for depression after hip fracture are possibly caused by the consequences of the event or a comorbid condition, such as cerebrovascular disease burden, cognitive impairment, frailty, and impaired functional status. In addition, new antidepressant prescriptions are 10 times the normal rate for older adults in the months after a hip fracture.
Many older users of antidepressants have a hip fracture event in their past, which could be caused by an untreated case of depression and an elevated risk of elevated fall or fracture, as suggested by Brännström et al., while other reasons could include off-label indications such as insomnia, poor motivation during rehabilitation therapy, pain, or hyperactive delirium.
“If individuals with untreated depression are at risk of falls and fractures, it follows that there would be an elevated rate of fractures before antidepressant use,” the authors wrote. “However, as discussed earlier, it is also important to recognize that, during the postfracture period, rightly or wrongly, antidepressants are prescribed at a high rate.”
Clinicians who treat these patients should not stop all antidepressant prescribing to this population. Instead, “a pragmatic preventive approach is warranted, starting with selecting the antidepressant, a cautious initial dose and dose-escalation schedule, a review of potentially interacting therapies ... and referral to fall prevention programs for patients with other risk factors for falls,” they wrote.
“For most older adults, the toll of untreated depression will likely outweigh the potential risks associated with antidepressant use.”
Dr. Iabroni is with the Toronto Rehabilitation Institute and the University of Toronto. He reported receiving fees from serving as a scientific adviser for Winterlight Labs. Dr. Maust is with the department of psychiatry at the University of Michigan, Ann Arbor. He reported no relevant conflicts of interest.
Older patients in a Swedish registry who took antidepressants had a greater incidence of hip fracture the year before beginning antidepressant therapy and the year after starting therapy, compared with individuals in a matched control group.
The use of antidepressants is associated with adverse events such as a higher risk of falls, wrote Jon Brännström, MD, and his colleagues in JAMA Psychiatry. Some evidence also suggests that antidepressants “might affect bone metabolism, thereby increasing the risk of hip fracture.”
To examine the relationship between antidepressants and hip fracture, Dr. Brännström and his colleagues performed a nationwide cohort study of 204,072 individuals in the Prescribed Drug Register of Sweden’s National Board of Health and Welfare. All of the individuals were aged at least 65 years (mean age, 80.1 years; 63.1% women) and filled a prescription for an antidepressant between July 2006 and December 2011. Selective serotonin reuptake inhibitors made up 62.6% of the antidepressants used.
Patients who filled an antidepressant prescription during that time period were matched with a control group of individuals by birth year and gender and were studied the year before and after beginning antidepressant therapy.
In the year after initiating antidepressant therapy, there was a 3.5% incidence rate for hip fractures, compared with 1.3% in the control group.
After adjusting the results using a conditional logistic regression model, the highest rate of hip fracture among antidepressant users occurred between 16 days and 30 days prior to filling the prescription (odds ratio, 5.76; 95% confidence interval, 4.73-7.01); this association persisted in further subgroup analyses based on age, reported Dr. Brännström, who is affiliated with the department of community medicine and rehabilitation and geriatric medicine at Umeå University (Sweden), and his colleagues.
They noted that, although the study included all Swedish individuals who filled prescriptions for antidepressants during the study period, there is an absence of primary care comorbidity data and indications for antidepressant use. In addition, the definition of high- and low-medication doses does not always match what is considered high and low therapeutically and the information that can be gleaned from merging data from several different registries was limited.
“These findings raise questions about associations between antidepressant use and hip fracture seen in previous observational studies,” Dr. Brännström and his colleagues wrote. “Further analysis of this association in treatment studies and examination of the incidence of hip fracture before and after the discontinuation of treatment is required and may shed further light on the possible residual risk associated with treatment.”
This study was funded by the Swedish Research Council. The authors reported no relevant conflicts of interest.
SOURCE: Brännström J et al. JAMA Psychiatry. 2019 Jan 2. doi: 10.1001/jamapsychiatry.2018.3679.
Older patients in a Swedish registry who took antidepressants had a greater incidence of hip fracture the year before beginning antidepressant therapy and the year after starting therapy, compared with individuals in a matched control group.
The use of antidepressants is associated with adverse events such as a higher risk of falls, wrote Jon Brännström, MD, and his colleagues in JAMA Psychiatry. Some evidence also suggests that antidepressants “might affect bone metabolism, thereby increasing the risk of hip fracture.”
To examine the relationship between antidepressants and hip fracture, Dr. Brännström and his colleagues performed a nationwide cohort study of 204,072 individuals in the Prescribed Drug Register of Sweden’s National Board of Health and Welfare. All of the individuals were aged at least 65 years (mean age, 80.1 years; 63.1% women) and filled a prescription for an antidepressant between July 2006 and December 2011. Selective serotonin reuptake inhibitors made up 62.6% of the antidepressants used.
Patients who filled an antidepressant prescription during that time period were matched with a control group of individuals by birth year and gender and were studied the year before and after beginning antidepressant therapy.
In the year after initiating antidepressant therapy, there was a 3.5% incidence rate for hip fractures, compared with 1.3% in the control group.
After adjusting the results using a conditional logistic regression model, the highest rate of hip fracture among antidepressant users occurred between 16 days and 30 days prior to filling the prescription (odds ratio, 5.76; 95% confidence interval, 4.73-7.01); this association persisted in further subgroup analyses based on age, reported Dr. Brännström, who is affiliated with the department of community medicine and rehabilitation and geriatric medicine at Umeå University (Sweden), and his colleagues.
They noted that, although the study included all Swedish individuals who filled prescriptions for antidepressants during the study period, there is an absence of primary care comorbidity data and indications for antidepressant use. In addition, the definition of high- and low-medication doses does not always match what is considered high and low therapeutically and the information that can be gleaned from merging data from several different registries was limited.
“These findings raise questions about associations between antidepressant use and hip fracture seen in previous observational studies,” Dr. Brännström and his colleagues wrote. “Further analysis of this association in treatment studies and examination of the incidence of hip fracture before and after the discontinuation of treatment is required and may shed further light on the possible residual risk associated with treatment.”
This study was funded by the Swedish Research Council. The authors reported no relevant conflicts of interest.
SOURCE: Brännström J et al. JAMA Psychiatry. 2019 Jan 2. doi: 10.1001/jamapsychiatry.2018.3679.
FROM JAMA PSYCHIATRY
Key clinical point: An association was found between greater hip fracture incidence for older individuals taking antidepressants in the year before beginning therapy and the year after starting therapy.
Major finding: Individuals who took antidepressants had a greater incidence of hip fractures in the year before (2.8% vs. 1.1%) and the year after (3.5% vs. 1.3%) beginning antidepressants, compared with individuals in a matched control group.
Study details: A nationwide cohort study of 408,144 individuals in the Prescribed Drugs Register of Sweden’s National Board of Health and Welfare who were aged 65 years or older.
Disclosures: This study was funded by the Swedish Research Council. The authors reported no relevant conflicts of interest.
Source: Brännström J et al. JAMA Psychiatry. 2019 Jan 2. doi: 10.1001/jamapsychiatry.2018.3679.
To prevent fractures, treating only women with osteoporosis is not enough
The conventional bone mineral density threshold for initiating treatment to prevent fragility fractures is a T-score of less than -2.5 (the World Health Organization criteria for osteoporosis).1 However, most fractures experienced by postmenopausal women occur not in osteoporotic women but in those with low bone mass (osteopenia).2
Investigators in New Zealand recently published the results of a randomized controlled trial they conducted to determine the efficacy of zoledronate (zoledronic acid) in preventing fractures in postmenopausal women.3 They enrolled women age 65 years or older with osteopenia of the hip and randomly assigned the participants to 4 intravenous infusions of 5 mg zoledronic acid or placebo at 18-month intervals for 6 years.
Zoledronic acid reduced fracture risk
The trial included 2,000 postmenopausal women (mean age at baseline, 71 years; 94% European ethnicity) with a T-score of -1.0 to -2.5 at either the total hip or the femoral neck on either side. Both hips were assessed. The women received either zoledronic acid treatment or placebo in a 1:1 ratio. Candidates were excluded if they regularly used bone-active drugs in the previous year.
Fragility fractures were noted in 190 women in the placebo group and in 122 women treated with zoledronic acid (hazard ratio [HR], 0.63; 95% confidence interval [CI], 0.50–0.79, P<.001). The number of women that would need to be treated to prevent the occurrence of a fracture in 1 woman was 15.
Compared with placebo, zoledronic acid also lowered the risk of nonvertebral, symptomatic, and vertebral fractures as well as height loss (P≤.003 for these 4 comparisons). Relatively few adverse events occurred with zoledronic acid treatment. No atypical femoral fractures or cases of osteonecrosis of the jaw occurred in either group.
Trial closes the knowledge gap regarding treatment thresholds
This trial’s findings underscore the importance of age as a risk factor for fragility fracture and clarify that pharmacologic treatment is appropriate not only for women with osteoporosis but also for older postmenopausal women with osteopenia.
As the authors point out, administration of zoledronic acid less often than annually can be highly effective in preventing fractures; they recommend future trials of administration of this intravenous bisphosphonate at intervals less frequent than 18 months. Although the absence of atypical femoral fractures or cases of osteonecrosis of the jaw is reassuring, the authors note that their trial was underpowered to assess these uncommon events.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- World Health Organization. WHO Scientific Group on the assessment of osteoporosis at primary health care level. Summary meeting report, Brussels, Belgium, 5-7 May 2004. https://www. who.int/chp/topics/Osteoporosis.pdf. Accessed November 19, 2018.
- Siris ES, Chen YT, Abbott TA, et al. Bone mineral density thresholds for pharmacological intervention to prevent fractures. Arch Intern Med. 2004;164:1108-1112.
- Reid IR, Horne AM, Mihov B, et al. Fracture prevention with zoledronate in older women with osteopenia. N Engl J Med. 2018. doi:10.1056/NEJMoa1808082.
The conventional bone mineral density threshold for initiating treatment to prevent fragility fractures is a T-score of less than -2.5 (the World Health Organization criteria for osteoporosis).1 However, most fractures experienced by postmenopausal women occur not in osteoporotic women but in those with low bone mass (osteopenia).2
Investigators in New Zealand recently published the results of a randomized controlled trial they conducted to determine the efficacy of zoledronate (zoledronic acid) in preventing fractures in postmenopausal women.3 They enrolled women age 65 years or older with osteopenia of the hip and randomly assigned the participants to 4 intravenous infusions of 5 mg zoledronic acid or placebo at 18-month intervals for 6 years.
Zoledronic acid reduced fracture risk
The trial included 2,000 postmenopausal women (mean age at baseline, 71 years; 94% European ethnicity) with a T-score of -1.0 to -2.5 at either the total hip or the femoral neck on either side. Both hips were assessed. The women received either zoledronic acid treatment or placebo in a 1:1 ratio. Candidates were excluded if they regularly used bone-active drugs in the previous year.
Fragility fractures were noted in 190 women in the placebo group and in 122 women treated with zoledronic acid (hazard ratio [HR], 0.63; 95% confidence interval [CI], 0.50–0.79, P<.001). The number of women that would need to be treated to prevent the occurrence of a fracture in 1 woman was 15.
Compared with placebo, zoledronic acid also lowered the risk of nonvertebral, symptomatic, and vertebral fractures as well as height loss (P≤.003 for these 4 comparisons). Relatively few adverse events occurred with zoledronic acid treatment. No atypical femoral fractures or cases of osteonecrosis of the jaw occurred in either group.
Trial closes the knowledge gap regarding treatment thresholds
This trial’s findings underscore the importance of age as a risk factor for fragility fracture and clarify that pharmacologic treatment is appropriate not only for women with osteoporosis but also for older postmenopausal women with osteopenia.
As the authors point out, administration of zoledronic acid less often than annually can be highly effective in preventing fractures; they recommend future trials of administration of this intravenous bisphosphonate at intervals less frequent than 18 months. Although the absence of atypical femoral fractures or cases of osteonecrosis of the jaw is reassuring, the authors note that their trial was underpowered to assess these uncommon events.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
The conventional bone mineral density threshold for initiating treatment to prevent fragility fractures is a T-score of less than -2.5 (the World Health Organization criteria for osteoporosis).1 However, most fractures experienced by postmenopausal women occur not in osteoporotic women but in those with low bone mass (osteopenia).2
Investigators in New Zealand recently published the results of a randomized controlled trial they conducted to determine the efficacy of zoledronate (zoledronic acid) in preventing fractures in postmenopausal women.3 They enrolled women age 65 years or older with osteopenia of the hip and randomly assigned the participants to 4 intravenous infusions of 5 mg zoledronic acid or placebo at 18-month intervals for 6 years.
Zoledronic acid reduced fracture risk
The trial included 2,000 postmenopausal women (mean age at baseline, 71 years; 94% European ethnicity) with a T-score of -1.0 to -2.5 at either the total hip or the femoral neck on either side. Both hips were assessed. The women received either zoledronic acid treatment or placebo in a 1:1 ratio. Candidates were excluded if they regularly used bone-active drugs in the previous year.
Fragility fractures were noted in 190 women in the placebo group and in 122 women treated with zoledronic acid (hazard ratio [HR], 0.63; 95% confidence interval [CI], 0.50–0.79, P<.001). The number of women that would need to be treated to prevent the occurrence of a fracture in 1 woman was 15.
Compared with placebo, zoledronic acid also lowered the risk of nonvertebral, symptomatic, and vertebral fractures as well as height loss (P≤.003 for these 4 comparisons). Relatively few adverse events occurred with zoledronic acid treatment. No atypical femoral fractures or cases of osteonecrosis of the jaw occurred in either group.
Trial closes the knowledge gap regarding treatment thresholds
This trial’s findings underscore the importance of age as a risk factor for fragility fracture and clarify that pharmacologic treatment is appropriate not only for women with osteoporosis but also for older postmenopausal women with osteopenia.
As the authors point out, administration of zoledronic acid less often than annually can be highly effective in preventing fractures; they recommend future trials of administration of this intravenous bisphosphonate at intervals less frequent than 18 months. Although the absence of atypical femoral fractures or cases of osteonecrosis of the jaw is reassuring, the authors note that their trial was underpowered to assess these uncommon events.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- World Health Organization. WHO Scientific Group on the assessment of osteoporosis at primary health care level. Summary meeting report, Brussels, Belgium, 5-7 May 2004. https://www. who.int/chp/topics/Osteoporosis.pdf. Accessed November 19, 2018.
- Siris ES, Chen YT, Abbott TA, et al. Bone mineral density thresholds for pharmacological intervention to prevent fractures. Arch Intern Med. 2004;164:1108-1112.
- Reid IR, Horne AM, Mihov B, et al. Fracture prevention with zoledronate in older women with osteopenia. N Engl J Med. 2018. doi:10.1056/NEJMoa1808082.
- World Health Organization. WHO Scientific Group on the assessment of osteoporosis at primary health care level. Summary meeting report, Brussels, Belgium, 5-7 May 2004. https://www. who.int/chp/topics/Osteoporosis.pdf. Accessed November 19, 2018.
- Siris ES, Chen YT, Abbott TA, et al. Bone mineral density thresholds for pharmacological intervention to prevent fractures. Arch Intern Med. 2004;164:1108-1112.
- Reid IR, Horne AM, Mihov B, et al. Fracture prevention with zoledronate in older women with osteopenia. N Engl J Med. 2018. doi:10.1056/NEJMoa1808082.
2018 Update on bone health
As ObGyns, we are the first-line health care providers for our menopausal patients in terms of identifying, preventing, and initiating treatment for women at risk for fragility fractures. Osteoporosis is probably the most important risk factor for bone health, although sarcopenia, frailty, poor eyesight, and falls also play a significant role in bone health and fragility fracture.
In 2005, more than 2 million incident fractures were reported in the United States, with a total cost of $17 billion.1 By 2025, annual fractures and costs are expected to rise by almost 50%. People who are 65 to 74 years of age will likely experience the largest increase in fracture—greater than 87%.1
Findings from the Women’s Health Initiative study showed that the number of women who had a clinical fracture in 1 year exceeded all the cases of myocardial infarction, stroke, and breast cancer combined.2 Furthermore, the morbidity and mortality rates for fractures are staggering. Thirty percent of women with a hip fracture will be dead within 1 year.3 So, although many patients fear developing breast cancer, and cardiovascular disease remains the number 1 cause of death, the impact of maintaining and protecting bone health cannot be emphasized enough.

_
WHI incidental findings: Hormone-treated menopausal women had decreased hip fracture rate
Manson JE, Aragaki AK, Rossouw JE, et al; WHI Investigators. Menopausal hormone therapy and long-term all-cause and cause-specific mortality: the Women’s Health Initiative randomized trials. JAMA. 2017;318:927-938.
Manson and colleagues examined the total and cause-specific cumulative mortality of the 2 Women’s Health Initiative (WHI) hormone therapy trials. This was an observational follow-up of US multiethnic postmenopausal women aged 50 to 79 years (mean age at baseline, 63.4 years) enrolled in 2 randomized clinical trials between 1993 and 1998 and followed up through December 31, 2014. A total of 27,347 women were randomly assigned to treatment.
Treatment groups
Depending on the presence or absence of a uterus, women received conjugated equine estrogens (CEE, 0.625 mg/d) plus medroxyprogesterone acetate (MPA, 2.5 mg/d) (n = 8,506) or placebo (n = 8,102) for a median of 5.6 years or CEE alone (n = 5,310) versus placebo (n = 5,429) for a median of 7.2 years. All-cause mortality (the primary outcome) and cause-specific mortality (cardiovascular disease mortality, cancer mortality, and other major causes of mortality) were analyzed in the 2 trials pooled and in each trial individually.
All-cause and cause-specific mortality findings
Mortality follow-up was available for more than 98% of participants. During the cumulative 18-year follow-up, 7,489 deaths occurred. In the overall pooled cohort, all-cause mortality in the hormone therapy group was 27.1% compared with 27.6% in the placebo group (hazard ratio [HR], 0.99 [95% confidence interval (CI), 0.94–1.03]). In the CEE plus MPA group, the HR was 1.02 (95% CI, 0.96–1.08). For those in the CEE-alone group, the HR was 0.94 (95% CI, 0.88–1.01).
In the pooled cohort for cardiovascular mortality, the HR was 1.00 (95% CI, 0.92–1.08 [8.9% with hormone therapy vs 9.0% with placebo]). For total cancer mortality, the HR was 1.03 (95% CI, 0.95–1.12 [8.2% with hormone therapy vs 8.0% with placebo]). For other causes, the HR was 0.95 (95% CI, 0.88–1.02 [10.0% with hormone therapy vs 10.7% with placebo]). Results did not differ significantly between trials.
Key takeaway
The study authors concluded that among postmenopausal women, hormone therapy with CEE plus MPA for a median of 5.6 years or with CEE alone for a median of 7.2 years was not associated with risk of all-cause, cardiovascular, or cancer mortality during a cumulative follow-up of 18 years.
Postmenopausal hormone therapy is arguably the most effective “bone drug” available. While all other antiresorptive agents show hip fracture efficacy only in subgroup analyses of the highest-risk patients (women with established osteoporosis, who often already have pre-existing vertebral fractures), the hormone-treated women in the WHI—who were not chosen for having low bone mass (in fact, dual-energy x-ray absorptiometry [DXA] scores were not even recorded)—still had a statistically significant decrease in hip fracture as an adverse event when compared with placebo-treated women. Increasing data on the long-term safety of hormone therapy in menopausal patients will perhaps encourage its greater use from a bone health perspective.
Continue to: Appropriate to defer DXA testing to age 65...
Appropriate to defer DXA testing to age 65 when baseline FRAX score is below treatment level
Gourlay ML, Overman RA, Fine JP, et al; Women’s Health Initiative Investigators. Time to clinically relevant fracture risk scores in postmenopausal women. Am J Med. 2017;130:862.e15-862.e23.
Gourlay ML, Fine JP, Preisser JS, et al; Study of Osteoporotic Fractures Research Group. Bone-density testing interval and transition to osteoporosis in older women. N Engl J Med. 2012;366:225-233.
Many clinicians used to (and still do) order bone mineral density (BMD) testing at 23-month intervals because that was what insurance would allow. Gourlay and colleagues previously published a study on BMD testing intervals and the time it takes to develop osteoporosis. I covered that information in previous Updates.4,5
To recap, Gourlay and colleagues studied 4,957 women, 67 years of age or older, with normal BMD or osteopenia and with no history of hip or clinical vertebral fracture or of treatment for osteoporosis; the women were followed prospectively for up to 15 years. The estimated time for 10% of women to make the transition to osteoporosis was 16.8 years for those with normal BMD, 4.7 years for those with moderate osteopenia, and 1.1 years for women with advanced osteopenia.
Today, FRAX is recommended to assess need for treatment
Older treatment recommendations involved determining various osteopenic BMD levels and the presence or absence of certain risk factors. More recently, the National Osteoporosis Foundation and many medical societies, including the American College of Obstetricians and Gynecologists, have recommended using the FRAX fracture prediction algorithm (available at https://www.sheffield.ac.uk/FRAX/) instead of T-scores to consider initiating pharmacotherapy.
The FRAX calculation tool uses information such as the country where the patient lives, age, sex, height, weight, history of previous fracture, parental fracture, current smoking, glucocorticoid use, rheumatoid arthritis, secondary osteoporosis, alcohol use of 3 or more units per day, and, if available, BMD determination at the femoral neck. It then yields the 10-year absolute risk of hip fracture and any major osteoporotic fracture for that individual or, more precisely, for an individual like that.
In the United States, accepted levels for cost-effective pharmacotherapy are a 10-year absolute risk of hip fracture of 3% or major osteoporotic fracture of 20%.
Continue to: Age also is a key factor in fracture risk assessment
Age also is a key factor in fracture risk assessment
Gourlay and colleagues more recently conducted a retrospective analysis of new occurrence of treatment-level fracture risk scores in postmenopausal women (50 years of age and older) before they received pharmacologic treatment and before they experienced a first hip or clinical vertebral fracture.
In 54,280 postmenopausal women aged 50 to 64 without a BMD test, the time for 10% to develop a treatment-level FRAX score could not be estimated accurately because of the rarity of treatment-level scores. In 6,096 women who had FRAX scores calculated with their BMD score, the estimated time to treatment-level FRAX was 7.6 years for those 65 to 69 and 5.1 years for 75 to 79 year olds. Furthermore, of 17,967 women aged 50 to 64 with a screening-level FRAX at baseline, only 100 (0.6%) experienced a hip or clinical vertebral fracture by age 65.
The investigators concluded that, “Postmenopausal women with sub-threshold fracture risk scores at baseline were unlikely to develop a treatment-level FRAX score between ages 50 and 64 years. After age 65, the increased incidence of treatment-level fracture risk scores, osteoporosis, and major osteoporotic fracture supports more frequent consideration of FRAX and bone mineral density testing.”
Many health care providers begin BMD testing early in menopause. Bone mass results may motivate patients to initiate healthy lifestyle choices, such as adequate dietary calcium, vitamin D supplementation, exercise, moderate alcohol use, smoking cessation, and fall prevention strategies. However, providers and their patients should be aware that if the fracture risk is beneath the threshold score at baseline, the risk of experiencing an osteoporotic fracture prior to age 65 is extremely low, and this should be taken into account before prescribing pharmacotherapy. Furthermore, as stated, FRAX can be performed without a DXA score. When the result is beneath a treatment level in a woman under 65, DXA testing may be deferred until age 65.
Continue to: USPSTF offers updated recommendations for osteoporosis screening
USPSTF offers updated recommendations for osteoporosis screening
US Preventive Services Task Force, Curry SJ, Krist AH, Owens DK, et al. Screening for osteoporosis to prevent fractures: US Preventive Services Task Force recommendation statement. JAMA. 2018;319:2521-2531.
The 2018 updated osteoporosis screening recommendations from the United States Preventative Services Task Force (USPSTF) may seem contradictory to the conclusions of Gourlay and colleagues discussed above. They are not.
The USPSTF authors point out that by 2020, about 12.3 million US individuals older than 50 years are expected to have osteoporosis. Osteoporotic fractures (especially hip fractures) are associated with limitations in ambulation, chronic pain and disability, loss of independence, and decreased quality of life. In fact, 21% to 30% of people who sustain a hip fracture die within 1 year. As the US population continues to age, the potential preventable burden will likely increase.
_
Evidence on bone measurement tests, risk assessment tools, and drug therapy efficacy
The USPSTF conducted an evidence review on screening for and treatment of osteoporotic fractures in women as well as risk assessment tools. The task force found the evidence convincing that bone measurement tests are accurate for detecting osteoporosis and predicting osteoporotic fractures. In addition, there is adequate evidence that clinical risk assessment tools are moderately accurate in identifying risk of osteoporosis and osteoporotic fractures. Furthermore, there is convincing evidence that drug therapies reduce subsequent fracture rates in postmenopausal women.
The USPSTF recommends the following:
- For women aged 65 and older, screen for osteoporosis with bone measurement testing to prevent osteoporotic fractures.
- For women younger than 65 who are at increased risk for osteoporosis based on formal clinical risk assessment tools, screen for osteoporosis with bone measurement testing to prevent osteoporotic fractures.
We all agree that women older than 65 years of age should be screened with DXA measurements of bone mass. The USPSTF says that in women under 65, a fracture assessment tool like FRAX, which does not require bone density testing to yield an individual’s absolute 10-year fracture risk, should be used to determine if bone mass measurement by DXA is, in fact, warranted. This recommendation is further supported by the article by Gourlay and colleagues, in which women aged 50 to 64 with subthreshold FRAX scores had a very low risk of fracture prior to age 65.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Burge R, Dawson-Hughes B, Solomon DH, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465-475.
- Cauley JA, Wampler NS, Barnhart JM, et al; Women’s Health Initiative Observational Study. Incidence of fractures compared to cardiovascular disease and breast cancer: the Women’s Health Initiative Observational Study. Osteoporos Int. 2008;19:1717-1723.
- Brauer CA, Coca-Perraillon M, Cutler DM, et al. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302:1573-1579.
- Goldstein SR. Update on osteoporosis. OBG Manag. 2012;24:16-21.
- Goldstein SR. 2017 update on bone health. OBG Manag. 2017;29-32, 48.
As ObGyns, we are the first-line health care providers for our menopausal patients in terms of identifying, preventing, and initiating treatment for women at risk for fragility fractures. Osteoporosis is probably the most important risk factor for bone health, although sarcopenia, frailty, poor eyesight, and falls also play a significant role in bone health and fragility fracture.
In 2005, more than 2 million incident fractures were reported in the United States, with a total cost of $17 billion.1 By 2025, annual fractures and costs are expected to rise by almost 50%. People who are 65 to 74 years of age will likely experience the largest increase in fracture—greater than 87%.1
Findings from the Women’s Health Initiative study showed that the number of women who had a clinical fracture in 1 year exceeded all the cases of myocardial infarction, stroke, and breast cancer combined.2 Furthermore, the morbidity and mortality rates for fractures are staggering. Thirty percent of women with a hip fracture will be dead within 1 year.3 So, although many patients fear developing breast cancer, and cardiovascular disease remains the number 1 cause of death, the impact of maintaining and protecting bone health cannot be emphasized enough.

_
WHI incidental findings: Hormone-treated menopausal women had decreased hip fracture rate
Manson JE, Aragaki AK, Rossouw JE, et al; WHI Investigators. Menopausal hormone therapy and long-term all-cause and cause-specific mortality: the Women’s Health Initiative randomized trials. JAMA. 2017;318:927-938.
Manson and colleagues examined the total and cause-specific cumulative mortality of the 2 Women’s Health Initiative (WHI) hormone therapy trials. This was an observational follow-up of US multiethnic postmenopausal women aged 50 to 79 years (mean age at baseline, 63.4 years) enrolled in 2 randomized clinical trials between 1993 and 1998 and followed up through December 31, 2014. A total of 27,347 women were randomly assigned to treatment.
Treatment groups
Depending on the presence or absence of a uterus, women received conjugated equine estrogens (CEE, 0.625 mg/d) plus medroxyprogesterone acetate (MPA, 2.5 mg/d) (n = 8,506) or placebo (n = 8,102) for a median of 5.6 years or CEE alone (n = 5,310) versus placebo (n = 5,429) for a median of 7.2 years. All-cause mortality (the primary outcome) and cause-specific mortality (cardiovascular disease mortality, cancer mortality, and other major causes of mortality) were analyzed in the 2 trials pooled and in each trial individually.
All-cause and cause-specific mortality findings
Mortality follow-up was available for more than 98% of participants. During the cumulative 18-year follow-up, 7,489 deaths occurred. In the overall pooled cohort, all-cause mortality in the hormone therapy group was 27.1% compared with 27.6% in the placebo group (hazard ratio [HR], 0.99 [95% confidence interval (CI), 0.94–1.03]). In the CEE plus MPA group, the HR was 1.02 (95% CI, 0.96–1.08). For those in the CEE-alone group, the HR was 0.94 (95% CI, 0.88–1.01).
In the pooled cohort for cardiovascular mortality, the HR was 1.00 (95% CI, 0.92–1.08 [8.9% with hormone therapy vs 9.0% with placebo]). For total cancer mortality, the HR was 1.03 (95% CI, 0.95–1.12 [8.2% with hormone therapy vs 8.0% with placebo]). For other causes, the HR was 0.95 (95% CI, 0.88–1.02 [10.0% with hormone therapy vs 10.7% with placebo]). Results did not differ significantly between trials.
Key takeaway
The study authors concluded that among postmenopausal women, hormone therapy with CEE plus MPA for a median of 5.6 years or with CEE alone for a median of 7.2 years was not associated with risk of all-cause, cardiovascular, or cancer mortality during a cumulative follow-up of 18 years.
Postmenopausal hormone therapy is arguably the most effective “bone drug” available. While all other antiresorptive agents show hip fracture efficacy only in subgroup analyses of the highest-risk patients (women with established osteoporosis, who often already have pre-existing vertebral fractures), the hormone-treated women in the WHI—who were not chosen for having low bone mass (in fact, dual-energy x-ray absorptiometry [DXA] scores were not even recorded)—still had a statistically significant decrease in hip fracture as an adverse event when compared with placebo-treated women. Increasing data on the long-term safety of hormone therapy in menopausal patients will perhaps encourage its greater use from a bone health perspective.
Continue to: Appropriate to defer DXA testing to age 65...
Appropriate to defer DXA testing to age 65 when baseline FRAX score is below treatment level
Gourlay ML, Overman RA, Fine JP, et al; Women’s Health Initiative Investigators. Time to clinically relevant fracture risk scores in postmenopausal women. Am J Med. 2017;130:862.e15-862.e23.
Gourlay ML, Fine JP, Preisser JS, et al; Study of Osteoporotic Fractures Research Group. Bone-density testing interval and transition to osteoporosis in older women. N Engl J Med. 2012;366:225-233.
Many clinicians used to (and still do) order bone mineral density (BMD) testing at 23-month intervals because that was what insurance would allow. Gourlay and colleagues previously published a study on BMD testing intervals and the time it takes to develop osteoporosis. I covered that information in previous Updates.4,5
To recap, Gourlay and colleagues studied 4,957 women, 67 years of age or older, with normal BMD or osteopenia and with no history of hip or clinical vertebral fracture or of treatment for osteoporosis; the women were followed prospectively for up to 15 years. The estimated time for 10% of women to make the transition to osteoporosis was 16.8 years for those with normal BMD, 4.7 years for those with moderate osteopenia, and 1.1 years for women with advanced osteopenia.
Today, FRAX is recommended to assess need for treatment
Older treatment recommendations involved determining various osteopenic BMD levels and the presence or absence of certain risk factors. More recently, the National Osteoporosis Foundation and many medical societies, including the American College of Obstetricians and Gynecologists, have recommended using the FRAX fracture prediction algorithm (available at https://www.sheffield.ac.uk/FRAX/) instead of T-scores to consider initiating pharmacotherapy.
The FRAX calculation tool uses information such as the country where the patient lives, age, sex, height, weight, history of previous fracture, parental fracture, current smoking, glucocorticoid use, rheumatoid arthritis, secondary osteoporosis, alcohol use of 3 or more units per day, and, if available, BMD determination at the femoral neck. It then yields the 10-year absolute risk of hip fracture and any major osteoporotic fracture for that individual or, more precisely, for an individual like that.
In the United States, accepted levels for cost-effective pharmacotherapy are a 10-year absolute risk of hip fracture of 3% or major osteoporotic fracture of 20%.
Continue to: Age also is a key factor in fracture risk assessment
Age also is a key factor in fracture risk assessment
Gourlay and colleagues more recently conducted a retrospective analysis of new occurrence of treatment-level fracture risk scores in postmenopausal women (50 years of age and older) before they received pharmacologic treatment and before they experienced a first hip or clinical vertebral fracture.
In 54,280 postmenopausal women aged 50 to 64 without a BMD test, the time for 10% to develop a treatment-level FRAX score could not be estimated accurately because of the rarity of treatment-level scores. In 6,096 women who had FRAX scores calculated with their BMD score, the estimated time to treatment-level FRAX was 7.6 years for those 65 to 69 and 5.1 years for 75 to 79 year olds. Furthermore, of 17,967 women aged 50 to 64 with a screening-level FRAX at baseline, only 100 (0.6%) experienced a hip or clinical vertebral fracture by age 65.
The investigators concluded that, “Postmenopausal women with sub-threshold fracture risk scores at baseline were unlikely to develop a treatment-level FRAX score between ages 50 and 64 years. After age 65, the increased incidence of treatment-level fracture risk scores, osteoporosis, and major osteoporotic fracture supports more frequent consideration of FRAX and bone mineral density testing.”
Many health care providers begin BMD testing early in menopause. Bone mass results may motivate patients to initiate healthy lifestyle choices, such as adequate dietary calcium, vitamin D supplementation, exercise, moderate alcohol use, smoking cessation, and fall prevention strategies. However, providers and their patients should be aware that if the fracture risk is beneath the threshold score at baseline, the risk of experiencing an osteoporotic fracture prior to age 65 is extremely low, and this should be taken into account before prescribing pharmacotherapy. Furthermore, as stated, FRAX can be performed without a DXA score. When the result is beneath a treatment level in a woman under 65, DXA testing may be deferred until age 65.
Continue to: USPSTF offers updated recommendations for osteoporosis screening
USPSTF offers updated recommendations for osteoporosis screening
US Preventive Services Task Force, Curry SJ, Krist AH, Owens DK, et al. Screening for osteoporosis to prevent fractures: US Preventive Services Task Force recommendation statement. JAMA. 2018;319:2521-2531.
The 2018 updated osteoporosis screening recommendations from the United States Preventative Services Task Force (USPSTF) may seem contradictory to the conclusions of Gourlay and colleagues discussed above. They are not.
The USPSTF authors point out that by 2020, about 12.3 million US individuals older than 50 years are expected to have osteoporosis. Osteoporotic fractures (especially hip fractures) are associated with limitations in ambulation, chronic pain and disability, loss of independence, and decreased quality of life. In fact, 21% to 30% of people who sustain a hip fracture die within 1 year. As the US population continues to age, the potential preventable burden will likely increase.
_
Evidence on bone measurement tests, risk assessment tools, and drug therapy efficacy
The USPSTF conducted an evidence review on screening for and treatment of osteoporotic fractures in women as well as risk assessment tools. The task force found the evidence convincing that bone measurement tests are accurate for detecting osteoporosis and predicting osteoporotic fractures. In addition, there is adequate evidence that clinical risk assessment tools are moderately accurate in identifying risk of osteoporosis and osteoporotic fractures. Furthermore, there is convincing evidence that drug therapies reduce subsequent fracture rates in postmenopausal women.
The USPSTF recommends the following:
- For women aged 65 and older, screen for osteoporosis with bone measurement testing to prevent osteoporotic fractures.
- For women younger than 65 who are at increased risk for osteoporosis based on formal clinical risk assessment tools, screen for osteoporosis with bone measurement testing to prevent osteoporotic fractures.
We all agree that women older than 65 years of age should be screened with DXA measurements of bone mass. The USPSTF says that in women under 65, a fracture assessment tool like FRAX, which does not require bone density testing to yield an individual’s absolute 10-year fracture risk, should be used to determine if bone mass measurement by DXA is, in fact, warranted. This recommendation is further supported by the article by Gourlay and colleagues, in which women aged 50 to 64 with subthreshold FRAX scores had a very low risk of fracture prior to age 65.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
As ObGyns, we are the first-line health care providers for our menopausal patients in terms of identifying, preventing, and initiating treatment for women at risk for fragility fractures. Osteoporosis is probably the most important risk factor for bone health, although sarcopenia, frailty, poor eyesight, and falls also play a significant role in bone health and fragility fracture.
In 2005, more than 2 million incident fractures were reported in the United States, with a total cost of $17 billion.1 By 2025, annual fractures and costs are expected to rise by almost 50%. People who are 65 to 74 years of age will likely experience the largest increase in fracture—greater than 87%.1
Findings from the Women’s Health Initiative study showed that the number of women who had a clinical fracture in 1 year exceeded all the cases of myocardial infarction, stroke, and breast cancer combined.2 Furthermore, the morbidity and mortality rates for fractures are staggering. Thirty percent of women with a hip fracture will be dead within 1 year.3 So, although many patients fear developing breast cancer, and cardiovascular disease remains the number 1 cause of death, the impact of maintaining and protecting bone health cannot be emphasized enough.

_
WHI incidental findings: Hormone-treated menopausal women had decreased hip fracture rate
Manson JE, Aragaki AK, Rossouw JE, et al; WHI Investigators. Menopausal hormone therapy and long-term all-cause and cause-specific mortality: the Women’s Health Initiative randomized trials. JAMA. 2017;318:927-938.
Manson and colleagues examined the total and cause-specific cumulative mortality of the 2 Women’s Health Initiative (WHI) hormone therapy trials. This was an observational follow-up of US multiethnic postmenopausal women aged 50 to 79 years (mean age at baseline, 63.4 years) enrolled in 2 randomized clinical trials between 1993 and 1998 and followed up through December 31, 2014. A total of 27,347 women were randomly assigned to treatment.
Treatment groups
Depending on the presence or absence of a uterus, women received conjugated equine estrogens (CEE, 0.625 mg/d) plus medroxyprogesterone acetate (MPA, 2.5 mg/d) (n = 8,506) or placebo (n = 8,102) for a median of 5.6 years or CEE alone (n = 5,310) versus placebo (n = 5,429) for a median of 7.2 years. All-cause mortality (the primary outcome) and cause-specific mortality (cardiovascular disease mortality, cancer mortality, and other major causes of mortality) were analyzed in the 2 trials pooled and in each trial individually.
All-cause and cause-specific mortality findings
Mortality follow-up was available for more than 98% of participants. During the cumulative 18-year follow-up, 7,489 deaths occurred. In the overall pooled cohort, all-cause mortality in the hormone therapy group was 27.1% compared with 27.6% in the placebo group (hazard ratio [HR], 0.99 [95% confidence interval (CI), 0.94–1.03]). In the CEE plus MPA group, the HR was 1.02 (95% CI, 0.96–1.08). For those in the CEE-alone group, the HR was 0.94 (95% CI, 0.88–1.01).
In the pooled cohort for cardiovascular mortality, the HR was 1.00 (95% CI, 0.92–1.08 [8.9% with hormone therapy vs 9.0% with placebo]). For total cancer mortality, the HR was 1.03 (95% CI, 0.95–1.12 [8.2% with hormone therapy vs 8.0% with placebo]). For other causes, the HR was 0.95 (95% CI, 0.88–1.02 [10.0% with hormone therapy vs 10.7% with placebo]). Results did not differ significantly between trials.
Key takeaway
The study authors concluded that among postmenopausal women, hormone therapy with CEE plus MPA for a median of 5.6 years or with CEE alone for a median of 7.2 years was not associated with risk of all-cause, cardiovascular, or cancer mortality during a cumulative follow-up of 18 years.
Postmenopausal hormone therapy is arguably the most effective “bone drug” available. While all other antiresorptive agents show hip fracture efficacy only in subgroup analyses of the highest-risk patients (women with established osteoporosis, who often already have pre-existing vertebral fractures), the hormone-treated women in the WHI—who were not chosen for having low bone mass (in fact, dual-energy x-ray absorptiometry [DXA] scores were not even recorded)—still had a statistically significant decrease in hip fracture as an adverse event when compared with placebo-treated women. Increasing data on the long-term safety of hormone therapy in menopausal patients will perhaps encourage its greater use from a bone health perspective.
Continue to: Appropriate to defer DXA testing to age 65...
Appropriate to defer DXA testing to age 65 when baseline FRAX score is below treatment level
Gourlay ML, Overman RA, Fine JP, et al; Women’s Health Initiative Investigators. Time to clinically relevant fracture risk scores in postmenopausal women. Am J Med. 2017;130:862.e15-862.e23.
Gourlay ML, Fine JP, Preisser JS, et al; Study of Osteoporotic Fractures Research Group. Bone-density testing interval and transition to osteoporosis in older women. N Engl J Med. 2012;366:225-233.
Many clinicians used to (and still do) order bone mineral density (BMD) testing at 23-month intervals because that was what insurance would allow. Gourlay and colleagues previously published a study on BMD testing intervals and the time it takes to develop osteoporosis. I covered that information in previous Updates.4,5
To recap, Gourlay and colleagues studied 4,957 women, 67 years of age or older, with normal BMD or osteopenia and with no history of hip or clinical vertebral fracture or of treatment for osteoporosis; the women were followed prospectively for up to 15 years. The estimated time for 10% of women to make the transition to osteoporosis was 16.8 years for those with normal BMD, 4.7 years for those with moderate osteopenia, and 1.1 years for women with advanced osteopenia.
Today, FRAX is recommended to assess need for treatment
Older treatment recommendations involved determining various osteopenic BMD levels and the presence or absence of certain risk factors. More recently, the National Osteoporosis Foundation and many medical societies, including the American College of Obstetricians and Gynecologists, have recommended using the FRAX fracture prediction algorithm (available at https://www.sheffield.ac.uk/FRAX/) instead of T-scores to consider initiating pharmacotherapy.
The FRAX calculation tool uses information such as the country where the patient lives, age, sex, height, weight, history of previous fracture, parental fracture, current smoking, glucocorticoid use, rheumatoid arthritis, secondary osteoporosis, alcohol use of 3 or more units per day, and, if available, BMD determination at the femoral neck. It then yields the 10-year absolute risk of hip fracture and any major osteoporotic fracture for that individual or, more precisely, for an individual like that.
In the United States, accepted levels for cost-effective pharmacotherapy are a 10-year absolute risk of hip fracture of 3% or major osteoporotic fracture of 20%.
Continue to: Age also is a key factor in fracture risk assessment
Age also is a key factor in fracture risk assessment
Gourlay and colleagues more recently conducted a retrospective analysis of new occurrence of treatment-level fracture risk scores in postmenopausal women (50 years of age and older) before they received pharmacologic treatment and before they experienced a first hip or clinical vertebral fracture.
In 54,280 postmenopausal women aged 50 to 64 without a BMD test, the time for 10% to develop a treatment-level FRAX score could not be estimated accurately because of the rarity of treatment-level scores. In 6,096 women who had FRAX scores calculated with their BMD score, the estimated time to treatment-level FRAX was 7.6 years for those 65 to 69 and 5.1 years for 75 to 79 year olds. Furthermore, of 17,967 women aged 50 to 64 with a screening-level FRAX at baseline, only 100 (0.6%) experienced a hip or clinical vertebral fracture by age 65.
The investigators concluded that, “Postmenopausal women with sub-threshold fracture risk scores at baseline were unlikely to develop a treatment-level FRAX score between ages 50 and 64 years. After age 65, the increased incidence of treatment-level fracture risk scores, osteoporosis, and major osteoporotic fracture supports more frequent consideration of FRAX and bone mineral density testing.”
Many health care providers begin BMD testing early in menopause. Bone mass results may motivate patients to initiate healthy lifestyle choices, such as adequate dietary calcium, vitamin D supplementation, exercise, moderate alcohol use, smoking cessation, and fall prevention strategies. However, providers and their patients should be aware that if the fracture risk is beneath the threshold score at baseline, the risk of experiencing an osteoporotic fracture prior to age 65 is extremely low, and this should be taken into account before prescribing pharmacotherapy. Furthermore, as stated, FRAX can be performed without a DXA score. When the result is beneath a treatment level in a woman under 65, DXA testing may be deferred until age 65.
Continue to: USPSTF offers updated recommendations for osteoporosis screening
USPSTF offers updated recommendations for osteoporosis screening
US Preventive Services Task Force, Curry SJ, Krist AH, Owens DK, et al. Screening for osteoporosis to prevent fractures: US Preventive Services Task Force recommendation statement. JAMA. 2018;319:2521-2531.
The 2018 updated osteoporosis screening recommendations from the United States Preventative Services Task Force (USPSTF) may seem contradictory to the conclusions of Gourlay and colleagues discussed above. They are not.
The USPSTF authors point out that by 2020, about 12.3 million US individuals older than 50 years are expected to have osteoporosis. Osteoporotic fractures (especially hip fractures) are associated with limitations in ambulation, chronic pain and disability, loss of independence, and decreased quality of life. In fact, 21% to 30% of people who sustain a hip fracture die within 1 year. As the US population continues to age, the potential preventable burden will likely increase.
_
Evidence on bone measurement tests, risk assessment tools, and drug therapy efficacy
The USPSTF conducted an evidence review on screening for and treatment of osteoporotic fractures in women as well as risk assessment tools. The task force found the evidence convincing that bone measurement tests are accurate for detecting osteoporosis and predicting osteoporotic fractures. In addition, there is adequate evidence that clinical risk assessment tools are moderately accurate in identifying risk of osteoporosis and osteoporotic fractures. Furthermore, there is convincing evidence that drug therapies reduce subsequent fracture rates in postmenopausal women.
The USPSTF recommends the following:
- For women aged 65 and older, screen for osteoporosis with bone measurement testing to prevent osteoporotic fractures.
- For women younger than 65 who are at increased risk for osteoporosis based on formal clinical risk assessment tools, screen for osteoporosis with bone measurement testing to prevent osteoporotic fractures.
We all agree that women older than 65 years of age should be screened with DXA measurements of bone mass. The USPSTF says that in women under 65, a fracture assessment tool like FRAX, which does not require bone density testing to yield an individual’s absolute 10-year fracture risk, should be used to determine if bone mass measurement by DXA is, in fact, warranted. This recommendation is further supported by the article by Gourlay and colleagues, in which women aged 50 to 64 with subthreshold FRAX scores had a very low risk of fracture prior to age 65.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Burge R, Dawson-Hughes B, Solomon DH, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465-475.
- Cauley JA, Wampler NS, Barnhart JM, et al; Women’s Health Initiative Observational Study. Incidence of fractures compared to cardiovascular disease and breast cancer: the Women’s Health Initiative Observational Study. Osteoporos Int. 2008;19:1717-1723.
- Brauer CA, Coca-Perraillon M, Cutler DM, et al. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302:1573-1579.
- Goldstein SR. Update on osteoporosis. OBG Manag. 2012;24:16-21.
- Goldstein SR. 2017 update on bone health. OBG Manag. 2017;29-32, 48.
- Burge R, Dawson-Hughes B, Solomon DH, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465-475.
- Cauley JA, Wampler NS, Barnhart JM, et al; Women’s Health Initiative Observational Study. Incidence of fractures compared to cardiovascular disease and breast cancer: the Women’s Health Initiative Observational Study. Osteoporos Int. 2008;19:1717-1723.
- Brauer CA, Coca-Perraillon M, Cutler DM, et al. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302:1573-1579.
- Goldstein SR. Update on osteoporosis. OBG Manag. 2012;24:16-21.
- Goldstein SR. 2017 update on bone health. OBG Manag. 2017;29-32, 48.
Denosumab effective against osteoporosis in TDT patients
Denosumab can be effective against osteoporosis caused by transfusion-dependent thalassemia (TDT), according to new research.
The study authors found that patients who received twice-yearly injections of denosumab experienced a significant increase in bone density and reduction in bone pain. Their findings were published in Blood Advances.
“Not only is denosumab associated with improved bone health and reduced pain, but its ease of administration may very well make this drug superior to bisphosphonates for the treatment of osteoporosis in patients with TDT and osteoporosis,” senior study author Evangelos Terpos, MD, of the National and Kapodistrian University of Athens, said in a statement.
For this phase 2b study, Dr. Terpos and his colleagues evaluated 63 patients with TDT and osteoporosis, randomized to receive 60 mg of denosumab (n = 32) or placebo (n = 31) on days 0 and 180 of a 12-month period. Patients in both arms also received daily supplements of calcium and vitamin D.
Baseline characteristics were largely similar between the treatment arms. However, the mean value of bone-specific alkaline phosphatase (bALP) was significantly lower in the placebo arm than the denosumab arm – 68.48 IU/L versus 85.45 IU/L (P = .013). And the mean value of the tartrate-resistant acid phosphatase isoform–5b (TRACP-5b) marker was significantly higher in the denosumab arm than in the placebo arm – 0.42 IU/L versus 0.16 IU/L (P = .026).
The researchers measured bone mineral density in the L1-L4 lumbar spine, wrist, and femoral neck. At 12 months, the mean increase in L1-L4 bone mineral density was 5.92% in the denosumab arm and 2.92% in the placebo arm (P = .043). The mean decrease in wrist bone mineral density was –0.26% and –3.92%, respectively (P = .035).
Femoral neck bone mineral density was increased in the denosumab arm (4.08%), compared with the placebo arm (1.96%), but the difference between the two groups was not statistically significant.
Patients in the denosumab arm had a significant reduction in bone pain at 12 months, according to the McGill-Melzack scoring system and the Huskisson visual analog scale (P less than .001 for both). There was no significant change in pain for patients in the placebo arm on either scale.
At 12 months, patients in the denosumab arm had experienced a significant reduction from baseline in several markers of bone remodeling, including soluble receptor activator of nuclear factor–kappa B ligand (sRANKL), osteoprotegerin (OPG), sRANKL/OPG ratio, C-terminal telopeptide of type I collagen (CTx), TRACP-5b, and bALP.
There were no significant changes in dickkopf-1, sclerostin, or osteocalcin in the denosumab arm.
In the placebo arm, patients had a significant increase from baseline in several markers of bone remodeling, including sRANKL, OPG, dickkopf-1, sclerostin, CTx, TRACP-5b, and bALP. There was no significant change from baseline in the sRANKL/OPG ratio or osteocalcin.
In all, there were 17 adverse events in 14 patients. There were three serious adverse events in the denosumab arm – pleural effusion (grade 3), atrial fibrillation (grade 3), and supraventricular tachycardia (grade 4). All three of these adverse events were considered unrelated to denosumab.
The study was funded by Amgen, which markets denosumab. The authors reported that they had no competing financial interests.
SOURCE: Terpos E et al. Blood Adv. 2018;2:2837-47.
Denosumab can be effective against osteoporosis caused by transfusion-dependent thalassemia (TDT), according to new research.
The study authors found that patients who received twice-yearly injections of denosumab experienced a significant increase in bone density and reduction in bone pain. Their findings were published in Blood Advances.
“Not only is denosumab associated with improved bone health and reduced pain, but its ease of administration may very well make this drug superior to bisphosphonates for the treatment of osteoporosis in patients with TDT and osteoporosis,” senior study author Evangelos Terpos, MD, of the National and Kapodistrian University of Athens, said in a statement.
For this phase 2b study, Dr. Terpos and his colleagues evaluated 63 patients with TDT and osteoporosis, randomized to receive 60 mg of denosumab (n = 32) or placebo (n = 31) on days 0 and 180 of a 12-month period. Patients in both arms also received daily supplements of calcium and vitamin D.
Baseline characteristics were largely similar between the treatment arms. However, the mean value of bone-specific alkaline phosphatase (bALP) was significantly lower in the placebo arm than the denosumab arm – 68.48 IU/L versus 85.45 IU/L (P = .013). And the mean value of the tartrate-resistant acid phosphatase isoform–5b (TRACP-5b) marker was significantly higher in the denosumab arm than in the placebo arm – 0.42 IU/L versus 0.16 IU/L (P = .026).
The researchers measured bone mineral density in the L1-L4 lumbar spine, wrist, and femoral neck. At 12 months, the mean increase in L1-L4 bone mineral density was 5.92% in the denosumab arm and 2.92% in the placebo arm (P = .043). The mean decrease in wrist bone mineral density was –0.26% and –3.92%, respectively (P = .035).
Femoral neck bone mineral density was increased in the denosumab arm (4.08%), compared with the placebo arm (1.96%), but the difference between the two groups was not statistically significant.
Patients in the denosumab arm had a significant reduction in bone pain at 12 months, according to the McGill-Melzack scoring system and the Huskisson visual analog scale (P less than .001 for both). There was no significant change in pain for patients in the placebo arm on either scale.
At 12 months, patients in the denosumab arm had experienced a significant reduction from baseline in several markers of bone remodeling, including soluble receptor activator of nuclear factor–kappa B ligand (sRANKL), osteoprotegerin (OPG), sRANKL/OPG ratio, C-terminal telopeptide of type I collagen (CTx), TRACP-5b, and bALP.
There were no significant changes in dickkopf-1, sclerostin, or osteocalcin in the denosumab arm.
In the placebo arm, patients had a significant increase from baseline in several markers of bone remodeling, including sRANKL, OPG, dickkopf-1, sclerostin, CTx, TRACP-5b, and bALP. There was no significant change from baseline in the sRANKL/OPG ratio or osteocalcin.
In all, there were 17 adverse events in 14 patients. There were three serious adverse events in the denosumab arm – pleural effusion (grade 3), atrial fibrillation (grade 3), and supraventricular tachycardia (grade 4). All three of these adverse events were considered unrelated to denosumab.
The study was funded by Amgen, which markets denosumab. The authors reported that they had no competing financial interests.
SOURCE: Terpos E et al. Blood Adv. 2018;2:2837-47.
Denosumab can be effective against osteoporosis caused by transfusion-dependent thalassemia (TDT), according to new research.
The study authors found that patients who received twice-yearly injections of denosumab experienced a significant increase in bone density and reduction in bone pain. Their findings were published in Blood Advances.
“Not only is denosumab associated with improved bone health and reduced pain, but its ease of administration may very well make this drug superior to bisphosphonates for the treatment of osteoporosis in patients with TDT and osteoporosis,” senior study author Evangelos Terpos, MD, of the National and Kapodistrian University of Athens, said in a statement.
For this phase 2b study, Dr. Terpos and his colleagues evaluated 63 patients with TDT and osteoporosis, randomized to receive 60 mg of denosumab (n = 32) or placebo (n = 31) on days 0 and 180 of a 12-month period. Patients in both arms also received daily supplements of calcium and vitamin D.
Baseline characteristics were largely similar between the treatment arms. However, the mean value of bone-specific alkaline phosphatase (bALP) was significantly lower in the placebo arm than the denosumab arm – 68.48 IU/L versus 85.45 IU/L (P = .013). And the mean value of the tartrate-resistant acid phosphatase isoform–5b (TRACP-5b) marker was significantly higher in the denosumab arm than in the placebo arm – 0.42 IU/L versus 0.16 IU/L (P = .026).
The researchers measured bone mineral density in the L1-L4 lumbar spine, wrist, and femoral neck. At 12 months, the mean increase in L1-L4 bone mineral density was 5.92% in the denosumab arm and 2.92% in the placebo arm (P = .043). The mean decrease in wrist bone mineral density was –0.26% and –3.92%, respectively (P = .035).
Femoral neck bone mineral density was increased in the denosumab arm (4.08%), compared with the placebo arm (1.96%), but the difference between the two groups was not statistically significant.
Patients in the denosumab arm had a significant reduction in bone pain at 12 months, according to the McGill-Melzack scoring system and the Huskisson visual analog scale (P less than .001 for both). There was no significant change in pain for patients in the placebo arm on either scale.
At 12 months, patients in the denosumab arm had experienced a significant reduction from baseline in several markers of bone remodeling, including soluble receptor activator of nuclear factor–kappa B ligand (sRANKL), osteoprotegerin (OPG), sRANKL/OPG ratio, C-terminal telopeptide of type I collagen (CTx), TRACP-5b, and bALP.
There were no significant changes in dickkopf-1, sclerostin, or osteocalcin in the denosumab arm.
In the placebo arm, patients had a significant increase from baseline in several markers of bone remodeling, including sRANKL, OPG, dickkopf-1, sclerostin, CTx, TRACP-5b, and bALP. There was no significant change from baseline in the sRANKL/OPG ratio or osteocalcin.
In all, there were 17 adverse events in 14 patients. There were three serious adverse events in the denosumab arm – pleural effusion (grade 3), atrial fibrillation (grade 3), and supraventricular tachycardia (grade 4). All three of these adverse events were considered unrelated to denosumab.
The study was funded by Amgen, which markets denosumab. The authors reported that they had no competing financial interests.
SOURCE: Terpos E et al. Blood Adv. 2018;2:2837-47.
FROM BLOOD ADVANCES
Key clinical point:
Major finding: The mean increase in L1-L4 bone mineral density was 5.92% in patients treated with denosumab, compared with 2.92% in patients who received placebo (P = .043).
Study details: A phase 2b study that included 63 patients.
Disclosures: The research was funded by Amgen. The authors reported having no competing financial interests.
Source: Terpos E et al. Blood Adv. 2018;2:2837-47.
Low BMD and spinal syndesmophytes predict radiographic progression in axSpA
Low bone mineral density and the presence of existing spinal syndesmophytes predict the formation of new spinal bony growths and radiographic progression in axial spondyloarthritis (axSpA) at 2 years, according to research conducted by Hyoung Rae Kim of the Catholic University of Korea, Seoul, South Korea, and colleagues.
The investigators noted that low bone mass in ankylosing spondyloarthritis (AS) had been linked in previous studies to spinal structural damage yet “despite the identification of this relationship, it is not yet known whether the presence of low bone mass can independently predict radiographic spinal progression in axSpA patients.”
In order to evaluate the association between low bone mass and the formation of new syndesmophytes and to investigate whether low bone mineral density (BMD) independently predicted radiographic progression in axSpA, the researchers enrolled 119 patients with definite axSpA into their study, published in Arthritis Research & Therapy.
They defined low BMD as z scores of less than or equal to –2.0 and spinal radiographic progression as worsening of the modified Stoke Ankylosing Spondylitis Spinal Score (mSASSS) by 2 or more points over the 2-year follow-up period.
Overall, 34 (29%) of the patients had syndesmophytes at baseline, 90 (76%) had radiographic sacroiliitis fulfilling the modified New York criteria for the classification of AS, and 19 (16%) had low BMD.
At 2 years, new syndesmophytes had developed in 22 (21%) of the patients. New syndesmophyte formation occurred in 15% of patients without low BMD and in 37% of patients with low BMD (P = .047).
In the multivariable analysis, current smoking (odds ratio, 3.0; 95% confidence interval, 1.1-7.7), the presence of syndesmophytes (OR, 4.6; 95% CI, 1.8-11.9); and low BMD at baseline (OR, 3.6; 95% CI, 1.2-11.2) were independently associated with significant spinal progression, the investigators reported.
The presence of baseline syndesmophytes and low BMD at any site (OR, 5.5; 95% CI, 2.0-15.2; and OR, 3.6; 95% CI, 1.1-11.8, respectively) was identified by the investigators as significant predictors of new syndesmophytes.
“The presence of a syndesmophyte at baseline and low BMD were predictors of the formation of new syndesmophytes and significant mSASSS progression. … This study is the first to demonstrate that low BMD predicts radiographic progression in axSpA,” they concluded.
The investigators noted that a potential driving mechanism for the ankylosing process was bone loss resulting from chronic inflammation and the associated changes in bone microarchitecture.
“The inflammatory process induces bone loss, which affects the microarchitecture in the trabecular bone, thereby leading to instability. Reduced bone strength triggers a stabilizing anabolic effort that results in bone formation,” they wrote.
“Our results suggest that successful anti-inflammatory treatment reduces inflammation and allows the bone metabolism to normalize, thereby taking away the compensatory anabolic response that leads to new bone formation in the cortical bone of the spine,” they said.
They noted that their study was limited by its small sample and their findings needed confirmation in larger cohorts of axSpA patients.
SOURCE: Arthritis Res Ther. 2018 Oct 16. doi: 10.1186/s13075-018-1731-8.
Low bone mineral density and the presence of existing spinal syndesmophytes predict the formation of new spinal bony growths and radiographic progression in axial spondyloarthritis (axSpA) at 2 years, according to research conducted by Hyoung Rae Kim of the Catholic University of Korea, Seoul, South Korea, and colleagues.
The investigators noted that low bone mass in ankylosing spondyloarthritis (AS) had been linked in previous studies to spinal structural damage yet “despite the identification of this relationship, it is not yet known whether the presence of low bone mass can independently predict radiographic spinal progression in axSpA patients.”
In order to evaluate the association between low bone mass and the formation of new syndesmophytes and to investigate whether low bone mineral density (BMD) independently predicted radiographic progression in axSpA, the researchers enrolled 119 patients with definite axSpA into their study, published in Arthritis Research & Therapy.
They defined low BMD as z scores of less than or equal to –2.0 and spinal radiographic progression as worsening of the modified Stoke Ankylosing Spondylitis Spinal Score (mSASSS) by 2 or more points over the 2-year follow-up period.
Overall, 34 (29%) of the patients had syndesmophytes at baseline, 90 (76%) had radiographic sacroiliitis fulfilling the modified New York criteria for the classification of AS, and 19 (16%) had low BMD.
At 2 years, new syndesmophytes had developed in 22 (21%) of the patients. New syndesmophyte formation occurred in 15% of patients without low BMD and in 37% of patients with low BMD (P = .047).
In the multivariable analysis, current smoking (odds ratio, 3.0; 95% confidence interval, 1.1-7.7), the presence of syndesmophytes (OR, 4.6; 95% CI, 1.8-11.9); and low BMD at baseline (OR, 3.6; 95% CI, 1.2-11.2) were independently associated with significant spinal progression, the investigators reported.
The presence of baseline syndesmophytes and low BMD at any site (OR, 5.5; 95% CI, 2.0-15.2; and OR, 3.6; 95% CI, 1.1-11.8, respectively) was identified by the investigators as significant predictors of new syndesmophytes.
“The presence of a syndesmophyte at baseline and low BMD were predictors of the formation of new syndesmophytes and significant mSASSS progression. … This study is the first to demonstrate that low BMD predicts radiographic progression in axSpA,” they concluded.
The investigators noted that a potential driving mechanism for the ankylosing process was bone loss resulting from chronic inflammation and the associated changes in bone microarchitecture.
“The inflammatory process induces bone loss, which affects the microarchitecture in the trabecular bone, thereby leading to instability. Reduced bone strength triggers a stabilizing anabolic effort that results in bone formation,” they wrote.
“Our results suggest that successful anti-inflammatory treatment reduces inflammation and allows the bone metabolism to normalize, thereby taking away the compensatory anabolic response that leads to new bone formation in the cortical bone of the spine,” they said.
They noted that their study was limited by its small sample and their findings needed confirmation in larger cohorts of axSpA patients.
SOURCE: Arthritis Res Ther. 2018 Oct 16. doi: 10.1186/s13075-018-1731-8.
Low bone mineral density and the presence of existing spinal syndesmophytes predict the formation of new spinal bony growths and radiographic progression in axial spondyloarthritis (axSpA) at 2 years, according to research conducted by Hyoung Rae Kim of the Catholic University of Korea, Seoul, South Korea, and colleagues.
The investigators noted that low bone mass in ankylosing spondyloarthritis (AS) had been linked in previous studies to spinal structural damage yet “despite the identification of this relationship, it is not yet known whether the presence of low bone mass can independently predict radiographic spinal progression in axSpA patients.”
In order to evaluate the association between low bone mass and the formation of new syndesmophytes and to investigate whether low bone mineral density (BMD) independently predicted radiographic progression in axSpA, the researchers enrolled 119 patients with definite axSpA into their study, published in Arthritis Research & Therapy.
They defined low BMD as z scores of less than or equal to –2.0 and spinal radiographic progression as worsening of the modified Stoke Ankylosing Spondylitis Spinal Score (mSASSS) by 2 or more points over the 2-year follow-up period.
Overall, 34 (29%) of the patients had syndesmophytes at baseline, 90 (76%) had radiographic sacroiliitis fulfilling the modified New York criteria for the classification of AS, and 19 (16%) had low BMD.
At 2 years, new syndesmophytes had developed in 22 (21%) of the patients. New syndesmophyte formation occurred in 15% of patients without low BMD and in 37% of patients with low BMD (P = .047).
In the multivariable analysis, current smoking (odds ratio, 3.0; 95% confidence interval, 1.1-7.7), the presence of syndesmophytes (OR, 4.6; 95% CI, 1.8-11.9); and low BMD at baseline (OR, 3.6; 95% CI, 1.2-11.2) were independently associated with significant spinal progression, the investigators reported.
The presence of baseline syndesmophytes and low BMD at any site (OR, 5.5; 95% CI, 2.0-15.2; and OR, 3.6; 95% CI, 1.1-11.8, respectively) was identified by the investigators as significant predictors of new syndesmophytes.
“The presence of a syndesmophyte at baseline and low BMD were predictors of the formation of new syndesmophytes and significant mSASSS progression. … This study is the first to demonstrate that low BMD predicts radiographic progression in axSpA,” they concluded.
The investigators noted that a potential driving mechanism for the ankylosing process was bone loss resulting from chronic inflammation and the associated changes in bone microarchitecture.
“The inflammatory process induces bone loss, which affects the microarchitecture in the trabecular bone, thereby leading to instability. Reduced bone strength triggers a stabilizing anabolic effort that results in bone formation,” they wrote.
“Our results suggest that successful anti-inflammatory treatment reduces inflammation and allows the bone metabolism to normalize, thereby taking away the compensatory anabolic response that leads to new bone formation in the cortical bone of the spine,” they said.
They noted that their study was limited by its small sample and their findings needed confirmation in larger cohorts of axSpA patients.
SOURCE: Arthritis Res Ther. 2018 Oct 16. doi: 10.1186/s13075-018-1731-8.
FROM ARTHRITIS RESEARCH & THERAPY
Key clinical point: Low bone mineral density and existing spinal syndesmophytes are risk factors for new syndesmophytes and radiographic progression in people with axial spondyloarthritis.
Major finding: The presence of syndesmophytes at baseline and low BMD were predictors of new syndesmophytes over the following 2 years (OR, 5.5; 95% CI, 2.0-15.2 and OR, 3.6; 95% CI, 1.1-11.8, respectively).
Study details: A longitudinal observational study of 119 consecutive patients with axial SpA aged under 50 years who fulfilled the imaging arm of the Assessment of SpondyloArthritis International Society axSpA criteria.
Disclosures: No specific funding was received from any public, commercial or not-for-profit bodies. No authors declared any conflicts of interest.
Source: Arthritis Res Ther. 2018 Oct 16. doi: 10.1186/s13075-018-1731-8.
Long-term follow-up results of ongoing trials highlighted at ACR 2018
A 5-year follow-up study comparing methods of meniscal tear management in patients with osteoarthritis kicks off the second Plenary Session on Monday, Oct. 22, at the annual meeting of the American College of Rheumatology.
Jeffrey N. Katz, MD, of Brigham and Women’s Hospital in Boston, and his colleagues conducted a long-term follow-up of patients from the METEOR study, the early results of which were presented at OARSI in 2017. Dr. Katz and his colleagues randomized patients with knee pain, meniscal tears, and OA changes on x-ray or MRI to physical therapy vs. physical therapy plus arthroscopic partial meniscectomy. After 5 years, pain relief was similar across treatment groups, supporting the short-term conclusion that these patients experience relief over time, irrespective of initial treatment. Overall, 25% of the patients had total knee replacement surgery during the follow-up period.
The session also includes a new presentation by Kenneth G. Saag, MD, of the University of Alabama at Birmingham of 2-year outcomes from a phase 3 trial of denosumab versus risedronate for glucocorticoid-induced osteoporosis that was first presented at EULAR this year.
At 2 years, denosumab proved superior for increasing spine and hip bone mineral density in osteoporosis patients, compared with risedronate, and demonstrated a similar safety profile.
In addition, attendees will hear updated long-term results from the SCOT trial of myeloablative autologous hematopoietic stem cell transplantation for scleroderma patients. Keith M. Sullivan, MD, of Duke University, Durham, N.C., and his colleagues found that the benefits of the treatment endured after 6-11 years, supporting results presented at ACR 2016.
A 5-year follow-up study comparing methods of meniscal tear management in patients with osteoarthritis kicks off the second Plenary Session on Monday, Oct. 22, at the annual meeting of the American College of Rheumatology.
Jeffrey N. Katz, MD, of Brigham and Women’s Hospital in Boston, and his colleagues conducted a long-term follow-up of patients from the METEOR study, the early results of which were presented at OARSI in 2017. Dr. Katz and his colleagues randomized patients with knee pain, meniscal tears, and OA changes on x-ray or MRI to physical therapy vs. physical therapy plus arthroscopic partial meniscectomy. After 5 years, pain relief was similar across treatment groups, supporting the short-term conclusion that these patients experience relief over time, irrespective of initial treatment. Overall, 25% of the patients had total knee replacement surgery during the follow-up period.
The session also includes a new presentation by Kenneth G. Saag, MD, of the University of Alabama at Birmingham of 2-year outcomes from a phase 3 trial of denosumab versus risedronate for glucocorticoid-induced osteoporosis that was first presented at EULAR this year.
At 2 years, denosumab proved superior for increasing spine and hip bone mineral density in osteoporosis patients, compared with risedronate, and demonstrated a similar safety profile.
In addition, attendees will hear updated long-term results from the SCOT trial of myeloablative autologous hematopoietic stem cell transplantation for scleroderma patients. Keith M. Sullivan, MD, of Duke University, Durham, N.C., and his colleagues found that the benefits of the treatment endured after 6-11 years, supporting results presented at ACR 2016.
A 5-year follow-up study comparing methods of meniscal tear management in patients with osteoarthritis kicks off the second Plenary Session on Monday, Oct. 22, at the annual meeting of the American College of Rheumatology.
Jeffrey N. Katz, MD, of Brigham and Women’s Hospital in Boston, and his colleagues conducted a long-term follow-up of patients from the METEOR study, the early results of which were presented at OARSI in 2017. Dr. Katz and his colleagues randomized patients with knee pain, meniscal tears, and OA changes on x-ray or MRI to physical therapy vs. physical therapy plus arthroscopic partial meniscectomy. After 5 years, pain relief was similar across treatment groups, supporting the short-term conclusion that these patients experience relief over time, irrespective of initial treatment. Overall, 25% of the patients had total knee replacement surgery during the follow-up period.
The session also includes a new presentation by Kenneth G. Saag, MD, of the University of Alabama at Birmingham of 2-year outcomes from a phase 3 trial of denosumab versus risedronate for glucocorticoid-induced osteoporosis that was first presented at EULAR this year.
At 2 years, denosumab proved superior for increasing spine and hip bone mineral density in osteoporosis patients, compared with risedronate, and demonstrated a similar safety profile.
In addition, attendees will hear updated long-term results from the SCOT trial of myeloablative autologous hematopoietic stem cell transplantation for scleroderma patients. Keith M. Sullivan, MD, of Duke University, Durham, N.C., and his colleagues found that the benefits of the treatment endured after 6-11 years, supporting results presented at ACR 2016.
REPORTING FROM THE ACR ANNUAL MEETING
Bisphosphonate holiday may help to reduce atypical femur fracture risk
, according to a study of more than 150,000 Southern California health plan members presented at the annual meeting of the American Society for Bone and Mineral Research in Montreal.
A second study in the same group of women found that higher bone mineral density levels before bisphosphonate treatment may put women at greater risk for these fractures.
“Our findings suggest really strongly that among women who have achieved some level of bisphosphonate exposure a drug holiday is certainly a reasonable approach to trying to balance the risk of these atypical fractures versus the benefit of preventing more typical, or classic, hip fractures,” said presenter Annette L. Adams, PhD, MPH, a research scientist with Kaiser Permanente Southern California, who was an author on both studies.
Atypical femur fractures (AFFs) occur below the trochanters in the femoral shaft area, around mid-thigh, Dr. Adams said. They appear different from other fractures, usually breaking in just two pieces transversely through the center of the bone, and occur with minimal to no trauma, she said.
“We’ve heard stories of women that are just sitting in a chair, and they stand up and their femur fractures,” Dr. Adams said. “Or they’re out in the garden on their knees, and they try to stand up and it fractures. These are not necessarily fall-related like many traditional hip fractures.”
The researchers observed a 44% reduction in women’s risk of AFFs in the first year of a so-called drug holiday, or discontinuation of bisphosphonates, after 3-5 years on treatment when compared with those who stayed on the medications (hazard ratio = 0.56; 95% confidence interval, 0.38-0.82). During the first to fourth years after discontinuation, AFF risk was decreased by 80% (HR = 0.20; 95% CI, 0.10-0.37), and after 4 years, AFF risk was reduced by 78% (HR = 0.22; 95% CI, 0.08-0.59) in comparison to bisphosphonate users.
Dr. Adams and her colleagues reviewed records from 152,934 women aged 50 or older who were members of Kaiser Permanente Southern California between Jan. 1, 2007, and Sept. 30, 2015. There were 185 AFFs overall (incidence rate 1.70 per 10,000 person-years).
The cohort included women who used a bisphosphonate and had at least one available pretreatment bone mineral density (BMD) total hip scan. AFFs were identified and verified by physician review of x-ray images for fractures occurring during the study period with ICD-9 codes for subtrochanteric or femoral shaft fractures. Women were considered to have discontinued bisphosphonates if there was a gap of over 3 months between the last bisphosphonate use and cohort entry anniversaries. Researchers included information on potential confounders of the association between discontinuation time and AFF such as age, race/ethnicity, smoking status, fracture history, duration of bisphosphonate use, discontinuation of glucocorticoid use, and pretreatment total hip T-score.
A second study in the same cohort consistently showed that women with higher pretreatment BMD had a larger risk of AFFs.
Researchers assessed the relationship of bisphosphonate duration to AFF risk before and after treatment, including pretreatment BMD in multivariate Cox models. In a multivariate model without pretreatment BMD, those with longer bisphosphonate duration had higher AFF risk. Compared to those taking the drug for less than 1 year, the relative hazard (RH) for 1-4 years of bisphosphonate use was 3 (95% CI, 1.4-7.3), for 4-8 years of bisphosphonate use was 15 (95% CI, 7-33), and for over 8 years was 37 (95% CI, 16-83).
Pretreatment BMD, when added to the model, did not attenuate the relationship of bisphosphonate duration and AFF risk. However, it showed those with higher BMD had a 40% increase in AFF risk per standard deviation of BMD increase (HR = 1.4; 95% CI, 1.2-1.7).
In those with normal pretreatment BMD (T-score greater than –1), the RH for 4-8 years of bisphosphonate use (versus less than 1 year) was 35, compared with 15 in those with osteopenic BMD (T-score –1 to –2.5) and 6 in those with osteoporotic BMD (T-score less than –2.5).
If confirmed in other studies, the results suggest that pretreatment BMD could impact clinical decisions around patient selection for bisphosphonate initiation and drug holidays, Dr. Adams said.
She reported receiving grant and research support from Merck.
SOURCES: Adams A et al. ASBMR 2018 Abstract 1005, and Black D et al. ASBMR 2018 Abstract 1007
, according to a study of more than 150,000 Southern California health plan members presented at the annual meeting of the American Society for Bone and Mineral Research in Montreal.
A second study in the same group of women found that higher bone mineral density levels before bisphosphonate treatment may put women at greater risk for these fractures.
“Our findings suggest really strongly that among women who have achieved some level of bisphosphonate exposure a drug holiday is certainly a reasonable approach to trying to balance the risk of these atypical fractures versus the benefit of preventing more typical, or classic, hip fractures,” said presenter Annette L. Adams, PhD, MPH, a research scientist with Kaiser Permanente Southern California, who was an author on both studies.
Atypical femur fractures (AFFs) occur below the trochanters in the femoral shaft area, around mid-thigh, Dr. Adams said. They appear different from other fractures, usually breaking in just two pieces transversely through the center of the bone, and occur with minimal to no trauma, she said.
“We’ve heard stories of women that are just sitting in a chair, and they stand up and their femur fractures,” Dr. Adams said. “Or they’re out in the garden on their knees, and they try to stand up and it fractures. These are not necessarily fall-related like many traditional hip fractures.”
The researchers observed a 44% reduction in women’s risk of AFFs in the first year of a so-called drug holiday, or discontinuation of bisphosphonates, after 3-5 years on treatment when compared with those who stayed on the medications (hazard ratio = 0.56; 95% confidence interval, 0.38-0.82). During the first to fourth years after discontinuation, AFF risk was decreased by 80% (HR = 0.20; 95% CI, 0.10-0.37), and after 4 years, AFF risk was reduced by 78% (HR = 0.22; 95% CI, 0.08-0.59) in comparison to bisphosphonate users.
Dr. Adams and her colleagues reviewed records from 152,934 women aged 50 or older who were members of Kaiser Permanente Southern California between Jan. 1, 2007, and Sept. 30, 2015. There were 185 AFFs overall (incidence rate 1.70 per 10,000 person-years).
The cohort included women who used a bisphosphonate and had at least one available pretreatment bone mineral density (BMD) total hip scan. AFFs were identified and verified by physician review of x-ray images for fractures occurring during the study period with ICD-9 codes for subtrochanteric or femoral shaft fractures. Women were considered to have discontinued bisphosphonates if there was a gap of over 3 months between the last bisphosphonate use and cohort entry anniversaries. Researchers included information on potential confounders of the association between discontinuation time and AFF such as age, race/ethnicity, smoking status, fracture history, duration of bisphosphonate use, discontinuation of glucocorticoid use, and pretreatment total hip T-score.
A second study in the same cohort consistently showed that women with higher pretreatment BMD had a larger risk of AFFs.
Researchers assessed the relationship of bisphosphonate duration to AFF risk before and after treatment, including pretreatment BMD in multivariate Cox models. In a multivariate model without pretreatment BMD, those with longer bisphosphonate duration had higher AFF risk. Compared to those taking the drug for less than 1 year, the relative hazard (RH) for 1-4 years of bisphosphonate use was 3 (95% CI, 1.4-7.3), for 4-8 years of bisphosphonate use was 15 (95% CI, 7-33), and for over 8 years was 37 (95% CI, 16-83).
Pretreatment BMD, when added to the model, did not attenuate the relationship of bisphosphonate duration and AFF risk. However, it showed those with higher BMD had a 40% increase in AFF risk per standard deviation of BMD increase (HR = 1.4; 95% CI, 1.2-1.7).
In those with normal pretreatment BMD (T-score greater than –1), the RH for 4-8 years of bisphosphonate use (versus less than 1 year) was 35, compared with 15 in those with osteopenic BMD (T-score –1 to –2.5) and 6 in those with osteoporotic BMD (T-score less than –2.5).
If confirmed in other studies, the results suggest that pretreatment BMD could impact clinical decisions around patient selection for bisphosphonate initiation and drug holidays, Dr. Adams said.
She reported receiving grant and research support from Merck.
SOURCES: Adams A et al. ASBMR 2018 Abstract 1005, and Black D et al. ASBMR 2018 Abstract 1007
, according to a study of more than 150,000 Southern California health plan members presented at the annual meeting of the American Society for Bone and Mineral Research in Montreal.
A second study in the same group of women found that higher bone mineral density levels before bisphosphonate treatment may put women at greater risk for these fractures.
“Our findings suggest really strongly that among women who have achieved some level of bisphosphonate exposure a drug holiday is certainly a reasonable approach to trying to balance the risk of these atypical fractures versus the benefit of preventing more typical, or classic, hip fractures,” said presenter Annette L. Adams, PhD, MPH, a research scientist with Kaiser Permanente Southern California, who was an author on both studies.
Atypical femur fractures (AFFs) occur below the trochanters in the femoral shaft area, around mid-thigh, Dr. Adams said. They appear different from other fractures, usually breaking in just two pieces transversely through the center of the bone, and occur with minimal to no trauma, she said.
“We’ve heard stories of women that are just sitting in a chair, and they stand up and their femur fractures,” Dr. Adams said. “Or they’re out in the garden on their knees, and they try to stand up and it fractures. These are not necessarily fall-related like many traditional hip fractures.”
The researchers observed a 44% reduction in women’s risk of AFFs in the first year of a so-called drug holiday, or discontinuation of bisphosphonates, after 3-5 years on treatment when compared with those who stayed on the medications (hazard ratio = 0.56; 95% confidence interval, 0.38-0.82). During the first to fourth years after discontinuation, AFF risk was decreased by 80% (HR = 0.20; 95% CI, 0.10-0.37), and after 4 years, AFF risk was reduced by 78% (HR = 0.22; 95% CI, 0.08-0.59) in comparison to bisphosphonate users.
Dr. Adams and her colleagues reviewed records from 152,934 women aged 50 or older who were members of Kaiser Permanente Southern California between Jan. 1, 2007, and Sept. 30, 2015. There were 185 AFFs overall (incidence rate 1.70 per 10,000 person-years).
The cohort included women who used a bisphosphonate and had at least one available pretreatment bone mineral density (BMD) total hip scan. AFFs were identified and verified by physician review of x-ray images for fractures occurring during the study period with ICD-9 codes for subtrochanteric or femoral shaft fractures. Women were considered to have discontinued bisphosphonates if there was a gap of over 3 months between the last bisphosphonate use and cohort entry anniversaries. Researchers included information on potential confounders of the association between discontinuation time and AFF such as age, race/ethnicity, smoking status, fracture history, duration of bisphosphonate use, discontinuation of glucocorticoid use, and pretreatment total hip T-score.
A second study in the same cohort consistently showed that women with higher pretreatment BMD had a larger risk of AFFs.
Researchers assessed the relationship of bisphosphonate duration to AFF risk before and after treatment, including pretreatment BMD in multivariate Cox models. In a multivariate model without pretreatment BMD, those with longer bisphosphonate duration had higher AFF risk. Compared to those taking the drug for less than 1 year, the relative hazard (RH) for 1-4 years of bisphosphonate use was 3 (95% CI, 1.4-7.3), for 4-8 years of bisphosphonate use was 15 (95% CI, 7-33), and for over 8 years was 37 (95% CI, 16-83).
Pretreatment BMD, when added to the model, did not attenuate the relationship of bisphosphonate duration and AFF risk. However, it showed those with higher BMD had a 40% increase in AFF risk per standard deviation of BMD increase (HR = 1.4; 95% CI, 1.2-1.7).
In those with normal pretreatment BMD (T-score greater than –1), the RH for 4-8 years of bisphosphonate use (versus less than 1 year) was 35, compared with 15 in those with osteopenic BMD (T-score –1 to –2.5) and 6 in those with osteoporotic BMD (T-score less than –2.5).
If confirmed in other studies, the results suggest that pretreatment BMD could impact clinical decisions around patient selection for bisphosphonate initiation and drug holidays, Dr. Adams said.
She reported receiving grant and research support from Merck.
SOURCES: Adams A et al. ASBMR 2018 Abstract 1005, and Black D et al. ASBMR 2018 Abstract 1007
REPORTING FROM ASBMR 2018