User login
For MD-IQ on Family Practice News, but a regular topic for Rheumatology News
EULAR: Steroid injection accuracy may not matter for OA knee pain relief
ROME – Ensuring that intra-articular injections are correctly placed does not appear to result in better pain management for knee osteoarthritis, according to research presented at the European Congress of Rheumatology.
“Accurate injection neither resulted in higher rate of response to treatment than inaccurate injection nor greater mean pain reduction,” said George Hirsch, Ph.D., of the Institute of Inflammation and Repair at the University of Manchester (England) and the Dudley Group NHS Foundation Trust.
Dr. Hirsch and his associates defined response to treatment as at least a 40% reduction in pain on the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), and the percentages who met that definition were similar among patients who had their injections correctly placed and those who did not at 3 weeks (57.7% vs. 63.4%, respectively; P = .0355) and 9 weeks (39.3% vs. 51.4%; P = .0148).
There also were no differences between mean pain reduction at 3 weeks (–110.7 mm vs. –116.9 mm on a visual analogue scale; P = .781) and 9 weeks (–65.2 mm vs. –92.8 mm; P = .247) between the patients with accurate and inaccurate intra-articular injection placement.
The researchers aimed to determine if injecting accurately into the knee could have an effect on patients’ pain outcomes because, despite the effectiveness of intra-articular corticosteroid injections (IACIs) for pain in knee OA, “responses to treatment vary.” In the poster presentation, Dr. Hirsch noted that uncertainty remained as to whether structural factors including accurate intra-articular placement mattered in regards to pain reduction.
The practical, prospective, observational study included 141 men and women with a mean age of 63.8 years who had been referred for IACI for their knee OA in a routine practice setting.
Before aspiration and injection into the affected knee(s) based on clinical examination, patients underwent careful x-ray and ultrasound assessment. Following injection, an air arthrosonogram was used to see if injections had entered the joint cavity.
Overall, just over half (53%) of patients were classed as responders at 3 weeks and 44% at 9 weeks, and a positive arthrosonogram was seen in 98 (70%).
In addition to no advantage for accurate injection placement on pain outcomes, there was no indication that individual physical factors mattered either. Mean measurements of sonographic effusion and synovial hypertrophy did not differ between responders and nonresponders at either time point assessed.
Similar findings also were seen for mean scores for power Doppler signal and individual radiographic features of osteoarthritis that included joint-space narrowing and presence of bone spurs.
“These results raise potential questions about the routine use of [ultrasound] to enhance or predict response to IACI in knee OA,” Dr. Hirsch said.
The authors reported having no financial disclosures.
ROME – Ensuring that intra-articular injections are correctly placed does not appear to result in better pain management for knee osteoarthritis, according to research presented at the European Congress of Rheumatology.
“Accurate injection neither resulted in higher rate of response to treatment than inaccurate injection nor greater mean pain reduction,” said George Hirsch, Ph.D., of the Institute of Inflammation and Repair at the University of Manchester (England) and the Dudley Group NHS Foundation Trust.
Dr. Hirsch and his associates defined response to treatment as at least a 40% reduction in pain on the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), and the percentages who met that definition were similar among patients who had their injections correctly placed and those who did not at 3 weeks (57.7% vs. 63.4%, respectively; P = .0355) and 9 weeks (39.3% vs. 51.4%; P = .0148).
There also were no differences between mean pain reduction at 3 weeks (–110.7 mm vs. –116.9 mm on a visual analogue scale; P = .781) and 9 weeks (–65.2 mm vs. –92.8 mm; P = .247) between the patients with accurate and inaccurate intra-articular injection placement.
The researchers aimed to determine if injecting accurately into the knee could have an effect on patients’ pain outcomes because, despite the effectiveness of intra-articular corticosteroid injections (IACIs) for pain in knee OA, “responses to treatment vary.” In the poster presentation, Dr. Hirsch noted that uncertainty remained as to whether structural factors including accurate intra-articular placement mattered in regards to pain reduction.
The practical, prospective, observational study included 141 men and women with a mean age of 63.8 years who had been referred for IACI for their knee OA in a routine practice setting.
Before aspiration and injection into the affected knee(s) based on clinical examination, patients underwent careful x-ray and ultrasound assessment. Following injection, an air arthrosonogram was used to see if injections had entered the joint cavity.
Overall, just over half (53%) of patients were classed as responders at 3 weeks and 44% at 9 weeks, and a positive arthrosonogram was seen in 98 (70%).
In addition to no advantage for accurate injection placement on pain outcomes, there was no indication that individual physical factors mattered either. Mean measurements of sonographic effusion and synovial hypertrophy did not differ between responders and nonresponders at either time point assessed.
Similar findings also were seen for mean scores for power Doppler signal and individual radiographic features of osteoarthritis that included joint-space narrowing and presence of bone spurs.
“These results raise potential questions about the routine use of [ultrasound] to enhance or predict response to IACI in knee OA,” Dr. Hirsch said.
The authors reported having no financial disclosures.
ROME – Ensuring that intra-articular injections are correctly placed does not appear to result in better pain management for knee osteoarthritis, according to research presented at the European Congress of Rheumatology.
“Accurate injection neither resulted in higher rate of response to treatment than inaccurate injection nor greater mean pain reduction,” said George Hirsch, Ph.D., of the Institute of Inflammation and Repair at the University of Manchester (England) and the Dudley Group NHS Foundation Trust.
Dr. Hirsch and his associates defined response to treatment as at least a 40% reduction in pain on the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), and the percentages who met that definition were similar among patients who had their injections correctly placed and those who did not at 3 weeks (57.7% vs. 63.4%, respectively; P = .0355) and 9 weeks (39.3% vs. 51.4%; P = .0148).
There also were no differences between mean pain reduction at 3 weeks (–110.7 mm vs. –116.9 mm on a visual analogue scale; P = .781) and 9 weeks (–65.2 mm vs. –92.8 mm; P = .247) between the patients with accurate and inaccurate intra-articular injection placement.
The researchers aimed to determine if injecting accurately into the knee could have an effect on patients’ pain outcomes because, despite the effectiveness of intra-articular corticosteroid injections (IACIs) for pain in knee OA, “responses to treatment vary.” In the poster presentation, Dr. Hirsch noted that uncertainty remained as to whether structural factors including accurate intra-articular placement mattered in regards to pain reduction.
The practical, prospective, observational study included 141 men and women with a mean age of 63.8 years who had been referred for IACI for their knee OA in a routine practice setting.
Before aspiration and injection into the affected knee(s) based on clinical examination, patients underwent careful x-ray and ultrasound assessment. Following injection, an air arthrosonogram was used to see if injections had entered the joint cavity.
Overall, just over half (53%) of patients were classed as responders at 3 weeks and 44% at 9 weeks, and a positive arthrosonogram was seen in 98 (70%).
In addition to no advantage for accurate injection placement on pain outcomes, there was no indication that individual physical factors mattered either. Mean measurements of sonographic effusion and synovial hypertrophy did not differ between responders and nonresponders at either time point assessed.
Similar findings also were seen for mean scores for power Doppler signal and individual radiographic features of osteoarthritis that included joint-space narrowing and presence of bone spurs.
“These results raise potential questions about the routine use of [ultrasound] to enhance or predict response to IACI in knee OA,” Dr. Hirsch said.
The authors reported having no financial disclosures.
AT THE EULAR 2015 CONGRESS
Key clinical point: Reductions in pain achieved with intra-articular corticosteroid injections were not influenced by the accuracy of injection.
Major finding: Response rates at 3 weeks (57.7% vs. 63.4%; P = .0355) and 9 weeks (39.3% vs. 51.4%; P = .0148) were similar for patients who did and did not have accurately placed intra-articular injections.
Data source: Nonrandomized, pragmatic, prospective, observational study of 141 patients with knee osteoarthritis receiving intra-articular corticosteroid injections for pain management.
Disclosures: The authors reported having no financial disclosures.
Tired knees
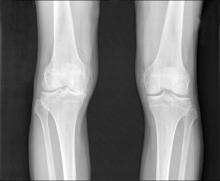
Last week, one of my patients presented with a BMI of 49 and two canes. Knee x-ray shows marked medial compartment narrowing bilaterally. We will inject her knees with steroids, but this will be temporary.
As the obesity epidemic continues to rage, native joints are rapidly being replaced with metal ones. Our pitiful homegrown joints were not designed to carry all this human weight. Joint forces in the hip and knee have been estimated to be 3 times body weight when walking on level ground and 6-10 times body weight when stooping or bending. Combine this with all the ‘screen time’ (average 8 hours a day for U.S. adults) and all the trips to the bathroom from the poorly controlled diabetes, and we are set up for needing a lot more orthopedic surgeons.
So should we push for surgery?
I am reluctant to immediately and eagerly pursue surgery based upon data from Ward et al. elucidating the increased risk for complications after joint surgery among patients with a BMI > 40 (J.Arthroplasty. 2015 Jun 3. pii: S0883-5403(15)00474-X. doi: 10.1016/j.arth.2015.03.045. [Epub ahead of print]). Data from the bariatric literature suggest that the risk of complications following joint replacement is lower if bariatric surgery is performed first. Weight loss as we look toward joint replacement is a good idea for both our orthopedic colleagues and our patients.
So we will work on weight loss first
In patients with osteoarthritis, a moderate amount of weight loss can significantly improve knee function. The short term efficacy of weight loss is comparable to joint replacement. But clinicians need to be wary of the “pain-exercise block”: patients telling us they cannot lose weight because the pain prevents them from exercising. I tell my patients that weight loss and weight maintenance can be managed effectively through dietary modification and that they do not have to run a marathon, they just need to walk if they can. But patients do not always want to hear this. Caloric restriction is psychologically painful for many. I remind them that 30 minutes of exercise can be undone in 30 seconds with a bar of chocolate, so we need to skip the chocolate bar if we do light exercise or forgo exercise altogether. Exercise is important for a million other reasons, but many of our patients can’t engage, especially when presenting with gait assist devices.
My patient and I started the discussion of bariatric surgery. In the meantime, we are going to try a trial of lorcaserin and hope the knees hold out. We are likely going to need more steroids.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no relevant financial disclosures about this article. Follow him on Twitter: @jonebbert.
Last week, one of my patients presented with a BMI of 49 and two canes. Knee x-ray shows marked medial compartment narrowing bilaterally. We will inject her knees with steroids, but this will be temporary.
As the obesity epidemic continues to rage, native joints are rapidly being replaced with metal ones. Our pitiful homegrown joints were not designed to carry all this human weight. Joint forces in the hip and knee have been estimated to be 3 times body weight when walking on level ground and 6-10 times body weight when stooping or bending. Combine this with all the ‘screen time’ (average 8 hours a day for U.S. adults) and all the trips to the bathroom from the poorly controlled diabetes, and we are set up for needing a lot more orthopedic surgeons.
So should we push for surgery?
I am reluctant to immediately and eagerly pursue surgery based upon data from Ward et al. elucidating the increased risk for complications after joint surgery among patients with a BMI > 40 (J.Arthroplasty. 2015 Jun 3. pii: S0883-5403(15)00474-X. doi: 10.1016/j.arth.2015.03.045. [Epub ahead of print]). Data from the bariatric literature suggest that the risk of complications following joint replacement is lower if bariatric surgery is performed first. Weight loss as we look toward joint replacement is a good idea for both our orthopedic colleagues and our patients.
So we will work on weight loss first
In patients with osteoarthritis, a moderate amount of weight loss can significantly improve knee function. The short term efficacy of weight loss is comparable to joint replacement. But clinicians need to be wary of the “pain-exercise block”: patients telling us they cannot lose weight because the pain prevents them from exercising. I tell my patients that weight loss and weight maintenance can be managed effectively through dietary modification and that they do not have to run a marathon, they just need to walk if they can. But patients do not always want to hear this. Caloric restriction is psychologically painful for many. I remind them that 30 minutes of exercise can be undone in 30 seconds with a bar of chocolate, so we need to skip the chocolate bar if we do light exercise or forgo exercise altogether. Exercise is important for a million other reasons, but many of our patients can’t engage, especially when presenting with gait assist devices.
My patient and I started the discussion of bariatric surgery. In the meantime, we are going to try a trial of lorcaserin and hope the knees hold out. We are likely going to need more steroids.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no relevant financial disclosures about this article. Follow him on Twitter: @jonebbert.
Last week, one of my patients presented with a BMI of 49 and two canes. Knee x-ray shows marked medial compartment narrowing bilaterally. We will inject her knees with steroids, but this will be temporary.
As the obesity epidemic continues to rage, native joints are rapidly being replaced with metal ones. Our pitiful homegrown joints were not designed to carry all this human weight. Joint forces in the hip and knee have been estimated to be 3 times body weight when walking on level ground and 6-10 times body weight when stooping or bending. Combine this with all the ‘screen time’ (average 8 hours a day for U.S. adults) and all the trips to the bathroom from the poorly controlled diabetes, and we are set up for needing a lot more orthopedic surgeons.
So should we push for surgery?
I am reluctant to immediately and eagerly pursue surgery based upon data from Ward et al. elucidating the increased risk for complications after joint surgery among patients with a BMI > 40 (J.Arthroplasty. 2015 Jun 3. pii: S0883-5403(15)00474-X. doi: 10.1016/j.arth.2015.03.045. [Epub ahead of print]). Data from the bariatric literature suggest that the risk of complications following joint replacement is lower if bariatric surgery is performed first. Weight loss as we look toward joint replacement is a good idea for both our orthopedic colleagues and our patients.
So we will work on weight loss first
In patients with osteoarthritis, a moderate amount of weight loss can significantly improve knee function. The short term efficacy of weight loss is comparable to joint replacement. But clinicians need to be wary of the “pain-exercise block”: patients telling us they cannot lose weight because the pain prevents them from exercising. I tell my patients that weight loss and weight maintenance can be managed effectively through dietary modification and that they do not have to run a marathon, they just need to walk if they can. But patients do not always want to hear this. Caloric restriction is psychologically painful for many. I remind them that 30 minutes of exercise can be undone in 30 seconds with a bar of chocolate, so we need to skip the chocolate bar if we do light exercise or forgo exercise altogether. Exercise is important for a million other reasons, but many of our patients can’t engage, especially when presenting with gait assist devices.
My patient and I started the discussion of bariatric surgery. In the meantime, we are going to try a trial of lorcaserin and hope the knees hold out. We are likely going to need more steroids.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no relevant financial disclosures about this article. Follow him on Twitter: @jonebbert.
Tai chi equivalent to physical therapy for knee OA
ROME – Tai chi is as effective as standard physical therapy in reducing pain and improving physical function and quality of life in patients with knee osteoarthritis, according to the results of a randomized, single-blind study reported at the European Congress of Rheumatology.
The primary outcome of change in the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain subscale score from baseline to 12 weeks was –167.2 mm in the patients randomized to the tai chi group vs. –143.0 mm in those who completed a standard physiotherapy program (P = .16).
“Future studies of ‘Eastern’ complementary medicine will further inform ‘Western’ medical treatment guidelines,” said Dr. Chenchen Wang, director of the Center for Complementary and Integrative Medicine at Tufts Medical Center in Boston. She noted that the study findings showed that tai chi could be a viable alternative to physical therapy for knee osteoarthritis (OA), which she called “a chronic disabling disease.”
Dr. Wang andher associates have previously shown that the classic Yang-style tai chi results in clinically important improvements in patients with fibromyalgia (N. Engl. J. Med. 2010;363:743-54). They have also previously reported beneficial effects in small numbers of patients with knee OA (Arthritis Rheum. 2009;61:1545–53). The present study findings replicate these results in a larger group of patients followed up for a longer period of time.
“This is the longest follow-up of tai chi for knee osteoarthritis to date,” Dr. Wang observed. It is also representative of a racially diverse population, she said. The study is ongoing but not recruiting participants and will continue to compare the effectiveness and cost-effectiveness of the Chinese martial art vs. standard-of-care physiotherapy for 1 year (BMC Complement. Altern. Med. 2014;14:333).Of 204 randomized patients with a mean age of 60 years and disease duration of 8 years, 167 (82%) completed the tai chi sessions and 12-week evaluation for the primary end point. In addition, three-quarters of patients completed 24 weeks and 69% completed 1 year of the intervention, showing the sustainability of the exercise program. Overall attendance was similar between the groups, at 74% for tai chi and 81% for physical therapy.
The 106 patients randomized to the tai chi group performed the martial art twice a week for 12 weeks while the 98 patients in the physical therapy group underwent twice-weekly sessions for the first 6 weeks, then continued with ”rigorously monitored” exercises at home for 12 additional weeks. Patients knew to which group they had been randomly assigned, but the study physician and outcomes assessments were blinded to the treatment allocation.
Similar benefits were seen for with both strategies for the secondary end points of physical function subscale of the WOMAC (P = .08), Patients’ Global Assessment (P = .06), and chronic pain self-efficacy (P = .22). There were also similar improvements in 6-minute (P = .76) and 20-meter (P = .40) walking tests.
Health-related quality of life measured using the Short Form 36 suggested a possible statistical advantage of tai chi over physical therapy for the physical but not mental component summary, with mean differences between the groups of 3.2 (P < .01) and 1.6 (P = .08), respectively. There was also a statistical difference in depression scores between the groups, but this may not be clinically significant, Dr. Wang observed.
“This study provides evidence to support both tai chi and physical therapy improve pain and physical function for patients with knee osteoarthritis,” she said. “Interestingly, we didn’t see any differences in effectiveness attributable to the four individual tai chi instructors.”
The National Center for Complementary and Integrative Health of the National Institutes of Health supported the study. Dr. Wang reported no relevant conflicts.
ROME – Tai chi is as effective as standard physical therapy in reducing pain and improving physical function and quality of life in patients with knee osteoarthritis, according to the results of a randomized, single-blind study reported at the European Congress of Rheumatology.
The primary outcome of change in the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain subscale score from baseline to 12 weeks was –167.2 mm in the patients randomized to the tai chi group vs. –143.0 mm in those who completed a standard physiotherapy program (P = .16).
“Future studies of ‘Eastern’ complementary medicine will further inform ‘Western’ medical treatment guidelines,” said Dr. Chenchen Wang, director of the Center for Complementary and Integrative Medicine at Tufts Medical Center in Boston. She noted that the study findings showed that tai chi could be a viable alternative to physical therapy for knee osteoarthritis (OA), which she called “a chronic disabling disease.”
Dr. Wang andher associates have previously shown that the classic Yang-style tai chi results in clinically important improvements in patients with fibromyalgia (N. Engl. J. Med. 2010;363:743-54). They have also previously reported beneficial effects in small numbers of patients with knee OA (Arthritis Rheum. 2009;61:1545–53). The present study findings replicate these results in a larger group of patients followed up for a longer period of time.
“This is the longest follow-up of tai chi for knee osteoarthritis to date,” Dr. Wang observed. It is also representative of a racially diverse population, she said. The study is ongoing but not recruiting participants and will continue to compare the effectiveness and cost-effectiveness of the Chinese martial art vs. standard-of-care physiotherapy for 1 year (BMC Complement. Altern. Med. 2014;14:333).Of 204 randomized patients with a mean age of 60 years and disease duration of 8 years, 167 (82%) completed the tai chi sessions and 12-week evaluation for the primary end point. In addition, three-quarters of patients completed 24 weeks and 69% completed 1 year of the intervention, showing the sustainability of the exercise program. Overall attendance was similar between the groups, at 74% for tai chi and 81% for physical therapy.
The 106 patients randomized to the tai chi group performed the martial art twice a week for 12 weeks while the 98 patients in the physical therapy group underwent twice-weekly sessions for the first 6 weeks, then continued with ”rigorously monitored” exercises at home for 12 additional weeks. Patients knew to which group they had been randomly assigned, but the study physician and outcomes assessments were blinded to the treatment allocation.
Similar benefits were seen for with both strategies for the secondary end points of physical function subscale of the WOMAC (P = .08), Patients’ Global Assessment (P = .06), and chronic pain self-efficacy (P = .22). There were also similar improvements in 6-minute (P = .76) and 20-meter (P = .40) walking tests.
Health-related quality of life measured using the Short Form 36 suggested a possible statistical advantage of tai chi over physical therapy for the physical but not mental component summary, with mean differences between the groups of 3.2 (P < .01) and 1.6 (P = .08), respectively. There was also a statistical difference in depression scores between the groups, but this may not be clinically significant, Dr. Wang observed.
“This study provides evidence to support both tai chi and physical therapy improve pain and physical function for patients with knee osteoarthritis,” she said. “Interestingly, we didn’t see any differences in effectiveness attributable to the four individual tai chi instructors.”
The National Center for Complementary and Integrative Health of the National Institutes of Health supported the study. Dr. Wang reported no relevant conflicts.
ROME – Tai chi is as effective as standard physical therapy in reducing pain and improving physical function and quality of life in patients with knee osteoarthritis, according to the results of a randomized, single-blind study reported at the European Congress of Rheumatology.
The primary outcome of change in the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain subscale score from baseline to 12 weeks was –167.2 mm in the patients randomized to the tai chi group vs. –143.0 mm in those who completed a standard physiotherapy program (P = .16).
“Future studies of ‘Eastern’ complementary medicine will further inform ‘Western’ medical treatment guidelines,” said Dr. Chenchen Wang, director of the Center for Complementary and Integrative Medicine at Tufts Medical Center in Boston. She noted that the study findings showed that tai chi could be a viable alternative to physical therapy for knee osteoarthritis (OA), which she called “a chronic disabling disease.”
Dr. Wang andher associates have previously shown that the classic Yang-style tai chi results in clinically important improvements in patients with fibromyalgia (N. Engl. J. Med. 2010;363:743-54). They have also previously reported beneficial effects in small numbers of patients with knee OA (Arthritis Rheum. 2009;61:1545–53). The present study findings replicate these results in a larger group of patients followed up for a longer period of time.
“This is the longest follow-up of tai chi for knee osteoarthritis to date,” Dr. Wang observed. It is also representative of a racially diverse population, she said. The study is ongoing but not recruiting participants and will continue to compare the effectiveness and cost-effectiveness of the Chinese martial art vs. standard-of-care physiotherapy for 1 year (BMC Complement. Altern. Med. 2014;14:333).Of 204 randomized patients with a mean age of 60 years and disease duration of 8 years, 167 (82%) completed the tai chi sessions and 12-week evaluation for the primary end point. In addition, three-quarters of patients completed 24 weeks and 69% completed 1 year of the intervention, showing the sustainability of the exercise program. Overall attendance was similar between the groups, at 74% for tai chi and 81% for physical therapy.
The 106 patients randomized to the tai chi group performed the martial art twice a week for 12 weeks while the 98 patients in the physical therapy group underwent twice-weekly sessions for the first 6 weeks, then continued with ”rigorously monitored” exercises at home for 12 additional weeks. Patients knew to which group they had been randomly assigned, but the study physician and outcomes assessments were blinded to the treatment allocation.
Similar benefits were seen for with both strategies for the secondary end points of physical function subscale of the WOMAC (P = .08), Patients’ Global Assessment (P = .06), and chronic pain self-efficacy (P = .22). There were also similar improvements in 6-minute (P = .76) and 20-meter (P = .40) walking tests.
Health-related quality of life measured using the Short Form 36 suggested a possible statistical advantage of tai chi over physical therapy for the physical but not mental component summary, with mean differences between the groups of 3.2 (P < .01) and 1.6 (P = .08), respectively. There was also a statistical difference in depression scores between the groups, but this may not be clinically significant, Dr. Wang observed.
“This study provides evidence to support both tai chi and physical therapy improve pain and physical function for patients with knee osteoarthritis,” she said. “Interestingly, we didn’t see any differences in effectiveness attributable to the four individual tai chi instructors.”
The National Center for Complementary and Integrative Health of the National Institutes of Health supported the study. Dr. Wang reported no relevant conflicts.
AT THE EULAR 2015 CONGRESS
Key clinical point: Tai chi may serve as an alternative to physical therapy for knee OA.
Major finding: The change in WOMAC score from baseline at 12 weeks was –167.2 mm in the patients randomized to the tai chi group vs. –143.0 mm in those who completed a standard physiotherapy program (P =.16).
Data source: Single-blind, 52-week randomized trial of twice-weekly tai chi vs. physical therapy for 12 weeks to alleviate knee pain in 204 patients with knee OA.
Disclosures: The National Center for Complementary and Integrative Health of the National Institutes of Health supported the study. Dr. Wang reported no relevant disclosures.
EULAR: Vitamin D supplementation fails to reduce knee OA pain
ROME – Vitamin D supplementation did not ease osteoarthritic knee pain measured using the Western Ontario and McMaster Universities Osteoarthritis Index in a 2-year, randomized, double-blind, placebo-controlled trial.
Results of the VIDEO (Vitamin D Effect on Osteoarthritis) study in patients with symptomatic knee osteoarthritis (OA) and low vitamin D levels also showed that replenishing vitamin D also had no effect on the loss of cartilage volume, although there might be a marginal benefit on bone marrow lesions (BMLs) and pain assessed using a visual analog scale (VAS).
“Vitamin D at 50,000 IU/month over 2 years did not meet the primary endpoint in this randomized, controlled trial,” said Jason Jin, a Ph.D. candidate at the Menzies Research Institute, University of Tasmania in Hobart, Australia, who presented the VIDEO study findings at the European Congress of Rheumatology.
He cited a recent commentary published in the Journal of the American Medical Association (JAMA 2015;313:1311-12) that looked at vitamin D research and clinical practice in which the authors said that “clinical enthusiasm for supplemental vitamin D has outpaced available evidence.” This seems to be true considering the results of this and other previous randomized trials, Mr. Jin observed.
“The background of this study is that, in the last decade, vitamin D has become a hot topic in osteoarthritis research and epidemiologic studies have found that vitamin D deficiency is very common in knee osteoarthritis patients,” he said. Low levels of vitamin D have been linked to increased knee pain, radiographic progression, and increased cartilage loss in OA.
Two prior randomized, controlled trials provided conflicting evidence, he highlighted, with one study showing that supplementation of 2,000 IU/day of vitamin D for 2 years had no effect on symptoms or knee structure (JAMA 2013;309:155-62) while another showed that a monthly dose of 60,000 IU for 1 year may be beneficial in terms of relieving pain and functional outcomes but longer follow-up was required (Clin. Orthop. Relat. Res. 2013;471:3556-62).
The VIDEO study was therefore designed to try to resolve some of the controversy and look at a larger group of patients for a longer period of time. The study’s hypothesis was that vitamin D might ease knee pain and perhaps have effect structural changes in patients with symptomatic knee OA who had low vitamin D levels. A low vitamin D level was defined as a serum measurement of 25(OH)D of 12.5-60 nmol/L (5-24 ng/mL) at baseline.
Of almost 600 patients screened, 413 were randomized, with 209 randomized to the oral vitamin D supplementation group and 204 to the matched placebo arm. Patients in each group had comparable characteristics at baseline, with a mean age of around 62 to 63 years. Half the patients were female. Baseline serum vitamin D levels were about 43 nmol/L (17.2 ng/mL). Virtually all (96%) of patients had radiographic evidence of knee OA, 97% had cartilage defects, and 80% had bone marrow lesions.
While serum levels of 25(OH)D were successfully increased in the supplemented patients over the course of the study, this did not translate into an improvement in the coprimary endpoint of a change in Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) knee pain over 24 months. The difference in WOMAC pain between the vitamin D and placebo groups was a nonsignifcant –14.8 (–49.9 vs. –35.1; P = .102). Vitamin D–supplemented patients did, however, report marginally less VAS pain (–14.8 vs. –9.4; P = .038).
Total tibial cartilage volume loss, the second coprimary endpoint, was not significantly different between the vitamin D and placebo groups, at around 121 and 150 mm3 per annum, with 2-year changes of –3.44% vs. –4.23% per annum (P = .132). The secondary endpoints of changes in tibiofemoral cartilage defects (0.29 vs. 0.47; P = .159) and tibiofemoral BMLs (–0.59 vs. –0.21; P = .087) were also not significantly different, but patients randomized to vitamin D supplementation had fewer increases in BMLs (17% vs. 27%; P = .03).
There was no concern over the safety of vitamin D supplementation, although more general side effects were noted in the vitamin D vs. the placebo group.
Commenting on the strengths and weaknesses of the study, Mr. Jin noted it was a large, multicenter, randomized, double-blind, placebo-controlled trial with a reasonably long follow-up. The patient group studied has good generalizability to those seen in everyday practice, he suggested, noting that the main limitation was the number of patients lost to follow-up because of noncompliance: 21 patients in the vitamin D group vs. 8 patients in the placebo group.
ROME – Vitamin D supplementation did not ease osteoarthritic knee pain measured using the Western Ontario and McMaster Universities Osteoarthritis Index in a 2-year, randomized, double-blind, placebo-controlled trial.
Results of the VIDEO (Vitamin D Effect on Osteoarthritis) study in patients with symptomatic knee osteoarthritis (OA) and low vitamin D levels also showed that replenishing vitamin D also had no effect on the loss of cartilage volume, although there might be a marginal benefit on bone marrow lesions (BMLs) and pain assessed using a visual analog scale (VAS).
“Vitamin D at 50,000 IU/month over 2 years did not meet the primary endpoint in this randomized, controlled trial,” said Jason Jin, a Ph.D. candidate at the Menzies Research Institute, University of Tasmania in Hobart, Australia, who presented the VIDEO study findings at the European Congress of Rheumatology.
He cited a recent commentary published in the Journal of the American Medical Association (JAMA 2015;313:1311-12) that looked at vitamin D research and clinical practice in which the authors said that “clinical enthusiasm for supplemental vitamin D has outpaced available evidence.” This seems to be true considering the results of this and other previous randomized trials, Mr. Jin observed.
“The background of this study is that, in the last decade, vitamin D has become a hot topic in osteoarthritis research and epidemiologic studies have found that vitamin D deficiency is very common in knee osteoarthritis patients,” he said. Low levels of vitamin D have been linked to increased knee pain, radiographic progression, and increased cartilage loss in OA.
Two prior randomized, controlled trials provided conflicting evidence, he highlighted, with one study showing that supplementation of 2,000 IU/day of vitamin D for 2 years had no effect on symptoms or knee structure (JAMA 2013;309:155-62) while another showed that a monthly dose of 60,000 IU for 1 year may be beneficial in terms of relieving pain and functional outcomes but longer follow-up was required (Clin. Orthop. Relat. Res. 2013;471:3556-62).
The VIDEO study was therefore designed to try to resolve some of the controversy and look at a larger group of patients for a longer period of time. The study’s hypothesis was that vitamin D might ease knee pain and perhaps have effect structural changes in patients with symptomatic knee OA who had low vitamin D levels. A low vitamin D level was defined as a serum measurement of 25(OH)D of 12.5-60 nmol/L (5-24 ng/mL) at baseline.
Of almost 600 patients screened, 413 were randomized, with 209 randomized to the oral vitamin D supplementation group and 204 to the matched placebo arm. Patients in each group had comparable characteristics at baseline, with a mean age of around 62 to 63 years. Half the patients were female. Baseline serum vitamin D levels were about 43 nmol/L (17.2 ng/mL). Virtually all (96%) of patients had radiographic evidence of knee OA, 97% had cartilage defects, and 80% had bone marrow lesions.
While serum levels of 25(OH)D were successfully increased in the supplemented patients over the course of the study, this did not translate into an improvement in the coprimary endpoint of a change in Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) knee pain over 24 months. The difference in WOMAC pain between the vitamin D and placebo groups was a nonsignifcant –14.8 (–49.9 vs. –35.1; P = .102). Vitamin D–supplemented patients did, however, report marginally less VAS pain (–14.8 vs. –9.4; P = .038).
Total tibial cartilage volume loss, the second coprimary endpoint, was not significantly different between the vitamin D and placebo groups, at around 121 and 150 mm3 per annum, with 2-year changes of –3.44% vs. –4.23% per annum (P = .132). The secondary endpoints of changes in tibiofemoral cartilage defects (0.29 vs. 0.47; P = .159) and tibiofemoral BMLs (–0.59 vs. –0.21; P = .087) were also not significantly different, but patients randomized to vitamin D supplementation had fewer increases in BMLs (17% vs. 27%; P = .03).
There was no concern over the safety of vitamin D supplementation, although more general side effects were noted in the vitamin D vs. the placebo group.
Commenting on the strengths and weaknesses of the study, Mr. Jin noted it was a large, multicenter, randomized, double-blind, placebo-controlled trial with a reasonably long follow-up. The patient group studied has good generalizability to those seen in everyday practice, he suggested, noting that the main limitation was the number of patients lost to follow-up because of noncompliance: 21 patients in the vitamin D group vs. 8 patients in the placebo group.
ROME – Vitamin D supplementation did not ease osteoarthritic knee pain measured using the Western Ontario and McMaster Universities Osteoarthritis Index in a 2-year, randomized, double-blind, placebo-controlled trial.
Results of the VIDEO (Vitamin D Effect on Osteoarthritis) study in patients with symptomatic knee osteoarthritis (OA) and low vitamin D levels also showed that replenishing vitamin D also had no effect on the loss of cartilage volume, although there might be a marginal benefit on bone marrow lesions (BMLs) and pain assessed using a visual analog scale (VAS).
“Vitamin D at 50,000 IU/month over 2 years did not meet the primary endpoint in this randomized, controlled trial,” said Jason Jin, a Ph.D. candidate at the Menzies Research Institute, University of Tasmania in Hobart, Australia, who presented the VIDEO study findings at the European Congress of Rheumatology.
He cited a recent commentary published in the Journal of the American Medical Association (JAMA 2015;313:1311-12) that looked at vitamin D research and clinical practice in which the authors said that “clinical enthusiasm for supplemental vitamin D has outpaced available evidence.” This seems to be true considering the results of this and other previous randomized trials, Mr. Jin observed.
“The background of this study is that, in the last decade, vitamin D has become a hot topic in osteoarthritis research and epidemiologic studies have found that vitamin D deficiency is very common in knee osteoarthritis patients,” he said. Low levels of vitamin D have been linked to increased knee pain, radiographic progression, and increased cartilage loss in OA.
Two prior randomized, controlled trials provided conflicting evidence, he highlighted, with one study showing that supplementation of 2,000 IU/day of vitamin D for 2 years had no effect on symptoms or knee structure (JAMA 2013;309:155-62) while another showed that a monthly dose of 60,000 IU for 1 year may be beneficial in terms of relieving pain and functional outcomes but longer follow-up was required (Clin. Orthop. Relat. Res. 2013;471:3556-62).
The VIDEO study was therefore designed to try to resolve some of the controversy and look at a larger group of patients for a longer period of time. The study’s hypothesis was that vitamin D might ease knee pain and perhaps have effect structural changes in patients with symptomatic knee OA who had low vitamin D levels. A low vitamin D level was defined as a serum measurement of 25(OH)D of 12.5-60 nmol/L (5-24 ng/mL) at baseline.
Of almost 600 patients screened, 413 were randomized, with 209 randomized to the oral vitamin D supplementation group and 204 to the matched placebo arm. Patients in each group had comparable characteristics at baseline, with a mean age of around 62 to 63 years. Half the patients were female. Baseline serum vitamin D levels were about 43 nmol/L (17.2 ng/mL). Virtually all (96%) of patients had radiographic evidence of knee OA, 97% had cartilage defects, and 80% had bone marrow lesions.
While serum levels of 25(OH)D were successfully increased in the supplemented patients over the course of the study, this did not translate into an improvement in the coprimary endpoint of a change in Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) knee pain over 24 months. The difference in WOMAC pain between the vitamin D and placebo groups was a nonsignifcant –14.8 (–49.9 vs. –35.1; P = .102). Vitamin D–supplemented patients did, however, report marginally less VAS pain (–14.8 vs. –9.4; P = .038).
Total tibial cartilage volume loss, the second coprimary endpoint, was not significantly different between the vitamin D and placebo groups, at around 121 and 150 mm3 per annum, with 2-year changes of –3.44% vs. –4.23% per annum (P = .132). The secondary endpoints of changes in tibiofemoral cartilage defects (0.29 vs. 0.47; P = .159) and tibiofemoral BMLs (–0.59 vs. –0.21; P = .087) were also not significantly different, but patients randomized to vitamin D supplementation had fewer increases in BMLs (17% vs. 27%; P = .03).
There was no concern over the safety of vitamin D supplementation, although more general side effects were noted in the vitamin D vs. the placebo group.
Commenting on the strengths and weaknesses of the study, Mr. Jin noted it was a large, multicenter, randomized, double-blind, placebo-controlled trial with a reasonably long follow-up. The patient group studied has good generalizability to those seen in everyday practice, he suggested, noting that the main limitation was the number of patients lost to follow-up because of noncompliance: 21 patients in the vitamin D group vs. 8 patients in the placebo group.
AT THE EULAR 2015 CONGRESS
Key clinical point: There appears to be no benefit of supplementing vitamin D to ease pain in symptomatic patients with knee osteoarthritis (OA) and low vitamin D levels.
Major finding: The difference in WOMAC pain between the vitamin D and placebo groups was a nonsignificant –14.8 (–49.9 vs. –35.1; P = .102).
Data source: A 2-year, multicenter, double-blind, placebo-controlled trial of 413 randomized patients with symptomatic knee OA and low vitamin D levels.
Disclosures: Mr. Jin reported having no conflicts of interest to disclose.
Joint distraction could preempt knee replacement for OA
ROME – Knee joint distraction – a method of relieving mechanical stress on the joint by temporarily pinning it – could help some patients with osteoarthritis avoid the need for a knee prosthesis, judging from preliminary findings from a randomized, controlled, comparative trial.
At 1-year follow-up, all subscales of the Knee Injury and Osteoarthritis Outcome Score (KOOS) and the Total KOOS score were significantly and progressively improved from baseline in patients who underwent knee distraction (P < .001). Overall the mean change in the Total KOOS score was not significantly different from that in the group of patients who underwent total knee replacement (TKR); although the KOOS subscale of quality of life did show greater improvement with the prosthesis than with distraction (P = .027), it was felt that this will “level out” when data on all 60 patients included in the trial are available. This research, performed at the UMC [University Medical Center] Utrecht and Sint Maartenskliniek in Woerden in the Netherlands, highlights how knee distraction may offer a valuable alternative to TKR, particularly in younger patients with OA, according to Simon Mastbergen, Ph.D., who studies tissue degeneration and regeneration in the department of rheumatology and clinical immunology at UMC Utrecht, and associates (Ann. Rheum. Dis. 2015;74:359-60).
“When you have a total knee prosthesis at a relatively young age, the outcome is not as successful as most people think,” Dr. Mastbergen said in an interview during a poster session at the European Congress of Rheumatology. Around 40% of TKRs are performed in people under the age of 65 years, he observed, and younger patients have a higher risk of revision failure because of mechanical failure as they tend to be more active than elderly patients with knee OA. Indeed, it’s been estimated that around 44% of younger patients who have TKR will need revision surgery at some point, and as secondary procedures are more difficult to perform and can be much more disabling “we need a joint-saving treatment.” Joint distraction is a surgical procedure that aims to gradually separate the two bony ends of a joint for a certain length of time. The method used by the Dutch team involved patients wearing an external frame bridging the knee that consisted of two long tubes with coiled springs inside with pins coming out that are inserted into the opposing soft tissue and bones and moved by about 5 mm each time. Patients wear the frame for 6-8 weeks and are encouraged to try to bear weight on the affected knee, with the aid of crutches if needed. The idea behind the method is that it will allow the joint to repair itself, and the team has already shown that cartilaginous tissue repair does indeed seem to occur (Cartilage 2013;21:1660-7).
Dr. Mastbergen noted that patients who underwent knee joint distraction in the study directly comparing it to TKR exhibited significant widening in the joint space, which is good because it indicates that cartilage has been regained. “We feel that knee joint distraction is an alternative for those [patients] who are ready for total knee prosthesis but are actually too young for [it],” he said.
Other randomized controlled trial data from the team was presented during an oral abstract session at the meeting (Ann. Rheum. Dis. 2015;74:108) and showed that knee joint distraction is also as good as high tibial osteotomy, which is another method aimed at relieving mechanical stress on the knee joint. The senior author of the team Floris Lafeber, Ph.D., who presented data on behalf of colleague Dr. Jan Ton van der Woude, noted that there were several similarities between the two procedures in that they were both joint saving and could potentially postpone TKR and had been shown to improve bone turnover and cartilaginous tissue repair.
To compare the two methods, the researchers studied almost 70 patients aged 65 years or younger with medial compartment knee OA who were indicated for high tibial osteotomy. Patients were randomized 2:1 to the two procedures, with 45 undergoing osteotomy and 22 knee joint distraction. Significant improvements in total Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), visual analog pain, and quality of life (EQ-5D) scores were seen in both groups when compared with the preoperative values (P < .05). None of the parameters showed any statistically significant difference between the two procedures at 1-year follow-up. The data led to the conclusion that knee joint distraction had a clinical benefit that was comparable to osteotomy.
However, both the minimum and mean joint space width showed a steeper increase in patients randomized to the knee joint distraction group, suggesting that cartilaginous tissue repair might be better with the latter method.
The potential clinical benefit of knee joint distraction was further highlighted in another poster from the team, presented by Dr. Natalia Kuchuk, which showed the effects of the procedure were maintained at 5-year follow-up. Importantly, 80% of the 20 patients studied in this open study still had their own knee joint. The mean age of patients at the time of distraction was 48.5 years. “In young patients, knee joint distraction effectively postpones total knee arthroplasty and is the only treatment which allows regeneration of cartilage,” she said in an interview.
Dr. Lafeber also commented in an interview on the practicalities of the procedure, which is still in its experimental phases. “It’s a rather an invasive procedure but if you compare it to a total knee replacement or high tibial osteotomy it’s less invasive,” he said.
“The surgical procedure takes about half an hour, we place a few pins through soft tissue and bone and the distraction tubes are placed mediolaterally to these pins, so in fact it’s less invasive than many of the other surgical techniques.” The distraction itself is not painful, he added, and actually alleviates OA pain but patients may need painkillers and perhaps antibiotics for short periods during the method.Next steps for the team are to follow up patients in the randomized trials for a longer period of time and refine the distraction device. “This is an off-the-shelf, ‘proof-of-concept’ device, and we are now developing a more patient-friendly, smaller, lighter frame device which is also easier to place by orthopedic surgeons,” Dr. Lafeber said. “Then we will do a comparison with the proof-of-concept device.”
Reumafonds (the Dutch Arthritis Foundation), ZonMw (The Netherlands Organization for Health Research and Development), UMC Utrecht, and Sint Maartinskliniek funded the research. Dr. Mastbergen, Dr. Lafeber, and Dr. Kuchuk had no disclosures to report.
ROME – Knee joint distraction – a method of relieving mechanical stress on the joint by temporarily pinning it – could help some patients with osteoarthritis avoid the need for a knee prosthesis, judging from preliminary findings from a randomized, controlled, comparative trial.
At 1-year follow-up, all subscales of the Knee Injury and Osteoarthritis Outcome Score (KOOS) and the Total KOOS score were significantly and progressively improved from baseline in patients who underwent knee distraction (P < .001). Overall the mean change in the Total KOOS score was not significantly different from that in the group of patients who underwent total knee replacement (TKR); although the KOOS subscale of quality of life did show greater improvement with the prosthesis than with distraction (P = .027), it was felt that this will “level out” when data on all 60 patients included in the trial are available. This research, performed at the UMC [University Medical Center] Utrecht and Sint Maartenskliniek in Woerden in the Netherlands, highlights how knee distraction may offer a valuable alternative to TKR, particularly in younger patients with OA, according to Simon Mastbergen, Ph.D., who studies tissue degeneration and regeneration in the department of rheumatology and clinical immunology at UMC Utrecht, and associates (Ann. Rheum. Dis. 2015;74:359-60).
“When you have a total knee prosthesis at a relatively young age, the outcome is not as successful as most people think,” Dr. Mastbergen said in an interview during a poster session at the European Congress of Rheumatology. Around 40% of TKRs are performed in people under the age of 65 years, he observed, and younger patients have a higher risk of revision failure because of mechanical failure as they tend to be more active than elderly patients with knee OA. Indeed, it’s been estimated that around 44% of younger patients who have TKR will need revision surgery at some point, and as secondary procedures are more difficult to perform and can be much more disabling “we need a joint-saving treatment.” Joint distraction is a surgical procedure that aims to gradually separate the two bony ends of a joint for a certain length of time. The method used by the Dutch team involved patients wearing an external frame bridging the knee that consisted of two long tubes with coiled springs inside with pins coming out that are inserted into the opposing soft tissue and bones and moved by about 5 mm each time. Patients wear the frame for 6-8 weeks and are encouraged to try to bear weight on the affected knee, with the aid of crutches if needed. The idea behind the method is that it will allow the joint to repair itself, and the team has already shown that cartilaginous tissue repair does indeed seem to occur (Cartilage 2013;21:1660-7).
Dr. Mastbergen noted that patients who underwent knee joint distraction in the study directly comparing it to TKR exhibited significant widening in the joint space, which is good because it indicates that cartilage has been regained. “We feel that knee joint distraction is an alternative for those [patients] who are ready for total knee prosthesis but are actually too young for [it],” he said.
Other randomized controlled trial data from the team was presented during an oral abstract session at the meeting (Ann. Rheum. Dis. 2015;74:108) and showed that knee joint distraction is also as good as high tibial osteotomy, which is another method aimed at relieving mechanical stress on the knee joint. The senior author of the team Floris Lafeber, Ph.D., who presented data on behalf of colleague Dr. Jan Ton van der Woude, noted that there were several similarities between the two procedures in that they were both joint saving and could potentially postpone TKR and had been shown to improve bone turnover and cartilaginous tissue repair.
To compare the two methods, the researchers studied almost 70 patients aged 65 years or younger with medial compartment knee OA who were indicated for high tibial osteotomy. Patients were randomized 2:1 to the two procedures, with 45 undergoing osteotomy and 22 knee joint distraction. Significant improvements in total Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), visual analog pain, and quality of life (EQ-5D) scores were seen in both groups when compared with the preoperative values (P < .05). None of the parameters showed any statistically significant difference between the two procedures at 1-year follow-up. The data led to the conclusion that knee joint distraction had a clinical benefit that was comparable to osteotomy.
However, both the minimum and mean joint space width showed a steeper increase in patients randomized to the knee joint distraction group, suggesting that cartilaginous tissue repair might be better with the latter method.
The potential clinical benefit of knee joint distraction was further highlighted in another poster from the team, presented by Dr. Natalia Kuchuk, which showed the effects of the procedure were maintained at 5-year follow-up. Importantly, 80% of the 20 patients studied in this open study still had their own knee joint. The mean age of patients at the time of distraction was 48.5 years. “In young patients, knee joint distraction effectively postpones total knee arthroplasty and is the only treatment which allows regeneration of cartilage,” she said in an interview.
Dr. Lafeber also commented in an interview on the practicalities of the procedure, which is still in its experimental phases. “It’s a rather an invasive procedure but if you compare it to a total knee replacement or high tibial osteotomy it’s less invasive,” he said.
“The surgical procedure takes about half an hour, we place a few pins through soft tissue and bone and the distraction tubes are placed mediolaterally to these pins, so in fact it’s less invasive than many of the other surgical techniques.” The distraction itself is not painful, he added, and actually alleviates OA pain but patients may need painkillers and perhaps antibiotics for short periods during the method.Next steps for the team are to follow up patients in the randomized trials for a longer period of time and refine the distraction device. “This is an off-the-shelf, ‘proof-of-concept’ device, and we are now developing a more patient-friendly, smaller, lighter frame device which is also easier to place by orthopedic surgeons,” Dr. Lafeber said. “Then we will do a comparison with the proof-of-concept device.”
Reumafonds (the Dutch Arthritis Foundation), ZonMw (The Netherlands Organization for Health Research and Development), UMC Utrecht, and Sint Maartinskliniek funded the research. Dr. Mastbergen, Dr. Lafeber, and Dr. Kuchuk had no disclosures to report.
ROME – Knee joint distraction – a method of relieving mechanical stress on the joint by temporarily pinning it – could help some patients with osteoarthritis avoid the need for a knee prosthesis, judging from preliminary findings from a randomized, controlled, comparative trial.
At 1-year follow-up, all subscales of the Knee Injury and Osteoarthritis Outcome Score (KOOS) and the Total KOOS score were significantly and progressively improved from baseline in patients who underwent knee distraction (P < .001). Overall the mean change in the Total KOOS score was not significantly different from that in the group of patients who underwent total knee replacement (TKR); although the KOOS subscale of quality of life did show greater improvement with the prosthesis than with distraction (P = .027), it was felt that this will “level out” when data on all 60 patients included in the trial are available. This research, performed at the UMC [University Medical Center] Utrecht and Sint Maartenskliniek in Woerden in the Netherlands, highlights how knee distraction may offer a valuable alternative to TKR, particularly in younger patients with OA, according to Simon Mastbergen, Ph.D., who studies tissue degeneration and regeneration in the department of rheumatology and clinical immunology at UMC Utrecht, and associates (Ann. Rheum. Dis. 2015;74:359-60).
“When you have a total knee prosthesis at a relatively young age, the outcome is not as successful as most people think,” Dr. Mastbergen said in an interview during a poster session at the European Congress of Rheumatology. Around 40% of TKRs are performed in people under the age of 65 years, he observed, and younger patients have a higher risk of revision failure because of mechanical failure as they tend to be more active than elderly patients with knee OA. Indeed, it’s been estimated that around 44% of younger patients who have TKR will need revision surgery at some point, and as secondary procedures are more difficult to perform and can be much more disabling “we need a joint-saving treatment.” Joint distraction is a surgical procedure that aims to gradually separate the two bony ends of a joint for a certain length of time. The method used by the Dutch team involved patients wearing an external frame bridging the knee that consisted of two long tubes with coiled springs inside with pins coming out that are inserted into the opposing soft tissue and bones and moved by about 5 mm each time. Patients wear the frame for 6-8 weeks and are encouraged to try to bear weight on the affected knee, with the aid of crutches if needed. The idea behind the method is that it will allow the joint to repair itself, and the team has already shown that cartilaginous tissue repair does indeed seem to occur (Cartilage 2013;21:1660-7).
Dr. Mastbergen noted that patients who underwent knee joint distraction in the study directly comparing it to TKR exhibited significant widening in the joint space, which is good because it indicates that cartilage has been regained. “We feel that knee joint distraction is an alternative for those [patients] who are ready for total knee prosthesis but are actually too young for [it],” he said.
Other randomized controlled trial data from the team was presented during an oral abstract session at the meeting (Ann. Rheum. Dis. 2015;74:108) and showed that knee joint distraction is also as good as high tibial osteotomy, which is another method aimed at relieving mechanical stress on the knee joint. The senior author of the team Floris Lafeber, Ph.D., who presented data on behalf of colleague Dr. Jan Ton van der Woude, noted that there were several similarities between the two procedures in that they were both joint saving and could potentially postpone TKR and had been shown to improve bone turnover and cartilaginous tissue repair.
To compare the two methods, the researchers studied almost 70 patients aged 65 years or younger with medial compartment knee OA who were indicated for high tibial osteotomy. Patients were randomized 2:1 to the two procedures, with 45 undergoing osteotomy and 22 knee joint distraction. Significant improvements in total Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), visual analog pain, and quality of life (EQ-5D) scores were seen in both groups when compared with the preoperative values (P < .05). None of the parameters showed any statistically significant difference between the two procedures at 1-year follow-up. The data led to the conclusion that knee joint distraction had a clinical benefit that was comparable to osteotomy.
However, both the minimum and mean joint space width showed a steeper increase in patients randomized to the knee joint distraction group, suggesting that cartilaginous tissue repair might be better with the latter method.
The potential clinical benefit of knee joint distraction was further highlighted in another poster from the team, presented by Dr. Natalia Kuchuk, which showed the effects of the procedure were maintained at 5-year follow-up. Importantly, 80% of the 20 patients studied in this open study still had their own knee joint. The mean age of patients at the time of distraction was 48.5 years. “In young patients, knee joint distraction effectively postpones total knee arthroplasty and is the only treatment which allows regeneration of cartilage,” she said in an interview.
Dr. Lafeber also commented in an interview on the practicalities of the procedure, which is still in its experimental phases. “It’s a rather an invasive procedure but if you compare it to a total knee replacement or high tibial osteotomy it’s less invasive,” he said.
“The surgical procedure takes about half an hour, we place a few pins through soft tissue and bone and the distraction tubes are placed mediolaterally to these pins, so in fact it’s less invasive than many of the other surgical techniques.” The distraction itself is not painful, he added, and actually alleviates OA pain but patients may need painkillers and perhaps antibiotics for short periods during the method.Next steps for the team are to follow up patients in the randomized trials for a longer period of time and refine the distraction device. “This is an off-the-shelf, ‘proof-of-concept’ device, and we are now developing a more patient-friendly, smaller, lighter frame device which is also easier to place by orthopedic surgeons,” Dr. Lafeber said. “Then we will do a comparison with the proof-of-concept device.”
Reumafonds (the Dutch Arthritis Foundation), ZonMw (The Netherlands Organization for Health Research and Development), UMC Utrecht, and Sint Maartinskliniek funded the research. Dr. Mastbergen, Dr. Lafeber, and Dr. Kuchuk had no disclosures to report.
AT THE EULAR 2015 CONGRESS
Key clinical point: Knee joint distraction could postpone the need for total knee replacement (TKR) in patients < 65 years and is the only treatment that allows regeneration of cartilage
Major finding: Total mean change in the Knee injury and Osteoarthritis Outcome Score (KOOS) at 1 year was 38 for knee joint distraction and 27 for TKR (P = NS).
Data source: Randomized controlled trial comparing knee joint distraction to total knee prosthesis in 60 patients with severe knee OA under 60 years of age.
Disclosures: Reumafonds (the Dutch Arthritis Foundation), ZonMw (The Netherlands Organization for Health Research and Development), UMC Utrect, and Sint Maartinskliniek funded the research. Dr. Mastbergen, Dr. Lafeber, and Dr. Kuchuk had no disclosures to report.
Harnessing the placebo effect in management of osteoarthritis
SEATTLE – When it comes to managing osteoarthritis, clinicians can use their interactions with patients to tap into a powerful placebo effect, according to Dr. Paul Dieppe, a professor of health and well-being at the University of Exeter, England.
“I am particularly excited to have the opportunity to talk to you about a phenomenology that I think is amongst the most important within medicine and an area that those of us interested in osteoarthritis could really exploit,” he said at the World Congress on Osteoarthritis. “We don’t have a treatment that’s better than placebo, so let’s use placebo.”
In the clinical trial context, the placebo effect – the response seen from giving a sham or dummy treatment, or in essence, doing nothing – has an effect size of about 0.5 for alleviating pain and stiffness from osteoarthritis (Ann. Rheum. Dis. 2008;67:1716-23). “That’s an effect size which is quite a lot bigger than the effect size of most of the standard interventions that we use, be they drug therapy, physical therapy, whatever. It’s not as big as joint replacement, although there we don’t have the appropriate data. But it is bigger than pretty much everything else. So ‘nothing’ is efficacious,” Dr. Dieppe commented.
On the other hand, effectiveness in the real-world setting is unknown and would require large pragmatic trials or Big Data analyses using registries. “But I think the effectiveness of ‘nothing’ is much, much greater than its efficacy in the very artificial circumstance of a clinical trial,” he said, a viewpoint based on his experience both as a clinician and as a patient with knee osteoarthritis.
“I prefer to call [the placebo effect] a healing response, and I’m not trying to be provocative using that term because I think we do have innate healing abilities in our bodies. I think that’s an evolutionary demand, and good interactions can activate that,” Dr. Dieppe maintained.
Compelling evidence suggests that healing does indeed work (Explore [NY] 2015;11:11-23). “We think that it’s mediated by focused attention with good intention of sensitive people,” he said. “Maybe that’s what a lot of you as therapists are actually doing. Maybe that is the basis of much of what we call the placebo effect.”
Clinicians should also be aware of the nocebo effect, what Dr. Dieppe referred to as the placebo effect’s evil twin, as it can negatively influence outcomes and is stronger (Am. J. Med. 2015;128:126-9). “The fact is that doing nothing ... can and often does make our patients much worse. This is most likely to occur when one or both people in a consultation are feeling unsafe or anxious. ... A lot of what we do in modern health care seems designed to make people anxious and to make them worse,” he elaborated at the meeting, which was sponsored by the Osteoarthritis Research Society International.
Many of the leading theories about the placebo and nocebo effects postulate that they relate to factors such as expectations or the release or blockage of natural endorphins. “These theories are basically saying that this is all about what’s going on in the brain of the patient,” Dr. Dieppe commented. “I think that’s wrong. ... It’s missing the point, completely, because the point is that this is about the quality of interactions between individuals. We are social beings, we are evolved as social beings, and our social interactions control a lot of what happens to us, not only psychologically but physiologically.”
He pointed to theories that instead focus on interactions, such as one pertaining to the concept of validation and invalidation (J. Clin. Psychol. 2006;62:459-80). “This theory goes beyond empathy and compassion, which are the usual sort of things evoked in this context, because you can be empathic and compassionate as much as you like, but if the patient in front of you doesn’t know you are being empathic or compassionate, then it’s no use at all. So validation, invalidation is more about have you successfully communicated that empathy and compassion to the other person or not. If you have, the person feels validated, they feel you genuinely do understand them, and you do genuinely care about them. If they are invalidated, they feel you haven’t understood them, and you don’t really care.” He added, “It depends very much on your behavior, as much as on what you say. Communication specialists tell us that 80% of communication to people is nonverbal.”
Another relevant theory here is the polyvagal theory of social interaction, which proposes that in addition to being hardwired for a fight or flight response, the autonomic nervous system is hardwired for a nurturing response (Cleve. Clin. J. Med. 2009;76 Suppl 2:S86-S90). Activation of this response has a calming physiologic effect and influences how messages are heard. “This nurturing response … is linked to communication strategies, so that you have to feel safe to be able to communicate well with another person,” Dr. Dieppe noted.
Taken together, these theories on interactions help explain “how we can make people better, how we can make people worse with ‘nothing,’ ” he maintained. “Of course, it’s not nothing – it’s the totality of our behavior with another person, and it’s crucial. And it can, in extreme cases, positively activate the innate healing response, or it can, as we often do sadly in clinical practice, activate an invalidation, fight-or-flight response, and make everything a lot worse.”
“There are colossal implications about how we behave when we are with patients,” Dr. Dieppe concluded. “I think basically, it’s just about our ability to be present for another human being in a nonjudgmental way. And that’s difficult, but that’s what we need to be able to do.”
SEATTLE – When it comes to managing osteoarthritis, clinicians can use their interactions with patients to tap into a powerful placebo effect, according to Dr. Paul Dieppe, a professor of health and well-being at the University of Exeter, England.
“I am particularly excited to have the opportunity to talk to you about a phenomenology that I think is amongst the most important within medicine and an area that those of us interested in osteoarthritis could really exploit,” he said at the World Congress on Osteoarthritis. “We don’t have a treatment that’s better than placebo, so let’s use placebo.”
In the clinical trial context, the placebo effect – the response seen from giving a sham or dummy treatment, or in essence, doing nothing – has an effect size of about 0.5 for alleviating pain and stiffness from osteoarthritis (Ann. Rheum. Dis. 2008;67:1716-23). “That’s an effect size which is quite a lot bigger than the effect size of most of the standard interventions that we use, be they drug therapy, physical therapy, whatever. It’s not as big as joint replacement, although there we don’t have the appropriate data. But it is bigger than pretty much everything else. So ‘nothing’ is efficacious,” Dr. Dieppe commented.
On the other hand, effectiveness in the real-world setting is unknown and would require large pragmatic trials or Big Data analyses using registries. “But I think the effectiveness of ‘nothing’ is much, much greater than its efficacy in the very artificial circumstance of a clinical trial,” he said, a viewpoint based on his experience both as a clinician and as a patient with knee osteoarthritis.
“I prefer to call [the placebo effect] a healing response, and I’m not trying to be provocative using that term because I think we do have innate healing abilities in our bodies. I think that’s an evolutionary demand, and good interactions can activate that,” Dr. Dieppe maintained.
Compelling evidence suggests that healing does indeed work (Explore [NY] 2015;11:11-23). “We think that it’s mediated by focused attention with good intention of sensitive people,” he said. “Maybe that’s what a lot of you as therapists are actually doing. Maybe that is the basis of much of what we call the placebo effect.”
Clinicians should also be aware of the nocebo effect, what Dr. Dieppe referred to as the placebo effect’s evil twin, as it can negatively influence outcomes and is stronger (Am. J. Med. 2015;128:126-9). “The fact is that doing nothing ... can and often does make our patients much worse. This is most likely to occur when one or both people in a consultation are feeling unsafe or anxious. ... A lot of what we do in modern health care seems designed to make people anxious and to make them worse,” he elaborated at the meeting, which was sponsored by the Osteoarthritis Research Society International.
Many of the leading theories about the placebo and nocebo effects postulate that they relate to factors such as expectations or the release or blockage of natural endorphins. “These theories are basically saying that this is all about what’s going on in the brain of the patient,” Dr. Dieppe commented. “I think that’s wrong. ... It’s missing the point, completely, because the point is that this is about the quality of interactions between individuals. We are social beings, we are evolved as social beings, and our social interactions control a lot of what happens to us, not only psychologically but physiologically.”
He pointed to theories that instead focus on interactions, such as one pertaining to the concept of validation and invalidation (J. Clin. Psychol. 2006;62:459-80). “This theory goes beyond empathy and compassion, which are the usual sort of things evoked in this context, because you can be empathic and compassionate as much as you like, but if the patient in front of you doesn’t know you are being empathic or compassionate, then it’s no use at all. So validation, invalidation is more about have you successfully communicated that empathy and compassion to the other person or not. If you have, the person feels validated, they feel you genuinely do understand them, and you do genuinely care about them. If they are invalidated, they feel you haven’t understood them, and you don’t really care.” He added, “It depends very much on your behavior, as much as on what you say. Communication specialists tell us that 80% of communication to people is nonverbal.”
Another relevant theory here is the polyvagal theory of social interaction, which proposes that in addition to being hardwired for a fight or flight response, the autonomic nervous system is hardwired for a nurturing response (Cleve. Clin. J. Med. 2009;76 Suppl 2:S86-S90). Activation of this response has a calming physiologic effect and influences how messages are heard. “This nurturing response … is linked to communication strategies, so that you have to feel safe to be able to communicate well with another person,” Dr. Dieppe noted.
Taken together, these theories on interactions help explain “how we can make people better, how we can make people worse with ‘nothing,’ ” he maintained. “Of course, it’s not nothing – it’s the totality of our behavior with another person, and it’s crucial. And it can, in extreme cases, positively activate the innate healing response, or it can, as we often do sadly in clinical practice, activate an invalidation, fight-or-flight response, and make everything a lot worse.”
“There are colossal implications about how we behave when we are with patients,” Dr. Dieppe concluded. “I think basically, it’s just about our ability to be present for another human being in a nonjudgmental way. And that’s difficult, but that’s what we need to be able to do.”
SEATTLE – When it comes to managing osteoarthritis, clinicians can use their interactions with patients to tap into a powerful placebo effect, according to Dr. Paul Dieppe, a professor of health and well-being at the University of Exeter, England.
“I am particularly excited to have the opportunity to talk to you about a phenomenology that I think is amongst the most important within medicine and an area that those of us interested in osteoarthritis could really exploit,” he said at the World Congress on Osteoarthritis. “We don’t have a treatment that’s better than placebo, so let’s use placebo.”
In the clinical trial context, the placebo effect – the response seen from giving a sham or dummy treatment, or in essence, doing nothing – has an effect size of about 0.5 for alleviating pain and stiffness from osteoarthritis (Ann. Rheum. Dis. 2008;67:1716-23). “That’s an effect size which is quite a lot bigger than the effect size of most of the standard interventions that we use, be they drug therapy, physical therapy, whatever. It’s not as big as joint replacement, although there we don’t have the appropriate data. But it is bigger than pretty much everything else. So ‘nothing’ is efficacious,” Dr. Dieppe commented.
On the other hand, effectiveness in the real-world setting is unknown and would require large pragmatic trials or Big Data analyses using registries. “But I think the effectiveness of ‘nothing’ is much, much greater than its efficacy in the very artificial circumstance of a clinical trial,” he said, a viewpoint based on his experience both as a clinician and as a patient with knee osteoarthritis.
“I prefer to call [the placebo effect] a healing response, and I’m not trying to be provocative using that term because I think we do have innate healing abilities in our bodies. I think that’s an evolutionary demand, and good interactions can activate that,” Dr. Dieppe maintained.
Compelling evidence suggests that healing does indeed work (Explore [NY] 2015;11:11-23). “We think that it’s mediated by focused attention with good intention of sensitive people,” he said. “Maybe that’s what a lot of you as therapists are actually doing. Maybe that is the basis of much of what we call the placebo effect.”
Clinicians should also be aware of the nocebo effect, what Dr. Dieppe referred to as the placebo effect’s evil twin, as it can negatively influence outcomes and is stronger (Am. J. Med. 2015;128:126-9). “The fact is that doing nothing ... can and often does make our patients much worse. This is most likely to occur when one or both people in a consultation are feeling unsafe or anxious. ... A lot of what we do in modern health care seems designed to make people anxious and to make them worse,” he elaborated at the meeting, which was sponsored by the Osteoarthritis Research Society International.
Many of the leading theories about the placebo and nocebo effects postulate that they relate to factors such as expectations or the release or blockage of natural endorphins. “These theories are basically saying that this is all about what’s going on in the brain of the patient,” Dr. Dieppe commented. “I think that’s wrong. ... It’s missing the point, completely, because the point is that this is about the quality of interactions between individuals. We are social beings, we are evolved as social beings, and our social interactions control a lot of what happens to us, not only psychologically but physiologically.”
He pointed to theories that instead focus on interactions, such as one pertaining to the concept of validation and invalidation (J. Clin. Psychol. 2006;62:459-80). “This theory goes beyond empathy and compassion, which are the usual sort of things evoked in this context, because you can be empathic and compassionate as much as you like, but if the patient in front of you doesn’t know you are being empathic or compassionate, then it’s no use at all. So validation, invalidation is more about have you successfully communicated that empathy and compassion to the other person or not. If you have, the person feels validated, they feel you genuinely do understand them, and you do genuinely care about them. If they are invalidated, they feel you haven’t understood them, and you don’t really care.” He added, “It depends very much on your behavior, as much as on what you say. Communication specialists tell us that 80% of communication to people is nonverbal.”
Another relevant theory here is the polyvagal theory of social interaction, which proposes that in addition to being hardwired for a fight or flight response, the autonomic nervous system is hardwired for a nurturing response (Cleve. Clin. J. Med. 2009;76 Suppl 2:S86-S90). Activation of this response has a calming physiologic effect and influences how messages are heard. “This nurturing response … is linked to communication strategies, so that you have to feel safe to be able to communicate well with another person,” Dr. Dieppe noted.
Taken together, these theories on interactions help explain “how we can make people better, how we can make people worse with ‘nothing,’ ” he maintained. “Of course, it’s not nothing – it’s the totality of our behavior with another person, and it’s crucial. And it can, in extreme cases, positively activate the innate healing response, or it can, as we often do sadly in clinical practice, activate an invalidation, fight-or-flight response, and make everything a lot worse.”
“There are colossal implications about how we behave when we are with patients,” Dr. Dieppe concluded. “I think basically, it’s just about our ability to be present for another human being in a nonjudgmental way. And that’s difficult, but that’s what we need to be able to do.”
AT OARSI 2015
Arthroscopic knee surgery offers no lasting pain benefit
Arthroscopic knee surgery in middle-aged or older patients with knee pain is associated with greater harm than good, according to a meta-analysis.
The analysis of nine randomized, controlled trials in 1,270 patients of arthroscopic surgery involving partial meniscectomy, debridement, or both showed a small but statistically significant benefit from the procedure – comparable to the pain-relieving effects of paracetamol – but which falls below significance after 12 months.
However, there were no significant improvements in knee function, and there were significant increases in the risk of deep vein thrombosis (4.13 events per 1,000 procedures) as well as infection, pulmonary embolism, and death, according to the paper published online June 16 in BMJ.
“Thus, middle-aged patients with knee pain and meniscal tears should be considered as having early-stage osteoarthritis and be treated according to clinical guidelines for knee osteoarthritis, starting with information, exercise, and often weight loss,” wrote Dr. Jonas B. Thorlund of the University of Southern Denmark, Odense, and coauthors (BMJ 2015, June 16 [doi:10.1136/bmj.h2747]).
The study was supported by the Swedish Research Council. One author declared personal fees from several pharmaceutical and medical companies and relevant journal editorship, while another declared fees from lectureships and books.
While randomized trials, uncontrolled observational studies, and surgeons’ own observations suggest that patients improve after arthroscopy, robust and bias-free trials that use placebo controls show that active treatment works no better than control treatment.
We may be close to a tipping point where the weight of evidence against arthroscopic knee surgery for pain is enough to overcome concerns about the quality of the studies, confirmation bias, and vested interests. When that point is reached, we should anticipate a swift reversal of established practice.
Dr. Andy Carr is from the Oxford University Institute of Musculoskeletal Sciences at the NIHR Oxford Musculoskeletal Biomedical Research Unit, Oxford, England. These comments are taken from an accompanying editorial (BMJ 2015, June 16 [doi:10.1136/bmj.h2983]). He declared research grants from NIHR and Arthritis Research UK.
While randomized trials, uncontrolled observational studies, and surgeons’ own observations suggest that patients improve after arthroscopy, robust and bias-free trials that use placebo controls show that active treatment works no better than control treatment.
We may be close to a tipping point where the weight of evidence against arthroscopic knee surgery for pain is enough to overcome concerns about the quality of the studies, confirmation bias, and vested interests. When that point is reached, we should anticipate a swift reversal of established practice.
Dr. Andy Carr is from the Oxford University Institute of Musculoskeletal Sciences at the NIHR Oxford Musculoskeletal Biomedical Research Unit, Oxford, England. These comments are taken from an accompanying editorial (BMJ 2015, June 16 [doi:10.1136/bmj.h2983]). He declared research grants from NIHR and Arthritis Research UK.
While randomized trials, uncontrolled observational studies, and surgeons’ own observations suggest that patients improve after arthroscopy, robust and bias-free trials that use placebo controls show that active treatment works no better than control treatment.
We may be close to a tipping point where the weight of evidence against arthroscopic knee surgery for pain is enough to overcome concerns about the quality of the studies, confirmation bias, and vested interests. When that point is reached, we should anticipate a swift reversal of established practice.
Dr. Andy Carr is from the Oxford University Institute of Musculoskeletal Sciences at the NIHR Oxford Musculoskeletal Biomedical Research Unit, Oxford, England. These comments are taken from an accompanying editorial (BMJ 2015, June 16 [doi:10.1136/bmj.h2983]). He declared research grants from NIHR and Arthritis Research UK.
Arthroscopic knee surgery in middle-aged or older patients with knee pain is associated with greater harm than good, according to a meta-analysis.
The analysis of nine randomized, controlled trials in 1,270 patients of arthroscopic surgery involving partial meniscectomy, debridement, or both showed a small but statistically significant benefit from the procedure – comparable to the pain-relieving effects of paracetamol – but which falls below significance after 12 months.
However, there were no significant improvements in knee function, and there were significant increases in the risk of deep vein thrombosis (4.13 events per 1,000 procedures) as well as infection, pulmonary embolism, and death, according to the paper published online June 16 in BMJ.
“Thus, middle-aged patients with knee pain and meniscal tears should be considered as having early-stage osteoarthritis and be treated according to clinical guidelines for knee osteoarthritis, starting with information, exercise, and often weight loss,” wrote Dr. Jonas B. Thorlund of the University of Southern Denmark, Odense, and coauthors (BMJ 2015, June 16 [doi:10.1136/bmj.h2747]).
The study was supported by the Swedish Research Council. One author declared personal fees from several pharmaceutical and medical companies and relevant journal editorship, while another declared fees from lectureships and books.
Arthroscopic knee surgery in middle-aged or older patients with knee pain is associated with greater harm than good, according to a meta-analysis.
The analysis of nine randomized, controlled trials in 1,270 patients of arthroscopic surgery involving partial meniscectomy, debridement, or both showed a small but statistically significant benefit from the procedure – comparable to the pain-relieving effects of paracetamol – but which falls below significance after 12 months.
However, there were no significant improvements in knee function, and there were significant increases in the risk of deep vein thrombosis (4.13 events per 1,000 procedures) as well as infection, pulmonary embolism, and death, according to the paper published online June 16 in BMJ.
“Thus, middle-aged patients with knee pain and meniscal tears should be considered as having early-stage osteoarthritis and be treated according to clinical guidelines for knee osteoarthritis, starting with information, exercise, and often weight loss,” wrote Dr. Jonas B. Thorlund of the University of Southern Denmark, Odense, and coauthors (BMJ 2015, June 16 [doi:10.1136/bmj.h2747]).
The study was supported by the Swedish Research Council. One author declared personal fees from several pharmaceutical and medical companies and relevant journal editorship, while another declared fees from lectureships and books.
FROM BMJ
Key clinical point: The potential harms of arthroscopic knee surgery in middle-aged or older patients with knee pain outweigh the benefits.
Major finding: Arthroscopic knee surgery is associated with a small but significant improvement in symptoms that disappears after 12 months.
Data source: Meta-analysis of nine randomized, controlled trials in 1,270 patients.
Disclosures: The study was supported by the Swedish Research Council. One author declared personal fees from several pharmaceutical and medical companies and relevant journal editorship, while another declared fees from lectureships and books.
EULAR: Hydroxychloroquine shows no benefit in hand osteoarthritis
ROME – Hydroxychloroquine should not be prescribed for patients with mild to moderate hand osteoarthritis (OA) according to data from a 24-week, randomized, multicenter, placebo-controlled trial.
The results of the Dutch study, presented at the European Congress of Rheumatology by Dr. Natalja M. Basoski of Maasstad Hospital, Rotterdam, the Netherlands, showed that hydroxychloroquine was no better than placebo at reducing patients’ pain and disability, or for improving their physical, social, or emotional well-being.
The primary outcome measure used was reduction in OA hand pain in the preceding 24 hours measured using a 100-mm visual analog scale (VAS) at the end of the study. The mean change in pain using the VAS over 24 weeks was a reduction of 1.3 mm in the hydroxychloroquine-treated patients versus a 0.10-mm rise in the patients who received placebo (P = .82).
There also was no change in the two secondary endpoints of change in total score of the Australian/Canadian Hand Osteoarthritis Index (AUSCAN) and the Arthritis Impact Measurement Scale 2 SF (AIMS2-SF) by the end of the treatment period. Mean changes in AUSCAN total scores were –0.42 and –0.25 (P = .49) and mean reductions in total AIMS2-SF scores were –0.17 and –0.076 (P = .68), comparing hydroxychloroquine with placebo, respectively.
“Osteoarthritis of the hand is one of the most common types of osteoarthritis, leading to pain, stiffness, and loss of function,” Dr. Basoski explained during a clinical science session looking at manifestations of the disease beyond the knee. “Unfortunately, current pharmacological treatment options are limited,” she added.
The underlying pathophysiological mechanisms of OA that primarily affect the hand are not clear, although inflammation is known to have a role, as in knee OA. Hydroxychloroquine is an established disease-modifying antirheumatoid drug that has shown benefit in patients with mild rheumatoid arthritis, which has led many rheumatologists to prescribe off label for the treatment of hand OA as well, Dr. Basoski observed in an interview. Data to support this are lacking, however, so this trial aimed to look at the potential symptom-modifying effects of the drug specifically in OA.
Over a 3-year period starting in July 2010, 202 patients with symptoms of primary mild to moderate hand OA of at least 1 years’ duration were recruited at six hospitals in the Netherlands and randomized to hydroxychloroquine 400 mg/day or matching placebo for 24 weeks. Six patients were lost to follow-up early on in the study, leaving 98 patients in each study arm who could be included in the intent-to-treat analysis. Of these, 22 hydroxychloroquine-treated and nine placebo-treated patients discontinued treatment, 10 and 5 in each group, respectively, because of adverse effects.
Dr. Basoski noted that patient characteristics were similar at baseline. Mean age was 57 years, and about 86% of participants were women. Hand OA was defined via American College of Rheumatology criteria and 86% and 91% of hydroxychloroquine- and placebo-treated patients had at least one joint with radiographic evidence of joint disease defined as a Kellgren-Lawrence score of ≥2.
“This is one of the studies that does not support the use of hydroxychloroquine in patients with OA of the hands and mild complaints,” she said in an interview. “It means that you should not prescribe it anymore, at least based on the results of this study.”
Further research is needed to see if there are some patients who might benefit or if it applies to other OA phenotypes, such as erosive hand OA. “More studies should be done, although in our second analysis after the study we tried to differentiate between very low pain and high pain and we still didn’t really see a difference,” she observed.
Erosive hand OA could be a different case, and results of an ongoing UK study should provide insight on whether hydroxychloroquine could be beneficial in these patients.
Although a similar number of patients treated with hydroxychloroquine or placebo in the trial experienced adverse events (21 vs. 24, respectively), there was an increase in allergic reactions (3 vs. 0) and rash or itching (8 vs. 3) with the active treatment.
With hydroxychloroquine seemingly out of the picture, at least in mild to moderate cases, Dr. Basoski advised on how she might treat a patient with primary hand OA. “I would try to start with paracetamol [acetaminophen] at the dose that is currently recommended, like 4 g/day, then eventually try to use opioids, as NSAIDs are not such a good thing to use in the long term.”
Dr. Basoski did not have any conflicts of interest to disclose.
ROME – Hydroxychloroquine should not be prescribed for patients with mild to moderate hand osteoarthritis (OA) according to data from a 24-week, randomized, multicenter, placebo-controlled trial.
The results of the Dutch study, presented at the European Congress of Rheumatology by Dr. Natalja M. Basoski of Maasstad Hospital, Rotterdam, the Netherlands, showed that hydroxychloroquine was no better than placebo at reducing patients’ pain and disability, or for improving their physical, social, or emotional well-being.
The primary outcome measure used was reduction in OA hand pain in the preceding 24 hours measured using a 100-mm visual analog scale (VAS) at the end of the study. The mean change in pain using the VAS over 24 weeks was a reduction of 1.3 mm in the hydroxychloroquine-treated patients versus a 0.10-mm rise in the patients who received placebo (P = .82).
There also was no change in the two secondary endpoints of change in total score of the Australian/Canadian Hand Osteoarthritis Index (AUSCAN) and the Arthritis Impact Measurement Scale 2 SF (AIMS2-SF) by the end of the treatment period. Mean changes in AUSCAN total scores were –0.42 and –0.25 (P = .49) and mean reductions in total AIMS2-SF scores were –0.17 and –0.076 (P = .68), comparing hydroxychloroquine with placebo, respectively.
“Osteoarthritis of the hand is one of the most common types of osteoarthritis, leading to pain, stiffness, and loss of function,” Dr. Basoski explained during a clinical science session looking at manifestations of the disease beyond the knee. “Unfortunately, current pharmacological treatment options are limited,” she added.
The underlying pathophysiological mechanisms of OA that primarily affect the hand are not clear, although inflammation is known to have a role, as in knee OA. Hydroxychloroquine is an established disease-modifying antirheumatoid drug that has shown benefit in patients with mild rheumatoid arthritis, which has led many rheumatologists to prescribe off label for the treatment of hand OA as well, Dr. Basoski observed in an interview. Data to support this are lacking, however, so this trial aimed to look at the potential symptom-modifying effects of the drug specifically in OA.
Over a 3-year period starting in July 2010, 202 patients with symptoms of primary mild to moderate hand OA of at least 1 years’ duration were recruited at six hospitals in the Netherlands and randomized to hydroxychloroquine 400 mg/day or matching placebo for 24 weeks. Six patients were lost to follow-up early on in the study, leaving 98 patients in each study arm who could be included in the intent-to-treat analysis. Of these, 22 hydroxychloroquine-treated and nine placebo-treated patients discontinued treatment, 10 and 5 in each group, respectively, because of adverse effects.
Dr. Basoski noted that patient characteristics were similar at baseline. Mean age was 57 years, and about 86% of participants were women. Hand OA was defined via American College of Rheumatology criteria and 86% and 91% of hydroxychloroquine- and placebo-treated patients had at least one joint with radiographic evidence of joint disease defined as a Kellgren-Lawrence score of ≥2.
“This is one of the studies that does not support the use of hydroxychloroquine in patients with OA of the hands and mild complaints,” she said in an interview. “It means that you should not prescribe it anymore, at least based on the results of this study.”
Further research is needed to see if there are some patients who might benefit or if it applies to other OA phenotypes, such as erosive hand OA. “More studies should be done, although in our second analysis after the study we tried to differentiate between very low pain and high pain and we still didn’t really see a difference,” she observed.
Erosive hand OA could be a different case, and results of an ongoing UK study should provide insight on whether hydroxychloroquine could be beneficial in these patients.
Although a similar number of patients treated with hydroxychloroquine or placebo in the trial experienced adverse events (21 vs. 24, respectively), there was an increase in allergic reactions (3 vs. 0) and rash or itching (8 vs. 3) with the active treatment.
With hydroxychloroquine seemingly out of the picture, at least in mild to moderate cases, Dr. Basoski advised on how she might treat a patient with primary hand OA. “I would try to start with paracetamol [acetaminophen] at the dose that is currently recommended, like 4 g/day, then eventually try to use opioids, as NSAIDs are not such a good thing to use in the long term.”
Dr. Basoski did not have any conflicts of interest to disclose.
ROME – Hydroxychloroquine should not be prescribed for patients with mild to moderate hand osteoarthritis (OA) according to data from a 24-week, randomized, multicenter, placebo-controlled trial.
The results of the Dutch study, presented at the European Congress of Rheumatology by Dr. Natalja M. Basoski of Maasstad Hospital, Rotterdam, the Netherlands, showed that hydroxychloroquine was no better than placebo at reducing patients’ pain and disability, or for improving their physical, social, or emotional well-being.
The primary outcome measure used was reduction in OA hand pain in the preceding 24 hours measured using a 100-mm visual analog scale (VAS) at the end of the study. The mean change in pain using the VAS over 24 weeks was a reduction of 1.3 mm in the hydroxychloroquine-treated patients versus a 0.10-mm rise in the patients who received placebo (P = .82).
There also was no change in the two secondary endpoints of change in total score of the Australian/Canadian Hand Osteoarthritis Index (AUSCAN) and the Arthritis Impact Measurement Scale 2 SF (AIMS2-SF) by the end of the treatment period. Mean changes in AUSCAN total scores were –0.42 and –0.25 (P = .49) and mean reductions in total AIMS2-SF scores were –0.17 and –0.076 (P = .68), comparing hydroxychloroquine with placebo, respectively.
“Osteoarthritis of the hand is one of the most common types of osteoarthritis, leading to pain, stiffness, and loss of function,” Dr. Basoski explained during a clinical science session looking at manifestations of the disease beyond the knee. “Unfortunately, current pharmacological treatment options are limited,” she added.
The underlying pathophysiological mechanisms of OA that primarily affect the hand are not clear, although inflammation is known to have a role, as in knee OA. Hydroxychloroquine is an established disease-modifying antirheumatoid drug that has shown benefit in patients with mild rheumatoid arthritis, which has led many rheumatologists to prescribe off label for the treatment of hand OA as well, Dr. Basoski observed in an interview. Data to support this are lacking, however, so this trial aimed to look at the potential symptom-modifying effects of the drug specifically in OA.
Over a 3-year period starting in July 2010, 202 patients with symptoms of primary mild to moderate hand OA of at least 1 years’ duration were recruited at six hospitals in the Netherlands and randomized to hydroxychloroquine 400 mg/day or matching placebo for 24 weeks. Six patients were lost to follow-up early on in the study, leaving 98 patients in each study arm who could be included in the intent-to-treat analysis. Of these, 22 hydroxychloroquine-treated and nine placebo-treated patients discontinued treatment, 10 and 5 in each group, respectively, because of adverse effects.
Dr. Basoski noted that patient characteristics were similar at baseline. Mean age was 57 years, and about 86% of participants were women. Hand OA was defined via American College of Rheumatology criteria and 86% and 91% of hydroxychloroquine- and placebo-treated patients had at least one joint with radiographic evidence of joint disease defined as a Kellgren-Lawrence score of ≥2.
“This is one of the studies that does not support the use of hydroxychloroquine in patients with OA of the hands and mild complaints,” she said in an interview. “It means that you should not prescribe it anymore, at least based on the results of this study.”
Further research is needed to see if there are some patients who might benefit or if it applies to other OA phenotypes, such as erosive hand OA. “More studies should be done, although in our second analysis after the study we tried to differentiate between very low pain and high pain and we still didn’t really see a difference,” she observed.
Erosive hand OA could be a different case, and results of an ongoing UK study should provide insight on whether hydroxychloroquine could be beneficial in these patients.
Although a similar number of patients treated with hydroxychloroquine or placebo in the trial experienced adverse events (21 vs. 24, respectively), there was an increase in allergic reactions (3 vs. 0) and rash or itching (8 vs. 3) with the active treatment.
With hydroxychloroquine seemingly out of the picture, at least in mild to moderate cases, Dr. Basoski advised on how she might treat a patient with primary hand OA. “I would try to start with paracetamol [acetaminophen] at the dose that is currently recommended, like 4 g/day, then eventually try to use opioids, as NSAIDs are not such a good thing to use in the long term.”
Dr. Basoski did not have any conflicts of interest to disclose.
AT THE EULAR 2015 CONGRESS
Key clinical point: Hydroxychloroquine should not be prescribed for mild to moderate primary hand osteoarthritis (OA).
Major finding: There was no significant change in pain (P = .82); disability (P = .49); or patient physical, social, and emotional well-being (P = .68) when comparing hydroxychloroquine with placebo.
Data source: A 24-week, randomized, multicenter, double-blind, placebo-controlled trial of 202 patients aged 40 years or older with mild to moderate primary hand OA.
Disclosures: Dr. Basoski had no conflicts of interest to disclose.
Amplified pain in knee osteoarthritis linked to insomnia, catastrophizing
Patients with knee osteoarthritis and poor sleep habits suffered greater central sensitization to pain than other individuals, especially if they tended to ruminate about their pain, a case-control study found.
The study is the largest to date to examine sleep, catastrophizing, and central sensitization in knee osteoarthritis, said Claudia Campbell, Ph.D., of Johns Hopkins University, Baltimore. “While we were underpowered to fully examine all possible data described, we hope that these data serve as a platform for future studies to adequately power themselves and explore potential differences.”
Patients with osteoarthritis often report poor sleep, and studies show that many of these patients also have central sensitization, or hyperexcitability of nociceptive nerve pathways, a phenomenon that tends to amplify and prolong pain. Catastrophizing – a “persistently negative cognitive affective style” in which patients feel helpless, and magnify and ruminate about their pain – predicts worse pain outcomes in osteoarthritis and other painful conditions, the investigators noted (Arthritis Care Res. 2015 June 4 [doi: 10.1002/acr.22609]).Dr. Campbell and her colleagues categorized 208 adults into four groups: those with insomnia and knee osteoarthritis, those with one or the other of the disorders, and those with neither condition (healthy controls). More than 70% of participants were female, and individuals with knee osteoarthritis were significantly older than the rest. The investigators matched the groups with knee osteoarthritis based on radiographic severity.
Quantitative sensory testing showed that patients with knee osteoarthritis and insomnia had significantly greater central sensitization, compared with healthy controls, the researchers reported. Low sleep efficiency (a measure of self-perceived sleep quality) was linked to heightened central sensitization, but only when patients scored more 7.4 on the 13-item Pain Catastrophizing Scale, they added. In all 56% of the sample met that threshold, as did 77% of participants who had both insomnia and knee osteoarthritis.
Central sensitization also correlated positively with clinical pain. “Clinical implications of these findings suggest that treatment options for osteoarthritis patients could include sleep and/or intervention for catastrophizing, both modifiable risk factors, [which] may aid in reducing central sensitization and decrease clinical pain,” the researchers noted.
The study was the first part of a randomized trial that is examining cognitive behavioral therapy for insomnia in patients with osteoarthritis.
The National Institutes of Arthritis and Musculoskeletal and Skin Disease and the National Institutes of Health supported the study. The investigators reported having no relevant conflicts of interest.
Patients with knee osteoarthritis and poor sleep habits suffered greater central sensitization to pain than other individuals, especially if they tended to ruminate about their pain, a case-control study found.
The study is the largest to date to examine sleep, catastrophizing, and central sensitization in knee osteoarthritis, said Claudia Campbell, Ph.D., of Johns Hopkins University, Baltimore. “While we were underpowered to fully examine all possible data described, we hope that these data serve as a platform for future studies to adequately power themselves and explore potential differences.”
Patients with osteoarthritis often report poor sleep, and studies show that many of these patients also have central sensitization, or hyperexcitability of nociceptive nerve pathways, a phenomenon that tends to amplify and prolong pain. Catastrophizing – a “persistently negative cognitive affective style” in which patients feel helpless, and magnify and ruminate about their pain – predicts worse pain outcomes in osteoarthritis and other painful conditions, the investigators noted (Arthritis Care Res. 2015 June 4 [doi: 10.1002/acr.22609]).Dr. Campbell and her colleagues categorized 208 adults into four groups: those with insomnia and knee osteoarthritis, those with one or the other of the disorders, and those with neither condition (healthy controls). More than 70% of participants were female, and individuals with knee osteoarthritis were significantly older than the rest. The investigators matched the groups with knee osteoarthritis based on radiographic severity.
Quantitative sensory testing showed that patients with knee osteoarthritis and insomnia had significantly greater central sensitization, compared with healthy controls, the researchers reported. Low sleep efficiency (a measure of self-perceived sleep quality) was linked to heightened central sensitization, but only when patients scored more 7.4 on the 13-item Pain Catastrophizing Scale, they added. In all 56% of the sample met that threshold, as did 77% of participants who had both insomnia and knee osteoarthritis.
Central sensitization also correlated positively with clinical pain. “Clinical implications of these findings suggest that treatment options for osteoarthritis patients could include sleep and/or intervention for catastrophizing, both modifiable risk factors, [which] may aid in reducing central sensitization and decrease clinical pain,” the researchers noted.
The study was the first part of a randomized trial that is examining cognitive behavioral therapy for insomnia in patients with osteoarthritis.
The National Institutes of Arthritis and Musculoskeletal and Skin Disease and the National Institutes of Health supported the study. The investigators reported having no relevant conflicts of interest.
Patients with knee osteoarthritis and poor sleep habits suffered greater central sensitization to pain than other individuals, especially if they tended to ruminate about their pain, a case-control study found.
The study is the largest to date to examine sleep, catastrophizing, and central sensitization in knee osteoarthritis, said Claudia Campbell, Ph.D., of Johns Hopkins University, Baltimore. “While we were underpowered to fully examine all possible data described, we hope that these data serve as a platform for future studies to adequately power themselves and explore potential differences.”
Patients with osteoarthritis often report poor sleep, and studies show that many of these patients also have central sensitization, or hyperexcitability of nociceptive nerve pathways, a phenomenon that tends to amplify and prolong pain. Catastrophizing – a “persistently negative cognitive affective style” in which patients feel helpless, and magnify and ruminate about their pain – predicts worse pain outcomes in osteoarthritis and other painful conditions, the investigators noted (Arthritis Care Res. 2015 June 4 [doi: 10.1002/acr.22609]).Dr. Campbell and her colleagues categorized 208 adults into four groups: those with insomnia and knee osteoarthritis, those with one or the other of the disorders, and those with neither condition (healthy controls). More than 70% of participants were female, and individuals with knee osteoarthritis were significantly older than the rest. The investigators matched the groups with knee osteoarthritis based on radiographic severity.
Quantitative sensory testing showed that patients with knee osteoarthritis and insomnia had significantly greater central sensitization, compared with healthy controls, the researchers reported. Low sleep efficiency (a measure of self-perceived sleep quality) was linked to heightened central sensitization, but only when patients scored more 7.4 on the 13-item Pain Catastrophizing Scale, they added. In all 56% of the sample met that threshold, as did 77% of participants who had both insomnia and knee osteoarthritis.
Central sensitization also correlated positively with clinical pain. “Clinical implications of these findings suggest that treatment options for osteoarthritis patients could include sleep and/or intervention for catastrophizing, both modifiable risk factors, [which] may aid in reducing central sensitization and decrease clinical pain,” the researchers noted.
The study was the first part of a randomized trial that is examining cognitive behavioral therapy for insomnia in patients with osteoarthritis.
The National Institutes of Arthritis and Musculoskeletal and Skin Disease and the National Institutes of Health supported the study. The investigators reported having no relevant conflicts of interest.
Key clinical point: Patients with knee osteoarthritis and insomnia suffered greater central sensitization, especially if they tended to ruminate about their pain.
Major finding: Patients with knee osteoarthritis and insomnia had significantly greater central sensitization compared with controls.
Data source: Case-control study of 208 adults.
Disclosures: The National Institutes of Health supported the research. The investigators reported having no relevant conflicts of interest.
OARSI: Set concrete walking goals in knee OA
SEATTLE – The pain of knee osteoarthritis is not exacerbated by regular exercise such as walking and may actually be relieved by it, according to several findings presented at the World Congress on Osteoarthritis.
“Physical activity is important for the reduction of knee pain and the prevention of functional limitation in knee osteoarthritis,” Daniel White, Sc.D., said.
“We should be recommending walking to people with painful knee osteoarthritis. Just as a preliminary goal, we can start with 3,000 steps per day and ultimately progress people to at least 6,000 steps per day,” he added.
National guidelines issued in 2008 for the general population call for at least 150 minutes per week of moderate to vigorous–intensity physical activity, according to Dr. White of the department of physical therapy at the University of Delaware in Newark. When that recommendation is applied to walking, which is the most common physical activity among older adults (Arthritis Care Res. 2014;66:139-46), it translates to a brisk pace that permits conversation but is exertional enough to cause sweating. Meeting the goal would mean approximately 100 steps per minute (Am. J. Prev. Med. 2009;36:410-5).
“The clinical hypothesis is that osteoarthritis pain is limiting your physical activity, but whether that has been empirically [established] has yet to be seen,” Dr. White said. For example, investigators for an Osteoarthritis Initiative study found that only 13% of men and 8% of women with knee osteoarthritis met the criteria for the national guideline (Arthritis Rheum. 2011;63:3372-82), but also noted that these values differed little from those of the general population. Data from the Multicenter Osteoarthritis Study found similarly low proportions, regardless of the presence of radiographic disease and the severity of knee pain (Arthritis Rheum. 2013;65:139-47). In a cohort that underwent total knee replacement, patients had more than 180% improvements in subjective pain and function at 6 months, yet their objectively measured time spent walking increased by only 5% (Clin. Orthop. Relat. Res. 2008;466:2201-8).
These findings suggest that osteoarthritis and pain may have a limited role in explaining physical inactivity, according to Dr. White. “An implication of this is that improvements in disease and pain may not lead to more physical activity; in other words, the pills you give to people to make them feel better or the exercises that they may do to improve their knee pain may not necessarily increase the amount of unstructured physical activity that people do on a day-to-day basis. Also, physical activity specifically may need to be targeted; you need to increase physical activity in a specific way rather than just expecting it to happen once the barriers of pain and disease are removed.”
Recommendations for physical activity must consider both potential risks and benefits, he noted. Data regarding its impact on structural changes in the knee are mixed. Conversely, there is substantial evidence that physical activity moderately reduces knee pain (Cochrane Database Syst Rev. 2015;1:CD004376) and lowers the likelihood of developing functional limitations in a dose-response manner (Arthritis Care Res. 2014;66:1328-36). And there are a variety of other health benefits, some of which may affect osteoarthritis, such as weight maintenance.
“In my mind, the benefits outweigh the risks for promoting physical activity in this patient population. And specifically, given that walking is the most common physical activity, from a clinical perspective, there is very strong evidence to recommend walking to this patient population,” Dr. White said at the meeting sponsored by the Osteoarthritis Research Society International.
He further endorsed use of a pedometer as a practical, objective way to measure this activity. “Regardless of what instrument or device you use, they all measure steps, and that is sort of the common denominator which is a very understandable outcome that patients can relate to, that clinicians understand,” he elaborated. Moreover, a meta-analysis has shown that interventions using pedometers achieve greater increases in walking (JAMA 2007;298:2296-304).
The above analysis of impact on functional limitations in people with knee osteoarthritis also helps to define target walking goals, according to Dr. White, who disclosed that he had no relevant conflicts of interest. The study showed that 95% of people who did not develop functional limitations walked at least 3,000 steps per day, and that 6,000 steps per day best discriminated between those who did and did not develop functional limitations.
Assuming that a moderate intensity of walking is 100 steps per minute, this step range translates to 30-60 minutes of walking per day, he said. As half of 60-year-olds in the general population already walk approximately 40-50 minutes daily as part of their usual activities (J. Gerontol. A Biol. Sci. Med. Sci. 2013;68:1426-32), they may need to add only 10 more minutes. And a recent report suggests that even people with severe knee osteoarthritis find this amount to be safe and feasible (Osteoarthritis Cartilage 2015 April 14 [doi:10.1016/j.joca.2015.04.001]).
SEATTLE – The pain of knee osteoarthritis is not exacerbated by regular exercise such as walking and may actually be relieved by it, according to several findings presented at the World Congress on Osteoarthritis.
“Physical activity is important for the reduction of knee pain and the prevention of functional limitation in knee osteoarthritis,” Daniel White, Sc.D., said.
“We should be recommending walking to people with painful knee osteoarthritis. Just as a preliminary goal, we can start with 3,000 steps per day and ultimately progress people to at least 6,000 steps per day,” he added.
National guidelines issued in 2008 for the general population call for at least 150 minutes per week of moderate to vigorous–intensity physical activity, according to Dr. White of the department of physical therapy at the University of Delaware in Newark. When that recommendation is applied to walking, which is the most common physical activity among older adults (Arthritis Care Res. 2014;66:139-46), it translates to a brisk pace that permits conversation but is exertional enough to cause sweating. Meeting the goal would mean approximately 100 steps per minute (Am. J. Prev. Med. 2009;36:410-5).
“The clinical hypothesis is that osteoarthritis pain is limiting your physical activity, but whether that has been empirically [established] has yet to be seen,” Dr. White said. For example, investigators for an Osteoarthritis Initiative study found that only 13% of men and 8% of women with knee osteoarthritis met the criteria for the national guideline (Arthritis Rheum. 2011;63:3372-82), but also noted that these values differed little from those of the general population. Data from the Multicenter Osteoarthritis Study found similarly low proportions, regardless of the presence of radiographic disease and the severity of knee pain (Arthritis Rheum. 2013;65:139-47). In a cohort that underwent total knee replacement, patients had more than 180% improvements in subjective pain and function at 6 months, yet their objectively measured time spent walking increased by only 5% (Clin. Orthop. Relat. Res. 2008;466:2201-8).
These findings suggest that osteoarthritis and pain may have a limited role in explaining physical inactivity, according to Dr. White. “An implication of this is that improvements in disease and pain may not lead to more physical activity; in other words, the pills you give to people to make them feel better or the exercises that they may do to improve their knee pain may not necessarily increase the amount of unstructured physical activity that people do on a day-to-day basis. Also, physical activity specifically may need to be targeted; you need to increase physical activity in a specific way rather than just expecting it to happen once the barriers of pain and disease are removed.”
Recommendations for physical activity must consider both potential risks and benefits, he noted. Data regarding its impact on structural changes in the knee are mixed. Conversely, there is substantial evidence that physical activity moderately reduces knee pain (Cochrane Database Syst Rev. 2015;1:CD004376) and lowers the likelihood of developing functional limitations in a dose-response manner (Arthritis Care Res. 2014;66:1328-36). And there are a variety of other health benefits, some of which may affect osteoarthritis, such as weight maintenance.
“In my mind, the benefits outweigh the risks for promoting physical activity in this patient population. And specifically, given that walking is the most common physical activity, from a clinical perspective, there is very strong evidence to recommend walking to this patient population,” Dr. White said at the meeting sponsored by the Osteoarthritis Research Society International.
He further endorsed use of a pedometer as a practical, objective way to measure this activity. “Regardless of what instrument or device you use, they all measure steps, and that is sort of the common denominator which is a very understandable outcome that patients can relate to, that clinicians understand,” he elaborated. Moreover, a meta-analysis has shown that interventions using pedometers achieve greater increases in walking (JAMA 2007;298:2296-304).
The above analysis of impact on functional limitations in people with knee osteoarthritis also helps to define target walking goals, according to Dr. White, who disclosed that he had no relevant conflicts of interest. The study showed that 95% of people who did not develop functional limitations walked at least 3,000 steps per day, and that 6,000 steps per day best discriminated between those who did and did not develop functional limitations.
Assuming that a moderate intensity of walking is 100 steps per minute, this step range translates to 30-60 minutes of walking per day, he said. As half of 60-year-olds in the general population already walk approximately 40-50 minutes daily as part of their usual activities (J. Gerontol. A Biol. Sci. Med. Sci. 2013;68:1426-32), they may need to add only 10 more minutes. And a recent report suggests that even people with severe knee osteoarthritis find this amount to be safe and feasible (Osteoarthritis Cartilage 2015 April 14 [doi:10.1016/j.joca.2015.04.001]).
SEATTLE – The pain of knee osteoarthritis is not exacerbated by regular exercise such as walking and may actually be relieved by it, according to several findings presented at the World Congress on Osteoarthritis.
“Physical activity is important for the reduction of knee pain and the prevention of functional limitation in knee osteoarthritis,” Daniel White, Sc.D., said.
“We should be recommending walking to people with painful knee osteoarthritis. Just as a preliminary goal, we can start with 3,000 steps per day and ultimately progress people to at least 6,000 steps per day,” he added.
National guidelines issued in 2008 for the general population call for at least 150 minutes per week of moderate to vigorous–intensity physical activity, according to Dr. White of the department of physical therapy at the University of Delaware in Newark. When that recommendation is applied to walking, which is the most common physical activity among older adults (Arthritis Care Res. 2014;66:139-46), it translates to a brisk pace that permits conversation but is exertional enough to cause sweating. Meeting the goal would mean approximately 100 steps per minute (Am. J. Prev. Med. 2009;36:410-5).
“The clinical hypothesis is that osteoarthritis pain is limiting your physical activity, but whether that has been empirically [established] has yet to be seen,” Dr. White said. For example, investigators for an Osteoarthritis Initiative study found that only 13% of men and 8% of women with knee osteoarthritis met the criteria for the national guideline (Arthritis Rheum. 2011;63:3372-82), but also noted that these values differed little from those of the general population. Data from the Multicenter Osteoarthritis Study found similarly low proportions, regardless of the presence of radiographic disease and the severity of knee pain (Arthritis Rheum. 2013;65:139-47). In a cohort that underwent total knee replacement, patients had more than 180% improvements in subjective pain and function at 6 months, yet their objectively measured time spent walking increased by only 5% (Clin. Orthop. Relat. Res. 2008;466:2201-8).
These findings suggest that osteoarthritis and pain may have a limited role in explaining physical inactivity, according to Dr. White. “An implication of this is that improvements in disease and pain may not lead to more physical activity; in other words, the pills you give to people to make them feel better or the exercises that they may do to improve their knee pain may not necessarily increase the amount of unstructured physical activity that people do on a day-to-day basis. Also, physical activity specifically may need to be targeted; you need to increase physical activity in a specific way rather than just expecting it to happen once the barriers of pain and disease are removed.”
Recommendations for physical activity must consider both potential risks and benefits, he noted. Data regarding its impact on structural changes in the knee are mixed. Conversely, there is substantial evidence that physical activity moderately reduces knee pain (Cochrane Database Syst Rev. 2015;1:CD004376) and lowers the likelihood of developing functional limitations in a dose-response manner (Arthritis Care Res. 2014;66:1328-36). And there are a variety of other health benefits, some of which may affect osteoarthritis, such as weight maintenance.
“In my mind, the benefits outweigh the risks for promoting physical activity in this patient population. And specifically, given that walking is the most common physical activity, from a clinical perspective, there is very strong evidence to recommend walking to this patient population,” Dr. White said at the meeting sponsored by the Osteoarthritis Research Society International.
He further endorsed use of a pedometer as a practical, objective way to measure this activity. “Regardless of what instrument or device you use, they all measure steps, and that is sort of the common denominator which is a very understandable outcome that patients can relate to, that clinicians understand,” he elaborated. Moreover, a meta-analysis has shown that interventions using pedometers achieve greater increases in walking (JAMA 2007;298:2296-304).
The above analysis of impact on functional limitations in people with knee osteoarthritis also helps to define target walking goals, according to Dr. White, who disclosed that he had no relevant conflicts of interest. The study showed that 95% of people who did not develop functional limitations walked at least 3,000 steps per day, and that 6,000 steps per day best discriminated between those who did and did not develop functional limitations.
Assuming that a moderate intensity of walking is 100 steps per minute, this step range translates to 30-60 minutes of walking per day, he said. As half of 60-year-olds in the general population already walk approximately 40-50 minutes daily as part of their usual activities (J. Gerontol. A Biol. Sci. Med. Sci. 2013;68:1426-32), they may need to add only 10 more minutes. And a recent report suggests that even people with severe knee osteoarthritis find this amount to be safe and feasible (Osteoarthritis Cartilage 2015 April 14 [doi:10.1016/j.joca.2015.04.001]).
EXPERT ANALYSIS FROM OARSI 2015