User login
Five times greater suicide risk for trans, gender-diverse teens in ED
WASHINGTON – , according to a study presented at the annual meeting of the American Academy of Pediatrics.
“The take-home message here is this study emphasizes the importance of universal screening to identify gender-diverse youth at risk,” Amanda Burnside, PhD, assistant professor of psychiatry and behavioral sciences at Ann and Robert H. Lurie Children’s Hospital of Chicago and Northwestern University, told attendees. “We really need to develop robust strategies and systems to link better mental health services.”
Suicide rates in transgender and gender-diverse youth are exceptionally high among youth in the U.S., Dr. Burnside said during her presentation. For example, the 2022 LGBTQ health survey from the Trevor Project found that much higher percentages of transgender and gender nonconforming youth had considered suicide in the past year compared with cisgender youth, even within the LGBTQ umbrella. Among nearly 34,000 LGBTQ youth aged 13-24, nearly half of trans females (48%) and more than half of trans males (59%) had considered suicide, compared with 28% of cisgender males and 37% of cisgender females. The rate among nonbinary/genderqueer individuals was 53%, and it was 48% for those questioning their gender.
Current methods of identifying trans and gender-diverse (TGD) youth in the hospital, however, may not actually be capturing the entire population.
“In health care settings, research involving TGD individuals has historically been limited to specialized clinic populations or youth with gender-specific diagnostic codes documented in the electronic medical record,” an approach that “likely significantly underestimates the prevalence of TGD youth in health care settings.” While at least one study has attempted to bridge this gap by searching the EMR for keywords, that study only tried to identify trans youth and not other youth on the gender diversity spectrum, such as nonbinary youth or those questioning their gender identity. Dr. Burnside and her colleagues therefore designed a study that used keywords to identify both trans youth and other gender-diverse youth who visited the ED so they could assess the rate of positive suicide screens in this population.
Underestimating the population at risk?
The researchers conducted a retrospective cross-sectional study of EMR data for all ED visits during which the patient underwent suicide screening. For the period of November 2019 to August 2022, they collected data on the screening results and the patient’s gender identity, age, race/ethnicity, insurance status, chief complaint in the ED and child opportunity index, which assess a youth’s access to resources based on geography. The suicide screener used was the Ask Suicide–Screening Questions (ASQ) tool.
The keywords they looked for in the EMR to identify trans and gender-diverse youth included transgender, pronouns, agender, gender dysphoria, male-to-female, female-to-male, nonbinary, preferred name, and they/them (captured as a complete term, not as “they” and “them” separately).
“If a keyword was present, the surrounding text was extracted and reviewed by two members of our team,” Dr. Burnside explained in her presentation. “We categorized keywords into either indicative of gender-diverse identity or not, and if it wasn’t clear based on the text extracted, we would conduct a manual chart review,” though that only occurred in about 3% of cases, she added.
Among 15,413 ED encounters with a suicide screen, the researchers identified 1,126 of these keywords in the EMR, among which 91.2% were classified as referring to a gender-diverse patient. Nearly all of the words were at least 90% effective in identify a gender-diverse youth, Dr. Burnside said, and all of the 197 instances of “they/them” were classified as gender diverse.
The accuracy was a little lower for the two keywords that appeared most frequently: For “pronouns,” 86.3% of 306 instances were classified as gender diverse, and for “transgender,” 83.1% of 207 instances were classified as gender diverse. Since some providers ask all patients their pronouns, the presence of “pronouns” in the EMR alone did not necessarily indicate the patient was gender diverse, Dr. Burnside said. A common reason the term “transgender” occurred in the EMR of non–gender diverse patients is that the department’s list of crisis resources includes transgender hotlines.
After identifying all the keywords, the researchers determined how many of these occurred in unique ED encounters and removed those with incomplete screening. Overall, they found 565 encounters by 399 gender-diverse individuals who had a suicide screening, representing 4.6% of total visits. This percentage is slightly lower than recent population-based estimates of gender-diverse youth, the researchers noted.
This population ranged from 8 to 23 years old, and 43% were publicly insured. The chief complaint for most of the patients (77.5%) was a mental health one. They were predominantly White (43%) or Hispanic (35%), with 10% Black youth, 4% Asian youth, and 8% youth who were “other” or two or more races. About half (52%) lived in a neighborhood with a “low” or “very low” child opportunity index.
Within this population, 81% of the patients screened positive on the suicide screening, compared with 23% positive screens across all ED visits. One in ten (10%) gender-diverse youth had active suicidal ideation, compared with 3.4% of the rest of the ED patient population. The researchers calculated that gender-diverse youth had 5.35 times greater odds of screening positive than cisgender youth in the ED (95% confidence interval [CI] 8.7-15.92). Further, a quarter (25%) of the trans and gender-diverse youth who screened positive for suicide risk had come to the ED for a primary complaint unrelated to mental health.
“We had a kid who came in because he broke his arm who had active suicidal ideation,” study coauthor Jennifer A. Hoffmann, MD, assistant professor of pediatrics at the Ann & Robert H. Lurie Children’s Hospital of Chicago and Northwestern University, mentioned after the presentation. That particular patient even had a suicide plan, but was identified as actively suicidal only because of the screening. In other cases, she said, a youth may come in with self-inflicted injuries, and while those are the primary complaint, they are linked with suicidal ideation.
Among the study’s limitations are that gender identity is not necessarily being systematically assessed during visits, misspellings might have missed some youth, and their search strategy has not yet been externally validated, though they plan to seek that.
“Overall, however, this study did demonstrate that keyword searching is a promising technique to identify and prioritize gender-diverse youth in health services research,” Dr. Burnside said. In addition to showing the feasibility of using a keyword search strategy for identifying gender-diverse youth, Dr. Burnside noted that 31% of the encounters were identified by just one of the keywords they used, “highlighting the importance of using a comprehensive list of keywords to identify gender-diverse youth.”
Uncovering valuable information
Jason Rafferty, MD, MPH, EdM, clinical assistant professor of pediatrics and of psychiatry and human behavior at Brown University, Providence, R.I., who attended the presentation, noted that the study provides information on a population that’s often difficult to get through traditional EMR research methods.
“A lot of medical record systems don’t have uniform ways of capturing [gender diversity], but what we know as providers is that kids are really struggling and that it’s not a surprise that we’re seeing these disparities with suicidality,” Dr. Rafferty said.
The study also provides more discrete estimates by age than what most other current research measures, which tends to be lifetime suicidality as opposed to suicidal thoughts or attempts within the past year, Dr. Rafferty added.
”What this shows is, for adolescents, the risk of suicide is something we need to be paying attention to. Because it’s not that it’s something that only happens in adults, this really dispels a lot of the misquoting of the data that’s out there.” That kind of information is valuable for determining resource allocation, he said. “A disparity like this really underlies the importance of mental health resources in this field,” he said.
Dr. Burnside, Dr. Hoffmann, and Dr. Rafferty had no disclosures, and no external funding sources were noted.
WASHINGTON – , according to a study presented at the annual meeting of the American Academy of Pediatrics.
“The take-home message here is this study emphasizes the importance of universal screening to identify gender-diverse youth at risk,” Amanda Burnside, PhD, assistant professor of psychiatry and behavioral sciences at Ann and Robert H. Lurie Children’s Hospital of Chicago and Northwestern University, told attendees. “We really need to develop robust strategies and systems to link better mental health services.”
Suicide rates in transgender and gender-diverse youth are exceptionally high among youth in the U.S., Dr. Burnside said during her presentation. For example, the 2022 LGBTQ health survey from the Trevor Project found that much higher percentages of transgender and gender nonconforming youth had considered suicide in the past year compared with cisgender youth, even within the LGBTQ umbrella. Among nearly 34,000 LGBTQ youth aged 13-24, nearly half of trans females (48%) and more than half of trans males (59%) had considered suicide, compared with 28% of cisgender males and 37% of cisgender females. The rate among nonbinary/genderqueer individuals was 53%, and it was 48% for those questioning their gender.
Current methods of identifying trans and gender-diverse (TGD) youth in the hospital, however, may not actually be capturing the entire population.
“In health care settings, research involving TGD individuals has historically been limited to specialized clinic populations or youth with gender-specific diagnostic codes documented in the electronic medical record,” an approach that “likely significantly underestimates the prevalence of TGD youth in health care settings.” While at least one study has attempted to bridge this gap by searching the EMR for keywords, that study only tried to identify trans youth and not other youth on the gender diversity spectrum, such as nonbinary youth or those questioning their gender identity. Dr. Burnside and her colleagues therefore designed a study that used keywords to identify both trans youth and other gender-diverse youth who visited the ED so they could assess the rate of positive suicide screens in this population.
Underestimating the population at risk?
The researchers conducted a retrospective cross-sectional study of EMR data for all ED visits during which the patient underwent suicide screening. For the period of November 2019 to August 2022, they collected data on the screening results and the patient’s gender identity, age, race/ethnicity, insurance status, chief complaint in the ED and child opportunity index, which assess a youth’s access to resources based on geography. The suicide screener used was the Ask Suicide–Screening Questions (ASQ) tool.
The keywords they looked for in the EMR to identify trans and gender-diverse youth included transgender, pronouns, agender, gender dysphoria, male-to-female, female-to-male, nonbinary, preferred name, and they/them (captured as a complete term, not as “they” and “them” separately).
“If a keyword was present, the surrounding text was extracted and reviewed by two members of our team,” Dr. Burnside explained in her presentation. “We categorized keywords into either indicative of gender-diverse identity or not, and if it wasn’t clear based on the text extracted, we would conduct a manual chart review,” though that only occurred in about 3% of cases, she added.
Among 15,413 ED encounters with a suicide screen, the researchers identified 1,126 of these keywords in the EMR, among which 91.2% were classified as referring to a gender-diverse patient. Nearly all of the words were at least 90% effective in identify a gender-diverse youth, Dr. Burnside said, and all of the 197 instances of “they/them” were classified as gender diverse.
The accuracy was a little lower for the two keywords that appeared most frequently: For “pronouns,” 86.3% of 306 instances were classified as gender diverse, and for “transgender,” 83.1% of 207 instances were classified as gender diverse. Since some providers ask all patients their pronouns, the presence of “pronouns” in the EMR alone did not necessarily indicate the patient was gender diverse, Dr. Burnside said. A common reason the term “transgender” occurred in the EMR of non–gender diverse patients is that the department’s list of crisis resources includes transgender hotlines.
After identifying all the keywords, the researchers determined how many of these occurred in unique ED encounters and removed those with incomplete screening. Overall, they found 565 encounters by 399 gender-diverse individuals who had a suicide screening, representing 4.6% of total visits. This percentage is slightly lower than recent population-based estimates of gender-diverse youth, the researchers noted.
This population ranged from 8 to 23 years old, and 43% were publicly insured. The chief complaint for most of the patients (77.5%) was a mental health one. They were predominantly White (43%) or Hispanic (35%), with 10% Black youth, 4% Asian youth, and 8% youth who were “other” or two or more races. About half (52%) lived in a neighborhood with a “low” or “very low” child opportunity index.
Within this population, 81% of the patients screened positive on the suicide screening, compared with 23% positive screens across all ED visits. One in ten (10%) gender-diverse youth had active suicidal ideation, compared with 3.4% of the rest of the ED patient population. The researchers calculated that gender-diverse youth had 5.35 times greater odds of screening positive than cisgender youth in the ED (95% confidence interval [CI] 8.7-15.92). Further, a quarter (25%) of the trans and gender-diverse youth who screened positive for suicide risk had come to the ED for a primary complaint unrelated to mental health.
“We had a kid who came in because he broke his arm who had active suicidal ideation,” study coauthor Jennifer A. Hoffmann, MD, assistant professor of pediatrics at the Ann & Robert H. Lurie Children’s Hospital of Chicago and Northwestern University, mentioned after the presentation. That particular patient even had a suicide plan, but was identified as actively suicidal only because of the screening. In other cases, she said, a youth may come in with self-inflicted injuries, and while those are the primary complaint, they are linked with suicidal ideation.
Among the study’s limitations are that gender identity is not necessarily being systematically assessed during visits, misspellings might have missed some youth, and their search strategy has not yet been externally validated, though they plan to seek that.
“Overall, however, this study did demonstrate that keyword searching is a promising technique to identify and prioritize gender-diverse youth in health services research,” Dr. Burnside said. In addition to showing the feasibility of using a keyword search strategy for identifying gender-diverse youth, Dr. Burnside noted that 31% of the encounters were identified by just one of the keywords they used, “highlighting the importance of using a comprehensive list of keywords to identify gender-diverse youth.”
Uncovering valuable information
Jason Rafferty, MD, MPH, EdM, clinical assistant professor of pediatrics and of psychiatry and human behavior at Brown University, Providence, R.I., who attended the presentation, noted that the study provides information on a population that’s often difficult to get through traditional EMR research methods.
“A lot of medical record systems don’t have uniform ways of capturing [gender diversity], but what we know as providers is that kids are really struggling and that it’s not a surprise that we’re seeing these disparities with suicidality,” Dr. Rafferty said.
The study also provides more discrete estimates by age than what most other current research measures, which tends to be lifetime suicidality as opposed to suicidal thoughts or attempts within the past year, Dr. Rafferty added.
”What this shows is, for adolescents, the risk of suicide is something we need to be paying attention to. Because it’s not that it’s something that only happens in adults, this really dispels a lot of the misquoting of the data that’s out there.” That kind of information is valuable for determining resource allocation, he said. “A disparity like this really underlies the importance of mental health resources in this field,” he said.
Dr. Burnside, Dr. Hoffmann, and Dr. Rafferty had no disclosures, and no external funding sources were noted.
WASHINGTON – , according to a study presented at the annual meeting of the American Academy of Pediatrics.
“The take-home message here is this study emphasizes the importance of universal screening to identify gender-diverse youth at risk,” Amanda Burnside, PhD, assistant professor of psychiatry and behavioral sciences at Ann and Robert H. Lurie Children’s Hospital of Chicago and Northwestern University, told attendees. “We really need to develop robust strategies and systems to link better mental health services.”
Suicide rates in transgender and gender-diverse youth are exceptionally high among youth in the U.S., Dr. Burnside said during her presentation. For example, the 2022 LGBTQ health survey from the Trevor Project found that much higher percentages of transgender and gender nonconforming youth had considered suicide in the past year compared with cisgender youth, even within the LGBTQ umbrella. Among nearly 34,000 LGBTQ youth aged 13-24, nearly half of trans females (48%) and more than half of trans males (59%) had considered suicide, compared with 28% of cisgender males and 37% of cisgender females. The rate among nonbinary/genderqueer individuals was 53%, and it was 48% for those questioning their gender.
Current methods of identifying trans and gender-diverse (TGD) youth in the hospital, however, may not actually be capturing the entire population.
“In health care settings, research involving TGD individuals has historically been limited to specialized clinic populations or youth with gender-specific diagnostic codes documented in the electronic medical record,” an approach that “likely significantly underestimates the prevalence of TGD youth in health care settings.” While at least one study has attempted to bridge this gap by searching the EMR for keywords, that study only tried to identify trans youth and not other youth on the gender diversity spectrum, such as nonbinary youth or those questioning their gender identity. Dr. Burnside and her colleagues therefore designed a study that used keywords to identify both trans youth and other gender-diverse youth who visited the ED so they could assess the rate of positive suicide screens in this population.
Underestimating the population at risk?
The researchers conducted a retrospective cross-sectional study of EMR data for all ED visits during which the patient underwent suicide screening. For the period of November 2019 to August 2022, they collected data on the screening results and the patient’s gender identity, age, race/ethnicity, insurance status, chief complaint in the ED and child opportunity index, which assess a youth’s access to resources based on geography. The suicide screener used was the Ask Suicide–Screening Questions (ASQ) tool.
The keywords they looked for in the EMR to identify trans and gender-diverse youth included transgender, pronouns, agender, gender dysphoria, male-to-female, female-to-male, nonbinary, preferred name, and they/them (captured as a complete term, not as “they” and “them” separately).
“If a keyword was present, the surrounding text was extracted and reviewed by two members of our team,” Dr. Burnside explained in her presentation. “We categorized keywords into either indicative of gender-diverse identity or not, and if it wasn’t clear based on the text extracted, we would conduct a manual chart review,” though that only occurred in about 3% of cases, she added.
Among 15,413 ED encounters with a suicide screen, the researchers identified 1,126 of these keywords in the EMR, among which 91.2% were classified as referring to a gender-diverse patient. Nearly all of the words were at least 90% effective in identify a gender-diverse youth, Dr. Burnside said, and all of the 197 instances of “they/them” were classified as gender diverse.
The accuracy was a little lower for the two keywords that appeared most frequently: For “pronouns,” 86.3% of 306 instances were classified as gender diverse, and for “transgender,” 83.1% of 207 instances were classified as gender diverse. Since some providers ask all patients their pronouns, the presence of “pronouns” in the EMR alone did not necessarily indicate the patient was gender diverse, Dr. Burnside said. A common reason the term “transgender” occurred in the EMR of non–gender diverse patients is that the department’s list of crisis resources includes transgender hotlines.
After identifying all the keywords, the researchers determined how many of these occurred in unique ED encounters and removed those with incomplete screening. Overall, they found 565 encounters by 399 gender-diverse individuals who had a suicide screening, representing 4.6% of total visits. This percentage is slightly lower than recent population-based estimates of gender-diverse youth, the researchers noted.
This population ranged from 8 to 23 years old, and 43% were publicly insured. The chief complaint for most of the patients (77.5%) was a mental health one. They were predominantly White (43%) or Hispanic (35%), with 10% Black youth, 4% Asian youth, and 8% youth who were “other” or two or more races. About half (52%) lived in a neighborhood with a “low” or “very low” child opportunity index.
Within this population, 81% of the patients screened positive on the suicide screening, compared with 23% positive screens across all ED visits. One in ten (10%) gender-diverse youth had active suicidal ideation, compared with 3.4% of the rest of the ED patient population. The researchers calculated that gender-diverse youth had 5.35 times greater odds of screening positive than cisgender youth in the ED (95% confidence interval [CI] 8.7-15.92). Further, a quarter (25%) of the trans and gender-diverse youth who screened positive for suicide risk had come to the ED for a primary complaint unrelated to mental health.
“We had a kid who came in because he broke his arm who had active suicidal ideation,” study coauthor Jennifer A. Hoffmann, MD, assistant professor of pediatrics at the Ann & Robert H. Lurie Children’s Hospital of Chicago and Northwestern University, mentioned after the presentation. That particular patient even had a suicide plan, but was identified as actively suicidal only because of the screening. In other cases, she said, a youth may come in with self-inflicted injuries, and while those are the primary complaint, they are linked with suicidal ideation.
Among the study’s limitations are that gender identity is not necessarily being systematically assessed during visits, misspellings might have missed some youth, and their search strategy has not yet been externally validated, though they plan to seek that.
“Overall, however, this study did demonstrate that keyword searching is a promising technique to identify and prioritize gender-diverse youth in health services research,” Dr. Burnside said. In addition to showing the feasibility of using a keyword search strategy for identifying gender-diverse youth, Dr. Burnside noted that 31% of the encounters were identified by just one of the keywords they used, “highlighting the importance of using a comprehensive list of keywords to identify gender-diverse youth.”
Uncovering valuable information
Jason Rafferty, MD, MPH, EdM, clinical assistant professor of pediatrics and of psychiatry and human behavior at Brown University, Providence, R.I., who attended the presentation, noted that the study provides information on a population that’s often difficult to get through traditional EMR research methods.
“A lot of medical record systems don’t have uniform ways of capturing [gender diversity], but what we know as providers is that kids are really struggling and that it’s not a surprise that we’re seeing these disparities with suicidality,” Dr. Rafferty said.
The study also provides more discrete estimates by age than what most other current research measures, which tends to be lifetime suicidality as opposed to suicidal thoughts or attempts within the past year, Dr. Rafferty added.
”What this shows is, for adolescents, the risk of suicide is something we need to be paying attention to. Because it’s not that it’s something that only happens in adults, this really dispels a lot of the misquoting of the data that’s out there.” That kind of information is valuable for determining resource allocation, he said. “A disparity like this really underlies the importance of mental health resources in this field,” he said.
Dr. Burnside, Dr. Hoffmann, and Dr. Rafferty had no disclosures, and no external funding sources were noted.
AT AAP 2023
Can thermal biofeedback reduce pain and anxiety?
TOPLINE:
A novel handheld tool may hold promise for reducing anxiety and pain and improving sleep quality, according to research presented at Lifestyle Medicine 2023, the annual meeting of the American College of Lifestyle Medicine.
METHODOLOGY:
- Franklin Somchith Ly, a PhD candidate in mechanical engineering at the University of California, Santa Barbara, developed , a product that assesses blood flow to the hand with an infrared temperature sensor and changes color as blood vessels expand during relaxation.
- Exercises such as intentional breathwork, visualization, and muscle relaxation change the color displayed by the device.
- Mr. Ly examined how measures of anxiety, sleep quality, and chronic pain changed after participants used the instrument. Ten participants completed a study assessing anxiety. Eight participants were enrolled in a sleep study where they completed biofeedback sessions before bed for 2 weeks, and 15 participants performed biofeedback twice daily and reported their levels of anxiety and pain.
TAKEAWAY:
- Anxiety scores decreased by about 22% on average (P < .001).
- Seven of the eight participants in the sleep study had improved scores on the Pittsburgh Sleep Quality Index, with an average improvement of nearly 30% (P < .05). Daytime dysfunction improved by 58% (P < .01).
- In the chronic pain study, about 60% of the 350 biofeedback sessions led to reduced pain.
IN PRACTICE:
“These portable devices may aid lifestyle management by alleviating anxiety, chronic pain, and enhancing daytime energy,” Mr. Ly said. “The results support their integration into lifestyle medicine and integrative medicine.”
SOURCE:
Mr. Ly presented the findings as a poster at Lifestyle Medicine 2023, which took place Oct. 29 to Nov. 1 in Denver and online.
LIMITATIONS:
The studies were open label and did not include control groups.
DISCLOSURES:
Mr. Ly is the founder of CalmStone, which markets a thermal biofeedback device. The research was supported by the Bill and Melinda Gates Foundation and the U.S. Army Research Office and Institute for Collaborative Biotechnologies.
A version of this article first appeared on Medscape.com.
TOPLINE:
A novel handheld tool may hold promise for reducing anxiety and pain and improving sleep quality, according to research presented at Lifestyle Medicine 2023, the annual meeting of the American College of Lifestyle Medicine.
METHODOLOGY:
- Franklin Somchith Ly, a PhD candidate in mechanical engineering at the University of California, Santa Barbara, developed , a product that assesses blood flow to the hand with an infrared temperature sensor and changes color as blood vessels expand during relaxation.
- Exercises such as intentional breathwork, visualization, and muscle relaxation change the color displayed by the device.
- Mr. Ly examined how measures of anxiety, sleep quality, and chronic pain changed after participants used the instrument. Ten participants completed a study assessing anxiety. Eight participants were enrolled in a sleep study where they completed biofeedback sessions before bed for 2 weeks, and 15 participants performed biofeedback twice daily and reported their levels of anxiety and pain.
TAKEAWAY:
- Anxiety scores decreased by about 22% on average (P < .001).
- Seven of the eight participants in the sleep study had improved scores on the Pittsburgh Sleep Quality Index, with an average improvement of nearly 30% (P < .05). Daytime dysfunction improved by 58% (P < .01).
- In the chronic pain study, about 60% of the 350 biofeedback sessions led to reduced pain.
IN PRACTICE:
“These portable devices may aid lifestyle management by alleviating anxiety, chronic pain, and enhancing daytime energy,” Mr. Ly said. “The results support their integration into lifestyle medicine and integrative medicine.”
SOURCE:
Mr. Ly presented the findings as a poster at Lifestyle Medicine 2023, which took place Oct. 29 to Nov. 1 in Denver and online.
LIMITATIONS:
The studies were open label and did not include control groups.
DISCLOSURES:
Mr. Ly is the founder of CalmStone, which markets a thermal biofeedback device. The research was supported by the Bill and Melinda Gates Foundation and the U.S. Army Research Office and Institute for Collaborative Biotechnologies.
A version of this article first appeared on Medscape.com.
TOPLINE:
A novel handheld tool may hold promise for reducing anxiety and pain and improving sleep quality, according to research presented at Lifestyle Medicine 2023, the annual meeting of the American College of Lifestyle Medicine.
METHODOLOGY:
- Franklin Somchith Ly, a PhD candidate in mechanical engineering at the University of California, Santa Barbara, developed , a product that assesses blood flow to the hand with an infrared temperature sensor and changes color as blood vessels expand during relaxation.
- Exercises such as intentional breathwork, visualization, and muscle relaxation change the color displayed by the device.
- Mr. Ly examined how measures of anxiety, sleep quality, and chronic pain changed after participants used the instrument. Ten participants completed a study assessing anxiety. Eight participants were enrolled in a sleep study where they completed biofeedback sessions before bed for 2 weeks, and 15 participants performed biofeedback twice daily and reported their levels of anxiety and pain.
TAKEAWAY:
- Anxiety scores decreased by about 22% on average (P < .001).
- Seven of the eight participants in the sleep study had improved scores on the Pittsburgh Sleep Quality Index, with an average improvement of nearly 30% (P < .05). Daytime dysfunction improved by 58% (P < .01).
- In the chronic pain study, about 60% of the 350 biofeedback sessions led to reduced pain.
IN PRACTICE:
“These portable devices may aid lifestyle management by alleviating anxiety, chronic pain, and enhancing daytime energy,” Mr. Ly said. “The results support their integration into lifestyle medicine and integrative medicine.”
SOURCE:
Mr. Ly presented the findings as a poster at Lifestyle Medicine 2023, which took place Oct. 29 to Nov. 1 in Denver and online.
LIMITATIONS:
The studies were open label and did not include control groups.
DISCLOSURES:
Mr. Ly is the founder of CalmStone, which markets a thermal biofeedback device. The research was supported by the Bill and Melinda Gates Foundation and the U.S. Army Research Office and Institute for Collaborative Biotechnologies.
A version of this article first appeared on Medscape.com.
Perinatal depression rarely stands alone
Mental health conditions are the leading cause of pregnancy-related death in Illinois (40%) and across the United States (21%).1,2 Funding bodies, such as the Agency for Healthcare Research and Quality3 and the Health Resources and Service Administration,4 have spotlights on improving screening and access to care for depression and substance use disorders (SUDs). However, the needs of individuals with multiple mental health conditions still often go unrecognized and unaddressed in perinatal health settings.
The U.S. Preventive Services Task Force recommends that all adults be screened for depression, alcohol use, and drug use, and will be recommending screening for anxiety.5,6 The American College of Obstetrics and Gynecology recommends screening for perinatal mental health conditions including depression, anxiety, bipolar disorder, acute postpartum psychosis, and suicidality; however, despite these recommendations, screening and treatment for comorbid mental health disorders during pregnancy and the postpartum is not standard practice.7
Addressing perinatal mental health is critical because untreated mental health conditions during the perinatal period can cause long-term adverse psychiatric and medical outcomes for the birthing person, the baby, and the family.8 This commentary highlights the importance of recognizing and screening for perinatal mental health comorbidities, improving referral rates for mental health treatment, and raising awareness of the importance of addressing rural perinatal mental health.
Perinatal mental health comorbidities
Major depressive disorder is the most common mental health condition during the perinatal period9 and is often comorbid.10-12 In “Perinatal mental health in low-income urban and rural patients: The importance of screening for comorbidities,” Craemer et al.13 reported that nearly half of the perinatal patients who screened positive for MDD also screened positive for at least one other mental health condition, among them general anxiety disorder (GAD), SUD, posttraumatic stress disorder (PTSD), and suicidality.
Many (9%) of the perinatal patients with MDD had a severe comorbidity profile characterized by four diagnoses – MDD, GAD, SUD, and PTSD. In routine medical care these comorbidities often go undetected even though the risk to mothers and babies increases with more severe mental health symptoms.8
The high frequency of perinatal mental health comorbidities Craemer et al.13 found demonstrates a compelling need for comorbid mental health screening during the perinatal period, particularly for low-income Black, Hispanic, and rural birthing persons. Positive screens for perinatal mental health disorders may reflect the onset of these disorders in pregnancy or the postpartum, or preexisting disorders that have gone undetected or untreated before pregnancy.
For many patients, the perinatal period is the first time they are screened for any mental health disorder; typically, they are screened solely for depression. Screening alone can have a positive impact on perinatal mental health. In fact, the USPSTF found that programs to screen perinatal patients, with or without treatment-related support, resulted in a 2%-9% absolute reduction in depression prevalence.14 However, screening for MDD is too infrequent for many reasons, including the logistics of integrating screening into the clinic workflow and limited provider availability, time, and training in mental health.
We recommend screening perinatal patients for mental health comorbidities. This recommendation may seem impractical given the lack of screening tools for comorbid mental health conditions; however, the Computerized Adaptive Test for Mental Health (CAT-MH), the validated tool15-17 used in this study, is an ideal option. CAT-MH is uniquely capable of screening for MDD, GAD, PTSD, SUD, and suicidality in one platform and is routinely used in diverse settings including the Veterans Administration,18 foster care,19 and universities.20 The main limitation of this more comprehensive screening is that it takes about 10 minutes per patient. However, CAT-MH is self-administered and can be done in the waiting room or on a mobile device prior to a clinic visit.
CAT-MH can also be easily integrated into clinical workflow when added to the Electronic Medical Record21, and is a more comprehensive tool than existing perinatal depression tools such as the Perinatal Health Questionaire-9 (PHQ-9) and Edinburgh Perinatal Depression Scale (EPDS).22 Another limitation is cost – currently $5.00 per assessment – however, this is less than routine blood work.23 If CAT-MH is not an option, we recommend a stepped approach of screening for GAD when perinatal patients screen positive for MDD, as this is the most common comorbidity profile. The GAD-7 is a free and widely available tool.24
Barriers to care
In Craemer et al,13 nearly two-thirds (64.9%) of perinatal patients with a positive screen did not receive a referral to follow-up care or a medication prescription. These low referral rates may reflect a variety of widely recognized barriers to care, including lack of referral options, provider and/or patient reluctance to pursue referrals, barriers to insurance coverage, or inadequate behavioral health infrastructure to ensure referral and diagnostic follow-up.
Further, rural residing perinatal patients are an underserved population that need more resources and screening. Despite an on-site behavioral specialist at the rural clinic, Craemer et al13 found a stark disparity in referral rates: referrals to treatment for a positive diagnosis was over two times less at the rural clinic (23.9%), compared with the urban clinics (51.6%). The most common treatment offered at the rural clinic was a prescription for medication (17.4%), while referral to follow-up care was the most common at the urban clinics (35.5%). Rural areas not only have a shortage of health care providers, but community members seeking mental health care often encounter greater stigma, compared with urban residents.25,26
These data highlight an unmet need for referrals to treatment for patients in rural communities, particularly in Illinois where the pregnancy-related mortality ratio attributable to mental health conditions is three times greater in rural areas, compared with those residing in urban Cook County (Chicago).2 Increasing access and availability to mental health treatment and prevention resources in Illinois, especially in rural areas, is an opportunity to prevent pregnancy-related mortality attributable to mental health conditions.
Overall, there is a critical need for screening for perinatal mental health comorbidities, increased attention to low rates of referral to mental health treatment, and investing in rural perinatal mental health. Addressing perinatal mental health disorders is key to decreasing the burden of maternal mortality, particularly in Illinois.
Ms. Craemer and Ms. Sayah are senior research specialists at the Center for Research on Women & Gender, University of Illinois at Chicago. Dr. Duffecy is a professor of clinical psychiatry at the University of Illinois at Chicago. Dr. Geller is a professor of obstetrics & gynecology and director of the Center for Research on Women & Gender, University of Illinois at Chicago. Dr. Maki is a professor of psychiatry, psychology, and obstetrics & gynecology at the University of Illinois at Chicago.
References
1. Trost S et al. Pregnancy-related deaths: Data from maternal mortality review committees in 36 states, 2017-2019. Atlanta: Centers for Disease Control and Prevention, U.S. Department of Health & Human Services, 2022.
2. Illinois Department of Public Health. Illinois maternal morbidity and mortality report 2016-2017. 2021.
3. AHRQ. Funding opportunities to address opioid and other substance use disorders. Updated 2023.
4. HRSA. Screening and treatment for maternal mental health and substance use disorders.
5. U.S. Preventive Services Task Force. Recommendations for primary care practice. Accessed May 26, 2023.
6. U.S. Preventive Services Task Force. Draft recommendation statement: Anxiety in adults: Screening. 2022.
7. ACOG. Screening and diagnosis of mental health conditions during pregnancy and postpartum. Clinical Practice Guideline. Number 4. 2023 June.
8. Meltzer-Brody S and Stuebe A. The long-term psychiatric and medical prognosis of perinatal mental illness. Best Pract Res Clin Obstet Gynaecol. 2014 Jan. doi: 10.1016/j.bpobgyn.2013.08.009.
9. Van Niel MS and Payne JL. Perinatal depression: A review. Cleve Clin J Med. 2020 May. doi: 10.3949/ccjm.87a.19054.
10. Wisner KL et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. 2013 May. doi: 10.1001/jamapsychiatry.2013.87.
11. Falah-Hassani K et al. The prevalence of antenatal and postnatal co-morbid anxiety and depression: A meta-analysis. Psychol Med. 2017 Sep. doi: 10.1017/S0033291717000617.
12. Pentecost R et al. Scoping review of the associations between perinatal substance use and perinatal depression and anxiety. J Obstet Gynecol Neonatal Nurs. 2021 Jul. doi: 10.1016/j.jogn.2021.02.008.
13. Craemer KA et al. Perinatal mental health in low-income urban and rural patients: The importance of screening for comorbidities. Gen Hosp Psychiatry. 2023 Jul-Aug. doi: 10.1016/j.genhosppsych.2023.05.007.
14. O’Connor E et al. Primary care screening for and treatment of depression in pregnant and postpartum women: Evidence report and systematic review for the U.S. Preventive Services Task Force. JAMA. 2016 Jan 26. doi: 10.1001/jama.2015.18948.
15. Kozhimannil KB et al. Racial and ethnic disparities in postpartum depression care among low-income women. Psychiatr Serv. 2011 Jun. doi: 10.1176/ps.62.6.pss6206_0619.
16. Wenzel ES et al. Depression and anxiety symptoms across pregnancy and the postpartum in low-income Black and Latina women. Arch Womens Ment Health. 2021 Dec. doi: 10.1007/s00737-021-01139-y.
17. Gibbons RD et al. Development of a computerized adaptive substance use disorder scale for screening and measurement: The CAT‐SUD. Addiction. 2020 Jul. doi: 10.1111/add.14938.
18. Brenner LA et al. Validation of a computerized adaptive test suicide scale (CAT-SS) among united states military veterans. PloS One. 2022 Jan 21. doi: 10.1371/journal.pone.0261920.
19. The Center for State Child Welfare Data. Using technology to diagnose and report on behavioral health challenges facing foster youth. 2018.
20. Kim JJ et al. The experience of depression, anxiety, and mania among perinatal women. Arch Womens Ment Health. 2016 Oct. doi: 10.1007/s00737-016-0632-6.
21. Tepper MC et al. Toward population health: Using a learning behavioral health system and measurement-based care to improve access, care, outcomes, and disparities. Community Ment Health J. 2022 Nov. doi: 10.1007/s10597-022-00957-3.
22. Wenzel E et al. Using computerised adaptive tests to screen for perinatal depression in underserved women of colour. Evid Based Ment Health. 2022 Feb. doi: 10.1136/ebmental-2021-300262.
23. Sanger-Katz M. They want it to be secret: How a common blood test can cost $11 or almost $1,000. New York Times. 2019 Apr 19.
24. Spitzer RL et al. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med. 2006 May 22. doi: 10.1001/archinte.166.10.1092.
25. Mollard E et al. An integrative review of postpartum depression in rural US communities. Arch Psychiatr Nurs. 2016 Jun. doi: 10.1016/j.apnu.2015.12.003.
26. Anglim AJ and Radke SM. Rural maternal health care outcomes, drivers, and patient perspectives. Clin Obstet Gynecol. 2022 Dec 1. doi: 10.1097/GRF.0000000000000753.
Mental health conditions are the leading cause of pregnancy-related death in Illinois (40%) and across the United States (21%).1,2 Funding bodies, such as the Agency for Healthcare Research and Quality3 and the Health Resources and Service Administration,4 have spotlights on improving screening and access to care for depression and substance use disorders (SUDs). However, the needs of individuals with multiple mental health conditions still often go unrecognized and unaddressed in perinatal health settings.
The U.S. Preventive Services Task Force recommends that all adults be screened for depression, alcohol use, and drug use, and will be recommending screening for anxiety.5,6 The American College of Obstetrics and Gynecology recommends screening for perinatal mental health conditions including depression, anxiety, bipolar disorder, acute postpartum psychosis, and suicidality; however, despite these recommendations, screening and treatment for comorbid mental health disorders during pregnancy and the postpartum is not standard practice.7
Addressing perinatal mental health is critical because untreated mental health conditions during the perinatal period can cause long-term adverse psychiatric and medical outcomes for the birthing person, the baby, and the family.8 This commentary highlights the importance of recognizing and screening for perinatal mental health comorbidities, improving referral rates for mental health treatment, and raising awareness of the importance of addressing rural perinatal mental health.
Perinatal mental health comorbidities
Major depressive disorder is the most common mental health condition during the perinatal period9 and is often comorbid.10-12 In “Perinatal mental health in low-income urban and rural patients: The importance of screening for comorbidities,” Craemer et al.13 reported that nearly half of the perinatal patients who screened positive for MDD also screened positive for at least one other mental health condition, among them general anxiety disorder (GAD), SUD, posttraumatic stress disorder (PTSD), and suicidality.
Many (9%) of the perinatal patients with MDD had a severe comorbidity profile characterized by four diagnoses – MDD, GAD, SUD, and PTSD. In routine medical care these comorbidities often go undetected even though the risk to mothers and babies increases with more severe mental health symptoms.8
The high frequency of perinatal mental health comorbidities Craemer et al.13 found demonstrates a compelling need for comorbid mental health screening during the perinatal period, particularly for low-income Black, Hispanic, and rural birthing persons. Positive screens for perinatal mental health disorders may reflect the onset of these disorders in pregnancy or the postpartum, or preexisting disorders that have gone undetected or untreated before pregnancy.
For many patients, the perinatal period is the first time they are screened for any mental health disorder; typically, they are screened solely for depression. Screening alone can have a positive impact on perinatal mental health. In fact, the USPSTF found that programs to screen perinatal patients, with or without treatment-related support, resulted in a 2%-9% absolute reduction in depression prevalence.14 However, screening for MDD is too infrequent for many reasons, including the logistics of integrating screening into the clinic workflow and limited provider availability, time, and training in mental health.
We recommend screening perinatal patients for mental health comorbidities. This recommendation may seem impractical given the lack of screening tools for comorbid mental health conditions; however, the Computerized Adaptive Test for Mental Health (CAT-MH), the validated tool15-17 used in this study, is an ideal option. CAT-MH is uniquely capable of screening for MDD, GAD, PTSD, SUD, and suicidality in one platform and is routinely used in diverse settings including the Veterans Administration,18 foster care,19 and universities.20 The main limitation of this more comprehensive screening is that it takes about 10 minutes per patient. However, CAT-MH is self-administered and can be done in the waiting room or on a mobile device prior to a clinic visit.
CAT-MH can also be easily integrated into clinical workflow when added to the Electronic Medical Record21, and is a more comprehensive tool than existing perinatal depression tools such as the Perinatal Health Questionaire-9 (PHQ-9) and Edinburgh Perinatal Depression Scale (EPDS).22 Another limitation is cost – currently $5.00 per assessment – however, this is less than routine blood work.23 If CAT-MH is not an option, we recommend a stepped approach of screening for GAD when perinatal patients screen positive for MDD, as this is the most common comorbidity profile. The GAD-7 is a free and widely available tool.24
Barriers to care
In Craemer et al,13 nearly two-thirds (64.9%) of perinatal patients with a positive screen did not receive a referral to follow-up care or a medication prescription. These low referral rates may reflect a variety of widely recognized barriers to care, including lack of referral options, provider and/or patient reluctance to pursue referrals, barriers to insurance coverage, or inadequate behavioral health infrastructure to ensure referral and diagnostic follow-up.
Further, rural residing perinatal patients are an underserved population that need more resources and screening. Despite an on-site behavioral specialist at the rural clinic, Craemer et al13 found a stark disparity in referral rates: referrals to treatment for a positive diagnosis was over two times less at the rural clinic (23.9%), compared with the urban clinics (51.6%). The most common treatment offered at the rural clinic was a prescription for medication (17.4%), while referral to follow-up care was the most common at the urban clinics (35.5%). Rural areas not only have a shortage of health care providers, but community members seeking mental health care often encounter greater stigma, compared with urban residents.25,26
These data highlight an unmet need for referrals to treatment for patients in rural communities, particularly in Illinois where the pregnancy-related mortality ratio attributable to mental health conditions is three times greater in rural areas, compared with those residing in urban Cook County (Chicago).2 Increasing access and availability to mental health treatment and prevention resources in Illinois, especially in rural areas, is an opportunity to prevent pregnancy-related mortality attributable to mental health conditions.
Overall, there is a critical need for screening for perinatal mental health comorbidities, increased attention to low rates of referral to mental health treatment, and investing in rural perinatal mental health. Addressing perinatal mental health disorders is key to decreasing the burden of maternal mortality, particularly in Illinois.
Ms. Craemer and Ms. Sayah are senior research specialists at the Center for Research on Women & Gender, University of Illinois at Chicago. Dr. Duffecy is a professor of clinical psychiatry at the University of Illinois at Chicago. Dr. Geller is a professor of obstetrics & gynecology and director of the Center for Research on Women & Gender, University of Illinois at Chicago. Dr. Maki is a professor of psychiatry, psychology, and obstetrics & gynecology at the University of Illinois at Chicago.
References
1. Trost S et al. Pregnancy-related deaths: Data from maternal mortality review committees in 36 states, 2017-2019. Atlanta: Centers for Disease Control and Prevention, U.S. Department of Health & Human Services, 2022.
2. Illinois Department of Public Health. Illinois maternal morbidity and mortality report 2016-2017. 2021.
3. AHRQ. Funding opportunities to address opioid and other substance use disorders. Updated 2023.
4. HRSA. Screening and treatment for maternal mental health and substance use disorders.
5. U.S. Preventive Services Task Force. Recommendations for primary care practice. Accessed May 26, 2023.
6. U.S. Preventive Services Task Force. Draft recommendation statement: Anxiety in adults: Screening. 2022.
7. ACOG. Screening and diagnosis of mental health conditions during pregnancy and postpartum. Clinical Practice Guideline. Number 4. 2023 June.
8. Meltzer-Brody S and Stuebe A. The long-term psychiatric and medical prognosis of perinatal mental illness. Best Pract Res Clin Obstet Gynaecol. 2014 Jan. doi: 10.1016/j.bpobgyn.2013.08.009.
9. Van Niel MS and Payne JL. Perinatal depression: A review. Cleve Clin J Med. 2020 May. doi: 10.3949/ccjm.87a.19054.
10. Wisner KL et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. 2013 May. doi: 10.1001/jamapsychiatry.2013.87.
11. Falah-Hassani K et al. The prevalence of antenatal and postnatal co-morbid anxiety and depression: A meta-analysis. Psychol Med. 2017 Sep. doi: 10.1017/S0033291717000617.
12. Pentecost R et al. Scoping review of the associations between perinatal substance use and perinatal depression and anxiety. J Obstet Gynecol Neonatal Nurs. 2021 Jul. doi: 10.1016/j.jogn.2021.02.008.
13. Craemer KA et al. Perinatal mental health in low-income urban and rural patients: The importance of screening for comorbidities. Gen Hosp Psychiatry. 2023 Jul-Aug. doi: 10.1016/j.genhosppsych.2023.05.007.
14. O’Connor E et al. Primary care screening for and treatment of depression in pregnant and postpartum women: Evidence report and systematic review for the U.S. Preventive Services Task Force. JAMA. 2016 Jan 26. doi: 10.1001/jama.2015.18948.
15. Kozhimannil KB et al. Racial and ethnic disparities in postpartum depression care among low-income women. Psychiatr Serv. 2011 Jun. doi: 10.1176/ps.62.6.pss6206_0619.
16. Wenzel ES et al. Depression and anxiety symptoms across pregnancy and the postpartum in low-income Black and Latina women. Arch Womens Ment Health. 2021 Dec. doi: 10.1007/s00737-021-01139-y.
17. Gibbons RD et al. Development of a computerized adaptive substance use disorder scale for screening and measurement: The CAT‐SUD. Addiction. 2020 Jul. doi: 10.1111/add.14938.
18. Brenner LA et al. Validation of a computerized adaptive test suicide scale (CAT-SS) among united states military veterans. PloS One. 2022 Jan 21. doi: 10.1371/journal.pone.0261920.
19. The Center for State Child Welfare Data. Using technology to diagnose and report on behavioral health challenges facing foster youth. 2018.
20. Kim JJ et al. The experience of depression, anxiety, and mania among perinatal women. Arch Womens Ment Health. 2016 Oct. doi: 10.1007/s00737-016-0632-6.
21. Tepper MC et al. Toward population health: Using a learning behavioral health system and measurement-based care to improve access, care, outcomes, and disparities. Community Ment Health J. 2022 Nov. doi: 10.1007/s10597-022-00957-3.
22. Wenzel E et al. Using computerised adaptive tests to screen for perinatal depression in underserved women of colour. Evid Based Ment Health. 2022 Feb. doi: 10.1136/ebmental-2021-300262.
23. Sanger-Katz M. They want it to be secret: How a common blood test can cost $11 or almost $1,000. New York Times. 2019 Apr 19.
24. Spitzer RL et al. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med. 2006 May 22. doi: 10.1001/archinte.166.10.1092.
25. Mollard E et al. An integrative review of postpartum depression in rural US communities. Arch Psychiatr Nurs. 2016 Jun. doi: 10.1016/j.apnu.2015.12.003.
26. Anglim AJ and Radke SM. Rural maternal health care outcomes, drivers, and patient perspectives. Clin Obstet Gynecol. 2022 Dec 1. doi: 10.1097/GRF.0000000000000753.
Mental health conditions are the leading cause of pregnancy-related death in Illinois (40%) and across the United States (21%).1,2 Funding bodies, such as the Agency for Healthcare Research and Quality3 and the Health Resources and Service Administration,4 have spotlights on improving screening and access to care for depression and substance use disorders (SUDs). However, the needs of individuals with multiple mental health conditions still often go unrecognized and unaddressed in perinatal health settings.
The U.S. Preventive Services Task Force recommends that all adults be screened for depression, alcohol use, and drug use, and will be recommending screening for anxiety.5,6 The American College of Obstetrics and Gynecology recommends screening for perinatal mental health conditions including depression, anxiety, bipolar disorder, acute postpartum psychosis, and suicidality; however, despite these recommendations, screening and treatment for comorbid mental health disorders during pregnancy and the postpartum is not standard practice.7
Addressing perinatal mental health is critical because untreated mental health conditions during the perinatal period can cause long-term adverse psychiatric and medical outcomes for the birthing person, the baby, and the family.8 This commentary highlights the importance of recognizing and screening for perinatal mental health comorbidities, improving referral rates for mental health treatment, and raising awareness of the importance of addressing rural perinatal mental health.
Perinatal mental health comorbidities
Major depressive disorder is the most common mental health condition during the perinatal period9 and is often comorbid.10-12 In “Perinatal mental health in low-income urban and rural patients: The importance of screening for comorbidities,” Craemer et al.13 reported that nearly half of the perinatal patients who screened positive for MDD also screened positive for at least one other mental health condition, among them general anxiety disorder (GAD), SUD, posttraumatic stress disorder (PTSD), and suicidality.
Many (9%) of the perinatal patients with MDD had a severe comorbidity profile characterized by four diagnoses – MDD, GAD, SUD, and PTSD. In routine medical care these comorbidities often go undetected even though the risk to mothers and babies increases with more severe mental health symptoms.8
The high frequency of perinatal mental health comorbidities Craemer et al.13 found demonstrates a compelling need for comorbid mental health screening during the perinatal period, particularly for low-income Black, Hispanic, and rural birthing persons. Positive screens for perinatal mental health disorders may reflect the onset of these disorders in pregnancy or the postpartum, or preexisting disorders that have gone undetected or untreated before pregnancy.
For many patients, the perinatal period is the first time they are screened for any mental health disorder; typically, they are screened solely for depression. Screening alone can have a positive impact on perinatal mental health. In fact, the USPSTF found that programs to screen perinatal patients, with or without treatment-related support, resulted in a 2%-9% absolute reduction in depression prevalence.14 However, screening for MDD is too infrequent for many reasons, including the logistics of integrating screening into the clinic workflow and limited provider availability, time, and training in mental health.
We recommend screening perinatal patients for mental health comorbidities. This recommendation may seem impractical given the lack of screening tools for comorbid mental health conditions; however, the Computerized Adaptive Test for Mental Health (CAT-MH), the validated tool15-17 used in this study, is an ideal option. CAT-MH is uniquely capable of screening for MDD, GAD, PTSD, SUD, and suicidality in one platform and is routinely used in diverse settings including the Veterans Administration,18 foster care,19 and universities.20 The main limitation of this more comprehensive screening is that it takes about 10 minutes per patient. However, CAT-MH is self-administered and can be done in the waiting room or on a mobile device prior to a clinic visit.
CAT-MH can also be easily integrated into clinical workflow when added to the Electronic Medical Record21, and is a more comprehensive tool than existing perinatal depression tools such as the Perinatal Health Questionaire-9 (PHQ-9) and Edinburgh Perinatal Depression Scale (EPDS).22 Another limitation is cost – currently $5.00 per assessment – however, this is less than routine blood work.23 If CAT-MH is not an option, we recommend a stepped approach of screening for GAD when perinatal patients screen positive for MDD, as this is the most common comorbidity profile. The GAD-7 is a free and widely available tool.24
Barriers to care
In Craemer et al,13 nearly two-thirds (64.9%) of perinatal patients with a positive screen did not receive a referral to follow-up care or a medication prescription. These low referral rates may reflect a variety of widely recognized barriers to care, including lack of referral options, provider and/or patient reluctance to pursue referrals, barriers to insurance coverage, or inadequate behavioral health infrastructure to ensure referral and diagnostic follow-up.
Further, rural residing perinatal patients are an underserved population that need more resources and screening. Despite an on-site behavioral specialist at the rural clinic, Craemer et al13 found a stark disparity in referral rates: referrals to treatment for a positive diagnosis was over two times less at the rural clinic (23.9%), compared with the urban clinics (51.6%). The most common treatment offered at the rural clinic was a prescription for medication (17.4%), while referral to follow-up care was the most common at the urban clinics (35.5%). Rural areas not only have a shortage of health care providers, but community members seeking mental health care often encounter greater stigma, compared with urban residents.25,26
These data highlight an unmet need for referrals to treatment for patients in rural communities, particularly in Illinois where the pregnancy-related mortality ratio attributable to mental health conditions is three times greater in rural areas, compared with those residing in urban Cook County (Chicago).2 Increasing access and availability to mental health treatment and prevention resources in Illinois, especially in rural areas, is an opportunity to prevent pregnancy-related mortality attributable to mental health conditions.
Overall, there is a critical need for screening for perinatal mental health comorbidities, increased attention to low rates of referral to mental health treatment, and investing in rural perinatal mental health. Addressing perinatal mental health disorders is key to decreasing the burden of maternal mortality, particularly in Illinois.
Ms. Craemer and Ms. Sayah are senior research specialists at the Center for Research on Women & Gender, University of Illinois at Chicago. Dr. Duffecy is a professor of clinical psychiatry at the University of Illinois at Chicago. Dr. Geller is a professor of obstetrics & gynecology and director of the Center for Research on Women & Gender, University of Illinois at Chicago. Dr. Maki is a professor of psychiatry, psychology, and obstetrics & gynecology at the University of Illinois at Chicago.
References
1. Trost S et al. Pregnancy-related deaths: Data from maternal mortality review committees in 36 states, 2017-2019. Atlanta: Centers for Disease Control and Prevention, U.S. Department of Health & Human Services, 2022.
2. Illinois Department of Public Health. Illinois maternal morbidity and mortality report 2016-2017. 2021.
3. AHRQ. Funding opportunities to address opioid and other substance use disorders. Updated 2023.
4. HRSA. Screening and treatment for maternal mental health and substance use disorders.
5. U.S. Preventive Services Task Force. Recommendations for primary care practice. Accessed May 26, 2023.
6. U.S. Preventive Services Task Force. Draft recommendation statement: Anxiety in adults: Screening. 2022.
7. ACOG. Screening and diagnosis of mental health conditions during pregnancy and postpartum. Clinical Practice Guideline. Number 4. 2023 June.
8. Meltzer-Brody S and Stuebe A. The long-term psychiatric and medical prognosis of perinatal mental illness. Best Pract Res Clin Obstet Gynaecol. 2014 Jan. doi: 10.1016/j.bpobgyn.2013.08.009.
9. Van Niel MS and Payne JL. Perinatal depression: A review. Cleve Clin J Med. 2020 May. doi: 10.3949/ccjm.87a.19054.
10. Wisner KL et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. 2013 May. doi: 10.1001/jamapsychiatry.2013.87.
11. Falah-Hassani K et al. The prevalence of antenatal and postnatal co-morbid anxiety and depression: A meta-analysis. Psychol Med. 2017 Sep. doi: 10.1017/S0033291717000617.
12. Pentecost R et al. Scoping review of the associations between perinatal substance use and perinatal depression and anxiety. J Obstet Gynecol Neonatal Nurs. 2021 Jul. doi: 10.1016/j.jogn.2021.02.008.
13. Craemer KA et al. Perinatal mental health in low-income urban and rural patients: The importance of screening for comorbidities. Gen Hosp Psychiatry. 2023 Jul-Aug. doi: 10.1016/j.genhosppsych.2023.05.007.
14. O’Connor E et al. Primary care screening for and treatment of depression in pregnant and postpartum women: Evidence report and systematic review for the U.S. Preventive Services Task Force. JAMA. 2016 Jan 26. doi: 10.1001/jama.2015.18948.
15. Kozhimannil KB et al. Racial and ethnic disparities in postpartum depression care among low-income women. Psychiatr Serv. 2011 Jun. doi: 10.1176/ps.62.6.pss6206_0619.
16. Wenzel ES et al. Depression and anxiety symptoms across pregnancy and the postpartum in low-income Black and Latina women. Arch Womens Ment Health. 2021 Dec. doi: 10.1007/s00737-021-01139-y.
17. Gibbons RD et al. Development of a computerized adaptive substance use disorder scale for screening and measurement: The CAT‐SUD. Addiction. 2020 Jul. doi: 10.1111/add.14938.
18. Brenner LA et al. Validation of a computerized adaptive test suicide scale (CAT-SS) among united states military veterans. PloS One. 2022 Jan 21. doi: 10.1371/journal.pone.0261920.
19. The Center for State Child Welfare Data. Using technology to diagnose and report on behavioral health challenges facing foster youth. 2018.
20. Kim JJ et al. The experience of depression, anxiety, and mania among perinatal women. Arch Womens Ment Health. 2016 Oct. doi: 10.1007/s00737-016-0632-6.
21. Tepper MC et al. Toward population health: Using a learning behavioral health system and measurement-based care to improve access, care, outcomes, and disparities. Community Ment Health J. 2022 Nov. doi: 10.1007/s10597-022-00957-3.
22. Wenzel E et al. Using computerised adaptive tests to screen for perinatal depression in underserved women of colour. Evid Based Ment Health. 2022 Feb. doi: 10.1136/ebmental-2021-300262.
23. Sanger-Katz M. They want it to be secret: How a common blood test can cost $11 or almost $1,000. New York Times. 2019 Apr 19.
24. Spitzer RL et al. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med. 2006 May 22. doi: 10.1001/archinte.166.10.1092.
25. Mollard E et al. An integrative review of postpartum depression in rural US communities. Arch Psychiatr Nurs. 2016 Jun. doi: 10.1016/j.apnu.2015.12.003.
26. Anglim AJ and Radke SM. Rural maternal health care outcomes, drivers, and patient perspectives. Clin Obstet Gynecol. 2022 Dec 1. doi: 10.1097/GRF.0000000000000753.
Serious mental illness tied to 50% higher all-cause mortality risk after COVID
TOPLINE:
METHODOLOGY:
- Investigators analyzed data from the Clinical Practice Research Datalink database, which contains health information on 13.5 million patients receiving care from family practices in England and Northern Ireland.
- The study included participants with SMI, including schizophrenia, schizoaffective disorder, and bipolar disorder.
- Participants were aged 5 years or older with a SARS-CoV-2 infection recorded between Feb. 1, 2020, and March 31, 2021, spanning two waves of the pandemic.
- Death rates among participants with SMI and COVID-19 (n = 7,150; 56% female) were compared with those in a control group of participants without SMI who had been diagnosed with COVID-19 (n = 650,000; 55% female).
TAKEAWAY:
- Participants with SMI and COVID-19 had a 53% higher risk for death than those in the non-SMI control group (adjusted hazard ratio, 1.53; 95% confidence interval, 1.39-1.68).
- Black Caribbean/Black African participants were more likely than White participants to die of COVID-19 (aHR, 1.22; 95% CI, 1.12-1.34), although ethnicity was not recorded in 30% of participants.
- After SARS-CoV-2 infection, for every additional multimorbid condition, the aHR for death increased by 6% in the SMI group and 16% in the non-SMI group (P = .001). Some of these conditions included hypertension, heart disease, diabetes, kidney disease, depression, and anxiety.
IN PRACTICE:
“From a public health perspective, our study has emphasized the need for early and timely preventative interventions (e.g. vaccination) for the SMI population. Future studies are needed to disentangle the complex biological and psychosocial factors, and health care pathways, that have led to the greater mortality rates in the SMI population,” the authors write.
SOURCE:
Jayati Das-Munshi, MD, of Kings College London, led the study, which was published online in the British Journal of Psychiatry. The study was funded by the Health Foundation.
LIMITATIONS:
COVID-19 may have been underdiagnosed or underreported in the records studied. Also, investigators did not have information about cause of death.
DISCLOSURES:
One author received funding from Janssen, GSK, and Takeda. All other authors declared no conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Investigators analyzed data from the Clinical Practice Research Datalink database, which contains health information on 13.5 million patients receiving care from family practices in England and Northern Ireland.
- The study included participants with SMI, including schizophrenia, schizoaffective disorder, and bipolar disorder.
- Participants were aged 5 years or older with a SARS-CoV-2 infection recorded between Feb. 1, 2020, and March 31, 2021, spanning two waves of the pandemic.
- Death rates among participants with SMI and COVID-19 (n = 7,150; 56% female) were compared with those in a control group of participants without SMI who had been diagnosed with COVID-19 (n = 650,000; 55% female).
TAKEAWAY:
- Participants with SMI and COVID-19 had a 53% higher risk for death than those in the non-SMI control group (adjusted hazard ratio, 1.53; 95% confidence interval, 1.39-1.68).
- Black Caribbean/Black African participants were more likely than White participants to die of COVID-19 (aHR, 1.22; 95% CI, 1.12-1.34), although ethnicity was not recorded in 30% of participants.
- After SARS-CoV-2 infection, for every additional multimorbid condition, the aHR for death increased by 6% in the SMI group and 16% in the non-SMI group (P = .001). Some of these conditions included hypertension, heart disease, diabetes, kidney disease, depression, and anxiety.
IN PRACTICE:
“From a public health perspective, our study has emphasized the need for early and timely preventative interventions (e.g. vaccination) for the SMI population. Future studies are needed to disentangle the complex biological and psychosocial factors, and health care pathways, that have led to the greater mortality rates in the SMI population,” the authors write.
SOURCE:
Jayati Das-Munshi, MD, of Kings College London, led the study, which was published online in the British Journal of Psychiatry. The study was funded by the Health Foundation.
LIMITATIONS:
COVID-19 may have been underdiagnosed or underreported in the records studied. Also, investigators did not have information about cause of death.
DISCLOSURES:
One author received funding from Janssen, GSK, and Takeda. All other authors declared no conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Investigators analyzed data from the Clinical Practice Research Datalink database, which contains health information on 13.5 million patients receiving care from family practices in England and Northern Ireland.
- The study included participants with SMI, including schizophrenia, schizoaffective disorder, and bipolar disorder.
- Participants were aged 5 years or older with a SARS-CoV-2 infection recorded between Feb. 1, 2020, and March 31, 2021, spanning two waves of the pandemic.
- Death rates among participants with SMI and COVID-19 (n = 7,150; 56% female) were compared with those in a control group of participants without SMI who had been diagnosed with COVID-19 (n = 650,000; 55% female).
TAKEAWAY:
- Participants with SMI and COVID-19 had a 53% higher risk for death than those in the non-SMI control group (adjusted hazard ratio, 1.53; 95% confidence interval, 1.39-1.68).
- Black Caribbean/Black African participants were more likely than White participants to die of COVID-19 (aHR, 1.22; 95% CI, 1.12-1.34), although ethnicity was not recorded in 30% of participants.
- After SARS-CoV-2 infection, for every additional multimorbid condition, the aHR for death increased by 6% in the SMI group and 16% in the non-SMI group (P = .001). Some of these conditions included hypertension, heart disease, diabetes, kidney disease, depression, and anxiety.
IN PRACTICE:
“From a public health perspective, our study has emphasized the need for early and timely preventative interventions (e.g. vaccination) for the SMI population. Future studies are needed to disentangle the complex biological and psychosocial factors, and health care pathways, that have led to the greater mortality rates in the SMI population,” the authors write.
SOURCE:
Jayati Das-Munshi, MD, of Kings College London, led the study, which was published online in the British Journal of Psychiatry. The study was funded by the Health Foundation.
LIMITATIONS:
COVID-19 may have been underdiagnosed or underreported in the records studied. Also, investigators did not have information about cause of death.
DISCLOSURES:
One author received funding from Janssen, GSK, and Takeda. All other authors declared no conflicts of interest.
A version of this article first appeared on Medscape.com.
Ketamine no better for depression than placebo?
TOPLINE:
results of a new study suggest, contradicting prior research. Although symptoms improved in both study groups, investigators say participants’ expectations of an improvement from ketamine may be driving that result.
METHODOLOGY:
- The randomized, placebo-controlled trial included 40 patients who had previously been diagnosed with MDD and who were scheduled for elective noncardiac, nonintracranial surgery.
- Participants completed pre- and postsurgery depression screenings with the Patient Health Questionnaire–8 (inclusion score was ≥ 12) and the Montgomery-Åsberg Depression Rating Scale (MADRS).
- Patients received an infusion of 0.5 mg/kg of saline (placebo group; n = 20) or ketamine (n = 20) during surgery, along with general anesthesia.
- At the end of a 14-day follow-up, patients were asked to guess whether they had received ketamine or placebo.
TAKEAWAY:
- MADRS scores dropped by around half 1 day after treatment, indicating an improvement in depressive symptoms in both the group that received ketamine (mean decrease from 25 to 12.6 points) and the group that received placebo (mean decrease from 30 to 15.3 points). There was no significant difference between the two.
- Participants in the ketamine and placebo groups also reported high rates of clinical response (60% and 50%, respectively) and remission (50% and 35%, respectively), again with no significant difference based on treatment with ketamine or placebo.
- Only 36.8% of participants accurately guessed their treatment group. Those who guessed they had received ketamine had higher MADRS scores than those who guessed they had received placebo or said they didn’t know (10.1 vs. 19.2 vs. 23.0).
- The ketamine group had a significantly shorter hospital stay (1.9 days) than the placebo group (4 days) (P = .02).
IN PRACTICE:
“Our primary findings differ from those of previous antidepressant trials with ketamine conducted without adequate masking, which find robust effects of ketamine,” the authors wrote, adding that “regardless of the intervention being tested, participant expectations of a positive outcome – also known as hope – may drive large decreases in depression symptoms seen in antidepressant trials.”
SOURCE:
Boris D. Heifets, MD, PhD, led the study, which was published online in Nature Mental Health. The study was funded by the Society for Neuroscience in Anesthesiology and Critical Care, the National Institutes of Health, and the Stanford School of Medicine Research Office.
LIMITATIONS:
The investigators did not measure participants’ treatment expectations prior to randomization and could not determine what effect participant expectancy bias may have had on the results. In addition, there was no assessment of the blind for anesthesiologists who administered the ketamine or placebo to patients.
DISCLOSURES:
Dr. Heifets is on the scientific advisory boards of Osmind and Journey Clinical and is a consultant to Clairvoyant Therapeutics and Vine Ventures.
A version of this article first appeared on Medscape.com.
TOPLINE:
results of a new study suggest, contradicting prior research. Although symptoms improved in both study groups, investigators say participants’ expectations of an improvement from ketamine may be driving that result.
METHODOLOGY:
- The randomized, placebo-controlled trial included 40 patients who had previously been diagnosed with MDD and who were scheduled for elective noncardiac, nonintracranial surgery.
- Participants completed pre- and postsurgery depression screenings with the Patient Health Questionnaire–8 (inclusion score was ≥ 12) and the Montgomery-Åsberg Depression Rating Scale (MADRS).
- Patients received an infusion of 0.5 mg/kg of saline (placebo group; n = 20) or ketamine (n = 20) during surgery, along with general anesthesia.
- At the end of a 14-day follow-up, patients were asked to guess whether they had received ketamine or placebo.
TAKEAWAY:
- MADRS scores dropped by around half 1 day after treatment, indicating an improvement in depressive symptoms in both the group that received ketamine (mean decrease from 25 to 12.6 points) and the group that received placebo (mean decrease from 30 to 15.3 points). There was no significant difference between the two.
- Participants in the ketamine and placebo groups also reported high rates of clinical response (60% and 50%, respectively) and remission (50% and 35%, respectively), again with no significant difference based on treatment with ketamine or placebo.
- Only 36.8% of participants accurately guessed their treatment group. Those who guessed they had received ketamine had higher MADRS scores than those who guessed they had received placebo or said they didn’t know (10.1 vs. 19.2 vs. 23.0).
- The ketamine group had a significantly shorter hospital stay (1.9 days) than the placebo group (4 days) (P = .02).
IN PRACTICE:
“Our primary findings differ from those of previous antidepressant trials with ketamine conducted without adequate masking, which find robust effects of ketamine,” the authors wrote, adding that “regardless of the intervention being tested, participant expectations of a positive outcome – also known as hope – may drive large decreases in depression symptoms seen in antidepressant trials.”
SOURCE:
Boris D. Heifets, MD, PhD, led the study, which was published online in Nature Mental Health. The study was funded by the Society for Neuroscience in Anesthesiology and Critical Care, the National Institutes of Health, and the Stanford School of Medicine Research Office.
LIMITATIONS:
The investigators did not measure participants’ treatment expectations prior to randomization and could not determine what effect participant expectancy bias may have had on the results. In addition, there was no assessment of the blind for anesthesiologists who administered the ketamine or placebo to patients.
DISCLOSURES:
Dr. Heifets is on the scientific advisory boards of Osmind and Journey Clinical and is a consultant to Clairvoyant Therapeutics and Vine Ventures.
A version of this article first appeared on Medscape.com.
TOPLINE:
results of a new study suggest, contradicting prior research. Although symptoms improved in both study groups, investigators say participants’ expectations of an improvement from ketamine may be driving that result.
METHODOLOGY:
- The randomized, placebo-controlled trial included 40 patients who had previously been diagnosed with MDD and who were scheduled for elective noncardiac, nonintracranial surgery.
- Participants completed pre- and postsurgery depression screenings with the Patient Health Questionnaire–8 (inclusion score was ≥ 12) and the Montgomery-Åsberg Depression Rating Scale (MADRS).
- Patients received an infusion of 0.5 mg/kg of saline (placebo group; n = 20) or ketamine (n = 20) during surgery, along with general anesthesia.
- At the end of a 14-day follow-up, patients were asked to guess whether they had received ketamine or placebo.
TAKEAWAY:
- MADRS scores dropped by around half 1 day after treatment, indicating an improvement in depressive symptoms in both the group that received ketamine (mean decrease from 25 to 12.6 points) and the group that received placebo (mean decrease from 30 to 15.3 points). There was no significant difference between the two.
- Participants in the ketamine and placebo groups also reported high rates of clinical response (60% and 50%, respectively) and remission (50% and 35%, respectively), again with no significant difference based on treatment with ketamine or placebo.
- Only 36.8% of participants accurately guessed their treatment group. Those who guessed they had received ketamine had higher MADRS scores than those who guessed they had received placebo or said they didn’t know (10.1 vs. 19.2 vs. 23.0).
- The ketamine group had a significantly shorter hospital stay (1.9 days) than the placebo group (4 days) (P = .02).
IN PRACTICE:
“Our primary findings differ from those of previous antidepressant trials with ketamine conducted without adequate masking, which find robust effects of ketamine,” the authors wrote, adding that “regardless of the intervention being tested, participant expectations of a positive outcome – also known as hope – may drive large decreases in depression symptoms seen in antidepressant trials.”
SOURCE:
Boris D. Heifets, MD, PhD, led the study, which was published online in Nature Mental Health. The study was funded by the Society for Neuroscience in Anesthesiology and Critical Care, the National Institutes of Health, and the Stanford School of Medicine Research Office.
LIMITATIONS:
The investigators did not measure participants’ treatment expectations prior to randomization and could not determine what effect participant expectancy bias may have had on the results. In addition, there was no assessment of the blind for anesthesiologists who administered the ketamine or placebo to patients.
DISCLOSURES:
Dr. Heifets is on the scientific advisory boards of Osmind and Journey Clinical and is a consultant to Clairvoyant Therapeutics and Vine Ventures.
A version of this article first appeared on Medscape.com.
Teens streaming on Twitch vulnerable to predators
WASHINGTON – Half of youth broadcasting live streams on the online platform Twitch revealed their real-world location, and nearly half provided their name to viewers, according to research presented at the annual meeting of the American Academy of Pediatrics. It took researchers less than 5 minutes – and sometimes as little as 12 seconds – to find minors in different video game categories, suggesting the environment offers opportunities to predators to gain sensitive information about minors, reported Fiona Dubrosa, BS, BA, a visiting scholar at Cohen Children’s Medical Center, New York, and colleagues.
A ‘clandestine, threatening digital environment’
the authors concluded. “The nature of live streaming makes it particularly dangerous, as there is no way to take back information that has been revealed or regulate content or viewers. Parents and pediatricians should be aware of the dangers presented by Twitch and other live-streaming platforms and counsel children on best practices for Internet safety.”
Twitch is an online streaming platform where people can watch creator’s live content, such as music performances or narrating real-time video game playing. The platform requires live streamers to be 13 years old with a valid email address or phone number to create an account, but no age restrictions or identification requirements exist for viewers, “potentially putting minors in danger of being watched, followed, and groomed by predators,” the researchers noted. They added that people following different streamers receive notifications when those streamers are live. Further, “viewers can donate money to streamers, which can make it easier for predators to manipulate, track, and encourage risky behaviors from minors.”
To better understand the risks the platform might pose to minors, the researchers searched for and analyzed popular video game live streams that appeared to be streamed by minors who had their cameras on and their faces visible. Then the researchers noted the name of the video game, the topics discussed by the streamers, the time it took to find minors under each game, and each streamer’s age, name, follower count, location, streaming schedule, and social media links for money donations.
The researchers analyzed 100 Twitch streamers who were minors, who had a combined 1,755,452 million followers. Nearly half the streamers (47%) provided their presumably real names, and half (50%) gave out their location. Nearly two-thirds (64%) linked other social media accounts they had and encouraged viewers to follow them. Detailed schedules of when they would be live were available for 38% of the streamers, and 37% of the minor streamers were accepting money donations.
Only 11% of the discussion on the streams revealed personal details, most often related to trying on different outfits for viewers and talking about real-world locations they liked to visit. The researchers needed anywhere from 12 seconds to 5 minutes to find a minor in each game category.
”Young users clearly feel a false sense of safety on the platform; a significant proportion were willing to reveal personal information despite having no knowledge of who might be listening,” the researchers said. “The donation system provides a menacing avenue for manipulation and continued exploitation of minors. Our findings reveal the need for stricter age limitations for streamers and more stringent identity verification of audience members on Twitch.”
Open-minded parental guidance is warranted
Jenny Radesky, MD, a developmental behavioral pediatrician and media researcher at University of Michigan Medicine, Ann Arbor, was not surprised that many teens live stream on Twitch since it’s a popular platform for video gaming, but she was surprised at how many revealed their locations and other personal details.
“I suspect that they do this to build closeness with their viewers, by seeming more authentic,” said Dr. Radesky, who was not involved in the study. “It is this type of parasocial relationship with influencers and gamers that keeps an audience engaged, and encourages future viewing and purchases.”
Their willingness to share personal details suggests it’s important to conduct qualitative research to find out how teen live streamers think about privacy risks, what privacy settings they can use and choose to use, and how they handle inappropriate contact from adults, Dr. Radesky said.
Meanwhile, parents should talk with their kids in an open-minded way about what platforms they use and what they like and dislike about them. She recommended parents read the Common Sense Media guide about different social platforms ”to understand what attracts kids to content on specific sites, what their pitfalls are, and what types of privacy and safety settings are available.”
“A child or teen is much more likely to be honest about negative experiences online if they think their parent will hear them out – not judge them or take away their tech. No teen wants to talk with a panicky parent,” Dr. Radesky said.
David Hill, MD, a hospitalist pediatrician for Goldsboro Pediatrics in Wayne County, North Carolina, who also specializes in media communication, said that Twitch is just one example of a social media platform where children can encounter a variety of dangers, including sometimes adult predators.
“This just highlights the importance of parents having an ongoing conversation with their children about how they use their social media platforms and ensuring, just as we do with learning to ride a bicycle or learning to drive a car, that they apply some basic rules of safety,” Dr. Hill said. Then it’s important to keep coming back to that conversation “again and again as they grow and change and as those platforms change to ensure that those kids are continuing to apply those rules consistently.
“The best way for parents to keep up is ask your kids,” he said. “They love to share. They love to teach. They love to be in a position to show you something, especially if it’s something that interests them.”
An example of a rule would be setting personal accounts to private, not public, by default, Dr. Radesky said. “When interviewed, teens often say that they feel intruded upon by older people ‘stalking’ them or trying to connect with them on social platforms,” so making an account private can reduce those opportunities.
For teens who specifically want to create content on social platforms, parent oversight is needed, she said, but she acknowledged it can be a lot of work. “This might take the form of talking about what a teen plans to post before they do, expectations for positive behaviors or language, plans for privacy settings (such as public vs. private accounts), and what to do with trolls or hateful comment,” she said. “Parents may want to follow their child’s account to check in on it.”
Useful advice
Dr. Radesky also provided a handful of talking points that pediatricians can use in talking with patients who use these platforms:
- Keep your account private to just your friends and people you want to interact with. There are a lot of people on the Internet that you don’t want intruding upon your social life.
- Maintain your feed and the accounts you follow to keep it positive, entertaining, and not a source of stress or self-doubt. Content creators are always trying to grab your attention in new ways, some of which are rude or dehumanizing, so don’t waste your time on things that bring you down.
- Talk about why you want to post or live stream. Is it to get reactions or feel validated? If so, can you find other ways to feel validated that don’t require performing for other people? Is it to share a special skill? If so, how do you keep your posts creative and community building rather than attention grabbing? And how can you keep your parents involved so that they can help you navigate challenges?”
Ms. Dubrosa and Dr. Hill had no disclosures. Dr. Radesky is a consultant for Melissa & Doug. No information on external funding was provided.
WASHINGTON – Half of youth broadcasting live streams on the online platform Twitch revealed their real-world location, and nearly half provided their name to viewers, according to research presented at the annual meeting of the American Academy of Pediatrics. It took researchers less than 5 minutes – and sometimes as little as 12 seconds – to find minors in different video game categories, suggesting the environment offers opportunities to predators to gain sensitive information about minors, reported Fiona Dubrosa, BS, BA, a visiting scholar at Cohen Children’s Medical Center, New York, and colleagues.
A ‘clandestine, threatening digital environment’
the authors concluded. “The nature of live streaming makes it particularly dangerous, as there is no way to take back information that has been revealed or regulate content or viewers. Parents and pediatricians should be aware of the dangers presented by Twitch and other live-streaming platforms and counsel children on best practices for Internet safety.”
Twitch is an online streaming platform where people can watch creator’s live content, such as music performances or narrating real-time video game playing. The platform requires live streamers to be 13 years old with a valid email address or phone number to create an account, but no age restrictions or identification requirements exist for viewers, “potentially putting minors in danger of being watched, followed, and groomed by predators,” the researchers noted. They added that people following different streamers receive notifications when those streamers are live. Further, “viewers can donate money to streamers, which can make it easier for predators to manipulate, track, and encourage risky behaviors from minors.”
To better understand the risks the platform might pose to minors, the researchers searched for and analyzed popular video game live streams that appeared to be streamed by minors who had their cameras on and their faces visible. Then the researchers noted the name of the video game, the topics discussed by the streamers, the time it took to find minors under each game, and each streamer’s age, name, follower count, location, streaming schedule, and social media links for money donations.
The researchers analyzed 100 Twitch streamers who were minors, who had a combined 1,755,452 million followers. Nearly half the streamers (47%) provided their presumably real names, and half (50%) gave out their location. Nearly two-thirds (64%) linked other social media accounts they had and encouraged viewers to follow them. Detailed schedules of when they would be live were available for 38% of the streamers, and 37% of the minor streamers were accepting money donations.
Only 11% of the discussion on the streams revealed personal details, most often related to trying on different outfits for viewers and talking about real-world locations they liked to visit. The researchers needed anywhere from 12 seconds to 5 minutes to find a minor in each game category.
”Young users clearly feel a false sense of safety on the platform; a significant proportion were willing to reveal personal information despite having no knowledge of who might be listening,” the researchers said. “The donation system provides a menacing avenue for manipulation and continued exploitation of minors. Our findings reveal the need for stricter age limitations for streamers and more stringent identity verification of audience members on Twitch.”
Open-minded parental guidance is warranted
Jenny Radesky, MD, a developmental behavioral pediatrician and media researcher at University of Michigan Medicine, Ann Arbor, was not surprised that many teens live stream on Twitch since it’s a popular platform for video gaming, but she was surprised at how many revealed their locations and other personal details.
“I suspect that they do this to build closeness with their viewers, by seeming more authentic,” said Dr. Radesky, who was not involved in the study. “It is this type of parasocial relationship with influencers and gamers that keeps an audience engaged, and encourages future viewing and purchases.”
Their willingness to share personal details suggests it’s important to conduct qualitative research to find out how teen live streamers think about privacy risks, what privacy settings they can use and choose to use, and how they handle inappropriate contact from adults, Dr. Radesky said.
Meanwhile, parents should talk with their kids in an open-minded way about what platforms they use and what they like and dislike about them. She recommended parents read the Common Sense Media guide about different social platforms ”to understand what attracts kids to content on specific sites, what their pitfalls are, and what types of privacy and safety settings are available.”
“A child or teen is much more likely to be honest about negative experiences online if they think their parent will hear them out – not judge them or take away their tech. No teen wants to talk with a panicky parent,” Dr. Radesky said.
David Hill, MD, a hospitalist pediatrician for Goldsboro Pediatrics in Wayne County, North Carolina, who also specializes in media communication, said that Twitch is just one example of a social media platform where children can encounter a variety of dangers, including sometimes adult predators.
“This just highlights the importance of parents having an ongoing conversation with their children about how they use their social media platforms and ensuring, just as we do with learning to ride a bicycle or learning to drive a car, that they apply some basic rules of safety,” Dr. Hill said. Then it’s important to keep coming back to that conversation “again and again as they grow and change and as those platforms change to ensure that those kids are continuing to apply those rules consistently.
“The best way for parents to keep up is ask your kids,” he said. “They love to share. They love to teach. They love to be in a position to show you something, especially if it’s something that interests them.”
An example of a rule would be setting personal accounts to private, not public, by default, Dr. Radesky said. “When interviewed, teens often say that they feel intruded upon by older people ‘stalking’ them or trying to connect with them on social platforms,” so making an account private can reduce those opportunities.
For teens who specifically want to create content on social platforms, parent oversight is needed, she said, but she acknowledged it can be a lot of work. “This might take the form of talking about what a teen plans to post before they do, expectations for positive behaviors or language, plans for privacy settings (such as public vs. private accounts), and what to do with trolls or hateful comment,” she said. “Parents may want to follow their child’s account to check in on it.”
Useful advice
Dr. Radesky also provided a handful of talking points that pediatricians can use in talking with patients who use these platforms:
- Keep your account private to just your friends and people you want to interact with. There are a lot of people on the Internet that you don’t want intruding upon your social life.
- Maintain your feed and the accounts you follow to keep it positive, entertaining, and not a source of stress or self-doubt. Content creators are always trying to grab your attention in new ways, some of which are rude or dehumanizing, so don’t waste your time on things that bring you down.
- Talk about why you want to post or live stream. Is it to get reactions or feel validated? If so, can you find other ways to feel validated that don’t require performing for other people? Is it to share a special skill? If so, how do you keep your posts creative and community building rather than attention grabbing? And how can you keep your parents involved so that they can help you navigate challenges?”
Ms. Dubrosa and Dr. Hill had no disclosures. Dr. Radesky is a consultant for Melissa & Doug. No information on external funding was provided.
WASHINGTON – Half of youth broadcasting live streams on the online platform Twitch revealed their real-world location, and nearly half provided their name to viewers, according to research presented at the annual meeting of the American Academy of Pediatrics. It took researchers less than 5 minutes – and sometimes as little as 12 seconds – to find minors in different video game categories, suggesting the environment offers opportunities to predators to gain sensitive information about minors, reported Fiona Dubrosa, BS, BA, a visiting scholar at Cohen Children’s Medical Center, New York, and colleagues.
A ‘clandestine, threatening digital environment’
the authors concluded. “The nature of live streaming makes it particularly dangerous, as there is no way to take back information that has been revealed or regulate content or viewers. Parents and pediatricians should be aware of the dangers presented by Twitch and other live-streaming platforms and counsel children on best practices for Internet safety.”
Twitch is an online streaming platform where people can watch creator’s live content, such as music performances or narrating real-time video game playing. The platform requires live streamers to be 13 years old with a valid email address or phone number to create an account, but no age restrictions or identification requirements exist for viewers, “potentially putting minors in danger of being watched, followed, and groomed by predators,” the researchers noted. They added that people following different streamers receive notifications when those streamers are live. Further, “viewers can donate money to streamers, which can make it easier for predators to manipulate, track, and encourage risky behaviors from minors.”
To better understand the risks the platform might pose to minors, the researchers searched for and analyzed popular video game live streams that appeared to be streamed by minors who had their cameras on and their faces visible. Then the researchers noted the name of the video game, the topics discussed by the streamers, the time it took to find minors under each game, and each streamer’s age, name, follower count, location, streaming schedule, and social media links for money donations.
The researchers analyzed 100 Twitch streamers who were minors, who had a combined 1,755,452 million followers. Nearly half the streamers (47%) provided their presumably real names, and half (50%) gave out their location. Nearly two-thirds (64%) linked other social media accounts they had and encouraged viewers to follow them. Detailed schedules of when they would be live were available for 38% of the streamers, and 37% of the minor streamers were accepting money donations.
Only 11% of the discussion on the streams revealed personal details, most often related to trying on different outfits for viewers and talking about real-world locations they liked to visit. The researchers needed anywhere from 12 seconds to 5 minutes to find a minor in each game category.
”Young users clearly feel a false sense of safety on the platform; a significant proportion were willing to reveal personal information despite having no knowledge of who might be listening,” the researchers said. “The donation system provides a menacing avenue for manipulation and continued exploitation of minors. Our findings reveal the need for stricter age limitations for streamers and more stringent identity verification of audience members on Twitch.”
Open-minded parental guidance is warranted
Jenny Radesky, MD, a developmental behavioral pediatrician and media researcher at University of Michigan Medicine, Ann Arbor, was not surprised that many teens live stream on Twitch since it’s a popular platform for video gaming, but she was surprised at how many revealed their locations and other personal details.
“I suspect that they do this to build closeness with their viewers, by seeming more authentic,” said Dr. Radesky, who was not involved in the study. “It is this type of parasocial relationship with influencers and gamers that keeps an audience engaged, and encourages future viewing and purchases.”
Their willingness to share personal details suggests it’s important to conduct qualitative research to find out how teen live streamers think about privacy risks, what privacy settings they can use and choose to use, and how they handle inappropriate contact from adults, Dr. Radesky said.
Meanwhile, parents should talk with their kids in an open-minded way about what platforms they use and what they like and dislike about them. She recommended parents read the Common Sense Media guide about different social platforms ”to understand what attracts kids to content on specific sites, what their pitfalls are, and what types of privacy and safety settings are available.”
“A child or teen is much more likely to be honest about negative experiences online if they think their parent will hear them out – not judge them or take away their tech. No teen wants to talk with a panicky parent,” Dr. Radesky said.
David Hill, MD, a hospitalist pediatrician for Goldsboro Pediatrics in Wayne County, North Carolina, who also specializes in media communication, said that Twitch is just one example of a social media platform where children can encounter a variety of dangers, including sometimes adult predators.
“This just highlights the importance of parents having an ongoing conversation with their children about how they use their social media platforms and ensuring, just as we do with learning to ride a bicycle or learning to drive a car, that they apply some basic rules of safety,” Dr. Hill said. Then it’s important to keep coming back to that conversation “again and again as they grow and change and as those platforms change to ensure that those kids are continuing to apply those rules consistently.
“The best way for parents to keep up is ask your kids,” he said. “They love to share. They love to teach. They love to be in a position to show you something, especially if it’s something that interests them.”
An example of a rule would be setting personal accounts to private, not public, by default, Dr. Radesky said. “When interviewed, teens often say that they feel intruded upon by older people ‘stalking’ them or trying to connect with them on social platforms,” so making an account private can reduce those opportunities.
For teens who specifically want to create content on social platforms, parent oversight is needed, she said, but she acknowledged it can be a lot of work. “This might take the form of talking about what a teen plans to post before they do, expectations for positive behaviors or language, plans for privacy settings (such as public vs. private accounts), and what to do with trolls or hateful comment,” she said. “Parents may want to follow their child’s account to check in on it.”
Useful advice
Dr. Radesky also provided a handful of talking points that pediatricians can use in talking with patients who use these platforms:
- Keep your account private to just your friends and people you want to interact with. There are a lot of people on the Internet that you don’t want intruding upon your social life.
- Maintain your feed and the accounts you follow to keep it positive, entertaining, and not a source of stress or self-doubt. Content creators are always trying to grab your attention in new ways, some of which are rude or dehumanizing, so don’t waste your time on things that bring you down.
- Talk about why you want to post or live stream. Is it to get reactions or feel validated? If so, can you find other ways to feel validated that don’t require performing for other people? Is it to share a special skill? If so, how do you keep your posts creative and community building rather than attention grabbing? And how can you keep your parents involved so that they can help you navigate challenges?”
Ms. Dubrosa and Dr. Hill had no disclosures. Dr. Radesky is a consultant for Melissa & Doug. No information on external funding was provided.
AT AAP 2023
Psychedelic therapy tied to reduced depression, anxiety
TOPLINE:
Perhaps most surprising to investigators, however, was that treatment was also associated with improved cognitive scores in the veterans, many of whom had traumatic brain injuries.
METHODOLOGY:
- Investigators reviewed clinical charts of 86 SOFVs who received psychedelic-assisted treatment at a therapeutic program in Mexico, 86% of whom sustained head injuries during deployment.
- On the first day of the study, participants received a single oral dose (10 mg/kg) of ibogaine hydrochloride in a group setting with two to five other attendees and spent the next day reflecting on their experience with program staff.
- On the third day, participants inhaled 5-MeO-DMT in three incremental doses for a total of 50 mg and were then invited to reflect on their experience both individually and with the group of peers who shared the experience.
- Follow-up surveys at 1, 3, and 6 months posttreatment between September 2019 to March 2021 measured symptoms of posttraumatic stress disorder, cognitive functioning, generalized anxiety disorder, depression, and quality of life.
TAKEAWAY:
- There were significant improvements in self-reported PTSD symptoms, depression, anxiety, insomnia severity, anger, and a large improvement in self-reported satisfaction with life (P < .001 for all).
- Participants reported significant increases in psychological flexibility (P < .001), cognitive functioning (P < .001), and postconcussive symptoms (P < .001).
- Treatment was also associated with a significant reduction in suicidal ideation from pretreatment to 1-month follow-up (P < .01).
IN PRACTICE:
“If consistently replicated, this could have major implications for the landscape of mental health care if people are able to experience significant and sustained healing with 3 days of intensive treatment, relative to our traditionally available interventions that require 8-12 weeks of weekly therapy (for example, gold standard talk therapies such as [prolonged exposure] or [cognitive processing therapy]), or daily use of a pharmacotherapy such as [a selective serotonin reuptake inhibitor] for months to years,” study authors write.
SOURCE:
Alan Kooi Davis, PhD, of the Center for Psychedelic Drug Research and Education at Ohio State University, led the study, which was published online in the American Journal of Drug and Alcohol Abuse.
LIMITATIONS:
Study assessments are based solely on self-report measures. Future research should implement carefully designed batteries that include both self-report and gold-standard clinician-administered measures to better capture symptom improvement and other information. The sample also lacked diversity with regard to race, religion, and socioeconomic status.
DISCLOSURES:
The study was funded by Veterans Exploring Treatment Solutions. Dr. Davis is a board member at Source Resource Foundation and a lead trainer at Fluence. Full disclosures are included in the original article.
A version of this article first appeared on Medscape.com.
TOPLINE:
Perhaps most surprising to investigators, however, was that treatment was also associated with improved cognitive scores in the veterans, many of whom had traumatic brain injuries.
METHODOLOGY:
- Investigators reviewed clinical charts of 86 SOFVs who received psychedelic-assisted treatment at a therapeutic program in Mexico, 86% of whom sustained head injuries during deployment.
- On the first day of the study, participants received a single oral dose (10 mg/kg) of ibogaine hydrochloride in a group setting with two to five other attendees and spent the next day reflecting on their experience with program staff.
- On the third day, participants inhaled 5-MeO-DMT in three incremental doses for a total of 50 mg and were then invited to reflect on their experience both individually and with the group of peers who shared the experience.
- Follow-up surveys at 1, 3, and 6 months posttreatment between September 2019 to March 2021 measured symptoms of posttraumatic stress disorder, cognitive functioning, generalized anxiety disorder, depression, and quality of life.
TAKEAWAY:
- There were significant improvements in self-reported PTSD symptoms, depression, anxiety, insomnia severity, anger, and a large improvement in self-reported satisfaction with life (P < .001 for all).
- Participants reported significant increases in psychological flexibility (P < .001), cognitive functioning (P < .001), and postconcussive symptoms (P < .001).
- Treatment was also associated with a significant reduction in suicidal ideation from pretreatment to 1-month follow-up (P < .01).
IN PRACTICE:
“If consistently replicated, this could have major implications for the landscape of mental health care if people are able to experience significant and sustained healing with 3 days of intensive treatment, relative to our traditionally available interventions that require 8-12 weeks of weekly therapy (for example, gold standard talk therapies such as [prolonged exposure] or [cognitive processing therapy]), or daily use of a pharmacotherapy such as [a selective serotonin reuptake inhibitor] for months to years,” study authors write.
SOURCE:
Alan Kooi Davis, PhD, of the Center for Psychedelic Drug Research and Education at Ohio State University, led the study, which was published online in the American Journal of Drug and Alcohol Abuse.
LIMITATIONS:
Study assessments are based solely on self-report measures. Future research should implement carefully designed batteries that include both self-report and gold-standard clinician-administered measures to better capture symptom improvement and other information. The sample also lacked diversity with regard to race, religion, and socioeconomic status.
DISCLOSURES:
The study was funded by Veterans Exploring Treatment Solutions. Dr. Davis is a board member at Source Resource Foundation and a lead trainer at Fluence. Full disclosures are included in the original article.
A version of this article first appeared on Medscape.com.
TOPLINE:
Perhaps most surprising to investigators, however, was that treatment was also associated with improved cognitive scores in the veterans, many of whom had traumatic brain injuries.
METHODOLOGY:
- Investigators reviewed clinical charts of 86 SOFVs who received psychedelic-assisted treatment at a therapeutic program in Mexico, 86% of whom sustained head injuries during deployment.
- On the first day of the study, participants received a single oral dose (10 mg/kg) of ibogaine hydrochloride in a group setting with two to five other attendees and spent the next day reflecting on their experience with program staff.
- On the third day, participants inhaled 5-MeO-DMT in three incremental doses for a total of 50 mg and were then invited to reflect on their experience both individually and with the group of peers who shared the experience.
- Follow-up surveys at 1, 3, and 6 months posttreatment between September 2019 to March 2021 measured symptoms of posttraumatic stress disorder, cognitive functioning, generalized anxiety disorder, depression, and quality of life.
TAKEAWAY:
- There were significant improvements in self-reported PTSD symptoms, depression, anxiety, insomnia severity, anger, and a large improvement in self-reported satisfaction with life (P < .001 for all).
- Participants reported significant increases in psychological flexibility (P < .001), cognitive functioning (P < .001), and postconcussive symptoms (P < .001).
- Treatment was also associated with a significant reduction in suicidal ideation from pretreatment to 1-month follow-up (P < .01).
IN PRACTICE:
“If consistently replicated, this could have major implications for the landscape of mental health care if people are able to experience significant and sustained healing with 3 days of intensive treatment, relative to our traditionally available interventions that require 8-12 weeks of weekly therapy (for example, gold standard talk therapies such as [prolonged exposure] or [cognitive processing therapy]), or daily use of a pharmacotherapy such as [a selective serotonin reuptake inhibitor] for months to years,” study authors write.
SOURCE:
Alan Kooi Davis, PhD, of the Center for Psychedelic Drug Research and Education at Ohio State University, led the study, which was published online in the American Journal of Drug and Alcohol Abuse.
LIMITATIONS:
Study assessments are based solely on self-report measures. Future research should implement carefully designed batteries that include both self-report and gold-standard clinician-administered measures to better capture symptom improvement and other information. The sample also lacked diversity with regard to race, religion, and socioeconomic status.
DISCLOSURES:
The study was funded by Veterans Exploring Treatment Solutions. Dr. Davis is a board member at Source Resource Foundation and a lead trainer at Fluence. Full disclosures are included in the original article.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF DRUG AND ALCOHOL ABUSE
Air pollution tied to postpartum depression
TOPLINE:
METHODOLOGY:
- Researchers analyzed data on 340,679 women who had singleton live births at Kaiser Permanente Southern California facilities between 2008 and 2016.
- Ambient air pollution exposures were assessed based on maternal residential addresses using monthly averages of particulate matter ≤ 2.5 mcm (PM2.5), PM ≤ 10 mcm (PM10), nitrogen dioxide, and ozone from Environmental Protection Agency monitoring stations.
- Constituents of PM2.5 (sulfate, nitrate, ammonium, organic matter, and black carbon) were obtained from models based on satellite, ground-based monitor, and chemical transport modeling data.
- Women with an Edinburgh Postnatal Depression Scale score of at least 10 during the first 6 months postpartum were referred for further assessment, including diagnosis and treatment.
TAKEAWAY:
- A total of 25,674 women had PPD (7.5%).
- Positive associations were observed between PPD ozone (adjusted odds ratio, 1.09), PM10 (aOR, 1.02), and PM2.5 (aOR, 1.02), with no statistically significant association with nitrogen dioxide.
- Among PM2.5 constituents, black carbon had the strongest association with PPD (OR 1.04).
- Overall, a higher risk of PPD was associated with ozone exposure during the entire pregnancy and postpartum periods and with PM exposure during the late pregnancy and postpartum periods.
IN PRACTICE:
“These findings suggest that long-term antepartum and postpartum air pollution exposure is a potentially modifiable environmental risk factor for PPD and an important public health issue to address for improved maternal mental health,” the authors wrote.
SOURCE:
The study, with first author Yi Sun, PhD, Chinese Academy of Medical Sciences and Peking Medical College, Beijing, was published online in JAMA Network Open.
LIMITATIONS:
Postpartum exposures were estimated using only maternal address at delivery, which may have led to exposure misclassification. Potential exposure misclassifications may also exist since indoor and personal exposure levels could not be estimated. Although several covariates were adjusted for, some residual or unmeasured covariates were inevitable due to data unavailability, such as psychiatric history, adverse life events, and marital status, which may affect mental health.
DISCLOSURES:
This study was supported by a grant from the National Institute of Environmental Health Sciences. The authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers analyzed data on 340,679 women who had singleton live births at Kaiser Permanente Southern California facilities between 2008 and 2016.
- Ambient air pollution exposures were assessed based on maternal residential addresses using monthly averages of particulate matter ≤ 2.5 mcm (PM2.5), PM ≤ 10 mcm (PM10), nitrogen dioxide, and ozone from Environmental Protection Agency monitoring stations.
- Constituents of PM2.5 (sulfate, nitrate, ammonium, organic matter, and black carbon) were obtained from models based on satellite, ground-based monitor, and chemical transport modeling data.
- Women with an Edinburgh Postnatal Depression Scale score of at least 10 during the first 6 months postpartum were referred for further assessment, including diagnosis and treatment.
TAKEAWAY:
- A total of 25,674 women had PPD (7.5%).
- Positive associations were observed between PPD ozone (adjusted odds ratio, 1.09), PM10 (aOR, 1.02), and PM2.5 (aOR, 1.02), with no statistically significant association with nitrogen dioxide.
- Among PM2.5 constituents, black carbon had the strongest association with PPD (OR 1.04).
- Overall, a higher risk of PPD was associated with ozone exposure during the entire pregnancy and postpartum periods and with PM exposure during the late pregnancy and postpartum periods.
IN PRACTICE:
“These findings suggest that long-term antepartum and postpartum air pollution exposure is a potentially modifiable environmental risk factor for PPD and an important public health issue to address for improved maternal mental health,” the authors wrote.
SOURCE:
The study, with first author Yi Sun, PhD, Chinese Academy of Medical Sciences and Peking Medical College, Beijing, was published online in JAMA Network Open.
LIMITATIONS:
Postpartum exposures were estimated using only maternal address at delivery, which may have led to exposure misclassification. Potential exposure misclassifications may also exist since indoor and personal exposure levels could not be estimated. Although several covariates were adjusted for, some residual or unmeasured covariates were inevitable due to data unavailability, such as psychiatric history, adverse life events, and marital status, which may affect mental health.
DISCLOSURES:
This study was supported by a grant from the National Institute of Environmental Health Sciences. The authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers analyzed data on 340,679 women who had singleton live births at Kaiser Permanente Southern California facilities between 2008 and 2016.
- Ambient air pollution exposures were assessed based on maternal residential addresses using monthly averages of particulate matter ≤ 2.5 mcm (PM2.5), PM ≤ 10 mcm (PM10), nitrogen dioxide, and ozone from Environmental Protection Agency monitoring stations.
- Constituents of PM2.5 (sulfate, nitrate, ammonium, organic matter, and black carbon) were obtained from models based on satellite, ground-based monitor, and chemical transport modeling data.
- Women with an Edinburgh Postnatal Depression Scale score of at least 10 during the first 6 months postpartum were referred for further assessment, including diagnosis and treatment.
TAKEAWAY:
- A total of 25,674 women had PPD (7.5%).
- Positive associations were observed between PPD ozone (adjusted odds ratio, 1.09), PM10 (aOR, 1.02), and PM2.5 (aOR, 1.02), with no statistically significant association with nitrogen dioxide.
- Among PM2.5 constituents, black carbon had the strongest association with PPD (OR 1.04).
- Overall, a higher risk of PPD was associated with ozone exposure during the entire pregnancy and postpartum periods and with PM exposure during the late pregnancy and postpartum periods.
IN PRACTICE:
“These findings suggest that long-term antepartum and postpartum air pollution exposure is a potentially modifiable environmental risk factor for PPD and an important public health issue to address for improved maternal mental health,” the authors wrote.
SOURCE:
The study, with first author Yi Sun, PhD, Chinese Academy of Medical Sciences and Peking Medical College, Beijing, was published online in JAMA Network Open.
LIMITATIONS:
Postpartum exposures were estimated using only maternal address at delivery, which may have led to exposure misclassification. Potential exposure misclassifications may also exist since indoor and personal exposure levels could not be estimated. Although several covariates were adjusted for, some residual or unmeasured covariates were inevitable due to data unavailability, such as psychiatric history, adverse life events, and marital status, which may affect mental health.
DISCLOSURES:
This study was supported by a grant from the National Institute of Environmental Health Sciences. The authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Teens have easy online access to Delta-8 cannabinoid products
WASHINGTON – , researchers reported at the 2023 annual meeting of the American Academy of Pediatrics. Most of the products identified came in bright, colorful, kid-friendly packaging and cost less than $10, the researchers found, and only 2 out of 45 sites had a third-party age verification requirement for purchases.
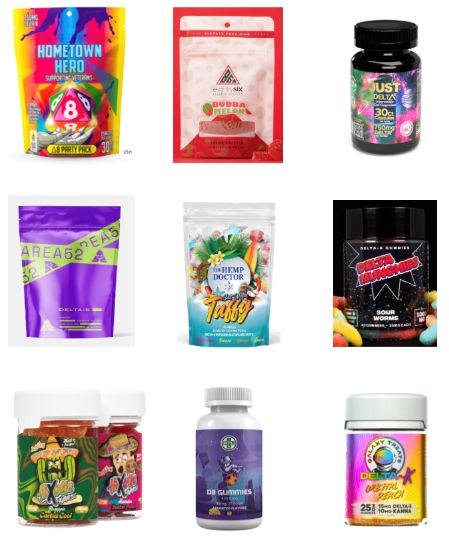
Delta-8 THC, also called D8, is a synthetically produced cannabinoid whose chemical structure and effects are nearly identical to traditional THC, the authors explained, and past research has found that D8 products, such as e-cigarettes, can contain toxic byproducts and contaminants.
”Since D8 is not traditional THC, minors may underestimate its strength and potential danger,” wrote lead author Abhijeet Grewal, BS, a research assistant at Cohen Children’s Medical Center, New York, and senior author Ruth Milanaik, DO, director of the Neonatal Neurodevelopmental Program at Cohen Children’s and a developmental/behavioral pediatrician at Northwell Health, also in New York. “Although traditional THC is a federally banned substance, D8 is legal on a federal level and less restricted on a state by state basis, making it easier for individuals to acquire D8.”
Easily accessible
During the first seven moments of 2021, 77% of reports of accidental exposure occurred in people under age 18, including some children who required ICU admission. The U.S. Food and Drug Administration also received 104 reports of adverse events from products containing D8 between December 2020-February 2022, and more than half of those required medical intervention.
To better understand how easy it is to access D8, the authors collected data on 45 websites they identified that sold D8. The researchers looked for age verification questions for accessing the site, third-party age certification, what kinds of products (edibles, smoke products, or tinctures) were sold, the price and dosage of the cheapest product, and examples of packaging, flavors, marketing claims, and warning statements at each site.
More than a third of the sites (36%) did not ask for customers’ age and almost none of the sites asked for proof: 96% of the sites lacked formal third-party age verification procedures. All but one of the sites sold D8 edibles, and most (82%) sold D8 vaping or smoking products. Only 42% sold tinctures, a mix of concentrated D8 with oil that’s orally consumed.
The cheapest product was priced under $5 on one-third of the sites and under $10 on another third of the sites. The cheapest product was between $10-20 on 16% of the sites while the remaining nine sites’ cheapest product was more than $20. In assessing only the cheapest D8 products on each site, nearly half (47%) contained 51 mg or more of D8, and 20% of the products didn’t report the dosage. Another 22% contained 41-50 mg of D8, and the remaining five products contained 20-40 mg.
Kid-friendly D8
More than half of the D8 products were sold in kid-friendly packaging – packages with bright, colorful designs and fonts that resemble candy or snack food, sometimes cartoon characters or fun items like dice on the packaging. Further, 24% of the websites did not include any warnings or other health information about D8.
“The low prices, high dosages available, and eye-popping packaging make these products extremely attractive to teens who are looking for a high,” the researchers concluded. They advised clinicians to talk with teen patients about the dangers of D8 and advocated for policymakers to more strictly regulate online distributors of D8 products, particularly in requiring age verification procedures and prohibiting kid-friendly packaging.
Megan Moreno, MD, MSEd, MPH, an adolescent medicine physician and researcher at the University of Wisconsin, Madison, School of Medicine and Public Health and UWHealthKids, was particularly struck by how eye-catching the packaging was. “The bright colors and font choices are really designed to attract adolescents,” commented Dr. Moreno, who was not involved in the study. But she was not surprised overall by the findings.
“Other studies have found that the cannabis industry leverages online tools and social media, alongside youth-friendly packaging, to attract youth to their products,” she said. “What is disappointing is that these companies do not use industry standard approaches, such as the alcohol industry, to age-gate their websites.”
It’s important for providers who care for adolescents to ask about substance use but to especially include questions about substances that teens might not think of as “drugs,” such as Delta 8, Dr. Moreno said.
“Prior research on other types of substance such as these has found that teens can think these are less dangerous versions of cannabis, so providing accurate information and asking about these products can prevent harm to kids,” Dr. Moreno said. Although this study focused on websites that sell D8 products, she said that “another important area of influence to consider is social media messaging around these products, which may drive traffic to the purchasing site.” It’s clear this industry is not going to self-regulate without policy changes, Dr. Moreno added, so she noted the importance of advocating for policy that regulates these sites.
Mr. Grewal, Dr. Milanaik and Dr. Moreno had no disclosures. No external funding sources were noted.
WASHINGTON – , researchers reported at the 2023 annual meeting of the American Academy of Pediatrics. Most of the products identified came in bright, colorful, kid-friendly packaging and cost less than $10, the researchers found, and only 2 out of 45 sites had a third-party age verification requirement for purchases.
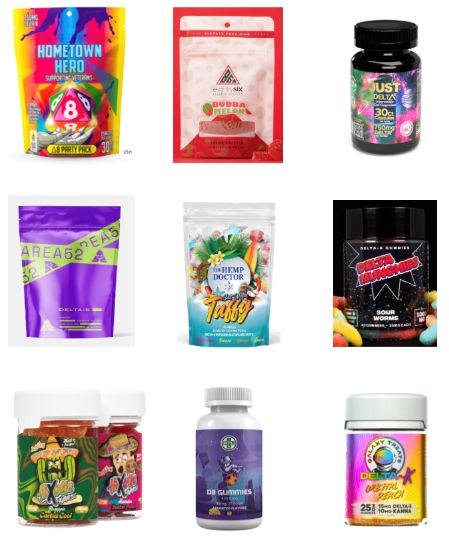
Delta-8 THC, also called D8, is a synthetically produced cannabinoid whose chemical structure and effects are nearly identical to traditional THC, the authors explained, and past research has found that D8 products, such as e-cigarettes, can contain toxic byproducts and contaminants.
”Since D8 is not traditional THC, minors may underestimate its strength and potential danger,” wrote lead author Abhijeet Grewal, BS, a research assistant at Cohen Children’s Medical Center, New York, and senior author Ruth Milanaik, DO, director of the Neonatal Neurodevelopmental Program at Cohen Children’s and a developmental/behavioral pediatrician at Northwell Health, also in New York. “Although traditional THC is a federally banned substance, D8 is legal on a federal level and less restricted on a state by state basis, making it easier for individuals to acquire D8.”
Easily accessible
During the first seven moments of 2021, 77% of reports of accidental exposure occurred in people under age 18, including some children who required ICU admission. The U.S. Food and Drug Administration also received 104 reports of adverse events from products containing D8 between December 2020-February 2022, and more than half of those required medical intervention.
To better understand how easy it is to access D8, the authors collected data on 45 websites they identified that sold D8. The researchers looked for age verification questions for accessing the site, third-party age certification, what kinds of products (edibles, smoke products, or tinctures) were sold, the price and dosage of the cheapest product, and examples of packaging, flavors, marketing claims, and warning statements at each site.
More than a third of the sites (36%) did not ask for customers’ age and almost none of the sites asked for proof: 96% of the sites lacked formal third-party age verification procedures. All but one of the sites sold D8 edibles, and most (82%) sold D8 vaping or smoking products. Only 42% sold tinctures, a mix of concentrated D8 with oil that’s orally consumed.
The cheapest product was priced under $5 on one-third of the sites and under $10 on another third of the sites. The cheapest product was between $10-20 on 16% of the sites while the remaining nine sites’ cheapest product was more than $20. In assessing only the cheapest D8 products on each site, nearly half (47%) contained 51 mg or more of D8, and 20% of the products didn’t report the dosage. Another 22% contained 41-50 mg of D8, and the remaining five products contained 20-40 mg.
Kid-friendly D8
More than half of the D8 products were sold in kid-friendly packaging – packages with bright, colorful designs and fonts that resemble candy or snack food, sometimes cartoon characters or fun items like dice on the packaging. Further, 24% of the websites did not include any warnings or other health information about D8.
“The low prices, high dosages available, and eye-popping packaging make these products extremely attractive to teens who are looking for a high,” the researchers concluded. They advised clinicians to talk with teen patients about the dangers of D8 and advocated for policymakers to more strictly regulate online distributors of D8 products, particularly in requiring age verification procedures and prohibiting kid-friendly packaging.
Megan Moreno, MD, MSEd, MPH, an adolescent medicine physician and researcher at the University of Wisconsin, Madison, School of Medicine and Public Health and UWHealthKids, was particularly struck by how eye-catching the packaging was. “The bright colors and font choices are really designed to attract adolescents,” commented Dr. Moreno, who was not involved in the study. But she was not surprised overall by the findings.
“Other studies have found that the cannabis industry leverages online tools and social media, alongside youth-friendly packaging, to attract youth to their products,” she said. “What is disappointing is that these companies do not use industry standard approaches, such as the alcohol industry, to age-gate their websites.”
It’s important for providers who care for adolescents to ask about substance use but to especially include questions about substances that teens might not think of as “drugs,” such as Delta 8, Dr. Moreno said.
“Prior research on other types of substance such as these has found that teens can think these are less dangerous versions of cannabis, so providing accurate information and asking about these products can prevent harm to kids,” Dr. Moreno said. Although this study focused on websites that sell D8 products, she said that “another important area of influence to consider is social media messaging around these products, which may drive traffic to the purchasing site.” It’s clear this industry is not going to self-regulate without policy changes, Dr. Moreno added, so she noted the importance of advocating for policy that regulates these sites.
Mr. Grewal, Dr. Milanaik and Dr. Moreno had no disclosures. No external funding sources were noted.
WASHINGTON – , researchers reported at the 2023 annual meeting of the American Academy of Pediatrics. Most of the products identified came in bright, colorful, kid-friendly packaging and cost less than $10, the researchers found, and only 2 out of 45 sites had a third-party age verification requirement for purchases.
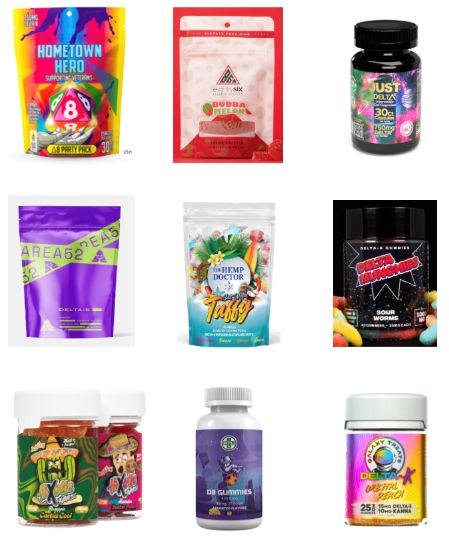
Delta-8 THC, also called D8, is a synthetically produced cannabinoid whose chemical structure and effects are nearly identical to traditional THC, the authors explained, and past research has found that D8 products, such as e-cigarettes, can contain toxic byproducts and contaminants.
”Since D8 is not traditional THC, minors may underestimate its strength and potential danger,” wrote lead author Abhijeet Grewal, BS, a research assistant at Cohen Children’s Medical Center, New York, and senior author Ruth Milanaik, DO, director of the Neonatal Neurodevelopmental Program at Cohen Children’s and a developmental/behavioral pediatrician at Northwell Health, also in New York. “Although traditional THC is a federally banned substance, D8 is legal on a federal level and less restricted on a state by state basis, making it easier for individuals to acquire D8.”
Easily accessible
During the first seven moments of 2021, 77% of reports of accidental exposure occurred in people under age 18, including some children who required ICU admission. The U.S. Food and Drug Administration also received 104 reports of adverse events from products containing D8 between December 2020-February 2022, and more than half of those required medical intervention.
To better understand how easy it is to access D8, the authors collected data on 45 websites they identified that sold D8. The researchers looked for age verification questions for accessing the site, third-party age certification, what kinds of products (edibles, smoke products, or tinctures) were sold, the price and dosage of the cheapest product, and examples of packaging, flavors, marketing claims, and warning statements at each site.
More than a third of the sites (36%) did not ask for customers’ age and almost none of the sites asked for proof: 96% of the sites lacked formal third-party age verification procedures. All but one of the sites sold D8 edibles, and most (82%) sold D8 vaping or smoking products. Only 42% sold tinctures, a mix of concentrated D8 with oil that’s orally consumed.
The cheapest product was priced under $5 on one-third of the sites and under $10 on another third of the sites. The cheapest product was between $10-20 on 16% of the sites while the remaining nine sites’ cheapest product was more than $20. In assessing only the cheapest D8 products on each site, nearly half (47%) contained 51 mg or more of D8, and 20% of the products didn’t report the dosage. Another 22% contained 41-50 mg of D8, and the remaining five products contained 20-40 mg.
Kid-friendly D8
More than half of the D8 products were sold in kid-friendly packaging – packages with bright, colorful designs and fonts that resemble candy or snack food, sometimes cartoon characters or fun items like dice on the packaging. Further, 24% of the websites did not include any warnings or other health information about D8.
“The low prices, high dosages available, and eye-popping packaging make these products extremely attractive to teens who are looking for a high,” the researchers concluded. They advised clinicians to talk with teen patients about the dangers of D8 and advocated for policymakers to more strictly regulate online distributors of D8 products, particularly in requiring age verification procedures and prohibiting kid-friendly packaging.
Megan Moreno, MD, MSEd, MPH, an adolescent medicine physician and researcher at the University of Wisconsin, Madison, School of Medicine and Public Health and UWHealthKids, was particularly struck by how eye-catching the packaging was. “The bright colors and font choices are really designed to attract adolescents,” commented Dr. Moreno, who was not involved in the study. But she was not surprised overall by the findings.
“Other studies have found that the cannabis industry leverages online tools and social media, alongside youth-friendly packaging, to attract youth to their products,” she said. “What is disappointing is that these companies do not use industry standard approaches, such as the alcohol industry, to age-gate their websites.”
It’s important for providers who care for adolescents to ask about substance use but to especially include questions about substances that teens might not think of as “drugs,” such as Delta 8, Dr. Moreno said.
“Prior research on other types of substance such as these has found that teens can think these are less dangerous versions of cannabis, so providing accurate information and asking about these products can prevent harm to kids,” Dr. Moreno said. Although this study focused on websites that sell D8 products, she said that “another important area of influence to consider is social media messaging around these products, which may drive traffic to the purchasing site.” It’s clear this industry is not going to self-regulate without policy changes, Dr. Moreno added, so she noted the importance of advocating for policy that regulates these sites.
Mr. Grewal, Dr. Milanaik and Dr. Moreno had no disclosures. No external funding sources were noted.
At AAP 2023
Is it time to scrap ultraprocessed foods?
Ultraprocessed foods (UPFs) make up nearly three-quarters of the entire U.S. food supply and about 60% of Americans’ daily caloric intake. A significant body of research has tied consumption of these foods – awash in added sugar, salt, fat, artificial colors, or preservatives – to cancer, diabetes, and heart disease.
Now, a growing number of studies also link them to poor brain health, including an increased risk of dementia, depression, and anxiety, and some experts are calling for public health policies aimed at reducing UPF consumption.
Under srutiny
A mainstay of diets in countries around the world, UPFs have come under increasing scrutiny because of their link to major diseases. The ingredients in UPFs add little or no nutritional value. Their primary function is to increase a product’s shelf life and palatability. Some recent evidence suggests these foods may be as addictive as tobacco. In addition, two pooled analysis studies using the Yale Food Addiction Scale showed that 14% of adults and 12% of children in the United States may have a UPF addiction.
The most widely used measure of what is, and what is not, a UPF was developed in 2009 by researchers in Brazil. The NOVA food classification system assigns food and beverages to one of four groups:
- Unprocessed and minimally processed foods, such as fruits, vegetables, milk, and meat.
- Processed culinary ingredients, including white sugar, butter, and oils derived from seeds, nuts, and fruits.
- Processed foods, such as tomato paste, bacon, canned tuna, and wine.
- Ultraprocessed foods, such as soda, ice cream, breakfast cereal, and prepackaged meals.
Those sounding the alarm about the potential harmful effects of UPFs are particularly concerned about their consumption by young people. The National Health and Nutrition Examination Survey showed that from 1999 to 2018, highly processed foods accounted for the majority of energy intake in those aged 2-19 years.
One of the most commonly used additives in UPFs, the artificial sweetener aspartame, garnered headlines this summer when the World Health Organization classified it as a likely carcinogen in humans. Aspartame is used in thousands of products, from soda to chewing gum to chewable vitamins.
The U.S. Food and Drug Administration strongly disagreed with the WHO’s position and is sticking by its recommended daily limit of 50 mg/kg of body weight – equivalent to 75 packets of the sweetener Equal – as safe for human consumption.
“Aspartame is one of the most studied food additives in the human food supply,” FDA officials said in a statement, adding that the agency found “significant shortcomings” in the studies the WHO used to justify the new classification. “FDA scientists do not have safety concerns when aspartame is used under the approved conditions.”
Increased attention to consumption of UPFs in general and aspartame particularly in recent years has yielded several studies pointing to the foods’ association with compromised brain health.
Link to depression, dementia
A recent report on UPF consumption and mental well-being among nearly 300,000 people across 70 countries showed that 53% of those who consumed UPFs several times a day were distressed or were struggling with their mental well-being, compared with 18% of those who rarely or never consumed UPFs.
Part of the Global Mind Project run by the nonprofit Sapien Labs in Arlington, Va., the report also showed that individuals with the highest rates of UPF consumption reported higher levels of confusion, slowed thinking, unwanted or obsessive thoughts, irritability, and feelings of sadness.
“There seems to be a much broader effect than just depression symptoms,” Tara Thiagarajan, PhD, founder and chief scientist of Sapien Labs and coauthor of the report, said in an interview.
The report, which has not been peer reviewed, comes on the heels of several other studies, including one from the Nurses Health Study II that showed that participants who consumed more than eight servings of UPFs daily had about a 50% higher depression risk, compared with those who consumed half that much.
“We found that UPFs in general, and artificial sweeteners and beverages in particular, were associated with increased risk,” said lead investigator Andrew T. Chan, MD, MPH, professor of medicine at Harvard Medical School and chief of the clinical and translational epidemiology unit, Massachusetts General Hospital, both in Boston.
“This was an interesting finding that correlates with data from animal studies that artificial sweeteners may trigger the transmission of particular signaling molecules in the brain that are important for mood,” he told this news organization.
Cognition may also be affected. An analysis of more than 72,000 people in the UK Biobank showed that those who consumed a high levels of UPFs were 50% more likely to develop dementia than those who consumed fewer processed foods. For every 10% increase in UPF consumption, the odds of developing any kind of dementia increased by 25%.
Another study of nearly 11,000 people showed that higher UPF consumption was associated with a significantly faster decline in executive and global cognitive function.
Epigenetic changes
While these and other studies suggest a link between UPF consumption and brain health, they are designed to demonstrate correlation. To date, no human study has proven that eating highly processed foods directly causes a decline in mental health or cognition.
Animal studies could provide that causal link. Earlier this year, researchers at Florida State University in Tallahassee reported learning and memory deficits in two groups of male mice that completed a maze test after being fed water mixed with aspartame for about 20% of their adult lives, compared with a group of mice that drank water only. Animals that ingested aspartame could finish the test, but it took them longer, and they needed help.
The amount of aspartame used in the study was just 7% and 15% of the FDA’s recommended maximum intake of aspartame (equivalent to two to four 8-ounce diet sodas daily).
Most intriguing was that offspring of the mice in the aspartame groups demonstrated the same levels of cognitive decline and anxiety as their fathers, even though they had never ingested the artificial sweetener. Researchers theorize that in addition to changes in brain gene expression, aspartame also caused epigenetic changes in germ cells.
“Epigenetic changes in germ cells due to environmental exposures are both good and bad,” lead investigator Pradeep G. Bhide, PhD, professor of developmental neuroscience and director of the Center for Brain Repair at FSU, told this news organization. “They are bad because the next generation is affected. But they’re good because as long as the exposure no longer occurs, 2 or 3 generations later, that’s gone.”
The mice, which lacked taste receptors for aspartame, were the same age and weight in all three groups. Because the only difference was exposure to the artificial sweetener, Dr. Bhide says it suggests a causal link.
“Extrapolation of data from well-controlled laboratory experiments in mice to humans is always risky,” Dr. Bhide said. “The extrapolations give us insights into what could happen rather than what will happen.”
Potential mechanisms
Although scientists can’t say for certain how UPFs affect brain health, there are several theories. UPFs may influence an inflammatory immune response, which has been linked to depression and dementia. Consumption of highly processed foods may also disrupt the gut microbiome, Dr. Chan said, which, in turn, may increase depression risk.
“This is an important potential mechanism linking ultraprocessed food to depression since there is emerging evidence that microbes in the gut have been linked with mood through their role in metabolizing and producing proteins that have activity in the brain,” he said.
In addition, with UPFs that contain aspartame, there could be a more direct link to brain function. In the gastrointestinal track, the sweetener is quickly broken down into methanol, aspartic acid, and phenylalanine. All three enter the bloodstream, cross the blood-brain barrier, and are neuroactive.
“Phenylalanine is a precursor for neurotransmitters in the brain, and aspartic acid activates the glutamate excitatory neurotransmitter receptor,” Dr. Bhide said. “The effects we’ve seen could be due to these metabolites that have a direct effect on the brain function.”
Time to act?
Some researchers are building a case for classifying UPFs as addictive substances. Others are calling for additional research on UPF safety that is conducted outside the food industry.
There has also been some discussion of placing warning labels on UPFs. However, there is disagreement about what information should be included and how consumers might interpret it. The question of which food products are UPFs and which are not also isn’t settled. The NOVA system may be widely used, but it still has its detractors who believe it misclassifies some healthy foods as ultraprocessed.
Dr. Chan and other experts say the research conducted thus far requires additional corroboration to inform appropriate public health interventions. That would likely take the form of a large, randomized trial with one group of participants eating a healthy diet and the other consuming large amounts of UPFs.
“This type of study is extremely challenging given the number of people that would have to be willing to participate and be willing to eat a very specific diet over a long period of time,” Dr. Chan said. “I am also not sure it would be ethical to assign people to such a diet, given what we already know about the potential health effects of UPFs.”
Dr. Thiagarajan and others have called on funding agencies to direct more grant monies toward studies of UPFs to better understand their effect on brain health.
“Given the magnitude of the problem and given that there is a fair bit of evidence that points to a potential causal link, then we damn well better put money into this and get to the bottom of it,” she said.
Others are looking to the FDA to increase the agency’s scrutiny of food additives. While some additives such as artificial sweeteners have a place in diets of people with diabetes or obesity, Dr. Bhide suggests it may be wise for healthy individuals to reduce their daily intake of UPFs.
“Our data raise this to a different level because of the transgenerational transmission, which has never been shown before,” he said. “We are saying that the FDA should look in preclinical models at germ cells and maybe transgenerational transmission before approving any food additive.”
A version of this article first appeared on Medscape.com.
Ultraprocessed foods (UPFs) make up nearly three-quarters of the entire U.S. food supply and about 60% of Americans’ daily caloric intake. A significant body of research has tied consumption of these foods – awash in added sugar, salt, fat, artificial colors, or preservatives – to cancer, diabetes, and heart disease.
Now, a growing number of studies also link them to poor brain health, including an increased risk of dementia, depression, and anxiety, and some experts are calling for public health policies aimed at reducing UPF consumption.
Under srutiny
A mainstay of diets in countries around the world, UPFs have come under increasing scrutiny because of their link to major diseases. The ingredients in UPFs add little or no nutritional value. Their primary function is to increase a product’s shelf life and palatability. Some recent evidence suggests these foods may be as addictive as tobacco. In addition, two pooled analysis studies using the Yale Food Addiction Scale showed that 14% of adults and 12% of children in the United States may have a UPF addiction.
The most widely used measure of what is, and what is not, a UPF was developed in 2009 by researchers in Brazil. The NOVA food classification system assigns food and beverages to one of four groups:
- Unprocessed and minimally processed foods, such as fruits, vegetables, milk, and meat.
- Processed culinary ingredients, including white sugar, butter, and oils derived from seeds, nuts, and fruits.
- Processed foods, such as tomato paste, bacon, canned tuna, and wine.
- Ultraprocessed foods, such as soda, ice cream, breakfast cereal, and prepackaged meals.
Those sounding the alarm about the potential harmful effects of UPFs are particularly concerned about their consumption by young people. The National Health and Nutrition Examination Survey showed that from 1999 to 2018, highly processed foods accounted for the majority of energy intake in those aged 2-19 years.
One of the most commonly used additives in UPFs, the artificial sweetener aspartame, garnered headlines this summer when the World Health Organization classified it as a likely carcinogen in humans. Aspartame is used in thousands of products, from soda to chewing gum to chewable vitamins.
The U.S. Food and Drug Administration strongly disagreed with the WHO’s position and is sticking by its recommended daily limit of 50 mg/kg of body weight – equivalent to 75 packets of the sweetener Equal – as safe for human consumption.
“Aspartame is one of the most studied food additives in the human food supply,” FDA officials said in a statement, adding that the agency found “significant shortcomings” in the studies the WHO used to justify the new classification. “FDA scientists do not have safety concerns when aspartame is used under the approved conditions.”
Increased attention to consumption of UPFs in general and aspartame particularly in recent years has yielded several studies pointing to the foods’ association with compromised brain health.
Link to depression, dementia
A recent report on UPF consumption and mental well-being among nearly 300,000 people across 70 countries showed that 53% of those who consumed UPFs several times a day were distressed or were struggling with their mental well-being, compared with 18% of those who rarely or never consumed UPFs.
Part of the Global Mind Project run by the nonprofit Sapien Labs in Arlington, Va., the report also showed that individuals with the highest rates of UPF consumption reported higher levels of confusion, slowed thinking, unwanted or obsessive thoughts, irritability, and feelings of sadness.
“There seems to be a much broader effect than just depression symptoms,” Tara Thiagarajan, PhD, founder and chief scientist of Sapien Labs and coauthor of the report, said in an interview.
The report, which has not been peer reviewed, comes on the heels of several other studies, including one from the Nurses Health Study II that showed that participants who consumed more than eight servings of UPFs daily had about a 50% higher depression risk, compared with those who consumed half that much.
“We found that UPFs in general, and artificial sweeteners and beverages in particular, were associated with increased risk,” said lead investigator Andrew T. Chan, MD, MPH, professor of medicine at Harvard Medical School and chief of the clinical and translational epidemiology unit, Massachusetts General Hospital, both in Boston.
“This was an interesting finding that correlates with data from animal studies that artificial sweeteners may trigger the transmission of particular signaling molecules in the brain that are important for mood,” he told this news organization.
Cognition may also be affected. An analysis of more than 72,000 people in the UK Biobank showed that those who consumed a high levels of UPFs were 50% more likely to develop dementia than those who consumed fewer processed foods. For every 10% increase in UPF consumption, the odds of developing any kind of dementia increased by 25%.
Another study of nearly 11,000 people showed that higher UPF consumption was associated with a significantly faster decline in executive and global cognitive function.
Epigenetic changes
While these and other studies suggest a link between UPF consumption and brain health, they are designed to demonstrate correlation. To date, no human study has proven that eating highly processed foods directly causes a decline in mental health or cognition.
Animal studies could provide that causal link. Earlier this year, researchers at Florida State University in Tallahassee reported learning and memory deficits in two groups of male mice that completed a maze test after being fed water mixed with aspartame for about 20% of their adult lives, compared with a group of mice that drank water only. Animals that ingested aspartame could finish the test, but it took them longer, and they needed help.
The amount of aspartame used in the study was just 7% and 15% of the FDA’s recommended maximum intake of aspartame (equivalent to two to four 8-ounce diet sodas daily).
Most intriguing was that offspring of the mice in the aspartame groups demonstrated the same levels of cognitive decline and anxiety as their fathers, even though they had never ingested the artificial sweetener. Researchers theorize that in addition to changes in brain gene expression, aspartame also caused epigenetic changes in germ cells.
“Epigenetic changes in germ cells due to environmental exposures are both good and bad,” lead investigator Pradeep G. Bhide, PhD, professor of developmental neuroscience and director of the Center for Brain Repair at FSU, told this news organization. “They are bad because the next generation is affected. But they’re good because as long as the exposure no longer occurs, 2 or 3 generations later, that’s gone.”
The mice, which lacked taste receptors for aspartame, were the same age and weight in all three groups. Because the only difference was exposure to the artificial sweetener, Dr. Bhide says it suggests a causal link.
“Extrapolation of data from well-controlled laboratory experiments in mice to humans is always risky,” Dr. Bhide said. “The extrapolations give us insights into what could happen rather than what will happen.”
Potential mechanisms
Although scientists can’t say for certain how UPFs affect brain health, there are several theories. UPFs may influence an inflammatory immune response, which has been linked to depression and dementia. Consumption of highly processed foods may also disrupt the gut microbiome, Dr. Chan said, which, in turn, may increase depression risk.
“This is an important potential mechanism linking ultraprocessed food to depression since there is emerging evidence that microbes in the gut have been linked with mood through their role in metabolizing and producing proteins that have activity in the brain,” he said.
In addition, with UPFs that contain aspartame, there could be a more direct link to brain function. In the gastrointestinal track, the sweetener is quickly broken down into methanol, aspartic acid, and phenylalanine. All three enter the bloodstream, cross the blood-brain barrier, and are neuroactive.
“Phenylalanine is a precursor for neurotransmitters in the brain, and aspartic acid activates the glutamate excitatory neurotransmitter receptor,” Dr. Bhide said. “The effects we’ve seen could be due to these metabolites that have a direct effect on the brain function.”
Time to act?
Some researchers are building a case for classifying UPFs as addictive substances. Others are calling for additional research on UPF safety that is conducted outside the food industry.
There has also been some discussion of placing warning labels on UPFs. However, there is disagreement about what information should be included and how consumers might interpret it. The question of which food products are UPFs and which are not also isn’t settled. The NOVA system may be widely used, but it still has its detractors who believe it misclassifies some healthy foods as ultraprocessed.
Dr. Chan and other experts say the research conducted thus far requires additional corroboration to inform appropriate public health interventions. That would likely take the form of a large, randomized trial with one group of participants eating a healthy diet and the other consuming large amounts of UPFs.
“This type of study is extremely challenging given the number of people that would have to be willing to participate and be willing to eat a very specific diet over a long period of time,” Dr. Chan said. “I am also not sure it would be ethical to assign people to such a diet, given what we already know about the potential health effects of UPFs.”
Dr. Thiagarajan and others have called on funding agencies to direct more grant monies toward studies of UPFs to better understand their effect on brain health.
“Given the magnitude of the problem and given that there is a fair bit of evidence that points to a potential causal link, then we damn well better put money into this and get to the bottom of it,” she said.
Others are looking to the FDA to increase the agency’s scrutiny of food additives. While some additives such as artificial sweeteners have a place in diets of people with diabetes or obesity, Dr. Bhide suggests it may be wise for healthy individuals to reduce their daily intake of UPFs.
“Our data raise this to a different level because of the transgenerational transmission, which has never been shown before,” he said. “We are saying that the FDA should look in preclinical models at germ cells and maybe transgenerational transmission before approving any food additive.”
A version of this article first appeared on Medscape.com.
Ultraprocessed foods (UPFs) make up nearly three-quarters of the entire U.S. food supply and about 60% of Americans’ daily caloric intake. A significant body of research has tied consumption of these foods – awash in added sugar, salt, fat, artificial colors, or preservatives – to cancer, diabetes, and heart disease.
Now, a growing number of studies also link them to poor brain health, including an increased risk of dementia, depression, and anxiety, and some experts are calling for public health policies aimed at reducing UPF consumption.
Under srutiny
A mainstay of diets in countries around the world, UPFs have come under increasing scrutiny because of their link to major diseases. The ingredients in UPFs add little or no nutritional value. Their primary function is to increase a product’s shelf life and palatability. Some recent evidence suggests these foods may be as addictive as tobacco. In addition, two pooled analysis studies using the Yale Food Addiction Scale showed that 14% of adults and 12% of children in the United States may have a UPF addiction.
The most widely used measure of what is, and what is not, a UPF was developed in 2009 by researchers in Brazil. The NOVA food classification system assigns food and beverages to one of four groups:
- Unprocessed and minimally processed foods, such as fruits, vegetables, milk, and meat.
- Processed culinary ingredients, including white sugar, butter, and oils derived from seeds, nuts, and fruits.
- Processed foods, such as tomato paste, bacon, canned tuna, and wine.
- Ultraprocessed foods, such as soda, ice cream, breakfast cereal, and prepackaged meals.
Those sounding the alarm about the potential harmful effects of UPFs are particularly concerned about their consumption by young people. The National Health and Nutrition Examination Survey showed that from 1999 to 2018, highly processed foods accounted for the majority of energy intake in those aged 2-19 years.
One of the most commonly used additives in UPFs, the artificial sweetener aspartame, garnered headlines this summer when the World Health Organization classified it as a likely carcinogen in humans. Aspartame is used in thousands of products, from soda to chewing gum to chewable vitamins.
The U.S. Food and Drug Administration strongly disagreed with the WHO’s position and is sticking by its recommended daily limit of 50 mg/kg of body weight – equivalent to 75 packets of the sweetener Equal – as safe for human consumption.
“Aspartame is one of the most studied food additives in the human food supply,” FDA officials said in a statement, adding that the agency found “significant shortcomings” in the studies the WHO used to justify the new classification. “FDA scientists do not have safety concerns when aspartame is used under the approved conditions.”
Increased attention to consumption of UPFs in general and aspartame particularly in recent years has yielded several studies pointing to the foods’ association with compromised brain health.
Link to depression, dementia
A recent report on UPF consumption and mental well-being among nearly 300,000 people across 70 countries showed that 53% of those who consumed UPFs several times a day were distressed or were struggling with their mental well-being, compared with 18% of those who rarely or never consumed UPFs.
Part of the Global Mind Project run by the nonprofit Sapien Labs in Arlington, Va., the report also showed that individuals with the highest rates of UPF consumption reported higher levels of confusion, slowed thinking, unwanted or obsessive thoughts, irritability, and feelings of sadness.
“There seems to be a much broader effect than just depression symptoms,” Tara Thiagarajan, PhD, founder and chief scientist of Sapien Labs and coauthor of the report, said in an interview.
The report, which has not been peer reviewed, comes on the heels of several other studies, including one from the Nurses Health Study II that showed that participants who consumed more than eight servings of UPFs daily had about a 50% higher depression risk, compared with those who consumed half that much.
“We found that UPFs in general, and artificial sweeteners and beverages in particular, were associated with increased risk,” said lead investigator Andrew T. Chan, MD, MPH, professor of medicine at Harvard Medical School and chief of the clinical and translational epidemiology unit, Massachusetts General Hospital, both in Boston.
“This was an interesting finding that correlates with data from animal studies that artificial sweeteners may trigger the transmission of particular signaling molecules in the brain that are important for mood,” he told this news organization.
Cognition may also be affected. An analysis of more than 72,000 people in the UK Biobank showed that those who consumed a high levels of UPFs were 50% more likely to develop dementia than those who consumed fewer processed foods. For every 10% increase in UPF consumption, the odds of developing any kind of dementia increased by 25%.
Another study of nearly 11,000 people showed that higher UPF consumption was associated with a significantly faster decline in executive and global cognitive function.
Epigenetic changes
While these and other studies suggest a link between UPF consumption and brain health, they are designed to demonstrate correlation. To date, no human study has proven that eating highly processed foods directly causes a decline in mental health or cognition.
Animal studies could provide that causal link. Earlier this year, researchers at Florida State University in Tallahassee reported learning and memory deficits in two groups of male mice that completed a maze test after being fed water mixed with aspartame for about 20% of their adult lives, compared with a group of mice that drank water only. Animals that ingested aspartame could finish the test, but it took them longer, and they needed help.
The amount of aspartame used in the study was just 7% and 15% of the FDA’s recommended maximum intake of aspartame (equivalent to two to four 8-ounce diet sodas daily).
Most intriguing was that offspring of the mice in the aspartame groups demonstrated the same levels of cognitive decline and anxiety as their fathers, even though they had never ingested the artificial sweetener. Researchers theorize that in addition to changes in brain gene expression, aspartame also caused epigenetic changes in germ cells.
“Epigenetic changes in germ cells due to environmental exposures are both good and bad,” lead investigator Pradeep G. Bhide, PhD, professor of developmental neuroscience and director of the Center for Brain Repair at FSU, told this news organization. “They are bad because the next generation is affected. But they’re good because as long as the exposure no longer occurs, 2 or 3 generations later, that’s gone.”
The mice, which lacked taste receptors for aspartame, were the same age and weight in all three groups. Because the only difference was exposure to the artificial sweetener, Dr. Bhide says it suggests a causal link.
“Extrapolation of data from well-controlled laboratory experiments in mice to humans is always risky,” Dr. Bhide said. “The extrapolations give us insights into what could happen rather than what will happen.”
Potential mechanisms
Although scientists can’t say for certain how UPFs affect brain health, there are several theories. UPFs may influence an inflammatory immune response, which has been linked to depression and dementia. Consumption of highly processed foods may also disrupt the gut microbiome, Dr. Chan said, which, in turn, may increase depression risk.
“This is an important potential mechanism linking ultraprocessed food to depression since there is emerging evidence that microbes in the gut have been linked with mood through their role in metabolizing and producing proteins that have activity in the brain,” he said.
In addition, with UPFs that contain aspartame, there could be a more direct link to brain function. In the gastrointestinal track, the sweetener is quickly broken down into methanol, aspartic acid, and phenylalanine. All three enter the bloodstream, cross the blood-brain barrier, and are neuroactive.
“Phenylalanine is a precursor for neurotransmitters in the brain, and aspartic acid activates the glutamate excitatory neurotransmitter receptor,” Dr. Bhide said. “The effects we’ve seen could be due to these metabolites that have a direct effect on the brain function.”
Time to act?
Some researchers are building a case for classifying UPFs as addictive substances. Others are calling for additional research on UPF safety that is conducted outside the food industry.
There has also been some discussion of placing warning labels on UPFs. However, there is disagreement about what information should be included and how consumers might interpret it. The question of which food products are UPFs and which are not also isn’t settled. The NOVA system may be widely used, but it still has its detractors who believe it misclassifies some healthy foods as ultraprocessed.
Dr. Chan and other experts say the research conducted thus far requires additional corroboration to inform appropriate public health interventions. That would likely take the form of a large, randomized trial with one group of participants eating a healthy diet and the other consuming large amounts of UPFs.
“This type of study is extremely challenging given the number of people that would have to be willing to participate and be willing to eat a very specific diet over a long period of time,” Dr. Chan said. “I am also not sure it would be ethical to assign people to such a diet, given what we already know about the potential health effects of UPFs.”
Dr. Thiagarajan and others have called on funding agencies to direct more grant monies toward studies of UPFs to better understand their effect on brain health.
“Given the magnitude of the problem and given that there is a fair bit of evidence that points to a potential causal link, then we damn well better put money into this and get to the bottom of it,” she said.
Others are looking to the FDA to increase the agency’s scrutiny of food additives. While some additives such as artificial sweeteners have a place in diets of people with diabetes or obesity, Dr. Bhide suggests it may be wise for healthy individuals to reduce their daily intake of UPFs.
“Our data raise this to a different level because of the transgenerational transmission, which has never been shown before,” he said. “We are saying that the FDA should look in preclinical models at germ cells and maybe transgenerational transmission before approving any food additive.”
A version of this article first appeared on Medscape.com.