User login
Benefit from cooling temps for cardiac arrest does not differ in randomized trial
The first randomized controlled trial to compare specific temperatures for therapeutic hypothermia in comatose survivors of out-of-hospital cardiac arrest showed no differences in major outcomes, according to a single-center, double-blind study.
In the CAPITAL-CHILL trial, cooling temperatures of 31° C and 34° C were compared to explore the hypothesis that a lower temperature would improve major outcomes, explained Michel Le May, MD.
No differences for the primary composite outcome of all-cause mortality or poor neurologic outcome at 180 days were observed, he reported at the annual scientific sessions of the American College of Cardiology.
The study was completed over a period of almost 7 years in patients presumed to have had an out-of-hospital cardiac arrest and who were unconscious when they reached a center affiliated with the Ottawa Heart Institute, where Dr. Le May directs the regional STEMI (ST-elevation myocardial infarction) program. The initial rhythm at the time of the cardiac arrest was not an entry criterion.
Of 389 patients enrolled, the intention-to-treat analysis included 184 randomized to a cooling temperature of 31° C group and 183 to a temperature of 34° C. The assigned target temperature, reached with an endovascular device, was known only by the managing nurses.
31° C and 34° C are equivalent
There was a small numerical disadvantage for the lower temperature assignment, but none reached statistical significance. This was true of the primary outcome (48.4% vs. 45.4% for the higher temperature) and its components of mortality (43.5% vs. 41.0%) and poor neurologic outcome (4.9% vs. 4.4%). Poor neurologic outcome was defined as a Disability Rating Scale score of greater than 5.
Deaths were most common in the early part of the 180-day follow-up in both arms. On a Kaplan-Meier survival graph, Dr. Le May showed curves that he characterized as “almost superimposable.”
There were no significant differences for any subgroup stratifications, such as age 75 years or older versus younger, males versus females, presence versus absence or an initial shockable rhythm, percutaneous coronary intervention (PCI) within 24 hours versus later, and STEMI versus non-STEMI. In these analyses, the higher temperature was associated with a potential trend for benefit among females and those with a shockable rhythm.
There was no signal for a difference in neurologic outcomes on the Disability Rating Scale or the Modified Rankin Scale. On the latter, for example, 46% of those in the 31° C group and 44% of these in the 34° C group had a score of four or greater at the end of follow-up.
The baseline characteristics of the two groups were similar. About 80% were male; the average age was roughly 62 years. More than 80% of the cardiac arrests were witnessed with CPR being administered by bystanders in nearly 70%. Nearly 40% had a STEMI.
Interventions were similar. Almost all patients underwent coronary angiography, of which nearly 60% received a percutaneous coronary intervention. More than 50% received a stent. The time from arrest to randomization was slightly longer in the 31° C group (228 vs. 204 minutes). The time to balloon inflation from arrival at the cardiac center was also slightly longer (73 vs. 60 minutes).
There was a trend for an increased rate of seizures in the 31° C group (12.5% vs. 7.1%; P = .08), but other secondary outcomes, including pneumonia (67.8% vs. 63.4%), renal replacement therapy (9.2% vs. 9.3%), and stroke (4.4% vs. 1.6%), were similar in the 31° C and 34° C groups, respectively.
Bleeding, whether measured by transfusion (19.6% vs. 22.4%) or TIMI major bleed (23.4% vs. 19.7%) were similar in the 31° C and 34° C groups, respectively. Thrombosis, whether measured by stent thrombosis (1.2% vs. 2.2%) or deep venous thrombosis (11.4% vs. 10.9%) were similar in these two groups, respectively.
The length of stay in the cardiac intensive care unit was significantly greater in the 31° C group (10 vs. 7 days; P = .004). Some of this increased length of stay can be attributed to the longer rewarming process required for the greater cooling, according to Dr. Le May, but he acknowledged that it is not clear this provides a full explanation.
More trials like CAPITAL-CHILL needed
The validity of these findings is supported by several strengths of the methodology, according to Jeanne E. Poole, MD, director of the arrhythmia service and electrophysiology laboratory, University of Washington, Seattle. This includes the reliance of an endovascular device, which can accelerate the time to the target temperature and assure the precision with which it is reached and maintained.
Dr. Poole did note that many of the primary and secondary measures, including the rates of stroke, seizures, and major bleeds, even though not significantly different, favored the higher temperature. The slightly longer door-to-balloon times might have been a factor. For the higher rate of pneumonia in the 31° C group, she questioned whether the longer period of ventilation linked to a longer period of rewarming might have been a factor.
However, Dr. Poole praised the CAPITAL-CHILL trial for drawing attention to a group of patients for whom survival rates remain “dismally low.” She indicated that these types of high-level trials are needed to look for strategies to improve outcomes.
Dr. Le May and Dr. Poole report no potential conflicts of interest.
The first randomized controlled trial to compare specific temperatures for therapeutic hypothermia in comatose survivors of out-of-hospital cardiac arrest showed no differences in major outcomes, according to a single-center, double-blind study.
In the CAPITAL-CHILL trial, cooling temperatures of 31° C and 34° C were compared to explore the hypothesis that a lower temperature would improve major outcomes, explained Michel Le May, MD.
No differences for the primary composite outcome of all-cause mortality or poor neurologic outcome at 180 days were observed, he reported at the annual scientific sessions of the American College of Cardiology.
The study was completed over a period of almost 7 years in patients presumed to have had an out-of-hospital cardiac arrest and who were unconscious when they reached a center affiliated with the Ottawa Heart Institute, where Dr. Le May directs the regional STEMI (ST-elevation myocardial infarction) program. The initial rhythm at the time of the cardiac arrest was not an entry criterion.
Of 389 patients enrolled, the intention-to-treat analysis included 184 randomized to a cooling temperature of 31° C group and 183 to a temperature of 34° C. The assigned target temperature, reached with an endovascular device, was known only by the managing nurses.
31° C and 34° C are equivalent
There was a small numerical disadvantage for the lower temperature assignment, but none reached statistical significance. This was true of the primary outcome (48.4% vs. 45.4% for the higher temperature) and its components of mortality (43.5% vs. 41.0%) and poor neurologic outcome (4.9% vs. 4.4%). Poor neurologic outcome was defined as a Disability Rating Scale score of greater than 5.
Deaths were most common in the early part of the 180-day follow-up in both arms. On a Kaplan-Meier survival graph, Dr. Le May showed curves that he characterized as “almost superimposable.”
There were no significant differences for any subgroup stratifications, such as age 75 years or older versus younger, males versus females, presence versus absence or an initial shockable rhythm, percutaneous coronary intervention (PCI) within 24 hours versus later, and STEMI versus non-STEMI. In these analyses, the higher temperature was associated with a potential trend for benefit among females and those with a shockable rhythm.
There was no signal for a difference in neurologic outcomes on the Disability Rating Scale or the Modified Rankin Scale. On the latter, for example, 46% of those in the 31° C group and 44% of these in the 34° C group had a score of four or greater at the end of follow-up.
The baseline characteristics of the two groups were similar. About 80% were male; the average age was roughly 62 years. More than 80% of the cardiac arrests were witnessed with CPR being administered by bystanders in nearly 70%. Nearly 40% had a STEMI.
Interventions were similar. Almost all patients underwent coronary angiography, of which nearly 60% received a percutaneous coronary intervention. More than 50% received a stent. The time from arrest to randomization was slightly longer in the 31° C group (228 vs. 204 minutes). The time to balloon inflation from arrival at the cardiac center was also slightly longer (73 vs. 60 minutes).
There was a trend for an increased rate of seizures in the 31° C group (12.5% vs. 7.1%; P = .08), but other secondary outcomes, including pneumonia (67.8% vs. 63.4%), renal replacement therapy (9.2% vs. 9.3%), and stroke (4.4% vs. 1.6%), were similar in the 31° C and 34° C groups, respectively.
Bleeding, whether measured by transfusion (19.6% vs. 22.4%) or TIMI major bleed (23.4% vs. 19.7%) were similar in the 31° C and 34° C groups, respectively. Thrombosis, whether measured by stent thrombosis (1.2% vs. 2.2%) or deep venous thrombosis (11.4% vs. 10.9%) were similar in these two groups, respectively.
The length of stay in the cardiac intensive care unit was significantly greater in the 31° C group (10 vs. 7 days; P = .004). Some of this increased length of stay can be attributed to the longer rewarming process required for the greater cooling, according to Dr. Le May, but he acknowledged that it is not clear this provides a full explanation.
More trials like CAPITAL-CHILL needed
The validity of these findings is supported by several strengths of the methodology, according to Jeanne E. Poole, MD, director of the arrhythmia service and electrophysiology laboratory, University of Washington, Seattle. This includes the reliance of an endovascular device, which can accelerate the time to the target temperature and assure the precision with which it is reached and maintained.
Dr. Poole did note that many of the primary and secondary measures, including the rates of stroke, seizures, and major bleeds, even though not significantly different, favored the higher temperature. The slightly longer door-to-balloon times might have been a factor. For the higher rate of pneumonia in the 31° C group, she questioned whether the longer period of ventilation linked to a longer period of rewarming might have been a factor.
However, Dr. Poole praised the CAPITAL-CHILL trial for drawing attention to a group of patients for whom survival rates remain “dismally low.” She indicated that these types of high-level trials are needed to look for strategies to improve outcomes.
Dr. Le May and Dr. Poole report no potential conflicts of interest.
The first randomized controlled trial to compare specific temperatures for therapeutic hypothermia in comatose survivors of out-of-hospital cardiac arrest showed no differences in major outcomes, according to a single-center, double-blind study.
In the CAPITAL-CHILL trial, cooling temperatures of 31° C and 34° C were compared to explore the hypothesis that a lower temperature would improve major outcomes, explained Michel Le May, MD.
No differences for the primary composite outcome of all-cause mortality or poor neurologic outcome at 180 days were observed, he reported at the annual scientific sessions of the American College of Cardiology.
The study was completed over a period of almost 7 years in patients presumed to have had an out-of-hospital cardiac arrest and who were unconscious when they reached a center affiliated with the Ottawa Heart Institute, where Dr. Le May directs the regional STEMI (ST-elevation myocardial infarction) program. The initial rhythm at the time of the cardiac arrest was not an entry criterion.
Of 389 patients enrolled, the intention-to-treat analysis included 184 randomized to a cooling temperature of 31° C group and 183 to a temperature of 34° C. The assigned target temperature, reached with an endovascular device, was known only by the managing nurses.
31° C and 34° C are equivalent
There was a small numerical disadvantage for the lower temperature assignment, but none reached statistical significance. This was true of the primary outcome (48.4% vs. 45.4% for the higher temperature) and its components of mortality (43.5% vs. 41.0%) and poor neurologic outcome (4.9% vs. 4.4%). Poor neurologic outcome was defined as a Disability Rating Scale score of greater than 5.
Deaths were most common in the early part of the 180-day follow-up in both arms. On a Kaplan-Meier survival graph, Dr. Le May showed curves that he characterized as “almost superimposable.”
There were no significant differences for any subgroup stratifications, such as age 75 years or older versus younger, males versus females, presence versus absence or an initial shockable rhythm, percutaneous coronary intervention (PCI) within 24 hours versus later, and STEMI versus non-STEMI. In these analyses, the higher temperature was associated with a potential trend for benefit among females and those with a shockable rhythm.
There was no signal for a difference in neurologic outcomes on the Disability Rating Scale or the Modified Rankin Scale. On the latter, for example, 46% of those in the 31° C group and 44% of these in the 34° C group had a score of four or greater at the end of follow-up.
The baseline characteristics of the two groups were similar. About 80% were male; the average age was roughly 62 years. More than 80% of the cardiac arrests were witnessed with CPR being administered by bystanders in nearly 70%. Nearly 40% had a STEMI.
Interventions were similar. Almost all patients underwent coronary angiography, of which nearly 60% received a percutaneous coronary intervention. More than 50% received a stent. The time from arrest to randomization was slightly longer in the 31° C group (228 vs. 204 minutes). The time to balloon inflation from arrival at the cardiac center was also slightly longer (73 vs. 60 minutes).
There was a trend for an increased rate of seizures in the 31° C group (12.5% vs. 7.1%; P = .08), but other secondary outcomes, including pneumonia (67.8% vs. 63.4%), renal replacement therapy (9.2% vs. 9.3%), and stroke (4.4% vs. 1.6%), were similar in the 31° C and 34° C groups, respectively.
Bleeding, whether measured by transfusion (19.6% vs. 22.4%) or TIMI major bleed (23.4% vs. 19.7%) were similar in the 31° C and 34° C groups, respectively. Thrombosis, whether measured by stent thrombosis (1.2% vs. 2.2%) or deep venous thrombosis (11.4% vs. 10.9%) were similar in these two groups, respectively.
The length of stay in the cardiac intensive care unit was significantly greater in the 31° C group (10 vs. 7 days; P = .004). Some of this increased length of stay can be attributed to the longer rewarming process required for the greater cooling, according to Dr. Le May, but he acknowledged that it is not clear this provides a full explanation.
More trials like CAPITAL-CHILL needed
The validity of these findings is supported by several strengths of the methodology, according to Jeanne E. Poole, MD, director of the arrhythmia service and electrophysiology laboratory, University of Washington, Seattle. This includes the reliance of an endovascular device, which can accelerate the time to the target temperature and assure the precision with which it is reached and maintained.
Dr. Poole did note that many of the primary and secondary measures, including the rates of stroke, seizures, and major bleeds, even though not significantly different, favored the higher temperature. The slightly longer door-to-balloon times might have been a factor. For the higher rate of pneumonia in the 31° C group, she questioned whether the longer period of ventilation linked to a longer period of rewarming might have been a factor.
However, Dr. Poole praised the CAPITAL-CHILL trial for drawing attention to a group of patients for whom survival rates remain “dismally low.” She indicated that these types of high-level trials are needed to look for strategies to improve outcomes.
Dr. Le May and Dr. Poole report no potential conflicts of interest.
FROM ACC 2021
Early aspirin withdrawal after PCI: More benefit for women?
A new analysis from the TWILIGHT study has shown that, in the high-risk population undergoing percutaneous coronary intervention (PCI) enrolled in the study, the benefits of early aspirin withdrawal and continuation on ticagrelor monotherapy were similar in women and men.
But there were some interesting observations in the analysis suggesting possible additional benefits of this strategy for women.
“These data support the use of ticagrelor monotherapy in women and men, and importantly show that the absolute risk reduction of bleeding was higher in women, as their bleeding rates were higher,” senior author Roxana Mehran, MD, the Zena and Michael A. Wiener Cardiovascular Institute, Icahn School of Medicine at Mount Sinai, New York, said in an interview.
“These data also support the need for prospective dual antiplatelet therapy deescalation studies in women,” Dr. Mehran added.
The main results of the TWILIGHT study showed that after a short period of dual antiplatelet therapy, a strategy of ticagrelor monotherapy, compared with continued dual therapy led to reduced bleeding without an increase in ischemic events among patients at high risk for bleeding or ischemic events after PCI.
The new gender-based analysis was presented by Birgit Vogel, MD, on May 15 at the annual scientific sessions of the American College of Cardiology. It was also published online in JAMA Cardiology to coincide with the ACC presentation.
Dr. Vogel, also from Wiener Cardiovascular Institute, explained that the current analysis was undertaken to investigate whether the TWILIGHT results varied in relation to sex, given that women are believed to have an increased risk for bleeding after PCI, compared with men.
“The current analysis showed that, while women did have a higher bleeding risk, compared to men, this was no longer significant after adjustment for baseline characteristics; and ischemic events were similar between the two sexes,” she reported.
“Results showed that withdrawing aspirin while continuing ticagrelor after 3 months of dual antiplatelet therapy was associated with a reduction in bleeding and preserved ischemic benefits in both women and men,” she added.
The TWILIGHT trial randomized 7,119 patients at high risk of ischemic or bleeding events who had undergone successful PCI with at least one drug-eluting stent and had completed 3 months of dual antiplatelet therapy to aspirin or placebo for an additional 12 months plus open-label ticagrelor.
The main results showed that the primary endpoint of Bleeding Academic Research Consortium (BARC) 2, 3, or 5 bleeding at 1 year was almost halved with ticagrelor monotherapy, occurring in 4% of these patients, compared with 7.1% of the ticagrelor/aspirin group (hazard ratio, 0.56). Ischemic events were similar in the two groups.
The current analysis focused on whether these effects varied in relation to sex.
Dr. Vogel noted that women made up 23.9% of the study population, were older than the men, and were more likely to have diabetes, chronic kidney disease, anemia and hypertension, while the men were more likely to be current smokers. Men had a higher incidence of coronary heart disease history, while women were more likely to have an ACS indication for PCI.
Unadjusted results showed a higher rate of BARC 2, 3, or 5 bleeding at 1 year in women (6.8%) versus men (5.2%), giving an HR of 1.32 (95% CI, 1.06-1.64).
But after adjustment for baseline characteristics, this became nonsignificant (HR, 1.20; 95% CI, 0.95-1.52).
Dr. Vogel pointed out that the most severe type of bleeding (BARC 3 and 5) was not attenuated as much by adjustment for baseline characteristics, with the HR reducing from 1.57 to 1.49.
The ischemic endpoint of death/stroke or MI was similar in men (4.0%) and women (3.5%), and this did not change after adjustment for baseline characteristics.
In terms of the two treatment groups, BARC 2, 3, or 5 bleeding was reduced to a similar extent with ticagrelor monotherapy in both men and women. This endpoint decreased from 8.6% in women on dual-antiplatelet therapy to 5.0% in women on ticagrelor alone (adjusted HR, 0.62) and from 6.6% to 3.7% in men (aHR, 0.57). But she noted that the absolute risk reduction in bleeding was greater in women (3.6%) versus men (2.9%).
“If we have a relative risk reduction in bleeding with early withdrawal of aspirin that is similar between the sexes but an overall higher risk of bleeding in women, that results in a greater absolute risk reduction,” Dr. Vogel commented.
The primary ischemic endpoint of death/MI/stroke was not increased in the ticagrelor group vs the dual antiplatelet group in either men (aHR, 1.06) or women (aHR, 1.04).
Greater reduction in mortality in women?
However, Dr. Vogel reported that there was a suggestion of a greater reduction in all-cause mortality with ticagrelor monotherapy in women versus men. “We found a significant interaction for treatment effect and sex for all-cause mortality, a prespecified endpoint, which was significantly lower in women treated with ticagrelor monotherapy, compared to dual antiplatelet therapy, but this was not the case in men.”
However, this observation was based on few events and should not be considered definitive, she added.
Dr. Vogel noted that the analysis had the limitations of the study not being powered to show differences in men versus women, and the results are only applicable to the population studied who were at high risk of bleeding post PCI.
Commenting on the study at the ACC session, Jacqueline Tamis-Holland, MD, associate professor of medicine at the Icahn School of Medicine at Mount Sinai, described the presentation as “very interesting.”
“We know that women notoriously have higher bleeding risk than men, but this particular study did not show a difference in bleeding risk after adjusting for other confounding variables,” she said.
“In fact, one would think that the relative benefit of a treatment designed to decrease bleeding would be more favorable to women, but this analysis didn’t show that,” she added.
Dr. Vogel replied that the HR of the most serious type of bleeding (BARC 3 and 5) in women versus men was only reduced minimally after adjustment for baseline characteristics, “which still makes us think that there are additional factors that might be important and contribute to an increased risk for bleeding and especially more serous types of bleeding in women.”
She pointed out that, while there was a similar risk reduction in bleeding in women and men, there was a potential mortality benefit in women. “The question is whether this mortality benefit is due to reduced bleeding that might be greater in women than men, and the reality is we don’t have a lot of data on that.”
Dr. Vogel added: “We know about the relationship between bleeding and mortality very well but the impact of sex on this is really not well investigated. It would be worth investigating this further to come up with bleeding reduction strategies for women because this is a really important issue.”
This work was supported by an investigator-initiated grant from AstraZeneca. Dr. Mehran reported grants and personal fees (paid to the institution) from Abbott, Abiomed, Bayer, Beth Israel Deaconess, Bristol-Myers Squibb, Chiesi, Concept Medical Research, Medtronic, Novartis and DSI Research; grants from Applied Therapeutics, AstraZeneca, Cerecor, CSL Behring, OrbusNeich, and Zoll; personal fees from Boston Scientific, California Institute for Regenerative Medicine, Cine-Med Research, Janssen Scientific Affairs, ACC, and WebMD; personal fees paid to the institution from CardiaWave, Duke University, and Idorsia Pharmaceuticals; serving as a consultant or committee or advisory board member for Society for Cardiovascular Angiography and Interventions, the American Medical Association, and Regeneron Pharmaceuticals; and owning stock in ControlRad, Elixir Medical, and STEL outside the submitted work. Dr. Vogel disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new analysis from the TWILIGHT study has shown that, in the high-risk population undergoing percutaneous coronary intervention (PCI) enrolled in the study, the benefits of early aspirin withdrawal and continuation on ticagrelor monotherapy were similar in women and men.
But there were some interesting observations in the analysis suggesting possible additional benefits of this strategy for women.
“These data support the use of ticagrelor monotherapy in women and men, and importantly show that the absolute risk reduction of bleeding was higher in women, as their bleeding rates were higher,” senior author Roxana Mehran, MD, the Zena and Michael A. Wiener Cardiovascular Institute, Icahn School of Medicine at Mount Sinai, New York, said in an interview.
“These data also support the need for prospective dual antiplatelet therapy deescalation studies in women,” Dr. Mehran added.
The main results of the TWILIGHT study showed that after a short period of dual antiplatelet therapy, a strategy of ticagrelor monotherapy, compared with continued dual therapy led to reduced bleeding without an increase in ischemic events among patients at high risk for bleeding or ischemic events after PCI.
The new gender-based analysis was presented by Birgit Vogel, MD, on May 15 at the annual scientific sessions of the American College of Cardiology. It was also published online in JAMA Cardiology to coincide with the ACC presentation.
Dr. Vogel, also from Wiener Cardiovascular Institute, explained that the current analysis was undertaken to investigate whether the TWILIGHT results varied in relation to sex, given that women are believed to have an increased risk for bleeding after PCI, compared with men.
“The current analysis showed that, while women did have a higher bleeding risk, compared to men, this was no longer significant after adjustment for baseline characteristics; and ischemic events were similar between the two sexes,” she reported.
“Results showed that withdrawing aspirin while continuing ticagrelor after 3 months of dual antiplatelet therapy was associated with a reduction in bleeding and preserved ischemic benefits in both women and men,” she added.
The TWILIGHT trial randomized 7,119 patients at high risk of ischemic or bleeding events who had undergone successful PCI with at least one drug-eluting stent and had completed 3 months of dual antiplatelet therapy to aspirin or placebo for an additional 12 months plus open-label ticagrelor.
The main results showed that the primary endpoint of Bleeding Academic Research Consortium (BARC) 2, 3, or 5 bleeding at 1 year was almost halved with ticagrelor monotherapy, occurring in 4% of these patients, compared with 7.1% of the ticagrelor/aspirin group (hazard ratio, 0.56). Ischemic events were similar in the two groups.
The current analysis focused on whether these effects varied in relation to sex.
Dr. Vogel noted that women made up 23.9% of the study population, were older than the men, and were more likely to have diabetes, chronic kidney disease, anemia and hypertension, while the men were more likely to be current smokers. Men had a higher incidence of coronary heart disease history, while women were more likely to have an ACS indication for PCI.
Unadjusted results showed a higher rate of BARC 2, 3, or 5 bleeding at 1 year in women (6.8%) versus men (5.2%), giving an HR of 1.32 (95% CI, 1.06-1.64).
But after adjustment for baseline characteristics, this became nonsignificant (HR, 1.20; 95% CI, 0.95-1.52).
Dr. Vogel pointed out that the most severe type of bleeding (BARC 3 and 5) was not attenuated as much by adjustment for baseline characteristics, with the HR reducing from 1.57 to 1.49.
The ischemic endpoint of death/stroke or MI was similar in men (4.0%) and women (3.5%), and this did not change after adjustment for baseline characteristics.
In terms of the two treatment groups, BARC 2, 3, or 5 bleeding was reduced to a similar extent with ticagrelor monotherapy in both men and women. This endpoint decreased from 8.6% in women on dual-antiplatelet therapy to 5.0% in women on ticagrelor alone (adjusted HR, 0.62) and from 6.6% to 3.7% in men (aHR, 0.57). But she noted that the absolute risk reduction in bleeding was greater in women (3.6%) versus men (2.9%).
“If we have a relative risk reduction in bleeding with early withdrawal of aspirin that is similar between the sexes but an overall higher risk of bleeding in women, that results in a greater absolute risk reduction,” Dr. Vogel commented.
The primary ischemic endpoint of death/MI/stroke was not increased in the ticagrelor group vs the dual antiplatelet group in either men (aHR, 1.06) or women (aHR, 1.04).
Greater reduction in mortality in women?
However, Dr. Vogel reported that there was a suggestion of a greater reduction in all-cause mortality with ticagrelor monotherapy in women versus men. “We found a significant interaction for treatment effect and sex for all-cause mortality, a prespecified endpoint, which was significantly lower in women treated with ticagrelor monotherapy, compared to dual antiplatelet therapy, but this was not the case in men.”
However, this observation was based on few events and should not be considered definitive, she added.
Dr. Vogel noted that the analysis had the limitations of the study not being powered to show differences in men versus women, and the results are only applicable to the population studied who were at high risk of bleeding post PCI.
Commenting on the study at the ACC session, Jacqueline Tamis-Holland, MD, associate professor of medicine at the Icahn School of Medicine at Mount Sinai, described the presentation as “very interesting.”
“We know that women notoriously have higher bleeding risk than men, but this particular study did not show a difference in bleeding risk after adjusting for other confounding variables,” she said.
“In fact, one would think that the relative benefit of a treatment designed to decrease bleeding would be more favorable to women, but this analysis didn’t show that,” she added.
Dr. Vogel replied that the HR of the most serious type of bleeding (BARC 3 and 5) in women versus men was only reduced minimally after adjustment for baseline characteristics, “which still makes us think that there are additional factors that might be important and contribute to an increased risk for bleeding and especially more serous types of bleeding in women.”
She pointed out that, while there was a similar risk reduction in bleeding in women and men, there was a potential mortality benefit in women. “The question is whether this mortality benefit is due to reduced bleeding that might be greater in women than men, and the reality is we don’t have a lot of data on that.”
Dr. Vogel added: “We know about the relationship between bleeding and mortality very well but the impact of sex on this is really not well investigated. It would be worth investigating this further to come up with bleeding reduction strategies for women because this is a really important issue.”
This work was supported by an investigator-initiated grant from AstraZeneca. Dr. Mehran reported grants and personal fees (paid to the institution) from Abbott, Abiomed, Bayer, Beth Israel Deaconess, Bristol-Myers Squibb, Chiesi, Concept Medical Research, Medtronic, Novartis and DSI Research; grants from Applied Therapeutics, AstraZeneca, Cerecor, CSL Behring, OrbusNeich, and Zoll; personal fees from Boston Scientific, California Institute for Regenerative Medicine, Cine-Med Research, Janssen Scientific Affairs, ACC, and WebMD; personal fees paid to the institution from CardiaWave, Duke University, and Idorsia Pharmaceuticals; serving as a consultant or committee or advisory board member for Society for Cardiovascular Angiography and Interventions, the American Medical Association, and Regeneron Pharmaceuticals; and owning stock in ControlRad, Elixir Medical, and STEL outside the submitted work. Dr. Vogel disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new analysis from the TWILIGHT study has shown that, in the high-risk population undergoing percutaneous coronary intervention (PCI) enrolled in the study, the benefits of early aspirin withdrawal and continuation on ticagrelor monotherapy were similar in women and men.
But there were some interesting observations in the analysis suggesting possible additional benefits of this strategy for women.
“These data support the use of ticagrelor monotherapy in women and men, and importantly show that the absolute risk reduction of bleeding was higher in women, as their bleeding rates were higher,” senior author Roxana Mehran, MD, the Zena and Michael A. Wiener Cardiovascular Institute, Icahn School of Medicine at Mount Sinai, New York, said in an interview.
“These data also support the need for prospective dual antiplatelet therapy deescalation studies in women,” Dr. Mehran added.
The main results of the TWILIGHT study showed that after a short period of dual antiplatelet therapy, a strategy of ticagrelor monotherapy, compared with continued dual therapy led to reduced bleeding without an increase in ischemic events among patients at high risk for bleeding or ischemic events after PCI.
The new gender-based analysis was presented by Birgit Vogel, MD, on May 15 at the annual scientific sessions of the American College of Cardiology. It was also published online in JAMA Cardiology to coincide with the ACC presentation.
Dr. Vogel, also from Wiener Cardiovascular Institute, explained that the current analysis was undertaken to investigate whether the TWILIGHT results varied in relation to sex, given that women are believed to have an increased risk for bleeding after PCI, compared with men.
“The current analysis showed that, while women did have a higher bleeding risk, compared to men, this was no longer significant after adjustment for baseline characteristics; and ischemic events were similar between the two sexes,” she reported.
“Results showed that withdrawing aspirin while continuing ticagrelor after 3 months of dual antiplatelet therapy was associated with a reduction in bleeding and preserved ischemic benefits in both women and men,” she added.
The TWILIGHT trial randomized 7,119 patients at high risk of ischemic or bleeding events who had undergone successful PCI with at least one drug-eluting stent and had completed 3 months of dual antiplatelet therapy to aspirin or placebo for an additional 12 months plus open-label ticagrelor.
The main results showed that the primary endpoint of Bleeding Academic Research Consortium (BARC) 2, 3, or 5 bleeding at 1 year was almost halved with ticagrelor monotherapy, occurring in 4% of these patients, compared with 7.1% of the ticagrelor/aspirin group (hazard ratio, 0.56). Ischemic events were similar in the two groups.
The current analysis focused on whether these effects varied in relation to sex.
Dr. Vogel noted that women made up 23.9% of the study population, were older than the men, and were more likely to have diabetes, chronic kidney disease, anemia and hypertension, while the men were more likely to be current smokers. Men had a higher incidence of coronary heart disease history, while women were more likely to have an ACS indication for PCI.
Unadjusted results showed a higher rate of BARC 2, 3, or 5 bleeding at 1 year in women (6.8%) versus men (5.2%), giving an HR of 1.32 (95% CI, 1.06-1.64).
But after adjustment for baseline characteristics, this became nonsignificant (HR, 1.20; 95% CI, 0.95-1.52).
Dr. Vogel pointed out that the most severe type of bleeding (BARC 3 and 5) was not attenuated as much by adjustment for baseline characteristics, with the HR reducing from 1.57 to 1.49.
The ischemic endpoint of death/stroke or MI was similar in men (4.0%) and women (3.5%), and this did not change after adjustment for baseline characteristics.
In terms of the two treatment groups, BARC 2, 3, or 5 bleeding was reduced to a similar extent with ticagrelor monotherapy in both men and women. This endpoint decreased from 8.6% in women on dual-antiplatelet therapy to 5.0% in women on ticagrelor alone (adjusted HR, 0.62) and from 6.6% to 3.7% in men (aHR, 0.57). But she noted that the absolute risk reduction in bleeding was greater in women (3.6%) versus men (2.9%).
“If we have a relative risk reduction in bleeding with early withdrawal of aspirin that is similar between the sexes but an overall higher risk of bleeding in women, that results in a greater absolute risk reduction,” Dr. Vogel commented.
The primary ischemic endpoint of death/MI/stroke was not increased in the ticagrelor group vs the dual antiplatelet group in either men (aHR, 1.06) or women (aHR, 1.04).
Greater reduction in mortality in women?
However, Dr. Vogel reported that there was a suggestion of a greater reduction in all-cause mortality with ticagrelor monotherapy in women versus men. “We found a significant interaction for treatment effect and sex for all-cause mortality, a prespecified endpoint, which was significantly lower in women treated with ticagrelor monotherapy, compared to dual antiplatelet therapy, but this was not the case in men.”
However, this observation was based on few events and should not be considered definitive, she added.
Dr. Vogel noted that the analysis had the limitations of the study not being powered to show differences in men versus women, and the results are only applicable to the population studied who were at high risk of bleeding post PCI.
Commenting on the study at the ACC session, Jacqueline Tamis-Holland, MD, associate professor of medicine at the Icahn School of Medicine at Mount Sinai, described the presentation as “very interesting.”
“We know that women notoriously have higher bleeding risk than men, but this particular study did not show a difference in bleeding risk after adjusting for other confounding variables,” she said.
“In fact, one would think that the relative benefit of a treatment designed to decrease bleeding would be more favorable to women, but this analysis didn’t show that,” she added.
Dr. Vogel replied that the HR of the most serious type of bleeding (BARC 3 and 5) in women versus men was only reduced minimally after adjustment for baseline characteristics, “which still makes us think that there are additional factors that might be important and contribute to an increased risk for bleeding and especially more serous types of bleeding in women.”
She pointed out that, while there was a similar risk reduction in bleeding in women and men, there was a potential mortality benefit in women. “The question is whether this mortality benefit is due to reduced bleeding that might be greater in women than men, and the reality is we don’t have a lot of data on that.”
Dr. Vogel added: “We know about the relationship between bleeding and mortality very well but the impact of sex on this is really not well investigated. It would be worth investigating this further to come up with bleeding reduction strategies for women because this is a really important issue.”
This work was supported by an investigator-initiated grant from AstraZeneca. Dr. Mehran reported grants and personal fees (paid to the institution) from Abbott, Abiomed, Bayer, Beth Israel Deaconess, Bristol-Myers Squibb, Chiesi, Concept Medical Research, Medtronic, Novartis and DSI Research; grants from Applied Therapeutics, AstraZeneca, Cerecor, CSL Behring, OrbusNeich, and Zoll; personal fees from Boston Scientific, California Institute for Regenerative Medicine, Cine-Med Research, Janssen Scientific Affairs, ACC, and WebMD; personal fees paid to the institution from CardiaWave, Duke University, and Idorsia Pharmaceuticals; serving as a consultant or committee or advisory board member for Society for Cardiovascular Angiography and Interventions, the American Medical Association, and Regeneron Pharmaceuticals; and owning stock in ControlRad, Elixir Medical, and STEL outside the submitted work. Dr. Vogel disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
SAFE-PAD: Endovascular paclitaxel-coated devices exonerated in real-world analysis
A cohort analysis using advanced strategies to minimize the impact of confounders has concluded that the current Food and Drug Administration warning about paclitaxel-coated devices used for femoropopliteal endovascular treatment should be lifted, according to investigators of a study called SAFE-PAD.
In early 2019, an FDA letter to clinicians warned that endovascular stents and balloons coated with paclitaxel might increase mortality, recounted the principal investigator of SAFE-PAD, Eric A. Secemsky, MD, director of vascular intervention, Beth Israel Deaconess Hospital, Boston.
An FDA advisory committee that was subsequently convened in 2019 did not elect to remove these devices from the market, but it did call for restrictions and for the collection of more safety data. In the absence of a clear mechanism of risk, and in the context of perceived problems with data suggesting harm, Dr. Secemsky said that there was interest in a conclusive answer.
The problem was that a randomized controlled trial, even if funding were available, was considered impractical, he noted in presenting SAFE-PAD at the annual scientific sessions of the American College of Cardiology.
In the initial meta-analysis that suggested an increased mortality risk, no risk was seen in the first year after exposure, and it climbed to only 3.5% after 2 years. As a result, the definitive 2-year study with sufficient power to produce conclusive results was an estimated 40,000 patients. Even if extended to 5 years, 20,000 patients would be needed, according to Dr. Secemsky.
SAFE-PAD born of collaboration
An alternative solution was required, which is why “we became engaged with the FDA to design a real-world study for use in making a regulatory decision,” Dr. Secemsky said.
SAFE-PAD, designed with feedback from the FDA, employed sophisticated methodologies to account for known and unknown confounding in the Medicare cohort data used for this study.
Of 168,553 Medicare fee-for-service patients undergoing femoropopliteal artery revascularization with a stent, a balloon, or both at 2,978 institutions, 70,584 (42%) were treated with a paclitaxel drug-coated device (DCD) and the remainder were managed with a non–drug-coated device (NDCD).
The groups were compared with a primary outcome of all-cause mortality in a design to evaluate DCD for noninferiority. Several secondary outcomes, such as repeated lower extremity revascularization, were also evaluated.
To create balanced groups, inverse probability of treatment weighting (IPTW) blinded to outcome was the primary analytic strategy. In addition, several sensitivity analyses were applied, including a technique that tests for the impact of a hypothetical variable that allows adjustment for an unknown confounder.
After a median follow-up of 2.7 years (longest more than 5 years), the cumulative mortality after weighting was 53.8% in the DCD group and 55.1% in the NDCD group. The 5% advantage for the DCD group (hazard ratio, 0.95; 95% confidence interval, 0.94-0.97) ensured noninferiority (P < .001).
On unweighted analysis, the mortality difference favoring DCD was even greater (HR, 0.85; 95% CI, 0.82–0.85).
None of the sensitivity analyses – including a multivariable Cox regression analysis, an instrumental variable analysis, and a falsification endpoints analysis that employed myocardial infarction, pneumonia, and heart failure – altered the conclusion. The hypothetical variable analysis produced the same result.
“A missing confounder would need to be more prevalent and more strongly associated to outcome than any measured variable in this analysis,” reported Dr. Secemsky, indicating that this ruled out essentially any probability of this occurring.
A subgroup analysis told the same story. By hazard ratio for the outcome of mortality, DCD was consistently favored over NDCD for groups characterized by low risk (HR, 0.98), stent implantation (HR, 0.97), receipt of balloon angioplasty alone (HR, 0.94), having critical limb ischemia (HR, 0.95) or no critical limb ischemia (HR, 0.97), and being managed inpatient (HR, 0.97) or outpatient (HR, 0.95).
The results of SAFE-PAD were simultaneously published with Dr. Secemsky’s ACC presentation.
Value of revascularization questioned
In an accompanying editorial, the coauthors Rita F. Redberg, MD, of the University of California, San Francisco, and Mary M. McDermott, MD, of Northwestern University, Chicago, reiterated the findings and the conclusions, but used the forum to draw attention to the low survival rates.
“Thus, while this well-done observational study provides new information,” they wrote, “a major conclusion should be that mortality is high among Medicare beneficiaries undergoing revascularization [for peripheral artery disease] with any devices.”
‘Very impressive’ methods
Marc P. Bonaca, MD, director of vascular research, University of Colorado at Denver, Aurora, called the methods to ensure the validity of the conclusions of this study “very impressive.” In situations where prospective randomized trials are impractical, he suggested that this type of approach might answer an unmet need.
“We have always desired the ability to look at these large datasets with a lot of power to answer important questions,” he said. While “the issue has always been residual confounding,” he expressed interest in further verifications that this type of methodology can serve as a template for data analysis to guide other regulatory decisions.
Dr. Secemsky reports financial relationships with Abbott, Bayer, Boston Scientific, Cook, CSI, Inari, Janssen, Medtronic, and Phillips. Dr. Redford reports no potential conflicts of interest. Dr. McDermott reports a financial relationship with Regeneron. Dr. Bonaca reports financial relationships with Amgen, AstraZeneca, Bayer, Janssen Merck, Novo Nordisk, Pfizer, and Sanofi.
A cohort analysis using advanced strategies to minimize the impact of confounders has concluded that the current Food and Drug Administration warning about paclitaxel-coated devices used for femoropopliteal endovascular treatment should be lifted, according to investigators of a study called SAFE-PAD.
In early 2019, an FDA letter to clinicians warned that endovascular stents and balloons coated with paclitaxel might increase mortality, recounted the principal investigator of SAFE-PAD, Eric A. Secemsky, MD, director of vascular intervention, Beth Israel Deaconess Hospital, Boston.
An FDA advisory committee that was subsequently convened in 2019 did not elect to remove these devices from the market, but it did call for restrictions and for the collection of more safety data. In the absence of a clear mechanism of risk, and in the context of perceived problems with data suggesting harm, Dr. Secemsky said that there was interest in a conclusive answer.
The problem was that a randomized controlled trial, even if funding were available, was considered impractical, he noted in presenting SAFE-PAD at the annual scientific sessions of the American College of Cardiology.
In the initial meta-analysis that suggested an increased mortality risk, no risk was seen in the first year after exposure, and it climbed to only 3.5% after 2 years. As a result, the definitive 2-year study with sufficient power to produce conclusive results was an estimated 40,000 patients. Even if extended to 5 years, 20,000 patients would be needed, according to Dr. Secemsky.
SAFE-PAD born of collaboration
An alternative solution was required, which is why “we became engaged with the FDA to design a real-world study for use in making a regulatory decision,” Dr. Secemsky said.
SAFE-PAD, designed with feedback from the FDA, employed sophisticated methodologies to account for known and unknown confounding in the Medicare cohort data used for this study.
Of 168,553 Medicare fee-for-service patients undergoing femoropopliteal artery revascularization with a stent, a balloon, or both at 2,978 institutions, 70,584 (42%) were treated with a paclitaxel drug-coated device (DCD) and the remainder were managed with a non–drug-coated device (NDCD).
The groups were compared with a primary outcome of all-cause mortality in a design to evaluate DCD for noninferiority. Several secondary outcomes, such as repeated lower extremity revascularization, were also evaluated.
To create balanced groups, inverse probability of treatment weighting (IPTW) blinded to outcome was the primary analytic strategy. In addition, several sensitivity analyses were applied, including a technique that tests for the impact of a hypothetical variable that allows adjustment for an unknown confounder.
After a median follow-up of 2.7 years (longest more than 5 years), the cumulative mortality after weighting was 53.8% in the DCD group and 55.1% in the NDCD group. The 5% advantage for the DCD group (hazard ratio, 0.95; 95% confidence interval, 0.94-0.97) ensured noninferiority (P < .001).
On unweighted analysis, the mortality difference favoring DCD was even greater (HR, 0.85; 95% CI, 0.82–0.85).
None of the sensitivity analyses – including a multivariable Cox regression analysis, an instrumental variable analysis, and a falsification endpoints analysis that employed myocardial infarction, pneumonia, and heart failure – altered the conclusion. The hypothetical variable analysis produced the same result.
“A missing confounder would need to be more prevalent and more strongly associated to outcome than any measured variable in this analysis,” reported Dr. Secemsky, indicating that this ruled out essentially any probability of this occurring.
A subgroup analysis told the same story. By hazard ratio for the outcome of mortality, DCD was consistently favored over NDCD for groups characterized by low risk (HR, 0.98), stent implantation (HR, 0.97), receipt of balloon angioplasty alone (HR, 0.94), having critical limb ischemia (HR, 0.95) or no critical limb ischemia (HR, 0.97), and being managed inpatient (HR, 0.97) or outpatient (HR, 0.95).
The results of SAFE-PAD were simultaneously published with Dr. Secemsky’s ACC presentation.
Value of revascularization questioned
In an accompanying editorial, the coauthors Rita F. Redberg, MD, of the University of California, San Francisco, and Mary M. McDermott, MD, of Northwestern University, Chicago, reiterated the findings and the conclusions, but used the forum to draw attention to the low survival rates.
“Thus, while this well-done observational study provides new information,” they wrote, “a major conclusion should be that mortality is high among Medicare beneficiaries undergoing revascularization [for peripheral artery disease] with any devices.”
‘Very impressive’ methods
Marc P. Bonaca, MD, director of vascular research, University of Colorado at Denver, Aurora, called the methods to ensure the validity of the conclusions of this study “very impressive.” In situations where prospective randomized trials are impractical, he suggested that this type of approach might answer an unmet need.
“We have always desired the ability to look at these large datasets with a lot of power to answer important questions,” he said. While “the issue has always been residual confounding,” he expressed interest in further verifications that this type of methodology can serve as a template for data analysis to guide other regulatory decisions.
Dr. Secemsky reports financial relationships with Abbott, Bayer, Boston Scientific, Cook, CSI, Inari, Janssen, Medtronic, and Phillips. Dr. Redford reports no potential conflicts of interest. Dr. McDermott reports a financial relationship with Regeneron. Dr. Bonaca reports financial relationships with Amgen, AstraZeneca, Bayer, Janssen Merck, Novo Nordisk, Pfizer, and Sanofi.
A cohort analysis using advanced strategies to minimize the impact of confounders has concluded that the current Food and Drug Administration warning about paclitaxel-coated devices used for femoropopliteal endovascular treatment should be lifted, according to investigators of a study called SAFE-PAD.
In early 2019, an FDA letter to clinicians warned that endovascular stents and balloons coated with paclitaxel might increase mortality, recounted the principal investigator of SAFE-PAD, Eric A. Secemsky, MD, director of vascular intervention, Beth Israel Deaconess Hospital, Boston.
An FDA advisory committee that was subsequently convened in 2019 did not elect to remove these devices from the market, but it did call for restrictions and for the collection of more safety data. In the absence of a clear mechanism of risk, and in the context of perceived problems with data suggesting harm, Dr. Secemsky said that there was interest in a conclusive answer.
The problem was that a randomized controlled trial, even if funding were available, was considered impractical, he noted in presenting SAFE-PAD at the annual scientific sessions of the American College of Cardiology.
In the initial meta-analysis that suggested an increased mortality risk, no risk was seen in the first year after exposure, and it climbed to only 3.5% after 2 years. As a result, the definitive 2-year study with sufficient power to produce conclusive results was an estimated 40,000 patients. Even if extended to 5 years, 20,000 patients would be needed, according to Dr. Secemsky.
SAFE-PAD born of collaboration
An alternative solution was required, which is why “we became engaged with the FDA to design a real-world study for use in making a regulatory decision,” Dr. Secemsky said.
SAFE-PAD, designed with feedback from the FDA, employed sophisticated methodologies to account for known and unknown confounding in the Medicare cohort data used for this study.
Of 168,553 Medicare fee-for-service patients undergoing femoropopliteal artery revascularization with a stent, a balloon, or both at 2,978 institutions, 70,584 (42%) were treated with a paclitaxel drug-coated device (DCD) and the remainder were managed with a non–drug-coated device (NDCD).
The groups were compared with a primary outcome of all-cause mortality in a design to evaluate DCD for noninferiority. Several secondary outcomes, such as repeated lower extremity revascularization, were also evaluated.
To create balanced groups, inverse probability of treatment weighting (IPTW) blinded to outcome was the primary analytic strategy. In addition, several sensitivity analyses were applied, including a technique that tests for the impact of a hypothetical variable that allows adjustment for an unknown confounder.
After a median follow-up of 2.7 years (longest more than 5 years), the cumulative mortality after weighting was 53.8% in the DCD group and 55.1% in the NDCD group. The 5% advantage for the DCD group (hazard ratio, 0.95; 95% confidence interval, 0.94-0.97) ensured noninferiority (P < .001).
On unweighted analysis, the mortality difference favoring DCD was even greater (HR, 0.85; 95% CI, 0.82–0.85).
None of the sensitivity analyses – including a multivariable Cox regression analysis, an instrumental variable analysis, and a falsification endpoints analysis that employed myocardial infarction, pneumonia, and heart failure – altered the conclusion. The hypothetical variable analysis produced the same result.
“A missing confounder would need to be more prevalent and more strongly associated to outcome than any measured variable in this analysis,” reported Dr. Secemsky, indicating that this ruled out essentially any probability of this occurring.
A subgroup analysis told the same story. By hazard ratio for the outcome of mortality, DCD was consistently favored over NDCD for groups characterized by low risk (HR, 0.98), stent implantation (HR, 0.97), receipt of balloon angioplasty alone (HR, 0.94), having critical limb ischemia (HR, 0.95) or no critical limb ischemia (HR, 0.97), and being managed inpatient (HR, 0.97) or outpatient (HR, 0.95).
The results of SAFE-PAD were simultaneously published with Dr. Secemsky’s ACC presentation.
Value of revascularization questioned
In an accompanying editorial, the coauthors Rita F. Redberg, MD, of the University of California, San Francisco, and Mary M. McDermott, MD, of Northwestern University, Chicago, reiterated the findings and the conclusions, but used the forum to draw attention to the low survival rates.
“Thus, while this well-done observational study provides new information,” they wrote, “a major conclusion should be that mortality is high among Medicare beneficiaries undergoing revascularization [for peripheral artery disease] with any devices.”
‘Very impressive’ methods
Marc P. Bonaca, MD, director of vascular research, University of Colorado at Denver, Aurora, called the methods to ensure the validity of the conclusions of this study “very impressive.” In situations where prospective randomized trials are impractical, he suggested that this type of approach might answer an unmet need.
“We have always desired the ability to look at these large datasets with a lot of power to answer important questions,” he said. While “the issue has always been residual confounding,” he expressed interest in further verifications that this type of methodology can serve as a template for data analysis to guide other regulatory decisions.
Dr. Secemsky reports financial relationships with Abbott, Bayer, Boston Scientific, Cook, CSI, Inari, Janssen, Medtronic, and Phillips. Dr. Redford reports no potential conflicts of interest. Dr. McDermott reports a financial relationship with Regeneron. Dr. Bonaca reports financial relationships with Amgen, AstraZeneca, Bayer, Janssen Merck, Novo Nordisk, Pfizer, and Sanofi.
FROM ACC 2021
Ultrasound renal denervation drops BP in patients on triple therapy
Renal denervation’s comeback as a potential treatment for patients with drug-resistant hypertension rolls on.
Renal denervation with ultrasound energy produced a significant, median 4.5–mm Hg incremental drop in daytime, ambulatory, systolic blood pressure, compared with sham-treatment after 2 months follow-up in a randomized study of 136 patients with drug-resistant hypertension maintained on a standardized, single-pill, triple-drug regimen during the study.
The results “confirm that ultrasound renal denervation can lower blood pressure across a spectrum of hypertension,” concluded Ajay J. Kirtane, MD, at the annual scientific sessions of the American College of Cardiology. Renal denervation procedures involve percutaneously placing an endovascular catheter bilaterally inside a patient’s renal arteries and using brief pulses of energy to ablate neurons involved in blood pressure regulation.
A former ‘hot concept’
“Renal denervation was a hot concept a number of years ago, but had been tested only in studies without a sham control,” and initial testing using sham controls failed to show a significant benefit from the intervention, noted Deepak L. Bhatt, MD, an interventional cardiologist and professor of medicine at Harvard Medical School in Boston who was not involved with the study. The significant reductions in systolic blood pressure reported with renal denervation, compared with control patients in this study, “are believable” because of inclusion of a true control cohort, he added. “This really exciting finding puts renal denervation squarely back on the map,” commented Dr. Bhatt during a press briefing.
Dr. Bhatt added that, while the median 4.5–mm Hg incremental reduction in daytime, ambulatory, systolic blood pressure, compared with control patients – the study’s primary endpoint – may seem modest, “in the world of hypertension it’s a meaningful reduction” that, if sustained over the long term, would be expected to produce meaningful cuts in adverse cardiovascular events such as heart failure, stroke, and MI.
“The question is whether the effects are durable,” highlighted Dr. Bhatt, who helped lead the first sham-controlled trial of renal denervation, SYMPLICITY HTN-3, which failed to show a significant blood pressure reduction, compared with controls using radiofrequency energy to ablate renal nerves. A more recent study that used a different radiofrequency catheter and sham controls showed a significant effect on reducing systolic blood pressure in the SPYRAL HTN-OFF MED Pivotal trial, which by design did not maintain patients on any antihypertensive medications following their renal denervation procedure.
Dr. Kirtane noted that, although the median systolic blood pressure reduction, compared with controls treated by a sham procedure, was 4.5 mm Hg, the total median systolic pressure reduction after 2 months in the actively treated patients was 8.0 mm Hg when compared with their baseline blood pressure.
Concurrently with his report the results also appeared in an article posted online (Lancet. 2021 May 16;doi: 10.1016/S0140-6736(21)00788-1).
Denervation coupled with a single, daily three-drug pill
The RADIANCE-HTN TRIO study ran at 53 centers in the United States and Europe, and randomized 136 adults with an office-measured blood pressure of at least 140/90 mm Hg despite being on a stable regimen of at least three antihypertensive drugs including a diuretic. The enrolled cohort averaged 52 years of age and had an average office-measured pressure of about 162/104 mm Hg despite being on an average of four agents, although only about a third of enrolled patients were on treatment with a mineralocorticoid-receptor antagonist (MRA) such as spironolactone.
At the time of enrollment and 4 weeks before their denervation procedure, all patients switched to a uniform drug regimen of a single, daily, oral pill containing the calcium channel blocker amlodipine, the angiotensin receptor blocker valsartan or olmesartan, and the diuretic hydrochlorothiazide with no other drug treatment allowed except for unusual, prespecified clinical circumstances. All patients remained on this drug regimen for the initial 2-month follow-up period unless their blood pressure exceeded 180/110 mm Hg during in-office measurement.
The denervation treatment was well tolerated, although patients reported brief, transient, and “minor” pain associated with the procedure that did not affect treatment blinding or have any lingering consequences, said Dr. Kirtane, professor of medicine at Columbia University Vagelos College of Physicians and Surgeons in New York.
A reason to use energy delivery by ultrasound rather than by radiofrequency to ablate nerves in the renal arteries is that the ultrasound approach exerts a more uniform effect, allowing effective treatment delivery without need for catheter repositioning into more distal branches of the renal arteries, said Dr. Kirtane, who is also an interventional cardiologist at NewYork-Presbyterian/Columbia University Irving Medical Center.
But each method has its advantages, he added.
He also conceded that additional questions need to be addressed regarding which patients are most appropriate for renal denervation. “We need to figure out in which patients we can apply a device-based treatment,” Dr. Kirtane said during the press briefing. Patients with what appears to be drug-resistant hypertension often do not receive treatment with a MRA because of adverse effects, and many of these patients are not usually assessed for primary aldosteronism.
In SYMPLICITY HTN-3, “about half the patients who were seemingly eligible became ineligible” when they started treatment with a MRA, noted Dr. Bhatt. “A little spironolactone can go a long way” toward resolving treatment-resistant hypertension in many patients, he said.
RADIANCE-HTN TRIO was sponsored by ReCor Medical, the company developing the tested ultrasound catheter. Dr. Kirtane has received travel expenses and meals from ReCor Medical and several other companies, and Columbia has received research funding from ReCor Medical and several other companies related to research he has conducted. Dr. Bhatt has no relationship with ReCor Medical. He has been a consultant to and received honoraria from K2P, Level Ex, and MJH Life Sciences; he has been an advisor to Cardax, Cereno Scientific, Myokardia, Novo Nordisk, Phase Bio, and PLx Pharma; and he has received research funding from numerous companies.
Renal denervation’s comeback as a potential treatment for patients with drug-resistant hypertension rolls on.
Renal denervation with ultrasound energy produced a significant, median 4.5–mm Hg incremental drop in daytime, ambulatory, systolic blood pressure, compared with sham-treatment after 2 months follow-up in a randomized study of 136 patients with drug-resistant hypertension maintained on a standardized, single-pill, triple-drug regimen during the study.
The results “confirm that ultrasound renal denervation can lower blood pressure across a spectrum of hypertension,” concluded Ajay J. Kirtane, MD, at the annual scientific sessions of the American College of Cardiology. Renal denervation procedures involve percutaneously placing an endovascular catheter bilaterally inside a patient’s renal arteries and using brief pulses of energy to ablate neurons involved in blood pressure regulation.
A former ‘hot concept’
“Renal denervation was a hot concept a number of years ago, but had been tested only in studies without a sham control,” and initial testing using sham controls failed to show a significant benefit from the intervention, noted Deepak L. Bhatt, MD, an interventional cardiologist and professor of medicine at Harvard Medical School in Boston who was not involved with the study. The significant reductions in systolic blood pressure reported with renal denervation, compared with control patients in this study, “are believable” because of inclusion of a true control cohort, he added. “This really exciting finding puts renal denervation squarely back on the map,” commented Dr. Bhatt during a press briefing.
Dr. Bhatt added that, while the median 4.5–mm Hg incremental reduction in daytime, ambulatory, systolic blood pressure, compared with control patients – the study’s primary endpoint – may seem modest, “in the world of hypertension it’s a meaningful reduction” that, if sustained over the long term, would be expected to produce meaningful cuts in adverse cardiovascular events such as heart failure, stroke, and MI.
“The question is whether the effects are durable,” highlighted Dr. Bhatt, who helped lead the first sham-controlled trial of renal denervation, SYMPLICITY HTN-3, which failed to show a significant blood pressure reduction, compared with controls using radiofrequency energy to ablate renal nerves. A more recent study that used a different radiofrequency catheter and sham controls showed a significant effect on reducing systolic blood pressure in the SPYRAL HTN-OFF MED Pivotal trial, which by design did not maintain patients on any antihypertensive medications following their renal denervation procedure.
Dr. Kirtane noted that, although the median systolic blood pressure reduction, compared with controls treated by a sham procedure, was 4.5 mm Hg, the total median systolic pressure reduction after 2 months in the actively treated patients was 8.0 mm Hg when compared with their baseline blood pressure.
Concurrently with his report the results also appeared in an article posted online (Lancet. 2021 May 16;doi: 10.1016/S0140-6736(21)00788-1).
Denervation coupled with a single, daily three-drug pill
The RADIANCE-HTN TRIO study ran at 53 centers in the United States and Europe, and randomized 136 adults with an office-measured blood pressure of at least 140/90 mm Hg despite being on a stable regimen of at least three antihypertensive drugs including a diuretic. The enrolled cohort averaged 52 years of age and had an average office-measured pressure of about 162/104 mm Hg despite being on an average of four agents, although only about a third of enrolled patients were on treatment with a mineralocorticoid-receptor antagonist (MRA) such as spironolactone.
At the time of enrollment and 4 weeks before their denervation procedure, all patients switched to a uniform drug regimen of a single, daily, oral pill containing the calcium channel blocker amlodipine, the angiotensin receptor blocker valsartan or olmesartan, and the diuretic hydrochlorothiazide with no other drug treatment allowed except for unusual, prespecified clinical circumstances. All patients remained on this drug regimen for the initial 2-month follow-up period unless their blood pressure exceeded 180/110 mm Hg during in-office measurement.
The denervation treatment was well tolerated, although patients reported brief, transient, and “minor” pain associated with the procedure that did not affect treatment blinding or have any lingering consequences, said Dr. Kirtane, professor of medicine at Columbia University Vagelos College of Physicians and Surgeons in New York.
A reason to use energy delivery by ultrasound rather than by radiofrequency to ablate nerves in the renal arteries is that the ultrasound approach exerts a more uniform effect, allowing effective treatment delivery without need for catheter repositioning into more distal branches of the renal arteries, said Dr. Kirtane, who is also an interventional cardiologist at NewYork-Presbyterian/Columbia University Irving Medical Center.
But each method has its advantages, he added.
He also conceded that additional questions need to be addressed regarding which patients are most appropriate for renal denervation. “We need to figure out in which patients we can apply a device-based treatment,” Dr. Kirtane said during the press briefing. Patients with what appears to be drug-resistant hypertension often do not receive treatment with a MRA because of adverse effects, and many of these patients are not usually assessed for primary aldosteronism.
In SYMPLICITY HTN-3, “about half the patients who were seemingly eligible became ineligible” when they started treatment with a MRA, noted Dr. Bhatt. “A little spironolactone can go a long way” toward resolving treatment-resistant hypertension in many patients, he said.
RADIANCE-HTN TRIO was sponsored by ReCor Medical, the company developing the tested ultrasound catheter. Dr. Kirtane has received travel expenses and meals from ReCor Medical and several other companies, and Columbia has received research funding from ReCor Medical and several other companies related to research he has conducted. Dr. Bhatt has no relationship with ReCor Medical. He has been a consultant to and received honoraria from K2P, Level Ex, and MJH Life Sciences; he has been an advisor to Cardax, Cereno Scientific, Myokardia, Novo Nordisk, Phase Bio, and PLx Pharma; and he has received research funding from numerous companies.
Renal denervation’s comeback as a potential treatment for patients with drug-resistant hypertension rolls on.
Renal denervation with ultrasound energy produced a significant, median 4.5–mm Hg incremental drop in daytime, ambulatory, systolic blood pressure, compared with sham-treatment after 2 months follow-up in a randomized study of 136 patients with drug-resistant hypertension maintained on a standardized, single-pill, triple-drug regimen during the study.
The results “confirm that ultrasound renal denervation can lower blood pressure across a spectrum of hypertension,” concluded Ajay J. Kirtane, MD, at the annual scientific sessions of the American College of Cardiology. Renal denervation procedures involve percutaneously placing an endovascular catheter bilaterally inside a patient’s renal arteries and using brief pulses of energy to ablate neurons involved in blood pressure regulation.
A former ‘hot concept’
“Renal denervation was a hot concept a number of years ago, but had been tested only in studies without a sham control,” and initial testing using sham controls failed to show a significant benefit from the intervention, noted Deepak L. Bhatt, MD, an interventional cardiologist and professor of medicine at Harvard Medical School in Boston who was not involved with the study. The significant reductions in systolic blood pressure reported with renal denervation, compared with control patients in this study, “are believable” because of inclusion of a true control cohort, he added. “This really exciting finding puts renal denervation squarely back on the map,” commented Dr. Bhatt during a press briefing.
Dr. Bhatt added that, while the median 4.5–mm Hg incremental reduction in daytime, ambulatory, systolic blood pressure, compared with control patients – the study’s primary endpoint – may seem modest, “in the world of hypertension it’s a meaningful reduction” that, if sustained over the long term, would be expected to produce meaningful cuts in adverse cardiovascular events such as heart failure, stroke, and MI.
“The question is whether the effects are durable,” highlighted Dr. Bhatt, who helped lead the first sham-controlled trial of renal denervation, SYMPLICITY HTN-3, which failed to show a significant blood pressure reduction, compared with controls using radiofrequency energy to ablate renal nerves. A more recent study that used a different radiofrequency catheter and sham controls showed a significant effect on reducing systolic blood pressure in the SPYRAL HTN-OFF MED Pivotal trial, which by design did not maintain patients on any antihypertensive medications following their renal denervation procedure.
Dr. Kirtane noted that, although the median systolic blood pressure reduction, compared with controls treated by a sham procedure, was 4.5 mm Hg, the total median systolic pressure reduction after 2 months in the actively treated patients was 8.0 mm Hg when compared with their baseline blood pressure.
Concurrently with his report the results also appeared in an article posted online (Lancet. 2021 May 16;doi: 10.1016/S0140-6736(21)00788-1).
Denervation coupled with a single, daily three-drug pill
The RADIANCE-HTN TRIO study ran at 53 centers in the United States and Europe, and randomized 136 adults with an office-measured blood pressure of at least 140/90 mm Hg despite being on a stable regimen of at least three antihypertensive drugs including a diuretic. The enrolled cohort averaged 52 years of age and had an average office-measured pressure of about 162/104 mm Hg despite being on an average of four agents, although only about a third of enrolled patients were on treatment with a mineralocorticoid-receptor antagonist (MRA) such as spironolactone.
At the time of enrollment and 4 weeks before their denervation procedure, all patients switched to a uniform drug regimen of a single, daily, oral pill containing the calcium channel blocker amlodipine, the angiotensin receptor blocker valsartan or olmesartan, and the diuretic hydrochlorothiazide with no other drug treatment allowed except for unusual, prespecified clinical circumstances. All patients remained on this drug regimen for the initial 2-month follow-up period unless their blood pressure exceeded 180/110 mm Hg during in-office measurement.
The denervation treatment was well tolerated, although patients reported brief, transient, and “minor” pain associated with the procedure that did not affect treatment blinding or have any lingering consequences, said Dr. Kirtane, professor of medicine at Columbia University Vagelos College of Physicians and Surgeons in New York.
A reason to use energy delivery by ultrasound rather than by radiofrequency to ablate nerves in the renal arteries is that the ultrasound approach exerts a more uniform effect, allowing effective treatment delivery without need for catheter repositioning into more distal branches of the renal arteries, said Dr. Kirtane, who is also an interventional cardiologist at NewYork-Presbyterian/Columbia University Irving Medical Center.
But each method has its advantages, he added.
He also conceded that additional questions need to be addressed regarding which patients are most appropriate for renal denervation. “We need to figure out in which patients we can apply a device-based treatment,” Dr. Kirtane said during the press briefing. Patients with what appears to be drug-resistant hypertension often do not receive treatment with a MRA because of adverse effects, and many of these patients are not usually assessed for primary aldosteronism.
In SYMPLICITY HTN-3, “about half the patients who were seemingly eligible became ineligible” when they started treatment with a MRA, noted Dr. Bhatt. “A little spironolactone can go a long way” toward resolving treatment-resistant hypertension in many patients, he said.
RADIANCE-HTN TRIO was sponsored by ReCor Medical, the company developing the tested ultrasound catheter. Dr. Kirtane has received travel expenses and meals from ReCor Medical and several other companies, and Columbia has received research funding from ReCor Medical and several other companies related to research he has conducted. Dr. Bhatt has no relationship with ReCor Medical. He has been a consultant to and received honoraria from K2P, Level Ex, and MJH Life Sciences; he has been an advisor to Cardax, Cereno Scientific, Myokardia, Novo Nordisk, Phase Bio, and PLx Pharma; and he has received research funding from numerous companies.
FROM ACC 2021
FLOWER-MI: FFR-guided complete revascularization shows no advantage in STEMI
For patients with ST-elevated myocardial infarction (STEMI) undergoing complete revascularization, percutaneous coronary interventions (PCI) guided by fractional flow reserve (FFR) relative to angiography-guided PCI do not result in significantly lower risk of death or events, according to data from the randomized FLOWER-MI trial.
Rather, the events at 1 year were numerically lower among those randomized to the angiography-guided approach, according to the principal investigator of the trial, Etienne Puymirat, MD, PhD.
Prior studies showing an advantage for FFR-guided PCI in patients with coronary syndromes provided the hypothesis that FFR-guided PCI would also be superior for guiding PCI in STEMI patients. In the multicenter FAME trial, for example, FFR-guided PCI for patients with multivessel disease was associated with fewer stent placements (P < .001) and a nearly 30% lower rate of events at 1 year (P = .02).
While the advantage of complete revascularization, meaning PCI treatment of nonculprit as well as culprit lesions, has already been shown to be a better strategy than treatment of culprit lesions alone, FLOWER-MI is the first large study to compare FFR to angiography for guiding this approach to STEMI patients with multivessel disease, said Dr. Puymirat of Hôpital Européen George Pompidou, Paris, at the annual scientific sessions of the American College of Cardiology.
In this trial, involving multiple centers in France, STEMI patients were eligible for randomization if they had successful PCI of a culprit lesion and 50% or greater stenosis in at least one additional nonculprit lesion. The complete revascularization, whether patients were randomized to PCI guided by angiography or FFR, was performed during the index hospital admission. Patient management and follow-up was otherwise the same.
After a small number of exclusions, the intention-to-treat populations were 577 patients in the angiography-guided group and 586 in the FFR-guided group. The characteristics of the groups were well matched with an average age of about 62 years and similar rates of risk factors, such as hypertension and diabetes.
Angiography guidance just as good
The primary outcome was a composite of all-cause mortality, nonfatal MI, and unplanned revascularization. By hazard ratio, the risk of having one of these events within 1 year of PCI was numerically greater, at 32 in the FFR-guided group and 24 in the angiography-guided group, but the difference was not statistically significant (1.32; P = .31).
However, the total rate of events was low (5.5% vs. 4.2% for the angiography-guided and FFR-guided groups, respectively) and the confidence intervals were wide (95% CI, 0.78-2.23). This was also true of the components of the primary outcome.
No signal for a difference between strategies could be derived from these components, which included a higher rate of MI in the FFR-guided group (3.1% vs. 1.7%) but a lower rate of death (1.5% vs. 1.7%).
Unplanned hospitalizations leading to revascularization rates were also low (1.9% and 2.6% for angiography-guided and FFR-guided PCI, respectively), although it was reported that the rate of revascularization for nonculprit lesions was about twice as high in the FFR group (53.3% vs. 27.3%).
At 1 year, there were also low rates and no significant differences in a list of secondary outcomes that included hospitalization for recurrent ischemia or heart failure, stent thrombosis, and revascularization. As within the primary composite outcome, no pattern could be seen in the secondary events, some of which were numerically more common in the FFR-guided group and some numerically lower.
In a cost-efficacy analysis, the median per-patient cost of the FFR-guided strategy was about 500 Euros ($607) greater (8,832 vs. 8,322; P < .01), leading Dr. Puymirat to conclude that “the use of FFR for nonculprit lesions appears to be less effective but more expensive,” at least by costs derived in France.
Lack of statistical power limits interpretation
The conclusion of FLOWER-MI is that FFR-guided PCI in complete revascularization of nonculprit lesions in STEMI patients is not superior to an angiography-guided approach, but Dr. Puymirat cautioned that the low number of events precludes a definitive message.
William Fearon, MD, professor of cardiovascular medicine at Stanford (Calif.) University Medical Center, agreed. Based on his calculations, the trial was substantially underpowered. Evaluating the details of treatment in the FFR group, Dr. Fearon pointed out that a nonculprit lesion with a FFR of 0.80 or less was identified in about 55% of patients. Ultimately, 66% in the FFR group received PCI, eliminating the key distinction between strategies for the majority of patients enrolled.
“Only about one-third of the FFR-guided patients, or about 200 patients, did not receive nonculprit PCI, and therefore only in this small group could we expect a difference in outcomes from the angio-guided group,” Dr. Fearon said.
Fewer stents were placed in the FFR-guided than angiography-guided group (1.01 vs. 1.5), but Dr. Fearon suggested that it would be very difficult to show a difference in risk of events in a study of this size when event rates at 1 year reached only about 5%.
In response, Dr. Puymirat acknowledged that the rate of events for this trial, which was designed in 2015, were lower than expected. In recalculating the power needed based on the rate of events observed in FLOWER-MI, he estimated that about 8,000 patients would have been needed to show a meaningful difference in these PCI strategies.
Dr. Puymirat reports financial relationships with more than a dozen pharmaceutical companies, including Abbott, which provided some of the funding for this trial. Dr. Fearon reports financial relationships with Abbott, CathWorks, HeartFlow, and Medtronic.
For patients with ST-elevated myocardial infarction (STEMI) undergoing complete revascularization, percutaneous coronary interventions (PCI) guided by fractional flow reserve (FFR) relative to angiography-guided PCI do not result in significantly lower risk of death or events, according to data from the randomized FLOWER-MI trial.
Rather, the events at 1 year were numerically lower among those randomized to the angiography-guided approach, according to the principal investigator of the trial, Etienne Puymirat, MD, PhD.
Prior studies showing an advantage for FFR-guided PCI in patients with coronary syndromes provided the hypothesis that FFR-guided PCI would also be superior for guiding PCI in STEMI patients. In the multicenter FAME trial, for example, FFR-guided PCI for patients with multivessel disease was associated with fewer stent placements (P < .001) and a nearly 30% lower rate of events at 1 year (P = .02).
While the advantage of complete revascularization, meaning PCI treatment of nonculprit as well as culprit lesions, has already been shown to be a better strategy than treatment of culprit lesions alone, FLOWER-MI is the first large study to compare FFR to angiography for guiding this approach to STEMI patients with multivessel disease, said Dr. Puymirat of Hôpital Européen George Pompidou, Paris, at the annual scientific sessions of the American College of Cardiology.
In this trial, involving multiple centers in France, STEMI patients were eligible for randomization if they had successful PCI of a culprit lesion and 50% or greater stenosis in at least one additional nonculprit lesion. The complete revascularization, whether patients were randomized to PCI guided by angiography or FFR, was performed during the index hospital admission. Patient management and follow-up was otherwise the same.
After a small number of exclusions, the intention-to-treat populations were 577 patients in the angiography-guided group and 586 in the FFR-guided group. The characteristics of the groups were well matched with an average age of about 62 years and similar rates of risk factors, such as hypertension and diabetes.
Angiography guidance just as good
The primary outcome was a composite of all-cause mortality, nonfatal MI, and unplanned revascularization. By hazard ratio, the risk of having one of these events within 1 year of PCI was numerically greater, at 32 in the FFR-guided group and 24 in the angiography-guided group, but the difference was not statistically significant (1.32; P = .31).
However, the total rate of events was low (5.5% vs. 4.2% for the angiography-guided and FFR-guided groups, respectively) and the confidence intervals were wide (95% CI, 0.78-2.23). This was also true of the components of the primary outcome.
No signal for a difference between strategies could be derived from these components, which included a higher rate of MI in the FFR-guided group (3.1% vs. 1.7%) but a lower rate of death (1.5% vs. 1.7%).
Unplanned hospitalizations leading to revascularization rates were also low (1.9% and 2.6% for angiography-guided and FFR-guided PCI, respectively), although it was reported that the rate of revascularization for nonculprit lesions was about twice as high in the FFR group (53.3% vs. 27.3%).
At 1 year, there were also low rates and no significant differences in a list of secondary outcomes that included hospitalization for recurrent ischemia or heart failure, stent thrombosis, and revascularization. As within the primary composite outcome, no pattern could be seen in the secondary events, some of which were numerically more common in the FFR-guided group and some numerically lower.
In a cost-efficacy analysis, the median per-patient cost of the FFR-guided strategy was about 500 Euros ($607) greater (8,832 vs. 8,322; P < .01), leading Dr. Puymirat to conclude that “the use of FFR for nonculprit lesions appears to be less effective but more expensive,” at least by costs derived in France.
Lack of statistical power limits interpretation
The conclusion of FLOWER-MI is that FFR-guided PCI in complete revascularization of nonculprit lesions in STEMI patients is not superior to an angiography-guided approach, but Dr. Puymirat cautioned that the low number of events precludes a definitive message.
William Fearon, MD, professor of cardiovascular medicine at Stanford (Calif.) University Medical Center, agreed. Based on his calculations, the trial was substantially underpowered. Evaluating the details of treatment in the FFR group, Dr. Fearon pointed out that a nonculprit lesion with a FFR of 0.80 or less was identified in about 55% of patients. Ultimately, 66% in the FFR group received PCI, eliminating the key distinction between strategies for the majority of patients enrolled.
“Only about one-third of the FFR-guided patients, or about 200 patients, did not receive nonculprit PCI, and therefore only in this small group could we expect a difference in outcomes from the angio-guided group,” Dr. Fearon said.
Fewer stents were placed in the FFR-guided than angiography-guided group (1.01 vs. 1.5), but Dr. Fearon suggested that it would be very difficult to show a difference in risk of events in a study of this size when event rates at 1 year reached only about 5%.
In response, Dr. Puymirat acknowledged that the rate of events for this trial, which was designed in 2015, were lower than expected. In recalculating the power needed based on the rate of events observed in FLOWER-MI, he estimated that about 8,000 patients would have been needed to show a meaningful difference in these PCI strategies.
Dr. Puymirat reports financial relationships with more than a dozen pharmaceutical companies, including Abbott, which provided some of the funding for this trial. Dr. Fearon reports financial relationships with Abbott, CathWorks, HeartFlow, and Medtronic.
For patients with ST-elevated myocardial infarction (STEMI) undergoing complete revascularization, percutaneous coronary interventions (PCI) guided by fractional flow reserve (FFR) relative to angiography-guided PCI do not result in significantly lower risk of death or events, according to data from the randomized FLOWER-MI trial.
Rather, the events at 1 year were numerically lower among those randomized to the angiography-guided approach, according to the principal investigator of the trial, Etienne Puymirat, MD, PhD.
Prior studies showing an advantage for FFR-guided PCI in patients with coronary syndromes provided the hypothesis that FFR-guided PCI would also be superior for guiding PCI in STEMI patients. In the multicenter FAME trial, for example, FFR-guided PCI for patients with multivessel disease was associated with fewer stent placements (P < .001) and a nearly 30% lower rate of events at 1 year (P = .02).
While the advantage of complete revascularization, meaning PCI treatment of nonculprit as well as culprit lesions, has already been shown to be a better strategy than treatment of culprit lesions alone, FLOWER-MI is the first large study to compare FFR to angiography for guiding this approach to STEMI patients with multivessel disease, said Dr. Puymirat of Hôpital Européen George Pompidou, Paris, at the annual scientific sessions of the American College of Cardiology.
In this trial, involving multiple centers in France, STEMI patients were eligible for randomization if they had successful PCI of a culprit lesion and 50% or greater stenosis in at least one additional nonculprit lesion. The complete revascularization, whether patients were randomized to PCI guided by angiography or FFR, was performed during the index hospital admission. Patient management and follow-up was otherwise the same.
After a small number of exclusions, the intention-to-treat populations were 577 patients in the angiography-guided group and 586 in the FFR-guided group. The characteristics of the groups were well matched with an average age of about 62 years and similar rates of risk factors, such as hypertension and diabetes.
Angiography guidance just as good
The primary outcome was a composite of all-cause mortality, nonfatal MI, and unplanned revascularization. By hazard ratio, the risk of having one of these events within 1 year of PCI was numerically greater, at 32 in the FFR-guided group and 24 in the angiography-guided group, but the difference was not statistically significant (1.32; P = .31).
However, the total rate of events was low (5.5% vs. 4.2% for the angiography-guided and FFR-guided groups, respectively) and the confidence intervals were wide (95% CI, 0.78-2.23). This was also true of the components of the primary outcome.
No signal for a difference between strategies could be derived from these components, which included a higher rate of MI in the FFR-guided group (3.1% vs. 1.7%) but a lower rate of death (1.5% vs. 1.7%).
Unplanned hospitalizations leading to revascularization rates were also low (1.9% and 2.6% for angiography-guided and FFR-guided PCI, respectively), although it was reported that the rate of revascularization for nonculprit lesions was about twice as high in the FFR group (53.3% vs. 27.3%).
At 1 year, there were also low rates and no significant differences in a list of secondary outcomes that included hospitalization for recurrent ischemia or heart failure, stent thrombosis, and revascularization. As within the primary composite outcome, no pattern could be seen in the secondary events, some of which were numerically more common in the FFR-guided group and some numerically lower.
In a cost-efficacy analysis, the median per-patient cost of the FFR-guided strategy was about 500 Euros ($607) greater (8,832 vs. 8,322; P < .01), leading Dr. Puymirat to conclude that “the use of FFR for nonculprit lesions appears to be less effective but more expensive,” at least by costs derived in France.
Lack of statistical power limits interpretation
The conclusion of FLOWER-MI is that FFR-guided PCI in complete revascularization of nonculprit lesions in STEMI patients is not superior to an angiography-guided approach, but Dr. Puymirat cautioned that the low number of events precludes a definitive message.
William Fearon, MD, professor of cardiovascular medicine at Stanford (Calif.) University Medical Center, agreed. Based on his calculations, the trial was substantially underpowered. Evaluating the details of treatment in the FFR group, Dr. Fearon pointed out that a nonculprit lesion with a FFR of 0.80 or less was identified in about 55% of patients. Ultimately, 66% in the FFR group received PCI, eliminating the key distinction between strategies for the majority of patients enrolled.
“Only about one-third of the FFR-guided patients, or about 200 patients, did not receive nonculprit PCI, and therefore only in this small group could we expect a difference in outcomes from the angio-guided group,” Dr. Fearon said.
Fewer stents were placed in the FFR-guided than angiography-guided group (1.01 vs. 1.5), but Dr. Fearon suggested that it would be very difficult to show a difference in risk of events in a study of this size when event rates at 1 year reached only about 5%.
In response, Dr. Puymirat acknowledged that the rate of events for this trial, which was designed in 2015, were lower than expected. In recalculating the power needed based on the rate of events observed in FLOWER-MI, he estimated that about 8,000 patients would have been needed to show a meaningful difference in these PCI strategies.
Dr. Puymirat reports financial relationships with more than a dozen pharmaceutical companies, including Abbott, which provided some of the funding for this trial. Dr. Fearon reports financial relationships with Abbott, CathWorks, HeartFlow, and Medtronic.
FROM ACC 2021
LAAOS III: Surgical LAA closure cuts AFib stroke risk by one third
Left atrial appendage occlusion performed at the time of other heart surgery reduces the risk for stroke by about one-third in high-risk patients with atrial fibrillation (AFib), according to results of the Left Atrial Appendage Occlusion Study III (LAAOS III).
At 3.8 years’ follow-up, the primary endpoint of ischemic stroke or systemic embolism occurred in 4.8% of patients randomly assigned to left atrial appendage occlusion (LAAO) and 7.0% of those with no occlusion. This translated into a 33% relative risk reduction (hazard ratio, 0.67; 95% confidence interval, 0.53-0.85; P = .001).
In a landmark analysis, the effect was present early on but was more pronounced after the first 30 days, reducing the relative risk by 42% (HR, 0.58; 95% CI, 0.42-0.80), the researchers report.
The reduction in ongoing stroke risk was on top of oral anticoagulation (OAC) and consistent across all subgroups, Richard Whitlock, MD, PhD, professor of surgery, McMaster University, Hamilton, Ont., reported in a late-breaking trial session at the annual scientific sessions of the American College of Cardiology.
The procedure was safe and added, on average, just 6 minutes to cardiopulmonary bypass time, according to the results, simultaneously published in the New England Journal of Medicine.
“Any patient who comes to the operating room who fits the profile of a LAAOS III patient – so has atrial fibrillation and an elevated stroke risk based on their CHA2DS2-VASc score – the appendage should come off,” he said in an interview.
Commenting during the formal discussion, panelist Michael J. Mack, MD, of Baylor Health Care System in Houston, said, “This is potentially a game-changing, practice-changing study” but asked if there are any patients who shouldn’t undergo LAAO, such as those with heart failure (HF).
Dr. Whitlock said about 10%-15% of patients coming for heart surgery have a history of AFib and “as surgeons, you do need to individualize therapy. If you have a very frail patient, have concerns about tissue quality, you really need to think about how you would occlude the left atrial appendage or if you would occlude.”
Reassuringly, he noted, the data show no increase in HF hospitalizations and a beneficial effect on stroke among patients with HF and those with low ejection fractions, below 50%.
Observational data on surgical occlusion have been inconsistent, and current guidelines offer a weak recommendation in patients with AFib who have a contraindication to long-term anticoagulation. This is the first study to definitively prove that ischemic stroke is reduced by managing the left atrial appendage, he said in an interview.
“The previous percutaneous trials failed to demonstrate that; they demonstrated noninferiority but it was driven primarily by the avoidance of hemorrhagic events or strokes through taking patients off oral anticoagulation,” he said.
The results should translate into a class I guideline recommendation, he added. “This opens up a new paradigm of treatment for atrial fibrillation and stroke prevention in that it is really the first study that has looked at the additive effects of managing the left atrial appendage in addition to oral anticoagulation, and it’s protective on top of oral anticoagulation. That is a paradigm shift.”
In an accompanying editorial, Richard L. Page, MD, University of Vermont in Burlington, said the trial provides no insight on the possible benefit of surgical occlusion in patients unable to receive anticoagulation or with a lower CHA2DS2-VASc score, but he agreed a class I recommendation is likely for the population studied.
“I hope and anticipate that the results of this paper will strengthen the guideline indications for surgical left atrial appendage occlusion and will increase the number of cardiac surgeons who routinely perform this add-on procedure,” he said. “While many already perform this procedure, cardiac surgeons should now feel more comfortable that surgical left atrial appendage occlusion is indicated and supported by high-quality randomized data.”
Unfortunately, LAAOS III does not answer the question of whether patients can come off anticoagulation, but it does show surgical occlusion provides added protection from strokes, which can be huge with atrial fibrillation, Dr. Whitlock said.
“I spoke with a patient today who is an active 66-year-old individual on a [direct oral anticoagulant], and his stroke risk has been further reduced by 30%-40%, so he was ecstatic to hear the results,” Dr. Whitlock said. “I think it’s peace of mind.”
Global, nonindustry effort
LAAOS III investigators at 105 centers in 27 countries enrolled 4,811 patients undergoing cardiac surgery (mean age, 71 years; 68% male) who had a CHA2DS2-VASc score of at least 2.
In all, 4,770 were randomly assigned to no LAAO or occlusion via the preferred technique of amputation with suture closure of the stump as well as stapler occlusion, or epicardial device closure with the AtriClip (AtriCure) or TigerPaw (Maquet Medical). The treating team, researchers, and patients were blinded to assignment.
Patients were followed every 6 months with a validated stroke questionnaire. The trial was stopped early by the data safety monitoring board after the second interim analysis.
The mean CHA2DS2-VASc score was 4.2, one-third of patients had permanent AFib, 9% had a history of stroke, and more than two-thirds underwent a valve procedure, which makes LAAOS III unique, as many previous trials excluded valvular AFib, Dr. Whitlock pointed out.
Operative outcomes in the LAAO and no-LAAO groups were as follows:
- Bypass time: mean, 119 minutes vs. 113 minutes.
- Cross-clamp time: mean, 86 minutes vs. 82 minutes.
- Chest tube output: median, 520 mL vs. 500 mL.
- Reoperation for bleeding: both, 4.0%.
- Prolonged hospitalization due to HF: 5 vs. 14 events.
- 30-day mortality: 3.7% vs 4.0%.
The primary safety outcome of HF hospitalization at 3.8 years occurred in 7.7% of patients with LAAO and 6.8% without occlusion (HR, 1.13; 95% CI, 0.92-1.40), despite concerns that taking off the appendage could worsen HF risk by impairing renal clearance of salt and water.
“There’s observational data on either side of the fence, so it was an important endpoint that people were concerned about,” Dr. Whitlock told this news organization. “We had a data collection firm dedicated to admission for heart failure to really tease that out and, in the end, we saw no adverse effect.”
Although rates of ischemic stroke at 3.8 years were lower with LAAO than without (4.2% vs. 6.6%; HR, 0.62; 95% CI, 0.48-0.80), there was no difference in systemic embolism (0.3% for both) or death (22.6% vs. 22.5%).
In LAAOS III, fewer than 2% of the deaths were attributed to stroke, which is consistent with large stroke registries, Dr. Whitlock said. “Stroke is not what causes people with atrial fibrillation to die; it’s actually the progression on to heart failure.”
The positive effect on stroke was consistent across all subgroups, including sex, age, rheumatic heart disease, type of OAC at baseline, CHA2DS2-VASc score (≤4 vs. >4), type of surgery, history of heart failure or hypertension, and prior stroke/transient ischemic attack/systemic embolism.
Panelist Anne B. Curtis, MD, State University of New York at Buffalo, expressed surprise that about half of patients at baseline were not receiving anticoagulation and questioned whether event rates varied among those who did and didn’t stay on OAC.
Dr. Whitlock noted that OAC is often underused in AFib and that analyses showed the effects were consistent whether patients were on or off anticoagulants.
The study was sponsored by the Population Health Research Institute, McMaster University. Dr. Whitlock reported no relevant disclosures. Dr. Curtis reported consultant fees/honoraria from Abbott, Janssen, Medtronic, Milestone Pharmaceuticals, and Sanofi Aventis, and data safety monitoring board participation for Medtronic.
A version of this article first appeared on Medscape.com.
Left atrial appendage occlusion performed at the time of other heart surgery reduces the risk for stroke by about one-third in high-risk patients with atrial fibrillation (AFib), according to results of the Left Atrial Appendage Occlusion Study III (LAAOS III).
At 3.8 years’ follow-up, the primary endpoint of ischemic stroke or systemic embolism occurred in 4.8% of patients randomly assigned to left atrial appendage occlusion (LAAO) and 7.0% of those with no occlusion. This translated into a 33% relative risk reduction (hazard ratio, 0.67; 95% confidence interval, 0.53-0.85; P = .001).
In a landmark analysis, the effect was present early on but was more pronounced after the first 30 days, reducing the relative risk by 42% (HR, 0.58; 95% CI, 0.42-0.80), the researchers report.
The reduction in ongoing stroke risk was on top of oral anticoagulation (OAC) and consistent across all subgroups, Richard Whitlock, MD, PhD, professor of surgery, McMaster University, Hamilton, Ont., reported in a late-breaking trial session at the annual scientific sessions of the American College of Cardiology.
The procedure was safe and added, on average, just 6 minutes to cardiopulmonary bypass time, according to the results, simultaneously published in the New England Journal of Medicine.
“Any patient who comes to the operating room who fits the profile of a LAAOS III patient – so has atrial fibrillation and an elevated stroke risk based on their CHA2DS2-VASc score – the appendage should come off,” he said in an interview.
Commenting during the formal discussion, panelist Michael J. Mack, MD, of Baylor Health Care System in Houston, said, “This is potentially a game-changing, practice-changing study” but asked if there are any patients who shouldn’t undergo LAAO, such as those with heart failure (HF).
Dr. Whitlock said about 10%-15% of patients coming for heart surgery have a history of AFib and “as surgeons, you do need to individualize therapy. If you have a very frail patient, have concerns about tissue quality, you really need to think about how you would occlude the left atrial appendage or if you would occlude.”
Reassuringly, he noted, the data show no increase in HF hospitalizations and a beneficial effect on stroke among patients with HF and those with low ejection fractions, below 50%.
Observational data on surgical occlusion have been inconsistent, and current guidelines offer a weak recommendation in patients with AFib who have a contraindication to long-term anticoagulation. This is the first study to definitively prove that ischemic stroke is reduced by managing the left atrial appendage, he said in an interview.
“The previous percutaneous trials failed to demonstrate that; they demonstrated noninferiority but it was driven primarily by the avoidance of hemorrhagic events or strokes through taking patients off oral anticoagulation,” he said.
The results should translate into a class I guideline recommendation, he added. “This opens up a new paradigm of treatment for atrial fibrillation and stroke prevention in that it is really the first study that has looked at the additive effects of managing the left atrial appendage in addition to oral anticoagulation, and it’s protective on top of oral anticoagulation. That is a paradigm shift.”
In an accompanying editorial, Richard L. Page, MD, University of Vermont in Burlington, said the trial provides no insight on the possible benefit of surgical occlusion in patients unable to receive anticoagulation or with a lower CHA2DS2-VASc score, but he agreed a class I recommendation is likely for the population studied.
“I hope and anticipate that the results of this paper will strengthen the guideline indications for surgical left atrial appendage occlusion and will increase the number of cardiac surgeons who routinely perform this add-on procedure,” he said. “While many already perform this procedure, cardiac surgeons should now feel more comfortable that surgical left atrial appendage occlusion is indicated and supported by high-quality randomized data.”
Unfortunately, LAAOS III does not answer the question of whether patients can come off anticoagulation, but it does show surgical occlusion provides added protection from strokes, which can be huge with atrial fibrillation, Dr. Whitlock said.
“I spoke with a patient today who is an active 66-year-old individual on a [direct oral anticoagulant], and his stroke risk has been further reduced by 30%-40%, so he was ecstatic to hear the results,” Dr. Whitlock said. “I think it’s peace of mind.”
Global, nonindustry effort
LAAOS III investigators at 105 centers in 27 countries enrolled 4,811 patients undergoing cardiac surgery (mean age, 71 years; 68% male) who had a CHA2DS2-VASc score of at least 2.
In all, 4,770 were randomly assigned to no LAAO or occlusion via the preferred technique of amputation with suture closure of the stump as well as stapler occlusion, or epicardial device closure with the AtriClip (AtriCure) or TigerPaw (Maquet Medical). The treating team, researchers, and patients were blinded to assignment.
Patients were followed every 6 months with a validated stroke questionnaire. The trial was stopped early by the data safety monitoring board after the second interim analysis.
The mean CHA2DS2-VASc score was 4.2, one-third of patients had permanent AFib, 9% had a history of stroke, and more than two-thirds underwent a valve procedure, which makes LAAOS III unique, as many previous trials excluded valvular AFib, Dr. Whitlock pointed out.
Operative outcomes in the LAAO and no-LAAO groups were as follows:
- Bypass time: mean, 119 minutes vs. 113 minutes.
- Cross-clamp time: mean, 86 minutes vs. 82 minutes.
- Chest tube output: median, 520 mL vs. 500 mL.
- Reoperation for bleeding: both, 4.0%.
- Prolonged hospitalization due to HF: 5 vs. 14 events.
- 30-day mortality: 3.7% vs 4.0%.
The primary safety outcome of HF hospitalization at 3.8 years occurred in 7.7% of patients with LAAO and 6.8% without occlusion (HR, 1.13; 95% CI, 0.92-1.40), despite concerns that taking off the appendage could worsen HF risk by impairing renal clearance of salt and water.
“There’s observational data on either side of the fence, so it was an important endpoint that people were concerned about,” Dr. Whitlock told this news organization. “We had a data collection firm dedicated to admission for heart failure to really tease that out and, in the end, we saw no adverse effect.”
Although rates of ischemic stroke at 3.8 years were lower with LAAO than without (4.2% vs. 6.6%; HR, 0.62; 95% CI, 0.48-0.80), there was no difference in systemic embolism (0.3% for both) or death (22.6% vs. 22.5%).
In LAAOS III, fewer than 2% of the deaths were attributed to stroke, which is consistent with large stroke registries, Dr. Whitlock said. “Stroke is not what causes people with atrial fibrillation to die; it’s actually the progression on to heart failure.”
The positive effect on stroke was consistent across all subgroups, including sex, age, rheumatic heart disease, type of OAC at baseline, CHA2DS2-VASc score (≤4 vs. >4), type of surgery, history of heart failure or hypertension, and prior stroke/transient ischemic attack/systemic embolism.
Panelist Anne B. Curtis, MD, State University of New York at Buffalo, expressed surprise that about half of patients at baseline were not receiving anticoagulation and questioned whether event rates varied among those who did and didn’t stay on OAC.
Dr. Whitlock noted that OAC is often underused in AFib and that analyses showed the effects were consistent whether patients were on or off anticoagulants.
The study was sponsored by the Population Health Research Institute, McMaster University. Dr. Whitlock reported no relevant disclosures. Dr. Curtis reported consultant fees/honoraria from Abbott, Janssen, Medtronic, Milestone Pharmaceuticals, and Sanofi Aventis, and data safety monitoring board participation for Medtronic.
A version of this article first appeared on Medscape.com.
Left atrial appendage occlusion performed at the time of other heart surgery reduces the risk for stroke by about one-third in high-risk patients with atrial fibrillation (AFib), according to results of the Left Atrial Appendage Occlusion Study III (LAAOS III).
At 3.8 years’ follow-up, the primary endpoint of ischemic stroke or systemic embolism occurred in 4.8% of patients randomly assigned to left atrial appendage occlusion (LAAO) and 7.0% of those with no occlusion. This translated into a 33% relative risk reduction (hazard ratio, 0.67; 95% confidence interval, 0.53-0.85; P = .001).
In a landmark analysis, the effect was present early on but was more pronounced after the first 30 days, reducing the relative risk by 42% (HR, 0.58; 95% CI, 0.42-0.80), the researchers report.
The reduction in ongoing stroke risk was on top of oral anticoagulation (OAC) and consistent across all subgroups, Richard Whitlock, MD, PhD, professor of surgery, McMaster University, Hamilton, Ont., reported in a late-breaking trial session at the annual scientific sessions of the American College of Cardiology.
The procedure was safe and added, on average, just 6 minutes to cardiopulmonary bypass time, according to the results, simultaneously published in the New England Journal of Medicine.
“Any patient who comes to the operating room who fits the profile of a LAAOS III patient – so has atrial fibrillation and an elevated stroke risk based on their CHA2DS2-VASc score – the appendage should come off,” he said in an interview.
Commenting during the formal discussion, panelist Michael J. Mack, MD, of Baylor Health Care System in Houston, said, “This is potentially a game-changing, practice-changing study” but asked if there are any patients who shouldn’t undergo LAAO, such as those with heart failure (HF).
Dr. Whitlock said about 10%-15% of patients coming for heart surgery have a history of AFib and “as surgeons, you do need to individualize therapy. If you have a very frail patient, have concerns about tissue quality, you really need to think about how you would occlude the left atrial appendage or if you would occlude.”
Reassuringly, he noted, the data show no increase in HF hospitalizations and a beneficial effect on stroke among patients with HF and those with low ejection fractions, below 50%.
Observational data on surgical occlusion have been inconsistent, and current guidelines offer a weak recommendation in patients with AFib who have a contraindication to long-term anticoagulation. This is the first study to definitively prove that ischemic stroke is reduced by managing the left atrial appendage, he said in an interview.
“The previous percutaneous trials failed to demonstrate that; they demonstrated noninferiority but it was driven primarily by the avoidance of hemorrhagic events or strokes through taking patients off oral anticoagulation,” he said.
The results should translate into a class I guideline recommendation, he added. “This opens up a new paradigm of treatment for atrial fibrillation and stroke prevention in that it is really the first study that has looked at the additive effects of managing the left atrial appendage in addition to oral anticoagulation, and it’s protective on top of oral anticoagulation. That is a paradigm shift.”
In an accompanying editorial, Richard L. Page, MD, University of Vermont in Burlington, said the trial provides no insight on the possible benefit of surgical occlusion in patients unable to receive anticoagulation or with a lower CHA2DS2-VASc score, but he agreed a class I recommendation is likely for the population studied.
“I hope and anticipate that the results of this paper will strengthen the guideline indications for surgical left atrial appendage occlusion and will increase the number of cardiac surgeons who routinely perform this add-on procedure,” he said. “While many already perform this procedure, cardiac surgeons should now feel more comfortable that surgical left atrial appendage occlusion is indicated and supported by high-quality randomized data.”
Unfortunately, LAAOS III does not answer the question of whether patients can come off anticoagulation, but it does show surgical occlusion provides added protection from strokes, which can be huge with atrial fibrillation, Dr. Whitlock said.
“I spoke with a patient today who is an active 66-year-old individual on a [direct oral anticoagulant], and his stroke risk has been further reduced by 30%-40%, so he was ecstatic to hear the results,” Dr. Whitlock said. “I think it’s peace of mind.”
Global, nonindustry effort
LAAOS III investigators at 105 centers in 27 countries enrolled 4,811 patients undergoing cardiac surgery (mean age, 71 years; 68% male) who had a CHA2DS2-VASc score of at least 2.
In all, 4,770 were randomly assigned to no LAAO or occlusion via the preferred technique of amputation with suture closure of the stump as well as stapler occlusion, or epicardial device closure with the AtriClip (AtriCure) or TigerPaw (Maquet Medical). The treating team, researchers, and patients were blinded to assignment.
Patients were followed every 6 months with a validated stroke questionnaire. The trial was stopped early by the data safety monitoring board after the second interim analysis.
The mean CHA2DS2-VASc score was 4.2, one-third of patients had permanent AFib, 9% had a history of stroke, and more than two-thirds underwent a valve procedure, which makes LAAOS III unique, as many previous trials excluded valvular AFib, Dr. Whitlock pointed out.
Operative outcomes in the LAAO and no-LAAO groups were as follows:
- Bypass time: mean, 119 minutes vs. 113 minutes.
- Cross-clamp time: mean, 86 minutes vs. 82 minutes.
- Chest tube output: median, 520 mL vs. 500 mL.
- Reoperation for bleeding: both, 4.0%.
- Prolonged hospitalization due to HF: 5 vs. 14 events.
- 30-day mortality: 3.7% vs 4.0%.
The primary safety outcome of HF hospitalization at 3.8 years occurred in 7.7% of patients with LAAO and 6.8% without occlusion (HR, 1.13; 95% CI, 0.92-1.40), despite concerns that taking off the appendage could worsen HF risk by impairing renal clearance of salt and water.
“There’s observational data on either side of the fence, so it was an important endpoint that people were concerned about,” Dr. Whitlock told this news organization. “We had a data collection firm dedicated to admission for heart failure to really tease that out and, in the end, we saw no adverse effect.”
Although rates of ischemic stroke at 3.8 years were lower with LAAO than without (4.2% vs. 6.6%; HR, 0.62; 95% CI, 0.48-0.80), there was no difference in systemic embolism (0.3% for both) or death (22.6% vs. 22.5%).
In LAAOS III, fewer than 2% of the deaths were attributed to stroke, which is consistent with large stroke registries, Dr. Whitlock said. “Stroke is not what causes people with atrial fibrillation to die; it’s actually the progression on to heart failure.”
The positive effect on stroke was consistent across all subgroups, including sex, age, rheumatic heart disease, type of OAC at baseline, CHA2DS2-VASc score (≤4 vs. >4), type of surgery, history of heart failure or hypertension, and prior stroke/transient ischemic attack/systemic embolism.
Panelist Anne B. Curtis, MD, State University of New York at Buffalo, expressed surprise that about half of patients at baseline were not receiving anticoagulation and questioned whether event rates varied among those who did and didn’t stay on OAC.
Dr. Whitlock noted that OAC is often underused in AFib and that analyses showed the effects were consistent whether patients were on or off anticoagulants.
The study was sponsored by the Population Health Research Institute, McMaster University. Dr. Whitlock reported no relevant disclosures. Dr. Curtis reported consultant fees/honoraria from Abbott, Janssen, Medtronic, Milestone Pharmaceuticals, and Sanofi Aventis, and data safety monitoring board participation for Medtronic.
A version of this article first appeared on Medscape.com.
FROM ACC 2021
ACC 21 looks to repeat success despite pandemic headwinds
The American College of Cardiology pulled off an impressive all-virtual meeting in March 2020, less than 3 weeks after canceling its in-person event and just 2 weeks after COVID-19 was declared a national emergency.
Optimistic plans for the annual scientific sessions of the American College of Cardiology (ACC 2021) to be a March hybrid affair in Atlanta pivoted not once, but twice, as the pandemic evolved, with the date pushed back 2 full months, to May 15-17, and the format revised to fully virtual.
“While this meeting is being delivered virtually, I think you’ll see there have been benefits in the time to plan and also the lessons that ACC has learned in virtual education over the past year. This has come together to really create a robust educational and scientific agenda,” ACC 2021 chair Pamela B. Morris, MD, said in a press conference focused on the upcoming meeting.
Over the 3 days, there will be more than 200 education sessions, 10 guideline-specific sessions, and 11 learning pathways that include core areas, but also special topics, such as COVID-19 and the emerging cardio-obstetrics subspecialty.
The meeting will be delivered through a new virtual education program built to optimize real-time interaction between faculty members and attendees, she said. A dedicated portal on the platform will allow attendees to interact virtually, for example, with presenters of the nearly 3,000 ePosters and 420 moderated posters.
For those suffering from Zoom fatigue, the increasingly popular Heart2Heart stage talks have also been converted to podcasts, which cover topics like gender equity in cardiology, the evolving role of advanced practice professionals, and “one of my favorites: art as a tool for healing,” said Dr. Morris, from the Medical University of South Carolina, Charleston. “Those sessions are really not to be missed.”
Reconnecting is an underlying theme of the meeting but the great divider will not be ignored. COVID-19 will be the focus of two 90-minute Intensive Sessions on Saturday, May 15, the first kicking off at 10:30 a.m. ET, with the Bishop Keynote lecture on bringing health equity to the frontline of cardiovascular care, followed by lessons learned during the pandemic, how to conduct clinical trials, and vaccine development.
The second session, set for 12:15 p.m., continues the “silver linings” theme, with case presentations on advances in telehealth, myocardial involvement, and thrombosis in COVID. For those wanting more, 18 abstracts are on tap in a 2-hour Spotlight on Special Topics session beginning at 2:30 p.m.
Asked about the pandemic’s effect on bringing science to fruition this past year, Dr. Morris said there’s no question it’s slowed some of the progress the cardiology community had made but, like clinical practice, “we’ve also surmounted many of those obstacles.”
“I think research has rebounded,” she said. “Just in terms of the number of abstracts and the quality of abstracts that were submitted this year, I don’t think there’s any question that we are right on par with previous years.”
Indeed, 5,258 abstracts from 76 countries were submitted, with more than 3,400 chosen for oral and poster presentation, including 25 late-breaking clinical trials to be presented in five sessions.
The late-breaking presentations and discussions will be prerecorded but speakers and panelists have been invited to be present during the streaming to answer live any questions that may arise in the chat box, ACC 2021 vice chair Douglas Drachman, MD, Massachusetts General Hospital, Boston, said in an interview.
Late-breaking clinical trials
The Joint ACC/JACC Late-Breaking Clinical Trials I (Saturday, May 15, 9:00 a.m.–-10:00 a.m.) kicks off with PARADISE-MI, the first head-to-head comparison of an angiotensin receptor neprilysin inhibitor (ARNI) and an ACE inhibitor in patients with reduced ejection fractions (EFs) after MI but no history of heart failure (HF), studying 200 mg sacubitril/valsartan (Entresto) versus 5 mg of ramipril, both twice daily, in 5,669 patients.
Sacubitril/valsartan was initially approved for HF with reduced EF and added a new indication to treat some HF patients with preserved EF. Novartis, however, recently told investors that although numerical trends consistently favored the ARNI over the ACE inhibitor ramipril, the phase 3 study failed to meet the primary endpoint for efficacy superiority of reducing the risk for cardiovascular (CV) death and HF events after an acute MI.
Second up is ADAPTABLE, which looks to close a surprising evidence gap over whether 81 mg or 325 mg daily is the optimal dose of the ubiquitously prescribed aspirin for secondary prevention in high-risk patients with established atherosclerotic CV disease.
The open-label, randomized study will look at efficacy and major bleeding over roughly 4 years in 15,000 patients within PCORnet, the National Patient-centered Clinical Research Network, a partnership of clinical research, health plan research, and patient-powered networks created to streamline patient-reported outcomes research.
“This study will not only give important clinical information for us, practically speaking, whether we should prescribe lower- or higher-dose aspirin, but it may also serve as a template for future pragmatic clinical trial design in the real world,” Dr. Drachman said during the press conference.
Up next is the 4,812-patient Canadian LAAOS III, the largest trial to examine the efficacy of left atrial appendage occlusion for stroke prevention in patients with atrial fibrillation (AFib) already undergoing cardiac surgery. The primary outcome is the first occurrence of stroke or systemic arterial embolism over an average follow-up of 4 years.
Percutaneous closure of the left atrial appendage (LAA) has been shown to reduce stroke in AFib patients at high-risk of bleeding on systemic anticoagulation. But these devices can be expensive and studies haven’t included patients who also have valvular heart disease, a group that actually comprises more than half of patients undergoing cardiac surgery who also have AFib, he noted.
At the same time, surgical LAA closure studies have been small and have had very mixed results. “There isn’t a large-scale rigorous assessment out there for these patients undergoing surgery, so I think this is going to be fascinating to see,” Dr. Drachman said.
The session closes with ATLANTIS, which looks to shed some light on the role of anticoagulation therapy in patients after transcatheter aortic valve replacement (TAVR or TAVI). POPular TAVI, presented at ACC 2020, showed aspirin alone was the preferred antithrombotic therapy over aspirin plus clopidogrel (Plavix) in patients not on oral anticoagulants, but the optimal anticoagulation regimen remains unsettled.
The French open-label, 1,510-patient ATLANTIS trial examined whether the novel oral anticoagulant apixaban (Eliquis) is superior in preventing CV events after TAVR, compared with antiplatelet therapy in patients without an indication for anticoagulation and compared with vitamin K antagonists in those receiving anticoagulants.
An ATLANTIS 4D CT substudy of valve thrombosis is also slated for Saturday’s Featured Clinical Research 1 session at 12:15 p.m. to 1:45 p.m..
Sunday LBCTs
Dr. Drachman highlighted a series of other late-breaking studies, including the global DARE-19 trial testing the diabetes and HF drug dapagliflozin (Farxiga) given with local standard-of-care therapy for 30 days in hospitalized COVID-19 patients with CV, metabolic, or renal risk factors.
Although sodium-glucose cotransporter-2 inhibitors have been white-hot of late, top-line results reported last month show dapagliflozin failed to achieve statistical significance for the primary endpoints of reducing organ dysfunction and all-cause mortality and for improving recovery. Details will be presented in the Joint ACC/JAMA Late-Breaking Clinical Trials II (Sunday, May 16, 8:00 a.m.-9:30 a.m.).
Two trials, FLOWER-MI and RADIANCE-HTN TRIO, were singled out in the Joint ACC/New England Journal of Medicine Late-Breaking Clinical Trials III (Sunday, May 16, 10:45 a.m.-12:00 p.m.). FLOWER-MI examines whether fractional flow reserve (FFR) is better than angiography to guide complete multivessel revascularization in ST-elevation MI patients with at least 50% stenosis in at least one nonculprit lesion requiring percutaneous coronary intervention (PCI). Recent studies have shown the superiority of FFR-guided PCI for nonculprit lesions, compared with culprit lesion treatment-only, but this is the first time FFR- and angiography-guided PCI have been compared in STEMI patients.
RADIANCE-HTN TRIO already tipped its hand, with top-line results reported in late 2020 showing that the trial met its primary efficacy endpoint of greater reduction in daytime blood pressure over 2 months with the Paradise endovascular ultrasound renal denervation system, compared with a sham procedure, in 136 patients with resistant hypertension, importantly, after being given a single pill containing a calcium channel blocker, angiotensin II receptor blocker, and diuretic.
Renal denervation for hypertension has been making something of a comeback, with the 2018 RADIANCE-HTN SOLO reporting better ambulatory blood pressure control with the Paradise system than with a sham procedure in the absence of antihypertensive agents. The device has been granted breakthrough device designation from the Food and Drug Administration for the treatment of hypertensive patients who are unable to sufficiently respond to or are intolerant of antihypertensive therapy.
Monday LBCTs
In the Late-Breaking Clinical Trials IV session (Monday, May 17, 8 a.m.–9:30 a.m.), Drachman called out a secondary analysis from GALATIC-HF looking at the impact of EF on the therapeutic effect of omecamtiv mecarbil. In last year’s primary analysis, the selective cardiac myosin activator produced a modest but significant reduction in HF events or CV death in 8,232 patients with HF and an EF of 35% or less.
Rounding out the list is the Canadian CAPITAL CHILL study of moderate versus mild therapeutic hypothermia in out-of-hospital cardiac arrest, to be presented in the final Late-Breaking Clinical Trials V session (Monday, May 17, 10:45 a.m.–12:00 p.m.).
The double-blind trial sought to determine whether neurologic outcomes at 6 months are improved by targeting a core temperature of 31 ˚C versus 34 ˚C after the return of spontaneous circulation in comatose survivors of out-of-hospital cardiac arrest.
“For me, I think this could really change practice and has personal relevance from experience with cardiac arrest survivors that I’ve known and care for very deeply,” Dr. Drachman said in an interview. “I think that there’s a lot of opportunity here as well.”
Asked what other trials have the potential to change practice, Dr. Drachman said FLOWER-MI holds particular interest because it looks at how to manage patients with STEMI with multiple lesions at the point of care.
“We’ve gained a lot of clarity from several other prior clinical trials, but this will help to answer the question in a slightly different way of saying: can you eyeball it, can you look at the angiogram and say whether or not that other, nonculprit lesion ought to be treated in the same hospitalization or should you really be using a pressure wire,” he said. “For me as an interventionalist, this is really important because when you finish up doing an intervention on a patient it might be the middle of the night and the patient may be more or less stable, but you’ve already exposed them to the risk of a procedure, should you then move on and do another aspect of the procedure to interrogate with a pressure wire a remaining narrowing? I think that’s very important; that’ll help me make decisions on a day-to-day basis.”
Dr. Drachman also cited RADIANCE-HTN TRIO because it employs an endovascular technique to control blood pressure in patients with hypertension, specifically those resistant to multiple drugs.
During the press conference, Dr. Morris, a preventive cardiologist, put her money on the ADAPTABLE study of aspirin dosing, reiterating that the unique trial design could inform future research, and on Sunday’s 8:45 a.m. late-breaking post hoc analysis from the STRENGTH trial that looks to pick up where the controversy over omega-3 fatty acid preparations left off at last year’s American Heart Association meeting.
A lack of benefit on CV event rates reported with Epanova, a high-dose combination of eicosapentaenoic acid (EPA) and docosahexaenoic acid, led to a contentious debate over how to reconcile STRENGTH with the findings from REDUCE-IT, which showed a 25% relative risk reduction in major CV events with the EPA product icosapent ethyl (Vascepa).
STRENGTH investigator Steven Nissen, MD, Cleveland Clinic, and REDUCE-IT investigator and session panelist Deepak Bhatt, MD, Brigham and Women’s Hospital, Boston, will share the virtual stage at ACC 2021, but Dr. Morris said the “good news” is both researchers know one another very well and “will really be focusing on no political issues, just the omega-3 fatty levels in the bloodstream and what does that mean in either trial.
“This is not designed to be a debate, point counterpoint,” she added.
For that, as all cardiologists and journalists know, there will be the wild and woolly #CardioTwitter sphere.
A version of this article first appeared on Medscape.com.
The American College of Cardiology pulled off an impressive all-virtual meeting in March 2020, less than 3 weeks after canceling its in-person event and just 2 weeks after COVID-19 was declared a national emergency.
Optimistic plans for the annual scientific sessions of the American College of Cardiology (ACC 2021) to be a March hybrid affair in Atlanta pivoted not once, but twice, as the pandemic evolved, with the date pushed back 2 full months, to May 15-17, and the format revised to fully virtual.
“While this meeting is being delivered virtually, I think you’ll see there have been benefits in the time to plan and also the lessons that ACC has learned in virtual education over the past year. This has come together to really create a robust educational and scientific agenda,” ACC 2021 chair Pamela B. Morris, MD, said in a press conference focused on the upcoming meeting.
Over the 3 days, there will be more than 200 education sessions, 10 guideline-specific sessions, and 11 learning pathways that include core areas, but also special topics, such as COVID-19 and the emerging cardio-obstetrics subspecialty.
The meeting will be delivered through a new virtual education program built to optimize real-time interaction between faculty members and attendees, she said. A dedicated portal on the platform will allow attendees to interact virtually, for example, with presenters of the nearly 3,000 ePosters and 420 moderated posters.
For those suffering from Zoom fatigue, the increasingly popular Heart2Heart stage talks have also been converted to podcasts, which cover topics like gender equity in cardiology, the evolving role of advanced practice professionals, and “one of my favorites: art as a tool for healing,” said Dr. Morris, from the Medical University of South Carolina, Charleston. “Those sessions are really not to be missed.”
Reconnecting is an underlying theme of the meeting but the great divider will not be ignored. COVID-19 will be the focus of two 90-minute Intensive Sessions on Saturday, May 15, the first kicking off at 10:30 a.m. ET, with the Bishop Keynote lecture on bringing health equity to the frontline of cardiovascular care, followed by lessons learned during the pandemic, how to conduct clinical trials, and vaccine development.
The second session, set for 12:15 p.m., continues the “silver linings” theme, with case presentations on advances in telehealth, myocardial involvement, and thrombosis in COVID. For those wanting more, 18 abstracts are on tap in a 2-hour Spotlight on Special Topics session beginning at 2:30 p.m.
Asked about the pandemic’s effect on bringing science to fruition this past year, Dr. Morris said there’s no question it’s slowed some of the progress the cardiology community had made but, like clinical practice, “we’ve also surmounted many of those obstacles.”
“I think research has rebounded,” she said. “Just in terms of the number of abstracts and the quality of abstracts that were submitted this year, I don’t think there’s any question that we are right on par with previous years.”
Indeed, 5,258 abstracts from 76 countries were submitted, with more than 3,400 chosen for oral and poster presentation, including 25 late-breaking clinical trials to be presented in five sessions.
The late-breaking presentations and discussions will be prerecorded but speakers and panelists have been invited to be present during the streaming to answer live any questions that may arise in the chat box, ACC 2021 vice chair Douglas Drachman, MD, Massachusetts General Hospital, Boston, said in an interview.
Late-breaking clinical trials
The Joint ACC/JACC Late-Breaking Clinical Trials I (Saturday, May 15, 9:00 a.m.–-10:00 a.m.) kicks off with PARADISE-MI, the first head-to-head comparison of an angiotensin receptor neprilysin inhibitor (ARNI) and an ACE inhibitor in patients with reduced ejection fractions (EFs) after MI but no history of heart failure (HF), studying 200 mg sacubitril/valsartan (Entresto) versus 5 mg of ramipril, both twice daily, in 5,669 patients.
Sacubitril/valsartan was initially approved for HF with reduced EF and added a new indication to treat some HF patients with preserved EF. Novartis, however, recently told investors that although numerical trends consistently favored the ARNI over the ACE inhibitor ramipril, the phase 3 study failed to meet the primary endpoint for efficacy superiority of reducing the risk for cardiovascular (CV) death and HF events after an acute MI.
Second up is ADAPTABLE, which looks to close a surprising evidence gap over whether 81 mg or 325 mg daily is the optimal dose of the ubiquitously prescribed aspirin for secondary prevention in high-risk patients with established atherosclerotic CV disease.
The open-label, randomized study will look at efficacy and major bleeding over roughly 4 years in 15,000 patients within PCORnet, the National Patient-centered Clinical Research Network, a partnership of clinical research, health plan research, and patient-powered networks created to streamline patient-reported outcomes research.
“This study will not only give important clinical information for us, practically speaking, whether we should prescribe lower- or higher-dose aspirin, but it may also serve as a template for future pragmatic clinical trial design in the real world,” Dr. Drachman said during the press conference.
Up next is the 4,812-patient Canadian LAAOS III, the largest trial to examine the efficacy of left atrial appendage occlusion for stroke prevention in patients with atrial fibrillation (AFib) already undergoing cardiac surgery. The primary outcome is the first occurrence of stroke or systemic arterial embolism over an average follow-up of 4 years.
Percutaneous closure of the left atrial appendage (LAA) has been shown to reduce stroke in AFib patients at high-risk of bleeding on systemic anticoagulation. But these devices can be expensive and studies haven’t included patients who also have valvular heart disease, a group that actually comprises more than half of patients undergoing cardiac surgery who also have AFib, he noted.
At the same time, surgical LAA closure studies have been small and have had very mixed results. “There isn’t a large-scale rigorous assessment out there for these patients undergoing surgery, so I think this is going to be fascinating to see,” Dr. Drachman said.
The session closes with ATLANTIS, which looks to shed some light on the role of anticoagulation therapy in patients after transcatheter aortic valve replacement (TAVR or TAVI). POPular TAVI, presented at ACC 2020, showed aspirin alone was the preferred antithrombotic therapy over aspirin plus clopidogrel (Plavix) in patients not on oral anticoagulants, but the optimal anticoagulation regimen remains unsettled.
The French open-label, 1,510-patient ATLANTIS trial examined whether the novel oral anticoagulant apixaban (Eliquis) is superior in preventing CV events after TAVR, compared with antiplatelet therapy in patients without an indication for anticoagulation and compared with vitamin K antagonists in those receiving anticoagulants.
An ATLANTIS 4D CT substudy of valve thrombosis is also slated for Saturday’s Featured Clinical Research 1 session at 12:15 p.m. to 1:45 p.m..
Sunday LBCTs
Dr. Drachman highlighted a series of other late-breaking studies, including the global DARE-19 trial testing the diabetes and HF drug dapagliflozin (Farxiga) given with local standard-of-care therapy for 30 days in hospitalized COVID-19 patients with CV, metabolic, or renal risk factors.
Although sodium-glucose cotransporter-2 inhibitors have been white-hot of late, top-line results reported last month show dapagliflozin failed to achieve statistical significance for the primary endpoints of reducing organ dysfunction and all-cause mortality and for improving recovery. Details will be presented in the Joint ACC/JAMA Late-Breaking Clinical Trials II (Sunday, May 16, 8:00 a.m.-9:30 a.m.).
Two trials, FLOWER-MI and RADIANCE-HTN TRIO, were singled out in the Joint ACC/New England Journal of Medicine Late-Breaking Clinical Trials III (Sunday, May 16, 10:45 a.m.-12:00 p.m.). FLOWER-MI examines whether fractional flow reserve (FFR) is better than angiography to guide complete multivessel revascularization in ST-elevation MI patients with at least 50% stenosis in at least one nonculprit lesion requiring percutaneous coronary intervention (PCI). Recent studies have shown the superiority of FFR-guided PCI for nonculprit lesions, compared with culprit lesion treatment-only, but this is the first time FFR- and angiography-guided PCI have been compared in STEMI patients.
RADIANCE-HTN TRIO already tipped its hand, with top-line results reported in late 2020 showing that the trial met its primary efficacy endpoint of greater reduction in daytime blood pressure over 2 months with the Paradise endovascular ultrasound renal denervation system, compared with a sham procedure, in 136 patients with resistant hypertension, importantly, after being given a single pill containing a calcium channel blocker, angiotensin II receptor blocker, and diuretic.
Renal denervation for hypertension has been making something of a comeback, with the 2018 RADIANCE-HTN SOLO reporting better ambulatory blood pressure control with the Paradise system than with a sham procedure in the absence of antihypertensive agents. The device has been granted breakthrough device designation from the Food and Drug Administration for the treatment of hypertensive patients who are unable to sufficiently respond to or are intolerant of antihypertensive therapy.
Monday LBCTs
In the Late-Breaking Clinical Trials IV session (Monday, May 17, 8 a.m.–9:30 a.m.), Drachman called out a secondary analysis from GALATIC-HF looking at the impact of EF on the therapeutic effect of omecamtiv mecarbil. In last year’s primary analysis, the selective cardiac myosin activator produced a modest but significant reduction in HF events or CV death in 8,232 patients with HF and an EF of 35% or less.
Rounding out the list is the Canadian CAPITAL CHILL study of moderate versus mild therapeutic hypothermia in out-of-hospital cardiac arrest, to be presented in the final Late-Breaking Clinical Trials V session (Monday, May 17, 10:45 a.m.–12:00 p.m.).
The double-blind trial sought to determine whether neurologic outcomes at 6 months are improved by targeting a core temperature of 31 ˚C versus 34 ˚C after the return of spontaneous circulation in comatose survivors of out-of-hospital cardiac arrest.
“For me, I think this could really change practice and has personal relevance from experience with cardiac arrest survivors that I’ve known and care for very deeply,” Dr. Drachman said in an interview. “I think that there’s a lot of opportunity here as well.”
Asked what other trials have the potential to change practice, Dr. Drachman said FLOWER-MI holds particular interest because it looks at how to manage patients with STEMI with multiple lesions at the point of care.
“We’ve gained a lot of clarity from several other prior clinical trials, but this will help to answer the question in a slightly different way of saying: can you eyeball it, can you look at the angiogram and say whether or not that other, nonculprit lesion ought to be treated in the same hospitalization or should you really be using a pressure wire,” he said. “For me as an interventionalist, this is really important because when you finish up doing an intervention on a patient it might be the middle of the night and the patient may be more or less stable, but you’ve already exposed them to the risk of a procedure, should you then move on and do another aspect of the procedure to interrogate with a pressure wire a remaining narrowing? I think that’s very important; that’ll help me make decisions on a day-to-day basis.”
Dr. Drachman also cited RADIANCE-HTN TRIO because it employs an endovascular technique to control blood pressure in patients with hypertension, specifically those resistant to multiple drugs.
During the press conference, Dr. Morris, a preventive cardiologist, put her money on the ADAPTABLE study of aspirin dosing, reiterating that the unique trial design could inform future research, and on Sunday’s 8:45 a.m. late-breaking post hoc analysis from the STRENGTH trial that looks to pick up where the controversy over omega-3 fatty acid preparations left off at last year’s American Heart Association meeting.
A lack of benefit on CV event rates reported with Epanova, a high-dose combination of eicosapentaenoic acid (EPA) and docosahexaenoic acid, led to a contentious debate over how to reconcile STRENGTH with the findings from REDUCE-IT, which showed a 25% relative risk reduction in major CV events with the EPA product icosapent ethyl (Vascepa).
STRENGTH investigator Steven Nissen, MD, Cleveland Clinic, and REDUCE-IT investigator and session panelist Deepak Bhatt, MD, Brigham and Women’s Hospital, Boston, will share the virtual stage at ACC 2021, but Dr. Morris said the “good news” is both researchers know one another very well and “will really be focusing on no political issues, just the omega-3 fatty levels in the bloodstream and what does that mean in either trial.
“This is not designed to be a debate, point counterpoint,” she added.
For that, as all cardiologists and journalists know, there will be the wild and woolly #CardioTwitter sphere.
A version of this article first appeared on Medscape.com.
The American College of Cardiology pulled off an impressive all-virtual meeting in March 2020, less than 3 weeks after canceling its in-person event and just 2 weeks after COVID-19 was declared a national emergency.
Optimistic plans for the annual scientific sessions of the American College of Cardiology (ACC 2021) to be a March hybrid affair in Atlanta pivoted not once, but twice, as the pandemic evolved, with the date pushed back 2 full months, to May 15-17, and the format revised to fully virtual.
“While this meeting is being delivered virtually, I think you’ll see there have been benefits in the time to plan and also the lessons that ACC has learned in virtual education over the past year. This has come together to really create a robust educational and scientific agenda,” ACC 2021 chair Pamela B. Morris, MD, said in a press conference focused on the upcoming meeting.
Over the 3 days, there will be more than 200 education sessions, 10 guideline-specific sessions, and 11 learning pathways that include core areas, but also special topics, such as COVID-19 and the emerging cardio-obstetrics subspecialty.
The meeting will be delivered through a new virtual education program built to optimize real-time interaction between faculty members and attendees, she said. A dedicated portal on the platform will allow attendees to interact virtually, for example, with presenters of the nearly 3,000 ePosters and 420 moderated posters.
For those suffering from Zoom fatigue, the increasingly popular Heart2Heart stage talks have also been converted to podcasts, which cover topics like gender equity in cardiology, the evolving role of advanced practice professionals, and “one of my favorites: art as a tool for healing,” said Dr. Morris, from the Medical University of South Carolina, Charleston. “Those sessions are really not to be missed.”
Reconnecting is an underlying theme of the meeting but the great divider will not be ignored. COVID-19 will be the focus of two 90-minute Intensive Sessions on Saturday, May 15, the first kicking off at 10:30 a.m. ET, with the Bishop Keynote lecture on bringing health equity to the frontline of cardiovascular care, followed by lessons learned during the pandemic, how to conduct clinical trials, and vaccine development.
The second session, set for 12:15 p.m., continues the “silver linings” theme, with case presentations on advances in telehealth, myocardial involvement, and thrombosis in COVID. For those wanting more, 18 abstracts are on tap in a 2-hour Spotlight on Special Topics session beginning at 2:30 p.m.
Asked about the pandemic’s effect on bringing science to fruition this past year, Dr. Morris said there’s no question it’s slowed some of the progress the cardiology community had made but, like clinical practice, “we’ve also surmounted many of those obstacles.”
“I think research has rebounded,” she said. “Just in terms of the number of abstracts and the quality of abstracts that were submitted this year, I don’t think there’s any question that we are right on par with previous years.”
Indeed, 5,258 abstracts from 76 countries were submitted, with more than 3,400 chosen for oral and poster presentation, including 25 late-breaking clinical trials to be presented in five sessions.
The late-breaking presentations and discussions will be prerecorded but speakers and panelists have been invited to be present during the streaming to answer live any questions that may arise in the chat box, ACC 2021 vice chair Douglas Drachman, MD, Massachusetts General Hospital, Boston, said in an interview.
Late-breaking clinical trials
The Joint ACC/JACC Late-Breaking Clinical Trials I (Saturday, May 15, 9:00 a.m.–-10:00 a.m.) kicks off with PARADISE-MI, the first head-to-head comparison of an angiotensin receptor neprilysin inhibitor (ARNI) and an ACE inhibitor in patients with reduced ejection fractions (EFs) after MI but no history of heart failure (HF), studying 200 mg sacubitril/valsartan (Entresto) versus 5 mg of ramipril, both twice daily, in 5,669 patients.
Sacubitril/valsartan was initially approved for HF with reduced EF and added a new indication to treat some HF patients with preserved EF. Novartis, however, recently told investors that although numerical trends consistently favored the ARNI over the ACE inhibitor ramipril, the phase 3 study failed to meet the primary endpoint for efficacy superiority of reducing the risk for cardiovascular (CV) death and HF events after an acute MI.
Second up is ADAPTABLE, which looks to close a surprising evidence gap over whether 81 mg or 325 mg daily is the optimal dose of the ubiquitously prescribed aspirin for secondary prevention in high-risk patients with established atherosclerotic CV disease.
The open-label, randomized study will look at efficacy and major bleeding over roughly 4 years in 15,000 patients within PCORnet, the National Patient-centered Clinical Research Network, a partnership of clinical research, health plan research, and patient-powered networks created to streamline patient-reported outcomes research.
“This study will not only give important clinical information for us, practically speaking, whether we should prescribe lower- or higher-dose aspirin, but it may also serve as a template for future pragmatic clinical trial design in the real world,” Dr. Drachman said during the press conference.
Up next is the 4,812-patient Canadian LAAOS III, the largest trial to examine the efficacy of left atrial appendage occlusion for stroke prevention in patients with atrial fibrillation (AFib) already undergoing cardiac surgery. The primary outcome is the first occurrence of stroke or systemic arterial embolism over an average follow-up of 4 years.
Percutaneous closure of the left atrial appendage (LAA) has been shown to reduce stroke in AFib patients at high-risk of bleeding on systemic anticoagulation. But these devices can be expensive and studies haven’t included patients who also have valvular heart disease, a group that actually comprises more than half of patients undergoing cardiac surgery who also have AFib, he noted.
At the same time, surgical LAA closure studies have been small and have had very mixed results. “There isn’t a large-scale rigorous assessment out there for these patients undergoing surgery, so I think this is going to be fascinating to see,” Dr. Drachman said.
The session closes with ATLANTIS, which looks to shed some light on the role of anticoagulation therapy in patients after transcatheter aortic valve replacement (TAVR or TAVI). POPular TAVI, presented at ACC 2020, showed aspirin alone was the preferred antithrombotic therapy over aspirin plus clopidogrel (Plavix) in patients not on oral anticoagulants, but the optimal anticoagulation regimen remains unsettled.
The French open-label, 1,510-patient ATLANTIS trial examined whether the novel oral anticoagulant apixaban (Eliquis) is superior in preventing CV events after TAVR, compared with antiplatelet therapy in patients without an indication for anticoagulation and compared with vitamin K antagonists in those receiving anticoagulants.
An ATLANTIS 4D CT substudy of valve thrombosis is also slated for Saturday’s Featured Clinical Research 1 session at 12:15 p.m. to 1:45 p.m..
Sunday LBCTs
Dr. Drachman highlighted a series of other late-breaking studies, including the global DARE-19 trial testing the diabetes and HF drug dapagliflozin (Farxiga) given with local standard-of-care therapy for 30 days in hospitalized COVID-19 patients with CV, metabolic, or renal risk factors.
Although sodium-glucose cotransporter-2 inhibitors have been white-hot of late, top-line results reported last month show dapagliflozin failed to achieve statistical significance for the primary endpoints of reducing organ dysfunction and all-cause mortality and for improving recovery. Details will be presented in the Joint ACC/JAMA Late-Breaking Clinical Trials II (Sunday, May 16, 8:00 a.m.-9:30 a.m.).
Two trials, FLOWER-MI and RADIANCE-HTN TRIO, were singled out in the Joint ACC/New England Journal of Medicine Late-Breaking Clinical Trials III (Sunday, May 16, 10:45 a.m.-12:00 p.m.). FLOWER-MI examines whether fractional flow reserve (FFR) is better than angiography to guide complete multivessel revascularization in ST-elevation MI patients with at least 50% stenosis in at least one nonculprit lesion requiring percutaneous coronary intervention (PCI). Recent studies have shown the superiority of FFR-guided PCI for nonculprit lesions, compared with culprit lesion treatment-only, but this is the first time FFR- and angiography-guided PCI have been compared in STEMI patients.
RADIANCE-HTN TRIO already tipped its hand, with top-line results reported in late 2020 showing that the trial met its primary efficacy endpoint of greater reduction in daytime blood pressure over 2 months with the Paradise endovascular ultrasound renal denervation system, compared with a sham procedure, in 136 patients with resistant hypertension, importantly, after being given a single pill containing a calcium channel blocker, angiotensin II receptor blocker, and diuretic.
Renal denervation for hypertension has been making something of a comeback, with the 2018 RADIANCE-HTN SOLO reporting better ambulatory blood pressure control with the Paradise system than with a sham procedure in the absence of antihypertensive agents. The device has been granted breakthrough device designation from the Food and Drug Administration for the treatment of hypertensive patients who are unable to sufficiently respond to or are intolerant of antihypertensive therapy.
Monday LBCTs
In the Late-Breaking Clinical Trials IV session (Monday, May 17, 8 a.m.–9:30 a.m.), Drachman called out a secondary analysis from GALATIC-HF looking at the impact of EF on the therapeutic effect of omecamtiv mecarbil. In last year’s primary analysis, the selective cardiac myosin activator produced a modest but significant reduction in HF events or CV death in 8,232 patients with HF and an EF of 35% or less.
Rounding out the list is the Canadian CAPITAL CHILL study of moderate versus mild therapeutic hypothermia in out-of-hospital cardiac arrest, to be presented in the final Late-Breaking Clinical Trials V session (Monday, May 17, 10:45 a.m.–12:00 p.m.).
The double-blind trial sought to determine whether neurologic outcomes at 6 months are improved by targeting a core temperature of 31 ˚C versus 34 ˚C after the return of spontaneous circulation in comatose survivors of out-of-hospital cardiac arrest.
“For me, I think this could really change practice and has personal relevance from experience with cardiac arrest survivors that I’ve known and care for very deeply,” Dr. Drachman said in an interview. “I think that there’s a lot of opportunity here as well.”
Asked what other trials have the potential to change practice, Dr. Drachman said FLOWER-MI holds particular interest because it looks at how to manage patients with STEMI with multiple lesions at the point of care.
“We’ve gained a lot of clarity from several other prior clinical trials, but this will help to answer the question in a slightly different way of saying: can you eyeball it, can you look at the angiogram and say whether or not that other, nonculprit lesion ought to be treated in the same hospitalization or should you really be using a pressure wire,” he said. “For me as an interventionalist, this is really important because when you finish up doing an intervention on a patient it might be the middle of the night and the patient may be more or less stable, but you’ve already exposed them to the risk of a procedure, should you then move on and do another aspect of the procedure to interrogate with a pressure wire a remaining narrowing? I think that’s very important; that’ll help me make decisions on a day-to-day basis.”
Dr. Drachman also cited RADIANCE-HTN TRIO because it employs an endovascular technique to control blood pressure in patients with hypertension, specifically those resistant to multiple drugs.
During the press conference, Dr. Morris, a preventive cardiologist, put her money on the ADAPTABLE study of aspirin dosing, reiterating that the unique trial design could inform future research, and on Sunday’s 8:45 a.m. late-breaking post hoc analysis from the STRENGTH trial that looks to pick up where the controversy over omega-3 fatty acid preparations left off at last year’s American Heart Association meeting.
A lack of benefit on CV event rates reported with Epanova, a high-dose combination of eicosapentaenoic acid (EPA) and docosahexaenoic acid, led to a contentious debate over how to reconcile STRENGTH with the findings from REDUCE-IT, which showed a 25% relative risk reduction in major CV events with the EPA product icosapent ethyl (Vascepa).
STRENGTH investigator Steven Nissen, MD, Cleveland Clinic, and REDUCE-IT investigator and session panelist Deepak Bhatt, MD, Brigham and Women’s Hospital, Boston, will share the virtual stage at ACC 2021, but Dr. Morris said the “good news” is both researchers know one another very well and “will really be focusing on no political issues, just the omega-3 fatty levels in the bloodstream and what does that mean in either trial.
“This is not designed to be a debate, point counterpoint,” she added.
For that, as all cardiologists and journalists know, there will be the wild and woolly #CardioTwitter sphere.
A version of this article first appeared on Medscape.com.
Fresh look at ISCHEMIA bolsters conservative message in stable CAD
The more complicated a primary endpoint, the greater a puzzle it can be for clinicians to interpret the results. It’s likely even tougher for patients, who don’t help choose the events studied in clinical trials yet are increasingly sharing in the management decisions they influence.
That creates an opening for a more patient-centered take on one of cardiology’s most influential recent studies, ISCHEMIA, which bolsters the case for conservative, med-oriented management over a more invasive initial strategy for patients with stable coronary artery disease (CAD) and positive stress tests, researchers said.
The new, prespecified analysis replaced the trial’s conventional primary endpoint of major adverse cardiac events (MACE) with one based on “days alive out of hospital” (DAOH) and found an early advantage for the conservative approach, with caveats.
Those assigned to the conservative arm benefited with more out-of-hospital days throughout the next 2 years than those in the invasive-management group, owing to the latter’s protocol-mandated early cath-lab work-up with possible revascularization. The difference averaged more than 6 days for much of that time.
But DAOH evened out for the two groups by the fourth year in the analysis of more than 5,000 patients.
Protocol-determined cath procedures accounted for 61% of hospitalizations in the invasively managed group. A secondary DAOH analysis that excluded such required hospital days, also prespecified, showed no meaningful difference between the two strategies over the 4 years, noted the report published online May 3 in JAMA Cardiology.
DOAH is ‘very, very important’
The DAOH metric has been a far less common consideration in clinical trials, compared with clinical events, yet in some ways it is as “hard” a metric as mortality, encompasses a broader range of outcomes, and may matter more to patients, it’s been argued.
“The thing patients most value is time at home. So they don’t want to be in the hospital, they don’t want to be away from friends, they want to do recreation, or they may want to work,” lead author Harvey D. White, DSc, Green Lane Cardiovascular Services, Auckland (New Zealand) City Hospital, University of Auckland, told this news organization.
“When we need to talk to patients – and we do need to talk to patients – to have a days-out-of-hospital metric is very, very important,” he said. It is not only patient focused, it’s “meaningful in terms of the seriousness of events,” in that length of hospitalization tracks with clinical severity, observed Dr. White, who is slated to present the analysis May 17 during the virtual American College of Cardiology 2021 scientific sessions.
As previously reported, ISCHEMIA showed no significant effect on the primary endpoint of cardiovascular mortality, MI, or hospitalization for unstable angina, heart failure, or resuscitated cardiac arrest by assignment group over a median 3.2 years. Angina and quality of life measures were improved for patients in the invasive arm.
With an invasive initial strategy, “What we know now is that you get nothing of an advantage in terms of the composite endpoint, and you’re going to spend 6 days more in the hospital in the first 2 years, for largely no benefit,” Dr. White said.
That outlook may apply out to 4 years, the analysis suggests, but could conceivably change if DAOH is reassessed later as the ISCHEMIA follow-up continues for what is now a planned total of 10 years.
Meanwhile, the current findings could enhance doctor-patient discussions about the trade-offs between the two strategies for individuals whose considerations will vary.
“This is a very helpful measure to understand the burden of an approach to the patient,” observed E. Magnus Ohman, MD, an interventional cardiologist at Duke University, Durham, N.C., who was not involved in the trial.
With DAOH as an endpoint, “you as a clinician get another aspect of understanding of a treatment’s impact on a multitude of endpoints.” Days out of hospital, he noted, encompasses the effects of clinical events that often go into composite clinical endpoints – not death, but including nonfatal MI, stroke, need for revascularization, and cardiovascular hospitalization.
To patients with stable CAD who ask whether the invasive approach has merits in their case, the DAOH finding “helps you to say, well, at the end of the day, you will probably be spending an equal amount of time in the hospital. Your price up front is a little bit higher, but over time, the group who gets conservative treatment will catch up.”
The DAOH outcome also avoids the limitations of an endpoint based on time to first event, “not the least of which,” said Dr. White, is that it counts only the first of what might be multiple events of varying clinical impact. Misleadingly, “you can have an event that’s a small troponin rise, but that becomes more important in a person than dying the next day.”
The DAOH analysis was based on 5,179 patients from 37 countries who averaged 64 years of age and of whom 23% were women. The endpoint considered only overnight stays in hospitals, skilled nursing facilities, rehabilitation centers, and nursing homes.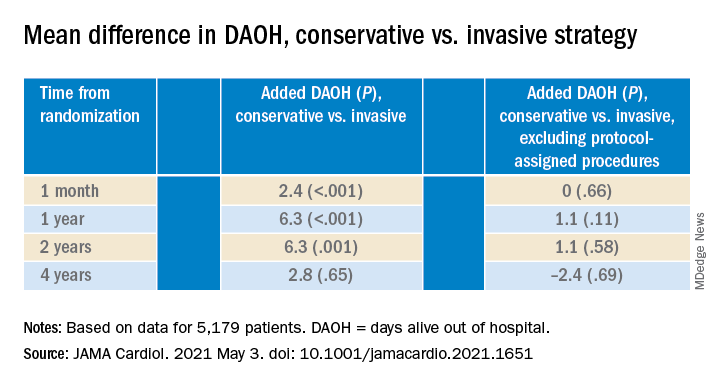
There were many more hospital or extended care facility stays overall in the invasive-management group, 4,002 versus 1,897 for those following the conservative strategy (P < .001), but the numbers flipped after excluding protocol-assigned procedures: 1,568 stays in the invasive group, compared with 1,897 (P = .001)
There were no associations between DAOH and Seattle Angina Questionnaire 7–Angina Frequency scores or DAOH interactions by age, sex, geographic region, or whether the patient had diabetes, prior MI, or heart failure, the report notes.
The primary ISCHEMIA analysis hinted at a possible long-term advantage for the invasive initial strategy in that event curves for the two arms crossed after 2-3 years, Dr. Ohman observed.
Based on that, for younger patients with stable CAD and ischemia at stress testing, “an investment of more hospital days early on might be worth it in the long run.” But ISCHEMIA, he said, “only suggests it, it doesn’t confirm it.”
The study was supported in part by grants from Arbor Pharmaceuticals and AstraZeneca. Devices or medications were provided by Abbott Vascular, Amgen, Arbor, AstraZeneca, Esperion, Medtronic, Merck Sharp & Dohme, Phillips, Omron Healthcare, and Sunovion. Dr. White disclosed receiving grants paid to his institution and fees for serving on a steering committee from Sanofi-Aventis, Regeneron, Eli Lilly, Omthera, American Regent, Eisai, DalCor, CSL Behring, Sanofi-Aventis Australia, and Esperion Therapeutics, and personal fees from Genentech and AstraZeneca. Dr. Ohman reported receiving grants from Abiomed and Cheisi USA, and consulting for Abiomed, Cara Therapeutics, Chiesi USA, Cytokinetics, Imbria Pharmaceuticals, Otsuka Pharmaceuticals, Milestone Pharmaceuticals, and XyloCor Therapeutics.
A version of this article first appeared on Medscape.com.
The more complicated a primary endpoint, the greater a puzzle it can be for clinicians to interpret the results. It’s likely even tougher for patients, who don’t help choose the events studied in clinical trials yet are increasingly sharing in the management decisions they influence.
That creates an opening for a more patient-centered take on one of cardiology’s most influential recent studies, ISCHEMIA, which bolsters the case for conservative, med-oriented management over a more invasive initial strategy for patients with stable coronary artery disease (CAD) and positive stress tests, researchers said.
The new, prespecified analysis replaced the trial’s conventional primary endpoint of major adverse cardiac events (MACE) with one based on “days alive out of hospital” (DAOH) and found an early advantage for the conservative approach, with caveats.
Those assigned to the conservative arm benefited with more out-of-hospital days throughout the next 2 years than those in the invasive-management group, owing to the latter’s protocol-mandated early cath-lab work-up with possible revascularization. The difference averaged more than 6 days for much of that time.
But DAOH evened out for the two groups by the fourth year in the analysis of more than 5,000 patients.
Protocol-determined cath procedures accounted for 61% of hospitalizations in the invasively managed group. A secondary DAOH analysis that excluded such required hospital days, also prespecified, showed no meaningful difference between the two strategies over the 4 years, noted the report published online May 3 in JAMA Cardiology.
DOAH is ‘very, very important’
The DAOH metric has been a far less common consideration in clinical trials, compared with clinical events, yet in some ways it is as “hard” a metric as mortality, encompasses a broader range of outcomes, and may matter more to patients, it’s been argued.
“The thing patients most value is time at home. So they don’t want to be in the hospital, they don’t want to be away from friends, they want to do recreation, or they may want to work,” lead author Harvey D. White, DSc, Green Lane Cardiovascular Services, Auckland (New Zealand) City Hospital, University of Auckland, told this news organization.
“When we need to talk to patients – and we do need to talk to patients – to have a days-out-of-hospital metric is very, very important,” he said. It is not only patient focused, it’s “meaningful in terms of the seriousness of events,” in that length of hospitalization tracks with clinical severity, observed Dr. White, who is slated to present the analysis May 17 during the virtual American College of Cardiology 2021 scientific sessions.
As previously reported, ISCHEMIA showed no significant effect on the primary endpoint of cardiovascular mortality, MI, or hospitalization for unstable angina, heart failure, or resuscitated cardiac arrest by assignment group over a median 3.2 years. Angina and quality of life measures were improved for patients in the invasive arm.
With an invasive initial strategy, “What we know now is that you get nothing of an advantage in terms of the composite endpoint, and you’re going to spend 6 days more in the hospital in the first 2 years, for largely no benefit,” Dr. White said.
That outlook may apply out to 4 years, the analysis suggests, but could conceivably change if DAOH is reassessed later as the ISCHEMIA follow-up continues for what is now a planned total of 10 years.
Meanwhile, the current findings could enhance doctor-patient discussions about the trade-offs between the two strategies for individuals whose considerations will vary.
“This is a very helpful measure to understand the burden of an approach to the patient,” observed E. Magnus Ohman, MD, an interventional cardiologist at Duke University, Durham, N.C., who was not involved in the trial.
With DAOH as an endpoint, “you as a clinician get another aspect of understanding of a treatment’s impact on a multitude of endpoints.” Days out of hospital, he noted, encompasses the effects of clinical events that often go into composite clinical endpoints – not death, but including nonfatal MI, stroke, need for revascularization, and cardiovascular hospitalization.
To patients with stable CAD who ask whether the invasive approach has merits in their case, the DAOH finding “helps you to say, well, at the end of the day, you will probably be spending an equal amount of time in the hospital. Your price up front is a little bit higher, but over time, the group who gets conservative treatment will catch up.”
The DAOH outcome also avoids the limitations of an endpoint based on time to first event, “not the least of which,” said Dr. White, is that it counts only the first of what might be multiple events of varying clinical impact. Misleadingly, “you can have an event that’s a small troponin rise, but that becomes more important in a person than dying the next day.”
The DAOH analysis was based on 5,179 patients from 37 countries who averaged 64 years of age and of whom 23% were women. The endpoint considered only overnight stays in hospitals, skilled nursing facilities, rehabilitation centers, and nursing homes.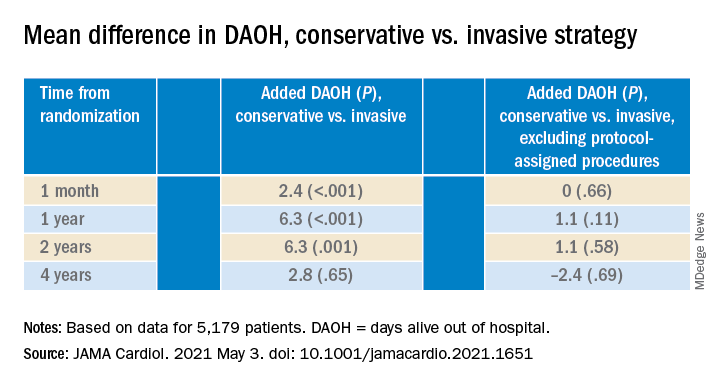
There were many more hospital or extended care facility stays overall in the invasive-management group, 4,002 versus 1,897 for those following the conservative strategy (P < .001), but the numbers flipped after excluding protocol-assigned procedures: 1,568 stays in the invasive group, compared with 1,897 (P = .001)
There were no associations between DAOH and Seattle Angina Questionnaire 7–Angina Frequency scores or DAOH interactions by age, sex, geographic region, or whether the patient had diabetes, prior MI, or heart failure, the report notes.
The primary ISCHEMIA analysis hinted at a possible long-term advantage for the invasive initial strategy in that event curves for the two arms crossed after 2-3 years, Dr. Ohman observed.
Based on that, for younger patients with stable CAD and ischemia at stress testing, “an investment of more hospital days early on might be worth it in the long run.” But ISCHEMIA, he said, “only suggests it, it doesn’t confirm it.”
The study was supported in part by grants from Arbor Pharmaceuticals and AstraZeneca. Devices or medications were provided by Abbott Vascular, Amgen, Arbor, AstraZeneca, Esperion, Medtronic, Merck Sharp & Dohme, Phillips, Omron Healthcare, and Sunovion. Dr. White disclosed receiving grants paid to his institution and fees for serving on a steering committee from Sanofi-Aventis, Regeneron, Eli Lilly, Omthera, American Regent, Eisai, DalCor, CSL Behring, Sanofi-Aventis Australia, and Esperion Therapeutics, and personal fees from Genentech and AstraZeneca. Dr. Ohman reported receiving grants from Abiomed and Cheisi USA, and consulting for Abiomed, Cara Therapeutics, Chiesi USA, Cytokinetics, Imbria Pharmaceuticals, Otsuka Pharmaceuticals, Milestone Pharmaceuticals, and XyloCor Therapeutics.
A version of this article first appeared on Medscape.com.
The more complicated a primary endpoint, the greater a puzzle it can be for clinicians to interpret the results. It’s likely even tougher for patients, who don’t help choose the events studied in clinical trials yet are increasingly sharing in the management decisions they influence.
That creates an opening for a more patient-centered take on one of cardiology’s most influential recent studies, ISCHEMIA, which bolsters the case for conservative, med-oriented management over a more invasive initial strategy for patients with stable coronary artery disease (CAD) and positive stress tests, researchers said.
The new, prespecified analysis replaced the trial’s conventional primary endpoint of major adverse cardiac events (MACE) with one based on “days alive out of hospital” (DAOH) and found an early advantage for the conservative approach, with caveats.
Those assigned to the conservative arm benefited with more out-of-hospital days throughout the next 2 years than those in the invasive-management group, owing to the latter’s protocol-mandated early cath-lab work-up with possible revascularization. The difference averaged more than 6 days for much of that time.
But DAOH evened out for the two groups by the fourth year in the analysis of more than 5,000 patients.
Protocol-determined cath procedures accounted for 61% of hospitalizations in the invasively managed group. A secondary DAOH analysis that excluded such required hospital days, also prespecified, showed no meaningful difference between the two strategies over the 4 years, noted the report published online May 3 in JAMA Cardiology.
DOAH is ‘very, very important’
The DAOH metric has been a far less common consideration in clinical trials, compared with clinical events, yet in some ways it is as “hard” a metric as mortality, encompasses a broader range of outcomes, and may matter more to patients, it’s been argued.
“The thing patients most value is time at home. So they don’t want to be in the hospital, they don’t want to be away from friends, they want to do recreation, or they may want to work,” lead author Harvey D. White, DSc, Green Lane Cardiovascular Services, Auckland (New Zealand) City Hospital, University of Auckland, told this news organization.
“When we need to talk to patients – and we do need to talk to patients – to have a days-out-of-hospital metric is very, very important,” he said. It is not only patient focused, it’s “meaningful in terms of the seriousness of events,” in that length of hospitalization tracks with clinical severity, observed Dr. White, who is slated to present the analysis May 17 during the virtual American College of Cardiology 2021 scientific sessions.
As previously reported, ISCHEMIA showed no significant effect on the primary endpoint of cardiovascular mortality, MI, or hospitalization for unstable angina, heart failure, or resuscitated cardiac arrest by assignment group over a median 3.2 years. Angina and quality of life measures were improved for patients in the invasive arm.
With an invasive initial strategy, “What we know now is that you get nothing of an advantage in terms of the composite endpoint, and you’re going to spend 6 days more in the hospital in the first 2 years, for largely no benefit,” Dr. White said.
That outlook may apply out to 4 years, the analysis suggests, but could conceivably change if DAOH is reassessed later as the ISCHEMIA follow-up continues for what is now a planned total of 10 years.
Meanwhile, the current findings could enhance doctor-patient discussions about the trade-offs between the two strategies for individuals whose considerations will vary.
“This is a very helpful measure to understand the burden of an approach to the patient,” observed E. Magnus Ohman, MD, an interventional cardiologist at Duke University, Durham, N.C., who was not involved in the trial.
With DAOH as an endpoint, “you as a clinician get another aspect of understanding of a treatment’s impact on a multitude of endpoints.” Days out of hospital, he noted, encompasses the effects of clinical events that often go into composite clinical endpoints – not death, but including nonfatal MI, stroke, need for revascularization, and cardiovascular hospitalization.
To patients with stable CAD who ask whether the invasive approach has merits in their case, the DAOH finding “helps you to say, well, at the end of the day, you will probably be spending an equal amount of time in the hospital. Your price up front is a little bit higher, but over time, the group who gets conservative treatment will catch up.”
The DAOH outcome also avoids the limitations of an endpoint based on time to first event, “not the least of which,” said Dr. White, is that it counts only the first of what might be multiple events of varying clinical impact. Misleadingly, “you can have an event that’s a small troponin rise, but that becomes more important in a person than dying the next day.”
The DAOH analysis was based on 5,179 patients from 37 countries who averaged 64 years of age and of whom 23% were women. The endpoint considered only overnight stays in hospitals, skilled nursing facilities, rehabilitation centers, and nursing homes.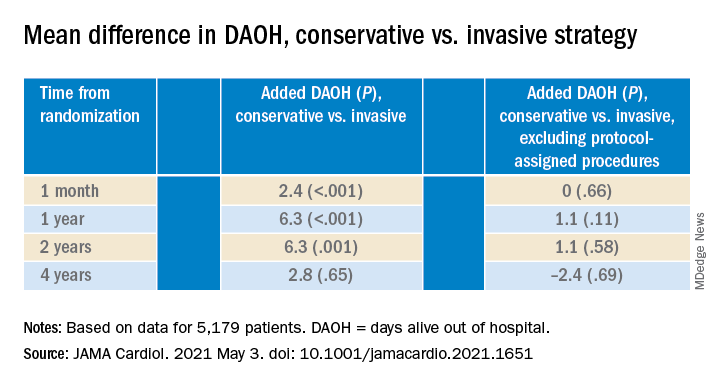
There were many more hospital or extended care facility stays overall in the invasive-management group, 4,002 versus 1,897 for those following the conservative strategy (P < .001), but the numbers flipped after excluding protocol-assigned procedures: 1,568 stays in the invasive group, compared with 1,897 (P = .001)
There were no associations between DAOH and Seattle Angina Questionnaire 7–Angina Frequency scores or DAOH interactions by age, sex, geographic region, or whether the patient had diabetes, prior MI, or heart failure, the report notes.
The primary ISCHEMIA analysis hinted at a possible long-term advantage for the invasive initial strategy in that event curves for the two arms crossed after 2-3 years, Dr. Ohman observed.
Based on that, for younger patients with stable CAD and ischemia at stress testing, “an investment of more hospital days early on might be worth it in the long run.” But ISCHEMIA, he said, “only suggests it, it doesn’t confirm it.”
The study was supported in part by grants from Arbor Pharmaceuticals and AstraZeneca. Devices or medications were provided by Abbott Vascular, Amgen, Arbor, AstraZeneca, Esperion, Medtronic, Merck Sharp & Dohme, Phillips, Omron Healthcare, and Sunovion. Dr. White disclosed receiving grants paid to his institution and fees for serving on a steering committee from Sanofi-Aventis, Regeneron, Eli Lilly, Omthera, American Regent, Eisai, DalCor, CSL Behring, Sanofi-Aventis Australia, and Esperion Therapeutics, and personal fees from Genentech and AstraZeneca. Dr. Ohman reported receiving grants from Abiomed and Cheisi USA, and consulting for Abiomed, Cara Therapeutics, Chiesi USA, Cytokinetics, Imbria Pharmaceuticals, Otsuka Pharmaceuticals, Milestone Pharmaceuticals, and XyloCor Therapeutics.
A version of this article first appeared on Medscape.com.
Infective endocarditis with stroke after TAVR has ‘dismal’ prognosis
Patients who suffer a stroke during hospitalization for infective endocarditis (IE) after transcatheter aortic valve replacement (TAVR) have a dismal prognosis, with more than half dying during the index hospitalization and two-thirds within the first year, a new study shows.
The study – the first to evaluate stroke as an IE-related complication following TAVR in a large multicenter cohort – is published in the May 11 issue of the Journal of the American College of Cardiology.
The authors, led by David del Val, MD, Quebec Heart & Lung Institute, Quebec City, explain that IE after TAVR is a rare but serious complication associated with a high mortality rate. Neurologic events, especially stroke, remain one of the most common and potentially disabling IE-related complications, but until now, no study has attempted to evaluate the predictors of stroke and outcomes in patients with IE following TAVR.
For the current study, the authors analyzed data from the Infectious Endocarditis after TAVR International Registry, including 569 patients who developed definite IE following TAVR from 59 centers in 11 countries.
Patients who experienced a stroke during IE admission were compared with patients who did not have a stroke.
Results showed that 57 patients (10%) had a stroke during IE hospitalization, with no differences in the causative microorganism between groups. Stroke patients had higher rates of acute renal failure, systemic embolization, and persistent bacteremia.
Factors associated with a higher risk for stroke during the index IE hospitalization included stroke before IE, moderate or higher residual aortic regurgitation after TAVR, balloon-expandable valves, IE within 30 days after TAVR, and vegetation size greater than 8 mm.
The stroke rate was 3.1% in patients with none of these risk factors; 6.1% with one risk factor; 13.1% with two risk factors; 28.9% with three risk factors, and 60% with four risk factors.
“The presence of such factors (particularly in combination) may be considered for determining an earlier and more aggressive (medical or surgical) treatment in these patients,” the researchers say.
IE patients with stroke had higher rates of in-hospital mortality (54.4% vs. 28.7%) and overall mortality at 1 year (66.3% vs. 45.6%).
Surgery rates were low (25%) even in the presence of stroke and failed to improve outcomes in this population.
Noting that consensus guidelines for managing patients with IE recommend surgery along with antibiotic treatment for patients developing systemic embolism, particularly stroke, the researchers say their findings suggest that such surgery recommendations may not be extrapolated to TAVR-IE patients, and specific guidelines are warranted for this particular population.
Furthermore, the possibility of early surgery in those patients with factors increasing the risk for stroke should be evaluated in future studies.
The authors note that TAVR has revolutionized the treatment of aortic stenosis and is currently moving toward less complex and younger patients with lower surgical risk. Despite the relatively low incidence of IE after TAVR, the number of procedures is expected to grow exponentially, increasing the number of patients at risk of developing this life-threatening complication. Therefore, detailed knowledge of this disease and its complications is essential to improve outcomes.
They point out that the 10% rate of stroke found in this study is substantially lower, compared with the largest surgical prosthetic-valve infective endocarditis registries, but they suggest that the unique clinical profile of TAVR patients may lead to an underdiagnosis of stroke, with a high proportion of elderly patients who more frequently present with nonspecific symptoms.
They conclude that “IE post-TAVR is associated with a poor prognosis with high in-hospital and late mortality rates. Our study reveals that patients with IE after TAVR complicated by stroke showed an even worse prognosis.”
“The progressive implementation of advanced imaging modalities for early IE diagnosis, especially nuclear imaging, may translate into a better prognosis in coming years. Close attention should be paid to early recognition of stroke-associated factors to improve clinical outcomes,” they add.
In an accompanying editorial, Vuyisile Nkomo, MD, Daniel DeSimone, MD, and William Miranda, MD, Mayo Clinic, Rochester, Minn., say the current study “highlights the devastating consequences of IE after TAVR and the even worse consequences when IE was associated with stroke.”
This points to the critical importance of efforts to prevent IE with appropriate antibiotic prophylaxis and addressing potential sources of infection (for example, dental screening) before invasive cardiac procedures.
“Patient education is critical in regard to recognizing early signs and symptoms of IE. In particular, patients must be informed to obtain blood cultures with any episode of fever, as identification of bacteremia is critical in the diagnosis of IE,” the editorialists comment.
Endocarditis should also be suspected in afebrile patients with increasing transcatheter heart valve gradients or new or worsening regurgitation, they state.
Multimodality imaging is important for the early diagnosis of IE to facilitate prompt antibiotic treatment and potentially decrease the risk for IE complications, especially systemic embolization, they add.
“Despite the unequivocal advances in the safety and periprocedural complications of TAVR, IE with and without stroke in this TAVR population remains a dreadful complication,” they conclude.
Dr. Del Val was supported by a research grant from the Fundación Alfonso Martin Escudero. The editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Patients who suffer a stroke during hospitalization for infective endocarditis (IE) after transcatheter aortic valve replacement (TAVR) have a dismal prognosis, with more than half dying during the index hospitalization and two-thirds within the first year, a new study shows.
The study – the first to evaluate stroke as an IE-related complication following TAVR in a large multicenter cohort – is published in the May 11 issue of the Journal of the American College of Cardiology.
The authors, led by David del Val, MD, Quebec Heart & Lung Institute, Quebec City, explain that IE after TAVR is a rare but serious complication associated with a high mortality rate. Neurologic events, especially stroke, remain one of the most common and potentially disabling IE-related complications, but until now, no study has attempted to evaluate the predictors of stroke and outcomes in patients with IE following TAVR.
For the current study, the authors analyzed data from the Infectious Endocarditis after TAVR International Registry, including 569 patients who developed definite IE following TAVR from 59 centers in 11 countries.
Patients who experienced a stroke during IE admission were compared with patients who did not have a stroke.
Results showed that 57 patients (10%) had a stroke during IE hospitalization, with no differences in the causative microorganism between groups. Stroke patients had higher rates of acute renal failure, systemic embolization, and persistent bacteremia.
Factors associated with a higher risk for stroke during the index IE hospitalization included stroke before IE, moderate or higher residual aortic regurgitation after TAVR, balloon-expandable valves, IE within 30 days after TAVR, and vegetation size greater than 8 mm.
The stroke rate was 3.1% in patients with none of these risk factors; 6.1% with one risk factor; 13.1% with two risk factors; 28.9% with three risk factors, and 60% with four risk factors.
“The presence of such factors (particularly in combination) may be considered for determining an earlier and more aggressive (medical or surgical) treatment in these patients,” the researchers say.
IE patients with stroke had higher rates of in-hospital mortality (54.4% vs. 28.7%) and overall mortality at 1 year (66.3% vs. 45.6%).
Surgery rates were low (25%) even in the presence of stroke and failed to improve outcomes in this population.
Noting that consensus guidelines for managing patients with IE recommend surgery along with antibiotic treatment for patients developing systemic embolism, particularly stroke, the researchers say their findings suggest that such surgery recommendations may not be extrapolated to TAVR-IE patients, and specific guidelines are warranted for this particular population.
Furthermore, the possibility of early surgery in those patients with factors increasing the risk for stroke should be evaluated in future studies.
The authors note that TAVR has revolutionized the treatment of aortic stenosis and is currently moving toward less complex and younger patients with lower surgical risk. Despite the relatively low incidence of IE after TAVR, the number of procedures is expected to grow exponentially, increasing the number of patients at risk of developing this life-threatening complication. Therefore, detailed knowledge of this disease and its complications is essential to improve outcomes.
They point out that the 10% rate of stroke found in this study is substantially lower, compared with the largest surgical prosthetic-valve infective endocarditis registries, but they suggest that the unique clinical profile of TAVR patients may lead to an underdiagnosis of stroke, with a high proportion of elderly patients who more frequently present with nonspecific symptoms.
They conclude that “IE post-TAVR is associated with a poor prognosis with high in-hospital and late mortality rates. Our study reveals that patients with IE after TAVR complicated by stroke showed an even worse prognosis.”
“The progressive implementation of advanced imaging modalities for early IE diagnosis, especially nuclear imaging, may translate into a better prognosis in coming years. Close attention should be paid to early recognition of stroke-associated factors to improve clinical outcomes,” they add.
In an accompanying editorial, Vuyisile Nkomo, MD, Daniel DeSimone, MD, and William Miranda, MD, Mayo Clinic, Rochester, Minn., say the current study “highlights the devastating consequences of IE after TAVR and the even worse consequences when IE was associated with stroke.”
This points to the critical importance of efforts to prevent IE with appropriate antibiotic prophylaxis and addressing potential sources of infection (for example, dental screening) before invasive cardiac procedures.
“Patient education is critical in regard to recognizing early signs and symptoms of IE. In particular, patients must be informed to obtain blood cultures with any episode of fever, as identification of bacteremia is critical in the diagnosis of IE,” the editorialists comment.
Endocarditis should also be suspected in afebrile patients with increasing transcatheter heart valve gradients or new or worsening regurgitation, they state.
Multimodality imaging is important for the early diagnosis of IE to facilitate prompt antibiotic treatment and potentially decrease the risk for IE complications, especially systemic embolization, they add.
“Despite the unequivocal advances in the safety and periprocedural complications of TAVR, IE with and without stroke in this TAVR population remains a dreadful complication,” they conclude.
Dr. Del Val was supported by a research grant from the Fundación Alfonso Martin Escudero. The editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Patients who suffer a stroke during hospitalization for infective endocarditis (IE) after transcatheter aortic valve replacement (TAVR) have a dismal prognosis, with more than half dying during the index hospitalization and two-thirds within the first year, a new study shows.
The study – the first to evaluate stroke as an IE-related complication following TAVR in a large multicenter cohort – is published in the May 11 issue of the Journal of the American College of Cardiology.
The authors, led by David del Val, MD, Quebec Heart & Lung Institute, Quebec City, explain that IE after TAVR is a rare but serious complication associated with a high mortality rate. Neurologic events, especially stroke, remain one of the most common and potentially disabling IE-related complications, but until now, no study has attempted to evaluate the predictors of stroke and outcomes in patients with IE following TAVR.
For the current study, the authors analyzed data from the Infectious Endocarditis after TAVR International Registry, including 569 patients who developed definite IE following TAVR from 59 centers in 11 countries.
Patients who experienced a stroke during IE admission were compared with patients who did not have a stroke.
Results showed that 57 patients (10%) had a stroke during IE hospitalization, with no differences in the causative microorganism between groups. Stroke patients had higher rates of acute renal failure, systemic embolization, and persistent bacteremia.
Factors associated with a higher risk for stroke during the index IE hospitalization included stroke before IE, moderate or higher residual aortic regurgitation after TAVR, balloon-expandable valves, IE within 30 days after TAVR, and vegetation size greater than 8 mm.
The stroke rate was 3.1% in patients with none of these risk factors; 6.1% with one risk factor; 13.1% with two risk factors; 28.9% with three risk factors, and 60% with four risk factors.
“The presence of such factors (particularly in combination) may be considered for determining an earlier and more aggressive (medical or surgical) treatment in these patients,” the researchers say.
IE patients with stroke had higher rates of in-hospital mortality (54.4% vs. 28.7%) and overall mortality at 1 year (66.3% vs. 45.6%).
Surgery rates were low (25%) even in the presence of stroke and failed to improve outcomes in this population.
Noting that consensus guidelines for managing patients with IE recommend surgery along with antibiotic treatment for patients developing systemic embolism, particularly stroke, the researchers say their findings suggest that such surgery recommendations may not be extrapolated to TAVR-IE patients, and specific guidelines are warranted for this particular population.
Furthermore, the possibility of early surgery in those patients with factors increasing the risk for stroke should be evaluated in future studies.
The authors note that TAVR has revolutionized the treatment of aortic stenosis and is currently moving toward less complex and younger patients with lower surgical risk. Despite the relatively low incidence of IE after TAVR, the number of procedures is expected to grow exponentially, increasing the number of patients at risk of developing this life-threatening complication. Therefore, detailed knowledge of this disease and its complications is essential to improve outcomes.
They point out that the 10% rate of stroke found in this study is substantially lower, compared with the largest surgical prosthetic-valve infective endocarditis registries, but they suggest that the unique clinical profile of TAVR patients may lead to an underdiagnosis of stroke, with a high proportion of elderly patients who more frequently present with nonspecific symptoms.
They conclude that “IE post-TAVR is associated with a poor prognosis with high in-hospital and late mortality rates. Our study reveals that patients with IE after TAVR complicated by stroke showed an even worse prognosis.”
“The progressive implementation of advanced imaging modalities for early IE diagnosis, especially nuclear imaging, may translate into a better prognosis in coming years. Close attention should be paid to early recognition of stroke-associated factors to improve clinical outcomes,” they add.
In an accompanying editorial, Vuyisile Nkomo, MD, Daniel DeSimone, MD, and William Miranda, MD, Mayo Clinic, Rochester, Minn., say the current study “highlights the devastating consequences of IE after TAVR and the even worse consequences when IE was associated with stroke.”
This points to the critical importance of efforts to prevent IE with appropriate antibiotic prophylaxis and addressing potential sources of infection (for example, dental screening) before invasive cardiac procedures.
“Patient education is critical in regard to recognizing early signs and symptoms of IE. In particular, patients must be informed to obtain blood cultures with any episode of fever, as identification of bacteremia is critical in the diagnosis of IE,” the editorialists comment.
Endocarditis should also be suspected in afebrile patients with increasing transcatheter heart valve gradients or new or worsening regurgitation, they state.
Multimodality imaging is important for the early diagnosis of IE to facilitate prompt antibiotic treatment and potentially decrease the risk for IE complications, especially systemic embolization, they add.
“Despite the unequivocal advances in the safety and periprocedural complications of TAVR, IE with and without stroke in this TAVR population remains a dreadful complication,” they conclude.
Dr. Del Val was supported by a research grant from the Fundación Alfonso Martin Escudero. The editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
VARC-3 sets goalpost for future aortic valve trials
The newly updated Valve Academic Research Consortium 3 (VARC-3) definitions and endpoints proposed for transcatheter and surgical aortic valve replacement (TAVR/SAVR) research aim to add more granularity and a patient focus to a rapidly evolving field, the authors say.
Work began in 2016 to update definitions in the document to be more contemporary, as TAVR matured over the last 10 years to include younger, lower-risk patients and began moving to long-term outcomes, lead author Philippe Généreux, MD, said in an interview.
“The main change in VARC-3 is really that we tried to define not only procedural outcome, both for TAVR and aortic valve replacement performed by surgery, but also more the long-term outcomes mainly based on the patient – so quality of life, bioprosthetic valve failure, how do we define a valve failure, and also the need for rehospitalization,” he said.
However, soon after the VARC-3 document was published on April 19, 2021, in the European Heart Journal and Journal of the American College of Cardiology, surgeons took to social media to highlight the writing committee’s financial ties to industry and to suggest some definitions were shaped to favor transcatheter approaches.
“There’s no doubt that the coauthors who participated in these guidelines are experts; nobody would argue about that but what we can argue, and I’m 100% sure about, is that we have experts outside the payroll of industry who are excellent and can be part of this guideline drafting in an unbiased way,” Victor Dayan, MD, adjunct professor of cardiac surgery, National Institute of Cardiac Surgery, Montevideo, Uruguay, said in an interview.
Although the American College of Physicians recommends guideline committee members with moderate- or high-level conflicts of interest recuse themselves from authorship, he noted that one author has received more than $2 million in fees from industry in the past 4-5 years.
In all, 20 of 23 authors were involved in PARTNER, SURTAVI, and PORTICO, and several also write clinical guidelines for the American College of Cardiology and American Heart Association. “So we have the same authors that are judge, jury, and attorney for these issues,” Dr. Dayan said.
In a comment, J. Rafael Sádaba, MD, PhD, interim secretary general for the European Association for Cardio-Thoracic Surgery, pointed out that only three committee members are surgeons and that author disclosures took up nearly a full page of the document. “Surely they would be able to find very capable physicians with far less conflicts of interest.”
Dr. Sádaba said the question to him is why professional societies like ACC and AHA don’t define the endpoints for the clinical trials that will inform their guidelines.
“One could say these people are there because they’re good scientists, trialists, but one at least has to ask why is this happening. Why are these people setting the rules for the trials they’re running?” said Dr. Sádaba, of the Royal Navarre Hospital, Pamplona, Spain.
Dr. Généreux dismissed the Twitter comments as coming from a handful of people who engage in conspiracy theories. The VARC-3 document, he said, was created with input from 75 experts, including Food and Drug Administration officials, and the final document was reviewed by the FDA and underwent rigorous peer review prior to publication.
“The question is: do you believe there is bias when people are involved in studies driven by the industry? Well, this is where we derive our science in this field,” he said. “We are very transparent and disclose our conflicts of interest [COI].”
Commenting further, Dr. Généreux added, “this was a very well-balanced group and to imply that because we work with industry, we don’t have the best interest of the patient in mind is wrong.”
Editor in chief of the EHJ, Filippo Crea, MD, PhD, Catholic University, Rome, said in an comment that “it is not surprising that most of the authors have experience in TAVR trials. All of the authors have carefully disclosed their COIs.”
He noted that the EHJ and JACC copublished the first VARC consensus in 2011, VARC-2 1 year later, and that VARC-3 was reviewed by four external reviewers and two editors and was accepted for publication after two revisions.
Asked about a shot on social media that the EHJ had long ago “sold its soul” to be the scientific “arm” of industry, Dr. Crea said allegations need to be substantiated by facts.
“The wide adoption of VARC definitions implies that they have been well accepted by the scientific community and that they have stood the test of time,” Dr. Crea said. “EHJ has a history of publishing high-quality science. We welcome robust arguments that may challenge previously published work. Readers who perceive gaps are encouraged to provide a detailed challenge and engage with the journal.”
Defining hospitalizations
One of the surgeons’ biggest concerns is that VARC-3 now defines hospitalization or rehospitalization as “any admission after the index hospitalization or study enrollment” for at least 24 hours, including an ED stay.
VARC-2 and SURTAVI defined hospitalizations as those for valve-related symptoms or worsening heart failure, whereas the newly reformulated definition of hospitalization was part of the main composite endpoint in the PARTNER-3 trial, along with stroke and mortality, that drove the superiority of TAVR over SAVR at 1 year for low-risk patients, Dr. Dayan noted.
“It’s not uncommon for patients who have cardiac surgery to come back for issues related to wound healing or mild pulmonary edema for a day or 2, and if you include these hospitalizations in the primary endpoint, it will dilute the real benefit of SAVR versus TAVR, which is mortality and stroke,” he added.
In choosing the broader definition, Dr. Généreux said they borrowed from heart failure studies that take a granular approach and account for every hospitalization, be it for a medication change or adjustment. “We cannot pick and choose which hospitalization we are going to consider or ignore.”
VARC-3 proposes criteria for identifying and diagnosing hypoattenuated leaflet thickening (HALT) and reduced leaflet motion and features a detailed chart of the new classification scheme for bioprosthetic valve dysfunction and failure.
Bioprosthetic valve dysfunction includes structural valve deterioration, nonstructural valve dysfunction (including abnormalities not intrinsic to the valve such as paravalvular regurgitation or prosthesis-patient mismatch), thrombosis, and endocarditis. VARC-3 proposes a five-class grading system for paravalvular regurgitation (mild, mild-moderate, moderate, moderate-severe, severe).
The document updates what the authors called a “previously vague definition” of valve thrombosis proposed in 2011 to now include “clinically significant” prosthetic valve thrombosis. This requires clinical sequelae of a thromboembolic event (stroke, transient ischemic attack, retinal occlusion, or other evidence of thromboembolism) or worsening valve stenosis/regurgitation and either hemodynamic valve deterioration stage 2 or 3 or confirmatory imaging (CT evidence of HALT or transesophageal echocardiographic findings). In the absence of symptoms/clinical sequelae, valve thrombosis (subclinical) can be diagnosed if there is hemodynamic valve deterioration stage 3 and confirmatory imaging.
Bioprosthetic valve failure is divided into three stages, with stage 1 taking into account clinical factors along with valve dysfunction, stage 2 being reintervention, and stage 3 being valve-related death.
“For us, bioprosthesis valve failure is not only the need for reintervention, but it’s also mortality, it’s also a significant increase in gradient or the occurrence of paravalvular leak,” said Dr. Généreux, of the Morristown (N.J.) Medical Center. “So it’s much more clinical.”
Stroke, myocardial infarction
VARC-3 provides detailed definitions of neurologic events and, in an attempt to harmonize with the Neurologic Academic Research Consortium, recommends combining assessment of neurologic symptoms with tissue-based criteria (pathology or neuroimaging, ideally diffusion-weighted MRI) to define stroke and other central nervous system injury.
It also recommends that assessment be performed 30-90 days after a neurologic event and that assessment of neurologic deficits for cerebral embolic protection trials be performed by a neurologist.
VARC-3 endorses the fourth Universal Definition of Myocardial Infarction for MI types 1-3, 4B, and 4C.
For periprocedural MI after percutaneous coronary intervention (PCI), coronary bypass graft surgery, TAVR, and SAVR, however, it endorses the modified Society for Cardiovascular Angiography and Interventions and Academic Research Consortium-2 definition, which uses troponin or creatine kinase-MB thresholds.
“Given that most current and future studies related to AVR strategies will involve long-term follow-up, with patients frequently suffering from coronary artery disease, VARC-3 believes that these definitions will allow the most appropriate characterization and classification of types of MI occurring in this population,” the committee wrote.
The decision comes after last year’s controversy surrounding the Abbott-sponsored EXCEL trial, which used a modified version of the SCAI definition for periprocedural MI as part of its primary composite endpoint of death, stroke, and MI.
Initial reports showed nearly twice the rate of periprocedural MI with cardiac surgery as with PCI, but after a BBC investigation involving leaked data and an onslaught of criticism from surgeons, later results using the third universal definition showed surgery had the advantage.
The debacle frayed relations between surgeons and interventionalists and prompted EACTS to withdraw its support for treatment recommendations for left main coronary artery disease.
Dr. Dayan applauded VARC-3 for incorporating more detailed information on stroke and neurologic events, but said the use of the SCAI definition in the final published document is in “total disregard” to the controversy generated among surgeons and interventionalists.
“The main concern for surgeons is defining periprocedural MI just by biochemical definitions, without any additional criteria like ECG, angiographic,” he said. “This is totally new and goes against what surgeons have been advocating for years around EXCEL.”
Dr. Sádaba was troubled by the definitions of MI and hospitalization, but also questioned other changes, like lumping vascular complications together with access-related complications. “The sense is a lot of what they’ve put here favors one type of intervention over the other.”
Dr. Généreux reported receiving consultant fees from Abbott Vascular, Abiomed, Boston Scientific, Cardinal Health, Cardiovascular System, Edwards Lifesciences, Medtronic, Opsens, Siemens, SoundBite Medical Solutions, Sig.Num, Saranas, Teleflex, Tryton Medical, and has equity in Pi-Cardia, Sig.Num, SoundBite Medical Solutions, Saranas, and Puzzle Medical. Dr. Crea reported receiving personal fees from Novartis, Bristol-Myers Squibb, Amgen, and AstraZeneca, and is a member of the advisory board of GlyCardial Diagnostics. Dr. Dayan and Dr. Sádaba reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
The newly updated Valve Academic Research Consortium 3 (VARC-3) definitions and endpoints proposed for transcatheter and surgical aortic valve replacement (TAVR/SAVR) research aim to add more granularity and a patient focus to a rapidly evolving field, the authors say.
Work began in 2016 to update definitions in the document to be more contemporary, as TAVR matured over the last 10 years to include younger, lower-risk patients and began moving to long-term outcomes, lead author Philippe Généreux, MD, said in an interview.
“The main change in VARC-3 is really that we tried to define not only procedural outcome, both for TAVR and aortic valve replacement performed by surgery, but also more the long-term outcomes mainly based on the patient – so quality of life, bioprosthetic valve failure, how do we define a valve failure, and also the need for rehospitalization,” he said.
However, soon after the VARC-3 document was published on April 19, 2021, in the European Heart Journal and Journal of the American College of Cardiology, surgeons took to social media to highlight the writing committee’s financial ties to industry and to suggest some definitions were shaped to favor transcatheter approaches.
“There’s no doubt that the coauthors who participated in these guidelines are experts; nobody would argue about that but what we can argue, and I’m 100% sure about, is that we have experts outside the payroll of industry who are excellent and can be part of this guideline drafting in an unbiased way,” Victor Dayan, MD, adjunct professor of cardiac surgery, National Institute of Cardiac Surgery, Montevideo, Uruguay, said in an interview.
Although the American College of Physicians recommends guideline committee members with moderate- or high-level conflicts of interest recuse themselves from authorship, he noted that one author has received more than $2 million in fees from industry in the past 4-5 years.
In all, 20 of 23 authors were involved in PARTNER, SURTAVI, and PORTICO, and several also write clinical guidelines for the American College of Cardiology and American Heart Association. “So we have the same authors that are judge, jury, and attorney for these issues,” Dr. Dayan said.
In a comment, J. Rafael Sádaba, MD, PhD, interim secretary general for the European Association for Cardio-Thoracic Surgery, pointed out that only three committee members are surgeons and that author disclosures took up nearly a full page of the document. “Surely they would be able to find very capable physicians with far less conflicts of interest.”
Dr. Sádaba said the question to him is why professional societies like ACC and AHA don’t define the endpoints for the clinical trials that will inform their guidelines.
“One could say these people are there because they’re good scientists, trialists, but one at least has to ask why is this happening. Why are these people setting the rules for the trials they’re running?” said Dr. Sádaba, of the Royal Navarre Hospital, Pamplona, Spain.
Dr. Généreux dismissed the Twitter comments as coming from a handful of people who engage in conspiracy theories. The VARC-3 document, he said, was created with input from 75 experts, including Food and Drug Administration officials, and the final document was reviewed by the FDA and underwent rigorous peer review prior to publication.
“The question is: do you believe there is bias when people are involved in studies driven by the industry? Well, this is where we derive our science in this field,” he said. “We are very transparent and disclose our conflicts of interest [COI].”
Commenting further, Dr. Généreux added, “this was a very well-balanced group and to imply that because we work with industry, we don’t have the best interest of the patient in mind is wrong.”
Editor in chief of the EHJ, Filippo Crea, MD, PhD, Catholic University, Rome, said in an comment that “it is not surprising that most of the authors have experience in TAVR trials. All of the authors have carefully disclosed their COIs.”
He noted that the EHJ and JACC copublished the first VARC consensus in 2011, VARC-2 1 year later, and that VARC-3 was reviewed by four external reviewers and two editors and was accepted for publication after two revisions.
Asked about a shot on social media that the EHJ had long ago “sold its soul” to be the scientific “arm” of industry, Dr. Crea said allegations need to be substantiated by facts.
“The wide adoption of VARC definitions implies that they have been well accepted by the scientific community and that they have stood the test of time,” Dr. Crea said. “EHJ has a history of publishing high-quality science. We welcome robust arguments that may challenge previously published work. Readers who perceive gaps are encouraged to provide a detailed challenge and engage with the journal.”
Defining hospitalizations
One of the surgeons’ biggest concerns is that VARC-3 now defines hospitalization or rehospitalization as “any admission after the index hospitalization or study enrollment” for at least 24 hours, including an ED stay.
VARC-2 and SURTAVI defined hospitalizations as those for valve-related symptoms or worsening heart failure, whereas the newly reformulated definition of hospitalization was part of the main composite endpoint in the PARTNER-3 trial, along with stroke and mortality, that drove the superiority of TAVR over SAVR at 1 year for low-risk patients, Dr. Dayan noted.
“It’s not uncommon for patients who have cardiac surgery to come back for issues related to wound healing or mild pulmonary edema for a day or 2, and if you include these hospitalizations in the primary endpoint, it will dilute the real benefit of SAVR versus TAVR, which is mortality and stroke,” he added.
In choosing the broader definition, Dr. Généreux said they borrowed from heart failure studies that take a granular approach and account for every hospitalization, be it for a medication change or adjustment. “We cannot pick and choose which hospitalization we are going to consider or ignore.”
VARC-3 proposes criteria for identifying and diagnosing hypoattenuated leaflet thickening (HALT) and reduced leaflet motion and features a detailed chart of the new classification scheme for bioprosthetic valve dysfunction and failure.
Bioprosthetic valve dysfunction includes structural valve deterioration, nonstructural valve dysfunction (including abnormalities not intrinsic to the valve such as paravalvular regurgitation or prosthesis-patient mismatch), thrombosis, and endocarditis. VARC-3 proposes a five-class grading system for paravalvular regurgitation (mild, mild-moderate, moderate, moderate-severe, severe).
The document updates what the authors called a “previously vague definition” of valve thrombosis proposed in 2011 to now include “clinically significant” prosthetic valve thrombosis. This requires clinical sequelae of a thromboembolic event (stroke, transient ischemic attack, retinal occlusion, or other evidence of thromboembolism) or worsening valve stenosis/regurgitation and either hemodynamic valve deterioration stage 2 or 3 or confirmatory imaging (CT evidence of HALT or transesophageal echocardiographic findings). In the absence of symptoms/clinical sequelae, valve thrombosis (subclinical) can be diagnosed if there is hemodynamic valve deterioration stage 3 and confirmatory imaging.
Bioprosthetic valve failure is divided into three stages, with stage 1 taking into account clinical factors along with valve dysfunction, stage 2 being reintervention, and stage 3 being valve-related death.
“For us, bioprosthesis valve failure is not only the need for reintervention, but it’s also mortality, it’s also a significant increase in gradient or the occurrence of paravalvular leak,” said Dr. Généreux, of the Morristown (N.J.) Medical Center. “So it’s much more clinical.”
Stroke, myocardial infarction
VARC-3 provides detailed definitions of neurologic events and, in an attempt to harmonize with the Neurologic Academic Research Consortium, recommends combining assessment of neurologic symptoms with tissue-based criteria (pathology or neuroimaging, ideally diffusion-weighted MRI) to define stroke and other central nervous system injury.
It also recommends that assessment be performed 30-90 days after a neurologic event and that assessment of neurologic deficits for cerebral embolic protection trials be performed by a neurologist.
VARC-3 endorses the fourth Universal Definition of Myocardial Infarction for MI types 1-3, 4B, and 4C.
For periprocedural MI after percutaneous coronary intervention (PCI), coronary bypass graft surgery, TAVR, and SAVR, however, it endorses the modified Society for Cardiovascular Angiography and Interventions and Academic Research Consortium-2 definition, which uses troponin or creatine kinase-MB thresholds.
“Given that most current and future studies related to AVR strategies will involve long-term follow-up, with patients frequently suffering from coronary artery disease, VARC-3 believes that these definitions will allow the most appropriate characterization and classification of types of MI occurring in this population,” the committee wrote.
The decision comes after last year’s controversy surrounding the Abbott-sponsored EXCEL trial, which used a modified version of the SCAI definition for periprocedural MI as part of its primary composite endpoint of death, stroke, and MI.
Initial reports showed nearly twice the rate of periprocedural MI with cardiac surgery as with PCI, but after a BBC investigation involving leaked data and an onslaught of criticism from surgeons, later results using the third universal definition showed surgery had the advantage.
The debacle frayed relations between surgeons and interventionalists and prompted EACTS to withdraw its support for treatment recommendations for left main coronary artery disease.
Dr. Dayan applauded VARC-3 for incorporating more detailed information on stroke and neurologic events, but said the use of the SCAI definition in the final published document is in “total disregard” to the controversy generated among surgeons and interventionalists.
“The main concern for surgeons is defining periprocedural MI just by biochemical definitions, without any additional criteria like ECG, angiographic,” he said. “This is totally new and goes against what surgeons have been advocating for years around EXCEL.”
Dr. Sádaba was troubled by the definitions of MI and hospitalization, but also questioned other changes, like lumping vascular complications together with access-related complications. “The sense is a lot of what they’ve put here favors one type of intervention over the other.”
Dr. Généreux reported receiving consultant fees from Abbott Vascular, Abiomed, Boston Scientific, Cardinal Health, Cardiovascular System, Edwards Lifesciences, Medtronic, Opsens, Siemens, SoundBite Medical Solutions, Sig.Num, Saranas, Teleflex, Tryton Medical, and has equity in Pi-Cardia, Sig.Num, SoundBite Medical Solutions, Saranas, and Puzzle Medical. Dr. Crea reported receiving personal fees from Novartis, Bristol-Myers Squibb, Amgen, and AstraZeneca, and is a member of the advisory board of GlyCardial Diagnostics. Dr. Dayan and Dr. Sádaba reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
The newly updated Valve Academic Research Consortium 3 (VARC-3) definitions and endpoints proposed for transcatheter and surgical aortic valve replacement (TAVR/SAVR) research aim to add more granularity and a patient focus to a rapidly evolving field, the authors say.
Work began in 2016 to update definitions in the document to be more contemporary, as TAVR matured over the last 10 years to include younger, lower-risk patients and began moving to long-term outcomes, lead author Philippe Généreux, MD, said in an interview.
“The main change in VARC-3 is really that we tried to define not only procedural outcome, both for TAVR and aortic valve replacement performed by surgery, but also more the long-term outcomes mainly based on the patient – so quality of life, bioprosthetic valve failure, how do we define a valve failure, and also the need for rehospitalization,” he said.
However, soon after the VARC-3 document was published on April 19, 2021, in the European Heart Journal and Journal of the American College of Cardiology, surgeons took to social media to highlight the writing committee’s financial ties to industry and to suggest some definitions were shaped to favor transcatheter approaches.
“There’s no doubt that the coauthors who participated in these guidelines are experts; nobody would argue about that but what we can argue, and I’m 100% sure about, is that we have experts outside the payroll of industry who are excellent and can be part of this guideline drafting in an unbiased way,” Victor Dayan, MD, adjunct professor of cardiac surgery, National Institute of Cardiac Surgery, Montevideo, Uruguay, said in an interview.
Although the American College of Physicians recommends guideline committee members with moderate- or high-level conflicts of interest recuse themselves from authorship, he noted that one author has received more than $2 million in fees from industry in the past 4-5 years.
In all, 20 of 23 authors were involved in PARTNER, SURTAVI, and PORTICO, and several also write clinical guidelines for the American College of Cardiology and American Heart Association. “So we have the same authors that are judge, jury, and attorney for these issues,” Dr. Dayan said.
In a comment, J. Rafael Sádaba, MD, PhD, interim secretary general for the European Association for Cardio-Thoracic Surgery, pointed out that only three committee members are surgeons and that author disclosures took up nearly a full page of the document. “Surely they would be able to find very capable physicians with far less conflicts of interest.”
Dr. Sádaba said the question to him is why professional societies like ACC and AHA don’t define the endpoints for the clinical trials that will inform their guidelines.
“One could say these people are there because they’re good scientists, trialists, but one at least has to ask why is this happening. Why are these people setting the rules for the trials they’re running?” said Dr. Sádaba, of the Royal Navarre Hospital, Pamplona, Spain.
Dr. Généreux dismissed the Twitter comments as coming from a handful of people who engage in conspiracy theories. The VARC-3 document, he said, was created with input from 75 experts, including Food and Drug Administration officials, and the final document was reviewed by the FDA and underwent rigorous peer review prior to publication.
“The question is: do you believe there is bias when people are involved in studies driven by the industry? Well, this is where we derive our science in this field,” he said. “We are very transparent and disclose our conflicts of interest [COI].”
Commenting further, Dr. Généreux added, “this was a very well-balanced group and to imply that because we work with industry, we don’t have the best interest of the patient in mind is wrong.”
Editor in chief of the EHJ, Filippo Crea, MD, PhD, Catholic University, Rome, said in an comment that “it is not surprising that most of the authors have experience in TAVR trials. All of the authors have carefully disclosed their COIs.”
He noted that the EHJ and JACC copublished the first VARC consensus in 2011, VARC-2 1 year later, and that VARC-3 was reviewed by four external reviewers and two editors and was accepted for publication after two revisions.
Asked about a shot on social media that the EHJ had long ago “sold its soul” to be the scientific “arm” of industry, Dr. Crea said allegations need to be substantiated by facts.
“The wide adoption of VARC definitions implies that they have been well accepted by the scientific community and that they have stood the test of time,” Dr. Crea said. “EHJ has a history of publishing high-quality science. We welcome robust arguments that may challenge previously published work. Readers who perceive gaps are encouraged to provide a detailed challenge and engage with the journal.”
Defining hospitalizations
One of the surgeons’ biggest concerns is that VARC-3 now defines hospitalization or rehospitalization as “any admission after the index hospitalization or study enrollment” for at least 24 hours, including an ED stay.
VARC-2 and SURTAVI defined hospitalizations as those for valve-related symptoms or worsening heart failure, whereas the newly reformulated definition of hospitalization was part of the main composite endpoint in the PARTNER-3 trial, along with stroke and mortality, that drove the superiority of TAVR over SAVR at 1 year for low-risk patients, Dr. Dayan noted.
“It’s not uncommon for patients who have cardiac surgery to come back for issues related to wound healing or mild pulmonary edema for a day or 2, and if you include these hospitalizations in the primary endpoint, it will dilute the real benefit of SAVR versus TAVR, which is mortality and stroke,” he added.
In choosing the broader definition, Dr. Généreux said they borrowed from heart failure studies that take a granular approach and account for every hospitalization, be it for a medication change or adjustment. “We cannot pick and choose which hospitalization we are going to consider or ignore.”
VARC-3 proposes criteria for identifying and diagnosing hypoattenuated leaflet thickening (HALT) and reduced leaflet motion and features a detailed chart of the new classification scheme for bioprosthetic valve dysfunction and failure.
Bioprosthetic valve dysfunction includes structural valve deterioration, nonstructural valve dysfunction (including abnormalities not intrinsic to the valve such as paravalvular regurgitation or prosthesis-patient mismatch), thrombosis, and endocarditis. VARC-3 proposes a five-class grading system for paravalvular regurgitation (mild, mild-moderate, moderate, moderate-severe, severe).
The document updates what the authors called a “previously vague definition” of valve thrombosis proposed in 2011 to now include “clinically significant” prosthetic valve thrombosis. This requires clinical sequelae of a thromboembolic event (stroke, transient ischemic attack, retinal occlusion, or other evidence of thromboembolism) or worsening valve stenosis/regurgitation and either hemodynamic valve deterioration stage 2 or 3 or confirmatory imaging (CT evidence of HALT or transesophageal echocardiographic findings). In the absence of symptoms/clinical sequelae, valve thrombosis (subclinical) can be diagnosed if there is hemodynamic valve deterioration stage 3 and confirmatory imaging.
Bioprosthetic valve failure is divided into three stages, with stage 1 taking into account clinical factors along with valve dysfunction, stage 2 being reintervention, and stage 3 being valve-related death.
“For us, bioprosthesis valve failure is not only the need for reintervention, but it’s also mortality, it’s also a significant increase in gradient or the occurrence of paravalvular leak,” said Dr. Généreux, of the Morristown (N.J.) Medical Center. “So it’s much more clinical.”
Stroke, myocardial infarction
VARC-3 provides detailed definitions of neurologic events and, in an attempt to harmonize with the Neurologic Academic Research Consortium, recommends combining assessment of neurologic symptoms with tissue-based criteria (pathology or neuroimaging, ideally diffusion-weighted MRI) to define stroke and other central nervous system injury.
It also recommends that assessment be performed 30-90 days after a neurologic event and that assessment of neurologic deficits for cerebral embolic protection trials be performed by a neurologist.
VARC-3 endorses the fourth Universal Definition of Myocardial Infarction for MI types 1-3, 4B, and 4C.
For periprocedural MI after percutaneous coronary intervention (PCI), coronary bypass graft surgery, TAVR, and SAVR, however, it endorses the modified Society for Cardiovascular Angiography and Interventions and Academic Research Consortium-2 definition, which uses troponin or creatine kinase-MB thresholds.
“Given that most current and future studies related to AVR strategies will involve long-term follow-up, with patients frequently suffering from coronary artery disease, VARC-3 believes that these definitions will allow the most appropriate characterization and classification of types of MI occurring in this population,” the committee wrote.
The decision comes after last year’s controversy surrounding the Abbott-sponsored EXCEL trial, which used a modified version of the SCAI definition for periprocedural MI as part of its primary composite endpoint of death, stroke, and MI.
Initial reports showed nearly twice the rate of periprocedural MI with cardiac surgery as with PCI, but after a BBC investigation involving leaked data and an onslaught of criticism from surgeons, later results using the third universal definition showed surgery had the advantage.
The debacle frayed relations between surgeons and interventionalists and prompted EACTS to withdraw its support for treatment recommendations for left main coronary artery disease.
Dr. Dayan applauded VARC-3 for incorporating more detailed information on stroke and neurologic events, but said the use of the SCAI definition in the final published document is in “total disregard” to the controversy generated among surgeons and interventionalists.
“The main concern for surgeons is defining periprocedural MI just by biochemical definitions, without any additional criteria like ECG, angiographic,” he said. “This is totally new and goes against what surgeons have been advocating for years around EXCEL.”
Dr. Sádaba was troubled by the definitions of MI and hospitalization, but also questioned other changes, like lumping vascular complications together with access-related complications. “The sense is a lot of what they’ve put here favors one type of intervention over the other.”
Dr. Généreux reported receiving consultant fees from Abbott Vascular, Abiomed, Boston Scientific, Cardinal Health, Cardiovascular System, Edwards Lifesciences, Medtronic, Opsens, Siemens, SoundBite Medical Solutions, Sig.Num, Saranas, Teleflex, Tryton Medical, and has equity in Pi-Cardia, Sig.Num, SoundBite Medical Solutions, Saranas, and Puzzle Medical. Dr. Crea reported receiving personal fees from Novartis, Bristol-Myers Squibb, Amgen, and AstraZeneca, and is a member of the advisory board of GlyCardial Diagnostics. Dr. Dayan and Dr. Sádaba reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.