User login
Critical illness-related corticosteroid insufficiency guidelines explained
SAN ANTONIO – When corticosteroids are used for septic shock, the dose should be low to moderate, the timing should be early, and the duration should be at least 3 days, said a speaker at the Critical Care Congress sponsored by the Society for Critical Care.
Dosing, timing, and duration are “three critical questions” critical care specialists face that are answered by the new critical illness–related corticosteroid insufficiency (CIRCI) guidelines, continued Stephen M. Pastores, MD, a cochair of the task force that developed guidelines for the diagnosis and management of CIRCI in critically ill patients.
During his presentation, Dr. Pastores limited his remarks to discussion of sepsis and septic shock with corticosteroids. He cautioned that, despite careful deliberations by the panel, the level of evidence behind some of the recommendations was “low to moderate and never high” and that not all task force members agreed with all recommendations.
“There were a lot of back and forth disagreements behind these recommendations,” said Dr. Pastores, who is the director of the critical care medicine fellowship training and research programs at Memorial Sloan Kettering Cancer Center, New York. “We only required 80% of the panelists to agree that these were the recommendations and statements that we were going to go by.”
The guidelines recommend against the use of corticosteroids in adult patients who have sepsis without shock, Dr. Pastores noted.
In contrast,
In an analysis of available data from randomized clinical trials including patients with septic shock, corticosteroids significantly reduced 28-day mortality when compared with placebo, Dr. Pastores said.
That survival benefit seems to be dependent on several factors: dose of the corticosteroids (hydrocortisone less than 400 mg/day), longer duration (at least 3 or more days), and severity of sepsis. “The more severe the sepsis, the more septic shock the patient was in, the more likely the corticosteroids were likely to help those patients,” Dr. Pastores explained.
Accordingly, the guidelines further suggest using long-course, low-dose corticosteroid treatment, namely intravenous hydrocortisone at no more than 400 mg/day for at least 3 days.
The expert panel specifically recommended hydrocortisone as the corticosteroid of choice in this setting, according to Dr. Pastores. That recommendation was based in part on a recent systematic review and meta-analysis showing that hydrocortisone, given as a bolus or an infusion, was more likely than placebo or methylprednisolone to result in shock reversal.
Dr. Pastores reported disclosures related to Theravance Biopharma, Bayer HealthCare Pharmaceuticals, Spectral Diagnostics, and Asahi-Kasei.
SAN ANTONIO – When corticosteroids are used for septic shock, the dose should be low to moderate, the timing should be early, and the duration should be at least 3 days, said a speaker at the Critical Care Congress sponsored by the Society for Critical Care.
Dosing, timing, and duration are “three critical questions” critical care specialists face that are answered by the new critical illness–related corticosteroid insufficiency (CIRCI) guidelines, continued Stephen M. Pastores, MD, a cochair of the task force that developed guidelines for the diagnosis and management of CIRCI in critically ill patients.
During his presentation, Dr. Pastores limited his remarks to discussion of sepsis and septic shock with corticosteroids. He cautioned that, despite careful deliberations by the panel, the level of evidence behind some of the recommendations was “low to moderate and never high” and that not all task force members agreed with all recommendations.
“There were a lot of back and forth disagreements behind these recommendations,” said Dr. Pastores, who is the director of the critical care medicine fellowship training and research programs at Memorial Sloan Kettering Cancer Center, New York. “We only required 80% of the panelists to agree that these were the recommendations and statements that we were going to go by.”
The guidelines recommend against the use of corticosteroids in adult patients who have sepsis without shock, Dr. Pastores noted.
In contrast,
In an analysis of available data from randomized clinical trials including patients with septic shock, corticosteroids significantly reduced 28-day mortality when compared with placebo, Dr. Pastores said.
That survival benefit seems to be dependent on several factors: dose of the corticosteroids (hydrocortisone less than 400 mg/day), longer duration (at least 3 or more days), and severity of sepsis. “The more severe the sepsis, the more septic shock the patient was in, the more likely the corticosteroids were likely to help those patients,” Dr. Pastores explained.
Accordingly, the guidelines further suggest using long-course, low-dose corticosteroid treatment, namely intravenous hydrocortisone at no more than 400 mg/day for at least 3 days.
The expert panel specifically recommended hydrocortisone as the corticosteroid of choice in this setting, according to Dr. Pastores. That recommendation was based in part on a recent systematic review and meta-analysis showing that hydrocortisone, given as a bolus or an infusion, was more likely than placebo or methylprednisolone to result in shock reversal.
Dr. Pastores reported disclosures related to Theravance Biopharma, Bayer HealthCare Pharmaceuticals, Spectral Diagnostics, and Asahi-Kasei.
SAN ANTONIO – When corticosteroids are used for septic shock, the dose should be low to moderate, the timing should be early, and the duration should be at least 3 days, said a speaker at the Critical Care Congress sponsored by the Society for Critical Care.
Dosing, timing, and duration are “three critical questions” critical care specialists face that are answered by the new critical illness–related corticosteroid insufficiency (CIRCI) guidelines, continued Stephen M. Pastores, MD, a cochair of the task force that developed guidelines for the diagnosis and management of CIRCI in critically ill patients.
During his presentation, Dr. Pastores limited his remarks to discussion of sepsis and septic shock with corticosteroids. He cautioned that, despite careful deliberations by the panel, the level of evidence behind some of the recommendations was “low to moderate and never high” and that not all task force members agreed with all recommendations.
“There were a lot of back and forth disagreements behind these recommendations,” said Dr. Pastores, who is the director of the critical care medicine fellowship training and research programs at Memorial Sloan Kettering Cancer Center, New York. “We only required 80% of the panelists to agree that these were the recommendations and statements that we were going to go by.”
The guidelines recommend against the use of corticosteroids in adult patients who have sepsis without shock, Dr. Pastores noted.
In contrast,
In an analysis of available data from randomized clinical trials including patients with septic shock, corticosteroids significantly reduced 28-day mortality when compared with placebo, Dr. Pastores said.
That survival benefit seems to be dependent on several factors: dose of the corticosteroids (hydrocortisone less than 400 mg/day), longer duration (at least 3 or more days), and severity of sepsis. “The more severe the sepsis, the more septic shock the patient was in, the more likely the corticosteroids were likely to help those patients,” Dr. Pastores explained.
Accordingly, the guidelines further suggest using long-course, low-dose corticosteroid treatment, namely intravenous hydrocortisone at no more than 400 mg/day for at least 3 days.
The expert panel specifically recommended hydrocortisone as the corticosteroid of choice in this setting, according to Dr. Pastores. That recommendation was based in part on a recent systematic review and meta-analysis showing that hydrocortisone, given as a bolus or an infusion, was more likely than placebo or methylprednisolone to result in shock reversal.
Dr. Pastores reported disclosures related to Theravance Biopharma, Bayer HealthCare Pharmaceuticals, Spectral Diagnostics, and Asahi-Kasei.
EXPERT ANALYSIS FROM THE CCC47
Prehospital antibiotics improved some aspects of sepsis care
SAN ANTONIO – according to results of a randomized trial.
Emergency medical service (EMS) personnel were able to recognize sepsis more quickly, obtain blood cultures, and give antibiotics after the training, reported investigator Prabath Nanayakkara, MD, PhD, FRCP, at the Society of Critical Care Medicine’s Critical Care Congress.
At 28 days, 120 patients (8%) in the prehospital antibiotics group had died, compared with 93 patients (8%) in the usual care group (relative risk, 0.95; 95% confidence interval, 0.74-1.24), according to the study’s results that were simultaneously published online in Lancet Respiratory Medicine.
The intervention group received antibiotics a median of 26 minutes prior to emergency department (ED) arrival. In the usual care group, median time to antibiotics after ED arrival was 70 minutes, versus 93 minutes prior to the sepsis recognition training (P = .142), the report further says.
“We do not advise prehospital antibiotics at the moment for patients with suspected sepsis,” Dr. Nanayakkara said, during his presentation at the conference.
Other countries might see different results, he cautioned.
In the Netherlands, ambulances reach the emergency scene within 15 minutes 93% of the time, and the average time from dispatch call to ED arrival is 40 minutes, Dr. Nanayakkara noted in the report.
“In part, due to the relatively short response times in the Netherlands, we don’t know if there are other countries with longer response times that would have other results, and whether they should use antibiotics in their ambulances,” Dr. Nanayakkara said in his presentation.
The study was the first-ever prospective randomized, controlled open-label trial to compare early prehospital antibiotics with standard care.
Before the study was started, EMS personnel at 10 large regional ambulance services serving 34 secondary or tertiary hospitals were trained in recognizing sepsis, the report says.
A total of 2,672 patients with suspected sepsis were included in the intention-to-treat analysis, of whom 1,535 were randomized to receive prehospital antibiotics and 1,137 to usual EMS care, which consisted of fluid resuscitation and supplementary oxygen.
The primary end point of the study was all-cause mortality at 28 days.
The negative mortality results of this trial are “not surprising,” given that the trial’s inclusion criteria allowed individuals with suspected infection but without organ dysfunction, said Jean-Louis Vincent, MD, PhD, of Erasmus Hospital, Brussels, in a related editorial appearing in the Lancet Respiratory Medicine (2018 Jan. doi: 10.1016/S2213-2600[17]30446-0).
Recent consensus definitions of sepsis recognize that sepsis is the association of an infection with some degree of organ dysfunction, according to Dr. Vincent.
“After this initial experience, I believe that a randomized, controlled trial could be done to assess the potential benefit of early antibiotic administration in the ambulance for patients with organ dysfunction associated with infection,” Dr. Vincent wrote in his editorial.
Dr. Nanayakkara and his coauthors declared no competing interests related to their study.
SOURCE: Alam N et al. Lancet Respir Med. 2018 Jan;6(1):40-50.
SAN ANTONIO – according to results of a randomized trial.
Emergency medical service (EMS) personnel were able to recognize sepsis more quickly, obtain blood cultures, and give antibiotics after the training, reported investigator Prabath Nanayakkara, MD, PhD, FRCP, at the Society of Critical Care Medicine’s Critical Care Congress.
At 28 days, 120 patients (8%) in the prehospital antibiotics group had died, compared with 93 patients (8%) in the usual care group (relative risk, 0.95; 95% confidence interval, 0.74-1.24), according to the study’s results that were simultaneously published online in Lancet Respiratory Medicine.
The intervention group received antibiotics a median of 26 minutes prior to emergency department (ED) arrival. In the usual care group, median time to antibiotics after ED arrival was 70 minutes, versus 93 minutes prior to the sepsis recognition training (P = .142), the report further says.
“We do not advise prehospital antibiotics at the moment for patients with suspected sepsis,” Dr. Nanayakkara said, during his presentation at the conference.
Other countries might see different results, he cautioned.
In the Netherlands, ambulances reach the emergency scene within 15 minutes 93% of the time, and the average time from dispatch call to ED arrival is 40 minutes, Dr. Nanayakkara noted in the report.
“In part, due to the relatively short response times in the Netherlands, we don’t know if there are other countries with longer response times that would have other results, and whether they should use antibiotics in their ambulances,” Dr. Nanayakkara said in his presentation.
The study was the first-ever prospective randomized, controlled open-label trial to compare early prehospital antibiotics with standard care.
Before the study was started, EMS personnel at 10 large regional ambulance services serving 34 secondary or tertiary hospitals were trained in recognizing sepsis, the report says.
A total of 2,672 patients with suspected sepsis were included in the intention-to-treat analysis, of whom 1,535 were randomized to receive prehospital antibiotics and 1,137 to usual EMS care, which consisted of fluid resuscitation and supplementary oxygen.
The primary end point of the study was all-cause mortality at 28 days.
The negative mortality results of this trial are “not surprising,” given that the trial’s inclusion criteria allowed individuals with suspected infection but without organ dysfunction, said Jean-Louis Vincent, MD, PhD, of Erasmus Hospital, Brussels, in a related editorial appearing in the Lancet Respiratory Medicine (2018 Jan. doi: 10.1016/S2213-2600[17]30446-0).
Recent consensus definitions of sepsis recognize that sepsis is the association of an infection with some degree of organ dysfunction, according to Dr. Vincent.
“After this initial experience, I believe that a randomized, controlled trial could be done to assess the potential benefit of early antibiotic administration in the ambulance for patients with organ dysfunction associated with infection,” Dr. Vincent wrote in his editorial.
Dr. Nanayakkara and his coauthors declared no competing interests related to their study.
SOURCE: Alam N et al. Lancet Respir Med. 2018 Jan;6(1):40-50.
SAN ANTONIO – according to results of a randomized trial.
Emergency medical service (EMS) personnel were able to recognize sepsis more quickly, obtain blood cultures, and give antibiotics after the training, reported investigator Prabath Nanayakkara, MD, PhD, FRCP, at the Society of Critical Care Medicine’s Critical Care Congress.
At 28 days, 120 patients (8%) in the prehospital antibiotics group had died, compared with 93 patients (8%) in the usual care group (relative risk, 0.95; 95% confidence interval, 0.74-1.24), according to the study’s results that were simultaneously published online in Lancet Respiratory Medicine.
The intervention group received antibiotics a median of 26 minutes prior to emergency department (ED) arrival. In the usual care group, median time to antibiotics after ED arrival was 70 minutes, versus 93 minutes prior to the sepsis recognition training (P = .142), the report further says.
“We do not advise prehospital antibiotics at the moment for patients with suspected sepsis,” Dr. Nanayakkara said, during his presentation at the conference.
Other countries might see different results, he cautioned.
In the Netherlands, ambulances reach the emergency scene within 15 minutes 93% of the time, and the average time from dispatch call to ED arrival is 40 minutes, Dr. Nanayakkara noted in the report.
“In part, due to the relatively short response times in the Netherlands, we don’t know if there are other countries with longer response times that would have other results, and whether they should use antibiotics in their ambulances,” Dr. Nanayakkara said in his presentation.
The study was the first-ever prospective randomized, controlled open-label trial to compare early prehospital antibiotics with standard care.
Before the study was started, EMS personnel at 10 large regional ambulance services serving 34 secondary or tertiary hospitals were trained in recognizing sepsis, the report says.
A total of 2,672 patients with suspected sepsis were included in the intention-to-treat analysis, of whom 1,535 were randomized to receive prehospital antibiotics and 1,137 to usual EMS care, which consisted of fluid resuscitation and supplementary oxygen.
The primary end point of the study was all-cause mortality at 28 days.
The negative mortality results of this trial are “not surprising,” given that the trial’s inclusion criteria allowed individuals with suspected infection but without organ dysfunction, said Jean-Louis Vincent, MD, PhD, of Erasmus Hospital, Brussels, in a related editorial appearing in the Lancet Respiratory Medicine (2018 Jan. doi: 10.1016/S2213-2600[17]30446-0).
Recent consensus definitions of sepsis recognize that sepsis is the association of an infection with some degree of organ dysfunction, according to Dr. Vincent.
“After this initial experience, I believe that a randomized, controlled trial could be done to assess the potential benefit of early antibiotic administration in the ambulance for patients with organ dysfunction associated with infection,” Dr. Vincent wrote in his editorial.
Dr. Nanayakkara and his coauthors declared no competing interests related to their study.
SOURCE: Alam N et al. Lancet Respir Med. 2018 Jan;6(1):40-50.
REPORTING FROM CCC47
Key clinical point: In patients with suspected sepsis, prehospital antibiotics delivered by EMS personnel improved some aspects of care, but did not reduce mortality.
Major finding: At 28 days, 120 patients (8%) in the prehospital antibiotics group had died, compared with 93 patients (8%) in the usual care group (relative risk, 0.95; 95% CI, 0.74-1.24).
Data source: Intention-to-treat analysis of 2,672 patients in a prospective randomized, controlled open-label trial comparing early prehospital antibiotics to standard care.
Disclosures: The study authors declared no competing interests related to the study.
Source: Alam N et al. Lancet Respir Med. 2018 Jan;6(1):40-50.
Hydrocortisone-fludrocortisone cuts deaths in septic shock
Hydrocortisone in combination with fludrocortisone significantly reduced 90-day mortality in septic shock patients in a double-blind, randomized, controlled trial.
Prior to this study, two large trials had displayed that corticosteroids were beneficial in improving hemodynamic status and organ function, but little was known about corticosteroids’ ability to increase survival in sepsis patients.
The study, named the Activated Protein C and Corticosteroids for Human Septic Shock (APROCCHSS) trial, was designed to assess the benefit/risk ratio of using activated protein C – drotrecogin alfa (activated) – and corticosteroids together or separately in septic shock patients. The original design of the study included Xigris (drotrecogin alfa) and was composed of four parallel groups, but Xigris was removed from the market in October of 2011, so the study continued with only two parallel groups.
A total of 1,241 patients experiencing chronic septic shock were recruited into the two double-blind, parallel groups, with patients in one group receiving hydrocortisone plus fludrocortisone and the other receiving placebos. The placebos used in this study were similar in appearance to the actual treatment drugs. The placebos for hydrocortisone and fludrocortisone were either parenteral mannitol (133.6 mg), disodium phosphate (8.73 mg), and sodium phosphate (0.92 mg) or tablets of microcrystalline cellulose (59.098 mg), respectively.
Hydrocortisone was given intravenously every 6 hours as a 50-mg intravenous bolus, and fludrocortisone was given once a day as a 50-mcg tablet through a nasogastric tube. Patients in ICUs who had septic shock for less than 24 hours were included in the study. Septic shock was identified by the presence of a clinically or microbiologically documented infection, a Sequential Organ Failure Assessment score of 3 or 4 for at least two organs and for at least 6 hours, and receipt of vasopressor therapy for at least 6 hours.
After 90 days, 264 of 614 of the patients (43%) in the hydrocortisone/fludrocortisone group and almost half (49.1%) of 627 patients in the placebo group had died (P = .03). The relative risk of death was 0.88 (95% confidence interval, 0.78-0.99), which favored the hydrocortisone/fludrocortisone group. The researchers also observed that death was significantly lower in the hydrocortisone/fludrocortisone group, compared with the placebo group, at time of ICU discharge (35.4% vs. 41.0%, respectively; P = .04).
While mortality was reduced, patients still experienced adverse events. 326 of 614 (53.1%) patients in the hydrocortisone/fludrocortisone group and 363 of 626 patients (58.0%) in the placebo group experienced at least one serious adverse event by day 180 (P = 0.08).
“Seven-day treatment with a 50-mg intravenous bolus of hydrocortisone every 6 hours and a daily dose of 50 mcg of oral fludrocortisone resulted in lower mortality at day 90 and at ICU and hospital discharge than placebo among adults with septic shock,” concluded Dr. Annane and his coauthors.
The majority of researchers had no relevant financial disclosures to report, while some doctors received grants and personal fees unrelated to this study. This study was funded in part by public grants from the French Ministry of Health.
SOURCE: Annana A et al. NEJM. 2018 Feb 28. doi: 10.1056/NEJMoa1705716.
The results of the Activated Protein C and Corticosteroids for Human Septic Shock (APROCCHSS) trial and the Adjunctive Corticosteroid Treatment in Critically Ill Patients with Septic Shock (ADRENAL), both reported in the latest issue of NEJM, are landmark studies detailing the largest analyses of hydrocortisone use in patients with septic shock.
Both of these trials were massive, with over 5,000 patients combined, which is much larger than all previous studies according to Anthony Suffredini, MD, of the National Institutes of Health. An additional useful feature of these trials was that they had clear criteria for entry into the study. These criteria included: “vasopressor-dependent shock and respiratory failure leading to the use of mechanical ventilation, details of antimicrobial therapy, assessment of survival at 90 days, and well-defined secondary outcomes and analyses of adverse events.”
The ADRENAL and APROCCHSS had vastly different 90-day mortality rates: ADRENAL had mortality rates of 27.9% with hydrocortisone and 28.8% with placebo (P = .50), while APROACCHSS had mortality rates of 43.0% with hydrocortisone plus fludrocortisone and 49.1% with placebo (P = .03). Despite this, they both display the beneficial effect anti-inflammatory therapies, such as hydrocortisone, have on secondary outcomes of shock reversal and the reduction in duration of mechanical ventilation. “It is unlikely that in the near future sufficiently powered trials will provide us with better data” than the ADRENAL and APROCCHSS trials, Dr. Suffredini wrote.
Dr. Suffredini made these comments in an editorial accompanying this study in the New England Journal of Medicine. He is the deputy chief of the critical care medicine department at the National Institutes of Health Clinical Center, and he has served on the executive committee of the Department of Veteran Affairs Cooperative Studies Program. He has no other relevant financial disclosures to report.
The results of the Activated Protein C and Corticosteroids for Human Septic Shock (APROCCHSS) trial and the Adjunctive Corticosteroid Treatment in Critically Ill Patients with Septic Shock (ADRENAL), both reported in the latest issue of NEJM, are landmark studies detailing the largest analyses of hydrocortisone use in patients with septic shock.
Both of these trials were massive, with over 5,000 patients combined, which is much larger than all previous studies according to Anthony Suffredini, MD, of the National Institutes of Health. An additional useful feature of these trials was that they had clear criteria for entry into the study. These criteria included: “vasopressor-dependent shock and respiratory failure leading to the use of mechanical ventilation, details of antimicrobial therapy, assessment of survival at 90 days, and well-defined secondary outcomes and analyses of adverse events.”
The ADRENAL and APROCCHSS had vastly different 90-day mortality rates: ADRENAL had mortality rates of 27.9% with hydrocortisone and 28.8% with placebo (P = .50), while APROACCHSS had mortality rates of 43.0% with hydrocortisone plus fludrocortisone and 49.1% with placebo (P = .03). Despite this, they both display the beneficial effect anti-inflammatory therapies, such as hydrocortisone, have on secondary outcomes of shock reversal and the reduction in duration of mechanical ventilation. “It is unlikely that in the near future sufficiently powered trials will provide us with better data” than the ADRENAL and APROCCHSS trials, Dr. Suffredini wrote.
Dr. Suffredini made these comments in an editorial accompanying this study in the New England Journal of Medicine. He is the deputy chief of the critical care medicine department at the National Institutes of Health Clinical Center, and he has served on the executive committee of the Department of Veteran Affairs Cooperative Studies Program. He has no other relevant financial disclosures to report.
The results of the Activated Protein C and Corticosteroids for Human Septic Shock (APROCCHSS) trial and the Adjunctive Corticosteroid Treatment in Critically Ill Patients with Septic Shock (ADRENAL), both reported in the latest issue of NEJM, are landmark studies detailing the largest analyses of hydrocortisone use in patients with septic shock.
Both of these trials were massive, with over 5,000 patients combined, which is much larger than all previous studies according to Anthony Suffredini, MD, of the National Institutes of Health. An additional useful feature of these trials was that they had clear criteria for entry into the study. These criteria included: “vasopressor-dependent shock and respiratory failure leading to the use of mechanical ventilation, details of antimicrobial therapy, assessment of survival at 90 days, and well-defined secondary outcomes and analyses of adverse events.”
The ADRENAL and APROCCHSS had vastly different 90-day mortality rates: ADRENAL had mortality rates of 27.9% with hydrocortisone and 28.8% with placebo (P = .50), while APROACCHSS had mortality rates of 43.0% with hydrocortisone plus fludrocortisone and 49.1% with placebo (P = .03). Despite this, they both display the beneficial effect anti-inflammatory therapies, such as hydrocortisone, have on secondary outcomes of shock reversal and the reduction in duration of mechanical ventilation. “It is unlikely that in the near future sufficiently powered trials will provide us with better data” than the ADRENAL and APROCCHSS trials, Dr. Suffredini wrote.
Dr. Suffredini made these comments in an editorial accompanying this study in the New England Journal of Medicine. He is the deputy chief of the critical care medicine department at the National Institutes of Health Clinical Center, and he has served on the executive committee of the Department of Veteran Affairs Cooperative Studies Program. He has no other relevant financial disclosures to report.
Hydrocortisone in combination with fludrocortisone significantly reduced 90-day mortality in septic shock patients in a double-blind, randomized, controlled trial.
Prior to this study, two large trials had displayed that corticosteroids were beneficial in improving hemodynamic status and organ function, but little was known about corticosteroids’ ability to increase survival in sepsis patients.
The study, named the Activated Protein C and Corticosteroids for Human Septic Shock (APROCCHSS) trial, was designed to assess the benefit/risk ratio of using activated protein C – drotrecogin alfa (activated) – and corticosteroids together or separately in septic shock patients. The original design of the study included Xigris (drotrecogin alfa) and was composed of four parallel groups, but Xigris was removed from the market in October of 2011, so the study continued with only two parallel groups.
A total of 1,241 patients experiencing chronic septic shock were recruited into the two double-blind, parallel groups, with patients in one group receiving hydrocortisone plus fludrocortisone and the other receiving placebos. The placebos used in this study were similar in appearance to the actual treatment drugs. The placebos for hydrocortisone and fludrocortisone were either parenteral mannitol (133.6 mg), disodium phosphate (8.73 mg), and sodium phosphate (0.92 mg) or tablets of microcrystalline cellulose (59.098 mg), respectively.
Hydrocortisone was given intravenously every 6 hours as a 50-mg intravenous bolus, and fludrocortisone was given once a day as a 50-mcg tablet through a nasogastric tube. Patients in ICUs who had septic shock for less than 24 hours were included in the study. Septic shock was identified by the presence of a clinically or microbiologically documented infection, a Sequential Organ Failure Assessment score of 3 or 4 for at least two organs and for at least 6 hours, and receipt of vasopressor therapy for at least 6 hours.
After 90 days, 264 of 614 of the patients (43%) in the hydrocortisone/fludrocortisone group and almost half (49.1%) of 627 patients in the placebo group had died (P = .03). The relative risk of death was 0.88 (95% confidence interval, 0.78-0.99), which favored the hydrocortisone/fludrocortisone group. The researchers also observed that death was significantly lower in the hydrocortisone/fludrocortisone group, compared with the placebo group, at time of ICU discharge (35.4% vs. 41.0%, respectively; P = .04).
While mortality was reduced, patients still experienced adverse events. 326 of 614 (53.1%) patients in the hydrocortisone/fludrocortisone group and 363 of 626 patients (58.0%) in the placebo group experienced at least one serious adverse event by day 180 (P = 0.08).
“Seven-day treatment with a 50-mg intravenous bolus of hydrocortisone every 6 hours and a daily dose of 50 mcg of oral fludrocortisone resulted in lower mortality at day 90 and at ICU and hospital discharge than placebo among adults with septic shock,” concluded Dr. Annane and his coauthors.
The majority of researchers had no relevant financial disclosures to report, while some doctors received grants and personal fees unrelated to this study. This study was funded in part by public grants from the French Ministry of Health.
SOURCE: Annana A et al. NEJM. 2018 Feb 28. doi: 10.1056/NEJMoa1705716.
Hydrocortisone in combination with fludrocortisone significantly reduced 90-day mortality in septic shock patients in a double-blind, randomized, controlled trial.
Prior to this study, two large trials had displayed that corticosteroids were beneficial in improving hemodynamic status and organ function, but little was known about corticosteroids’ ability to increase survival in sepsis patients.
The study, named the Activated Protein C and Corticosteroids for Human Septic Shock (APROCCHSS) trial, was designed to assess the benefit/risk ratio of using activated protein C – drotrecogin alfa (activated) – and corticosteroids together or separately in septic shock patients. The original design of the study included Xigris (drotrecogin alfa) and was composed of four parallel groups, but Xigris was removed from the market in October of 2011, so the study continued with only two parallel groups.
A total of 1,241 patients experiencing chronic septic shock were recruited into the two double-blind, parallel groups, with patients in one group receiving hydrocortisone plus fludrocortisone and the other receiving placebos. The placebos used in this study were similar in appearance to the actual treatment drugs. The placebos for hydrocortisone and fludrocortisone were either parenteral mannitol (133.6 mg), disodium phosphate (8.73 mg), and sodium phosphate (0.92 mg) or tablets of microcrystalline cellulose (59.098 mg), respectively.
Hydrocortisone was given intravenously every 6 hours as a 50-mg intravenous bolus, and fludrocortisone was given once a day as a 50-mcg tablet through a nasogastric tube. Patients in ICUs who had septic shock for less than 24 hours were included in the study. Septic shock was identified by the presence of a clinically or microbiologically documented infection, a Sequential Organ Failure Assessment score of 3 or 4 for at least two organs and for at least 6 hours, and receipt of vasopressor therapy for at least 6 hours.
After 90 days, 264 of 614 of the patients (43%) in the hydrocortisone/fludrocortisone group and almost half (49.1%) of 627 patients in the placebo group had died (P = .03). The relative risk of death was 0.88 (95% confidence interval, 0.78-0.99), which favored the hydrocortisone/fludrocortisone group. The researchers also observed that death was significantly lower in the hydrocortisone/fludrocortisone group, compared with the placebo group, at time of ICU discharge (35.4% vs. 41.0%, respectively; P = .04).
While mortality was reduced, patients still experienced adverse events. 326 of 614 (53.1%) patients in the hydrocortisone/fludrocortisone group and 363 of 626 patients (58.0%) in the placebo group experienced at least one serious adverse event by day 180 (P = 0.08).
“Seven-day treatment with a 50-mg intravenous bolus of hydrocortisone every 6 hours and a daily dose of 50 mcg of oral fludrocortisone resulted in lower mortality at day 90 and at ICU and hospital discharge than placebo among adults with septic shock,” concluded Dr. Annane and his coauthors.
The majority of researchers had no relevant financial disclosures to report, while some doctors received grants and personal fees unrelated to this study. This study was funded in part by public grants from the French Ministry of Health.
SOURCE: Annana A et al. NEJM. 2018 Feb 28. doi: 10.1056/NEJMoa1705716.
FROM NEJM
Key clinical point: Hydrocortisone in combination with fludrocortisone significantly reduced 90-day mortality in septic shock patients.
Major finding: Mortality rates were lower in patients treated with hydrocortisone plus fludrocortisone, compared with patients treated with placebos (43% vs. 49.1%, respectively; P = .03).
Study details: A randomized, double-blind study of 1,241 patients with septic shock.
Disclosures: The majority of researchers had no relevant financial disclosures to report, while some doctors received grants and personal fees unrelated to this study. This study was funded in part by public grants from the French Ministry of Health.
Source: Annane A et al. NEJM. 2018 Feb 28. doi: 10.1056/NEJMoa1705716.
New C. difficile guidelines recommend fecal microbiota transplants
.
The updated Clinical Practice Guidelines for Clostridium difficile Infection in Adults and Children, published in the Feb. 15 edition of Clinical Infectious Diseases (doi: 10.1093/cid/cix1085), address changes in management and diagnosis of the infection, and include recommendations for pediatric infection. The guidelines from the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America were lasted published in 2010.
One of the strongest recommendations was on the use of FMTs to treat recurrent C. difficile infection after the failure of antibiotic therapy.
“Anecdotal treatment success rates of fecal microbiota transplantation for recurrent CDI [C. difficile infection] have been high regardless of route of instillation of feces, and have ranged between 77% and 94% with administration via the proximal small bowel; the highest success rates (80%-100%) have been associated with instillation of feces via the colon,” they wrote.
The guidelines also addressed what the authors described as the “evolving controversy” over the best methods for diagnosis, pointing out that there is little consensus about the best laboratory testing method.
“Given these various conundrums and the paucity of large prospective studies, the recommendations, while strong in some instances, are based upon a very low to low quality of evidence,” the authors said.
That aside, they advised that patients with unexplained and new-onset diarrhea (three or more unformed stools in 24 hours) were the preferred target population for testing for C. difficile infection. The most sensitive method of diagnosis in patients with clinical symptoms likely to be C. difficile infection was a nucleic acid amplification test, or a multistep algorithm, rather than a toxin test alone.
The guidelines committee also strongly advised against repeat testing within 7 days during the same episode of diarrhea, and against testing stool from asymptomatic patients, except for the purpose of epidemiologic study. They also noted there was insufficient evidence for the use of biologic markers such as fecal lactoferrin as an adjunct to testing.
The guidelines’ authors found there was not enough evidence to recommend discontinuing proton pump inhibitors to reduce the incidence of C. difficile infection, despite epidemiologic evidence of an association between proton pump inhibitor use and C. difficile infection. Similarly, there was a lack of evidence for the use of probiotics for primary prevention, but the authors noted that meta-analyses suggest probiotics may help prevent C. difficile infection in patients on antibiotics without a history of C. difficile infection.
With respect to antibiotic treatment, they recommended that patients diagnosed with C. difficile infection should first discontinue the inciting antibiotic treatment and then begin therapy with either vancomycin or fidaxomicin. For recurrent infection, they advised a tapered and pulsed regimen of oral vancomycin or a 10-day course of fidaxomicin. If patients had received metronidazole for the primary episode, they should be given a standard 10-day course of vancomycin for recurrent infection, the authors said.
In terms of diagnosis and management of pediatric C. difficile, the guidelines advised against routinely testing infants under 2 years of age with diarrhea, as the rate of C. difficile colonization even among asymptomatic infants can be higher than 40%. Even in children older than age 2, there was only a “weak” recommendation for C. difficile testing in patients with prolonged or worsening diarrhea and other risk factors such as inflammatory bowel disease or recent antibiotic exposure.
Children with a first episode or first recurrence of nonsevere C. difficile should be treated with either metronidazole or vancomycin, the authors wrote, but in the case of more severe illness or second recurrence, oral vancomycin was preferred over metronidazole.
The authors also suggested clinicians consider FMTs for children with recurrent infection that had failed to respond to antibiotics, but noted the quality of evidence for this was very low.
The guidelines were funded by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Six authors declared grants, consultancies, board positions, and other payments from the pharmaceutical industry outside the submitted work. One author also held patents relating to the treatment and prevention of C. difficile infection.
SOURCE: McDonald CL et al. Clin Infect Dis. 2018 Feb 15. doi: 10.1093/cid/cix1085.
.
The updated Clinical Practice Guidelines for Clostridium difficile Infection in Adults and Children, published in the Feb. 15 edition of Clinical Infectious Diseases (doi: 10.1093/cid/cix1085), address changes in management and diagnosis of the infection, and include recommendations for pediatric infection. The guidelines from the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America were lasted published in 2010.
One of the strongest recommendations was on the use of FMTs to treat recurrent C. difficile infection after the failure of antibiotic therapy.
“Anecdotal treatment success rates of fecal microbiota transplantation for recurrent CDI [C. difficile infection] have been high regardless of route of instillation of feces, and have ranged between 77% and 94% with administration via the proximal small bowel; the highest success rates (80%-100%) have been associated with instillation of feces via the colon,” they wrote.
The guidelines also addressed what the authors described as the “evolving controversy” over the best methods for diagnosis, pointing out that there is little consensus about the best laboratory testing method.
“Given these various conundrums and the paucity of large prospective studies, the recommendations, while strong in some instances, are based upon a very low to low quality of evidence,” the authors said.
That aside, they advised that patients with unexplained and new-onset diarrhea (three or more unformed stools in 24 hours) were the preferred target population for testing for C. difficile infection. The most sensitive method of diagnosis in patients with clinical symptoms likely to be C. difficile infection was a nucleic acid amplification test, or a multistep algorithm, rather than a toxin test alone.
The guidelines committee also strongly advised against repeat testing within 7 days during the same episode of diarrhea, and against testing stool from asymptomatic patients, except for the purpose of epidemiologic study. They also noted there was insufficient evidence for the use of biologic markers such as fecal lactoferrin as an adjunct to testing.
The guidelines’ authors found there was not enough evidence to recommend discontinuing proton pump inhibitors to reduce the incidence of C. difficile infection, despite epidemiologic evidence of an association between proton pump inhibitor use and C. difficile infection. Similarly, there was a lack of evidence for the use of probiotics for primary prevention, but the authors noted that meta-analyses suggest probiotics may help prevent C. difficile infection in patients on antibiotics without a history of C. difficile infection.
With respect to antibiotic treatment, they recommended that patients diagnosed with C. difficile infection should first discontinue the inciting antibiotic treatment and then begin therapy with either vancomycin or fidaxomicin. For recurrent infection, they advised a tapered and pulsed regimen of oral vancomycin or a 10-day course of fidaxomicin. If patients had received metronidazole for the primary episode, they should be given a standard 10-day course of vancomycin for recurrent infection, the authors said.
In terms of diagnosis and management of pediatric C. difficile, the guidelines advised against routinely testing infants under 2 years of age with diarrhea, as the rate of C. difficile colonization even among asymptomatic infants can be higher than 40%. Even in children older than age 2, there was only a “weak” recommendation for C. difficile testing in patients with prolonged or worsening diarrhea and other risk factors such as inflammatory bowel disease or recent antibiotic exposure.
Children with a first episode or first recurrence of nonsevere C. difficile should be treated with either metronidazole or vancomycin, the authors wrote, but in the case of more severe illness or second recurrence, oral vancomycin was preferred over metronidazole.
The authors also suggested clinicians consider FMTs for children with recurrent infection that had failed to respond to antibiotics, but noted the quality of evidence for this was very low.
The guidelines were funded by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Six authors declared grants, consultancies, board positions, and other payments from the pharmaceutical industry outside the submitted work. One author also held patents relating to the treatment and prevention of C. difficile infection.
SOURCE: McDonald CL et al. Clin Infect Dis. 2018 Feb 15. doi: 10.1093/cid/cix1085.
.
The updated Clinical Practice Guidelines for Clostridium difficile Infection in Adults and Children, published in the Feb. 15 edition of Clinical Infectious Diseases (doi: 10.1093/cid/cix1085), address changes in management and diagnosis of the infection, and include recommendations for pediatric infection. The guidelines from the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America were lasted published in 2010.
One of the strongest recommendations was on the use of FMTs to treat recurrent C. difficile infection after the failure of antibiotic therapy.
“Anecdotal treatment success rates of fecal microbiota transplantation for recurrent CDI [C. difficile infection] have been high regardless of route of instillation of feces, and have ranged between 77% and 94% with administration via the proximal small bowel; the highest success rates (80%-100%) have been associated with instillation of feces via the colon,” they wrote.
The guidelines also addressed what the authors described as the “evolving controversy” over the best methods for diagnosis, pointing out that there is little consensus about the best laboratory testing method.
“Given these various conundrums and the paucity of large prospective studies, the recommendations, while strong in some instances, are based upon a very low to low quality of evidence,” the authors said.
That aside, they advised that patients with unexplained and new-onset diarrhea (three or more unformed stools in 24 hours) were the preferred target population for testing for C. difficile infection. The most sensitive method of diagnosis in patients with clinical symptoms likely to be C. difficile infection was a nucleic acid amplification test, or a multistep algorithm, rather than a toxin test alone.
The guidelines committee also strongly advised against repeat testing within 7 days during the same episode of diarrhea, and against testing stool from asymptomatic patients, except for the purpose of epidemiologic study. They also noted there was insufficient evidence for the use of biologic markers such as fecal lactoferrin as an adjunct to testing.
The guidelines’ authors found there was not enough evidence to recommend discontinuing proton pump inhibitors to reduce the incidence of C. difficile infection, despite epidemiologic evidence of an association between proton pump inhibitor use and C. difficile infection. Similarly, there was a lack of evidence for the use of probiotics for primary prevention, but the authors noted that meta-analyses suggest probiotics may help prevent C. difficile infection in patients on antibiotics without a history of C. difficile infection.
With respect to antibiotic treatment, they recommended that patients diagnosed with C. difficile infection should first discontinue the inciting antibiotic treatment and then begin therapy with either vancomycin or fidaxomicin. For recurrent infection, they advised a tapered and pulsed regimen of oral vancomycin or a 10-day course of fidaxomicin. If patients had received metronidazole for the primary episode, they should be given a standard 10-day course of vancomycin for recurrent infection, the authors said.
In terms of diagnosis and management of pediatric C. difficile, the guidelines advised against routinely testing infants under 2 years of age with diarrhea, as the rate of C. difficile colonization even among asymptomatic infants can be higher than 40%. Even in children older than age 2, there was only a “weak” recommendation for C. difficile testing in patients with prolonged or worsening diarrhea and other risk factors such as inflammatory bowel disease or recent antibiotic exposure.
Children with a first episode or first recurrence of nonsevere C. difficile should be treated with either metronidazole or vancomycin, the authors wrote, but in the case of more severe illness or second recurrence, oral vancomycin was preferred over metronidazole.
The authors also suggested clinicians consider FMTs for children with recurrent infection that had failed to respond to antibiotics, but noted the quality of evidence for this was very low.
The guidelines were funded by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Six authors declared grants, consultancies, board positions, and other payments from the pharmaceutical industry outside the submitted work. One author also held patents relating to the treatment and prevention of C. difficile infection.
SOURCE: McDonald CL et al. Clin Infect Dis. 2018 Feb 15. doi: 10.1093/cid/cix1085.
FROM CLINICAL INFECTIOUS DISEASES
Key clinical point: Fecal microbiota transplants should be considered for use in patients with recurrent Clostridium difficile infection that has not responded to antibiotic therapy.
Major finding: One of the strongest recommendations in the new guidelines on C. difficile infection is to consider use of fecal microbiota transplants in patients with recurrent infection.
Data source: Clinical practice guidelines.
Disclosures: The guidelines were funded by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Six authors declared grants, consultancies, board positions, and other payments from the pharmaceutical industry outside the submitted work. One author also held patents relating to the treatment and prevention of C. difficile infection.
Source: McDonald CL et al. Clin Infect Dis. 2018 Feb 15. doi: 10.1093/cid/cix1085.
FDA issues safety alert for loperamide
The Food and Drug Administration announced Jan. 30 that is has issued a MedWatch safety alert on the use of the over-the-counter (OTC) antidiarrhea drug, loperamide.
Currently, the FDA is working with manufacturers to use blister packs or other single-dose packaging and to limit the number of doses in a package.
The alert comes after receiving continuous reports of serious heart problems and deaths with the use of much higher than recommended doses of loperamide, mainly among people who are intentionally misusing or abusing the product, regardless of the addition of a warning to the medicine label and a previous communication. The FDA states that loperamide is a safe drug when used as directed.
Loperamide is approved to help control symptoms of diarrhea. The maximum recommended daily dose for adults is 8 mg per day for OTC use and 16 mg per day for prescription use. It acts on opioid receptors in the gut to slow the movement in the intestines and decrease the number of bowel movements.
It is noted that much higher than recommended doses of loperamide, either intentionally or unintentionally, can result in serious cardiac adverse events, including QT interval prolongation, torsade de pointes or other ventricular arrhythmias, syncope, and cardiac arrest. Health care professionals and patients can report adverse events or side effects related to the use of these products to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program.
In 2016, the FDA issued a Drug Safety Communication and added warnings about serious heart problems to the drug label of prescription loperamide and to the Drug Facts label of OTC loperamide products. The FDA is working to evaluate this safety issue and will update the public when more information is available.
Read the full safety alert here.
The Food and Drug Administration announced Jan. 30 that is has issued a MedWatch safety alert on the use of the over-the-counter (OTC) antidiarrhea drug, loperamide.
Currently, the FDA is working with manufacturers to use blister packs or other single-dose packaging and to limit the number of doses in a package.
The alert comes after receiving continuous reports of serious heart problems and deaths with the use of much higher than recommended doses of loperamide, mainly among people who are intentionally misusing or abusing the product, regardless of the addition of a warning to the medicine label and a previous communication. The FDA states that loperamide is a safe drug when used as directed.
Loperamide is approved to help control symptoms of diarrhea. The maximum recommended daily dose for adults is 8 mg per day for OTC use and 16 mg per day for prescription use. It acts on opioid receptors in the gut to slow the movement in the intestines and decrease the number of bowel movements.
It is noted that much higher than recommended doses of loperamide, either intentionally or unintentionally, can result in serious cardiac adverse events, including QT interval prolongation, torsade de pointes or other ventricular arrhythmias, syncope, and cardiac arrest. Health care professionals and patients can report adverse events or side effects related to the use of these products to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program.
In 2016, the FDA issued a Drug Safety Communication and added warnings about serious heart problems to the drug label of prescription loperamide and to the Drug Facts label of OTC loperamide products. The FDA is working to evaluate this safety issue and will update the public when more information is available.
Read the full safety alert here.
The Food and Drug Administration announced Jan. 30 that is has issued a MedWatch safety alert on the use of the over-the-counter (OTC) antidiarrhea drug, loperamide.
Currently, the FDA is working with manufacturers to use blister packs or other single-dose packaging and to limit the number of doses in a package.
The alert comes after receiving continuous reports of serious heart problems and deaths with the use of much higher than recommended doses of loperamide, mainly among people who are intentionally misusing or abusing the product, regardless of the addition of a warning to the medicine label and a previous communication. The FDA states that loperamide is a safe drug when used as directed.
Loperamide is approved to help control symptoms of diarrhea. The maximum recommended daily dose for adults is 8 mg per day for OTC use and 16 mg per day for prescription use. It acts on opioid receptors in the gut to slow the movement in the intestines and decrease the number of bowel movements.
It is noted that much higher than recommended doses of loperamide, either intentionally or unintentionally, can result in serious cardiac adverse events, including QT interval prolongation, torsade de pointes or other ventricular arrhythmias, syncope, and cardiac arrest. Health care professionals and patients can report adverse events or side effects related to the use of these products to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program.
In 2016, the FDA issued a Drug Safety Communication and added warnings about serious heart problems to the drug label of prescription loperamide and to the Drug Facts label of OTC loperamide products. The FDA is working to evaluate this safety issue and will update the public when more information is available.
Read the full safety alert here.
Zika-linked birth defects climbing in U.S. hot spots
The prevalence of birth defects strongly linked with congenital Zika virus infection increased 21% from the first to the second half of 2016 in areas of the United States with local, endemic transmission: Puerto Rico, south Florida, and southern Texas, according to a report in the Jan. 26 edition of Morbidity and Mortality Weekly Report.
In those areas, complications strongly associated with Zika – including microcephaly; brain and eye abnormalities; and neurogenic hip dislocation, clubfoot, hearing loss, and arthrogryposis – jumped from 2.0 to 2.4 cases per 1,000 live births, with 140 cases in the first half of the year and 169 cases in the second (P = .009). Microcephaly and brain abnormalities were the most common problems.
In places with less than one confirmed Zika case from travel per 100,000 residents, such as Hawaii and Utah, the prevalence of birth defects strongly linked to Zika actually dropped from 2.8 cases per 1,000 live births to 2.4 in 2016.
The 15 U.S. jurisdictions in the study included nearly 1 million live births, representing approximately one fourth of the total live births in the United States in 2016. The live birth rate was 92% among the 2,962 infants and fetuses with Zika-associated birth defects.
All the jurisdictions had existing birth defects surveillance systems that quickly adapted to monitor for potential Zika defects. However, although strongly associated with Zika, there’s no guarantee that the birth defects in the study were actually caused by the virus, the researchers noted.
“These data will help communities plan for needed resources to care for affected patients and families and can serve as a foundation for linking and evaluating health and developmental outcomes of affected children,” said the investigators, led by Augustina Delaney, PhD, of the National Center on Birth Defects and Developmental Disabilities at the Centers for Disease Control and Prevention in Atlanta.
The work was the first population-based birth defect surveillance report for Zika. The CDC follows confirmed Zika cases in pregnant women and their offspring closely, but only a small portion of women are actually tested, so there’s likely far more cases of congenital Zika infection than show up in registries. Despite its limits, birth defect surveillance likely provides a more accurate picture of the actual extent of the problem.
It’s not known why Zika-linked birth defects dropped off in areas with low or no travel-associated cases. “However ... further case ascertainment from the final quarter of 2016 is anticipated in all jurisdictions,” so the numbers could change, the authors said.
They had no conflicts of interest.
SOURCE: Delaney A, et. al. MMWR Morb Mortal Wkly Rep. 2018 Jan 26;67(3):91-6
Although these birth defects are not specific to congenital Zika virus infection, only those defects found previously to be most closely aligned with congenital Zika infection had increased prevalence.
It is critical that public health surveillance programs continue reporting the occurrence of these birth defects to monitor for trends following the Zika virus outbreak.
Brenda Fitzgerald , MD, is the director of the Centers for Disease Control and Prevention in Atlanta. Coleen A. Boyle , PhD, is the director of the CDC National Center on Birth Defects and Developmental Disabilities, and Margaret Honein , PhD, is chief of the agency’s Birth Defects Branch. They made their comments Jan. 25 in JAMA, and had no conflicts of interest (Jama. 2018 Jan 25. doi: 10.1001/jama.2018.0126).
Although these birth defects are not specific to congenital Zika virus infection, only those defects found previously to be most closely aligned with congenital Zika infection had increased prevalence.
It is critical that public health surveillance programs continue reporting the occurrence of these birth defects to monitor for trends following the Zika virus outbreak.
Brenda Fitzgerald , MD, is the director of the Centers for Disease Control and Prevention in Atlanta. Coleen A. Boyle , PhD, is the director of the CDC National Center on Birth Defects and Developmental Disabilities, and Margaret Honein , PhD, is chief of the agency’s Birth Defects Branch. They made their comments Jan. 25 in JAMA, and had no conflicts of interest (Jama. 2018 Jan 25. doi: 10.1001/jama.2018.0126).
Although these birth defects are not specific to congenital Zika virus infection, only those defects found previously to be most closely aligned with congenital Zika infection had increased prevalence.
It is critical that public health surveillance programs continue reporting the occurrence of these birth defects to monitor for trends following the Zika virus outbreak.
Brenda Fitzgerald , MD, is the director of the Centers for Disease Control and Prevention in Atlanta. Coleen A. Boyle , PhD, is the director of the CDC National Center on Birth Defects and Developmental Disabilities, and Margaret Honein , PhD, is chief of the agency’s Birth Defects Branch. They made their comments Jan. 25 in JAMA, and had no conflicts of interest (Jama. 2018 Jan 25. doi: 10.1001/jama.2018.0126).
The prevalence of birth defects strongly linked with congenital Zika virus infection increased 21% from the first to the second half of 2016 in areas of the United States with local, endemic transmission: Puerto Rico, south Florida, and southern Texas, according to a report in the Jan. 26 edition of Morbidity and Mortality Weekly Report.
In those areas, complications strongly associated with Zika – including microcephaly; brain and eye abnormalities; and neurogenic hip dislocation, clubfoot, hearing loss, and arthrogryposis – jumped from 2.0 to 2.4 cases per 1,000 live births, with 140 cases in the first half of the year and 169 cases in the second (P = .009). Microcephaly and brain abnormalities were the most common problems.
In places with less than one confirmed Zika case from travel per 100,000 residents, such as Hawaii and Utah, the prevalence of birth defects strongly linked to Zika actually dropped from 2.8 cases per 1,000 live births to 2.4 in 2016.
The 15 U.S. jurisdictions in the study included nearly 1 million live births, representing approximately one fourth of the total live births in the United States in 2016. The live birth rate was 92% among the 2,962 infants and fetuses with Zika-associated birth defects.
All the jurisdictions had existing birth defects surveillance systems that quickly adapted to monitor for potential Zika defects. However, although strongly associated with Zika, there’s no guarantee that the birth defects in the study were actually caused by the virus, the researchers noted.
“These data will help communities plan for needed resources to care for affected patients and families and can serve as a foundation for linking and evaluating health and developmental outcomes of affected children,” said the investigators, led by Augustina Delaney, PhD, of the National Center on Birth Defects and Developmental Disabilities at the Centers for Disease Control and Prevention in Atlanta.
The work was the first population-based birth defect surveillance report for Zika. The CDC follows confirmed Zika cases in pregnant women and their offspring closely, but only a small portion of women are actually tested, so there’s likely far more cases of congenital Zika infection than show up in registries. Despite its limits, birth defect surveillance likely provides a more accurate picture of the actual extent of the problem.
It’s not known why Zika-linked birth defects dropped off in areas with low or no travel-associated cases. “However ... further case ascertainment from the final quarter of 2016 is anticipated in all jurisdictions,” so the numbers could change, the authors said.
They had no conflicts of interest.
SOURCE: Delaney A, et. al. MMWR Morb Mortal Wkly Rep. 2018 Jan 26;67(3):91-6
The prevalence of birth defects strongly linked with congenital Zika virus infection increased 21% from the first to the second half of 2016 in areas of the United States with local, endemic transmission: Puerto Rico, south Florida, and southern Texas, according to a report in the Jan. 26 edition of Morbidity and Mortality Weekly Report.
In those areas, complications strongly associated with Zika – including microcephaly; brain and eye abnormalities; and neurogenic hip dislocation, clubfoot, hearing loss, and arthrogryposis – jumped from 2.0 to 2.4 cases per 1,000 live births, with 140 cases in the first half of the year and 169 cases in the second (P = .009). Microcephaly and brain abnormalities were the most common problems.
In places with less than one confirmed Zika case from travel per 100,000 residents, such as Hawaii and Utah, the prevalence of birth defects strongly linked to Zika actually dropped from 2.8 cases per 1,000 live births to 2.4 in 2016.
The 15 U.S. jurisdictions in the study included nearly 1 million live births, representing approximately one fourth of the total live births in the United States in 2016. The live birth rate was 92% among the 2,962 infants and fetuses with Zika-associated birth defects.
All the jurisdictions had existing birth defects surveillance systems that quickly adapted to monitor for potential Zika defects. However, although strongly associated with Zika, there’s no guarantee that the birth defects in the study were actually caused by the virus, the researchers noted.
“These data will help communities plan for needed resources to care for affected patients and families and can serve as a foundation for linking and evaluating health and developmental outcomes of affected children,” said the investigators, led by Augustina Delaney, PhD, of the National Center on Birth Defects and Developmental Disabilities at the Centers for Disease Control and Prevention in Atlanta.
The work was the first population-based birth defect surveillance report for Zika. The CDC follows confirmed Zika cases in pregnant women and their offspring closely, but only a small portion of women are actually tested, so there’s likely far more cases of congenital Zika infection than show up in registries. Despite its limits, birth defect surveillance likely provides a more accurate picture of the actual extent of the problem.
It’s not known why Zika-linked birth defects dropped off in areas with low or no travel-associated cases. “However ... further case ascertainment from the final quarter of 2016 is anticipated in all jurisdictions,” so the numbers could change, the authors said.
They had no conflicts of interest.
SOURCE: Delaney A, et. al. MMWR Morb Mortal Wkly Rep. 2018 Jan 26;67(3):91-6
FROM MMWR
Key clinical point: Although microcephaly and other birth defects strongly associated with Zika virus are holding steady or even decreasing elsewhere in the United States, there was an uptick in 2016 in areas with endemic transmission.
Major finding: The prevalence of birth defects strongly related to congenital Zika virus infection increased 21% from the first to the second half of 2016 in southern Texas, south Florida, and Puerto Rico.
Study details: Birth defects surveillance in about a quarter of the infants born in the United States in 2016.
Disclosures: The investigators had no conflicts of interest.
Source: Delaney A, et. al. MMWR Morb Mortal Wkly Rep. 2018 Jan 26;67(3):91-6
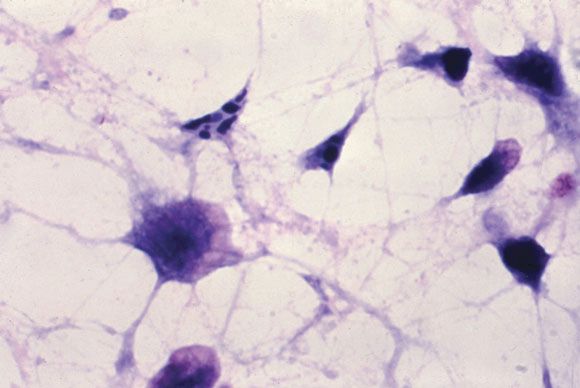
Chikungunya virus goes undetected despite chronic arthritis in 25% of patients after 20 months
Up to a quarter of patients infected with chikungunya virus who reported joint pain as one of their initial symptoms continue to have joint pain after 20 months of follow-up, and evidence suggests that the persistent joint symptoms are not related to the continued presence of the virus in synovial fluid, according to two studies of patients infected during the 2014-2015 Colombian epidemic.
In the first large-scale, cross-sectional follow-up of a prospective cohort from the Colombian epidemic, Aileen Chang, MD, of George Washington University, Washington, and her colleagues at multiple other institutions reported persistent joint pain and multiple swollen and/or tender joints after 20 months in 123 of 485 Colombian patients who initially had joint pain with their Chikungunya virus infection (CHIKV) diagnosis. In their report in Arthritis & Rheumatology, they said that increased initial viral load and severe initial joint pain were predictors of persistent arthritis, which is consistent with the work of other researchers.
Dr. Chang worked with a variety of coinvestigators, some of whom were also involved in the larger symptom follow-up study, to conduct this Study of Chikungunya Arthritis Mechanisms in the Americas (CAMA). They collected synovial fluid and blood plasma from these 38 patients as well as 10 healthy controls who were serologically negative for CHIKV and never had arthritis, and analyzed the fluid and plasma for signs of CHIKV. They assessed viral RNA via quantitative reverse transcription polymerase chain reaction (qRT-PCR) testing, looked at viral proteins via mass spectrometry, and did viral cultures.
All samples from the 38 patients in the study were negative for CHIKV in two separate qRT-PCR assays. To determine if low-level viremia was present in synovial fluid samples, the samples were added to cell cultures to expand viral replication. No viral growth was found after three attempts and 10 days of culture. Conversely, controls with low quantities of virus (about 1 plaque-forming unit per well) yielded growth and detection of the virus.
Patients with CHIKV-associated arthritis also had no significant increase in rheumatoid arthritis markers or C-reactive protein. In fact, plasma markers for rheumatoid arthritis were found in only a fraction of patients with CHIKV arthritis: rheumatoid factor (RF) IgM antibody in 9%, RF IgG antibody in 12%, and anti–cyclic citrullinated peptide in 0%.
The more probable potential mechanisms through which CHIKV could cause persistent arthritis symptoms is through the presence of persistent CHIKV or viral antigens at low enough levels in the synovial tissue that it is undetectable in the synovial fluid, Dr. Chang and her associates suggested. There is also a possibility of epigenetic changes to the host DNA, altering host gene transcription. Other epigenetic changes, like epigenetic imprinting, could be possible in macrophages, leading to more aggressive cell behavior, they said. Unlikelier scenarios would be the presence of seronegative RA in these patients or, alternatively, the presence of seronegative RA indicating prior infection with CHIKV or other arthritogenic viruses.
Whatever mechanisms are causing CHIKV-associated arthritis, “these study findings may have important clinical relevance for CHIKV in the Americas. Since there is no current standard of care guidance for the treatment of CHIKV arthritis, some patients are currently being treated with immunosuppressant medications such as methotrexate, hydroxychloroquine, etanercept, adalimumab, sulfasalazine, fingolimod, abatacept, and tofacitinib,” Dr. Chang and her colleagues wrote. “This practice could be potentially harmful in the setting of replicating virus in the synovium as it could permit reemergence of a systemic viral infection.”
The CAMA study has several important limitations , the investigators said, the first being that during collection of synovial fluid, 0-20 mL of saline solution were used to flush the joints, which could have affected the ability to detect virus in the samples. In an attempt to mitigate this, the researchers cultured 0.5-1.5 mL of sampled synovial fluid to expand any replication-competent virus present in the sample, used two complementary PCR assays to detect nucleic acids, and a proteomic approach to look for viral proteins.
The researchers acknowledged that despite these measures, “proving the absence of a target is difficult, and we recognize that it is possible that our approach failed to detect low-level viral antigen; however, our orthogonal approach clearly demonstrates that if viral antigen exists in the synovial fluid, it is at extremely low levels.” They advised that future studies may want to use synovial biopsies rather than extracted fluid.
The investigators also did not include patients who had previously been infected by CHIKV without chronic arthritis. This issue was compounded by the lack of age- and sex-matched healthy controls.
All researchers involved in the studies reported no financial conflicts of interest. The studies were supported by various grants from the National Institutes of Health and the Rheumatology Research Foundation.
SOURCE: Chang A et al. Arthritis Rheumatol. 2017 Dec 20. doi: 10.1002/art.40383 and Chang A et al. Arthritis Rheumatol. 2017 Dec 20. doi: 10.1002/art.40384
Up to a quarter of patients infected with chikungunya virus who reported joint pain as one of their initial symptoms continue to have joint pain after 20 months of follow-up, and evidence suggests that the persistent joint symptoms are not related to the continued presence of the virus in synovial fluid, according to two studies of patients infected during the 2014-2015 Colombian epidemic.
In the first large-scale, cross-sectional follow-up of a prospective cohort from the Colombian epidemic, Aileen Chang, MD, of George Washington University, Washington, and her colleagues at multiple other institutions reported persistent joint pain and multiple swollen and/or tender joints after 20 months in 123 of 485 Colombian patients who initially had joint pain with their Chikungunya virus infection (CHIKV) diagnosis. In their report in Arthritis & Rheumatology, they said that increased initial viral load and severe initial joint pain were predictors of persistent arthritis, which is consistent with the work of other researchers.
Dr. Chang worked with a variety of coinvestigators, some of whom were also involved in the larger symptom follow-up study, to conduct this Study of Chikungunya Arthritis Mechanisms in the Americas (CAMA). They collected synovial fluid and blood plasma from these 38 patients as well as 10 healthy controls who were serologically negative for CHIKV and never had arthritis, and analyzed the fluid and plasma for signs of CHIKV. They assessed viral RNA via quantitative reverse transcription polymerase chain reaction (qRT-PCR) testing, looked at viral proteins via mass spectrometry, and did viral cultures.
All samples from the 38 patients in the study were negative for CHIKV in two separate qRT-PCR assays. To determine if low-level viremia was present in synovial fluid samples, the samples were added to cell cultures to expand viral replication. No viral growth was found after three attempts and 10 days of culture. Conversely, controls with low quantities of virus (about 1 plaque-forming unit per well) yielded growth and detection of the virus.
Patients with CHIKV-associated arthritis also had no significant increase in rheumatoid arthritis markers or C-reactive protein. In fact, plasma markers for rheumatoid arthritis were found in only a fraction of patients with CHIKV arthritis: rheumatoid factor (RF) IgM antibody in 9%, RF IgG antibody in 12%, and anti–cyclic citrullinated peptide in 0%.
The more probable potential mechanisms through which CHIKV could cause persistent arthritis symptoms is through the presence of persistent CHIKV or viral antigens at low enough levels in the synovial tissue that it is undetectable in the synovial fluid, Dr. Chang and her associates suggested. There is also a possibility of epigenetic changes to the host DNA, altering host gene transcription. Other epigenetic changes, like epigenetic imprinting, could be possible in macrophages, leading to more aggressive cell behavior, they said. Unlikelier scenarios would be the presence of seronegative RA in these patients or, alternatively, the presence of seronegative RA indicating prior infection with CHIKV or other arthritogenic viruses.
Whatever mechanisms are causing CHIKV-associated arthritis, “these study findings may have important clinical relevance for CHIKV in the Americas. Since there is no current standard of care guidance for the treatment of CHIKV arthritis, some patients are currently being treated with immunosuppressant medications such as methotrexate, hydroxychloroquine, etanercept, adalimumab, sulfasalazine, fingolimod, abatacept, and tofacitinib,” Dr. Chang and her colleagues wrote. “This practice could be potentially harmful in the setting of replicating virus in the synovium as it could permit reemergence of a systemic viral infection.”
The CAMA study has several important limitations , the investigators said, the first being that during collection of synovial fluid, 0-20 mL of saline solution were used to flush the joints, which could have affected the ability to detect virus in the samples. In an attempt to mitigate this, the researchers cultured 0.5-1.5 mL of sampled synovial fluid to expand any replication-competent virus present in the sample, used two complementary PCR assays to detect nucleic acids, and a proteomic approach to look for viral proteins.
The researchers acknowledged that despite these measures, “proving the absence of a target is difficult, and we recognize that it is possible that our approach failed to detect low-level viral antigen; however, our orthogonal approach clearly demonstrates that if viral antigen exists in the synovial fluid, it is at extremely low levels.” They advised that future studies may want to use synovial biopsies rather than extracted fluid.
The investigators also did not include patients who had previously been infected by CHIKV without chronic arthritis. This issue was compounded by the lack of age- and sex-matched healthy controls.
All researchers involved in the studies reported no financial conflicts of interest. The studies were supported by various grants from the National Institutes of Health and the Rheumatology Research Foundation.
SOURCE: Chang A et al. Arthritis Rheumatol. 2017 Dec 20. doi: 10.1002/art.40383 and Chang A et al. Arthritis Rheumatol. 2017 Dec 20. doi: 10.1002/art.40384
Up to a quarter of patients infected with chikungunya virus who reported joint pain as one of their initial symptoms continue to have joint pain after 20 months of follow-up, and evidence suggests that the persistent joint symptoms are not related to the continued presence of the virus in synovial fluid, according to two studies of patients infected during the 2014-2015 Colombian epidemic.
In the first large-scale, cross-sectional follow-up of a prospective cohort from the Colombian epidemic, Aileen Chang, MD, of George Washington University, Washington, and her colleagues at multiple other institutions reported persistent joint pain and multiple swollen and/or tender joints after 20 months in 123 of 485 Colombian patients who initially had joint pain with their Chikungunya virus infection (CHIKV) diagnosis. In their report in Arthritis & Rheumatology, they said that increased initial viral load and severe initial joint pain were predictors of persistent arthritis, which is consistent with the work of other researchers.
Dr. Chang worked with a variety of coinvestigators, some of whom were also involved in the larger symptom follow-up study, to conduct this Study of Chikungunya Arthritis Mechanisms in the Americas (CAMA). They collected synovial fluid and blood plasma from these 38 patients as well as 10 healthy controls who were serologically negative for CHIKV and never had arthritis, and analyzed the fluid and plasma for signs of CHIKV. They assessed viral RNA via quantitative reverse transcription polymerase chain reaction (qRT-PCR) testing, looked at viral proteins via mass spectrometry, and did viral cultures.
All samples from the 38 patients in the study were negative for CHIKV in two separate qRT-PCR assays. To determine if low-level viremia was present in synovial fluid samples, the samples were added to cell cultures to expand viral replication. No viral growth was found after three attempts and 10 days of culture. Conversely, controls with low quantities of virus (about 1 plaque-forming unit per well) yielded growth and detection of the virus.
Patients with CHIKV-associated arthritis also had no significant increase in rheumatoid arthritis markers or C-reactive protein. In fact, plasma markers for rheumatoid arthritis were found in only a fraction of patients with CHIKV arthritis: rheumatoid factor (RF) IgM antibody in 9%, RF IgG antibody in 12%, and anti–cyclic citrullinated peptide in 0%.
The more probable potential mechanisms through which CHIKV could cause persistent arthritis symptoms is through the presence of persistent CHIKV or viral antigens at low enough levels in the synovial tissue that it is undetectable in the synovial fluid, Dr. Chang and her associates suggested. There is also a possibility of epigenetic changes to the host DNA, altering host gene transcription. Other epigenetic changes, like epigenetic imprinting, could be possible in macrophages, leading to more aggressive cell behavior, they said. Unlikelier scenarios would be the presence of seronegative RA in these patients or, alternatively, the presence of seronegative RA indicating prior infection with CHIKV or other arthritogenic viruses.
Whatever mechanisms are causing CHIKV-associated arthritis, “these study findings may have important clinical relevance for CHIKV in the Americas. Since there is no current standard of care guidance for the treatment of CHIKV arthritis, some patients are currently being treated with immunosuppressant medications such as methotrexate, hydroxychloroquine, etanercept, adalimumab, sulfasalazine, fingolimod, abatacept, and tofacitinib,” Dr. Chang and her colleagues wrote. “This practice could be potentially harmful in the setting of replicating virus in the synovium as it could permit reemergence of a systemic viral infection.”
The CAMA study has several important limitations , the investigators said, the first being that during collection of synovial fluid, 0-20 mL of saline solution were used to flush the joints, which could have affected the ability to detect virus in the samples. In an attempt to mitigate this, the researchers cultured 0.5-1.5 mL of sampled synovial fluid to expand any replication-competent virus present in the sample, used two complementary PCR assays to detect nucleic acids, and a proteomic approach to look for viral proteins.
The researchers acknowledged that despite these measures, “proving the absence of a target is difficult, and we recognize that it is possible that our approach failed to detect low-level viral antigen; however, our orthogonal approach clearly demonstrates that if viral antigen exists in the synovial fluid, it is at extremely low levels.” They advised that future studies may want to use synovial biopsies rather than extracted fluid.
The investigators also did not include patients who had previously been infected by CHIKV without chronic arthritis. This issue was compounded by the lack of age- and sex-matched healthy controls.
All researchers involved in the studies reported no financial conflicts of interest. The studies were supported by various grants from the National Institutes of Health and the Rheumatology Research Foundation.
SOURCE: Chang A et al. Arthritis Rheumatol. 2017 Dec 20. doi: 10.1002/art.40383 and Chang A et al. Arthritis Rheumatol. 2017 Dec 20. doi: 10.1002/art.40384
FROM ARTHRITIS & RHEUMATOLOGY
Key clinical point:
Major finding: No signs of persistent CHIKV infection can be found in synovial fluid or blood plasma from patients with chronic arthritis after CHIKV.
Study details: Cross-sectional studies of 485 Colombian patients who had clinical CHIKV and associated arthritis symptoms in 2014-2015 and another 38 patients who underwent further synovial fluid and blood plasma testing after a median of 22 months.
Disclosures: All researchers involved in the studies reported no financial conflicts of interest. The studies were supported by various grants from the National Institutes of Health and the Rheumatology Research Foundation.
Source: Chang A et al. Arthritis Rheumatol. 2017 Dec 20. doi: 10.1002/art.40383 and Chang A et al. Arthritis Rheumatol. 2017 Dec 20. doi: 10.1002/art.40384.
Corynebacterium in the gut can trigger Parkinson’s disease
SAN DIEGO – The presence of Corynebacterium in the gut microbiome of people with two G alleles at the rs356219 single nucleotide polymorphism locus of the alpha-synuclein gene was associated with 100% probability of having Parkinson’s disease in a study conducted by the NeuroGenetics Research Consortium.
If the finding is replicated, it means that Corynebacterium is the trigger for Parkinson’s disease (PD) in people with the GG genotype. The GG signature at rs356219 is the strongest genetic risk factor for PD identified to date, but it’s not necessarily strong enough to cause the disease on its own. “It definitely needs a trigger,” and there’s a good chance that Corynebacterium is it, said senior investigator Haydeh Payami, PhD, professor of neurology and genomics at the University of Alabama, Birmingham.
Her team genotyped SNCA rs356219 from blood samples in 197 middle-aged PD patients and 115 age-matched controls. They also extracted DNA from stool samples to see what bacteria were in their gut and then looked for interactions between rs356219 genotype, gut microbiome, and PD risk.
The medical literature has been full of hints for a while now that PD might be set off by something going wrong in the gastrointestinal tract. Colonic inflammation, alpha-synuclein pathology in the gut, and dysbiosis of the gut microbiome in PD are among the many clues. The goal of the work was to find the link between PD and its GI aberrations.
Ninety genera were identified in the stool samples, but “no matter how you looked at the data, whichever method you used, one [genus] kept coming up” for interaction with the rs356219 genotype, “and that was Corynebacterium,” Dr. Payami said.
As in past studies, the rs356219 AA genotype did not increase the odds of PD, and there was no difference in microbiome abundance between PD patients and controls. The GA genotype increased the odds slightly without Corynebacterium, but it increased the odds more than fivefold when Corynebacterium was in the gut (odds ratio, 5.9; P = .04). If people had GG plus Corynebacterium, however, “you nailed it,” Dr. Payami said: The odds of developing PD were infinite (P = .0003).
Corynebacterium was more abundant in GA subjects with PD than GA subjects without PD, but it was by far the most abundant in GG subjects, and every person who had the GG genotype and gut Corynebacterium also had PD.
Corynebacterium are gram-positive, aerobic bacilli commonly found on the skin. Some members of the genus are opportunistic pathogens. It’s not clear how they get incorporated into the gut microbiome, or if they can be wiped out selectively in the gut with antibiotics or probiotics.
Perhaps Corynebacterium in the GI tract induces expression of alpha-synuclein protein, a major component of PD Lewy bodies that’s known to travel from the gut to the brain. Maybe the amount expressed depends on how many Gs people have in rs356219. Perhaps “if you have two Gs, you get so much alpha-synuclein that’s there’s no turning back, and it’s enough to cause PD,” Dr. Payami said.
The study was led by Zachary Wallen, a PhD candidate in Dr. Payami’s lab, and presented by him at the annual meeting of the American Neurological Association. The work was supported by the National Institutes of Health. Dr. Payami and Mr. Wallen had no industry disclosures.
SOURCE: Wallen Z et al. ANA 2017 abstract number S268
SAN DIEGO – The presence of Corynebacterium in the gut microbiome of people with two G alleles at the rs356219 single nucleotide polymorphism locus of the alpha-synuclein gene was associated with 100% probability of having Parkinson’s disease in a study conducted by the NeuroGenetics Research Consortium.
If the finding is replicated, it means that Corynebacterium is the trigger for Parkinson’s disease (PD) in people with the GG genotype. The GG signature at rs356219 is the strongest genetic risk factor for PD identified to date, but it’s not necessarily strong enough to cause the disease on its own. “It definitely needs a trigger,” and there’s a good chance that Corynebacterium is it, said senior investigator Haydeh Payami, PhD, professor of neurology and genomics at the University of Alabama, Birmingham.
Her team genotyped SNCA rs356219 from blood samples in 197 middle-aged PD patients and 115 age-matched controls. They also extracted DNA from stool samples to see what bacteria were in their gut and then looked for interactions between rs356219 genotype, gut microbiome, and PD risk.
The medical literature has been full of hints for a while now that PD might be set off by something going wrong in the gastrointestinal tract. Colonic inflammation, alpha-synuclein pathology in the gut, and dysbiosis of the gut microbiome in PD are among the many clues. The goal of the work was to find the link between PD and its GI aberrations.
Ninety genera were identified in the stool samples, but “no matter how you looked at the data, whichever method you used, one [genus] kept coming up” for interaction with the rs356219 genotype, “and that was Corynebacterium,” Dr. Payami said.
As in past studies, the rs356219 AA genotype did not increase the odds of PD, and there was no difference in microbiome abundance between PD patients and controls. The GA genotype increased the odds slightly without Corynebacterium, but it increased the odds more than fivefold when Corynebacterium was in the gut (odds ratio, 5.9; P = .04). If people had GG plus Corynebacterium, however, “you nailed it,” Dr. Payami said: The odds of developing PD were infinite (P = .0003).
Corynebacterium was more abundant in GA subjects with PD than GA subjects without PD, but it was by far the most abundant in GG subjects, and every person who had the GG genotype and gut Corynebacterium also had PD.
Corynebacterium are gram-positive, aerobic bacilli commonly found on the skin. Some members of the genus are opportunistic pathogens. It’s not clear how they get incorporated into the gut microbiome, or if they can be wiped out selectively in the gut with antibiotics or probiotics.
Perhaps Corynebacterium in the GI tract induces expression of alpha-synuclein protein, a major component of PD Lewy bodies that’s known to travel from the gut to the brain. Maybe the amount expressed depends on how many Gs people have in rs356219. Perhaps “if you have two Gs, you get so much alpha-synuclein that’s there’s no turning back, and it’s enough to cause PD,” Dr. Payami said.
The study was led by Zachary Wallen, a PhD candidate in Dr. Payami’s lab, and presented by him at the annual meeting of the American Neurological Association. The work was supported by the National Institutes of Health. Dr. Payami and Mr. Wallen had no industry disclosures.
SOURCE: Wallen Z et al. ANA 2017 abstract number S268
SAN DIEGO – The presence of Corynebacterium in the gut microbiome of people with two G alleles at the rs356219 single nucleotide polymorphism locus of the alpha-synuclein gene was associated with 100% probability of having Parkinson’s disease in a study conducted by the NeuroGenetics Research Consortium.
If the finding is replicated, it means that Corynebacterium is the trigger for Parkinson’s disease (PD) in people with the GG genotype. The GG signature at rs356219 is the strongest genetic risk factor for PD identified to date, but it’s not necessarily strong enough to cause the disease on its own. “It definitely needs a trigger,” and there’s a good chance that Corynebacterium is it, said senior investigator Haydeh Payami, PhD, professor of neurology and genomics at the University of Alabama, Birmingham.
Her team genotyped SNCA rs356219 from blood samples in 197 middle-aged PD patients and 115 age-matched controls. They also extracted DNA from stool samples to see what bacteria were in their gut and then looked for interactions between rs356219 genotype, gut microbiome, and PD risk.
The medical literature has been full of hints for a while now that PD might be set off by something going wrong in the gastrointestinal tract. Colonic inflammation, alpha-synuclein pathology in the gut, and dysbiosis of the gut microbiome in PD are among the many clues. The goal of the work was to find the link between PD and its GI aberrations.
Ninety genera were identified in the stool samples, but “no matter how you looked at the data, whichever method you used, one [genus] kept coming up” for interaction with the rs356219 genotype, “and that was Corynebacterium,” Dr. Payami said.
As in past studies, the rs356219 AA genotype did not increase the odds of PD, and there was no difference in microbiome abundance between PD patients and controls. The GA genotype increased the odds slightly without Corynebacterium, but it increased the odds more than fivefold when Corynebacterium was in the gut (odds ratio, 5.9; P = .04). If people had GG plus Corynebacterium, however, “you nailed it,” Dr. Payami said: The odds of developing PD were infinite (P = .0003).
Corynebacterium was more abundant in GA subjects with PD than GA subjects without PD, but it was by far the most abundant in GG subjects, and every person who had the GG genotype and gut Corynebacterium also had PD.
Corynebacterium are gram-positive, aerobic bacilli commonly found on the skin. Some members of the genus are opportunistic pathogens. It’s not clear how they get incorporated into the gut microbiome, or if they can be wiped out selectively in the gut with antibiotics or probiotics.
Perhaps Corynebacterium in the GI tract induces expression of alpha-synuclein protein, a major component of PD Lewy bodies that’s known to travel from the gut to the brain. Maybe the amount expressed depends on how many Gs people have in rs356219. Perhaps “if you have two Gs, you get so much alpha-synuclein that’s there’s no turning back, and it’s enough to cause PD,” Dr. Payami said.
The study was led by Zachary Wallen, a PhD candidate in Dr. Payami’s lab, and presented by him at the annual meeting of the American Neurological Association. The work was supported by the National Institutes of Health. Dr. Payami and Mr. Wallen had no industry disclosures.
SOURCE: Wallen Z et al. ANA 2017 abstract number S268
REPORTING FROM ANA 2017
Key clinical point: in genetically susceptible people.
Major finding: Those who have Corynebacterium in their gut microbiome plus two G alleles at the rs356219 locus of the alpha-synuclein gene have infinite odds of developing PD (P = .0003).
Study details: A case-control study involving 197 middle-aged PD patients and 115 age-matched controls.
Disclosures: The work was supported by the National Institutes of Health. The lead and senior investigators had no industry disclosures.
Source: Wallen Z et al. ANA 2017 abstract number S268
Staph bloodstream infection algorithm shortens treatment course
SAN DIEGO – By standardizing antibiotic treatment for simple and uncomplicated staphylococcal bloodstream infections (BSI), an algorithm effectively shortens therapy and simplifies decision making, according to results of a multinational randomized trial.
“The data from the study confirm that the algorithm achieves more with less and verify that shorter antibiotic courses are sufficient,” reported Thomas L. Holland, MD, an infectious disease specialist at Duke University Hospital in Durham, N.C.
In this study, the patients randomized to algorithm treatment received vancomycin (or daptomycin in allergic or intolerant patients), which was administered for periods of duration based on clinical features. In those randomized to SOC, the choice and duration of antibiotics were left to the discretion of the treating physician without restrictions.
In those with simple staphylococcal BSI, the algorithm called for no further antibiotics beyond what had already been administered empirically prior to randomization. Key features of simple coagulase-negative staphylococcal (CONS) BSIs include absence of fever or evidence of metastatic infection, as well as no more than one positive follow-up blood culture. The key features of simple Staphylococcus aureus BSI are similar. However, no positive blood cultures are required for S. aureus BSI to be classified as simple.
“In the algorithm arm, no antibiotics were given to those with simple staphylococcal BSI unless antibiotics had been given prior to randomization,” Dr. Holland explained, but he acknowledged that empiric antibiotics prior to randomization reflect “clinical reality.”
In those with uncomplicated rather than simple staphylococcal BSI, vancomycin was given for 5 days to those with CONS BSI and for 14 days to those with S. aureus BSI. In those who were randomized and then subsequently found to have a complicated infection, defined as multiple positive blood cultures or evidence of metastatic infection, patients received as few as 7 days or as many as 28 days of antibiotics, “reflecting the heterogeneity of these infections,” Dr. Holland reported at an annual scientific meeting on infectious diseases.
The coprimary endpoints were treatment success at test of cure and treatment safety, both of which were adjudicated by an external committee consisting of infectious disease specialists blinded to the therapy.
There were 509 patients from 16 sites in both the United States and Spain. CONS BSIs represented approximately 75% of patients in both arms. The complicated staphylococcal infections, which also were evenly distributed in the two arms, were included in the intention-to-treat analysis. Of complicated staphylococcal infections in this study, the pathogen was CONS in 34 instances and S. aureus in 37.
Treatment success was achieved in 82.0% and 81.5% of patients in the algorithm and SOC arms, respectively. Significant adverse events occurred in 32.9% and 28.3% of patients, respectively. Neither difference approached statistical significance.
“In other words, the algorithm was as effective and safe as standard of care,” Dr. Holland confirmed.
However, the median duration of treatment was reduced substantially for those randomized to the algorithm arm, compared with that seen in the standard of care arm. Among evaluable patients without complicated BSI, the mean duration of therapy was 4.4 days in the algorithm group vs. 6.2 days in the SOC group (P = .003). Most of this nearly 2-day reduction in treatment was achieved in uncomplicated CONS BSI patients. In this group, the mean days of treatment were 5.3 days and 8.4 days for the algorithm and SOC groups, respectively. In the uncomplicated S. aureus group, the reduction (from 15.9 to 15.3 days) was not significant.
“The study has several messages. For one, it suggests that patients who meet the criteria of simple staphylococcal BSI can be managed safely with monitoring alone. In addition, this study “provides the best evidence to date that 14 days of vancomycin from the first negative blood culture is sufficient in uncomplicated S. aureus bloodstream infections,” Dr. Holland stated.
“For many, these data will validate what they are already doing,” said Dr. Holland, who reported that the algorithm is now being applied routinely at his institution. “The value is that we now have a randomized trial to demonstrate that shorter therapy can be provided in uncomplicated staphylococcal blood stream infections without increasing risk of serious adverse events.”
SAN DIEGO – By standardizing antibiotic treatment for simple and uncomplicated staphylococcal bloodstream infections (BSI), an algorithm effectively shortens therapy and simplifies decision making, according to results of a multinational randomized trial.
“The data from the study confirm that the algorithm achieves more with less and verify that shorter antibiotic courses are sufficient,” reported Thomas L. Holland, MD, an infectious disease specialist at Duke University Hospital in Durham, N.C.
In this study, the patients randomized to algorithm treatment received vancomycin (or daptomycin in allergic or intolerant patients), which was administered for periods of duration based on clinical features. In those randomized to SOC, the choice and duration of antibiotics were left to the discretion of the treating physician without restrictions.
In those with simple staphylococcal BSI, the algorithm called for no further antibiotics beyond what had already been administered empirically prior to randomization. Key features of simple coagulase-negative staphylococcal (CONS) BSIs include absence of fever or evidence of metastatic infection, as well as no more than one positive follow-up blood culture. The key features of simple Staphylococcus aureus BSI are similar. However, no positive blood cultures are required for S. aureus BSI to be classified as simple.
“In the algorithm arm, no antibiotics were given to those with simple staphylococcal BSI unless antibiotics had been given prior to randomization,” Dr. Holland explained, but he acknowledged that empiric antibiotics prior to randomization reflect “clinical reality.”
In those with uncomplicated rather than simple staphylococcal BSI, vancomycin was given for 5 days to those with CONS BSI and for 14 days to those with S. aureus BSI. In those who were randomized and then subsequently found to have a complicated infection, defined as multiple positive blood cultures or evidence of metastatic infection, patients received as few as 7 days or as many as 28 days of antibiotics, “reflecting the heterogeneity of these infections,” Dr. Holland reported at an annual scientific meeting on infectious diseases.
The coprimary endpoints were treatment success at test of cure and treatment safety, both of which were adjudicated by an external committee consisting of infectious disease specialists blinded to the therapy.
There were 509 patients from 16 sites in both the United States and Spain. CONS BSIs represented approximately 75% of patients in both arms. The complicated staphylococcal infections, which also were evenly distributed in the two arms, were included in the intention-to-treat analysis. Of complicated staphylococcal infections in this study, the pathogen was CONS in 34 instances and S. aureus in 37.
Treatment success was achieved in 82.0% and 81.5% of patients in the algorithm and SOC arms, respectively. Significant adverse events occurred in 32.9% and 28.3% of patients, respectively. Neither difference approached statistical significance.
“In other words, the algorithm was as effective and safe as standard of care,” Dr. Holland confirmed.
However, the median duration of treatment was reduced substantially for those randomized to the algorithm arm, compared with that seen in the standard of care arm. Among evaluable patients without complicated BSI, the mean duration of therapy was 4.4 days in the algorithm group vs. 6.2 days in the SOC group (P = .003). Most of this nearly 2-day reduction in treatment was achieved in uncomplicated CONS BSI patients. In this group, the mean days of treatment were 5.3 days and 8.4 days for the algorithm and SOC groups, respectively. In the uncomplicated S. aureus group, the reduction (from 15.9 to 15.3 days) was not significant.
“The study has several messages. For one, it suggests that patients who meet the criteria of simple staphylococcal BSI can be managed safely with monitoring alone. In addition, this study “provides the best evidence to date that 14 days of vancomycin from the first negative blood culture is sufficient in uncomplicated S. aureus bloodstream infections,” Dr. Holland stated.
“For many, these data will validate what they are already doing,” said Dr. Holland, who reported that the algorithm is now being applied routinely at his institution. “The value is that we now have a randomized trial to demonstrate that shorter therapy can be provided in uncomplicated staphylococcal blood stream infections without increasing risk of serious adverse events.”
SAN DIEGO – By standardizing antibiotic treatment for simple and uncomplicated staphylococcal bloodstream infections (BSI), an algorithm effectively shortens therapy and simplifies decision making, according to results of a multinational randomized trial.
“The data from the study confirm that the algorithm achieves more with less and verify that shorter antibiotic courses are sufficient,” reported Thomas L. Holland, MD, an infectious disease specialist at Duke University Hospital in Durham, N.C.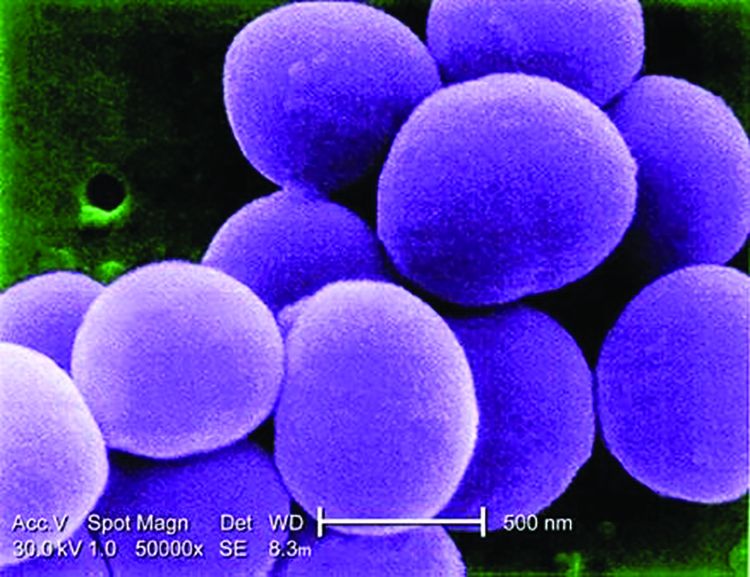
In this study, the patients randomized to algorithm treatment received vancomycin (or daptomycin in allergic or intolerant patients), which was administered for periods of duration based on clinical features. In those randomized to SOC, the choice and duration of antibiotics were left to the discretion of the treating physician without restrictions.
In those with simple staphylococcal BSI, the algorithm called for no further antibiotics beyond what had already been administered empirically prior to randomization. Key features of simple coagulase-negative staphylococcal (CONS) BSIs include absence of fever or evidence of metastatic infection, as well as no more than one positive follow-up blood culture. The key features of simple Staphylococcus aureus BSI are similar. However, no positive blood cultures are required for S. aureus BSI to be classified as simple.
“In the algorithm arm, no antibiotics were given to those with simple staphylococcal BSI unless antibiotics had been given prior to randomization,” Dr. Holland explained, but he acknowledged that empiric antibiotics prior to randomization reflect “clinical reality.”
In those with uncomplicated rather than simple staphylococcal BSI, vancomycin was given for 5 days to those with CONS BSI and for 14 days to those with S. aureus BSI. In those who were randomized and then subsequently found to have a complicated infection, defined as multiple positive blood cultures or evidence of metastatic infection, patients received as few as 7 days or as many as 28 days of antibiotics, “reflecting the heterogeneity of these infections,” Dr. Holland reported at an annual scientific meeting on infectious diseases.
The coprimary endpoints were treatment success at test of cure and treatment safety, both of which were adjudicated by an external committee consisting of infectious disease specialists blinded to the therapy.
There were 509 patients from 16 sites in both the United States and Spain. CONS BSIs represented approximately 75% of patients in both arms. The complicated staphylococcal infections, which also were evenly distributed in the two arms, were included in the intention-to-treat analysis. Of complicated staphylococcal infections in this study, the pathogen was CONS in 34 instances and S. aureus in 37.
Treatment success was achieved in 82.0% and 81.5% of patients in the algorithm and SOC arms, respectively. Significant adverse events occurred in 32.9% and 28.3% of patients, respectively. Neither difference approached statistical significance.
“In other words, the algorithm was as effective and safe as standard of care,” Dr. Holland confirmed.
However, the median duration of treatment was reduced substantially for those randomized to the algorithm arm, compared with that seen in the standard of care arm. Among evaluable patients without complicated BSI, the mean duration of therapy was 4.4 days in the algorithm group vs. 6.2 days in the SOC group (P = .003). Most of this nearly 2-day reduction in treatment was achieved in uncomplicated CONS BSI patients. In this group, the mean days of treatment were 5.3 days and 8.4 days for the algorithm and SOC groups, respectively. In the uncomplicated S. aureus group, the reduction (from 15.9 to 15.3 days) was not significant.
“The study has several messages. For one, it suggests that patients who meet the criteria of simple staphylococcal BSI can be managed safely with monitoring alone. In addition, this study “provides the best evidence to date that 14 days of vancomycin from the first negative blood culture is sufficient in uncomplicated S. aureus bloodstream infections,” Dr. Holland stated.
“For many, these data will validate what they are already doing,” said Dr. Holland, who reported that the algorithm is now being applied routinely at his institution. “The value is that we now have a randomized trial to demonstrate that shorter therapy can be provided in uncomplicated staphylococcal blood stream infections without increasing risk of serious adverse events.”
AT ID WEEK 2017
Key clinical point:
Major finding: With no change in outcome or differences in adverse events, the algorithm reduced average antibiotic duration by 1.9 days (P = .003).
Data source: A randomized, prospective, multicenter trial of 509 patients randomized at 16 sites in the United States and Spain.
Disclosures: Dr. Holland reports no financial relationships relevant to this study.
Post-Ebola syndrome includes neurologic sequelae
SAN DIEGO – Add neurologic issues to the growing list of medical problems faced by survivors of Ebola virus.
Among 153 Liberian patients about a year out from their acute illness, “there were only a handful who didn’t have” some lingering neurologic problem. “The most commonly reported ongoing symptoms were headache and memory loss. A couple of people had seizures possibly related to Ebola.” Depression, anxiety, and posttraumatic stress disorder were common, said neurologist Jeanne Billioux, MD, a clinical fellow at the National Institute of Neurological Disorders and Stroke, Bethesda, Md.
Almost two-thirds of the patients had abnormal neurologic exams. The most common findings were tremors, pathological reflexes, mild dysmetria, and abnormalities of eye pursuits and saccades, plus nystagmus. The findings were statistically significant, compared with 81 close contacts, generally household members, who served as controls in the ongoing natural history study, which was presented at the annual meeting of the American Neurological Association.
What’s become clear in the wake of the recent outbreak in West Africa, by far the worst to date with over 28,000 cases and more than 11,000 deaths, is that there is a post-Ebola syndrome that includes ophthalmologic, cardiac, and rheumatologic problems. It now appears that “neurologic sequelae are a part of it,” as well, she said.
The natural history study – dubbed the Partnership for Research on Ebola Virus in Liberia (PREVAIL III) – is a collaboration between the National Institutes of Health and the Ministry of Health of Liberia, one of the hardest-hit countries; the neurology investigation is just one component of the study, which includes about 1,500 patients overall.
Serology testing confirmed that cases truly did have Ebola, and the controls did not. After the first evaluation a year or so after the acute illness, patients have been followed up every 6 months, with some out to about 3 years.
Although patients aren’t back to normal, the good news is that their symptoms and exams are improving. “We started with only 6 who had no symptoms; now we have 15. Headaches are getting better; memory is getting better. It’s wonderful,” Dr. Billioux said.
The patients were asked to recall their acute symptoms during their first study visit. Many reported headaches, weakness, altered mental status, and cranial nerve symptoms. About 2% described convulsions or strokelike symptoms, and about 25% described symptoms consistent with meningitis.
It’s unclear how the virus affected the CNS, which isn’t considered to be a target organ. Perhaps fluid loss from severe diarrhea led to cerebral hypoperfusion. The cytokine storm during the acute phase might also have played a role. The virus has, however, been isolated from cerebral spinal fluid and, although uncommon, there are the reports of meningitis symptoms, so perhaps it does have direct CNS effects. Much remains to be learned.
Both cases and controls were a mean of about 35 years old, and evenly split between the sexes; 108 patients (70.6%) spent more than 2 weeks in an Ebola treatment unit.
The work was funded by the National Institutes of Health. Dr. Billioux had no disclosures.
SAN DIEGO – Add neurologic issues to the growing list of medical problems faced by survivors of Ebola virus.
Among 153 Liberian patients about a year out from their acute illness, “there were only a handful who didn’t have” some lingering neurologic problem. “The most commonly reported ongoing symptoms were headache and memory loss. A couple of people had seizures possibly related to Ebola.” Depression, anxiety, and posttraumatic stress disorder were common, said neurologist Jeanne Billioux, MD, a clinical fellow at the National Institute of Neurological Disorders and Stroke, Bethesda, Md.
Almost two-thirds of the patients had abnormal neurologic exams. The most common findings were tremors, pathological reflexes, mild dysmetria, and abnormalities of eye pursuits and saccades, plus nystagmus. The findings were statistically significant, compared with 81 close contacts, generally household members, who served as controls in the ongoing natural history study, which was presented at the annual meeting of the American Neurological Association.
What’s become clear in the wake of the recent outbreak in West Africa, by far the worst to date with over 28,000 cases and more than 11,000 deaths, is that there is a post-Ebola syndrome that includes ophthalmologic, cardiac, and rheumatologic problems. It now appears that “neurologic sequelae are a part of it,” as well, she said.
The natural history study – dubbed the Partnership for Research on Ebola Virus in Liberia (PREVAIL III) – is a collaboration between the National Institutes of Health and the Ministry of Health of Liberia, one of the hardest-hit countries; the neurology investigation is just one component of the study, which includes about 1,500 patients overall.
Serology testing confirmed that cases truly did have Ebola, and the controls did not. After the first evaluation a year or so after the acute illness, patients have been followed up every 6 months, with some out to about 3 years.
Although patients aren’t back to normal, the good news is that their symptoms and exams are improving. “We started with only 6 who had no symptoms; now we have 15. Headaches are getting better; memory is getting better. It’s wonderful,” Dr. Billioux said.
The patients were asked to recall their acute symptoms during their first study visit. Many reported headaches, weakness, altered mental status, and cranial nerve symptoms. About 2% described convulsions or strokelike symptoms, and about 25% described symptoms consistent with meningitis.
It’s unclear how the virus affected the CNS, which isn’t considered to be a target organ. Perhaps fluid loss from severe diarrhea led to cerebral hypoperfusion. The cytokine storm during the acute phase might also have played a role. The virus has, however, been isolated from cerebral spinal fluid and, although uncommon, there are the reports of meningitis symptoms, so perhaps it does have direct CNS effects. Much remains to be learned.
Both cases and controls were a mean of about 35 years old, and evenly split between the sexes; 108 patients (70.6%) spent more than 2 weeks in an Ebola treatment unit.
The work was funded by the National Institutes of Health. Dr. Billioux had no disclosures.
SAN DIEGO – Add neurologic issues to the growing list of medical problems faced by survivors of Ebola virus.
Among 153 Liberian patients about a year out from their acute illness, “there were only a handful who didn’t have” some lingering neurologic problem. “The most commonly reported ongoing symptoms were headache and memory loss. A couple of people had seizures possibly related to Ebola.” Depression, anxiety, and posttraumatic stress disorder were common, said neurologist Jeanne Billioux, MD, a clinical fellow at the National Institute of Neurological Disorders and Stroke, Bethesda, Md.
Almost two-thirds of the patients had abnormal neurologic exams. The most common findings were tremors, pathological reflexes, mild dysmetria, and abnormalities of eye pursuits and saccades, plus nystagmus. The findings were statistically significant, compared with 81 close contacts, generally household members, who served as controls in the ongoing natural history study, which was presented at the annual meeting of the American Neurological Association.
What’s become clear in the wake of the recent outbreak in West Africa, by far the worst to date with over 28,000 cases and more than 11,000 deaths, is that there is a post-Ebola syndrome that includes ophthalmologic, cardiac, and rheumatologic problems. It now appears that “neurologic sequelae are a part of it,” as well, she said.
The natural history study – dubbed the Partnership for Research on Ebola Virus in Liberia (PREVAIL III) – is a collaboration between the National Institutes of Health and the Ministry of Health of Liberia, one of the hardest-hit countries; the neurology investigation is just one component of the study, which includes about 1,500 patients overall.
Serology testing confirmed that cases truly did have Ebola, and the controls did not. After the first evaluation a year or so after the acute illness, patients have been followed up every 6 months, with some out to about 3 years.
Although patients aren’t back to normal, the good news is that their symptoms and exams are improving. “We started with only 6 who had no symptoms; now we have 15. Headaches are getting better; memory is getting better. It’s wonderful,” Dr. Billioux said.
The patients were asked to recall their acute symptoms during their first study visit. Many reported headaches, weakness, altered mental status, and cranial nerve symptoms. About 2% described convulsions or strokelike symptoms, and about 25% described symptoms consistent with meningitis.
It’s unclear how the virus affected the CNS, which isn’t considered to be a target organ. Perhaps fluid loss from severe diarrhea led to cerebral hypoperfusion. The cytokine storm during the acute phase might also have played a role. The virus has, however, been isolated from cerebral spinal fluid and, although uncommon, there are the reports of meningitis symptoms, so perhaps it does have direct CNS effects. Much remains to be learned.
Both cases and controls were a mean of about 35 years old, and evenly split between the sexes; 108 patients (70.6%) spent more than 2 weeks in an Ebola treatment unit.
The work was funded by the National Institutes of Health. Dr. Billioux had no disclosures.
AT ANA 2017
Key clinical point:
Major finding: A year after their acute infection, almost two-thirds of Ebola survivors had abnormal neurologic exams.
Data source: Natural history study involving 153 patients
Disclosures: The work was funded by the National Institutes of Health. The lead investigator had no disclosures.