User login
Study Reveals Tumor Blood Vessels Cluster in Beltlike Zones
Digital pathology has made it possible to measure microscopic objects, such as blood vessels in tumor tissue and then visualize them in density maps, showing hotspot regions. But for many applications in histopathology, there is no clear-cut definition of the hotspots, say researchers from Heidelberg University in Germany. Thus, most tumor models “implicitly assume” that blood vessels are equally abundant in different parts of a tumor. But the researchers’ new computational approach to mapping angiogenesis in colorectal cancer (CRC) could change that assumption.
Related: In Rare Case Colorectal Cancer Causes Thrombus
Their method analyzes blood vessels based on spatial statistics, identifying all hotspot areas that are unlikely to occur by chance. The researchers found that in nearly all cases, the blood vessels grouped in a distinctive beltlike pattern. In 33 of 34 untreated colorectal tumor samples, the blood vessels were aggregated at the interface of tumor tissue to the intestinal wall. The researchers found similar “hypervascularized” zones at the boundaries of liver tissue in 100% of the samples of CRC liver metastases. Ultimately, they describe a new model of tumor vascularization: a highly vascularized zone about 1.5-mm wide close to the intestinal lumen in CRC primary tumors and a highly vascularized zone approximately 1-mm wide close to the invasion front in CRC liver metastases.
Related: Colorectal Screening: Available but Underused
Their model has immediate and far-reaching implications, the researchers say. For instance, because vascular patterns determine how chemotherapeutic drugs are distributed in tumor tissue, it is likely that these drugs reach the luminal side of CRC tumors much easier than they reach the the basolateral side. Their new information also could be used in timing surgery, since the tumor parts of the deep invasion front may be less sensitive to chemotherapy. The researchers suggest that using their model could help optimize treatment in any number of ways: explaining early symptoms like gastrointestinal bleeding, the architecture of CRC, metastasis, and opening new pathways for investigation.
Source:
Kather JN, Zöllner FG, Schad LR. PLoS One. 2017;12(3):e0171378.
doi: 10.1371/journal.pone.0171378.
Digital pathology has made it possible to measure microscopic objects, such as blood vessels in tumor tissue and then visualize them in density maps, showing hotspot regions. But for many applications in histopathology, there is no clear-cut definition of the hotspots, say researchers from Heidelberg University in Germany. Thus, most tumor models “implicitly assume” that blood vessels are equally abundant in different parts of a tumor. But the researchers’ new computational approach to mapping angiogenesis in colorectal cancer (CRC) could change that assumption.
Related: In Rare Case Colorectal Cancer Causes Thrombus
Their method analyzes blood vessels based on spatial statistics, identifying all hotspot areas that are unlikely to occur by chance. The researchers found that in nearly all cases, the blood vessels grouped in a distinctive beltlike pattern. In 33 of 34 untreated colorectal tumor samples, the blood vessels were aggregated at the interface of tumor tissue to the intestinal wall. The researchers found similar “hypervascularized” zones at the boundaries of liver tissue in 100% of the samples of CRC liver metastases. Ultimately, they describe a new model of tumor vascularization: a highly vascularized zone about 1.5-mm wide close to the intestinal lumen in CRC primary tumors and a highly vascularized zone approximately 1-mm wide close to the invasion front in CRC liver metastases.
Related: Colorectal Screening: Available but Underused
Their model has immediate and far-reaching implications, the researchers say. For instance, because vascular patterns determine how chemotherapeutic drugs are distributed in tumor tissue, it is likely that these drugs reach the luminal side of CRC tumors much easier than they reach the the basolateral side. Their new information also could be used in timing surgery, since the tumor parts of the deep invasion front may be less sensitive to chemotherapy. The researchers suggest that using their model could help optimize treatment in any number of ways: explaining early symptoms like gastrointestinal bleeding, the architecture of CRC, metastasis, and opening new pathways for investigation.
Source:
Kather JN, Zöllner FG, Schad LR. PLoS One. 2017;12(3):e0171378.
doi: 10.1371/journal.pone.0171378.
Digital pathology has made it possible to measure microscopic objects, such as blood vessels in tumor tissue and then visualize them in density maps, showing hotspot regions. But for many applications in histopathology, there is no clear-cut definition of the hotspots, say researchers from Heidelberg University in Germany. Thus, most tumor models “implicitly assume” that blood vessels are equally abundant in different parts of a tumor. But the researchers’ new computational approach to mapping angiogenesis in colorectal cancer (CRC) could change that assumption.
Related: In Rare Case Colorectal Cancer Causes Thrombus
Their method analyzes blood vessels based on spatial statistics, identifying all hotspot areas that are unlikely to occur by chance. The researchers found that in nearly all cases, the blood vessels grouped in a distinctive beltlike pattern. In 33 of 34 untreated colorectal tumor samples, the blood vessels were aggregated at the interface of tumor tissue to the intestinal wall. The researchers found similar “hypervascularized” zones at the boundaries of liver tissue in 100% of the samples of CRC liver metastases. Ultimately, they describe a new model of tumor vascularization: a highly vascularized zone about 1.5-mm wide close to the intestinal lumen in CRC primary tumors and a highly vascularized zone approximately 1-mm wide close to the invasion front in CRC liver metastases.
Related: Colorectal Screening: Available but Underused
Their model has immediate and far-reaching implications, the researchers say. For instance, because vascular patterns determine how chemotherapeutic drugs are distributed in tumor tissue, it is likely that these drugs reach the luminal side of CRC tumors much easier than they reach the the basolateral side. Their new information also could be used in timing surgery, since the tumor parts of the deep invasion front may be less sensitive to chemotherapy. The researchers suggest that using their model could help optimize treatment in any number of ways: explaining early symptoms like gastrointestinal bleeding, the architecture of CRC, metastasis, and opening new pathways for investigation.
Source:
Kather JN, Zöllner FG, Schad LR. PLoS One. 2017;12(3):e0171378.
doi: 10.1371/journal.pone.0171378.
In Rare Case Colorectal Cancer Causes Thrombus
A 46-year-old woman went to her family doctor after 3 months of abdominal bloating, fatigue, nausea, vomiting, anorexia, and weight loss. Ultrasound imaging revealed hepatic lesions and a mass in the colon; she was diagnosed with colon cancer. The cancer had metastasized to an extent that complete resection wasn’t possible, so she received palliative-intent therapy for the next 18 months.
Related: Colorectal Screening: Available but Underused
Initially, the patient responded to the treatment but then presented to the emergency department (ED) with a severe headache. A CT scan revealed that the cancer had spread to her brain. However, this time resection was possible, and she recovered well.
Three weeks later the patient was back in the ED with an infection. A new CT scan showed no evidence of abscess (one of the differential diagnoses). A transthoracic echocardiogram showed a right atrial lesion, and further imaging confirmed a lesion in the right atrium. “Unexpectedly,” her clinicians reported, the lesion originated from the distal inferior vena cava (IVC): She had shown no signs of symptoms of pulmonary embolus or occlusion of the IVC.
Tumor thrombus is rarely reported with colorectal cancer cases, so the patient’s clinicians at first thought the mass in the IVC was bland thrombus, managed with anticoagulation alone. The clinicians felt that the assumption was reasonable, given the link between malignancy and venous thromboembolism; also because the patient had an indwelling central venous catheter. Contrast-enhanced CT scan and contrast-enhanced ultrasound, however, supported the diagnosis of tumor thrombus.
Due to the rarity of tumor thrombus in colorectal cancer, there are no guidelines for diagnosis and management, the clinicians say. In the patient’s case, consultation with cardiologists, radiologists, and gastrointestinal specialists at the cancer center resulted in an offer to extract the thrombus, but the risks and the fact that she was asymptomatic led the patient to decline. She was instead restarted on palliative chemotherapy with heparin in case part of the thrombus was indeed bland thrombus.
The patient’s condition deteriorated over the next 3 months. She and her team agreed that supportive care at home was best. The patient still had no symptoms from the tumor thrombus when she died.
Related: Cancer Prevention and Gastrointestinal Risk
Autopsy supported the suspicion that the original lesion was partly tumor thrombus and partly bland thrombus, reduced by anticoagulation. But autopsy results revealed no embolization of tumor thrombus or bland thrombus into the pulmonary arteries, although there were extensive metastases in the brain, lung, liver, adrenals, and ovaries. Ultimately, the patient’s death was attributed not to the tumor thrombus that extended into the right atrium but to multiorgan failure due to cancer--validating the decisions to not choose surgery for the thrombus.
Source:
Meyers D, Nixon NA, Franko A, Ng D, Tam VC. BMJ Case Rep. 2017;2017:pii:bcr2016218107.
doi: 10.1136/bcr-2016-218107.
A 46-year-old woman went to her family doctor after 3 months of abdominal bloating, fatigue, nausea, vomiting, anorexia, and weight loss. Ultrasound imaging revealed hepatic lesions and a mass in the colon; she was diagnosed with colon cancer. The cancer had metastasized to an extent that complete resection wasn’t possible, so she received palliative-intent therapy for the next 18 months.
Related: Colorectal Screening: Available but Underused
Initially, the patient responded to the treatment but then presented to the emergency department (ED) with a severe headache. A CT scan revealed that the cancer had spread to her brain. However, this time resection was possible, and she recovered well.
Three weeks later the patient was back in the ED with an infection. A new CT scan showed no evidence of abscess (one of the differential diagnoses). A transthoracic echocardiogram showed a right atrial lesion, and further imaging confirmed a lesion in the right atrium. “Unexpectedly,” her clinicians reported, the lesion originated from the distal inferior vena cava (IVC): She had shown no signs of symptoms of pulmonary embolus or occlusion of the IVC.
Tumor thrombus is rarely reported with colorectal cancer cases, so the patient’s clinicians at first thought the mass in the IVC was bland thrombus, managed with anticoagulation alone. The clinicians felt that the assumption was reasonable, given the link between malignancy and venous thromboembolism; also because the patient had an indwelling central venous catheter. Contrast-enhanced CT scan and contrast-enhanced ultrasound, however, supported the diagnosis of tumor thrombus.
Due to the rarity of tumor thrombus in colorectal cancer, there are no guidelines for diagnosis and management, the clinicians say. In the patient’s case, consultation with cardiologists, radiologists, and gastrointestinal specialists at the cancer center resulted in an offer to extract the thrombus, but the risks and the fact that she was asymptomatic led the patient to decline. She was instead restarted on palliative chemotherapy with heparin in case part of the thrombus was indeed bland thrombus.
The patient’s condition deteriorated over the next 3 months. She and her team agreed that supportive care at home was best. The patient still had no symptoms from the tumor thrombus when she died.
Related: Cancer Prevention and Gastrointestinal Risk
Autopsy supported the suspicion that the original lesion was partly tumor thrombus and partly bland thrombus, reduced by anticoagulation. But autopsy results revealed no embolization of tumor thrombus or bland thrombus into the pulmonary arteries, although there were extensive metastases in the brain, lung, liver, adrenals, and ovaries. Ultimately, the patient’s death was attributed not to the tumor thrombus that extended into the right atrium but to multiorgan failure due to cancer--validating the decisions to not choose surgery for the thrombus.
Source:
Meyers D, Nixon NA, Franko A, Ng D, Tam VC. BMJ Case Rep. 2017;2017:pii:bcr2016218107.
doi: 10.1136/bcr-2016-218107.
A 46-year-old woman went to her family doctor after 3 months of abdominal bloating, fatigue, nausea, vomiting, anorexia, and weight loss. Ultrasound imaging revealed hepatic lesions and a mass in the colon; she was diagnosed with colon cancer. The cancer had metastasized to an extent that complete resection wasn’t possible, so she received palliative-intent therapy for the next 18 months.
Related: Colorectal Screening: Available but Underused
Initially, the patient responded to the treatment but then presented to the emergency department (ED) with a severe headache. A CT scan revealed that the cancer had spread to her brain. However, this time resection was possible, and she recovered well.
Three weeks later the patient was back in the ED with an infection. A new CT scan showed no evidence of abscess (one of the differential diagnoses). A transthoracic echocardiogram showed a right atrial lesion, and further imaging confirmed a lesion in the right atrium. “Unexpectedly,” her clinicians reported, the lesion originated from the distal inferior vena cava (IVC): She had shown no signs of symptoms of pulmonary embolus or occlusion of the IVC.
Tumor thrombus is rarely reported with colorectal cancer cases, so the patient’s clinicians at first thought the mass in the IVC was bland thrombus, managed with anticoagulation alone. The clinicians felt that the assumption was reasonable, given the link between malignancy and venous thromboembolism; also because the patient had an indwelling central venous catheter. Contrast-enhanced CT scan and contrast-enhanced ultrasound, however, supported the diagnosis of tumor thrombus.
Due to the rarity of tumor thrombus in colorectal cancer, there are no guidelines for diagnosis and management, the clinicians say. In the patient’s case, consultation with cardiologists, radiologists, and gastrointestinal specialists at the cancer center resulted in an offer to extract the thrombus, but the risks and the fact that she was asymptomatic led the patient to decline. She was instead restarted on palliative chemotherapy with heparin in case part of the thrombus was indeed bland thrombus.
The patient’s condition deteriorated over the next 3 months. She and her team agreed that supportive care at home was best. The patient still had no symptoms from the tumor thrombus when she died.
Related: Cancer Prevention and Gastrointestinal Risk
Autopsy supported the suspicion that the original lesion was partly tumor thrombus and partly bland thrombus, reduced by anticoagulation. But autopsy results revealed no embolization of tumor thrombus or bland thrombus into the pulmonary arteries, although there were extensive metastases in the brain, lung, liver, adrenals, and ovaries. Ultimately, the patient’s death was attributed not to the tumor thrombus that extended into the right atrium but to multiorgan failure due to cancer--validating the decisions to not choose surgery for the thrombus.
Source:
Meyers D, Nixon NA, Franko A, Ng D, Tam VC. BMJ Case Rep. 2017;2017:pii:bcr2016218107.
doi: 10.1136/bcr-2016-218107.
Transanal TME comparable to open, lap approaches to rectal cancer
HOUSTON – Transanal total mesorectal excision can consistently achieve good pathological results for obtaining specimens in rectal cancer, and overcome the shortcomings of the open and laparoscopic approaches to rectal cancer surgery, particularly in the distal part of the rectum where obtaining quality specimens can be technically challenging, researchers at the Hospital Clinic of Barcelona have found.
Reporting at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons, Jacqueline van Laarhoven, MD, PhD, said, “Pathologically, transanal total mesorectal excision [TME] provides good results on integrity of the mesorectum, negative circumferential and distal resection margins, and lymph nodes per specimen.” This study represents the first results of a relatively large, single-institution cohort, Dr. van Laarhoven said.
The study involved 187 patients with mid- or low-rectal cancer who had transanal TME from November 2011 to June 2016. Dr. van Laarhoven explained that obtaining high-quality specimens is an important prognostic factor for determining locoregional recurrence in rectal cancer. The study analyzed results of excised specimens in the mesorectum, circumferential and distal resected margins, and lymph nodes, and compared outcomes with those in two randomized clinical trials of both open and laparoscopic TME – the COLOR II (Lancet Oncol. 2013;14:210-8) and COREAN trials (Lancet Oncol. 2014;15:767-74) – where applicable.
In the Barcelona study population, 63.1% had tumors in the midrectum and 36.9% in the low rectum. Transanal TME yielded complete mesorectal quality in 95.7% of cases, almost-complete quality in 1.6% and incomplete in 1.1%, but comparison with COLOR II and COREAN trials was difficult because of differing inclusion criteria, Dr. van Laarhoven said.
Mean distal margin was 2.1 cm in midrectal cancer with a positive distal resection margin in 3.2%. In low-rectal cancer, the mean distal margin was 1.1 cm with a positive distal resection margin in 7.8%. Dr. van Laarhoven noted the overall circumferential resection margin (CRM) was 8.6% in this study, compared with 8.3% overall for the COREAN trial. As for COLOR II, the overall rate for positive CRM in mid- and low-rectal tumors was around 9%, Dr. van Laarhoven said, but in the open group the positive CRM was 3% in the midrectal excisions and 22% in low-rectal disease.
With regard to lymph nodes, the Barcelona study reported a median of 14 per specimen, with a range of 11 to 18, Dr. van Laarhoven said. However, in nonirradiated patients, the median was 15 per specimen. “This is consistent with the fact that neoadjuvant radiotherapy leads to a decrease in the lymph-node harvest,” she said. “These results are comparable to the COREAN and the COLOR II trials.”
Sixty-two percent of patients received neoadjuvant chemoradiotherapy, 3.2% received radiotherapy only, and 2.1% chemotherapy only.
On preoperative staging, 3.2% had T1 tumors, 20.3% T2, 67.9% T3, and 7.5% T4. The overall positive CRM (less than 1 mm) was 8.6% (including T4 tumors).
Postoperative pathological staging showed complete remission in 16% of patients, pT1 in 6.4%, pT2 in 28.9%, pT3 in 42.8%, pT4 in 2.7%, and pTis in 1.6%.
Dr. van Laarhoven commented, “As the quality of the surgical treatment is a surrogate marker for survival, transanal TME can be regarded as an oncologically safe method to treat patients with rectal cancer.”
Dr. van Laarhoven reported having no financial disclosures.
HOUSTON – Transanal total mesorectal excision can consistently achieve good pathological results for obtaining specimens in rectal cancer, and overcome the shortcomings of the open and laparoscopic approaches to rectal cancer surgery, particularly in the distal part of the rectum where obtaining quality specimens can be technically challenging, researchers at the Hospital Clinic of Barcelona have found.
Reporting at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons, Jacqueline van Laarhoven, MD, PhD, said, “Pathologically, transanal total mesorectal excision [TME] provides good results on integrity of the mesorectum, negative circumferential and distal resection margins, and lymph nodes per specimen.” This study represents the first results of a relatively large, single-institution cohort, Dr. van Laarhoven said.
The study involved 187 patients with mid- or low-rectal cancer who had transanal TME from November 2011 to June 2016. Dr. van Laarhoven explained that obtaining high-quality specimens is an important prognostic factor for determining locoregional recurrence in rectal cancer. The study analyzed results of excised specimens in the mesorectum, circumferential and distal resected margins, and lymph nodes, and compared outcomes with those in two randomized clinical trials of both open and laparoscopic TME – the COLOR II (Lancet Oncol. 2013;14:210-8) and COREAN trials (Lancet Oncol. 2014;15:767-74) – where applicable.
In the Barcelona study population, 63.1% had tumors in the midrectum and 36.9% in the low rectum. Transanal TME yielded complete mesorectal quality in 95.7% of cases, almost-complete quality in 1.6% and incomplete in 1.1%, but comparison with COLOR II and COREAN trials was difficult because of differing inclusion criteria, Dr. van Laarhoven said.
Mean distal margin was 2.1 cm in midrectal cancer with a positive distal resection margin in 3.2%. In low-rectal cancer, the mean distal margin was 1.1 cm with a positive distal resection margin in 7.8%. Dr. van Laarhoven noted the overall circumferential resection margin (CRM) was 8.6% in this study, compared with 8.3% overall for the COREAN trial. As for COLOR II, the overall rate for positive CRM in mid- and low-rectal tumors was around 9%, Dr. van Laarhoven said, but in the open group the positive CRM was 3% in the midrectal excisions and 22% in low-rectal disease.
With regard to lymph nodes, the Barcelona study reported a median of 14 per specimen, with a range of 11 to 18, Dr. van Laarhoven said. However, in nonirradiated patients, the median was 15 per specimen. “This is consistent with the fact that neoadjuvant radiotherapy leads to a decrease in the lymph-node harvest,” she said. “These results are comparable to the COREAN and the COLOR II trials.”
Sixty-two percent of patients received neoadjuvant chemoradiotherapy, 3.2% received radiotherapy only, and 2.1% chemotherapy only.
On preoperative staging, 3.2% had T1 tumors, 20.3% T2, 67.9% T3, and 7.5% T4. The overall positive CRM (less than 1 mm) was 8.6% (including T4 tumors).
Postoperative pathological staging showed complete remission in 16% of patients, pT1 in 6.4%, pT2 in 28.9%, pT3 in 42.8%, pT4 in 2.7%, and pTis in 1.6%.
Dr. van Laarhoven commented, “As the quality of the surgical treatment is a surrogate marker for survival, transanal TME can be regarded as an oncologically safe method to treat patients with rectal cancer.”
Dr. van Laarhoven reported having no financial disclosures.
HOUSTON – Transanal total mesorectal excision can consistently achieve good pathological results for obtaining specimens in rectal cancer, and overcome the shortcomings of the open and laparoscopic approaches to rectal cancer surgery, particularly in the distal part of the rectum where obtaining quality specimens can be technically challenging, researchers at the Hospital Clinic of Barcelona have found.
Reporting at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons, Jacqueline van Laarhoven, MD, PhD, said, “Pathologically, transanal total mesorectal excision [TME] provides good results on integrity of the mesorectum, negative circumferential and distal resection margins, and lymph nodes per specimen.” This study represents the first results of a relatively large, single-institution cohort, Dr. van Laarhoven said.
The study involved 187 patients with mid- or low-rectal cancer who had transanal TME from November 2011 to June 2016. Dr. van Laarhoven explained that obtaining high-quality specimens is an important prognostic factor for determining locoregional recurrence in rectal cancer. The study analyzed results of excised specimens in the mesorectum, circumferential and distal resected margins, and lymph nodes, and compared outcomes with those in two randomized clinical trials of both open and laparoscopic TME – the COLOR II (Lancet Oncol. 2013;14:210-8) and COREAN trials (Lancet Oncol. 2014;15:767-74) – where applicable.
In the Barcelona study population, 63.1% had tumors in the midrectum and 36.9% in the low rectum. Transanal TME yielded complete mesorectal quality in 95.7% of cases, almost-complete quality in 1.6% and incomplete in 1.1%, but comparison with COLOR II and COREAN trials was difficult because of differing inclusion criteria, Dr. van Laarhoven said.
Mean distal margin was 2.1 cm in midrectal cancer with a positive distal resection margin in 3.2%. In low-rectal cancer, the mean distal margin was 1.1 cm with a positive distal resection margin in 7.8%. Dr. van Laarhoven noted the overall circumferential resection margin (CRM) was 8.6% in this study, compared with 8.3% overall for the COREAN trial. As for COLOR II, the overall rate for positive CRM in mid- and low-rectal tumors was around 9%, Dr. van Laarhoven said, but in the open group the positive CRM was 3% in the midrectal excisions and 22% in low-rectal disease.
With regard to lymph nodes, the Barcelona study reported a median of 14 per specimen, with a range of 11 to 18, Dr. van Laarhoven said. However, in nonirradiated patients, the median was 15 per specimen. “This is consistent with the fact that neoadjuvant radiotherapy leads to a decrease in the lymph-node harvest,” she said. “These results are comparable to the COREAN and the COLOR II trials.”
Sixty-two percent of patients received neoadjuvant chemoradiotherapy, 3.2% received radiotherapy only, and 2.1% chemotherapy only.
On preoperative staging, 3.2% had T1 tumors, 20.3% T2, 67.9% T3, and 7.5% T4. The overall positive CRM (less than 1 mm) was 8.6% (including T4 tumors).
Postoperative pathological staging showed complete remission in 16% of patients, pT1 in 6.4%, pT2 in 28.9%, pT3 in 42.8%, pT4 in 2.7%, and pTis in 1.6%.
Dr. van Laarhoven commented, “As the quality of the surgical treatment is a surrogate marker for survival, transanal TME can be regarded as an oncologically safe method to treat patients with rectal cancer.”
Dr. van Laarhoven reported having no financial disclosures.
AT SAGES 2017
Key clinical point: Transanal total mesorectal excision (TME) is a viable alternative to open or laparoscopic TME in cancers of the low and midrectum.
Major finding: Postoperative pathological staging showed complete remission in 16%, with pT1 in 6.4%, pT2 in 28.9%, pT3 in 42.8%, pT4 in 2.7%, and pTis in 1.6%.
Data source: Analysis of 187 patients prospectively enrolled in a standardized database who had transanal TME from November 2011 to June 2016 at a single center.
Disclosures: Dr. van Laarhoven reported having no financial disclosures.
Disease site determines QOL, pain in recurrent rectal cancer
SEATTLE – Disease anatomy is the main determinant of subsequent quality of life (QOL) in patients with locally recurrent rectal cancer at both base line and in the long term, according to findings presented at the annual Society of Surgical Oncology Cancer Symposium.
Posterior recurrences were associated with the worst QOL scores and the most severe pain.
Recurrent rectal cancer is a morbid disease state, leading to pain and disability. “Patients experience a multitude of symptoms, including disability as a result of tumor growth in a confined space in the pelvis and invasion of adjacent organs as well as complications from surgery and neoadjuvant treatment,” said lead author Dr. Tarik Sammour of the University of Texas MD Anderson Cancer Center in Houston.
He noted, however, that “it is not all doom and gloom.” Survival outcomes have been improving in this population, with the median 5-year survival now approaching 40%-50%.
“Decade by decade, the 5-year survival outcomes are increasing,” explained Dr. Sammour.
Increasing survival also begs the question: “Are we helping patients or affording them the option of living longer with pain and disability? In other words, we need to measure patient-centered outcomes,” he said.
Data for recurrent rectal cancer are very limited, particularly when it comes to measuring patient outcomes. Most studies have been retrospective in design, making it difficult to gauge symptoms and quality of life.
The majority of studies also have focused on surgery, have short follow-up times, and may be missing data.
“Very few measure baseline quality of life, so it makes it difficult to measure trajectories,” Dr. Sammour said. “So overall we don’t know very much about the quality of life of these patients, so we thought to remedy that with a prospective study.”
Dr. Sammour and his colleagues examined the longitudinal trajectory of cancer survivorship in recurrent rectal cancer over a 7-year period. A total of 104 patients diagnosed with recurrent rectal cancer were enrolled between 2008 and 2015, and they prospectively self reported QOL using the validated EORTC QLQ-C30 and EORTC QLQ-CR29. Pain was measured by the Brief Pain Inventory.
Symptoms were measured at baseline and then every 6 months for 5 years or until death.
Within this cohort, 73 (70.2%) patients were amenable to salvage surgery with curative intent. A variety of types of surgery were performed, and R0 resection was achieved in 75% of cases.
The 30-day complication rate was 49% (21% with grade 3/4), and 5-year disease-free survival was 40%. There was no immediate mortality from the surgery.
When looking at differences between patients who underwent surgery and those who didn’t, there was a significant difference in the location of the disease. The nonsurgical group was more likely to have posterior recurrences (26%) than was the surgical group (19%).
“This makes sense since these are more difficult to achieve a R0 result with, so it may be less likely that they were offered the procedure,” Dr. Sammour said.
There was also a significant difference in estimated 5-year survival. Overall survival was 7.7% in the nonsurgical group vs. 50.9% in the surgical group (P less than .0001), and cancer-specific survival was 11.5% vs. 59.6% (P less than .0001).
As for pain and QOL scores, there were no differences between groups at baseline.
“So when they arrived at clinic they had roughly equivalent quality of life,” he said.
At follow-up, male patients were more likely to experience severe pain, but “we felt it was due to the anatomical location. Men have a narrower pelvis and don’t have the luxury of a uterus to protect the genitourinary organs,” he explained. “We suspect this may have played a role in the severity of their pain.”
Patients with posterior recurrences also had worse pain, and this was true for both surgical and nonsurgical patients.
The only determinant for QOL in those who underwent surgery was a positive margin (global health score 70.4 for negative margin and 61.9 for positive margins [P = .024]), but otherwise there were no differences by type of surgery or postoperative complications.
At a median follow-up of 33 months, patients who underwent surgery showed gradual sustained improvement in QOL but not pain scores.
“We were encouraged to see improvement,” concluded Dr. Sammour. “Surgery does improve quality of life in resectable cases.”
No funding source was disclosed. Dr. Sammour and his coauthors had no disclosures.
SEATTLE – Disease anatomy is the main determinant of subsequent quality of life (QOL) in patients with locally recurrent rectal cancer at both base line and in the long term, according to findings presented at the annual Society of Surgical Oncology Cancer Symposium.
Posterior recurrences were associated with the worst QOL scores and the most severe pain.
Recurrent rectal cancer is a morbid disease state, leading to pain and disability. “Patients experience a multitude of symptoms, including disability as a result of tumor growth in a confined space in the pelvis and invasion of adjacent organs as well as complications from surgery and neoadjuvant treatment,” said lead author Dr. Tarik Sammour of the University of Texas MD Anderson Cancer Center in Houston.
He noted, however, that “it is not all doom and gloom.” Survival outcomes have been improving in this population, with the median 5-year survival now approaching 40%-50%.
“Decade by decade, the 5-year survival outcomes are increasing,” explained Dr. Sammour.
Increasing survival also begs the question: “Are we helping patients or affording them the option of living longer with pain and disability? In other words, we need to measure patient-centered outcomes,” he said.
Data for recurrent rectal cancer are very limited, particularly when it comes to measuring patient outcomes. Most studies have been retrospective in design, making it difficult to gauge symptoms and quality of life.
The majority of studies also have focused on surgery, have short follow-up times, and may be missing data.
“Very few measure baseline quality of life, so it makes it difficult to measure trajectories,” Dr. Sammour said. “So overall we don’t know very much about the quality of life of these patients, so we thought to remedy that with a prospective study.”
Dr. Sammour and his colleagues examined the longitudinal trajectory of cancer survivorship in recurrent rectal cancer over a 7-year period. A total of 104 patients diagnosed with recurrent rectal cancer were enrolled between 2008 and 2015, and they prospectively self reported QOL using the validated EORTC QLQ-C30 and EORTC QLQ-CR29. Pain was measured by the Brief Pain Inventory.
Symptoms were measured at baseline and then every 6 months for 5 years or until death.
Within this cohort, 73 (70.2%) patients were amenable to salvage surgery with curative intent. A variety of types of surgery were performed, and R0 resection was achieved in 75% of cases.
The 30-day complication rate was 49% (21% with grade 3/4), and 5-year disease-free survival was 40%. There was no immediate mortality from the surgery.
When looking at differences between patients who underwent surgery and those who didn’t, there was a significant difference in the location of the disease. The nonsurgical group was more likely to have posterior recurrences (26%) than was the surgical group (19%).
“This makes sense since these are more difficult to achieve a R0 result with, so it may be less likely that they were offered the procedure,” Dr. Sammour said.
There was also a significant difference in estimated 5-year survival. Overall survival was 7.7% in the nonsurgical group vs. 50.9% in the surgical group (P less than .0001), and cancer-specific survival was 11.5% vs. 59.6% (P less than .0001).
As for pain and QOL scores, there were no differences between groups at baseline.
“So when they arrived at clinic they had roughly equivalent quality of life,” he said.
At follow-up, male patients were more likely to experience severe pain, but “we felt it was due to the anatomical location. Men have a narrower pelvis and don’t have the luxury of a uterus to protect the genitourinary organs,” he explained. “We suspect this may have played a role in the severity of their pain.”
Patients with posterior recurrences also had worse pain, and this was true for both surgical and nonsurgical patients.
The only determinant for QOL in those who underwent surgery was a positive margin (global health score 70.4 for negative margin and 61.9 for positive margins [P = .024]), but otherwise there were no differences by type of surgery or postoperative complications.
At a median follow-up of 33 months, patients who underwent surgery showed gradual sustained improvement in QOL but not pain scores.
“We were encouraged to see improvement,” concluded Dr. Sammour. “Surgery does improve quality of life in resectable cases.”
No funding source was disclosed. Dr. Sammour and his coauthors had no disclosures.
SEATTLE – Disease anatomy is the main determinant of subsequent quality of life (QOL) in patients with locally recurrent rectal cancer at both base line and in the long term, according to findings presented at the annual Society of Surgical Oncology Cancer Symposium.
Posterior recurrences were associated with the worst QOL scores and the most severe pain.
Recurrent rectal cancer is a morbid disease state, leading to pain and disability. “Patients experience a multitude of symptoms, including disability as a result of tumor growth in a confined space in the pelvis and invasion of adjacent organs as well as complications from surgery and neoadjuvant treatment,” said lead author Dr. Tarik Sammour of the University of Texas MD Anderson Cancer Center in Houston.
He noted, however, that “it is not all doom and gloom.” Survival outcomes have been improving in this population, with the median 5-year survival now approaching 40%-50%.
“Decade by decade, the 5-year survival outcomes are increasing,” explained Dr. Sammour.
Increasing survival also begs the question: “Are we helping patients or affording them the option of living longer with pain and disability? In other words, we need to measure patient-centered outcomes,” he said.
Data for recurrent rectal cancer are very limited, particularly when it comes to measuring patient outcomes. Most studies have been retrospective in design, making it difficult to gauge symptoms and quality of life.
The majority of studies also have focused on surgery, have short follow-up times, and may be missing data.
“Very few measure baseline quality of life, so it makes it difficult to measure trajectories,” Dr. Sammour said. “So overall we don’t know very much about the quality of life of these patients, so we thought to remedy that with a prospective study.”
Dr. Sammour and his colleagues examined the longitudinal trajectory of cancer survivorship in recurrent rectal cancer over a 7-year period. A total of 104 patients diagnosed with recurrent rectal cancer were enrolled between 2008 and 2015, and they prospectively self reported QOL using the validated EORTC QLQ-C30 and EORTC QLQ-CR29. Pain was measured by the Brief Pain Inventory.
Symptoms were measured at baseline and then every 6 months for 5 years or until death.
Within this cohort, 73 (70.2%) patients were amenable to salvage surgery with curative intent. A variety of types of surgery were performed, and R0 resection was achieved in 75% of cases.
The 30-day complication rate was 49% (21% with grade 3/4), and 5-year disease-free survival was 40%. There was no immediate mortality from the surgery.
When looking at differences between patients who underwent surgery and those who didn’t, there was a significant difference in the location of the disease. The nonsurgical group was more likely to have posterior recurrences (26%) than was the surgical group (19%).
“This makes sense since these are more difficult to achieve a R0 result with, so it may be less likely that they were offered the procedure,” Dr. Sammour said.
There was also a significant difference in estimated 5-year survival. Overall survival was 7.7% in the nonsurgical group vs. 50.9% in the surgical group (P less than .0001), and cancer-specific survival was 11.5% vs. 59.6% (P less than .0001).
As for pain and QOL scores, there were no differences between groups at baseline.
“So when they arrived at clinic they had roughly equivalent quality of life,” he said.
At follow-up, male patients were more likely to experience severe pain, but “we felt it was due to the anatomical location. Men have a narrower pelvis and don’t have the luxury of a uterus to protect the genitourinary organs,” he explained. “We suspect this may have played a role in the severity of their pain.”
Patients with posterior recurrences also had worse pain, and this was true for both surgical and nonsurgical patients.
The only determinant for QOL in those who underwent surgery was a positive margin (global health score 70.4 for negative margin and 61.9 for positive margins [P = .024]), but otherwise there were no differences by type of surgery or postoperative complications.
At a median follow-up of 33 months, patients who underwent surgery showed gradual sustained improvement in QOL but not pain scores.
“We were encouraged to see improvement,” concluded Dr. Sammour. “Surgery does improve quality of life in resectable cases.”
No funding source was disclosed. Dr. Sammour and his coauthors had no disclosures.
AT SSO 2017
Key clinical point: Posterior recurrence in recurrent rectal cancer was associated with worst quality of life and pain.
Major finding: Surgery improved overall survival (7.7% in the nonsurgical group vs. 50.9% in the surgical group [P less than .0001]) and quality of life.
Data source: Prospective study involved 104 patients with recurrent rectal cancer.
Disclosures: No funding source was disclosed. Dr. Sammour and his coauthors had no disclosures.
Colonic Diaphragm Disease: An Important NSAID Complication to Know
Colonic diaphragm disease (CDD) is a rare but serious complication of nonsteroidal anti‐inflammatory drug (NSAID) use in which diaphragm‐like strictures develop in the large and/or small intestines. There have been about 100 reported cases of CDD since this finding was first reported in the medical literature in 1989.1,2 However, given the frequency of NSAID use, providers should consider this diagnosis.
Case Report
An 85-year‐old woman presented to the emergency department (ED) with generalized weakness, occult positive stool, and severe anemia requiring blood transfusions. Eight months prior, she had presented to her primary care physician (PCP) for a routine visit and was found to have anemia. She was referred to gastroenterology by her PCP for an upper endoscopy but refused the referral despite clear warnings of the potential for serious complications. She was started on ferrous sulfate 325 mg po tid at that time. The patient’s hemoglobin (Hbg) levels ranged from 10.8 to 11.2 g/dL prior to her ED presentation, and random fecal occult blood testing had been negative.
In the ED, the patient reported no abdominal pain, nausea emesis or constipation. Her past medical history was significant for compensated diastolic heart failure, paroxysmal atrial fibrillation controlled by medication, and chronic lumbago. The patient had been prescribed NSAIDs for 10 years for the chronic lumbago diagnosis; however, she was inconsistent in taking this medication until more recent years. Surgical history included a hysterectomy and back surgeries in the distant past. She had no symptoms or history of inflammatory bowel disease. The patient’s medications included both the oral and topical forms of diclofenac, conjugated estrogen, nitroglycerin, amlodipine, hydrocodone bitartrate and acetaminophen 5 mg once daily, amiodarone, diazepam, valsartan, furosemide, oxycodone 5 mg nightly prn for severe pain, and ferrous sulfate 325 mg.
Significant laboratory results in the ED included a Hbg level of 8.3 g/dL; a ferritin level of 11.9 ng/mL, and a serum iron level of 12 mg/dL. A computerized tomography scan of the abdomen and pelvis was normal. The patient was admitted, received a blood transfusion, and a gastroenterology consult was obtained for an upper and lower endoscopy. Although copy was normal, the colonoscopy revealed evidence of CDD of the ascending colon.
Colonic Diaphragm Disease
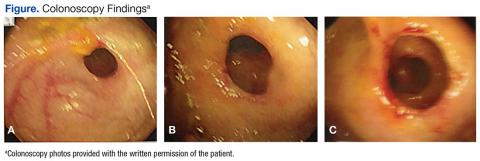
The gross findings seen on this patient’s colonoscopy showed evidence of the development of an internal colonic stricture from the fibrous overgrowth of the diaphragm (Figures A, B, & C). The narrow lumen is exhibited particularly well in Figure A in the upper left image. The external surface of the intestine appears normal.
Presentation and Evaluation
The presenting symptoms of CDD can vary and include abdominal pain, vomiting, lower gastrointestinal bleeding, anemia, and intestinal obstruction/perforation. Evidence seems to suggest a greater association with use of the oxicams (meloxicam, piroxicam) or diclofenac.1,2 Some researchers have suggested an association with long‐acting NSAID formulations.1 The use of misoprostol or proton pump inhibitors does not seem to lessen the chance of stricture formulation.2 Cox‐2 inhibitors are less likely players in the development of CDD.2 Most diaphragms in the large colon have been noted in the cecum, ascending and transverse colon, though descending colonic lesions have been documented as well.1
The incidence of CDD is higher among women and occurs most often in the seventh decade of life. Correlation with the duration of NSAID use prior to disease onset varies widely, with studies documenting disease onset from 3 months to 5 years after initiating consistent NSAID use.1 The patient in this case study was prescribed NSAIDs for almost 10 years, although she had poor adherence. One study also notes a possible association of CYP2C9*3 genetic polymorphism with the propensity to develop CDD. This finding is particularly interesting since NSAIDs are principally metabolized by CYP2C9 in the liver. CYP2C9 polymorphisms are thought to induce higher plasma concentrations of NSAIDs over time, which may lead to the formation of colonic diaphragms.2
Endoscopy with biopsy is the diagnostic modality of choice. Use of capsule endoscopy is limited because the capsule may not be able to pass through narrow stricture walls.
Pathology and Histology
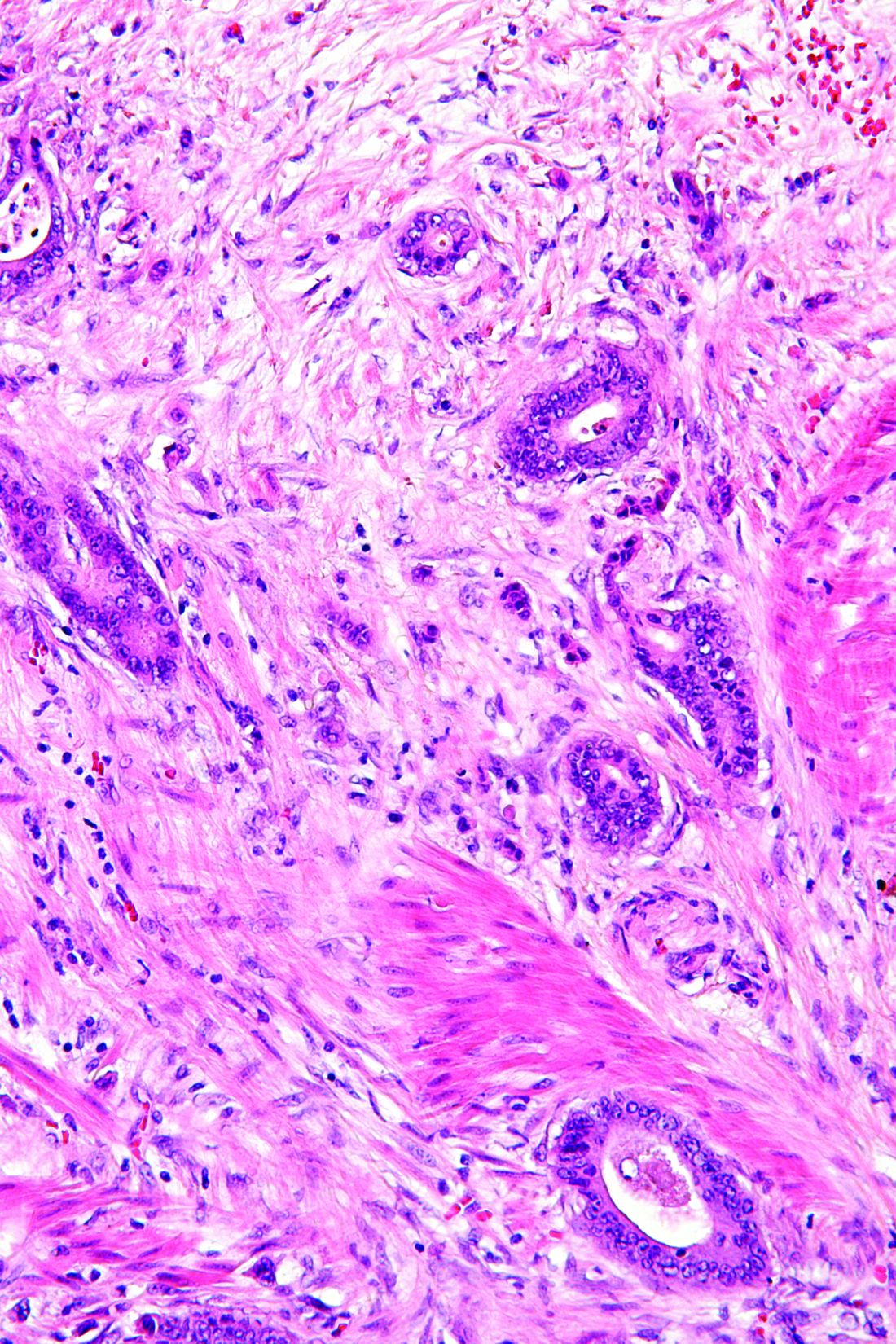
The mechanism by which NSAIDs induce the formation of colonic diaphragms may be related to these medications’ effects on mucosal integrity, vasoconstriction, and vascular spasm. These effects may lead to “erosions, ulceration, and diaphragm-like strictures.”3
The primary histologic feature of these strictures is submucosal fibrosis with an intact muscularis propria. Prominent features also include areas of ulceration and granulation.1 The widened submucosa results in annular constriction of the intestinal lumen with disorganized bundles of smooth muscle, unmyelinated nerve bundles, scattered ganglion cells, and blood vessels. This morphology can resemble a node or mass.4 The mucosa is typically normal.5 Conditions such as vascular and neuromuscular hamartoma can resemble CDD. Interestingly, the fibrous changes in CDD have been noted apart from NSAID use, leading to speculation that diaphragm formation may be a result of injury and not exclusively a reaction to NSAID use.5
Treatment
Recommendations include NSAID withdrawal, endoscopic/fluoroscopic dilatation, and surgical resection. Outcomes with these treatment approaches have been highly variable. For some patients, NSAID withdrawal alone or following resection has resulted in success. However, even with withdrawal of NSAIDs, symptoms may improve, although the histologic findings of CDD may not be reversed.3,6 In one case report, a colonic stricture persisted endoscopically after NSAID withdrawal but resolved after a 20-week course of prednisone.7
Conclusion
Despite NSAID cessation, the patient in this case study presented a month later with an acute bowel obstruction. The bowel obstruction responded to conservative treatment, and the patient declined surgical intervention. The patient was readmitted again 4 months later with an acute bowel obstruction, and underwent an emergent colonic resection. The pathology report was consistent with CDD. In the 3 years since the resection, the patient has had no recurrences and continues to avoid all NSAIDs. She has refused a follow-up postresection colonoscopy.
1. Munipalle PC, Garud T, Light D. Diaphragmatic disease of the colon: systematic review. Colorectal Dis. 2013;15(9):1063-1069.
2. Ishihara M, Ohmiya N, Nakamura M, et al. Risk factors of symptomatic NSAID-induced small intestinal injury and diaphragm disease. Aliment Pharmacol Ther. 2014;40(5):538-547.
3. Keeling AN, Davis JL, Williams A, Sabharwal T, Adam A. Fluoroscopically guided balloon dilation of NSAID-induced colonic diaphragm. J Vasc Interv Radiol. 2007;18(8):1060-1062.
4. Yousfi MM, De Petris G, Leighton JA, et al. Diaphragm disease after use of nonsteroidal anti-inflammatory agents: first report of diagnosis with capsule endoscopy. J Clin Gastroenterol. 2004;38(8):686-691.
5. Pilgrim S, Velchuru V, Waters G, Tsiamis A, Lal R. Diaphragm disease and small bowel enteropathy due to nonsteroidal anti-inflammatory drugs: a surgical perspective. Colorectal Dis. 2011;13(4):463-466.
6. Munipalle PC, Little M, Garud T, Henderson D. NSAID-induced diaphragmatic disease of the colon. BMJ Case Rep. 2013;2013:pii:bcr2012008448.
7. Penner RM, Williams CN. Resolution of multiple severe nonsteroidal anti-inflammatory drug-induced colonic strictures with prednisone therapy: a case report and review of the literature. Can J Gastroenterol. 2003;17(8):497-500.
Colonic diaphragm disease (CDD) is a rare but serious complication of nonsteroidal anti‐inflammatory drug (NSAID) use in which diaphragm‐like strictures develop in the large and/or small intestines. There have been about 100 reported cases of CDD since this finding was first reported in the medical literature in 1989.1,2 However, given the frequency of NSAID use, providers should consider this diagnosis.
Case Report
An 85-year‐old woman presented to the emergency department (ED) with generalized weakness, occult positive stool, and severe anemia requiring blood transfusions. Eight months prior, she had presented to her primary care physician (PCP) for a routine visit and was found to have anemia. She was referred to gastroenterology by her PCP for an upper endoscopy but refused the referral despite clear warnings of the potential for serious complications. She was started on ferrous sulfate 325 mg po tid at that time. The patient’s hemoglobin (Hbg) levels ranged from 10.8 to 11.2 g/dL prior to her ED presentation, and random fecal occult blood testing had been negative.
In the ED, the patient reported no abdominal pain, nausea emesis or constipation. Her past medical history was significant for compensated diastolic heart failure, paroxysmal atrial fibrillation controlled by medication, and chronic lumbago. The patient had been prescribed NSAIDs for 10 years for the chronic lumbago diagnosis; however, she was inconsistent in taking this medication until more recent years. Surgical history included a hysterectomy and back surgeries in the distant past. She had no symptoms or history of inflammatory bowel disease. The patient’s medications included both the oral and topical forms of diclofenac, conjugated estrogen, nitroglycerin, amlodipine, hydrocodone bitartrate and acetaminophen 5 mg once daily, amiodarone, diazepam, valsartan, furosemide, oxycodone 5 mg nightly prn for severe pain, and ferrous sulfate 325 mg.
Significant laboratory results in the ED included a Hbg level of 8.3 g/dL; a ferritin level of 11.9 ng/mL, and a serum iron level of 12 mg/dL. A computerized tomography scan of the abdomen and pelvis was normal. The patient was admitted, received a blood transfusion, and a gastroenterology consult was obtained for an upper and lower endoscopy. Although copy was normal, the colonoscopy revealed evidence of CDD of the ascending colon.
Colonic Diaphragm Disease
The gross findings seen on this patient’s colonoscopy showed evidence of the development of an internal colonic stricture from the fibrous overgrowth of the diaphragm (Figures A, B, & C). The narrow lumen is exhibited particularly well in Figure A in the upper left image. The external surface of the intestine appears normal.
Presentation and Evaluation
The presenting symptoms of CDD can vary and include abdominal pain, vomiting, lower gastrointestinal bleeding, anemia, and intestinal obstruction/perforation. Evidence seems to suggest a greater association with use of the oxicams (meloxicam, piroxicam) or diclofenac.1,2 Some researchers have suggested an association with long‐acting NSAID formulations.1 The use of misoprostol or proton pump inhibitors does not seem to lessen the chance of stricture formulation.2 Cox‐2 inhibitors are less likely players in the development of CDD.2 Most diaphragms in the large colon have been noted in the cecum, ascending and transverse colon, though descending colonic lesions have been documented as well.1
The incidence of CDD is higher among women and occurs most often in the seventh decade of life. Correlation with the duration of NSAID use prior to disease onset varies widely, with studies documenting disease onset from 3 months to 5 years after initiating consistent NSAID use.1 The patient in this case study was prescribed NSAIDs for almost 10 years, although she had poor adherence. One study also notes a possible association of CYP2C9*3 genetic polymorphism with the propensity to develop CDD. This finding is particularly interesting since NSAIDs are principally metabolized by CYP2C9 in the liver. CYP2C9 polymorphisms are thought to induce higher plasma concentrations of NSAIDs over time, which may lead to the formation of colonic diaphragms.2
Endoscopy with biopsy is the diagnostic modality of choice. Use of capsule endoscopy is limited because the capsule may not be able to pass through narrow stricture walls.
Pathology and Histology
The mechanism by which NSAIDs induce the formation of colonic diaphragms may be related to these medications’ effects on mucosal integrity, vasoconstriction, and vascular spasm. These effects may lead to “erosions, ulceration, and diaphragm-like strictures.”3
The primary histologic feature of these strictures is submucosal fibrosis with an intact muscularis propria. Prominent features also include areas of ulceration and granulation.1 The widened submucosa results in annular constriction of the intestinal lumen with disorganized bundles of smooth muscle, unmyelinated nerve bundles, scattered ganglion cells, and blood vessels. This morphology can resemble a node or mass.4 The mucosa is typically normal.5 Conditions such as vascular and neuromuscular hamartoma can resemble CDD. Interestingly, the fibrous changes in CDD have been noted apart from NSAID use, leading to speculation that diaphragm formation may be a result of injury and not exclusively a reaction to NSAID use.5
Treatment
Recommendations include NSAID withdrawal, endoscopic/fluoroscopic dilatation, and surgical resection. Outcomes with these treatment approaches have been highly variable. For some patients, NSAID withdrawal alone or following resection has resulted in success. However, even with withdrawal of NSAIDs, symptoms may improve, although the histologic findings of CDD may not be reversed.3,6 In one case report, a colonic stricture persisted endoscopically after NSAID withdrawal but resolved after a 20-week course of prednisone.7
Conclusion
Despite NSAID cessation, the patient in this case study presented a month later with an acute bowel obstruction. The bowel obstruction responded to conservative treatment, and the patient declined surgical intervention. The patient was readmitted again 4 months later with an acute bowel obstruction, and underwent an emergent colonic resection. The pathology report was consistent with CDD. In the 3 years since the resection, the patient has had no recurrences and continues to avoid all NSAIDs. She has refused a follow-up postresection colonoscopy.
Colonic diaphragm disease (CDD) is a rare but serious complication of nonsteroidal anti‐inflammatory drug (NSAID) use in which diaphragm‐like strictures develop in the large and/or small intestines. There have been about 100 reported cases of CDD since this finding was first reported in the medical literature in 1989.1,2 However, given the frequency of NSAID use, providers should consider this diagnosis.
Case Report
An 85-year‐old woman presented to the emergency department (ED) with generalized weakness, occult positive stool, and severe anemia requiring blood transfusions. Eight months prior, she had presented to her primary care physician (PCP) for a routine visit and was found to have anemia. She was referred to gastroenterology by her PCP for an upper endoscopy but refused the referral despite clear warnings of the potential for serious complications. She was started on ferrous sulfate 325 mg po tid at that time. The patient’s hemoglobin (Hbg) levels ranged from 10.8 to 11.2 g/dL prior to her ED presentation, and random fecal occult blood testing had been negative.
In the ED, the patient reported no abdominal pain, nausea emesis or constipation. Her past medical history was significant for compensated diastolic heart failure, paroxysmal atrial fibrillation controlled by medication, and chronic lumbago. The patient had been prescribed NSAIDs for 10 years for the chronic lumbago diagnosis; however, she was inconsistent in taking this medication until more recent years. Surgical history included a hysterectomy and back surgeries in the distant past. She had no symptoms or history of inflammatory bowel disease. The patient’s medications included both the oral and topical forms of diclofenac, conjugated estrogen, nitroglycerin, amlodipine, hydrocodone bitartrate and acetaminophen 5 mg once daily, amiodarone, diazepam, valsartan, furosemide, oxycodone 5 mg nightly prn for severe pain, and ferrous sulfate 325 mg.
Significant laboratory results in the ED included a Hbg level of 8.3 g/dL; a ferritin level of 11.9 ng/mL, and a serum iron level of 12 mg/dL. A computerized tomography scan of the abdomen and pelvis was normal. The patient was admitted, received a blood transfusion, and a gastroenterology consult was obtained for an upper and lower endoscopy. Although copy was normal, the colonoscopy revealed evidence of CDD of the ascending colon.
Colonic Diaphragm Disease
The gross findings seen on this patient’s colonoscopy showed evidence of the development of an internal colonic stricture from the fibrous overgrowth of the diaphragm (Figures A, B, & C). The narrow lumen is exhibited particularly well in Figure A in the upper left image. The external surface of the intestine appears normal.
Presentation and Evaluation
The presenting symptoms of CDD can vary and include abdominal pain, vomiting, lower gastrointestinal bleeding, anemia, and intestinal obstruction/perforation. Evidence seems to suggest a greater association with use of the oxicams (meloxicam, piroxicam) or diclofenac.1,2 Some researchers have suggested an association with long‐acting NSAID formulations.1 The use of misoprostol or proton pump inhibitors does not seem to lessen the chance of stricture formulation.2 Cox‐2 inhibitors are less likely players in the development of CDD.2 Most diaphragms in the large colon have been noted in the cecum, ascending and transverse colon, though descending colonic lesions have been documented as well.1
The incidence of CDD is higher among women and occurs most often in the seventh decade of life. Correlation with the duration of NSAID use prior to disease onset varies widely, with studies documenting disease onset from 3 months to 5 years after initiating consistent NSAID use.1 The patient in this case study was prescribed NSAIDs for almost 10 years, although she had poor adherence. One study also notes a possible association of CYP2C9*3 genetic polymorphism with the propensity to develop CDD. This finding is particularly interesting since NSAIDs are principally metabolized by CYP2C9 in the liver. CYP2C9 polymorphisms are thought to induce higher plasma concentrations of NSAIDs over time, which may lead to the formation of colonic diaphragms.2
Endoscopy with biopsy is the diagnostic modality of choice. Use of capsule endoscopy is limited because the capsule may not be able to pass through narrow stricture walls.
Pathology and Histology
The mechanism by which NSAIDs induce the formation of colonic diaphragms may be related to these medications’ effects on mucosal integrity, vasoconstriction, and vascular spasm. These effects may lead to “erosions, ulceration, and diaphragm-like strictures.”3
The primary histologic feature of these strictures is submucosal fibrosis with an intact muscularis propria. Prominent features also include areas of ulceration and granulation.1 The widened submucosa results in annular constriction of the intestinal lumen with disorganized bundles of smooth muscle, unmyelinated nerve bundles, scattered ganglion cells, and blood vessels. This morphology can resemble a node or mass.4 The mucosa is typically normal.5 Conditions such as vascular and neuromuscular hamartoma can resemble CDD. Interestingly, the fibrous changes in CDD have been noted apart from NSAID use, leading to speculation that diaphragm formation may be a result of injury and not exclusively a reaction to NSAID use.5
Treatment
Recommendations include NSAID withdrawal, endoscopic/fluoroscopic dilatation, and surgical resection. Outcomes with these treatment approaches have been highly variable. For some patients, NSAID withdrawal alone or following resection has resulted in success. However, even with withdrawal of NSAIDs, symptoms may improve, although the histologic findings of CDD may not be reversed.3,6 In one case report, a colonic stricture persisted endoscopically after NSAID withdrawal but resolved after a 20-week course of prednisone.7
Conclusion
Despite NSAID cessation, the patient in this case study presented a month later with an acute bowel obstruction. The bowel obstruction responded to conservative treatment, and the patient declined surgical intervention. The patient was readmitted again 4 months later with an acute bowel obstruction, and underwent an emergent colonic resection. The pathology report was consistent with CDD. In the 3 years since the resection, the patient has had no recurrences and continues to avoid all NSAIDs. She has refused a follow-up postresection colonoscopy.
1. Munipalle PC, Garud T, Light D. Diaphragmatic disease of the colon: systematic review. Colorectal Dis. 2013;15(9):1063-1069.
2. Ishihara M, Ohmiya N, Nakamura M, et al. Risk factors of symptomatic NSAID-induced small intestinal injury and diaphragm disease. Aliment Pharmacol Ther. 2014;40(5):538-547.
3. Keeling AN, Davis JL, Williams A, Sabharwal T, Adam A. Fluoroscopically guided balloon dilation of NSAID-induced colonic diaphragm. J Vasc Interv Radiol. 2007;18(8):1060-1062.
4. Yousfi MM, De Petris G, Leighton JA, et al. Diaphragm disease after use of nonsteroidal anti-inflammatory agents: first report of diagnosis with capsule endoscopy. J Clin Gastroenterol. 2004;38(8):686-691.
5. Pilgrim S, Velchuru V, Waters G, Tsiamis A, Lal R. Diaphragm disease and small bowel enteropathy due to nonsteroidal anti-inflammatory drugs: a surgical perspective. Colorectal Dis. 2011;13(4):463-466.
6. Munipalle PC, Little M, Garud T, Henderson D. NSAID-induced diaphragmatic disease of the colon. BMJ Case Rep. 2013;2013:pii:bcr2012008448.
7. Penner RM, Williams CN. Resolution of multiple severe nonsteroidal anti-inflammatory drug-induced colonic strictures with prednisone therapy: a case report and review of the literature. Can J Gastroenterol. 2003;17(8):497-500.
1. Munipalle PC, Garud T, Light D. Diaphragmatic disease of the colon: systematic review. Colorectal Dis. 2013;15(9):1063-1069.
2. Ishihara M, Ohmiya N, Nakamura M, et al. Risk factors of symptomatic NSAID-induced small intestinal injury and diaphragm disease. Aliment Pharmacol Ther. 2014;40(5):538-547.
3. Keeling AN, Davis JL, Williams A, Sabharwal T, Adam A. Fluoroscopically guided balloon dilation of NSAID-induced colonic diaphragm. J Vasc Interv Radiol. 2007;18(8):1060-1062.
4. Yousfi MM, De Petris G, Leighton JA, et al. Diaphragm disease after use of nonsteroidal anti-inflammatory agents: first report of diagnosis with capsule endoscopy. J Clin Gastroenterol. 2004;38(8):686-691.
5. Pilgrim S, Velchuru V, Waters G, Tsiamis A, Lal R. Diaphragm disease and small bowel enteropathy due to nonsteroidal anti-inflammatory drugs: a surgical perspective. Colorectal Dis. 2011;13(4):463-466.
6. Munipalle PC, Little M, Garud T, Henderson D. NSAID-induced diaphragmatic disease of the colon. BMJ Case Rep. 2013;2013:pii:bcr2012008448.
7. Penner RM, Williams CN. Resolution of multiple severe nonsteroidal anti-inflammatory drug-induced colonic strictures with prednisone therapy: a case report and review of the literature. Can J Gastroenterol. 2003;17(8):497-500.
Cardiovascular disease most common cause of death in CRC survivors
SEATTLE – Improvements in diagnosis and treatment have lengthened the survival time of patients with colorectal cancer, but the majority of deaths from CRC occur within the first 5 years.
According to new findings presented at the annual Society of Surgical Oncology Cancer Symposium, CRC as a cause of death is surpassed by cardiovascular disease (CVD) and second primary cancers as time goes on.
Dr. Lewis explained that CRC as a cause of death begins to plateau over time and other causes become more important.
“As time goes on, colorectal cancer becomes less prominent, and by year 8, cardiovascular death surpasses it. By year 10, colorectal cancer is surpassed by second cancers and neurologic diseases.”
Information about long-term health problems in long-term colorectal cancer survivors is limited. To address this, Dr. Lewis and his colleagues sought to understand the trends and causes of death over time.
They analyzed causes of death in CRC patients who have survived 5 years and longer using the California Cancer Registry (2000-2011) that is linked to inpatient records. From this database, 139,743 patients with CRC were identified, with 97,604 (69.8%) having been treated for disease originating from the colon and 42,139 (30.2%) from the rectum.
The median age of the patients at the time of presentation was 68 years; at 5 years after diagnosis, 70 years; and at 10 years, 74 years. The 5-year overall survival was 59.1%, and it was during that 5 years that 95% of cancer-specific deaths occurred.
During the first 5 years, the major cause of death was CRC, accounting for nearly two-thirds of the mortality (n = 38,992, 65.4%). This was followed by cardiovascular disease (n = 7,140, 12.0%), second primary cancer (n = 3,775, 6.3%), neurologic disease (n = 2,329, 3.9%), and pulmonary disease (n = 2,307, 3.9%).
The most common second primary malignancies affecting CRC survivors were lung and hematologic cancers, followed by pancreatic and liver cancers.
Overall, in long-term survivors, cardiovascular disease was the major cause of death (n = 2,163, 24.0%) although nearly as many deaths were due to CRC (2,094, 23.2%). This was followed by neurologic disease (n = 1,174, 13.0%), secondary primary cancer (n = 1,146, 12.7%), and pulmonary disease (n = 765, 8.5%).
There was no funding source disclosed in the abstract. Dr. Lewis had no disclosures.
SEATTLE – Improvements in diagnosis and treatment have lengthened the survival time of patients with colorectal cancer, but the majority of deaths from CRC occur within the first 5 years.
According to new findings presented at the annual Society of Surgical Oncology Cancer Symposium, CRC as a cause of death is surpassed by cardiovascular disease (CVD) and second primary cancers as time goes on.
Dr. Lewis explained that CRC as a cause of death begins to plateau over time and other causes become more important.
“As time goes on, colorectal cancer becomes less prominent, and by year 8, cardiovascular death surpasses it. By year 10, colorectal cancer is surpassed by second cancers and neurologic diseases.”
Information about long-term health problems in long-term colorectal cancer survivors is limited. To address this, Dr. Lewis and his colleagues sought to understand the trends and causes of death over time.
They analyzed causes of death in CRC patients who have survived 5 years and longer using the California Cancer Registry (2000-2011) that is linked to inpatient records. From this database, 139,743 patients with CRC were identified, with 97,604 (69.8%) having been treated for disease originating from the colon and 42,139 (30.2%) from the rectum.
The median age of the patients at the time of presentation was 68 years; at 5 years after diagnosis, 70 years; and at 10 years, 74 years. The 5-year overall survival was 59.1%, and it was during that 5 years that 95% of cancer-specific deaths occurred.
During the first 5 years, the major cause of death was CRC, accounting for nearly two-thirds of the mortality (n = 38,992, 65.4%). This was followed by cardiovascular disease (n = 7,140, 12.0%), second primary cancer (n = 3,775, 6.3%), neurologic disease (n = 2,329, 3.9%), and pulmonary disease (n = 2,307, 3.9%).
The most common second primary malignancies affecting CRC survivors were lung and hematologic cancers, followed by pancreatic and liver cancers.
Overall, in long-term survivors, cardiovascular disease was the major cause of death (n = 2,163, 24.0%) although nearly as many deaths were due to CRC (2,094, 23.2%). This was followed by neurologic disease (n = 1,174, 13.0%), secondary primary cancer (n = 1,146, 12.7%), and pulmonary disease (n = 765, 8.5%).
There was no funding source disclosed in the abstract. Dr. Lewis had no disclosures.
SEATTLE – Improvements in diagnosis and treatment have lengthened the survival time of patients with colorectal cancer, but the majority of deaths from CRC occur within the first 5 years.
According to new findings presented at the annual Society of Surgical Oncology Cancer Symposium, CRC as a cause of death is surpassed by cardiovascular disease (CVD) and second primary cancers as time goes on.
Dr. Lewis explained that CRC as a cause of death begins to plateau over time and other causes become more important.
“As time goes on, colorectal cancer becomes less prominent, and by year 8, cardiovascular death surpasses it. By year 10, colorectal cancer is surpassed by second cancers and neurologic diseases.”
Information about long-term health problems in long-term colorectal cancer survivors is limited. To address this, Dr. Lewis and his colleagues sought to understand the trends and causes of death over time.
They analyzed causes of death in CRC patients who have survived 5 years and longer using the California Cancer Registry (2000-2011) that is linked to inpatient records. From this database, 139,743 patients with CRC were identified, with 97,604 (69.8%) having been treated for disease originating from the colon and 42,139 (30.2%) from the rectum.
The median age of the patients at the time of presentation was 68 years; at 5 years after diagnosis, 70 years; and at 10 years, 74 years. The 5-year overall survival was 59.1%, and it was during that 5 years that 95% of cancer-specific deaths occurred.
During the first 5 years, the major cause of death was CRC, accounting for nearly two-thirds of the mortality (n = 38,992, 65.4%). This was followed by cardiovascular disease (n = 7,140, 12.0%), second primary cancer (n = 3,775, 6.3%), neurologic disease (n = 2,329, 3.9%), and pulmonary disease (n = 2,307, 3.9%).
The most common second primary malignancies affecting CRC survivors were lung and hematologic cancers, followed by pancreatic and liver cancers.
Overall, in long-term survivors, cardiovascular disease was the major cause of death (n = 2,163, 24.0%) although nearly as many deaths were due to CRC (2,094, 23.2%). This was followed by neurologic disease (n = 1,174, 13.0%), secondary primary cancer (n = 1,146, 12.7%), and pulmonary disease (n = 765, 8.5%).
There was no funding source disclosed in the abstract. Dr. Lewis had no disclosures.
AT SSO 2017
Key clinical point: Long-term colorectal cancer survivors generally will die from other causes.
Major finding: By year 8, cardiovascular disease surpasses colorectal cancer in survivors, as the leading cause of death.
Data source: Large cancer registry with almost 140,000 colorectal cancer patients.
Disclosures: There was no funding source disclosed in the abstract. Dr. Lewis had no disclosures.
Molecular Profiles Guide Colorectal Cancer Treatment
Colorectal cancer (CRC) is the third leading cause of cancer-related death in veterans, despite significant advances in treatment options.1,2 Over the past 20 years, the median survival of patients with metastatic CRC (mCRC), has improved with the most recent clinical trials demonstrating a median overall survival (OS) of up to 29 months.3
In addition to standard chemotherapeutic regimens using 5-fluorouracil, oxaliplatin, and irinotecan, biologic therapies have resulted in improved OS for patients with mCRC. These therapies include the human vascular endothelial growth factor (VEGF) monoclonal antibody bevacizumab and the epidermal growth factor receptor (EGFR) monoclonal antibodies cetuximab and panitumumab. Additional agents, including aflibercept, ramucirumab, regorafenib, and TAS-102, also have been FDA approved for mCRC, though the OS benefit for these agents as part of the series of standard-of-care treatments is less clear.
Investigators continue to determine subtypes of CRC to further advance treatment options. The histologic classification of colon cancers is actually a collection of multiple cancer subtypes. Each subtype possesses a unique biology largely dependent on the mutations present within the cancer. Recent data, reviewed below, indicate predictive and prognostic benefits to understanding the unique mutational profile of mCRC. Here, the authors present a brief updated summary of these biomarkers and a discussion of treatment strategies.
Resistance to Anti-EGFR Therapies
KRAS and NRAS are members of the RAS family of oncogenes. Activating mutations in these genes results in the propagation of growth factor signals independent of EGFR. The most common KRAS mutations are found in exon 2 (codon 12 or 13). Numerous studies over the past 10 years have confirmed that KRAS mutations at exon 2 predict resistance to cetuximab and panitumumab.4-11 Since at least 2009, restricting use of cetuximab and panitumumab has been the standard of care for patients with KRAS exon 2 wild-type cancers.12
Recent investigations have indicated a predictive role for extended-spectrum KRAS and NRAS mutations (KRAS mutations at exons 2, 3, and 4 and NRAS mutations at exons 2, 3, and 4). In the OPUS clinical trial, patients whose cancers possessed extended-spectrum RAS mutations received no benefit with the addition of cetuximab to standard chemotherapy in response rate (RR), progression-free survival (PFS), or OS compared with standard chemotherapy alone.13 Interestingly, median OS was shorter for those treated with cetuximab when a RAS mutation was present, though the difference was not statistically significant. Additional studies also have confirmed similar benefits in different settings.8,14-18
The CALGB/SWOG 80405 phase 3 clinical trial investigated the first-line use of biologic therapies in combination with standard chemotherapy. The extendedspectrum RAS testing from this study now has been presented.3,19 In the RAS wild-type population, the median OS was 31.2 months in the chemotherapy plus bevacizumab arm and 32.0 months in the chemotherapy plus cetuximab arm (no significant difference). No difference in PFS was observed. A significant improvement in the RR was seen in the cetuximab arm for the RAS wild-type population.
Predictive Biomarkers
BRAF is an oncogene in the RAF gene family that encodes a serine-threonine protein kinase found in the Ras-Raf-MAPK cascade. About 10% of CRC harbor a BRAF mutation.20,21 The most significant and prevalent mutation occurs at the kinase domain from the single substitution V600E. Numerous clinical studies have suggested the presence of this mutation as a predictor of resistance to anti-EGFR therapies and a marker of poor prognosis.6,17,22-25 In a retrospective analysis of RAS and BRAF mutation status of PRIME study data, patients without RAS and BRAF mutations showed significantly better OS and PFS when treated with FOLFOX4 (5-fluorouracil, oxaliplatin, and leucovorin) plus panitumumab, compared with FOLFOX4 alone.8 The presence of BRAF mutations in RAS wild-type patients resulted in a worse outcome. Treatment with anti-EGFR therapy did not significantly improve median PFS or OS.
PIK3CA mutations. Phosphoinositide 3-kinase (PI3K) is a lipid kinase important for multiple cellular processes including cell growth, proliferation, survival, and apoptosis. PIK3CA encodes the catalytic subunit and is mutant in about 20% of mCRC.26 The PI3K is downstream of EGFR signaling; activation of this pathway in the setting of an oncogenic mutation might lead to resistance to anti-EGFR therapies. Sartore-Bianchi and colleagues examined 110 patients with mCRC treated with either panitumumab or cetuximab.27 Of these, 15 patient cancers featured PIK3CA mutations, and none of these responded to anti-EGFR therapies. In addition, preclinical studies have demonstrated that targeting CRC downstream of PI3K might result in significant treatment benefit.28,29
Human epidermal growth factor receptor 2 (HER2) amplification. A subpopulation of CRC with amplification of HER2, a growth factor receptor commonly used in selecting treatment options in breast cancer, has recently been described. The HERACLES phase 2 study evaluated dual HER2 targeting with lapatinib and trastuzumab in therapy-refractory mCRC with HER2 amplification.30 A RR of 35% was observed in this treatment-refractory population.
BRAF mutations. In addition to predicting a poor prognosis and resistance to EGFR-directed therapies, BRAF mutations might be predictive of treatment response using combination regimens containing RAF inhibitors. A recent phase 1B study of a combination therapy using the BRAF inhibitor vemurafenib with irinotecan and cetuximab observed a partial RR of 35%.31 This is being investigated further in the Southwest Oncology Group 1406 phase 2 trial.
Mismatch repair deficiency. Detection of microsatellite instability or the presence of mismatch repair deficiency has become standard-of-care testing for CRC. This is important for the detection of Lynch syndrome and predicting potential resistance to adjuvant 5-fluorouracil in the adjuvant setting.32,33 A recent clinical trial has demonstrated benefits for the use of programmed death 1 (PD-1) inhibitors in the setting of mismatch repair deficiency, including a RR of 40% and PFS of 5.4 months.34
Discussion
Metastatic CRC is now better understood as a collection of multiple cancer subtypes based on mutational profile. This improved understanding of the biology of CRC is altering treatment strategies to a precision medicine-based approach. It is now the standard of care for all patients with mCRC to have the cancers assayed for mutations in KRAS (exons 2, 3, and 4), NRAS (exons 2, 3, and 4), and BRAF. Anti-EGFR therapies should not be used for patients with RAS or BRAF mutations outside of a clinical trial because of a demonstrated lack of benefit in all lines of therapy. Currently, there is no evidence that these mutations significantly alter the response to the approved anti-angiogenic agents bevacizumab, aflibercept, ramucirumab, and regorafenib.
The timing of EGFR-directed therapies for patients with wild-type KRAS, NRAS, and BRAF is still being debated. According to the available data, first-line treatment with anti-EGFR agents in combination with FOLFOX or FOLFIRI (5-fluorouracil, irinotecan, and leucovorin) should be considered for all patients with KRAS, NRAS, and BRAF wild-type mCRCs. The toxicities of anti-EGFR therapies also should be considered for this setting, as some patients find that the acneiform rash, fatigue, nausea, and diarrhea that occur with these agents can have a negative impact on quality of life. As there is no improvement in OS with first-line anti-EGFR therapies for these patients, the increased toxicity from these agents limits their use. In addition, patients with mCRC with known PIK3CA mutation should consider use of EGFR-directed therapies only in the later line setting.
Research is focused on how to best use the mutational profile of the tumor to tailor therapies for mCRC. High-quality, large-volume data sets will become more important as molecular subtypes of cancer become more narrowly defined and less common. Further investigations are needed to look for other markers of resistance and to identify biomarkers predictive of treatment sensitivity.
This is an exciting time in the treatment of many cancers, especially mCRC, which significantly impacts the veteran population, because routine DNA sequencing of patient samples has allowed for rapid advances in the realization of precision medicine. This allows for improved patient selection to reduce costs and toxicities while increasing the benefit for veterans.
Acknowledgments
This work was supported by the National Institutes of Health (P30 CA014520, Core Grant, University of Wisconsin Carbone Cancer Center).
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies.
Click here to read the digital edition.
1. Landrum MB, Keating NL, Lamont EB, et al. Survival of older patients with cancer in the Veterans Health Administration versus fee-for-service Medicare. J Clin Oncol. 2012;30(10):1072-1079.
2. Hynes DM, Tarlov E, Durazo-Arvizu R, et al. Surgery and adjuvant chemotherapy use among veterans with colon cancer: insights from a California study. J Clin Oncol. 2010;28(15):2571-2576.
3. Venook AP, Niedzwiecki D, Lenz H-J, et al; Cancer and Leukemia Group B (Alliance), SWOG, and ECOG. CALGB/SWOG 80405: Phase III trial of irinotecan/5-FU/leucovorin (FOLFIRI) or oxaliplatin/5-FU/leucovorin (mFOLFOX6) with bevacizumab (BV) or cetuximab (CET) for patients (pts) with KRAS wild-type (wt) untreated metastatic adenocarcinoma of the colon or rectum (MCRC). J Clin Oncol. 2014;32(suppl 18):Abstract LBA3.
4. Benvenuti S, Sartore-Bianchi A, Di Nicolantonio F, et al. Oncogenic activation of the RAS/RAF signaling pathway impairs the response of metastatic colorectal cancers to anti-epidermal growth factor receptor antibody therapies. Cancer Res. 2007;67(6):2643-2648.
5. Bokemeyer C, Bondarenko I, Hartmann JT, et al. Efficacy according to biomarker status of cetuximab plus FOLFOX-4 as first-line treatment for metastatic colorectal cancer: the OPUS study. Ann Oncol. 2011;22(7):1535-1546.
6. De Roock W, Claes B, Bernasconi D, et al. Effects of KRAS, BRAF, NRAS, and PIK3CA mutations on the efficacy of cetuximab plus chemotherapy in chemotherapy-refractory metastatic colorectal cancer: a retrospective consortium analysis. Lancet Oncol. 2010;11(8):753-7562.
7. Di Fiore F, Blanchard F, Charbonnier F, et al. Clinical relevance of KRAS mutation detection in metastatic colorectal cancer treated by cetuximab plus chemotherapy. Br J Cancer. 2007;96(8):1166-1169.
8. Douillard JY, Oliner KS, Siena S, et al. Panitumumab-FOLFOX4 treatment and RAS mutations in colorectal cancer. N Engl J Med. 2013;369(11):1023-1034.
9. Lièvre A, Bachet JB, Boige V, et al. KRAS mutations as an independent prognostic factor in patients with advanced colorectal cancer treated with cetuximab. J Clin Oncol. 2008;26(3):374-379.
10. Lièvre A, Bachet JB, Le Corre D, et al. KRAS mutation status is predictive of response to cetuximab therapy in colorectal cancer. Cancer Res. 2006;66(8):3992-3995.
11. Van Cutsem E, Köhne CH, Hitre E, et al. Cetuximab and chemotherapy as initial treatment for metastatic colorectal cancer. N Engl J Med. 2009;360(14):1408-1417.
12. Allegra CJ, Jessup JM, Somerfield MR, et al. American Society of Clinical Oncology provisional clinical opinion: testing for KRAS gene mutations in patients with metastatic colorectal carcinoma to predict response to anti-epidermal growth factor receptor monoclonal antibody therapy. J Clin Oncol. 2009;27(12):2091-2096.
13. Tejpar S, Lenz HJ, Kohne CH, et al. Effect of KRAS and NRAS mutations on treatment outcomes in patients with metastatic colorectal cancer (mCRC) treated first-line with cetuximab plus FOLFOX4: new results from the OPUS study. J Clin Oncol. 2014;32(suppl 3):LBA444.
14. Abad A, Massuti B, Gravalos C, et al. Panitumumab plus FOLFOX4 or panitumumab plus FOLFIRI in subjects with wild-type KRAS (exon 2) colorectal cancer and multiple or unresectable liver-limited metastases: data from the randomized, phase II planet study. Ann Oncol. 2014;25(suppl 2):ii7-ii18.
15. Schwartzberg LS, Rivera F, Karthaus M, et al. PEAK: a randomized, multicenter phase II study of panitumumab plus modified fluorouracil, leucovorin, and oxaliplatin (mFOLFOX6) or bevacizumab plus mFOLFOX6 in patients with previously untreated, unresectable, wild-type KRAS exon 2 metastatic colorectal cancer. J Clin Oncol. 2014;32(21):2240-2247.
16. Peeters M, Oliner K, Price T, et al. KRAS/NRAS and BRAF mutations in the 20050181 study of panitumumab plus FOLFIRI for the 2nd-line treatment of metastatic colorectal cancer: updated analysis. Ann Oncol. 2014;25(suppl 2):ii5.
17. Bokemeyer C, Van Cutsem E, Rougier P, et al. Addition of cetuximab to chemotherapy as first-line treatment for KRAS wild-type metastatic colorectal cancer: pooled analysis of the CRYSTAL and OPUS randomised clinical trials. Eur J Cancer. 2012;48(10):1466-1475.
18. Van Cutsem E, Lenz HJ, Köhne CH, et al. Fluorouracil, leucovorin, and irinotecan plus cetuximab treatment and RAS mutations in colorectal cancer. J Clin Oncol. 2015;33(7):692-700.
19. ESMO. ESMO 2014: results from the CALGB/SWOG 80405 and FIRE-3 (AIO KRK-0306) studies in all RAS wild type population. ESMO website. http://www.esmo.org/Conferences/Past-Conferences/ESMO-2014-Congress/News-Articles/Results-From-the-CALGB-SWOG-80405-and-FIRE-3-AIO-KRK -0306-Studies-In-All-RAS-Wild-Type-Population. Updated September 29, 2014. Accessed April 6, 2016.
20. Davies H, Bignell GR, Cox C, et al. Mutations of the BRAF gene in human cancer. Nature. 2002;417(6892):949-954.
21. Samowitz WS, Sweeney C, Herrick J, Albertsen H, Levin TR, Murtaugh MA, Wolff RK, Slattery ML. Poor survival associated with the BRAF V600E mutation in microsatellite-stable colon cancers. Cancer Res. 2005;65(14):6063-6069.
22. Di Nicolantonio F, Martini M, Molinari F, et al. Wild-type BRAF is required for response to panitumumab or cetuximab in metastatic colorectal cancer. J Clin Oncol. 2008;26(35):5705-5712.
23. Laurent-Puig P, Cayre A, Manceau G, et al. Analysis of PTEN, BRAF, and EGFR status in determining benefit from cetuximab therapy in wild-type KRAS metastatic colon cancer. J Clin Oncol. 2009;27(35):5924-5930.
24. Richman SD, Seymour MT, Chambers P, et al. KRAS and BRAF mutations in advanced colorectal cancer are associated with poor prognosis but do not preclude benefit from oxaliplatin or irinotecan: results from the MRC FOCUS trial. J Clin Oncol. 2009;27(35):5931-5937.
25. Tveit KM, Guren T, et al. Phase III trial of cetuximab with continuous or intermittent fluorouracil, leucovorin, and oxaliplatin (Nordic FLOX) versus FLOX alone in first-line treatment of metastatic colorectal cancer: The NORDIC-VII study. J Clin Oncol. 2012;30(15):1755-1762.
26. Samuels Y, Wang Z, Bardelli A, et al. High frequency of mutations of the PIK3CA gene in human cancers. Science. 2004;304(5670):554.
27. Sartore-Bianchi A, Martini M, Molinari F, et al. PIK3CA mutations in colorectal cancer are associated with clinical resistance to EGFR-targeted monoclonal antibodies. Cancer Res. 2009;69(5):1851-1857.
28. Deming DA, Leystra AA, Farhoud M, et al. mTOR inhibition elicits a dramatic response in PI3K-dependent colon cancers. PLoS One. 2013;8(4):e60709.
29. Yueh AE, Payne SN, Leystra AA, et al. Colon cancer tumorigenesis initiated by the H1047R mutant PI3K. PLoS One. 2016;11(2):e0148730.
30. Siena S, Sartore-Bianchi A, Lonardi S, et al. Trastuzumab and lapatinib in HER2-amplified metastatic colorectal cancer patients (mCRC): the HERACLES trial. J Clin Oncol. 2015;33(suppl 15):3508.
31. Hong DS, Morris VK, El Osta BE, et al. Phase Ib study of vemurafenib in combination with irinotecan and cetuximab in patients with BRAF-mutated metastatic colorectal cancer and advanced cancers. J Clin Oncol. 2015;33(suppl 15):3511.
32. Benatti P, Gafà R, Barana D, et al. Microsatellite instability and colorectal cancer prognosis. Clin Cancer Res. 2005;11(23):8332-8340.
33. Funkhouser WK, Jr, Lubin IM, Monzon FA, et al. Relevance, pathogenesis, and testing algorithm for mismatch repair-defective colorectal carcinomas: a report of the association for molecular pathology. J Mol Diagn. 2012;14(2):91-103.
34. Le DT, Uram JN, Wang H, et al. PD-1 blockade in tumors with mismatch-repair
deficiency. N Engl J Med. 2015;372(26):2509-2520.
Colorectal cancer (CRC) is the third leading cause of cancer-related death in veterans, despite significant advances in treatment options.1,2 Over the past 20 years, the median survival of patients with metastatic CRC (mCRC), has improved with the most recent clinical trials demonstrating a median overall survival (OS) of up to 29 months.3
In addition to standard chemotherapeutic regimens using 5-fluorouracil, oxaliplatin, and irinotecan, biologic therapies have resulted in improved OS for patients with mCRC. These therapies include the human vascular endothelial growth factor (VEGF) monoclonal antibody bevacizumab and the epidermal growth factor receptor (EGFR) monoclonal antibodies cetuximab and panitumumab. Additional agents, including aflibercept, ramucirumab, regorafenib, and TAS-102, also have been FDA approved for mCRC, though the OS benefit for these agents as part of the series of standard-of-care treatments is less clear.
Investigators continue to determine subtypes of CRC to further advance treatment options. The histologic classification of colon cancers is actually a collection of multiple cancer subtypes. Each subtype possesses a unique biology largely dependent on the mutations present within the cancer. Recent data, reviewed below, indicate predictive and prognostic benefits to understanding the unique mutational profile of mCRC. Here, the authors present a brief updated summary of these biomarkers and a discussion of treatment strategies.
Resistance to Anti-EGFR Therapies
KRAS and NRAS are members of the RAS family of oncogenes. Activating mutations in these genes results in the propagation of growth factor signals independent of EGFR. The most common KRAS mutations are found in exon 2 (codon 12 or 13). Numerous studies over the past 10 years have confirmed that KRAS mutations at exon 2 predict resistance to cetuximab and panitumumab.4-11 Since at least 2009, restricting use of cetuximab and panitumumab has been the standard of care for patients with KRAS exon 2 wild-type cancers.12
Recent investigations have indicated a predictive role for extended-spectrum KRAS and NRAS mutations (KRAS mutations at exons 2, 3, and 4 and NRAS mutations at exons 2, 3, and 4). In the OPUS clinical trial, patients whose cancers possessed extended-spectrum RAS mutations received no benefit with the addition of cetuximab to standard chemotherapy in response rate (RR), progression-free survival (PFS), or OS compared with standard chemotherapy alone.13 Interestingly, median OS was shorter for those treated with cetuximab when a RAS mutation was present, though the difference was not statistically significant. Additional studies also have confirmed similar benefits in different settings.8,14-18
The CALGB/SWOG 80405 phase 3 clinical trial investigated the first-line use of biologic therapies in combination with standard chemotherapy. The extendedspectrum RAS testing from this study now has been presented.3,19 In the RAS wild-type population, the median OS was 31.2 months in the chemotherapy plus bevacizumab arm and 32.0 months in the chemotherapy plus cetuximab arm (no significant difference). No difference in PFS was observed. A significant improvement in the RR was seen in the cetuximab arm for the RAS wild-type population.
Predictive Biomarkers
BRAF is an oncogene in the RAF gene family that encodes a serine-threonine protein kinase found in the Ras-Raf-MAPK cascade. About 10% of CRC harbor a BRAF mutation.20,21 The most significant and prevalent mutation occurs at the kinase domain from the single substitution V600E. Numerous clinical studies have suggested the presence of this mutation as a predictor of resistance to anti-EGFR therapies and a marker of poor prognosis.6,17,22-25 In a retrospective analysis of RAS and BRAF mutation status of PRIME study data, patients without RAS and BRAF mutations showed significantly better OS and PFS when treated with FOLFOX4 (5-fluorouracil, oxaliplatin, and leucovorin) plus panitumumab, compared with FOLFOX4 alone.8 The presence of BRAF mutations in RAS wild-type patients resulted in a worse outcome. Treatment with anti-EGFR therapy did not significantly improve median PFS or OS.
PIK3CA mutations. Phosphoinositide 3-kinase (PI3K) is a lipid kinase important for multiple cellular processes including cell growth, proliferation, survival, and apoptosis. PIK3CA encodes the catalytic subunit and is mutant in about 20% of mCRC.26 The PI3K is downstream of EGFR signaling; activation of this pathway in the setting of an oncogenic mutation might lead to resistance to anti-EGFR therapies. Sartore-Bianchi and colleagues examined 110 patients with mCRC treated with either panitumumab or cetuximab.27 Of these, 15 patient cancers featured PIK3CA mutations, and none of these responded to anti-EGFR therapies. In addition, preclinical studies have demonstrated that targeting CRC downstream of PI3K might result in significant treatment benefit.28,29
Human epidermal growth factor receptor 2 (HER2) amplification. A subpopulation of CRC with amplification of HER2, a growth factor receptor commonly used in selecting treatment options in breast cancer, has recently been described. The HERACLES phase 2 study evaluated dual HER2 targeting with lapatinib and trastuzumab in therapy-refractory mCRC with HER2 amplification.30 A RR of 35% was observed in this treatment-refractory population.
BRAF mutations. In addition to predicting a poor prognosis and resistance to EGFR-directed therapies, BRAF mutations might be predictive of treatment response using combination regimens containing RAF inhibitors. A recent phase 1B study of a combination therapy using the BRAF inhibitor vemurafenib with irinotecan and cetuximab observed a partial RR of 35%.31 This is being investigated further in the Southwest Oncology Group 1406 phase 2 trial.
Mismatch repair deficiency. Detection of microsatellite instability or the presence of mismatch repair deficiency has become standard-of-care testing for CRC. This is important for the detection of Lynch syndrome and predicting potential resistance to adjuvant 5-fluorouracil in the adjuvant setting.32,33 A recent clinical trial has demonstrated benefits for the use of programmed death 1 (PD-1) inhibitors in the setting of mismatch repair deficiency, including a RR of 40% and PFS of 5.4 months.34
Discussion
Metastatic CRC is now better understood as a collection of multiple cancer subtypes based on mutational profile. This improved understanding of the biology of CRC is altering treatment strategies to a precision medicine-based approach. It is now the standard of care for all patients with mCRC to have the cancers assayed for mutations in KRAS (exons 2, 3, and 4), NRAS (exons 2, 3, and 4), and BRAF. Anti-EGFR therapies should not be used for patients with RAS or BRAF mutations outside of a clinical trial because of a demonstrated lack of benefit in all lines of therapy. Currently, there is no evidence that these mutations significantly alter the response to the approved anti-angiogenic agents bevacizumab, aflibercept, ramucirumab, and regorafenib.
The timing of EGFR-directed therapies for patients with wild-type KRAS, NRAS, and BRAF is still being debated. According to the available data, first-line treatment with anti-EGFR agents in combination with FOLFOX or FOLFIRI (5-fluorouracil, irinotecan, and leucovorin) should be considered for all patients with KRAS, NRAS, and BRAF wild-type mCRCs. The toxicities of anti-EGFR therapies also should be considered for this setting, as some patients find that the acneiform rash, fatigue, nausea, and diarrhea that occur with these agents can have a negative impact on quality of life. As there is no improvement in OS with first-line anti-EGFR therapies for these patients, the increased toxicity from these agents limits their use. In addition, patients with mCRC with known PIK3CA mutation should consider use of EGFR-directed therapies only in the later line setting.
Research is focused on how to best use the mutational profile of the tumor to tailor therapies for mCRC. High-quality, large-volume data sets will become more important as molecular subtypes of cancer become more narrowly defined and less common. Further investigations are needed to look for other markers of resistance and to identify biomarkers predictive of treatment sensitivity.
This is an exciting time in the treatment of many cancers, especially mCRC, which significantly impacts the veteran population, because routine DNA sequencing of patient samples has allowed for rapid advances in the realization of precision medicine. This allows for improved patient selection to reduce costs and toxicities while increasing the benefit for veterans.
Acknowledgments
This work was supported by the National Institutes of Health (P30 CA014520, Core Grant, University of Wisconsin Carbone Cancer Center).
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies.
Click here to read the digital edition.
Colorectal cancer (CRC) is the third leading cause of cancer-related death in veterans, despite significant advances in treatment options.1,2 Over the past 20 years, the median survival of patients with metastatic CRC (mCRC), has improved with the most recent clinical trials demonstrating a median overall survival (OS) of up to 29 months.3
In addition to standard chemotherapeutic regimens using 5-fluorouracil, oxaliplatin, and irinotecan, biologic therapies have resulted in improved OS for patients with mCRC. These therapies include the human vascular endothelial growth factor (VEGF) monoclonal antibody bevacizumab and the epidermal growth factor receptor (EGFR) monoclonal antibodies cetuximab and panitumumab. Additional agents, including aflibercept, ramucirumab, regorafenib, and TAS-102, also have been FDA approved for mCRC, though the OS benefit for these agents as part of the series of standard-of-care treatments is less clear.
Investigators continue to determine subtypes of CRC to further advance treatment options. The histologic classification of colon cancers is actually a collection of multiple cancer subtypes. Each subtype possesses a unique biology largely dependent on the mutations present within the cancer. Recent data, reviewed below, indicate predictive and prognostic benefits to understanding the unique mutational profile of mCRC. Here, the authors present a brief updated summary of these biomarkers and a discussion of treatment strategies.
Resistance to Anti-EGFR Therapies
KRAS and NRAS are members of the RAS family of oncogenes. Activating mutations in these genes results in the propagation of growth factor signals independent of EGFR. The most common KRAS mutations are found in exon 2 (codon 12 or 13). Numerous studies over the past 10 years have confirmed that KRAS mutations at exon 2 predict resistance to cetuximab and panitumumab.4-11 Since at least 2009, restricting use of cetuximab and panitumumab has been the standard of care for patients with KRAS exon 2 wild-type cancers.12
Recent investigations have indicated a predictive role for extended-spectrum KRAS and NRAS mutations (KRAS mutations at exons 2, 3, and 4 and NRAS mutations at exons 2, 3, and 4). In the OPUS clinical trial, patients whose cancers possessed extended-spectrum RAS mutations received no benefit with the addition of cetuximab to standard chemotherapy in response rate (RR), progression-free survival (PFS), or OS compared with standard chemotherapy alone.13 Interestingly, median OS was shorter for those treated with cetuximab when a RAS mutation was present, though the difference was not statistically significant. Additional studies also have confirmed similar benefits in different settings.8,14-18
The CALGB/SWOG 80405 phase 3 clinical trial investigated the first-line use of biologic therapies in combination with standard chemotherapy. The extendedspectrum RAS testing from this study now has been presented.3,19 In the RAS wild-type population, the median OS was 31.2 months in the chemotherapy plus bevacizumab arm and 32.0 months in the chemotherapy plus cetuximab arm (no significant difference). No difference in PFS was observed. A significant improvement in the RR was seen in the cetuximab arm for the RAS wild-type population.
Predictive Biomarkers
BRAF is an oncogene in the RAF gene family that encodes a serine-threonine protein kinase found in the Ras-Raf-MAPK cascade. About 10% of CRC harbor a BRAF mutation.20,21 The most significant and prevalent mutation occurs at the kinase domain from the single substitution V600E. Numerous clinical studies have suggested the presence of this mutation as a predictor of resistance to anti-EGFR therapies and a marker of poor prognosis.6,17,22-25 In a retrospective analysis of RAS and BRAF mutation status of PRIME study data, patients without RAS and BRAF mutations showed significantly better OS and PFS when treated with FOLFOX4 (5-fluorouracil, oxaliplatin, and leucovorin) plus panitumumab, compared with FOLFOX4 alone.8 The presence of BRAF mutations in RAS wild-type patients resulted in a worse outcome. Treatment with anti-EGFR therapy did not significantly improve median PFS or OS.
PIK3CA mutations. Phosphoinositide 3-kinase (PI3K) is a lipid kinase important for multiple cellular processes including cell growth, proliferation, survival, and apoptosis. PIK3CA encodes the catalytic subunit and is mutant in about 20% of mCRC.26 The PI3K is downstream of EGFR signaling; activation of this pathway in the setting of an oncogenic mutation might lead to resistance to anti-EGFR therapies. Sartore-Bianchi and colleagues examined 110 patients with mCRC treated with either panitumumab or cetuximab.27 Of these, 15 patient cancers featured PIK3CA mutations, and none of these responded to anti-EGFR therapies. In addition, preclinical studies have demonstrated that targeting CRC downstream of PI3K might result in significant treatment benefit.28,29
Human epidermal growth factor receptor 2 (HER2) amplification. A subpopulation of CRC with amplification of HER2, a growth factor receptor commonly used in selecting treatment options in breast cancer, has recently been described. The HERACLES phase 2 study evaluated dual HER2 targeting with lapatinib and trastuzumab in therapy-refractory mCRC with HER2 amplification.30 A RR of 35% was observed in this treatment-refractory population.
BRAF mutations. In addition to predicting a poor prognosis and resistance to EGFR-directed therapies, BRAF mutations might be predictive of treatment response using combination regimens containing RAF inhibitors. A recent phase 1B study of a combination therapy using the BRAF inhibitor vemurafenib with irinotecan and cetuximab observed a partial RR of 35%.31 This is being investigated further in the Southwest Oncology Group 1406 phase 2 trial.
Mismatch repair deficiency. Detection of microsatellite instability or the presence of mismatch repair deficiency has become standard-of-care testing for CRC. This is important for the detection of Lynch syndrome and predicting potential resistance to adjuvant 5-fluorouracil in the adjuvant setting.32,33 A recent clinical trial has demonstrated benefits for the use of programmed death 1 (PD-1) inhibitors in the setting of mismatch repair deficiency, including a RR of 40% and PFS of 5.4 months.34
Discussion
Metastatic CRC is now better understood as a collection of multiple cancer subtypes based on mutational profile. This improved understanding of the biology of CRC is altering treatment strategies to a precision medicine-based approach. It is now the standard of care for all patients with mCRC to have the cancers assayed for mutations in KRAS (exons 2, 3, and 4), NRAS (exons 2, 3, and 4), and BRAF. Anti-EGFR therapies should not be used for patients with RAS or BRAF mutations outside of a clinical trial because of a demonstrated lack of benefit in all lines of therapy. Currently, there is no evidence that these mutations significantly alter the response to the approved anti-angiogenic agents bevacizumab, aflibercept, ramucirumab, and regorafenib.
The timing of EGFR-directed therapies for patients with wild-type KRAS, NRAS, and BRAF is still being debated. According to the available data, first-line treatment with anti-EGFR agents in combination with FOLFOX or FOLFIRI (5-fluorouracil, irinotecan, and leucovorin) should be considered for all patients with KRAS, NRAS, and BRAF wild-type mCRCs. The toxicities of anti-EGFR therapies also should be considered for this setting, as some patients find that the acneiform rash, fatigue, nausea, and diarrhea that occur with these agents can have a negative impact on quality of life. As there is no improvement in OS with first-line anti-EGFR therapies for these patients, the increased toxicity from these agents limits their use. In addition, patients with mCRC with known PIK3CA mutation should consider use of EGFR-directed therapies only in the later line setting.
Research is focused on how to best use the mutational profile of the tumor to tailor therapies for mCRC. High-quality, large-volume data sets will become more important as molecular subtypes of cancer become more narrowly defined and less common. Further investigations are needed to look for other markers of resistance and to identify biomarkers predictive of treatment sensitivity.
This is an exciting time in the treatment of many cancers, especially mCRC, which significantly impacts the veteran population, because routine DNA sequencing of patient samples has allowed for rapid advances in the realization of precision medicine. This allows for improved patient selection to reduce costs and toxicities while increasing the benefit for veterans.
Acknowledgments
This work was supported by the National Institutes of Health (P30 CA014520, Core Grant, University of Wisconsin Carbone Cancer Center).
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies.
Click here to read the digital edition.
1. Landrum MB, Keating NL, Lamont EB, et al. Survival of older patients with cancer in the Veterans Health Administration versus fee-for-service Medicare. J Clin Oncol. 2012;30(10):1072-1079.
2. Hynes DM, Tarlov E, Durazo-Arvizu R, et al. Surgery and adjuvant chemotherapy use among veterans with colon cancer: insights from a California study. J Clin Oncol. 2010;28(15):2571-2576.
3. Venook AP, Niedzwiecki D, Lenz H-J, et al; Cancer and Leukemia Group B (Alliance), SWOG, and ECOG. CALGB/SWOG 80405: Phase III trial of irinotecan/5-FU/leucovorin (FOLFIRI) or oxaliplatin/5-FU/leucovorin (mFOLFOX6) with bevacizumab (BV) or cetuximab (CET) for patients (pts) with KRAS wild-type (wt) untreated metastatic adenocarcinoma of the colon or rectum (MCRC). J Clin Oncol. 2014;32(suppl 18):Abstract LBA3.
4. Benvenuti S, Sartore-Bianchi A, Di Nicolantonio F, et al. Oncogenic activation of the RAS/RAF signaling pathway impairs the response of metastatic colorectal cancers to anti-epidermal growth factor receptor antibody therapies. Cancer Res. 2007;67(6):2643-2648.
5. Bokemeyer C, Bondarenko I, Hartmann JT, et al. Efficacy according to biomarker status of cetuximab plus FOLFOX-4 as first-line treatment for metastatic colorectal cancer: the OPUS study. Ann Oncol. 2011;22(7):1535-1546.
6. De Roock W, Claes B, Bernasconi D, et al. Effects of KRAS, BRAF, NRAS, and PIK3CA mutations on the efficacy of cetuximab plus chemotherapy in chemotherapy-refractory metastatic colorectal cancer: a retrospective consortium analysis. Lancet Oncol. 2010;11(8):753-7562.
7. Di Fiore F, Blanchard F, Charbonnier F, et al. Clinical relevance of KRAS mutation detection in metastatic colorectal cancer treated by cetuximab plus chemotherapy. Br J Cancer. 2007;96(8):1166-1169.
8. Douillard JY, Oliner KS, Siena S, et al. Panitumumab-FOLFOX4 treatment and RAS mutations in colorectal cancer. N Engl J Med. 2013;369(11):1023-1034.
9. Lièvre A, Bachet JB, Boige V, et al. KRAS mutations as an independent prognostic factor in patients with advanced colorectal cancer treated with cetuximab. J Clin Oncol. 2008;26(3):374-379.
10. Lièvre A, Bachet JB, Le Corre D, et al. KRAS mutation status is predictive of response to cetuximab therapy in colorectal cancer. Cancer Res. 2006;66(8):3992-3995.
11. Van Cutsem E, Köhne CH, Hitre E, et al. Cetuximab and chemotherapy as initial treatment for metastatic colorectal cancer. N Engl J Med. 2009;360(14):1408-1417.
12. Allegra CJ, Jessup JM, Somerfield MR, et al. American Society of Clinical Oncology provisional clinical opinion: testing for KRAS gene mutations in patients with metastatic colorectal carcinoma to predict response to anti-epidermal growth factor receptor monoclonal antibody therapy. J Clin Oncol. 2009;27(12):2091-2096.
13. Tejpar S, Lenz HJ, Kohne CH, et al. Effect of KRAS and NRAS mutations on treatment outcomes in patients with metastatic colorectal cancer (mCRC) treated first-line with cetuximab plus FOLFOX4: new results from the OPUS study. J Clin Oncol. 2014;32(suppl 3):LBA444.
14. Abad A, Massuti B, Gravalos C, et al. Panitumumab plus FOLFOX4 or panitumumab plus FOLFIRI in subjects with wild-type KRAS (exon 2) colorectal cancer and multiple or unresectable liver-limited metastases: data from the randomized, phase II planet study. Ann Oncol. 2014;25(suppl 2):ii7-ii18.
15. Schwartzberg LS, Rivera F, Karthaus M, et al. PEAK: a randomized, multicenter phase II study of panitumumab plus modified fluorouracil, leucovorin, and oxaliplatin (mFOLFOX6) or bevacizumab plus mFOLFOX6 in patients with previously untreated, unresectable, wild-type KRAS exon 2 metastatic colorectal cancer. J Clin Oncol. 2014;32(21):2240-2247.
16. Peeters M, Oliner K, Price T, et al. KRAS/NRAS and BRAF mutations in the 20050181 study of panitumumab plus FOLFIRI for the 2nd-line treatment of metastatic colorectal cancer: updated analysis. Ann Oncol. 2014;25(suppl 2):ii5.
17. Bokemeyer C, Van Cutsem E, Rougier P, et al. Addition of cetuximab to chemotherapy as first-line treatment for KRAS wild-type metastatic colorectal cancer: pooled analysis of the CRYSTAL and OPUS randomised clinical trials. Eur J Cancer. 2012;48(10):1466-1475.
18. Van Cutsem E, Lenz HJ, Köhne CH, et al. Fluorouracil, leucovorin, and irinotecan plus cetuximab treatment and RAS mutations in colorectal cancer. J Clin Oncol. 2015;33(7):692-700.
19. ESMO. ESMO 2014: results from the CALGB/SWOG 80405 and FIRE-3 (AIO KRK-0306) studies in all RAS wild type population. ESMO website. http://www.esmo.org/Conferences/Past-Conferences/ESMO-2014-Congress/News-Articles/Results-From-the-CALGB-SWOG-80405-and-FIRE-3-AIO-KRK -0306-Studies-In-All-RAS-Wild-Type-Population. Updated September 29, 2014. Accessed April 6, 2016.
20. Davies H, Bignell GR, Cox C, et al. Mutations of the BRAF gene in human cancer. Nature. 2002;417(6892):949-954.
21. Samowitz WS, Sweeney C, Herrick J, Albertsen H, Levin TR, Murtaugh MA, Wolff RK, Slattery ML. Poor survival associated with the BRAF V600E mutation in microsatellite-stable colon cancers. Cancer Res. 2005;65(14):6063-6069.
22. Di Nicolantonio F, Martini M, Molinari F, et al. Wild-type BRAF is required for response to panitumumab or cetuximab in metastatic colorectal cancer. J Clin Oncol. 2008;26(35):5705-5712.
23. Laurent-Puig P, Cayre A, Manceau G, et al. Analysis of PTEN, BRAF, and EGFR status in determining benefit from cetuximab therapy in wild-type KRAS metastatic colon cancer. J Clin Oncol. 2009;27(35):5924-5930.
24. Richman SD, Seymour MT, Chambers P, et al. KRAS and BRAF mutations in advanced colorectal cancer are associated with poor prognosis but do not preclude benefit from oxaliplatin or irinotecan: results from the MRC FOCUS trial. J Clin Oncol. 2009;27(35):5931-5937.
25. Tveit KM, Guren T, et al. Phase III trial of cetuximab with continuous or intermittent fluorouracil, leucovorin, and oxaliplatin (Nordic FLOX) versus FLOX alone in first-line treatment of metastatic colorectal cancer: The NORDIC-VII study. J Clin Oncol. 2012;30(15):1755-1762.
26. Samuels Y, Wang Z, Bardelli A, et al. High frequency of mutations of the PIK3CA gene in human cancers. Science. 2004;304(5670):554.
27. Sartore-Bianchi A, Martini M, Molinari F, et al. PIK3CA mutations in colorectal cancer are associated with clinical resistance to EGFR-targeted monoclonal antibodies. Cancer Res. 2009;69(5):1851-1857.
28. Deming DA, Leystra AA, Farhoud M, et al. mTOR inhibition elicits a dramatic response in PI3K-dependent colon cancers. PLoS One. 2013;8(4):e60709.
29. Yueh AE, Payne SN, Leystra AA, et al. Colon cancer tumorigenesis initiated by the H1047R mutant PI3K. PLoS One. 2016;11(2):e0148730.
30. Siena S, Sartore-Bianchi A, Lonardi S, et al. Trastuzumab and lapatinib in HER2-amplified metastatic colorectal cancer patients (mCRC): the HERACLES trial. J Clin Oncol. 2015;33(suppl 15):3508.
31. Hong DS, Morris VK, El Osta BE, et al. Phase Ib study of vemurafenib in combination with irinotecan and cetuximab in patients with BRAF-mutated metastatic colorectal cancer and advanced cancers. J Clin Oncol. 2015;33(suppl 15):3511.
32. Benatti P, Gafà R, Barana D, et al. Microsatellite instability and colorectal cancer prognosis. Clin Cancer Res. 2005;11(23):8332-8340.
33. Funkhouser WK, Jr, Lubin IM, Monzon FA, et al. Relevance, pathogenesis, and testing algorithm for mismatch repair-defective colorectal carcinomas: a report of the association for molecular pathology. J Mol Diagn. 2012;14(2):91-103.
34. Le DT, Uram JN, Wang H, et al. PD-1 blockade in tumors with mismatch-repair
deficiency. N Engl J Med. 2015;372(26):2509-2520.
1. Landrum MB, Keating NL, Lamont EB, et al. Survival of older patients with cancer in the Veterans Health Administration versus fee-for-service Medicare. J Clin Oncol. 2012;30(10):1072-1079.
2. Hynes DM, Tarlov E, Durazo-Arvizu R, et al. Surgery and adjuvant chemotherapy use among veterans with colon cancer: insights from a California study. J Clin Oncol. 2010;28(15):2571-2576.
3. Venook AP, Niedzwiecki D, Lenz H-J, et al; Cancer and Leukemia Group B (Alliance), SWOG, and ECOG. CALGB/SWOG 80405: Phase III trial of irinotecan/5-FU/leucovorin (FOLFIRI) or oxaliplatin/5-FU/leucovorin (mFOLFOX6) with bevacizumab (BV) or cetuximab (CET) for patients (pts) with KRAS wild-type (wt) untreated metastatic adenocarcinoma of the colon or rectum (MCRC). J Clin Oncol. 2014;32(suppl 18):Abstract LBA3.
4. Benvenuti S, Sartore-Bianchi A, Di Nicolantonio F, et al. Oncogenic activation of the RAS/RAF signaling pathway impairs the response of metastatic colorectal cancers to anti-epidermal growth factor receptor antibody therapies. Cancer Res. 2007;67(6):2643-2648.
5. Bokemeyer C, Bondarenko I, Hartmann JT, et al. Efficacy according to biomarker status of cetuximab plus FOLFOX-4 as first-line treatment for metastatic colorectal cancer: the OPUS study. Ann Oncol. 2011;22(7):1535-1546.
6. De Roock W, Claes B, Bernasconi D, et al. Effects of KRAS, BRAF, NRAS, and PIK3CA mutations on the efficacy of cetuximab plus chemotherapy in chemotherapy-refractory metastatic colorectal cancer: a retrospective consortium analysis. Lancet Oncol. 2010;11(8):753-7562.
7. Di Fiore F, Blanchard F, Charbonnier F, et al. Clinical relevance of KRAS mutation detection in metastatic colorectal cancer treated by cetuximab plus chemotherapy. Br J Cancer. 2007;96(8):1166-1169.
8. Douillard JY, Oliner KS, Siena S, et al. Panitumumab-FOLFOX4 treatment and RAS mutations in colorectal cancer. N Engl J Med. 2013;369(11):1023-1034.
9. Lièvre A, Bachet JB, Boige V, et al. KRAS mutations as an independent prognostic factor in patients with advanced colorectal cancer treated with cetuximab. J Clin Oncol. 2008;26(3):374-379.
10. Lièvre A, Bachet JB, Le Corre D, et al. KRAS mutation status is predictive of response to cetuximab therapy in colorectal cancer. Cancer Res. 2006;66(8):3992-3995.
11. Van Cutsem E, Köhne CH, Hitre E, et al. Cetuximab and chemotherapy as initial treatment for metastatic colorectal cancer. N Engl J Med. 2009;360(14):1408-1417.
12. Allegra CJ, Jessup JM, Somerfield MR, et al. American Society of Clinical Oncology provisional clinical opinion: testing for KRAS gene mutations in patients with metastatic colorectal carcinoma to predict response to anti-epidermal growth factor receptor monoclonal antibody therapy. J Clin Oncol. 2009;27(12):2091-2096.
13. Tejpar S, Lenz HJ, Kohne CH, et al. Effect of KRAS and NRAS mutations on treatment outcomes in patients with metastatic colorectal cancer (mCRC) treated first-line with cetuximab plus FOLFOX4: new results from the OPUS study. J Clin Oncol. 2014;32(suppl 3):LBA444.
14. Abad A, Massuti B, Gravalos C, et al. Panitumumab plus FOLFOX4 or panitumumab plus FOLFIRI in subjects with wild-type KRAS (exon 2) colorectal cancer and multiple or unresectable liver-limited metastases: data from the randomized, phase II planet study. Ann Oncol. 2014;25(suppl 2):ii7-ii18.
15. Schwartzberg LS, Rivera F, Karthaus M, et al. PEAK: a randomized, multicenter phase II study of panitumumab plus modified fluorouracil, leucovorin, and oxaliplatin (mFOLFOX6) or bevacizumab plus mFOLFOX6 in patients with previously untreated, unresectable, wild-type KRAS exon 2 metastatic colorectal cancer. J Clin Oncol. 2014;32(21):2240-2247.
16. Peeters M, Oliner K, Price T, et al. KRAS/NRAS and BRAF mutations in the 20050181 study of panitumumab plus FOLFIRI for the 2nd-line treatment of metastatic colorectal cancer: updated analysis. Ann Oncol. 2014;25(suppl 2):ii5.
17. Bokemeyer C, Van Cutsem E, Rougier P, et al. Addition of cetuximab to chemotherapy as first-line treatment for KRAS wild-type metastatic colorectal cancer: pooled analysis of the CRYSTAL and OPUS randomised clinical trials. Eur J Cancer. 2012;48(10):1466-1475.
18. Van Cutsem E, Lenz HJ, Köhne CH, et al. Fluorouracil, leucovorin, and irinotecan plus cetuximab treatment and RAS mutations in colorectal cancer. J Clin Oncol. 2015;33(7):692-700.
19. ESMO. ESMO 2014: results from the CALGB/SWOG 80405 and FIRE-3 (AIO KRK-0306) studies in all RAS wild type population. ESMO website. http://www.esmo.org/Conferences/Past-Conferences/ESMO-2014-Congress/News-Articles/Results-From-the-CALGB-SWOG-80405-and-FIRE-3-AIO-KRK -0306-Studies-In-All-RAS-Wild-Type-Population. Updated September 29, 2014. Accessed April 6, 2016.
20. Davies H, Bignell GR, Cox C, et al. Mutations of the BRAF gene in human cancer. Nature. 2002;417(6892):949-954.
21. Samowitz WS, Sweeney C, Herrick J, Albertsen H, Levin TR, Murtaugh MA, Wolff RK, Slattery ML. Poor survival associated with the BRAF V600E mutation in microsatellite-stable colon cancers. Cancer Res. 2005;65(14):6063-6069.
22. Di Nicolantonio F, Martini M, Molinari F, et al. Wild-type BRAF is required for response to panitumumab or cetuximab in metastatic colorectal cancer. J Clin Oncol. 2008;26(35):5705-5712.
23. Laurent-Puig P, Cayre A, Manceau G, et al. Analysis of PTEN, BRAF, and EGFR status in determining benefit from cetuximab therapy in wild-type KRAS metastatic colon cancer. J Clin Oncol. 2009;27(35):5924-5930.
24. Richman SD, Seymour MT, Chambers P, et al. KRAS and BRAF mutations in advanced colorectal cancer are associated with poor prognosis but do not preclude benefit from oxaliplatin or irinotecan: results from the MRC FOCUS trial. J Clin Oncol. 2009;27(35):5931-5937.
25. Tveit KM, Guren T, et al. Phase III trial of cetuximab with continuous or intermittent fluorouracil, leucovorin, and oxaliplatin (Nordic FLOX) versus FLOX alone in first-line treatment of metastatic colorectal cancer: The NORDIC-VII study. J Clin Oncol. 2012;30(15):1755-1762.
26. Samuels Y, Wang Z, Bardelli A, et al. High frequency of mutations of the PIK3CA gene in human cancers. Science. 2004;304(5670):554.
27. Sartore-Bianchi A, Martini M, Molinari F, et al. PIK3CA mutations in colorectal cancer are associated with clinical resistance to EGFR-targeted monoclonal antibodies. Cancer Res. 2009;69(5):1851-1857.
28. Deming DA, Leystra AA, Farhoud M, et al. mTOR inhibition elicits a dramatic response in PI3K-dependent colon cancers. PLoS One. 2013;8(4):e60709.
29. Yueh AE, Payne SN, Leystra AA, et al. Colon cancer tumorigenesis initiated by the H1047R mutant PI3K. PLoS One. 2016;11(2):e0148730.
30. Siena S, Sartore-Bianchi A, Lonardi S, et al. Trastuzumab and lapatinib in HER2-amplified metastatic colorectal cancer patients (mCRC): the HERACLES trial. J Clin Oncol. 2015;33(suppl 15):3508.
31. Hong DS, Morris VK, El Osta BE, et al. Phase Ib study of vemurafenib in combination with irinotecan and cetuximab in patients with BRAF-mutated metastatic colorectal cancer and advanced cancers. J Clin Oncol. 2015;33(suppl 15):3511.
32. Benatti P, Gafà R, Barana D, et al. Microsatellite instability and colorectal cancer prognosis. Clin Cancer Res. 2005;11(23):8332-8340.
33. Funkhouser WK, Jr, Lubin IM, Monzon FA, et al. Relevance, pathogenesis, and testing algorithm for mismatch repair-defective colorectal carcinomas: a report of the association for molecular pathology. J Mol Diagn. 2012;14(2):91-103.
34. Le DT, Uram JN, Wang H, et al. PD-1 blockade in tumors with mismatch-repair
deficiency. N Engl J Med. 2015;372(26):2509-2520.
Updated SSI prevention guidance highlights glucose control, MRSA
The guidelines for controlling surgical site infections have been updated to reflect evidence-based findings of a collaboration between surgeons and infection control experts from the American College of Surgeons, the ACS National Surgical Quality Improvement Program, and the Surgical Infection Society.
Updated strategies to reduce the risk of surgical site infections (SSIs) include perioperative glucose control in all patients and the use of oral antibiotics as an element of colon procedures, according to guidelines published in Journal of the American College of Surgeons (J Am Coll Surg. 2017;224:59-74).
Surgical site infections now account for 20% of all hospital-acquired infections, wrote lead author Kristen A. Ban, MD, a surgical resident at Loyola University Medical Center, Maywood, Ill., and her colleagues.
The most recent guidelines for preventing surgical site infections came from the Centers for Disease Control and Prevention in 1999; “the CDC has been working on an update since 2011, but this has been incredibly slow,” E. Patchen Dellinger, MD, of the University of Washington, Seattle, one of the guidelines’ authors, said in an interview. “A publication should be coming out sometime this year, but in the meantime, it was useful to have something for clinicians to refer to,” he said.
The researchers used PubMed to review specific topics in the SSI literature and address knowledge gaps.
Based on their findings, the new guidelines add recommendations to previous versions that address SSI prevention in the prehospital setting, at the hospital, and after discharge. The level of evidence to support each guideline varies; the researchers strongly recommend certain points, such as perioperative glucose control for all patients, not only those with diabetes; other recommendations such as postoperative showering 12 hours after surgery vs. delayed showering are left to the surgeon’s discretion.
“The changes/new recommendations since the 1999 guideline include the recommendation for the use of oral antibiotics with mechanical bowel prep for colon operations (in combination with intravenous prophylactic antibiotics), the control of perioperative glucose levels in ALL patients (not just diabetics), the maintenance of normothermia in the OR, the use of wound protectors for clean-contaminated cases, the use of antimicrobial sutures, and the use of increased FiO2 levels for intubated patients,” Dr. Dellinger said. These new elements also will be recommended when the updated CDC guidelines are released, and already have been recommended in recent guidelines from the World Health Organization, he added.
Guidelines for prehospital interventions include smoking cessation 4-6 weeks before surgery, preoperative bathing with chlorhexidine, glucose control for diabetes patients, MRSA screening, and bowel preparation (combining mechanical and antibiotic) for all elective colectomies.
Recommended hospital interventions include the following:
• Intraoperative normothermia.
• Use of wound protectors in open abdominal surgery.
• Use of triclosan antibiotic sutures.
• Supplemental oxygen.
• Antibiotic prophylaxis when indicated.
• Glucose control for all patients perioperatively.
• Hair removal only when necessary, avoiding a razor if possible.
• Alcohol-based skin preparation when possible.
• Surgical hand scrub.
• Facility scrub laundering and use of a skull cap if minimal hair is exposed.
• Use of double gloves and changing gloves before incision closure in colorectal cases.
• Use of new instruments for closure in colorectal cases.
• Purse string closure of stoma sites.
• Use of topical antibiotics as part of wound care.
• Using wound vacuum therapy over stapled skin.
Data on interventions after hospital discharge that may reduce SSI incidence are limited, the researchers said. No specific wound care protocols or surveillance methods have been identified. However, “promising new methods of surveillance are being explored, many of which use smartphone technology to help patients send their surgeon daily photos or updates,” they noted.
“Strategies to decrease SSI are multimodal and occur across a range of settings under the supervision of numerous providers,” the researchers wrote. “Ensuring high compliance with these risk-reduction strategies is crucial to the success of SSI reduction efforts,” they added.
However, changes to surgical practice don’t happen overnight, Dr. Dellinger said. “If all of these are actually adapted it should decrease SSI rates in all areas,” he noted. “Oral antibiotics for colorectal cases and glucose control for all patients will probably make the biggest benefit if actually adopted,” he said.
“We could use some better studies on the precise timing of parenteral prophylactic antibiotics,” said Dr. Dellinger. “One such study has been submitted from Switzerland and should be published sometime this year. Hard evidence on the best timing is missing although observational data allows some of us to come to conclusions on that,” he said. “Additional studies on perioperative oxygenation where fluid management and temperature management are better controlled would be helpful, and more and better studies are need for antimicrobial sutures,” he added.
The authors had nothing to disclose relevant to the scope of the guidelines. Outside the scope of this work, Dr. Dellinger disclosed serving on the advisory boards for 3M, Melinta, and Theravance, as well as receiving a grant from Motif for a clinical trial of iclaprim vs. vancomycin for the treatment of skin and soft tissue infections.
The guidelines for controlling surgical site infections have been updated to reflect evidence-based findings of a collaboration between surgeons and infection control experts from the American College of Surgeons, the ACS National Surgical Quality Improvement Program, and the Surgical Infection Society.
Updated strategies to reduce the risk of surgical site infections (SSIs) include perioperative glucose control in all patients and the use of oral antibiotics as an element of colon procedures, according to guidelines published in Journal of the American College of Surgeons (J Am Coll Surg. 2017;224:59-74).
Surgical site infections now account for 20% of all hospital-acquired infections, wrote lead author Kristen A. Ban, MD, a surgical resident at Loyola University Medical Center, Maywood, Ill., and her colleagues.
The most recent guidelines for preventing surgical site infections came from the Centers for Disease Control and Prevention in 1999; “the CDC has been working on an update since 2011, but this has been incredibly slow,” E. Patchen Dellinger, MD, of the University of Washington, Seattle, one of the guidelines’ authors, said in an interview. “A publication should be coming out sometime this year, but in the meantime, it was useful to have something for clinicians to refer to,” he said.
The researchers used PubMed to review specific topics in the SSI literature and address knowledge gaps.
Based on their findings, the new guidelines add recommendations to previous versions that address SSI prevention in the prehospital setting, at the hospital, and after discharge. The level of evidence to support each guideline varies; the researchers strongly recommend certain points, such as perioperative glucose control for all patients, not only those with diabetes; other recommendations such as postoperative showering 12 hours after surgery vs. delayed showering are left to the surgeon’s discretion.
“The changes/new recommendations since the 1999 guideline include the recommendation for the use of oral antibiotics with mechanical bowel prep for colon operations (in combination with intravenous prophylactic antibiotics), the control of perioperative glucose levels in ALL patients (not just diabetics), the maintenance of normothermia in the OR, the use of wound protectors for clean-contaminated cases, the use of antimicrobial sutures, and the use of increased FiO2 levels for intubated patients,” Dr. Dellinger said. These new elements also will be recommended when the updated CDC guidelines are released, and already have been recommended in recent guidelines from the World Health Organization, he added.
Guidelines for prehospital interventions include smoking cessation 4-6 weeks before surgery, preoperative bathing with chlorhexidine, glucose control for diabetes patients, MRSA screening, and bowel preparation (combining mechanical and antibiotic) for all elective colectomies.
Recommended hospital interventions include the following:
• Intraoperative normothermia.
• Use of wound protectors in open abdominal surgery.
• Use of triclosan antibiotic sutures.
• Supplemental oxygen.
• Antibiotic prophylaxis when indicated.
• Glucose control for all patients perioperatively.
• Hair removal only when necessary, avoiding a razor if possible.
• Alcohol-based skin preparation when possible.
• Surgical hand scrub.
• Facility scrub laundering and use of a skull cap if minimal hair is exposed.
• Use of double gloves and changing gloves before incision closure in colorectal cases.
• Use of new instruments for closure in colorectal cases.
• Purse string closure of stoma sites.
• Use of topical antibiotics as part of wound care.
• Using wound vacuum therapy over stapled skin.
Data on interventions after hospital discharge that may reduce SSI incidence are limited, the researchers said. No specific wound care protocols or surveillance methods have been identified. However, “promising new methods of surveillance are being explored, many of which use smartphone technology to help patients send their surgeon daily photos or updates,” they noted.
“Strategies to decrease SSI are multimodal and occur across a range of settings under the supervision of numerous providers,” the researchers wrote. “Ensuring high compliance with these risk-reduction strategies is crucial to the success of SSI reduction efforts,” they added.
However, changes to surgical practice don’t happen overnight, Dr. Dellinger said. “If all of these are actually adapted it should decrease SSI rates in all areas,” he noted. “Oral antibiotics for colorectal cases and glucose control for all patients will probably make the biggest benefit if actually adopted,” he said.
“We could use some better studies on the precise timing of parenteral prophylactic antibiotics,” said Dr. Dellinger. “One such study has been submitted from Switzerland and should be published sometime this year. Hard evidence on the best timing is missing although observational data allows some of us to come to conclusions on that,” he said. “Additional studies on perioperative oxygenation where fluid management and temperature management are better controlled would be helpful, and more and better studies are need for antimicrobial sutures,” he added.
The authors had nothing to disclose relevant to the scope of the guidelines. Outside the scope of this work, Dr. Dellinger disclosed serving on the advisory boards for 3M, Melinta, and Theravance, as well as receiving a grant from Motif for a clinical trial of iclaprim vs. vancomycin for the treatment of skin and soft tissue infections.
The guidelines for controlling surgical site infections have been updated to reflect evidence-based findings of a collaboration between surgeons and infection control experts from the American College of Surgeons, the ACS National Surgical Quality Improvement Program, and the Surgical Infection Society.
Updated strategies to reduce the risk of surgical site infections (SSIs) include perioperative glucose control in all patients and the use of oral antibiotics as an element of colon procedures, according to guidelines published in Journal of the American College of Surgeons (J Am Coll Surg. 2017;224:59-74).
Surgical site infections now account for 20% of all hospital-acquired infections, wrote lead author Kristen A. Ban, MD, a surgical resident at Loyola University Medical Center, Maywood, Ill., and her colleagues.
The most recent guidelines for preventing surgical site infections came from the Centers for Disease Control and Prevention in 1999; “the CDC has been working on an update since 2011, but this has been incredibly slow,” E. Patchen Dellinger, MD, of the University of Washington, Seattle, one of the guidelines’ authors, said in an interview. “A publication should be coming out sometime this year, but in the meantime, it was useful to have something for clinicians to refer to,” he said.
The researchers used PubMed to review specific topics in the SSI literature and address knowledge gaps.
Based on their findings, the new guidelines add recommendations to previous versions that address SSI prevention in the prehospital setting, at the hospital, and after discharge. The level of evidence to support each guideline varies; the researchers strongly recommend certain points, such as perioperative glucose control for all patients, not only those with diabetes; other recommendations such as postoperative showering 12 hours after surgery vs. delayed showering are left to the surgeon’s discretion.
“The changes/new recommendations since the 1999 guideline include the recommendation for the use of oral antibiotics with mechanical bowel prep for colon operations (in combination with intravenous prophylactic antibiotics), the control of perioperative glucose levels in ALL patients (not just diabetics), the maintenance of normothermia in the OR, the use of wound protectors for clean-contaminated cases, the use of antimicrobial sutures, and the use of increased FiO2 levels for intubated patients,” Dr. Dellinger said. These new elements also will be recommended when the updated CDC guidelines are released, and already have been recommended in recent guidelines from the World Health Organization, he added.
Guidelines for prehospital interventions include smoking cessation 4-6 weeks before surgery, preoperative bathing with chlorhexidine, glucose control for diabetes patients, MRSA screening, and bowel preparation (combining mechanical and antibiotic) for all elective colectomies.
Recommended hospital interventions include the following:
• Intraoperative normothermia.
• Use of wound protectors in open abdominal surgery.
• Use of triclosan antibiotic sutures.
• Supplemental oxygen.
• Antibiotic prophylaxis when indicated.
• Glucose control for all patients perioperatively.
• Hair removal only when necessary, avoiding a razor if possible.
• Alcohol-based skin preparation when possible.
• Surgical hand scrub.
• Facility scrub laundering and use of a skull cap if minimal hair is exposed.
• Use of double gloves and changing gloves before incision closure in colorectal cases.
• Use of new instruments for closure in colorectal cases.
• Purse string closure of stoma sites.
• Use of topical antibiotics as part of wound care.
• Using wound vacuum therapy over stapled skin.
Data on interventions after hospital discharge that may reduce SSI incidence are limited, the researchers said. No specific wound care protocols or surveillance methods have been identified. However, “promising new methods of surveillance are being explored, many of which use smartphone technology to help patients send their surgeon daily photos or updates,” they noted.
“Strategies to decrease SSI are multimodal and occur across a range of settings under the supervision of numerous providers,” the researchers wrote. “Ensuring high compliance with these risk-reduction strategies is crucial to the success of SSI reduction efforts,” they added.
However, changes to surgical practice don’t happen overnight, Dr. Dellinger said. “If all of these are actually adapted it should decrease SSI rates in all areas,” he noted. “Oral antibiotics for colorectal cases and glucose control for all patients will probably make the biggest benefit if actually adopted,” he said.
“We could use some better studies on the precise timing of parenteral prophylactic antibiotics,” said Dr. Dellinger. “One such study has been submitted from Switzerland and should be published sometime this year. Hard evidence on the best timing is missing although observational data allows some of us to come to conclusions on that,” he said. “Additional studies on perioperative oxygenation where fluid management and temperature management are better controlled would be helpful, and more and better studies are need for antimicrobial sutures,” he added.
The authors had nothing to disclose relevant to the scope of the guidelines. Outside the scope of this work, Dr. Dellinger disclosed serving on the advisory boards for 3M, Melinta, and Theravance, as well as receiving a grant from Motif for a clinical trial of iclaprim vs. vancomycin for the treatment of skin and soft tissue infections.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
Intrathecal hydromorphone boosts post-op pain control
LAS VEGAS – Intrathecal hydromorphone, administered alone or with lidocaine, effectively controlled pain and decreased postoperative opioid use after colorectal surgery in a retrospective study.
The technique was so effective that 28% of patients required no postoperative opioids at all, Amit Merchea, MD, said at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
The intrathecal analgesic was part of an enhanced recovery pathway (ERP) for patients undergoing elective colorectal surgery at the Mayo Clinic, Jacksonville, Fla., where Dr. Merchea practices colorectal surgery.
Morphine has been the gold standard for this approach, he said. Dr. Merchea and his colleagues investigated the use of hydromorphone in 601 patients who underwent open or minimally invasive colorectal surgery at the Mayo Clinic from 2012 to 2013.
The patients were a median of 52 years old. The surgical approach was almost evenly split between open and laparoscopic. The median length of hospital stay was 3 days. All received intrathecal hydromorphone either alone (91%) or with a local anesthetic (9%).
Everyone was on the same presurgical and postsurgical pain control regimen, which consisted of celecoxib, gabapentin, and acetaminophen before surgery, followed by nonsteroidal anti-inflammatories and acetaminophen, with oxycodone as needed, after surgery.
Overall, the procedure was well tolerated, with seven cases of pruritus requiring Nubain (nalbuphine), one case of respiratory depression that required naloxone, and one postdural headache that required a patch. The rate of ileus was 16%.
At 4 hours, the median pain score was 3 on a 1- to 10-point scale. At 24 hours, it was a median of 4. By 48 hours, the median pain score was 6. This increase is to be expected as the hydrocodone exists in the intrathecal space for up to 36 hours, Dr. Merchea noted.
The median total oral morphine equivalent (OME) was 24; 170 patients (28%) needed no opioid medications after surgery.
He also presented outcomes by infusion composition. There was no difference in the rate of ileus among those who had hydromorphone alone and those who had it with lidocaine. The length of stay was 3 vs. 3.5 days, respectively. The only significant difference in pain scores was the 48-hour maximum, which was a median of 7 in the combination group and 6 in the hydromorphone-only group.
The combination group, however, required more postoperative opioids (33.8 vs. 22.5 OMEs). Significantly more patients in the hydromorphone-only group were able to go without any postoperative opioids (30% vs. 15%).
Dr. Merchea also broke down the results by hydromorphone dosage, but there were no significant differences in ileus rate, length of stay, or pain scores correlated with dosage. However, those who received higher doses were significantly more likely to need more postoperative opioids than those who had lower doses.
Session moderator Peter Muscarella, MD, of Montefiore Medical Center, New York, asked whether the intrathecal infusion was associated with hypotension. “Some of these procedures with epidural analgesics intraoperatively, we have seen shifts in blood pressure that result in excess fluid administration, sometimes leading to tissue complications.”
Dr. Merchea said hypotension was not an outcome of this trial, but that he has looked at it before. “We have previously reported that epidural analgesia was associated with a 15% occurrence of hypotension, but it had no clinical impact and didn’t warrant giving any additional fluids.”
Dr. Merchea had no relevant financial disclosures.
[email protected]
On Twitter @Alz_Gal
LAS VEGAS – Intrathecal hydromorphone, administered alone or with lidocaine, effectively controlled pain and decreased postoperative opioid use after colorectal surgery in a retrospective study.
The technique was so effective that 28% of patients required no postoperative opioids at all, Amit Merchea, MD, said at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
The intrathecal analgesic was part of an enhanced recovery pathway (ERP) for patients undergoing elective colorectal surgery at the Mayo Clinic, Jacksonville, Fla., where Dr. Merchea practices colorectal surgery.
Morphine has been the gold standard for this approach, he said. Dr. Merchea and his colleagues investigated the use of hydromorphone in 601 patients who underwent open or minimally invasive colorectal surgery at the Mayo Clinic from 2012 to 2013.
The patients were a median of 52 years old. The surgical approach was almost evenly split between open and laparoscopic. The median length of hospital stay was 3 days. All received intrathecal hydromorphone either alone (91%) or with a local anesthetic (9%).
Everyone was on the same presurgical and postsurgical pain control regimen, which consisted of celecoxib, gabapentin, and acetaminophen before surgery, followed by nonsteroidal anti-inflammatories and acetaminophen, with oxycodone as needed, after surgery.
Overall, the procedure was well tolerated, with seven cases of pruritus requiring Nubain (nalbuphine), one case of respiratory depression that required naloxone, and one postdural headache that required a patch. The rate of ileus was 16%.
At 4 hours, the median pain score was 3 on a 1- to 10-point scale. At 24 hours, it was a median of 4. By 48 hours, the median pain score was 6. This increase is to be expected as the hydrocodone exists in the intrathecal space for up to 36 hours, Dr. Merchea noted.
The median total oral morphine equivalent (OME) was 24; 170 patients (28%) needed no opioid medications after surgery.
He also presented outcomes by infusion composition. There was no difference in the rate of ileus among those who had hydromorphone alone and those who had it with lidocaine. The length of stay was 3 vs. 3.5 days, respectively. The only significant difference in pain scores was the 48-hour maximum, which was a median of 7 in the combination group and 6 in the hydromorphone-only group.
The combination group, however, required more postoperative opioids (33.8 vs. 22.5 OMEs). Significantly more patients in the hydromorphone-only group were able to go without any postoperative opioids (30% vs. 15%).
Dr. Merchea also broke down the results by hydromorphone dosage, but there were no significant differences in ileus rate, length of stay, or pain scores correlated with dosage. However, those who received higher doses were significantly more likely to need more postoperative opioids than those who had lower doses.
Session moderator Peter Muscarella, MD, of Montefiore Medical Center, New York, asked whether the intrathecal infusion was associated with hypotension. “Some of these procedures with epidural analgesics intraoperatively, we have seen shifts in blood pressure that result in excess fluid administration, sometimes leading to tissue complications.”
Dr. Merchea said hypotension was not an outcome of this trial, but that he has looked at it before. “We have previously reported that epidural analgesia was associated with a 15% occurrence of hypotension, but it had no clinical impact and didn’t warrant giving any additional fluids.”
Dr. Merchea had no relevant financial disclosures.
[email protected]
On Twitter @Alz_Gal
LAS VEGAS – Intrathecal hydromorphone, administered alone or with lidocaine, effectively controlled pain and decreased postoperative opioid use after colorectal surgery in a retrospective study.
The technique was so effective that 28% of patients required no postoperative opioids at all, Amit Merchea, MD, said at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
The intrathecal analgesic was part of an enhanced recovery pathway (ERP) for patients undergoing elective colorectal surgery at the Mayo Clinic, Jacksonville, Fla., where Dr. Merchea practices colorectal surgery.
Morphine has been the gold standard for this approach, he said. Dr. Merchea and his colleagues investigated the use of hydromorphone in 601 patients who underwent open or minimally invasive colorectal surgery at the Mayo Clinic from 2012 to 2013.
The patients were a median of 52 years old. The surgical approach was almost evenly split between open and laparoscopic. The median length of hospital stay was 3 days. All received intrathecal hydromorphone either alone (91%) or with a local anesthetic (9%).
Everyone was on the same presurgical and postsurgical pain control regimen, which consisted of celecoxib, gabapentin, and acetaminophen before surgery, followed by nonsteroidal anti-inflammatories and acetaminophen, with oxycodone as needed, after surgery.
Overall, the procedure was well tolerated, with seven cases of pruritus requiring Nubain (nalbuphine), one case of respiratory depression that required naloxone, and one postdural headache that required a patch. The rate of ileus was 16%.
At 4 hours, the median pain score was 3 on a 1- to 10-point scale. At 24 hours, it was a median of 4. By 48 hours, the median pain score was 6. This increase is to be expected as the hydrocodone exists in the intrathecal space for up to 36 hours, Dr. Merchea noted.
The median total oral morphine equivalent (OME) was 24; 170 patients (28%) needed no opioid medications after surgery.
He also presented outcomes by infusion composition. There was no difference in the rate of ileus among those who had hydromorphone alone and those who had it with lidocaine. The length of stay was 3 vs. 3.5 days, respectively. The only significant difference in pain scores was the 48-hour maximum, which was a median of 7 in the combination group and 6 in the hydromorphone-only group.
The combination group, however, required more postoperative opioids (33.8 vs. 22.5 OMEs). Significantly more patients in the hydromorphone-only group were able to go without any postoperative opioids (30% vs. 15%).
Dr. Merchea also broke down the results by hydromorphone dosage, but there were no significant differences in ileus rate, length of stay, or pain scores correlated with dosage. However, those who received higher doses were significantly more likely to need more postoperative opioids than those who had lower doses.
Session moderator Peter Muscarella, MD, of Montefiore Medical Center, New York, asked whether the intrathecal infusion was associated with hypotension. “Some of these procedures with epidural analgesics intraoperatively, we have seen shifts in blood pressure that result in excess fluid administration, sometimes leading to tissue complications.”
Dr. Merchea said hypotension was not an outcome of this trial, but that he has looked at it before. “We have previously reported that epidural analgesia was associated with a 15% occurrence of hypotension, but it had no clinical impact and didn’t warrant giving any additional fluids.”
Dr. Merchea had no relevant financial disclosures.
[email protected]
On Twitter @Alz_Gal
AT THE ACADEMIC SURGICAL CONGRESS
Key clinical point:
Major finding: About a quarter of patients (28%) needed no postoperative opioids.
Data source: A retrospective study of 601 patients.
Disclosures: Dr. Merchea had no relevant financial disclosures.
Adjuvant chemotherapy overused in young patients with colon cancer
Adjuvant chemotherapy may be overused among younger patients with colon cancer, without clear evidence of survival benefit over surgery alone, according to a report in JAMA Surgery.
Using data from 3,143 patients with histologically confirmed primary colon adenocarcinoma in the U.S. Department of Defense’s Central Cancer Registry and Military Heath System medical claims databases, researchers compared overall survival in those who underwent surgery and adjuvant chemotherapy to those who underwent surgery alone.
They found patients aged 18-49 years were up to eight times more likely to receive postoperative systemic chemotherapy across all tumor stages compared to patients aged 65-75 years. The odds ratios ranged from 7.98 for stage I tumors to 2.30 for stage III tumors (JAMA Surgery 2017, Jan 25. doi:10.1001/jamasurg.2016.5050).
“Furthermore, young and middle-aged adults were 2.5 times more likely to receive multiagent chemotherapy regimens and most patients with information on chemotherapy regimens underwent multiagent regimens, suggesting a tendency toward more intense treatments,” wrote Janna Manjelievskaia, MPH, of Walter Reed National Military Medical Center, and coauthors.*
However, they found that there was no significant difference in survival between those who had surgery and chemotherapy compared to those who had surgery alone, across age groups and tumor stage.
They did note greater overall survival among middle-aged patients with stage I and stage IV disease who were treated with surgery alone, compared to their older counterparts. Younger patients with stage III disease who received surgery alone also had slightly better survival than did older patients.
“The study suggests that more use of chemotherapy in younger patients did not result in additional survival benefits,” the authors wrote.
While national guidelines advise that selected patients with stage II disease – those with inadequately sampled nodes, T3 lesions or poorly differentiated histology – can be considered for adjuvant chemotherapy, the authors argued there is no solid evidence for the effectiveness of chemotherapy in these patients.
“Patients with cancer who receive chemotherapy are vulnerable to its toxicity and adverse effects and may have reduced quality of life,” they wrote. “As a result, patients may undergo decreased physical, functional, emotional, and social well-being, although these changes might be mitigated over time.”
Given the additional economic and financial cost of adjuvant chemotherapy, the authors called for further research to evaluate the appropriate use of chemotherapy in colon cancer.
The John P. Murtha Cancer Center, Walter Reed National Military Medical Center, and the National Cancer Institute supported the study. No conflicts of interest were declared.
* This story was updated on 2/6/2107
The study by Manjelievskaia et al. is a call for action, and invites contemplation and in-depth study. Appropriate treatment is vital for a patient’s survival, but excess treatment may increase complications and is a poor stewardship of health care funds.
Further investigation of the discrepancies in stage II would be worthwhile, and additional research on the age discrepancies in stage I disease would not only be interesting but also mandatory. Colorectal cancer tumor boards frequently concentrate on the complex care of rectal cancer and metastatic colon cancer. This is also a clear call for improved oversight of chemotherapy for colon cancer.
Tonia M. Young-Fadok, MD, is at the Mayo Clinic, Phoenix, Ariz. These comments are exerpts from an accompanying editorial (JAMA Surg. 2017, Jan 25. doi: 10.1001/jamasurg.2016.5051). No conflicts of interest were declared.
The study by Manjelievskaia et al. is a call for action, and invites contemplation and in-depth study. Appropriate treatment is vital for a patient’s survival, but excess treatment may increase complications and is a poor stewardship of health care funds.
Further investigation of the discrepancies in stage II would be worthwhile, and additional research on the age discrepancies in stage I disease would not only be interesting but also mandatory. Colorectal cancer tumor boards frequently concentrate on the complex care of rectal cancer and metastatic colon cancer. This is also a clear call for improved oversight of chemotherapy for colon cancer.
Tonia M. Young-Fadok, MD, is at the Mayo Clinic, Phoenix, Ariz. These comments are exerpts from an accompanying editorial (JAMA Surg. 2017, Jan 25. doi: 10.1001/jamasurg.2016.5051). No conflicts of interest were declared.
The study by Manjelievskaia et al. is a call for action, and invites contemplation and in-depth study. Appropriate treatment is vital for a patient’s survival, but excess treatment may increase complications and is a poor stewardship of health care funds.
Further investigation of the discrepancies in stage II would be worthwhile, and additional research on the age discrepancies in stage I disease would not only be interesting but also mandatory. Colorectal cancer tumor boards frequently concentrate on the complex care of rectal cancer and metastatic colon cancer. This is also a clear call for improved oversight of chemotherapy for colon cancer.
Tonia M. Young-Fadok, MD, is at the Mayo Clinic, Phoenix, Ariz. These comments are exerpts from an accompanying editorial (JAMA Surg. 2017, Jan 25. doi: 10.1001/jamasurg.2016.5051). No conflicts of interest were declared.
Adjuvant chemotherapy may be overused among younger patients with colon cancer, without clear evidence of survival benefit over surgery alone, according to a report in JAMA Surgery.
Using data from 3,143 patients with histologically confirmed primary colon adenocarcinoma in the U.S. Department of Defense’s Central Cancer Registry and Military Heath System medical claims databases, researchers compared overall survival in those who underwent surgery and adjuvant chemotherapy to those who underwent surgery alone.
They found patients aged 18-49 years were up to eight times more likely to receive postoperative systemic chemotherapy across all tumor stages compared to patients aged 65-75 years. The odds ratios ranged from 7.98 for stage I tumors to 2.30 for stage III tumors (JAMA Surgery 2017, Jan 25. doi:10.1001/jamasurg.2016.5050).
“Furthermore, young and middle-aged adults were 2.5 times more likely to receive multiagent chemotherapy regimens and most patients with information on chemotherapy regimens underwent multiagent regimens, suggesting a tendency toward more intense treatments,” wrote Janna Manjelievskaia, MPH, of Walter Reed National Military Medical Center, and coauthors.*
However, they found that there was no significant difference in survival between those who had surgery and chemotherapy compared to those who had surgery alone, across age groups and tumor stage.
They did note greater overall survival among middle-aged patients with stage I and stage IV disease who were treated with surgery alone, compared to their older counterparts. Younger patients with stage III disease who received surgery alone also had slightly better survival than did older patients.
“The study suggests that more use of chemotherapy in younger patients did not result in additional survival benefits,” the authors wrote.
While national guidelines advise that selected patients with stage II disease – those with inadequately sampled nodes, T3 lesions or poorly differentiated histology – can be considered for adjuvant chemotherapy, the authors argued there is no solid evidence for the effectiveness of chemotherapy in these patients.
“Patients with cancer who receive chemotherapy are vulnerable to its toxicity and adverse effects and may have reduced quality of life,” they wrote. “As a result, patients may undergo decreased physical, functional, emotional, and social well-being, although these changes might be mitigated over time.”
Given the additional economic and financial cost of adjuvant chemotherapy, the authors called for further research to evaluate the appropriate use of chemotherapy in colon cancer.
The John P. Murtha Cancer Center, Walter Reed National Military Medical Center, and the National Cancer Institute supported the study. No conflicts of interest were declared.
* This story was updated on 2/6/2107
Adjuvant chemotherapy may be overused among younger patients with colon cancer, without clear evidence of survival benefit over surgery alone, according to a report in JAMA Surgery.
Using data from 3,143 patients with histologically confirmed primary colon adenocarcinoma in the U.S. Department of Defense’s Central Cancer Registry and Military Heath System medical claims databases, researchers compared overall survival in those who underwent surgery and adjuvant chemotherapy to those who underwent surgery alone.
They found patients aged 18-49 years were up to eight times more likely to receive postoperative systemic chemotherapy across all tumor stages compared to patients aged 65-75 years. The odds ratios ranged from 7.98 for stage I tumors to 2.30 for stage III tumors (JAMA Surgery 2017, Jan 25. doi:10.1001/jamasurg.2016.5050).
“Furthermore, young and middle-aged adults were 2.5 times more likely to receive multiagent chemotherapy regimens and most patients with information on chemotherapy regimens underwent multiagent regimens, suggesting a tendency toward more intense treatments,” wrote Janna Manjelievskaia, MPH, of Walter Reed National Military Medical Center, and coauthors.*
However, they found that there was no significant difference in survival between those who had surgery and chemotherapy compared to those who had surgery alone, across age groups and tumor stage.
They did note greater overall survival among middle-aged patients with stage I and stage IV disease who were treated with surgery alone, compared to their older counterparts. Younger patients with stage III disease who received surgery alone also had slightly better survival than did older patients.
“The study suggests that more use of chemotherapy in younger patients did not result in additional survival benefits,” the authors wrote.
While national guidelines advise that selected patients with stage II disease – those with inadequately sampled nodes, T3 lesions or poorly differentiated histology – can be considered for adjuvant chemotherapy, the authors argued there is no solid evidence for the effectiveness of chemotherapy in these patients.
“Patients with cancer who receive chemotherapy are vulnerable to its toxicity and adverse effects and may have reduced quality of life,” they wrote. “As a result, patients may undergo decreased physical, functional, emotional, and social well-being, although these changes might be mitigated over time.”
Given the additional economic and financial cost of adjuvant chemotherapy, the authors called for further research to evaluate the appropriate use of chemotherapy in colon cancer.
The John P. Murtha Cancer Center, Walter Reed National Military Medical Center, and the National Cancer Institute supported the study. No conflicts of interest were declared.
* This story was updated on 2/6/2107
FROM JAMA SURGERY
Key clinical point: Adjuvant chemotherapy may be overused among younger patients with colon cancer, without clear evidence of a survival benefit over surgery alone.
Major finding: Younger patients with colon cancer are between two and eight times more likely to have adjuvant chemotherapy in addition to surgery compared to older patients with colon cancer.
Data source: A cohort study of 3,143 patients with histologically confirmed primary colon adenocarcinoma.
Disclosures: The John P. Murtha Cancer Center, Walter Reed National Military Medical Center, and the National Cancer Institute supported the study. No conflicts of interest were declared.