User login
Efficacy and Toxicity of XELOX vs FOLFOX in Adjuvant and Metastatic Treatment of Colorectal Cancer in Veterans
Purpose: To determine the efficacy and toxicity of fluorouracil/leucovorin/oxaliplatin (FOLFOX) vs capecitabine/oxaliplatin (XELOX or CAPOX) in the treatment of colorectal cancer (CRC) in both the adjuvant (aCRC) and metastatic (mCRC) setting in Veterans at the Southern Arizona Veteran Affairs Health Care System (SAVAHCS).
Methods: A retrospective chart review was conducted to collect efficacy and toxicity data. Subjects were included based on age, treatment setting, and regimen in the preset 5-year period, and appropriate diagnosis via International Classification of Diseases-Revision 9 (ICD-9) codes. Efficacy was measured via 1-year disease-free survival (DFS) for aCRC, progression-free survival (PFS) for mCRC, and overall survival (OS) for both settings.
Results: A total of 79 subjects were initially evaluatedwith 51 and 54 all-male subjects included in the efficacy and toxicity analysis, respectively. Mean range of age was 63-72 years old. Subjects were divided into four groups: FOLFOX aCRC (N = 17) and mCRC (N = 19), XELOX aCRC (N = 10) and mCRC (N = 8). No difference was found in 1-year DFS and OS between aCRC treatment groups, and PFS between mCRC groups. A higher incidence of 1-year OS with FOLFOX in the mCRC setting was noted (P = .03). No difference was found in the incidence of most of the toxicities between FOLFOX and XELOX, except a higher incidence of hand-foot syndrome was seen in XELOX (P = .0007) treated patients.
Conclusions: In this patient population, the efficacy between FOLFOX and XELOX in aCRC and mCRC was similar, while toxicity was slightly more prevalent with XELOX treatment due to increased hand-foot syndrome incidence. These findings are consistent with the results reported by previous larger prospective clinical trials.
Purpose: To determine the efficacy and toxicity of fluorouracil/leucovorin/oxaliplatin (FOLFOX) vs capecitabine/oxaliplatin (XELOX or CAPOX) in the treatment of colorectal cancer (CRC) in both the adjuvant (aCRC) and metastatic (mCRC) setting in Veterans at the Southern Arizona Veteran Affairs Health Care System (SAVAHCS).
Methods: A retrospective chart review was conducted to collect efficacy and toxicity data. Subjects were included based on age, treatment setting, and regimen in the preset 5-year period, and appropriate diagnosis via International Classification of Diseases-Revision 9 (ICD-9) codes. Efficacy was measured via 1-year disease-free survival (DFS) for aCRC, progression-free survival (PFS) for mCRC, and overall survival (OS) for both settings.
Results: A total of 79 subjects were initially evaluatedwith 51 and 54 all-male subjects included in the efficacy and toxicity analysis, respectively. Mean range of age was 63-72 years old. Subjects were divided into four groups: FOLFOX aCRC (N = 17) and mCRC (N = 19), XELOX aCRC (N = 10) and mCRC (N = 8). No difference was found in 1-year DFS and OS between aCRC treatment groups, and PFS between mCRC groups. A higher incidence of 1-year OS with FOLFOX in the mCRC setting was noted (P = .03). No difference was found in the incidence of most of the toxicities between FOLFOX and XELOX, except a higher incidence of hand-foot syndrome was seen in XELOX (P = .0007) treated patients.
Conclusions: In this patient population, the efficacy between FOLFOX and XELOX in aCRC and mCRC was similar, while toxicity was slightly more prevalent with XELOX treatment due to increased hand-foot syndrome incidence. These findings are consistent with the results reported by previous larger prospective clinical trials.
Purpose: To determine the efficacy and toxicity of fluorouracil/leucovorin/oxaliplatin (FOLFOX) vs capecitabine/oxaliplatin (XELOX or CAPOX) in the treatment of colorectal cancer (CRC) in both the adjuvant (aCRC) and metastatic (mCRC) setting in Veterans at the Southern Arizona Veteran Affairs Health Care System (SAVAHCS).
Methods: A retrospective chart review was conducted to collect efficacy and toxicity data. Subjects were included based on age, treatment setting, and regimen in the preset 5-year period, and appropriate diagnosis via International Classification of Diseases-Revision 9 (ICD-9) codes. Efficacy was measured via 1-year disease-free survival (DFS) for aCRC, progression-free survival (PFS) for mCRC, and overall survival (OS) for both settings.
Results: A total of 79 subjects were initially evaluatedwith 51 and 54 all-male subjects included in the efficacy and toxicity analysis, respectively. Mean range of age was 63-72 years old. Subjects were divided into four groups: FOLFOX aCRC (N = 17) and mCRC (N = 19), XELOX aCRC (N = 10) and mCRC (N = 8). No difference was found in 1-year DFS and OS between aCRC treatment groups, and PFS between mCRC groups. A higher incidence of 1-year OS with FOLFOX in the mCRC setting was noted (P = .03). No difference was found in the incidence of most of the toxicities between FOLFOX and XELOX, except a higher incidence of hand-foot syndrome was seen in XELOX (P = .0007) treated patients.
Conclusions: In this patient population, the efficacy between FOLFOX and XELOX in aCRC and mCRC was similar, while toxicity was slightly more prevalent with XELOX treatment due to increased hand-foot syndrome incidence. These findings are consistent with the results reported by previous larger prospective clinical trials.
Assessing the Efficacy of Prostate Cancer Therapies in Veterans at the James J. Peters VAMC
Background: Oncologists evaluating tumor size after anticancer therapy in patients observe the net result of 2 phenomena: regression of the sensitive tumor fraction and growth of the resistant fraction occurring simultaneously at rates that are constant. We have employed simple mathematical models with single and multi-institutional data sets to estimate 2 exponential rate constants: one for tumor regression or decay (d) and one for tumor growth (g). We have (1) established that g correlates with overall survival; (2) demonstrated changes in g after treatment is discontinued; and (3) benchmarked effectiveness in small 20 to 30 patient cohorts to reference data sets from randomized phase 3 trials. Our approach is novel and not another modification of PSA doubling time or velocity, which cannot estimate regression or growth rates while a patient receives therapy. It allows us to determine treatment efficacy regardless of the interval between measurements, which often varies in clinical practice. Our ultimate goals are to establish a reliable method to assess efficacy, provide support for clinical decisions and increase access to clinical trials.
Methods: For the current study we applied our methodology to assess treatment effectiveness among Veterans with prostate cancer (PC) at the J.J. Peters VAMC. To do this we captured serial PSA values and dates when treatment with abiraterone and enzalutamide were started and stopped.
Results: Our initial analysis has examined data from twenty Veterans with PC. The majority had received abiraterone first followed by enzalutamide. With both therapies we found excellent fit of data. Despite wide variations in assessment intervals, g could be calculated in all patients. The median g on abiraterone (0.00086) was fourfold slower than on enzalutamide (0.0035), a statistically significant difference (P = .022). In individual patients we demonstrated comparable g values on abiraterone and enzalutamide in some, but increased g in half the patients when switched to enzalutamide.
Conclusions: Using observational data and a novel method to assess efficacy, we have compared the effectiveness of PC therapies administered to Veterans. Our VAMC data will be benchmarked against publicly available data from registration trials.
Background: Oncologists evaluating tumor size after anticancer therapy in patients observe the net result of 2 phenomena: regression of the sensitive tumor fraction and growth of the resistant fraction occurring simultaneously at rates that are constant. We have employed simple mathematical models with single and multi-institutional data sets to estimate 2 exponential rate constants: one for tumor regression or decay (d) and one for tumor growth (g). We have (1) established that g correlates with overall survival; (2) demonstrated changes in g after treatment is discontinued; and (3) benchmarked effectiveness in small 20 to 30 patient cohorts to reference data sets from randomized phase 3 trials. Our approach is novel and not another modification of PSA doubling time or velocity, which cannot estimate regression or growth rates while a patient receives therapy. It allows us to determine treatment efficacy regardless of the interval between measurements, which often varies in clinical practice. Our ultimate goals are to establish a reliable method to assess efficacy, provide support for clinical decisions and increase access to clinical trials.
Methods: For the current study we applied our methodology to assess treatment effectiveness among Veterans with prostate cancer (PC) at the J.J. Peters VAMC. To do this we captured serial PSA values and dates when treatment with abiraterone and enzalutamide were started and stopped.
Results: Our initial analysis has examined data from twenty Veterans with PC. The majority had received abiraterone first followed by enzalutamide. With both therapies we found excellent fit of data. Despite wide variations in assessment intervals, g could be calculated in all patients. The median g on abiraterone (0.00086) was fourfold slower than on enzalutamide (0.0035), a statistically significant difference (P = .022). In individual patients we demonstrated comparable g values on abiraterone and enzalutamide in some, but increased g in half the patients when switched to enzalutamide.
Conclusions: Using observational data and a novel method to assess efficacy, we have compared the effectiveness of PC therapies administered to Veterans. Our VAMC data will be benchmarked against publicly available data from registration trials.
Background: Oncologists evaluating tumor size after anticancer therapy in patients observe the net result of 2 phenomena: regression of the sensitive tumor fraction and growth of the resistant fraction occurring simultaneously at rates that are constant. We have employed simple mathematical models with single and multi-institutional data sets to estimate 2 exponential rate constants: one for tumor regression or decay (d) and one for tumor growth (g). We have (1) established that g correlates with overall survival; (2) demonstrated changes in g after treatment is discontinued; and (3) benchmarked effectiveness in small 20 to 30 patient cohorts to reference data sets from randomized phase 3 trials. Our approach is novel and not another modification of PSA doubling time or velocity, which cannot estimate regression or growth rates while a patient receives therapy. It allows us to determine treatment efficacy regardless of the interval between measurements, which often varies in clinical practice. Our ultimate goals are to establish a reliable method to assess efficacy, provide support for clinical decisions and increase access to clinical trials.
Methods: For the current study we applied our methodology to assess treatment effectiveness among Veterans with prostate cancer (PC) at the J.J. Peters VAMC. To do this we captured serial PSA values and dates when treatment with abiraterone and enzalutamide were started and stopped.
Results: Our initial analysis has examined data from twenty Veterans with PC. The majority had received abiraterone first followed by enzalutamide. With both therapies we found excellent fit of data. Despite wide variations in assessment intervals, g could be calculated in all patients. The median g on abiraterone (0.00086) was fourfold slower than on enzalutamide (0.0035), a statistically significant difference (P = .022). In individual patients we demonstrated comparable g values on abiraterone and enzalutamide in some, but increased g in half the patients when switched to enzalutamide.
Conclusions: Using observational data and a novel method to assess efficacy, we have compared the effectiveness of PC therapies administered to Veterans. Our VAMC data will be benchmarked against publicly available data from registration trials.
Application of Extracellular Matrix to Reinforce Bowel Anstomoses in Colorectal Surgery: Does It Make a Difference in Clinically Significant Leaks?
Purpose: Evaluate the impact of extracellular matrix on bowel anastomotic complications.
Background: The incidence of anastomotic leak is 1-33%. It remains the most feared colorectal surgical complication leading to sepsis and death. Anastomotic leaks alter bowel function and overall cancer survival.
Methods: We retrospectively reviewed a single surgeon’s experience at our VAMC. From January 1, 2012 to December 1, 2014, 50 patients had bowel anastomoses performed without reinforcement. Due to complications, we began using extracellular matrix as reinforcement for all bowel anastomoses. From October 31, 2014 to May 19, 2017, 66 reinforced bowel anastomoses were performed.
Results: 50 anastomoses were completed in the first 23 months. 12 ileostomy reversals/small bowel anastomoses were completed without leaks. 12 ileo-colonic anastomoses resulted in 1 abscess requiring interventional radiology drainage for several months, which ultimately healed. 13 left-sided anastomoses were completed without complication. 13 low anterior anastomoses were performed: 2 leaks resulted in 2 patients after chemoradiation despite fecal diversion. 1 resulted in a complete stenosis and remains diverted. The second underwent revision with colo-anal pull through and resulted in complete stenosis requiring completion APR. Neither returned to bowel continuity.
After bowel reinforcement was begun, 66 bowel anastomoses were completed in 31 months. 9 ileostomy reversal/small bowel anastomoses were completed, without leaks. 33 ileo-colonic anastomoses resulted without leaks. 9 left-sided anastomoses were completed resulting in 2 leaks: both were suture repaired and had fecal diversion. Neither resulted in stenosis. 1 has returned to bowel continuity and the other is pending. 9 Low anterior anastomoses were performed: 3 leaks resulted in 3 patients. 1 required completion APR due to low location. The remaining 2 were
treated with drainage and fecal diversion. However, both healed without stenosis and were restored to bowel continuity.
Conclusions: Many new technologies have been investigated to reduce anastomotic complications. None have proven to work effectively. In our experience, extracellular matrix as reinforcement agent showed a trend in limiting the severity of the anastomotic leak and furthermore appears to limit progression to stenosis and affords return to bowel continuity: improving surgical quality outcomes.
Purpose: Evaluate the impact of extracellular matrix on bowel anastomotic complications.
Background: The incidence of anastomotic leak is 1-33%. It remains the most feared colorectal surgical complication leading to sepsis and death. Anastomotic leaks alter bowel function and overall cancer survival.
Methods: We retrospectively reviewed a single surgeon’s experience at our VAMC. From January 1, 2012 to December 1, 2014, 50 patients had bowel anastomoses performed without reinforcement. Due to complications, we began using extracellular matrix as reinforcement for all bowel anastomoses. From October 31, 2014 to May 19, 2017, 66 reinforced bowel anastomoses were performed.
Results: 50 anastomoses were completed in the first 23 months. 12 ileostomy reversals/small bowel anastomoses were completed without leaks. 12 ileo-colonic anastomoses resulted in 1 abscess requiring interventional radiology drainage for several months, which ultimately healed. 13 left-sided anastomoses were completed without complication. 13 low anterior anastomoses were performed: 2 leaks resulted in 2 patients after chemoradiation despite fecal diversion. 1 resulted in a complete stenosis and remains diverted. The second underwent revision with colo-anal pull through and resulted in complete stenosis requiring completion APR. Neither returned to bowel continuity.
After bowel reinforcement was begun, 66 bowel anastomoses were completed in 31 months. 9 ileostomy reversal/small bowel anastomoses were completed, without leaks. 33 ileo-colonic anastomoses resulted without leaks. 9 left-sided anastomoses were completed resulting in 2 leaks: both were suture repaired and had fecal diversion. Neither resulted in stenosis. 1 has returned to bowel continuity and the other is pending. 9 Low anterior anastomoses were performed: 3 leaks resulted in 3 patients. 1 required completion APR due to low location. The remaining 2 were
treated with drainage and fecal diversion. However, both healed without stenosis and were restored to bowel continuity.
Conclusions: Many new technologies have been investigated to reduce anastomotic complications. None have proven to work effectively. In our experience, extracellular matrix as reinforcement agent showed a trend in limiting the severity of the anastomotic leak and furthermore appears to limit progression to stenosis and affords return to bowel continuity: improving surgical quality outcomes.
Purpose: Evaluate the impact of extracellular matrix on bowel anastomotic complications.
Background: The incidence of anastomotic leak is 1-33%. It remains the most feared colorectal surgical complication leading to sepsis and death. Anastomotic leaks alter bowel function and overall cancer survival.
Methods: We retrospectively reviewed a single surgeon’s experience at our VAMC. From January 1, 2012 to December 1, 2014, 50 patients had bowel anastomoses performed without reinforcement. Due to complications, we began using extracellular matrix as reinforcement for all bowel anastomoses. From October 31, 2014 to May 19, 2017, 66 reinforced bowel anastomoses were performed.
Results: 50 anastomoses were completed in the first 23 months. 12 ileostomy reversals/small bowel anastomoses were completed without leaks. 12 ileo-colonic anastomoses resulted in 1 abscess requiring interventional radiology drainage for several months, which ultimately healed. 13 left-sided anastomoses were completed without complication. 13 low anterior anastomoses were performed: 2 leaks resulted in 2 patients after chemoradiation despite fecal diversion. 1 resulted in a complete stenosis and remains diverted. The second underwent revision with colo-anal pull through and resulted in complete stenosis requiring completion APR. Neither returned to bowel continuity.
After bowel reinforcement was begun, 66 bowel anastomoses were completed in 31 months. 9 ileostomy reversal/small bowel anastomoses were completed, without leaks. 33 ileo-colonic anastomoses resulted without leaks. 9 left-sided anastomoses were completed resulting in 2 leaks: both were suture repaired and had fecal diversion. Neither resulted in stenosis. 1 has returned to bowel continuity and the other is pending. 9 Low anterior anastomoses were performed: 3 leaks resulted in 3 patients. 1 required completion APR due to low location. The remaining 2 were
treated with drainage and fecal diversion. However, both healed without stenosis and were restored to bowel continuity.
Conclusions: Many new technologies have been investigated to reduce anastomotic complications. None have proven to work effectively. In our experience, extracellular matrix as reinforcement agent showed a trend in limiting the severity of the anastomotic leak and furthermore appears to limit progression to stenosis and affords return to bowel continuity: improving surgical quality outcomes.
Hypertension Among Veterans Affairs Colorectal Cancer Survivors: A Matched Case-Control Analysis
Purpose: We sought to: (1) determine the odds of colorectal cancer (CRC) survivors being diagnosed with hypertension 2 years post-CRC diagnosis; (2) assess differences in blood pressure (BP) control one year post-CRC diagnosis; and (3) assess differences in antihypertensive medication adherence one year post-CRC diagnosis, all relative to matched non-cancer controls.
Background: CRC and hypertension share common risk factors. Because CRC survivors often transition from oncology-led care to primary care, it is important to know whether they have differential prevalence of hypertension for chronic disease management.
Methods: We used the national VA Central Cancer Registry to identify patients diagnosed with non-metastatic CRC from 10/1/2008 to 12/31/2012 who had ≥ 1 primary care or oncology visit in the previous year. Up to 3 non-cancer controls were identified for each CRC survivor through electronic health records matched on age, race, sex, copayment status, geographic region, distance to VA healthcare, body mass index, number of outpatient visits (≥ 3 vs. fewer), and pre-existing hypertension, hyperlipidemia, and diabetes. We used logistic regression to calculate odds ratios (OR) and confidence intervals (CI) for being diagnosed with, and control of, hypertension between CRC survivors and controls. We calculated Medication Possession Ratio (MPR), a pharmacy refill-based adherence measure, for patients prescribed metoprolol tartrate.
Results: 9,758 patients with CRC were matched to 29,066 controls. The cohort was predominantly white (79.5%) men (97.8%), mean age of 66.8 years. Compared to matched controls, CRC survivors had 60% higher odds of being diagnosed with hypertension (OR = 1.59, 95% CI, = 1.51-1.67) one year post-diagnosis (69.4% CRC survivors have hypertension). CRC survivors experienced lower odds of BP control (OR = 0.89, 95% CI, 0.85-0.94); antihypertensive medication adherence was lower (relative MPR difference 7%) compared with matched non-cancer controls.
Implications: Compared to patients without a history of cancer, CRC survivors have higher odds of being diagnosed with hypertension, worse BP control, and worse antihypertension medication adherence. A critical component of survivorship care for CRC patients is management of hypertension to reduce CVD risk.
Purpose: We sought to: (1) determine the odds of colorectal cancer (CRC) survivors being diagnosed with hypertension 2 years post-CRC diagnosis; (2) assess differences in blood pressure (BP) control one year post-CRC diagnosis; and (3) assess differences in antihypertensive medication adherence one year post-CRC diagnosis, all relative to matched non-cancer controls.
Background: CRC and hypertension share common risk factors. Because CRC survivors often transition from oncology-led care to primary care, it is important to know whether they have differential prevalence of hypertension for chronic disease management.
Methods: We used the national VA Central Cancer Registry to identify patients diagnosed with non-metastatic CRC from 10/1/2008 to 12/31/2012 who had ≥ 1 primary care or oncology visit in the previous year. Up to 3 non-cancer controls were identified for each CRC survivor through electronic health records matched on age, race, sex, copayment status, geographic region, distance to VA healthcare, body mass index, number of outpatient visits (≥ 3 vs. fewer), and pre-existing hypertension, hyperlipidemia, and diabetes. We used logistic regression to calculate odds ratios (OR) and confidence intervals (CI) for being diagnosed with, and control of, hypertension between CRC survivors and controls. We calculated Medication Possession Ratio (MPR), a pharmacy refill-based adherence measure, for patients prescribed metoprolol tartrate.
Results: 9,758 patients with CRC were matched to 29,066 controls. The cohort was predominantly white (79.5%) men (97.8%), mean age of 66.8 years. Compared to matched controls, CRC survivors had 60% higher odds of being diagnosed with hypertension (OR = 1.59, 95% CI, = 1.51-1.67) one year post-diagnosis (69.4% CRC survivors have hypertension). CRC survivors experienced lower odds of BP control (OR = 0.89, 95% CI, 0.85-0.94); antihypertensive medication adherence was lower (relative MPR difference 7%) compared with matched non-cancer controls.
Implications: Compared to patients without a history of cancer, CRC survivors have higher odds of being diagnosed with hypertension, worse BP control, and worse antihypertension medication adherence. A critical component of survivorship care for CRC patients is management of hypertension to reduce CVD risk.
Purpose: We sought to: (1) determine the odds of colorectal cancer (CRC) survivors being diagnosed with hypertension 2 years post-CRC diagnosis; (2) assess differences in blood pressure (BP) control one year post-CRC diagnosis; and (3) assess differences in antihypertensive medication adherence one year post-CRC diagnosis, all relative to matched non-cancer controls.
Background: CRC and hypertension share common risk factors. Because CRC survivors often transition from oncology-led care to primary care, it is important to know whether they have differential prevalence of hypertension for chronic disease management.
Methods: We used the national VA Central Cancer Registry to identify patients diagnosed with non-metastatic CRC from 10/1/2008 to 12/31/2012 who had ≥ 1 primary care or oncology visit in the previous year. Up to 3 non-cancer controls were identified for each CRC survivor through electronic health records matched on age, race, sex, copayment status, geographic region, distance to VA healthcare, body mass index, number of outpatient visits (≥ 3 vs. fewer), and pre-existing hypertension, hyperlipidemia, and diabetes. We used logistic regression to calculate odds ratios (OR) and confidence intervals (CI) for being diagnosed with, and control of, hypertension between CRC survivors and controls. We calculated Medication Possession Ratio (MPR), a pharmacy refill-based adherence measure, for patients prescribed metoprolol tartrate.
Results: 9,758 patients with CRC were matched to 29,066 controls. The cohort was predominantly white (79.5%) men (97.8%), mean age of 66.8 years. Compared to matched controls, CRC survivors had 60% higher odds of being diagnosed with hypertension (OR = 1.59, 95% CI, = 1.51-1.67) one year post-diagnosis (69.4% CRC survivors have hypertension). CRC survivors experienced lower odds of BP control (OR = 0.89, 95% CI, 0.85-0.94); antihypertensive medication adherence was lower (relative MPR difference 7%) compared with matched non-cancer controls.
Implications: Compared to patients without a history of cancer, CRC survivors have higher odds of being diagnosed with hypertension, worse BP control, and worse antihypertension medication adherence. A critical component of survivorship care for CRC patients is management of hypertension to reduce CVD risk.
Comprehensive guidelines released for enhanced colorectal surgery recovery
New guidelines for enhanced recovery from colon and rectal surgery highlight the small steps that can add up to big improvements in patient outcomes.
“I think one of the most surprising aspects” of the guidelines – a joint effort from the American Society of Colon and Rectal Surgeons (ASCRS) and the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) – “is how enhanced recovery in many ways involves all the little things,” said senior author Scott Steele, MD, FACS, chairman of the department of colorectal surgery at the Cleveland Clinic (Dis Colon Rectum. 2017 Aug;60[8]:761-84. doi: 10.1097/DCR.0000000000000883). The guideline includes 24 literature-based recommendations covering everything from preoperative stoma counseling to postop chewing gum, all rated by quality of evidence.
“Many are easy to incorporate into day-to-day practice: getting [patients] out of bed, avoiding nasogastric tubes, not giving as much IV fluid as we used to, having patients take oral food and drink right after surgery, and having nursing/anesthesia/surgeons all on the same page and understanding that ... multidisciplinary, multisetting care leads to the best outcomes,” he said.
ASCRS and SAGES joined forces after noting that previous guidelines for enhanced recovery – perhaps better known as enhanced recovery after surgery, or ERAS, protocols – are dated, including studies only up to 2012; much has been published since then.
Preop measures
Some of the new recommendations encourage closer patient involvement with care. For instance, the groups strongly recommend discussing goals and discharge criteria with patients before surgery. Recent work has found that compliance and success go up when patients understand what’s going on, and length of stay and complications go down. For similar reasons, stoma education, stoma marking, and counseling on avoiding dehydration should happen preoperatively.
Meanwhile, “although there appear to be no meaningful benefits of [mechanical bowel prep (MBP)] alone in terms of complications,” the groups made a weak recommendation for MBP plus oral antibiotics before surgery. “A meta-analysis of seven RCTs comparing MBP with [antibiotics] versus MBP alone showed a reduction in total surgical site infection and incisional site infection,” they noted.
ASCRS and SAGES strongly recommended that patients drink clear fluids in the 2 hours before surgery, and also recommended carbohydrate loading – specifically drinks high in complex carbohydrates – in nondiabetic patients to attenuate insulin resistance induced by surgery and starvation.
The groups also recommended preset orders to standardize care, and care bundles to reduce surgical site infections. Measures could include preop chlorhexidine showers, ertapenem (Invanz) within an hour of incision, gown and glove changes before fascial closure, and washing incisions with chlorhexidine during recovery.
Pain control
“A multimodal, opioid-sparing, pain management plan should be ... implemented before the induction of anesthesia” for earlier return of bowel function and shorter lengths of stay, they said in a strong recommendation. “One of the simplest techniques to limit opioid intake is to schedule narcotic alternatives, such as oral acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), and gabapentin, rather than giving them on an as-needed basis.” The risk of anastomotic leaks with NSAIDs appears to be most pronounced when patients are on them for more than 3 days.
Wound infiltration and abdominal trunk blocks with liposomal bupivacaine have shown promising results, as well. “Limited data demonstrate that the (TAP) block with a local anesthetic [is] associated with decreased length of stay ... TAP blocks performed before surgery appear to provide better analgesia than TAP blocks performed at the end,” the groups said.
ASCRS and SAGES strongly recommended thoracic epidural analgesia for open colorectal cases, but not for routine use in laparoscopic cases. “The modest analgesic benefits provided by TEA do not support a faster recovery in laparoscopic surgery,” they said, noting that at least in open cases, infusion of a local anesthetic and a lipophilic opioid seems to work better than either option alone.
They also strongly recommended that surgery teams preempt postop nausea and vomiting. Dexamethasone at anesthesia induction and ondansetron at emergence is a common option for patients at risk. Others include total intravenous anesthesia, intravenous acetaminophen, and gabapentin.
Fluid management
Intraoperative crystalloids have to be managed to avoid volume overload and its bad effects. “A maintenance infusion of 1.5-2 mL/kg/h of balanced crystalloid solution is sufficient to cover the needs derived from salt water homeostasis during major abdominal surgery,” ASCRS and SAGES said in a strong recommendation.
“The neuroendocrine response induced by surgical trauma leads to a physiologic reduction of urine output that, in the absence of other signs of hypovolemia, should not trigger additional fluid administration.” Also, “crystalloid or colloid preloading does not prevent hypotension induced by neuraxial blockade ... hypotension induced by epidural analgesia should be managed by reducing the epidural infusion rate and with small doses of vasopressors” – not IV fluids – “so long at the patient is normovolemic,” they noted.
Intravenous fluids should be stopped after recovery room discharge, and clear fluids encouraged as soon as patients can tolerate them.
Postop care
ASCRS and SAGES made strong recommendations for minimally invasive surgery when possible, and for avoiding intra-abdominal drains and nasogastric tubes, both recommendations that support current practice in many places. NG tubes can push oral intake back 2 days, and there’s no evidence that abdominal drains prevent anastomotic leaks, plus there can be complications with both.
The groups also strongly recommended early and progressive patient mobilization to shorten length of stay, and a regular diet immediately after surgery.
As for the chewing gum, “sham feeding (i.e., chewing sugar-free gum for [at least] 10 minutes 3-4 times per day) after colorectal surgery is safe, results in small improvements in GI recovery” – flatus and bowel moments happen sooner – “and may be associated with a reduction in the length of hospital stay.” The groups strongly recommended it based on high-quality evidence
Alvimopan was also a strong recommendation to reverse increased GI transit time and constipation from opioids after open cases. “Several RCTs and pooled post hoc analyses showed accelerated time to recovery of GI function with 6- and 12-mg doses compared with placebo and a significantly shorter hospital length of stay in the alvimopan 12-mg group.” It’s unclear at this point, however, if alvimopan has a role in laparoscopic cases, the groups said.
To reduce the risk of urinary tract infections, they said urinary catheters should be pulled within 24 hours of elective colonic or upper rectal resection not involving a vesicular fistula, and within 48 hours of midrectal/lower rectal resections, which carry a greater risk of urinary retention.
ASCRS and SAGES funded the work. Seven of the 10 authors, including Dr. Steele, had no financial disclosures. One author is a speaker for Pacira Pharmaceuticals, and her institution has received unrestricted educational grants from the company. Another author reported grant support from Medtronic and Merck, maker of alvimopan and ertapenem, and a third reported collaborations with Medtronic and Johnson & Johnson.
New guidelines for enhanced recovery from colon and rectal surgery highlight the small steps that can add up to big improvements in patient outcomes.
“I think one of the most surprising aspects” of the guidelines – a joint effort from the American Society of Colon and Rectal Surgeons (ASCRS) and the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) – “is how enhanced recovery in many ways involves all the little things,” said senior author Scott Steele, MD, FACS, chairman of the department of colorectal surgery at the Cleveland Clinic (Dis Colon Rectum. 2017 Aug;60[8]:761-84. doi: 10.1097/DCR.0000000000000883). The guideline includes 24 literature-based recommendations covering everything from preoperative stoma counseling to postop chewing gum, all rated by quality of evidence.
“Many are easy to incorporate into day-to-day practice: getting [patients] out of bed, avoiding nasogastric tubes, not giving as much IV fluid as we used to, having patients take oral food and drink right after surgery, and having nursing/anesthesia/surgeons all on the same page and understanding that ... multidisciplinary, multisetting care leads to the best outcomes,” he said.
ASCRS and SAGES joined forces after noting that previous guidelines for enhanced recovery – perhaps better known as enhanced recovery after surgery, or ERAS, protocols – are dated, including studies only up to 2012; much has been published since then.
Preop measures
Some of the new recommendations encourage closer patient involvement with care. For instance, the groups strongly recommend discussing goals and discharge criteria with patients before surgery. Recent work has found that compliance and success go up when patients understand what’s going on, and length of stay and complications go down. For similar reasons, stoma education, stoma marking, and counseling on avoiding dehydration should happen preoperatively.
Meanwhile, “although there appear to be no meaningful benefits of [mechanical bowel prep (MBP)] alone in terms of complications,” the groups made a weak recommendation for MBP plus oral antibiotics before surgery. “A meta-analysis of seven RCTs comparing MBP with [antibiotics] versus MBP alone showed a reduction in total surgical site infection and incisional site infection,” they noted.
ASCRS and SAGES strongly recommended that patients drink clear fluids in the 2 hours before surgery, and also recommended carbohydrate loading – specifically drinks high in complex carbohydrates – in nondiabetic patients to attenuate insulin resistance induced by surgery and starvation.
The groups also recommended preset orders to standardize care, and care bundles to reduce surgical site infections. Measures could include preop chlorhexidine showers, ertapenem (Invanz) within an hour of incision, gown and glove changes before fascial closure, and washing incisions with chlorhexidine during recovery.
Pain control
“A multimodal, opioid-sparing, pain management plan should be ... implemented before the induction of anesthesia” for earlier return of bowel function and shorter lengths of stay, they said in a strong recommendation. “One of the simplest techniques to limit opioid intake is to schedule narcotic alternatives, such as oral acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), and gabapentin, rather than giving them on an as-needed basis.” The risk of anastomotic leaks with NSAIDs appears to be most pronounced when patients are on them for more than 3 days.
Wound infiltration and abdominal trunk blocks with liposomal bupivacaine have shown promising results, as well. “Limited data demonstrate that the (TAP) block with a local anesthetic [is] associated with decreased length of stay ... TAP blocks performed before surgery appear to provide better analgesia than TAP blocks performed at the end,” the groups said.
ASCRS and SAGES strongly recommended thoracic epidural analgesia for open colorectal cases, but not for routine use in laparoscopic cases. “The modest analgesic benefits provided by TEA do not support a faster recovery in laparoscopic surgery,” they said, noting that at least in open cases, infusion of a local anesthetic and a lipophilic opioid seems to work better than either option alone.
They also strongly recommended that surgery teams preempt postop nausea and vomiting. Dexamethasone at anesthesia induction and ondansetron at emergence is a common option for patients at risk. Others include total intravenous anesthesia, intravenous acetaminophen, and gabapentin.
Fluid management
Intraoperative crystalloids have to be managed to avoid volume overload and its bad effects. “A maintenance infusion of 1.5-2 mL/kg/h of balanced crystalloid solution is sufficient to cover the needs derived from salt water homeostasis during major abdominal surgery,” ASCRS and SAGES said in a strong recommendation.
“The neuroendocrine response induced by surgical trauma leads to a physiologic reduction of urine output that, in the absence of other signs of hypovolemia, should not trigger additional fluid administration.” Also, “crystalloid or colloid preloading does not prevent hypotension induced by neuraxial blockade ... hypotension induced by epidural analgesia should be managed by reducing the epidural infusion rate and with small doses of vasopressors” – not IV fluids – “so long at the patient is normovolemic,” they noted.
Intravenous fluids should be stopped after recovery room discharge, and clear fluids encouraged as soon as patients can tolerate them.
Postop care
ASCRS and SAGES made strong recommendations for minimally invasive surgery when possible, and for avoiding intra-abdominal drains and nasogastric tubes, both recommendations that support current practice in many places. NG tubes can push oral intake back 2 days, and there’s no evidence that abdominal drains prevent anastomotic leaks, plus there can be complications with both.
The groups also strongly recommended early and progressive patient mobilization to shorten length of stay, and a regular diet immediately after surgery.
As for the chewing gum, “sham feeding (i.e., chewing sugar-free gum for [at least] 10 minutes 3-4 times per day) after colorectal surgery is safe, results in small improvements in GI recovery” – flatus and bowel moments happen sooner – “and may be associated with a reduction in the length of hospital stay.” The groups strongly recommended it based on high-quality evidence
Alvimopan was also a strong recommendation to reverse increased GI transit time and constipation from opioids after open cases. “Several RCTs and pooled post hoc analyses showed accelerated time to recovery of GI function with 6- and 12-mg doses compared with placebo and a significantly shorter hospital length of stay in the alvimopan 12-mg group.” It’s unclear at this point, however, if alvimopan has a role in laparoscopic cases, the groups said.
To reduce the risk of urinary tract infections, they said urinary catheters should be pulled within 24 hours of elective colonic or upper rectal resection not involving a vesicular fistula, and within 48 hours of midrectal/lower rectal resections, which carry a greater risk of urinary retention.
ASCRS and SAGES funded the work. Seven of the 10 authors, including Dr. Steele, had no financial disclosures. One author is a speaker for Pacira Pharmaceuticals, and her institution has received unrestricted educational grants from the company. Another author reported grant support from Medtronic and Merck, maker of alvimopan and ertapenem, and a third reported collaborations with Medtronic and Johnson & Johnson.
New guidelines for enhanced recovery from colon and rectal surgery highlight the small steps that can add up to big improvements in patient outcomes.
“I think one of the most surprising aspects” of the guidelines – a joint effort from the American Society of Colon and Rectal Surgeons (ASCRS) and the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) – “is how enhanced recovery in many ways involves all the little things,” said senior author Scott Steele, MD, FACS, chairman of the department of colorectal surgery at the Cleveland Clinic (Dis Colon Rectum. 2017 Aug;60[8]:761-84. doi: 10.1097/DCR.0000000000000883). The guideline includes 24 literature-based recommendations covering everything from preoperative stoma counseling to postop chewing gum, all rated by quality of evidence.
“Many are easy to incorporate into day-to-day practice: getting [patients] out of bed, avoiding nasogastric tubes, not giving as much IV fluid as we used to, having patients take oral food and drink right after surgery, and having nursing/anesthesia/surgeons all on the same page and understanding that ... multidisciplinary, multisetting care leads to the best outcomes,” he said.
ASCRS and SAGES joined forces after noting that previous guidelines for enhanced recovery – perhaps better known as enhanced recovery after surgery, or ERAS, protocols – are dated, including studies only up to 2012; much has been published since then.
Preop measures
Some of the new recommendations encourage closer patient involvement with care. For instance, the groups strongly recommend discussing goals and discharge criteria with patients before surgery. Recent work has found that compliance and success go up when patients understand what’s going on, and length of stay and complications go down. For similar reasons, stoma education, stoma marking, and counseling on avoiding dehydration should happen preoperatively.
Meanwhile, “although there appear to be no meaningful benefits of [mechanical bowel prep (MBP)] alone in terms of complications,” the groups made a weak recommendation for MBP plus oral antibiotics before surgery. “A meta-analysis of seven RCTs comparing MBP with [antibiotics] versus MBP alone showed a reduction in total surgical site infection and incisional site infection,” they noted.
ASCRS and SAGES strongly recommended that patients drink clear fluids in the 2 hours before surgery, and also recommended carbohydrate loading – specifically drinks high in complex carbohydrates – in nondiabetic patients to attenuate insulin resistance induced by surgery and starvation.
The groups also recommended preset orders to standardize care, and care bundles to reduce surgical site infections. Measures could include preop chlorhexidine showers, ertapenem (Invanz) within an hour of incision, gown and glove changes before fascial closure, and washing incisions with chlorhexidine during recovery.
Pain control
“A multimodal, opioid-sparing, pain management plan should be ... implemented before the induction of anesthesia” for earlier return of bowel function and shorter lengths of stay, they said in a strong recommendation. “One of the simplest techniques to limit opioid intake is to schedule narcotic alternatives, such as oral acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), and gabapentin, rather than giving them on an as-needed basis.” The risk of anastomotic leaks with NSAIDs appears to be most pronounced when patients are on them for more than 3 days.
Wound infiltration and abdominal trunk blocks with liposomal bupivacaine have shown promising results, as well. “Limited data demonstrate that the (TAP) block with a local anesthetic [is] associated with decreased length of stay ... TAP blocks performed before surgery appear to provide better analgesia than TAP blocks performed at the end,” the groups said.
ASCRS and SAGES strongly recommended thoracic epidural analgesia for open colorectal cases, but not for routine use in laparoscopic cases. “The modest analgesic benefits provided by TEA do not support a faster recovery in laparoscopic surgery,” they said, noting that at least in open cases, infusion of a local anesthetic and a lipophilic opioid seems to work better than either option alone.
They also strongly recommended that surgery teams preempt postop nausea and vomiting. Dexamethasone at anesthesia induction and ondansetron at emergence is a common option for patients at risk. Others include total intravenous anesthesia, intravenous acetaminophen, and gabapentin.
Fluid management
Intraoperative crystalloids have to be managed to avoid volume overload and its bad effects. “A maintenance infusion of 1.5-2 mL/kg/h of balanced crystalloid solution is sufficient to cover the needs derived from salt water homeostasis during major abdominal surgery,” ASCRS and SAGES said in a strong recommendation.
“The neuroendocrine response induced by surgical trauma leads to a physiologic reduction of urine output that, in the absence of other signs of hypovolemia, should not trigger additional fluid administration.” Also, “crystalloid or colloid preloading does not prevent hypotension induced by neuraxial blockade ... hypotension induced by epidural analgesia should be managed by reducing the epidural infusion rate and with small doses of vasopressors” – not IV fluids – “so long at the patient is normovolemic,” they noted.
Intravenous fluids should be stopped after recovery room discharge, and clear fluids encouraged as soon as patients can tolerate them.
Postop care
ASCRS and SAGES made strong recommendations for minimally invasive surgery when possible, and for avoiding intra-abdominal drains and nasogastric tubes, both recommendations that support current practice in many places. NG tubes can push oral intake back 2 days, and there’s no evidence that abdominal drains prevent anastomotic leaks, plus there can be complications with both.
The groups also strongly recommended early and progressive patient mobilization to shorten length of stay, and a regular diet immediately after surgery.
As for the chewing gum, “sham feeding (i.e., chewing sugar-free gum for [at least] 10 minutes 3-4 times per day) after colorectal surgery is safe, results in small improvements in GI recovery” – flatus and bowel moments happen sooner – “and may be associated with a reduction in the length of hospital stay.” The groups strongly recommended it based on high-quality evidence
Alvimopan was also a strong recommendation to reverse increased GI transit time and constipation from opioids after open cases. “Several RCTs and pooled post hoc analyses showed accelerated time to recovery of GI function with 6- and 12-mg doses compared with placebo and a significantly shorter hospital length of stay in the alvimopan 12-mg group.” It’s unclear at this point, however, if alvimopan has a role in laparoscopic cases, the groups said.
To reduce the risk of urinary tract infections, they said urinary catheters should be pulled within 24 hours of elective colonic or upper rectal resection not involving a vesicular fistula, and within 48 hours of midrectal/lower rectal resections, which carry a greater risk of urinary retention.
ASCRS and SAGES funded the work. Seven of the 10 authors, including Dr. Steele, had no financial disclosures. One author is a speaker for Pacira Pharmaceuticals, and her institution has received unrestricted educational grants from the company. Another author reported grant support from Medtronic and Merck, maker of alvimopan and ertapenem, and a third reported collaborations with Medtronic and Johnson & Johnson.
FROM DISEASES OF THE COLON AND RECTUM
VA cohort study: Individualize SSI prophylaxis based on patient factors
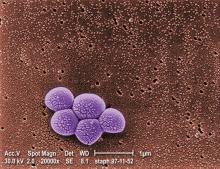
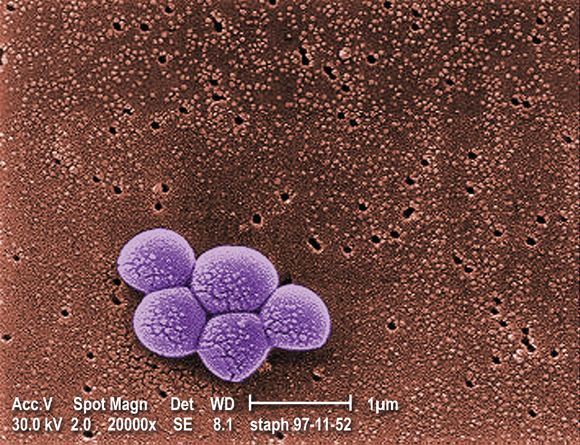
The combined use of vancomycin and a beta-lactam antibiotic for prophylaxis against surgical site infections is associated with both benefits and harms, according to findings from a national propensity-score–adjusted retrospective cohort study.
For example, the combination treatment reduced surgical site infections (SSIs) 30 days after cardiac surgical procedures but increased the risk of postoperative acute kidney injury (AKI) in some patients, Westyn Branch-Elliman, MD, of the VA Boston Healthcare System and her colleagues reported online July 10 in PLOS Medicine.
Among cardiac surgery patients, the incidence of surgical site infections was significantly lower for the 6,953 patients treated with both drugs vs. the 12,834 treated with a single agent (0.95% vs. 1.48%), the investigators found (PLOS Med. 2017 Jul 10. doi: 10.1371/journal.pmed.1002340).
SSI benefit with combination therapy
“After controlling for age, diabetes, ASA [American Society of Anesthesiologists] score, mupirocin administration, current smoking status, and preoperative MRSA [methicillin-resistant Staphylococcus aureus] colonization status, receipt of combination antimicrobial prophylaxis was associated with reduced SSI risk following cardiac surgical procedures (adjusted risk ratio, 0.61),” they wrote, noting that, when combination therapy was compared with either of the agents alone, the associations were similar and that no association between SSI reduction and the combination regimen was seen for the other types of surgical procedures assessed.
Secondary analyses showed that, among the cardiac patients, differences in the rates of SSIs were seen based on MRSA status in patients undergoing cardiac surgery. Among MRSA-colonized patients, SSIs occurred in 8 of 346 patients (2.3%) who received combination prophylaxis vs. 4 of 100 patients (4%) who received vancomycin alone (aRR, 0.53), and, among MRSA-negative and MRSA-unknown cardiac surgery patients, SSIs occurred in 58 of 6,607 patients (0.88%) receiving combination prophylaxis and 146 of 10,215 patients (1.4%) receiving a beta-lactam alone (aRR, 0.60).
“Among MRSA-colonized patients undergoing cardiac surgery, the associated absolute risk reduction for SSI was approximately triple that of the absolute risk reduction in MRSA-negative or -unknown patients, with a [number needed to treat] to prevent 1 SSI of 53 for the MRSA-colonized group, compared with 176 for the MRSA-negative or -unknown groups,” they wrote.
The incidence of Clostridium difficile infection was similar in both exposure groups (0.72% and 0.81% with combination and single agent prophylaxis, respectively).
Higher AKI risk with combination therapy
“In contrast, combination versus single prophylaxis was associated with higher relative risk of AKI in the 7-day postoperative period after adjusting for prophylaxis regimen duration, age, diabetes, ASA score, and smoking,” they said.
The rate of AKI was 23.75% among patients receiving combination prophylaxis, compared with 20.79% and 13.93% among those receiving vancomycin alone and a beta-lactam alone, respectively.
Significant associations between absolute risk of AKI and receipt of combination regimens were seen across all types of procedures, the investigators said.
“Overall, the NNH [number needed to harm] to cause one episode of AKI in cardiac surgery patients receiving combination therapy was 22, and, for stage 3 AKI, 167. The NNH associated with one additional episode of any postoperative AKI after receipt of combination therapy was 76 following orthopedic procedures and 25 following vascular surgical procedures,” they said.
The optimal approach for preventing SSIs is unclear. Although the multidisciplinary Clinical Practice Guidelines for Antimicrobial Prophylaxis in Surgery recommend single agent prophylaxis most often, with a beta-lactam antibiotic, for most surgical procedures, the use of vancomycin alone is a consideration in MRSA-colonized patients and in centers with a high MRSA incidence, and combination prophylaxis with a beta-lactam plus vancomycin is increasing. However, the relative risks and benefit of this strategy have not been carefully studied, the investigators said.
Thus, the investigators used a propensity-adjusted, log-binomial regression model stratified by type of surgical procedure among the cases identified in the Veterans Affairs cohort to assess the association between SSIs and receipt of combination prophylaxis versus single agent prophylaxis.
Though limited by the observational study design and by factors such as a predominantly male and slightly older and more rural population, the findings suggest that “clinicians may need to individualize prophylaxis strategy based on patient-specific factors that influence the risk-versus-benefit equation,” they said, concluding that “future studies are needed to evaluate the utility of MRSA screening protocols for optimizing and individualizing surgical prophylaxis regimen.”
This study was funded by Veterans Affairs Health Services Research and Development. Dr. Branch-Elliman reported having no disclosures. One other author, Eli Perencevich, MD, received an investigator initiated Grant from Merck Pharmaceuticals in 2013.
The combined use of vancomycin and a beta-lactam antibiotic for prophylaxis against surgical site infections is associated with both benefits and harms, according to findings from a national propensity-score–adjusted retrospective cohort study.
For example, the combination treatment reduced surgical site infections (SSIs) 30 days after cardiac surgical procedures but increased the risk of postoperative acute kidney injury (AKI) in some patients, Westyn Branch-Elliman, MD, of the VA Boston Healthcare System and her colleagues reported online July 10 in PLOS Medicine.
Among cardiac surgery patients, the incidence of surgical site infections was significantly lower for the 6,953 patients treated with both drugs vs. the 12,834 treated with a single agent (0.95% vs. 1.48%), the investigators found (PLOS Med. 2017 Jul 10. doi: 10.1371/journal.pmed.1002340).
SSI benefit with combination therapy
“After controlling for age, diabetes, ASA [American Society of Anesthesiologists] score, mupirocin administration, current smoking status, and preoperative MRSA [methicillin-resistant Staphylococcus aureus] colonization status, receipt of combination antimicrobial prophylaxis was associated with reduced SSI risk following cardiac surgical procedures (adjusted risk ratio, 0.61),” they wrote, noting that, when combination therapy was compared with either of the agents alone, the associations were similar and that no association between SSI reduction and the combination regimen was seen for the other types of surgical procedures assessed.
Secondary analyses showed that, among the cardiac patients, differences in the rates of SSIs were seen based on MRSA status in patients undergoing cardiac surgery. Among MRSA-colonized patients, SSIs occurred in 8 of 346 patients (2.3%) who received combination prophylaxis vs. 4 of 100 patients (4%) who received vancomycin alone (aRR, 0.53), and, among MRSA-negative and MRSA-unknown cardiac surgery patients, SSIs occurred in 58 of 6,607 patients (0.88%) receiving combination prophylaxis and 146 of 10,215 patients (1.4%) receiving a beta-lactam alone (aRR, 0.60).
“Among MRSA-colonized patients undergoing cardiac surgery, the associated absolute risk reduction for SSI was approximately triple that of the absolute risk reduction in MRSA-negative or -unknown patients, with a [number needed to treat] to prevent 1 SSI of 53 for the MRSA-colonized group, compared with 176 for the MRSA-negative or -unknown groups,” they wrote.
The incidence of Clostridium difficile infection was similar in both exposure groups (0.72% and 0.81% with combination and single agent prophylaxis, respectively).
Higher AKI risk with combination therapy
“In contrast, combination versus single prophylaxis was associated with higher relative risk of AKI in the 7-day postoperative period after adjusting for prophylaxis regimen duration, age, diabetes, ASA score, and smoking,” they said.
The rate of AKI was 23.75% among patients receiving combination prophylaxis, compared with 20.79% and 13.93% among those receiving vancomycin alone and a beta-lactam alone, respectively.
Significant associations between absolute risk of AKI and receipt of combination regimens were seen across all types of procedures, the investigators said.
“Overall, the NNH [number needed to harm] to cause one episode of AKI in cardiac surgery patients receiving combination therapy was 22, and, for stage 3 AKI, 167. The NNH associated with one additional episode of any postoperative AKI after receipt of combination therapy was 76 following orthopedic procedures and 25 following vascular surgical procedures,” they said.
The optimal approach for preventing SSIs is unclear. Although the multidisciplinary Clinical Practice Guidelines for Antimicrobial Prophylaxis in Surgery recommend single agent prophylaxis most often, with a beta-lactam antibiotic, for most surgical procedures, the use of vancomycin alone is a consideration in MRSA-colonized patients and in centers with a high MRSA incidence, and combination prophylaxis with a beta-lactam plus vancomycin is increasing. However, the relative risks and benefit of this strategy have not been carefully studied, the investigators said.
Thus, the investigators used a propensity-adjusted, log-binomial regression model stratified by type of surgical procedure among the cases identified in the Veterans Affairs cohort to assess the association between SSIs and receipt of combination prophylaxis versus single agent prophylaxis.
Though limited by the observational study design and by factors such as a predominantly male and slightly older and more rural population, the findings suggest that “clinicians may need to individualize prophylaxis strategy based on patient-specific factors that influence the risk-versus-benefit equation,” they said, concluding that “future studies are needed to evaluate the utility of MRSA screening protocols for optimizing and individualizing surgical prophylaxis regimen.”
This study was funded by Veterans Affairs Health Services Research and Development. Dr. Branch-Elliman reported having no disclosures. One other author, Eli Perencevich, MD, received an investigator initiated Grant from Merck Pharmaceuticals in 2013.
The combined use of vancomycin and a beta-lactam antibiotic for prophylaxis against surgical site infections is associated with both benefits and harms, according to findings from a national propensity-score–adjusted retrospective cohort study.
For example, the combination treatment reduced surgical site infections (SSIs) 30 days after cardiac surgical procedures but increased the risk of postoperative acute kidney injury (AKI) in some patients, Westyn Branch-Elliman, MD, of the VA Boston Healthcare System and her colleagues reported online July 10 in PLOS Medicine.
Among cardiac surgery patients, the incidence of surgical site infections was significantly lower for the 6,953 patients treated with both drugs vs. the 12,834 treated with a single agent (0.95% vs. 1.48%), the investigators found (PLOS Med. 2017 Jul 10. doi: 10.1371/journal.pmed.1002340).
SSI benefit with combination therapy
“After controlling for age, diabetes, ASA [American Society of Anesthesiologists] score, mupirocin administration, current smoking status, and preoperative MRSA [methicillin-resistant Staphylococcus aureus] colonization status, receipt of combination antimicrobial prophylaxis was associated with reduced SSI risk following cardiac surgical procedures (adjusted risk ratio, 0.61),” they wrote, noting that, when combination therapy was compared with either of the agents alone, the associations were similar and that no association between SSI reduction and the combination regimen was seen for the other types of surgical procedures assessed.
Secondary analyses showed that, among the cardiac patients, differences in the rates of SSIs were seen based on MRSA status in patients undergoing cardiac surgery. Among MRSA-colonized patients, SSIs occurred in 8 of 346 patients (2.3%) who received combination prophylaxis vs. 4 of 100 patients (4%) who received vancomycin alone (aRR, 0.53), and, among MRSA-negative and MRSA-unknown cardiac surgery patients, SSIs occurred in 58 of 6,607 patients (0.88%) receiving combination prophylaxis and 146 of 10,215 patients (1.4%) receiving a beta-lactam alone (aRR, 0.60).
“Among MRSA-colonized patients undergoing cardiac surgery, the associated absolute risk reduction for SSI was approximately triple that of the absolute risk reduction in MRSA-negative or -unknown patients, with a [number needed to treat] to prevent 1 SSI of 53 for the MRSA-colonized group, compared with 176 for the MRSA-negative or -unknown groups,” they wrote.
The incidence of Clostridium difficile infection was similar in both exposure groups (0.72% and 0.81% with combination and single agent prophylaxis, respectively).
Higher AKI risk with combination therapy
“In contrast, combination versus single prophylaxis was associated with higher relative risk of AKI in the 7-day postoperative period after adjusting for prophylaxis regimen duration, age, diabetes, ASA score, and smoking,” they said.
The rate of AKI was 23.75% among patients receiving combination prophylaxis, compared with 20.79% and 13.93% among those receiving vancomycin alone and a beta-lactam alone, respectively.
Significant associations between absolute risk of AKI and receipt of combination regimens were seen across all types of procedures, the investigators said.
“Overall, the NNH [number needed to harm] to cause one episode of AKI in cardiac surgery patients receiving combination therapy was 22, and, for stage 3 AKI, 167. The NNH associated with one additional episode of any postoperative AKI after receipt of combination therapy was 76 following orthopedic procedures and 25 following vascular surgical procedures,” they said.
The optimal approach for preventing SSIs is unclear. Although the multidisciplinary Clinical Practice Guidelines for Antimicrobial Prophylaxis in Surgery recommend single agent prophylaxis most often, with a beta-lactam antibiotic, for most surgical procedures, the use of vancomycin alone is a consideration in MRSA-colonized patients and in centers with a high MRSA incidence, and combination prophylaxis with a beta-lactam plus vancomycin is increasing. However, the relative risks and benefit of this strategy have not been carefully studied, the investigators said.
Thus, the investigators used a propensity-adjusted, log-binomial regression model stratified by type of surgical procedure among the cases identified in the Veterans Affairs cohort to assess the association between SSIs and receipt of combination prophylaxis versus single agent prophylaxis.
Though limited by the observational study design and by factors such as a predominantly male and slightly older and more rural population, the findings suggest that “clinicians may need to individualize prophylaxis strategy based on patient-specific factors that influence the risk-versus-benefit equation,” they said, concluding that “future studies are needed to evaluate the utility of MRSA screening protocols for optimizing and individualizing surgical prophylaxis regimen.”
This study was funded by Veterans Affairs Health Services Research and Development. Dr. Branch-Elliman reported having no disclosures. One other author, Eli Perencevich, MD, received an investigator initiated Grant from Merck Pharmaceuticals in 2013.
FROM PLOS MEDICINE
Key clinical point:
Major finding: The SSI incidence was 0.95% vs. 1.48% with combination vs. single agent–therapy in cardiac surgery patients. Acute kidney injuries occurred in 23.75% of all surgery patients receiving combination prophylaxis, compared with 20.79% and 13.93% with vancomycin or a beta-lactam, respectively.
Data source: A retrospective cohort study of more than 70,000 surgical procedures.
Disclosures: This study was funded by Veterans Affairs Health Services Research and Development. Dr. Branch-Elliman reported having no disclosures. One other author, Eli Perencevich, MD, received an investigator initiated grant from Merck Pharmaceuticals in 2013.
Multidisciplinary bundle drives drop in colorectal SSIs
NEW YORK – Facing an “unacceptably high” rate of surgical site infections associated with colorectal surgery at their community hospital, surgeons searched for solutions. They created a perioperative bundle of interventions that ultimately dropped their infection rates enough to achieve the highest ranking in the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP).
“The Centers for Disease Control and Prevention recommends we use a robust surveillance program to monitor surgical site infection data. The system gives us feedback, and that will [help us] reduce surgical site infection (SSI) risk,” said Christopher Wolff, MD, a PGY4 resident at the Cleveland Clinic Akron General Hospital. “NSQIP and the National Healthcare Safety Network from the CDC are two programs that do just that.”
The effort paid off, with the number of SSIs going from 16 cases in 2013 to 10 cases in 2014 and then 5 cases in 2015. Since the bundle was implemented in the last quarter of 2014, “we’ve seen a consistent downtrend since that point in our total infections, and we kept that in the background of a consistent number of cases.
“We have good outcomes by incidence, but that is not the whole story,” Dr. Wolff said. “With respect to colorectal infections, we are now performing in the ‘exemplary’ category, compared with our peers” according to the ACS NSQIP data. In addition, “we are performing at or below the SIR [standardized infection ratio] or expected number consistently since the implementation.”
The bundle addresses actions in five domains: preoperative, anesthesia, operating room, post–anesthesia care unit, and postoperative floor interventions. Preoperative elements include patient education, use of chlorhexidine wipes before surgery, and antibiotics noted on the chart, for example. Additional features include prewarming preoperatively and maintaining normothermia, requiring all surgeons scrub traditionally instead of “foaming,” use of wound protectors in the OR, and close monitoring of blood glucose in diabetics postoperatively. “There also is education of floor nurses on how to take care of these patients specifically,” Dr. Wolff noted.
To identify these areas for improvement, Dr. Wolff and his colleagues initially reviewed the literature to find individual and bundle elements demonstrated to improve outcomes. Then, a surgeon group “think tank” discussed the possibilities. However, reaching agreement was not easy, Dr. Wolff said. “They had a hard time agreeing on best practices, even within our own specialty. We did finally come to a consensus.
“We took those bundled protocols through to other areas and said ‘here are the things we want you to work on, things we want you to improve.’ That did not necessarily go over so well,” Dr. Wolff said. Because of resistance from their colleagues, they changed strategies. “We brought other people to the table and changed our work groups from being surgeons only to [being] a multidisciplinary team.”
The process took months and months of deliberation. It’s important to have a champion behind the project, said Dr. Wolff. “I have to thank my chairman, Mark C. Horattas, MD, FACS, who had the vision to see this through.
“We implemented tried-and-true measures to reduce surgical site infections. We did so in a team manner and had multidisciplinary buy-in, and that created a culture change in our program over time,” Dr. Wolff said.
This study also shows, Dr. Wolff added, that “a successful multidisciplinary quality improvement program can be implemented in a community hospital setting.”
Going forward, continuous monitoring will identify any areas that need improvement over time. The preoperative bundle also will be integrated into an Enhanced Recovery After Surgery protocol.
The Akron Hospital is now ranked by ACS NSQIP in the top 10% of hospitals for their colorectal SSI rate. “It’s nice to meet someone in the first decile,” session moderator Timothy D. Jackson, MD, FACS, of the University of Toronto said after Dr. Wolff’s presentation. “I’ve never done that before, and I took notes for what to do at my hospital.”
Dr. Wolff had no relevant financial disclosures.
NEW YORK – Facing an “unacceptably high” rate of surgical site infections associated with colorectal surgery at their community hospital, surgeons searched for solutions. They created a perioperative bundle of interventions that ultimately dropped their infection rates enough to achieve the highest ranking in the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP).
“The Centers for Disease Control and Prevention recommends we use a robust surveillance program to monitor surgical site infection data. The system gives us feedback, and that will [help us] reduce surgical site infection (SSI) risk,” said Christopher Wolff, MD, a PGY4 resident at the Cleveland Clinic Akron General Hospital. “NSQIP and the National Healthcare Safety Network from the CDC are two programs that do just that.”
The effort paid off, with the number of SSIs going from 16 cases in 2013 to 10 cases in 2014 and then 5 cases in 2015. Since the bundle was implemented in the last quarter of 2014, “we’ve seen a consistent downtrend since that point in our total infections, and we kept that in the background of a consistent number of cases.
“We have good outcomes by incidence, but that is not the whole story,” Dr. Wolff said. “With respect to colorectal infections, we are now performing in the ‘exemplary’ category, compared with our peers” according to the ACS NSQIP data. In addition, “we are performing at or below the SIR [standardized infection ratio] or expected number consistently since the implementation.”
The bundle addresses actions in five domains: preoperative, anesthesia, operating room, post–anesthesia care unit, and postoperative floor interventions. Preoperative elements include patient education, use of chlorhexidine wipes before surgery, and antibiotics noted on the chart, for example. Additional features include prewarming preoperatively and maintaining normothermia, requiring all surgeons scrub traditionally instead of “foaming,” use of wound protectors in the OR, and close monitoring of blood glucose in diabetics postoperatively. “There also is education of floor nurses on how to take care of these patients specifically,” Dr. Wolff noted.
To identify these areas for improvement, Dr. Wolff and his colleagues initially reviewed the literature to find individual and bundle elements demonstrated to improve outcomes. Then, a surgeon group “think tank” discussed the possibilities. However, reaching agreement was not easy, Dr. Wolff said. “They had a hard time agreeing on best practices, even within our own specialty. We did finally come to a consensus.
“We took those bundled protocols through to other areas and said ‘here are the things we want you to work on, things we want you to improve.’ That did not necessarily go over so well,” Dr. Wolff said. Because of resistance from their colleagues, they changed strategies. “We brought other people to the table and changed our work groups from being surgeons only to [being] a multidisciplinary team.”
The process took months and months of deliberation. It’s important to have a champion behind the project, said Dr. Wolff. “I have to thank my chairman, Mark C. Horattas, MD, FACS, who had the vision to see this through.
“We implemented tried-and-true measures to reduce surgical site infections. We did so in a team manner and had multidisciplinary buy-in, and that created a culture change in our program over time,” Dr. Wolff said.
This study also shows, Dr. Wolff added, that “a successful multidisciplinary quality improvement program can be implemented in a community hospital setting.”
Going forward, continuous monitoring will identify any areas that need improvement over time. The preoperative bundle also will be integrated into an Enhanced Recovery After Surgery protocol.
The Akron Hospital is now ranked by ACS NSQIP in the top 10% of hospitals for their colorectal SSI rate. “It’s nice to meet someone in the first decile,” session moderator Timothy D. Jackson, MD, FACS, of the University of Toronto said after Dr. Wolff’s presentation. “I’ve never done that before, and I took notes for what to do at my hospital.”
Dr. Wolff had no relevant financial disclosures.
NEW YORK – Facing an “unacceptably high” rate of surgical site infections associated with colorectal surgery at their community hospital, surgeons searched for solutions. They created a perioperative bundle of interventions that ultimately dropped their infection rates enough to achieve the highest ranking in the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP).
“The Centers for Disease Control and Prevention recommends we use a robust surveillance program to monitor surgical site infection data. The system gives us feedback, and that will [help us] reduce surgical site infection (SSI) risk,” said Christopher Wolff, MD, a PGY4 resident at the Cleveland Clinic Akron General Hospital. “NSQIP and the National Healthcare Safety Network from the CDC are two programs that do just that.”
The effort paid off, with the number of SSIs going from 16 cases in 2013 to 10 cases in 2014 and then 5 cases in 2015. Since the bundle was implemented in the last quarter of 2014, “we’ve seen a consistent downtrend since that point in our total infections, and we kept that in the background of a consistent number of cases.
“We have good outcomes by incidence, but that is not the whole story,” Dr. Wolff said. “With respect to colorectal infections, we are now performing in the ‘exemplary’ category, compared with our peers” according to the ACS NSQIP data. In addition, “we are performing at or below the SIR [standardized infection ratio] or expected number consistently since the implementation.”
The bundle addresses actions in five domains: preoperative, anesthesia, operating room, post–anesthesia care unit, and postoperative floor interventions. Preoperative elements include patient education, use of chlorhexidine wipes before surgery, and antibiotics noted on the chart, for example. Additional features include prewarming preoperatively and maintaining normothermia, requiring all surgeons scrub traditionally instead of “foaming,” use of wound protectors in the OR, and close monitoring of blood glucose in diabetics postoperatively. “There also is education of floor nurses on how to take care of these patients specifically,” Dr. Wolff noted.
To identify these areas for improvement, Dr. Wolff and his colleagues initially reviewed the literature to find individual and bundle elements demonstrated to improve outcomes. Then, a surgeon group “think tank” discussed the possibilities. However, reaching agreement was not easy, Dr. Wolff said. “They had a hard time agreeing on best practices, even within our own specialty. We did finally come to a consensus.
“We took those bundled protocols through to other areas and said ‘here are the things we want you to work on, things we want you to improve.’ That did not necessarily go over so well,” Dr. Wolff said. Because of resistance from their colleagues, they changed strategies. “We brought other people to the table and changed our work groups from being surgeons only to [being] a multidisciplinary team.”
The process took months and months of deliberation. It’s important to have a champion behind the project, said Dr. Wolff. “I have to thank my chairman, Mark C. Horattas, MD, FACS, who had the vision to see this through.
“We implemented tried-and-true measures to reduce surgical site infections. We did so in a team manner and had multidisciplinary buy-in, and that created a culture change in our program over time,” Dr. Wolff said.
This study also shows, Dr. Wolff added, that “a successful multidisciplinary quality improvement program can be implemented in a community hospital setting.”
Going forward, continuous monitoring will identify any areas that need improvement over time. The preoperative bundle also will be integrated into an Enhanced Recovery After Surgery protocol.
The Akron Hospital is now ranked by ACS NSQIP in the top 10% of hospitals for their colorectal SSI rate. “It’s nice to meet someone in the first decile,” session moderator Timothy D. Jackson, MD, FACS, of the University of Toronto said after Dr. Wolff’s presentation. “I’ve never done that before, and I took notes for what to do at my hospital.”
Dr. Wolff had no relevant financial disclosures.
AT THE ACS QUALITY AND SAFETY CONFERENCE
Key clinical point: A multidisciplinary team initiative successfully reduced surgical site infections after colorectal surgery in a community hospital.
Major finding: The number of annual SSIs dropped from 16 in the calendar year before the intervention to 5 afterward.
Data source: Comparison of SSI rates before and after a bundled intervention in late 2014.
Disclosures: Dr. Wolff had no relevant financial disclosures.
Outcomes improved with ERAS pathway tailored to colorectal surgery
NEW YORK – A protocol that standardizes care before, during, and after colorectal surgery cut average hospital stays from almost 6 days to less than 3, reduced complications, and slashed costs an estimated $11,227 per procedure.
“We decided to take a look at our own data, and we saw that a couple of variables were higher than we wanted them to be,” said Deepa Bhat, MD, a second year surgery resident at Advocate Illinois Masonic Medical Center in Chicago. Length of stay was one. Colorectal surgery patients were staying in the hospital an average 5.65 days, for example.
Their surgical site infection rate also warranted attention, Dr. Bhat said during a poster session at the American College of Surgeons Quality and Safety Conference. The overall complication rate was 6.45%.
“So, we decided to implement this enhanced recovery pathway in the hope that it would, one, get patients out of the hospital faster and allow them to recover at home and, two, decrease the rate of complications, including surgical site infections.”
Prior to the protocol, individual surgeons chose when to initiate fluids, when to discharge a patient, and many other preoperative factors. “Now, care is standardized so that every patient experiences the same pre-, intra-, and postoperative protocol, which leads to better outcomes,” Dr. Bhat said.
The multidisciplinary Enhanced Recovery After Colorectal Surgery (ERACS) pathway also now emphasizes more patient education prior to surgery. “The patients go into surgery having a very clear idea of what they can expect, such as how their pain will be controlled, when they can start liquids, and what their expectations are for ambulation,” she said. “By making patients active participants in their own care, they tend to do better.”
The investigators studied 246 elective colorectal surgery patients at their large, urban, community teaching hospital. They compared outcomes in 2014, versus 2015, to gauge the effectiveness of the ERACS. “The change in length of stay was really rather remarkable,” Dr. Bhat said. In fact, the typical number of days in the hospital decreased by about half from 5.65 to 2.89 days, a statistically significant difference (P less than .0001).
Historically, “the whole reason we don’t send patients home sooner is we’re worried they’re going to bounce right back, and that’s an issue for the 30-day readmission rate,” Dr. Bhat said. However, the enhanced recovery protocol was designed to minimize that risk, and the study verified that it works. “We wanted to show that you can send patients home safely and also not worry that they would come back more often.”
Patient satisfaction seems higher too. Dr. Bhat added, “Who doesn’t feel better at home?”
“It is pretty remarkable that you can send somebody home in less than 3 days and they don’t come back to the hospital with complications, versus having them stay double that amount of time,” Dr. Bhat said. The direct variable cost was approximately $3,705 lower with the ERACS, and total hospitalization costs decreased by up to $11,227 per patient. For the institution overall, that outcome translated into savings of approximately $1 million for the year.
Dr. Bhat continues to see increasing gains from the protocol ERACS since the study period ended. “Our enhanced recovery pathway is getting better and better and more efficient.” The institution is now looking to expand enhanced recovery protocols to other types of surgery.
Dr. Deepa Bhat had no relevant financial disclosures.
NEW YORK – A protocol that standardizes care before, during, and after colorectal surgery cut average hospital stays from almost 6 days to less than 3, reduced complications, and slashed costs an estimated $11,227 per procedure.
“We decided to take a look at our own data, and we saw that a couple of variables were higher than we wanted them to be,” said Deepa Bhat, MD, a second year surgery resident at Advocate Illinois Masonic Medical Center in Chicago. Length of stay was one. Colorectal surgery patients were staying in the hospital an average 5.65 days, for example.
Their surgical site infection rate also warranted attention, Dr. Bhat said during a poster session at the American College of Surgeons Quality and Safety Conference. The overall complication rate was 6.45%.
“So, we decided to implement this enhanced recovery pathway in the hope that it would, one, get patients out of the hospital faster and allow them to recover at home and, two, decrease the rate of complications, including surgical site infections.”
Prior to the protocol, individual surgeons chose when to initiate fluids, when to discharge a patient, and many other preoperative factors. “Now, care is standardized so that every patient experiences the same pre-, intra-, and postoperative protocol, which leads to better outcomes,” Dr. Bhat said.
The multidisciplinary Enhanced Recovery After Colorectal Surgery (ERACS) pathway also now emphasizes more patient education prior to surgery. “The patients go into surgery having a very clear idea of what they can expect, such as how their pain will be controlled, when they can start liquids, and what their expectations are for ambulation,” she said. “By making patients active participants in their own care, they tend to do better.”
The investigators studied 246 elective colorectal surgery patients at their large, urban, community teaching hospital. They compared outcomes in 2014, versus 2015, to gauge the effectiveness of the ERACS. “The change in length of stay was really rather remarkable,” Dr. Bhat said. In fact, the typical number of days in the hospital decreased by about half from 5.65 to 2.89 days, a statistically significant difference (P less than .0001).
Historically, “the whole reason we don’t send patients home sooner is we’re worried they’re going to bounce right back, and that’s an issue for the 30-day readmission rate,” Dr. Bhat said. However, the enhanced recovery protocol was designed to minimize that risk, and the study verified that it works. “We wanted to show that you can send patients home safely and also not worry that they would come back more often.”
Patient satisfaction seems higher too. Dr. Bhat added, “Who doesn’t feel better at home?”
“It is pretty remarkable that you can send somebody home in less than 3 days and they don’t come back to the hospital with complications, versus having them stay double that amount of time,” Dr. Bhat said. The direct variable cost was approximately $3,705 lower with the ERACS, and total hospitalization costs decreased by up to $11,227 per patient. For the institution overall, that outcome translated into savings of approximately $1 million for the year.
Dr. Bhat continues to see increasing gains from the protocol ERACS since the study period ended. “Our enhanced recovery pathway is getting better and better and more efficient.” The institution is now looking to expand enhanced recovery protocols to other types of surgery.
Dr. Deepa Bhat had no relevant financial disclosures.
NEW YORK – A protocol that standardizes care before, during, and after colorectal surgery cut average hospital stays from almost 6 days to less than 3, reduced complications, and slashed costs an estimated $11,227 per procedure.
“We decided to take a look at our own data, and we saw that a couple of variables were higher than we wanted them to be,” said Deepa Bhat, MD, a second year surgery resident at Advocate Illinois Masonic Medical Center in Chicago. Length of stay was one. Colorectal surgery patients were staying in the hospital an average 5.65 days, for example.
Their surgical site infection rate also warranted attention, Dr. Bhat said during a poster session at the American College of Surgeons Quality and Safety Conference. The overall complication rate was 6.45%.
“So, we decided to implement this enhanced recovery pathway in the hope that it would, one, get patients out of the hospital faster and allow them to recover at home and, two, decrease the rate of complications, including surgical site infections.”
Prior to the protocol, individual surgeons chose when to initiate fluids, when to discharge a patient, and many other preoperative factors. “Now, care is standardized so that every patient experiences the same pre-, intra-, and postoperative protocol, which leads to better outcomes,” Dr. Bhat said.
The multidisciplinary Enhanced Recovery After Colorectal Surgery (ERACS) pathway also now emphasizes more patient education prior to surgery. “The patients go into surgery having a very clear idea of what they can expect, such as how their pain will be controlled, when they can start liquids, and what their expectations are for ambulation,” she said. “By making patients active participants in their own care, they tend to do better.”
The investigators studied 246 elective colorectal surgery patients at their large, urban, community teaching hospital. They compared outcomes in 2014, versus 2015, to gauge the effectiveness of the ERACS. “The change in length of stay was really rather remarkable,” Dr. Bhat said. In fact, the typical number of days in the hospital decreased by about half from 5.65 to 2.89 days, a statistically significant difference (P less than .0001).
Historically, “the whole reason we don’t send patients home sooner is we’re worried they’re going to bounce right back, and that’s an issue for the 30-day readmission rate,” Dr. Bhat said. However, the enhanced recovery protocol was designed to minimize that risk, and the study verified that it works. “We wanted to show that you can send patients home safely and also not worry that they would come back more often.”
Patient satisfaction seems higher too. Dr. Bhat added, “Who doesn’t feel better at home?”
“It is pretty remarkable that you can send somebody home in less than 3 days and they don’t come back to the hospital with complications, versus having them stay double that amount of time,” Dr. Bhat said. The direct variable cost was approximately $3,705 lower with the ERACS, and total hospitalization costs decreased by up to $11,227 per patient. For the institution overall, that outcome translated into savings of approximately $1 million for the year.
Dr. Bhat continues to see increasing gains from the protocol ERACS since the study period ended. “Our enhanced recovery pathway is getting better and better and more efficient.” The institution is now looking to expand enhanced recovery protocols to other types of surgery.
Dr. Deepa Bhat had no relevant financial disclosures.
AT THE ACS QUALITY AND SAFETY CONFERENCE
Key clinical point: An Enhanced Recovery After Colorectal Surgery (ERACS) protocol cut colorectal surgical site infections and reduced length of stay.
Major finding: The intervention decreased the hospital stays from an average of 6 days to 3 days and saved an estimated $11,227 per surgery.
Data source: A retrospective study of 246 patients undergoing elective colorectal surgery at a large, urban, community teaching hospital.
Disclosures: Dr. Deepa Bhat had no relevant financial disclosures.
Prior resections increase anastomotic leak risk in Crohn’s
SEATTLE – The risk of anastomotic leaks after bowel resection for Crohn’s disease is more than three times higher in patients who have had prior resections, according to a review of 206 patients at Lahey Hospital and Medical Center in Burlington, Mass.
There were 20 anastomotic leaks within 30 days of resection in those patients, giving an overall leakage rate of 10%. Among the 123 patients who were having their first resection, however, the rate was 5% (6/123). The risk jumped to 17% in the 83 who had prior resections (14/83) and 23% (7) among the 30 patients who had two or more prior resections, which is “substantially higher than we talk about in the clinic when we are counseling these people,” said lead investigator Forrest Johnston, MD, a colorectal surgery fellow at Lahey.
The findings are important because prior resections have not, until now, been formally recognized as a risk factor for anastomotic leaks, and repeat resections are common in Crohn’s. “When you see patients for repeat intestinal resections, you have to look at them as a higher risk population in terms of your counseling and algorithms,” Dr. Johnston said at the American Society of Colon and Rectal Surgeons annual meeting. In addition, to mitigate the increased risk, Crohn’s patients who have repeat resections need additional attention to correct modifiable risk factors before surgery, such as steroid use and malnutrition. “Some of these patients are pushed through the clinic,” but “they deserve a bit more time.”
The heightened risk is also “another factor that might tip you one way or another” in choosing surgical options. “It’s certainly something to think about,” he said.
The new and prior resection patients in the study were well matched in terms of known risk factors for leakage, including age, sex, preoperative serum albumin, and use of immune suppressing medications. “The increased risk of leak is not explained by preoperative nutritional status or medication use,” Dr. Johnston said.
Estimated blood loss, OR time, types of procedures, hand-sewn versus stapled anastomoses, and other surgical variables were also similar.
The lack of significant differences between the groups raises the question of why repeat resections leak more. “That’s the million dollar question. My thought is that repeat resections indicate a greater severity of Crohn’s disease. I think there’s microvascular disease that’s affecting their tissue integrity, but we don’t appreciate it at the time of their anastomosis. If it was obvious at the time of surgery, patients wouldn’t be put together. They’d just get a stoma and be done with it,” Dr. Johnston said
About 80% of both first-time and repeat procedures were ileocolic resections secondary to obstruction, generally without bowel prep. Repeat procedures were performed a mean of 15 years after the first operation. Most initial resections were done laparoscopically, and a good portion of repeat procedures were open. Anorectal cases were excluded from the analysis.
Dr. Johnston said his team looked into the issue after noticing that repeat patients “seemed to leak a little bit more than we expected.”
The investigators had no conflicts of interest.
SEATTLE – The risk of anastomotic leaks after bowel resection for Crohn’s disease is more than three times higher in patients who have had prior resections, according to a review of 206 patients at Lahey Hospital and Medical Center in Burlington, Mass.
There were 20 anastomotic leaks within 30 days of resection in those patients, giving an overall leakage rate of 10%. Among the 123 patients who were having their first resection, however, the rate was 5% (6/123). The risk jumped to 17% in the 83 who had prior resections (14/83) and 23% (7) among the 30 patients who had two or more prior resections, which is “substantially higher than we talk about in the clinic when we are counseling these people,” said lead investigator Forrest Johnston, MD, a colorectal surgery fellow at Lahey.
The findings are important because prior resections have not, until now, been formally recognized as a risk factor for anastomotic leaks, and repeat resections are common in Crohn’s. “When you see patients for repeat intestinal resections, you have to look at them as a higher risk population in terms of your counseling and algorithms,” Dr. Johnston said at the American Society of Colon and Rectal Surgeons annual meeting. In addition, to mitigate the increased risk, Crohn’s patients who have repeat resections need additional attention to correct modifiable risk factors before surgery, such as steroid use and malnutrition. “Some of these patients are pushed through the clinic,” but “they deserve a bit more time.”
The heightened risk is also “another factor that might tip you one way or another” in choosing surgical options. “It’s certainly something to think about,” he said.
The new and prior resection patients in the study were well matched in terms of known risk factors for leakage, including age, sex, preoperative serum albumin, and use of immune suppressing medications. “The increased risk of leak is not explained by preoperative nutritional status or medication use,” Dr. Johnston said.
Estimated blood loss, OR time, types of procedures, hand-sewn versus stapled anastomoses, and other surgical variables were also similar.
The lack of significant differences between the groups raises the question of why repeat resections leak more. “That’s the million dollar question. My thought is that repeat resections indicate a greater severity of Crohn’s disease. I think there’s microvascular disease that’s affecting their tissue integrity, but we don’t appreciate it at the time of their anastomosis. If it was obvious at the time of surgery, patients wouldn’t be put together. They’d just get a stoma and be done with it,” Dr. Johnston said
About 80% of both first-time and repeat procedures were ileocolic resections secondary to obstruction, generally without bowel prep. Repeat procedures were performed a mean of 15 years after the first operation. Most initial resections were done laparoscopically, and a good portion of repeat procedures were open. Anorectal cases were excluded from the analysis.
Dr. Johnston said his team looked into the issue after noticing that repeat patients “seemed to leak a little bit more than we expected.”
The investigators had no conflicts of interest.
SEATTLE – The risk of anastomotic leaks after bowel resection for Crohn’s disease is more than three times higher in patients who have had prior resections, according to a review of 206 patients at Lahey Hospital and Medical Center in Burlington, Mass.
There were 20 anastomotic leaks within 30 days of resection in those patients, giving an overall leakage rate of 10%. Among the 123 patients who were having their first resection, however, the rate was 5% (6/123). The risk jumped to 17% in the 83 who had prior resections (14/83) and 23% (7) among the 30 patients who had two or more prior resections, which is “substantially higher than we talk about in the clinic when we are counseling these people,” said lead investigator Forrest Johnston, MD, a colorectal surgery fellow at Lahey.
The findings are important because prior resections have not, until now, been formally recognized as a risk factor for anastomotic leaks, and repeat resections are common in Crohn’s. “When you see patients for repeat intestinal resections, you have to look at them as a higher risk population in terms of your counseling and algorithms,” Dr. Johnston said at the American Society of Colon and Rectal Surgeons annual meeting. In addition, to mitigate the increased risk, Crohn’s patients who have repeat resections need additional attention to correct modifiable risk factors before surgery, such as steroid use and malnutrition. “Some of these patients are pushed through the clinic,” but “they deserve a bit more time.”
The heightened risk is also “another factor that might tip you one way or another” in choosing surgical options. “It’s certainly something to think about,” he said.
The new and prior resection patients in the study were well matched in terms of known risk factors for leakage, including age, sex, preoperative serum albumin, and use of immune suppressing medications. “The increased risk of leak is not explained by preoperative nutritional status or medication use,” Dr. Johnston said.
Estimated blood loss, OR time, types of procedures, hand-sewn versus stapled anastomoses, and other surgical variables were also similar.
The lack of significant differences between the groups raises the question of why repeat resections leak more. “That’s the million dollar question. My thought is that repeat resections indicate a greater severity of Crohn’s disease. I think there’s microvascular disease that’s affecting their tissue integrity, but we don’t appreciate it at the time of their anastomosis. If it was obvious at the time of surgery, patients wouldn’t be put together. They’d just get a stoma and be done with it,” Dr. Johnston said
About 80% of both first-time and repeat procedures were ileocolic resections secondary to obstruction, generally without bowel prep. Repeat procedures were performed a mean of 15 years after the first operation. Most initial resections were done laparoscopically, and a good portion of repeat procedures were open. Anorectal cases were excluded from the analysis.
Dr. Johnston said his team looked into the issue after noticing that repeat patients “seemed to leak a little bit more than we expected.”
The investigators had no conflicts of interest.
AT ASCRS 2017
Key clinical point:
Major finding: The number of prior resections correlated almost perfectly with an increasing risk of anastomotic leakage (r = 0.998); the odds ratio for leakage with prior resection, compared with initial resection, was 3.5 (95% confidence interval, 1.3-9.4; P less than .005).
Data source: A review of 206 Crohn’ patients.
Disclosures: The investigators had no conflicts of interest.
Loop ileostomy tops colectomy for IBD rescue
SEATTLE – Diverting loop ileostomies save patients with inflammatory bowel disease (IBD) with severe colitis from rushed total abdominal colectomies, buying time for patient optimization before surgery, and perhaps even saving colons, according to a report from the University of California, Los Angeles.
Urgent colectomy is the standard of care, but it’s a big operation when patients aren’t doing well. Immunosuppression, malnutrition, and other problems lead to high rates of complications.
In 2013, UCLA physicians decided to try rescue diverting loop ileostomies (DLIs), a relatively quick, minimally invasive option to temporarily divert the fecal stream, instead. The idea is to give the colon a chance to heal and the patient another shot at medical management and recovery before definitive surgery. There’s even a chance of colon salvage.
The approach has been working well at UCLA. Investigators previously reported good results for their first eight patients. They presented updated results for the series – now up to 34 patients – at the annual meeting of the American Society of Colon and Rectal Surgeons.
So far, DLI allowed 91% of patients (31/34) to avoid urgent total colectomies. It’s “a safe alternative. Patients undergoing DLI have acceptably low complication rates and most are afforded time for medical and nutritional optimization prior to proceeding with their definitive surgical care,” said presenter Tara Russell, MD, a UCLA surgery resident.
“Currently, [almost every] patient presenting with acute colitis who we aren’t able to get to the point of discharge with medical optimization” is now offered rescue DLI at the university, and patients have been eager for a chance at avoiding total colectomy. The only patients who are not offered DLI are those with, for instance, fulminant toxic megacolon, Dr. Russell said.
The DLI approach failed in just 2 of the 18 ulcerative colitis patients and 1 of the 16 Crohn’s patients in the series. All three went on to emergent total colectomies 11-53 days after the procedure.
The majority of DLI patients tolerated oral intake by postop day 1, and the median time to resuming a regular diet was 2 days. Most people were discharged within a day or 2 of diversion, and a few took longer to achieve medical rescue. Almost 90% had an improvement in nutritional status, and over 80% went on to elective laparoscopic definitive procedures or colon salvage.
Two patients had postop wound infections, “but there were no other complications” with DLI, Dr. Russell said.
All DLIs were performed with a single-incision laparoscopic approach and took an average of about a half hour. Most of the diversions were in the right lower abdominal quadrant.
The mean age of the patients was 36 years, with a range of 16-81 years. Just over half were men. Of 21 patients who met systemic inflammatory response syndrome criteria at the time of operation, 13 (62%) resolved within 24 hours of DLI.
SEATTLE – Diverting loop ileostomies save patients with inflammatory bowel disease (IBD) with severe colitis from rushed total abdominal colectomies, buying time for patient optimization before surgery, and perhaps even saving colons, according to a report from the University of California, Los Angeles.
Urgent colectomy is the standard of care, but it’s a big operation when patients aren’t doing well. Immunosuppression, malnutrition, and other problems lead to high rates of complications.
In 2013, UCLA physicians decided to try rescue diverting loop ileostomies (DLIs), a relatively quick, minimally invasive option to temporarily divert the fecal stream, instead. The idea is to give the colon a chance to heal and the patient another shot at medical management and recovery before definitive surgery. There’s even a chance of colon salvage.
The approach has been working well at UCLA. Investigators previously reported good results for their first eight patients. They presented updated results for the series – now up to 34 patients – at the annual meeting of the American Society of Colon and Rectal Surgeons.
So far, DLI allowed 91% of patients (31/34) to avoid urgent total colectomies. It’s “a safe alternative. Patients undergoing DLI have acceptably low complication rates and most are afforded time for medical and nutritional optimization prior to proceeding with their definitive surgical care,” said presenter Tara Russell, MD, a UCLA surgery resident.
“Currently, [almost every] patient presenting with acute colitis who we aren’t able to get to the point of discharge with medical optimization” is now offered rescue DLI at the university, and patients have been eager for a chance at avoiding total colectomy. The only patients who are not offered DLI are those with, for instance, fulminant toxic megacolon, Dr. Russell said.
The DLI approach failed in just 2 of the 18 ulcerative colitis patients and 1 of the 16 Crohn’s patients in the series. All three went on to emergent total colectomies 11-53 days after the procedure.
The majority of DLI patients tolerated oral intake by postop day 1, and the median time to resuming a regular diet was 2 days. Most people were discharged within a day or 2 of diversion, and a few took longer to achieve medical rescue. Almost 90% had an improvement in nutritional status, and over 80% went on to elective laparoscopic definitive procedures or colon salvage.
Two patients had postop wound infections, “but there were no other complications” with DLI, Dr. Russell said.
All DLIs were performed with a single-incision laparoscopic approach and took an average of about a half hour. Most of the diversions were in the right lower abdominal quadrant.
The mean age of the patients was 36 years, with a range of 16-81 years. Just over half were men. Of 21 patients who met systemic inflammatory response syndrome criteria at the time of operation, 13 (62%) resolved within 24 hours of DLI.
SEATTLE – Diverting loop ileostomies save patients with inflammatory bowel disease (IBD) with severe colitis from rushed total abdominal colectomies, buying time for patient optimization before surgery, and perhaps even saving colons, according to a report from the University of California, Los Angeles.
Urgent colectomy is the standard of care, but it’s a big operation when patients aren’t doing well. Immunosuppression, malnutrition, and other problems lead to high rates of complications.
In 2013, UCLA physicians decided to try rescue diverting loop ileostomies (DLIs), a relatively quick, minimally invasive option to temporarily divert the fecal stream, instead. The idea is to give the colon a chance to heal and the patient another shot at medical management and recovery before definitive surgery. There’s even a chance of colon salvage.
The approach has been working well at UCLA. Investigators previously reported good results for their first eight patients. They presented updated results for the series – now up to 34 patients – at the annual meeting of the American Society of Colon and Rectal Surgeons.
So far, DLI allowed 91% of patients (31/34) to avoid urgent total colectomies. It’s “a safe alternative. Patients undergoing DLI have acceptably low complication rates and most are afforded time for medical and nutritional optimization prior to proceeding with their definitive surgical care,” said presenter Tara Russell, MD, a UCLA surgery resident.
“Currently, [almost every] patient presenting with acute colitis who we aren’t able to get to the point of discharge with medical optimization” is now offered rescue DLI at the university, and patients have been eager for a chance at avoiding total colectomy. The only patients who are not offered DLI are those with, for instance, fulminant toxic megacolon, Dr. Russell said.
The DLI approach failed in just 2 of the 18 ulcerative colitis patients and 1 of the 16 Crohn’s patients in the series. All three went on to emergent total colectomies 11-53 days after the procedure.
The majority of DLI patients tolerated oral intake by postop day 1, and the median time to resuming a regular diet was 2 days. Most people were discharged within a day or 2 of diversion, and a few took longer to achieve medical rescue. Almost 90% had an improvement in nutritional status, and over 80% went on to elective laparoscopic definitive procedures or colon salvage.
Two patients had postop wound infections, “but there were no other complications” with DLI, Dr. Russell said.
All DLIs were performed with a single-incision laparoscopic approach and took an average of about a half hour. Most of the diversions were in the right lower abdominal quadrant.
The mean age of the patients was 36 years, with a range of 16-81 years. Just over half were men. Of 21 patients who met systemic inflammatory response syndrome criteria at the time of operation, 13 (62%) resolved within 24 hours of DLI.
AT ASCRS 2017
Key clinical point:
Major finding: DLI allowed 91% of patients (31/34) to avoid urgent total colectomies.
Data source: A report on 34 patients with severe, acute inflammatory bowel disease colitis.
Disclosures: The presenter had no disclosures.