User login
New TAVI Platform Adds More Valve Sizes to Choose From
PARIS — Intermediate valve sizes are at least as safe and effective as the standard sizes now available for transcatheter aortic valve implantation (TAVI), according to an international randomized trial.
In a head-to-head comparison, the LANDMARK trial looked at valves from the new balloon-expandable Myval® by Merril Life Sciences and compared them with the balloon-expandable Sapien® from Edwards Lifesciences and the self-expanding Evolut® valve from Medtronic.
The new Myval platform offers multiple valves sized at 1.5 mm intervals, while the other two have valves that are generally sized at intervals of 3.0 mm.
at the Congress of the European Association of Percutaneous Coronary Interventions 2024.
The LANDMARK Trial
The trial enrolled 768 patients at 31 sites in 16 countries. They were randomized in a 1:1 fashion to the new platform or to one of the standards to compare the concept of intermediate valves with contemporary standards.
Seven sizes of Myval valves were used in the study, ranging from 20 mm to 29 mm at 1.5 mm increments. Two more sizes, 30.5 mm and 32.0 mm, were not included in this analysis but are being following in a registry.
The study also used Sapien valves sized 20 mm, 23 mm, 26 mm, and 29 mm and Evolut valves sized 26 mm, 29 mm, and 34 mm. There is also a 23 mm Evolut valve available, but it was not selected by any of the participating investigators.
Of the 336 patients given Myval valves, 48% were an intermediate size not available on one of the other platforms.
For the primary composite efficacy and safety endpoint of all-cause mortality, fatal or nonfatal strokes, VARC 3 or 4 bleeding, acute kidney injury, major vascular injury, moderate or greater valve regurgitation, or conduction disturbances requiring a new permanent pacemaker, the difference in absolute risk was slightly lower in the Myval arm, at 24.7% vs 27.0%, but not statistically significant. With that numerical difference favoring the Myval platform, noninferiority was demonstrated at 30 days with a high level of statistical significance, Dr. Serruys reported.
When each endpoint, with the composite primary endpoint, was evaluated separately in a secondary analysis, all-cause mortality and stroke incidence were identical in the two arms.
Major bleeding and acute kidney injury were nonsignificantly more common in the Myval group, while the incidence of moderate or greater valve regurgitation, placement of a new permanent pacemaker, and major vascular complications were nonsignificantly less common.
Precise Matching
The effective orifice area was consistently higher in the group receiving an intermediate valve relative to a Sapien valve. This was not significant for the 20 mm valve size, but it did reach statistical significance for the rest of the sizes. In contrast, there was no significant difference with the Evolut series.
The data suggest that intermediate sizes “enable precise and appropriate matching of devices to an individual anatomy,” at least relative to Sapien, said Dr. Serruys.
Martin Leon, MD, of Columbia University in New York, called LANDMARK an important step for considering how comparative trials should be conducted in the future.
However, he challenged the idea that this study compared devices for both safety and efficacy. Despite the evidence it provides on device and procedural safety over the short-term, he said few conclusions can be drawn about comparative efficacy after just 30 days. Rather, the true comparative value of the trial will be derived from “rigorous late follow-up,” he said.
Longer Follow-Up to Come
Dr. Serruys acknowledged that the differences seen after 30 days have uncertain relevance to longer-term outcomes. He is planning to conduct a 10-year follow-up that “will unravel whether the documented effective orifice area of the Myval platform will have a beneficial impact on long-term patient prognosis and valve durability,” he said.
Leon agreed that, so far, these data do suggest superior hemodynamic performance with the intermediate sizing relative to valves in the Sapien platform, but the same cannot be said for the Evolut platform, and he pointed out that pooling data from the two platforms for the primary endpoint “makes comparisons difficult.”
And with about half of patients still fitted with the sizes already available, he said a deeper understanding was needed of how “adjustment strategies,” such as oversizing, affect long-term outcomes relative to platforms, such as Myval, with more valve sizes.
A version of this article appeared on Medscape.com.
PARIS — Intermediate valve sizes are at least as safe and effective as the standard sizes now available for transcatheter aortic valve implantation (TAVI), according to an international randomized trial.
In a head-to-head comparison, the LANDMARK trial looked at valves from the new balloon-expandable Myval® by Merril Life Sciences and compared them with the balloon-expandable Sapien® from Edwards Lifesciences and the self-expanding Evolut® valve from Medtronic.
The new Myval platform offers multiple valves sized at 1.5 mm intervals, while the other two have valves that are generally sized at intervals of 3.0 mm.
at the Congress of the European Association of Percutaneous Coronary Interventions 2024.
The LANDMARK Trial
The trial enrolled 768 patients at 31 sites in 16 countries. They were randomized in a 1:1 fashion to the new platform or to one of the standards to compare the concept of intermediate valves with contemporary standards.
Seven sizes of Myval valves were used in the study, ranging from 20 mm to 29 mm at 1.5 mm increments. Two more sizes, 30.5 mm and 32.0 mm, were not included in this analysis but are being following in a registry.
The study also used Sapien valves sized 20 mm, 23 mm, 26 mm, and 29 mm and Evolut valves sized 26 mm, 29 mm, and 34 mm. There is also a 23 mm Evolut valve available, but it was not selected by any of the participating investigators.
Of the 336 patients given Myval valves, 48% were an intermediate size not available on one of the other platforms.
For the primary composite efficacy and safety endpoint of all-cause mortality, fatal or nonfatal strokes, VARC 3 or 4 bleeding, acute kidney injury, major vascular injury, moderate or greater valve regurgitation, or conduction disturbances requiring a new permanent pacemaker, the difference in absolute risk was slightly lower in the Myval arm, at 24.7% vs 27.0%, but not statistically significant. With that numerical difference favoring the Myval platform, noninferiority was demonstrated at 30 days with a high level of statistical significance, Dr. Serruys reported.
When each endpoint, with the composite primary endpoint, was evaluated separately in a secondary analysis, all-cause mortality and stroke incidence were identical in the two arms.
Major bleeding and acute kidney injury were nonsignificantly more common in the Myval group, while the incidence of moderate or greater valve regurgitation, placement of a new permanent pacemaker, and major vascular complications were nonsignificantly less common.
Precise Matching
The effective orifice area was consistently higher in the group receiving an intermediate valve relative to a Sapien valve. This was not significant for the 20 mm valve size, but it did reach statistical significance for the rest of the sizes. In contrast, there was no significant difference with the Evolut series.
The data suggest that intermediate sizes “enable precise and appropriate matching of devices to an individual anatomy,” at least relative to Sapien, said Dr. Serruys.
Martin Leon, MD, of Columbia University in New York, called LANDMARK an important step for considering how comparative trials should be conducted in the future.
However, he challenged the idea that this study compared devices for both safety and efficacy. Despite the evidence it provides on device and procedural safety over the short-term, he said few conclusions can be drawn about comparative efficacy after just 30 days. Rather, the true comparative value of the trial will be derived from “rigorous late follow-up,” he said.
Longer Follow-Up to Come
Dr. Serruys acknowledged that the differences seen after 30 days have uncertain relevance to longer-term outcomes. He is planning to conduct a 10-year follow-up that “will unravel whether the documented effective orifice area of the Myval platform will have a beneficial impact on long-term patient prognosis and valve durability,” he said.
Leon agreed that, so far, these data do suggest superior hemodynamic performance with the intermediate sizing relative to valves in the Sapien platform, but the same cannot be said for the Evolut platform, and he pointed out that pooling data from the two platforms for the primary endpoint “makes comparisons difficult.”
And with about half of patients still fitted with the sizes already available, he said a deeper understanding was needed of how “adjustment strategies,” such as oversizing, affect long-term outcomes relative to platforms, such as Myval, with more valve sizes.
A version of this article appeared on Medscape.com.
PARIS — Intermediate valve sizes are at least as safe and effective as the standard sizes now available for transcatheter aortic valve implantation (TAVI), according to an international randomized trial.
In a head-to-head comparison, the LANDMARK trial looked at valves from the new balloon-expandable Myval® by Merril Life Sciences and compared them with the balloon-expandable Sapien® from Edwards Lifesciences and the self-expanding Evolut® valve from Medtronic.
The new Myval platform offers multiple valves sized at 1.5 mm intervals, while the other two have valves that are generally sized at intervals of 3.0 mm.
at the Congress of the European Association of Percutaneous Coronary Interventions 2024.
The LANDMARK Trial
The trial enrolled 768 patients at 31 sites in 16 countries. They were randomized in a 1:1 fashion to the new platform or to one of the standards to compare the concept of intermediate valves with contemporary standards.
Seven sizes of Myval valves were used in the study, ranging from 20 mm to 29 mm at 1.5 mm increments. Two more sizes, 30.5 mm and 32.0 mm, were not included in this analysis but are being following in a registry.
The study also used Sapien valves sized 20 mm, 23 mm, 26 mm, and 29 mm and Evolut valves sized 26 mm, 29 mm, and 34 mm. There is also a 23 mm Evolut valve available, but it was not selected by any of the participating investigators.
Of the 336 patients given Myval valves, 48% were an intermediate size not available on one of the other platforms.
For the primary composite efficacy and safety endpoint of all-cause mortality, fatal or nonfatal strokes, VARC 3 or 4 bleeding, acute kidney injury, major vascular injury, moderate or greater valve regurgitation, or conduction disturbances requiring a new permanent pacemaker, the difference in absolute risk was slightly lower in the Myval arm, at 24.7% vs 27.0%, but not statistically significant. With that numerical difference favoring the Myval platform, noninferiority was demonstrated at 30 days with a high level of statistical significance, Dr. Serruys reported.
When each endpoint, with the composite primary endpoint, was evaluated separately in a secondary analysis, all-cause mortality and stroke incidence were identical in the two arms.
Major bleeding and acute kidney injury were nonsignificantly more common in the Myval group, while the incidence of moderate or greater valve regurgitation, placement of a new permanent pacemaker, and major vascular complications were nonsignificantly less common.
Precise Matching
The effective orifice area was consistently higher in the group receiving an intermediate valve relative to a Sapien valve. This was not significant for the 20 mm valve size, but it did reach statistical significance for the rest of the sizes. In contrast, there was no significant difference with the Evolut series.
The data suggest that intermediate sizes “enable precise and appropriate matching of devices to an individual anatomy,” at least relative to Sapien, said Dr. Serruys.
Martin Leon, MD, of Columbia University in New York, called LANDMARK an important step for considering how comparative trials should be conducted in the future.
However, he challenged the idea that this study compared devices for both safety and efficacy. Despite the evidence it provides on device and procedural safety over the short-term, he said few conclusions can be drawn about comparative efficacy after just 30 days. Rather, the true comparative value of the trial will be derived from “rigorous late follow-up,” he said.
Longer Follow-Up to Come
Dr. Serruys acknowledged that the differences seen after 30 days have uncertain relevance to longer-term outcomes. He is planning to conduct a 10-year follow-up that “will unravel whether the documented effective orifice area of the Myval platform will have a beneficial impact on long-term patient prognosis and valve durability,” he said.
Leon agreed that, so far, these data do suggest superior hemodynamic performance with the intermediate sizing relative to valves in the Sapien platform, but the same cannot be said for the Evolut platform, and he pointed out that pooling data from the two platforms for the primary endpoint “makes comparisons difficult.”
And with about half of patients still fitted with the sizes already available, he said a deeper understanding was needed of how “adjustment strategies,” such as oversizing, affect long-term outcomes relative to platforms, such as Myval, with more valve sizes.
A version of this article appeared on Medscape.com.
FROM EUROPCR 2024
Guidelines on Rapid Blood Pressure Reduction in Acute Ischemic Stroke Challenged
BASEL, SWITZERLAND — New findings challenge the practice of rapidly lowering blood pressure (BP) in acute ischemic stroke to allow for speedy thrombolysis.
The observational cluster study showed that , even though this meant fewer patient received thrombolysis.
“We found insufficient evidence to recommend active blood pressure lowering in patients with ischemic stroke who have blood pressure levels exceeding the guidelines but are otherwise eligible for thrombolytic therapy,” said senior study author Nyika D. Kruyt, MD, PhD, Leiden University Medical Center, the Netherlands.
“Our results suggest that if the blood pressure is too high for thrombolysis, then it is best to wait and only treat with thrombolysis if the blood pressure drops spontaneously,” Dr. Kruyt said.
The findings were presented at the European Stroke Organisation Conference (ESOC) annual meeting and published online in The Lancet Neurology.
Guidelines Without Evidence?
Owing to concerns about high BP increasing the risk for intracerebral hemorrhage after thrombolysis, the original trials evaluating thrombolysis in stroke set an arbitrary threshold of 185/110 mm Hg, which has been incorporated into stroke guidelines. These trials cautioned against lowering BP rapidly, which is not included in guidelines.
Most stroke centers therefore tend to rapidly lower BP in patients who have values greater than 185/110 mm Hg and who are otherwise eligible for thrombolysis, investigators noted. Because thrombolysis is more effective the earlier it is administered, there is some urgency to reduce the BP quickly when patients first arrive at the hospital.
“But there has never been any evidence for the lowering of blood pressure with IV [intravenous] antihypertensives before thrombolysis, and some centers have never adopted this approach because of concerns that a rapid decline in blood pressure may reduce perfusion of the brain at a time when there is already ischemia present,” Dr. Kruyt noted.
However, if BP is lowered quickly, there is a greater chance that patients will not be able to receive thrombolysis because the 4.5-hour time limit could be exceeded.
For the prospective, observational TRUTH study, researchers compared outcomes in 853 patients treated at 27 stroke centers in the Netherlands with an active BP-lowering strategy vs 199 patients treated at 10 hospitals with no such strategy.
Baseline characteristics of participants in the two groups were similar.
Results showed a strong trend toward worse outcomes in participants whose BP was lowered, with an adjusted odds ratio (aOR) for a shift toward a worse 90-day functional outcome on the modified Rankin Scale of 1.27 (95% CI, 0.96-1.68).
This was despite the fact that many more patients whose BP was reduced received thrombolysis (94% vs 52% of those with no BP lowering) and had shorter times to treatment, with average door-to-needle times of 35 minutes (vs 47 minutes among those with no BP lowering).
Symptomatic intracranial hemorrhage occurred in 5% of the active BP-lowering group versus 3% of those who did not have their BP lowered (aOR, 1.28; 95% CI, 0.62-2.62).
Reconsider Guidelines?
These results are consistent with those from the INTERACT4 trial, which was also presented at the ESOC 2024 meeting. That trial showed a harmful effect of lowering BP in the ambulance in patients with acute ischemic stroke, but a beneficial effect in patients with hemorrhagic stroke.
“I think the guidelines need to be reconsidered after these studies and we should refrain from active blood pressure–lowering in patients with acute ischemic stroke,” Dr. Kruyt said.
But he acknowledged that not rapidly lowering BP will mean fewer patients will be able to receive thrombolysis within the 4.5-hour treatment window.
Dr. Kruyt estimated that the combination of being eligible for thrombolysis, with the only exclusion criterion being BP greater than 185/110 mm Hg, applies to about 10%-15% of patients.
“If we have a watch-and-wait policy, then about half of those patients will still get treated with thrombolysis within in the 4.5-hour limit but later than if blood pressure was reduced with IV antihypertensives,” he added.
Dr. Kruyt noted that there has never been a randomized trial on the practice of BP lowering in order to be able to administer thrombolysis.
“The 185/110 mm Hg blood pressure level is an arbitrary threshold that was chosen for the original thrombolysis stroke trials,” he said. “I believe we need trials to investigate whether we can give thrombolysis safely to patients with higher blood pressure levels than this, without needing to rapidly reduce the pressure.”
Caution Advised
Discussing the TRUTH study at the ESOC meeting, Guillaume Turc, MD, professor of neurology at Sainte-Anne Hospital, Paris, said he thought the findings were “very thought provoking.”
Simona Sacco, MD, professor of neurology at the University of L’Aquila, Italy, said the result was surprising, but she advised caution in acting on this finding.
“I don’t think this study can change practice or guidelines as it is not a randomized trial. Yes, it can generate a hypothesis, but we need more research before changing clinical practice,” she said.
In an accompanying editorial, Verónica Olavarría, MD, Clínica Alemana Universidad del Desarrollo, Santiago, Chile, also suggested the trial should be interpreted cautiously because there was “insufficient evidence for a definitive conclusion.”
But Dr. Kruyt noted that even though the TRUTH study was not a randomized trial, the results are in line with those of recent randomized trials such as INTERACT4.
He added that the ENCHANTED trial also showed no benefit of intensive BP management immediately after thrombolysis in mild to moderate stroke and even suggested harm in severe stroke. And other trials (OPTIMAL-BP and ENCHANTED2/MT) have shown worse outcomes with BP lowering in patients with acute ischemic stroke undergoing thrombectomy.
“All these studies are showing similar signals throughout the whole timeline in acute ischemic stroke. The results are very much in line with each other. I think this strengthens our findings,” Dr. Kruyt said.
“With this data, I think the guidelines should be revised, and until randomized data become available showing that reducing blood pressure in acute ischemic stroke patients in order for them to receive early thrombolysis is beneficial, then we should refrain from doing so,” he added.
INTERACT4 investigator Craig Anderson, MD, George Institute for Global Health, Sydney, New South Wales, Australia, agreed.
“The TRUTH study gives the same message as INTERACT4. They are completely in line with each other, both suggesting harm with blood pressure lowering in acute ischemic stroke. These two together are going to rattle the cage around blood pressure control in acute ischemic stroke patients,” Dr. Anderson said.
The TRUTH study was funded by a grant from Fonds NutsOhra. Dr. Kruyt reported no relevant financial disclosures. Dr. Olavarría reported receiving a grant from Boehringer Ingelheim for the RECCA registry and honoraria from Novo Nordisk.
A version of this article appeared on Medscape.com.
BASEL, SWITZERLAND — New findings challenge the practice of rapidly lowering blood pressure (BP) in acute ischemic stroke to allow for speedy thrombolysis.
The observational cluster study showed that , even though this meant fewer patient received thrombolysis.
“We found insufficient evidence to recommend active blood pressure lowering in patients with ischemic stroke who have blood pressure levels exceeding the guidelines but are otherwise eligible for thrombolytic therapy,” said senior study author Nyika D. Kruyt, MD, PhD, Leiden University Medical Center, the Netherlands.
“Our results suggest that if the blood pressure is too high for thrombolysis, then it is best to wait and only treat with thrombolysis if the blood pressure drops spontaneously,” Dr. Kruyt said.
The findings were presented at the European Stroke Organisation Conference (ESOC) annual meeting and published online in The Lancet Neurology.
Guidelines Without Evidence?
Owing to concerns about high BP increasing the risk for intracerebral hemorrhage after thrombolysis, the original trials evaluating thrombolysis in stroke set an arbitrary threshold of 185/110 mm Hg, which has been incorporated into stroke guidelines. These trials cautioned against lowering BP rapidly, which is not included in guidelines.
Most stroke centers therefore tend to rapidly lower BP in patients who have values greater than 185/110 mm Hg and who are otherwise eligible for thrombolysis, investigators noted. Because thrombolysis is more effective the earlier it is administered, there is some urgency to reduce the BP quickly when patients first arrive at the hospital.
“But there has never been any evidence for the lowering of blood pressure with IV [intravenous] antihypertensives before thrombolysis, and some centers have never adopted this approach because of concerns that a rapid decline in blood pressure may reduce perfusion of the brain at a time when there is already ischemia present,” Dr. Kruyt noted.
However, if BP is lowered quickly, there is a greater chance that patients will not be able to receive thrombolysis because the 4.5-hour time limit could be exceeded.
For the prospective, observational TRUTH study, researchers compared outcomes in 853 patients treated at 27 stroke centers in the Netherlands with an active BP-lowering strategy vs 199 patients treated at 10 hospitals with no such strategy.
Baseline characteristics of participants in the two groups were similar.
Results showed a strong trend toward worse outcomes in participants whose BP was lowered, with an adjusted odds ratio (aOR) for a shift toward a worse 90-day functional outcome on the modified Rankin Scale of 1.27 (95% CI, 0.96-1.68).
This was despite the fact that many more patients whose BP was reduced received thrombolysis (94% vs 52% of those with no BP lowering) and had shorter times to treatment, with average door-to-needle times of 35 minutes (vs 47 minutes among those with no BP lowering).
Symptomatic intracranial hemorrhage occurred in 5% of the active BP-lowering group versus 3% of those who did not have their BP lowered (aOR, 1.28; 95% CI, 0.62-2.62).
Reconsider Guidelines?
These results are consistent with those from the INTERACT4 trial, which was also presented at the ESOC 2024 meeting. That trial showed a harmful effect of lowering BP in the ambulance in patients with acute ischemic stroke, but a beneficial effect in patients with hemorrhagic stroke.
“I think the guidelines need to be reconsidered after these studies and we should refrain from active blood pressure–lowering in patients with acute ischemic stroke,” Dr. Kruyt said.
But he acknowledged that not rapidly lowering BP will mean fewer patients will be able to receive thrombolysis within the 4.5-hour treatment window.
Dr. Kruyt estimated that the combination of being eligible for thrombolysis, with the only exclusion criterion being BP greater than 185/110 mm Hg, applies to about 10%-15% of patients.
“If we have a watch-and-wait policy, then about half of those patients will still get treated with thrombolysis within in the 4.5-hour limit but later than if blood pressure was reduced with IV antihypertensives,” he added.
Dr. Kruyt noted that there has never been a randomized trial on the practice of BP lowering in order to be able to administer thrombolysis.
“The 185/110 mm Hg blood pressure level is an arbitrary threshold that was chosen for the original thrombolysis stroke trials,” he said. “I believe we need trials to investigate whether we can give thrombolysis safely to patients with higher blood pressure levels than this, without needing to rapidly reduce the pressure.”
Caution Advised
Discussing the TRUTH study at the ESOC meeting, Guillaume Turc, MD, professor of neurology at Sainte-Anne Hospital, Paris, said he thought the findings were “very thought provoking.”
Simona Sacco, MD, professor of neurology at the University of L’Aquila, Italy, said the result was surprising, but she advised caution in acting on this finding.
“I don’t think this study can change practice or guidelines as it is not a randomized trial. Yes, it can generate a hypothesis, but we need more research before changing clinical practice,” she said.
In an accompanying editorial, Verónica Olavarría, MD, Clínica Alemana Universidad del Desarrollo, Santiago, Chile, also suggested the trial should be interpreted cautiously because there was “insufficient evidence for a definitive conclusion.”
But Dr. Kruyt noted that even though the TRUTH study was not a randomized trial, the results are in line with those of recent randomized trials such as INTERACT4.
He added that the ENCHANTED trial also showed no benefit of intensive BP management immediately after thrombolysis in mild to moderate stroke and even suggested harm in severe stroke. And other trials (OPTIMAL-BP and ENCHANTED2/MT) have shown worse outcomes with BP lowering in patients with acute ischemic stroke undergoing thrombectomy.
“All these studies are showing similar signals throughout the whole timeline in acute ischemic stroke. The results are very much in line with each other. I think this strengthens our findings,” Dr. Kruyt said.
“With this data, I think the guidelines should be revised, and until randomized data become available showing that reducing blood pressure in acute ischemic stroke patients in order for them to receive early thrombolysis is beneficial, then we should refrain from doing so,” he added.
INTERACT4 investigator Craig Anderson, MD, George Institute for Global Health, Sydney, New South Wales, Australia, agreed.
“The TRUTH study gives the same message as INTERACT4. They are completely in line with each other, both suggesting harm with blood pressure lowering in acute ischemic stroke. These two together are going to rattle the cage around blood pressure control in acute ischemic stroke patients,” Dr. Anderson said.
The TRUTH study was funded by a grant from Fonds NutsOhra. Dr. Kruyt reported no relevant financial disclosures. Dr. Olavarría reported receiving a grant from Boehringer Ingelheim for the RECCA registry and honoraria from Novo Nordisk.
A version of this article appeared on Medscape.com.
BASEL, SWITZERLAND — New findings challenge the practice of rapidly lowering blood pressure (BP) in acute ischemic stroke to allow for speedy thrombolysis.
The observational cluster study showed that , even though this meant fewer patient received thrombolysis.
“We found insufficient evidence to recommend active blood pressure lowering in patients with ischemic stroke who have blood pressure levels exceeding the guidelines but are otherwise eligible for thrombolytic therapy,” said senior study author Nyika D. Kruyt, MD, PhD, Leiden University Medical Center, the Netherlands.
“Our results suggest that if the blood pressure is too high for thrombolysis, then it is best to wait and only treat with thrombolysis if the blood pressure drops spontaneously,” Dr. Kruyt said.
The findings were presented at the European Stroke Organisation Conference (ESOC) annual meeting and published online in The Lancet Neurology.
Guidelines Without Evidence?
Owing to concerns about high BP increasing the risk for intracerebral hemorrhage after thrombolysis, the original trials evaluating thrombolysis in stroke set an arbitrary threshold of 185/110 mm Hg, which has been incorporated into stroke guidelines. These trials cautioned against lowering BP rapidly, which is not included in guidelines.
Most stroke centers therefore tend to rapidly lower BP in patients who have values greater than 185/110 mm Hg and who are otherwise eligible for thrombolysis, investigators noted. Because thrombolysis is more effective the earlier it is administered, there is some urgency to reduce the BP quickly when patients first arrive at the hospital.
“But there has never been any evidence for the lowering of blood pressure with IV [intravenous] antihypertensives before thrombolysis, and some centers have never adopted this approach because of concerns that a rapid decline in blood pressure may reduce perfusion of the brain at a time when there is already ischemia present,” Dr. Kruyt noted.
However, if BP is lowered quickly, there is a greater chance that patients will not be able to receive thrombolysis because the 4.5-hour time limit could be exceeded.
For the prospective, observational TRUTH study, researchers compared outcomes in 853 patients treated at 27 stroke centers in the Netherlands with an active BP-lowering strategy vs 199 patients treated at 10 hospitals with no such strategy.
Baseline characteristics of participants in the two groups were similar.
Results showed a strong trend toward worse outcomes in participants whose BP was lowered, with an adjusted odds ratio (aOR) for a shift toward a worse 90-day functional outcome on the modified Rankin Scale of 1.27 (95% CI, 0.96-1.68).
This was despite the fact that many more patients whose BP was reduced received thrombolysis (94% vs 52% of those with no BP lowering) and had shorter times to treatment, with average door-to-needle times of 35 minutes (vs 47 minutes among those with no BP lowering).
Symptomatic intracranial hemorrhage occurred in 5% of the active BP-lowering group versus 3% of those who did not have their BP lowered (aOR, 1.28; 95% CI, 0.62-2.62).
Reconsider Guidelines?
These results are consistent with those from the INTERACT4 trial, which was also presented at the ESOC 2024 meeting. That trial showed a harmful effect of lowering BP in the ambulance in patients with acute ischemic stroke, but a beneficial effect in patients with hemorrhagic stroke.
“I think the guidelines need to be reconsidered after these studies and we should refrain from active blood pressure–lowering in patients with acute ischemic stroke,” Dr. Kruyt said.
But he acknowledged that not rapidly lowering BP will mean fewer patients will be able to receive thrombolysis within the 4.5-hour treatment window.
Dr. Kruyt estimated that the combination of being eligible for thrombolysis, with the only exclusion criterion being BP greater than 185/110 mm Hg, applies to about 10%-15% of patients.
“If we have a watch-and-wait policy, then about half of those patients will still get treated with thrombolysis within in the 4.5-hour limit but later than if blood pressure was reduced with IV antihypertensives,” he added.
Dr. Kruyt noted that there has never been a randomized trial on the practice of BP lowering in order to be able to administer thrombolysis.
“The 185/110 mm Hg blood pressure level is an arbitrary threshold that was chosen for the original thrombolysis stroke trials,” he said. “I believe we need trials to investigate whether we can give thrombolysis safely to patients with higher blood pressure levels than this, without needing to rapidly reduce the pressure.”
Caution Advised
Discussing the TRUTH study at the ESOC meeting, Guillaume Turc, MD, professor of neurology at Sainte-Anne Hospital, Paris, said he thought the findings were “very thought provoking.”
Simona Sacco, MD, professor of neurology at the University of L’Aquila, Italy, said the result was surprising, but she advised caution in acting on this finding.
“I don’t think this study can change practice or guidelines as it is not a randomized trial. Yes, it can generate a hypothesis, but we need more research before changing clinical practice,” she said.
In an accompanying editorial, Verónica Olavarría, MD, Clínica Alemana Universidad del Desarrollo, Santiago, Chile, also suggested the trial should be interpreted cautiously because there was “insufficient evidence for a definitive conclusion.”
But Dr. Kruyt noted that even though the TRUTH study was not a randomized trial, the results are in line with those of recent randomized trials such as INTERACT4.
He added that the ENCHANTED trial also showed no benefit of intensive BP management immediately after thrombolysis in mild to moderate stroke and even suggested harm in severe stroke. And other trials (OPTIMAL-BP and ENCHANTED2/MT) have shown worse outcomes with BP lowering in patients with acute ischemic stroke undergoing thrombectomy.
“All these studies are showing similar signals throughout the whole timeline in acute ischemic stroke. The results are very much in line with each other. I think this strengthens our findings,” Dr. Kruyt said.
“With this data, I think the guidelines should be revised, and until randomized data become available showing that reducing blood pressure in acute ischemic stroke patients in order for them to receive early thrombolysis is beneficial, then we should refrain from doing so,” he added.
INTERACT4 investigator Craig Anderson, MD, George Institute for Global Health, Sydney, New South Wales, Australia, agreed.
“The TRUTH study gives the same message as INTERACT4. They are completely in line with each other, both suggesting harm with blood pressure lowering in acute ischemic stroke. These two together are going to rattle the cage around blood pressure control in acute ischemic stroke patients,” Dr. Anderson said.
The TRUTH study was funded by a grant from Fonds NutsOhra. Dr. Kruyt reported no relevant financial disclosures. Dr. Olavarría reported receiving a grant from Boehringer Ingelheim for the RECCA registry and honoraria from Novo Nordisk.
A version of this article appeared on Medscape.com.
FROM ESOC 2024
IV Thrombolysis Offers No Benefit for Mild Stroke
BASEL, SWITZERLAND — , a new trial has concluded.
Results from the randomized controlled trial TEMPO-2 showed no benefit from treatment with tenecteplase following ischemic stroke. In addition, investigators found a small increased risk for symptomatic intracranial hemorrhage (ICH) and more deaths in the tenecteplase group compared with the control group.
The research suggests that although it makes sense to open up vessels in patients with minor stroke, they didn’t do better with thrombolysis.
“This is not the result we were hoping for, but I think the question of whether to treat these minor stroke patients who are not disabled has now been answered,” said lead investigator Shelagh B. Coutts, MD, University of Calgary, Alberta, Canada.
“After these results, I think we should scan these patients, admit them, give them dual antiplatelet therapy and IV fluids, and watch them like a hawk. If they deteriorate, we can intervene at that point.”
The findings were presented at the European Stroke Organization Conference (ESOC) 2024 annual meeting and published online simultaneously in The Lancet.
Very Little Data
Up to half of patients with ischemic stroke initially present with minimal symptoms, which are not disabling, investigators noted. Despite having low scores on the National Institutes of Health Stroke Scale (NIHSS) that typically range from 0 to 5, a third of these patients are dead or disabled at 90-day follow-up if thrombolysis is withheld.
Patients with minor deficits and evidence of an intracranial occlusion are a subpopulation at a high risk for early neurological deterioration, which most often occurs within the first 24 hours after presentation.
However, many physicians have concerns about giving thrombolysis to these patients because of the potential harm from bleeding in the absence of major deficits, and most trials of thrombolysis have excluded patients with minor stroke. That leaves very little high-quality data to guide practice for these patients.
Two previous studies have compared alteplase with antiplatelet agents in minor stroke, but no trial has specifically looked at the subset of patients with minor stroke who have intracranial occlusion. The TEMPO-2 trial was conducted to evaluate the use of tenecteplase in this patient population.
The multicenter, parallel group, open-label study was conducted at 48 hospitals in Australia, Austria, Brazil, Canada, Finland, Ireland, New Zealand, Singapore, Spain, and the United Kingdom.
The trial included patients with minor acute ischemic stroke (NIHSS score of 0-5) and intracranial occlusion or focal perfusion abnormality who were within 12 hours from stroke onset.
Patients received IV tenecteplase (0.25 mg/kg) or non-thrombolytic standard of care (control). Most patients in the control group were treated with dual antiplatelet therapy with aspirin and clopidogrel (57%) or aspirin monotherapy (23%).
The trial was stopped early for futility after 886 patients had been enrolled. The median NIHSS score was 2.
The primary outcome — a return to baseline functioning on the modified Rankin Scale score at 90 days — occurred in 75% of the control group and in 72% of the tenecteplase group (risk ratio [RR], 0.96; P = .29).
Although there were significantly more patients with early recanalization and an NIHSS score of 0 at day 5 or discharge after tenecteplase treatment, this did not translate into improved functional outcomes at 90 days.
More patients died in the tenecteplase group compared with the control group (5% vs 1%; adjusted hazard ratio, 3.8; P = .0085).
There were eight (2%) symptomatic ICHs in the tenecteplase group versus two (< 1%) in the control group (RR, 4.2; P = .059).
The ICH rate was not different in patients treated after 4.5 hours versus before 4.5 hours. The subgroup of patients treated at 4.5-12.0 hours showed weaker evidence of better outcomes with thrombolysis than those treated before 4.5 hours, suggesting that the 12-hour window for TEMPO-2 did not explain the absence of benefit seen with tenecteplase.
Patients in the control group did better than expected, which may have been the result of chance, patient selection, or greater use of dual antiplatelet therapy, researchers noted.
Despite higher recanalization rates in the tenecteplase group (48% vs 22%), there was no change in the rate of stroke progression between groups, with an 8% rate of progression seen overall in the study.
Noting that previous studies have shown that patients with minor stroke and intracranial occlusion are at a risk for both progression and disability, the authors suggested that good supportive care may have improved outcomes in both groups.
More Trials Needed
Commenting on the study at the ESOC meeting, Urs Fischer, MD, Basel University Hospital, Switzerland, said “What should we do for patients with mild stroke with vessel occlusion has been a huge unanswered question. The TEMPO-2 study did not show a benefit with thrombolysis, and there was a tendency toward an increased risk of ICH. This is an important finding.”
In an accompanying editorial, Simona Sacco, MD, University of L’Aquila, Italy, and Guillaume Turc, MD, Université Paris Cité, France, noted that different minor ischemic stroke populations pose different therapeutic challenges.
Observational data suggest a benefit of endovascular treatment for minor stroke with large vessel occlusion, and dedicated randomized controlled trials in this group are ongoing, they added.
Early dual antiplatelet treatment is now the recommended treatment of minor stroke and should therefore be the active comparator for non-cardioembolic strokes in future trials.
While TEMPO-2 did not prove that tenecteplase is better than the standard of care for the acute treatment of minor stroke, Dr. Sacco and Dr. Turc said the study confirms that tenecteplase is associated with a high rate of recanalization.
“Fast recanalization with intravenous thrombolysis, endovascular treatment, proper patient selection, and combination with dual antiplatelet treatment or early initiation of anticoagulants may translate into tangible clinical benefits for patients with minor ischemic stroke, which should be tested in future studies,” they wrote.
This trial was funded by grants from the Canadian Institutes of Health Research, Heart and Stroke Foundation of Canada, and the British Heart Foundation. Boehringer Ingelheim provided tenecteplase for the study. Dr. Coutts reported no conflicts of interest. Dr. Sacco reported receiving grants for research from Novartis and Uriach; consulting fees from Novartis, Allergan-AbbVie, Teva, Lilly, Lundbeck, Pfizer, Novo Nordisk, Abbott, and AstraZeneca; payment for lectures from Novartis, Allergan-AbbVie, Teva, Lilly, Lundbeck, Pfizer, Novo Nordisk, Abbott, and AstraZeneca; and support for attending conferences from Lilly, Novartis, Teva, Lundbeck, and Pfizer. She is president elect of the European Stroke Organization and editor-in-chief of Cephalalgia. Dr. Turc reported payment for lectures from Guerbet France, is a member of the scientific advisory board of AI-Stroke, and is the Secretary General of the European Stroke Organisation.
A version of this article appeared on Medscape.com.
BASEL, SWITZERLAND — , a new trial has concluded.
Results from the randomized controlled trial TEMPO-2 showed no benefit from treatment with tenecteplase following ischemic stroke. In addition, investigators found a small increased risk for symptomatic intracranial hemorrhage (ICH) and more deaths in the tenecteplase group compared with the control group.
The research suggests that although it makes sense to open up vessels in patients with minor stroke, they didn’t do better with thrombolysis.
“This is not the result we were hoping for, but I think the question of whether to treat these minor stroke patients who are not disabled has now been answered,” said lead investigator Shelagh B. Coutts, MD, University of Calgary, Alberta, Canada.
“After these results, I think we should scan these patients, admit them, give them dual antiplatelet therapy and IV fluids, and watch them like a hawk. If they deteriorate, we can intervene at that point.”
The findings were presented at the European Stroke Organization Conference (ESOC) 2024 annual meeting and published online simultaneously in The Lancet.
Very Little Data
Up to half of patients with ischemic stroke initially present with minimal symptoms, which are not disabling, investigators noted. Despite having low scores on the National Institutes of Health Stroke Scale (NIHSS) that typically range from 0 to 5, a third of these patients are dead or disabled at 90-day follow-up if thrombolysis is withheld.
Patients with minor deficits and evidence of an intracranial occlusion are a subpopulation at a high risk for early neurological deterioration, which most often occurs within the first 24 hours after presentation.
However, many physicians have concerns about giving thrombolysis to these patients because of the potential harm from bleeding in the absence of major deficits, and most trials of thrombolysis have excluded patients with minor stroke. That leaves very little high-quality data to guide practice for these patients.
Two previous studies have compared alteplase with antiplatelet agents in minor stroke, but no trial has specifically looked at the subset of patients with minor stroke who have intracranial occlusion. The TEMPO-2 trial was conducted to evaluate the use of tenecteplase in this patient population.
The multicenter, parallel group, open-label study was conducted at 48 hospitals in Australia, Austria, Brazil, Canada, Finland, Ireland, New Zealand, Singapore, Spain, and the United Kingdom.
The trial included patients with minor acute ischemic stroke (NIHSS score of 0-5) and intracranial occlusion or focal perfusion abnormality who were within 12 hours from stroke onset.
Patients received IV tenecteplase (0.25 mg/kg) or non-thrombolytic standard of care (control). Most patients in the control group were treated with dual antiplatelet therapy with aspirin and clopidogrel (57%) or aspirin monotherapy (23%).
The trial was stopped early for futility after 886 patients had been enrolled. The median NIHSS score was 2.
The primary outcome — a return to baseline functioning on the modified Rankin Scale score at 90 days — occurred in 75% of the control group and in 72% of the tenecteplase group (risk ratio [RR], 0.96; P = .29).
Although there were significantly more patients with early recanalization and an NIHSS score of 0 at day 5 or discharge after tenecteplase treatment, this did not translate into improved functional outcomes at 90 days.
More patients died in the tenecteplase group compared with the control group (5% vs 1%; adjusted hazard ratio, 3.8; P = .0085).
There were eight (2%) symptomatic ICHs in the tenecteplase group versus two (< 1%) in the control group (RR, 4.2; P = .059).
The ICH rate was not different in patients treated after 4.5 hours versus before 4.5 hours. The subgroup of patients treated at 4.5-12.0 hours showed weaker evidence of better outcomes with thrombolysis than those treated before 4.5 hours, suggesting that the 12-hour window for TEMPO-2 did not explain the absence of benefit seen with tenecteplase.
Patients in the control group did better than expected, which may have been the result of chance, patient selection, or greater use of dual antiplatelet therapy, researchers noted.
Despite higher recanalization rates in the tenecteplase group (48% vs 22%), there was no change in the rate of stroke progression between groups, with an 8% rate of progression seen overall in the study.
Noting that previous studies have shown that patients with minor stroke and intracranial occlusion are at a risk for both progression and disability, the authors suggested that good supportive care may have improved outcomes in both groups.
More Trials Needed
Commenting on the study at the ESOC meeting, Urs Fischer, MD, Basel University Hospital, Switzerland, said “What should we do for patients with mild stroke with vessel occlusion has been a huge unanswered question. The TEMPO-2 study did not show a benefit with thrombolysis, and there was a tendency toward an increased risk of ICH. This is an important finding.”
In an accompanying editorial, Simona Sacco, MD, University of L’Aquila, Italy, and Guillaume Turc, MD, Université Paris Cité, France, noted that different minor ischemic stroke populations pose different therapeutic challenges.
Observational data suggest a benefit of endovascular treatment for minor stroke with large vessel occlusion, and dedicated randomized controlled trials in this group are ongoing, they added.
Early dual antiplatelet treatment is now the recommended treatment of minor stroke and should therefore be the active comparator for non-cardioembolic strokes in future trials.
While TEMPO-2 did not prove that tenecteplase is better than the standard of care for the acute treatment of minor stroke, Dr. Sacco and Dr. Turc said the study confirms that tenecteplase is associated with a high rate of recanalization.
“Fast recanalization with intravenous thrombolysis, endovascular treatment, proper patient selection, and combination with dual antiplatelet treatment or early initiation of anticoagulants may translate into tangible clinical benefits for patients with minor ischemic stroke, which should be tested in future studies,” they wrote.
This trial was funded by grants from the Canadian Institutes of Health Research, Heart and Stroke Foundation of Canada, and the British Heart Foundation. Boehringer Ingelheim provided tenecteplase for the study. Dr. Coutts reported no conflicts of interest. Dr. Sacco reported receiving grants for research from Novartis and Uriach; consulting fees from Novartis, Allergan-AbbVie, Teva, Lilly, Lundbeck, Pfizer, Novo Nordisk, Abbott, and AstraZeneca; payment for lectures from Novartis, Allergan-AbbVie, Teva, Lilly, Lundbeck, Pfizer, Novo Nordisk, Abbott, and AstraZeneca; and support for attending conferences from Lilly, Novartis, Teva, Lundbeck, and Pfizer. She is president elect of the European Stroke Organization and editor-in-chief of Cephalalgia. Dr. Turc reported payment for lectures from Guerbet France, is a member of the scientific advisory board of AI-Stroke, and is the Secretary General of the European Stroke Organisation.
A version of this article appeared on Medscape.com.
BASEL, SWITZERLAND — , a new trial has concluded.
Results from the randomized controlled trial TEMPO-2 showed no benefit from treatment with tenecteplase following ischemic stroke. In addition, investigators found a small increased risk for symptomatic intracranial hemorrhage (ICH) and more deaths in the tenecteplase group compared with the control group.
The research suggests that although it makes sense to open up vessels in patients with minor stroke, they didn’t do better with thrombolysis.
“This is not the result we were hoping for, but I think the question of whether to treat these minor stroke patients who are not disabled has now been answered,” said lead investigator Shelagh B. Coutts, MD, University of Calgary, Alberta, Canada.
“After these results, I think we should scan these patients, admit them, give them dual antiplatelet therapy and IV fluids, and watch them like a hawk. If they deteriorate, we can intervene at that point.”
The findings were presented at the European Stroke Organization Conference (ESOC) 2024 annual meeting and published online simultaneously in The Lancet.
Very Little Data
Up to half of patients with ischemic stroke initially present with minimal symptoms, which are not disabling, investigators noted. Despite having low scores on the National Institutes of Health Stroke Scale (NIHSS) that typically range from 0 to 5, a third of these patients are dead or disabled at 90-day follow-up if thrombolysis is withheld.
Patients with minor deficits and evidence of an intracranial occlusion are a subpopulation at a high risk for early neurological deterioration, which most often occurs within the first 24 hours after presentation.
However, many physicians have concerns about giving thrombolysis to these patients because of the potential harm from bleeding in the absence of major deficits, and most trials of thrombolysis have excluded patients with minor stroke. That leaves very little high-quality data to guide practice for these patients.
Two previous studies have compared alteplase with antiplatelet agents in minor stroke, but no trial has specifically looked at the subset of patients with minor stroke who have intracranial occlusion. The TEMPO-2 trial was conducted to evaluate the use of tenecteplase in this patient population.
The multicenter, parallel group, open-label study was conducted at 48 hospitals in Australia, Austria, Brazil, Canada, Finland, Ireland, New Zealand, Singapore, Spain, and the United Kingdom.
The trial included patients with minor acute ischemic stroke (NIHSS score of 0-5) and intracranial occlusion or focal perfusion abnormality who were within 12 hours from stroke onset.
Patients received IV tenecteplase (0.25 mg/kg) or non-thrombolytic standard of care (control). Most patients in the control group were treated with dual antiplatelet therapy with aspirin and clopidogrel (57%) or aspirin monotherapy (23%).
The trial was stopped early for futility after 886 patients had been enrolled. The median NIHSS score was 2.
The primary outcome — a return to baseline functioning on the modified Rankin Scale score at 90 days — occurred in 75% of the control group and in 72% of the tenecteplase group (risk ratio [RR], 0.96; P = .29).
Although there were significantly more patients with early recanalization and an NIHSS score of 0 at day 5 or discharge after tenecteplase treatment, this did not translate into improved functional outcomes at 90 days.
More patients died in the tenecteplase group compared with the control group (5% vs 1%; adjusted hazard ratio, 3.8; P = .0085).
There were eight (2%) symptomatic ICHs in the tenecteplase group versus two (< 1%) in the control group (RR, 4.2; P = .059).
The ICH rate was not different in patients treated after 4.5 hours versus before 4.5 hours. The subgroup of patients treated at 4.5-12.0 hours showed weaker evidence of better outcomes with thrombolysis than those treated before 4.5 hours, suggesting that the 12-hour window for TEMPO-2 did not explain the absence of benefit seen with tenecteplase.
Patients in the control group did better than expected, which may have been the result of chance, patient selection, or greater use of dual antiplatelet therapy, researchers noted.
Despite higher recanalization rates in the tenecteplase group (48% vs 22%), there was no change in the rate of stroke progression between groups, with an 8% rate of progression seen overall in the study.
Noting that previous studies have shown that patients with minor stroke and intracranial occlusion are at a risk for both progression and disability, the authors suggested that good supportive care may have improved outcomes in both groups.
More Trials Needed
Commenting on the study at the ESOC meeting, Urs Fischer, MD, Basel University Hospital, Switzerland, said “What should we do for patients with mild stroke with vessel occlusion has been a huge unanswered question. The TEMPO-2 study did not show a benefit with thrombolysis, and there was a tendency toward an increased risk of ICH. This is an important finding.”
In an accompanying editorial, Simona Sacco, MD, University of L’Aquila, Italy, and Guillaume Turc, MD, Université Paris Cité, France, noted that different minor ischemic stroke populations pose different therapeutic challenges.
Observational data suggest a benefit of endovascular treatment for minor stroke with large vessel occlusion, and dedicated randomized controlled trials in this group are ongoing, they added.
Early dual antiplatelet treatment is now the recommended treatment of minor stroke and should therefore be the active comparator for non-cardioembolic strokes in future trials.
While TEMPO-2 did not prove that tenecteplase is better than the standard of care for the acute treatment of minor stroke, Dr. Sacco and Dr. Turc said the study confirms that tenecteplase is associated with a high rate of recanalization.
“Fast recanalization with intravenous thrombolysis, endovascular treatment, proper patient selection, and combination with dual antiplatelet treatment or early initiation of anticoagulants may translate into tangible clinical benefits for patients with minor ischemic stroke, which should be tested in future studies,” they wrote.
This trial was funded by grants from the Canadian Institutes of Health Research, Heart and Stroke Foundation of Canada, and the British Heart Foundation. Boehringer Ingelheim provided tenecteplase for the study. Dr. Coutts reported no conflicts of interest. Dr. Sacco reported receiving grants for research from Novartis and Uriach; consulting fees from Novartis, Allergan-AbbVie, Teva, Lilly, Lundbeck, Pfizer, Novo Nordisk, Abbott, and AstraZeneca; payment for lectures from Novartis, Allergan-AbbVie, Teva, Lilly, Lundbeck, Pfizer, Novo Nordisk, Abbott, and AstraZeneca; and support for attending conferences from Lilly, Novartis, Teva, Lundbeck, and Pfizer. She is president elect of the European Stroke Organization and editor-in-chief of Cephalalgia. Dr. Turc reported payment for lectures from Guerbet France, is a member of the scientific advisory board of AI-Stroke, and is the Secretary General of the European Stroke Organisation.
A version of this article appeared on Medscape.com.
FROM ESOC 2024
New Data to Change Practice on BP Control in Acute Stroke: INTERACT4
BASEL, SWITZERLAND — Early reduction of blood pressure has a beneficial effect in hemorrhagic stroke but a detrimental effect in ischemic stroke, new trial data show. The findings could shake up recommendations on control of blood pressure in acute stroke patients.
“This is the first time that we have randomized evidence of blood pressure control prior to reperfusion in ischemic stroke patients, and our data will challenge the current guidelines that recommend lowering blood pressure to below 180 mm Hg systolic in these patients,” said study coauthor Craig Anderson, MD, George Institute for Global Health, Sydney, Australia.
“And this study also clearly shows for the first time that getting blood pressure under control in hemorrhagic stroke patients in the first couple of hours has definitive benefits,” he added.
The findings were presented on May 16 at the European Stroke Organization Conference (ESOC) annual meeting and published online simultaneously in The New England Journal of Medicine.
A Test of Early BP Control
The trial was conducted to test the strategy of very early blood pressure control during patient transport in an ambulance after acute stroke, which investigators suspected could benefit patients with both types of stroke.
The hypothesis was that this would reduce bleeding in the brain for those with hemorrhagic stroke. For ischemic stroke patients, it was thought this strategy would speed up administration of thrombolysis, because guidelines recommend bringing blood pressure under control before thrombolysis.
For the INTERACT4 trial, which was conducted in China, 2404 patients with suspected acute stroke and elevated systolic blood pressure (≥ 150 mm Hg) who were assessed in the ambulance within 2 hours after symptom onset were randomized to receive immediate treatment with intravenous urapidil to lower the systolic blood pressure or usual blood pressure management (usual care group).
The median time between symptom onset and randomization was 61 minutes, and the mean blood pressure at randomization was 178/98 mm Hg.
Stroke was subsequently confirmed by imaging in 2240 patients, of whom 46% had a hemorrhagic stroke and 54% an ischemic stroke.
At the time of arrival at the hospital, the mean systolic blood pressure in the intervention group was 158 mm Hg, compared with 170 mm Hg in the usual care group.
The primary efficacy outcome was functional status as assessed by modified Rankin scale score at 90 days.
Overall, there was no difference between the two groups in terms of functional outcome scores (common odds ratio [OR], 1.00; 95% CI, 0.87-1.15), and the incidence of serious adverse events was similar.
But the study showed very different results in patients with hemorrhagic stroke vs those with ischemic stroke.
‘Slam-Dunk’ Effect
Anderson has led several previous trials of blood pressure control in stroke patients, some of which have suggested benefit of lowering blood pressure in those with hemorrhagic stroke, but he says the results of the current trial are more clear-cut.
“We have never seen such a slam-dunk effect as there was in INTERACT4,” Dr. Anderson said. “Not only did we show that early reduction of blood pressure in hemorrhagic stroke patients improved functional outcome, it also reduced bleeding in the brain, improved survival and quality of life, and reduced surgery and infection complications. That’s quite remarkable.”
The findings offer “clear evidence that for patients with hemorrhagic stroke, we must get the blood pressure under control as soon as possible and introduce systems of care to ensure this happens,” he added.
The reason for the clear findings in the current trial is probably the treatment time, Dr. Anderson said.
“This is the first trial in which blood pressure has been controlled in the ambulance and occurred much earlier than in the previous trials.”
Challenging Ischemic Stroke Guidelines
The INTERACT4 results in ischemic stroke patients are likely to be more controversial.
“Our results are clearly challenging longstanding beliefs around blood pressure control in ischemic stroke prior to thrombolysis,” Dr. Anderson said.
Current guidelines recommend a blood pressure < 185 mm Hg systolic before initiation of thrombolysis because of concerns about intracerebral hemorrhage, he noted. Often, blood pressure is lowered rapidly down to much lower levels in order give thrombolysis quickly.
“Our results suggest this may not be a good idea,” Dr. Anderson said. “I think these data will shake us up a bit and make us more cautious about reducing blood pressure in these patients. Personally, I wouldn’t touch the blood pressure at all in ischemic stroke patients after these results.”
He said the mechanisms behind the different stroke types would explain the results.
“If a patient is bleeding, it makes sense that higher blood pressure would make that worse,” Dr. Anderson said. “But when a patient has a blocked artery and ischemia in the brain, it seems likely that the extra pressure is needed to keep oxygen delivery to the ischemic tissue.”
Accurate Diagnosis Necessary
Because it is not possible to make an accurate diagnosis between ischemic and hemorrhagic stroke without a CT scan, Dr. Anderson stressed that at the present time, no action on blood pressure can be taken in the ambulance.
“There is a lot of interest in developing a lightweight brain scanner to be used in ambulances, but this won’t be routinely available for several years,” he said. “So for now, quick diagnosis of the type of stroke that is occurring on the patient’s arrival at the emergency department and, for hemorrhagic stroke patients, swift action to control blood pressure at this point is critical to preserving brain function.”
Commenting on the INTERACT4 results at the ESOC meeting, Simona Sacco, MD, professor of neurology at the University of L’Aquila, Italy, said this was a very important trial that would impact clinical practice.
“The data really reinforce that hemorrhagic stroke patients must have their blood pressure reduced as soon as possible,” she stated.
Dr. Sacco said the trial emphasizes the need to be able to distinguish between a hemorrhagic and ischemic stroke in a prehospital setting and supports the introduction of more mobile stroke units carrying CT scanners and calls for the development of biomarkers that can allow rapid differentiation between the two conditions.
In an accompanying editorial, Jonathan Edlow, MD, Department of Emergency Medicine, Beth Israel Deaconess Medical Center, Boston, points out several aspects of the trial that may potentially limit the generalizability of the findings. These include use of urapidil as the antihypertensive agent, which is unavailable in the United States; all patients being of Han Chinese ethnicity; and an unusually high sensitivity of initial CT scans in detecting visible signs of ischemia or infarction in patients in acute ischemic stroke.
“These findings should be considered hypothesis-generating, and they make the case for validation of the trial results in other settings,” Dr. Edlow wrote.
The INTERACT4 trial was funded by the National Health and Medical Research Council of Australia, the George Institute for Global Health, several Chinese healthcare institutions, and Takeda Pharmaceuticals China. Disclosures for study and editorial authors are provided in the original articles.
A version of this article appeared on Medscape.com.
BASEL, SWITZERLAND — Early reduction of blood pressure has a beneficial effect in hemorrhagic stroke but a detrimental effect in ischemic stroke, new trial data show. The findings could shake up recommendations on control of blood pressure in acute stroke patients.
“This is the first time that we have randomized evidence of blood pressure control prior to reperfusion in ischemic stroke patients, and our data will challenge the current guidelines that recommend lowering blood pressure to below 180 mm Hg systolic in these patients,” said study coauthor Craig Anderson, MD, George Institute for Global Health, Sydney, Australia.
“And this study also clearly shows for the first time that getting blood pressure under control in hemorrhagic stroke patients in the first couple of hours has definitive benefits,” he added.
The findings were presented on May 16 at the European Stroke Organization Conference (ESOC) annual meeting and published online simultaneously in The New England Journal of Medicine.
A Test of Early BP Control
The trial was conducted to test the strategy of very early blood pressure control during patient transport in an ambulance after acute stroke, which investigators suspected could benefit patients with both types of stroke.
The hypothesis was that this would reduce bleeding in the brain for those with hemorrhagic stroke. For ischemic stroke patients, it was thought this strategy would speed up administration of thrombolysis, because guidelines recommend bringing blood pressure under control before thrombolysis.
For the INTERACT4 trial, which was conducted in China, 2404 patients with suspected acute stroke and elevated systolic blood pressure (≥ 150 mm Hg) who were assessed in the ambulance within 2 hours after symptom onset were randomized to receive immediate treatment with intravenous urapidil to lower the systolic blood pressure or usual blood pressure management (usual care group).
The median time between symptom onset and randomization was 61 minutes, and the mean blood pressure at randomization was 178/98 mm Hg.
Stroke was subsequently confirmed by imaging in 2240 patients, of whom 46% had a hemorrhagic stroke and 54% an ischemic stroke.
At the time of arrival at the hospital, the mean systolic blood pressure in the intervention group was 158 mm Hg, compared with 170 mm Hg in the usual care group.
The primary efficacy outcome was functional status as assessed by modified Rankin scale score at 90 days.
Overall, there was no difference between the two groups in terms of functional outcome scores (common odds ratio [OR], 1.00; 95% CI, 0.87-1.15), and the incidence of serious adverse events was similar.
But the study showed very different results in patients with hemorrhagic stroke vs those with ischemic stroke.
‘Slam-Dunk’ Effect
Anderson has led several previous trials of blood pressure control in stroke patients, some of which have suggested benefit of lowering blood pressure in those with hemorrhagic stroke, but he says the results of the current trial are more clear-cut.
“We have never seen such a slam-dunk effect as there was in INTERACT4,” Dr. Anderson said. “Not only did we show that early reduction of blood pressure in hemorrhagic stroke patients improved functional outcome, it also reduced bleeding in the brain, improved survival and quality of life, and reduced surgery and infection complications. That’s quite remarkable.”
The findings offer “clear evidence that for patients with hemorrhagic stroke, we must get the blood pressure under control as soon as possible and introduce systems of care to ensure this happens,” he added.
The reason for the clear findings in the current trial is probably the treatment time, Dr. Anderson said.
“This is the first trial in which blood pressure has been controlled in the ambulance and occurred much earlier than in the previous trials.”
Challenging Ischemic Stroke Guidelines
The INTERACT4 results in ischemic stroke patients are likely to be more controversial.
“Our results are clearly challenging longstanding beliefs around blood pressure control in ischemic stroke prior to thrombolysis,” Dr. Anderson said.
Current guidelines recommend a blood pressure < 185 mm Hg systolic before initiation of thrombolysis because of concerns about intracerebral hemorrhage, he noted. Often, blood pressure is lowered rapidly down to much lower levels in order give thrombolysis quickly.
“Our results suggest this may not be a good idea,” Dr. Anderson said. “I think these data will shake us up a bit and make us more cautious about reducing blood pressure in these patients. Personally, I wouldn’t touch the blood pressure at all in ischemic stroke patients after these results.”
He said the mechanisms behind the different stroke types would explain the results.
“If a patient is bleeding, it makes sense that higher blood pressure would make that worse,” Dr. Anderson said. “But when a patient has a blocked artery and ischemia in the brain, it seems likely that the extra pressure is needed to keep oxygen delivery to the ischemic tissue.”
Accurate Diagnosis Necessary
Because it is not possible to make an accurate diagnosis between ischemic and hemorrhagic stroke without a CT scan, Dr. Anderson stressed that at the present time, no action on blood pressure can be taken in the ambulance.
“There is a lot of interest in developing a lightweight brain scanner to be used in ambulances, but this won’t be routinely available for several years,” he said. “So for now, quick diagnosis of the type of stroke that is occurring on the patient’s arrival at the emergency department and, for hemorrhagic stroke patients, swift action to control blood pressure at this point is critical to preserving brain function.”
Commenting on the INTERACT4 results at the ESOC meeting, Simona Sacco, MD, professor of neurology at the University of L’Aquila, Italy, said this was a very important trial that would impact clinical practice.
“The data really reinforce that hemorrhagic stroke patients must have their blood pressure reduced as soon as possible,” she stated.
Dr. Sacco said the trial emphasizes the need to be able to distinguish between a hemorrhagic and ischemic stroke in a prehospital setting and supports the introduction of more mobile stroke units carrying CT scanners and calls for the development of biomarkers that can allow rapid differentiation between the two conditions.
In an accompanying editorial, Jonathan Edlow, MD, Department of Emergency Medicine, Beth Israel Deaconess Medical Center, Boston, points out several aspects of the trial that may potentially limit the generalizability of the findings. These include use of urapidil as the antihypertensive agent, which is unavailable in the United States; all patients being of Han Chinese ethnicity; and an unusually high sensitivity of initial CT scans in detecting visible signs of ischemia or infarction in patients in acute ischemic stroke.
“These findings should be considered hypothesis-generating, and they make the case for validation of the trial results in other settings,” Dr. Edlow wrote.
The INTERACT4 trial was funded by the National Health and Medical Research Council of Australia, the George Institute for Global Health, several Chinese healthcare institutions, and Takeda Pharmaceuticals China. Disclosures for study and editorial authors are provided in the original articles.
A version of this article appeared on Medscape.com.
BASEL, SWITZERLAND — Early reduction of blood pressure has a beneficial effect in hemorrhagic stroke but a detrimental effect in ischemic stroke, new trial data show. The findings could shake up recommendations on control of blood pressure in acute stroke patients.
“This is the first time that we have randomized evidence of blood pressure control prior to reperfusion in ischemic stroke patients, and our data will challenge the current guidelines that recommend lowering blood pressure to below 180 mm Hg systolic in these patients,” said study coauthor Craig Anderson, MD, George Institute for Global Health, Sydney, Australia.
“And this study also clearly shows for the first time that getting blood pressure under control in hemorrhagic stroke patients in the first couple of hours has definitive benefits,” he added.
The findings were presented on May 16 at the European Stroke Organization Conference (ESOC) annual meeting and published online simultaneously in The New England Journal of Medicine.
A Test of Early BP Control
The trial was conducted to test the strategy of very early blood pressure control during patient transport in an ambulance after acute stroke, which investigators suspected could benefit patients with both types of stroke.
The hypothesis was that this would reduce bleeding in the brain for those with hemorrhagic stroke. For ischemic stroke patients, it was thought this strategy would speed up administration of thrombolysis, because guidelines recommend bringing blood pressure under control before thrombolysis.
For the INTERACT4 trial, which was conducted in China, 2404 patients with suspected acute stroke and elevated systolic blood pressure (≥ 150 mm Hg) who were assessed in the ambulance within 2 hours after symptom onset were randomized to receive immediate treatment with intravenous urapidil to lower the systolic blood pressure or usual blood pressure management (usual care group).
The median time between symptom onset and randomization was 61 minutes, and the mean blood pressure at randomization was 178/98 mm Hg.
Stroke was subsequently confirmed by imaging in 2240 patients, of whom 46% had a hemorrhagic stroke and 54% an ischemic stroke.
At the time of arrival at the hospital, the mean systolic blood pressure in the intervention group was 158 mm Hg, compared with 170 mm Hg in the usual care group.
The primary efficacy outcome was functional status as assessed by modified Rankin scale score at 90 days.
Overall, there was no difference between the two groups in terms of functional outcome scores (common odds ratio [OR], 1.00; 95% CI, 0.87-1.15), and the incidence of serious adverse events was similar.
But the study showed very different results in patients with hemorrhagic stroke vs those with ischemic stroke.
‘Slam-Dunk’ Effect
Anderson has led several previous trials of blood pressure control in stroke patients, some of which have suggested benefit of lowering blood pressure in those with hemorrhagic stroke, but he says the results of the current trial are more clear-cut.
“We have never seen such a slam-dunk effect as there was in INTERACT4,” Dr. Anderson said. “Not only did we show that early reduction of blood pressure in hemorrhagic stroke patients improved functional outcome, it also reduced bleeding in the brain, improved survival and quality of life, and reduced surgery and infection complications. That’s quite remarkable.”
The findings offer “clear evidence that for patients with hemorrhagic stroke, we must get the blood pressure under control as soon as possible and introduce systems of care to ensure this happens,” he added.
The reason for the clear findings in the current trial is probably the treatment time, Dr. Anderson said.
“This is the first trial in which blood pressure has been controlled in the ambulance and occurred much earlier than in the previous trials.”
Challenging Ischemic Stroke Guidelines
The INTERACT4 results in ischemic stroke patients are likely to be more controversial.
“Our results are clearly challenging longstanding beliefs around blood pressure control in ischemic stroke prior to thrombolysis,” Dr. Anderson said.
Current guidelines recommend a blood pressure < 185 mm Hg systolic before initiation of thrombolysis because of concerns about intracerebral hemorrhage, he noted. Often, blood pressure is lowered rapidly down to much lower levels in order give thrombolysis quickly.
“Our results suggest this may not be a good idea,” Dr. Anderson said. “I think these data will shake us up a bit and make us more cautious about reducing blood pressure in these patients. Personally, I wouldn’t touch the blood pressure at all in ischemic stroke patients after these results.”
He said the mechanisms behind the different stroke types would explain the results.
“If a patient is bleeding, it makes sense that higher blood pressure would make that worse,” Dr. Anderson said. “But when a patient has a blocked artery and ischemia in the brain, it seems likely that the extra pressure is needed to keep oxygen delivery to the ischemic tissue.”
Accurate Diagnosis Necessary
Because it is not possible to make an accurate diagnosis between ischemic and hemorrhagic stroke without a CT scan, Dr. Anderson stressed that at the present time, no action on blood pressure can be taken in the ambulance.
“There is a lot of interest in developing a lightweight brain scanner to be used in ambulances, but this won’t be routinely available for several years,” he said. “So for now, quick diagnosis of the type of stroke that is occurring on the patient’s arrival at the emergency department and, for hemorrhagic stroke patients, swift action to control blood pressure at this point is critical to preserving brain function.”
Commenting on the INTERACT4 results at the ESOC meeting, Simona Sacco, MD, professor of neurology at the University of L’Aquila, Italy, said this was a very important trial that would impact clinical practice.
“The data really reinforce that hemorrhagic stroke patients must have their blood pressure reduced as soon as possible,” she stated.
Dr. Sacco said the trial emphasizes the need to be able to distinguish between a hemorrhagic and ischemic stroke in a prehospital setting and supports the introduction of more mobile stroke units carrying CT scanners and calls for the development of biomarkers that can allow rapid differentiation between the two conditions.
In an accompanying editorial, Jonathan Edlow, MD, Department of Emergency Medicine, Beth Israel Deaconess Medical Center, Boston, points out several aspects of the trial that may potentially limit the generalizability of the findings. These include use of urapidil as the antihypertensive agent, which is unavailable in the United States; all patients being of Han Chinese ethnicity; and an unusually high sensitivity of initial CT scans in detecting visible signs of ischemia or infarction in patients in acute ischemic stroke.
“These findings should be considered hypothesis-generating, and they make the case for validation of the trial results in other settings,” Dr. Edlow wrote.
The INTERACT4 trial was funded by the National Health and Medical Research Council of Australia, the George Institute for Global Health, several Chinese healthcare institutions, and Takeda Pharmaceuticals China. Disclosures for study and editorial authors are provided in the original articles.
A version of this article appeared on Medscape.com.
What Health Risks Do Microplastics Pose?
The annual production of plastic worldwide has increased exponentially from about 2 million tons in 1950 to 460 million tons in 2019, and current levels are expected to triple by 2060.
Plastic contains more than 10,000 chemicals, including carcinogenic substances and endocrine disruptors. Plastic and associated chemicals are responsible for widespread pollution, contaminating aquatic (marine and freshwater), terrestrial, and atmospheric environments globally.
Atmospheric concentrations of plastic particles are on the rise, to the extent that in a remote station in the Eastern Alps in Austria, the contribution of micro- and nanoplastics (MNPs) to organic matter was comparable to data collected at an urban site.
The ocean is the ultimate destination for much of the plastic. All oceans, on the surface and in the depths, contain plastic, which is even found in polar sea ice. Many plastics seem to resist decomposition in the ocean and could persist in the environment for decades. Macro- and microplastic (MP) particles have been identified in hundreds of marine species, including species consumed by humans.
The quantity and fate of MP particles (> 10 µm) and smaller nanoplastics (< 10 µm) in aquatic environments are poorly understood, but what is most concerning is their ability to cross biologic barriers and the potential harm associated with their mobility in biologic systems.
MNP Exposure
MNPs can originate from a wide variety of sources, including food, beverages, and food product packaging. Water bottles represent a significant source of ingestible MNPs for people in their daily lives. Recent estimates, using stimulated Raman scattering imaging, documented a concentration of MNP of approximately 2.4 ± 1.3 × 105 particles per liter of bottled water. Around 90% are nanoplastics, which is two to three orders of magnitude higher than previously reported results for larger MPs.
MNPs enter the body primarily through ingestion or inhalation. For example, MNPs can be ingested by drinking liquids or eating food that has been stored or heated in plastic containers from which they have leaked or by using toothpaste that contains them. Infants are exposed to MPs from artificial milk preparation in polypropylene baby bottles, with higher levels than previously detected and ranging from 14,600 to 4,550,000 particles per capita per day.
MNP and Biologic Systems
The possible formation of hetero-aggregates between nanoplastics and natural organic matter has long been recognized as a potential challenge in the analysis of nanoplastics and can influence toxicologic results in biologic exposure. The direct visualization of such hetero-aggregates in real-world samples supports these concerns, but the analysis of MNPs with traditional techniques remains challenging. Unlike engineered nanoparticles (prepared in the laboratory as model systems), the nanoplastics in the environment are label-free and exhibit significant heterogeneity in chemical composition and morphology.
A systematic analysis of evidence on the toxic effects of MNPs on murine models, however, showed that 52.78% of biologic endpoints (related to glucose metabolism, reproduction, oxidative stress, and lipid metabolism) were significantly affected by MNP exposure.
Between Risk and Toxicity
MNP can enter the body in vivo through the digestive tract, respiratory tract, and skin contact. On average, humans could ingest from 0.1 to 5 g of MNP per week through various exposure routes.
MNPs are a potential risk factor for cardiovascular diseases, as suggested by a recent study on 257 patients with carotid atheromatous plaques. In 58.4% of cases, polyvinyl chloride was detected in the carotid artery plaque, with an average level of 5.2 ± 2.4 μg/mg of plaque. Patients with MNPs inside the atheroma had a higher risk (relative risk, 4.53) for a composite cardiovascular event of myocardial infarction, stroke, or death from any cause at 34 months of follow-up than participants where MNPs were not detectable inside the atheromatous plaque.
The potential link between inflammatory bowel disease (IBD) and MPs has been hypothesized by a study that reported a higher fecal MP concentration in patients with IBD than in healthy individuals. Fecal MP level was correlated with disease severity.
However, these studies have not demonstrated a causal relationship between MNPs and disease, and the way MNPs may influence cellular functions and induce stress responses is not yet well understood.
Future Scenarios
Current evidence confirms the fragmentation of plastic beyond the micrometer level and has unequivocally detected nanoplastics in real samples. As with many other particle distributions of the same size in the natural world, there are substantially more nanoplastics, despite their invisibility with conventional imaging techniques, than particles larger than the micron size.
The initial results of studies on MNPs in humans will stimulate future research on the amounts of MNPs that accumulate in tissue over a person’s lifetime. Researchers also will examine how the particles’ characteristics, including their chemical composition, size, and shape, can influence organs and tissues.
The way MNPs can cause harm, including through effects on the immune system and microbiome, will need to be clarified by investigating possible direct cytotoxic effects, consistent with the introductory statement of the Organization for Economic Cooperation and Development global policy forum on plastics, which states, “Plastic pollution is one of the great environmental challenges of the 21st century, causing wide-ranging damage to ecosystems and human health.”
This story was translated from Univadis Italy, which is part of the Medscape professional network, using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
The annual production of plastic worldwide has increased exponentially from about 2 million tons in 1950 to 460 million tons in 2019, and current levels are expected to triple by 2060.
Plastic contains more than 10,000 chemicals, including carcinogenic substances and endocrine disruptors. Plastic and associated chemicals are responsible for widespread pollution, contaminating aquatic (marine and freshwater), terrestrial, and atmospheric environments globally.
Atmospheric concentrations of plastic particles are on the rise, to the extent that in a remote station in the Eastern Alps in Austria, the contribution of micro- and nanoplastics (MNPs) to organic matter was comparable to data collected at an urban site.
The ocean is the ultimate destination for much of the plastic. All oceans, on the surface and in the depths, contain plastic, which is even found in polar sea ice. Many plastics seem to resist decomposition in the ocean and could persist in the environment for decades. Macro- and microplastic (MP) particles have been identified in hundreds of marine species, including species consumed by humans.
The quantity and fate of MP particles (> 10 µm) and smaller nanoplastics (< 10 µm) in aquatic environments are poorly understood, but what is most concerning is their ability to cross biologic barriers and the potential harm associated with their mobility in biologic systems.
MNP Exposure
MNPs can originate from a wide variety of sources, including food, beverages, and food product packaging. Water bottles represent a significant source of ingestible MNPs for people in their daily lives. Recent estimates, using stimulated Raman scattering imaging, documented a concentration of MNP of approximately 2.4 ± 1.3 × 105 particles per liter of bottled water. Around 90% are nanoplastics, which is two to three orders of magnitude higher than previously reported results for larger MPs.
MNPs enter the body primarily through ingestion or inhalation. For example, MNPs can be ingested by drinking liquids or eating food that has been stored or heated in plastic containers from which they have leaked or by using toothpaste that contains them. Infants are exposed to MPs from artificial milk preparation in polypropylene baby bottles, with higher levels than previously detected and ranging from 14,600 to 4,550,000 particles per capita per day.
MNP and Biologic Systems
The possible formation of hetero-aggregates between nanoplastics and natural organic matter has long been recognized as a potential challenge in the analysis of nanoplastics and can influence toxicologic results in biologic exposure. The direct visualization of such hetero-aggregates in real-world samples supports these concerns, but the analysis of MNPs with traditional techniques remains challenging. Unlike engineered nanoparticles (prepared in the laboratory as model systems), the nanoplastics in the environment are label-free and exhibit significant heterogeneity in chemical composition and morphology.
A systematic analysis of evidence on the toxic effects of MNPs on murine models, however, showed that 52.78% of biologic endpoints (related to glucose metabolism, reproduction, oxidative stress, and lipid metabolism) were significantly affected by MNP exposure.
Between Risk and Toxicity
MNP can enter the body in vivo through the digestive tract, respiratory tract, and skin contact. On average, humans could ingest from 0.1 to 5 g of MNP per week through various exposure routes.
MNPs are a potential risk factor for cardiovascular diseases, as suggested by a recent study on 257 patients with carotid atheromatous plaques. In 58.4% of cases, polyvinyl chloride was detected in the carotid artery plaque, with an average level of 5.2 ± 2.4 μg/mg of plaque. Patients with MNPs inside the atheroma had a higher risk (relative risk, 4.53) for a composite cardiovascular event of myocardial infarction, stroke, or death from any cause at 34 months of follow-up than participants where MNPs were not detectable inside the atheromatous plaque.
The potential link between inflammatory bowel disease (IBD) and MPs has been hypothesized by a study that reported a higher fecal MP concentration in patients with IBD than in healthy individuals. Fecal MP level was correlated with disease severity.
However, these studies have not demonstrated a causal relationship between MNPs and disease, and the way MNPs may influence cellular functions and induce stress responses is not yet well understood.
Future Scenarios
Current evidence confirms the fragmentation of plastic beyond the micrometer level and has unequivocally detected nanoplastics in real samples. As with many other particle distributions of the same size in the natural world, there are substantially more nanoplastics, despite their invisibility with conventional imaging techniques, than particles larger than the micron size.
The initial results of studies on MNPs in humans will stimulate future research on the amounts of MNPs that accumulate in tissue over a person’s lifetime. Researchers also will examine how the particles’ characteristics, including their chemical composition, size, and shape, can influence organs and tissues.
The way MNPs can cause harm, including through effects on the immune system and microbiome, will need to be clarified by investigating possible direct cytotoxic effects, consistent with the introductory statement of the Organization for Economic Cooperation and Development global policy forum on plastics, which states, “Plastic pollution is one of the great environmental challenges of the 21st century, causing wide-ranging damage to ecosystems and human health.”
This story was translated from Univadis Italy, which is part of the Medscape professional network, using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
The annual production of plastic worldwide has increased exponentially from about 2 million tons in 1950 to 460 million tons in 2019, and current levels are expected to triple by 2060.
Plastic contains more than 10,000 chemicals, including carcinogenic substances and endocrine disruptors. Plastic and associated chemicals are responsible for widespread pollution, contaminating aquatic (marine and freshwater), terrestrial, and atmospheric environments globally.
Atmospheric concentrations of plastic particles are on the rise, to the extent that in a remote station in the Eastern Alps in Austria, the contribution of micro- and nanoplastics (MNPs) to organic matter was comparable to data collected at an urban site.
The ocean is the ultimate destination for much of the plastic. All oceans, on the surface and in the depths, contain plastic, which is even found in polar sea ice. Many plastics seem to resist decomposition in the ocean and could persist in the environment for decades. Macro- and microplastic (MP) particles have been identified in hundreds of marine species, including species consumed by humans.
The quantity and fate of MP particles (> 10 µm) and smaller nanoplastics (< 10 µm) in aquatic environments are poorly understood, but what is most concerning is their ability to cross biologic barriers and the potential harm associated with their mobility in biologic systems.
MNP Exposure
MNPs can originate from a wide variety of sources, including food, beverages, and food product packaging. Water bottles represent a significant source of ingestible MNPs for people in their daily lives. Recent estimates, using stimulated Raman scattering imaging, documented a concentration of MNP of approximately 2.4 ± 1.3 × 105 particles per liter of bottled water. Around 90% are nanoplastics, which is two to three orders of magnitude higher than previously reported results for larger MPs.
MNPs enter the body primarily through ingestion or inhalation. For example, MNPs can be ingested by drinking liquids or eating food that has been stored or heated in plastic containers from which they have leaked or by using toothpaste that contains them. Infants are exposed to MPs from artificial milk preparation in polypropylene baby bottles, with higher levels than previously detected and ranging from 14,600 to 4,550,000 particles per capita per day.
MNP and Biologic Systems
The possible formation of hetero-aggregates between nanoplastics and natural organic matter has long been recognized as a potential challenge in the analysis of nanoplastics and can influence toxicologic results in biologic exposure. The direct visualization of such hetero-aggregates in real-world samples supports these concerns, but the analysis of MNPs with traditional techniques remains challenging. Unlike engineered nanoparticles (prepared in the laboratory as model systems), the nanoplastics in the environment are label-free and exhibit significant heterogeneity in chemical composition and morphology.
A systematic analysis of evidence on the toxic effects of MNPs on murine models, however, showed that 52.78% of biologic endpoints (related to glucose metabolism, reproduction, oxidative stress, and lipid metabolism) were significantly affected by MNP exposure.
Between Risk and Toxicity
MNP can enter the body in vivo through the digestive tract, respiratory tract, and skin contact. On average, humans could ingest from 0.1 to 5 g of MNP per week through various exposure routes.
MNPs are a potential risk factor for cardiovascular diseases, as suggested by a recent study on 257 patients with carotid atheromatous plaques. In 58.4% of cases, polyvinyl chloride was detected in the carotid artery plaque, with an average level of 5.2 ± 2.4 μg/mg of plaque. Patients with MNPs inside the atheroma had a higher risk (relative risk, 4.53) for a composite cardiovascular event of myocardial infarction, stroke, or death from any cause at 34 months of follow-up than participants where MNPs were not detectable inside the atheromatous plaque.
The potential link between inflammatory bowel disease (IBD) and MPs has been hypothesized by a study that reported a higher fecal MP concentration in patients with IBD than in healthy individuals. Fecal MP level was correlated with disease severity.
However, these studies have not demonstrated a causal relationship between MNPs and disease, and the way MNPs may influence cellular functions and induce stress responses is not yet well understood.
Future Scenarios
Current evidence confirms the fragmentation of plastic beyond the micrometer level and has unequivocally detected nanoplastics in real samples. As with many other particle distributions of the same size in the natural world, there are substantially more nanoplastics, despite their invisibility with conventional imaging techniques, than particles larger than the micron size.
The initial results of studies on MNPs in humans will stimulate future research on the amounts of MNPs that accumulate in tissue over a person’s lifetime. Researchers also will examine how the particles’ characteristics, including their chemical composition, size, and shape, can influence organs and tissues.
The way MNPs can cause harm, including through effects on the immune system and microbiome, will need to be clarified by investigating possible direct cytotoxic effects, consistent with the introductory statement of the Organization for Economic Cooperation and Development global policy forum on plastics, which states, “Plastic pollution is one of the great environmental challenges of the 21st century, causing wide-ranging damage to ecosystems and human health.”
This story was translated from Univadis Italy, which is part of the Medscape professional network, using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Vigilance Needed in Gout Treatment to Reduce CVD Risks
NEW YORK — Urate, the culprit of gout, affects the vasculature in multiple ways that can raise cardiovascular risk (CV) in an individual with gout, and following guidelines for gout treatment, including the use of colchicine, can be the key to reducing those risks.
“Guideline-concordant gout treatment, which is essentially an anti-inflammatory urate-lowering strategy, at least improves arterial physiology and likely reduces cardiovascular risk,” Michael H. Pillinger, MD, told attendees at the 4th Annual Cardiometabolic Risk in Inflammatory Conditions conference. Dr. Pillinger is professor of medicine and biochemistry and molecular pharmacology at New York University Grossman School of Medicine, New York City, who has published multiple studies on gout.
He cited evidence that has shown soluble urate stimulates the production of C-reactive protein (CRP), which is a predictor of cardiovascular disease (CVD). Another study, in which Dr. Pillinger participated, demonstrated that gout patients have impaired vascular endothelial function associated with a chronic, low-level inflammatory state, he said.
“There’s good evidence that urate itself affects the vasculature in multiple ways, and I suspect this may be a model for other metabolic effects on vasculature,” Dr. Pillinger said. “Patients with gout have abnormal endothelium in ways that really convey vascular risk.”
Gout, Inflammation, and CVD
However, for rheumatologists to study the association between gout-related inflammation and CVD is “very, very hard,” Dr. Pillinger added. “But I do think that the mechanisms by which gout induces biological changes in the vasculature may provide insights into cardiovascular disease in general.”
One way to evaluate the effects of gout on the endothelium in the clinic is to measure flow-mediated dilation. This technique involves placing an ultrasound probe over the brachial artery and measuring the baseline artery diameter. Then, with the blood pressure cuff over the forearm, inflate it to reduce flow, then release the cuff and measure the brachial artery diameter after the endothelium releases vasodilators.
Dr. Pillinger and colleagues evaluated this technique in 34 patients with gout and 64 controls and found that patients with gout had an almost 50% decrease in flow-mediated dilation, he said. “Interestingly, the higher the urate, the worse the flow; the more the inflammation, the worse the flow, so seemingly corresponding with the severity of the gout,” he said. That raised an obvious question, Dr. Pillinger continued: “If you can treat the gout, can you improve the flow-mediated dilation?”
His group answered that question with a study in 38 previously untreated patients with gout, giving them colchicine 0.6 mg twice daily for a month plus a urate-lowering xanthine oxidase inhibitor (allopurinol or febuxostat) to treat them to a target urate level of < 6 mg/dL. “We saw an increase in endothelial function, and it normalized,” Dr. Pillinger said.
However, some study participants didn’t respond. “They were people with well-established other cardiovascular comorbidities — hypertension, hyperlipidemia,” he said. “I think some people just have vessels that are too damaged to get at them just by fixing their gout problem or their inflammation.”
That means patients with gout need to be treated with colchicine early on to avoid CV problems, Dr. Pillinger added. “We ought to get to them before they have the other problems,” he said.
Managing gout, and the concomitant CV problems, requires vigilance both during and in between flares, Dr. Pillinger said after his presentation.
“We have always taught that patients between flares basically look like people with no gout, but we do know now that patients with gout between flares tend to have what you might call ‘subclinical’ inflammation: CRPs and ESRs [erythrocyte sedimentation rates] that are higher than those of the general population, though not so excessive that they might grab attention,” he said. “We also know that many, if not all, patients between flares have urate deposited in or around their joints, but how these two relate is not fully established.”
Better treatment within 3 months of an acute gout flare may reduce the risk for CV events, he said, but that’s based on speculation more so than clinical data.
Potential Benefits of Targeting Inflammation
“More chronically, we know from the cardiologists’ studies that anti-inflammatory therapy should reduce risk in the high-risk general population,” Dr. Pillinger said. “There are no prospective studies confirming that this approach will work among gout patients, but there is no reason why it shouldn’t work — except perhaps that gout patients may have higher inflammation than the general population and also have more comorbidities, so they could perhaps be more resistant.”
Dr. Pillinger said that his group’s studies and another led by Daniel Solomon, MD, at Brigham and Women’s Hospital in Boston, have indicated that anti-inflammatory strategies in gout will lower CV risk.
“And interestingly,” he added, “our data suggest that colchicine use may lower risk not only in high-risk gout patients but also in gout patients who start with no CAD [coronary artery disease] but who seem to have less incident CAD on colchicine. I see this as identifying that gout patients are intrinsically at high risk for CAD, even if they don’t actually have any, so they represent a population for whom lowering chronic inflammation may help prevent incident disease.”
Dr. Pillinger provided more evidence that the understanding of the relationship between gout, gout flares, and CV risk is evolving, said Michael S. Garshick, MD, who attended the conference and is head of the Cardio-Rheumatology Program at NYU Langone, New York City.
“There’s epidemiologic evidence supporting the association,” Dr. Garshick told this news organization after the conference. “We think that most conditions with immune system activation do tend to have an increased risk of some form of cardiovascular disease, but I think the relationship with gout has been highly underpublicized.”
Many patients with gout tend to have a higher prevalence of traditional cardiometabolic issues, which may compound the relationship, Dr. Garshick added. “However, I would argue that with this patient subset that it doesn’t matter because gout patients have a higher risk of traditional risk factors, and you have to [treat-to-target] those traditional risk factors.”
While the clinical evidence of a link between gout and atherosclerosis may not be conclusive, enough circumstantial evidence exists to believe that treating gout will reduce CV risks, he said. “Some of the imaging techniques do suggest that gouty crystals [are] in the atherosclerotic plaque of gout patients,” Dr. Garshick added. Dr. Pillinger’s work, he said, “is showing us that there are different pathways to develop atherosclerosis.”
Dr. Pillinger disclosed relationships with Federation Bio, Fortress Biotech, Amgen, Scilex, Hikma Pharmaceuticals, LG Chem, and Olatec Therapeutics. Dr. Garshick disclosed relationships with Kiniksa Pharmaceuticals, Agepha Pharma, Bristol Myers Squibb, and Horizon Therapeutics.
A version of this article appeared on Medscape.com.
NEW YORK — Urate, the culprit of gout, affects the vasculature in multiple ways that can raise cardiovascular risk (CV) in an individual with gout, and following guidelines for gout treatment, including the use of colchicine, can be the key to reducing those risks.
“Guideline-concordant gout treatment, which is essentially an anti-inflammatory urate-lowering strategy, at least improves arterial physiology and likely reduces cardiovascular risk,” Michael H. Pillinger, MD, told attendees at the 4th Annual Cardiometabolic Risk in Inflammatory Conditions conference. Dr. Pillinger is professor of medicine and biochemistry and molecular pharmacology at New York University Grossman School of Medicine, New York City, who has published multiple studies on gout.
He cited evidence that has shown soluble urate stimulates the production of C-reactive protein (CRP), which is a predictor of cardiovascular disease (CVD). Another study, in which Dr. Pillinger participated, demonstrated that gout patients have impaired vascular endothelial function associated with a chronic, low-level inflammatory state, he said.
“There’s good evidence that urate itself affects the vasculature in multiple ways, and I suspect this may be a model for other metabolic effects on vasculature,” Dr. Pillinger said. “Patients with gout have abnormal endothelium in ways that really convey vascular risk.”
Gout, Inflammation, and CVD
However, for rheumatologists to study the association between gout-related inflammation and CVD is “very, very hard,” Dr. Pillinger added. “But I do think that the mechanisms by which gout induces biological changes in the vasculature may provide insights into cardiovascular disease in general.”
One way to evaluate the effects of gout on the endothelium in the clinic is to measure flow-mediated dilation. This technique involves placing an ultrasound probe over the brachial artery and measuring the baseline artery diameter. Then, with the blood pressure cuff over the forearm, inflate it to reduce flow, then release the cuff and measure the brachial artery diameter after the endothelium releases vasodilators.
Dr. Pillinger and colleagues evaluated this technique in 34 patients with gout and 64 controls and found that patients with gout had an almost 50% decrease in flow-mediated dilation, he said. “Interestingly, the higher the urate, the worse the flow; the more the inflammation, the worse the flow, so seemingly corresponding with the severity of the gout,” he said. That raised an obvious question, Dr. Pillinger continued: “If you can treat the gout, can you improve the flow-mediated dilation?”
His group answered that question with a study in 38 previously untreated patients with gout, giving them colchicine 0.6 mg twice daily for a month plus a urate-lowering xanthine oxidase inhibitor (allopurinol or febuxostat) to treat them to a target urate level of < 6 mg/dL. “We saw an increase in endothelial function, and it normalized,” Dr. Pillinger said.
However, some study participants didn’t respond. “They were people with well-established other cardiovascular comorbidities — hypertension, hyperlipidemia,” he said. “I think some people just have vessels that are too damaged to get at them just by fixing their gout problem or their inflammation.”
That means patients with gout need to be treated with colchicine early on to avoid CV problems, Dr. Pillinger added. “We ought to get to them before they have the other problems,” he said.
Managing gout, and the concomitant CV problems, requires vigilance both during and in between flares, Dr. Pillinger said after his presentation.
“We have always taught that patients between flares basically look like people with no gout, but we do know now that patients with gout between flares tend to have what you might call ‘subclinical’ inflammation: CRPs and ESRs [erythrocyte sedimentation rates] that are higher than those of the general population, though not so excessive that they might grab attention,” he said. “We also know that many, if not all, patients between flares have urate deposited in or around their joints, but how these two relate is not fully established.”
Better treatment within 3 months of an acute gout flare may reduce the risk for CV events, he said, but that’s based on speculation more so than clinical data.
Potential Benefits of Targeting Inflammation
“More chronically, we know from the cardiologists’ studies that anti-inflammatory therapy should reduce risk in the high-risk general population,” Dr. Pillinger said. “There are no prospective studies confirming that this approach will work among gout patients, but there is no reason why it shouldn’t work — except perhaps that gout patients may have higher inflammation than the general population and also have more comorbidities, so they could perhaps be more resistant.”
Dr. Pillinger said that his group’s studies and another led by Daniel Solomon, MD, at Brigham and Women’s Hospital in Boston, have indicated that anti-inflammatory strategies in gout will lower CV risk.
“And interestingly,” he added, “our data suggest that colchicine use may lower risk not only in high-risk gout patients but also in gout patients who start with no CAD [coronary artery disease] but who seem to have less incident CAD on colchicine. I see this as identifying that gout patients are intrinsically at high risk for CAD, even if they don’t actually have any, so they represent a population for whom lowering chronic inflammation may help prevent incident disease.”
Dr. Pillinger provided more evidence that the understanding of the relationship between gout, gout flares, and CV risk is evolving, said Michael S. Garshick, MD, who attended the conference and is head of the Cardio-Rheumatology Program at NYU Langone, New York City.
“There’s epidemiologic evidence supporting the association,” Dr. Garshick told this news organization after the conference. “We think that most conditions with immune system activation do tend to have an increased risk of some form of cardiovascular disease, but I think the relationship with gout has been highly underpublicized.”
Many patients with gout tend to have a higher prevalence of traditional cardiometabolic issues, which may compound the relationship, Dr. Garshick added. “However, I would argue that with this patient subset that it doesn’t matter because gout patients have a higher risk of traditional risk factors, and you have to [treat-to-target] those traditional risk factors.”
While the clinical evidence of a link between gout and atherosclerosis may not be conclusive, enough circumstantial evidence exists to believe that treating gout will reduce CV risks, he said. “Some of the imaging techniques do suggest that gouty crystals [are] in the atherosclerotic plaque of gout patients,” Dr. Garshick added. Dr. Pillinger’s work, he said, “is showing us that there are different pathways to develop atherosclerosis.”
Dr. Pillinger disclosed relationships with Federation Bio, Fortress Biotech, Amgen, Scilex, Hikma Pharmaceuticals, LG Chem, and Olatec Therapeutics. Dr. Garshick disclosed relationships with Kiniksa Pharmaceuticals, Agepha Pharma, Bristol Myers Squibb, and Horizon Therapeutics.
A version of this article appeared on Medscape.com.
NEW YORK — Urate, the culprit of gout, affects the vasculature in multiple ways that can raise cardiovascular risk (CV) in an individual with gout, and following guidelines for gout treatment, including the use of colchicine, can be the key to reducing those risks.
“Guideline-concordant gout treatment, which is essentially an anti-inflammatory urate-lowering strategy, at least improves arterial physiology and likely reduces cardiovascular risk,” Michael H. Pillinger, MD, told attendees at the 4th Annual Cardiometabolic Risk in Inflammatory Conditions conference. Dr. Pillinger is professor of medicine and biochemistry and molecular pharmacology at New York University Grossman School of Medicine, New York City, who has published multiple studies on gout.
He cited evidence that has shown soluble urate stimulates the production of C-reactive protein (CRP), which is a predictor of cardiovascular disease (CVD). Another study, in which Dr. Pillinger participated, demonstrated that gout patients have impaired vascular endothelial function associated with a chronic, low-level inflammatory state, he said.
“There’s good evidence that urate itself affects the vasculature in multiple ways, and I suspect this may be a model for other metabolic effects on vasculature,” Dr. Pillinger said. “Patients with gout have abnormal endothelium in ways that really convey vascular risk.”
Gout, Inflammation, and CVD
However, for rheumatologists to study the association between gout-related inflammation and CVD is “very, very hard,” Dr. Pillinger added. “But I do think that the mechanisms by which gout induces biological changes in the vasculature may provide insights into cardiovascular disease in general.”
One way to evaluate the effects of gout on the endothelium in the clinic is to measure flow-mediated dilation. This technique involves placing an ultrasound probe over the brachial artery and measuring the baseline artery diameter. Then, with the blood pressure cuff over the forearm, inflate it to reduce flow, then release the cuff and measure the brachial artery diameter after the endothelium releases vasodilators.
Dr. Pillinger and colleagues evaluated this technique in 34 patients with gout and 64 controls and found that patients with gout had an almost 50% decrease in flow-mediated dilation, he said. “Interestingly, the higher the urate, the worse the flow; the more the inflammation, the worse the flow, so seemingly corresponding with the severity of the gout,” he said. That raised an obvious question, Dr. Pillinger continued: “If you can treat the gout, can you improve the flow-mediated dilation?”
His group answered that question with a study in 38 previously untreated patients with gout, giving them colchicine 0.6 mg twice daily for a month plus a urate-lowering xanthine oxidase inhibitor (allopurinol or febuxostat) to treat them to a target urate level of < 6 mg/dL. “We saw an increase in endothelial function, and it normalized,” Dr. Pillinger said.
However, some study participants didn’t respond. “They were people with well-established other cardiovascular comorbidities — hypertension, hyperlipidemia,” he said. “I think some people just have vessels that are too damaged to get at them just by fixing their gout problem or their inflammation.”
That means patients with gout need to be treated with colchicine early on to avoid CV problems, Dr. Pillinger added. “We ought to get to them before they have the other problems,” he said.
Managing gout, and the concomitant CV problems, requires vigilance both during and in between flares, Dr. Pillinger said after his presentation.
“We have always taught that patients between flares basically look like people with no gout, but we do know now that patients with gout between flares tend to have what you might call ‘subclinical’ inflammation: CRPs and ESRs [erythrocyte sedimentation rates] that are higher than those of the general population, though not so excessive that they might grab attention,” he said. “We also know that many, if not all, patients between flares have urate deposited in or around their joints, but how these two relate is not fully established.”
Better treatment within 3 months of an acute gout flare may reduce the risk for CV events, he said, but that’s based on speculation more so than clinical data.
Potential Benefits of Targeting Inflammation
“More chronically, we know from the cardiologists’ studies that anti-inflammatory therapy should reduce risk in the high-risk general population,” Dr. Pillinger said. “There are no prospective studies confirming that this approach will work among gout patients, but there is no reason why it shouldn’t work — except perhaps that gout patients may have higher inflammation than the general population and also have more comorbidities, so they could perhaps be more resistant.”
Dr. Pillinger said that his group’s studies and another led by Daniel Solomon, MD, at Brigham and Women’s Hospital in Boston, have indicated that anti-inflammatory strategies in gout will lower CV risk.
“And interestingly,” he added, “our data suggest that colchicine use may lower risk not only in high-risk gout patients but also in gout patients who start with no CAD [coronary artery disease] but who seem to have less incident CAD on colchicine. I see this as identifying that gout patients are intrinsically at high risk for CAD, even if they don’t actually have any, so they represent a population for whom lowering chronic inflammation may help prevent incident disease.”
Dr. Pillinger provided more evidence that the understanding of the relationship between gout, gout flares, and CV risk is evolving, said Michael S. Garshick, MD, who attended the conference and is head of the Cardio-Rheumatology Program at NYU Langone, New York City.
“There’s epidemiologic evidence supporting the association,” Dr. Garshick told this news organization after the conference. “We think that most conditions with immune system activation do tend to have an increased risk of some form of cardiovascular disease, but I think the relationship with gout has been highly underpublicized.”
Many patients with gout tend to have a higher prevalence of traditional cardiometabolic issues, which may compound the relationship, Dr. Garshick added. “However, I would argue that with this patient subset that it doesn’t matter because gout patients have a higher risk of traditional risk factors, and you have to [treat-to-target] those traditional risk factors.”
While the clinical evidence of a link between gout and atherosclerosis may not be conclusive, enough circumstantial evidence exists to believe that treating gout will reduce CV risks, he said. “Some of the imaging techniques do suggest that gouty crystals [are] in the atherosclerotic plaque of gout patients,” Dr. Garshick added. Dr. Pillinger’s work, he said, “is showing us that there are different pathways to develop atherosclerosis.”
Dr. Pillinger disclosed relationships with Federation Bio, Fortress Biotech, Amgen, Scilex, Hikma Pharmaceuticals, LG Chem, and Olatec Therapeutics. Dr. Garshick disclosed relationships with Kiniksa Pharmaceuticals, Agepha Pharma, Bristol Myers Squibb, and Horizon Therapeutics.
A version of this article appeared on Medscape.com.
Serious Mental Illness Tied to Multiple Physical Illnesses
Serious mental illness (SMI), including bipolar disorder or schizophrenia spectrum disorders, is associated with a twofold increased risk for comorbid physical illness, results of a new meta-analysis showed.
“Although treatment of physical and mental health remains siloed in many health services globally, the high prevalence of physical multimorbidity attests to the urgent need for integrated care models that address both physical and mental health outcomes in people with severe mental illness,” the authors, led by Sean Halstead, MD, of The University of Queensland Medical School in Brisbane, Australia, wrote.
The findings were published online in The Lancet Psychiatry.
Shorter Lifespan?
SMI is associated with reduced life expectancy, and experts speculate that additional chronic illnesses — whether physical or psychiatric — may underlie this association.
While previous research has paired SMI with comorbid physical illnesses, the researchers noted that this study is the first to focus on both physical and psychiatric multimorbidity in individuals with SMI.
The investigators conducted a meta-analysis of 82 observational studies comprising 1.6 million individuals with SMI and 13.2 million control subjects to determine the risk for physical or psychiatric multimorbidity.
Studies were included if participants were diagnosed with either a schizophrenia spectrum disorder or bipolar disorder, and the study assessed either physical multimorbidity (at least two physical health conditions) or psychiatric multimorbidity (at least three psychiatric conditions), including the initial SMI.
Investigators found that individuals with SMI had more than a twofold increased risk for physical multimorbidity than those without SMI (odds ratio [OR], 2.40; 95% CI, 1.57-3.65; P = .0009).
Physical multimorbidity, which included cardiovascular, endocrine, neurological rental, gastrointestinal, musculoskeletal, and infectious disorders, was prevalent at similar rates in both schizophrenia spectrum disorder and bipolar disorder.
The ratio of physical multimorbidity was about four times higher in younger populations with SMI (mean age ≤ 40; OR, 3.99; 95% CI, 1.43-11.10) than in older populations (mean age > 40; OR, 1.55; 95% CI, 0.96-2.51; subgroup differences, P = .0013).
In terms of absolute prevalence, 25% of those with SMI had a physical multimorbidity, and 14% had a psychiatric multimorbidity, which were primarily anxiety and substance use disorders.
Investigators speculated that physical multimorbidity in SMI could stem from side effects of psychotropic medications, which are known to cause rapid cardiometabolic changes, including weight gain. In addition, lifestyle factors or nonmodifiable risk factors could also contribute to physical multimorbidity.
The study’s limitations included its small sample sizes for subgroup analyses and insufficient analysis for significant covariates, including smoking rates and symptom severity.
“While health services and treatment guidelines often operate on the assumption that individuals have a single principal diagnosis, these results attest to the clinical complexity many people with severe mental illness face in relation to burden of chronic disease,” the investigators wrote. They added that a greater understanding of the epidemiological manifestations of multimorbidity in SMI is “imperative.”
There was no source of funding for this study. Dr. Halstead is supported by the Australian Research Training Program scholarship. Other disclosures were noted in the original article.
A version of this article appeared on Medscape.com .
Serious mental illness (SMI), including bipolar disorder or schizophrenia spectrum disorders, is associated with a twofold increased risk for comorbid physical illness, results of a new meta-analysis showed.
“Although treatment of physical and mental health remains siloed in many health services globally, the high prevalence of physical multimorbidity attests to the urgent need for integrated care models that address both physical and mental health outcomes in people with severe mental illness,” the authors, led by Sean Halstead, MD, of The University of Queensland Medical School in Brisbane, Australia, wrote.
The findings were published online in The Lancet Psychiatry.
Shorter Lifespan?
SMI is associated with reduced life expectancy, and experts speculate that additional chronic illnesses — whether physical or psychiatric — may underlie this association.
While previous research has paired SMI with comorbid physical illnesses, the researchers noted that this study is the first to focus on both physical and psychiatric multimorbidity in individuals with SMI.
The investigators conducted a meta-analysis of 82 observational studies comprising 1.6 million individuals with SMI and 13.2 million control subjects to determine the risk for physical or psychiatric multimorbidity.
Studies were included if participants were diagnosed with either a schizophrenia spectrum disorder or bipolar disorder, and the study assessed either physical multimorbidity (at least two physical health conditions) or psychiatric multimorbidity (at least three psychiatric conditions), including the initial SMI.
Investigators found that individuals with SMI had more than a twofold increased risk for physical multimorbidity than those without SMI (odds ratio [OR], 2.40; 95% CI, 1.57-3.65; P = .0009).
Physical multimorbidity, which included cardiovascular, endocrine, neurological rental, gastrointestinal, musculoskeletal, and infectious disorders, was prevalent at similar rates in both schizophrenia spectrum disorder and bipolar disorder.
The ratio of physical multimorbidity was about four times higher in younger populations with SMI (mean age ≤ 40; OR, 3.99; 95% CI, 1.43-11.10) than in older populations (mean age > 40; OR, 1.55; 95% CI, 0.96-2.51; subgroup differences, P = .0013).
In terms of absolute prevalence, 25% of those with SMI had a physical multimorbidity, and 14% had a psychiatric multimorbidity, which were primarily anxiety and substance use disorders.
Investigators speculated that physical multimorbidity in SMI could stem from side effects of psychotropic medications, which are known to cause rapid cardiometabolic changes, including weight gain. In addition, lifestyle factors or nonmodifiable risk factors could also contribute to physical multimorbidity.
The study’s limitations included its small sample sizes for subgroup analyses and insufficient analysis for significant covariates, including smoking rates and symptom severity.
“While health services and treatment guidelines often operate on the assumption that individuals have a single principal diagnosis, these results attest to the clinical complexity many people with severe mental illness face in relation to burden of chronic disease,” the investigators wrote. They added that a greater understanding of the epidemiological manifestations of multimorbidity in SMI is “imperative.”
There was no source of funding for this study. Dr. Halstead is supported by the Australian Research Training Program scholarship. Other disclosures were noted in the original article.
A version of this article appeared on Medscape.com .
Serious mental illness (SMI), including bipolar disorder or schizophrenia spectrum disorders, is associated with a twofold increased risk for comorbid physical illness, results of a new meta-analysis showed.
“Although treatment of physical and mental health remains siloed in many health services globally, the high prevalence of physical multimorbidity attests to the urgent need for integrated care models that address both physical and mental health outcomes in people with severe mental illness,” the authors, led by Sean Halstead, MD, of The University of Queensland Medical School in Brisbane, Australia, wrote.
The findings were published online in The Lancet Psychiatry.
Shorter Lifespan?
SMI is associated with reduced life expectancy, and experts speculate that additional chronic illnesses — whether physical or psychiatric — may underlie this association.
While previous research has paired SMI with comorbid physical illnesses, the researchers noted that this study is the first to focus on both physical and psychiatric multimorbidity in individuals with SMI.
The investigators conducted a meta-analysis of 82 observational studies comprising 1.6 million individuals with SMI and 13.2 million control subjects to determine the risk for physical or psychiatric multimorbidity.
Studies were included if participants were diagnosed with either a schizophrenia spectrum disorder or bipolar disorder, and the study assessed either physical multimorbidity (at least two physical health conditions) or psychiatric multimorbidity (at least three psychiatric conditions), including the initial SMI.
Investigators found that individuals with SMI had more than a twofold increased risk for physical multimorbidity than those without SMI (odds ratio [OR], 2.40; 95% CI, 1.57-3.65; P = .0009).
Physical multimorbidity, which included cardiovascular, endocrine, neurological rental, gastrointestinal, musculoskeletal, and infectious disorders, was prevalent at similar rates in both schizophrenia spectrum disorder and bipolar disorder.
The ratio of physical multimorbidity was about four times higher in younger populations with SMI (mean age ≤ 40; OR, 3.99; 95% CI, 1.43-11.10) than in older populations (mean age > 40; OR, 1.55; 95% CI, 0.96-2.51; subgroup differences, P = .0013).
In terms of absolute prevalence, 25% of those with SMI had a physical multimorbidity, and 14% had a psychiatric multimorbidity, which were primarily anxiety and substance use disorders.
Investigators speculated that physical multimorbidity in SMI could stem from side effects of psychotropic medications, which are known to cause rapid cardiometabolic changes, including weight gain. In addition, lifestyle factors or nonmodifiable risk factors could also contribute to physical multimorbidity.
The study’s limitations included its small sample sizes for subgroup analyses and insufficient analysis for significant covariates, including smoking rates and symptom severity.
“While health services and treatment guidelines often operate on the assumption that individuals have a single principal diagnosis, these results attest to the clinical complexity many people with severe mental illness face in relation to burden of chronic disease,” the investigators wrote. They added that a greater understanding of the epidemiological manifestations of multimorbidity in SMI is “imperative.”
There was no source of funding for this study. Dr. Halstead is supported by the Australian Research Training Program scholarship. Other disclosures were noted in the original article.
A version of this article appeared on Medscape.com .
FROM THE LANCET PSYCHIATRY
Don’t Leave CVD Risk in RA Undertreated Despite Unresolved Questions
NEW YORK — Patients with rheumatoid arthritis (RA) carry a high risk for cardiovascular events, but mounting clinical evidence suggests they’re being undertreated to manage that risk. Rheumatologists should consider a patient with RA’s cardiovascular disease (CVD) status before deciding on RA treatments, a researcher of cardiometabolic disorders advised.
“The ORAL Surveillance trial suggests that we need to consider cardiovascular risk factors and maybe do additional screening in these patients before we use RA therapies,” Jon T. Giles, MD, PhD, director of the Cedars-Sinai Inflammatory Arthritis Clinical Center at Cedars-Sinai in Los Angeles, told attendees at the 4th Annual Cardiometabolic Risk in Inflammatory Conditions conference.
Underuse of Statins
ORAL Surveillance enrolled 4362 patients with RA aged 50 years and older with at least one cardiovascular risk factor. About 23% of all patients were taking statins, as were about half of patients with a history of atherosclerotic CVD (ASCVD).
“A lot of those people should have been on statins,” Dr. Giles said in an interview. “Not because of their RA but because of their risk factors, and then RA brings it up another notch.” In the population with ASCVD, Dr. Giles added, “It should have been more like 70% and 80%. If we’re talking about a disease that has enhanced cardiovascular risk, then the adoption of standard care that you would do for anybody in the general population should be at that standard and maybe above.”
Multiple studies have documented the underlying risk for CVD events, CV mortality, and subclinical atherosclerosis in people with RA, Dr. Giles noted in his presentation. Physiologically, the RA-specific risk factors most linked to CVD risk are systemic inflammation/cytokine excess and specific circulating T-cell and intermediate monocyte subsets, or both, Dr. Giles said.
Disease-Modifying Antirheumatic Drugs (DMARDs) and CVD Risk
Likewise, research in the past decade has linked methotrexate and tumor necrosis factor (TNF) inhibitors to reduced ASCVD events in RA. Another study showed that abatacept had an effect similar to that of etanercept in patients with RA, and the ENTRACTE trial, for which Dr. Giles was the lead author, demonstrated that tocilizumab matched etanercept in reducing CV events.
The ORAL Surveillance investigators also reported that patients with RA who were receiving the Janus kinase (JAK) inhibitor tofacitinib had a higher risk for major adverse cardiovascular events and cancers than those on TNF therapy, Dr. Giles noted. While statins in combination with JAK inhibitors may have the potential to provide a balance for controlling CV risk in patients with RA, he said later that the potential of JAK inhibitors in reducing CVD risk in RA “is still unsettled.”
The ongoing TARGET trial is further evaluating the impact of DMARDs on vascular inflammation in RA, said Dr. Giles, who’s also a trial principal investigator. TARGET is randomizing 115 patients with RA who didn’t respond to methotrexate to a TNF inhibitor or the addition of sulfasalazine and hydroxychloroquine to their methotrexate. Patients can be on low-intensity but not high-intensity statin therapy, Dr. Giles said.
TARGET results reported last year demonstrated an 8% decrease in arterial fluorodeoxyglucose (FDG) uptake on PET-CT in both treatment arms. Previous studies, Dr. Giles noted, have shown a potential link between FDG and histologic markers of inflammation. “An 8% decrease in vascular FDG is in line with what you would expect from statin treatment,” he said.
TARGET results published in April showed that a measure of a cluster of 12 cytokines and other inflammatory mediators, known as the multibiomarker disease activity (MBDA) score and marketed under the brand name Vectra DA, may help determine arterial FDG uptake. “Those who had a low MBDA score at week 24 actually had the greatest reduction in the arterial FDG,” he said.
Those results were driven entirely by low serum amyloid A (SAA) levels, Dr. Giles said. Those same results didn’t hold for patients in whom SAA and C-reactive protein were correlated.
“So, there’s more to come here,” Dr. Giles said. “We’re looking at other, much larger biomarker panels.”
Nonetheless, he said, sufficient evidence exists to conclude that treating RA to target reduces CV events. “The idea is that at every visit that you see an RA patient, you measure their disease activity, and if they’re not at the target of low disease activity or remission, then you change their therapy to improve that,” he said in an interview.
But an evidence-based guideline is needed to improve coverage of CVD risks in patients with RA, Dr. Giles said. “There is a movement afoot” for a guideline, he said. “If you just did what is supposed to happen for a general population, you would make some improvements. The risk-benefit [ratio] for statins for people with RA has been looked at, and it’s very favorable.”
Unanswered Questions
Dr. Giles noted that the ORAL Surveillance trial has left a number of questions unanswered about the role of JAK inhibitors in managing CVD risk in patients with RA. “The issue that we’re trying to ask is, is it just the TNF inhibitors may be better? Is this a subpopulation issue, or was it just bad luck from the purposes of this one trial? Granted, it was a very large trial, but you can still have luck in terms of getting an effect that’s not accurate.”
Dr. Giles’ “gut feeling” on JAK inhibitors is that they’re not causing harm, but that they’re not as effective as TNF inhibitors in ameliorating CV risks in patients with RA.
Michael S. Garshick, MD, who attended the conference and is head of the cardio-rheumatology program at NYU Langone Health, concurred that a number of unanswered questions persist over the treatment of CVD risk in RA — and autoimmune disease in general.
“I think we’re still trying to prove that DMARDs reduce cardiovascular risk in autoimmune conditions,” he said. “The epidemiologic data would suggest, yes, that inflammation prevention is beneficial for cardiovascular disease, but the TARGET trial suggested that vascular inflammation improved by treating RA, but that biologic therapy wasn’t better than traditional triple therapy.”
Other questions remain unanswered, Dr. Garshick said.
“Is there a specific immunotherapy that is most beneficial to reduce heart disease in patients with an autoimmune condition, whether it’s rheumatoid arthritis, psoriasis, or lupus?”
Dr. Garshick said he’s specifically interested in the residual risk that exists after treating the autoimmunity. “Do you still have a higher risk for heart disease, and if so, why? Is there something else going on that we can’t see?”
The biggest unanswered question, he said, is “How can we do a better job of recognizing heart disease risk in these patients? That’s the low-hanging fruit that people are studying, but across many of those studies, patients have higher rates of blood pressure, cholesterol issues, obesity, diabetes, and many times, we’re not adequately treating these comorbidities.”
That, Dr. Garshick said, may be a result of physician fatigue. “And so [treatment of these comorbidities is] kicked down the road for a year or years,” he added.
Dr. Giles disclosed financial relationships with Pfizer, AbbVie, Eli Lilly, and Novartis. Dr. Garshick disclosed relationships with Kiniksa Pharmaceuticals, Agepha Pharma, Bristol Myers Squibb, and Horizon Therapeutics.
A version of this article appeared on Medscape.com.
NEW YORK — Patients with rheumatoid arthritis (RA) carry a high risk for cardiovascular events, but mounting clinical evidence suggests they’re being undertreated to manage that risk. Rheumatologists should consider a patient with RA’s cardiovascular disease (CVD) status before deciding on RA treatments, a researcher of cardiometabolic disorders advised.
“The ORAL Surveillance trial suggests that we need to consider cardiovascular risk factors and maybe do additional screening in these patients before we use RA therapies,” Jon T. Giles, MD, PhD, director of the Cedars-Sinai Inflammatory Arthritis Clinical Center at Cedars-Sinai in Los Angeles, told attendees at the 4th Annual Cardiometabolic Risk in Inflammatory Conditions conference.
Underuse of Statins
ORAL Surveillance enrolled 4362 patients with RA aged 50 years and older with at least one cardiovascular risk factor. About 23% of all patients were taking statins, as were about half of patients with a history of atherosclerotic CVD (ASCVD).
“A lot of those people should have been on statins,” Dr. Giles said in an interview. “Not because of their RA but because of their risk factors, and then RA brings it up another notch.” In the population with ASCVD, Dr. Giles added, “It should have been more like 70% and 80%. If we’re talking about a disease that has enhanced cardiovascular risk, then the adoption of standard care that you would do for anybody in the general population should be at that standard and maybe above.”
Multiple studies have documented the underlying risk for CVD events, CV mortality, and subclinical atherosclerosis in people with RA, Dr. Giles noted in his presentation. Physiologically, the RA-specific risk factors most linked to CVD risk are systemic inflammation/cytokine excess and specific circulating T-cell and intermediate monocyte subsets, or both, Dr. Giles said.
Disease-Modifying Antirheumatic Drugs (DMARDs) and CVD Risk
Likewise, research in the past decade has linked methotrexate and tumor necrosis factor (TNF) inhibitors to reduced ASCVD events in RA. Another study showed that abatacept had an effect similar to that of etanercept in patients with RA, and the ENTRACTE trial, for which Dr. Giles was the lead author, demonstrated that tocilizumab matched etanercept in reducing CV events.
The ORAL Surveillance investigators also reported that patients with RA who were receiving the Janus kinase (JAK) inhibitor tofacitinib had a higher risk for major adverse cardiovascular events and cancers than those on TNF therapy, Dr. Giles noted. While statins in combination with JAK inhibitors may have the potential to provide a balance for controlling CV risk in patients with RA, he said later that the potential of JAK inhibitors in reducing CVD risk in RA “is still unsettled.”
The ongoing TARGET trial is further evaluating the impact of DMARDs on vascular inflammation in RA, said Dr. Giles, who’s also a trial principal investigator. TARGET is randomizing 115 patients with RA who didn’t respond to methotrexate to a TNF inhibitor or the addition of sulfasalazine and hydroxychloroquine to their methotrexate. Patients can be on low-intensity but not high-intensity statin therapy, Dr. Giles said.
TARGET results reported last year demonstrated an 8% decrease in arterial fluorodeoxyglucose (FDG) uptake on PET-CT in both treatment arms. Previous studies, Dr. Giles noted, have shown a potential link between FDG and histologic markers of inflammation. “An 8% decrease in vascular FDG is in line with what you would expect from statin treatment,” he said.
TARGET results published in April showed that a measure of a cluster of 12 cytokines and other inflammatory mediators, known as the multibiomarker disease activity (MBDA) score and marketed under the brand name Vectra DA, may help determine arterial FDG uptake. “Those who had a low MBDA score at week 24 actually had the greatest reduction in the arterial FDG,” he said.
Those results were driven entirely by low serum amyloid A (SAA) levels, Dr. Giles said. Those same results didn’t hold for patients in whom SAA and C-reactive protein were correlated.
“So, there’s more to come here,” Dr. Giles said. “We’re looking at other, much larger biomarker panels.”
Nonetheless, he said, sufficient evidence exists to conclude that treating RA to target reduces CV events. “The idea is that at every visit that you see an RA patient, you measure their disease activity, and if they’re not at the target of low disease activity or remission, then you change their therapy to improve that,” he said in an interview.
But an evidence-based guideline is needed to improve coverage of CVD risks in patients with RA, Dr. Giles said. “There is a movement afoot” for a guideline, he said. “If you just did what is supposed to happen for a general population, you would make some improvements. The risk-benefit [ratio] for statins for people with RA has been looked at, and it’s very favorable.”
Unanswered Questions
Dr. Giles noted that the ORAL Surveillance trial has left a number of questions unanswered about the role of JAK inhibitors in managing CVD risk in patients with RA. “The issue that we’re trying to ask is, is it just the TNF inhibitors may be better? Is this a subpopulation issue, or was it just bad luck from the purposes of this one trial? Granted, it was a very large trial, but you can still have luck in terms of getting an effect that’s not accurate.”
Dr. Giles’ “gut feeling” on JAK inhibitors is that they’re not causing harm, but that they’re not as effective as TNF inhibitors in ameliorating CV risks in patients with RA.
Michael S. Garshick, MD, who attended the conference and is head of the cardio-rheumatology program at NYU Langone Health, concurred that a number of unanswered questions persist over the treatment of CVD risk in RA — and autoimmune disease in general.
“I think we’re still trying to prove that DMARDs reduce cardiovascular risk in autoimmune conditions,” he said. “The epidemiologic data would suggest, yes, that inflammation prevention is beneficial for cardiovascular disease, but the TARGET trial suggested that vascular inflammation improved by treating RA, but that biologic therapy wasn’t better than traditional triple therapy.”
Other questions remain unanswered, Dr. Garshick said.
“Is there a specific immunotherapy that is most beneficial to reduce heart disease in patients with an autoimmune condition, whether it’s rheumatoid arthritis, psoriasis, or lupus?”
Dr. Garshick said he’s specifically interested in the residual risk that exists after treating the autoimmunity. “Do you still have a higher risk for heart disease, and if so, why? Is there something else going on that we can’t see?”
The biggest unanswered question, he said, is “How can we do a better job of recognizing heart disease risk in these patients? That’s the low-hanging fruit that people are studying, but across many of those studies, patients have higher rates of blood pressure, cholesterol issues, obesity, diabetes, and many times, we’re not adequately treating these comorbidities.”
That, Dr. Garshick said, may be a result of physician fatigue. “And so [treatment of these comorbidities is] kicked down the road for a year or years,” he added.
Dr. Giles disclosed financial relationships with Pfizer, AbbVie, Eli Lilly, and Novartis. Dr. Garshick disclosed relationships with Kiniksa Pharmaceuticals, Agepha Pharma, Bristol Myers Squibb, and Horizon Therapeutics.
A version of this article appeared on Medscape.com.
NEW YORK — Patients with rheumatoid arthritis (RA) carry a high risk for cardiovascular events, but mounting clinical evidence suggests they’re being undertreated to manage that risk. Rheumatologists should consider a patient with RA’s cardiovascular disease (CVD) status before deciding on RA treatments, a researcher of cardiometabolic disorders advised.
“The ORAL Surveillance trial suggests that we need to consider cardiovascular risk factors and maybe do additional screening in these patients before we use RA therapies,” Jon T. Giles, MD, PhD, director of the Cedars-Sinai Inflammatory Arthritis Clinical Center at Cedars-Sinai in Los Angeles, told attendees at the 4th Annual Cardiometabolic Risk in Inflammatory Conditions conference.
Underuse of Statins
ORAL Surveillance enrolled 4362 patients with RA aged 50 years and older with at least one cardiovascular risk factor. About 23% of all patients were taking statins, as were about half of patients with a history of atherosclerotic CVD (ASCVD).
“A lot of those people should have been on statins,” Dr. Giles said in an interview. “Not because of their RA but because of their risk factors, and then RA brings it up another notch.” In the population with ASCVD, Dr. Giles added, “It should have been more like 70% and 80%. If we’re talking about a disease that has enhanced cardiovascular risk, then the adoption of standard care that you would do for anybody in the general population should be at that standard and maybe above.”
Multiple studies have documented the underlying risk for CVD events, CV mortality, and subclinical atherosclerosis in people with RA, Dr. Giles noted in his presentation. Physiologically, the RA-specific risk factors most linked to CVD risk are systemic inflammation/cytokine excess and specific circulating T-cell and intermediate monocyte subsets, or both, Dr. Giles said.
Disease-Modifying Antirheumatic Drugs (DMARDs) and CVD Risk
Likewise, research in the past decade has linked methotrexate and tumor necrosis factor (TNF) inhibitors to reduced ASCVD events in RA. Another study showed that abatacept had an effect similar to that of etanercept in patients with RA, and the ENTRACTE trial, for which Dr. Giles was the lead author, demonstrated that tocilizumab matched etanercept in reducing CV events.
The ORAL Surveillance investigators also reported that patients with RA who were receiving the Janus kinase (JAK) inhibitor tofacitinib had a higher risk for major adverse cardiovascular events and cancers than those on TNF therapy, Dr. Giles noted. While statins in combination with JAK inhibitors may have the potential to provide a balance for controlling CV risk in patients with RA, he said later that the potential of JAK inhibitors in reducing CVD risk in RA “is still unsettled.”
The ongoing TARGET trial is further evaluating the impact of DMARDs on vascular inflammation in RA, said Dr. Giles, who’s also a trial principal investigator. TARGET is randomizing 115 patients with RA who didn’t respond to methotrexate to a TNF inhibitor or the addition of sulfasalazine and hydroxychloroquine to their methotrexate. Patients can be on low-intensity but not high-intensity statin therapy, Dr. Giles said.
TARGET results reported last year demonstrated an 8% decrease in arterial fluorodeoxyglucose (FDG) uptake on PET-CT in both treatment arms. Previous studies, Dr. Giles noted, have shown a potential link between FDG and histologic markers of inflammation. “An 8% decrease in vascular FDG is in line with what you would expect from statin treatment,” he said.
TARGET results published in April showed that a measure of a cluster of 12 cytokines and other inflammatory mediators, known as the multibiomarker disease activity (MBDA) score and marketed under the brand name Vectra DA, may help determine arterial FDG uptake. “Those who had a low MBDA score at week 24 actually had the greatest reduction in the arterial FDG,” he said.
Those results were driven entirely by low serum amyloid A (SAA) levels, Dr. Giles said. Those same results didn’t hold for patients in whom SAA and C-reactive protein were correlated.
“So, there’s more to come here,” Dr. Giles said. “We’re looking at other, much larger biomarker panels.”
Nonetheless, he said, sufficient evidence exists to conclude that treating RA to target reduces CV events. “The idea is that at every visit that you see an RA patient, you measure their disease activity, and if they’re not at the target of low disease activity or remission, then you change their therapy to improve that,” he said in an interview.
But an evidence-based guideline is needed to improve coverage of CVD risks in patients with RA, Dr. Giles said. “There is a movement afoot” for a guideline, he said. “If you just did what is supposed to happen for a general population, you would make some improvements. The risk-benefit [ratio] for statins for people with RA has been looked at, and it’s very favorable.”
Unanswered Questions
Dr. Giles noted that the ORAL Surveillance trial has left a number of questions unanswered about the role of JAK inhibitors in managing CVD risk in patients with RA. “The issue that we’re trying to ask is, is it just the TNF inhibitors may be better? Is this a subpopulation issue, or was it just bad luck from the purposes of this one trial? Granted, it was a very large trial, but you can still have luck in terms of getting an effect that’s not accurate.”
Dr. Giles’ “gut feeling” on JAK inhibitors is that they’re not causing harm, but that they’re not as effective as TNF inhibitors in ameliorating CV risks in patients with RA.
Michael S. Garshick, MD, who attended the conference and is head of the cardio-rheumatology program at NYU Langone Health, concurred that a number of unanswered questions persist over the treatment of CVD risk in RA — and autoimmune disease in general.
“I think we’re still trying to prove that DMARDs reduce cardiovascular risk in autoimmune conditions,” he said. “The epidemiologic data would suggest, yes, that inflammation prevention is beneficial for cardiovascular disease, but the TARGET trial suggested that vascular inflammation improved by treating RA, but that biologic therapy wasn’t better than traditional triple therapy.”
Other questions remain unanswered, Dr. Garshick said.
“Is there a specific immunotherapy that is most beneficial to reduce heart disease in patients with an autoimmune condition, whether it’s rheumatoid arthritis, psoriasis, or lupus?”
Dr. Garshick said he’s specifically interested in the residual risk that exists after treating the autoimmunity. “Do you still have a higher risk for heart disease, and if so, why? Is there something else going on that we can’t see?”
The biggest unanswered question, he said, is “How can we do a better job of recognizing heart disease risk in these patients? That’s the low-hanging fruit that people are studying, but across many of those studies, patients have higher rates of blood pressure, cholesterol issues, obesity, diabetes, and many times, we’re not adequately treating these comorbidities.”
That, Dr. Garshick said, may be a result of physician fatigue. “And so [treatment of these comorbidities is] kicked down the road for a year or years,” he added.
Dr. Giles disclosed financial relationships with Pfizer, AbbVie, Eli Lilly, and Novartis. Dr. Garshick disclosed relationships with Kiniksa Pharmaceuticals, Agepha Pharma, Bristol Myers Squibb, and Horizon Therapeutics.
A version of this article appeared on Medscape.com.
CPAP Underperforms: The Sequel
A few months ago, I posted a column on continuous positive airway pressure (CPAP) with the title, “CPAP Oversells and Underperforms.” To date, it has 299 likes and 90 comments, which are almost all negative. I’m glad to see that it’s generated interest, and I’d like to address some of the themes expressed in the posts.
Most comments were personal testimonies to the miracles of CPAP. These are important, and the point deserves emphasis. CPAP can provide significant improvements in daytime sleepiness and quality of life. I closed the original piece by acknowledging this important fact. Readers can be forgiven for missing it given that the title and text were otherwise disparaging of CPAP.
But several comments warrant a more in-depth discussion. The original piece focuses on CPAP and cardiovascular (CV) outcomes but made no mention of atrial fibrillation (AF) or ejection fraction (EF). The effects of CPAP on each are touted by cardiologists and PAP-pushers alike and are drivers of frequent referrals. It›s my fault for omitting them from the discussion.
AF is easy. The data is identical to all other things CPAP and CV. Based on biologic plausibility alone, the likelihood of a relationship between AF and obstructive sleep apnea (OSA) is similar to the odds that the Celtics raise an 18th banner come June. There’s hypoxia, intrathoracic pressure swings, sympathetic surges, and sleep state disruptions. It’s easy to get from there to arrhythmogenesis. There’s lots of observational noise, too, but no randomized proof that CPAP alters this relationship.
I found four randomized controlled trials (RCTs) that tested CPAP’s effect on AF. I’ll save you the suspense; they were all negative. One even found a signal for more adverse events in the CPAP group. These studies have several positive qualities: They enrolled patients with moderate to severe sleep apnea and high oxygen desaturation indices, adherence averaged more than 4 hours across all groups in all trials, and the methods for assessing the AF outcomes differed slightly. There’s also a lot not to like: The sample sizes were small, only one trial enrolled “sleepy” patients (as assessed by the Epworth Sleepiness Score), and follow-up was short.
To paraphrase Carl Sagan, “absence of evidence does not equal evidence of absence.” As a statistician would say, type II error cannot be excluded by these RCTs. In medicine, however, the burden of proof falls on demonstrating efficacy. If we treat before concluding that a therapy works, we risk wasting time, money, medical resources, and the most precious of patient commodities: the energy required for behavior change. In their response to letters to the editor, the authors of the third RCT summarize the CPAP, AF, and CV disease data far better than I ever could. They sound the same words of caution and come out against screening patients with AF for OSA.
The story for CPAP’s effects on EF is similar though muddier. The American College of Cardiology (ACC)/American Heart Association (AHA) guidelines for heart failure cite a meta-analysis showing that CPAP improves left ventricular EF. In 2019, the American Academy of Sleep Medicine (AASM) CPAP guidelines included a systematic review and meta-analysis that found that CPAP has no effect on left ventricular EF in patients with or without heart failure.
There are a million reasons why two systematic reviews on the same topic might come to different conclusions. In this case, the included studies only partially overlap, and broadly speaking, it appears the authors made trade-offs. The review cited by the ACC/AHA had broader inclusion and significantly more patients and paid for it in heterogeneity (I2 in the 80%-90% range). The AASM analysis achieved 0% heterogeneity but limited inclusion to fewer than 100 patients. Across both, the improvement in EF was 2%- 5% at a minimally clinically important difference of 4%. Hardly convincing.
In summary, the road to negative trials and patient harm has always been paved with observational signal and biologic plausibility. Throw in some intellectual and academic bias, and you’ve created the perfect storm of therapeutic overconfidence.
Dr. Holley is a professor in the department of medicine, Uniformed Services University, Bethesda, Maryland, and a physician at Pulmonary/Sleep and Critical Care Medicine, MedStar Washington Hospital Center, Washington. He disclosed ties to Metapharm Inc., CHEST College, and WebMD.
A version of this article appeared on Medscape.com .
A few months ago, I posted a column on continuous positive airway pressure (CPAP) with the title, “CPAP Oversells and Underperforms.” To date, it has 299 likes and 90 comments, which are almost all negative. I’m glad to see that it’s generated interest, and I’d like to address some of the themes expressed in the posts.
Most comments were personal testimonies to the miracles of CPAP. These are important, and the point deserves emphasis. CPAP can provide significant improvements in daytime sleepiness and quality of life. I closed the original piece by acknowledging this important fact. Readers can be forgiven for missing it given that the title and text were otherwise disparaging of CPAP.
But several comments warrant a more in-depth discussion. The original piece focuses on CPAP and cardiovascular (CV) outcomes but made no mention of atrial fibrillation (AF) or ejection fraction (EF). The effects of CPAP on each are touted by cardiologists and PAP-pushers alike and are drivers of frequent referrals. It›s my fault for omitting them from the discussion.
AF is easy. The data is identical to all other things CPAP and CV. Based on biologic plausibility alone, the likelihood of a relationship between AF and obstructive sleep apnea (OSA) is similar to the odds that the Celtics raise an 18th banner come June. There’s hypoxia, intrathoracic pressure swings, sympathetic surges, and sleep state disruptions. It’s easy to get from there to arrhythmogenesis. There’s lots of observational noise, too, but no randomized proof that CPAP alters this relationship.
I found four randomized controlled trials (RCTs) that tested CPAP’s effect on AF. I’ll save you the suspense; they were all negative. One even found a signal for more adverse events in the CPAP group. These studies have several positive qualities: They enrolled patients with moderate to severe sleep apnea and high oxygen desaturation indices, adherence averaged more than 4 hours across all groups in all trials, and the methods for assessing the AF outcomes differed slightly. There’s also a lot not to like: The sample sizes were small, only one trial enrolled “sleepy” patients (as assessed by the Epworth Sleepiness Score), and follow-up was short.
To paraphrase Carl Sagan, “absence of evidence does not equal evidence of absence.” As a statistician would say, type II error cannot be excluded by these RCTs. In medicine, however, the burden of proof falls on demonstrating efficacy. If we treat before concluding that a therapy works, we risk wasting time, money, medical resources, and the most precious of patient commodities: the energy required for behavior change. In their response to letters to the editor, the authors of the third RCT summarize the CPAP, AF, and CV disease data far better than I ever could. They sound the same words of caution and come out against screening patients with AF for OSA.
The story for CPAP’s effects on EF is similar though muddier. The American College of Cardiology (ACC)/American Heart Association (AHA) guidelines for heart failure cite a meta-analysis showing that CPAP improves left ventricular EF. In 2019, the American Academy of Sleep Medicine (AASM) CPAP guidelines included a systematic review and meta-analysis that found that CPAP has no effect on left ventricular EF in patients with or without heart failure.
There are a million reasons why two systematic reviews on the same topic might come to different conclusions. In this case, the included studies only partially overlap, and broadly speaking, it appears the authors made trade-offs. The review cited by the ACC/AHA had broader inclusion and significantly more patients and paid for it in heterogeneity (I2 in the 80%-90% range). The AASM analysis achieved 0% heterogeneity but limited inclusion to fewer than 100 patients. Across both, the improvement in EF was 2%- 5% at a minimally clinically important difference of 4%. Hardly convincing.
In summary, the road to negative trials and patient harm has always been paved with observational signal and biologic plausibility. Throw in some intellectual and academic bias, and you’ve created the perfect storm of therapeutic overconfidence.
Dr. Holley is a professor in the department of medicine, Uniformed Services University, Bethesda, Maryland, and a physician at Pulmonary/Sleep and Critical Care Medicine, MedStar Washington Hospital Center, Washington. He disclosed ties to Metapharm Inc., CHEST College, and WebMD.
A version of this article appeared on Medscape.com .
A few months ago, I posted a column on continuous positive airway pressure (CPAP) with the title, “CPAP Oversells and Underperforms.” To date, it has 299 likes and 90 comments, which are almost all negative. I’m glad to see that it’s generated interest, and I’d like to address some of the themes expressed in the posts.
Most comments were personal testimonies to the miracles of CPAP. These are important, and the point deserves emphasis. CPAP can provide significant improvements in daytime sleepiness and quality of life. I closed the original piece by acknowledging this important fact. Readers can be forgiven for missing it given that the title and text were otherwise disparaging of CPAP.
But several comments warrant a more in-depth discussion. The original piece focuses on CPAP and cardiovascular (CV) outcomes but made no mention of atrial fibrillation (AF) or ejection fraction (EF). The effects of CPAP on each are touted by cardiologists and PAP-pushers alike and are drivers of frequent referrals. It›s my fault for omitting them from the discussion.
AF is easy. The data is identical to all other things CPAP and CV. Based on biologic plausibility alone, the likelihood of a relationship between AF and obstructive sleep apnea (OSA) is similar to the odds that the Celtics raise an 18th banner come June. There’s hypoxia, intrathoracic pressure swings, sympathetic surges, and sleep state disruptions. It’s easy to get from there to arrhythmogenesis. There’s lots of observational noise, too, but no randomized proof that CPAP alters this relationship.
I found four randomized controlled trials (RCTs) that tested CPAP’s effect on AF. I’ll save you the suspense; they were all negative. One even found a signal for more adverse events in the CPAP group. These studies have several positive qualities: They enrolled patients with moderate to severe sleep apnea and high oxygen desaturation indices, adherence averaged more than 4 hours across all groups in all trials, and the methods for assessing the AF outcomes differed slightly. There’s also a lot not to like: The sample sizes were small, only one trial enrolled “sleepy” patients (as assessed by the Epworth Sleepiness Score), and follow-up was short.
To paraphrase Carl Sagan, “absence of evidence does not equal evidence of absence.” As a statistician would say, type II error cannot be excluded by these RCTs. In medicine, however, the burden of proof falls on demonstrating efficacy. If we treat before concluding that a therapy works, we risk wasting time, money, medical resources, and the most precious of patient commodities: the energy required for behavior change. In their response to letters to the editor, the authors of the third RCT summarize the CPAP, AF, and CV disease data far better than I ever could. They sound the same words of caution and come out against screening patients with AF for OSA.
The story for CPAP’s effects on EF is similar though muddier. The American College of Cardiology (ACC)/American Heart Association (AHA) guidelines for heart failure cite a meta-analysis showing that CPAP improves left ventricular EF. In 2019, the American Academy of Sleep Medicine (AASM) CPAP guidelines included a systematic review and meta-analysis that found that CPAP has no effect on left ventricular EF in patients with or without heart failure.
There are a million reasons why two systematic reviews on the same topic might come to different conclusions. In this case, the included studies only partially overlap, and broadly speaking, it appears the authors made trade-offs. The review cited by the ACC/AHA had broader inclusion and significantly more patients and paid for it in heterogeneity (I2 in the 80%-90% range). The AASM analysis achieved 0% heterogeneity but limited inclusion to fewer than 100 patients. Across both, the improvement in EF was 2%- 5% at a minimally clinically important difference of 4%. Hardly convincing.
In summary, the road to negative trials and patient harm has always been paved with observational signal and biologic plausibility. Throw in some intellectual and academic bias, and you’ve created the perfect storm of therapeutic overconfidence.
Dr. Holley is a professor in the department of medicine, Uniformed Services University, Bethesda, Maryland, and a physician at Pulmonary/Sleep and Critical Care Medicine, MedStar Washington Hospital Center, Washington. He disclosed ties to Metapharm Inc., CHEST College, and WebMD.
A version of this article appeared on Medscape.com .
Why Cardiac Biomarkers Don’t Help Predict Heart Disease
This transcript has been edited for clarity.
It’s the counterintuitive stuff in epidemiology that always really interests me. One intuition many of us have is that if a risk factor is significantly associated with an outcome, knowledge of that risk factor would help to predict that outcome. Makes sense. Feels right.
But it’s not right. Not always.
Here’s a fake example to illustrate my point. Let’s say we have 10,000 individuals who we follow for 10 years and 2000 of them die. (It’s been a rough decade.) At baseline, I measured a novel biomarker, the Perry Factor, in everyone. To keep it simple, the Perry Factor has only two values: 0 or 1.
I then do a standard associational analysis and find that individuals who are positive for the Perry Factor have a 40-fold higher odds of death than those who are negative for it. I am beginning to reconsider ascribing my good name to this biomarker. This is a highly statistically significant result — a P value <.001.
Clearly, knowledge of the Perry Factor should help me predict who will die in the cohort. I evaluate predictive power using a metric called the area under the receiver operating characteristic curve (AUC, referred to as the C-statistic in time-to-event studies). It tells you, given two people — one who dies and one who doesn’t — how frequently you “pick” the right person, given the knowledge of their Perry Factor.
A C-statistic of 0.5, or 50%, would mean the Perry Factor gives you no better results than a coin flip; it’s chance. A C-statistic of 1 is perfect prediction. So, what will the C-statistic be, given the incredibly strong association of the Perry Factor with outcomes? 0.9? 0.95?
0.5024. Almost useless.

Let’s figure out why strength of association and usefulness for prediction are not always the same thing.
I constructed my fake Perry Factor dataset quite carefully to illustrate this point. Let me show you what happened. What you see here is a breakdown of the patients in my fake study. You can see that just 11 of them were Perry Factor positive, but 10 of those 11 ended up dying.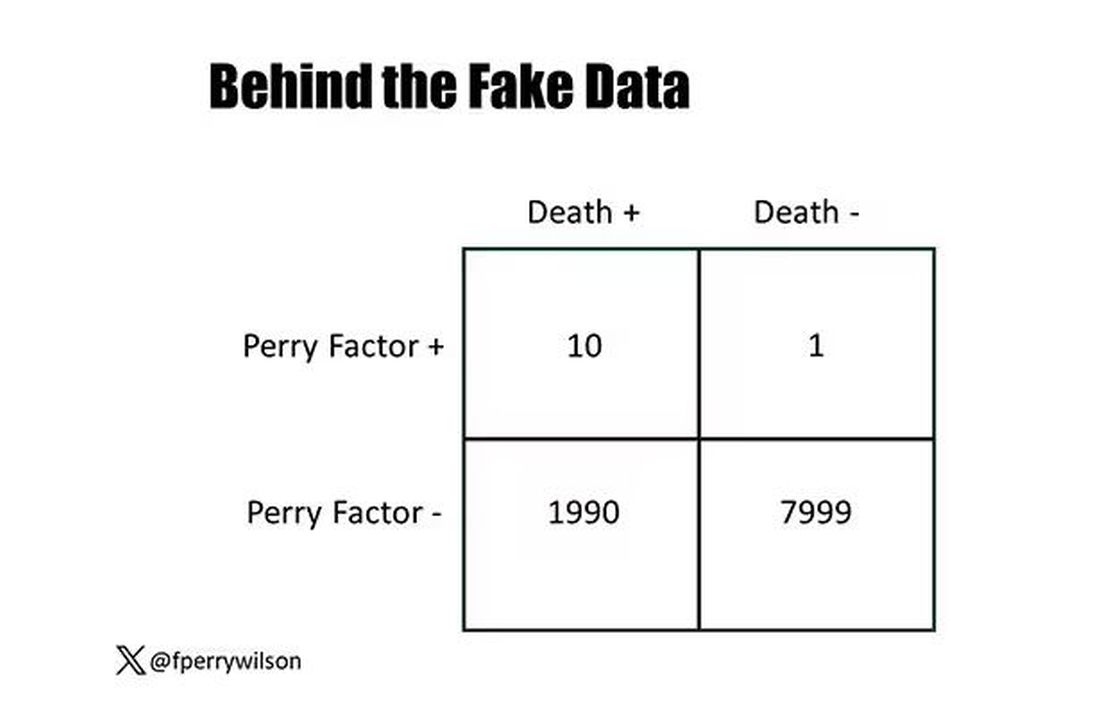
That’s quite unlikely by chance alone. It really does appear that if you have Perry Factor, your risk for death is much higher. But the reason that Perry Factor is a bad predictor is because it is so rare in the population. Sure, you can use it to correctly predict the outcome of 10 of the 11 people who have it, but the vast majority of people don’t have Perry Factor. It’s useless to distinguish who will die vs who will live in that population.
Why have I spent so much time trying to reverse our intuition that strength of association and strength of predictive power must be related? Because it helps to explain this paper, “Prognostic Value of Cardiovascular Biomarkers in the Population,” appearing in JAMA, which is a very nice piece of work trying to help us better predict cardiovascular disease.
I don’t need to tell you that cardiovascular disease is the number-one killer in this country and most of the world. I don’t need to tell you that we have really good preventive therapies and lifestyle interventions that can reduce the risk. But it would be nice to know in whom, specifically, we should use those interventions.
Cardiovascular risk scores, to date, are pretty simple. The most common one in use in the United States, the pooled cohort risk equation, has nine variables, two of which require a cholesterol panel and one a blood pressure test. It’s easy and it’s pretty accurate.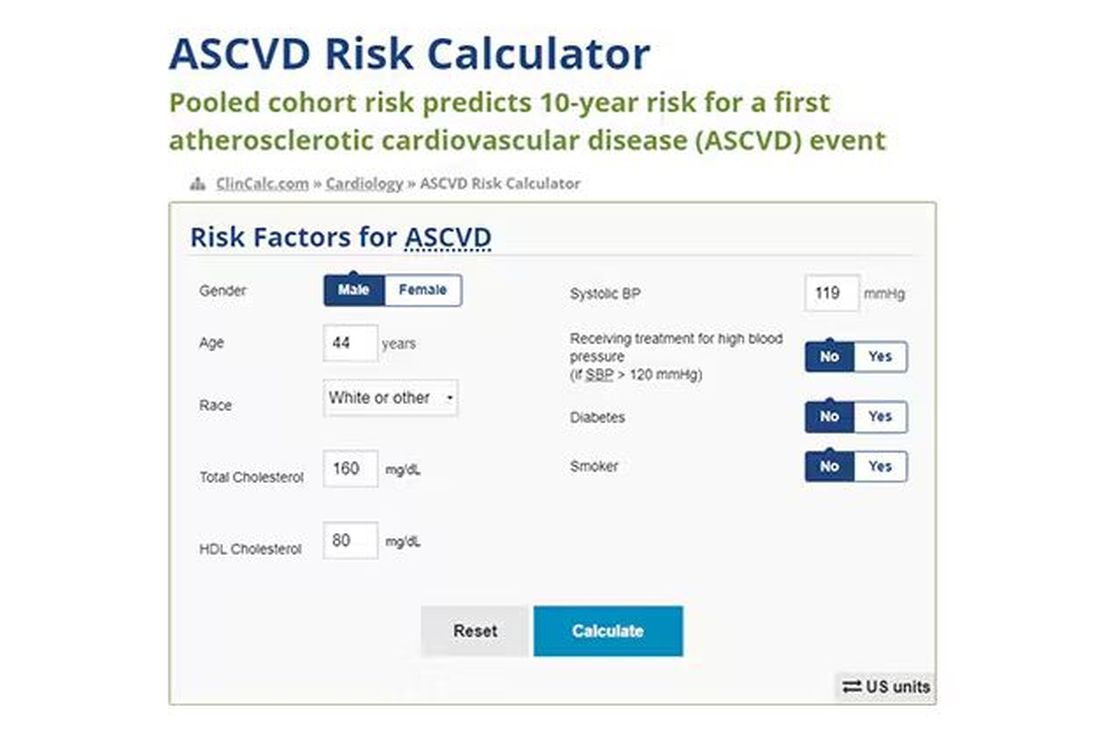
Using the score from the pooled cohort risk calculator, you get a C-statistic as high as 0.82 when applied to Black women, a low of 0.71 when applied to Black men. Non-Black individuals are in the middle. Not bad. But, clearly, not perfect.
And aren’t we in the era of big data, the era of personalized medicine? We have dozens, maybe hundreds, of quantifiable biomarkers that are associated with subsequent heart disease. Surely, by adding these biomarkers into the risk equation, we can improve prediction. Right?
The JAMA study includes 164,054 patients pooled from 28 cohort studies from 12 countries. All the studies measured various key biomarkers at baseline and followed their participants for cardiovascular events like heart attack, stroke, coronary revascularization, and so on.
The biomarkers in question are really the big guns in this space: troponin, a marker of stress on the heart muscle; NT-proBNP, a marker of stretch on the heart muscle; and C-reactive protein, a marker of inflammation. In every case, higher levels of these markers at baseline were associated with a higher risk for cardiovascular disease in the future.
Troponin T, shown here, has a basically linear risk with subsequent cardiovascular disease.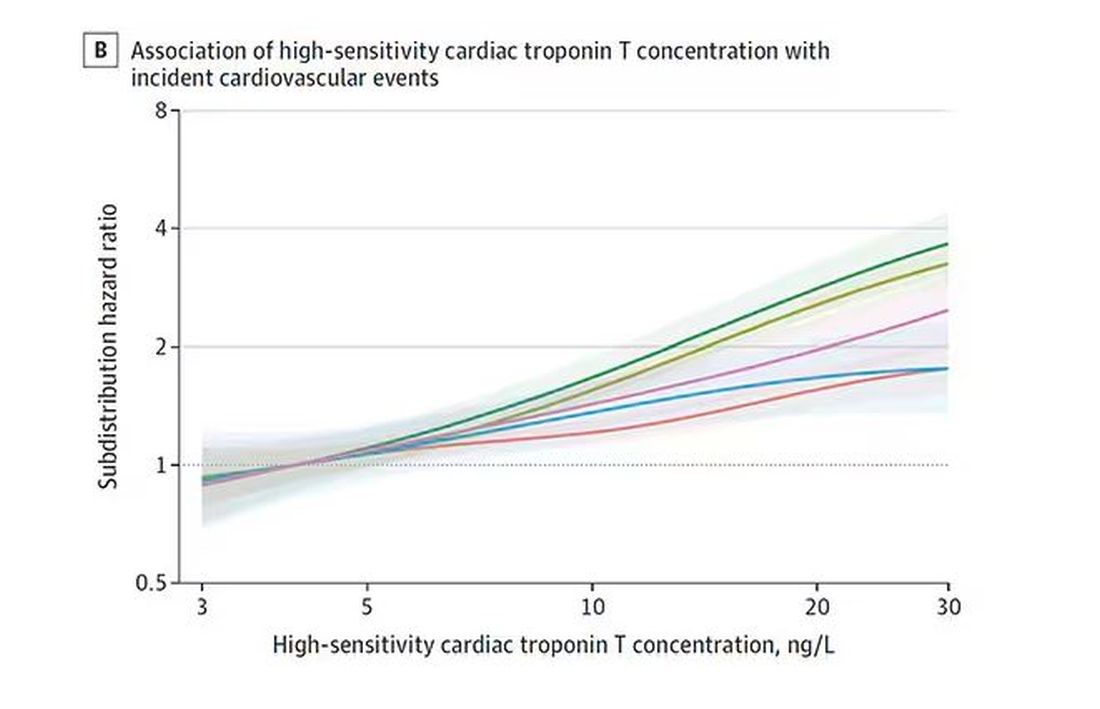
BNP seems to demonstrate more of a threshold effect, where levels above 60 start to associate with problems.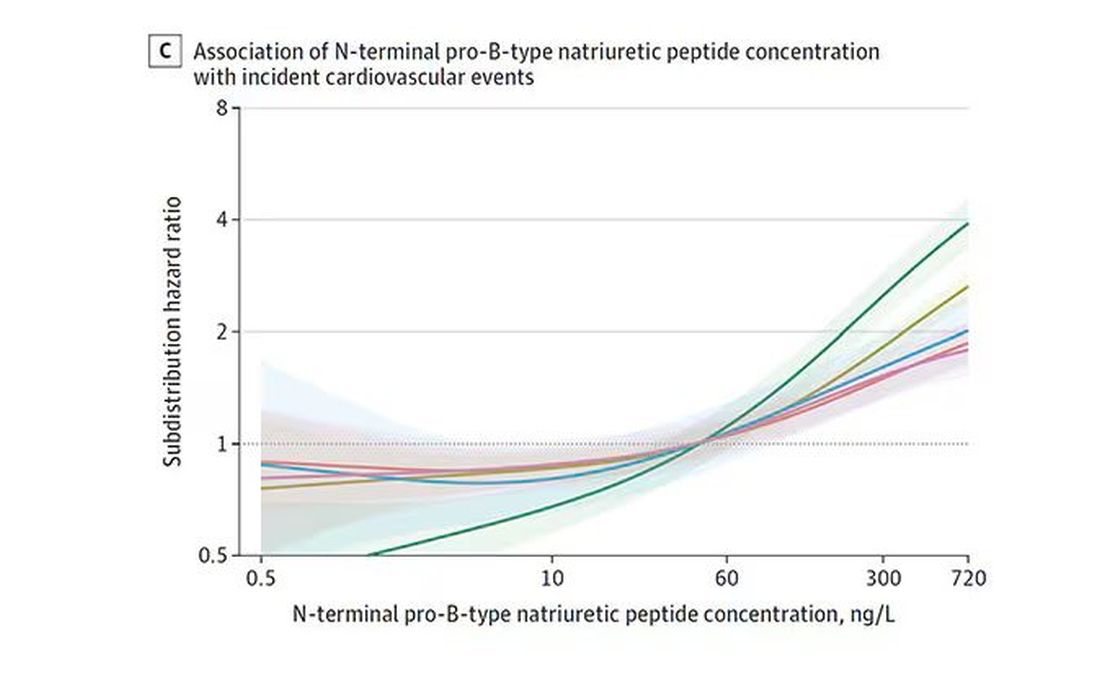
And CRP does a similar thing, with levels above 1.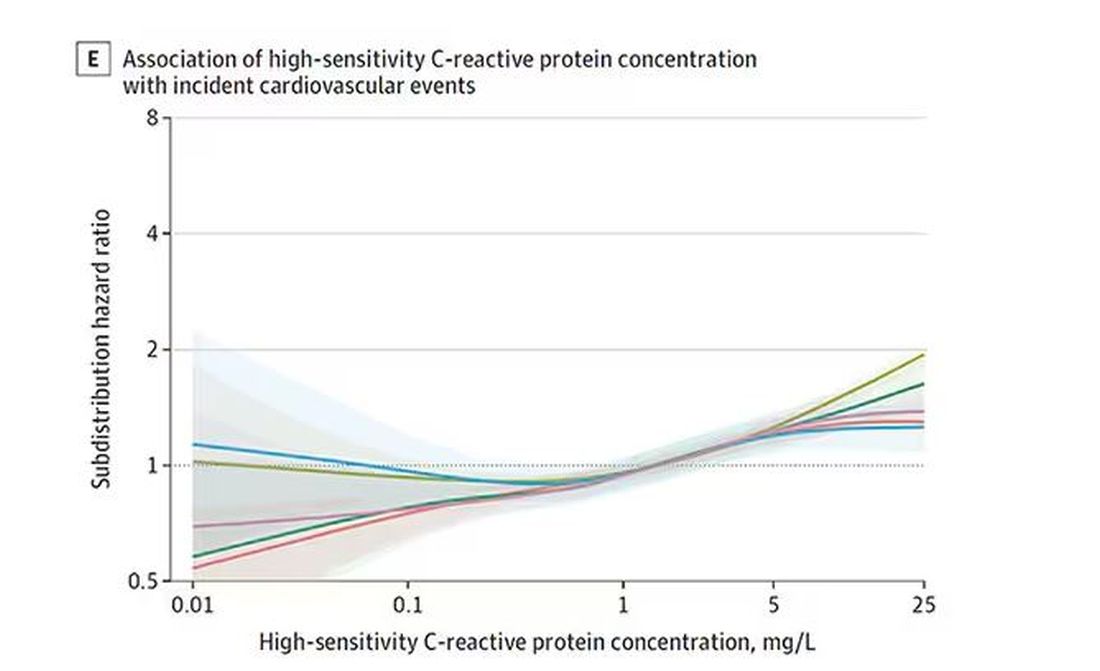
All of these findings were statistically significant. If you have higher levels of one or more of these biomarkers, you are more likely to have cardiovascular disease in the future.
Of course, our old friend the pooled cohort risk equation is still here — in the background — requiring just that one blood test and measurement of blood pressure. Let’s talk about predictive power.
The pooled cohort risk equation score, in this study, had a C-statistic of 0.812.
By adding troponin, BNP, and CRP to the equation, the new C-statistic is 0.819. Barely any change.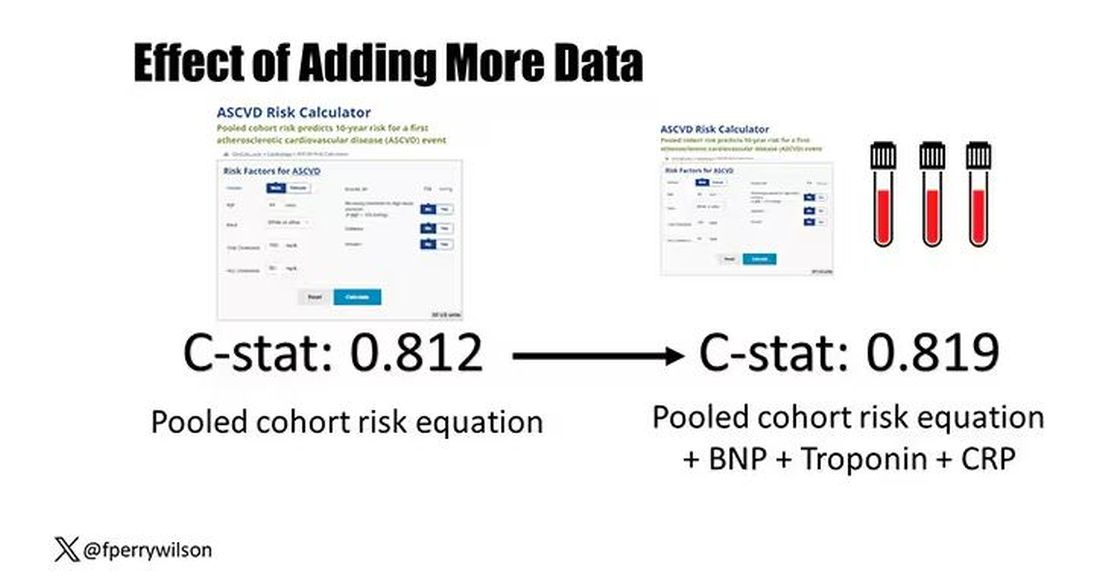
Now, the authors looked at different types of prediction here. The greatest improvement in the AUC was seen when they tried to predict heart failure within 1 year of measurement; there the AUC improved by 0.04. But the presence of BNP as a biomarker and the short time window of 1 year makes me wonder whether this is really prediction at all or whether they were essentially just diagnosing people with existing heart failure.
Why does this happen? Why do these promising biomarkers, clearly associated with bad outcomes, fail to improve our ability to predict the future? I already gave one example, which has to do with how the markers are distributed in the population. But even more relevant here is that the new markers will only improve prediction insofar as they are not already represented in the old predictive model.
Of course, BNP, for example, wasn’t in the old model. But smoking was. Diabetes was. Blood pressure was. All of that data might actually tell you something about the patient’s BNP through their mutual correlation. And improvement in prediction requires new information.
This is actually why I consider this a really successful study. We need to do studies like this to help us find what those new sources of information might be.
We will never get to a C-statistic of 1. Perfect prediction is the domain of palm readers and astrophysicists. But better prediction is always possible through data. The big question, of course, is which data?
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
It’s the counterintuitive stuff in epidemiology that always really interests me. One intuition many of us have is that if a risk factor is significantly associated with an outcome, knowledge of that risk factor would help to predict that outcome. Makes sense. Feels right.
But it’s not right. Not always.
Here’s a fake example to illustrate my point. Let’s say we have 10,000 individuals who we follow for 10 years and 2000 of them die. (It’s been a rough decade.) At baseline, I measured a novel biomarker, the Perry Factor, in everyone. To keep it simple, the Perry Factor has only two values: 0 or 1.
I then do a standard associational analysis and find that individuals who are positive for the Perry Factor have a 40-fold higher odds of death than those who are negative for it. I am beginning to reconsider ascribing my good name to this biomarker. This is a highly statistically significant result — a P value <.001.
Clearly, knowledge of the Perry Factor should help me predict who will die in the cohort. I evaluate predictive power using a metric called the area under the receiver operating characteristic curve (AUC, referred to as the C-statistic in time-to-event studies). It tells you, given two people — one who dies and one who doesn’t — how frequently you “pick” the right person, given the knowledge of their Perry Factor.
A C-statistic of 0.5, or 50%, would mean the Perry Factor gives you no better results than a coin flip; it’s chance. A C-statistic of 1 is perfect prediction. So, what will the C-statistic be, given the incredibly strong association of the Perry Factor with outcomes? 0.9? 0.95?
0.5024. Almost useless.

Let’s figure out why strength of association and usefulness for prediction are not always the same thing.
I constructed my fake Perry Factor dataset quite carefully to illustrate this point. Let me show you what happened. What you see here is a breakdown of the patients in my fake study. You can see that just 11 of them were Perry Factor positive, but 10 of those 11 ended up dying.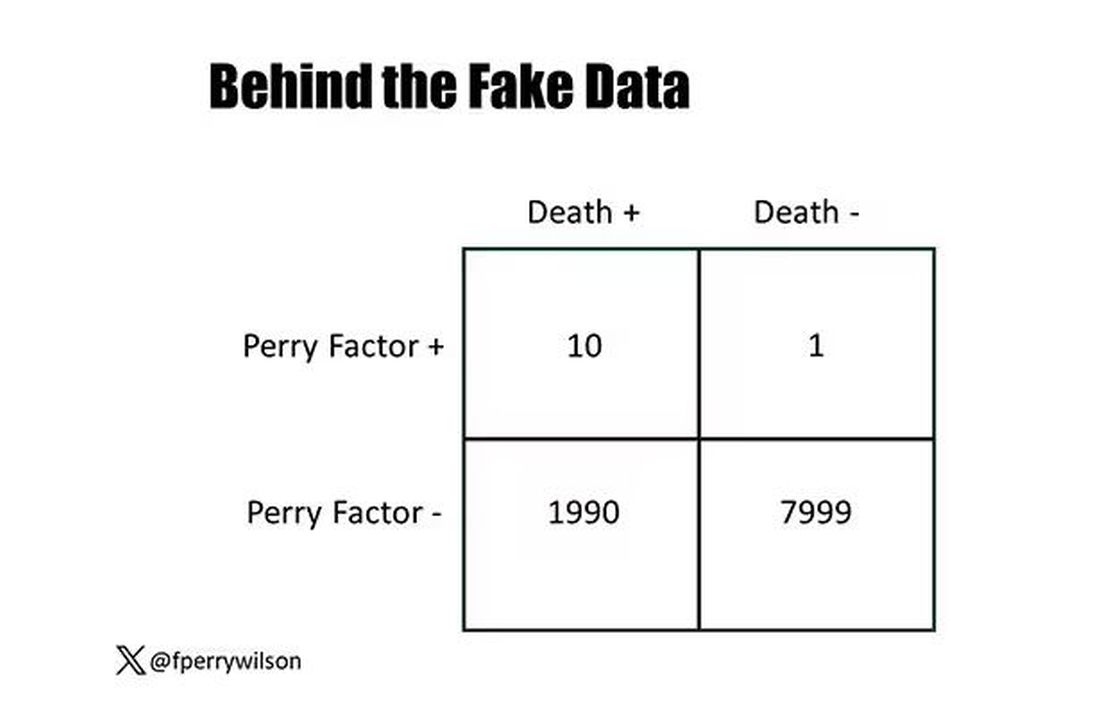
That’s quite unlikely by chance alone. It really does appear that if you have Perry Factor, your risk for death is much higher. But the reason that Perry Factor is a bad predictor is because it is so rare in the population. Sure, you can use it to correctly predict the outcome of 10 of the 11 people who have it, but the vast majority of people don’t have Perry Factor. It’s useless to distinguish who will die vs who will live in that population.
Why have I spent so much time trying to reverse our intuition that strength of association and strength of predictive power must be related? Because it helps to explain this paper, “Prognostic Value of Cardiovascular Biomarkers in the Population,” appearing in JAMA, which is a very nice piece of work trying to help us better predict cardiovascular disease.
I don’t need to tell you that cardiovascular disease is the number-one killer in this country and most of the world. I don’t need to tell you that we have really good preventive therapies and lifestyle interventions that can reduce the risk. But it would be nice to know in whom, specifically, we should use those interventions.
Cardiovascular risk scores, to date, are pretty simple. The most common one in use in the United States, the pooled cohort risk equation, has nine variables, two of which require a cholesterol panel and one a blood pressure test. It’s easy and it’s pretty accurate.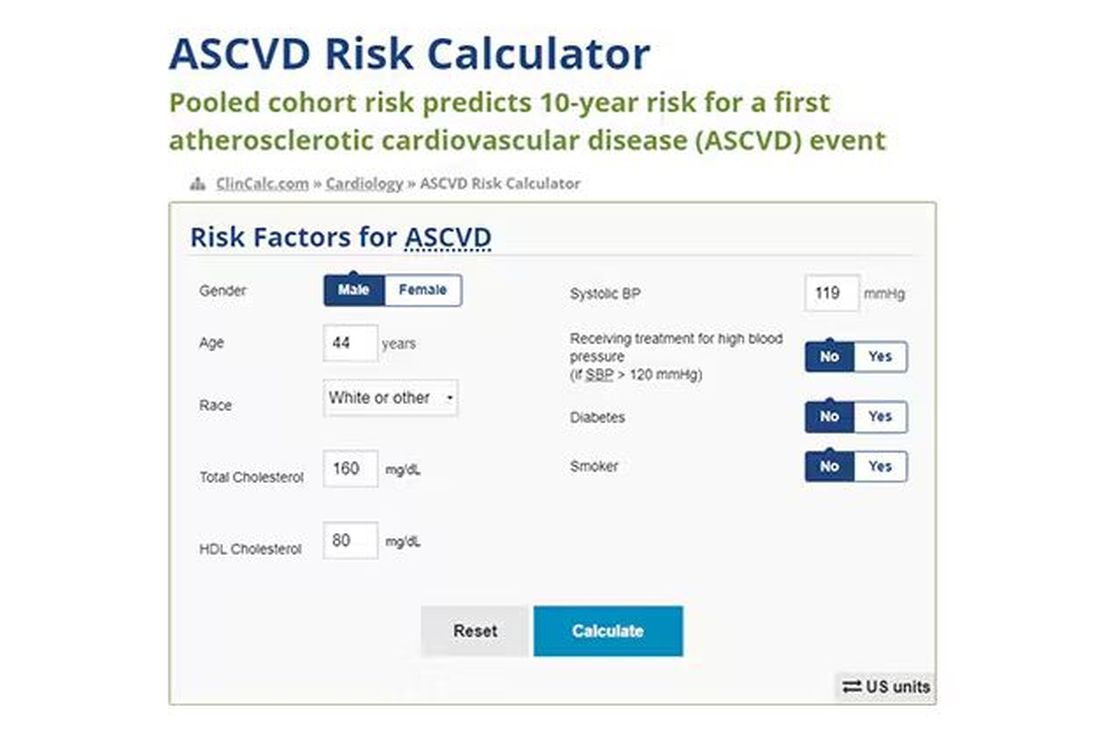
Using the score from the pooled cohort risk calculator, you get a C-statistic as high as 0.82 when applied to Black women, a low of 0.71 when applied to Black men. Non-Black individuals are in the middle. Not bad. But, clearly, not perfect.
And aren’t we in the era of big data, the era of personalized medicine? We have dozens, maybe hundreds, of quantifiable biomarkers that are associated with subsequent heart disease. Surely, by adding these biomarkers into the risk equation, we can improve prediction. Right?
The JAMA study includes 164,054 patients pooled from 28 cohort studies from 12 countries. All the studies measured various key biomarkers at baseline and followed their participants for cardiovascular events like heart attack, stroke, coronary revascularization, and so on.
The biomarkers in question are really the big guns in this space: troponin, a marker of stress on the heart muscle; NT-proBNP, a marker of stretch on the heart muscle; and C-reactive protein, a marker of inflammation. In every case, higher levels of these markers at baseline were associated with a higher risk for cardiovascular disease in the future.
Troponin T, shown here, has a basically linear risk with subsequent cardiovascular disease.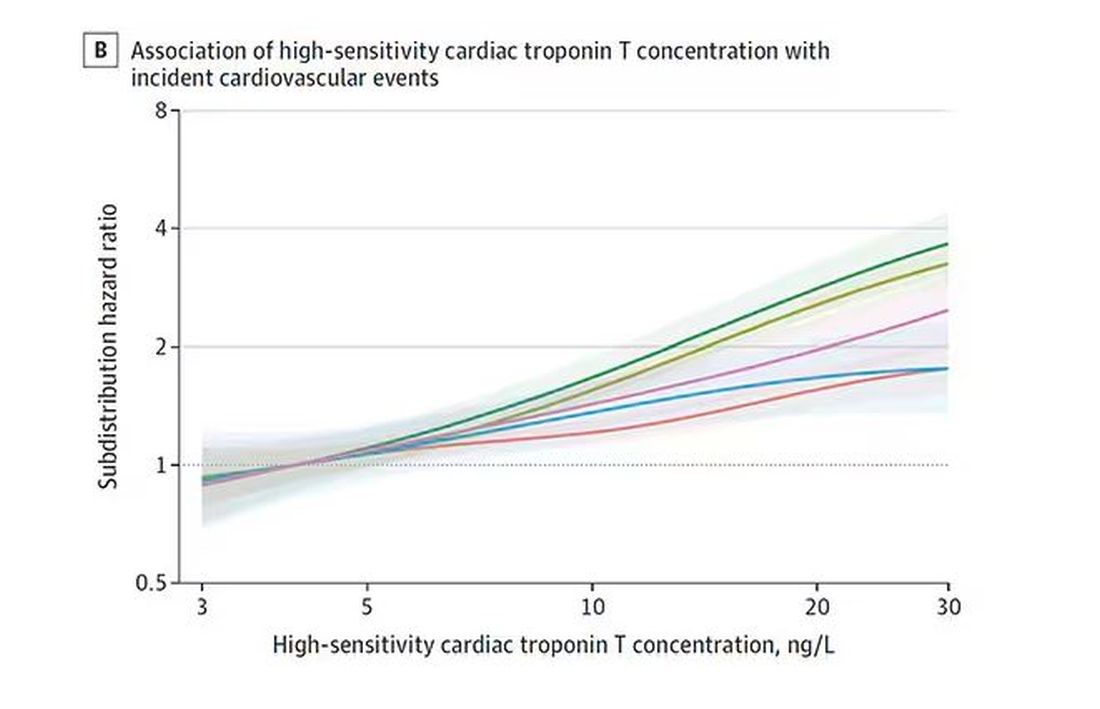
BNP seems to demonstrate more of a threshold effect, where levels above 60 start to associate with problems.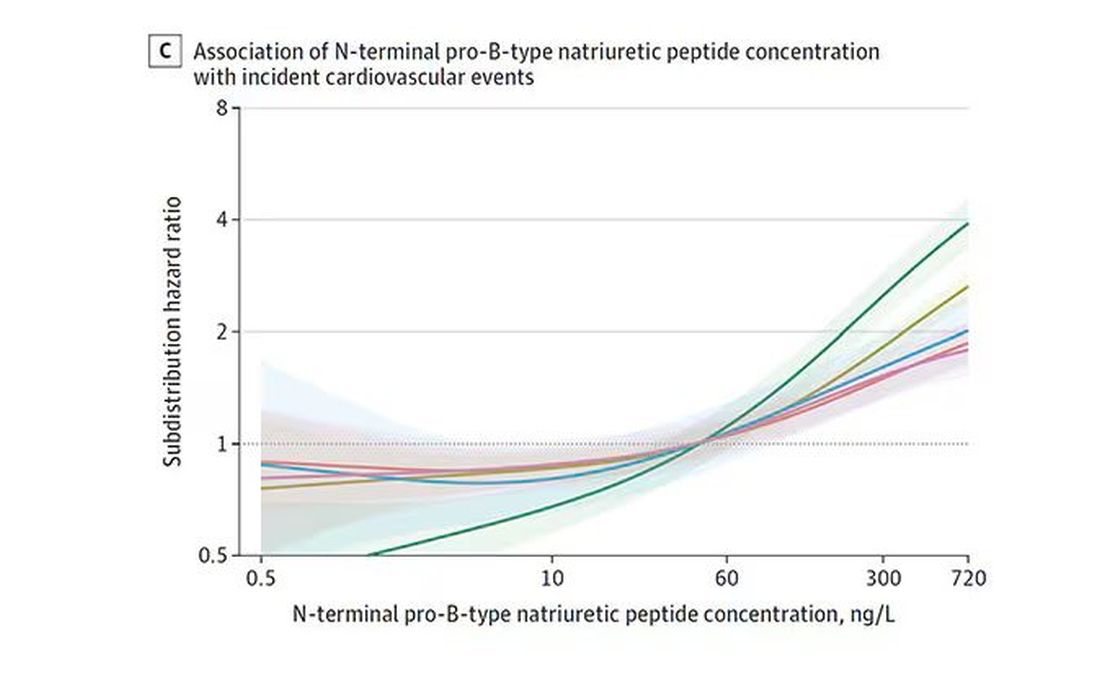
And CRP does a similar thing, with levels above 1.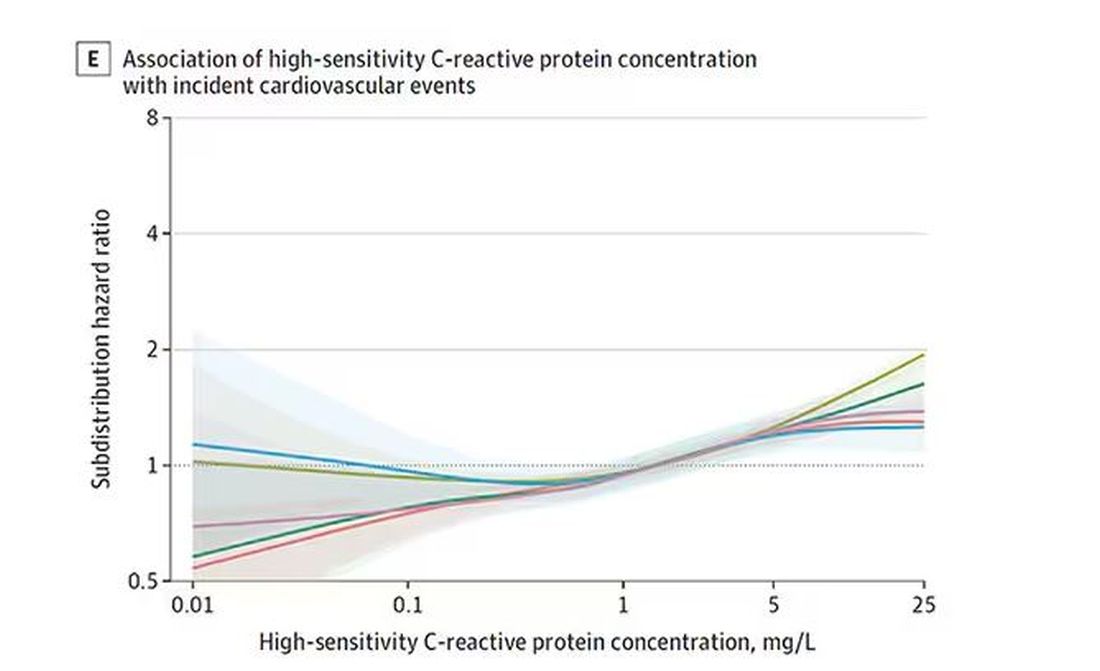
All of these findings were statistically significant. If you have higher levels of one or more of these biomarkers, you are more likely to have cardiovascular disease in the future.
Of course, our old friend the pooled cohort risk equation is still here — in the background — requiring just that one blood test and measurement of blood pressure. Let’s talk about predictive power.
The pooled cohort risk equation score, in this study, had a C-statistic of 0.812.
By adding troponin, BNP, and CRP to the equation, the new C-statistic is 0.819. Barely any change.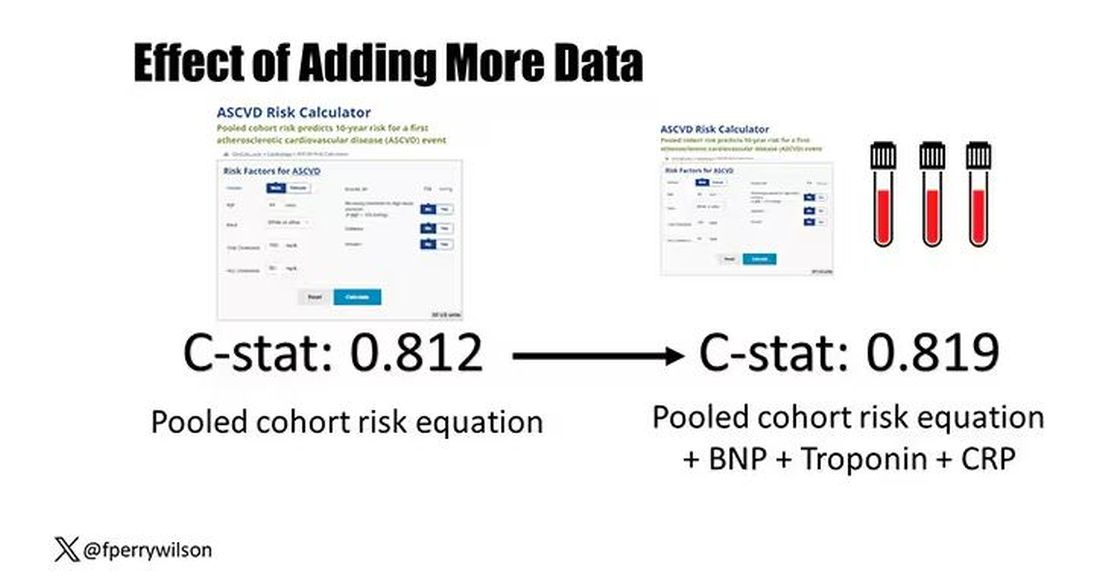
Now, the authors looked at different types of prediction here. The greatest improvement in the AUC was seen when they tried to predict heart failure within 1 year of measurement; there the AUC improved by 0.04. But the presence of BNP as a biomarker and the short time window of 1 year makes me wonder whether this is really prediction at all or whether they were essentially just diagnosing people with existing heart failure.
Why does this happen? Why do these promising biomarkers, clearly associated with bad outcomes, fail to improve our ability to predict the future? I already gave one example, which has to do with how the markers are distributed in the population. But even more relevant here is that the new markers will only improve prediction insofar as they are not already represented in the old predictive model.
Of course, BNP, for example, wasn’t in the old model. But smoking was. Diabetes was. Blood pressure was. All of that data might actually tell you something about the patient’s BNP through their mutual correlation. And improvement in prediction requires new information.
This is actually why I consider this a really successful study. We need to do studies like this to help us find what those new sources of information might be.
We will never get to a C-statistic of 1. Perfect prediction is the domain of palm readers and astrophysicists. But better prediction is always possible through data. The big question, of course, is which data?
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
It’s the counterintuitive stuff in epidemiology that always really interests me. One intuition many of us have is that if a risk factor is significantly associated with an outcome, knowledge of that risk factor would help to predict that outcome. Makes sense. Feels right.
But it’s not right. Not always.
Here’s a fake example to illustrate my point. Let’s say we have 10,000 individuals who we follow for 10 years and 2000 of them die. (It’s been a rough decade.) At baseline, I measured a novel biomarker, the Perry Factor, in everyone. To keep it simple, the Perry Factor has only two values: 0 or 1.
I then do a standard associational analysis and find that individuals who are positive for the Perry Factor have a 40-fold higher odds of death than those who are negative for it. I am beginning to reconsider ascribing my good name to this biomarker. This is a highly statistically significant result — a P value <.001.
Clearly, knowledge of the Perry Factor should help me predict who will die in the cohort. I evaluate predictive power using a metric called the area under the receiver operating characteristic curve (AUC, referred to as the C-statistic in time-to-event studies). It tells you, given two people — one who dies and one who doesn’t — how frequently you “pick” the right person, given the knowledge of their Perry Factor.
A C-statistic of 0.5, or 50%, would mean the Perry Factor gives you no better results than a coin flip; it’s chance. A C-statistic of 1 is perfect prediction. So, what will the C-statistic be, given the incredibly strong association of the Perry Factor with outcomes? 0.9? 0.95?
0.5024. Almost useless.

Let’s figure out why strength of association and usefulness for prediction are not always the same thing.
I constructed my fake Perry Factor dataset quite carefully to illustrate this point. Let me show you what happened. What you see here is a breakdown of the patients in my fake study. You can see that just 11 of them were Perry Factor positive, but 10 of those 11 ended up dying.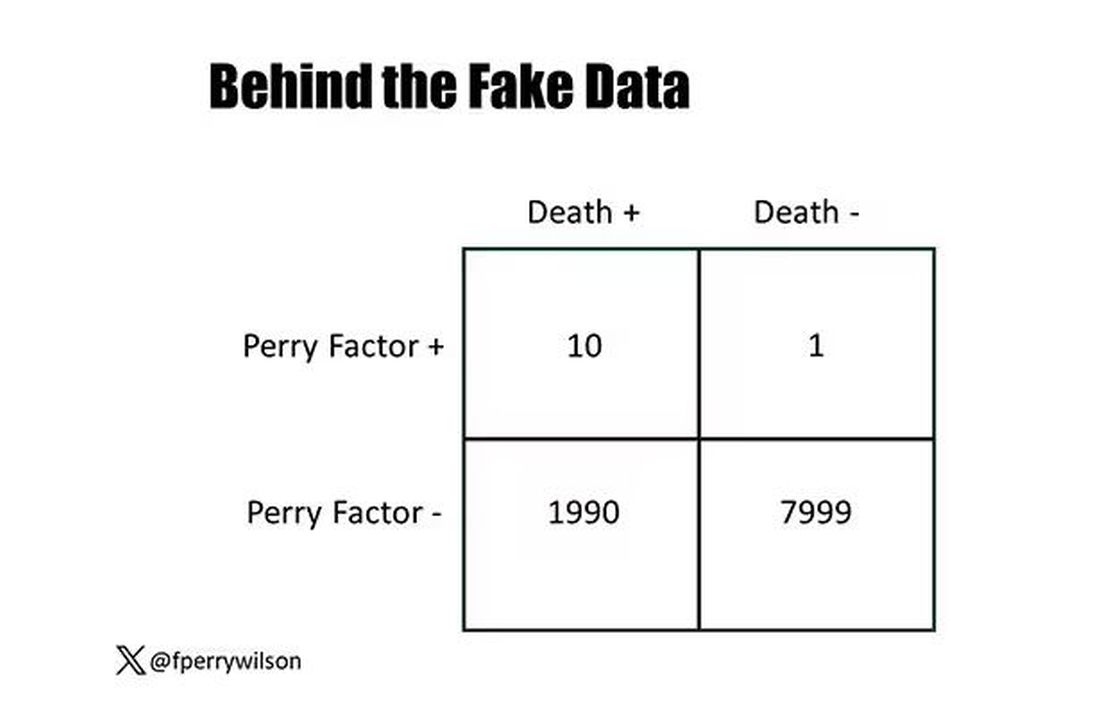
That’s quite unlikely by chance alone. It really does appear that if you have Perry Factor, your risk for death is much higher. But the reason that Perry Factor is a bad predictor is because it is so rare in the population. Sure, you can use it to correctly predict the outcome of 10 of the 11 people who have it, but the vast majority of people don’t have Perry Factor. It’s useless to distinguish who will die vs who will live in that population.
Why have I spent so much time trying to reverse our intuition that strength of association and strength of predictive power must be related? Because it helps to explain this paper, “Prognostic Value of Cardiovascular Biomarkers in the Population,” appearing in JAMA, which is a very nice piece of work trying to help us better predict cardiovascular disease.
I don’t need to tell you that cardiovascular disease is the number-one killer in this country and most of the world. I don’t need to tell you that we have really good preventive therapies and lifestyle interventions that can reduce the risk. But it would be nice to know in whom, specifically, we should use those interventions.
Cardiovascular risk scores, to date, are pretty simple. The most common one in use in the United States, the pooled cohort risk equation, has nine variables, two of which require a cholesterol panel and one a blood pressure test. It’s easy and it’s pretty accurate.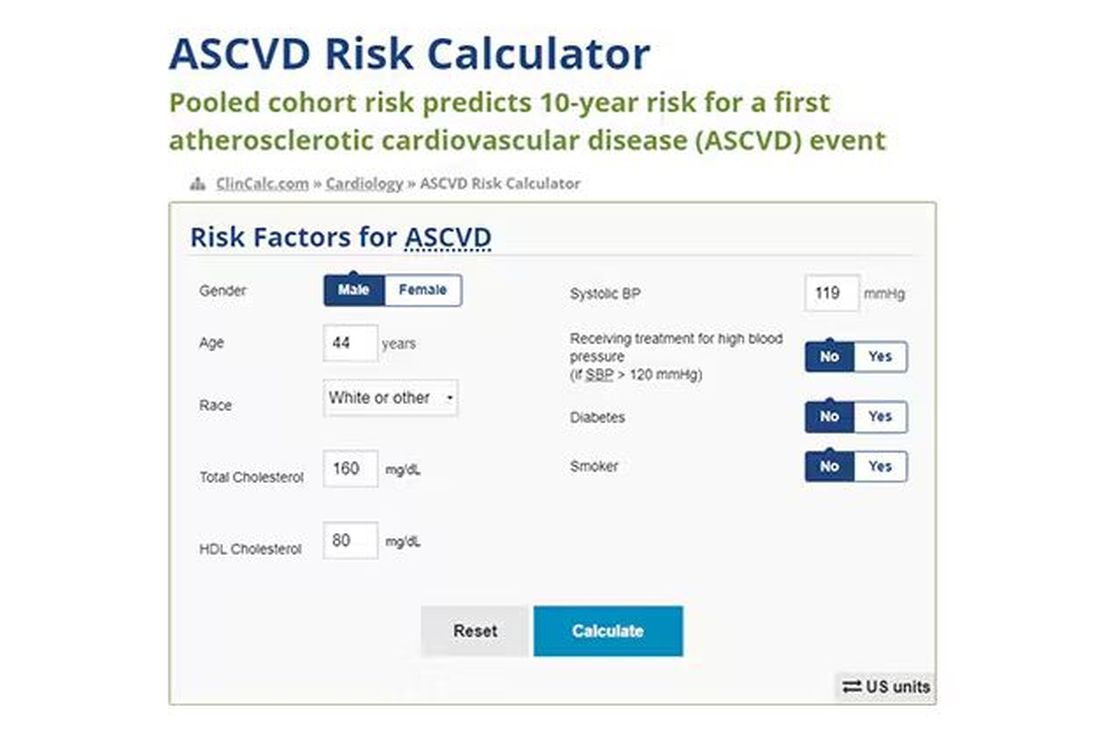
Using the score from the pooled cohort risk calculator, you get a C-statistic as high as 0.82 when applied to Black women, a low of 0.71 when applied to Black men. Non-Black individuals are in the middle. Not bad. But, clearly, not perfect.
And aren’t we in the era of big data, the era of personalized medicine? We have dozens, maybe hundreds, of quantifiable biomarkers that are associated with subsequent heart disease. Surely, by adding these biomarkers into the risk equation, we can improve prediction. Right?
The JAMA study includes 164,054 patients pooled from 28 cohort studies from 12 countries. All the studies measured various key biomarkers at baseline and followed their participants for cardiovascular events like heart attack, stroke, coronary revascularization, and so on.
The biomarkers in question are really the big guns in this space: troponin, a marker of stress on the heart muscle; NT-proBNP, a marker of stretch on the heart muscle; and C-reactive protein, a marker of inflammation. In every case, higher levels of these markers at baseline were associated with a higher risk for cardiovascular disease in the future.
Troponin T, shown here, has a basically linear risk with subsequent cardiovascular disease.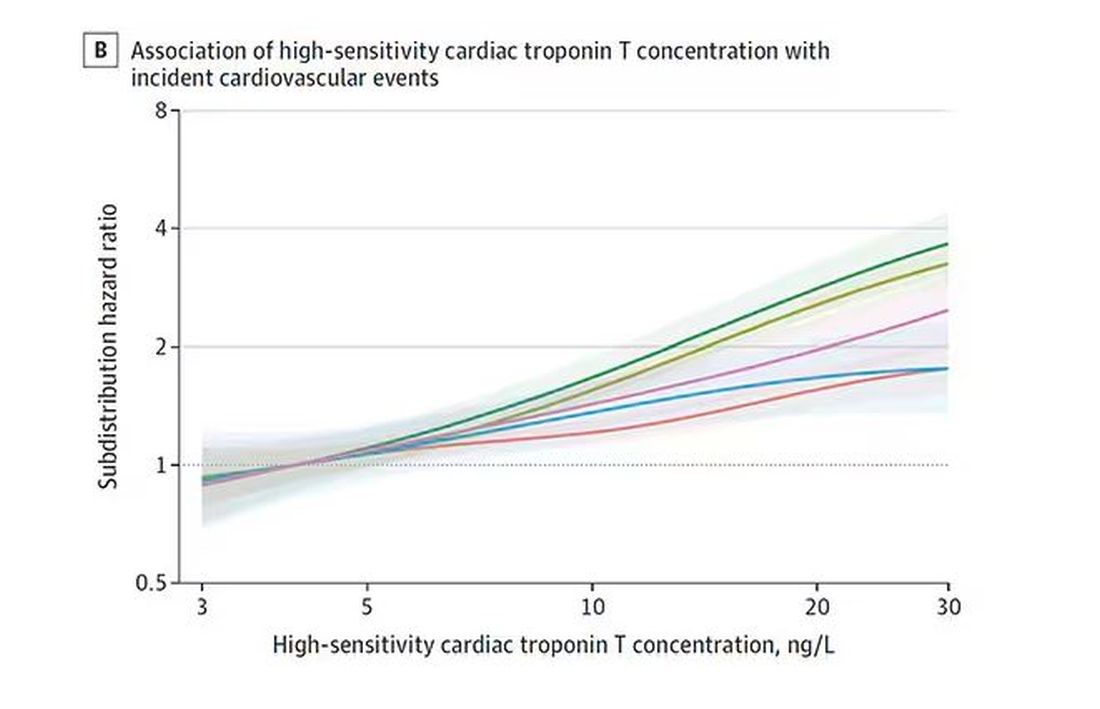
BNP seems to demonstrate more of a threshold effect, where levels above 60 start to associate with problems.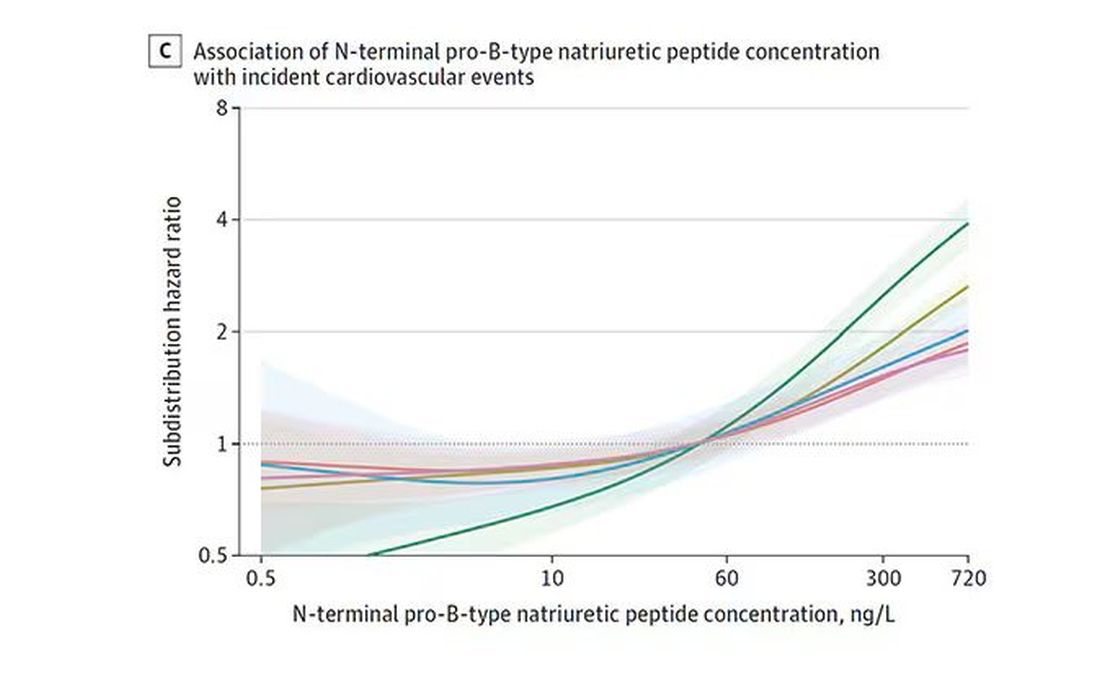
And CRP does a similar thing, with levels above 1.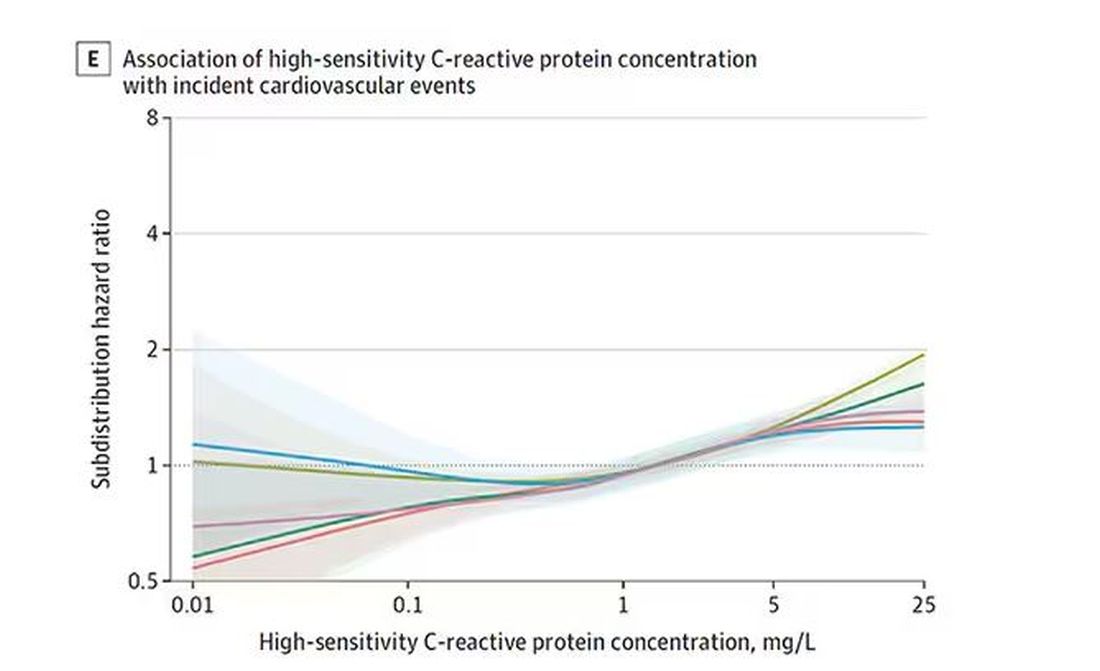
All of these findings were statistically significant. If you have higher levels of one or more of these biomarkers, you are more likely to have cardiovascular disease in the future.
Of course, our old friend the pooled cohort risk equation is still here — in the background — requiring just that one blood test and measurement of blood pressure. Let’s talk about predictive power.
The pooled cohort risk equation score, in this study, had a C-statistic of 0.812.
By adding troponin, BNP, and CRP to the equation, the new C-statistic is 0.819. Barely any change.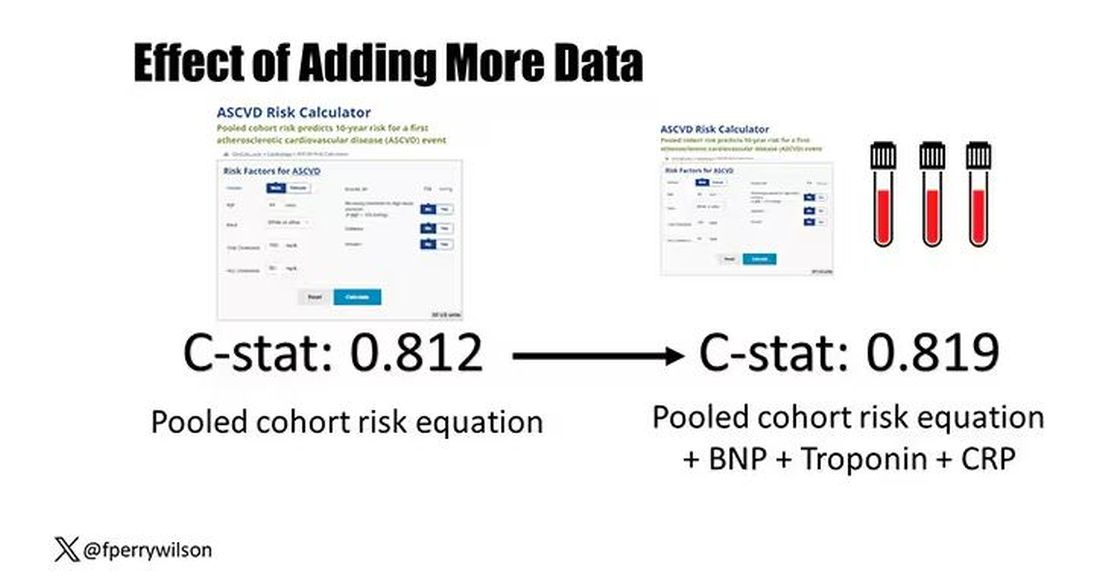
Now, the authors looked at different types of prediction here. The greatest improvement in the AUC was seen when they tried to predict heart failure within 1 year of measurement; there the AUC improved by 0.04. But the presence of BNP as a biomarker and the short time window of 1 year makes me wonder whether this is really prediction at all or whether they were essentially just diagnosing people with existing heart failure.
Why does this happen? Why do these promising biomarkers, clearly associated with bad outcomes, fail to improve our ability to predict the future? I already gave one example, which has to do with how the markers are distributed in the population. But even more relevant here is that the new markers will only improve prediction insofar as they are not already represented in the old predictive model.
Of course, BNP, for example, wasn’t in the old model. But smoking was. Diabetes was. Blood pressure was. All of that data might actually tell you something about the patient’s BNP through their mutual correlation. And improvement in prediction requires new information.
This is actually why I consider this a really successful study. We need to do studies like this to help us find what those new sources of information might be.
We will never get to a C-statistic of 1. Perfect prediction is the domain of palm readers and astrophysicists. But better prediction is always possible through data. The big question, of course, is which data?
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.




