User login
FDA panel rejects vernakalant bid for AFib cardioversion indication
for cardioversion of recent-onset atrial fibrillation (AFib).
It was the second time before an FDA advisory panel for vernakalant (Brinavess, Correvio International Sàrl), which the agency had declined to approve in 2008 due to safety concerns. That time, however, its advisors had given the agency a decidedly positive recommendation.
Since then, registry data collected for the drug’s resubmission seemed only to raise further safety issues, especially evidence that a single infusion may cause severe hypotension and suppress left ventricular function.
Some members of the Cardiovascular and Renal Drugs Advisory Committee (CRDAC), including a number who voted against approval, expressed hopes for further research aimed at identifying specific AFib patient groups who might safely benefit from vernakalant.
Of note, the drug has long been available for AFib cardioversion in Europe, where there are a number of other pharmacologic options, and was recently approved in Canada.
“We do recognize there’s a significant clinical need here,” observed Paul M. Ridker, MD, MPH, of Harvard Medical School and Brigham and Women’s Hospital Boston, a CRDAC panelist.
The results of the safety study that Correvio presented to the panel were “pretty marginal,” Dr. Ridker said. Given the negative safety signals and the available cardioversion alternatives, he questioned whether vernakalant represented a “substantial advance versus just another option. Right now, I’m not convinced it’s a substantial advance.”
FDA representatives were skeptical about vernakalant when they walked into the meeting room, as noted in briefing documents they had circulated beforehand. The drug’s safety experience under consideration included one case of ventricular arrhythmia and cardiogenic shock in a treated patient without apparent structural heart disease, who subsequently died. That case was much discussed throughout the meeting.
In its resubmission of vernakalant to regulators, Correvio also pointed to a significant unmet need for AFib cardioversion options in the United States, given the few alternatives.
For example, ibutilide is FDA-approved for recent-onset AFib or atrial flutter; but as the company and panelists noted, the drug isn’t often used for that indication. Patients with recent-onset AFib are often put on rate-control meds without cardioversion. Or clinicians may resort to electrical cardioversion, which can be logistically cumbersome and require anesthesia and generally a hospital stay.
Oral or intravenous amiodarone and oral dofetilide, flecainide, and propafenone are guideline-recommended but not actually FDA-approved for recent-onset AFib, the company noted.
Correvio made its “pre-infusion checklist” a core feature of its case. It was designed to guide selection of patients for vernakalant cardioversion based on contraindications such as a systolic blood pressure under 100 mm Hg, severe heart failure, aortic stenosis, severe bradycardia or heart block, or a prolonged QT interval.
In his presentation to the panel, FDA medical officer Preston Dunnmon, MD, said the safety results from the SPECTRUM registry, another main pillar of support for the vernakalant resubmission, “are not reassuring.”
As reasons, Dr. Dunnmon cited likely patient-selection bias and its high proportion of patients who were not prospectively enrolled; 21% were retrospectively entered from records.
Moreover, “the proposed preinfusion checklist will not reliably predict which subjects will experience serious cardiovascular adverse events with vernakalant,” he said.
“Vernakalant has induced harm that cannot be reliably predicted, prevented, or in some cases, treated. In contrast to vernakalant, electrical cardioversion and ibutilide pharmacologic cardioversion can cause adverse events, but these are transient and treatable,” he said.
Many on the panel agreed. “I thought the totality of evidence supported the hypothesis that this drug has a potential for a fatal side effect in a disease that you can live with, potentially, and that there are other treatments for,” said Julia B. Lewis, MD, Vanderbilt Medical Center, Nashville, Tenn., who chaired the CRDAC panel.
“The drug clearly converts atrial fibrillation, although it’s only transient,” observed John H. Alexander, MD, MHSc, Duke University, Durham, N.C., one of the two panelists who voted to recommend approval of vernakalant.
“And, there clearly is a serious safety signal in some populations of patients,” he agreed. “However, I was more reassured by the SPECTRUM data.” There is likely to be a low-risk group of patients for whom vernakalant could represent an important option that “outweighs the relatively low risk of serious complications,” Dr. Alexander said.
“So more work needs to be done to clarify who are the low risk patients where it would be favorable.”
Panelist Matthew Needleman, MD, Walter Reed National Military Medical Center, Bethesda, Md., also voted in favor of approval.
“We’ve all known patients with normal ejection fractions who keep coming in with symptomatic atrial fib, want to get out of it quickly, and get back to their lives. So having an option like this I think would be good for a very select group of patients,” Dr. Needleman said.
But the preinfusion checklist and other potential ways to select low-risk patients for vernakalant could potentially backfire, warned John M. Mandrola, MD, Baptist Medical Associates, Louisville, Ky., from the panel.
The FDA representatives had presented evidence that the drug can seriously depress ventricular function, and that the lower cardiac output is what leads to hypotension, he elaborated in an interview after the meeting.
If the checklist is used to exclude hemodynamically unstable patients from receiving vernakalant, he said, “Then you’re really giving this drug to relatively healthy patients for convenience, to decrease hospitalization or the hospital stay.”
The signal for substantial harm, Dr. Mandrola said, has to be balanced against that modest benefit.
Moreover, those in whom the drug doesn’t work may be left in a worse situation, he proposed. Only about half of patients are successfully converted on vernakalant, the company and FDA data suggested. The other half of patients who don’t achieve sinus rhythm on the drug still must face the significant hazards of depressed ejection fraction and hypotension, a high price to pay for an unsuccessful treatment.
Dr. Mandrola is Chief Cardiology Correspondent for theheart.org | Medscape Cardiology; his disclosure statement states no relevant financial relationships.
This article first appeared on Medscape.com.
for cardioversion of recent-onset atrial fibrillation (AFib).
It was the second time before an FDA advisory panel for vernakalant (Brinavess, Correvio International Sàrl), which the agency had declined to approve in 2008 due to safety concerns. That time, however, its advisors had given the agency a decidedly positive recommendation.
Since then, registry data collected for the drug’s resubmission seemed only to raise further safety issues, especially evidence that a single infusion may cause severe hypotension and suppress left ventricular function.
Some members of the Cardiovascular and Renal Drugs Advisory Committee (CRDAC), including a number who voted against approval, expressed hopes for further research aimed at identifying specific AFib patient groups who might safely benefit from vernakalant.
Of note, the drug has long been available for AFib cardioversion in Europe, where there are a number of other pharmacologic options, and was recently approved in Canada.
“We do recognize there’s a significant clinical need here,” observed Paul M. Ridker, MD, MPH, of Harvard Medical School and Brigham and Women’s Hospital Boston, a CRDAC panelist.
The results of the safety study that Correvio presented to the panel were “pretty marginal,” Dr. Ridker said. Given the negative safety signals and the available cardioversion alternatives, he questioned whether vernakalant represented a “substantial advance versus just another option. Right now, I’m not convinced it’s a substantial advance.”
FDA representatives were skeptical about vernakalant when they walked into the meeting room, as noted in briefing documents they had circulated beforehand. The drug’s safety experience under consideration included one case of ventricular arrhythmia and cardiogenic shock in a treated patient without apparent structural heart disease, who subsequently died. That case was much discussed throughout the meeting.
In its resubmission of vernakalant to regulators, Correvio also pointed to a significant unmet need for AFib cardioversion options in the United States, given the few alternatives.
For example, ibutilide is FDA-approved for recent-onset AFib or atrial flutter; but as the company and panelists noted, the drug isn’t often used for that indication. Patients with recent-onset AFib are often put on rate-control meds without cardioversion. Or clinicians may resort to electrical cardioversion, which can be logistically cumbersome and require anesthesia and generally a hospital stay.
Oral or intravenous amiodarone and oral dofetilide, flecainide, and propafenone are guideline-recommended but not actually FDA-approved for recent-onset AFib, the company noted.
Correvio made its “pre-infusion checklist” a core feature of its case. It was designed to guide selection of patients for vernakalant cardioversion based on contraindications such as a systolic blood pressure under 100 mm Hg, severe heart failure, aortic stenosis, severe bradycardia or heart block, or a prolonged QT interval.
In his presentation to the panel, FDA medical officer Preston Dunnmon, MD, said the safety results from the SPECTRUM registry, another main pillar of support for the vernakalant resubmission, “are not reassuring.”
As reasons, Dr. Dunnmon cited likely patient-selection bias and its high proportion of patients who were not prospectively enrolled; 21% were retrospectively entered from records.
Moreover, “the proposed preinfusion checklist will not reliably predict which subjects will experience serious cardiovascular adverse events with vernakalant,” he said.
“Vernakalant has induced harm that cannot be reliably predicted, prevented, or in some cases, treated. In contrast to vernakalant, electrical cardioversion and ibutilide pharmacologic cardioversion can cause adverse events, but these are transient and treatable,” he said.
Many on the panel agreed. “I thought the totality of evidence supported the hypothesis that this drug has a potential for a fatal side effect in a disease that you can live with, potentially, and that there are other treatments for,” said Julia B. Lewis, MD, Vanderbilt Medical Center, Nashville, Tenn., who chaired the CRDAC panel.
“The drug clearly converts atrial fibrillation, although it’s only transient,” observed John H. Alexander, MD, MHSc, Duke University, Durham, N.C., one of the two panelists who voted to recommend approval of vernakalant.
“And, there clearly is a serious safety signal in some populations of patients,” he agreed. “However, I was more reassured by the SPECTRUM data.” There is likely to be a low-risk group of patients for whom vernakalant could represent an important option that “outweighs the relatively low risk of serious complications,” Dr. Alexander said.
“So more work needs to be done to clarify who are the low risk patients where it would be favorable.”
Panelist Matthew Needleman, MD, Walter Reed National Military Medical Center, Bethesda, Md., also voted in favor of approval.
“We’ve all known patients with normal ejection fractions who keep coming in with symptomatic atrial fib, want to get out of it quickly, and get back to their lives. So having an option like this I think would be good for a very select group of patients,” Dr. Needleman said.
But the preinfusion checklist and other potential ways to select low-risk patients for vernakalant could potentially backfire, warned John M. Mandrola, MD, Baptist Medical Associates, Louisville, Ky., from the panel.
The FDA representatives had presented evidence that the drug can seriously depress ventricular function, and that the lower cardiac output is what leads to hypotension, he elaborated in an interview after the meeting.
If the checklist is used to exclude hemodynamically unstable patients from receiving vernakalant, he said, “Then you’re really giving this drug to relatively healthy patients for convenience, to decrease hospitalization or the hospital stay.”
The signal for substantial harm, Dr. Mandrola said, has to be balanced against that modest benefit.
Moreover, those in whom the drug doesn’t work may be left in a worse situation, he proposed. Only about half of patients are successfully converted on vernakalant, the company and FDA data suggested. The other half of patients who don’t achieve sinus rhythm on the drug still must face the significant hazards of depressed ejection fraction and hypotension, a high price to pay for an unsuccessful treatment.
Dr. Mandrola is Chief Cardiology Correspondent for theheart.org | Medscape Cardiology; his disclosure statement states no relevant financial relationships.
This article first appeared on Medscape.com.
for cardioversion of recent-onset atrial fibrillation (AFib).
It was the second time before an FDA advisory panel for vernakalant (Brinavess, Correvio International Sàrl), which the agency had declined to approve in 2008 due to safety concerns. That time, however, its advisors had given the agency a decidedly positive recommendation.
Since then, registry data collected for the drug’s resubmission seemed only to raise further safety issues, especially evidence that a single infusion may cause severe hypotension and suppress left ventricular function.
Some members of the Cardiovascular and Renal Drugs Advisory Committee (CRDAC), including a number who voted against approval, expressed hopes for further research aimed at identifying specific AFib patient groups who might safely benefit from vernakalant.
Of note, the drug has long been available for AFib cardioversion in Europe, where there are a number of other pharmacologic options, and was recently approved in Canada.
“We do recognize there’s a significant clinical need here,” observed Paul M. Ridker, MD, MPH, of Harvard Medical School and Brigham and Women’s Hospital Boston, a CRDAC panelist.
The results of the safety study that Correvio presented to the panel were “pretty marginal,” Dr. Ridker said. Given the negative safety signals and the available cardioversion alternatives, he questioned whether vernakalant represented a “substantial advance versus just another option. Right now, I’m not convinced it’s a substantial advance.”
FDA representatives were skeptical about vernakalant when they walked into the meeting room, as noted in briefing documents they had circulated beforehand. The drug’s safety experience under consideration included one case of ventricular arrhythmia and cardiogenic shock in a treated patient without apparent structural heart disease, who subsequently died. That case was much discussed throughout the meeting.
In its resubmission of vernakalant to regulators, Correvio also pointed to a significant unmet need for AFib cardioversion options in the United States, given the few alternatives.
For example, ibutilide is FDA-approved for recent-onset AFib or atrial flutter; but as the company and panelists noted, the drug isn’t often used for that indication. Patients with recent-onset AFib are often put on rate-control meds without cardioversion. Or clinicians may resort to electrical cardioversion, which can be logistically cumbersome and require anesthesia and generally a hospital stay.
Oral or intravenous amiodarone and oral dofetilide, flecainide, and propafenone are guideline-recommended but not actually FDA-approved for recent-onset AFib, the company noted.
Correvio made its “pre-infusion checklist” a core feature of its case. It was designed to guide selection of patients for vernakalant cardioversion based on contraindications such as a systolic blood pressure under 100 mm Hg, severe heart failure, aortic stenosis, severe bradycardia or heart block, or a prolonged QT interval.
In his presentation to the panel, FDA medical officer Preston Dunnmon, MD, said the safety results from the SPECTRUM registry, another main pillar of support for the vernakalant resubmission, “are not reassuring.”
As reasons, Dr. Dunnmon cited likely patient-selection bias and its high proportion of patients who were not prospectively enrolled; 21% were retrospectively entered from records.
Moreover, “the proposed preinfusion checklist will not reliably predict which subjects will experience serious cardiovascular adverse events with vernakalant,” he said.
“Vernakalant has induced harm that cannot be reliably predicted, prevented, or in some cases, treated. In contrast to vernakalant, electrical cardioversion and ibutilide pharmacologic cardioversion can cause adverse events, but these are transient and treatable,” he said.
Many on the panel agreed. “I thought the totality of evidence supported the hypothesis that this drug has a potential for a fatal side effect in a disease that you can live with, potentially, and that there are other treatments for,” said Julia B. Lewis, MD, Vanderbilt Medical Center, Nashville, Tenn., who chaired the CRDAC panel.
“The drug clearly converts atrial fibrillation, although it’s only transient,” observed John H. Alexander, MD, MHSc, Duke University, Durham, N.C., one of the two panelists who voted to recommend approval of vernakalant.
“And, there clearly is a serious safety signal in some populations of patients,” he agreed. “However, I was more reassured by the SPECTRUM data.” There is likely to be a low-risk group of patients for whom vernakalant could represent an important option that “outweighs the relatively low risk of serious complications,” Dr. Alexander said.
“So more work needs to be done to clarify who are the low risk patients where it would be favorable.”
Panelist Matthew Needleman, MD, Walter Reed National Military Medical Center, Bethesda, Md., also voted in favor of approval.
“We’ve all known patients with normal ejection fractions who keep coming in with symptomatic atrial fib, want to get out of it quickly, and get back to their lives. So having an option like this I think would be good for a very select group of patients,” Dr. Needleman said.
But the preinfusion checklist and other potential ways to select low-risk patients for vernakalant could potentially backfire, warned John M. Mandrola, MD, Baptist Medical Associates, Louisville, Ky., from the panel.
The FDA representatives had presented evidence that the drug can seriously depress ventricular function, and that the lower cardiac output is what leads to hypotension, he elaborated in an interview after the meeting.
If the checklist is used to exclude hemodynamically unstable patients from receiving vernakalant, he said, “Then you’re really giving this drug to relatively healthy patients for convenience, to decrease hospitalization or the hospital stay.”
The signal for substantial harm, Dr. Mandrola said, has to be balanced against that modest benefit.
Moreover, those in whom the drug doesn’t work may be left in a worse situation, he proposed. Only about half of patients are successfully converted on vernakalant, the company and FDA data suggested. The other half of patients who don’t achieve sinus rhythm on the drug still must face the significant hazards of depressed ejection fraction and hypotension, a high price to pay for an unsuccessful treatment.
Dr. Mandrola is Chief Cardiology Correspondent for theheart.org | Medscape Cardiology; his disclosure statement states no relevant financial relationships.
This article first appeared on Medscape.com.
Genetic test stratified AFib patients with low CHA2DS2-VASc scores
PHILADELPHIA – A 32-gene screening test for stroke risk identified a subgroup of atrial fibrillation (AFib) patients with an elevated rate of ischemic strokes despite having a low stroke risk by conventional criteria by their CHA2DS2-VASc score in a post-hoc analysis of more than 11,000 patients enrolled in a recent drug trial.
Overall, AFib patients in the highest tertile for genetic risk based on a 32 gene-loci test had a 31% increase rate of ischemic stroke during a median 2.8 years of follow-up compared with patients in the tertile with the lowest risk based on the 32-loci screen, Nicholas A. Marston, MD, said at the American Heart Association scientific sessions. This suggested that the genetic test had roughly the same association with an increased stroke risk as several components of the CHA2DS2-VASc score, such as female sex, an age of 65-74 years old, or having heart failure as a comorbidity, each of which links with an increased risk for ischemic stroke of about 31%-38%, Dr. Marston noted.
The genetic test produced even sharper discrimination among the patients with the lowest stroke risk as measured by their CHA2DS2-VASc score (Circulation. 2012 Aug 14;126[7]: 860-5). Among the slightly more than 3,000 patients in the study with a CHA2DS2-VASc score of three or less, those in the subgroup with the highest risk by the 32-loci screen had a stroke rate during follow-up that was 76% higher than those in the low or intermediate tertile for their genetic score. Among the 796 patients with a CHA2DS2-VASc score of just 1 or 2, those who also fell into the highest level of risk on the 32-loci screen had a stroke rate 3.5-fold higher than those with a similar CHA2DS2-VASc score but in the low and intermediate tertiles by the 32-loci screen.
The additional risk prediction provided by the 32-loci test was statistically significant in the analysis of the 3,071 patients with a CHA2DS2-VASc score of 3 or less after adjustment for age, sex, ancestry, and the individual components of the CHA2DS2-VASc score, which includes factors such as hypertension, diabetes, and heart failure, said Dr. Marston, a cardiologist at Brigham and Women’s Hospital in Boston. The 3.5-fold elevation among patients with a high genetic-risk score in the cohort of 796 patients with a CHA2DS2-VASc score of 1 or 2 just missed statistical significance (P = .06), possibly because the number of patients in the analysis was relatively low. Future research should explore the predictive value of the genetic risk score in patients with a CHA2DS2-VASc score of 0 or 1, the “group where therapeutic decisions could be altered” depending on the genetic risk score, he explained.
Dr. Marston and his associates used data collected in the ENGAGE AF-TIMI 48 (Effective Anticoagulation with Factor Xa Next Generation in Atrial Fibrillation–Thrombolysis in Myocardial Infarction 48) trial, which was designed to assess the safety and efficacy of the direct-acting oral anticoagulant edoxaban in patients with AFib (New Engl J Med. 2013 Nov 28; 369[21]: 2091-2104). The 32-loci panel to measure a person’s genetic risk for stroke came from a 2018 report by a multinational team of researchers (Nature Genetics. 2018 Apr;50[4]: 524-37). The new analysis applied this 32-loci genetic test panel to 11.164 unrelated AFib patients with European ancestry from the ENGAGE AF-TIMIT 48 database. They divided this cohort into tertiles based on having a low, intermediate, or high stroke risk as assessed by the 32-loci genetic test. The analysis focused on patients enrolled in the trial who had European ancestry because the 32-loci screening test relied predominantly on data collected from people with this genetic background, Dr. Marston said.
SOURCE: Marston NA et al. AHA 2019, Abstract 336.
PHILADELPHIA – A 32-gene screening test for stroke risk identified a subgroup of atrial fibrillation (AFib) patients with an elevated rate of ischemic strokes despite having a low stroke risk by conventional criteria by their CHA2DS2-VASc score in a post-hoc analysis of more than 11,000 patients enrolled in a recent drug trial.
Overall, AFib patients in the highest tertile for genetic risk based on a 32 gene-loci test had a 31% increase rate of ischemic stroke during a median 2.8 years of follow-up compared with patients in the tertile with the lowest risk based on the 32-loci screen, Nicholas A. Marston, MD, said at the American Heart Association scientific sessions. This suggested that the genetic test had roughly the same association with an increased stroke risk as several components of the CHA2DS2-VASc score, such as female sex, an age of 65-74 years old, or having heart failure as a comorbidity, each of which links with an increased risk for ischemic stroke of about 31%-38%, Dr. Marston noted.
The genetic test produced even sharper discrimination among the patients with the lowest stroke risk as measured by their CHA2DS2-VASc score (Circulation. 2012 Aug 14;126[7]: 860-5). Among the slightly more than 3,000 patients in the study with a CHA2DS2-VASc score of three or less, those in the subgroup with the highest risk by the 32-loci screen had a stroke rate during follow-up that was 76% higher than those in the low or intermediate tertile for their genetic score. Among the 796 patients with a CHA2DS2-VASc score of just 1 or 2, those who also fell into the highest level of risk on the 32-loci screen had a stroke rate 3.5-fold higher than those with a similar CHA2DS2-VASc score but in the low and intermediate tertiles by the 32-loci screen.
The additional risk prediction provided by the 32-loci test was statistically significant in the analysis of the 3,071 patients with a CHA2DS2-VASc score of 3 or less after adjustment for age, sex, ancestry, and the individual components of the CHA2DS2-VASc score, which includes factors such as hypertension, diabetes, and heart failure, said Dr. Marston, a cardiologist at Brigham and Women’s Hospital in Boston. The 3.5-fold elevation among patients with a high genetic-risk score in the cohort of 796 patients with a CHA2DS2-VASc score of 1 or 2 just missed statistical significance (P = .06), possibly because the number of patients in the analysis was relatively low. Future research should explore the predictive value of the genetic risk score in patients with a CHA2DS2-VASc score of 0 or 1, the “group where therapeutic decisions could be altered” depending on the genetic risk score, he explained.
Dr. Marston and his associates used data collected in the ENGAGE AF-TIMI 48 (Effective Anticoagulation with Factor Xa Next Generation in Atrial Fibrillation–Thrombolysis in Myocardial Infarction 48) trial, which was designed to assess the safety and efficacy of the direct-acting oral anticoagulant edoxaban in patients with AFib (New Engl J Med. 2013 Nov 28; 369[21]: 2091-2104). The 32-loci panel to measure a person’s genetic risk for stroke came from a 2018 report by a multinational team of researchers (Nature Genetics. 2018 Apr;50[4]: 524-37). The new analysis applied this 32-loci genetic test panel to 11.164 unrelated AFib patients with European ancestry from the ENGAGE AF-TIMIT 48 database. They divided this cohort into tertiles based on having a low, intermediate, or high stroke risk as assessed by the 32-loci genetic test. The analysis focused on patients enrolled in the trial who had European ancestry because the 32-loci screening test relied predominantly on data collected from people with this genetic background, Dr. Marston said.
SOURCE: Marston NA et al. AHA 2019, Abstract 336.
PHILADELPHIA – A 32-gene screening test for stroke risk identified a subgroup of atrial fibrillation (AFib) patients with an elevated rate of ischemic strokes despite having a low stroke risk by conventional criteria by their CHA2DS2-VASc score in a post-hoc analysis of more than 11,000 patients enrolled in a recent drug trial.
Overall, AFib patients in the highest tertile for genetic risk based on a 32 gene-loci test had a 31% increase rate of ischemic stroke during a median 2.8 years of follow-up compared with patients in the tertile with the lowest risk based on the 32-loci screen, Nicholas A. Marston, MD, said at the American Heart Association scientific sessions. This suggested that the genetic test had roughly the same association with an increased stroke risk as several components of the CHA2DS2-VASc score, such as female sex, an age of 65-74 years old, or having heart failure as a comorbidity, each of which links with an increased risk for ischemic stroke of about 31%-38%, Dr. Marston noted.
The genetic test produced even sharper discrimination among the patients with the lowest stroke risk as measured by their CHA2DS2-VASc score (Circulation. 2012 Aug 14;126[7]: 860-5). Among the slightly more than 3,000 patients in the study with a CHA2DS2-VASc score of three or less, those in the subgroup with the highest risk by the 32-loci screen had a stroke rate during follow-up that was 76% higher than those in the low or intermediate tertile for their genetic score. Among the 796 patients with a CHA2DS2-VASc score of just 1 or 2, those who also fell into the highest level of risk on the 32-loci screen had a stroke rate 3.5-fold higher than those with a similar CHA2DS2-VASc score but in the low and intermediate tertiles by the 32-loci screen.
The additional risk prediction provided by the 32-loci test was statistically significant in the analysis of the 3,071 patients with a CHA2DS2-VASc score of 3 or less after adjustment for age, sex, ancestry, and the individual components of the CHA2DS2-VASc score, which includes factors such as hypertension, diabetes, and heart failure, said Dr. Marston, a cardiologist at Brigham and Women’s Hospital in Boston. The 3.5-fold elevation among patients with a high genetic-risk score in the cohort of 796 patients with a CHA2DS2-VASc score of 1 or 2 just missed statistical significance (P = .06), possibly because the number of patients in the analysis was relatively low. Future research should explore the predictive value of the genetic risk score in patients with a CHA2DS2-VASc score of 0 or 1, the “group where therapeutic decisions could be altered” depending on the genetic risk score, he explained.
Dr. Marston and his associates used data collected in the ENGAGE AF-TIMI 48 (Effective Anticoagulation with Factor Xa Next Generation in Atrial Fibrillation–Thrombolysis in Myocardial Infarction 48) trial, which was designed to assess the safety and efficacy of the direct-acting oral anticoagulant edoxaban in patients with AFib (New Engl J Med. 2013 Nov 28; 369[21]: 2091-2104). The 32-loci panel to measure a person’s genetic risk for stroke came from a 2018 report by a multinational team of researchers (Nature Genetics. 2018 Apr;50[4]: 524-37). The new analysis applied this 32-loci genetic test panel to 11.164 unrelated AFib patients with European ancestry from the ENGAGE AF-TIMIT 48 database. They divided this cohort into tertiles based on having a low, intermediate, or high stroke risk as assessed by the 32-loci genetic test. The analysis focused on patients enrolled in the trial who had European ancestry because the 32-loci screening test relied predominantly on data collected from people with this genetic background, Dr. Marston said.
SOURCE: Marston NA et al. AHA 2019, Abstract 336.
REPORTING FROM AHA 2019
Uncertain generalizability limits AFib ablation in HFrEF
Despite several reports of dramatic efficacy and reasonable safety using catheter ablation of atrial fibrillation (AFib) in patients with heart failure, many clinicians, including many heart failure specialists, remain skeptical about whether existing evidence supports using ablation routinely in selected heart failure patients.
Though concerns vary, one core stumbling block is inadequate confidence that the ablation outcomes reported from studies represent the benefit that the average American heart failure patient might expect to receive from ablation done outside of a study. A related issue is whether atrial fibrillation ablation in patients with heart failure is cost effective, especially at sites that did not participate in the published studies.
The first part of this article discussed the building evidence that radiofrequency catheter ablation of atrial fibrillation (AFib) can produce striking reductions in all-cause mortality of nearly 50%, and a greater than one-third cut in cardiovascular hospitalizations in patients with heart failure with reduced ejection fraction (HFrEF), according to one recent meta-analysis (Circ Arrhythm Electrophysiol. 2019 Sep;12[9]:e007414). A key question about the implications of these findings is their generalizability.
“Experience is an issue, and I agree that not every operator should do it. A common perception is that ablation doesn’t work, but that mindset is changing,” said Luigi Di Biase, MD, director of arrhythmia services at Montefiore Medical Center and professor of medicine at Albert Einstein College of Medicine in New York. He noted that some apparent ablations failures happen because the treatment is used too late. “Ablation will fail if it is done too late. Think about using ablation earlier,” he advised. “The earlier you ablate, the earlier you reduce the AFib burden and the sooner the patient benefits. Ablation is a cost-effective, first-line strategy for younger patients with paroxysmal AFib. The unanswered question is whether it is cost effective for patients who have both AFib and heart failure. It may be, because in addition to the mortality benefit, there are likely savings from a lower rate of hospitalizations. A clearer picture should emerge from the cost-effectiveness analysis of CASTLE-AF.”
CASTLE-AF (Catheter Ablation Versus Standard Conventional Therapy in Patients With Left Ventricular Dysfunction and Atrial Fibrillation), which randomized patients with heart failure and AFib to ablation or medical management (N Engl J Med. 2018 Feb 1;378[5]:417-27), is one of the highest-profile studies reported so far showing AFib ablation’s efficacy in patients with heart failure. However, it has drawn skepticism over its generalizability because of its long enrollment period of 8 years despite running at 33 worldwide sites, and by its winnowing of 3,013 patients assessed down to the 398 actually enrolled and 363 randomized and included in the efficacy analysis.
“CASTLE-HF showed a remarkable benefit. The problem was that it took years and years to enroll the patients,” commented Mariell Jessup, MD, a heart failure specialist and chief science and medical officer of the American Heart Association in Dallas.
At the annual congress of the European Society of Cardiology in September 2019, French researchers reported data that supported the generalizability of the CASTLE-AF findings. The study used data collected from 252,395 patients in the French national hospital-discharge database during 2010-2018 who had diagnoses of both heart failure and AFib. Among these patients, 1,384 underwent catheter ablation and the remaining 251,011 were managed without ablation.
During a median follow-up of 537 days (about 1.5 years), the incidence of both all-cause death and heart failure hospitalization were both significantly lower in the ablated patients. The ablated patients were also much younger and were more often men, but both groups had several prevalent comorbidities at roughly similar rates. To better match the groups, the French researchers ran both a multivariate analysis, and then an even more intensively adjusting propensity-score analysis that compared the ablated patients with 1,384 closely matched patients from the nonablated group. Both analyses showed substantial incremental benefit from ablation. In the propensity score–matched analysis, ablation was linked with a relative 66% cut in all-cause death, and a relative 71% reduction in heart failure hospitalizations, compared with the patients who did not undergo ablation, reported Arnaud Bisson, MD, a cardiologist at the University of Tours (France).
Another recent assessment of the generalizability of the AFib ablation trial findings used data from nearly 184,000 U.S. patients treated for AFib during 2009-2016 in an administrative database, including more than 12,000 treated with ablation. This analysis did not take into account the coexistence of heart failure. After propensity-score matching of the ablated patients with a similar subgroup of those managed medically, the results showed a 25% relative cut in the combined primary endpoint used in the CABANA (Catheter Ablation vs. Anti-Arrhythmic Drug Therapy for Atrial Fibrillation Trial) study (JAMA. 2019 Mar 15;321[134]:1261-74). Among the 74% of ablated patients who met the enrollment criteria for CABANA, the primary endpoint reduction was even greater, a 30% drop relative to matched patients who did not undergo ablation (Eur Heart J. 2019 Apr 21;40[16]:1257-64).
“Professional societies are working to clarify best practices for procedural volume, outcomes, etc.,” said Jonathan P. Piccini, MD, a cardiac electrophysiologist at Duke University, Durham, N.C., and a CABANA coinvestigator. “There are some data on ablation cost effectiveness, and they generally favor” positive cost efficacy, with more analyses now in progress,” he noted in an interview.
Many unanswered questions remain about AFib in heart failure patients and how aggressively to use ablation to treat it. Most of the data so far have come from patients with HFrEF, and so most experts consider AFib ablation in patients with heart failure with preserved ejection fraction (HFpEF) a big unknown, although nearly 80% of the heart failure patients enrolled in CABANA (the largest randomized trial of AFib ablation with more than 2,200 patients) had left ventricular ejection fraction of 50% or greater, which translates into HFpEF. Another gray area is how to think about asymptomatic (also called subclinical) AFib and whether that warrants ablation in heart failure patients. The presence or absence of symptoms is a major consideration because the traditional indication for ablation has been to reduce or eliminate symptoms like palpitations, a step that can substantially improve patients’ quality of life as well as their left ventricular function. The indication to ablate asymptomatic AFib for the purpose of improving survival and reducing hospitalizations is the new and controversial concept. Yet it has been embraced by some heart failure physicians.
“Whether or not AFib is symptomatic doesn’t matter” in a heart failure patient, said Maria Rosa Costanzo, MD, a heart failure physician at Edward Heart Hospital in Naperville, Ill. “A patient with AFib doesn’t get the atrial contribution to cardiac output. When we look deeper, a patient with ‘asymptomatic’ AFib often has symptoms, such as new fatigue or obstructive sleep apnea, so when you see a patient with asymptomatic AFib look for sleep apnea, a trigger for AFib,” Dr. Costanzo advised. “Sleep apnea, AFib, and heart failure form a triad” that often clusters in patients, and the three conditions interact in a vicious circle of reinforcing comorbidities, she said in an interview.
The cardiac electrophysiology and arrhythmia community clearly realizes that catheter ablation of AFib, in patients with or without heart failure, has many unaddressed questions about who should administer it and who should undergo it. In March 2019, the National Heart, Lung, and Blood Institute held a workshop on AFib ablation. “Numerous knowledge gaps remain” about the best way to use ablation, said a summary of the workshop (Circulation. 2019 Nov 20;doi: 10.1161/CIRCULATIONAHA.119.042706). Among the research needs highlighted by the workshop was “more definitive studies ... to delineate the impact of AFib ablation on outcomes in patients with heart failure with preserved ejection fraction.” The workshop recommended establishing a national U.S. registry for AFib ablations with a reliable source of funding, as well as “establishing the cause-effect relationship between ventricular dysfunction and AFib, and the potential moderating role of atrial structure and function.” The workshop also raised the possibility of sham-controlled assessments of AFib ablation, while conceding that enrollment into such trials would probably be very challenging.
The upshot is that, even while ablation advocates agree on the need for more study, clinicians are using AFib ablation on a growing number of heart failure patients (as well as on growing numbers of patients with AFib but without heart failure), with a focus on treating those who “have refractory symptoms or evidence of tachycardia-induced cardiomyopathy,” said Dr. Piccini. Extending that to a first-line, class I indication for heart failure patients seems to need more data, and also needs clinicians to collectively raise their comfort level with the ablation concept. If results from additional studies now underway support the dramatic efficacy and reasonable safety that’s already been seen with ablation, then increased comfort should follow.
CABANA received funding from Biosense Webster, Boston Scientific, Medtronic, and St. Jude. CASTLE-AF was funded by Biotronik. Dr. Di Biase, Dr. Jessup, and Dr. Bisson had no disclosures. Dr. Piccini has been a consultant to Allergan, Biotronik, Medtronic, Phillips, and Sanofi Aventis; he has received research funding from Abbott, ARCA, Boston Scientific, Gilead, and Johnson & Johnson; and he had a financial relationship with GlaxoSmithKline. Dr. Costanzo has been a consultant to Abbott.
This is part 2 of a 2-part story. See part 1 here.
Despite several reports of dramatic efficacy and reasonable safety using catheter ablation of atrial fibrillation (AFib) in patients with heart failure, many clinicians, including many heart failure specialists, remain skeptical about whether existing evidence supports using ablation routinely in selected heart failure patients.
Though concerns vary, one core stumbling block is inadequate confidence that the ablation outcomes reported from studies represent the benefit that the average American heart failure patient might expect to receive from ablation done outside of a study. A related issue is whether atrial fibrillation ablation in patients with heart failure is cost effective, especially at sites that did not participate in the published studies.
The first part of this article discussed the building evidence that radiofrequency catheter ablation of atrial fibrillation (AFib) can produce striking reductions in all-cause mortality of nearly 50%, and a greater than one-third cut in cardiovascular hospitalizations in patients with heart failure with reduced ejection fraction (HFrEF), according to one recent meta-analysis (Circ Arrhythm Electrophysiol. 2019 Sep;12[9]:e007414). A key question about the implications of these findings is their generalizability.
“Experience is an issue, and I agree that not every operator should do it. A common perception is that ablation doesn’t work, but that mindset is changing,” said Luigi Di Biase, MD, director of arrhythmia services at Montefiore Medical Center and professor of medicine at Albert Einstein College of Medicine in New York. He noted that some apparent ablations failures happen because the treatment is used too late. “Ablation will fail if it is done too late. Think about using ablation earlier,” he advised. “The earlier you ablate, the earlier you reduce the AFib burden and the sooner the patient benefits. Ablation is a cost-effective, first-line strategy for younger patients with paroxysmal AFib. The unanswered question is whether it is cost effective for patients who have both AFib and heart failure. It may be, because in addition to the mortality benefit, there are likely savings from a lower rate of hospitalizations. A clearer picture should emerge from the cost-effectiveness analysis of CASTLE-AF.”
CASTLE-AF (Catheter Ablation Versus Standard Conventional Therapy in Patients With Left Ventricular Dysfunction and Atrial Fibrillation), which randomized patients with heart failure and AFib to ablation or medical management (N Engl J Med. 2018 Feb 1;378[5]:417-27), is one of the highest-profile studies reported so far showing AFib ablation’s efficacy in patients with heart failure. However, it has drawn skepticism over its generalizability because of its long enrollment period of 8 years despite running at 33 worldwide sites, and by its winnowing of 3,013 patients assessed down to the 398 actually enrolled and 363 randomized and included in the efficacy analysis.
“CASTLE-HF showed a remarkable benefit. The problem was that it took years and years to enroll the patients,” commented Mariell Jessup, MD, a heart failure specialist and chief science and medical officer of the American Heart Association in Dallas.
At the annual congress of the European Society of Cardiology in September 2019, French researchers reported data that supported the generalizability of the CASTLE-AF findings. The study used data collected from 252,395 patients in the French national hospital-discharge database during 2010-2018 who had diagnoses of both heart failure and AFib. Among these patients, 1,384 underwent catheter ablation and the remaining 251,011 were managed without ablation.
During a median follow-up of 537 days (about 1.5 years), the incidence of both all-cause death and heart failure hospitalization were both significantly lower in the ablated patients. The ablated patients were also much younger and were more often men, but both groups had several prevalent comorbidities at roughly similar rates. To better match the groups, the French researchers ran both a multivariate analysis, and then an even more intensively adjusting propensity-score analysis that compared the ablated patients with 1,384 closely matched patients from the nonablated group. Both analyses showed substantial incremental benefit from ablation. In the propensity score–matched analysis, ablation was linked with a relative 66% cut in all-cause death, and a relative 71% reduction in heart failure hospitalizations, compared with the patients who did not undergo ablation, reported Arnaud Bisson, MD, a cardiologist at the University of Tours (France).
Another recent assessment of the generalizability of the AFib ablation trial findings used data from nearly 184,000 U.S. patients treated for AFib during 2009-2016 in an administrative database, including more than 12,000 treated with ablation. This analysis did not take into account the coexistence of heart failure. After propensity-score matching of the ablated patients with a similar subgroup of those managed medically, the results showed a 25% relative cut in the combined primary endpoint used in the CABANA (Catheter Ablation vs. Anti-Arrhythmic Drug Therapy for Atrial Fibrillation Trial) study (JAMA. 2019 Mar 15;321[134]:1261-74). Among the 74% of ablated patients who met the enrollment criteria for CABANA, the primary endpoint reduction was even greater, a 30% drop relative to matched patients who did not undergo ablation (Eur Heart J. 2019 Apr 21;40[16]:1257-64).
“Professional societies are working to clarify best practices for procedural volume, outcomes, etc.,” said Jonathan P. Piccini, MD, a cardiac electrophysiologist at Duke University, Durham, N.C., and a CABANA coinvestigator. “There are some data on ablation cost effectiveness, and they generally favor” positive cost efficacy, with more analyses now in progress,” he noted in an interview.
Many unanswered questions remain about AFib in heart failure patients and how aggressively to use ablation to treat it. Most of the data so far have come from patients with HFrEF, and so most experts consider AFib ablation in patients with heart failure with preserved ejection fraction (HFpEF) a big unknown, although nearly 80% of the heart failure patients enrolled in CABANA (the largest randomized trial of AFib ablation with more than 2,200 patients) had left ventricular ejection fraction of 50% or greater, which translates into HFpEF. Another gray area is how to think about asymptomatic (also called subclinical) AFib and whether that warrants ablation in heart failure patients. The presence or absence of symptoms is a major consideration because the traditional indication for ablation has been to reduce or eliminate symptoms like palpitations, a step that can substantially improve patients’ quality of life as well as their left ventricular function. The indication to ablate asymptomatic AFib for the purpose of improving survival and reducing hospitalizations is the new and controversial concept. Yet it has been embraced by some heart failure physicians.
“Whether or not AFib is symptomatic doesn’t matter” in a heart failure patient, said Maria Rosa Costanzo, MD, a heart failure physician at Edward Heart Hospital in Naperville, Ill. “A patient with AFib doesn’t get the atrial contribution to cardiac output. When we look deeper, a patient with ‘asymptomatic’ AFib often has symptoms, such as new fatigue or obstructive sleep apnea, so when you see a patient with asymptomatic AFib look for sleep apnea, a trigger for AFib,” Dr. Costanzo advised. “Sleep apnea, AFib, and heart failure form a triad” that often clusters in patients, and the three conditions interact in a vicious circle of reinforcing comorbidities, she said in an interview.
The cardiac electrophysiology and arrhythmia community clearly realizes that catheter ablation of AFib, in patients with or without heart failure, has many unaddressed questions about who should administer it and who should undergo it. In March 2019, the National Heart, Lung, and Blood Institute held a workshop on AFib ablation. “Numerous knowledge gaps remain” about the best way to use ablation, said a summary of the workshop (Circulation. 2019 Nov 20;doi: 10.1161/CIRCULATIONAHA.119.042706). Among the research needs highlighted by the workshop was “more definitive studies ... to delineate the impact of AFib ablation on outcomes in patients with heart failure with preserved ejection fraction.” The workshop recommended establishing a national U.S. registry for AFib ablations with a reliable source of funding, as well as “establishing the cause-effect relationship between ventricular dysfunction and AFib, and the potential moderating role of atrial structure and function.” The workshop also raised the possibility of sham-controlled assessments of AFib ablation, while conceding that enrollment into such trials would probably be very challenging.
The upshot is that, even while ablation advocates agree on the need for more study, clinicians are using AFib ablation on a growing number of heart failure patients (as well as on growing numbers of patients with AFib but without heart failure), with a focus on treating those who “have refractory symptoms or evidence of tachycardia-induced cardiomyopathy,” said Dr. Piccini. Extending that to a first-line, class I indication for heart failure patients seems to need more data, and also needs clinicians to collectively raise their comfort level with the ablation concept. If results from additional studies now underway support the dramatic efficacy and reasonable safety that’s already been seen with ablation, then increased comfort should follow.
CABANA received funding from Biosense Webster, Boston Scientific, Medtronic, and St. Jude. CASTLE-AF was funded by Biotronik. Dr. Di Biase, Dr. Jessup, and Dr. Bisson had no disclosures. Dr. Piccini has been a consultant to Allergan, Biotronik, Medtronic, Phillips, and Sanofi Aventis; he has received research funding from Abbott, ARCA, Boston Scientific, Gilead, and Johnson & Johnson; and he had a financial relationship with GlaxoSmithKline. Dr. Costanzo has been a consultant to Abbott.
This is part 2 of a 2-part story. See part 1 here.
Despite several reports of dramatic efficacy and reasonable safety using catheter ablation of atrial fibrillation (AFib) in patients with heart failure, many clinicians, including many heart failure specialists, remain skeptical about whether existing evidence supports using ablation routinely in selected heart failure patients.
Though concerns vary, one core stumbling block is inadequate confidence that the ablation outcomes reported from studies represent the benefit that the average American heart failure patient might expect to receive from ablation done outside of a study. A related issue is whether atrial fibrillation ablation in patients with heart failure is cost effective, especially at sites that did not participate in the published studies.
The first part of this article discussed the building evidence that radiofrequency catheter ablation of atrial fibrillation (AFib) can produce striking reductions in all-cause mortality of nearly 50%, and a greater than one-third cut in cardiovascular hospitalizations in patients with heart failure with reduced ejection fraction (HFrEF), according to one recent meta-analysis (Circ Arrhythm Electrophysiol. 2019 Sep;12[9]:e007414). A key question about the implications of these findings is their generalizability.
“Experience is an issue, and I agree that not every operator should do it. A common perception is that ablation doesn’t work, but that mindset is changing,” said Luigi Di Biase, MD, director of arrhythmia services at Montefiore Medical Center and professor of medicine at Albert Einstein College of Medicine in New York. He noted that some apparent ablations failures happen because the treatment is used too late. “Ablation will fail if it is done too late. Think about using ablation earlier,” he advised. “The earlier you ablate, the earlier you reduce the AFib burden and the sooner the patient benefits. Ablation is a cost-effective, first-line strategy for younger patients with paroxysmal AFib. The unanswered question is whether it is cost effective for patients who have both AFib and heart failure. It may be, because in addition to the mortality benefit, there are likely savings from a lower rate of hospitalizations. A clearer picture should emerge from the cost-effectiveness analysis of CASTLE-AF.”
CASTLE-AF (Catheter Ablation Versus Standard Conventional Therapy in Patients With Left Ventricular Dysfunction and Atrial Fibrillation), which randomized patients with heart failure and AFib to ablation or medical management (N Engl J Med. 2018 Feb 1;378[5]:417-27), is one of the highest-profile studies reported so far showing AFib ablation’s efficacy in patients with heart failure. However, it has drawn skepticism over its generalizability because of its long enrollment period of 8 years despite running at 33 worldwide sites, and by its winnowing of 3,013 patients assessed down to the 398 actually enrolled and 363 randomized and included in the efficacy analysis.
“CASTLE-HF showed a remarkable benefit. The problem was that it took years and years to enroll the patients,” commented Mariell Jessup, MD, a heart failure specialist and chief science and medical officer of the American Heart Association in Dallas.
At the annual congress of the European Society of Cardiology in September 2019, French researchers reported data that supported the generalizability of the CASTLE-AF findings. The study used data collected from 252,395 patients in the French national hospital-discharge database during 2010-2018 who had diagnoses of both heart failure and AFib. Among these patients, 1,384 underwent catheter ablation and the remaining 251,011 were managed without ablation.
During a median follow-up of 537 days (about 1.5 years), the incidence of both all-cause death and heart failure hospitalization were both significantly lower in the ablated patients. The ablated patients were also much younger and were more often men, but both groups had several prevalent comorbidities at roughly similar rates. To better match the groups, the French researchers ran both a multivariate analysis, and then an even more intensively adjusting propensity-score analysis that compared the ablated patients with 1,384 closely matched patients from the nonablated group. Both analyses showed substantial incremental benefit from ablation. In the propensity score–matched analysis, ablation was linked with a relative 66% cut in all-cause death, and a relative 71% reduction in heart failure hospitalizations, compared with the patients who did not undergo ablation, reported Arnaud Bisson, MD, a cardiologist at the University of Tours (France).
Another recent assessment of the generalizability of the AFib ablation trial findings used data from nearly 184,000 U.S. patients treated for AFib during 2009-2016 in an administrative database, including more than 12,000 treated with ablation. This analysis did not take into account the coexistence of heart failure. After propensity-score matching of the ablated patients with a similar subgroup of those managed medically, the results showed a 25% relative cut in the combined primary endpoint used in the CABANA (Catheter Ablation vs. Anti-Arrhythmic Drug Therapy for Atrial Fibrillation Trial) study (JAMA. 2019 Mar 15;321[134]:1261-74). Among the 74% of ablated patients who met the enrollment criteria for CABANA, the primary endpoint reduction was even greater, a 30% drop relative to matched patients who did not undergo ablation (Eur Heart J. 2019 Apr 21;40[16]:1257-64).
“Professional societies are working to clarify best practices for procedural volume, outcomes, etc.,” said Jonathan P. Piccini, MD, a cardiac electrophysiologist at Duke University, Durham, N.C., and a CABANA coinvestigator. “There are some data on ablation cost effectiveness, and they generally favor” positive cost efficacy, with more analyses now in progress,” he noted in an interview.
Many unanswered questions remain about AFib in heart failure patients and how aggressively to use ablation to treat it. Most of the data so far have come from patients with HFrEF, and so most experts consider AFib ablation in patients with heart failure with preserved ejection fraction (HFpEF) a big unknown, although nearly 80% of the heart failure patients enrolled in CABANA (the largest randomized trial of AFib ablation with more than 2,200 patients) had left ventricular ejection fraction of 50% or greater, which translates into HFpEF. Another gray area is how to think about asymptomatic (also called subclinical) AFib and whether that warrants ablation in heart failure patients. The presence or absence of symptoms is a major consideration because the traditional indication for ablation has been to reduce or eliminate symptoms like palpitations, a step that can substantially improve patients’ quality of life as well as their left ventricular function. The indication to ablate asymptomatic AFib for the purpose of improving survival and reducing hospitalizations is the new and controversial concept. Yet it has been embraced by some heart failure physicians.
“Whether or not AFib is symptomatic doesn’t matter” in a heart failure patient, said Maria Rosa Costanzo, MD, a heart failure physician at Edward Heart Hospital in Naperville, Ill. “A patient with AFib doesn’t get the atrial contribution to cardiac output. When we look deeper, a patient with ‘asymptomatic’ AFib often has symptoms, such as new fatigue or obstructive sleep apnea, so when you see a patient with asymptomatic AFib look for sleep apnea, a trigger for AFib,” Dr. Costanzo advised. “Sleep apnea, AFib, and heart failure form a triad” that often clusters in patients, and the three conditions interact in a vicious circle of reinforcing comorbidities, she said in an interview.
The cardiac electrophysiology and arrhythmia community clearly realizes that catheter ablation of AFib, in patients with or without heart failure, has many unaddressed questions about who should administer it and who should undergo it. In March 2019, the National Heart, Lung, and Blood Institute held a workshop on AFib ablation. “Numerous knowledge gaps remain” about the best way to use ablation, said a summary of the workshop (Circulation. 2019 Nov 20;doi: 10.1161/CIRCULATIONAHA.119.042706). Among the research needs highlighted by the workshop was “more definitive studies ... to delineate the impact of AFib ablation on outcomes in patients with heart failure with preserved ejection fraction.” The workshop recommended establishing a national U.S. registry for AFib ablations with a reliable source of funding, as well as “establishing the cause-effect relationship between ventricular dysfunction and AFib, and the potential moderating role of atrial structure and function.” The workshop also raised the possibility of sham-controlled assessments of AFib ablation, while conceding that enrollment into such trials would probably be very challenging.
The upshot is that, even while ablation advocates agree on the need for more study, clinicians are using AFib ablation on a growing number of heart failure patients (as well as on growing numbers of patients with AFib but without heart failure), with a focus on treating those who “have refractory symptoms or evidence of tachycardia-induced cardiomyopathy,” said Dr. Piccini. Extending that to a first-line, class I indication for heart failure patients seems to need more data, and also needs clinicians to collectively raise their comfort level with the ablation concept. If results from additional studies now underway support the dramatic efficacy and reasonable safety that’s already been seen with ablation, then increased comfort should follow.
CABANA received funding from Biosense Webster, Boston Scientific, Medtronic, and St. Jude. CASTLE-AF was funded by Biotronik. Dr. Di Biase, Dr. Jessup, and Dr. Bisson had no disclosures. Dr. Piccini has been a consultant to Allergan, Biotronik, Medtronic, Phillips, and Sanofi Aventis; he has received research funding from Abbott, ARCA, Boston Scientific, Gilead, and Johnson & Johnson; and he had a financial relationship with GlaxoSmithKline. Dr. Costanzo has been a consultant to Abbott.
This is part 2 of a 2-part story. See part 1 here.
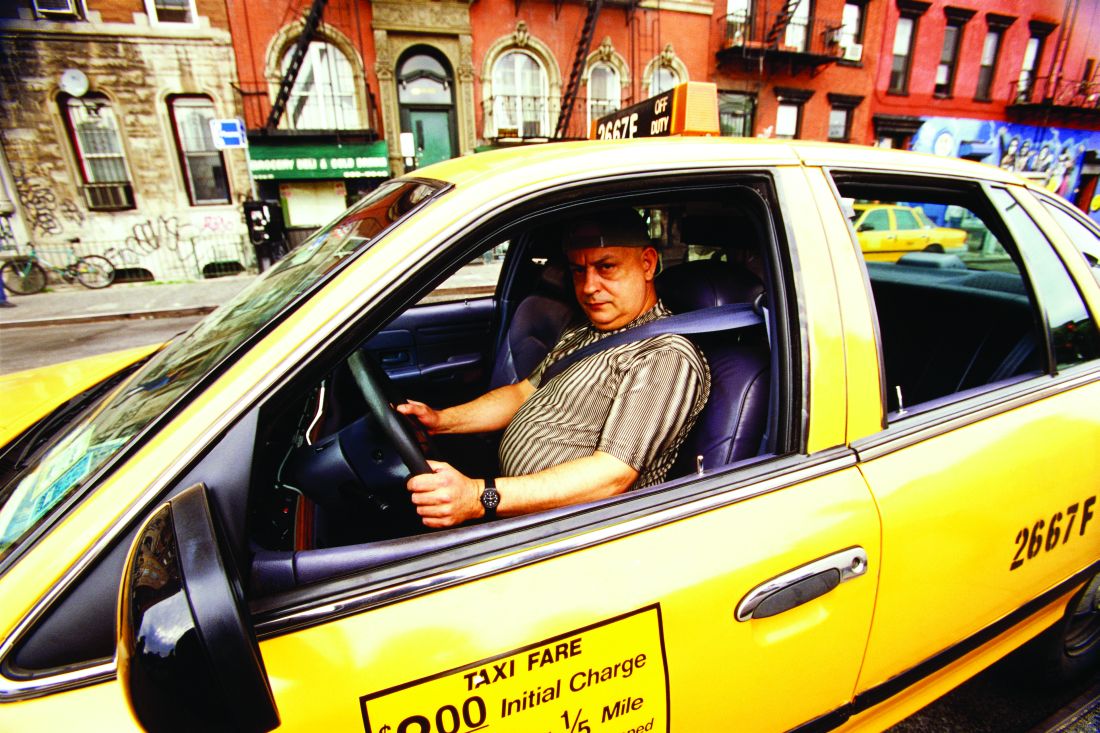
Cardiac arrests peak with pollution in Japan
PHILADELPHIA – Out-of-hospital cardiac arrests spike with daily counts of emissions-related particulate matter – a key contributor to urban smog – and particularly affect men and people older than age 75, according to results of a nationwide Japanese study presented at the American Heart Association scientific sessions.
“Short-term exposure to particulate pollutants is a potential trigger for cardiac-origin, out-of-hospital cardiac arrest [OHCA] onset in Japan,” said Sunao Kojima, MD, a professor at Kawasaki Medical School in Kurashiki, Japan.
The study used the All-Japan Utstein Registry of OHCA throughout all 47 prefectures in Japan. The analysis then applied prefecture-specific estimates of PM2.5 – particulate matter that measures 2.5 mcm in average diameter – using a time-stratified, case-crossover design. By comparison, PM2.5 is about 1/40th the diameter of human hair (approximately 100 mcm) and about 1/12th that of cedar pollen (30 mcm).
“Increased OHCAs incidence correlated with the average increase in PM2.5 concentrations over those observed 1 day before cardiac arrest,” Dr. Kojima said.
What’s noteworthy about the Utstein registry, Dr. Kojima said, is that emergency medical service personnel in Japan are not authorized to terminate resuscitation efforts, so most OHCA patients are transported to the nearest hospital and are thus counted in the registry.
From a total count of 1.4 million EMS-assessed OHCAs from 2005 through 2016, the study focused on 103,189 bystander-witnessed events from April 2011 through 2016. The analysis further divided that population into three groups: those presenting with initial ventricular fibrillation/pulseless ventricular tachycardia (20,848); those without initial VF/pulseless VT (80,110); and those with initial cardiac rhythm of unknown origin (2,231).
“The pathways linking PM2.5 exposure with OHCA remain unknown, but several mechanisms have been suspected,” Dr. Kojima said. “A major mechanism is thought to be associated with oxidative stress and systemic inflammation.”
The average daily concentration for PM2.5 was 13.9/m3 across all of Japan, Dr. Kojima said, with the highest concentrations in western Japan (16.3/m3). A 10-mcg/m3 increase in the average PM2.5 concentrations on the day of OHCA from the previous day (lag 0-1) was associated with a 1.6% increase in OHCAs (95% confidence interval, 0.1-3.1%), he said.
“Increased PM2.5 concentrations were closely associated with OHCA incidence, even when adjusted for other pollutants, such as ozone, nitrogen dioxide, sulfur dioxide, and lag 0-1,” Dr. Kojima said.
The incidence for PM2.5-related OHCA was higher for people age 75 and older and for men, during the warm season and in the central region. In the central region, the incidence increased around 6% for every 10-mcg/m3 day-to-day increase in the average PM2.5 compared to less than 1% increases in the eastern and western regions, Dr. Kojima said.
PM2.5 levels also seemed to influence outcomes depending on the origin of the OHCA, he said. Patients with VF/pulseless VT and pulseless electrical activity had better outcomes than did those with asystole. Increased PM2.5 levels were linked with lower rates of restoration of spontaneous circulation, 1-month survival, and 1-month survival with minimal neurological impairment, he said. Patients who had chest-compression-only CPR seemed to do significantly better than did those who had chest compression with rescue breathing, he said.
“There may be room for further discussion regarding the impact of performing rescue breathing in CPR and the consequent effects of short-term PM2.5 exposure on patients with cardiac origin,” he said.
Dr. Kojima has no financial relationships to disclose. The study received funding from the Japan Ministry of the Environment, Japan Society for the Promotion of Science, and Foundation for Total Health Promotion, Japan.
SOURCE: Kojima S. AHA 2019, Session FS.AOS.F1.
PHILADELPHIA – Out-of-hospital cardiac arrests spike with daily counts of emissions-related particulate matter – a key contributor to urban smog – and particularly affect men and people older than age 75, according to results of a nationwide Japanese study presented at the American Heart Association scientific sessions.
“Short-term exposure to particulate pollutants is a potential trigger for cardiac-origin, out-of-hospital cardiac arrest [OHCA] onset in Japan,” said Sunao Kojima, MD, a professor at Kawasaki Medical School in Kurashiki, Japan.
The study used the All-Japan Utstein Registry of OHCA throughout all 47 prefectures in Japan. The analysis then applied prefecture-specific estimates of PM2.5 – particulate matter that measures 2.5 mcm in average diameter – using a time-stratified, case-crossover design. By comparison, PM2.5 is about 1/40th the diameter of human hair (approximately 100 mcm) and about 1/12th that of cedar pollen (30 mcm).
“Increased OHCAs incidence correlated with the average increase in PM2.5 concentrations over those observed 1 day before cardiac arrest,” Dr. Kojima said.
What’s noteworthy about the Utstein registry, Dr. Kojima said, is that emergency medical service personnel in Japan are not authorized to terminate resuscitation efforts, so most OHCA patients are transported to the nearest hospital and are thus counted in the registry.
From a total count of 1.4 million EMS-assessed OHCAs from 2005 through 2016, the study focused on 103,189 bystander-witnessed events from April 2011 through 2016. The analysis further divided that population into three groups: those presenting with initial ventricular fibrillation/pulseless ventricular tachycardia (20,848); those without initial VF/pulseless VT (80,110); and those with initial cardiac rhythm of unknown origin (2,231).
“The pathways linking PM2.5 exposure with OHCA remain unknown, but several mechanisms have been suspected,” Dr. Kojima said. “A major mechanism is thought to be associated with oxidative stress and systemic inflammation.”
The average daily concentration for PM2.5 was 13.9/m3 across all of Japan, Dr. Kojima said, with the highest concentrations in western Japan (16.3/m3). A 10-mcg/m3 increase in the average PM2.5 concentrations on the day of OHCA from the previous day (lag 0-1) was associated with a 1.6% increase in OHCAs (95% confidence interval, 0.1-3.1%), he said.
“Increased PM2.5 concentrations were closely associated with OHCA incidence, even when adjusted for other pollutants, such as ozone, nitrogen dioxide, sulfur dioxide, and lag 0-1,” Dr. Kojima said.
The incidence for PM2.5-related OHCA was higher for people age 75 and older and for men, during the warm season and in the central region. In the central region, the incidence increased around 6% for every 10-mcg/m3 day-to-day increase in the average PM2.5 compared to less than 1% increases in the eastern and western regions, Dr. Kojima said.
PM2.5 levels also seemed to influence outcomes depending on the origin of the OHCA, he said. Patients with VF/pulseless VT and pulseless electrical activity had better outcomes than did those with asystole. Increased PM2.5 levels were linked with lower rates of restoration of spontaneous circulation, 1-month survival, and 1-month survival with minimal neurological impairment, he said. Patients who had chest-compression-only CPR seemed to do significantly better than did those who had chest compression with rescue breathing, he said.
“There may be room for further discussion regarding the impact of performing rescue breathing in CPR and the consequent effects of short-term PM2.5 exposure on patients with cardiac origin,” he said.
Dr. Kojima has no financial relationships to disclose. The study received funding from the Japan Ministry of the Environment, Japan Society for the Promotion of Science, and Foundation for Total Health Promotion, Japan.
SOURCE: Kojima S. AHA 2019, Session FS.AOS.F1.
PHILADELPHIA – Out-of-hospital cardiac arrests spike with daily counts of emissions-related particulate matter – a key contributor to urban smog – and particularly affect men and people older than age 75, according to results of a nationwide Japanese study presented at the American Heart Association scientific sessions.
“Short-term exposure to particulate pollutants is a potential trigger for cardiac-origin, out-of-hospital cardiac arrest [OHCA] onset in Japan,” said Sunao Kojima, MD, a professor at Kawasaki Medical School in Kurashiki, Japan.
The study used the All-Japan Utstein Registry of OHCA throughout all 47 prefectures in Japan. The analysis then applied prefecture-specific estimates of PM2.5 – particulate matter that measures 2.5 mcm in average diameter – using a time-stratified, case-crossover design. By comparison, PM2.5 is about 1/40th the diameter of human hair (approximately 100 mcm) and about 1/12th that of cedar pollen (30 mcm).
“Increased OHCAs incidence correlated with the average increase in PM2.5 concentrations over those observed 1 day before cardiac arrest,” Dr. Kojima said.
What’s noteworthy about the Utstein registry, Dr. Kojima said, is that emergency medical service personnel in Japan are not authorized to terminate resuscitation efforts, so most OHCA patients are transported to the nearest hospital and are thus counted in the registry.
From a total count of 1.4 million EMS-assessed OHCAs from 2005 through 2016, the study focused on 103,189 bystander-witnessed events from April 2011 through 2016. The analysis further divided that population into three groups: those presenting with initial ventricular fibrillation/pulseless ventricular tachycardia (20,848); those without initial VF/pulseless VT (80,110); and those with initial cardiac rhythm of unknown origin (2,231).
“The pathways linking PM2.5 exposure with OHCA remain unknown, but several mechanisms have been suspected,” Dr. Kojima said. “A major mechanism is thought to be associated with oxidative stress and systemic inflammation.”
The average daily concentration for PM2.5 was 13.9/m3 across all of Japan, Dr. Kojima said, with the highest concentrations in western Japan (16.3/m3). A 10-mcg/m3 increase in the average PM2.5 concentrations on the day of OHCA from the previous day (lag 0-1) was associated with a 1.6% increase in OHCAs (95% confidence interval, 0.1-3.1%), he said.
“Increased PM2.5 concentrations were closely associated with OHCA incidence, even when adjusted for other pollutants, such as ozone, nitrogen dioxide, sulfur dioxide, and lag 0-1,” Dr. Kojima said.
The incidence for PM2.5-related OHCA was higher for people age 75 and older and for men, during the warm season and in the central region. In the central region, the incidence increased around 6% for every 10-mcg/m3 day-to-day increase in the average PM2.5 compared to less than 1% increases in the eastern and western regions, Dr. Kojima said.
PM2.5 levels also seemed to influence outcomes depending on the origin of the OHCA, he said. Patients with VF/pulseless VT and pulseless electrical activity had better outcomes than did those with asystole. Increased PM2.5 levels were linked with lower rates of restoration of spontaneous circulation, 1-month survival, and 1-month survival with minimal neurological impairment, he said. Patients who had chest-compression-only CPR seemed to do significantly better than did those who had chest compression with rescue breathing, he said.
“There may be room for further discussion regarding the impact of performing rescue breathing in CPR and the consequent effects of short-term PM2.5 exposure on patients with cardiac origin,” he said.
Dr. Kojima has no financial relationships to disclose. The study received funding from the Japan Ministry of the Environment, Japan Society for the Promotion of Science, and Foundation for Total Health Promotion, Japan.
SOURCE: Kojima S. AHA 2019, Session FS.AOS.F1.
REPORTING FROM AHA 2019
Evidence builds for AFib ablation’s efficacy in heart failure
Roughly a third of patients with heart failure also have atrial fibrillation, a comorbid combination notorious for working synergistically to worsen a patient’s quality of life and life expectancy.
During the past year, radiofrequency catheter ablation of atrial fibrillation in patients with both conditions has gathered steam as a way to intervene in at least selected patients, driven by study results that featured attention-grabbing reductions in death and cardiovascular hospitalizations.
The evidence favoring catheter ablation of atrial fibrillation (AFib) in patients with heart failure, particularly patients with heart failure with reduced ejection fraction (HFrEF), ramped up in 2019, spurred largely by a subgroup analysis from the CABANA trial, the largest randomized comparison by far of AFib ablation with antiarrhythmic drug treatment with 2,204 patients.
The past few months also featured release of two meta-analyses that took the CABANA results into account plus findings from about a dozen earlier randomized studies. Both meta-analyses, as well as the heart failure analysis from CABANA, all point in one direction, as stated in the conclusion of one of the meta-analyses: “In patients with AFib, catheter ablation is associated with all-cause mortality benefit, compared with medical therapy, that is driven by patients with AFib and HFrEF. Catheter ablation is safe and reduces cardiovascular hospitalizations and recurrences of atrial arrhythmias” both in patients with paroxysmal and persistent AFib,” wrote Stavros Stavrakis, MD, and his associates in their systematic review of 18 randomized, controlled trials of catheter ablation of AFib in a total of 4,464 patients with or without heart failure (Circ Arrhythm Electrophysiol. 2019 Sep;12[9]: e007414).
Despite these new data and analyses, clinicians seem to have very mixed reactions. Some call for an upgraded recommendation by professional societies that would support more aggressive use of AFib ablation in heart failure patients, and the anecdotal impressions of people who manage these patients are that ablation procedures have recently increased. But others advise caution, and note that in their opinion the efficacy data remain preliminary; the procedure has safety, logistical, and economic concerns; and questions remain about the ability of all active ablation programs to consistently deliver the results seen in published trials.
The meta-analysis led by Dr. Stavrakis showed that catheter ablation of AFib cut all-cause mortality during follow-up by a statistically significant 31%, compared with medical therapy, in all patients regardless of their heart failure status. But in patients with HFrEF, the reduction was 48%, along with a 38% cut in cardiovascular hospitalizations. In contrast, patients without heart failure who underwent AFib ablation showed no significant change in their all-cause mortality, compared with medical management of these patients.
“Based both on our meta-analysis and the CABANA data, patients with AFib most likely to benefit from ablation are patients younger than 65 and those with heart failure,” summed up Dr. Stavrakis, a cardiac electrophysiologist at the Heart Rhythm Institute of the University of Oklahoma in Oklahoma City.
The second meta-analysis, which initially appeared in July, analyzed data from 11 randomized trials of catheter ablations compared with anti-arrhythmic medical therapy for rate or rhythm control with in a total of 3,598 patients who all had heart failure, again including the patients enrolled in the CABANA study. The results showed a significant 49% relative drop in all cause mortality with ablation compared with medical treatment, and a statistically significant 56% cut in hospitalizations, as well as a significant, nearly 7% average, absolute improvement in left ventricular ejection fraction, plus benefits for preventing arrhythmia recurrence and improving quality of life (Eur Heart J. 2019 Jul 11. doi: 10.1093/eurheartj/ehz443).
“The magnitude of the effect seen in the meta-analysis, a 49% reduction in total mortality and a 56% reduction in hospitalizations, is rather staggering, and is larger than typically quoted for other medical interventions or device therapy in heart failure. The treatment effect was uniform among studies, and entirely compatible with the changes in left ventricular function, exercise capacity, and heart failure symptoms. Therefore, although more data are desirable, there are already arguably sufficient data to understand a great deal regarding the impact of a fib ablation,” commented Ross J. Hunter, MRCP, a cardiac electrophysiologist at Barts Heart Centre in London, and his associates in an editorial about this meta-analysis (Eur Heart J. 2019 Oct 22. doi: 10.1093/eurheartj/ehz704).
The heart failure analysis of CABANA (Catheter Ablation vs. Anti-Arrhythmic Drug Therapy for Atrial Fibrillation Trial) itself also showed striking findings when first reported at the annual scientific sessions of the Heart Rhythm Society last May. In presentations he made at this meeting, Douglas L. Packer, MD, CABANA’s lead investigator, reported details of a prespecified subgroup analysis of the 778 patients enrolled in CABANA who had heart failure at baseline, slightly more than a third of the total study enrollment. This was more than double the number of patients identified as specifically having heart failure at entry in the initial publication of CABANA’s findings (JAMA. 2019 Mar 15;321[134]:1261-74). Comparison of the 378 patients with heart failure and randomized to undergo ablation with the 400 with heart failure randomized to medical treatment showed a 36% reduction in the study’s primary, composite endpoint relative to the control group in an intention-to-treat analysis, and a 43% relative cut in all-cause mortality during follow-up, Dr. Packer reported at the May meeting. (As of early November 2019, these results had not yet appeared in a published article.) In contrast, in the 1,422 CABANA patients randomized who did not have heart failure, ablation produced results for these endpoints that were similar to and not statistically different from the outcomes in patients treated medically, said Dr. Packer, a cardiac electrophysiologist and professor of medicine at the Mayo Clinic in Rochester, Minn.
The CABANA results added to what had been previously reported from two other landmark studies that documented incremental efficacy of AFib ablation compared with medical treatment in patients with heart failure: The AATAC (Ablation vs Amiodarone for Treatment of AFib in Patients With Congestive HF and an Implanted Device) study, which randomized 203 patients (Circulation. 2016 Apr 26;133[17]:1637-44), and CASTLE-AF (Catheter Ablation vs. Standard Conventional Therapy in Patients with Left Ventricular Dysfunction and Atrial Fibrillation) trial, which randomized 363 patients (N Engl J Med. 2018 Feb 1;378[5]:417-27). These three studies contributed the most patients and outcomes to the two recent meta-analyses.
“The CASTLE-AF and AATAC trials both showed improved cardiovascular outcomes with ablation in patients with heart failure and AFib. The meta-analysis [by Dr. Stavrakis and his associates] and CABANA subgroup analysis further support use of catheter ablation to improve the outcomes in these patients,” noted Jonathan P. Piccini, MD, a cardiac electrophysiologist at Duke University, Durham, N.C., and a CABANA coinvestigator.
“The CABANA trial was very important because it confirmed the safety of catheter ablation, and more importantly suggested that patients with heart failure may benefit the most [from AFib ablation]. The evidence is very strong to advocate ablation as first-line therapy for selected patients with heart failure. Perhaps the optimal patients are those with [New York Heart Association] class I-III or ambulatory class IV heart failure who are on optimized, guideline-directed medical therapy. We have enough data to make this a class I recommendation. The question that remains is whether this is a cost effective strategy. Because it lowers rehospitalization and death, I suspect it is,” said Luigi Di Biase, MD, lead investigator of AATAC, and director of arrhythmia services at Montefiore Medical Center and professor of medicine at Albert Einstein College of Medicine, both in New York.
Opinions differ on AFib ablation’s role
Despite this expansive assessment of the current status of AFib ablation for patients with heart failure from Dr. Di Biase and shared by others, another camp of cardiologists currently sees ablation as having more limited current utility, as recommended earlier this year by a guideline-update panel representing the American Heart Association, the American College of Cardiology, and the Heart Rhythm Society. The guideline update included this new recommendation for how to use AFib ablation in heart failure patients: “AF catheter ablation may be reasonable in selected patients with symptomatic AFib and heart failure with reduced left ventricular ejection fraction to potentially lower mortality rate and reduce hospitalization for heart failure,” a class IIb recommendation. (J Am Coll Cardiol. 2019 Jul 9;74[1]:104-32). The guideline’s text cited the findings from AATAC and CASTLE-AF, but qualified both studies as “relatively small” and with “highly selected patient populations.” The guideline also incorporated the CABANA results into its considerations (although they may not have had the full analysis in heart failure patients available during their deliberations), but cited the study’s main limitation: CABANA failed to show a statistically significant difference in the primary endpoint in its primary, intention-to-treat analysis, which meant that by the strict statistical criteria that trialists apply to study findings, all other endpoints analyzed using CABANA’s are merely “hypothesis generating” and not definitive.
Questions about the extent of patient selection required to see a clear clinical-endpoint benefit from AFib ablation in heart failure patients, as well as the flawed validity of the CABANA results for making unqualified practice recommendation are the main arguments advanced by experts who caution against broader and more routine ablations.
“The findings from the heart failure subgroup of CABANA are hypothesis generating rather than definitive. Even with the recent meta-analysis, uncertainty remains regarding the ability of catheter ablation to improve outcomes beyond reducing AFib-related symptoms,” commented Gregg Fonarow, MD, a heart failure physician and professor of medicine at the University of California, Los Angeles.
“CASTLE-HF had fewer than 100 deaths combined in both arms, which means very unstable results. We don’t know a lot of detail about the heart failure patients in CABANA, and overall we do not have much data from patients with heart failure with preserved ejection fraction [HFpEF],” said Javed Butler, MD, a heart failure physician and professor and chairman of medicine at the University of Mississippi in Jackson. Dr. Butler also voiced his concerns (shared by other heart failure specialists) about the safety of ablation in heart failure patients, noting that “many patients require multiple ablations; many burns result in scarring and can worsen atrial function. In short, ablation of AFib is probably good for selected patients, but to have a class 1 recommendation, we need much larger trials with well-phenotyped heart failure patients,” Dr. Butler said in an interview.
“The totality of data still captures a relatively small number of patients. CASTLE-HF took 8 years to enroll fewer than 400 patients, and the results showed some heterogeneity. Study patients were a decade younger than average HFrEF patients in the community, and thus the effectiveness and safety of catheter ablation in people with more comorbidity and frailty remains in question. Certain HFrEF patients may be less likely to benefit, such as those with amyloid cardiomyopathy. And with the increasing availability of other treatments for HFrEF such as sacubitril/valsartan, dapagliflozin, and MitraClip, it is less clear how catheter ablation would [benefit patients] on top of what is now current best therapy,” said Larry Allen, MD, a heart failure physician and professor of medicine at the University of Colorado in Aurora.
“With these limitations and the fact that catheter ablation is not a simple procedure, a large randomized, controlled trial of ablation, compared with no ablation, in a wide range of HFrEF patients on contemporary therapy would be welcome,” Dr. Allen said. “Given the prevalence of heart failure and AFib and the potential positive and negative implications of catheter ablation running such a trial seems critical for patients and for society.”
“For ablation of AFib in heart failure to become a class I recommendation there will need to be results from larger randomized studies,” summed up Dr. Stavrakis. The meta-analysis that he coauthored noted that “the benefits of catheter ablation for AFib in HFrEF patients have been consistently shown for over a decade now; however, the uptake of this procedure by clinicians in practice has been slow.”
Despite this history of reticence and ongoing caution about ablation, some cardiology experts see the indications for AFib ablation in heart failure steadily creeping forward, buoyed by a safety record that has more benign than ablation’s reputation suggests.
The CABANA results showed that “ablation is remarkably safe in the hands of experienced clinicians, with risks comparable to anti-arrhythmic drugs,” said Peter R. Kowey, MD, a specialist in treating AFib and professor of medicine at Thomas Jefferson University in Philadelphia, who made this assessment during a talk at an AFib meeting in early 2019. Dr. Kowey’s take on what the CABANA safety data showed contrasts with the impression of other cardiologists who are wary of perceived dangers from ablation.
“Ablation comes with a lot of morbidity and mortality. It’s not that the idea of ablation is wrong, but the ability to do it without a lot of adverse effects. ... We’re not quite there yet,” said Douglas L. Mann, MD, a heart failure physician and professor of medicine and chief of the cardiovascular division at Washington University in St. Louis.
“If I had a patient with HFrEF and AFib who was really sick, I’m not so sure I’d send them for ablation, which is not a simple procedure. The patients we tend to send for ablation are selected. Ablation is a big undertaking in patients who are already sick, and it’s expensive. I don’t think the data we have now will change the consensus view, but every heart failure physician is sending some patients for AFib ablation. People are turning to AFib ablation earlier than before. I think the consensus is that ablation is for symptoms or poor rate control, not for better outcomes,” said Mariell Jessup, MD, a heart failure specialist and chief science and medical officer of the American Heart Association in Dallas.
However, this caution about safety and skepticism over efficacy may be dissipating as experience with ablation accumulates.
“CASTLE-AF and other data, including evidence for the apparent isolation of beta-blocker benefit to patients in sinus rhythm, have made me much more proactive about considering catheter ablation in my HFrEF patients. I think many other cardiologists have a similar view,” said Dr. Allen in an interview.
“A lot [of heart failure] patients are [being] referred for ablation, depending on the practice, setting, the local availability of electrophysiologists, and patient interest in ablation,” said Dr. Butler.
“We have no absolutely compelling data, but the data we have all point in the same direction. Like most, I am becoming convinced that AFib ablation in heart failure patients is a very valuable method for managing patients, but I can’t point to one study that was conclusive. Results from lots of studies show that it is likely, and when you add them all together it looks indisputable,” commented A. John Camm, MD, an atrial fibrillation specialist and professor of clinical cardiology at St. George’s University in London. “The findings put a responsibility on cardiologists to assess patients with heart failure for AFib. But there are nothing like enough resources to deal with all the patients who have heart failure who also have AFib.”
A rough estimate of just the U.S. volume of patients with heart failure and AFib is likely in the ball park of 2 million people (a third of the estimated 6 million American currently living with heart failure), and with the prevalence of each of these disorders rising precipitously (more than 5 million Americans have AFib) the confluence of the two should also show a steady increase. “It will take a major change in our concept of heart failure management to really address this. Potentially it would mean a large increase in the number of RF ablations of AFib, but the resources for that are not now present,” Dr. Camm said in an interview.
The attractions of catheter ablation also stand in contrast to the limitations of alternative treatments. Ablation is effective in a majority of patients for reducing AFib burden, both the frequency and duration of AFib episodes, and safety issues are mostly limited to the procedural and immediate postprocedural periods. The drugs available for trying to control AFib are beta-blockers, which provide rate control and can help prevent AFib onset, and rhythm-controlling anti-arrhythmic drugs like amiodarone, which have substantial limitations in both their ability to prevent arrhythmia recurrences as well as for safety.
“Most of the conventional antiarrhythmic drugs are contraindicated, frequently ineffective, or not well tolerated in patients with HFrEF. Catheter ablation of AFib provides an increasingly important option for rhythm control in these patients without using antiarrhythmic drugs,” Dr. Di Biase and his associates wrote in a recent review of AFib ablation in heart failure patients (Eur Heart J. 2019 Feb 21;40[8]:663-71).
“The guidelines that are controversial still make amiodarone a class I drug even though it’s been associated with serious side effects and has been shown in several heart failure trials to increase mortality. I can’t believe that ablation is a class IIb recommendation while a drug like amiodarone is a class I recommendation,” Dr. Di Biase said.
And although beta-blockers are a mainstay of heart failure treatment, once AFib becomes established they are less useful for maintaining sinus rhythm. “Beta-blockers provide effective rate control, but they can’t convert patients to sinus rhythm [once AFib begins], and there is no convincing evidence that patients on beta-blockers stay in sinus rhythm longer. You can’t just say: the patient is on a beta-blocker so I’ve done my best,” noted Dr. Jessup.
CABANA received funding from Biosense Webster, Boston Scientific, Medtronic, and St. Jude. Dr. Stavrakis, Dr, Jessup, and Dr. Di Biase. Dr. Hunter has received research funding, educational grants, and speakers fees from Biosense Webster and Medtronic. Dr. Packer had received honoraria from Biotronik and MediaSphere Medical and research support from several companies. Dr. Piccini has been a consultant to Allergan, Biotronik, Medtronic, Phillips, and Sanofi Aventis, he has received research funding from Abbott, ARCA biopharma, Boston Scientific, Gilead, and Johnson & Johnson, and he had a financial relationship with GlaxoSmithKline. Dr. Fonarow has been a consultant to Abbott, Amgen, Bayer, Janssen, and Novartis. Dr. Butler has been a consultant to several companies. Dr. Allen has been a consultant to Boston Scientific, Janssen, and Novartis. Dr. Kowey has been a consultant to several companies. Dr. Mann has been a consultant to Bristol-Myers Squibb, Corvia, and Novartis, and an adviser to miRagen. Dr. Camm has been a consultant to several companies.
This is part one of a two-part article.
Roughly a third of patients with heart failure also have atrial fibrillation, a comorbid combination notorious for working synergistically to worsen a patient’s quality of life and life expectancy.
During the past year, radiofrequency catheter ablation of atrial fibrillation in patients with both conditions has gathered steam as a way to intervene in at least selected patients, driven by study results that featured attention-grabbing reductions in death and cardiovascular hospitalizations.
The evidence favoring catheter ablation of atrial fibrillation (AFib) in patients with heart failure, particularly patients with heart failure with reduced ejection fraction (HFrEF), ramped up in 2019, spurred largely by a subgroup analysis from the CABANA trial, the largest randomized comparison by far of AFib ablation with antiarrhythmic drug treatment with 2,204 patients.
The past few months also featured release of two meta-analyses that took the CABANA results into account plus findings from about a dozen earlier randomized studies. Both meta-analyses, as well as the heart failure analysis from CABANA, all point in one direction, as stated in the conclusion of one of the meta-analyses: “In patients with AFib, catheter ablation is associated with all-cause mortality benefit, compared with medical therapy, that is driven by patients with AFib and HFrEF. Catheter ablation is safe and reduces cardiovascular hospitalizations and recurrences of atrial arrhythmias” both in patients with paroxysmal and persistent AFib,” wrote Stavros Stavrakis, MD, and his associates in their systematic review of 18 randomized, controlled trials of catheter ablation of AFib in a total of 4,464 patients with or without heart failure (Circ Arrhythm Electrophysiol. 2019 Sep;12[9]: e007414).
Despite these new data and analyses, clinicians seem to have very mixed reactions. Some call for an upgraded recommendation by professional societies that would support more aggressive use of AFib ablation in heart failure patients, and the anecdotal impressions of people who manage these patients are that ablation procedures have recently increased. But others advise caution, and note that in their opinion the efficacy data remain preliminary; the procedure has safety, logistical, and economic concerns; and questions remain about the ability of all active ablation programs to consistently deliver the results seen in published trials.
The meta-analysis led by Dr. Stavrakis showed that catheter ablation of AFib cut all-cause mortality during follow-up by a statistically significant 31%, compared with medical therapy, in all patients regardless of their heart failure status. But in patients with HFrEF, the reduction was 48%, along with a 38% cut in cardiovascular hospitalizations. In contrast, patients without heart failure who underwent AFib ablation showed no significant change in their all-cause mortality, compared with medical management of these patients.
“Based both on our meta-analysis and the CABANA data, patients with AFib most likely to benefit from ablation are patients younger than 65 and those with heart failure,” summed up Dr. Stavrakis, a cardiac electrophysiologist at the Heart Rhythm Institute of the University of Oklahoma in Oklahoma City.
The second meta-analysis, which initially appeared in July, analyzed data from 11 randomized trials of catheter ablations compared with anti-arrhythmic medical therapy for rate or rhythm control with in a total of 3,598 patients who all had heart failure, again including the patients enrolled in the CABANA study. The results showed a significant 49% relative drop in all cause mortality with ablation compared with medical treatment, and a statistically significant 56% cut in hospitalizations, as well as a significant, nearly 7% average, absolute improvement in left ventricular ejection fraction, plus benefits for preventing arrhythmia recurrence and improving quality of life (Eur Heart J. 2019 Jul 11. doi: 10.1093/eurheartj/ehz443).
“The magnitude of the effect seen in the meta-analysis, a 49% reduction in total mortality and a 56% reduction in hospitalizations, is rather staggering, and is larger than typically quoted for other medical interventions or device therapy in heart failure. The treatment effect was uniform among studies, and entirely compatible with the changes in left ventricular function, exercise capacity, and heart failure symptoms. Therefore, although more data are desirable, there are already arguably sufficient data to understand a great deal regarding the impact of a fib ablation,” commented Ross J. Hunter, MRCP, a cardiac electrophysiologist at Barts Heart Centre in London, and his associates in an editorial about this meta-analysis (Eur Heart J. 2019 Oct 22. doi: 10.1093/eurheartj/ehz704).
The heart failure analysis of CABANA (Catheter Ablation vs. Anti-Arrhythmic Drug Therapy for Atrial Fibrillation Trial) itself also showed striking findings when first reported at the annual scientific sessions of the Heart Rhythm Society last May. In presentations he made at this meeting, Douglas L. Packer, MD, CABANA’s lead investigator, reported details of a prespecified subgroup analysis of the 778 patients enrolled in CABANA who had heart failure at baseline, slightly more than a third of the total study enrollment. This was more than double the number of patients identified as specifically having heart failure at entry in the initial publication of CABANA’s findings (JAMA. 2019 Mar 15;321[134]:1261-74). Comparison of the 378 patients with heart failure and randomized to undergo ablation with the 400 with heart failure randomized to medical treatment showed a 36% reduction in the study’s primary, composite endpoint relative to the control group in an intention-to-treat analysis, and a 43% relative cut in all-cause mortality during follow-up, Dr. Packer reported at the May meeting. (As of early November 2019, these results had not yet appeared in a published article.) In contrast, in the 1,422 CABANA patients randomized who did not have heart failure, ablation produced results for these endpoints that were similar to and not statistically different from the outcomes in patients treated medically, said Dr. Packer, a cardiac electrophysiologist and professor of medicine at the Mayo Clinic in Rochester, Minn.
The CABANA results added to what had been previously reported from two other landmark studies that documented incremental efficacy of AFib ablation compared with medical treatment in patients with heart failure: The AATAC (Ablation vs Amiodarone for Treatment of AFib in Patients With Congestive HF and an Implanted Device) study, which randomized 203 patients (Circulation. 2016 Apr 26;133[17]:1637-44), and CASTLE-AF (Catheter Ablation vs. Standard Conventional Therapy in Patients with Left Ventricular Dysfunction and Atrial Fibrillation) trial, which randomized 363 patients (N Engl J Med. 2018 Feb 1;378[5]:417-27). These three studies contributed the most patients and outcomes to the two recent meta-analyses.
“The CASTLE-AF and AATAC trials both showed improved cardiovascular outcomes with ablation in patients with heart failure and AFib. The meta-analysis [by Dr. Stavrakis and his associates] and CABANA subgroup analysis further support use of catheter ablation to improve the outcomes in these patients,” noted Jonathan P. Piccini, MD, a cardiac electrophysiologist at Duke University, Durham, N.C., and a CABANA coinvestigator.
“The CABANA trial was very important because it confirmed the safety of catheter ablation, and more importantly suggested that patients with heart failure may benefit the most [from AFib ablation]. The evidence is very strong to advocate ablation as first-line therapy for selected patients with heart failure. Perhaps the optimal patients are those with [New York Heart Association] class I-III or ambulatory class IV heart failure who are on optimized, guideline-directed medical therapy. We have enough data to make this a class I recommendation. The question that remains is whether this is a cost effective strategy. Because it lowers rehospitalization and death, I suspect it is,” said Luigi Di Biase, MD, lead investigator of AATAC, and director of arrhythmia services at Montefiore Medical Center and professor of medicine at Albert Einstein College of Medicine, both in New York.
Opinions differ on AFib ablation’s role
Despite this expansive assessment of the current status of AFib ablation for patients with heart failure from Dr. Di Biase and shared by others, another camp of cardiologists currently sees ablation as having more limited current utility, as recommended earlier this year by a guideline-update panel representing the American Heart Association, the American College of Cardiology, and the Heart Rhythm Society. The guideline update included this new recommendation for how to use AFib ablation in heart failure patients: “AF catheter ablation may be reasonable in selected patients with symptomatic AFib and heart failure with reduced left ventricular ejection fraction to potentially lower mortality rate and reduce hospitalization for heart failure,” a class IIb recommendation. (J Am Coll Cardiol. 2019 Jul 9;74[1]:104-32). The guideline’s text cited the findings from AATAC and CASTLE-AF, but qualified both studies as “relatively small” and with “highly selected patient populations.” The guideline also incorporated the CABANA results into its considerations (although they may not have had the full analysis in heart failure patients available during their deliberations), but cited the study’s main limitation: CABANA failed to show a statistically significant difference in the primary endpoint in its primary, intention-to-treat analysis, which meant that by the strict statistical criteria that trialists apply to study findings, all other endpoints analyzed using CABANA’s are merely “hypothesis generating” and not definitive.
Questions about the extent of patient selection required to see a clear clinical-endpoint benefit from AFib ablation in heart failure patients, as well as the flawed validity of the CABANA results for making unqualified practice recommendation are the main arguments advanced by experts who caution against broader and more routine ablations.
“The findings from the heart failure subgroup of CABANA are hypothesis generating rather than definitive. Even with the recent meta-analysis, uncertainty remains regarding the ability of catheter ablation to improve outcomes beyond reducing AFib-related symptoms,” commented Gregg Fonarow, MD, a heart failure physician and professor of medicine at the University of California, Los Angeles.
“CASTLE-HF had fewer than 100 deaths combined in both arms, which means very unstable results. We don’t know a lot of detail about the heart failure patients in CABANA, and overall we do not have much data from patients with heart failure with preserved ejection fraction [HFpEF],” said Javed Butler, MD, a heart failure physician and professor and chairman of medicine at the University of Mississippi in Jackson. Dr. Butler also voiced his concerns (shared by other heart failure specialists) about the safety of ablation in heart failure patients, noting that “many patients require multiple ablations; many burns result in scarring and can worsen atrial function. In short, ablation of AFib is probably good for selected patients, but to have a class 1 recommendation, we need much larger trials with well-phenotyped heart failure patients,” Dr. Butler said in an interview.
“The totality of data still captures a relatively small number of patients. CASTLE-HF took 8 years to enroll fewer than 400 patients, and the results showed some heterogeneity. Study patients were a decade younger than average HFrEF patients in the community, and thus the effectiveness and safety of catheter ablation in people with more comorbidity and frailty remains in question. Certain HFrEF patients may be less likely to benefit, such as those with amyloid cardiomyopathy. And with the increasing availability of other treatments for HFrEF such as sacubitril/valsartan, dapagliflozin, and MitraClip, it is less clear how catheter ablation would [benefit patients] on top of what is now current best therapy,” said Larry Allen, MD, a heart failure physician and professor of medicine at the University of Colorado in Aurora.
“With these limitations and the fact that catheter ablation is not a simple procedure, a large randomized, controlled trial of ablation, compared with no ablation, in a wide range of HFrEF patients on contemporary therapy would be welcome,” Dr. Allen said. “Given the prevalence of heart failure and AFib and the potential positive and negative implications of catheter ablation running such a trial seems critical for patients and for society.”
“For ablation of AFib in heart failure to become a class I recommendation there will need to be results from larger randomized studies,” summed up Dr. Stavrakis. The meta-analysis that he coauthored noted that “the benefits of catheter ablation for AFib in HFrEF patients have been consistently shown for over a decade now; however, the uptake of this procedure by clinicians in practice has been slow.”
Despite this history of reticence and ongoing caution about ablation, some cardiology experts see the indications for AFib ablation in heart failure steadily creeping forward, buoyed by a safety record that has more benign than ablation’s reputation suggests.
The CABANA results showed that “ablation is remarkably safe in the hands of experienced clinicians, with risks comparable to anti-arrhythmic drugs,” said Peter R. Kowey, MD, a specialist in treating AFib and professor of medicine at Thomas Jefferson University in Philadelphia, who made this assessment during a talk at an AFib meeting in early 2019. Dr. Kowey’s take on what the CABANA safety data showed contrasts with the impression of other cardiologists who are wary of perceived dangers from ablation.
“Ablation comes with a lot of morbidity and mortality. It’s not that the idea of ablation is wrong, but the ability to do it without a lot of adverse effects. ... We’re not quite there yet,” said Douglas L. Mann, MD, a heart failure physician and professor of medicine and chief of the cardiovascular division at Washington University in St. Louis.
“If I had a patient with HFrEF and AFib who was really sick, I’m not so sure I’d send them for ablation, which is not a simple procedure. The patients we tend to send for ablation are selected. Ablation is a big undertaking in patients who are already sick, and it’s expensive. I don’t think the data we have now will change the consensus view, but every heart failure physician is sending some patients for AFib ablation. People are turning to AFib ablation earlier than before. I think the consensus is that ablation is for symptoms or poor rate control, not for better outcomes,” said Mariell Jessup, MD, a heart failure specialist and chief science and medical officer of the American Heart Association in Dallas.
However, this caution about safety and skepticism over efficacy may be dissipating as experience with ablation accumulates.
“CASTLE-AF and other data, including evidence for the apparent isolation of beta-blocker benefit to patients in sinus rhythm, have made me much more proactive about considering catheter ablation in my HFrEF patients. I think many other cardiologists have a similar view,” said Dr. Allen in an interview.
“A lot [of heart failure] patients are [being] referred for ablation, depending on the practice, setting, the local availability of electrophysiologists, and patient interest in ablation,” said Dr. Butler.
“We have no absolutely compelling data, but the data we have all point in the same direction. Like most, I am becoming convinced that AFib ablation in heart failure patients is a very valuable method for managing patients, but I can’t point to one study that was conclusive. Results from lots of studies show that it is likely, and when you add them all together it looks indisputable,” commented A. John Camm, MD, an atrial fibrillation specialist and professor of clinical cardiology at St. George’s University in London. “The findings put a responsibility on cardiologists to assess patients with heart failure for AFib. But there are nothing like enough resources to deal with all the patients who have heart failure who also have AFib.”
A rough estimate of just the U.S. volume of patients with heart failure and AFib is likely in the ball park of 2 million people (a third of the estimated 6 million American currently living with heart failure), and with the prevalence of each of these disorders rising precipitously (more than 5 million Americans have AFib) the confluence of the two should also show a steady increase. “It will take a major change in our concept of heart failure management to really address this. Potentially it would mean a large increase in the number of RF ablations of AFib, but the resources for that are not now present,” Dr. Camm said in an interview.
The attractions of catheter ablation also stand in contrast to the limitations of alternative treatments. Ablation is effective in a majority of patients for reducing AFib burden, both the frequency and duration of AFib episodes, and safety issues are mostly limited to the procedural and immediate postprocedural periods. The drugs available for trying to control AFib are beta-blockers, which provide rate control and can help prevent AFib onset, and rhythm-controlling anti-arrhythmic drugs like amiodarone, which have substantial limitations in both their ability to prevent arrhythmia recurrences as well as for safety.
“Most of the conventional antiarrhythmic drugs are contraindicated, frequently ineffective, or not well tolerated in patients with HFrEF. Catheter ablation of AFib provides an increasingly important option for rhythm control in these patients without using antiarrhythmic drugs,” Dr. Di Biase and his associates wrote in a recent review of AFib ablation in heart failure patients (Eur Heart J. 2019 Feb 21;40[8]:663-71).
“The guidelines that are controversial still make amiodarone a class I drug even though it’s been associated with serious side effects and has been shown in several heart failure trials to increase mortality. I can’t believe that ablation is a class IIb recommendation while a drug like amiodarone is a class I recommendation,” Dr. Di Biase said.
And although beta-blockers are a mainstay of heart failure treatment, once AFib becomes established they are less useful for maintaining sinus rhythm. “Beta-blockers provide effective rate control, but they can’t convert patients to sinus rhythm [once AFib begins], and there is no convincing evidence that patients on beta-blockers stay in sinus rhythm longer. You can’t just say: the patient is on a beta-blocker so I’ve done my best,” noted Dr. Jessup.
CABANA received funding from Biosense Webster, Boston Scientific, Medtronic, and St. Jude. Dr. Stavrakis, Dr, Jessup, and Dr. Di Biase. Dr. Hunter has received research funding, educational grants, and speakers fees from Biosense Webster and Medtronic. Dr. Packer had received honoraria from Biotronik and MediaSphere Medical and research support from several companies. Dr. Piccini has been a consultant to Allergan, Biotronik, Medtronic, Phillips, and Sanofi Aventis, he has received research funding from Abbott, ARCA biopharma, Boston Scientific, Gilead, and Johnson & Johnson, and he had a financial relationship with GlaxoSmithKline. Dr. Fonarow has been a consultant to Abbott, Amgen, Bayer, Janssen, and Novartis. Dr. Butler has been a consultant to several companies. Dr. Allen has been a consultant to Boston Scientific, Janssen, and Novartis. Dr. Kowey has been a consultant to several companies. Dr. Mann has been a consultant to Bristol-Myers Squibb, Corvia, and Novartis, and an adviser to miRagen. Dr. Camm has been a consultant to several companies.
This is part one of a two-part article.
Roughly a third of patients with heart failure also have atrial fibrillation, a comorbid combination notorious for working synergistically to worsen a patient’s quality of life and life expectancy.
During the past year, radiofrequency catheter ablation of atrial fibrillation in patients with both conditions has gathered steam as a way to intervene in at least selected patients, driven by study results that featured attention-grabbing reductions in death and cardiovascular hospitalizations.
The evidence favoring catheter ablation of atrial fibrillation (AFib) in patients with heart failure, particularly patients with heart failure with reduced ejection fraction (HFrEF), ramped up in 2019, spurred largely by a subgroup analysis from the CABANA trial, the largest randomized comparison by far of AFib ablation with antiarrhythmic drug treatment with 2,204 patients.
The past few months also featured release of two meta-analyses that took the CABANA results into account plus findings from about a dozen earlier randomized studies. Both meta-analyses, as well as the heart failure analysis from CABANA, all point in one direction, as stated in the conclusion of one of the meta-analyses: “In patients with AFib, catheter ablation is associated with all-cause mortality benefit, compared with medical therapy, that is driven by patients with AFib and HFrEF. Catheter ablation is safe and reduces cardiovascular hospitalizations and recurrences of atrial arrhythmias” both in patients with paroxysmal and persistent AFib,” wrote Stavros Stavrakis, MD, and his associates in their systematic review of 18 randomized, controlled trials of catheter ablation of AFib in a total of 4,464 patients with or without heart failure (Circ Arrhythm Electrophysiol. 2019 Sep;12[9]: e007414).
Despite these new data and analyses, clinicians seem to have very mixed reactions. Some call for an upgraded recommendation by professional societies that would support more aggressive use of AFib ablation in heart failure patients, and the anecdotal impressions of people who manage these patients are that ablation procedures have recently increased. But others advise caution, and note that in their opinion the efficacy data remain preliminary; the procedure has safety, logistical, and economic concerns; and questions remain about the ability of all active ablation programs to consistently deliver the results seen in published trials.
The meta-analysis led by Dr. Stavrakis showed that catheter ablation of AFib cut all-cause mortality during follow-up by a statistically significant 31%, compared with medical therapy, in all patients regardless of their heart failure status. But in patients with HFrEF, the reduction was 48%, along with a 38% cut in cardiovascular hospitalizations. In contrast, patients without heart failure who underwent AFib ablation showed no significant change in their all-cause mortality, compared with medical management of these patients.
“Based both on our meta-analysis and the CABANA data, patients with AFib most likely to benefit from ablation are patients younger than 65 and those with heart failure,” summed up Dr. Stavrakis, a cardiac electrophysiologist at the Heart Rhythm Institute of the University of Oklahoma in Oklahoma City.
The second meta-analysis, which initially appeared in July, analyzed data from 11 randomized trials of catheter ablations compared with anti-arrhythmic medical therapy for rate or rhythm control with in a total of 3,598 patients who all had heart failure, again including the patients enrolled in the CABANA study. The results showed a significant 49% relative drop in all cause mortality with ablation compared with medical treatment, and a statistically significant 56% cut in hospitalizations, as well as a significant, nearly 7% average, absolute improvement in left ventricular ejection fraction, plus benefits for preventing arrhythmia recurrence and improving quality of life (Eur Heart J. 2019 Jul 11. doi: 10.1093/eurheartj/ehz443).
“The magnitude of the effect seen in the meta-analysis, a 49% reduction in total mortality and a 56% reduction in hospitalizations, is rather staggering, and is larger than typically quoted for other medical interventions or device therapy in heart failure. The treatment effect was uniform among studies, and entirely compatible with the changes in left ventricular function, exercise capacity, and heart failure symptoms. Therefore, although more data are desirable, there are already arguably sufficient data to understand a great deal regarding the impact of a fib ablation,” commented Ross J. Hunter, MRCP, a cardiac electrophysiologist at Barts Heart Centre in London, and his associates in an editorial about this meta-analysis (Eur Heart J. 2019 Oct 22. doi: 10.1093/eurheartj/ehz704).
The heart failure analysis of CABANA (Catheter Ablation vs. Anti-Arrhythmic Drug Therapy for Atrial Fibrillation Trial) itself also showed striking findings when first reported at the annual scientific sessions of the Heart Rhythm Society last May. In presentations he made at this meeting, Douglas L. Packer, MD, CABANA’s lead investigator, reported details of a prespecified subgroup analysis of the 778 patients enrolled in CABANA who had heart failure at baseline, slightly more than a third of the total study enrollment. This was more than double the number of patients identified as specifically having heart failure at entry in the initial publication of CABANA’s findings (JAMA. 2019 Mar 15;321[134]:1261-74). Comparison of the 378 patients with heart failure and randomized to undergo ablation with the 400 with heart failure randomized to medical treatment showed a 36% reduction in the study’s primary, composite endpoint relative to the control group in an intention-to-treat analysis, and a 43% relative cut in all-cause mortality during follow-up, Dr. Packer reported at the May meeting. (As of early November 2019, these results had not yet appeared in a published article.) In contrast, in the 1,422 CABANA patients randomized who did not have heart failure, ablation produced results for these endpoints that were similar to and not statistically different from the outcomes in patients treated medically, said Dr. Packer, a cardiac electrophysiologist and professor of medicine at the Mayo Clinic in Rochester, Minn.
The CABANA results added to what had been previously reported from two other landmark studies that documented incremental efficacy of AFib ablation compared with medical treatment in patients with heart failure: The AATAC (Ablation vs Amiodarone for Treatment of AFib in Patients With Congestive HF and an Implanted Device) study, which randomized 203 patients (Circulation. 2016 Apr 26;133[17]:1637-44), and CASTLE-AF (Catheter Ablation vs. Standard Conventional Therapy in Patients with Left Ventricular Dysfunction and Atrial Fibrillation) trial, which randomized 363 patients (N Engl J Med. 2018 Feb 1;378[5]:417-27). These three studies contributed the most patients and outcomes to the two recent meta-analyses.
“The CASTLE-AF and AATAC trials both showed improved cardiovascular outcomes with ablation in patients with heart failure and AFib. The meta-analysis [by Dr. Stavrakis and his associates] and CABANA subgroup analysis further support use of catheter ablation to improve the outcomes in these patients,” noted Jonathan P. Piccini, MD, a cardiac electrophysiologist at Duke University, Durham, N.C., and a CABANA coinvestigator.
“The CABANA trial was very important because it confirmed the safety of catheter ablation, and more importantly suggested that patients with heart failure may benefit the most [from AFib ablation]. The evidence is very strong to advocate ablation as first-line therapy for selected patients with heart failure. Perhaps the optimal patients are those with [New York Heart Association] class I-III or ambulatory class IV heart failure who are on optimized, guideline-directed medical therapy. We have enough data to make this a class I recommendation. The question that remains is whether this is a cost effective strategy. Because it lowers rehospitalization and death, I suspect it is,” said Luigi Di Biase, MD, lead investigator of AATAC, and director of arrhythmia services at Montefiore Medical Center and professor of medicine at Albert Einstein College of Medicine, both in New York.
Opinions differ on AFib ablation’s role
Despite this expansive assessment of the current status of AFib ablation for patients with heart failure from Dr. Di Biase and shared by others, another camp of cardiologists currently sees ablation as having more limited current utility, as recommended earlier this year by a guideline-update panel representing the American Heart Association, the American College of Cardiology, and the Heart Rhythm Society. The guideline update included this new recommendation for how to use AFib ablation in heart failure patients: “AF catheter ablation may be reasonable in selected patients with symptomatic AFib and heart failure with reduced left ventricular ejection fraction to potentially lower mortality rate and reduce hospitalization for heart failure,” a class IIb recommendation. (J Am Coll Cardiol. 2019 Jul 9;74[1]:104-32). The guideline’s text cited the findings from AATAC and CASTLE-AF, but qualified both studies as “relatively small” and with “highly selected patient populations.” The guideline also incorporated the CABANA results into its considerations (although they may not have had the full analysis in heart failure patients available during their deliberations), but cited the study’s main limitation: CABANA failed to show a statistically significant difference in the primary endpoint in its primary, intention-to-treat analysis, which meant that by the strict statistical criteria that trialists apply to study findings, all other endpoints analyzed using CABANA’s are merely “hypothesis generating” and not definitive.
Questions about the extent of patient selection required to see a clear clinical-endpoint benefit from AFib ablation in heart failure patients, as well as the flawed validity of the CABANA results for making unqualified practice recommendation are the main arguments advanced by experts who caution against broader and more routine ablations.
“The findings from the heart failure subgroup of CABANA are hypothesis generating rather than definitive. Even with the recent meta-analysis, uncertainty remains regarding the ability of catheter ablation to improve outcomes beyond reducing AFib-related symptoms,” commented Gregg Fonarow, MD, a heart failure physician and professor of medicine at the University of California, Los Angeles.
“CASTLE-HF had fewer than 100 deaths combined in both arms, which means very unstable results. We don’t know a lot of detail about the heart failure patients in CABANA, and overall we do not have much data from patients with heart failure with preserved ejection fraction [HFpEF],” said Javed Butler, MD, a heart failure physician and professor and chairman of medicine at the University of Mississippi in Jackson. Dr. Butler also voiced his concerns (shared by other heart failure specialists) about the safety of ablation in heart failure patients, noting that “many patients require multiple ablations; many burns result in scarring and can worsen atrial function. In short, ablation of AFib is probably good for selected patients, but to have a class 1 recommendation, we need much larger trials with well-phenotyped heart failure patients,” Dr. Butler said in an interview.
“The totality of data still captures a relatively small number of patients. CASTLE-HF took 8 years to enroll fewer than 400 patients, and the results showed some heterogeneity. Study patients were a decade younger than average HFrEF patients in the community, and thus the effectiveness and safety of catheter ablation in people with more comorbidity and frailty remains in question. Certain HFrEF patients may be less likely to benefit, such as those with amyloid cardiomyopathy. And with the increasing availability of other treatments for HFrEF such as sacubitril/valsartan, dapagliflozin, and MitraClip, it is less clear how catheter ablation would [benefit patients] on top of what is now current best therapy,” said Larry Allen, MD, a heart failure physician and professor of medicine at the University of Colorado in Aurora.
“With these limitations and the fact that catheter ablation is not a simple procedure, a large randomized, controlled trial of ablation, compared with no ablation, in a wide range of HFrEF patients on contemporary therapy would be welcome,” Dr. Allen said. “Given the prevalence of heart failure and AFib and the potential positive and negative implications of catheter ablation running such a trial seems critical for patients and for society.”
“For ablation of AFib in heart failure to become a class I recommendation there will need to be results from larger randomized studies,” summed up Dr. Stavrakis. The meta-analysis that he coauthored noted that “the benefits of catheter ablation for AFib in HFrEF patients have been consistently shown for over a decade now; however, the uptake of this procedure by clinicians in practice has been slow.”
Despite this history of reticence and ongoing caution about ablation, some cardiology experts see the indications for AFib ablation in heart failure steadily creeping forward, buoyed by a safety record that has more benign than ablation’s reputation suggests.
The CABANA results showed that “ablation is remarkably safe in the hands of experienced clinicians, with risks comparable to anti-arrhythmic drugs,” said Peter R. Kowey, MD, a specialist in treating AFib and professor of medicine at Thomas Jefferson University in Philadelphia, who made this assessment during a talk at an AFib meeting in early 2019. Dr. Kowey’s take on what the CABANA safety data showed contrasts with the impression of other cardiologists who are wary of perceived dangers from ablation.
“Ablation comes with a lot of morbidity and mortality. It’s not that the idea of ablation is wrong, but the ability to do it without a lot of adverse effects. ... We’re not quite there yet,” said Douglas L. Mann, MD, a heart failure physician and professor of medicine and chief of the cardiovascular division at Washington University in St. Louis.
“If I had a patient with HFrEF and AFib who was really sick, I’m not so sure I’d send them for ablation, which is not a simple procedure. The patients we tend to send for ablation are selected. Ablation is a big undertaking in patients who are already sick, and it’s expensive. I don’t think the data we have now will change the consensus view, but every heart failure physician is sending some patients for AFib ablation. People are turning to AFib ablation earlier than before. I think the consensus is that ablation is for symptoms or poor rate control, not for better outcomes,” said Mariell Jessup, MD, a heart failure specialist and chief science and medical officer of the American Heart Association in Dallas.
However, this caution about safety and skepticism over efficacy may be dissipating as experience with ablation accumulates.
“CASTLE-AF and other data, including evidence for the apparent isolation of beta-blocker benefit to patients in sinus rhythm, have made me much more proactive about considering catheter ablation in my HFrEF patients. I think many other cardiologists have a similar view,” said Dr. Allen in an interview.
“A lot [of heart failure] patients are [being] referred for ablation, depending on the practice, setting, the local availability of electrophysiologists, and patient interest in ablation,” said Dr. Butler.
“We have no absolutely compelling data, but the data we have all point in the same direction. Like most, I am becoming convinced that AFib ablation in heart failure patients is a very valuable method for managing patients, but I can’t point to one study that was conclusive. Results from lots of studies show that it is likely, and when you add them all together it looks indisputable,” commented A. John Camm, MD, an atrial fibrillation specialist and professor of clinical cardiology at St. George’s University in London. “The findings put a responsibility on cardiologists to assess patients with heart failure for AFib. But there are nothing like enough resources to deal with all the patients who have heart failure who also have AFib.”
A rough estimate of just the U.S. volume of patients with heart failure and AFib is likely in the ball park of 2 million people (a third of the estimated 6 million American currently living with heart failure), and with the prevalence of each of these disorders rising precipitously (more than 5 million Americans have AFib) the confluence of the two should also show a steady increase. “It will take a major change in our concept of heart failure management to really address this. Potentially it would mean a large increase in the number of RF ablations of AFib, but the resources for that are not now present,” Dr. Camm said in an interview.
The attractions of catheter ablation also stand in contrast to the limitations of alternative treatments. Ablation is effective in a majority of patients for reducing AFib burden, both the frequency and duration of AFib episodes, and safety issues are mostly limited to the procedural and immediate postprocedural periods. The drugs available for trying to control AFib are beta-blockers, which provide rate control and can help prevent AFib onset, and rhythm-controlling anti-arrhythmic drugs like amiodarone, which have substantial limitations in both their ability to prevent arrhythmia recurrences as well as for safety.
“Most of the conventional antiarrhythmic drugs are contraindicated, frequently ineffective, or not well tolerated in patients with HFrEF. Catheter ablation of AFib provides an increasingly important option for rhythm control in these patients without using antiarrhythmic drugs,” Dr. Di Biase and his associates wrote in a recent review of AFib ablation in heart failure patients (Eur Heart J. 2019 Feb 21;40[8]:663-71).
“The guidelines that are controversial still make amiodarone a class I drug even though it’s been associated with serious side effects and has been shown in several heart failure trials to increase mortality. I can’t believe that ablation is a class IIb recommendation while a drug like amiodarone is a class I recommendation,” Dr. Di Biase said.
And although beta-blockers are a mainstay of heart failure treatment, once AFib becomes established they are less useful for maintaining sinus rhythm. “Beta-blockers provide effective rate control, but they can’t convert patients to sinus rhythm [once AFib begins], and there is no convincing evidence that patients on beta-blockers stay in sinus rhythm longer. You can’t just say: the patient is on a beta-blocker so I’ve done my best,” noted Dr. Jessup.
CABANA received funding from Biosense Webster, Boston Scientific, Medtronic, and St. Jude. Dr. Stavrakis, Dr, Jessup, and Dr. Di Biase. Dr. Hunter has received research funding, educational grants, and speakers fees from Biosense Webster and Medtronic. Dr. Packer had received honoraria from Biotronik and MediaSphere Medical and research support from several companies. Dr. Piccini has been a consultant to Allergan, Biotronik, Medtronic, Phillips, and Sanofi Aventis, he has received research funding from Abbott, ARCA biopharma, Boston Scientific, Gilead, and Johnson & Johnson, and he had a financial relationship with GlaxoSmithKline. Dr. Fonarow has been a consultant to Abbott, Amgen, Bayer, Janssen, and Novartis. Dr. Butler has been a consultant to several companies. Dr. Allen has been a consultant to Boston Scientific, Janssen, and Novartis. Dr. Kowey has been a consultant to several companies. Dr. Mann has been a consultant to Bristol-Myers Squibb, Corvia, and Novartis, and an adviser to miRagen. Dr. Camm has been a consultant to several companies.
This is part one of a two-part article.
ATTEST: AFib ablation slows progression to persistence
PARIS – Radiofrequency catheter ablation of atrial fibrillation is not only a more definitive rhythm control treatment than antiarrhythmic drugs, but it’s also much more effective at slowing progression of AFib from paroxysmal to persistent, according to results from a randomized trial in 255 patients.
The multicenter study, ATTEST, randomized patients with paroxysmal AFib to radiofrequency catheter ablation or medical management and found that, during up to 3 years of follow-up, ablation cut the incidence of progression to persistent AFib by 89%, compared with medically managed patients, a statistically significant difference that documented a previously unappreciated benefit of catheter ablation: the ability to slow AFib progression, Karl-Heinz Kuck, MD, said at the annual congress of the European Society of Cardiology.
“This was never looked at before.” Assessing progression to persistent AFib is “a new endpoint for ablation” and an important one because progression from paroxysmal to persistent AFib has been associated with increased mortality, increased strokes, and increased hospitalizations,” said Dr. Kuck, a professor and cardiologist at the Asklepios Clinic St. Georg in Hamburg, Germany. If the findings are confirmed, “it may introduce a new indication for catheter ablation” in patients with paroxysmal AFib, Dr. Kuck said in an interview.
ATTEST (Atrial Fibrillation Progression Trial) enrolled patients at 30 sites worldwide who were at least 60 years old, had been diagnosed with paroxysmal AFib for at least 2 years, had at least two AFib episodes within 6 months of enrollment, and had not fully responded to one or two rhythm- or rate-control drugs. The 255 patients enrolled averaged 68 years of age, 58% were women, their median duration of AFib was slightly greater than 4 years, and on average patients had six to seven episodes during the prior 6 months. Enrollment into the study stopped sooner than planned because of slow recruitment, which topped out at 79% of the goal. Enrolled patients underwent weekly screening by transtelephonic monitoring for an AFib episode of at least 30 seconds during 3-9 months after entry, and then they had monthly screening. Patients positive for AFib on screening underwent a week of daily transtelephonic monitoring to determine whether their AFib persisted. The study’s primary endpoint was development of an AFib episode that lasted at least 7 days or for at least 2 days followed by cardioversion, which the investigators defined as persistent AFib.
The results showed that after 1 year development of persistent AFib occurred in 1% of the 128 patients assigned to receive ablation (102 actually underwent ablation) and in 7% of 127 patients assigned to drug management, with 123 patients who followed the treatment protocol. After 2 years of follow-up, the cumulative rate of progression to persistent AFib was 2% after ablation and 12% with medical treatment, and after 3 years, the respective rates of progression were 2% and 18%. The between-group differences were statistically significant at all three follow-up intervals, Dr. Kuck reported. Analysis of only patients who followed their assigned protocol showed similar results, as did an analysis that used the definition of persistent AFib advanced by the Heart Rhythm Society in 2017 (Heart Rhythm. 2017 Oct;14[10]:e275-e444).
The advantage of ablation for deferring progression was consistent in all subgroups analyzed, with no signal of interaction by age, sex, or other subgroup definitions. The rate of serious adverse events was “low,” occurring in 12% of the ablated patients and in 5% of controls. The need for two or more ablations was also “low,” Dr Kuck said, with 17% of patients requiring a second procedure. The results additionally showed that ablation also led to a lower rate of any AFib recurrence, regardless of whether or not it met the definition of persistent AFib. Any AFib recurrence occurred in 57% of the ablated patients and in 85% of those managed medically during 3 years of follow-up, a statistically significant difference.
Although the mechanism by which ablation slowed AFib progression is not known, Dr. Kuck suggested that it may relate to a reduction in the frequency and duration of AFib recurrences. “I believe that AFib burden is the key. If AFib episodes last a few days, then the likelihood of progressing to episodes that last 7 days is much higher than when an episode only lasts a few minutes,” he explained. “We’re opening a new perspective that looks beyond managing AFib symptoms” using ablation.
ATTEST was funded by Biosense Webster, a company that markets catheter ablation devices. Dr. Kuck has been a consultant to Biosense Webster, as well as to Abbott, Boston Scientific, Edwards, and Medtronic.
The ATTEST design and results are important because the study’s findings provide a good complement to the previously reported outcomes from the CASTLE-AF study, which randomized 363 patients with mostly persistent AFib (and heart failure) to catheter ablation of the AFib or medical management. The CASTLE-HF results showed that ablation was much more effective for reducing death from any cause and heart failure hospitalizations (N Engl J Med. 2018 Feb 1;378[5]:417-27). In other words, catheter ablation was the superior treatment for persistent AFib, the type of AFib diagnosed in about two-thirds of the patients enrolled in CASTLE-AF.
Thorsten Lewalter, MD, an arrhythmia specialist and professor at Peter Osypka Heart Center in Munich, made these comments in an interview. He has received personal fees from Abbott, Bayer, Boehringer Ingelheim, Boston Scientific, Daiichi Sankyo, and Pfizer.
The ATTEST design and results are important because the study’s findings provide a good complement to the previously reported outcomes from the CASTLE-AF study, which randomized 363 patients with mostly persistent AFib (and heart failure) to catheter ablation of the AFib or medical management. The CASTLE-HF results showed that ablation was much more effective for reducing death from any cause and heart failure hospitalizations (N Engl J Med. 2018 Feb 1;378[5]:417-27). In other words, catheter ablation was the superior treatment for persistent AFib, the type of AFib diagnosed in about two-thirds of the patients enrolled in CASTLE-AF.
Thorsten Lewalter, MD, an arrhythmia specialist and professor at Peter Osypka Heart Center in Munich, made these comments in an interview. He has received personal fees from Abbott, Bayer, Boehringer Ingelheim, Boston Scientific, Daiichi Sankyo, and Pfizer.
The ATTEST design and results are important because the study’s findings provide a good complement to the previously reported outcomes from the CASTLE-AF study, which randomized 363 patients with mostly persistent AFib (and heart failure) to catheter ablation of the AFib or medical management. The CASTLE-HF results showed that ablation was much more effective for reducing death from any cause and heart failure hospitalizations (N Engl J Med. 2018 Feb 1;378[5]:417-27). In other words, catheter ablation was the superior treatment for persistent AFib, the type of AFib diagnosed in about two-thirds of the patients enrolled in CASTLE-AF.
Thorsten Lewalter, MD, an arrhythmia specialist and professor at Peter Osypka Heart Center in Munich, made these comments in an interview. He has received personal fees from Abbott, Bayer, Boehringer Ingelheim, Boston Scientific, Daiichi Sankyo, and Pfizer.
PARIS – Radiofrequency catheter ablation of atrial fibrillation is not only a more definitive rhythm control treatment than antiarrhythmic drugs, but it’s also much more effective at slowing progression of AFib from paroxysmal to persistent, according to results from a randomized trial in 255 patients.
The multicenter study, ATTEST, randomized patients with paroxysmal AFib to radiofrequency catheter ablation or medical management and found that, during up to 3 years of follow-up, ablation cut the incidence of progression to persistent AFib by 89%, compared with medically managed patients, a statistically significant difference that documented a previously unappreciated benefit of catheter ablation: the ability to slow AFib progression, Karl-Heinz Kuck, MD, said at the annual congress of the European Society of Cardiology.
“This was never looked at before.” Assessing progression to persistent AFib is “a new endpoint for ablation” and an important one because progression from paroxysmal to persistent AFib has been associated with increased mortality, increased strokes, and increased hospitalizations,” said Dr. Kuck, a professor and cardiologist at the Asklepios Clinic St. Georg in Hamburg, Germany. If the findings are confirmed, “it may introduce a new indication for catheter ablation” in patients with paroxysmal AFib, Dr. Kuck said in an interview.
ATTEST (Atrial Fibrillation Progression Trial) enrolled patients at 30 sites worldwide who were at least 60 years old, had been diagnosed with paroxysmal AFib for at least 2 years, had at least two AFib episodes within 6 months of enrollment, and had not fully responded to one or two rhythm- or rate-control drugs. The 255 patients enrolled averaged 68 years of age, 58% were women, their median duration of AFib was slightly greater than 4 years, and on average patients had six to seven episodes during the prior 6 months. Enrollment into the study stopped sooner than planned because of slow recruitment, which topped out at 79% of the goal. Enrolled patients underwent weekly screening by transtelephonic monitoring for an AFib episode of at least 30 seconds during 3-9 months after entry, and then they had monthly screening. Patients positive for AFib on screening underwent a week of daily transtelephonic monitoring to determine whether their AFib persisted. The study’s primary endpoint was development of an AFib episode that lasted at least 7 days or for at least 2 days followed by cardioversion, which the investigators defined as persistent AFib.
The results showed that after 1 year development of persistent AFib occurred in 1% of the 128 patients assigned to receive ablation (102 actually underwent ablation) and in 7% of 127 patients assigned to drug management, with 123 patients who followed the treatment protocol. After 2 years of follow-up, the cumulative rate of progression to persistent AFib was 2% after ablation and 12% with medical treatment, and after 3 years, the respective rates of progression were 2% and 18%. The between-group differences were statistically significant at all three follow-up intervals, Dr. Kuck reported. Analysis of only patients who followed their assigned protocol showed similar results, as did an analysis that used the definition of persistent AFib advanced by the Heart Rhythm Society in 2017 (Heart Rhythm. 2017 Oct;14[10]:e275-e444).
The advantage of ablation for deferring progression was consistent in all subgroups analyzed, with no signal of interaction by age, sex, or other subgroup definitions. The rate of serious adverse events was “low,” occurring in 12% of the ablated patients and in 5% of controls. The need for two or more ablations was also “low,” Dr Kuck said, with 17% of patients requiring a second procedure. The results additionally showed that ablation also led to a lower rate of any AFib recurrence, regardless of whether or not it met the definition of persistent AFib. Any AFib recurrence occurred in 57% of the ablated patients and in 85% of those managed medically during 3 years of follow-up, a statistically significant difference.
Although the mechanism by which ablation slowed AFib progression is not known, Dr. Kuck suggested that it may relate to a reduction in the frequency and duration of AFib recurrences. “I believe that AFib burden is the key. If AFib episodes last a few days, then the likelihood of progressing to episodes that last 7 days is much higher than when an episode only lasts a few minutes,” he explained. “We’re opening a new perspective that looks beyond managing AFib symptoms” using ablation.
ATTEST was funded by Biosense Webster, a company that markets catheter ablation devices. Dr. Kuck has been a consultant to Biosense Webster, as well as to Abbott, Boston Scientific, Edwards, and Medtronic.
PARIS – Radiofrequency catheter ablation of atrial fibrillation is not only a more definitive rhythm control treatment than antiarrhythmic drugs, but it’s also much more effective at slowing progression of AFib from paroxysmal to persistent, according to results from a randomized trial in 255 patients.
The multicenter study, ATTEST, randomized patients with paroxysmal AFib to radiofrequency catheter ablation or medical management and found that, during up to 3 years of follow-up, ablation cut the incidence of progression to persistent AFib by 89%, compared with medically managed patients, a statistically significant difference that documented a previously unappreciated benefit of catheter ablation: the ability to slow AFib progression, Karl-Heinz Kuck, MD, said at the annual congress of the European Society of Cardiology.
“This was never looked at before.” Assessing progression to persistent AFib is “a new endpoint for ablation” and an important one because progression from paroxysmal to persistent AFib has been associated with increased mortality, increased strokes, and increased hospitalizations,” said Dr. Kuck, a professor and cardiologist at the Asklepios Clinic St. Georg in Hamburg, Germany. If the findings are confirmed, “it may introduce a new indication for catheter ablation” in patients with paroxysmal AFib, Dr. Kuck said in an interview.
ATTEST (Atrial Fibrillation Progression Trial) enrolled patients at 30 sites worldwide who were at least 60 years old, had been diagnosed with paroxysmal AFib for at least 2 years, had at least two AFib episodes within 6 months of enrollment, and had not fully responded to one or two rhythm- or rate-control drugs. The 255 patients enrolled averaged 68 years of age, 58% were women, their median duration of AFib was slightly greater than 4 years, and on average patients had six to seven episodes during the prior 6 months. Enrollment into the study stopped sooner than planned because of slow recruitment, which topped out at 79% of the goal. Enrolled patients underwent weekly screening by transtelephonic monitoring for an AFib episode of at least 30 seconds during 3-9 months after entry, and then they had monthly screening. Patients positive for AFib on screening underwent a week of daily transtelephonic monitoring to determine whether their AFib persisted. The study’s primary endpoint was development of an AFib episode that lasted at least 7 days or for at least 2 days followed by cardioversion, which the investigators defined as persistent AFib.
The results showed that after 1 year development of persistent AFib occurred in 1% of the 128 patients assigned to receive ablation (102 actually underwent ablation) and in 7% of 127 patients assigned to drug management, with 123 patients who followed the treatment protocol. After 2 years of follow-up, the cumulative rate of progression to persistent AFib was 2% after ablation and 12% with medical treatment, and after 3 years, the respective rates of progression were 2% and 18%. The between-group differences were statistically significant at all three follow-up intervals, Dr. Kuck reported. Analysis of only patients who followed their assigned protocol showed similar results, as did an analysis that used the definition of persistent AFib advanced by the Heart Rhythm Society in 2017 (Heart Rhythm. 2017 Oct;14[10]:e275-e444).
The advantage of ablation for deferring progression was consistent in all subgroups analyzed, with no signal of interaction by age, sex, or other subgroup definitions. The rate of serious adverse events was “low,” occurring in 12% of the ablated patients and in 5% of controls. The need for two or more ablations was also “low,” Dr Kuck said, with 17% of patients requiring a second procedure. The results additionally showed that ablation also led to a lower rate of any AFib recurrence, regardless of whether or not it met the definition of persistent AFib. Any AFib recurrence occurred in 57% of the ablated patients and in 85% of those managed medically during 3 years of follow-up, a statistically significant difference.
Although the mechanism by which ablation slowed AFib progression is not known, Dr. Kuck suggested that it may relate to a reduction in the frequency and duration of AFib recurrences. “I believe that AFib burden is the key. If AFib episodes last a few days, then the likelihood of progressing to episodes that last 7 days is much higher than when an episode only lasts a few minutes,” he explained. “We’re opening a new perspective that looks beyond managing AFib symptoms” using ablation.
ATTEST was funded by Biosense Webster, a company that markets catheter ablation devices. Dr. Kuck has been a consultant to Biosense Webster, as well as to Abbott, Boston Scientific, Edwards, and Medtronic.
REPORTING FROM THE ESC 2019 CONGRESS
Getting high heightens stroke, arrhythmia risks
Stoners, beware: , and people with cannabis use disorder are at a 50% greater risk of being hospitalized for arrhythmias, according to new research presented at the American Heart Association Scientific Sessions 2019.
An analysis of pooled data on nearly 44,000 participants in a cross-sectional survey showed that, among the 13.6% who reported using marijuana within the last 30 days, the adjusted odds ratio for young-onset stroke (aged 18-44 years), compared with non-users, was 2.75, reported Tarang Parekh, MBBS, a health policy researcher of George Mason University in Fairfax, Va., and colleagues.
In a separate study, a retrospective analysis of national inpatient data showed that people diagnosed with cannabis use disorder – a pathological pattern of impaired control, social impairment, risky behavior or physiological adaptation similar in nature to alcoholism – had a 47%-52% increased likelihood of hospitalization for an arrhythmia, reported Rikinkumar S. Patel, MD, a psychiatry resident at Griffin Memorial Hospital in Norman, Okla.
“As these [cannabis] products become increasingly used across the country, getting clearer, scientifically rigorous data is going to be important as we try to understand the overall health effects of cannabis,” said AHA President Robert Harrington, MD, of Stanford (Calif.) University in a statement.
Currently, use of both medical and recreational marijuana is fully legal in 11 U.S. states and the District of Columbia. Medical marijuana is legal with recreational use decriminalized (or penalties reduced) in 28 other states, and totally illegal in 11 other states, according to employee screening firm DISA Global Solutions.
Stroke study
In an oral presentation with simultaneous publication in the AHA journal Stroke, Dr. Parekh and colleagues presented an analysis of pooled data from the Behavioral Risk Factor Surveillance System (BRFSS), a nationally representative cross-sectional survey collected by the Centers for Disease Control and Prevention in 2016 and 2017.
They looked at baseline sociodemographic data and created multivariable logistic regression models with state fixed effects to determine whether marijuana use within the last 30 days was associated with young-onset stroke.
They identified 43,860 participants representing a weighted sample of 35.5 million Americans. Of the sample, 63.3% were male, and 13.6 % of all participants reported using marijuana in the last 30 days.
They found in an unadjusted model that marijuana users had an odds ratio for stroke, compared with nonusers, of 1.59 (P less than.1), and in a model adjusted for demographic factors (gender, race, ethnicity, and education) the OR increased to 1.76 (P less than .05).
When they threw risk behavior into the model (physical activity, body mass index, heavy drinking, and cigarette smoking), they saw that the OR for stroke shot up to 2.75 (P less than .01).
“Physicians should ask patients if they use cannabis and counsel them about its potential stroke risk as part of regular doctor visits,” Dr. Parekh said in a statement.
Arrhythmias study
Based on recent studies suggesting that cannabis use may trigger cardiovascular events, Dr. Patel and colleagues studied whether cannabis use disorder may be related to arrhythmias, approaching the question through hospital records.
“The effects of using cannabis are seen within 15 minutes and last for around 3 hours. At lower doses, it is linked to a rapid heartbeat. At higher doses, it is linked to a too-slow heartbeat,” he said in a statement.
Dr. Patel and colleagues conducted a retrospective analysis of the Nationwide Inpatient Sample from 2010-2014, a period during which medical marijuana became legal in several states and recreational marijuana became legal in Colorado and Washington. The sample is a database maintained by the Healthcare Cost and Utilization Project of the U.S. Office of Disease Prevention and Health Promotion.
They identified 570,557 patients aged 15-54 years with a primary diagnosis of arrhythmia, and compared them with a sample of 67,662,082 patients hospitalized with no arrhythmia diagnosed during the same period.
They found a 2.6% incidence of cannabis use disorder among patients hospitalized for arrhythmias. Patients with cannabis use disorder tended to be younger (15- to 24-years-old; OR, 4.23), male (OR, 1.70) and African American (OR, 2.70).
In regression analysis adjusted for demographics and comorbidities, cannabis use disorder was associated with higher odds of arrhythmia hospitalization in young patients, at 1.28 times among 15- to 24-year-olds (95% confidence interval, 1.229-1.346) and 1.52 times for 25- to 34-year-olds (95% CI, 1.469-1.578).
“As medical and recreational cannabis is legalized in many states, it is important to know the difference between therapeutic cannabis dosing for medical purposes and the consequences of cannabis abuse. We urgently need additional research to understand these issues,” Dr. Patel said.
“It’s not proving that there’s a direct link, but it’s raising a suggestion in an observational analysis that [this] indeed might be the case. What that means for clinicians is that, if you’re seeing a patient who is presenting with a symptomatic arrhythmia, adding cannabis usage to your list of questions as you begin to try to understand possible precipitating factors for this arrhythmia seems to be a reasonable thing to do,” Dr. Harrington commented.
Stoners, beware: , and people with cannabis use disorder are at a 50% greater risk of being hospitalized for arrhythmias, according to new research presented at the American Heart Association Scientific Sessions 2019.
An analysis of pooled data on nearly 44,000 participants in a cross-sectional survey showed that, among the 13.6% who reported using marijuana within the last 30 days, the adjusted odds ratio for young-onset stroke (aged 18-44 years), compared with non-users, was 2.75, reported Tarang Parekh, MBBS, a health policy researcher of George Mason University in Fairfax, Va., and colleagues.
In a separate study, a retrospective analysis of national inpatient data showed that people diagnosed with cannabis use disorder – a pathological pattern of impaired control, social impairment, risky behavior or physiological adaptation similar in nature to alcoholism – had a 47%-52% increased likelihood of hospitalization for an arrhythmia, reported Rikinkumar S. Patel, MD, a psychiatry resident at Griffin Memorial Hospital in Norman, Okla.
“As these [cannabis] products become increasingly used across the country, getting clearer, scientifically rigorous data is going to be important as we try to understand the overall health effects of cannabis,” said AHA President Robert Harrington, MD, of Stanford (Calif.) University in a statement.
Currently, use of both medical and recreational marijuana is fully legal in 11 U.S. states and the District of Columbia. Medical marijuana is legal with recreational use decriminalized (or penalties reduced) in 28 other states, and totally illegal in 11 other states, according to employee screening firm DISA Global Solutions.
Stroke study
In an oral presentation with simultaneous publication in the AHA journal Stroke, Dr. Parekh and colleagues presented an analysis of pooled data from the Behavioral Risk Factor Surveillance System (BRFSS), a nationally representative cross-sectional survey collected by the Centers for Disease Control and Prevention in 2016 and 2017.
They looked at baseline sociodemographic data and created multivariable logistic regression models with state fixed effects to determine whether marijuana use within the last 30 days was associated with young-onset stroke.
They identified 43,860 participants representing a weighted sample of 35.5 million Americans. Of the sample, 63.3% were male, and 13.6 % of all participants reported using marijuana in the last 30 days.
They found in an unadjusted model that marijuana users had an odds ratio for stroke, compared with nonusers, of 1.59 (P less than.1), and in a model adjusted for demographic factors (gender, race, ethnicity, and education) the OR increased to 1.76 (P less than .05).
When they threw risk behavior into the model (physical activity, body mass index, heavy drinking, and cigarette smoking), they saw that the OR for stroke shot up to 2.75 (P less than .01).
“Physicians should ask patients if they use cannabis and counsel them about its potential stroke risk as part of regular doctor visits,” Dr. Parekh said in a statement.
Arrhythmias study
Based on recent studies suggesting that cannabis use may trigger cardiovascular events, Dr. Patel and colleagues studied whether cannabis use disorder may be related to arrhythmias, approaching the question through hospital records.
“The effects of using cannabis are seen within 15 minutes and last for around 3 hours. At lower doses, it is linked to a rapid heartbeat. At higher doses, it is linked to a too-slow heartbeat,” he said in a statement.
Dr. Patel and colleagues conducted a retrospective analysis of the Nationwide Inpatient Sample from 2010-2014, a period during which medical marijuana became legal in several states and recreational marijuana became legal in Colorado and Washington. The sample is a database maintained by the Healthcare Cost and Utilization Project of the U.S. Office of Disease Prevention and Health Promotion.
They identified 570,557 patients aged 15-54 years with a primary diagnosis of arrhythmia, and compared them with a sample of 67,662,082 patients hospitalized with no arrhythmia diagnosed during the same period.
They found a 2.6% incidence of cannabis use disorder among patients hospitalized for arrhythmias. Patients with cannabis use disorder tended to be younger (15- to 24-years-old; OR, 4.23), male (OR, 1.70) and African American (OR, 2.70).
In regression analysis adjusted for demographics and comorbidities, cannabis use disorder was associated with higher odds of arrhythmia hospitalization in young patients, at 1.28 times among 15- to 24-year-olds (95% confidence interval, 1.229-1.346) and 1.52 times for 25- to 34-year-olds (95% CI, 1.469-1.578).
“As medical and recreational cannabis is legalized in many states, it is important to know the difference between therapeutic cannabis dosing for medical purposes and the consequences of cannabis abuse. We urgently need additional research to understand these issues,” Dr. Patel said.
“It’s not proving that there’s a direct link, but it’s raising a suggestion in an observational analysis that [this] indeed might be the case. What that means for clinicians is that, if you’re seeing a patient who is presenting with a symptomatic arrhythmia, adding cannabis usage to your list of questions as you begin to try to understand possible precipitating factors for this arrhythmia seems to be a reasonable thing to do,” Dr. Harrington commented.
Stoners, beware: , and people with cannabis use disorder are at a 50% greater risk of being hospitalized for arrhythmias, according to new research presented at the American Heart Association Scientific Sessions 2019.
An analysis of pooled data on nearly 44,000 participants in a cross-sectional survey showed that, among the 13.6% who reported using marijuana within the last 30 days, the adjusted odds ratio for young-onset stroke (aged 18-44 years), compared with non-users, was 2.75, reported Tarang Parekh, MBBS, a health policy researcher of George Mason University in Fairfax, Va., and colleagues.
In a separate study, a retrospective analysis of national inpatient data showed that people diagnosed with cannabis use disorder – a pathological pattern of impaired control, social impairment, risky behavior or physiological adaptation similar in nature to alcoholism – had a 47%-52% increased likelihood of hospitalization for an arrhythmia, reported Rikinkumar S. Patel, MD, a psychiatry resident at Griffin Memorial Hospital in Norman, Okla.
“As these [cannabis] products become increasingly used across the country, getting clearer, scientifically rigorous data is going to be important as we try to understand the overall health effects of cannabis,” said AHA President Robert Harrington, MD, of Stanford (Calif.) University in a statement.
Currently, use of both medical and recreational marijuana is fully legal in 11 U.S. states and the District of Columbia. Medical marijuana is legal with recreational use decriminalized (or penalties reduced) in 28 other states, and totally illegal in 11 other states, according to employee screening firm DISA Global Solutions.
Stroke study
In an oral presentation with simultaneous publication in the AHA journal Stroke, Dr. Parekh and colleagues presented an analysis of pooled data from the Behavioral Risk Factor Surveillance System (BRFSS), a nationally representative cross-sectional survey collected by the Centers for Disease Control and Prevention in 2016 and 2017.
They looked at baseline sociodemographic data and created multivariable logistic regression models with state fixed effects to determine whether marijuana use within the last 30 days was associated with young-onset stroke.
They identified 43,860 participants representing a weighted sample of 35.5 million Americans. Of the sample, 63.3% were male, and 13.6 % of all participants reported using marijuana in the last 30 days.
They found in an unadjusted model that marijuana users had an odds ratio for stroke, compared with nonusers, of 1.59 (P less than.1), and in a model adjusted for demographic factors (gender, race, ethnicity, and education) the OR increased to 1.76 (P less than .05).
When they threw risk behavior into the model (physical activity, body mass index, heavy drinking, and cigarette smoking), they saw that the OR for stroke shot up to 2.75 (P less than .01).
“Physicians should ask patients if they use cannabis and counsel them about its potential stroke risk as part of regular doctor visits,” Dr. Parekh said in a statement.
Arrhythmias study
Based on recent studies suggesting that cannabis use may trigger cardiovascular events, Dr. Patel and colleagues studied whether cannabis use disorder may be related to arrhythmias, approaching the question through hospital records.
“The effects of using cannabis are seen within 15 minutes and last for around 3 hours. At lower doses, it is linked to a rapid heartbeat. At higher doses, it is linked to a too-slow heartbeat,” he said in a statement.
Dr. Patel and colleagues conducted a retrospective analysis of the Nationwide Inpatient Sample from 2010-2014, a period during which medical marijuana became legal in several states and recreational marijuana became legal in Colorado and Washington. The sample is a database maintained by the Healthcare Cost and Utilization Project of the U.S. Office of Disease Prevention and Health Promotion.
They identified 570,557 patients aged 15-54 years with a primary diagnosis of arrhythmia, and compared them with a sample of 67,662,082 patients hospitalized with no arrhythmia diagnosed during the same period.
They found a 2.6% incidence of cannabis use disorder among patients hospitalized for arrhythmias. Patients with cannabis use disorder tended to be younger (15- to 24-years-old; OR, 4.23), male (OR, 1.70) and African American (OR, 2.70).
In regression analysis adjusted for demographics and comorbidities, cannabis use disorder was associated with higher odds of arrhythmia hospitalization in young patients, at 1.28 times among 15- to 24-year-olds (95% confidence interval, 1.229-1.346) and 1.52 times for 25- to 34-year-olds (95% CI, 1.469-1.578).
“As medical and recreational cannabis is legalized in many states, it is important to know the difference between therapeutic cannabis dosing for medical purposes and the consequences of cannabis abuse. We urgently need additional research to understand these issues,” Dr. Patel said.
“It’s not proving that there’s a direct link, but it’s raising a suggestion in an observational analysis that [this] indeed might be the case. What that means for clinicians is that, if you’re seeing a patient who is presenting with a symptomatic arrhythmia, adding cannabis usage to your list of questions as you begin to try to understand possible precipitating factors for this arrhythmia seems to be a reasonable thing to do,” Dr. Harrington commented.
REPORTING FROM AHA 2019
Patients frequently drive too soon after ICD implantation
PARIS – Fewer than half of commercial drivers who received implantable cardioverter-defibrillators (ICDs) recalled being told they should never drive professionally again, according to a recent Danish survey. Further, about a third of patients overall reported that they began driving soon after they received an ICD, during the period when guidelines recommend refraining from driving.
“These devices, they save lives – so what’s not to like?” lead investigator Jenny Bjerre, MD, asked at the annual congress of the European Society of Cardiology. “Well, if you are a patient qualifying for an ICD, you also automatically qualify for some driving restrictions.” These are put in place because of the concern for an arrhythmia causing a loss of consciousness behind the wheel, she said.
A European consensus statement calls for a 3-month driving moratorium when an ICD is implanted for secondary prevention or after an appropriate ICD shock, and a 4-week restriction when an ICD is placed for primary prevention. All these restrictions apply to personal driver’s licenses; anyone with an ICD is permanently restricted from commercial driving according to the consensus statement, said Dr. Bjerre, of the University Hospital, Copenhagen.
“As you can imagine, these restrictions are not that popular with the patients,” she said. She related the story of a patient, a taxi driver who had returned to a full range of physically taxing activities after his ICD implantation, but whose livelihood had been taken away from him.
Dr. Bjerre said she sought to understand the perspective of this patient, who said, “Sometimes I wish I hadn’t been resuscitated!” She saw that the loss of freedom and a meaningful occupation had profoundly affected the daily life of this patient, and she became curious about adherence to driving restrictions in patients with ICDs.
Using the nationwide Danish medical record database, Dr. Bjerre and her colleagues looked at a nationwide cohort of ICD patients to see they remembered hearing about restrictions on personal and commercial driving activities after ICD implantation. They also investigated adherence to restrictions, and sought to identify what factors were associated with nonadherence.
The questionnaire developed by Dr. Bjerre and her colleagues was made available to the ICD cohort both electronically and in a paper version. Questionnaires received were linked with a variety of nationwide registries through each participant’s unique national identification number, she explained. They obtained information about comorbidities, pharmacotherapies, and socioeconomic status. Not only did this linkage give more precise and complete data than would a questionnaire alone, but it also allowed the investigators to see how responders differed from nonresponders – important in questionnaire research, said Dr. Bjerre.
The investigators were able to locate and distribute questionnaires to a total of 3,913 living adults who had received first-time ICDs during the 3-year study period. In the end, even after excluding 31 responses for missing data, 2,741 responses were used for analysis – a response rate of over 70%.
The median age of respondents was 67, and 83% were male. About half – 46% – of respondents had an ICD implanted for primary prevention. Compared with those who did respond, said Dr. Bjerre, the nonresponders “were younger, sicker, more likely to be female, had lower socioeconomic status, and were less likely to be on guideline-directed therapy.”
Over 90% of respondents held a private driver’s license at the time of their ICD implantation, and just 7% were actively using a commercial license prior to implantation. Participants had a variety of commercial driving occupations, including driving trucks, buses, and taxis.
“Only 43% of primary prevention patients and 64% of secondary prevention patients stated that they had been informed about any driving restrictions,” said Dr. Bjerre. The figure was slightly better for patients after an ICD shock was delivered – 72% of these patients recalled hearing about driving restrictions.
“Among professional drivers – who are never supposed to drive again – only 45% said they had been informed about any professional driving restrictions,” she added.
What did patients report about their actual driving behaviors? Of patients receiving an ICD for primary prevention, 34% resumed driving within one week of ICD implantation. For those receiving an ICD for secondary prevention and those who had received an appropriate ICD shock, 43% and 30%, respectively, began driving before the recommended 3 months had elapsed.
The driving behavior of those with commercial licenses didn’t differ from the cohort as a whole: 35% of this group had resumed commercial driving.
In all the study’s subgroups, nonadherence to driving restrictions was more likely if the participant didn’t recall having been informed of the restrictions, with an odds ratio (OR) of 3.34 for nonadherence. However, noted Dr. Bjerre, at least 20% of patients in all subgroups who said they’d been told not to drive still resumed driving in contravention of restrictions. “So it seems that information can’t explain everything,” she said.
Additional predictors of nonadherence included male sex, with an OR of 1.53, being the only driver in the household (OR 1.29), and being at least 60 years old (OR, 1.20). Those receiving an ICD for secondary prevention had an OR of 2.20 for nonadherence, as well.
The study had a large cohort of real-life ICD patients and the response rate was high, said Dr. Bjerre. However, there was a risk of recall bias; additionally, nonresponders differed from responders, limiting full generalizability of the data. Finally, she observed that participants may have given the answers they thought were socially desirable.
“I want to get back to our friend the taxi driver,” who was adherent to restrictions, but who kept wanting to know what the actual chances were that he’d harm someone if he resumed driving. Realizing she couldn’t give him a very precise answer, Dr. Bjerre concluded, “I do think we owe it to our patients to provide more evidence on the absolute risk of traffic accidents in these patients.”
Dr. Bjerre reported that she had no conflicts of interest.
PARIS – Fewer than half of commercial drivers who received implantable cardioverter-defibrillators (ICDs) recalled being told they should never drive professionally again, according to a recent Danish survey. Further, about a third of patients overall reported that they began driving soon after they received an ICD, during the period when guidelines recommend refraining from driving.
“These devices, they save lives – so what’s not to like?” lead investigator Jenny Bjerre, MD, asked at the annual congress of the European Society of Cardiology. “Well, if you are a patient qualifying for an ICD, you also automatically qualify for some driving restrictions.” These are put in place because of the concern for an arrhythmia causing a loss of consciousness behind the wheel, she said.
A European consensus statement calls for a 3-month driving moratorium when an ICD is implanted for secondary prevention or after an appropriate ICD shock, and a 4-week restriction when an ICD is placed for primary prevention. All these restrictions apply to personal driver’s licenses; anyone with an ICD is permanently restricted from commercial driving according to the consensus statement, said Dr. Bjerre, of the University Hospital, Copenhagen.
“As you can imagine, these restrictions are not that popular with the patients,” she said. She related the story of a patient, a taxi driver who had returned to a full range of physically taxing activities after his ICD implantation, but whose livelihood had been taken away from him.
Dr. Bjerre said she sought to understand the perspective of this patient, who said, “Sometimes I wish I hadn’t been resuscitated!” She saw that the loss of freedom and a meaningful occupation had profoundly affected the daily life of this patient, and she became curious about adherence to driving restrictions in patients with ICDs.
Using the nationwide Danish medical record database, Dr. Bjerre and her colleagues looked at a nationwide cohort of ICD patients to see they remembered hearing about restrictions on personal and commercial driving activities after ICD implantation. They also investigated adherence to restrictions, and sought to identify what factors were associated with nonadherence.
The questionnaire developed by Dr. Bjerre and her colleagues was made available to the ICD cohort both electronically and in a paper version. Questionnaires received were linked with a variety of nationwide registries through each participant’s unique national identification number, she explained. They obtained information about comorbidities, pharmacotherapies, and socioeconomic status. Not only did this linkage give more precise and complete data than would a questionnaire alone, but it also allowed the investigators to see how responders differed from nonresponders – important in questionnaire research, said Dr. Bjerre.
The investigators were able to locate and distribute questionnaires to a total of 3,913 living adults who had received first-time ICDs during the 3-year study period. In the end, even after excluding 31 responses for missing data, 2,741 responses were used for analysis – a response rate of over 70%.
The median age of respondents was 67, and 83% were male. About half – 46% – of respondents had an ICD implanted for primary prevention. Compared with those who did respond, said Dr. Bjerre, the nonresponders “were younger, sicker, more likely to be female, had lower socioeconomic status, and were less likely to be on guideline-directed therapy.”
Over 90% of respondents held a private driver’s license at the time of their ICD implantation, and just 7% were actively using a commercial license prior to implantation. Participants had a variety of commercial driving occupations, including driving trucks, buses, and taxis.
“Only 43% of primary prevention patients and 64% of secondary prevention patients stated that they had been informed about any driving restrictions,” said Dr. Bjerre. The figure was slightly better for patients after an ICD shock was delivered – 72% of these patients recalled hearing about driving restrictions.
“Among professional drivers – who are never supposed to drive again – only 45% said they had been informed about any professional driving restrictions,” she added.
What did patients report about their actual driving behaviors? Of patients receiving an ICD for primary prevention, 34% resumed driving within one week of ICD implantation. For those receiving an ICD for secondary prevention and those who had received an appropriate ICD shock, 43% and 30%, respectively, began driving before the recommended 3 months had elapsed.
The driving behavior of those with commercial licenses didn’t differ from the cohort as a whole: 35% of this group had resumed commercial driving.
In all the study’s subgroups, nonadherence to driving restrictions was more likely if the participant didn’t recall having been informed of the restrictions, with an odds ratio (OR) of 3.34 for nonadherence. However, noted Dr. Bjerre, at least 20% of patients in all subgroups who said they’d been told not to drive still resumed driving in contravention of restrictions. “So it seems that information can’t explain everything,” she said.
Additional predictors of nonadherence included male sex, with an OR of 1.53, being the only driver in the household (OR 1.29), and being at least 60 years old (OR, 1.20). Those receiving an ICD for secondary prevention had an OR of 2.20 for nonadherence, as well.
The study had a large cohort of real-life ICD patients and the response rate was high, said Dr. Bjerre. However, there was a risk of recall bias; additionally, nonresponders differed from responders, limiting full generalizability of the data. Finally, she observed that participants may have given the answers they thought were socially desirable.
“I want to get back to our friend the taxi driver,” who was adherent to restrictions, but who kept wanting to know what the actual chances were that he’d harm someone if he resumed driving. Realizing she couldn’t give him a very precise answer, Dr. Bjerre concluded, “I do think we owe it to our patients to provide more evidence on the absolute risk of traffic accidents in these patients.”
Dr. Bjerre reported that she had no conflicts of interest.
PARIS – Fewer than half of commercial drivers who received implantable cardioverter-defibrillators (ICDs) recalled being told they should never drive professionally again, according to a recent Danish survey. Further, about a third of patients overall reported that they began driving soon after they received an ICD, during the period when guidelines recommend refraining from driving.
“These devices, they save lives – so what’s not to like?” lead investigator Jenny Bjerre, MD, asked at the annual congress of the European Society of Cardiology. “Well, if you are a patient qualifying for an ICD, you also automatically qualify for some driving restrictions.” These are put in place because of the concern for an arrhythmia causing a loss of consciousness behind the wheel, she said.
A European consensus statement calls for a 3-month driving moratorium when an ICD is implanted for secondary prevention or after an appropriate ICD shock, and a 4-week restriction when an ICD is placed for primary prevention. All these restrictions apply to personal driver’s licenses; anyone with an ICD is permanently restricted from commercial driving according to the consensus statement, said Dr. Bjerre, of the University Hospital, Copenhagen.
“As you can imagine, these restrictions are not that popular with the patients,” she said. She related the story of a patient, a taxi driver who had returned to a full range of physically taxing activities after his ICD implantation, but whose livelihood had been taken away from him.
Dr. Bjerre said she sought to understand the perspective of this patient, who said, “Sometimes I wish I hadn’t been resuscitated!” She saw that the loss of freedom and a meaningful occupation had profoundly affected the daily life of this patient, and she became curious about adherence to driving restrictions in patients with ICDs.
Using the nationwide Danish medical record database, Dr. Bjerre and her colleagues looked at a nationwide cohort of ICD patients to see they remembered hearing about restrictions on personal and commercial driving activities after ICD implantation. They also investigated adherence to restrictions, and sought to identify what factors were associated with nonadherence.
The questionnaire developed by Dr. Bjerre and her colleagues was made available to the ICD cohort both electronically and in a paper version. Questionnaires received were linked with a variety of nationwide registries through each participant’s unique national identification number, she explained. They obtained information about comorbidities, pharmacotherapies, and socioeconomic status. Not only did this linkage give more precise and complete data than would a questionnaire alone, but it also allowed the investigators to see how responders differed from nonresponders – important in questionnaire research, said Dr. Bjerre.
The investigators were able to locate and distribute questionnaires to a total of 3,913 living adults who had received first-time ICDs during the 3-year study period. In the end, even after excluding 31 responses for missing data, 2,741 responses were used for analysis – a response rate of over 70%.
The median age of respondents was 67, and 83% were male. About half – 46% – of respondents had an ICD implanted for primary prevention. Compared with those who did respond, said Dr. Bjerre, the nonresponders “were younger, sicker, more likely to be female, had lower socioeconomic status, and were less likely to be on guideline-directed therapy.”
Over 90% of respondents held a private driver’s license at the time of their ICD implantation, and just 7% were actively using a commercial license prior to implantation. Participants had a variety of commercial driving occupations, including driving trucks, buses, and taxis.
“Only 43% of primary prevention patients and 64% of secondary prevention patients stated that they had been informed about any driving restrictions,” said Dr. Bjerre. The figure was slightly better for patients after an ICD shock was delivered – 72% of these patients recalled hearing about driving restrictions.
“Among professional drivers – who are never supposed to drive again – only 45% said they had been informed about any professional driving restrictions,” she added.
What did patients report about their actual driving behaviors? Of patients receiving an ICD for primary prevention, 34% resumed driving within one week of ICD implantation. For those receiving an ICD for secondary prevention and those who had received an appropriate ICD shock, 43% and 30%, respectively, began driving before the recommended 3 months had elapsed.
The driving behavior of those with commercial licenses didn’t differ from the cohort as a whole: 35% of this group had resumed commercial driving.
In all the study’s subgroups, nonadherence to driving restrictions was more likely if the participant didn’t recall having been informed of the restrictions, with an odds ratio (OR) of 3.34 for nonadherence. However, noted Dr. Bjerre, at least 20% of patients in all subgroups who said they’d been told not to drive still resumed driving in contravention of restrictions. “So it seems that information can’t explain everything,” she said.
Additional predictors of nonadherence included male sex, with an OR of 1.53, being the only driver in the household (OR 1.29), and being at least 60 years old (OR, 1.20). Those receiving an ICD for secondary prevention had an OR of 2.20 for nonadherence, as well.
The study had a large cohort of real-life ICD patients and the response rate was high, said Dr. Bjerre. However, there was a risk of recall bias; additionally, nonresponders differed from responders, limiting full generalizability of the data. Finally, she observed that participants may have given the answers they thought were socially desirable.
“I want to get back to our friend the taxi driver,” who was adherent to restrictions, but who kept wanting to know what the actual chances were that he’d harm someone if he resumed driving. Realizing she couldn’t give him a very precise answer, Dr. Bjerre concluded, “I do think we owe it to our patients to provide more evidence on the absolute risk of traffic accidents in these patients.”
Dr. Bjerre reported that she had no conflicts of interest.
REPORTING FROM ESC CONGRESS 2019
Native Americans appear to be at increased risk for AFib
Over 4 years, atrial fibrillation (AFib) developed significantly more often in a group of Native Americans men than it did among other racial and ethnic groups, a large longitudinal cohort study has found.
The overall incidence among Native Americans was 7.49 per 1,000 person-years – significantly higher than the incidence in a comparator cohort of black, white, Asian, and Hispanic men, Gregory M. Marcus, MD, of the University of California, San Francisco, and colleagues wrote in a research letter published in Circulation.
“We were surprised to find that American Indians experienced a higher risk of atrial fibrillation, compared to every other racial and ethnic group,” Dr. Marcus said in a press release that accompanied the study. “Understanding the mechanisms and factors by which American Indians experience this higher risk may help investigators better understand the fundamental causes of atrial fibrillation that prove useful to everyone at risk for AFib, regardless of their race or ethnicity.”
The team plumbed the Healthcare Cost and Utilization Project (HCUP) California state databases for information on more than 16 million cases of AFib that occurred during 2005-2011. Native Americans comprised just 0.6% of the cohort. Most of the patients (57.2%) were white; 8% were black, 25.6% Hispanic, and 8.6% Asian. After targeting only new-onset cases, there were 344,469 incident AFib episodes over a median follow-up of 4.1 years.
The overall incidence of AFib in Native Americans was 7.49 per 1,000 person-years, significantly higher than the 6.89 per 1000 person-years observed in the rest of the cohort ( P less than .0001). The difference remained significant even after the team controlled for age, sex, income, and heart and other diseases. Nor was it altered by a sensitivity analysis that controlled for place of presentation and patients who were aged at least 35 years with at least two encounters with medical facilities.
In an interaction analysis, the increased risk appeared to be driven by higher rates of diabetes and chronic kidney disease, the authors wrote.
“This may suggest that the presence of these two processes contributes some pathophysiology related to AF[ib] risk that may be similar to the heightened risk inherent among American Indians,” they wrote. “It is also important to note that there was no evidence of any other statistically significant interactions despite the inclusion of millions of patients.”
Supporting data for these associations were not included in the research letter.
The authors noted some limitations of their study. Race or ethnicity were self-reported and could not be independently confirmed, so there was no way to tease out the effects in multiracial patients. Also, the database didn’t record outpatient encounters, which might result in some selection bias.
“Last, because this was an observational study, these results should not be interpreted as evidence of causal effect,” they noted.
“In conclusion, we observed that American Indians had a higher risk of atrial fibrillation, compared with all other racial and ethnic group. The heightened risk … in American Indians persisted after multivariable adjustment for known conventional confounders and mediators, suggesting that an unidentified characteristic, including possible genetic or environmental factors, may be responsible,” the investigators wrote.
The HCUP database is supported by the Agency for Healthcare Research and Quality. Dr. Marcus reported receiving research support from Jawbone, Medtronic, Eight, and Baylis Medical, and is a consultant for and holds equity in InCarda Therapeutics. The other authors reported no conflicts of interest.
SOURCE: Marcus GM et al. Circulation. 2019 Oct 21. doi:10.1161/CIRCULATIONAHA.119.042882.
Over 4 years, atrial fibrillation (AFib) developed significantly more often in a group of Native Americans men than it did among other racial and ethnic groups, a large longitudinal cohort study has found.
The overall incidence among Native Americans was 7.49 per 1,000 person-years – significantly higher than the incidence in a comparator cohort of black, white, Asian, and Hispanic men, Gregory M. Marcus, MD, of the University of California, San Francisco, and colleagues wrote in a research letter published in Circulation.
“We were surprised to find that American Indians experienced a higher risk of atrial fibrillation, compared to every other racial and ethnic group,” Dr. Marcus said in a press release that accompanied the study. “Understanding the mechanisms and factors by which American Indians experience this higher risk may help investigators better understand the fundamental causes of atrial fibrillation that prove useful to everyone at risk for AFib, regardless of their race or ethnicity.”
The team plumbed the Healthcare Cost and Utilization Project (HCUP) California state databases for information on more than 16 million cases of AFib that occurred during 2005-2011. Native Americans comprised just 0.6% of the cohort. Most of the patients (57.2%) were white; 8% were black, 25.6% Hispanic, and 8.6% Asian. After targeting only new-onset cases, there were 344,469 incident AFib episodes over a median follow-up of 4.1 years.
The overall incidence of AFib in Native Americans was 7.49 per 1,000 person-years, significantly higher than the 6.89 per 1000 person-years observed in the rest of the cohort ( P less than .0001). The difference remained significant even after the team controlled for age, sex, income, and heart and other diseases. Nor was it altered by a sensitivity analysis that controlled for place of presentation and patients who were aged at least 35 years with at least two encounters with medical facilities.
In an interaction analysis, the increased risk appeared to be driven by higher rates of diabetes and chronic kidney disease, the authors wrote.
“This may suggest that the presence of these two processes contributes some pathophysiology related to AF[ib] risk that may be similar to the heightened risk inherent among American Indians,” they wrote. “It is also important to note that there was no evidence of any other statistically significant interactions despite the inclusion of millions of patients.”
Supporting data for these associations were not included in the research letter.
The authors noted some limitations of their study. Race or ethnicity were self-reported and could not be independently confirmed, so there was no way to tease out the effects in multiracial patients. Also, the database didn’t record outpatient encounters, which might result in some selection bias.
“Last, because this was an observational study, these results should not be interpreted as evidence of causal effect,” they noted.
“In conclusion, we observed that American Indians had a higher risk of atrial fibrillation, compared with all other racial and ethnic group. The heightened risk … in American Indians persisted after multivariable adjustment for known conventional confounders and mediators, suggesting that an unidentified characteristic, including possible genetic or environmental factors, may be responsible,” the investigators wrote.
The HCUP database is supported by the Agency for Healthcare Research and Quality. Dr. Marcus reported receiving research support from Jawbone, Medtronic, Eight, and Baylis Medical, and is a consultant for and holds equity in InCarda Therapeutics. The other authors reported no conflicts of interest.
SOURCE: Marcus GM et al. Circulation. 2019 Oct 21. doi:10.1161/CIRCULATIONAHA.119.042882.
Over 4 years, atrial fibrillation (AFib) developed significantly more often in a group of Native Americans men than it did among other racial and ethnic groups, a large longitudinal cohort study has found.
The overall incidence among Native Americans was 7.49 per 1,000 person-years – significantly higher than the incidence in a comparator cohort of black, white, Asian, and Hispanic men, Gregory M. Marcus, MD, of the University of California, San Francisco, and colleagues wrote in a research letter published in Circulation.
“We were surprised to find that American Indians experienced a higher risk of atrial fibrillation, compared to every other racial and ethnic group,” Dr. Marcus said in a press release that accompanied the study. “Understanding the mechanisms and factors by which American Indians experience this higher risk may help investigators better understand the fundamental causes of atrial fibrillation that prove useful to everyone at risk for AFib, regardless of their race or ethnicity.”
The team plumbed the Healthcare Cost and Utilization Project (HCUP) California state databases for information on more than 16 million cases of AFib that occurred during 2005-2011. Native Americans comprised just 0.6% of the cohort. Most of the patients (57.2%) were white; 8% were black, 25.6% Hispanic, and 8.6% Asian. After targeting only new-onset cases, there were 344,469 incident AFib episodes over a median follow-up of 4.1 years.
The overall incidence of AFib in Native Americans was 7.49 per 1,000 person-years, significantly higher than the 6.89 per 1000 person-years observed in the rest of the cohort ( P less than .0001). The difference remained significant even after the team controlled for age, sex, income, and heart and other diseases. Nor was it altered by a sensitivity analysis that controlled for place of presentation and patients who were aged at least 35 years with at least two encounters with medical facilities.
In an interaction analysis, the increased risk appeared to be driven by higher rates of diabetes and chronic kidney disease, the authors wrote.
“This may suggest that the presence of these two processes contributes some pathophysiology related to AF[ib] risk that may be similar to the heightened risk inherent among American Indians,” they wrote. “It is also important to note that there was no evidence of any other statistically significant interactions despite the inclusion of millions of patients.”
Supporting data for these associations were not included in the research letter.
The authors noted some limitations of their study. Race or ethnicity were self-reported and could not be independently confirmed, so there was no way to tease out the effects in multiracial patients. Also, the database didn’t record outpatient encounters, which might result in some selection bias.
“Last, because this was an observational study, these results should not be interpreted as evidence of causal effect,” they noted.
“In conclusion, we observed that American Indians had a higher risk of atrial fibrillation, compared with all other racial and ethnic group. The heightened risk … in American Indians persisted after multivariable adjustment for known conventional confounders and mediators, suggesting that an unidentified characteristic, including possible genetic or environmental factors, may be responsible,” the investigators wrote.
The HCUP database is supported by the Agency for Healthcare Research and Quality. Dr. Marcus reported receiving research support from Jawbone, Medtronic, Eight, and Baylis Medical, and is a consultant for and holds equity in InCarda Therapeutics. The other authors reported no conflicts of interest.
SOURCE: Marcus GM et al. Circulation. 2019 Oct 21. doi:10.1161/CIRCULATIONAHA.119.042882.
FROM CIRCULATION
Regular drinking a greater AFib risk than binge drinking
Regular low-level alcohol consumption may be a bigger risk factor for new-onset atrial fibrillation than binge drinking, according to a paper published online in EP Europace.
Alcohol consumption is known to have a dose-dependent association with the risk of new-onset atrial fibrillation (AFib), but the mechanism underlying this association was not clear, according to Yun Gi Kim, MD, from the Seoul National University (South Korea), and coauthors.
They analyzed data from the Korean National Health Insurance Service database for 9,776,956 individuals without atrial fibrillation at baseline, including health survey information about their alcohol consumption.
Overall, 51.3% of the study population were classified as nondrinkers, 32.1% were mild drinkers – defined as up to 105 g of alcohol consumed per week – 9.7% were moderate drinkers consuming 105-210 g/week, and 6.9% were heavy drinkers consuming 210 g or more per week.
The analysis revealed that heavy drinkers had the highest risk for new-onset AFib – 21.5% higher than mild drinkers – while nondrinkers had an 8.6% higher risk and moderate drinkers had a 7.7% higher risk, compared with mild drinkers.
It also showed an association between the number of drinking sessions per week and the development of new-onset atrial fibrillation. Individuals who only drank once per week had the lowest risk of AFib while those who drank every day had the highest.
“Although weekly alcohol intake was associated with the risk of new-onset [AFib], such association was lost when drinking frequency was included in the multivariate model,” the authors wrote.
They found a significant inverse relationship between the amount of alcohol consumed per drinking session, and the risk of new-onset AFib, such that individuals who consumed low amounts of alcohol per session had a higher risk, and the risk decreased as higher amounts were consumed.
“Regardless of whether weekly alcohol intake exceeded 210 g, the frequency of drinking was significantly associated with risk of new-onset [AFib],” they reported. “Patients who drink everyday represented the highest-risk group and those who drink once per week were the lowest-risk group for new-onset [AFib] in this investigation, respectively.”
The authors speculated that if alcohol consumption can trigger AFib, then multiple drinking episodes per week, regardless of amount, might trigger more episodes of AFib and potentially lead to the development of overt, new-onset disease. They also suggested that frequent drinking could lead to regular sleep disturbance, which might also contribute to the link with atrial fibrillation.
The study was supported by Korea University, Korea University Anam Hospital, Republic of Korea, the National Research Foundation of Korea, the Ministry of Education and the Ministry of Science, ICT, and Future Planning. No conflicts of interest were declared.
SOURCE: Kim YG et al. EP Europace. 2019 Oct 17. doi: 10.1093/europace/euz256.
Regular low-level alcohol consumption may be a bigger risk factor for new-onset atrial fibrillation than binge drinking, according to a paper published online in EP Europace.
Alcohol consumption is known to have a dose-dependent association with the risk of new-onset atrial fibrillation (AFib), but the mechanism underlying this association was not clear, according to Yun Gi Kim, MD, from the Seoul National University (South Korea), and coauthors.
They analyzed data from the Korean National Health Insurance Service database for 9,776,956 individuals without atrial fibrillation at baseline, including health survey information about their alcohol consumption.
Overall, 51.3% of the study population were classified as nondrinkers, 32.1% were mild drinkers – defined as up to 105 g of alcohol consumed per week – 9.7% were moderate drinkers consuming 105-210 g/week, and 6.9% were heavy drinkers consuming 210 g or more per week.
The analysis revealed that heavy drinkers had the highest risk for new-onset AFib – 21.5% higher than mild drinkers – while nondrinkers had an 8.6% higher risk and moderate drinkers had a 7.7% higher risk, compared with mild drinkers.
It also showed an association between the number of drinking sessions per week and the development of new-onset atrial fibrillation. Individuals who only drank once per week had the lowest risk of AFib while those who drank every day had the highest.
“Although weekly alcohol intake was associated with the risk of new-onset [AFib], such association was lost when drinking frequency was included in the multivariate model,” the authors wrote.
They found a significant inverse relationship between the amount of alcohol consumed per drinking session, and the risk of new-onset AFib, such that individuals who consumed low amounts of alcohol per session had a higher risk, and the risk decreased as higher amounts were consumed.
“Regardless of whether weekly alcohol intake exceeded 210 g, the frequency of drinking was significantly associated with risk of new-onset [AFib],” they reported. “Patients who drink everyday represented the highest-risk group and those who drink once per week were the lowest-risk group for new-onset [AFib] in this investigation, respectively.”
The authors speculated that if alcohol consumption can trigger AFib, then multiple drinking episodes per week, regardless of amount, might trigger more episodes of AFib and potentially lead to the development of overt, new-onset disease. They also suggested that frequent drinking could lead to regular sleep disturbance, which might also contribute to the link with atrial fibrillation.
The study was supported by Korea University, Korea University Anam Hospital, Republic of Korea, the National Research Foundation of Korea, the Ministry of Education and the Ministry of Science, ICT, and Future Planning. No conflicts of interest were declared.
SOURCE: Kim YG et al. EP Europace. 2019 Oct 17. doi: 10.1093/europace/euz256.
Regular low-level alcohol consumption may be a bigger risk factor for new-onset atrial fibrillation than binge drinking, according to a paper published online in EP Europace.
Alcohol consumption is known to have a dose-dependent association with the risk of new-onset atrial fibrillation (AFib), but the mechanism underlying this association was not clear, according to Yun Gi Kim, MD, from the Seoul National University (South Korea), and coauthors.
They analyzed data from the Korean National Health Insurance Service database for 9,776,956 individuals without atrial fibrillation at baseline, including health survey information about their alcohol consumption.
Overall, 51.3% of the study population were classified as nondrinkers, 32.1% were mild drinkers – defined as up to 105 g of alcohol consumed per week – 9.7% were moderate drinkers consuming 105-210 g/week, and 6.9% were heavy drinkers consuming 210 g or more per week.
The analysis revealed that heavy drinkers had the highest risk for new-onset AFib – 21.5% higher than mild drinkers – while nondrinkers had an 8.6% higher risk and moderate drinkers had a 7.7% higher risk, compared with mild drinkers.
It also showed an association between the number of drinking sessions per week and the development of new-onset atrial fibrillation. Individuals who only drank once per week had the lowest risk of AFib while those who drank every day had the highest.
“Although weekly alcohol intake was associated with the risk of new-onset [AFib], such association was lost when drinking frequency was included in the multivariate model,” the authors wrote.
They found a significant inverse relationship between the amount of alcohol consumed per drinking session, and the risk of new-onset AFib, such that individuals who consumed low amounts of alcohol per session had a higher risk, and the risk decreased as higher amounts were consumed.
“Regardless of whether weekly alcohol intake exceeded 210 g, the frequency of drinking was significantly associated with risk of new-onset [AFib],” they reported. “Patients who drink everyday represented the highest-risk group and those who drink once per week were the lowest-risk group for new-onset [AFib] in this investigation, respectively.”
The authors speculated that if alcohol consumption can trigger AFib, then multiple drinking episodes per week, regardless of amount, might trigger more episodes of AFib and potentially lead to the development of overt, new-onset disease. They also suggested that frequent drinking could lead to regular sleep disturbance, which might also contribute to the link with atrial fibrillation.
The study was supported by Korea University, Korea University Anam Hospital, Republic of Korea, the National Research Foundation of Korea, the Ministry of Education and the Ministry of Science, ICT, and Future Planning. No conflicts of interest were declared.
SOURCE: Kim YG et al. EP Europace. 2019 Oct 17. doi: 10.1093/europace/euz256.
FROM EP EUROPACE