User login
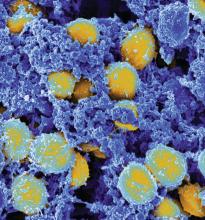
Clinical Trial: The Checklist to Prevent MRSA Surgical Site Infections
who are undergoing or have undergone cardiac surgery or total joint arthroplasty.
The Department of Veteran Affairs has previously implemented the VA MRSA Prevention Initiative, which successfully reduced patient-to-patient MRSA transmission; however, this initiative does not prevent most MRSA surgical site infections, which are spread differently. The VA has developed a new checklist which will be tested in this study aimed at reducing MRSA surgical site infections (SSIs), and will be implemented at 10 VA medical centers.
The primary outcome measure is superficial and deep/organ space MRSA infections within 90 days of operation. Secondary outcome measures include superficial and deep/organ space MRSA infections within 1 year of operation, presurgical bundle and individual bundle components compliance for 30 days prior to operation, length of postoperative stay, all-cause mortality 1 year after surgery, readmission within 90 days of surgery, and mupirocin and chlorhexidine resistance 30 days presurgery to 90 days postsurgery.
The study will end in April 2019. More than 10,000 people are expected to be included in the final analysis.
Find more information on the study page at Clinicaltrials.gov.
who are undergoing or have undergone cardiac surgery or total joint arthroplasty.
The Department of Veteran Affairs has previously implemented the VA MRSA Prevention Initiative, which successfully reduced patient-to-patient MRSA transmission; however, this initiative does not prevent most MRSA surgical site infections, which are spread differently. The VA has developed a new checklist which will be tested in this study aimed at reducing MRSA surgical site infections (SSIs), and will be implemented at 10 VA medical centers.
The primary outcome measure is superficial and deep/organ space MRSA infections within 90 days of operation. Secondary outcome measures include superficial and deep/organ space MRSA infections within 1 year of operation, presurgical bundle and individual bundle components compliance for 30 days prior to operation, length of postoperative stay, all-cause mortality 1 year after surgery, readmission within 90 days of surgery, and mupirocin and chlorhexidine resistance 30 days presurgery to 90 days postsurgery.
The study will end in April 2019. More than 10,000 people are expected to be included in the final analysis.
Find more information on the study page at Clinicaltrials.gov.
who are undergoing or have undergone cardiac surgery or total joint arthroplasty.
The Department of Veteran Affairs has previously implemented the VA MRSA Prevention Initiative, which successfully reduced patient-to-patient MRSA transmission; however, this initiative does not prevent most MRSA surgical site infections, which are spread differently. The VA has developed a new checklist which will be tested in this study aimed at reducing MRSA surgical site infections (SSIs), and will be implemented at 10 VA medical centers.
The primary outcome measure is superficial and deep/organ space MRSA infections within 90 days of operation. Secondary outcome measures include superficial and deep/organ space MRSA infections within 1 year of operation, presurgical bundle and individual bundle components compliance for 30 days prior to operation, length of postoperative stay, all-cause mortality 1 year after surgery, readmission within 90 days of surgery, and mupirocin and chlorhexidine resistance 30 days presurgery to 90 days postsurgery.
The study will end in April 2019. More than 10,000 people are expected to be included in the final analysis.
Find more information on the study page at Clinicaltrials.gov.
FROM CLINICALTRIALS.GOV
Risks identified for drug-resistant bacteremia in cirrhosis
In patients hospitalized with cirrhosis, biliary cirrhosis, recent health care exposure, nonwhite race, and cultures taken more than 48 hours after admission all independently predicted that bacteremia would be caused by multidrug-resistant organisms (MDROs), according to a medical record review at CHI St. Luke’s Medical Center, an 850-bed tertiary care center in Houston.
“These variables along with severity of infection and liver disease may help clinicians identify patients who will benefit most from broader-spectrum empiric antimicrobial therapy,” wrote the investigators, led by Jennifer Addo Smith, PharmD, of St. Luke’s, in the Journal of Clinical Gastroenterology.
But local epidemiology remains important. “Although a gram-positive agent (e.g., vancomycin) and a carbapenem-sparing gram-negative agent (e.g., ceftriaxone, cefepime) are reasonable empiric agents at our center, other centers with different resistance patterns may warrant different empiric therapy. Given the low prevalence of VRE [vancomycin-resistant Enterococcus] in this study ... and E. faecium in other studies (4%-7%), an empiric agent active against VRE does not seem to be routinely required,” they said.
The team looked into the issue because there hasn’t been much investigation in the United States of the role of multidrug resistant organisms in bacteremia among patients hospitalized with cirrhosis.
Thirty patients in the study had bacteremia caused by MDROs while 60 had bacteremia from non-MDROs, giving a 33% prevalence of MDRO bacteremia, which was consistent with previous, mostly European studies.
Enterobacteriaceae (43%), Staphylococcus aureus (18%), Streptococcus spp. (11%), Enterococcus spp. (10%), and nonfermenting gram-negative bacilli (6%) were the main causes of bacteremia overall.
Among the 30 MDRO cases, methicillin-resistant S. aureus was isolated in seven (23%); methicillin-resistant coagulase-negative Staphylococci in four (13%); fluoroquinolone-resistant Enterobacteriaceae in nine (30%); extended spectrum beta-lactamase–producing Enterobacteriaceae in three (10%), and VRE in two (7%). No carbapenemase-producing gram-negative bacteria were identified.
The predictors of MDRO bacteremia emerged on multivariate analysis and included biliary cirrhosis (adjusted odds ratio, 11.75; 95% confidence interval, 2.08-66.32); recent health care exposure (aOR, 9.81; 95% CI, 2.15-44.88); blood cultures obtained 48 hours after hospital admission (aOR, 6.02; 95% CI, 1.70-21.40) and nonwhite race (aOR , 3.35; 95% CI, 1.19-9.38).
Blood cultures past 48 hours and recent health care exposure – generally hospitalization within the past 90 days – were likely surrogates for nosocomial infection.
The link with biliary cirrhosis is unclear. “Compared with other cirrhotic patients, perhaps patients with PBC [primary biliary cholangitis] have had more cumulative antimicrobial exposure because of [their] higher risk for UTIs [urinary tract infections] and therefore are at increased risk for MDROs,” they wrote.
The median age in the study was 59 years. Half of the patients were white; 46% were women. Hepatitis C was the most common cause of cirrhosis, followed by alcohol.
MDRO was defined in the study as bacteria not susceptible to at least one antibiotic in at least three antimicrobial categories; 90 cirrhosis patients without bacteremia served as controls.
The funding source was not reported. Dr. Addo Smith had no disclosures.
SOURCE: Smith JA et al. J Clin Gastroenterol. 2017 Nov 23. doi: 10.1097/MCG.0000000000000964.
*This story was updated on 1/10/2018.
In patients hospitalized with cirrhosis, biliary cirrhosis, recent health care exposure, nonwhite race, and cultures taken more than 48 hours after admission all independently predicted that bacteremia would be caused by multidrug-resistant organisms (MDROs), according to a medical record review at CHI St. Luke’s Medical Center, an 850-bed tertiary care center in Houston.
“These variables along with severity of infection and liver disease may help clinicians identify patients who will benefit most from broader-spectrum empiric antimicrobial therapy,” wrote the investigators, led by Jennifer Addo Smith, PharmD, of St. Luke’s, in the Journal of Clinical Gastroenterology.
But local epidemiology remains important. “Although a gram-positive agent (e.g., vancomycin) and a carbapenem-sparing gram-negative agent (e.g., ceftriaxone, cefepime) are reasonable empiric agents at our center, other centers with different resistance patterns may warrant different empiric therapy. Given the low prevalence of VRE [vancomycin-resistant Enterococcus] in this study ... and E. faecium in other studies (4%-7%), an empiric agent active against VRE does not seem to be routinely required,” they said.
The team looked into the issue because there hasn’t been much investigation in the United States of the role of multidrug resistant organisms in bacteremia among patients hospitalized with cirrhosis.
Thirty patients in the study had bacteremia caused by MDROs while 60 had bacteremia from non-MDROs, giving a 33% prevalence of MDRO bacteremia, which was consistent with previous, mostly European studies.
Enterobacteriaceae (43%), Staphylococcus aureus (18%), Streptococcus spp. (11%), Enterococcus spp. (10%), and nonfermenting gram-negative bacilli (6%) were the main causes of bacteremia overall.
Among the 30 MDRO cases, methicillin-resistant S. aureus was isolated in seven (23%); methicillin-resistant coagulase-negative Staphylococci in four (13%); fluoroquinolone-resistant Enterobacteriaceae in nine (30%); extended spectrum beta-lactamase–producing Enterobacteriaceae in three (10%), and VRE in two (7%). No carbapenemase-producing gram-negative bacteria were identified.
The predictors of MDRO bacteremia emerged on multivariate analysis and included biliary cirrhosis (adjusted odds ratio, 11.75; 95% confidence interval, 2.08-66.32); recent health care exposure (aOR, 9.81; 95% CI, 2.15-44.88); blood cultures obtained 48 hours after hospital admission (aOR, 6.02; 95% CI, 1.70-21.40) and nonwhite race (aOR , 3.35; 95% CI, 1.19-9.38).
Blood cultures past 48 hours and recent health care exposure – generally hospitalization within the past 90 days – were likely surrogates for nosocomial infection.
The link with biliary cirrhosis is unclear. “Compared with other cirrhotic patients, perhaps patients with PBC [primary biliary cholangitis] have had more cumulative antimicrobial exposure because of [their] higher risk for UTIs [urinary tract infections] and therefore are at increased risk for MDROs,” they wrote.
The median age in the study was 59 years. Half of the patients were white; 46% were women. Hepatitis C was the most common cause of cirrhosis, followed by alcohol.
MDRO was defined in the study as bacteria not susceptible to at least one antibiotic in at least three antimicrobial categories; 90 cirrhosis patients without bacteremia served as controls.
The funding source was not reported. Dr. Addo Smith had no disclosures.
SOURCE: Smith JA et al. J Clin Gastroenterol. 2017 Nov 23. doi: 10.1097/MCG.0000000000000964.
*This story was updated on 1/10/2018.
In patients hospitalized with cirrhosis, biliary cirrhosis, recent health care exposure, nonwhite race, and cultures taken more than 48 hours after admission all independently predicted that bacteremia would be caused by multidrug-resistant organisms (MDROs), according to a medical record review at CHI St. Luke’s Medical Center, an 850-bed tertiary care center in Houston.
“These variables along with severity of infection and liver disease may help clinicians identify patients who will benefit most from broader-spectrum empiric antimicrobial therapy,” wrote the investigators, led by Jennifer Addo Smith, PharmD, of St. Luke’s, in the Journal of Clinical Gastroenterology.
But local epidemiology remains important. “Although a gram-positive agent (e.g., vancomycin) and a carbapenem-sparing gram-negative agent (e.g., ceftriaxone, cefepime) are reasonable empiric agents at our center, other centers with different resistance patterns may warrant different empiric therapy. Given the low prevalence of VRE [vancomycin-resistant Enterococcus] in this study ... and E. faecium in other studies (4%-7%), an empiric agent active against VRE does not seem to be routinely required,” they said.
The team looked into the issue because there hasn’t been much investigation in the United States of the role of multidrug resistant organisms in bacteremia among patients hospitalized with cirrhosis.
Thirty patients in the study had bacteremia caused by MDROs while 60 had bacteremia from non-MDROs, giving a 33% prevalence of MDRO bacteremia, which was consistent with previous, mostly European studies.
Enterobacteriaceae (43%), Staphylococcus aureus (18%), Streptococcus spp. (11%), Enterococcus spp. (10%), and nonfermenting gram-negative bacilli (6%) were the main causes of bacteremia overall.
Among the 30 MDRO cases, methicillin-resistant S. aureus was isolated in seven (23%); methicillin-resistant coagulase-negative Staphylococci in four (13%); fluoroquinolone-resistant Enterobacteriaceae in nine (30%); extended spectrum beta-lactamase–producing Enterobacteriaceae in three (10%), and VRE in two (7%). No carbapenemase-producing gram-negative bacteria were identified.
The predictors of MDRO bacteremia emerged on multivariate analysis and included biliary cirrhosis (adjusted odds ratio, 11.75; 95% confidence interval, 2.08-66.32); recent health care exposure (aOR, 9.81; 95% CI, 2.15-44.88); blood cultures obtained 48 hours after hospital admission (aOR, 6.02; 95% CI, 1.70-21.40) and nonwhite race (aOR , 3.35; 95% CI, 1.19-9.38).
Blood cultures past 48 hours and recent health care exposure – generally hospitalization within the past 90 days – were likely surrogates for nosocomial infection.
The link with biliary cirrhosis is unclear. “Compared with other cirrhotic patients, perhaps patients with PBC [primary biliary cholangitis] have had more cumulative antimicrobial exposure because of [their] higher risk for UTIs [urinary tract infections] and therefore are at increased risk for MDROs,” they wrote.
The median age in the study was 59 years. Half of the patients were white; 46% were women. Hepatitis C was the most common cause of cirrhosis, followed by alcohol.
MDRO was defined in the study as bacteria not susceptible to at least one antibiotic in at least three antimicrobial categories; 90 cirrhosis patients without bacteremia served as controls.
The funding source was not reported. Dr. Addo Smith had no disclosures.
SOURCE: Smith JA et al. J Clin Gastroenterol. 2017 Nov 23. doi: 10.1097/MCG.0000000000000964.
*This story was updated on 1/10/2018.
FROM THE JOURNAL OF CLINICAL GASTROENTEROLOGY
Key clinical point: In patients hospitalized with cirrhosis, nonwhite race, biliary involvement, recent health care exposure, and cultures taken more than 48 hours after hospital admission all independently predicted that bacteremia would be caused by multidrug-resistant organisms.
Major finding: The predictors of multidrug-resistant organism bacteremia emerged on multivariate analysis and included biliary cirrhosis (aOR 11.75; 95% CI, 2.08-66.32); recent health care exposure (aOR 9.81; 95% CI, 2.15-44.88); and blood cultures obtained 48 hours after hospital admission (aOR 6.02; 95% CI, 1.70-21.40).
Study details: Review of 90 cirrhotic patients with bacteremia, plus 90 controls.
Disclosures: The lead investigator had no disclosures.
Source: Smith JA et al. J Clin Gastroenterol. 2017 Nov 23. doi: 10.1097/MCG.0000000000000964.
FDA bans 24 ingredients from OTC health care antiseptic products
in hospital settings and other health care situations outside the hospital, the U.S. Food and Drug Administration announced in a final rule.
The affected products include health care personnel hand washes and hand rubs, surgical hand scrubs and hand rubs, and patient antiseptic skin preparations. The final rule was published Dec. 20 in the Federal Register and becomes effective in December 2018.
The agency determined that a deferral is warranted for six health care antiseptic active ingredients – benzalkonium chloride, benzethonium chloride, chloroxylenol, alcohol, isopropyl alcohol, and povidone-iodine – to allow more time for interested parties to complete the studies necessary to fill the safety and effectiveness data gaps identified for these ingredients.
“The FDA expects that this information may help better inform us on antiseptic resistance and antibiotic cross-resistance in the health care setting,” FDA Commissioner Scott Gottlieb, MD, said in a statement. “Importantly, this doesn’t mean that products containing these six ingredients are ineffective or unsafe. These antiseptic products remain an important resource in health care settings. Personnel should continue to use these products consistent with infection control guidelines while the additional data are gathered.”
No additional data was provided for another 24 products, which were deemed not generally recognized as safe and effective. The minimum data needed to demonstrate safety for all health care antiseptic active ingredients fall into four broad categories: human safety studies, nonclinical safety studies (developmental and reproductive toxicity studies and carcinogenicity studies), data to characterize potential hormonal effects, and data to evaluate the development of antimicrobial resistance, the final rule states.
The FDA noted that manufacturers started to remove nearly all of these 24 active ingredients from their products following a 2015 proposed rule. Triclosan is currently being used in available products.
The active ingredients affected are chlorhexidine gluconate; cloflucarban; fluorosalan; hexachlorophene; hexylresorcinol; iodophors (iodine-containing ingredients including iodine complex [ammonium ether sulfate and polyoxyethylene sorbitan monolaurate], iodine complex [phosphate ester of alkylaryloxy polyethylene glycol], iodine tincture USP, iodine topical solution USP, nonylphenoxypoly [ethyleneoxy] ethanoliodine, poloxamer–iodine complex, undecoylium chloride iodine complex); mercufenol chloride; methylbenzethonium chloride; phenol; secondary amyltricresols; sodium oxychlorosene; tribromsalan; triclocarban; triclosan; triple dye; combination of calomel, oxyquinoline benzoate, triethanolamine, and phenol derivative; and combination of mercufenol chloride and secondary amyltricresols in 50% alcohol.
If manufacturers want to use one or more of these 24 active ingredients in future OTC health care antiseptic drug products, those products will be considered new drugs for which a new drug application approval will be required, the agency said.
The rule does not affect health care antiseptics that are currently marketed under new drug applications and abbreviated new drug applications.
FDA’s action follows a similar final rule published Sept. 6, 2016, which removed triclosan and 18 other active ingredients from consumer antiseptic products.
in hospital settings and other health care situations outside the hospital, the U.S. Food and Drug Administration announced in a final rule.
The affected products include health care personnel hand washes and hand rubs, surgical hand scrubs and hand rubs, and patient antiseptic skin preparations. The final rule was published Dec. 20 in the Federal Register and becomes effective in December 2018.
The agency determined that a deferral is warranted for six health care antiseptic active ingredients – benzalkonium chloride, benzethonium chloride, chloroxylenol, alcohol, isopropyl alcohol, and povidone-iodine – to allow more time for interested parties to complete the studies necessary to fill the safety and effectiveness data gaps identified for these ingredients.
“The FDA expects that this information may help better inform us on antiseptic resistance and antibiotic cross-resistance in the health care setting,” FDA Commissioner Scott Gottlieb, MD, said in a statement. “Importantly, this doesn’t mean that products containing these six ingredients are ineffective or unsafe. These antiseptic products remain an important resource in health care settings. Personnel should continue to use these products consistent with infection control guidelines while the additional data are gathered.”
No additional data was provided for another 24 products, which were deemed not generally recognized as safe and effective. The minimum data needed to demonstrate safety for all health care antiseptic active ingredients fall into four broad categories: human safety studies, nonclinical safety studies (developmental and reproductive toxicity studies and carcinogenicity studies), data to characterize potential hormonal effects, and data to evaluate the development of antimicrobial resistance, the final rule states.
The FDA noted that manufacturers started to remove nearly all of these 24 active ingredients from their products following a 2015 proposed rule. Triclosan is currently being used in available products.
The active ingredients affected are chlorhexidine gluconate; cloflucarban; fluorosalan; hexachlorophene; hexylresorcinol; iodophors (iodine-containing ingredients including iodine complex [ammonium ether sulfate and polyoxyethylene sorbitan monolaurate], iodine complex [phosphate ester of alkylaryloxy polyethylene glycol], iodine tincture USP, iodine topical solution USP, nonylphenoxypoly [ethyleneoxy] ethanoliodine, poloxamer–iodine complex, undecoylium chloride iodine complex); mercufenol chloride; methylbenzethonium chloride; phenol; secondary amyltricresols; sodium oxychlorosene; tribromsalan; triclocarban; triclosan; triple dye; combination of calomel, oxyquinoline benzoate, triethanolamine, and phenol derivative; and combination of mercufenol chloride and secondary amyltricresols in 50% alcohol.
If manufacturers want to use one or more of these 24 active ingredients in future OTC health care antiseptic drug products, those products will be considered new drugs for which a new drug application approval will be required, the agency said.
The rule does not affect health care antiseptics that are currently marketed under new drug applications and abbreviated new drug applications.
FDA’s action follows a similar final rule published Sept. 6, 2016, which removed triclosan and 18 other active ingredients from consumer antiseptic products.
in hospital settings and other health care situations outside the hospital, the U.S. Food and Drug Administration announced in a final rule.
The affected products include health care personnel hand washes and hand rubs, surgical hand scrubs and hand rubs, and patient antiseptic skin preparations. The final rule was published Dec. 20 in the Federal Register and becomes effective in December 2018.
The agency determined that a deferral is warranted for six health care antiseptic active ingredients – benzalkonium chloride, benzethonium chloride, chloroxylenol, alcohol, isopropyl alcohol, and povidone-iodine – to allow more time for interested parties to complete the studies necessary to fill the safety and effectiveness data gaps identified for these ingredients.
“The FDA expects that this information may help better inform us on antiseptic resistance and antibiotic cross-resistance in the health care setting,” FDA Commissioner Scott Gottlieb, MD, said in a statement. “Importantly, this doesn’t mean that products containing these six ingredients are ineffective or unsafe. These antiseptic products remain an important resource in health care settings. Personnel should continue to use these products consistent with infection control guidelines while the additional data are gathered.”
No additional data was provided for another 24 products, which were deemed not generally recognized as safe and effective. The minimum data needed to demonstrate safety for all health care antiseptic active ingredients fall into four broad categories: human safety studies, nonclinical safety studies (developmental and reproductive toxicity studies and carcinogenicity studies), data to characterize potential hormonal effects, and data to evaluate the development of antimicrobial resistance, the final rule states.
The FDA noted that manufacturers started to remove nearly all of these 24 active ingredients from their products following a 2015 proposed rule. Triclosan is currently being used in available products.
The active ingredients affected are chlorhexidine gluconate; cloflucarban; fluorosalan; hexachlorophene; hexylresorcinol; iodophors (iodine-containing ingredients including iodine complex [ammonium ether sulfate and polyoxyethylene sorbitan monolaurate], iodine complex [phosphate ester of alkylaryloxy polyethylene glycol], iodine tincture USP, iodine topical solution USP, nonylphenoxypoly [ethyleneoxy] ethanoliodine, poloxamer–iodine complex, undecoylium chloride iodine complex); mercufenol chloride; methylbenzethonium chloride; phenol; secondary amyltricresols; sodium oxychlorosene; tribromsalan; triclocarban; triclosan; triple dye; combination of calomel, oxyquinoline benzoate, triethanolamine, and phenol derivative; and combination of mercufenol chloride and secondary amyltricresols in 50% alcohol.
If manufacturers want to use one or more of these 24 active ingredients in future OTC health care antiseptic drug products, those products will be considered new drugs for which a new drug application approval will be required, the agency said.
The rule does not affect health care antiseptics that are currently marketed under new drug applications and abbreviated new drug applications.
FDA’s action follows a similar final rule published Sept. 6, 2016, which removed triclosan and 18 other active ingredients from consumer antiseptic products.
Fecal microbiota transplants by oral capsule noninferior to colonoscopy
Fecal microbiota transplantation (FMT) using oral capsules as the delivery method has been shown to be noninferior to delivery using colonoscopy for the treatment of Clostridium difficile infection, but with a significantly lower price tag.
In an unblended noninferiority trial, published in the Nov. 28 issue of JAMA, 116 adults with at least three documented episodes of C. difficile infection were randomized to either 360 mL of fecal slurry delivered to the cecum via colonoscopy or to 40 capsules of processed fecal microbiota swallowed under direct observation.
Dina Kao, MD, of the department of medicine at the University of Alberta, Edmonton, and coauthors commented that the response rate with the capsules was higher than that seen in other studies of fecal microbiota capsules, which they suggested may partly be due to the larger amount of donor stool used in the study: 80-100 g, compared with 17 g and 25 g used in other studies.
“The higher efficacy observed in this study suggests a dose-dependent response to FMT, and a benefit of bowel lavage prior to FMT, because residual vancomycin was detected up to 8 days despite its discontinuation,” they wrote.
Both treatment modalities achieved similar quality of life improvements. Both groups reported major improvements in domains including physical and emotional health, physical and social functioning, and general health, with no significant differences between the two arms of the study.
The cost per treatment in the colonoscopy group was $874 per patient, compared with $308 per patient in the capsule group.
“Although colonoscopy delivery is more invasive, resource intensive, costly, and inconvenient for patients, it has the advantage of identifying alternative diagnoses,” the authors wrote. “Conversely, when FMT is given by oral capsules, it can be administered in an office setting, which could substantially reduce cost and wait time.”
Both groups also showed significantly improved gut microbiota diversity, which approached that of the donor just 1 week after administration of the treatment.
While 30% of patients characterized FMTs as “unpleasant, gross, or disgusting,” 79% of participants said the unpleasantness was the same or less than anticipated, and 97% said they would undergo the same treatment by the same delivery method again if needed.
However, significantly more patients in the capsule group described their experience as “not at all unpleasant,” compared with the colonoscopy group (66% vs. 44%; 95% CI, 3%-40%; P = .01).
There were no colonic perforations seen in the colonoscopy group, and no infectious complications relating to the treatment in either group. One patient in each group died of underlying cardiopulmonary illness that was unrelated to the treatment, and the rate of minor adverse events was 5.4% in the capsule group and 12.5% in the colonoscopy group.
The authors acknowledged that the lack of a placebo group in the study meant they were not able to measure the size of the effect of fecal microbiota transplantation by either route. One earlier trial had also shown a placebo response rate of 45%.
The study was funded by Alberta Health Services and the University of Alberta Hospital Foundation. Four authors declared grants and other funding from the study funder and the pharmaceutical industry.
Clostridium difficile infection costs the U.S. health care system an estimated $1.5 billion each year, with 450,000 cases reported annually, 20% of which involve a recurrence of the infection. Fecal microbiota transplantation is increasingly being used as a treatment, but more widespread adoption is limited partly by the logistical difficulties of delivery.
This study offers encouraging data on delivery of fecal microbiota transplants via capsule, which may reduce barriers to adoption of this treatment; however, there are still some questions to be answered about the treatment’s efficacy, such as the timing of delivery and the relative importance of stool components.
There are also other approaches that should be considered in future research on C. difficile infection, including the use of vancomycin tapers with and without “chasers” of fidaxomicin/rifaximin, the use of defined microbial communities, and the use of sterile, fecal-derived products, which may even supplant standard fecal microbial transplants in the future.
Krishna Rao, MD, Vincent B. Young, MD, PhD, and Preeti N. Malani, MD, are with the division of infectious diseases in the department of internal medicine at the University of Michigan, Ann Arbor. These comments are taken from an accompanying editorial (JAMA. 2017 Nov 28;381:1979-80. doi: 10.1001/jama.2017.17969). Dr. Young reported consulting fees from Vedanta, Merck, and Finch Therapeutics and grants from MedImmune. No other disclosures were reported.
Clostridium difficile infection costs the U.S. health care system an estimated $1.5 billion each year, with 450,000 cases reported annually, 20% of which involve a recurrence of the infection. Fecal microbiota transplantation is increasingly being used as a treatment, but more widespread adoption is limited partly by the logistical difficulties of delivery.
This study offers encouraging data on delivery of fecal microbiota transplants via capsule, which may reduce barriers to adoption of this treatment; however, there are still some questions to be answered about the treatment’s efficacy, such as the timing of delivery and the relative importance of stool components.
There are also other approaches that should be considered in future research on C. difficile infection, including the use of vancomycin tapers with and without “chasers” of fidaxomicin/rifaximin, the use of defined microbial communities, and the use of sterile, fecal-derived products, which may even supplant standard fecal microbial transplants in the future.
Krishna Rao, MD, Vincent B. Young, MD, PhD, and Preeti N. Malani, MD, are with the division of infectious diseases in the department of internal medicine at the University of Michigan, Ann Arbor. These comments are taken from an accompanying editorial (JAMA. 2017 Nov 28;381:1979-80. doi: 10.1001/jama.2017.17969). Dr. Young reported consulting fees from Vedanta, Merck, and Finch Therapeutics and grants from MedImmune. No other disclosures were reported.
Clostridium difficile infection costs the U.S. health care system an estimated $1.5 billion each year, with 450,000 cases reported annually, 20% of which involve a recurrence of the infection. Fecal microbiota transplantation is increasingly being used as a treatment, but more widespread adoption is limited partly by the logistical difficulties of delivery.
This study offers encouraging data on delivery of fecal microbiota transplants via capsule, which may reduce barriers to adoption of this treatment; however, there are still some questions to be answered about the treatment’s efficacy, such as the timing of delivery and the relative importance of stool components.
There are also other approaches that should be considered in future research on C. difficile infection, including the use of vancomycin tapers with and without “chasers” of fidaxomicin/rifaximin, the use of defined microbial communities, and the use of sterile, fecal-derived products, which may even supplant standard fecal microbial transplants in the future.
Krishna Rao, MD, Vincent B. Young, MD, PhD, and Preeti N. Malani, MD, are with the division of infectious diseases in the department of internal medicine at the University of Michigan, Ann Arbor. These comments are taken from an accompanying editorial (JAMA. 2017 Nov 28;381:1979-80. doi: 10.1001/jama.2017.17969). Dr. Young reported consulting fees from Vedanta, Merck, and Finch Therapeutics and grants from MedImmune. No other disclosures were reported.
Fecal microbiota transplantation (FMT) using oral capsules as the delivery method has been shown to be noninferior to delivery using colonoscopy for the treatment of Clostridium difficile infection, but with a significantly lower price tag.
In an unblended noninferiority trial, published in the Nov. 28 issue of JAMA, 116 adults with at least three documented episodes of C. difficile infection were randomized to either 360 mL of fecal slurry delivered to the cecum via colonoscopy or to 40 capsules of processed fecal microbiota swallowed under direct observation.
Dina Kao, MD, of the department of medicine at the University of Alberta, Edmonton, and coauthors commented that the response rate with the capsules was higher than that seen in other studies of fecal microbiota capsules, which they suggested may partly be due to the larger amount of donor stool used in the study: 80-100 g, compared with 17 g and 25 g used in other studies.
“The higher efficacy observed in this study suggests a dose-dependent response to FMT, and a benefit of bowel lavage prior to FMT, because residual vancomycin was detected up to 8 days despite its discontinuation,” they wrote.
Both treatment modalities achieved similar quality of life improvements. Both groups reported major improvements in domains including physical and emotional health, physical and social functioning, and general health, with no significant differences between the two arms of the study.
The cost per treatment in the colonoscopy group was $874 per patient, compared with $308 per patient in the capsule group.
“Although colonoscopy delivery is more invasive, resource intensive, costly, and inconvenient for patients, it has the advantage of identifying alternative diagnoses,” the authors wrote. “Conversely, when FMT is given by oral capsules, it can be administered in an office setting, which could substantially reduce cost and wait time.”
Both groups also showed significantly improved gut microbiota diversity, which approached that of the donor just 1 week after administration of the treatment.
While 30% of patients characterized FMTs as “unpleasant, gross, or disgusting,” 79% of participants said the unpleasantness was the same or less than anticipated, and 97% said they would undergo the same treatment by the same delivery method again if needed.
However, significantly more patients in the capsule group described their experience as “not at all unpleasant,” compared with the colonoscopy group (66% vs. 44%; 95% CI, 3%-40%; P = .01).
There were no colonic perforations seen in the colonoscopy group, and no infectious complications relating to the treatment in either group. One patient in each group died of underlying cardiopulmonary illness that was unrelated to the treatment, and the rate of minor adverse events was 5.4% in the capsule group and 12.5% in the colonoscopy group.
The authors acknowledged that the lack of a placebo group in the study meant they were not able to measure the size of the effect of fecal microbiota transplantation by either route. One earlier trial had also shown a placebo response rate of 45%.
The study was funded by Alberta Health Services and the University of Alberta Hospital Foundation. Four authors declared grants and other funding from the study funder and the pharmaceutical industry.
Fecal microbiota transplantation (FMT) using oral capsules as the delivery method has been shown to be noninferior to delivery using colonoscopy for the treatment of Clostridium difficile infection, but with a significantly lower price tag.
In an unblended noninferiority trial, published in the Nov. 28 issue of JAMA, 116 adults with at least three documented episodes of C. difficile infection were randomized to either 360 mL of fecal slurry delivered to the cecum via colonoscopy or to 40 capsules of processed fecal microbiota swallowed under direct observation.
Dina Kao, MD, of the department of medicine at the University of Alberta, Edmonton, and coauthors commented that the response rate with the capsules was higher than that seen in other studies of fecal microbiota capsules, which they suggested may partly be due to the larger amount of donor stool used in the study: 80-100 g, compared with 17 g and 25 g used in other studies.
“The higher efficacy observed in this study suggests a dose-dependent response to FMT, and a benefit of bowel lavage prior to FMT, because residual vancomycin was detected up to 8 days despite its discontinuation,” they wrote.
Both treatment modalities achieved similar quality of life improvements. Both groups reported major improvements in domains including physical and emotional health, physical and social functioning, and general health, with no significant differences between the two arms of the study.
The cost per treatment in the colonoscopy group was $874 per patient, compared with $308 per patient in the capsule group.
“Although colonoscopy delivery is more invasive, resource intensive, costly, and inconvenient for patients, it has the advantage of identifying alternative diagnoses,” the authors wrote. “Conversely, when FMT is given by oral capsules, it can be administered in an office setting, which could substantially reduce cost and wait time.”
Both groups also showed significantly improved gut microbiota diversity, which approached that of the donor just 1 week after administration of the treatment.
While 30% of patients characterized FMTs as “unpleasant, gross, or disgusting,” 79% of participants said the unpleasantness was the same or less than anticipated, and 97% said they would undergo the same treatment by the same delivery method again if needed.
However, significantly more patients in the capsule group described their experience as “not at all unpleasant,” compared with the colonoscopy group (66% vs. 44%; 95% CI, 3%-40%; P = .01).
There were no colonic perforations seen in the colonoscopy group, and no infectious complications relating to the treatment in either group. One patient in each group died of underlying cardiopulmonary illness that was unrelated to the treatment, and the rate of minor adverse events was 5.4% in the capsule group and 12.5% in the colonoscopy group.
The authors acknowledged that the lack of a placebo group in the study meant they were not able to measure the size of the effect of fecal microbiota transplantation by either route. One earlier trial had also shown a placebo response rate of 45%.
The study was funded by Alberta Health Services and the University of Alberta Hospital Foundation. Four authors declared grants and other funding from the study funder and the pharmaceutical industry.
FROM JAMA
Key clinical point: Delivering fecal microbiota transplants using oral capsules is noninferior to delivery via colonoscopy in the treatment of Clostridium difficile infection.
Major finding: The rates of resolution of recurrent C. difficile infection with fecal microbiota transplants are similar for delivery via oral capsule or via colonoscopy.
Data source: A randomized, unblended noninferiority trial in 116 adults with recurrent C. difficile infection.
Disclosures: The study was funded by Alberta Health Services and the University of Alberta Hospital Foundation. Four authors declared grants and other funding from the study funder and the pharmaceutical industry.
SHORT TAKES
Cardiac testing of Emergency Department patients with chest pain leads to increased revascularization without reduction in admissions for acute MI
Retrospective cohort study of ED patients presenting with chest pain but without evidence of ischemia, shows that non-invasive cardiac testing of these patients lead to more coronary angiograms (92.1 per 1,000 patients) within 30 days, but no significant reduction of admissions for acute MI at 1 year (remained 7.8 per 1,000 patients tested).
Citation: Sandhu AT, Heidenreich PA, Bhattacharya J, Bundorf MK. Cardiovascular Testing and Clinical Outcomes in Emergency Department Patients With Chest Pain. JAMA Intern Med. Published online 2017 June 26. doi: 10.1001/jamainternmed.2017.2432.
Facebook star ratings and “likes” correlate with patient satisfaction scores
In a cross-sectional analysis of 136 New York State hospitals, the study found increased Facebook star ratings correlated (P less than .003) with overall increased HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) score (21/23 HCAHPS). HCAHPS measures also positively correlated (P less than .05) with adjusted number of “likes” on Facebook but to a lesser degree (3/21 HCAHPS). Neither star ratings nor number of “likes” correlate with Medicare spending or 30-day all-cause readmission rate.
Citation: Campbell L, Yue L. Are Facebook user ratings associated with hospital cost, quality, and patient satisfaction? BMJ Qual Saf. 2017 July 19. doi:10.1136/bmjqs-2016-006291.
Candida auris remains an ongoing health care facility transmission risk
Multidrug-resistant fungus Candida auris is an emerging pathogen and a transmission risk across health care facilities. From June 2016 through May 2017, 77 cases of clinical infection have been reported to the Centers for Disease Control and Prevention from seven states, though most (90%) cases are clustered in the New York City metropolitan area. Most patients had multiple medical conditions and extensive health care facility exposure. The CDC recommends contact precautions, private rooming, daily and terminal cleaning with disinfectant active against Clostridium difficile spores, and notification to receiving health care facilities about C. auris colonization or infection on transfer to help reduce the spread of C. auris throughout the United States.
Citation: Tsay S, Welsh RM, Adams EH, et al. Notes from the Field: Ongoing Transmission of Candida auris in Health Care Facilities – United States, June 2016–May 2017. MMWR Morb Mortal Wkly Rep. 2017;66:51415.
Cardiac testing of Emergency Department patients with chest pain leads to increased revascularization without reduction in admissions for acute MI
Retrospective cohort study of ED patients presenting with chest pain but without evidence of ischemia, shows that non-invasive cardiac testing of these patients lead to more coronary angiograms (92.1 per 1,000 patients) within 30 days, but no significant reduction of admissions for acute MI at 1 year (remained 7.8 per 1,000 patients tested).
Citation: Sandhu AT, Heidenreich PA, Bhattacharya J, Bundorf MK. Cardiovascular Testing and Clinical Outcomes in Emergency Department Patients With Chest Pain. JAMA Intern Med. Published online 2017 June 26. doi: 10.1001/jamainternmed.2017.2432.
Facebook star ratings and “likes” correlate with patient satisfaction scores
In a cross-sectional analysis of 136 New York State hospitals, the study found increased Facebook star ratings correlated (P less than .003) with overall increased HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) score (21/23 HCAHPS). HCAHPS measures also positively correlated (P less than .05) with adjusted number of “likes” on Facebook but to a lesser degree (3/21 HCAHPS). Neither star ratings nor number of “likes” correlate with Medicare spending or 30-day all-cause readmission rate.
Citation: Campbell L, Yue L. Are Facebook user ratings associated with hospital cost, quality, and patient satisfaction? BMJ Qual Saf. 2017 July 19. doi:10.1136/bmjqs-2016-006291.
Candida auris remains an ongoing health care facility transmission risk
Multidrug-resistant fungus Candida auris is an emerging pathogen and a transmission risk across health care facilities. From June 2016 through May 2017, 77 cases of clinical infection have been reported to the Centers for Disease Control and Prevention from seven states, though most (90%) cases are clustered in the New York City metropolitan area. Most patients had multiple medical conditions and extensive health care facility exposure. The CDC recommends contact precautions, private rooming, daily and terminal cleaning with disinfectant active against Clostridium difficile spores, and notification to receiving health care facilities about C. auris colonization or infection on transfer to help reduce the spread of C. auris throughout the United States.
Citation: Tsay S, Welsh RM, Adams EH, et al. Notes from the Field: Ongoing Transmission of Candida auris in Health Care Facilities – United States, June 2016–May 2017. MMWR Morb Mortal Wkly Rep. 2017;66:51415.
Cardiac testing of Emergency Department patients with chest pain leads to increased revascularization without reduction in admissions for acute MI
Retrospective cohort study of ED patients presenting with chest pain but without evidence of ischemia, shows that non-invasive cardiac testing of these patients lead to more coronary angiograms (92.1 per 1,000 patients) within 30 days, but no significant reduction of admissions for acute MI at 1 year (remained 7.8 per 1,000 patients tested).
Citation: Sandhu AT, Heidenreich PA, Bhattacharya J, Bundorf MK. Cardiovascular Testing and Clinical Outcomes in Emergency Department Patients With Chest Pain. JAMA Intern Med. Published online 2017 June 26. doi: 10.1001/jamainternmed.2017.2432.
Facebook star ratings and “likes” correlate with patient satisfaction scores
In a cross-sectional analysis of 136 New York State hospitals, the study found increased Facebook star ratings correlated (P less than .003) with overall increased HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) score (21/23 HCAHPS). HCAHPS measures also positively correlated (P less than .05) with adjusted number of “likes” on Facebook but to a lesser degree (3/21 HCAHPS). Neither star ratings nor number of “likes” correlate with Medicare spending or 30-day all-cause readmission rate.
Citation: Campbell L, Yue L. Are Facebook user ratings associated with hospital cost, quality, and patient satisfaction? BMJ Qual Saf. 2017 July 19. doi:10.1136/bmjqs-2016-006291.
Candida auris remains an ongoing health care facility transmission risk
Multidrug-resistant fungus Candida auris is an emerging pathogen and a transmission risk across health care facilities. From June 2016 through May 2017, 77 cases of clinical infection have been reported to the Centers for Disease Control and Prevention from seven states, though most (90%) cases are clustered in the New York City metropolitan area. Most patients had multiple medical conditions and extensive health care facility exposure. The CDC recommends contact precautions, private rooming, daily and terminal cleaning with disinfectant active against Clostridium difficile spores, and notification to receiving health care facilities about C. auris colonization or infection on transfer to help reduce the spread of C. auris throughout the United States.
Citation: Tsay S, Welsh RM, Adams EH, et al. Notes from the Field: Ongoing Transmission of Candida auris in Health Care Facilities – United States, June 2016–May 2017. MMWR Morb Mortal Wkly Rep. 2017;66:51415.
Pediatric hospitalists take on the challenge of antibiotic stewardship
When Carol Glaser, MD, was in training, the philosophy around antibiotic prescribing often went something like this: “Ten days of antibiotics is good, but let’s do a few more days just to be sure,” she said.
Today, however, the new mantra is “less is more.” Dr. Glaser is an experienced pediatric infectious disease physician and the lead physician for pediatric antimicrobial stewardship at The Permanente Medical Group, Kaiser Permanente, at the Oakland (Calif.) Medical Center. While antibiotic stewardship is an issue relevant to nearly all hospitalists, for pediatric patients, the considerations can be unique and particularly serious.
Dr. Shah, a pediatric infectious disease physician at Cincinnati Children’s Hospital, spoke last spring at HM17, the Society of Hospital Medicine’s annual meeting. His talk drew from issues raised on pediatric hospital medicine electronic mailing lists and from audience questions. These centered on decisions regarding the use of intravenous versus oral antibiotics for pediatric patients – or what he refers to as intravenous-to-oral conversion – as well as antibiotic treatment duration.
“For many conditions in pediatrics, we used to treat with intravenous antibiotics initially – and sometimes for the entire course – and now we’re using oral antibiotics for the entire course,” Dr. Shah said. He noted that urinary tract infections were once treated with IV antibiotics in the hospital but are now routinely treated orally in an outpatient setting.
Dr. Shah cited two studies, both of which he coauthored as part of the Pediatric Research in Inpatient Settings Network, which compared intravenous versus oral antibiotics treatments given after discharge: The first, published in JAMA Pediatrics in 2014, examined treatment for osteomyelitis, while the second, which focused on complicated pneumonia, was published in Pediatrics in 2016.1,2
Both were observational, retrospective studies involving more than 2,000 children across more than 30 hospitals. The JAMA Pediatrics study found that roughly half of the patients were discharged with a peripherally inserted central catheter (PICC) line, and half were prescribed oral antibiotics. In some hospitals, 100% of patients were sent home with a PICC line, and in others, all children were sent home on oral antibiotics. Although treatment failure rates were the same for both groups, 15% of the patients sent home with a PICC line had to return to the emergency department because of PICC-related complications. Some were hospitalized.1
The Pediatrics study found less variation in PICC versus oral antibiotic use across hospitals for patients with complicated pneumonia, but the treatment failure rate was slightly higher for PICC patients at 3.2%, compared with 2.6% for those on oral antibiotics. This difference, however, was not statistically significant. PICC-related complications were observed in 7.1% of patients with PICC lines also were more likely to experience adverse drug reactions, compared with patients on oral antibiotics.2
“PICC lines have some advantages, particularly when children are unable or unwilling to take oral antibiotics, but they also have risks” said Dr. Shah. “If outcomes are equivalent, why would you subject patients to the risks of a catheter? And, every time they get a fever at home with a PICC line, they need urgent evaluation for the possibility of a catheter-associated bacterial infection. There is an emotional cost, as well, to taking care of catheters in the home setting.”
Additionally, economic pressures are compelling hospitals to reduce costs and resource utilization while maintaining or improving the quality of care, Dr. Shah pointed out. “Hospitalists do many things well, and quality improvement is one of those areas. That approach really aligns with antimicrobial stewardship, and there is greater incentive with episode-based payment models and financial penalties for excess readmissions. Reducing post-discharge IV antibiotic use aligns with stewardship goals and reduces the likelihood of hospital readmissions.”
The hospital medicine division at Dr. Shah’s hospital helped assemble a multidisciplinary team involving emergency physicians, pharmacists, nursing staff, hospitalists, and infectious disease physicians to encourage the use of appropriate, narrow-spectrum antibiotics and reduce the duration of antibiotic therapies. For example, skin and soft-tissue infections that were once treated for 10-14 days are now sufficiently treated in 5-7days. These efforts to improve outcomes through better adherence to evidence-based practices, including better stewardship, earned the team the SHM Teamwork in Quality Improvement Award in 2014.
“Quality improvement is really about changing the system, and hospitalists, who excel in QI, are poised to help drive antimicrobial stewardship efforts,” Dr. Shah said.
At Oakland Medical Center, Dr. Glaser helped implement handshake rounds, an idea they adopted from a group in Colorado. Every day, with every patient, the antimicrobial stewardship team meets with representatives of the teams – pediatric intensive care, the wards, the NICU, and others – to review antibiotic treatment plans for the choice of antimicrobial drug, for the duration of treatment, and for specific conditions. “We work really closely with hospitalists and our strong pediatric pharmacy team every day to ask: ‘Do we have the right dose? Do we really need to use this antibiotic?’ ” Dr. Glaser said.
Last year, she also worked to incorporate antimicrobial stewardship principles into the hospital’s residency program. “I think the most important thing we’re doing is changing the culture,” she said. “For these young physicians, we’re giving them the knowledge to empower them rather than telling them what to do and giving them a better, fundamental understanding of infectious disease.”
For instance, most pediatric respiratory illnesses are caused by a virus, yet physicians will still prescribe antibiotics for a host of reasons – including the expectations of parents, the guesswork that can go into diagnosing a young patient who cannot describe what is wrong, and the fear that children will get sicker if an antibiotic is not started early.
“A lot of it is figuring out the best approach with the least amount of side effects but covering what we need to cover for a given patient,” she said.
A number of physicians from Dr. Glaser’s team presented stewardship data from their hospital at the July 2017 Pediatric Hospital Medicine meeting in Nashville, demonstrating that, overall, they are using fewer antibiotics and that fewer of those used are broad spectrum. This satisfies the “pillars of stewardship,” Dr. Glaser said. Use antibiotics only when you need them, use them only as long as you need, and then make sure you use the most narrow-spectrum antibiotic you possibly can, she said.
Oakland Medical Center has benefited from a strong commitment to antimicrobial stewardship efforts, Dr. Glaser said, noting that many programs may lack such support, a problem that can be one of the biggest hurdles antimicrobial stewardship efforts face. The support at her hospital “has been an immense help in getting our program to where it is today.”
References
1. Keren R, Shah SS, Srivastava R, et al. Comparative effectiveness of intravenous vs oral antibiotics for postdischarge treatment of acute osteomyelitis in children. JAMA Pediatr. 2015 Feb:169(2):120-8.
2. Shah SS, Srivastava R, Wu S, et al. Intravenous versus oral antibiotics for postdischarge treatment of complicated pneumonia. Pediatrics. 2016 Dec;138(6). pii: e20161692.
When Carol Glaser, MD, was in training, the philosophy around antibiotic prescribing often went something like this: “Ten days of antibiotics is good, but let’s do a few more days just to be sure,” she said.
Today, however, the new mantra is “less is more.” Dr. Glaser is an experienced pediatric infectious disease physician and the lead physician for pediatric antimicrobial stewardship at The Permanente Medical Group, Kaiser Permanente, at the Oakland (Calif.) Medical Center. While antibiotic stewardship is an issue relevant to nearly all hospitalists, for pediatric patients, the considerations can be unique and particularly serious.
Dr. Shah, a pediatric infectious disease physician at Cincinnati Children’s Hospital, spoke last spring at HM17, the Society of Hospital Medicine’s annual meeting. His talk drew from issues raised on pediatric hospital medicine electronic mailing lists and from audience questions. These centered on decisions regarding the use of intravenous versus oral antibiotics for pediatric patients – or what he refers to as intravenous-to-oral conversion – as well as antibiotic treatment duration.
“For many conditions in pediatrics, we used to treat with intravenous antibiotics initially – and sometimes for the entire course – and now we’re using oral antibiotics for the entire course,” Dr. Shah said. He noted that urinary tract infections were once treated with IV antibiotics in the hospital but are now routinely treated orally in an outpatient setting.
Dr. Shah cited two studies, both of which he coauthored as part of the Pediatric Research in Inpatient Settings Network, which compared intravenous versus oral antibiotics treatments given after discharge: The first, published in JAMA Pediatrics in 2014, examined treatment for osteomyelitis, while the second, which focused on complicated pneumonia, was published in Pediatrics in 2016.1,2
Both were observational, retrospective studies involving more than 2,000 children across more than 30 hospitals. The JAMA Pediatrics study found that roughly half of the patients were discharged with a peripherally inserted central catheter (PICC) line, and half were prescribed oral antibiotics. In some hospitals, 100% of patients were sent home with a PICC line, and in others, all children were sent home on oral antibiotics. Although treatment failure rates were the same for both groups, 15% of the patients sent home with a PICC line had to return to the emergency department because of PICC-related complications. Some were hospitalized.1
The Pediatrics study found less variation in PICC versus oral antibiotic use across hospitals for patients with complicated pneumonia, but the treatment failure rate was slightly higher for PICC patients at 3.2%, compared with 2.6% for those on oral antibiotics. This difference, however, was not statistically significant. PICC-related complications were observed in 7.1% of patients with PICC lines also were more likely to experience adverse drug reactions, compared with patients on oral antibiotics.2
“PICC lines have some advantages, particularly when children are unable or unwilling to take oral antibiotics, but they also have risks” said Dr. Shah. “If outcomes are equivalent, why would you subject patients to the risks of a catheter? And, every time they get a fever at home with a PICC line, they need urgent evaluation for the possibility of a catheter-associated bacterial infection. There is an emotional cost, as well, to taking care of catheters in the home setting.”
Additionally, economic pressures are compelling hospitals to reduce costs and resource utilization while maintaining or improving the quality of care, Dr. Shah pointed out. “Hospitalists do many things well, and quality improvement is one of those areas. That approach really aligns with antimicrobial stewardship, and there is greater incentive with episode-based payment models and financial penalties for excess readmissions. Reducing post-discharge IV antibiotic use aligns with stewardship goals and reduces the likelihood of hospital readmissions.”
The hospital medicine division at Dr. Shah’s hospital helped assemble a multidisciplinary team involving emergency physicians, pharmacists, nursing staff, hospitalists, and infectious disease physicians to encourage the use of appropriate, narrow-spectrum antibiotics and reduce the duration of antibiotic therapies. For example, skin and soft-tissue infections that were once treated for 10-14 days are now sufficiently treated in 5-7days. These efforts to improve outcomes through better adherence to evidence-based practices, including better stewardship, earned the team the SHM Teamwork in Quality Improvement Award in 2014.
“Quality improvement is really about changing the system, and hospitalists, who excel in QI, are poised to help drive antimicrobial stewardship efforts,” Dr. Shah said.
At Oakland Medical Center, Dr. Glaser helped implement handshake rounds, an idea they adopted from a group in Colorado. Every day, with every patient, the antimicrobial stewardship team meets with representatives of the teams – pediatric intensive care, the wards, the NICU, and others – to review antibiotic treatment plans for the choice of antimicrobial drug, for the duration of treatment, and for specific conditions. “We work really closely with hospitalists and our strong pediatric pharmacy team every day to ask: ‘Do we have the right dose? Do we really need to use this antibiotic?’ ” Dr. Glaser said.
Last year, she also worked to incorporate antimicrobial stewardship principles into the hospital’s residency program. “I think the most important thing we’re doing is changing the culture,” she said. “For these young physicians, we’re giving them the knowledge to empower them rather than telling them what to do and giving them a better, fundamental understanding of infectious disease.”
For instance, most pediatric respiratory illnesses are caused by a virus, yet physicians will still prescribe antibiotics for a host of reasons – including the expectations of parents, the guesswork that can go into diagnosing a young patient who cannot describe what is wrong, and the fear that children will get sicker if an antibiotic is not started early.
“A lot of it is figuring out the best approach with the least amount of side effects but covering what we need to cover for a given patient,” she said.
A number of physicians from Dr. Glaser’s team presented stewardship data from their hospital at the July 2017 Pediatric Hospital Medicine meeting in Nashville, demonstrating that, overall, they are using fewer antibiotics and that fewer of those used are broad spectrum. This satisfies the “pillars of stewardship,” Dr. Glaser said. Use antibiotics only when you need them, use them only as long as you need, and then make sure you use the most narrow-spectrum antibiotic you possibly can, she said.
Oakland Medical Center has benefited from a strong commitment to antimicrobial stewardship efforts, Dr. Glaser said, noting that many programs may lack such support, a problem that can be one of the biggest hurdles antimicrobial stewardship efforts face. The support at her hospital “has been an immense help in getting our program to where it is today.”
References
1. Keren R, Shah SS, Srivastava R, et al. Comparative effectiveness of intravenous vs oral antibiotics for postdischarge treatment of acute osteomyelitis in children. JAMA Pediatr. 2015 Feb:169(2):120-8.
2. Shah SS, Srivastava R, Wu S, et al. Intravenous versus oral antibiotics for postdischarge treatment of complicated pneumonia. Pediatrics. 2016 Dec;138(6). pii: e20161692.
When Carol Glaser, MD, was in training, the philosophy around antibiotic prescribing often went something like this: “Ten days of antibiotics is good, but let’s do a few more days just to be sure,” she said.
Today, however, the new mantra is “less is more.” Dr. Glaser is an experienced pediatric infectious disease physician and the lead physician for pediatric antimicrobial stewardship at The Permanente Medical Group, Kaiser Permanente, at the Oakland (Calif.) Medical Center. While antibiotic stewardship is an issue relevant to nearly all hospitalists, for pediatric patients, the considerations can be unique and particularly serious.
Dr. Shah, a pediatric infectious disease physician at Cincinnati Children’s Hospital, spoke last spring at HM17, the Society of Hospital Medicine’s annual meeting. His talk drew from issues raised on pediatric hospital medicine electronic mailing lists and from audience questions. These centered on decisions regarding the use of intravenous versus oral antibiotics for pediatric patients – or what he refers to as intravenous-to-oral conversion – as well as antibiotic treatment duration.
“For many conditions in pediatrics, we used to treat with intravenous antibiotics initially – and sometimes for the entire course – and now we’re using oral antibiotics for the entire course,” Dr. Shah said. He noted that urinary tract infections were once treated with IV antibiotics in the hospital but are now routinely treated orally in an outpatient setting.
Dr. Shah cited two studies, both of which he coauthored as part of the Pediatric Research in Inpatient Settings Network, which compared intravenous versus oral antibiotics treatments given after discharge: The first, published in JAMA Pediatrics in 2014, examined treatment for osteomyelitis, while the second, which focused on complicated pneumonia, was published in Pediatrics in 2016.1,2
Both were observational, retrospective studies involving more than 2,000 children across more than 30 hospitals. The JAMA Pediatrics study found that roughly half of the patients were discharged with a peripherally inserted central catheter (PICC) line, and half were prescribed oral antibiotics. In some hospitals, 100% of patients were sent home with a PICC line, and in others, all children were sent home on oral antibiotics. Although treatment failure rates were the same for both groups, 15% of the patients sent home with a PICC line had to return to the emergency department because of PICC-related complications. Some were hospitalized.1
The Pediatrics study found less variation in PICC versus oral antibiotic use across hospitals for patients with complicated pneumonia, but the treatment failure rate was slightly higher for PICC patients at 3.2%, compared with 2.6% for those on oral antibiotics. This difference, however, was not statistically significant. PICC-related complications were observed in 7.1% of patients with PICC lines also were more likely to experience adverse drug reactions, compared with patients on oral antibiotics.2
“PICC lines have some advantages, particularly when children are unable or unwilling to take oral antibiotics, but they also have risks” said Dr. Shah. “If outcomes are equivalent, why would you subject patients to the risks of a catheter? And, every time they get a fever at home with a PICC line, they need urgent evaluation for the possibility of a catheter-associated bacterial infection. There is an emotional cost, as well, to taking care of catheters in the home setting.”
Additionally, economic pressures are compelling hospitals to reduce costs and resource utilization while maintaining or improving the quality of care, Dr. Shah pointed out. “Hospitalists do many things well, and quality improvement is one of those areas. That approach really aligns with antimicrobial stewardship, and there is greater incentive with episode-based payment models and financial penalties for excess readmissions. Reducing post-discharge IV antibiotic use aligns with stewardship goals and reduces the likelihood of hospital readmissions.”
The hospital medicine division at Dr. Shah’s hospital helped assemble a multidisciplinary team involving emergency physicians, pharmacists, nursing staff, hospitalists, and infectious disease physicians to encourage the use of appropriate, narrow-spectrum antibiotics and reduce the duration of antibiotic therapies. For example, skin and soft-tissue infections that were once treated for 10-14 days are now sufficiently treated in 5-7days. These efforts to improve outcomes through better adherence to evidence-based practices, including better stewardship, earned the team the SHM Teamwork in Quality Improvement Award in 2014.
“Quality improvement is really about changing the system, and hospitalists, who excel in QI, are poised to help drive antimicrobial stewardship efforts,” Dr. Shah said.
At Oakland Medical Center, Dr. Glaser helped implement handshake rounds, an idea they adopted from a group in Colorado. Every day, with every patient, the antimicrobial stewardship team meets with representatives of the teams – pediatric intensive care, the wards, the NICU, and others – to review antibiotic treatment plans for the choice of antimicrobial drug, for the duration of treatment, and for specific conditions. “We work really closely with hospitalists and our strong pediatric pharmacy team every day to ask: ‘Do we have the right dose? Do we really need to use this antibiotic?’ ” Dr. Glaser said.
Last year, she also worked to incorporate antimicrobial stewardship principles into the hospital’s residency program. “I think the most important thing we’re doing is changing the culture,” she said. “For these young physicians, we’re giving them the knowledge to empower them rather than telling them what to do and giving them a better, fundamental understanding of infectious disease.”
For instance, most pediatric respiratory illnesses are caused by a virus, yet physicians will still prescribe antibiotics for a host of reasons – including the expectations of parents, the guesswork that can go into diagnosing a young patient who cannot describe what is wrong, and the fear that children will get sicker if an antibiotic is not started early.
“A lot of it is figuring out the best approach with the least amount of side effects but covering what we need to cover for a given patient,” she said.
A number of physicians from Dr. Glaser’s team presented stewardship data from their hospital at the July 2017 Pediatric Hospital Medicine meeting in Nashville, demonstrating that, overall, they are using fewer antibiotics and that fewer of those used are broad spectrum. This satisfies the “pillars of stewardship,” Dr. Glaser said. Use antibiotics only when you need them, use them only as long as you need, and then make sure you use the most narrow-spectrum antibiotic you possibly can, she said.
Oakland Medical Center has benefited from a strong commitment to antimicrobial stewardship efforts, Dr. Glaser said, noting that many programs may lack such support, a problem that can be one of the biggest hurdles antimicrobial stewardship efforts face. The support at her hospital “has been an immense help in getting our program to where it is today.”
References
1. Keren R, Shah SS, Srivastava R, et al. Comparative effectiveness of intravenous vs oral antibiotics for postdischarge treatment of acute osteomyelitis in children. JAMA Pediatr. 2015 Feb:169(2):120-8.
2. Shah SS, Srivastava R, Wu S, et al. Intravenous versus oral antibiotics for postdischarge treatment of complicated pneumonia. Pediatrics. 2016 Dec;138(6). pii: e20161692.
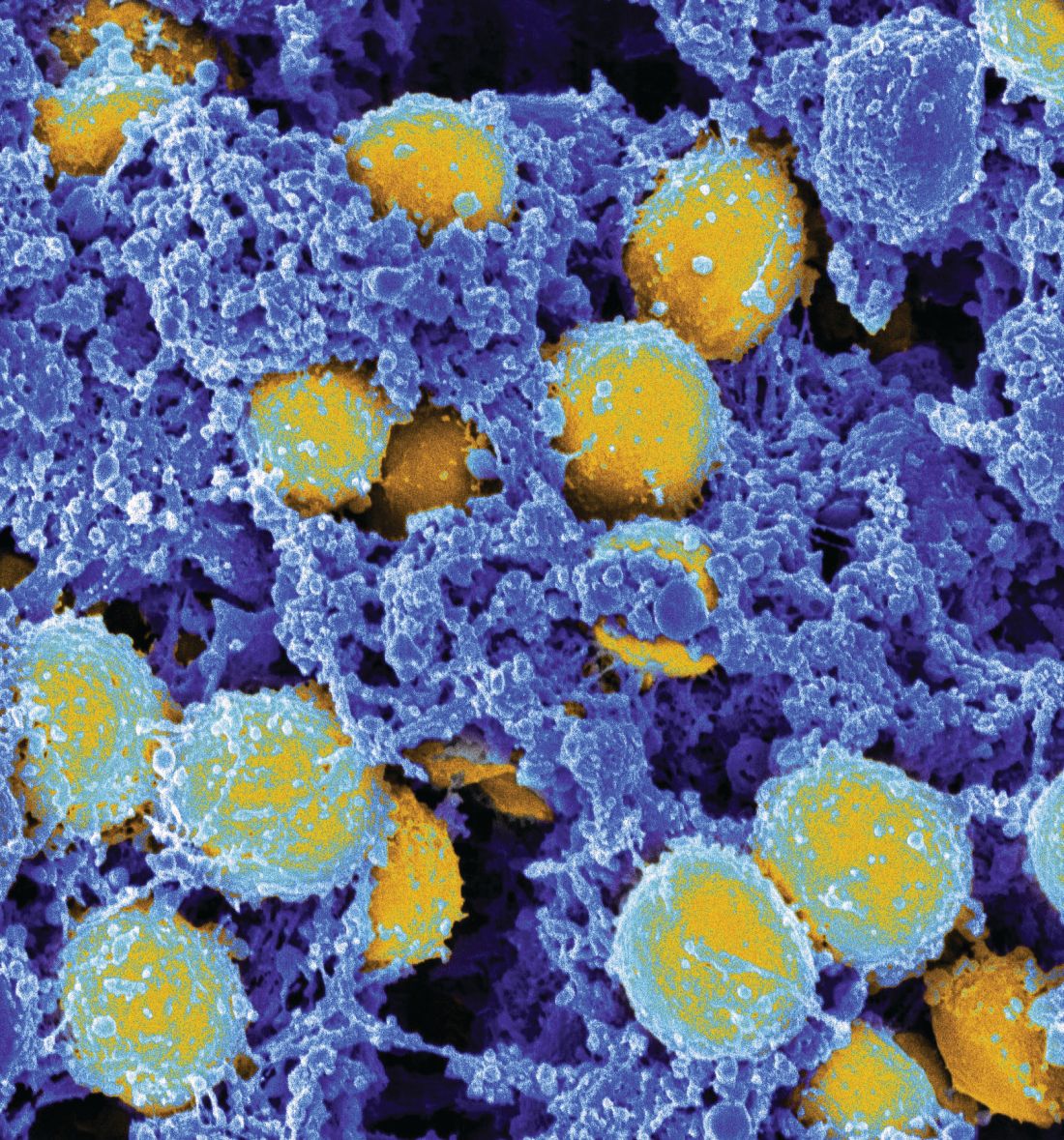
Involving experts in S. aureus bacteremia treatment reduces mortality
SAN DIEGO – Thirty-day mortality associated with Staphylococcus aureus bacteremia is reduced if there is guidance from either an antimicrobial stewardship team (AST) or an infectious disease consultant (IDC), according to a multivariate experience at Yale New Haven Hospital presented at an annual scientific meeting on infectious diseases.
“This has been a hot area, because there have been a lot of recent studies suggesting that expert infectious disease advice improves care, but not every study has associated expert advice with a mortality benefit,” said Jacqueline Sherbuk, MD, a fellow in the division of infectious diseases and international health at the University of Virginia, Charlottesville. She was a resident at Yale University when this study was conducted.
In this study, the impact of an IDC on outcome in patients with S. aureus bacteremia was evaluated relative to no expert advice. By itself, an IDC was associated with improved adherence to standards of care for S. aureus bacteremia management, but the reduction in mortality was not statistically significant for those who received IDC guidance relative to those who did not.
“Given that patient care may be guided by consultations from the AST independent of IDC, we looked at the overall impact of expert opinion versus no expert involvement, and this achieved significance on multivariate analysis,” Dr. Sherbuk reported.
For adherence to guidelines, IDC guidance was better than no expert advice on multiple measures, including proportion obtaining an echocardiogram (89% vs. 67%; P less than .001), appropriate definitive antibiotics (98% vs. 80%; P less than .001), and appropriate treatment duration (92% vs. 35%; P less than .001). However, the advantage for 30-day mortality rates was only a trend (11% vs. 21%, P = .07). It was only when patients who received IDC guidance or a consultation from the AST were combined that the difference climbed to significance (11% vs. 23%; P = .04).
“On multivariate analysis, the OR [odds ratio] was substantial, predicting a 60% reduction [OR 0.40; P = .03) in 30-day mortality for expert advice vs. no expert advice,” Dr. Sherbuk reported.
In this retrospective observational study, 261 unique cases of S. aureus bacteremia cases in adult patients established with positive blood cultures were evaluated. The cases were collected over a 1-year period at Yale New Haven Hospital. After exclusion of those who died within 3 days of the initial positive culture or who were transferred to other facilities, 236 were included in this analysis.
IDC guidance, which is not required for S. aureus bacteremia at Yale New Haven Hospital, was provided for 74.5% of the patients. Another 4% of patients received guidance from the AST, which is an independent service often provided prior to IDC guidance, according to Dr. Sherbuk.
Relapse (3% vs. 5%) and reinfection (6% vs. 4%) rates were low in both those who did and did not receive expert advice, respectively. These rates were not significantly different. On multivariate analysis, the two factors associated with increased 30-day mortality were patient age greater than 60 years and sepsis based on sequential organ failure assessment.
Several previous studies have associated IDC advice with improved outcomes in S. aureus bacteremia, according to Dr. Sherbuk, but this study suggests that the AST “can be a meaningful adjunct” to IDC guidance to improve outcomes. She noted that several other sets of data presented at this year’s ID Week also associated AST with improved infection management.
SAN DIEGO – Thirty-day mortality associated with Staphylococcus aureus bacteremia is reduced if there is guidance from either an antimicrobial stewardship team (AST) or an infectious disease consultant (IDC), according to a multivariate experience at Yale New Haven Hospital presented at an annual scientific meeting on infectious diseases.
“This has been a hot area, because there have been a lot of recent studies suggesting that expert infectious disease advice improves care, but not every study has associated expert advice with a mortality benefit,” said Jacqueline Sherbuk, MD, a fellow in the division of infectious diseases and international health at the University of Virginia, Charlottesville. She was a resident at Yale University when this study was conducted.
In this study, the impact of an IDC on outcome in patients with S. aureus bacteremia was evaluated relative to no expert advice. By itself, an IDC was associated with improved adherence to standards of care for S. aureus bacteremia management, but the reduction in mortality was not statistically significant for those who received IDC guidance relative to those who did not.
“Given that patient care may be guided by consultations from the AST independent of IDC, we looked at the overall impact of expert opinion versus no expert involvement, and this achieved significance on multivariate analysis,” Dr. Sherbuk reported.
For adherence to guidelines, IDC guidance was better than no expert advice on multiple measures, including proportion obtaining an echocardiogram (89% vs. 67%; P less than .001), appropriate definitive antibiotics (98% vs. 80%; P less than .001), and appropriate treatment duration (92% vs. 35%; P less than .001). However, the advantage for 30-day mortality rates was only a trend (11% vs. 21%, P = .07). It was only when patients who received IDC guidance or a consultation from the AST were combined that the difference climbed to significance (11% vs. 23%; P = .04).
“On multivariate analysis, the OR [odds ratio] was substantial, predicting a 60% reduction [OR 0.40; P = .03) in 30-day mortality for expert advice vs. no expert advice,” Dr. Sherbuk reported.
In this retrospective observational study, 261 unique cases of S. aureus bacteremia cases in adult patients established with positive blood cultures were evaluated. The cases were collected over a 1-year period at Yale New Haven Hospital. After exclusion of those who died within 3 days of the initial positive culture or who were transferred to other facilities, 236 were included in this analysis.
IDC guidance, which is not required for S. aureus bacteremia at Yale New Haven Hospital, was provided for 74.5% of the patients. Another 4% of patients received guidance from the AST, which is an independent service often provided prior to IDC guidance, according to Dr. Sherbuk.
Relapse (3% vs. 5%) and reinfection (6% vs. 4%) rates were low in both those who did and did not receive expert advice, respectively. These rates were not significantly different. On multivariate analysis, the two factors associated with increased 30-day mortality were patient age greater than 60 years and sepsis based on sequential organ failure assessment.
Several previous studies have associated IDC advice with improved outcomes in S. aureus bacteremia, according to Dr. Sherbuk, but this study suggests that the AST “can be a meaningful adjunct” to IDC guidance to improve outcomes. She noted that several other sets of data presented at this year’s ID Week also associated AST with improved infection management.
SAN DIEGO – Thirty-day mortality associated with Staphylococcus aureus bacteremia is reduced if there is guidance from either an antimicrobial stewardship team (AST) or an infectious disease consultant (IDC), according to a multivariate experience at Yale New Haven Hospital presented at an annual scientific meeting on infectious diseases.
“This has been a hot area, because there have been a lot of recent studies suggesting that expert infectious disease advice improves care, but not every study has associated expert advice with a mortality benefit,” said Jacqueline Sherbuk, MD, a fellow in the division of infectious diseases and international health at the University of Virginia, Charlottesville. She was a resident at Yale University when this study was conducted.
In this study, the impact of an IDC on outcome in patients with S. aureus bacteremia was evaluated relative to no expert advice. By itself, an IDC was associated with improved adherence to standards of care for S. aureus bacteremia management, but the reduction in mortality was not statistically significant for those who received IDC guidance relative to those who did not.
“Given that patient care may be guided by consultations from the AST independent of IDC, we looked at the overall impact of expert opinion versus no expert involvement, and this achieved significance on multivariate analysis,” Dr. Sherbuk reported.
For adherence to guidelines, IDC guidance was better than no expert advice on multiple measures, including proportion obtaining an echocardiogram (89% vs. 67%; P less than .001), appropriate definitive antibiotics (98% vs. 80%; P less than .001), and appropriate treatment duration (92% vs. 35%; P less than .001). However, the advantage for 30-day mortality rates was only a trend (11% vs. 21%, P = .07). It was only when patients who received IDC guidance or a consultation from the AST were combined that the difference climbed to significance (11% vs. 23%; P = .04).
“On multivariate analysis, the OR [odds ratio] was substantial, predicting a 60% reduction [OR 0.40; P = .03) in 30-day mortality for expert advice vs. no expert advice,” Dr. Sherbuk reported.
In this retrospective observational study, 261 unique cases of S. aureus bacteremia cases in adult patients established with positive blood cultures were evaluated. The cases were collected over a 1-year period at Yale New Haven Hospital. After exclusion of those who died within 3 days of the initial positive culture or who were transferred to other facilities, 236 were included in this analysis.
IDC guidance, which is not required for S. aureus bacteremia at Yale New Haven Hospital, was provided for 74.5% of the patients. Another 4% of patients received guidance from the AST, which is an independent service often provided prior to IDC guidance, according to Dr. Sherbuk.
Relapse (3% vs. 5%) and reinfection (6% vs. 4%) rates were low in both those who did and did not receive expert advice, respectively. These rates were not significantly different. On multivariate analysis, the two factors associated with increased 30-day mortality were patient age greater than 60 years and sepsis based on sequential organ failure assessment.
Several previous studies have associated IDC advice with improved outcomes in S. aureus bacteremia, according to Dr. Sherbuk, but this study suggests that the AST “can be a meaningful adjunct” to IDC guidance to improve outcomes. She noted that several other sets of data presented at this year’s ID Week also associated AST with improved infection management.
AT ID WEEK 2017
Key clinical point:
Major finding: For those receiving expert involvement in S. aureus bacteremia management, the odds ratio for 30-day mortality was reduced 60% (OR 0.40; P = .03) on multivariate analysis.
Data source: Retrospective, single-center study exploring the management of 236 S. aureus bacteremia cases in adult patients.
Disclosures: Dr. Sherbuk reported no financial relationships relevant to this study.
Thirty-one percent of multidrug-resistant infections were community acquired
SAN DIEGO – Thirty-one percent of multidrug-resistant infections were acquired from the community in a prospective single-center study of a regional hospital.
“Multidrug-resistant organisms have escaped the hospital,” Nicholas A. Turner, MD, of Duke University Medical Center, Durham, N.C., and his associates wrote in a poster presented at an annual scientific meeting on infectious diseases. “Community acquisition of multidrug-resistant organisms [MDROs] is increasing, not just within referral centers but also community hospitals. Providers will need to be increasingly aware of this trend.”
Infections of MDROs cause about 2,000,000 illnesses and 23,000 deaths annually in the United States, according to the Centers for Disease Control and Prevention. Until recently, MDROs were considered a plague of hospitals. Amid reports of increasing levels of community acquisition, the researchers studied adults admitted to a 202-bed regional hospital between 2013 and 2016. They defined MDROs as infections of methicillin-resistant Staphylococcus aureus (MRSA), gram-negative bacteria resistant to more than three antimicrobial classes, vancomycin-resistant Enterococcus (VRE), or diarrhea with a positive stool culture for Clostridium difficile.
A total of 285 patients had MDROs. Clostridium difficile (45%) and MRSA (35%) were most common. In all, 88 (31%) MDROs were community-acquired – that is, diagnosed within 48 hours of admission in patients who were not on dialysis, did not live in a long-term care facility, and had not been hospitalized for more than 48 hours in the past 90 days. A total of 36% of MRSA and multidrug-resistant gram-negative infections were community acquired, as were 25% of Clostridium difficile infections. There were only 10 VRE infections, of which none were community-acquired.
After the researchers controlled for clinical and demographic variables, the only significant predictor of community-acquired MDRO was cancer (odds ratio [OR], 2.3; 95% confidence interval [CI], 1.02-5.2). Surgery within the previous 12 months was significantly associated with hospital-acquired MDRO (OR, 0.16; 95% CI, 0.05-0.5).
Traditional risk factors for community-acquired MRSA or C. difficile infection did not achieve statistical significance in the multivariable analysis, the researchers noted. “Similar to data from large tertiary care centers, our findings suggest that MDROs are increasingly acquired in the community setting, even at smaller regional hospitals,” they concluded. “Further study is needed to track the expansion of MDROs in the community setting.”
Dr. Turner reported having no conflicts of interest.
SAN DIEGO – Thirty-one percent of multidrug-resistant infections were acquired from the community in a prospective single-center study of a regional hospital.
“Multidrug-resistant organisms have escaped the hospital,” Nicholas A. Turner, MD, of Duke University Medical Center, Durham, N.C., and his associates wrote in a poster presented at an annual scientific meeting on infectious diseases. “Community acquisition of multidrug-resistant organisms [MDROs] is increasing, not just within referral centers but also community hospitals. Providers will need to be increasingly aware of this trend.”
Infections of MDROs cause about 2,000,000 illnesses and 23,000 deaths annually in the United States, according to the Centers for Disease Control and Prevention. Until recently, MDROs were considered a plague of hospitals. Amid reports of increasing levels of community acquisition, the researchers studied adults admitted to a 202-bed regional hospital between 2013 and 2016. They defined MDROs as infections of methicillin-resistant Staphylococcus aureus (MRSA), gram-negative bacteria resistant to more than three antimicrobial classes, vancomycin-resistant Enterococcus (VRE), or diarrhea with a positive stool culture for Clostridium difficile.
A total of 285 patients had MDROs. Clostridium difficile (45%) and MRSA (35%) were most common. In all, 88 (31%) MDROs were community-acquired – that is, diagnosed within 48 hours of admission in patients who were not on dialysis, did not live in a long-term care facility, and had not been hospitalized for more than 48 hours in the past 90 days. A total of 36% of MRSA and multidrug-resistant gram-negative infections were community acquired, as were 25% of Clostridium difficile infections. There were only 10 VRE infections, of which none were community-acquired.
After the researchers controlled for clinical and demographic variables, the only significant predictor of community-acquired MDRO was cancer (odds ratio [OR], 2.3; 95% confidence interval [CI], 1.02-5.2). Surgery within the previous 12 months was significantly associated with hospital-acquired MDRO (OR, 0.16; 95% CI, 0.05-0.5).
Traditional risk factors for community-acquired MRSA or C. difficile infection did not achieve statistical significance in the multivariable analysis, the researchers noted. “Similar to data from large tertiary care centers, our findings suggest that MDROs are increasingly acquired in the community setting, even at smaller regional hospitals,” they concluded. “Further study is needed to track the expansion of MDROs in the community setting.”
Dr. Turner reported having no conflicts of interest.
SAN DIEGO – Thirty-one percent of multidrug-resistant infections were acquired from the community in a prospective single-center study of a regional hospital.
“Multidrug-resistant organisms have escaped the hospital,” Nicholas A. Turner, MD, of Duke University Medical Center, Durham, N.C., and his associates wrote in a poster presented at an annual scientific meeting on infectious diseases. “Community acquisition of multidrug-resistant organisms [MDROs] is increasing, not just within referral centers but also community hospitals. Providers will need to be increasingly aware of this trend.”
Infections of MDROs cause about 2,000,000 illnesses and 23,000 deaths annually in the United States, according to the Centers for Disease Control and Prevention. Until recently, MDROs were considered a plague of hospitals. Amid reports of increasing levels of community acquisition, the researchers studied adults admitted to a 202-bed regional hospital between 2013 and 2016. They defined MDROs as infections of methicillin-resistant Staphylococcus aureus (MRSA), gram-negative bacteria resistant to more than three antimicrobial classes, vancomycin-resistant Enterococcus (VRE), or diarrhea with a positive stool culture for Clostridium difficile.
A total of 285 patients had MDROs. Clostridium difficile (45%) and MRSA (35%) were most common. In all, 88 (31%) MDROs were community-acquired – that is, diagnosed within 48 hours of admission in patients who were not on dialysis, did not live in a long-term care facility, and had not been hospitalized for more than 48 hours in the past 90 days. A total of 36% of MRSA and multidrug-resistant gram-negative infections were community acquired, as were 25% of Clostridium difficile infections. There were only 10 VRE infections, of which none were community-acquired.
After the researchers controlled for clinical and demographic variables, the only significant predictor of community-acquired MDRO was cancer (odds ratio [OR], 2.3; 95% confidence interval [CI], 1.02-5.2). Surgery within the previous 12 months was significantly associated with hospital-acquired MDRO (OR, 0.16; 95% CI, 0.05-0.5).
Traditional risk factors for community-acquired MRSA or C. difficile infection did not achieve statistical significance in the multivariable analysis, the researchers noted. “Similar to data from large tertiary care centers, our findings suggest that MDROs are increasingly acquired in the community setting, even at smaller regional hospitals,” they concluded. “Further study is needed to track the expansion of MDROs in the community setting.”
Dr. Turner reported having no conflicts of interest.
AT IDWEEK 2017
Key clinical point: Multidrug resistant infections are increasingly being acquired in communities.
Major finding:
Data source: A prospective study of 285 patients with multidrug-resistant infections at a 202-bed hospital.
Disclosures: Dr. Turner reported having no conflicts of interest.
Ciprofloxacin cured gyrA wild-type Neisseria gonorrhoeae infections
SAN DIEGO – Ciprofloxacin cured 100% of gyrase A wild-type Neisseria gonorrhoeae infections, and physicians prescribed it significantly more frequently when they received electronic reminders of test results and recommendations, in a single-center study.
“Recent reports of untreatable gonorrhea have caused great concern. Treatment with ceftriaxone may be a major driver of resistance, and reducing its use may curb the emergence of resistant infections,” Lao-Tzu Allan-Blitz, a medical student at the David Geffen School of Medicine at the University of California, Los Angeles, said at an annual scientific meeting on infectious diseases.
The Centers for Disease Control and Prevention ranks multidrug-resistant N. gonorrhoeae third among all drug-resistant threats in the United States, Mr. Allan-Blitz noted during an oral presentation at the meeting. Beginning in the late 1990s, strains of N. gonorrhoeae developed resistance to sulfanilamides, penicillin, tetracycline, and fluoroquinolones, leaving only the extended-spectrum cephalosporins for empiric treatment. Recent reports of cephalosporin-resistant N. gonorrhoeae in other countries have raised the specter of untreatable gonorrhea.
Because antimicrobial resistance can shift in response to selective pressure, experts are exploring the use of antibiotics once considered ineffective for treating N. gonorrhoeae infections. At UCLA, researchers developed a real-time reverse transcription polymerase chain reaction test for a mutation of codon 91 in the gyrase A (gyrA) gene in N. gonorrhoeae that reliably predicts resistance to ciprofloxacin.
Test results take 24-48 hours. The test is not Food and Drug Administration approved but has been validated in accordance with Clinical Laboratory Improvement Amendments, Mr. Allan-Blitz said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
In November 2015, UCLA Health began gyrA genotyping all N. gonorrhoeae positive specimens, and in May 2016, it began sending providers electronic reminders of genotype results and treatment recommendations. For gyrA wild-type infections, UCLA Health recommends 500 mg oral ciprofloxacin, Mr. Allan-Blitz said.
Initial test-of-cure data are promising. All 25 patients with wild-type infections who received ciprofloxacin and returned 7-90 days later tested negative for N. gonorrhoeae. Culture sites included the urethra (seven cases), pharynx (seven cases), rectum (seven cases), and genitals (four cases), Mr. Allan-Blitz said. “Prior studies have demonstrated that reminder notifications improve uptake of antimicrobial stewardship,” he said. “Other health centers should consider implementing the gyrA assay, and using reminder notifications may improve uptake by providers.”
The National Institutes of Health provided funding. The investigators reported having no conflicts of interest.
SAN DIEGO – Ciprofloxacin cured 100% of gyrase A wild-type Neisseria gonorrhoeae infections, and physicians prescribed it significantly more frequently when they received electronic reminders of test results and recommendations, in a single-center study.
“Recent reports of untreatable gonorrhea have caused great concern. Treatment with ceftriaxone may be a major driver of resistance, and reducing its use may curb the emergence of resistant infections,” Lao-Tzu Allan-Blitz, a medical student at the David Geffen School of Medicine at the University of California, Los Angeles, said at an annual scientific meeting on infectious diseases.
The Centers for Disease Control and Prevention ranks multidrug-resistant N. gonorrhoeae third among all drug-resistant threats in the United States, Mr. Allan-Blitz noted during an oral presentation at the meeting. Beginning in the late 1990s, strains of N. gonorrhoeae developed resistance to sulfanilamides, penicillin, tetracycline, and fluoroquinolones, leaving only the extended-spectrum cephalosporins for empiric treatment. Recent reports of cephalosporin-resistant N. gonorrhoeae in other countries have raised the specter of untreatable gonorrhea.
Because antimicrobial resistance can shift in response to selective pressure, experts are exploring the use of antibiotics once considered ineffective for treating N. gonorrhoeae infections. At UCLA, researchers developed a real-time reverse transcription polymerase chain reaction test for a mutation of codon 91 in the gyrase A (gyrA) gene in N. gonorrhoeae that reliably predicts resistance to ciprofloxacin.
Test results take 24-48 hours. The test is not Food and Drug Administration approved but has been validated in accordance with Clinical Laboratory Improvement Amendments, Mr. Allan-Blitz said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
In November 2015, UCLA Health began gyrA genotyping all N. gonorrhoeae positive specimens, and in May 2016, it began sending providers electronic reminders of genotype results and treatment recommendations. For gyrA wild-type infections, UCLA Health recommends 500 mg oral ciprofloxacin, Mr. Allan-Blitz said.
Initial test-of-cure data are promising. All 25 patients with wild-type infections who received ciprofloxacin and returned 7-90 days later tested negative for N. gonorrhoeae. Culture sites included the urethra (seven cases), pharynx (seven cases), rectum (seven cases), and genitals (four cases), Mr. Allan-Blitz said. “Prior studies have demonstrated that reminder notifications improve uptake of antimicrobial stewardship,” he said. “Other health centers should consider implementing the gyrA assay, and using reminder notifications may improve uptake by providers.”
The National Institutes of Health provided funding. The investigators reported having no conflicts of interest.
SAN DIEGO – Ciprofloxacin cured 100% of gyrase A wild-type Neisseria gonorrhoeae infections, and physicians prescribed it significantly more frequently when they received electronic reminders of test results and recommendations, in a single-center study.
“Recent reports of untreatable gonorrhea have caused great concern. Treatment with ceftriaxone may be a major driver of resistance, and reducing its use may curb the emergence of resistant infections,” Lao-Tzu Allan-Blitz, a medical student at the David Geffen School of Medicine at the University of California, Los Angeles, said at an annual scientific meeting on infectious diseases.
The Centers for Disease Control and Prevention ranks multidrug-resistant N. gonorrhoeae third among all drug-resistant threats in the United States, Mr. Allan-Blitz noted during an oral presentation at the meeting. Beginning in the late 1990s, strains of N. gonorrhoeae developed resistance to sulfanilamides, penicillin, tetracycline, and fluoroquinolones, leaving only the extended-spectrum cephalosporins for empiric treatment. Recent reports of cephalosporin-resistant N. gonorrhoeae in other countries have raised the specter of untreatable gonorrhea.
Because antimicrobial resistance can shift in response to selective pressure, experts are exploring the use of antibiotics once considered ineffective for treating N. gonorrhoeae infections. At UCLA, researchers developed a real-time reverse transcription polymerase chain reaction test for a mutation of codon 91 in the gyrase A (gyrA) gene in N. gonorrhoeae that reliably predicts resistance to ciprofloxacin.
Test results take 24-48 hours. The test is not Food and Drug Administration approved but has been validated in accordance with Clinical Laboratory Improvement Amendments, Mr. Allan-Blitz said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
In November 2015, UCLA Health began gyrA genotyping all N. gonorrhoeae positive specimens, and in May 2016, it began sending providers electronic reminders of genotype results and treatment recommendations. For gyrA wild-type infections, UCLA Health recommends 500 mg oral ciprofloxacin, Mr. Allan-Blitz said.
Initial test-of-cure data are promising. All 25 patients with wild-type infections who received ciprofloxacin and returned 7-90 days later tested negative for N. gonorrhoeae. Culture sites included the urethra (seven cases), pharynx (seven cases), rectum (seven cases), and genitals (four cases), Mr. Allan-Blitz said. “Prior studies have demonstrated that reminder notifications improve uptake of antimicrobial stewardship,” he said. “Other health centers should consider implementing the gyrA assay, and using reminder notifications may improve uptake by providers.”
The National Institutes of Health provided funding. The investigators reported having no conflicts of interest.
AT IDWEEK 2017
Key clinical point:
Major finding: The cure rate was 100% among 25 patients who received ciprofloxacin for wild-type gyrA gonorrhea.
Data source: A single-center study of 582 patients with gonorrhea.
Disclosures: The National Institutes of Health provided funding. The investigators reported having no conflicts of interest.
Delayed appropriate therapy affects outcomes in patients at risk for CRE infections
SAN DIEGO – Among patients with serious infections due to Enterobacteriaceae, delayed appropriate therapy has a stronger association with outcomes, relative to presence of carbapenem-resistant Enterobacteriaceae, according to an analysis of national hospital data.
“We need to reconsider how we approach patients with serious Gram-negative infections,” lead study author Thomas Lodise, PharmD, PhD, said at an annual scientific meeting on infectious diseases. “We kind of take this wait-and-see approach in infectious diseases; we wait a couple of days, then we get aggressive. You would never do this in oncology. I don’t know how many more studies we need to show that early therapy matters. We talk about antibiotic stewardship. One of the fundamental pillars of stewardship is getting it right the first time, and we fail to do this in the majority of patients with serious Gram-negative infections.”

At the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society, he noted that delayed appropriate therapy is associated with increased rates of clinical failure and mortality, longer lengths of stay, longer durations of antibiotic treatment, and greater in-hospital costs. “Similarly, patients with infections caused by carbapenem-resistant Enterobacteriaceae (CRE) have poorer outcomes, such as increased risk of mortality or of being discharged to a long-term care facility, compared with patients with infections caused by carbapenem-susceptible Enterobacteriaceae isolates,” said Dr. Lodise of the Albany (N.Y.) College of Pharmacy and Health Sciences. “Although CRE and delayed appropriate therapy have both been associated with worse outcomes, the impact of each of these factors on clinical and economic outcomes is not well understood.”
In an effort to assess the independent and combined impact of CRE and delayed appropriate therapy on clinical and economic outcomes among hospitalized U.S. patients with serious infections due to Enterobacteriaceae, Dr. Lodise and his associates drew from the Premier Hospital Database, which includes information for about 500 acute-care hospitals in the United States, including the 150 hospitals that provided admission records and microbiological data assessed in the current analysis.
The researchers evaluated adults hospitalized between July 2011 and September 2014. The index date was defined as the earliest culture positive for at least one Gram-negative bacteria of interest, and patients were stratified based on whether the pathogen was CRE or non-CRE. Appropriate therapy was defined as receipt of an antibiotic regimen with microbiological activity against all pathogens identified within the index culture on the index date or within the subsequent 2-day period. All subsequent receipt of such therapy was defined as delayed appropriate therapy.
In all, 50,069 patients with a mean age of 66 years were included in the study. Of these, 514 (1%) harbored infections caused by CRE, and 49,555 (99%) had infections caused by a pathogen other than CRE. Multivariate adjusted analysis revealed significant differences between the CRE group and the non-CRE group in duration of antibiotic therapy (a mean of 8.5 days vs. 7.5 days, respectively); length of stay (a mean of 8.4 days vs. 7.6 days), and in-hospital cost (a mean of $19,816 vs. a mean of $15,165; P less than .01 for all associations). In addition, CRE patients were less likely to be discharged home (odds ratio [OR], .3) and more likely to die in the hospital or be discharged to hospice (OR, 2.2).
When outcomes of patients infections due to Enterobacteriaceae species were stratified by timing of appropriate therapy (timely vs. delayed) and CRE status (CRE vs. non-CRE), without exception the burden of serious infections was least among patients with infections due to non-CRE who received timely appropriate therapy, and greatest among patients with infections due to CRE in whom appropriate therapy was delayed. A gradient effect was observed across strata, and weighted towards timing of receipt of initial therapy. For example, the mean LOS post index culture date rank was lowest among non-CRE patients who received timely appropriate therapy (a mean of 5 days) and greatest among patients infected with CRE who received delayed appropriate therapy (a mean of 8.8 days). Similarly, mean in-hospital costs post index culture date rank was lowest among non-CRE patients who received timely appropriate therapy (a mean of $9,875) and greatest among patients infected with CRE who received delayed appropriate therapy (a mean of $25,506).
“This study demonstrates the importance of early identification of patients at risk for delayed appropriate therapy, through the use of clinical criteria for risk stratification or rapid diagnostic tools,” Dr. Lodise concluded. “The findings also highlight the need to shift current treatment practices away from antibiotic escalation strategies that contribute to delayed appropriate therapy and toward early aggressive, appropriate therapy in patients at risk for CRE infection.”
Allergan funded the study. Dr. Lodise disclosed that he has received consulting fees or honoraria from Allergan. He has also been a consultant for Merck, Achaogen, Zavante, and The Medicines Company.
SAN DIEGO – Among patients with serious infections due to Enterobacteriaceae, delayed appropriate therapy has a stronger association with outcomes, relative to presence of carbapenem-resistant Enterobacteriaceae, according to an analysis of national hospital data.
“We need to reconsider how we approach patients with serious Gram-negative infections,” lead study author Thomas Lodise, PharmD, PhD, said at an annual scientific meeting on infectious diseases. “We kind of take this wait-and-see approach in infectious diseases; we wait a couple of days, then we get aggressive. You would never do this in oncology. I don’t know how many more studies we need to show that early therapy matters. We talk about antibiotic stewardship. One of the fundamental pillars of stewardship is getting it right the first time, and we fail to do this in the majority of patients with serious Gram-negative infections.”

At the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society, he noted that delayed appropriate therapy is associated with increased rates of clinical failure and mortality, longer lengths of stay, longer durations of antibiotic treatment, and greater in-hospital costs. “Similarly, patients with infections caused by carbapenem-resistant Enterobacteriaceae (CRE) have poorer outcomes, such as increased risk of mortality or of being discharged to a long-term care facility, compared with patients with infections caused by carbapenem-susceptible Enterobacteriaceae isolates,” said Dr. Lodise of the Albany (N.Y.) College of Pharmacy and Health Sciences. “Although CRE and delayed appropriate therapy have both been associated with worse outcomes, the impact of each of these factors on clinical and economic outcomes is not well understood.”
In an effort to assess the independent and combined impact of CRE and delayed appropriate therapy on clinical and economic outcomes among hospitalized U.S. patients with serious infections due to Enterobacteriaceae, Dr. Lodise and his associates drew from the Premier Hospital Database, which includes information for about 500 acute-care hospitals in the United States, including the 150 hospitals that provided admission records and microbiological data assessed in the current analysis.
The researchers evaluated adults hospitalized between July 2011 and September 2014. The index date was defined as the earliest culture positive for at least one Gram-negative bacteria of interest, and patients were stratified based on whether the pathogen was CRE or non-CRE. Appropriate therapy was defined as receipt of an antibiotic regimen with microbiological activity against all pathogens identified within the index culture on the index date or within the subsequent 2-day period. All subsequent receipt of such therapy was defined as delayed appropriate therapy.
In all, 50,069 patients with a mean age of 66 years were included in the study. Of these, 514 (1%) harbored infections caused by CRE, and 49,555 (99%) had infections caused by a pathogen other than CRE. Multivariate adjusted analysis revealed significant differences between the CRE group and the non-CRE group in duration of antibiotic therapy (a mean of 8.5 days vs. 7.5 days, respectively); length of stay (a mean of 8.4 days vs. 7.6 days), and in-hospital cost (a mean of $19,816 vs. a mean of $15,165; P less than .01 for all associations). In addition, CRE patients were less likely to be discharged home (odds ratio [OR], .3) and more likely to die in the hospital or be discharged to hospice (OR, 2.2).
When outcomes of patients infections due to Enterobacteriaceae species were stratified by timing of appropriate therapy (timely vs. delayed) and CRE status (CRE vs. non-CRE), without exception the burden of serious infections was least among patients with infections due to non-CRE who received timely appropriate therapy, and greatest among patients with infections due to CRE in whom appropriate therapy was delayed. A gradient effect was observed across strata, and weighted towards timing of receipt of initial therapy. For example, the mean LOS post index culture date rank was lowest among non-CRE patients who received timely appropriate therapy (a mean of 5 days) and greatest among patients infected with CRE who received delayed appropriate therapy (a mean of 8.8 days). Similarly, mean in-hospital costs post index culture date rank was lowest among non-CRE patients who received timely appropriate therapy (a mean of $9,875) and greatest among patients infected with CRE who received delayed appropriate therapy (a mean of $25,506).
“This study demonstrates the importance of early identification of patients at risk for delayed appropriate therapy, through the use of clinical criteria for risk stratification or rapid diagnostic tools,” Dr. Lodise concluded. “The findings also highlight the need to shift current treatment practices away from antibiotic escalation strategies that contribute to delayed appropriate therapy and toward early aggressive, appropriate therapy in patients at risk for CRE infection.”
Allergan funded the study. Dr. Lodise disclosed that he has received consulting fees or honoraria from Allergan. He has also been a consultant for Merck, Achaogen, Zavante, and The Medicines Company.
SAN DIEGO – Among patients with serious infections due to Enterobacteriaceae, delayed appropriate therapy has a stronger association with outcomes, relative to presence of carbapenem-resistant Enterobacteriaceae, according to an analysis of national hospital data.
“We need to reconsider how we approach patients with serious Gram-negative infections,” lead study author Thomas Lodise, PharmD, PhD, said at an annual scientific meeting on infectious diseases. “We kind of take this wait-and-see approach in infectious diseases; we wait a couple of days, then we get aggressive. You would never do this in oncology. I don’t know how many more studies we need to show that early therapy matters. We talk about antibiotic stewardship. One of the fundamental pillars of stewardship is getting it right the first time, and we fail to do this in the majority of patients with serious Gram-negative infections.”

At the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society, he noted that delayed appropriate therapy is associated with increased rates of clinical failure and mortality, longer lengths of stay, longer durations of antibiotic treatment, and greater in-hospital costs. “Similarly, patients with infections caused by carbapenem-resistant Enterobacteriaceae (CRE) have poorer outcomes, such as increased risk of mortality or of being discharged to a long-term care facility, compared with patients with infections caused by carbapenem-susceptible Enterobacteriaceae isolates,” said Dr. Lodise of the Albany (N.Y.) College of Pharmacy and Health Sciences. “Although CRE and delayed appropriate therapy have both been associated with worse outcomes, the impact of each of these factors on clinical and economic outcomes is not well understood.”
In an effort to assess the independent and combined impact of CRE and delayed appropriate therapy on clinical and economic outcomes among hospitalized U.S. patients with serious infections due to Enterobacteriaceae, Dr. Lodise and his associates drew from the Premier Hospital Database, which includes information for about 500 acute-care hospitals in the United States, including the 150 hospitals that provided admission records and microbiological data assessed in the current analysis.
The researchers evaluated adults hospitalized between July 2011 and September 2014. The index date was defined as the earliest culture positive for at least one Gram-negative bacteria of interest, and patients were stratified based on whether the pathogen was CRE or non-CRE. Appropriate therapy was defined as receipt of an antibiotic regimen with microbiological activity against all pathogens identified within the index culture on the index date or within the subsequent 2-day period. All subsequent receipt of such therapy was defined as delayed appropriate therapy.
In all, 50,069 patients with a mean age of 66 years were included in the study. Of these, 514 (1%) harbored infections caused by CRE, and 49,555 (99%) had infections caused by a pathogen other than CRE. Multivariate adjusted analysis revealed significant differences between the CRE group and the non-CRE group in duration of antibiotic therapy (a mean of 8.5 days vs. 7.5 days, respectively); length of stay (a mean of 8.4 days vs. 7.6 days), and in-hospital cost (a mean of $19,816 vs. a mean of $15,165; P less than .01 for all associations). In addition, CRE patients were less likely to be discharged home (odds ratio [OR], .3) and more likely to die in the hospital or be discharged to hospice (OR, 2.2).
When outcomes of patients infections due to Enterobacteriaceae species were stratified by timing of appropriate therapy (timely vs. delayed) and CRE status (CRE vs. non-CRE), without exception the burden of serious infections was least among patients with infections due to non-CRE who received timely appropriate therapy, and greatest among patients with infections due to CRE in whom appropriate therapy was delayed. A gradient effect was observed across strata, and weighted towards timing of receipt of initial therapy. For example, the mean LOS post index culture date rank was lowest among non-CRE patients who received timely appropriate therapy (a mean of 5 days) and greatest among patients infected with CRE who received delayed appropriate therapy (a mean of 8.8 days). Similarly, mean in-hospital costs post index culture date rank was lowest among non-CRE patients who received timely appropriate therapy (a mean of $9,875) and greatest among patients infected with CRE who received delayed appropriate therapy (a mean of $25,506).
“This study demonstrates the importance of early identification of patients at risk for delayed appropriate therapy, through the use of clinical criteria for risk stratification or rapid diagnostic tools,” Dr. Lodise concluded. “The findings also highlight the need to shift current treatment practices away from antibiotic escalation strategies that contribute to delayed appropriate therapy and toward early aggressive, appropriate therapy in patients at risk for CRE infection.”
Allergan funded the study. Dr. Lodise disclosed that he has received consulting fees or honoraria from Allergan. He has also been a consultant for Merck, Achaogen, Zavante, and The Medicines Company.
REPORTING FROM ID WEEK 2017
Key clinical point:
Major finding: The mean LOS post index culture date rank was lowest among non-CRE patients who received timely appropriate therapy (a mean of 5 days) and greatest among patients infected with CRE who received delayed appropriate therapy (a mean of 8.8 days).
Study details: An analysis of 50,069 adults hospitalized with serious infections due to Enterobacteriaceae between July 2011 and September 2014.
Disclosures: Allergan funded the study. Dr. Lodise disclosed that he has received consulting fees or honoraria from Allergan. He also has been a consultant for Merck, Achaogen, Zavante, and The Medicines Company.