User login
Negative symptoms of schizophrenia: An update
The negative symptoms of schizophrenia have been recognized for 100 years. Characterized by a loss of a function that should be present, negative symptoms include anhedonia, asociality, amotivation, and affective blunting. Individuals with schizophrenia who have a preponderance of negative symptoms (“deficit syndrome”) may comprise a special subset of patients. Compared with positive symptoms, negative symptoms are associated with worse global functioning and worse response to antipsychotic medication. Treatment of negative symptoms is challenging. Secondary negative symptoms—those that simulate or resemble primary negative symptoms but are attributable to another cause, such as major depressive disorder or the adverse effects of antipsychotic medication—need to be ruled out. Emerging evidence suggests that newer antipsychotics with novel mechanisms might be effective in treating negative symptoms. Antidepressants might also play a role.
This article describes types of negative symptoms, their clinical relevance, neuroanatomical and neurotransmission factors associated with negative symptoms, and current and future treatment options.
Modest improvements with antipsychotics
Schizophrenia affects an estimated 1% of the population.1 Antipsychotic medication has been the mainstay of schizophrenia treatment since
All antipsychotics are believed to exert their therapeutic effects by blocking dopamine (D2) receptors and are effective in ameliorating the positive symptoms of schizophrenia, including hallucinations, delusions, bizarre behavior, disordered thinking, and agitation.1 Early research had suggested that SGAs might also reduce the negative symptoms of schizophrenia, perhaps because they also block serotonin 2A receptors, a property thought to broaden their therapeutic profile. Over time, it became clear that neither FGAs nor SGAs conferred an advantage in treating negative symptoms, and that the observed improvements were modest.2-5 However, recent research suggests that several newer antipsychotics might be effective in targeting negative symptoms.2,6,7
History of negative symptoms
In the early 20th century, Swiss psychiatrist Eugen Bleuler coined the term schizophrenia to emphasize the cognitive impairment that occurs in patients with this illness, and which he conceptualized as a fragmenting of the psychic process.8 He believed that certain symptoms were fundamental to the illness, and described affective blunting, disturbance of association (ie, distorted thinking) autism (ie, impaired relationships), and ambivalence (ie, fragmented emotional responses). He viewed hallucinations and delusions as accessory symptoms because they were not unique to schizophrenia but were also found in other disorders (eg, mood disorders). Bleuler’s ideas took root, and generations of psychiatrists were taught his fundamental symptoms (“the 4 A’s”), the forerunner of today’s negative symptoms. Later, other experts chose to emphasize psychotic symptoms as most characteristic of schizophrenia, including Schneider’s “first-rank symptoms,” such as voices conversing or delusions of passivity.9
Negative symptoms were rediscovered in the 1970s and 1980s by psychiatric researchers interested in descriptive phenomenology.10,11 Research confirmed the presence of a positive dimension in schizophrenia characterized by the loss of boundaries between the patient and the real world (eg, hallucinations, delusions), and a negative dimension characterized by the loss of a function that should be present, such as alogia and asociality. These experts carefully described negative symptoms and created scales to measure them, including the Scale for the Assessment of Negative Symptoms (SANS),12 the Positive and Negative Syndrome Scale (PANSS),13 the Brief Negative Symptom Scale (BNSS),14 and the 16-item Negative Symptom Assessment (NSA-16).15 Contemporaneous to this work, a “deficit syndrome” was identified among patients with schizophrenia with prominent negative symptoms. The deficit syndrome is found in 25% to 30% of chronic cases.16 Negative symptoms are very common in patients with schizophrenia (Table 19).8,17
Early editions of the DSM defined schizophrenia mainly on the basis of disturbance of cognition, mood, and behavior, and a retreat from reality. With the publication of DSM-III in 1980, and in subsequent editions, schizophrenia was redefined as a relatively severe psychotic illness in which positive and negative symptoms were present, thereby acknowledging the importance of Bleuler’s fundamental symptoms. In DSM-5, negative symptoms are described as accounting for “a substantial portion of the morbidity associated with schizophrenia but are less prominent in other psychotic disorders.”18
Continue to: Types of negative symptoms
Types of negative symptoms
The following symptoms fall within the negative dimension19:
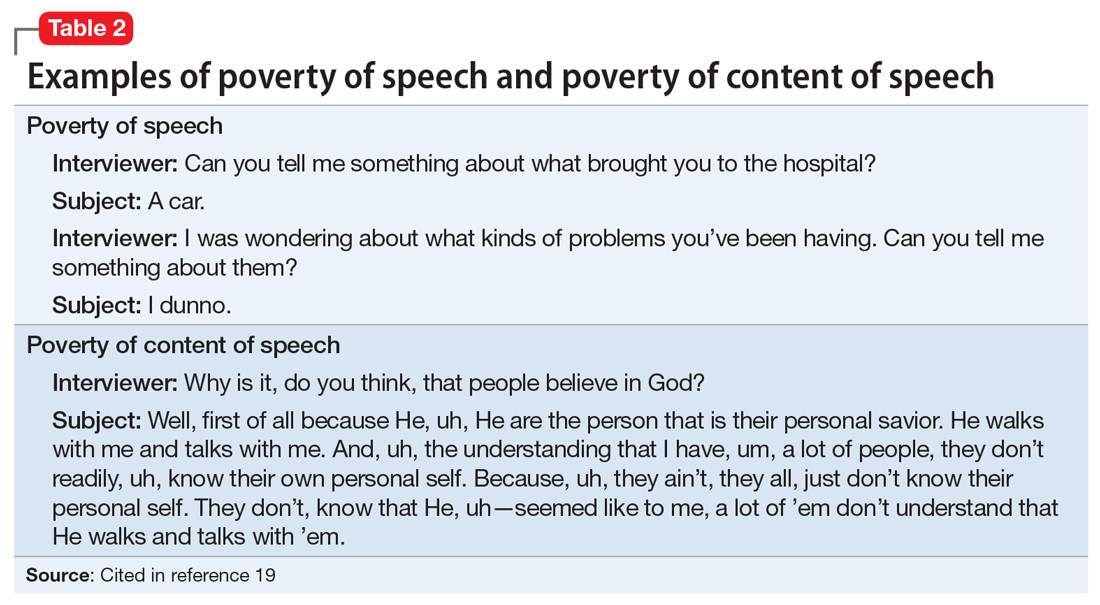
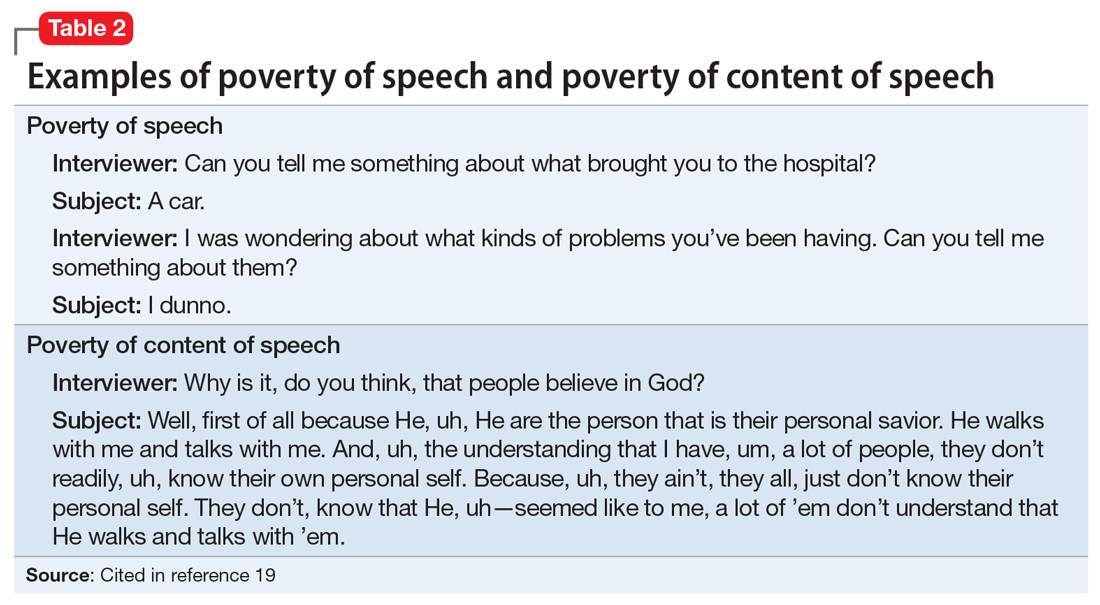
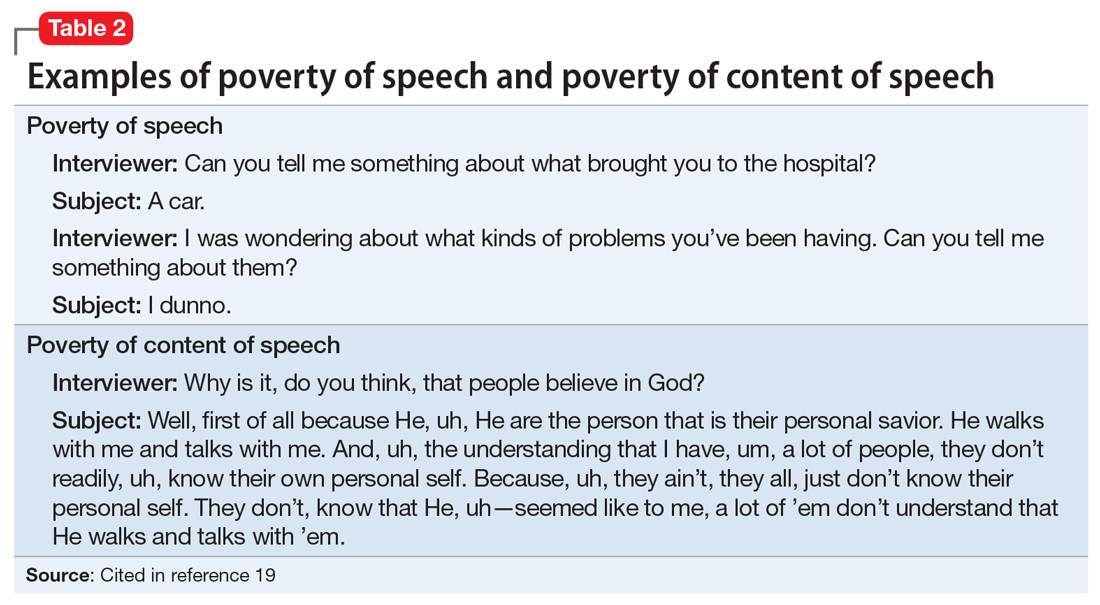
Alogia refers to the impoverished thinking and cognition that often occur in patients with schizophrenia. The patient’s thinking processes seem empty, turgid, or slow, as inferred from the patient’s speech. The 2 major manifestations of alogia are poverty of speech (nonfluent empty speech) and poverty of content of speech (fluent but empty speech). Examples of each appear in Table 2.19
Affective flattening or blunting manifests as a general impoverishment of emotional expression, reactivity, and feeling. Affective flattening can be assessed through observing a patient’s behavior and responsiveness during the interview.
Avolition-apathy manifests itself as a lack of energy and drive. Patients become inert and are unable to mobilize themselves to initiate or persist in completing many kinds of tasks.
Anhedonia-asociality encompasses the patient’s difficulties in experiencing interest or pleasure. It may express itself as a loss of interest in pleasurable activities, an inability to experience pleasure when participating in activities normally considered pleasurable, or a lack of involvement in social relationships.
Continue to: Attention
Attention is often poor in patients with severe mental illnesses. The patient may have trouble focusing his/her attention or may be able to focus only sporadically and erratically. He/she may ignore attempts to converse with him/her, wander away during an activity or a task, or appear to be inattentive when engaged in formal testing or interviewing.
Clinical relevance of negative symptoms
According to DSM-5, “Negative symptoms are more closely related to prognosis than are positive symptoms and tend to be the most persistent.”18 Research has shown that, compared with positive symptoms, negative symptoms are associated with greater impairment in overall functioning, social interaction, interpersonal relationships, economic functioning, and recreational activities.1,3,5 Negative symptoms also are associated with poorer response to medication and a positive family history of schizophrenia. Research shows that negative symptoms are persistent over time, and, in fact, become more prominent as the patient ages, whereas positive symptoms become less prominent.20
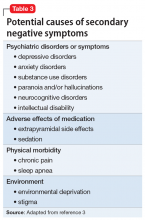
Secondary negative symptoms
Potential secondary causes of negative symptoms should be ruled out before concluding that the negative symptoms are due to schizophrenia.3 What might appear to be a negative symptom of schizophrenia, such as poor motivation or flattened affect, could be due to the presence of major depressive disorder. Such symptoms might resolve with treatment. Alternatively, a patient could have developed pseudoparkinsonism from antipsychotic medication and display unchanging facial expression and decreased spontaneous movements. These symptoms could resolve by adding
The neuroanatomy of negative symptoms
Although the neuroanatomical basis of negative symptoms has not been determined, neuroimaging studies have provided important clues.3 Structural brain imaging has consistently shown that negative symptoms in patients with schizophrenia correlate with decreased prefrontal white matter volume, anterior cingulate volume, insular cortex volume, left temporal cortex volume, and ventricular enlargement. Interestingly, volume loss starts before the appearance of negative symptoms.21,22 Functional imaging has shown that negative symptoms correlate with reduced cerebral blood perfusion in frontal, prefrontal, posterior cingulate, thalamus, parietal, and striatal regions.21,22 These findings may help explain the apathy, failure to initiate activities, and impaired social relatedness in patients with schizophrenia.
Neurotransmission and negative symptoms
Some experts have hypothesized that lowered cortical dopamine transmission in mesocortical pathways could give rise to negative symptoms, whereas excess transmission in subcortical structures leads to positive symptoms.23 There is also evidence for a noradrenalin deficiency based on the finding that low levels of cerebrospinal fluid 3-methoxy-4-hydroxyphenylglycol (MHPG), a noradrenaline metabolite, correlates with greater negative symptom severity.24 The presence of a serotonin deficiency has been proposed based on evidence that negative symptoms might be mitigated by serotonergic agents.25 More recently, some experts have posited that the dopamine D3 receptor might be involved in the etiology of negative symptoms. The dopamine D3 receptor activity is expressed in brain regions thought to control reward, emotions, and motivation.2 Newer medications with novel mechanisms suggest that other neurotransmitter pathways could be involved.6,7
Continue to: Treatment options
Treatment options
Treating negative symptoms remains challenging and there are no clear answers. When they were introduced in the 1990s, SGAs were initially thought to be superior to FGAs in targeting negative symptoms. Subsequent research, including recent reviews and meta-analyses, has shown that SGAs are not superior to FGAs in treating negative symptoms, and the effect of either medication class on negative symptoms is modest.2-5 One exception is amisulpride (not available in the United States), which is known to antagonize D2 and D3 receptors. A meta-analysis of the efficacy of antipsychotics in schizophrenia showed that amisulpride was significantly more effective than placebo in treating negative symptoms in 590 patients who received the medication.26 The authors suggested that amisulpride was effective due to its binding to presynaptic receptors in the frontal cortex, thereby enhancing dopamine transmission in this region.
Cariprazine, which acts as a partial agonist at the D2 and D3 receptors, with a 10-fold affinity for the D3 receptor, also has shown promise in treating negative symptoms.2 In a clinical trial of 460 patients with predominant negative symptoms, treatment with cariprazine led to a greater reduction in negative symptoms than
Other promising agentsinclude
Antidepressants also could be effective in reducing negative symptoms.3 A meta-analysis of randomized controlled trials evaluating the use of antidepressants as adjuncts to antipsychotic medications showed that adding an antidepressant was effective in reducing negative symptoms.29 The mechanism by which an antidepressant might cause a reduction in negative symptoms is uncertain, and it is possible that the antidepressant might treat depressive symptoms that are causing or contributing to the negative symptoms.
Bottom Line
Negative symptoms in patients with schizophrenia are associated with a worse functional outcome and poorer response to antipsychotic medication than positive symptoms. First- and second-generation antipsychotics are largely ineffective in consistently treating negative symptoms. Antipsychotic medications that target the D3 receptor might be more effective. Roluperidone, which targets serotonin 2A and sigma receptors, and SEP-363856, which targets TAAR1 and serotonin 1A receptors, are being studied for their effects on negative symptoms.
Continue to: Related Resources
Related Resources
- Galderisi S, Färden A, Kaiser S. Dissecting negative symptoms of schizophrenia: History, assessment, pathophysiological mechanisms and treatment. Schizophr Res. 2017;186:1-2.
- Rabinowitz J. Treating negative symptoms of schizophrenia. Current Psychiatry. 2018;17(12):19-23.
Drug Brand Names
Benztropine • Cogentin
Cariprazine • Vraylar
Chlorpromazine • Promapar, Thorazine
Risperidone • Risperdal
1. Owen MJ, Sawa A, Mortensen PD. Schizophrenia. Lancet. 2016;388(10039):86-97.
2. Cerviri G, Gesi C, Mencacci C. Pharmacological treatment of negative symptoms in schizophrenia: update and proposal of a clinical algorithm. Neuropsychiatr Dis Treat. 2019;15:1525-1535.
3. Mitra S, Mahintamani T, Kavoor AR, et al. Negative symptoms in schizophrenia. Ind Psychiatr J. 2016;25(2):135-144.
4. Fusa-Poli P, Papanastasiou E, Stahl D, et al. Treatments of negative symptoms in schizophrenia: meta-analysis of 168 randomized placebo-controlled trials. Schizophr Bull. 2015;41(4):892-899.
5. Remington G, Foussias G, Fervaha G, et al. Treating negative symptoms: an update. Curr Treat Options Psych. 2016;3:133-150.
6. Harvey PD, Saoud JB, Luthringer R, et al. Effects of roluperidone (MIN-101) on two dimensions of negative symptoms factor score: reduced emotional experience and reduced emotional expression. Schizophr Res. 2020;215:352-356.
7. Dedic N, Jones PG, Hopkins SC, et al. SEP-363856, a novel psychotropic agent with a unique, non-D2 receptor mechanism of action. J Psychopharmacol Exp Ther. 2019;371(1):1-14.
8. Bleuler E. Dementia praecox or the group of schizophrenia. New York, New York: International Universities Press; 1950.
9. Andreasen NC. The diagnosis of schizophrenia. Schizophr Bull. 1987;13(1):9-22.
10. Andreasen NC. Thought, language, and communication disorders I. Clinical assessment, definition of terms, and evaluation of their reliability. Arch Gen Psychiatry. 1979;36(12):1315-1321.
11. Crow TJ. Molecular pathology of schizophrenia: more than one disease process? Br Med J. 1980;280(6207):66-68.
12. Andreasen NC, Olsen S. Negative v positive schizophrenia. Definition and validation. Arch Gen Psychiatry. 1982;39(7):789-794.
13. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261-276.
14. Kirkpatrick B, Strauss GP, Nguyen L, et al. The brief negative symptom scale: psychometric properties. Schizophr Bull. 2011;37(2):300-305.
15. Axelrod BN, Goldman RS, Alphs LD. Validation of the 16-item Negative Symptoms Assessment. J Psychiatr Res. 1993;27(3):253-258.
16. Carpenter WT Jr, Heinrichs DW, Wagman AM. Deficit and nondeficit forms of schizophrenia: the concept. Am J Psychiatry. 1988;145(5):578-583.
17. Bobes J, Arango C, Garcia-Garcia M, et al. Prevalence of negative symptoms in outpatients with schizophrenia spectrum disorders treated with antipsychotics in routine clinical practice: findings from the CLAMORS Study. J Clin Psychiatry. 2010;71(3):280-286.
18. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
19. Black DW, Andreasen NC. Interviewing and assessment. In: Introductory textbook of psychiatry, 7th ed. Black DW, Andreasen NC, eds. Washington, DC: American Psychiatric Publishing; 2020:15-53.
20. Pfohl B, Winokur G. The micropsychopathology of hebephrenic/catatonic schizophrenia. J Nerv Ment Dis. 1983;171(5):296-300.
21. Hovington CL, Lepage M. Neurocognition and neuroimaging of persistent negative symptoms of schizophrenia. Expert Rev Neurother. 2012;12(1):53-69.
22. Winograd-Gurvich C, Fitzgerald PB, Georgiou-Karistianis N, et al. A review of schizophrenia, melancholic depression and Parkinson’s disease. Brain Res Bull. 2006;70(4-6):312-321.
23. Toda M, Abi-Dargham A. Dopamine hypothesis of schizophrenia: making sense of it all. Curr Psychiatry Rep. 2007;9(4):329-336.
24. Yoshimura R, Hori H, Katsuki A, et al. Serum levels of brain-derived neurotrophic factor (BDNF), proBDNF, and plasma 3-methoxy-4-hydroxyphenylglycol levels in chronic schizophrenia. Ann Gen Psychiatry. 2016;15:1.
25. Moller HJ. Management of negative symptoms of schizophrenia: new treatment options. CNS Drugs. 2003;17(11):793-823.
26. Leucht S. Amisulpride: a selective dopamine antagonist and atypical antipsychotic: results of a meta-analysis of randomized controlled trials. Int J Neuropsychopharmacol. 2004;7(suppl 1):S15-S20. doi: 10.1017/S1461145704004109.
27. Nemeth G, Laszlovszky I, Czobor P, et al. Cariprazine versus risperidone monotherapy for treatment of predominant negative symptoms in patients with schizophrenia: a randomized, double-blind, controlled trial. Lancet. 2017;389(10074):1103-1113.
28. Neill JC, Grayson, Kiss B, et al. Effects of cariprazine, a novel antipsychotic, on cognitive deficit and negative symptoms in a rodent model of schizophrenia symptomatology. Eur Neuropsychopharmacol. 2016;26(1):3-14.
29. Helfer B, Samara MT, Huhn M, et al. Efficacy and safety of antidepressants added to antipsychotics for schizophrenia: a systematic review and meta-analysis. Am J Psychiatry. 2016;173(9):876-886.
The negative symptoms of schizophrenia have been recognized for 100 years. Characterized by a loss of a function that should be present, negative symptoms include anhedonia, asociality, amotivation, and affective blunting. Individuals with schizophrenia who have a preponderance of negative symptoms (“deficit syndrome”) may comprise a special subset of patients. Compared with positive symptoms, negative symptoms are associated with worse global functioning and worse response to antipsychotic medication. Treatment of negative symptoms is challenging. Secondary negative symptoms—those that simulate or resemble primary negative symptoms but are attributable to another cause, such as major depressive disorder or the adverse effects of antipsychotic medication—need to be ruled out. Emerging evidence suggests that newer antipsychotics with novel mechanisms might be effective in treating negative symptoms. Antidepressants might also play a role.
This article describes types of negative symptoms, their clinical relevance, neuroanatomical and neurotransmission factors associated with negative symptoms, and current and future treatment options.
Modest improvements with antipsychotics
Schizophrenia affects an estimated 1% of the population.1 Antipsychotic medication has been the mainstay of schizophrenia treatment since
All antipsychotics are believed to exert their therapeutic effects by blocking dopamine (D2) receptors and are effective in ameliorating the positive symptoms of schizophrenia, including hallucinations, delusions, bizarre behavior, disordered thinking, and agitation.1 Early research had suggested that SGAs might also reduce the negative symptoms of schizophrenia, perhaps because they also block serotonin 2A receptors, a property thought to broaden their therapeutic profile. Over time, it became clear that neither FGAs nor SGAs conferred an advantage in treating negative symptoms, and that the observed improvements were modest.2-5 However, recent research suggests that several newer antipsychotics might be effective in targeting negative symptoms.2,6,7
History of negative symptoms
In the early 20th century, Swiss psychiatrist Eugen Bleuler coined the term schizophrenia to emphasize the cognitive impairment that occurs in patients with this illness, and which he conceptualized as a fragmenting of the psychic process.8 He believed that certain symptoms were fundamental to the illness, and described affective blunting, disturbance of association (ie, distorted thinking) autism (ie, impaired relationships), and ambivalence (ie, fragmented emotional responses). He viewed hallucinations and delusions as accessory symptoms because they were not unique to schizophrenia but were also found in other disorders (eg, mood disorders). Bleuler’s ideas took root, and generations of psychiatrists were taught his fundamental symptoms (“the 4 A’s”), the forerunner of today’s negative symptoms. Later, other experts chose to emphasize psychotic symptoms as most characteristic of schizophrenia, including Schneider’s “first-rank symptoms,” such as voices conversing or delusions of passivity.9
Negative symptoms were rediscovered in the 1970s and 1980s by psychiatric researchers interested in descriptive phenomenology.10,11 Research confirmed the presence of a positive dimension in schizophrenia characterized by the loss of boundaries between the patient and the real world (eg, hallucinations, delusions), and a negative dimension characterized by the loss of a function that should be present, such as alogia and asociality. These experts carefully described negative symptoms and created scales to measure them, including the Scale for the Assessment of Negative Symptoms (SANS),12 the Positive and Negative Syndrome Scale (PANSS),13 the Brief Negative Symptom Scale (BNSS),14 and the 16-item Negative Symptom Assessment (NSA-16).15 Contemporaneous to this work, a “deficit syndrome” was identified among patients with schizophrenia with prominent negative symptoms. The deficit syndrome is found in 25% to 30% of chronic cases.16 Negative symptoms are very common in patients with schizophrenia (Table 19).8,17
Early editions of the DSM defined schizophrenia mainly on the basis of disturbance of cognition, mood, and behavior, and a retreat from reality. With the publication of DSM-III in 1980, and in subsequent editions, schizophrenia was redefined as a relatively severe psychotic illness in which positive and negative symptoms were present, thereby acknowledging the importance of Bleuler’s fundamental symptoms. In DSM-5, negative symptoms are described as accounting for “a substantial portion of the morbidity associated with schizophrenia but are less prominent in other psychotic disorders.”18
Continue to: Types of negative symptoms
Types of negative symptoms
The following symptoms fall within the negative dimension19:
Alogia refers to the impoverished thinking and cognition that often occur in patients with schizophrenia. The patient’s thinking processes seem empty, turgid, or slow, as inferred from the patient’s speech. The 2 major manifestations of alogia are poverty of speech (nonfluent empty speech) and poverty of content of speech (fluent but empty speech). Examples of each appear in Table 2.19
Affective flattening or blunting manifests as a general impoverishment of emotional expression, reactivity, and feeling. Affective flattening can be assessed through observing a patient’s behavior and responsiveness during the interview.
Avolition-apathy manifests itself as a lack of energy and drive. Patients become inert and are unable to mobilize themselves to initiate or persist in completing many kinds of tasks.
Anhedonia-asociality encompasses the patient’s difficulties in experiencing interest or pleasure. It may express itself as a loss of interest in pleasurable activities, an inability to experience pleasure when participating in activities normally considered pleasurable, or a lack of involvement in social relationships.
Continue to: Attention
Attention is often poor in patients with severe mental illnesses. The patient may have trouble focusing his/her attention or may be able to focus only sporadically and erratically. He/she may ignore attempts to converse with him/her, wander away during an activity or a task, or appear to be inattentive when engaged in formal testing or interviewing.
Clinical relevance of negative symptoms
According to DSM-5, “Negative symptoms are more closely related to prognosis than are positive symptoms and tend to be the most persistent.”18 Research has shown that, compared with positive symptoms, negative symptoms are associated with greater impairment in overall functioning, social interaction, interpersonal relationships, economic functioning, and recreational activities.1,3,5 Negative symptoms also are associated with poorer response to medication and a positive family history of schizophrenia. Research shows that negative symptoms are persistent over time, and, in fact, become more prominent as the patient ages, whereas positive symptoms become less prominent.20
Secondary negative symptoms
Potential secondary causes of negative symptoms should be ruled out before concluding that the negative symptoms are due to schizophrenia.3 What might appear to be a negative symptom of schizophrenia, such as poor motivation or flattened affect, could be due to the presence of major depressive disorder. Such symptoms might resolve with treatment. Alternatively, a patient could have developed pseudoparkinsonism from antipsychotic medication and display unchanging facial expression and decreased spontaneous movements. These symptoms could resolve by adding
The neuroanatomy of negative symptoms
Although the neuroanatomical basis of negative symptoms has not been determined, neuroimaging studies have provided important clues.3 Structural brain imaging has consistently shown that negative symptoms in patients with schizophrenia correlate with decreased prefrontal white matter volume, anterior cingulate volume, insular cortex volume, left temporal cortex volume, and ventricular enlargement. Interestingly, volume loss starts before the appearance of negative symptoms.21,22 Functional imaging has shown that negative symptoms correlate with reduced cerebral blood perfusion in frontal, prefrontal, posterior cingulate, thalamus, parietal, and striatal regions.21,22 These findings may help explain the apathy, failure to initiate activities, and impaired social relatedness in patients with schizophrenia.
Neurotransmission and negative symptoms
Some experts have hypothesized that lowered cortical dopamine transmission in mesocortical pathways could give rise to negative symptoms, whereas excess transmission in subcortical structures leads to positive symptoms.23 There is also evidence for a noradrenalin deficiency based on the finding that low levels of cerebrospinal fluid 3-methoxy-4-hydroxyphenylglycol (MHPG), a noradrenaline metabolite, correlates with greater negative symptom severity.24 The presence of a serotonin deficiency has been proposed based on evidence that negative symptoms might be mitigated by serotonergic agents.25 More recently, some experts have posited that the dopamine D3 receptor might be involved in the etiology of negative symptoms. The dopamine D3 receptor activity is expressed in brain regions thought to control reward, emotions, and motivation.2 Newer medications with novel mechanisms suggest that other neurotransmitter pathways could be involved.6,7
Continue to: Treatment options
Treatment options
Treating negative symptoms remains challenging and there are no clear answers. When they were introduced in the 1990s, SGAs were initially thought to be superior to FGAs in targeting negative symptoms. Subsequent research, including recent reviews and meta-analyses, has shown that SGAs are not superior to FGAs in treating negative symptoms, and the effect of either medication class on negative symptoms is modest.2-5 One exception is amisulpride (not available in the United States), which is known to antagonize D2 and D3 receptors. A meta-analysis of the efficacy of antipsychotics in schizophrenia showed that amisulpride was significantly more effective than placebo in treating negative symptoms in 590 patients who received the medication.26 The authors suggested that amisulpride was effective due to its binding to presynaptic receptors in the frontal cortex, thereby enhancing dopamine transmission in this region.
Cariprazine, which acts as a partial agonist at the D2 and D3 receptors, with a 10-fold affinity for the D3 receptor, also has shown promise in treating negative symptoms.2 In a clinical trial of 460 patients with predominant negative symptoms, treatment with cariprazine led to a greater reduction in negative symptoms than
Other promising agentsinclude
Antidepressants also could be effective in reducing negative symptoms.3 A meta-analysis of randomized controlled trials evaluating the use of antidepressants as adjuncts to antipsychotic medications showed that adding an antidepressant was effective in reducing negative symptoms.29 The mechanism by which an antidepressant might cause a reduction in negative symptoms is uncertain, and it is possible that the antidepressant might treat depressive symptoms that are causing or contributing to the negative symptoms.
Bottom Line
Negative symptoms in patients with schizophrenia are associated with a worse functional outcome and poorer response to antipsychotic medication than positive symptoms. First- and second-generation antipsychotics are largely ineffective in consistently treating negative symptoms. Antipsychotic medications that target the D3 receptor might be more effective. Roluperidone, which targets serotonin 2A and sigma receptors, and SEP-363856, which targets TAAR1 and serotonin 1A receptors, are being studied for their effects on negative symptoms.
Continue to: Related Resources
Related Resources
- Galderisi S, Färden A, Kaiser S. Dissecting negative symptoms of schizophrenia: History, assessment, pathophysiological mechanisms and treatment. Schizophr Res. 2017;186:1-2.
- Rabinowitz J. Treating negative symptoms of schizophrenia. Current Psychiatry. 2018;17(12):19-23.
Drug Brand Names
Benztropine • Cogentin
Cariprazine • Vraylar
Chlorpromazine • Promapar, Thorazine
Risperidone • Risperdal
The negative symptoms of schizophrenia have been recognized for 100 years. Characterized by a loss of a function that should be present, negative symptoms include anhedonia, asociality, amotivation, and affective blunting. Individuals with schizophrenia who have a preponderance of negative symptoms (“deficit syndrome”) may comprise a special subset of patients. Compared with positive symptoms, negative symptoms are associated with worse global functioning and worse response to antipsychotic medication. Treatment of negative symptoms is challenging. Secondary negative symptoms—those that simulate or resemble primary negative symptoms but are attributable to another cause, such as major depressive disorder or the adverse effects of antipsychotic medication—need to be ruled out. Emerging evidence suggests that newer antipsychotics with novel mechanisms might be effective in treating negative symptoms. Antidepressants might also play a role.
This article describes types of negative symptoms, their clinical relevance, neuroanatomical and neurotransmission factors associated with negative symptoms, and current and future treatment options.
Modest improvements with antipsychotics
Schizophrenia affects an estimated 1% of the population.1 Antipsychotic medication has been the mainstay of schizophrenia treatment since
All antipsychotics are believed to exert their therapeutic effects by blocking dopamine (D2) receptors and are effective in ameliorating the positive symptoms of schizophrenia, including hallucinations, delusions, bizarre behavior, disordered thinking, and agitation.1 Early research had suggested that SGAs might also reduce the negative symptoms of schizophrenia, perhaps because they also block serotonin 2A receptors, a property thought to broaden their therapeutic profile. Over time, it became clear that neither FGAs nor SGAs conferred an advantage in treating negative symptoms, and that the observed improvements were modest.2-5 However, recent research suggests that several newer antipsychotics might be effective in targeting negative symptoms.2,6,7
History of negative symptoms
In the early 20th century, Swiss psychiatrist Eugen Bleuler coined the term schizophrenia to emphasize the cognitive impairment that occurs in patients with this illness, and which he conceptualized as a fragmenting of the psychic process.8 He believed that certain symptoms were fundamental to the illness, and described affective blunting, disturbance of association (ie, distorted thinking) autism (ie, impaired relationships), and ambivalence (ie, fragmented emotional responses). He viewed hallucinations and delusions as accessory symptoms because they were not unique to schizophrenia but were also found in other disorders (eg, mood disorders). Bleuler’s ideas took root, and generations of psychiatrists were taught his fundamental symptoms (“the 4 A’s”), the forerunner of today’s negative symptoms. Later, other experts chose to emphasize psychotic symptoms as most characteristic of schizophrenia, including Schneider’s “first-rank symptoms,” such as voices conversing or delusions of passivity.9
Negative symptoms were rediscovered in the 1970s and 1980s by psychiatric researchers interested in descriptive phenomenology.10,11 Research confirmed the presence of a positive dimension in schizophrenia characterized by the loss of boundaries between the patient and the real world (eg, hallucinations, delusions), and a negative dimension characterized by the loss of a function that should be present, such as alogia and asociality. These experts carefully described negative symptoms and created scales to measure them, including the Scale for the Assessment of Negative Symptoms (SANS),12 the Positive and Negative Syndrome Scale (PANSS),13 the Brief Negative Symptom Scale (BNSS),14 and the 16-item Negative Symptom Assessment (NSA-16).15 Contemporaneous to this work, a “deficit syndrome” was identified among patients with schizophrenia with prominent negative symptoms. The deficit syndrome is found in 25% to 30% of chronic cases.16 Negative symptoms are very common in patients with schizophrenia (Table 19).8,17
Early editions of the DSM defined schizophrenia mainly on the basis of disturbance of cognition, mood, and behavior, and a retreat from reality. With the publication of DSM-III in 1980, and in subsequent editions, schizophrenia was redefined as a relatively severe psychotic illness in which positive and negative symptoms were present, thereby acknowledging the importance of Bleuler’s fundamental symptoms. In DSM-5, negative symptoms are described as accounting for “a substantial portion of the morbidity associated with schizophrenia but are less prominent in other psychotic disorders.”18
Continue to: Types of negative symptoms
Types of negative symptoms
The following symptoms fall within the negative dimension19:
Alogia refers to the impoverished thinking and cognition that often occur in patients with schizophrenia. The patient’s thinking processes seem empty, turgid, or slow, as inferred from the patient’s speech. The 2 major manifestations of alogia are poverty of speech (nonfluent empty speech) and poverty of content of speech (fluent but empty speech). Examples of each appear in Table 2.19
Affective flattening or blunting manifests as a general impoverishment of emotional expression, reactivity, and feeling. Affective flattening can be assessed through observing a patient’s behavior and responsiveness during the interview.
Avolition-apathy manifests itself as a lack of energy and drive. Patients become inert and are unable to mobilize themselves to initiate or persist in completing many kinds of tasks.
Anhedonia-asociality encompasses the patient’s difficulties in experiencing interest or pleasure. It may express itself as a loss of interest in pleasurable activities, an inability to experience pleasure when participating in activities normally considered pleasurable, or a lack of involvement in social relationships.
Continue to: Attention
Attention is often poor in patients with severe mental illnesses. The patient may have trouble focusing his/her attention or may be able to focus only sporadically and erratically. He/she may ignore attempts to converse with him/her, wander away during an activity or a task, or appear to be inattentive when engaged in formal testing or interviewing.
Clinical relevance of negative symptoms
According to DSM-5, “Negative symptoms are more closely related to prognosis than are positive symptoms and tend to be the most persistent.”18 Research has shown that, compared with positive symptoms, negative symptoms are associated with greater impairment in overall functioning, social interaction, interpersonal relationships, economic functioning, and recreational activities.1,3,5 Negative symptoms also are associated with poorer response to medication and a positive family history of schizophrenia. Research shows that negative symptoms are persistent over time, and, in fact, become more prominent as the patient ages, whereas positive symptoms become less prominent.20
Secondary negative symptoms
Potential secondary causes of negative symptoms should be ruled out before concluding that the negative symptoms are due to schizophrenia.3 What might appear to be a negative symptom of schizophrenia, such as poor motivation or flattened affect, could be due to the presence of major depressive disorder. Such symptoms might resolve with treatment. Alternatively, a patient could have developed pseudoparkinsonism from antipsychotic medication and display unchanging facial expression and decreased spontaneous movements. These symptoms could resolve by adding
The neuroanatomy of negative symptoms
Although the neuroanatomical basis of negative symptoms has not been determined, neuroimaging studies have provided important clues.3 Structural brain imaging has consistently shown that negative symptoms in patients with schizophrenia correlate with decreased prefrontal white matter volume, anterior cingulate volume, insular cortex volume, left temporal cortex volume, and ventricular enlargement. Interestingly, volume loss starts before the appearance of negative symptoms.21,22 Functional imaging has shown that negative symptoms correlate with reduced cerebral blood perfusion in frontal, prefrontal, posterior cingulate, thalamus, parietal, and striatal regions.21,22 These findings may help explain the apathy, failure to initiate activities, and impaired social relatedness in patients with schizophrenia.
Neurotransmission and negative symptoms
Some experts have hypothesized that lowered cortical dopamine transmission in mesocortical pathways could give rise to negative symptoms, whereas excess transmission in subcortical structures leads to positive symptoms.23 There is also evidence for a noradrenalin deficiency based on the finding that low levels of cerebrospinal fluid 3-methoxy-4-hydroxyphenylglycol (MHPG), a noradrenaline metabolite, correlates with greater negative symptom severity.24 The presence of a serotonin deficiency has been proposed based on evidence that negative symptoms might be mitigated by serotonergic agents.25 More recently, some experts have posited that the dopamine D3 receptor might be involved in the etiology of negative symptoms. The dopamine D3 receptor activity is expressed in brain regions thought to control reward, emotions, and motivation.2 Newer medications with novel mechanisms suggest that other neurotransmitter pathways could be involved.6,7
Continue to: Treatment options
Treatment options
Treating negative symptoms remains challenging and there are no clear answers. When they were introduced in the 1990s, SGAs were initially thought to be superior to FGAs in targeting negative symptoms. Subsequent research, including recent reviews and meta-analyses, has shown that SGAs are not superior to FGAs in treating negative symptoms, and the effect of either medication class on negative symptoms is modest.2-5 One exception is amisulpride (not available in the United States), which is known to antagonize D2 and D3 receptors. A meta-analysis of the efficacy of antipsychotics in schizophrenia showed that amisulpride was significantly more effective than placebo in treating negative symptoms in 590 patients who received the medication.26 The authors suggested that amisulpride was effective due to its binding to presynaptic receptors in the frontal cortex, thereby enhancing dopamine transmission in this region.
Cariprazine, which acts as a partial agonist at the D2 and D3 receptors, with a 10-fold affinity for the D3 receptor, also has shown promise in treating negative symptoms.2 In a clinical trial of 460 patients with predominant negative symptoms, treatment with cariprazine led to a greater reduction in negative symptoms than
Other promising agentsinclude
Antidepressants also could be effective in reducing negative symptoms.3 A meta-analysis of randomized controlled trials evaluating the use of antidepressants as adjuncts to antipsychotic medications showed that adding an antidepressant was effective in reducing negative symptoms.29 The mechanism by which an antidepressant might cause a reduction in negative symptoms is uncertain, and it is possible that the antidepressant might treat depressive symptoms that are causing or contributing to the negative symptoms.
Bottom Line
Negative symptoms in patients with schizophrenia are associated with a worse functional outcome and poorer response to antipsychotic medication than positive symptoms. First- and second-generation antipsychotics are largely ineffective in consistently treating negative symptoms. Antipsychotic medications that target the D3 receptor might be more effective. Roluperidone, which targets serotonin 2A and sigma receptors, and SEP-363856, which targets TAAR1 and serotonin 1A receptors, are being studied for their effects on negative symptoms.
Continue to: Related Resources
Related Resources
- Galderisi S, Färden A, Kaiser S. Dissecting negative symptoms of schizophrenia: History, assessment, pathophysiological mechanisms and treatment. Schizophr Res. 2017;186:1-2.
- Rabinowitz J. Treating negative symptoms of schizophrenia. Current Psychiatry. 2018;17(12):19-23.
Drug Brand Names
Benztropine • Cogentin
Cariprazine • Vraylar
Chlorpromazine • Promapar, Thorazine
Risperidone • Risperdal
1. Owen MJ, Sawa A, Mortensen PD. Schizophrenia. Lancet. 2016;388(10039):86-97.
2. Cerviri G, Gesi C, Mencacci C. Pharmacological treatment of negative symptoms in schizophrenia: update and proposal of a clinical algorithm. Neuropsychiatr Dis Treat. 2019;15:1525-1535.
3. Mitra S, Mahintamani T, Kavoor AR, et al. Negative symptoms in schizophrenia. Ind Psychiatr J. 2016;25(2):135-144.
4. Fusa-Poli P, Papanastasiou E, Stahl D, et al. Treatments of negative symptoms in schizophrenia: meta-analysis of 168 randomized placebo-controlled trials. Schizophr Bull. 2015;41(4):892-899.
5. Remington G, Foussias G, Fervaha G, et al. Treating negative symptoms: an update. Curr Treat Options Psych. 2016;3:133-150.
6. Harvey PD, Saoud JB, Luthringer R, et al. Effects of roluperidone (MIN-101) on two dimensions of negative symptoms factor score: reduced emotional experience and reduced emotional expression. Schizophr Res. 2020;215:352-356.
7. Dedic N, Jones PG, Hopkins SC, et al. SEP-363856, a novel psychotropic agent with a unique, non-D2 receptor mechanism of action. J Psychopharmacol Exp Ther. 2019;371(1):1-14.
8. Bleuler E. Dementia praecox or the group of schizophrenia. New York, New York: International Universities Press; 1950.
9. Andreasen NC. The diagnosis of schizophrenia. Schizophr Bull. 1987;13(1):9-22.
10. Andreasen NC. Thought, language, and communication disorders I. Clinical assessment, definition of terms, and evaluation of their reliability. Arch Gen Psychiatry. 1979;36(12):1315-1321.
11. Crow TJ. Molecular pathology of schizophrenia: more than one disease process? Br Med J. 1980;280(6207):66-68.
12. Andreasen NC, Olsen S. Negative v positive schizophrenia. Definition and validation. Arch Gen Psychiatry. 1982;39(7):789-794.
13. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261-276.
14. Kirkpatrick B, Strauss GP, Nguyen L, et al. The brief negative symptom scale: psychometric properties. Schizophr Bull. 2011;37(2):300-305.
15. Axelrod BN, Goldman RS, Alphs LD. Validation of the 16-item Negative Symptoms Assessment. J Psychiatr Res. 1993;27(3):253-258.
16. Carpenter WT Jr, Heinrichs DW, Wagman AM. Deficit and nondeficit forms of schizophrenia: the concept. Am J Psychiatry. 1988;145(5):578-583.
17. Bobes J, Arango C, Garcia-Garcia M, et al. Prevalence of negative symptoms in outpatients with schizophrenia spectrum disorders treated with antipsychotics in routine clinical practice: findings from the CLAMORS Study. J Clin Psychiatry. 2010;71(3):280-286.
18. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
19. Black DW, Andreasen NC. Interviewing and assessment. In: Introductory textbook of psychiatry, 7th ed. Black DW, Andreasen NC, eds. Washington, DC: American Psychiatric Publishing; 2020:15-53.
20. Pfohl B, Winokur G. The micropsychopathology of hebephrenic/catatonic schizophrenia. J Nerv Ment Dis. 1983;171(5):296-300.
21. Hovington CL, Lepage M. Neurocognition and neuroimaging of persistent negative symptoms of schizophrenia. Expert Rev Neurother. 2012;12(1):53-69.
22. Winograd-Gurvich C, Fitzgerald PB, Georgiou-Karistianis N, et al. A review of schizophrenia, melancholic depression and Parkinson’s disease. Brain Res Bull. 2006;70(4-6):312-321.
23. Toda M, Abi-Dargham A. Dopamine hypothesis of schizophrenia: making sense of it all. Curr Psychiatry Rep. 2007;9(4):329-336.
24. Yoshimura R, Hori H, Katsuki A, et al. Serum levels of brain-derived neurotrophic factor (BDNF), proBDNF, and plasma 3-methoxy-4-hydroxyphenylglycol levels in chronic schizophrenia. Ann Gen Psychiatry. 2016;15:1.
25. Moller HJ. Management of negative symptoms of schizophrenia: new treatment options. CNS Drugs. 2003;17(11):793-823.
26. Leucht S. Amisulpride: a selective dopamine antagonist and atypical antipsychotic: results of a meta-analysis of randomized controlled trials. Int J Neuropsychopharmacol. 2004;7(suppl 1):S15-S20. doi: 10.1017/S1461145704004109.
27. Nemeth G, Laszlovszky I, Czobor P, et al. Cariprazine versus risperidone monotherapy for treatment of predominant negative symptoms in patients with schizophrenia: a randomized, double-blind, controlled trial. Lancet. 2017;389(10074):1103-1113.
28. Neill JC, Grayson, Kiss B, et al. Effects of cariprazine, a novel antipsychotic, on cognitive deficit and negative symptoms in a rodent model of schizophrenia symptomatology. Eur Neuropsychopharmacol. 2016;26(1):3-14.
29. Helfer B, Samara MT, Huhn M, et al. Efficacy and safety of antidepressants added to antipsychotics for schizophrenia: a systematic review and meta-analysis. Am J Psychiatry. 2016;173(9):876-886.
1. Owen MJ, Sawa A, Mortensen PD. Schizophrenia. Lancet. 2016;388(10039):86-97.
2. Cerviri G, Gesi C, Mencacci C. Pharmacological treatment of negative symptoms in schizophrenia: update and proposal of a clinical algorithm. Neuropsychiatr Dis Treat. 2019;15:1525-1535.
3. Mitra S, Mahintamani T, Kavoor AR, et al. Negative symptoms in schizophrenia. Ind Psychiatr J. 2016;25(2):135-144.
4. Fusa-Poli P, Papanastasiou E, Stahl D, et al. Treatments of negative symptoms in schizophrenia: meta-analysis of 168 randomized placebo-controlled trials. Schizophr Bull. 2015;41(4):892-899.
5. Remington G, Foussias G, Fervaha G, et al. Treating negative symptoms: an update. Curr Treat Options Psych. 2016;3:133-150.
6. Harvey PD, Saoud JB, Luthringer R, et al. Effects of roluperidone (MIN-101) on two dimensions of negative symptoms factor score: reduced emotional experience and reduced emotional expression. Schizophr Res. 2020;215:352-356.
7. Dedic N, Jones PG, Hopkins SC, et al. SEP-363856, a novel psychotropic agent with a unique, non-D2 receptor mechanism of action. J Psychopharmacol Exp Ther. 2019;371(1):1-14.
8. Bleuler E. Dementia praecox or the group of schizophrenia. New York, New York: International Universities Press; 1950.
9. Andreasen NC. The diagnosis of schizophrenia. Schizophr Bull. 1987;13(1):9-22.
10. Andreasen NC. Thought, language, and communication disorders I. Clinical assessment, definition of terms, and evaluation of their reliability. Arch Gen Psychiatry. 1979;36(12):1315-1321.
11. Crow TJ. Molecular pathology of schizophrenia: more than one disease process? Br Med J. 1980;280(6207):66-68.
12. Andreasen NC, Olsen S. Negative v positive schizophrenia. Definition and validation. Arch Gen Psychiatry. 1982;39(7):789-794.
13. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261-276.
14. Kirkpatrick B, Strauss GP, Nguyen L, et al. The brief negative symptom scale: psychometric properties. Schizophr Bull. 2011;37(2):300-305.
15. Axelrod BN, Goldman RS, Alphs LD. Validation of the 16-item Negative Symptoms Assessment. J Psychiatr Res. 1993;27(3):253-258.
16. Carpenter WT Jr, Heinrichs DW, Wagman AM. Deficit and nondeficit forms of schizophrenia: the concept. Am J Psychiatry. 1988;145(5):578-583.
17. Bobes J, Arango C, Garcia-Garcia M, et al. Prevalence of negative symptoms in outpatients with schizophrenia spectrum disorders treated with antipsychotics in routine clinical practice: findings from the CLAMORS Study. J Clin Psychiatry. 2010;71(3):280-286.
18. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
19. Black DW, Andreasen NC. Interviewing and assessment. In: Introductory textbook of psychiatry, 7th ed. Black DW, Andreasen NC, eds. Washington, DC: American Psychiatric Publishing; 2020:15-53.
20. Pfohl B, Winokur G. The micropsychopathology of hebephrenic/catatonic schizophrenia. J Nerv Ment Dis. 1983;171(5):296-300.
21. Hovington CL, Lepage M. Neurocognition and neuroimaging of persistent negative symptoms of schizophrenia. Expert Rev Neurother. 2012;12(1):53-69.
22. Winograd-Gurvich C, Fitzgerald PB, Georgiou-Karistianis N, et al. A review of schizophrenia, melancholic depression and Parkinson’s disease. Brain Res Bull. 2006;70(4-6):312-321.
23. Toda M, Abi-Dargham A. Dopamine hypothesis of schizophrenia: making sense of it all. Curr Psychiatry Rep. 2007;9(4):329-336.
24. Yoshimura R, Hori H, Katsuki A, et al. Serum levels of brain-derived neurotrophic factor (BDNF), proBDNF, and plasma 3-methoxy-4-hydroxyphenylglycol levels in chronic schizophrenia. Ann Gen Psychiatry. 2016;15:1.
25. Moller HJ. Management of negative symptoms of schizophrenia: new treatment options. CNS Drugs. 2003;17(11):793-823.
26. Leucht S. Amisulpride: a selective dopamine antagonist and atypical antipsychotic: results of a meta-analysis of randomized controlled trials. Int J Neuropsychopharmacol. 2004;7(suppl 1):S15-S20. doi: 10.1017/S1461145704004109.
27. Nemeth G, Laszlovszky I, Czobor P, et al. Cariprazine versus risperidone monotherapy for treatment of predominant negative symptoms in patients with schizophrenia: a randomized, double-blind, controlled trial. Lancet. 2017;389(10074):1103-1113.
28. Neill JC, Grayson, Kiss B, et al. Effects of cariprazine, a novel antipsychotic, on cognitive deficit and negative symptoms in a rodent model of schizophrenia symptomatology. Eur Neuropsychopharmacol. 2016;26(1):3-14.
29. Helfer B, Samara MT, Huhn M, et al. Efficacy and safety of antidepressants added to antipsychotics for schizophrenia: a systematic review and meta-analysis. Am J Psychiatry. 2016;173(9):876-886.
Evaluating patients’ decision-making capacity during COVID-19
The coronavirus disease 2019 (COVID-19) pandemic has introduced many new clinical challenges. Consider the patient with fever and dyspnea who tests positive for COVID-19 but does not believe in COVID-19 and wants to leave the hospital against medical advice (AMA). Or the patient with numerous cardiovascular risk factors and crushing substernal chest pain who is too afraid of contracting COVID-19 to come to the emergency department. These challenging clinical scenarios can be addressed in the context of decision-making capacity (DMC), for which our medical colleagues often call upon psychiatrists to assist. This article reviews the framework for DMC assessment, describes how COVID-19 affects DMC assessment, and discusses approaches to these scenarios using the DMC framework.
Review of decision-making capacity
Assessment of DMC is a fundamental clinical skill. It allows a physician to balance autonomy with beneficence and non-maleficence. An autonomous decision is a decision that is made intentionally, with understanding, and without controlling influences (these are the elements of informed consent).1 However, if a patient cannot make a decision with intention and understanding, then beneficence and non-maleficence must prevail in order to protect the patient. Capacity assessments evaluate a patient’s ability to make an intentional and understood choice.
In order to prove capacity, a patient must demonstrate 4 functional abilities:
- choice refers to the ability to communicate a relatively stable choice2,3
- understanding refers to the ability to convey information about the illness, risks/benefits of the chosen intervention, and risks/benefits of alternative options.2,3 Understanding measures objective information about the medical situation
- appreciation refers to the patient’s ability to apply that information to his/her own life.2,3 Appreciation requires insight into having the illness and the ability to anticipate how one’s life would be impacted by one’s condition and choice. This is where life experiences and values come into play
- reasoning is intimately tied to appreciation. It refers to the ability to explain how the decision was made and which factors were most important.2,3
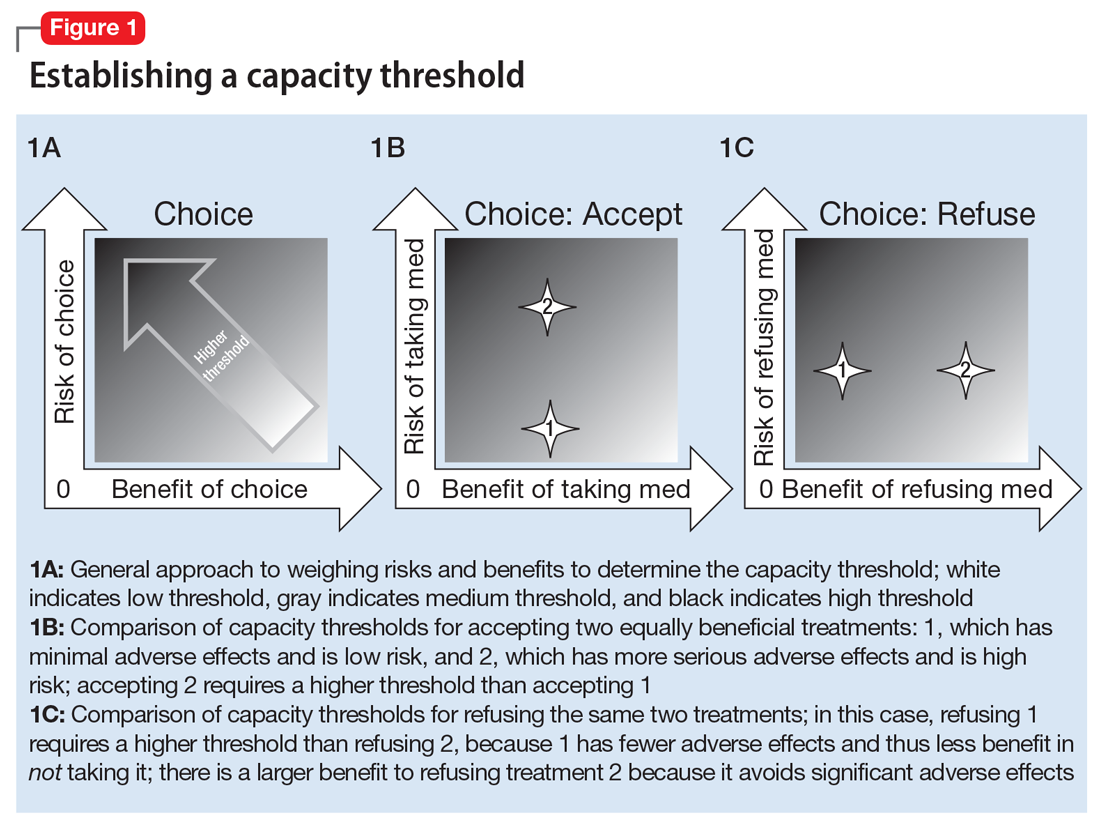
Most clinicians and ethicists endorse a “threshold” approach to decisional capacity, which specifies that the level of evidence required to prove capacity depends on the gravity of the medical situation (Figure 1A).1,4,5 The gravity of the situation is based on the risk/benefit analysis. Consider two treatments with equal benefit: one has minimal adverse effects (gastrointestinal upset) and the second has significant adverse effects (myelosuppression). Accepting the first treatment requires less intentionality and understanding than accepting the second because the risk is much lower and thus has a lower capacity threshold (Figure 1B). The capacity to refuse these treatments results in the opposite ranking (Figure 1C).
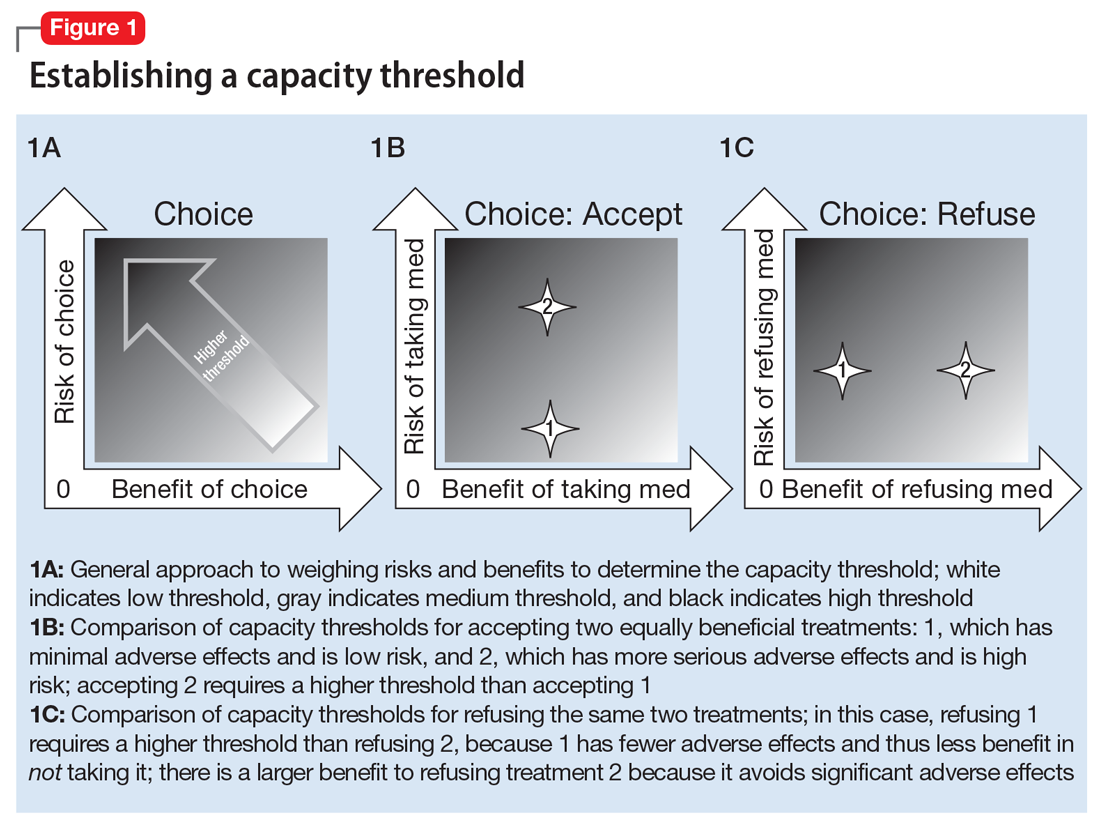
Establishing a threshold helps guide the physician in determining how robust the patient’s responses must be to have decisional capacity. For a high-threshold decision, the patient must have a well-developed and highly detailed level of understanding, appreciation, and reasoning.
How COVID-19 affects assessment of decision-making capacity
Three characteristics of the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and COVID-19 illness impact decision-making assessment:
- high level of contagiousness
- high health-care utilization
- the uncertainty about its clinical course and outcomes.
The high level of contagiousness stems from this virus’s estimated basic reproduction number (R0) of 2.2 to 5.7 (which indicates the expected number of cases from any single case), its long incubation period, and the potential for asymptomatic and pre-symptomatic shedding.6-9 Decision-making capacity assessments must therefore consider community-level effects in the risk/benefit analysis. Because SARS-CoV-2 is a new virus affecting humans, it can easily overwhelm existing hospital systems. This happened in Wuhan, China; Lombardy, Italy; and New York. In a stressed system, physicians will have to factor health-care utilization into the risk/benefit analysis. Finally, because this is a novel virus, there is still considerable uncertainty about the epidemiology, clinical course, and outcomes.10 The minimal dose of virus needed to cause illness is unknown. Patients can deteriorate quickly and unpredictably into needing ventilator support.11 Treatment options are limited, and many candidates are being investigated.12 This uncertainty hinders physicians’ ability to accurately estimate risks and benefits for an individual patient when discussing various medical decisions. As our understanding of SARS-CoV-2 improves, this uncertainty will lessen.
Continue to: Effects of the sociopolitical climate
Effects of the sociopolitical climate
In the United States, the COVID-19 pandemic emerged during a time of deep sociopolitical divide. Accordingly, beliefs about viral infectivity, severity of illness, and precautionary measures have varied. Some politicians, media outlets, and physicians have shared information that contradicts guidelines and recommendations from mainstream national and international medical and scientific organizations. Patients who subscribe to these reports and beliefs may not meet the threshold for understanding, appreciation, or reasoning. For example, if a patient’s beliefs about the virus depart from well-established medical evidence, they would technically lack understanding. The usual remedy for addressing misunderstanding is education and time. However, because of the divisiveness of the sociopolitical climate, the limited time physicians have with patients, and the fact that many DMC assessments will occur in acute-care settings, it may be difficult or near impossible to correct the misunderstanding.
The sociopolitical climate and its accompanying potentially erroneous or imbalanced narrative may thus directly impact patients’ understanding, appreciation, and reasoning. However, it can be problematic to declare incapacity in a patient whose understanding, appreciation, and reasoning arise from widely shared and relatively fixed sociopolitical values. Additionally, some clinicians and ethicists might object to declaring incapacity in a patient with no underlying mental or neurologic dysfunction. The United States has a functional approach to capacity, based solely on meeting criteria for the 4 functional abilities.3,13 Mental or neurologic dysfunction is not legally required in the United States, but in practice, the consideration of incapacity is often closely linked to some form of cognitive impairment.14 Other countries do make dysfunction a specific criterion; for example, the United Kingdom dictates that mental incapacity can only occur in someone with “impairment of, or a disturbance in the functioning of, the mind or brain.”15
Leaving against medical advice
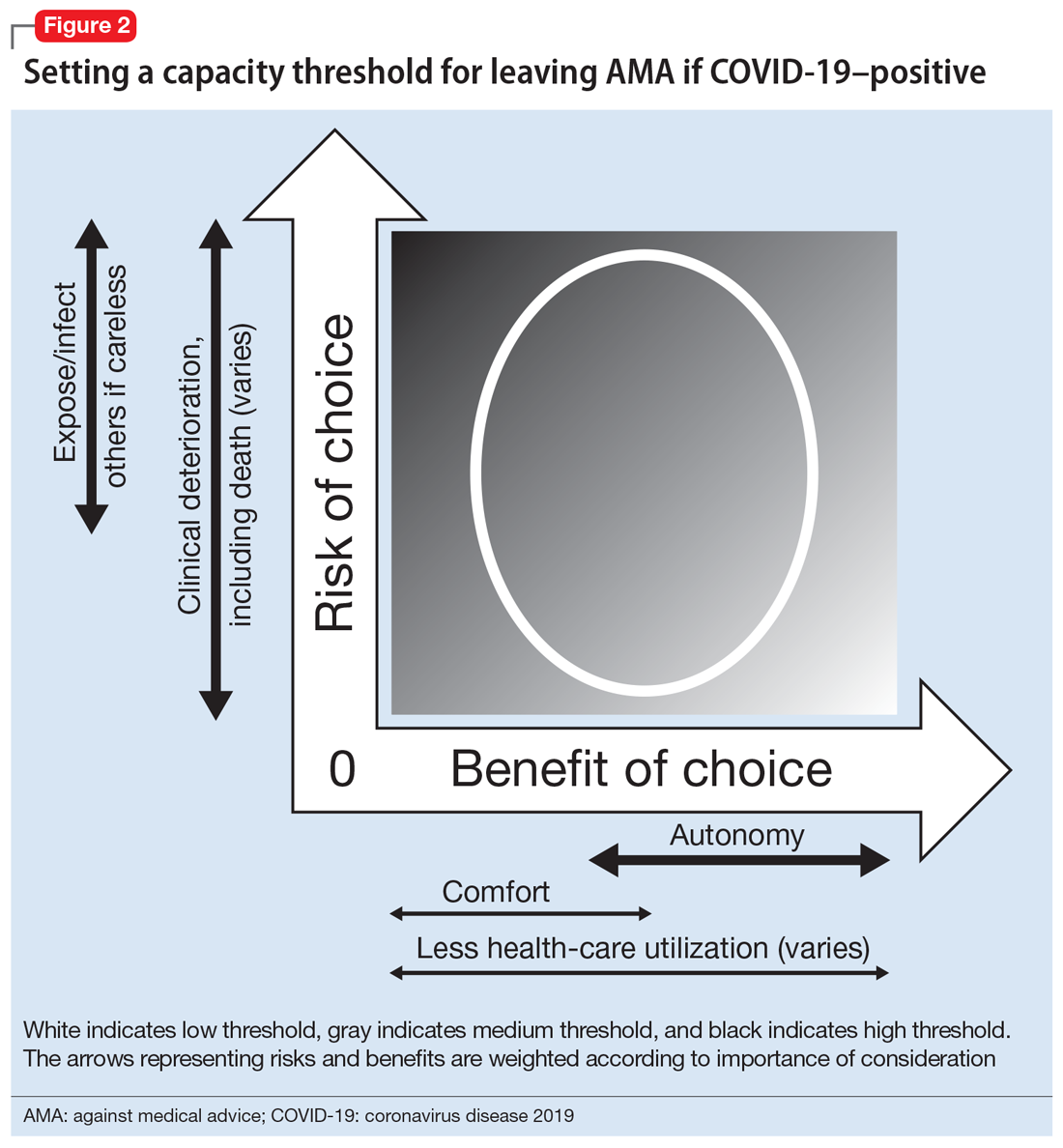
In the case of a patient who is COVID-19–positive, symptomatic, and wants to leave AMA, the threshold is automatically elevated because of societal-level risks (the risk of potential exposure or infection of others if a patient who is COVID-19–positive is not properly isolated). Furthermore, the individual risk of the patient leaving AMA depends on his/her age, comorbidities, and current clinical status; because of the uncertainty and rapid deterioration seen with COVID-19 illness, the calculated risk may actually be higher than for a non-COVID-19–related illness. Thus, in order to leave AMA, the patient’s responses must be fairly robust (Figure 2). Table 1 describes the information needed for robust understanding, appreciation, and reasoning.
For patients who do not meet this threshold, it is important to determine why. If a patient has a psychiatric condition that not only impacts DMC but also meets criteria for a psychiatric hold (ie, an imminent risk of harm to self or others), a psychiatric hold should be placed. If the patient does not meet the threshold because of altered mental status or some other neurologic or cognitive comorbidity, a medical hold should be placed. Most states do not have an explicit legal basis for a medical hold, although it does fall under the incapacity laws in the United States; in the absence of a surrogate, declaration of medical emergency can also be used if applicable.16,17 As a caveat, it can be difficult to detain someone on a medical hold because security officers may be afraid to physically detain someone without explicit legal paperwork.17
If a patient does not meet the capacity threshold but there does not seem to be a psychiatric, neurologic, or cognitive explanation, several options are possible. The first step would be to assess whether the patient is amenable to further discussion and compromise. A nonjudgmental and nonconfrontational approach that aims to further clarify the patient’s perspective and identify shared goals is key. Any plan that lowers the risks sufficiently would allow the patient to leave by lowering the capacity threshold. Enlisting the support of family and friends can be helpful. If this does not work, theoretically the patient should be detained in the hospital. Practically speaking, this may be difficult or unadvised. First, as described above, security officers may refuse to physically detain the patient.17 Second, the patient’s legally mandated surrogate may espouse similar COVID-related views as the patient; thus, this approach may not help keep the patient in the hospital. If the physician has serious concern about the risk of the patient leaving, he/she would have to consult the facility’s Ethics and Legal staff to determine capacity of the surrogate. Third, it can be problematic to declare incapacity in a patient whose understanding, appreciation, and reasoning arise from widely shared and relatively fixed sociopolitical values. In the current sociopolitical climate, involuntary detention may elicit a political backlash. Using medical detention for impending deterioration of clinical status would be more acceptable than using medical detention for isolation. Presently, there are no such laws for patients with COVID-19 (although this is not without precedent, as with active tuberculosis or Ebola18,19), but individual jurisdictions may have isolation or quarantine orders; the local health department could be contacted and may evaluate on a case-by-case basis.
Continue to: Refusing to seek medical care
Refusing to seek medical care
Anecdotally, many physicians have reported an increase in patients who are refusing clinic- or hospital-based treatment for a medical condition because they fear they may catch the virus. Although this is not strictly a capacity case—there is little recourse for action if a patient is refusing treatment from home (unless the patient requires a psychiatric hold or already has a guardian for medical decisions)—the same elements of thresholds apply and can be helpful in guiding conversations with the patient.
For the patient, the benefits of staying at home are to avoid potentially exposing themselves and the members of their household to the virus and COVID-19 illness. The risks of staying home include progression of the patient’s primary illness, which could lead to increased morbidity and mortality. Staying home has an ancillary benefit to the community of reducing health-care utilization, but at the risk of increasing utilization in the future.
The risk/benefit profile is shown on the thresholds graph in Figure 3. There is considerable variability. It is helpful to stratify the risk of progression of the primary condition as low (can be postponed indefinitely with minimal risk), medium (can be postponed for a short amount of time; risk of increased morbidity with ongoing delay and possibly increased mortality), or high (cannot be postponed; will have greater morbidity and/or higher risk of mortality). Because of the uncertainty about COVID-19, it is harder to quantify the benefits of refusing care and staying at home, although older patients and patients with underlying health issues are at higher risk of severe illness and death.20 However, by taking appropriate precautions when seeking care, viral exposure and risk of infection can be mitigated.
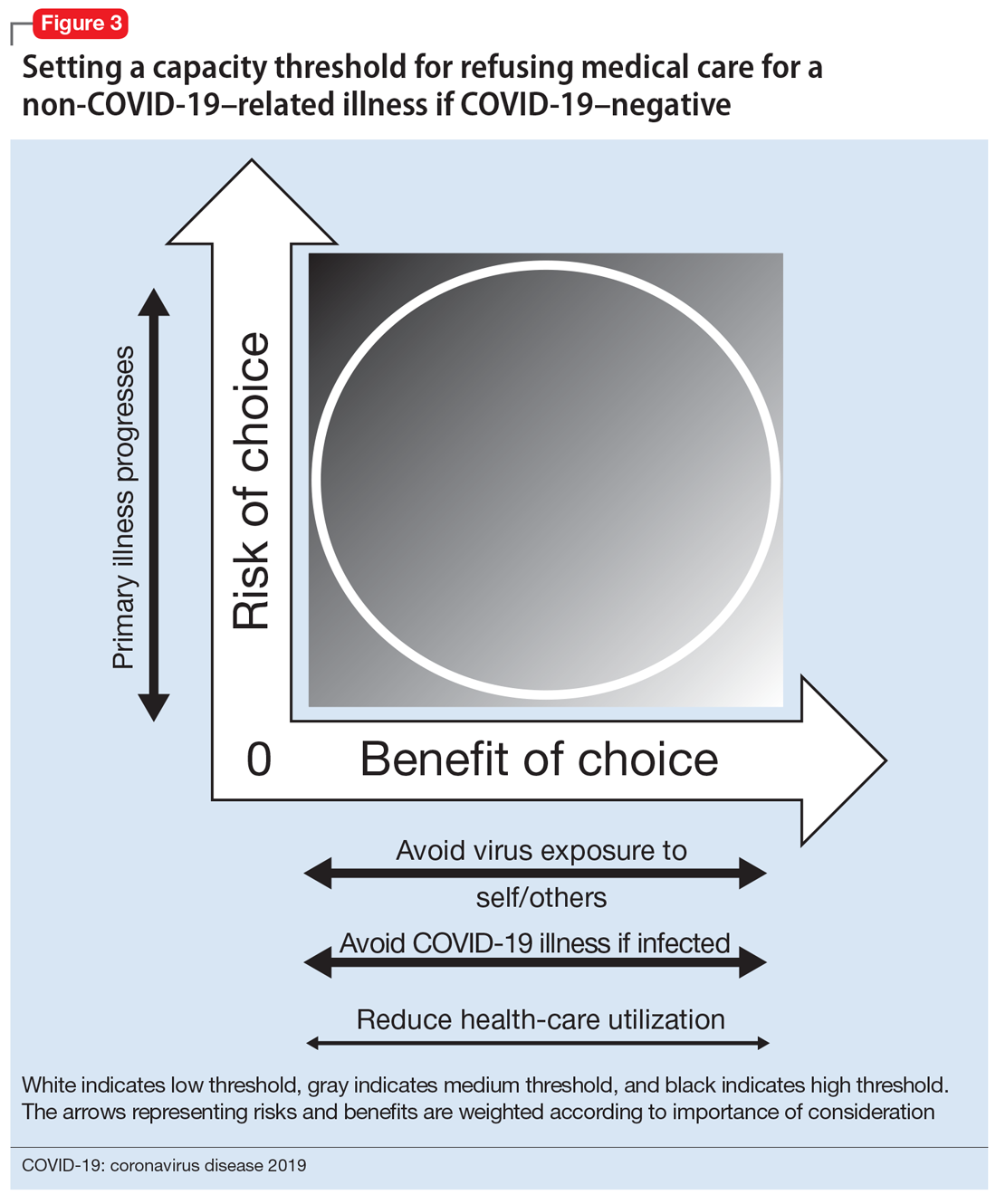
This risk/benefit analysis will help set the threshold for whether staying at home is reasonable or whether it would incur more risk of harm. If the latter, then the physician must elicit the patient’s understanding, appreciation, and reasoning related to their current medical condition and COVID-19. It is likely they are undervaluing the former and overvaluing the latter. Table 2 lists important points to cover during these discussions.
Although there is no legal recourse to force patients at home to come to the clinic or hospital for medical treatment, there are several possible strategies to motivate them to do so. One is to ask patients how likely (on a scale of 0 to 100) they think they are to contract COVID-19 if they came for evaluation/treatment, and how likely they feel they are to experience a bad outcome from their primary condition. Then, after providing psychoeducation about their primary medical condition and COVID-19–related precautions and risk, repeat this question. Another strategy is to empathize with the patient’s fears while also expressing concern about the primary medical condition and connecting with the patient on the shared desire to protect his/her health. A third is to draw a risk/benefit diagram (similar to Figure 3) or reassure the patient by describing the ways in which the clinic or hospital is minimizing exposure and infection risk. A final strategy is to enlist the help of the patient’s family or friends.
Continue to: Bottom Line
Bottom Line
In order to have decision-making capacity, a patient must demonstrate choice, understanding, appreciation, and reasoning. The degree of understanding, appreciation, and reasoning required depends on the capacity threshold, which is determined by a risk/benefit analysis. Conducting a risk/benefit analysis during the coronavirus disease 2019 (COVID-19) pandemic requires consideration of societallevel factors (such as contagiousness to others and health-care utilization) and is complicated by a wide range of uncertainties and divisive sociopolitical views regarding COVID-19.
Related Resources
- Appelbaum PS. Clinical practice. Assessment of patients’ competence to consent to treatment. N Engl J Med. 2007;357(18):1834-1840.
- Ryznar E, Hamaoka D, Lloyd RB. Capacity evaluations. https://admsep.org/csi-emodules.php?c=capacity&v=y. Accessed March 30, 2020.
Acknowledgments
The author thanks Drs. Awais Aftab, Zackary D. Berger, and R. Brett Lloyd for their helpful discussions on the topic.
1. Beauchamp TL, Childress JF. Principles of biomedical ethics. 7th ed. New York, NY: Oxford University Press; 2013.
2. Appelbaum PS, Grisso T. Assessing patients’ capacities to consent to treatment. N Engl J Med. 1988;319(25):1635-1638.
3. Appelbaum PS. Clinical practice. Assessment of patients’ competence to consent to treatment. N Engl J Med. 2007;357(18):1834-1840.
4. Magid M, Dodd ML, Bostwick MJ, et al. Is your patient making the ‘wrong’ treatment choice? Current Psychiatry. 2006;5(3):13-20.
5. Ryznar E, Hamaoka D, Lloyd RB. Capacity evaluations. Association of Directors of Medical Student Education in Psychiatry. 2020. https://admsep.org/csi-emodules.php?c=capacity&v=y. Accessed March 30, 2020.
6. Sanche S, Lin YT, Xu C, et al. High contagiousness and rapid spread of severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis. 2020;26(7):1470-1477.
7. Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199-1207.
8. Wölfel R, Corman VM, Guggemos W, et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581(7809):465-469.
9. Mizumoto K, Kagaya K, Zarebski A, et al. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Euro Surveill. 2020;25(10):2000180. doi: 10.2807/1560-7917.ES.2020.25.10.2000180.
10. Lipsitch M, Swerdlow DL, Finelli L. Defining the epidemiology of Covid-19 — studies needed. N Engl J Med. 2020;382(13):1194-1196.
11. Goh KJ, Choong MC, Cheong EH, et al. Rapid progression to acute respiratory distress syndrome: review of current understanding of critical illness from COVID-19 infection. Ann Acad Med Singapore. 2020;49(3):108-118.
12. Asai A, Konno M, Ozaki M, et al. COVID-19 drug discovery using intensive approaches. Int J Mol Sci. 2020;21(8):2839.
13. Siegel AM, Barnwell AS, Sisti DA. Assessing decision-making capacity: a primer for the development of hospital practice guidelines. HEC Forum. 2014;26(2):159-168.
14. Karlawish J. Assessment of decision-making capacity in adults. UpToDate. https://www.uptodate.com/contents/assessment-of-decision-making-capacity-in-adults. Updated February 24, 2020. Accessed May 27, 2020.
15. Mental Capacity Act 2005. Chapter 9. http://www.legislation.gov.uk/ukpga/2005/9/part/1. Accessed May 27, 2020.
16. Kersten C. The doctor as jailer: medical detention of non-psychiatric patients. J Law Biosci. 2019;6(1):310-316.
17. Cheung EH, Heldt J, Strouse T, et al. The medical incapacity hold: a policy on the involuntary medical hospitalization of patients who lack decisional capacity. Psychosomatics. 2018;59(2):169-176.
18. Parmet WE, Sinha MS. Covid-19 - the law and limits of quarantine. N Engl J Med. 2020;382(15):e28.
19. Coker R, Thomas M, Lock K, et al. Detention and the evolving threat of tuberculosis: evidence, ethics, and law. J Law Med Ethics. 2007;35(4):609-615.
20. Garg S, Kim L, Whitaker M, et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 — COVID-NET, 14 States, March 1–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(15):458-464.
The coronavirus disease 2019 (COVID-19) pandemic has introduced many new clinical challenges. Consider the patient with fever and dyspnea who tests positive for COVID-19 but does not believe in COVID-19 and wants to leave the hospital against medical advice (AMA). Or the patient with numerous cardiovascular risk factors and crushing substernal chest pain who is too afraid of contracting COVID-19 to come to the emergency department. These challenging clinical scenarios can be addressed in the context of decision-making capacity (DMC), for which our medical colleagues often call upon psychiatrists to assist. This article reviews the framework for DMC assessment, describes how COVID-19 affects DMC assessment, and discusses approaches to these scenarios using the DMC framework.
Review of decision-making capacity
Assessment of DMC is a fundamental clinical skill. It allows a physician to balance autonomy with beneficence and non-maleficence. An autonomous decision is a decision that is made intentionally, with understanding, and without controlling influences (these are the elements of informed consent).1 However, if a patient cannot make a decision with intention and understanding, then beneficence and non-maleficence must prevail in order to protect the patient. Capacity assessments evaluate a patient’s ability to make an intentional and understood choice.
In order to prove capacity, a patient must demonstrate 4 functional abilities:
- choice refers to the ability to communicate a relatively stable choice2,3
- understanding refers to the ability to convey information about the illness, risks/benefits of the chosen intervention, and risks/benefits of alternative options.2,3 Understanding measures objective information about the medical situation
- appreciation refers to the patient’s ability to apply that information to his/her own life.2,3 Appreciation requires insight into having the illness and the ability to anticipate how one’s life would be impacted by one’s condition and choice. This is where life experiences and values come into play
- reasoning is intimately tied to appreciation. It refers to the ability to explain how the decision was made and which factors were most important.2,3
Most clinicians and ethicists endorse a “threshold” approach to decisional capacity, which specifies that the level of evidence required to prove capacity depends on the gravity of the medical situation (Figure 1A).1,4,5 The gravity of the situation is based on the risk/benefit analysis. Consider two treatments with equal benefit: one has minimal adverse effects (gastrointestinal upset) and the second has significant adverse effects (myelosuppression). Accepting the first treatment requires less intentionality and understanding than accepting the second because the risk is much lower and thus has a lower capacity threshold (Figure 1B). The capacity to refuse these treatments results in the opposite ranking (Figure 1C).
Establishing a threshold helps guide the physician in determining how robust the patient’s responses must be to have decisional capacity. For a high-threshold decision, the patient must have a well-developed and highly detailed level of understanding, appreciation, and reasoning.
How COVID-19 affects assessment of decision-making capacity
Three characteristics of the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and COVID-19 illness impact decision-making assessment:
- high level of contagiousness
- high health-care utilization
- the uncertainty about its clinical course and outcomes.
The high level of contagiousness stems from this virus’s estimated basic reproduction number (R0) of 2.2 to 5.7 (which indicates the expected number of cases from any single case), its long incubation period, and the potential for asymptomatic and pre-symptomatic shedding.6-9 Decision-making capacity assessments must therefore consider community-level effects in the risk/benefit analysis. Because SARS-CoV-2 is a new virus affecting humans, it can easily overwhelm existing hospital systems. This happened in Wuhan, China; Lombardy, Italy; and New York. In a stressed system, physicians will have to factor health-care utilization into the risk/benefit analysis. Finally, because this is a novel virus, there is still considerable uncertainty about the epidemiology, clinical course, and outcomes.10 The minimal dose of virus needed to cause illness is unknown. Patients can deteriorate quickly and unpredictably into needing ventilator support.11 Treatment options are limited, and many candidates are being investigated.12 This uncertainty hinders physicians’ ability to accurately estimate risks and benefits for an individual patient when discussing various medical decisions. As our understanding of SARS-CoV-2 improves, this uncertainty will lessen.
Continue to: Effects of the sociopolitical climate
Effects of the sociopolitical climate
In the United States, the COVID-19 pandemic emerged during a time of deep sociopolitical divide. Accordingly, beliefs about viral infectivity, severity of illness, and precautionary measures have varied. Some politicians, media outlets, and physicians have shared information that contradicts guidelines and recommendations from mainstream national and international medical and scientific organizations. Patients who subscribe to these reports and beliefs may not meet the threshold for understanding, appreciation, or reasoning. For example, if a patient’s beliefs about the virus depart from well-established medical evidence, they would technically lack understanding. The usual remedy for addressing misunderstanding is education and time. However, because of the divisiveness of the sociopolitical climate, the limited time physicians have with patients, and the fact that many DMC assessments will occur in acute-care settings, it may be difficult or near impossible to correct the misunderstanding.
The sociopolitical climate and its accompanying potentially erroneous or imbalanced narrative may thus directly impact patients’ understanding, appreciation, and reasoning. However, it can be problematic to declare incapacity in a patient whose understanding, appreciation, and reasoning arise from widely shared and relatively fixed sociopolitical values. Additionally, some clinicians and ethicists might object to declaring incapacity in a patient with no underlying mental or neurologic dysfunction. The United States has a functional approach to capacity, based solely on meeting criteria for the 4 functional abilities.3,13 Mental or neurologic dysfunction is not legally required in the United States, but in practice, the consideration of incapacity is often closely linked to some form of cognitive impairment.14 Other countries do make dysfunction a specific criterion; for example, the United Kingdom dictates that mental incapacity can only occur in someone with “impairment of, or a disturbance in the functioning of, the mind or brain.”15
Leaving against medical advice
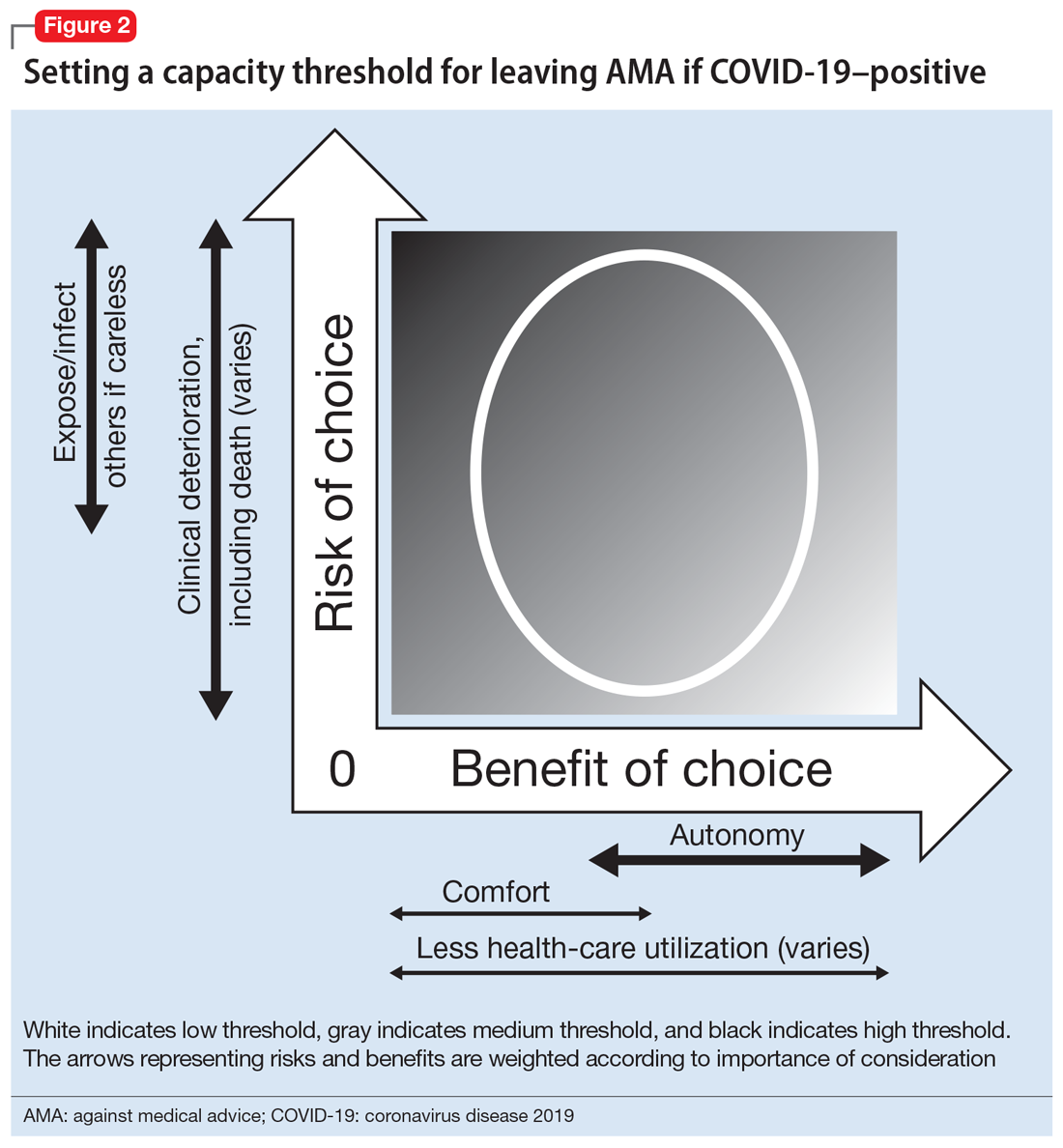
In the case of a patient who is COVID-19–positive, symptomatic, and wants to leave AMA, the threshold is automatically elevated because of societal-level risks (the risk of potential exposure or infection of others if a patient who is COVID-19–positive is not properly isolated). Furthermore, the individual risk of the patient leaving AMA depends on his/her age, comorbidities, and current clinical status; because of the uncertainty and rapid deterioration seen with COVID-19 illness, the calculated risk may actually be higher than for a non-COVID-19–related illness. Thus, in order to leave AMA, the patient’s responses must be fairly robust (Figure 2). Table 1 describes the information needed for robust understanding, appreciation, and reasoning.
For patients who do not meet this threshold, it is important to determine why. If a patient has a psychiatric condition that not only impacts DMC but also meets criteria for a psychiatric hold (ie, an imminent risk of harm to self or others), a psychiatric hold should be placed. If the patient does not meet the threshold because of altered mental status or some other neurologic or cognitive comorbidity, a medical hold should be placed. Most states do not have an explicit legal basis for a medical hold, although it does fall under the incapacity laws in the United States; in the absence of a surrogate, declaration of medical emergency can also be used if applicable.16,17 As a caveat, it can be difficult to detain someone on a medical hold because security officers may be afraid to physically detain someone without explicit legal paperwork.17
If a patient does not meet the capacity threshold but there does not seem to be a psychiatric, neurologic, or cognitive explanation, several options are possible. The first step would be to assess whether the patient is amenable to further discussion and compromise. A nonjudgmental and nonconfrontational approach that aims to further clarify the patient’s perspective and identify shared goals is key. Any plan that lowers the risks sufficiently would allow the patient to leave by lowering the capacity threshold. Enlisting the support of family and friends can be helpful. If this does not work, theoretically the patient should be detained in the hospital. Practically speaking, this may be difficult or unadvised. First, as described above, security officers may refuse to physically detain the patient.17 Second, the patient’s legally mandated surrogate may espouse similar COVID-related views as the patient; thus, this approach may not help keep the patient in the hospital. If the physician has serious concern about the risk of the patient leaving, he/she would have to consult the facility’s Ethics and Legal staff to determine capacity of the surrogate. Third, it can be problematic to declare incapacity in a patient whose understanding, appreciation, and reasoning arise from widely shared and relatively fixed sociopolitical values. In the current sociopolitical climate, involuntary detention may elicit a political backlash. Using medical detention for impending deterioration of clinical status would be more acceptable than using medical detention for isolation. Presently, there are no such laws for patients with COVID-19 (although this is not without precedent, as with active tuberculosis or Ebola18,19), but individual jurisdictions may have isolation or quarantine orders; the local health department could be contacted and may evaluate on a case-by-case basis.
Continue to: Refusing to seek medical care
Refusing to seek medical care
Anecdotally, many physicians have reported an increase in patients who are refusing clinic- or hospital-based treatment for a medical condition because they fear they may catch the virus. Although this is not strictly a capacity case—there is little recourse for action if a patient is refusing treatment from home (unless the patient requires a psychiatric hold or already has a guardian for medical decisions)—the same elements of thresholds apply and can be helpful in guiding conversations with the patient.
For the patient, the benefits of staying at home are to avoid potentially exposing themselves and the members of their household to the virus and COVID-19 illness. The risks of staying home include progression of the patient’s primary illness, which could lead to increased morbidity and mortality. Staying home has an ancillary benefit to the community of reducing health-care utilization, but at the risk of increasing utilization in the future.
The risk/benefit profile is shown on the thresholds graph in Figure 3. There is considerable variability. It is helpful to stratify the risk of progression of the primary condition as low (can be postponed indefinitely with minimal risk), medium (can be postponed for a short amount of time; risk of increased morbidity with ongoing delay and possibly increased mortality), or high (cannot be postponed; will have greater morbidity and/or higher risk of mortality). Because of the uncertainty about COVID-19, it is harder to quantify the benefits of refusing care and staying at home, although older patients and patients with underlying health issues are at higher risk of severe illness and death.20 However, by taking appropriate precautions when seeking care, viral exposure and risk of infection can be mitigated.
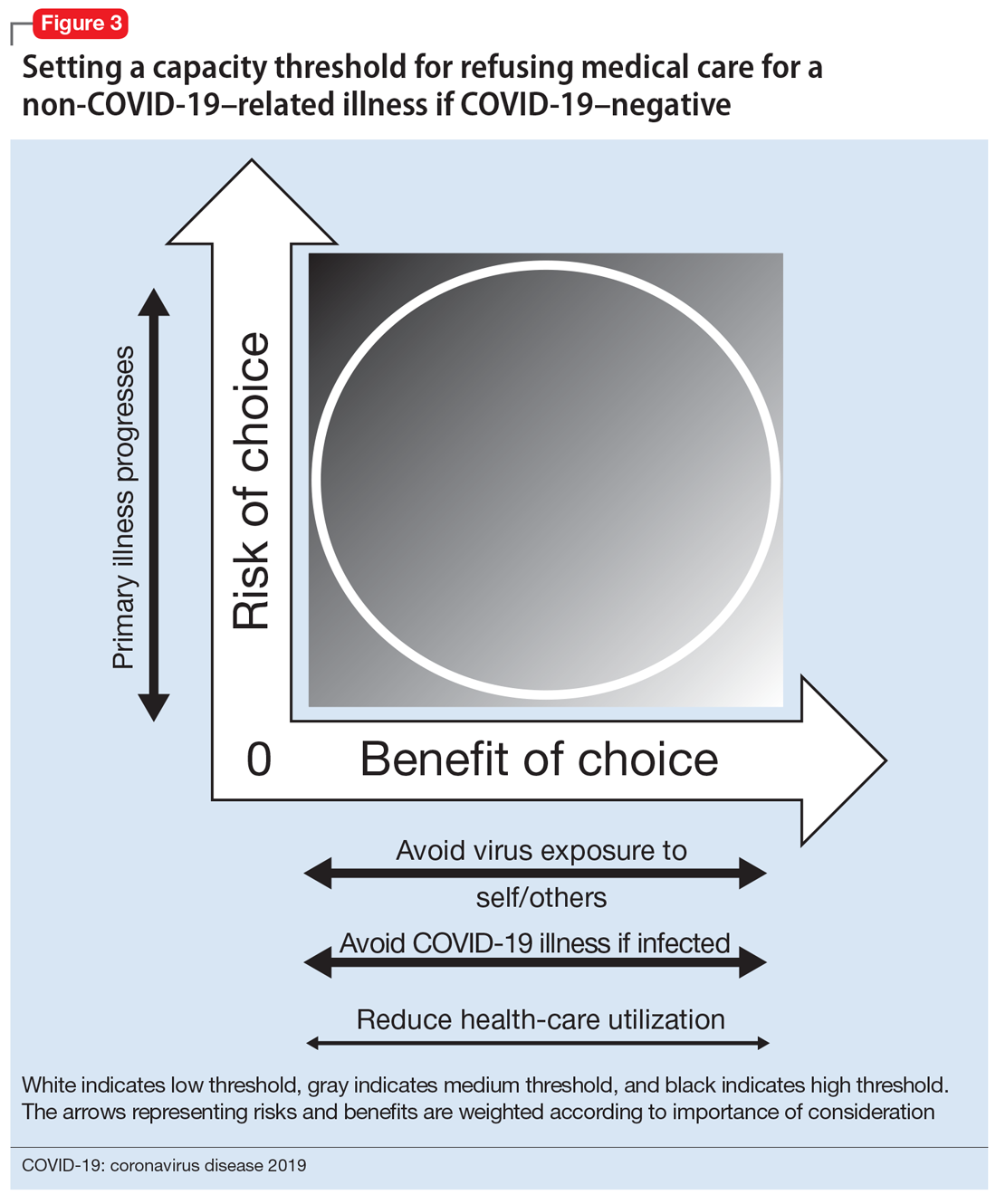
This risk/benefit analysis will help set the threshold for whether staying at home is reasonable or whether it would incur more risk of harm. If the latter, then the physician must elicit the patient’s understanding, appreciation, and reasoning related to their current medical condition and COVID-19. It is likely they are undervaluing the former and overvaluing the latter. Table 2 lists important points to cover during these discussions.
Although there is no legal recourse to force patients at home to come to the clinic or hospital for medical treatment, there are several possible strategies to motivate them to do so. One is to ask patients how likely (on a scale of 0 to 100) they think they are to contract COVID-19 if they came for evaluation/treatment, and how likely they feel they are to experience a bad outcome from their primary condition. Then, after providing psychoeducation about their primary medical condition and COVID-19–related precautions and risk, repeat this question. Another strategy is to empathize with the patient’s fears while also expressing concern about the primary medical condition and connecting with the patient on the shared desire to protect his/her health. A third is to draw a risk/benefit diagram (similar to Figure 3) or reassure the patient by describing the ways in which the clinic or hospital is minimizing exposure and infection risk. A final strategy is to enlist the help of the patient’s family or friends.
Continue to: Bottom Line
Bottom Line
In order to have decision-making capacity, a patient must demonstrate choice, understanding, appreciation, and reasoning. The degree of understanding, appreciation, and reasoning required depends on the capacity threshold, which is determined by a risk/benefit analysis. Conducting a risk/benefit analysis during the coronavirus disease 2019 (COVID-19) pandemic requires consideration of societallevel factors (such as contagiousness to others and health-care utilization) and is complicated by a wide range of uncertainties and divisive sociopolitical views regarding COVID-19.
Related Resources
- Appelbaum PS. Clinical practice. Assessment of patients’ competence to consent to treatment. N Engl J Med. 2007;357(18):1834-1840.
- Ryznar E, Hamaoka D, Lloyd RB. Capacity evaluations. https://admsep.org/csi-emodules.php?c=capacity&v=y. Accessed March 30, 2020.
Acknowledgments
The author thanks Drs. Awais Aftab, Zackary D. Berger, and R. Brett Lloyd for their helpful discussions on the topic.
The coronavirus disease 2019 (COVID-19) pandemic has introduced many new clinical challenges. Consider the patient with fever and dyspnea who tests positive for COVID-19 but does not believe in COVID-19 and wants to leave the hospital against medical advice (AMA). Or the patient with numerous cardiovascular risk factors and crushing substernal chest pain who is too afraid of contracting COVID-19 to come to the emergency department. These challenging clinical scenarios can be addressed in the context of decision-making capacity (DMC), for which our medical colleagues often call upon psychiatrists to assist. This article reviews the framework for DMC assessment, describes how COVID-19 affects DMC assessment, and discusses approaches to these scenarios using the DMC framework.
Review of decision-making capacity
Assessment of DMC is a fundamental clinical skill. It allows a physician to balance autonomy with beneficence and non-maleficence. An autonomous decision is a decision that is made intentionally, with understanding, and without controlling influences (these are the elements of informed consent).1 However, if a patient cannot make a decision with intention and understanding, then beneficence and non-maleficence must prevail in order to protect the patient. Capacity assessments evaluate a patient’s ability to make an intentional and understood choice.
In order to prove capacity, a patient must demonstrate 4 functional abilities:
- choice refers to the ability to communicate a relatively stable choice2,3
- understanding refers to the ability to convey information about the illness, risks/benefits of the chosen intervention, and risks/benefits of alternative options.2,3 Understanding measures objective information about the medical situation
- appreciation refers to the patient’s ability to apply that information to his/her own life.2,3 Appreciation requires insight into having the illness and the ability to anticipate how one’s life would be impacted by one’s condition and choice. This is where life experiences and values come into play
- reasoning is intimately tied to appreciation. It refers to the ability to explain how the decision was made and which factors were most important.2,3
Most clinicians and ethicists endorse a “threshold” approach to decisional capacity, which specifies that the level of evidence required to prove capacity depends on the gravity of the medical situation (Figure 1A).1,4,5 The gravity of the situation is based on the risk/benefit analysis. Consider two treatments with equal benefit: one has minimal adverse effects (gastrointestinal upset) and the second has significant adverse effects (myelosuppression). Accepting the first treatment requires less intentionality and understanding than accepting the second because the risk is much lower and thus has a lower capacity threshold (Figure 1B). The capacity to refuse these treatments results in the opposite ranking (Figure 1C).
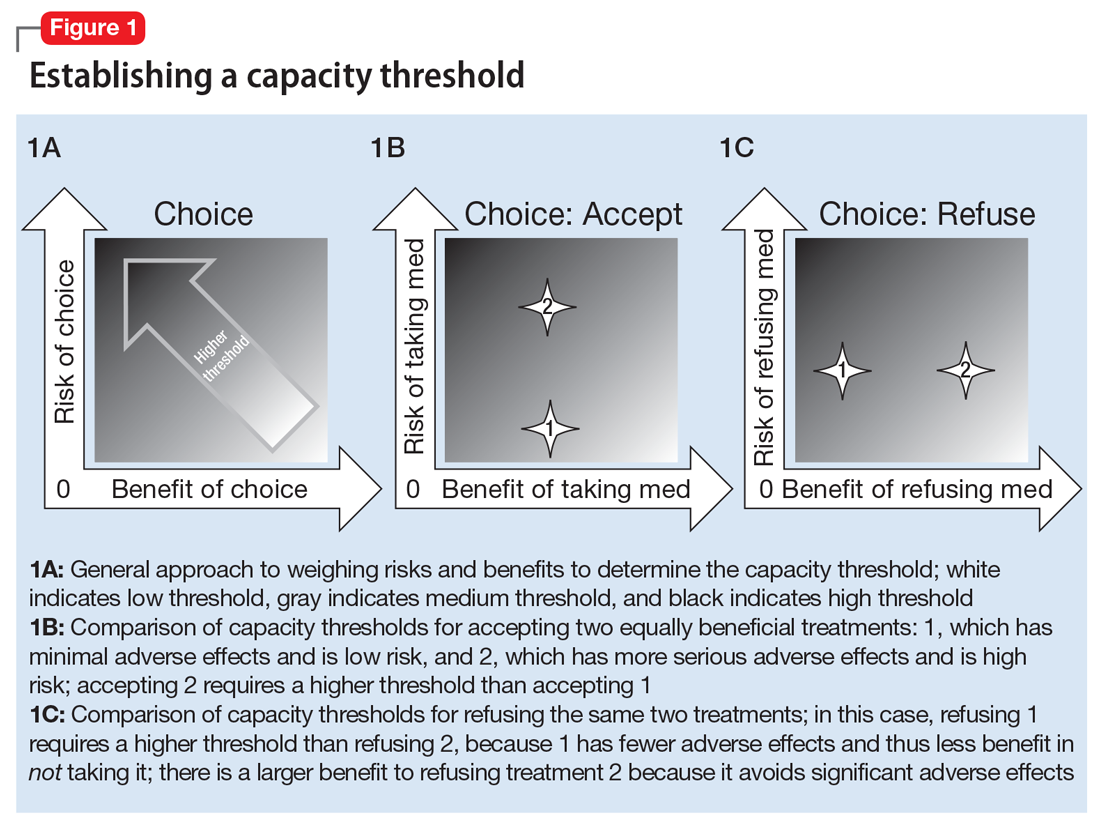
Establishing a threshold helps guide the physician in determining how robust the patient’s responses must be to have decisional capacity. For a high-threshold decision, the patient must have a well-developed and highly detailed level of understanding, appreciation, and reasoning.
How COVID-19 affects assessment of decision-making capacity
Three characteristics of the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and COVID-19 illness impact decision-making assessment:
- high level of contagiousness
- high health-care utilization
- the uncertainty about its clinical course and outcomes.
The high level of contagiousness stems from this virus’s estimated basic reproduction number (R0) of 2.2 to 5.7 (which indicates the expected number of cases from any single case), its long incubation period, and the potential for asymptomatic and pre-symptomatic shedding.6-9 Decision-making capacity assessments must therefore consider community-level effects in the risk/benefit analysis. Because SARS-CoV-2 is a new virus affecting humans, it can easily overwhelm existing hospital systems. This happened in Wuhan, China; Lombardy, Italy; and New York. In a stressed system, physicians will have to factor health-care utilization into the risk/benefit analysis. Finally, because this is a novel virus, there is still considerable uncertainty about the epidemiology, clinical course, and outcomes.10 The minimal dose of virus needed to cause illness is unknown. Patients can deteriorate quickly and unpredictably into needing ventilator support.11 Treatment options are limited, and many candidates are being investigated.12 This uncertainty hinders physicians’ ability to accurately estimate risks and benefits for an individual patient when discussing various medical decisions. As our understanding of SARS-CoV-2 improves, this uncertainty will lessen.
Continue to: Effects of the sociopolitical climate
Effects of the sociopolitical climate
In the United States, the COVID-19 pandemic emerged during a time of deep sociopolitical divide. Accordingly, beliefs about viral infectivity, severity of illness, and precautionary measures have varied. Some politicians, media outlets, and physicians have shared information that contradicts guidelines and recommendations from mainstream national and international medical and scientific organizations. Patients who subscribe to these reports and beliefs may not meet the threshold for understanding, appreciation, or reasoning. For example, if a patient’s beliefs about the virus depart from well-established medical evidence, they would technically lack understanding. The usual remedy for addressing misunderstanding is education and time. However, because of the divisiveness of the sociopolitical climate, the limited time physicians have with patients, and the fact that many DMC assessments will occur in acute-care settings, it may be difficult or near impossible to correct the misunderstanding.
The sociopolitical climate and its accompanying potentially erroneous or imbalanced narrative may thus directly impact patients’ understanding, appreciation, and reasoning. However, it can be problematic to declare incapacity in a patient whose understanding, appreciation, and reasoning arise from widely shared and relatively fixed sociopolitical values. Additionally, some clinicians and ethicists might object to declaring incapacity in a patient with no underlying mental or neurologic dysfunction. The United States has a functional approach to capacity, based solely on meeting criteria for the 4 functional abilities.3,13 Mental or neurologic dysfunction is not legally required in the United States, but in practice, the consideration of incapacity is often closely linked to some form of cognitive impairment.14 Other countries do make dysfunction a specific criterion; for example, the United Kingdom dictates that mental incapacity can only occur in someone with “impairment of, or a disturbance in the functioning of, the mind or brain.”15
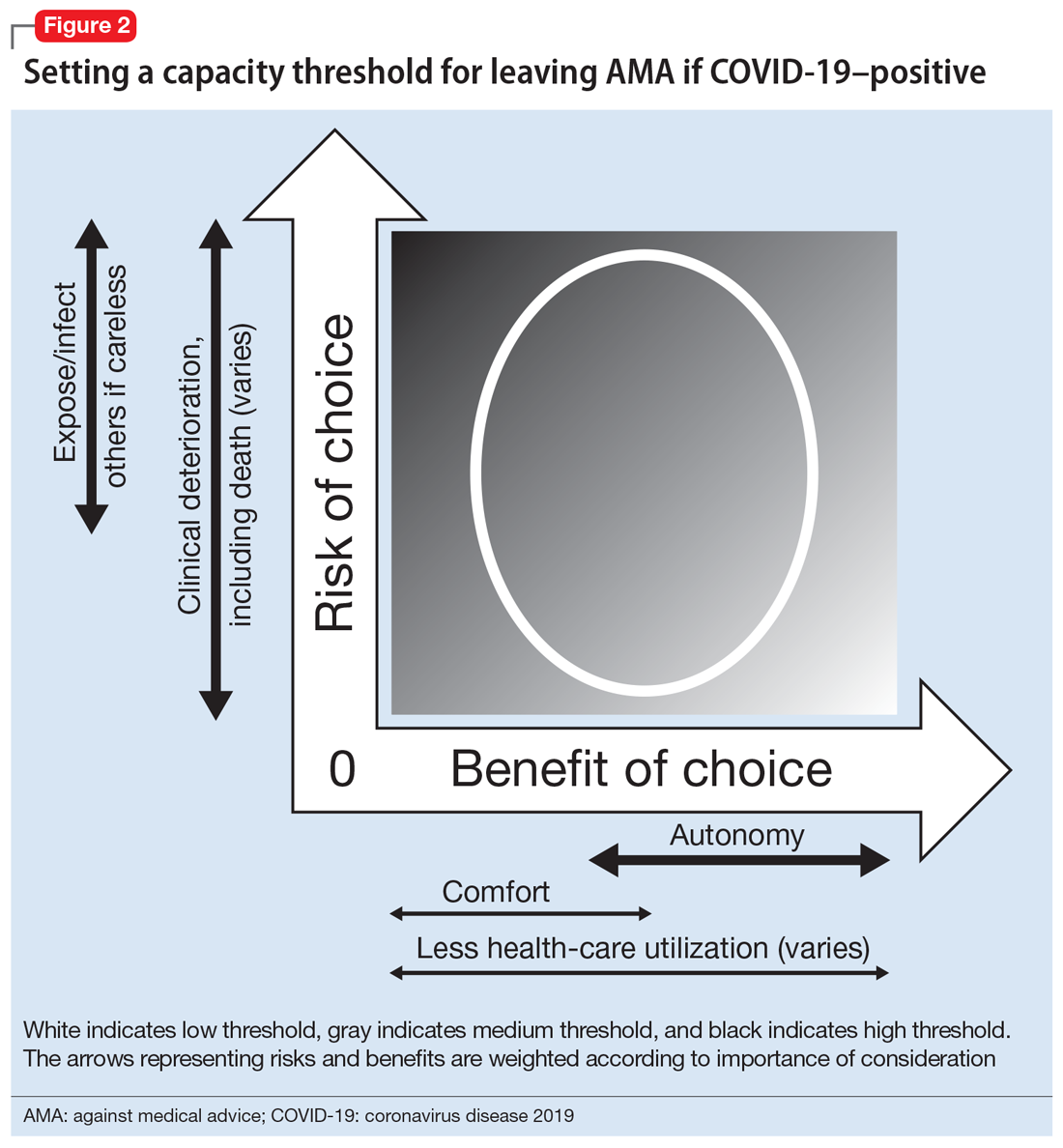
Leaving against medical advice
In the case of a patient who is COVID-19–positive, symptomatic, and wants to leave AMA, the threshold is automatically elevated because of societal-level risks (the risk of potential exposure or infection of others if a patient who is COVID-19–positive is not properly isolated). Furthermore, the individual risk of the patient leaving AMA depends on his/her age, comorbidities, and current clinical status; because of the uncertainty and rapid deterioration seen with COVID-19 illness, the calculated risk may actually be higher than for a non-COVID-19–related illness. Thus, in order to leave AMA, the patient’s responses must be fairly robust (Figure 2). Table 1 describes the information needed for robust understanding, appreciation, and reasoning.
For patients who do not meet this threshold, it is important to determine why. If a patient has a psychiatric condition that not only impacts DMC but also meets criteria for a psychiatric hold (ie, an imminent risk of harm to self or others), a psychiatric hold should be placed. If the patient does not meet the threshold because of altered mental status or some other neurologic or cognitive comorbidity, a medical hold should be placed. Most states do not have an explicit legal basis for a medical hold, although it does fall under the incapacity laws in the United States; in the absence of a surrogate, declaration of medical emergency can also be used if applicable.16,17 As a caveat, it can be difficult to detain someone on a medical hold because security officers may be afraid to physically detain someone without explicit legal paperwork.17
If a patient does not meet the capacity threshold but there does not seem to be a psychiatric, neurologic, or cognitive explanation, several options are possible. The first step would be to assess whether the patient is amenable to further discussion and compromise. A nonjudgmental and nonconfrontational approach that aims to further clarify the patient’s perspective and identify shared goals is key. Any plan that lowers the risks sufficiently would allow the patient to leave by lowering the capacity threshold. Enlisting the support of family and friends can be helpful. If this does not work, theoretically the patient should be detained in the hospital. Practically speaking, this may be difficult or unadvised. First, as described above, security officers may refuse to physically detain the patient.17 Second, the patient’s legally mandated surrogate may espouse similar COVID-related views as the patient; thus, this approach may not help keep the patient in the hospital. If the physician has serious concern about the risk of the patient leaving, he/she would have to consult the facility’s Ethics and Legal staff to determine capacity of the surrogate. Third, it can be problematic to declare incapacity in a patient whose understanding, appreciation, and reasoning arise from widely shared and relatively fixed sociopolitical values. In the current sociopolitical climate, involuntary detention may elicit a political backlash. Using medical detention for impending deterioration of clinical status would be more acceptable than using medical detention for isolation. Presently, there are no such laws for patients with COVID-19 (although this is not without precedent, as with active tuberculosis or Ebola18,19), but individual jurisdictions may have isolation or quarantine orders; the local health department could be contacted and may evaluate on a case-by-case basis.
Continue to: Refusing to seek medical care
Refusing to seek medical care
Anecdotally, many physicians have reported an increase in patients who are refusing clinic- or hospital-based treatment for a medical condition because they fear they may catch the virus. Although this is not strictly a capacity case—there is little recourse for action if a patient is refusing treatment from home (unless the patient requires a psychiatric hold or already has a guardian for medical decisions)—the same elements of thresholds apply and can be helpful in guiding conversations with the patient.
For the patient, the benefits of staying at home are to avoid potentially exposing themselves and the members of their household to the virus and COVID-19 illness. The risks of staying home include progression of the patient’s primary illness, which could lead to increased morbidity and mortality. Staying home has an ancillary benefit to the community of reducing health-care utilization, but at the risk of increasing utilization in the future.
The risk/benefit profile is shown on the thresholds graph in Figure 3. There is considerable variability. It is helpful to stratify the risk of progression of the primary condition as low (can be postponed indefinitely with minimal risk), medium (can be postponed for a short amount of time; risk of increased morbidity with ongoing delay and possibly increased mortality), or high (cannot be postponed; will have greater morbidity and/or higher risk of mortality). Because of the uncertainty about COVID-19, it is harder to quantify the benefits of refusing care and staying at home, although older patients and patients with underlying health issues are at higher risk of severe illness and death.20 However, by taking appropriate precautions when seeking care, viral exposure and risk of infection can be mitigated.
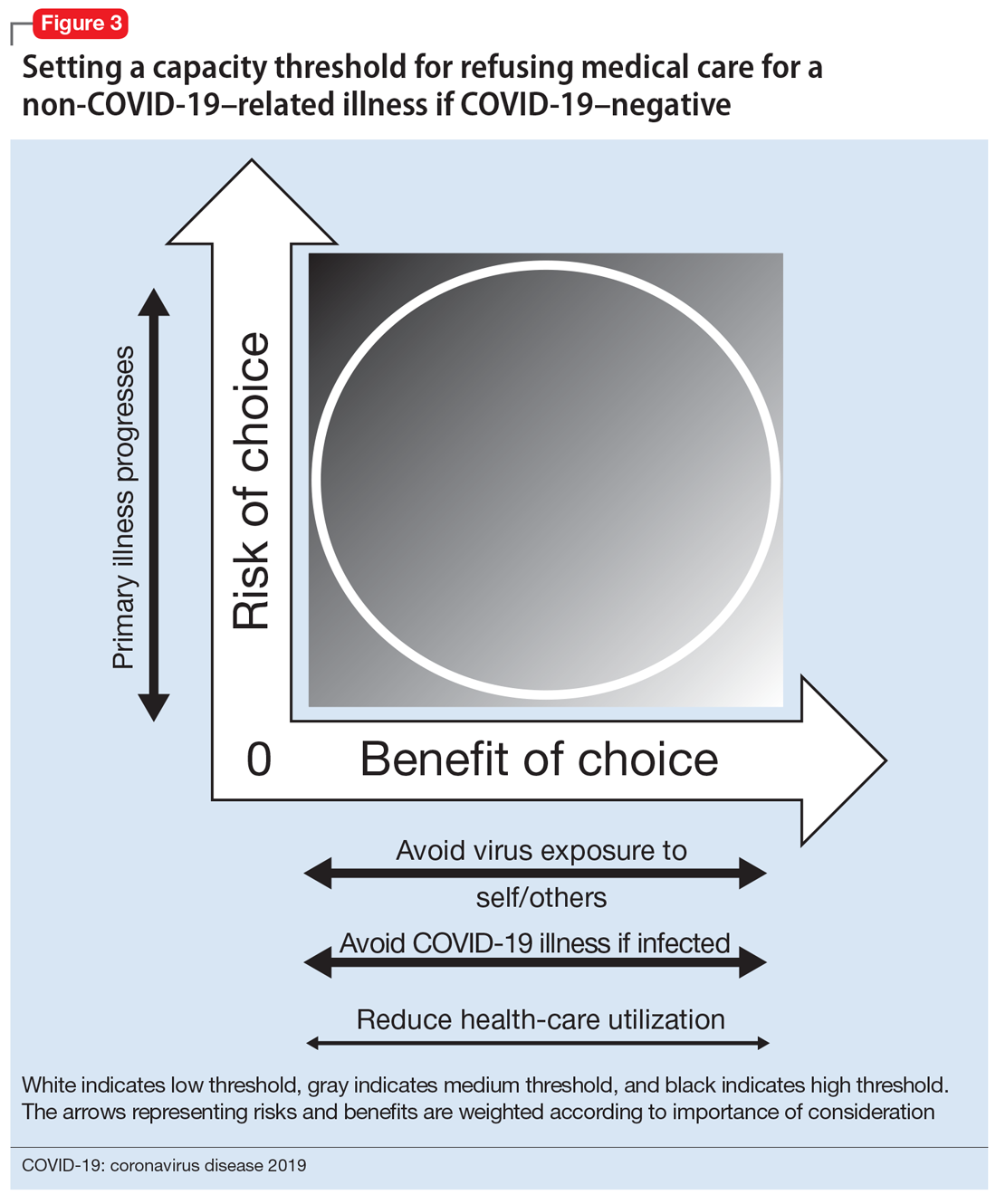
This risk/benefit analysis will help set the threshold for whether staying at home is reasonable or whether it would incur more risk of harm. If the latter, then the physician must elicit the patient’s understanding, appreciation, and reasoning related to their current medical condition and COVID-19. It is likely they are undervaluing the former and overvaluing the latter. Table 2 lists important points to cover during these discussions.
Although there is no legal recourse to force patients at home to come to the clinic or hospital for medical treatment, there are several possible strategies to motivate them to do so. One is to ask patients how likely (on a scale of 0 to 100) they think they are to contract COVID-19 if they came for evaluation/treatment, and how likely they feel they are to experience a bad outcome from their primary condition. Then, after providing psychoeducation about their primary medical condition and COVID-19–related precautions and risk, repeat this question. Another strategy is to empathize with the patient’s fears while also expressing concern about the primary medical condition and connecting with the patient on the shared desire to protect his/her health. A third is to draw a risk/benefit diagram (similar to Figure 3) or reassure the patient by describing the ways in which the clinic or hospital is minimizing exposure and infection risk. A final strategy is to enlist the help of the patient’s family or friends.
Continue to: Bottom Line
Bottom Line
In order to have decision-making capacity, a patient must demonstrate choice, understanding, appreciation, and reasoning. The degree of understanding, appreciation, and reasoning required depends on the capacity threshold, which is determined by a risk/benefit analysis. Conducting a risk/benefit analysis during the coronavirus disease 2019 (COVID-19) pandemic requires consideration of societallevel factors (such as contagiousness to others and health-care utilization) and is complicated by a wide range of uncertainties and divisive sociopolitical views regarding COVID-19.
Related Resources
- Appelbaum PS. Clinical practice. Assessment of patients’ competence to consent to treatment. N Engl J Med. 2007;357(18):1834-1840.
- Ryznar E, Hamaoka D, Lloyd RB. Capacity evaluations. https://admsep.org/csi-emodules.php?c=capacity&v=y. Accessed March 30, 2020.
Acknowledgments
The author thanks Drs. Awais Aftab, Zackary D. Berger, and R. Brett Lloyd for their helpful discussions on the topic.
1. Beauchamp TL, Childress JF. Principles of biomedical ethics. 7th ed. New York, NY: Oxford University Press; 2013.
2. Appelbaum PS, Grisso T. Assessing patients’ capacities to consent to treatment. N Engl J Med. 1988;319(25):1635-1638.
3. Appelbaum PS. Clinical practice. Assessment of patients’ competence to consent to treatment. N Engl J Med. 2007;357(18):1834-1840.
4. Magid M, Dodd ML, Bostwick MJ, et al. Is your patient making the ‘wrong’ treatment choice? Current Psychiatry. 2006;5(3):13-20.
5. Ryznar E, Hamaoka D, Lloyd RB. Capacity evaluations. Association of Directors of Medical Student Education in Psychiatry. 2020. https://admsep.org/csi-emodules.php?c=capacity&v=y. Accessed March 30, 2020.
6. Sanche S, Lin YT, Xu C, et al. High contagiousness and rapid spread of severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis. 2020;26(7):1470-1477.
7. Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199-1207.
8. Wölfel R, Corman VM, Guggemos W, et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581(7809):465-469.
9. Mizumoto K, Kagaya K, Zarebski A, et al. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Euro Surveill. 2020;25(10):2000180. doi: 10.2807/1560-7917.ES.2020.25.10.2000180.
10. Lipsitch M, Swerdlow DL, Finelli L. Defining the epidemiology of Covid-19 — studies needed. N Engl J Med. 2020;382(13):1194-1196.
11. Goh KJ, Choong MC, Cheong EH, et al. Rapid progression to acute respiratory distress syndrome: review of current understanding of critical illness from COVID-19 infection. Ann Acad Med Singapore. 2020;49(3):108-118.
12. Asai A, Konno M, Ozaki M, et al. COVID-19 drug discovery using intensive approaches. Int J Mol Sci. 2020;21(8):2839.
13. Siegel AM, Barnwell AS, Sisti DA. Assessing decision-making capacity: a primer for the development of hospital practice guidelines. HEC Forum. 2014;26(2):159-168.
14. Karlawish J. Assessment of decision-making capacity in adults. UpToDate. https://www.uptodate.com/contents/assessment-of-decision-making-capacity-in-adults. Updated February 24, 2020. Accessed May 27, 2020.
15. Mental Capacity Act 2005. Chapter 9. http://www.legislation.gov.uk/ukpga/2005/9/part/1. Accessed May 27, 2020.
16. Kersten C. The doctor as jailer: medical detention of non-psychiatric patients. J Law Biosci. 2019;6(1):310-316.
17. Cheung EH, Heldt J, Strouse T, et al. The medical incapacity hold: a policy on the involuntary medical hospitalization of patients who lack decisional capacity. Psychosomatics. 2018;59(2):169-176.
18. Parmet WE, Sinha MS. Covid-19 - the law and limits of quarantine. N Engl J Med. 2020;382(15):e28.
19. Coker R, Thomas M, Lock K, et al. Detention and the evolving threat of tuberculosis: evidence, ethics, and law. J Law Med Ethics. 2007;35(4):609-615.
20. Garg S, Kim L, Whitaker M, et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 — COVID-NET, 14 States, March 1–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(15):458-464.
1. Beauchamp TL, Childress JF. Principles of biomedical ethics. 7th ed. New York, NY: Oxford University Press; 2013.
2. Appelbaum PS, Grisso T. Assessing patients’ capacities to consent to treatment. N Engl J Med. 1988;319(25):1635-1638.
3. Appelbaum PS. Clinical practice. Assessment of patients’ competence to consent to treatment. N Engl J Med. 2007;357(18):1834-1840.
4. Magid M, Dodd ML, Bostwick MJ, et al. Is your patient making the ‘wrong’ treatment choice? Current Psychiatry. 2006;5(3):13-20.
5. Ryznar E, Hamaoka D, Lloyd RB. Capacity evaluations. Association of Directors of Medical Student Education in Psychiatry. 2020. https://admsep.org/csi-emodules.php?c=capacity&v=y. Accessed March 30, 2020.
6. Sanche S, Lin YT, Xu C, et al. High contagiousness and rapid spread of severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis. 2020;26(7):1470-1477.
7. Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199-1207.
8. Wölfel R, Corman VM, Guggemos W, et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581(7809):465-469.
9. Mizumoto K, Kagaya K, Zarebski A, et al. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Euro Surveill. 2020;25(10):2000180. doi: 10.2807/1560-7917.ES.2020.25.10.2000180.
10. Lipsitch M, Swerdlow DL, Finelli L. Defining the epidemiology of Covid-19 — studies needed. N Engl J Med. 2020;382(13):1194-1196.
11. Goh KJ, Choong MC, Cheong EH, et al. Rapid progression to acute respiratory distress syndrome: review of current understanding of critical illness from COVID-19 infection. Ann Acad Med Singapore. 2020;49(3):108-118.
12. Asai A, Konno M, Ozaki M, et al. COVID-19 drug discovery using intensive approaches. Int J Mol Sci. 2020;21(8):2839.
13. Siegel AM, Barnwell AS, Sisti DA. Assessing decision-making capacity: a primer for the development of hospital practice guidelines. HEC Forum. 2014;26(2):159-168.
14. Karlawish J. Assessment of decision-making capacity in adults. UpToDate. https://www.uptodate.com/contents/assessment-of-decision-making-capacity-in-adults. Updated February 24, 2020. Accessed May 27, 2020.
15. Mental Capacity Act 2005. Chapter 9. http://www.legislation.gov.uk/ukpga/2005/9/part/1. Accessed May 27, 2020.
16. Kersten C. The doctor as jailer: medical detention of non-psychiatric patients. J Law Biosci. 2019;6(1):310-316.
17. Cheung EH, Heldt J, Strouse T, et al. The medical incapacity hold: a policy on the involuntary medical hospitalization of patients who lack decisional capacity. Psychosomatics. 2018;59(2):169-176.
18. Parmet WE, Sinha MS. Covid-19 - the law and limits of quarantine. N Engl J Med. 2020;382(15):e28.
19. Coker R, Thomas M, Lock K, et al. Detention and the evolving threat of tuberculosis: evidence, ethics, and law. J Law Med Ethics. 2007;35(4):609-615.
20. Garg S, Kim L, Whitaker M, et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 — COVID-NET, 14 States, March 1–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(15):458-464.
Legal concerns after a patient suicide
Most psychiatrists will care for at least one patient who dies by suicide. Many clinicians consider this to be one of the most stressful and formative events of their careers, prompting strong emotions, logistical questions, and legal concerns. Because the aftermath of a patient suicide can be difficult, we offer guidance on how to cope with such events, and specifically how to address the legal concerns.
Attend to self-care. “At a cardiac arrest, the first procedure is to take your own pulse.” This advice, from Samuel Shem’s The House of God, highlights the importance of self-awareness during highly stressful events.1 When facing the aftermath of a patient suicide, be sure to attend to your own needs, such as eating, staying hydrated, and getting enough sleep. Identify and reach out to your support systems, such as friends and family. Your colleagues can be a source of support, both formally or informally. Reaching out to other psychiatrists, who likely have their own experience with patient suicide, can help process the event. A support group consisting of other psychiatrists also may be beneficial. Finally, avoid blaming yourself. Although you might perceive your patient’s suicide as a personal failing, suicide is notoriously difficult to predict and an unfortunate reality of working in this specialty.
Report the event. Follow your institution’s guidelines for reporting adverse events. You may be required to inform your supervisor, the risk management department, legal services, your malpractice provider, and/or the police. Your risk management department and malpractice provider may have their own regulations and recommendations.
Review the case. Institutions often have established processes for reviewing adverse events and, if applicable, suggesting constructive feedback or general quality improvements. A review process may provide an opportunity to look for potential negligence that could be an issue if there is a malpractice suit. Ideally, such processes are constructive and a time for reflection, rather than punitive or blaming. Trainees may find their supervisors’ presence and guidance to be particularly helpful during this review process.
Assess malpractice risk. Although psychiatrists have a relatively low risk of being sued for malpractice, many lawsuits against psychiatrists occur after a completed patient suicide.2 In a successful malpractice suit, the plaintiff needs to establish all 4 “Ds” of medical malpractice:
1) Duty, or an established physician–patient relationship
2) Damages from an adverse event
3) Dereliction of duty (negligence)
4) Direct causality between the deviation and the damages.
In the event of a patient suicide, both a doctor–patient relationship (duty) and an adverse outcome (damages) exist.3 Establishing dereliction of duty and direct causality rests on the plaintiff to prove. Good documentation can serve as evidence against accusations of negligence.3
Typically, a patient’s medical record will be used as evidence in a malpractice suit. After a suicide, do not alter this record, such as by editing your past assessments of the patient. If an addendum must be made, such as to document a conversation with suicide survivors (family and friends of the deceased), be sure to label it as such with the current date. An addendum should contain only facts; avoid adding information that attempts to explain your patient’s suicide, justifying or apologizing for past treatment decisions, or otherwise editorializing.
Continue to: Consider reaching out to suicide survivors
Consider reaching out to suicide survivors. The Health Insurance Portability and Accountability Act permits clinicians to use their best judgment when identifying individuals to contact and deciding what information to share after a patient’s death.4 Some states and practice settings have stricter confidentiality laws. Consider seeking legal counsel before interacting with suicide survivors.
Suicide survivors may experience feelings such as guilt, shame, and anger, and these feelings may lead suicide survivors to file a malpractice suit.3 Speaking with suicide survivors can help to address these feelings and potentially decrease the likelihood of them pursuing a malpractice suit. In addition, suicide survivors are at high risk for developing mental health issues, including suicidality. Contacting them can be an opportunity to encourage them to seek mental health treatment. It is important to clarify that any recommendations you provide in such situations do not constitute a doctor–patient relationship.
Should you offer an apology? Consider seeking legal counsel if you wish to apologize. Some states have “apology laws” that render a clinician’s apologetic statements inadmissible if a malpractice suit should occur.5 These laws might include empathic statements (“I’m sorry for your loss”) or disclosures of error (“I’m sorry for causing your loss”).5 It is unclear whether these laws affect the likelihood and/or outcome of malpractice suits.5
Focus on empathy. Experiencing a patient suicide can be one of the most challenging events in a psychiatrist’s career. Empathy is crucial, both towards the suicide survivors and to oneself.
1. Shem S. The House of God. New York, NY: Berkley Books; 2010.
2. Schaffer AC, Jena AB, Seabury SA, et al. Rates and characteristics of paid malpractice claims among US physicians by specialty, 1992-2014. JAMA Intern Med. 2017;177(5):710-719.
3. Gutheil TG, Appelbaum PS. Clinical handbook of psychiatry and the law, 3rd ed. Baltimore, MD: Lippincott Williams & Wilkins; 2000.
4. Office of Civil Rights. How can a covered entity determine if a person is a family member prior to an individual’s death. US Department of Health and Human Services. https://www.hhs.gov/hipaa/for-professionals/faq/1505/how-can-a-covered-entity-determine-whether-a-person-is-a-family-member/index.html. Accessed September 9, 2020.
5. McMichael BJ, Van Horn RL, Viscusi WK. “Sorry” is never enough: how state apology laws fail to reduce medical malpractice liability risk. Stanford Law Rev. 2019;71(2):341-409.
Most psychiatrists will care for at least one patient who dies by suicide. Many clinicians consider this to be one of the most stressful and formative events of their careers, prompting strong emotions, logistical questions, and legal concerns. Because the aftermath of a patient suicide can be difficult, we offer guidance on how to cope with such events, and specifically how to address the legal concerns.
Attend to self-care. “At a cardiac arrest, the first procedure is to take your own pulse.” This advice, from Samuel Shem’s The House of God, highlights the importance of self-awareness during highly stressful events.1 When facing the aftermath of a patient suicide, be sure to attend to your own needs, such as eating, staying hydrated, and getting enough sleep. Identify and reach out to your support systems, such as friends and family. Your colleagues can be a source of support, both formally or informally. Reaching out to other psychiatrists, who likely have their own experience with patient suicide, can help process the event. A support group consisting of other psychiatrists also may be beneficial. Finally, avoid blaming yourself. Although you might perceive your patient’s suicide as a personal failing, suicide is notoriously difficult to predict and an unfortunate reality of working in this specialty.
Report the event. Follow your institution’s guidelines for reporting adverse events. You may be required to inform your supervisor, the risk management department, legal services, your malpractice provider, and/or the police. Your risk management department and malpractice provider may have their own regulations and recommendations.
Review the case. Institutions often have established processes for reviewing adverse events and, if applicable, suggesting constructive feedback or general quality improvements. A review process may provide an opportunity to look for potential negligence that could be an issue if there is a malpractice suit. Ideally, such processes are constructive and a time for reflection, rather than punitive or blaming. Trainees may find their supervisors’ presence and guidance to be particularly helpful during this review process.
Assess malpractice risk. Although psychiatrists have a relatively low risk of being sued for malpractice, many lawsuits against psychiatrists occur after a completed patient suicide.2 In a successful malpractice suit, the plaintiff needs to establish all 4 “Ds” of medical malpractice:
1) Duty, or an established physician–patient relationship
2) Damages from an adverse event
3) Dereliction of duty (negligence)
4) Direct causality between the deviation and the damages.
In the event of a patient suicide, both a doctor–patient relationship (duty) and an adverse outcome (damages) exist.3 Establishing dereliction of duty and direct causality rests on the plaintiff to prove. Good documentation can serve as evidence against accusations of negligence.3
Typically, a patient’s medical record will be used as evidence in a malpractice suit. After a suicide, do not alter this record, such as by editing your past assessments of the patient. If an addendum must be made, such as to document a conversation with suicide survivors (family and friends of the deceased), be sure to label it as such with the current date. An addendum should contain only facts; avoid adding information that attempts to explain your patient’s suicide, justifying or apologizing for past treatment decisions, or otherwise editorializing.
Continue to: Consider reaching out to suicide survivors
Consider reaching out to suicide survivors. The Health Insurance Portability and Accountability Act permits clinicians to use their best judgment when identifying individuals to contact and deciding what information to share after a patient’s death.4 Some states and practice settings have stricter confidentiality laws. Consider seeking legal counsel before interacting with suicide survivors.
Suicide survivors may experience feelings such as guilt, shame, and anger, and these feelings may lead suicide survivors to file a malpractice suit.3 Speaking with suicide survivors can help to address these feelings and potentially decrease the likelihood of them pursuing a malpractice suit. In addition, suicide survivors are at high risk for developing mental health issues, including suicidality. Contacting them can be an opportunity to encourage them to seek mental health treatment. It is important to clarify that any recommendations you provide in such situations do not constitute a doctor–patient relationship.
Should you offer an apology? Consider seeking legal counsel if you wish to apologize. Some states have “apology laws” that render a clinician’s apologetic statements inadmissible if a malpractice suit should occur.5 These laws might include empathic statements (“I’m sorry for your loss”) or disclosures of error (“I’m sorry for causing your loss”).5 It is unclear whether these laws affect the likelihood and/or outcome of malpractice suits.5
Focus on empathy. Experiencing a patient suicide can be one of the most challenging events in a psychiatrist’s career. Empathy is crucial, both towards the suicide survivors and to oneself.
Most psychiatrists will care for at least one patient who dies by suicide. Many clinicians consider this to be one of the most stressful and formative events of their careers, prompting strong emotions, logistical questions, and legal concerns. Because the aftermath of a patient suicide can be difficult, we offer guidance on how to cope with such events, and specifically how to address the legal concerns.
Attend to self-care. “At a cardiac arrest, the first procedure is to take your own pulse.” This advice, from Samuel Shem’s The House of God, highlights the importance of self-awareness during highly stressful events.1 When facing the aftermath of a patient suicide, be sure to attend to your own needs, such as eating, staying hydrated, and getting enough sleep. Identify and reach out to your support systems, such as friends and family. Your colleagues can be a source of support, both formally or informally. Reaching out to other psychiatrists, who likely have their own experience with patient suicide, can help process the event. A support group consisting of other psychiatrists also may be beneficial. Finally, avoid blaming yourself. Although you might perceive your patient’s suicide as a personal failing, suicide is notoriously difficult to predict and an unfortunate reality of working in this specialty.
Report the event. Follow your institution’s guidelines for reporting adverse events. You may be required to inform your supervisor, the risk management department, legal services, your malpractice provider, and/or the police. Your risk management department and malpractice provider may have their own regulations and recommendations.
Review the case. Institutions often have established processes for reviewing adverse events and, if applicable, suggesting constructive feedback or general quality improvements. A review process may provide an opportunity to look for potential negligence that could be an issue if there is a malpractice suit. Ideally, such processes are constructive and a time for reflection, rather than punitive or blaming. Trainees may find their supervisors’ presence and guidance to be particularly helpful during this review process.
Assess malpractice risk. Although psychiatrists have a relatively low risk of being sued for malpractice, many lawsuits against psychiatrists occur after a completed patient suicide.2 In a successful malpractice suit, the plaintiff needs to establish all 4 “Ds” of medical malpractice:
1) Duty, or an established physician–patient relationship
2) Damages from an adverse event
3) Dereliction of duty (negligence)
4) Direct causality between the deviation and the damages.
In the event of a patient suicide, both a doctor–patient relationship (duty) and an adverse outcome (damages) exist.3 Establishing dereliction of duty and direct causality rests on the plaintiff to prove. Good documentation can serve as evidence against accusations of negligence.3
Typically, a patient’s medical record will be used as evidence in a malpractice suit. After a suicide, do not alter this record, such as by editing your past assessments of the patient. If an addendum must be made, such as to document a conversation with suicide survivors (family and friends of the deceased), be sure to label it as such with the current date. An addendum should contain only facts; avoid adding information that attempts to explain your patient’s suicide, justifying or apologizing for past treatment decisions, or otherwise editorializing.
Continue to: Consider reaching out to suicide survivors
Consider reaching out to suicide survivors. The Health Insurance Portability and Accountability Act permits clinicians to use their best judgment when identifying individuals to contact and deciding what information to share after a patient’s death.4 Some states and practice settings have stricter confidentiality laws. Consider seeking legal counsel before interacting with suicide survivors.
Suicide survivors may experience feelings such as guilt, shame, and anger, and these feelings may lead suicide survivors to file a malpractice suit.3 Speaking with suicide survivors can help to address these feelings and potentially decrease the likelihood of them pursuing a malpractice suit. In addition, suicide survivors are at high risk for developing mental health issues, including suicidality. Contacting them can be an opportunity to encourage them to seek mental health treatment. It is important to clarify that any recommendations you provide in such situations do not constitute a doctor–patient relationship.
Should you offer an apology? Consider seeking legal counsel if you wish to apologize. Some states have “apology laws” that render a clinician’s apologetic statements inadmissible if a malpractice suit should occur.5 These laws might include empathic statements (“I’m sorry for your loss”) or disclosures of error (“I’m sorry for causing your loss”).5 It is unclear whether these laws affect the likelihood and/or outcome of malpractice suits.5
Focus on empathy. Experiencing a patient suicide can be one of the most challenging events in a psychiatrist’s career. Empathy is crucial, both towards the suicide survivors and to oneself.
1. Shem S. The House of God. New York, NY: Berkley Books; 2010.
2. Schaffer AC, Jena AB, Seabury SA, et al. Rates and characteristics of paid malpractice claims among US physicians by specialty, 1992-2014. JAMA Intern Med. 2017;177(5):710-719.
3. Gutheil TG, Appelbaum PS. Clinical handbook of psychiatry and the law, 3rd ed. Baltimore, MD: Lippincott Williams & Wilkins; 2000.
4. Office of Civil Rights. How can a covered entity determine if a person is a family member prior to an individual’s death. US Department of Health and Human Services. https://www.hhs.gov/hipaa/for-professionals/faq/1505/how-can-a-covered-entity-determine-whether-a-person-is-a-family-member/index.html. Accessed September 9, 2020.
5. McMichael BJ, Van Horn RL, Viscusi WK. “Sorry” is never enough: how state apology laws fail to reduce medical malpractice liability risk. Stanford Law Rev. 2019;71(2):341-409.
1. Shem S. The House of God. New York, NY: Berkley Books; 2010.
2. Schaffer AC, Jena AB, Seabury SA, et al. Rates and characteristics of paid malpractice claims among US physicians by specialty, 1992-2014. JAMA Intern Med. 2017;177(5):710-719.
3. Gutheil TG, Appelbaum PS. Clinical handbook of psychiatry and the law, 3rd ed. Baltimore, MD: Lippincott Williams & Wilkins; 2000.
4. Office of Civil Rights. How can a covered entity determine if a person is a family member prior to an individual’s death. US Department of Health and Human Services. https://www.hhs.gov/hipaa/for-professionals/faq/1505/how-can-a-covered-entity-determine-whether-a-person-is-a-family-member/index.html. Accessed September 9, 2020.
5. McMichael BJ, Van Horn RL, Viscusi WK. “Sorry” is never enough: how state apology laws fail to reduce medical malpractice liability risk. Stanford Law Rev. 2019;71(2):341-409.
Cannabis-derived compounds: What you need to know
Cannabis-derived compounds, such as cannabidiol (CBD), are popping up like weeds (so to speak) in retail and online stores, and are being marketed for a wide range of purported health benefits, most of which are unsubstantiated. Cannabidiol—a chemical component of the Cannabis sativa plant (marijuana)—does not produce intoxication or euphoria (ie, the “high”) that comes from delta-9-tetrahydrocannabinol (THC), which is the psychoactive component of marijuana.1 Cannabidiol has become popular partly due to increased cultural acceptance of marijuana. In a 2019 Pew Research Center survey, 67% of Americans supported marijuana legalization.2
In addition, changing laws have increased the interest in and availability of CBD. The Agricultural Improvement Act of 2018 legalized hemp, which is defined as cannabis and cannabis-derived compounds with significantly low concentrations of THC (<0.3% on a dry weight basis).1,3 However, this act also preserved the FDA’s authority to regulate products containing cannabis and cannabis-derived compounds.1
With the recent emphasis on CBD, it is easy to forget that the FDA has approved a few medications that are derived from or related to cannabis. In this article, I review the current FDA-approved cannabis-related treatments and their indications, and concerns regarding CBD products.
FDA-approved treatments
To date, the FDA has not approved cannabis for the treatment of any medical or psychiatric condition. However, the FDA has approved 1 cannabis-derived medication (CBD) and 2 cannabis-related medications (dronabinol and nabilone) for specific indications (these medications are available by prescription only):
Cannabidiol (brand name: Epidiolex) is approved for the treatment of seizures associated with Lennox-Gastaut syndrome or Dravet syndrome in patients age ≥2, and for the treatment of seizures associated with tuberous sclerosis complex in patients age ≥1.1,4 There are no other FDA-approved medications that contain CBD.
Dronabinol (brand names: Marinol and Syndros) is an antiemetic agent that contains synthetic THC. It is approved for treating or preventing nausea and vomiting caused by cancer medications and for increasing the appetite of individuals with AIDS.1
Nabilone (brand name: Cesamet) is a synthetic compound that is structurally similar to THC. It is approved for treating or preventing nausea and vomiting caused by cancer medications.1
Continue to: Questionable claims about CBD
Questionable claims about CBD
Some manufacturers market CBD products as having a variety of health benefits for both humans and pets, but most of these claims are unsubstantiated.1 The FDA has issued warning letters to several manufacturers who have marketed CBD products as producing therapeutic effects.5
Under the Federal Food, Drug, and Cosmetic Act, any products intended to have a therapeutic effect are considered drugs, and unapproved drugs cannot be distributed or sold in interstate commerce.1 Cannabidiol products cannot be sold as dietary supplements.1 In addition, food products containing CBD cannot be introduced or delivered for introduction into interstate commerce.1 Many CBD products do not contain the amount of CBD advertised, and some contain contaminants such as pesticides and heavy metals.1 Also, CBD products can affect the therapeutic effectiveness of prescription medications.
Discuss CBD with your patients
Ask your patients if they use CBD and, if so, find out which product(s), the quantity and frequency of use, and any effects they have experienced from using them. Patients can report any adverse effects from CBD products to the FDA’s MedWatch program (www.accessdata.fda.gov/scripts/medwatch/). Tell your patients that there is limited or inconclusive evidence regarding the therapeutic efficacy of over-the-counter CBD products for any medical or psychiatric condition. Encourage your patients to be open with you about using these products, so you can make appropriate treatment decisions.
1. US Food and Drug Administration. FDA regulation of cannabis and cannabis-derived products, including cannabidiol (CBD). https://www.fda.gov/news-events/public-health-focus/fda-regulation-cannabis-and-cannabis-derived-products-questions-and-answers. Updated August 3, 2020. Accessed September 1, 2020.
2. Daniller A. Two-thirds of Americans support marijuana legalization. Pew Research Center. https://www.pewresearch.org/fact-tank/2018/10/08/americans-support-marijuana-legalization/. Updated November 14, 2019. Accessed September 1, 2020.
3. Agricultural Improvement Act of 2018, HR 2—115th Cong, Public L No. 115-334 (2018). https://www.congress.gov/bill/115th-congress/house-bill/2/text?overview=closed. Accessed September 1, 2020.
4. US Food and Drug Administration. FDA approves new indication for drug containing an active ingredient derived from cannabis to treat seizures in rare genetic disease. https://www.fda.gov/news-events/press-announcements/fda-approves-new-indication-drug-containing-active-ingredient-derived-cannabis-treat-seizures-rare. Published July 31, 2020. Accessed September 1, 2020.
5. US Food and Drug Administration. Warning letters and test results for cannabidiol-related products. https://www.fda.gov/news-events/public-health-focus/warning-letters-and-test-results-cannabidiol-related-products. Updated August 20, 2020. Accessed September 1, 2020.
Cannabis-derived compounds, such as cannabidiol (CBD), are popping up like weeds (so to speak) in retail and online stores, and are being marketed for a wide range of purported health benefits, most of which are unsubstantiated. Cannabidiol—a chemical component of the Cannabis sativa plant (marijuana)—does not produce intoxication or euphoria (ie, the “high”) that comes from delta-9-tetrahydrocannabinol (THC), which is the psychoactive component of marijuana.1 Cannabidiol has become popular partly due to increased cultural acceptance of marijuana. In a 2019 Pew Research Center survey, 67% of Americans supported marijuana legalization.2
In addition, changing laws have increased the interest in and availability of CBD. The Agricultural Improvement Act of 2018 legalized hemp, which is defined as cannabis and cannabis-derived compounds with significantly low concentrations of THC (<0.3% on a dry weight basis).1,3 However, this act also preserved the FDA’s authority to regulate products containing cannabis and cannabis-derived compounds.1
With the recent emphasis on CBD, it is easy to forget that the FDA has approved a few medications that are derived from or related to cannabis. In this article, I review the current FDA-approved cannabis-related treatments and their indications, and concerns regarding CBD products.
FDA-approved treatments
To date, the FDA has not approved cannabis for the treatment of any medical or psychiatric condition. However, the FDA has approved 1 cannabis-derived medication (CBD) and 2 cannabis-related medications (dronabinol and nabilone) for specific indications (these medications are available by prescription only):
Cannabidiol (brand name: Epidiolex) is approved for the treatment of seizures associated with Lennox-Gastaut syndrome or Dravet syndrome in patients age ≥2, and for the treatment of seizures associated with tuberous sclerosis complex in patients age ≥1.1,4 There are no other FDA-approved medications that contain CBD.
Dronabinol (brand names: Marinol and Syndros) is an antiemetic agent that contains synthetic THC. It is approved for treating or preventing nausea and vomiting caused by cancer medications and for increasing the appetite of individuals with AIDS.1
Nabilone (brand name: Cesamet) is a synthetic compound that is structurally similar to THC. It is approved for treating or preventing nausea and vomiting caused by cancer medications.1
Continue to: Questionable claims about CBD
Questionable claims about CBD
Some manufacturers market CBD products as having a variety of health benefits for both humans and pets, but most of these claims are unsubstantiated.1 The FDA has issued warning letters to several manufacturers who have marketed CBD products as producing therapeutic effects.5
Under the Federal Food, Drug, and Cosmetic Act, any products intended to have a therapeutic effect are considered drugs, and unapproved drugs cannot be distributed or sold in interstate commerce.1 Cannabidiol products cannot be sold as dietary supplements.1 In addition, food products containing CBD cannot be introduced or delivered for introduction into interstate commerce.1 Many CBD products do not contain the amount of CBD advertised, and some contain contaminants such as pesticides and heavy metals.1 Also, CBD products can affect the therapeutic effectiveness of prescription medications.
Discuss CBD with your patients
Ask your patients if they use CBD and, if so, find out which product(s), the quantity and frequency of use, and any effects they have experienced from using them. Patients can report any adverse effects from CBD products to the FDA’s MedWatch program (www.accessdata.fda.gov/scripts/medwatch/). Tell your patients that there is limited or inconclusive evidence regarding the therapeutic efficacy of over-the-counter CBD products for any medical or psychiatric condition. Encourage your patients to be open with you about using these products, so you can make appropriate treatment decisions.
Cannabis-derived compounds, such as cannabidiol (CBD), are popping up like weeds (so to speak) in retail and online stores, and are being marketed for a wide range of purported health benefits, most of which are unsubstantiated. Cannabidiol—a chemical component of the Cannabis sativa plant (marijuana)—does not produce intoxication or euphoria (ie, the “high”) that comes from delta-9-tetrahydrocannabinol (THC), which is the psychoactive component of marijuana.1 Cannabidiol has become popular partly due to increased cultural acceptance of marijuana. In a 2019 Pew Research Center survey, 67% of Americans supported marijuana legalization.2
In addition, changing laws have increased the interest in and availability of CBD. The Agricultural Improvement Act of 2018 legalized hemp, which is defined as cannabis and cannabis-derived compounds with significantly low concentrations of THC (<0.3% on a dry weight basis).1,3 However, this act also preserved the FDA’s authority to regulate products containing cannabis and cannabis-derived compounds.1
With the recent emphasis on CBD, it is easy to forget that the FDA has approved a few medications that are derived from or related to cannabis. In this article, I review the current FDA-approved cannabis-related treatments and their indications, and concerns regarding CBD products.
FDA-approved treatments
To date, the FDA has not approved cannabis for the treatment of any medical or psychiatric condition. However, the FDA has approved 1 cannabis-derived medication (CBD) and 2 cannabis-related medications (dronabinol and nabilone) for specific indications (these medications are available by prescription only):
Cannabidiol (brand name: Epidiolex) is approved for the treatment of seizures associated with Lennox-Gastaut syndrome or Dravet syndrome in patients age ≥2, and for the treatment of seizures associated with tuberous sclerosis complex in patients age ≥1.1,4 There are no other FDA-approved medications that contain CBD.
Dronabinol (brand names: Marinol and Syndros) is an antiemetic agent that contains synthetic THC. It is approved for treating or preventing nausea and vomiting caused by cancer medications and for increasing the appetite of individuals with AIDS.1
Nabilone (brand name: Cesamet) is a synthetic compound that is structurally similar to THC. It is approved for treating or preventing nausea and vomiting caused by cancer medications.1
Continue to: Questionable claims about CBD
Questionable claims about CBD
Some manufacturers market CBD products as having a variety of health benefits for both humans and pets, but most of these claims are unsubstantiated.1 The FDA has issued warning letters to several manufacturers who have marketed CBD products as producing therapeutic effects.5
Under the Federal Food, Drug, and Cosmetic Act, any products intended to have a therapeutic effect are considered drugs, and unapproved drugs cannot be distributed or sold in interstate commerce.1 Cannabidiol products cannot be sold as dietary supplements.1 In addition, food products containing CBD cannot be introduced or delivered for introduction into interstate commerce.1 Many CBD products do not contain the amount of CBD advertised, and some contain contaminants such as pesticides and heavy metals.1 Also, CBD products can affect the therapeutic effectiveness of prescription medications.
Discuss CBD with your patients
Ask your patients if they use CBD and, if so, find out which product(s), the quantity and frequency of use, and any effects they have experienced from using them. Patients can report any adverse effects from CBD products to the FDA’s MedWatch program (www.accessdata.fda.gov/scripts/medwatch/). Tell your patients that there is limited or inconclusive evidence regarding the therapeutic efficacy of over-the-counter CBD products for any medical or psychiatric condition. Encourage your patients to be open with you about using these products, so you can make appropriate treatment decisions.
1. US Food and Drug Administration. FDA regulation of cannabis and cannabis-derived products, including cannabidiol (CBD). https://www.fda.gov/news-events/public-health-focus/fda-regulation-cannabis-and-cannabis-derived-products-questions-and-answers. Updated August 3, 2020. Accessed September 1, 2020.
2. Daniller A. Two-thirds of Americans support marijuana legalization. Pew Research Center. https://www.pewresearch.org/fact-tank/2018/10/08/americans-support-marijuana-legalization/. Updated November 14, 2019. Accessed September 1, 2020.
3. Agricultural Improvement Act of 2018, HR 2—115th Cong, Public L No. 115-334 (2018). https://www.congress.gov/bill/115th-congress/house-bill/2/text?overview=closed. Accessed September 1, 2020.
4. US Food and Drug Administration. FDA approves new indication for drug containing an active ingredient derived from cannabis to treat seizures in rare genetic disease. https://www.fda.gov/news-events/press-announcements/fda-approves-new-indication-drug-containing-active-ingredient-derived-cannabis-treat-seizures-rare. Published July 31, 2020. Accessed September 1, 2020.
5. US Food and Drug Administration. Warning letters and test results for cannabidiol-related products. https://www.fda.gov/news-events/public-health-focus/warning-letters-and-test-results-cannabidiol-related-products. Updated August 20, 2020. Accessed September 1, 2020.
1. US Food and Drug Administration. FDA regulation of cannabis and cannabis-derived products, including cannabidiol (CBD). https://www.fda.gov/news-events/public-health-focus/fda-regulation-cannabis-and-cannabis-derived-products-questions-and-answers. Updated August 3, 2020. Accessed September 1, 2020.
2. Daniller A. Two-thirds of Americans support marijuana legalization. Pew Research Center. https://www.pewresearch.org/fact-tank/2018/10/08/americans-support-marijuana-legalization/. Updated November 14, 2019. Accessed September 1, 2020.
3. Agricultural Improvement Act of 2018, HR 2—115th Cong, Public L No. 115-334 (2018). https://www.congress.gov/bill/115th-congress/house-bill/2/text?overview=closed. Accessed September 1, 2020.
4. US Food and Drug Administration. FDA approves new indication for drug containing an active ingredient derived from cannabis to treat seizures in rare genetic disease. https://www.fda.gov/news-events/press-announcements/fda-approves-new-indication-drug-containing-active-ingredient-derived-cannabis-treat-seizures-rare. Published July 31, 2020. Accessed September 1, 2020.
5. US Food and Drug Administration. Warning letters and test results for cannabidiol-related products. https://www.fda.gov/news-events/public-health-focus/warning-letters-and-test-results-cannabidiol-related-products. Updated August 20, 2020. Accessed September 1, 2020.
A STEEEP Hill to Climb: A Scoping Review of Assessments of Individual Hospitalist Performance
Healthcare quality is defined as the extent to which healthcare services result in desired outcomes.1 Quality of care depends on how the healthcare system’s various components, including healthcare practitioners, interact to meet each patient’s needs.2 These components can be shaped to achieve desired outcomes through rules, incentives, and other approaches, but influencing the behaviors of each component, such as the performance of hospitalists, requires defining goals for performance and implementing measurement approaches to assess progress toward these goals.
One set of principles to define goals for quality and guide assessment of desired behaviors is the multidimensional STEEEP framework. This framework, created by the Institute of Medicine, identifies six domains of quality: Safe, Timely, Effective, Efficient, Equitable, and Patient Centered.2 Briefly, “Safe” means avoiding injuries to patients, “Timely” means reducing waits and delays in care, “Effective” means providing care based on evidence, “Efficient” means avoiding waste, “Equitable” means ensuring quality does not vary based on personal characteristics such as race and gender, and “Patient Centered” means providing care that is responsive to patients’ values and preferences. The STEEEP domains are not coequal; rather, they ensure that quality is considered broadly, while avoiding errors such as measuring only an intervention’s impact on effectiveness but not assessing its impact on multiple domains of quality, such as how patient centered, efficient (cost effective), or equitable the resulting care is.
Based on our review of the literature, a multidimensional framework like STEEEP has not been used in defining and assessing the quality of individual hospitalists’ performance. Some quality metrics at the hospital level impact several dimensions simultaneously, such as door to balloon time for acute myocardial infarction, which measures effectiveness and timeliness of care. Programs like pay-for-performance, Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS), and the Merit-Based Incentive Payment System (MIPS) have tied reimbursement to assessments aligned with several STEEEP domains at both individual and institutional levels but lack a holistic approach to quality.3-6 The every-other-year State of Hospital Medicine Report, the most widely used description of individual hospitalist performance, reports group-level performance including relative value units and whether groups are accountable for measures of quality such as performance on core measures, timely documentation, and “citizenship” (eg, committee participation or academic work).7 While these are useful benchmarks, the report focuses on performance at the group level. Concurrently, several academic groups have described more complete dashboards or scorecards to assess individual hospitalist performance, primarily designed to facilitate comparison across hospitalist groups or to incentivize overall group performance.8-10 However, these efforts are not guided by an overarching framework and are structured after traditional academic models with components related to teaching and scholarship, which may not translate to nonacademic environments. Finally, the Core Competencies for Hospital Medicine outlines some goals for hospitalist performance but does not speak to specific measurement approaches.11
Overall, assessing individual hospitalist performance is hindered by lack of consensus on important concepts to measure, a limited number of valid measures, and challenges in data collection such as resource limitations and feasibility. Developing and refining measures grounded in the STEEEP framework may provide a more comprehensive assessment of hospitalist quality and identify approaches to improve overall health outcomes. Comparative data could help individual hospitalists improve performance; leaders of hospitalist groups could use this data to guide faculty development and advancement as they ensure quality care at the individual, group, and system levels.
To better inform quality measurement of individual hospitalists, we sought to identify existing publications on individual hospitalist quality. Our goal was to define the published literature about quality measurement at the individual hospitalist level, relate these publications to domains of quality defined by the STEEEP framework, and identify directions for assessment or further research that could affect the overall quality of care.
METHODS
We conducted a scoping review following methods outlined by Arksey and O’Malley12 and Tricco.13 The goal of a scoping review is to map the extent of research within a specific field. This methodology is well suited to characterizing the existing research related to the quality of hospitalist care at the individual level. A protocol for the scoping review was not registered.
Evidence Search
A systematic search for published, English-language literature on hospitalist care was conducted in Medline (Ovid; 1946 - June 4, 2019) on June 5, 2019. The search used a combination of keywords and controlled vocabulary for the concept of hospitalists or hospital medicine. The search strategy used in this review is described in the Appendix. In addition, a hand search of reference lists of articles was used to discover publications not identified in the database searches.
Study Selection
All references were uploaded to Covidence systematic review software (www.covidence.org; Covidence), and duplicates were removed. Four reviewers (A.D., B.C., L.H., R.Q.) conducted title and abstract, as well as full-text, review to identify studies that measured differences in the performance of hospitalists at the individual level. Any disagreements among reviewers were resolved by consensus. Articles included both adult and pediatric populations. Articles that focused on group-level outcomes could be included if nonpooled data at the individual level was also reported. Studies were excluded if they did not focus on individual quality of care indicators or were not published in English.
Data Charting and Synthesis
We extracted the following information using a standardized data collection form: author, title, year of publication, study design, intervention, and outcome measures. Original manuscripts were accessed as needed to supplement analysis. Critical appraisal of individual studies was not conducted in this review because the goal of this review was to analyze which quality indicators have been studied and how they were measured. Articles were then coded for their alignment to the STEEEP framework by two reviewers (AD and BC). After initial coding was conducted, the reviewers met to consolidate codes and resolve any disagreement by consensus. The results of the analysis were summarized in both text and tabular format with studies grouped by focus of assessment with each one’s methods of assessment listed.
RESULTS
Results of the search strategy are shown in the Figure. The search retrieved a total of 2,363 references of which 113 were duplicates, leaving 2,250 to be screened. After title and abstract and full-text screening, 42 studies were included in the review. The final 42 studies were coded for alignment with the STEEEP framework. The Table displays the focus of assessment and methods of assessment within each STEEEP domain.
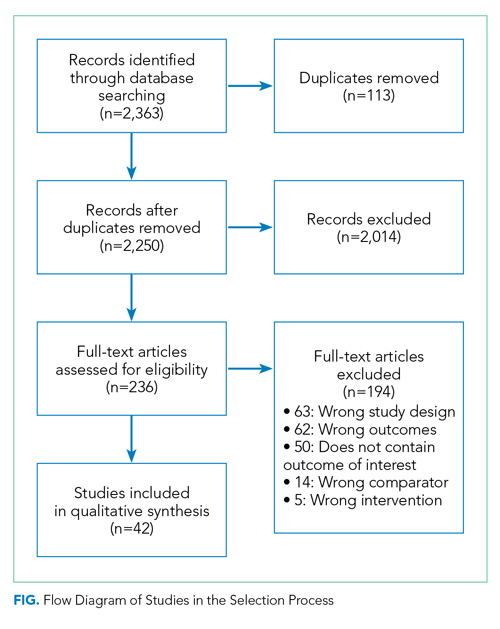
Eighteen studies were coded into a single domain while the rest were coded into at least two domains. The domain Patient Centered was coded as having the most studies (n = 23), followed by the domain of Safe (n = 15). Timely, Effective, and Efficient domains had 11, 9, and 12 studies, respectively. No studies were coded into the domain of Equitable.
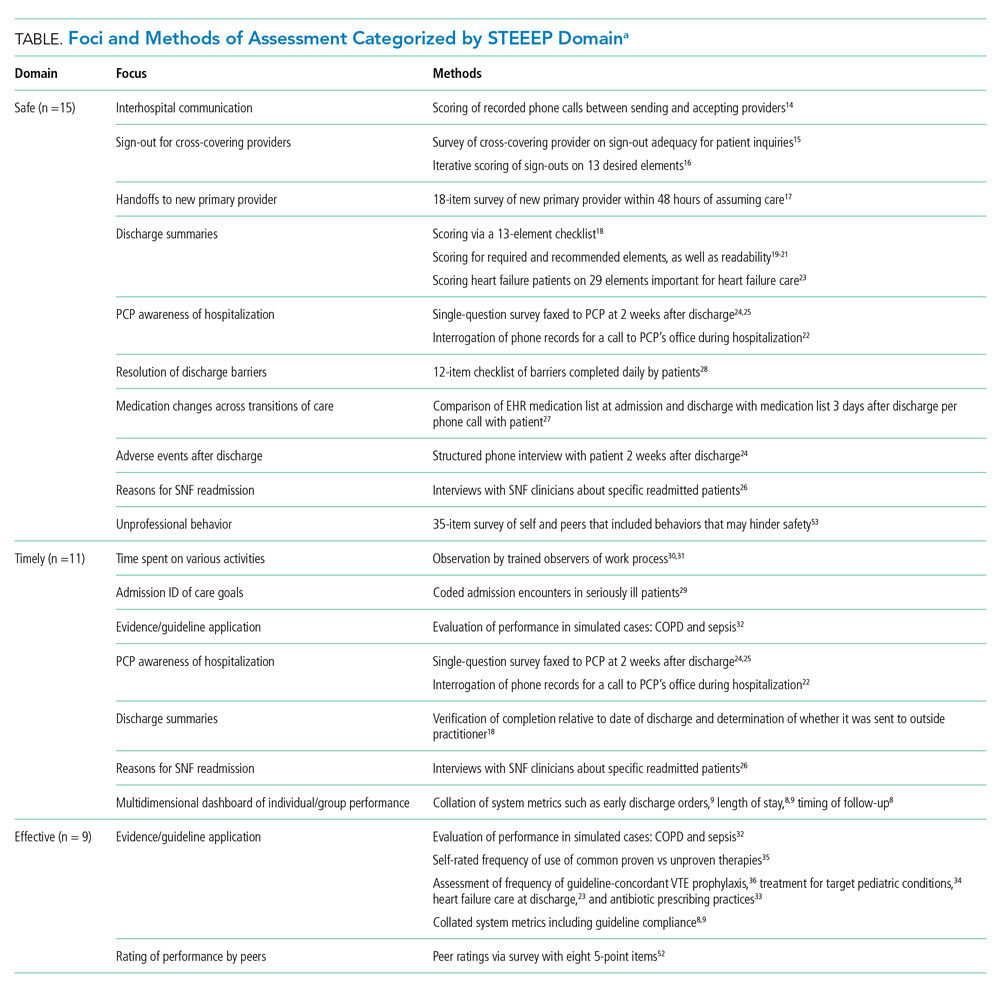
Safe
Nearly all studies coded into the Safe domain focused on transitions of care. These included transfers into a hospital from other hospitals,14 transitions of care to cross-covering providers15,16 and new primary providers,17 and transition out from the acute care setting.18-28 Measures of hospital discharge included measures of both processes18-22 and outcomes.23-27 Methods of assessment varied from use of trained observers or scorers to surveys of individuals and colleagues about performance. Though a few leveraged informatics,22,27 all approaches relied on human interaction, and none were automated.

Timely
All studies coded into the Timely domain were coded into at least one other domain. For example, Anderson et al looked at how hospitalists communicated about potential life-limiting illness at the time of hospital admission and the subsequent effects on plans of care29; this was coded as both Timely and Patient Centered. Likewise, another group of studies centered on application of evidence-based guidelines, such as giving antibiotics within a certain time interval for sepsis and were coded as both Timely and Effective. Another set of authors described dashboards or scorecards that captured a number of group-level metrics of processes of care that span STEEEP domains and may be applicable to individuals, including Fox et al for pediatrics8 and Hwa et al for an adult academic hospitalist group.9 Methods of assessment varied widely across studies and included observations in the clinical environment,28,30,31 performance in simulations,32 and surveys about performance.22-26 A handful of approaches were more automated and made use of informatics8,9,22 or data collected for other health system purposes.8,9
Effective
Effectiveness was most often assessed through adherence to consensus and evidence-based guidelines. Examples included processes of care related to sepsis, venous thromboembolism prophylaxis, COPD, heart failure, pediatric asthma, and antibiotic appropriateness.8,9,23,32-36 Through the review, multiple other studies that included group-level measures of effectiveness for a variety of health conditions were excluded because data on individual-level variation were not reported. Methods of assessment included expert review of cases or discharge summaries, compliance with core measures, performance in simulation, and self-assessment on practice behaviors. Other than those efforts aligned with institutional data collection, most approaches were resource intensive.
Efficient
As with those in the Timely domain, most studies coded into the Efficient domain were coded into at least one other domain. One exception measured unnecessary daily lab work and both showed provider-level variation and demonstrated improvement in quality based on an intervention.37 Another paper coded into the Effective domain evaluated adherence to components of the Choosing Wisely® recommendations.34 In addition to these two studies focusing on cost efficacy, other studies coded to this domain assessed concepts such as ensuring more efficient care from other providers by optimizing transitions of care15-17 and clarifying patients’ goals for care.38 Although integrating insurer information into care plans is emphasized in the Core Competencies of Hospital Medicine,11 this concept was not represented in any of the identified articles. Methods of assessment varied and mostly relied on observation of behaviors or survey of providers. Several approaches were more automated or used Medicare claims data to assess the efficiency of individual providers relative to peers.34,37,39
Equitable
Among the studies reviewed, none were coded into the Equitable domain despite care of vulnerable populations being identified as a core competency of hospital medicine.40
Patient Centered
Studies coded to the Patient Centered domain assessed hospitalist performance through ratings of patient satisfaction,8,9,41-44 rating of communication between hospitalists and patients,19-21,29,45-51 identification of patient preferences,38,52 outcomes of patient-centered care activities,27,28 and peer ratings.53,54 Authors applied several theoretical constructs to these assessments including shared decision-making,50 etiquette-based medicine,47,48 empathetic responsiveness,45 agreement about the goals of care between the patient and healthcare team members,52 and lapses in professionalism.53 Studies often crossed STEEEP domains, such as those assessing quality of discharge information provided to patients, which were coded as both Safe and Patient Centered.19-21 In addition to coded or observed performance in the clinical setting, studies in this domain also used patient ratings as a method of assessment.8,9,28,41-44,49,50 Only a few of these approaches aligned with existing performance measures of health systems and were more automated.8,9
DISCUSSION
This scoping review of performance data for individual hospitalists coded to the STEEEP framework identified robust areas in the published literature, as well as opportunities to develop new approaches or refine existing measures. Transitions of care, both intrahospital and at discharge, and adherence to evidence-based guidelines are areas for which current research has created a foundation for care that is Safe, Timely, Effective, and Efficient. The Patient Centered domain also has several measures described, though the conceptual underpinnings are heterogeneous, and consensus appears necessary to compare performance across groups. No studies were coded to the Equitable domain. Across domains, approaches to measurement varied in resource intensity from simple ones, like integrating existing data collected by hospitals, to more complex ones, like shadowing physicians or coding interactions.
Methods of assessment coded into the Safe domain focused on communication and, less so, patient outcomes around transitions of care. Transitions of care that were evaluated included transfer of patients into a new facility, sign-out to new physicians for both cross-cover responsibilities and for newly assuming the role of primary attending, and discharge from the hospital. Most measures rated the quality of communication, although several23-27 examined patient outcomes. Approaches that survey individuals downstream from a transition of care15,17,24-26 may be the simplest and most feasible approach to implement in the future but, as described to date, do not include all transitions of care and may miss patient outcomes. Important core competencies for hospital medicine under the Safe domain that were not identified in this review include areas such as diagnostic error, hospital-acquired infections, error reporting, and medication safety.11 These are potential areas for future measure development.
The assessments in many studies were coded across more than one domain; for example, measures of the application of evidence-based guidelines were coded into domains of Effective, Timely, Efficient, and others. Applying the six domains of the STEEEP framework revealed the multidimensional outcomes of hospitalist work and could guide more meaningful quality assessments of individual hospitalist performance. For example, assessing adherence to evidence-based guidelines, as well as consideration of the Core Competencies of Hospital Medicine and recommendations of the Choosing Wisely® campaign, are promising areas for measurement and may align with existing hospital metrics. Notably, several reviewed studies measured group-level adherence to guidelines but were excluded because they did not examine variation at the individual level. Future measures based on evidence-based guidelines could center on the Effective domain while also integrating assessment of domains such as Efficient, Timely, and Patient Centered and, in so doing, provide a richer assessment of the diverse aspects of quality.
Several other approaches in the domains of Timely, Effective, and Efficient were described only in a few studies yet deserve consideration for further development. Two time-motion studies30,31 were coded into the domains of Timely and Efficient and would be cumbersome in regular practice but, with advances in wearable technology and electronic health records, could become more feasible in the future. Another approach used Medicare payment data to detect provider-level variation.39 Potentially, “big data” could be analyzed in other ways to compare the performance of individual hospitalists.
The lack of studies coded into the Equitable domain may seem surprising, but the Institute for Healthcare Improvement identifies Equitable as the “forgotten aim” of the STEEEP framework. This organization has developed a guide for health care organizations to promote equitable care.55 While this guide focuses mostly on organizational-level actions, some are focused on individual providers, such as training in implicit bias. Future research should seek to identify disparities in care by individual providers and develop interventions to address any discovered gaps.
The “Patient Centered” domain was the most frequently coded and had the most heterogeneous underpinnings for assessment. Studies varied widely in terminology and conceptual foundations. The field would benefit from future work to identify how “Patient Centered” care might be more clearly conceptualized, guided by comparative studies among different assessment approaches to define those most valid and feasible.
The overarching goal for measuring individual hospitalist quality should be to improve the delivery of patient care in a supportive and formative way. To further this goal, adding or expanding on metrics identified in this article may provide a more complete description of performance. As a future direction, groups should consider partnering with one another to define measurement approaches, collaborate with existing data sources, and even share deidentified individual data to establish performance benchmarks at the individual and group levels.
While this study used broad search terms to support completeness, the search process could have missed important studies. Grey literature, non–English language studies, and industry reports were not included in this review. Groups may also be using other assessments of individual hospitalist performance that are not published in the peer-reviewed literature. Coding of study assessments was achieved through consensus reconciliation; other coders might have classified studies differently.
CONCLUSION
This scoping review describes the peer-reviewed literature of individual hospitalist performance and is the first to link it to the STEEEP quality framework. Assessments of transitions of care, evidence-based care, and cost-effective care are exemplars in the published literature. Patient-centered care is well studied but assessed in a heterogeneous fashion. Assessments of equity in care are notably absent. The STEEEP framework provides a model to structure assessment of individual performance. Future research should build on this framework to define meaningful assessment approaches that are actionable and improve the welfare of our patients and our system.
Disclosures
The authors have nothing to disclose.
1. Quality of Care: A Process for Making Strategic Choices in Health Systems. World Health Organization; 2006.
2. Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. National Academies Press; 2001. Accessed December 20, 2019. http://www.ncbi.nlm.nih.gov/books/NBK222274/
3. Wadhera RK, Joynt Maddox KE, Wasfy JH, Haneuse S, Shen C, Yeh RW. Association of the hospital readmissions reduction program with mortality among Medicare beneficiaries hospitalized for heart failure, acute myocardial infarction, and pneumonia. JAMA. 2018;320(24):2542-2552. https://doi.org/10.1001/jama.2018.19232
4. Kondo KK, Damberg CL, Mendelson A, et al. Implementation processes and pay for performance in healthcare: a systematic review. J Gen Intern Med. 2016;31(Suppl 1):61-69. https://doi.org/10.1007/s11606-015-3567-0
5. Fung CH, Lim Y-W, Mattke S, Damberg C, Shekelle PG. Systematic review: the evidence that publishing patient care performance data improves quality of care. Ann Intern Med. 2008;148(2):111-123. https://doi.org/10.7326/0003-4819-148-2-200801150-00006
6. Jha AK, Orav EJ, Epstein AM. Public reporting of discharge planning and rates of readmissions. N Engl J Med. 2009;361(27):2637-2645. https://doi.org/10.1056/NEJMsa0904859
7. Society of Hospital Medicine. State of Hospital Medicine Report; 2018. Accessed December 20, 2019. https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/
8. Hwa M, Sharpe BA, Wachter RM. Development and implementation of a balanced scorecard in an academic hospitalist group. J Hosp Med. 2013;8(3):148-153. https://doi.org/10.1002/jhm.2006
9. Fox LA, Walsh KE, Schainker EG. The creation of a pediatric hospital medicine dashboard: performance assessment for improvement. Hosp Pediatr. 2016;6(7):412-419. https://doi.org/10.1542/hpeds.2015-0222
10. Hain PD, Daru J, Robbins E, et al. A proposed dashboard for pediatric hospital medicine groups. Hosp Pediatr. 2012;2(2):59-68. https://doi.org/10.1542/hpeds.2012-0004
11. Nichani S, Crocker J, Fitterman N, Lukela M. Updating the core competencies in hospital medicine--2017 revision: introduction and methodology. J Hosp Med. 2017;12(4):283-287. https://doi.org/10.12788/jhm.2715
12. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19-32. https://doi.org/10.1080/1364557032000119616
13. Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467-473. https://doi.org/10.7326/m18-0850
14. Borofsky JS, Bartsch JC, Howard AB, Repp AB. Quality of interhospital transfer communication practices and association with adverse events on an internal medicine hospitalist service. J Healthc Qual. 2017;39(3):177-185. https://doi.org/10.1097/01.JHQ.0000462682.32512.ad
15. Fogerty RL, Schoenfeld A, Salim Al-Damluji M, Horwitz LI. Effectiveness of written hospitalist sign-outs in answering overnight inquiries. J Hosp Med. 2013;8(11):609-614. https://doi.org10.1002/jhm.2090
16. Miller DM, Schapira MM, Visotcky AM, et al. Changes in written sign-out composition across hospitalization. J Hosp Med. 2015;10(8):534-536. https://doi.org/10.1002/jhm.2390
17. Hinami K, Farnan JM, Meltzer DO, Arora VM. Understanding communication during hospitalist service changes: a mixed methods study. J Hosp Med. 2009;4(9):535-540. https://doi.org/10.1002/jhm.523
18. Horwitz LI, Jenq GY, Brewster UC, et al. Comprehensive quality of discharge summaries at an academic medical center. J Hosp Med. 2013;8(8):436-443. https://doi.org10.1002/jhm.2021
19. Sarzynski E, Hashmi H, Subramanian J, et al. Opportunities to improve clinical summaries for patients at hospital discharge. BMJ Qual Saf. 2017;26(5):372-380. https://doi.org/10.1136/bmjqs-2015-005201
20. Unaka NI, Statile A, Haney J, Beck AF, Brady PW, Jerardi KE. Assessment of readability, understandability, and completeness of pediatric hospital medicine discharge instructions. J Hosp Med. 2017;12(2):98-101. https://doi.org/10.12788/jhm.2688
21. Unaka N, Statile A, Jerardi K, et al. Improving the readability of pediatric hospital medicine discharge instructions. J Hosp Med. 2017;12(7):551-557. https://doi.org/10.12788/jhm.2770
22. Zackoff MW, Graham C, Warrick D, et al. Increasing PCP and hospital medicine physician verbal communication during hospital admissions. Hosp Pediatr. 2018;8(4):220-226. https://doi.org/10.1542/hpeds.2017-0119
23. Salata BM, Sterling MR, Beecy AN, et al. Discharge processes and 30-day readmission rates of patients hospitalized for heart failure on general medicine and cardiology services. Am J Cardiol. 2018;121(9):1076-1080. https://doi.org/10.1016/j.amjcard.2018.01.027
24. Arora VM, Prochaska ML, Farnan JM, et al. Problems after discharge and understanding of communication with their primary care physicians among hospitalized seniors: a mixed methods study. J Hosp Med. 2010;5(7):385-391. https://doi.org/10.1002/jhm.668
25. Bell CM, Schnipper JL, Auerbach AD, et al. Association of communication between hospital-based physicians and primary care providers with patient outcomes. J Gen Intern Med. 2009;24(3):381-386. https://doi.org/10.1007/s11606-008-0882-8
26. Clark B, Baron K, Tynan-McKiernan K, Britton M, Minges K, Chaudhry S. Perspectives of clinicians at skilled nursing facilities on 30-day hospital readmissions: a qualitative study. J Hosp Med. 2017;12(8):632-638. https://doi.org/10.12788/jhm.2785
27. Harris CM, Sridharan A, Landis R, Howell E, Wright S. What happens to the medication regimens of older adults during and after an acute hospitalization? J Patient Saf. 2013;9(3):150-153. https://doi.org/10.1097/PTS.0b013e318286f87d
28. Harrison JD, Greysen RS, Jacolbia R, Nguyen A, Auerbach AD. Not ready, not set...discharge: patient-reported barriers to discharge readiness at an academic medical center. J Hosp Med. 2016;11(9):610-614. https://doi.org/10.1002/jhm.2591
29. Anderson WG, Kools S, Lyndon A. Dancing around death: hospitalist-patient communication about serious illness. Qual Health Res. 2013;23(1):3-13. https://doi.org/10.1177/1049732312461728
30. Tipping MD, Forth VE, Magill DB, Englert K, Williams MV. Systematic review of time studies evaluating physicians in the hospital setting. J Hosp Med. 2010;5(6):353-359. https://doi.org/10.1002/jhm.647
31. Tipping MD, Forth VE, O’Leary KJ, et al. Where did the day go?--a time-motion study of hospitalists. J Hosp Med. 2010;5(6):323-328. https://doi.org/10.1002/jhm.790
32. Bergmann S, Tran M, Robison K, et al. Standardising hospitalist practice in sepsis and COPD care. BMJ Qual Saf. 2019;28(10):800-808. https://doi.org/10.1136/bmjqs-2018-008829
33. Kisuule F, Wright S, Barreto J, Zenilman J. Improving antibiotic utilization among hospitalists: a pilot academic detailing project with a public health approach. J Hosp Med. 2008;3(1):64-70. https://doi.org/10.1002/jhm.278
34. Reyes M, Paulus E, Hronek C, et al. Choosing Wisely campaign: report card and achievable benchmarks of care for children’s hospitals. Hosp Pediatr. 2017;7(11):633-641. https://doi.org/10.1542/hpeds.2017-0029
35. Landrigan CP, Conway PH, Stucky ER, et al. Variation in pediatric hospitalists’ use of proven and unproven therapies: a study from the Pediatric Research in Inpatient Settings (PRIS) network. J Hosp Med. 2008;3(4):292-298. https://doi.org/10.1002/jhm.347
36. Michtalik HJ, Carolan HT, Haut ER, et al. Use of provider-level dashboards and pay-for-performance in venous thromboprophylaxis. J Hosp Med. 2015;10(3):172-178. https://doi.org/10.1002/jhm.2303
37. Johnson DP, Lind C, Parker SE, et al. Toward high-value care: a quality improvement initiative to reduce unnecessary repeat complete blood counts and basic metabolic panels on a pediatric hospitalist service. Hosp Pediatr. 2016;6(1):1-8. https://doi.org/10.1542/hpeds.2015-0099
38. Auerbach AD, Katz R, Pantilat SZ, et al. Factors associated with discussion of care plans and code status at the time of hospital admission: results from the Multicenter Hospitalist Study. J Hosp Med. 2008;3(6):437-445. https://doi.org/10.1002/jhm.369
39. Tsugawa Y, Jha AK, Newhouse JP, Zaslavsky AM, Jena AB. Variation in physician spending and association with patient outcomes. JAMA Intern Med. 2017;177(5):675-682. https://doi.org/10.1001/jamainternmed.2017.0059
40. Nichani S, Fitterman N, Lukela M, Crocker J. Equitable allocation of resources. 2017 hospital medicine revised core competencies. J Hosp Med. 2017;12(4):S62. https://doi.org/10.12788/jhm.3016
41. Blanden AR, Rohr RE. Cognitive interview techniques reveal specific behaviors and issues that could affect patient satisfaction relative to hospitalists. J Hosp Med. 2009;4(9):E1-E6. https://doi.org/10.1002/jhm.524
42. Torok H, Ghazarian SR, Kotwal S, Landis R, Wright S, Howell E. Development and validation of the tool to assess inpatient satisfaction with care from hospitalists. J Hosp Med. 2014;9(9):553-558. https://doi.org/10.1002/jhm.2220
43. Torok H, Kotwal S, Landis R, Ozumba U, Howell E, Wright S. Providing feedback on clinical performance to hospitalists: Experience using a new metric tool to assess inpatient satisfaction with care from hospitalists. J Contin Educ Health Prof. 2016;36(1):61-68. https://doi.org/10.1097/CEH.0000000000000060
44. Indovina K, Keniston A, Reid M, et al. Real-time patient experience surveys of hospitalized medical patients. J Hosp Med. 2016;11(4):251-256. https://doi.org/10.1002/jhm.2533
45. Weiss R, Vittinghoff E, Fang MC, et al. Associations of physician empathy with patient anxiety and ratings of communication in hospital admission encounters. J Hosp Med. 2017;12(10):805-810. https://doi.org/10.12788/jhm.2828
46. Apker J, Baker M, Shank S, Hatten K, VanSweden S. Optimizing hospitalist-patient communication: an observation study of medical encounter quality. Jt Comm J Qual Patient Saf. 2018;44(4):196-203. https://doi.org/10.1016/j.jcjq.2017.08.011
47. Kotwal S, Torok H, Khaliq W, Landis R, Howell E, Wright S. Comportment and communication patterns among hospitalist physicians: insight gleaned through observation. South Med J. 2015;108(8):496-501. https://doi.org/10.14423/SMJ.0000000000000328
48. Tackett S, Tad-y D, Rios R, Kisuule F, Wright S. Appraising the practice of etiquette-based medicine in the inpatient setting. J Gen Intern Med. 2013;28(7):908-913. https://doi.org/10.1007/s11606-012-2328-6
49. Ferranti DE, Makoul G, Forth VE, Rauworth J, Lee J, Williams MV. Assessing patient perceptions of hospitalist communication skills using the Communication Assessment Tool (CAT). J Hosp Med. 2010;5(9):522-527. https://doi.org/10.1002/jhm.787
50. Blankenburg R, Hilton JF, Yuan P, et al. Shared decision-making during inpatient rounds: opportunities for improvement in patient engagement and communication. J Hosp Med. 2018;13(7):453-461. https://doi.org/10.12788/jhm.2909
51. Chang D, Mann M, Sommer T, Fallar R, Weinberg A, Friedman E. Using standardized patients to assess hospitalist communication skills. J Hosp Med. 2017;12(7):562-566. https://doi.org/10.12788/jhm.2772
52. Figueroa JF, Schnipper JL, McNally K, Stade D, Lipsitz SR, Dalal AK. How often are hospitalized patients and providers on the same page with regard to the patient’s primary recovery goal for hospitalization? J Hosp Med. 2016;11(9):615-619. https://doi.org/10.1002/jhm.2569
53. Reddy ST, Iwaz JA, Didwania AK, et al. Participation in unprofessional behaviors among hospitalists: a multicenter study. J Hosp Med. 2012;7(7):543-550. https://doi.org/10.1002/jhm.1946
54. Bhogal HK, Howe E, Torok H, Knight AM, Howell E, Wright S. Peer assessment of professional performance by hospitalist physicians. South Med J. 2012;105(5):254-258. https://doi.org/10.1097/SMJ.0b013e318252d602
55. Wyatt R, Laderman M, Botwinick L, Mate K, Whittington J. Achieving health equity: a guide for health care organizations. IHI White Paper. Institute for Healthcare Improvement; 2016. https://www.ihi.org
Healthcare quality is defined as the extent to which healthcare services result in desired outcomes.1 Quality of care depends on how the healthcare system’s various components, including healthcare practitioners, interact to meet each patient’s needs.2 These components can be shaped to achieve desired outcomes through rules, incentives, and other approaches, but influencing the behaviors of each component, such as the performance of hospitalists, requires defining goals for performance and implementing measurement approaches to assess progress toward these goals.
One set of principles to define goals for quality and guide assessment of desired behaviors is the multidimensional STEEEP framework. This framework, created by the Institute of Medicine, identifies six domains of quality: Safe, Timely, Effective, Efficient, Equitable, and Patient Centered.2 Briefly, “Safe” means avoiding injuries to patients, “Timely” means reducing waits and delays in care, “Effective” means providing care based on evidence, “Efficient” means avoiding waste, “Equitable” means ensuring quality does not vary based on personal characteristics such as race and gender, and “Patient Centered” means providing care that is responsive to patients’ values and preferences. The STEEEP domains are not coequal; rather, they ensure that quality is considered broadly, while avoiding errors such as measuring only an intervention’s impact on effectiveness but not assessing its impact on multiple domains of quality, such as how patient centered, efficient (cost effective), or equitable the resulting care is.
Based on our review of the literature, a multidimensional framework like STEEEP has not been used in defining and assessing the quality of individual hospitalists’ performance. Some quality metrics at the hospital level impact several dimensions simultaneously, such as door to balloon time for acute myocardial infarction, which measures effectiveness and timeliness of care. Programs like pay-for-performance, Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS), and the Merit-Based Incentive Payment System (MIPS) have tied reimbursement to assessments aligned with several STEEEP domains at both individual and institutional levels but lack a holistic approach to quality.3-6 The every-other-year State of Hospital Medicine Report, the most widely used description of individual hospitalist performance, reports group-level performance including relative value units and whether groups are accountable for measures of quality such as performance on core measures, timely documentation, and “citizenship” (eg, committee participation or academic work).7 While these are useful benchmarks, the report focuses on performance at the group level. Concurrently, several academic groups have described more complete dashboards or scorecards to assess individual hospitalist performance, primarily designed to facilitate comparison across hospitalist groups or to incentivize overall group performance.8-10 However, these efforts are not guided by an overarching framework and are structured after traditional academic models with components related to teaching and scholarship, which may not translate to nonacademic environments. Finally, the Core Competencies for Hospital Medicine outlines some goals for hospitalist performance but does not speak to specific measurement approaches.11
Overall, assessing individual hospitalist performance is hindered by lack of consensus on important concepts to measure, a limited number of valid measures, and challenges in data collection such as resource limitations and feasibility. Developing and refining measures grounded in the STEEEP framework may provide a more comprehensive assessment of hospitalist quality and identify approaches to improve overall health outcomes. Comparative data could help individual hospitalists improve performance; leaders of hospitalist groups could use this data to guide faculty development and advancement as they ensure quality care at the individual, group, and system levels.
To better inform quality measurement of individual hospitalists, we sought to identify existing publications on individual hospitalist quality. Our goal was to define the published literature about quality measurement at the individual hospitalist level, relate these publications to domains of quality defined by the STEEEP framework, and identify directions for assessment or further research that could affect the overall quality of care.
METHODS
We conducted a scoping review following methods outlined by Arksey and O’Malley12 and Tricco.13 The goal of a scoping review is to map the extent of research within a specific field. This methodology is well suited to characterizing the existing research related to the quality of hospitalist care at the individual level. A protocol for the scoping review was not registered.
Evidence Search
A systematic search for published, English-language literature on hospitalist care was conducted in Medline (Ovid; 1946 - June 4, 2019) on June 5, 2019. The search used a combination of keywords and controlled vocabulary for the concept of hospitalists or hospital medicine. The search strategy used in this review is described in the Appendix. In addition, a hand search of reference lists of articles was used to discover publications not identified in the database searches.
Study Selection
All references were uploaded to Covidence systematic review software (www.covidence.org; Covidence), and duplicates were removed. Four reviewers (A.D., B.C., L.H., R.Q.) conducted title and abstract, as well as full-text, review to identify studies that measured differences in the performance of hospitalists at the individual level. Any disagreements among reviewers were resolved by consensus. Articles included both adult and pediatric populations. Articles that focused on group-level outcomes could be included if nonpooled data at the individual level was also reported. Studies were excluded if they did not focus on individual quality of care indicators or were not published in English.
Data Charting and Synthesis
We extracted the following information using a standardized data collection form: author, title, year of publication, study design, intervention, and outcome measures. Original manuscripts were accessed as needed to supplement analysis. Critical appraisal of individual studies was not conducted in this review because the goal of this review was to analyze which quality indicators have been studied and how they were measured. Articles were then coded for their alignment to the STEEEP framework by two reviewers (AD and BC). After initial coding was conducted, the reviewers met to consolidate codes and resolve any disagreement by consensus. The results of the analysis were summarized in both text and tabular format with studies grouped by focus of assessment with each one’s methods of assessment listed.
RESULTS
Results of the search strategy are shown in the Figure. The search retrieved a total of 2,363 references of which 113 were duplicates, leaving 2,250 to be screened. After title and abstract and full-text screening, 42 studies were included in the review. The final 42 studies were coded for alignment with the STEEEP framework. The Table displays the focus of assessment and methods of assessment within each STEEEP domain.
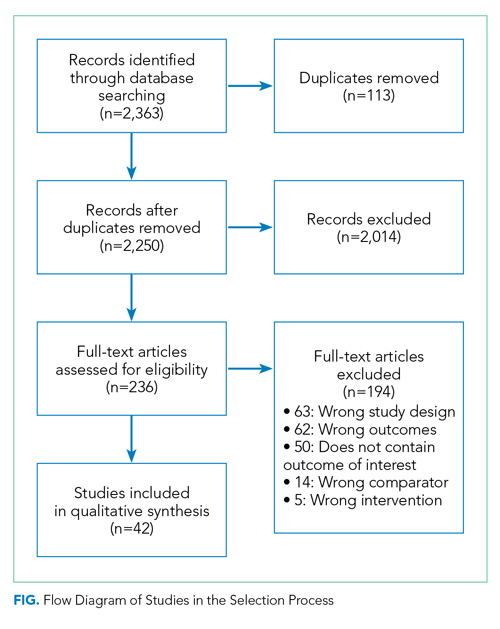
Eighteen studies were coded into a single domain while the rest were coded into at least two domains. The domain Patient Centered was coded as having the most studies (n = 23), followed by the domain of Safe (n = 15). Timely, Effective, and Efficient domains had 11, 9, and 12 studies, respectively. No studies were coded into the domain of Equitable.
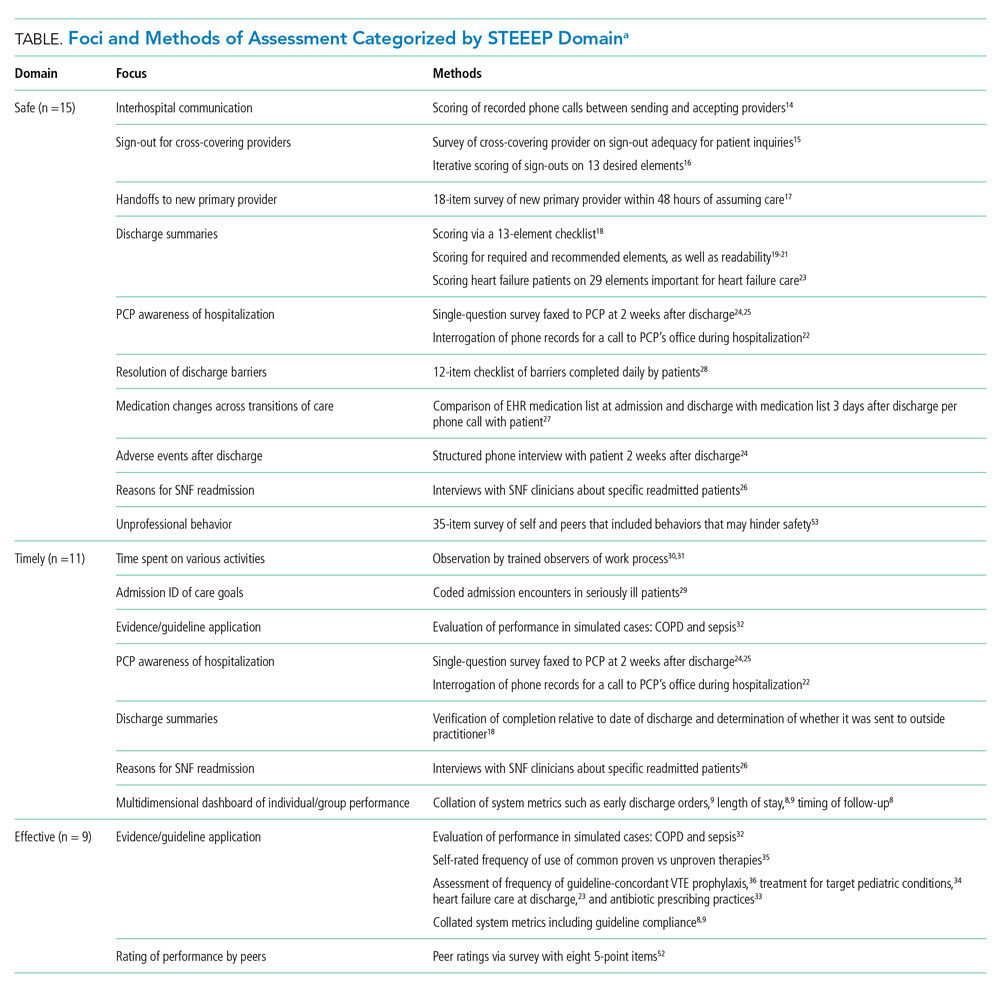
Safe
Nearly all studies coded into the Safe domain focused on transitions of care. These included transfers into a hospital from other hospitals,14 transitions of care to cross-covering providers15,16 and new primary providers,17 and transition out from the acute care setting.18-28 Measures of hospital discharge included measures of both processes18-22 and outcomes.23-27 Methods of assessment varied from use of trained observers or scorers to surveys of individuals and colleagues about performance. Though a few leveraged informatics,22,27 all approaches relied on human interaction, and none were automated.

Timely
All studies coded into the Timely domain were coded into at least one other domain. For example, Anderson et al looked at how hospitalists communicated about potential life-limiting illness at the time of hospital admission and the subsequent effects on plans of care29; this was coded as both Timely and Patient Centered. Likewise, another group of studies centered on application of evidence-based guidelines, such as giving antibiotics within a certain time interval for sepsis and were coded as both Timely and Effective. Another set of authors described dashboards or scorecards that captured a number of group-level metrics of processes of care that span STEEEP domains and may be applicable to individuals, including Fox et al for pediatrics8 and Hwa et al for an adult academic hospitalist group.9 Methods of assessment varied widely across studies and included observations in the clinical environment,28,30,31 performance in simulations,32 and surveys about performance.22-26 A handful of approaches were more automated and made use of informatics8,9,22 or data collected for other health system purposes.8,9
Effective
Effectiveness was most often assessed through adherence to consensus and evidence-based guidelines. Examples included processes of care related to sepsis, venous thromboembolism prophylaxis, COPD, heart failure, pediatric asthma, and antibiotic appropriateness.8,9,23,32-36 Through the review, multiple other studies that included group-level measures of effectiveness for a variety of health conditions were excluded because data on individual-level variation were not reported. Methods of assessment included expert review of cases or discharge summaries, compliance with core measures, performance in simulation, and self-assessment on practice behaviors. Other than those efforts aligned with institutional data collection, most approaches were resource intensive.
Efficient
As with those in the Timely domain, most studies coded into the Efficient domain were coded into at least one other domain. One exception measured unnecessary daily lab work and both showed provider-level variation and demonstrated improvement in quality based on an intervention.37 Another paper coded into the Effective domain evaluated adherence to components of the Choosing Wisely® recommendations.34 In addition to these two studies focusing on cost efficacy, other studies coded to this domain assessed concepts such as ensuring more efficient care from other providers by optimizing transitions of care15-17 and clarifying patients’ goals for care.38 Although integrating insurer information into care plans is emphasized in the Core Competencies of Hospital Medicine,11 this concept was not represented in any of the identified articles. Methods of assessment varied and mostly relied on observation of behaviors or survey of providers. Several approaches were more automated or used Medicare claims data to assess the efficiency of individual providers relative to peers.34,37,39
Equitable
Among the studies reviewed, none were coded into the Equitable domain despite care of vulnerable populations being identified as a core competency of hospital medicine.40
Patient Centered
Studies coded to the Patient Centered domain assessed hospitalist performance through ratings of patient satisfaction,8,9,41-44 rating of communication between hospitalists and patients,19-21,29,45-51 identification of patient preferences,38,52 outcomes of patient-centered care activities,27,28 and peer ratings.53,54 Authors applied several theoretical constructs to these assessments including shared decision-making,50 etiquette-based medicine,47,48 empathetic responsiveness,45 agreement about the goals of care between the patient and healthcare team members,52 and lapses in professionalism.53 Studies often crossed STEEEP domains, such as those assessing quality of discharge information provided to patients, which were coded as both Safe and Patient Centered.19-21 In addition to coded or observed performance in the clinical setting, studies in this domain also used patient ratings as a method of assessment.8,9,28,41-44,49,50 Only a few of these approaches aligned with existing performance measures of health systems and were more automated.8,9
DISCUSSION
This scoping review of performance data for individual hospitalists coded to the STEEEP framework identified robust areas in the published literature, as well as opportunities to develop new approaches or refine existing measures. Transitions of care, both intrahospital and at discharge, and adherence to evidence-based guidelines are areas for which current research has created a foundation for care that is Safe, Timely, Effective, and Efficient. The Patient Centered domain also has several measures described, though the conceptual underpinnings are heterogeneous, and consensus appears necessary to compare performance across groups. No studies were coded to the Equitable domain. Across domains, approaches to measurement varied in resource intensity from simple ones, like integrating existing data collected by hospitals, to more complex ones, like shadowing physicians or coding interactions.
Methods of assessment coded into the Safe domain focused on communication and, less so, patient outcomes around transitions of care. Transitions of care that were evaluated included transfer of patients into a new facility, sign-out to new physicians for both cross-cover responsibilities and for newly assuming the role of primary attending, and discharge from the hospital. Most measures rated the quality of communication, although several23-27 examined patient outcomes. Approaches that survey individuals downstream from a transition of care15,17,24-26 may be the simplest and most feasible approach to implement in the future but, as described to date, do not include all transitions of care and may miss patient outcomes. Important core competencies for hospital medicine under the Safe domain that were not identified in this review include areas such as diagnostic error, hospital-acquired infections, error reporting, and medication safety.11 These are potential areas for future measure development.
The assessments in many studies were coded across more than one domain; for example, measures of the application of evidence-based guidelines were coded into domains of Effective, Timely, Efficient, and others. Applying the six domains of the STEEEP framework revealed the multidimensional outcomes of hospitalist work and could guide more meaningful quality assessments of individual hospitalist performance. For example, assessing adherence to evidence-based guidelines, as well as consideration of the Core Competencies of Hospital Medicine and recommendations of the Choosing Wisely® campaign, are promising areas for measurement and may align with existing hospital metrics. Notably, several reviewed studies measured group-level adherence to guidelines but were excluded because they did not examine variation at the individual level. Future measures based on evidence-based guidelines could center on the Effective domain while also integrating assessment of domains such as Efficient, Timely, and Patient Centered and, in so doing, provide a richer assessment of the diverse aspects of quality.
Several other approaches in the domains of Timely, Effective, and Efficient were described only in a few studies yet deserve consideration for further development. Two time-motion studies30,31 were coded into the domains of Timely and Efficient and would be cumbersome in regular practice but, with advances in wearable technology and electronic health records, could become more feasible in the future. Another approach used Medicare payment data to detect provider-level variation.39 Potentially, “big data” could be analyzed in other ways to compare the performance of individual hospitalists.
The lack of studies coded into the Equitable domain may seem surprising, but the Institute for Healthcare Improvement identifies Equitable as the “forgotten aim” of the STEEEP framework. This organization has developed a guide for health care organizations to promote equitable care.55 While this guide focuses mostly on organizational-level actions, some are focused on individual providers, such as training in implicit bias. Future research should seek to identify disparities in care by individual providers and develop interventions to address any discovered gaps.
The “Patient Centered” domain was the most frequently coded and had the most heterogeneous underpinnings for assessment. Studies varied widely in terminology and conceptual foundations. The field would benefit from future work to identify how “Patient Centered” care might be more clearly conceptualized, guided by comparative studies among different assessment approaches to define those most valid and feasible.
The overarching goal for measuring individual hospitalist quality should be to improve the delivery of patient care in a supportive and formative way. To further this goal, adding or expanding on metrics identified in this article may provide a more complete description of performance. As a future direction, groups should consider partnering with one another to define measurement approaches, collaborate with existing data sources, and even share deidentified individual data to establish performance benchmarks at the individual and group levels.
While this study used broad search terms to support completeness, the search process could have missed important studies. Grey literature, non–English language studies, and industry reports were not included in this review. Groups may also be using other assessments of individual hospitalist performance that are not published in the peer-reviewed literature. Coding of study assessments was achieved through consensus reconciliation; other coders might have classified studies differently.
CONCLUSION
This scoping review describes the peer-reviewed literature of individual hospitalist performance and is the first to link it to the STEEEP quality framework. Assessments of transitions of care, evidence-based care, and cost-effective care are exemplars in the published literature. Patient-centered care is well studied but assessed in a heterogeneous fashion. Assessments of equity in care are notably absent. The STEEEP framework provides a model to structure assessment of individual performance. Future research should build on this framework to define meaningful assessment approaches that are actionable and improve the welfare of our patients and our system.
Disclosures
The authors have nothing to disclose.
Healthcare quality is defined as the extent to which healthcare services result in desired outcomes.1 Quality of care depends on how the healthcare system’s various components, including healthcare practitioners, interact to meet each patient’s needs.2 These components can be shaped to achieve desired outcomes through rules, incentives, and other approaches, but influencing the behaviors of each component, such as the performance of hospitalists, requires defining goals for performance and implementing measurement approaches to assess progress toward these goals.
One set of principles to define goals for quality and guide assessment of desired behaviors is the multidimensional STEEEP framework. This framework, created by the Institute of Medicine, identifies six domains of quality: Safe, Timely, Effective, Efficient, Equitable, and Patient Centered.2 Briefly, “Safe” means avoiding injuries to patients, “Timely” means reducing waits and delays in care, “Effective” means providing care based on evidence, “Efficient” means avoiding waste, “Equitable” means ensuring quality does not vary based on personal characteristics such as race and gender, and “Patient Centered” means providing care that is responsive to patients’ values and preferences. The STEEEP domains are not coequal; rather, they ensure that quality is considered broadly, while avoiding errors such as measuring only an intervention’s impact on effectiveness but not assessing its impact on multiple domains of quality, such as how patient centered, efficient (cost effective), or equitable the resulting care is.
Based on our review of the literature, a multidimensional framework like STEEEP has not been used in defining and assessing the quality of individual hospitalists’ performance. Some quality metrics at the hospital level impact several dimensions simultaneously, such as door to balloon time for acute myocardial infarction, which measures effectiveness and timeliness of care. Programs like pay-for-performance, Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS), and the Merit-Based Incentive Payment System (MIPS) have tied reimbursement to assessments aligned with several STEEEP domains at both individual and institutional levels but lack a holistic approach to quality.3-6 The every-other-year State of Hospital Medicine Report, the most widely used description of individual hospitalist performance, reports group-level performance including relative value units and whether groups are accountable for measures of quality such as performance on core measures, timely documentation, and “citizenship” (eg, committee participation or academic work).7 While these are useful benchmarks, the report focuses on performance at the group level. Concurrently, several academic groups have described more complete dashboards or scorecards to assess individual hospitalist performance, primarily designed to facilitate comparison across hospitalist groups or to incentivize overall group performance.8-10 However, these efforts are not guided by an overarching framework and are structured after traditional academic models with components related to teaching and scholarship, which may not translate to nonacademic environments. Finally, the Core Competencies for Hospital Medicine outlines some goals for hospitalist performance but does not speak to specific measurement approaches.11
Overall, assessing individual hospitalist performance is hindered by lack of consensus on important concepts to measure, a limited number of valid measures, and challenges in data collection such as resource limitations and feasibility. Developing and refining measures grounded in the STEEEP framework may provide a more comprehensive assessment of hospitalist quality and identify approaches to improve overall health outcomes. Comparative data could help individual hospitalists improve performance; leaders of hospitalist groups could use this data to guide faculty development and advancement as they ensure quality care at the individual, group, and system levels.
To better inform quality measurement of individual hospitalists, we sought to identify existing publications on individual hospitalist quality. Our goal was to define the published literature about quality measurement at the individual hospitalist level, relate these publications to domains of quality defined by the STEEEP framework, and identify directions for assessment or further research that could affect the overall quality of care.
METHODS
We conducted a scoping review following methods outlined by Arksey and O’Malley12 and Tricco.13 The goal of a scoping review is to map the extent of research within a specific field. This methodology is well suited to characterizing the existing research related to the quality of hospitalist care at the individual level. A protocol for the scoping review was not registered.
Evidence Search
A systematic search for published, English-language literature on hospitalist care was conducted in Medline (Ovid; 1946 - June 4, 2019) on June 5, 2019. The search used a combination of keywords and controlled vocabulary for the concept of hospitalists or hospital medicine. The search strategy used in this review is described in the Appendix. In addition, a hand search of reference lists of articles was used to discover publications not identified in the database searches.
Study Selection
All references were uploaded to Covidence systematic review software (www.covidence.org; Covidence), and duplicates were removed. Four reviewers (A.D., B.C., L.H., R.Q.) conducted title and abstract, as well as full-text, review to identify studies that measured differences in the performance of hospitalists at the individual level. Any disagreements among reviewers were resolved by consensus. Articles included both adult and pediatric populations. Articles that focused on group-level outcomes could be included if nonpooled data at the individual level was also reported. Studies were excluded if they did not focus on individual quality of care indicators or were not published in English.
Data Charting and Synthesis
We extracted the following information using a standardized data collection form: author, title, year of publication, study design, intervention, and outcome measures. Original manuscripts were accessed as needed to supplement analysis. Critical appraisal of individual studies was not conducted in this review because the goal of this review was to analyze which quality indicators have been studied and how they were measured. Articles were then coded for their alignment to the STEEEP framework by two reviewers (AD and BC). After initial coding was conducted, the reviewers met to consolidate codes and resolve any disagreement by consensus. The results of the analysis were summarized in both text and tabular format with studies grouped by focus of assessment with each one’s methods of assessment listed.
RESULTS
Results of the search strategy are shown in the Figure. The search retrieved a total of 2,363 references of which 113 were duplicates, leaving 2,250 to be screened. After title and abstract and full-text screening, 42 studies were included in the review. The final 42 studies were coded for alignment with the STEEEP framework. The Table displays the focus of assessment and methods of assessment within each STEEEP domain.
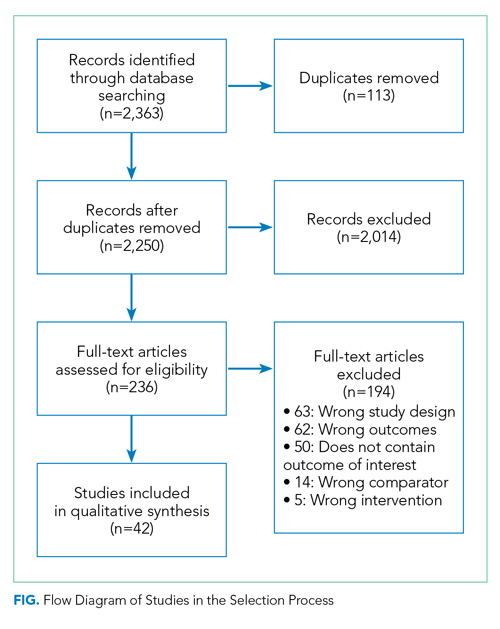
Eighteen studies were coded into a single domain while the rest were coded into at least two domains. The domain Patient Centered was coded as having the most studies (n = 23), followed by the domain of Safe (n = 15). Timely, Effective, and Efficient domains had 11, 9, and 12 studies, respectively. No studies were coded into the domain of Equitable.
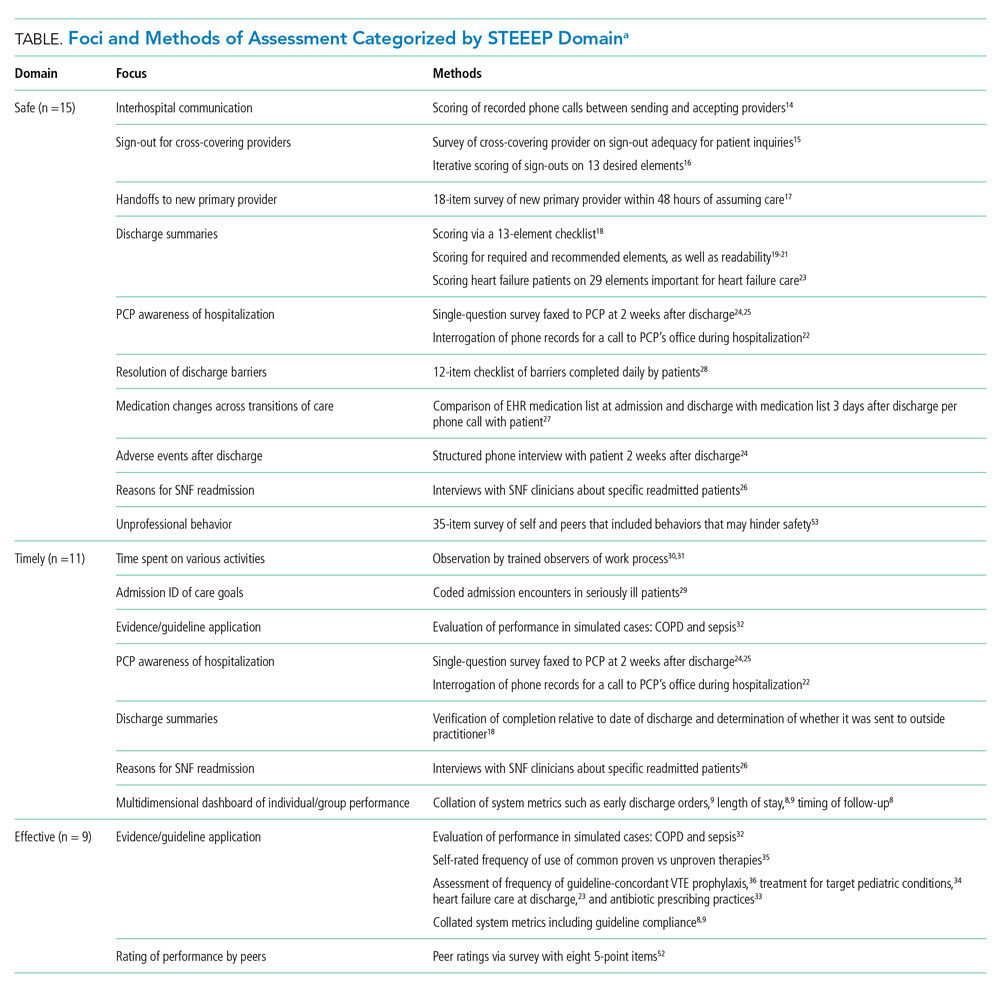
Safe
Nearly all studies coded into the Safe domain focused on transitions of care. These included transfers into a hospital from other hospitals,14 transitions of care to cross-covering providers15,16 and new primary providers,17 and transition out from the acute care setting.18-28 Measures of hospital discharge included measures of both processes18-22 and outcomes.23-27 Methods of assessment varied from use of trained observers or scorers to surveys of individuals and colleagues about performance. Though a few leveraged informatics,22,27 all approaches relied on human interaction, and none were automated.

Timely
All studies coded into the Timely domain were coded into at least one other domain. For example, Anderson et al looked at how hospitalists communicated about potential life-limiting illness at the time of hospital admission and the subsequent effects on plans of care29; this was coded as both Timely and Patient Centered. Likewise, another group of studies centered on application of evidence-based guidelines, such as giving antibiotics within a certain time interval for sepsis and were coded as both Timely and Effective. Another set of authors described dashboards or scorecards that captured a number of group-level metrics of processes of care that span STEEEP domains and may be applicable to individuals, including Fox et al for pediatrics8 and Hwa et al for an adult academic hospitalist group.9 Methods of assessment varied widely across studies and included observations in the clinical environment,28,30,31 performance in simulations,32 and surveys about performance.22-26 A handful of approaches were more automated and made use of informatics8,9,22 or data collected for other health system purposes.8,9
Effective
Effectiveness was most often assessed through adherence to consensus and evidence-based guidelines. Examples included processes of care related to sepsis, venous thromboembolism prophylaxis, COPD, heart failure, pediatric asthma, and antibiotic appropriateness.8,9,23,32-36 Through the review, multiple other studies that included group-level measures of effectiveness for a variety of health conditions were excluded because data on individual-level variation were not reported. Methods of assessment included expert review of cases or discharge summaries, compliance with core measures, performance in simulation, and self-assessment on practice behaviors. Other than those efforts aligned with institutional data collection, most approaches were resource intensive.
Efficient
As with those in the Timely domain, most studies coded into the Efficient domain were coded into at least one other domain. One exception measured unnecessary daily lab work and both showed provider-level variation and demonstrated improvement in quality based on an intervention.37 Another paper coded into the Effective domain evaluated adherence to components of the Choosing Wisely® recommendations.34 In addition to these two studies focusing on cost efficacy, other studies coded to this domain assessed concepts such as ensuring more efficient care from other providers by optimizing transitions of care15-17 and clarifying patients’ goals for care.38 Although integrating insurer information into care plans is emphasized in the Core Competencies of Hospital Medicine,11 this concept was not represented in any of the identified articles. Methods of assessment varied and mostly relied on observation of behaviors or survey of providers. Several approaches were more automated or used Medicare claims data to assess the efficiency of individual providers relative to peers.34,37,39
Equitable
Among the studies reviewed, none were coded into the Equitable domain despite care of vulnerable populations being identified as a core competency of hospital medicine.40
Patient Centered
Studies coded to the Patient Centered domain assessed hospitalist performance through ratings of patient satisfaction,8,9,41-44 rating of communication between hospitalists and patients,19-21,29,45-51 identification of patient preferences,38,52 outcomes of patient-centered care activities,27,28 and peer ratings.53,54 Authors applied several theoretical constructs to these assessments including shared decision-making,50 etiquette-based medicine,47,48 empathetic responsiveness,45 agreement about the goals of care between the patient and healthcare team members,52 and lapses in professionalism.53 Studies often crossed STEEEP domains, such as those assessing quality of discharge information provided to patients, which were coded as both Safe and Patient Centered.19-21 In addition to coded or observed performance in the clinical setting, studies in this domain also used patient ratings as a method of assessment.8,9,28,41-44,49,50 Only a few of these approaches aligned with existing performance measures of health systems and were more automated.8,9
DISCUSSION
This scoping review of performance data for individual hospitalists coded to the STEEEP framework identified robust areas in the published literature, as well as opportunities to develop new approaches or refine existing measures. Transitions of care, both intrahospital and at discharge, and adherence to evidence-based guidelines are areas for which current research has created a foundation for care that is Safe, Timely, Effective, and Efficient. The Patient Centered domain also has several measures described, though the conceptual underpinnings are heterogeneous, and consensus appears necessary to compare performance across groups. No studies were coded to the Equitable domain. Across domains, approaches to measurement varied in resource intensity from simple ones, like integrating existing data collected by hospitals, to more complex ones, like shadowing physicians or coding interactions.
Methods of assessment coded into the Safe domain focused on communication and, less so, patient outcomes around transitions of care. Transitions of care that were evaluated included transfer of patients into a new facility, sign-out to new physicians for both cross-cover responsibilities and for newly assuming the role of primary attending, and discharge from the hospital. Most measures rated the quality of communication, although several23-27 examined patient outcomes. Approaches that survey individuals downstream from a transition of care15,17,24-26 may be the simplest and most feasible approach to implement in the future but, as described to date, do not include all transitions of care and may miss patient outcomes. Important core competencies for hospital medicine under the Safe domain that were not identified in this review include areas such as diagnostic error, hospital-acquired infections, error reporting, and medication safety.11 These are potential areas for future measure development.
The assessments in many studies were coded across more than one domain; for example, measures of the application of evidence-based guidelines were coded into domains of Effective, Timely, Efficient, and others. Applying the six domains of the STEEEP framework revealed the multidimensional outcomes of hospitalist work and could guide more meaningful quality assessments of individual hospitalist performance. For example, assessing adherence to evidence-based guidelines, as well as consideration of the Core Competencies of Hospital Medicine and recommendations of the Choosing Wisely® campaign, are promising areas for measurement and may align with existing hospital metrics. Notably, several reviewed studies measured group-level adherence to guidelines but were excluded because they did not examine variation at the individual level. Future measures based on evidence-based guidelines could center on the Effective domain while also integrating assessment of domains such as Efficient, Timely, and Patient Centered and, in so doing, provide a richer assessment of the diverse aspects of quality.
Several other approaches in the domains of Timely, Effective, and Efficient were described only in a few studies yet deserve consideration for further development. Two time-motion studies30,31 were coded into the domains of Timely and Efficient and would be cumbersome in regular practice but, with advances in wearable technology and electronic health records, could become more feasible in the future. Another approach used Medicare payment data to detect provider-level variation.39 Potentially, “big data” could be analyzed in other ways to compare the performance of individual hospitalists.
The lack of studies coded into the Equitable domain may seem surprising, but the Institute for Healthcare Improvement identifies Equitable as the “forgotten aim” of the STEEEP framework. This organization has developed a guide for health care organizations to promote equitable care.55 While this guide focuses mostly on organizational-level actions, some are focused on individual providers, such as training in implicit bias. Future research should seek to identify disparities in care by individual providers and develop interventions to address any discovered gaps.
The “Patient Centered” domain was the most frequently coded and had the most heterogeneous underpinnings for assessment. Studies varied widely in terminology and conceptual foundations. The field would benefit from future work to identify how “Patient Centered” care might be more clearly conceptualized, guided by comparative studies among different assessment approaches to define those most valid and feasible.
The overarching goal for measuring individual hospitalist quality should be to improve the delivery of patient care in a supportive and formative way. To further this goal, adding or expanding on metrics identified in this article may provide a more complete description of performance. As a future direction, groups should consider partnering with one another to define measurement approaches, collaborate with existing data sources, and even share deidentified individual data to establish performance benchmarks at the individual and group levels.
While this study used broad search terms to support completeness, the search process could have missed important studies. Grey literature, non–English language studies, and industry reports were not included in this review. Groups may also be using other assessments of individual hospitalist performance that are not published in the peer-reviewed literature. Coding of study assessments was achieved through consensus reconciliation; other coders might have classified studies differently.
CONCLUSION
This scoping review describes the peer-reviewed literature of individual hospitalist performance and is the first to link it to the STEEEP quality framework. Assessments of transitions of care, evidence-based care, and cost-effective care are exemplars in the published literature. Patient-centered care is well studied but assessed in a heterogeneous fashion. Assessments of equity in care are notably absent. The STEEEP framework provides a model to structure assessment of individual performance. Future research should build on this framework to define meaningful assessment approaches that are actionable and improve the welfare of our patients and our system.
Disclosures
The authors have nothing to disclose.
1. Quality of Care: A Process for Making Strategic Choices in Health Systems. World Health Organization; 2006.
2. Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. National Academies Press; 2001. Accessed December 20, 2019. http://www.ncbi.nlm.nih.gov/books/NBK222274/
3. Wadhera RK, Joynt Maddox KE, Wasfy JH, Haneuse S, Shen C, Yeh RW. Association of the hospital readmissions reduction program with mortality among Medicare beneficiaries hospitalized for heart failure, acute myocardial infarction, and pneumonia. JAMA. 2018;320(24):2542-2552. https://doi.org/10.1001/jama.2018.19232
4. Kondo KK, Damberg CL, Mendelson A, et al. Implementation processes and pay for performance in healthcare: a systematic review. J Gen Intern Med. 2016;31(Suppl 1):61-69. https://doi.org/10.1007/s11606-015-3567-0
5. Fung CH, Lim Y-W, Mattke S, Damberg C, Shekelle PG. Systematic review: the evidence that publishing patient care performance data improves quality of care. Ann Intern Med. 2008;148(2):111-123. https://doi.org/10.7326/0003-4819-148-2-200801150-00006
6. Jha AK, Orav EJ, Epstein AM. Public reporting of discharge planning and rates of readmissions. N Engl J Med. 2009;361(27):2637-2645. https://doi.org/10.1056/NEJMsa0904859
7. Society of Hospital Medicine. State of Hospital Medicine Report; 2018. Accessed December 20, 2019. https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/
8. Hwa M, Sharpe BA, Wachter RM. Development and implementation of a balanced scorecard in an academic hospitalist group. J Hosp Med. 2013;8(3):148-153. https://doi.org/10.1002/jhm.2006
9. Fox LA, Walsh KE, Schainker EG. The creation of a pediatric hospital medicine dashboard: performance assessment for improvement. Hosp Pediatr. 2016;6(7):412-419. https://doi.org/10.1542/hpeds.2015-0222
10. Hain PD, Daru J, Robbins E, et al. A proposed dashboard for pediatric hospital medicine groups. Hosp Pediatr. 2012;2(2):59-68. https://doi.org/10.1542/hpeds.2012-0004
11. Nichani S, Crocker J, Fitterman N, Lukela M. Updating the core competencies in hospital medicine--2017 revision: introduction and methodology. J Hosp Med. 2017;12(4):283-287. https://doi.org/10.12788/jhm.2715
12. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19-32. https://doi.org/10.1080/1364557032000119616
13. Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467-473. https://doi.org/10.7326/m18-0850
14. Borofsky JS, Bartsch JC, Howard AB, Repp AB. Quality of interhospital transfer communication practices and association with adverse events on an internal medicine hospitalist service. J Healthc Qual. 2017;39(3):177-185. https://doi.org/10.1097/01.JHQ.0000462682.32512.ad
15. Fogerty RL, Schoenfeld A, Salim Al-Damluji M, Horwitz LI. Effectiveness of written hospitalist sign-outs in answering overnight inquiries. J Hosp Med. 2013;8(11):609-614. https://doi.org10.1002/jhm.2090
16. Miller DM, Schapira MM, Visotcky AM, et al. Changes in written sign-out composition across hospitalization. J Hosp Med. 2015;10(8):534-536. https://doi.org/10.1002/jhm.2390
17. Hinami K, Farnan JM, Meltzer DO, Arora VM. Understanding communication during hospitalist service changes: a mixed methods study. J Hosp Med. 2009;4(9):535-540. https://doi.org/10.1002/jhm.523
18. Horwitz LI, Jenq GY, Brewster UC, et al. Comprehensive quality of discharge summaries at an academic medical center. J Hosp Med. 2013;8(8):436-443. https://doi.org10.1002/jhm.2021
19. Sarzynski E, Hashmi H, Subramanian J, et al. Opportunities to improve clinical summaries for patients at hospital discharge. BMJ Qual Saf. 2017;26(5):372-380. https://doi.org/10.1136/bmjqs-2015-005201
20. Unaka NI, Statile A, Haney J, Beck AF, Brady PW, Jerardi KE. Assessment of readability, understandability, and completeness of pediatric hospital medicine discharge instructions. J Hosp Med. 2017;12(2):98-101. https://doi.org/10.12788/jhm.2688
21. Unaka N, Statile A, Jerardi K, et al. Improving the readability of pediatric hospital medicine discharge instructions. J Hosp Med. 2017;12(7):551-557. https://doi.org/10.12788/jhm.2770
22. Zackoff MW, Graham C, Warrick D, et al. Increasing PCP and hospital medicine physician verbal communication during hospital admissions. Hosp Pediatr. 2018;8(4):220-226. https://doi.org/10.1542/hpeds.2017-0119
23. Salata BM, Sterling MR, Beecy AN, et al. Discharge processes and 30-day readmission rates of patients hospitalized for heart failure on general medicine and cardiology services. Am J Cardiol. 2018;121(9):1076-1080. https://doi.org/10.1016/j.amjcard.2018.01.027
24. Arora VM, Prochaska ML, Farnan JM, et al. Problems after discharge and understanding of communication with their primary care physicians among hospitalized seniors: a mixed methods study. J Hosp Med. 2010;5(7):385-391. https://doi.org/10.1002/jhm.668
25. Bell CM, Schnipper JL, Auerbach AD, et al. Association of communication between hospital-based physicians and primary care providers with patient outcomes. J Gen Intern Med. 2009;24(3):381-386. https://doi.org/10.1007/s11606-008-0882-8
26. Clark B, Baron K, Tynan-McKiernan K, Britton M, Minges K, Chaudhry S. Perspectives of clinicians at skilled nursing facilities on 30-day hospital readmissions: a qualitative study. J Hosp Med. 2017;12(8):632-638. https://doi.org/10.12788/jhm.2785
27. Harris CM, Sridharan A, Landis R, Howell E, Wright S. What happens to the medication regimens of older adults during and after an acute hospitalization? J Patient Saf. 2013;9(3):150-153. https://doi.org/10.1097/PTS.0b013e318286f87d
28. Harrison JD, Greysen RS, Jacolbia R, Nguyen A, Auerbach AD. Not ready, not set...discharge: patient-reported barriers to discharge readiness at an academic medical center. J Hosp Med. 2016;11(9):610-614. https://doi.org/10.1002/jhm.2591
29. Anderson WG, Kools S, Lyndon A. Dancing around death: hospitalist-patient communication about serious illness. Qual Health Res. 2013;23(1):3-13. https://doi.org/10.1177/1049732312461728
30. Tipping MD, Forth VE, Magill DB, Englert K, Williams MV. Systematic review of time studies evaluating physicians in the hospital setting. J Hosp Med. 2010;5(6):353-359. https://doi.org/10.1002/jhm.647
31. Tipping MD, Forth VE, O’Leary KJ, et al. Where did the day go?--a time-motion study of hospitalists. J Hosp Med. 2010;5(6):323-328. https://doi.org/10.1002/jhm.790
32. Bergmann S, Tran M, Robison K, et al. Standardising hospitalist practice in sepsis and COPD care. BMJ Qual Saf. 2019;28(10):800-808. https://doi.org/10.1136/bmjqs-2018-008829
33. Kisuule F, Wright S, Barreto J, Zenilman J. Improving antibiotic utilization among hospitalists: a pilot academic detailing project with a public health approach. J Hosp Med. 2008;3(1):64-70. https://doi.org/10.1002/jhm.278
34. Reyes M, Paulus E, Hronek C, et al. Choosing Wisely campaign: report card and achievable benchmarks of care for children’s hospitals. Hosp Pediatr. 2017;7(11):633-641. https://doi.org/10.1542/hpeds.2017-0029
35. Landrigan CP, Conway PH, Stucky ER, et al. Variation in pediatric hospitalists’ use of proven and unproven therapies: a study from the Pediatric Research in Inpatient Settings (PRIS) network. J Hosp Med. 2008;3(4):292-298. https://doi.org/10.1002/jhm.347
36. Michtalik HJ, Carolan HT, Haut ER, et al. Use of provider-level dashboards and pay-for-performance in venous thromboprophylaxis. J Hosp Med. 2015;10(3):172-178. https://doi.org/10.1002/jhm.2303
37. Johnson DP, Lind C, Parker SE, et al. Toward high-value care: a quality improvement initiative to reduce unnecessary repeat complete blood counts and basic metabolic panels on a pediatric hospitalist service. Hosp Pediatr. 2016;6(1):1-8. https://doi.org/10.1542/hpeds.2015-0099
38. Auerbach AD, Katz R, Pantilat SZ, et al. Factors associated with discussion of care plans and code status at the time of hospital admission: results from the Multicenter Hospitalist Study. J Hosp Med. 2008;3(6):437-445. https://doi.org/10.1002/jhm.369
39. Tsugawa Y, Jha AK, Newhouse JP, Zaslavsky AM, Jena AB. Variation in physician spending and association with patient outcomes. JAMA Intern Med. 2017;177(5):675-682. https://doi.org/10.1001/jamainternmed.2017.0059
40. Nichani S, Fitterman N, Lukela M, Crocker J. Equitable allocation of resources. 2017 hospital medicine revised core competencies. J Hosp Med. 2017;12(4):S62. https://doi.org/10.12788/jhm.3016
41. Blanden AR, Rohr RE. Cognitive interview techniques reveal specific behaviors and issues that could affect patient satisfaction relative to hospitalists. J Hosp Med. 2009;4(9):E1-E6. https://doi.org/10.1002/jhm.524
42. Torok H, Ghazarian SR, Kotwal S, Landis R, Wright S, Howell E. Development and validation of the tool to assess inpatient satisfaction with care from hospitalists. J Hosp Med. 2014;9(9):553-558. https://doi.org/10.1002/jhm.2220
43. Torok H, Kotwal S, Landis R, Ozumba U, Howell E, Wright S. Providing feedback on clinical performance to hospitalists: Experience using a new metric tool to assess inpatient satisfaction with care from hospitalists. J Contin Educ Health Prof. 2016;36(1):61-68. https://doi.org/10.1097/CEH.0000000000000060
44. Indovina K, Keniston A, Reid M, et al. Real-time patient experience surveys of hospitalized medical patients. J Hosp Med. 2016;11(4):251-256. https://doi.org/10.1002/jhm.2533
45. Weiss R, Vittinghoff E, Fang MC, et al. Associations of physician empathy with patient anxiety and ratings of communication in hospital admission encounters. J Hosp Med. 2017;12(10):805-810. https://doi.org/10.12788/jhm.2828
46. Apker J, Baker M, Shank S, Hatten K, VanSweden S. Optimizing hospitalist-patient communication: an observation study of medical encounter quality. Jt Comm J Qual Patient Saf. 2018;44(4):196-203. https://doi.org/10.1016/j.jcjq.2017.08.011
47. Kotwal S, Torok H, Khaliq W, Landis R, Howell E, Wright S. Comportment and communication patterns among hospitalist physicians: insight gleaned through observation. South Med J. 2015;108(8):496-501. https://doi.org/10.14423/SMJ.0000000000000328
48. Tackett S, Tad-y D, Rios R, Kisuule F, Wright S. Appraising the practice of etiquette-based medicine in the inpatient setting. J Gen Intern Med. 2013;28(7):908-913. https://doi.org/10.1007/s11606-012-2328-6
49. Ferranti DE, Makoul G, Forth VE, Rauworth J, Lee J, Williams MV. Assessing patient perceptions of hospitalist communication skills using the Communication Assessment Tool (CAT). J Hosp Med. 2010;5(9):522-527. https://doi.org/10.1002/jhm.787
50. Blankenburg R, Hilton JF, Yuan P, et al. Shared decision-making during inpatient rounds: opportunities for improvement in patient engagement and communication. J Hosp Med. 2018;13(7):453-461. https://doi.org/10.12788/jhm.2909
51. Chang D, Mann M, Sommer T, Fallar R, Weinberg A, Friedman E. Using standardized patients to assess hospitalist communication skills. J Hosp Med. 2017;12(7):562-566. https://doi.org/10.12788/jhm.2772
52. Figueroa JF, Schnipper JL, McNally K, Stade D, Lipsitz SR, Dalal AK. How often are hospitalized patients and providers on the same page with regard to the patient’s primary recovery goal for hospitalization? J Hosp Med. 2016;11(9):615-619. https://doi.org/10.1002/jhm.2569
53. Reddy ST, Iwaz JA, Didwania AK, et al. Participation in unprofessional behaviors among hospitalists: a multicenter study. J Hosp Med. 2012;7(7):543-550. https://doi.org/10.1002/jhm.1946
54. Bhogal HK, Howe E, Torok H, Knight AM, Howell E, Wright S. Peer assessment of professional performance by hospitalist physicians. South Med J. 2012;105(5):254-258. https://doi.org/10.1097/SMJ.0b013e318252d602
55. Wyatt R, Laderman M, Botwinick L, Mate K, Whittington J. Achieving health equity: a guide for health care organizations. IHI White Paper. Institute for Healthcare Improvement; 2016. https://www.ihi.org
1. Quality of Care: A Process for Making Strategic Choices in Health Systems. World Health Organization; 2006.
2. Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. National Academies Press; 2001. Accessed December 20, 2019. http://www.ncbi.nlm.nih.gov/books/NBK222274/
3. Wadhera RK, Joynt Maddox KE, Wasfy JH, Haneuse S, Shen C, Yeh RW. Association of the hospital readmissions reduction program with mortality among Medicare beneficiaries hospitalized for heart failure, acute myocardial infarction, and pneumonia. JAMA. 2018;320(24):2542-2552. https://doi.org/10.1001/jama.2018.19232
4. Kondo KK, Damberg CL, Mendelson A, et al. Implementation processes and pay for performance in healthcare: a systematic review. J Gen Intern Med. 2016;31(Suppl 1):61-69. https://doi.org/10.1007/s11606-015-3567-0
5. Fung CH, Lim Y-W, Mattke S, Damberg C, Shekelle PG. Systematic review: the evidence that publishing patient care performance data improves quality of care. Ann Intern Med. 2008;148(2):111-123. https://doi.org/10.7326/0003-4819-148-2-200801150-00006
6. Jha AK, Orav EJ, Epstein AM. Public reporting of discharge planning and rates of readmissions. N Engl J Med. 2009;361(27):2637-2645. https://doi.org/10.1056/NEJMsa0904859
7. Society of Hospital Medicine. State of Hospital Medicine Report; 2018. Accessed December 20, 2019. https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/
8. Hwa M, Sharpe BA, Wachter RM. Development and implementation of a balanced scorecard in an academic hospitalist group. J Hosp Med. 2013;8(3):148-153. https://doi.org/10.1002/jhm.2006
9. Fox LA, Walsh KE, Schainker EG. The creation of a pediatric hospital medicine dashboard: performance assessment for improvement. Hosp Pediatr. 2016;6(7):412-419. https://doi.org/10.1542/hpeds.2015-0222
10. Hain PD, Daru J, Robbins E, et al. A proposed dashboard for pediatric hospital medicine groups. Hosp Pediatr. 2012;2(2):59-68. https://doi.org/10.1542/hpeds.2012-0004
11. Nichani S, Crocker J, Fitterman N, Lukela M. Updating the core competencies in hospital medicine--2017 revision: introduction and methodology. J Hosp Med. 2017;12(4):283-287. https://doi.org/10.12788/jhm.2715
12. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19-32. https://doi.org/10.1080/1364557032000119616
13. Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467-473. https://doi.org/10.7326/m18-0850
14. Borofsky JS, Bartsch JC, Howard AB, Repp AB. Quality of interhospital transfer communication practices and association with adverse events on an internal medicine hospitalist service. J Healthc Qual. 2017;39(3):177-185. https://doi.org/10.1097/01.JHQ.0000462682.32512.ad
15. Fogerty RL, Schoenfeld A, Salim Al-Damluji M, Horwitz LI. Effectiveness of written hospitalist sign-outs in answering overnight inquiries. J Hosp Med. 2013;8(11):609-614. https://doi.org10.1002/jhm.2090
16. Miller DM, Schapira MM, Visotcky AM, et al. Changes in written sign-out composition across hospitalization. J Hosp Med. 2015;10(8):534-536. https://doi.org/10.1002/jhm.2390
17. Hinami K, Farnan JM, Meltzer DO, Arora VM. Understanding communication during hospitalist service changes: a mixed methods study. J Hosp Med. 2009;4(9):535-540. https://doi.org/10.1002/jhm.523
18. Horwitz LI, Jenq GY, Brewster UC, et al. Comprehensive quality of discharge summaries at an academic medical center. J Hosp Med. 2013;8(8):436-443. https://doi.org10.1002/jhm.2021
19. Sarzynski E, Hashmi H, Subramanian J, et al. Opportunities to improve clinical summaries for patients at hospital discharge. BMJ Qual Saf. 2017;26(5):372-380. https://doi.org/10.1136/bmjqs-2015-005201
20. Unaka NI, Statile A, Haney J, Beck AF, Brady PW, Jerardi KE. Assessment of readability, understandability, and completeness of pediatric hospital medicine discharge instructions. J Hosp Med. 2017;12(2):98-101. https://doi.org/10.12788/jhm.2688
21. Unaka N, Statile A, Jerardi K, et al. Improving the readability of pediatric hospital medicine discharge instructions. J Hosp Med. 2017;12(7):551-557. https://doi.org/10.12788/jhm.2770
22. Zackoff MW, Graham C, Warrick D, et al. Increasing PCP and hospital medicine physician verbal communication during hospital admissions. Hosp Pediatr. 2018;8(4):220-226. https://doi.org/10.1542/hpeds.2017-0119
23. Salata BM, Sterling MR, Beecy AN, et al. Discharge processes and 30-day readmission rates of patients hospitalized for heart failure on general medicine and cardiology services. Am J Cardiol. 2018;121(9):1076-1080. https://doi.org/10.1016/j.amjcard.2018.01.027
24. Arora VM, Prochaska ML, Farnan JM, et al. Problems after discharge and understanding of communication with their primary care physicians among hospitalized seniors: a mixed methods study. J Hosp Med. 2010;5(7):385-391. https://doi.org/10.1002/jhm.668
25. Bell CM, Schnipper JL, Auerbach AD, et al. Association of communication between hospital-based physicians and primary care providers with patient outcomes. J Gen Intern Med. 2009;24(3):381-386. https://doi.org/10.1007/s11606-008-0882-8
26. Clark B, Baron K, Tynan-McKiernan K, Britton M, Minges K, Chaudhry S. Perspectives of clinicians at skilled nursing facilities on 30-day hospital readmissions: a qualitative study. J Hosp Med. 2017;12(8):632-638. https://doi.org/10.12788/jhm.2785
27. Harris CM, Sridharan A, Landis R, Howell E, Wright S. What happens to the medication regimens of older adults during and after an acute hospitalization? J Patient Saf. 2013;9(3):150-153. https://doi.org/10.1097/PTS.0b013e318286f87d
28. Harrison JD, Greysen RS, Jacolbia R, Nguyen A, Auerbach AD. Not ready, not set...discharge: patient-reported barriers to discharge readiness at an academic medical center. J Hosp Med. 2016;11(9):610-614. https://doi.org/10.1002/jhm.2591
29. Anderson WG, Kools S, Lyndon A. Dancing around death: hospitalist-patient communication about serious illness. Qual Health Res. 2013;23(1):3-13. https://doi.org/10.1177/1049732312461728
30. Tipping MD, Forth VE, Magill DB, Englert K, Williams MV. Systematic review of time studies evaluating physicians in the hospital setting. J Hosp Med. 2010;5(6):353-359. https://doi.org/10.1002/jhm.647
31. Tipping MD, Forth VE, O’Leary KJ, et al. Where did the day go?--a time-motion study of hospitalists. J Hosp Med. 2010;5(6):323-328. https://doi.org/10.1002/jhm.790
32. Bergmann S, Tran M, Robison K, et al. Standardising hospitalist practice in sepsis and COPD care. BMJ Qual Saf. 2019;28(10):800-808. https://doi.org/10.1136/bmjqs-2018-008829
33. Kisuule F, Wright S, Barreto J, Zenilman J. Improving antibiotic utilization among hospitalists: a pilot academic detailing project with a public health approach. J Hosp Med. 2008;3(1):64-70. https://doi.org/10.1002/jhm.278
34. Reyes M, Paulus E, Hronek C, et al. Choosing Wisely campaign: report card and achievable benchmarks of care for children’s hospitals. Hosp Pediatr. 2017;7(11):633-641. https://doi.org/10.1542/hpeds.2017-0029
35. Landrigan CP, Conway PH, Stucky ER, et al. Variation in pediatric hospitalists’ use of proven and unproven therapies: a study from the Pediatric Research in Inpatient Settings (PRIS) network. J Hosp Med. 2008;3(4):292-298. https://doi.org/10.1002/jhm.347
36. Michtalik HJ, Carolan HT, Haut ER, et al. Use of provider-level dashboards and pay-for-performance in venous thromboprophylaxis. J Hosp Med. 2015;10(3):172-178. https://doi.org/10.1002/jhm.2303
37. Johnson DP, Lind C, Parker SE, et al. Toward high-value care: a quality improvement initiative to reduce unnecessary repeat complete blood counts and basic metabolic panels on a pediatric hospitalist service. Hosp Pediatr. 2016;6(1):1-8. https://doi.org/10.1542/hpeds.2015-0099
38. Auerbach AD, Katz R, Pantilat SZ, et al. Factors associated with discussion of care plans and code status at the time of hospital admission: results from the Multicenter Hospitalist Study. J Hosp Med. 2008;3(6):437-445. https://doi.org/10.1002/jhm.369
39. Tsugawa Y, Jha AK, Newhouse JP, Zaslavsky AM, Jena AB. Variation in physician spending and association with patient outcomes. JAMA Intern Med. 2017;177(5):675-682. https://doi.org/10.1001/jamainternmed.2017.0059
40. Nichani S, Fitterman N, Lukela M, Crocker J. Equitable allocation of resources. 2017 hospital medicine revised core competencies. J Hosp Med. 2017;12(4):S62. https://doi.org/10.12788/jhm.3016
41. Blanden AR, Rohr RE. Cognitive interview techniques reveal specific behaviors and issues that could affect patient satisfaction relative to hospitalists. J Hosp Med. 2009;4(9):E1-E6. https://doi.org/10.1002/jhm.524
42. Torok H, Ghazarian SR, Kotwal S, Landis R, Wright S, Howell E. Development and validation of the tool to assess inpatient satisfaction with care from hospitalists. J Hosp Med. 2014;9(9):553-558. https://doi.org/10.1002/jhm.2220
43. Torok H, Kotwal S, Landis R, Ozumba U, Howell E, Wright S. Providing feedback on clinical performance to hospitalists: Experience using a new metric tool to assess inpatient satisfaction with care from hospitalists. J Contin Educ Health Prof. 2016;36(1):61-68. https://doi.org/10.1097/CEH.0000000000000060
44. Indovina K, Keniston A, Reid M, et al. Real-time patient experience surveys of hospitalized medical patients. J Hosp Med. 2016;11(4):251-256. https://doi.org/10.1002/jhm.2533
45. Weiss R, Vittinghoff E, Fang MC, et al. Associations of physician empathy with patient anxiety and ratings of communication in hospital admission encounters. J Hosp Med. 2017;12(10):805-810. https://doi.org/10.12788/jhm.2828
46. Apker J, Baker M, Shank S, Hatten K, VanSweden S. Optimizing hospitalist-patient communication: an observation study of medical encounter quality. Jt Comm J Qual Patient Saf. 2018;44(4):196-203. https://doi.org/10.1016/j.jcjq.2017.08.011
47. Kotwal S, Torok H, Khaliq W, Landis R, Howell E, Wright S. Comportment and communication patterns among hospitalist physicians: insight gleaned through observation. South Med J. 2015;108(8):496-501. https://doi.org/10.14423/SMJ.0000000000000328
48. Tackett S, Tad-y D, Rios R, Kisuule F, Wright S. Appraising the practice of etiquette-based medicine in the inpatient setting. J Gen Intern Med. 2013;28(7):908-913. https://doi.org/10.1007/s11606-012-2328-6
49. Ferranti DE, Makoul G, Forth VE, Rauworth J, Lee J, Williams MV. Assessing patient perceptions of hospitalist communication skills using the Communication Assessment Tool (CAT). J Hosp Med. 2010;5(9):522-527. https://doi.org/10.1002/jhm.787
50. Blankenburg R, Hilton JF, Yuan P, et al. Shared decision-making during inpatient rounds: opportunities for improvement in patient engagement and communication. J Hosp Med. 2018;13(7):453-461. https://doi.org/10.12788/jhm.2909
51. Chang D, Mann M, Sommer T, Fallar R, Weinberg A, Friedman E. Using standardized patients to assess hospitalist communication skills. J Hosp Med. 2017;12(7):562-566. https://doi.org/10.12788/jhm.2772
52. Figueroa JF, Schnipper JL, McNally K, Stade D, Lipsitz SR, Dalal AK. How often are hospitalized patients and providers on the same page with regard to the patient’s primary recovery goal for hospitalization? J Hosp Med. 2016;11(9):615-619. https://doi.org/10.1002/jhm.2569
53. Reddy ST, Iwaz JA, Didwania AK, et al. Participation in unprofessional behaviors among hospitalists: a multicenter study. J Hosp Med. 2012;7(7):543-550. https://doi.org/10.1002/jhm.1946
54. Bhogal HK, Howe E, Torok H, Knight AM, Howell E, Wright S. Peer assessment of professional performance by hospitalist physicians. South Med J. 2012;105(5):254-258. https://doi.org/10.1097/SMJ.0b013e318252d602
55. Wyatt R, Laderman M, Botwinick L, Mate K, Whittington J. Achieving health equity: a guide for health care organizations. IHI White Paper. Institute for Healthcare Improvement; 2016. https://www.ihi.org
© 2020 Society of Hospital Medicine
Helping older adults overcome the challenges of technology
Technology is pervasive, and for many people, it is central to their daily activities. Younger people who have been exposed to technology for their entire lives take this for granted, but older individuals often have had much less experience with it. Many technological developments that are now a part of most people’s daily life, such as personal computers, cell phones, and automated teller machines (ATMs), have occurred in the past 4 decades, with the pace accelerating in the last 15 to 20 years.
Such changes have had a substantial impact on older adults who were never exposed to these technologies during their working life. For example, an 85-year-old person who retired at age 65 would probably have not been exposed to wireless internet prior to retirement. Therefore, all of the tasks that they are now required to complete online would have been performed in other ways. Banking, accessing instruction manuals for new devices, and even scheduling and confirming health care appointments and accessing medical records all now require individuals to have a level of technological skills that many older individuals find challenging. At times, this can limit their ability to complete routine daily activities, and also can have clinical implications (Table).
Fortunately, there are strategies clinicians can use to help their older patients face these challenges. In this article, we describe the cognitive domains associated with learning technological skills, how aging affects these domains, and what can be done to help older adults improve their technological skills.
Limited training on how to use new technology
Technological skills are similar to any other skills in one critical way: they need to be learned. At the same time, technological skills also differ from many other skills, such as playing a musical instrument, because of the constant updating of devices, programs, and applications. When smartphones or computers update their operating systems, the visual appearance of the screen and the way that tasks are performed also can change. Buttons can move and sequences of commands can be altered. Updates often happen with little or no notice, and users may need to navigate a completely different device landscape in order to perform tasks that they had previously mastered.
In addition, the creators/distributors of technology typically provide little training or documentation. Further, institutions such as banks or health care systems frequently do not provide any specific training for using their systems. For example, when patients are required to use technology to refill prescriptions, typically there is no training available on how the system operates.
Cognitive domains associated with technological skills
Because there are minimal opportunities to receive training in how to use most aspects of technology, users have to be able to learn by exposure and experience. This requires several different cognitive abilities to work together. In a recent review, Harvey1 described cognition and cognitive assessment in the general population, with a focus on cognitive domains. Here we discuss several of these domains in terms of the relationship to real-world functional tasks and discuss their importance for mastering technology.
Reasoning and problem solving. Because most technological devices and applications are designed to be “intuitive,” the user needs to be able to adopt a sequential approach to learning the task. For example, using the internet to refill a prescription requires several steps:
- accessing the internet
- finding the pharmacy web site
- establishing a user ID and password
- navigating the web site to the prescriptions section
- identifying the correct prescription
- requesting the refill
- selecting the pickup date and time.
Continue to: After navigating these steps...
After navigating these steps, an individual still needs other cognitive abilities to refill other prescriptions later. However, executive functioning is also critical for maintaining organization across different technological demands. For example, web sites have different password rules and require frequent changes without re-using old passwords, so it becomes critical to maintain an organized list of web site addresses and their passwords.
Refilling a prescription with a telephone voice menu also requires a series of steps. Typically, this process is simpler than an internet refill, because no log-in information is necessary. However, it still requires a structured series of tasks.
Working memory refers to the ability to hold information in consciousness long enough to operate on it. At each step of the navigation process, the user needs to remember which steps he/she has already completed, because repeating steps can slow down the process or lead to error messages. Thus, remembering which steps have been completed is as critical for performing tasks as is correctly understanding the anticipated sequence of steps. Further, when a password is forgotten, the user needs to remember the newly provided password.
Working memory can be spatial as well. For example, most web sites do not display a password while it is being entered, which eliminates spatial working memory from the equation. Thus, the ability to remember which characters have been entered and which still need to be entered is necessary.
Episodic memory is the process of learning and retaining newly presented verbal or spatial information as well as recalling it later for adaptive use. After successfully using a new technology, it is critical to be able to remember what to do the next time it is used. This includes both recalling how to access the technology (including the web address, user ID, and password), recalling the steps needed to be performed and their sequence, and recognizing the buttons and instructions presented onscreen.
Continue to: Procedural memory
Procedural memory is memory for motor acts and sequences. For instance, remembering how to ride a bicycle is a procedural memory, as is the ability to perform motor acts in sequence, such as peeling, cutting, and cooking vegetables. Interestingly, procedural memory can be spared in individuals with major challenges in episodic memory, such as those with amnestic conditions or cortical dementia. Thus, it may be possible for people to continue to perform technology-based skills despite declines in episodic memory. Many current technological functional tasks have fixed sequences of events that, if remembered, can lead to increased efficiency and higher chances of success in performance of functional tasks.
Prospective memory is the ability to remember to perform tasks in the future. This can include event-related tasks (eg, enter your password before trying to make a hotel reservation on a web site) or time-related tasks (eg, refill your prescriptions next Friday). Technology can actually facilitate prospective memory by providing reminders to individuals, such as alarms for appointments. However, prospective memory is required to initially set up such alarms, and setting up confusing or incorrect alarms can impede task performance.
Processing speed is the ability to perform cognitively demanding tasks under time constraints. Traditional processing speed tasks include coding and sorting tasks, which require processing new information and effort for relatively short periods of time. In our research, we discovered that processing speed measured with traditional tests was strongly correlated with the time required to perform functional tasks such as an ATM banking task.2,3 This correlation makes sense in terms of the fact that many real-world functional tasks with technology often have a series of sequential demands that must be accomplished before progression to the next task.
Manual dexterity is also important for using technology. Many electronic devices have small, touch screen-based keyboards. Being able to touch the correct key requires dexterity and can be made more difficult by age-related vision changes, a tremor, or reduced sensation in extremities.
Cognitive changes and aging
It is normal for certain cognitive abilities to change with aging. There are a set of cognitive skills that are generally stable from early adulthood until the early “senescent” period. Some of these skills decline normatively after age 60 to 65, or earlier in some individuals. These include processing new information, solving new problems, and learning and remembering information. Referred to as “fluid intelligence,” these abilities show age-related decline during healthy aging, and even greater decline in individuals with age-related cognitive conditions.
Continue to: On the other hand...
On the other hand, some cognitive abilities do not decline with aging. These include previously acquired knowledge, such as vocabulary and mathematics skills, as well as factual information, such as academic information and the faces of familiar people. These are referred to as “crystallized intelligence,” and there is limited evidence that they decline with age. In fact, these abilities do not decline until the moderately severe stage of cortical dementias, and are commonly used to index premorbid cognitive functioning and cognitive reserve.
Why is this distinction between fluid intelligence and crystallized intelligence important? As noted above, many older people do not have early-life experience with technology. Thus, their crystallized intelligence, which is not as vulnerable to decline with aging, does not include information about how to perform many technological tasks. In contrast to today’s adolescents and young adults, older adults’ academic history typically does not include using smartphones, doing homework via Google Docs, or having homework and classwork assigned via the internet.
Learning how to use new technology requires fluid intelligence, and these abilities are less efficient in older adults. So for many older people, technological tasks can be complex and unfamiliar, and the skills needed to learn how to perform them are also more limited, even in comparison to older adults’ own ability when younger. Because many technology-based activities require concurrent performance of multiple tasks, older adults are at a disadvantage.4 It is not surprising, therefore, that a subset of older adults rate their technology skills as weak, and technology-based tasks as challenging or anxiety-provoking.
However, studies show most older adults’ attitudes toward technology remain largely positive, and that they are capable of attaining the necessary skills to use information and communication technology.4,5 An individual’s perception of his/her age, age-related beliefs, and self-efficacy are associated not only with attitudes toward technology, but possibly with cognition itself.6
Education level and socioeconomic factors also influence a person’s ability to become proficient in using technology.7-9 In fact, socioeconomic factors are more strongly related to access to the internet than age. Many older adults have internet access, but this access does not always translate into full use of its services.
Continue to: The Box...
The Box10-22 describes some of the effects of aging on the brain, and how these changes are reflected in cognitive abilities.
Box
The global baseline intensity of human brain activity, determined by indirectly measuring blood oxygenation, decreases with age.10 Multiple domains of fluid cognition decline with age; these cognitive abilities include processing speed,11,12 working memory,11 episodic memory,11 and executive function.11 Expected neuroanatomic changes of aging include a decrease in cerebral grey matter volume as well as decreased white matter integrity, which is associated with diminished executive function and impaired working memory.13 Processing speed is associated with increased white matter microstructure during neurodevelopment.14 Diminished processing speed in older adults also may predict increased mortality risk.15 Individuals with advanced age may have augmented difficulty with episodic memory, especially when they are required to integrate information from more than one source.11 Diminished hippocampal volume13 and reduced activity of the middle frontal gyrus are associated with age-related decline in episodic memory retrieval.10 Working memory16 is known to share a neurocircuitry overlap with attention processes.17 Working memory capacity also is closely associated with other cognitive functions, such as shifting and inhibition.10 Enhanced cerebellar activity is related to working memory; increased cerebellar activity is likely due to compensatory recruitment of neurons due to reduced activity in the superior frontal gyrus.10 The superior frontal gyrus contributes to both working memory as well as executive processing.10
Although the cognitive decline associated with aging is inevitable, individuals who experience cognitive decline at an increased rate are predisposed to worse outcomes. One longitudinal cohort study found that adults in their 8th and 9th decades of life with preserved cognitive function had a lower risk of disability and death.18
On the other hand, crystallized cognitive functions such as semantic memory,13 shortterm memory,13 and emotion regulation16 remain largely intact throughout the aging process. Semantic memory, a subtype of episodic memory, is related to associated facts or interpretations of previous occurrences.19 This type of memory is detached from an individual’s personal experience.20 Semantic memory loss classically presents with anomia and detectable lesions in the anterior and temporal lobes.20 Emotion regulation deficits are not a part of normal aging; in fact, emotional well-being is known to either improve or remain consistent with age.21 Emotional experiences in patients of advanced age may be more complex and unique in comparison to other cognitive abilities.22
The role of cognitive training
Existing interventions for helping older adults improve their technology proficiency generally focus on improving cognition, and not necessarily on addressing skills learning. Skills learning and cognition are related; however, the brain depends on neural plasticity for skills learning, whereas cognitive declines are a result of gradual and functional worsening of memory, processing speed, executive functioning, and attention.23 Interventions such as cognitive strategy training are capable of altering brain neurocircuitry to improve attention and memory.10,11 Other interventions known to improve cognition include exercise10 and processing speed training.24 On the other hand, skills learning is more effectively targeted by interventions that focus on stimulating realistic environments to mimic activities of daily living that involve technology.
Studies have consistently demonstrated cognitive improvements associated with computerized cognitive training (CCT). The Advanced Cognitive Training for Independent and Vital Elderly (ACTIVE) study was designed to evaluate the efficacy of cognitive training in 2,832 healthy adults age >65 across 6 recruitment sites in the United States.25 Participants were randomized to a control group (no treatment) or to 1 of 3 treatment groups:
- memory strategy training (instructor-led, not computerized)
- reasoning training (instructor-led, not computerized)
- speed training (no instructor, adaptive computerized training).
Each treatment group received 10 sessions of classroom-based training (1 hour each, twice per week for 5 weeks). Following the intervention, participants who had completed ≥8 sessions were randomized to receive 4 booster sessions at 11 and 35 months after the initial training, or no booster sessions.
Each cognitive training program significantly improved performance on within-domain cognitive tests relative to the control group. Effect sizes were large immediately following training; they declined over time, but were still significant at 10-year follow-up. As hypothesized, training effects did not generalize to neuropsychological tests in other training domains. The booster subgroup of speed training showed improved performance on a separate functional speed measure at 2-year26 and 5-year follow-up.27 Each condition showed slower decline in instrumental activities of daily living relative to the control group.
Continue to: The Figure...
The Figure shows the type of stimuli presented in the speed training, a procedure where individuals are taught high-speed multitasking by having to identify and locate visual information quickly in a divided-attention format. A stimulus appears in the center of the screen—either a car or a truck—and at the same time, a “Route 66” sign appears in the periphery. For every successful response, the next stimulus is presented at a shorter duration after every successful response, and more slowly after errors.
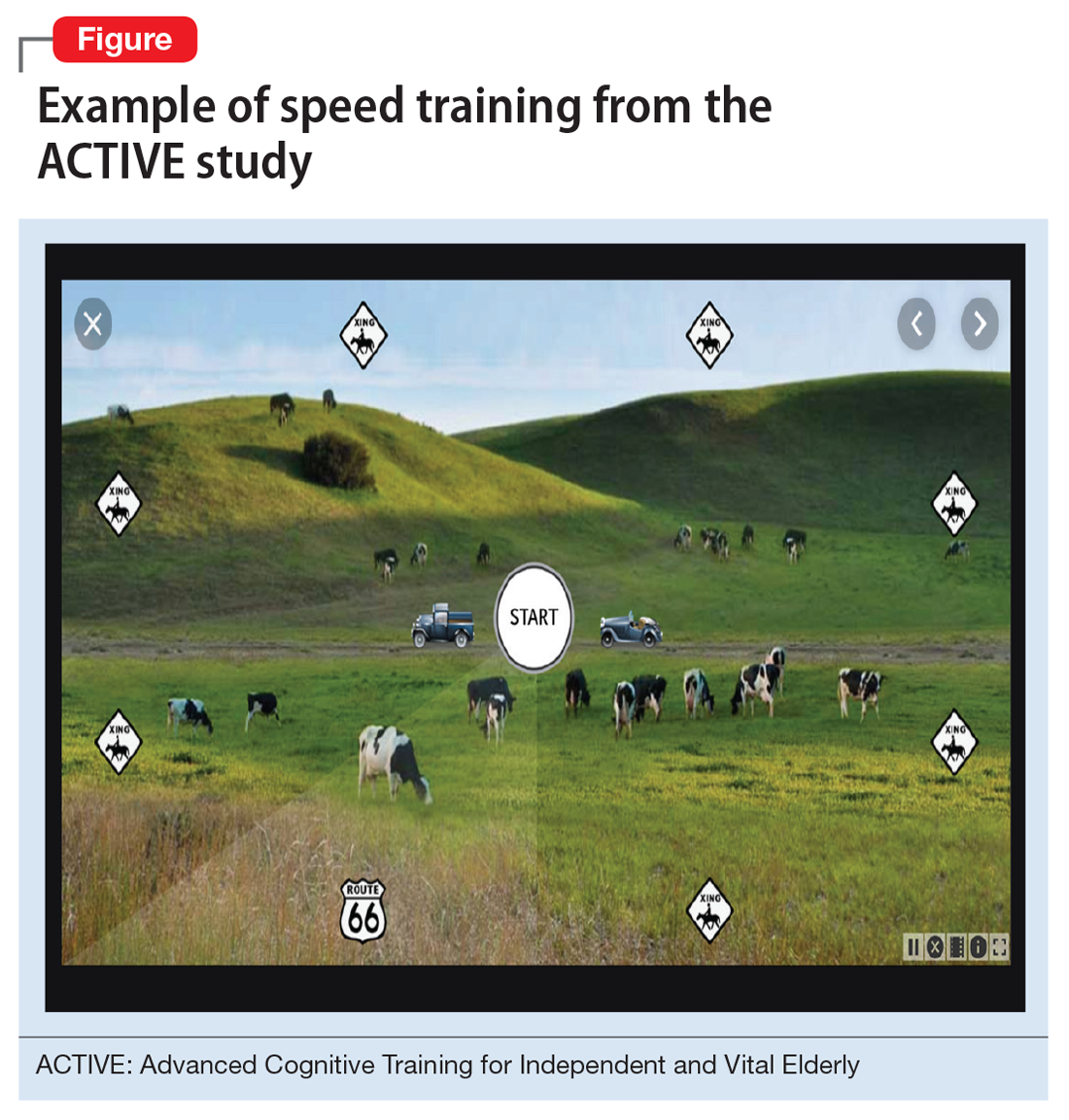
Secondary outcome analyses demonstrated that for older adults, speed training reduced rates of driving cessation,27 improved driving habits, and lowered the incidence of at-fault crashes28 (based on motor vehicle records). Speed training also resulted in improvements in health-related quality of life,29,30 depression,31 locus of control,32 and medical expenditures.33 An analysis of 10-year outcomes34 found that speed training was associated with a 29% reduction in risk of developing of dementia, while the other 2 interventions were not. However, despite these multiple areas of benefit, there was no evidence that new functional skills were acquired as a result of the training.26-34
Functional skills training
While there is a long history of using functional skills training to help patients with schizophrenia, for healthy older people, there are considerably more challenges. First, aging is not a disease. Consequently, functional skills training is typically not covered by health insurance. Second, functional skills training delivered by a human trainer can be expensive and is not readily available. Finally, there are no real curricula for training functional skills, particularly those that are device-based (phone, tablet, or computer).
Recently, researchers have developed a functional skills assessment and training program that was originally piloted as a fixed difficulty simulation as described in 2 studies by Czaja et al.2,3 The original assessment was used to compare healthy control individuals with people with mild cognitive impairment (MCI) or schizophrenia. Most recently, training modules for 6 different technology-based functional tasks have been developed and piloted in samples of healthy controls and patients with MCI in a randomized trial.35 Half of the participants in each of the 2 groups were randomized to receive speed training similar to the ACTIVE study, and the other half received skills training alone. All participants were trained for 24 sessions over 12 weeks or until they mastered all 6 simulations.
Both patients with MCI and healthy controls improved in all 6 simulations. Although patients with MCI were considerably less efficient at baseline, their training gains per session were equivalent to that of healthy controls. Finally, concurrent cognitive training increased the efficiency of skills training. At the end of the study, functional gains were the same for people in both groups randomized to either condition, even though individuals in the combined cognitive and skills training interventions received only half as much skills training time.
Continue to: What to tell patients
What to tell patients
Older patients might ask their clinicians what they can do to “exercise their brain.” Let them know that CCT has been shown to improve cognitive performance in healthy older people, and that there are several evidence-based, commercially available products for this purpose. Two such self-administrable systems with supportive data are BrainHQ (www.brainhq.com) and Happy Neuron (www.happy-neuron.com). Explain that it is likely that the best strategy is a combination of cognitive and functional skills training. One commercially available functional skills training program with supportive data is i-Function (www.i-Function.com). (Editor’s note: One of the authors, PDH, is an employee of i-Function, Inc.)
Bottom Line
Clinicians should ensure older patients that they have the cognitive capacity to learn new technology-related functional skills, and that such patients have the opportunity to learn these skills. Clinicians need to be able to identify people who are at high risk of not being able to adhere to instructions and suggestions that require interactions with technology. Treatment options include computerized cognitive training and functional skills training.
Related Resources
- Hill NT, Mowszowski L, Naismith SL, et al. Computerized cognitive training in older adults with mild cognitive impairment or dementia: a systematic review and metaanalysis. Am J Psychiatry. 2017;174(4):329-340.
- Harvey PD, McGurk SR, Mahncke H, et al. Controversies in computerized cognitive training. Biol Psychiatry Cogn Neurosci Neuroimaging. 2018;3(11):907-915.
1. Harvey PD. Domains of cognition and their assessment. Dialogues Clin Neuro. 2019;21(3):227-237.
2. Czaja SJ, Loewenstein DA, Sabbag SA, et al. A novel method for direct assessment of everyday competence among older adults. J Alzheimers Dis. 2017;57(4):1229-1238.
3. Czaja SJ, Loewenstein DA, Lee CC, et al. Assessing functional performance using computer-based simulations of everyday activities. Schizophr Res. 2017;183:130-136.
4. Tsai HS, Shillair R, Cotten SR. Social support and “playing around”: an examination of how older adults acquire digital literacy with tablet computers. J Appl Gerontol. 2017;36(1):29-55.
5. Cabrita M, Tabak M, Vollenbroek-Hutten MM. Older adults’ attitudes toward ambulatory technology to support monitoring and coaching of healthy behaviors: qualitative study. JMIR Aging. 2019;2(1):e10476. doi: 10.2196/10476.
6. Lim KY, Chang KJ, Kim HJ, et al. P.5.a.010 association between memory age identity and cognition in the elderly. Eur Neuropsychopharmacol. 2010;20(suppl 3):S555.
7. Moraes C, Pinto JA Jr, Lopes MA, et al. Impact of sociodemographic and health variables on mini-mental state examination in a community-based sample of older people. Eur Arch Psychiatry Clin Neurosci. 2010;260(7):535-542.
8. Freitas S, Simões MR, Alves L, et al. The relevance of sociodemographic and health variables on MMSE normative data. Appl Neuropsychol Adult. 2015;22(4):311-319.
9. Han C, Jo SA, Jo I, et al. An adaptation of the Korean mini-mental state examination (K-MMSE) in elderly Koreans: demographic influence and population-based norms (the AGE study). Arch Gerontol Geriatr. 2008;47(3):302-310.
10. Yin S, Zhu X, Li R, et al. Intervention-induced enhancement in intrinsic brain activity in healthy older adults. Sci Rep. 2014;4:7309.
11. Bender AR, Prindle JJ, Brandmaier AM, et al. White matter and memory in healthy adults: coupled changes over two years. Neuroimage. 2016;131:193-204.
12. Guye S, von Bastian CC. Working memory training in older adults: Bayesian evidence supporting the absence of transfer. Psychol Aging. 2017;32(8):732-746.
13. Taki Y, Kinomura S, Sato K, et al. Correlation between gray/white matter volume and cognition in healthy elderly people. Brain Cogn. 2011;75(2):170-176.
14. Cassidy AR, White MT, DeMaso DR, et al. Processing speed, executive function, and academic achievement in children with dextro-transposition of the great arteries: Testing a longitudinal developmental cascade model. Neuropsychology. 2016;30(7):874-885.
15. Aichele S, Rabbitt P, Ghisletta P. Life span decrements in fluid intelligence and processing speed predict mortality risk. Psychol Aging. 2015;30(3):598-612.
16. Eich TS, Castel AD. The cognitive control of emotional versus value-based information in younger and older adults. Psychol Aging. 2016;31(5):503-512.
17. Rolle CE, Anguera JA, Skinner SN, et al. Enhancing spatial attention and working memory in younger and older adults. J Cogn Neurosci. 2017;29(9):1483-1497.
18. Yaffe K, Lindquist K, Vittinghoff E, et al. The effect of maintaining cognition on risk of disability and death. J Am Geriatr Soc. 2010;58(5):889-894.
19. Madore KP, Schacter DL. An episodic specificity induction enhances means-end problem solving in young and older adults. Psychol Aging. 2014;29(4):913-924.
20. Matthews BR. Memory dysfunction. Continuum (Minneap Minn). 2015;21(3 Behavioral Neurology and Neuropsychiatry):613-626.
21. Mather M. The emotion paradox in the aging brain. Ann N Y Acad Sci. 2012;1251(1):33-49.
22. Gurera JW, Isaacowitz DM. Emotion regulation and emotion perception in aging: A perspective on age-related differences and similarities. Prog Brain Res. 2019;247:329-351.
23. Cai L, Chan JS, Yan JH, et al. Brain plasticity and motor practice in cognitive aging. Front Aging Neurosci. 2014;6:31.
24. Cassetta BD, Tomfohr-Madsen LM, Goghari VM. A randomized controlled trial of working memory and processing speed training in schizophrenia. Psychol Med. 2019;49(12):2009-2019.
25. Ball K, Berch DB, Helmers KF, et al. Effects of cognitive training interventions with older adults: a randomized controlled trial. JAMA. 2002;288(18):2271-2281.
26. Rebok GW, Ball K, Guey LT, et al. Ten-year effects of the advanced cognitive training for independent and vital elderly cognitive training trial on cognition and everyday functioning in older adults. J Am Geriatr Soc. 2014;62(1):16-24.
27. Edwards JD, Delahunt PB, Mahncke HW. Cognitive speed of processing training delays driving cessation. J Gerontol A Biol Sci Med Sci. 2009;64(12):1262-1267.
28. Ball K, Edwards JD, Ross LA, et al. Cognitive training decreases motor vehicle collision involvement of older drivers. J Am Geriatr Soc. 2010;58(11):2107-2113.
29. Wolinsky FD, Unverzagt FW, Smith DM, et al. The effects of the ACTIVE cognitive training trial on clinically relevant declines in health-related quality of life. J Gerontol B Psychol Sci Soc Sci. 2006;61(5):S281-S287.
30. Wolinsky FD, Unverzagt FW, Smith DM, et al. The ACTIVE cognitive training trial and health-related quality of life: protection that lasts for 5 years. J Gerontol A Biol Sci Med Sci. 2006;61(12):1324-1329.
31. Wolinsky FD, Vander Weg MW, Martin R, et al. The effect of speed-of-processing training on depressive symptoms in ACTIVE. J Gerontol A Biol Sci Med Sci. 2009;64(4):468-472.
32. Wolinsky FD, Vander Weg MW, Martin R, et al. Does cognitive training improve internal locus of control among older adults? J Gerontol B Psychol Sci Soc Sci. 2010;65(5):591-598.
33. Wolinsky FD, Mahncke HW, Kosinski M, et al. The ACTIVE cognitive training trial and predicted medical expenditures. BMC Health Serv Res. 2009;9:109.
34. Edwards JD, Xu H, Clark DO, et al. Speed of processing training results in lower risk of dementia. Alzheimers Dement (N Y). 2017;3(4):603-611.
35. Harvey PD, Tibiriçá L, Kallestrup P, et al. A computerized functional skills assessment and training program targeting technology based everyday functional skills. J Vis Exp. 2020;156:e60330. doi: 10.3791/60330.
Technology is pervasive, and for many people, it is central to their daily activities. Younger people who have been exposed to technology for their entire lives take this for granted, but older individuals often have had much less experience with it. Many technological developments that are now a part of most people’s daily life, such as personal computers, cell phones, and automated teller machines (ATMs), have occurred in the past 4 decades, with the pace accelerating in the last 15 to 20 years.
Such changes have had a substantial impact on older adults who were never exposed to these technologies during their working life. For example, an 85-year-old person who retired at age 65 would probably have not been exposed to wireless internet prior to retirement. Therefore, all of the tasks that they are now required to complete online would have been performed in other ways. Banking, accessing instruction manuals for new devices, and even scheduling and confirming health care appointments and accessing medical records all now require individuals to have a level of technological skills that many older individuals find challenging. At times, this can limit their ability to complete routine daily activities, and also can have clinical implications (Table).
Fortunately, there are strategies clinicians can use to help their older patients face these challenges. In this article, we describe the cognitive domains associated with learning technological skills, how aging affects these domains, and what can be done to help older adults improve their technological skills.
Limited training on how to use new technology
Technological skills are similar to any other skills in one critical way: they need to be learned. At the same time, technological skills also differ from many other skills, such as playing a musical instrument, because of the constant updating of devices, programs, and applications. When smartphones or computers update their operating systems, the visual appearance of the screen and the way that tasks are performed also can change. Buttons can move and sequences of commands can be altered. Updates often happen with little or no notice, and users may need to navigate a completely different device landscape in order to perform tasks that they had previously mastered.
In addition, the creators/distributors of technology typically provide little training or documentation. Further, institutions such as banks or health care systems frequently do not provide any specific training for using their systems. For example, when patients are required to use technology to refill prescriptions, typically there is no training available on how the system operates.
Cognitive domains associated with technological skills
Because there are minimal opportunities to receive training in how to use most aspects of technology, users have to be able to learn by exposure and experience. This requires several different cognitive abilities to work together. In a recent review, Harvey1 described cognition and cognitive assessment in the general population, with a focus on cognitive domains. Here we discuss several of these domains in terms of the relationship to real-world functional tasks and discuss their importance for mastering technology.
Reasoning and problem solving. Because most technological devices and applications are designed to be “intuitive,” the user needs to be able to adopt a sequential approach to learning the task. For example, using the internet to refill a prescription requires several steps:
- accessing the internet
- finding the pharmacy web site
- establishing a user ID and password
- navigating the web site to the prescriptions section
- identifying the correct prescription
- requesting the refill
- selecting the pickup date and time.
Continue to: After navigating these steps...
After navigating these steps, an individual still needs other cognitive abilities to refill other prescriptions later. However, executive functioning is also critical for maintaining organization across different technological demands. For example, web sites have different password rules and require frequent changes without re-using old passwords, so it becomes critical to maintain an organized list of web site addresses and their passwords.
Refilling a prescription with a telephone voice menu also requires a series of steps. Typically, this process is simpler than an internet refill, because no log-in information is necessary. However, it still requires a structured series of tasks.
Working memory refers to the ability to hold information in consciousness long enough to operate on it. At each step of the navigation process, the user needs to remember which steps he/she has already completed, because repeating steps can slow down the process or lead to error messages. Thus, remembering which steps have been completed is as critical for performing tasks as is correctly understanding the anticipated sequence of steps. Further, when a password is forgotten, the user needs to remember the newly provided password.
Working memory can be spatial as well. For example, most web sites do not display a password while it is being entered, which eliminates spatial working memory from the equation. Thus, the ability to remember which characters have been entered and which still need to be entered is necessary.
Episodic memory is the process of learning and retaining newly presented verbal or spatial information as well as recalling it later for adaptive use. After successfully using a new technology, it is critical to be able to remember what to do the next time it is used. This includes both recalling how to access the technology (including the web address, user ID, and password), recalling the steps needed to be performed and their sequence, and recognizing the buttons and instructions presented onscreen.
Continue to: Procedural memory
Procedural memory is memory for motor acts and sequences. For instance, remembering how to ride a bicycle is a procedural memory, as is the ability to perform motor acts in sequence, such as peeling, cutting, and cooking vegetables. Interestingly, procedural memory can be spared in individuals with major challenges in episodic memory, such as those with amnestic conditions or cortical dementia. Thus, it may be possible for people to continue to perform technology-based skills despite declines in episodic memory. Many current technological functional tasks have fixed sequences of events that, if remembered, can lead to increased efficiency and higher chances of success in performance of functional tasks.
Prospective memory is the ability to remember to perform tasks in the future. This can include event-related tasks (eg, enter your password before trying to make a hotel reservation on a web site) or time-related tasks (eg, refill your prescriptions next Friday). Technology can actually facilitate prospective memory by providing reminders to individuals, such as alarms for appointments. However, prospective memory is required to initially set up such alarms, and setting up confusing or incorrect alarms can impede task performance.
Processing speed is the ability to perform cognitively demanding tasks under time constraints. Traditional processing speed tasks include coding and sorting tasks, which require processing new information and effort for relatively short periods of time. In our research, we discovered that processing speed measured with traditional tests was strongly correlated with the time required to perform functional tasks such as an ATM banking task.2,3 This correlation makes sense in terms of the fact that many real-world functional tasks with technology often have a series of sequential demands that must be accomplished before progression to the next task.
Manual dexterity is also important for using technology. Many electronic devices have small, touch screen-based keyboards. Being able to touch the correct key requires dexterity and can be made more difficult by age-related vision changes, a tremor, or reduced sensation in extremities.
Cognitive changes and aging
It is normal for certain cognitive abilities to change with aging. There are a set of cognitive skills that are generally stable from early adulthood until the early “senescent” period. Some of these skills decline normatively after age 60 to 65, or earlier in some individuals. These include processing new information, solving new problems, and learning and remembering information. Referred to as “fluid intelligence,” these abilities show age-related decline during healthy aging, and even greater decline in individuals with age-related cognitive conditions.
Continue to: On the other hand...
On the other hand, some cognitive abilities do not decline with aging. These include previously acquired knowledge, such as vocabulary and mathematics skills, as well as factual information, such as academic information and the faces of familiar people. These are referred to as “crystallized intelligence,” and there is limited evidence that they decline with age. In fact, these abilities do not decline until the moderately severe stage of cortical dementias, and are commonly used to index premorbid cognitive functioning and cognitive reserve.
Why is this distinction between fluid intelligence and crystallized intelligence important? As noted above, many older people do not have early-life experience with technology. Thus, their crystallized intelligence, which is not as vulnerable to decline with aging, does not include information about how to perform many technological tasks. In contrast to today’s adolescents and young adults, older adults’ academic history typically does not include using smartphones, doing homework via Google Docs, or having homework and classwork assigned via the internet.
Learning how to use new technology requires fluid intelligence, and these abilities are less efficient in older adults. So for many older people, technological tasks can be complex and unfamiliar, and the skills needed to learn how to perform them are also more limited, even in comparison to older adults’ own ability when younger. Because many technology-based activities require concurrent performance of multiple tasks, older adults are at a disadvantage.4 It is not surprising, therefore, that a subset of older adults rate their technology skills as weak, and technology-based tasks as challenging or anxiety-provoking.
However, studies show most older adults’ attitudes toward technology remain largely positive, and that they are capable of attaining the necessary skills to use information and communication technology.4,5 An individual’s perception of his/her age, age-related beliefs, and self-efficacy are associated not only with attitudes toward technology, but possibly with cognition itself.6
Education level and socioeconomic factors also influence a person’s ability to become proficient in using technology.7-9 In fact, socioeconomic factors are more strongly related to access to the internet than age. Many older adults have internet access, but this access does not always translate into full use of its services.
Continue to: The Box...
The Box10-22 describes some of the effects of aging on the brain, and how these changes are reflected in cognitive abilities.
Box
The global baseline intensity of human brain activity, determined by indirectly measuring blood oxygenation, decreases with age.10 Multiple domains of fluid cognition decline with age; these cognitive abilities include processing speed,11,12 working memory,11 episodic memory,11 and executive function.11 Expected neuroanatomic changes of aging include a decrease in cerebral grey matter volume as well as decreased white matter integrity, which is associated with diminished executive function and impaired working memory.13 Processing speed is associated with increased white matter microstructure during neurodevelopment.14 Diminished processing speed in older adults also may predict increased mortality risk.15 Individuals with advanced age may have augmented difficulty with episodic memory, especially when they are required to integrate information from more than one source.11 Diminished hippocampal volume13 and reduced activity of the middle frontal gyrus are associated with age-related decline in episodic memory retrieval.10 Working memory16 is known to share a neurocircuitry overlap with attention processes.17 Working memory capacity also is closely associated with other cognitive functions, such as shifting and inhibition.10 Enhanced cerebellar activity is related to working memory; increased cerebellar activity is likely due to compensatory recruitment of neurons due to reduced activity in the superior frontal gyrus.10 The superior frontal gyrus contributes to both working memory as well as executive processing.10
Although the cognitive decline associated with aging is inevitable, individuals who experience cognitive decline at an increased rate are predisposed to worse outcomes. One longitudinal cohort study found that adults in their 8th and 9th decades of life with preserved cognitive function had a lower risk of disability and death.18
On the other hand, crystallized cognitive functions such as semantic memory,13 shortterm memory,13 and emotion regulation16 remain largely intact throughout the aging process. Semantic memory, a subtype of episodic memory, is related to associated facts or interpretations of previous occurrences.19 This type of memory is detached from an individual’s personal experience.20 Semantic memory loss classically presents with anomia and detectable lesions in the anterior and temporal lobes.20 Emotion regulation deficits are not a part of normal aging; in fact, emotional well-being is known to either improve or remain consistent with age.21 Emotional experiences in patients of advanced age may be more complex and unique in comparison to other cognitive abilities.22
The role of cognitive training
Existing interventions for helping older adults improve their technology proficiency generally focus on improving cognition, and not necessarily on addressing skills learning. Skills learning and cognition are related; however, the brain depends on neural plasticity for skills learning, whereas cognitive declines are a result of gradual and functional worsening of memory, processing speed, executive functioning, and attention.23 Interventions such as cognitive strategy training are capable of altering brain neurocircuitry to improve attention and memory.10,11 Other interventions known to improve cognition include exercise10 and processing speed training.24 On the other hand, skills learning is more effectively targeted by interventions that focus on stimulating realistic environments to mimic activities of daily living that involve technology.
Studies have consistently demonstrated cognitive improvements associated with computerized cognitive training (CCT). The Advanced Cognitive Training for Independent and Vital Elderly (ACTIVE) study was designed to evaluate the efficacy of cognitive training in 2,832 healthy adults age >65 across 6 recruitment sites in the United States.25 Participants were randomized to a control group (no treatment) or to 1 of 3 treatment groups:
- memory strategy training (instructor-led, not computerized)
- reasoning training (instructor-led, not computerized)
- speed training (no instructor, adaptive computerized training).
Each treatment group received 10 sessions of classroom-based training (1 hour each, twice per week for 5 weeks). Following the intervention, participants who had completed ≥8 sessions were randomized to receive 4 booster sessions at 11 and 35 months after the initial training, or no booster sessions.
Each cognitive training program significantly improved performance on within-domain cognitive tests relative to the control group. Effect sizes were large immediately following training; they declined over time, but were still significant at 10-year follow-up. As hypothesized, training effects did not generalize to neuropsychological tests in other training domains. The booster subgroup of speed training showed improved performance on a separate functional speed measure at 2-year26 and 5-year follow-up.27 Each condition showed slower decline in instrumental activities of daily living relative to the control group.
Continue to: The Figure...
The Figure shows the type of stimuli presented in the speed training, a procedure where individuals are taught high-speed multitasking by having to identify and locate visual information quickly in a divided-attention format. A stimulus appears in the center of the screen—either a car or a truck—and at the same time, a “Route 66” sign appears in the periphery. For every successful response, the next stimulus is presented at a shorter duration after every successful response, and more slowly after errors.
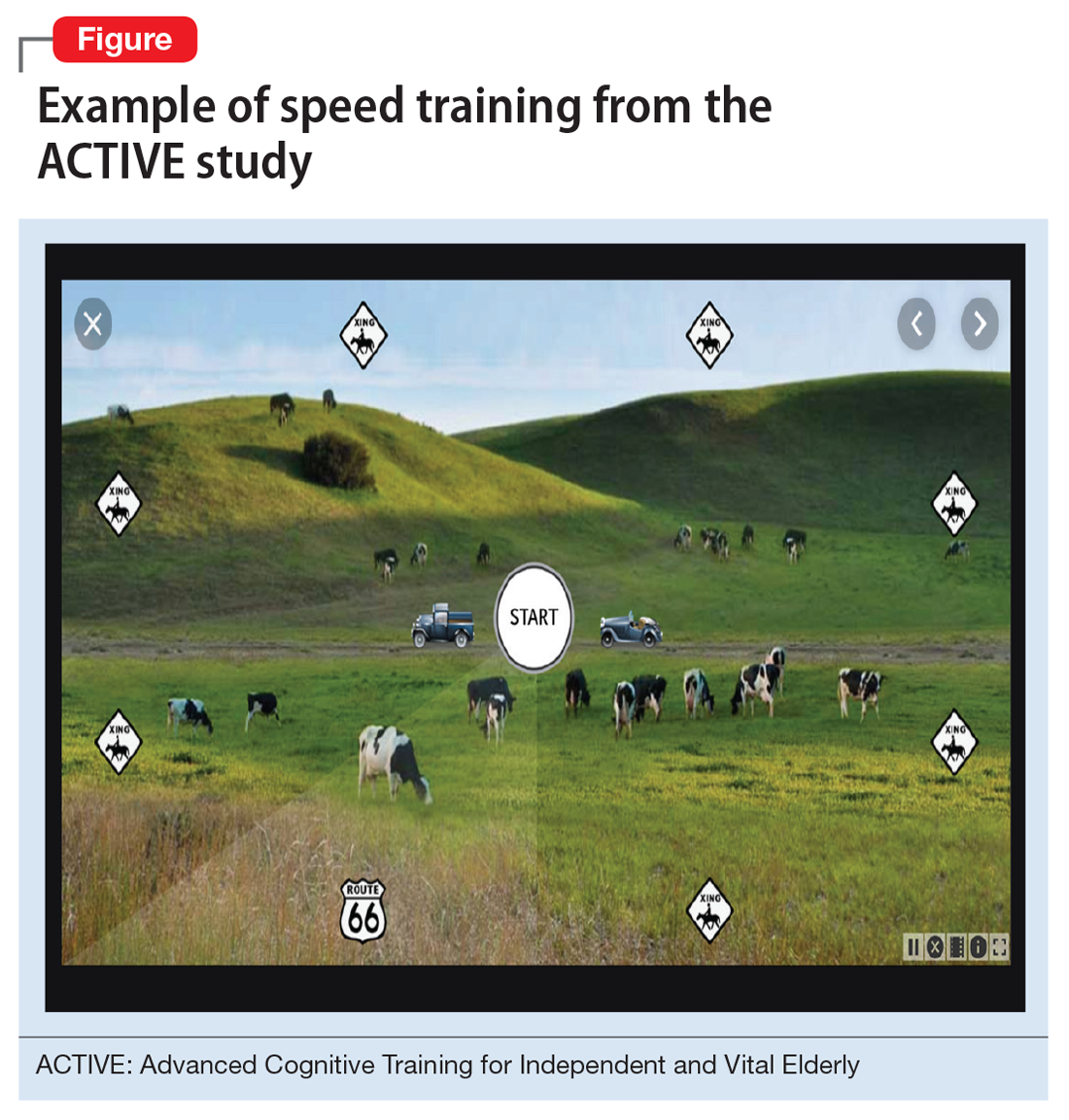
Secondary outcome analyses demonstrated that for older adults, speed training reduced rates of driving cessation,27 improved driving habits, and lowered the incidence of at-fault crashes28 (based on motor vehicle records). Speed training also resulted in improvements in health-related quality of life,29,30 depression,31 locus of control,32 and medical expenditures.33 An analysis of 10-year outcomes34 found that speed training was associated with a 29% reduction in risk of developing of dementia, while the other 2 interventions were not. However, despite these multiple areas of benefit, there was no evidence that new functional skills were acquired as a result of the training.26-34
Functional skills training
While there is a long history of using functional skills training to help patients with schizophrenia, for healthy older people, there are considerably more challenges. First, aging is not a disease. Consequently, functional skills training is typically not covered by health insurance. Second, functional skills training delivered by a human trainer can be expensive and is not readily available. Finally, there are no real curricula for training functional skills, particularly those that are device-based (phone, tablet, or computer).
Recently, researchers have developed a functional skills assessment and training program that was originally piloted as a fixed difficulty simulation as described in 2 studies by Czaja et al.2,3 The original assessment was used to compare healthy control individuals with people with mild cognitive impairment (MCI) or schizophrenia. Most recently, training modules for 6 different technology-based functional tasks have been developed and piloted in samples of healthy controls and patients with MCI in a randomized trial.35 Half of the participants in each of the 2 groups were randomized to receive speed training similar to the ACTIVE study, and the other half received skills training alone. All participants were trained for 24 sessions over 12 weeks or until they mastered all 6 simulations.
Both patients with MCI and healthy controls improved in all 6 simulations. Although patients with MCI were considerably less efficient at baseline, their training gains per session were equivalent to that of healthy controls. Finally, concurrent cognitive training increased the efficiency of skills training. At the end of the study, functional gains were the same for people in both groups randomized to either condition, even though individuals in the combined cognitive and skills training interventions received only half as much skills training time.
Continue to: What to tell patients
What to tell patients
Older patients might ask their clinicians what they can do to “exercise their brain.” Let them know that CCT has been shown to improve cognitive performance in healthy older people, and that there are several evidence-based, commercially available products for this purpose. Two such self-administrable systems with supportive data are BrainHQ (www.brainhq.com) and Happy Neuron (www.happy-neuron.com). Explain that it is likely that the best strategy is a combination of cognitive and functional skills training. One commercially available functional skills training program with supportive data is i-Function (www.i-Function.com). (Editor’s note: One of the authors, PDH, is an employee of i-Function, Inc.)
Bottom Line
Clinicians should ensure older patients that they have the cognitive capacity to learn new technology-related functional skills, and that such patients have the opportunity to learn these skills. Clinicians need to be able to identify people who are at high risk of not being able to adhere to instructions and suggestions that require interactions with technology. Treatment options include computerized cognitive training and functional skills training.
Related Resources
- Hill NT, Mowszowski L, Naismith SL, et al. Computerized cognitive training in older adults with mild cognitive impairment or dementia: a systematic review and metaanalysis. Am J Psychiatry. 2017;174(4):329-340.
- Harvey PD, McGurk SR, Mahncke H, et al. Controversies in computerized cognitive training. Biol Psychiatry Cogn Neurosci Neuroimaging. 2018;3(11):907-915.
Technology is pervasive, and for many people, it is central to their daily activities. Younger people who have been exposed to technology for their entire lives take this for granted, but older individuals often have had much less experience with it. Many technological developments that are now a part of most people’s daily life, such as personal computers, cell phones, and automated teller machines (ATMs), have occurred in the past 4 decades, with the pace accelerating in the last 15 to 20 years.
Such changes have had a substantial impact on older adults who were never exposed to these technologies during their working life. For example, an 85-year-old person who retired at age 65 would probably have not been exposed to wireless internet prior to retirement. Therefore, all of the tasks that they are now required to complete online would have been performed in other ways. Banking, accessing instruction manuals for new devices, and even scheduling and confirming health care appointments and accessing medical records all now require individuals to have a level of technological skills that many older individuals find challenging. At times, this can limit their ability to complete routine daily activities, and also can have clinical implications (Table).
Fortunately, there are strategies clinicians can use to help their older patients face these challenges. In this article, we describe the cognitive domains associated with learning technological skills, how aging affects these domains, and what can be done to help older adults improve their technological skills.
Limited training on how to use new technology
Technological skills are similar to any other skills in one critical way: they need to be learned. At the same time, technological skills also differ from many other skills, such as playing a musical instrument, because of the constant updating of devices, programs, and applications. When smartphones or computers update their operating systems, the visual appearance of the screen and the way that tasks are performed also can change. Buttons can move and sequences of commands can be altered. Updates often happen with little or no notice, and users may need to navigate a completely different device landscape in order to perform tasks that they had previously mastered.
In addition, the creators/distributors of technology typically provide little training or documentation. Further, institutions such as banks or health care systems frequently do not provide any specific training for using their systems. For example, when patients are required to use technology to refill prescriptions, typically there is no training available on how the system operates.
Cognitive domains associated with technological skills
Because there are minimal opportunities to receive training in how to use most aspects of technology, users have to be able to learn by exposure and experience. This requires several different cognitive abilities to work together. In a recent review, Harvey1 described cognition and cognitive assessment in the general population, with a focus on cognitive domains. Here we discuss several of these domains in terms of the relationship to real-world functional tasks and discuss their importance for mastering technology.
Reasoning and problem solving. Because most technological devices and applications are designed to be “intuitive,” the user needs to be able to adopt a sequential approach to learning the task. For example, using the internet to refill a prescription requires several steps:
- accessing the internet
- finding the pharmacy web site
- establishing a user ID and password
- navigating the web site to the prescriptions section
- identifying the correct prescription
- requesting the refill
- selecting the pickup date and time.
Continue to: After navigating these steps...
After navigating these steps, an individual still needs other cognitive abilities to refill other prescriptions later. However, executive functioning is also critical for maintaining organization across different technological demands. For example, web sites have different password rules and require frequent changes without re-using old passwords, so it becomes critical to maintain an organized list of web site addresses and their passwords.
Refilling a prescription with a telephone voice menu also requires a series of steps. Typically, this process is simpler than an internet refill, because no log-in information is necessary. However, it still requires a structured series of tasks.
Working memory refers to the ability to hold information in consciousness long enough to operate on it. At each step of the navigation process, the user needs to remember which steps he/she has already completed, because repeating steps can slow down the process or lead to error messages. Thus, remembering which steps have been completed is as critical for performing tasks as is correctly understanding the anticipated sequence of steps. Further, when a password is forgotten, the user needs to remember the newly provided password.
Working memory can be spatial as well. For example, most web sites do not display a password while it is being entered, which eliminates spatial working memory from the equation. Thus, the ability to remember which characters have been entered and which still need to be entered is necessary.
Episodic memory is the process of learning and retaining newly presented verbal or spatial information as well as recalling it later for adaptive use. After successfully using a new technology, it is critical to be able to remember what to do the next time it is used. This includes both recalling how to access the technology (including the web address, user ID, and password), recalling the steps needed to be performed and their sequence, and recognizing the buttons and instructions presented onscreen.
Continue to: Procedural memory
Procedural memory is memory for motor acts and sequences. For instance, remembering how to ride a bicycle is a procedural memory, as is the ability to perform motor acts in sequence, such as peeling, cutting, and cooking vegetables. Interestingly, procedural memory can be spared in individuals with major challenges in episodic memory, such as those with amnestic conditions or cortical dementia. Thus, it may be possible for people to continue to perform technology-based skills despite declines in episodic memory. Many current technological functional tasks have fixed sequences of events that, if remembered, can lead to increased efficiency and higher chances of success in performance of functional tasks.
Prospective memory is the ability to remember to perform tasks in the future. This can include event-related tasks (eg, enter your password before trying to make a hotel reservation on a web site) or time-related tasks (eg, refill your prescriptions next Friday). Technology can actually facilitate prospective memory by providing reminders to individuals, such as alarms for appointments. However, prospective memory is required to initially set up such alarms, and setting up confusing or incorrect alarms can impede task performance.
Processing speed is the ability to perform cognitively demanding tasks under time constraints. Traditional processing speed tasks include coding and sorting tasks, which require processing new information and effort for relatively short periods of time. In our research, we discovered that processing speed measured with traditional tests was strongly correlated with the time required to perform functional tasks such as an ATM banking task.2,3 This correlation makes sense in terms of the fact that many real-world functional tasks with technology often have a series of sequential demands that must be accomplished before progression to the next task.
Manual dexterity is also important for using technology. Many electronic devices have small, touch screen-based keyboards. Being able to touch the correct key requires dexterity and can be made more difficult by age-related vision changes, a tremor, or reduced sensation in extremities.
Cognitive changes and aging
It is normal for certain cognitive abilities to change with aging. There are a set of cognitive skills that are generally stable from early adulthood until the early “senescent” period. Some of these skills decline normatively after age 60 to 65, or earlier in some individuals. These include processing new information, solving new problems, and learning and remembering information. Referred to as “fluid intelligence,” these abilities show age-related decline during healthy aging, and even greater decline in individuals with age-related cognitive conditions.
Continue to: On the other hand...
On the other hand, some cognitive abilities do not decline with aging. These include previously acquired knowledge, such as vocabulary and mathematics skills, as well as factual information, such as academic information and the faces of familiar people. These are referred to as “crystallized intelligence,” and there is limited evidence that they decline with age. In fact, these abilities do not decline until the moderately severe stage of cortical dementias, and are commonly used to index premorbid cognitive functioning and cognitive reserve.
Why is this distinction between fluid intelligence and crystallized intelligence important? As noted above, many older people do not have early-life experience with technology. Thus, their crystallized intelligence, which is not as vulnerable to decline with aging, does not include information about how to perform many technological tasks. In contrast to today’s adolescents and young adults, older adults’ academic history typically does not include using smartphones, doing homework via Google Docs, or having homework and classwork assigned via the internet.
Learning how to use new technology requires fluid intelligence, and these abilities are less efficient in older adults. So for many older people, technological tasks can be complex and unfamiliar, and the skills needed to learn how to perform them are also more limited, even in comparison to older adults’ own ability when younger. Because many technology-based activities require concurrent performance of multiple tasks, older adults are at a disadvantage.4 It is not surprising, therefore, that a subset of older adults rate their technology skills as weak, and technology-based tasks as challenging or anxiety-provoking.
However, studies show most older adults’ attitudes toward technology remain largely positive, and that they are capable of attaining the necessary skills to use information and communication technology.4,5 An individual’s perception of his/her age, age-related beliefs, and self-efficacy are associated not only with attitudes toward technology, but possibly with cognition itself.6
Education level and socioeconomic factors also influence a person’s ability to become proficient in using technology.7-9 In fact, socioeconomic factors are more strongly related to access to the internet than age. Many older adults have internet access, but this access does not always translate into full use of its services.
Continue to: The Box...
The Box10-22 describes some of the effects of aging on the brain, and how these changes are reflected in cognitive abilities.
Box
The global baseline intensity of human brain activity, determined by indirectly measuring blood oxygenation, decreases with age.10 Multiple domains of fluid cognition decline with age; these cognitive abilities include processing speed,11,12 working memory,11 episodic memory,11 and executive function.11 Expected neuroanatomic changes of aging include a decrease in cerebral grey matter volume as well as decreased white matter integrity, which is associated with diminished executive function and impaired working memory.13 Processing speed is associated with increased white matter microstructure during neurodevelopment.14 Diminished processing speed in older adults also may predict increased mortality risk.15 Individuals with advanced age may have augmented difficulty with episodic memory, especially when they are required to integrate information from more than one source.11 Diminished hippocampal volume13 and reduced activity of the middle frontal gyrus are associated with age-related decline in episodic memory retrieval.10 Working memory16 is known to share a neurocircuitry overlap with attention processes.17 Working memory capacity also is closely associated with other cognitive functions, such as shifting and inhibition.10 Enhanced cerebellar activity is related to working memory; increased cerebellar activity is likely due to compensatory recruitment of neurons due to reduced activity in the superior frontal gyrus.10 The superior frontal gyrus contributes to both working memory as well as executive processing.10
Although the cognitive decline associated with aging is inevitable, individuals who experience cognitive decline at an increased rate are predisposed to worse outcomes. One longitudinal cohort study found that adults in their 8th and 9th decades of life with preserved cognitive function had a lower risk of disability and death.18
On the other hand, crystallized cognitive functions such as semantic memory,13 shortterm memory,13 and emotion regulation16 remain largely intact throughout the aging process. Semantic memory, a subtype of episodic memory, is related to associated facts or interpretations of previous occurrences.19 This type of memory is detached from an individual’s personal experience.20 Semantic memory loss classically presents with anomia and detectable lesions in the anterior and temporal lobes.20 Emotion regulation deficits are not a part of normal aging; in fact, emotional well-being is known to either improve or remain consistent with age.21 Emotional experiences in patients of advanced age may be more complex and unique in comparison to other cognitive abilities.22
The role of cognitive training
Existing interventions for helping older adults improve their technology proficiency generally focus on improving cognition, and not necessarily on addressing skills learning. Skills learning and cognition are related; however, the brain depends on neural plasticity for skills learning, whereas cognitive declines are a result of gradual and functional worsening of memory, processing speed, executive functioning, and attention.23 Interventions such as cognitive strategy training are capable of altering brain neurocircuitry to improve attention and memory.10,11 Other interventions known to improve cognition include exercise10 and processing speed training.24 On the other hand, skills learning is more effectively targeted by interventions that focus on stimulating realistic environments to mimic activities of daily living that involve technology.
Studies have consistently demonstrated cognitive improvements associated with computerized cognitive training (CCT). The Advanced Cognitive Training for Independent and Vital Elderly (ACTIVE) study was designed to evaluate the efficacy of cognitive training in 2,832 healthy adults age >65 across 6 recruitment sites in the United States.25 Participants were randomized to a control group (no treatment) or to 1 of 3 treatment groups:
- memory strategy training (instructor-led, not computerized)
- reasoning training (instructor-led, not computerized)
- speed training (no instructor, adaptive computerized training).
Each treatment group received 10 sessions of classroom-based training (1 hour each, twice per week for 5 weeks). Following the intervention, participants who had completed ≥8 sessions were randomized to receive 4 booster sessions at 11 and 35 months after the initial training, or no booster sessions.
Each cognitive training program significantly improved performance on within-domain cognitive tests relative to the control group. Effect sizes were large immediately following training; they declined over time, but were still significant at 10-year follow-up. As hypothesized, training effects did not generalize to neuropsychological tests in other training domains. The booster subgroup of speed training showed improved performance on a separate functional speed measure at 2-year26 and 5-year follow-up.27 Each condition showed slower decline in instrumental activities of daily living relative to the control group.
Continue to: The Figure...
The Figure shows the type of stimuli presented in the speed training, a procedure where individuals are taught high-speed multitasking by having to identify and locate visual information quickly in a divided-attention format. A stimulus appears in the center of the screen—either a car or a truck—and at the same time, a “Route 66” sign appears in the periphery. For every successful response, the next stimulus is presented at a shorter duration after every successful response, and more slowly after errors.
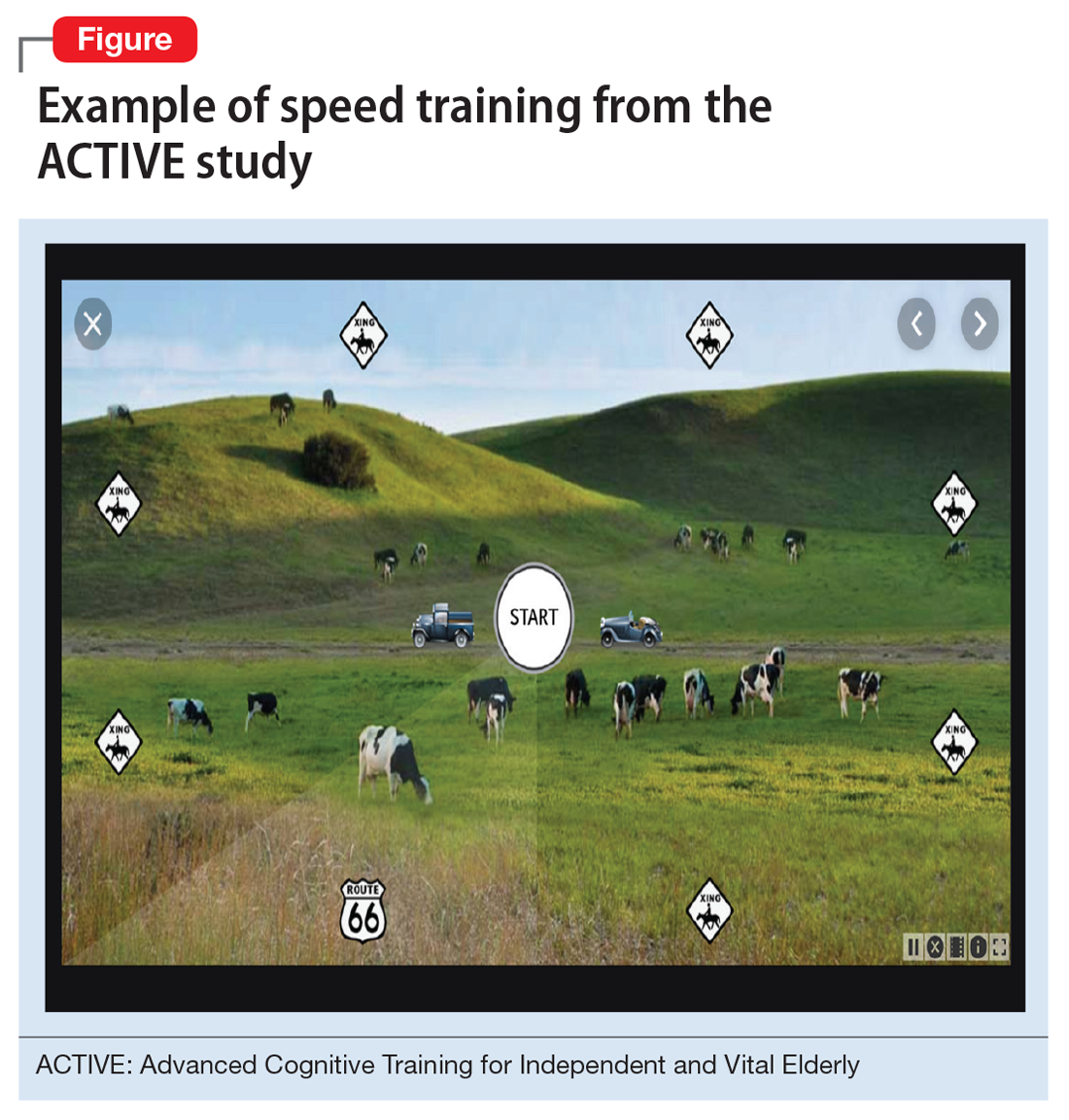
Secondary outcome analyses demonstrated that for older adults, speed training reduced rates of driving cessation,27 improved driving habits, and lowered the incidence of at-fault crashes28 (based on motor vehicle records). Speed training also resulted in improvements in health-related quality of life,29,30 depression,31 locus of control,32 and medical expenditures.33 An analysis of 10-year outcomes34 found that speed training was associated with a 29% reduction in risk of developing of dementia, while the other 2 interventions were not. However, despite these multiple areas of benefit, there was no evidence that new functional skills were acquired as a result of the training.26-34
Functional skills training
While there is a long history of using functional skills training to help patients with schizophrenia, for healthy older people, there are considerably more challenges. First, aging is not a disease. Consequently, functional skills training is typically not covered by health insurance. Second, functional skills training delivered by a human trainer can be expensive and is not readily available. Finally, there are no real curricula for training functional skills, particularly those that are device-based (phone, tablet, or computer).
Recently, researchers have developed a functional skills assessment and training program that was originally piloted as a fixed difficulty simulation as described in 2 studies by Czaja et al.2,3 The original assessment was used to compare healthy control individuals with people with mild cognitive impairment (MCI) or schizophrenia. Most recently, training modules for 6 different technology-based functional tasks have been developed and piloted in samples of healthy controls and patients with MCI in a randomized trial.35 Half of the participants in each of the 2 groups were randomized to receive speed training similar to the ACTIVE study, and the other half received skills training alone. All participants were trained for 24 sessions over 12 weeks or until they mastered all 6 simulations.
Both patients with MCI and healthy controls improved in all 6 simulations. Although patients with MCI were considerably less efficient at baseline, their training gains per session were equivalent to that of healthy controls. Finally, concurrent cognitive training increased the efficiency of skills training. At the end of the study, functional gains were the same for people in both groups randomized to either condition, even though individuals in the combined cognitive and skills training interventions received only half as much skills training time.
Continue to: What to tell patients
What to tell patients
Older patients might ask their clinicians what they can do to “exercise their brain.” Let them know that CCT has been shown to improve cognitive performance in healthy older people, and that there are several evidence-based, commercially available products for this purpose. Two such self-administrable systems with supportive data are BrainHQ (www.brainhq.com) and Happy Neuron (www.happy-neuron.com). Explain that it is likely that the best strategy is a combination of cognitive and functional skills training. One commercially available functional skills training program with supportive data is i-Function (www.i-Function.com). (Editor’s note: One of the authors, PDH, is an employee of i-Function, Inc.)
Bottom Line
Clinicians should ensure older patients that they have the cognitive capacity to learn new technology-related functional skills, and that such patients have the opportunity to learn these skills. Clinicians need to be able to identify people who are at high risk of not being able to adhere to instructions and suggestions that require interactions with technology. Treatment options include computerized cognitive training and functional skills training.
Related Resources
- Hill NT, Mowszowski L, Naismith SL, et al. Computerized cognitive training in older adults with mild cognitive impairment or dementia: a systematic review and metaanalysis. Am J Psychiatry. 2017;174(4):329-340.
- Harvey PD, McGurk SR, Mahncke H, et al. Controversies in computerized cognitive training. Biol Psychiatry Cogn Neurosci Neuroimaging. 2018;3(11):907-915.
1. Harvey PD. Domains of cognition and their assessment. Dialogues Clin Neuro. 2019;21(3):227-237.
2. Czaja SJ, Loewenstein DA, Sabbag SA, et al. A novel method for direct assessment of everyday competence among older adults. J Alzheimers Dis. 2017;57(4):1229-1238.
3. Czaja SJ, Loewenstein DA, Lee CC, et al. Assessing functional performance using computer-based simulations of everyday activities. Schizophr Res. 2017;183:130-136.
4. Tsai HS, Shillair R, Cotten SR. Social support and “playing around”: an examination of how older adults acquire digital literacy with tablet computers. J Appl Gerontol. 2017;36(1):29-55.
5. Cabrita M, Tabak M, Vollenbroek-Hutten MM. Older adults’ attitudes toward ambulatory technology to support monitoring and coaching of healthy behaviors: qualitative study. JMIR Aging. 2019;2(1):e10476. doi: 10.2196/10476.
6. Lim KY, Chang KJ, Kim HJ, et al. P.5.a.010 association between memory age identity and cognition in the elderly. Eur Neuropsychopharmacol. 2010;20(suppl 3):S555.
7. Moraes C, Pinto JA Jr, Lopes MA, et al. Impact of sociodemographic and health variables on mini-mental state examination in a community-based sample of older people. Eur Arch Psychiatry Clin Neurosci. 2010;260(7):535-542.
8. Freitas S, Simões MR, Alves L, et al. The relevance of sociodemographic and health variables on MMSE normative data. Appl Neuropsychol Adult. 2015;22(4):311-319.
9. Han C, Jo SA, Jo I, et al. An adaptation of the Korean mini-mental state examination (K-MMSE) in elderly Koreans: demographic influence and population-based norms (the AGE study). Arch Gerontol Geriatr. 2008;47(3):302-310.
10. Yin S, Zhu X, Li R, et al. Intervention-induced enhancement in intrinsic brain activity in healthy older adults. Sci Rep. 2014;4:7309.
11. Bender AR, Prindle JJ, Brandmaier AM, et al. White matter and memory in healthy adults: coupled changes over two years. Neuroimage. 2016;131:193-204.
12. Guye S, von Bastian CC. Working memory training in older adults: Bayesian evidence supporting the absence of transfer. Psychol Aging. 2017;32(8):732-746.
13. Taki Y, Kinomura S, Sato K, et al. Correlation between gray/white matter volume and cognition in healthy elderly people. Brain Cogn. 2011;75(2):170-176.
14. Cassidy AR, White MT, DeMaso DR, et al. Processing speed, executive function, and academic achievement in children with dextro-transposition of the great arteries: Testing a longitudinal developmental cascade model. Neuropsychology. 2016;30(7):874-885.
15. Aichele S, Rabbitt P, Ghisletta P. Life span decrements in fluid intelligence and processing speed predict mortality risk. Psychol Aging. 2015;30(3):598-612.
16. Eich TS, Castel AD. The cognitive control of emotional versus value-based information in younger and older adults. Psychol Aging. 2016;31(5):503-512.
17. Rolle CE, Anguera JA, Skinner SN, et al. Enhancing spatial attention and working memory in younger and older adults. J Cogn Neurosci. 2017;29(9):1483-1497.
18. Yaffe K, Lindquist K, Vittinghoff E, et al. The effect of maintaining cognition on risk of disability and death. J Am Geriatr Soc. 2010;58(5):889-894.
19. Madore KP, Schacter DL. An episodic specificity induction enhances means-end problem solving in young and older adults. Psychol Aging. 2014;29(4):913-924.
20. Matthews BR. Memory dysfunction. Continuum (Minneap Minn). 2015;21(3 Behavioral Neurology and Neuropsychiatry):613-626.
21. Mather M. The emotion paradox in the aging brain. Ann N Y Acad Sci. 2012;1251(1):33-49.
22. Gurera JW, Isaacowitz DM. Emotion regulation and emotion perception in aging: A perspective on age-related differences and similarities. Prog Brain Res. 2019;247:329-351.
23. Cai L, Chan JS, Yan JH, et al. Brain plasticity and motor practice in cognitive aging. Front Aging Neurosci. 2014;6:31.
24. Cassetta BD, Tomfohr-Madsen LM, Goghari VM. A randomized controlled trial of working memory and processing speed training in schizophrenia. Psychol Med. 2019;49(12):2009-2019.
25. Ball K, Berch DB, Helmers KF, et al. Effects of cognitive training interventions with older adults: a randomized controlled trial. JAMA. 2002;288(18):2271-2281.
26. Rebok GW, Ball K, Guey LT, et al. Ten-year effects of the advanced cognitive training for independent and vital elderly cognitive training trial on cognition and everyday functioning in older adults. J Am Geriatr Soc. 2014;62(1):16-24.
27. Edwards JD, Delahunt PB, Mahncke HW. Cognitive speed of processing training delays driving cessation. J Gerontol A Biol Sci Med Sci. 2009;64(12):1262-1267.
28. Ball K, Edwards JD, Ross LA, et al. Cognitive training decreases motor vehicle collision involvement of older drivers. J Am Geriatr Soc. 2010;58(11):2107-2113.
29. Wolinsky FD, Unverzagt FW, Smith DM, et al. The effects of the ACTIVE cognitive training trial on clinically relevant declines in health-related quality of life. J Gerontol B Psychol Sci Soc Sci. 2006;61(5):S281-S287.
30. Wolinsky FD, Unverzagt FW, Smith DM, et al. The ACTIVE cognitive training trial and health-related quality of life: protection that lasts for 5 years. J Gerontol A Biol Sci Med Sci. 2006;61(12):1324-1329.
31. Wolinsky FD, Vander Weg MW, Martin R, et al. The effect of speed-of-processing training on depressive symptoms in ACTIVE. J Gerontol A Biol Sci Med Sci. 2009;64(4):468-472.
32. Wolinsky FD, Vander Weg MW, Martin R, et al. Does cognitive training improve internal locus of control among older adults? J Gerontol B Psychol Sci Soc Sci. 2010;65(5):591-598.
33. Wolinsky FD, Mahncke HW, Kosinski M, et al. The ACTIVE cognitive training trial and predicted medical expenditures. BMC Health Serv Res. 2009;9:109.
34. Edwards JD, Xu H, Clark DO, et al. Speed of processing training results in lower risk of dementia. Alzheimers Dement (N Y). 2017;3(4):603-611.
35. Harvey PD, Tibiriçá L, Kallestrup P, et al. A computerized functional skills assessment and training program targeting technology based everyday functional skills. J Vis Exp. 2020;156:e60330. doi: 10.3791/60330.
1. Harvey PD. Domains of cognition and their assessment. Dialogues Clin Neuro. 2019;21(3):227-237.
2. Czaja SJ, Loewenstein DA, Sabbag SA, et al. A novel method for direct assessment of everyday competence among older adults. J Alzheimers Dis. 2017;57(4):1229-1238.
3. Czaja SJ, Loewenstein DA, Lee CC, et al. Assessing functional performance using computer-based simulations of everyday activities. Schizophr Res. 2017;183:130-136.
4. Tsai HS, Shillair R, Cotten SR. Social support and “playing around”: an examination of how older adults acquire digital literacy with tablet computers. J Appl Gerontol. 2017;36(1):29-55.
5. Cabrita M, Tabak M, Vollenbroek-Hutten MM. Older adults’ attitudes toward ambulatory technology to support monitoring and coaching of healthy behaviors: qualitative study. JMIR Aging. 2019;2(1):e10476. doi: 10.2196/10476.
6. Lim KY, Chang KJ, Kim HJ, et al. P.5.a.010 association between memory age identity and cognition in the elderly. Eur Neuropsychopharmacol. 2010;20(suppl 3):S555.
7. Moraes C, Pinto JA Jr, Lopes MA, et al. Impact of sociodemographic and health variables on mini-mental state examination in a community-based sample of older people. Eur Arch Psychiatry Clin Neurosci. 2010;260(7):535-542.
8. Freitas S, Simões MR, Alves L, et al. The relevance of sociodemographic and health variables on MMSE normative data. Appl Neuropsychol Adult. 2015;22(4):311-319.
9. Han C, Jo SA, Jo I, et al. An adaptation of the Korean mini-mental state examination (K-MMSE) in elderly Koreans: demographic influence and population-based norms (the AGE study). Arch Gerontol Geriatr. 2008;47(3):302-310.
10. Yin S, Zhu X, Li R, et al. Intervention-induced enhancement in intrinsic brain activity in healthy older adults. Sci Rep. 2014;4:7309.
11. Bender AR, Prindle JJ, Brandmaier AM, et al. White matter and memory in healthy adults: coupled changes over two years. Neuroimage. 2016;131:193-204.
12. Guye S, von Bastian CC. Working memory training in older adults: Bayesian evidence supporting the absence of transfer. Psychol Aging. 2017;32(8):732-746.
13. Taki Y, Kinomura S, Sato K, et al. Correlation between gray/white matter volume and cognition in healthy elderly people. Brain Cogn. 2011;75(2):170-176.
14. Cassidy AR, White MT, DeMaso DR, et al. Processing speed, executive function, and academic achievement in children with dextro-transposition of the great arteries: Testing a longitudinal developmental cascade model. Neuropsychology. 2016;30(7):874-885.
15. Aichele S, Rabbitt P, Ghisletta P. Life span decrements in fluid intelligence and processing speed predict mortality risk. Psychol Aging. 2015;30(3):598-612.
16. Eich TS, Castel AD. The cognitive control of emotional versus value-based information in younger and older adults. Psychol Aging. 2016;31(5):503-512.
17. Rolle CE, Anguera JA, Skinner SN, et al. Enhancing spatial attention and working memory in younger and older adults. J Cogn Neurosci. 2017;29(9):1483-1497.
18. Yaffe K, Lindquist K, Vittinghoff E, et al. The effect of maintaining cognition on risk of disability and death. J Am Geriatr Soc. 2010;58(5):889-894.
19. Madore KP, Schacter DL. An episodic specificity induction enhances means-end problem solving in young and older adults. Psychol Aging. 2014;29(4):913-924.
20. Matthews BR. Memory dysfunction. Continuum (Minneap Minn). 2015;21(3 Behavioral Neurology and Neuropsychiatry):613-626.
21. Mather M. The emotion paradox in the aging brain. Ann N Y Acad Sci. 2012;1251(1):33-49.
22. Gurera JW, Isaacowitz DM. Emotion regulation and emotion perception in aging: A perspective on age-related differences and similarities. Prog Brain Res. 2019;247:329-351.
23. Cai L, Chan JS, Yan JH, et al. Brain plasticity and motor practice in cognitive aging. Front Aging Neurosci. 2014;6:31.
24. Cassetta BD, Tomfohr-Madsen LM, Goghari VM. A randomized controlled trial of working memory and processing speed training in schizophrenia. Psychol Med. 2019;49(12):2009-2019.
25. Ball K, Berch DB, Helmers KF, et al. Effects of cognitive training interventions with older adults: a randomized controlled trial. JAMA. 2002;288(18):2271-2281.
26. Rebok GW, Ball K, Guey LT, et al. Ten-year effects of the advanced cognitive training for independent and vital elderly cognitive training trial on cognition and everyday functioning in older adults. J Am Geriatr Soc. 2014;62(1):16-24.
27. Edwards JD, Delahunt PB, Mahncke HW. Cognitive speed of processing training delays driving cessation. J Gerontol A Biol Sci Med Sci. 2009;64(12):1262-1267.
28. Ball K, Edwards JD, Ross LA, et al. Cognitive training decreases motor vehicle collision involvement of older drivers. J Am Geriatr Soc. 2010;58(11):2107-2113.
29. Wolinsky FD, Unverzagt FW, Smith DM, et al. The effects of the ACTIVE cognitive training trial on clinically relevant declines in health-related quality of life. J Gerontol B Psychol Sci Soc Sci. 2006;61(5):S281-S287.
30. Wolinsky FD, Unverzagt FW, Smith DM, et al. The ACTIVE cognitive training trial and health-related quality of life: protection that lasts for 5 years. J Gerontol A Biol Sci Med Sci. 2006;61(12):1324-1329.
31. Wolinsky FD, Vander Weg MW, Martin R, et al. The effect of speed-of-processing training on depressive symptoms in ACTIVE. J Gerontol A Biol Sci Med Sci. 2009;64(4):468-472.
32. Wolinsky FD, Vander Weg MW, Martin R, et al. Does cognitive training improve internal locus of control among older adults? J Gerontol B Psychol Sci Soc Sci. 2010;65(5):591-598.
33. Wolinsky FD, Mahncke HW, Kosinski M, et al. The ACTIVE cognitive training trial and predicted medical expenditures. BMC Health Serv Res. 2009;9:109.
34. Edwards JD, Xu H, Clark DO, et al. Speed of processing training results in lower risk of dementia. Alzheimers Dement (N Y). 2017;3(4):603-611.
35. Harvey PD, Tibiriçá L, Kallestrup P, et al. A computerized functional skills assessment and training program targeting technology based everyday functional skills. J Vis Exp. 2020;156:e60330. doi: 10.3791/60330.
COVID-19 and patients with serious mental illness
“This whole thing is not about heroism. It’s about decency. It may seem a ridiculous idea, but the only way to fight the plague is with decency . ”
– Albert Camus, La Peste (1947)1
Severe acute respiratory syndrome (SARS), H1N1 swine flu, Ebola, Zika, and Middle East respiratory syndrome (MERS): the 21st century has already been witness to several serious infectious outbreaks and pandemics,2 but none has been as deadly and consequential as the current one. The ongoing SARS-coronavirus-2 (SARS-CoV-2) pandemic is shaping not only current psychiatric care but the future of psychiatry. Now that we are beyond the initial stages of the coronavirus disease 2019 (COVID-19) pandemic, when psychiatrists had a crash course in disaster psychiatry, our attention must shift to rebuilding and managing disillusionment and other psychological fallout of the intense early days.3
In this article, we offer guidance to psychiatrists caring for patients with serious mental illness (SMI) during the SARS-CoV-2 pandemic. Patients with SMI are easily forgotten as other issues (eg, preserving ICU capacity) overshadow the already historically neglected needs of this impoverished group.4 From both human and public-health perspectives, this inattention is a mistake. Assuring psychiatric stability is critically important to prevent the spread of COVID-19 in marginalized communities comprised of individuals who are poor, members of racial minorities, and others who already experience health disparities.5 Without controlling transmission in these groups, the pandemic will not be sufficiently contained.
We begin by highlighting general principles of pandemic management because caring for patients with SMI does not occur in a vacuum. Infectious outbreaks require not only helping those who need direct medical care because they are infected, but also managing populations that are at risk of getting infected, including health care and other essential workers.
Principles of pandemic management
Delivery of medical care during a pandemic differs from routine care. An effective disaster response requires collaboration and coordination among public-health, treatment, and emergency systems. Many institutions shift to an incident management system and crisis leadership, with clear lines of authority to coordinate responders and build medical surge capacity. Such a top-down leadership approach must plan and allow for the emergence of other credible leaders and for the restoration of people’s agency.
Unfortunately, adaptive capacity may be limited, especially in the public sector and psychiatric care system, where resources are already poor. Particularly early in a pandemic, services considered non-essential—which includes most psychiatric outpatient care—can become unavailable. A major effort is needed to prevent the psychiatric care system from contracting further, as happened during 9/11.6 Additionally, “essential” cannot be conflated with “emergent,” as can easily occur in extreme circumstances. Early and sustained efforts are required to ensure that patients with SMI who may be teetering on the edge of emergency status do not slip off that edge, especially when the emergency medical system is operating over capacity.
A comprehensive outbreak response must consider that a pandemic is not only a medical crisis but a mental health crisis and a communication emergency.7 Mental health clinicians need to provide accurate information and help patients cope with their fears.
Continue to: Psychological aspects of pandemics
Psychological aspects of pandemics. Previous infectious outbreaks have reaffirmed that mental health plays an outsized role during epidemics. Chaos, uncertainty, fear of death, and loss of income and housing cause prolonged stress and exact a psychological toll.
Adverse psychological impacts include expectable, normal reactions such as stress-induced anxiety or insomnia. In addition, new-onset psychiatric illnesses or exacerbations of existing ones may emerge.8 As disillusionment and demoralization appear in the wake of the acute phase, with persistently high unemployment, suicide prevention becomes an important goal.9
Pandemics lead to expectable behavioral responses (eg, increases in substance use and interpersonal conflict). Fear-based decisions may result in unhelpful behavior, such as hoarding medications (which may result in shortages) or dangerous, unsupervised use of unproven medications (eg, hydroxychloroquine). Trust is needed to accept public-health measures, and recommendations (eg, wearing masks) must be culturally informed to be credible and effective.
Because people are affected differently, at individual, cultural, and socioeconomic levels, they will view the situation differently. For many people, secondary stressors (eg, job loss) may be more disastrous than the primary medical event (ie, the pandemic). This distinction is critical because concrete financial help, not psychiatric care, is needed. Sometimes, even when a psychiatric disorder such as SMI or major neurocognitive disorder is present, the illusion of an acute decompensation can be created by the loss of social and structural supports that previously scaffolded a person’s life.
Mental illness prevention. Community mental-health surveillance is important to monitor for distress, psychiatric symptoms, health-risk behaviors, risk and safety perception, and preparedness. Clinicians must be ready to normalize expectable and temporary distress, while recognizing when that distress becomes pathological. This may be difficult in patients with SMI who often already have reduced stress tolerance or problem-based coping skills.10
Continue to: Psychological first aid...
Psychological first aid (PFA) is a standard intervention recommended by the World Health Organization for most individuals following a disaster; it is evidence-informed and has face validity.11 Intended to relieve distress by creating an environment that is safe, calm, and connected, PFA fosters self-efficacy and hope. While PFA is a form of universal prevention, it is not designed for patients with SMI, is not a psychiatric intervention, and is not provided by clinicians. Its principles, however, can easily be applied to patients with SMI to prevent distressing symptoms from becoming a relapse.
Communication. Good risk and crisis communication are critical because individual and population behavior will be governed by the perception of risk and fear, and not by facts. Failure to manage the “infodemic”7—with its misinformation, contradictory messages, and rumors—jeopardizes infection control if patients become paralyzed by uncertainty and fear. Scapegoating occurs easily during times of threat, and society must contain the parallel epidemic of xenophobia based on stigma and misinformation.12
Decision-making under uncertainty is not perfect and subject to revision as better information becomes available. Pointing this out to the public is delicate but essential to curtail skepticism and mistrust when policies are adjusted in response to new circumstances and knowledge.
Mistrust of an authority’s legitimacy and fear-based decisions lead to lack of cooperation with public-health measures, which can undermine an effective response to the pandemic. Travel restrictions or quarantine measures will not be followed if individuals question their importance. Like the general public, patients need education and clear communication to address their fear of contagion, dangers posed to family (and pets), and mistrust of authority and government. A lack of appreciation of the seriousness of the pandemic and individual responsibility may need to be addressed. Two important measures to accomplish this are steering patients to reputable sources of information and advising that they limit media exposure.
Resilience-building. Community and workplace resilience are important aspects of making it through a disaster as best as possible. Resilience is not innate and fixed; it must be deliberately built.13 Choosing an attitude of post-traumatic growth over the victim narrative is a helpful stance. Practicing self-care (rest, nutrition, exercise) and self-compassion (self-kindness, common humanity, mindfulness) is good advice for patients and caregivers alike.
Continue to: Workforce protection
Workforce protection. Compared to other disasters, infectious outbreaks disproportionally affect the medical community, and care delivery is at stake. While psychological and psychiatric needs may increase during a pandemic, services often contract, day programs and clinics close, teams are reduced to skeleton crews, and only emergency psychiatric care is available. Workforce protection is critical to avoid illness or simple absenteeism due to mistrust of protective measures.
Only a well-briefed, well-led, well-supported, and adequately resourced workforce is going to be effective in managing this public-health emergency. Burnout and moral injury are feared long-term consequences for health care workers that need to be proactively addressed.14 As opposed to other forms of disasters, managing your own fears about safety is important. Clinicians and their patients sit in the proverbial same boat.
Ethics. The anticipated need to ration life-saving care (eg, ventilators) has been at the forefront of ethical concerns.15 In psychiatry, the question of involuntary public-health interventions for uncooperative psychiatric patients sits uncomfortably between public-health ethics and human rights, and is an opportunity for collaboration with public-health and infectious-disease colleagues.
Redeployed clinicians and those working under substandard conditions may be concerned about civil liability due to a modified standard of care during a crisis. Some clinicians may ask if their duty to care must override their natural instinct to protect themselves. There is a lot of room for resentment in these circumstances. Redeployed or otherwise “conscripted” clinicians may resent administrators, especially those administering from the safety of their homes. Those “left behind” to work in potentially precarious circumstances may resent their absent colleagues. Moreover, these front-line clinicians may have been forced to make ethical decisions for which they were not prepared.16 Maintaining morale is far from trivial, not just during the pandemic, but afterward, when (and if) the entire workforce is reunited. All parties need to be mindful of how their actions and decisions impact and are perceived by others, both in the hospital and at home.
Managing patients with SMI during COVID-19
Patients with SMI are potentially hard hit by COVID-19 due to a “tragic” epidemiologic triad of agent-host-environment: SARS-CoV-2 is a highly infectious agent affecting patients with SMI who are vulnerable hosts in permissive environments (Figure).
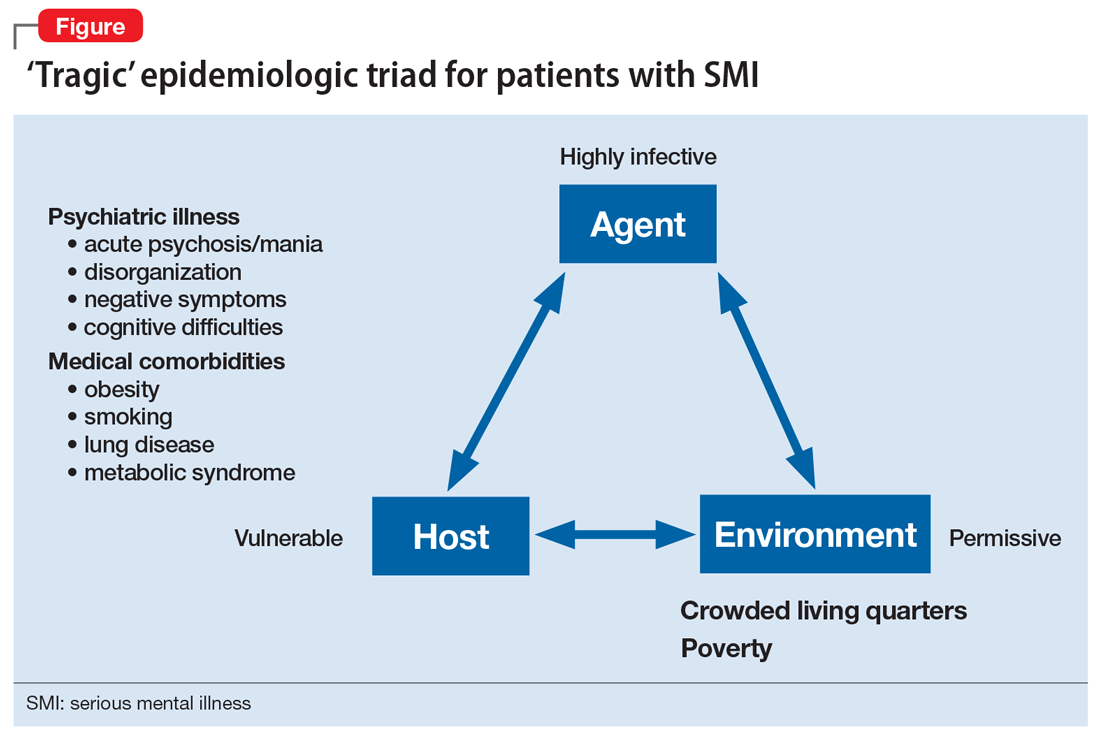
Continue to: While not as infectious as measles...
While not as infectious as measles, COVID-19 is more infectious than the seasonal flu virus.17 It can lead to uncontrolled infection within a short period of time, particularly in enclosed settings. Outbreaks have occurred readily on cruise ships and aircraft carriers as well as in nursing homes, homeless shelters, prisons, and group homes.
Patients with SMI are vulnerable hosts because they have many of the medical risk factors18 that portend a poor prognosis if they become infected, including pre-existing lung conditions and heart disease19 as well as diabetes and obesity.20 Obesity likely creates a hyperinflammatory state and a decrease in vital capacity. Patient-related behavioral factors include poor early-symptom reporting and ineffective infection control.
Unfavorable social determinants of health include not only poverty but crowded housing that is a perfect incubator for COVID-19.
Priority treatment goals. The overarching goal during a pandemic is to keep patients with SMI in psychiatric treatment and prevent them from disengaging from care in the service of infection control. Urgent tasks include infection control, relapse prevention, and preventing treatment disengagement and loneliness.
Infection control. As trusted sources of information, psychiatrists can play an important role in infection control in several important ways:
- educating patients about infection-control measures and public-health recommendations
- helping patients understand what testing can accomplish and when to pursue it
- encouraging protective health behaviors (eg, hand washing, mask wearing, physical distancing)
- assessing patients’ risk appreciation
- assessing for and addressing obstacles to implementing and complying with infection-control measures
- explaining contact tracing
- providing reassurance.
Continue to: Materials and explanations...
Materials and explanations must be adapted for patient understanding.
Patients with disorganization or cognitive disturbances may have difficulties cooperating or problem-solving. Patients with negative symptoms may be inappropriately unconcerned and also inaccurately report symptoms that suggest COVID-19. Acute psychosis or mania can prevent patients from complying with public-health efforts. Some measures may be difficult to implement if the means are simply not there (eg, physical distancing in a crowded apartment). Previously open settings (eg, group homes) have had to develop new mechanisms under the primacy of infection control. Inpatient units—traditionally places where community, shared healing, and group therapy are prized—have had to decrease maximum occupancy, limit the number of patients attending groups, and discourage or outrightly prohibit social interaction (eg, dining together).
Relapse prevention. Patients who take maintenance medications need to be supported. A manic or psychotic relapse during a pandemic puts patients at risk of acquiring and spreading COVID-19. “Treatment as prevention” is a slogan from human immunodeficiency virus (HIV) care that captures the importance of antiretroviral treatment to prevent medical complications from HIV, and also to reduce infecting other people. By analogy, psychiatric treatment for patients with SMI can prevent psychiatric instability and thereby control viral transmission. Avoiding sending psychiatric patients to a potentially stressed acute-care system is important.
Psychosocial support. Clinics need to ensure that patients continue to engage in care beyond medication-taking to proactively prevent psychiatric exacerbations. Healthful, resilience-building behaviors should be encouraged while monitoring and counseling against maladaptive ones (eg, increased substance use). Supporting patients emotionally and helping them solve problems are critical, particularly for those who are subjected to quarantine or isolation. Obviously, in these latter situations, outreach will be necessary and may require creative delivery systems and dedicated clinicians for patients who lack access to the technology necessary for virtual visits. Havens and Ghaemi21 have suggested that a good therapeutic alliance can be viewed as a mood stabilizer. Helping patients grieve losses (loved ones, jobs, sense of safety) may be an important part of support.
Even before COVID-19, loneliness was a major factor for patients with schizophrenia.22 A psychiatric clinic is one aspect of a person with SMI’s social network; during the initial phase of the pandemic, many clinics and treatment programs closed. Patients for whom clinics structure and anchor their activities are at high risk of disconnecting from treatment, staying at home, and becoming lonely.
Continue to: Caregivers are always important...
Caregivers are always important to SMI patients, but they may assume an even bigger role during this pandemic. Some patients may have moved in with a relative, after years of living on their own. In other cases, stable caregiver relationships may be disrupted due to COVID-19–related sickness in the caregiver; if not addressed, this can result in a patient’s clinical decompensation. Clinicians should take the opportunity to understand who a patient’s caregivers are (group home staff, families) and rekindle clinical contact with them. Relationships with caregivers that may have been on “autopilot” during normal times are opportunities for welcome support and guidance, to the benefit of both patients and caregivers.
Table 1 summarizes clinical tasks that need to be kept in mind when conducting clinic visits during COVID-19 in order to achieve the high-priority treatment goals of infection control, relapse prevention, and psychosocial support.
Differential diagnosis. Neuropsychiatric syndromes have long been observed in influenza pandemics,23 due both to direct viral effects and to the effects of critical illness on the brain. Two core symptoms of COVID-19—anosmia and ageusia—suggest that COVID-19 can directly affect the brain. While neurologic manifestations are common,24 it remains unclear to what extent COVID-19 can directly “cause” psychiatric symptoms, or if such symptoms are the result of cytokines25 or other medical processes (eg, thromboembolism).26 Psychosis due to COVID-19 may, in some cases, represent a stress-related brief psychotic disorder.27
Hospitalized patients who have recovered from COVID-19 may have experienced prolonged sedation and severe delirium in an ICU.28 Complications such as posttraumatic stress disorder,29 hypoperfusion-related brain injuries, or other long-term cognitive difficulties may result. In previous flu epidemics, patients developed serious neurologic complications such as post-encephalitic Parkinson’s disease.30
Any person subjected to isolation or quarantine is at risk for psychiatric complications.31 Patients with SMI who live in group homes may be particularly susceptible to new rules, including no-visitor policies.
Continue to: Outpatients whose primary disorder...
Outpatients whose primary disorder is well controlled may, like anyone else, struggle with the effects of the pandemic. It is necessary to carefully differentiate non-specific symptoms associated with stress from the emergence of a new disorder resulting from stress.32 For some patients, grief or adjustment disorders should be considered. Prolonged stress and uncertainty may eventually lead to an exacerbation of a primary disorder, particularly if the situation (eg, financial loss) does not improve or worsens. Demoralization and suicidal thinking need to be monitored. Relapse or increased use of alcohol or other substances as a response to stress may also complicate the clinical picture.33 Last, smoking cessation as a major treatment goal in general should be re-emphasized and not ignored during the ongoing pandemic.34
Table 2 summarizes psychiatric symptoms that need to be considered when managing a patient with SMI during this pandemic.
Treatment tools
Psychopharmacology. Even though crisis-mode prescribing may be necessary, the safe use of psychotropics remains the goal of psychiatric prescribing. Access to medications becomes a larger consideration; for many patients, a 90-day supply may be indicated. Review of polypharmacy, including for pneumonia risk, should be undertaken. Preventing drooling (eg, from sedation, clozapine, extrapyramidal symptoms [EPS]) will decrease aspiration risk.
In general, treatment of psychiatric symptoms in a patient with COVID-19 follows usual guidelines. The best treatment for COVID-19 patients with delirium, however, remains to be established, particularly how to manage severe agitation.28 Pharmacodynamic and pharmacokinetic drug–drug interactions between psychotropics and antiviral treatments for COVID-19 (eg, QTc prolongation) can be expected and need to be reviewed.35 For stress-related anxiety, judicious pharmacotherapy can be helpful. Diazepam given at the earliest signs of a psychotic relapse may stave off a relapse for patients with schizophrenia.36 Even if permitted under relaxed prescribing rules during a public-health emergency, prescribing controlled substances without seeing patients in person requires additional thought. In some cases, adjusting the primary medication to buffer against stress may be preferred (eg, adjusting an antipsychotic in a patient on maintenance treatment for schizophrenia, particularly if a low-dose strategy is pursued).
Clozapine requires registry-based prescribing and bloodwork (“no blood, no drug”). The use of clozapine during this public-health emergency has been made easier because of FDA guidance that allows clozapine to be dispensed without blood work if obtaining blood work is not possible (eg, a patient is quarantined) or can be accomplished only at substantial risk to patients and the population at large. Under certain conditions, clozapine can be dispensed safely and in a way that is consistent with infection prevention. Clozapine-treated patients admitted with COVID-19 should be monitored for clozapine toxicity and the clozapine dose adjusted.37 A consensus statement consistent with the FDA and clinical considerations for using clozapine during COVID-19 is summarized in Table 3.38
Continue to: Long-acting injectable antipsychotics...
Long-acting injectable antipsychotics (LAIs) pose a problem because they require in-person visits. Ideally, during a pandemic, patients should be seen in person as frequently as medically necessary but as infrequently as possible to limit exposure of both patients and staff. Table 4 provides some clinical recommendations on how to use LAIs during the pandemic.39
Supportive psychotherapy may be the most important tool we have in helping patients with loss and uncertainty during these challenging months.40 Simply staying in contact with patients plays a major role in preventing care discontinuity. Even routine interactions have become stressful, with everyone wearing a mask that partially obscures the face. People with impaired hearing may find it even more difficult to understand you.
Education, problem-solving, and a directive, encouraging style are major tools of supportive psychotherapy to reduce symptoms and increase adaptive skills. Clarify that social distancing refers to physical, not emotional, distancing. The judicious and temporary use of anxiolytics is appropriate to reduce anxiety. Concrete help and problem-solving (eg, filling out forms) are examples of proactive crisis intervention.
Telepsychiatry emerged in the pandemic’s early days as the default mode of practice in order to limit in-person contacts.41 Like all new technology, telepsychiatry brings progress and peril.42 While it has gone surprisingly well for most, the “digital divide” does not afford all patients access to the needed technology. The long-term effectiveness and acceptance of telehealth remain to be seen. (Editor’s Note: For more about this topic, see “Telepsychiatry: What you need to know.”
Lessons learned and outlook
Infectious outbreaks have historically inflicted long-term disruptions on societies and altered the course of history. However, each disaster is unique, and lessons from previous disasters may only partially apply.43 We do not yet know how this one will end, including how long it will take for the world’s economies to recover. If nothing else, the current public-health emergency has brought to the forefront what psychiatrists have always known: health disparities are partially responsible for different disease risks (in this case, the risk of getting infected with SARS-CoV-2).5 It may not be a coincidence that the Black Lives Matter movement is becoming a major impetus for social change at a time when the pandemic is exposing health-care inequalities.
Continue to: Some areas of the country...
Some areas of the country succeeded in reducing infections and limiting community spread, which ushered in an uneasy sense of normalcy even while the pandemic continues. At least for now, these locales can focus on rebuilding and preparing for expectable fluctuations in disease activity, including the arrival of the annual flu season on top of COVID-19.44 Recovery is not a return to the status quo ante but building stronger communities—“building back better.”45 Unless there is a continuum of care, shortcomings in one sector will have ripple effects through the entire system, particularly for psychiatric care for patients with SMI, which was inadequate before the pandemic.
Ensuring access to critical care was a priority during the pandemic’s early phase but came at the price of deferring other types of care, such as routine primary care; the coming months will see the downstream consequences of this approach,46 including for patients with SMI.
In the meantime, doing our job as clinicians, as Camus’s fictitious Dr. Bernard Rieux from the epigraph responds when asked how to define decency, may be the best we can do in these times. This includes contributing to and molding our field’s future and fostering a sense of agency in our patients and in ourselves. Major goals will be to preserve lessons learned, maintain flexibility, and avoid a return to unhelpful overregulation and payment models that do not reflect the flexible, person-centered care so important for patients with SMI.47
Bottom Line
During a pandemic, patients with serious mental illness may be easily forgotten as other issues overshadow the needs of this impoverished group. During a pandemic, the priority treatment goals for these patients are infection control, relapse prevention, and preventing treatment disengagement and loneliness. A pandemic requires changes in how patients with serious mental illness will receive psychopharmacology and psychotherapy.
Related Resources
- Huremović D (ed). Psychiatry of pandemics: a mental health response to infection outbreak. Cham, Switzerland: Springer Nature Switzerland AG; 2019.
- Ursano RJ, Fullerton CS, Weisaeth L, et al (eds). Textbook of disaster psychiatry. 2nd ed. Cambridge, UK: Cambridge University Press; 2017.
- Centers for Disease Control and Prevention. Coronavirus (COVID-19). https://www.cdc.gov/coronavirus/2019-ncov/index.html.
- American Psychiatric Association. Coronavirus resources. https://www.psychiatry.org/psychiatrists/covid-19-coronavirus.
- SMI Adviser. Make informed decisions related to COVID-19 and mental health. https://smiadviser.org/about/covid.
Drug Brand Names
Clozapine • Clozaril
Diazepam • Valium
Hydroxychloroquine • Plaquenil
1. Camus A. La peste. Paris, France: Éditions Gallimard; 1947.
2. Huremovic
3. Substance Abuse and Mental Health Services Administration. Phases of disaster. https://www.samhsa.gov/dtac/recovering-disasters/phases-disaster. Updated June 17, 2020. Accessed August 7, 2020.
4. Geller J. COVID-19 and advocacy—the good and the unacceptable. Psychiatric News. https://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2020.5b13. Published May 7, 2020. Accessed August 7, 2020.
5. Webb Hooper M, Nápoles AM, Perez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA. 2020;323(24):2466-2467.
6. Sederer LI, Lanzara CB, Essock SM, et al. Lessons learned from the New York State mental health response to the September 11, 2001, attacks. Psychiatr Serv. 2011;62(9):1085-1089.
7. World Health Organization. Infodemic management – infodemiology. https://www.who.int/teams/risk-communication/infodemic-management. Accessed August 7, 2020.
8. Zhou J, Liu L, Xue P, et al. Mental health response to the COVID-19 outbreak in China. Am J Psychiatry. 2020;117(7):574-575.
9. Kawohl W, Nordt C. COVID-19, unemployment, and suicide. Lancet Psychiatry. 2020;7(5):389-390.
10. Yao H, Chen JH, Xu YF. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry. 2020;7(4):e21. doi: 10.1016/S2215-0366(20)30090-0.
11. Minihan E, Gavin B, Kelly BD, et al. Covid-19, mental health and psychological first aid. Ir J Psychol Med. 2020:1-12.
12. Adja KYC, Golinelli D, Lenzi J, et al. Pandemics and social stigma: who’s next? Italy’s experience with COVID-19. Public Health. 2020;185:39-41.
13. Rosenberg AR. Cultivating deliberate resilience during the coronavirus disease 2019 pandemic [published online April 14, 2020]. JAMA Pediatr. doi: 10.1001/jamapediatrics.2020.1436.
14. Dean W, Talbot SG, Caplan A. Clarifying the language of clinician distress [published online January 31, 2020]. JAMA. doi: 10.1001/jama.2019.21576.
15. Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. 2020;382(21):2049-2055.
16. Rosenbaum L. Facing Covid-19 in Italy - ethics, logistics, and therapeutics on the epidemic’s front line. N Engl J Med. 2020;382(20):1873-1875.
17. Viceconte G, Petrosillo N. COVID-19 R0: magic number or conundrum? Infect Dis Rep. 2020;12(1):8516.
18. de Hert M, Schreurs V, Vancampfort D, van Winkel R. Metabolic syndrome in people with schizophrenia: a review. World Psychiatry. 2009;8(1):15-22.
19. Chen R, Liang W, Jiang M, et al. Risk factors of fatal outcome in hospitalized subjects with coronavirus disease 2019 from a nationwide analysis in China. Chest. 2020;158(1):97-105.
20. Finer N, Garnett SP, Bruun JM. COVID-19 and obesity. Clin Obes. 2020;10(3):e12365. doi: 10.1111/cob.12365.
21. Havens LL, Ghaemi SN. Existential despair and bipolar disorder: the therapeutic alliance as a mood stabilizer. Am J Psychother. 2005;59(2):137-147.
22. Trémeau F, Antonius D, Malaspina D, et al. Loneliness in schizophrenia and its possible correlates. An exploratory study. Psychiatry Res. 2016;246:211-217.
23. Menninger KA. Psychoses associated with influenza: I. General data: statistical analysis. JAMA. 1919;72(4):235-241.
24. Asadi-Pooya AA, Simani L. Central nervous system manifestations of COVID-19: a systematic review. J Neurol Sci. 2020;413:116832. doi: 10.1016/j.jns.2020.116832.
25. Ferrando SJ, Klepacz L, Lynch S, et al. COVID-19 psychosis: a potential new neuropsychiatric condition triggered by novel coronavirus infection and the inflammatory response? [published online May 19, 2020]. Psychosomatics. doi: 10.1016/j.psym.2020.05.012.
26. Troyer EA, Kohn JN, Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav Immun. 2020;87:34-39.
27. Martin Jr. EB. Brief psychotic disorder triggered by fear of coronavirus? Psychiatric Times. https://www.psychiatrictimes.com/view/brief-psychotic-disorder-triggered-fear-coronavirus-small-case-series. Published May 8, 2020. Accessed August 7, 2020.
28. Sher Y, Rabkin B, Maldonado JR, et al. COVID-19-associated hyperactive intensive care unit delirium with proposed pathophysiology and treatment: a case report [published online May 19, 2020]. Psychosomatics. doi: 10.1016/j.psym.2020.05.007.
29. Wolters AE, Peelen LM, Welling MC, et al. Long-term mental health problems after delirium in the ICU. Crit Care Med. 2016;44(10):1808-1813.
30. Toovey S. Influenza-associated central nervous system dysfunction: a literature review. Travel Med Infect Dis. 2008;6(3):114-124.
31. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912-920.
32. Maercker A, Brewin CR, Bryant RA, et al. Diagnosis and classification of disorders specifically associated with stress: proposals for ICD-11. World Psychiatry. 2013;12(3):198-206.
33. Ornell F, Moura HF, Scherer JN, et al. The COVID-19 pandemic and its impact on substance use: implications for prevention and treatment. Psychiatry Res. 2020;289:113096. doi: 10.1016/j.psychres.2020.113096.
34. Berlin I, Thomas D, Le Faou AL, Cornuz J. COVID-19 and smoking [published online April 3, 2020]. Nicotine Tob Res. https://doi.org/10.1093/ntr/ntaa059.
35. Back D, Marzolini C, Hodge C, et al. COVID-19 treatment in patients with comorbidities: awareness of drug-drug interactions [published online May 8, 2020]. Br J Clin Pharmacol. doi: 10.1111/bcp.14358.
36. Carpenter WT Jr., Buchanan RW, Kirkpatrick B, et al. Diazepam treatment of early signs of exacerbation in schizophrenia. Am J Psychiatry. 1999;156(2):299-303.
37. Dotson S, Hartvigsen N, Wesner T, et al. Clozapine toxicity in the setting of COVID-19 [published online May 30, 2020]. Psychosomatics. doi: 10.1016/j.psym.2020.05.025.
38. Siskind D, Honer WG, Clark S, et al. Consensus statement on the use of clozapine during the COVID-19 pandemic. J Psychiatry Neurosci. 2020;45(3):222-223.
39. Schnitzer K, MacLaurin S, Freudenreich O. Long-acting injectable antipsychotics during the COVID-19 pandemic. Current Psychiatry. In press.
40. Winston A, Rosenthal RN, Pinsker H. Learning supportive psychotherapy: an illustrated guide. Washington, DC: American Psychiatric Publishing; 2012.
41. Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382(18):1679-1681.
42. Jordan A, Dixon LB. Considerations for telepsychiatry service implementation in the era of COVID-19. Psychiatr Serv. 2020;71(6):643-644.
43. DePierro J, Lowe S, Katz C. Lessons learned from 9/11: mental health perspectives on the COVID-19 pandemic. Psychiatry Res. 2020;288:113024.
44. Hussain S. Immunization and vaccination. In: Huremovic
45. Epping-Jordan JE, van Ommeren M, Ashour HN, et al. Beyond the crisis: building back better mental health care in 10 emergency-affected areas using a longer-term perspective. Int J Ment Health Syst. 2015;9:15.
46. Rosenbaum L. The untold toll - the pandemic’s effects on patients without Covid-19. N Engl J Med. 2020;382(24):2368-2371.
47. Bartels SJ, Baggett TP, Freudenreich O, et al. COVID-19 emergency reforms in Massachusetts to support behavioral health care and reduce mortality of people with serious mental illness [published online June 3, 2020]. Psychiatr Serv. doi: 10.1176/appi.ps.202000244.
“This whole thing is not about heroism. It’s about decency. It may seem a ridiculous idea, but the only way to fight the plague is with decency . ”
– Albert Camus, La Peste (1947)1
Severe acute respiratory syndrome (SARS), H1N1 swine flu, Ebola, Zika, and Middle East respiratory syndrome (MERS): the 21st century has already been witness to several serious infectious outbreaks and pandemics,2 but none has been as deadly and consequential as the current one. The ongoing SARS-coronavirus-2 (SARS-CoV-2) pandemic is shaping not only current psychiatric care but the future of psychiatry. Now that we are beyond the initial stages of the coronavirus disease 2019 (COVID-19) pandemic, when psychiatrists had a crash course in disaster psychiatry, our attention must shift to rebuilding and managing disillusionment and other psychological fallout of the intense early days.3
In this article, we offer guidance to psychiatrists caring for patients with serious mental illness (SMI) during the SARS-CoV-2 pandemic. Patients with SMI are easily forgotten as other issues (eg, preserving ICU capacity) overshadow the already historically neglected needs of this impoverished group.4 From both human and public-health perspectives, this inattention is a mistake. Assuring psychiatric stability is critically important to prevent the spread of COVID-19 in marginalized communities comprised of individuals who are poor, members of racial minorities, and others who already experience health disparities.5 Without controlling transmission in these groups, the pandemic will not be sufficiently contained.
We begin by highlighting general principles of pandemic management because caring for patients with SMI does not occur in a vacuum. Infectious outbreaks require not only helping those who need direct medical care because they are infected, but also managing populations that are at risk of getting infected, including health care and other essential workers.
Principles of pandemic management
Delivery of medical care during a pandemic differs from routine care. An effective disaster response requires collaboration and coordination among public-health, treatment, and emergency systems. Many institutions shift to an incident management system and crisis leadership, with clear lines of authority to coordinate responders and build medical surge capacity. Such a top-down leadership approach must plan and allow for the emergence of other credible leaders and for the restoration of people’s agency.
Unfortunately, adaptive capacity may be limited, especially in the public sector and psychiatric care system, where resources are already poor. Particularly early in a pandemic, services considered non-essential—which includes most psychiatric outpatient care—can become unavailable. A major effort is needed to prevent the psychiatric care system from contracting further, as happened during 9/11.6 Additionally, “essential” cannot be conflated with “emergent,” as can easily occur in extreme circumstances. Early and sustained efforts are required to ensure that patients with SMI who may be teetering on the edge of emergency status do not slip off that edge, especially when the emergency medical system is operating over capacity.
A comprehensive outbreak response must consider that a pandemic is not only a medical crisis but a mental health crisis and a communication emergency.7 Mental health clinicians need to provide accurate information and help patients cope with their fears.
Continue to: Psychological aspects of pandemics
Psychological aspects of pandemics. Previous infectious outbreaks have reaffirmed that mental health plays an outsized role during epidemics. Chaos, uncertainty, fear of death, and loss of income and housing cause prolonged stress and exact a psychological toll.
Adverse psychological impacts include expectable, normal reactions such as stress-induced anxiety or insomnia. In addition, new-onset psychiatric illnesses or exacerbations of existing ones may emerge.8 As disillusionment and demoralization appear in the wake of the acute phase, with persistently high unemployment, suicide prevention becomes an important goal.9
Pandemics lead to expectable behavioral responses (eg, increases in substance use and interpersonal conflict). Fear-based decisions may result in unhelpful behavior, such as hoarding medications (which may result in shortages) or dangerous, unsupervised use of unproven medications (eg, hydroxychloroquine). Trust is needed to accept public-health measures, and recommendations (eg, wearing masks) must be culturally informed to be credible and effective.
Because people are affected differently, at individual, cultural, and socioeconomic levels, they will view the situation differently. For many people, secondary stressors (eg, job loss) may be more disastrous than the primary medical event (ie, the pandemic). This distinction is critical because concrete financial help, not psychiatric care, is needed. Sometimes, even when a psychiatric disorder such as SMI or major neurocognitive disorder is present, the illusion of an acute decompensation can be created by the loss of social and structural supports that previously scaffolded a person’s life.
Mental illness prevention. Community mental-health surveillance is important to monitor for distress, psychiatric symptoms, health-risk behaviors, risk and safety perception, and preparedness. Clinicians must be ready to normalize expectable and temporary distress, while recognizing when that distress becomes pathological. This may be difficult in patients with SMI who often already have reduced stress tolerance or problem-based coping skills.10
Continue to: Psychological first aid...
Psychological first aid (PFA) is a standard intervention recommended by the World Health Organization for most individuals following a disaster; it is evidence-informed and has face validity.11 Intended to relieve distress by creating an environment that is safe, calm, and connected, PFA fosters self-efficacy and hope. While PFA is a form of universal prevention, it is not designed for patients with SMI, is not a psychiatric intervention, and is not provided by clinicians. Its principles, however, can easily be applied to patients with SMI to prevent distressing symptoms from becoming a relapse.
Communication. Good risk and crisis communication are critical because individual and population behavior will be governed by the perception of risk and fear, and not by facts. Failure to manage the “infodemic”7—with its misinformation, contradictory messages, and rumors—jeopardizes infection control if patients become paralyzed by uncertainty and fear. Scapegoating occurs easily during times of threat, and society must contain the parallel epidemic of xenophobia based on stigma and misinformation.12
Decision-making under uncertainty is not perfect and subject to revision as better information becomes available. Pointing this out to the public is delicate but essential to curtail skepticism and mistrust when policies are adjusted in response to new circumstances and knowledge.
Mistrust of an authority’s legitimacy and fear-based decisions lead to lack of cooperation with public-health measures, which can undermine an effective response to the pandemic. Travel restrictions or quarantine measures will not be followed if individuals question their importance. Like the general public, patients need education and clear communication to address their fear of contagion, dangers posed to family (and pets), and mistrust of authority and government. A lack of appreciation of the seriousness of the pandemic and individual responsibility may need to be addressed. Two important measures to accomplish this are steering patients to reputable sources of information and advising that they limit media exposure.
Resilience-building. Community and workplace resilience are important aspects of making it through a disaster as best as possible. Resilience is not innate and fixed; it must be deliberately built.13 Choosing an attitude of post-traumatic growth over the victim narrative is a helpful stance. Practicing self-care (rest, nutrition, exercise) and self-compassion (self-kindness, common humanity, mindfulness) is good advice for patients and caregivers alike.
Continue to: Workforce protection
Workforce protection. Compared to other disasters, infectious outbreaks disproportionally affect the medical community, and care delivery is at stake. While psychological and psychiatric needs may increase during a pandemic, services often contract, day programs and clinics close, teams are reduced to skeleton crews, and only emergency psychiatric care is available. Workforce protection is critical to avoid illness or simple absenteeism due to mistrust of protective measures.
Only a well-briefed, well-led, well-supported, and adequately resourced workforce is going to be effective in managing this public-health emergency. Burnout and moral injury are feared long-term consequences for health care workers that need to be proactively addressed.14 As opposed to other forms of disasters, managing your own fears about safety is important. Clinicians and their patients sit in the proverbial same boat.
Ethics. The anticipated need to ration life-saving care (eg, ventilators) has been at the forefront of ethical concerns.15 In psychiatry, the question of involuntary public-health interventions for uncooperative psychiatric patients sits uncomfortably between public-health ethics and human rights, and is an opportunity for collaboration with public-health and infectious-disease colleagues.
Redeployed clinicians and those working under substandard conditions may be concerned about civil liability due to a modified standard of care during a crisis. Some clinicians may ask if their duty to care must override their natural instinct to protect themselves. There is a lot of room for resentment in these circumstances. Redeployed or otherwise “conscripted” clinicians may resent administrators, especially those administering from the safety of their homes. Those “left behind” to work in potentially precarious circumstances may resent their absent colleagues. Moreover, these front-line clinicians may have been forced to make ethical decisions for which they were not prepared.16 Maintaining morale is far from trivial, not just during the pandemic, but afterward, when (and if) the entire workforce is reunited. All parties need to be mindful of how their actions and decisions impact and are perceived by others, both in the hospital and at home.
Managing patients with SMI during COVID-19
Patients with SMI are potentially hard hit by COVID-19 due to a “tragic” epidemiologic triad of agent-host-environment: SARS-CoV-2 is a highly infectious agent affecting patients with SMI who are vulnerable hosts in permissive environments (Figure).
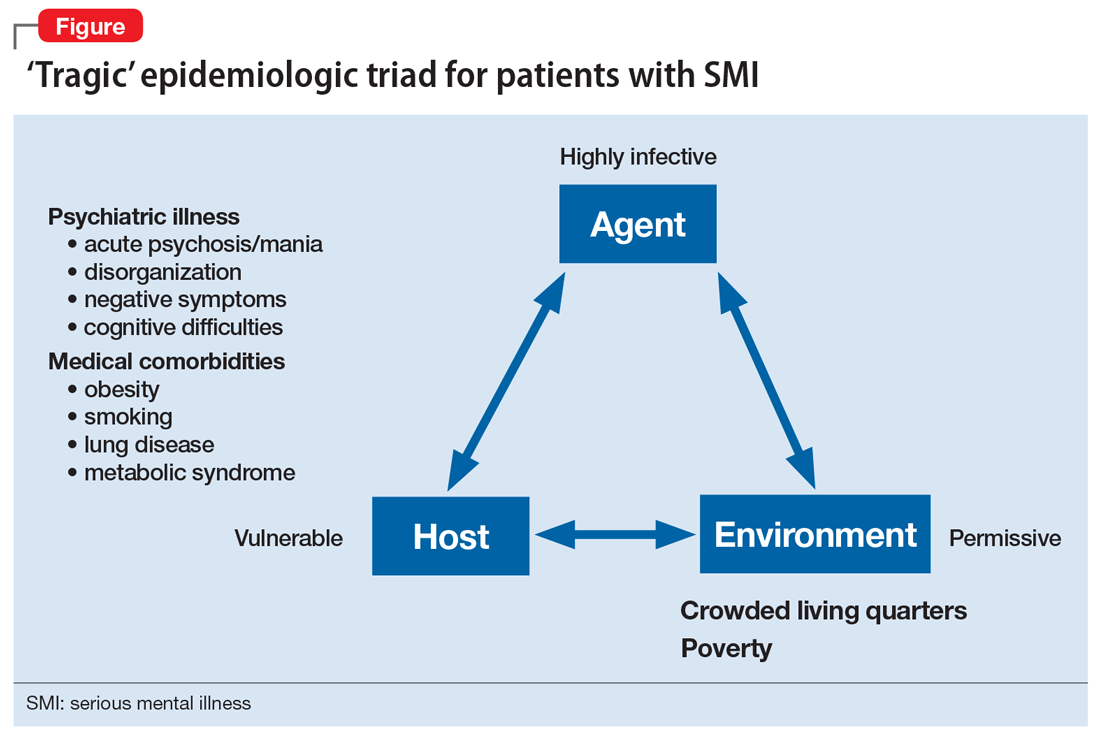
Continue to: While not as infectious as measles...
While not as infectious as measles, COVID-19 is more infectious than the seasonal flu virus.17 It can lead to uncontrolled infection within a short period of time, particularly in enclosed settings. Outbreaks have occurred readily on cruise ships and aircraft carriers as well as in nursing homes, homeless shelters, prisons, and group homes.
Patients with SMI are vulnerable hosts because they have many of the medical risk factors18 that portend a poor prognosis if they become infected, including pre-existing lung conditions and heart disease19 as well as diabetes and obesity.20 Obesity likely creates a hyperinflammatory state and a decrease in vital capacity. Patient-related behavioral factors include poor early-symptom reporting and ineffective infection control.
Unfavorable social determinants of health include not only poverty but crowded housing that is a perfect incubator for COVID-19.
Priority treatment goals. The overarching goal during a pandemic is to keep patients with SMI in psychiatric treatment and prevent them from disengaging from care in the service of infection control. Urgent tasks include infection control, relapse prevention, and preventing treatment disengagement and loneliness.
Infection control. As trusted sources of information, psychiatrists can play an important role in infection control in several important ways:
- educating patients about infection-control measures and public-health recommendations
- helping patients understand what testing can accomplish and when to pursue it
- encouraging protective health behaviors (eg, hand washing, mask wearing, physical distancing)
- assessing patients’ risk appreciation
- assessing for and addressing obstacles to implementing and complying with infection-control measures
- explaining contact tracing
- providing reassurance.
Continue to: Materials and explanations...
Materials and explanations must be adapted for patient understanding.
Patients with disorganization or cognitive disturbances may have difficulties cooperating or problem-solving. Patients with negative symptoms may be inappropriately unconcerned and also inaccurately report symptoms that suggest COVID-19. Acute psychosis or mania can prevent patients from complying with public-health efforts. Some measures may be difficult to implement if the means are simply not there (eg, physical distancing in a crowded apartment). Previously open settings (eg, group homes) have had to develop new mechanisms under the primacy of infection control. Inpatient units—traditionally places where community, shared healing, and group therapy are prized—have had to decrease maximum occupancy, limit the number of patients attending groups, and discourage or outrightly prohibit social interaction (eg, dining together).
Relapse prevention. Patients who take maintenance medications need to be supported. A manic or psychotic relapse during a pandemic puts patients at risk of acquiring and spreading COVID-19. “Treatment as prevention” is a slogan from human immunodeficiency virus (HIV) care that captures the importance of antiretroviral treatment to prevent medical complications from HIV, and also to reduce infecting other people. By analogy, psychiatric treatment for patients with SMI can prevent psychiatric instability and thereby control viral transmission. Avoiding sending psychiatric patients to a potentially stressed acute-care system is important.
Psychosocial support. Clinics need to ensure that patients continue to engage in care beyond medication-taking to proactively prevent psychiatric exacerbations. Healthful, resilience-building behaviors should be encouraged while monitoring and counseling against maladaptive ones (eg, increased substance use). Supporting patients emotionally and helping them solve problems are critical, particularly for those who are subjected to quarantine or isolation. Obviously, in these latter situations, outreach will be necessary and may require creative delivery systems and dedicated clinicians for patients who lack access to the technology necessary for virtual visits. Havens and Ghaemi21 have suggested that a good therapeutic alliance can be viewed as a mood stabilizer. Helping patients grieve losses (loved ones, jobs, sense of safety) may be an important part of support.
Even before COVID-19, loneliness was a major factor for patients with schizophrenia.22 A psychiatric clinic is one aspect of a person with SMI’s social network; during the initial phase of the pandemic, many clinics and treatment programs closed. Patients for whom clinics structure and anchor their activities are at high risk of disconnecting from treatment, staying at home, and becoming lonely.
Continue to: Caregivers are always important...
Caregivers are always important to SMI patients, but they may assume an even bigger role during this pandemic. Some patients may have moved in with a relative, after years of living on their own. In other cases, stable caregiver relationships may be disrupted due to COVID-19–related sickness in the caregiver; if not addressed, this can result in a patient’s clinical decompensation. Clinicians should take the opportunity to understand who a patient’s caregivers are (group home staff, families) and rekindle clinical contact with them. Relationships with caregivers that may have been on “autopilot” during normal times are opportunities for welcome support and guidance, to the benefit of both patients and caregivers.
Table 1 summarizes clinical tasks that need to be kept in mind when conducting clinic visits during COVID-19 in order to achieve the high-priority treatment goals of infection control, relapse prevention, and psychosocial support.
Differential diagnosis. Neuropsychiatric syndromes have long been observed in influenza pandemics,23 due both to direct viral effects and to the effects of critical illness on the brain. Two core symptoms of COVID-19—anosmia and ageusia—suggest that COVID-19 can directly affect the brain. While neurologic manifestations are common,24 it remains unclear to what extent COVID-19 can directly “cause” psychiatric symptoms, or if such symptoms are the result of cytokines25 or other medical processes (eg, thromboembolism).26 Psychosis due to COVID-19 may, in some cases, represent a stress-related brief psychotic disorder.27
Hospitalized patients who have recovered from COVID-19 may have experienced prolonged sedation and severe delirium in an ICU.28 Complications such as posttraumatic stress disorder,29 hypoperfusion-related brain injuries, or other long-term cognitive difficulties may result. In previous flu epidemics, patients developed serious neurologic complications such as post-encephalitic Parkinson’s disease.30
Any person subjected to isolation or quarantine is at risk for psychiatric complications.31 Patients with SMI who live in group homes may be particularly susceptible to new rules, including no-visitor policies.
Continue to: Outpatients whose primary disorder...
Outpatients whose primary disorder is well controlled may, like anyone else, struggle with the effects of the pandemic. It is necessary to carefully differentiate non-specific symptoms associated with stress from the emergence of a new disorder resulting from stress.32 For some patients, grief or adjustment disorders should be considered. Prolonged stress and uncertainty may eventually lead to an exacerbation of a primary disorder, particularly if the situation (eg, financial loss) does not improve or worsens. Demoralization and suicidal thinking need to be monitored. Relapse or increased use of alcohol or other substances as a response to stress may also complicate the clinical picture.33 Last, smoking cessation as a major treatment goal in general should be re-emphasized and not ignored during the ongoing pandemic.34
Table 2 summarizes psychiatric symptoms that need to be considered when managing a patient with SMI during this pandemic.
Treatment tools
Psychopharmacology. Even though crisis-mode prescribing may be necessary, the safe use of psychotropics remains the goal of psychiatric prescribing. Access to medications becomes a larger consideration; for many patients, a 90-day supply may be indicated. Review of polypharmacy, including for pneumonia risk, should be undertaken. Preventing drooling (eg, from sedation, clozapine, extrapyramidal symptoms [EPS]) will decrease aspiration risk.
In general, treatment of psychiatric symptoms in a patient with COVID-19 follows usual guidelines. The best treatment for COVID-19 patients with delirium, however, remains to be established, particularly how to manage severe agitation.28 Pharmacodynamic and pharmacokinetic drug–drug interactions between psychotropics and antiviral treatments for COVID-19 (eg, QTc prolongation) can be expected and need to be reviewed.35 For stress-related anxiety, judicious pharmacotherapy can be helpful. Diazepam given at the earliest signs of a psychotic relapse may stave off a relapse for patients with schizophrenia.36 Even if permitted under relaxed prescribing rules during a public-health emergency, prescribing controlled substances without seeing patients in person requires additional thought. In some cases, adjusting the primary medication to buffer against stress may be preferred (eg, adjusting an antipsychotic in a patient on maintenance treatment for schizophrenia, particularly if a low-dose strategy is pursued).
Clozapine requires registry-based prescribing and bloodwork (“no blood, no drug”). The use of clozapine during this public-health emergency has been made easier because of FDA guidance that allows clozapine to be dispensed without blood work if obtaining blood work is not possible (eg, a patient is quarantined) or can be accomplished only at substantial risk to patients and the population at large. Under certain conditions, clozapine can be dispensed safely and in a way that is consistent with infection prevention. Clozapine-treated patients admitted with COVID-19 should be monitored for clozapine toxicity and the clozapine dose adjusted.37 A consensus statement consistent with the FDA and clinical considerations for using clozapine during COVID-19 is summarized in Table 3.38
Continue to: Long-acting injectable antipsychotics...
Long-acting injectable antipsychotics (LAIs) pose a problem because they require in-person visits. Ideally, during a pandemic, patients should be seen in person as frequently as medically necessary but as infrequently as possible to limit exposure of both patients and staff. Table 4 provides some clinical recommendations on how to use LAIs during the pandemic.39
Supportive psychotherapy may be the most important tool we have in helping patients with loss and uncertainty during these challenging months.40 Simply staying in contact with patients plays a major role in preventing care discontinuity. Even routine interactions have become stressful, with everyone wearing a mask that partially obscures the face. People with impaired hearing may find it even more difficult to understand you.
Education, problem-solving, and a directive, encouraging style are major tools of supportive psychotherapy to reduce symptoms and increase adaptive skills. Clarify that social distancing refers to physical, not emotional, distancing. The judicious and temporary use of anxiolytics is appropriate to reduce anxiety. Concrete help and problem-solving (eg, filling out forms) are examples of proactive crisis intervention.
Telepsychiatry emerged in the pandemic’s early days as the default mode of practice in order to limit in-person contacts.41 Like all new technology, telepsychiatry brings progress and peril.42 While it has gone surprisingly well for most, the “digital divide” does not afford all patients access to the needed technology. The long-term effectiveness and acceptance of telehealth remain to be seen. (Editor’s Note: For more about this topic, see “Telepsychiatry: What you need to know.”
Lessons learned and outlook
Infectious outbreaks have historically inflicted long-term disruptions on societies and altered the course of history. However, each disaster is unique, and lessons from previous disasters may only partially apply.43 We do not yet know how this one will end, including how long it will take for the world’s economies to recover. If nothing else, the current public-health emergency has brought to the forefront what psychiatrists have always known: health disparities are partially responsible for different disease risks (in this case, the risk of getting infected with SARS-CoV-2).5 It may not be a coincidence that the Black Lives Matter movement is becoming a major impetus for social change at a time when the pandemic is exposing health-care inequalities.
Continue to: Some areas of the country...
Some areas of the country succeeded in reducing infections and limiting community spread, which ushered in an uneasy sense of normalcy even while the pandemic continues. At least for now, these locales can focus on rebuilding and preparing for expectable fluctuations in disease activity, including the arrival of the annual flu season on top of COVID-19.44 Recovery is not a return to the status quo ante but building stronger communities—“building back better.”45 Unless there is a continuum of care, shortcomings in one sector will have ripple effects through the entire system, particularly for psychiatric care for patients with SMI, which was inadequate before the pandemic.
Ensuring access to critical care was a priority during the pandemic’s early phase but came at the price of deferring other types of care, such as routine primary care; the coming months will see the downstream consequences of this approach,46 including for patients with SMI.
In the meantime, doing our job as clinicians, as Camus’s fictitious Dr. Bernard Rieux from the epigraph responds when asked how to define decency, may be the best we can do in these times. This includes contributing to and molding our field’s future and fostering a sense of agency in our patients and in ourselves. Major goals will be to preserve lessons learned, maintain flexibility, and avoid a return to unhelpful overregulation and payment models that do not reflect the flexible, person-centered care so important for patients with SMI.47
Bottom Line
During a pandemic, patients with serious mental illness may be easily forgotten as other issues overshadow the needs of this impoverished group. During a pandemic, the priority treatment goals for these patients are infection control, relapse prevention, and preventing treatment disengagement and loneliness. A pandemic requires changes in how patients with serious mental illness will receive psychopharmacology and psychotherapy.
Related Resources
- Huremović D (ed). Psychiatry of pandemics: a mental health response to infection outbreak. Cham, Switzerland: Springer Nature Switzerland AG; 2019.
- Ursano RJ, Fullerton CS, Weisaeth L, et al (eds). Textbook of disaster psychiatry. 2nd ed. Cambridge, UK: Cambridge University Press; 2017.
- Centers for Disease Control and Prevention. Coronavirus (COVID-19). https://www.cdc.gov/coronavirus/2019-ncov/index.html.
- American Psychiatric Association. Coronavirus resources. https://www.psychiatry.org/psychiatrists/covid-19-coronavirus.
- SMI Adviser. Make informed decisions related to COVID-19 and mental health. https://smiadviser.org/about/covid.
Drug Brand Names
Clozapine • Clozaril
Diazepam • Valium
Hydroxychloroquine • Plaquenil
“This whole thing is not about heroism. It’s about decency. It may seem a ridiculous idea, but the only way to fight the plague is with decency . ”
– Albert Camus, La Peste (1947)1
Severe acute respiratory syndrome (SARS), H1N1 swine flu, Ebola, Zika, and Middle East respiratory syndrome (MERS): the 21st century has already been witness to several serious infectious outbreaks and pandemics,2 but none has been as deadly and consequential as the current one. The ongoing SARS-coronavirus-2 (SARS-CoV-2) pandemic is shaping not only current psychiatric care but the future of psychiatry. Now that we are beyond the initial stages of the coronavirus disease 2019 (COVID-19) pandemic, when psychiatrists had a crash course in disaster psychiatry, our attention must shift to rebuilding and managing disillusionment and other psychological fallout of the intense early days.3
In this article, we offer guidance to psychiatrists caring for patients with serious mental illness (SMI) during the SARS-CoV-2 pandemic. Patients with SMI are easily forgotten as other issues (eg, preserving ICU capacity) overshadow the already historically neglected needs of this impoverished group.4 From both human and public-health perspectives, this inattention is a mistake. Assuring psychiatric stability is critically important to prevent the spread of COVID-19 in marginalized communities comprised of individuals who are poor, members of racial minorities, and others who already experience health disparities.5 Without controlling transmission in these groups, the pandemic will not be sufficiently contained.
We begin by highlighting general principles of pandemic management because caring for patients with SMI does not occur in a vacuum. Infectious outbreaks require not only helping those who need direct medical care because they are infected, but also managing populations that are at risk of getting infected, including health care and other essential workers.
Principles of pandemic management
Delivery of medical care during a pandemic differs from routine care. An effective disaster response requires collaboration and coordination among public-health, treatment, and emergency systems. Many institutions shift to an incident management system and crisis leadership, with clear lines of authority to coordinate responders and build medical surge capacity. Such a top-down leadership approach must plan and allow for the emergence of other credible leaders and for the restoration of people’s agency.
Unfortunately, adaptive capacity may be limited, especially in the public sector and psychiatric care system, where resources are already poor. Particularly early in a pandemic, services considered non-essential—which includes most psychiatric outpatient care—can become unavailable. A major effort is needed to prevent the psychiatric care system from contracting further, as happened during 9/11.6 Additionally, “essential” cannot be conflated with “emergent,” as can easily occur in extreme circumstances. Early and sustained efforts are required to ensure that patients with SMI who may be teetering on the edge of emergency status do not slip off that edge, especially when the emergency medical system is operating over capacity.
A comprehensive outbreak response must consider that a pandemic is not only a medical crisis but a mental health crisis and a communication emergency.7 Mental health clinicians need to provide accurate information and help patients cope with their fears.
Continue to: Psychological aspects of pandemics
Psychological aspects of pandemics. Previous infectious outbreaks have reaffirmed that mental health plays an outsized role during epidemics. Chaos, uncertainty, fear of death, and loss of income and housing cause prolonged stress and exact a psychological toll.
Adverse psychological impacts include expectable, normal reactions such as stress-induced anxiety or insomnia. In addition, new-onset psychiatric illnesses or exacerbations of existing ones may emerge.8 As disillusionment and demoralization appear in the wake of the acute phase, with persistently high unemployment, suicide prevention becomes an important goal.9
Pandemics lead to expectable behavioral responses (eg, increases in substance use and interpersonal conflict). Fear-based decisions may result in unhelpful behavior, such as hoarding medications (which may result in shortages) or dangerous, unsupervised use of unproven medications (eg, hydroxychloroquine). Trust is needed to accept public-health measures, and recommendations (eg, wearing masks) must be culturally informed to be credible and effective.
Because people are affected differently, at individual, cultural, and socioeconomic levels, they will view the situation differently. For many people, secondary stressors (eg, job loss) may be more disastrous than the primary medical event (ie, the pandemic). This distinction is critical because concrete financial help, not psychiatric care, is needed. Sometimes, even when a psychiatric disorder such as SMI or major neurocognitive disorder is present, the illusion of an acute decompensation can be created by the loss of social and structural supports that previously scaffolded a person’s life.
Mental illness prevention. Community mental-health surveillance is important to monitor for distress, psychiatric symptoms, health-risk behaviors, risk and safety perception, and preparedness. Clinicians must be ready to normalize expectable and temporary distress, while recognizing when that distress becomes pathological. This may be difficult in patients with SMI who often already have reduced stress tolerance or problem-based coping skills.10
Continue to: Psychological first aid...
Psychological first aid (PFA) is a standard intervention recommended by the World Health Organization for most individuals following a disaster; it is evidence-informed and has face validity.11 Intended to relieve distress by creating an environment that is safe, calm, and connected, PFA fosters self-efficacy and hope. While PFA is a form of universal prevention, it is not designed for patients with SMI, is not a psychiatric intervention, and is not provided by clinicians. Its principles, however, can easily be applied to patients with SMI to prevent distressing symptoms from becoming a relapse.
Communication. Good risk and crisis communication are critical because individual and population behavior will be governed by the perception of risk and fear, and not by facts. Failure to manage the “infodemic”7—with its misinformation, contradictory messages, and rumors—jeopardizes infection control if patients become paralyzed by uncertainty and fear. Scapegoating occurs easily during times of threat, and society must contain the parallel epidemic of xenophobia based on stigma and misinformation.12
Decision-making under uncertainty is not perfect and subject to revision as better information becomes available. Pointing this out to the public is delicate but essential to curtail skepticism and mistrust when policies are adjusted in response to new circumstances and knowledge.
Mistrust of an authority’s legitimacy and fear-based decisions lead to lack of cooperation with public-health measures, which can undermine an effective response to the pandemic. Travel restrictions or quarantine measures will not be followed if individuals question their importance. Like the general public, patients need education and clear communication to address their fear of contagion, dangers posed to family (and pets), and mistrust of authority and government. A lack of appreciation of the seriousness of the pandemic and individual responsibility may need to be addressed. Two important measures to accomplish this are steering patients to reputable sources of information and advising that they limit media exposure.
Resilience-building. Community and workplace resilience are important aspects of making it through a disaster as best as possible. Resilience is not innate and fixed; it must be deliberately built.13 Choosing an attitude of post-traumatic growth over the victim narrative is a helpful stance. Practicing self-care (rest, nutrition, exercise) and self-compassion (self-kindness, common humanity, mindfulness) is good advice for patients and caregivers alike.
Continue to: Workforce protection
Workforce protection. Compared to other disasters, infectious outbreaks disproportionally affect the medical community, and care delivery is at stake. While psychological and psychiatric needs may increase during a pandemic, services often contract, day programs and clinics close, teams are reduced to skeleton crews, and only emergency psychiatric care is available. Workforce protection is critical to avoid illness or simple absenteeism due to mistrust of protective measures.
Only a well-briefed, well-led, well-supported, and adequately resourced workforce is going to be effective in managing this public-health emergency. Burnout and moral injury are feared long-term consequences for health care workers that need to be proactively addressed.14 As opposed to other forms of disasters, managing your own fears about safety is important. Clinicians and their patients sit in the proverbial same boat.
Ethics. The anticipated need to ration life-saving care (eg, ventilators) has been at the forefront of ethical concerns.15 In psychiatry, the question of involuntary public-health interventions for uncooperative psychiatric patients sits uncomfortably between public-health ethics and human rights, and is an opportunity for collaboration with public-health and infectious-disease colleagues.
Redeployed clinicians and those working under substandard conditions may be concerned about civil liability due to a modified standard of care during a crisis. Some clinicians may ask if their duty to care must override their natural instinct to protect themselves. There is a lot of room for resentment in these circumstances. Redeployed or otherwise “conscripted” clinicians may resent administrators, especially those administering from the safety of their homes. Those “left behind” to work in potentially precarious circumstances may resent their absent colleagues. Moreover, these front-line clinicians may have been forced to make ethical decisions for which they were not prepared.16 Maintaining morale is far from trivial, not just during the pandemic, but afterward, when (and if) the entire workforce is reunited. All parties need to be mindful of how their actions and decisions impact and are perceived by others, both in the hospital and at home.
Managing patients with SMI during COVID-19
Patients with SMI are potentially hard hit by COVID-19 due to a “tragic” epidemiologic triad of agent-host-environment: SARS-CoV-2 is a highly infectious agent affecting patients with SMI who are vulnerable hosts in permissive environments (Figure).
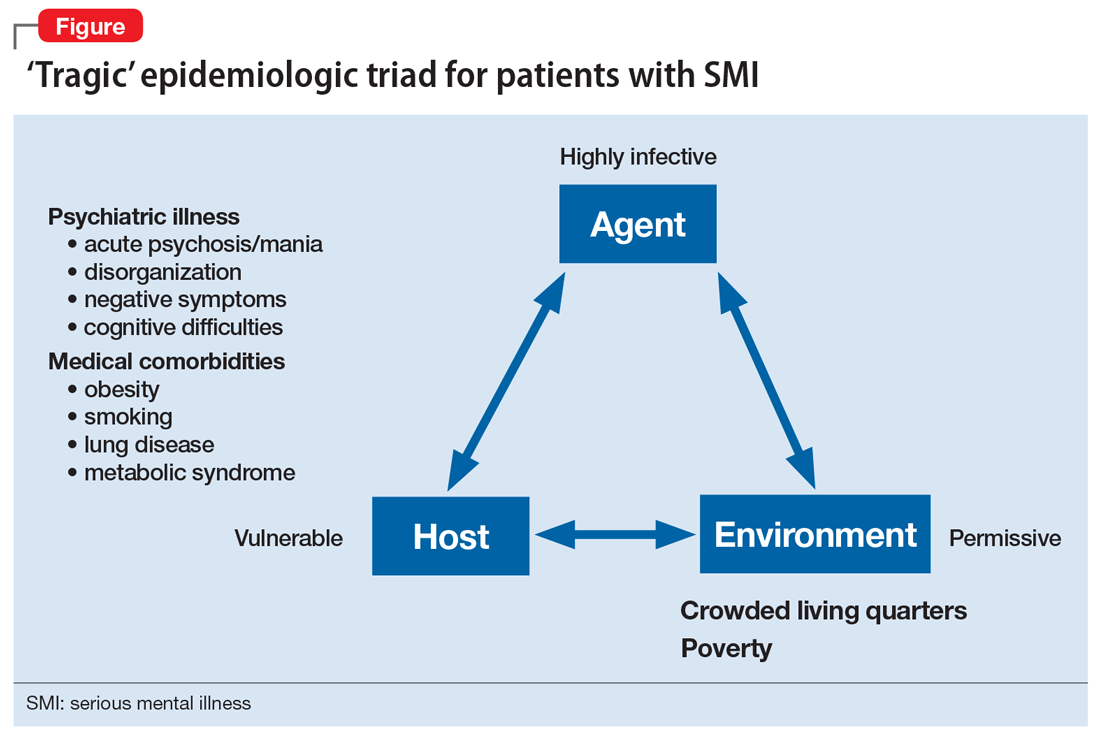
Continue to: While not as infectious as measles...
While not as infectious as measles, COVID-19 is more infectious than the seasonal flu virus.17 It can lead to uncontrolled infection within a short period of time, particularly in enclosed settings. Outbreaks have occurred readily on cruise ships and aircraft carriers as well as in nursing homes, homeless shelters, prisons, and group homes.
Patients with SMI are vulnerable hosts because they have many of the medical risk factors18 that portend a poor prognosis if they become infected, including pre-existing lung conditions and heart disease19 as well as diabetes and obesity.20 Obesity likely creates a hyperinflammatory state and a decrease in vital capacity. Patient-related behavioral factors include poor early-symptom reporting and ineffective infection control.
Unfavorable social determinants of health include not only poverty but crowded housing that is a perfect incubator for COVID-19.
Priority treatment goals. The overarching goal during a pandemic is to keep patients with SMI in psychiatric treatment and prevent them from disengaging from care in the service of infection control. Urgent tasks include infection control, relapse prevention, and preventing treatment disengagement and loneliness.
Infection control. As trusted sources of information, psychiatrists can play an important role in infection control in several important ways:
- educating patients about infection-control measures and public-health recommendations
- helping patients understand what testing can accomplish and when to pursue it
- encouraging protective health behaviors (eg, hand washing, mask wearing, physical distancing)
- assessing patients’ risk appreciation
- assessing for and addressing obstacles to implementing and complying with infection-control measures
- explaining contact tracing
- providing reassurance.
Continue to: Materials and explanations...
Materials and explanations must be adapted for patient understanding.
Patients with disorganization or cognitive disturbances may have difficulties cooperating or problem-solving. Patients with negative symptoms may be inappropriately unconcerned and also inaccurately report symptoms that suggest COVID-19. Acute psychosis or mania can prevent patients from complying with public-health efforts. Some measures may be difficult to implement if the means are simply not there (eg, physical distancing in a crowded apartment). Previously open settings (eg, group homes) have had to develop new mechanisms under the primacy of infection control. Inpatient units—traditionally places where community, shared healing, and group therapy are prized—have had to decrease maximum occupancy, limit the number of patients attending groups, and discourage or outrightly prohibit social interaction (eg, dining together).
Relapse prevention. Patients who take maintenance medications need to be supported. A manic or psychotic relapse during a pandemic puts patients at risk of acquiring and spreading COVID-19. “Treatment as prevention” is a slogan from human immunodeficiency virus (HIV) care that captures the importance of antiretroviral treatment to prevent medical complications from HIV, and also to reduce infecting other people. By analogy, psychiatric treatment for patients with SMI can prevent psychiatric instability and thereby control viral transmission. Avoiding sending psychiatric patients to a potentially stressed acute-care system is important.
Psychosocial support. Clinics need to ensure that patients continue to engage in care beyond medication-taking to proactively prevent psychiatric exacerbations. Healthful, resilience-building behaviors should be encouraged while monitoring and counseling against maladaptive ones (eg, increased substance use). Supporting patients emotionally and helping them solve problems are critical, particularly for those who are subjected to quarantine or isolation. Obviously, in these latter situations, outreach will be necessary and may require creative delivery systems and dedicated clinicians for patients who lack access to the technology necessary for virtual visits. Havens and Ghaemi21 have suggested that a good therapeutic alliance can be viewed as a mood stabilizer. Helping patients grieve losses (loved ones, jobs, sense of safety) may be an important part of support.
Even before COVID-19, loneliness was a major factor for patients with schizophrenia.22 A psychiatric clinic is one aspect of a person with SMI’s social network; during the initial phase of the pandemic, many clinics and treatment programs closed. Patients for whom clinics structure and anchor their activities are at high risk of disconnecting from treatment, staying at home, and becoming lonely.
Continue to: Caregivers are always important...
Caregivers are always important to SMI patients, but they may assume an even bigger role during this pandemic. Some patients may have moved in with a relative, after years of living on their own. In other cases, stable caregiver relationships may be disrupted due to COVID-19–related sickness in the caregiver; if not addressed, this can result in a patient’s clinical decompensation. Clinicians should take the opportunity to understand who a patient’s caregivers are (group home staff, families) and rekindle clinical contact with them. Relationships with caregivers that may have been on “autopilot” during normal times are opportunities for welcome support and guidance, to the benefit of both patients and caregivers.
Table 1 summarizes clinical tasks that need to be kept in mind when conducting clinic visits during COVID-19 in order to achieve the high-priority treatment goals of infection control, relapse prevention, and psychosocial support.
Differential diagnosis. Neuropsychiatric syndromes have long been observed in influenza pandemics,23 due both to direct viral effects and to the effects of critical illness on the brain. Two core symptoms of COVID-19—anosmia and ageusia—suggest that COVID-19 can directly affect the brain. While neurologic manifestations are common,24 it remains unclear to what extent COVID-19 can directly “cause” psychiatric symptoms, or if such symptoms are the result of cytokines25 or other medical processes (eg, thromboembolism).26 Psychosis due to COVID-19 may, in some cases, represent a stress-related brief psychotic disorder.27
Hospitalized patients who have recovered from COVID-19 may have experienced prolonged sedation and severe delirium in an ICU.28 Complications such as posttraumatic stress disorder,29 hypoperfusion-related brain injuries, or other long-term cognitive difficulties may result. In previous flu epidemics, patients developed serious neurologic complications such as post-encephalitic Parkinson’s disease.30
Any person subjected to isolation or quarantine is at risk for psychiatric complications.31 Patients with SMI who live in group homes may be particularly susceptible to new rules, including no-visitor policies.
Continue to: Outpatients whose primary disorder...
Outpatients whose primary disorder is well controlled may, like anyone else, struggle with the effects of the pandemic. It is necessary to carefully differentiate non-specific symptoms associated with stress from the emergence of a new disorder resulting from stress.32 For some patients, grief or adjustment disorders should be considered. Prolonged stress and uncertainty may eventually lead to an exacerbation of a primary disorder, particularly if the situation (eg, financial loss) does not improve or worsens. Demoralization and suicidal thinking need to be monitored. Relapse or increased use of alcohol or other substances as a response to stress may also complicate the clinical picture.33 Last, smoking cessation as a major treatment goal in general should be re-emphasized and not ignored during the ongoing pandemic.34
Table 2 summarizes psychiatric symptoms that need to be considered when managing a patient with SMI during this pandemic.
Treatment tools
Psychopharmacology. Even though crisis-mode prescribing may be necessary, the safe use of psychotropics remains the goal of psychiatric prescribing. Access to medications becomes a larger consideration; for many patients, a 90-day supply may be indicated. Review of polypharmacy, including for pneumonia risk, should be undertaken. Preventing drooling (eg, from sedation, clozapine, extrapyramidal symptoms [EPS]) will decrease aspiration risk.
In general, treatment of psychiatric symptoms in a patient with COVID-19 follows usual guidelines. The best treatment for COVID-19 patients with delirium, however, remains to be established, particularly how to manage severe agitation.28 Pharmacodynamic and pharmacokinetic drug–drug interactions between psychotropics and antiviral treatments for COVID-19 (eg, QTc prolongation) can be expected and need to be reviewed.35 For stress-related anxiety, judicious pharmacotherapy can be helpful. Diazepam given at the earliest signs of a psychotic relapse may stave off a relapse for patients with schizophrenia.36 Even if permitted under relaxed prescribing rules during a public-health emergency, prescribing controlled substances without seeing patients in person requires additional thought. In some cases, adjusting the primary medication to buffer against stress may be preferred (eg, adjusting an antipsychotic in a patient on maintenance treatment for schizophrenia, particularly if a low-dose strategy is pursued).
Clozapine requires registry-based prescribing and bloodwork (“no blood, no drug”). The use of clozapine during this public-health emergency has been made easier because of FDA guidance that allows clozapine to be dispensed without blood work if obtaining blood work is not possible (eg, a patient is quarantined) or can be accomplished only at substantial risk to patients and the population at large. Under certain conditions, clozapine can be dispensed safely and in a way that is consistent with infection prevention. Clozapine-treated patients admitted with COVID-19 should be monitored for clozapine toxicity and the clozapine dose adjusted.37 A consensus statement consistent with the FDA and clinical considerations for using clozapine during COVID-19 is summarized in Table 3.38
Continue to: Long-acting injectable antipsychotics...
Long-acting injectable antipsychotics (LAIs) pose a problem because they require in-person visits. Ideally, during a pandemic, patients should be seen in person as frequently as medically necessary but as infrequently as possible to limit exposure of both patients and staff. Table 4 provides some clinical recommendations on how to use LAIs during the pandemic.39
Supportive psychotherapy may be the most important tool we have in helping patients with loss and uncertainty during these challenging months.40 Simply staying in contact with patients plays a major role in preventing care discontinuity. Even routine interactions have become stressful, with everyone wearing a mask that partially obscures the face. People with impaired hearing may find it even more difficult to understand you.
Education, problem-solving, and a directive, encouraging style are major tools of supportive psychotherapy to reduce symptoms and increase adaptive skills. Clarify that social distancing refers to physical, not emotional, distancing. The judicious and temporary use of anxiolytics is appropriate to reduce anxiety. Concrete help and problem-solving (eg, filling out forms) are examples of proactive crisis intervention.
Telepsychiatry emerged in the pandemic’s early days as the default mode of practice in order to limit in-person contacts.41 Like all new technology, telepsychiatry brings progress and peril.42 While it has gone surprisingly well for most, the “digital divide” does not afford all patients access to the needed technology. The long-term effectiveness and acceptance of telehealth remain to be seen. (Editor’s Note: For more about this topic, see “Telepsychiatry: What you need to know.”
Lessons learned and outlook
Infectious outbreaks have historically inflicted long-term disruptions on societies and altered the course of history. However, each disaster is unique, and lessons from previous disasters may only partially apply.43 We do not yet know how this one will end, including how long it will take for the world’s economies to recover. If nothing else, the current public-health emergency has brought to the forefront what psychiatrists have always known: health disparities are partially responsible for different disease risks (in this case, the risk of getting infected with SARS-CoV-2).5 It may not be a coincidence that the Black Lives Matter movement is becoming a major impetus for social change at a time when the pandemic is exposing health-care inequalities.
Continue to: Some areas of the country...
Some areas of the country succeeded in reducing infections and limiting community spread, which ushered in an uneasy sense of normalcy even while the pandemic continues. At least for now, these locales can focus on rebuilding and preparing for expectable fluctuations in disease activity, including the arrival of the annual flu season on top of COVID-19.44 Recovery is not a return to the status quo ante but building stronger communities—“building back better.”45 Unless there is a continuum of care, shortcomings in one sector will have ripple effects through the entire system, particularly for psychiatric care for patients with SMI, which was inadequate before the pandemic.
Ensuring access to critical care was a priority during the pandemic’s early phase but came at the price of deferring other types of care, such as routine primary care; the coming months will see the downstream consequences of this approach,46 including for patients with SMI.
In the meantime, doing our job as clinicians, as Camus’s fictitious Dr. Bernard Rieux from the epigraph responds when asked how to define decency, may be the best we can do in these times. This includes contributing to and molding our field’s future and fostering a sense of agency in our patients and in ourselves. Major goals will be to preserve lessons learned, maintain flexibility, and avoid a return to unhelpful overregulation and payment models that do not reflect the flexible, person-centered care so important for patients with SMI.47
Bottom Line
During a pandemic, patients with serious mental illness may be easily forgotten as other issues overshadow the needs of this impoverished group. During a pandemic, the priority treatment goals for these patients are infection control, relapse prevention, and preventing treatment disengagement and loneliness. A pandemic requires changes in how patients with serious mental illness will receive psychopharmacology and psychotherapy.
Related Resources
- Huremović D (ed). Psychiatry of pandemics: a mental health response to infection outbreak. Cham, Switzerland: Springer Nature Switzerland AG; 2019.
- Ursano RJ, Fullerton CS, Weisaeth L, et al (eds). Textbook of disaster psychiatry. 2nd ed. Cambridge, UK: Cambridge University Press; 2017.
- Centers for Disease Control and Prevention. Coronavirus (COVID-19). https://www.cdc.gov/coronavirus/2019-ncov/index.html.
- American Psychiatric Association. Coronavirus resources. https://www.psychiatry.org/psychiatrists/covid-19-coronavirus.
- SMI Adviser. Make informed decisions related to COVID-19 and mental health. https://smiadviser.org/about/covid.
Drug Brand Names
Clozapine • Clozaril
Diazepam • Valium
Hydroxychloroquine • Plaquenil
1. Camus A. La peste. Paris, France: Éditions Gallimard; 1947.
2. Huremovic
3. Substance Abuse and Mental Health Services Administration. Phases of disaster. https://www.samhsa.gov/dtac/recovering-disasters/phases-disaster. Updated June 17, 2020. Accessed August 7, 2020.
4. Geller J. COVID-19 and advocacy—the good and the unacceptable. Psychiatric News. https://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2020.5b13. Published May 7, 2020. Accessed August 7, 2020.
5. Webb Hooper M, Nápoles AM, Perez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA. 2020;323(24):2466-2467.
6. Sederer LI, Lanzara CB, Essock SM, et al. Lessons learned from the New York State mental health response to the September 11, 2001, attacks. Psychiatr Serv. 2011;62(9):1085-1089.
7. World Health Organization. Infodemic management – infodemiology. https://www.who.int/teams/risk-communication/infodemic-management. Accessed August 7, 2020.
8. Zhou J, Liu L, Xue P, et al. Mental health response to the COVID-19 outbreak in China. Am J Psychiatry. 2020;117(7):574-575.
9. Kawohl W, Nordt C. COVID-19, unemployment, and suicide. Lancet Psychiatry. 2020;7(5):389-390.
10. Yao H, Chen JH, Xu YF. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry. 2020;7(4):e21. doi: 10.1016/S2215-0366(20)30090-0.
11. Minihan E, Gavin B, Kelly BD, et al. Covid-19, mental health and psychological first aid. Ir J Psychol Med. 2020:1-12.
12. Adja KYC, Golinelli D, Lenzi J, et al. Pandemics and social stigma: who’s next? Italy’s experience with COVID-19. Public Health. 2020;185:39-41.
13. Rosenberg AR. Cultivating deliberate resilience during the coronavirus disease 2019 pandemic [published online April 14, 2020]. JAMA Pediatr. doi: 10.1001/jamapediatrics.2020.1436.
14. Dean W, Talbot SG, Caplan A. Clarifying the language of clinician distress [published online January 31, 2020]. JAMA. doi: 10.1001/jama.2019.21576.
15. Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. 2020;382(21):2049-2055.
16. Rosenbaum L. Facing Covid-19 in Italy - ethics, logistics, and therapeutics on the epidemic’s front line. N Engl J Med. 2020;382(20):1873-1875.
17. Viceconte G, Petrosillo N. COVID-19 R0: magic number or conundrum? Infect Dis Rep. 2020;12(1):8516.
18. de Hert M, Schreurs V, Vancampfort D, van Winkel R. Metabolic syndrome in people with schizophrenia: a review. World Psychiatry. 2009;8(1):15-22.
19. Chen R, Liang W, Jiang M, et al. Risk factors of fatal outcome in hospitalized subjects with coronavirus disease 2019 from a nationwide analysis in China. Chest. 2020;158(1):97-105.
20. Finer N, Garnett SP, Bruun JM. COVID-19 and obesity. Clin Obes. 2020;10(3):e12365. doi: 10.1111/cob.12365.
21. Havens LL, Ghaemi SN. Existential despair and bipolar disorder: the therapeutic alliance as a mood stabilizer. Am J Psychother. 2005;59(2):137-147.
22. Trémeau F, Antonius D, Malaspina D, et al. Loneliness in schizophrenia and its possible correlates. An exploratory study. Psychiatry Res. 2016;246:211-217.
23. Menninger KA. Psychoses associated with influenza: I. General data: statistical analysis. JAMA. 1919;72(4):235-241.
24. Asadi-Pooya AA, Simani L. Central nervous system manifestations of COVID-19: a systematic review. J Neurol Sci. 2020;413:116832. doi: 10.1016/j.jns.2020.116832.
25. Ferrando SJ, Klepacz L, Lynch S, et al. COVID-19 psychosis: a potential new neuropsychiatric condition triggered by novel coronavirus infection and the inflammatory response? [published online May 19, 2020]. Psychosomatics. doi: 10.1016/j.psym.2020.05.012.
26. Troyer EA, Kohn JN, Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav Immun. 2020;87:34-39.
27. Martin Jr. EB. Brief psychotic disorder triggered by fear of coronavirus? Psychiatric Times. https://www.psychiatrictimes.com/view/brief-psychotic-disorder-triggered-fear-coronavirus-small-case-series. Published May 8, 2020. Accessed August 7, 2020.
28. Sher Y, Rabkin B, Maldonado JR, et al. COVID-19-associated hyperactive intensive care unit delirium with proposed pathophysiology and treatment: a case report [published online May 19, 2020]. Psychosomatics. doi: 10.1016/j.psym.2020.05.007.
29. Wolters AE, Peelen LM, Welling MC, et al. Long-term mental health problems after delirium in the ICU. Crit Care Med. 2016;44(10):1808-1813.
30. Toovey S. Influenza-associated central nervous system dysfunction: a literature review. Travel Med Infect Dis. 2008;6(3):114-124.
31. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912-920.
32. Maercker A, Brewin CR, Bryant RA, et al. Diagnosis and classification of disorders specifically associated with stress: proposals for ICD-11. World Psychiatry. 2013;12(3):198-206.
33. Ornell F, Moura HF, Scherer JN, et al. The COVID-19 pandemic and its impact on substance use: implications for prevention and treatment. Psychiatry Res. 2020;289:113096. doi: 10.1016/j.psychres.2020.113096.
34. Berlin I, Thomas D, Le Faou AL, Cornuz J. COVID-19 and smoking [published online April 3, 2020]. Nicotine Tob Res. https://doi.org/10.1093/ntr/ntaa059.
35. Back D, Marzolini C, Hodge C, et al. COVID-19 treatment in patients with comorbidities: awareness of drug-drug interactions [published online May 8, 2020]. Br J Clin Pharmacol. doi: 10.1111/bcp.14358.
36. Carpenter WT Jr., Buchanan RW, Kirkpatrick B, et al. Diazepam treatment of early signs of exacerbation in schizophrenia. Am J Psychiatry. 1999;156(2):299-303.
37. Dotson S, Hartvigsen N, Wesner T, et al. Clozapine toxicity in the setting of COVID-19 [published online May 30, 2020]. Psychosomatics. doi: 10.1016/j.psym.2020.05.025.
38. Siskind D, Honer WG, Clark S, et al. Consensus statement on the use of clozapine during the COVID-19 pandemic. J Psychiatry Neurosci. 2020;45(3):222-223.
39. Schnitzer K, MacLaurin S, Freudenreich O. Long-acting injectable antipsychotics during the COVID-19 pandemic. Current Psychiatry. In press.
40. Winston A, Rosenthal RN, Pinsker H. Learning supportive psychotherapy: an illustrated guide. Washington, DC: American Psychiatric Publishing; 2012.
41. Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382(18):1679-1681.
42. Jordan A, Dixon LB. Considerations for telepsychiatry service implementation in the era of COVID-19. Psychiatr Serv. 2020;71(6):643-644.
43. DePierro J, Lowe S, Katz C. Lessons learned from 9/11: mental health perspectives on the COVID-19 pandemic. Psychiatry Res. 2020;288:113024.
44. Hussain S. Immunization and vaccination. In: Huremovic
45. Epping-Jordan JE, van Ommeren M, Ashour HN, et al. Beyond the crisis: building back better mental health care in 10 emergency-affected areas using a longer-term perspective. Int J Ment Health Syst. 2015;9:15.
46. Rosenbaum L. The untold toll - the pandemic’s effects on patients without Covid-19. N Engl J Med. 2020;382(24):2368-2371.
47. Bartels SJ, Baggett TP, Freudenreich O, et al. COVID-19 emergency reforms in Massachusetts to support behavioral health care and reduce mortality of people with serious mental illness [published online June 3, 2020]. Psychiatr Serv. doi: 10.1176/appi.ps.202000244.
1. Camus A. La peste. Paris, France: Éditions Gallimard; 1947.
2. Huremovic
3. Substance Abuse and Mental Health Services Administration. Phases of disaster. https://www.samhsa.gov/dtac/recovering-disasters/phases-disaster. Updated June 17, 2020. Accessed August 7, 2020.
4. Geller J. COVID-19 and advocacy—the good and the unacceptable. Psychiatric News. https://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2020.5b13. Published May 7, 2020. Accessed August 7, 2020.
5. Webb Hooper M, Nápoles AM, Perez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA. 2020;323(24):2466-2467.
6. Sederer LI, Lanzara CB, Essock SM, et al. Lessons learned from the New York State mental health response to the September 11, 2001, attacks. Psychiatr Serv. 2011;62(9):1085-1089.
7. World Health Organization. Infodemic management – infodemiology. https://www.who.int/teams/risk-communication/infodemic-management. Accessed August 7, 2020.
8. Zhou J, Liu L, Xue P, et al. Mental health response to the COVID-19 outbreak in China. Am J Psychiatry. 2020;117(7):574-575.
9. Kawohl W, Nordt C. COVID-19, unemployment, and suicide. Lancet Psychiatry. 2020;7(5):389-390.
10. Yao H, Chen JH, Xu YF. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry. 2020;7(4):e21. doi: 10.1016/S2215-0366(20)30090-0.
11. Minihan E, Gavin B, Kelly BD, et al. Covid-19, mental health and psychological first aid. Ir J Psychol Med. 2020:1-12.
12. Adja KYC, Golinelli D, Lenzi J, et al. Pandemics and social stigma: who’s next? Italy’s experience with COVID-19. Public Health. 2020;185:39-41.
13. Rosenberg AR. Cultivating deliberate resilience during the coronavirus disease 2019 pandemic [published online April 14, 2020]. JAMA Pediatr. doi: 10.1001/jamapediatrics.2020.1436.
14. Dean W, Talbot SG, Caplan A. Clarifying the language of clinician distress [published online January 31, 2020]. JAMA. doi: 10.1001/jama.2019.21576.
15. Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. 2020;382(21):2049-2055.
16. Rosenbaum L. Facing Covid-19 in Italy - ethics, logistics, and therapeutics on the epidemic’s front line. N Engl J Med. 2020;382(20):1873-1875.
17. Viceconte G, Petrosillo N. COVID-19 R0: magic number or conundrum? Infect Dis Rep. 2020;12(1):8516.
18. de Hert M, Schreurs V, Vancampfort D, van Winkel R. Metabolic syndrome in people with schizophrenia: a review. World Psychiatry. 2009;8(1):15-22.
19. Chen R, Liang W, Jiang M, et al. Risk factors of fatal outcome in hospitalized subjects with coronavirus disease 2019 from a nationwide analysis in China. Chest. 2020;158(1):97-105.
20. Finer N, Garnett SP, Bruun JM. COVID-19 and obesity. Clin Obes. 2020;10(3):e12365. doi: 10.1111/cob.12365.
21. Havens LL, Ghaemi SN. Existential despair and bipolar disorder: the therapeutic alliance as a mood stabilizer. Am J Psychother. 2005;59(2):137-147.
22. Trémeau F, Antonius D, Malaspina D, et al. Loneliness in schizophrenia and its possible correlates. An exploratory study. Psychiatry Res. 2016;246:211-217.
23. Menninger KA. Psychoses associated with influenza: I. General data: statistical analysis. JAMA. 1919;72(4):235-241.
24. Asadi-Pooya AA, Simani L. Central nervous system manifestations of COVID-19: a systematic review. J Neurol Sci. 2020;413:116832. doi: 10.1016/j.jns.2020.116832.
25. Ferrando SJ, Klepacz L, Lynch S, et al. COVID-19 psychosis: a potential new neuropsychiatric condition triggered by novel coronavirus infection and the inflammatory response? [published online May 19, 2020]. Psychosomatics. doi: 10.1016/j.psym.2020.05.012.
26. Troyer EA, Kohn JN, Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav Immun. 2020;87:34-39.
27. Martin Jr. EB. Brief psychotic disorder triggered by fear of coronavirus? Psychiatric Times. https://www.psychiatrictimes.com/view/brief-psychotic-disorder-triggered-fear-coronavirus-small-case-series. Published May 8, 2020. Accessed August 7, 2020.
28. Sher Y, Rabkin B, Maldonado JR, et al. COVID-19-associated hyperactive intensive care unit delirium with proposed pathophysiology and treatment: a case report [published online May 19, 2020]. Psychosomatics. doi: 10.1016/j.psym.2020.05.007.
29. Wolters AE, Peelen LM, Welling MC, et al. Long-term mental health problems after delirium in the ICU. Crit Care Med. 2016;44(10):1808-1813.
30. Toovey S. Influenza-associated central nervous system dysfunction: a literature review. Travel Med Infect Dis. 2008;6(3):114-124.
31. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912-920.
32. Maercker A, Brewin CR, Bryant RA, et al. Diagnosis and classification of disorders specifically associated with stress: proposals for ICD-11. World Psychiatry. 2013;12(3):198-206.
33. Ornell F, Moura HF, Scherer JN, et al. The COVID-19 pandemic and its impact on substance use: implications for prevention and treatment. Psychiatry Res. 2020;289:113096. doi: 10.1016/j.psychres.2020.113096.
34. Berlin I, Thomas D, Le Faou AL, Cornuz J. COVID-19 and smoking [published online April 3, 2020]. Nicotine Tob Res. https://doi.org/10.1093/ntr/ntaa059.
35. Back D, Marzolini C, Hodge C, et al. COVID-19 treatment in patients with comorbidities: awareness of drug-drug interactions [published online May 8, 2020]. Br J Clin Pharmacol. doi: 10.1111/bcp.14358.
36. Carpenter WT Jr., Buchanan RW, Kirkpatrick B, et al. Diazepam treatment of early signs of exacerbation in schizophrenia. Am J Psychiatry. 1999;156(2):299-303.
37. Dotson S, Hartvigsen N, Wesner T, et al. Clozapine toxicity in the setting of COVID-19 [published online May 30, 2020]. Psychosomatics. doi: 10.1016/j.psym.2020.05.025.
38. Siskind D, Honer WG, Clark S, et al. Consensus statement on the use of clozapine during the COVID-19 pandemic. J Psychiatry Neurosci. 2020;45(3):222-223.
39. Schnitzer K, MacLaurin S, Freudenreich O. Long-acting injectable antipsychotics during the COVID-19 pandemic. Current Psychiatry. In press.
40. Winston A, Rosenthal RN, Pinsker H. Learning supportive psychotherapy: an illustrated guide. Washington, DC: American Psychiatric Publishing; 2012.
41. Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382(18):1679-1681.
42. Jordan A, Dixon LB. Considerations for telepsychiatry service implementation in the era of COVID-19. Psychiatr Serv. 2020;71(6):643-644.
43. DePierro J, Lowe S, Katz C. Lessons learned from 9/11: mental health perspectives on the COVID-19 pandemic. Psychiatry Res. 2020;288:113024.
44. Hussain S. Immunization and vaccination. In: Huremovic
45. Epping-Jordan JE, van Ommeren M, Ashour HN, et al. Beyond the crisis: building back better mental health care in 10 emergency-affected areas using a longer-term perspective. Int J Ment Health Syst. 2015;9:15.
46. Rosenbaum L. The untold toll - the pandemic’s effects on patients without Covid-19. N Engl J Med. 2020;382(24):2368-2371.
47. Bartels SJ, Baggett TP, Freudenreich O, et al. COVID-19 emergency reforms in Massachusetts to support behavioral health care and reduce mortality of people with serious mental illness [published online June 3, 2020]. Psychiatr Serv. doi: 10.1176/appi.ps.202000244.
Cognitive-behavioral therapy for insomnia: A review of 8 studies
The prevalence of insomnia in the general population is approximately 6% to 10%.1 In addition, an estimated 30% of the general population may have symptoms of insomnia without meeting the diagnostic criteria.2 As a disorder, insomnia is characterized by a persistent difficulty initiating or maintaining sleep, or early morning awakening with inability to return to sleep, that has been present for at least 3 months. Additionally, the sleep difficulties must occur at least 3 nights a week, result in impaired daytime functioning, and cause significant distress.1
Cognitive-behavioral therapy for insomnia (CBT-I) is an effective treatment, supported by several systematic reviews and meta-analyses.3-5 In the short term, CBT-I is as effective as pharmacotherapy.6 However, CBT-I is the preferred treatment for chronic insomnia, according to recommendations in European and American guidelines.7,8
Here we review 8 recent studies that examined CBT-I. These studies are summarized in the Table.9-16
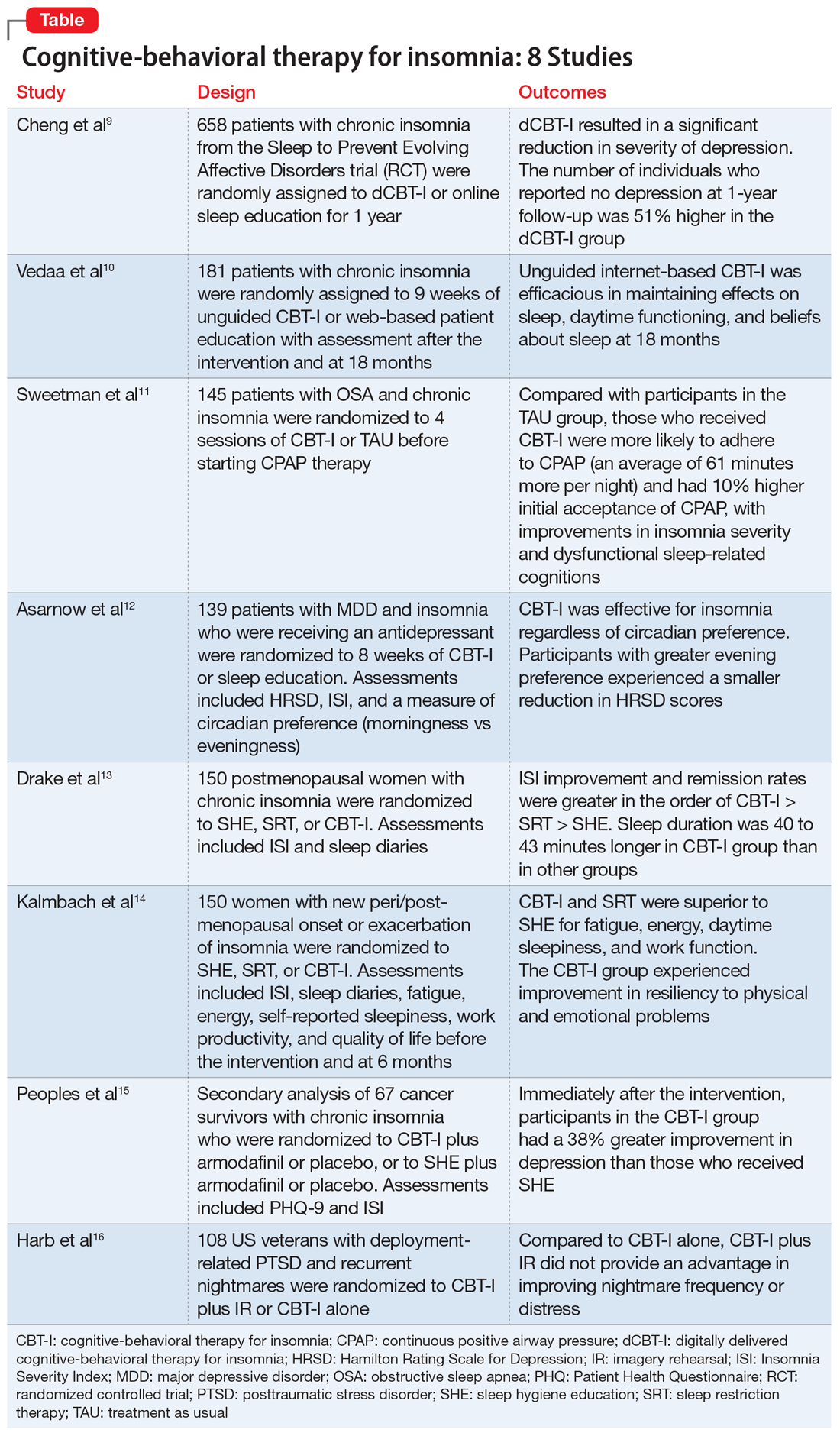
1. Cheng P, Kalmbach DA, Tallent G, et al. Depression prevention via digital cognitive behavioral therapy for insomnia: a randomized controlled trial. Sleep. 2019;42(10):zsz150. doi: 10.1093/sleep/zsz150.
Although CBT-I is a first-line treatment for chronic insomnia, it is underutilized in clinical practice primarily due to limited availability. Because few clinicians are certified in CBT-I, it has become necessary to develop alternative modes of delivery for CBT-I, such as fully automated, internet-delivered approaches to reach more patients with insomnia. Digital CBT-I (dCBT-I) is comparable to in-person CBT-I in improving insomnia symptoms and reducing concurrent depressive symptoms with insomnia. It is unclear if unguided, internet-delivered CBT-I is effective for achieving remission from depression or preventing depression in the long term. Chen et al9 examined the efficacy of dCBT-I in reducing and preventing depression over a 1-year follow-up.
Study design
- Participants from various centers in Southeastern Michigan were recruited between 2016 and 2017. Data was obtained from the Sleep to Prevent Evolving Affective Disorders (SPREAD) trial.
- Participants who met DSM-5 criteria for chronic insomnia disorder were randomized to dCBT-I (n = 358) using the Sleepio digital CBT program via the internet or to online sleep education (n = 300).
- The primary outcome was depression, measured using the Quick Inventory of Depressive Symptomatology-Self Report (QIDS-SR-16) at 1-year follow-up. Depression incidence was also tested against insomnia treatment response.
Outcomes
- The severity of depression was significantly lower at 1-year follow-up in the dCBT-I group compared with the control group.
- The dCBT-I group showed a 51% higher remission rate than the control group at 1-year follow-up.
- The incidence of moderate to severe depression in individuals with minimal to no depression at baseline was halved at 1 year after receiving dCBT-I treatment compared with the control group.
Continue to: Conclusion
Conclusion
- dCBT-I can improve depression and insomnia and has a sustained antidepressant effect.
- dCBT-I is effective for preventing depression. In other words, the risk of developing depression is decreased when dCBT-I is used to treat insomnia in individuals with minimal to no depression at baseline.
2. Vedaa Ø, Hagatun S, Kallestad H, et al. Long-term effects of an unguided online cognitive behavioral therapy for chronic insomnia. J Clin Sleep Med. 2019;15(1):101-110.
dCBT-I is effective for treating insomnia in the short term; however, little is known about the long-term effectiveness of dCBT-I on sleep and daytime symptoms. Vedaa et al10 evaluated the efficacy of dCBT-I at 18 months after the intervention.
Study design
- In this randomized controlled trial (RCT), the efficacy of unguided, internet-delivered CBT-I (n = 95) was compared with web-based patient education (n = 86) for patients with chronic insomnia.
- Participants were assessed at baseline, after a 9-week intervention period, and at 6-month follow-up. Participants in the internet CBT-I group were reassessed at 18 months after the intervention using online questionnaires, including the Insomnia Severity Index (ISI), Bergen Insomnia Scale (BIS), Brief Dysfunctional Beliefs and Attitudes Scale, Hospital Anxiety and Depression Scale, Chalder Fatigue Questionnaire, and sleep diaries.
Outcomes
- At 18 months, significant improvements were noted from baseline ISI and BIS scores and in levels of daytime fatigue, as well as psychological distress and beliefs about sleep.
- Sleep diary variables—including sleep onset latency, time awake during the night (wake time after sleep onset), early morning awakening, total sleep time, and sleep efficiency—showed significant improvement from baseline to 18-month follow-up (at least moderate effect size).
- Improvements were maintained from the completion of the 9-week intervention to follow-up at 18 months.
Continue to: Conclusion
Conclusion
- Fully-automated, internet-based CBT-I is efficacious in maintaining positive effects on sleep and daytime functioning up to 18 months after completing treatment.
3. Sweetman A, Lack L, Catcheside PG, et al. Cognitive and behavioral therapy for insomnia increases the use of continuous positive airway pressure therapy in obstructive sleep apnea participants with comorbid insomnia: a randomized clinical trial. Sleep. 2019;42(12):zsz178. doi: 10.1093/sleep/zsz178.
Comorbid insomnia and sleep apnea (COMISA) can affect a patient’s ability to accept and comply with continuous positive airway pressure (CPAP) therapy. Providing adequate treatment for these patients can be challenging.
Sweetman et al11 evaluated the acceptance and use of CPAP in patients with obstructive sleep apnea and chronic insomnia following initial treatment with CBT-I compared with treatment as usual (TAU).
Study design
- In this RCT, 145 participants with COMISA were randomized to 4 sessions of CBT-I or TAU before starting CPAP therapy until 6 months after randomization.
- Primary outcomes were objective CPAP adherence and objective sleep efficiency at the end of 6 months.
- Secondary outcomes were CPAP acceptance/rejection, changes in sleep parameters, global insomnia severity, and daytime impairments at 6 months.
Continue to: Outcomes
Outcomes
- The CBT-I group had higher initial CPAP acceptance and greater average nightly adherence to CPAP (61 minutes more) than the TAU group.
- Significant improvements were noted in global insomnia severity, nighttime insomnia complaints, and dysfunctional sleep-related cognitions at 6 months in the CBT-I group compared with TAU.
- No differences between the 2 groups were noted in sleep diary parameters or daytime impairments at 6 months.
Conclusions
- Patients with COMISA can benefit from receiving CBT-I before starting CPAP therapy because CBT-I can improve immediate acceptance of CPAP and may help to maintain adherence to CPAP over time.
- Patients with sleep apnea should be evaluated for comorbid insomnia, and CBT-I should be considered before starting CPAP treatment.
4. Asarnow LD, Bei B, Krystal A, et al. Circadian preference as a moderator of depression outcome following cognitive behavioral therapy for insomnia plus antidepressant medications: a report from the TRIAD study. J Clin Sleep Med. 2019;15(4):573-580.
The Treatment of Insomnia and Depression (TRIAD) study reported the effects of combining antidepressants with CBT-I in patients with major depressive disorder (MDD) and insomnia. Asarnow et al12 examined the moderation of circadian preference in the reduction of depression and insomnia symptoms severity during the same trial.
Study design
- In this RCT, 139 participants with MDD and insomnia were treated with an antidepressant (escitalopram, sertraline, or desvenlafaxine) and randomized to 8 weeks of CBT-I or control therapy (sleep education).
- Measurements used were Composite Scale of Morningness for circadian preference (morningness vs eveningness), depression severity with the Hamilton Rating Scale for Depression, and insomnia severity using the ISI.
Continue to: Outcomes
Outcomes
- CBT-I was effective for insomnia regardless of circadian preference.
- A smaller reduction in depression scores was noted in participants with greater evening preference.
- Depression outcomes were better among participants with evening preference if they were assigned to CBT-I vs control therapy.
- The control therapy (sleep education) was particularly ineffective in reducing depression symptoms in participants with evening preference.
Conclusion
- Individuals with MDD and insomnia and an evening preference are at an increased risk for poor response to antidepressants alone.
- Outcomes for both depression and insomnia improve if CBT-I is combined with antidepressants.
- Offering sleep education alone is not sufficient.
5. Drake CL, Kalmbach DA, Arnedt JT, et al. Treating chronic insomnia in postmenopausal women: a randomized clinical trial comparing cognitive-behavioral therapy for insomnia, sleep restriction therapy, and sleep hygiene education. Sleep. 2019;42(2):zsy217. doi: 10.1093/sleep/zsy217.
Postmenopausal women with sleep disturbances experience higher medical and psychiatric comorbidities, and have higher alcohol consumption and stress levels than postmenopausal women with good sleep. Nonpharmacologic insomnia treatments with durable effects are imperative for postmenopausal women because they are safer than pharmacologic approaches. Although CBT-I is the recommended first-line treatment for chronic insomnia, its application in menopause-related insomnia is limited. Drake et al13 evaluated the efficacy of CBT-I in menopause-related insomnia compared with sleep restriction therapy (SRT) and sleep hygiene education (SHE).
Study design
- This RCT was conducted at a health system with 6 hospitals in Michigan.
- Postmenopausal women who met DSM-5 criteria for chronic insomnia disorder (n = 150) were randomized into 1 of 3 groups: SHE, SRT, or CBT-I.
- Primary outcome measures were ISI scores and sleep diaries that documented multiple sleep parameters, including sleep onset latency, wake time after sleep onset, number of awakenings in the middle of the night, time in bed, total sleep time, and sleep efficiency. These were measured at baseline, after completion of treatment, and 6 months after treatment.
Continue to: Outcomes
Outcomes
- Both CBT-I and SRT outperformed SHE on the ISI and for most of the sleep parameters on sleep diaries immediately after treatment completion and at 6 months after treatment.
- Total sleep time was 40 to 43 minutes longer in the CBT-I group than in the SRT and SHE groups at 6-month follow-up.
- Remission rates (sleep onset latency ≤30 minutes, wake time after sleep onset ≤30 minutes, sleep efficiency ≥85%) were significantly higher in CBT-I group (CBT-I > SRT > SHE).
Conclusion
- Sleep hygiene education as a standalone treatment is not useful for treating chronic insomnia.
- Both CBT-I and SRT are efficacious for menopause-related insomnia.
- CBT-I may be a better option than SRT because it produces higher remission rates and better long-term outcomes.
6. Kalmbach DA, Cheng P, Arnedt JT, et al. Improving daytime functioning, work performance, and quality of life in postmenopausal women with insomnia: comparing cognitive behavioral therapy for insomnia, sleep restriction therapy, and sleep hygiene education. J Clin Sleep Med. 2019;15(7):999-1010.
CBT-I has shown efficacy in the treatment of insomnia in postmenopausal women. In this study, Kalmbach et al14 compared 3 nonpharmacologic modalities—CBT-I, SRT, and SHE—for the treatment of menopause-related insomnia and daytime impairment.
Study design
- In this RCT, 150 participants with new peri- and post-menopausal onset or exacerbation of insomnia were randomized to 1 of 3 groups: SHE, SRT, or CBT-I.
- Participants were assessed at baseline, after treatment completion, and at 6-month follow-up using the ISI, sleep diaries, Fatigue Severity Scale, Epworth Sleepiness Scale, Work Productivity and Activity Impairment Questionnaire, and 36-item Medical Outcomes Study Short Form Health Survey.
Continue to: Outcomes
Outcomes
- In both the CBT-I and SRT groups, significant improvements were noted in fatigue, energy, daytime sleepiness, and work function after treatment completion and at 6-month follow-up.
- Improvements were noted in emotional well-being and resiliency to physical and emotional problems in the CBT-I group at 6 months.
- Improvements in overall general health and social functioning, less pain, and fewer hot flashes were reported by postmenopausal women who remitted from insomnia; however, these benefits were not directly related to any specific treatment modality.
Conclusion
- CBT-I and SRT are superior to SHE for improving daytime functioning, and some aspects of life quality and work productivity, in postmenopausal women with insomnia.
- CBT-I may be superior to SRT in producing larger improvements in fatigue, energy level, and daytime sleep propensity.
- CBT-I can improve emotional well-being and resilience to emotional problems in postmenopausal women with insomnia.
7. Peoples AR, Garland SN, Pigeon WR, et al. Cognitive behavioral therapy for insomnia reduces depression in cancer survivors. J Clin Sleep Med. 2019;15(1):129-137.
Depression is common in patients with cancer and is usually associated with comorbid insomnia. Depression has significant effect on treatment compliance, coping with illness, and quality of life. Peoples et al15 examined the effects of CBT-I on depression in cancer survivors.
Study design
- This was a secondary analysis of a multicenter, randomized, placebo-controlled trial that evaluated interventions for cancer survivors with chronic insomnia in which the primary outcome measure was insomnia severity.
- Cancer survivors (n = 67) were randomized to CBT-I plus armodafinil or placebo or to SHE plus armodafinil or placebo.
- The Patient Health Questionnaire-9 (PHQ-9) and ISI were used to measure depression and insomnia at baseline, after 7-weeks of intervention, and at 3 months postintervention.
Continue to: Outcomes
Outcomes
- Immediately after completing the intervention, cancer survivors treated with CBT-I had significantly less depression (38% greater improvement in depression) compared with those who received SHE (control group).
- In the CBT-I group, 23% of cancer survivors achieved a clinically important reduction (5-point reduction on PHQ-9 total score) in depression at postintervention compared with 6% of those in the control group.
- At 3 months after the intervention, only 14% of cancer survivors in CBT-I group reported depression (PHQ-9 score >4), whereas 47% of those in the control group (SHE) reported depression.
Conclusion
- CBT-I improves both depression and insomnia in cancer survivors, and the improvements are sustained at 3 months after completing treatment.
- Improvement in insomnia severity appears to mediate the positive effects of CBT-I on depression.
8. Harb GC, Cook JM, Phelps AJ, et al. Randomized controlled trial of imagery rehearsal for posttraumatic nightmares in combat veterans. J Clin Sleep Med. 2019;15(5):757-767.
The American Academy of Sleep Medicine recommends imagery rehearsal (IR) therapy, which incorporates some components of CBT-I, for the treatment of recurrent posttraumatic stress disorder (PTSD)–related nightmares. In this study, Harb et al16 compared CBT-I plus IR to CBT-I alone for the treatment of nightmares in veterans with combat-related PTSD.
Study design
- This RCT included male and female US veterans (n = 108) deployed to Iraq and Afghanistan with current PTSD and recurrent nightmares related to deployment.
- Participants were randomized to 6 sessions of CBT-I plus IR or CBT-I alone.
- Primary outcome measures included frequency of nightmares and distress associated with nightmares.
Continue to: Outcomes
Outcomes
- A significant improvement in nightmares was noted in both groups (29% of participants showed a clinically-significant reduction in nightmare frequency and 22% of participants achieved remission).
- CBT-I plus IR was not superior to CBT-I only at postintervention and at 6-month follow-up.
Conclusion
- Both IR and CBT-I demonstrated efficacy for decreasing nightmare frequency and distress.
- Combining IR and CBT-I may not provide a synergistic advantage over CBT-I alone for treating PTSD-related nightmares in veterans.
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
2. Morin CM, LeBlanc M, Daley M, et al. Epidemiology of insomnia: prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Med. 2006;7(2):123-130.
3. Trauer JM, Qian MY, Doyle JS, et al. Cognitive behavioral therapy for chronic insomnia: a systematic review and meta-analysis. Ann Intern Med. 2015;163(3):191-204.
4. Wu JQ, Appleman ER, Salazar RD, et al. Cognitive behavioral therapy for insomnia comorbid with psychiatric and medical conditions: a meta-analysis. JAMA Intern Med. 2015;175(9):1461-1472.
5. van Straten A, van der Zweerde T, Kleiboer A, et al. Cognitive and behavioral therapies in the treatment of insomnia: a meta-analysis. Sleep Med Rev. 2018;38:3-16.
6. Smith MT, Perlis ML, Park A, et al. Comparative meta-analysis of pharmacotherapy and behavior therapy for persistent insomnia. Am J Psychiatry. 2002;159(1):5-11.
7. Qaseem A, Kansagara D, Forciea MA, et al. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016;165(2):125-133.
8. Riemann D, Baglioni C, Bassetti C, et al. European guideline for the diagnosis and treatment of insomnia. J Sleep Res. 2017;26(6):675-700.
9. Cheng P, Kalmbach DA, Tallent G, et al. Depression prevention via digital cognitive behavioral therapy for insomnia: a randomized controlled trial. Sleep. 2019;42(10):zsz150. doi: 10.1093/sleep/zsz150.
10. Vedaa Ø, Hagatun S, Kallestad H, et al. Long-term effects of an unguided online cognitive behavioral therapy for chronic insomnia. J Clin Sleep Med. 2019;15(1):101-110.
11. Sweetman A, Lack L, Catcheside PG, et al. Cognitive and behavioral therapy for insomnia increases the use of continuous positive airway pressure therapy in obstructive sleep apnea participants with comorbid insomnia: a randomized clinical trial. Sleep. 2019;42(12):zsz178. doi: 10.1093/sleep/zsz178.
12. Asarnow LD, Bei B, Krystal A, et al. Circadian preference as a moderator of depression outcome following cognitive behavioral therapy for insomnia plus antidepressant medications: a report from the TRIAD study. J Clin Sleep Med. 2019;15(4):573-580.
13. Drake CL, Kalmbach DA, Arnedt JT, et al. Treating chronic insomnia in postmenopausal women: a randomized clinical trial comparing cognitive-behavioral therapy for insomnia, sleep restriction therapy, and sleep hygiene education. Sleep. 2019;42(2):zsy217. doi: 10.1093/sleep/zsy217.
14. Kalmbach DA, Cheng P, Arnedt JT, et al. Improving daytime functioning, work performance, and quality of life in postmenopausal women with insomnia: comparing cognitive behavioral therapy for insomnia, sleep restriction therapy, and sleep hygiene education. J Clin Sleep Med. 2019;15(7):999-1010.
15. Peoples AR, Garland SN, Pigeon WR, et al. Cognitive behavioral therapy for insomnia reduces depression in cancer survivors. J Clin Sleep Med. 2019;15(1):129-137.
16. Harb GC, Cook JM, Phelps AJ, et al. Randomized controlled trial of imagery rehearsal for posttraumatic nightmares in combat veterans. J Clin Sleep Med. 2019;15(5):757-767.
The prevalence of insomnia in the general population is approximately 6% to 10%.1 In addition, an estimated 30% of the general population may have symptoms of insomnia without meeting the diagnostic criteria.2 As a disorder, insomnia is characterized by a persistent difficulty initiating or maintaining sleep, or early morning awakening with inability to return to sleep, that has been present for at least 3 months. Additionally, the sleep difficulties must occur at least 3 nights a week, result in impaired daytime functioning, and cause significant distress.1
Cognitive-behavioral therapy for insomnia (CBT-I) is an effective treatment, supported by several systematic reviews and meta-analyses.3-5 In the short term, CBT-I is as effective as pharmacotherapy.6 However, CBT-I is the preferred treatment for chronic insomnia, according to recommendations in European and American guidelines.7,8
Here we review 8 recent studies that examined CBT-I. These studies are summarized in the Table.9-16
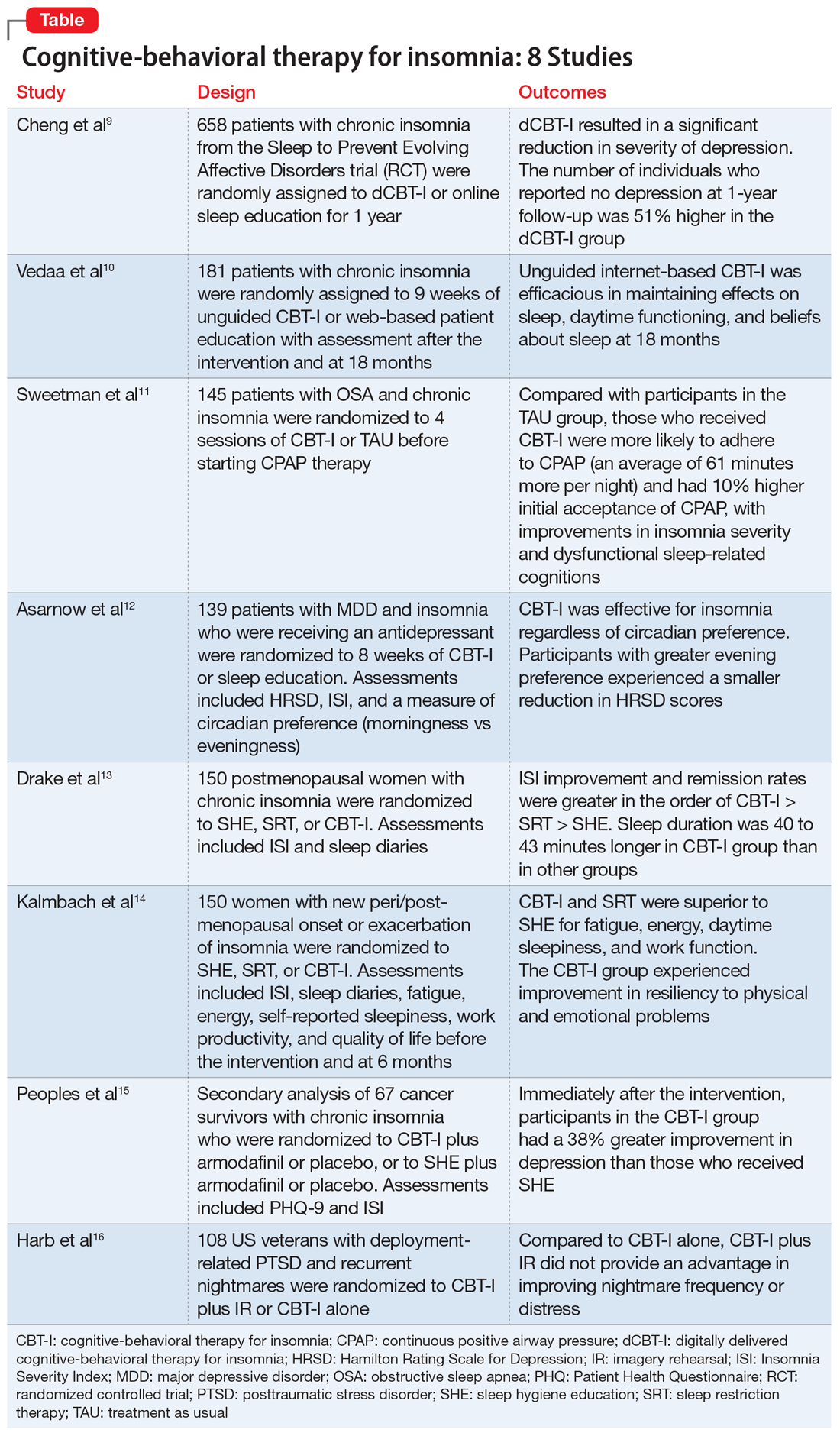
1. Cheng P, Kalmbach DA, Tallent G, et al. Depression prevention via digital cognitive behavioral therapy for insomnia: a randomized controlled trial. Sleep. 2019;42(10):zsz150. doi: 10.1093/sleep/zsz150.
Although CBT-I is a first-line treatment for chronic insomnia, it is underutilized in clinical practice primarily due to limited availability. Because few clinicians are certified in CBT-I, it has become necessary to develop alternative modes of delivery for CBT-I, such as fully automated, internet-delivered approaches to reach more patients with insomnia. Digital CBT-I (dCBT-I) is comparable to in-person CBT-I in improving insomnia symptoms and reducing concurrent depressive symptoms with insomnia. It is unclear if unguided, internet-delivered CBT-I is effective for achieving remission from depression or preventing depression in the long term. Chen et al9 examined the efficacy of dCBT-I in reducing and preventing depression over a 1-year follow-up.
Study design
- Participants from various centers in Southeastern Michigan were recruited between 2016 and 2017. Data was obtained from the Sleep to Prevent Evolving Affective Disorders (SPREAD) trial.
- Participants who met DSM-5 criteria for chronic insomnia disorder were randomized to dCBT-I (n = 358) using the Sleepio digital CBT program via the internet or to online sleep education (n = 300).
- The primary outcome was depression, measured using the Quick Inventory of Depressive Symptomatology-Self Report (QIDS-SR-16) at 1-year follow-up. Depression incidence was also tested against insomnia treatment response.
Outcomes
- The severity of depression was significantly lower at 1-year follow-up in the dCBT-I group compared with the control group.
- The dCBT-I group showed a 51% higher remission rate than the control group at 1-year follow-up.
- The incidence of moderate to severe depression in individuals with minimal to no depression at baseline was halved at 1 year after receiving dCBT-I treatment compared with the control group.
Continue to: Conclusion
Conclusion
- dCBT-I can improve depression and insomnia and has a sustained antidepressant effect.
- dCBT-I is effective for preventing depression. In other words, the risk of developing depression is decreased when dCBT-I is used to treat insomnia in individuals with minimal to no depression at baseline.
2. Vedaa Ø, Hagatun S, Kallestad H, et al. Long-term effects of an unguided online cognitive behavioral therapy for chronic insomnia. J Clin Sleep Med. 2019;15(1):101-110.
dCBT-I is effective for treating insomnia in the short term; however, little is known about the long-term effectiveness of dCBT-I on sleep and daytime symptoms. Vedaa et al10 evaluated the efficacy of dCBT-I at 18 months after the intervention.
Study design
- In this randomized controlled trial (RCT), the efficacy of unguided, internet-delivered CBT-I (n = 95) was compared with web-based patient education (n = 86) for patients with chronic insomnia.
- Participants were assessed at baseline, after a 9-week intervention period, and at 6-month follow-up. Participants in the internet CBT-I group were reassessed at 18 months after the intervention using online questionnaires, including the Insomnia Severity Index (ISI), Bergen Insomnia Scale (BIS), Brief Dysfunctional Beliefs and Attitudes Scale, Hospital Anxiety and Depression Scale, Chalder Fatigue Questionnaire, and sleep diaries.
Outcomes
- At 18 months, significant improvements were noted from baseline ISI and BIS scores and in levels of daytime fatigue, as well as psychological distress and beliefs about sleep.
- Sleep diary variables—including sleep onset latency, time awake during the night (wake time after sleep onset), early morning awakening, total sleep time, and sleep efficiency—showed significant improvement from baseline to 18-month follow-up (at least moderate effect size).
- Improvements were maintained from the completion of the 9-week intervention to follow-up at 18 months.
Continue to: Conclusion
Conclusion
- Fully-automated, internet-based CBT-I is efficacious in maintaining positive effects on sleep and daytime functioning up to 18 months after completing treatment.
3. Sweetman A, Lack L, Catcheside PG, et al. Cognitive and behavioral therapy for insomnia increases the use of continuous positive airway pressure therapy in obstructive sleep apnea participants with comorbid insomnia: a randomized clinical trial. Sleep. 2019;42(12):zsz178. doi: 10.1093/sleep/zsz178.
Comorbid insomnia and sleep apnea (COMISA) can affect a patient’s ability to accept and comply with continuous positive airway pressure (CPAP) therapy. Providing adequate treatment for these patients can be challenging.
Sweetman et al11 evaluated the acceptance and use of CPAP in patients with obstructive sleep apnea and chronic insomnia following initial treatment with CBT-I compared with treatment as usual (TAU).
Study design
- In this RCT, 145 participants with COMISA were randomized to 4 sessions of CBT-I or TAU before starting CPAP therapy until 6 months after randomization.
- Primary outcomes were objective CPAP adherence and objective sleep efficiency at the end of 6 months.
- Secondary outcomes were CPAP acceptance/rejection, changes in sleep parameters, global insomnia severity, and daytime impairments at 6 months.
Continue to: Outcomes
Outcomes
- The CBT-I group had higher initial CPAP acceptance and greater average nightly adherence to CPAP (61 minutes more) than the TAU group.
- Significant improvements were noted in global insomnia severity, nighttime insomnia complaints, and dysfunctional sleep-related cognitions at 6 months in the CBT-I group compared with TAU.
- No differences between the 2 groups were noted in sleep diary parameters or daytime impairments at 6 months.
Conclusions
- Patients with COMISA can benefit from receiving CBT-I before starting CPAP therapy because CBT-I can improve immediate acceptance of CPAP and may help to maintain adherence to CPAP over time.
- Patients with sleep apnea should be evaluated for comorbid insomnia, and CBT-I should be considered before starting CPAP treatment.
4. Asarnow LD, Bei B, Krystal A, et al. Circadian preference as a moderator of depression outcome following cognitive behavioral therapy for insomnia plus antidepressant medications: a report from the TRIAD study. J Clin Sleep Med. 2019;15(4):573-580.
The Treatment of Insomnia and Depression (TRIAD) study reported the effects of combining antidepressants with CBT-I in patients with major depressive disorder (MDD) and insomnia. Asarnow et al12 examined the moderation of circadian preference in the reduction of depression and insomnia symptoms severity during the same trial.
Study design
- In this RCT, 139 participants with MDD and insomnia were treated with an antidepressant (escitalopram, sertraline, or desvenlafaxine) and randomized to 8 weeks of CBT-I or control therapy (sleep education).
- Measurements used were Composite Scale of Morningness for circadian preference (morningness vs eveningness), depression severity with the Hamilton Rating Scale for Depression, and insomnia severity using the ISI.
Continue to: Outcomes
Outcomes
- CBT-I was effective for insomnia regardless of circadian preference.
- A smaller reduction in depression scores was noted in participants with greater evening preference.
- Depression outcomes were better among participants with evening preference if they were assigned to CBT-I vs control therapy.
- The control therapy (sleep education) was particularly ineffective in reducing depression symptoms in participants with evening preference.
Conclusion
- Individuals with MDD and insomnia and an evening preference are at an increased risk for poor response to antidepressants alone.
- Outcomes for both depression and insomnia improve if CBT-I is combined with antidepressants.
- Offering sleep education alone is not sufficient.
5. Drake CL, Kalmbach DA, Arnedt JT, et al. Treating chronic insomnia in postmenopausal women: a randomized clinical trial comparing cognitive-behavioral therapy for insomnia, sleep restriction therapy, and sleep hygiene education. Sleep. 2019;42(2):zsy217. doi: 10.1093/sleep/zsy217.
Postmenopausal women with sleep disturbances experience higher medical and psychiatric comorbidities, and have higher alcohol consumption and stress levels than postmenopausal women with good sleep. Nonpharmacologic insomnia treatments with durable effects are imperative for postmenopausal women because they are safer than pharmacologic approaches. Although CBT-I is the recommended first-line treatment for chronic insomnia, its application in menopause-related insomnia is limited. Drake et al13 evaluated the efficacy of CBT-I in menopause-related insomnia compared with sleep restriction therapy (SRT) and sleep hygiene education (SHE).
Study design
- This RCT was conducted at a health system with 6 hospitals in Michigan.
- Postmenopausal women who met DSM-5 criteria for chronic insomnia disorder (n = 150) were randomized into 1 of 3 groups: SHE, SRT, or CBT-I.
- Primary outcome measures were ISI scores and sleep diaries that documented multiple sleep parameters, including sleep onset latency, wake time after sleep onset, number of awakenings in the middle of the night, time in bed, total sleep time, and sleep efficiency. These were measured at baseline, after completion of treatment, and 6 months after treatment.
Continue to: Outcomes
Outcomes
- Both CBT-I and SRT outperformed SHE on the ISI and for most of the sleep parameters on sleep diaries immediately after treatment completion and at 6 months after treatment.
- Total sleep time was 40 to 43 minutes longer in the CBT-I group than in the SRT and SHE groups at 6-month follow-up.
- Remission rates (sleep onset latency ≤30 minutes, wake time after sleep onset ≤30 minutes, sleep efficiency ≥85%) were significantly higher in CBT-I group (CBT-I > SRT > SHE).
Conclusion
- Sleep hygiene education as a standalone treatment is not useful for treating chronic insomnia.
- Both CBT-I and SRT are efficacious for menopause-related insomnia.
- CBT-I may be a better option than SRT because it produces higher remission rates and better long-term outcomes.
6. Kalmbach DA, Cheng P, Arnedt JT, et al. Improving daytime functioning, work performance, and quality of life in postmenopausal women with insomnia: comparing cognitive behavioral therapy for insomnia, sleep restriction therapy, and sleep hygiene education. J Clin Sleep Med. 2019;15(7):999-1010.
CBT-I has shown efficacy in the treatment of insomnia in postmenopausal women. In this study, Kalmbach et al14 compared 3 nonpharmacologic modalities—CBT-I, SRT, and SHE—for the treatment of menopause-related insomnia and daytime impairment.
Study design
- In this RCT, 150 participants with new peri- and post-menopausal onset or exacerbation of insomnia were randomized to 1 of 3 groups: SHE, SRT, or CBT-I.
- Participants were assessed at baseline, after treatment completion, and at 6-month follow-up using the ISI, sleep diaries, Fatigue Severity Scale, Epworth Sleepiness Scale, Work Productivity and Activity Impairment Questionnaire, and 36-item Medical Outcomes Study Short Form Health Survey.
Continue to: Outcomes
Outcomes
- In both the CBT-I and SRT groups, significant improvements were noted in fatigue, energy, daytime sleepiness, and work function after treatment completion and at 6-month follow-up.
- Improvements were noted in emotional well-being and resiliency to physical and emotional problems in the CBT-I group at 6 months.
- Improvements in overall general health and social functioning, less pain, and fewer hot flashes were reported by postmenopausal women who remitted from insomnia; however, these benefits were not directly related to any specific treatment modality.
Conclusion
- CBT-I and SRT are superior to SHE for improving daytime functioning, and some aspects of life quality and work productivity, in postmenopausal women with insomnia.
- CBT-I may be superior to SRT in producing larger improvements in fatigue, energy level, and daytime sleep propensity.
- CBT-I can improve emotional well-being and resilience to emotional problems in postmenopausal women with insomnia.
7. Peoples AR, Garland SN, Pigeon WR, et al. Cognitive behavioral therapy for insomnia reduces depression in cancer survivors. J Clin Sleep Med. 2019;15(1):129-137.
Depression is common in patients with cancer and is usually associated with comorbid insomnia. Depression has significant effect on treatment compliance, coping with illness, and quality of life. Peoples et al15 examined the effects of CBT-I on depression in cancer survivors.
Study design
- This was a secondary analysis of a multicenter, randomized, placebo-controlled trial that evaluated interventions for cancer survivors with chronic insomnia in which the primary outcome measure was insomnia severity.
- Cancer survivors (n = 67) were randomized to CBT-I plus armodafinil or placebo or to SHE plus armodafinil or placebo.
- The Patient Health Questionnaire-9 (PHQ-9) and ISI were used to measure depression and insomnia at baseline, after 7-weeks of intervention, and at 3 months postintervention.
Continue to: Outcomes
Outcomes
- Immediately after completing the intervention, cancer survivors treated with CBT-I had significantly less depression (38% greater improvement in depression) compared with those who received SHE (control group).
- In the CBT-I group, 23% of cancer survivors achieved a clinically important reduction (5-point reduction on PHQ-9 total score) in depression at postintervention compared with 6% of those in the control group.
- At 3 months after the intervention, only 14% of cancer survivors in CBT-I group reported depression (PHQ-9 score >4), whereas 47% of those in the control group (SHE) reported depression.
Conclusion
- CBT-I improves both depression and insomnia in cancer survivors, and the improvements are sustained at 3 months after completing treatment.
- Improvement in insomnia severity appears to mediate the positive effects of CBT-I on depression.
8. Harb GC, Cook JM, Phelps AJ, et al. Randomized controlled trial of imagery rehearsal for posttraumatic nightmares in combat veterans. J Clin Sleep Med. 2019;15(5):757-767.
The American Academy of Sleep Medicine recommends imagery rehearsal (IR) therapy, which incorporates some components of CBT-I, for the treatment of recurrent posttraumatic stress disorder (PTSD)–related nightmares. In this study, Harb et al16 compared CBT-I plus IR to CBT-I alone for the treatment of nightmares in veterans with combat-related PTSD.
Study design
- This RCT included male and female US veterans (n = 108) deployed to Iraq and Afghanistan with current PTSD and recurrent nightmares related to deployment.
- Participants were randomized to 6 sessions of CBT-I plus IR or CBT-I alone.
- Primary outcome measures included frequency of nightmares and distress associated with nightmares.
Continue to: Outcomes
Outcomes
- A significant improvement in nightmares was noted in both groups (29% of participants showed a clinically-significant reduction in nightmare frequency and 22% of participants achieved remission).
- CBT-I plus IR was not superior to CBT-I only at postintervention and at 6-month follow-up.
Conclusion
- Both IR and CBT-I demonstrated efficacy for decreasing nightmare frequency and distress.
- Combining IR and CBT-I may not provide a synergistic advantage over CBT-I alone for treating PTSD-related nightmares in veterans.
The prevalence of insomnia in the general population is approximately 6% to 10%.1 In addition, an estimated 30% of the general population may have symptoms of insomnia without meeting the diagnostic criteria.2 As a disorder, insomnia is characterized by a persistent difficulty initiating or maintaining sleep, or early morning awakening with inability to return to sleep, that has been present for at least 3 months. Additionally, the sleep difficulties must occur at least 3 nights a week, result in impaired daytime functioning, and cause significant distress.1
Cognitive-behavioral therapy for insomnia (CBT-I) is an effective treatment, supported by several systematic reviews and meta-analyses.3-5 In the short term, CBT-I is as effective as pharmacotherapy.6 However, CBT-I is the preferred treatment for chronic insomnia, according to recommendations in European and American guidelines.7,8
Here we review 8 recent studies that examined CBT-I. These studies are summarized in the Table.9-16
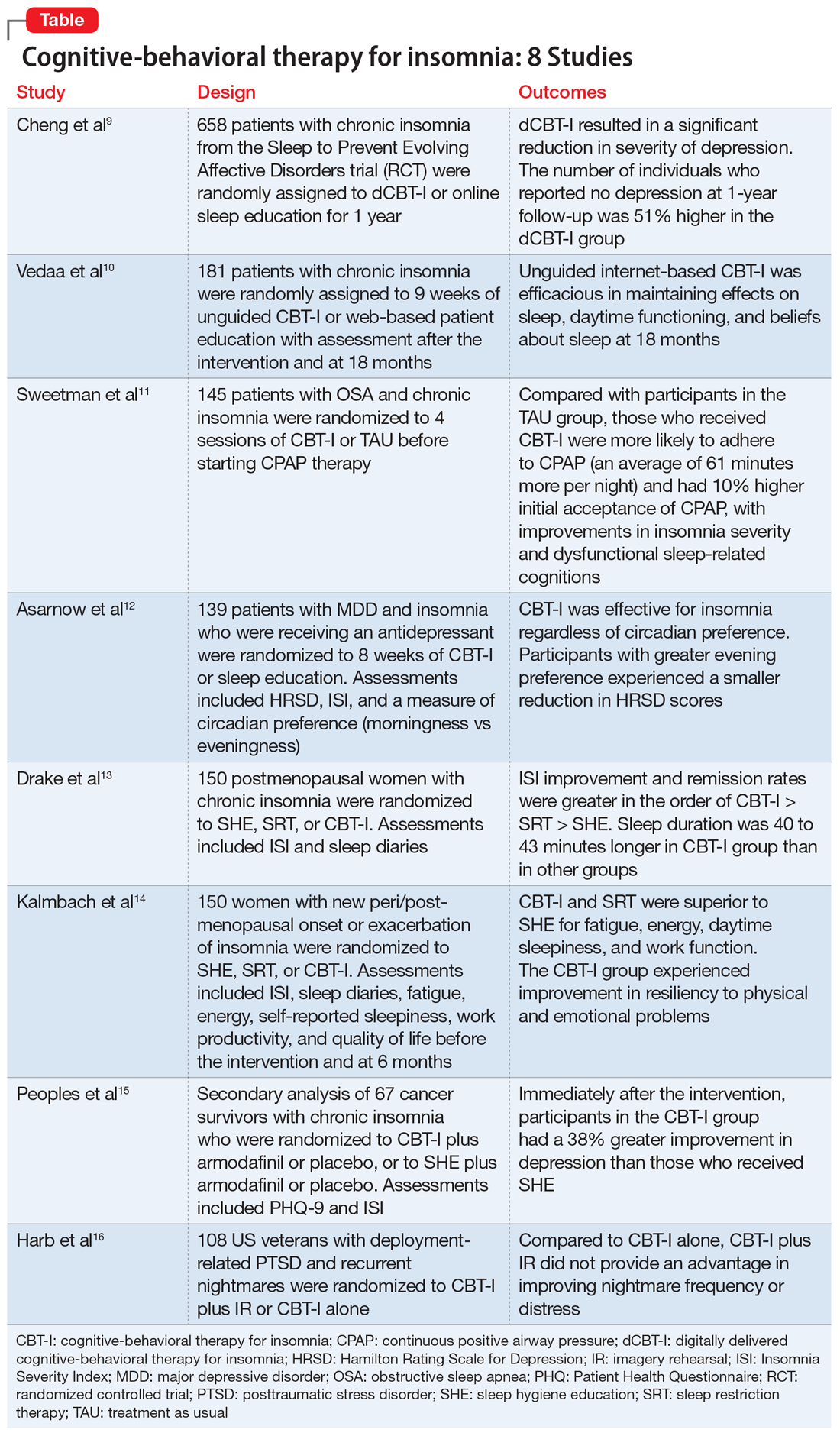
1. Cheng P, Kalmbach DA, Tallent G, et al. Depression prevention via digital cognitive behavioral therapy for insomnia: a randomized controlled trial. Sleep. 2019;42(10):zsz150. doi: 10.1093/sleep/zsz150.
Although CBT-I is a first-line treatment for chronic insomnia, it is underutilized in clinical practice primarily due to limited availability. Because few clinicians are certified in CBT-I, it has become necessary to develop alternative modes of delivery for CBT-I, such as fully automated, internet-delivered approaches to reach more patients with insomnia. Digital CBT-I (dCBT-I) is comparable to in-person CBT-I in improving insomnia symptoms and reducing concurrent depressive symptoms with insomnia. It is unclear if unguided, internet-delivered CBT-I is effective for achieving remission from depression or preventing depression in the long term. Chen et al9 examined the efficacy of dCBT-I in reducing and preventing depression over a 1-year follow-up.
Study design
- Participants from various centers in Southeastern Michigan were recruited between 2016 and 2017. Data was obtained from the Sleep to Prevent Evolving Affective Disorders (SPREAD) trial.
- Participants who met DSM-5 criteria for chronic insomnia disorder were randomized to dCBT-I (n = 358) using the Sleepio digital CBT program via the internet or to online sleep education (n = 300).
- The primary outcome was depression, measured using the Quick Inventory of Depressive Symptomatology-Self Report (QIDS-SR-16) at 1-year follow-up. Depression incidence was also tested against insomnia treatment response.
Outcomes
- The severity of depression was significantly lower at 1-year follow-up in the dCBT-I group compared with the control group.
- The dCBT-I group showed a 51% higher remission rate than the control group at 1-year follow-up.
- The incidence of moderate to severe depression in individuals with minimal to no depression at baseline was halved at 1 year after receiving dCBT-I treatment compared with the control group.
Continue to: Conclusion
Conclusion
- dCBT-I can improve depression and insomnia and has a sustained antidepressant effect.
- dCBT-I is effective for preventing depression. In other words, the risk of developing depression is decreased when dCBT-I is used to treat insomnia in individuals with minimal to no depression at baseline.
2. Vedaa Ø, Hagatun S, Kallestad H, et al. Long-term effects of an unguided online cognitive behavioral therapy for chronic insomnia. J Clin Sleep Med. 2019;15(1):101-110.
dCBT-I is effective for treating insomnia in the short term; however, little is known about the long-term effectiveness of dCBT-I on sleep and daytime symptoms. Vedaa et al10 evaluated the efficacy of dCBT-I at 18 months after the intervention.
Study design
- In this randomized controlled trial (RCT), the efficacy of unguided, internet-delivered CBT-I (n = 95) was compared with web-based patient education (n = 86) for patients with chronic insomnia.
- Participants were assessed at baseline, after a 9-week intervention period, and at 6-month follow-up. Participants in the internet CBT-I group were reassessed at 18 months after the intervention using online questionnaires, including the Insomnia Severity Index (ISI), Bergen Insomnia Scale (BIS), Brief Dysfunctional Beliefs and Attitudes Scale, Hospital Anxiety and Depression Scale, Chalder Fatigue Questionnaire, and sleep diaries.
Outcomes
- At 18 months, significant improvements were noted from baseline ISI and BIS scores and in levels of daytime fatigue, as well as psychological distress and beliefs about sleep.
- Sleep diary variables—including sleep onset latency, time awake during the night (wake time after sleep onset), early morning awakening, total sleep time, and sleep efficiency—showed significant improvement from baseline to 18-month follow-up (at least moderate effect size).
- Improvements were maintained from the completion of the 9-week intervention to follow-up at 18 months.
Continue to: Conclusion
Conclusion
- Fully-automated, internet-based CBT-I is efficacious in maintaining positive effects on sleep and daytime functioning up to 18 months after completing treatment.
3. Sweetman A, Lack L, Catcheside PG, et al. Cognitive and behavioral therapy for insomnia increases the use of continuous positive airway pressure therapy in obstructive sleep apnea participants with comorbid insomnia: a randomized clinical trial. Sleep. 2019;42(12):zsz178. doi: 10.1093/sleep/zsz178.
Comorbid insomnia and sleep apnea (COMISA) can affect a patient’s ability to accept and comply with continuous positive airway pressure (CPAP) therapy. Providing adequate treatment for these patients can be challenging.
Sweetman et al11 evaluated the acceptance and use of CPAP in patients with obstructive sleep apnea and chronic insomnia following initial treatment with CBT-I compared with treatment as usual (TAU).
Study design
- In this RCT, 145 participants with COMISA were randomized to 4 sessions of CBT-I or TAU before starting CPAP therapy until 6 months after randomization.
- Primary outcomes were objective CPAP adherence and objective sleep efficiency at the end of 6 months.
- Secondary outcomes were CPAP acceptance/rejection, changes in sleep parameters, global insomnia severity, and daytime impairments at 6 months.
Continue to: Outcomes
Outcomes
- The CBT-I group had higher initial CPAP acceptance and greater average nightly adherence to CPAP (61 minutes more) than the TAU group.
- Significant improvements were noted in global insomnia severity, nighttime insomnia complaints, and dysfunctional sleep-related cognitions at 6 months in the CBT-I group compared with TAU.
- No differences between the 2 groups were noted in sleep diary parameters or daytime impairments at 6 months.
Conclusions
- Patients with COMISA can benefit from receiving CBT-I before starting CPAP therapy because CBT-I can improve immediate acceptance of CPAP and may help to maintain adherence to CPAP over time.
- Patients with sleep apnea should be evaluated for comorbid insomnia, and CBT-I should be considered before starting CPAP treatment.
4. Asarnow LD, Bei B, Krystal A, et al. Circadian preference as a moderator of depression outcome following cognitive behavioral therapy for insomnia plus antidepressant medications: a report from the TRIAD study. J Clin Sleep Med. 2019;15(4):573-580.
The Treatment of Insomnia and Depression (TRIAD) study reported the effects of combining antidepressants with CBT-I in patients with major depressive disorder (MDD) and insomnia. Asarnow et al12 examined the moderation of circadian preference in the reduction of depression and insomnia symptoms severity during the same trial.
Study design
- In this RCT, 139 participants with MDD and insomnia were treated with an antidepressant (escitalopram, sertraline, or desvenlafaxine) and randomized to 8 weeks of CBT-I or control therapy (sleep education).
- Measurements used were Composite Scale of Morningness for circadian preference (morningness vs eveningness), depression severity with the Hamilton Rating Scale for Depression, and insomnia severity using the ISI.
Continue to: Outcomes
Outcomes
- CBT-I was effective for insomnia regardless of circadian preference.
- A smaller reduction in depression scores was noted in participants with greater evening preference.
- Depression outcomes were better among participants with evening preference if they were assigned to CBT-I vs control therapy.
- The control therapy (sleep education) was particularly ineffective in reducing depression symptoms in participants with evening preference.
Conclusion
- Individuals with MDD and insomnia and an evening preference are at an increased risk for poor response to antidepressants alone.
- Outcomes for both depression and insomnia improve if CBT-I is combined with antidepressants.
- Offering sleep education alone is not sufficient.
5. Drake CL, Kalmbach DA, Arnedt JT, et al. Treating chronic insomnia in postmenopausal women: a randomized clinical trial comparing cognitive-behavioral therapy for insomnia, sleep restriction therapy, and sleep hygiene education. Sleep. 2019;42(2):zsy217. doi: 10.1093/sleep/zsy217.
Postmenopausal women with sleep disturbances experience higher medical and psychiatric comorbidities, and have higher alcohol consumption and stress levels than postmenopausal women with good sleep. Nonpharmacologic insomnia treatments with durable effects are imperative for postmenopausal women because they are safer than pharmacologic approaches. Although CBT-I is the recommended first-line treatment for chronic insomnia, its application in menopause-related insomnia is limited. Drake et al13 evaluated the efficacy of CBT-I in menopause-related insomnia compared with sleep restriction therapy (SRT) and sleep hygiene education (SHE).
Study design
- This RCT was conducted at a health system with 6 hospitals in Michigan.
- Postmenopausal women who met DSM-5 criteria for chronic insomnia disorder (n = 150) were randomized into 1 of 3 groups: SHE, SRT, or CBT-I.
- Primary outcome measures were ISI scores and sleep diaries that documented multiple sleep parameters, including sleep onset latency, wake time after sleep onset, number of awakenings in the middle of the night, time in bed, total sleep time, and sleep efficiency. These were measured at baseline, after completion of treatment, and 6 months after treatment.
Continue to: Outcomes
Outcomes
- Both CBT-I and SRT outperformed SHE on the ISI and for most of the sleep parameters on sleep diaries immediately after treatment completion and at 6 months after treatment.
- Total sleep time was 40 to 43 minutes longer in the CBT-I group than in the SRT and SHE groups at 6-month follow-up.
- Remission rates (sleep onset latency ≤30 minutes, wake time after sleep onset ≤30 minutes, sleep efficiency ≥85%) were significantly higher in CBT-I group (CBT-I > SRT > SHE).
Conclusion
- Sleep hygiene education as a standalone treatment is not useful for treating chronic insomnia.
- Both CBT-I and SRT are efficacious for menopause-related insomnia.
- CBT-I may be a better option than SRT because it produces higher remission rates and better long-term outcomes.
6. Kalmbach DA, Cheng P, Arnedt JT, et al. Improving daytime functioning, work performance, and quality of life in postmenopausal women with insomnia: comparing cognitive behavioral therapy for insomnia, sleep restriction therapy, and sleep hygiene education. J Clin Sleep Med. 2019;15(7):999-1010.
CBT-I has shown efficacy in the treatment of insomnia in postmenopausal women. In this study, Kalmbach et al14 compared 3 nonpharmacologic modalities—CBT-I, SRT, and SHE—for the treatment of menopause-related insomnia and daytime impairment.
Study design
- In this RCT, 150 participants with new peri- and post-menopausal onset or exacerbation of insomnia were randomized to 1 of 3 groups: SHE, SRT, or CBT-I.
- Participants were assessed at baseline, after treatment completion, and at 6-month follow-up using the ISI, sleep diaries, Fatigue Severity Scale, Epworth Sleepiness Scale, Work Productivity and Activity Impairment Questionnaire, and 36-item Medical Outcomes Study Short Form Health Survey.
Continue to: Outcomes
Outcomes
- In both the CBT-I and SRT groups, significant improvements were noted in fatigue, energy, daytime sleepiness, and work function after treatment completion and at 6-month follow-up.
- Improvements were noted in emotional well-being and resiliency to physical and emotional problems in the CBT-I group at 6 months.
- Improvements in overall general health and social functioning, less pain, and fewer hot flashes were reported by postmenopausal women who remitted from insomnia; however, these benefits were not directly related to any specific treatment modality.
Conclusion
- CBT-I and SRT are superior to SHE for improving daytime functioning, and some aspects of life quality and work productivity, in postmenopausal women with insomnia.
- CBT-I may be superior to SRT in producing larger improvements in fatigue, energy level, and daytime sleep propensity.
- CBT-I can improve emotional well-being and resilience to emotional problems in postmenopausal women with insomnia.
7. Peoples AR, Garland SN, Pigeon WR, et al. Cognitive behavioral therapy for insomnia reduces depression in cancer survivors. J Clin Sleep Med. 2019;15(1):129-137.
Depression is common in patients with cancer and is usually associated with comorbid insomnia. Depression has significant effect on treatment compliance, coping with illness, and quality of life. Peoples et al15 examined the effects of CBT-I on depression in cancer survivors.
Study design
- This was a secondary analysis of a multicenter, randomized, placebo-controlled trial that evaluated interventions for cancer survivors with chronic insomnia in which the primary outcome measure was insomnia severity.
- Cancer survivors (n = 67) were randomized to CBT-I plus armodafinil or placebo or to SHE plus armodafinil or placebo.
- The Patient Health Questionnaire-9 (PHQ-9) and ISI were used to measure depression and insomnia at baseline, after 7-weeks of intervention, and at 3 months postintervention.
Continue to: Outcomes
Outcomes
- Immediately after completing the intervention, cancer survivors treated with CBT-I had significantly less depression (38% greater improvement in depression) compared with those who received SHE (control group).
- In the CBT-I group, 23% of cancer survivors achieved a clinically important reduction (5-point reduction on PHQ-9 total score) in depression at postintervention compared with 6% of those in the control group.
- At 3 months after the intervention, only 14% of cancer survivors in CBT-I group reported depression (PHQ-9 score >4), whereas 47% of those in the control group (SHE) reported depression.
Conclusion
- CBT-I improves both depression and insomnia in cancer survivors, and the improvements are sustained at 3 months after completing treatment.
- Improvement in insomnia severity appears to mediate the positive effects of CBT-I on depression.
8. Harb GC, Cook JM, Phelps AJ, et al. Randomized controlled trial of imagery rehearsal for posttraumatic nightmares in combat veterans. J Clin Sleep Med. 2019;15(5):757-767.
The American Academy of Sleep Medicine recommends imagery rehearsal (IR) therapy, which incorporates some components of CBT-I, for the treatment of recurrent posttraumatic stress disorder (PTSD)–related nightmares. In this study, Harb et al16 compared CBT-I plus IR to CBT-I alone for the treatment of nightmares in veterans with combat-related PTSD.
Study design
- This RCT included male and female US veterans (n = 108) deployed to Iraq and Afghanistan with current PTSD and recurrent nightmares related to deployment.
- Participants were randomized to 6 sessions of CBT-I plus IR or CBT-I alone.
- Primary outcome measures included frequency of nightmares and distress associated with nightmares.
Continue to: Outcomes
Outcomes
- A significant improvement in nightmares was noted in both groups (29% of participants showed a clinically-significant reduction in nightmare frequency and 22% of participants achieved remission).
- CBT-I plus IR was not superior to CBT-I only at postintervention and at 6-month follow-up.
Conclusion
- Both IR and CBT-I demonstrated efficacy for decreasing nightmare frequency and distress.
- Combining IR and CBT-I may not provide a synergistic advantage over CBT-I alone for treating PTSD-related nightmares in veterans.
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
2. Morin CM, LeBlanc M, Daley M, et al. Epidemiology of insomnia: prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Med. 2006;7(2):123-130.
3. Trauer JM, Qian MY, Doyle JS, et al. Cognitive behavioral therapy for chronic insomnia: a systematic review and meta-analysis. Ann Intern Med. 2015;163(3):191-204.
4. Wu JQ, Appleman ER, Salazar RD, et al. Cognitive behavioral therapy for insomnia comorbid with psychiatric and medical conditions: a meta-analysis. JAMA Intern Med. 2015;175(9):1461-1472.
5. van Straten A, van der Zweerde T, Kleiboer A, et al. Cognitive and behavioral therapies in the treatment of insomnia: a meta-analysis. Sleep Med Rev. 2018;38:3-16.
6. Smith MT, Perlis ML, Park A, et al. Comparative meta-analysis of pharmacotherapy and behavior therapy for persistent insomnia. Am J Psychiatry. 2002;159(1):5-11.
7. Qaseem A, Kansagara D, Forciea MA, et al. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016;165(2):125-133.
8. Riemann D, Baglioni C, Bassetti C, et al. European guideline for the diagnosis and treatment of insomnia. J Sleep Res. 2017;26(6):675-700.
9. Cheng P, Kalmbach DA, Tallent G, et al. Depression prevention via digital cognitive behavioral therapy for insomnia: a randomized controlled trial. Sleep. 2019;42(10):zsz150. doi: 10.1093/sleep/zsz150.
10. Vedaa Ø, Hagatun S, Kallestad H, et al. Long-term effects of an unguided online cognitive behavioral therapy for chronic insomnia. J Clin Sleep Med. 2019;15(1):101-110.
11. Sweetman A, Lack L, Catcheside PG, et al. Cognitive and behavioral therapy for insomnia increases the use of continuous positive airway pressure therapy in obstructive sleep apnea participants with comorbid insomnia: a randomized clinical trial. Sleep. 2019;42(12):zsz178. doi: 10.1093/sleep/zsz178.
12. Asarnow LD, Bei B, Krystal A, et al. Circadian preference as a moderator of depression outcome following cognitive behavioral therapy for insomnia plus antidepressant medications: a report from the TRIAD study. J Clin Sleep Med. 2019;15(4):573-580.
13. Drake CL, Kalmbach DA, Arnedt JT, et al. Treating chronic insomnia in postmenopausal women: a randomized clinical trial comparing cognitive-behavioral therapy for insomnia, sleep restriction therapy, and sleep hygiene education. Sleep. 2019;42(2):zsy217. doi: 10.1093/sleep/zsy217.
14. Kalmbach DA, Cheng P, Arnedt JT, et al. Improving daytime functioning, work performance, and quality of life in postmenopausal women with insomnia: comparing cognitive behavioral therapy for insomnia, sleep restriction therapy, and sleep hygiene education. J Clin Sleep Med. 2019;15(7):999-1010.
15. Peoples AR, Garland SN, Pigeon WR, et al. Cognitive behavioral therapy for insomnia reduces depression in cancer survivors. J Clin Sleep Med. 2019;15(1):129-137.
16. Harb GC, Cook JM, Phelps AJ, et al. Randomized controlled trial of imagery rehearsal for posttraumatic nightmares in combat veterans. J Clin Sleep Med. 2019;15(5):757-767.
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
2. Morin CM, LeBlanc M, Daley M, et al. Epidemiology of insomnia: prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Med. 2006;7(2):123-130.
3. Trauer JM, Qian MY, Doyle JS, et al. Cognitive behavioral therapy for chronic insomnia: a systematic review and meta-analysis. Ann Intern Med. 2015;163(3):191-204.
4. Wu JQ, Appleman ER, Salazar RD, et al. Cognitive behavioral therapy for insomnia comorbid with psychiatric and medical conditions: a meta-analysis. JAMA Intern Med. 2015;175(9):1461-1472.
5. van Straten A, van der Zweerde T, Kleiboer A, et al. Cognitive and behavioral therapies in the treatment of insomnia: a meta-analysis. Sleep Med Rev. 2018;38:3-16.
6. Smith MT, Perlis ML, Park A, et al. Comparative meta-analysis of pharmacotherapy and behavior therapy for persistent insomnia. Am J Psychiatry. 2002;159(1):5-11.
7. Qaseem A, Kansagara D, Forciea MA, et al. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016;165(2):125-133.
8. Riemann D, Baglioni C, Bassetti C, et al. European guideline for the diagnosis and treatment of insomnia. J Sleep Res. 2017;26(6):675-700.
9. Cheng P, Kalmbach DA, Tallent G, et al. Depression prevention via digital cognitive behavioral therapy for insomnia: a randomized controlled trial. Sleep. 2019;42(10):zsz150. doi: 10.1093/sleep/zsz150.
10. Vedaa Ø, Hagatun S, Kallestad H, et al. Long-term effects of an unguided online cognitive behavioral therapy for chronic insomnia. J Clin Sleep Med. 2019;15(1):101-110.
11. Sweetman A, Lack L, Catcheside PG, et al. Cognitive and behavioral therapy for insomnia increases the use of continuous positive airway pressure therapy in obstructive sleep apnea participants with comorbid insomnia: a randomized clinical trial. Sleep. 2019;42(12):zsz178. doi: 10.1093/sleep/zsz178.
12. Asarnow LD, Bei B, Krystal A, et al. Circadian preference as a moderator of depression outcome following cognitive behavioral therapy for insomnia plus antidepressant medications: a report from the TRIAD study. J Clin Sleep Med. 2019;15(4):573-580.
13. Drake CL, Kalmbach DA, Arnedt JT, et al. Treating chronic insomnia in postmenopausal women: a randomized clinical trial comparing cognitive-behavioral therapy for insomnia, sleep restriction therapy, and sleep hygiene education. Sleep. 2019;42(2):zsy217. doi: 10.1093/sleep/zsy217.
14. Kalmbach DA, Cheng P, Arnedt JT, et al. Improving daytime functioning, work performance, and quality of life in postmenopausal women with insomnia: comparing cognitive behavioral therapy for insomnia, sleep restriction therapy, and sleep hygiene education. J Clin Sleep Med. 2019;15(7):999-1010.
15. Peoples AR, Garland SN, Pigeon WR, et al. Cognitive behavioral therapy for insomnia reduces depression in cancer survivors. J Clin Sleep Med. 2019;15(1):129-137.
16. Harb GC, Cook JM, Phelps AJ, et al. Randomized controlled trial of imagery rehearsal for posttraumatic nightmares in combat veterans. J Clin Sleep Med. 2019;15(5):757-767.
Off-label prescribing: How to limit your liability
The FDA defines “off-label” prescribing as prescribing an FDA-approved medication for an unapproved use, such as for an unapproved clinical indication, for a higher-than-approved dose, or for a patient who is not part of the FDA-approved population (eg, children or geriatric patients).1 Off-label prescribing is common in psychiatry; approximately 13% of psychiatry patients are prescribed off-label psychotropic medications.2 The American Psychiatric Association strongly supports “the autonomous clinical decision-making authority of a physician” and “a physician’s lawful use of an FDA-approved drug product or medical device for an off-label indication when such use is based upon sound scientific evidence in conjunction with sound medical judgment.”3 Because many psychiatric diagnoses have no FDA-approved medications, off-label prescribing often may be a psychiatrist’s only pharmacologic option.
Unfortunately, off-label prescribing can increase a psychiatrist’s risk for liability when treatment falls short of patients’ expectations, or when patients allege that they were injured by the use of an off-label medication. Off-label prescribing does not automatically lead to losing a malpractice suit because the FDA states that physicians can prescribe approved medications for any scientifically supported use, including off-label.1 Medical malpractice lawsuits alleging negligence in prescribing practices, such as off-label prescribing, typically include allegations against the psychiatrist for failure to4:
- adequately assess the patient
- consult the patient’s medical records
- obtain informed consent from the patient
- appropriately prescribe a medication for the clinical indication, dosage, patient’s age, etc.
- monitor for adverse effects and therapeutic effectiveness.
Steps to minimize your risk
When prescribing a medication off-label, the following approaches can help reduce your liability risk:
Conduct a comprehensive clinical assessment. This should include requesting and reviewing your patient’s medical records.
Explain your motivation. Explain to your patient how prescribing an off-label medication can directly benefit him/her. Make it clear that you are not conducting experimental research by prescribing off-label because some patients might perceive this as a covert form of research.
Know the medications you prescribe. Although this sounds obvious, psychiatrists should thoroughly understand how each medication they prescribe is likely to clinically affect their patient. This information is available from many sources, including the FDA’s medication information sheets and the manufacturer’s medication package inserts. If possible, make sure that your off-label prescribing is supported by reputable, peer-reviewed literature.
Obtain informed consent. Tell your patient that the medication you are recommending is being prescribed off-label. Discuss the medication’s risks, benefits, adverse effects, associated “black-box” warnings, off-label uses, and alternatives to the off-label medication.4 Allow time for the patient to ask questions about these treatments.
Continue to: Document all steps
Document all steps. There is an adage in medicine that “If it’s not written, it wasn’t done.” To help reduce your liability risk when prescribing off-label, be sure to document the following4:
- your clinical assessment
- information you gleaned from the patient’s medical records
- your review of information regarding both therapeutic and adverse effects of the medication you want to prescribe
- your discussion of informed consent, including documentation that the patient is aware that the medication is being prescribed off-label
- your clinical rationale for why the off-label medication is in the patient’s best interest.
Also, document the steps you take to monitor for adverse events and therapeutic effectiveness.4 Overall, the goal of documentation should be to support the adequate continuing care of our patients.
1. US Food and Drug Administration. Understanding unapproved use of approved drugs “off label.” https://www.fda.gov/patients/learn-about-expanded-access-and-other-treatment-options/understanding-unapproved-use-approved-drugs-label. Updated February 5, 2018. Accessed August 6, 2020.
2. Vijay A, Becker JE, Ross JS. Patterns and predictors of off-label prescription of psychiatric drugs. PLoS One. 2018;13(7):e0198363. doi: 10.1371/journal.pone.0198363.
3. McLeer S, Mawhinney J; Council on Healthcare Systems and Financing. Position statement on off-label treatments. American Psychiatric Association. https://www.psychiatry.org/File%20Library/About-APA/Organization-Documents-Policies/Policies/Position-2016-Off-Label-Treatment.pdf. Published July 2016. Accessed August 6, 2020.
4. Funicelli A. What to consider when prescribing off-label. Psychiatric News. 2019;54(14):12.
The FDA defines “off-label” prescribing as prescribing an FDA-approved medication for an unapproved use, such as for an unapproved clinical indication, for a higher-than-approved dose, or for a patient who is not part of the FDA-approved population (eg, children or geriatric patients).1 Off-label prescribing is common in psychiatry; approximately 13% of psychiatry patients are prescribed off-label psychotropic medications.2 The American Psychiatric Association strongly supports “the autonomous clinical decision-making authority of a physician” and “a physician’s lawful use of an FDA-approved drug product or medical device for an off-label indication when such use is based upon sound scientific evidence in conjunction with sound medical judgment.”3 Because many psychiatric diagnoses have no FDA-approved medications, off-label prescribing often may be a psychiatrist’s only pharmacologic option.
Unfortunately, off-label prescribing can increase a psychiatrist’s risk for liability when treatment falls short of patients’ expectations, or when patients allege that they were injured by the use of an off-label medication. Off-label prescribing does not automatically lead to losing a malpractice suit because the FDA states that physicians can prescribe approved medications for any scientifically supported use, including off-label.1 Medical malpractice lawsuits alleging negligence in prescribing practices, such as off-label prescribing, typically include allegations against the psychiatrist for failure to4:
- adequately assess the patient
- consult the patient’s medical records
- obtain informed consent from the patient
- appropriately prescribe a medication for the clinical indication, dosage, patient’s age, etc.
- monitor for adverse effects and therapeutic effectiveness.
Steps to minimize your risk
When prescribing a medication off-label, the following approaches can help reduce your liability risk:
Conduct a comprehensive clinical assessment. This should include requesting and reviewing your patient’s medical records.
Explain your motivation. Explain to your patient how prescribing an off-label medication can directly benefit him/her. Make it clear that you are not conducting experimental research by prescribing off-label because some patients might perceive this as a covert form of research.
Know the medications you prescribe. Although this sounds obvious, psychiatrists should thoroughly understand how each medication they prescribe is likely to clinically affect their patient. This information is available from many sources, including the FDA’s medication information sheets and the manufacturer’s medication package inserts. If possible, make sure that your off-label prescribing is supported by reputable, peer-reviewed literature.
Obtain informed consent. Tell your patient that the medication you are recommending is being prescribed off-label. Discuss the medication’s risks, benefits, adverse effects, associated “black-box” warnings, off-label uses, and alternatives to the off-label medication.4 Allow time for the patient to ask questions about these treatments.
Continue to: Document all steps
Document all steps. There is an adage in medicine that “If it’s not written, it wasn’t done.” To help reduce your liability risk when prescribing off-label, be sure to document the following4:
- your clinical assessment
- information you gleaned from the patient’s medical records
- your review of information regarding both therapeutic and adverse effects of the medication you want to prescribe
- your discussion of informed consent, including documentation that the patient is aware that the medication is being prescribed off-label
- your clinical rationale for why the off-label medication is in the patient’s best interest.
Also, document the steps you take to monitor for adverse events and therapeutic effectiveness.4 Overall, the goal of documentation should be to support the adequate continuing care of our patients.
The FDA defines “off-label” prescribing as prescribing an FDA-approved medication for an unapproved use, such as for an unapproved clinical indication, for a higher-than-approved dose, or for a patient who is not part of the FDA-approved population (eg, children or geriatric patients).1 Off-label prescribing is common in psychiatry; approximately 13% of psychiatry patients are prescribed off-label psychotropic medications.2 The American Psychiatric Association strongly supports “the autonomous clinical decision-making authority of a physician” and “a physician’s lawful use of an FDA-approved drug product or medical device for an off-label indication when such use is based upon sound scientific evidence in conjunction with sound medical judgment.”3 Because many psychiatric diagnoses have no FDA-approved medications, off-label prescribing often may be a psychiatrist’s only pharmacologic option.
Unfortunately, off-label prescribing can increase a psychiatrist’s risk for liability when treatment falls short of patients’ expectations, or when patients allege that they were injured by the use of an off-label medication. Off-label prescribing does not automatically lead to losing a malpractice suit because the FDA states that physicians can prescribe approved medications for any scientifically supported use, including off-label.1 Medical malpractice lawsuits alleging negligence in prescribing practices, such as off-label prescribing, typically include allegations against the psychiatrist for failure to4:
- adequately assess the patient
- consult the patient’s medical records
- obtain informed consent from the patient
- appropriately prescribe a medication for the clinical indication, dosage, patient’s age, etc.
- monitor for adverse effects and therapeutic effectiveness.
Steps to minimize your risk
When prescribing a medication off-label, the following approaches can help reduce your liability risk:
Conduct a comprehensive clinical assessment. This should include requesting and reviewing your patient’s medical records.
Explain your motivation. Explain to your patient how prescribing an off-label medication can directly benefit him/her. Make it clear that you are not conducting experimental research by prescribing off-label because some patients might perceive this as a covert form of research.
Know the medications you prescribe. Although this sounds obvious, psychiatrists should thoroughly understand how each medication they prescribe is likely to clinically affect their patient. This information is available from many sources, including the FDA’s medication information sheets and the manufacturer’s medication package inserts. If possible, make sure that your off-label prescribing is supported by reputable, peer-reviewed literature.
Obtain informed consent. Tell your patient that the medication you are recommending is being prescribed off-label. Discuss the medication’s risks, benefits, adverse effects, associated “black-box” warnings, off-label uses, and alternatives to the off-label medication.4 Allow time for the patient to ask questions about these treatments.
Continue to: Document all steps
Document all steps. There is an adage in medicine that “If it’s not written, it wasn’t done.” To help reduce your liability risk when prescribing off-label, be sure to document the following4:
- your clinical assessment
- information you gleaned from the patient’s medical records
- your review of information regarding both therapeutic and adverse effects of the medication you want to prescribe
- your discussion of informed consent, including documentation that the patient is aware that the medication is being prescribed off-label
- your clinical rationale for why the off-label medication is in the patient’s best interest.
Also, document the steps you take to monitor for adverse events and therapeutic effectiveness.4 Overall, the goal of documentation should be to support the adequate continuing care of our patients.
1. US Food and Drug Administration. Understanding unapproved use of approved drugs “off label.” https://www.fda.gov/patients/learn-about-expanded-access-and-other-treatment-options/understanding-unapproved-use-approved-drugs-label. Updated February 5, 2018. Accessed August 6, 2020.
2. Vijay A, Becker JE, Ross JS. Patterns and predictors of off-label prescription of psychiatric drugs. PLoS One. 2018;13(7):e0198363. doi: 10.1371/journal.pone.0198363.
3. McLeer S, Mawhinney J; Council on Healthcare Systems and Financing. Position statement on off-label treatments. American Psychiatric Association. https://www.psychiatry.org/File%20Library/About-APA/Organization-Documents-Policies/Policies/Position-2016-Off-Label-Treatment.pdf. Published July 2016. Accessed August 6, 2020.
4. Funicelli A. What to consider when prescribing off-label. Psychiatric News. 2019;54(14):12.
1. US Food and Drug Administration. Understanding unapproved use of approved drugs “off label.” https://www.fda.gov/patients/learn-about-expanded-access-and-other-treatment-options/understanding-unapproved-use-approved-drugs-label. Updated February 5, 2018. Accessed August 6, 2020.
2. Vijay A, Becker JE, Ross JS. Patterns and predictors of off-label prescription of psychiatric drugs. PLoS One. 2018;13(7):e0198363. doi: 10.1371/journal.pone.0198363.
3. McLeer S, Mawhinney J; Council on Healthcare Systems and Financing. Position statement on off-label treatments. American Psychiatric Association. https://www.psychiatry.org/File%20Library/About-APA/Organization-Documents-Policies/Policies/Position-2016-Off-Label-Treatment.pdf. Published July 2016. Accessed August 6, 2020.
4. Funicelli A. What to consider when prescribing off-label. Psychiatric News. 2019;54(14):12.