User login
The Hospitalist only
SHM Forms Hospitalist IT Task Force
Do you speak geek? If you haven’t already, you may hear that phrase or something similar in the halls of your hospital or institution.
As hospitals face the challenge of implementing computerized physician order entry (CPOE) and electronic medical records (EMRs), many hospitals are turning to hospitalists to help guide them through the complex and daunting task of translating a critical initiative into an information technology (IT) success story. More and more, hospitalists are asked to play any number of roles in leading their institution to the IT Promised Land. Are you one of these people? Do you want to be? Not sure how to get started or where to turn for help? Look no further—SHM is here to help.
Late last year, SHM convened a small group of hospitalists with extensive IT experience. The meeting led to the formation of SHM’s new Hospitalist IT Task Force and a list of initiatives to help those of you interested in bridging the gap between the hospital and IT. In addition to this laundry list of ideas, the group described a set of roles a hospitalist can play in facilitating a CPOE or other IT project. Hospitalists involved in IT can act as:
Communicators: There are gaps in knowledge and understanding between physicians and IT staff. Medical staff members might not understand the IT vocabulary/processes, while the IT staff might not be familiar with medical vocabulary/processes. Hospitalists must translate the clinical needs of the hospital for the IT community when implementing programs like CPOE.
Champions: Every project needs a champion to have a chance at success. Knowledgeable hospitalists can communicate the value of IT initiatives to the hospital and drive these projects to a positive conclusion. Hospitalists understand the implications of transitioning from a paper to electronic environment and can engage the right people and resources to support these initiatives.
Experienced leaders (power users): There is a growing community of hospitalists who have implemented CPOE/EMR and other IT initiatives. They have been in the trenches. They know what works and what doesn’t, and they understand the pros and cons of different solutions. They are power users of medical IT and possess significant knowledge that can help others.
Reviewers: Each hospital has to select a technical solution that fits its administrative and clinical needs. The hospital will evaluate multiple options and selecting the appropriate solution. Hospitalists who play the roles of communicator, champion, and/or experienced leader can be valuable when solutions are being reviewed and evaluated.
Have you served in one of these roles? Would you like to get more involved in IT? SHM’s Hospitalist IT Task Force is exploring different ways to assist our members. Potential initiatives include:
- Developing an online resource of articles, reference material, and Web sites that provide guidance and support related to IT in a hospital setting;
- Holding an open forum at Hospital Medicine 2008, SHM’s Annual Meeting from April 3-5 in San Diego, to discuss the roles, challenges, successes, and pitfalls encountered in IT initiatives; and
- Creating other educational vehicles for hospitalists working with IT in their hospital.
The success of an IT project depends on having the right people at the table. They are committed to success, they make open and honest contributions, and they work to align the needs of the organization with the capabilities of the technical solution by taking users’ needs into full consideration.
SHM’s Hospitalist IT Task Force is working to develop the right solutions to help you improve your hospital or project. If you are one of our hospitalist IT users and have an opinion, idea, or experience you would like to share, we would like to hear from you. Contact the Hospitalist IT Task Force at [email protected]. TH
Do you speak geek? If you haven’t already, you may hear that phrase or something similar in the halls of your hospital or institution.
As hospitals face the challenge of implementing computerized physician order entry (CPOE) and electronic medical records (EMRs), many hospitals are turning to hospitalists to help guide them through the complex and daunting task of translating a critical initiative into an information technology (IT) success story. More and more, hospitalists are asked to play any number of roles in leading their institution to the IT Promised Land. Are you one of these people? Do you want to be? Not sure how to get started or where to turn for help? Look no further—SHM is here to help.
Late last year, SHM convened a small group of hospitalists with extensive IT experience. The meeting led to the formation of SHM’s new Hospitalist IT Task Force and a list of initiatives to help those of you interested in bridging the gap between the hospital and IT. In addition to this laundry list of ideas, the group described a set of roles a hospitalist can play in facilitating a CPOE or other IT project. Hospitalists involved in IT can act as:
Communicators: There are gaps in knowledge and understanding between physicians and IT staff. Medical staff members might not understand the IT vocabulary/processes, while the IT staff might not be familiar with medical vocabulary/processes. Hospitalists must translate the clinical needs of the hospital for the IT community when implementing programs like CPOE.
Champions: Every project needs a champion to have a chance at success. Knowledgeable hospitalists can communicate the value of IT initiatives to the hospital and drive these projects to a positive conclusion. Hospitalists understand the implications of transitioning from a paper to electronic environment and can engage the right people and resources to support these initiatives.
Experienced leaders (power users): There is a growing community of hospitalists who have implemented CPOE/EMR and other IT initiatives. They have been in the trenches. They know what works and what doesn’t, and they understand the pros and cons of different solutions. They are power users of medical IT and possess significant knowledge that can help others.
Reviewers: Each hospital has to select a technical solution that fits its administrative and clinical needs. The hospital will evaluate multiple options and selecting the appropriate solution. Hospitalists who play the roles of communicator, champion, and/or experienced leader can be valuable when solutions are being reviewed and evaluated.
Have you served in one of these roles? Would you like to get more involved in IT? SHM’s Hospitalist IT Task Force is exploring different ways to assist our members. Potential initiatives include:
- Developing an online resource of articles, reference material, and Web sites that provide guidance and support related to IT in a hospital setting;
- Holding an open forum at Hospital Medicine 2008, SHM’s Annual Meeting from April 3-5 in San Diego, to discuss the roles, challenges, successes, and pitfalls encountered in IT initiatives; and
- Creating other educational vehicles for hospitalists working with IT in their hospital.
The success of an IT project depends on having the right people at the table. They are committed to success, they make open and honest contributions, and they work to align the needs of the organization with the capabilities of the technical solution by taking users’ needs into full consideration.
SHM’s Hospitalist IT Task Force is working to develop the right solutions to help you improve your hospital or project. If you are one of our hospitalist IT users and have an opinion, idea, or experience you would like to share, we would like to hear from you. Contact the Hospitalist IT Task Force at [email protected]. TH
Do you speak geek? If you haven’t already, you may hear that phrase or something similar in the halls of your hospital or institution.
As hospitals face the challenge of implementing computerized physician order entry (CPOE) and electronic medical records (EMRs), many hospitals are turning to hospitalists to help guide them through the complex and daunting task of translating a critical initiative into an information technology (IT) success story. More and more, hospitalists are asked to play any number of roles in leading their institution to the IT Promised Land. Are you one of these people? Do you want to be? Not sure how to get started or where to turn for help? Look no further—SHM is here to help.
Late last year, SHM convened a small group of hospitalists with extensive IT experience. The meeting led to the formation of SHM’s new Hospitalist IT Task Force and a list of initiatives to help those of you interested in bridging the gap between the hospital and IT. In addition to this laundry list of ideas, the group described a set of roles a hospitalist can play in facilitating a CPOE or other IT project. Hospitalists involved in IT can act as:
Communicators: There are gaps in knowledge and understanding between physicians and IT staff. Medical staff members might not understand the IT vocabulary/processes, while the IT staff might not be familiar with medical vocabulary/processes. Hospitalists must translate the clinical needs of the hospital for the IT community when implementing programs like CPOE.
Champions: Every project needs a champion to have a chance at success. Knowledgeable hospitalists can communicate the value of IT initiatives to the hospital and drive these projects to a positive conclusion. Hospitalists understand the implications of transitioning from a paper to electronic environment and can engage the right people and resources to support these initiatives.
Experienced leaders (power users): There is a growing community of hospitalists who have implemented CPOE/EMR and other IT initiatives. They have been in the trenches. They know what works and what doesn’t, and they understand the pros and cons of different solutions. They are power users of medical IT and possess significant knowledge that can help others.
Reviewers: Each hospital has to select a technical solution that fits its administrative and clinical needs. The hospital will evaluate multiple options and selecting the appropriate solution. Hospitalists who play the roles of communicator, champion, and/or experienced leader can be valuable when solutions are being reviewed and evaluated.
Have you served in one of these roles? Would you like to get more involved in IT? SHM’s Hospitalist IT Task Force is exploring different ways to assist our members. Potential initiatives include:
- Developing an online resource of articles, reference material, and Web sites that provide guidance and support related to IT in a hospital setting;
- Holding an open forum at Hospital Medicine 2008, SHM’s Annual Meeting from April 3-5 in San Diego, to discuss the roles, challenges, successes, and pitfalls encountered in IT initiatives; and
- Creating other educational vehicles for hospitalists working with IT in their hospital.
The success of an IT project depends on having the right people at the table. They are committed to success, they make open and honest contributions, and they work to align the needs of the organization with the capabilities of the technical solution by taking users’ needs into full consideration.
SHM’s Hospitalist IT Task Force is working to develop the right solutions to help you improve your hospital or project. If you are one of our hospitalist IT users and have an opinion, idea, or experience you would like to share, we would like to hear from you. Contact the Hospitalist IT Task Force at [email protected]. TH
Inside SHM Quality Summit
In October, SHM embarked on the exciting endeavor of gathering leaders in education, research, standards, and clinical practice to begin developing ideas for furthering quality improvement initiatives in hospital medicine.
At the one-day Quality Summit in Chicago, participants were asked to consider and discuss their “big-picture” vision for improving quality care in hospitals. The meeting was led by Janet Nagamine, MD, chair of SHM’s Hospital Quality Patient Safety (HQPS) Committee, and Larry Wellikson, MD, the CEO of SHM.
As Dr. Nagamine opened the meeting, she expressed both the great excitement and angst that comes with undertaking such a huge initiative as creating a quality road map for SHM. Explaining that the day was to be devoted to determining vision, Dr. Wellikson further clarified that the goal of the summit was to set priorities and create strategies for moving forward.
Russell Holman, MD, SHM’s president, expressed appreciation for the wealth of experience and background of the attendees and encouraged participants to think as visionaries. Dr. Holman remarked on SHM’s devotion to a higher calling centered on looking at patient care as being inclusive and collaborative. The group was urged to put forth their best thinking to advance the quality and safety agenda.
Pre-work for the summit focused on bringing attendees up to speed with all SHM’s initiatives related to quality improvement. To understand the scope and breadth of work undertaken by SHM, each participant was asked to thoroughly examine the most updated Resource Rooms (Web-based, interactive learning tools) and to look at a comprehensive list of organizations with whom SHM is involved. Armed with a complete picture of what SHM has done, the group was expected to think about plans for progress.
Participants worked in large and small groups to generate themes to pursue in quality endeavors.
The group agreed on the benefit of expanding SHM’s resources in education and implementation.
A generally supported theme was that training in quality improvement should be offered in medical schools and residency and fellowship programs. Additionally, those who have experience with quality improvement can benefit from additional support with implementing projects. Discussions focused on SHM’s success with educational opportunities by creating multidisciplinary teams and focusing on putting principles into practice (e.g., the Venous Thromboembolism Prevention Collaborative).
Additionally, small groups identified the potential for SHM to further the national hospital quality and patient-safety agenda by expanding research efforts into national networks. SHM’s relationships with national organizations and leaders in the quality arena were a focal point of discussion. One small group was devoted entirely to developing an innovative care collaborative comprising national leaders in nursing, pharmacy, quality, and patient care.
One noteworthy conclusion attendees could draw at the end of the summit was that SHM functions with great excitement and initiative. From leadership to members, volunteers, and staff, SHM is not an organization that rests on accomplishments but one that uses progress as a launch pad for continued improvement.
The people making decisions about quality endeavors to pursue have front-line experience and are in touch with what will improve patient care.
It was evident that while no one person or organization has all the answers, SHM is willing to do what it takes in terms of trying new things and forging new relationships.
Hospital Medicine Fast Facts 10 Key Metrics for Monitoring Hospitalist Performance
- Volume data: Measurements indicating “volume of services” provided by a hospitalist group or by individual hospitalists. Volume data, in general terms, are counts of services performed by hospitalists.
- Case mix: A tool used to characterize the clinical complexity of the patients treated by the hospital medicine group (and comparison groups). The goal of case mix is to allow “apples to apples” comparisons.
- Patient satisfaction: A survey-based measure often considered an element of quality outcomes. Surveys, often designed and administered by vendors, are typically designed to measure a patient’s perception of his or her overall hospital experience.
- Length of stay: The number of days of inpatient care utilized by a patient or a group of patients.
- Hospital cost: Measures the money expended by a hospital to care for its patients, most often expressed as cost per unit of service (e.g., cost per patient day or cost per discharge).
- Productivity measures: Objective qualifications of physician productivity (e.g., encounters, Relative Value Units).
- Provider satisfaction: The most common metric addresses referring-physician satisfaction and uses a survey to measure perceptions of their overall experience with the hospital medicine program (e.g., the care of their patient and interactions with the hospitalists). Other providers could be monitored for satisfaction, including specialists and nurses.
- Mortality: A measure of the number of patient deaths over a defined time period. Typically, the observed mortality metric is compared with expected mortality.
- Readmission rate: Describes how often patients admitted to the hospital by a physician or practice are admitted again, within a defined period following discharge.
- Joint Commission Core Measures: These are evidence-based, standardized “core” measures to track the performance of hospitals in providing quality healthcare. Four diagnoses are included: acute myocardial infarction, congestive heart failure, community-acquired pneumonia, and pregnancy and related conditions.
To download “Measuring Hospitalist Performance: Metrics, Reports, and Dashboards.” Visit the “SHM Initiatives” section at www.hospitalmedicine.org.
In October, SHM embarked on the exciting endeavor of gathering leaders in education, research, standards, and clinical practice to begin developing ideas for furthering quality improvement initiatives in hospital medicine.
At the one-day Quality Summit in Chicago, participants were asked to consider and discuss their “big-picture” vision for improving quality care in hospitals. The meeting was led by Janet Nagamine, MD, chair of SHM’s Hospital Quality Patient Safety (HQPS) Committee, and Larry Wellikson, MD, the CEO of SHM.
As Dr. Nagamine opened the meeting, she expressed both the great excitement and angst that comes with undertaking such a huge initiative as creating a quality road map for SHM. Explaining that the day was to be devoted to determining vision, Dr. Wellikson further clarified that the goal of the summit was to set priorities and create strategies for moving forward.
Russell Holman, MD, SHM’s president, expressed appreciation for the wealth of experience and background of the attendees and encouraged participants to think as visionaries. Dr. Holman remarked on SHM’s devotion to a higher calling centered on looking at patient care as being inclusive and collaborative. The group was urged to put forth their best thinking to advance the quality and safety agenda.
Pre-work for the summit focused on bringing attendees up to speed with all SHM’s initiatives related to quality improvement. To understand the scope and breadth of work undertaken by SHM, each participant was asked to thoroughly examine the most updated Resource Rooms (Web-based, interactive learning tools) and to look at a comprehensive list of organizations with whom SHM is involved. Armed with a complete picture of what SHM has done, the group was expected to think about plans for progress.
Participants worked in large and small groups to generate themes to pursue in quality endeavors.
The group agreed on the benefit of expanding SHM’s resources in education and implementation.
A generally supported theme was that training in quality improvement should be offered in medical schools and residency and fellowship programs. Additionally, those who have experience with quality improvement can benefit from additional support with implementing projects. Discussions focused on SHM’s success with educational opportunities by creating multidisciplinary teams and focusing on putting principles into practice (e.g., the Venous Thromboembolism Prevention Collaborative).
Additionally, small groups identified the potential for SHM to further the national hospital quality and patient-safety agenda by expanding research efforts into national networks. SHM’s relationships with national organizations and leaders in the quality arena were a focal point of discussion. One small group was devoted entirely to developing an innovative care collaborative comprising national leaders in nursing, pharmacy, quality, and patient care.
One noteworthy conclusion attendees could draw at the end of the summit was that SHM functions with great excitement and initiative. From leadership to members, volunteers, and staff, SHM is not an organization that rests on accomplishments but one that uses progress as a launch pad for continued improvement.
The people making decisions about quality endeavors to pursue have front-line experience and are in touch with what will improve patient care.
It was evident that while no one person or organization has all the answers, SHM is willing to do what it takes in terms of trying new things and forging new relationships.
Hospital Medicine Fast Facts 10 Key Metrics for Monitoring Hospitalist Performance
- Volume data: Measurements indicating “volume of services” provided by a hospitalist group or by individual hospitalists. Volume data, in general terms, are counts of services performed by hospitalists.
- Case mix: A tool used to characterize the clinical complexity of the patients treated by the hospital medicine group (and comparison groups). The goal of case mix is to allow “apples to apples” comparisons.
- Patient satisfaction: A survey-based measure often considered an element of quality outcomes. Surveys, often designed and administered by vendors, are typically designed to measure a patient’s perception of his or her overall hospital experience.
- Length of stay: The number of days of inpatient care utilized by a patient or a group of patients.
- Hospital cost: Measures the money expended by a hospital to care for its patients, most often expressed as cost per unit of service (e.g., cost per patient day or cost per discharge).
- Productivity measures: Objective qualifications of physician productivity (e.g., encounters, Relative Value Units).
- Provider satisfaction: The most common metric addresses referring-physician satisfaction and uses a survey to measure perceptions of their overall experience with the hospital medicine program (e.g., the care of their patient and interactions with the hospitalists). Other providers could be monitored for satisfaction, including specialists and nurses.
- Mortality: A measure of the number of patient deaths over a defined time period. Typically, the observed mortality metric is compared with expected mortality.
- Readmission rate: Describes how often patients admitted to the hospital by a physician or practice are admitted again, within a defined period following discharge.
- Joint Commission Core Measures: These are evidence-based, standardized “core” measures to track the performance of hospitals in providing quality healthcare. Four diagnoses are included: acute myocardial infarction, congestive heart failure, community-acquired pneumonia, and pregnancy and related conditions.
To download “Measuring Hospitalist Performance: Metrics, Reports, and Dashboards.” Visit the “SHM Initiatives” section at www.hospitalmedicine.org.
In October, SHM embarked on the exciting endeavor of gathering leaders in education, research, standards, and clinical practice to begin developing ideas for furthering quality improvement initiatives in hospital medicine.
At the one-day Quality Summit in Chicago, participants were asked to consider and discuss their “big-picture” vision for improving quality care in hospitals. The meeting was led by Janet Nagamine, MD, chair of SHM’s Hospital Quality Patient Safety (HQPS) Committee, and Larry Wellikson, MD, the CEO of SHM.
As Dr. Nagamine opened the meeting, she expressed both the great excitement and angst that comes with undertaking such a huge initiative as creating a quality road map for SHM. Explaining that the day was to be devoted to determining vision, Dr. Wellikson further clarified that the goal of the summit was to set priorities and create strategies for moving forward.
Russell Holman, MD, SHM’s president, expressed appreciation for the wealth of experience and background of the attendees and encouraged participants to think as visionaries. Dr. Holman remarked on SHM’s devotion to a higher calling centered on looking at patient care as being inclusive and collaborative. The group was urged to put forth their best thinking to advance the quality and safety agenda.
Pre-work for the summit focused on bringing attendees up to speed with all SHM’s initiatives related to quality improvement. To understand the scope and breadth of work undertaken by SHM, each participant was asked to thoroughly examine the most updated Resource Rooms (Web-based, interactive learning tools) and to look at a comprehensive list of organizations with whom SHM is involved. Armed with a complete picture of what SHM has done, the group was expected to think about plans for progress.
Participants worked in large and small groups to generate themes to pursue in quality endeavors.
The group agreed on the benefit of expanding SHM’s resources in education and implementation.
A generally supported theme was that training in quality improvement should be offered in medical schools and residency and fellowship programs. Additionally, those who have experience with quality improvement can benefit from additional support with implementing projects. Discussions focused on SHM’s success with educational opportunities by creating multidisciplinary teams and focusing on putting principles into practice (e.g., the Venous Thromboembolism Prevention Collaborative).
Additionally, small groups identified the potential for SHM to further the national hospital quality and patient-safety agenda by expanding research efforts into national networks. SHM’s relationships with national organizations and leaders in the quality arena were a focal point of discussion. One small group was devoted entirely to developing an innovative care collaborative comprising national leaders in nursing, pharmacy, quality, and patient care.
One noteworthy conclusion attendees could draw at the end of the summit was that SHM functions with great excitement and initiative. From leadership to members, volunteers, and staff, SHM is not an organization that rests on accomplishments but one that uses progress as a launch pad for continued improvement.
The people making decisions about quality endeavors to pursue have front-line experience and are in touch with what will improve patient care.
It was evident that while no one person or organization has all the answers, SHM is willing to do what it takes in terms of trying new things and forging new relationships.
Hospital Medicine Fast Facts 10 Key Metrics for Monitoring Hospitalist Performance
- Volume data: Measurements indicating “volume of services” provided by a hospitalist group or by individual hospitalists. Volume data, in general terms, are counts of services performed by hospitalists.
- Case mix: A tool used to characterize the clinical complexity of the patients treated by the hospital medicine group (and comparison groups). The goal of case mix is to allow “apples to apples” comparisons.
- Patient satisfaction: A survey-based measure often considered an element of quality outcomes. Surveys, often designed and administered by vendors, are typically designed to measure a patient’s perception of his or her overall hospital experience.
- Length of stay: The number of days of inpatient care utilized by a patient or a group of patients.
- Hospital cost: Measures the money expended by a hospital to care for its patients, most often expressed as cost per unit of service (e.g., cost per patient day or cost per discharge).
- Productivity measures: Objective qualifications of physician productivity (e.g., encounters, Relative Value Units).
- Provider satisfaction: The most common metric addresses referring-physician satisfaction and uses a survey to measure perceptions of their overall experience with the hospital medicine program (e.g., the care of their patient and interactions with the hospitalists). Other providers could be monitored for satisfaction, including specialists and nurses.
- Mortality: A measure of the number of patient deaths over a defined time period. Typically, the observed mortality metric is compared with expected mortality.
- Readmission rate: Describes how often patients admitted to the hospital by a physician or practice are admitted again, within a defined period following discharge.
- Joint Commission Core Measures: These are evidence-based, standardized “core” measures to track the performance of hospitals in providing quality healthcare. Four diagnoses are included: acute myocardial infarction, congestive heart failure, community-acquired pneumonia, and pregnancy and related conditions.
To download “Measuring Hospitalist Performance: Metrics, Reports, and Dashboards.” Visit the “SHM Initiatives” section at www.hospitalmedicine.org.
What pre-operative cardiac evaluation of patients undergoing intermediate-risk surgery is most appropriate?
Case
The orthopedic service asks you to evaluate a 76-year-old woman with a hip fracture. She has diabetes, hypertension, and hyperlipidemia but no known coronary artery disease (CAD). She says she can carry a bag of groceries up one flight of stairs without chest symptoms.
Her physical exam is significant only for a shortened, internally rotated right hip. Her blood pressure is 160/88 mm/hg, her pulse is 75 beats per minute, and her respiratory rate is 16 breaths a minute with an oxygen saturation of 95% on one liter. Her creatinine is 1.2 mg/dL, and her fasting glucose is 106 mg/dL. An electrocardiogram reveals normal sinus rhythm without evidence of prior myocardial infarction (MI).
Her medications are lisinopril, atorvastatin, aspirin, fluoxetine, and diazepam. She is scheduled for the operating room tomorrow. What is the best strategy to evaluate and minimize her perioperative cardiac risk, and does it include a beta-blocker?
Overview
There are many ways to identify patients at risk for perioperative cardiac complications—but few simple, safe, evidence-based means of mitigating risk.1
Over the past 10 years, the general approach has been that preoperative revascularization is beneficial in a limited number of clinical scenarios. Further, beta-blockers reduce risk in nearly all other high- and intermediate-risk patients. Unfortunately, routine perioperative administration of beta-blockers to intermediate-risk patients is not supported by trial evidence and may expose these patients to increased risk of adverse outcomes—including death and stroke.
Review of the Data
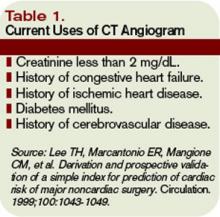
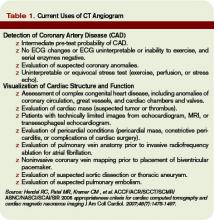
Intermediate-risk patients: Inter-mediate risk patients have recently been redefined as patients with a Revised Cardiac Risk Index (RCRI) score of two or one (See Table 1, p. 27).2,3 Older guidelines suggested noninvasive testing for such patients if they had poor functional capacity (less than four metabolic equivalents [METS]) and were undergoing intermediate-risk surgery, including orthopedic, peritoneal, and thoracic procedures.
Unfortunately, this situation is common, leading to frequent testing and unclear benefit to patients. Omission of a noninvasive evaluation in intermediate-risk orthopedic surgery patients is not associated with an increase in perioperative cardiac events.4 Most events occur in patients who did not meet criteria for preoperative testing.
The 2007 ACC/AHA Guidelines for Perioperative Evaluation and Care address this by recommending noninvasive testing only “if it will change management.” But they offer little guidance in unclear clinical situations, such as the urgent hip-fracture repair needed by our patient.
Preoperative revascularization: While it makes intuitive sense that preoperative revascularization of high-risk patients would decrease their risk of perioperative cardiac complications, evidence countering this idea is nearly definitive. In a study by McFalls, revascularization prior to major vascular surgery did not decrease the risk of perioperative MI or 30-day mortality; however, it delayed the surgical procedure, even in patients with high-risk noninvasive test results.5,6 It is generally accepted that if these high-risk patients can safely undergo major vascular surgery without revascularization, a lower-risk patient such as ours can do so at even lower risk.
In these trials, revascularization occurred in addition to medical management of coronary disease, including aspirin, statin, and—particularly in the study by Poldermans,6 where beta-blockers were started and titrated well before surgery—beta-blocker therapy.
Patients with active cardiac symptoms or signs or uncharacterized anginal symptoms should have elective surgery delayed. However, delay is rarely an option for the hospitalist, who is typically asked to address a patient’s risk shortly before urgent or emergent surgery. These difficult situations require one to weigh the cardiac risk of surgery in a patient who is not optimized versus the risk of delaying surgery to address the more urgent cardiac situation.
Timing of perioperative percutaneous intervention: For patients with coronary artery disease (CAD) or coronary lesions, the interval between percutaneous revascularization (via stent or percutaneous transluminal coronary angioplasty [PTCA]) and surgery affects rates of postoperative cardiac events.7
The recommended interval between stent placement and noncardiac surgery for patients receiving bare-metal and drug-eluting stents is six weeks and one year, respectively.8 Surgery within two weeks of stent placement can carry mortality rates as high as 40%, and this risk appears to decrease out to one year.9,10 If a new stent is in place, any potential benefit appears to be offset by the increased risk of in-stent thrombosis with subsequent MI and possible death. PTCA may not be a safe alternative, although some recommend using PTCA if the patient has unstable cardiac symptoms and needs urgent/emergent surgery.11
Perioperative discontinuation of dual antiplatelet agents (e.g., clopidogrel and aspirin) is common and appears to increase thrombosis risk. This presents a challenge when patients with recent stent placement present for urgent surgery. Minimizing the interruption of dual antiplatelet therapy is the most important intervention a hospitalist can perform. Interruption is associated with increased risk of stent thrombosis, MI, and death. If clopidogrel must be discontinued in the perioperative period, continuation of aspirin is recommended and intravenous glycoprotein 2b/3a inhibitors can be considered.12
Perioperative beta-blocker: Studies on the outcomes of perioperative beta blockade strongly suggested benefits initially. But a number of randomized trials in the past three years have not shown a positive effect.
In a landmark study published in 1996, Mangano showed that initiation of beta blockade just prior to surgery reduced perioperative MI and cardiac death in a mixed surgical population.13 Similar findings were seen with initiation of beta-blocker one month prior to vascular surgery.14 Additionally, higher doses of beta-blocker and lower heart rates in the perioperative period seem to be associated with decreased troponin release.15 Finally, perioperative beta blockade was associated with decreased mortality in high-risk patients (RCRI of three or greater), but higher mortality in lower-risk patients (e.g., RCRI of zero or one).16
More recent data reveal less benefit for perioperative beta blockade. Yang, et al., suggested that initiation of beta-blockers just prior to surgery did not decrease postoperative cardiac complications in vascular surgery patients.17 Similar results were found in a cohort of diabetic patients undergoing major surgery.18 A subsequent meta-analysis concluded that, in the aggregate, perioperative beta blockade was neither beneficial nor harmful.19
Further data have shown increased mortality with perioperative beta blockade in low-risk patients. Most recently, an abstract from the largest randomized controlled trial to date, the POISE study, suggested that preoperative beta blockade decreased MI and cardiac death, but increased the risk of stroke and produced higher overall mortality.20
It is challenging to reconcile this newer evidence with the previous data. While it seems intuitive that blunting the catecholamine response would minimize cardiac workload and therefore decrease perioperative infarcts, surgical patients are also at risk for poor pain control, sepsis, hypovolemia, and venous thromboembolism. Beta blockade can obscure their clinical manifestations, delaying diagnosis or complicating therapy. Inconsistencies among studies and published guidelines make them difficult to apply broadly, particularly with the intermediate-risk patient. Finally, perioperative beta blockade is poorly defined in terms of timing of initiation, target heart rate, and duration of postoperative use.
Until more definitive trial data are published, it seems most prudent to continue beta-blockers in patients already using them. Start them as far in advance of surgery as possible in patients with high-risk features (such as a positive stress test). After surgery, pay close attention to volume status, pain, signs of sepsis, or other noncardiac complications.
Back to the Case
As per the 2007 ACC/AHA guidelines, this patient with one clinical risk factor (diabetes) and good functional capacity can proceed to the operating room without further intervention. While it is likely a patient with diabetes and hyperlipidemia has some degree of CAD, including possible vulnerable plaques, the best medical evidence offers little to decrease her operative cardiac risk. Perioperative beta blockade is not indicated at her level of risk (RCRI of one) given the inconsistent benefits and possible harm to patients like this seen in trials to date.
If she were limited in terms of functional capacity (i.e., less than four METS), the 2007 ACC/AHA algorithm suggests preoperative noninvasive testing “if it would change management.”
How might a positive stress test change management in this case? Revascularization with stenting in close proximity to noncardiac surgery is not safe, and there appears to be no benefit to preoperative revascularization before high-risk vascular surgery. However, ischemia on preoperative testing is an indication for a beta-blocker. A brief delay in her surgery to allow dose titration and use of telemetry monitoring after surgery would increase the safety of beta-blockers after surgery. How long to continue beta-blockers is an open question, but at least 30 days would seem adequate, tapering rather than abruptly discontinuing the dose. TH
Dr. Carter is an assistant professor of medicine at the University of Colorado Denver in the Section of Hospital Medicine, where he directs the Medicine Consult Service. Dr. Auerbach is an associate professor of medicine in residence, associate director of the general medicine research fellowship, director of quality improvement for the UCSF Department of Medicine, and director of the surgical care Improvement program at UCSF. His research interests include perioperative medicine and quality improvement.
References
- Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation. 1999;100(10):1043-1049.
- Eagle KA, Berger PB, Calkins H, et al. ACC/AHA Guideline update for perioperative cardiovascular evaluation for noncardiac surgery—executive summary. Circulation 2002;105:1257-1267.
- Fleischer LA, Beckman JA, Brown KA, et al. ACC/AHA Guidelines on Perioperative Cardiovascular Evaluation and Care for noncardiac surgery: executive summary. Circulation. 2007;116:1971-1996.
- Salerno SM, Carlson DW, Soh EK, et al. Impact of perioperative cardiac assessment guidelines on management of orthopedic surgery patients. Am J Med. 2007;120(2):185.
- McFalls EO, Ward HB, Moritz TE, et al. Coronary artery revascularization before elective major vascular surgery. N Engl J Med. 2004;351:2795-2804.
- Poldermans D, Schouten O, Vidakovic R, et al. A clinical randomized trial to evaluate the safety of a noninvasive approach in high-risk patients undergoing major vascular surgery: The DECREASE-V Pilot Study. J Am Coll Cardiol. 2007;49(17):1763-1769.
- Wilson, SH, Fasseas P, Orford JL, et al. Clinical outcomes of patients undergoing non-cardiac surgery in the two months following coronary stenting. J Am Coll Cardiol. 2003;42(2):234-240.
- Grines, CL, Bonow RO, Casey DE Jr, et al. Prevention of premature discontinuation of dual antiplatelet therapy in patients with coronary artery stents. Circulation. 2007; 115:813-818.
- Kaluza GL, Joseph J, Lee JR, et al. Catastrophic outcomes of noncardiac surgery soon after coronary stenting. Am J Coll Cardiol. 2000;35(5):1288-1294.
- Schouten O, Bax JJ, Damen J, et al. Coronary stent placement immediately before non cardiac surgery: a potential risk? Anesthesiology 106(5);2007:1067.
- Leibowitz D, Cohen M, Planer D, et al. Comparison of cardiovascular risk of noncardiac surgery following coronary angioplasty with versus without stenting. Am J Cardiol. 2006;97(8):1188-1191.
- Auerbach A, Goldman L. Assessing and reducing the cardiac risk of noncardiac surgery. Circulation 2006;113:1361-1376.
- Mangano DT, Layug EL, Wallace A, et al. Effect of atenolol on mortality and cardiovascular morbidity after noncardiac surgery. N Engl J Med. 1996;335(23):1713-1720.
- Poldermans D, Boersma E, Bax JJ, et al. The effect of bisoprolol on perioperative mortality and myocardial infarction in high-risk patients undergoing vascular surgery. N Engl J Med. 1999;341(24):1789-1794.
- Feringa HH, Bax JJ, Boersma E, et al. High dose b-blockers and tight heart rate control reduce myocardial ischemia and troponin T release in vascular surgery patients. Circulation. 2006;114(supp):I344.
- Lindenauer PK Pekow P, Wang K, et al. Perioperative beta-blocker therapy and mortality after major noncardiac surgery. N Engl J Med. 2005;353(4):349-361.
- Yang H, Raymer K, Butler R, et al. The effects of perioperative beta blockade: results of the Metoprolol after Vascular Surgery (MaVS) study, a randomized controlled trial. Am Heart J. 2006;152(5):983-990.
- Juul AB, Wetterslev J, Gluud C, et al. Effect of perioperative ß blockade in patients with diabetes undergoing major non-cardiac surgery: randomized placebo controlled, blinded multicentre trial. BMJ. 2006 June;332:1482.
- Devereaux PJ, Beattie WS, Choi PT, et al. How strong is the evidence for the use of perioperative ß blockers in noncardiac surgery? Systematic review and meta-analysis of randomized controlled trials. BMJ. 2005;331:313.
- Devereaux PJ. POISE Abstract. American Heart Association Annual Scientific Session, Orlando, Fla., November 2007.
Case
The orthopedic service asks you to evaluate a 76-year-old woman with a hip fracture. She has diabetes, hypertension, and hyperlipidemia but no known coronary artery disease (CAD). She says she can carry a bag of groceries up one flight of stairs without chest symptoms.
Her physical exam is significant only for a shortened, internally rotated right hip. Her blood pressure is 160/88 mm/hg, her pulse is 75 beats per minute, and her respiratory rate is 16 breaths a minute with an oxygen saturation of 95% on one liter. Her creatinine is 1.2 mg/dL, and her fasting glucose is 106 mg/dL. An electrocardiogram reveals normal sinus rhythm without evidence of prior myocardial infarction (MI).
Her medications are lisinopril, atorvastatin, aspirin, fluoxetine, and diazepam. She is scheduled for the operating room tomorrow. What is the best strategy to evaluate and minimize her perioperative cardiac risk, and does it include a beta-blocker?
Overview
There are many ways to identify patients at risk for perioperative cardiac complications—but few simple, safe, evidence-based means of mitigating risk.1
Over the past 10 years, the general approach has been that preoperative revascularization is beneficial in a limited number of clinical scenarios. Further, beta-blockers reduce risk in nearly all other high- and intermediate-risk patients. Unfortunately, routine perioperative administration of beta-blockers to intermediate-risk patients is not supported by trial evidence and may expose these patients to increased risk of adverse outcomes—including death and stroke.
Review of the Data
Intermediate-risk patients: Inter-mediate risk patients have recently been redefined as patients with a Revised Cardiac Risk Index (RCRI) score of two or one (See Table 1, p. 27).2,3 Older guidelines suggested noninvasive testing for such patients if they had poor functional capacity (less than four metabolic equivalents [METS]) and were undergoing intermediate-risk surgery, including orthopedic, peritoneal, and thoracic procedures.
Unfortunately, this situation is common, leading to frequent testing and unclear benefit to patients. Omission of a noninvasive evaluation in intermediate-risk orthopedic surgery patients is not associated with an increase in perioperative cardiac events.4 Most events occur in patients who did not meet criteria for preoperative testing.
The 2007 ACC/AHA Guidelines for Perioperative Evaluation and Care address this by recommending noninvasive testing only “if it will change management.” But they offer little guidance in unclear clinical situations, such as the urgent hip-fracture repair needed by our patient.
Preoperative revascularization: While it makes intuitive sense that preoperative revascularization of high-risk patients would decrease their risk of perioperative cardiac complications, evidence countering this idea is nearly definitive. In a study by McFalls, revascularization prior to major vascular surgery did not decrease the risk of perioperative MI or 30-day mortality; however, it delayed the surgical procedure, even in patients with high-risk noninvasive test results.5,6 It is generally accepted that if these high-risk patients can safely undergo major vascular surgery without revascularization, a lower-risk patient such as ours can do so at even lower risk.
In these trials, revascularization occurred in addition to medical management of coronary disease, including aspirin, statin, and—particularly in the study by Poldermans,6 where beta-blockers were started and titrated well before surgery—beta-blocker therapy.
Patients with active cardiac symptoms or signs or uncharacterized anginal symptoms should have elective surgery delayed. However, delay is rarely an option for the hospitalist, who is typically asked to address a patient’s risk shortly before urgent or emergent surgery. These difficult situations require one to weigh the cardiac risk of surgery in a patient who is not optimized versus the risk of delaying surgery to address the more urgent cardiac situation.
Timing of perioperative percutaneous intervention: For patients with coronary artery disease (CAD) or coronary lesions, the interval between percutaneous revascularization (via stent or percutaneous transluminal coronary angioplasty [PTCA]) and surgery affects rates of postoperative cardiac events.7
The recommended interval between stent placement and noncardiac surgery for patients receiving bare-metal and drug-eluting stents is six weeks and one year, respectively.8 Surgery within two weeks of stent placement can carry mortality rates as high as 40%, and this risk appears to decrease out to one year.9,10 If a new stent is in place, any potential benefit appears to be offset by the increased risk of in-stent thrombosis with subsequent MI and possible death. PTCA may not be a safe alternative, although some recommend using PTCA if the patient has unstable cardiac symptoms and needs urgent/emergent surgery.11
Perioperative discontinuation of dual antiplatelet agents (e.g., clopidogrel and aspirin) is common and appears to increase thrombosis risk. This presents a challenge when patients with recent stent placement present for urgent surgery. Minimizing the interruption of dual antiplatelet therapy is the most important intervention a hospitalist can perform. Interruption is associated with increased risk of stent thrombosis, MI, and death. If clopidogrel must be discontinued in the perioperative period, continuation of aspirin is recommended and intravenous glycoprotein 2b/3a inhibitors can be considered.12
Perioperative beta-blocker: Studies on the outcomes of perioperative beta blockade strongly suggested benefits initially. But a number of randomized trials in the past three years have not shown a positive effect.
In a landmark study published in 1996, Mangano showed that initiation of beta blockade just prior to surgery reduced perioperative MI and cardiac death in a mixed surgical population.13 Similar findings were seen with initiation of beta-blocker one month prior to vascular surgery.14 Additionally, higher doses of beta-blocker and lower heart rates in the perioperative period seem to be associated with decreased troponin release.15 Finally, perioperative beta blockade was associated with decreased mortality in high-risk patients (RCRI of three or greater), but higher mortality in lower-risk patients (e.g., RCRI of zero or one).16
More recent data reveal less benefit for perioperative beta blockade. Yang, et al., suggested that initiation of beta-blockers just prior to surgery did not decrease postoperative cardiac complications in vascular surgery patients.17 Similar results were found in a cohort of diabetic patients undergoing major surgery.18 A subsequent meta-analysis concluded that, in the aggregate, perioperative beta blockade was neither beneficial nor harmful.19
Further data have shown increased mortality with perioperative beta blockade in low-risk patients. Most recently, an abstract from the largest randomized controlled trial to date, the POISE study, suggested that preoperative beta blockade decreased MI and cardiac death, but increased the risk of stroke and produced higher overall mortality.20
It is challenging to reconcile this newer evidence with the previous data. While it seems intuitive that blunting the catecholamine response would minimize cardiac workload and therefore decrease perioperative infarcts, surgical patients are also at risk for poor pain control, sepsis, hypovolemia, and venous thromboembolism. Beta blockade can obscure their clinical manifestations, delaying diagnosis or complicating therapy. Inconsistencies among studies and published guidelines make them difficult to apply broadly, particularly with the intermediate-risk patient. Finally, perioperative beta blockade is poorly defined in terms of timing of initiation, target heart rate, and duration of postoperative use.
Until more definitive trial data are published, it seems most prudent to continue beta-blockers in patients already using them. Start them as far in advance of surgery as possible in patients with high-risk features (such as a positive stress test). After surgery, pay close attention to volume status, pain, signs of sepsis, or other noncardiac complications.
Back to the Case
As per the 2007 ACC/AHA guidelines, this patient with one clinical risk factor (diabetes) and good functional capacity can proceed to the operating room without further intervention. While it is likely a patient with diabetes and hyperlipidemia has some degree of CAD, including possible vulnerable plaques, the best medical evidence offers little to decrease her operative cardiac risk. Perioperative beta blockade is not indicated at her level of risk (RCRI of one) given the inconsistent benefits and possible harm to patients like this seen in trials to date.
If she were limited in terms of functional capacity (i.e., less than four METS), the 2007 ACC/AHA algorithm suggests preoperative noninvasive testing “if it would change management.”
How might a positive stress test change management in this case? Revascularization with stenting in close proximity to noncardiac surgery is not safe, and there appears to be no benefit to preoperative revascularization before high-risk vascular surgery. However, ischemia on preoperative testing is an indication for a beta-blocker. A brief delay in her surgery to allow dose titration and use of telemetry monitoring after surgery would increase the safety of beta-blockers after surgery. How long to continue beta-blockers is an open question, but at least 30 days would seem adequate, tapering rather than abruptly discontinuing the dose. TH
Dr. Carter is an assistant professor of medicine at the University of Colorado Denver in the Section of Hospital Medicine, where he directs the Medicine Consult Service. Dr. Auerbach is an associate professor of medicine in residence, associate director of the general medicine research fellowship, director of quality improvement for the UCSF Department of Medicine, and director of the surgical care Improvement program at UCSF. His research interests include perioperative medicine and quality improvement.
References
- Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation. 1999;100(10):1043-1049.
- Eagle KA, Berger PB, Calkins H, et al. ACC/AHA Guideline update for perioperative cardiovascular evaluation for noncardiac surgery—executive summary. Circulation 2002;105:1257-1267.
- Fleischer LA, Beckman JA, Brown KA, et al. ACC/AHA Guidelines on Perioperative Cardiovascular Evaluation and Care for noncardiac surgery: executive summary. Circulation. 2007;116:1971-1996.
- Salerno SM, Carlson DW, Soh EK, et al. Impact of perioperative cardiac assessment guidelines on management of orthopedic surgery patients. Am J Med. 2007;120(2):185.
- McFalls EO, Ward HB, Moritz TE, et al. Coronary artery revascularization before elective major vascular surgery. N Engl J Med. 2004;351:2795-2804.
- Poldermans D, Schouten O, Vidakovic R, et al. A clinical randomized trial to evaluate the safety of a noninvasive approach in high-risk patients undergoing major vascular surgery: The DECREASE-V Pilot Study. J Am Coll Cardiol. 2007;49(17):1763-1769.
- Wilson, SH, Fasseas P, Orford JL, et al. Clinical outcomes of patients undergoing non-cardiac surgery in the two months following coronary stenting. J Am Coll Cardiol. 2003;42(2):234-240.
- Grines, CL, Bonow RO, Casey DE Jr, et al. Prevention of premature discontinuation of dual antiplatelet therapy in patients with coronary artery stents. Circulation. 2007; 115:813-818.
- Kaluza GL, Joseph J, Lee JR, et al. Catastrophic outcomes of noncardiac surgery soon after coronary stenting. Am J Coll Cardiol. 2000;35(5):1288-1294.
- Schouten O, Bax JJ, Damen J, et al. Coronary stent placement immediately before non cardiac surgery: a potential risk? Anesthesiology 106(5);2007:1067.
- Leibowitz D, Cohen M, Planer D, et al. Comparison of cardiovascular risk of noncardiac surgery following coronary angioplasty with versus without stenting. Am J Cardiol. 2006;97(8):1188-1191.
- Auerbach A, Goldman L. Assessing and reducing the cardiac risk of noncardiac surgery. Circulation 2006;113:1361-1376.
- Mangano DT, Layug EL, Wallace A, et al. Effect of atenolol on mortality and cardiovascular morbidity after noncardiac surgery. N Engl J Med. 1996;335(23):1713-1720.
- Poldermans D, Boersma E, Bax JJ, et al. The effect of bisoprolol on perioperative mortality and myocardial infarction in high-risk patients undergoing vascular surgery. N Engl J Med. 1999;341(24):1789-1794.
- Feringa HH, Bax JJ, Boersma E, et al. High dose b-blockers and tight heart rate control reduce myocardial ischemia and troponin T release in vascular surgery patients. Circulation. 2006;114(supp):I344.
- Lindenauer PK Pekow P, Wang K, et al. Perioperative beta-blocker therapy and mortality after major noncardiac surgery. N Engl J Med. 2005;353(4):349-361.
- Yang H, Raymer K, Butler R, et al. The effects of perioperative beta blockade: results of the Metoprolol after Vascular Surgery (MaVS) study, a randomized controlled trial. Am Heart J. 2006;152(5):983-990.
- Juul AB, Wetterslev J, Gluud C, et al. Effect of perioperative ß blockade in patients with diabetes undergoing major non-cardiac surgery: randomized placebo controlled, blinded multicentre trial. BMJ. 2006 June;332:1482.
- Devereaux PJ, Beattie WS, Choi PT, et al. How strong is the evidence for the use of perioperative ß blockers in noncardiac surgery? Systematic review and meta-analysis of randomized controlled trials. BMJ. 2005;331:313.
- Devereaux PJ. POISE Abstract. American Heart Association Annual Scientific Session, Orlando, Fla., November 2007.
Case
The orthopedic service asks you to evaluate a 76-year-old woman with a hip fracture. She has diabetes, hypertension, and hyperlipidemia but no known coronary artery disease (CAD). She says she can carry a bag of groceries up one flight of stairs without chest symptoms.
Her physical exam is significant only for a shortened, internally rotated right hip. Her blood pressure is 160/88 mm/hg, her pulse is 75 beats per minute, and her respiratory rate is 16 breaths a minute with an oxygen saturation of 95% on one liter. Her creatinine is 1.2 mg/dL, and her fasting glucose is 106 mg/dL. An electrocardiogram reveals normal sinus rhythm without evidence of prior myocardial infarction (MI).
Her medications are lisinopril, atorvastatin, aspirin, fluoxetine, and diazepam. She is scheduled for the operating room tomorrow. What is the best strategy to evaluate and minimize her perioperative cardiac risk, and does it include a beta-blocker?
Overview
There are many ways to identify patients at risk for perioperative cardiac complications—but few simple, safe, evidence-based means of mitigating risk.1
Over the past 10 years, the general approach has been that preoperative revascularization is beneficial in a limited number of clinical scenarios. Further, beta-blockers reduce risk in nearly all other high- and intermediate-risk patients. Unfortunately, routine perioperative administration of beta-blockers to intermediate-risk patients is not supported by trial evidence and may expose these patients to increased risk of adverse outcomes—including death and stroke.
Review of the Data
Intermediate-risk patients: Inter-mediate risk patients have recently been redefined as patients with a Revised Cardiac Risk Index (RCRI) score of two or one (See Table 1, p. 27).2,3 Older guidelines suggested noninvasive testing for such patients if they had poor functional capacity (less than four metabolic equivalents [METS]) and were undergoing intermediate-risk surgery, including orthopedic, peritoneal, and thoracic procedures.
Unfortunately, this situation is common, leading to frequent testing and unclear benefit to patients. Omission of a noninvasive evaluation in intermediate-risk orthopedic surgery patients is not associated with an increase in perioperative cardiac events.4 Most events occur in patients who did not meet criteria for preoperative testing.
The 2007 ACC/AHA Guidelines for Perioperative Evaluation and Care address this by recommending noninvasive testing only “if it will change management.” But they offer little guidance in unclear clinical situations, such as the urgent hip-fracture repair needed by our patient.
Preoperative revascularization: While it makes intuitive sense that preoperative revascularization of high-risk patients would decrease their risk of perioperative cardiac complications, evidence countering this idea is nearly definitive. In a study by McFalls, revascularization prior to major vascular surgery did not decrease the risk of perioperative MI or 30-day mortality; however, it delayed the surgical procedure, even in patients with high-risk noninvasive test results.5,6 It is generally accepted that if these high-risk patients can safely undergo major vascular surgery without revascularization, a lower-risk patient such as ours can do so at even lower risk.
In these trials, revascularization occurred in addition to medical management of coronary disease, including aspirin, statin, and—particularly in the study by Poldermans,6 where beta-blockers were started and titrated well before surgery—beta-blocker therapy.
Patients with active cardiac symptoms or signs or uncharacterized anginal symptoms should have elective surgery delayed. However, delay is rarely an option for the hospitalist, who is typically asked to address a patient’s risk shortly before urgent or emergent surgery. These difficult situations require one to weigh the cardiac risk of surgery in a patient who is not optimized versus the risk of delaying surgery to address the more urgent cardiac situation.
Timing of perioperative percutaneous intervention: For patients with coronary artery disease (CAD) or coronary lesions, the interval between percutaneous revascularization (via stent or percutaneous transluminal coronary angioplasty [PTCA]) and surgery affects rates of postoperative cardiac events.7
The recommended interval between stent placement and noncardiac surgery for patients receiving bare-metal and drug-eluting stents is six weeks and one year, respectively.8 Surgery within two weeks of stent placement can carry mortality rates as high as 40%, and this risk appears to decrease out to one year.9,10 If a new stent is in place, any potential benefit appears to be offset by the increased risk of in-stent thrombosis with subsequent MI and possible death. PTCA may not be a safe alternative, although some recommend using PTCA if the patient has unstable cardiac symptoms and needs urgent/emergent surgery.11
Perioperative discontinuation of dual antiplatelet agents (e.g., clopidogrel and aspirin) is common and appears to increase thrombosis risk. This presents a challenge when patients with recent stent placement present for urgent surgery. Minimizing the interruption of dual antiplatelet therapy is the most important intervention a hospitalist can perform. Interruption is associated with increased risk of stent thrombosis, MI, and death. If clopidogrel must be discontinued in the perioperative period, continuation of aspirin is recommended and intravenous glycoprotein 2b/3a inhibitors can be considered.12
Perioperative beta-blocker: Studies on the outcomes of perioperative beta blockade strongly suggested benefits initially. But a number of randomized trials in the past three years have not shown a positive effect.
In a landmark study published in 1996, Mangano showed that initiation of beta blockade just prior to surgery reduced perioperative MI and cardiac death in a mixed surgical population.13 Similar findings were seen with initiation of beta-blocker one month prior to vascular surgery.14 Additionally, higher doses of beta-blocker and lower heart rates in the perioperative period seem to be associated with decreased troponin release.15 Finally, perioperative beta blockade was associated with decreased mortality in high-risk patients (RCRI of three or greater), but higher mortality in lower-risk patients (e.g., RCRI of zero or one).16
More recent data reveal less benefit for perioperative beta blockade. Yang, et al., suggested that initiation of beta-blockers just prior to surgery did not decrease postoperative cardiac complications in vascular surgery patients.17 Similar results were found in a cohort of diabetic patients undergoing major surgery.18 A subsequent meta-analysis concluded that, in the aggregate, perioperative beta blockade was neither beneficial nor harmful.19
Further data have shown increased mortality with perioperative beta blockade in low-risk patients. Most recently, an abstract from the largest randomized controlled trial to date, the POISE study, suggested that preoperative beta blockade decreased MI and cardiac death, but increased the risk of stroke and produced higher overall mortality.20
It is challenging to reconcile this newer evidence with the previous data. While it seems intuitive that blunting the catecholamine response would minimize cardiac workload and therefore decrease perioperative infarcts, surgical patients are also at risk for poor pain control, sepsis, hypovolemia, and venous thromboembolism. Beta blockade can obscure their clinical manifestations, delaying diagnosis or complicating therapy. Inconsistencies among studies and published guidelines make them difficult to apply broadly, particularly with the intermediate-risk patient. Finally, perioperative beta blockade is poorly defined in terms of timing of initiation, target heart rate, and duration of postoperative use.
Until more definitive trial data are published, it seems most prudent to continue beta-blockers in patients already using them. Start them as far in advance of surgery as possible in patients with high-risk features (such as a positive stress test). After surgery, pay close attention to volume status, pain, signs of sepsis, or other noncardiac complications.
Back to the Case
As per the 2007 ACC/AHA guidelines, this patient with one clinical risk factor (diabetes) and good functional capacity can proceed to the operating room without further intervention. While it is likely a patient with diabetes and hyperlipidemia has some degree of CAD, including possible vulnerable plaques, the best medical evidence offers little to decrease her operative cardiac risk. Perioperative beta blockade is not indicated at her level of risk (RCRI of one) given the inconsistent benefits and possible harm to patients like this seen in trials to date.
If she were limited in terms of functional capacity (i.e., less than four METS), the 2007 ACC/AHA algorithm suggests preoperative noninvasive testing “if it would change management.”
How might a positive stress test change management in this case? Revascularization with stenting in close proximity to noncardiac surgery is not safe, and there appears to be no benefit to preoperative revascularization before high-risk vascular surgery. However, ischemia on preoperative testing is an indication for a beta-blocker. A brief delay in her surgery to allow dose titration and use of telemetry monitoring after surgery would increase the safety of beta-blockers after surgery. How long to continue beta-blockers is an open question, but at least 30 days would seem adequate, tapering rather than abruptly discontinuing the dose. TH
Dr. Carter is an assistant professor of medicine at the University of Colorado Denver in the Section of Hospital Medicine, where he directs the Medicine Consult Service. Dr. Auerbach is an associate professor of medicine in residence, associate director of the general medicine research fellowship, director of quality improvement for the UCSF Department of Medicine, and director of the surgical care Improvement program at UCSF. His research interests include perioperative medicine and quality improvement.
References
- Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation. 1999;100(10):1043-1049.
- Eagle KA, Berger PB, Calkins H, et al. ACC/AHA Guideline update for perioperative cardiovascular evaluation for noncardiac surgery—executive summary. Circulation 2002;105:1257-1267.
- Fleischer LA, Beckman JA, Brown KA, et al. ACC/AHA Guidelines on Perioperative Cardiovascular Evaluation and Care for noncardiac surgery: executive summary. Circulation. 2007;116:1971-1996.
- Salerno SM, Carlson DW, Soh EK, et al. Impact of perioperative cardiac assessment guidelines on management of orthopedic surgery patients. Am J Med. 2007;120(2):185.
- McFalls EO, Ward HB, Moritz TE, et al. Coronary artery revascularization before elective major vascular surgery. N Engl J Med. 2004;351:2795-2804.
- Poldermans D, Schouten O, Vidakovic R, et al. A clinical randomized trial to evaluate the safety of a noninvasive approach in high-risk patients undergoing major vascular surgery: The DECREASE-V Pilot Study. J Am Coll Cardiol. 2007;49(17):1763-1769.
- Wilson, SH, Fasseas P, Orford JL, et al. Clinical outcomes of patients undergoing non-cardiac surgery in the two months following coronary stenting. J Am Coll Cardiol. 2003;42(2):234-240.
- Grines, CL, Bonow RO, Casey DE Jr, et al. Prevention of premature discontinuation of dual antiplatelet therapy in patients with coronary artery stents. Circulation. 2007; 115:813-818.
- Kaluza GL, Joseph J, Lee JR, et al. Catastrophic outcomes of noncardiac surgery soon after coronary stenting. Am J Coll Cardiol. 2000;35(5):1288-1294.
- Schouten O, Bax JJ, Damen J, et al. Coronary stent placement immediately before non cardiac surgery: a potential risk? Anesthesiology 106(5);2007:1067.
- Leibowitz D, Cohen M, Planer D, et al. Comparison of cardiovascular risk of noncardiac surgery following coronary angioplasty with versus without stenting. Am J Cardiol. 2006;97(8):1188-1191.
- Auerbach A, Goldman L. Assessing and reducing the cardiac risk of noncardiac surgery. Circulation 2006;113:1361-1376.
- Mangano DT, Layug EL, Wallace A, et al. Effect of atenolol on mortality and cardiovascular morbidity after noncardiac surgery. N Engl J Med. 1996;335(23):1713-1720.
- Poldermans D, Boersma E, Bax JJ, et al. The effect of bisoprolol on perioperative mortality and myocardial infarction in high-risk patients undergoing vascular surgery. N Engl J Med. 1999;341(24):1789-1794.
- Feringa HH, Bax JJ, Boersma E, et al. High dose b-blockers and tight heart rate control reduce myocardial ischemia and troponin T release in vascular surgery patients. Circulation. 2006;114(supp):I344.
- Lindenauer PK Pekow P, Wang K, et al. Perioperative beta-blocker therapy and mortality after major noncardiac surgery. N Engl J Med. 2005;353(4):349-361.
- Yang H, Raymer K, Butler R, et al. The effects of perioperative beta blockade: results of the Metoprolol after Vascular Surgery (MaVS) study, a randomized controlled trial. Am Heart J. 2006;152(5):983-990.
- Juul AB, Wetterslev J, Gluud C, et al. Effect of perioperative ß blockade in patients with diabetes undergoing major non-cardiac surgery: randomized placebo controlled, blinded multicentre trial. BMJ. 2006 June;332:1482.
- Devereaux PJ, Beattie WS, Choi PT, et al. How strong is the evidence for the use of perioperative ß blockers in noncardiac surgery? Systematic review and meta-analysis of randomized controlled trials. BMJ. 2005;331:313.
- Devereaux PJ. POISE Abstract. American Heart Association Annual Scientific Session, Orlando, Fla., November 2007.
Deposition Minefield
One day, you’re sitting in your office when a stranger appears and asks, “Are you Dr. Smith?” When you say yes, the stranger hands you a sheaf of papers. You open the papers and see you’ve been “commanded” to attend a deposition at a lawyer’s office next week. How do you prepare?
The Basics
Black’s Law Dictionary gives a long definition of a deposition. But the shorter, more practical definition is that a deposition is a witness’s sworn out-of-court testimony. When a physician gives a deposition in a lawyer’s office, this testimony has the same legal effect as though the physician were testifying in court.
Lawyers typically view depositions as one of two types:
- Discovery depositions: These allow lawyers to discover the substance of a witness’s testimony before trial. They can touch upon a number of subjects that seem tangential to the case. A lawyer taking a discovery deposition is putting together the pieces of the case and may or may not ask the witness to testify at trial; and
- Perpetuation depositions: These let lawyers present the testimony of a witness who cannot appear at trial. Perpetuation depositions substitute for the examinations and cross-examinations that would normally occur in the courtroom. Perpetuation depositions are generally shorter and more focused than discovery depositions.
In all depositions, lawyers ask questions of the witness and can object to legally improper questions. The lawyers can ask the witness to refer to documents or other exhibits during the deposition. A court reporter will transcribe the questions and answers and condense them into a written transcript. A judge is normally not present for a deposition but can be called during the deposition to make rulings.
Know Your Role
Perhaps the most important thing you can do in preparing for a deposition is understand your role in the lawsuit. Generally, physicians serve in one of three potential roles as deponents:
Medical malpractice defendant: When a patient sues a physician for malpractice, the patient’s attorney normally will take the physician’s deposition. In this highly adversarial process, the patient’s attorney attempts to demonstrate that the physician’s negligence injured the patient. A physician being deposed as a defendant must prepare by meeting with his attorney and reviewing the issues likely to arise during the proceedings. If you are a defendant in a lawsuit, you must set aside adequate time to prepare for the deposition with your attorney;
Retained expert witness: The rules of evidence allow people with specialized knowledge to testify as experts in fields normally beyond the average juror’s experience. Because they have specialized knowledge, experts are allowed to state opinions in their testimony, such as whether a physician’s conduct complied with the applicable standards of care. Attorneys generally hire expert witnesses to present opinions in a case and will provide a summary of the expert’s testimony before the deposition; and
Treating physician: Many physicians are deposed concerning the care they provided to a patient in lawsuits that implicate the patient’s health (auto accident, work injury, disability suit). These depositions focus on the substance of treatment, the patient’s medical condition, and the patient’s prognosis. The physician normally does not have any interest in how the lawsuit is resolved. A treating physician is often compensated for his time in the deposition, even though he was not retained as an expert to testify in the lawsuit.
Golden Rules
Because depositions are stressful, lawyers ask witnesses to remember only three rules.
Tell the truth: Your only job as a witness is to tell the truth. If you follow this rule, you have discharged your obligation to the legal system.
However, keep some things in mind when telling the truth. In particular, your ability to tell the truth is subject to the limitations of your memory and the fact that your deposition may be occurring several years after you provided care. “I don’t know” and “I don’t remember” are absolutely acceptable answers in a deposition. In fact, they are preferable to inaccurate or untruthful testimony. If reviewing a document (such as the patient’s medical records) will help you provide accurate and truthful testimony, don’t be shy about asking to review them. In any situation where you are guessing or providing your best recollection, make sure the lawyer knows you are doing your best but that you can’t remember all the details.
Make sure you understand the question: This rule seems self-evident, but many lawyers ask convoluted or compound questions. Lawyers may also use language unfamiliar to you as an outsider to the legal process. For example, when lawyers use the phrase “standard of care,” it has a fairly precise definition (it is an action a reasonably careful physician would undertake under the same or similar circumstances). Ask for clarification of any question that is not clear. It’s the lawyer’s job to ask an understandable question, not the physician’s job to answer a question that doesn’t make sense. Be extra careful when the opposing lawyer objects to a question. While the lawyer’s objection does not relieve you from answering, it should signal you that the question is potentially flawed or beyond the scope of your knowledge.
Answer only what you’re asked: Invariably, physicians struggle most when they don’t focus their answers on the question posed to them.
The majority of questions in a deposition can be answered “Yes,” “No,” “I don’t know,” and “I don’t remember.” Yet many physicians tend to volunteer additional information to explain their answers. Because lawyers are trained to recognize and follow up on nonresponsive answers, the physician’s deposition becomes longer and more challenging. To provide a better answer, don’t think out loud. Ponder the question and mentally prepare your answer. Doing so lets you respond more precisely. Answer only the question you are asked. If there is an area that needs more explanation, the other party’s attorney (or your attorney) will have an opportunity to allow you to clarify the record.
To help you follow the rules, use this decision tree during your deposition (see Figure 1, left).
Regardless of the purpose of a deposition or your perceived role in it, consult with an attorney before being deposed. Even if you believe you are being deposed only as a treating provider, a deposition could lead to potential claims or raise concerns about your records. If served with a subpoena, contact your insurance company, which may retain an attorney to assist you. TH
Patrick O’Rourke works in the Office of University Counsel, Department of Litigation, University of Colorado, Denver.
One day, you’re sitting in your office when a stranger appears and asks, “Are you Dr. Smith?” When you say yes, the stranger hands you a sheaf of papers. You open the papers and see you’ve been “commanded” to attend a deposition at a lawyer’s office next week. How do you prepare?
The Basics
Black’s Law Dictionary gives a long definition of a deposition. But the shorter, more practical definition is that a deposition is a witness’s sworn out-of-court testimony. When a physician gives a deposition in a lawyer’s office, this testimony has the same legal effect as though the physician were testifying in court.
Lawyers typically view depositions as one of two types:
- Discovery depositions: These allow lawyers to discover the substance of a witness’s testimony before trial. They can touch upon a number of subjects that seem tangential to the case. A lawyer taking a discovery deposition is putting together the pieces of the case and may or may not ask the witness to testify at trial; and
- Perpetuation depositions: These let lawyers present the testimony of a witness who cannot appear at trial. Perpetuation depositions substitute for the examinations and cross-examinations that would normally occur in the courtroom. Perpetuation depositions are generally shorter and more focused than discovery depositions.
In all depositions, lawyers ask questions of the witness and can object to legally improper questions. The lawyers can ask the witness to refer to documents or other exhibits during the deposition. A court reporter will transcribe the questions and answers and condense them into a written transcript. A judge is normally not present for a deposition but can be called during the deposition to make rulings.
Know Your Role
Perhaps the most important thing you can do in preparing for a deposition is understand your role in the lawsuit. Generally, physicians serve in one of three potential roles as deponents:
Medical malpractice defendant: When a patient sues a physician for malpractice, the patient’s attorney normally will take the physician’s deposition. In this highly adversarial process, the patient’s attorney attempts to demonstrate that the physician’s negligence injured the patient. A physician being deposed as a defendant must prepare by meeting with his attorney and reviewing the issues likely to arise during the proceedings. If you are a defendant in a lawsuit, you must set aside adequate time to prepare for the deposition with your attorney;
Retained expert witness: The rules of evidence allow people with specialized knowledge to testify as experts in fields normally beyond the average juror’s experience. Because they have specialized knowledge, experts are allowed to state opinions in their testimony, such as whether a physician’s conduct complied with the applicable standards of care. Attorneys generally hire expert witnesses to present opinions in a case and will provide a summary of the expert’s testimony before the deposition; and
Treating physician: Many physicians are deposed concerning the care they provided to a patient in lawsuits that implicate the patient’s health (auto accident, work injury, disability suit). These depositions focus on the substance of treatment, the patient’s medical condition, and the patient’s prognosis. The physician normally does not have any interest in how the lawsuit is resolved. A treating physician is often compensated for his time in the deposition, even though he was not retained as an expert to testify in the lawsuit.
Golden Rules
Because depositions are stressful, lawyers ask witnesses to remember only three rules.
Tell the truth: Your only job as a witness is to tell the truth. If you follow this rule, you have discharged your obligation to the legal system.
However, keep some things in mind when telling the truth. In particular, your ability to tell the truth is subject to the limitations of your memory and the fact that your deposition may be occurring several years after you provided care. “I don’t know” and “I don’t remember” are absolutely acceptable answers in a deposition. In fact, they are preferable to inaccurate or untruthful testimony. If reviewing a document (such as the patient’s medical records) will help you provide accurate and truthful testimony, don’t be shy about asking to review them. In any situation where you are guessing or providing your best recollection, make sure the lawyer knows you are doing your best but that you can’t remember all the details.
Make sure you understand the question: This rule seems self-evident, but many lawyers ask convoluted or compound questions. Lawyers may also use language unfamiliar to you as an outsider to the legal process. For example, when lawyers use the phrase “standard of care,” it has a fairly precise definition (it is an action a reasonably careful physician would undertake under the same or similar circumstances). Ask for clarification of any question that is not clear. It’s the lawyer’s job to ask an understandable question, not the physician’s job to answer a question that doesn’t make sense. Be extra careful when the opposing lawyer objects to a question. While the lawyer’s objection does not relieve you from answering, it should signal you that the question is potentially flawed or beyond the scope of your knowledge.
Answer only what you’re asked: Invariably, physicians struggle most when they don’t focus their answers on the question posed to them.
The majority of questions in a deposition can be answered “Yes,” “No,” “I don’t know,” and “I don’t remember.” Yet many physicians tend to volunteer additional information to explain their answers. Because lawyers are trained to recognize and follow up on nonresponsive answers, the physician’s deposition becomes longer and more challenging. To provide a better answer, don’t think out loud. Ponder the question and mentally prepare your answer. Doing so lets you respond more precisely. Answer only the question you are asked. If there is an area that needs more explanation, the other party’s attorney (or your attorney) will have an opportunity to allow you to clarify the record.
To help you follow the rules, use this decision tree during your deposition (see Figure 1, left).
Regardless of the purpose of a deposition or your perceived role in it, consult with an attorney before being deposed. Even if you believe you are being deposed only as a treating provider, a deposition could lead to potential claims or raise concerns about your records. If served with a subpoena, contact your insurance company, which may retain an attorney to assist you. TH
Patrick O’Rourke works in the Office of University Counsel, Department of Litigation, University of Colorado, Denver.
One day, you’re sitting in your office when a stranger appears and asks, “Are you Dr. Smith?” When you say yes, the stranger hands you a sheaf of papers. You open the papers and see you’ve been “commanded” to attend a deposition at a lawyer’s office next week. How do you prepare?
The Basics
Black’s Law Dictionary gives a long definition of a deposition. But the shorter, more practical definition is that a deposition is a witness’s sworn out-of-court testimony. When a physician gives a deposition in a lawyer’s office, this testimony has the same legal effect as though the physician were testifying in court.
Lawyers typically view depositions as one of two types:
- Discovery depositions: These allow lawyers to discover the substance of a witness’s testimony before trial. They can touch upon a number of subjects that seem tangential to the case. A lawyer taking a discovery deposition is putting together the pieces of the case and may or may not ask the witness to testify at trial; and
- Perpetuation depositions: These let lawyers present the testimony of a witness who cannot appear at trial. Perpetuation depositions substitute for the examinations and cross-examinations that would normally occur in the courtroom. Perpetuation depositions are generally shorter and more focused than discovery depositions.
In all depositions, lawyers ask questions of the witness and can object to legally improper questions. The lawyers can ask the witness to refer to documents or other exhibits during the deposition. A court reporter will transcribe the questions and answers and condense them into a written transcript. A judge is normally not present for a deposition but can be called during the deposition to make rulings.
Know Your Role
Perhaps the most important thing you can do in preparing for a deposition is understand your role in the lawsuit. Generally, physicians serve in one of three potential roles as deponents:
Medical malpractice defendant: When a patient sues a physician for malpractice, the patient’s attorney normally will take the physician’s deposition. In this highly adversarial process, the patient’s attorney attempts to demonstrate that the physician’s negligence injured the patient. A physician being deposed as a defendant must prepare by meeting with his attorney and reviewing the issues likely to arise during the proceedings. If you are a defendant in a lawsuit, you must set aside adequate time to prepare for the deposition with your attorney;
Retained expert witness: The rules of evidence allow people with specialized knowledge to testify as experts in fields normally beyond the average juror’s experience. Because they have specialized knowledge, experts are allowed to state opinions in their testimony, such as whether a physician’s conduct complied with the applicable standards of care. Attorneys generally hire expert witnesses to present opinions in a case and will provide a summary of the expert’s testimony before the deposition; and
Treating physician: Many physicians are deposed concerning the care they provided to a patient in lawsuits that implicate the patient’s health (auto accident, work injury, disability suit). These depositions focus on the substance of treatment, the patient’s medical condition, and the patient’s prognosis. The physician normally does not have any interest in how the lawsuit is resolved. A treating physician is often compensated for his time in the deposition, even though he was not retained as an expert to testify in the lawsuit.
Golden Rules
Because depositions are stressful, lawyers ask witnesses to remember only three rules.
Tell the truth: Your only job as a witness is to tell the truth. If you follow this rule, you have discharged your obligation to the legal system.
However, keep some things in mind when telling the truth. In particular, your ability to tell the truth is subject to the limitations of your memory and the fact that your deposition may be occurring several years after you provided care. “I don’t know” and “I don’t remember” are absolutely acceptable answers in a deposition. In fact, they are preferable to inaccurate or untruthful testimony. If reviewing a document (such as the patient’s medical records) will help you provide accurate and truthful testimony, don’t be shy about asking to review them. In any situation where you are guessing or providing your best recollection, make sure the lawyer knows you are doing your best but that you can’t remember all the details.
Make sure you understand the question: This rule seems self-evident, but many lawyers ask convoluted or compound questions. Lawyers may also use language unfamiliar to you as an outsider to the legal process. For example, when lawyers use the phrase “standard of care,” it has a fairly precise definition (it is an action a reasonably careful physician would undertake under the same or similar circumstances). Ask for clarification of any question that is not clear. It’s the lawyer’s job to ask an understandable question, not the physician’s job to answer a question that doesn’t make sense. Be extra careful when the opposing lawyer objects to a question. While the lawyer’s objection does not relieve you from answering, it should signal you that the question is potentially flawed or beyond the scope of your knowledge.
Answer only what you’re asked: Invariably, physicians struggle most when they don’t focus their answers on the question posed to them.
The majority of questions in a deposition can be answered “Yes,” “No,” “I don’t know,” and “I don’t remember.” Yet many physicians tend to volunteer additional information to explain their answers. Because lawyers are trained to recognize and follow up on nonresponsive answers, the physician’s deposition becomes longer and more challenging. To provide a better answer, don’t think out loud. Ponder the question and mentally prepare your answer. Doing so lets you respond more precisely. Answer only the question you are asked. If there is an area that needs more explanation, the other party’s attorney (or your attorney) will have an opportunity to allow you to clarify the record.
To help you follow the rules, use this decision tree during your deposition (see Figure 1, left).
Regardless of the purpose of a deposition or your perceived role in it, consult with an attorney before being deposed. Even if you believe you are being deposed only as a treating provider, a deposition could lead to potential claims or raise concerns about your records. If served with a subpoena, contact your insurance company, which may retain an attorney to assist you. TH
Patrick O’Rourke works in the Office of University Counsel, Department of Litigation, University of Colorado, Denver.
Plan for Discharge
Discharge planning typically begins at the time of admission. Physicians and hospital staff manage the patient’s acute issues throughout the stay while simultaneously trying to anticipate the patient’s discharge needs. Physicians capture these associated efforts by reporting discharge day management codes 99238 or 99239.
Code Use
Use of discharge day management codes 99238-99239 is reserved for the admitting physician/group, unless a formal transfer of care occurs (e.g., patient is transferred from the intensive care unit by the critical care physician to the medical-surgical floor on the hospitalist’s service).
Report one discharge code per hospitalization, but only when the service occurs after the initial date of admission. Codes 99238 or 99239 are not permitted for use when the patient is admitted and discharged on the same calendar date. When this occurs, the physician selects from 99221-99223 (initial inpatient care) or 99234-99236 (admission and discharge on the same day). Choose 99234-99238 when the patient stay is eight or more hours on the same calendar day and the insurer accepts these codes.
Documentation must also reflect two components of service: the corresponding elements of both the admission and discharge. Alternately, if the patient stays less than eight hours, or the insurer does not recognize 99234-99236 (admission and discharge on the same day), report 9922x (initial inpatient care) as appropriate.
Don’t mistakenly report discharge services for merely dictating the discharge summary. Discharge day management, as with most payable evaluation and management (E/M) services, requires a face-to-face visit between the physician and the patient on discharge day.
The entire visit need not take place at the bedside and may include other discharge-related elements performed on the patient’s unit/floor such as discussions with other healthcare professionals, patient/caregiver instruction and coordination of follow-up care. The discharge code description indicates that a final examination of the patient is included, but only “as appropriate.” In other words, an exam may not occur, or may not be documented, yet this does not preclude the physician from reporting 99238-99239. However, inclusion of the exam in the discharge day documentation is the best way to justify that a face-to-face service occurred on discharge day. This may be included in the discharge summary or a separate progress note in the medical record.
Time-Based Service
Discharge day management codes reflect the time accumulated on a calendar date, ending when the patient physically leaves the hospital. Services performed in a location other than the patient’s unit/floor (e.g., dictating the discharge summary from the outpatient office), do not count toward the cumulative time. Additionally, discharge-related services performed by residents, students or ancillary staff (i.e., registered nurses), such as reviewing instructions with the patient, do not count toward the discharge service time.
To support the discharge day management claim, documentation should reference the discharge status and other clinically relevant information. Time is not required when documenting 99238 because this service code constitutes any amount of time up to and including 30 minutes. When reporting 99239, documentation must include the physician’s cumulative service time (more than 30 minutes).
Medicare currently initiates a prepayment review (i.e., request for documentation to review the service prior to any payment consideration) for claims involving 99239. Failure to respond to the prepayment request or failure to include the time component in the documentation often results in claim denial. Payment can be recovered only through the appeal process or claim correction, when applicable.
Rules For Surgery
Surgeons are prohibited from separately reporting inpatient postoperative services related to the surgery, including discharge day management (99238-99239). Additionally, when the surgeon admits a patient to the hospital and discharge services are performed postoperatively by the hospitalist, discharge day management is included in the surgical package.
The reasons are two-fold: If the surgeon transfers the remaining inpatient care to the hospitalist, these discharge services are considered part of the global surgical package.
If no transfer occurs (as the surgeon is typically responsible and paid for all care up to 90 days following surgery), only the admitting physician/group (i.e., the surgeon) may report discharge day management codes 99238-99239.
In the latter scenario, the hospitalist reports subsequent hospital care (99231-99233) for all medically necessary services involving the patient’s medical management, even if provided on the day of discharge.
Pronouncement of Death
One of the most underreported services involves pronouncement of death. A physician who performs this service may qualify to report discharge day management code 99238-99239. To pronounce death, the physician must examine the patient, thus satisfying the face-to-face visit requirement.
Additionally, the physician may have to coordinate the necessary services, speak with family members or other healthcare providers, and fill out the necessary documentation.
If performed on the patient’s unit/floor, these services count toward the cumulative discharge service time. Documentation must include the time (if reporting 99239) as well as the patient’s discharge status and clinically relevant information. Completion of the death certificate alone is not sufficient for billing. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Discharge planning typically begins at the time of admission. Physicians and hospital staff manage the patient’s acute issues throughout the stay while simultaneously trying to anticipate the patient’s discharge needs. Physicians capture these associated efforts by reporting discharge day management codes 99238 or 99239.
Code Use
Use of discharge day management codes 99238-99239 is reserved for the admitting physician/group, unless a formal transfer of care occurs (e.g., patient is transferred from the intensive care unit by the critical care physician to the medical-surgical floor on the hospitalist’s service).
Report one discharge code per hospitalization, but only when the service occurs after the initial date of admission. Codes 99238 or 99239 are not permitted for use when the patient is admitted and discharged on the same calendar date. When this occurs, the physician selects from 99221-99223 (initial inpatient care) or 99234-99236 (admission and discharge on the same day). Choose 99234-99238 when the patient stay is eight or more hours on the same calendar day and the insurer accepts these codes.
Documentation must also reflect two components of service: the corresponding elements of both the admission and discharge. Alternately, if the patient stays less than eight hours, or the insurer does not recognize 99234-99236 (admission and discharge on the same day), report 9922x (initial inpatient care) as appropriate.
Don’t mistakenly report discharge services for merely dictating the discharge summary. Discharge day management, as with most payable evaluation and management (E/M) services, requires a face-to-face visit between the physician and the patient on discharge day.
The entire visit need not take place at the bedside and may include other discharge-related elements performed on the patient’s unit/floor such as discussions with other healthcare professionals, patient/caregiver instruction and coordination of follow-up care. The discharge code description indicates that a final examination of the patient is included, but only “as appropriate.” In other words, an exam may not occur, or may not be documented, yet this does not preclude the physician from reporting 99238-99239. However, inclusion of the exam in the discharge day documentation is the best way to justify that a face-to-face service occurred on discharge day. This may be included in the discharge summary or a separate progress note in the medical record.
Time-Based Service
Discharge day management codes reflect the time accumulated on a calendar date, ending when the patient physically leaves the hospital. Services performed in a location other than the patient’s unit/floor (e.g., dictating the discharge summary from the outpatient office), do not count toward the cumulative time. Additionally, discharge-related services performed by residents, students or ancillary staff (i.e., registered nurses), such as reviewing instructions with the patient, do not count toward the discharge service time.
To support the discharge day management claim, documentation should reference the discharge status and other clinically relevant information. Time is not required when documenting 99238 because this service code constitutes any amount of time up to and including 30 minutes. When reporting 99239, documentation must include the physician’s cumulative service time (more than 30 minutes).
Medicare currently initiates a prepayment review (i.e., request for documentation to review the service prior to any payment consideration) for claims involving 99239. Failure to respond to the prepayment request or failure to include the time component in the documentation often results in claim denial. Payment can be recovered only through the appeal process or claim correction, when applicable.
Rules For Surgery
Surgeons are prohibited from separately reporting inpatient postoperative services related to the surgery, including discharge day management (99238-99239). Additionally, when the surgeon admits a patient to the hospital and discharge services are performed postoperatively by the hospitalist, discharge day management is included in the surgical package.
The reasons are two-fold: If the surgeon transfers the remaining inpatient care to the hospitalist, these discharge services are considered part of the global surgical package.
If no transfer occurs (as the surgeon is typically responsible and paid for all care up to 90 days following surgery), only the admitting physician/group (i.e., the surgeon) may report discharge day management codes 99238-99239.
In the latter scenario, the hospitalist reports subsequent hospital care (99231-99233) for all medically necessary services involving the patient’s medical management, even if provided on the day of discharge.
Pronouncement of Death
One of the most underreported services involves pronouncement of death. A physician who performs this service may qualify to report discharge day management code 99238-99239. To pronounce death, the physician must examine the patient, thus satisfying the face-to-face visit requirement.
Additionally, the physician may have to coordinate the necessary services, speak with family members or other healthcare providers, and fill out the necessary documentation.
If performed on the patient’s unit/floor, these services count toward the cumulative discharge service time. Documentation must include the time (if reporting 99239) as well as the patient’s discharge status and clinically relevant information. Completion of the death certificate alone is not sufficient for billing. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Discharge planning typically begins at the time of admission. Physicians and hospital staff manage the patient’s acute issues throughout the stay while simultaneously trying to anticipate the patient’s discharge needs. Physicians capture these associated efforts by reporting discharge day management codes 99238 or 99239.
Code Use
Use of discharge day management codes 99238-99239 is reserved for the admitting physician/group, unless a formal transfer of care occurs (e.g., patient is transferred from the intensive care unit by the critical care physician to the medical-surgical floor on the hospitalist’s service).
Report one discharge code per hospitalization, but only when the service occurs after the initial date of admission. Codes 99238 or 99239 are not permitted for use when the patient is admitted and discharged on the same calendar date. When this occurs, the physician selects from 99221-99223 (initial inpatient care) or 99234-99236 (admission and discharge on the same day). Choose 99234-99238 when the patient stay is eight or more hours on the same calendar day and the insurer accepts these codes.
Documentation must also reflect two components of service: the corresponding elements of both the admission and discharge. Alternately, if the patient stays less than eight hours, or the insurer does not recognize 99234-99236 (admission and discharge on the same day), report 9922x (initial inpatient care) as appropriate.
Don’t mistakenly report discharge services for merely dictating the discharge summary. Discharge day management, as with most payable evaluation and management (E/M) services, requires a face-to-face visit between the physician and the patient on discharge day.
The entire visit need not take place at the bedside and may include other discharge-related elements performed on the patient’s unit/floor such as discussions with other healthcare professionals, patient/caregiver instruction and coordination of follow-up care. The discharge code description indicates that a final examination of the patient is included, but only “as appropriate.” In other words, an exam may not occur, or may not be documented, yet this does not preclude the physician from reporting 99238-99239. However, inclusion of the exam in the discharge day documentation is the best way to justify that a face-to-face service occurred on discharge day. This may be included in the discharge summary or a separate progress note in the medical record.
Time-Based Service
Discharge day management codes reflect the time accumulated on a calendar date, ending when the patient physically leaves the hospital. Services performed in a location other than the patient’s unit/floor (e.g., dictating the discharge summary from the outpatient office), do not count toward the cumulative time. Additionally, discharge-related services performed by residents, students or ancillary staff (i.e., registered nurses), such as reviewing instructions with the patient, do not count toward the discharge service time.
To support the discharge day management claim, documentation should reference the discharge status and other clinically relevant information. Time is not required when documenting 99238 because this service code constitutes any amount of time up to and including 30 minutes. When reporting 99239, documentation must include the physician’s cumulative service time (more than 30 minutes).
Medicare currently initiates a prepayment review (i.e., request for documentation to review the service prior to any payment consideration) for claims involving 99239. Failure to respond to the prepayment request or failure to include the time component in the documentation often results in claim denial. Payment can be recovered only through the appeal process or claim correction, when applicable.
Rules For Surgery
Surgeons are prohibited from separately reporting inpatient postoperative services related to the surgery, including discharge day management (99238-99239). Additionally, when the surgeon admits a patient to the hospital and discharge services are performed postoperatively by the hospitalist, discharge day management is included in the surgical package.
The reasons are two-fold: If the surgeon transfers the remaining inpatient care to the hospitalist, these discharge services are considered part of the global surgical package.
If no transfer occurs (as the surgeon is typically responsible and paid for all care up to 90 days following surgery), only the admitting physician/group (i.e., the surgeon) may report discharge day management codes 99238-99239.
In the latter scenario, the hospitalist reports subsequent hospital care (99231-99233) for all medically necessary services involving the patient’s medical management, even if provided on the day of discharge.
Pronouncement of Death
One of the most underreported services involves pronouncement of death. A physician who performs this service may qualify to report discharge day management code 99238-99239. To pronounce death, the physician must examine the patient, thus satisfying the face-to-face visit requirement.
Additionally, the physician may have to coordinate the necessary services, speak with family members or other healthcare providers, and fill out the necessary documentation.
If performed on the patient’s unit/floor, these services count toward the cumulative discharge service time. Documentation must include the time (if reporting 99239) as well as the patient’s discharge status and clinically relevant information. Completion of the death certificate alone is not sufficient for billing. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
AHRQ in the Lead
What exactly is the Agency for Healthcare Research and Quality (AHRQ), and why are hospitalists urged to increase its portion of the federal budget pie each year?
According to its mission statement, the AHRQ is “the lead federal agency charged with improving the quality, safety, efficiency, and effectiveness of healthcare for all Americans.” This includes supporting high-quality, impartial research that specifically improves healthcare quality, reduces costs, advances patient safety, decreases medical errors, eliminates healthcare disparities, and broadens access to essential services.
“Supporting AHRQ is supporting an unbiased government organization that’s clearly on the side of patient safety, and that gets important information out fast,” says Andrew Fishmann, MD, FCCP, FACP, a member of AHRQ’s National Advisory Council and director of intensive care at Good Samaritan Hospital in Los Angeles. “Where’s the argument?”
Fight over Funding
The argument is over money, plain and simple. Each year, medical associations like SHM push for increased federal funding for AHRQ so the agency’s research can be expanded. And each year, Congress refuses those increases. Lawmakers have granted a slight boost in funding: Since 2002, AHRQ’s budget has increased by $2 million, or 6.7%.
Proponents of AHRQ believe precarious funding levels threaten the agency’s ability to achieve its essential mission. Last year, SHM lobbied for an increase in federal funding for AHRQ to $350 million in fiscal year 2008—$31 million more than the agency’s fiscal 2007 budget. By late 2007, Congress was weighing an increase of $329 million, plus $5 million targeted for comparative-effectiveness research.
“Think of AHRQ compared to the $28 billion that NIH gets,” says Dr. Fishmann. “[AHRQ’s] is a small budget relative to what they do.”
How much does AHRQ need to provide adequate research information? The answer is, apparently, as much as they can get. There are countless areas in healthcare the agency could address.
“If they got $500 million, could they spend it?” asks Dr. Fishmann. “Yes. They could look at the top 20 diseases instead of the top 10.”
What AHRQ Does
Regardless of the final budget amount they receive, AHRQ spends roughly 80% on grants and contracts focused on improving healthcare.
“AHRQ doesn’t do its own research or create its own data,” explains Dr. Fishmann. Rather, AHRQ conducts and supports health services research in leading academic institutions, hospitals, and other settings. In 2005, two hospitalists received separate grants for projects that have already had an effect on hospital medicine. Greg Maynard, MD, MS, division chief of hospital medicine at University of California San Diego School of Medicine, used AHRQ funds for an intervention project to prevent hospital-acquired venous thromboembolism (VTE). Dr. Maynard’s project continued to grow since that grant and has yielded key findings such as a risk-assessment model for VTE. Data and lessons learned are available in the VTE Resource Room on SHM’s Web site at www.hospitalmedicine.org/ResourceRoomRedesign/RR_LandingPage.cfm.
Asked why he went after AHRQ funding, Dr. Maynard explains: “AHRQ is one of the few [funding] agencies that focuses on the realm of implementation—that impact the patient immediately. It was a perfect marriage of what we wanted to do.” The other AHRQ-funded hospital medicine project was conducted by Mark V. Williams, MD, FACP, professor and chief, division of hospital medicine at Northwestern University Feinberg School of Medicine in Chicago, and editor of the Journal of Hospital Medicine. Working for Emory University’s hospital medicine program in Atlanta at the time, Dr. Williams used the grant to create a “discharge bundle” of patient safety interventions such as medication reconciliation and patient-centered education to improve patient safety transitions out of the hospital setting.
“We would not have been able to conduct the study without the support of AHRQ,” says Dr. Williams. “We certainly need more research funds such as this. AHRQ is the primary federal agency funding health services research—however, they receive less than 5% of the funding that goes to NIH and fund more basic science-oriented research. As few as one in 10 grants submitted to AHRQ are actually funded.”
Like Dr. Maynard’s work on VTE prevention, the injection of AHRQ funds also allowed Dr. Williams’ project to continue and grow. “With support from the Society of Hospital Medicine, we have been quite fortunate to utilize the momentum from the AHRQ Patient Safe-[Discharge] grant to obtain a $1.4 million grant from the John A. Hartford Grant to develop a discharge toolkit and facilitate implementation of it at hundreds of hospital,” he explains. “The BOOST [Better Outcomes for Older adults through Safe Transitions] project aims to improve care delivery to older adults at hospitals across America as they transition from the hospital to home.”
Additional research is developed in AHRQ’s Centers for Education and Research in Therapeutics (CERTS). Each of the 11 CERTS has a specific charge and gathers data on the benefits, risks, and cost-effectiveness of therapeutic products such as drugs, medical devices, and biological products.
AHRQ disseminates current healthcare data quickly and more effectively than private channels. “They look at healthcare as a whole,” explains Dr. Fishmann. “For five years, they’ve published the annual National Quality Report and the National Disparity Report. They try to zero in on information to share with the public and with physicians, including all issues related to patient safety. They allow anyone access to the information: One market is hospitalists.”
AHRQ and Hospitalists
Of course, the research and information that AHRQ provides is vital to all physicians. But Dr. Fishmann believes hospitalists find the agency particularly valuable.
“SHM perceives AHRQ as their champion,” he says. “It’s a great partnership: AHRQ documents the value of having hospitalists. SHM provides an efficient way to disseminate new information relevant to hospitals.”
Many essential data and resources for physicians can be found on AHRQ’s Web site at www.ahrq.gov.
“The average hospitalist already uses this site, but I don’t think the average resident does,” says Dr. Fishmann. “I hope everyone knows about it.” TH
Jane Jerrard has written for The Hospitalist since 2005.
What exactly is the Agency for Healthcare Research and Quality (AHRQ), and why are hospitalists urged to increase its portion of the federal budget pie each year?
According to its mission statement, the AHRQ is “the lead federal agency charged with improving the quality, safety, efficiency, and effectiveness of healthcare for all Americans.” This includes supporting high-quality, impartial research that specifically improves healthcare quality, reduces costs, advances patient safety, decreases medical errors, eliminates healthcare disparities, and broadens access to essential services.
“Supporting AHRQ is supporting an unbiased government organization that’s clearly on the side of patient safety, and that gets important information out fast,” says Andrew Fishmann, MD, FCCP, FACP, a member of AHRQ’s National Advisory Council and director of intensive care at Good Samaritan Hospital in Los Angeles. “Where’s the argument?”
Fight over Funding
The argument is over money, plain and simple. Each year, medical associations like SHM push for increased federal funding for AHRQ so the agency’s research can be expanded. And each year, Congress refuses those increases. Lawmakers have granted a slight boost in funding: Since 2002, AHRQ’s budget has increased by $2 million, or 6.7%.
Proponents of AHRQ believe precarious funding levels threaten the agency’s ability to achieve its essential mission. Last year, SHM lobbied for an increase in federal funding for AHRQ to $350 million in fiscal year 2008—$31 million more than the agency’s fiscal 2007 budget. By late 2007, Congress was weighing an increase of $329 million, plus $5 million targeted for comparative-effectiveness research.
“Think of AHRQ compared to the $28 billion that NIH gets,” says Dr. Fishmann. “[AHRQ’s] is a small budget relative to what they do.”
How much does AHRQ need to provide adequate research information? The answer is, apparently, as much as they can get. There are countless areas in healthcare the agency could address.
“If they got $500 million, could they spend it?” asks Dr. Fishmann. “Yes. They could look at the top 20 diseases instead of the top 10.”
What AHRQ Does
Regardless of the final budget amount they receive, AHRQ spends roughly 80% on grants and contracts focused on improving healthcare.
“AHRQ doesn’t do its own research or create its own data,” explains Dr. Fishmann. Rather, AHRQ conducts and supports health services research in leading academic institutions, hospitals, and other settings. In 2005, two hospitalists received separate grants for projects that have already had an effect on hospital medicine. Greg Maynard, MD, MS, division chief of hospital medicine at University of California San Diego School of Medicine, used AHRQ funds for an intervention project to prevent hospital-acquired venous thromboembolism (VTE). Dr. Maynard’s project continued to grow since that grant and has yielded key findings such as a risk-assessment model for VTE. Data and lessons learned are available in the VTE Resource Room on SHM’s Web site at www.hospitalmedicine.org/ResourceRoomRedesign/RR_LandingPage.cfm.
Asked why he went after AHRQ funding, Dr. Maynard explains: “AHRQ is one of the few [funding] agencies that focuses on the realm of implementation—that impact the patient immediately. It was a perfect marriage of what we wanted to do.” The other AHRQ-funded hospital medicine project was conducted by Mark V. Williams, MD, FACP, professor and chief, division of hospital medicine at Northwestern University Feinberg School of Medicine in Chicago, and editor of the Journal of Hospital Medicine. Working for Emory University’s hospital medicine program in Atlanta at the time, Dr. Williams used the grant to create a “discharge bundle” of patient safety interventions such as medication reconciliation and patient-centered education to improve patient safety transitions out of the hospital setting.
“We would not have been able to conduct the study without the support of AHRQ,” says Dr. Williams. “We certainly need more research funds such as this. AHRQ is the primary federal agency funding health services research—however, they receive less than 5% of the funding that goes to NIH and fund more basic science-oriented research. As few as one in 10 grants submitted to AHRQ are actually funded.”
Like Dr. Maynard’s work on VTE prevention, the injection of AHRQ funds also allowed Dr. Williams’ project to continue and grow. “With support from the Society of Hospital Medicine, we have been quite fortunate to utilize the momentum from the AHRQ Patient Safe-[Discharge] grant to obtain a $1.4 million grant from the John A. Hartford Grant to develop a discharge toolkit and facilitate implementation of it at hundreds of hospital,” he explains. “The BOOST [Better Outcomes for Older adults through Safe Transitions] project aims to improve care delivery to older adults at hospitals across America as they transition from the hospital to home.”
Additional research is developed in AHRQ’s Centers for Education and Research in Therapeutics (CERTS). Each of the 11 CERTS has a specific charge and gathers data on the benefits, risks, and cost-effectiveness of therapeutic products such as drugs, medical devices, and biological products.
AHRQ disseminates current healthcare data quickly and more effectively than private channels. “They look at healthcare as a whole,” explains Dr. Fishmann. “For five years, they’ve published the annual National Quality Report and the National Disparity Report. They try to zero in on information to share with the public and with physicians, including all issues related to patient safety. They allow anyone access to the information: One market is hospitalists.”
AHRQ and Hospitalists
Of course, the research and information that AHRQ provides is vital to all physicians. But Dr. Fishmann believes hospitalists find the agency particularly valuable.
“SHM perceives AHRQ as their champion,” he says. “It’s a great partnership: AHRQ documents the value of having hospitalists. SHM provides an efficient way to disseminate new information relevant to hospitals.”
Many essential data and resources for physicians can be found on AHRQ’s Web site at www.ahrq.gov.
“The average hospitalist already uses this site, but I don’t think the average resident does,” says Dr. Fishmann. “I hope everyone knows about it.” TH
Jane Jerrard has written for The Hospitalist since 2005.
What exactly is the Agency for Healthcare Research and Quality (AHRQ), and why are hospitalists urged to increase its portion of the federal budget pie each year?
According to its mission statement, the AHRQ is “the lead federal agency charged with improving the quality, safety, efficiency, and effectiveness of healthcare for all Americans.” This includes supporting high-quality, impartial research that specifically improves healthcare quality, reduces costs, advances patient safety, decreases medical errors, eliminates healthcare disparities, and broadens access to essential services.
“Supporting AHRQ is supporting an unbiased government organization that’s clearly on the side of patient safety, and that gets important information out fast,” says Andrew Fishmann, MD, FCCP, FACP, a member of AHRQ’s National Advisory Council and director of intensive care at Good Samaritan Hospital in Los Angeles. “Where’s the argument?”
Fight over Funding
The argument is over money, plain and simple. Each year, medical associations like SHM push for increased federal funding for AHRQ so the agency’s research can be expanded. And each year, Congress refuses those increases. Lawmakers have granted a slight boost in funding: Since 2002, AHRQ’s budget has increased by $2 million, or 6.7%.
Proponents of AHRQ believe precarious funding levels threaten the agency’s ability to achieve its essential mission. Last year, SHM lobbied for an increase in federal funding for AHRQ to $350 million in fiscal year 2008—$31 million more than the agency’s fiscal 2007 budget. By late 2007, Congress was weighing an increase of $329 million, plus $5 million targeted for comparative-effectiveness research.
“Think of AHRQ compared to the $28 billion that NIH gets,” says Dr. Fishmann. “[AHRQ’s] is a small budget relative to what they do.”
How much does AHRQ need to provide adequate research information? The answer is, apparently, as much as they can get. There are countless areas in healthcare the agency could address.
“If they got $500 million, could they spend it?” asks Dr. Fishmann. “Yes. They could look at the top 20 diseases instead of the top 10.”
What AHRQ Does
Regardless of the final budget amount they receive, AHRQ spends roughly 80% on grants and contracts focused on improving healthcare.
“AHRQ doesn’t do its own research or create its own data,” explains Dr. Fishmann. Rather, AHRQ conducts and supports health services research in leading academic institutions, hospitals, and other settings. In 2005, two hospitalists received separate grants for projects that have already had an effect on hospital medicine. Greg Maynard, MD, MS, division chief of hospital medicine at University of California San Diego School of Medicine, used AHRQ funds for an intervention project to prevent hospital-acquired venous thromboembolism (VTE). Dr. Maynard’s project continued to grow since that grant and has yielded key findings such as a risk-assessment model for VTE. Data and lessons learned are available in the VTE Resource Room on SHM’s Web site at www.hospitalmedicine.org/ResourceRoomRedesign/RR_LandingPage.cfm.
Asked why he went after AHRQ funding, Dr. Maynard explains: “AHRQ is one of the few [funding] agencies that focuses on the realm of implementation—that impact the patient immediately. It was a perfect marriage of what we wanted to do.” The other AHRQ-funded hospital medicine project was conducted by Mark V. Williams, MD, FACP, professor and chief, division of hospital medicine at Northwestern University Feinberg School of Medicine in Chicago, and editor of the Journal of Hospital Medicine. Working for Emory University’s hospital medicine program in Atlanta at the time, Dr. Williams used the grant to create a “discharge bundle” of patient safety interventions such as medication reconciliation and patient-centered education to improve patient safety transitions out of the hospital setting.
“We would not have been able to conduct the study without the support of AHRQ,” says Dr. Williams. “We certainly need more research funds such as this. AHRQ is the primary federal agency funding health services research—however, they receive less than 5% of the funding that goes to NIH and fund more basic science-oriented research. As few as one in 10 grants submitted to AHRQ are actually funded.”
Like Dr. Maynard’s work on VTE prevention, the injection of AHRQ funds also allowed Dr. Williams’ project to continue and grow. “With support from the Society of Hospital Medicine, we have been quite fortunate to utilize the momentum from the AHRQ Patient Safe-[Discharge] grant to obtain a $1.4 million grant from the John A. Hartford Grant to develop a discharge toolkit and facilitate implementation of it at hundreds of hospital,” he explains. “The BOOST [Better Outcomes for Older adults through Safe Transitions] project aims to improve care delivery to older adults at hospitals across America as they transition from the hospital to home.”
Additional research is developed in AHRQ’s Centers for Education and Research in Therapeutics (CERTS). Each of the 11 CERTS has a specific charge and gathers data on the benefits, risks, and cost-effectiveness of therapeutic products such as drugs, medical devices, and biological products.
AHRQ disseminates current healthcare data quickly and more effectively than private channels. “They look at healthcare as a whole,” explains Dr. Fishmann. “For five years, they’ve published the annual National Quality Report and the National Disparity Report. They try to zero in on information to share with the public and with physicians, including all issues related to patient safety. They allow anyone access to the information: One market is hospitalists.”
AHRQ and Hospitalists
Of course, the research and information that AHRQ provides is vital to all physicians. But Dr. Fishmann believes hospitalists find the agency particularly valuable.
“SHM perceives AHRQ as their champion,” he says. “It’s a great partnership: AHRQ documents the value of having hospitalists. SHM provides an efficient way to disseminate new information relevant to hospitals.”
Many essential data and resources for physicians can be found on AHRQ’s Web site at www.ahrq.gov.
“The average hospitalist already uses this site, but I don’t think the average resident does,” says Dr. Fishmann. “I hope everyone knows about it.” TH
Jane Jerrard has written for The Hospitalist since 2005.
Medical Mediation
How many conflicts do you witness during your average shift? How many are you embroiled in? Are any of them resolved amicably? How many can you resolve?
“Everyone does conflict resolution on some level,” says Leonard J. Marcus, PhD, director of the Program for Health Care Negotiation and Conflict Resolution, Harvard School of Public Health in Cambridge, Mass. “If you’re in a relationship, if you have kids—we all do it. The difference is that hospitalists do it as part of their professional work, and that requires a different level of complexity.” Dr. Marcus teaches conflict resolution skills in SHM’s Leadership Academy.
Everyone’s Best Interest
Dr. Marcus’ colleague and associate director of his program is Barry C. Dorn, MD, MHCM. Dr. Dorn clarifies: “Conflict is not bad. But unresolved conflict can be costly.”
A good leader can—and should—resolve problems on his team for the sake of the team, the project or work, and the hospital. Understanding that is easy—it’s how to end the problem that can be tricky.
“There are two poles to conflict resolution,” explains Dr. Marcus. “Positional bargaining is the adversarial win-lose approach to problem solving, and many people believe that’s the only way to resolve a conflict. However, interest-based negotiation focuses on what different people want to accomplish. It’s what we call a collaborative, cooperative approach—it’s gain-gain negotiating.”
How Hard Can It Be?
As Dr. Marcus says, everyone resolves conflicts. So is training in how to go about it really necessary?
“Absolutely,” asserts Dr. Dorn. “[Hospitalist leaders] need some sort of training, though a lot of it can be self-taught. I think this training is the most important thing a physician can do. The stresses and rapid changes in healthcare today make people crazy. It’s not just hospitalists—all physicians have conflicts with other groups. That conflict takes its toll; it’s a tremendous waste of time and energy. And it’s very costly to an institution to have people constantly at odds.”
Dr. Marcus agrees. “Given the role of the hospitalist, having specific skills training in conflict resolution is a huge plus,” he says. “They regularly face challenges in engaging other departments and other physicians, which can lead to turf wars and territoriality. They have to go beyond the simple ability to resolve conflicts and get to the core of the issue quickly. That’s where the training comes in.”
Conflicts among Peers
To further complicate the conflicts they face, hospitalists often find themselves managing a group of peers as committee chairs or lead researchers. They don’t have the title or authority to tell fellow hospitalists, other physicians, hospital staff, and administrators what to do. This can lead to some delicate conflict resolution.
“They’re dealing with people who lead individual silos within the healthcare system,” says Dr. Dorn. “And when someone else wants to step into their silo, it makes you and them uncomfortable. Leaders have to make others feel comfortable and learn to speak their language. Hospitalists have to lead across silos as well as within their own silo [of hospital medicine]; then they have to lead up, because hospital administrators have a lot of control. There are many nuances to leadership.”
As group leaders, hospitalists may face a wide range of conflicts, says Dr. Marcus, “from differences of opinion to resistance to downright draw-the-line-in-the-sand and get out of my way. The other piece is that some issues are clinical, whether between physicians, between physician and patient or family member, and some are administrative or managerial. Hospitalists are at the hub of all those issues; they serve as the fulcrum.”
According to Dr. Dorn, physician-physician conflicts can be disagreements of opinion, of training, of personality, and of reimbursement issues. “Physicians are very concerned with reimbursement—they want to know what it is going to cost them in time and money,” he explains.
For a hospitalist serving as a committee chair, says Dr. Dorn, “The critical thing is that when they assume these positions without authority, the only way to make it work is to increase their level of influence. The level of influence over authority is the indication of a good leader.”
You can acquire the necessary influence by learning solid conflict resolution skills.
Resolve to Study
There are a number of resources available for hospitalists interested in studying conflict resolution. Drs. Dorn and Marcus have co-written a book on the subject, Renegotiating Health Care: Resolving Conflict to Build Collaboration. “The conflicts we deal with [in the book] are right at the core of what’s going on in healthcare right now,” Dr. Marcus says.
Dr. Dorn also recommends some general books on resolving conflict. “Most of conflict resolution is interest-based negotiation, and the father of interest-based negotiation is Roger Fisher,” he says. “With Bill Ury, he wrote Getting to Yes. I think a better book for physicians is Getting Past No. It’s very simple and concise. These are basic books on conflict resolution.”
For a more detailed textbook, Dr. Dorn suggests The Mediation Process: Practical Strategies for Resolving Conflicts by Chris Moore. “This is the definitive text,” he says. “I also like Difficult Conversations by Stone, Patton, and Heen.”
Whether you’re in a leadership role or a hospitalist doing straight clinical work, successfully resolving conflicts on the job can be a much-appreciated skill. “[Conflict resolution training] will make your life so much easier, so much more pleasant,” promises Dr. Dorn. TH
Jane Jerrard writes “Public Policy” for The Hospitalist.
How many conflicts do you witness during your average shift? How many are you embroiled in? Are any of them resolved amicably? How many can you resolve?
“Everyone does conflict resolution on some level,” says Leonard J. Marcus, PhD, director of the Program for Health Care Negotiation and Conflict Resolution, Harvard School of Public Health in Cambridge, Mass. “If you’re in a relationship, if you have kids—we all do it. The difference is that hospitalists do it as part of their professional work, and that requires a different level of complexity.” Dr. Marcus teaches conflict resolution skills in SHM’s Leadership Academy.
Everyone’s Best Interest
Dr. Marcus’ colleague and associate director of his program is Barry C. Dorn, MD, MHCM. Dr. Dorn clarifies: “Conflict is not bad. But unresolved conflict can be costly.”
A good leader can—and should—resolve problems on his team for the sake of the team, the project or work, and the hospital. Understanding that is easy—it’s how to end the problem that can be tricky.
“There are two poles to conflict resolution,” explains Dr. Marcus. “Positional bargaining is the adversarial win-lose approach to problem solving, and many people believe that’s the only way to resolve a conflict. However, interest-based negotiation focuses on what different people want to accomplish. It’s what we call a collaborative, cooperative approach—it’s gain-gain negotiating.”
How Hard Can It Be?
As Dr. Marcus says, everyone resolves conflicts. So is training in how to go about it really necessary?
“Absolutely,” asserts Dr. Dorn. “[Hospitalist leaders] need some sort of training, though a lot of it can be self-taught. I think this training is the most important thing a physician can do. The stresses and rapid changes in healthcare today make people crazy. It’s not just hospitalists—all physicians have conflicts with other groups. That conflict takes its toll; it’s a tremendous waste of time and energy. And it’s very costly to an institution to have people constantly at odds.”
Dr. Marcus agrees. “Given the role of the hospitalist, having specific skills training in conflict resolution is a huge plus,” he says. “They regularly face challenges in engaging other departments and other physicians, which can lead to turf wars and territoriality. They have to go beyond the simple ability to resolve conflicts and get to the core of the issue quickly. That’s where the training comes in.”
Conflicts among Peers
To further complicate the conflicts they face, hospitalists often find themselves managing a group of peers as committee chairs or lead researchers. They don’t have the title or authority to tell fellow hospitalists, other physicians, hospital staff, and administrators what to do. This can lead to some delicate conflict resolution.
“They’re dealing with people who lead individual silos within the healthcare system,” says Dr. Dorn. “And when someone else wants to step into their silo, it makes you and them uncomfortable. Leaders have to make others feel comfortable and learn to speak their language. Hospitalists have to lead across silos as well as within their own silo [of hospital medicine]; then they have to lead up, because hospital administrators have a lot of control. There are many nuances to leadership.”
As group leaders, hospitalists may face a wide range of conflicts, says Dr. Marcus, “from differences of opinion to resistance to downright draw-the-line-in-the-sand and get out of my way. The other piece is that some issues are clinical, whether between physicians, between physician and patient or family member, and some are administrative or managerial. Hospitalists are at the hub of all those issues; they serve as the fulcrum.”
According to Dr. Dorn, physician-physician conflicts can be disagreements of opinion, of training, of personality, and of reimbursement issues. “Physicians are very concerned with reimbursement—they want to know what it is going to cost them in time and money,” he explains.
For a hospitalist serving as a committee chair, says Dr. Dorn, “The critical thing is that when they assume these positions without authority, the only way to make it work is to increase their level of influence. The level of influence over authority is the indication of a good leader.”
You can acquire the necessary influence by learning solid conflict resolution skills.
Resolve to Study
There are a number of resources available for hospitalists interested in studying conflict resolution. Drs. Dorn and Marcus have co-written a book on the subject, Renegotiating Health Care: Resolving Conflict to Build Collaboration. “The conflicts we deal with [in the book] are right at the core of what’s going on in healthcare right now,” Dr. Marcus says.
Dr. Dorn also recommends some general books on resolving conflict. “Most of conflict resolution is interest-based negotiation, and the father of interest-based negotiation is Roger Fisher,” he says. “With Bill Ury, he wrote Getting to Yes. I think a better book for physicians is Getting Past No. It’s very simple and concise. These are basic books on conflict resolution.”
For a more detailed textbook, Dr. Dorn suggests The Mediation Process: Practical Strategies for Resolving Conflicts by Chris Moore. “This is the definitive text,” he says. “I also like Difficult Conversations by Stone, Patton, and Heen.”
Whether you’re in a leadership role or a hospitalist doing straight clinical work, successfully resolving conflicts on the job can be a much-appreciated skill. “[Conflict resolution training] will make your life so much easier, so much more pleasant,” promises Dr. Dorn. TH
Jane Jerrard writes “Public Policy” for The Hospitalist.
How many conflicts do you witness during your average shift? How many are you embroiled in? Are any of them resolved amicably? How many can you resolve?
“Everyone does conflict resolution on some level,” says Leonard J. Marcus, PhD, director of the Program for Health Care Negotiation and Conflict Resolution, Harvard School of Public Health in Cambridge, Mass. “If you’re in a relationship, if you have kids—we all do it. The difference is that hospitalists do it as part of their professional work, and that requires a different level of complexity.” Dr. Marcus teaches conflict resolution skills in SHM’s Leadership Academy.
Everyone’s Best Interest
Dr. Marcus’ colleague and associate director of his program is Barry C. Dorn, MD, MHCM. Dr. Dorn clarifies: “Conflict is not bad. But unresolved conflict can be costly.”
A good leader can—and should—resolve problems on his team for the sake of the team, the project or work, and the hospital. Understanding that is easy—it’s how to end the problem that can be tricky.
“There are two poles to conflict resolution,” explains Dr. Marcus. “Positional bargaining is the adversarial win-lose approach to problem solving, and many people believe that’s the only way to resolve a conflict. However, interest-based negotiation focuses on what different people want to accomplish. It’s what we call a collaborative, cooperative approach—it’s gain-gain negotiating.”
How Hard Can It Be?
As Dr. Marcus says, everyone resolves conflicts. So is training in how to go about it really necessary?
“Absolutely,” asserts Dr. Dorn. “[Hospitalist leaders] need some sort of training, though a lot of it can be self-taught. I think this training is the most important thing a physician can do. The stresses and rapid changes in healthcare today make people crazy. It’s not just hospitalists—all physicians have conflicts with other groups. That conflict takes its toll; it’s a tremendous waste of time and energy. And it’s very costly to an institution to have people constantly at odds.”
Dr. Marcus agrees. “Given the role of the hospitalist, having specific skills training in conflict resolution is a huge plus,” he says. “They regularly face challenges in engaging other departments and other physicians, which can lead to turf wars and territoriality. They have to go beyond the simple ability to resolve conflicts and get to the core of the issue quickly. That’s where the training comes in.”
Conflicts among Peers
To further complicate the conflicts they face, hospitalists often find themselves managing a group of peers as committee chairs or lead researchers. They don’t have the title or authority to tell fellow hospitalists, other physicians, hospital staff, and administrators what to do. This can lead to some delicate conflict resolution.
“They’re dealing with people who lead individual silos within the healthcare system,” says Dr. Dorn. “And when someone else wants to step into their silo, it makes you and them uncomfortable. Leaders have to make others feel comfortable and learn to speak their language. Hospitalists have to lead across silos as well as within their own silo [of hospital medicine]; then they have to lead up, because hospital administrators have a lot of control. There are many nuances to leadership.”
As group leaders, hospitalists may face a wide range of conflicts, says Dr. Marcus, “from differences of opinion to resistance to downright draw-the-line-in-the-sand and get out of my way. The other piece is that some issues are clinical, whether between physicians, between physician and patient or family member, and some are administrative or managerial. Hospitalists are at the hub of all those issues; they serve as the fulcrum.”
According to Dr. Dorn, physician-physician conflicts can be disagreements of opinion, of training, of personality, and of reimbursement issues. “Physicians are very concerned with reimbursement—they want to know what it is going to cost them in time and money,” he explains.
For a hospitalist serving as a committee chair, says Dr. Dorn, “The critical thing is that when they assume these positions without authority, the only way to make it work is to increase their level of influence. The level of influence over authority is the indication of a good leader.”
You can acquire the necessary influence by learning solid conflict resolution skills.
Resolve to Study
There are a number of resources available for hospitalists interested in studying conflict resolution. Drs. Dorn and Marcus have co-written a book on the subject, Renegotiating Health Care: Resolving Conflict to Build Collaboration. “The conflicts we deal with [in the book] are right at the core of what’s going on in healthcare right now,” Dr. Marcus says.
Dr. Dorn also recommends some general books on resolving conflict. “Most of conflict resolution is interest-based negotiation, and the father of interest-based negotiation is Roger Fisher,” he says. “With Bill Ury, he wrote Getting to Yes. I think a better book for physicians is Getting Past No. It’s very simple and concise. These are basic books on conflict resolution.”
For a more detailed textbook, Dr. Dorn suggests The Mediation Process: Practical Strategies for Resolving Conflicts by Chris Moore. “This is the definitive text,” he says. “I also like Difficult Conversations by Stone, Patton, and Heen.”
Whether you’re in a leadership role or a hospitalist doing straight clinical work, successfully resolving conflicts on the job can be a much-appreciated skill. “[Conflict resolution training] will make your life so much easier, so much more pleasant,” promises Dr. Dorn. TH
Jane Jerrard writes “Public Policy” for The Hospitalist.
Hail Fellows
Because hospital medicine is still a new specialty, the finer points of hospitalist education and training are being developed. According to two papers in this month’s Journal of Hospital Medicine, students, hospitalists, employers—even patients—are eager for programs that allow hospitalists to hone their skills.
In one study, investigators at the University of California, San Francisco (UCSF), designed a program for third-year medical students and pharmacy graduate students emphasizing the issues involved in making the transition from inpatient to outpatient care.
Patients often are overwhelmed by the change, and the situation is ripe for miscommunication and error. Students accustomed to seeing these individuals only in the hospital often underestimate the challenges patients confront when they leave the hospital with a bewildering array of instructions and medications.
Medical students also receive little exposure to the roles of caregivers from other fields, yet good transitional care involves professionals from several disciplines. The authors, led by Cindy Lai, MD, assistant clinical professor of medicine at UCSF, reason that “training students in interdisciplinary collaboration may improve their ability to provide quality care.”
They designed an inpatient medicine clerkship curriculum in which teams of medical and pharmacy students paid a home visit to a patient they had cared for in the hospital. After the visits, the students wrote summary letters to each patient’s primary care physician.
The home visits lasted one to two hours and in general consisted of an introduction to the patient’s living quarters, a review of symptoms and medication, a brief physical examination, and a home tour to check for relevant issues such as safety hazards or the patient’s ability to function independently. Students quickly discovered the visits consisted of much more than that.
“Across the board, the response that came back was the ability to view the patient as a person,” says Heather Nye, MD, PhD, assistant clinical professor of internal medicine and one of the authors of the study. Students found it inspiring to see patients as people in control of their surroundings and also were surprised how well or poorly some people did away from the hospital.
They learned how to maximize their interaction with the pharmacy students and how to anticipate problems patients might encounter at home, such as taking medicines appropriately or scheduling and keeping follow-up appointments.
Apparently, the lessons went both ways, with some patients inviting students to stay for dinner or dessert. “That human aspect was one of the most profound features of the visits,” Dr. Nye says.
She acknowledges that scheduling home visits regularly would require a commitment of time and money that is simply not feasible in today’s environment, especially after medical school. But she urged that instruction in transitional and interdisciplinary care be incorporated into the curriculum whenever possible. “We all understand that safe discharges require multiple disciplines,” she said. “It’s never too early to start teaching about transitional care.”
Medical school training is especially important because students and residents who specialize in hospital medicine will find fellowships in short supply. The few that exist function more to train educators rather than practicing physicians.
—Philip Goodman, MD, professor of internal medicine and biomedical engineering, University of Nevada, Reno, School of Medicine
This despite the fact hospital medicine has grown at a near-exponential pace, from 2000 practitioners in 1998 to 15,000 in 2005, with 30,000 projected by 2010.
Practicing hospitalists and residents Philip Goodman, MD, MS, and Andrius Januska, BS, of the University of Nevada, Reno, School of Medicine set about to gauge the value of and interest in a practical fellowship in hospital medicine to employers. They sent questionnaires to employers and practicing hospitalists. Of 103 employers, two-thirds indicated they would offer fellowship graduates a signing bonus or salary premium ranging from $10,000 to more than $20,000.
Of 101 practicing hospitalists, 58% felt a clinical fellowship probably or strongly would be a good career move. Further, 91% said it would at least possibly be a good move. And 57% of the residents thinking of a career in hospital medicine said they would consider a one-year clinical fellowship if one were available.
“I was surprised at how strongly practicing hospitalists, most of whom are not academics, supported the value of an intense year of clinical hospital medicine fellowship training,” says Dr. Goodman, professor of internal medicine and biomedical engineering. “Most felt that graduating internal medicine residents ‘probably’ or ‘strongly’ should consider such fellowship training. I had expected a more neutral response, reflecting a balanced response bias of those with strong feelings at either extreme.”
Such training can offer new physicians a chance to develop expertise and leadership capabilities that might otherwise require years of on-the-job experience, he explains. Fellowship training also might elevate hospitalists to a level of prestige equaling that of other subspecialties, he says.
Ironically, the specialty’s rapid growth is probably slowing the establishment of fellowship programs, because residents can command annual salaries of $160,000 to $200,000 upon graduation with no special fellowship training. But a few months into it, they often realize a fellowship would have helped them master some of the unique aspects of hospital medicine, such as process of care, communication, productivity and medicolegal insight, and quality improvement, Dr. Goodman notes.
The University of Nevada will start training its first six hospitalist fellows next year. “I wouldn’t be surprised if most applicants were those who had recently taken hospitalist positions but realized the professional impact a year of polishing school can provide,” he says. TH
Norra MacReady is a medical writer based in California.
Because hospital medicine is still a new specialty, the finer points of hospitalist education and training are being developed. According to two papers in this month’s Journal of Hospital Medicine, students, hospitalists, employers—even patients—are eager for programs that allow hospitalists to hone their skills.
In one study, investigators at the University of California, San Francisco (UCSF), designed a program for third-year medical students and pharmacy graduate students emphasizing the issues involved in making the transition from inpatient to outpatient care.
Patients often are overwhelmed by the change, and the situation is ripe for miscommunication and error. Students accustomed to seeing these individuals only in the hospital often underestimate the challenges patients confront when they leave the hospital with a bewildering array of instructions and medications.
Medical students also receive little exposure to the roles of caregivers from other fields, yet good transitional care involves professionals from several disciplines. The authors, led by Cindy Lai, MD, assistant clinical professor of medicine at UCSF, reason that “training students in interdisciplinary collaboration may improve their ability to provide quality care.”
They designed an inpatient medicine clerkship curriculum in which teams of medical and pharmacy students paid a home visit to a patient they had cared for in the hospital. After the visits, the students wrote summary letters to each patient’s primary care physician.
The home visits lasted one to two hours and in general consisted of an introduction to the patient’s living quarters, a review of symptoms and medication, a brief physical examination, and a home tour to check for relevant issues such as safety hazards or the patient’s ability to function independently. Students quickly discovered the visits consisted of much more than that.
“Across the board, the response that came back was the ability to view the patient as a person,” says Heather Nye, MD, PhD, assistant clinical professor of internal medicine and one of the authors of the study. Students found it inspiring to see patients as people in control of their surroundings and also were surprised how well or poorly some people did away from the hospital.
They learned how to maximize their interaction with the pharmacy students and how to anticipate problems patients might encounter at home, such as taking medicines appropriately or scheduling and keeping follow-up appointments.
Apparently, the lessons went both ways, with some patients inviting students to stay for dinner or dessert. “That human aspect was one of the most profound features of the visits,” Dr. Nye says.
She acknowledges that scheduling home visits regularly would require a commitment of time and money that is simply not feasible in today’s environment, especially after medical school. But she urged that instruction in transitional and interdisciplinary care be incorporated into the curriculum whenever possible. “We all understand that safe discharges require multiple disciplines,” she said. “It’s never too early to start teaching about transitional care.”
Medical school training is especially important because students and residents who specialize in hospital medicine will find fellowships in short supply. The few that exist function more to train educators rather than practicing physicians.
—Philip Goodman, MD, professor of internal medicine and biomedical engineering, University of Nevada, Reno, School of Medicine
This despite the fact hospital medicine has grown at a near-exponential pace, from 2000 practitioners in 1998 to 15,000 in 2005, with 30,000 projected by 2010.
Practicing hospitalists and residents Philip Goodman, MD, MS, and Andrius Januska, BS, of the University of Nevada, Reno, School of Medicine set about to gauge the value of and interest in a practical fellowship in hospital medicine to employers. They sent questionnaires to employers and practicing hospitalists. Of 103 employers, two-thirds indicated they would offer fellowship graduates a signing bonus or salary premium ranging from $10,000 to more than $20,000.
Of 101 practicing hospitalists, 58% felt a clinical fellowship probably or strongly would be a good career move. Further, 91% said it would at least possibly be a good move. And 57% of the residents thinking of a career in hospital medicine said they would consider a one-year clinical fellowship if one were available.
“I was surprised at how strongly practicing hospitalists, most of whom are not academics, supported the value of an intense year of clinical hospital medicine fellowship training,” says Dr. Goodman, professor of internal medicine and biomedical engineering. “Most felt that graduating internal medicine residents ‘probably’ or ‘strongly’ should consider such fellowship training. I had expected a more neutral response, reflecting a balanced response bias of those with strong feelings at either extreme.”
Such training can offer new physicians a chance to develop expertise and leadership capabilities that might otherwise require years of on-the-job experience, he explains. Fellowship training also might elevate hospitalists to a level of prestige equaling that of other subspecialties, he says.
Ironically, the specialty’s rapid growth is probably slowing the establishment of fellowship programs, because residents can command annual salaries of $160,000 to $200,000 upon graduation with no special fellowship training. But a few months into it, they often realize a fellowship would have helped them master some of the unique aspects of hospital medicine, such as process of care, communication, productivity and medicolegal insight, and quality improvement, Dr. Goodman notes.
The University of Nevada will start training its first six hospitalist fellows next year. “I wouldn’t be surprised if most applicants were those who had recently taken hospitalist positions but realized the professional impact a year of polishing school can provide,” he says. TH
Norra MacReady is a medical writer based in California.
Because hospital medicine is still a new specialty, the finer points of hospitalist education and training are being developed. According to two papers in this month’s Journal of Hospital Medicine, students, hospitalists, employers—even patients—are eager for programs that allow hospitalists to hone their skills.
In one study, investigators at the University of California, San Francisco (UCSF), designed a program for third-year medical students and pharmacy graduate students emphasizing the issues involved in making the transition from inpatient to outpatient care.
Patients often are overwhelmed by the change, and the situation is ripe for miscommunication and error. Students accustomed to seeing these individuals only in the hospital often underestimate the challenges patients confront when they leave the hospital with a bewildering array of instructions and medications.
Medical students also receive little exposure to the roles of caregivers from other fields, yet good transitional care involves professionals from several disciplines. The authors, led by Cindy Lai, MD, assistant clinical professor of medicine at UCSF, reason that “training students in interdisciplinary collaboration may improve their ability to provide quality care.”
They designed an inpatient medicine clerkship curriculum in which teams of medical and pharmacy students paid a home visit to a patient they had cared for in the hospital. After the visits, the students wrote summary letters to each patient’s primary care physician.
The home visits lasted one to two hours and in general consisted of an introduction to the patient’s living quarters, a review of symptoms and medication, a brief physical examination, and a home tour to check for relevant issues such as safety hazards or the patient’s ability to function independently. Students quickly discovered the visits consisted of much more than that.
“Across the board, the response that came back was the ability to view the patient as a person,” says Heather Nye, MD, PhD, assistant clinical professor of internal medicine and one of the authors of the study. Students found it inspiring to see patients as people in control of their surroundings and also were surprised how well or poorly some people did away from the hospital.
They learned how to maximize their interaction with the pharmacy students and how to anticipate problems patients might encounter at home, such as taking medicines appropriately or scheduling and keeping follow-up appointments.
Apparently, the lessons went both ways, with some patients inviting students to stay for dinner or dessert. “That human aspect was one of the most profound features of the visits,” Dr. Nye says.
She acknowledges that scheduling home visits regularly would require a commitment of time and money that is simply not feasible in today’s environment, especially after medical school. But she urged that instruction in transitional and interdisciplinary care be incorporated into the curriculum whenever possible. “We all understand that safe discharges require multiple disciplines,” she said. “It’s never too early to start teaching about transitional care.”
Medical school training is especially important because students and residents who specialize in hospital medicine will find fellowships in short supply. The few that exist function more to train educators rather than practicing physicians.
—Philip Goodman, MD, professor of internal medicine and biomedical engineering, University of Nevada, Reno, School of Medicine
This despite the fact hospital medicine has grown at a near-exponential pace, from 2000 practitioners in 1998 to 15,000 in 2005, with 30,000 projected by 2010.
Practicing hospitalists and residents Philip Goodman, MD, MS, and Andrius Januska, BS, of the University of Nevada, Reno, School of Medicine set about to gauge the value of and interest in a practical fellowship in hospital medicine to employers. They sent questionnaires to employers and practicing hospitalists. Of 103 employers, two-thirds indicated they would offer fellowship graduates a signing bonus or salary premium ranging from $10,000 to more than $20,000.
Of 101 practicing hospitalists, 58% felt a clinical fellowship probably or strongly would be a good career move. Further, 91% said it would at least possibly be a good move. And 57% of the residents thinking of a career in hospital medicine said they would consider a one-year clinical fellowship if one were available.
“I was surprised at how strongly practicing hospitalists, most of whom are not academics, supported the value of an intense year of clinical hospital medicine fellowship training,” says Dr. Goodman, professor of internal medicine and biomedical engineering. “Most felt that graduating internal medicine residents ‘probably’ or ‘strongly’ should consider such fellowship training. I had expected a more neutral response, reflecting a balanced response bias of those with strong feelings at either extreme.”
Such training can offer new physicians a chance to develop expertise and leadership capabilities that might otherwise require years of on-the-job experience, he explains. Fellowship training also might elevate hospitalists to a level of prestige equaling that of other subspecialties, he says.
Ironically, the specialty’s rapid growth is probably slowing the establishment of fellowship programs, because residents can command annual salaries of $160,000 to $200,000 upon graduation with no special fellowship training. But a few months into it, they often realize a fellowship would have helped them master some of the unique aspects of hospital medicine, such as process of care, communication, productivity and medicolegal insight, and quality improvement, Dr. Goodman notes.
The University of Nevada will start training its first six hospitalist fellows next year. “I wouldn’t be surprised if most applicants were those who had recently taken hospitalist positions but realized the professional impact a year of polishing school can provide,” he says. TH
Norra MacReady is a medical writer based in California.
Liver Risks Abound
Drug-induced liver injury (DILI) or hepatotoxicity accounts for more than 50% of all cases of acute liver failure. DILI, often life-threatening, is the leading cause of patient referral for liver transplantation.1,2
DILI is an important diagnostic challenge for the treating clinician because of its presentation, which is often a diagnosis of exclusion. Determination of all potential causes of hepatic injury need to be assessed through onset of symptoms and a careful drug history (including prescription and over-the-counter medication, dietary supplements, and complementary and alternative therapies).3
DILI has brought an increase in Food and Drug Administration (FDA) “black box” warnings. Among the drugs affected are ketoconazole, pemoline, tolcapone, valproate sodium, and zalcitabine.4
A number of drugs have been withdrawn from the U.S. market after DILI or interactions with those that are hepatically metabolized, such as:
- Astemizole (cardiotoxicity);
- Bromfenac sodium, cisapride (cardiotoxicity);
- Felbamate, mibefradil (cardiotoxicity);
- Temafloxacin (abnormal liver function tests, as well as renal failure and other serious adverse events);
- Terfenadine (cardiotoxicity);
- Troglitazone; and
- Trovafloxacin mesylate.
One of the most common causes of DILI is intentional or unintentional overdose with acetaminophen.
DILI has been classified into two major types: cholestatic and hepatocellular, or cytolytic injury. In cholestatic liver injury, the serum alkaline phosphatase (ALP) is elevated; total bilirubin level (TBL) and the alanine aminotransferase (ALT) may also be elevated. In hepatocellular injury, initial elevation is noted in the ALT.
There may also be overlap in the pattern of injury (mixed-pattern injury) whereby ALP and ALT are elevated. These patterns of injury may be defined further by the degree of enzyme elevation, such as an ALT level of three or more times the upper limit of normal (ULN), an ALP level two or more times ULN, and TBL two or more times ULN if associated with an elevation of ALP or ALT.
Hepatotoxicity is often predictable—but not always. When predictable, the reaction is usually dose-dependent, such as in the case of acetaminophen. These reactions usually occur shortly after a threshold for toxicity has been reached. Unpredictable reactions can occur days or months after exposure, usually without warning. Hypersensitivity reactions are often delayed and occur upon repeated exposure to the agent. Symptoms of immunologic injury may include rash, fever, or eosinophilia. More severe forms include Stevens-Johnson syndrome, toxic epidermal necrolysis, or cytopenias. Reactions are more severe upon repeat exposure or rechallenge of the offending agent.
Symptomatology
Patients usually present with vague symptoms that may include nausea, anorexia, fatigue, right upper-quadrant discomfort, jaundice, or dark urine. Patients with cholestatic liver disease may also present with pruritus.
Any of these along with laboratory evidence of liver injury should indicate further investigation into possible DILI. Impaired hepatic function such as increased prothrombin time and encephalopathy (signs of acute liver failure) indicate severe hepatic injury.
The Agents
Common causes of hepatocellular injury include: acetaminophen, fluoxetine, highly active antiretroviral therapies, kava kava (other herbal products), non-steroidal anti-inflammatory drugs, paroxetine, rifampin, risperidone, statins, trazodone, and troglitazone.
Common causes of cholestatic injury include: ampicillin-clavulanic acid, anabolic steroids, chlorpromazine, clopidogrel, estrogens, mirtazapine, terbinafine, and tricyclics.
Common causes of mixed-pattern injury include: amitriptyline, azathioprine, captopril, carbamazepine, enalapril, erythromycins, flutamide, phenytoin, sulfonamides, trazodone, and trimethoprim-sulfamethoxazole.
Most cases of non-fulminant hepatitis will improve upon cessation of offending or potentially offending agent(s). Assess hepatic injury immediately via continuously obtained biochemical tests.
Consult a hepatologist or gastroenterologist immediately if jaundice, impaired hepatic function or clinical signs of acute hepatic failure (e.g., encephalopathy) are evident.
Report all cases of potential DILI to the FDA’s adverse events reporting program, Medwatch, at www.fda.gov/ medwatch or by calling (800) 332-1088. For patients receiving potentially hepatotoxic agents, liver function test monitoring is recommended following a baseline assessment. Some agents require monthly rather than periodic monitoring. For a list of some agents that require hepatic monitoring and the recommended frequency, visit www.factsandcomparisons.com/assets/hospitalpharm/feb2002_HepSp.pdf.5 TH
Michele B. Kaufman is a freelance medical writer based in New York City.
References
- Nathwani RA, Kaplowitz N. Drug hepatotoxicity. Clin Liver Dis. 2006;10:207-217.
- Navarro VJ, Senior JR. Drug-related hepatotoxicity. N Engl J Med. 2006;354(7):731-739.
- Hepatic Toxicity Possibly Associated with Kava-Containing Products—United States, Germany, and Switzerland, 1999-2002. MMWR Weekly, Nov. 29, 2002/51(47):1065-1067. Available at: www.cdc.gov/MMWR/previews/mmwrhtml/mm5147a1.htm. Last accessed Nov. 5, 2007.
- Lasser KE, Allen PD, Woolhandler SJ, et al. Timing of new black box warnings and withdrawals for prescription medications. JAMA. 2002;287:17:2215-2220.
- Tice SA, Parr D. Medications that require hepatic monitoring. Hospital Pharmacy 2004;39(6):595-606.
Drug-induced liver injury (DILI) or hepatotoxicity accounts for more than 50% of all cases of acute liver failure. DILI, often life-threatening, is the leading cause of patient referral for liver transplantation.1,2
DILI is an important diagnostic challenge for the treating clinician because of its presentation, which is often a diagnosis of exclusion. Determination of all potential causes of hepatic injury need to be assessed through onset of symptoms and a careful drug history (including prescription and over-the-counter medication, dietary supplements, and complementary and alternative therapies).3
DILI has brought an increase in Food and Drug Administration (FDA) “black box” warnings. Among the drugs affected are ketoconazole, pemoline, tolcapone, valproate sodium, and zalcitabine.4
A number of drugs have been withdrawn from the U.S. market after DILI or interactions with those that are hepatically metabolized, such as:
- Astemizole (cardiotoxicity);
- Bromfenac sodium, cisapride (cardiotoxicity);
- Felbamate, mibefradil (cardiotoxicity);
- Temafloxacin (abnormal liver function tests, as well as renal failure and other serious adverse events);
- Terfenadine (cardiotoxicity);
- Troglitazone; and
- Trovafloxacin mesylate.
One of the most common causes of DILI is intentional or unintentional overdose with acetaminophen.
DILI has been classified into two major types: cholestatic and hepatocellular, or cytolytic injury. In cholestatic liver injury, the serum alkaline phosphatase (ALP) is elevated; total bilirubin level (TBL) and the alanine aminotransferase (ALT) may also be elevated. In hepatocellular injury, initial elevation is noted in the ALT.
There may also be overlap in the pattern of injury (mixed-pattern injury) whereby ALP and ALT are elevated. These patterns of injury may be defined further by the degree of enzyme elevation, such as an ALT level of three or more times the upper limit of normal (ULN), an ALP level two or more times ULN, and TBL two or more times ULN if associated with an elevation of ALP or ALT.
Hepatotoxicity is often predictable—but not always. When predictable, the reaction is usually dose-dependent, such as in the case of acetaminophen. These reactions usually occur shortly after a threshold for toxicity has been reached. Unpredictable reactions can occur days or months after exposure, usually without warning. Hypersensitivity reactions are often delayed and occur upon repeated exposure to the agent. Symptoms of immunologic injury may include rash, fever, or eosinophilia. More severe forms include Stevens-Johnson syndrome, toxic epidermal necrolysis, or cytopenias. Reactions are more severe upon repeat exposure or rechallenge of the offending agent.
Symptomatology
Patients usually present with vague symptoms that may include nausea, anorexia, fatigue, right upper-quadrant discomfort, jaundice, or dark urine. Patients with cholestatic liver disease may also present with pruritus.
Any of these along with laboratory evidence of liver injury should indicate further investigation into possible DILI. Impaired hepatic function such as increased prothrombin time and encephalopathy (signs of acute liver failure) indicate severe hepatic injury.
The Agents
Common causes of hepatocellular injury include: acetaminophen, fluoxetine, highly active antiretroviral therapies, kava kava (other herbal products), non-steroidal anti-inflammatory drugs, paroxetine, rifampin, risperidone, statins, trazodone, and troglitazone.
Common causes of cholestatic injury include: ampicillin-clavulanic acid, anabolic steroids, chlorpromazine, clopidogrel, estrogens, mirtazapine, terbinafine, and tricyclics.
Common causes of mixed-pattern injury include: amitriptyline, azathioprine, captopril, carbamazepine, enalapril, erythromycins, flutamide, phenytoin, sulfonamides, trazodone, and trimethoprim-sulfamethoxazole.
Most cases of non-fulminant hepatitis will improve upon cessation of offending or potentially offending agent(s). Assess hepatic injury immediately via continuously obtained biochemical tests.
Consult a hepatologist or gastroenterologist immediately if jaundice, impaired hepatic function or clinical signs of acute hepatic failure (e.g., encephalopathy) are evident.
Report all cases of potential DILI to the FDA’s adverse events reporting program, Medwatch, at www.fda.gov/ medwatch or by calling (800) 332-1088. For patients receiving potentially hepatotoxic agents, liver function test monitoring is recommended following a baseline assessment. Some agents require monthly rather than periodic monitoring. For a list of some agents that require hepatic monitoring and the recommended frequency, visit www.factsandcomparisons.com/assets/hospitalpharm/feb2002_HepSp.pdf.5 TH
Michele B. Kaufman is a freelance medical writer based in New York City.
References
- Nathwani RA, Kaplowitz N. Drug hepatotoxicity. Clin Liver Dis. 2006;10:207-217.
- Navarro VJ, Senior JR. Drug-related hepatotoxicity. N Engl J Med. 2006;354(7):731-739.
- Hepatic Toxicity Possibly Associated with Kava-Containing Products—United States, Germany, and Switzerland, 1999-2002. MMWR Weekly, Nov. 29, 2002/51(47):1065-1067. Available at: www.cdc.gov/MMWR/previews/mmwrhtml/mm5147a1.htm. Last accessed Nov. 5, 2007.
- Lasser KE, Allen PD, Woolhandler SJ, et al. Timing of new black box warnings and withdrawals for prescription medications. JAMA. 2002;287:17:2215-2220.
- Tice SA, Parr D. Medications that require hepatic monitoring. Hospital Pharmacy 2004;39(6):595-606.
Drug-induced liver injury (DILI) or hepatotoxicity accounts for more than 50% of all cases of acute liver failure. DILI, often life-threatening, is the leading cause of patient referral for liver transplantation.1,2
DILI is an important diagnostic challenge for the treating clinician because of its presentation, which is often a diagnosis of exclusion. Determination of all potential causes of hepatic injury need to be assessed through onset of symptoms and a careful drug history (including prescription and over-the-counter medication, dietary supplements, and complementary and alternative therapies).3
DILI has brought an increase in Food and Drug Administration (FDA) “black box” warnings. Among the drugs affected are ketoconazole, pemoline, tolcapone, valproate sodium, and zalcitabine.4
A number of drugs have been withdrawn from the U.S. market after DILI or interactions with those that are hepatically metabolized, such as:
- Astemizole (cardiotoxicity);
- Bromfenac sodium, cisapride (cardiotoxicity);
- Felbamate, mibefradil (cardiotoxicity);
- Temafloxacin (abnormal liver function tests, as well as renal failure and other serious adverse events);
- Terfenadine (cardiotoxicity);
- Troglitazone; and
- Trovafloxacin mesylate.
One of the most common causes of DILI is intentional or unintentional overdose with acetaminophen.
DILI has been classified into two major types: cholestatic and hepatocellular, or cytolytic injury. In cholestatic liver injury, the serum alkaline phosphatase (ALP) is elevated; total bilirubin level (TBL) and the alanine aminotransferase (ALT) may also be elevated. In hepatocellular injury, initial elevation is noted in the ALT.
There may also be overlap in the pattern of injury (mixed-pattern injury) whereby ALP and ALT are elevated. These patterns of injury may be defined further by the degree of enzyme elevation, such as an ALT level of three or more times the upper limit of normal (ULN), an ALP level two or more times ULN, and TBL two or more times ULN if associated with an elevation of ALP or ALT.
Hepatotoxicity is often predictable—but not always. When predictable, the reaction is usually dose-dependent, such as in the case of acetaminophen. These reactions usually occur shortly after a threshold for toxicity has been reached. Unpredictable reactions can occur days or months after exposure, usually without warning. Hypersensitivity reactions are often delayed and occur upon repeated exposure to the agent. Symptoms of immunologic injury may include rash, fever, or eosinophilia. More severe forms include Stevens-Johnson syndrome, toxic epidermal necrolysis, or cytopenias. Reactions are more severe upon repeat exposure or rechallenge of the offending agent.
Symptomatology
Patients usually present with vague symptoms that may include nausea, anorexia, fatigue, right upper-quadrant discomfort, jaundice, or dark urine. Patients with cholestatic liver disease may also present with pruritus.
Any of these along with laboratory evidence of liver injury should indicate further investigation into possible DILI. Impaired hepatic function such as increased prothrombin time and encephalopathy (signs of acute liver failure) indicate severe hepatic injury.
The Agents
Common causes of hepatocellular injury include: acetaminophen, fluoxetine, highly active antiretroviral therapies, kava kava (other herbal products), non-steroidal anti-inflammatory drugs, paroxetine, rifampin, risperidone, statins, trazodone, and troglitazone.
Common causes of cholestatic injury include: ampicillin-clavulanic acid, anabolic steroids, chlorpromazine, clopidogrel, estrogens, mirtazapine, terbinafine, and tricyclics.
Common causes of mixed-pattern injury include: amitriptyline, azathioprine, captopril, carbamazepine, enalapril, erythromycins, flutamide, phenytoin, sulfonamides, trazodone, and trimethoprim-sulfamethoxazole.
Most cases of non-fulminant hepatitis will improve upon cessation of offending or potentially offending agent(s). Assess hepatic injury immediately via continuously obtained biochemical tests.
Consult a hepatologist or gastroenterologist immediately if jaundice, impaired hepatic function or clinical signs of acute hepatic failure (e.g., encephalopathy) are evident.
Report all cases of potential DILI to the FDA’s adverse events reporting program, Medwatch, at www.fda.gov/ medwatch or by calling (800) 332-1088. For patients receiving potentially hepatotoxic agents, liver function test monitoring is recommended following a baseline assessment. Some agents require monthly rather than periodic monitoring. For a list of some agents that require hepatic monitoring and the recommended frequency, visit www.factsandcomparisons.com/assets/hospitalpharm/feb2002_HepSp.pdf.5 TH
Michele B. Kaufman is a freelance medical writer based in New York City.
References
- Nathwani RA, Kaplowitz N. Drug hepatotoxicity. Clin Liver Dis. 2006;10:207-217.
- Navarro VJ, Senior JR. Drug-related hepatotoxicity. N Engl J Med. 2006;354(7):731-739.
- Hepatic Toxicity Possibly Associated with Kava-Containing Products—United States, Germany, and Switzerland, 1999-2002. MMWR Weekly, Nov. 29, 2002/51(47):1065-1067. Available at: www.cdc.gov/MMWR/previews/mmwrhtml/mm5147a1.htm. Last accessed Nov. 5, 2007.
- Lasser KE, Allen PD, Woolhandler SJ, et al. Timing of new black box warnings and withdrawals for prescription medications. JAMA. 2002;287:17:2215-2220.
- Tice SA, Parr D. Medications that require hepatic monitoring. Hospital Pharmacy 2004;39(6):595-606.
Can CT coronary angiography effectively rule out coronary disease in a patient admitted with chest pain?
Case
A 58-year-old male with a past medical history significant for hypertension and hypercholesterolemia presents four hours after acute onset of substernal chest pain that rates eight on a scale of 10. There is no radiation of the pain or associated dyspnea. He describes diaphoresis and nausea. Cardiac enzymes are negative on admission, and the electrocardiogram (ECG) is unchanged. Can computed tomography (CT) coronary angiography effectively rule out coronary disease in this patient admitted with chest pain?
Overview
Approximately 5 million patients presented to U.S. hospitals in 2002 for evaluation of chest pain.1 Less than a third of these patients were ultimately diagnosed with acute coronary syndrome.2 Current strategies to differentiate acute coronary syndrome from non-cardiac causes of chest pain have included electrocardiography, cardiac enzymes, exercise treadmill, echocardiography, and nuclear perfusion.
Unfortunately, each of these modalities has false positive and negative rates that result in a significant number of patients undergoing further evaluation for coronary artery stenosis. Although coronary angiography is the current gold standard to evaluate coronary luminal obstruction, it has many drawbacks. It is costly and inconvenient for patients, invasive, and demonstrates only the later stages of atherosclerosis—not which plaques are prone to rupture. All these limitations necessitate a search for a non-invasive evaluation of the coronary vasculature.
Because 64-slice CT scanners allow for visualization of the cardiac anatomy and coronary vasculature without catheters, there has been increasing interest in this modality to evaluate for coronary artery stenosis in low- to intermediate-risk patients presenting with chest pain. Comparative studies have found it allows for faster, safer evaluation of chest pain with sensitivity and specificity comparable to traditional angiography and a negative predictive value superior to nuclear imaging.3,4
Additional advantages include easy access to CT scanners over cardiac catheterization facilities; 88% of community hospitals with six or more beds had CT scanners in 2004. Further, turnaround is faster (15 to 20 minutes for the CT angiography versus six to eight hours of observation after cardiac catheterization). Also, physicians can simultaneously exclude other life-threatening causes of chest pain including aortic dissection and pulmonary embolus.5 Finally, CT angiography is less expensive (about $800 to $1,000) than invasive coronary angiography (approximately $3,000 to $4,000).6
Review of the Data
Patients undergoing CT angiography require a target heart rate of less than 70 beats per minute. Oral or intravenous beta-blockers are typically given prior to the procedure.
Nitroglycerin 0.4-0.8 mg is also administered sublingually to enhance visualization of the coronary vasculature.
Pulse, ECG, and blood pressure are monitored throughout the imaging process. Initially, a non-contrast scan is performed for coronary artery calcium (CAC) scoring. This is followed by angiography using a bolus of iodinated contrast. At this time, multislice cardiac scanning is synchronized with an ECG (i.e., gating the scan) and images are obtained during diastole.
Two types of CT are capable of obtaining the necessary high-speed images. Electron-beam CT (EBCT) and helical or spiral CT scanning. Multidetector helical CT (MDCT) or multislice CT (MSCT) is an evolution of helical CT. MDCT is available in four-, eight-, 16-, 32-, or 64-slice. Interpretation of the imaging uses the American College of Cardiology nomenclature: no stenosis, insignificant stenosis (less than 50% of coronary luminal diameter), significant stenosis (more than 50%), and total occlusion.
The presence of CAC has been shown in numerous studies to have prognostic significance for cardiac events and death. An elevated CAC score more accurately predicts coronary heart disease (CHD) risk in adults with an initial Framingham risk score between 10% and 19%. In addition, compared with a CAC score of zero, a score of more than 300 was predictive of CHD risk.7
Some studies suggest negative CAC scores alone are enough to risk-stratify patients presenting with chest pain, reporting sensitivities between 96% and 100% for the detection of significant cardiac events.8
Clinical studies of CT angiography typically consist of patients already selected to receive traditional invasive coronary angiography. Initial reports by Leschka, et al., showed sensitivity and specificity of 94% and 97%, respectively, with positive predictive values and negative predictive values of 87% and 99%.9
Additionally, a meta-analysis revealed multislice computed tomography (MSCT) for the diagnosis of CHD was highly sensitive (95% to 100%) for the detection of significant CHD. Specificity was 100% with the 64-slice MSCT and only slightly lower with the four- and 16-slice scanners (87%). A positive predictive value of 66% and negative predictive value of 98% for the presence of significant coronary stenosis have also been reported.10
Gallagher, et al., and previous studies comparing CT angiography with traditional invasive coronary angiography suggest further testing, such as stress nuclear imaging for any patient with stenosis more than 25% or CCS of greater than 100 and further recommends cardiac catheterization of any patient with greater than 70% stenosis by MSCT.
The utility of CT coronary angiography in the evaluation of patients presenting to the ED with chest pain was studied by Goldstein and peers.11 A randomized trial was conducted with patients admitted with chest pain or anginal equivalent, considered to be at low risk for CAD. Patients with negative cardiac enzymes and non-diagnostic ECG were assigned to either MSCCT or myocardial perfusion scan. CT angiography was adequate to diagnose or exclude CAD as the cause of chest pain in 75% of patients. The remaining 25% of patients had additional nuclear stress imaging. Average cost of the MDCT cohort was $1,586 compared with $1,872 for standard diagnostic evaluation. The time required for diagnosis was significantly shorter in the CT cohort: 3.4 hours, compared with 15 hours in the standard group.
An ongoing study at Beaumont Hospital in Royal Oak, Mich., is evaluating the length of stay and cost of care in patients presenting to the ED with chest pain. Patients are randomized to standard evaluation with serial enzymes, ECG, and nuclear perfusion testing or 64-slice CT angiography, plus coronary calcium score. Preliminary results presented at the 2006 American College of Cardiology Annual Scientific Session regarding the initial 200 patients showed a shorter length of stay and lower cost of care with similar patient outcomes in the group that underwent CT angiography.12
A large randomized controlled trial, Coronary Computed Tomography for Systematic Triage of Acute Chest Pain Patients to Treatment (CT-STAT), is planned to definitively study the use of coronary CT angiography in low-risk patients with chest pain. The large-scale study will involve 750 patients in 15 U.S. hospitals.
CT angiography remains limited despite many recent advances. A stable rhythm is a prerequisite, precluding use in patients with atrial fibrillation or frequent extra-systoles. Also, the required dose of 80 cc to 100 cc of iodinated contrast puts patients at risk for contrast-induced nephropathy, especially those with renal insufficiency.
Finally, radiation exposure is higher than that required for cardiac catheterization.13 Coronary calcification interferes with the images obtained by CT. Therefore, patients with heavy coronary calcium burden (CAC more than 400) may have reduced specificity and negative predictive value. Because this calcification increases with age, the diagnostic accuracy of CT angiography may decrease with age.
Morbidly obese patients may also have decreased image quality. Raff. et al., found significant stenosis in patients with normal body-mass index (BMI) (less than 25 kg/m2). Sensitivity, specificity, and positive and negative predictive values were all 100% and remained accurate in overweight patients. When BMI was more than 30, sensitivity and specificity were reduced to 90% and 86%, respectively.
Visualization of the coronary artery within a stent may be less accurate with CT angiography due to beam artifact, but evaluation of native coronary arteries and bypass grafts maintain similar sensitivity and specificity in these patients.14 A final concern is that CT angiography is only diagnostic. Although only 25% to 30% of diagnostic cardiac catheterizations reveal disease that meets criteria for stent placement, the study is redundant in these high-risk patients, who likely will be referred for traditional coronary angiography with stenting.
Back to the Case
The patient underwent nuclear stress testing the morning following admission. He had minimal attenuation in the infero-lateral distribution. A 64-slice CT angiogram was obtained, and images of the coronary anatomy demonstrated no plaque. The patient was reassured, and no further cardiac imaging was pursued. TH
Dr. Jenkins is an associate clinical professor and associate chief of hospital medicine in the Department of Family Medicine and Community Health at the University of Massachusetts medical school, Worcester.
References
- Statistics CNCH, ed. National Hospital Ambulatory Medical Care Survey: 2002 Emergency Department Summary, 2004. Available at www.cdc.gov/nchs/pressroom/04facts/emergencydept.htm. Last accessed Nov. 8, 2007.
- Kohn MA, Kwan E, Gupta M, et al. Prevalence of acute myocardial infarction and other serious diagnoses in patients presenting to an urban emergency department with chest pain. J Emerg Med. 2005;29(4):383-390.
- Stein PD, Beemath A, Kayali F, et al. Multidetector computed tomography for the diagnosis of coronary artery disease: a systematic review. Am J Med. 2006;119(3):203-216.
- Gallagher MJ, Ross MA, Raff G, et al. The diagnostic accuracy of 64-slice computed tomography coronary angiography compared with stress nuclear imaging in emergency department low-risk chest pain patients. Ann of Emerg Med. 200;49(2):125-136.
- AHA Hospital Statistics, 2006 Edition. Chicago: American Hospital Association; 2006:158, 161.
- Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, HCUPnet. Available at www.ahrq.gov/data/hcup. Last accessed Nov. 8, 2007.
- Greenland P, LaBree L, Azen SP, et al. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA. 2004;291(2):210-215.
- Kondos GT, Hoff JA, Sevrkov A, et al. Electron-beam tomography coronary artery calcium and cardiac events: a 37-month follow-up of 5,635 initially asymptomatic low- to intermediate-risk adults. Circulation. 2003;107(20):2571-2676.
- Leschka S, Alkadhi H, Plass A, et al. Accuracy of MSCT coronary angiography with 64-slice technology: first experience. Eur Heart J. 2005;177:1482-1487.
- Raff GL, Gallagher MJ, O’Neill WW, et al. Diagnostic accuracy of noninvasive coronary angiography using 64-slice spiral computed tomography. J Am Coll Cardiol. 2005;46:552-557.
- Goldstein JA, Gallagher MJ, O’Neill WW, et al. A randomized controlled trial of multi-slice coronary computed tomography for evaluation of acute chest pain. J Am Coll Cardiol. 2007;49(8):863-871.
- Raff GL, Gallagher MJ, O’Neill WW. Immediate coronary artery computed tomographic angiography rapidly and definitively excludes coronary artery disease in low-risk acute chest pain. Abstract 807-8. 55th Annual Scientific Session of the American College of Cardiology, March 11-14, 2006.
- de Feyter PJ, Nieman K. Noninvasive multi-slice computed tomography coronary angiography: an emerging clinical modality. J Am Coll Cardiol. 2004;44(6):1238-1240.
- Garcia MJ. Noninvasive coronary angiography: hype or new paradigm? J Am Med Assoc. 2005; 293:2531-2533.
Case
A 58-year-old male with a past medical history significant for hypertension and hypercholesterolemia presents four hours after acute onset of substernal chest pain that rates eight on a scale of 10. There is no radiation of the pain or associated dyspnea. He describes diaphoresis and nausea. Cardiac enzymes are negative on admission, and the electrocardiogram (ECG) is unchanged. Can computed tomography (CT) coronary angiography effectively rule out coronary disease in this patient admitted with chest pain?
Overview
Approximately 5 million patients presented to U.S. hospitals in 2002 for evaluation of chest pain.1 Less than a third of these patients were ultimately diagnosed with acute coronary syndrome.2 Current strategies to differentiate acute coronary syndrome from non-cardiac causes of chest pain have included electrocardiography, cardiac enzymes, exercise treadmill, echocardiography, and nuclear perfusion.
Unfortunately, each of these modalities has false positive and negative rates that result in a significant number of patients undergoing further evaluation for coronary artery stenosis. Although coronary angiography is the current gold standard to evaluate coronary luminal obstruction, it has many drawbacks. It is costly and inconvenient for patients, invasive, and demonstrates only the later stages of atherosclerosis—not which plaques are prone to rupture. All these limitations necessitate a search for a non-invasive evaluation of the coronary vasculature.
Because 64-slice CT scanners allow for visualization of the cardiac anatomy and coronary vasculature without catheters, there has been increasing interest in this modality to evaluate for coronary artery stenosis in low- to intermediate-risk patients presenting with chest pain. Comparative studies have found it allows for faster, safer evaluation of chest pain with sensitivity and specificity comparable to traditional angiography and a negative predictive value superior to nuclear imaging.3,4
Additional advantages include easy access to CT scanners over cardiac catheterization facilities; 88% of community hospitals with six or more beds had CT scanners in 2004. Further, turnaround is faster (15 to 20 minutes for the CT angiography versus six to eight hours of observation after cardiac catheterization). Also, physicians can simultaneously exclude other life-threatening causes of chest pain including aortic dissection and pulmonary embolus.5 Finally, CT angiography is less expensive (about $800 to $1,000) than invasive coronary angiography (approximately $3,000 to $4,000).6
Review of the Data
Patients undergoing CT angiography require a target heart rate of less than 70 beats per minute. Oral or intravenous beta-blockers are typically given prior to the procedure.
Nitroglycerin 0.4-0.8 mg is also administered sublingually to enhance visualization of the coronary vasculature.
Pulse, ECG, and blood pressure are monitored throughout the imaging process. Initially, a non-contrast scan is performed for coronary artery calcium (CAC) scoring. This is followed by angiography using a bolus of iodinated contrast. At this time, multislice cardiac scanning is synchronized with an ECG (i.e., gating the scan) and images are obtained during diastole.
Two types of CT are capable of obtaining the necessary high-speed images. Electron-beam CT (EBCT) and helical or spiral CT scanning. Multidetector helical CT (MDCT) or multislice CT (MSCT) is an evolution of helical CT. MDCT is available in four-, eight-, 16-, 32-, or 64-slice. Interpretation of the imaging uses the American College of Cardiology nomenclature: no stenosis, insignificant stenosis (less than 50% of coronary luminal diameter), significant stenosis (more than 50%), and total occlusion.
The presence of CAC has been shown in numerous studies to have prognostic significance for cardiac events and death. An elevated CAC score more accurately predicts coronary heart disease (CHD) risk in adults with an initial Framingham risk score between 10% and 19%. In addition, compared with a CAC score of zero, a score of more than 300 was predictive of CHD risk.7
Some studies suggest negative CAC scores alone are enough to risk-stratify patients presenting with chest pain, reporting sensitivities between 96% and 100% for the detection of significant cardiac events.8
Clinical studies of CT angiography typically consist of patients already selected to receive traditional invasive coronary angiography. Initial reports by Leschka, et al., showed sensitivity and specificity of 94% and 97%, respectively, with positive predictive values and negative predictive values of 87% and 99%.9
Additionally, a meta-analysis revealed multislice computed tomography (MSCT) for the diagnosis of CHD was highly sensitive (95% to 100%) for the detection of significant CHD. Specificity was 100% with the 64-slice MSCT and only slightly lower with the four- and 16-slice scanners (87%). A positive predictive value of 66% and negative predictive value of 98% for the presence of significant coronary stenosis have also been reported.10
Gallagher, et al., and previous studies comparing CT angiography with traditional invasive coronary angiography suggest further testing, such as stress nuclear imaging for any patient with stenosis more than 25% or CCS of greater than 100 and further recommends cardiac catheterization of any patient with greater than 70% stenosis by MSCT.
The utility of CT coronary angiography in the evaluation of patients presenting to the ED with chest pain was studied by Goldstein and peers.11 A randomized trial was conducted with patients admitted with chest pain or anginal equivalent, considered to be at low risk for CAD. Patients with negative cardiac enzymes and non-diagnostic ECG were assigned to either MSCCT or myocardial perfusion scan. CT angiography was adequate to diagnose or exclude CAD as the cause of chest pain in 75% of patients. The remaining 25% of patients had additional nuclear stress imaging. Average cost of the MDCT cohort was $1,586 compared with $1,872 for standard diagnostic evaluation. The time required for diagnosis was significantly shorter in the CT cohort: 3.4 hours, compared with 15 hours in the standard group.
An ongoing study at Beaumont Hospital in Royal Oak, Mich., is evaluating the length of stay and cost of care in patients presenting to the ED with chest pain. Patients are randomized to standard evaluation with serial enzymes, ECG, and nuclear perfusion testing or 64-slice CT angiography, plus coronary calcium score. Preliminary results presented at the 2006 American College of Cardiology Annual Scientific Session regarding the initial 200 patients showed a shorter length of stay and lower cost of care with similar patient outcomes in the group that underwent CT angiography.12
A large randomized controlled trial, Coronary Computed Tomography for Systematic Triage of Acute Chest Pain Patients to Treatment (CT-STAT), is planned to definitively study the use of coronary CT angiography in low-risk patients with chest pain. The large-scale study will involve 750 patients in 15 U.S. hospitals.
CT angiography remains limited despite many recent advances. A stable rhythm is a prerequisite, precluding use in patients with atrial fibrillation or frequent extra-systoles. Also, the required dose of 80 cc to 100 cc of iodinated contrast puts patients at risk for contrast-induced nephropathy, especially those with renal insufficiency.
Finally, radiation exposure is higher than that required for cardiac catheterization.13 Coronary calcification interferes with the images obtained by CT. Therefore, patients with heavy coronary calcium burden (CAC more than 400) may have reduced specificity and negative predictive value. Because this calcification increases with age, the diagnostic accuracy of CT angiography may decrease with age.
Morbidly obese patients may also have decreased image quality. Raff. et al., found significant stenosis in patients with normal body-mass index (BMI) (less than 25 kg/m2). Sensitivity, specificity, and positive and negative predictive values were all 100% and remained accurate in overweight patients. When BMI was more than 30, sensitivity and specificity were reduced to 90% and 86%, respectively.
Visualization of the coronary artery within a stent may be less accurate with CT angiography due to beam artifact, but evaluation of native coronary arteries and bypass grafts maintain similar sensitivity and specificity in these patients.14 A final concern is that CT angiography is only diagnostic. Although only 25% to 30% of diagnostic cardiac catheterizations reveal disease that meets criteria for stent placement, the study is redundant in these high-risk patients, who likely will be referred for traditional coronary angiography with stenting.
Back to the Case
The patient underwent nuclear stress testing the morning following admission. He had minimal attenuation in the infero-lateral distribution. A 64-slice CT angiogram was obtained, and images of the coronary anatomy demonstrated no plaque. The patient was reassured, and no further cardiac imaging was pursued. TH
Dr. Jenkins is an associate clinical professor and associate chief of hospital medicine in the Department of Family Medicine and Community Health at the University of Massachusetts medical school, Worcester.
References
- Statistics CNCH, ed. National Hospital Ambulatory Medical Care Survey: 2002 Emergency Department Summary, 2004. Available at www.cdc.gov/nchs/pressroom/04facts/emergencydept.htm. Last accessed Nov. 8, 2007.
- Kohn MA, Kwan E, Gupta M, et al. Prevalence of acute myocardial infarction and other serious diagnoses in patients presenting to an urban emergency department with chest pain. J Emerg Med. 2005;29(4):383-390.
- Stein PD, Beemath A, Kayali F, et al. Multidetector computed tomography for the diagnosis of coronary artery disease: a systematic review. Am J Med. 2006;119(3):203-216.
- Gallagher MJ, Ross MA, Raff G, et al. The diagnostic accuracy of 64-slice computed tomography coronary angiography compared with stress nuclear imaging in emergency department low-risk chest pain patients. Ann of Emerg Med. 200;49(2):125-136.
- AHA Hospital Statistics, 2006 Edition. Chicago: American Hospital Association; 2006:158, 161.
- Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, HCUPnet. Available at www.ahrq.gov/data/hcup. Last accessed Nov. 8, 2007.
- Greenland P, LaBree L, Azen SP, et al. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA. 2004;291(2):210-215.
- Kondos GT, Hoff JA, Sevrkov A, et al. Electron-beam tomography coronary artery calcium and cardiac events: a 37-month follow-up of 5,635 initially asymptomatic low- to intermediate-risk adults. Circulation. 2003;107(20):2571-2676.
- Leschka S, Alkadhi H, Plass A, et al. Accuracy of MSCT coronary angiography with 64-slice technology: first experience. Eur Heart J. 2005;177:1482-1487.
- Raff GL, Gallagher MJ, O’Neill WW, et al. Diagnostic accuracy of noninvasive coronary angiography using 64-slice spiral computed tomography. J Am Coll Cardiol. 2005;46:552-557.
- Goldstein JA, Gallagher MJ, O’Neill WW, et al. A randomized controlled trial of multi-slice coronary computed tomography for evaluation of acute chest pain. J Am Coll Cardiol. 2007;49(8):863-871.
- Raff GL, Gallagher MJ, O’Neill WW. Immediate coronary artery computed tomographic angiography rapidly and definitively excludes coronary artery disease in low-risk acute chest pain. Abstract 807-8. 55th Annual Scientific Session of the American College of Cardiology, March 11-14, 2006.
- de Feyter PJ, Nieman K. Noninvasive multi-slice computed tomography coronary angiography: an emerging clinical modality. J Am Coll Cardiol. 2004;44(6):1238-1240.
- Garcia MJ. Noninvasive coronary angiography: hype or new paradigm? J Am Med Assoc. 2005; 293:2531-2533.
Case
A 58-year-old male with a past medical history significant for hypertension and hypercholesterolemia presents four hours after acute onset of substernal chest pain that rates eight on a scale of 10. There is no radiation of the pain or associated dyspnea. He describes diaphoresis and nausea. Cardiac enzymes are negative on admission, and the electrocardiogram (ECG) is unchanged. Can computed tomography (CT) coronary angiography effectively rule out coronary disease in this patient admitted with chest pain?
Overview
Approximately 5 million patients presented to U.S. hospitals in 2002 for evaluation of chest pain.1 Less than a third of these patients were ultimately diagnosed with acute coronary syndrome.2 Current strategies to differentiate acute coronary syndrome from non-cardiac causes of chest pain have included electrocardiography, cardiac enzymes, exercise treadmill, echocardiography, and nuclear perfusion.
Unfortunately, each of these modalities has false positive and negative rates that result in a significant number of patients undergoing further evaluation for coronary artery stenosis. Although coronary angiography is the current gold standard to evaluate coronary luminal obstruction, it has many drawbacks. It is costly and inconvenient for patients, invasive, and demonstrates only the later stages of atherosclerosis—not which plaques are prone to rupture. All these limitations necessitate a search for a non-invasive evaluation of the coronary vasculature.
Because 64-slice CT scanners allow for visualization of the cardiac anatomy and coronary vasculature without catheters, there has been increasing interest in this modality to evaluate for coronary artery stenosis in low- to intermediate-risk patients presenting with chest pain. Comparative studies have found it allows for faster, safer evaluation of chest pain with sensitivity and specificity comparable to traditional angiography and a negative predictive value superior to nuclear imaging.3,4
Additional advantages include easy access to CT scanners over cardiac catheterization facilities; 88% of community hospitals with six or more beds had CT scanners in 2004. Further, turnaround is faster (15 to 20 minutes for the CT angiography versus six to eight hours of observation after cardiac catheterization). Also, physicians can simultaneously exclude other life-threatening causes of chest pain including aortic dissection and pulmonary embolus.5 Finally, CT angiography is less expensive (about $800 to $1,000) than invasive coronary angiography (approximately $3,000 to $4,000).6
Review of the Data
Patients undergoing CT angiography require a target heart rate of less than 70 beats per minute. Oral or intravenous beta-blockers are typically given prior to the procedure.
Nitroglycerin 0.4-0.8 mg is also administered sublingually to enhance visualization of the coronary vasculature.
Pulse, ECG, and blood pressure are monitored throughout the imaging process. Initially, a non-contrast scan is performed for coronary artery calcium (CAC) scoring. This is followed by angiography using a bolus of iodinated contrast. At this time, multislice cardiac scanning is synchronized with an ECG (i.e., gating the scan) and images are obtained during diastole.
Two types of CT are capable of obtaining the necessary high-speed images. Electron-beam CT (EBCT) and helical or spiral CT scanning. Multidetector helical CT (MDCT) or multislice CT (MSCT) is an evolution of helical CT. MDCT is available in four-, eight-, 16-, 32-, or 64-slice. Interpretation of the imaging uses the American College of Cardiology nomenclature: no stenosis, insignificant stenosis (less than 50% of coronary luminal diameter), significant stenosis (more than 50%), and total occlusion.
The presence of CAC has been shown in numerous studies to have prognostic significance for cardiac events and death. An elevated CAC score more accurately predicts coronary heart disease (CHD) risk in adults with an initial Framingham risk score between 10% and 19%. In addition, compared with a CAC score of zero, a score of more than 300 was predictive of CHD risk.7
Some studies suggest negative CAC scores alone are enough to risk-stratify patients presenting with chest pain, reporting sensitivities between 96% and 100% for the detection of significant cardiac events.8
Clinical studies of CT angiography typically consist of patients already selected to receive traditional invasive coronary angiography. Initial reports by Leschka, et al., showed sensitivity and specificity of 94% and 97%, respectively, with positive predictive values and negative predictive values of 87% and 99%.9
Additionally, a meta-analysis revealed multislice computed tomography (MSCT) for the diagnosis of CHD was highly sensitive (95% to 100%) for the detection of significant CHD. Specificity was 100% with the 64-slice MSCT and only slightly lower with the four- and 16-slice scanners (87%). A positive predictive value of 66% and negative predictive value of 98% for the presence of significant coronary stenosis have also been reported.10
Gallagher, et al., and previous studies comparing CT angiography with traditional invasive coronary angiography suggest further testing, such as stress nuclear imaging for any patient with stenosis more than 25% or CCS of greater than 100 and further recommends cardiac catheterization of any patient with greater than 70% stenosis by MSCT.
The utility of CT coronary angiography in the evaluation of patients presenting to the ED with chest pain was studied by Goldstein and peers.11 A randomized trial was conducted with patients admitted with chest pain or anginal equivalent, considered to be at low risk for CAD. Patients with negative cardiac enzymes and non-diagnostic ECG were assigned to either MSCCT or myocardial perfusion scan. CT angiography was adequate to diagnose or exclude CAD as the cause of chest pain in 75% of patients. The remaining 25% of patients had additional nuclear stress imaging. Average cost of the MDCT cohort was $1,586 compared with $1,872 for standard diagnostic evaluation. The time required for diagnosis was significantly shorter in the CT cohort: 3.4 hours, compared with 15 hours in the standard group.
An ongoing study at Beaumont Hospital in Royal Oak, Mich., is evaluating the length of stay and cost of care in patients presenting to the ED with chest pain. Patients are randomized to standard evaluation with serial enzymes, ECG, and nuclear perfusion testing or 64-slice CT angiography, plus coronary calcium score. Preliminary results presented at the 2006 American College of Cardiology Annual Scientific Session regarding the initial 200 patients showed a shorter length of stay and lower cost of care with similar patient outcomes in the group that underwent CT angiography.12
A large randomized controlled trial, Coronary Computed Tomography for Systematic Triage of Acute Chest Pain Patients to Treatment (CT-STAT), is planned to definitively study the use of coronary CT angiography in low-risk patients with chest pain. The large-scale study will involve 750 patients in 15 U.S. hospitals.
CT angiography remains limited despite many recent advances. A stable rhythm is a prerequisite, precluding use in patients with atrial fibrillation or frequent extra-systoles. Also, the required dose of 80 cc to 100 cc of iodinated contrast puts patients at risk for contrast-induced nephropathy, especially those with renal insufficiency.
Finally, radiation exposure is higher than that required for cardiac catheterization.13 Coronary calcification interferes with the images obtained by CT. Therefore, patients with heavy coronary calcium burden (CAC more than 400) may have reduced specificity and negative predictive value. Because this calcification increases with age, the diagnostic accuracy of CT angiography may decrease with age.
Morbidly obese patients may also have decreased image quality. Raff. et al., found significant stenosis in patients with normal body-mass index (BMI) (less than 25 kg/m2). Sensitivity, specificity, and positive and negative predictive values were all 100% and remained accurate in overweight patients. When BMI was more than 30, sensitivity and specificity were reduced to 90% and 86%, respectively.
Visualization of the coronary artery within a stent may be less accurate with CT angiography due to beam artifact, but evaluation of native coronary arteries and bypass grafts maintain similar sensitivity and specificity in these patients.14 A final concern is that CT angiography is only diagnostic. Although only 25% to 30% of diagnostic cardiac catheterizations reveal disease that meets criteria for stent placement, the study is redundant in these high-risk patients, who likely will be referred for traditional coronary angiography with stenting.
Back to the Case
The patient underwent nuclear stress testing the morning following admission. He had minimal attenuation in the infero-lateral distribution. A 64-slice CT angiogram was obtained, and images of the coronary anatomy demonstrated no plaque. The patient was reassured, and no further cardiac imaging was pursued. TH
Dr. Jenkins is an associate clinical professor and associate chief of hospital medicine in the Department of Family Medicine and Community Health at the University of Massachusetts medical school, Worcester.
References
- Statistics CNCH, ed. National Hospital Ambulatory Medical Care Survey: 2002 Emergency Department Summary, 2004. Available at www.cdc.gov/nchs/pressroom/04facts/emergencydept.htm. Last accessed Nov. 8, 2007.
- Kohn MA, Kwan E, Gupta M, et al. Prevalence of acute myocardial infarction and other serious diagnoses in patients presenting to an urban emergency department with chest pain. J Emerg Med. 2005;29(4):383-390.
- Stein PD, Beemath A, Kayali F, et al. Multidetector computed tomography for the diagnosis of coronary artery disease: a systematic review. Am J Med. 2006;119(3):203-216.
- Gallagher MJ, Ross MA, Raff G, et al. The diagnostic accuracy of 64-slice computed tomography coronary angiography compared with stress nuclear imaging in emergency department low-risk chest pain patients. Ann of Emerg Med. 200;49(2):125-136.
- AHA Hospital Statistics, 2006 Edition. Chicago: American Hospital Association; 2006:158, 161.
- Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, HCUPnet. Available at www.ahrq.gov/data/hcup. Last accessed Nov. 8, 2007.
- Greenland P, LaBree L, Azen SP, et al. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA. 2004;291(2):210-215.
- Kondos GT, Hoff JA, Sevrkov A, et al. Electron-beam tomography coronary artery calcium and cardiac events: a 37-month follow-up of 5,635 initially asymptomatic low- to intermediate-risk adults. Circulation. 2003;107(20):2571-2676.
- Leschka S, Alkadhi H, Plass A, et al. Accuracy of MSCT coronary angiography with 64-slice technology: first experience. Eur Heart J. 2005;177:1482-1487.
- Raff GL, Gallagher MJ, O’Neill WW, et al. Diagnostic accuracy of noninvasive coronary angiography using 64-slice spiral computed tomography. J Am Coll Cardiol. 2005;46:552-557.
- Goldstein JA, Gallagher MJ, O’Neill WW, et al. A randomized controlled trial of multi-slice coronary computed tomography for evaluation of acute chest pain. J Am Coll Cardiol. 2007;49(8):863-871.
- Raff GL, Gallagher MJ, O’Neill WW. Immediate coronary artery computed tomographic angiography rapidly and definitively excludes coronary artery disease in low-risk acute chest pain. Abstract 807-8. 55th Annual Scientific Session of the American College of Cardiology, March 11-14, 2006.
- de Feyter PJ, Nieman K. Noninvasive multi-slice computed tomography coronary angiography: an emerging clinical modality. J Am Coll Cardiol. 2004;44(6):1238-1240.
- Garcia MJ. Noninvasive coronary angiography: hype or new paradigm? J Am Med Assoc. 2005; 293:2531-2533.