User login
The Hospitalist only
Subtle Skills
Hospitalists with a hunger for taking on administrative roles often pursue an advanced degree. But whether it’s to assume a leadership role or just do a better job, it’s the not-altogether-obvious skills that can help hospitalists improve their careers and job satisfaction.
By refining communication styles, being receptive to mentoring, or learning how to influence decision-makers, hospitalists can convey competence to their peers and superiors. Intangible strengths such as these will help the hospitalist who wishes to carve a niche as a quality-improvement researcher, director of a medical education clerkship, patient safety officer, or medical director.
Who Needs What
The administrative skills hospitalists need depend on their career goals. Those who reflect on their career goals, identify their core values, and consider what is feasible at different stages in their lives can more quickly build the abilities they’ll need. This self-awareness is perhaps the first skill to develop.
The setting and practice model hospitalists work in also influences which skills they may need.
“Although the skills needed in different settings may be fundamentally the same, the politics differ between a community hospital and a teaching hospital,” says Sayeed Khan, MD, director of the hospitalist program of Lakeside Medical Group. “Communication skills may be even more crucial in a community hospital, where it’s less understood what a hospitalist is.” Such ability to educate people in Hospitalist 101 is yet another skill a savvy administrator or administrator-to-be should hone.
Hospitalists also need to understand quality control and other measures—and what the numbers mean.
For example, says Dr. Khan, it’s valuable to know:
- What it means to have good bed days at the end of the month and an average length of stay of 3.3 days;
- How that compares with other groups in other hospitals; and
- The implications of those measures in terms of outcomes, dollar costs, and savings to the hospital as well as the group—and how that translates for the patient.
“Those are the types of figures that many hospitalists don’t really understand,” says Dr. Khan.
But hospitalists can learn by observing and studying. “I’m a good example of that in that I do not have a formal business background,” Dr. Khan says. “Along with the literature, networking with other people, particularly at the SHM annual meeting, can help hospitalists gain a better understanding of what these numbers mean and what the benchmarks are.”
He believes administrative skills can be divided into two categories: those related to metrics (the math behind what hospitalists do) and those related to patient care.
In regard to patient care, effective committee participation is an administrative ability that can influence the standard of care. For example, Dr. Khan is participating in committee work in the area of maintaining patients’ glycemic control.
“Historically, that issue was not well addressed,” he says. It is now recognized that patients who have tight glycemic control do much better while hospitalized, irrespective of whether they have diabetes. “But it’s difficult to get other clinicians to change their practice styles,” says Dr. Khan. “You can implement change in your own practice, and others can learn by example. But if you are on a committee that designs new protocols and those get implemented, then you’ve directly changed how medicine is practiced at that hospital.”
Being able to win buy-in for your ideas makes that possible. “Purely speaking, committee participation is not an administrative role,” says Dr. Khan. “But it is an administrative skill in that it is outside the scope of what’s normally required for a hospitalist.”
Get Help
Honing one’s receptivity to mentorship is another vital ability for the upwardly mobile hospitalist. Mentors can direct inexperienced physicians to resources that may help them develop proficiency. A mentor who has grappled with the same issues can help open doors to opportunities hospitalists may not know about.
As she reflects on her early career, when she had no mentors and no administrative experience, Sylvia C.W. McKean, MD, realizes she could have used guidance and advocacy. Effective mentorship helps hospitalists reach their goals faster with fewer impediments, she says.
“Mentorship is critical,” says Dr. McKean, medical director, Brigham and Women’s Hospital/Faulkner Hospitalist Service of Brigham and Women’s Hospital in Boston. “But knowing how to receive the information you’re getting and how to apply it to your own specific professional goals can really help you develop the skills that will help you move your career forward. Informal mentorship is one area where there has been less opportunity for women in the past, resulting in more promotions for men.”
Other skills women may especially need are learning the written and unwritten rules of promotion, being more assertive in finding out what they are, and developing diplomacy—including learning to say no with finesse.
“The reality is that if you are in an environment that has predominantly male leadership, it is important for [a woman] to have male advocates to support whatever it is that you are trying to do,” says Dr. McKean. “In some instances they may have to speak for you.”
Efficiency and setting priorities are also important skills.
“I learned very early on that efficiency was critical to managing several roles—administrative, patient care, and raising three boys,” says Dr. McKean. “There were some things, however, that in retrospect I did not need to do. For example, I did my own home-improvement tasks instead of hiring someone else to do them. For women in particular, you don’t have to be a super everything. At different phases in your life your priorities will vary. Get help so that you’re not spending time doing tasks that don’t further your goals.”
Communication
Facility with communication, of course, is paramount in every aspect of medicine. Being poised, articulate, concise, and persuasive to get your message across, says Dr. McKean, goes a long way toward advancing one’s career.
“It took me a long time to realize this,” says Dr. McKean. “For example, whenever I generated reports I tried to have as much information in there as possible because I thought it would look like I was very knowledgeable. A one-page document that summarizes the key points is often more effective in getting people’s attention.”
Another subset of communication is skill at public speaking, which may lead to being invited to give lectures.
Dr. Khan believes shy, less-articulate clinicians can begin to improve their public speaking by serving on committees. “Unless the committee is a committee of two, that is the appropriate forum to begin voicing your opinions and expertise on a particular matter,” he says. “There’s a certain comfort level built into that because you’re not necessarily speaking on a topic you are unfamiliar with.”
Another intangible administrative skill, he says, is the ability to deal with people from different walks of life. Some highly placed hospital administrators don’t have clinical backgrounds and will require explanations of clinical situations that mesh with their business understanding.
Time Management
Organization is a critical administrative skill no matter what career path a hospitalist follows.
“As hospitalists we are typically juggling more than one thing at one time,” Dr. Khan says. “As a hospitalist who is involved in administrative tasks, if you’re not organized, that is a path to failure.”
Strive to hire the right people for clerical and administrative staff positions. They will fill in the weak spots to keep you on track and present a good image as your front person. But having a good clerical or administrative assistant doesn’t let you off the hook; you, too, must demonstrate solid time management. Make sure you take good notes at committees, quickly access data or documentation, and research and report back well.
The Interpersonal
Robert L. Benak, MD, a hospitalist and medical director of Champlain Valley Physicians Hospital (CVPH) Medical Center, a 341-bed acute care hospital and 54-bed skilled nursing facility in Plattsburgh, N.Y., thinks the most important intangible skills involve managing relationships.
Again, self-reflection helps. “Understand what your personality is like on a calm day and what it is like on a stressful day,” he says.
He says it’s critical to be able to negotiate with others. “Understanding what lies underneath, what common and different interests the two negotiating partners have helps you focus on getting the best compromise of conflicting interests to resolve a disagreement in an amicable and effective way,” he says.
Dr. Benak, who joined SHM around the time his group started in October 2006, thanks the SHM Leadership Academy for strengthening his interpersonal skills. He has tried to bring home what he learned to his group of five hospitalists.
Recently, he had to determine whether to designate a patient with abdominal pain as a surgical or medical patient. Dr. Benak invoked his “ability to sit down with the orthopedic surgeon and general surgeon, recognizing that they’ve got legitimate interests and concerns, as do I, and figuring out what works well for us, and more importantly, what works best for the patient.”
That ability to compromise is indispensable to growth as a hospitalist, he says.
“I was a chemistry major in college and loved working with concrete, though sometimes complicated, problems where you’re either right or you’re wrong,” he says. “I’ve come to see that giving up being right, and giving up any sense of entitlement I may feel in having the principal position, are skills. Even if you think the other person is being unreasonable, you have to accept that as a fact and figure out how to cope with that in a way that is a credit to yourself and your program.” TH
Andrea Sattinger is a medical writer based in North Carolina.
Hospitalists with a hunger for taking on administrative roles often pursue an advanced degree. But whether it’s to assume a leadership role or just do a better job, it’s the not-altogether-obvious skills that can help hospitalists improve their careers and job satisfaction.
By refining communication styles, being receptive to mentoring, or learning how to influence decision-makers, hospitalists can convey competence to their peers and superiors. Intangible strengths such as these will help the hospitalist who wishes to carve a niche as a quality-improvement researcher, director of a medical education clerkship, patient safety officer, or medical director.
Who Needs What
The administrative skills hospitalists need depend on their career goals. Those who reflect on their career goals, identify their core values, and consider what is feasible at different stages in their lives can more quickly build the abilities they’ll need. This self-awareness is perhaps the first skill to develop.
The setting and practice model hospitalists work in also influences which skills they may need.
“Although the skills needed in different settings may be fundamentally the same, the politics differ between a community hospital and a teaching hospital,” says Sayeed Khan, MD, director of the hospitalist program of Lakeside Medical Group. “Communication skills may be even more crucial in a community hospital, where it’s less understood what a hospitalist is.” Such ability to educate people in Hospitalist 101 is yet another skill a savvy administrator or administrator-to-be should hone.
Hospitalists also need to understand quality control and other measures—and what the numbers mean.
For example, says Dr. Khan, it’s valuable to know:
- What it means to have good bed days at the end of the month and an average length of stay of 3.3 days;
- How that compares with other groups in other hospitals; and
- The implications of those measures in terms of outcomes, dollar costs, and savings to the hospital as well as the group—and how that translates for the patient.
“Those are the types of figures that many hospitalists don’t really understand,” says Dr. Khan.
But hospitalists can learn by observing and studying. “I’m a good example of that in that I do not have a formal business background,” Dr. Khan says. “Along with the literature, networking with other people, particularly at the SHM annual meeting, can help hospitalists gain a better understanding of what these numbers mean and what the benchmarks are.”
He believes administrative skills can be divided into two categories: those related to metrics (the math behind what hospitalists do) and those related to patient care.
In regard to patient care, effective committee participation is an administrative ability that can influence the standard of care. For example, Dr. Khan is participating in committee work in the area of maintaining patients’ glycemic control.
“Historically, that issue was not well addressed,” he says. It is now recognized that patients who have tight glycemic control do much better while hospitalized, irrespective of whether they have diabetes. “But it’s difficult to get other clinicians to change their practice styles,” says Dr. Khan. “You can implement change in your own practice, and others can learn by example. But if you are on a committee that designs new protocols and those get implemented, then you’ve directly changed how medicine is practiced at that hospital.”
Being able to win buy-in for your ideas makes that possible. “Purely speaking, committee participation is not an administrative role,” says Dr. Khan. “But it is an administrative skill in that it is outside the scope of what’s normally required for a hospitalist.”
Get Help
Honing one’s receptivity to mentorship is another vital ability for the upwardly mobile hospitalist. Mentors can direct inexperienced physicians to resources that may help them develop proficiency. A mentor who has grappled with the same issues can help open doors to opportunities hospitalists may not know about.
As she reflects on her early career, when she had no mentors and no administrative experience, Sylvia C.W. McKean, MD, realizes she could have used guidance and advocacy. Effective mentorship helps hospitalists reach their goals faster with fewer impediments, she says.
“Mentorship is critical,” says Dr. McKean, medical director, Brigham and Women’s Hospital/Faulkner Hospitalist Service of Brigham and Women’s Hospital in Boston. “But knowing how to receive the information you’re getting and how to apply it to your own specific professional goals can really help you develop the skills that will help you move your career forward. Informal mentorship is one area where there has been less opportunity for women in the past, resulting in more promotions for men.”
Other skills women may especially need are learning the written and unwritten rules of promotion, being more assertive in finding out what they are, and developing diplomacy—including learning to say no with finesse.
“The reality is that if you are in an environment that has predominantly male leadership, it is important for [a woman] to have male advocates to support whatever it is that you are trying to do,” says Dr. McKean. “In some instances they may have to speak for you.”
Efficiency and setting priorities are also important skills.
“I learned very early on that efficiency was critical to managing several roles—administrative, patient care, and raising three boys,” says Dr. McKean. “There were some things, however, that in retrospect I did not need to do. For example, I did my own home-improvement tasks instead of hiring someone else to do them. For women in particular, you don’t have to be a super everything. At different phases in your life your priorities will vary. Get help so that you’re not spending time doing tasks that don’t further your goals.”
Communication
Facility with communication, of course, is paramount in every aspect of medicine. Being poised, articulate, concise, and persuasive to get your message across, says Dr. McKean, goes a long way toward advancing one’s career.
“It took me a long time to realize this,” says Dr. McKean. “For example, whenever I generated reports I tried to have as much information in there as possible because I thought it would look like I was very knowledgeable. A one-page document that summarizes the key points is often more effective in getting people’s attention.”
Another subset of communication is skill at public speaking, which may lead to being invited to give lectures.
Dr. Khan believes shy, less-articulate clinicians can begin to improve their public speaking by serving on committees. “Unless the committee is a committee of two, that is the appropriate forum to begin voicing your opinions and expertise on a particular matter,” he says. “There’s a certain comfort level built into that because you’re not necessarily speaking on a topic you are unfamiliar with.”
Another intangible administrative skill, he says, is the ability to deal with people from different walks of life. Some highly placed hospital administrators don’t have clinical backgrounds and will require explanations of clinical situations that mesh with their business understanding.
Time Management
Organization is a critical administrative skill no matter what career path a hospitalist follows.
“As hospitalists we are typically juggling more than one thing at one time,” Dr. Khan says. “As a hospitalist who is involved in administrative tasks, if you’re not organized, that is a path to failure.”
Strive to hire the right people for clerical and administrative staff positions. They will fill in the weak spots to keep you on track and present a good image as your front person. But having a good clerical or administrative assistant doesn’t let you off the hook; you, too, must demonstrate solid time management. Make sure you take good notes at committees, quickly access data or documentation, and research and report back well.
The Interpersonal
Robert L. Benak, MD, a hospitalist and medical director of Champlain Valley Physicians Hospital (CVPH) Medical Center, a 341-bed acute care hospital and 54-bed skilled nursing facility in Plattsburgh, N.Y., thinks the most important intangible skills involve managing relationships.
Again, self-reflection helps. “Understand what your personality is like on a calm day and what it is like on a stressful day,” he says.
He says it’s critical to be able to negotiate with others. “Understanding what lies underneath, what common and different interests the two negotiating partners have helps you focus on getting the best compromise of conflicting interests to resolve a disagreement in an amicable and effective way,” he says.
Dr. Benak, who joined SHM around the time his group started in October 2006, thanks the SHM Leadership Academy for strengthening his interpersonal skills. He has tried to bring home what he learned to his group of five hospitalists.
Recently, he had to determine whether to designate a patient with abdominal pain as a surgical or medical patient. Dr. Benak invoked his “ability to sit down with the orthopedic surgeon and general surgeon, recognizing that they’ve got legitimate interests and concerns, as do I, and figuring out what works well for us, and more importantly, what works best for the patient.”
That ability to compromise is indispensable to growth as a hospitalist, he says.
“I was a chemistry major in college and loved working with concrete, though sometimes complicated, problems where you’re either right or you’re wrong,” he says. “I’ve come to see that giving up being right, and giving up any sense of entitlement I may feel in having the principal position, are skills. Even if you think the other person is being unreasonable, you have to accept that as a fact and figure out how to cope with that in a way that is a credit to yourself and your program.” TH
Andrea Sattinger is a medical writer based in North Carolina.
Hospitalists with a hunger for taking on administrative roles often pursue an advanced degree. But whether it’s to assume a leadership role or just do a better job, it’s the not-altogether-obvious skills that can help hospitalists improve their careers and job satisfaction.
By refining communication styles, being receptive to mentoring, or learning how to influence decision-makers, hospitalists can convey competence to their peers and superiors. Intangible strengths such as these will help the hospitalist who wishes to carve a niche as a quality-improvement researcher, director of a medical education clerkship, patient safety officer, or medical director.
Who Needs What
The administrative skills hospitalists need depend on their career goals. Those who reflect on their career goals, identify their core values, and consider what is feasible at different stages in their lives can more quickly build the abilities they’ll need. This self-awareness is perhaps the first skill to develop.
The setting and practice model hospitalists work in also influences which skills they may need.
“Although the skills needed in different settings may be fundamentally the same, the politics differ between a community hospital and a teaching hospital,” says Sayeed Khan, MD, director of the hospitalist program of Lakeside Medical Group. “Communication skills may be even more crucial in a community hospital, where it’s less understood what a hospitalist is.” Such ability to educate people in Hospitalist 101 is yet another skill a savvy administrator or administrator-to-be should hone.
Hospitalists also need to understand quality control and other measures—and what the numbers mean.
For example, says Dr. Khan, it’s valuable to know:
- What it means to have good bed days at the end of the month and an average length of stay of 3.3 days;
- How that compares with other groups in other hospitals; and
- The implications of those measures in terms of outcomes, dollar costs, and savings to the hospital as well as the group—and how that translates for the patient.
“Those are the types of figures that many hospitalists don’t really understand,” says Dr. Khan.
But hospitalists can learn by observing and studying. “I’m a good example of that in that I do not have a formal business background,” Dr. Khan says. “Along with the literature, networking with other people, particularly at the SHM annual meeting, can help hospitalists gain a better understanding of what these numbers mean and what the benchmarks are.”
He believes administrative skills can be divided into two categories: those related to metrics (the math behind what hospitalists do) and those related to patient care.
In regard to patient care, effective committee participation is an administrative ability that can influence the standard of care. For example, Dr. Khan is participating in committee work in the area of maintaining patients’ glycemic control.
“Historically, that issue was not well addressed,” he says. It is now recognized that patients who have tight glycemic control do much better while hospitalized, irrespective of whether they have diabetes. “But it’s difficult to get other clinicians to change their practice styles,” says Dr. Khan. “You can implement change in your own practice, and others can learn by example. But if you are on a committee that designs new protocols and those get implemented, then you’ve directly changed how medicine is practiced at that hospital.”
Being able to win buy-in for your ideas makes that possible. “Purely speaking, committee participation is not an administrative role,” says Dr. Khan. “But it is an administrative skill in that it is outside the scope of what’s normally required for a hospitalist.”
Get Help
Honing one’s receptivity to mentorship is another vital ability for the upwardly mobile hospitalist. Mentors can direct inexperienced physicians to resources that may help them develop proficiency. A mentor who has grappled with the same issues can help open doors to opportunities hospitalists may not know about.
As she reflects on her early career, when she had no mentors and no administrative experience, Sylvia C.W. McKean, MD, realizes she could have used guidance and advocacy. Effective mentorship helps hospitalists reach their goals faster with fewer impediments, she says.
“Mentorship is critical,” says Dr. McKean, medical director, Brigham and Women’s Hospital/Faulkner Hospitalist Service of Brigham and Women’s Hospital in Boston. “But knowing how to receive the information you’re getting and how to apply it to your own specific professional goals can really help you develop the skills that will help you move your career forward. Informal mentorship is one area where there has been less opportunity for women in the past, resulting in more promotions for men.”
Other skills women may especially need are learning the written and unwritten rules of promotion, being more assertive in finding out what they are, and developing diplomacy—including learning to say no with finesse.
“The reality is that if you are in an environment that has predominantly male leadership, it is important for [a woman] to have male advocates to support whatever it is that you are trying to do,” says Dr. McKean. “In some instances they may have to speak for you.”
Efficiency and setting priorities are also important skills.
“I learned very early on that efficiency was critical to managing several roles—administrative, patient care, and raising three boys,” says Dr. McKean. “There were some things, however, that in retrospect I did not need to do. For example, I did my own home-improvement tasks instead of hiring someone else to do them. For women in particular, you don’t have to be a super everything. At different phases in your life your priorities will vary. Get help so that you’re not spending time doing tasks that don’t further your goals.”
Communication
Facility with communication, of course, is paramount in every aspect of medicine. Being poised, articulate, concise, and persuasive to get your message across, says Dr. McKean, goes a long way toward advancing one’s career.
“It took me a long time to realize this,” says Dr. McKean. “For example, whenever I generated reports I tried to have as much information in there as possible because I thought it would look like I was very knowledgeable. A one-page document that summarizes the key points is often more effective in getting people’s attention.”
Another subset of communication is skill at public speaking, which may lead to being invited to give lectures.
Dr. Khan believes shy, less-articulate clinicians can begin to improve their public speaking by serving on committees. “Unless the committee is a committee of two, that is the appropriate forum to begin voicing your opinions and expertise on a particular matter,” he says. “There’s a certain comfort level built into that because you’re not necessarily speaking on a topic you are unfamiliar with.”
Another intangible administrative skill, he says, is the ability to deal with people from different walks of life. Some highly placed hospital administrators don’t have clinical backgrounds and will require explanations of clinical situations that mesh with their business understanding.
Time Management
Organization is a critical administrative skill no matter what career path a hospitalist follows.
“As hospitalists we are typically juggling more than one thing at one time,” Dr. Khan says. “As a hospitalist who is involved in administrative tasks, if you’re not organized, that is a path to failure.”
Strive to hire the right people for clerical and administrative staff positions. They will fill in the weak spots to keep you on track and present a good image as your front person. But having a good clerical or administrative assistant doesn’t let you off the hook; you, too, must demonstrate solid time management. Make sure you take good notes at committees, quickly access data or documentation, and research and report back well.
The Interpersonal
Robert L. Benak, MD, a hospitalist and medical director of Champlain Valley Physicians Hospital (CVPH) Medical Center, a 341-bed acute care hospital and 54-bed skilled nursing facility in Plattsburgh, N.Y., thinks the most important intangible skills involve managing relationships.
Again, self-reflection helps. “Understand what your personality is like on a calm day and what it is like on a stressful day,” he says.
He says it’s critical to be able to negotiate with others. “Understanding what lies underneath, what common and different interests the two negotiating partners have helps you focus on getting the best compromise of conflicting interests to resolve a disagreement in an amicable and effective way,” he says.
Dr. Benak, who joined SHM around the time his group started in October 2006, thanks the SHM Leadership Academy for strengthening his interpersonal skills. He has tried to bring home what he learned to his group of five hospitalists.
Recently, he had to determine whether to designate a patient with abdominal pain as a surgical or medical patient. Dr. Benak invoked his “ability to sit down with the orthopedic surgeon and general surgeon, recognizing that they’ve got legitimate interests and concerns, as do I, and figuring out what works well for us, and more importantly, what works best for the patient.”
That ability to compromise is indispensable to growth as a hospitalist, he says.
“I was a chemistry major in college and loved working with concrete, though sometimes complicated, problems where you’re either right or you’re wrong,” he says. “I’ve come to see that giving up being right, and giving up any sense of entitlement I may feel in having the principal position, are skills. Even if you think the other person is being unreasonable, you have to accept that as a fact and figure out how to cope with that in a way that is a credit to yourself and your program.” TH
Andrea Sattinger is a medical writer based in North Carolina.
Hospitalists on Top
Many technically skilled professionals—including computer programmers, stockbrokers, or hospitalists—aspire to the executive suite.
The burgeoning field of hospital medicine offers especially enticing rewards for business-minded doctors, inducing frontline leaders to trade the white coat for wing tips and a shot at the top.
The pinnacle can be stratospheric. Adam Singer, MD, CEO of California-based IPC-The Hospitalist Company, traded his white coat for the so-called C suite. He has since filed an initial public offering that should produce $105 million for IPC’s stakeholders.
There’s also lots of room for hospitalists with more modest executive aspirations. The skills acquired by good hospitalists—thoroughness, the ability to solve complex problems, critical thinking, strong motivation, sound work ethic, and teamwork—serve physician executives well. Some physicians back into the executive suite once they realize they’re attracted to the business end of medicine. Those are the clinicians who volunteer to do the group’s scheduling or find that they enjoy negotiating contracts with new hires and payers. Others pursue a personal road map to the C suite.
Balancing Act
The biggest decision facing a hospitalist with managerial aspirations is whether to relinquish patient care.
“For most of your career you must remain active clinically, even though your time is disjointed because you’re intensely needed in both clinical and administrative areas,” says Andrew Urbach, MD, medical director of clinical excellence and service at Children’s Hospital of Pittsburgh. He manages both by constantly adapting. His time had been evenly split between clinical and administrative duties until July, when he cut back on his clinical duties. He now spends one week every quarter as a hospitalist and a half-day a week at the clinic. “It’s difficult balancing both, and reaching the highest level of excellence in two areas is demanding,” he says. “But the best hospitalist managers continue to see patients to maintain credibility with their peers.”
Stacy Goldsholl, MD, president of Knoxville, Tenn.-based Team Health, Hospital Medicine Division, was a staff hospitalist who ceded clinical work for a managerial career. After a three-year stint as a hospitalist with Covenant HealthCare’s hospital medicine program at Covenant Medical Center in Saginaw, Mich., her mentors recruited her to “jump around the country starting hospitalist programs during 2004 and 2005,” she says. “I was in the right place at the right time, and I had the confidence to move my agenda in a diplomatic way and with humor.”
Dr. Goldsholl reluctantly gave up clinical responsibilities three years ago. “It’s all about balance in my life,” she says. “It was a conscious decision to give up patient care. I miss it, but I wanted to take my career to a national level. I travel a great deal, which isn’t compatible with patient care.”
Business School
Hospitalists attracted to management often realize they need more business schooling, says Kevin Shulman, MD, MBA, professor of medicine and management at Duke University Medical Center and the Fuqua School of Business in Durham, N.C.
“The issues in medical training are clinical, not organizational,” he says. “As you move up in administration you don’t have business skills you need. When doctors feel frustrated about not being effective organizationally, that’s when they think about business school.”
Edward Ogata, MD, MBA, chief medical officer of Children’s Memorial Hospital in Chicago, and a pediatric neonatologist, realized how useful an MBA would be as he moved from clinical work to management. “I went back to school for an MBA at Northwestern University Kellogg School of Management 27 years after graduating from medical school,” he says. Pushed by the healthcare market into negotiating managed-care contracts in the 1980s, Dr. Ogata realized he knew little about accounting and finance. The always-precarious financial situations of children’s hospitals encouraged him to get the business skills to cope.
At Kellogg, in Chicago, Dr. Ogata was assigned homework and teamwork with executives from Motorola, Lucent, and GE. The first year was difficult because he was still covering call and juggling administrative tasks. He got up at 4 a.m. every day to study. Armed with business skills, Dr. Ogata feels better equipped to meet the financial and administrative needs of his inner-city hospital. “We’re not in a nice suburb with a favorable payer mix, and a hospital isn’t really a business in the conventional sense,’’ he notes. “But we are committed to doing the best.”
For Joy Drass, MD, MBA, a critical care trauma surgeon for 13 years and president of Georgetown University Hospital in Washington, D.C., methodically performing clinical tasks prepared her for top management. She assumed the presidency of the troubled hospital in 2001, one year after MedStar Health in Columbia, Md., acquired it. The hospital had recorded losses in excess of $200 million before MedStar stepped in.
“Many skills I developed as a critical care physician had an absolute application in this stressed organization,” she says. “In medicine, it’s called triage. In business, it’s prioritizing. You look at a situation and quickly set goals to get from point A to point B, encourage team work, and develop structures to support people when they are struggling through uncertainty.” Skills she learned as a graduate of the Wharton business school in Philadelphia helped her stabilize hospital operations, improve customer service and revenue collection, and develop a long-term strategic plan to improve the hospital’s chances of survival.
Varied Paths
Some hospitalists acquire business smarts from instinct and experience. When he was 13 years old, Dr. Urbach ran his family’s retail business for weeks at a time when his parents were away.
“I’ve had no formal [business] school training, but my entrepreneurial instincts and management skills were honed early in life,” he says.
Team Health’s Dr. Goldsholl intended to get a formal MBA, but was too busy. “SHM’s Leadership Academy and other programs gave me management skills, and I chose CME credits in business and management areas,” she says. “I’m also more of an experiential than a classroom learner. Mentoring and other informal settings work for me.”
Michael Ruhlen, MD, MHM, Toledo (Ohio) Children’s Hospital corporate vice president of medical informatics and vice president of medical affairs, made a successful if not easy move from clinician to manager. Acting as a hospitalist seven years before the discipline was named in 1996, he developed systematic, data-driven clinical pathways and trained other would-be pediatric hospitalists in acute care pediatrics. In 2001 he was the first recipient of the National Association of Inpatient Physician’s Award for Outstanding Service in Hospital Medicine. The award recognized his managerial skill in building a hospitalist program from scratch.
Unlike hospitalists who are moving from well-defined clinical tracks to managerial roles, Dr. Ruhlen operated in uncharted territory in his first decade as a hospitalist. From the beginning of his hospitalist career, Dr. Ruhlen’s business head identified volume-dependent competency as critical to clinical and financial success. “I saw how to create time and quality efficiencies,” he explains. “If you do one or two lumbar punctures a year, you might stick a child five or six times. Doing a higher volume of procedures led to smoother operations.”
Recognizing the complexities of hospital management, Dr. Ruhlen returned to school to sharpen his management skills. He chose the Harvard School of Public Health’s master’s in healthcare management over an MBA because, as he puts it, “I’m interested in managing a hospital, not running Campbell’s Soup.” As a hospitalist executive, he works on improving the hospital’s IT systems, developing new physician leaders, and taking the lead on change management and patient safety issues. He also has been tapped twice to serve as acting hospital president.
Medicine as Business
Hospitalists enjoy an array of career choices. Those who savor the pure joy of clinical work can continue on that path, while others can choose a career in management; some can blend both. No matter what their career paths, healthcare’s increasing complexity will keep them fully occupied.
“As medicine grows more complex, students spend their time mastering clinical issues,” Dr. Shulman notes. “Many third-year med students don’t even know the difference between Medicaid and Medicare. As they practice as hospitalists and want to move up the administrative ranks, they will acquire the general business skills that will help them be effective and reshape healthcare policy.” TH
Marlene Piturro is a medical writer based in New York.
Many technically skilled professionals—including computer programmers, stockbrokers, or hospitalists—aspire to the executive suite.
The burgeoning field of hospital medicine offers especially enticing rewards for business-minded doctors, inducing frontline leaders to trade the white coat for wing tips and a shot at the top.
The pinnacle can be stratospheric. Adam Singer, MD, CEO of California-based IPC-The Hospitalist Company, traded his white coat for the so-called C suite. He has since filed an initial public offering that should produce $105 million for IPC’s stakeholders.
There’s also lots of room for hospitalists with more modest executive aspirations. The skills acquired by good hospitalists—thoroughness, the ability to solve complex problems, critical thinking, strong motivation, sound work ethic, and teamwork—serve physician executives well. Some physicians back into the executive suite once they realize they’re attracted to the business end of medicine. Those are the clinicians who volunteer to do the group’s scheduling or find that they enjoy negotiating contracts with new hires and payers. Others pursue a personal road map to the C suite.
Balancing Act
The biggest decision facing a hospitalist with managerial aspirations is whether to relinquish patient care.
“For most of your career you must remain active clinically, even though your time is disjointed because you’re intensely needed in both clinical and administrative areas,” says Andrew Urbach, MD, medical director of clinical excellence and service at Children’s Hospital of Pittsburgh. He manages both by constantly adapting. His time had been evenly split between clinical and administrative duties until July, when he cut back on his clinical duties. He now spends one week every quarter as a hospitalist and a half-day a week at the clinic. “It’s difficult balancing both, and reaching the highest level of excellence in two areas is demanding,” he says. “But the best hospitalist managers continue to see patients to maintain credibility with their peers.”
Stacy Goldsholl, MD, president of Knoxville, Tenn.-based Team Health, Hospital Medicine Division, was a staff hospitalist who ceded clinical work for a managerial career. After a three-year stint as a hospitalist with Covenant HealthCare’s hospital medicine program at Covenant Medical Center in Saginaw, Mich., her mentors recruited her to “jump around the country starting hospitalist programs during 2004 and 2005,” she says. “I was in the right place at the right time, and I had the confidence to move my agenda in a diplomatic way and with humor.”
Dr. Goldsholl reluctantly gave up clinical responsibilities three years ago. “It’s all about balance in my life,” she says. “It was a conscious decision to give up patient care. I miss it, but I wanted to take my career to a national level. I travel a great deal, which isn’t compatible with patient care.”
Business School
Hospitalists attracted to management often realize they need more business schooling, says Kevin Shulman, MD, MBA, professor of medicine and management at Duke University Medical Center and the Fuqua School of Business in Durham, N.C.
“The issues in medical training are clinical, not organizational,” he says. “As you move up in administration you don’t have business skills you need. When doctors feel frustrated about not being effective organizationally, that’s when they think about business school.”
Edward Ogata, MD, MBA, chief medical officer of Children’s Memorial Hospital in Chicago, and a pediatric neonatologist, realized how useful an MBA would be as he moved from clinical work to management. “I went back to school for an MBA at Northwestern University Kellogg School of Management 27 years after graduating from medical school,” he says. Pushed by the healthcare market into negotiating managed-care contracts in the 1980s, Dr. Ogata realized he knew little about accounting and finance. The always-precarious financial situations of children’s hospitals encouraged him to get the business skills to cope.
At Kellogg, in Chicago, Dr. Ogata was assigned homework and teamwork with executives from Motorola, Lucent, and GE. The first year was difficult because he was still covering call and juggling administrative tasks. He got up at 4 a.m. every day to study. Armed with business skills, Dr. Ogata feels better equipped to meet the financial and administrative needs of his inner-city hospital. “We’re not in a nice suburb with a favorable payer mix, and a hospital isn’t really a business in the conventional sense,’’ he notes. “But we are committed to doing the best.”
For Joy Drass, MD, MBA, a critical care trauma surgeon for 13 years and president of Georgetown University Hospital in Washington, D.C., methodically performing clinical tasks prepared her for top management. She assumed the presidency of the troubled hospital in 2001, one year after MedStar Health in Columbia, Md., acquired it. The hospital had recorded losses in excess of $200 million before MedStar stepped in.
“Many skills I developed as a critical care physician had an absolute application in this stressed organization,” she says. “In medicine, it’s called triage. In business, it’s prioritizing. You look at a situation and quickly set goals to get from point A to point B, encourage team work, and develop structures to support people when they are struggling through uncertainty.” Skills she learned as a graduate of the Wharton business school in Philadelphia helped her stabilize hospital operations, improve customer service and revenue collection, and develop a long-term strategic plan to improve the hospital’s chances of survival.
Varied Paths
Some hospitalists acquire business smarts from instinct and experience. When he was 13 years old, Dr. Urbach ran his family’s retail business for weeks at a time when his parents were away.
“I’ve had no formal [business] school training, but my entrepreneurial instincts and management skills were honed early in life,” he says.
Team Health’s Dr. Goldsholl intended to get a formal MBA, but was too busy. “SHM’s Leadership Academy and other programs gave me management skills, and I chose CME credits in business and management areas,” she says. “I’m also more of an experiential than a classroom learner. Mentoring and other informal settings work for me.”
Michael Ruhlen, MD, MHM, Toledo (Ohio) Children’s Hospital corporate vice president of medical informatics and vice president of medical affairs, made a successful if not easy move from clinician to manager. Acting as a hospitalist seven years before the discipline was named in 1996, he developed systematic, data-driven clinical pathways and trained other would-be pediatric hospitalists in acute care pediatrics. In 2001 he was the first recipient of the National Association of Inpatient Physician’s Award for Outstanding Service in Hospital Medicine. The award recognized his managerial skill in building a hospitalist program from scratch.
Unlike hospitalists who are moving from well-defined clinical tracks to managerial roles, Dr. Ruhlen operated in uncharted territory in his first decade as a hospitalist. From the beginning of his hospitalist career, Dr. Ruhlen’s business head identified volume-dependent competency as critical to clinical and financial success. “I saw how to create time and quality efficiencies,” he explains. “If you do one or two lumbar punctures a year, you might stick a child five or six times. Doing a higher volume of procedures led to smoother operations.”
Recognizing the complexities of hospital management, Dr. Ruhlen returned to school to sharpen his management skills. He chose the Harvard School of Public Health’s master’s in healthcare management over an MBA because, as he puts it, “I’m interested in managing a hospital, not running Campbell’s Soup.” As a hospitalist executive, he works on improving the hospital’s IT systems, developing new physician leaders, and taking the lead on change management and patient safety issues. He also has been tapped twice to serve as acting hospital president.
Medicine as Business
Hospitalists enjoy an array of career choices. Those who savor the pure joy of clinical work can continue on that path, while others can choose a career in management; some can blend both. No matter what their career paths, healthcare’s increasing complexity will keep them fully occupied.
“As medicine grows more complex, students spend their time mastering clinical issues,” Dr. Shulman notes. “Many third-year med students don’t even know the difference between Medicaid and Medicare. As they practice as hospitalists and want to move up the administrative ranks, they will acquire the general business skills that will help them be effective and reshape healthcare policy.” TH
Marlene Piturro is a medical writer based in New York.
Many technically skilled professionals—including computer programmers, stockbrokers, or hospitalists—aspire to the executive suite.
The burgeoning field of hospital medicine offers especially enticing rewards for business-minded doctors, inducing frontline leaders to trade the white coat for wing tips and a shot at the top.
The pinnacle can be stratospheric. Adam Singer, MD, CEO of California-based IPC-The Hospitalist Company, traded his white coat for the so-called C suite. He has since filed an initial public offering that should produce $105 million for IPC’s stakeholders.
There’s also lots of room for hospitalists with more modest executive aspirations. The skills acquired by good hospitalists—thoroughness, the ability to solve complex problems, critical thinking, strong motivation, sound work ethic, and teamwork—serve physician executives well. Some physicians back into the executive suite once they realize they’re attracted to the business end of medicine. Those are the clinicians who volunteer to do the group’s scheduling or find that they enjoy negotiating contracts with new hires and payers. Others pursue a personal road map to the C suite.
Balancing Act
The biggest decision facing a hospitalist with managerial aspirations is whether to relinquish patient care.
“For most of your career you must remain active clinically, even though your time is disjointed because you’re intensely needed in both clinical and administrative areas,” says Andrew Urbach, MD, medical director of clinical excellence and service at Children’s Hospital of Pittsburgh. He manages both by constantly adapting. His time had been evenly split between clinical and administrative duties until July, when he cut back on his clinical duties. He now spends one week every quarter as a hospitalist and a half-day a week at the clinic. “It’s difficult balancing both, and reaching the highest level of excellence in two areas is demanding,” he says. “But the best hospitalist managers continue to see patients to maintain credibility with their peers.”
Stacy Goldsholl, MD, president of Knoxville, Tenn.-based Team Health, Hospital Medicine Division, was a staff hospitalist who ceded clinical work for a managerial career. After a three-year stint as a hospitalist with Covenant HealthCare’s hospital medicine program at Covenant Medical Center in Saginaw, Mich., her mentors recruited her to “jump around the country starting hospitalist programs during 2004 and 2005,” she says. “I was in the right place at the right time, and I had the confidence to move my agenda in a diplomatic way and with humor.”
Dr. Goldsholl reluctantly gave up clinical responsibilities three years ago. “It’s all about balance in my life,” she says. “It was a conscious decision to give up patient care. I miss it, but I wanted to take my career to a national level. I travel a great deal, which isn’t compatible with patient care.”
Business School
Hospitalists attracted to management often realize they need more business schooling, says Kevin Shulman, MD, MBA, professor of medicine and management at Duke University Medical Center and the Fuqua School of Business in Durham, N.C.
“The issues in medical training are clinical, not organizational,” he says. “As you move up in administration you don’t have business skills you need. When doctors feel frustrated about not being effective organizationally, that’s when they think about business school.”
Edward Ogata, MD, MBA, chief medical officer of Children’s Memorial Hospital in Chicago, and a pediatric neonatologist, realized how useful an MBA would be as he moved from clinical work to management. “I went back to school for an MBA at Northwestern University Kellogg School of Management 27 years after graduating from medical school,” he says. Pushed by the healthcare market into negotiating managed-care contracts in the 1980s, Dr. Ogata realized he knew little about accounting and finance. The always-precarious financial situations of children’s hospitals encouraged him to get the business skills to cope.
At Kellogg, in Chicago, Dr. Ogata was assigned homework and teamwork with executives from Motorola, Lucent, and GE. The first year was difficult because he was still covering call and juggling administrative tasks. He got up at 4 a.m. every day to study. Armed with business skills, Dr. Ogata feels better equipped to meet the financial and administrative needs of his inner-city hospital. “We’re not in a nice suburb with a favorable payer mix, and a hospital isn’t really a business in the conventional sense,’’ he notes. “But we are committed to doing the best.”
For Joy Drass, MD, MBA, a critical care trauma surgeon for 13 years and president of Georgetown University Hospital in Washington, D.C., methodically performing clinical tasks prepared her for top management. She assumed the presidency of the troubled hospital in 2001, one year after MedStar Health in Columbia, Md., acquired it. The hospital had recorded losses in excess of $200 million before MedStar stepped in.
“Many skills I developed as a critical care physician had an absolute application in this stressed organization,” she says. “In medicine, it’s called triage. In business, it’s prioritizing. You look at a situation and quickly set goals to get from point A to point B, encourage team work, and develop structures to support people when they are struggling through uncertainty.” Skills she learned as a graduate of the Wharton business school in Philadelphia helped her stabilize hospital operations, improve customer service and revenue collection, and develop a long-term strategic plan to improve the hospital’s chances of survival.
Varied Paths
Some hospitalists acquire business smarts from instinct and experience. When he was 13 years old, Dr. Urbach ran his family’s retail business for weeks at a time when his parents were away.
“I’ve had no formal [business] school training, but my entrepreneurial instincts and management skills were honed early in life,” he says.
Team Health’s Dr. Goldsholl intended to get a formal MBA, but was too busy. “SHM’s Leadership Academy and other programs gave me management skills, and I chose CME credits in business and management areas,” she says. “I’m also more of an experiential than a classroom learner. Mentoring and other informal settings work for me.”
Michael Ruhlen, MD, MHM, Toledo (Ohio) Children’s Hospital corporate vice president of medical informatics and vice president of medical affairs, made a successful if not easy move from clinician to manager. Acting as a hospitalist seven years before the discipline was named in 1996, he developed systematic, data-driven clinical pathways and trained other would-be pediatric hospitalists in acute care pediatrics. In 2001 he was the first recipient of the National Association of Inpatient Physician’s Award for Outstanding Service in Hospital Medicine. The award recognized his managerial skill in building a hospitalist program from scratch.
Unlike hospitalists who are moving from well-defined clinical tracks to managerial roles, Dr. Ruhlen operated in uncharted territory in his first decade as a hospitalist. From the beginning of his hospitalist career, Dr. Ruhlen’s business head identified volume-dependent competency as critical to clinical and financial success. “I saw how to create time and quality efficiencies,” he explains. “If you do one or two lumbar punctures a year, you might stick a child five or six times. Doing a higher volume of procedures led to smoother operations.”
Recognizing the complexities of hospital management, Dr. Ruhlen returned to school to sharpen his management skills. He chose the Harvard School of Public Health’s master’s in healthcare management over an MBA because, as he puts it, “I’m interested in managing a hospital, not running Campbell’s Soup.” As a hospitalist executive, he works on improving the hospital’s IT systems, developing new physician leaders, and taking the lead on change management and patient safety issues. He also has been tapped twice to serve as acting hospital president.
Medicine as Business
Hospitalists enjoy an array of career choices. Those who savor the pure joy of clinical work can continue on that path, while others can choose a career in management; some can blend both. No matter what their career paths, healthcare’s increasing complexity will keep them fully occupied.
“As medicine grows more complex, students spend their time mastering clinical issues,” Dr. Shulman notes. “Many third-year med students don’t even know the difference between Medicaid and Medicare. As they practice as hospitalists and want to move up the administrative ranks, they will acquire the general business skills that will help them be effective and reshape healthcare policy.” TH
Marlene Piturro is a medical writer based in New York.
Report Critical Care
Hospitalists often encounter patients who are or could become critically ill. The increased efforts while caring for these patients are best captured through critical-care service codes 99291 and 99292.
Although these codes yield higher reimbursement ($204.15 and $102.45, respectively, per national Medicare average payment), they are reported only under certain circumstances. The physician’s documentation must include enough detail to support critical-care claims: the patient’s condition, the nature of the physician’s care, and the time spent rendering care. Documentation of any other pertinent information is strongly encouraged because these services often come under payer scrutiny.
Condition and Care
A patient’s condition must meet the established criteria before the service qualifies as critical care. More specifically, the patient must have a critical illness or injury that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition.
The physician’s personal attention (i.e., care involving one critically ill patient at a time) is essential for rendering the highly complex decisions necessary to prevent the patient’s decline if left untreated. Given the seriousness of the patient’s condition, the physician is expected to focus only on the patient for whom critical-care time is reported.
Duration
Critical care is a time-based service. It constitutes the physician’s time spent providing direct care at the bedside and gathering and reviewing data on the patient’s unit or floor.
If the physician is not immediately available to the patient, the time associated with indirect care (e.g., reviewing data, calling the family from the office) is not counted in the overall critical-care service.
The physician keeps tracks of his/her total critical-care time throughout the day. A new period of critical-care time begins each calendar day. There is no prohibition against reporting multiple hours or days of critical care, as long as the patient’s condition prompts the service and documentation supports it.
Code 99291 represents the first “hour” of critical care, which physicians may report after accumulating the first 30 minutes of care. Alternately, physician management of the patient involving less than 30 minutes of critical-care time on a given day must be reported with the appropriate evaluation and management (E/M) code:
- Initial inpatient service (99221-99223);
- Subsequent hospital care (99231-99233); or
- Inpatient consultation (99251-99255).
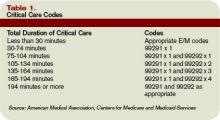
Once the physician achieves 75 minutes of critical-care time, he/she reports 99292 for the additional “30 minutes” of care beyond the first hour. Never report 99292 alone on the claim form. Code 99292 is considered an “add-on” code, which means it must be reported in addition to a primary code. Code 99291 is always the primary code (reported once per physician/group per day) for critical-care services. Code 99292 can be reported in multiple units per physician/group per day according to the number of minutes spent after the initial hour (see Table 1, p. 30).
Service Inclusions
Critical care involves highly complex decision making to manage the patient’s condition. This includes the physician’s performance and/or interpretation of labs, diagnostic studies, and procedures inherent in critical care.
Therefore, do not report the following services when billing 99291-99292:
- Cardiac output measurements (93561, 93562);
- Chest X-rays (71010, 71015, 71020);
- Pulse oximetry (94760, 94761, 94762); and
- Blood gases (multiple codes).
Further, don’t report interpretation of data stored in computers:
- Electrocardiograms, blood pressures, hematologic data (99090);
- Gastric intubation (43752, 91105);
- Temporary transcutaneous pacing (92953);
- Ventilation management (94002-94004, 94660, 94662); and
- Vascular access procedures (36000, 36410, 36415, 36591, 36600).
Any other service or procedure provided by the physician can be billed in addition to 99291-99292.
Be sure not to add separately billable procedure time into the physician’s total critical-care time. A notation in the medical record should reflect this (e.g., time spent inserting a central line is not included in today’s critical-care time).
Location
Because a patient can become seriously ill in any setting, physicians often provide critical-care services in emergency departments (EDs) and on standard medical-surgical floors before the patient is transferred to the intensive care unit (ICU).
Bed location alone does not determine critical-care reporting. Patients assigned to an ICU might be critically ill or injured and meet the “condition” requirements for 99291-99292.
However, the care provided may not meet the remaining requirements. According to the American Medical Association’s Current Procedural Terminology 2008 (Professional Edition) and the Medicare Claims Processing Manual, payment can be made for critical-care services provided in any location as long as the care provided meets the definition of critical care. Services for a patient who is not critically ill and unstable but who happens to be receiving care in a critical-care, intensive-care, or other specialized-care unit are reported using subsequent hospital care codes 99231-99233 or hospital consultation codes 99251-99255. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Hospitalists often encounter patients who are or could become critically ill. The increased efforts while caring for these patients are best captured through critical-care service codes 99291 and 99292.
Although these codes yield higher reimbursement ($204.15 and $102.45, respectively, per national Medicare average payment), they are reported only under certain circumstances. The physician’s documentation must include enough detail to support critical-care claims: the patient’s condition, the nature of the physician’s care, and the time spent rendering care. Documentation of any other pertinent information is strongly encouraged because these services often come under payer scrutiny.
Condition and Care
A patient’s condition must meet the established criteria before the service qualifies as critical care. More specifically, the patient must have a critical illness or injury that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition.
The physician’s personal attention (i.e., care involving one critically ill patient at a time) is essential for rendering the highly complex decisions necessary to prevent the patient’s decline if left untreated. Given the seriousness of the patient’s condition, the physician is expected to focus only on the patient for whom critical-care time is reported.
Duration
Critical care is a time-based service. It constitutes the physician’s time spent providing direct care at the bedside and gathering and reviewing data on the patient’s unit or floor.
If the physician is not immediately available to the patient, the time associated with indirect care (e.g., reviewing data, calling the family from the office) is not counted in the overall critical-care service.
The physician keeps tracks of his/her total critical-care time throughout the day. A new period of critical-care time begins each calendar day. There is no prohibition against reporting multiple hours or days of critical care, as long as the patient’s condition prompts the service and documentation supports it.
Code 99291 represents the first “hour” of critical care, which physicians may report after accumulating the first 30 minutes of care. Alternately, physician management of the patient involving less than 30 minutes of critical-care time on a given day must be reported with the appropriate evaluation and management (E/M) code:
- Initial inpatient service (99221-99223);
- Subsequent hospital care (99231-99233); or
- Inpatient consultation (99251-99255).
Once the physician achieves 75 minutes of critical-care time, he/she reports 99292 for the additional “30 minutes” of care beyond the first hour. Never report 99292 alone on the claim form. Code 99292 is considered an “add-on” code, which means it must be reported in addition to a primary code. Code 99291 is always the primary code (reported once per physician/group per day) for critical-care services. Code 99292 can be reported in multiple units per physician/group per day according to the number of minutes spent after the initial hour (see Table 1, p. 30).
Service Inclusions
Critical care involves highly complex decision making to manage the patient’s condition. This includes the physician’s performance and/or interpretation of labs, diagnostic studies, and procedures inherent in critical care.
Therefore, do not report the following services when billing 99291-99292:
- Cardiac output measurements (93561, 93562);
- Chest X-rays (71010, 71015, 71020);
- Pulse oximetry (94760, 94761, 94762); and
- Blood gases (multiple codes).
Further, don’t report interpretation of data stored in computers:
- Electrocardiograms, blood pressures, hematologic data (99090);
- Gastric intubation (43752, 91105);
- Temporary transcutaneous pacing (92953);
- Ventilation management (94002-94004, 94660, 94662); and
- Vascular access procedures (36000, 36410, 36415, 36591, 36600).
Any other service or procedure provided by the physician can be billed in addition to 99291-99292.
Be sure not to add separately billable procedure time into the physician’s total critical-care time. A notation in the medical record should reflect this (e.g., time spent inserting a central line is not included in today’s critical-care time).
Location
Because a patient can become seriously ill in any setting, physicians often provide critical-care services in emergency departments (EDs) and on standard medical-surgical floors before the patient is transferred to the intensive care unit (ICU).
Bed location alone does not determine critical-care reporting. Patients assigned to an ICU might be critically ill or injured and meet the “condition” requirements for 99291-99292.
However, the care provided may not meet the remaining requirements. According to the American Medical Association’s Current Procedural Terminology 2008 (Professional Edition) and the Medicare Claims Processing Manual, payment can be made for critical-care services provided in any location as long as the care provided meets the definition of critical care. Services for a patient who is not critically ill and unstable but who happens to be receiving care in a critical-care, intensive-care, or other specialized-care unit are reported using subsequent hospital care codes 99231-99233 or hospital consultation codes 99251-99255. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Hospitalists often encounter patients who are or could become critically ill. The increased efforts while caring for these patients are best captured through critical-care service codes 99291 and 99292.
Although these codes yield higher reimbursement ($204.15 and $102.45, respectively, per national Medicare average payment), they are reported only under certain circumstances. The physician’s documentation must include enough detail to support critical-care claims: the patient’s condition, the nature of the physician’s care, and the time spent rendering care. Documentation of any other pertinent information is strongly encouraged because these services often come under payer scrutiny.
Condition and Care
A patient’s condition must meet the established criteria before the service qualifies as critical care. More specifically, the patient must have a critical illness or injury that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition.
The physician’s personal attention (i.e., care involving one critically ill patient at a time) is essential for rendering the highly complex decisions necessary to prevent the patient’s decline if left untreated. Given the seriousness of the patient’s condition, the physician is expected to focus only on the patient for whom critical-care time is reported.
Duration
Critical care is a time-based service. It constitutes the physician’s time spent providing direct care at the bedside and gathering and reviewing data on the patient’s unit or floor.
If the physician is not immediately available to the patient, the time associated with indirect care (e.g., reviewing data, calling the family from the office) is not counted in the overall critical-care service.
The physician keeps tracks of his/her total critical-care time throughout the day. A new period of critical-care time begins each calendar day. There is no prohibition against reporting multiple hours or days of critical care, as long as the patient’s condition prompts the service and documentation supports it.
Code 99291 represents the first “hour” of critical care, which physicians may report after accumulating the first 30 minutes of care. Alternately, physician management of the patient involving less than 30 minutes of critical-care time on a given day must be reported with the appropriate evaluation and management (E/M) code:
- Initial inpatient service (99221-99223);
- Subsequent hospital care (99231-99233); or
- Inpatient consultation (99251-99255).
Once the physician achieves 75 minutes of critical-care time, he/she reports 99292 for the additional “30 minutes” of care beyond the first hour. Never report 99292 alone on the claim form. Code 99292 is considered an “add-on” code, which means it must be reported in addition to a primary code. Code 99291 is always the primary code (reported once per physician/group per day) for critical-care services. Code 99292 can be reported in multiple units per physician/group per day according to the number of minutes spent after the initial hour (see Table 1, p. 30).
Service Inclusions
Critical care involves highly complex decision making to manage the patient’s condition. This includes the physician’s performance and/or interpretation of labs, diagnostic studies, and procedures inherent in critical care.
Therefore, do not report the following services when billing 99291-99292:
- Cardiac output measurements (93561, 93562);
- Chest X-rays (71010, 71015, 71020);
- Pulse oximetry (94760, 94761, 94762); and
- Blood gases (multiple codes).
Further, don’t report interpretation of data stored in computers:
- Electrocardiograms, blood pressures, hematologic data (99090);
- Gastric intubation (43752, 91105);
- Temporary transcutaneous pacing (92953);
- Ventilation management (94002-94004, 94660, 94662); and
- Vascular access procedures (36000, 36410, 36415, 36591, 36600).
Any other service or procedure provided by the physician can be billed in addition to 99291-99292.
Be sure not to add separately billable procedure time into the physician’s total critical-care time. A notation in the medical record should reflect this (e.g., time spent inserting a central line is not included in today’s critical-care time).
Location
Because a patient can become seriously ill in any setting, physicians often provide critical-care services in emergency departments (EDs) and on standard medical-surgical floors before the patient is transferred to the intensive care unit (ICU).
Bed location alone does not determine critical-care reporting. Patients assigned to an ICU might be critically ill or injured and meet the “condition” requirements for 99291-99292.
However, the care provided may not meet the remaining requirements. According to the American Medical Association’s Current Procedural Terminology 2008 (Professional Edition) and the Medicare Claims Processing Manual, payment can be made for critical-care services provided in any location as long as the care provided meets the definition of critical care. Services for a patient who is not critically ill and unstable but who happens to be receiving care in a critical-care, intensive-care, or other specialized-care unit are reported using subsequent hospital care codes 99231-99233 or hospital consultation codes 99251-99255. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
The OIG Aftermath
An increase in uninsured patients who show up in emergency departments (EDs), physician specialty shortages, and a physician population unwilling to take call all have led to a now-common practice: hospitals pay physician-specialists for on-call coverage of their EDs.
Though essential for providing adequate emergency care, this hospital-physician arrangement can violate anti-kickback laws. But recently, one hospital’s payments to on-call physicians was given an official federal stamp of approval. What does this official statement mean for hospital medicine groups and the hospitalists they employ?
Origins of the Opinion
In September 2007, the Office of the Inspector General (OIG) issued an advisory opinion that a hospital that pays physicians for providing on-call and indigent care services in the ED does not violate the federal anti-kickback statute.
An unnamed medical center requested the opinion and submitted details on the comprehensive, detailed program it had created to ensure coverage of the ED.
The hospital’s program includes varied payment structures for staff physicians based on their participation in an on-call schedule for the ED and provision of inpatient follow-up care to patients seen while on call, among other actions.
The program applies to 18 specialties including hospitalists, and all participating physicians receive a per-diem payment for each on-call day.
Lou Glaser, partner at law firm of Sonnenschein Nath & Rosenthal, LLP, in Chicago, wrote the request.
“In this particular case, the hospital extended the program to nearly every specialty on the staff,” he explains. “Few hospitals have gone that far. But my client wanted to ensure that this program was appropriate and, if questioned, wanted to be able to say that they did everything possible to set up an appropriate program. They also, to the extent that if the OIG said no, wanted to be able to tell their physicians that they tried everything possible” to set up a fair payment system.
Ron Greeno, MD, FCCP, chief medical officer at Cogent Healthcare in Irvine, Calif., and a member of SHM’s Public Policy Committee, is surprised the opinion was requested.
“It came out of the blue,” he says. “We weren’t worrying about it.” He believes the shortage of physicians willing to provide on-call care in the ED—particularly to uninsured patients—forces hospitals to create similar payment structures.
“The opinion basically says the OIG doesn’t frown on the current practice,” Dr. Greeno says. “There’s no reason they would—and if they did, it would mean a staffing crisis for all hospitals.” Part of this potential crisis includes care for uninsured patients, for which the hospital isn’t compensated.
Uninsured Patients
A pivotal point in the OIG opinion and in the problems hospitals have with ED on-call staffing is payment for care of uninsured patients—especially those who require an on-call physician at the ED in the middle of the night.
“My client wanted a solution to this, a solution that ensured their indigent patients would receive care from all necessary specialties,” says Glaser.
The payment program created by Glaser’s client hospitals was structured to include care for indigent patients. “The OIG latched on to that for a number of reasons,” says Glaser. “But basically it shows that physicians are being paid for something that they would not otherwise be paid for.”
Effect on Hospitalists
Though the OIG opinion doesn’t change status quo for most, it provides valuable guidance on what the government considers an acceptable plan for covering on-call shortages. Criteria outlined in the opinion include:
- There must be a clear, demonstrated need for the on-call service;
- Participating physicians would otherwise be un- or under-compensated for a meaningful portion of their work, such as caring for uninsured admissions;
- Participating physicians deliver defined added value such as better outcomes, or participation in quality initiatives; and
- Reimbursement reflects market value.
Because most hospitalists are employed by or supported by the hospital for which they are on call, they are entirely exempt from anti-kickback issues. Therefore, the OIG opinion won’t affect their on-call payments.
“The opinion obviously isn’t geared toward any specialty,” Glaser points out. “In fact, the OIG noted that the hospital could not select specific groups and try to steer money toward those. That said, hospitalists are in a slightly different position than other medical staff. They maintain their practice at the hospital, and depend on that for their volume and income.”
If your hospital medicine group is not supported primarily by the hospital, how can you ensure your on-call payments are legally acceptable?
First, have a lawyer review your arrangements. While the onus for staying within the bounds of the law is on hospitals, it’s important for every hospital medicine group to have local legal experts examine their current or proposed payment structure for on-call and indigent care.
“Any time a hospital gives money to a doctor, [he or she] is subject to scrutiny,” says Dr. Greeno. “This has to be legally vetted.”
Second, document your own payment system. “There was a great deal of discussion in the request for opinion on how the hospital established its payment structure,” says Glaser. “The opinion shows the importance of having a well-documented process for establishing the rates to be paid, and showing that that’s fair.”
You can start your review of your own payment program by downloading a comprehensive overview of the OIG advisory opinion at SHM’s Web site, www.hospitalmedicine.org.
“For most of us who have been minding their p’s and q’s, [the opinion] doesn’t require any changes,” Dr. Greeno stresses. However, hospital medicine directors should stay on the safe side and check any on-call payment programs you might be participating in. TH
Jane Jerrard has written for The Hospitalist since 2005.
An increase in uninsured patients who show up in emergency departments (EDs), physician specialty shortages, and a physician population unwilling to take call all have led to a now-common practice: hospitals pay physician-specialists for on-call coverage of their EDs.
Though essential for providing adequate emergency care, this hospital-physician arrangement can violate anti-kickback laws. But recently, one hospital’s payments to on-call physicians was given an official federal stamp of approval. What does this official statement mean for hospital medicine groups and the hospitalists they employ?
Origins of the Opinion
In September 2007, the Office of the Inspector General (OIG) issued an advisory opinion that a hospital that pays physicians for providing on-call and indigent care services in the ED does not violate the federal anti-kickback statute.
An unnamed medical center requested the opinion and submitted details on the comprehensive, detailed program it had created to ensure coverage of the ED.
The hospital’s program includes varied payment structures for staff physicians based on their participation in an on-call schedule for the ED and provision of inpatient follow-up care to patients seen while on call, among other actions.
The program applies to 18 specialties including hospitalists, and all participating physicians receive a per-diem payment for each on-call day.
Lou Glaser, partner at law firm of Sonnenschein Nath & Rosenthal, LLP, in Chicago, wrote the request.
“In this particular case, the hospital extended the program to nearly every specialty on the staff,” he explains. “Few hospitals have gone that far. But my client wanted to ensure that this program was appropriate and, if questioned, wanted to be able to say that they did everything possible to set up an appropriate program. They also, to the extent that if the OIG said no, wanted to be able to tell their physicians that they tried everything possible” to set up a fair payment system.
Ron Greeno, MD, FCCP, chief medical officer at Cogent Healthcare in Irvine, Calif., and a member of SHM’s Public Policy Committee, is surprised the opinion was requested.
“It came out of the blue,” he says. “We weren’t worrying about it.” He believes the shortage of physicians willing to provide on-call care in the ED—particularly to uninsured patients—forces hospitals to create similar payment structures.
“The opinion basically says the OIG doesn’t frown on the current practice,” Dr. Greeno says. “There’s no reason they would—and if they did, it would mean a staffing crisis for all hospitals.” Part of this potential crisis includes care for uninsured patients, for which the hospital isn’t compensated.
Uninsured Patients
A pivotal point in the OIG opinion and in the problems hospitals have with ED on-call staffing is payment for care of uninsured patients—especially those who require an on-call physician at the ED in the middle of the night.
“My client wanted a solution to this, a solution that ensured their indigent patients would receive care from all necessary specialties,” says Glaser.
The payment program created by Glaser’s client hospitals was structured to include care for indigent patients. “The OIG latched on to that for a number of reasons,” says Glaser. “But basically it shows that physicians are being paid for something that they would not otherwise be paid for.”
Effect on Hospitalists
Though the OIG opinion doesn’t change status quo for most, it provides valuable guidance on what the government considers an acceptable plan for covering on-call shortages. Criteria outlined in the opinion include:
- There must be a clear, demonstrated need for the on-call service;
- Participating physicians would otherwise be un- or under-compensated for a meaningful portion of their work, such as caring for uninsured admissions;
- Participating physicians deliver defined added value such as better outcomes, or participation in quality initiatives; and
- Reimbursement reflects market value.
Because most hospitalists are employed by or supported by the hospital for which they are on call, they are entirely exempt from anti-kickback issues. Therefore, the OIG opinion won’t affect their on-call payments.
“The opinion obviously isn’t geared toward any specialty,” Glaser points out. “In fact, the OIG noted that the hospital could not select specific groups and try to steer money toward those. That said, hospitalists are in a slightly different position than other medical staff. They maintain their practice at the hospital, and depend on that for their volume and income.”
If your hospital medicine group is not supported primarily by the hospital, how can you ensure your on-call payments are legally acceptable?
First, have a lawyer review your arrangements. While the onus for staying within the bounds of the law is on hospitals, it’s important for every hospital medicine group to have local legal experts examine their current or proposed payment structure for on-call and indigent care.
“Any time a hospital gives money to a doctor, [he or she] is subject to scrutiny,” says Dr. Greeno. “This has to be legally vetted.”
Second, document your own payment system. “There was a great deal of discussion in the request for opinion on how the hospital established its payment structure,” says Glaser. “The opinion shows the importance of having a well-documented process for establishing the rates to be paid, and showing that that’s fair.”
You can start your review of your own payment program by downloading a comprehensive overview of the OIG advisory opinion at SHM’s Web site, www.hospitalmedicine.org.
“For most of us who have been minding their p’s and q’s, [the opinion] doesn’t require any changes,” Dr. Greeno stresses. However, hospital medicine directors should stay on the safe side and check any on-call payment programs you might be participating in. TH
Jane Jerrard has written for The Hospitalist since 2005.
An increase in uninsured patients who show up in emergency departments (EDs), physician specialty shortages, and a physician population unwilling to take call all have led to a now-common practice: hospitals pay physician-specialists for on-call coverage of their EDs.
Though essential for providing adequate emergency care, this hospital-physician arrangement can violate anti-kickback laws. But recently, one hospital’s payments to on-call physicians was given an official federal stamp of approval. What does this official statement mean for hospital medicine groups and the hospitalists they employ?
Origins of the Opinion
In September 2007, the Office of the Inspector General (OIG) issued an advisory opinion that a hospital that pays physicians for providing on-call and indigent care services in the ED does not violate the federal anti-kickback statute.
An unnamed medical center requested the opinion and submitted details on the comprehensive, detailed program it had created to ensure coverage of the ED.
The hospital’s program includes varied payment structures for staff physicians based on their participation in an on-call schedule for the ED and provision of inpatient follow-up care to patients seen while on call, among other actions.
The program applies to 18 specialties including hospitalists, and all participating physicians receive a per-diem payment for each on-call day.
Lou Glaser, partner at law firm of Sonnenschein Nath & Rosenthal, LLP, in Chicago, wrote the request.
“In this particular case, the hospital extended the program to nearly every specialty on the staff,” he explains. “Few hospitals have gone that far. But my client wanted to ensure that this program was appropriate and, if questioned, wanted to be able to say that they did everything possible to set up an appropriate program. They also, to the extent that if the OIG said no, wanted to be able to tell their physicians that they tried everything possible” to set up a fair payment system.
Ron Greeno, MD, FCCP, chief medical officer at Cogent Healthcare in Irvine, Calif., and a member of SHM’s Public Policy Committee, is surprised the opinion was requested.
“It came out of the blue,” he says. “We weren’t worrying about it.” He believes the shortage of physicians willing to provide on-call care in the ED—particularly to uninsured patients—forces hospitals to create similar payment structures.
“The opinion basically says the OIG doesn’t frown on the current practice,” Dr. Greeno says. “There’s no reason they would—and if they did, it would mean a staffing crisis for all hospitals.” Part of this potential crisis includes care for uninsured patients, for which the hospital isn’t compensated.
Uninsured Patients
A pivotal point in the OIG opinion and in the problems hospitals have with ED on-call staffing is payment for care of uninsured patients—especially those who require an on-call physician at the ED in the middle of the night.
“My client wanted a solution to this, a solution that ensured their indigent patients would receive care from all necessary specialties,” says Glaser.
The payment program created by Glaser’s client hospitals was structured to include care for indigent patients. “The OIG latched on to that for a number of reasons,” says Glaser. “But basically it shows that physicians are being paid for something that they would not otherwise be paid for.”
Effect on Hospitalists
Though the OIG opinion doesn’t change status quo for most, it provides valuable guidance on what the government considers an acceptable plan for covering on-call shortages. Criteria outlined in the opinion include:
- There must be a clear, demonstrated need for the on-call service;
- Participating physicians would otherwise be un- or under-compensated for a meaningful portion of their work, such as caring for uninsured admissions;
- Participating physicians deliver defined added value such as better outcomes, or participation in quality initiatives; and
- Reimbursement reflects market value.
Because most hospitalists are employed by or supported by the hospital for which they are on call, they are entirely exempt from anti-kickback issues. Therefore, the OIG opinion won’t affect their on-call payments.
“The opinion obviously isn’t geared toward any specialty,” Glaser points out. “In fact, the OIG noted that the hospital could not select specific groups and try to steer money toward those. That said, hospitalists are in a slightly different position than other medical staff. They maintain their practice at the hospital, and depend on that for their volume and income.”
If your hospital medicine group is not supported primarily by the hospital, how can you ensure your on-call payments are legally acceptable?
First, have a lawyer review your arrangements. While the onus for staying within the bounds of the law is on hospitals, it’s important for every hospital medicine group to have local legal experts examine their current or proposed payment structure for on-call and indigent care.
“Any time a hospital gives money to a doctor, [he or she] is subject to scrutiny,” says Dr. Greeno. “This has to be legally vetted.”
Second, document your own payment system. “There was a great deal of discussion in the request for opinion on how the hospital established its payment structure,” says Glaser. “The opinion shows the importance of having a well-documented process for establishing the rates to be paid, and showing that that’s fair.”
You can start your review of your own payment program by downloading a comprehensive overview of the OIG advisory opinion at SHM’s Web site, www.hospitalmedicine.org.
“For most of us who have been minding their p’s and q’s, [the opinion] doesn’t require any changes,” Dr. Greeno stresses. However, hospital medicine directors should stay on the safe side and check any on-call payment programs you might be participating in. TH
Jane Jerrard has written for The Hospitalist since 2005.
Your First Chair Job
An increase in uninsured patients who show up in emergency departments (EDs), physician specialty shortages, and a physician population unwilling to take call all have led to a now-common practice: hospitals pay physician-specialists for on-call coverage of their EDs.
Though essential for providing adequate emergency care, this hospital-physician arrangement can violate anti-kickback laws. But recently, one hospital’s payments to on-call physicians was given an official federal stamp of approval. What does this official statement mean for hospital medicine groups and the hospitalists they employ?
Origins of the Opinion
In September 2007, the Office of the Inspector General (OIG) issued an advisory opinion that a hospital that pays physicians for providing on-call and indigent care services in the ED does not violate the federal anti-kickback statute.
An unnamed medical center requested the opinion and submitted details on the comprehensive, detailed program it had created to ensure coverage of the ED.
The hospital’s program includes varied payment structures for staff physicians based on their participation in an on-call schedule for the ED and provision of inpatient follow-up care to patients seen while on call, among other actions.
The program applies to 18 specialties including hospitalists, and all participating physicians receive a per-diem payment for each on-call day.
Lou Glaser, partner at law firm of Sonnenschein Nath & Rosenthal, LLP, in Chicago, wrote the request.
“In this particular case, the hospital extended the program to nearly every specialty on the staff,” he explains. “Few hospitals have gone that far. But my client wanted to ensure that this program was appropriate and, if questioned, wanted to be able to say that they did everything possible to set up an appropriate program. They also, to the extent that if the OIG said no, wanted to be able to tell their physicians that they tried everything possible” to set up a fair payment system.
Ron Greeno, MD, FCCP, chief medical officer at Cogent Healthcare in Irvine, Calif., and a member of SHM’s Public Policy Committee, is surprised the opinion was requested.
“It came out of the blue,” he says. “We weren’t worrying about it.” He believes the shortage of physicians willing to provide on-call care in the ED—particularly to uninsured patients—forces hospitals to create similar payment structures.
“The opinion basically says the OIG doesn’t frown on the current practice,” Dr. Greeno says. “There’s no reason they would—and if they did, it would mean a staffing crisis for all hospitals.” Part of this potential crisis includes care for uninsured patients, for which the hospital isn’t compensated.
Uninsured Patients
A pivotal point in the OIG opinion and in the problems hospitals have with ED on-call staffing is payment for care of uninsured patients—especially those who require an on-call physician at the ED in the middle of the night.
“My client wanted a solution to this, a solution that ensured their indigent patients would receive care from all necessary specialties,” says Glaser.
The payment program created by Glaser’s client hospitals was structured to include care for indigent patients. “The OIG latched on to that for a number of reasons,” says Glaser. “But basically it shows that physicians are being paid for something that they would not otherwise be paid for.”
Effect on Hospitalists
Though the OIG opinion doesn’t change status quo for most, it provides valuable guidance on what the government considers an acceptable plan for covering on-call shortages. Criteria outlined in the opinion include:
- There must be a clear, demonstrated need for the on-call service;
- Participating physicians would otherwise be un- or under-compensated for a meaningful portion of their work, such as caring for uninsured admissions;
- Participating physicians deliver defined added value such as better outcomes, or participation in quality initiatives; and
- Reimbursement reflects market value.
Because most hospitalists are employed by or supported by the hospital for which they are on call, they are entirely exempt from anti-kickback issues. Therefore, the OIG opinion won’t affect their on-call payments.
“The opinion obviously isn’t geared toward any specialty,” Glaser points out. “In fact, the OIG noted that the hospital could not select specific groups and try to steer money toward those. That said, hospitalists are in a slightly different position than other medical staff. They maintain their practice at the hospital, and depend on that for their volume and income.”
If your hospital medicine group is not supported primarily by the hospital, how can you ensure your on-call payments are legally acceptable?
First, have a lawyer review your arrangements. While the onus for staying within the bounds of the law is on hospitals, it’s important for every hospital medicine group to have local legal experts examine their current or proposed payment structure for on-call and indigent care.
“Any time a hospital gives money to a doctor, [he or she] is subject to scrutiny,” says Dr. Greeno. “This has to be legally vetted.”
Second, document your own payment system. “There was a great deal of discussion in the request for opinion on how the hospital established its payment structure,” says Glaser. “The opinion shows the importance of having a well-documented process for establishing the rates to be paid, and showing that that’s fair.”
You can start your review of your own payment program by downloading a comprehensive overview of the OIG advisory opinion at SHM’s Web site, www.hospitalmedicine.org.
“For most of us who have been minding their p’s and q’s, [the opinion] doesn’t require any changes,” Dr. Greeno stresses. However, hospital medicine directors should stay on the safe side and check any on-call payment programs you might be participating in. TH
Jane Jerrard has written for The Hospitalist since 2005.
An increase in uninsured patients who show up in emergency departments (EDs), physician specialty shortages, and a physician population unwilling to take call all have led to a now-common practice: hospitals pay physician-specialists for on-call coverage of their EDs.
Though essential for providing adequate emergency care, this hospital-physician arrangement can violate anti-kickback laws. But recently, one hospital’s payments to on-call physicians was given an official federal stamp of approval. What does this official statement mean for hospital medicine groups and the hospitalists they employ?
Origins of the Opinion
In September 2007, the Office of the Inspector General (OIG) issued an advisory opinion that a hospital that pays physicians for providing on-call and indigent care services in the ED does not violate the federal anti-kickback statute.
An unnamed medical center requested the opinion and submitted details on the comprehensive, detailed program it had created to ensure coverage of the ED.
The hospital’s program includes varied payment structures for staff physicians based on their participation in an on-call schedule for the ED and provision of inpatient follow-up care to patients seen while on call, among other actions.
The program applies to 18 specialties including hospitalists, and all participating physicians receive a per-diem payment for each on-call day.
Lou Glaser, partner at law firm of Sonnenschein Nath & Rosenthal, LLP, in Chicago, wrote the request.
“In this particular case, the hospital extended the program to nearly every specialty on the staff,” he explains. “Few hospitals have gone that far. But my client wanted to ensure that this program was appropriate and, if questioned, wanted to be able to say that they did everything possible to set up an appropriate program. They also, to the extent that if the OIG said no, wanted to be able to tell their physicians that they tried everything possible” to set up a fair payment system.
Ron Greeno, MD, FCCP, chief medical officer at Cogent Healthcare in Irvine, Calif., and a member of SHM’s Public Policy Committee, is surprised the opinion was requested.
“It came out of the blue,” he says. “We weren’t worrying about it.” He believes the shortage of physicians willing to provide on-call care in the ED—particularly to uninsured patients—forces hospitals to create similar payment structures.
“The opinion basically says the OIG doesn’t frown on the current practice,” Dr. Greeno says. “There’s no reason they would—and if they did, it would mean a staffing crisis for all hospitals.” Part of this potential crisis includes care for uninsured patients, for which the hospital isn’t compensated.
Uninsured Patients
A pivotal point in the OIG opinion and in the problems hospitals have with ED on-call staffing is payment for care of uninsured patients—especially those who require an on-call physician at the ED in the middle of the night.
“My client wanted a solution to this, a solution that ensured their indigent patients would receive care from all necessary specialties,” says Glaser.
The payment program created by Glaser’s client hospitals was structured to include care for indigent patients. “The OIG latched on to that for a number of reasons,” says Glaser. “But basically it shows that physicians are being paid for something that they would not otherwise be paid for.”
Effect on Hospitalists
Though the OIG opinion doesn’t change status quo for most, it provides valuable guidance on what the government considers an acceptable plan for covering on-call shortages. Criteria outlined in the opinion include:
- There must be a clear, demonstrated need for the on-call service;
- Participating physicians would otherwise be un- or under-compensated for a meaningful portion of their work, such as caring for uninsured admissions;
- Participating physicians deliver defined added value such as better outcomes, or participation in quality initiatives; and
- Reimbursement reflects market value.
Because most hospitalists are employed by or supported by the hospital for which they are on call, they are entirely exempt from anti-kickback issues. Therefore, the OIG opinion won’t affect their on-call payments.
“The opinion obviously isn’t geared toward any specialty,” Glaser points out. “In fact, the OIG noted that the hospital could not select specific groups and try to steer money toward those. That said, hospitalists are in a slightly different position than other medical staff. They maintain their practice at the hospital, and depend on that for their volume and income.”
If your hospital medicine group is not supported primarily by the hospital, how can you ensure your on-call payments are legally acceptable?
First, have a lawyer review your arrangements. While the onus for staying within the bounds of the law is on hospitals, it’s important for every hospital medicine group to have local legal experts examine their current or proposed payment structure for on-call and indigent care.
“Any time a hospital gives money to a doctor, [he or she] is subject to scrutiny,” says Dr. Greeno. “This has to be legally vetted.”
Second, document your own payment system. “There was a great deal of discussion in the request for opinion on how the hospital established its payment structure,” says Glaser. “The opinion shows the importance of having a well-documented process for establishing the rates to be paid, and showing that that’s fair.”
You can start your review of your own payment program by downloading a comprehensive overview of the OIG advisory opinion at SHM’s Web site, www.hospitalmedicine.org.
“For most of us who have been minding their p’s and q’s, [the opinion] doesn’t require any changes,” Dr. Greeno stresses. However, hospital medicine directors should stay on the safe side and check any on-call payment programs you might be participating in. TH
Jane Jerrard has written for The Hospitalist since 2005.
An increase in uninsured patients who show up in emergency departments (EDs), physician specialty shortages, and a physician population unwilling to take call all have led to a now-common practice: hospitals pay physician-specialists for on-call coverage of their EDs.
Though essential for providing adequate emergency care, this hospital-physician arrangement can violate anti-kickback laws. But recently, one hospital’s payments to on-call physicians was given an official federal stamp of approval. What does this official statement mean for hospital medicine groups and the hospitalists they employ?
Origins of the Opinion
In September 2007, the Office of the Inspector General (OIG) issued an advisory opinion that a hospital that pays physicians for providing on-call and indigent care services in the ED does not violate the federal anti-kickback statute.
An unnamed medical center requested the opinion and submitted details on the comprehensive, detailed program it had created to ensure coverage of the ED.
The hospital’s program includes varied payment structures for staff physicians based on their participation in an on-call schedule for the ED and provision of inpatient follow-up care to patients seen while on call, among other actions.
The program applies to 18 specialties including hospitalists, and all participating physicians receive a per-diem payment for each on-call day.
Lou Glaser, partner at law firm of Sonnenschein Nath & Rosenthal, LLP, in Chicago, wrote the request.
“In this particular case, the hospital extended the program to nearly every specialty on the staff,” he explains. “Few hospitals have gone that far. But my client wanted to ensure that this program was appropriate and, if questioned, wanted to be able to say that they did everything possible to set up an appropriate program. They also, to the extent that if the OIG said no, wanted to be able to tell their physicians that they tried everything possible” to set up a fair payment system.
Ron Greeno, MD, FCCP, chief medical officer at Cogent Healthcare in Irvine, Calif., and a member of SHM’s Public Policy Committee, is surprised the opinion was requested.
“It came out of the blue,” he says. “We weren’t worrying about it.” He believes the shortage of physicians willing to provide on-call care in the ED—particularly to uninsured patients—forces hospitals to create similar payment structures.
“The opinion basically says the OIG doesn’t frown on the current practice,” Dr. Greeno says. “There’s no reason they would—and if they did, it would mean a staffing crisis for all hospitals.” Part of this potential crisis includes care for uninsured patients, for which the hospital isn’t compensated.
Uninsured Patients
A pivotal point in the OIG opinion and in the problems hospitals have with ED on-call staffing is payment for care of uninsured patients—especially those who require an on-call physician at the ED in the middle of the night.
“My client wanted a solution to this, a solution that ensured their indigent patients would receive care from all necessary specialties,” says Glaser.
The payment program created by Glaser’s client hospitals was structured to include care for indigent patients. “The OIG latched on to that for a number of reasons,” says Glaser. “But basically it shows that physicians are being paid for something that they would not otherwise be paid for.”
Effect on Hospitalists
Though the OIG opinion doesn’t change status quo for most, it provides valuable guidance on what the government considers an acceptable plan for covering on-call shortages. Criteria outlined in the opinion include:
- There must be a clear, demonstrated need for the on-call service;
- Participating physicians would otherwise be un- or under-compensated for a meaningful portion of their work, such as caring for uninsured admissions;
- Participating physicians deliver defined added value such as better outcomes, or participation in quality initiatives; and
- Reimbursement reflects market value.
Because most hospitalists are employed by or supported by the hospital for which they are on call, they are entirely exempt from anti-kickback issues. Therefore, the OIG opinion won’t affect their on-call payments.
“The opinion obviously isn’t geared toward any specialty,” Glaser points out. “In fact, the OIG noted that the hospital could not select specific groups and try to steer money toward those. That said, hospitalists are in a slightly different position than other medical staff. They maintain their practice at the hospital, and depend on that for their volume and income.”
If your hospital medicine group is not supported primarily by the hospital, how can you ensure your on-call payments are legally acceptable?
First, have a lawyer review your arrangements. While the onus for staying within the bounds of the law is on hospitals, it’s important for every hospital medicine group to have local legal experts examine their current or proposed payment structure for on-call and indigent care.
“Any time a hospital gives money to a doctor, [he or she] is subject to scrutiny,” says Dr. Greeno. “This has to be legally vetted.”
Second, document your own payment system. “There was a great deal of discussion in the request for opinion on how the hospital established its payment structure,” says Glaser. “The opinion shows the importance of having a well-documented process for establishing the rates to be paid, and showing that that’s fair.”
You can start your review of your own payment program by downloading a comprehensive overview of the OIG advisory opinion at SHM’s Web site, www.hospitalmedicine.org.
“For most of us who have been minding their p’s and q’s, [the opinion] doesn’t require any changes,” Dr. Greeno stresses. However, hospital medicine directors should stay on the safe side and check any on-call payment programs you might be participating in. TH
Jane Jerrard has written for The Hospitalist since 2005.
Teamwork Triumphs
Hospitalists regularly list daily workload and long working hours among their top concerns—but some of their tasks can be delegated to another member of the healthcare team.
“There is a perception that a lot of the activities hospitalists spend their time on don’t need to be done by a hospitalist,” said Kevin O’Leary, MD, assistant professor of medicine and associate division chief, Division of Hospital Medicine, Northwestern University Feinberg School of Medicine in Chicago.
For example, at Northwestern, hospitalists engage in discharge activities, case management, and communication with families. All this can be performed by someone else with clinical training, Dr. O’Leary says. The hospital has unit-based care coordinators (UCCs), but they follow all patients on a 30-bed unit and do not go on rounds with the hospitalists. “Their duties were more aligned with the hospital’s interests than the hospitalists’,” Dr. O’Leary explains. He and his colleagues decided to study the effect of assigning hospitalist care coordinators (HCCs) to work with hospitalists exclusively. Their findings are featured in this month’s Journal of Hospital Medicine.
The study covered the 12 weeks from September 2006, through November 2006. During that time, half the hospitalists on duty each week were randomly assigned to work with an HCC, while the other hospitalists continued working in their usual fashion. The HCCs performed the same duties as the UCCs, plus additional ones such as obtaining outside medical records and attending to more discharge details (see Table 1, below). All the HCCs were registered nurses who performed only team-related duties for the duration of the study.
The hospitalists and HCCs rounded together each morning as a team. They collaborated on the daily plan of care and decided on specific duties for each team member to accomplish. Essentially, the HCCs “allowed the physicians to focus more on clinical rather than ancillary issues,” Dr. O’Leary notes.
Activities related to the discharge process were a key feature of the HCC role. Among other things, they started discharge, arranged for home care, and wrote instructions. “We think that if this program is adopted long-term, HCCs could be key in planning the discharge process to improve patient safety,” Dr. O’Leary says. “For example, they could call patients at home to make sure they’re taking their medication.”
At the end of each week, the hospitalists completed an on-line survey measuring their satisfaction with the program and its effects on their efficiency. Patients also were contacted seven to 14 days after discharge and asked about their satisfaction with the discharge process.
Five hospitalists were on duty on any given week, for a total 60 hospitalist weeks. Of those, hospitalist-HCC teams accounted for 31 weeks (52%), and control hospitalists the remaining 29 (48%). Of the 31 hospitalists who completed a team week, 28 (90%) reported that the team approach improved their efficiency and job satisfaction. They singled out activities relating to communication with nurses and those associated with discharge planning and execution as particularly benefiting from the presence of an HCC.
“One of the advantages that hospitalists told us about working with the HCC was that it allowed them to be in two places at once,” Dr. O’Leary says. “[For example,] if a new admission came in before they were done with morning rounds, the hospitalist could begin the admission while the HCC looked in on their old patients. Or, if two admissions came at once, the hospitalist could begin to admit one of the patients while the HCC gathered background information on the second.
“Also, having an extra pair of hands was incredibly helpful on rounds for patients who had wounds that needed to be undressed and examined, or for helping to turn or move patients who were otherwise difficult to examine.”
The HCCs were not formally surveyed, but all said they would rather continue as team members than return to their old duties.
Of 71 patients who completed the discharge satisfaction interview, 44 (62%) were cared for by a hospitalist-HCC team, but their satisfaction levels were no different from those reported by patients cared for by control hospitalists.
There was also a suggestion that the addition of the HCC lowered costs and shortened length of stay. Patients cared for by a team incurred an unadjusted mean cost of $10,052.96 +/-$11,708.73, compared with an unadjusted mean cost of $11,703.19 +/-$20,455.78 incurred by the control patients (p=0.008). Unadjusted mean length of stay was 4.70 +/-4.15 days for patients cared for by a team, compared with 5.07 +/- 3.99 for patients seen by control hospitalists (p=0.005). Both findings lost significance on multivariate regression analysis, but the hospital is planning a longer study with a larger sample size to see if truly significant differences emerge.
The HCCs helped in two basic ways, Dr. O’Leary concludes. They lightened the physicians’ workload, and they were able to add a nurse’s perspective to patient care. For example, if the hospitalist wrote an order for a diuretic, the HCC could alert the unit nurse to check the computer for the order. “They had a unique ability to see what the nurses needed to know, because they were nurses themselves,” he says.
Hospitalists aren’t the only physicians who could benefit from this arrangement, he adds. “For physicians in a lot of specialties, there are lots of activities that don’t necessarily need to be done by the doctor. The right support would make them happier and more efficient.”TH
Norra MacReady is a medical writer based in California.
Hospitalists regularly list daily workload and long working hours among their top concerns—but some of their tasks can be delegated to another member of the healthcare team.
“There is a perception that a lot of the activities hospitalists spend their time on don’t need to be done by a hospitalist,” said Kevin O’Leary, MD, assistant professor of medicine and associate division chief, Division of Hospital Medicine, Northwestern University Feinberg School of Medicine in Chicago.
For example, at Northwestern, hospitalists engage in discharge activities, case management, and communication with families. All this can be performed by someone else with clinical training, Dr. O’Leary says. The hospital has unit-based care coordinators (UCCs), but they follow all patients on a 30-bed unit and do not go on rounds with the hospitalists. “Their duties were more aligned with the hospital’s interests than the hospitalists’,” Dr. O’Leary explains. He and his colleagues decided to study the effect of assigning hospitalist care coordinators (HCCs) to work with hospitalists exclusively. Their findings are featured in this month’s Journal of Hospital Medicine.
The study covered the 12 weeks from September 2006, through November 2006. During that time, half the hospitalists on duty each week were randomly assigned to work with an HCC, while the other hospitalists continued working in their usual fashion. The HCCs performed the same duties as the UCCs, plus additional ones such as obtaining outside medical records and attending to more discharge details (see Table 1, below). All the HCCs were registered nurses who performed only team-related duties for the duration of the study.
The hospitalists and HCCs rounded together each morning as a team. They collaborated on the daily plan of care and decided on specific duties for each team member to accomplish. Essentially, the HCCs “allowed the physicians to focus more on clinical rather than ancillary issues,” Dr. O’Leary notes.
Activities related to the discharge process were a key feature of the HCC role. Among other things, they started discharge, arranged for home care, and wrote instructions. “We think that if this program is adopted long-term, HCCs could be key in planning the discharge process to improve patient safety,” Dr. O’Leary says. “For example, they could call patients at home to make sure they’re taking their medication.”
At the end of each week, the hospitalists completed an on-line survey measuring their satisfaction with the program and its effects on their efficiency. Patients also were contacted seven to 14 days after discharge and asked about their satisfaction with the discharge process.
Five hospitalists were on duty on any given week, for a total 60 hospitalist weeks. Of those, hospitalist-HCC teams accounted for 31 weeks (52%), and control hospitalists the remaining 29 (48%). Of the 31 hospitalists who completed a team week, 28 (90%) reported that the team approach improved their efficiency and job satisfaction. They singled out activities relating to communication with nurses and those associated with discharge planning and execution as particularly benefiting from the presence of an HCC.
“One of the advantages that hospitalists told us about working with the HCC was that it allowed them to be in two places at once,” Dr. O’Leary says. “[For example,] if a new admission came in before they were done with morning rounds, the hospitalist could begin the admission while the HCC looked in on their old patients. Or, if two admissions came at once, the hospitalist could begin to admit one of the patients while the HCC gathered background information on the second.
“Also, having an extra pair of hands was incredibly helpful on rounds for patients who had wounds that needed to be undressed and examined, or for helping to turn or move patients who were otherwise difficult to examine.”
The HCCs were not formally surveyed, but all said they would rather continue as team members than return to their old duties.
Of 71 patients who completed the discharge satisfaction interview, 44 (62%) were cared for by a hospitalist-HCC team, but their satisfaction levels were no different from those reported by patients cared for by control hospitalists.
There was also a suggestion that the addition of the HCC lowered costs and shortened length of stay. Patients cared for by a team incurred an unadjusted mean cost of $10,052.96 +/-$11,708.73, compared with an unadjusted mean cost of $11,703.19 +/-$20,455.78 incurred by the control patients (p=0.008). Unadjusted mean length of stay was 4.70 +/-4.15 days for patients cared for by a team, compared with 5.07 +/- 3.99 for patients seen by control hospitalists (p=0.005). Both findings lost significance on multivariate regression analysis, but the hospital is planning a longer study with a larger sample size to see if truly significant differences emerge.
The HCCs helped in two basic ways, Dr. O’Leary concludes. They lightened the physicians’ workload, and they were able to add a nurse’s perspective to patient care. For example, if the hospitalist wrote an order for a diuretic, the HCC could alert the unit nurse to check the computer for the order. “They had a unique ability to see what the nurses needed to know, because they were nurses themselves,” he says.
Hospitalists aren’t the only physicians who could benefit from this arrangement, he adds. “For physicians in a lot of specialties, there are lots of activities that don’t necessarily need to be done by the doctor. The right support would make them happier and more efficient.”TH
Norra MacReady is a medical writer based in California.
Hospitalists regularly list daily workload and long working hours among their top concerns—but some of their tasks can be delegated to another member of the healthcare team.
“There is a perception that a lot of the activities hospitalists spend their time on don’t need to be done by a hospitalist,” said Kevin O’Leary, MD, assistant professor of medicine and associate division chief, Division of Hospital Medicine, Northwestern University Feinberg School of Medicine in Chicago.
For example, at Northwestern, hospitalists engage in discharge activities, case management, and communication with families. All this can be performed by someone else with clinical training, Dr. O’Leary says. The hospital has unit-based care coordinators (UCCs), but they follow all patients on a 30-bed unit and do not go on rounds with the hospitalists. “Their duties were more aligned with the hospital’s interests than the hospitalists’,” Dr. O’Leary explains. He and his colleagues decided to study the effect of assigning hospitalist care coordinators (HCCs) to work with hospitalists exclusively. Their findings are featured in this month’s Journal of Hospital Medicine.
The study covered the 12 weeks from September 2006, through November 2006. During that time, half the hospitalists on duty each week were randomly assigned to work with an HCC, while the other hospitalists continued working in their usual fashion. The HCCs performed the same duties as the UCCs, plus additional ones such as obtaining outside medical records and attending to more discharge details (see Table 1, below). All the HCCs were registered nurses who performed only team-related duties for the duration of the study.
The hospitalists and HCCs rounded together each morning as a team. They collaborated on the daily plan of care and decided on specific duties for each team member to accomplish. Essentially, the HCCs “allowed the physicians to focus more on clinical rather than ancillary issues,” Dr. O’Leary notes.
Activities related to the discharge process were a key feature of the HCC role. Among other things, they started discharge, arranged for home care, and wrote instructions. “We think that if this program is adopted long-term, HCCs could be key in planning the discharge process to improve patient safety,” Dr. O’Leary says. “For example, they could call patients at home to make sure they’re taking their medication.”
At the end of each week, the hospitalists completed an on-line survey measuring their satisfaction with the program and its effects on their efficiency. Patients also were contacted seven to 14 days after discharge and asked about their satisfaction with the discharge process.
Five hospitalists were on duty on any given week, for a total 60 hospitalist weeks. Of those, hospitalist-HCC teams accounted for 31 weeks (52%), and control hospitalists the remaining 29 (48%). Of the 31 hospitalists who completed a team week, 28 (90%) reported that the team approach improved their efficiency and job satisfaction. They singled out activities relating to communication with nurses and those associated with discharge planning and execution as particularly benefiting from the presence of an HCC.
“One of the advantages that hospitalists told us about working with the HCC was that it allowed them to be in two places at once,” Dr. O’Leary says. “[For example,] if a new admission came in before they were done with morning rounds, the hospitalist could begin the admission while the HCC looked in on their old patients. Or, if two admissions came at once, the hospitalist could begin to admit one of the patients while the HCC gathered background information on the second.
“Also, having an extra pair of hands was incredibly helpful on rounds for patients who had wounds that needed to be undressed and examined, or for helping to turn or move patients who were otherwise difficult to examine.”
The HCCs were not formally surveyed, but all said they would rather continue as team members than return to their old duties.
Of 71 patients who completed the discharge satisfaction interview, 44 (62%) were cared for by a hospitalist-HCC team, but their satisfaction levels were no different from those reported by patients cared for by control hospitalists.
There was also a suggestion that the addition of the HCC lowered costs and shortened length of stay. Patients cared for by a team incurred an unadjusted mean cost of $10,052.96 +/-$11,708.73, compared with an unadjusted mean cost of $11,703.19 +/-$20,455.78 incurred by the control patients (p=0.008). Unadjusted mean length of stay was 4.70 +/-4.15 days for patients cared for by a team, compared with 5.07 +/- 3.99 for patients seen by control hospitalists (p=0.005). Both findings lost significance on multivariate regression analysis, but the hospital is planning a longer study with a larger sample size to see if truly significant differences emerge.
The HCCs helped in two basic ways, Dr. O’Leary concludes. They lightened the physicians’ workload, and they were able to add a nurse’s perspective to patient care. For example, if the hospitalist wrote an order for a diuretic, the HCC could alert the unit nurse to check the computer for the order. “They had a unique ability to see what the nurses needed to know, because they were nurses themselves,” he says.
Hospitalists aren’t the only physicians who could benefit from this arrangement, he adds. “For physicians in a lot of specialties, there are lots of activities that don’t necessarily need to be done by the doctor. The right support would make them happier and more efficient.”TH
Norra MacReady is a medical writer based in California.
Combat Adverse Effects
A serious adverse drug event (ADE) is defined as one that causes death, disability, or permanent damage, hospitalization (initial or prolonged), or birth defects.
According to Moore, et al., the number of serious ADEs has increased significantly since 1998 through 2005, according to reports in the Food and Drug Administration (FDA) adverse event reporting system, also known as MedWatch.1 During that time, 467,809 serious ADEs were reported, and the annual number of reports had increased from 34,966 to 89,842.
The number of fatal ADEs increased in that period as well, from 4,419 to 15,109. Further, ADEs related to biotech drugs increased 15.8-fold. The most commonly reported classes with serious ADEs included anti-tumor necrosis factor drugs, interferons, and insulins. Drugs associated with ADEs included some that had been withdrawn from the U.S. market over safety concerns, as well as products that remained on the market.
On Sept. 27, the FDA Amendments Act of 2007 was passed. The measure includes the Prescription Drug User Fee Act (PDUFA), which authorizes the FDA to collect fees from drug makers to supplement funding for the drug-review process.2 A key revision now lets the agency require—not just request—that drug companies perform phase four clinical studies. The PDUFA also includes additional staff for reviewing medical devices. Additional stipulations are that the FDA will:
- Assess signals of serious risk related to drug use as they arise;
- Identify unexpected serious risks;
- Identify when post-marketing studies are needed; and
- Quickly submit a supplement proposing changes to the approved labeling of a drug to reflect new safety information, including changes to boxed warnings, contraindications, warnings, precautions, or adverse reactions within 30 days of identification.
This legislation has brought a number of new warnings on FDA-approved products.
The Warnings
A study in the May 2007 issue of Lancet Infectious Diseases noted higher all-cause mortality in patients treated with cefepime (Maxipime) compared with other beta-lactam antibiotics.3 Cefepime is FDA approved for the treatment of infections caused by susceptible gram-positive and gram-negative micro-organisms. The risk ratio (RR) was 1.26 (95% confidence interval [CI] 1.08–1.49) for cefepime and for the subgroup of patients with febrile neutropenia (RR 1.42 [95% CI 1.09–1.84]). The FDA is reviewing safety data and has requested additional data from Bristol-Myers Squibb to further evaluate the risk of death in cefepime-treated patients. The FDA asks healthcare professionals to report adverse events from cefepime and other agents to MedWatch at www.fda.gov/medwatch/report.htm.
A new warning regarding the pregnancy category and teratogenic effects has been added to the label of mycophenolic acid (MPA) delayed-release tablets (Myfortic). The FDA notes that use of MPA during pregnancy is associated with increased risks of pregnancy loss and congenital malformations, thereby changing the pregnancy category to D (positive evidence of fetal risk) from C (risk of fetal harm cannot be ruled out).
The MPA warnings and precautions sections also have changed. Results from postmarketing data from the U.S. National Transplantation Pregnancy Registry and additional postmarketing data collected in women exposed to systemic mycophenolate mofetil (MMF) during pregnancy brought these revisions. MMF is converted to the active ingredient in MPA following intravenous or oral administration. A patient planning to get pregnant should not use MMF/MPA unless she cannot be treated with other immunosuppressant drugs. Additionally, female patients of childbearing potential must receive contraceptive counseling and use contraception while on this agent. Remember, not only transplant patients receive MMF/MPA; patients with lupus nephritis also use it.
On Nov. 27, the Pediatric Advisory Committee of the FDA recommended changing the label of the two neuraminidase inhibitors, oseltamivir (Tamiflu) and zanamivir (Relenza), to reflect the potential for neuropsychiatric effects (mostly in children). Last year, Roche revised the oseltamivir label to add warnings of potential confusion and self-injury with the product. According to the FDA, about five patients died as a result of these neuropsychiatric effects, and nearly 600 cases of psychiatric problems were reported.
On Nov. 14, the FDA added to the black box label of rosiglitazone (Avandia) regarding an increased risk of myocardial infarction. The warning states that a recent meta-analysis of 42 clinical studies (mean duration six months, n=14,237) mostly comparing rosiglitazone with placebo, showed it to be associated with an increased risk of myocardial ischemic events. Further, three other studies (mean duration 41 months; n=14,067), comparing rosiglitazone with other oral antidiabetic agents or placebo, have not confirmed or excluded this risk. The available data on the risk of myocardial ischemia are currently inconclusive.
The FDA has asked that GlaxoSmithKline conduct extensive long-term, post-marketing trials to determine rosiglitazone’s cardiovascular safety. A study of this type, is a direct result of the new PDUFA legislation. The trial is expected to begin after July and end by 2014. Updates to the warnings, precautions, and indications sections were also added to the label. For example, rosiglitazone is not recommended for heart disease patients who are taking nitrates, nor is it recommended in combination with insulin.
Finally, the FDA is evaluating postmarketing adverse event reports for varenicline (Chantix) describing suicidal ideation, suicide, and aggressive and erratic behavior in patients taking it for smoking cessation. While the review proceeds, physicians are advised to evaluate patients for behavior and mood disorders, as well as drowsiness. In patients taking varenicline, caution is advised while driving or operating machinery until the patient’s response to it is known. TH
Michele B. Kaufman is a freelance medical writer based in New York City.
References
- Moore TJ, Cohen MJ, Furberg CD. Serious adverse drug events reported to the Food and Drug Administration, 1998-2005. Arch Intern Med. 2007;167:1752-1759.
- Wechsler J. No shortage of recommendations for PDUFA IV as Congress and professional organizations weigh in on drug safety. Formulary 2007;42:264-265.
- Yahav D, Paul M, Fraser A, Sarid N, Leibovici L. Efficacy and safety of cefepime: a systematic review and meta-analysis. Lancet Infect Dis. 2007 May;7(5):338-348.
A serious adverse drug event (ADE) is defined as one that causes death, disability, or permanent damage, hospitalization (initial or prolonged), or birth defects.
According to Moore, et al., the number of serious ADEs has increased significantly since 1998 through 2005, according to reports in the Food and Drug Administration (FDA) adverse event reporting system, also known as MedWatch.1 During that time, 467,809 serious ADEs were reported, and the annual number of reports had increased from 34,966 to 89,842.
The number of fatal ADEs increased in that period as well, from 4,419 to 15,109. Further, ADEs related to biotech drugs increased 15.8-fold. The most commonly reported classes with serious ADEs included anti-tumor necrosis factor drugs, interferons, and insulins. Drugs associated with ADEs included some that had been withdrawn from the U.S. market over safety concerns, as well as products that remained on the market.
On Sept. 27, the FDA Amendments Act of 2007 was passed. The measure includes the Prescription Drug User Fee Act (PDUFA), which authorizes the FDA to collect fees from drug makers to supplement funding for the drug-review process.2 A key revision now lets the agency require—not just request—that drug companies perform phase four clinical studies. The PDUFA also includes additional staff for reviewing medical devices. Additional stipulations are that the FDA will:
- Assess signals of serious risk related to drug use as they arise;
- Identify unexpected serious risks;
- Identify when post-marketing studies are needed; and
- Quickly submit a supplement proposing changes to the approved labeling of a drug to reflect new safety information, including changes to boxed warnings, contraindications, warnings, precautions, or adverse reactions within 30 days of identification.
This legislation has brought a number of new warnings on FDA-approved products.
The Warnings
A study in the May 2007 issue of Lancet Infectious Diseases noted higher all-cause mortality in patients treated with cefepime (Maxipime) compared with other beta-lactam antibiotics.3 Cefepime is FDA approved for the treatment of infections caused by susceptible gram-positive and gram-negative micro-organisms. The risk ratio (RR) was 1.26 (95% confidence interval [CI] 1.08–1.49) for cefepime and for the subgroup of patients with febrile neutropenia (RR 1.42 [95% CI 1.09–1.84]). The FDA is reviewing safety data and has requested additional data from Bristol-Myers Squibb to further evaluate the risk of death in cefepime-treated patients. The FDA asks healthcare professionals to report adverse events from cefepime and other agents to MedWatch at www.fda.gov/medwatch/report.htm.
A new warning regarding the pregnancy category and teratogenic effects has been added to the label of mycophenolic acid (MPA) delayed-release tablets (Myfortic). The FDA notes that use of MPA during pregnancy is associated with increased risks of pregnancy loss and congenital malformations, thereby changing the pregnancy category to D (positive evidence of fetal risk) from C (risk of fetal harm cannot be ruled out).
The MPA warnings and precautions sections also have changed. Results from postmarketing data from the U.S. National Transplantation Pregnancy Registry and additional postmarketing data collected in women exposed to systemic mycophenolate mofetil (MMF) during pregnancy brought these revisions. MMF is converted to the active ingredient in MPA following intravenous or oral administration. A patient planning to get pregnant should not use MMF/MPA unless she cannot be treated with other immunosuppressant drugs. Additionally, female patients of childbearing potential must receive contraceptive counseling and use contraception while on this agent. Remember, not only transplant patients receive MMF/MPA; patients with lupus nephritis also use it.
On Nov. 27, the Pediatric Advisory Committee of the FDA recommended changing the label of the two neuraminidase inhibitors, oseltamivir (Tamiflu) and zanamivir (Relenza), to reflect the potential for neuropsychiatric effects (mostly in children). Last year, Roche revised the oseltamivir label to add warnings of potential confusion and self-injury with the product. According to the FDA, about five patients died as a result of these neuropsychiatric effects, and nearly 600 cases of psychiatric problems were reported.
On Nov. 14, the FDA added to the black box label of rosiglitazone (Avandia) regarding an increased risk of myocardial infarction. The warning states that a recent meta-analysis of 42 clinical studies (mean duration six months, n=14,237) mostly comparing rosiglitazone with placebo, showed it to be associated with an increased risk of myocardial ischemic events. Further, three other studies (mean duration 41 months; n=14,067), comparing rosiglitazone with other oral antidiabetic agents or placebo, have not confirmed or excluded this risk. The available data on the risk of myocardial ischemia are currently inconclusive.
The FDA has asked that GlaxoSmithKline conduct extensive long-term, post-marketing trials to determine rosiglitazone’s cardiovascular safety. A study of this type, is a direct result of the new PDUFA legislation. The trial is expected to begin after July and end by 2014. Updates to the warnings, precautions, and indications sections were also added to the label. For example, rosiglitazone is not recommended for heart disease patients who are taking nitrates, nor is it recommended in combination with insulin.
Finally, the FDA is evaluating postmarketing adverse event reports for varenicline (Chantix) describing suicidal ideation, suicide, and aggressive and erratic behavior in patients taking it for smoking cessation. While the review proceeds, physicians are advised to evaluate patients for behavior and mood disorders, as well as drowsiness. In patients taking varenicline, caution is advised while driving or operating machinery until the patient’s response to it is known. TH
Michele B. Kaufman is a freelance medical writer based in New York City.
References
- Moore TJ, Cohen MJ, Furberg CD. Serious adverse drug events reported to the Food and Drug Administration, 1998-2005. Arch Intern Med. 2007;167:1752-1759.
- Wechsler J. No shortage of recommendations for PDUFA IV as Congress and professional organizations weigh in on drug safety. Formulary 2007;42:264-265.
- Yahav D, Paul M, Fraser A, Sarid N, Leibovici L. Efficacy and safety of cefepime: a systematic review and meta-analysis. Lancet Infect Dis. 2007 May;7(5):338-348.
A serious adverse drug event (ADE) is defined as one that causes death, disability, or permanent damage, hospitalization (initial or prolonged), or birth defects.
According to Moore, et al., the number of serious ADEs has increased significantly since 1998 through 2005, according to reports in the Food and Drug Administration (FDA) adverse event reporting system, also known as MedWatch.1 During that time, 467,809 serious ADEs were reported, and the annual number of reports had increased from 34,966 to 89,842.
The number of fatal ADEs increased in that period as well, from 4,419 to 15,109. Further, ADEs related to biotech drugs increased 15.8-fold. The most commonly reported classes with serious ADEs included anti-tumor necrosis factor drugs, interferons, and insulins. Drugs associated with ADEs included some that had been withdrawn from the U.S. market over safety concerns, as well as products that remained on the market.
On Sept. 27, the FDA Amendments Act of 2007 was passed. The measure includes the Prescription Drug User Fee Act (PDUFA), which authorizes the FDA to collect fees from drug makers to supplement funding for the drug-review process.2 A key revision now lets the agency require—not just request—that drug companies perform phase four clinical studies. The PDUFA also includes additional staff for reviewing medical devices. Additional stipulations are that the FDA will:
- Assess signals of serious risk related to drug use as they arise;
- Identify unexpected serious risks;
- Identify when post-marketing studies are needed; and
- Quickly submit a supplement proposing changes to the approved labeling of a drug to reflect new safety information, including changes to boxed warnings, contraindications, warnings, precautions, or adverse reactions within 30 days of identification.
This legislation has brought a number of new warnings on FDA-approved products.
The Warnings
A study in the May 2007 issue of Lancet Infectious Diseases noted higher all-cause mortality in patients treated with cefepime (Maxipime) compared with other beta-lactam antibiotics.3 Cefepime is FDA approved for the treatment of infections caused by susceptible gram-positive and gram-negative micro-organisms. The risk ratio (RR) was 1.26 (95% confidence interval [CI] 1.08–1.49) for cefepime and for the subgroup of patients with febrile neutropenia (RR 1.42 [95% CI 1.09–1.84]). The FDA is reviewing safety data and has requested additional data from Bristol-Myers Squibb to further evaluate the risk of death in cefepime-treated patients. The FDA asks healthcare professionals to report adverse events from cefepime and other agents to MedWatch at www.fda.gov/medwatch/report.htm.
A new warning regarding the pregnancy category and teratogenic effects has been added to the label of mycophenolic acid (MPA) delayed-release tablets (Myfortic). The FDA notes that use of MPA during pregnancy is associated with increased risks of pregnancy loss and congenital malformations, thereby changing the pregnancy category to D (positive evidence of fetal risk) from C (risk of fetal harm cannot be ruled out).
The MPA warnings and precautions sections also have changed. Results from postmarketing data from the U.S. National Transplantation Pregnancy Registry and additional postmarketing data collected in women exposed to systemic mycophenolate mofetil (MMF) during pregnancy brought these revisions. MMF is converted to the active ingredient in MPA following intravenous or oral administration. A patient planning to get pregnant should not use MMF/MPA unless she cannot be treated with other immunosuppressant drugs. Additionally, female patients of childbearing potential must receive contraceptive counseling and use contraception while on this agent. Remember, not only transplant patients receive MMF/MPA; patients with lupus nephritis also use it.
On Nov. 27, the Pediatric Advisory Committee of the FDA recommended changing the label of the two neuraminidase inhibitors, oseltamivir (Tamiflu) and zanamivir (Relenza), to reflect the potential for neuropsychiatric effects (mostly in children). Last year, Roche revised the oseltamivir label to add warnings of potential confusion and self-injury with the product. According to the FDA, about five patients died as a result of these neuropsychiatric effects, and nearly 600 cases of psychiatric problems were reported.
On Nov. 14, the FDA added to the black box label of rosiglitazone (Avandia) regarding an increased risk of myocardial infarction. The warning states that a recent meta-analysis of 42 clinical studies (mean duration six months, n=14,237) mostly comparing rosiglitazone with placebo, showed it to be associated with an increased risk of myocardial ischemic events. Further, three other studies (mean duration 41 months; n=14,067), comparing rosiglitazone with other oral antidiabetic agents or placebo, have not confirmed or excluded this risk. The available data on the risk of myocardial ischemia are currently inconclusive.
The FDA has asked that GlaxoSmithKline conduct extensive long-term, post-marketing trials to determine rosiglitazone’s cardiovascular safety. A study of this type, is a direct result of the new PDUFA legislation. The trial is expected to begin after July and end by 2014. Updates to the warnings, precautions, and indications sections were also added to the label. For example, rosiglitazone is not recommended for heart disease patients who are taking nitrates, nor is it recommended in combination with insulin.
Finally, the FDA is evaluating postmarketing adverse event reports for varenicline (Chantix) describing suicidal ideation, suicide, and aggressive and erratic behavior in patients taking it for smoking cessation. While the review proceeds, physicians are advised to evaluate patients for behavior and mood disorders, as well as drowsiness. In patients taking varenicline, caution is advised while driving or operating machinery until the patient’s response to it is known. TH
Michele B. Kaufman is a freelance medical writer based in New York City.
References
- Moore TJ, Cohen MJ, Furberg CD. Serious adverse drug events reported to the Food and Drug Administration, 1998-2005. Arch Intern Med. 2007;167:1752-1759.
- Wechsler J. No shortage of recommendations for PDUFA IV as Congress and professional organizations weigh in on drug safety. Formulary 2007;42:264-265.
- Yahav D, Paul M, Fraser A, Sarid N, Leibovici L. Efficacy and safety of cefepime: a systematic review and meta-analysis. Lancet Infect Dis. 2007 May;7(5):338-348.
In the Literature
LITERATURE AT A GLANCE
Use this guide to find the abstracts below that correspond to these recent clinical findings
- 24-hour TIA clinic improves outcomes.
- More rapid treatment after TIA and minor stroke reduce risk for recurrent stroke.
- Prasugrel more efficacious than clopidogrel in acute coronary syndrome, but with higher bleeding rates.
- Zoledronic acid use after hip fracture repair reduces probability of new fractures.
- No benefit in quality measures and resource use for surgical patients receiving medical consultation.
- Pediatric RRTs reduce mortality rate.
- Influenza vaccinations prevent hospitalization, death among elderly.
- Chlorhexidine bathing reduces catheter-associated bloodstream infections.
- Chlorhexidine-based antiseptic solution reduces rates of catheter-associated infections
Would 24-hour Hospital Clinic Reduce LOS, Stroke Risk?
Background: Transient ischemic attacks (TIA) precede up to 25% of completed strokes and can provide opportunity for critical intervention if identified early. A specialty clinic with immediate access to imaging facilities could provide early identification and intervention.
Study design: Cohort study statistical analysis of data.
Setting: SOS-TIA hospital clinic in Paris.
Synopsis: A leaflet about TIA with a toll-free telephone number for SOS-TIA was sent to 15,000 family doctors, cardiologists, neurologists, and ophthalmologists in Paris. Between January 2003 and December 2005, 1,085 patients with suspected TIA were admitted to the clinic. The median duration of symptoms was 15 minutes. All patients were started on a stroke-prevention program, 5% had urgent carotid revascularization, and 5% were treated for atrial fibrillation with anticoagulants. Further, 74% of all patients seen were sent home the same day. The 90-day stroke rate was 1.24%; the rate predicted was 5.96%. Limitations of the study included selective patient recruitment from family doctors and office-based specialists. Also, the study lacked a randomized control group.
Bottom line: Prompt evaluation and treatment of patients in a dedicated TIA clinic is associated with a lower stroke risk. The TIA clinic also may lower costs via decreased length of hospital stay.
Citation: Lavallee P, Meseguer E, Abboud H, et al. A transient ischemic attack clinic with round the clock access (SOS-TIA): feasibility and effects. Lancet Neurol. 2007;6(11):953-960.
Can Early Treatment after TIA or Minor Stroke Reduce Risk of Early Recurrent Stroke?
Background: In the week following a TIA or a minor stroke, the risk of recurrent stroke grows to 10%. These warning events provide a limited window of opportunity for prevention. Several treatments are effective in stroke prevention following TIA or minor ischemic stroke if identified early. These include aspirin, other antiplatelet agents, blood-pressure (BP) medications, statins, anticoagulation for atrial fibrillation, and endarterectomy.
Study design: Prospective before-versus-after study (Oxford Vascular Study, or OXVASC) within population-based incidence study.
Setting:: The study population was located in primary care practices in the United Kingdom.
Synopsis: The OXVASC study looked at 1,278 patients who presented with TIA or stroke: 607 were referred directly to the hospital, 620 were referred for outpatient assessment, and 51 were not referred to secondary care. In phase 1, a daily TIA and minor stroke clinic was introduced. Collaborating primary care physicians were asked to refer all patients suspected of having TIA and minor stroke. Phase 1 took place between April 1, 2002, and Sept. 30, 2004. The treatment protocol recommended aspirin in patients not already on anti-platelet therapy (75 mg daily) or clopidogrel if aspirin was contraindicated; simvastatin (40 mg daily); BP lowering agents unless systolic BP less than 130 mm Hg; and anticoagulation as required.
In phase 2, from Oct. 1, 2004, to March 31, 2007, a clinic was established at which no appointments were necessary, treatment was initiated immediately, and diagnosis was confirmed. Patients were assessed in the same way as in phase 1, but all those considered to have had a TIA or stroke were given aspirin 300 mg together with a prescription of any other study medication to start the same day. A loading dose of clopidogrel 300 mg was also prescribed. The 90-day risk if recurrent stroke in the patients referred to the study clinic was 10.3% in phase 1 and 2.1% in phase 2.
Bottom line: Early treatment after TIA or minor stroke was associated with an 80% reduction in the risk of recurrent stroke.
Citation: Rothwell PM, Giles MF, Chandratheva A, et al. Effect of urgent treatment of transient ischemic attack (TIA) and minor stroke on early recurrent stroke (EXPRESS study): a prospective population-based sequential comparison. Lancet 2007;370:1432-1442.
How Does Prasugrel Compare With Clopidogrel in Acute Coronary Syndrome?
Background: Short-term and long-term benefits of a dual anti-platelet therapy for patients with acute coronary syndromes and/or PTCA has been well established but limited by recurrent atherothrombatic events and safety issues.
Study design: Double-blind, randomized study.
Setting: Triton-TIMI 38 Study Group.
Synopsis: This study randomly assigned 13,608 patients with acute coronary syndromes from 30 countries to a treatment group between November 2004 and January 2007. The study protocol used a loading dose of prasugrel (60 mg) within 72 hours before randomization and one hour after cardiac catheterization.
After percutaneous coronary intervention (PCI) patients received maintenance doses of either prasugrel (10 mg) or clopidogrel (75 mg) daily. Daily aspirin (75-162 mg) was required. The outcome of this study showed a significant reduction in the rate of ischemic end points (nonfatal myocardial infarction, stroke, and death) and stent re-thrombosis with prasugrel over clopidogrel. This was theorized to be due to the more rapid onset of antiplatelet effect with prasugrel and improved inhibition of platelet aggregation. Bleeding episodes were more frequent in the prasugrel group. Limitations of the study included the choice of vessels treated, devices used, and adjunctive medication administered to support PCI. All were left to the discretion of the treating physician.
Bottom line: Prasugrel therapy was significantly better than clopidogrel but with an increased risk of major bleeding.
Citation: Wiviott SD, Braunwald E, McCabe CH, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007;357:2001-2015.
Can the Rate of New Hip Fracture Be Reduced with Zoledronic Acid?
Background: Mortality is markedly increased following hip fractures, and medical interventions exist to improve clinical outcomes.
Study design: Randomized, double-blind, placebo-controlled trial.
Setting: International, multicenter trial involving patients with recent hip fracture.
Synopsis: This study, know as the HORIZON trial, involved 2,127 patients. Of those, 1,065 (mean age of 74.5) were assigned to receive yearly infusions of 5 mg IV zoledronic acid within 90 days after surgical hip fracture repair. Meantime, 1,062 were assigned to receive placebo.
All patients received supplemental vitamin D and calcium. The median follow-up was 1.9 years, and the primary end point was a new clinical fracture. The rate of any new clinical fracture was 8.6% in the zoledronic acid group and 13.9% in the placebo group. This represents a 35% relative risk reduction with zoledronic acid.
Limitations of the study included a slightly younger and healthier patient population with hip fracture than the general population.
Bottom line: An annual infusion of zoledronic acid within 90 days after repair of hip fracture was associated with reduced new fractures and improved survival.
Citation: Lyles KW, Colon-Emeric CS, Magaziner JS, et al. Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med. 2007;357:1799-1809.
Does Peri-operative Consultation Improve Post-operative Outcome, Reduce Hospital Cost?
Background: Hospitalist-surgical co-management of the surgical inpatient is a model of care enjoying increasing interest. However, there is little published evidence of the effectiveness of this model.
Study design: Retrospective chart review.
Setting: Surgical service of academic teaching hospital.
Synopsis: Of 1,282 surgical patients, 9.1% underwent perioperative medical consultation in a retrospective review. Based on a number of measurement variables (post-operative serum glucose, venous thromboembolism [VTE] prophylaxis, use of perioperative beta-blockers), consulted patients had the same outcome, length of stay and cost as did non-consulted patients. This was, however, a retrospective observational study, using chart abstraction and administrative techniques. This introduces considerable weakness to the validity of the findings.
Bottom line:: In a retrospective study, no value was found to the use of peri-operative medical consultation of surgical patients in a large academic teaching hospital. Because of the weakness in study design, no conclusion can be drawn regarding the true effectiveness of perioperative medical consultation of the surgical patient.
Citation: Auerbach AD, Rasic MA, Sehgal N, Ide B, Stone B, Maselli J. Opportunity missed: medical consultation, resource use, and quality of care of patients undergoing major surgery. Arch Intern Med. 2007 Nov 26;167(21):2338-2344.
Does an RRT Save Children Outside the ICU?
Background: The Institute for Healthcare Improvement initiative known as the 100,000 lives campaign recommended six strategies to decrease preventable inpatient deaths. Implementation of a rapid response team (RRT) was one such strategy.
Study design: Cohort study design.
Setting: A 264-bed academic children’s hospital, between Jan. 1, 2001, and March 31, 2007.
Synopsis:
A total of 22,037 patient admissions and 102,537 patient days were evaluated pre-intervention, and 7,257 admissions and 34,420 patient days were evaluated post-intervention. Once the RRT was implemented, the mean morality rate decreased by 18% and the mean monthly code rate per 1,000 patient days were decreased by 71.2%. Study limitations included small differences in gender and race between pre-intervention and post-intervention populations.
This study is the first published study of pediatric inpatients to show significant reductions in both hospital wide mortality rate and code rate outside the intensive-care unit (ICU) setting after implementation of an RRT.
Bottom line: In an era of widely publicized hospital-related patient deaths the use of a pediatric RRT appears associated with reductions in inpatient codes and mortality.
Citation: Sharek PJ, Parast LM, Leong K, et al. Effect of a rapid response team on hospital-wide mortality and code rates outside the ICU in a children’s hospital. JAMA. 2007;298(19):2267-2274.
Does Influenza Vaccine Reduce Hospitalization, Death among Community Elderly?
Background: Most studies assessing the overall effectiveness of the influenza vaccine cover only a few influenza seasons. The need for long-term assessment was determined. Data were extracted retrospectively from HMO databases.
Study design: Retrospective (regression) analysis of pooled data.
Setting: One U.S. health maintenance organization. Data were pooled from 18 cohorts of community-dwelling elderly members of the HMO from 1990-2000.Synopsis: This study reviewed the effectiveness of influenza vaccine among patients 65 and older in community dwelling HMO members.
The study analyzed 713,872 person seasons over a 10-year period. The regression analysis revealed that influenza vaccination was associated with a 27% reduction in hospitalization for pneumonia/influenza and a 48% reduction in risk of death. The study was limited by inclusion of HMO enrollees only and may not have evaluated the vaccine effectiveness among the frailest elderly (e.g., nursing home dwellers). The study may have also been limited by misclassification of vaccination status.
Bottom line: Hospitalizations and deaths are prevented by influenza vaccination.
Citation: Nichol KL, Nordin JD, Nelson DB, Mullooly JP, Hak E. Effectiveness of influenza vaccine in the community dwelling elderly. N Engl J Med. 2007, 357; 1373-1381.
Is There a Simple, Effective Strategy to Reduce Primary Blood Stream Infections?
Background: An estimated 80,000 patients in U.S. ICUs incur catheter-associated bloodstream infections (BSIs). Reduction in BSI risk is the focus of several recent patient safety initiatives.
Study design: Two-arm, crossover clinical trial.
Setting: 22-bed medical ICU in Chicago.
Synopsis: This study took place over 52 weeks and involved 836 MICU patients. The patients were located in two ICUs at Cook County Hospital. One hospital unit was selected to serve as the intervention unit during which patients were bathed daily with 2% chlorhexidine gluconate (CHG)-impregnated washcloths. Patients in the concurrent control unit were bathed daily with soap and water. Outcome measures included incidences of primary BSIs and clinical sepsis (primary outcomes) and incidences of other infections (secondary outcomes). There were 4.1 vs. 10.4 primary infections per 1,000 patient days in the CHG intervention patients. Limitations in the CHG arm of the study were that patients had a slightly longer length of stay.
Bottom line: Daily cleansing of MICU patients with CHG-impregnated cloths is a simple and effective strategy to reduce primary BSIs.
Citation: Bleasdale SC, Trick WE, Gonzalez IM, Lyles RD, Hayden MK, Weinstein RA. Effectiveness of chlorhexidine bathing to reduce catheter-associated bloodstream infections in medical intensive care unit patients. Arch Intern Med. 2007;167:2073-2079.
Is There a Better Way to Prevent Central Venous Catheter-related Infections?
Background: The Centers for Disease Control and Prevention (CDC) has identified catheter-associated adverse events, including bloodstream infections, as one of its seven safety challenges. The CDC has set a goal to reduce these events by 50% in five years. This is the first study comparing chlorhexidine-based solutions and alcohol-based povidone-iodine solutions for skin disinfection at central venous catheter-insertion sites.
Study design: Randomized comparison study.
Setting: Surgical ICU of University Hospital of Poitiers, France.
Synopsis: This study randomized 538 catheters inserted in the ICU to the two antiseptic groups. The trial was conducted from May 14, 2004, through June 29, 2006. Before catheter insertion, the skin was disinfected twice with the assigned solution. Catheters were removed aseptically, and the distal 5 cm was placed in a sterile tube for subsequent culture in the microbiology lab.
The microbiologists were unaware of the type of antiseptic solution used. In all, 481 catheters produced culture results. The chlorhexidine-based solution was associated with a 50% decrease in catheter colonization. The study couldn’t be conducted in a blinded manner because the two solutions are different colors.
Bottom line: Chlorhexidine-based solutions should be used as a replacement for povidone-iodine formulations to prevent central venous catheter-related infections.
Citation: Mimoz O, Villeminey S, Ragot S, et al. Chlorhexidine-based antiseptic solution vs. alcohol-based povidone-iodine for central venous catheter care. Arch Intern Med. 2007;167:2066-2072. TH
LITERATURE AT A GLANCE
Use this guide to find the abstracts below that correspond to these recent clinical findings
- 24-hour TIA clinic improves outcomes.
- More rapid treatment after TIA and minor stroke reduce risk for recurrent stroke.
- Prasugrel more efficacious than clopidogrel in acute coronary syndrome, but with higher bleeding rates.
- Zoledronic acid use after hip fracture repair reduces probability of new fractures.
- No benefit in quality measures and resource use for surgical patients receiving medical consultation.
- Pediatric RRTs reduce mortality rate.
- Influenza vaccinations prevent hospitalization, death among elderly.
- Chlorhexidine bathing reduces catheter-associated bloodstream infections.
- Chlorhexidine-based antiseptic solution reduces rates of catheter-associated infections
Would 24-hour Hospital Clinic Reduce LOS, Stroke Risk?
Background: Transient ischemic attacks (TIA) precede up to 25% of completed strokes and can provide opportunity for critical intervention if identified early. A specialty clinic with immediate access to imaging facilities could provide early identification and intervention.
Study design: Cohort study statistical analysis of data.
Setting: SOS-TIA hospital clinic in Paris.
Synopsis: A leaflet about TIA with a toll-free telephone number for SOS-TIA was sent to 15,000 family doctors, cardiologists, neurologists, and ophthalmologists in Paris. Between January 2003 and December 2005, 1,085 patients with suspected TIA were admitted to the clinic. The median duration of symptoms was 15 minutes. All patients were started on a stroke-prevention program, 5% had urgent carotid revascularization, and 5% were treated for atrial fibrillation with anticoagulants. Further, 74% of all patients seen were sent home the same day. The 90-day stroke rate was 1.24%; the rate predicted was 5.96%. Limitations of the study included selective patient recruitment from family doctors and office-based specialists. Also, the study lacked a randomized control group.
Bottom line: Prompt evaluation and treatment of patients in a dedicated TIA clinic is associated with a lower stroke risk. The TIA clinic also may lower costs via decreased length of hospital stay.
Citation: Lavallee P, Meseguer E, Abboud H, et al. A transient ischemic attack clinic with round the clock access (SOS-TIA): feasibility and effects. Lancet Neurol. 2007;6(11):953-960.
Can Early Treatment after TIA or Minor Stroke Reduce Risk of Early Recurrent Stroke?
Background: In the week following a TIA or a minor stroke, the risk of recurrent stroke grows to 10%. These warning events provide a limited window of opportunity for prevention. Several treatments are effective in stroke prevention following TIA or minor ischemic stroke if identified early. These include aspirin, other antiplatelet agents, blood-pressure (BP) medications, statins, anticoagulation for atrial fibrillation, and endarterectomy.
Study design: Prospective before-versus-after study (Oxford Vascular Study, or OXVASC) within population-based incidence study.
Setting:: The study population was located in primary care practices in the United Kingdom.
Synopsis: The OXVASC study looked at 1,278 patients who presented with TIA or stroke: 607 were referred directly to the hospital, 620 were referred for outpatient assessment, and 51 were not referred to secondary care. In phase 1, a daily TIA and minor stroke clinic was introduced. Collaborating primary care physicians were asked to refer all patients suspected of having TIA and minor stroke. Phase 1 took place between April 1, 2002, and Sept. 30, 2004. The treatment protocol recommended aspirin in patients not already on anti-platelet therapy (75 mg daily) or clopidogrel if aspirin was contraindicated; simvastatin (40 mg daily); BP lowering agents unless systolic BP less than 130 mm Hg; and anticoagulation as required.
In phase 2, from Oct. 1, 2004, to March 31, 2007, a clinic was established at which no appointments were necessary, treatment was initiated immediately, and diagnosis was confirmed. Patients were assessed in the same way as in phase 1, but all those considered to have had a TIA or stroke were given aspirin 300 mg together with a prescription of any other study medication to start the same day. A loading dose of clopidogrel 300 mg was also prescribed. The 90-day risk if recurrent stroke in the patients referred to the study clinic was 10.3% in phase 1 and 2.1% in phase 2.
Bottom line: Early treatment after TIA or minor stroke was associated with an 80% reduction in the risk of recurrent stroke.
Citation: Rothwell PM, Giles MF, Chandratheva A, et al. Effect of urgent treatment of transient ischemic attack (TIA) and minor stroke on early recurrent stroke (EXPRESS study): a prospective population-based sequential comparison. Lancet 2007;370:1432-1442.
How Does Prasugrel Compare With Clopidogrel in Acute Coronary Syndrome?
Background: Short-term and long-term benefits of a dual anti-platelet therapy for patients with acute coronary syndromes and/or PTCA has been well established but limited by recurrent atherothrombatic events and safety issues.
Study design: Double-blind, randomized study.
Setting: Triton-TIMI 38 Study Group.
Synopsis: This study randomly assigned 13,608 patients with acute coronary syndromes from 30 countries to a treatment group between November 2004 and January 2007. The study protocol used a loading dose of prasugrel (60 mg) within 72 hours before randomization and one hour after cardiac catheterization.
After percutaneous coronary intervention (PCI) patients received maintenance doses of either prasugrel (10 mg) or clopidogrel (75 mg) daily. Daily aspirin (75-162 mg) was required. The outcome of this study showed a significant reduction in the rate of ischemic end points (nonfatal myocardial infarction, stroke, and death) and stent re-thrombosis with prasugrel over clopidogrel. This was theorized to be due to the more rapid onset of antiplatelet effect with prasugrel and improved inhibition of platelet aggregation. Bleeding episodes were more frequent in the prasugrel group. Limitations of the study included the choice of vessels treated, devices used, and adjunctive medication administered to support PCI. All were left to the discretion of the treating physician.
Bottom line: Prasugrel therapy was significantly better than clopidogrel but with an increased risk of major bleeding.
Citation: Wiviott SD, Braunwald E, McCabe CH, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007;357:2001-2015.
Can the Rate of New Hip Fracture Be Reduced with Zoledronic Acid?
Background: Mortality is markedly increased following hip fractures, and medical interventions exist to improve clinical outcomes.
Study design: Randomized, double-blind, placebo-controlled trial.
Setting: International, multicenter trial involving patients with recent hip fracture.
Synopsis: This study, know as the HORIZON trial, involved 2,127 patients. Of those, 1,065 (mean age of 74.5) were assigned to receive yearly infusions of 5 mg IV zoledronic acid within 90 days after surgical hip fracture repair. Meantime, 1,062 were assigned to receive placebo.
All patients received supplemental vitamin D and calcium. The median follow-up was 1.9 years, and the primary end point was a new clinical fracture. The rate of any new clinical fracture was 8.6% in the zoledronic acid group and 13.9% in the placebo group. This represents a 35% relative risk reduction with zoledronic acid.
Limitations of the study included a slightly younger and healthier patient population with hip fracture than the general population.
Bottom line: An annual infusion of zoledronic acid within 90 days after repair of hip fracture was associated with reduced new fractures and improved survival.
Citation: Lyles KW, Colon-Emeric CS, Magaziner JS, et al. Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med. 2007;357:1799-1809.
Does Peri-operative Consultation Improve Post-operative Outcome, Reduce Hospital Cost?
Background: Hospitalist-surgical co-management of the surgical inpatient is a model of care enjoying increasing interest. However, there is little published evidence of the effectiveness of this model.
Study design: Retrospective chart review.
Setting: Surgical service of academic teaching hospital.
Synopsis: Of 1,282 surgical patients, 9.1% underwent perioperative medical consultation in a retrospective review. Based on a number of measurement variables (post-operative serum glucose, venous thromboembolism [VTE] prophylaxis, use of perioperative beta-blockers), consulted patients had the same outcome, length of stay and cost as did non-consulted patients. This was, however, a retrospective observational study, using chart abstraction and administrative techniques. This introduces considerable weakness to the validity of the findings.
Bottom line:: In a retrospective study, no value was found to the use of peri-operative medical consultation of surgical patients in a large academic teaching hospital. Because of the weakness in study design, no conclusion can be drawn regarding the true effectiveness of perioperative medical consultation of the surgical patient.
Citation: Auerbach AD, Rasic MA, Sehgal N, Ide B, Stone B, Maselli J. Opportunity missed: medical consultation, resource use, and quality of care of patients undergoing major surgery. Arch Intern Med. 2007 Nov 26;167(21):2338-2344.
Does an RRT Save Children Outside the ICU?
Background: The Institute for Healthcare Improvement initiative known as the 100,000 lives campaign recommended six strategies to decrease preventable inpatient deaths. Implementation of a rapid response team (RRT) was one such strategy.
Study design: Cohort study design.
Setting: A 264-bed academic children’s hospital, between Jan. 1, 2001, and March 31, 2007.
Synopsis:
A total of 22,037 patient admissions and 102,537 patient days were evaluated pre-intervention, and 7,257 admissions and 34,420 patient days were evaluated post-intervention. Once the RRT was implemented, the mean morality rate decreased by 18% and the mean monthly code rate per 1,000 patient days were decreased by 71.2%. Study limitations included small differences in gender and race between pre-intervention and post-intervention populations.
This study is the first published study of pediatric inpatients to show significant reductions in both hospital wide mortality rate and code rate outside the intensive-care unit (ICU) setting after implementation of an RRT.
Bottom line: In an era of widely publicized hospital-related patient deaths the use of a pediatric RRT appears associated with reductions in inpatient codes and mortality.
Citation: Sharek PJ, Parast LM, Leong K, et al. Effect of a rapid response team on hospital-wide mortality and code rates outside the ICU in a children’s hospital. JAMA. 2007;298(19):2267-2274.
Does Influenza Vaccine Reduce Hospitalization, Death among Community Elderly?
Background: Most studies assessing the overall effectiveness of the influenza vaccine cover only a few influenza seasons. The need for long-term assessment was determined. Data were extracted retrospectively from HMO databases.
Study design: Retrospective (regression) analysis of pooled data.
Setting: One U.S. health maintenance organization. Data were pooled from 18 cohorts of community-dwelling elderly members of the HMO from 1990-2000.Synopsis: This study reviewed the effectiveness of influenza vaccine among patients 65 and older in community dwelling HMO members.
The study analyzed 713,872 person seasons over a 10-year period. The regression analysis revealed that influenza vaccination was associated with a 27% reduction in hospitalization for pneumonia/influenza and a 48% reduction in risk of death. The study was limited by inclusion of HMO enrollees only and may not have evaluated the vaccine effectiveness among the frailest elderly (e.g., nursing home dwellers). The study may have also been limited by misclassification of vaccination status.
Bottom line: Hospitalizations and deaths are prevented by influenza vaccination.
Citation: Nichol KL, Nordin JD, Nelson DB, Mullooly JP, Hak E. Effectiveness of influenza vaccine in the community dwelling elderly. N Engl J Med. 2007, 357; 1373-1381.
Is There a Simple, Effective Strategy to Reduce Primary Blood Stream Infections?
Background: An estimated 80,000 patients in U.S. ICUs incur catheter-associated bloodstream infections (BSIs). Reduction in BSI risk is the focus of several recent patient safety initiatives.
Study design: Two-arm, crossover clinical trial.
Setting: 22-bed medical ICU in Chicago.
Synopsis: This study took place over 52 weeks and involved 836 MICU patients. The patients were located in two ICUs at Cook County Hospital. One hospital unit was selected to serve as the intervention unit during which patients were bathed daily with 2% chlorhexidine gluconate (CHG)-impregnated washcloths. Patients in the concurrent control unit were bathed daily with soap and water. Outcome measures included incidences of primary BSIs and clinical sepsis (primary outcomes) and incidences of other infections (secondary outcomes). There were 4.1 vs. 10.4 primary infections per 1,000 patient days in the CHG intervention patients. Limitations in the CHG arm of the study were that patients had a slightly longer length of stay.
Bottom line: Daily cleansing of MICU patients with CHG-impregnated cloths is a simple and effective strategy to reduce primary BSIs.
Citation: Bleasdale SC, Trick WE, Gonzalez IM, Lyles RD, Hayden MK, Weinstein RA. Effectiveness of chlorhexidine bathing to reduce catheter-associated bloodstream infections in medical intensive care unit patients. Arch Intern Med. 2007;167:2073-2079.
Is There a Better Way to Prevent Central Venous Catheter-related Infections?
Background: The Centers for Disease Control and Prevention (CDC) has identified catheter-associated adverse events, including bloodstream infections, as one of its seven safety challenges. The CDC has set a goal to reduce these events by 50% in five years. This is the first study comparing chlorhexidine-based solutions and alcohol-based povidone-iodine solutions for skin disinfection at central venous catheter-insertion sites.
Study design: Randomized comparison study.
Setting: Surgical ICU of University Hospital of Poitiers, France.
Synopsis: This study randomized 538 catheters inserted in the ICU to the two antiseptic groups. The trial was conducted from May 14, 2004, through June 29, 2006. Before catheter insertion, the skin was disinfected twice with the assigned solution. Catheters were removed aseptically, and the distal 5 cm was placed in a sterile tube for subsequent culture in the microbiology lab.
The microbiologists were unaware of the type of antiseptic solution used. In all, 481 catheters produced culture results. The chlorhexidine-based solution was associated with a 50% decrease in catheter colonization. The study couldn’t be conducted in a blinded manner because the two solutions are different colors.
Bottom line: Chlorhexidine-based solutions should be used as a replacement for povidone-iodine formulations to prevent central venous catheter-related infections.
Citation: Mimoz O, Villeminey S, Ragot S, et al. Chlorhexidine-based antiseptic solution vs. alcohol-based povidone-iodine for central venous catheter care. Arch Intern Med. 2007;167:2066-2072. TH
LITERATURE AT A GLANCE
Use this guide to find the abstracts below that correspond to these recent clinical findings
- 24-hour TIA clinic improves outcomes.
- More rapid treatment after TIA and minor stroke reduce risk for recurrent stroke.
- Prasugrel more efficacious than clopidogrel in acute coronary syndrome, but with higher bleeding rates.
- Zoledronic acid use after hip fracture repair reduces probability of new fractures.
- No benefit in quality measures and resource use for surgical patients receiving medical consultation.
- Pediatric RRTs reduce mortality rate.
- Influenza vaccinations prevent hospitalization, death among elderly.
- Chlorhexidine bathing reduces catheter-associated bloodstream infections.
- Chlorhexidine-based antiseptic solution reduces rates of catheter-associated infections
Would 24-hour Hospital Clinic Reduce LOS, Stroke Risk?
Background: Transient ischemic attacks (TIA) precede up to 25% of completed strokes and can provide opportunity for critical intervention if identified early. A specialty clinic with immediate access to imaging facilities could provide early identification and intervention.
Study design: Cohort study statistical analysis of data.
Setting: SOS-TIA hospital clinic in Paris.
Synopsis: A leaflet about TIA with a toll-free telephone number for SOS-TIA was sent to 15,000 family doctors, cardiologists, neurologists, and ophthalmologists in Paris. Between January 2003 and December 2005, 1,085 patients with suspected TIA were admitted to the clinic. The median duration of symptoms was 15 minutes. All patients were started on a stroke-prevention program, 5% had urgent carotid revascularization, and 5% were treated for atrial fibrillation with anticoagulants. Further, 74% of all patients seen were sent home the same day. The 90-day stroke rate was 1.24%; the rate predicted was 5.96%. Limitations of the study included selective patient recruitment from family doctors and office-based specialists. Also, the study lacked a randomized control group.
Bottom line: Prompt evaluation and treatment of patients in a dedicated TIA clinic is associated with a lower stroke risk. The TIA clinic also may lower costs via decreased length of hospital stay.
Citation: Lavallee P, Meseguer E, Abboud H, et al. A transient ischemic attack clinic with round the clock access (SOS-TIA): feasibility and effects. Lancet Neurol. 2007;6(11):953-960.
Can Early Treatment after TIA or Minor Stroke Reduce Risk of Early Recurrent Stroke?
Background: In the week following a TIA or a minor stroke, the risk of recurrent stroke grows to 10%. These warning events provide a limited window of opportunity for prevention. Several treatments are effective in stroke prevention following TIA or minor ischemic stroke if identified early. These include aspirin, other antiplatelet agents, blood-pressure (BP) medications, statins, anticoagulation for atrial fibrillation, and endarterectomy.
Study design: Prospective before-versus-after study (Oxford Vascular Study, or OXVASC) within population-based incidence study.
Setting:: The study population was located in primary care practices in the United Kingdom.
Synopsis: The OXVASC study looked at 1,278 patients who presented with TIA or stroke: 607 were referred directly to the hospital, 620 were referred for outpatient assessment, and 51 were not referred to secondary care. In phase 1, a daily TIA and minor stroke clinic was introduced. Collaborating primary care physicians were asked to refer all patients suspected of having TIA and minor stroke. Phase 1 took place between April 1, 2002, and Sept. 30, 2004. The treatment protocol recommended aspirin in patients not already on anti-platelet therapy (75 mg daily) or clopidogrel if aspirin was contraindicated; simvastatin (40 mg daily); BP lowering agents unless systolic BP less than 130 mm Hg; and anticoagulation as required.
In phase 2, from Oct. 1, 2004, to March 31, 2007, a clinic was established at which no appointments were necessary, treatment was initiated immediately, and diagnosis was confirmed. Patients were assessed in the same way as in phase 1, but all those considered to have had a TIA or stroke were given aspirin 300 mg together with a prescription of any other study medication to start the same day. A loading dose of clopidogrel 300 mg was also prescribed. The 90-day risk if recurrent stroke in the patients referred to the study clinic was 10.3% in phase 1 and 2.1% in phase 2.
Bottom line: Early treatment after TIA or minor stroke was associated with an 80% reduction in the risk of recurrent stroke.
Citation: Rothwell PM, Giles MF, Chandratheva A, et al. Effect of urgent treatment of transient ischemic attack (TIA) and minor stroke on early recurrent stroke (EXPRESS study): a prospective population-based sequential comparison. Lancet 2007;370:1432-1442.
How Does Prasugrel Compare With Clopidogrel in Acute Coronary Syndrome?
Background: Short-term and long-term benefits of a dual anti-platelet therapy for patients with acute coronary syndromes and/or PTCA has been well established but limited by recurrent atherothrombatic events and safety issues.
Study design: Double-blind, randomized study.
Setting: Triton-TIMI 38 Study Group.
Synopsis: This study randomly assigned 13,608 patients with acute coronary syndromes from 30 countries to a treatment group between November 2004 and January 2007. The study protocol used a loading dose of prasugrel (60 mg) within 72 hours before randomization and one hour after cardiac catheterization.
After percutaneous coronary intervention (PCI) patients received maintenance doses of either prasugrel (10 mg) or clopidogrel (75 mg) daily. Daily aspirin (75-162 mg) was required. The outcome of this study showed a significant reduction in the rate of ischemic end points (nonfatal myocardial infarction, stroke, and death) and stent re-thrombosis with prasugrel over clopidogrel. This was theorized to be due to the more rapid onset of antiplatelet effect with prasugrel and improved inhibition of platelet aggregation. Bleeding episodes were more frequent in the prasugrel group. Limitations of the study included the choice of vessels treated, devices used, and adjunctive medication administered to support PCI. All were left to the discretion of the treating physician.
Bottom line: Prasugrel therapy was significantly better than clopidogrel but with an increased risk of major bleeding.
Citation: Wiviott SD, Braunwald E, McCabe CH, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007;357:2001-2015.
Can the Rate of New Hip Fracture Be Reduced with Zoledronic Acid?
Background: Mortality is markedly increased following hip fractures, and medical interventions exist to improve clinical outcomes.
Study design: Randomized, double-blind, placebo-controlled trial.
Setting: International, multicenter trial involving patients with recent hip fracture.
Synopsis: This study, know as the HORIZON trial, involved 2,127 patients. Of those, 1,065 (mean age of 74.5) were assigned to receive yearly infusions of 5 mg IV zoledronic acid within 90 days after surgical hip fracture repair. Meantime, 1,062 were assigned to receive placebo.
All patients received supplemental vitamin D and calcium. The median follow-up was 1.9 years, and the primary end point was a new clinical fracture. The rate of any new clinical fracture was 8.6% in the zoledronic acid group and 13.9% in the placebo group. This represents a 35% relative risk reduction with zoledronic acid.
Limitations of the study included a slightly younger and healthier patient population with hip fracture than the general population.
Bottom line: An annual infusion of zoledronic acid within 90 days after repair of hip fracture was associated with reduced new fractures and improved survival.
Citation: Lyles KW, Colon-Emeric CS, Magaziner JS, et al. Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med. 2007;357:1799-1809.
Does Peri-operative Consultation Improve Post-operative Outcome, Reduce Hospital Cost?
Background: Hospitalist-surgical co-management of the surgical inpatient is a model of care enjoying increasing interest. However, there is little published evidence of the effectiveness of this model.
Study design: Retrospective chart review.
Setting: Surgical service of academic teaching hospital.
Synopsis: Of 1,282 surgical patients, 9.1% underwent perioperative medical consultation in a retrospective review. Based on a number of measurement variables (post-operative serum glucose, venous thromboembolism [VTE] prophylaxis, use of perioperative beta-blockers), consulted patients had the same outcome, length of stay and cost as did non-consulted patients. This was, however, a retrospective observational study, using chart abstraction and administrative techniques. This introduces considerable weakness to the validity of the findings.
Bottom line:: In a retrospective study, no value was found to the use of peri-operative medical consultation of surgical patients in a large academic teaching hospital. Because of the weakness in study design, no conclusion can be drawn regarding the true effectiveness of perioperative medical consultation of the surgical patient.
Citation: Auerbach AD, Rasic MA, Sehgal N, Ide B, Stone B, Maselli J. Opportunity missed: medical consultation, resource use, and quality of care of patients undergoing major surgery. Arch Intern Med. 2007 Nov 26;167(21):2338-2344.
Does an RRT Save Children Outside the ICU?
Background: The Institute for Healthcare Improvement initiative known as the 100,000 lives campaign recommended six strategies to decrease preventable inpatient deaths. Implementation of a rapid response team (RRT) was one such strategy.
Study design: Cohort study design.
Setting: A 264-bed academic children’s hospital, between Jan. 1, 2001, and March 31, 2007.
Synopsis:
A total of 22,037 patient admissions and 102,537 patient days were evaluated pre-intervention, and 7,257 admissions and 34,420 patient days were evaluated post-intervention. Once the RRT was implemented, the mean morality rate decreased by 18% and the mean monthly code rate per 1,000 patient days were decreased by 71.2%. Study limitations included small differences in gender and race between pre-intervention and post-intervention populations.
This study is the first published study of pediatric inpatients to show significant reductions in both hospital wide mortality rate and code rate outside the intensive-care unit (ICU) setting after implementation of an RRT.
Bottom line: In an era of widely publicized hospital-related patient deaths the use of a pediatric RRT appears associated with reductions in inpatient codes and mortality.
Citation: Sharek PJ, Parast LM, Leong K, et al. Effect of a rapid response team on hospital-wide mortality and code rates outside the ICU in a children’s hospital. JAMA. 2007;298(19):2267-2274.
Does Influenza Vaccine Reduce Hospitalization, Death among Community Elderly?
Background: Most studies assessing the overall effectiveness of the influenza vaccine cover only a few influenza seasons. The need for long-term assessment was determined. Data were extracted retrospectively from HMO databases.
Study design: Retrospective (regression) analysis of pooled data.
Setting: One U.S. health maintenance organization. Data were pooled from 18 cohorts of community-dwelling elderly members of the HMO from 1990-2000.Synopsis: This study reviewed the effectiveness of influenza vaccine among patients 65 and older in community dwelling HMO members.
The study analyzed 713,872 person seasons over a 10-year period. The regression analysis revealed that influenza vaccination was associated with a 27% reduction in hospitalization for pneumonia/influenza and a 48% reduction in risk of death. The study was limited by inclusion of HMO enrollees only and may not have evaluated the vaccine effectiveness among the frailest elderly (e.g., nursing home dwellers). The study may have also been limited by misclassification of vaccination status.
Bottom line: Hospitalizations and deaths are prevented by influenza vaccination.
Citation: Nichol KL, Nordin JD, Nelson DB, Mullooly JP, Hak E. Effectiveness of influenza vaccine in the community dwelling elderly. N Engl J Med. 2007, 357; 1373-1381.
Is There a Simple, Effective Strategy to Reduce Primary Blood Stream Infections?
Background: An estimated 80,000 patients in U.S. ICUs incur catheter-associated bloodstream infections (BSIs). Reduction in BSI risk is the focus of several recent patient safety initiatives.
Study design: Two-arm, crossover clinical trial.
Setting: 22-bed medical ICU in Chicago.
Synopsis: This study took place over 52 weeks and involved 836 MICU patients. The patients were located in two ICUs at Cook County Hospital. One hospital unit was selected to serve as the intervention unit during which patients were bathed daily with 2% chlorhexidine gluconate (CHG)-impregnated washcloths. Patients in the concurrent control unit were bathed daily with soap and water. Outcome measures included incidences of primary BSIs and clinical sepsis (primary outcomes) and incidences of other infections (secondary outcomes). There were 4.1 vs. 10.4 primary infections per 1,000 patient days in the CHG intervention patients. Limitations in the CHG arm of the study were that patients had a slightly longer length of stay.
Bottom line: Daily cleansing of MICU patients with CHG-impregnated cloths is a simple and effective strategy to reduce primary BSIs.
Citation: Bleasdale SC, Trick WE, Gonzalez IM, Lyles RD, Hayden MK, Weinstein RA. Effectiveness of chlorhexidine bathing to reduce catheter-associated bloodstream infections in medical intensive care unit patients. Arch Intern Med. 2007;167:2073-2079.
Is There a Better Way to Prevent Central Venous Catheter-related Infections?
Background: The Centers for Disease Control and Prevention (CDC) has identified catheter-associated adverse events, including bloodstream infections, as one of its seven safety challenges. The CDC has set a goal to reduce these events by 50% in five years. This is the first study comparing chlorhexidine-based solutions and alcohol-based povidone-iodine solutions for skin disinfection at central venous catheter-insertion sites.
Study design: Randomized comparison study.
Setting: Surgical ICU of University Hospital of Poitiers, France.
Synopsis: This study randomized 538 catheters inserted in the ICU to the two antiseptic groups. The trial was conducted from May 14, 2004, through June 29, 2006. Before catheter insertion, the skin was disinfected twice with the assigned solution. Catheters were removed aseptically, and the distal 5 cm was placed in a sterile tube for subsequent culture in the microbiology lab.
The microbiologists were unaware of the type of antiseptic solution used. In all, 481 catheters produced culture results. The chlorhexidine-based solution was associated with a 50% decrease in catheter colonization. The study couldn’t be conducted in a blinded manner because the two solutions are different colors.
Bottom line: Chlorhexidine-based solutions should be used as a replacement for povidone-iodine formulations to prevent central venous catheter-related infections.
Citation: Mimoz O, Villeminey S, Ragot S, et al. Chlorhexidine-based antiseptic solution vs. alcohol-based povidone-iodine for central venous catheter care. Arch Intern Med. 2007;167:2066-2072. TH
SHM Takes on VTE
Venous thromboembolic (VTE) disease, ranging from asymptomatic deep-vein thrombosis (DVT) to massive pulmonary embolism (PE), is a significant cause of morbidity and mortality in hospitalized patients. Almost all hospitalized patients are at risk for VTE, and the literature suggests approximately half of all VTEs are hospital-acquired.
Hospitalists are ideally positioned to reduce the incidence of preventable VTEs, both by using known best practices to improve care delivered to their own patients, and, more importantly, by leading hospitalwide efforts that improve care for all patients at their home institutions.
In recognition of this important clinical issue and the role hospitalists can play in addressing it, SHM launched the VTE Prevention Collaborative (VTEPC) in January 2007. The program offers individualized assistance to hospitalists wishing to take the lead in this area.
The VTEPC offers two technical assistance options. Individuals interested in securing ongoing support for their planned or active VTE prevention projects can enroll in the mentoring program. This allows a full year of access to and support from SHM mentors with VTE and quality-improvement (QI) expertise. Mentoring occurs in eight telephone calls, during which mentors offer individualized assistance on any topics, tasks, or barriers commonly encountered in designing, implementing, and evaluating a VTE prevention project.
An on-site consultation program is designed for individuals interested in securing expert evaluation and input on a VTE prevention program but who don’t feel they need ongoing, longitudinal support. In this program, SHM consultants with VTE and QI expertise visit applicants’ hospitals to evaluate active or planned VTE prevention programs. The consultation visits feature a structured evaluation of the site’s strengths and resources, barriers to improvement, and the design and function of active or proposed VTE prevention interventions.
For both programs, support and instruction are organized around the VTE QI workbook, “Preventing Hospital-Acquired Venous Thromboembolism: A Guide for Effective Quality Improvement,” SHM’s step-by-step guide for developing a VTE prevention program. SHM secured the services of Greg Maynard, MD, and Jason Stein, MD, to provide mentoring and conduct consultation visits. Drs. Maynard and Stein have led successful local VTE prevention QI projects, hold QI leadership positions, and have taught QI and VTE prevention principals to local and national audiences. Dr. Maynard is head of the Division of Hospital Medicine and associate clinical professor of medicine at the University of California, San Diego. Dr. Stein is a hospitalist at Atlanta’s Emory University Hospital, assistant professor of medicine at Emory University School of Medicine, and director of quality improvement for the Emory Hospital Medicine Unit.
Both were also instrumental in developing SHM’s online VTE Resource Room and the VTE QI workbook.
Strong Responses
Twenty-seven hospitalists enrolled in the VTEPC in its first year of operation, 24 in the mentoring program and three in the consultation program.
Enrollees have broad experience in VTE prevention and QI. Some enrollees have been in practice for two years, others more than 25 years. Some fill QI leadership roles in their hospitals or hospital medicine groups. For others the VTE prevention project is their first experience leading a QI effort. Regional representation (19 states), hospital system representation (18 systems), hospital size (135 to 700 staffed beds), and hospital type (academic centers, community teaching hospitals, and community hospitals) are also broad. One enrollee works at a long-term acute care hospital, all others work at acute-care hospitals.
What They Said
Participants in the mentoring and consultation programs have reported that the support they’ve received has been enormously helpful.
According to feedback from one participant, support from the mentoring program made the potentially overwhelming prospect of launching a hospitalwide improvement effort much more manageable: “The prospect of launching a multihospital VTE Prevention Protocol was extremely daunting; however, with the help of my SHM mentor, we stand ready to pilot the program within the week. Our mentor carefully constructed a step-by-step process that allowed me to investigate the scope of the problem at the local level and develop a protocol that was embraced by our administration and physicians. He supplied me with resources and knowledge that allowed me to successfully handle multiple obstacles that arose along the way. What we have accomplished will have an enormous impact on the quality of care that we provide for our patients.”
Other participants have reported that having access to objective input from an external expert can help transform a slow-developing or ineffective prevention program. As one participant put it: “Mentoring through SHM’s VTE Prevention Collaborative has been an invaluable experience. Through monthly phone calls and frequent e-mails, our mentor focused our previously ineffective efforts and guided us to develop a streamlined tool that was custom-fit to the workflow at our hospital. He has saved us tremendous frustrations by directing us to the appropriate resources in our institution to accomplish tasks we would have attempted ourselves. Since our first phone call, he has been both our coach and cheerleader. The processes and techniques that he has taught us are applicable to every quality endeavor we engage in.”
What Impressed Experts
Drs. Maynard and Stein have been enormously impressed by what VTEPC members have achieved. “What is most impressive to me is how all these hospitalist project leaders in different settings are overcoming a wide variety of intuitional barriers, medical staff barriers, infrastructure barriers—all the obstacles that can challenge the typical big QI project,” says Dr. Maynard. He notes that not only are participants utilizing all the basic QI principles in all the ways that were outlined in the QI workbook, but they also are coming up with innovations and approaches beyond what the workbook authors envisioned.
“We learn from them as they come up with innovations to meet their own challenges,” Dr. Stein says. “It shows the resilience and flexibility of the QI framework. If you really work in your local setting on these things with the improvement framework in mind you can get by almost any barrier.” Drs. Maynard and Stein have noted that participants have been able to design and implement VTE prevention programs at a pace that far outstrips what the two mentors achieved at their home institutions.
Many participants have found real-time ways to identify patients who are not on prophylaxis but should be. At many sites, identification begins with a report generated by the hospital’s inpatient pharmacy service, which typically shows the anti-coagulation regimen for each patient in a given hospital ward. The floor pharmacist or nurse can identify who is not on prophylaxis, assess risk factors and contraindications, and act to mitigate the situation—for example, by placing a call to the patient’s attending physician. Other sites have developed more sophisticated reports that capture information about relative risk for DVT and the absence or presence of contraindications to pharmacologic prophylaxis; these features reduce the effort required to investigate each case.
How to Learn More
The Quality Track at the 2008 Annual Meeting (April 3-5 at the Manchester Hyatt, San Diego, Calif.) includes a session on the “VTE Collaborative Experience” (1-2:25 p.m. April 4). Drs. Maynard and Stein will discuss the initiative, as will collaborative members, who will describe key successes and innovations that furthered their efforts to establish effective VTE prevention programs. Questions about the VTEPC and the Annual Meeting session can be directed to [email protected].
Update on Hand-Offs
SHM task force continues to refine transitions-of-care checklist
by Shannon Roach
Among hospitalists and other organizations, there has been an increasing interest surrounding the improvement of the quality of patient care, especially within transitions of care and patient discharge. As the leader in the hospital medicine field, SHM continues to support and lead initiatives for the improvement of care as related to patient discharge and transitions. Last year’s creation of the Hand-Offs Communication Task Force (HCTF) has upheld SHM’s position of being dedicated to the promotion of the highest quality care for all hospitalized patients.
Derived from members of the Hospital Quality and Patient Safety Committee and the Education Committee, this task force was led by Vineet Arora, MD, MA, assistant professor of medicine, University of Chicago. Collaborating with her were Preetha Basaviah, MD, clinical instructor, Stanford University Medical Center in Calif.; Dan Dressler, MD, instructor of medicine, Emory University School of Medicine in Atlanta; Lakshmi Halasyamani, MD, associate chairperson of the Department of Internal Medicine at St. Joseph Mercy Hospital in Ann Arbor, Mich.; Sunil Kripalani, MD, MSc, an instructor at Emory University in Atlanta; and Efren Manjarrez, MD, assistant clinical professor of medicine at the Miller School of Medicine, University of Miami.
This team set out to create a formally recognized set of recommendations for ensuring optimum communication and continuity of care at the end of a medical professional’s shift or a patient’s change in service.
The task force’s first step was to determine what information was available as a basis for these recommendations. Though data were limited, the group decided that recommendations for effective hand-offs would be broken into three categories: program policy, verbal exchange, and content exchange.
As the need for more evidence-based data for the improvement of in-hospital hand-offs became clear, the group decided a valuable follow-up approach for these recommendations would be to incorporate a research agenda into the findings. This proposal suggests a need for a rigorous evaluation of these recommendations, with an emphasis on controlled interventions. It also encourages the development of patient-based outcomes sensitive to hand-off quality.
As a test run for these recommendations, the HCTF presented its findings at Hospital Medicine 2007 in Dallas. Their session “Developing Communications and Hand-Off Standards for Hospitalists” drew a passionate response. During this session they unveiled a checklist outlining the important elements of an in-hospital physician hand-off. Attendees were encouraged to offer feedback and vote on proposed hand-off elements. They also were encouraged to submit suggestions if they believed something was missing.
Using that feedback, the group produced a final draft of recommendations and distributed it to a multidisciplinary team of experts for a final review. On the panel were Linda Bell, RN, MSN; Emily Patterson, PhD; Erik Van Eaton, MD; and Arpana Vidyarthi, MD. These experts reflect the perspective of nonphysician members of the hospital community, representing the interests of technology, nursing, human factors research, and hospital medicine. They reviewed the paper and hand-off recommendations by participating in conference calls in which they were asked to comment on questions regarding the working paper. These discussions gave the task force invaluable, candid feedback adopted into the working paper to create a more robust set of recommendations.
The final product was reviewed by SHM’s Board of Directors in January; a dissemination plan is in progress. If these recommendations are endorsed by an institution or a hospitalist group, they will act as a guide to ensure the coordination of hand-offs and the mangement of important clinical care issues.
Through their research and interactions with a large number of individuals concerned with this issue, the HCTF discovered that the quality improvement of patient transitions is a complex, global issue. They believe this checklist of hand-off elements is essential to these efforts.
Venous thromboembolic (VTE) disease, ranging from asymptomatic deep-vein thrombosis (DVT) to massive pulmonary embolism (PE), is a significant cause of morbidity and mortality in hospitalized patients. Almost all hospitalized patients are at risk for VTE, and the literature suggests approximately half of all VTEs are hospital-acquired.
Hospitalists are ideally positioned to reduce the incidence of preventable VTEs, both by using known best practices to improve care delivered to their own patients, and, more importantly, by leading hospitalwide efforts that improve care for all patients at their home institutions.
In recognition of this important clinical issue and the role hospitalists can play in addressing it, SHM launched the VTE Prevention Collaborative (VTEPC) in January 2007. The program offers individualized assistance to hospitalists wishing to take the lead in this area.
The VTEPC offers two technical assistance options. Individuals interested in securing ongoing support for their planned or active VTE prevention projects can enroll in the mentoring program. This allows a full year of access to and support from SHM mentors with VTE and quality-improvement (QI) expertise. Mentoring occurs in eight telephone calls, during which mentors offer individualized assistance on any topics, tasks, or barriers commonly encountered in designing, implementing, and evaluating a VTE prevention project.
An on-site consultation program is designed for individuals interested in securing expert evaluation and input on a VTE prevention program but who don’t feel they need ongoing, longitudinal support. In this program, SHM consultants with VTE and QI expertise visit applicants’ hospitals to evaluate active or planned VTE prevention programs. The consultation visits feature a structured evaluation of the site’s strengths and resources, barriers to improvement, and the design and function of active or proposed VTE prevention interventions.
For both programs, support and instruction are organized around the VTE QI workbook, “Preventing Hospital-Acquired Venous Thromboembolism: A Guide for Effective Quality Improvement,” SHM’s step-by-step guide for developing a VTE prevention program. SHM secured the services of Greg Maynard, MD, and Jason Stein, MD, to provide mentoring and conduct consultation visits. Drs. Maynard and Stein have led successful local VTE prevention QI projects, hold QI leadership positions, and have taught QI and VTE prevention principals to local and national audiences. Dr. Maynard is head of the Division of Hospital Medicine and associate clinical professor of medicine at the University of California, San Diego. Dr. Stein is a hospitalist at Atlanta’s Emory University Hospital, assistant professor of medicine at Emory University School of Medicine, and director of quality improvement for the Emory Hospital Medicine Unit.
Both were also instrumental in developing SHM’s online VTE Resource Room and the VTE QI workbook.
Strong Responses
Twenty-seven hospitalists enrolled in the VTEPC in its first year of operation, 24 in the mentoring program and three in the consultation program.
Enrollees have broad experience in VTE prevention and QI. Some enrollees have been in practice for two years, others more than 25 years. Some fill QI leadership roles in their hospitals or hospital medicine groups. For others the VTE prevention project is their first experience leading a QI effort. Regional representation (19 states), hospital system representation (18 systems), hospital size (135 to 700 staffed beds), and hospital type (academic centers, community teaching hospitals, and community hospitals) are also broad. One enrollee works at a long-term acute care hospital, all others work at acute-care hospitals.
What They Said
Participants in the mentoring and consultation programs have reported that the support they’ve received has been enormously helpful.
According to feedback from one participant, support from the mentoring program made the potentially overwhelming prospect of launching a hospitalwide improvement effort much more manageable: “The prospect of launching a multihospital VTE Prevention Protocol was extremely daunting; however, with the help of my SHM mentor, we stand ready to pilot the program within the week. Our mentor carefully constructed a step-by-step process that allowed me to investigate the scope of the problem at the local level and develop a protocol that was embraced by our administration and physicians. He supplied me with resources and knowledge that allowed me to successfully handle multiple obstacles that arose along the way. What we have accomplished will have an enormous impact on the quality of care that we provide for our patients.”
Other participants have reported that having access to objective input from an external expert can help transform a slow-developing or ineffective prevention program. As one participant put it: “Mentoring through SHM’s VTE Prevention Collaborative has been an invaluable experience. Through monthly phone calls and frequent e-mails, our mentor focused our previously ineffective efforts and guided us to develop a streamlined tool that was custom-fit to the workflow at our hospital. He has saved us tremendous frustrations by directing us to the appropriate resources in our institution to accomplish tasks we would have attempted ourselves. Since our first phone call, he has been both our coach and cheerleader. The processes and techniques that he has taught us are applicable to every quality endeavor we engage in.”
What Impressed Experts
Drs. Maynard and Stein have been enormously impressed by what VTEPC members have achieved. “What is most impressive to me is how all these hospitalist project leaders in different settings are overcoming a wide variety of intuitional barriers, medical staff barriers, infrastructure barriers—all the obstacles that can challenge the typical big QI project,” says Dr. Maynard. He notes that not only are participants utilizing all the basic QI principles in all the ways that were outlined in the QI workbook, but they also are coming up with innovations and approaches beyond what the workbook authors envisioned.
“We learn from them as they come up with innovations to meet their own challenges,” Dr. Stein says. “It shows the resilience and flexibility of the QI framework. If you really work in your local setting on these things with the improvement framework in mind you can get by almost any barrier.” Drs. Maynard and Stein have noted that participants have been able to design and implement VTE prevention programs at a pace that far outstrips what the two mentors achieved at their home institutions.
Many participants have found real-time ways to identify patients who are not on prophylaxis but should be. At many sites, identification begins with a report generated by the hospital’s inpatient pharmacy service, which typically shows the anti-coagulation regimen for each patient in a given hospital ward. The floor pharmacist or nurse can identify who is not on prophylaxis, assess risk factors and contraindications, and act to mitigate the situation—for example, by placing a call to the patient’s attending physician. Other sites have developed more sophisticated reports that capture information about relative risk for DVT and the absence or presence of contraindications to pharmacologic prophylaxis; these features reduce the effort required to investigate each case.
How to Learn More
The Quality Track at the 2008 Annual Meeting (April 3-5 at the Manchester Hyatt, San Diego, Calif.) includes a session on the “VTE Collaborative Experience” (1-2:25 p.m. April 4). Drs. Maynard and Stein will discuss the initiative, as will collaborative members, who will describe key successes and innovations that furthered their efforts to establish effective VTE prevention programs. Questions about the VTEPC and the Annual Meeting session can be directed to [email protected].
Update on Hand-Offs
SHM task force continues to refine transitions-of-care checklist
by Shannon Roach
Among hospitalists and other organizations, there has been an increasing interest surrounding the improvement of the quality of patient care, especially within transitions of care and patient discharge. As the leader in the hospital medicine field, SHM continues to support and lead initiatives for the improvement of care as related to patient discharge and transitions. Last year’s creation of the Hand-Offs Communication Task Force (HCTF) has upheld SHM’s position of being dedicated to the promotion of the highest quality care for all hospitalized patients.
Derived from members of the Hospital Quality and Patient Safety Committee and the Education Committee, this task force was led by Vineet Arora, MD, MA, assistant professor of medicine, University of Chicago. Collaborating with her were Preetha Basaviah, MD, clinical instructor, Stanford University Medical Center in Calif.; Dan Dressler, MD, instructor of medicine, Emory University School of Medicine in Atlanta; Lakshmi Halasyamani, MD, associate chairperson of the Department of Internal Medicine at St. Joseph Mercy Hospital in Ann Arbor, Mich.; Sunil Kripalani, MD, MSc, an instructor at Emory University in Atlanta; and Efren Manjarrez, MD, assistant clinical professor of medicine at the Miller School of Medicine, University of Miami.
This team set out to create a formally recognized set of recommendations for ensuring optimum communication and continuity of care at the end of a medical professional’s shift or a patient’s change in service.
The task force’s first step was to determine what information was available as a basis for these recommendations. Though data were limited, the group decided that recommendations for effective hand-offs would be broken into three categories: program policy, verbal exchange, and content exchange.
As the need for more evidence-based data for the improvement of in-hospital hand-offs became clear, the group decided a valuable follow-up approach for these recommendations would be to incorporate a research agenda into the findings. This proposal suggests a need for a rigorous evaluation of these recommendations, with an emphasis on controlled interventions. It also encourages the development of patient-based outcomes sensitive to hand-off quality.
As a test run for these recommendations, the HCTF presented its findings at Hospital Medicine 2007 in Dallas. Their session “Developing Communications and Hand-Off Standards for Hospitalists” drew a passionate response. During this session they unveiled a checklist outlining the important elements of an in-hospital physician hand-off. Attendees were encouraged to offer feedback and vote on proposed hand-off elements. They also were encouraged to submit suggestions if they believed something was missing.
Using that feedback, the group produced a final draft of recommendations and distributed it to a multidisciplinary team of experts for a final review. On the panel were Linda Bell, RN, MSN; Emily Patterson, PhD; Erik Van Eaton, MD; and Arpana Vidyarthi, MD. These experts reflect the perspective of nonphysician members of the hospital community, representing the interests of technology, nursing, human factors research, and hospital medicine. They reviewed the paper and hand-off recommendations by participating in conference calls in which they were asked to comment on questions regarding the working paper. These discussions gave the task force invaluable, candid feedback adopted into the working paper to create a more robust set of recommendations.
The final product was reviewed by SHM’s Board of Directors in January; a dissemination plan is in progress. If these recommendations are endorsed by an institution or a hospitalist group, they will act as a guide to ensure the coordination of hand-offs and the mangement of important clinical care issues.
Through their research and interactions with a large number of individuals concerned with this issue, the HCTF discovered that the quality improvement of patient transitions is a complex, global issue. They believe this checklist of hand-off elements is essential to these efforts.
Venous thromboembolic (VTE) disease, ranging from asymptomatic deep-vein thrombosis (DVT) to massive pulmonary embolism (PE), is a significant cause of morbidity and mortality in hospitalized patients. Almost all hospitalized patients are at risk for VTE, and the literature suggests approximately half of all VTEs are hospital-acquired.
Hospitalists are ideally positioned to reduce the incidence of preventable VTEs, both by using known best practices to improve care delivered to their own patients, and, more importantly, by leading hospitalwide efforts that improve care for all patients at their home institutions.
In recognition of this important clinical issue and the role hospitalists can play in addressing it, SHM launched the VTE Prevention Collaborative (VTEPC) in January 2007. The program offers individualized assistance to hospitalists wishing to take the lead in this area.
The VTEPC offers two technical assistance options. Individuals interested in securing ongoing support for their planned or active VTE prevention projects can enroll in the mentoring program. This allows a full year of access to and support from SHM mentors with VTE and quality-improvement (QI) expertise. Mentoring occurs in eight telephone calls, during which mentors offer individualized assistance on any topics, tasks, or barriers commonly encountered in designing, implementing, and evaluating a VTE prevention project.
An on-site consultation program is designed for individuals interested in securing expert evaluation and input on a VTE prevention program but who don’t feel they need ongoing, longitudinal support. In this program, SHM consultants with VTE and QI expertise visit applicants’ hospitals to evaluate active or planned VTE prevention programs. The consultation visits feature a structured evaluation of the site’s strengths and resources, barriers to improvement, and the design and function of active or proposed VTE prevention interventions.
For both programs, support and instruction are organized around the VTE QI workbook, “Preventing Hospital-Acquired Venous Thromboembolism: A Guide for Effective Quality Improvement,” SHM’s step-by-step guide for developing a VTE prevention program. SHM secured the services of Greg Maynard, MD, and Jason Stein, MD, to provide mentoring and conduct consultation visits. Drs. Maynard and Stein have led successful local VTE prevention QI projects, hold QI leadership positions, and have taught QI and VTE prevention principals to local and national audiences. Dr. Maynard is head of the Division of Hospital Medicine and associate clinical professor of medicine at the University of California, San Diego. Dr. Stein is a hospitalist at Atlanta’s Emory University Hospital, assistant professor of medicine at Emory University School of Medicine, and director of quality improvement for the Emory Hospital Medicine Unit.
Both were also instrumental in developing SHM’s online VTE Resource Room and the VTE QI workbook.
Strong Responses
Twenty-seven hospitalists enrolled in the VTEPC in its first year of operation, 24 in the mentoring program and three in the consultation program.
Enrollees have broad experience in VTE prevention and QI. Some enrollees have been in practice for two years, others more than 25 years. Some fill QI leadership roles in their hospitals or hospital medicine groups. For others the VTE prevention project is their first experience leading a QI effort. Regional representation (19 states), hospital system representation (18 systems), hospital size (135 to 700 staffed beds), and hospital type (academic centers, community teaching hospitals, and community hospitals) are also broad. One enrollee works at a long-term acute care hospital, all others work at acute-care hospitals.
What They Said
Participants in the mentoring and consultation programs have reported that the support they’ve received has been enormously helpful.
According to feedback from one participant, support from the mentoring program made the potentially overwhelming prospect of launching a hospitalwide improvement effort much more manageable: “The prospect of launching a multihospital VTE Prevention Protocol was extremely daunting; however, with the help of my SHM mentor, we stand ready to pilot the program within the week. Our mentor carefully constructed a step-by-step process that allowed me to investigate the scope of the problem at the local level and develop a protocol that was embraced by our administration and physicians. He supplied me with resources and knowledge that allowed me to successfully handle multiple obstacles that arose along the way. What we have accomplished will have an enormous impact on the quality of care that we provide for our patients.”
Other participants have reported that having access to objective input from an external expert can help transform a slow-developing or ineffective prevention program. As one participant put it: “Mentoring through SHM’s VTE Prevention Collaborative has been an invaluable experience. Through monthly phone calls and frequent e-mails, our mentor focused our previously ineffective efforts and guided us to develop a streamlined tool that was custom-fit to the workflow at our hospital. He has saved us tremendous frustrations by directing us to the appropriate resources in our institution to accomplish tasks we would have attempted ourselves. Since our first phone call, he has been both our coach and cheerleader. The processes and techniques that he has taught us are applicable to every quality endeavor we engage in.”
What Impressed Experts
Drs. Maynard and Stein have been enormously impressed by what VTEPC members have achieved. “What is most impressive to me is how all these hospitalist project leaders in different settings are overcoming a wide variety of intuitional barriers, medical staff barriers, infrastructure barriers—all the obstacles that can challenge the typical big QI project,” says Dr. Maynard. He notes that not only are participants utilizing all the basic QI principles in all the ways that were outlined in the QI workbook, but they also are coming up with innovations and approaches beyond what the workbook authors envisioned.
“We learn from them as they come up with innovations to meet their own challenges,” Dr. Stein says. “It shows the resilience and flexibility of the QI framework. If you really work in your local setting on these things with the improvement framework in mind you can get by almost any barrier.” Drs. Maynard and Stein have noted that participants have been able to design and implement VTE prevention programs at a pace that far outstrips what the two mentors achieved at their home institutions.
Many participants have found real-time ways to identify patients who are not on prophylaxis but should be. At many sites, identification begins with a report generated by the hospital’s inpatient pharmacy service, which typically shows the anti-coagulation regimen for each patient in a given hospital ward. The floor pharmacist or nurse can identify who is not on prophylaxis, assess risk factors and contraindications, and act to mitigate the situation—for example, by placing a call to the patient’s attending physician. Other sites have developed more sophisticated reports that capture information about relative risk for DVT and the absence or presence of contraindications to pharmacologic prophylaxis; these features reduce the effort required to investigate each case.
How to Learn More
The Quality Track at the 2008 Annual Meeting (April 3-5 at the Manchester Hyatt, San Diego, Calif.) includes a session on the “VTE Collaborative Experience” (1-2:25 p.m. April 4). Drs. Maynard and Stein will discuss the initiative, as will collaborative members, who will describe key successes and innovations that furthered their efforts to establish effective VTE prevention programs. Questions about the VTEPC and the Annual Meeting session can be directed to [email protected].
Update on Hand-Offs
SHM task force continues to refine transitions-of-care checklist
by Shannon Roach
Among hospitalists and other organizations, there has been an increasing interest surrounding the improvement of the quality of patient care, especially within transitions of care and patient discharge. As the leader in the hospital medicine field, SHM continues to support and lead initiatives for the improvement of care as related to patient discharge and transitions. Last year’s creation of the Hand-Offs Communication Task Force (HCTF) has upheld SHM’s position of being dedicated to the promotion of the highest quality care for all hospitalized patients.
Derived from members of the Hospital Quality and Patient Safety Committee and the Education Committee, this task force was led by Vineet Arora, MD, MA, assistant professor of medicine, University of Chicago. Collaborating with her were Preetha Basaviah, MD, clinical instructor, Stanford University Medical Center in Calif.; Dan Dressler, MD, instructor of medicine, Emory University School of Medicine in Atlanta; Lakshmi Halasyamani, MD, associate chairperson of the Department of Internal Medicine at St. Joseph Mercy Hospital in Ann Arbor, Mich.; Sunil Kripalani, MD, MSc, an instructor at Emory University in Atlanta; and Efren Manjarrez, MD, assistant clinical professor of medicine at the Miller School of Medicine, University of Miami.
This team set out to create a formally recognized set of recommendations for ensuring optimum communication and continuity of care at the end of a medical professional’s shift or a patient’s change in service.
The task force’s first step was to determine what information was available as a basis for these recommendations. Though data were limited, the group decided that recommendations for effective hand-offs would be broken into three categories: program policy, verbal exchange, and content exchange.
As the need for more evidence-based data for the improvement of in-hospital hand-offs became clear, the group decided a valuable follow-up approach for these recommendations would be to incorporate a research agenda into the findings. This proposal suggests a need for a rigorous evaluation of these recommendations, with an emphasis on controlled interventions. It also encourages the development of patient-based outcomes sensitive to hand-off quality.
As a test run for these recommendations, the HCTF presented its findings at Hospital Medicine 2007 in Dallas. Their session “Developing Communications and Hand-Off Standards for Hospitalists” drew a passionate response. During this session they unveiled a checklist outlining the important elements of an in-hospital physician hand-off. Attendees were encouraged to offer feedback and vote on proposed hand-off elements. They also were encouraged to submit suggestions if they believed something was missing.
Using that feedback, the group produced a final draft of recommendations and distributed it to a multidisciplinary team of experts for a final review. On the panel were Linda Bell, RN, MSN; Emily Patterson, PhD; Erik Van Eaton, MD; and Arpana Vidyarthi, MD. These experts reflect the perspective of nonphysician members of the hospital community, representing the interests of technology, nursing, human factors research, and hospital medicine. They reviewed the paper and hand-off recommendations by participating in conference calls in which they were asked to comment on questions regarding the working paper. These discussions gave the task force invaluable, candid feedback adopted into the working paper to create a more robust set of recommendations.
The final product was reviewed by SHM’s Board of Directors in January; a dissemination plan is in progress. If these recommendations are endorsed by an institution or a hospitalist group, they will act as a guide to ensure the coordination of hand-offs and the mangement of important clinical care issues.
Through their research and interactions with a large number of individuals concerned with this issue, the HCTF discovered that the quality improvement of patient transitions is a complex, global issue. They believe this checklist of hand-off elements is essential to these efforts.
In the Literature
In This Edition
- Statin and beta-blocker use reduces probability of long-term mortality after vascular surgery.
- Low-probability clinical assessment does not exclude pulmonary embolism.
- Upper-extremity DVT is increasing and warrants more aggressive treatment.
- Intensive clinical case management reduces length of hospital stay in CAP.
- Daily chest radiographs have low diagnostic and therapeutic value in the ICU.
- CDAD is associated with high 30-day mortality rate in the ICU setting.
- Frequent nocturnal hemodialysis reduces left ventricular mass and blood pressure.
- Glycemic control in hospitalized patients remains suboptimal.
- Carvedilol fails to show benefit for children with heart failure.
Does Ambulatory Use of Statins, Beta-blockers Reduce Mortality After Vascular Surgery?
Background: Mortality for vascular surgery remains high. Considering promising new data on use of perioperative statins, the question is, does use of statins and/or beta-blockers within 30 days of surgery reduce long-term mortality? Long-term post-operative mortality has not commonly been reported.
Study design: A retrospective observational cohort study.
Setting: Five Veterans Affairs (VA) medical centers in four western states.
Synopsis: Data were gathered from the regional Department of Veterans Affairs administrative and relational database for the 3,062 patients who had vascular surgery at five VA medical centers from January 1998 to March 2005. All had decreased long-term mortality after vascular surgery when they started taking beta-blockers or statins or both within 30 days before or after surgery, compared with patients taking neither drug. Higher-risk patients benefited the most from combination therapy with statins and beta-blockers, with a 33% reduction in mortality after two years.
Study results were limited by several factors, most related to the study’s retrospective nature. There were differences between users and non-users of statins and beta-blockers. Use of the medications was not random, only 1% of study participants were women, and perhaps most importantly, information regarding tobacco use was available for only 47% of the patients.
Bottom Line: The use of statins and beta-blockers in combination should be considered for all patients undergoing vascular surgery.
Citation: Barrett TW, Mori M, DeBoer D. Association of ambulatory use of statins and beta-blockers with long-term mortality after vascular surgery. J Hosp Med. 2007; 2(4):241-252.
What Are the Presenting Characteristics of Patients with PE?
Background: The identification of patients who should undergo diagnostic testing for pulmonary embolism (PE) rests on the identification of clinical signs and symptoms. Because these findings are frequently subtle, diagnosis of PE is often delayed or missed.
Study design: Prospective multicenter study.
Setting: Eight academic centers, using a study focusing on inpatients and outpatients.
Synopsis: The most common clinical symptoms associated with PE were the hemoptysis/pleuritic chest pain syndrome (44%) and uncomplicated dyspnea (36%). Circulatory collapse was uncommon (8%). The most common presenting signs were tachypnea (57%), orthopnea (36%), tachycardia (26%), decreased breath sounds (21%), and crackles (21%). Neither oxygen saturation nor the A-a gradient provides useful diagnostic value in excluding PE.
Compared with segmental pulmonary artery embolism, proximal pulmonary emboli more often presented with typical signs and symptoms. Dyspnea, tachypnea, or pleuritic chest pain occurred in 77% of patients with segmental artery embolism.
Bottom Line: Because symptoms may be mild or even absent, a high level of clinical suspicion is critical for identifying patients in whom further diagnostic testing for pulmonary embolism is warranted.
Citation: Stein PD, Afzal B, Fadi M, et al. Clinical characteristics of patients with acute pulmonary embolism: Data from PIOPED II. Am J Med. 2007;120:871-879.
What Incidence, Risk Factors, and Outcomes Are Associated with Upper-Extremity DVT?
Background: The incidence of upper-extremity deep-vein thrombosis (DVT) is increasing although the risk factors and clinical outcomes are not as well established as for lower-extremity DVT.
Study design: Retrospective observational study.
Setting: Twelve hospitals serving the community of Worchester, Mass.
Synopsis: In this study of 483 people with DVT, the incidence of lower-extremity DVT was six times as common as upper-extremity DVT. The risk factor most strongly associated with upper-extremity DVT was a history of a recent indwelling central venous catheter. In this study, patients with upper-extremity DVT (69) were less likely to receive long-term anticoagulation with warfarin (Coumadin) than patients with lower-extremity DVT, although there were no differences in observed outcomes.
Recurrent upper-extremity DVT occurred in 10 of the 69 patients. Only one patient (1.5%) with an upper-extremity DVT suffered a PE, compared with 15% of patients with lower-extremity DVT.
There was not a significant incidence of PE associated with upper-extremity DVT in this study because of the low number of cases of upper-extremity DVTs (n=69). But hospitalists should not use the data to infer that upper-extremity DVT is a benign condition not requiring aggressive treatment.
Bottom Line: Upper-extremity DVT is strongly associated with central venous catheters. Further study is needed to define its appropriate treatment, possible prophylaxis, and associated morbidity.
Citation: Spencer FA, Emery C, Lessard D, et al. Upper extremity deep vein thrombosis: a community-based perspective. Am J Med. 2007;120:678-684.
What Are Hospital Mortality Risk Factors among Critically Ill CDAD Patients?
Background: C. difficile-associated disease (CDAD) is an important hospital-acquired infection among critically ill patients. Risk factors for hospital mortality in critically ill patients with CDAD have not previously been identified.
Study design: A retrospective, single-center, observational, cohort study.
Setting: A 1,200-bed urban teaching facility.
Synopsis: During a two-year period, all patients in the ICU setting with a diagnosis of CDAD were evaluated. CDAD was defined by the presence of diarrhea or pseudomembranous colitis and a positive assay finding for C. difficile toxin A, toxin B, or both.
A crude 30-day mortality rate of 36.7% was found for patients with CDAD in the ICU setting. Significant risk factors for 30-day mortality included greater severity of illness, the presence of septic shock, and having CDAD develop on the hospital ward prior to ICU transfer. Mortality attributable to CDAD was relatively low (6.1%). CDAD was associated with an excess LOS in the ICU (2.2 days) and hospital LOS (4.5 days).
Bottom Line: CDAD is associated with high 30-day mortality rate but no less attributable mortality. Preventing horizontal transmission in the hospital may reduce mortality.
Citation: Kenneally C, Rosini JM, Skrupky LP, et al. Analysis of 30-day mortality for C. difficile-associated disease in the ICU setting. Chest. 2007;132:418-424.
Do Standardized Order Sets, Intensive Case Management Reduce LOS in CAP Patients?
Background: Community-acquired pneumonia (CAP) results in significant costs to the healthcare system. Length of stay (LOS) affects cost as well as risk for hospital-acquired medical complications. CAP studies have found that guideline adherence improves outcomes such as mortality but does not reduce LOS.
Study design: Sequential course of study with three consecutive blocks of patients.
Setting: Single-institution teaching hospital.
Synopsis: Three consecutive blocks of approximately 110 patients were enrolled. Block 1 patients underwent treatment not guided by order sets or case management. For block 2 patients, clinicians were reminded to use the order sets. If the care processes were not completed, case managers (trained medical residents) would intervene. Emphasis was placed on prompting for timely conversion to oral antibiotics and discharge.
For block 3 patients, clinicians were reminded to use order sets, but no case management was involved. Among the groups, no difference in pneumonia severity or time to clinical stability was found. The mean LOS was 8.8 days in block 1, 5.3 days in block 2, and 7.3 days in block 3.
Order sets (block 3) reduced LOS by 1.5 days (p=0.01) over conventional therapy (block 1). Order sets combined with case management (block 2) reduced LOS by 3.5 days (p<0.001) over conventional therapy.
Bottom Line: Standardized order sets combined with intensive case management reduce LOS in CAP. However, the cost effectiveness and long-term application of this approach are uncertain.
Citation: Fishbane S, Niederman MS, Daly C, et al. The impact of standardized order sets and intensive clinical case management on outcomes in community-acquired pneumonia. Arch Intern Med. 2007;167:1664-1669.
Do Daily Chest Radiographs Have Diagnostic, Therapeutic Value in Medical-Surgical ICUs?
Background: The American College of Radiology recommends daily chest radiographs (CXR) on patients in the intensive care unit (ICU), regardless of the patient’s clinical status. Previous non-blinded studies suggested CXR should be obtained in the ICU only when clinically indicated but did not address the utility of routine daily CXR in finding unsuspected pathology.
Study design: Prospective controlled study.
Setting: University-affiliated hospital ICU in the Netherlands.
Synopsis: For one year, 1,780 daily routine CXR on 559 ICU admissions were reviewed by a radiologist and blinded to the attending physician, who could view radiographs ordered with a clinical indication.
Daily CXR assisted in a diagnosis in 4.4% of cases, most frequently detecting infiltrates or tracheal tube malposition. These findings resulted in a change in clinical management in only 1.9% of the total. For the following six months, daily CXR was abandoned and data were collected on ICU length of stay, readmission, mortality, and cost. The study was not powered to detect differences between the two groups.
This is an observational study that does not provide outcome data on routine daily CXR in either specific disease states or on general ICU patients. Also, the mixed medical-surgical ICU setting may be difficult to generalize to some hospitalists’ practices.
Bottom Line: Routine daily CXR in the medical-surgical ICU has a low diagnostic and therapeutic value.
Citation: Hendrikse KA, Gratama JW, Jove W, et al. Low value of routine chest radiographs in a mixed medical-surgical ICU. Chest. 2007;132:823-828.
Does Frequent Nocturnal Hemodialysis Reduce LV Mass in Patients with ESRD?
Background: Left ventricle (LV) hypertrophy, heart failure, and sudden cardiac death are responsible for significant morbidity and mortality in patients with end-stage renal disease (ESRD). In the general population, reduction of LV mass lowers risk of major cardiovascular events. Some evidence suggests that nocturnal hemodialysis reduces LV mass and blood pressure, and improves mineral metabolism.
Study design: Small randomized controlled trial.
Setting: Two university medical centers in Alberta, Canada.
Synopsis: Fifty-two hemodialysis patients were randomized to receive nocturnal hemodialysis six times weekly or conventional hemodialysis three times weekly. Cardiovascular magnetic resonance imaging assessed LV mass at the beginning and end of six months. Secondary outcomes included health-related quality of life, predialysis systolic blood pressure, and calcium-phosphate product.
LV mass decreased with nocturnal hemodialysis (p=.04). Average systolic blood pressure dropped 7 mm Hg despite antihypertensive medication reductions or discontinuation in many patients receiving nocturnal hemodialysis. The calcium-phosphate product decreased, thus reducing the need for phosphate binders and calcium supplementation. No significant effect on health-related quality of life was found in the primary analysis; however, a small improvement was seen in the nocturnal hemodialysis arm when comparing values from the time of randomization and six months.
The outcomes measured were not validated in patients with ESRD. The dose of dialysis was not compared between the two groups. Confidence intervals were wide and the duration of follow-up limited. The study was underpowered for differences in mortality, quality of life, or adverse event rates.
Bottom Line: Frequent nocturnal hemodialysis may improve cardiovascular outcomes, reduce the need for medications, and enhance quality of life for patients with ESRD having the physical and mental capacity to perform it safely.
Citation: Culleton BF, Walsh M, Klarenbach SW, et al. Effect of frequent nocturnal hemodialysis vs. conventional hemodialysis on left ventricular mass and quality of life. JAMA. 2007;298(11):1291-1299.
Is Glycemic Control in Non-critically Ill Hospitalized Patients Adequate?
Background: In-hospital hyperglycemia is associated with adverse outcomes. Recent guidelines support tight glycemic control for most hospitalized patient populations. Little is known about the current practice of glycemic control in non-critically ill patients.
Study design: Retrospective cohort analysis.
Setting: A 200-bed tertiary-care U.S. teaching hospital.
Synopsis: Hospital databases were reviewed for 2,916 non-critically ill patients discharged after three days with a diagnosis of diabetes or hyperglycemia. Glycemic control was assessed by blood glucose (BG) measurement during the first 24 hours, BG prior to discharge, and overall hospital stay.
Hyperglycemia (BG more than 200 mg/dL) occurred in 20% to 25% of patients throughout the hospital stay or during the first or final 24 hours. The same percentage had at least one hypoglycemic episode (BG less than 70 mg/dL). Most patients received insulin, either alone or in combination with oral agents. Of those, 58% received short-acting bolus insulin, while only 42% were treated with basal-bolus insulin regimens. Insulin administered during the first and the final 24 hours increased in 54% of patients, decreased in 39%, and remained unchanged in 7%. Almost one-third had reductions in insulin therapy despite persistent hyperglycemia.
This single-site study did not distinguish between pre-existing diabetes, unrecognized diabetes, or stress-induced hyperglycemia. The electronic databases did not permit analysis of clinical decision-making behavior or the nutritional support utilized to explain the findings.
Bottom Line: Glycemic control in non-critically ill hospitalized patients appears limited by failure to change treatment when indicated (clinical inertia) and diminution of treatment despite ongoing hyperglycemia (negative therapeutic momentum).
Citation: Cook CV, Castro JC, Schmidt RE, et al. Diabetes care in hospitalized noncritically ill patients: More evidence for clinical inertia and negative therapeutic momentum. J Hosp Med. 2007;2:203-211.
Does Carvedilol Significantly Improve Outcomes in Youths with Symptomatic Systolic Heart Failure?
Background: Although beta-blockers improve symptoms and survival in adults with heart failure, little is known about these medications in children and adolescents. Treatment recommendations in children and adolescents with heart failure usually must be extrapolated from the results of clinical trials conducted in adults.
Study design: A multicenter, randomized, double-blind placebo controlled study.
Setting: 26 U.S. hospitals.
Synopsis: 161 children and adolescents with symptomatic systolic heart failure on conventional heart failure medications were randomized in a 1:1:1 ratio to twice-daily dosing with placebo, low-dose carvedilol (Coreg) or high-dose carvedilol for eight months. Patients were determined to have a response of worsened, improved, or unchanged, based on variables involving a change in New York Heart Association class, hospitalization requiring IV medications, or withdrawal from the study for treatment failure or lack of therapeutic response.
Carvedilol had no significant effect on the primary end points above, although there may have been some difference in benefit based on ventricular morphology. Because fewer patients overall experienced worsening of their heart failure than expected and because of the high rate of spontaneous improvement seen, the study may have been underpowered. Randomized clinical trials in pediatrics are exceedingly rare, and trials that are done routinely have study populations far smaller than this one.
Bottom Line: Carvedilol has not been shown to benefit children and adolescents with symptomatic systolic heart failure.
Citation: Shaddy RE, Boucek MM, Hsu DT, et al. Carvedilol for children and adolescents with heart failure: a randomized controlled trial. JAMA. 2007; 298(10):1171-1179. TH
In This Edition
- Statin and beta-blocker use reduces probability of long-term mortality after vascular surgery.
- Low-probability clinical assessment does not exclude pulmonary embolism.
- Upper-extremity DVT is increasing and warrants more aggressive treatment.
- Intensive clinical case management reduces length of hospital stay in CAP.
- Daily chest radiographs have low diagnostic and therapeutic value in the ICU.
- CDAD is associated with high 30-day mortality rate in the ICU setting.
- Frequent nocturnal hemodialysis reduces left ventricular mass and blood pressure.
- Glycemic control in hospitalized patients remains suboptimal.
- Carvedilol fails to show benefit for children with heart failure.
Does Ambulatory Use of Statins, Beta-blockers Reduce Mortality After Vascular Surgery?
Background: Mortality for vascular surgery remains high. Considering promising new data on use of perioperative statins, the question is, does use of statins and/or beta-blockers within 30 days of surgery reduce long-term mortality? Long-term post-operative mortality has not commonly been reported.
Study design: A retrospective observational cohort study.
Setting: Five Veterans Affairs (VA) medical centers in four western states.
Synopsis: Data were gathered from the regional Department of Veterans Affairs administrative and relational database for the 3,062 patients who had vascular surgery at five VA medical centers from January 1998 to March 2005. All had decreased long-term mortality after vascular surgery when they started taking beta-blockers or statins or both within 30 days before or after surgery, compared with patients taking neither drug. Higher-risk patients benefited the most from combination therapy with statins and beta-blockers, with a 33% reduction in mortality after two years.
Study results were limited by several factors, most related to the study’s retrospective nature. There were differences between users and non-users of statins and beta-blockers. Use of the medications was not random, only 1% of study participants were women, and perhaps most importantly, information regarding tobacco use was available for only 47% of the patients.
Bottom Line: The use of statins and beta-blockers in combination should be considered for all patients undergoing vascular surgery.
Citation: Barrett TW, Mori M, DeBoer D. Association of ambulatory use of statins and beta-blockers with long-term mortality after vascular surgery. J Hosp Med. 2007; 2(4):241-252.
What Are the Presenting Characteristics of Patients with PE?
Background: The identification of patients who should undergo diagnostic testing for pulmonary embolism (PE) rests on the identification of clinical signs and symptoms. Because these findings are frequently subtle, diagnosis of PE is often delayed or missed.
Study design: Prospective multicenter study.
Setting: Eight academic centers, using a study focusing on inpatients and outpatients.
Synopsis: The most common clinical symptoms associated with PE were the hemoptysis/pleuritic chest pain syndrome (44%) and uncomplicated dyspnea (36%). Circulatory collapse was uncommon (8%). The most common presenting signs were tachypnea (57%), orthopnea (36%), tachycardia (26%), decreased breath sounds (21%), and crackles (21%). Neither oxygen saturation nor the A-a gradient provides useful diagnostic value in excluding PE.
Compared with segmental pulmonary artery embolism, proximal pulmonary emboli more often presented with typical signs and symptoms. Dyspnea, tachypnea, or pleuritic chest pain occurred in 77% of patients with segmental artery embolism.
Bottom Line: Because symptoms may be mild or even absent, a high level of clinical suspicion is critical for identifying patients in whom further diagnostic testing for pulmonary embolism is warranted.
Citation: Stein PD, Afzal B, Fadi M, et al. Clinical characteristics of patients with acute pulmonary embolism: Data from PIOPED II. Am J Med. 2007;120:871-879.
What Incidence, Risk Factors, and Outcomes Are Associated with Upper-Extremity DVT?
Background: The incidence of upper-extremity deep-vein thrombosis (DVT) is increasing although the risk factors and clinical outcomes are not as well established as for lower-extremity DVT.
Study design: Retrospective observational study.
Setting: Twelve hospitals serving the community of Worchester, Mass.
Synopsis: In this study of 483 people with DVT, the incidence of lower-extremity DVT was six times as common as upper-extremity DVT. The risk factor most strongly associated with upper-extremity DVT was a history of a recent indwelling central venous catheter. In this study, patients with upper-extremity DVT (69) were less likely to receive long-term anticoagulation with warfarin (Coumadin) than patients with lower-extremity DVT, although there were no differences in observed outcomes.
Recurrent upper-extremity DVT occurred in 10 of the 69 patients. Only one patient (1.5%) with an upper-extremity DVT suffered a PE, compared with 15% of patients with lower-extremity DVT.
There was not a significant incidence of PE associated with upper-extremity DVT in this study because of the low number of cases of upper-extremity DVTs (n=69). But hospitalists should not use the data to infer that upper-extremity DVT is a benign condition not requiring aggressive treatment.
Bottom Line: Upper-extremity DVT is strongly associated with central venous catheters. Further study is needed to define its appropriate treatment, possible prophylaxis, and associated morbidity.
Citation: Spencer FA, Emery C, Lessard D, et al. Upper extremity deep vein thrombosis: a community-based perspective. Am J Med. 2007;120:678-684.
What Are Hospital Mortality Risk Factors among Critically Ill CDAD Patients?
Background: C. difficile-associated disease (CDAD) is an important hospital-acquired infection among critically ill patients. Risk factors for hospital mortality in critically ill patients with CDAD have not previously been identified.
Study design: A retrospective, single-center, observational, cohort study.
Setting: A 1,200-bed urban teaching facility.
Synopsis: During a two-year period, all patients in the ICU setting with a diagnosis of CDAD were evaluated. CDAD was defined by the presence of diarrhea or pseudomembranous colitis and a positive assay finding for C. difficile toxin A, toxin B, or both.
A crude 30-day mortality rate of 36.7% was found for patients with CDAD in the ICU setting. Significant risk factors for 30-day mortality included greater severity of illness, the presence of septic shock, and having CDAD develop on the hospital ward prior to ICU transfer. Mortality attributable to CDAD was relatively low (6.1%). CDAD was associated with an excess LOS in the ICU (2.2 days) and hospital LOS (4.5 days).
Bottom Line: CDAD is associated with high 30-day mortality rate but no less attributable mortality. Preventing horizontal transmission in the hospital may reduce mortality.
Citation: Kenneally C, Rosini JM, Skrupky LP, et al. Analysis of 30-day mortality for C. difficile-associated disease in the ICU setting. Chest. 2007;132:418-424.
Do Standardized Order Sets, Intensive Case Management Reduce LOS in CAP Patients?
Background: Community-acquired pneumonia (CAP) results in significant costs to the healthcare system. Length of stay (LOS) affects cost as well as risk for hospital-acquired medical complications. CAP studies have found that guideline adherence improves outcomes such as mortality but does not reduce LOS.
Study design: Sequential course of study with three consecutive blocks of patients.
Setting: Single-institution teaching hospital.
Synopsis: Three consecutive blocks of approximately 110 patients were enrolled. Block 1 patients underwent treatment not guided by order sets or case management. For block 2 patients, clinicians were reminded to use the order sets. If the care processes were not completed, case managers (trained medical residents) would intervene. Emphasis was placed on prompting for timely conversion to oral antibiotics and discharge.
For block 3 patients, clinicians were reminded to use order sets, but no case management was involved. Among the groups, no difference in pneumonia severity or time to clinical stability was found. The mean LOS was 8.8 days in block 1, 5.3 days in block 2, and 7.3 days in block 3.
Order sets (block 3) reduced LOS by 1.5 days (p=0.01) over conventional therapy (block 1). Order sets combined with case management (block 2) reduced LOS by 3.5 days (p<0.001) over conventional therapy.
Bottom Line: Standardized order sets combined with intensive case management reduce LOS in CAP. However, the cost effectiveness and long-term application of this approach are uncertain.
Citation: Fishbane S, Niederman MS, Daly C, et al. The impact of standardized order sets and intensive clinical case management on outcomes in community-acquired pneumonia. Arch Intern Med. 2007;167:1664-1669.
Do Daily Chest Radiographs Have Diagnostic, Therapeutic Value in Medical-Surgical ICUs?
Background: The American College of Radiology recommends daily chest radiographs (CXR) on patients in the intensive care unit (ICU), regardless of the patient’s clinical status. Previous non-blinded studies suggested CXR should be obtained in the ICU only when clinically indicated but did not address the utility of routine daily CXR in finding unsuspected pathology.
Study design: Prospective controlled study.
Setting: University-affiliated hospital ICU in the Netherlands.
Synopsis: For one year, 1,780 daily routine CXR on 559 ICU admissions were reviewed by a radiologist and blinded to the attending physician, who could view radiographs ordered with a clinical indication.
Daily CXR assisted in a diagnosis in 4.4% of cases, most frequently detecting infiltrates or tracheal tube malposition. These findings resulted in a change in clinical management in only 1.9% of the total. For the following six months, daily CXR was abandoned and data were collected on ICU length of stay, readmission, mortality, and cost. The study was not powered to detect differences between the two groups.
This is an observational study that does not provide outcome data on routine daily CXR in either specific disease states or on general ICU patients. Also, the mixed medical-surgical ICU setting may be difficult to generalize to some hospitalists’ practices.
Bottom Line: Routine daily CXR in the medical-surgical ICU has a low diagnostic and therapeutic value.
Citation: Hendrikse KA, Gratama JW, Jove W, et al. Low value of routine chest radiographs in a mixed medical-surgical ICU. Chest. 2007;132:823-828.
Does Frequent Nocturnal Hemodialysis Reduce LV Mass in Patients with ESRD?
Background: Left ventricle (LV) hypertrophy, heart failure, and sudden cardiac death are responsible for significant morbidity and mortality in patients with end-stage renal disease (ESRD). In the general population, reduction of LV mass lowers risk of major cardiovascular events. Some evidence suggests that nocturnal hemodialysis reduces LV mass and blood pressure, and improves mineral metabolism.
Study design: Small randomized controlled trial.
Setting: Two university medical centers in Alberta, Canada.
Synopsis: Fifty-two hemodialysis patients were randomized to receive nocturnal hemodialysis six times weekly or conventional hemodialysis three times weekly. Cardiovascular magnetic resonance imaging assessed LV mass at the beginning and end of six months. Secondary outcomes included health-related quality of life, predialysis systolic blood pressure, and calcium-phosphate product.
LV mass decreased with nocturnal hemodialysis (p=.04). Average systolic blood pressure dropped 7 mm Hg despite antihypertensive medication reductions or discontinuation in many patients receiving nocturnal hemodialysis. The calcium-phosphate product decreased, thus reducing the need for phosphate binders and calcium supplementation. No significant effect on health-related quality of life was found in the primary analysis; however, a small improvement was seen in the nocturnal hemodialysis arm when comparing values from the time of randomization and six months.
The outcomes measured were not validated in patients with ESRD. The dose of dialysis was not compared between the two groups. Confidence intervals were wide and the duration of follow-up limited. The study was underpowered for differences in mortality, quality of life, or adverse event rates.
Bottom Line: Frequent nocturnal hemodialysis may improve cardiovascular outcomes, reduce the need for medications, and enhance quality of life for patients with ESRD having the physical and mental capacity to perform it safely.
Citation: Culleton BF, Walsh M, Klarenbach SW, et al. Effect of frequent nocturnal hemodialysis vs. conventional hemodialysis on left ventricular mass and quality of life. JAMA. 2007;298(11):1291-1299.
Is Glycemic Control in Non-critically Ill Hospitalized Patients Adequate?
Background: In-hospital hyperglycemia is associated with adverse outcomes. Recent guidelines support tight glycemic control for most hospitalized patient populations. Little is known about the current practice of glycemic control in non-critically ill patients.
Study design: Retrospective cohort analysis.
Setting: A 200-bed tertiary-care U.S. teaching hospital.
Synopsis: Hospital databases were reviewed for 2,916 non-critically ill patients discharged after three days with a diagnosis of diabetes or hyperglycemia. Glycemic control was assessed by blood glucose (BG) measurement during the first 24 hours, BG prior to discharge, and overall hospital stay.
Hyperglycemia (BG more than 200 mg/dL) occurred in 20% to 25% of patients throughout the hospital stay or during the first or final 24 hours. The same percentage had at least one hypoglycemic episode (BG less than 70 mg/dL). Most patients received insulin, either alone or in combination with oral agents. Of those, 58% received short-acting bolus insulin, while only 42% were treated with basal-bolus insulin regimens. Insulin administered during the first and the final 24 hours increased in 54% of patients, decreased in 39%, and remained unchanged in 7%. Almost one-third had reductions in insulin therapy despite persistent hyperglycemia.
This single-site study did not distinguish between pre-existing diabetes, unrecognized diabetes, or stress-induced hyperglycemia. The electronic databases did not permit analysis of clinical decision-making behavior or the nutritional support utilized to explain the findings.
Bottom Line: Glycemic control in non-critically ill hospitalized patients appears limited by failure to change treatment when indicated (clinical inertia) and diminution of treatment despite ongoing hyperglycemia (negative therapeutic momentum).
Citation: Cook CV, Castro JC, Schmidt RE, et al. Diabetes care in hospitalized noncritically ill patients: More evidence for clinical inertia and negative therapeutic momentum. J Hosp Med. 2007;2:203-211.
Does Carvedilol Significantly Improve Outcomes in Youths with Symptomatic Systolic Heart Failure?
Background: Although beta-blockers improve symptoms and survival in adults with heart failure, little is known about these medications in children and adolescents. Treatment recommendations in children and adolescents with heart failure usually must be extrapolated from the results of clinical trials conducted in adults.
Study design: A multicenter, randomized, double-blind placebo controlled study.
Setting: 26 U.S. hospitals.
Synopsis: 161 children and adolescents with symptomatic systolic heart failure on conventional heart failure medications were randomized in a 1:1:1 ratio to twice-daily dosing with placebo, low-dose carvedilol (Coreg) or high-dose carvedilol for eight months. Patients were determined to have a response of worsened, improved, or unchanged, based on variables involving a change in New York Heart Association class, hospitalization requiring IV medications, or withdrawal from the study for treatment failure or lack of therapeutic response.
Carvedilol had no significant effect on the primary end points above, although there may have been some difference in benefit based on ventricular morphology. Because fewer patients overall experienced worsening of their heart failure than expected and because of the high rate of spontaneous improvement seen, the study may have been underpowered. Randomized clinical trials in pediatrics are exceedingly rare, and trials that are done routinely have study populations far smaller than this one.
Bottom Line: Carvedilol has not been shown to benefit children and adolescents with symptomatic systolic heart failure.
Citation: Shaddy RE, Boucek MM, Hsu DT, et al. Carvedilol for children and adolescents with heart failure: a randomized controlled trial. JAMA. 2007; 298(10):1171-1179. TH
In This Edition
- Statin and beta-blocker use reduces probability of long-term mortality after vascular surgery.
- Low-probability clinical assessment does not exclude pulmonary embolism.
- Upper-extremity DVT is increasing and warrants more aggressive treatment.
- Intensive clinical case management reduces length of hospital stay in CAP.
- Daily chest radiographs have low diagnostic and therapeutic value in the ICU.
- CDAD is associated with high 30-day mortality rate in the ICU setting.
- Frequent nocturnal hemodialysis reduces left ventricular mass and blood pressure.
- Glycemic control in hospitalized patients remains suboptimal.
- Carvedilol fails to show benefit for children with heart failure.
Does Ambulatory Use of Statins, Beta-blockers Reduce Mortality After Vascular Surgery?
Background: Mortality for vascular surgery remains high. Considering promising new data on use of perioperative statins, the question is, does use of statins and/or beta-blockers within 30 days of surgery reduce long-term mortality? Long-term post-operative mortality has not commonly been reported.
Study design: A retrospective observational cohort study.
Setting: Five Veterans Affairs (VA) medical centers in four western states.
Synopsis: Data were gathered from the regional Department of Veterans Affairs administrative and relational database for the 3,062 patients who had vascular surgery at five VA medical centers from January 1998 to March 2005. All had decreased long-term mortality after vascular surgery when they started taking beta-blockers or statins or both within 30 days before or after surgery, compared with patients taking neither drug. Higher-risk patients benefited the most from combination therapy with statins and beta-blockers, with a 33% reduction in mortality after two years.
Study results were limited by several factors, most related to the study’s retrospective nature. There were differences between users and non-users of statins and beta-blockers. Use of the medications was not random, only 1% of study participants were women, and perhaps most importantly, information regarding tobacco use was available for only 47% of the patients.
Bottom Line: The use of statins and beta-blockers in combination should be considered for all patients undergoing vascular surgery.
Citation: Barrett TW, Mori M, DeBoer D. Association of ambulatory use of statins and beta-blockers with long-term mortality after vascular surgery. J Hosp Med. 2007; 2(4):241-252.
What Are the Presenting Characteristics of Patients with PE?
Background: The identification of patients who should undergo diagnostic testing for pulmonary embolism (PE) rests on the identification of clinical signs and symptoms. Because these findings are frequently subtle, diagnosis of PE is often delayed or missed.
Study design: Prospective multicenter study.
Setting: Eight academic centers, using a study focusing on inpatients and outpatients.
Synopsis: The most common clinical symptoms associated with PE were the hemoptysis/pleuritic chest pain syndrome (44%) and uncomplicated dyspnea (36%). Circulatory collapse was uncommon (8%). The most common presenting signs were tachypnea (57%), orthopnea (36%), tachycardia (26%), decreased breath sounds (21%), and crackles (21%). Neither oxygen saturation nor the A-a gradient provides useful diagnostic value in excluding PE.
Compared with segmental pulmonary artery embolism, proximal pulmonary emboli more often presented with typical signs and symptoms. Dyspnea, tachypnea, or pleuritic chest pain occurred in 77% of patients with segmental artery embolism.
Bottom Line: Because symptoms may be mild or even absent, a high level of clinical suspicion is critical for identifying patients in whom further diagnostic testing for pulmonary embolism is warranted.
Citation: Stein PD, Afzal B, Fadi M, et al. Clinical characteristics of patients with acute pulmonary embolism: Data from PIOPED II. Am J Med. 2007;120:871-879.
What Incidence, Risk Factors, and Outcomes Are Associated with Upper-Extremity DVT?
Background: The incidence of upper-extremity deep-vein thrombosis (DVT) is increasing although the risk factors and clinical outcomes are not as well established as for lower-extremity DVT.
Study design: Retrospective observational study.
Setting: Twelve hospitals serving the community of Worchester, Mass.
Synopsis: In this study of 483 people with DVT, the incidence of lower-extremity DVT was six times as common as upper-extremity DVT. The risk factor most strongly associated with upper-extremity DVT was a history of a recent indwelling central venous catheter. In this study, patients with upper-extremity DVT (69) were less likely to receive long-term anticoagulation with warfarin (Coumadin) than patients with lower-extremity DVT, although there were no differences in observed outcomes.
Recurrent upper-extremity DVT occurred in 10 of the 69 patients. Only one patient (1.5%) with an upper-extremity DVT suffered a PE, compared with 15% of patients with lower-extremity DVT.
There was not a significant incidence of PE associated with upper-extremity DVT in this study because of the low number of cases of upper-extremity DVTs (n=69). But hospitalists should not use the data to infer that upper-extremity DVT is a benign condition not requiring aggressive treatment.
Bottom Line: Upper-extremity DVT is strongly associated with central venous catheters. Further study is needed to define its appropriate treatment, possible prophylaxis, and associated morbidity.
Citation: Spencer FA, Emery C, Lessard D, et al. Upper extremity deep vein thrombosis: a community-based perspective. Am J Med. 2007;120:678-684.
What Are Hospital Mortality Risk Factors among Critically Ill CDAD Patients?
Background: C. difficile-associated disease (CDAD) is an important hospital-acquired infection among critically ill patients. Risk factors for hospital mortality in critically ill patients with CDAD have not previously been identified.
Study design: A retrospective, single-center, observational, cohort study.
Setting: A 1,200-bed urban teaching facility.
Synopsis: During a two-year period, all patients in the ICU setting with a diagnosis of CDAD were evaluated. CDAD was defined by the presence of diarrhea or pseudomembranous colitis and a positive assay finding for C. difficile toxin A, toxin B, or both.
A crude 30-day mortality rate of 36.7% was found for patients with CDAD in the ICU setting. Significant risk factors for 30-day mortality included greater severity of illness, the presence of septic shock, and having CDAD develop on the hospital ward prior to ICU transfer. Mortality attributable to CDAD was relatively low (6.1%). CDAD was associated with an excess LOS in the ICU (2.2 days) and hospital LOS (4.5 days).
Bottom Line: CDAD is associated with high 30-day mortality rate but no less attributable mortality. Preventing horizontal transmission in the hospital may reduce mortality.
Citation: Kenneally C, Rosini JM, Skrupky LP, et al. Analysis of 30-day mortality for C. difficile-associated disease in the ICU setting. Chest. 2007;132:418-424.
Do Standardized Order Sets, Intensive Case Management Reduce LOS in CAP Patients?
Background: Community-acquired pneumonia (CAP) results in significant costs to the healthcare system. Length of stay (LOS) affects cost as well as risk for hospital-acquired medical complications. CAP studies have found that guideline adherence improves outcomes such as mortality but does not reduce LOS.
Study design: Sequential course of study with three consecutive blocks of patients.
Setting: Single-institution teaching hospital.
Synopsis: Three consecutive blocks of approximately 110 patients were enrolled. Block 1 patients underwent treatment not guided by order sets or case management. For block 2 patients, clinicians were reminded to use the order sets. If the care processes were not completed, case managers (trained medical residents) would intervene. Emphasis was placed on prompting for timely conversion to oral antibiotics and discharge.
For block 3 patients, clinicians were reminded to use order sets, but no case management was involved. Among the groups, no difference in pneumonia severity or time to clinical stability was found. The mean LOS was 8.8 days in block 1, 5.3 days in block 2, and 7.3 days in block 3.
Order sets (block 3) reduced LOS by 1.5 days (p=0.01) over conventional therapy (block 1). Order sets combined with case management (block 2) reduced LOS by 3.5 days (p<0.001) over conventional therapy.
Bottom Line: Standardized order sets combined with intensive case management reduce LOS in CAP. However, the cost effectiveness and long-term application of this approach are uncertain.
Citation: Fishbane S, Niederman MS, Daly C, et al. The impact of standardized order sets and intensive clinical case management on outcomes in community-acquired pneumonia. Arch Intern Med. 2007;167:1664-1669.
Do Daily Chest Radiographs Have Diagnostic, Therapeutic Value in Medical-Surgical ICUs?
Background: The American College of Radiology recommends daily chest radiographs (CXR) on patients in the intensive care unit (ICU), regardless of the patient’s clinical status. Previous non-blinded studies suggested CXR should be obtained in the ICU only when clinically indicated but did not address the utility of routine daily CXR in finding unsuspected pathology.
Study design: Prospective controlled study.
Setting: University-affiliated hospital ICU in the Netherlands.
Synopsis: For one year, 1,780 daily routine CXR on 559 ICU admissions were reviewed by a radiologist and blinded to the attending physician, who could view radiographs ordered with a clinical indication.
Daily CXR assisted in a diagnosis in 4.4% of cases, most frequently detecting infiltrates or tracheal tube malposition. These findings resulted in a change in clinical management in only 1.9% of the total. For the following six months, daily CXR was abandoned and data were collected on ICU length of stay, readmission, mortality, and cost. The study was not powered to detect differences between the two groups.
This is an observational study that does not provide outcome data on routine daily CXR in either specific disease states or on general ICU patients. Also, the mixed medical-surgical ICU setting may be difficult to generalize to some hospitalists’ practices.
Bottom Line: Routine daily CXR in the medical-surgical ICU has a low diagnostic and therapeutic value.
Citation: Hendrikse KA, Gratama JW, Jove W, et al. Low value of routine chest radiographs in a mixed medical-surgical ICU. Chest. 2007;132:823-828.
Does Frequent Nocturnal Hemodialysis Reduce LV Mass in Patients with ESRD?
Background: Left ventricle (LV) hypertrophy, heart failure, and sudden cardiac death are responsible for significant morbidity and mortality in patients with end-stage renal disease (ESRD). In the general population, reduction of LV mass lowers risk of major cardiovascular events. Some evidence suggests that nocturnal hemodialysis reduces LV mass and blood pressure, and improves mineral metabolism.
Study design: Small randomized controlled trial.
Setting: Two university medical centers in Alberta, Canada.
Synopsis: Fifty-two hemodialysis patients were randomized to receive nocturnal hemodialysis six times weekly or conventional hemodialysis three times weekly. Cardiovascular magnetic resonance imaging assessed LV mass at the beginning and end of six months. Secondary outcomes included health-related quality of life, predialysis systolic blood pressure, and calcium-phosphate product.
LV mass decreased with nocturnal hemodialysis (p=.04). Average systolic blood pressure dropped 7 mm Hg despite antihypertensive medication reductions or discontinuation in many patients receiving nocturnal hemodialysis. The calcium-phosphate product decreased, thus reducing the need for phosphate binders and calcium supplementation. No significant effect on health-related quality of life was found in the primary analysis; however, a small improvement was seen in the nocturnal hemodialysis arm when comparing values from the time of randomization and six months.
The outcomes measured were not validated in patients with ESRD. The dose of dialysis was not compared between the two groups. Confidence intervals were wide and the duration of follow-up limited. The study was underpowered for differences in mortality, quality of life, or adverse event rates.
Bottom Line: Frequent nocturnal hemodialysis may improve cardiovascular outcomes, reduce the need for medications, and enhance quality of life for patients with ESRD having the physical and mental capacity to perform it safely.
Citation: Culleton BF, Walsh M, Klarenbach SW, et al. Effect of frequent nocturnal hemodialysis vs. conventional hemodialysis on left ventricular mass and quality of life. JAMA. 2007;298(11):1291-1299.
Is Glycemic Control in Non-critically Ill Hospitalized Patients Adequate?
Background: In-hospital hyperglycemia is associated with adverse outcomes. Recent guidelines support tight glycemic control for most hospitalized patient populations. Little is known about the current practice of glycemic control in non-critically ill patients.
Study design: Retrospective cohort analysis.
Setting: A 200-bed tertiary-care U.S. teaching hospital.
Synopsis: Hospital databases were reviewed for 2,916 non-critically ill patients discharged after three days with a diagnosis of diabetes or hyperglycemia. Glycemic control was assessed by blood glucose (BG) measurement during the first 24 hours, BG prior to discharge, and overall hospital stay.
Hyperglycemia (BG more than 200 mg/dL) occurred in 20% to 25% of patients throughout the hospital stay or during the first or final 24 hours. The same percentage had at least one hypoglycemic episode (BG less than 70 mg/dL). Most patients received insulin, either alone or in combination with oral agents. Of those, 58% received short-acting bolus insulin, while only 42% were treated with basal-bolus insulin regimens. Insulin administered during the first and the final 24 hours increased in 54% of patients, decreased in 39%, and remained unchanged in 7%. Almost one-third had reductions in insulin therapy despite persistent hyperglycemia.
This single-site study did not distinguish between pre-existing diabetes, unrecognized diabetes, or stress-induced hyperglycemia. The electronic databases did not permit analysis of clinical decision-making behavior or the nutritional support utilized to explain the findings.
Bottom Line: Glycemic control in non-critically ill hospitalized patients appears limited by failure to change treatment when indicated (clinical inertia) and diminution of treatment despite ongoing hyperglycemia (negative therapeutic momentum).
Citation: Cook CV, Castro JC, Schmidt RE, et al. Diabetes care in hospitalized noncritically ill patients: More evidence for clinical inertia and negative therapeutic momentum. J Hosp Med. 2007;2:203-211.
Does Carvedilol Significantly Improve Outcomes in Youths with Symptomatic Systolic Heart Failure?
Background: Although beta-blockers improve symptoms and survival in adults with heart failure, little is known about these medications in children and adolescents. Treatment recommendations in children and adolescents with heart failure usually must be extrapolated from the results of clinical trials conducted in adults.
Study design: A multicenter, randomized, double-blind placebo controlled study.
Setting: 26 U.S. hospitals.
Synopsis: 161 children and adolescents with symptomatic systolic heart failure on conventional heart failure medications were randomized in a 1:1:1 ratio to twice-daily dosing with placebo, low-dose carvedilol (Coreg) or high-dose carvedilol for eight months. Patients were determined to have a response of worsened, improved, or unchanged, based on variables involving a change in New York Heart Association class, hospitalization requiring IV medications, or withdrawal from the study for treatment failure or lack of therapeutic response.
Carvedilol had no significant effect on the primary end points above, although there may have been some difference in benefit based on ventricular morphology. Because fewer patients overall experienced worsening of their heart failure than expected and because of the high rate of spontaneous improvement seen, the study may have been underpowered. Randomized clinical trials in pediatrics are exceedingly rare, and trials that are done routinely have study populations far smaller than this one.
Bottom Line: Carvedilol has not been shown to benefit children and adolescents with symptomatic systolic heart failure.
Citation: Shaddy RE, Boucek MM, Hsu DT, et al. Carvedilol for children and adolescents with heart failure: a randomized controlled trial. JAMA. 2007; 298(10):1171-1179. TH