User login
Mass on upper chest
The pathology report indicated that the patient had squamous cell carcinoma (SCC) of the lung, a diagnosis that was consistent with an x-ray and computed tomography (CT) scan that were also done.
Lung cancer is a malignant neoplasm of the lung arising from the respiratory epithelium (bronchi, bronchioles/alveoli). The 4 major cell types responsible for 88% of cases are:
○ adenocarcinoma (including bronchoalveolar)—32% of cases
○ squamous cell carcinoma—29% of cases
○ small cell (or oat cell) carcinoma—18% of cases
○ large cell (or large cell anaplastic)—9% of cases.
Smoking is the major risk factor for lung cancer; a smoking history (current or former) is present in 90% of cases, with a risk ratio (RR) of 13 (passive smoke exposure has a RR of 1.5). Skin nodules from lung cancer metastases may not be painful but are a poor prognostic sign.
Any time spent helping your patients quit smoking may help avert a fatal outcome. In this case, the patient opted not to receive treatment. She passed away 10 months later.
Photos courtesy of Leonard Chow, MD, Ross Lawler, MD, and David Kasper, DO. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Lung cancer. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:355-364.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
The pathology report indicated that the patient had squamous cell carcinoma (SCC) of the lung, a diagnosis that was consistent with an x-ray and computed tomography (CT) scan that were also done.
Lung cancer is a malignant neoplasm of the lung arising from the respiratory epithelium (bronchi, bronchioles/alveoli). The 4 major cell types responsible for 88% of cases are:
○ adenocarcinoma (including bronchoalveolar)—32% of cases
○ squamous cell carcinoma—29% of cases
○ small cell (or oat cell) carcinoma—18% of cases
○ large cell (or large cell anaplastic)—9% of cases.
Smoking is the major risk factor for lung cancer; a smoking history (current or former) is present in 90% of cases, with a risk ratio (RR) of 13 (passive smoke exposure has a RR of 1.5). Skin nodules from lung cancer metastases may not be painful but are a poor prognostic sign.
Any time spent helping your patients quit smoking may help avert a fatal outcome. In this case, the patient opted not to receive treatment. She passed away 10 months later.
Photos courtesy of Leonard Chow, MD, Ross Lawler, MD, and David Kasper, DO. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Lung cancer. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:355-364.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
The pathology report indicated that the patient had squamous cell carcinoma (SCC) of the lung, a diagnosis that was consistent with an x-ray and computed tomography (CT) scan that were also done.
Lung cancer is a malignant neoplasm of the lung arising from the respiratory epithelium (bronchi, bronchioles/alveoli). The 4 major cell types responsible for 88% of cases are:
○ adenocarcinoma (including bronchoalveolar)—32% of cases
○ squamous cell carcinoma—29% of cases
○ small cell (or oat cell) carcinoma—18% of cases
○ large cell (or large cell anaplastic)—9% of cases.
Smoking is the major risk factor for lung cancer; a smoking history (current or former) is present in 90% of cases, with a risk ratio (RR) of 13 (passive smoke exposure has a RR of 1.5). Skin nodules from lung cancer metastases may not be painful but are a poor prognostic sign.
Any time spent helping your patients quit smoking may help avert a fatal outcome. In this case, the patient opted not to receive treatment. She passed away 10 months later.
Photos courtesy of Leonard Chow, MD, Ross Lawler, MD, and David Kasper, DO. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Lung cancer. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:355-364.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
Sores in neck
The FP suspected scrofuloderma from tuberculosis (TB), and referred him to the local health department, where an advanced practice nurse ensured that he got a chest x-ray and an acid-fast bacillus (AFB) stain and culture. The chest x-ray was clear, but the AFB studies showed Mycobacterium tuberculosis. The patient was started on 4 TB drugs—isoniazid, rifampin, pyrazinamide, and ethambutol—while awaiting sensitivities.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith, M. Tuberculosis. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:310-319.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
The FP suspected scrofuloderma from tuberculosis (TB), and referred him to the local health department, where an advanced practice nurse ensured that he got a chest x-ray and an acid-fast bacillus (AFB) stain and culture. The chest x-ray was clear, but the AFB studies showed Mycobacterium tuberculosis. The patient was started on 4 TB drugs—isoniazid, rifampin, pyrazinamide, and ethambutol—while awaiting sensitivities.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith, M. Tuberculosis. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:310-319.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
The FP suspected scrofuloderma from tuberculosis (TB), and referred him to the local health department, where an advanced practice nurse ensured that he got a chest x-ray and an acid-fast bacillus (AFB) stain and culture. The chest x-ray was clear, but the AFB studies showed Mycobacterium tuberculosis. The patient was started on 4 TB drugs—isoniazid, rifampin, pyrazinamide, and ethambutol—while awaiting sensitivities.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith, M. Tuberculosis. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:310-319.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
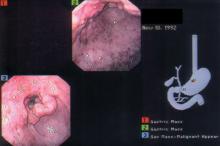
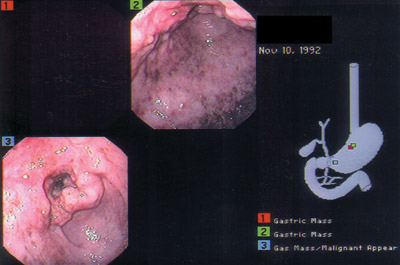
Difficulty eating
The biopsy revealed that the patient had an adenocarcinoma.
The median age at diagnosis is 70 years and median age at death from gastric cancer is 73 years. High rates of stomach cancer occur in Japan, China, Chile, and Ireland. Eighty-five percent of stomach cancers are adenocarcinomas; 15% are lymphomas and GI stromal tumors.
Most tumors are thought to arise from ingestion of nitrates that are converted by bacteria to carcinogens. Sources include foods that are dried, smoked, and salted. Helicobacter pylori infection may contribute to carcinogenicity by creating gastritis, loss of acidity, and bacterial growth. Two important prognostic factors are depth of invasion through the gastric wall (less than T2 [tumor invades muscularis propria]) and the presence or absence of regional lymph node involvement.
In this case, liver metastases were found and the patient decided to not undergo chemotherapy. He died at home after 6 months of hospice care.
Figure courtesy of Michael Harper, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith, M. Gastric cancer. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:371-376.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
The biopsy revealed that the patient had an adenocarcinoma.
The median age at diagnosis is 70 years and median age at death from gastric cancer is 73 years. High rates of stomach cancer occur in Japan, China, Chile, and Ireland. Eighty-five percent of stomach cancers are adenocarcinomas; 15% are lymphomas and GI stromal tumors.
Most tumors are thought to arise from ingestion of nitrates that are converted by bacteria to carcinogens. Sources include foods that are dried, smoked, and salted. Helicobacter pylori infection may contribute to carcinogenicity by creating gastritis, loss of acidity, and bacterial growth. Two important prognostic factors are depth of invasion through the gastric wall (less than T2 [tumor invades muscularis propria]) and the presence or absence of regional lymph node involvement.
In this case, liver metastases were found and the patient decided to not undergo chemotherapy. He died at home after 6 months of hospice care.
Figure courtesy of Michael Harper, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith, M. Gastric cancer. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:371-376.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
The biopsy revealed that the patient had an adenocarcinoma.
The median age at diagnosis is 70 years and median age at death from gastric cancer is 73 years. High rates of stomach cancer occur in Japan, China, Chile, and Ireland. Eighty-five percent of stomach cancers are adenocarcinomas; 15% are lymphomas and GI stromal tumors.
Most tumors are thought to arise from ingestion of nitrates that are converted by bacteria to carcinogens. Sources include foods that are dried, smoked, and salted. Helicobacter pylori infection may contribute to carcinogenicity by creating gastritis, loss of acidity, and bacterial growth. Two important prognostic factors are depth of invasion through the gastric wall (less than T2 [tumor invades muscularis propria]) and the presence or absence of regional lymph node involvement.
In this case, liver metastases were found and the patient decided to not undergo chemotherapy. He died at home after 6 months of hospice care.
Figure courtesy of Michael Harper, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith, M. Gastric cancer. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:371-376.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
Persistent cough
The physician recognized this as a typical presentation of primary pulmonary tuberculosis (TB).
TB is a bacterial infection caused by M tuberculosis, an obligate intracellular pathogen that is aerobic, acid fast, and nonencapsulated. More than 8 million cases occur annually around the world, with nearly 2 million TB-related deaths. In 2010, the multiple-drug resistant TB rate in the United States was 1.2% (88 cases)—a rate that remains relatively stable. Based on the 2010 data, 60% of US cases of M tuberculosis occurred in foreign-born individuals.
Prophylactic treatment of those with latent TB (infection without active disease—diagnosed by tuberculin skin test conversion from negative to positive or by an interferon gamma release assay performed on blood) can reduce the risk of active TB by 90% or more.
TB is transmitted by aerosolized respiratory droplet nuclei. TB usually localizes to the middle and upper lung zones accompanied by hilar and paratracheal lymphadenopathy (as the tubercle bacilli spread from lung to lymphatic vessels). Early nonspecific signs and symptoms include fever, night sweats, fatigue, anorexia, weight loss. On exam, crackles or rhonchi will be present. Later, patients develop a nonproductive cough (lasting 2-3 weeks) or a cough with purulent sputum. Patients with extensive disease may develop dyspnea or acute respiratory distress syndrome.
Initial treatment centers on administering the following 4 medications together for 2 months: isoniazid (INH), rifampin, pyrazinamide, and ethambutol. This is followed by a 4-month continuation phase with INH and rifampin.
In this case, the patient was admitted to a private room with negative pressure; the patient’s sputum was sent for acid-fast bacillus (AFB) stain and cultures. The results showed acid-fast bacilli consistent with Mycobacterium spp. While culture results were pending, the patient was started on the 4 anti-tuberculosis drug regimen. Fortunately, the sputum culture result showed pan susceptible Mycobacterium tuberculosis, and his treatment continued with directly observed therapy through the local city health department.
Figure courtesy of Carlos Santiago Restrepo, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith, M. Tuberculosis. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:310-319.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
The physician recognized this as a typical presentation of primary pulmonary tuberculosis (TB).
TB is a bacterial infection caused by M tuberculosis, an obligate intracellular pathogen that is aerobic, acid fast, and nonencapsulated. More than 8 million cases occur annually around the world, with nearly 2 million TB-related deaths. In 2010, the multiple-drug resistant TB rate in the United States was 1.2% (88 cases)—a rate that remains relatively stable. Based on the 2010 data, 60% of US cases of M tuberculosis occurred in foreign-born individuals.
Prophylactic treatment of those with latent TB (infection without active disease—diagnosed by tuberculin skin test conversion from negative to positive or by an interferon gamma release assay performed on blood) can reduce the risk of active TB by 90% or more.
TB is transmitted by aerosolized respiratory droplet nuclei. TB usually localizes to the middle and upper lung zones accompanied by hilar and paratracheal lymphadenopathy (as the tubercle bacilli spread from lung to lymphatic vessels). Early nonspecific signs and symptoms include fever, night sweats, fatigue, anorexia, weight loss. On exam, crackles or rhonchi will be present. Later, patients develop a nonproductive cough (lasting 2-3 weeks) or a cough with purulent sputum. Patients with extensive disease may develop dyspnea or acute respiratory distress syndrome.
Initial treatment centers on administering the following 4 medications together for 2 months: isoniazid (INH), rifampin, pyrazinamide, and ethambutol. This is followed by a 4-month continuation phase with INH and rifampin.
In this case, the patient was admitted to a private room with negative pressure; the patient’s sputum was sent for acid-fast bacillus (AFB) stain and cultures. The results showed acid-fast bacilli consistent with Mycobacterium spp. While culture results were pending, the patient was started on the 4 anti-tuberculosis drug regimen. Fortunately, the sputum culture result showed pan susceptible Mycobacterium tuberculosis, and his treatment continued with directly observed therapy through the local city health department.
Figure courtesy of Carlos Santiago Restrepo, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith, M. Tuberculosis. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:310-319.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
The physician recognized this as a typical presentation of primary pulmonary tuberculosis (TB).
TB is a bacterial infection caused by M tuberculosis, an obligate intracellular pathogen that is aerobic, acid fast, and nonencapsulated. More than 8 million cases occur annually around the world, with nearly 2 million TB-related deaths. In 2010, the multiple-drug resistant TB rate in the United States was 1.2% (88 cases)—a rate that remains relatively stable. Based on the 2010 data, 60% of US cases of M tuberculosis occurred in foreign-born individuals.
Prophylactic treatment of those with latent TB (infection without active disease—diagnosed by tuberculin skin test conversion from negative to positive or by an interferon gamma release assay performed on blood) can reduce the risk of active TB by 90% or more.
TB is transmitted by aerosolized respiratory droplet nuclei. TB usually localizes to the middle and upper lung zones accompanied by hilar and paratracheal lymphadenopathy (as the tubercle bacilli spread from lung to lymphatic vessels). Early nonspecific signs and symptoms include fever, night sweats, fatigue, anorexia, weight loss. On exam, crackles or rhonchi will be present. Later, patients develop a nonproductive cough (lasting 2-3 weeks) or a cough with purulent sputum. Patients with extensive disease may develop dyspnea or acute respiratory distress syndrome.
Initial treatment centers on administering the following 4 medications together for 2 months: isoniazid (INH), rifampin, pyrazinamide, and ethambutol. This is followed by a 4-month continuation phase with INH and rifampin.
In this case, the patient was admitted to a private room with negative pressure; the patient’s sputum was sent for acid-fast bacillus (AFB) stain and cultures. The results showed acid-fast bacilli consistent with Mycobacterium spp. While culture results were pending, the patient was started on the 4 anti-tuberculosis drug regimen. Fortunately, the sputum culture result showed pan susceptible Mycobacterium tuberculosis, and his treatment continued with directly observed therapy through the local city health department.
Figure courtesy of Carlos Santiago Restrepo, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith, M. Tuberculosis. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:310-319.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
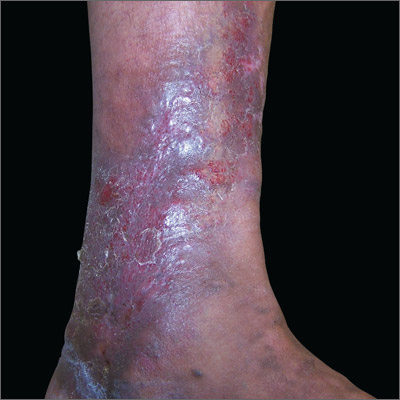
Rash on lower leg
The FP diagnosed lipodermatosclerosis, venous stasis dermatitis, and venous insufficiency in this patient. All of the skin changes were secondary to the venous insufficiency.
Venous insufficiency, or improperly functioning valves in the venous system, can lead to a variety of symptoms, including heaviness and/or swelling in the legs with prolonged standing, leg fatigue or aching, bleeding from leg varices, skin changes, and ulcerations.
Venous insufficiency occurs more frequently in women than in men. Varicose veins are notable only in half of patients with venous insufficiency. Venous insufficiency is typically a result of valvular dysfunction, which may be primary or secondary (the result of trauma or deep venous thrombosis). It may affect the deep system (eg, femoral vein), superficial system (eg, saphenous vein), or both. Dysfunction leads to a loss of compartmentalization of veins, which results in distention and increased pressure. Increased pressure in veins is transmitted to the microvasculature, leading to basement membrane thickening, increased capillary elongation, and visual skin changes.
In this case, the FP recommended graduated compression hose to treat the venous insufficiency. Compression hose treat symptoms—not underlying pathophysiology. The skin changes were treated with 0.1% triamcinolone ointment to improve the symptoms and decrease the dermatitis. (The pigmentary changes and atrophy are not reversible.)
The FP also discussed other treatment options, including endovenous ablation or stripping and ligation if the superficial system is involved. Endovenous therapy uses radiofrequency or laser energy to ablate the vein. Because the vein is usually accessed with a needle under ultrasound guidance, an incision is avoided.
Photo courtesy of Maureen Sheehan, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Sheehan M. Venous insufficiency. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine, 2nd ed. New York, NY: McGraw-Hill; 2013:295-298.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
The FP diagnosed lipodermatosclerosis, venous stasis dermatitis, and venous insufficiency in this patient. All of the skin changes were secondary to the venous insufficiency.
Venous insufficiency, or improperly functioning valves in the venous system, can lead to a variety of symptoms, including heaviness and/or swelling in the legs with prolonged standing, leg fatigue or aching, bleeding from leg varices, skin changes, and ulcerations.
Venous insufficiency occurs more frequently in women than in men. Varicose veins are notable only in half of patients with venous insufficiency. Venous insufficiency is typically a result of valvular dysfunction, which may be primary or secondary (the result of trauma or deep venous thrombosis). It may affect the deep system (eg, femoral vein), superficial system (eg, saphenous vein), or both. Dysfunction leads to a loss of compartmentalization of veins, which results in distention and increased pressure. Increased pressure in veins is transmitted to the microvasculature, leading to basement membrane thickening, increased capillary elongation, and visual skin changes.
In this case, the FP recommended graduated compression hose to treat the venous insufficiency. Compression hose treat symptoms—not underlying pathophysiology. The skin changes were treated with 0.1% triamcinolone ointment to improve the symptoms and decrease the dermatitis. (The pigmentary changes and atrophy are not reversible.)
The FP also discussed other treatment options, including endovenous ablation or stripping and ligation if the superficial system is involved. Endovenous therapy uses radiofrequency or laser energy to ablate the vein. Because the vein is usually accessed with a needle under ultrasound guidance, an incision is avoided.
Photo courtesy of Maureen Sheehan, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Sheehan M. Venous insufficiency. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine, 2nd ed. New York, NY: McGraw-Hill; 2013:295-298.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
The FP diagnosed lipodermatosclerosis, venous stasis dermatitis, and venous insufficiency in this patient. All of the skin changes were secondary to the venous insufficiency.
Venous insufficiency, or improperly functioning valves in the venous system, can lead to a variety of symptoms, including heaviness and/or swelling in the legs with prolonged standing, leg fatigue or aching, bleeding from leg varices, skin changes, and ulcerations.
Venous insufficiency occurs more frequently in women than in men. Varicose veins are notable only in half of patients with venous insufficiency. Venous insufficiency is typically a result of valvular dysfunction, which may be primary or secondary (the result of trauma or deep venous thrombosis). It may affect the deep system (eg, femoral vein), superficial system (eg, saphenous vein), or both. Dysfunction leads to a loss of compartmentalization of veins, which results in distention and increased pressure. Increased pressure in veins is transmitted to the microvasculature, leading to basement membrane thickening, increased capillary elongation, and visual skin changes.
In this case, the FP recommended graduated compression hose to treat the venous insufficiency. Compression hose treat symptoms—not underlying pathophysiology. The skin changes were treated with 0.1% triamcinolone ointment to improve the symptoms and decrease the dermatitis. (The pigmentary changes and atrophy are not reversible.)
The FP also discussed other treatment options, including endovenous ablation or stripping and ligation if the superficial system is involved. Endovenous therapy uses radiofrequency or laser energy to ablate the vein. Because the vein is usually accessed with a needle under ultrasound guidance, an incision is avoided.
Photo courtesy of Maureen Sheehan, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Sheehan M. Venous insufficiency. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine, 2nd ed. New York, NY: McGraw-Hill; 2013:295-298.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
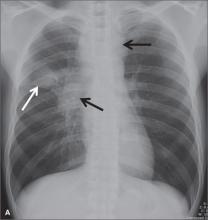
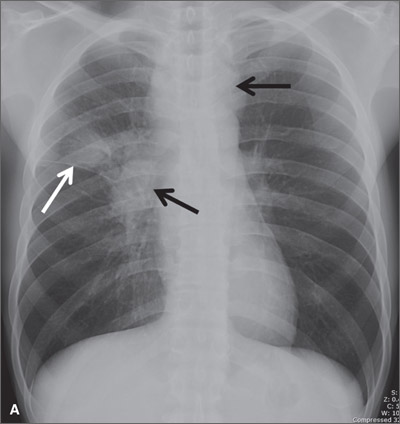
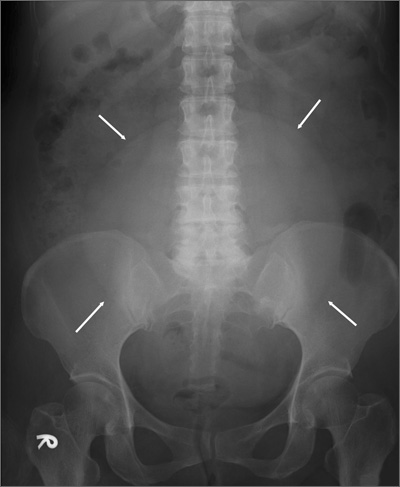
Teenager with shortness of breath and hypoxia
A 19-year-old male complaining of shortness of breath was transferred from our facility’s urgent care unit to our emergency department. He had a 2-week history of hemoptysis and vomiting, and over the previous week, he had developed mild hematemesis. His other symptoms included left thigh, flank, and upper quadrant pain; left chest pain exacerbated by exertion, light-headedness, and palpitations. He said that over the past 8 months, he’d been tired and lost some weight.
His blood pressure was 138/77 mm Hg, pulse was 142 beats per min, respiratory rate was 22 breaths per min, and oxygen saturation was 93% on room air. The physical exam revealed normal breath sounds and a diffusely tender abdomen. We ordered a chest X-ray (FIGURE).
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Metastatic testicular cancer
The chest x-ray showed multiple bilateral discrete nodules throughout all of the lung fields. These findings, along with the age of the patient, prompted the radiologist to suspect metastatic testicular cancer. An examination of the patient’s scrotum revealed an 11-cm mass encompassing the patient’s left testicle. When asked about the mass, the patient acknowledged that it had been there for about 8 months.
A rare cancer seen in younger men
Although relatively uncommon, testicular cancer accounts for 1% to 2% of all tumors in men.1 If caught it is highly treatable.
Testicular cancer is classified into germ cell tumors (which our patient had) and sex cord-stromal tumors. Germ cell tumors are the most common malignancy in men ages 15 to 44 years, and have a 95% cure rate when identified early and promptly treated.2,3 Sex cordstromal tumors are more common in pediatric patients and are more often benign.2
Diagnosis usually is made clinically and pathologically at resection. Left untreated, testicular cancer spreads via the lymphatic system to the retroperitoneal lymph nodes and through the bloodstream to the lungs (predominantly),4 as well as to bone, the liver, and the brain. Metastatic testicular cancer to the lungs, liver, and retroperitoneum occurs in advanced disease and has a poor prognosis.4,5
Differential diagnosis includes pneumonia, septic emboli
The differential diagnosis includes atypical pneumonia, septic emboli (ie, endocarditis or Lemierre’s syndrome), or sarcoidosis. Patients with atypical pneumonia often present with a cough, fever, and malaise. Patients with septic emboli will have an x-ray that looks similar to that of our patient. Their signs and symptoms will include malaise, shortness of breath, hypoxia, tachycardia, and tachypnea. Risk factors and physical exam findings might include a history of intravenous drug abuse (endocarditis) or deep tissue neck infection (Lemierre’s syndrome). Sarcoidosis can be a challenging diagnosis without further study.
Successful treatment hinges on early detection
Treatment for testicular cancer often is successful if the condition is localized.
The choice of treatment depends on tumor type and stage. Options include orchiectomy, retroperitoneal lymph node dissection, chemotherapy, and radiation.2-5 After being diagnosed with testicular cancer 95% of patients live for 5 or more years.6 For localized testicular cancer, the 5-year survival rate is 99%.6
An eye toward prevention. The US Preventive Services Task Force recommends against screening with clinical examination or testicular self examination7; however, some clinicians support regular screening and self examinations.
When silence is deadly
Although physicians expect that patients will disclose obvious physical manifestations of disease, we know that this is not always the case. Patients often have barriers to care, including their own reluctance to share certain types of information with a provider.
Our patient. After we diagnosed metastatic testicular cancer in our patient, he was transferred to the medical intensive care unit. His overall clinical status declined and he died 14 days later.
1. Manecksha RP, Fitzpatrick JM. Epidemiology of testicular cancer. BJU Int. 2009;104(9 pt B):1329-1333.
2. Schultz KA, Schneider DT, Pashankar F, et al. Management of ovarian and testicular sex cord-stromal tumors in children and adolescents. J Pediatr Hematol Oncol. 2012;34 suppl 2:S55-S63.
3. Sohaib SA, Koh DM, Husband JE. The role of imaging in the diagnosis, staging, and management of testicular cancer. AJR Am J Roentgenol. 2008;191:387-395.
4. Viatori M. Testicular cancer. Semin Oncol Nurs. 2012;28:180-189.
5. Mannuel H, Mitikiri N, Khan M, et al. Testicular germ cell tumors: biology and clinical update. Curr Opin Oncol. 2012;24:266-271.
6. SEER Stat Fact Sheets: Testis Cancer. National Cancer Institute Web site. Available at: http://seer.cancer.gov/statfacts/html/testis.html. Accessed May 20, 2014.
7. Screening for testicular cancer. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf10/testicular/testicuprs.htm. Accessed May 21, 2014.
A 19-year-old male complaining of shortness of breath was transferred from our facility’s urgent care unit to our emergency department. He had a 2-week history of hemoptysis and vomiting, and over the previous week, he had developed mild hematemesis. His other symptoms included left thigh, flank, and upper quadrant pain; left chest pain exacerbated by exertion, light-headedness, and palpitations. He said that over the past 8 months, he’d been tired and lost some weight.
His blood pressure was 138/77 mm Hg, pulse was 142 beats per min, respiratory rate was 22 breaths per min, and oxygen saturation was 93% on room air. The physical exam revealed normal breath sounds and a diffusely tender abdomen. We ordered a chest X-ray (FIGURE).
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Metastatic testicular cancer
The chest x-ray showed multiple bilateral discrete nodules throughout all of the lung fields. These findings, along with the age of the patient, prompted the radiologist to suspect metastatic testicular cancer. An examination of the patient’s scrotum revealed an 11-cm mass encompassing the patient’s left testicle. When asked about the mass, the patient acknowledged that it had been there for about 8 months.
A rare cancer seen in younger men
Although relatively uncommon, testicular cancer accounts for 1% to 2% of all tumors in men.1 If caught it is highly treatable.
Testicular cancer is classified into germ cell tumors (which our patient had) and sex cord-stromal tumors. Germ cell tumors are the most common malignancy in men ages 15 to 44 years, and have a 95% cure rate when identified early and promptly treated.2,3 Sex cordstromal tumors are more common in pediatric patients and are more often benign.2
Diagnosis usually is made clinically and pathologically at resection. Left untreated, testicular cancer spreads via the lymphatic system to the retroperitoneal lymph nodes and through the bloodstream to the lungs (predominantly),4 as well as to bone, the liver, and the brain. Metastatic testicular cancer to the lungs, liver, and retroperitoneum occurs in advanced disease and has a poor prognosis.4,5
Differential diagnosis includes pneumonia, septic emboli
The differential diagnosis includes atypical pneumonia, septic emboli (ie, endocarditis or Lemierre’s syndrome), or sarcoidosis. Patients with atypical pneumonia often present with a cough, fever, and malaise. Patients with septic emboli will have an x-ray that looks similar to that of our patient. Their signs and symptoms will include malaise, shortness of breath, hypoxia, tachycardia, and tachypnea. Risk factors and physical exam findings might include a history of intravenous drug abuse (endocarditis) or deep tissue neck infection (Lemierre’s syndrome). Sarcoidosis can be a challenging diagnosis without further study.
Successful treatment hinges on early detection
Treatment for testicular cancer often is successful if the condition is localized.
The choice of treatment depends on tumor type and stage. Options include orchiectomy, retroperitoneal lymph node dissection, chemotherapy, and radiation.2-5 After being diagnosed with testicular cancer 95% of patients live for 5 or more years.6 For localized testicular cancer, the 5-year survival rate is 99%.6
An eye toward prevention. The US Preventive Services Task Force recommends against screening with clinical examination or testicular self examination7; however, some clinicians support regular screening and self examinations.
When silence is deadly
Although physicians expect that patients will disclose obvious physical manifestations of disease, we know that this is not always the case. Patients often have barriers to care, including their own reluctance to share certain types of information with a provider.
Our patient. After we diagnosed metastatic testicular cancer in our patient, he was transferred to the medical intensive care unit. His overall clinical status declined and he died 14 days later.
A 19-year-old male complaining of shortness of breath was transferred from our facility’s urgent care unit to our emergency department. He had a 2-week history of hemoptysis and vomiting, and over the previous week, he had developed mild hematemesis. His other symptoms included left thigh, flank, and upper quadrant pain; left chest pain exacerbated by exertion, light-headedness, and palpitations. He said that over the past 8 months, he’d been tired and lost some weight.
His blood pressure was 138/77 mm Hg, pulse was 142 beats per min, respiratory rate was 22 breaths per min, and oxygen saturation was 93% on room air. The physical exam revealed normal breath sounds and a diffusely tender abdomen. We ordered a chest X-ray (FIGURE).
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Metastatic testicular cancer
The chest x-ray showed multiple bilateral discrete nodules throughout all of the lung fields. These findings, along with the age of the patient, prompted the radiologist to suspect metastatic testicular cancer. An examination of the patient’s scrotum revealed an 11-cm mass encompassing the patient’s left testicle. When asked about the mass, the patient acknowledged that it had been there for about 8 months.
A rare cancer seen in younger men
Although relatively uncommon, testicular cancer accounts for 1% to 2% of all tumors in men.1 If caught it is highly treatable.
Testicular cancer is classified into germ cell tumors (which our patient had) and sex cord-stromal tumors. Germ cell tumors are the most common malignancy in men ages 15 to 44 years, and have a 95% cure rate when identified early and promptly treated.2,3 Sex cordstromal tumors are more common in pediatric patients and are more often benign.2
Diagnosis usually is made clinically and pathologically at resection. Left untreated, testicular cancer spreads via the lymphatic system to the retroperitoneal lymph nodes and through the bloodstream to the lungs (predominantly),4 as well as to bone, the liver, and the brain. Metastatic testicular cancer to the lungs, liver, and retroperitoneum occurs in advanced disease and has a poor prognosis.4,5
Differential diagnosis includes pneumonia, septic emboli
The differential diagnosis includes atypical pneumonia, septic emboli (ie, endocarditis or Lemierre’s syndrome), or sarcoidosis. Patients with atypical pneumonia often present with a cough, fever, and malaise. Patients with septic emboli will have an x-ray that looks similar to that of our patient. Their signs and symptoms will include malaise, shortness of breath, hypoxia, tachycardia, and tachypnea. Risk factors and physical exam findings might include a history of intravenous drug abuse (endocarditis) or deep tissue neck infection (Lemierre’s syndrome). Sarcoidosis can be a challenging diagnosis without further study.
Successful treatment hinges on early detection
Treatment for testicular cancer often is successful if the condition is localized.
The choice of treatment depends on tumor type and stage. Options include orchiectomy, retroperitoneal lymph node dissection, chemotherapy, and radiation.2-5 After being diagnosed with testicular cancer 95% of patients live for 5 or more years.6 For localized testicular cancer, the 5-year survival rate is 99%.6
An eye toward prevention. The US Preventive Services Task Force recommends against screening with clinical examination or testicular self examination7; however, some clinicians support regular screening and self examinations.
When silence is deadly
Although physicians expect that patients will disclose obvious physical manifestations of disease, we know that this is not always the case. Patients often have barriers to care, including their own reluctance to share certain types of information with a provider.
Our patient. After we diagnosed metastatic testicular cancer in our patient, he was transferred to the medical intensive care unit. His overall clinical status declined and he died 14 days later.
1. Manecksha RP, Fitzpatrick JM. Epidemiology of testicular cancer. BJU Int. 2009;104(9 pt B):1329-1333.
2. Schultz KA, Schneider DT, Pashankar F, et al. Management of ovarian and testicular sex cord-stromal tumors in children and adolescents. J Pediatr Hematol Oncol. 2012;34 suppl 2:S55-S63.
3. Sohaib SA, Koh DM, Husband JE. The role of imaging in the diagnosis, staging, and management of testicular cancer. AJR Am J Roentgenol. 2008;191:387-395.
4. Viatori M. Testicular cancer. Semin Oncol Nurs. 2012;28:180-189.
5. Mannuel H, Mitikiri N, Khan M, et al. Testicular germ cell tumors: biology and clinical update. Curr Opin Oncol. 2012;24:266-271.
6. SEER Stat Fact Sheets: Testis Cancer. National Cancer Institute Web site. Available at: http://seer.cancer.gov/statfacts/html/testis.html. Accessed May 20, 2014.
7. Screening for testicular cancer. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf10/testicular/testicuprs.htm. Accessed May 21, 2014.
1. Manecksha RP, Fitzpatrick JM. Epidemiology of testicular cancer. BJU Int. 2009;104(9 pt B):1329-1333.
2. Schultz KA, Schneider DT, Pashankar F, et al. Management of ovarian and testicular sex cord-stromal tumors in children and adolescents. J Pediatr Hematol Oncol. 2012;34 suppl 2:S55-S63.
3. Sohaib SA, Koh DM, Husband JE. The role of imaging in the diagnosis, staging, and management of testicular cancer. AJR Am J Roentgenol. 2008;191:387-395.
4. Viatori M. Testicular cancer. Semin Oncol Nurs. 2012;28:180-189.
5. Mannuel H, Mitikiri N, Khan M, et al. Testicular germ cell tumors: biology and clinical update. Curr Opin Oncol. 2012;24:266-271.
6. SEER Stat Fact Sheets: Testis Cancer. National Cancer Institute Web site. Available at: http://seer.cancer.gov/statfacts/html/testis.html. Accessed May 20, 2014.
7. Screening for testicular cancer. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf10/testicular/testicuprs.htm. Accessed May 21, 2014.
Large pelvic mass
This patient had a large uterine fibroid. Also known as a leiomyoma, a uterine fibroid is a benign tumor that is composed of smooth muscle tissue and fibrous connective tissue. It is the most common pelvic tumor found in the female body. Unlike cancerous tumors, fibroids usually grow slowly and do not break away or invade other parts of the body.
Based on its position within the uterus, a fibroid can be submucosal, intramural, or subserosal. Uterine fibroids are usually diagnosed based on a clinical history and pelvic examination; the presence of a fibroid is confirmed by ultrasound, magnetic resonance imaging, computed tomography, saline infusion sonography, or hysterosalpingography.
Small fibroids that are asymptomatic or cause only minor problems are not usually treated. However, if a fibroid is large or results in pain or excessive bleeding, further management may be needed. Management of fibroids may be surgical or nonsurgical (hormones). Factors that affect management choices include the patient’s desire to become pregnant or preserve her uterus, symptom severity, and tumor characteristics.
This patient’s physicians originally suspected malignancy, so they consulted a gynecologist for a sonographic examination. The ultrasound revealed a heterogeneous mass with calcification. The patient underwent a hysterectomy.
The solitary soft tissue mass that was removed measured 13 cm in diameter and weighted 2100 g. Histopathological analysis revealed that the fibroid was made up of myometrium and fibrous connective tissue. After hospital discharge, the patient resumed all of her normal activities with no recurrence.
Adapted from: Chang CF, Ke CY, Lin JG. Photo Rounds: large pelvic mass in a 46-year-old woman. J Fam Pract. 2013;62:581-584.
This patient had a large uterine fibroid. Also known as a leiomyoma, a uterine fibroid is a benign tumor that is composed of smooth muscle tissue and fibrous connective tissue. It is the most common pelvic tumor found in the female body. Unlike cancerous tumors, fibroids usually grow slowly and do not break away or invade other parts of the body.
Based on its position within the uterus, a fibroid can be submucosal, intramural, or subserosal. Uterine fibroids are usually diagnosed based on a clinical history and pelvic examination; the presence of a fibroid is confirmed by ultrasound, magnetic resonance imaging, computed tomography, saline infusion sonography, or hysterosalpingography.
Small fibroids that are asymptomatic or cause only minor problems are not usually treated. However, if a fibroid is large or results in pain or excessive bleeding, further management may be needed. Management of fibroids may be surgical or nonsurgical (hormones). Factors that affect management choices include the patient’s desire to become pregnant or preserve her uterus, symptom severity, and tumor characteristics.
This patient’s physicians originally suspected malignancy, so they consulted a gynecologist for a sonographic examination. The ultrasound revealed a heterogeneous mass with calcification. The patient underwent a hysterectomy.
The solitary soft tissue mass that was removed measured 13 cm in diameter and weighted 2100 g. Histopathological analysis revealed that the fibroid was made up of myometrium and fibrous connective tissue. After hospital discharge, the patient resumed all of her normal activities with no recurrence.
Adapted from: Chang CF, Ke CY, Lin JG. Photo Rounds: large pelvic mass in a 46-year-old woman. J Fam Pract. 2013;62:581-584.
This patient had a large uterine fibroid. Also known as a leiomyoma, a uterine fibroid is a benign tumor that is composed of smooth muscle tissue and fibrous connective tissue. It is the most common pelvic tumor found in the female body. Unlike cancerous tumors, fibroids usually grow slowly and do not break away or invade other parts of the body.
Based on its position within the uterus, a fibroid can be submucosal, intramural, or subserosal. Uterine fibroids are usually diagnosed based on a clinical history and pelvic examination; the presence of a fibroid is confirmed by ultrasound, magnetic resonance imaging, computed tomography, saline infusion sonography, or hysterosalpingography.
Small fibroids that are asymptomatic or cause only minor problems are not usually treated. However, if a fibroid is large or results in pain or excessive bleeding, further management may be needed. Management of fibroids may be surgical or nonsurgical (hormones). Factors that affect management choices include the patient’s desire to become pregnant or preserve her uterus, symptom severity, and tumor characteristics.
This patient’s physicians originally suspected malignancy, so they consulted a gynecologist for a sonographic examination. The ultrasound revealed a heterogeneous mass with calcification. The patient underwent a hysterectomy.
The solitary soft tissue mass that was removed measured 13 cm in diameter and weighted 2100 g. Histopathological analysis revealed that the fibroid was made up of myometrium and fibrous connective tissue. After hospital discharge, the patient resumed all of her normal activities with no recurrence.
Adapted from: Chang CF, Ke CY, Lin JG. Photo Rounds: large pelvic mass in a 46-year-old woman. J Fam Pract. 2013;62:581-584.
White patch on tongue
This patient was given a diagnosis of leukoplakia and the biopsy indicated that the lesion was premalignant.
The World Health Organization defines leukoplakia as “white plaques of questionable risk” in cases where other known diseases that don’t carry an increased risk for cancer have been excluded. For all types of leukoplakia, the risk of malignant transformation is approximately 1%, with a much higher risk associated with leukoplakias that contain red spots and/or rough spots.
Smoking and alcohol exposure are major risk factors for leukoplakia and create a synergistic effect when combined. Human papillomavirus (HPV) is a recognized risk factor for oropharyngeal cancer, but its association with leukoplakia is undetermined.
All leukoplakias should be excised and biopsied to determine the presence of epithelia dysplasia, carcinoma in situ, or squamous cell carcinoma. In this case, the patient was told that he needed to stop smoking and drinking. He was also referred to an oral surgeon for further evaluation of the dysplasia.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Huber M, Gonsalves W. Leukoplakia. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:249-252.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
This patient was given a diagnosis of leukoplakia and the biopsy indicated that the lesion was premalignant.
The World Health Organization defines leukoplakia as “white plaques of questionable risk” in cases where other known diseases that don’t carry an increased risk for cancer have been excluded. For all types of leukoplakia, the risk of malignant transformation is approximately 1%, with a much higher risk associated with leukoplakias that contain red spots and/or rough spots.
Smoking and alcohol exposure are major risk factors for leukoplakia and create a synergistic effect when combined. Human papillomavirus (HPV) is a recognized risk factor for oropharyngeal cancer, but its association with leukoplakia is undetermined.
All leukoplakias should be excised and biopsied to determine the presence of epithelia dysplasia, carcinoma in situ, or squamous cell carcinoma. In this case, the patient was told that he needed to stop smoking and drinking. He was also referred to an oral surgeon for further evaluation of the dysplasia.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Huber M, Gonsalves W. Leukoplakia. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:249-252.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
This patient was given a diagnosis of leukoplakia and the biopsy indicated that the lesion was premalignant.
The World Health Organization defines leukoplakia as “white plaques of questionable risk” in cases where other known diseases that don’t carry an increased risk for cancer have been excluded. For all types of leukoplakia, the risk of malignant transformation is approximately 1%, with a much higher risk associated with leukoplakias that contain red spots and/or rough spots.
Smoking and alcohol exposure are major risk factors for leukoplakia and create a synergistic effect when combined. Human papillomavirus (HPV) is a recognized risk factor for oropharyngeal cancer, but its association with leukoplakia is undetermined.
All leukoplakias should be excised and biopsied to determine the presence of epithelia dysplasia, carcinoma in situ, or squamous cell carcinoma. In this case, the patient was told that he needed to stop smoking and drinking. He was also referred to an oral surgeon for further evaluation of the dysplasia.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Huber M, Gonsalves W. Leukoplakia. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:249-252.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
Lesion on side of tongue
A punch biopsy revealed that the patient had a squamous cell carcinoma (SCC).
Fully two-thirds of oropharyngeal cancers (OPCs) will present with advanced disease at the time of diagnosis. Ninety percent of OPCs are of the squamous cell type. Reports in the literature suggest that clinicians may be missing early disease by not conducting thorough soft-tissue examinations on a routine basis. However, the fact that more than 35% of patients do not see a dentist on a routine basis likely contributes to the diagnostic delay. The 5-year survival rate for OPC is 62% for whites and 42% for blacks.
Tobacco use is the major risk factor for OPC and is implicated in approximately 75% of cases. Alcohol use is also a major risk factor. The combined use of tobacco and alcohol increases the risk of OPC far more than either alone. Human papillomavirus (especially HPV 16) is a newly recognized major risk factor for carcinomas affecting the lingual and palatine tonsils.
The principal therapeutic modalities for OPC are surgery, radiotherapy, and chemotherapy. This patient was referred to a head and neck surgeon.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Huber M, Gonsalves W. Oropharyngeal cancer. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:253-256.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
A punch biopsy revealed that the patient had a squamous cell carcinoma (SCC).
Fully two-thirds of oropharyngeal cancers (OPCs) will present with advanced disease at the time of diagnosis. Ninety percent of OPCs are of the squamous cell type. Reports in the literature suggest that clinicians may be missing early disease by not conducting thorough soft-tissue examinations on a routine basis. However, the fact that more than 35% of patients do not see a dentist on a routine basis likely contributes to the diagnostic delay. The 5-year survival rate for OPC is 62% for whites and 42% for blacks.
Tobacco use is the major risk factor for OPC and is implicated in approximately 75% of cases. Alcohol use is also a major risk factor. The combined use of tobacco and alcohol increases the risk of OPC far more than either alone. Human papillomavirus (especially HPV 16) is a newly recognized major risk factor for carcinomas affecting the lingual and palatine tonsils.
The principal therapeutic modalities for OPC are surgery, radiotherapy, and chemotherapy. This patient was referred to a head and neck surgeon.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Huber M, Gonsalves W. Oropharyngeal cancer. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:253-256.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
A punch biopsy revealed that the patient had a squamous cell carcinoma (SCC).
Fully two-thirds of oropharyngeal cancers (OPCs) will present with advanced disease at the time of diagnosis. Ninety percent of OPCs are of the squamous cell type. Reports in the literature suggest that clinicians may be missing early disease by not conducting thorough soft-tissue examinations on a routine basis. However, the fact that more than 35% of patients do not see a dentist on a routine basis likely contributes to the diagnostic delay. The 5-year survival rate for OPC is 62% for whites and 42% for blacks.
Tobacco use is the major risk factor for OPC and is implicated in approximately 75% of cases. Alcohol use is also a major risk factor. The combined use of tobacco and alcohol increases the risk of OPC far more than either alone. Human papillomavirus (especially HPV 16) is a newly recognized major risk factor for carcinomas affecting the lingual and palatine tonsils.
The principal therapeutic modalities for OPC are surgery, radiotherapy, and chemotherapy. This patient was referred to a head and neck surgeon.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Huber M, Gonsalves W. Oropharyngeal cancer. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:253-256.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
Lesions on tongue
The family physician recognized his condition as recurrent aphthous ulcers (RAS) with giant ulcers.
Aphthous ulcers are painful ulcerations in the mouth, which can be single, multiple, occasional, or recurrent. These ulcers can be small or large but are uniformly painful and may interfere with eating, speaking, and swallowing. While the precise etiology of RAS is unclear, the following are risk factors:
- oral trauma
- stress and anxiety
- systemic diseases (eg, Celiac disease, Crohn’s disease, Behçet’s syndrome, human immunodeficiency virus, reactive arthritis)
- medications (nonsteroidal anti-inflammatory drugs, beta-blockers, angiotensin-converting enzyme inhibitors)
- vitamin deficiencies (eg, zinc, iron, B12, folate)
- food and chemical sensitivities.
Topical corticosteroids, such as fluocinonide gel or dexamethasone elixir, can promote healing and lessen the severity of RAS. Patients should be instructed to dab the area of the ulcer dry, apply the gel, paste, or cream after rinsing, and avoid eating or drinking for at least 30 minutes.
Amlexanox 5% paste (Aphthasol) reduces ulcer size, pain duration, and healing time. It is a nonprescription paste that is applied directly to ulcers 4 times a day until the ulcers heal. Lidocaine 1% cream applied to aphthous ulcers was found to reduce pain intensity compared to a placebo cream. In severe RAS cases, systemic therapy with oral steroids, montelukast, colchicine, or pentoxifylline should be considered.
In this case, no underlying systemic disease was found. The patient was started on oral prednisone on the first visit and given dexamethasone oral elixir to swish and swallow. Within one week, the patient was able to eat and drink liquids comfortably and began regaining his lost weight. Long-term management of his problem will likely require use of montelukast, colchicine, or pentoxifylline to taper him off prednisone without recurrences.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Usatine R, Gonsalves W. Aphthous ulcer. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:244-248.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
The family physician recognized his condition as recurrent aphthous ulcers (RAS) with giant ulcers.
Aphthous ulcers are painful ulcerations in the mouth, which can be single, multiple, occasional, or recurrent. These ulcers can be small or large but are uniformly painful and may interfere with eating, speaking, and swallowing. While the precise etiology of RAS is unclear, the following are risk factors:
- oral trauma
- stress and anxiety
- systemic diseases (eg, Celiac disease, Crohn’s disease, Behçet’s syndrome, human immunodeficiency virus, reactive arthritis)
- medications (nonsteroidal anti-inflammatory drugs, beta-blockers, angiotensin-converting enzyme inhibitors)
- vitamin deficiencies (eg, zinc, iron, B12, folate)
- food and chemical sensitivities.
Topical corticosteroids, such as fluocinonide gel or dexamethasone elixir, can promote healing and lessen the severity of RAS. Patients should be instructed to dab the area of the ulcer dry, apply the gel, paste, or cream after rinsing, and avoid eating or drinking for at least 30 minutes.
Amlexanox 5% paste (Aphthasol) reduces ulcer size, pain duration, and healing time. It is a nonprescription paste that is applied directly to ulcers 4 times a day until the ulcers heal. Lidocaine 1% cream applied to aphthous ulcers was found to reduce pain intensity compared to a placebo cream. In severe RAS cases, systemic therapy with oral steroids, montelukast, colchicine, or pentoxifylline should be considered.
In this case, no underlying systemic disease was found. The patient was started on oral prednisone on the first visit and given dexamethasone oral elixir to swish and swallow. Within one week, the patient was able to eat and drink liquids comfortably and began regaining his lost weight. Long-term management of his problem will likely require use of montelukast, colchicine, or pentoxifylline to taper him off prednisone without recurrences.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Usatine R, Gonsalves W. Aphthous ulcer. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:244-248.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
The family physician recognized his condition as recurrent aphthous ulcers (RAS) with giant ulcers.
Aphthous ulcers are painful ulcerations in the mouth, which can be single, multiple, occasional, or recurrent. These ulcers can be small or large but are uniformly painful and may interfere with eating, speaking, and swallowing. While the precise etiology of RAS is unclear, the following are risk factors:
- oral trauma
- stress and anxiety
- systemic diseases (eg, Celiac disease, Crohn’s disease, Behçet’s syndrome, human immunodeficiency virus, reactive arthritis)
- medications (nonsteroidal anti-inflammatory drugs, beta-blockers, angiotensin-converting enzyme inhibitors)
- vitamin deficiencies (eg, zinc, iron, B12, folate)
- food and chemical sensitivities.
Topical corticosteroids, such as fluocinonide gel or dexamethasone elixir, can promote healing and lessen the severity of RAS. Patients should be instructed to dab the area of the ulcer dry, apply the gel, paste, or cream after rinsing, and avoid eating or drinking for at least 30 minutes.
Amlexanox 5% paste (Aphthasol) reduces ulcer size, pain duration, and healing time. It is a nonprescription paste that is applied directly to ulcers 4 times a day until the ulcers heal. Lidocaine 1% cream applied to aphthous ulcers was found to reduce pain intensity compared to a placebo cream. In severe RAS cases, systemic therapy with oral steroids, montelukast, colchicine, or pentoxifylline should be considered.
In this case, no underlying systemic disease was found. The patient was started on oral prednisone on the first visit and given dexamethasone oral elixir to swish and swallow. Within one week, the patient was able to eat and drink liquids comfortably and began regaining his lost weight. Long-term management of his problem will likely require use of montelukast, colchicine, or pentoxifylline to taper him off prednisone without recurrences.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Usatine R, Gonsalves W. Aphthous ulcer. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:244-248.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/