User login
In Memoriam
Dr. Christopher D. Spradley, FCCP, died July 17, 2015. Dr. Spradley was a member of the Critical Care NetWork and also served as a moderator for the CHEST e-Community. He served as the director of the Medical Intensive Care Unit at Scott & White Hospital in Temple, Texas, and was also director of the hospital’s Pulmonary Hypertension Center. Dr. Spradley attended Texas A&M University System Health Science Center College of Medicine to earn his Doctor of Medicine, and after a residency in internal medicine at Scott & White Hospital, he became a fellow in Pulmonary, Critical Care, and Sleep Medicine at Scott & White. He specialized in critical care medicine, PAH, diseases of the chest, sleep disorders, and palliative care. Our condolences go out to the Spradley family and friends.
Dr. Christopher D. Spradley, FCCP, died July 17, 2015. Dr. Spradley was a member of the Critical Care NetWork and also served as a moderator for the CHEST e-Community. He served as the director of the Medical Intensive Care Unit at Scott & White Hospital in Temple, Texas, and was also director of the hospital’s Pulmonary Hypertension Center. Dr. Spradley attended Texas A&M University System Health Science Center College of Medicine to earn his Doctor of Medicine, and after a residency in internal medicine at Scott & White Hospital, he became a fellow in Pulmonary, Critical Care, and Sleep Medicine at Scott & White. He specialized in critical care medicine, PAH, diseases of the chest, sleep disorders, and palliative care. Our condolences go out to the Spradley family and friends.
Dr. Christopher D. Spradley, FCCP, died July 17, 2015. Dr. Spradley was a member of the Critical Care NetWork and also served as a moderator for the CHEST e-Community. He served as the director of the Medical Intensive Care Unit at Scott & White Hospital in Temple, Texas, and was also director of the hospital’s Pulmonary Hypertension Center. Dr. Spradley attended Texas A&M University System Health Science Center College of Medicine to earn his Doctor of Medicine, and after a residency in internal medicine at Scott & White Hospital, he became a fellow in Pulmonary, Critical Care, and Sleep Medicine at Scott & White. He specialized in critical care medicine, PAH, diseases of the chest, sleep disorders, and palliative care. Our condolences go out to the Spradley family and friends.
CHEST Fellow Receives ASTRO Honor
The American Society for Radiation Oncology (ASTRO) has selected leading surgeon and researcher Jack A. Roth, MD, FCCP, as the 2015 Honorary Member, the highest honor ASTRO bestows on distinguished cancer researchers, scientists, and leaders in disciplines other than radiation oncology, radiobiology, or radiation physics. Dr. Roth will be inducted as the 2015 ASTRO Honorary Member during the Awards Ceremony in October, at ASTRO’s 57th Annual Meeting, in San Antonio.
Dr. Roth is professor, Department of Thoracic and Cardiovascular Surgery, Division of Surgery, MD Anderson Cancer Center, Houston, and chief, Section of Thoracic Molecular Oncology, Department of Thoracic and Cardiovascular Surgery, Division of Surgery, MD Anderson Cancer Center, Houston.
He cited his and colleagues’ study “Stereotactic ablative radiotherapy versus lobectomy for operable stage I non-small-cell lung cancer: a pooled analysis of two randomized trials,” published in Lancet Oncology in May 2015, as his most recent career highlight. Dr. Roth was an early innovator in the development of gene therapy for cancer, and led the first tumor suppressor gene therapy clinical trials approved by the National Institutes of Health Recombinant DNA Advisory Committee and the U.S. Food and Drug Administration. His work was the first gene therapy in cancer approved for human use.
The American Society for Radiation Oncology (ASTRO) has selected leading surgeon and researcher Jack A. Roth, MD, FCCP, as the 2015 Honorary Member, the highest honor ASTRO bestows on distinguished cancer researchers, scientists, and leaders in disciplines other than radiation oncology, radiobiology, or radiation physics. Dr. Roth will be inducted as the 2015 ASTRO Honorary Member during the Awards Ceremony in October, at ASTRO’s 57th Annual Meeting, in San Antonio.
Dr. Roth is professor, Department of Thoracic and Cardiovascular Surgery, Division of Surgery, MD Anderson Cancer Center, Houston, and chief, Section of Thoracic Molecular Oncology, Department of Thoracic and Cardiovascular Surgery, Division of Surgery, MD Anderson Cancer Center, Houston.
He cited his and colleagues’ study “Stereotactic ablative radiotherapy versus lobectomy for operable stage I non-small-cell lung cancer: a pooled analysis of two randomized trials,” published in Lancet Oncology in May 2015, as his most recent career highlight. Dr. Roth was an early innovator in the development of gene therapy for cancer, and led the first tumor suppressor gene therapy clinical trials approved by the National Institutes of Health Recombinant DNA Advisory Committee and the U.S. Food and Drug Administration. His work was the first gene therapy in cancer approved for human use.
The American Society for Radiation Oncology (ASTRO) has selected leading surgeon and researcher Jack A. Roth, MD, FCCP, as the 2015 Honorary Member, the highest honor ASTRO bestows on distinguished cancer researchers, scientists, and leaders in disciplines other than radiation oncology, radiobiology, or radiation physics. Dr. Roth will be inducted as the 2015 ASTRO Honorary Member during the Awards Ceremony in October, at ASTRO’s 57th Annual Meeting, in San Antonio.
Dr. Roth is professor, Department of Thoracic and Cardiovascular Surgery, Division of Surgery, MD Anderson Cancer Center, Houston, and chief, Section of Thoracic Molecular Oncology, Department of Thoracic and Cardiovascular Surgery, Division of Surgery, MD Anderson Cancer Center, Houston.
He cited his and colleagues’ study “Stereotactic ablative radiotherapy versus lobectomy for operable stage I non-small-cell lung cancer: a pooled analysis of two randomized trials,” published in Lancet Oncology in May 2015, as his most recent career highlight. Dr. Roth was an early innovator in the development of gene therapy for cancer, and led the first tumor suppressor gene therapy clinical trials approved by the National Institutes of Health Recombinant DNA Advisory Committee and the U.S. Food and Drug Administration. His work was the first gene therapy in cancer approved for human use.
From the EVP/CEO: Cultivating future leaders
At CHEST, cultivating future leaders in chest medicine is of paramount importance to us. Our members who desire to become leaders are prepared to advance our goals and initiatives, as well as become leaders within their own communities and institutions. That’s why we work to inspire, train, mentor, and galvanize new leaders.
When looking for leaders, volunteers, and faculty for CHEST, we most often draw from our own CHEST community—identifying members interested in engaging with us to help build the future of our organization and advance chest medicine. Knowing each person’s path to leadership is different, we have undertaken a new initiative, CHEST Academies, to help identify and provide essential training and development for future leaders.
Over the past several years, the Leadership Development Task Force supported these efforts by launching a mentorship program, an annual leadership development course, and a standard approach to preparing leaders and volunteers for their role in the organization. Our new Academies Work Group, following on the successes of the Leadership Development Task Force, will carry this work forward and further develop training opportunities in education, faculty training, guideline development, and leadership. The work group initially will focus on two distinct tracks: faculty development and leadership development.
The work group has made fast progress, and I’m happy to share that CHEST Annual Meeting 2015 will mark the launch of our first course tracks being offered as part of the new CHEST Academies. These tracks are direct pathways to the latest training for leaders in health care and for faculty in chest medicine. Core competencies to be included in the tracks include:
• Leadership—personal characteristics, communication, teamwork, finance, and strategic planning
• Faculty—educational goals and objectives, gap analysis and needs assessment, point of care and large group teaching, and instructional methods
I want to personally thank our current and past CHEST leadership for their contributions toward our success, the Academies Work Group for moving this opportunity forward, and those pioneers who will participate in our first CHEST Academies offerings at CHEST 2015.
This is only the beginning. Because we value our leaders and want to help them to succeed personally and professionally, we’re committed to continuing to develop and offer year-round opportunities for leadership and faculty development. Members also can access additional resources for leadership development in the Get Involved section on chestnet.org.
I welcome your input on how we can continue to advance professional development within our CHEST community. As always, feel free to connect with me to share your ideas. I invite you to follow me on Twitter, @PMarkowskiACCP, or look for me at CHEST 2015, October 24-28, in Montréal.
At CHEST, cultivating future leaders in chest medicine is of paramount importance to us. Our members who desire to become leaders are prepared to advance our goals and initiatives, as well as become leaders within their own communities and institutions. That’s why we work to inspire, train, mentor, and galvanize new leaders.
When looking for leaders, volunteers, and faculty for CHEST, we most often draw from our own CHEST community—identifying members interested in engaging with us to help build the future of our organization and advance chest medicine. Knowing each person’s path to leadership is different, we have undertaken a new initiative, CHEST Academies, to help identify and provide essential training and development for future leaders.
Over the past several years, the Leadership Development Task Force supported these efforts by launching a mentorship program, an annual leadership development course, and a standard approach to preparing leaders and volunteers for their role in the organization. Our new Academies Work Group, following on the successes of the Leadership Development Task Force, will carry this work forward and further develop training opportunities in education, faculty training, guideline development, and leadership. The work group initially will focus on two distinct tracks: faculty development and leadership development.
The work group has made fast progress, and I’m happy to share that CHEST Annual Meeting 2015 will mark the launch of our first course tracks being offered as part of the new CHEST Academies. These tracks are direct pathways to the latest training for leaders in health care and for faculty in chest medicine. Core competencies to be included in the tracks include:
• Leadership—personal characteristics, communication, teamwork, finance, and strategic planning
• Faculty—educational goals and objectives, gap analysis and needs assessment, point of care and large group teaching, and instructional methods
I want to personally thank our current and past CHEST leadership for their contributions toward our success, the Academies Work Group for moving this opportunity forward, and those pioneers who will participate in our first CHEST Academies offerings at CHEST 2015.
This is only the beginning. Because we value our leaders and want to help them to succeed personally and professionally, we’re committed to continuing to develop and offer year-round opportunities for leadership and faculty development. Members also can access additional resources for leadership development in the Get Involved section on chestnet.org.
I welcome your input on how we can continue to advance professional development within our CHEST community. As always, feel free to connect with me to share your ideas. I invite you to follow me on Twitter, @PMarkowskiACCP, or look for me at CHEST 2015, October 24-28, in Montréal.
At CHEST, cultivating future leaders in chest medicine is of paramount importance to us. Our members who desire to become leaders are prepared to advance our goals and initiatives, as well as become leaders within their own communities and institutions. That’s why we work to inspire, train, mentor, and galvanize new leaders.
When looking for leaders, volunteers, and faculty for CHEST, we most often draw from our own CHEST community—identifying members interested in engaging with us to help build the future of our organization and advance chest medicine. Knowing each person’s path to leadership is different, we have undertaken a new initiative, CHEST Academies, to help identify and provide essential training and development for future leaders.
Over the past several years, the Leadership Development Task Force supported these efforts by launching a mentorship program, an annual leadership development course, and a standard approach to preparing leaders and volunteers for their role in the organization. Our new Academies Work Group, following on the successes of the Leadership Development Task Force, will carry this work forward and further develop training opportunities in education, faculty training, guideline development, and leadership. The work group initially will focus on two distinct tracks: faculty development and leadership development.
The work group has made fast progress, and I’m happy to share that CHEST Annual Meeting 2015 will mark the launch of our first course tracks being offered as part of the new CHEST Academies. These tracks are direct pathways to the latest training for leaders in health care and for faculty in chest medicine. Core competencies to be included in the tracks include:
• Leadership—personal characteristics, communication, teamwork, finance, and strategic planning
• Faculty—educational goals and objectives, gap analysis and needs assessment, point of care and large group teaching, and instructional methods
I want to personally thank our current and past CHEST leadership for their contributions toward our success, the Academies Work Group for moving this opportunity forward, and those pioneers who will participate in our first CHEST Academies offerings at CHEST 2015.
This is only the beginning. Because we value our leaders and want to help them to succeed personally and professionally, we’re committed to continuing to develop and offer year-round opportunities for leadership and faculty development. Members also can access additional resources for leadership development in the Get Involved section on chestnet.org.
I welcome your input on how we can continue to advance professional development within our CHEST community. As always, feel free to connect with me to share your ideas. I invite you to follow me on Twitter, @PMarkowskiACCP, or look for me at CHEST 2015, October 24-28, in Montréal.
NAMDRC tackles archaic home mechanical ventilation Medicare rules
Under current Medicare law and regulations, the Center for Medicare and Medicaid Services (CMS) has a confusing mix of rules that is complicated to understand and certainly contrary to the current standards of practice. Earlier this year, NAMDRC, CHEST, and about a dozen other societies wrote to CMS citing problems:
• Medicare does not recognize FDA classifications of devices as ventilators. Therefore, while one agency within the Department of Health & Human Services is specifically charged with the responsibility for determining safety and efficacy of medical devices and providing strict rules for labeling, a sister agency in the same department is not bound to accept those determinations. This has the effect of CMS stating that “just because FDA calls a device a ventilator does not make it a ventilator.”
This bizarre scenario is undoubtedly tied to a current statute that requires CMS to pay for certain ventilators under the “frequent and substantial servicing” payment methodology rather than the “capped rental” payment methodology. If CMS believes it might pay too much for home mechanical ventilators, it simply says that the worrisome device is actually a “respiratory assist device,” a term it has created for payment purposes.
• In 2001, CMS issued a Decision Memo that has the effect of signaling that in order to receive home mechanical ventilation, there must be the presence of an artificial airway AND removal of the device would lead to death. This principle is fraught with problems from various perspectives. First, even though the memo explicitly states “contractor discretion,” the key Medicare contractors have repeatedly signaled they have no flexibility and must adhere to that principle.
Secondly, with the advent of noninvasive mechanical ventilation, CMS created codes for processing such devices through the payment system, even though the 2001 Decision Memo refers to the need for an artificial airway. The inconsistency in these policies have led to confusion from ordering physicians and suppliers as well.
• Now, in 2015, the state-of-the-art of home mechanical ventilation is a world apart from 2001, and no policies have been updated related to home mechanical ventilation. Respiratory assist devices (RADs) or bilevel devices to everyone except Medicare recipients, are part of the problem. Because access to RADs are covered by very strict, inflexible Medicare rules, physicians and suppliers often find it easier to prescribe a ventilator for treatment of respiratory failure.
Possible solutions: Crafting solutions might seem relatively easy, but we want to ensure that rules we might agree to today need to be flexible enough to address innovations 2, 3, or 5 years from now. Therefore, the pathway of a national coverage determination (NCD) might not be the best approach because once an NCD is set into policy, it is a challenging effort to modify it, even if CMS agrees that problems with the relatively new policy need adjustment. Therefore, NAMDRC is working with other societies to craft some important principles and shape those principles into new policies that CMS could adopt outside of the NCD framework. Those principles include the following:
• A specific definition of “respiratory failure” that can be used to guide physicians, suppliers, and payers. Under this principle, if a diagnosis of respiratory failure meets the clinical definition and the physician certifies the medical necessity of treating respiratory failure, part of the treatment plan, by definition, includes a home mechanical ventilator.
• We see little need to distinguish between invasive and noninvasive home mechanical ventilation for coverage purposes. The principle outlined in the 2001 Decision Memo is outdated and no one genuinely believes that, by definition, the most critically ill must have a trach in order to survive. Let the physician determine the best approach; and in the case of many patients, particularly in the neuromuscular arena, a patient might use invasive mechanical ventilation nocturnally and noninvasive ventilation at other times. Importantly, most devices today can accommodate either approach.
• CMS’s RAD policy should be reshaped to provide greater flexibility to ensure that bilevel devices are available to those patients where less intensive therapy is appropriate.
We are hopeful that a revamped set of policies could be in place by the end of the year or early in 2016.
Under current Medicare law and regulations, the Center for Medicare and Medicaid Services (CMS) has a confusing mix of rules that is complicated to understand and certainly contrary to the current standards of practice. Earlier this year, NAMDRC, CHEST, and about a dozen other societies wrote to CMS citing problems:
• Medicare does not recognize FDA classifications of devices as ventilators. Therefore, while one agency within the Department of Health & Human Services is specifically charged with the responsibility for determining safety and efficacy of medical devices and providing strict rules for labeling, a sister agency in the same department is not bound to accept those determinations. This has the effect of CMS stating that “just because FDA calls a device a ventilator does not make it a ventilator.”
This bizarre scenario is undoubtedly tied to a current statute that requires CMS to pay for certain ventilators under the “frequent and substantial servicing” payment methodology rather than the “capped rental” payment methodology. If CMS believes it might pay too much for home mechanical ventilators, it simply says that the worrisome device is actually a “respiratory assist device,” a term it has created for payment purposes.
• In 2001, CMS issued a Decision Memo that has the effect of signaling that in order to receive home mechanical ventilation, there must be the presence of an artificial airway AND removal of the device would lead to death. This principle is fraught with problems from various perspectives. First, even though the memo explicitly states “contractor discretion,” the key Medicare contractors have repeatedly signaled they have no flexibility and must adhere to that principle.
Secondly, with the advent of noninvasive mechanical ventilation, CMS created codes for processing such devices through the payment system, even though the 2001 Decision Memo refers to the need for an artificial airway. The inconsistency in these policies have led to confusion from ordering physicians and suppliers as well.
• Now, in 2015, the state-of-the-art of home mechanical ventilation is a world apart from 2001, and no policies have been updated related to home mechanical ventilation. Respiratory assist devices (RADs) or bilevel devices to everyone except Medicare recipients, are part of the problem. Because access to RADs are covered by very strict, inflexible Medicare rules, physicians and suppliers often find it easier to prescribe a ventilator for treatment of respiratory failure.
Possible solutions: Crafting solutions might seem relatively easy, but we want to ensure that rules we might agree to today need to be flexible enough to address innovations 2, 3, or 5 years from now. Therefore, the pathway of a national coverage determination (NCD) might not be the best approach because once an NCD is set into policy, it is a challenging effort to modify it, even if CMS agrees that problems with the relatively new policy need adjustment. Therefore, NAMDRC is working with other societies to craft some important principles and shape those principles into new policies that CMS could adopt outside of the NCD framework. Those principles include the following:
• A specific definition of “respiratory failure” that can be used to guide physicians, suppliers, and payers. Under this principle, if a diagnosis of respiratory failure meets the clinical definition and the physician certifies the medical necessity of treating respiratory failure, part of the treatment plan, by definition, includes a home mechanical ventilator.
• We see little need to distinguish between invasive and noninvasive home mechanical ventilation for coverage purposes. The principle outlined in the 2001 Decision Memo is outdated and no one genuinely believes that, by definition, the most critically ill must have a trach in order to survive. Let the physician determine the best approach; and in the case of many patients, particularly in the neuromuscular arena, a patient might use invasive mechanical ventilation nocturnally and noninvasive ventilation at other times. Importantly, most devices today can accommodate either approach.
• CMS’s RAD policy should be reshaped to provide greater flexibility to ensure that bilevel devices are available to those patients where less intensive therapy is appropriate.
We are hopeful that a revamped set of policies could be in place by the end of the year or early in 2016.
Under current Medicare law and regulations, the Center for Medicare and Medicaid Services (CMS) has a confusing mix of rules that is complicated to understand and certainly contrary to the current standards of practice. Earlier this year, NAMDRC, CHEST, and about a dozen other societies wrote to CMS citing problems:
• Medicare does not recognize FDA classifications of devices as ventilators. Therefore, while one agency within the Department of Health & Human Services is specifically charged with the responsibility for determining safety and efficacy of medical devices and providing strict rules for labeling, a sister agency in the same department is not bound to accept those determinations. This has the effect of CMS stating that “just because FDA calls a device a ventilator does not make it a ventilator.”
This bizarre scenario is undoubtedly tied to a current statute that requires CMS to pay for certain ventilators under the “frequent and substantial servicing” payment methodology rather than the “capped rental” payment methodology. If CMS believes it might pay too much for home mechanical ventilators, it simply says that the worrisome device is actually a “respiratory assist device,” a term it has created for payment purposes.
• In 2001, CMS issued a Decision Memo that has the effect of signaling that in order to receive home mechanical ventilation, there must be the presence of an artificial airway AND removal of the device would lead to death. This principle is fraught with problems from various perspectives. First, even though the memo explicitly states “contractor discretion,” the key Medicare contractors have repeatedly signaled they have no flexibility and must adhere to that principle.
Secondly, with the advent of noninvasive mechanical ventilation, CMS created codes for processing such devices through the payment system, even though the 2001 Decision Memo refers to the need for an artificial airway. The inconsistency in these policies have led to confusion from ordering physicians and suppliers as well.
• Now, in 2015, the state-of-the-art of home mechanical ventilation is a world apart from 2001, and no policies have been updated related to home mechanical ventilation. Respiratory assist devices (RADs) or bilevel devices to everyone except Medicare recipients, are part of the problem. Because access to RADs are covered by very strict, inflexible Medicare rules, physicians and suppliers often find it easier to prescribe a ventilator for treatment of respiratory failure.
Possible solutions: Crafting solutions might seem relatively easy, but we want to ensure that rules we might agree to today need to be flexible enough to address innovations 2, 3, or 5 years from now. Therefore, the pathway of a national coverage determination (NCD) might not be the best approach because once an NCD is set into policy, it is a challenging effort to modify it, even if CMS agrees that problems with the relatively new policy need adjustment. Therefore, NAMDRC is working with other societies to craft some important principles and shape those principles into new policies that CMS could adopt outside of the NCD framework. Those principles include the following:
• A specific definition of “respiratory failure” that can be used to guide physicians, suppliers, and payers. Under this principle, if a diagnosis of respiratory failure meets the clinical definition and the physician certifies the medical necessity of treating respiratory failure, part of the treatment plan, by definition, includes a home mechanical ventilator.
• We see little need to distinguish between invasive and noninvasive home mechanical ventilation for coverage purposes. The principle outlined in the 2001 Decision Memo is outdated and no one genuinely believes that, by definition, the most critically ill must have a trach in order to survive. Let the physician determine the best approach; and in the case of many patients, particularly in the neuromuscular arena, a patient might use invasive mechanical ventilation nocturnally and noninvasive ventilation at other times. Importantly, most devices today can accommodate either approach.
• CMS’s RAD policy should be reshaped to provide greater flexibility to ensure that bilevel devices are available to those patients where less intensive therapy is appropriate.
We are hopeful that a revamped set of policies could be in place by the end of the year or early in 2016.
From the President: Ah, Summer...A Good Season to Readdress Work-Life Balance
There is something about the summertime that promotes appreciation for slower pace and reflection. Whether it’s the cool sand between your toes, an amazing vista after a vigorous hike, or the midmorning laughter of your kids on vacation – these joyful activities help reinvigorate. Reflecting back on 30 summers as an academic pulmonary and critical care physician, I think it may be more important than ever for us to take a moment to contemplate work-life balance in medicine, and, perhaps, our specialty in particular.
We all work hard, and most of us would enter a career in medicine again, and even sign up for the same specialty again. We value the work we do, particularly, the opportunity to improve the lives of our patients and generally find the work stimulating, rewarding, and even exciting. Additionally, we in pulmonary and critical care, and related fields, are accustomed to the stresses of high intensity, fast-pace, high-stakes work, as well as long and often undesirable work hours, including weekends and nights. There are certainly many more individuals in the hospital at night than a decade ago. Additionally, recent years have brought a rapid increase in the proportion of our time working as clinicians devoted to documentation and other non-patient care tasks. All told, the potential for work-related stress is certainly not decreasing.
Individuals who work in the ICU and similar work environments are accustomed to stress. It is part of the territory. To a point, short-term stress can actually be useful, as it tends to enhance focus and efficiency. Burnout, however, is a maladaptive response to excessive stress in the workplace and is characterized by emotional, mental, and physical exhaustion. Classically, burnout is defined as having three dimensions: emotional exhaustion, depersonalization, and diminished personal accomplishment. Importantly, development of burnout in a health-care worker has potential adverse consequences for the individual, the work environment, and our patients. Workers with burnout are more likely to have depression, alcohol and substance abuse, and various health disorders, and, often, leave the profession early. Behaviors of a burned out individual can be disruptive, contributing to staff dissatisfaction and excessive turnover. Finally, burnout has been associated with increased rates of medical errors, lower patient satisfaction, and reduced quality of care. Clearly, preventing and ameliorating burnout is an important target.
There is a growing body of evidence1-4 that serious burnout is commonplace among ICU workers. From a broad perspective, burnout is more common, and satisfaction with work/life balance less common, among physicians compared with the general population. Not surprisingly, among both physicians and nurses, the ICU as a workplace is associated with higher-than-average rates of burnout. There are now numerous survey-based multicenter studies that indicate approximately one-third to one-half of ICU workers have severe burnout.1-4 Look to your left. Look to your right. Chances are that one of you has significant burnout.
Particularly noteworthy is a recent online survey of physicians performed by Medscape4 in which 52% of intensivists described themselves as having serious burnout – the largest proportion among all 25 medical specialties reported. Perhaps more distressing, intensivists had among the lowest proportion of respondents who described themselves as “very happy” when describing their satisfaction at work and home. Finally, intensivists had the lowest proportion, among 25 medical specialties, of self-described health as “excellent” or “very good.”
We should all be concerned that these findings collectively paint a picture of a specialty at risk. It is important for us to consider why burnout occurs and what can be done about it. Specifically, which individuals are at increased risk? Are there identifiable factors that might be modified to reduce the likelihood of developing burnout? Are there individual and organizational approaches to identify individuals with burnout syndrome and mitigate its effects? Finally, are there opportunities for key stakeholders, including administrators and policymakers, to become better informed as to this emerging epidemic?
Several studies1,3 have now identified independent, potentially modifiable risk factors for burnout of intensivists, as well as ICU nurses. Common themes have emerged and include the following: (a) the quality of working relationships; (b) end-of-life issues; (c) organizational factors; and (d) personal characteristics. Perhaps the most consistently noted factor is that of interpersonal conflicts, those among physicians, nurses, and patients and family members. ICU physicians and nurses with burnout more commonly described conflict with their colleagues and with the other key members of the ICU team. Suboptimal communication is often at the root of conflict, and there are opportunities for enhancing communications and creating a supportive and trusting environment among ICU health-care workers.
The relationships that physicians and nurses have with critically ill or injured patients, and, perhaps, more commonly with family members, can be highly stressful. Again, promoting understanding and healthy communication proactively can pay dividends in regards to stress mitigation. This ties in with the added challenges of end-of-life situations in which emotions often run high, and calm, thoughtful communication is of critical importance. Surveys indicate1,3 that end-of-life issues impact our ICU nursing colleagues even more significantly, perhaps in part because of their many hours of direct contact with patients and families at the bedside.
From a unit organizational perspective, studies indicate1,5 that an excessively heavy work schedule is an important risk factor for physicians. In particular, the number of night shifts per month, and the time since the last nonworking week, were independent risk factors for burnout in one study. In a prospective randomized trial,5 a continuous intensivist schedule of 14 consecutive days was associated with higher burnout, greater job distress, and more work-life imbalance than a schedule with weekend cross-coverage. Inclusion of nonclinical work, such as research, teaching, or administrative activities, or work in a different clinical setting, appears to be protective regarding burnout. Unit and practice leaders and administrators have an opportunity to influence scheduling and nonclinical activities to reduce burnout.
Individuals who seem to be higher risk for developing burnout tend to have perfectionist and controlling tendencies, pessimistic views, and an inability to express emotions or to delegate. Individuals with supportive relationships and those who are able to personally manage difficult situations effectively, ie, are “resilient,” tend to avoid burnout more effectively.
Strategies to manage burnout in the ICU focus on prevention, early identification of the individual with burnout, and mitigation of burnout (often employing the same techniques as for prevention). Preventive strategies include both individual and organizational approaches. Individual approaches include awareness and self-monitoring, willingness to accept help from others, lifestyle management, stress management, anger management, “mindfulness,” and development of resilience. Individual approaches are often promoted in an organization setting. Such programs are increasingly used for medical students and residents but must become more ingrained in clinical practice settings.
Organizational approaches include prospective identification and monitoring of worker well-being as a quality indicator, emphasis on teamwork, attention to high stress areas (such as the ICU), deliberate management of the work environment to address overwork, support for a healthy work environment in regards to respectful relationships and communication, and many others.
What can the American College of Chest Physicians do to help alleviate burnout and enhance work-life balance among our members? I’m pleased to report that CHEST is leading an important project conducted by members of the Critical Care Societies Collaborative (CCSC), that includes leaders and experts from the American Association of Critical-Care Nurses (AACN), the American Thoracic Society (ATS), the Society of Critical Care Medicine (SCCM), and CHEST. Key goals of this task force are to raise awareness and set the stage for interventions to reduce burnout in the ICU through publication of a review and call to action in multiple journals; sponsorship of educational sessions at our annual meetings; and development and posting of additional Web-based tools and resources. While critical care workers are certainly aware of the importance and prevalence of ICU burnout, an important aim is to raise awareness among other key groups, including policymakers, administrators, and funding agencies.
In conclusion, please take a moment during this month of August to pause and consider your own work-life balance and how, together, we can enhance not just the health of our patients but also the personal well-being and long productive career among those who care for the critically ill and injured.
References
1. Embriaco NE, Azoulay K, Barrau N et al. High level of burnout in intensivists: prevalence and associated factors. Am J Respir Crit Care Med. 2007;175[7]:686-692.
2. Merlani PM, Verdon A, Businger G, Domenighetti H, Parggerm H, Ricou B. Burnout in ICU caregivers: a multicenter study of factors associated to centers. Am J Respir Crit Care Med. 2011;184[10]:1140-1146.
3. Poncet MCP, Toullic L, Papazian N, et al. Burnout syndrome in critical care nursing staff. Am J Respir Crit Care Med. 2007;175[7]:698-704.
4. www.medscape.com/features/slideshow/lifestyle/2013/critical-care#7
5. Ali NA, Hammersley J, Hoffmann SP, et al. Continuity of care in intensive care units: a cluster-randomized trial of intensivist staffing. Am J Respir Crit Care Med. 2011;184[7]:803-808.
There is something about the summertime that promotes appreciation for slower pace and reflection. Whether it’s the cool sand between your toes, an amazing vista after a vigorous hike, or the midmorning laughter of your kids on vacation – these joyful activities help reinvigorate. Reflecting back on 30 summers as an academic pulmonary and critical care physician, I think it may be more important than ever for us to take a moment to contemplate work-life balance in medicine, and, perhaps, our specialty in particular.
We all work hard, and most of us would enter a career in medicine again, and even sign up for the same specialty again. We value the work we do, particularly, the opportunity to improve the lives of our patients and generally find the work stimulating, rewarding, and even exciting. Additionally, we in pulmonary and critical care, and related fields, are accustomed to the stresses of high intensity, fast-pace, high-stakes work, as well as long and often undesirable work hours, including weekends and nights. There are certainly many more individuals in the hospital at night than a decade ago. Additionally, recent years have brought a rapid increase in the proportion of our time working as clinicians devoted to documentation and other non-patient care tasks. All told, the potential for work-related stress is certainly not decreasing.
Individuals who work in the ICU and similar work environments are accustomed to stress. It is part of the territory. To a point, short-term stress can actually be useful, as it tends to enhance focus and efficiency. Burnout, however, is a maladaptive response to excessive stress in the workplace and is characterized by emotional, mental, and physical exhaustion. Classically, burnout is defined as having three dimensions: emotional exhaustion, depersonalization, and diminished personal accomplishment. Importantly, development of burnout in a health-care worker has potential adverse consequences for the individual, the work environment, and our patients. Workers with burnout are more likely to have depression, alcohol and substance abuse, and various health disorders, and, often, leave the profession early. Behaviors of a burned out individual can be disruptive, contributing to staff dissatisfaction and excessive turnover. Finally, burnout has been associated with increased rates of medical errors, lower patient satisfaction, and reduced quality of care. Clearly, preventing and ameliorating burnout is an important target.
There is a growing body of evidence1-4 that serious burnout is commonplace among ICU workers. From a broad perspective, burnout is more common, and satisfaction with work/life balance less common, among physicians compared with the general population. Not surprisingly, among both physicians and nurses, the ICU as a workplace is associated with higher-than-average rates of burnout. There are now numerous survey-based multicenter studies that indicate approximately one-third to one-half of ICU workers have severe burnout.1-4 Look to your left. Look to your right. Chances are that one of you has significant burnout.
Particularly noteworthy is a recent online survey of physicians performed by Medscape4 in which 52% of intensivists described themselves as having serious burnout – the largest proportion among all 25 medical specialties reported. Perhaps more distressing, intensivists had among the lowest proportion of respondents who described themselves as “very happy” when describing their satisfaction at work and home. Finally, intensivists had the lowest proportion, among 25 medical specialties, of self-described health as “excellent” or “very good.”
We should all be concerned that these findings collectively paint a picture of a specialty at risk. It is important for us to consider why burnout occurs and what can be done about it. Specifically, which individuals are at increased risk? Are there identifiable factors that might be modified to reduce the likelihood of developing burnout? Are there individual and organizational approaches to identify individuals with burnout syndrome and mitigate its effects? Finally, are there opportunities for key stakeholders, including administrators and policymakers, to become better informed as to this emerging epidemic?
Several studies1,3 have now identified independent, potentially modifiable risk factors for burnout of intensivists, as well as ICU nurses. Common themes have emerged and include the following: (a) the quality of working relationships; (b) end-of-life issues; (c) organizational factors; and (d) personal characteristics. Perhaps the most consistently noted factor is that of interpersonal conflicts, those among physicians, nurses, and patients and family members. ICU physicians and nurses with burnout more commonly described conflict with their colleagues and with the other key members of the ICU team. Suboptimal communication is often at the root of conflict, and there are opportunities for enhancing communications and creating a supportive and trusting environment among ICU health-care workers.
The relationships that physicians and nurses have with critically ill or injured patients, and, perhaps, more commonly with family members, can be highly stressful. Again, promoting understanding and healthy communication proactively can pay dividends in regards to stress mitigation. This ties in with the added challenges of end-of-life situations in which emotions often run high, and calm, thoughtful communication is of critical importance. Surveys indicate1,3 that end-of-life issues impact our ICU nursing colleagues even more significantly, perhaps in part because of their many hours of direct contact with patients and families at the bedside.
From a unit organizational perspective, studies indicate1,5 that an excessively heavy work schedule is an important risk factor for physicians. In particular, the number of night shifts per month, and the time since the last nonworking week, were independent risk factors for burnout in one study. In a prospective randomized trial,5 a continuous intensivist schedule of 14 consecutive days was associated with higher burnout, greater job distress, and more work-life imbalance than a schedule with weekend cross-coverage. Inclusion of nonclinical work, such as research, teaching, or administrative activities, or work in a different clinical setting, appears to be protective regarding burnout. Unit and practice leaders and administrators have an opportunity to influence scheduling and nonclinical activities to reduce burnout.
Individuals who seem to be higher risk for developing burnout tend to have perfectionist and controlling tendencies, pessimistic views, and an inability to express emotions or to delegate. Individuals with supportive relationships and those who are able to personally manage difficult situations effectively, ie, are “resilient,” tend to avoid burnout more effectively.
Strategies to manage burnout in the ICU focus on prevention, early identification of the individual with burnout, and mitigation of burnout (often employing the same techniques as for prevention). Preventive strategies include both individual and organizational approaches. Individual approaches include awareness and self-monitoring, willingness to accept help from others, lifestyle management, stress management, anger management, “mindfulness,” and development of resilience. Individual approaches are often promoted in an organization setting. Such programs are increasingly used for medical students and residents but must become more ingrained in clinical practice settings.
Organizational approaches include prospective identification and monitoring of worker well-being as a quality indicator, emphasis on teamwork, attention to high stress areas (such as the ICU), deliberate management of the work environment to address overwork, support for a healthy work environment in regards to respectful relationships and communication, and many others.
What can the American College of Chest Physicians do to help alleviate burnout and enhance work-life balance among our members? I’m pleased to report that CHEST is leading an important project conducted by members of the Critical Care Societies Collaborative (CCSC), that includes leaders and experts from the American Association of Critical-Care Nurses (AACN), the American Thoracic Society (ATS), the Society of Critical Care Medicine (SCCM), and CHEST. Key goals of this task force are to raise awareness and set the stage for interventions to reduce burnout in the ICU through publication of a review and call to action in multiple journals; sponsorship of educational sessions at our annual meetings; and development and posting of additional Web-based tools and resources. While critical care workers are certainly aware of the importance and prevalence of ICU burnout, an important aim is to raise awareness among other key groups, including policymakers, administrators, and funding agencies.
In conclusion, please take a moment during this month of August to pause and consider your own work-life balance and how, together, we can enhance not just the health of our patients but also the personal well-being and long productive career among those who care for the critically ill and injured.
References
1. Embriaco NE, Azoulay K, Barrau N et al. High level of burnout in intensivists: prevalence and associated factors. Am J Respir Crit Care Med. 2007;175[7]:686-692.
2. Merlani PM, Verdon A, Businger G, Domenighetti H, Parggerm H, Ricou B. Burnout in ICU caregivers: a multicenter study of factors associated to centers. Am J Respir Crit Care Med. 2011;184[10]:1140-1146.
3. Poncet MCP, Toullic L, Papazian N, et al. Burnout syndrome in critical care nursing staff. Am J Respir Crit Care Med. 2007;175[7]:698-704.
4. www.medscape.com/features/slideshow/lifestyle/2013/critical-care#7
5. Ali NA, Hammersley J, Hoffmann SP, et al. Continuity of care in intensive care units: a cluster-randomized trial of intensivist staffing. Am J Respir Crit Care Med. 2011;184[7]:803-808.
There is something about the summertime that promotes appreciation for slower pace and reflection. Whether it’s the cool sand between your toes, an amazing vista after a vigorous hike, or the midmorning laughter of your kids on vacation – these joyful activities help reinvigorate. Reflecting back on 30 summers as an academic pulmonary and critical care physician, I think it may be more important than ever for us to take a moment to contemplate work-life balance in medicine, and, perhaps, our specialty in particular.
We all work hard, and most of us would enter a career in medicine again, and even sign up for the same specialty again. We value the work we do, particularly, the opportunity to improve the lives of our patients and generally find the work stimulating, rewarding, and even exciting. Additionally, we in pulmonary and critical care, and related fields, are accustomed to the stresses of high intensity, fast-pace, high-stakes work, as well as long and often undesirable work hours, including weekends and nights. There are certainly many more individuals in the hospital at night than a decade ago. Additionally, recent years have brought a rapid increase in the proportion of our time working as clinicians devoted to documentation and other non-patient care tasks. All told, the potential for work-related stress is certainly not decreasing.
Individuals who work in the ICU and similar work environments are accustomed to stress. It is part of the territory. To a point, short-term stress can actually be useful, as it tends to enhance focus and efficiency. Burnout, however, is a maladaptive response to excessive stress in the workplace and is characterized by emotional, mental, and physical exhaustion. Classically, burnout is defined as having three dimensions: emotional exhaustion, depersonalization, and diminished personal accomplishment. Importantly, development of burnout in a health-care worker has potential adverse consequences for the individual, the work environment, and our patients. Workers with burnout are more likely to have depression, alcohol and substance abuse, and various health disorders, and, often, leave the profession early. Behaviors of a burned out individual can be disruptive, contributing to staff dissatisfaction and excessive turnover. Finally, burnout has been associated with increased rates of medical errors, lower patient satisfaction, and reduced quality of care. Clearly, preventing and ameliorating burnout is an important target.
There is a growing body of evidence1-4 that serious burnout is commonplace among ICU workers. From a broad perspective, burnout is more common, and satisfaction with work/life balance less common, among physicians compared with the general population. Not surprisingly, among both physicians and nurses, the ICU as a workplace is associated with higher-than-average rates of burnout. There are now numerous survey-based multicenter studies that indicate approximately one-third to one-half of ICU workers have severe burnout.1-4 Look to your left. Look to your right. Chances are that one of you has significant burnout.
Particularly noteworthy is a recent online survey of physicians performed by Medscape4 in which 52% of intensivists described themselves as having serious burnout – the largest proportion among all 25 medical specialties reported. Perhaps more distressing, intensivists had among the lowest proportion of respondents who described themselves as “very happy” when describing their satisfaction at work and home. Finally, intensivists had the lowest proportion, among 25 medical specialties, of self-described health as “excellent” or “very good.”
We should all be concerned that these findings collectively paint a picture of a specialty at risk. It is important for us to consider why burnout occurs and what can be done about it. Specifically, which individuals are at increased risk? Are there identifiable factors that might be modified to reduce the likelihood of developing burnout? Are there individual and organizational approaches to identify individuals with burnout syndrome and mitigate its effects? Finally, are there opportunities for key stakeholders, including administrators and policymakers, to become better informed as to this emerging epidemic?
Several studies1,3 have now identified independent, potentially modifiable risk factors for burnout of intensivists, as well as ICU nurses. Common themes have emerged and include the following: (a) the quality of working relationships; (b) end-of-life issues; (c) organizational factors; and (d) personal characteristics. Perhaps the most consistently noted factor is that of interpersonal conflicts, those among physicians, nurses, and patients and family members. ICU physicians and nurses with burnout more commonly described conflict with their colleagues and with the other key members of the ICU team. Suboptimal communication is often at the root of conflict, and there are opportunities for enhancing communications and creating a supportive and trusting environment among ICU health-care workers.
The relationships that physicians and nurses have with critically ill or injured patients, and, perhaps, more commonly with family members, can be highly stressful. Again, promoting understanding and healthy communication proactively can pay dividends in regards to stress mitigation. This ties in with the added challenges of end-of-life situations in which emotions often run high, and calm, thoughtful communication is of critical importance. Surveys indicate1,3 that end-of-life issues impact our ICU nursing colleagues even more significantly, perhaps in part because of their many hours of direct contact with patients and families at the bedside.
From a unit organizational perspective, studies indicate1,5 that an excessively heavy work schedule is an important risk factor for physicians. In particular, the number of night shifts per month, and the time since the last nonworking week, were independent risk factors for burnout in one study. In a prospective randomized trial,5 a continuous intensivist schedule of 14 consecutive days was associated with higher burnout, greater job distress, and more work-life imbalance than a schedule with weekend cross-coverage. Inclusion of nonclinical work, such as research, teaching, or administrative activities, or work in a different clinical setting, appears to be protective regarding burnout. Unit and practice leaders and administrators have an opportunity to influence scheduling and nonclinical activities to reduce burnout.
Individuals who seem to be higher risk for developing burnout tend to have perfectionist and controlling tendencies, pessimistic views, and an inability to express emotions or to delegate. Individuals with supportive relationships and those who are able to personally manage difficult situations effectively, ie, are “resilient,” tend to avoid burnout more effectively.
Strategies to manage burnout in the ICU focus on prevention, early identification of the individual with burnout, and mitigation of burnout (often employing the same techniques as for prevention). Preventive strategies include both individual and organizational approaches. Individual approaches include awareness and self-monitoring, willingness to accept help from others, lifestyle management, stress management, anger management, “mindfulness,” and development of resilience. Individual approaches are often promoted in an organization setting. Such programs are increasingly used for medical students and residents but must become more ingrained in clinical practice settings.
Organizational approaches include prospective identification and monitoring of worker well-being as a quality indicator, emphasis on teamwork, attention to high stress areas (such as the ICU), deliberate management of the work environment to address overwork, support for a healthy work environment in regards to respectful relationships and communication, and many others.
What can the American College of Chest Physicians do to help alleviate burnout and enhance work-life balance among our members? I’m pleased to report that CHEST is leading an important project conducted by members of the Critical Care Societies Collaborative (CCSC), that includes leaders and experts from the American Association of Critical-Care Nurses (AACN), the American Thoracic Society (ATS), the Society of Critical Care Medicine (SCCM), and CHEST. Key goals of this task force are to raise awareness and set the stage for interventions to reduce burnout in the ICU through publication of a review and call to action in multiple journals; sponsorship of educational sessions at our annual meetings; and development and posting of additional Web-based tools and resources. While critical care workers are certainly aware of the importance and prevalence of ICU burnout, an important aim is to raise awareness among other key groups, including policymakers, administrators, and funding agencies.
In conclusion, please take a moment during this month of August to pause and consider your own work-life balance and how, together, we can enhance not just the health of our patients but also the personal well-being and long productive career among those who care for the critically ill and injured.
References
1. Embriaco NE, Azoulay K, Barrau N et al. High level of burnout in intensivists: prevalence and associated factors. Am J Respir Crit Care Med. 2007;175[7]:686-692.
2. Merlani PM, Verdon A, Businger G, Domenighetti H, Parggerm H, Ricou B. Burnout in ICU caregivers: a multicenter study of factors associated to centers. Am J Respir Crit Care Med. 2011;184[10]:1140-1146.
3. Poncet MCP, Toullic L, Papazian N, et al. Burnout syndrome in critical care nursing staff. Am J Respir Crit Care Med. 2007;175[7]:698-704.
4. www.medscape.com/features/slideshow/lifestyle/2013/critical-care#7
5. Ali NA, Hammersley J, Hoffmann SP, et al. Continuity of care in intensive care units: a cluster-randomized trial of intensivist staffing. Am J Respir Crit Care Med. 2011;184[7]:803-808.
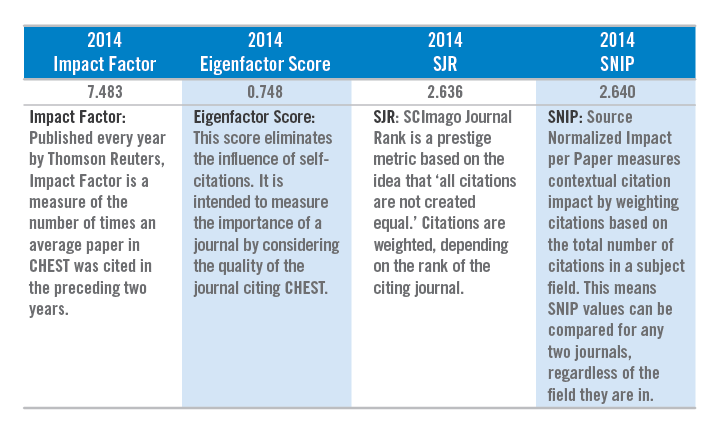
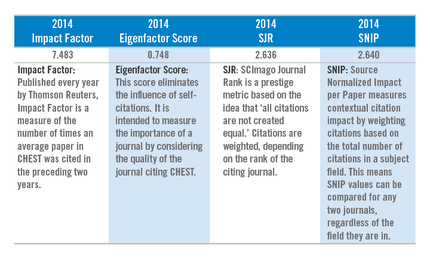
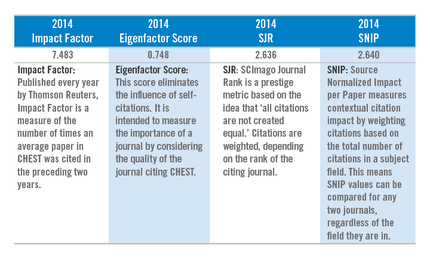
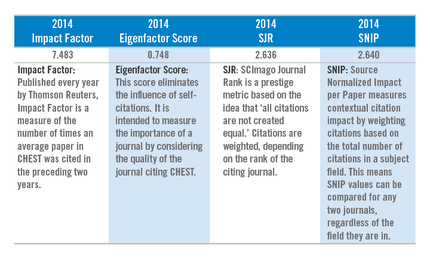
Impact Factor Highest in CHEST’s History
The new Thomson Reuters Journal Citation Report Impact Factor (IF) numbers for this past year were recently released, and we are pleased to announce that the CHEST IF for 2014 has increased from 7.132 to 7.483, once again setting a record for CHEST. In addition, CHEST’s Eigenfactor Score (a measure that eliminates the influence of self-citations) for 2014 is 0.748, which ranks CHEST as 2nd in both the Respiratory and Critical Care categories of the Journal Citation Reports.
Highlights:
Impact Factor*
◦ 4.9% increase from 2013, rising from 7.132 to 7.483
◦ Continues as 2nd among 27 journals in Critical Care
◦ Now ranked 5th among 54 journals in Respiratory Medicine
Eigenfactor Score**
◦ Now ranked 2nd in both the Respiratory and Critical Care categories of the Journal Citation Reports
SJR
◦ Ranked in the top 5 in both Pulmonary and Respiratory Medicine and Critical and Intensive Care Medicine
SNIP
◦ Ranked 3rd in Critical Care and Intensive Care Medicine
◦ Ranked 4th in both Cardiology and Cardiovascular Medicine and Pulmonary and Respiratory Medicine
* Journal Citation Reports ®, published by Thomson Reuters, 2015. ** Eigenfactor® published by Eigenfactor ® Project.
The new Thomson Reuters Journal Citation Report Impact Factor (IF) numbers for this past year were recently released, and we are pleased to announce that the CHEST IF for 2014 has increased from 7.132 to 7.483, once again setting a record for CHEST. In addition, CHEST’s Eigenfactor Score (a measure that eliminates the influence of self-citations) for 2014 is 0.748, which ranks CHEST as 2nd in both the Respiratory and Critical Care categories of the Journal Citation Reports.
Highlights:
Impact Factor*
◦ 4.9% increase from 2013, rising from 7.132 to 7.483
◦ Continues as 2nd among 27 journals in Critical Care
◦ Now ranked 5th among 54 journals in Respiratory Medicine
Eigenfactor Score**
◦ Now ranked 2nd in both the Respiratory and Critical Care categories of the Journal Citation Reports
SJR
◦ Ranked in the top 5 in both Pulmonary and Respiratory Medicine and Critical and Intensive Care Medicine
SNIP
◦ Ranked 3rd in Critical Care and Intensive Care Medicine
◦ Ranked 4th in both Cardiology and Cardiovascular Medicine and Pulmonary and Respiratory Medicine
* Journal Citation Reports ®, published by Thomson Reuters, 2015. ** Eigenfactor® published by Eigenfactor ® Project.
The new Thomson Reuters Journal Citation Report Impact Factor (IF) numbers for this past year were recently released, and we are pleased to announce that the CHEST IF for 2014 has increased from 7.132 to 7.483, once again setting a record for CHEST. In addition, CHEST’s Eigenfactor Score (a measure that eliminates the influence of self-citations) for 2014 is 0.748, which ranks CHEST as 2nd in both the Respiratory and Critical Care categories of the Journal Citation Reports.
Highlights:
Impact Factor*
◦ 4.9% increase from 2013, rising from 7.132 to 7.483
◦ Continues as 2nd among 27 journals in Critical Care
◦ Now ranked 5th among 54 journals in Respiratory Medicine
Eigenfactor Score**
◦ Now ranked 2nd in both the Respiratory and Critical Care categories of the Journal Citation Reports
SJR
◦ Ranked in the top 5 in both Pulmonary and Respiratory Medicine and Critical and Intensive Care Medicine
SNIP
◦ Ranked 3rd in Critical Care and Intensive Care Medicine
◦ Ranked 4th in both Cardiology and Cardiovascular Medicine and Pulmonary and Respiratory Medicine
* Journal Citation Reports ®, published by Thomson Reuters, 2015. ** Eigenfactor® published by Eigenfactor ® Project.
Satisfy Your Educational Needs, Your Taste Buds with CHEST 2015 in Montréal
Smoked meats, bagels, poutine, duck confit, couscous...Montréal has it all! When you travel to Montréal, October 24-28, for the CHEST Annual Meeting 2015, expect to fill up on assorted clinical education opportunities and diverse cuisine.
While Montréal offers high end French fare, casual plates at diners, and everything in between, the city is best known for some simple staples.
Bagels are iconic in Montréal. These special bagels are hand - rolled, blanched in honey water, and baked in a wood-burning oven. You can taste these Montréal classics at St- Viateur Bagel or Fairmount Bagel. The bagel shops are located a block apart in the Mile End neighborhood of Montréal.
Smoked meat is also popular in Montréal. Many restaurants serve smoked meat sandwiches, but if you want to take a foodie’s tour of the city, Schwartz’s is the place to go. Founded in 1928, this deli dishes up a classic brisket on rye with a smear of yellow mustard. You can find this landmark in the Le Plateau-Mont-Royal neighborhood.
And you can’t visit Québec without feasting on some poutine. Indulge with some Foie Gras Poutine, fried French fries in duck fat with a slab of foie gras on top. Find this dish at Au Pied de Cochon, chef Martin Picard’s restaurant, located in the Le Plateau-Mont-Royal neighborhood.
We checked in with our favorite local Montréalers, CHEST members, and here are some of their favorite spots:
• Bouillon Bilk - Treat yourself to a fine-dining experience with delicious contemporary cuisine, focusing on seafood. located at 1595 Boulevard Saint-Laurent, Montréal, H2X 2S9
• le Majestique - This restaurant and bar offers many small plate options and cocktails. located at 4105 Boulevard Saint-Laurent, Montréal, QC H2W
• Brasserie T - Catch a show at the nearby Place des Arts, and then treat yourself to this French cuisine. located at 1425 Rue Jeanne-Mance, Montréal, QC H2X 2J4
• Graziella - Located 10 minutes walking distance from the Palais des Congres, this restaurant is known for their upscale Italian dishes. located at 116 Rue McGill, Montréal, QC H2Y 2E5
• Le filet - This hot spot features glam decor and creative seafood-focused dishes along with a seasonal terrace. located at 219, ave. Mont-Royal Ouest, Montréal, QC H2T 2T2
• Pasta Casareccia - Try fresh homemade pastas and sauces at this trattoria with an attached deli. located at 5849 Rue Sherbrooke Ouest, Montréal, QC H4A 1X4
Montréal is sure to satisfy your taste buds with its wide variety of culinary options. CHEST 2015 will also offer you a variety of educational options including hands-on simulation, case- and problem-based presentations, small-group interactive discussions, lectures, self-study opportunities, and more. CHEST 2015 is dedicated to delivering the latest information in pulmonary, critical care, and sleep medicine to you, ensuring you make the best decisions with your patients. Register by August 31 to pay the lowest fees. Learn more at chestmeeting.chestnet.org.
Smoked meats, bagels, poutine, duck confit, couscous...Montréal has it all! When you travel to Montréal, October 24-28, for the CHEST Annual Meeting 2015, expect to fill up on assorted clinical education opportunities and diverse cuisine.
While Montréal offers high end French fare, casual plates at diners, and everything in between, the city is best known for some simple staples.
Bagels are iconic in Montréal. These special bagels are hand - rolled, blanched in honey water, and baked in a wood-burning oven. You can taste these Montréal classics at St- Viateur Bagel or Fairmount Bagel. The bagel shops are located a block apart in the Mile End neighborhood of Montréal.
Smoked meat is also popular in Montréal. Many restaurants serve smoked meat sandwiches, but if you want to take a foodie’s tour of the city, Schwartz’s is the place to go. Founded in 1928, this deli dishes up a classic brisket on rye with a smear of yellow mustard. You can find this landmark in the Le Plateau-Mont-Royal neighborhood.
And you can’t visit Québec without feasting on some poutine. Indulge with some Foie Gras Poutine, fried French fries in duck fat with a slab of foie gras on top. Find this dish at Au Pied de Cochon, chef Martin Picard’s restaurant, located in the Le Plateau-Mont-Royal neighborhood.
We checked in with our favorite local Montréalers, CHEST members, and here are some of their favorite spots:
• Bouillon Bilk - Treat yourself to a fine-dining experience with delicious contemporary cuisine, focusing on seafood. located at 1595 Boulevard Saint-Laurent, Montréal, H2X 2S9
• le Majestique - This restaurant and bar offers many small plate options and cocktails. located at 4105 Boulevard Saint-Laurent, Montréal, QC H2W
• Brasserie T - Catch a show at the nearby Place des Arts, and then treat yourself to this French cuisine. located at 1425 Rue Jeanne-Mance, Montréal, QC H2X 2J4
• Graziella - Located 10 minutes walking distance from the Palais des Congres, this restaurant is known for their upscale Italian dishes. located at 116 Rue McGill, Montréal, QC H2Y 2E5
• Le filet - This hot spot features glam decor and creative seafood-focused dishes along with a seasonal terrace. located at 219, ave. Mont-Royal Ouest, Montréal, QC H2T 2T2
• Pasta Casareccia - Try fresh homemade pastas and sauces at this trattoria with an attached deli. located at 5849 Rue Sherbrooke Ouest, Montréal, QC H4A 1X4
Montréal is sure to satisfy your taste buds with its wide variety of culinary options. CHEST 2015 will also offer you a variety of educational options including hands-on simulation, case- and problem-based presentations, small-group interactive discussions, lectures, self-study opportunities, and more. CHEST 2015 is dedicated to delivering the latest information in pulmonary, critical care, and sleep medicine to you, ensuring you make the best decisions with your patients. Register by August 31 to pay the lowest fees. Learn more at chestmeeting.chestnet.org.
Smoked meats, bagels, poutine, duck confit, couscous...Montréal has it all! When you travel to Montréal, October 24-28, for the CHEST Annual Meeting 2015, expect to fill up on assorted clinical education opportunities and diverse cuisine.
While Montréal offers high end French fare, casual plates at diners, and everything in between, the city is best known for some simple staples.
Bagels are iconic in Montréal. These special bagels are hand - rolled, blanched in honey water, and baked in a wood-burning oven. You can taste these Montréal classics at St- Viateur Bagel or Fairmount Bagel. The bagel shops are located a block apart in the Mile End neighborhood of Montréal.
Smoked meat is also popular in Montréal. Many restaurants serve smoked meat sandwiches, but if you want to take a foodie’s tour of the city, Schwartz’s is the place to go. Founded in 1928, this deli dishes up a classic brisket on rye with a smear of yellow mustard. You can find this landmark in the Le Plateau-Mont-Royal neighborhood.
And you can’t visit Québec without feasting on some poutine. Indulge with some Foie Gras Poutine, fried French fries in duck fat with a slab of foie gras on top. Find this dish at Au Pied de Cochon, chef Martin Picard’s restaurant, located in the Le Plateau-Mont-Royal neighborhood.
We checked in with our favorite local Montréalers, CHEST members, and here are some of their favorite spots:
• Bouillon Bilk - Treat yourself to a fine-dining experience with delicious contemporary cuisine, focusing on seafood. located at 1595 Boulevard Saint-Laurent, Montréal, H2X 2S9
• le Majestique - This restaurant and bar offers many small plate options and cocktails. located at 4105 Boulevard Saint-Laurent, Montréal, QC H2W
• Brasserie T - Catch a show at the nearby Place des Arts, and then treat yourself to this French cuisine. located at 1425 Rue Jeanne-Mance, Montréal, QC H2X 2J4
• Graziella - Located 10 minutes walking distance from the Palais des Congres, this restaurant is known for their upscale Italian dishes. located at 116 Rue McGill, Montréal, QC H2Y 2E5
• Le filet - This hot spot features glam decor and creative seafood-focused dishes along with a seasonal terrace. located at 219, ave. Mont-Royal Ouest, Montréal, QC H2T 2T2
• Pasta Casareccia - Try fresh homemade pastas and sauces at this trattoria with an attached deli. located at 5849 Rue Sherbrooke Ouest, Montréal, QC H4A 1X4
Montréal is sure to satisfy your taste buds with its wide variety of culinary options. CHEST 2015 will also offer you a variety of educational options including hands-on simulation, case- and problem-based presentations, small-group interactive discussions, lectures, self-study opportunities, and more. CHEST 2015 is dedicated to delivering the latest information in pulmonary, critical care, and sleep medicine to you, ensuring you make the best decisions with your patients. Register by August 31 to pay the lowest fees. Learn more at chestmeeting.chestnet.org.
Catching up with our Past Presidents EDWARD C. ROSENOW III, MD, MS, MASTER FCCP
Where are they now? What have they been up to? CHEST’s Past Presidents each forged the way for the many successes of the American College of Chest Physicians (CHEST), leading to enhanced patient care around the globe. Their outstanding leadership and vision are evidenced today in many of CHEST’s current initiatives, and now it is time to check in with these past leaders to give us a look at what’s new in their lives.
It is a privilege and an honor to be asked to reminisce about my life experiences after my year as president of the College. I think we accomplished a lot during that year, with the completion of the new American College of Chest Physicians’ headquarters in Northbrook and the College’s participation in effecting the ban on smoking on domestic airline flights.
I retired in 1996 but continued to be very active in teaching and writing as I still am. Mayo’s emeritus center is right in the middle of the campus that I go to three or four mornings a week; this keeps me in touch with a number of friends, encountering many of them regularly. I go to lunch several times a week with old friends, as well as with pre-med students, fellows, my former secretary, and allied health personnel that I worked with for decades. One group comprises pulmonary colleagues that I have worked with for 4 decades. I would urge my fellow retirees to do the same. It will help you stay ‘young’! And you have to get out of the house, even in cold winter months. I teach year 2 medical students in their clinic at the Salvation Army. One of my greatest pleasures is mentoring pre-med students as well as residents/fellows and even young staff. Try it, you’ll love it
I am working on my fourth book, and this is very stimulating. My first one was self-published in 2006 and titled The Art of Living….The Art of Medicine. This was followed by a 900+ slide compilation on a CD titled Mayo Clinic Challenging Images for Pulmonary Board Review. I’m currently working on two more: The Interpretation of CXRs by a Nonradiologist—this will be for primary care physicians and even nurse primary care providers. Hopefully, Mayo will publish this on to our education website. It is currently also being translated into Mandarin. Finally, one that only an old man could write, and that is The Making of the Physician, beginning with the pre-med student going up through leadership of departments and divisions.
My two grandchildren are awesome and mean the world to me. Christian was MVP for the Minnesota State High School Baseball All Stars and Kate has twice won the doubles in the Minnesota State High School Tennis Championships.
I thank the College for all it has given me!
Where are they now? What have they been up to? CHEST’s Past Presidents each forged the way for the many successes of the American College of Chest Physicians (CHEST), leading to enhanced patient care around the globe. Their outstanding leadership and vision are evidenced today in many of CHEST’s current initiatives, and now it is time to check in with these past leaders to give us a look at what’s new in their lives.
It is a privilege and an honor to be asked to reminisce about my life experiences after my year as president of the College. I think we accomplished a lot during that year, with the completion of the new American College of Chest Physicians’ headquarters in Northbrook and the College’s participation in effecting the ban on smoking on domestic airline flights.
I retired in 1996 but continued to be very active in teaching and writing as I still am. Mayo’s emeritus center is right in the middle of the campus that I go to three or four mornings a week; this keeps me in touch with a number of friends, encountering many of them regularly. I go to lunch several times a week with old friends, as well as with pre-med students, fellows, my former secretary, and allied health personnel that I worked with for decades. One group comprises pulmonary colleagues that I have worked with for 4 decades. I would urge my fellow retirees to do the same. It will help you stay ‘young’! And you have to get out of the house, even in cold winter months. I teach year 2 medical students in their clinic at the Salvation Army. One of my greatest pleasures is mentoring pre-med students as well as residents/fellows and even young staff. Try it, you’ll love it
I am working on my fourth book, and this is very stimulating. My first one was self-published in 2006 and titled The Art of Living….The Art of Medicine. This was followed by a 900+ slide compilation on a CD titled Mayo Clinic Challenging Images for Pulmonary Board Review. I’m currently working on two more: The Interpretation of CXRs by a Nonradiologist—this will be for primary care physicians and even nurse primary care providers. Hopefully, Mayo will publish this on to our education website. It is currently also being translated into Mandarin. Finally, one that only an old man could write, and that is The Making of the Physician, beginning with the pre-med student going up through leadership of departments and divisions.
My two grandchildren are awesome and mean the world to me. Christian was MVP for the Minnesota State High School Baseball All Stars and Kate has twice won the doubles in the Minnesota State High School Tennis Championships.
I thank the College for all it has given me!
Where are they now? What have they been up to? CHEST’s Past Presidents each forged the way for the many successes of the American College of Chest Physicians (CHEST), leading to enhanced patient care around the globe. Their outstanding leadership and vision are evidenced today in many of CHEST’s current initiatives, and now it is time to check in with these past leaders to give us a look at what’s new in their lives.
It is a privilege and an honor to be asked to reminisce about my life experiences after my year as president of the College. I think we accomplished a lot during that year, with the completion of the new American College of Chest Physicians’ headquarters in Northbrook and the College’s participation in effecting the ban on smoking on domestic airline flights.
I retired in 1996 but continued to be very active in teaching and writing as I still am. Mayo’s emeritus center is right in the middle of the campus that I go to three or four mornings a week; this keeps me in touch with a number of friends, encountering many of them regularly. I go to lunch several times a week with old friends, as well as with pre-med students, fellows, my former secretary, and allied health personnel that I worked with for decades. One group comprises pulmonary colleagues that I have worked with for 4 decades. I would urge my fellow retirees to do the same. It will help you stay ‘young’! And you have to get out of the house, even in cold winter months. I teach year 2 medical students in their clinic at the Salvation Army. One of my greatest pleasures is mentoring pre-med students as well as residents/fellows and even young staff. Try it, you’ll love it
I am working on my fourth book, and this is very stimulating. My first one was self-published in 2006 and titled The Art of Living….The Art of Medicine. This was followed by a 900+ slide compilation on a CD titled Mayo Clinic Challenging Images for Pulmonary Board Review. I’m currently working on two more: The Interpretation of CXRs by a Nonradiologist—this will be for primary care physicians and even nurse primary care providers. Hopefully, Mayo will publish this on to our education website. It is currently also being translated into Mandarin. Finally, one that only an old man could write, and that is The Making of the Physician, beginning with the pre-med student going up through leadership of departments and divisions.
My two grandchildren are awesome and mean the world to me. Christian was MVP for the Minnesota State High School Baseball All Stars and Kate has twice won the doubles in the Minnesota State High School Tennis Championships.
I thank the College for all it has given me!
1-Day Registration for CHEST 2015: Come for the Day or Make a Weekend of It
If you’d like to attend the CHEST Annual Meeting 2015 but have trouble scheduling time away from your practice, consider the 1-day registration. Register for any given day, Sunday through Wednesday. Or, attend for the weekend by registering for a postgraduate course on Saturday and 1 day on Sunday. If you come for the weekend, consider bringing your family. You won’t be alone—there’s so much to do for everyone in Montréal.
Postgraduate Courses
Saturday, October 24
Attend a postgraduate course for an intensive learning experience. Postgraduate courses include:
• A Case-Based Review of Cutting-Edge Critical Care: What’s Happened Since You Left Fellowship?
• Advanced Critical Care Echocardiography
• Cardiopulmonary Exercise Testing 2015: An Evidence- and Case-Based Update
• Pulmonary Medicine 2015: Year in Review and Clinical Update
• Sleep Medicine 2015: Year in Review and Clinical Update
Program Highlights
CHEST 2015 is your connection to focused clinical education that will help optimize your patient care. The relevant sessions and community of innovative problem-solvers in attendance will be sure to inspire and energize you and your career. Don’t miss these highlights:
Interdisciplinary Programs
Bring your entire care team to attend programs that will address clinical issues across the disciplines. Session speakers will represent each role and present from their perspective, so your group can collectively experience practical, relevant updates. Sessions will combine lecture-based, case-based, and hands-on learning opportunities.
CHEST Simulation Center
Practice your clinical skills in a hands-on learning environment. Work with expert faculty to sharpen your skills and apply your knowledge using real equipment and simulators.
General Sessions
Choose from hundreds of sessions, offered in a variety of instructional formats, including hands-on simulation, interactive case-based presentations, small-group discussions, and a rich variety of self-study modules and educational games.
Exhibit Hall
Don’t miss the showcase of diagnostic and treatment solutions for optimal patient care.
Explore Montréal!
Montréal is known for its warm camaraderie and joie de vivre!
You’ll enjoy this friendly city—a melting pot of ethnicities, languages, cuisines, and ideas. Explore Montréal’s history in Old Montréal, take in a hockey game at the Bell Centre, breathe in the fresh air at Mount Royal, or enjoy a wide variety of classic Montréal foods. During your free time at CHEST 2015, you’ll want to check out everything that Montréal has to offer.
Learn more about Montréal at tourisme-montreal.org, and find information about CHEST 2015 at chestmeeting.chestnet.org.
If you’d like to attend the CHEST Annual Meeting 2015 but have trouble scheduling time away from your practice, consider the 1-day registration. Register for any given day, Sunday through Wednesday. Or, attend for the weekend by registering for a postgraduate course on Saturday and 1 day on Sunday. If you come for the weekend, consider bringing your family. You won’t be alone—there’s so much to do for everyone in Montréal.
Postgraduate Courses
Saturday, October 24
Attend a postgraduate course for an intensive learning experience. Postgraduate courses include:
• A Case-Based Review of Cutting-Edge Critical Care: What’s Happened Since You Left Fellowship?
• Advanced Critical Care Echocardiography
• Cardiopulmonary Exercise Testing 2015: An Evidence- and Case-Based Update
• Pulmonary Medicine 2015: Year in Review and Clinical Update
• Sleep Medicine 2015: Year in Review and Clinical Update
Program Highlights
CHEST 2015 is your connection to focused clinical education that will help optimize your patient care. The relevant sessions and community of innovative problem-solvers in attendance will be sure to inspire and energize you and your career. Don’t miss these highlights:
Interdisciplinary Programs
Bring your entire care team to attend programs that will address clinical issues across the disciplines. Session speakers will represent each role and present from their perspective, so your group can collectively experience practical, relevant updates. Sessions will combine lecture-based, case-based, and hands-on learning opportunities.
CHEST Simulation Center
Practice your clinical skills in a hands-on learning environment. Work with expert faculty to sharpen your skills and apply your knowledge using real equipment and simulators.
General Sessions
Choose from hundreds of sessions, offered in a variety of instructional formats, including hands-on simulation, interactive case-based presentations, small-group discussions, and a rich variety of self-study modules and educational games.
Exhibit Hall
Don’t miss the showcase of diagnostic and treatment solutions for optimal patient care.
Explore Montréal!
Montréal is known for its warm camaraderie and joie de vivre!
You’ll enjoy this friendly city—a melting pot of ethnicities, languages, cuisines, and ideas. Explore Montréal’s history in Old Montréal, take in a hockey game at the Bell Centre, breathe in the fresh air at Mount Royal, or enjoy a wide variety of classic Montréal foods. During your free time at CHEST 2015, you’ll want to check out everything that Montréal has to offer.
Learn more about Montréal at tourisme-montreal.org, and find information about CHEST 2015 at chestmeeting.chestnet.org.
If you’d like to attend the CHEST Annual Meeting 2015 but have trouble scheduling time away from your practice, consider the 1-day registration. Register for any given day, Sunday through Wednesday. Or, attend for the weekend by registering for a postgraduate course on Saturday and 1 day on Sunday. If you come for the weekend, consider bringing your family. You won’t be alone—there’s so much to do for everyone in Montréal.
Postgraduate Courses
Saturday, October 24
Attend a postgraduate course for an intensive learning experience. Postgraduate courses include:
• A Case-Based Review of Cutting-Edge Critical Care: What’s Happened Since You Left Fellowship?
• Advanced Critical Care Echocardiography
• Cardiopulmonary Exercise Testing 2015: An Evidence- and Case-Based Update
• Pulmonary Medicine 2015: Year in Review and Clinical Update
• Sleep Medicine 2015: Year in Review and Clinical Update
Program Highlights
CHEST 2015 is your connection to focused clinical education that will help optimize your patient care. The relevant sessions and community of innovative problem-solvers in attendance will be sure to inspire and energize you and your career. Don’t miss these highlights:
Interdisciplinary Programs
Bring your entire care team to attend programs that will address clinical issues across the disciplines. Session speakers will represent each role and present from their perspective, so your group can collectively experience practical, relevant updates. Sessions will combine lecture-based, case-based, and hands-on learning opportunities.
CHEST Simulation Center
Practice your clinical skills in a hands-on learning environment. Work with expert faculty to sharpen your skills and apply your knowledge using real equipment and simulators.
General Sessions
Choose from hundreds of sessions, offered in a variety of instructional formats, including hands-on simulation, interactive case-based presentations, small-group discussions, and a rich variety of self-study modules and educational games.
Exhibit Hall
Don’t miss the showcase of diagnostic and treatment solutions for optimal patient care.
Explore Montréal!
Montréal is known for its warm camaraderie and joie de vivre!
You’ll enjoy this friendly city—a melting pot of ethnicities, languages, cuisines, and ideas. Explore Montréal’s history in Old Montréal, take in a hockey game at the Bell Centre, breathe in the fresh air at Mount Royal, or enjoy a wide variety of classic Montréal foods. During your free time at CHEST 2015, you’ll want to check out everything that Montréal has to offer.
Learn more about Montréal at tourisme-montreal.org, and find information about CHEST 2015 at chestmeeting.chestnet.org.
ABIM Incorporates Diplomate Recommendations Into MOC Program
We wanted to provide the pulmonary disease community with an update on the work ABIM has been doing to transform and improve its Maintenance of Certification (MOC) program. Recently, the Pulmonary Disease Board and Pulmonary Disease Board Exam Committee held a joint meeting in Philadelphia to discuss their roles in ensuring we continue to work closely with the physician community to enhance the MOC program, including the exam.
An important part of the work ABIM as a whole is undertaking is listening to the community so that it can design an MOC program that physicians find more meaningful and relevant. Tangible expressions of this listening are evident in the significant program changes announced by ABIM’s Board of Directors.
A few of the changes, among the others announced, include:
• Recognizing more activities for MOC credit. In an effort to better link MOC with activities that physicians are already doing to stay current, by the end of 2015, ABIM will begin to accept a wider variety of approved CME activities for MOC points and streamline the process for its medical society partners to submit new activities. ABIM is interested in finding ways to recognize meaningful clinical work that you do in your practices to earn CME credit and is particularly interested in recognizing CME activities for which there is evidence that they drive learning and/or change practice.
• New exam Score Report. Results of all examinations beginning with the spring 2015 MOC exam administration will be released in a new, electronic format. For years, ABIM has heard that diplomates want more specific feedback on exam performance. The new Score Report was redesigned and created with the feedback and guidance of ABIM board-certified physicians, including many members of ABIM governance and community physicians. This collaboration led ABIM to the design of a new Score Report, which offers:
• Clearer graphical explanations of exam performance
• More detailed feedback on questions missed
• Less technical jargon in explaining the report
• Links to more in-depth information on the ABIM website
• Updates to the Internal Medicine MOC exam blueprint. Over the past 4 months, the Internal Medicine Board, the Internal Medicine Board Exam Committee, and ABIM staff worked with a representative sample of practicing general internists to review and update the IM MOC exam blueprint. Internists rated blueprint topics for frequency in practice and rated the relative importance of tasks (eg, diagnosis) performed in relation to each of those topics. Their ratings will now inform the exam assembly process for the fall 2015 IM MOC exam. This process will be used in the future for other disciplines, including pulmonary disease.
We encourage you to visit the Transforming ABIM blog to view sample pages from the new Score Report, learn more about how ABIM collaborated with physicians to update the internal medicine MOC exam blueprint and read further about how ABIM came to the decision to change its website reporting language. In addition to the information on the exam Score Report and new blueprint, the blog also provides updates about ABIM’s ongoing discussions with the community, upcoming opportunities to provide input, and more information regarding the changes mentioned above. Subscribe to the blog.
Another way ABIM is collaborating with the physician community is through Assessment 2020, a task force commissioned by the ABIM Board of Directors to develop a vision for the future of assessment for certification (initial and maintenance) in internal medicine and associated subspecialties. The task force is comprised of experts with diverse areas of expertise including assessment, medicine, health policy, education and technology. Visit the site to learn more about how Assessment 2020 is engaging clinicians, patients and other important members of the community to provide feedback on the skills physicians need to deliver the highest quality of care. Additionally, read how ABIM is putting this feedback into action as we look for ways to innovate and enhance the exam experience.
Also, as you might be aware, earlier this year, ABIM suspended the Practice Assessment, Patient Voice, and Patient Safety requirements for at least 2 years. This means that physicians participating in the MOC program are not required to complete these requirements but should still work toward completing the existing Medical Knowledge and MOC exam requirements for their certifications. To learn more about your specific requirements and deadlines, log into www.abim.org to view your MOC Status Report.
We look forward to sharing more updates with you as we continue our work of ensuring the relevancy of MOC to pulmonary disease physicians across the country.
We wanted to provide the pulmonary disease community with an update on the work ABIM has been doing to transform and improve its Maintenance of Certification (MOC) program. Recently, the Pulmonary Disease Board and Pulmonary Disease Board Exam Committee held a joint meeting in Philadelphia to discuss their roles in ensuring we continue to work closely with the physician community to enhance the MOC program, including the exam.
An important part of the work ABIM as a whole is undertaking is listening to the community so that it can design an MOC program that physicians find more meaningful and relevant. Tangible expressions of this listening are evident in the significant program changes announced by ABIM’s Board of Directors.
A few of the changes, among the others announced, include:
• Recognizing more activities for MOC credit. In an effort to better link MOC with activities that physicians are already doing to stay current, by the end of 2015, ABIM will begin to accept a wider variety of approved CME activities for MOC points and streamline the process for its medical society partners to submit new activities. ABIM is interested in finding ways to recognize meaningful clinical work that you do in your practices to earn CME credit and is particularly interested in recognizing CME activities for which there is evidence that they drive learning and/or change practice.
• New exam Score Report. Results of all examinations beginning with the spring 2015 MOC exam administration will be released in a new, electronic format. For years, ABIM has heard that diplomates want more specific feedback on exam performance. The new Score Report was redesigned and created with the feedback and guidance of ABIM board-certified physicians, including many members of ABIM governance and community physicians. This collaboration led ABIM to the design of a new Score Report, which offers:
• Clearer graphical explanations of exam performance
• More detailed feedback on questions missed
• Less technical jargon in explaining the report
• Links to more in-depth information on the ABIM website
• Updates to the Internal Medicine MOC exam blueprint. Over the past 4 months, the Internal Medicine Board, the Internal Medicine Board Exam Committee, and ABIM staff worked with a representative sample of practicing general internists to review and update the IM MOC exam blueprint. Internists rated blueprint topics for frequency in practice and rated the relative importance of tasks (eg, diagnosis) performed in relation to each of those topics. Their ratings will now inform the exam assembly process for the fall 2015 IM MOC exam. This process will be used in the future for other disciplines, including pulmonary disease.
We encourage you to visit the Transforming ABIM blog to view sample pages from the new Score Report, learn more about how ABIM collaborated with physicians to update the internal medicine MOC exam blueprint and read further about how ABIM came to the decision to change its website reporting language. In addition to the information on the exam Score Report and new blueprint, the blog also provides updates about ABIM’s ongoing discussions with the community, upcoming opportunities to provide input, and more information regarding the changes mentioned above. Subscribe to the blog.
Another way ABIM is collaborating with the physician community is through Assessment 2020, a task force commissioned by the ABIM Board of Directors to develop a vision for the future of assessment for certification (initial and maintenance) in internal medicine and associated subspecialties. The task force is comprised of experts with diverse areas of expertise including assessment, medicine, health policy, education and technology. Visit the site to learn more about how Assessment 2020 is engaging clinicians, patients and other important members of the community to provide feedback on the skills physicians need to deliver the highest quality of care. Additionally, read how ABIM is putting this feedback into action as we look for ways to innovate and enhance the exam experience.
Also, as you might be aware, earlier this year, ABIM suspended the Practice Assessment, Patient Voice, and Patient Safety requirements for at least 2 years. This means that physicians participating in the MOC program are not required to complete these requirements but should still work toward completing the existing Medical Knowledge and MOC exam requirements for their certifications. To learn more about your specific requirements and deadlines, log into www.abim.org to view your MOC Status Report.
We look forward to sharing more updates with you as we continue our work of ensuring the relevancy of MOC to pulmonary disease physicians across the country.
We wanted to provide the pulmonary disease community with an update on the work ABIM has been doing to transform and improve its Maintenance of Certification (MOC) program. Recently, the Pulmonary Disease Board and Pulmonary Disease Board Exam Committee held a joint meeting in Philadelphia to discuss their roles in ensuring we continue to work closely with the physician community to enhance the MOC program, including the exam.
An important part of the work ABIM as a whole is undertaking is listening to the community so that it can design an MOC program that physicians find more meaningful and relevant. Tangible expressions of this listening are evident in the significant program changes announced by ABIM’s Board of Directors.
A few of the changes, among the others announced, include:
• Recognizing more activities for MOC credit. In an effort to better link MOC with activities that physicians are already doing to stay current, by the end of 2015, ABIM will begin to accept a wider variety of approved CME activities for MOC points and streamline the process for its medical society partners to submit new activities. ABIM is interested in finding ways to recognize meaningful clinical work that you do in your practices to earn CME credit and is particularly interested in recognizing CME activities for which there is evidence that they drive learning and/or change practice.
• New exam Score Report. Results of all examinations beginning with the spring 2015 MOC exam administration will be released in a new, electronic format. For years, ABIM has heard that diplomates want more specific feedback on exam performance. The new Score Report was redesigned and created with the feedback and guidance of ABIM board-certified physicians, including many members of ABIM governance and community physicians. This collaboration led ABIM to the design of a new Score Report, which offers:
• Clearer graphical explanations of exam performance
• More detailed feedback on questions missed
• Less technical jargon in explaining the report
• Links to more in-depth information on the ABIM website
• Updates to the Internal Medicine MOC exam blueprint. Over the past 4 months, the Internal Medicine Board, the Internal Medicine Board Exam Committee, and ABIM staff worked with a representative sample of practicing general internists to review and update the IM MOC exam blueprint. Internists rated blueprint topics for frequency in practice and rated the relative importance of tasks (eg, diagnosis) performed in relation to each of those topics. Their ratings will now inform the exam assembly process for the fall 2015 IM MOC exam. This process will be used in the future for other disciplines, including pulmonary disease.
We encourage you to visit the Transforming ABIM blog to view sample pages from the new Score Report, learn more about how ABIM collaborated with physicians to update the internal medicine MOC exam blueprint and read further about how ABIM came to the decision to change its website reporting language. In addition to the information on the exam Score Report and new blueprint, the blog also provides updates about ABIM’s ongoing discussions with the community, upcoming opportunities to provide input, and more information regarding the changes mentioned above. Subscribe to the blog.
Another way ABIM is collaborating with the physician community is through Assessment 2020, a task force commissioned by the ABIM Board of Directors to develop a vision for the future of assessment for certification (initial and maintenance) in internal medicine and associated subspecialties. The task force is comprised of experts with diverse areas of expertise including assessment, medicine, health policy, education and technology. Visit the site to learn more about how Assessment 2020 is engaging clinicians, patients and other important members of the community to provide feedback on the skills physicians need to deliver the highest quality of care. Additionally, read how ABIM is putting this feedback into action as we look for ways to innovate and enhance the exam experience.
Also, as you might be aware, earlier this year, ABIM suspended the Practice Assessment, Patient Voice, and Patient Safety requirements for at least 2 years. This means that physicians participating in the MOC program are not required to complete these requirements but should still work toward completing the existing Medical Knowledge and MOC exam requirements for their certifications. To learn more about your specific requirements and deadlines, log into www.abim.org to view your MOC Status Report.
We look forward to sharing more updates with you as we continue our work of ensuring the relevancy of MOC to pulmonary disease physicians across the country.