User login
Fellow in HM
One of the best things about working in the membership department is seeing the passion and commitment our members have for the success of our specialty. You also get to hear about what is needed to elevate our field to the next level.
Throughout the past 10 years, hospitalists have been asking for a unique designation that clearly identifies those physicians whose career is committed to hospital medicine. SHM wants you to know that we have heard you and have responded to this need by creating a Fellowship in Hospital Medicine (FHM) program.
Hospitalists who earn their FHM designation will have a demonstrated commitment to hospital medicine, systems change, and quality improvement principals. There will be three designations available, each with increasingly more challenging selection criteria:
- Fellow in Hospital Medicine (FHM);
- Senior Fellow in Hospital Medicine (SFHM); and
- Master in Hospital Medicine (MHM).
Application requirements include:
- Five years as a practicing hospitalist;
- Demonstration of competencies tied to the SHM Core Competencies in Hospital Medicine, including systems improvement, quality initiatives, and clinical excellence; and
- Endorsement by two active SHM members.
Applications for Fellow in Hospital Medicine will be available this fall, and the first class will be inducted at Hospital Medicine 2009 in Chicago.
One of the best things about working in the membership department is seeing the passion and commitment our members have for the success of our specialty. You also get to hear about what is needed to elevate our field to the next level.
Throughout the past 10 years, hospitalists have been asking for a unique designation that clearly identifies those physicians whose career is committed to hospital medicine. SHM wants you to know that we have heard you and have responded to this need by creating a Fellowship in Hospital Medicine (FHM) program.
Hospitalists who earn their FHM designation will have a demonstrated commitment to hospital medicine, systems change, and quality improvement principals. There will be three designations available, each with increasingly more challenging selection criteria:
- Fellow in Hospital Medicine (FHM);
- Senior Fellow in Hospital Medicine (SFHM); and
- Master in Hospital Medicine (MHM).
Application requirements include:
- Five years as a practicing hospitalist;
- Demonstration of competencies tied to the SHM Core Competencies in Hospital Medicine, including systems improvement, quality initiatives, and clinical excellence; and
- Endorsement by two active SHM members.
Applications for Fellow in Hospital Medicine will be available this fall, and the first class will be inducted at Hospital Medicine 2009 in Chicago.
One of the best things about working in the membership department is seeing the passion and commitment our members have for the success of our specialty. You also get to hear about what is needed to elevate our field to the next level.
Throughout the past 10 years, hospitalists have been asking for a unique designation that clearly identifies those physicians whose career is committed to hospital medicine. SHM wants you to know that we have heard you and have responded to this need by creating a Fellowship in Hospital Medicine (FHM) program.
Hospitalists who earn their FHM designation will have a demonstrated commitment to hospital medicine, systems change, and quality improvement principals. There will be three designations available, each with increasingly more challenging selection criteria:
- Fellow in Hospital Medicine (FHM);
- Senior Fellow in Hospital Medicine (SFHM); and
- Master in Hospital Medicine (MHM).
Application requirements include:
- Five years as a practicing hospitalist;
- Demonstration of competencies tied to the SHM Core Competencies in Hospital Medicine, including systems improvement, quality initiatives, and clinical excellence; and
- Endorsement by two active SHM members.
Applications for Fellow in Hospital Medicine will be available this fall, and the first class will be inducted at Hospital Medicine 2009 in Chicago.
Malpractice Chronicle
Reprinted with permission from Medical Malpractice Verdicts, Settlements and Experts, Lewis Laska, Editor, (800) 298-6288.
Cesarean Delivery Too Late to Prevent Uterine Rupture
A pregnant woman with hypertension and associated medical concerns was admitted to the hospital for induction of labor. She had previously undergone a cesarean delivery.
Synthetic oxytocin was started. That evening, dinoprostone was administered, and synthetic oxytocin was substituted for it the following morning.
That afternoon, the patient complained of severe uterine pain. She was 3.0 cm dilated and 60% effaced; she was then given butorphanol tartrate.
Because labor was not progressing, the defendant obstetrician decided to perform a cesarean delivery, then left with the nurse to attend to another patient. When the nurse returned, she noted that the fetal heart rate tracing had become dangerously slow, and she paged the obstetrician.
By the time he arrived, the membranes had ruptured. A fetal scalp electrode was placed, revealing a fetal heart rate of 70 beats/min. A "stat" cesarean delivery was ordered.
Twenty-four minutes elapsed from the time the fetal heart rate anomaly was noted to the time the incision was made. The uterus was found to have ruptured; the infant, a boy, was floating in the woman's abdominal cavity under her diaphragm. He was resuscitated and transferred to a children's hospital, where he was diagnosed with hypoxic ischemic encephalopathy and choreoathetoid cerebral palsy.
The plaintiff charged the defendants with negligence in failing to perform the surgery earlier. The defendants denied any negligence and contended that the woman's complaints of pain were not extraordinary.
According to a published account, a defense verdict was returned.
Conflicting Accounts About ED Referral for Man With Back Pain
After being given prescriptions for carisoprodol and hydrocodone with acetaminophen for back pain, a 26-year-old man returned to Dr. S., the defendant primary care physician, complaining of unremitting pain. Dr. S., who had been treating the plaintiff for staph infections, suspected a spinal epidural abscess. He prescribed naproxen, referred the patient to a laboratory for blood testing, and directed him to go to the emergency department (ED) if the pain worsened or if he developed neurologic symptoms.
That evening, the man's pain worsened, and he was taken to the ED. The ED physician considered a differential diagnosis that included epidural abscess. After consulting with the on-call primary care physician, the ED physician wrote holding orders for admission to the hospital. Very early the next morning, the patient complained to a nurse that he could not move his legs. Morphine was administered, and he slept for seven hours.
When he awoke, a nurse checked his status and reported that the patient was flaccid and paralyzed from the umbilicus down. Dr. S. came to see the plaintiff at about 11:00 am and discovered that he was paralyzed. Dr. S. ordered CT, then changed the order to one for MRI. In the hospital history, Dr. S. dictated that he had directed the patient to report to the ED the previous afternoon, but that he had refused.
The MRI revealed a large epidural abscess. Laminectomy was performed, and the abscess was removed.
The plaintiff never regained function in his legs, bowel, or bladder. He continued to experience spasms that were strong enough to eject him from his wheelchair.
The plaintiff alleged negligence by Dr. S., the hospital, and the ED physicians. The hospital and ED physicians settled for $1.25 million prior to trial.
At trial, the plaintiff claimed that Dr. S. had failed to properly refer him to the ED.
The defendant claimed that even if the plaintiff had been sent to the ED, he might not have undergone MRI and received treatment before paralysis developed. Dr. S. claimed that the hospital physicians and staff had delayed the diagnosis and treatment of the epidural abscess. He also claimed that he had instructed the plaintiff to go to the ED immediately because he might be at risk for paralysis, but the plaintiff had refused. Dr. S. argued that he ordered the blood work and prescribed naproxen only after the plaintiff refused to go to the ED. The plaintiff denied that Dr. S. had told him to go to the ED or risk paralysis.
According to a published account, a verdict of $9,420,840 was returned. Calculation of credit for the settlements and application of the 1975 Medical Injury Compensation Reform Act were pending.
Did Acne Medication Cause IBD?
For four months, a 14-year-old boy was treated with isotretinoin for acne. During this time, he noticed that he had chapped lips and achy knees.
Within the following year, the patient began to experience severe gastrointestinal pain, which was ultimately diagnosed as inflammatory bowel disease (IBD). Eventually, he underwent partial removal of his rectum and almost his entire colon.
After years of using a colostomy bag, the patient underwent surgery to connect the remains of his colon and anus, but there was not enough left of his colon to draw out excess water, and he now has permanent diarrhea.
The plaintiff claimed that the labeling for isotretinoin provided insufficient warning regarding the risk of bowel disease. The defendant manufacturer claimed that isotretinoin labeling had warned about IBD as a possible adverse effect for more than 20 years. The company also maintained that there is no significant scientific evidence to prove that the medication causes IBD.
According to a published report, a $2,619,000 verdict was returned.
Symptoms Should Have Prompted Repeat Urinalysis
In September 2002, a 62-year-old man with a 30-year history of smoking went to the defendant, his primary care physician, with a complaint of urinary symptoms. He had not undergone a general physical examination in three years.
Laboratory work was ordered. Red and white blood cells, protein, and bacteria were found in the urinalysis. The blood chemistry panel revealed elevated total cholesterol, slightly elevated glucose, and findings indicating a hereditary red blood cell abnormality.
During a subsequent phone call, the primary care physician made a diagnosis of urinary tract infection and prescribed antibiotics. The patient told the physician that he was experiencing discomfort and pain during urination. Whether the patient was advised to return for repeat laboratory studies once he had completed the prescribed antibiotics was later disputed.
In March 2003, the man presented to a gastroenterologist for a screening colonoscopy, as recommended by the defendant in September 2002. The man mentioned to the gastroenterologist that he was experiencing urinary discomfort and frequency. The gastroenterologist ordered urinalysis, and red and white blood cells, bacteria, and protein were found once again. Ten days later, the patient visited a urologist, who performed a cystoscopy and made a diagnosis of bladder cancer. Surgery revealed that the cancer had metastasized into a lymph node.
The patient underwent chemotherapy, but in early 2006 the cancer recurred in his liver and hip joint. He died in March 2006.
The plaintiff, the decedent's widow, alleged negligence by the defendant primary care physician in failing to repeat the urinalysis (she claimed to have overheard the phone conversation in question and denied hearing any such instruction) and in failing to stress the importance of returning for repeat urinalysis. The plaintiff claimed that if the cancer had been diagnosed earlier, her husband would have had a high probability of survival.
The defendant maintained that the decedent had been treated properly and that the defendant's advice to repeat the urinalysis had been ignored. The defendant also claimed that he was not required to inform the decedent of any risk for bladder cancer. Additionally, the defendant claimed that the decedent had an extremely aggressive, high-grade bladder cancer that had most likely metastasized before September 2002.
According to a published account, a defense verdict was returned.
Reprinted with permission from Medical Malpractice Verdicts, Settlements and Experts, Lewis Laska, Editor, (800) 298-6288.
Cesarean Delivery Too Late to Prevent Uterine Rupture
A pregnant woman with hypertension and associated medical concerns was admitted to the hospital for induction of labor. She had previously undergone a cesarean delivery.
Synthetic oxytocin was started. That evening, dinoprostone was administered, and synthetic oxytocin was substituted for it the following morning.
That afternoon, the patient complained of severe uterine pain. She was 3.0 cm dilated and 60% effaced; she was then given butorphanol tartrate.
Because labor was not progressing, the defendant obstetrician decided to perform a cesarean delivery, then left with the nurse to attend to another patient. When the nurse returned, she noted that the fetal heart rate tracing had become dangerously slow, and she paged the obstetrician.
By the time he arrived, the membranes had ruptured. A fetal scalp electrode was placed, revealing a fetal heart rate of 70 beats/min. A "stat" cesarean delivery was ordered.
Twenty-four minutes elapsed from the time the fetal heart rate anomaly was noted to the time the incision was made. The uterus was found to have ruptured; the infant, a boy, was floating in the woman's abdominal cavity under her diaphragm. He was resuscitated and transferred to a children's hospital, where he was diagnosed with hypoxic ischemic encephalopathy and choreoathetoid cerebral palsy.
The plaintiff charged the defendants with negligence in failing to perform the surgery earlier. The defendants denied any negligence and contended that the woman's complaints of pain were not extraordinary.
According to a published account, a defense verdict was returned.
Conflicting Accounts About ED Referral for Man With Back Pain
After being given prescriptions for carisoprodol and hydrocodone with acetaminophen for back pain, a 26-year-old man returned to Dr. S., the defendant primary care physician, complaining of unremitting pain. Dr. S., who had been treating the plaintiff for staph infections, suspected a spinal epidural abscess. He prescribed naproxen, referred the patient to a laboratory for blood testing, and directed him to go to the emergency department (ED) if the pain worsened or if he developed neurologic symptoms.
That evening, the man's pain worsened, and he was taken to the ED. The ED physician considered a differential diagnosis that included epidural abscess. After consulting with the on-call primary care physician, the ED physician wrote holding orders for admission to the hospital. Very early the next morning, the patient complained to a nurse that he could not move his legs. Morphine was administered, and he slept for seven hours.
When he awoke, a nurse checked his status and reported that the patient was flaccid and paralyzed from the umbilicus down. Dr. S. came to see the plaintiff at about 11:00 am and discovered that he was paralyzed. Dr. S. ordered CT, then changed the order to one for MRI. In the hospital history, Dr. S. dictated that he had directed the patient to report to the ED the previous afternoon, but that he had refused.
The MRI revealed a large epidural abscess. Laminectomy was performed, and the abscess was removed.
The plaintiff never regained function in his legs, bowel, or bladder. He continued to experience spasms that were strong enough to eject him from his wheelchair.
The plaintiff alleged negligence by Dr. S., the hospital, and the ED physicians. The hospital and ED physicians settled for $1.25 million prior to trial.
At trial, the plaintiff claimed that Dr. S. had failed to properly refer him to the ED.
The defendant claimed that even if the plaintiff had been sent to the ED, he might not have undergone MRI and received treatment before paralysis developed. Dr. S. claimed that the hospital physicians and staff had delayed the diagnosis and treatment of the epidural abscess. He also claimed that he had instructed the plaintiff to go to the ED immediately because he might be at risk for paralysis, but the plaintiff had refused. Dr. S. argued that he ordered the blood work and prescribed naproxen only after the plaintiff refused to go to the ED. The plaintiff denied that Dr. S. had told him to go to the ED or risk paralysis.
According to a published account, a verdict of $9,420,840 was returned. Calculation of credit for the settlements and application of the 1975 Medical Injury Compensation Reform Act were pending.
Did Acne Medication Cause IBD?
For four months, a 14-year-old boy was treated with isotretinoin for acne. During this time, he noticed that he had chapped lips and achy knees.
Within the following year, the patient began to experience severe gastrointestinal pain, which was ultimately diagnosed as inflammatory bowel disease (IBD). Eventually, he underwent partial removal of his rectum and almost his entire colon.
After years of using a colostomy bag, the patient underwent surgery to connect the remains of his colon and anus, but there was not enough left of his colon to draw out excess water, and he now has permanent diarrhea.
The plaintiff claimed that the labeling for isotretinoin provided insufficient warning regarding the risk of bowel disease. The defendant manufacturer claimed that isotretinoin labeling had warned about IBD as a possible adverse effect for more than 20 years. The company also maintained that there is no significant scientific evidence to prove that the medication causes IBD.
According to a published report, a $2,619,000 verdict was returned.
Symptoms Should Have Prompted Repeat Urinalysis
In September 2002, a 62-year-old man with a 30-year history of smoking went to the defendant, his primary care physician, with a complaint of urinary symptoms. He had not undergone a general physical examination in three years.
Laboratory work was ordered. Red and white blood cells, protein, and bacteria were found in the urinalysis. The blood chemistry panel revealed elevated total cholesterol, slightly elevated glucose, and findings indicating a hereditary red blood cell abnormality.
During a subsequent phone call, the primary care physician made a diagnosis of urinary tract infection and prescribed antibiotics. The patient told the physician that he was experiencing discomfort and pain during urination. Whether the patient was advised to return for repeat laboratory studies once he had completed the prescribed antibiotics was later disputed.
In March 2003, the man presented to a gastroenterologist for a screening colonoscopy, as recommended by the defendant in September 2002. The man mentioned to the gastroenterologist that he was experiencing urinary discomfort and frequency. The gastroenterologist ordered urinalysis, and red and white blood cells, bacteria, and protein were found once again. Ten days later, the patient visited a urologist, who performed a cystoscopy and made a diagnosis of bladder cancer. Surgery revealed that the cancer had metastasized into a lymph node.
The patient underwent chemotherapy, but in early 2006 the cancer recurred in his liver and hip joint. He died in March 2006.
The plaintiff, the decedent's widow, alleged negligence by the defendant primary care physician in failing to repeat the urinalysis (she claimed to have overheard the phone conversation in question and denied hearing any such instruction) and in failing to stress the importance of returning for repeat urinalysis. The plaintiff claimed that if the cancer had been diagnosed earlier, her husband would have had a high probability of survival.
The defendant maintained that the decedent had been treated properly and that the defendant's advice to repeat the urinalysis had been ignored. The defendant also claimed that he was not required to inform the decedent of any risk for bladder cancer. Additionally, the defendant claimed that the decedent had an extremely aggressive, high-grade bladder cancer that had most likely metastasized before September 2002.
According to a published account, a defense verdict was returned.
Reprinted with permission from Medical Malpractice Verdicts, Settlements and Experts, Lewis Laska, Editor, (800) 298-6288.
Cesarean Delivery Too Late to Prevent Uterine Rupture
A pregnant woman with hypertension and associated medical concerns was admitted to the hospital for induction of labor. She had previously undergone a cesarean delivery.
Synthetic oxytocin was started. That evening, dinoprostone was administered, and synthetic oxytocin was substituted for it the following morning.
That afternoon, the patient complained of severe uterine pain. She was 3.0 cm dilated and 60% effaced; she was then given butorphanol tartrate.
Because labor was not progressing, the defendant obstetrician decided to perform a cesarean delivery, then left with the nurse to attend to another patient. When the nurse returned, she noted that the fetal heart rate tracing had become dangerously slow, and she paged the obstetrician.
By the time he arrived, the membranes had ruptured. A fetal scalp electrode was placed, revealing a fetal heart rate of 70 beats/min. A "stat" cesarean delivery was ordered.
Twenty-four minutes elapsed from the time the fetal heart rate anomaly was noted to the time the incision was made. The uterus was found to have ruptured; the infant, a boy, was floating in the woman's abdominal cavity under her diaphragm. He was resuscitated and transferred to a children's hospital, where he was diagnosed with hypoxic ischemic encephalopathy and choreoathetoid cerebral palsy.
The plaintiff charged the defendants with negligence in failing to perform the surgery earlier. The defendants denied any negligence and contended that the woman's complaints of pain were not extraordinary.
According to a published account, a defense verdict was returned.
Conflicting Accounts About ED Referral for Man With Back Pain
After being given prescriptions for carisoprodol and hydrocodone with acetaminophen for back pain, a 26-year-old man returned to Dr. S., the defendant primary care physician, complaining of unremitting pain. Dr. S., who had been treating the plaintiff for staph infections, suspected a spinal epidural abscess. He prescribed naproxen, referred the patient to a laboratory for blood testing, and directed him to go to the emergency department (ED) if the pain worsened or if he developed neurologic symptoms.
That evening, the man's pain worsened, and he was taken to the ED. The ED physician considered a differential diagnosis that included epidural abscess. After consulting with the on-call primary care physician, the ED physician wrote holding orders for admission to the hospital. Very early the next morning, the patient complained to a nurse that he could not move his legs. Morphine was administered, and he slept for seven hours.
When he awoke, a nurse checked his status and reported that the patient was flaccid and paralyzed from the umbilicus down. Dr. S. came to see the plaintiff at about 11:00 am and discovered that he was paralyzed. Dr. S. ordered CT, then changed the order to one for MRI. In the hospital history, Dr. S. dictated that he had directed the patient to report to the ED the previous afternoon, but that he had refused.
The MRI revealed a large epidural abscess. Laminectomy was performed, and the abscess was removed.
The plaintiff never regained function in his legs, bowel, or bladder. He continued to experience spasms that were strong enough to eject him from his wheelchair.
The plaintiff alleged negligence by Dr. S., the hospital, and the ED physicians. The hospital and ED physicians settled for $1.25 million prior to trial.
At trial, the plaintiff claimed that Dr. S. had failed to properly refer him to the ED.
The defendant claimed that even if the plaintiff had been sent to the ED, he might not have undergone MRI and received treatment before paralysis developed. Dr. S. claimed that the hospital physicians and staff had delayed the diagnosis and treatment of the epidural abscess. He also claimed that he had instructed the plaintiff to go to the ED immediately because he might be at risk for paralysis, but the plaintiff had refused. Dr. S. argued that he ordered the blood work and prescribed naproxen only after the plaintiff refused to go to the ED. The plaintiff denied that Dr. S. had told him to go to the ED or risk paralysis.
According to a published account, a verdict of $9,420,840 was returned. Calculation of credit for the settlements and application of the 1975 Medical Injury Compensation Reform Act were pending.
Did Acne Medication Cause IBD?
For four months, a 14-year-old boy was treated with isotretinoin for acne. During this time, he noticed that he had chapped lips and achy knees.
Within the following year, the patient began to experience severe gastrointestinal pain, which was ultimately diagnosed as inflammatory bowel disease (IBD). Eventually, he underwent partial removal of his rectum and almost his entire colon.
After years of using a colostomy bag, the patient underwent surgery to connect the remains of his colon and anus, but there was not enough left of his colon to draw out excess water, and he now has permanent diarrhea.
The plaintiff claimed that the labeling for isotretinoin provided insufficient warning regarding the risk of bowel disease. The defendant manufacturer claimed that isotretinoin labeling had warned about IBD as a possible adverse effect for more than 20 years. The company also maintained that there is no significant scientific evidence to prove that the medication causes IBD.
According to a published report, a $2,619,000 verdict was returned.
Symptoms Should Have Prompted Repeat Urinalysis
In September 2002, a 62-year-old man with a 30-year history of smoking went to the defendant, his primary care physician, with a complaint of urinary symptoms. He had not undergone a general physical examination in three years.
Laboratory work was ordered. Red and white blood cells, protein, and bacteria were found in the urinalysis. The blood chemistry panel revealed elevated total cholesterol, slightly elevated glucose, and findings indicating a hereditary red blood cell abnormality.
During a subsequent phone call, the primary care physician made a diagnosis of urinary tract infection and prescribed antibiotics. The patient told the physician that he was experiencing discomfort and pain during urination. Whether the patient was advised to return for repeat laboratory studies once he had completed the prescribed antibiotics was later disputed.
In March 2003, the man presented to a gastroenterologist for a screening colonoscopy, as recommended by the defendant in September 2002. The man mentioned to the gastroenterologist that he was experiencing urinary discomfort and frequency. The gastroenterologist ordered urinalysis, and red and white blood cells, bacteria, and protein were found once again. Ten days later, the patient visited a urologist, who performed a cystoscopy and made a diagnosis of bladder cancer. Surgery revealed that the cancer had metastasized into a lymph node.
The patient underwent chemotherapy, but in early 2006 the cancer recurred in his liver and hip joint. He died in March 2006.
The plaintiff, the decedent's widow, alleged negligence by the defendant primary care physician in failing to repeat the urinalysis (she claimed to have overheard the phone conversation in question and denied hearing any such instruction) and in failing to stress the importance of returning for repeat urinalysis. The plaintiff claimed that if the cancer had been diagnosed earlier, her husband would have had a high probability of survival.
The defendant maintained that the decedent had been treated properly and that the defendant's advice to repeat the urinalysis had been ignored. The defendant also claimed that he was not required to inform the decedent of any risk for bladder cancer. Additionally, the defendant claimed that the decedent had an extremely aggressive, high-grade bladder cancer that had most likely metastasized before September 2002.
According to a published account, a defense verdict was returned.
10 Ways to Help Your Case
Even following the best practices, some patients will suffer adverse outcomes—and some of those patients will bring a lawsuit. Knowing that some of you either are defending claims against you or that you may have to defend a claim in the future, we wanted to provide you with a bit of practical advice that may ease the burden of litigation.
1) Engage: Many physicians want to put a lawsuit out of their mind and “let the lawyer handle it.” Just as a patient can’t cure a cancer by ignoring it, avoiding a lawsuit is not going to make it go away.
While much of the legal work takes place on a day-to-day basis without your participation, you need to remember that this is your lawsuit, not your lawyer’s lawsuit. If you do not engage with your lawyer and help the lawyer shape the defense, your lawyer may end up presenting the wrong theories. More importantly, spending time with your lawyer will help them understand your personality and the way you interact with your patients. If your lawyer doesn’t know you very well, it’s very difficult for the lawyer to build rapport between you and the jurors, who ultimately will determine the outcome of the lawsuit.
2) Teach: Many defense lawyers have picked up a fair amount of medical knowledge during our careers, but few of us have practiced medicine. As you certainly know, the fact that your lawyer has read surgical textbooks doesn’t make them qualified to perform surgery.
Because you have cared for thousands of patients, you know more about your area of medical expertise than we can ever hope to gain in the course of defending a lawsuit. Teach us the medicine that will enable us to understand how and why you made important decisions while caring for the plaintiff. Ultimately, our success at trial depends on our ability to convince juries that your decisions were thoughtful and reasonable, but we can’t do that without your help.
3) Select: In almost every medical malpractice case, the parties will endorse physicians to provide the jury with expert testimony about the medical issues. These experts become important witnesses because they help the jury understand the relevant standards of care and determine whether an allegedly negligent act caused the plaintiff to suffer an injury.
You probably know the well-respected practitioners in your field who would make credible and persuasive witnesses. Help us identify them and persuade them to serve as experts on your behalf.
4) Prepare: During the course of a lawsuit, one of the most critical events is your deposition. During your deposition, the opposing lawyer will attempt to “lock you in” on the key issues in the case and prevent you from changing your testimony at the time of trial. Consequently, you have to be well prepared for your deposition, both in terms of knowing the facts of the plaintiff’s care (which may have been rendered several years earlier) and in knowing the medical principles that applied to the plaintiff’s care.
You must demand your lawyer adequately prepare you for the deposition by reviewing these matters and preparing you for the deposition process. You need to understand how lawyers frame questions in the hopes of obtaining responses that will come back to haunt you. If you haven’t devoted the time and energy necessary for you to understand and feel comfortable with the process before sitting down for the deposition, you’re in trouble.
5) Attend: Your deposition is the only event before trial that you legally are required to attend. As a defendant, however, you have a right to attend any other deposition that takes place before trial, including the deposition of the plaintiffs and the opposing experts.
If you attend the plaintiff’s deposition, you will have the firsthand ability to hear that person’s story, and you then have the ability to suggest areas where your lawyer can challenge the plaintiff’s recollection. If you attend the opposing expert’s deposition, you similarly have the ability to hear that person’s criticisms, and you can suggest areas where your lawyer can challenge the factual or medical basis for the opinions.
6) Demonstrate: Contrary to television depictions, a trial can be a long and boring process, particularly when there’s nothing to capture the jury’s attention. Jurors have a hard time following a witness’s testimony when it consists solely of questions and answers.
This problem can be compounded when the testimony consists of technical medical information. To prevent boredom and inattention, we want to engage the jurors—and you can help us do it. Give us props, whether in the form of anatomic models, instruments used during the procedure, photographs, charts, or animations that will allow us to capture the jury’s imagination.
7) Communicate: Lawyers and doctors work in different environments. For example, you have the ability to order a test and receive the results within hours, but lawyers generally have weeks to respond to an opposing party’s requests for information. Doctors often receive results that are quantifiable and measurable—but ambiguity and nuance are a lawyer’s stock in trade.
You will be frustrated as you go through the litigation, and you need to have clear and open channels of communication with your lawyer.
Just as your patients depend upon you to orient them within an unfamiliar and frightening environment, your lawyer should help you understand what’s happening in your case. If you don’t have enough information to make intelligent decisions, you should ask for more.
8) Trust: While it’s vital to engage in the process and understand how the lawsuit is proceeding, you need to remember you are not a lawyer. There will be times when your lawyer will have to make judgment calls, and you need to give your lawyer the ability to make those decisions.
Please don’t misunderstand: You have a right to make informed decisions, but a lawyer will make hundreds of judgment calls in the course of a trial, such as whether to dismiss a potential juror, pursue a certain line of questioning with a witness, or introduce a particular exhibit. Some of your lawyer’s recommendations may seem counterintuitive to you, but the courtroom is our operating room.
9) Defend: Most jurors come to the courtroom with some skepticism of medical malpractice claims. One of the reasons for this skepticism is jurors generally like their own physicians and want to believe the medical system functions properly. When they hear a plaintiff’s claim that they were injured through medical negligence, they want the physicians involved in the care to explain how the injury occurred and why it wasn’t the physicians’ fault.
You need to be able to stand up, look the jurors in the eye, explain that your care was appropriate, and withstand an attorney’s attempts to impeach your credibility. If you are unwilling to stand up and fight for yourself and your care, there’s little reason to expect the jurors will fight on your behalf once they begin their deliberations.
10) Relax: This may be the most important tip of all. Lawsuits impose a tremendous amount of stress upon all of the participants, but especially upon a physician whose care is under fire.
We’ve represented physicians who have become so stressed and frustrated by the litigation process that it has overwhelmed them and harmed their ability to provide high-quality care for their ongoing patients.
Some physicians resort to alcohol or other substances to cope with stress. This is the worst possible scenario because it increases the likelihood that you will face another lawsuit in the future.
You need to recognize the stress imposed by a lawsuit, take care of yourself, take care of your practice, and seek help when appropriate. Almost every state has a peer-counseling program for physicians that offers specialized and confidential assistance for physicians. Contact your local medical association for a referral to one of these organizations. TH
Patrick O’Rourke works in the Office of University Counsel, Department of Litigation, University of Colorado, Denver.
Even following the best practices, some patients will suffer adverse outcomes—and some of those patients will bring a lawsuit. Knowing that some of you either are defending claims against you or that you may have to defend a claim in the future, we wanted to provide you with a bit of practical advice that may ease the burden of litigation.
1) Engage: Many physicians want to put a lawsuit out of their mind and “let the lawyer handle it.” Just as a patient can’t cure a cancer by ignoring it, avoiding a lawsuit is not going to make it go away.
While much of the legal work takes place on a day-to-day basis without your participation, you need to remember that this is your lawsuit, not your lawyer’s lawsuit. If you do not engage with your lawyer and help the lawyer shape the defense, your lawyer may end up presenting the wrong theories. More importantly, spending time with your lawyer will help them understand your personality and the way you interact with your patients. If your lawyer doesn’t know you very well, it’s very difficult for the lawyer to build rapport between you and the jurors, who ultimately will determine the outcome of the lawsuit.
2) Teach: Many defense lawyers have picked up a fair amount of medical knowledge during our careers, but few of us have practiced medicine. As you certainly know, the fact that your lawyer has read surgical textbooks doesn’t make them qualified to perform surgery.
Because you have cared for thousands of patients, you know more about your area of medical expertise than we can ever hope to gain in the course of defending a lawsuit. Teach us the medicine that will enable us to understand how and why you made important decisions while caring for the plaintiff. Ultimately, our success at trial depends on our ability to convince juries that your decisions were thoughtful and reasonable, but we can’t do that without your help.
3) Select: In almost every medical malpractice case, the parties will endorse physicians to provide the jury with expert testimony about the medical issues. These experts become important witnesses because they help the jury understand the relevant standards of care and determine whether an allegedly negligent act caused the plaintiff to suffer an injury.
You probably know the well-respected practitioners in your field who would make credible and persuasive witnesses. Help us identify them and persuade them to serve as experts on your behalf.
4) Prepare: During the course of a lawsuit, one of the most critical events is your deposition. During your deposition, the opposing lawyer will attempt to “lock you in” on the key issues in the case and prevent you from changing your testimony at the time of trial. Consequently, you have to be well prepared for your deposition, both in terms of knowing the facts of the plaintiff’s care (which may have been rendered several years earlier) and in knowing the medical principles that applied to the plaintiff’s care.
You must demand your lawyer adequately prepare you for the deposition by reviewing these matters and preparing you for the deposition process. You need to understand how lawyers frame questions in the hopes of obtaining responses that will come back to haunt you. If you haven’t devoted the time and energy necessary for you to understand and feel comfortable with the process before sitting down for the deposition, you’re in trouble.
5) Attend: Your deposition is the only event before trial that you legally are required to attend. As a defendant, however, you have a right to attend any other deposition that takes place before trial, including the deposition of the plaintiffs and the opposing experts.
If you attend the plaintiff’s deposition, you will have the firsthand ability to hear that person’s story, and you then have the ability to suggest areas where your lawyer can challenge the plaintiff’s recollection. If you attend the opposing expert’s deposition, you similarly have the ability to hear that person’s criticisms, and you can suggest areas where your lawyer can challenge the factual or medical basis for the opinions.
6) Demonstrate: Contrary to television depictions, a trial can be a long and boring process, particularly when there’s nothing to capture the jury’s attention. Jurors have a hard time following a witness’s testimony when it consists solely of questions and answers.
This problem can be compounded when the testimony consists of technical medical information. To prevent boredom and inattention, we want to engage the jurors—and you can help us do it. Give us props, whether in the form of anatomic models, instruments used during the procedure, photographs, charts, or animations that will allow us to capture the jury’s imagination.
7) Communicate: Lawyers and doctors work in different environments. For example, you have the ability to order a test and receive the results within hours, but lawyers generally have weeks to respond to an opposing party’s requests for information. Doctors often receive results that are quantifiable and measurable—but ambiguity and nuance are a lawyer’s stock in trade.
You will be frustrated as you go through the litigation, and you need to have clear and open channels of communication with your lawyer.
Just as your patients depend upon you to orient them within an unfamiliar and frightening environment, your lawyer should help you understand what’s happening in your case. If you don’t have enough information to make intelligent decisions, you should ask for more.
8) Trust: While it’s vital to engage in the process and understand how the lawsuit is proceeding, you need to remember you are not a lawyer. There will be times when your lawyer will have to make judgment calls, and you need to give your lawyer the ability to make those decisions.
Please don’t misunderstand: You have a right to make informed decisions, but a lawyer will make hundreds of judgment calls in the course of a trial, such as whether to dismiss a potential juror, pursue a certain line of questioning with a witness, or introduce a particular exhibit. Some of your lawyer’s recommendations may seem counterintuitive to you, but the courtroom is our operating room.
9) Defend: Most jurors come to the courtroom with some skepticism of medical malpractice claims. One of the reasons for this skepticism is jurors generally like their own physicians and want to believe the medical system functions properly. When they hear a plaintiff’s claim that they were injured through medical negligence, they want the physicians involved in the care to explain how the injury occurred and why it wasn’t the physicians’ fault.
You need to be able to stand up, look the jurors in the eye, explain that your care was appropriate, and withstand an attorney’s attempts to impeach your credibility. If you are unwilling to stand up and fight for yourself and your care, there’s little reason to expect the jurors will fight on your behalf once they begin their deliberations.
10) Relax: This may be the most important tip of all. Lawsuits impose a tremendous amount of stress upon all of the participants, but especially upon a physician whose care is under fire.
We’ve represented physicians who have become so stressed and frustrated by the litigation process that it has overwhelmed them and harmed their ability to provide high-quality care for their ongoing patients.
Some physicians resort to alcohol or other substances to cope with stress. This is the worst possible scenario because it increases the likelihood that you will face another lawsuit in the future.
You need to recognize the stress imposed by a lawsuit, take care of yourself, take care of your practice, and seek help when appropriate. Almost every state has a peer-counseling program for physicians that offers specialized and confidential assistance for physicians. Contact your local medical association for a referral to one of these organizations. TH
Patrick O’Rourke works in the Office of University Counsel, Department of Litigation, University of Colorado, Denver.
Even following the best practices, some patients will suffer adverse outcomes—and some of those patients will bring a lawsuit. Knowing that some of you either are defending claims against you or that you may have to defend a claim in the future, we wanted to provide you with a bit of practical advice that may ease the burden of litigation.
1) Engage: Many physicians want to put a lawsuit out of their mind and “let the lawyer handle it.” Just as a patient can’t cure a cancer by ignoring it, avoiding a lawsuit is not going to make it go away.
While much of the legal work takes place on a day-to-day basis without your participation, you need to remember that this is your lawsuit, not your lawyer’s lawsuit. If you do not engage with your lawyer and help the lawyer shape the defense, your lawyer may end up presenting the wrong theories. More importantly, spending time with your lawyer will help them understand your personality and the way you interact with your patients. If your lawyer doesn’t know you very well, it’s very difficult for the lawyer to build rapport between you and the jurors, who ultimately will determine the outcome of the lawsuit.
2) Teach: Many defense lawyers have picked up a fair amount of medical knowledge during our careers, but few of us have practiced medicine. As you certainly know, the fact that your lawyer has read surgical textbooks doesn’t make them qualified to perform surgery.
Because you have cared for thousands of patients, you know more about your area of medical expertise than we can ever hope to gain in the course of defending a lawsuit. Teach us the medicine that will enable us to understand how and why you made important decisions while caring for the plaintiff. Ultimately, our success at trial depends on our ability to convince juries that your decisions were thoughtful and reasonable, but we can’t do that without your help.
3) Select: In almost every medical malpractice case, the parties will endorse physicians to provide the jury with expert testimony about the medical issues. These experts become important witnesses because they help the jury understand the relevant standards of care and determine whether an allegedly negligent act caused the plaintiff to suffer an injury.
You probably know the well-respected practitioners in your field who would make credible and persuasive witnesses. Help us identify them and persuade them to serve as experts on your behalf.
4) Prepare: During the course of a lawsuit, one of the most critical events is your deposition. During your deposition, the opposing lawyer will attempt to “lock you in” on the key issues in the case and prevent you from changing your testimony at the time of trial. Consequently, you have to be well prepared for your deposition, both in terms of knowing the facts of the plaintiff’s care (which may have been rendered several years earlier) and in knowing the medical principles that applied to the plaintiff’s care.
You must demand your lawyer adequately prepare you for the deposition by reviewing these matters and preparing you for the deposition process. You need to understand how lawyers frame questions in the hopes of obtaining responses that will come back to haunt you. If you haven’t devoted the time and energy necessary for you to understand and feel comfortable with the process before sitting down for the deposition, you’re in trouble.
5) Attend: Your deposition is the only event before trial that you legally are required to attend. As a defendant, however, you have a right to attend any other deposition that takes place before trial, including the deposition of the plaintiffs and the opposing experts.
If you attend the plaintiff’s deposition, you will have the firsthand ability to hear that person’s story, and you then have the ability to suggest areas where your lawyer can challenge the plaintiff’s recollection. If you attend the opposing expert’s deposition, you similarly have the ability to hear that person’s criticisms, and you can suggest areas where your lawyer can challenge the factual or medical basis for the opinions.
6) Demonstrate: Contrary to television depictions, a trial can be a long and boring process, particularly when there’s nothing to capture the jury’s attention. Jurors have a hard time following a witness’s testimony when it consists solely of questions and answers.
This problem can be compounded when the testimony consists of technical medical information. To prevent boredom and inattention, we want to engage the jurors—and you can help us do it. Give us props, whether in the form of anatomic models, instruments used during the procedure, photographs, charts, or animations that will allow us to capture the jury’s imagination.
7) Communicate: Lawyers and doctors work in different environments. For example, you have the ability to order a test and receive the results within hours, but lawyers generally have weeks to respond to an opposing party’s requests for information. Doctors often receive results that are quantifiable and measurable—but ambiguity and nuance are a lawyer’s stock in trade.
You will be frustrated as you go through the litigation, and you need to have clear and open channels of communication with your lawyer.
Just as your patients depend upon you to orient them within an unfamiliar and frightening environment, your lawyer should help you understand what’s happening in your case. If you don’t have enough information to make intelligent decisions, you should ask for more.
8) Trust: While it’s vital to engage in the process and understand how the lawsuit is proceeding, you need to remember you are not a lawyer. There will be times when your lawyer will have to make judgment calls, and you need to give your lawyer the ability to make those decisions.
Please don’t misunderstand: You have a right to make informed decisions, but a lawyer will make hundreds of judgment calls in the course of a trial, such as whether to dismiss a potential juror, pursue a certain line of questioning with a witness, or introduce a particular exhibit. Some of your lawyer’s recommendations may seem counterintuitive to you, but the courtroom is our operating room.
9) Defend: Most jurors come to the courtroom with some skepticism of medical malpractice claims. One of the reasons for this skepticism is jurors generally like their own physicians and want to believe the medical system functions properly. When they hear a plaintiff’s claim that they were injured through medical negligence, they want the physicians involved in the care to explain how the injury occurred and why it wasn’t the physicians’ fault.
You need to be able to stand up, look the jurors in the eye, explain that your care was appropriate, and withstand an attorney’s attempts to impeach your credibility. If you are unwilling to stand up and fight for yourself and your care, there’s little reason to expect the jurors will fight on your behalf once they begin their deliberations.
10) Relax: This may be the most important tip of all. Lawsuits impose a tremendous amount of stress upon all of the participants, but especially upon a physician whose care is under fire.
We’ve represented physicians who have become so stressed and frustrated by the litigation process that it has overwhelmed them and harmed their ability to provide high-quality care for their ongoing patients.
Some physicians resort to alcohol or other substances to cope with stress. This is the worst possible scenario because it increases the likelihood that you will face another lawsuit in the future.
You need to recognize the stress imposed by a lawsuit, take care of yourself, take care of your practice, and seek help when appropriate. Almost every state has a peer-counseling program for physicians that offers specialized and confidential assistance for physicians. Contact your local medical association for a referral to one of these organizations. TH
Patrick O’Rourke works in the Office of University Counsel, Department of Litigation, University of Colorado, Denver.
Document Your Decisions
For all the differences highlighted in my April and May columns studying the 1995 and 1997 documentation guidelines set forth by the Centers for Medicare and Medicaid Services (CMS) and the American Medical Association (AMA), decision making remains consistent in both.
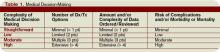
Physician documentation addresses the complexity of the patient’s condition in terms of the number of diagnoses and/or treatment options, the amount and/or complexity of data ordered/reviewed, and the risk of complications/morbidity/mortality. The “diagnoses” and “data” categories follow a point system (see Table 1, below) determined by local Medicare contractors, whereas the “risk” category utilizes a universal table to define medical and/or procedural risks for the patient. The final result of complexity is classified as straightforward, low, moderate, or high.
A complete and accurate description of the patient’s condition should be conveyed through the plan of care. While acuity and severity may be inferred by a physician’s colleagues from particular pieces of information included in the record (e.g., critical lab values), the importance of this information may be lost on auditors and medical record reviewers. This article will assist in explaining the categories of medical decision making, as well as provide documentation tips to best represent patient complexity.
Diagnoses, Care Options
The plan of care outlines problems the physician personally manages and those that affect their management options, even if another physician directly oversees the problem. For example, the hospitalist may primarily manage a patient’s diabetes while the nephrologist manages renal insufficiency. Since the renal insufficiency may affect the hospitalist’s plan for diabetic management, the hospitalist receives credit for the documented renal insufficiency diagnosis and hospitalist-related care plan.
Physicians should address all problems in the documentation for each encounter regardless of any changes to the treatment plan. Credit is provided for each problem that has an associated plan, even if the plan states “continue same treatment.” Additional credit is provided when the treatment to be “continued” is referenced somewhere in the progress note (e.g., in the history).
The amount of credit varies depending upon the problem type. An established problem, defined as having a care plan established by the physician or someone from the same group practice during the current hospitalization, is considered less complex than an undiagnosed new problem for which a prognosis cannot be determined. Severity of the problem affects the weight of complexity. A stable, improving problem is not as complex as a progressing problem.
When documenting diagnoses/treatment options:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined; and
- Indicate the management/treatment option(s) for each problem.
When documentation indicates a continuation of current management options (e.g., “continue meds”), be sure the management options to be continued are noted somewhere in the progress note for that encounter (e.g., medication list).
Data Ordered/Reviewed
“Data” order/review comes in many forms: pathology/laboratory testing, radiology, and medicine-based diagnostics. Although an intuitive part of medical practice, the data section of the progress note is often underdocumented by physicians. Pertinent orders or results may be noted in the visit record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note.
When documenting amount and/or complexity of data:
- Specify tests ordered and rationale in the physician’s progress note or make an entry that refers to another auditor-accessible location for ordered tests and studies;
- Test review may be documented by including a brief entry in the progress note (e.g., “decreased Hgb” or “CXR shows NAD”), or by dating and initialing the report;
- Physicians receive credit for reviewing old records or obtaining history from someone other than the patient, when necessary, as long as a summary of the review or discussion is documented in the medical record; and
- Indicate when images, tracings, or specimens are “personally reviewed” by the physician.
Discussion of unexpected or contradictory test results with the performing physician should be summarized in the medical record.
Risks of Complication
Risk is viewed in light of the patient’s presenting problem, diagnostic procedures ordered, and management options selected.
Risk is graded as minimal, low, moderate, and high with corresponding items that help to differentiate each level (see Table 2, right). The single highest item in any given risk category determines the risk level.
Chronic conditions and invasive procedures expose the patient to more risk than acute, uncomplicated illnesses or non-invasive procedures, respectively. As in the diagnoses/treatment options category, a stable or improving problem poses less risk than a progressing problem. Medication risk varies with the type and degree of potential adverse effects associated with each medication.
When documenting risk:
- Indicate status of all problems in the plan of care; identify them as stable, worsening, exacerbating (mild or severe), etc.;
- Document all diagnostic procedures being considered;
- Identify surgical risk factors involving co-morbid conditions, when appropriate; and
- Associate the labs ordered to monitor for toxicity with the corresponding. medication (e.g., “Continue coumadin, monitor PT/INR”). A patient maintains the same level of risk for a given medication whether the dosage is increased, decreased, or continued without change.
Determine Complexity
To determine the final complexity of medical decision making, two of three categories must be met. For example, if a physician satisfies the requirements for “multiple” diagnoses/treatment options, “minimal” data, and “high” risk, the physician achieves moderate complexity decision-making.
Remember that decision-making is just one of three components of evaluation and management services, along with history and exam.
Determining the final visit level (e.g., 9922x) depends upon each of these three key components for initial hospital care and consultations, and two key components for subsequent hospital care. However, medical decision making always should drive visit level selection as it is the best representation of medical necessity for the service involved.
Contributory Factors
In addition to the three categories of medical decision making, a payer (e.g., TrailblazerHealth) may consider contributory factors when determining patient complexity and selecting visit levels.
For example, the nature of the presenting problem may play a role when reviewing claims for subsequent hospital care codes (99231-99233). Found in the code descriptors of the CPT manual, problems are identified as:
- 99231: Stable, recovering or improving;
- 99232: Responding inadequately to therapy or developed a minor complication; and
- 99233: Unstable or has developed a significant complication or a significant new problem.
Although this is not a general requirement, it represents a locally established standard for reviewing claims for medical necessity. It should not be used exclusively to determine the visit level.
Be sure to query your payer’s policy via written communication or Web site posting (e.g., www.trailblazerhealth.com/Publications/Job%20Aid/medical%20necessity.pdf) for guidance on how payers review documentation. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
For all the differences highlighted in my April and May columns studying the 1995 and 1997 documentation guidelines set forth by the Centers for Medicare and Medicaid Services (CMS) and the American Medical Association (AMA), decision making remains consistent in both.
Physician documentation addresses the complexity of the patient’s condition in terms of the number of diagnoses and/or treatment options, the amount and/or complexity of data ordered/reviewed, and the risk of complications/morbidity/mortality. The “diagnoses” and “data” categories follow a point system (see Table 1, below) determined by local Medicare contractors, whereas the “risk” category utilizes a universal table to define medical and/or procedural risks for the patient. The final result of complexity is classified as straightforward, low, moderate, or high.
A complete and accurate description of the patient’s condition should be conveyed through the plan of care. While acuity and severity may be inferred by a physician’s colleagues from particular pieces of information included in the record (e.g., critical lab values), the importance of this information may be lost on auditors and medical record reviewers. This article will assist in explaining the categories of medical decision making, as well as provide documentation tips to best represent patient complexity.
Diagnoses, Care Options
The plan of care outlines problems the physician personally manages and those that affect their management options, even if another physician directly oversees the problem. For example, the hospitalist may primarily manage a patient’s diabetes while the nephrologist manages renal insufficiency. Since the renal insufficiency may affect the hospitalist’s plan for diabetic management, the hospitalist receives credit for the documented renal insufficiency diagnosis and hospitalist-related care plan.
Physicians should address all problems in the documentation for each encounter regardless of any changes to the treatment plan. Credit is provided for each problem that has an associated plan, even if the plan states “continue same treatment.” Additional credit is provided when the treatment to be “continued” is referenced somewhere in the progress note (e.g., in the history).
The amount of credit varies depending upon the problem type. An established problem, defined as having a care plan established by the physician or someone from the same group practice during the current hospitalization, is considered less complex than an undiagnosed new problem for which a prognosis cannot be determined. Severity of the problem affects the weight of complexity. A stable, improving problem is not as complex as a progressing problem.
When documenting diagnoses/treatment options:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined; and
- Indicate the management/treatment option(s) for each problem.
When documentation indicates a continuation of current management options (e.g., “continue meds”), be sure the management options to be continued are noted somewhere in the progress note for that encounter (e.g., medication list).
Data Ordered/Reviewed
“Data” order/review comes in many forms: pathology/laboratory testing, radiology, and medicine-based diagnostics. Although an intuitive part of medical practice, the data section of the progress note is often underdocumented by physicians. Pertinent orders or results may be noted in the visit record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note.
When documenting amount and/or complexity of data:
- Specify tests ordered and rationale in the physician’s progress note or make an entry that refers to another auditor-accessible location for ordered tests and studies;
- Test review may be documented by including a brief entry in the progress note (e.g., “decreased Hgb” or “CXR shows NAD”), or by dating and initialing the report;
- Physicians receive credit for reviewing old records or obtaining history from someone other than the patient, when necessary, as long as a summary of the review or discussion is documented in the medical record; and
- Indicate when images, tracings, or specimens are “personally reviewed” by the physician.
Discussion of unexpected or contradictory test results with the performing physician should be summarized in the medical record.
Risks of Complication
Risk is viewed in light of the patient’s presenting problem, diagnostic procedures ordered, and management options selected.
Risk is graded as minimal, low, moderate, and high with corresponding items that help to differentiate each level (see Table 2, right). The single highest item in any given risk category determines the risk level.
Chronic conditions and invasive procedures expose the patient to more risk than acute, uncomplicated illnesses or non-invasive procedures, respectively. As in the diagnoses/treatment options category, a stable or improving problem poses less risk than a progressing problem. Medication risk varies with the type and degree of potential adverse effects associated with each medication.
When documenting risk:
- Indicate status of all problems in the plan of care; identify them as stable, worsening, exacerbating (mild or severe), etc.;
- Document all diagnostic procedures being considered;
- Identify surgical risk factors involving co-morbid conditions, when appropriate; and
- Associate the labs ordered to monitor for toxicity with the corresponding. medication (e.g., “Continue coumadin, monitor PT/INR”). A patient maintains the same level of risk for a given medication whether the dosage is increased, decreased, or continued without change.
Determine Complexity
To determine the final complexity of medical decision making, two of three categories must be met. For example, if a physician satisfies the requirements for “multiple” diagnoses/treatment options, “minimal” data, and “high” risk, the physician achieves moderate complexity decision-making.
Remember that decision-making is just one of three components of evaluation and management services, along with history and exam.
Determining the final visit level (e.g., 9922x) depends upon each of these three key components for initial hospital care and consultations, and two key components for subsequent hospital care. However, medical decision making always should drive visit level selection as it is the best representation of medical necessity for the service involved.
Contributory Factors
In addition to the three categories of medical decision making, a payer (e.g., TrailblazerHealth) may consider contributory factors when determining patient complexity and selecting visit levels.
For example, the nature of the presenting problem may play a role when reviewing claims for subsequent hospital care codes (99231-99233). Found in the code descriptors of the CPT manual, problems are identified as:
- 99231: Stable, recovering or improving;
- 99232: Responding inadequately to therapy or developed a minor complication; and
- 99233: Unstable or has developed a significant complication or a significant new problem.
Although this is not a general requirement, it represents a locally established standard for reviewing claims for medical necessity. It should not be used exclusively to determine the visit level.
Be sure to query your payer’s policy via written communication or Web site posting (e.g., www.trailblazerhealth.com/Publications/Job%20Aid/medical%20necessity.pdf) for guidance on how payers review documentation. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
For all the differences highlighted in my April and May columns studying the 1995 and 1997 documentation guidelines set forth by the Centers for Medicare and Medicaid Services (CMS) and the American Medical Association (AMA), decision making remains consistent in both.
Physician documentation addresses the complexity of the patient’s condition in terms of the number of diagnoses and/or treatment options, the amount and/or complexity of data ordered/reviewed, and the risk of complications/morbidity/mortality. The “diagnoses” and “data” categories follow a point system (see Table 1, below) determined by local Medicare contractors, whereas the “risk” category utilizes a universal table to define medical and/or procedural risks for the patient. The final result of complexity is classified as straightforward, low, moderate, or high.
A complete and accurate description of the patient’s condition should be conveyed through the plan of care. While acuity and severity may be inferred by a physician’s colleagues from particular pieces of information included in the record (e.g., critical lab values), the importance of this information may be lost on auditors and medical record reviewers. This article will assist in explaining the categories of medical decision making, as well as provide documentation tips to best represent patient complexity.
Diagnoses, Care Options
The plan of care outlines problems the physician personally manages and those that affect their management options, even if another physician directly oversees the problem. For example, the hospitalist may primarily manage a patient’s diabetes while the nephrologist manages renal insufficiency. Since the renal insufficiency may affect the hospitalist’s plan for diabetic management, the hospitalist receives credit for the documented renal insufficiency diagnosis and hospitalist-related care plan.
Physicians should address all problems in the documentation for each encounter regardless of any changes to the treatment plan. Credit is provided for each problem that has an associated plan, even if the plan states “continue same treatment.” Additional credit is provided when the treatment to be “continued” is referenced somewhere in the progress note (e.g., in the history).
The amount of credit varies depending upon the problem type. An established problem, defined as having a care plan established by the physician or someone from the same group practice during the current hospitalization, is considered less complex than an undiagnosed new problem for which a prognosis cannot be determined. Severity of the problem affects the weight of complexity. A stable, improving problem is not as complex as a progressing problem.
When documenting diagnoses/treatment options:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined; and
- Indicate the management/treatment option(s) for each problem.
When documentation indicates a continuation of current management options (e.g., “continue meds”), be sure the management options to be continued are noted somewhere in the progress note for that encounter (e.g., medication list).
Data Ordered/Reviewed
“Data” order/review comes in many forms: pathology/laboratory testing, radiology, and medicine-based diagnostics. Although an intuitive part of medical practice, the data section of the progress note is often underdocumented by physicians. Pertinent orders or results may be noted in the visit record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note.
When documenting amount and/or complexity of data:
- Specify tests ordered and rationale in the physician’s progress note or make an entry that refers to another auditor-accessible location for ordered tests and studies;
- Test review may be documented by including a brief entry in the progress note (e.g., “decreased Hgb” or “CXR shows NAD”), or by dating and initialing the report;
- Physicians receive credit for reviewing old records or obtaining history from someone other than the patient, when necessary, as long as a summary of the review or discussion is documented in the medical record; and
- Indicate when images, tracings, or specimens are “personally reviewed” by the physician.
Discussion of unexpected or contradictory test results with the performing physician should be summarized in the medical record.
Risks of Complication
Risk is viewed in light of the patient’s presenting problem, diagnostic procedures ordered, and management options selected.
Risk is graded as minimal, low, moderate, and high with corresponding items that help to differentiate each level (see Table 2, right). The single highest item in any given risk category determines the risk level.
Chronic conditions and invasive procedures expose the patient to more risk than acute, uncomplicated illnesses or non-invasive procedures, respectively. As in the diagnoses/treatment options category, a stable or improving problem poses less risk than a progressing problem. Medication risk varies with the type and degree of potential adverse effects associated with each medication.
When documenting risk:
- Indicate status of all problems in the plan of care; identify them as stable, worsening, exacerbating (mild or severe), etc.;
- Document all diagnostic procedures being considered;
- Identify surgical risk factors involving co-morbid conditions, when appropriate; and
- Associate the labs ordered to monitor for toxicity with the corresponding. medication (e.g., “Continue coumadin, monitor PT/INR”). A patient maintains the same level of risk for a given medication whether the dosage is increased, decreased, or continued without change.
Determine Complexity
To determine the final complexity of medical decision making, two of three categories must be met. For example, if a physician satisfies the requirements for “multiple” diagnoses/treatment options, “minimal” data, and “high” risk, the physician achieves moderate complexity decision-making.
Remember that decision-making is just one of three components of evaluation and management services, along with history and exam.
Determining the final visit level (e.g., 9922x) depends upon each of these three key components for initial hospital care and consultations, and two key components for subsequent hospital care. However, medical decision making always should drive visit level selection as it is the best representation of medical necessity for the service involved.
Contributory Factors
In addition to the three categories of medical decision making, a payer (e.g., TrailblazerHealth) may consider contributory factors when determining patient complexity and selecting visit levels.
For example, the nature of the presenting problem may play a role when reviewing claims for subsequent hospital care codes (99231-99233). Found in the code descriptors of the CPT manual, problems are identified as:
- 99231: Stable, recovering or improving;
- 99232: Responding inadequately to therapy or developed a minor complication; and
- 99233: Unstable or has developed a significant complication or a significant new problem.
Although this is not a general requirement, it represents a locally established standard for reviewing claims for medical necessity. It should not be used exclusively to determine the visit level.
Be sure to query your payer’s policy via written communication or Web site posting (e.g., www.trailblazerhealth.com/Publications/Job%20Aid/medical%20necessity.pdf) for guidance on how payers review documentation. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
Are Patients Satisfied?
Have you seen what your discharged patients are saying about your hospital?
Now that patient satisfaction data is public, you can rest assured others are looking at how your facility stacks up against neighboring hospitals on doctor communication, pain management, and more.
As of late March, patient satisfaction information is available on the Centers for Medicare and Medicaid Services (CMS) Hospital Compare consumer Web site (www.hospitalcompare.hhs.gov). This allows for a new level of transparency about the quality of care hospitals provide.
“This is an opportunity,” says Mark V. Williams, MD, director of the hospital medicine program at Northwestern University’s Feinberg School of Medicine in Chicago.
“Hospitalists ought to look up the information on their hospitals and, if they’re not doing well, go to their administrators and say they want to help bring those standings up.”
Satisfaction Defined
What is patient satisfaction? The Hospital Compare site terms this information “Survey of Patients’ Hospital Experiences” and offers a straight percentage of patient satisfaction for 10 areas, including these summary measures:
- How well nurses and doctors in the hospital communicated with the patient;
- How responsive hospital staff were to the patient’s needs;
- How well hospital staff helped the patient manage pain;
- How well the staff communicated with the patient about medicines; and
- Whether pertinent information was provided when the patient was discharged.
Additional items address the cleanliness and quietness of the patient’s room, as well as the patient’s overall rating of the hospital and whether the patient would recommend the hospital to others.
About the Survey
The CMS patient satisfaction percentages are compiled from hospital responses to the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS). This is the first national, standardized, publicly reported survey of patients’ perspectives of hospital care.
Under CMS’ Reporting Hospital Quality Data Annual Payment Update program, hospitals subject to Inpatient Prospective Payment System (IPPS) payment provisions must collect and submit HCAHPS data to receive their full IPPS annual payment update. Other hospitals can voluntarily participate, but there is no incentive payment.
Hospitals administer the survey to a random sample of their adult Medicare patients (across medical conditions) anywhere from 48 hours to six weeks after discharge. They are allowed to conduct the survey by mail, telephone, mail with telephone follow-up, or active interactive voice recognition, and they either can integrate the HCAHPS questions with their own patient satisfaction survey or use HCAHPS by itself. Hospitals must survey patients throughout each month of the year.
CMS began reporting HCAHPS data in March on responses of patients discharged between October 2006 and June 2007. Results will be published quarterly and will comprise the most recent four quarters of data.
To the Rescue
How will this new aspect of transparency affect hospitalists?
“Hospitals are now going to be publicly exposed, as it were, and there will be increasing pressure on how to optimize these measures,” says Dr. Williams.
For this, they are likely to turn to their hospitalists. “Especially since hospitals spend so much money on supporting their hospital medicine programs, they’re going to want to see some return on that money in the form of improvement in these numbers.”
Although the data were added to Hospital Compare for the education of current and future patients, “I don’t think consumers look at this data at all,” Dr. Williams notes. “However, I think hospitals look at it, and they’ll use it to advertise [when they have impressive ratings on measures]. On these questions, hospitals are going to begin competing with each other.”
Hospitalists should be able to help their hospitals improve on specific ratings, just as they help with current quality and outcome measures.
“A lot of hospital medicine programs have already used patient satisfaction as a metric, with their own surveys,” Dr. Williams points out.
One patient satisfaction measure in particular can be addressed by hospitalists. “For HCAHPS, discharge is the component [with the lowest scores],” says Dr. Williams. “Obviously hospitalists can have a big impact on improving those numbers.”
Your own path to improving patient satisfaction is clear: Start by checking your hospital’s numbers on Hospital Compare—and remember those numbers can change quarterly. Consider how to boost satisfaction rates for some of those measures and get the buy-in you need to make changes that will bring the percentages up and keep them up. TH
Jane Jerrard is a medical writer based in Chicago.
Have you seen what your discharged patients are saying about your hospital?
Now that patient satisfaction data is public, you can rest assured others are looking at how your facility stacks up against neighboring hospitals on doctor communication, pain management, and more.
As of late March, patient satisfaction information is available on the Centers for Medicare and Medicaid Services (CMS) Hospital Compare consumer Web site (www.hospitalcompare.hhs.gov). This allows for a new level of transparency about the quality of care hospitals provide.
“This is an opportunity,” says Mark V. Williams, MD, director of the hospital medicine program at Northwestern University’s Feinberg School of Medicine in Chicago.
“Hospitalists ought to look up the information on their hospitals and, if they’re not doing well, go to their administrators and say they want to help bring those standings up.”
Satisfaction Defined
What is patient satisfaction? The Hospital Compare site terms this information “Survey of Patients’ Hospital Experiences” and offers a straight percentage of patient satisfaction for 10 areas, including these summary measures:
- How well nurses and doctors in the hospital communicated with the patient;
- How responsive hospital staff were to the patient’s needs;
- How well hospital staff helped the patient manage pain;
- How well the staff communicated with the patient about medicines; and
- Whether pertinent information was provided when the patient was discharged.
Additional items address the cleanliness and quietness of the patient’s room, as well as the patient’s overall rating of the hospital and whether the patient would recommend the hospital to others.
About the Survey
The CMS patient satisfaction percentages are compiled from hospital responses to the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS). This is the first national, standardized, publicly reported survey of patients’ perspectives of hospital care.
Under CMS’ Reporting Hospital Quality Data Annual Payment Update program, hospitals subject to Inpatient Prospective Payment System (IPPS) payment provisions must collect and submit HCAHPS data to receive their full IPPS annual payment update. Other hospitals can voluntarily participate, but there is no incentive payment.
Hospitals administer the survey to a random sample of their adult Medicare patients (across medical conditions) anywhere from 48 hours to six weeks after discharge. They are allowed to conduct the survey by mail, telephone, mail with telephone follow-up, or active interactive voice recognition, and they either can integrate the HCAHPS questions with their own patient satisfaction survey or use HCAHPS by itself. Hospitals must survey patients throughout each month of the year.
CMS began reporting HCAHPS data in March on responses of patients discharged between October 2006 and June 2007. Results will be published quarterly and will comprise the most recent four quarters of data.
To the Rescue
How will this new aspect of transparency affect hospitalists?
“Hospitals are now going to be publicly exposed, as it were, and there will be increasing pressure on how to optimize these measures,” says Dr. Williams.
For this, they are likely to turn to their hospitalists. “Especially since hospitals spend so much money on supporting their hospital medicine programs, they’re going to want to see some return on that money in the form of improvement in these numbers.”
Although the data were added to Hospital Compare for the education of current and future patients, “I don’t think consumers look at this data at all,” Dr. Williams notes. “However, I think hospitals look at it, and they’ll use it to advertise [when they have impressive ratings on measures]. On these questions, hospitals are going to begin competing with each other.”
Hospitalists should be able to help their hospitals improve on specific ratings, just as they help with current quality and outcome measures.
“A lot of hospital medicine programs have already used patient satisfaction as a metric, with their own surveys,” Dr. Williams points out.
One patient satisfaction measure in particular can be addressed by hospitalists. “For HCAHPS, discharge is the component [with the lowest scores],” says Dr. Williams. “Obviously hospitalists can have a big impact on improving those numbers.”
Your own path to improving patient satisfaction is clear: Start by checking your hospital’s numbers on Hospital Compare—and remember those numbers can change quarterly. Consider how to boost satisfaction rates for some of those measures and get the buy-in you need to make changes that will bring the percentages up and keep them up. TH
Jane Jerrard is a medical writer based in Chicago.
Have you seen what your discharged patients are saying about your hospital?
Now that patient satisfaction data is public, you can rest assured others are looking at how your facility stacks up against neighboring hospitals on doctor communication, pain management, and more.
As of late March, patient satisfaction information is available on the Centers for Medicare and Medicaid Services (CMS) Hospital Compare consumer Web site (www.hospitalcompare.hhs.gov). This allows for a new level of transparency about the quality of care hospitals provide.
“This is an opportunity,” says Mark V. Williams, MD, director of the hospital medicine program at Northwestern University’s Feinberg School of Medicine in Chicago.
“Hospitalists ought to look up the information on their hospitals and, if they’re not doing well, go to their administrators and say they want to help bring those standings up.”
Satisfaction Defined
What is patient satisfaction? The Hospital Compare site terms this information “Survey of Patients’ Hospital Experiences” and offers a straight percentage of patient satisfaction for 10 areas, including these summary measures:
- How well nurses and doctors in the hospital communicated with the patient;
- How responsive hospital staff were to the patient’s needs;
- How well hospital staff helped the patient manage pain;
- How well the staff communicated with the patient about medicines; and
- Whether pertinent information was provided when the patient was discharged.
Additional items address the cleanliness and quietness of the patient’s room, as well as the patient’s overall rating of the hospital and whether the patient would recommend the hospital to others.
About the Survey
The CMS patient satisfaction percentages are compiled from hospital responses to the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS). This is the first national, standardized, publicly reported survey of patients’ perspectives of hospital care.
Under CMS’ Reporting Hospital Quality Data Annual Payment Update program, hospitals subject to Inpatient Prospective Payment System (IPPS) payment provisions must collect and submit HCAHPS data to receive their full IPPS annual payment update. Other hospitals can voluntarily participate, but there is no incentive payment.
Hospitals administer the survey to a random sample of their adult Medicare patients (across medical conditions) anywhere from 48 hours to six weeks after discharge. They are allowed to conduct the survey by mail, telephone, mail with telephone follow-up, or active interactive voice recognition, and they either can integrate the HCAHPS questions with their own patient satisfaction survey or use HCAHPS by itself. Hospitals must survey patients throughout each month of the year.
CMS began reporting HCAHPS data in March on responses of patients discharged between October 2006 and June 2007. Results will be published quarterly and will comprise the most recent four quarters of data.
To the Rescue
How will this new aspect of transparency affect hospitalists?
“Hospitals are now going to be publicly exposed, as it were, and there will be increasing pressure on how to optimize these measures,” says Dr. Williams.
For this, they are likely to turn to their hospitalists. “Especially since hospitals spend so much money on supporting their hospital medicine programs, they’re going to want to see some return on that money in the form of improvement in these numbers.”
Although the data were added to Hospital Compare for the education of current and future patients, “I don’t think consumers look at this data at all,” Dr. Williams notes. “However, I think hospitals look at it, and they’ll use it to advertise [when they have impressive ratings on measures]. On these questions, hospitals are going to begin competing with each other.”
Hospitalists should be able to help their hospitals improve on specific ratings, just as they help with current quality and outcome measures.
“A lot of hospital medicine programs have already used patient satisfaction as a metric, with their own surveys,” Dr. Williams points out.
One patient satisfaction measure in particular can be addressed by hospitalists. “For HCAHPS, discharge is the component [with the lowest scores],” says Dr. Williams. “Obviously hospitalists can have a big impact on improving those numbers.”
Your own path to improving patient satisfaction is clear: Start by checking your hospital’s numbers on Hospital Compare—and remember those numbers can change quarterly. Consider how to boost satisfaction rates for some of those measures and get the buy-in you need to make changes that will bring the percentages up and keep them up. TH
Jane Jerrard is a medical writer based in Chicago.
Stop Drug-Induced Lupus
The chronic inflammatory disease lupus, usually traced to environmental and genetic causes, also can be drug-induced (DILE). It occurs in patients differently than systemic lupus erythematosus (SLE).
DILE tends to strike:
- Older patients (ages 50-70);
- Men more than women; and
- Whites more than blacks.
It was first described in 1945 as a side effect of sulfadiazine. Between 15,000 and 20,000 cases of drug-induced lupus erythematosus (DILE) occur yearly. Symptoms usually appear within three to six months of taking an offending drug.1 However, it also can occur within two years of receiving a triggering drug.2,3 The reaction usually resolves within days or months after removal of the offending medication. Care must be taken to correctly diagnose DILE and differentiate it from the systemic autoimmune disease SLE.
DILE arises mainly from the production of autoantibodies in reaction to certain drugs.4 Patients may also have a genetic predisposition, particularly for agents that are metabolically acetylated (e.g., hydralazine, procainamide). DILE is likely to appear more rapidly in patients who are slow acetylators. These patients include those with the HLA-DR4 or HLA-DR0301 genes, the complement C4 null allele, and females.
DILE symptoms include anorexia, arthralgia, fever, lymphadenopathy, malaise, myalgia, rash, serositis, and weight loss.5 The rash usually presents as polycyclic, with scaling and erythema in sun-exposed areas. Serologic findings include a positive antinuclear antibody (ANA) in 75% or more of patients and anti-histone antibodies. Levels of C3/C4 are usually normal. Antibodies to anti-double stranded DNA (anti-ds DNA) are rare, in contrast to SLE where C3/C4 levels usually decrease and anti-ds DNA is usually (50%-70%) positive. An elevated erythrocyte sedimentation rate (ESR 80%) may also be present. The absence of renal or central nervous system involvement is more suggestive of DILE. Renal effects occur in 5% to 10% of hydralazine-induced DILE cases, and renal deaths have been reported in rare cases.
The Agents
Many agents can cause DILE. A large number of these agents rarely are used in present-day medicine. The more commonly used agents/classes include:
- Carbamazepine;
- Diltiazem;
- Docetaxel;
- Hydralazine;
- Isoniazid;
- Minocycline;
- Procainamide; and
- Sulfasalazine.
Other agents that may possibly cause DILE include:
- Anti-tumor necrosis factor agents (adalimumab, etanercept, infliximab);
- Bupropion;
- Fluorouracil;
- Interferon;
- Lisinopril;
- Non-steroidal anti-inflammatory agents;
- Propylthiouracil;
- Statins; and
- Terbinafine.
Diagnosis is made by confirming the patient has:
- One or more clinical symptoms;
- A positive ANA;
- No SLE history prior to using the suspected agent;
- Not taken the drug anytime from three weeks to two years before the symptoms appeared; and
- Clinical resolution occurs rapidly upon “suspected drug” discontinuation.
A complete blood count should be obtained to evaluate for anemia (rare in DILE, common in SLE). Liver function tests, blood urea nitrogen, creatinine, and urinalysis can be performed to evaluate for other complications.
DILE usually resolves following drug discontinuation, but severe cases may require low doses of systemic corticosteroids. TH
Michele B Kaufman, PharmD, BSc, is a registered pharmacist based in New York City.
References
- Vasoo S. Drug-induced lupus: an update. Lupus 2006;15:757-761.
- Kauffman CL. Lupus erythematosus, drug-induced. eMedicine 2007. Available at www.emedicine.com/derm/TOPIC107.htm. Accessed April 8, 2008.
- MedlinePlus. www.nlm.nih.gov/medlineplus/ print/ency/article/000446.htm. Accessed April 8, 2008.
- Schur PH, Rose BD. Drug-induced lupus 2008; Patients UpToDate Version 16.1. Available www.uptodate.com/patients/content/topic.do;jsessionid=1934E0AFFCBBB588269DBFEE5F96BDF4.1002?topicKey=~kU3CGByPyaH&selectedTitle=2~103&source=search_result. Accessed April 8, 2008.
- Borchers A, Keen CL, Gershwin ME. Drug-induced lupus. Ann NY Acad Sci. 2007;1108:166-182.
The chronic inflammatory disease lupus, usually traced to environmental and genetic causes, also can be drug-induced (DILE). It occurs in patients differently than systemic lupus erythematosus (SLE).
DILE tends to strike:
- Older patients (ages 50-70);
- Men more than women; and
- Whites more than blacks.
It was first described in 1945 as a side effect of sulfadiazine. Between 15,000 and 20,000 cases of drug-induced lupus erythematosus (DILE) occur yearly. Symptoms usually appear within three to six months of taking an offending drug.1 However, it also can occur within two years of receiving a triggering drug.2,3 The reaction usually resolves within days or months after removal of the offending medication. Care must be taken to correctly diagnose DILE and differentiate it from the systemic autoimmune disease SLE.
DILE arises mainly from the production of autoantibodies in reaction to certain drugs.4 Patients may also have a genetic predisposition, particularly for agents that are metabolically acetylated (e.g., hydralazine, procainamide). DILE is likely to appear more rapidly in patients who are slow acetylators. These patients include those with the HLA-DR4 or HLA-DR0301 genes, the complement C4 null allele, and females.
DILE symptoms include anorexia, arthralgia, fever, lymphadenopathy, malaise, myalgia, rash, serositis, and weight loss.5 The rash usually presents as polycyclic, with scaling and erythema in sun-exposed areas. Serologic findings include a positive antinuclear antibody (ANA) in 75% or more of patients and anti-histone antibodies. Levels of C3/C4 are usually normal. Antibodies to anti-double stranded DNA (anti-ds DNA) are rare, in contrast to SLE where C3/C4 levels usually decrease and anti-ds DNA is usually (50%-70%) positive. An elevated erythrocyte sedimentation rate (ESR 80%) may also be present. The absence of renal or central nervous system involvement is more suggestive of DILE. Renal effects occur in 5% to 10% of hydralazine-induced DILE cases, and renal deaths have been reported in rare cases.
The Agents
Many agents can cause DILE. A large number of these agents rarely are used in present-day medicine. The more commonly used agents/classes include:
- Carbamazepine;
- Diltiazem;
- Docetaxel;
- Hydralazine;
- Isoniazid;
- Minocycline;
- Procainamide; and
- Sulfasalazine.
Other agents that may possibly cause DILE include:
- Anti-tumor necrosis factor agents (adalimumab, etanercept, infliximab);
- Bupropion;
- Fluorouracil;
- Interferon;
- Lisinopril;
- Non-steroidal anti-inflammatory agents;
- Propylthiouracil;
- Statins; and
- Terbinafine.
Diagnosis is made by confirming the patient has:
- One or more clinical symptoms;
- A positive ANA;
- No SLE history prior to using the suspected agent;
- Not taken the drug anytime from three weeks to two years before the symptoms appeared; and
- Clinical resolution occurs rapidly upon “suspected drug” discontinuation.
A complete blood count should be obtained to evaluate for anemia (rare in DILE, common in SLE). Liver function tests, blood urea nitrogen, creatinine, and urinalysis can be performed to evaluate for other complications.
DILE usually resolves following drug discontinuation, but severe cases may require low doses of systemic corticosteroids. TH
Michele B Kaufman, PharmD, BSc, is a registered pharmacist based in New York City.
References
- Vasoo S. Drug-induced lupus: an update. Lupus 2006;15:757-761.
- Kauffman CL. Lupus erythematosus, drug-induced. eMedicine 2007. Available at www.emedicine.com/derm/TOPIC107.htm. Accessed April 8, 2008.
- MedlinePlus. www.nlm.nih.gov/medlineplus/ print/ency/article/000446.htm. Accessed April 8, 2008.
- Schur PH, Rose BD. Drug-induced lupus 2008; Patients UpToDate Version 16.1. Available www.uptodate.com/patients/content/topic.do;jsessionid=1934E0AFFCBBB588269DBFEE5F96BDF4.1002?topicKey=~kU3CGByPyaH&selectedTitle=2~103&source=search_result. Accessed April 8, 2008.
- Borchers A, Keen CL, Gershwin ME. Drug-induced lupus. Ann NY Acad Sci. 2007;1108:166-182.
The chronic inflammatory disease lupus, usually traced to environmental and genetic causes, also can be drug-induced (DILE). It occurs in patients differently than systemic lupus erythematosus (SLE).
DILE tends to strike:
- Older patients (ages 50-70);
- Men more than women; and
- Whites more than blacks.
It was first described in 1945 as a side effect of sulfadiazine. Between 15,000 and 20,000 cases of drug-induced lupus erythematosus (DILE) occur yearly. Symptoms usually appear within three to six months of taking an offending drug.1 However, it also can occur within two years of receiving a triggering drug.2,3 The reaction usually resolves within days or months after removal of the offending medication. Care must be taken to correctly diagnose DILE and differentiate it from the systemic autoimmune disease SLE.
DILE arises mainly from the production of autoantibodies in reaction to certain drugs.4 Patients may also have a genetic predisposition, particularly for agents that are metabolically acetylated (e.g., hydralazine, procainamide). DILE is likely to appear more rapidly in patients who are slow acetylators. These patients include those with the HLA-DR4 or HLA-DR0301 genes, the complement C4 null allele, and females.
DILE symptoms include anorexia, arthralgia, fever, lymphadenopathy, malaise, myalgia, rash, serositis, and weight loss.5 The rash usually presents as polycyclic, with scaling and erythema in sun-exposed areas. Serologic findings include a positive antinuclear antibody (ANA) in 75% or more of patients and anti-histone antibodies. Levels of C3/C4 are usually normal. Antibodies to anti-double stranded DNA (anti-ds DNA) are rare, in contrast to SLE where C3/C4 levels usually decrease and anti-ds DNA is usually (50%-70%) positive. An elevated erythrocyte sedimentation rate (ESR 80%) may also be present. The absence of renal or central nervous system involvement is more suggestive of DILE. Renal effects occur in 5% to 10% of hydralazine-induced DILE cases, and renal deaths have been reported in rare cases.
The Agents
Many agents can cause DILE. A large number of these agents rarely are used in present-day medicine. The more commonly used agents/classes include:
- Carbamazepine;
- Diltiazem;
- Docetaxel;
- Hydralazine;
- Isoniazid;
- Minocycline;
- Procainamide; and
- Sulfasalazine.
Other agents that may possibly cause DILE include:
- Anti-tumor necrosis factor agents (adalimumab, etanercept, infliximab);
- Bupropion;
- Fluorouracil;
- Interferon;
- Lisinopril;
- Non-steroidal anti-inflammatory agents;
- Propylthiouracil;
- Statins; and
- Terbinafine.
Diagnosis is made by confirming the patient has:
- One or more clinical symptoms;
- A positive ANA;
- No SLE history prior to using the suspected agent;
- Not taken the drug anytime from three weeks to two years before the symptoms appeared; and
- Clinical resolution occurs rapidly upon “suspected drug” discontinuation.
A complete blood count should be obtained to evaluate for anemia (rare in DILE, common in SLE). Liver function tests, blood urea nitrogen, creatinine, and urinalysis can be performed to evaluate for other complications.
DILE usually resolves following drug discontinuation, but severe cases may require low doses of systemic corticosteroids. TH
Michele B Kaufman, PharmD, BSc, is a registered pharmacist based in New York City.
References
- Vasoo S. Drug-induced lupus: an update. Lupus 2006;15:757-761.
- Kauffman CL. Lupus erythematosus, drug-induced. eMedicine 2007. Available at www.emedicine.com/derm/TOPIC107.htm. Accessed April 8, 2008.
- MedlinePlus. www.nlm.nih.gov/medlineplus/ print/ency/article/000446.htm. Accessed April 8, 2008.
- Schur PH, Rose BD. Drug-induced lupus 2008; Patients UpToDate Version 16.1. Available www.uptodate.com/patients/content/topic.do;jsessionid=1934E0AFFCBBB588269DBFEE5F96BDF4.1002?topicKey=~kU3CGByPyaH&selectedTitle=2~103&source=search_result. Accessed April 8, 2008.
- Borchers A, Keen CL, Gershwin ME. Drug-induced lupus. Ann NY Acad Sci. 2007;1108:166-182.
In the Literature
Literature at a Glance
A guide to this month’s studies.
- Adverse events are common after stopping clopidogrel following acute coronary syndrome.
- Treatment intensification with insulin improves inpatient glucose control.
- Pressure for early antibiotic administration leads to inaccuracy of pneumonia diagnosis.
- Multifaceted ventilation strategy no better than low-tidal-volume protocol.
- Higher PEEP ventilation strategy reduces duration of ventilation but not mortality.
- N-acetylcysteine reduces contrast-induced nephropathy.
- Vasopressin is no better than norepinephrine in patients with septic shock.
- Hospital patients desire greater participation in decision-making.
- Outcomes of patients with upper- or lower-extremity DVT are similar.
- Oral and IV steroids may be equally effective in COPD exacerbation.
What is Frequency, Timing of Adverse Events After Stopping Clopidogrel in ACS Patients?
Background: Clopidogrel is recommended in treatment of acute coronary syndrome (ACS) with or without stent placement. A rebound hypercoagulable state may occur following clopidogrel cessation, but this has not been investigated previously.
Study design: Retrospective cohort.
Setting: 127 VA medical centers.
Synopsis: Data were collected as part of the Veterans Health Administration Cardiac Care Follow-up Clinical Study from October 2003 through March 2005 on all patients with acute myocardial infarction (MI) or unstable angina who were discharged with clopidogrel treatment (3,137 patients). The analysis assessed the incidence and timing of adverse events after stopping clopidogrel among medically treated patients and among those treated with percutaneous coronary intervention (PCI).
In adjusted analyses among medically treated patients, the risk of death or acute MI in the first 90 days after clopidogrel cessation was 1.98 times higher, compared with the interval from 91-180 days. Among patients who received PCI (usually with a bare-metal stent), the risk was 1.82 times higher in the first 90 days. The clustering of events shortly after clopidogrel cessation support the possibility of a rebound hypercoagulable state.
Bottom line: In patients with ACS who received medical management or PCI, there was a higher rate of adverse events in the first 90 days after clopidogrel cessation.
Citation: Ho PM, Peterson ED, Wang L, et al. Incidence of death and acute myocardial infarction associated with stopping clopidorel after acute coronary syndrome. JAMA 2008;299(5):532-539.
What is the Relationship Between Treatment Intensification, Blood Pressure Changes in Diabetes Patients?
Background: Hyperglycemia is common in hospitalized patients with diabetes and associated with poor outcomes. Prior research on treatment intensification has focused on the intensive care unit or outpatient setting. The effect of treatment intensification in the inpatient (non-ICU) setting is not known.
Study design: Retrospective cohort.
Setting: 734-bed teaching hospital in Boston.
Synopsis: Between January 2003 and August 2004, data on blood glucose and daily pharmacologic management were gathered from electronic sources on 3,613 inpatients with diabetes. Inpatient hyperglycemia (glucose more than 180 mg/dL) occurred at least once in 2,980 (82.5%) hospitalizations.
Intensification of antihyperglycemic therapy occurred after only 22% of hospital days with hyperglycemia. Intensification included scheduled insulin, sliding scale insulin, and oral antihyperglycemic medications. Intensification of sliding scale insulin, as well as scheduled insulin, but not oral medications, was associated with a significant (12.2 mg/dL and 11.1 mg/dL respectively) average daily reduction in bedside glucose. Hypoglycemia was documented in 2.2% of days after intensification of antihyperglycemic treatment.
Bottom line: Inpatient hyperglycemia is common, and treatment intensification should be considered more often among hospitalized patients with diabetes.
Citation: Matheny ME, Shubina M, Kimmel ZM, Pendergrass ML, Turchin A. Treatment intensification and blood glucose control among hospitalized diabetic patients. J Gen Intern Med. 2008;23(2):184-189.
Does Four-Hour Antibiotic Goal Negatively Affect Accuracy of CAP Diagnosis?
Background: A period of less than our hour from emergency department presentation to first antibiotic dose is a core quality measure for community-acquired pneumonia (CAP). Time pressures might reduce the accuracy of pneumonia diagnosis and lead to unnecessary antibiotic administration.
Study design: Retrospective cohort.
Setting: 365-bed university-affiliated community hospital in Baltimore.
Synopsis: Patients admitted with an initial diagnosis of CAP were studied when the time to first antibiotic dose (TFAD) quality standard was eight hours (n=255) and later when the goal TFAD was four hours (n=293).
At admission, under the eight-hour goal, 45.9% of patients met prespecified diagnostic criteria for CAP, compared with 33.8% of patients under the four-hour goal (odds ratio [OR]=0.61, p=0.004). At discharge, 74.5% of patients had a diagnosis of pneumonia with an eight-hour TFAD standard, vs. 66.9% with a four-hour standard (p=0.05). The most common alternate diagnoses were acute bronchitis, heart failure, and COPD exacerbation.
No significant difference in antibiotic-associated adverse drug events, morbidity, or mortality were detected. Importantly, the goal TFAD reduction did not significantly increase the percentage of patients who received antibiotics within four hours (81.6% when the goal was within eight hours, vs. 85.3% when the goal was within four hours, p=0.21). The study is limited by its retrospective nature and the absence of gold standards for the diagnosis of CAP.
Bottom line: Greater pressure to administer antibiotics early in suspected cases of CAP may decrease diagnostic accuracy, without substantially improving antibiotic administration time.
Citation: Welker JA, Huston M, McCue JD. Antibiotic timing and errors in diagnosing pneumonia. Arch Intern Med. 2008;168(4):351-356.
Do Recruitment Maneuvers and High PEEP Reduce All-cause Hospital Mortality in Acute Lung Injury, ARDS?
Background: Low-tidal-volume ventilation reduces mortality in acute lung injury and acute respiratory distress syndrome (ARDS). Adding methods to open collapsed lung, such as employing recruitment maneuvers or using higher positive end-expiratory pressures (PEEP), may further reduce mortality.
Study design: Randomized controlled trial with blinded analysis. Patients were randomized to ventilation using the ARDS Network protocol (tidal volume of 6 ml/kg predicted body weight, assist control ventilation, low PEEP) vs. a higher PEEP intervention algorithm (using pressure control ventilation but still using 6 ml/kg tidal volume).
Setting: 30 intensive-care units in Canada, Australia, and Saudi Arabia.
Synopsis: Despite higher PEEP in the experimental group (14.6 cm H2O, SD 3.4) vs. the control group (9.8 cm H2O, SD 2.7) during the first 72 hours (p<0.001), there was no difference in all-cause hospital mortality or barotrauma between the two groups. The experimental group did, however, have a lower frequency of refractory hypoxemia (4.6% vs. 10.2%, 95% confidence interval [CI] 0.34-0.86, p=0.01).
At the end of the trial, a difference in the number of patients allocated to each group was noted. Investigation uncovered a programming error that disrupted the specified randomization blocks. Sensitivity analyses, which were not described, indicated that this error did not undermine randomization.
Bottom line: The addition of recruitment maneuvers and high PEEP to low-tidal-volume ventilation in acute lung injury and acute respiratory distress syndrome improved oxygenation but did not lower mortality.
Citation: Meade MO, Cook DJ, Guyatt GH, et al. Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome. A randomized controlled trial. JAMA 2008;299(6):637-645.
Does a Ventilation Strategy Setting PEEP to Increase Alveolar Recruitment, Limit Hyperinflation Improve 28-day Mortality in Acute Lung Injury, ARDS?
Background: The need for lung protection in patients with acute lung injury or acute respiratory distress syndrome (ARDS) is accepted. The optimal level of positive end-expiratory pressure (PEEP) to provide protection yet allow alveolar expansion is debated
Study design: Unblinded, randomized controlled trial. Patients were randomized to standard low tidal volume ventilation with low PEEP or low tidal volume ventilation with higher PEEP (intervention group). PEEP was increased in the intervention group to attain a plateau pressure of 28-30 cm H2O
Setting: 37 intensive care units in France.
Synopsis: Though PEEP, total PEEP, and plateau pressure were considerably higher in the experimental group, there was no difference in 28-day mortality compared with the control group, 27.8% vs. 31.2% (95% CI 0.90-1.40, p=0.31). There was, however, an increase in the number of ventilator-free days (seven vs. three, p=0.04) and organ-failure-free days (six vs. two, p=0.04) in the experimental group compared with the control group. Criteria were used to evaluate patients for readiness for extubation, but the differential application of PEEP between arms may have altered the timing of these evaluations in the two arms and may be at least partly responsible for the difference in ventilator-free days.
Throughout patient recruitment, the primary end point was monitored, resulting in 18 interim analyses of the data. No statistical adjustments were made for these frequent examinations of the data.
Bottom line: The use of higher PEEP and maximum plateau pressure to increase alveolar recruitment while limiting hyperinflation results in more ventilator-free and organ failure-free days in patients with acute lung injury and ARDS. These maneuvers do not, however, alter mortality.
Citation: Mercat A, Richard JCM, Vielle B, et al. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome. A randomized controlled trial. JAMA 2008;299(6):646-655.
What are the Effects of N-acetylcysteine, Theophylline, Other Agents on Preventing Contrast-induced Nephropathy
Background: Contrast-induced nephropathy is the third-most common cause of new acute renal failure in hospitalized patients, occurring in up to 25% of patients with renal impairment, diabetes, heart failure, advanced age, or concurrent use of nephrotoxic drugs. Clinicians use different agents to reduce the risk, including intravenous hydration, N-acetylcysteine, theophylline, fenoldopam, dopamine, furosemide, mannitol, and bicarbonate.
Study design: Meta-analysis of randomized controlled trials.
Setting: 41 studies involving 6,379 patients, published internationally between 1994 and 2006.
Synopsis: All but one study evaluated patients undergoing cardiac catheterization, and 34 trials evaluated patients with impaired renal function. N-acetylcysteine significantly reduced the risk of contrast-induced nephropathy more than saline hydration alone (risk ratio [RR]=0.62, 95% CI 0.44 to 0.88). Theophylline may have renoprotective effects but the findings were not statistically significant (RR=0.49, 95% CI 0.23 to 1.06). Ascorbic acid and bicarbonate significantly reduced nephropathy, though only one study was found for each. The other agents evaluated did not significantly reduce risk. Furosemide increased the risk (RR=3.27, 95% CI 1.48 to 7.26).
Bottom line: N-acetylcycteine is an effective agent for prevention of contrast-induced nephropathy, and it has the added benefits of low cost, few side effects, and rare drug interactions.
Citation: Kelly AM, Dwamena B, Cronin P, Bernstein SJ, Carlos RC. Meta-analysis: effectiveness of drugs for preventing contrast-induced nephropathy. Ann Intern Med. 2008;148(4):284-294.
Compared With Norepinephrine, Does Vasopressin Infusion Improve Mortality in Septic Shock Patients?
Background: Vasopressin is commonly used to support blood pressure in patients with septic shock. It has been shown to restore vascular tone, maintain blood pressure, and decrease catecholamine requirements, but its effect on mortality is uncertain.
Study design: Randomized, double-blind trial.
Setting: 27 centers in Canada, Australia, and the United States.
Synopsis: Patients with septic shock who required at least 5 mcg/min of norepinephrine were randomized to receive either low-dose vasopressin infusion (0.01 to 0.03 U/min) or norepinephrine (5 to 15 mcg/min). There was no significant difference in mortality at 28 days (35.4% for vasopressin vs. 39.3% for norepinephrine, p=0.26) or at 90 days (43.9% vs. 49.6%, p=0.11). The vasopressin group had lower heart rate and norepinephrine requirements. There were no significant differences in the frequency of adverse events.
However, since mean blood pressure at baseline was 72-73 mmHg, study patients did not necessarily have catecholamine unresponsive shock. Also, the mean time from meeting criteria for study entry to infusion of the drug was 12 hours, longer than the six-hour time period identified as important in studies of early goal-directed therapy. This may have limited the effectiveness of vasopressin infusion.
Bottom line: Low-dose vasopressin as compared with norepinephrine did not improve mortality in patients with septic shock.
Citation: Russell JA, Walley KR, Singer J, et al. Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med. 2008;358(9):877-887.
How Much do Hospitalized Patients Want to Participate in Decisions on Therapies of Varying Risk, Benefit?
Background: Obtaining informed consent is required for invasive procedures, but most non-invasive medical treatments are performed without discussing the risks, benefits, and alternatives with patients.
Study design: Questionnaire with four scenarios.
Setting: Medical wards in a Connecticut hospital.
Synopsis: Among the 210 patients studied, about one-fourth wanted physicians to obtain their permission “no matter what” even for mundane therapies like potassium supplementation (24%) or diuretic administration (28%). When presented with a higher risk scenario, such as thrombolysis with a greater than 20% chance of hemorrhage, 40.8% of patients definitely wanted to participate in decision-making.
Younger patients (age 65 or younger) were more likely to want to participate in decision-making. For each scenario, at least 85% of patients noted they would like to be consulted about the decision “no matter what” or if time allowed. Importantly, patients expressed these preferences in response to written scenarios that did not provide detailed information about the risks and benefits. Further, patients did not receive explanations of the logistical hurdles of trying to obtain patient input for each decision.
Bottom line: The great majority of patients in this study wished to participate in decision making for hypothetical medical treatments, especially if time allowed. At least 24% always wanted to be consulted, even about mundane therapies like potassium supplementation.
Citation: Upadhyay S, Beck A, Rishi A, Amoateng-Adjepong Y, Manthous CA. Patients’ predilections regarding informed consent for hospital treatments. J Hosp Med. 2008; 3(1):6-11.
What are the Clinical Characteristics, Treatments, and Three-month Outcomes of Patients With Upper-extremity DVT
Background: Anticoagulation is the treatment of choice for upper-extremity deep venous thrombosis (DVT). However, no large studies have characterized the nature, management, and prognosis of upper-extremity DVT.
Study design: Prospective registry of consecutive patients (RIETE registry).
Setting: International multicenter study (124 centers in Spain, France, Italy, Israel, and Argentina).
Synopsis: Among the 11,564 registry patients with acute DVT, 512 (4.4%) were noted to have upper-extremity DVT. Cancer was more common and immobility was less common with upper-extremity DVT. Initially, most patients (91%) were treated with low-molecular-weight heparin (LMWH). For long-term therapy, 75% of patients with cancer received LMWH, and 76% of patients without cancer were given oral vitamin K antagonists. At diagnosis, only 9% of patients with upper-extremity DVT had clinically apparent pulmonary embolism (PE) versus 29% of those with lower-extremity DVT. During the three-month follow-up, the incidence of PE, fatal PE, recurrent DVT, and bleeding was similar for upper- and lower-extremity DVT. Mortality was higher in patients with upper-extremity DVT, which in multivariable analyses, was explained by the higher prevalence of cancer in that group.
Bottom line: Because the incidence of recurrent DVT/PE, fatal PE, or major bleeding is similar between upper and lower extremity DVT, therapy should not differ.
Citation: Muñoz FJ, Mismetti P, Poggio R, et al. Clinical outcome of patients with upper-extremity deep vein thrombosis. Chest 2008;133(1):143-148.
Are Oral Steroids as Effective as IV Steroids in Patients With COPD Exacerbation?
Background: Oral prednisolone has near 100% bioavailability following oral administration. Although current guidelines suggest using oral steroids in the treatment of COPD exacerbation, the optimal route of administration has not been studied rigorously.
Study design: Non-inferiority, double-blinded, randomized controlled trial.
Setting: Single hospital in the Netherlands.
Synopsis: Patients were randomized to receive either a five-day course of IV or oral prednisolone 60 mg, followed by an oral prednisolone taper. All received nebulized ipratropium and albuterol four times daily, as well as oral amoxicillin/clavulanate (or doxycycline if allergic). The primary outcome was treatment failure, which included death, ICU admission, hospital readmission for COPD, or treatment intensification during 90-day follow-up.
Non-inferiority was defined as a treatment failure rate for oral steroids not more than 15% worse than the treatment failure rate for IV steroids. The study design called for 256 patients to provide adequate (80%) power for the primary analysis. However, only 210 were enrolled due to slow recruitment, and 17 withdrew consent or did not meet study entry criteria.
The intention-to-treat analysis showed no significant difference between oral and IV steroids in the treatment failure rate (56.3% vs. 61.7%, respectively). Results of the per-protocol analysis were similar. However, insufficient power and poor patient accounting raise questions about the validity of the results.
Bottom line: Oral steroids appeared no worse than IV steroids in the treatment of COPD exacerbation, but the study was underpowered, which prevents definitive conclusions.
Citation: De Jong YP, Uil SM, Grotjohan HP, et al. Oral or IV prednisolone in the treatment of COPD exacerbations. A randomized, controlled, double-blind study. Chest 2007;132(6):1741-1747. TH
Literature at a Glance
A guide to this month’s studies.
- Adverse events are common after stopping clopidogrel following acute coronary syndrome.
- Treatment intensification with insulin improves inpatient glucose control.
- Pressure for early antibiotic administration leads to inaccuracy of pneumonia diagnosis.
- Multifaceted ventilation strategy no better than low-tidal-volume protocol.
- Higher PEEP ventilation strategy reduces duration of ventilation but not mortality.
- N-acetylcysteine reduces contrast-induced nephropathy.
- Vasopressin is no better than norepinephrine in patients with septic shock.
- Hospital patients desire greater participation in decision-making.
- Outcomes of patients with upper- or lower-extremity DVT are similar.
- Oral and IV steroids may be equally effective in COPD exacerbation.
What is Frequency, Timing of Adverse Events After Stopping Clopidogrel in ACS Patients?
Background: Clopidogrel is recommended in treatment of acute coronary syndrome (ACS) with or without stent placement. A rebound hypercoagulable state may occur following clopidogrel cessation, but this has not been investigated previously.
Study design: Retrospective cohort.
Setting: 127 VA medical centers.
Synopsis: Data were collected as part of the Veterans Health Administration Cardiac Care Follow-up Clinical Study from October 2003 through March 2005 on all patients with acute myocardial infarction (MI) or unstable angina who were discharged with clopidogrel treatment (3,137 patients). The analysis assessed the incidence and timing of adverse events after stopping clopidogrel among medically treated patients and among those treated with percutaneous coronary intervention (PCI).
In adjusted analyses among medically treated patients, the risk of death or acute MI in the first 90 days after clopidogrel cessation was 1.98 times higher, compared with the interval from 91-180 days. Among patients who received PCI (usually with a bare-metal stent), the risk was 1.82 times higher in the first 90 days. The clustering of events shortly after clopidogrel cessation support the possibility of a rebound hypercoagulable state.
Bottom line: In patients with ACS who received medical management or PCI, there was a higher rate of adverse events in the first 90 days after clopidogrel cessation.
Citation: Ho PM, Peterson ED, Wang L, et al. Incidence of death and acute myocardial infarction associated with stopping clopidorel after acute coronary syndrome. JAMA 2008;299(5):532-539.
What is the Relationship Between Treatment Intensification, Blood Pressure Changes in Diabetes Patients?
Background: Hyperglycemia is common in hospitalized patients with diabetes and associated with poor outcomes. Prior research on treatment intensification has focused on the intensive care unit or outpatient setting. The effect of treatment intensification in the inpatient (non-ICU) setting is not known.
Study design: Retrospective cohort.
Setting: 734-bed teaching hospital in Boston.
Synopsis: Between January 2003 and August 2004, data on blood glucose and daily pharmacologic management were gathered from electronic sources on 3,613 inpatients with diabetes. Inpatient hyperglycemia (glucose more than 180 mg/dL) occurred at least once in 2,980 (82.5%) hospitalizations.
Intensification of antihyperglycemic therapy occurred after only 22% of hospital days with hyperglycemia. Intensification included scheduled insulin, sliding scale insulin, and oral antihyperglycemic medications. Intensification of sliding scale insulin, as well as scheduled insulin, but not oral medications, was associated with a significant (12.2 mg/dL and 11.1 mg/dL respectively) average daily reduction in bedside glucose. Hypoglycemia was documented in 2.2% of days after intensification of antihyperglycemic treatment.
Bottom line: Inpatient hyperglycemia is common, and treatment intensification should be considered more often among hospitalized patients with diabetes.
Citation: Matheny ME, Shubina M, Kimmel ZM, Pendergrass ML, Turchin A. Treatment intensification and blood glucose control among hospitalized diabetic patients. J Gen Intern Med. 2008;23(2):184-189.
Does Four-Hour Antibiotic Goal Negatively Affect Accuracy of CAP Diagnosis?
Background: A period of less than our hour from emergency department presentation to first antibiotic dose is a core quality measure for community-acquired pneumonia (CAP). Time pressures might reduce the accuracy of pneumonia diagnosis and lead to unnecessary antibiotic administration.
Study design: Retrospective cohort.
Setting: 365-bed university-affiliated community hospital in Baltimore.
Synopsis: Patients admitted with an initial diagnosis of CAP were studied when the time to first antibiotic dose (TFAD) quality standard was eight hours (n=255) and later when the goal TFAD was four hours (n=293).
At admission, under the eight-hour goal, 45.9% of patients met prespecified diagnostic criteria for CAP, compared with 33.8% of patients under the four-hour goal (odds ratio [OR]=0.61, p=0.004). At discharge, 74.5% of patients had a diagnosis of pneumonia with an eight-hour TFAD standard, vs. 66.9% with a four-hour standard (p=0.05). The most common alternate diagnoses were acute bronchitis, heart failure, and COPD exacerbation.
No significant difference in antibiotic-associated adverse drug events, morbidity, or mortality were detected. Importantly, the goal TFAD reduction did not significantly increase the percentage of patients who received antibiotics within four hours (81.6% when the goal was within eight hours, vs. 85.3% when the goal was within four hours, p=0.21). The study is limited by its retrospective nature and the absence of gold standards for the diagnosis of CAP.
Bottom line: Greater pressure to administer antibiotics early in suspected cases of CAP may decrease diagnostic accuracy, without substantially improving antibiotic administration time.
Citation: Welker JA, Huston M, McCue JD. Antibiotic timing and errors in diagnosing pneumonia. Arch Intern Med. 2008;168(4):351-356.
Do Recruitment Maneuvers and High PEEP Reduce All-cause Hospital Mortality in Acute Lung Injury, ARDS?
Background: Low-tidal-volume ventilation reduces mortality in acute lung injury and acute respiratory distress syndrome (ARDS). Adding methods to open collapsed lung, such as employing recruitment maneuvers or using higher positive end-expiratory pressures (PEEP), may further reduce mortality.
Study design: Randomized controlled trial with blinded analysis. Patients were randomized to ventilation using the ARDS Network protocol (tidal volume of 6 ml/kg predicted body weight, assist control ventilation, low PEEP) vs. a higher PEEP intervention algorithm (using pressure control ventilation but still using 6 ml/kg tidal volume).
Setting: 30 intensive-care units in Canada, Australia, and Saudi Arabia.
Synopsis: Despite higher PEEP in the experimental group (14.6 cm H2O, SD 3.4) vs. the control group (9.8 cm H2O, SD 2.7) during the first 72 hours (p<0.001), there was no difference in all-cause hospital mortality or barotrauma between the two groups. The experimental group did, however, have a lower frequency of refractory hypoxemia (4.6% vs. 10.2%, 95% confidence interval [CI] 0.34-0.86, p=0.01).
At the end of the trial, a difference in the number of patients allocated to each group was noted. Investigation uncovered a programming error that disrupted the specified randomization blocks. Sensitivity analyses, which were not described, indicated that this error did not undermine randomization.
Bottom line: The addition of recruitment maneuvers and high PEEP to low-tidal-volume ventilation in acute lung injury and acute respiratory distress syndrome improved oxygenation but did not lower mortality.
Citation: Meade MO, Cook DJ, Guyatt GH, et al. Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome. A randomized controlled trial. JAMA 2008;299(6):637-645.
Does a Ventilation Strategy Setting PEEP to Increase Alveolar Recruitment, Limit Hyperinflation Improve 28-day Mortality in Acute Lung Injury, ARDS?
Background: The need for lung protection in patients with acute lung injury or acute respiratory distress syndrome (ARDS) is accepted. The optimal level of positive end-expiratory pressure (PEEP) to provide protection yet allow alveolar expansion is debated
Study design: Unblinded, randomized controlled trial. Patients were randomized to standard low tidal volume ventilation with low PEEP or low tidal volume ventilation with higher PEEP (intervention group). PEEP was increased in the intervention group to attain a plateau pressure of 28-30 cm H2O
Setting: 37 intensive care units in France.
Synopsis: Though PEEP, total PEEP, and plateau pressure were considerably higher in the experimental group, there was no difference in 28-day mortality compared with the control group, 27.8% vs. 31.2% (95% CI 0.90-1.40, p=0.31). There was, however, an increase in the number of ventilator-free days (seven vs. three, p=0.04) and organ-failure-free days (six vs. two, p=0.04) in the experimental group compared with the control group. Criteria were used to evaluate patients for readiness for extubation, but the differential application of PEEP between arms may have altered the timing of these evaluations in the two arms and may be at least partly responsible for the difference in ventilator-free days.
Throughout patient recruitment, the primary end point was monitored, resulting in 18 interim analyses of the data. No statistical adjustments were made for these frequent examinations of the data.
Bottom line: The use of higher PEEP and maximum plateau pressure to increase alveolar recruitment while limiting hyperinflation results in more ventilator-free and organ failure-free days in patients with acute lung injury and ARDS. These maneuvers do not, however, alter mortality.
Citation: Mercat A, Richard JCM, Vielle B, et al. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome. A randomized controlled trial. JAMA 2008;299(6):646-655.
What are the Effects of N-acetylcysteine, Theophylline, Other Agents on Preventing Contrast-induced Nephropathy
Background: Contrast-induced nephropathy is the third-most common cause of new acute renal failure in hospitalized patients, occurring in up to 25% of patients with renal impairment, diabetes, heart failure, advanced age, or concurrent use of nephrotoxic drugs. Clinicians use different agents to reduce the risk, including intravenous hydration, N-acetylcysteine, theophylline, fenoldopam, dopamine, furosemide, mannitol, and bicarbonate.
Study design: Meta-analysis of randomized controlled trials.
Setting: 41 studies involving 6,379 patients, published internationally between 1994 and 2006.
Synopsis: All but one study evaluated patients undergoing cardiac catheterization, and 34 trials evaluated patients with impaired renal function. N-acetylcysteine significantly reduced the risk of contrast-induced nephropathy more than saline hydration alone (risk ratio [RR]=0.62, 95% CI 0.44 to 0.88). Theophylline may have renoprotective effects but the findings were not statistically significant (RR=0.49, 95% CI 0.23 to 1.06). Ascorbic acid and bicarbonate significantly reduced nephropathy, though only one study was found for each. The other agents evaluated did not significantly reduce risk. Furosemide increased the risk (RR=3.27, 95% CI 1.48 to 7.26).
Bottom line: N-acetylcycteine is an effective agent for prevention of contrast-induced nephropathy, and it has the added benefits of low cost, few side effects, and rare drug interactions.
Citation: Kelly AM, Dwamena B, Cronin P, Bernstein SJ, Carlos RC. Meta-analysis: effectiveness of drugs for preventing contrast-induced nephropathy. Ann Intern Med. 2008;148(4):284-294.
Compared With Norepinephrine, Does Vasopressin Infusion Improve Mortality in Septic Shock Patients?
Background: Vasopressin is commonly used to support blood pressure in patients with septic shock. It has been shown to restore vascular tone, maintain blood pressure, and decrease catecholamine requirements, but its effect on mortality is uncertain.
Study design: Randomized, double-blind trial.
Setting: 27 centers in Canada, Australia, and the United States.
Synopsis: Patients with septic shock who required at least 5 mcg/min of norepinephrine were randomized to receive either low-dose vasopressin infusion (0.01 to 0.03 U/min) or norepinephrine (5 to 15 mcg/min). There was no significant difference in mortality at 28 days (35.4% for vasopressin vs. 39.3% for norepinephrine, p=0.26) or at 90 days (43.9% vs. 49.6%, p=0.11). The vasopressin group had lower heart rate and norepinephrine requirements. There were no significant differences in the frequency of adverse events.
However, since mean blood pressure at baseline was 72-73 mmHg, study patients did not necessarily have catecholamine unresponsive shock. Also, the mean time from meeting criteria for study entry to infusion of the drug was 12 hours, longer than the six-hour time period identified as important in studies of early goal-directed therapy. This may have limited the effectiveness of vasopressin infusion.
Bottom line: Low-dose vasopressin as compared with norepinephrine did not improve mortality in patients with septic shock.
Citation: Russell JA, Walley KR, Singer J, et al. Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med. 2008;358(9):877-887.
How Much do Hospitalized Patients Want to Participate in Decisions on Therapies of Varying Risk, Benefit?
Background: Obtaining informed consent is required for invasive procedures, but most non-invasive medical treatments are performed without discussing the risks, benefits, and alternatives with patients.
Study design: Questionnaire with four scenarios.
Setting: Medical wards in a Connecticut hospital.
Synopsis: Among the 210 patients studied, about one-fourth wanted physicians to obtain their permission “no matter what” even for mundane therapies like potassium supplementation (24%) or diuretic administration (28%). When presented with a higher risk scenario, such as thrombolysis with a greater than 20% chance of hemorrhage, 40.8% of patients definitely wanted to participate in decision-making.
Younger patients (age 65 or younger) were more likely to want to participate in decision-making. For each scenario, at least 85% of patients noted they would like to be consulted about the decision “no matter what” or if time allowed. Importantly, patients expressed these preferences in response to written scenarios that did not provide detailed information about the risks and benefits. Further, patients did not receive explanations of the logistical hurdles of trying to obtain patient input for each decision.
Bottom line: The great majority of patients in this study wished to participate in decision making for hypothetical medical treatments, especially if time allowed. At least 24% always wanted to be consulted, even about mundane therapies like potassium supplementation.
Citation: Upadhyay S, Beck A, Rishi A, Amoateng-Adjepong Y, Manthous CA. Patients’ predilections regarding informed consent for hospital treatments. J Hosp Med. 2008; 3(1):6-11.
What are the Clinical Characteristics, Treatments, and Three-month Outcomes of Patients With Upper-extremity DVT
Background: Anticoagulation is the treatment of choice for upper-extremity deep venous thrombosis (DVT). However, no large studies have characterized the nature, management, and prognosis of upper-extremity DVT.
Study design: Prospective registry of consecutive patients (RIETE registry).
Setting: International multicenter study (124 centers in Spain, France, Italy, Israel, and Argentina).
Synopsis: Among the 11,564 registry patients with acute DVT, 512 (4.4%) were noted to have upper-extremity DVT. Cancer was more common and immobility was less common with upper-extremity DVT. Initially, most patients (91%) were treated with low-molecular-weight heparin (LMWH). For long-term therapy, 75% of patients with cancer received LMWH, and 76% of patients without cancer were given oral vitamin K antagonists. At diagnosis, only 9% of patients with upper-extremity DVT had clinically apparent pulmonary embolism (PE) versus 29% of those with lower-extremity DVT. During the three-month follow-up, the incidence of PE, fatal PE, recurrent DVT, and bleeding was similar for upper- and lower-extremity DVT. Mortality was higher in patients with upper-extremity DVT, which in multivariable analyses, was explained by the higher prevalence of cancer in that group.
Bottom line: Because the incidence of recurrent DVT/PE, fatal PE, or major bleeding is similar between upper and lower extremity DVT, therapy should not differ.
Citation: Muñoz FJ, Mismetti P, Poggio R, et al. Clinical outcome of patients with upper-extremity deep vein thrombosis. Chest 2008;133(1):143-148.
Are Oral Steroids as Effective as IV Steroids in Patients With COPD Exacerbation?
Background: Oral prednisolone has near 100% bioavailability following oral administration. Although current guidelines suggest using oral steroids in the treatment of COPD exacerbation, the optimal route of administration has not been studied rigorously.
Study design: Non-inferiority, double-blinded, randomized controlled trial.
Setting: Single hospital in the Netherlands.
Synopsis: Patients were randomized to receive either a five-day course of IV or oral prednisolone 60 mg, followed by an oral prednisolone taper. All received nebulized ipratropium and albuterol four times daily, as well as oral amoxicillin/clavulanate (or doxycycline if allergic). The primary outcome was treatment failure, which included death, ICU admission, hospital readmission for COPD, or treatment intensification during 90-day follow-up.
Non-inferiority was defined as a treatment failure rate for oral steroids not more than 15% worse than the treatment failure rate for IV steroids. The study design called for 256 patients to provide adequate (80%) power for the primary analysis. However, only 210 were enrolled due to slow recruitment, and 17 withdrew consent or did not meet study entry criteria.
The intention-to-treat analysis showed no significant difference between oral and IV steroids in the treatment failure rate (56.3% vs. 61.7%, respectively). Results of the per-protocol analysis were similar. However, insufficient power and poor patient accounting raise questions about the validity of the results.
Bottom line: Oral steroids appeared no worse than IV steroids in the treatment of COPD exacerbation, but the study was underpowered, which prevents definitive conclusions.
Citation: De Jong YP, Uil SM, Grotjohan HP, et al. Oral or IV prednisolone in the treatment of COPD exacerbations. A randomized, controlled, double-blind study. Chest 2007;132(6):1741-1747. TH
Literature at a Glance
A guide to this month’s studies.
- Adverse events are common after stopping clopidogrel following acute coronary syndrome.
- Treatment intensification with insulin improves inpatient glucose control.
- Pressure for early antibiotic administration leads to inaccuracy of pneumonia diagnosis.
- Multifaceted ventilation strategy no better than low-tidal-volume protocol.
- Higher PEEP ventilation strategy reduces duration of ventilation but not mortality.
- N-acetylcysteine reduces contrast-induced nephropathy.
- Vasopressin is no better than norepinephrine in patients with septic shock.
- Hospital patients desire greater participation in decision-making.
- Outcomes of patients with upper- or lower-extremity DVT are similar.
- Oral and IV steroids may be equally effective in COPD exacerbation.
What is Frequency, Timing of Adverse Events After Stopping Clopidogrel in ACS Patients?
Background: Clopidogrel is recommended in treatment of acute coronary syndrome (ACS) with or without stent placement. A rebound hypercoagulable state may occur following clopidogrel cessation, but this has not been investigated previously.
Study design: Retrospective cohort.
Setting: 127 VA medical centers.
Synopsis: Data were collected as part of the Veterans Health Administration Cardiac Care Follow-up Clinical Study from October 2003 through March 2005 on all patients with acute myocardial infarction (MI) or unstable angina who were discharged with clopidogrel treatment (3,137 patients). The analysis assessed the incidence and timing of adverse events after stopping clopidogrel among medically treated patients and among those treated with percutaneous coronary intervention (PCI).
In adjusted analyses among medically treated patients, the risk of death or acute MI in the first 90 days after clopidogrel cessation was 1.98 times higher, compared with the interval from 91-180 days. Among patients who received PCI (usually with a bare-metal stent), the risk was 1.82 times higher in the first 90 days. The clustering of events shortly after clopidogrel cessation support the possibility of a rebound hypercoagulable state.
Bottom line: In patients with ACS who received medical management or PCI, there was a higher rate of adverse events in the first 90 days after clopidogrel cessation.
Citation: Ho PM, Peterson ED, Wang L, et al. Incidence of death and acute myocardial infarction associated with stopping clopidorel after acute coronary syndrome. JAMA 2008;299(5):532-539.
What is the Relationship Between Treatment Intensification, Blood Pressure Changes in Diabetes Patients?
Background: Hyperglycemia is common in hospitalized patients with diabetes and associated with poor outcomes. Prior research on treatment intensification has focused on the intensive care unit or outpatient setting. The effect of treatment intensification in the inpatient (non-ICU) setting is not known.
Study design: Retrospective cohort.
Setting: 734-bed teaching hospital in Boston.
Synopsis: Between January 2003 and August 2004, data on blood glucose and daily pharmacologic management were gathered from electronic sources on 3,613 inpatients with diabetes. Inpatient hyperglycemia (glucose more than 180 mg/dL) occurred at least once in 2,980 (82.5%) hospitalizations.
Intensification of antihyperglycemic therapy occurred after only 22% of hospital days with hyperglycemia. Intensification included scheduled insulin, sliding scale insulin, and oral antihyperglycemic medications. Intensification of sliding scale insulin, as well as scheduled insulin, but not oral medications, was associated with a significant (12.2 mg/dL and 11.1 mg/dL respectively) average daily reduction in bedside glucose. Hypoglycemia was documented in 2.2% of days after intensification of antihyperglycemic treatment.
Bottom line: Inpatient hyperglycemia is common, and treatment intensification should be considered more often among hospitalized patients with diabetes.
Citation: Matheny ME, Shubina M, Kimmel ZM, Pendergrass ML, Turchin A. Treatment intensification and blood glucose control among hospitalized diabetic patients. J Gen Intern Med. 2008;23(2):184-189.
Does Four-Hour Antibiotic Goal Negatively Affect Accuracy of CAP Diagnosis?
Background: A period of less than our hour from emergency department presentation to first antibiotic dose is a core quality measure for community-acquired pneumonia (CAP). Time pressures might reduce the accuracy of pneumonia diagnosis and lead to unnecessary antibiotic administration.
Study design: Retrospective cohort.
Setting: 365-bed university-affiliated community hospital in Baltimore.
Synopsis: Patients admitted with an initial diagnosis of CAP were studied when the time to first antibiotic dose (TFAD) quality standard was eight hours (n=255) and later when the goal TFAD was four hours (n=293).
At admission, under the eight-hour goal, 45.9% of patients met prespecified diagnostic criteria for CAP, compared with 33.8% of patients under the four-hour goal (odds ratio [OR]=0.61, p=0.004). At discharge, 74.5% of patients had a diagnosis of pneumonia with an eight-hour TFAD standard, vs. 66.9% with a four-hour standard (p=0.05). The most common alternate diagnoses were acute bronchitis, heart failure, and COPD exacerbation.
No significant difference in antibiotic-associated adverse drug events, morbidity, or mortality were detected. Importantly, the goal TFAD reduction did not significantly increase the percentage of patients who received antibiotics within four hours (81.6% when the goal was within eight hours, vs. 85.3% when the goal was within four hours, p=0.21). The study is limited by its retrospective nature and the absence of gold standards for the diagnosis of CAP.
Bottom line: Greater pressure to administer antibiotics early in suspected cases of CAP may decrease diagnostic accuracy, without substantially improving antibiotic administration time.
Citation: Welker JA, Huston M, McCue JD. Antibiotic timing and errors in diagnosing pneumonia. Arch Intern Med. 2008;168(4):351-356.
Do Recruitment Maneuvers and High PEEP Reduce All-cause Hospital Mortality in Acute Lung Injury, ARDS?
Background: Low-tidal-volume ventilation reduces mortality in acute lung injury and acute respiratory distress syndrome (ARDS). Adding methods to open collapsed lung, such as employing recruitment maneuvers or using higher positive end-expiratory pressures (PEEP), may further reduce mortality.
Study design: Randomized controlled trial with blinded analysis. Patients were randomized to ventilation using the ARDS Network protocol (tidal volume of 6 ml/kg predicted body weight, assist control ventilation, low PEEP) vs. a higher PEEP intervention algorithm (using pressure control ventilation but still using 6 ml/kg tidal volume).
Setting: 30 intensive-care units in Canada, Australia, and Saudi Arabia.
Synopsis: Despite higher PEEP in the experimental group (14.6 cm H2O, SD 3.4) vs. the control group (9.8 cm H2O, SD 2.7) during the first 72 hours (p<0.001), there was no difference in all-cause hospital mortality or barotrauma between the two groups. The experimental group did, however, have a lower frequency of refractory hypoxemia (4.6% vs. 10.2%, 95% confidence interval [CI] 0.34-0.86, p=0.01).
At the end of the trial, a difference in the number of patients allocated to each group was noted. Investigation uncovered a programming error that disrupted the specified randomization blocks. Sensitivity analyses, which were not described, indicated that this error did not undermine randomization.
Bottom line: The addition of recruitment maneuvers and high PEEP to low-tidal-volume ventilation in acute lung injury and acute respiratory distress syndrome improved oxygenation but did not lower mortality.
Citation: Meade MO, Cook DJ, Guyatt GH, et al. Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome. A randomized controlled trial. JAMA 2008;299(6):637-645.
Does a Ventilation Strategy Setting PEEP to Increase Alveolar Recruitment, Limit Hyperinflation Improve 28-day Mortality in Acute Lung Injury, ARDS?
Background: The need for lung protection in patients with acute lung injury or acute respiratory distress syndrome (ARDS) is accepted. The optimal level of positive end-expiratory pressure (PEEP) to provide protection yet allow alveolar expansion is debated
Study design: Unblinded, randomized controlled trial. Patients were randomized to standard low tidal volume ventilation with low PEEP or low tidal volume ventilation with higher PEEP (intervention group). PEEP was increased in the intervention group to attain a plateau pressure of 28-30 cm H2O
Setting: 37 intensive care units in France.
Synopsis: Though PEEP, total PEEP, and plateau pressure were considerably higher in the experimental group, there was no difference in 28-day mortality compared with the control group, 27.8% vs. 31.2% (95% CI 0.90-1.40, p=0.31). There was, however, an increase in the number of ventilator-free days (seven vs. three, p=0.04) and organ-failure-free days (six vs. two, p=0.04) in the experimental group compared with the control group. Criteria were used to evaluate patients for readiness for extubation, but the differential application of PEEP between arms may have altered the timing of these evaluations in the two arms and may be at least partly responsible for the difference in ventilator-free days.
Throughout patient recruitment, the primary end point was monitored, resulting in 18 interim analyses of the data. No statistical adjustments were made for these frequent examinations of the data.
Bottom line: The use of higher PEEP and maximum plateau pressure to increase alveolar recruitment while limiting hyperinflation results in more ventilator-free and organ failure-free days in patients with acute lung injury and ARDS. These maneuvers do not, however, alter mortality.
Citation: Mercat A, Richard JCM, Vielle B, et al. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome. A randomized controlled trial. JAMA 2008;299(6):646-655.
What are the Effects of N-acetylcysteine, Theophylline, Other Agents on Preventing Contrast-induced Nephropathy
Background: Contrast-induced nephropathy is the third-most common cause of new acute renal failure in hospitalized patients, occurring in up to 25% of patients with renal impairment, diabetes, heart failure, advanced age, or concurrent use of nephrotoxic drugs. Clinicians use different agents to reduce the risk, including intravenous hydration, N-acetylcysteine, theophylline, fenoldopam, dopamine, furosemide, mannitol, and bicarbonate.
Study design: Meta-analysis of randomized controlled trials.
Setting: 41 studies involving 6,379 patients, published internationally between 1994 and 2006.
Synopsis: All but one study evaluated patients undergoing cardiac catheterization, and 34 trials evaluated patients with impaired renal function. N-acetylcysteine significantly reduced the risk of contrast-induced nephropathy more than saline hydration alone (risk ratio [RR]=0.62, 95% CI 0.44 to 0.88). Theophylline may have renoprotective effects but the findings were not statistically significant (RR=0.49, 95% CI 0.23 to 1.06). Ascorbic acid and bicarbonate significantly reduced nephropathy, though only one study was found for each. The other agents evaluated did not significantly reduce risk. Furosemide increased the risk (RR=3.27, 95% CI 1.48 to 7.26).
Bottom line: N-acetylcycteine is an effective agent for prevention of contrast-induced nephropathy, and it has the added benefits of low cost, few side effects, and rare drug interactions.
Citation: Kelly AM, Dwamena B, Cronin P, Bernstein SJ, Carlos RC. Meta-analysis: effectiveness of drugs for preventing contrast-induced nephropathy. Ann Intern Med. 2008;148(4):284-294.
Compared With Norepinephrine, Does Vasopressin Infusion Improve Mortality in Septic Shock Patients?
Background: Vasopressin is commonly used to support blood pressure in patients with septic shock. It has been shown to restore vascular tone, maintain blood pressure, and decrease catecholamine requirements, but its effect on mortality is uncertain.
Study design: Randomized, double-blind trial.
Setting: 27 centers in Canada, Australia, and the United States.
Synopsis: Patients with septic shock who required at least 5 mcg/min of norepinephrine were randomized to receive either low-dose vasopressin infusion (0.01 to 0.03 U/min) or norepinephrine (5 to 15 mcg/min). There was no significant difference in mortality at 28 days (35.4% for vasopressin vs. 39.3% for norepinephrine, p=0.26) or at 90 days (43.9% vs. 49.6%, p=0.11). The vasopressin group had lower heart rate and norepinephrine requirements. There were no significant differences in the frequency of adverse events.
However, since mean blood pressure at baseline was 72-73 mmHg, study patients did not necessarily have catecholamine unresponsive shock. Also, the mean time from meeting criteria for study entry to infusion of the drug was 12 hours, longer than the six-hour time period identified as important in studies of early goal-directed therapy. This may have limited the effectiveness of vasopressin infusion.
Bottom line: Low-dose vasopressin as compared with norepinephrine did not improve mortality in patients with septic shock.
Citation: Russell JA, Walley KR, Singer J, et al. Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med. 2008;358(9):877-887.
How Much do Hospitalized Patients Want to Participate in Decisions on Therapies of Varying Risk, Benefit?
Background: Obtaining informed consent is required for invasive procedures, but most non-invasive medical treatments are performed without discussing the risks, benefits, and alternatives with patients.
Study design: Questionnaire with four scenarios.
Setting: Medical wards in a Connecticut hospital.
Synopsis: Among the 210 patients studied, about one-fourth wanted physicians to obtain their permission “no matter what” even for mundane therapies like potassium supplementation (24%) or diuretic administration (28%). When presented with a higher risk scenario, such as thrombolysis with a greater than 20% chance of hemorrhage, 40.8% of patients definitely wanted to participate in decision-making.
Younger patients (age 65 or younger) were more likely to want to participate in decision-making. For each scenario, at least 85% of patients noted they would like to be consulted about the decision “no matter what” or if time allowed. Importantly, patients expressed these preferences in response to written scenarios that did not provide detailed information about the risks and benefits. Further, patients did not receive explanations of the logistical hurdles of trying to obtain patient input for each decision.
Bottom line: The great majority of patients in this study wished to participate in decision making for hypothetical medical treatments, especially if time allowed. At least 24% always wanted to be consulted, even about mundane therapies like potassium supplementation.
Citation: Upadhyay S, Beck A, Rishi A, Amoateng-Adjepong Y, Manthous CA. Patients’ predilections regarding informed consent for hospital treatments. J Hosp Med. 2008; 3(1):6-11.
What are the Clinical Characteristics, Treatments, and Three-month Outcomes of Patients With Upper-extremity DVT
Background: Anticoagulation is the treatment of choice for upper-extremity deep venous thrombosis (DVT). However, no large studies have characterized the nature, management, and prognosis of upper-extremity DVT.
Study design: Prospective registry of consecutive patients (RIETE registry).
Setting: International multicenter study (124 centers in Spain, France, Italy, Israel, and Argentina).
Synopsis: Among the 11,564 registry patients with acute DVT, 512 (4.4%) were noted to have upper-extremity DVT. Cancer was more common and immobility was less common with upper-extremity DVT. Initially, most patients (91%) were treated with low-molecular-weight heparin (LMWH). For long-term therapy, 75% of patients with cancer received LMWH, and 76% of patients without cancer were given oral vitamin K antagonists. At diagnosis, only 9% of patients with upper-extremity DVT had clinically apparent pulmonary embolism (PE) versus 29% of those with lower-extremity DVT. During the three-month follow-up, the incidence of PE, fatal PE, recurrent DVT, and bleeding was similar for upper- and lower-extremity DVT. Mortality was higher in patients with upper-extremity DVT, which in multivariable analyses, was explained by the higher prevalence of cancer in that group.
Bottom line: Because the incidence of recurrent DVT/PE, fatal PE, or major bleeding is similar between upper and lower extremity DVT, therapy should not differ.
Citation: Muñoz FJ, Mismetti P, Poggio R, et al. Clinical outcome of patients with upper-extremity deep vein thrombosis. Chest 2008;133(1):143-148.
Are Oral Steroids as Effective as IV Steroids in Patients With COPD Exacerbation?
Background: Oral prednisolone has near 100% bioavailability following oral administration. Although current guidelines suggest using oral steroids in the treatment of COPD exacerbation, the optimal route of administration has not been studied rigorously.
Study design: Non-inferiority, double-blinded, randomized controlled trial.
Setting: Single hospital in the Netherlands.
Synopsis: Patients were randomized to receive either a five-day course of IV or oral prednisolone 60 mg, followed by an oral prednisolone taper. All received nebulized ipratropium and albuterol four times daily, as well as oral amoxicillin/clavulanate (or doxycycline if allergic). The primary outcome was treatment failure, which included death, ICU admission, hospital readmission for COPD, or treatment intensification during 90-day follow-up.
Non-inferiority was defined as a treatment failure rate for oral steroids not more than 15% worse than the treatment failure rate for IV steroids. The study design called for 256 patients to provide adequate (80%) power for the primary analysis. However, only 210 were enrolled due to slow recruitment, and 17 withdrew consent or did not meet study entry criteria.
The intention-to-treat analysis showed no significant difference between oral and IV steroids in the treatment failure rate (56.3% vs. 61.7%, respectively). Results of the per-protocol analysis were similar. However, insufficient power and poor patient accounting raise questions about the validity of the results.
Bottom line: Oral steroids appeared no worse than IV steroids in the treatment of COPD exacerbation, but the study was underpowered, which prevents definitive conclusions.
Citation: De Jong YP, Uil SM, Grotjohan HP, et al. Oral or IV prednisolone in the treatment of COPD exacerbations. A randomized, controlled, double-blind study. Chest 2007;132(6):1741-1747. TH
Performance and Standards Committee Furthers SHM’s Quality Mission
The Performance and Standards Task Force (PSTF) was formed in May 2006 when SHM leadership recognized the need for a coordinated approach to working with other organizations in the quality arena.
A task force normally would have a beginning and an end to its scope of work. However, PSTF’s ongoing mission has matured, becoming more and more engaged in quality activities. In late fall 2007, the time had come for the PSTF to evolve into SHM’s Performance and Standards Committee (PSC).
What We Do
As SHM’s senior adviser for quality standards and compliance, I continue to work with PSC Chair Patrick Torcson, MD, along with senior staff and leadership of the Public Policy Committee (PPC), to monitor the national performance and quality landscape. The PSC, which engages with national organizations and is charged with developing performance measures and building consensus, also works to develop relationships with other professional medical societies and organizations.
Recognizing the need to communicate more frequently on SHM quality/policy issues related to quality improvement and patient safety, the PSC has also forged a stronger tie with the Hospital Quality and Patient Safety Committee (HQPSC) and was represented in the HQPSC-led Quality Summit in October.
Through the PSC, SHM has worked to influence performance measure development, consensus, and the endorsement process by joining the AMA Physician Consortium for Performance Improvement (PCPI) and the National Quality Forum (NQF).
Broader Reach
SHM members have contributed to the process by participating in activities relevant to hospital medicine and building relationships with senior staff and leadership within these national stakeholder groups.
The PCPI is committed to enhancing quality of care and patient safety by taking the lead in the development, testing, and maintaining evidence-based clinical performance measures and performance measurement resources for physicians. The NQF is a nonprofit organization charged by Congress to endorse consensus-based national standards for measurement and public reporting of healthcare performance data. Beginning in 2006, the PCPI and NQF have worked to influence the development of physician-level performance measures as part of the CMS Physician Quality Reporting Initiative (PQRI). Joining the PCPI has given SHM the opportunity to participate with other organizations on expert work groups to develop performance measures. SHM has been involved in performance measure development for topics such as geriatrics, emergency medicine, outpatient parenteral antimicrobial therapy, and anesthesiology issues including perioperative normothermia and critical care.
Many of these measures have been included in the PQRI program. SHM submitted feedback during public comment periods on measures related to perioperative care and chronic kidney disease. Most importantly, PCPI participation has given SHM high visibility among measurement stakeholder groups, including CMS and NQF. This has raised the acceptance of hospital medicine as a specialty, as well as the influence and credibility of SHM as a professional society.
As a collaborative effort on behalf of SHM, the PSC and PPC drafted and submitted a comment letter on the 2008 Centers for Medicare and Medicaid Studies (CMS) Proposed Rule regarding the future of the PQRI. SHM has supported the CMS value-based purchasing initiative and the PQRI in general. The PSC recommended that CMS and national stakeholder groups like the PCPI and NQF re-evaluate the denominators of several measures, existing and proposed, to make them applicable to the inpatient setting for hospitalist reporting.
PSC senior staff attended the PCPI meeting in Chicago last October and met with Susan Nedza, MD, of the CMS Special Program Office, Value-Based Purchasing, to express SHM’s appreciation of increased CMS recognition of hospitalists through its quality initiatives. This also was an opportunity to receive input on additional ways hospitalists can become engaged in the 2008 PQRI and other CMS quality efforts.
PQRI Success
In early November, Dr. Nedza and her staff, Dr. Torcson, and SHM senior staff met via conference call to discuss the preliminary results of the 2007 PQRI and exchange thoughts on the program related to hospitalists. A concern for hospitalists was the intent for the PQRI to include performance measures for each of the 39 medical specialties recognized by CMS; hospitalists were lumped under general internal medicine. By working closely with CMS and the PCPI, SHM succeeded in achieving denominator specification changes for additional relevant measures to become available for hospitalist reporting through the 2007 PQRI.
Soon thereafter, the CMS Final Rule on Physician Payment was released, indicating that 10 of the 11 measures available for hospitalist reporting in the 2007 PQRI also were to be included for 2008. “Beta-blocker on Arrival for Acute Myocardial Infarction” was the one measure no longer part of the 2008 PQRI. One new measure available for hospitalist reporting in 2008 is measure No. 75, “Prevention of Ventilator-Associated Pneumonia—Head Elevation,” for which hospitalists can report using a critical care code.
The 2007 PQRI included the following measures on which hospitalists could report:
- No. 5: “Heart Failure: Angiotensin-Converting Enzyme (ACE) Inhibitor or Angiotensin Receptor Blocker (ARB) Therapy for Left Ventricular Systolic Dysfunction (LVSD)”;
- No. 6: “Oral Antiplatelet Therapy Prescribed for Patients with Coronary Artery Disease”;
- No. 7: “Beta-blocker Therapy for CAD Patients with Prior Myocardial Infarction”;
- No. 29: “Beta-blocker at Time of Arrival for Acute Myocardial Infarction”;
- No. 31: “Stroke and Stroke Rehabilitation: Deep Vein Thrombosis Prophylaxis”;
- No. 32: “Stroke and Stroke Rehabilitation: Discharged on Antiplatelet Therapy”;
- No. 33: “Stroke and Stroke Rehabilitation: Anticoagulant Therapy Prescribed for Atrial Fibrillation at Discharge”;
- No. 34: “Stroke and Stroke Rehabilitation: Tissue Plasminogen Activator Considered”;
- No. 35: “Stroke and Stroke Rehabilitation: Screening for Dysphagia”;
- No. 36: “Stroke and Stroke Rehabilitation: Consideration of Rehabilitation Services”; and
- No. 47: “Documentation of an Advanced Care Plan.”
After the final specifications for the 2008 PQRI were released, there was a proposal for denominator specification changes that would preclude inpatient reporting for many of the measures relevant and available to hospitalists in 2007. The PSC again worked closely with the PCPI and relevant professional organizations to preserve the measure specifications for the 2008 PQRI to allow inpatient and thus hospitalist reporting. This experience has further enhanced productive SHM relationships with the PCPI and CMS.
The PSC has an ongoing commitment to recommend SHM members for appointments to PCPI expert measure workgroups, depending on the topic. For example, SHM was recently asked to identify a member to join a newly forming asthma measures workgroup that will be looking to develop inpatient measures. SHM will be notified when a palliative care measures workgroup is being formed.
Senior staff and leadership will meet PCPI senior staff to discuss formation of an expert workgroup on care transitions measures. This work group will be co-chaired by SHM and the American College of Physicians (ACP) and include societies such as the Society of General Internal Medicine (SGIM), the American Geriatrics Society (AGS), and others engaged in the development of the transitions of care consensus document in summer 2007. The work group also will refer to the principles and standards that resulted from the ABIM Foundation’s Stepping Up to the Plate (SUTTP) Alliance as a resource in its development of measures.
Looking ahead to the 2009 PQRI, the PSC has requested measure specification changes to the following PQRI measures:
- No. 56: “Vital Signs for Community Acquired Pneumonia”;
- No. 57: “Oxygenation Assessment for Community Acquired Pneumonia”;
- No. 58: “Assessment of Mental Status for Community Acquired Pneumonia”; and
- No. 59: “Empiric Antibiotic for Community Acquired Pneumonia.”
These measures harmonize with the Joint Commission’s core measures and are relevant for hospitalist performance reporting.
With the NQF
On Sept. 26-28, PSC member Greg Seymann represented SHM at NQF’s 8th Annual Meeting in Washington, D.C. This meeting featured plenary sessions focusing on issues at the forefront of policy discussions related to quality of care including:
- Chronic care episodes across care settings;
- Medications and quality;
- Medicare performance monitoring and payment initiatives;
- Moving performance measures into electronic health record requirements; and
- Nursing leadership in measurement activities and achieving higher performance.
- In the first quarter of 2008, the PSC has:
- Reviewed and commented on NQF’s “National Voluntary Consensus Standards for Hospital Care: Additional Priorities–2007, Part 2”;
- Sent a representative to the steering committee for the National Voluntary Consensus Clinician-Level Perioperative Care Standards meeting;
- Submitted nominees for the National Voluntary Consensus Standards for Emergency Care Phase II steering committee and the Prevention and Management of Stroke Across the Continuum steering committee (our nominee was accepted for the latter);
- Reviewed and commented on the National Voluntary Consensus Standards for Prevention and
- Care of Venous Thromboembolism: Performance Measures/Phase II; and;
- Has sent senior leadership and staff to the NQF Spring Meeting and Implementation Conference on Care Coordination.
In the Works
The PSC and the HQPSC submitted a comment letter on CMS’ selection of hospital-acquired conditions and present on admission indicator reporting for 2009. SHM supported CMS’ efforts to improve the quality of care for hospitalized patients by preventing avoidable hospital-acquired conditions and outlining its concerns regarding unintended consequences as relates to the various conditions.
With its new status as the PSC, this enthusiastic and committed group is preparing to extend its mission and scope of work in 2008.
The PSC plans to restructure and serve as expert liaisons for internal and external activities. This not only will empower committee members to become more engaged in our performance agenda, but also allow them to serve as key contacts for staff when monitoring the ever-growing landscape of performance measurement, quality, and policy. TH
The Performance and Standards Task Force (PSTF) was formed in May 2006 when SHM leadership recognized the need for a coordinated approach to working with other organizations in the quality arena.
A task force normally would have a beginning and an end to its scope of work. However, PSTF’s ongoing mission has matured, becoming more and more engaged in quality activities. In late fall 2007, the time had come for the PSTF to evolve into SHM’s Performance and Standards Committee (PSC).
What We Do
As SHM’s senior adviser for quality standards and compliance, I continue to work with PSC Chair Patrick Torcson, MD, along with senior staff and leadership of the Public Policy Committee (PPC), to monitor the national performance and quality landscape. The PSC, which engages with national organizations and is charged with developing performance measures and building consensus, also works to develop relationships with other professional medical societies and organizations.
Recognizing the need to communicate more frequently on SHM quality/policy issues related to quality improvement and patient safety, the PSC has also forged a stronger tie with the Hospital Quality and Patient Safety Committee (HQPSC) and was represented in the HQPSC-led Quality Summit in October.
Through the PSC, SHM has worked to influence performance measure development, consensus, and the endorsement process by joining the AMA Physician Consortium for Performance Improvement (PCPI) and the National Quality Forum (NQF).
Broader Reach
SHM members have contributed to the process by participating in activities relevant to hospital medicine and building relationships with senior staff and leadership within these national stakeholder groups.
The PCPI is committed to enhancing quality of care and patient safety by taking the lead in the development, testing, and maintaining evidence-based clinical performance measures and performance measurement resources for physicians. The NQF is a nonprofit organization charged by Congress to endorse consensus-based national standards for measurement and public reporting of healthcare performance data. Beginning in 2006, the PCPI and NQF have worked to influence the development of physician-level performance measures as part of the CMS Physician Quality Reporting Initiative (PQRI). Joining the PCPI has given SHM the opportunity to participate with other organizations on expert work groups to develop performance measures. SHM has been involved in performance measure development for topics such as geriatrics, emergency medicine, outpatient parenteral antimicrobial therapy, and anesthesiology issues including perioperative normothermia and critical care.
Many of these measures have been included in the PQRI program. SHM submitted feedback during public comment periods on measures related to perioperative care and chronic kidney disease. Most importantly, PCPI participation has given SHM high visibility among measurement stakeholder groups, including CMS and NQF. This has raised the acceptance of hospital medicine as a specialty, as well as the influence and credibility of SHM as a professional society.
As a collaborative effort on behalf of SHM, the PSC and PPC drafted and submitted a comment letter on the 2008 Centers for Medicare and Medicaid Studies (CMS) Proposed Rule regarding the future of the PQRI. SHM has supported the CMS value-based purchasing initiative and the PQRI in general. The PSC recommended that CMS and national stakeholder groups like the PCPI and NQF re-evaluate the denominators of several measures, existing and proposed, to make them applicable to the inpatient setting for hospitalist reporting.
PSC senior staff attended the PCPI meeting in Chicago last October and met with Susan Nedza, MD, of the CMS Special Program Office, Value-Based Purchasing, to express SHM’s appreciation of increased CMS recognition of hospitalists through its quality initiatives. This also was an opportunity to receive input on additional ways hospitalists can become engaged in the 2008 PQRI and other CMS quality efforts.
PQRI Success
In early November, Dr. Nedza and her staff, Dr. Torcson, and SHM senior staff met via conference call to discuss the preliminary results of the 2007 PQRI and exchange thoughts on the program related to hospitalists. A concern for hospitalists was the intent for the PQRI to include performance measures for each of the 39 medical specialties recognized by CMS; hospitalists were lumped under general internal medicine. By working closely with CMS and the PCPI, SHM succeeded in achieving denominator specification changes for additional relevant measures to become available for hospitalist reporting through the 2007 PQRI.
Soon thereafter, the CMS Final Rule on Physician Payment was released, indicating that 10 of the 11 measures available for hospitalist reporting in the 2007 PQRI also were to be included for 2008. “Beta-blocker on Arrival for Acute Myocardial Infarction” was the one measure no longer part of the 2008 PQRI. One new measure available for hospitalist reporting in 2008 is measure No. 75, “Prevention of Ventilator-Associated Pneumonia—Head Elevation,” for which hospitalists can report using a critical care code.
The 2007 PQRI included the following measures on which hospitalists could report:
- No. 5: “Heart Failure: Angiotensin-Converting Enzyme (ACE) Inhibitor or Angiotensin Receptor Blocker (ARB) Therapy for Left Ventricular Systolic Dysfunction (LVSD)”;
- No. 6: “Oral Antiplatelet Therapy Prescribed for Patients with Coronary Artery Disease”;
- No. 7: “Beta-blocker Therapy for CAD Patients with Prior Myocardial Infarction”;
- No. 29: “Beta-blocker at Time of Arrival for Acute Myocardial Infarction”;
- No. 31: “Stroke and Stroke Rehabilitation: Deep Vein Thrombosis Prophylaxis”;
- No. 32: “Stroke and Stroke Rehabilitation: Discharged on Antiplatelet Therapy”;
- No. 33: “Stroke and Stroke Rehabilitation: Anticoagulant Therapy Prescribed for Atrial Fibrillation at Discharge”;
- No. 34: “Stroke and Stroke Rehabilitation: Tissue Plasminogen Activator Considered”;
- No. 35: “Stroke and Stroke Rehabilitation: Screening for Dysphagia”;
- No. 36: “Stroke and Stroke Rehabilitation: Consideration of Rehabilitation Services”; and
- No. 47: “Documentation of an Advanced Care Plan.”
After the final specifications for the 2008 PQRI were released, there was a proposal for denominator specification changes that would preclude inpatient reporting for many of the measures relevant and available to hospitalists in 2007. The PSC again worked closely with the PCPI and relevant professional organizations to preserve the measure specifications for the 2008 PQRI to allow inpatient and thus hospitalist reporting. This experience has further enhanced productive SHM relationships with the PCPI and CMS.
The PSC has an ongoing commitment to recommend SHM members for appointments to PCPI expert measure workgroups, depending on the topic. For example, SHM was recently asked to identify a member to join a newly forming asthma measures workgroup that will be looking to develop inpatient measures. SHM will be notified when a palliative care measures workgroup is being formed.
Senior staff and leadership will meet PCPI senior staff to discuss formation of an expert workgroup on care transitions measures. This work group will be co-chaired by SHM and the American College of Physicians (ACP) and include societies such as the Society of General Internal Medicine (SGIM), the American Geriatrics Society (AGS), and others engaged in the development of the transitions of care consensus document in summer 2007. The work group also will refer to the principles and standards that resulted from the ABIM Foundation’s Stepping Up to the Plate (SUTTP) Alliance as a resource in its development of measures.
Looking ahead to the 2009 PQRI, the PSC has requested measure specification changes to the following PQRI measures:
- No. 56: “Vital Signs for Community Acquired Pneumonia”;
- No. 57: “Oxygenation Assessment for Community Acquired Pneumonia”;
- No. 58: “Assessment of Mental Status for Community Acquired Pneumonia”; and
- No. 59: “Empiric Antibiotic for Community Acquired Pneumonia.”
These measures harmonize with the Joint Commission’s core measures and are relevant for hospitalist performance reporting.
With the NQF
On Sept. 26-28, PSC member Greg Seymann represented SHM at NQF’s 8th Annual Meeting in Washington, D.C. This meeting featured plenary sessions focusing on issues at the forefront of policy discussions related to quality of care including:
- Chronic care episodes across care settings;
- Medications and quality;
- Medicare performance monitoring and payment initiatives;
- Moving performance measures into electronic health record requirements; and
- Nursing leadership in measurement activities and achieving higher performance.
- In the first quarter of 2008, the PSC has:
- Reviewed and commented on NQF’s “National Voluntary Consensus Standards for Hospital Care: Additional Priorities–2007, Part 2”;
- Sent a representative to the steering committee for the National Voluntary Consensus Clinician-Level Perioperative Care Standards meeting;
- Submitted nominees for the National Voluntary Consensus Standards for Emergency Care Phase II steering committee and the Prevention and Management of Stroke Across the Continuum steering committee (our nominee was accepted for the latter);
- Reviewed and commented on the National Voluntary Consensus Standards for Prevention and
- Care of Venous Thromboembolism: Performance Measures/Phase II; and;
- Has sent senior leadership and staff to the NQF Spring Meeting and Implementation Conference on Care Coordination.
In the Works
The PSC and the HQPSC submitted a comment letter on CMS’ selection of hospital-acquired conditions and present on admission indicator reporting for 2009. SHM supported CMS’ efforts to improve the quality of care for hospitalized patients by preventing avoidable hospital-acquired conditions and outlining its concerns regarding unintended consequences as relates to the various conditions.
With its new status as the PSC, this enthusiastic and committed group is preparing to extend its mission and scope of work in 2008.
The PSC plans to restructure and serve as expert liaisons for internal and external activities. This not only will empower committee members to become more engaged in our performance agenda, but also allow them to serve as key contacts for staff when monitoring the ever-growing landscape of performance measurement, quality, and policy. TH
The Performance and Standards Task Force (PSTF) was formed in May 2006 when SHM leadership recognized the need for a coordinated approach to working with other organizations in the quality arena.
A task force normally would have a beginning and an end to its scope of work. However, PSTF’s ongoing mission has matured, becoming more and more engaged in quality activities. In late fall 2007, the time had come for the PSTF to evolve into SHM’s Performance and Standards Committee (PSC).
What We Do
As SHM’s senior adviser for quality standards and compliance, I continue to work with PSC Chair Patrick Torcson, MD, along with senior staff and leadership of the Public Policy Committee (PPC), to monitor the national performance and quality landscape. The PSC, which engages with national organizations and is charged with developing performance measures and building consensus, also works to develop relationships with other professional medical societies and organizations.
Recognizing the need to communicate more frequently on SHM quality/policy issues related to quality improvement and patient safety, the PSC has also forged a stronger tie with the Hospital Quality and Patient Safety Committee (HQPSC) and was represented in the HQPSC-led Quality Summit in October.
Through the PSC, SHM has worked to influence performance measure development, consensus, and the endorsement process by joining the AMA Physician Consortium for Performance Improvement (PCPI) and the National Quality Forum (NQF).
Broader Reach
SHM members have contributed to the process by participating in activities relevant to hospital medicine and building relationships with senior staff and leadership within these national stakeholder groups.
The PCPI is committed to enhancing quality of care and patient safety by taking the lead in the development, testing, and maintaining evidence-based clinical performance measures and performance measurement resources for physicians. The NQF is a nonprofit organization charged by Congress to endorse consensus-based national standards for measurement and public reporting of healthcare performance data. Beginning in 2006, the PCPI and NQF have worked to influence the development of physician-level performance measures as part of the CMS Physician Quality Reporting Initiative (PQRI). Joining the PCPI has given SHM the opportunity to participate with other organizations on expert work groups to develop performance measures. SHM has been involved in performance measure development for topics such as geriatrics, emergency medicine, outpatient parenteral antimicrobial therapy, and anesthesiology issues including perioperative normothermia and critical care.
Many of these measures have been included in the PQRI program. SHM submitted feedback during public comment periods on measures related to perioperative care and chronic kidney disease. Most importantly, PCPI participation has given SHM high visibility among measurement stakeholder groups, including CMS and NQF. This has raised the acceptance of hospital medicine as a specialty, as well as the influence and credibility of SHM as a professional society.
As a collaborative effort on behalf of SHM, the PSC and PPC drafted and submitted a comment letter on the 2008 Centers for Medicare and Medicaid Studies (CMS) Proposed Rule regarding the future of the PQRI. SHM has supported the CMS value-based purchasing initiative and the PQRI in general. The PSC recommended that CMS and national stakeholder groups like the PCPI and NQF re-evaluate the denominators of several measures, existing and proposed, to make them applicable to the inpatient setting for hospitalist reporting.
PSC senior staff attended the PCPI meeting in Chicago last October and met with Susan Nedza, MD, of the CMS Special Program Office, Value-Based Purchasing, to express SHM’s appreciation of increased CMS recognition of hospitalists through its quality initiatives. This also was an opportunity to receive input on additional ways hospitalists can become engaged in the 2008 PQRI and other CMS quality efforts.
PQRI Success
In early November, Dr. Nedza and her staff, Dr. Torcson, and SHM senior staff met via conference call to discuss the preliminary results of the 2007 PQRI and exchange thoughts on the program related to hospitalists. A concern for hospitalists was the intent for the PQRI to include performance measures for each of the 39 medical specialties recognized by CMS; hospitalists were lumped under general internal medicine. By working closely with CMS and the PCPI, SHM succeeded in achieving denominator specification changes for additional relevant measures to become available for hospitalist reporting through the 2007 PQRI.
Soon thereafter, the CMS Final Rule on Physician Payment was released, indicating that 10 of the 11 measures available for hospitalist reporting in the 2007 PQRI also were to be included for 2008. “Beta-blocker on Arrival for Acute Myocardial Infarction” was the one measure no longer part of the 2008 PQRI. One new measure available for hospitalist reporting in 2008 is measure No. 75, “Prevention of Ventilator-Associated Pneumonia—Head Elevation,” for which hospitalists can report using a critical care code.
The 2007 PQRI included the following measures on which hospitalists could report:
- No. 5: “Heart Failure: Angiotensin-Converting Enzyme (ACE) Inhibitor or Angiotensin Receptor Blocker (ARB) Therapy for Left Ventricular Systolic Dysfunction (LVSD)”;
- No. 6: “Oral Antiplatelet Therapy Prescribed for Patients with Coronary Artery Disease”;
- No. 7: “Beta-blocker Therapy for CAD Patients with Prior Myocardial Infarction”;
- No. 29: “Beta-blocker at Time of Arrival for Acute Myocardial Infarction”;
- No. 31: “Stroke and Stroke Rehabilitation: Deep Vein Thrombosis Prophylaxis”;
- No. 32: “Stroke and Stroke Rehabilitation: Discharged on Antiplatelet Therapy”;
- No. 33: “Stroke and Stroke Rehabilitation: Anticoagulant Therapy Prescribed for Atrial Fibrillation at Discharge”;
- No. 34: “Stroke and Stroke Rehabilitation: Tissue Plasminogen Activator Considered”;
- No. 35: “Stroke and Stroke Rehabilitation: Screening for Dysphagia”;
- No. 36: “Stroke and Stroke Rehabilitation: Consideration of Rehabilitation Services”; and
- No. 47: “Documentation of an Advanced Care Plan.”
After the final specifications for the 2008 PQRI were released, there was a proposal for denominator specification changes that would preclude inpatient reporting for many of the measures relevant and available to hospitalists in 2007. The PSC again worked closely with the PCPI and relevant professional organizations to preserve the measure specifications for the 2008 PQRI to allow inpatient and thus hospitalist reporting. This experience has further enhanced productive SHM relationships with the PCPI and CMS.
The PSC has an ongoing commitment to recommend SHM members for appointments to PCPI expert measure workgroups, depending on the topic. For example, SHM was recently asked to identify a member to join a newly forming asthma measures workgroup that will be looking to develop inpatient measures. SHM will be notified when a palliative care measures workgroup is being formed.
Senior staff and leadership will meet PCPI senior staff to discuss formation of an expert workgroup on care transitions measures. This work group will be co-chaired by SHM and the American College of Physicians (ACP) and include societies such as the Society of General Internal Medicine (SGIM), the American Geriatrics Society (AGS), and others engaged in the development of the transitions of care consensus document in summer 2007. The work group also will refer to the principles and standards that resulted from the ABIM Foundation’s Stepping Up to the Plate (SUTTP) Alliance as a resource in its development of measures.
Looking ahead to the 2009 PQRI, the PSC has requested measure specification changes to the following PQRI measures:
- No. 56: “Vital Signs for Community Acquired Pneumonia”;
- No. 57: “Oxygenation Assessment for Community Acquired Pneumonia”;
- No. 58: “Assessment of Mental Status for Community Acquired Pneumonia”; and
- No. 59: “Empiric Antibiotic for Community Acquired Pneumonia.”
These measures harmonize with the Joint Commission’s core measures and are relevant for hospitalist performance reporting.
With the NQF
On Sept. 26-28, PSC member Greg Seymann represented SHM at NQF’s 8th Annual Meeting in Washington, D.C. This meeting featured plenary sessions focusing on issues at the forefront of policy discussions related to quality of care including:
- Chronic care episodes across care settings;
- Medications and quality;
- Medicare performance monitoring and payment initiatives;
- Moving performance measures into electronic health record requirements; and
- Nursing leadership in measurement activities and achieving higher performance.
- In the first quarter of 2008, the PSC has:
- Reviewed and commented on NQF’s “National Voluntary Consensus Standards for Hospital Care: Additional Priorities–2007, Part 2”;
- Sent a representative to the steering committee for the National Voluntary Consensus Clinician-Level Perioperative Care Standards meeting;
- Submitted nominees for the National Voluntary Consensus Standards for Emergency Care Phase II steering committee and the Prevention and Management of Stroke Across the Continuum steering committee (our nominee was accepted for the latter);
- Reviewed and commented on the National Voluntary Consensus Standards for Prevention and
- Care of Venous Thromboembolism: Performance Measures/Phase II; and;
- Has sent senior leadership and staff to the NQF Spring Meeting and Implementation Conference on Care Coordination.
In the Works
The PSC and the HQPSC submitted a comment letter on CMS’ selection of hospital-acquired conditions and present on admission indicator reporting for 2009. SHM supported CMS’ efforts to improve the quality of care for hospitalized patients by preventing avoidable hospital-acquired conditions and outlining its concerns regarding unintended consequences as relates to the various conditions.
With its new status as the PSC, this enthusiastic and committed group is preparing to extend its mission and scope of work in 2008.
The PSC plans to restructure and serve as expert liaisons for internal and external activities. This not only will empower committee members to become more engaged in our performance agenda, but also allow them to serve as key contacts for staff when monitoring the ever-growing landscape of performance measurement, quality, and policy. TH
VTE Collaborative Succeeding
It has been nearly 18 months since SHM launched the VTE Prevention Collaborative, which offers individualized assistance to hospitalists wishing to take the lead on reducing the incidence of preventable, hospital-acquired VTE at their sites.
The collaborative features two technical assistance options: a full year of distance mentoring or a one-day evaluation and consultation visit to the enrollee’s hospital. The project is led by Gregory Maynard, MD, and Jason Stein, MD. Both are stellar clinicians with quality improvement (QI) expertise and experience leading VTE prevention efforts. Dr. Maynard is head of the Division of Hospital Medicine and associate clinical professor of medicine at the University of California-San Diego. Dr. Stein is a hospitalist at Atlanta’s Emory University Hospital, assistant professor of Medicine at Emory University School of Medicine, and director of Quality Improvement for the Emory Hospital Medicine Unit.
Though we expect to continue working with sites enrolled in the mentoring program for many more months, the collaborative has been in place long enough that we can start evaluating outcomes and thinking about what we’ve learned.
In all, 35 hospitals so far have enrolled in the collaborative: three in the consultation program and 32 in the mentoring program. Because the participants enrolled in the mentoring program generally were starting from an earlier point in the QI process (i.e., thinking about starting a project vs. trying to improve an existing effort), we’ve focused our evaluation attention on them.
At the time of enrollment, 33% of these sites were thinking of starting a VTE-prevention project, 42% had an active QI project but had not yet implemented any interventions, and 25% had an active QI project and had implemented an intervention (i.e., a new order set or risk-assessment protocol).
We surveyed the 21 sites that have been involved in the mentoring program for at least six months, asking about the status of their VTE-prevention project and their experiences working with SHM mentors. So far, 15 have responded to the survey, and the results are quite interesting.
Since becoming involved with the collaborative, nearly every participant had made significant progress with their project:
- 94% had redesigned the processes for assessing VTE risk and bleeding risk and providing appropriate prophylaxis;
- 100% had selected a VTE risk assessment model, and 88% had developed prophylaxis recommendations for each level of risk;
- 100% had defined absolute and relative contraindications to pharmacologic prophylaxis and recommendations for what to do if they exist;
- 100% had developed order sets or protocols that encourage initial assessment of VTE risk and provision of appropriate prophylaxis; and
- 75% had developed order sets or protocols in use at their hospitals.
All seven sites that had a baseline figure that could be used for comparison reported their current rate of appropriate VTE prophylaxis is higher than it was before they became involved in the collaborative.
We asked participants to identify the topics with which they were helped by their mentors. The responses showed the breadth of issues that need attention to create a successful QI project. The topics covered and percentage of enrollees who sought help with them include:
- Defining the goals, aims and scope of your project, 93%;
- Redesigning your VTE prevention process, 87%;
- Developing risk assessment and prophylaxis recommendations, 87%;
- Developing order sets and protocols, 87%;
- Data collection and measurement, 87%;
- Piloting and revising risk assessment tools, order sets and protocols, 60%;
- Securing institutional support for your project, 47%;
- Assembling your project team, 47%;
- Mapping the original (pre-collaborative involvement) VTE prevention process at your site, 40%;
- Identifying and securing support from key stakeholders, 33%; and
- Developing educational/outreach strategies or materials, 27%.
Data collection and measurement remain a central issue for most participants. Nearly every mentoring call (mentors and participants speak once a month for the first six months of enrollment and every three months thereafter) focused at least in part on figuring out how to develop baseline data, monitor adherence to a new protocol, and determine if clinical outcomes were improving.
Of note, 100% of respondents said they would recommend the collaborative to others.
Hospitalists and QI
An impressive 67% of respondents indicated their work on the VTE project has helped identify them as a QI leader in their hospital or within their hospital medicine group. More impressively, 93% are working on or have signed up to work on other QI efforts.
The range of topics participants are turning their attention to are amazingly varied: acute coronary syndromes, heart failure, sepsis, glycemic control, pneumonia, delirium prevention, therapeutic hypothermia, hand washing, core measures, Joint Commission certification for a number of diagnoses/processes, do-not-resuscitate documentation/ordering, medication reconciliation, SCIP, hand-off communications, and computerized physician order entry. Or, as one respondent put it, “too many projects to name.”
While it is heartening that success in one area is being leveraged in other areas, a sobering reality is that only 7% of these folks have allotted time to pursue QI projects – all others do QI work on a volunteer basis, in addition to existing clinical and administrative responsibilities.
QI work is fun and rewarding but also time-consuming and at times, difficult and lonely. Heroic volunteerism is not necessarily a bad thing—many hospitalists are passionate about improving care and contributing to the hospitals where they work. Too much volunteerism leads to burnout and ultimately is not sustainable. Perhaps a mentoring emphasis should be helping people recognize and quantify the value of their efforts, and developing the negotiation skills that would help secure funding for their work.
What’s Next?
Drs. Maynard and Stein are among the SHM members with an interest in VTE who have convened the VTE Advisory Board. Under the leadership of Sylvia McKean, MD, the advisory board is exploring ways SHM can continue its work to promote the prevention, diagnosis and treatment of VTE.
Areas of interest include working with health systems, as opposed to individual hospitals, as a means of rapidly spreading tools and processes that promote assessment of VTE risk and administration of appropriate prophylaxis. The VTE collaborative team was thrilled to welcome five Veterans Affairs (VA) hospitals into the collaborative. It is hoped this group will succeed not only in developing successful local VTE prevention efforts, but also will develop a framework and set of tools that can be exported to all VA sites. Leveraging commonly used health IT systems is another exciting option for rapidly disseminating the tools and materials the collaborative’s members have developed.
It has been nearly 18 months since SHM launched the VTE Prevention Collaborative, which offers individualized assistance to hospitalists wishing to take the lead on reducing the incidence of preventable, hospital-acquired VTE at their sites.
The collaborative features two technical assistance options: a full year of distance mentoring or a one-day evaluation and consultation visit to the enrollee’s hospital. The project is led by Gregory Maynard, MD, and Jason Stein, MD. Both are stellar clinicians with quality improvement (QI) expertise and experience leading VTE prevention efforts. Dr. Maynard is head of the Division of Hospital Medicine and associate clinical professor of medicine at the University of California-San Diego. Dr. Stein is a hospitalist at Atlanta’s Emory University Hospital, assistant professor of Medicine at Emory University School of Medicine, and director of Quality Improvement for the Emory Hospital Medicine Unit.
Though we expect to continue working with sites enrolled in the mentoring program for many more months, the collaborative has been in place long enough that we can start evaluating outcomes and thinking about what we’ve learned.
In all, 35 hospitals so far have enrolled in the collaborative: three in the consultation program and 32 in the mentoring program. Because the participants enrolled in the mentoring program generally were starting from an earlier point in the QI process (i.e., thinking about starting a project vs. trying to improve an existing effort), we’ve focused our evaluation attention on them.
At the time of enrollment, 33% of these sites were thinking of starting a VTE-prevention project, 42% had an active QI project but had not yet implemented any interventions, and 25% had an active QI project and had implemented an intervention (i.e., a new order set or risk-assessment protocol).
We surveyed the 21 sites that have been involved in the mentoring program for at least six months, asking about the status of their VTE-prevention project and their experiences working with SHM mentors. So far, 15 have responded to the survey, and the results are quite interesting.
Since becoming involved with the collaborative, nearly every participant had made significant progress with their project:
- 94% had redesigned the processes for assessing VTE risk and bleeding risk and providing appropriate prophylaxis;
- 100% had selected a VTE risk assessment model, and 88% had developed prophylaxis recommendations for each level of risk;
- 100% had defined absolute and relative contraindications to pharmacologic prophylaxis and recommendations for what to do if they exist;
- 100% had developed order sets or protocols that encourage initial assessment of VTE risk and provision of appropriate prophylaxis; and
- 75% had developed order sets or protocols in use at their hospitals.
All seven sites that had a baseline figure that could be used for comparison reported their current rate of appropriate VTE prophylaxis is higher than it was before they became involved in the collaborative.
We asked participants to identify the topics with which they were helped by their mentors. The responses showed the breadth of issues that need attention to create a successful QI project. The topics covered and percentage of enrollees who sought help with them include:
- Defining the goals, aims and scope of your project, 93%;
- Redesigning your VTE prevention process, 87%;
- Developing risk assessment and prophylaxis recommendations, 87%;
- Developing order sets and protocols, 87%;
- Data collection and measurement, 87%;
- Piloting and revising risk assessment tools, order sets and protocols, 60%;
- Securing institutional support for your project, 47%;
- Assembling your project team, 47%;
- Mapping the original (pre-collaborative involvement) VTE prevention process at your site, 40%;
- Identifying and securing support from key stakeholders, 33%; and
- Developing educational/outreach strategies or materials, 27%.
Data collection and measurement remain a central issue for most participants. Nearly every mentoring call (mentors and participants speak once a month for the first six months of enrollment and every three months thereafter) focused at least in part on figuring out how to develop baseline data, monitor adherence to a new protocol, and determine if clinical outcomes were improving.
Of note, 100% of respondents said they would recommend the collaborative to others.
Hospitalists and QI
An impressive 67% of respondents indicated their work on the VTE project has helped identify them as a QI leader in their hospital or within their hospital medicine group. More impressively, 93% are working on or have signed up to work on other QI efforts.
The range of topics participants are turning their attention to are amazingly varied: acute coronary syndromes, heart failure, sepsis, glycemic control, pneumonia, delirium prevention, therapeutic hypothermia, hand washing, core measures, Joint Commission certification for a number of diagnoses/processes, do-not-resuscitate documentation/ordering, medication reconciliation, SCIP, hand-off communications, and computerized physician order entry. Or, as one respondent put it, “too many projects to name.”
While it is heartening that success in one area is being leveraged in other areas, a sobering reality is that only 7% of these folks have allotted time to pursue QI projects – all others do QI work on a volunteer basis, in addition to existing clinical and administrative responsibilities.
QI work is fun and rewarding but also time-consuming and at times, difficult and lonely. Heroic volunteerism is not necessarily a bad thing—many hospitalists are passionate about improving care and contributing to the hospitals where they work. Too much volunteerism leads to burnout and ultimately is not sustainable. Perhaps a mentoring emphasis should be helping people recognize and quantify the value of their efforts, and developing the negotiation skills that would help secure funding for their work.
What’s Next?
Drs. Maynard and Stein are among the SHM members with an interest in VTE who have convened the VTE Advisory Board. Under the leadership of Sylvia McKean, MD, the advisory board is exploring ways SHM can continue its work to promote the prevention, diagnosis and treatment of VTE.
Areas of interest include working with health systems, as opposed to individual hospitals, as a means of rapidly spreading tools and processes that promote assessment of VTE risk and administration of appropriate prophylaxis. The VTE collaborative team was thrilled to welcome five Veterans Affairs (VA) hospitals into the collaborative. It is hoped this group will succeed not only in developing successful local VTE prevention efforts, but also will develop a framework and set of tools that can be exported to all VA sites. Leveraging commonly used health IT systems is another exciting option for rapidly disseminating the tools and materials the collaborative’s members have developed.
It has been nearly 18 months since SHM launched the VTE Prevention Collaborative, which offers individualized assistance to hospitalists wishing to take the lead on reducing the incidence of preventable, hospital-acquired VTE at their sites.
The collaborative features two technical assistance options: a full year of distance mentoring or a one-day evaluation and consultation visit to the enrollee’s hospital. The project is led by Gregory Maynard, MD, and Jason Stein, MD. Both are stellar clinicians with quality improvement (QI) expertise and experience leading VTE prevention efforts. Dr. Maynard is head of the Division of Hospital Medicine and associate clinical professor of medicine at the University of California-San Diego. Dr. Stein is a hospitalist at Atlanta’s Emory University Hospital, assistant professor of Medicine at Emory University School of Medicine, and director of Quality Improvement for the Emory Hospital Medicine Unit.
Though we expect to continue working with sites enrolled in the mentoring program for many more months, the collaborative has been in place long enough that we can start evaluating outcomes and thinking about what we’ve learned.
In all, 35 hospitals so far have enrolled in the collaborative: three in the consultation program and 32 in the mentoring program. Because the participants enrolled in the mentoring program generally were starting from an earlier point in the QI process (i.e., thinking about starting a project vs. trying to improve an existing effort), we’ve focused our evaluation attention on them.
At the time of enrollment, 33% of these sites were thinking of starting a VTE-prevention project, 42% had an active QI project but had not yet implemented any interventions, and 25% had an active QI project and had implemented an intervention (i.e., a new order set or risk-assessment protocol).
We surveyed the 21 sites that have been involved in the mentoring program for at least six months, asking about the status of their VTE-prevention project and their experiences working with SHM mentors. So far, 15 have responded to the survey, and the results are quite interesting.
Since becoming involved with the collaborative, nearly every participant had made significant progress with their project:
- 94% had redesigned the processes for assessing VTE risk and bleeding risk and providing appropriate prophylaxis;
- 100% had selected a VTE risk assessment model, and 88% had developed prophylaxis recommendations for each level of risk;
- 100% had defined absolute and relative contraindications to pharmacologic prophylaxis and recommendations for what to do if they exist;
- 100% had developed order sets or protocols that encourage initial assessment of VTE risk and provision of appropriate prophylaxis; and
- 75% had developed order sets or protocols in use at their hospitals.
All seven sites that had a baseline figure that could be used for comparison reported their current rate of appropriate VTE prophylaxis is higher than it was before they became involved in the collaborative.
We asked participants to identify the topics with which they were helped by their mentors. The responses showed the breadth of issues that need attention to create a successful QI project. The topics covered and percentage of enrollees who sought help with them include:
- Defining the goals, aims and scope of your project, 93%;
- Redesigning your VTE prevention process, 87%;
- Developing risk assessment and prophylaxis recommendations, 87%;
- Developing order sets and protocols, 87%;
- Data collection and measurement, 87%;
- Piloting and revising risk assessment tools, order sets and protocols, 60%;
- Securing institutional support for your project, 47%;
- Assembling your project team, 47%;
- Mapping the original (pre-collaborative involvement) VTE prevention process at your site, 40%;
- Identifying and securing support from key stakeholders, 33%; and
- Developing educational/outreach strategies or materials, 27%.
Data collection and measurement remain a central issue for most participants. Nearly every mentoring call (mentors and participants speak once a month for the first six months of enrollment and every three months thereafter) focused at least in part on figuring out how to develop baseline data, monitor adherence to a new protocol, and determine if clinical outcomes were improving.
Of note, 100% of respondents said they would recommend the collaborative to others.
Hospitalists and QI
An impressive 67% of respondents indicated their work on the VTE project has helped identify them as a QI leader in their hospital or within their hospital medicine group. More impressively, 93% are working on or have signed up to work on other QI efforts.
The range of topics participants are turning their attention to are amazingly varied: acute coronary syndromes, heart failure, sepsis, glycemic control, pneumonia, delirium prevention, therapeutic hypothermia, hand washing, core measures, Joint Commission certification for a number of diagnoses/processes, do-not-resuscitate documentation/ordering, medication reconciliation, SCIP, hand-off communications, and computerized physician order entry. Or, as one respondent put it, “too many projects to name.”
While it is heartening that success in one area is being leveraged in other areas, a sobering reality is that only 7% of these folks have allotted time to pursue QI projects – all others do QI work on a volunteer basis, in addition to existing clinical and administrative responsibilities.
QI work is fun and rewarding but also time-consuming and at times, difficult and lonely. Heroic volunteerism is not necessarily a bad thing—many hospitalists are passionate about improving care and contributing to the hospitals where they work. Too much volunteerism leads to burnout and ultimately is not sustainable. Perhaps a mentoring emphasis should be helping people recognize and quantify the value of their efforts, and developing the negotiation skills that would help secure funding for their work.
What’s Next?
Drs. Maynard and Stein are among the SHM members with an interest in VTE who have convened the VTE Advisory Board. Under the leadership of Sylvia McKean, MD, the advisory board is exploring ways SHM can continue its work to promote the prevention, diagnosis and treatment of VTE.
Areas of interest include working with health systems, as opposed to individual hospitals, as a means of rapidly spreading tools and processes that promote assessment of VTE risk and administration of appropriate prophylaxis. The VTE collaborative team was thrilled to welcome five Veterans Affairs (VA) hospitals into the collaborative. It is hoped this group will succeed not only in developing successful local VTE prevention efforts, but also will develop a framework and set of tools that can be exported to all VA sites. Leveraging commonly used health IT systems is another exciting option for rapidly disseminating the tools and materials the collaborative’s members have developed.
What is the best intervention to help hospitalized patients quit smoking?
Case
A 56-year-old male with a 60-pack-a-year history of cigarette smoking is admitted to the telemetry unit with an initial assessment of acute coronary syndrome. Because there is a no-smoking policy in the hospital, he is willing to comply but is concerned about tobacco withdrawal symptoms.
Overview
As of 2006, approximately 20.8% of U.S. adults smoke cigarettes.1 Responsible for approximately 438,000 deaths annually, cigarette smoking is the most important preventable cause of death and disease in the U.S.2
Smoking cessation reduces the risk of tobacco-related diseases; the potential health benefits are numerous. This is most evident in the reduction of cardiovascular disease events upon tobacco abstinence.3 Yet, it remains a constant struggle for smokers to quit and stay abstinent.
The main barrier to quitting is nicotine addiction, which causes tolerance and physical dependence. Upon cessation of tobacco use, withdrawal symptoms, such as irritability, restlessness, impatience, and depression may occur within a few hours, peak within the first several days, and then wane during the next few months.
The crucial time frame to prevent relapse is the first week of cessation. For smokers to stay off cigarettes, they must break from routines, behaviors, or cues that trigger the urge to smoke.4
Among patients with acute myocardial infarction (AMI) in a study done by Van Spall, et al., 39% of them still smoked.5 Indeed, smoking is associated with 1.5 to three times increased relative risk of AMI, and hospitalists increasingly must manage cardiovascular disease patients’ tobacco dependence during their hospital stay.
Intervention strategies: Methods for smoking cessation need to target two aspects that support tobacco use—physical and psychological factors. High-intensity counseling and systematic behavioral intervention followed by sustained contact—in person or by phone up to one month after discharge—are effective behavioral interventions for sustained tobacco cessation.6 Pharmacotherapy also helps when added to high-intensity counseling of a hospitalized patient. It especially is beneficial for controlling withdrawal symptoms.
In addition, with policies prohibiting smoking in almost all U.S. hospitals, temporary tobacco abstinence promotes smoking cessation for hospitalized patients. Unfortunately, most hospitalized patients go back to smoking soon after discharge. Hospitalization may be the opportune time to help patients try to quit and avoid relapse.
Some hospitals feature inpatient smoking cessation programs in which nurse practitioners and counselors educate and counsel patients. It is highly recommended that a multidisciplinary team be involved in a tobacco cessation program catered to an individual patient’s needs. However, most hospitals have no such program. Nevertheless, the hospitalist can help a patient with brief or low-intensity tobacco cessation counseling, pharmacotherapy for nicotine withdrawal symptom control if clinically indicated, and follow-up upon discharge for relapse prevention.
Counseling: Smoking cessation counseling in the hospital after an AMI has been found to be associated with a relative risk reduction of mortality by 37% in one year. The hospitalist should give a two-minute cessation message as the first step. If tobacco cessation counselors or nurse practitioners are available, their additional counseling also may improve outcomes of smoking cessation therapies.7 However, if no established inpatient tobacco cessation program is available to the hospitalist, the following may be used to aid in physician counseling of the hospitalized cardiac patient:
The first step in treating tobacco dependence is to identify and assess tobacco use status.
Tobacco users willing to quit should be treated using the 5 A’s (Ask, Advise, Assess, Assist, and Arrange) (see Figure 1, p. 30). Tobacco users not willing to quit at the time of interaction should be treated using the 5 R’s for motivational intervention:
- Relevance (indicate why quitting is personally relevant);
- Risks (have patient identify potentially negative consequences of smoking);
- Rewards (have patient identify potential benefits of quitting smoking);
- Roadblocks (have patient identify potential barriers to smoking cessation and provide patient problem-solving techniques and pharmacotherapy to overcome the barriers); and
- Repetition (repeat motivational intervention to unmotivated patient each visit).
Further, former smokers who recently quit using tobacco should be given relapse prevention treatment.8 For the hospitalized smoker with acute cardiovascular disease, providing bedside counseling, enhancing self-coping behavior change, and arranging follow-up after discharge to maintain behavior change can help sustain tobacco abstinence.
Pharmacotherapy: The most important purpose of pharmacotherapy for smoking cessation is to reduce withdrawal symptoms and cigarette cravings. Public Health Service clinical guidelines for smoking cessation mention five first-line agents. These are sustained-release bupropion and four nicotine-replacement therapies (NRT): transdermal patch, gum, nasal spray, and vapor inhaler. Further, there are two second-line agents: clonidine and nortriptyline. Since the clinical guidelines’ release in 2000, the Food and Drug Administration has approved a fifth NRT product, the nicotine lozenge, in 2002, and a partial nicotine agonist, varenicline, in 2006 (see Table 1, right).9,10
Current guidelines recommend that NRT be used with caution in patients with unstable angina, serious arrhythmias, or an MI within the previous two weeks due to limited supportive data on the safety of use in these patients.11 The transdermal patch delivers nicotine at a slow and constant rate in contrast to the other forms of NRT and has been used safely in patients with stable coronary artery disease. However, the use of any NRT, including the patch, in acute cardiovascular disease is not advised due to the nicotine-mediated hemodynamic effects, such as increase heart rate and arterial vasoconstriction, which lead to increased myocardial workload.
Sustained-release bupropion generally is well tolerated by hospitalized patients with cardiovascular disease, but there may be a delay in control of withdrawal symptoms. In addition, blood pressure must be monitored especially if combined with NRT as there have been anecdotal reports of increase in blood pressure with bupropion alone.12 Bupropion must be used cautiously in patients with recent MI. Other contraindications include history of seizure, conditions that potentially can increase risk for convulsions, and use of monoamine oxidase inhibitors (MAOI) within 14 days.
The new drug varenicline has not been studied in hospitalized patients or patients with acute coronary syndrome. However, since it does not have any important hemodynamic effects, it may be useful in this setting and in selected patients with close monitoring for mood changes since there have been anecdotal case reports of psychotic events in patients with underlying psychiatric disorders.13 Its routine use currently is not recommended.
Follow-up after discharge: Pharmacotherapy may be added for withdrawal control, as well as relapse prevention for the hospitalized patient who recently quit smoking. However, inclusion of intensive tobacco cessation counseling during the hospital stay is the most effective intervention given the setting and patient condition, and follow-up support up to at least one month after discharge has been found to be more effective in sustaining tobacco abstinence than pharmacotherapy alone. In order to maximize long-term quit rates among patients who recently abstained from smoking, the hospitalist should arrange access to ongoing outpatient post-discharge support and tobacco cessation treatment.
Back to the Case
After appropriate cardiac testing, the patient was found to have a non-cardiac etiology for his symptoms. From the start of his hospital stay, he was counseled by the hospitalist and started on sustained-release bupropion, but withdrawal symptoms and cravings persisted.
Prior to his discharge home, the patient wanted to discontinue bupropion and be provided an alternative. The patient was given a nicotine patch, and a follow-up appointment at the tobacco cessation clinic within one week of discharge from the hospital was arranged. The patient has been compliant with his quit-smoking treatment and has followed-up for continued tobacco cessation counseling. He hasn’t smoked cigarettes for a year. TH
Dr. Palisoc is a preventive medicine resident at the University of Colorado Denver. Dr. Prochazka works at the Denver VA and is a professor of medicine at the University of Colorado Denver.
References
- CDC. Cigarette Smoking Among Adults, United States, 2006. MMWR Morbidity Mortality Wkly Rep. 2007;56(44):1157-1161. Available at www.cdc.gov/mmwr/preview/mmwrhtml/mm5644a2.htm. Last accessed March 4, 2008.
- CDC. Annual Smoking-Attributable Mortality, Years of Potential Life Lost, and Productivity, United States, 1997-2001. MMWR Morbidity Mortality Wkly Rep. 2005;54(25):625-628.
- Thomson CC, Rigotti NA. Hospital- and clinic-based smoking cessation interventions for smokers with cardiovascular disease. Prog Cardiovasc Dis. 2003;45(6):459-479.
- Rigotti NA. Treatment of tobacco use and dependence. N Engl J Med. 2002;346(7):506-512.
- Van Spall HGC, Chong A, Tu JV. Inpatient smoking-cessation counseling and all-cause mortality in patients with acute myocardial infarction. Am Heart J. 2007;154(2):213-220.
- Rigotti NA, Munafo MR, Stead LF. Interventions for smoking cessation in hospitalized patients. Cochrane Database Syst Rev. 2007;Issue 3.
- Ludvig J, Miner B, and Eisenberg, MJ. Smoking cessation in patients with coronary artery disease. Am Heart J. 2005;149(4):565-572.
- Fiore MC, Bailey WC, Cohen SJ, et al. Treating tobacco use and dependence: clinical practice guideline. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service 2000.
- Rigotti NA, Thorndike AN, Regan S, et al. Bupropion for smokers hospitalized with acute cardiovascular disease. Am J Med. 2006;199:1080-1087.
- Jorenby DE, Hays JT, Rigotti NA, et al. Efficacy of varenicline, an alpha4beta2 nicotinic acetylcholine receptor partial agonist, vs. placebo or sustained-release bupropion for smoking cessation: a randomized controlled trial. JAMA. 2006;296(1):56-63.
- Joseph AM, Fu SS. Safety issues in pharmacotherapy for smoking in patients with cardiovascular disease. Prog Cardiovasc Dis. 2003;45(6):429-441.
- FDA. Prescribing information of Zyban (bupropion hydrochloride) sustained release tablets. June 2007. Available at www.fda.gov/medwatch/safety/2007/ Aug_PI/Zyban_PI.pdf. Last accessed March 6, 2008.
- FDA. Early Communication About an Ongoing Safety Review: Varenicline (marketed as Chantix). November 2007. Available at www.fda.gov/cder/drug/early_comm/varenicline.htm. Last accessed March 6, 2008.
Case
A 56-year-old male with a 60-pack-a-year history of cigarette smoking is admitted to the telemetry unit with an initial assessment of acute coronary syndrome. Because there is a no-smoking policy in the hospital, he is willing to comply but is concerned about tobacco withdrawal symptoms.
Overview
As of 2006, approximately 20.8% of U.S. adults smoke cigarettes.1 Responsible for approximately 438,000 deaths annually, cigarette smoking is the most important preventable cause of death and disease in the U.S.2
Smoking cessation reduces the risk of tobacco-related diseases; the potential health benefits are numerous. This is most evident in the reduction of cardiovascular disease events upon tobacco abstinence.3 Yet, it remains a constant struggle for smokers to quit and stay abstinent.
The main barrier to quitting is nicotine addiction, which causes tolerance and physical dependence. Upon cessation of tobacco use, withdrawal symptoms, such as irritability, restlessness, impatience, and depression may occur within a few hours, peak within the first several days, and then wane during the next few months.
The crucial time frame to prevent relapse is the first week of cessation. For smokers to stay off cigarettes, they must break from routines, behaviors, or cues that trigger the urge to smoke.4
Among patients with acute myocardial infarction (AMI) in a study done by Van Spall, et al., 39% of them still smoked.5 Indeed, smoking is associated with 1.5 to three times increased relative risk of AMI, and hospitalists increasingly must manage cardiovascular disease patients’ tobacco dependence during their hospital stay.
Intervention strategies: Methods for smoking cessation need to target two aspects that support tobacco use—physical and psychological factors. High-intensity counseling and systematic behavioral intervention followed by sustained contact—in person or by phone up to one month after discharge—are effective behavioral interventions for sustained tobacco cessation.6 Pharmacotherapy also helps when added to high-intensity counseling of a hospitalized patient. It especially is beneficial for controlling withdrawal symptoms.
In addition, with policies prohibiting smoking in almost all U.S. hospitals, temporary tobacco abstinence promotes smoking cessation for hospitalized patients. Unfortunately, most hospitalized patients go back to smoking soon after discharge. Hospitalization may be the opportune time to help patients try to quit and avoid relapse.
Some hospitals feature inpatient smoking cessation programs in which nurse practitioners and counselors educate and counsel patients. It is highly recommended that a multidisciplinary team be involved in a tobacco cessation program catered to an individual patient’s needs. However, most hospitals have no such program. Nevertheless, the hospitalist can help a patient with brief or low-intensity tobacco cessation counseling, pharmacotherapy for nicotine withdrawal symptom control if clinically indicated, and follow-up upon discharge for relapse prevention.
Counseling: Smoking cessation counseling in the hospital after an AMI has been found to be associated with a relative risk reduction of mortality by 37% in one year. The hospitalist should give a two-minute cessation message as the first step. If tobacco cessation counselors or nurse practitioners are available, their additional counseling also may improve outcomes of smoking cessation therapies.7 However, if no established inpatient tobacco cessation program is available to the hospitalist, the following may be used to aid in physician counseling of the hospitalized cardiac patient:
The first step in treating tobacco dependence is to identify and assess tobacco use status.
Tobacco users willing to quit should be treated using the 5 A’s (Ask, Advise, Assess, Assist, and Arrange) (see Figure 1, p. 30). Tobacco users not willing to quit at the time of interaction should be treated using the 5 R’s for motivational intervention:
- Relevance (indicate why quitting is personally relevant);
- Risks (have patient identify potentially negative consequences of smoking);
- Rewards (have patient identify potential benefits of quitting smoking);
- Roadblocks (have patient identify potential barriers to smoking cessation and provide patient problem-solving techniques and pharmacotherapy to overcome the barriers); and
- Repetition (repeat motivational intervention to unmotivated patient each visit).
Further, former smokers who recently quit using tobacco should be given relapse prevention treatment.8 For the hospitalized smoker with acute cardiovascular disease, providing bedside counseling, enhancing self-coping behavior change, and arranging follow-up after discharge to maintain behavior change can help sustain tobacco abstinence.
Pharmacotherapy: The most important purpose of pharmacotherapy for smoking cessation is to reduce withdrawal symptoms and cigarette cravings. Public Health Service clinical guidelines for smoking cessation mention five first-line agents. These are sustained-release bupropion and four nicotine-replacement therapies (NRT): transdermal patch, gum, nasal spray, and vapor inhaler. Further, there are two second-line agents: clonidine and nortriptyline. Since the clinical guidelines’ release in 2000, the Food and Drug Administration has approved a fifth NRT product, the nicotine lozenge, in 2002, and a partial nicotine agonist, varenicline, in 2006 (see Table 1, right).9,10
Current guidelines recommend that NRT be used with caution in patients with unstable angina, serious arrhythmias, or an MI within the previous two weeks due to limited supportive data on the safety of use in these patients.11 The transdermal patch delivers nicotine at a slow and constant rate in contrast to the other forms of NRT and has been used safely in patients with stable coronary artery disease. However, the use of any NRT, including the patch, in acute cardiovascular disease is not advised due to the nicotine-mediated hemodynamic effects, such as increase heart rate and arterial vasoconstriction, which lead to increased myocardial workload.
Sustained-release bupropion generally is well tolerated by hospitalized patients with cardiovascular disease, but there may be a delay in control of withdrawal symptoms. In addition, blood pressure must be monitored especially if combined with NRT as there have been anecdotal reports of increase in blood pressure with bupropion alone.12 Bupropion must be used cautiously in patients with recent MI. Other contraindications include history of seizure, conditions that potentially can increase risk for convulsions, and use of monoamine oxidase inhibitors (MAOI) within 14 days.
The new drug varenicline has not been studied in hospitalized patients or patients with acute coronary syndrome. However, since it does not have any important hemodynamic effects, it may be useful in this setting and in selected patients with close monitoring for mood changes since there have been anecdotal case reports of psychotic events in patients with underlying psychiatric disorders.13 Its routine use currently is not recommended.
Follow-up after discharge: Pharmacotherapy may be added for withdrawal control, as well as relapse prevention for the hospitalized patient who recently quit smoking. However, inclusion of intensive tobacco cessation counseling during the hospital stay is the most effective intervention given the setting and patient condition, and follow-up support up to at least one month after discharge has been found to be more effective in sustaining tobacco abstinence than pharmacotherapy alone. In order to maximize long-term quit rates among patients who recently abstained from smoking, the hospitalist should arrange access to ongoing outpatient post-discharge support and tobacco cessation treatment.
Back to the Case
After appropriate cardiac testing, the patient was found to have a non-cardiac etiology for his symptoms. From the start of his hospital stay, he was counseled by the hospitalist and started on sustained-release bupropion, but withdrawal symptoms and cravings persisted.
Prior to his discharge home, the patient wanted to discontinue bupropion and be provided an alternative. The patient was given a nicotine patch, and a follow-up appointment at the tobacco cessation clinic within one week of discharge from the hospital was arranged. The patient has been compliant with his quit-smoking treatment and has followed-up for continued tobacco cessation counseling. He hasn’t smoked cigarettes for a year. TH
Dr. Palisoc is a preventive medicine resident at the University of Colorado Denver. Dr. Prochazka works at the Denver VA and is a professor of medicine at the University of Colorado Denver.
References
- CDC. Cigarette Smoking Among Adults, United States, 2006. MMWR Morbidity Mortality Wkly Rep. 2007;56(44):1157-1161. Available at www.cdc.gov/mmwr/preview/mmwrhtml/mm5644a2.htm. Last accessed March 4, 2008.
- CDC. Annual Smoking-Attributable Mortality, Years of Potential Life Lost, and Productivity, United States, 1997-2001. MMWR Morbidity Mortality Wkly Rep. 2005;54(25):625-628.
- Thomson CC, Rigotti NA. Hospital- and clinic-based smoking cessation interventions for smokers with cardiovascular disease. Prog Cardiovasc Dis. 2003;45(6):459-479.
- Rigotti NA. Treatment of tobacco use and dependence. N Engl J Med. 2002;346(7):506-512.
- Van Spall HGC, Chong A, Tu JV. Inpatient smoking-cessation counseling and all-cause mortality in patients with acute myocardial infarction. Am Heart J. 2007;154(2):213-220.
- Rigotti NA, Munafo MR, Stead LF. Interventions for smoking cessation in hospitalized patients. Cochrane Database Syst Rev. 2007;Issue 3.
- Ludvig J, Miner B, and Eisenberg, MJ. Smoking cessation in patients with coronary artery disease. Am Heart J. 2005;149(4):565-572.
- Fiore MC, Bailey WC, Cohen SJ, et al. Treating tobacco use and dependence: clinical practice guideline. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service 2000.
- Rigotti NA, Thorndike AN, Regan S, et al. Bupropion for smokers hospitalized with acute cardiovascular disease. Am J Med. 2006;199:1080-1087.
- Jorenby DE, Hays JT, Rigotti NA, et al. Efficacy of varenicline, an alpha4beta2 nicotinic acetylcholine receptor partial agonist, vs. placebo or sustained-release bupropion for smoking cessation: a randomized controlled trial. JAMA. 2006;296(1):56-63.
- Joseph AM, Fu SS. Safety issues in pharmacotherapy for smoking in patients with cardiovascular disease. Prog Cardiovasc Dis. 2003;45(6):429-441.
- FDA. Prescribing information of Zyban (bupropion hydrochloride) sustained release tablets. June 2007. Available at www.fda.gov/medwatch/safety/2007/ Aug_PI/Zyban_PI.pdf. Last accessed March 6, 2008.
- FDA. Early Communication About an Ongoing Safety Review: Varenicline (marketed as Chantix). November 2007. Available at www.fda.gov/cder/drug/early_comm/varenicline.htm. Last accessed March 6, 2008.
Case
A 56-year-old male with a 60-pack-a-year history of cigarette smoking is admitted to the telemetry unit with an initial assessment of acute coronary syndrome. Because there is a no-smoking policy in the hospital, he is willing to comply but is concerned about tobacco withdrawal symptoms.
Overview
As of 2006, approximately 20.8% of U.S. adults smoke cigarettes.1 Responsible for approximately 438,000 deaths annually, cigarette smoking is the most important preventable cause of death and disease in the U.S.2
Smoking cessation reduces the risk of tobacco-related diseases; the potential health benefits are numerous. This is most evident in the reduction of cardiovascular disease events upon tobacco abstinence.3 Yet, it remains a constant struggle for smokers to quit and stay abstinent.
The main barrier to quitting is nicotine addiction, which causes tolerance and physical dependence. Upon cessation of tobacco use, withdrawal symptoms, such as irritability, restlessness, impatience, and depression may occur within a few hours, peak within the first several days, and then wane during the next few months.
The crucial time frame to prevent relapse is the first week of cessation. For smokers to stay off cigarettes, they must break from routines, behaviors, or cues that trigger the urge to smoke.4
Among patients with acute myocardial infarction (AMI) in a study done by Van Spall, et al., 39% of them still smoked.5 Indeed, smoking is associated with 1.5 to three times increased relative risk of AMI, and hospitalists increasingly must manage cardiovascular disease patients’ tobacco dependence during their hospital stay.
Intervention strategies: Methods for smoking cessation need to target two aspects that support tobacco use—physical and psychological factors. High-intensity counseling and systematic behavioral intervention followed by sustained contact—in person or by phone up to one month after discharge—are effective behavioral interventions for sustained tobacco cessation.6 Pharmacotherapy also helps when added to high-intensity counseling of a hospitalized patient. It especially is beneficial for controlling withdrawal symptoms.
In addition, with policies prohibiting smoking in almost all U.S. hospitals, temporary tobacco abstinence promotes smoking cessation for hospitalized patients. Unfortunately, most hospitalized patients go back to smoking soon after discharge. Hospitalization may be the opportune time to help patients try to quit and avoid relapse.
Some hospitals feature inpatient smoking cessation programs in which nurse practitioners and counselors educate and counsel patients. It is highly recommended that a multidisciplinary team be involved in a tobacco cessation program catered to an individual patient’s needs. However, most hospitals have no such program. Nevertheless, the hospitalist can help a patient with brief or low-intensity tobacco cessation counseling, pharmacotherapy for nicotine withdrawal symptom control if clinically indicated, and follow-up upon discharge for relapse prevention.
Counseling: Smoking cessation counseling in the hospital after an AMI has been found to be associated with a relative risk reduction of mortality by 37% in one year. The hospitalist should give a two-minute cessation message as the first step. If tobacco cessation counselors or nurse practitioners are available, their additional counseling also may improve outcomes of smoking cessation therapies.7 However, if no established inpatient tobacco cessation program is available to the hospitalist, the following may be used to aid in physician counseling of the hospitalized cardiac patient:
The first step in treating tobacco dependence is to identify and assess tobacco use status.
Tobacco users willing to quit should be treated using the 5 A’s (Ask, Advise, Assess, Assist, and Arrange) (see Figure 1, p. 30). Tobacco users not willing to quit at the time of interaction should be treated using the 5 R’s for motivational intervention:
- Relevance (indicate why quitting is personally relevant);
- Risks (have patient identify potentially negative consequences of smoking);
- Rewards (have patient identify potential benefits of quitting smoking);
- Roadblocks (have patient identify potential barriers to smoking cessation and provide patient problem-solving techniques and pharmacotherapy to overcome the barriers); and
- Repetition (repeat motivational intervention to unmotivated patient each visit).
Further, former smokers who recently quit using tobacco should be given relapse prevention treatment.8 For the hospitalized smoker with acute cardiovascular disease, providing bedside counseling, enhancing self-coping behavior change, and arranging follow-up after discharge to maintain behavior change can help sustain tobacco abstinence.
Pharmacotherapy: The most important purpose of pharmacotherapy for smoking cessation is to reduce withdrawal symptoms and cigarette cravings. Public Health Service clinical guidelines for smoking cessation mention five first-line agents. These are sustained-release bupropion and four nicotine-replacement therapies (NRT): transdermal patch, gum, nasal spray, and vapor inhaler. Further, there are two second-line agents: clonidine and nortriptyline. Since the clinical guidelines’ release in 2000, the Food and Drug Administration has approved a fifth NRT product, the nicotine lozenge, in 2002, and a partial nicotine agonist, varenicline, in 2006 (see Table 1, right).9,10
Current guidelines recommend that NRT be used with caution in patients with unstable angina, serious arrhythmias, or an MI within the previous two weeks due to limited supportive data on the safety of use in these patients.11 The transdermal patch delivers nicotine at a slow and constant rate in contrast to the other forms of NRT and has been used safely in patients with stable coronary artery disease. However, the use of any NRT, including the patch, in acute cardiovascular disease is not advised due to the nicotine-mediated hemodynamic effects, such as increase heart rate and arterial vasoconstriction, which lead to increased myocardial workload.
Sustained-release bupropion generally is well tolerated by hospitalized patients with cardiovascular disease, but there may be a delay in control of withdrawal symptoms. In addition, blood pressure must be monitored especially if combined with NRT as there have been anecdotal reports of increase in blood pressure with bupropion alone.12 Bupropion must be used cautiously in patients with recent MI. Other contraindications include history of seizure, conditions that potentially can increase risk for convulsions, and use of monoamine oxidase inhibitors (MAOI) within 14 days.
The new drug varenicline has not been studied in hospitalized patients or patients with acute coronary syndrome. However, since it does not have any important hemodynamic effects, it may be useful in this setting and in selected patients with close monitoring for mood changes since there have been anecdotal case reports of psychotic events in patients with underlying psychiatric disorders.13 Its routine use currently is not recommended.
Follow-up after discharge: Pharmacotherapy may be added for withdrawal control, as well as relapse prevention for the hospitalized patient who recently quit smoking. However, inclusion of intensive tobacco cessation counseling during the hospital stay is the most effective intervention given the setting and patient condition, and follow-up support up to at least one month after discharge has been found to be more effective in sustaining tobacco abstinence than pharmacotherapy alone. In order to maximize long-term quit rates among patients who recently abstained from smoking, the hospitalist should arrange access to ongoing outpatient post-discharge support and tobacco cessation treatment.
Back to the Case
After appropriate cardiac testing, the patient was found to have a non-cardiac etiology for his symptoms. From the start of his hospital stay, he was counseled by the hospitalist and started on sustained-release bupropion, but withdrawal symptoms and cravings persisted.
Prior to his discharge home, the patient wanted to discontinue bupropion and be provided an alternative. The patient was given a nicotine patch, and a follow-up appointment at the tobacco cessation clinic within one week of discharge from the hospital was arranged. The patient has been compliant with his quit-smoking treatment and has followed-up for continued tobacco cessation counseling. He hasn’t smoked cigarettes for a year. TH
Dr. Palisoc is a preventive medicine resident at the University of Colorado Denver. Dr. Prochazka works at the Denver VA and is a professor of medicine at the University of Colorado Denver.
References
- CDC. Cigarette Smoking Among Adults, United States, 2006. MMWR Morbidity Mortality Wkly Rep. 2007;56(44):1157-1161. Available at www.cdc.gov/mmwr/preview/mmwrhtml/mm5644a2.htm. Last accessed March 4, 2008.
- CDC. Annual Smoking-Attributable Mortality, Years of Potential Life Lost, and Productivity, United States, 1997-2001. MMWR Morbidity Mortality Wkly Rep. 2005;54(25):625-628.
- Thomson CC, Rigotti NA. Hospital- and clinic-based smoking cessation interventions for smokers with cardiovascular disease. Prog Cardiovasc Dis. 2003;45(6):459-479.
- Rigotti NA. Treatment of tobacco use and dependence. N Engl J Med. 2002;346(7):506-512.
- Van Spall HGC, Chong A, Tu JV. Inpatient smoking-cessation counseling and all-cause mortality in patients with acute myocardial infarction. Am Heart J. 2007;154(2):213-220.
- Rigotti NA, Munafo MR, Stead LF. Interventions for smoking cessation in hospitalized patients. Cochrane Database Syst Rev. 2007;Issue 3.
- Ludvig J, Miner B, and Eisenberg, MJ. Smoking cessation in patients with coronary artery disease. Am Heart J. 2005;149(4):565-572.
- Fiore MC, Bailey WC, Cohen SJ, et al. Treating tobacco use and dependence: clinical practice guideline. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service 2000.
- Rigotti NA, Thorndike AN, Regan S, et al. Bupropion for smokers hospitalized with acute cardiovascular disease. Am J Med. 2006;199:1080-1087.
- Jorenby DE, Hays JT, Rigotti NA, et al. Efficacy of varenicline, an alpha4beta2 nicotinic acetylcholine receptor partial agonist, vs. placebo or sustained-release bupropion for smoking cessation: a randomized controlled trial. JAMA. 2006;296(1):56-63.
- Joseph AM, Fu SS. Safety issues in pharmacotherapy for smoking in patients with cardiovascular disease. Prog Cardiovasc Dis. 2003;45(6):429-441.
- FDA. Prescribing information of Zyban (bupropion hydrochloride) sustained release tablets. June 2007. Available at www.fda.gov/medwatch/safety/2007/ Aug_PI/Zyban_PI.pdf. Last accessed March 6, 2008.
- FDA. Early Communication About an Ongoing Safety Review: Varenicline (marketed as Chantix). November 2007. Available at www.fda.gov/cder/drug/early_comm/varenicline.htm. Last accessed March 6, 2008.