User login
Malpractice minute: June POLL RESULTS
Could a patient’s violent act have been prevented?
A man under outpatient care of the state’s regional behavioral health authority was diagnosed with schizophrenia, paranoid type. He killed his developmentally disabled niece, age 26. The niece’s family claimed the death could have been prevented if the man was civilly committed or heavily medicated. Was the behavioral health authority liable?
⋥ LIABLE: 11% ⋥ NOT LIABLE: 89%
What did the court decide?
The mother was found to be 39% at fault, the patient 11% at fault, and the behavioral health authority 50% at fault for the woman’s death and paid half of the verdict amount to the parents. A $101,740 verdict was returned for the niece’s mother and a $100,625 verdict was returned for the father.
Cases are selected by Current Psychiatry from Medical Malpractice Verdicts, Settlements & Experts, with permission of its editor, Lewis Laska of Nashville, TN (www.verdictslaska.com). Information may be incomplete in some instances, but these cases represent clinical situations that typically result in litigation.
Could a patient’s violent act have been prevented?
A man under outpatient care of the state’s regional behavioral health authority was diagnosed with schizophrenia, paranoid type. He killed his developmentally disabled niece, age 26. The niece’s family claimed the death could have been prevented if the man was civilly committed or heavily medicated. Was the behavioral health authority liable?
⋥ LIABLE: 11% ⋥ NOT LIABLE: 89%
What did the court decide?
The mother was found to be 39% at fault, the patient 11% at fault, and the behavioral health authority 50% at fault for the woman’s death and paid half of the verdict amount to the parents. A $101,740 verdict was returned for the niece’s mother and a $100,625 verdict was returned for the father.
Could a patient’s violent act have been prevented?
A man under outpatient care of the state’s regional behavioral health authority was diagnosed with schizophrenia, paranoid type. He killed his developmentally disabled niece, age 26. The niece’s family claimed the death could have been prevented if the man was civilly committed or heavily medicated. Was the behavioral health authority liable?
⋥ LIABLE: 11% ⋥ NOT LIABLE: 89%
What did the court decide?
The mother was found to be 39% at fault, the patient 11% at fault, and the behavioral health authority 50% at fault for the woman’s death and paid half of the verdict amount to the parents. A $101,740 verdict was returned for the niece’s mother and a $100,625 verdict was returned for the father.
Cases are selected by Current Psychiatry from Medical Malpractice Verdicts, Settlements & Experts, with permission of its editor, Lewis Laska of Nashville, TN (www.verdictslaska.com). Information may be incomplete in some instances, but these cases represent clinical situations that typically result in litigation.
Cases are selected by Current Psychiatry from Medical Malpractice Verdicts, Settlements & Experts, with permission of its editor, Lewis Laska of Nashville, TN (www.verdictslaska.com). Information may be incomplete in some instances, but these cases represent clinical situations that typically result in litigation.
Divorce, custody, and parental consent for psychiatric treatment
Dear Dr. Mossman:
I treat children and adolescents in an acute inpatient setting. Sometimes a child of divorced parents—call him “Johnny”—is admitted to the hospital by one parent—for example the mother—but she doesn’t inform the father. Although the parents have joint custody, Mom doesn’t want me to contact Dad.
I tell Mom that I’d like to get clinical information and consent from Dad, but she refuses, saying, “This will make me look bad, and my ex-husband will try to take emergency custody of Johnny.” My hospital’s legal department says consent from both parents isn’t needed.
These scenarios always leave me feeling upset and confused. I’d appreciate clarification on how to handle these matters.—Submitted by “Dr. K”
Knowing the correct legal answer to a question often doesn’t supply the best clinical solution for your patient. Dr. K received a legally sound response from hospital administrators: a parent who has legal custody may authorize medical treatment for a minor child without first asking or informing the other parent. But Dr. K feels unsatisfied because the hospital didn’t provide what Dr. K sought: a clinically sound answer.
This article reviews custody arrangements and the legal rights they give divorced parents. Also, we will discuss the mother’s concerns and explain why—despite her fears—notifying and involving Johnny’s father can be important, even when it’s not legally required.
- Submit your malpractice-related questions to Dr. Mossman at [email protected].
- Include your name, address, and practice location. If your question is chosen for publication, your name can be withheld by request.
- All readers who submit questions will be included in quarterly drawings for a $50 gift certificate for Professional Risk Management Services, Inc’s online market-place of risk management publications and resources (www.prms.com).
Custody and urgent treatment
A minor—defined in most states as a person younger than age 18—legally cannot give consent for medical care except in limited circumstances, such as contraceptive care.1,2 When a minor undergoes psychiatric hospitalization, physicians usually must obtain consent from the minor’s legal custodian.
Married parents both have legal custody of their children. They also have equal rights to spend time with their children and make major decisions about their welfare, such as authorizing medical care. When parents divorce, these rights must be reassigned in a court-approved divorce decree. Table 1 explains some key terms used to describe custody arrangements after divorce.2,3
Several decades ago, children—especially those younger age 10—usually remained with their mothers, who received sole legal custody; fathers typically had visitation privileges.4 Now, however, most states’ statutes presume that divorced mothers and fathers will have joint legal custody.3
Joint legal custody lets both parents retain their individual legal authority to make decisions on behalf of minor children, although the children may spend most of their time in the physical custody of 1 parent. This means that when urgent medical care is needed—such as a psychiatric hospitalization—1 parent’s consent is sufficient legal authorization for treatment.1,2
What if a child’s parent claims to have legal custody, but the doctor isn’t sure? A doctor who in good faith relies on a parent’s statement can properly provide urgent treatment without delving into custody arrangements.2 In many states, noncustodial parents may authorize treatment in urgent situations—and even some nonurgent ones—if they happen to have physical control of the child when care is needed, such as during a visit.1
Table 1
Child custody: Key legal terms
| Term | Refers to |
|---|---|
| Custody arrangement | The specified times each parent will spend with a minor child and which parent(s) can make major decisions about a child’s welfare |
| Legal custody | A parent’s right to make major decisions about a child’s welfare, including medical care |
| Visitation | The child’s means of maintaining contact with a noncustodial parent |
| Physical custody | Who has physical possession of the child at a particular time, such as during visitation |
| Sole legal custody | A custody arrangement in which only one parent retains the right to make major decisions for the child |
| Joint legal custody | A custody arrangement in which both parents retain the right to make major decisions affecting the child |
| Modification of custody | A legal process in which a court changes a previous custody order |
| Source: Adapted from references 2,3 | |
Nonurgent treatment
After receiving urgent treatment, psychiatric patients typically need continuing, nonurgent care. Dr. K’s inquiry may be anticipating this scenario. In general, parents with joint custody have an equal right to authorize nonurgent care for their children, and Johnny’s treatment could proceed with only Mom’s consent.1 However, if Dr. K knows or has reason to think that Johnny’s father would refuse to give consent for ongoing, nonurgent psychiatric care, providing treatment over the father’s objection may be legally questionable. Under some joint legal custody agreements, both parents need to give consent for medical care and receive clinical information about their children.2
Moreover, trying to treat Johnny in the face of Dad’s explicit objection may be clinically unwise. Unfortunately, many couples’ conflicts are not resolved by divorce, and children can become pawns in ongoing postmarital battles. Such situations can exacerbate children’s emotional problems, which is the opposite of what Dr. K hopes to do for Johnny.
What can Dr. K do?
Address a parent’s fears. Few parents are at their levelheaded best when their children need psychiatric hospitalization. To help Mom and Johnny, Dr. K can point out these things:
- Many states, such as Ohio,5 give Dad the right to learn about Johnny’s treatment and access to treatment records.
- Sooner or later, Dad will find out about the hospitalization. The next time Johnny visits his father, he’ll probably tell Dad what happened. In a few weeks, Dad may receive insurance paperwork or a bill from the hospital.
- Dad may be far more upset and prone to retaliate if he finds out later and is excluded from Johnny’s treatment than if he is notified immediately and gets to participate in his son’s care.
- Realistically, Dad cannot take Johnny away because Mom has arranged for appropriate medical care. If hospitalization is indicated, Mom’s failure to get treatment for Johnny could be grounds for Dad to claim she’s an unfit parent.
Why both parents are needed
Johnny’s hospital care probably will benefit from Dad’s involvement for several reasons (Table 2).
More information. Child and adolescent psychiatrists agree that in most clinical situations it helps to obtain information from as many sources as possible.6-9 Johnny’s father might have crucial information relevant to diagnosis or treatment, such as family history details that Mom doesn’t know.
Debiasing. If Johnny spends time living with both parents, Dr. K should know how often symptoms appear in both environments. Dad’s perspective may be vital, but when postdivorce relationships are strained, what parents convey about each other can be biased. Getting information directly from both parents will give Dr. K a more realistic picture of the child’s environment and psychosocial stressors.7
Treatment planning. After a psychiatric hospitalization, both parents should be aware of Johnny’s diagnosis and treatment. Johnny may need careful supervision for recurrence of symptoms, such as suicidal or homicidal ideation, that can have life-threatening implications.
Medication management. If Johnny is taking medication, he’ll need to receive it regularly. Missing medication when Johnny is with Dad would reduce effectiveness and in some cases could be dangerous. Both parents also should know about possible side effects so they can provide good monitoring.
Psychotherapy. Often, family therapy is an important element of a child’s recovery and will achieve optimum results only if all family members participate. Also, children need consistency. If a behavioral plan is part of Johnny’s treatment, Mom and Dad will need to agree on the rules and implement them consistently at both homes.
Table 2
Why both parents’ input is valuable
| More information from different perspectives concerning behavior in a variety of contexts and settings |
| Less biased information |
| Better treatment planning |
| Better medication management |
| More effective therapy |
Work with parents
When one divorced parent is reluctant to inform the other about their child’s hospitalization, you can respond empathically to fears and concerns. Despite mental health professionals’ best efforts, psychiatric illness still generates feelings of stigma and shame. Divorced parents often feel guilty about the stress the divorce has brought to their children, and they may consciously or unconsciously blame themselves for their child’s illness. In the midst of an ongoing custody dispute, the parent initiating a psychiatric hospitalization may feel especially vulnerable and reluctant to inform the other parent about what’s happening.
Being attuned to these issues will help you address and normalize a parent’s fears. Parents should know that a court could support their seeking treatment for their children’s illness, and they could be contributing to medical neglect if they do not seek this treatment.
In rare instances, not informing the other parent may be the best clinical decision. In situations involving child abuse or extreme domestic violence, a parent’s learning about the hospitalization could create safety issues. In most instances, however, both Mom and Dad will see their child soon after hospitalization, so one parent cannot hope to conceal a hospitalization for very long. Involving both parents from the outset usually will give the child and his family the best shot at a positive outcome.
1. Berger JE. Consent by proxy for nonurgent pediatric care. Pediatrics 2003;112:1186-95.
2. Quinn KM, Weiner BA. Legal rights of children. In: Weiner BA, Wettstein RM, eds. Legal issues in mental health care. New York, NY: Plenum Press; 1993:309-47.
3. Kelly JB. The determination of child custody. Future Child 1994;4:121-242.
4. Melton GB, Petrila J, Poythress NG, Slobogin C. Psychological evaluations for the courts: a handbook for mental health professionals and lawyers. 3rd ed. New York, NY: Guilford Press; 2007.
5. Ohio Rev Code § 3109. 051(H).
6. American Academy of Child and Adolescent Psychiatry. Practice parameters for the psychiatric assessment of children and adolescents. J Am Acad Child Adolesc Psychiatry 1997;36(10 suppl):4S-20S.
7. American Academy of Child and Adolescent Psychiatry. Practice parameter for the assessment of the family. J Am Acad Child Adolesc Psychiatry 2007;46:922-37.
8. Bostic JQ, King RA. Clinical assessment of children and adolescents: content and structure. In: Martin A, Volkmar FR, eds. Lewis’s child and adolescent psychiatry: a comprehensive textbook. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:323-44.
9. Weston CG, Klykylo WM. The initial psychiatric evaluation of children and adolescents. In: Tasman A, Kay J, Lieberman J, eds. Psychiatry. 3rd ed. London, UK: John Wiley & Sons; 2008:546-54.
Dear Dr. Mossman:
I treat children and adolescents in an acute inpatient setting. Sometimes a child of divorced parents—call him “Johnny”—is admitted to the hospital by one parent—for example the mother—but she doesn’t inform the father. Although the parents have joint custody, Mom doesn’t want me to contact Dad.
I tell Mom that I’d like to get clinical information and consent from Dad, but she refuses, saying, “This will make me look bad, and my ex-husband will try to take emergency custody of Johnny.” My hospital’s legal department says consent from both parents isn’t needed.
These scenarios always leave me feeling upset and confused. I’d appreciate clarification on how to handle these matters.—Submitted by “Dr. K”
Knowing the correct legal answer to a question often doesn’t supply the best clinical solution for your patient. Dr. K received a legally sound response from hospital administrators: a parent who has legal custody may authorize medical treatment for a minor child without first asking or informing the other parent. But Dr. K feels unsatisfied because the hospital didn’t provide what Dr. K sought: a clinically sound answer.
This article reviews custody arrangements and the legal rights they give divorced parents. Also, we will discuss the mother’s concerns and explain why—despite her fears—notifying and involving Johnny’s father can be important, even when it’s not legally required.
- Submit your malpractice-related questions to Dr. Mossman at [email protected].
- Include your name, address, and practice location. If your question is chosen for publication, your name can be withheld by request.
- All readers who submit questions will be included in quarterly drawings for a $50 gift certificate for Professional Risk Management Services, Inc’s online market-place of risk management publications and resources (www.prms.com).
Custody and urgent treatment
A minor—defined in most states as a person younger than age 18—legally cannot give consent for medical care except in limited circumstances, such as contraceptive care.1,2 When a minor undergoes psychiatric hospitalization, physicians usually must obtain consent from the minor’s legal custodian.
Married parents both have legal custody of their children. They also have equal rights to spend time with their children and make major decisions about their welfare, such as authorizing medical care. When parents divorce, these rights must be reassigned in a court-approved divorce decree. Table 1 explains some key terms used to describe custody arrangements after divorce.2,3
Several decades ago, children—especially those younger age 10—usually remained with their mothers, who received sole legal custody; fathers typically had visitation privileges.4 Now, however, most states’ statutes presume that divorced mothers and fathers will have joint legal custody.3
Joint legal custody lets both parents retain their individual legal authority to make decisions on behalf of minor children, although the children may spend most of their time in the physical custody of 1 parent. This means that when urgent medical care is needed—such as a psychiatric hospitalization—1 parent’s consent is sufficient legal authorization for treatment.1,2
What if a child’s parent claims to have legal custody, but the doctor isn’t sure? A doctor who in good faith relies on a parent’s statement can properly provide urgent treatment without delving into custody arrangements.2 In many states, noncustodial parents may authorize treatment in urgent situations—and even some nonurgent ones—if they happen to have physical control of the child when care is needed, such as during a visit.1
Table 1
Child custody: Key legal terms
| Term | Refers to |
|---|---|
| Custody arrangement | The specified times each parent will spend with a minor child and which parent(s) can make major decisions about a child’s welfare |
| Legal custody | A parent’s right to make major decisions about a child’s welfare, including medical care |
| Visitation | The child’s means of maintaining contact with a noncustodial parent |
| Physical custody | Who has physical possession of the child at a particular time, such as during visitation |
| Sole legal custody | A custody arrangement in which only one parent retains the right to make major decisions for the child |
| Joint legal custody | A custody arrangement in which both parents retain the right to make major decisions affecting the child |
| Modification of custody | A legal process in which a court changes a previous custody order |
| Source: Adapted from references 2,3 | |
Nonurgent treatment
After receiving urgent treatment, psychiatric patients typically need continuing, nonurgent care. Dr. K’s inquiry may be anticipating this scenario. In general, parents with joint custody have an equal right to authorize nonurgent care for their children, and Johnny’s treatment could proceed with only Mom’s consent.1 However, if Dr. K knows or has reason to think that Johnny’s father would refuse to give consent for ongoing, nonurgent psychiatric care, providing treatment over the father’s objection may be legally questionable. Under some joint legal custody agreements, both parents need to give consent for medical care and receive clinical information about their children.2
Moreover, trying to treat Johnny in the face of Dad’s explicit objection may be clinically unwise. Unfortunately, many couples’ conflicts are not resolved by divorce, and children can become pawns in ongoing postmarital battles. Such situations can exacerbate children’s emotional problems, which is the opposite of what Dr. K hopes to do for Johnny.
What can Dr. K do?
Address a parent’s fears. Few parents are at their levelheaded best when their children need psychiatric hospitalization. To help Mom and Johnny, Dr. K can point out these things:
- Many states, such as Ohio,5 give Dad the right to learn about Johnny’s treatment and access to treatment records.
- Sooner or later, Dad will find out about the hospitalization. The next time Johnny visits his father, he’ll probably tell Dad what happened. In a few weeks, Dad may receive insurance paperwork or a bill from the hospital.
- Dad may be far more upset and prone to retaliate if he finds out later and is excluded from Johnny’s treatment than if he is notified immediately and gets to participate in his son’s care.
- Realistically, Dad cannot take Johnny away because Mom has arranged for appropriate medical care. If hospitalization is indicated, Mom’s failure to get treatment for Johnny could be grounds for Dad to claim she’s an unfit parent.
Why both parents are needed
Johnny’s hospital care probably will benefit from Dad’s involvement for several reasons (Table 2).
More information. Child and adolescent psychiatrists agree that in most clinical situations it helps to obtain information from as many sources as possible.6-9 Johnny’s father might have crucial information relevant to diagnosis or treatment, such as family history details that Mom doesn’t know.
Debiasing. If Johnny spends time living with both parents, Dr. K should know how often symptoms appear in both environments. Dad’s perspective may be vital, but when postdivorce relationships are strained, what parents convey about each other can be biased. Getting information directly from both parents will give Dr. K a more realistic picture of the child’s environment and psychosocial stressors.7
Treatment planning. After a psychiatric hospitalization, both parents should be aware of Johnny’s diagnosis and treatment. Johnny may need careful supervision for recurrence of symptoms, such as suicidal or homicidal ideation, that can have life-threatening implications.
Medication management. If Johnny is taking medication, he’ll need to receive it regularly. Missing medication when Johnny is with Dad would reduce effectiveness and in some cases could be dangerous. Both parents also should know about possible side effects so they can provide good monitoring.
Psychotherapy. Often, family therapy is an important element of a child’s recovery and will achieve optimum results only if all family members participate. Also, children need consistency. If a behavioral plan is part of Johnny’s treatment, Mom and Dad will need to agree on the rules and implement them consistently at both homes.
Table 2
Why both parents’ input is valuable
| More information from different perspectives concerning behavior in a variety of contexts and settings |
| Less biased information |
| Better treatment planning |
| Better medication management |
| More effective therapy |
Work with parents
When one divorced parent is reluctant to inform the other about their child’s hospitalization, you can respond empathically to fears and concerns. Despite mental health professionals’ best efforts, psychiatric illness still generates feelings of stigma and shame. Divorced parents often feel guilty about the stress the divorce has brought to their children, and they may consciously or unconsciously blame themselves for their child’s illness. In the midst of an ongoing custody dispute, the parent initiating a psychiatric hospitalization may feel especially vulnerable and reluctant to inform the other parent about what’s happening.
Being attuned to these issues will help you address and normalize a parent’s fears. Parents should know that a court could support their seeking treatment for their children’s illness, and they could be contributing to medical neglect if they do not seek this treatment.
In rare instances, not informing the other parent may be the best clinical decision. In situations involving child abuse or extreme domestic violence, a parent’s learning about the hospitalization could create safety issues. In most instances, however, both Mom and Dad will see their child soon after hospitalization, so one parent cannot hope to conceal a hospitalization for very long. Involving both parents from the outset usually will give the child and his family the best shot at a positive outcome.
Dear Dr. Mossman:
I treat children and adolescents in an acute inpatient setting. Sometimes a child of divorced parents—call him “Johnny”—is admitted to the hospital by one parent—for example the mother—but she doesn’t inform the father. Although the parents have joint custody, Mom doesn’t want me to contact Dad.
I tell Mom that I’d like to get clinical information and consent from Dad, but she refuses, saying, “This will make me look bad, and my ex-husband will try to take emergency custody of Johnny.” My hospital’s legal department says consent from both parents isn’t needed.
These scenarios always leave me feeling upset and confused. I’d appreciate clarification on how to handle these matters.—Submitted by “Dr. K”
Knowing the correct legal answer to a question often doesn’t supply the best clinical solution for your patient. Dr. K received a legally sound response from hospital administrators: a parent who has legal custody may authorize medical treatment for a minor child without first asking or informing the other parent. But Dr. K feels unsatisfied because the hospital didn’t provide what Dr. K sought: a clinically sound answer.
This article reviews custody arrangements and the legal rights they give divorced parents. Also, we will discuss the mother’s concerns and explain why—despite her fears—notifying and involving Johnny’s father can be important, even when it’s not legally required.
- Submit your malpractice-related questions to Dr. Mossman at [email protected].
- Include your name, address, and practice location. If your question is chosen for publication, your name can be withheld by request.
- All readers who submit questions will be included in quarterly drawings for a $50 gift certificate for Professional Risk Management Services, Inc’s online market-place of risk management publications and resources (www.prms.com).
Custody and urgent treatment
A minor—defined in most states as a person younger than age 18—legally cannot give consent for medical care except in limited circumstances, such as contraceptive care.1,2 When a minor undergoes psychiatric hospitalization, physicians usually must obtain consent from the minor’s legal custodian.
Married parents both have legal custody of their children. They also have equal rights to spend time with their children and make major decisions about their welfare, such as authorizing medical care. When parents divorce, these rights must be reassigned in a court-approved divorce decree. Table 1 explains some key terms used to describe custody arrangements after divorce.2,3
Several decades ago, children—especially those younger age 10—usually remained with their mothers, who received sole legal custody; fathers typically had visitation privileges.4 Now, however, most states’ statutes presume that divorced mothers and fathers will have joint legal custody.3
Joint legal custody lets both parents retain their individual legal authority to make decisions on behalf of minor children, although the children may spend most of their time in the physical custody of 1 parent. This means that when urgent medical care is needed—such as a psychiatric hospitalization—1 parent’s consent is sufficient legal authorization for treatment.1,2
What if a child’s parent claims to have legal custody, but the doctor isn’t sure? A doctor who in good faith relies on a parent’s statement can properly provide urgent treatment without delving into custody arrangements.2 In many states, noncustodial parents may authorize treatment in urgent situations—and even some nonurgent ones—if they happen to have physical control of the child when care is needed, such as during a visit.1
Table 1
Child custody: Key legal terms
| Term | Refers to |
|---|---|
| Custody arrangement | The specified times each parent will spend with a minor child and which parent(s) can make major decisions about a child’s welfare |
| Legal custody | A parent’s right to make major decisions about a child’s welfare, including medical care |
| Visitation | The child’s means of maintaining contact with a noncustodial parent |
| Physical custody | Who has physical possession of the child at a particular time, such as during visitation |
| Sole legal custody | A custody arrangement in which only one parent retains the right to make major decisions for the child |
| Joint legal custody | A custody arrangement in which both parents retain the right to make major decisions affecting the child |
| Modification of custody | A legal process in which a court changes a previous custody order |
| Source: Adapted from references 2,3 | |
Nonurgent treatment
After receiving urgent treatment, psychiatric patients typically need continuing, nonurgent care. Dr. K’s inquiry may be anticipating this scenario. In general, parents with joint custody have an equal right to authorize nonurgent care for their children, and Johnny’s treatment could proceed with only Mom’s consent.1 However, if Dr. K knows or has reason to think that Johnny’s father would refuse to give consent for ongoing, nonurgent psychiatric care, providing treatment over the father’s objection may be legally questionable. Under some joint legal custody agreements, both parents need to give consent for medical care and receive clinical information about their children.2
Moreover, trying to treat Johnny in the face of Dad’s explicit objection may be clinically unwise. Unfortunately, many couples’ conflicts are not resolved by divorce, and children can become pawns in ongoing postmarital battles. Such situations can exacerbate children’s emotional problems, which is the opposite of what Dr. K hopes to do for Johnny.
What can Dr. K do?
Address a parent’s fears. Few parents are at their levelheaded best when their children need psychiatric hospitalization. To help Mom and Johnny, Dr. K can point out these things:
- Many states, such as Ohio,5 give Dad the right to learn about Johnny’s treatment and access to treatment records.
- Sooner or later, Dad will find out about the hospitalization. The next time Johnny visits his father, he’ll probably tell Dad what happened. In a few weeks, Dad may receive insurance paperwork or a bill from the hospital.
- Dad may be far more upset and prone to retaliate if he finds out later and is excluded from Johnny’s treatment than if he is notified immediately and gets to participate in his son’s care.
- Realistically, Dad cannot take Johnny away because Mom has arranged for appropriate medical care. If hospitalization is indicated, Mom’s failure to get treatment for Johnny could be grounds for Dad to claim she’s an unfit parent.
Why both parents are needed
Johnny’s hospital care probably will benefit from Dad’s involvement for several reasons (Table 2).
More information. Child and adolescent psychiatrists agree that in most clinical situations it helps to obtain information from as many sources as possible.6-9 Johnny’s father might have crucial information relevant to diagnosis or treatment, such as family history details that Mom doesn’t know.
Debiasing. If Johnny spends time living with both parents, Dr. K should know how often symptoms appear in both environments. Dad’s perspective may be vital, but when postdivorce relationships are strained, what parents convey about each other can be biased. Getting information directly from both parents will give Dr. K a more realistic picture of the child’s environment and psychosocial stressors.7
Treatment planning. After a psychiatric hospitalization, both parents should be aware of Johnny’s diagnosis and treatment. Johnny may need careful supervision for recurrence of symptoms, such as suicidal or homicidal ideation, that can have life-threatening implications.
Medication management. If Johnny is taking medication, he’ll need to receive it regularly. Missing medication when Johnny is with Dad would reduce effectiveness and in some cases could be dangerous. Both parents also should know about possible side effects so they can provide good monitoring.
Psychotherapy. Often, family therapy is an important element of a child’s recovery and will achieve optimum results only if all family members participate. Also, children need consistency. If a behavioral plan is part of Johnny’s treatment, Mom and Dad will need to agree on the rules and implement them consistently at both homes.
Table 2
Why both parents’ input is valuable
| More information from different perspectives concerning behavior in a variety of contexts and settings |
| Less biased information |
| Better treatment planning |
| Better medication management |
| More effective therapy |
Work with parents
When one divorced parent is reluctant to inform the other about their child’s hospitalization, you can respond empathically to fears and concerns. Despite mental health professionals’ best efforts, psychiatric illness still generates feelings of stigma and shame. Divorced parents often feel guilty about the stress the divorce has brought to their children, and they may consciously or unconsciously blame themselves for their child’s illness. In the midst of an ongoing custody dispute, the parent initiating a psychiatric hospitalization may feel especially vulnerable and reluctant to inform the other parent about what’s happening.
Being attuned to these issues will help you address and normalize a parent’s fears. Parents should know that a court could support their seeking treatment for their children’s illness, and they could be contributing to medical neglect if they do not seek this treatment.
In rare instances, not informing the other parent may be the best clinical decision. In situations involving child abuse or extreme domestic violence, a parent’s learning about the hospitalization could create safety issues. In most instances, however, both Mom and Dad will see their child soon after hospitalization, so one parent cannot hope to conceal a hospitalization for very long. Involving both parents from the outset usually will give the child and his family the best shot at a positive outcome.
1. Berger JE. Consent by proxy for nonurgent pediatric care. Pediatrics 2003;112:1186-95.
2. Quinn KM, Weiner BA. Legal rights of children. In: Weiner BA, Wettstein RM, eds. Legal issues in mental health care. New York, NY: Plenum Press; 1993:309-47.
3. Kelly JB. The determination of child custody. Future Child 1994;4:121-242.
4. Melton GB, Petrila J, Poythress NG, Slobogin C. Psychological evaluations for the courts: a handbook for mental health professionals and lawyers. 3rd ed. New York, NY: Guilford Press; 2007.
5. Ohio Rev Code § 3109. 051(H).
6. American Academy of Child and Adolescent Psychiatry. Practice parameters for the psychiatric assessment of children and adolescents. J Am Acad Child Adolesc Psychiatry 1997;36(10 suppl):4S-20S.
7. American Academy of Child and Adolescent Psychiatry. Practice parameter for the assessment of the family. J Am Acad Child Adolesc Psychiatry 2007;46:922-37.
8. Bostic JQ, King RA. Clinical assessment of children and adolescents: content and structure. In: Martin A, Volkmar FR, eds. Lewis’s child and adolescent psychiatry: a comprehensive textbook. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:323-44.
9. Weston CG, Klykylo WM. The initial psychiatric evaluation of children and adolescents. In: Tasman A, Kay J, Lieberman J, eds. Psychiatry. 3rd ed. London, UK: John Wiley & Sons; 2008:546-54.
1. Berger JE. Consent by proxy for nonurgent pediatric care. Pediatrics 2003;112:1186-95.
2. Quinn KM, Weiner BA. Legal rights of children. In: Weiner BA, Wettstein RM, eds. Legal issues in mental health care. New York, NY: Plenum Press; 1993:309-47.
3. Kelly JB. The determination of child custody. Future Child 1994;4:121-242.
4. Melton GB, Petrila J, Poythress NG, Slobogin C. Psychological evaluations for the courts: a handbook for mental health professionals and lawyers. 3rd ed. New York, NY: Guilford Press; 2007.
5. Ohio Rev Code § 3109. 051(H).
6. American Academy of Child and Adolescent Psychiatry. Practice parameters for the psychiatric assessment of children and adolescents. J Am Acad Child Adolesc Psychiatry 1997;36(10 suppl):4S-20S.
7. American Academy of Child and Adolescent Psychiatry. Practice parameter for the assessment of the family. J Am Acad Child Adolesc Psychiatry 2007;46:922-37.
8. Bostic JQ, King RA. Clinical assessment of children and adolescents: content and structure. In: Martin A, Volkmar FR, eds. Lewis’s child and adolescent psychiatry: a comprehensive textbook. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:323-44.
9. Weston CG, Klykylo WM. The initial psychiatric evaluation of children and adolescents. In: Tasman A, Kay J, Lieberman J, eds. Psychiatry. 3rd ed. London, UK: John Wiley & Sons; 2008:546-54.
We’re Hiring
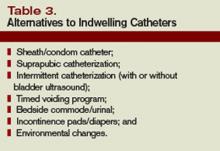
At the 2008 SHM Annual Meeting in San Diego, I had the pleasure of serving as moderator for a panel commenting on the opportunities and challenges faced by hospitalists. I’m not sure how well our predictions will withstand the test of time, but two things came up that I’ll discuss here:
1) Nearly every group is recruiting, and many seem to think the hospitalist shortage will last throughout the careers of those in practice today.
2) Nearly all hospitalist groups are looking for more doctors. I asked the approximately 1,600 in attendance how many are recruiting for more hospitalists. Nearly every hand in the room shot up. It was impressive; one friend (Bob Reynolds) told me he was sitting in the back and could feel a breeze in the room from all the hands being raised. Only about three hands went up when I asked how many thought their staffing was adequate.
Bear in mind that based on the show of hands nearly every group in the country is recruiting. Many groups are looking to add three to six hospitalists this year alone. This is on top of the average group growing about 20% to 25% the past two years, based on my study of data from the “Society of Hospital Medicine 2007-08 Survey: The Authoritative Source on the State of the Hospitalist Movement.” The survey showed the number of FTE doctors in the average hospitalist group grew from a median six to eight hospitalists (the average went from eight to 9.7).
Hospital medicine is the fastest-growing field in the history of American medicine, and it looks like the demand for hospitalists may be increasing even faster than the supply.
I was tempted to ask for a show of hands from doctors at the meeting who were looking for a hospitalist position, but feared it could disrupt the whole conference as those seeking new doctors pounced on the potential candidates in a piranha-like feeding frenzy. So there is good news for anyone interested in joining a hospitalist group: You should have a lot of choices. If you’re recruiting, you’d better get to work to make sure you have really good plan. Let me offer a few ideas.
Never stop recruiting. Dr. Greg Mappin, VPMA at Self Regional Hospital in Greenwood, S.C., told me his philosophy is to “recruit forever, and hire when necessary.” I agree.
You should build and maintain a robust candidate pipeline by ensuring your practice maintains a high level of visibility before your best source of new doctors. The best source for most groups is the closest residency training program, though other nearby hospitalist or outpatient practices might be a secondary source of new manpower.
I suggest you engage residents by hosting a dinner near their hospital once or twice a year and inviting all second- and third-year residents to attend regardless of their interest in becoming hospitalists. You might do this even in years you may not need to add hospitalists to ensure your dinner becomes a regular event for them and to ensure they’re very familiar with your program. Some hospitals develop night and weekend moonlighting programs that employ nearby residents, which increases the chance some will join the practice upon completion of their training.
Ensure all hospitalists—especially the group leader—actively participate in recruiting. Your hospital or medical group’s physician recruiter can be a terrific asset. He/she can provide advice regarding how to find candidates, arranging interviews, etc. Yet, it is critical for the hospitalist group leader to actively communicate with every candidate, including responding to every inquiry within a day or so.
Too many group leaders make a big mistake by waiting many days to respond to new inquiries, or letting the recruiter handle all communication in advance of an interview. During the interview, be sure the candidate spends time with many of the current group members and provides contact information for every group member in case the candidate would like to call any who weren’t available on the interview day. Consider providing the candidate with a copy of the group schedule, any orientation documents you have, and other such printed materials to review after the visit.
Recruit specifically for short-term members of your practice. Despite concerns about turnover, I think it is reasonable to actively pursue candidates who may have as little as two years to work in your practice. For example, they may plan to move to another town (e.g., when their spouse finishes training) or start fellowship training. In my experience, at least half of new doctors who plan to be a hospitalist for only a year or two will choose to stay on long term.
If you want your classified ad to stand out, think about writing one that specifically targets short-term hospitalists. It could say something like: “Do you have only two years to work as a hospitalist? Then this is the place for you.” You even could add benefits, such as tuition to attend conferences that would be of value for the doctor regardless of their future specialty or practice setting. If you desperately need additional doctors, get creative in recruiting those who plan to stay with you for only a couple years. I’m confident some will end up staying long term.
Continue “recruiting” the doctors in your practice. For a number of reasons, hospitalist turnover may be higher than most other specialties. So it is particularly important to take steps to minimize it. SHM’s white paper on hospitalist career satisfaction (“A Challenge for a New Specialty: A White Paper on Hospitalist Career Satisfaction”) offers observations and valuable suggestions for any practice. Find it under the “Publications” link on SHM’s Web site, www. hospitalmedicine.org.
No End to Shortage
Now back to that panel discussion at SHM’s Annual Meeting in April. I asked the panelists what things would be like if in 10 years the demand for hospitalists decreased, and the supply finally caught up with and ultimately exceeded demand.
I thought this could be a provocative question that would lead to a discussion about how much of our current situation, such as recent increases in hospital financial support provided per hospitalist, are due to the current hospitalist shortage. Will hospitals decrease their support if there is ever an excess of hospitalists?
No one was buying it. Everyone was convinced that despite the incredible growth in numbers of doctors practicing as hospitalists, the demand for hospitalists will continue to grow even faster than the supply. Panelist Ron Greeno, MD, FCCP, chief medical officer of Cogent Healthcare in Irvine, Calif., thought this hospitalist shortage would continue throughout our lifetime. I’m not sure how long Ron thinks he (or I) will live, but that’s a pretty bold prediction.
It looks like the current intense recruiting environment is here to stay for a long time. Every practice should be thinking about how best to manage it. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
At the 2008 SHM Annual Meeting in San Diego, I had the pleasure of serving as moderator for a panel commenting on the opportunities and challenges faced by hospitalists. I’m not sure how well our predictions will withstand the test of time, but two things came up that I’ll discuss here:
1) Nearly every group is recruiting, and many seem to think the hospitalist shortage will last throughout the careers of those in practice today.
2) Nearly all hospitalist groups are looking for more doctors. I asked the approximately 1,600 in attendance how many are recruiting for more hospitalists. Nearly every hand in the room shot up. It was impressive; one friend (Bob Reynolds) told me he was sitting in the back and could feel a breeze in the room from all the hands being raised. Only about three hands went up when I asked how many thought their staffing was adequate.
Bear in mind that based on the show of hands nearly every group in the country is recruiting. Many groups are looking to add three to six hospitalists this year alone. This is on top of the average group growing about 20% to 25% the past two years, based on my study of data from the “Society of Hospital Medicine 2007-08 Survey: The Authoritative Source on the State of the Hospitalist Movement.” The survey showed the number of FTE doctors in the average hospitalist group grew from a median six to eight hospitalists (the average went from eight to 9.7).
Hospital medicine is the fastest-growing field in the history of American medicine, and it looks like the demand for hospitalists may be increasing even faster than the supply.
I was tempted to ask for a show of hands from doctors at the meeting who were looking for a hospitalist position, but feared it could disrupt the whole conference as those seeking new doctors pounced on the potential candidates in a piranha-like feeding frenzy. So there is good news for anyone interested in joining a hospitalist group: You should have a lot of choices. If you’re recruiting, you’d better get to work to make sure you have really good plan. Let me offer a few ideas.
Never stop recruiting. Dr. Greg Mappin, VPMA at Self Regional Hospital in Greenwood, S.C., told me his philosophy is to “recruit forever, and hire when necessary.” I agree.
You should build and maintain a robust candidate pipeline by ensuring your practice maintains a high level of visibility before your best source of new doctors. The best source for most groups is the closest residency training program, though other nearby hospitalist or outpatient practices might be a secondary source of new manpower.
I suggest you engage residents by hosting a dinner near their hospital once or twice a year and inviting all second- and third-year residents to attend regardless of their interest in becoming hospitalists. You might do this even in years you may not need to add hospitalists to ensure your dinner becomes a regular event for them and to ensure they’re very familiar with your program. Some hospitals develop night and weekend moonlighting programs that employ nearby residents, which increases the chance some will join the practice upon completion of their training.
Ensure all hospitalists—especially the group leader—actively participate in recruiting. Your hospital or medical group’s physician recruiter can be a terrific asset. He/she can provide advice regarding how to find candidates, arranging interviews, etc. Yet, it is critical for the hospitalist group leader to actively communicate with every candidate, including responding to every inquiry within a day or so.
Too many group leaders make a big mistake by waiting many days to respond to new inquiries, or letting the recruiter handle all communication in advance of an interview. During the interview, be sure the candidate spends time with many of the current group members and provides contact information for every group member in case the candidate would like to call any who weren’t available on the interview day. Consider providing the candidate with a copy of the group schedule, any orientation documents you have, and other such printed materials to review after the visit.
Recruit specifically for short-term members of your practice. Despite concerns about turnover, I think it is reasonable to actively pursue candidates who may have as little as two years to work in your practice. For example, they may plan to move to another town (e.g., when their spouse finishes training) or start fellowship training. In my experience, at least half of new doctors who plan to be a hospitalist for only a year or two will choose to stay on long term.
If you want your classified ad to stand out, think about writing one that specifically targets short-term hospitalists. It could say something like: “Do you have only two years to work as a hospitalist? Then this is the place for you.” You even could add benefits, such as tuition to attend conferences that would be of value for the doctor regardless of their future specialty or practice setting. If you desperately need additional doctors, get creative in recruiting those who plan to stay with you for only a couple years. I’m confident some will end up staying long term.
Continue “recruiting” the doctors in your practice. For a number of reasons, hospitalist turnover may be higher than most other specialties. So it is particularly important to take steps to minimize it. SHM’s white paper on hospitalist career satisfaction (“A Challenge for a New Specialty: A White Paper on Hospitalist Career Satisfaction”) offers observations and valuable suggestions for any practice. Find it under the “Publications” link on SHM’s Web site, www. hospitalmedicine.org.
No End to Shortage
Now back to that panel discussion at SHM’s Annual Meeting in April. I asked the panelists what things would be like if in 10 years the demand for hospitalists decreased, and the supply finally caught up with and ultimately exceeded demand.
I thought this could be a provocative question that would lead to a discussion about how much of our current situation, such as recent increases in hospital financial support provided per hospitalist, are due to the current hospitalist shortage. Will hospitals decrease their support if there is ever an excess of hospitalists?
No one was buying it. Everyone was convinced that despite the incredible growth in numbers of doctors practicing as hospitalists, the demand for hospitalists will continue to grow even faster than the supply. Panelist Ron Greeno, MD, FCCP, chief medical officer of Cogent Healthcare in Irvine, Calif., thought this hospitalist shortage would continue throughout our lifetime. I’m not sure how long Ron thinks he (or I) will live, but that’s a pretty bold prediction.
It looks like the current intense recruiting environment is here to stay for a long time. Every practice should be thinking about how best to manage it. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
At the 2008 SHM Annual Meeting in San Diego, I had the pleasure of serving as moderator for a panel commenting on the opportunities and challenges faced by hospitalists. I’m not sure how well our predictions will withstand the test of time, but two things came up that I’ll discuss here:
1) Nearly every group is recruiting, and many seem to think the hospitalist shortage will last throughout the careers of those in practice today.
2) Nearly all hospitalist groups are looking for more doctors. I asked the approximately 1,600 in attendance how many are recruiting for more hospitalists. Nearly every hand in the room shot up. It was impressive; one friend (Bob Reynolds) told me he was sitting in the back and could feel a breeze in the room from all the hands being raised. Only about three hands went up when I asked how many thought their staffing was adequate.
Bear in mind that based on the show of hands nearly every group in the country is recruiting. Many groups are looking to add three to six hospitalists this year alone. This is on top of the average group growing about 20% to 25% the past two years, based on my study of data from the “Society of Hospital Medicine 2007-08 Survey: The Authoritative Source on the State of the Hospitalist Movement.” The survey showed the number of FTE doctors in the average hospitalist group grew from a median six to eight hospitalists (the average went from eight to 9.7).
Hospital medicine is the fastest-growing field in the history of American medicine, and it looks like the demand for hospitalists may be increasing even faster than the supply.
I was tempted to ask for a show of hands from doctors at the meeting who were looking for a hospitalist position, but feared it could disrupt the whole conference as those seeking new doctors pounced on the potential candidates in a piranha-like feeding frenzy. So there is good news for anyone interested in joining a hospitalist group: You should have a lot of choices. If you’re recruiting, you’d better get to work to make sure you have really good plan. Let me offer a few ideas.
Never stop recruiting. Dr. Greg Mappin, VPMA at Self Regional Hospital in Greenwood, S.C., told me his philosophy is to “recruit forever, and hire when necessary.” I agree.
You should build and maintain a robust candidate pipeline by ensuring your practice maintains a high level of visibility before your best source of new doctors. The best source for most groups is the closest residency training program, though other nearby hospitalist or outpatient practices might be a secondary source of new manpower.
I suggest you engage residents by hosting a dinner near their hospital once or twice a year and inviting all second- and third-year residents to attend regardless of their interest in becoming hospitalists. You might do this even in years you may not need to add hospitalists to ensure your dinner becomes a regular event for them and to ensure they’re very familiar with your program. Some hospitals develop night and weekend moonlighting programs that employ nearby residents, which increases the chance some will join the practice upon completion of their training.
Ensure all hospitalists—especially the group leader—actively participate in recruiting. Your hospital or medical group’s physician recruiter can be a terrific asset. He/she can provide advice regarding how to find candidates, arranging interviews, etc. Yet, it is critical for the hospitalist group leader to actively communicate with every candidate, including responding to every inquiry within a day or so.
Too many group leaders make a big mistake by waiting many days to respond to new inquiries, or letting the recruiter handle all communication in advance of an interview. During the interview, be sure the candidate spends time with many of the current group members and provides contact information for every group member in case the candidate would like to call any who weren’t available on the interview day. Consider providing the candidate with a copy of the group schedule, any orientation documents you have, and other such printed materials to review after the visit.
Recruit specifically for short-term members of your practice. Despite concerns about turnover, I think it is reasonable to actively pursue candidates who may have as little as two years to work in your practice. For example, they may plan to move to another town (e.g., when their spouse finishes training) or start fellowship training. In my experience, at least half of new doctors who plan to be a hospitalist for only a year or two will choose to stay on long term.
If you want your classified ad to stand out, think about writing one that specifically targets short-term hospitalists. It could say something like: “Do you have only two years to work as a hospitalist? Then this is the place for you.” You even could add benefits, such as tuition to attend conferences that would be of value for the doctor regardless of their future specialty or practice setting. If you desperately need additional doctors, get creative in recruiting those who plan to stay with you for only a couple years. I’m confident some will end up staying long term.
Continue “recruiting” the doctors in your practice. For a number of reasons, hospitalist turnover may be higher than most other specialties. So it is particularly important to take steps to minimize it. SHM’s white paper on hospitalist career satisfaction (“A Challenge for a New Specialty: A White Paper on Hospitalist Career Satisfaction”) offers observations and valuable suggestions for any practice. Find it under the “Publications” link on SHM’s Web site, www. hospitalmedicine.org.
No End to Shortage
Now back to that panel discussion at SHM’s Annual Meeting in April. I asked the panelists what things would be like if in 10 years the demand for hospitalists decreased, and the supply finally caught up with and ultimately exceeded demand.
I thought this could be a provocative question that would lead to a discussion about how much of our current situation, such as recent increases in hospital financial support provided per hospitalist, are due to the current hospitalist shortage. Will hospitals decrease their support if there is ever an excess of hospitalists?
No one was buying it. Everyone was convinced that despite the incredible growth in numbers of doctors practicing as hospitalists, the demand for hospitalists will continue to grow even faster than the supply. Panelist Ron Greeno, MD, FCCP, chief medical officer of Cogent Healthcare in Irvine, Calif., thought this hospitalist shortage would continue throughout our lifetime. I’m not sure how long Ron thinks he (or I) will live, but that’s a pretty bold prediction.
It looks like the current intense recruiting environment is here to stay for a long time. Every practice should be thinking about how best to manage it. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
How can we Reduce Indwelling Urinary Catheter Use and Complications?
Case
A 68-year-old male with a history of Alzheimer’s dementia and incontinence presents with failure to thrive. A Foley catheter is placed due to the patient’s incontinence and fall risk. Three days after admission while awaiting placement in a skilled nursing facility (SNF), he develops a urinary tract infection (UTI) complicated by delirium delaying his transfer to the SNF. What could have been done to prevent this complication?
Overview
It has been 50 years since Beeson, et al., recognized the potential harms stemming from urethral catheterization and penned an editorial to the American Journal of Medicine titled “The case against the catheter.”1
Since then, there has been considerable exploration of ways to limit urethral catheterization and ultimately decrease catheter-associated urinary tract infections (CAUTIs). Unfortunately, little progress has been made; indwelling urinary catheters remain ubiquitous in hospitals and CAUTIs remain the most common hospital-acquired infection in the United States.2 Given the emphasis on the quality and costs of healthcare, it is an opportune time to revisit catheter management and use as a way to combat the clinical and economic consequences of CAUTIs.
Clinicians may be lulled into thinking the clinical impact of CAUTI is less than that of other nosocomial infections. However, beyond the obvious patient harm from UTIs, associated bacteremia, and even death, the public health implications of CAUTI cannot be denied. Urinary tract infections constitute 40% of all nosocomial infections; accounting for an estimated 1 million cases annually.3 Further, 80% of all UTIs are associated with indwelling catheter use.
On average, nosocomial UTI necessitates one extra hospital day per patient, or approximately one million excess hospital days per year.4 Pooled cost analysis shows that UTIs consume an additional $400-$1,700 per event, or an estimated $425 million per year in the United States.5,6 Clearly, we cannot wait another 50 years to address this problem.
Review of the Data
Catheter duration as a risk factor for CAUTI: The indwelling catheter creates a portal of entry into a usually sterile body cavity and provides a surface on which microorganisms can colonize. At a finite rate of colonization—the incidence of bacteriuria is 3% to 10% per catheter day—the duration of urinary catheterization becomes the strongest predictor of catheter-associated bacteriuria.7 Even in relatively short-term catheter use of two to 10 days, the pooled cumulative incidence of developing bacteriuria is 26%.
Given the magnitude of these numbers, it should be no surprise that after one month of catheterization, bacteriuria develops in almost all patients. Twenty-four percent of patients with bacteriuria develop symptomatic UTIs with close to 5% suffering bacteremia. Consequently, nosocomial UTIs cause 15% of all hospital-acquired bacteremia.
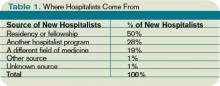
Optimal catheter management: The easiest and most effective means to prevent CAUTI is to limit the use of urinary catheters to clearly identified medical indications (see Table 1, above). However, as simple as this prevention practice may sound, studies have demonstrated that as many as 20% of patients have indwelling catheters initially placed for unjustified or even unknown medical indications.8 Additionally, continued catheter use is inappropriate in one-third to one-half of all catheter days.9 These data confirm misuse and overuse of indwelling urinary catheters in the hospital setting is common.
In 1981, the Centers for Disease Control and Prevention (CDC) recognized the importance of addressing this situation and published a guideline to aid prevention of CAUTIs.10 The CDC urged the limitation of catheter use to a carefully selected patient population. Furthermore, the report strongly stressed the importance of catheter removal as soon as possible and advised against the use of catheters solely for the convenience of healthcare workers.
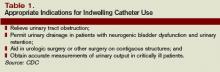
Evidence-based techniques for insertion and catheter care also were outlined in the guideline (see Table 2, p. 31). However, these recommendations have been poorly implemented, likely due to the competing priorities of providers and the difficulty operationalizing the guidelines. Additionally, evidence from the intervening 25 years has not yet been incorporated into the guideline, although a revision currently is underway.
Until that revision is complete, the Joanna Briggs Institute guideline published in 2001 addresses some of the same management techniques and incorporates newer evidence.11 Of note, practices that have been discredited due to contradictory evidence include aggressive meatal cleaning, bladder irrigation, and the application of antimicrobial agents in the drainage bag.12
Strategies to reduce unnecessary catheter days: One of the remediable reasons for catheter misuse lies in the fact physicians often are unaware of the presence of an indwelling catheter in their hospitalized patients.
Saint, et al., showed physicians were unaware of catheterization in 28% of their patients and that attending physicians were less conscious of a patient’s catheter status than residents, interns, or medical students.13 Further, the “forgotten” catheters were more likely to be unnecessary than those remembered by the healthcare team.
This information has prompted the use of various computer-based and multidisciplinary feedback protocols to readdress and re-evaluate the need for continued catheterization in a patient. For example, a study at the VAMC Puget Sound demonstrated that having a computerized order protocol for urinary catheters significantly increased the rate of documentation as well as decreased the duration of catheterization by an average of three days.14
Similar interventions to encourage early catheter removal have included daily reminders from nursing staff, allowing a nurse to discontinue catheter use independent of a physician’s order, and feedback in which nursing staff is educated about the incidence of UTI.15-17 All these relatively simple interventions showed significant improvement in the catheter removal rate and incidence of CAUTIs as well as documented cost savings.
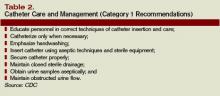
Alternatives to indwelling catheters: In addition to efforts to decrease catheter days, alternatives to the indwelling catheters also should be explored. One such alternative method is intermittent catheterization.
Several studies in postoperative patients with hip fractures have demonstrated that the development of UTI is lower with intermittent catheterization when compared with indwelling catheterization.18 Nevertheless, since the risk of bacteriuria is 1% to 3% per episode of catheterization, after a few weeks the majority of patients will have bacteriuria. However, as the bulk of this bacteriuria often is asymptomatic, intermittent catheterization may still be an improvement. This is particularly true in postoperative patients undergoing rehabilitation and those patients only requiring catheterization for a limited number of days.
More recent studies have evaluated the use of bedside bladder ultrasound in an attempt to determine when intermittent catheterization is needed and thereby limit its use compared with standard timed catheterization. Frederickson, et al., demonstrated that this intervention resulted in significantly fewer catheterizations in surgical patients, thus delaying or avoiding the need for catheterization in 81% of the cases.19 Given this drastic improvement, it is no surprise bladder ultrasound use reduced the rates of UTI.20
External condom catheters present another alternative to indwelling catheter use but the outcomes data is conflicting. While the risk of bacteriuria is approximately 12% per month, this rate becomes increasingly higher with frequent manipulation of the condom catheter. 21,22
Two parallel cohort studies in a VA nursing home showed the incidence of symptomatic UTI to be 2.5 times greater in men with an indwelling catheter than those with a condom catheter.23 On the other hand, a cross-sectional Danish study reported higher rates of UTI with external condom catheters than urethral catheters in hospitalized patients.24 Complications from condom catheters include phimosis and local skin maceration, necessitating meticulous care with the use of these devices. Although the data surrounding external catheterization is somewhat contradictory, this device warrants consideration in incontinent males without urinary tract obstruction.
There are several other alternatives to urethral catheterization (see Table 3, p. 31), many of which have excellent face validity even in the absence of rigorous evidence.
Antimicrobial catheters: The development of antimicrobial urinary catheters, including silver-alloy and nitrofurazone-coated catheters, has been greeted with much excitement, however, the jury is still out about their best use. A 2006 systematic literature review reported that in comparison to standard catheters, antimicrobial catheters can delay or even prevent the development of bacteriuria with short-term usage.25
However, not all antimicrobial catheters are equally effective; assorted studies lack data about clinically relevant endpoints such as prevention of symptomatic UTI, bloodstream infection or death.26, 27 In addition, there are no good trials comparing nitrofurazone to silver-alloy catheters. Therefore, the level of excitement surrounding antimicrobial catheters—particularly silver-alloy catheters—must be tempered by the additional costs incurred by their use.
To date, the cost-effectiveness of antimicrobial catheters has not been demonstrated. Although additional research in this topic is still needed, some experts currently recommend the consideration of silver-alloy catheters in patients at the highest risk for developing serious consequences from UTIs.
Efforts to reduce CAUTI: In response to significant public interest in hospital-acquired infections including CAUTI, the federal government and many state governments are beginning to demand change. In August 2007, the Centers for Medicare and Medicaid Services instituted a mandate making hospitals financially responsible for selected preventable hospital-acquired harms, including CAUTIs.28 In addition, beginning with Pennsylvania in 2006, several states have mandated public reporting of hospital-acquired infections.29
Given the available information about CAUTI prevalence, risks, and preventive techniques, it is surprising the majority of hospitals in the United States have not taken appropriate measures to limit indwelling catheter use. A recent study by Saint, et al., demonstrated the startling fact that only a minority of hospitals monitor the use of urethral catheters in their patients.30
Among study hospitals, there was no widely used technique to prevent CAUTI including evidence-based practices such as daily catheter reminders. The results of this investigation illustrate the urgent need for a national strategy to reduce CAUTI. Until that time, however, hospital-based physicians must take the lead to champion collaborative efforts, to promote evidence-based catheter use.
Back to the Case
As incontinence and fall risk are not medically appropriate indications for a urethral catheter, a Foley catheter should not have been utilized. Alternatives to indwelling catheterization in this patient would include a bedside commode with nursing assistance, a timed voiding program, intermittent catheterization with or without bladder ultrasound, incontinence pads, or a condom catheter.
Attentiveness to the appropriate medical indications for catheter use, familiarity with catheter alternatives, and recognition of the clinical and economic impact of CAUTI may have prevented this patient’s UTI-induced delirium and facilitated his early transfer to SNF. TH
Dr. Wald is a getriatric hospitalist and assistant professor of medicine at the University of Colorado, Denver. Dr. Furfari is a hospital medicine fellow at the University of Colorado Denver.
References
- Beeson PB. The case against the catheter. Am J Med. 1958;24:1-3.
- Saint S. Clinical and economic consequences of nosocomial catheter-related bacteriuria. Am J Infect Control. 2000;28:68-75.
- Sedor J, Mulholland SG. Hospital-acquired UTIs associated with the indwelling catheter. Urol Clin North Am. 1999;26:821-828.
- Foxman B. Epidemiology of UTI: Incidence, morbidity and economic costs. Am J Med. 2002;113(1A):5S-13S.
- Tambyah PA, Knasinski V, Maki D. The direct costs of nosocomial catheter-associated UTI in the era of managed care. Infect Control Hosp Epidemiol. 2002;23:27-31.
- Jarvis, WR. Selected aspects of socioeconomic impact of nosocomial infections. Infect Control Hosp Epidemiol. 1996;17:552-557.
- Warren JW. Catheter-associated urinary tract infections. Infect Dis Clin North Am. 1997;11:609-622.
- Jain P, Parada JP, David A, Smith L. Overuse of the indwelling urinary catheter in hospitalized medical patients. Arch Internal Med. 1995;155:1425-1429.
- Hartstein AI, Garber SB, Ward TT, Jones SR, Morthland VH. Nosocomial urinary tract infection: a prospective evaluation of 108 catheterized patients. Infect Control. 1981;2:380-386.
- Wong E. Guideline for prevention of catheter-associated urinary tract infections. Center for Disease Control and Prevention 1981. Available at: www.cdc.gov/ncidod/dhqp/gl_catheter_assoc.html . Accessed May 8, 2008.
- Joanna Briggs Institute. Management of short term indwelling urethral catheters to prevent urinary tract infections. 2000;4(1):ISSN 1329-1874.
- Burke JP, Garibaldi RA, Britt MR, Jacobson JA, Conti M, Alling DW. Prevention of catheter-associated urinary tract infections. Am J Med. 1981;70:655-658.
- Saint S, Wiese J, Amory JK, et al. Are physicians aware of which of their patients have indwelling urinary catheters? Am J Med. 2000;109:476-480.
- Cornia PB, Amory JK, Fraser S, Saint S, Lipsky BA. Computer-based order entry decreases duration of indwelling urinary catheterization in hospitalized patients. Am J Med. 2003;114:404-406.
- Huang WC, Wann SR, Lin SL, et al. Catheter-associated urinary tract infections in intensive care units can be reduced by prompting physicians to remove unnecessary catheters. Infect Control Hosp Epidemiol. 2004;25(11):974-978.
- Topal J, Conklin S, Camp K, Morris TB, Herbert P. Prevention of nosocomial catheter-associated urinary tract infections through computerized feedback to physicians and a nurse-directed protocol. Am J Med Qual. 2005;20(3):121-126.
- Goetz AM, Kedzuf S, Wagener M, Muder R. Feedback to nursing staff as an intervention to reduce catheter-associated urinary tract infections. Am J Infect Control. 1999;27(5):402-404.
- Johansson I, Athlin E, Frykholm L, Bolinder H, Larsson G. Intermittent versus indwelling catheters for older patients with hip fractures. J Clin Nurs. 2002;11:651-656.
- Frederickson M, Neitzel JJ, Miller EH, Reuter S, Graner T, Heller J. The implementation of bedside bladder ultrasound technology: Effects of patient and cost postoperative outcomes in tertiary care. Orthop Nurs. 2000;19(3):79-87.
- Slappendel R, Weber EWG. Non-invasive measurement of bladder volume as an indication for bladder catheterization after orthopedic surgery and its effect on urinary tract infections. Eur J Anesthesiol. 1999;16:503-506.
- Hirsh D, Fainstein V, Musher DM. Do condom catheter collecting systems cause urinary tract infections? JAMA. 1979;242:340-341.
- Wong ES. Guideline for prevention of catheter-associated urinary tract infections. Am J Infect Control. 1983;11:28-36.
- Saint S, Lipsky BA. Preventing catheter-related bacteriuria. Should We? Can We? How? Arch Internal Med. 1999;159:800-808.
- Zimakoff J, Stickler DJ, Pontoppidan B, Larsen SO. Bladder management and urinary tract infection in Danish hospitals, nursing homes and home care: A national prevalence study. Infect Control Hosp Epidemiol. 1996;17(4):215-221.
- Johnson JR, Kuskowski MA, Wilt TJ. Systematic Review: Antimicrobial urinary catheters to prevent catheter-associated urinary tract infections in hospitalized patients. Ann Internal Med. 2006;144(2):116-126.
- Saint S, Elmore JG, Sullivan SD, Emerson SS, Koepsell TD. The efficacy of silver alloy-coated urinary catheters in preventing urinary tract infections; a meta-analysis. Am J Med. 1998;105(3):236-241.
- Bronahan J, Jull A, Tracy C. Cochrane incontinence group. Types of urethral catheters for management of short-term voiding problems in hospitalized adults. Cochrane Database Syst Rev. 2004;1:CD004013.
- Wald HL, Kramer AM. Nonpayment for harms resulting from medical care. JAMA. 2007;298(23):2782-2784.
- Goldstein J. Hospital infections’ cost tallied. The Philadelphia Inquirer. Nov. 15, 2006.
- Saint S, Kowalski CP, Kaufman SR, et al. Preventing hospital-acquired urinary tract infection in the United States: A national study. Clin Infect Dis. 2008;46(2):243-250.
Case
A 68-year-old male with a history of Alzheimer’s dementia and incontinence presents with failure to thrive. A Foley catheter is placed due to the patient’s incontinence and fall risk. Three days after admission while awaiting placement in a skilled nursing facility (SNF), he develops a urinary tract infection (UTI) complicated by delirium delaying his transfer to the SNF. What could have been done to prevent this complication?
Overview
It has been 50 years since Beeson, et al., recognized the potential harms stemming from urethral catheterization and penned an editorial to the American Journal of Medicine titled “The case against the catheter.”1
Since then, there has been considerable exploration of ways to limit urethral catheterization and ultimately decrease catheter-associated urinary tract infections (CAUTIs). Unfortunately, little progress has been made; indwelling urinary catheters remain ubiquitous in hospitals and CAUTIs remain the most common hospital-acquired infection in the United States.2 Given the emphasis on the quality and costs of healthcare, it is an opportune time to revisit catheter management and use as a way to combat the clinical and economic consequences of CAUTIs.
Clinicians may be lulled into thinking the clinical impact of CAUTI is less than that of other nosocomial infections. However, beyond the obvious patient harm from UTIs, associated bacteremia, and even death, the public health implications of CAUTI cannot be denied. Urinary tract infections constitute 40% of all nosocomial infections; accounting for an estimated 1 million cases annually.3 Further, 80% of all UTIs are associated with indwelling catheter use.
On average, nosocomial UTI necessitates one extra hospital day per patient, or approximately one million excess hospital days per year.4 Pooled cost analysis shows that UTIs consume an additional $400-$1,700 per event, or an estimated $425 million per year in the United States.5,6 Clearly, we cannot wait another 50 years to address this problem.
Review of the Data
Catheter duration as a risk factor for CAUTI: The indwelling catheter creates a portal of entry into a usually sterile body cavity and provides a surface on which microorganisms can colonize. At a finite rate of colonization—the incidence of bacteriuria is 3% to 10% per catheter day—the duration of urinary catheterization becomes the strongest predictor of catheter-associated bacteriuria.7 Even in relatively short-term catheter use of two to 10 days, the pooled cumulative incidence of developing bacteriuria is 26%.
Given the magnitude of these numbers, it should be no surprise that after one month of catheterization, bacteriuria develops in almost all patients. Twenty-four percent of patients with bacteriuria develop symptomatic UTIs with close to 5% suffering bacteremia. Consequently, nosocomial UTIs cause 15% of all hospital-acquired bacteremia.
Optimal catheter management: The easiest and most effective means to prevent CAUTI is to limit the use of urinary catheters to clearly identified medical indications (see Table 1, above). However, as simple as this prevention practice may sound, studies have demonstrated that as many as 20% of patients have indwelling catheters initially placed for unjustified or even unknown medical indications.8 Additionally, continued catheter use is inappropriate in one-third to one-half of all catheter days.9 These data confirm misuse and overuse of indwelling urinary catheters in the hospital setting is common.
In 1981, the Centers for Disease Control and Prevention (CDC) recognized the importance of addressing this situation and published a guideline to aid prevention of CAUTIs.10 The CDC urged the limitation of catheter use to a carefully selected patient population. Furthermore, the report strongly stressed the importance of catheter removal as soon as possible and advised against the use of catheters solely for the convenience of healthcare workers.
Evidence-based techniques for insertion and catheter care also were outlined in the guideline (see Table 2, p. 31). However, these recommendations have been poorly implemented, likely due to the competing priorities of providers and the difficulty operationalizing the guidelines. Additionally, evidence from the intervening 25 years has not yet been incorporated into the guideline, although a revision currently is underway.
Until that revision is complete, the Joanna Briggs Institute guideline published in 2001 addresses some of the same management techniques and incorporates newer evidence.11 Of note, practices that have been discredited due to contradictory evidence include aggressive meatal cleaning, bladder irrigation, and the application of antimicrobial agents in the drainage bag.12
Strategies to reduce unnecessary catheter days: One of the remediable reasons for catheter misuse lies in the fact physicians often are unaware of the presence of an indwelling catheter in their hospitalized patients.
Saint, et al., showed physicians were unaware of catheterization in 28% of their patients and that attending physicians were less conscious of a patient’s catheter status than residents, interns, or medical students.13 Further, the “forgotten” catheters were more likely to be unnecessary than those remembered by the healthcare team.
This information has prompted the use of various computer-based and multidisciplinary feedback protocols to readdress and re-evaluate the need for continued catheterization in a patient. For example, a study at the VAMC Puget Sound demonstrated that having a computerized order protocol for urinary catheters significantly increased the rate of documentation as well as decreased the duration of catheterization by an average of three days.14
Similar interventions to encourage early catheter removal have included daily reminders from nursing staff, allowing a nurse to discontinue catheter use independent of a physician’s order, and feedback in which nursing staff is educated about the incidence of UTI.15-17 All these relatively simple interventions showed significant improvement in the catheter removal rate and incidence of CAUTIs as well as documented cost savings.
Alternatives to indwelling catheters: In addition to efforts to decrease catheter days, alternatives to the indwelling catheters also should be explored. One such alternative method is intermittent catheterization.
Several studies in postoperative patients with hip fractures have demonstrated that the development of UTI is lower with intermittent catheterization when compared with indwelling catheterization.18 Nevertheless, since the risk of bacteriuria is 1% to 3% per episode of catheterization, after a few weeks the majority of patients will have bacteriuria. However, as the bulk of this bacteriuria often is asymptomatic, intermittent catheterization may still be an improvement. This is particularly true in postoperative patients undergoing rehabilitation and those patients only requiring catheterization for a limited number of days.
More recent studies have evaluated the use of bedside bladder ultrasound in an attempt to determine when intermittent catheterization is needed and thereby limit its use compared with standard timed catheterization. Frederickson, et al., demonstrated that this intervention resulted in significantly fewer catheterizations in surgical patients, thus delaying or avoiding the need for catheterization in 81% of the cases.19 Given this drastic improvement, it is no surprise bladder ultrasound use reduced the rates of UTI.20
External condom catheters present another alternative to indwelling catheter use but the outcomes data is conflicting. While the risk of bacteriuria is approximately 12% per month, this rate becomes increasingly higher with frequent manipulation of the condom catheter. 21,22
Two parallel cohort studies in a VA nursing home showed the incidence of symptomatic UTI to be 2.5 times greater in men with an indwelling catheter than those with a condom catheter.23 On the other hand, a cross-sectional Danish study reported higher rates of UTI with external condom catheters than urethral catheters in hospitalized patients.24 Complications from condom catheters include phimosis and local skin maceration, necessitating meticulous care with the use of these devices. Although the data surrounding external catheterization is somewhat contradictory, this device warrants consideration in incontinent males without urinary tract obstruction.
There are several other alternatives to urethral catheterization (see Table 3, p. 31), many of which have excellent face validity even in the absence of rigorous evidence.
Antimicrobial catheters: The development of antimicrobial urinary catheters, including silver-alloy and nitrofurazone-coated catheters, has been greeted with much excitement, however, the jury is still out about their best use. A 2006 systematic literature review reported that in comparison to standard catheters, antimicrobial catheters can delay or even prevent the development of bacteriuria with short-term usage.25
However, not all antimicrobial catheters are equally effective; assorted studies lack data about clinically relevant endpoints such as prevention of symptomatic UTI, bloodstream infection or death.26, 27 In addition, there are no good trials comparing nitrofurazone to silver-alloy catheters. Therefore, the level of excitement surrounding antimicrobial catheters—particularly silver-alloy catheters—must be tempered by the additional costs incurred by their use.
To date, the cost-effectiveness of antimicrobial catheters has not been demonstrated. Although additional research in this topic is still needed, some experts currently recommend the consideration of silver-alloy catheters in patients at the highest risk for developing serious consequences from UTIs.
Efforts to reduce CAUTI: In response to significant public interest in hospital-acquired infections including CAUTI, the federal government and many state governments are beginning to demand change. In August 2007, the Centers for Medicare and Medicaid Services instituted a mandate making hospitals financially responsible for selected preventable hospital-acquired harms, including CAUTIs.28 In addition, beginning with Pennsylvania in 2006, several states have mandated public reporting of hospital-acquired infections.29
Given the available information about CAUTI prevalence, risks, and preventive techniques, it is surprising the majority of hospitals in the United States have not taken appropriate measures to limit indwelling catheter use. A recent study by Saint, et al., demonstrated the startling fact that only a minority of hospitals monitor the use of urethral catheters in their patients.30
Among study hospitals, there was no widely used technique to prevent CAUTI including evidence-based practices such as daily catheter reminders. The results of this investigation illustrate the urgent need for a national strategy to reduce CAUTI. Until that time, however, hospital-based physicians must take the lead to champion collaborative efforts, to promote evidence-based catheter use.
Back to the Case
As incontinence and fall risk are not medically appropriate indications for a urethral catheter, a Foley catheter should not have been utilized. Alternatives to indwelling catheterization in this patient would include a bedside commode with nursing assistance, a timed voiding program, intermittent catheterization with or without bladder ultrasound, incontinence pads, or a condom catheter.
Attentiveness to the appropriate medical indications for catheter use, familiarity with catheter alternatives, and recognition of the clinical and economic impact of CAUTI may have prevented this patient’s UTI-induced delirium and facilitated his early transfer to SNF. TH
Dr. Wald is a getriatric hospitalist and assistant professor of medicine at the University of Colorado, Denver. Dr. Furfari is a hospital medicine fellow at the University of Colorado Denver.
References
- Beeson PB. The case against the catheter. Am J Med. 1958;24:1-3.
- Saint S. Clinical and economic consequences of nosocomial catheter-related bacteriuria. Am J Infect Control. 2000;28:68-75.
- Sedor J, Mulholland SG. Hospital-acquired UTIs associated with the indwelling catheter. Urol Clin North Am. 1999;26:821-828.
- Foxman B. Epidemiology of UTI: Incidence, morbidity and economic costs. Am J Med. 2002;113(1A):5S-13S.
- Tambyah PA, Knasinski V, Maki D. The direct costs of nosocomial catheter-associated UTI in the era of managed care. Infect Control Hosp Epidemiol. 2002;23:27-31.
- Jarvis, WR. Selected aspects of socioeconomic impact of nosocomial infections. Infect Control Hosp Epidemiol. 1996;17:552-557.
- Warren JW. Catheter-associated urinary tract infections. Infect Dis Clin North Am. 1997;11:609-622.
- Jain P, Parada JP, David A, Smith L. Overuse of the indwelling urinary catheter in hospitalized medical patients. Arch Internal Med. 1995;155:1425-1429.
- Hartstein AI, Garber SB, Ward TT, Jones SR, Morthland VH. Nosocomial urinary tract infection: a prospective evaluation of 108 catheterized patients. Infect Control. 1981;2:380-386.
- Wong E. Guideline for prevention of catheter-associated urinary tract infections. Center for Disease Control and Prevention 1981. Available at: www.cdc.gov/ncidod/dhqp/gl_catheter_assoc.html . Accessed May 8, 2008.
- Joanna Briggs Institute. Management of short term indwelling urethral catheters to prevent urinary tract infections. 2000;4(1):ISSN 1329-1874.
- Burke JP, Garibaldi RA, Britt MR, Jacobson JA, Conti M, Alling DW. Prevention of catheter-associated urinary tract infections. Am J Med. 1981;70:655-658.
- Saint S, Wiese J, Amory JK, et al. Are physicians aware of which of their patients have indwelling urinary catheters? Am J Med. 2000;109:476-480.
- Cornia PB, Amory JK, Fraser S, Saint S, Lipsky BA. Computer-based order entry decreases duration of indwelling urinary catheterization in hospitalized patients. Am J Med. 2003;114:404-406.
- Huang WC, Wann SR, Lin SL, et al. Catheter-associated urinary tract infections in intensive care units can be reduced by prompting physicians to remove unnecessary catheters. Infect Control Hosp Epidemiol. 2004;25(11):974-978.
- Topal J, Conklin S, Camp K, Morris TB, Herbert P. Prevention of nosocomial catheter-associated urinary tract infections through computerized feedback to physicians and a nurse-directed protocol. Am J Med Qual. 2005;20(3):121-126.
- Goetz AM, Kedzuf S, Wagener M, Muder R. Feedback to nursing staff as an intervention to reduce catheter-associated urinary tract infections. Am J Infect Control. 1999;27(5):402-404.
- Johansson I, Athlin E, Frykholm L, Bolinder H, Larsson G. Intermittent versus indwelling catheters for older patients with hip fractures. J Clin Nurs. 2002;11:651-656.
- Frederickson M, Neitzel JJ, Miller EH, Reuter S, Graner T, Heller J. The implementation of bedside bladder ultrasound technology: Effects of patient and cost postoperative outcomes in tertiary care. Orthop Nurs. 2000;19(3):79-87.
- Slappendel R, Weber EWG. Non-invasive measurement of bladder volume as an indication for bladder catheterization after orthopedic surgery and its effect on urinary tract infections. Eur J Anesthesiol. 1999;16:503-506.
- Hirsh D, Fainstein V, Musher DM. Do condom catheter collecting systems cause urinary tract infections? JAMA. 1979;242:340-341.
- Wong ES. Guideline for prevention of catheter-associated urinary tract infections. Am J Infect Control. 1983;11:28-36.
- Saint S, Lipsky BA. Preventing catheter-related bacteriuria. Should We? Can We? How? Arch Internal Med. 1999;159:800-808.
- Zimakoff J, Stickler DJ, Pontoppidan B, Larsen SO. Bladder management and urinary tract infection in Danish hospitals, nursing homes and home care: A national prevalence study. Infect Control Hosp Epidemiol. 1996;17(4):215-221.
- Johnson JR, Kuskowski MA, Wilt TJ. Systematic Review: Antimicrobial urinary catheters to prevent catheter-associated urinary tract infections in hospitalized patients. Ann Internal Med. 2006;144(2):116-126.
- Saint S, Elmore JG, Sullivan SD, Emerson SS, Koepsell TD. The efficacy of silver alloy-coated urinary catheters in preventing urinary tract infections; a meta-analysis. Am J Med. 1998;105(3):236-241.
- Bronahan J, Jull A, Tracy C. Cochrane incontinence group. Types of urethral catheters for management of short-term voiding problems in hospitalized adults. Cochrane Database Syst Rev. 2004;1:CD004013.
- Wald HL, Kramer AM. Nonpayment for harms resulting from medical care. JAMA. 2007;298(23):2782-2784.
- Goldstein J. Hospital infections’ cost tallied. The Philadelphia Inquirer. Nov. 15, 2006.
- Saint S, Kowalski CP, Kaufman SR, et al. Preventing hospital-acquired urinary tract infection in the United States: A national study. Clin Infect Dis. 2008;46(2):243-250.
Case
A 68-year-old male with a history of Alzheimer’s dementia and incontinence presents with failure to thrive. A Foley catheter is placed due to the patient’s incontinence and fall risk. Three days after admission while awaiting placement in a skilled nursing facility (SNF), he develops a urinary tract infection (UTI) complicated by delirium delaying his transfer to the SNF. What could have been done to prevent this complication?
Overview
It has been 50 years since Beeson, et al., recognized the potential harms stemming from urethral catheterization and penned an editorial to the American Journal of Medicine titled “The case against the catheter.”1
Since then, there has been considerable exploration of ways to limit urethral catheterization and ultimately decrease catheter-associated urinary tract infections (CAUTIs). Unfortunately, little progress has been made; indwelling urinary catheters remain ubiquitous in hospitals and CAUTIs remain the most common hospital-acquired infection in the United States.2 Given the emphasis on the quality and costs of healthcare, it is an opportune time to revisit catheter management and use as a way to combat the clinical and economic consequences of CAUTIs.
Clinicians may be lulled into thinking the clinical impact of CAUTI is less than that of other nosocomial infections. However, beyond the obvious patient harm from UTIs, associated bacteremia, and even death, the public health implications of CAUTI cannot be denied. Urinary tract infections constitute 40% of all nosocomial infections; accounting for an estimated 1 million cases annually.3 Further, 80% of all UTIs are associated with indwelling catheter use.
On average, nosocomial UTI necessitates one extra hospital day per patient, or approximately one million excess hospital days per year.4 Pooled cost analysis shows that UTIs consume an additional $400-$1,700 per event, or an estimated $425 million per year in the United States.5,6 Clearly, we cannot wait another 50 years to address this problem.
Review of the Data
Catheter duration as a risk factor for CAUTI: The indwelling catheter creates a portal of entry into a usually sterile body cavity and provides a surface on which microorganisms can colonize. At a finite rate of colonization—the incidence of bacteriuria is 3% to 10% per catheter day—the duration of urinary catheterization becomes the strongest predictor of catheter-associated bacteriuria.7 Even in relatively short-term catheter use of two to 10 days, the pooled cumulative incidence of developing bacteriuria is 26%.
Given the magnitude of these numbers, it should be no surprise that after one month of catheterization, bacteriuria develops in almost all patients. Twenty-four percent of patients with bacteriuria develop symptomatic UTIs with close to 5% suffering bacteremia. Consequently, nosocomial UTIs cause 15% of all hospital-acquired bacteremia.
Optimal catheter management: The easiest and most effective means to prevent CAUTI is to limit the use of urinary catheters to clearly identified medical indications (see Table 1, above). However, as simple as this prevention practice may sound, studies have demonstrated that as many as 20% of patients have indwelling catheters initially placed for unjustified or even unknown medical indications.8 Additionally, continued catheter use is inappropriate in one-third to one-half of all catheter days.9 These data confirm misuse and overuse of indwelling urinary catheters in the hospital setting is common.
In 1981, the Centers for Disease Control and Prevention (CDC) recognized the importance of addressing this situation and published a guideline to aid prevention of CAUTIs.10 The CDC urged the limitation of catheter use to a carefully selected patient population. Furthermore, the report strongly stressed the importance of catheter removal as soon as possible and advised against the use of catheters solely for the convenience of healthcare workers.
Evidence-based techniques for insertion and catheter care also were outlined in the guideline (see Table 2, p. 31). However, these recommendations have been poorly implemented, likely due to the competing priorities of providers and the difficulty operationalizing the guidelines. Additionally, evidence from the intervening 25 years has not yet been incorporated into the guideline, although a revision currently is underway.
Until that revision is complete, the Joanna Briggs Institute guideline published in 2001 addresses some of the same management techniques and incorporates newer evidence.11 Of note, practices that have been discredited due to contradictory evidence include aggressive meatal cleaning, bladder irrigation, and the application of antimicrobial agents in the drainage bag.12
Strategies to reduce unnecessary catheter days: One of the remediable reasons for catheter misuse lies in the fact physicians often are unaware of the presence of an indwelling catheter in their hospitalized patients.
Saint, et al., showed physicians were unaware of catheterization in 28% of their patients and that attending physicians were less conscious of a patient’s catheter status than residents, interns, or medical students.13 Further, the “forgotten” catheters were more likely to be unnecessary than those remembered by the healthcare team.
This information has prompted the use of various computer-based and multidisciplinary feedback protocols to readdress and re-evaluate the need for continued catheterization in a patient. For example, a study at the VAMC Puget Sound demonstrated that having a computerized order protocol for urinary catheters significantly increased the rate of documentation as well as decreased the duration of catheterization by an average of three days.14
Similar interventions to encourage early catheter removal have included daily reminders from nursing staff, allowing a nurse to discontinue catheter use independent of a physician’s order, and feedback in which nursing staff is educated about the incidence of UTI.15-17 All these relatively simple interventions showed significant improvement in the catheter removal rate and incidence of CAUTIs as well as documented cost savings.
Alternatives to indwelling catheters: In addition to efforts to decrease catheter days, alternatives to the indwelling catheters also should be explored. One such alternative method is intermittent catheterization.
Several studies in postoperative patients with hip fractures have demonstrated that the development of UTI is lower with intermittent catheterization when compared with indwelling catheterization.18 Nevertheless, since the risk of bacteriuria is 1% to 3% per episode of catheterization, after a few weeks the majority of patients will have bacteriuria. However, as the bulk of this bacteriuria often is asymptomatic, intermittent catheterization may still be an improvement. This is particularly true in postoperative patients undergoing rehabilitation and those patients only requiring catheterization for a limited number of days.
More recent studies have evaluated the use of bedside bladder ultrasound in an attempt to determine when intermittent catheterization is needed and thereby limit its use compared with standard timed catheterization. Frederickson, et al., demonstrated that this intervention resulted in significantly fewer catheterizations in surgical patients, thus delaying or avoiding the need for catheterization in 81% of the cases.19 Given this drastic improvement, it is no surprise bladder ultrasound use reduced the rates of UTI.20
External condom catheters present another alternative to indwelling catheter use but the outcomes data is conflicting. While the risk of bacteriuria is approximately 12% per month, this rate becomes increasingly higher with frequent manipulation of the condom catheter. 21,22
Two parallel cohort studies in a VA nursing home showed the incidence of symptomatic UTI to be 2.5 times greater in men with an indwelling catheter than those with a condom catheter.23 On the other hand, a cross-sectional Danish study reported higher rates of UTI with external condom catheters than urethral catheters in hospitalized patients.24 Complications from condom catheters include phimosis and local skin maceration, necessitating meticulous care with the use of these devices. Although the data surrounding external catheterization is somewhat contradictory, this device warrants consideration in incontinent males without urinary tract obstruction.
There are several other alternatives to urethral catheterization (see Table 3, p. 31), many of which have excellent face validity even in the absence of rigorous evidence.
Antimicrobial catheters: The development of antimicrobial urinary catheters, including silver-alloy and nitrofurazone-coated catheters, has been greeted with much excitement, however, the jury is still out about their best use. A 2006 systematic literature review reported that in comparison to standard catheters, antimicrobial catheters can delay or even prevent the development of bacteriuria with short-term usage.25
However, not all antimicrobial catheters are equally effective; assorted studies lack data about clinically relevant endpoints such as prevention of symptomatic UTI, bloodstream infection or death.26, 27 In addition, there are no good trials comparing nitrofurazone to silver-alloy catheters. Therefore, the level of excitement surrounding antimicrobial catheters—particularly silver-alloy catheters—must be tempered by the additional costs incurred by their use.
To date, the cost-effectiveness of antimicrobial catheters has not been demonstrated. Although additional research in this topic is still needed, some experts currently recommend the consideration of silver-alloy catheters in patients at the highest risk for developing serious consequences from UTIs.
Efforts to reduce CAUTI: In response to significant public interest in hospital-acquired infections including CAUTI, the federal government and many state governments are beginning to demand change. In August 2007, the Centers for Medicare and Medicaid Services instituted a mandate making hospitals financially responsible for selected preventable hospital-acquired harms, including CAUTIs.28 In addition, beginning with Pennsylvania in 2006, several states have mandated public reporting of hospital-acquired infections.29
Given the available information about CAUTI prevalence, risks, and preventive techniques, it is surprising the majority of hospitals in the United States have not taken appropriate measures to limit indwelling catheter use. A recent study by Saint, et al., demonstrated the startling fact that only a minority of hospitals monitor the use of urethral catheters in their patients.30
Among study hospitals, there was no widely used technique to prevent CAUTI including evidence-based practices such as daily catheter reminders. The results of this investigation illustrate the urgent need for a national strategy to reduce CAUTI. Until that time, however, hospital-based physicians must take the lead to champion collaborative efforts, to promote evidence-based catheter use.
Back to the Case
As incontinence and fall risk are not medically appropriate indications for a urethral catheter, a Foley catheter should not have been utilized. Alternatives to indwelling catheterization in this patient would include a bedside commode with nursing assistance, a timed voiding program, intermittent catheterization with or without bladder ultrasound, incontinence pads, or a condom catheter.
Attentiveness to the appropriate medical indications for catheter use, familiarity with catheter alternatives, and recognition of the clinical and economic impact of CAUTI may have prevented this patient’s UTI-induced delirium and facilitated his early transfer to SNF. TH
Dr. Wald is a getriatric hospitalist and assistant professor of medicine at the University of Colorado, Denver. Dr. Furfari is a hospital medicine fellow at the University of Colorado Denver.
References
- Beeson PB. The case against the catheter. Am J Med. 1958;24:1-3.
- Saint S. Clinical and economic consequences of nosocomial catheter-related bacteriuria. Am J Infect Control. 2000;28:68-75.
- Sedor J, Mulholland SG. Hospital-acquired UTIs associated with the indwelling catheter. Urol Clin North Am. 1999;26:821-828.
- Foxman B. Epidemiology of UTI: Incidence, morbidity and economic costs. Am J Med. 2002;113(1A):5S-13S.
- Tambyah PA, Knasinski V, Maki D. The direct costs of nosocomial catheter-associated UTI in the era of managed care. Infect Control Hosp Epidemiol. 2002;23:27-31.
- Jarvis, WR. Selected aspects of socioeconomic impact of nosocomial infections. Infect Control Hosp Epidemiol. 1996;17:552-557.
- Warren JW. Catheter-associated urinary tract infections. Infect Dis Clin North Am. 1997;11:609-622.
- Jain P, Parada JP, David A, Smith L. Overuse of the indwelling urinary catheter in hospitalized medical patients. Arch Internal Med. 1995;155:1425-1429.
- Hartstein AI, Garber SB, Ward TT, Jones SR, Morthland VH. Nosocomial urinary tract infection: a prospective evaluation of 108 catheterized patients. Infect Control. 1981;2:380-386.
- Wong E. Guideline for prevention of catheter-associated urinary tract infections. Center for Disease Control and Prevention 1981. Available at: www.cdc.gov/ncidod/dhqp/gl_catheter_assoc.html . Accessed May 8, 2008.
- Joanna Briggs Institute. Management of short term indwelling urethral catheters to prevent urinary tract infections. 2000;4(1):ISSN 1329-1874.
- Burke JP, Garibaldi RA, Britt MR, Jacobson JA, Conti M, Alling DW. Prevention of catheter-associated urinary tract infections. Am J Med. 1981;70:655-658.
- Saint S, Wiese J, Amory JK, et al. Are physicians aware of which of their patients have indwelling urinary catheters? Am J Med. 2000;109:476-480.
- Cornia PB, Amory JK, Fraser S, Saint S, Lipsky BA. Computer-based order entry decreases duration of indwelling urinary catheterization in hospitalized patients. Am J Med. 2003;114:404-406.
- Huang WC, Wann SR, Lin SL, et al. Catheter-associated urinary tract infections in intensive care units can be reduced by prompting physicians to remove unnecessary catheters. Infect Control Hosp Epidemiol. 2004;25(11):974-978.
- Topal J, Conklin S, Camp K, Morris TB, Herbert P. Prevention of nosocomial catheter-associated urinary tract infections through computerized feedback to physicians and a nurse-directed protocol. Am J Med Qual. 2005;20(3):121-126.
- Goetz AM, Kedzuf S, Wagener M, Muder R. Feedback to nursing staff as an intervention to reduce catheter-associated urinary tract infections. Am J Infect Control. 1999;27(5):402-404.
- Johansson I, Athlin E, Frykholm L, Bolinder H, Larsson G. Intermittent versus indwelling catheters for older patients with hip fractures. J Clin Nurs. 2002;11:651-656.
- Frederickson M, Neitzel JJ, Miller EH, Reuter S, Graner T, Heller J. The implementation of bedside bladder ultrasound technology: Effects of patient and cost postoperative outcomes in tertiary care. Orthop Nurs. 2000;19(3):79-87.
- Slappendel R, Weber EWG. Non-invasive measurement of bladder volume as an indication for bladder catheterization after orthopedic surgery and its effect on urinary tract infections. Eur J Anesthesiol. 1999;16:503-506.
- Hirsh D, Fainstein V, Musher DM. Do condom catheter collecting systems cause urinary tract infections? JAMA. 1979;242:340-341.
- Wong ES. Guideline for prevention of catheter-associated urinary tract infections. Am J Infect Control. 1983;11:28-36.
- Saint S, Lipsky BA. Preventing catheter-related bacteriuria. Should We? Can We? How? Arch Internal Med. 1999;159:800-808.
- Zimakoff J, Stickler DJ, Pontoppidan B, Larsen SO. Bladder management and urinary tract infection in Danish hospitals, nursing homes and home care: A national prevalence study. Infect Control Hosp Epidemiol. 1996;17(4):215-221.
- Johnson JR, Kuskowski MA, Wilt TJ. Systematic Review: Antimicrobial urinary catheters to prevent catheter-associated urinary tract infections in hospitalized patients. Ann Internal Med. 2006;144(2):116-126.
- Saint S, Elmore JG, Sullivan SD, Emerson SS, Koepsell TD. The efficacy of silver alloy-coated urinary catheters in preventing urinary tract infections; a meta-analysis. Am J Med. 1998;105(3):236-241.
- Bronahan J, Jull A, Tracy C. Cochrane incontinence group. Types of urethral catheters for management of short-term voiding problems in hospitalized adults. Cochrane Database Syst Rev. 2004;1:CD004013.
- Wald HL, Kramer AM. Nonpayment for harms resulting from medical care. JAMA. 2007;298(23):2782-2784.
- Goldstein J. Hospital infections’ cost tallied. The Philadelphia Inquirer. Nov. 15, 2006.
- Saint S, Kowalski CP, Kaufman SR, et al. Preventing hospital-acquired urinary tract infection in the United States: A national study. Clin Infect Dis. 2008;46(2):243-250.
Bill by Time Spent on Case
In my recent columns, I addressed documentation guidelines with respect to the three key components: history, exam, and medical decision-making. However, time is considered the fourth key component.
Time-based billing places significant emphasis on the duration of the hospitalist-patient encounter more so than the detail or quality of the documentation. This month, I’ll focus on the guidelines for reporting inpatient hospital services based on time.
Counseling, Coordination
Hospitalists try to make their rounds as efficient as possible while still upholding a high standard of care. It is not unusual for a patient encounter to vary from the norm of updating the history, performing the necessary exam, and implementing the plan.
In fact, hospitalists often counsel patients with newly diagnosed conditions or when treatment options seem extensive and complicated. Based on these circumstances, physicians can document only a brief history and exam or none at all, since the bulk of the encounter focuses on medical decision-making, counseling, and coordination of care. Despite the minimal documentation compared with other physician services, it still is possible to report something more than the lowest service level (e.g., subsequent hospital care, 99231).
To use time as the determining factor for the visit level, more than 50% of the total visit time must involve counseling/coordination of care. The total visit time encompasses both the face-to-face time spent with the patient at the bedside and the additional time spent on the unit/floor reviewing data, obtaining relevant patient information, and discussing the case with other involved healthcare providers. Physicians providing care in academic settings cannot contribute teaching time toward the total visit time. Further, only the attending physician’s time counts.
Documentation
Hospitalists must document events during the patient encounter. There may be little or no history and an exam and counseling may dominate the entire visit.
Physicians must document both the counseling/coordination of care time and total visit time. The format may vary: “Total visit time = 25 minutes; more than 50% spent counseling/coordinating care,” or “20 of 25 minutes spent counseling/coordinating care.” Any given payer may prefer one documentation style over another. It always is best to query payers and review their documentation standards to determine the local preference.
In addition to the time, physicians must document the medical decision-making and details of the counseling/coordination of care. For example, patients with newly diagnosed diabetes need to be educated about their condition, lifestyle, and medication requirements. Physicians should include information regarding these factors in their progress notes as necessary.
Family Discussions
As noted in my previous article on critical care services (March 2008, p. 18), family discussions can contribute toward counseling/coordination of care time when:
- The patient is unable or clinically incompetent to participate in discussions;
- Time is spent on the unit/floor with family members or surrogate decision makers obtaining a medical history, reviewing the patient’s condition or prognosis, or discussing treatment or limitation(s) of treatment; or
- The conversation bears directly on the management of the patient.
Prolonged Care
A physician makes his rounds in the morning. He cares for a 72-year-old female with diabetes, end-stage renal disease, and hypertension. In the afternoon, he returns to find the family waiting with questions. He spends an additional 30 minutes speaking at the bedside with the patient and family. The additional afternoon effort may be captured as prolonged care if both services are documented appropriately.
For inpatient services, CPT defines code 99356 as the first hour of prolonged physician services requiring face-to-face patient contact beyond the usual services (reportable after the initial 30 minutes). Code 99357 is used for each additional 30 minutes of prolonged care beyond the first hour (reportable after the first 15 minutes of each additional segment). Both codes are considered add-on codes and cannot be reported alone on a claim form; a primary code must be reported. Code 99357 must be used with 99356, and 99356 must be reported with one of the following inpatient service [primary] codes: 99221-99223, 99231-99233, or 99251-99255.
Prolonged care employs the concept of threshold time. This means total face-to-face physician visit time must exceed the time requirements associated with the primary codes by 30 minutes (e.g., 99232 plus 99356 = 25 minutes plus 30 minutes = 55 total face-to-face attending visit minutes). Accordingly, the physician must document the total face-to-face time spent during each portion of care in two separate notes or in one cumulative note. Be aware that this varies from the standard reporting of counseling and/or coordination of care time in that the physician must meet the threshold face-to-face-time requirements (see Table 1, left), making prolonged care services inefficient. When two providers from the same group practice split the threshold time (e.g., physician A provided morning rounds, and physician B spoke with the family in the afternoon), only one physician can report the cumulative service. To reiterate, 99356 must be reported on the same invoice as the primary visit code (e.g., 99232). Be sure once again to query payers, because most non-Medicare insurers do not recognize these codes. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
In my recent columns, I addressed documentation guidelines with respect to the three key components: history, exam, and medical decision-making. However, time is considered the fourth key component.
Time-based billing places significant emphasis on the duration of the hospitalist-patient encounter more so than the detail or quality of the documentation. This month, I’ll focus on the guidelines for reporting inpatient hospital services based on time.
Counseling, Coordination
Hospitalists try to make their rounds as efficient as possible while still upholding a high standard of care. It is not unusual for a patient encounter to vary from the norm of updating the history, performing the necessary exam, and implementing the plan.
In fact, hospitalists often counsel patients with newly diagnosed conditions or when treatment options seem extensive and complicated. Based on these circumstances, physicians can document only a brief history and exam or none at all, since the bulk of the encounter focuses on medical decision-making, counseling, and coordination of care. Despite the minimal documentation compared with other physician services, it still is possible to report something more than the lowest service level (e.g., subsequent hospital care, 99231).
To use time as the determining factor for the visit level, more than 50% of the total visit time must involve counseling/coordination of care. The total visit time encompasses both the face-to-face time spent with the patient at the bedside and the additional time spent on the unit/floor reviewing data, obtaining relevant patient information, and discussing the case with other involved healthcare providers. Physicians providing care in academic settings cannot contribute teaching time toward the total visit time. Further, only the attending physician’s time counts.
Documentation
Hospitalists must document events during the patient encounter. There may be little or no history and an exam and counseling may dominate the entire visit.
Physicians must document both the counseling/coordination of care time and total visit time. The format may vary: “Total visit time = 25 minutes; more than 50% spent counseling/coordinating care,” or “20 of 25 minutes spent counseling/coordinating care.” Any given payer may prefer one documentation style over another. It always is best to query payers and review their documentation standards to determine the local preference.
In addition to the time, physicians must document the medical decision-making and details of the counseling/coordination of care. For example, patients with newly diagnosed diabetes need to be educated about their condition, lifestyle, and medication requirements. Physicians should include information regarding these factors in their progress notes as necessary.
Family Discussions
As noted in my previous article on critical care services (March 2008, p. 18), family discussions can contribute toward counseling/coordination of care time when:
- The patient is unable or clinically incompetent to participate in discussions;
- Time is spent on the unit/floor with family members or surrogate decision makers obtaining a medical history, reviewing the patient’s condition or prognosis, or discussing treatment or limitation(s) of treatment; or
- The conversation bears directly on the management of the patient.
Prolonged Care
A physician makes his rounds in the morning. He cares for a 72-year-old female with diabetes, end-stage renal disease, and hypertension. In the afternoon, he returns to find the family waiting with questions. He spends an additional 30 minutes speaking at the bedside with the patient and family. The additional afternoon effort may be captured as prolonged care if both services are documented appropriately.
For inpatient services, CPT defines code 99356 as the first hour of prolonged physician services requiring face-to-face patient contact beyond the usual services (reportable after the initial 30 minutes). Code 99357 is used for each additional 30 minutes of prolonged care beyond the first hour (reportable after the first 15 minutes of each additional segment). Both codes are considered add-on codes and cannot be reported alone on a claim form; a primary code must be reported. Code 99357 must be used with 99356, and 99356 must be reported with one of the following inpatient service [primary] codes: 99221-99223, 99231-99233, or 99251-99255.
Prolonged care employs the concept of threshold time. This means total face-to-face physician visit time must exceed the time requirements associated with the primary codes by 30 minutes (e.g., 99232 plus 99356 = 25 minutes plus 30 minutes = 55 total face-to-face attending visit minutes). Accordingly, the physician must document the total face-to-face time spent during each portion of care in two separate notes or in one cumulative note. Be aware that this varies from the standard reporting of counseling and/or coordination of care time in that the physician must meet the threshold face-to-face-time requirements (see Table 1, left), making prolonged care services inefficient. When two providers from the same group practice split the threshold time (e.g., physician A provided morning rounds, and physician B spoke with the family in the afternoon), only one physician can report the cumulative service. To reiterate, 99356 must be reported on the same invoice as the primary visit code (e.g., 99232). Be sure once again to query payers, because most non-Medicare insurers do not recognize these codes. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
In my recent columns, I addressed documentation guidelines with respect to the three key components: history, exam, and medical decision-making. However, time is considered the fourth key component.
Time-based billing places significant emphasis on the duration of the hospitalist-patient encounter more so than the detail or quality of the documentation. This month, I’ll focus on the guidelines for reporting inpatient hospital services based on time.
Counseling, Coordination
Hospitalists try to make their rounds as efficient as possible while still upholding a high standard of care. It is not unusual for a patient encounter to vary from the norm of updating the history, performing the necessary exam, and implementing the plan.
In fact, hospitalists often counsel patients with newly diagnosed conditions or when treatment options seem extensive and complicated. Based on these circumstances, physicians can document only a brief history and exam or none at all, since the bulk of the encounter focuses on medical decision-making, counseling, and coordination of care. Despite the minimal documentation compared with other physician services, it still is possible to report something more than the lowest service level (e.g., subsequent hospital care, 99231).
To use time as the determining factor for the visit level, more than 50% of the total visit time must involve counseling/coordination of care. The total visit time encompasses both the face-to-face time spent with the patient at the bedside and the additional time spent on the unit/floor reviewing data, obtaining relevant patient information, and discussing the case with other involved healthcare providers. Physicians providing care in academic settings cannot contribute teaching time toward the total visit time. Further, only the attending physician’s time counts.
Documentation
Hospitalists must document events during the patient encounter. There may be little or no history and an exam and counseling may dominate the entire visit.
Physicians must document both the counseling/coordination of care time and total visit time. The format may vary: “Total visit time = 25 minutes; more than 50% spent counseling/coordinating care,” or “20 of 25 minutes spent counseling/coordinating care.” Any given payer may prefer one documentation style over another. It always is best to query payers and review their documentation standards to determine the local preference.
In addition to the time, physicians must document the medical decision-making and details of the counseling/coordination of care. For example, patients with newly diagnosed diabetes need to be educated about their condition, lifestyle, and medication requirements. Physicians should include information regarding these factors in their progress notes as necessary.
Family Discussions
As noted in my previous article on critical care services (March 2008, p. 18), family discussions can contribute toward counseling/coordination of care time when:
- The patient is unable or clinically incompetent to participate in discussions;
- Time is spent on the unit/floor with family members or surrogate decision makers obtaining a medical history, reviewing the patient’s condition or prognosis, or discussing treatment or limitation(s) of treatment; or
- The conversation bears directly on the management of the patient.
Prolonged Care
A physician makes his rounds in the morning. He cares for a 72-year-old female with diabetes, end-stage renal disease, and hypertension. In the afternoon, he returns to find the family waiting with questions. He spends an additional 30 minutes speaking at the bedside with the patient and family. The additional afternoon effort may be captured as prolonged care if both services are documented appropriately.
For inpatient services, CPT defines code 99356 as the first hour of prolonged physician services requiring face-to-face patient contact beyond the usual services (reportable after the initial 30 minutes). Code 99357 is used for each additional 30 minutes of prolonged care beyond the first hour (reportable after the first 15 minutes of each additional segment). Both codes are considered add-on codes and cannot be reported alone on a claim form; a primary code must be reported. Code 99357 must be used with 99356, and 99356 must be reported with one of the following inpatient service [primary] codes: 99221-99223, 99231-99233, or 99251-99255.
Prolonged care employs the concept of threshold time. This means total face-to-face physician visit time must exceed the time requirements associated with the primary codes by 30 minutes (e.g., 99232 plus 99356 = 25 minutes plus 30 minutes = 55 total face-to-face attending visit minutes). Accordingly, the physician must document the total face-to-face time spent during each portion of care in two separate notes or in one cumulative note. Be aware that this varies from the standard reporting of counseling and/or coordination of care time in that the physician must meet the threshold face-to-face-time requirements (see Table 1, left), making prolonged care services inefficient. When two providers from the same group practice split the threshold time (e.g., physician A provided morning rounds, and physician B spoke with the family in the afternoon), only one physician can report the cumulative service. To reiterate, 99356 must be reported on the same invoice as the primary visit code (e.g., 99232). Be sure once again to query payers, because most non-Medicare insurers do not recognize these codes. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
Medicare too Costly?
In April, the Centers for Medicare and Medicaid (CMS) published its proposed Inpatient Prospective Payment System (IPPS) rule for fiscal year 2009. The rule contains many important components, including additional categories of hospital-acquired conditions (HACs) that no longer will earn higher Medicare payment.
The good news is that under the proposed rule, Medicare payments to hospitals would increase by nearly $4 billion. However, the requirements to earn that are causing concern among some individuals and organizations, including SHM.
This year, CMS announced it would begin withholding additional payments for eight specific HACs, including some “never events”—a practice that won’t take effect until October (May 2008, p. 25). Now, the agency proposes to add nine more. Why double these restrictions so soon?
—Gregory Maynard, MD, MSc, division chief of hospital medicine, University of California, San Diego
“I think it’s a combination of things,” says Gregory Maynard, MD, MSc, division chief of hospital medicine at the University of California, San Diego Medical Center. “Medicare is trying hard to find things that will improve quality and reduce costs, and there are many ways you can do both.”
CMS will pay the lesser Medicare Severity DRG (MS-DRG) amount if the complication was acquired at the hospital and the patient has no other complications or comorbidities.
“It’s not that Medicare won’t pay for the hospital stay—they won’t pay for that condition as a co-morbidity,” explains Dr. Maynard.
- The new HACs include:
- Surgical site infections following certain elective surgeries;
- Legionnaires’ disease;
- Glycemic control for diabetes;
- Iatrogenic pneumothorax;
- Delirium;
- Ventilator-associated pneumonia;
- Deep-vein thrombosis/pulmonary embolism (DVT/PE);
- Staphylococcus aureus septicemia; and
- Clostridium difficile-associated disease.
Unlike the original eight HACs, these proposed conditions are raising questions.
“The first round of conditions, such as objects left in during surgery, those are obvious and people can buy into them,” Dr. Maynard says. Regarding the proposed additions, he says, “Some of these are just out there.”
He singled out a couple of the new HACs. “DVT is a pet of mine, because we’ve done a lot of work in that area,’’ he notes. “We have good information about what patients are on when they develop DVTs or PEs, and we know that very, very few patients who do were neglected.”
As for C diff.-associated disease, he points out: “C diff.-associated diarrhea—that’s tough to totally avoid. In spite of a perfect process, it will still happen.”
SHM sent a letter to CMS regarding specific concerns with three HACs, stating: “SHM supports the CMS initiative to improve the quality of care for hospitalized patients by preventing avoidable hospital-acquired conditions as proposed in the Final Rule for fiscal year 2008. We have concerns about the conditions selected for FY 2009 and the potential for creating unintended consequences through the inclusion of these conditions.”
Dr. Maynard and others fear the new HACs will lead to the addition of processes and other expenses. “I can’t speak totally for SHM,” he says. “I know they support transparency—but you have to think carefully about the process of transparency. There are unintended consequences, like testing everyone who comes in the door for certain conditions, and even treating a condition that doesn’t need to be treated.”
In an April 28 post on his blog “Wachter’s World” (www.wachtersworld.org) Robert Wachter, MD, professor and associate chairman of the Department of Medicine at the University of California, San Francisco, says: “This new list is a case of too far, too fast. … I can’t argue with the premise—many of the [adverse events] on this list are no doubt partly preventable with more religious implementation of certain safety practices (for example, for C diff., avoiding unnecessary antibiotics and adhering to strict infection control practices with suspected cases). But they are nowhere near ready for prime time. Adoption of this new list will lead to all kinds of gaming, [present on admission] shenanigans, wasted effort on preventive strategies with no supportive evidence, and nasty unintended consequences.”
Too Many Measures?
The proposed rule also will significantly increase quality data reporting requirements for hospitals. The rule adds 43 quality measures to the existing 30, so hospitals would need to report on 73 measures to qualify for a full update to their FY 2009 payment rates. The new measures include:
- Surgical Care Improvement Project (one new measure);
- Hospital readmissions (three new measures);
- Nursing care (four new measures);
- Patient safety indicators developed by the Agency for Healthcare Research and Quality (AHRQ) (five new measures);
- Inpatient quality indicators by AHRQ (four new measures);
- Venous thromboembolism (six new measures);
- Stroke measures (five new measures); and
- Cardiac surgery measures (15 new measures).
Critics of the rule believe reporting on 73 measures is unreasonable—and perhaps impossible for smaller hospitals. In a statement released by the American Hospital Association (AHA), Nancy Foster, the AHA’s vice president for quality and patient safety. says, “… we are dismayed that CMS has proposed to add a long and confusing list of measures to those on which hospitals must report to get their full update.” Foster recommends CMS only include measures endorsed by the National Quality Forum as appropriate national standards and adopted by the Hospital Quality Alliance as useful for public reporting on hospital quality of care.
In the Middle
As with previous CMS programs and rules, the increased reporting requirements will mean a continued role for hospitalists.
“This will put hospitalists in the middle even more than they are now,” predicts Dr. Maynard. “It could be good—increasing their role of communicating and training hospital staff and leading quality improvement initiatives—or it could come down to a blame game. Hospitalists are taking care of half the patients in the hospital these days, so if something goes wrong, it may be seen as their fault.”
Read more about the proposed rule online at www.cms.hhs.gov. CMS will respond to comments in a final rule to be issued by Aug 1. TH
Jane Jerrard is a medical writer based in Chicago.
In April, the Centers for Medicare and Medicaid (CMS) published its proposed Inpatient Prospective Payment System (IPPS) rule for fiscal year 2009. The rule contains many important components, including additional categories of hospital-acquired conditions (HACs) that no longer will earn higher Medicare payment.
The good news is that under the proposed rule, Medicare payments to hospitals would increase by nearly $4 billion. However, the requirements to earn that are causing concern among some individuals and organizations, including SHM.
This year, CMS announced it would begin withholding additional payments for eight specific HACs, including some “never events”—a practice that won’t take effect until October (May 2008, p. 25). Now, the agency proposes to add nine more. Why double these restrictions so soon?
—Gregory Maynard, MD, MSc, division chief of hospital medicine, University of California, San Diego
“I think it’s a combination of things,” says Gregory Maynard, MD, MSc, division chief of hospital medicine at the University of California, San Diego Medical Center. “Medicare is trying hard to find things that will improve quality and reduce costs, and there are many ways you can do both.”
CMS will pay the lesser Medicare Severity DRG (MS-DRG) amount if the complication was acquired at the hospital and the patient has no other complications or comorbidities.
“It’s not that Medicare won’t pay for the hospital stay—they won’t pay for that condition as a co-morbidity,” explains Dr. Maynard.
- The new HACs include:
- Surgical site infections following certain elective surgeries;
- Legionnaires’ disease;
- Glycemic control for diabetes;
- Iatrogenic pneumothorax;
- Delirium;
- Ventilator-associated pneumonia;
- Deep-vein thrombosis/pulmonary embolism (DVT/PE);
- Staphylococcus aureus septicemia; and
- Clostridium difficile-associated disease.
Unlike the original eight HACs, these proposed conditions are raising questions.
“The first round of conditions, such as objects left in during surgery, those are obvious and people can buy into them,” Dr. Maynard says. Regarding the proposed additions, he says, “Some of these are just out there.”
He singled out a couple of the new HACs. “DVT is a pet of mine, because we’ve done a lot of work in that area,’’ he notes. “We have good information about what patients are on when they develop DVTs or PEs, and we know that very, very few patients who do were neglected.”
As for C diff.-associated disease, he points out: “C diff.-associated diarrhea—that’s tough to totally avoid. In spite of a perfect process, it will still happen.”
SHM sent a letter to CMS regarding specific concerns with three HACs, stating: “SHM supports the CMS initiative to improve the quality of care for hospitalized patients by preventing avoidable hospital-acquired conditions as proposed in the Final Rule for fiscal year 2008. We have concerns about the conditions selected for FY 2009 and the potential for creating unintended consequences through the inclusion of these conditions.”
Dr. Maynard and others fear the new HACs will lead to the addition of processes and other expenses. “I can’t speak totally for SHM,” he says. “I know they support transparency—but you have to think carefully about the process of transparency. There are unintended consequences, like testing everyone who comes in the door for certain conditions, and even treating a condition that doesn’t need to be treated.”
In an April 28 post on his blog “Wachter’s World” (www.wachtersworld.org) Robert Wachter, MD, professor and associate chairman of the Department of Medicine at the University of California, San Francisco, says: “This new list is a case of too far, too fast. … I can’t argue with the premise—many of the [adverse events] on this list are no doubt partly preventable with more religious implementation of certain safety practices (for example, for C diff., avoiding unnecessary antibiotics and adhering to strict infection control practices with suspected cases). But they are nowhere near ready for prime time. Adoption of this new list will lead to all kinds of gaming, [present on admission] shenanigans, wasted effort on preventive strategies with no supportive evidence, and nasty unintended consequences.”
Too Many Measures?
The proposed rule also will significantly increase quality data reporting requirements for hospitals. The rule adds 43 quality measures to the existing 30, so hospitals would need to report on 73 measures to qualify for a full update to their FY 2009 payment rates. The new measures include:
- Surgical Care Improvement Project (one new measure);
- Hospital readmissions (three new measures);
- Nursing care (four new measures);
- Patient safety indicators developed by the Agency for Healthcare Research and Quality (AHRQ) (five new measures);
- Inpatient quality indicators by AHRQ (four new measures);
- Venous thromboembolism (six new measures);
- Stroke measures (five new measures); and
- Cardiac surgery measures (15 new measures).
Critics of the rule believe reporting on 73 measures is unreasonable—and perhaps impossible for smaller hospitals. In a statement released by the American Hospital Association (AHA), Nancy Foster, the AHA’s vice president for quality and patient safety. says, “… we are dismayed that CMS has proposed to add a long and confusing list of measures to those on which hospitals must report to get their full update.” Foster recommends CMS only include measures endorsed by the National Quality Forum as appropriate national standards and adopted by the Hospital Quality Alliance as useful for public reporting on hospital quality of care.
In the Middle
As with previous CMS programs and rules, the increased reporting requirements will mean a continued role for hospitalists.
“This will put hospitalists in the middle even more than they are now,” predicts Dr. Maynard. “It could be good—increasing their role of communicating and training hospital staff and leading quality improvement initiatives—or it could come down to a blame game. Hospitalists are taking care of half the patients in the hospital these days, so if something goes wrong, it may be seen as their fault.”
Read more about the proposed rule online at www.cms.hhs.gov. CMS will respond to comments in a final rule to be issued by Aug 1. TH
Jane Jerrard is a medical writer based in Chicago.
In April, the Centers for Medicare and Medicaid (CMS) published its proposed Inpatient Prospective Payment System (IPPS) rule for fiscal year 2009. The rule contains many important components, including additional categories of hospital-acquired conditions (HACs) that no longer will earn higher Medicare payment.
The good news is that under the proposed rule, Medicare payments to hospitals would increase by nearly $4 billion. However, the requirements to earn that are causing concern among some individuals and organizations, including SHM.
This year, CMS announced it would begin withholding additional payments for eight specific HACs, including some “never events”—a practice that won’t take effect until October (May 2008, p. 25). Now, the agency proposes to add nine more. Why double these restrictions so soon?
—Gregory Maynard, MD, MSc, division chief of hospital medicine, University of California, San Diego
“I think it’s a combination of things,” says Gregory Maynard, MD, MSc, division chief of hospital medicine at the University of California, San Diego Medical Center. “Medicare is trying hard to find things that will improve quality and reduce costs, and there are many ways you can do both.”
CMS will pay the lesser Medicare Severity DRG (MS-DRG) amount if the complication was acquired at the hospital and the patient has no other complications or comorbidities.
“It’s not that Medicare won’t pay for the hospital stay—they won’t pay for that condition as a co-morbidity,” explains Dr. Maynard.
- The new HACs include:
- Surgical site infections following certain elective surgeries;
- Legionnaires’ disease;
- Glycemic control for diabetes;
- Iatrogenic pneumothorax;
- Delirium;
- Ventilator-associated pneumonia;
- Deep-vein thrombosis/pulmonary embolism (DVT/PE);
- Staphylococcus aureus septicemia; and
- Clostridium difficile-associated disease.
Unlike the original eight HACs, these proposed conditions are raising questions.
“The first round of conditions, such as objects left in during surgery, those are obvious and people can buy into them,” Dr. Maynard says. Regarding the proposed additions, he says, “Some of these are just out there.”
He singled out a couple of the new HACs. “DVT is a pet of mine, because we’ve done a lot of work in that area,’’ he notes. “We have good information about what patients are on when they develop DVTs or PEs, and we know that very, very few patients who do were neglected.”
As for C diff.-associated disease, he points out: “C diff.-associated diarrhea—that’s tough to totally avoid. In spite of a perfect process, it will still happen.”
SHM sent a letter to CMS regarding specific concerns with three HACs, stating: “SHM supports the CMS initiative to improve the quality of care for hospitalized patients by preventing avoidable hospital-acquired conditions as proposed in the Final Rule for fiscal year 2008. We have concerns about the conditions selected for FY 2009 and the potential for creating unintended consequences through the inclusion of these conditions.”
Dr. Maynard and others fear the new HACs will lead to the addition of processes and other expenses. “I can’t speak totally for SHM,” he says. “I know they support transparency—but you have to think carefully about the process of transparency. There are unintended consequences, like testing everyone who comes in the door for certain conditions, and even treating a condition that doesn’t need to be treated.”
In an April 28 post on his blog “Wachter’s World” (www.wachtersworld.org) Robert Wachter, MD, professor and associate chairman of the Department of Medicine at the University of California, San Francisco, says: “This new list is a case of too far, too fast. … I can’t argue with the premise—many of the [adverse events] on this list are no doubt partly preventable with more religious implementation of certain safety practices (for example, for C diff., avoiding unnecessary antibiotics and adhering to strict infection control practices with suspected cases). But they are nowhere near ready for prime time. Adoption of this new list will lead to all kinds of gaming, [present on admission] shenanigans, wasted effort on preventive strategies with no supportive evidence, and nasty unintended consequences.”
Too Many Measures?
The proposed rule also will significantly increase quality data reporting requirements for hospitals. The rule adds 43 quality measures to the existing 30, so hospitals would need to report on 73 measures to qualify for a full update to their FY 2009 payment rates. The new measures include:
- Surgical Care Improvement Project (one new measure);
- Hospital readmissions (three new measures);
- Nursing care (four new measures);
- Patient safety indicators developed by the Agency for Healthcare Research and Quality (AHRQ) (five new measures);
- Inpatient quality indicators by AHRQ (four new measures);
- Venous thromboembolism (six new measures);
- Stroke measures (five new measures); and
- Cardiac surgery measures (15 new measures).
Critics of the rule believe reporting on 73 measures is unreasonable—and perhaps impossible for smaller hospitals. In a statement released by the American Hospital Association (AHA), Nancy Foster, the AHA’s vice president for quality and patient safety. says, “… we are dismayed that CMS has proposed to add a long and confusing list of measures to those on which hospitals must report to get their full update.” Foster recommends CMS only include measures endorsed by the National Quality Forum as appropriate national standards and adopted by the Hospital Quality Alliance as useful for public reporting on hospital quality of care.
In the Middle
As with previous CMS programs and rules, the increased reporting requirements will mean a continued role for hospitalists.
“This will put hospitalists in the middle even more than they are now,” predicts Dr. Maynard. “It could be good—increasing their role of communicating and training hospital staff and leading quality improvement initiatives—or it could come down to a blame game. Hospitalists are taking care of half the patients in the hospital these days, so if something goes wrong, it may be seen as their fault.”
Read more about the proposed rule online at www.cms.hhs.gov. CMS will respond to comments in a final rule to be issued by Aug 1. TH
Jane Jerrard is a medical writer based in Chicago.
Change Jobs Wisely
In today’s wide-open job market, hospitalists can pick a plum position anywhere in the United States. With promising opportunities in sunny Hawaii, bustling New York City, and everywhere in between—likely including your own hometown—the temptation to move to a warmer climate, kid-friendly small town, or bigger paycheck may be irresistible.
Michael-Anthony Williams, MD, chief medical officer for the Rocky Mountain Region of Sound Inpatient Physicians, has hired hospitalists who come to Denver from across the country.
“Market competition [for hospitalists] is definitely fierce and will remain so,” he says. “But no matter where you’re looking or what you’re searching for, you need to get a sense of the group you’ll be joining.”
Sameer Badlani, MD, hospitalist and instructor at the University of Chicago, agrees location should come second to the job itself. “You have to do a lot of introspection and decide what you’re looking for,” he cautions. “If you’re unhappy, ask yourself why a new job would be different.”
After taking this advice into account, consider the challenges and opportunities of starting life anew somewhere else.
Reasons to Relocate
Why think about moving in the first place?
“Money might be the biggest reason,” speculates Dr. Badlani. “The only way to make significantly more money is to become a partner in the practice. I’d say if you’re a hospitalist who’s relocating, you should definitely try to become a partner.”
Another reason to consider moving might be family reasons. “If a spouse gets a job offer in a different city, it’s easy for the hospitalist to move there and find a job,” Dr. Badlani points out. “With the economy the way it is, I think that more and more you’ll see spouses’ jobs influencing where hospitalists relocate.”
Some hospitalists move because they are drawn to a certain region or lifestyle. Dr. Williams says. “We certainly see people who target geography as playing a big role in their job search.”
If you fall into this category, be careful to do your research to discover the realities of your dream location.
“I’d advise that you make more than one trip to a place if you’ve never lived there before,” Dr. Badlani says. “See exactly what it means to live there. Visit the hospital medicine group more than once. Go out with a real estate agent and look at houses.”
—Sameer Badlani, MD, hospitalist and instructor, University of Chicago
Timing Is Everything
Once you’ve decided you are interested in moving—or have to move—get started with your location scouting and your job search.
“You should start looking [for a job] even earlier when you’re relocating,” Dr. Badlani advises. “And be sure to tell your supervisor that you’re thinking of relocating. This seems like a bad idea to some people, but it will be worse if you wait and give two weeks’ notice. That is unfair to your employer and your colleagues who will have to cover your work, and you will end up burning your bridges.” He recommends telling your current employer while interviewing for next year. If you’re already deep into your search, that should be about six or seven months in advance, he says.
“Your current employer will appreciate it, and they may even try to make some changes in order to keep you,” Dr. Badlani says.
Try to negotiate to keep your transition dates flexible. Your plans to move may not go as smoothly as you’d like. “Recently, we’ve seen a couple of people have a tough time selling their house before they move,” Dr. Williams says. “If you live in a tough real estate market, you might want to see if your new employer can be flexible on your start date.”
Consider Cost of Living
As you compare compensation offered by hospital medicine practices in different parts of the country—or even different parts of the same county—consider cost of living in each area.
“If you make $150,000 in Tulsa, Oklahoma, (then you need to make) $210,000 in Chicago,” Dr. Badlani says, who has worked in both cities. Cost of living, he adds, “can be misleading. Do your research and find out housing costs for the area. Online calculators only give approximations; make sure you compare housing in desirable areas of the city, not across the board.”
In addition, Dr. Badlani says, “If you choose a smaller town, it’s likely that you can get paid more—because they need you more—and live in a cheaper place. And you’ll find more opportunities in a smaller town because there are fewer doctors.”
The biggest challenge when comparing jobs is assessing the work required to make that salary, Dr. Williams adds. “Find out how many shifts per month you’ll work to earn it, and how many patients you’ll see per shift,” he suggests.
Relocation, Negotiation
Before you start negotiating a new contract, Dr. Badlani advises you first look at your current one to see what you’re walking away from.
“Every place has a golden handcuff,” he says. “The University of Chicago gives you three years before you’re fully vested in your retirement benefits; I know an Oklahoma hospital where it takes seven years. Leave before you’re vested and you could lose thousands of dollars in employer contributions. You have to ask, will your new job help you recover that quickly? Can you get a signing bonus that’s equal to all or most of what you’re walking away from, or the promise of a partnership? Try to mitigate that loss with other opportunities.
“Places like Kaiser Permanente offer money to help with a down payment for a house—that’s their version of a golden handcuff. If you stay in the job long enough, that becomes a free loan.”
Dr. Williams adds: “Will the group cover your moving expenses? That’s a lot of money. Also check on the state’s licensing fees and how long it will take to get your license—it varies greatly from state to state.”
While you’re interviewing, keep the negotiation process in mind: “I would never tell a recruiter or prospective employer all the reasons why I’m moving,” Dr. Badlani says. “You don’t want to show how interested you are. It’s a game you have to play. Be sure to say you’re looking at other opportunities and other towns.”
Finally, weigh your options against the rest of the market—and against what your peers are getting in terms of compensation and benefits.
“Talk to your friends and try to figure out what the best deal is,” Dr. Badlani says.
Although you can choose a hospitalist position anywhere in the country, the most important thing to consider is the group you’re joining. If it is not a good fit for your values and personality, then the state you’ve decided to move to will be one of discontent. TH
Jane Jerrard also writes “Public Policy” for The Hospitalist.
In today’s wide-open job market, hospitalists can pick a plum position anywhere in the United States. With promising opportunities in sunny Hawaii, bustling New York City, and everywhere in between—likely including your own hometown—the temptation to move to a warmer climate, kid-friendly small town, or bigger paycheck may be irresistible.
Michael-Anthony Williams, MD, chief medical officer for the Rocky Mountain Region of Sound Inpatient Physicians, has hired hospitalists who come to Denver from across the country.
“Market competition [for hospitalists] is definitely fierce and will remain so,” he says. “But no matter where you’re looking or what you’re searching for, you need to get a sense of the group you’ll be joining.”
Sameer Badlani, MD, hospitalist and instructor at the University of Chicago, agrees location should come second to the job itself. “You have to do a lot of introspection and decide what you’re looking for,” he cautions. “If you’re unhappy, ask yourself why a new job would be different.”
After taking this advice into account, consider the challenges and opportunities of starting life anew somewhere else.
Reasons to Relocate
Why think about moving in the first place?
“Money might be the biggest reason,” speculates Dr. Badlani. “The only way to make significantly more money is to become a partner in the practice. I’d say if you’re a hospitalist who’s relocating, you should definitely try to become a partner.”
Another reason to consider moving might be family reasons. “If a spouse gets a job offer in a different city, it’s easy for the hospitalist to move there and find a job,” Dr. Badlani points out. “With the economy the way it is, I think that more and more you’ll see spouses’ jobs influencing where hospitalists relocate.”
Some hospitalists move because they are drawn to a certain region or lifestyle. Dr. Williams says. “We certainly see people who target geography as playing a big role in their job search.”
If you fall into this category, be careful to do your research to discover the realities of your dream location.
“I’d advise that you make more than one trip to a place if you’ve never lived there before,” Dr. Badlani says. “See exactly what it means to live there. Visit the hospital medicine group more than once. Go out with a real estate agent and look at houses.”
—Sameer Badlani, MD, hospitalist and instructor, University of Chicago
Timing Is Everything
Once you’ve decided you are interested in moving—or have to move—get started with your location scouting and your job search.
“You should start looking [for a job] even earlier when you’re relocating,” Dr. Badlani advises. “And be sure to tell your supervisor that you’re thinking of relocating. This seems like a bad idea to some people, but it will be worse if you wait and give two weeks’ notice. That is unfair to your employer and your colleagues who will have to cover your work, and you will end up burning your bridges.” He recommends telling your current employer while interviewing for next year. If you’re already deep into your search, that should be about six or seven months in advance, he says.
“Your current employer will appreciate it, and they may even try to make some changes in order to keep you,” Dr. Badlani says.
Try to negotiate to keep your transition dates flexible. Your plans to move may not go as smoothly as you’d like. “Recently, we’ve seen a couple of people have a tough time selling their house before they move,” Dr. Williams says. “If you live in a tough real estate market, you might want to see if your new employer can be flexible on your start date.”
Consider Cost of Living
As you compare compensation offered by hospital medicine practices in different parts of the country—or even different parts of the same county—consider cost of living in each area.
“If you make $150,000 in Tulsa, Oklahoma, (then you need to make) $210,000 in Chicago,” Dr. Badlani says, who has worked in both cities. Cost of living, he adds, “can be misleading. Do your research and find out housing costs for the area. Online calculators only give approximations; make sure you compare housing in desirable areas of the city, not across the board.”
In addition, Dr. Badlani says, “If you choose a smaller town, it’s likely that you can get paid more—because they need you more—and live in a cheaper place. And you’ll find more opportunities in a smaller town because there are fewer doctors.”
The biggest challenge when comparing jobs is assessing the work required to make that salary, Dr. Williams adds. “Find out how many shifts per month you’ll work to earn it, and how many patients you’ll see per shift,” he suggests.
Relocation, Negotiation
Before you start negotiating a new contract, Dr. Badlani advises you first look at your current one to see what you’re walking away from.
“Every place has a golden handcuff,” he says. “The University of Chicago gives you three years before you’re fully vested in your retirement benefits; I know an Oklahoma hospital where it takes seven years. Leave before you’re vested and you could lose thousands of dollars in employer contributions. You have to ask, will your new job help you recover that quickly? Can you get a signing bonus that’s equal to all or most of what you’re walking away from, or the promise of a partnership? Try to mitigate that loss with other opportunities.
“Places like Kaiser Permanente offer money to help with a down payment for a house—that’s their version of a golden handcuff. If you stay in the job long enough, that becomes a free loan.”
Dr. Williams adds: “Will the group cover your moving expenses? That’s a lot of money. Also check on the state’s licensing fees and how long it will take to get your license—it varies greatly from state to state.”
While you’re interviewing, keep the negotiation process in mind: “I would never tell a recruiter or prospective employer all the reasons why I’m moving,” Dr. Badlani says. “You don’t want to show how interested you are. It’s a game you have to play. Be sure to say you’re looking at other opportunities and other towns.”
Finally, weigh your options against the rest of the market—and against what your peers are getting in terms of compensation and benefits.
“Talk to your friends and try to figure out what the best deal is,” Dr. Badlani says.
Although you can choose a hospitalist position anywhere in the country, the most important thing to consider is the group you’re joining. If it is not a good fit for your values and personality, then the state you’ve decided to move to will be one of discontent. TH
Jane Jerrard also writes “Public Policy” for The Hospitalist.
In today’s wide-open job market, hospitalists can pick a plum position anywhere in the United States. With promising opportunities in sunny Hawaii, bustling New York City, and everywhere in between—likely including your own hometown—the temptation to move to a warmer climate, kid-friendly small town, or bigger paycheck may be irresistible.
Michael-Anthony Williams, MD, chief medical officer for the Rocky Mountain Region of Sound Inpatient Physicians, has hired hospitalists who come to Denver from across the country.
“Market competition [for hospitalists] is definitely fierce and will remain so,” he says. “But no matter where you’re looking or what you’re searching for, you need to get a sense of the group you’ll be joining.”
Sameer Badlani, MD, hospitalist and instructor at the University of Chicago, agrees location should come second to the job itself. “You have to do a lot of introspection and decide what you’re looking for,” he cautions. “If you’re unhappy, ask yourself why a new job would be different.”
After taking this advice into account, consider the challenges and opportunities of starting life anew somewhere else.
Reasons to Relocate
Why think about moving in the first place?
“Money might be the biggest reason,” speculates Dr. Badlani. “The only way to make significantly more money is to become a partner in the practice. I’d say if you’re a hospitalist who’s relocating, you should definitely try to become a partner.”
Another reason to consider moving might be family reasons. “If a spouse gets a job offer in a different city, it’s easy for the hospitalist to move there and find a job,” Dr. Badlani points out. “With the economy the way it is, I think that more and more you’ll see spouses’ jobs influencing where hospitalists relocate.”
Some hospitalists move because they are drawn to a certain region or lifestyle. Dr. Williams says. “We certainly see people who target geography as playing a big role in their job search.”
If you fall into this category, be careful to do your research to discover the realities of your dream location.
“I’d advise that you make more than one trip to a place if you’ve never lived there before,” Dr. Badlani says. “See exactly what it means to live there. Visit the hospital medicine group more than once. Go out with a real estate agent and look at houses.”
—Sameer Badlani, MD, hospitalist and instructor, University of Chicago
Timing Is Everything
Once you’ve decided you are interested in moving—or have to move—get started with your location scouting and your job search.
“You should start looking [for a job] even earlier when you’re relocating,” Dr. Badlani advises. “And be sure to tell your supervisor that you’re thinking of relocating. This seems like a bad idea to some people, but it will be worse if you wait and give two weeks’ notice. That is unfair to your employer and your colleagues who will have to cover your work, and you will end up burning your bridges.” He recommends telling your current employer while interviewing for next year. If you’re already deep into your search, that should be about six or seven months in advance, he says.
“Your current employer will appreciate it, and they may even try to make some changes in order to keep you,” Dr. Badlani says.
Try to negotiate to keep your transition dates flexible. Your plans to move may not go as smoothly as you’d like. “Recently, we’ve seen a couple of people have a tough time selling their house before they move,” Dr. Williams says. “If you live in a tough real estate market, you might want to see if your new employer can be flexible on your start date.”
Consider Cost of Living
As you compare compensation offered by hospital medicine practices in different parts of the country—or even different parts of the same county—consider cost of living in each area.
“If you make $150,000 in Tulsa, Oklahoma, (then you need to make) $210,000 in Chicago,” Dr. Badlani says, who has worked in both cities. Cost of living, he adds, “can be misleading. Do your research and find out housing costs for the area. Online calculators only give approximations; make sure you compare housing in desirable areas of the city, not across the board.”
In addition, Dr. Badlani says, “If you choose a smaller town, it’s likely that you can get paid more—because they need you more—and live in a cheaper place. And you’ll find more opportunities in a smaller town because there are fewer doctors.”
The biggest challenge when comparing jobs is assessing the work required to make that salary, Dr. Williams adds. “Find out how many shifts per month you’ll work to earn it, and how many patients you’ll see per shift,” he suggests.
Relocation, Negotiation
Before you start negotiating a new contract, Dr. Badlani advises you first look at your current one to see what you’re walking away from.
“Every place has a golden handcuff,” he says. “The University of Chicago gives you three years before you’re fully vested in your retirement benefits; I know an Oklahoma hospital where it takes seven years. Leave before you’re vested and you could lose thousands of dollars in employer contributions. You have to ask, will your new job help you recover that quickly? Can you get a signing bonus that’s equal to all or most of what you’re walking away from, or the promise of a partnership? Try to mitigate that loss with other opportunities.
“Places like Kaiser Permanente offer money to help with a down payment for a house—that’s their version of a golden handcuff. If you stay in the job long enough, that becomes a free loan.”
Dr. Williams adds: “Will the group cover your moving expenses? That’s a lot of money. Also check on the state’s licensing fees and how long it will take to get your license—it varies greatly from state to state.”
While you’re interviewing, keep the negotiation process in mind: “I would never tell a recruiter or prospective employer all the reasons why I’m moving,” Dr. Badlani says. “You don’t want to show how interested you are. It’s a game you have to play. Be sure to say you’re looking at other opportunities and other towns.”
Finally, weigh your options against the rest of the market—and against what your peers are getting in terms of compensation and benefits.
“Talk to your friends and try to figure out what the best deal is,” Dr. Badlani says.
Although you can choose a hospitalist position anywhere in the country, the most important thing to consider is the group you’re joining. If it is not a good fit for your values and personality, then the state you’ve decided to move to will be one of discontent. TH
Jane Jerrard also writes “Public Policy” for The Hospitalist.
The Specialist Advantage
The speed at which hospital medicine is growing is leaving many hospitalists in uncharted waters as they try to balance clinical practice and academic activities such as teaching, quality improvement, and research.
“Hospitalists often have great ideas but lack the resources to carry them out,” said Scott Flanders, MD, SHM president-elect, clinical associate professor of internal medicine, and director of the hospitalist program at the University of Michigan Health System, Ann Arbor.
Also, hospitalists do not always recognize the role of the subspecialist in diagnosing and treating complex patients—nor the advantages those specialists bring to designing and supporting clinical research. Given the nature of their education, specialists have a deeper understanding than hospitalists of the pathophysiologic concepts and scientific principles underlying important clinical questions, and are more likely to have had fellowship training that includes clinical research experience. They’re likely to be more adept at navigating outside bureaucracies to obtain grants for disease-based investigation.
All in all, specialist participation in hospital-based clinical research projects may improve project feasibility, increase the chances of obtaining money, and allow for wider dissemination of the results than if these projects had been undertaken by hospitalists alone.
“At large institutions, having hospitalists partner with clinical subspecialists could enhance patient enrollment and enhance funding opportunities, because subspecialists have a lot of credibility with funding agencies,” Dr. Flanders says.
Yet, clinical research programs performed by hospitalists and hospital medicine programs still are in an embryonic stage. In this month’s issue of the Journal of Hospital Medicine, he and his colleagues describe a new program for accelerating clinical and translational research by having hospitalists team with subspecialist physicians and other healthcare professionals to ask and answer novel research questions.
SHARP Solution
In the Specialist-Hospitalist Allied Research Program (SHARP), an academic hospitalist and an academic cardiologist serve as principle and co-principle investigators, respectively. Together, they direct a team of supporting personnel, including a hospitalist investigator, clinical research nurse, research associate, and clinical epidemiologist.
The program began in 2006, with the goal of facilitating multicenter, intervention-based clinical trials. Other aims include enhancing patient participation and supporting pilot projects that would generate enough data to attract money for more in-depth studies. The program is paid for three years by the department of internal medicine with revenues generated for the hospital medicine division.
Through SHARP, there will be “a pool of dollars to support a program and provide an infrastructure for a project,” Dr. Flanders says. “Otherwise, each new project would require a new team to find funding [and] perform data analysis.”
SHARP is, in part, an acknowledgment of the increasingly complex nature of clinical research, Dr. Flanders says. “Many big research projects involve more than one specialty, so there will always be a need to collaborate.”
In a sense, the program is an extension of what hospitalists do already. “Hospitalist work in general is often collaborative and team-based,” Dr. Flanders notes. “We frequently work with nurses and other hospital-based staff members.”
How it Works
A steering committee chaired by the two principle investigators and consisting of academic administrators from the University of Michigan will identify appropriate research projects, determine the best allocation of resources, and help the team overcome the bureaucratic hurdles that inevitably arise in any project that includes multiple departments and institutions.
The program has two opening projects. One is aimed at reducing the incidence of false-positive blood cultures. Right now, as many as half of all the blood cultures that test positive at the University of Michigan turn out to be contaminated. The SHARP team has started a randomized, controlled trial to compare the effects of several different skin antiseptics on the false-positive rate, and ultimately will test more than 12,000 blood culture sets. Other key outcomes will be the quantity of additional diagnostic testing generated by positive cultures, use of resources, and associated costs. Mortality and length of stay also will be examined as secondary outcomes.
The second study has been completed, and data analysis has begun. It examined the role of an inpatient clinical pharmacist in preventing medication errors related to hospital discharge among elderly patients.
“In our experience at the University of Michigan, patients frequently have medication-related adverse events after discharge because they do not understand what medications they should be taking, what they are used for, how to manage side effects, or whom to call with problems,” Dr. Flanders and his colleagues wrote. “In addition, predictable medication-related issues (such as ability to pay for a medicine or expected serum electrolyte changes with newly added medications) are not universally anticipated.”
The pharmacist divided his time between a non-resident hospitalist service and a resident general medicine service, focusing on high-risk patients older than 65. Those patients received pre-discharge counseling and post-discharge follow-up calls from the pharmacist within 72 hours and 30 days of leaving the hospital. The key outcomes include medication issues and actions taken by the pharmacist at or after discharge, as well as clinical outcomes such as emergency department visits, readmission rates, and healthcare-related costs.
So far, the biggest challenge faced by the hospitalists interested in SHARP simply has been finding enough hours in the day for it. One of the program’s goals is to generate grant money to hire supporting staff, but right now the doctors must participate on their own time. Nevertheless, says Dr. Flanders, the response to the program has been positive. “It facilitates the small, difficult steps [in funding and implementing research] along the way,” he says. “People have been pleasantly surprised that it works as well as it does.”TH
Norra MacReady is a medical writer based in California.
The speed at which hospital medicine is growing is leaving many hospitalists in uncharted waters as they try to balance clinical practice and academic activities such as teaching, quality improvement, and research.
“Hospitalists often have great ideas but lack the resources to carry them out,” said Scott Flanders, MD, SHM president-elect, clinical associate professor of internal medicine, and director of the hospitalist program at the University of Michigan Health System, Ann Arbor.
Also, hospitalists do not always recognize the role of the subspecialist in diagnosing and treating complex patients—nor the advantages those specialists bring to designing and supporting clinical research. Given the nature of their education, specialists have a deeper understanding than hospitalists of the pathophysiologic concepts and scientific principles underlying important clinical questions, and are more likely to have had fellowship training that includes clinical research experience. They’re likely to be more adept at navigating outside bureaucracies to obtain grants for disease-based investigation.
All in all, specialist participation in hospital-based clinical research projects may improve project feasibility, increase the chances of obtaining money, and allow for wider dissemination of the results than if these projects had been undertaken by hospitalists alone.
“At large institutions, having hospitalists partner with clinical subspecialists could enhance patient enrollment and enhance funding opportunities, because subspecialists have a lot of credibility with funding agencies,” Dr. Flanders says.
Yet, clinical research programs performed by hospitalists and hospital medicine programs still are in an embryonic stage. In this month’s issue of the Journal of Hospital Medicine, he and his colleagues describe a new program for accelerating clinical and translational research by having hospitalists team with subspecialist physicians and other healthcare professionals to ask and answer novel research questions.
SHARP Solution
In the Specialist-Hospitalist Allied Research Program (SHARP), an academic hospitalist and an academic cardiologist serve as principle and co-principle investigators, respectively. Together, they direct a team of supporting personnel, including a hospitalist investigator, clinical research nurse, research associate, and clinical epidemiologist.
The program began in 2006, with the goal of facilitating multicenter, intervention-based clinical trials. Other aims include enhancing patient participation and supporting pilot projects that would generate enough data to attract money for more in-depth studies. The program is paid for three years by the department of internal medicine with revenues generated for the hospital medicine division.
Through SHARP, there will be “a pool of dollars to support a program and provide an infrastructure for a project,” Dr. Flanders says. “Otherwise, each new project would require a new team to find funding [and] perform data analysis.”
SHARP is, in part, an acknowledgment of the increasingly complex nature of clinical research, Dr. Flanders says. “Many big research projects involve more than one specialty, so there will always be a need to collaborate.”
In a sense, the program is an extension of what hospitalists do already. “Hospitalist work in general is often collaborative and team-based,” Dr. Flanders notes. “We frequently work with nurses and other hospital-based staff members.”
How it Works
A steering committee chaired by the two principle investigators and consisting of academic administrators from the University of Michigan will identify appropriate research projects, determine the best allocation of resources, and help the team overcome the bureaucratic hurdles that inevitably arise in any project that includes multiple departments and institutions.
The program has two opening projects. One is aimed at reducing the incidence of false-positive blood cultures. Right now, as many as half of all the blood cultures that test positive at the University of Michigan turn out to be contaminated. The SHARP team has started a randomized, controlled trial to compare the effects of several different skin antiseptics on the false-positive rate, and ultimately will test more than 12,000 blood culture sets. Other key outcomes will be the quantity of additional diagnostic testing generated by positive cultures, use of resources, and associated costs. Mortality and length of stay also will be examined as secondary outcomes.
The second study has been completed, and data analysis has begun. It examined the role of an inpatient clinical pharmacist in preventing medication errors related to hospital discharge among elderly patients.
“In our experience at the University of Michigan, patients frequently have medication-related adverse events after discharge because they do not understand what medications they should be taking, what they are used for, how to manage side effects, or whom to call with problems,” Dr. Flanders and his colleagues wrote. “In addition, predictable medication-related issues (such as ability to pay for a medicine or expected serum electrolyte changes with newly added medications) are not universally anticipated.”
The pharmacist divided his time between a non-resident hospitalist service and a resident general medicine service, focusing on high-risk patients older than 65. Those patients received pre-discharge counseling and post-discharge follow-up calls from the pharmacist within 72 hours and 30 days of leaving the hospital. The key outcomes include medication issues and actions taken by the pharmacist at or after discharge, as well as clinical outcomes such as emergency department visits, readmission rates, and healthcare-related costs.
So far, the biggest challenge faced by the hospitalists interested in SHARP simply has been finding enough hours in the day for it. One of the program’s goals is to generate grant money to hire supporting staff, but right now the doctors must participate on their own time. Nevertheless, says Dr. Flanders, the response to the program has been positive. “It facilitates the small, difficult steps [in funding and implementing research] along the way,” he says. “People have been pleasantly surprised that it works as well as it does.”TH
Norra MacReady is a medical writer based in California.
The speed at which hospital medicine is growing is leaving many hospitalists in uncharted waters as they try to balance clinical practice and academic activities such as teaching, quality improvement, and research.
“Hospitalists often have great ideas but lack the resources to carry them out,” said Scott Flanders, MD, SHM president-elect, clinical associate professor of internal medicine, and director of the hospitalist program at the University of Michigan Health System, Ann Arbor.
Also, hospitalists do not always recognize the role of the subspecialist in diagnosing and treating complex patients—nor the advantages those specialists bring to designing and supporting clinical research. Given the nature of their education, specialists have a deeper understanding than hospitalists of the pathophysiologic concepts and scientific principles underlying important clinical questions, and are more likely to have had fellowship training that includes clinical research experience. They’re likely to be more adept at navigating outside bureaucracies to obtain grants for disease-based investigation.
All in all, specialist participation in hospital-based clinical research projects may improve project feasibility, increase the chances of obtaining money, and allow for wider dissemination of the results than if these projects had been undertaken by hospitalists alone.
“At large institutions, having hospitalists partner with clinical subspecialists could enhance patient enrollment and enhance funding opportunities, because subspecialists have a lot of credibility with funding agencies,” Dr. Flanders says.
Yet, clinical research programs performed by hospitalists and hospital medicine programs still are in an embryonic stage. In this month’s issue of the Journal of Hospital Medicine, he and his colleagues describe a new program for accelerating clinical and translational research by having hospitalists team with subspecialist physicians and other healthcare professionals to ask and answer novel research questions.
SHARP Solution
In the Specialist-Hospitalist Allied Research Program (SHARP), an academic hospitalist and an academic cardiologist serve as principle and co-principle investigators, respectively. Together, they direct a team of supporting personnel, including a hospitalist investigator, clinical research nurse, research associate, and clinical epidemiologist.
The program began in 2006, with the goal of facilitating multicenter, intervention-based clinical trials. Other aims include enhancing patient participation and supporting pilot projects that would generate enough data to attract money for more in-depth studies. The program is paid for three years by the department of internal medicine with revenues generated for the hospital medicine division.
Through SHARP, there will be “a pool of dollars to support a program and provide an infrastructure for a project,” Dr. Flanders says. “Otherwise, each new project would require a new team to find funding [and] perform data analysis.”
SHARP is, in part, an acknowledgment of the increasingly complex nature of clinical research, Dr. Flanders says. “Many big research projects involve more than one specialty, so there will always be a need to collaborate.”
In a sense, the program is an extension of what hospitalists do already. “Hospitalist work in general is often collaborative and team-based,” Dr. Flanders notes. “We frequently work with nurses and other hospital-based staff members.”
How it Works
A steering committee chaired by the two principle investigators and consisting of academic administrators from the University of Michigan will identify appropriate research projects, determine the best allocation of resources, and help the team overcome the bureaucratic hurdles that inevitably arise in any project that includes multiple departments and institutions.
The program has two opening projects. One is aimed at reducing the incidence of false-positive blood cultures. Right now, as many as half of all the blood cultures that test positive at the University of Michigan turn out to be contaminated. The SHARP team has started a randomized, controlled trial to compare the effects of several different skin antiseptics on the false-positive rate, and ultimately will test more than 12,000 blood culture sets. Other key outcomes will be the quantity of additional diagnostic testing generated by positive cultures, use of resources, and associated costs. Mortality and length of stay also will be examined as secondary outcomes.
The second study has been completed, and data analysis has begun. It examined the role of an inpatient clinical pharmacist in preventing medication errors related to hospital discharge among elderly patients.
“In our experience at the University of Michigan, patients frequently have medication-related adverse events after discharge because they do not understand what medications they should be taking, what they are used for, how to manage side effects, or whom to call with problems,” Dr. Flanders and his colleagues wrote. “In addition, predictable medication-related issues (such as ability to pay for a medicine or expected serum electrolyte changes with newly added medications) are not universally anticipated.”
The pharmacist divided his time between a non-resident hospitalist service and a resident general medicine service, focusing on high-risk patients older than 65. Those patients received pre-discharge counseling and post-discharge follow-up calls from the pharmacist within 72 hours and 30 days of leaving the hospital. The key outcomes include medication issues and actions taken by the pharmacist at or after discharge, as well as clinical outcomes such as emergency department visits, readmission rates, and healthcare-related costs.
So far, the biggest challenge faced by the hospitalists interested in SHARP simply has been finding enough hours in the day for it. One of the program’s goals is to generate grant money to hire supporting staff, but right now the doctors must participate on their own time. Nevertheless, says Dr. Flanders, the response to the program has been positive. “It facilitates the small, difficult steps [in funding and implementing research] along the way,” he says. “People have been pleasantly surprised that it works as well as it does.”TH
Norra MacReady is a medical writer based in California.
In the Literature
Literature at a Glance
A guide to this month’s studies.
- Survival of in-hospital cardiac arrest decreases during nights and weekends.
- C-reactive protein levels predict severity and complications in community-acquired pneumonia.
- Adherence to current guidelines improves outcome in treatment of prosthetic joint infection.
- Sodium phosphate bowel prep use is associated with a decline in GFR.
- Minimally interrupted cardiac resuscitation improves survival.
- Lower aPTT increases risk for future VTE.
- Warfarin combined with antiplatelet therapy increases hemorrhage rate.
- Creatinine rise during MI hospitalization is associated with long-term risk of death and ESRD.
- Communication improves patient adherence to beta-blockers after MI.
Does Time of Day Affect Survival of Cardiac Arrest Patients?
Background: In-hospital cardiac arrest is a major public health problem. Small studies have demonstrated survival after cardiac arrest is worse at night as compared with all other times. Multiple hypothesis are proffered for this decreased survival, including less effective detection and treatment of the warning signs of impending arrest during the night hours.
Study design: Prospective registry.
Setting: 507 hospitals participating through the National Registry of Cardiopulmonary Resuscitation.
Synopsis: 86,748 consecutive, inpatient cardiac arrests were reported from Jan. 1, 2000, through Feb. 1, 2007, including 58,593 cases during day/evening hours and 28,155 cases during night hours.
Rates of survival to discharge (14.7 % vs. 19.8%), survival at 24 hours (28.9% vs. 35.4%), and favorable neurological outcomes (11.0% vs. 15.2%) were substantially lower during the night compared with day/evening (all p values < 0.001). The first documented rhythm at night was more frequently asystole as opposed to ventricular fibrillation during the day/evening. There also was a higher survival rate with cardiac arrests during day/evening hours occurring on weekdays compared with weekends (odds ratio [OR] 1.15). There was no difference in survival rates between weekdays or weekends among cardiac arrests occurring during the night hours.
Bottom line: Survival rates for in-hospital cardiac arrest are lower during nights and weekends, which may relate to differential physician and hospital staffing patterns during these hours.
Citation: Peberdy MA, Ornato JP, Larkin GL et al. Survival from in-hospital cardiac arrest during nights and weekends. JAMA 2008;299:785-792.
Can CRP Identify Risk in CAP Patients?
Background: Small initial studies suggest an elevated C-reactive protein (CRP) is relatively nonspecific but may have a role in predicting disease severity in community-acquired pneumonia (CAP).
Study design: Prospective study.
Setting: Large academic center in the United Kingdom.
Synopsis: In this study of 570 patients over a two-year time period, all patients presenting to the hospital with a diagnosis of CAP and the absence of exclusion criteria were evaluated. CRP was measured on admission and repeated on day four of hospitalization.
Low CRP levels (less than 100 mg/L) were independently associated with a reduced risk of 30-day mortality (OR 0.18; p=0.03), need for invasive ventilation and/or inotropic support (OR 0.21; p=0.002), and complicated pneumonia (OR 0.05; p=0.003). In addition, the failure of CRP to fall by 50% or more at day four of hospitalization was associated with an increased risk of 30-day mortality (OR 24.5; p<0.0001), need for mechanical ventilation and/or inotropic support (OR 7.1; p<0.0001), and complicated pneumonia (OR 15.4; p<0.0001).
Patients with chronic lung disease, immunosuppression, active malignancy or hospital-acquired pneumonia were excluded from the study and the conclusions cannot be extrapolated to these higher risk populations.
Bottom line: C-reactive protein is an independent marker of severity in CAP, and low levels can be used as an adjunct to clinical judgment to help identify patients who may be safely discharged from the hospital.
Citation: Chalmers JD, Singanayagam A, Hill AT. C-reactive protein is an independent predictor of severity in community-acquired pneumonia. Am J of Med. 2008;121:219-225.
Do Aggressive Surgical Intervention and Antimicrobial Treatment Improve Outcomes in Patients Suffering PJI?
Background: Prosthetic joint infection (PJI) is a severe complication, causing significant morbidity and healthcare costs. A recent article put forth up to date guidelines for the management of PJI. The purpose of this current study was to evaluate the external clinical validity of these treatment recommendations.
Study design: Retrospective cohort analysis.
Setting: 1,000-bed tertiary care center in Switzerland.
Synopsis: 68 consecutive episodes of PJI from January 1995 through December 2004 were reviewed. Patients with polymicrobial infections and with treatment failures prior to referral to this center were included.
The success rate for treatment of PJI was highest (67%) when the surgical strategy met current recommendations and antimicrobial treatment was adequate or partially adequate. The preferred surgical strategy was a two-stage exchange. The risk of treatment failure was higher for PJI treated with a surgical strategy other than that recommended (hazard ratio [HR] 2.34, p=0.01) and for PJIs treated with antibiotics not corresponding to recommendations (HR 3.45, p=0.002).
This study was limited by its small sample size and retrospective nature. Patients were not randomized, and cure rates for PJI were significantly lower than in prior published studies.
Bottom line: Treatment of PJI in higher risk populations in accordance with currently recommended surgical and antimicrobial treatment recommendations is associated with better outcomes and cure rates.
Citation: Betsch BY, Eggli S, Siebenrock KA, Tauber MG, Muhlemann K. Treatment of joint prosthesis infection in accordance with current recommendations improves outcome. Clin Infect Dis. 2008;46:1221-1226.
Do Oral Sodium Phosphate Drugs in Large Bowel Prep for Endoscopy Worsen Renal Function?
Background: Proper bowel preparation is essential for adequate colonoscopy and flexible sigmoidoscopy. Oral agents that are most commonly used for bowel preparation are sodium phosphate drugs, polyethylglycol and magnesium citrate. Sodium phosphate drugs are often preferred because of the decreased amount of fluid necessary for bowel preparation.
Study design: Retrospective study.
Setting: Scott and White Clinic, Temple, Texas.
Synopsis: Researchers compared 286 patients receiving an oral sodium phosphate solution for colonoscopy bowel preparation with 125 patients with similar comorbidities who received a non-sodium phosphate solution for bowel preparation. All patients had normal baseline creatinine levels.
The baseline, six-month, and one-year glomerular filtration rates (GFR) were compared between the two groups. GFR declined from 79 to 73 to 71 ml/min/1.73 m2 in the study group vs. 76 to 74 to 74 ml/min/1.73 m2 in the control group for the baseline, six-month, and one-year time periods, respectively.
This is an observational study and thus limited by its non-randomized nature. Sodium phosphate has a black-box warning in stage four and five chronic kidney disease because of its deleterious effect on renal function and the potential for inducing electrolyte abnormalities. Given the findings of this study and the availability of other effective preps alternative regimens should be considered for colonic preparation.
Bottom line: Oral sodium phosphate drugs may cause an acute and chronic decline in renal function as measured by the GFR.
Citation: Khurana A, McLean L, Atkinson S, Foulks C. The effect of oral sodium phosphate drug products on renal function in adults is undergoing bowel endoscopy. Arch Intern Med. 2008; 168(6):593-597.
Does MICR Improve Survival-to-hospital Discharge vs. Traditional CPR and ACLS in Cardiac Arrest Outside the Hospital?
Background: Minimally interrupted cardiac resuscitation (MICR), also known as cardiocerebral resuscitation, is hypothesized to increase survival compared with traditional CPR and advanced cardiac life support (ACLS) in out-of-hospital cardiac arrest. In MICR, 200 “pre-shock” chest compressions (100 compressions/minute) are initially given. The rhythm is then analyzed, with a single shock given if indicated.
Study design: Prospective study.
Setting: Two cities in Arizona.
Synopsis: Using data in the Save Heart in Arizona Registry and Education (SHARE) program, outcomes of 218 individuals with cardiac arrest receiving traditional CPR/ACLS were compared to 668 individuals after MICR training was instituted in the same two metropolitan cities. Survival-to-hospital discharge increased from 1.8% (4/218) before MICR training to 5.4% (36/668) after MICR training. The authors then compared the outcomes of 1,799 individuals with cardiac arrest resuscitated by emergency medical services (EMS) who did not receive training in MICR to 661 individuals who received MICR training over the same period. Survival-to-hospital discharge was 9.1% (60/601) in the patients cared from by EMS that received MICR training versus 3.8% (69/1730) in their non-MICR trained colleagues.
This study is limited by its observational nature and lack of randomization. Surprisingly, more individuals were intubated in the MICR groups. For hospitalists, the results could have a dramatic affect on cardiac arrest survival and lead to future changes to CPR/ACLS protocols.
Bottom line: MICR has a significant impact on survival in out-of-hospital cardiac arrest as compared with traditional CPR and ACLS.
Citation: Bobrow B, Clark L, Ewy G, et al. Minimally interrupted cardiac resuscitation by emergency medical services for out-of-hospital cardiac arrest. JAMA. 2008;299(10):1158-1165.
Does Lower aPTT Increase Future VTE Independent of Other Pro-coagulant Factors?
Background: Certain factors, such as obesity, D-dimer levels, and factor V Leiden gene mutations, increase the risk of future venous thromboembolism (VTE) events. This study sought to determine whether lower baseline levels of activated partial thromboplastin time aPTT also increase this risk.
Study design: Prospective multicenter cohort study.
Setting: Longitudinal Investigation of Thromboembolism Etiology research study (Atherosclerosis Risk in Communities portion) in four U.S. communities.
Synopsis: 13,880 individuals with baseline aPTT measurements were followed for 13 years for future VTE events. Of those, 260 developed a VTE of which 111 were described as idiopathic. Individuals in the lowest two quartiles of aPTT compared with the highest fourth quartile had a 2.4-fold and 1.9-fold increase in the risk of VTE, respectively. A lower aPTT further increased the risk of VTE when associated with obesity, elevated D-dimer level, and particularly factor V Leiden.
This study was limited by the relatively small number of VTE events. It also did not clarify whether aPTT measurements in high-risk groups such as those with positive family history of VTE were useful for predicting risk of future VTE. For hospitalists, patients with a lower initial aPTT may warrant more aggressive inpatient DVT prophylaxis.
Bottom line: aPTT below the median level increases the risk of future VTE events, especially if associated with obesity, elevated D-dimer levels, and/or factor V Leiden.
Citation: Zakai NA, Ohira T, White R, Folsom A, Cushman M. Activated partial thromboplastin time and risk of future venous thromboembolism. Am J of Med. 2008;121:231-238.
What Bleeding Outcomes are Associated with Using Warfarin with Antiplatelet Agents?
Background: Despite a high prevalence of combining antiplatelet and warfarin therapy, the timing, safety, and efficacy of this strategy remain controversial.
Study design: Retrospective cohort study.
Setting: Kaiser Permanente Colorado.
Synopsis: Using a pharmacy database, the authors identified 2,560 patients receiving warfarin alone (monotherapy cohort) and 1,623 patients receiving warfarin combined with antiplatelet agents (combination therapy cohort).
In the combination therapy cohort, aspirin was the most common antiplatelet agent (37%) followed by clopidogrel (13%) and dipyridamole (2%). During a six-month period, the combination therapy cohort had a 4.2% risk of hemorrhage and a 2.0% risk of major hemorrhage. Warfarin monotherapy was associated with a 2% risk of hemorrhage and 0.9% risk of major hemorrhage.
At baseline, the combination therapy patients were twice as likely to have diabetes or congestive heart failure and four times as likely to have coronary artery disease. In both cohorts, the most common reason for warfarin therapy was atrial fibrillation.
Since this was a retrospective investigation, hospitalists should be careful about drawing conclusions from this study alone, but are reminded to discuss risks carefully and engage in shared decision-making with patients when using combined warfarin and antiplatelet therapy.
Bottom line: Warfarin use in combination with antiplatelet therapy is associated with more than double the risk of bleeding compared with warfarin monotherapy.
Citation: Johnson SG, Rogers K, Delate T, Witt DM. Outcomes associated with combined antiplatelet and anticoagulant therapy. Chest. 2008;133:948-954.
Does a Rise in Serum Creatinine Affect Post-hospitalization Mortality and ESRD in Elderly MI Patients?
Background: Previous studies found an association between small changes in serum creatinine during hospitalization and short-term mortality. Data has shown patients experiencing a rise in creatinine at the time of CABG have increased in-hospital and long-term follow-up mortality.
Study design: Retrospective cohort study
Setting: Nationwide Medicare database of acute MI hospitalizations.
Synopsis: The authors reviewed outcomes data for 87,094 patients hospitalized for acute myocardial infarction (MI) from 1994-1995 with follow-up data through 2004. Patients were classified into groups with no rise in creatinine during hospitalization and those with rises of 0.1 mg/dL, 0.2 mg/dL, 0.3-0.5 mg/dL, and 0.6-3 mg/dL.
Compared with patients with no rise in creatinine, a rise of 0.1 mg/dL was associated with an adjusted hazard ratio of 1.45 for end-stage renal disease (ESRD) and 1.14 for post-hospitalization death during long-term follow-up. An incremental increase in poor outcomes was seen with more dramatic increases in creatinine, with patients in the group with a 0.6-3 mg/dL rise in creatinine having an adjusted hazard ratio of 3.26 for ESRD and 1.39 for post-hospitalization death. Among patients with a creatinine rise, the absolute risk of mortality (15% annually) was greater than that of ESRD (0.3% annually).
Hospitalists should note limitations of this retrospective study, including its restriction to hospitalized elderly patients.
Bottom line: Even small rises in serum creatinine during acute hospitalization for MI are associated with long-term risk for death and ESRD in elderly patients.
Citation: Newsome BB, Warnock DG, McClellan WM, et al. Long-term risk of mortality and end-stage renal disease among the elderly after small increases in serum creatinine level during hospitalization for acute myocardial infarction. Arch Intern Med. 2008;168(6):609-616.
Does Direct-to-patient Communication Improve Adherence to Beta-blocker Therapy Following an MI?
Background: The joint American Heart Association and American College of Cardiology guidelines have specific treatment recommendations regarding care of a patient post-myocardial infarction (MI). A key component of this regimen is beta-blocker therapy. Beta-blockers routinely are prescribed at hospital discharge following MI; however, patient adherence has been shown to decline substantially over time.
Study design: Cluster randomized control trial.
Setting: Four health maintenance organizations in Boston, Minneapolis, Atlanta, and Portland, Ore.
Synopsis: 836 post-MI patients were given a beta-blocker prescription upon discharge from the hospital. The intervention group received two mailed communications. The first was a personalized, simply worded letter from a health plan physician-administrator, followed two months later by a similar letter with a brochure. Mailers were low cost and easily replicable; they addressed the importance of these medications, the risks of non-adherence, and adverse effects.
The primary outcome measure was beta-blocker adherence. Medication adherence was analyzed as a continuous measure and as a monthly proportion of days covered (PDC) of 80% or greater. Across all months of follow-up, a mean of 64.8% of intervention patients had a PDC of more than 80% compared with 58.5% of control group patients (number needed to treat=16). The intervention group was 17% more likely to have a PDC of 80% or greater over the entire post-intervention period.
These interventions were studied in a prepaid integrated care delivery system—limiting generalization to other insurance types. Nevertheless, finding ways to improve patient compliance and decrease recurrent cardiac events is liking to result in cost saving to any healthcare plan.
Bottom line: A low-cost direct-to-patient communication effort can have a positive effect on beta-blocker adherence following MI.
Citation: Smith DH, Kramer JM, Perrin N, et al. A randomized trial of direct-to-patient communication to enhance adherence to beta-blocker therapy following myocardial infarction. Arch Intern Med. 2008;168(5):477-483. TH
Literature at a Glance
A guide to this month’s studies.
- Survival of in-hospital cardiac arrest decreases during nights and weekends.
- C-reactive protein levels predict severity and complications in community-acquired pneumonia.
- Adherence to current guidelines improves outcome in treatment of prosthetic joint infection.
- Sodium phosphate bowel prep use is associated with a decline in GFR.
- Minimally interrupted cardiac resuscitation improves survival.
- Lower aPTT increases risk for future VTE.
- Warfarin combined with antiplatelet therapy increases hemorrhage rate.
- Creatinine rise during MI hospitalization is associated with long-term risk of death and ESRD.
- Communication improves patient adherence to beta-blockers after MI.
Does Time of Day Affect Survival of Cardiac Arrest Patients?
Background: In-hospital cardiac arrest is a major public health problem. Small studies have demonstrated survival after cardiac arrest is worse at night as compared with all other times. Multiple hypothesis are proffered for this decreased survival, including less effective detection and treatment of the warning signs of impending arrest during the night hours.
Study design: Prospective registry.
Setting: 507 hospitals participating through the National Registry of Cardiopulmonary Resuscitation.
Synopsis: 86,748 consecutive, inpatient cardiac arrests were reported from Jan. 1, 2000, through Feb. 1, 2007, including 58,593 cases during day/evening hours and 28,155 cases during night hours.
Rates of survival to discharge (14.7 % vs. 19.8%), survival at 24 hours (28.9% vs. 35.4%), and favorable neurological outcomes (11.0% vs. 15.2%) were substantially lower during the night compared with day/evening (all p values < 0.001). The first documented rhythm at night was more frequently asystole as opposed to ventricular fibrillation during the day/evening. There also was a higher survival rate with cardiac arrests during day/evening hours occurring on weekdays compared with weekends (odds ratio [OR] 1.15). There was no difference in survival rates between weekdays or weekends among cardiac arrests occurring during the night hours.
Bottom line: Survival rates for in-hospital cardiac arrest are lower during nights and weekends, which may relate to differential physician and hospital staffing patterns during these hours.
Citation: Peberdy MA, Ornato JP, Larkin GL et al. Survival from in-hospital cardiac arrest during nights and weekends. JAMA 2008;299:785-792.
Can CRP Identify Risk in CAP Patients?
Background: Small initial studies suggest an elevated C-reactive protein (CRP) is relatively nonspecific but may have a role in predicting disease severity in community-acquired pneumonia (CAP).
Study design: Prospective study.
Setting: Large academic center in the United Kingdom.
Synopsis: In this study of 570 patients over a two-year time period, all patients presenting to the hospital with a diagnosis of CAP and the absence of exclusion criteria were evaluated. CRP was measured on admission and repeated on day four of hospitalization.
Low CRP levels (less than 100 mg/L) were independently associated with a reduced risk of 30-day mortality (OR 0.18; p=0.03), need for invasive ventilation and/or inotropic support (OR 0.21; p=0.002), and complicated pneumonia (OR 0.05; p=0.003). In addition, the failure of CRP to fall by 50% or more at day four of hospitalization was associated with an increased risk of 30-day mortality (OR 24.5; p<0.0001), need for mechanical ventilation and/or inotropic support (OR 7.1; p<0.0001), and complicated pneumonia (OR 15.4; p<0.0001).
Patients with chronic lung disease, immunosuppression, active malignancy or hospital-acquired pneumonia were excluded from the study and the conclusions cannot be extrapolated to these higher risk populations.
Bottom line: C-reactive protein is an independent marker of severity in CAP, and low levels can be used as an adjunct to clinical judgment to help identify patients who may be safely discharged from the hospital.
Citation: Chalmers JD, Singanayagam A, Hill AT. C-reactive protein is an independent predictor of severity in community-acquired pneumonia. Am J of Med. 2008;121:219-225.
Do Aggressive Surgical Intervention and Antimicrobial Treatment Improve Outcomes in Patients Suffering PJI?
Background: Prosthetic joint infection (PJI) is a severe complication, causing significant morbidity and healthcare costs. A recent article put forth up to date guidelines for the management of PJI. The purpose of this current study was to evaluate the external clinical validity of these treatment recommendations.
Study design: Retrospective cohort analysis.
Setting: 1,000-bed tertiary care center in Switzerland.
Synopsis: 68 consecutive episodes of PJI from January 1995 through December 2004 were reviewed. Patients with polymicrobial infections and with treatment failures prior to referral to this center were included.
The success rate for treatment of PJI was highest (67%) when the surgical strategy met current recommendations and antimicrobial treatment was adequate or partially adequate. The preferred surgical strategy was a two-stage exchange. The risk of treatment failure was higher for PJI treated with a surgical strategy other than that recommended (hazard ratio [HR] 2.34, p=0.01) and for PJIs treated with antibiotics not corresponding to recommendations (HR 3.45, p=0.002).
This study was limited by its small sample size and retrospective nature. Patients were not randomized, and cure rates for PJI were significantly lower than in prior published studies.
Bottom line: Treatment of PJI in higher risk populations in accordance with currently recommended surgical and antimicrobial treatment recommendations is associated with better outcomes and cure rates.
Citation: Betsch BY, Eggli S, Siebenrock KA, Tauber MG, Muhlemann K. Treatment of joint prosthesis infection in accordance with current recommendations improves outcome. Clin Infect Dis. 2008;46:1221-1226.
Do Oral Sodium Phosphate Drugs in Large Bowel Prep for Endoscopy Worsen Renal Function?
Background: Proper bowel preparation is essential for adequate colonoscopy and flexible sigmoidoscopy. Oral agents that are most commonly used for bowel preparation are sodium phosphate drugs, polyethylglycol and magnesium citrate. Sodium phosphate drugs are often preferred because of the decreased amount of fluid necessary for bowel preparation.
Study design: Retrospective study.
Setting: Scott and White Clinic, Temple, Texas.
Synopsis: Researchers compared 286 patients receiving an oral sodium phosphate solution for colonoscopy bowel preparation with 125 patients with similar comorbidities who received a non-sodium phosphate solution for bowel preparation. All patients had normal baseline creatinine levels.
The baseline, six-month, and one-year glomerular filtration rates (GFR) were compared between the two groups. GFR declined from 79 to 73 to 71 ml/min/1.73 m2 in the study group vs. 76 to 74 to 74 ml/min/1.73 m2 in the control group for the baseline, six-month, and one-year time periods, respectively.
This is an observational study and thus limited by its non-randomized nature. Sodium phosphate has a black-box warning in stage four and five chronic kidney disease because of its deleterious effect on renal function and the potential for inducing electrolyte abnormalities. Given the findings of this study and the availability of other effective preps alternative regimens should be considered for colonic preparation.
Bottom line: Oral sodium phosphate drugs may cause an acute and chronic decline in renal function as measured by the GFR.
Citation: Khurana A, McLean L, Atkinson S, Foulks C. The effect of oral sodium phosphate drug products on renal function in adults is undergoing bowel endoscopy. Arch Intern Med. 2008; 168(6):593-597.
Does MICR Improve Survival-to-hospital Discharge vs. Traditional CPR and ACLS in Cardiac Arrest Outside the Hospital?
Background: Minimally interrupted cardiac resuscitation (MICR), also known as cardiocerebral resuscitation, is hypothesized to increase survival compared with traditional CPR and advanced cardiac life support (ACLS) in out-of-hospital cardiac arrest. In MICR, 200 “pre-shock” chest compressions (100 compressions/minute) are initially given. The rhythm is then analyzed, with a single shock given if indicated.
Study design: Prospective study.
Setting: Two cities in Arizona.
Synopsis: Using data in the Save Heart in Arizona Registry and Education (SHARE) program, outcomes of 218 individuals with cardiac arrest receiving traditional CPR/ACLS were compared to 668 individuals after MICR training was instituted in the same two metropolitan cities. Survival-to-hospital discharge increased from 1.8% (4/218) before MICR training to 5.4% (36/668) after MICR training. The authors then compared the outcomes of 1,799 individuals with cardiac arrest resuscitated by emergency medical services (EMS) who did not receive training in MICR to 661 individuals who received MICR training over the same period. Survival-to-hospital discharge was 9.1% (60/601) in the patients cared from by EMS that received MICR training versus 3.8% (69/1730) in their non-MICR trained colleagues.
This study is limited by its observational nature and lack of randomization. Surprisingly, more individuals were intubated in the MICR groups. For hospitalists, the results could have a dramatic affect on cardiac arrest survival and lead to future changes to CPR/ACLS protocols.
Bottom line: MICR has a significant impact on survival in out-of-hospital cardiac arrest as compared with traditional CPR and ACLS.
Citation: Bobrow B, Clark L, Ewy G, et al. Minimally interrupted cardiac resuscitation by emergency medical services for out-of-hospital cardiac arrest. JAMA. 2008;299(10):1158-1165.
Does Lower aPTT Increase Future VTE Independent of Other Pro-coagulant Factors?
Background: Certain factors, such as obesity, D-dimer levels, and factor V Leiden gene mutations, increase the risk of future venous thromboembolism (VTE) events. This study sought to determine whether lower baseline levels of activated partial thromboplastin time aPTT also increase this risk.
Study design: Prospective multicenter cohort study.
Setting: Longitudinal Investigation of Thromboembolism Etiology research study (Atherosclerosis Risk in Communities portion) in four U.S. communities.
Synopsis: 13,880 individuals with baseline aPTT measurements were followed for 13 years for future VTE events. Of those, 260 developed a VTE of which 111 were described as idiopathic. Individuals in the lowest two quartiles of aPTT compared with the highest fourth quartile had a 2.4-fold and 1.9-fold increase in the risk of VTE, respectively. A lower aPTT further increased the risk of VTE when associated with obesity, elevated D-dimer level, and particularly factor V Leiden.
This study was limited by the relatively small number of VTE events. It also did not clarify whether aPTT measurements in high-risk groups such as those with positive family history of VTE were useful for predicting risk of future VTE. For hospitalists, patients with a lower initial aPTT may warrant more aggressive inpatient DVT prophylaxis.
Bottom line: aPTT below the median level increases the risk of future VTE events, especially if associated with obesity, elevated D-dimer levels, and/or factor V Leiden.
Citation: Zakai NA, Ohira T, White R, Folsom A, Cushman M. Activated partial thromboplastin time and risk of future venous thromboembolism. Am J of Med. 2008;121:231-238.
What Bleeding Outcomes are Associated with Using Warfarin with Antiplatelet Agents?
Background: Despite a high prevalence of combining antiplatelet and warfarin therapy, the timing, safety, and efficacy of this strategy remain controversial.
Study design: Retrospective cohort study.
Setting: Kaiser Permanente Colorado.
Synopsis: Using a pharmacy database, the authors identified 2,560 patients receiving warfarin alone (monotherapy cohort) and 1,623 patients receiving warfarin combined with antiplatelet agents (combination therapy cohort).
In the combination therapy cohort, aspirin was the most common antiplatelet agent (37%) followed by clopidogrel (13%) and dipyridamole (2%). During a six-month period, the combination therapy cohort had a 4.2% risk of hemorrhage and a 2.0% risk of major hemorrhage. Warfarin monotherapy was associated with a 2% risk of hemorrhage and 0.9% risk of major hemorrhage.
At baseline, the combination therapy patients were twice as likely to have diabetes or congestive heart failure and four times as likely to have coronary artery disease. In both cohorts, the most common reason for warfarin therapy was atrial fibrillation.
Since this was a retrospective investigation, hospitalists should be careful about drawing conclusions from this study alone, but are reminded to discuss risks carefully and engage in shared decision-making with patients when using combined warfarin and antiplatelet therapy.
Bottom line: Warfarin use in combination with antiplatelet therapy is associated with more than double the risk of bleeding compared with warfarin monotherapy.
Citation: Johnson SG, Rogers K, Delate T, Witt DM. Outcomes associated with combined antiplatelet and anticoagulant therapy. Chest. 2008;133:948-954.
Does a Rise in Serum Creatinine Affect Post-hospitalization Mortality and ESRD in Elderly MI Patients?
Background: Previous studies found an association between small changes in serum creatinine during hospitalization and short-term mortality. Data has shown patients experiencing a rise in creatinine at the time of CABG have increased in-hospital and long-term follow-up mortality.
Study design: Retrospective cohort study
Setting: Nationwide Medicare database of acute MI hospitalizations.
Synopsis: The authors reviewed outcomes data for 87,094 patients hospitalized for acute myocardial infarction (MI) from 1994-1995 with follow-up data through 2004. Patients were classified into groups with no rise in creatinine during hospitalization and those with rises of 0.1 mg/dL, 0.2 mg/dL, 0.3-0.5 mg/dL, and 0.6-3 mg/dL.
Compared with patients with no rise in creatinine, a rise of 0.1 mg/dL was associated with an adjusted hazard ratio of 1.45 for end-stage renal disease (ESRD) and 1.14 for post-hospitalization death during long-term follow-up. An incremental increase in poor outcomes was seen with more dramatic increases in creatinine, with patients in the group with a 0.6-3 mg/dL rise in creatinine having an adjusted hazard ratio of 3.26 for ESRD and 1.39 for post-hospitalization death. Among patients with a creatinine rise, the absolute risk of mortality (15% annually) was greater than that of ESRD (0.3% annually).
Hospitalists should note limitations of this retrospective study, including its restriction to hospitalized elderly patients.
Bottom line: Even small rises in serum creatinine during acute hospitalization for MI are associated with long-term risk for death and ESRD in elderly patients.
Citation: Newsome BB, Warnock DG, McClellan WM, et al. Long-term risk of mortality and end-stage renal disease among the elderly after small increases in serum creatinine level during hospitalization for acute myocardial infarction. Arch Intern Med. 2008;168(6):609-616.
Does Direct-to-patient Communication Improve Adherence to Beta-blocker Therapy Following an MI?
Background: The joint American Heart Association and American College of Cardiology guidelines have specific treatment recommendations regarding care of a patient post-myocardial infarction (MI). A key component of this regimen is beta-blocker therapy. Beta-blockers routinely are prescribed at hospital discharge following MI; however, patient adherence has been shown to decline substantially over time.
Study design: Cluster randomized control trial.
Setting: Four health maintenance organizations in Boston, Minneapolis, Atlanta, and Portland, Ore.
Synopsis: 836 post-MI patients were given a beta-blocker prescription upon discharge from the hospital. The intervention group received two mailed communications. The first was a personalized, simply worded letter from a health plan physician-administrator, followed two months later by a similar letter with a brochure. Mailers were low cost and easily replicable; they addressed the importance of these medications, the risks of non-adherence, and adverse effects.
The primary outcome measure was beta-blocker adherence. Medication adherence was analyzed as a continuous measure and as a monthly proportion of days covered (PDC) of 80% or greater. Across all months of follow-up, a mean of 64.8% of intervention patients had a PDC of more than 80% compared with 58.5% of control group patients (number needed to treat=16). The intervention group was 17% more likely to have a PDC of 80% or greater over the entire post-intervention period.
These interventions were studied in a prepaid integrated care delivery system—limiting generalization to other insurance types. Nevertheless, finding ways to improve patient compliance and decrease recurrent cardiac events is liking to result in cost saving to any healthcare plan.
Bottom line: A low-cost direct-to-patient communication effort can have a positive effect on beta-blocker adherence following MI.
Citation: Smith DH, Kramer JM, Perrin N, et al. A randomized trial of direct-to-patient communication to enhance adherence to beta-blocker therapy following myocardial infarction. Arch Intern Med. 2008;168(5):477-483. TH
Literature at a Glance
A guide to this month’s studies.
- Survival of in-hospital cardiac arrest decreases during nights and weekends.
- C-reactive protein levels predict severity and complications in community-acquired pneumonia.
- Adherence to current guidelines improves outcome in treatment of prosthetic joint infection.
- Sodium phosphate bowel prep use is associated with a decline in GFR.
- Minimally interrupted cardiac resuscitation improves survival.
- Lower aPTT increases risk for future VTE.
- Warfarin combined with antiplatelet therapy increases hemorrhage rate.
- Creatinine rise during MI hospitalization is associated with long-term risk of death and ESRD.
- Communication improves patient adherence to beta-blockers after MI.
Does Time of Day Affect Survival of Cardiac Arrest Patients?
Background: In-hospital cardiac arrest is a major public health problem. Small studies have demonstrated survival after cardiac arrest is worse at night as compared with all other times. Multiple hypothesis are proffered for this decreased survival, including less effective detection and treatment of the warning signs of impending arrest during the night hours.
Study design: Prospective registry.
Setting: 507 hospitals participating through the National Registry of Cardiopulmonary Resuscitation.
Synopsis: 86,748 consecutive, inpatient cardiac arrests were reported from Jan. 1, 2000, through Feb. 1, 2007, including 58,593 cases during day/evening hours and 28,155 cases during night hours.
Rates of survival to discharge (14.7 % vs. 19.8%), survival at 24 hours (28.9% vs. 35.4%), and favorable neurological outcomes (11.0% vs. 15.2%) were substantially lower during the night compared with day/evening (all p values < 0.001). The first documented rhythm at night was more frequently asystole as opposed to ventricular fibrillation during the day/evening. There also was a higher survival rate with cardiac arrests during day/evening hours occurring on weekdays compared with weekends (odds ratio [OR] 1.15). There was no difference in survival rates between weekdays or weekends among cardiac arrests occurring during the night hours.
Bottom line: Survival rates for in-hospital cardiac arrest are lower during nights and weekends, which may relate to differential physician and hospital staffing patterns during these hours.
Citation: Peberdy MA, Ornato JP, Larkin GL et al. Survival from in-hospital cardiac arrest during nights and weekends. JAMA 2008;299:785-792.
Can CRP Identify Risk in CAP Patients?
Background: Small initial studies suggest an elevated C-reactive protein (CRP) is relatively nonspecific but may have a role in predicting disease severity in community-acquired pneumonia (CAP).
Study design: Prospective study.
Setting: Large academic center in the United Kingdom.
Synopsis: In this study of 570 patients over a two-year time period, all patients presenting to the hospital with a diagnosis of CAP and the absence of exclusion criteria were evaluated. CRP was measured on admission and repeated on day four of hospitalization.
Low CRP levels (less than 100 mg/L) were independently associated with a reduced risk of 30-day mortality (OR 0.18; p=0.03), need for invasive ventilation and/or inotropic support (OR 0.21; p=0.002), and complicated pneumonia (OR 0.05; p=0.003). In addition, the failure of CRP to fall by 50% or more at day four of hospitalization was associated with an increased risk of 30-day mortality (OR 24.5; p<0.0001), need for mechanical ventilation and/or inotropic support (OR 7.1; p<0.0001), and complicated pneumonia (OR 15.4; p<0.0001).
Patients with chronic lung disease, immunosuppression, active malignancy or hospital-acquired pneumonia were excluded from the study and the conclusions cannot be extrapolated to these higher risk populations.
Bottom line: C-reactive protein is an independent marker of severity in CAP, and low levels can be used as an adjunct to clinical judgment to help identify patients who may be safely discharged from the hospital.
Citation: Chalmers JD, Singanayagam A, Hill AT. C-reactive protein is an independent predictor of severity in community-acquired pneumonia. Am J of Med. 2008;121:219-225.
Do Aggressive Surgical Intervention and Antimicrobial Treatment Improve Outcomes in Patients Suffering PJI?
Background: Prosthetic joint infection (PJI) is a severe complication, causing significant morbidity and healthcare costs. A recent article put forth up to date guidelines for the management of PJI. The purpose of this current study was to evaluate the external clinical validity of these treatment recommendations.
Study design: Retrospective cohort analysis.
Setting: 1,000-bed tertiary care center in Switzerland.
Synopsis: 68 consecutive episodes of PJI from January 1995 through December 2004 were reviewed. Patients with polymicrobial infections and with treatment failures prior to referral to this center were included.
The success rate for treatment of PJI was highest (67%) when the surgical strategy met current recommendations and antimicrobial treatment was adequate or partially adequate. The preferred surgical strategy was a two-stage exchange. The risk of treatment failure was higher for PJI treated with a surgical strategy other than that recommended (hazard ratio [HR] 2.34, p=0.01) and for PJIs treated with antibiotics not corresponding to recommendations (HR 3.45, p=0.002).
This study was limited by its small sample size and retrospective nature. Patients were not randomized, and cure rates for PJI were significantly lower than in prior published studies.
Bottom line: Treatment of PJI in higher risk populations in accordance with currently recommended surgical and antimicrobial treatment recommendations is associated with better outcomes and cure rates.
Citation: Betsch BY, Eggli S, Siebenrock KA, Tauber MG, Muhlemann K. Treatment of joint prosthesis infection in accordance with current recommendations improves outcome. Clin Infect Dis. 2008;46:1221-1226.
Do Oral Sodium Phosphate Drugs in Large Bowel Prep for Endoscopy Worsen Renal Function?
Background: Proper bowel preparation is essential for adequate colonoscopy and flexible sigmoidoscopy. Oral agents that are most commonly used for bowel preparation are sodium phosphate drugs, polyethylglycol and magnesium citrate. Sodium phosphate drugs are often preferred because of the decreased amount of fluid necessary for bowel preparation.
Study design: Retrospective study.
Setting: Scott and White Clinic, Temple, Texas.
Synopsis: Researchers compared 286 patients receiving an oral sodium phosphate solution for colonoscopy bowel preparation with 125 patients with similar comorbidities who received a non-sodium phosphate solution for bowel preparation. All patients had normal baseline creatinine levels.
The baseline, six-month, and one-year glomerular filtration rates (GFR) were compared between the two groups. GFR declined from 79 to 73 to 71 ml/min/1.73 m2 in the study group vs. 76 to 74 to 74 ml/min/1.73 m2 in the control group for the baseline, six-month, and one-year time periods, respectively.
This is an observational study and thus limited by its non-randomized nature. Sodium phosphate has a black-box warning in stage four and five chronic kidney disease because of its deleterious effect on renal function and the potential for inducing electrolyte abnormalities. Given the findings of this study and the availability of other effective preps alternative regimens should be considered for colonic preparation.
Bottom line: Oral sodium phosphate drugs may cause an acute and chronic decline in renal function as measured by the GFR.
Citation: Khurana A, McLean L, Atkinson S, Foulks C. The effect of oral sodium phosphate drug products on renal function in adults is undergoing bowel endoscopy. Arch Intern Med. 2008; 168(6):593-597.
Does MICR Improve Survival-to-hospital Discharge vs. Traditional CPR and ACLS in Cardiac Arrest Outside the Hospital?
Background: Minimally interrupted cardiac resuscitation (MICR), also known as cardiocerebral resuscitation, is hypothesized to increase survival compared with traditional CPR and advanced cardiac life support (ACLS) in out-of-hospital cardiac arrest. In MICR, 200 “pre-shock” chest compressions (100 compressions/minute) are initially given. The rhythm is then analyzed, with a single shock given if indicated.
Study design: Prospective study.
Setting: Two cities in Arizona.
Synopsis: Using data in the Save Heart in Arizona Registry and Education (SHARE) program, outcomes of 218 individuals with cardiac arrest receiving traditional CPR/ACLS were compared to 668 individuals after MICR training was instituted in the same two metropolitan cities. Survival-to-hospital discharge increased from 1.8% (4/218) before MICR training to 5.4% (36/668) after MICR training. The authors then compared the outcomes of 1,799 individuals with cardiac arrest resuscitated by emergency medical services (EMS) who did not receive training in MICR to 661 individuals who received MICR training over the same period. Survival-to-hospital discharge was 9.1% (60/601) in the patients cared from by EMS that received MICR training versus 3.8% (69/1730) in their non-MICR trained colleagues.
This study is limited by its observational nature and lack of randomization. Surprisingly, more individuals were intubated in the MICR groups. For hospitalists, the results could have a dramatic affect on cardiac arrest survival and lead to future changes to CPR/ACLS protocols.
Bottom line: MICR has a significant impact on survival in out-of-hospital cardiac arrest as compared with traditional CPR and ACLS.
Citation: Bobrow B, Clark L, Ewy G, et al. Minimally interrupted cardiac resuscitation by emergency medical services for out-of-hospital cardiac arrest. JAMA. 2008;299(10):1158-1165.
Does Lower aPTT Increase Future VTE Independent of Other Pro-coagulant Factors?
Background: Certain factors, such as obesity, D-dimer levels, and factor V Leiden gene mutations, increase the risk of future venous thromboembolism (VTE) events. This study sought to determine whether lower baseline levels of activated partial thromboplastin time aPTT also increase this risk.
Study design: Prospective multicenter cohort study.
Setting: Longitudinal Investigation of Thromboembolism Etiology research study (Atherosclerosis Risk in Communities portion) in four U.S. communities.
Synopsis: 13,880 individuals with baseline aPTT measurements were followed for 13 years for future VTE events. Of those, 260 developed a VTE of which 111 were described as idiopathic. Individuals in the lowest two quartiles of aPTT compared with the highest fourth quartile had a 2.4-fold and 1.9-fold increase in the risk of VTE, respectively. A lower aPTT further increased the risk of VTE when associated with obesity, elevated D-dimer level, and particularly factor V Leiden.
This study was limited by the relatively small number of VTE events. It also did not clarify whether aPTT measurements in high-risk groups such as those with positive family history of VTE were useful for predicting risk of future VTE. For hospitalists, patients with a lower initial aPTT may warrant more aggressive inpatient DVT prophylaxis.
Bottom line: aPTT below the median level increases the risk of future VTE events, especially if associated with obesity, elevated D-dimer levels, and/or factor V Leiden.
Citation: Zakai NA, Ohira T, White R, Folsom A, Cushman M. Activated partial thromboplastin time and risk of future venous thromboembolism. Am J of Med. 2008;121:231-238.
What Bleeding Outcomes are Associated with Using Warfarin with Antiplatelet Agents?
Background: Despite a high prevalence of combining antiplatelet and warfarin therapy, the timing, safety, and efficacy of this strategy remain controversial.
Study design: Retrospective cohort study.
Setting: Kaiser Permanente Colorado.
Synopsis: Using a pharmacy database, the authors identified 2,560 patients receiving warfarin alone (monotherapy cohort) and 1,623 patients receiving warfarin combined with antiplatelet agents (combination therapy cohort).
In the combination therapy cohort, aspirin was the most common antiplatelet agent (37%) followed by clopidogrel (13%) and dipyridamole (2%). During a six-month period, the combination therapy cohort had a 4.2% risk of hemorrhage and a 2.0% risk of major hemorrhage. Warfarin monotherapy was associated with a 2% risk of hemorrhage and 0.9% risk of major hemorrhage.
At baseline, the combination therapy patients were twice as likely to have diabetes or congestive heart failure and four times as likely to have coronary artery disease. In both cohorts, the most common reason for warfarin therapy was atrial fibrillation.
Since this was a retrospective investigation, hospitalists should be careful about drawing conclusions from this study alone, but are reminded to discuss risks carefully and engage in shared decision-making with patients when using combined warfarin and antiplatelet therapy.
Bottom line: Warfarin use in combination with antiplatelet therapy is associated with more than double the risk of bleeding compared with warfarin monotherapy.
Citation: Johnson SG, Rogers K, Delate T, Witt DM. Outcomes associated with combined antiplatelet and anticoagulant therapy. Chest. 2008;133:948-954.
Does a Rise in Serum Creatinine Affect Post-hospitalization Mortality and ESRD in Elderly MI Patients?
Background: Previous studies found an association between small changes in serum creatinine during hospitalization and short-term mortality. Data has shown patients experiencing a rise in creatinine at the time of CABG have increased in-hospital and long-term follow-up mortality.
Study design: Retrospective cohort study
Setting: Nationwide Medicare database of acute MI hospitalizations.
Synopsis: The authors reviewed outcomes data for 87,094 patients hospitalized for acute myocardial infarction (MI) from 1994-1995 with follow-up data through 2004. Patients were classified into groups with no rise in creatinine during hospitalization and those with rises of 0.1 mg/dL, 0.2 mg/dL, 0.3-0.5 mg/dL, and 0.6-3 mg/dL.
Compared with patients with no rise in creatinine, a rise of 0.1 mg/dL was associated with an adjusted hazard ratio of 1.45 for end-stage renal disease (ESRD) and 1.14 for post-hospitalization death during long-term follow-up. An incremental increase in poor outcomes was seen with more dramatic increases in creatinine, with patients in the group with a 0.6-3 mg/dL rise in creatinine having an adjusted hazard ratio of 3.26 for ESRD and 1.39 for post-hospitalization death. Among patients with a creatinine rise, the absolute risk of mortality (15% annually) was greater than that of ESRD (0.3% annually).
Hospitalists should note limitations of this retrospective study, including its restriction to hospitalized elderly patients.
Bottom line: Even small rises in serum creatinine during acute hospitalization for MI are associated with long-term risk for death and ESRD in elderly patients.
Citation: Newsome BB, Warnock DG, McClellan WM, et al. Long-term risk of mortality and end-stage renal disease among the elderly after small increases in serum creatinine level during hospitalization for acute myocardial infarction. Arch Intern Med. 2008;168(6):609-616.
Does Direct-to-patient Communication Improve Adherence to Beta-blocker Therapy Following an MI?
Background: The joint American Heart Association and American College of Cardiology guidelines have specific treatment recommendations regarding care of a patient post-myocardial infarction (MI). A key component of this regimen is beta-blocker therapy. Beta-blockers routinely are prescribed at hospital discharge following MI; however, patient adherence has been shown to decline substantially over time.
Study design: Cluster randomized control trial.
Setting: Four health maintenance organizations in Boston, Minneapolis, Atlanta, and Portland, Ore.
Synopsis: 836 post-MI patients were given a beta-blocker prescription upon discharge from the hospital. The intervention group received two mailed communications. The first was a personalized, simply worded letter from a health plan physician-administrator, followed two months later by a similar letter with a brochure. Mailers were low cost and easily replicable; they addressed the importance of these medications, the risks of non-adherence, and adverse effects.
The primary outcome measure was beta-blocker adherence. Medication adherence was analyzed as a continuous measure and as a monthly proportion of days covered (PDC) of 80% or greater. Across all months of follow-up, a mean of 64.8% of intervention patients had a PDC of more than 80% compared with 58.5% of control group patients (number needed to treat=16). The intervention group was 17% more likely to have a PDC of 80% or greater over the entire post-intervention period.
These interventions were studied in a prepaid integrated care delivery system—limiting generalization to other insurance types. Nevertheless, finding ways to improve patient compliance and decrease recurrent cardiac events is liking to result in cost saving to any healthcare plan.
Bottom line: A low-cost direct-to-patient communication effort can have a positive effect on beta-blocker adherence following MI.
Citation: Smith DH, Kramer JM, Perrin N, et al. A randomized trial of direct-to-patient communication to enhance adherence to beta-blocker therapy following myocardial infarction. Arch Intern Med. 2008;168(5):477-483. TH
SHM Explores Social Networks
Dear John Q. Hospitalist,
Recently, a pair of college students in our office presented an impressive summary of Web 2.0, including Facebook.com and LinkedIn.com, to the rest of the SHM staff.
As I listened to their presentation and heard the energy in their voices, I couldn’t help but think about my initial experience and excitement with the World Wide Web. Instead of doing homework, I spent many late nights searching the Internet looking for more information to help me create my first Web page. After countless hours of coding and debugging, as well as throwing the keyboard a time or two, I published my Web page and became a part of the Internet. I was hooked.
After listening to these students I was inspired to check out LinkedIn.com and create my own LinkedIn profile. While I did not stay up until the very early morning sending invites or completing every part of my profile, I found connections to old colleagues, college friends, high school buddies, and family members. Today, I eagerly await the flood of e-mail from people accepting me as a friend in their network, some of them members of SHM. I am hooked again.
Seeing SHM members on LinkedIn got me thinking about how SHM might use social networking technology. I think there is an opportunity here to create an interactive resource that will empower hospitalists to find other hospitalists, make connections, and build their own networks. I’m interested in getting your perspective. Do you think our members will use this type of an online resource?
Many social networking sites on the Internet grew out of individuals in an academic setting trying to find ways to connect with each other. I would imagine many of our student and resident members already are using social networking sites. Do you think this is the case? If so, what features and functions of a social networking tool do you think are most important? Is that different from a third-year resident, or a hospitalist who has been practicing hospital medicine for a number of years?
I know I have thrown a bunch of questions at you, so let me share with you some ideas and maybe we can begin a dialogue that will help SHM find ways in which we can leverage social networking and other Web 2.0 tools.
One of the tasks in creating a LinkedIn account is selecting the college or institution you attended and the years in which you attended. Immediately after setting up my account I was able to see the names of other alumni who attended my university during my four years and invite old friends to join my network. I can envision a scenario where an SHM member indicates which medical school he or she attended and is able to see a list of other colleagues who attended at the same time.
For the general member, someone who hasn’t attended a meeting, participated in a committee, or been more actively engaged in SHM, an online network might be a first step to increased involvement with SHM. Members could use this site to connect with other hospitalists in their area and share their interests and experience with others.
Along the way, they might learn about an SHM initiative they are interested in and connect with another hospitalist who working on this project and begin to have a dialogue. Throughout time, this person builds their network and establishes new connections. When it’s time to register for next year’s SHM Annual Meeting in Chicago, they already know a few faces in the crowd—and maybe a couple of them have become friends.
These are just a couple of ways I think SHM and our members might benefit from social networking. I am confident there are many, many more ways this technology can help our members and the hospital medicine community. What do you think? I would love to hear your thoughts and ideas. E-mail me at [email protected]. TH
Dear John Q. Hospitalist,
Recently, a pair of college students in our office presented an impressive summary of Web 2.0, including Facebook.com and LinkedIn.com, to the rest of the SHM staff.
As I listened to their presentation and heard the energy in their voices, I couldn’t help but think about my initial experience and excitement with the World Wide Web. Instead of doing homework, I spent many late nights searching the Internet looking for more information to help me create my first Web page. After countless hours of coding and debugging, as well as throwing the keyboard a time or two, I published my Web page and became a part of the Internet. I was hooked.
After listening to these students I was inspired to check out LinkedIn.com and create my own LinkedIn profile. While I did not stay up until the very early morning sending invites or completing every part of my profile, I found connections to old colleagues, college friends, high school buddies, and family members. Today, I eagerly await the flood of e-mail from people accepting me as a friend in their network, some of them members of SHM. I am hooked again.
Seeing SHM members on LinkedIn got me thinking about how SHM might use social networking technology. I think there is an opportunity here to create an interactive resource that will empower hospitalists to find other hospitalists, make connections, and build their own networks. I’m interested in getting your perspective. Do you think our members will use this type of an online resource?
Many social networking sites on the Internet grew out of individuals in an academic setting trying to find ways to connect with each other. I would imagine many of our student and resident members already are using social networking sites. Do you think this is the case? If so, what features and functions of a social networking tool do you think are most important? Is that different from a third-year resident, or a hospitalist who has been practicing hospital medicine for a number of years?
I know I have thrown a bunch of questions at you, so let me share with you some ideas and maybe we can begin a dialogue that will help SHM find ways in which we can leverage social networking and other Web 2.0 tools.
One of the tasks in creating a LinkedIn account is selecting the college or institution you attended and the years in which you attended. Immediately after setting up my account I was able to see the names of other alumni who attended my university during my four years and invite old friends to join my network. I can envision a scenario where an SHM member indicates which medical school he or she attended and is able to see a list of other colleagues who attended at the same time.
For the general member, someone who hasn’t attended a meeting, participated in a committee, or been more actively engaged in SHM, an online network might be a first step to increased involvement with SHM. Members could use this site to connect with other hospitalists in their area and share their interests and experience with others.
Along the way, they might learn about an SHM initiative they are interested in and connect with another hospitalist who working on this project and begin to have a dialogue. Throughout time, this person builds their network and establishes new connections. When it’s time to register for next year’s SHM Annual Meeting in Chicago, they already know a few faces in the crowd—and maybe a couple of them have become friends.
These are just a couple of ways I think SHM and our members might benefit from social networking. I am confident there are many, many more ways this technology can help our members and the hospital medicine community. What do you think? I would love to hear your thoughts and ideas. E-mail me at [email protected]. TH
Dear John Q. Hospitalist,
Recently, a pair of college students in our office presented an impressive summary of Web 2.0, including Facebook.com and LinkedIn.com, to the rest of the SHM staff.
As I listened to their presentation and heard the energy in their voices, I couldn’t help but think about my initial experience and excitement with the World Wide Web. Instead of doing homework, I spent many late nights searching the Internet looking for more information to help me create my first Web page. After countless hours of coding and debugging, as well as throwing the keyboard a time or two, I published my Web page and became a part of the Internet. I was hooked.
After listening to these students I was inspired to check out LinkedIn.com and create my own LinkedIn profile. While I did not stay up until the very early morning sending invites or completing every part of my profile, I found connections to old colleagues, college friends, high school buddies, and family members. Today, I eagerly await the flood of e-mail from people accepting me as a friend in their network, some of them members of SHM. I am hooked again.
Seeing SHM members on LinkedIn got me thinking about how SHM might use social networking technology. I think there is an opportunity here to create an interactive resource that will empower hospitalists to find other hospitalists, make connections, and build their own networks. I’m interested in getting your perspective. Do you think our members will use this type of an online resource?
Many social networking sites on the Internet grew out of individuals in an academic setting trying to find ways to connect with each other. I would imagine many of our student and resident members already are using social networking sites. Do you think this is the case? If so, what features and functions of a social networking tool do you think are most important? Is that different from a third-year resident, or a hospitalist who has been practicing hospital medicine for a number of years?
I know I have thrown a bunch of questions at you, so let me share with you some ideas and maybe we can begin a dialogue that will help SHM find ways in which we can leverage social networking and other Web 2.0 tools.
One of the tasks in creating a LinkedIn account is selecting the college or institution you attended and the years in which you attended. Immediately after setting up my account I was able to see the names of other alumni who attended my university during my four years and invite old friends to join my network. I can envision a scenario where an SHM member indicates which medical school he or she attended and is able to see a list of other colleagues who attended at the same time.
For the general member, someone who hasn’t attended a meeting, participated in a committee, or been more actively engaged in SHM, an online network might be a first step to increased involvement with SHM. Members could use this site to connect with other hospitalists in their area and share their interests and experience with others.
Along the way, they might learn about an SHM initiative they are interested in and connect with another hospitalist who working on this project and begin to have a dialogue. Throughout time, this person builds their network and establishes new connections. When it’s time to register for next year’s SHM Annual Meeting in Chicago, they already know a few faces in the crowd—and maybe a couple of them have become friends.
These are just a couple of ways I think SHM and our members might benefit from social networking. I am confident there are many, many more ways this technology can help our members and the hospital medicine community. What do you think? I would love to hear your thoughts and ideas. E-mail me at [email protected]. TH