User login
Transsexualism: Clinical guide to gender identity disorder
Adults with gender identity disorder (GID)—commonly termed transsexualism—may seek psychiatric assessment and treatment for a variety of reasons. Some—but not all—might be candidates for hormone replacement therapies or sex reassignment surgery (SRS). For those with gender dysphoria, psychological assessment and psychotherapy are suggested and sometimes required.
Your role in the GID patient’s gender exploration and transition must be tailored to his or her gender identity and individual circumstances. For patients who are not candidates for surgery or cannot afford it, you may assist in exploring options for living with one’s gender identity.
WHAT IS GID?
Gender identity disorder is a rare, complex condition in which individuals of unambiguous genotype and phenotype identify with the opposite gender. One in 54,000 individuals are estimated to have GID:
- 75% are biologic males desiring reassignment to female gender (MTF)
- 25% are females desiring to be male (FTM).1
Table 1
DSM-IV-TR criteria for gender identity disorder
| Criterion A | A strong and persistent cross-gender identification defined as the desire to be or the insistence that one is of the other sex (must not be merely a desire for any perceived cultural advantages of being the other sex) |
| Criterion B | Persistent discomfort with one’s assigned sex or a sense of inappropriateness in the gender role of that sex |
| Criterion C | The disturbance is not concurrent with a physical intersex condition (such as partial androgen insensitivity syndrome or congenital adrenal hyperplasia) |
| Criterion D | The disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning |
| Source: Reference 2 | |
ICD-10 diagnoses for gender identity disorder in adults
| Diagnosis | Criteria |
|---|---|
| Transsexualism |
|
| Dual-role transvestism |
|
| Other gender identity disorders | No specific criteria; could be used for persons with an intersexed condition |
| Gender identify disorder, unspecified | No specific criteria; could be used for persons with an intersexed condition |
| Source: Adapted from International Classification of Diseases, 10th ed. (ICD-10) | |
Epidemiologic studies of GID are rare, but in a survey by Rachlin et al4 of 23 MTFs and 70 FTMs:
- most underwent hormone therapy (64% of MTFs, 80% of FTMs) and/or name change (45% of MTFs, 72% of FTMs)
- none of the MTFs had breast augmentation, whereas 52% of FTMs had undergone mastectomy and reconstruction and another 33% were actively planning it
- 3% of FTMs had genital surgery, 16% were planning it, and 29% had decided definitely not to have it
- 9% of MTFs decided definitely not to have genital surgery; 23% had undergone genital surgery, and another 35% were actively planning it.
Biologic basis. GID’s cause remains unknown. Organic differences in brain anatomy have been identified in patients with GID. Zhou et al6 showed that the volume of the central subdivision of the bed nucleus of the stria terminalis (BSTc)—a brain area essential for sexual behavior—is larger in men than in women. A female-sized BSTc was found in MTF GID patients.
Research, mainly on biologic boys, indicates that GIDs are usually associated with behavioral difficulties, relationship problems with peers and parents, and—most notably—separation anxiety disorder.7 An audit of the files of 124 children and adolescents with GID showed that 42% experienced loss of one or both parents, mainly through separation.8
Psychiatric comorbidity. Studies using standardized diagnostic instruments to assess psychiatric comorbidity in GID are rare. A study of 31 patients with GID found that many met diagnostic criteria for lifetime psychiatric comorbidity, including:
- 71% for Axis I disorders (primarily mood and anxiety disorders)
- 42% for comorbid personality disorders, primarily a cluster B diagnosis
- 45% for substance-related disorders
- 6.5% for psychotic disorders
- 3.2% for eating disorders.9
TREATING PATIENTS WITH GID
Psychotherapy. GID treatment decisions are made without clear prospective data. Standards of care are determined by the World Professional Association for Transgender Health (WPATH).12 Psychotherapy is often given before SRS but is not required. The therapist is left to determine the treatment terms and goals.
Your role in treating patients with GID goes beyond making an accurate diagnosis, identifying comorbid psychopathology, and instituting a treatment plan. Other tasks include:
- counseling the patient about the range of treatment options and their implications
- engaging in psychotherapy
- ascertaining eligibility and readiness for hormones and surgical therapy
- making formal recommendations to medical and surgical colleagues
- documenting the patient’s relevant history in a letter of recommendation
- educating support systems
- being available for follow-up.
Candidates for triadic therapy. For appropriately screened adults with severe GID, the therapeutic approach relies on triadic therapy:
- a 3-phase approach centered around real-life experience in the desired role
- hormones of the desired gender
- and surgery to change the genitalia and secondary sex characteristics.
HORMONE THERAPY
WPATH has established eligibility and readiness criteria for HRT in patients with GID (Table 3). Administering cross-sex hormones (testosterone in women; estrogens in men) brings about important physical changes as well as psychological relief. The prescribing physician need not be an endocrinologist but should become well-versed in relevant data.
Table 3
WPATH criteria for hormone replacement therapy*
| Eligibility criteria 3 criteria exist |
|
| Readiness criteria All 3 must exist |
|
| Source: World Professional Association for Transgender Health (WPATH) | |
Table 4
Sample hormonal regimens for transsexual patients*
| Medication | Starting dose | Subsequent dose | When to change doses | |
|---|---|---|---|---|
| Female to male | Testosterone enanthanate or testosterone cypionate | 200 mg IM every 2 weeks | 100 to 150 mg IM every 2 weeks | After masculinization complete and/or oophorectomy/hysterectomy |
| Transdermal testosterone | 5 mg to skin every day | Usually stays the same | Little data exist on efficacy; effective for maintenance, and may be less efficacious during transition | |
| Male to female | Conjugated estrogens | 1.25 mg/d (or 0.625 mg/d for smokers) | 2.5 mg/d (Do not increase in smokers) | To obtain best clinical results, or if testosterone is not suppressed After sexual reassignment surgery, dose may be decreased without losing secondary sexual characteristics |
| OR oral estradiol | 1 mg/d | 2 mg/d | ||
| OR transdermal estradiol | 0.1 mg patch/week | Two 0.1 mg patches/week | ||
| Spironolactone | 200 mg/d | May discontinue | After sexual assignment surgery | |
| Medroxyprogesterone† | 10 mg/d | May increase to 20 to 40 mg/d (usually not needed) | If testosterone is not suppressed and patient/doctor does not want to increase estrogen | |
| OR micronized progesterone | 100 mg bid | May discontinue after breast development is complete | Micronized progesterone is more costly but may lessen side effects of anxiety, as compared with medroxyprogesterone | |
| * Professional consensus does not exist regarding the most efficacious and safest dosing regimens for gender transition. This table reflects reasonable starting and maintenance doses that are supported in the (admittedly less than optimal) medical literature, and reflect the author’s opinion and practice. This table is not meant to include all possible hormone regimens, only several of the most commonly used medications. | ||||
| † Professional consensus does not exist regarding progesterone’s role in MTF transition. | ||||
| Adapted and reprinted with permission from Table VII in Oriel KA. Medical care of transsexual patients. J Gay Lesbian Med Asso 2000;4(4):193. | ||||
Transdermal testosterone is an option for biologic females who are leery of injections.13 Patches result in stable testosterone levels in the male range but may cause skin irritation in >50% of patients. Use transdermal estrogen in males with clotting abnormalities or who are age >40.
Medical workup. Basic medical monitoring includes serial physical examinations, vital signs, weight measurements, laboratory assessment, and screening for pelvic malignancies.
For biologic males receiving estrogen, pretreatment laboratory assessment includes free testosterone, fasting glucose, liver function tests, and complete blood count, with reassessment at 6 and 12 months and annually thereafter. Obtain pretreatment prolactin levels and repeat annually. If hyperprolactinemia fails to develop within 3 years, no further measurements are necessary. Monitor for breast and prostate cancer, and instruct patients to perform self-breast exams. Following orchiectomy, estrogen doses can be reduced by one-third to one-half.
For biologic women receiving androgen, obtain pretreatment liver function tests and complete blood count, then reassess at 6 months, 12 months, and annually thereafter. Do yearly liver palpation examinations.
Physiologic changes. Biologic males treated with estrogens can expect breast growth, redistribution of fat in keeping with female habitus, decreased upper body strength, decreased body hair, retardation of male pattern balding, diminished testicular size, and decrease in erection firmness and frequency. MTF transsexuals require electrolysis to remove facial hair, as HRT does not do this.
Biologic females treated with testosterone can expect deepening of the voice, clitoral enlargement, mild breast atrophy, increased facial and body hair and male-pattern baldness, increased upper body strength, weight gain, and decreased hip fat.
With effective and continuous dosages, most changes begin in 2 to 4 months, start becoming irreversible in 6 to 12 months, start to level off in 2 years, and are mostly complete in 5 years. Men with insufficient breast growth following HRT may pursue breast augmentation surgery.
Voice changes. Hormone therapy generally is presumed to “masculinize” the voice of FTM transsexuals. In one series, after initiation of hormone therapy, 12 of 16 (75%) FTM transsexuals believed they had a voice that always would be considered masculine.14,15
For MTF transsexuals, no surgical technique of pitch elevation is satisfactorily safe and effective. The most widely used—cricothyroid approximation—may not be long-lasting and can decrease range, loudness, and vocal quality.13
HRT COMPLICATIONS
Medical complications. Biologic males treated with estrogens and progestins may be at increased risk for blood clotting, benign pituitary prolactinomas, infertility, weight gain, liver disease, gallstones, somnolence, hypertension, and diabetes mellitus.
Biologic females treated with testosterone may be at increased risk for acne, cardiovascular disease from shifts of lipid profiles to male patterns, benign and malignant liver tumors, and hepatic dysfunction.
Psychiatric issues. Physical masculinization occurs much more rapidly and results in a more convincing opposite sex appearance in FTMs than feminization does in MTFs.16,17 Behaving masculine may be more socially acceptable for women and therefore easier than it is for men to behave convincingly feminine without being characterized.
Cross-sex hormones contribute to the expression of sex-dimorphic behaviors in adulthood.18,19 Estrogen appears to influence affect intensity, whereas androgens influence aggression and sexual motivation. Earlier studies established that untreated MTFs and FTMs do not differ in sex hormone levels from their biologic counterparts.20,21
After 3 months of HRT, transsexuals’ sex hormones are in the range of their identified sex. FTMs treated with androgens become more prone to aggression and exhibit increased sexual motivation and arousability associated with an overall dampened affect. MTFs treated with estrogen show decreased irritability and sexual arousability.22
SEX REASSIGNMENT SURGERY
The cost of SRS often is prohibitive. Patients may turn to the Internet or foreign venues for hormone therapy and surgical procedures. Thailand is a popular overseas destination, where the average cost for MTF surgery is approximately $6,000 to $9,000. In the United States the cost of counseling, hormones, electrolysis, and surgeries is typically $30,000 to $40,000.23
Surgical options are not limited to genital reassignment but include mammoplasty (breast augmentation for MTF), chest reduction surgery (FTM), trachea shave surgery, forehead/brow ridge contouring, chin and jaw contouring, scalp advancement surgery, cheek implant surgery, alarplasty (nasal base resection to narrow a nose), and chin contouring.
Some insurance companies assert that transsexual procedures are not medically necessary and are declining coverage. WPATH contends that sex reassignment is effective and medically indicated in severe GID.
Postsurgical outcomes. Patients who are emotionally healthy, have adequate social support, and attain reasonable cosmetic results are most satisfied with life after SRS.24 In studies of GID patients, the best predictor of postoperative psychopathology was poor surgical results.25
FTMs are transformed through the use of hormones and generally are not perceived as visibly different from other men. Genital surgery is often seen as a final step in completing the transition to the identified gender.
FTMs may elect to have their female reproductive organs removed, along with construction of male external genitalia through phalloplasty or metoidioplasty. The decision to pursue surgery and the type of procedure depend on peer influence.26 Although a phalloplasty does not provide a fully functioning and completely authentic-appearing penis, most FTMs report being satisfied with life after surgery and have few regrets.27-31
Long-term postoperative follow-up by the surgeon and mental health professional is associated with good psychosocial outcome.
Legal considerations. An individual’s new surgically created gender can cause legal complications in jurisdictions that do not recognize the new gender. Some states are amending laws to make allowances for these advances in medical science.32
- World Professional Association For Transgender Health. (formerly the Harry Benjamin International Gender Dysphoria Association [HBIGDA]). www.hbigda.org. Includes a directory of transgender organizations.
- North American gender programs and service centers
CAMH Gender Identity Clinic. Toronto, Ontario, Canada
Gender Identity Project, New York, NY
Gendercare Gender Clinic (Web clinic for gender variance). www.gendercare.com.
Ingersoll Gender Center, Seattle, Washington
Johns Hopkins Center for Sexual Health & Medicine, Baltimore, Maryland
Program in Human Sexuality, Transgender Services at the University of Minnesota - Sexology organizations and information
American Association of Sex Educators, Counselors, and Therapists. www.aasect.org.
Kinsey Institute at Indiana University. www.indiana.edu/%7Ekinsey.
Sexuality Information and Education Council of the United States. www.siecus.org.
Social Science Research Council. www.ssrc.org.
Society for the Scientific Study of Sexuality. www.sexscience.org.
- Conjugated equine estrogens • Premarin
- Estradiol (oral) • Estrace
- Estradiol (transdermal) • Climara
- Medroxyprogesterone (oral) • Provera
- Medroxyprogesterone (IM) • Depo-Provera
- Micronized progesterone • Prometrium
- Spironolactone • Aldactone
The author reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Laden M, Walinder J, Lundstrom B. Prevalence, incidence and sex ratio of transsexualism. Acta Psychiatr Scand 1996;93(4):221-3.
2. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
3. World Health Organization (WHO). The ICD-10 classification of mental and behavioural disorders: diagnostic criteria for research. Geneva; 1993.
4. Rachlin K. Transgender individuals’ experiences of psychotherapy. Int J Transgender 2002;6-1.
5. Pfäfflin F, Junge A. Thirty years of international follow-up studies after sex reassignment surgery: a comprehensive review, 1961-1991. Dusseldorf: Symposium Publishing; 1998.
6. Zhou JN, Hofman MA, Gooren LJ, Swaab DF. A sex difference in the human brain and its relation to transsexuality. Nature 1995;378(6552):68-70.
7. Coates S, Pearson ES. Extreme boyhood femininity: isolated behavior or pervasive disorder? J Am Acad Child Psychiatry 1985;24(6):702-9.
8. Zucker KJ. Associated psychopathology in children with gender identity disorders. In: DiCeglie D, Freedman D, eds. A stranger in my own body: atypical gender identity development and mental health. London: Karnac Books; 1998.
9. Hepp U, Kramer B, Schnyder U, et al. Psychiatric comorbidity in gender identity disorder. J Psychosom Res 2005;58(3):259-61.
10. Cole S, Denny D, Eyler A, Samons S. Issues in transgender. In: Szuchman L, Muscarella F, eds. Psychological perspective on human sexuality. New York: John Wiley; 2000.
11. Jones B, Hill M. Mental health issues in lesbian, gay, bisexual, and transgender communities. Rev Psychol 2002;21:15-31.
12. Harry Benjamin international gender association standards of care for gender identity disorders, 6th version. Minneapolis, MN: The Harry Benjamin International Gender Dysphoria Association; 2001.
13. Assecheman J, Gooren LJG. Hormone treatment in transsexuals: interdisciplinary approaches in clinical management. J Psychol Human Sex 1992;5(4):39-54.
14. Van Borsel J, De Cuypere G, Van den Berghe H. Physical appearance and voice in male-to-female transsexuals. J Voice 2001;15(4):570-5.
15. Van Borsel J, De Cuypere G, Rubens R, Destaerke B. Voice problems in female-to-male transsexuals. Int J Lang Commun Disord 2000;35(3):427-42.
16. Spiegel J, Jalisi S. Contemporary diagnosis and management of head and neck cancer. Otolaryngol Clin North Am 2005;38(1):xiii-xiv.
17. Meyer WJ, 3rd, Webb A, Stuart CA, et al. Physical and hormonal evaluation of transsexual patients: a longitudinal study. Arch Sex Behav 1986;15(2):121-38.
18. Archer J. The influence of testosterone on human aggression. Br J Psychol 1991;82(Pt 1):1-28.
19. Van de Poll ME, Van Goozen SHM. Hypothalamic involvement in sexuality and hostility: comparative psychologic aspects. In: Swaab DF, Mirmiran M, Ravid R, Van Leeuwen FW, eds. The human hypothalamus in health and disease, progress in research. Amsterdam: Elsevier; 1992;343-61.
20. Spijkstra JJ, Spinder T, Gooren LJ. Short-term patterns of pulsatile luteinizing hormone secretion do not differ between male-to-female transsexuals and heterosexual men. Psychoneuroendocrinology 1988;13(3):279-83.
21. Spinder J, Spijkstra JJ, Gooren LJ, Burger CW. Pulsatile luteinizing hormone release and ovarian steroid levels in female-to-male transsexuals compared to heterosexual women. Psychoneuroendocrinology 1989;14(1-2):97-102.
22. Slabbekoorn D, Van Goozen S, Gooren L, Cohen-Kettenis P. Effects of cross-sex hormone treatment on emotionality in transsexuals. Int J Transgender [serial online] 2001;5(3). Available at: http://www.symposion.com/ijt/ijtvo05no03_02.htm. Accessed January 11, 2007.
23. Conway L. Vaginoplasty: male to female sex reassignment surgery: historical notes, descriptions, photos, and links. Available at: http://ai.eecs.umich.edu/people/conway/TS/SRS.html. Accessed January 12, 2007.
24. Bodlund O, Kullgren G. Transsexualism-general outcome and prognostic factors: a five-year follow-up study of nineteen transsexuals in the process of changing sex. Arch Sex Behav 1996;25(3):303-16.
25. Ross MW, Need JA. Effects of adequacy of gender reassignment surgery on psychologic adjustment: a followup of fourteen male-to-female patients. Arch Sex Behav 1989;18(2):145-53.
26. Rachlin K. Factors which influence individual’s decisions when considering female-to-male genital reconstructive surgery. Int J Transgender [serial online];1999;3(3). Available at: http://www.symposion.com/ijt/ijt990302.htm. Accessed January 11, 2007.
27. Lundstrom B, Pauly I, Walinder J. Outcome of sex reassignment surgery. Acta Psychiatr Scand 1984;70(4):289-94.
28. Kuiper B, Cohen-Kettenis P. Sex reassignment surgery: a study of 141 Dutch transsexuals. Arch Sex Behav 1988;17(5):439-57.
29. Green R, Fleming D. Transsexual surgery followup: status in the 1990s. Ann Rev Sex Res 1990;7:351-69.
30. Tsoi WF. Follow-up study of transsexuals after sex-reassignment surgery. Singapore Med J 1993;34(6):515-7.
31. Tsoi WF. Male to female transsexuals: a comparison. Singapore Med J 1992;33(2):182-5.
32. Harish D, Sharma BR. Medical advances in transsexualism and the legal implications. Am J Forensic Med Pathol 2003;24(1):100-5.
Adults with gender identity disorder (GID)—commonly termed transsexualism—may seek psychiatric assessment and treatment for a variety of reasons. Some—but not all—might be candidates for hormone replacement therapies or sex reassignment surgery (SRS). For those with gender dysphoria, psychological assessment and psychotherapy are suggested and sometimes required.
Your role in the GID patient’s gender exploration and transition must be tailored to his or her gender identity and individual circumstances. For patients who are not candidates for surgery or cannot afford it, you may assist in exploring options for living with one’s gender identity.
WHAT IS GID?
Gender identity disorder is a rare, complex condition in which individuals of unambiguous genotype and phenotype identify with the opposite gender. One in 54,000 individuals are estimated to have GID:
- 75% are biologic males desiring reassignment to female gender (MTF)
- 25% are females desiring to be male (FTM).1
Table 1
DSM-IV-TR criteria for gender identity disorder
| Criterion A | A strong and persistent cross-gender identification defined as the desire to be or the insistence that one is of the other sex (must not be merely a desire for any perceived cultural advantages of being the other sex) |
| Criterion B | Persistent discomfort with one’s assigned sex or a sense of inappropriateness in the gender role of that sex |
| Criterion C | The disturbance is not concurrent with a physical intersex condition (such as partial androgen insensitivity syndrome or congenital adrenal hyperplasia) |
| Criterion D | The disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning |
| Source: Reference 2 | |
ICD-10 diagnoses for gender identity disorder in adults
| Diagnosis | Criteria |
|---|---|
| Transsexualism |
|
| Dual-role transvestism |
|
| Other gender identity disorders | No specific criteria; could be used for persons with an intersexed condition |
| Gender identify disorder, unspecified | No specific criteria; could be used for persons with an intersexed condition |
| Source: Adapted from International Classification of Diseases, 10th ed. (ICD-10) | |
Epidemiologic studies of GID are rare, but in a survey by Rachlin et al4 of 23 MTFs and 70 FTMs:
- most underwent hormone therapy (64% of MTFs, 80% of FTMs) and/or name change (45% of MTFs, 72% of FTMs)
- none of the MTFs had breast augmentation, whereas 52% of FTMs had undergone mastectomy and reconstruction and another 33% were actively planning it
- 3% of FTMs had genital surgery, 16% were planning it, and 29% had decided definitely not to have it
- 9% of MTFs decided definitely not to have genital surgery; 23% had undergone genital surgery, and another 35% were actively planning it.
Biologic basis. GID’s cause remains unknown. Organic differences in brain anatomy have been identified in patients with GID. Zhou et al6 showed that the volume of the central subdivision of the bed nucleus of the stria terminalis (BSTc)—a brain area essential for sexual behavior—is larger in men than in women. A female-sized BSTc was found in MTF GID patients.
Research, mainly on biologic boys, indicates that GIDs are usually associated with behavioral difficulties, relationship problems with peers and parents, and—most notably—separation anxiety disorder.7 An audit of the files of 124 children and adolescents with GID showed that 42% experienced loss of one or both parents, mainly through separation.8
Psychiatric comorbidity. Studies using standardized diagnostic instruments to assess psychiatric comorbidity in GID are rare. A study of 31 patients with GID found that many met diagnostic criteria for lifetime psychiatric comorbidity, including:
- 71% for Axis I disorders (primarily mood and anxiety disorders)
- 42% for comorbid personality disorders, primarily a cluster B diagnosis
- 45% for substance-related disorders
- 6.5% for psychotic disorders
- 3.2% for eating disorders.9
TREATING PATIENTS WITH GID
Psychotherapy. GID treatment decisions are made without clear prospective data. Standards of care are determined by the World Professional Association for Transgender Health (WPATH).12 Psychotherapy is often given before SRS but is not required. The therapist is left to determine the treatment terms and goals.
Your role in treating patients with GID goes beyond making an accurate diagnosis, identifying comorbid psychopathology, and instituting a treatment plan. Other tasks include:
- counseling the patient about the range of treatment options and their implications
- engaging in psychotherapy
- ascertaining eligibility and readiness for hormones and surgical therapy
- making formal recommendations to medical and surgical colleagues
- documenting the patient’s relevant history in a letter of recommendation
- educating support systems
- being available for follow-up.
Candidates for triadic therapy. For appropriately screened adults with severe GID, the therapeutic approach relies on triadic therapy:
- a 3-phase approach centered around real-life experience in the desired role
- hormones of the desired gender
- and surgery to change the genitalia and secondary sex characteristics.
HORMONE THERAPY
WPATH has established eligibility and readiness criteria for HRT in patients with GID (Table 3). Administering cross-sex hormones (testosterone in women; estrogens in men) brings about important physical changes as well as psychological relief. The prescribing physician need not be an endocrinologist but should become well-versed in relevant data.
Table 3
WPATH criteria for hormone replacement therapy*
| Eligibility criteria 3 criteria exist |
|
| Readiness criteria All 3 must exist |
|
| Source: World Professional Association for Transgender Health (WPATH) | |
Table 4
Sample hormonal regimens for transsexual patients*
| Medication | Starting dose | Subsequent dose | When to change doses | |
|---|---|---|---|---|
| Female to male | Testosterone enanthanate or testosterone cypionate | 200 mg IM every 2 weeks | 100 to 150 mg IM every 2 weeks | After masculinization complete and/or oophorectomy/hysterectomy |
| Transdermal testosterone | 5 mg to skin every day | Usually stays the same | Little data exist on efficacy; effective for maintenance, and may be less efficacious during transition | |
| Male to female | Conjugated estrogens | 1.25 mg/d (or 0.625 mg/d for smokers) | 2.5 mg/d (Do not increase in smokers) | To obtain best clinical results, or if testosterone is not suppressed After sexual reassignment surgery, dose may be decreased without losing secondary sexual characteristics |
| OR oral estradiol | 1 mg/d | 2 mg/d | ||
| OR transdermal estradiol | 0.1 mg patch/week | Two 0.1 mg patches/week | ||
| Spironolactone | 200 mg/d | May discontinue | After sexual assignment surgery | |
| Medroxyprogesterone† | 10 mg/d | May increase to 20 to 40 mg/d (usually not needed) | If testosterone is not suppressed and patient/doctor does not want to increase estrogen | |
| OR micronized progesterone | 100 mg bid | May discontinue after breast development is complete | Micronized progesterone is more costly but may lessen side effects of anxiety, as compared with medroxyprogesterone | |
| * Professional consensus does not exist regarding the most efficacious and safest dosing regimens for gender transition. This table reflects reasonable starting and maintenance doses that are supported in the (admittedly less than optimal) medical literature, and reflect the author’s opinion and practice. This table is not meant to include all possible hormone regimens, only several of the most commonly used medications. | ||||
| † Professional consensus does not exist regarding progesterone’s role in MTF transition. | ||||
| Adapted and reprinted with permission from Table VII in Oriel KA. Medical care of transsexual patients. J Gay Lesbian Med Asso 2000;4(4):193. | ||||
Transdermal testosterone is an option for biologic females who are leery of injections.13 Patches result in stable testosterone levels in the male range but may cause skin irritation in >50% of patients. Use transdermal estrogen in males with clotting abnormalities or who are age >40.
Medical workup. Basic medical monitoring includes serial physical examinations, vital signs, weight measurements, laboratory assessment, and screening for pelvic malignancies.
For biologic males receiving estrogen, pretreatment laboratory assessment includes free testosterone, fasting glucose, liver function tests, and complete blood count, with reassessment at 6 and 12 months and annually thereafter. Obtain pretreatment prolactin levels and repeat annually. If hyperprolactinemia fails to develop within 3 years, no further measurements are necessary. Monitor for breast and prostate cancer, and instruct patients to perform self-breast exams. Following orchiectomy, estrogen doses can be reduced by one-third to one-half.
For biologic women receiving androgen, obtain pretreatment liver function tests and complete blood count, then reassess at 6 months, 12 months, and annually thereafter. Do yearly liver palpation examinations.
Physiologic changes. Biologic males treated with estrogens can expect breast growth, redistribution of fat in keeping with female habitus, decreased upper body strength, decreased body hair, retardation of male pattern balding, diminished testicular size, and decrease in erection firmness and frequency. MTF transsexuals require electrolysis to remove facial hair, as HRT does not do this.
Biologic females treated with testosterone can expect deepening of the voice, clitoral enlargement, mild breast atrophy, increased facial and body hair and male-pattern baldness, increased upper body strength, weight gain, and decreased hip fat.
With effective and continuous dosages, most changes begin in 2 to 4 months, start becoming irreversible in 6 to 12 months, start to level off in 2 years, and are mostly complete in 5 years. Men with insufficient breast growth following HRT may pursue breast augmentation surgery.
Voice changes. Hormone therapy generally is presumed to “masculinize” the voice of FTM transsexuals. In one series, after initiation of hormone therapy, 12 of 16 (75%) FTM transsexuals believed they had a voice that always would be considered masculine.14,15
For MTF transsexuals, no surgical technique of pitch elevation is satisfactorily safe and effective. The most widely used—cricothyroid approximation—may not be long-lasting and can decrease range, loudness, and vocal quality.13
HRT COMPLICATIONS
Medical complications. Biologic males treated with estrogens and progestins may be at increased risk for blood clotting, benign pituitary prolactinomas, infertility, weight gain, liver disease, gallstones, somnolence, hypertension, and diabetes mellitus.
Biologic females treated with testosterone may be at increased risk for acne, cardiovascular disease from shifts of lipid profiles to male patterns, benign and malignant liver tumors, and hepatic dysfunction.
Psychiatric issues. Physical masculinization occurs much more rapidly and results in a more convincing opposite sex appearance in FTMs than feminization does in MTFs.16,17 Behaving masculine may be more socially acceptable for women and therefore easier than it is for men to behave convincingly feminine without being characterized.
Cross-sex hormones contribute to the expression of sex-dimorphic behaviors in adulthood.18,19 Estrogen appears to influence affect intensity, whereas androgens influence aggression and sexual motivation. Earlier studies established that untreated MTFs and FTMs do not differ in sex hormone levels from their biologic counterparts.20,21
After 3 months of HRT, transsexuals’ sex hormones are in the range of their identified sex. FTMs treated with androgens become more prone to aggression and exhibit increased sexual motivation and arousability associated with an overall dampened affect. MTFs treated with estrogen show decreased irritability and sexual arousability.22
SEX REASSIGNMENT SURGERY
The cost of SRS often is prohibitive. Patients may turn to the Internet or foreign venues for hormone therapy and surgical procedures. Thailand is a popular overseas destination, where the average cost for MTF surgery is approximately $6,000 to $9,000. In the United States the cost of counseling, hormones, electrolysis, and surgeries is typically $30,000 to $40,000.23
Surgical options are not limited to genital reassignment but include mammoplasty (breast augmentation for MTF), chest reduction surgery (FTM), trachea shave surgery, forehead/brow ridge contouring, chin and jaw contouring, scalp advancement surgery, cheek implant surgery, alarplasty (nasal base resection to narrow a nose), and chin contouring.
Some insurance companies assert that transsexual procedures are not medically necessary and are declining coverage. WPATH contends that sex reassignment is effective and medically indicated in severe GID.
Postsurgical outcomes. Patients who are emotionally healthy, have adequate social support, and attain reasonable cosmetic results are most satisfied with life after SRS.24 In studies of GID patients, the best predictor of postoperative psychopathology was poor surgical results.25
FTMs are transformed through the use of hormones and generally are not perceived as visibly different from other men. Genital surgery is often seen as a final step in completing the transition to the identified gender.
FTMs may elect to have their female reproductive organs removed, along with construction of male external genitalia through phalloplasty or metoidioplasty. The decision to pursue surgery and the type of procedure depend on peer influence.26 Although a phalloplasty does not provide a fully functioning and completely authentic-appearing penis, most FTMs report being satisfied with life after surgery and have few regrets.27-31
Long-term postoperative follow-up by the surgeon and mental health professional is associated with good psychosocial outcome.
Legal considerations. An individual’s new surgically created gender can cause legal complications in jurisdictions that do not recognize the new gender. Some states are amending laws to make allowances for these advances in medical science.32
- World Professional Association For Transgender Health. (formerly the Harry Benjamin International Gender Dysphoria Association [HBIGDA]). www.hbigda.org. Includes a directory of transgender organizations.
- North American gender programs and service centers
CAMH Gender Identity Clinic. Toronto, Ontario, Canada
Gender Identity Project, New York, NY
Gendercare Gender Clinic (Web clinic for gender variance). www.gendercare.com.
Ingersoll Gender Center, Seattle, Washington
Johns Hopkins Center for Sexual Health & Medicine, Baltimore, Maryland
Program in Human Sexuality, Transgender Services at the University of Minnesota - Sexology organizations and information
American Association of Sex Educators, Counselors, and Therapists. www.aasect.org.
Kinsey Institute at Indiana University. www.indiana.edu/%7Ekinsey.
Sexuality Information and Education Council of the United States. www.siecus.org.
Social Science Research Council. www.ssrc.org.
Society for the Scientific Study of Sexuality. www.sexscience.org.
- Conjugated equine estrogens • Premarin
- Estradiol (oral) • Estrace
- Estradiol (transdermal) • Climara
- Medroxyprogesterone (oral) • Provera
- Medroxyprogesterone (IM) • Depo-Provera
- Micronized progesterone • Prometrium
- Spironolactone • Aldactone
The author reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Adults with gender identity disorder (GID)—commonly termed transsexualism—may seek psychiatric assessment and treatment for a variety of reasons. Some—but not all—might be candidates for hormone replacement therapies or sex reassignment surgery (SRS). For those with gender dysphoria, psychological assessment and psychotherapy are suggested and sometimes required.
Your role in the GID patient’s gender exploration and transition must be tailored to his or her gender identity and individual circumstances. For patients who are not candidates for surgery or cannot afford it, you may assist in exploring options for living with one’s gender identity.
WHAT IS GID?
Gender identity disorder is a rare, complex condition in which individuals of unambiguous genotype and phenotype identify with the opposite gender. One in 54,000 individuals are estimated to have GID:
- 75% are biologic males desiring reassignment to female gender (MTF)
- 25% are females desiring to be male (FTM).1
Table 1
DSM-IV-TR criteria for gender identity disorder
| Criterion A | A strong and persistent cross-gender identification defined as the desire to be or the insistence that one is of the other sex (must not be merely a desire for any perceived cultural advantages of being the other sex) |
| Criterion B | Persistent discomfort with one’s assigned sex or a sense of inappropriateness in the gender role of that sex |
| Criterion C | The disturbance is not concurrent with a physical intersex condition (such as partial androgen insensitivity syndrome or congenital adrenal hyperplasia) |
| Criterion D | The disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning |
| Source: Reference 2 | |
ICD-10 diagnoses for gender identity disorder in adults
| Diagnosis | Criteria |
|---|---|
| Transsexualism |
|
| Dual-role transvestism |
|
| Other gender identity disorders | No specific criteria; could be used for persons with an intersexed condition |
| Gender identify disorder, unspecified | No specific criteria; could be used for persons with an intersexed condition |
| Source: Adapted from International Classification of Diseases, 10th ed. (ICD-10) | |
Epidemiologic studies of GID are rare, but in a survey by Rachlin et al4 of 23 MTFs and 70 FTMs:
- most underwent hormone therapy (64% of MTFs, 80% of FTMs) and/or name change (45% of MTFs, 72% of FTMs)
- none of the MTFs had breast augmentation, whereas 52% of FTMs had undergone mastectomy and reconstruction and another 33% were actively planning it
- 3% of FTMs had genital surgery, 16% were planning it, and 29% had decided definitely not to have it
- 9% of MTFs decided definitely not to have genital surgery; 23% had undergone genital surgery, and another 35% were actively planning it.
Biologic basis. GID’s cause remains unknown. Organic differences in brain anatomy have been identified in patients with GID. Zhou et al6 showed that the volume of the central subdivision of the bed nucleus of the stria terminalis (BSTc)—a brain area essential for sexual behavior—is larger in men than in women. A female-sized BSTc was found in MTF GID patients.
Research, mainly on biologic boys, indicates that GIDs are usually associated with behavioral difficulties, relationship problems with peers and parents, and—most notably—separation anxiety disorder.7 An audit of the files of 124 children and adolescents with GID showed that 42% experienced loss of one or both parents, mainly through separation.8
Psychiatric comorbidity. Studies using standardized diagnostic instruments to assess psychiatric comorbidity in GID are rare. A study of 31 patients with GID found that many met diagnostic criteria for lifetime psychiatric comorbidity, including:
- 71% for Axis I disorders (primarily mood and anxiety disorders)
- 42% for comorbid personality disorders, primarily a cluster B diagnosis
- 45% for substance-related disorders
- 6.5% for psychotic disorders
- 3.2% for eating disorders.9
TREATING PATIENTS WITH GID
Psychotherapy. GID treatment decisions are made without clear prospective data. Standards of care are determined by the World Professional Association for Transgender Health (WPATH).12 Psychotherapy is often given before SRS but is not required. The therapist is left to determine the treatment terms and goals.
Your role in treating patients with GID goes beyond making an accurate diagnosis, identifying comorbid psychopathology, and instituting a treatment plan. Other tasks include:
- counseling the patient about the range of treatment options and their implications
- engaging in psychotherapy
- ascertaining eligibility and readiness for hormones and surgical therapy
- making formal recommendations to medical and surgical colleagues
- documenting the patient’s relevant history in a letter of recommendation
- educating support systems
- being available for follow-up.
Candidates for triadic therapy. For appropriately screened adults with severe GID, the therapeutic approach relies on triadic therapy:
- a 3-phase approach centered around real-life experience in the desired role
- hormones of the desired gender
- and surgery to change the genitalia and secondary sex characteristics.
HORMONE THERAPY
WPATH has established eligibility and readiness criteria for HRT in patients with GID (Table 3). Administering cross-sex hormones (testosterone in women; estrogens in men) brings about important physical changes as well as psychological relief. The prescribing physician need not be an endocrinologist but should become well-versed in relevant data.
Table 3
WPATH criteria for hormone replacement therapy*
| Eligibility criteria 3 criteria exist |
|
| Readiness criteria All 3 must exist |
|
| Source: World Professional Association for Transgender Health (WPATH) | |
Table 4
Sample hormonal regimens for transsexual patients*
| Medication | Starting dose | Subsequent dose | When to change doses | |
|---|---|---|---|---|
| Female to male | Testosterone enanthanate or testosterone cypionate | 200 mg IM every 2 weeks | 100 to 150 mg IM every 2 weeks | After masculinization complete and/or oophorectomy/hysterectomy |
| Transdermal testosterone | 5 mg to skin every day | Usually stays the same | Little data exist on efficacy; effective for maintenance, and may be less efficacious during transition | |
| Male to female | Conjugated estrogens | 1.25 mg/d (or 0.625 mg/d for smokers) | 2.5 mg/d (Do not increase in smokers) | To obtain best clinical results, or if testosterone is not suppressed After sexual reassignment surgery, dose may be decreased without losing secondary sexual characteristics |
| OR oral estradiol | 1 mg/d | 2 mg/d | ||
| OR transdermal estradiol | 0.1 mg patch/week | Two 0.1 mg patches/week | ||
| Spironolactone | 200 mg/d | May discontinue | After sexual assignment surgery | |
| Medroxyprogesterone† | 10 mg/d | May increase to 20 to 40 mg/d (usually not needed) | If testosterone is not suppressed and patient/doctor does not want to increase estrogen | |
| OR micronized progesterone | 100 mg bid | May discontinue after breast development is complete | Micronized progesterone is more costly but may lessen side effects of anxiety, as compared with medroxyprogesterone | |
| * Professional consensus does not exist regarding the most efficacious and safest dosing regimens for gender transition. This table reflects reasonable starting and maintenance doses that are supported in the (admittedly less than optimal) medical literature, and reflect the author’s opinion and practice. This table is not meant to include all possible hormone regimens, only several of the most commonly used medications. | ||||
| † Professional consensus does not exist regarding progesterone’s role in MTF transition. | ||||
| Adapted and reprinted with permission from Table VII in Oriel KA. Medical care of transsexual patients. J Gay Lesbian Med Asso 2000;4(4):193. | ||||
Transdermal testosterone is an option for biologic females who are leery of injections.13 Patches result in stable testosterone levels in the male range but may cause skin irritation in >50% of patients. Use transdermal estrogen in males with clotting abnormalities or who are age >40.
Medical workup. Basic medical monitoring includes serial physical examinations, vital signs, weight measurements, laboratory assessment, and screening for pelvic malignancies.
For biologic males receiving estrogen, pretreatment laboratory assessment includes free testosterone, fasting glucose, liver function tests, and complete blood count, with reassessment at 6 and 12 months and annually thereafter. Obtain pretreatment prolactin levels and repeat annually. If hyperprolactinemia fails to develop within 3 years, no further measurements are necessary. Monitor for breast and prostate cancer, and instruct patients to perform self-breast exams. Following orchiectomy, estrogen doses can be reduced by one-third to one-half.
For biologic women receiving androgen, obtain pretreatment liver function tests and complete blood count, then reassess at 6 months, 12 months, and annually thereafter. Do yearly liver palpation examinations.
Physiologic changes. Biologic males treated with estrogens can expect breast growth, redistribution of fat in keeping with female habitus, decreased upper body strength, decreased body hair, retardation of male pattern balding, diminished testicular size, and decrease in erection firmness and frequency. MTF transsexuals require electrolysis to remove facial hair, as HRT does not do this.
Biologic females treated with testosterone can expect deepening of the voice, clitoral enlargement, mild breast atrophy, increased facial and body hair and male-pattern baldness, increased upper body strength, weight gain, and decreased hip fat.
With effective and continuous dosages, most changes begin in 2 to 4 months, start becoming irreversible in 6 to 12 months, start to level off in 2 years, and are mostly complete in 5 years. Men with insufficient breast growth following HRT may pursue breast augmentation surgery.
Voice changes. Hormone therapy generally is presumed to “masculinize” the voice of FTM transsexuals. In one series, after initiation of hormone therapy, 12 of 16 (75%) FTM transsexuals believed they had a voice that always would be considered masculine.14,15
For MTF transsexuals, no surgical technique of pitch elevation is satisfactorily safe and effective. The most widely used—cricothyroid approximation—may not be long-lasting and can decrease range, loudness, and vocal quality.13
HRT COMPLICATIONS
Medical complications. Biologic males treated with estrogens and progestins may be at increased risk for blood clotting, benign pituitary prolactinomas, infertility, weight gain, liver disease, gallstones, somnolence, hypertension, and diabetes mellitus.
Biologic females treated with testosterone may be at increased risk for acne, cardiovascular disease from shifts of lipid profiles to male patterns, benign and malignant liver tumors, and hepatic dysfunction.
Psychiatric issues. Physical masculinization occurs much more rapidly and results in a more convincing opposite sex appearance in FTMs than feminization does in MTFs.16,17 Behaving masculine may be more socially acceptable for women and therefore easier than it is for men to behave convincingly feminine without being characterized.
Cross-sex hormones contribute to the expression of sex-dimorphic behaviors in adulthood.18,19 Estrogen appears to influence affect intensity, whereas androgens influence aggression and sexual motivation. Earlier studies established that untreated MTFs and FTMs do not differ in sex hormone levels from their biologic counterparts.20,21
After 3 months of HRT, transsexuals’ sex hormones are in the range of their identified sex. FTMs treated with androgens become more prone to aggression and exhibit increased sexual motivation and arousability associated with an overall dampened affect. MTFs treated with estrogen show decreased irritability and sexual arousability.22
SEX REASSIGNMENT SURGERY
The cost of SRS often is prohibitive. Patients may turn to the Internet or foreign venues for hormone therapy and surgical procedures. Thailand is a popular overseas destination, where the average cost for MTF surgery is approximately $6,000 to $9,000. In the United States the cost of counseling, hormones, electrolysis, and surgeries is typically $30,000 to $40,000.23
Surgical options are not limited to genital reassignment but include mammoplasty (breast augmentation for MTF), chest reduction surgery (FTM), trachea shave surgery, forehead/brow ridge contouring, chin and jaw contouring, scalp advancement surgery, cheek implant surgery, alarplasty (nasal base resection to narrow a nose), and chin contouring.
Some insurance companies assert that transsexual procedures are not medically necessary and are declining coverage. WPATH contends that sex reassignment is effective and medically indicated in severe GID.
Postsurgical outcomes. Patients who are emotionally healthy, have adequate social support, and attain reasonable cosmetic results are most satisfied with life after SRS.24 In studies of GID patients, the best predictor of postoperative psychopathology was poor surgical results.25
FTMs are transformed through the use of hormones and generally are not perceived as visibly different from other men. Genital surgery is often seen as a final step in completing the transition to the identified gender.
FTMs may elect to have their female reproductive organs removed, along with construction of male external genitalia through phalloplasty or metoidioplasty. The decision to pursue surgery and the type of procedure depend on peer influence.26 Although a phalloplasty does not provide a fully functioning and completely authentic-appearing penis, most FTMs report being satisfied with life after surgery and have few regrets.27-31
Long-term postoperative follow-up by the surgeon and mental health professional is associated with good psychosocial outcome.
Legal considerations. An individual’s new surgically created gender can cause legal complications in jurisdictions that do not recognize the new gender. Some states are amending laws to make allowances for these advances in medical science.32
- World Professional Association For Transgender Health. (formerly the Harry Benjamin International Gender Dysphoria Association [HBIGDA]). www.hbigda.org. Includes a directory of transgender organizations.
- North American gender programs and service centers
CAMH Gender Identity Clinic. Toronto, Ontario, Canada
Gender Identity Project, New York, NY
Gendercare Gender Clinic (Web clinic for gender variance). www.gendercare.com.
Ingersoll Gender Center, Seattle, Washington
Johns Hopkins Center for Sexual Health & Medicine, Baltimore, Maryland
Program in Human Sexuality, Transgender Services at the University of Minnesota - Sexology organizations and information
American Association of Sex Educators, Counselors, and Therapists. www.aasect.org.
Kinsey Institute at Indiana University. www.indiana.edu/%7Ekinsey.
Sexuality Information and Education Council of the United States. www.siecus.org.
Social Science Research Council. www.ssrc.org.
Society for the Scientific Study of Sexuality. www.sexscience.org.
- Conjugated equine estrogens • Premarin
- Estradiol (oral) • Estrace
- Estradiol (transdermal) • Climara
- Medroxyprogesterone (oral) • Provera
- Medroxyprogesterone (IM) • Depo-Provera
- Micronized progesterone • Prometrium
- Spironolactone • Aldactone
The author reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Laden M, Walinder J, Lundstrom B. Prevalence, incidence and sex ratio of transsexualism. Acta Psychiatr Scand 1996;93(4):221-3.
2. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
3. World Health Organization (WHO). The ICD-10 classification of mental and behavioural disorders: diagnostic criteria for research. Geneva; 1993.
4. Rachlin K. Transgender individuals’ experiences of psychotherapy. Int J Transgender 2002;6-1.
5. Pfäfflin F, Junge A. Thirty years of international follow-up studies after sex reassignment surgery: a comprehensive review, 1961-1991. Dusseldorf: Symposium Publishing; 1998.
6. Zhou JN, Hofman MA, Gooren LJ, Swaab DF. A sex difference in the human brain and its relation to transsexuality. Nature 1995;378(6552):68-70.
7. Coates S, Pearson ES. Extreme boyhood femininity: isolated behavior or pervasive disorder? J Am Acad Child Psychiatry 1985;24(6):702-9.
8. Zucker KJ. Associated psychopathology in children with gender identity disorders. In: DiCeglie D, Freedman D, eds. A stranger in my own body: atypical gender identity development and mental health. London: Karnac Books; 1998.
9. Hepp U, Kramer B, Schnyder U, et al. Psychiatric comorbidity in gender identity disorder. J Psychosom Res 2005;58(3):259-61.
10. Cole S, Denny D, Eyler A, Samons S. Issues in transgender. In: Szuchman L, Muscarella F, eds. Psychological perspective on human sexuality. New York: John Wiley; 2000.
11. Jones B, Hill M. Mental health issues in lesbian, gay, bisexual, and transgender communities. Rev Psychol 2002;21:15-31.
12. Harry Benjamin international gender association standards of care for gender identity disorders, 6th version. Minneapolis, MN: The Harry Benjamin International Gender Dysphoria Association; 2001.
13. Assecheman J, Gooren LJG. Hormone treatment in transsexuals: interdisciplinary approaches in clinical management. J Psychol Human Sex 1992;5(4):39-54.
14. Van Borsel J, De Cuypere G, Van den Berghe H. Physical appearance and voice in male-to-female transsexuals. J Voice 2001;15(4):570-5.
15. Van Borsel J, De Cuypere G, Rubens R, Destaerke B. Voice problems in female-to-male transsexuals. Int J Lang Commun Disord 2000;35(3):427-42.
16. Spiegel J, Jalisi S. Contemporary diagnosis and management of head and neck cancer. Otolaryngol Clin North Am 2005;38(1):xiii-xiv.
17. Meyer WJ, 3rd, Webb A, Stuart CA, et al. Physical and hormonal evaluation of transsexual patients: a longitudinal study. Arch Sex Behav 1986;15(2):121-38.
18. Archer J. The influence of testosterone on human aggression. Br J Psychol 1991;82(Pt 1):1-28.
19. Van de Poll ME, Van Goozen SHM. Hypothalamic involvement in sexuality and hostility: comparative psychologic aspects. In: Swaab DF, Mirmiran M, Ravid R, Van Leeuwen FW, eds. The human hypothalamus in health and disease, progress in research. Amsterdam: Elsevier; 1992;343-61.
20. Spijkstra JJ, Spinder T, Gooren LJ. Short-term patterns of pulsatile luteinizing hormone secretion do not differ between male-to-female transsexuals and heterosexual men. Psychoneuroendocrinology 1988;13(3):279-83.
21. Spinder J, Spijkstra JJ, Gooren LJ, Burger CW. Pulsatile luteinizing hormone release and ovarian steroid levels in female-to-male transsexuals compared to heterosexual women. Psychoneuroendocrinology 1989;14(1-2):97-102.
22. Slabbekoorn D, Van Goozen S, Gooren L, Cohen-Kettenis P. Effects of cross-sex hormone treatment on emotionality in transsexuals. Int J Transgender [serial online] 2001;5(3). Available at: http://www.symposion.com/ijt/ijtvo05no03_02.htm. Accessed January 11, 2007.
23. Conway L. Vaginoplasty: male to female sex reassignment surgery: historical notes, descriptions, photos, and links. Available at: http://ai.eecs.umich.edu/people/conway/TS/SRS.html. Accessed January 12, 2007.
24. Bodlund O, Kullgren G. Transsexualism-general outcome and prognostic factors: a five-year follow-up study of nineteen transsexuals in the process of changing sex. Arch Sex Behav 1996;25(3):303-16.
25. Ross MW, Need JA. Effects of adequacy of gender reassignment surgery on psychologic adjustment: a followup of fourteen male-to-female patients. Arch Sex Behav 1989;18(2):145-53.
26. Rachlin K. Factors which influence individual’s decisions when considering female-to-male genital reconstructive surgery. Int J Transgender [serial online];1999;3(3). Available at: http://www.symposion.com/ijt/ijt990302.htm. Accessed January 11, 2007.
27. Lundstrom B, Pauly I, Walinder J. Outcome of sex reassignment surgery. Acta Psychiatr Scand 1984;70(4):289-94.
28. Kuiper B, Cohen-Kettenis P. Sex reassignment surgery: a study of 141 Dutch transsexuals. Arch Sex Behav 1988;17(5):439-57.
29. Green R, Fleming D. Transsexual surgery followup: status in the 1990s. Ann Rev Sex Res 1990;7:351-69.
30. Tsoi WF. Follow-up study of transsexuals after sex-reassignment surgery. Singapore Med J 1993;34(6):515-7.
31. Tsoi WF. Male to female transsexuals: a comparison. Singapore Med J 1992;33(2):182-5.
32. Harish D, Sharma BR. Medical advances in transsexualism and the legal implications. Am J Forensic Med Pathol 2003;24(1):100-5.
1. Laden M, Walinder J, Lundstrom B. Prevalence, incidence and sex ratio of transsexualism. Acta Psychiatr Scand 1996;93(4):221-3.
2. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
3. World Health Organization (WHO). The ICD-10 classification of mental and behavioural disorders: diagnostic criteria for research. Geneva; 1993.
4. Rachlin K. Transgender individuals’ experiences of psychotherapy. Int J Transgender 2002;6-1.
5. Pfäfflin F, Junge A. Thirty years of international follow-up studies after sex reassignment surgery: a comprehensive review, 1961-1991. Dusseldorf: Symposium Publishing; 1998.
6. Zhou JN, Hofman MA, Gooren LJ, Swaab DF. A sex difference in the human brain and its relation to transsexuality. Nature 1995;378(6552):68-70.
7. Coates S, Pearson ES. Extreme boyhood femininity: isolated behavior or pervasive disorder? J Am Acad Child Psychiatry 1985;24(6):702-9.
8. Zucker KJ. Associated psychopathology in children with gender identity disorders. In: DiCeglie D, Freedman D, eds. A stranger in my own body: atypical gender identity development and mental health. London: Karnac Books; 1998.
9. Hepp U, Kramer B, Schnyder U, et al. Psychiatric comorbidity in gender identity disorder. J Psychosom Res 2005;58(3):259-61.
10. Cole S, Denny D, Eyler A, Samons S. Issues in transgender. In: Szuchman L, Muscarella F, eds. Psychological perspective on human sexuality. New York: John Wiley; 2000.
11. Jones B, Hill M. Mental health issues in lesbian, gay, bisexual, and transgender communities. Rev Psychol 2002;21:15-31.
12. Harry Benjamin international gender association standards of care for gender identity disorders, 6th version. Minneapolis, MN: The Harry Benjamin International Gender Dysphoria Association; 2001.
13. Assecheman J, Gooren LJG. Hormone treatment in transsexuals: interdisciplinary approaches in clinical management. J Psychol Human Sex 1992;5(4):39-54.
14. Van Borsel J, De Cuypere G, Van den Berghe H. Physical appearance and voice in male-to-female transsexuals. J Voice 2001;15(4):570-5.
15. Van Borsel J, De Cuypere G, Rubens R, Destaerke B. Voice problems in female-to-male transsexuals. Int J Lang Commun Disord 2000;35(3):427-42.
16. Spiegel J, Jalisi S. Contemporary diagnosis and management of head and neck cancer. Otolaryngol Clin North Am 2005;38(1):xiii-xiv.
17. Meyer WJ, 3rd, Webb A, Stuart CA, et al. Physical and hormonal evaluation of transsexual patients: a longitudinal study. Arch Sex Behav 1986;15(2):121-38.
18. Archer J. The influence of testosterone on human aggression. Br J Psychol 1991;82(Pt 1):1-28.
19. Van de Poll ME, Van Goozen SHM. Hypothalamic involvement in sexuality and hostility: comparative psychologic aspects. In: Swaab DF, Mirmiran M, Ravid R, Van Leeuwen FW, eds. The human hypothalamus in health and disease, progress in research. Amsterdam: Elsevier; 1992;343-61.
20. Spijkstra JJ, Spinder T, Gooren LJ. Short-term patterns of pulsatile luteinizing hormone secretion do not differ between male-to-female transsexuals and heterosexual men. Psychoneuroendocrinology 1988;13(3):279-83.
21. Spinder J, Spijkstra JJ, Gooren LJ, Burger CW. Pulsatile luteinizing hormone release and ovarian steroid levels in female-to-male transsexuals compared to heterosexual women. Psychoneuroendocrinology 1989;14(1-2):97-102.
22. Slabbekoorn D, Van Goozen S, Gooren L, Cohen-Kettenis P. Effects of cross-sex hormone treatment on emotionality in transsexuals. Int J Transgender [serial online] 2001;5(3). Available at: http://www.symposion.com/ijt/ijtvo05no03_02.htm. Accessed January 11, 2007.
23. Conway L. Vaginoplasty: male to female sex reassignment surgery: historical notes, descriptions, photos, and links. Available at: http://ai.eecs.umich.edu/people/conway/TS/SRS.html. Accessed January 12, 2007.
24. Bodlund O, Kullgren G. Transsexualism-general outcome and prognostic factors: a five-year follow-up study of nineteen transsexuals in the process of changing sex. Arch Sex Behav 1996;25(3):303-16.
25. Ross MW, Need JA. Effects of adequacy of gender reassignment surgery on psychologic adjustment: a followup of fourteen male-to-female patients. Arch Sex Behav 1989;18(2):145-53.
26. Rachlin K. Factors which influence individual’s decisions when considering female-to-male genital reconstructive surgery. Int J Transgender [serial online];1999;3(3). Available at: http://www.symposion.com/ijt/ijt990302.htm. Accessed January 11, 2007.
27. Lundstrom B, Pauly I, Walinder J. Outcome of sex reassignment surgery. Acta Psychiatr Scand 1984;70(4):289-94.
28. Kuiper B, Cohen-Kettenis P. Sex reassignment surgery: a study of 141 Dutch transsexuals. Arch Sex Behav 1988;17(5):439-57.
29. Green R, Fleming D. Transsexual surgery followup: status in the 1990s. Ann Rev Sex Res 1990;7:351-69.
30. Tsoi WF. Follow-up study of transsexuals after sex-reassignment surgery. Singapore Med J 1993;34(6):515-7.
31. Tsoi WF. Male to female transsexuals: a comparison. Singapore Med J 1992;33(2):182-5.
32. Harish D, Sharma BR. Medical advances in transsexualism and the legal implications. Am J Forensic Med Pathol 2003;24(1):100-5.
Antipsychotics equivalent? CUtLASS renews the debate
When treating chronic psychotic disorders, U.S. psychiatrists generally prefer second-generation antipsychotics (SGAs) to first-generation antipsychotics (FGAs) because of widely held views1,2 that SGAs:
- are more effective for negative and cognitive symptoms
- produce fewer troublesome side effects
- help patients realize a better quality of life.
These beliefs have been challenged by two large-scale, government-supported studies: the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) in the United States3-6 and more recently the Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study (CUtLASS) from the United Kingdom.7,8
CATIE and CUtLASS data suggest that the SGA advantage has been exaggerated, if in fact such an advantage exists. Other Current Psychiatry articles for the clinical practitioner have discussed the CATIE findings.9-11 This article addresses the CUtLASS results in the context of the trial’s methodology, using information from the primary publications7,8 and technical report.12
Cutlass study
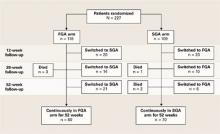
Design. CUtLASS included 2 “bands” (Table 1):
- Band 1 compared the clinical usefulness and cost effectiveness of FGAs and SGAs in treating schizophrenia7
- Band 2 compared the effectiveness of clozapine versus other SGAs in treating refractory schizophrenia.8
CUtLASS Band 1 was not as extensive in scope as CATIE, and its design had some important differences (Table 2). Patients were referred for participation because their psychiatrists were considering a change in antipsychotic medication to address adverse effects or inadequate response. Fewer patients were recruited than expected—40% of the planned sample during 30 months of recruitment—but researchers considered the size sufficient to compare the effectiveness of FGAs and SGAs.
Patients were randomly assigned to treatment with an antipsychotic class, either:
- an FGA (1 of 11 options—including 5 depot formulations—chosen by the treating clinician)
- or an SGA (risperidone, olanzapine, quetiapine, or amisulpride, also chosen by the clinician).
Physicians and patients were not blinded to the medications used. They could choose medications within patients’ assigned classes and switch as needed in ways that mimicked clinical practice. Trained assessors, who were blinded to the medications being used, evaluated the patients after 12, 26, and 52 weeks.
Quality of life was the primary outcome measure.13 Secondary measures included symptoms, side effects, patient satisfaction, and cost of care.
Band 1 results. Patients assigned to the SGA or FGA classes showed no significant differences in quality of life measures or schizophrenia symptoms. If anything, the findings slightly favored the FGAs.
Patient satisfaction and overall cost of care were similar, and rates of extrapyramidal symptoms (EPS), tardive dyskinesia, and akathisia did not differ significantly.
Clozapine comparison. In CUtLASS band 2, a different sample of 136 schizophrenia patients who had responded poorly to ≥2 antipsychotics was randomly assigned to clozapine or one of the above four SGAs. During the 1-year comparison trial, clozapine:
- was found to be significantly more effective (P=0.01) in managing patients’ symptoms, as measured by total Positive and Negative Syndrome Scale (PANSS) score
- showed a trend (P=0.08) towards providing these treatment-resistant patients with a better quality of life.8
Table 1
Summary of CUtLASS trial design and results
Band 1
|
Band 2
|
| CUtLASS: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study |
| FGA: First-generation antipsychotic |
| PANSS: Positive and Negative Syndrome Scale |
| SGA: Second-generation antipsychotic |
Table 2
Comparing designs of the CUtLASS and CATIE schizophrenia trials
| CUtLASS | CATIE | |
|---|---|---|
| Trial duration | 12 months | 18 months |
| Clinical sites | 14 (United Kingdom) | 57 (United States) |
| Number of Subjects | 227 | 1,460 |
| Gender and age | 68% male; mean age 41 | 74% male; mean age 41 |
| Mental illness duration (mean) | 14 years | 16 years |
| Diagnosis | 75% schizophrenia | 100% schizophrenia |
| First-episode patients included? | Yes (13% of sample) | No |
| % of patients receiving antipsychotics at enrollment | 99% | 74% |
| Baseline PANSS score (mean) | 82% FGAs; 40% depot | 15% FGAs; <5% depot |
| Baseline PANSS score | 72.2 | 75.7 |
| Baseline EPS scores | Low | Low |
| Antipsychotic options in randomization | 2 classes (SGA or FGA) (50% of subjects assigned to an FGA) | 4 SGAs, 1 FGA (20% of subjects assigned to an FGA) |
| % of subjects given sulpiride | 49% | 0% |
| Administration methodology | Medication blinded to raters but not to patients and physicians | Medication blinded to patients and physicians |
| Primary outcome | Quality of life | Discontinuation of medication |
| Long-acting antipsychotic option? | Yes | No |
| Antipsychotic switching | All patients switched agents; 49% changed antipsychotic class | 15% stayed on some agent |
| CATIE: Clinical Antipsychotic Trials of Intervention Effectiveness | ||
| CUtLASS: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study | ||
| EPS: Extrapyramidal symptom | ||
| FGA: First-generation antipsychotic | ||
| PANSS: Positive and Negative Syndrome Scale | ||
| SGA: Second-generation antipsychotic | ||
Comparing catie, cutlass data
The CUtLASS findings are not identical to those of CATIE phase 114 but are remarkably similar: no differences in effectiveness were seen between FGAs and SGA when treating patients with chronic schizophrenia.15,16
CUtLASS investigators concluded that “in people with schizophrenia whose medication is changed for clinical reasons, there is no disadvantage across 1 year in terms of quality of life, symptoms, or associated costs of care in using FGAs rather than nonclozapine SGAs.”7
By confirming CATIE’s results, is CUtLASS the final word on antipsychotic treatment of chronic schizophrenia? Or is it just another piece of the puzzle? CATIE and CUtLASS add much to our knowledge, but methodologic “flies in the ointment” plague all clinical trials. We must consider potential biases and confounding factors to properly interpret and apply their findings.
Although the CUtLASS trial was well-constructed and executed, its conclusions—like those of CATIE—merit careful scrutiny. Its patient recruitment methods and study design involved choices and compromises that are appropriate to evaluate17,18 as we weigh CUtLASS’ contribution to the SGA/FGA debate (Table 3).
Table 3
‘Flies in the ointment’ of the CUtLASS trial design
| Who was studied |
|
| What was compared |
|
| Other Issues |
|
| CUtLASS: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study | |
| EPS: Extrapyramidal symptom | |
| FGA: First-generation antipsychotic | |
| SGA: Second-generation antipsychotic | |
Who was studied?
Selection questions. CUtLASS researchers had problems recruiting patients for their study, in part because clinicians were reluctant to expose their patients to a 50% probability of being assigned to an FGA. Only 40% of the targeted sample was recruited, and participating clinicians referred only 20% to 37% of their eligible patients to the study.12 Thus, one could ask:
- Were enrolled subjects truly representative of the population from which they were drawn?
- Or did selection bias result in a disproportionate inclusion of individuals with certain characteristics?
Is it possible, for example, that clinicians preferentially referred medication-noncompliant patients to CUtLASS because they believed the benefits of depot FGAs—such as more assured adherence—would compensate for the potential benefits of SGAs—better efficacy/tolerability?19
Treatment resistance. Although patients were randomly assigned to FGAs or SGAs, a significantly greater proportion of those whose antipsychotics were being changed because of treatment resistance were assigned to receive SGAs. Treatment resistance was one reason that 88% of subjects in the SGA arm were referred to the trial, compared with 70% of subjects in the FGA arm (P<0.01).12 The extent to which this differential assignment may have biased results against SGAs is unclear.
EPS risk. CUtLASS-1 patients had been ill a mean of 14 years and had low baseline EPS rates despite receiving long-term antipsychotics (primarily FGAs). Even so, FGAs and SGAs showed similar rates of akathisia and other EPS. Thus—as with the CATIE results—the extent to which CUtLASS-1 findings may apply beyond chronic schizophrenia patients at relatively low risk for EPS is unclear.11,17
Impact of switching. Although patients were referred to CUtLASS because of adverse effects or inadequate response to one or more antipsychotics, they were only moderately ill (mean PANSS total score 72)20 and probably were deriving some benefit from their baseline antipsychotics. Before randomization, 82% of patients were receiving an FGA and 19% an SGA. Consequently, a far larger percentage of patients in the SGA group had to switch to a different medication class as the trial began.
As observed in CATIE, switching antipsychotics often has short-term negative consequences for patients,21 although switching classes (as in CUtLASS) may have had a different impact than switching individual antipsychotics (as in CATIE). If unequal antipsychotic switching rates in the two arms differentially affected patients’ quality of life, we would expect to see this effect emerge at the 12-week assessment, which is precisely where the greatest difference in Quality of Life Scale (QLS)13 scores appeared.
The mean QLS score for patients in the SGA arm was 2.6 points lower than in the FGA group at 12 weeks. This difference disappeared and, in fact, reversed at 26 weeks, but this 12-week effect had a strong impact on results of the 52-week intent-to-treat analysis. CUtLASS—like CATIE—might exemplify the risks of switching patients from treatment with partially effective antipsychotics.22
What was compared?
Classes vs individual drugs. The decision in CUtLASS-1 to compare antipsychotic classes rather than individual agents makes it difficult to interpret its findings. Antipsychotics are not homogeneous; clear differences exist within both the SGA and FGA classes in terms of individual agents’ efficacy and tolerability, and each SGA has a reasonably well-established and different side-effect profile.23
Sulpiride was the most commonly used FGA in CUtLASS-1 (by 49% of FGA patients). Sulpiride has some unusual attributes—such as lower EPS liability—and is not available in the United States. Thus, including this agent might have affected how applicable CUtLASS findings are to clinical practice in the United States.
Oral vs depot delivery. Individuals assigned to an FGA could receive either oral or long-acting depot medication, whereas those assigned to an SGA could receive only oral medication. At baseline, 84 of 227 CUtLASS-1 participants were receiving a depot antipsychotic, which was discontinued during randomization in 72 patients. During the 1-year study, the number of patients receiving a depot antipsychotic tripled from 12 to 35, suggesting the usefulness of long-acting agents in this population.19
Cross-class switching. Although participating physicians and their patients were urged to stay within assigned antipsychotic classes at least for the first 12 weeks and ideally for 1 year, a high rate of cross-class switching occurred (Figure). At the 52-week assessment, 51 of 118 patients (43%) in the intent-to-treat FGA group were receiving SGAs instead.
The CUtLASS authors’ assert that the trial refutes the hypothesis that using SGAs is superior to using FGAs in improving quality of life. This conclusion is difficult to justify when so many patients assigned to the FGA class actually were receiving SGAs. The conclusion is further weakened if differential switching rates put SGAs at a disadvantage in the first 12 weeks of the trial.
A more accurate conclusion of the intent-to-treat comparison appears in the technical report: “There was no statistically significant difference in terms of quality of life or symptoms over 1 year in commencing [italics added] conventional antipsychotic drugs rather than new atypical drugs.”12
Figure CUtLASS-1: Did switching rate affect trial outcome?
The high rate of cross-class medication switching in CUtLASS-1 may have weakened the study’s conclusion that virtually no difference in effectiveness exists between first- and second-generation antipsychotics. At the 52-week assessment, 51 of 118 patients (43%) in the intent-to-treat FGA group were receiving SGAs instead. Not shown in the figure is that 4 of the total 55 patients who switched from FGAs to SGAs had switched back to FGAs by the 52-week assessment.
CUtLASS: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study
FGA: First-generation antipsychotic
SGA: Second-generation antipsychotic
Source: Adapted from reference 7, Figure 1
Clinical implications
Notwithstanding these cautionary notes, CUtLASS-1 findings add to the questions raised by CATIE about the relative effectiveness of SGAs and FGAs. At a minimum, the data indicate that the SGA advantage has been overstated or oversimplified and that FGAs may be suitable options for meeting the needs of some patients with psychosis (particularly those at low risk for EPS).
Depot antipsychotics. CUtLASS also suggests a wider role for long-acting antipsychotics in chronic psychotic disorders, beyond treating patients with severe nonadherence.19,23 The number of patients receiving long-acting agents tripled over the 1-year study.12
Clozapine. Both CATIE and CUtLASS-2 confirmed clozapine’s superior efficacy for patients with treatment-resistant psychotic illness (Table 4). CUtLASS-2 also reaffirmed the challenges of clozapine’s metabolic and other side effects, such as sedation, hypotension, and hypersalivation.
All-cause discontinuation was significantly higher (P<0.05) in patients taking clozapine (73%) than in those taking other SGAs (52%). Even so, clozapine-group patients achieved significantly greater symptom reduction and tended toward a higher quality of life than other SGA-group patients.
Table 4
Clinical ‘pearls’ from the CUtLASS trial data
|
| CUtLASS: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study |
| EPS: Extrapyramidal symptom |
| FGA: First-generation antipsychotic |
| SGA: Second-generation antipsychotic |
Overview. In conclusion, one can reasonably conclude from analyzing the CATIE and CUtLASS data that:
- FGA-SGA differences are not as great as previously thought.
- Substantial differences exist among agents within both antipsychotic classes, particularly in side effect profiles.
- Neither study disproves the following presumed benefit of SGAs: that compared with FGAs, SGAs provide an equivalent antipsychotic effect and pose a lower risk of problems related to unmitigated dopamine blockade—such as EPS, dysphoria, bradyphrenia, neuroleptic-induced deficit syndrome, and tardive dyskinesia.11
- To use antipsychotics effectively and optimize individual treatment, consider the CATIE and CUtLASS trials in the contexts of their designs and the results of other studies of patients with chronic schizophrenia.
Related resources
- Heres S, Davis J, Maino K, et al. Why olanzapine beats risperidone, risperidone beats quetiapine, and quetiapine beats olanzapine: An exploratory analysis of head-head comparison studies of second-generation antipsychotics. Am J Psychiatry 2006;163:185-94.
Drug brand names
- Clozapine • Clozaril
- Quetiapine • Seroquel
- Olanzapine • Zyprexa
- Risperidone • Risperdal
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Kane JM, Leucht S, Carpenter D, et al. Expert consensus guideline series: optimizing pharmacologic treatment of psychotic disorders. J Clin Psychiatry 2003;64(suppl 12):1-100.
2. Tandon R, Fleischhacker WW. Comparative efficacy of antipsychotics in the treatment of schizophrenia: a critical assessment. Schizophr Res 2005;79:145-55.
3. Lieberman JA, Stroup TS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med 2005;353:1209-23.
4. McEvoy JP, Lieberman JA, Stroup TS, et al. Effectiveness of clozapine versus olanzapine, quetiapine, and risperidone in patients with chronic schizophrenia who did not respond to prior antipsychotic treatment. Am J Psychiatry 2006;163:600-10.
5. Stroup TS, Lieberman JA, McEvoy JP, et al. Effectiveness of olanzapine, quetiapine, risperidone, and ziprasidone in patients with chronic schizophrenia following discontinuation of a previous atypical antipsychotic. Am J Psychiatry 2006;163:611-22.
6. Rosenheck RA, Leslie DL, Sindelar J, et al. Cost-effectiveness of second-generation antipsychotics and perphenazine in a randomized trial of treatment for chronic schizophrenia. Am J Psychiatry 2006;163:2080-9.
7. Jones PB, Barnes T, Davies L, et al. Randomized controlled trial of the effect on quality of life of second- vs first-generation antipsychotic drugs in schizophrenia: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study (CUtLASS). Arch Gen Psychiatry 2006;63:1079-87.
8. Lewis SW, Barnes TRE, Davies L, et al. Randomised controlled trial of effect of prescription of clozapine versus other second-generation antipsychotic drugs in resistant schizophrenia. Schizophr Bull 2006;32:715-23.
9. Nasrallah HA. CATIE’s surprises: in antipsychotics’ square-off, were there winners or losers? Current Psychiatry 2006;5(2):49-65.
10. Buckley PF. Which antipsychotic do I choose next? CATIE phase 2 offers insights on efficacy and tolerability. Current Psychiatry 2006;5(9):27-43.
11. Tandon R, Constantine R. Avoiding EPS is key to realizing ‘atypical’ benefits. Current Psychiatry 2006;5(11):35-45.
12. Lewis SW, Davies L, Jones PB, et al. Randomised controlled trials of conventional antipsychotic versus new atypical drugs, and new atypical drugs versus clozapine, in people with schizophrenia responding poorly to, or intolerant of, current drug treatment. Health Technology Assessment 2006;10(#17):1-182.Available at http://www.hta.ac.uk/project/1078.asp. Accessed January 3, 2007.
13. Heinrichs DW, Hanlon TE, Carpenter WT. The Quality of Life Scale: an instrument for assessing the schizophrenic deficit syndrome. Schizophr Bull 1984;10:388-98.
14. Tandon R, Davis JM, Carpenter WT. CATIE, CUtLASS, and the FGA-SGA debate (letter). Arch Gen Psychiatry 2007 (in press).
15. Lieberman J. Comparative effectiveness of antipsychotic drugs: a commentary on the Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study and Clinical Antipsychotic Trials of Intervention Effectiveness. Arch Gen Psychiatry 2006;63:1069-72.
16. Rosenheck RA. Outcomes, costs, and policy caution: a commentary on the Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study. Arch Gen Psychiatry 2006;63:1074-6.
17. Tandon R. Comparative effectiveness of antipsychotics in the treatment of schizophrenia: what CATIE tells us—Parts 1 and 2. International Drug Therapy Newsletter 2006;41(7,9):51-8,67-74.
18. Meltzer HY, Bobo WV. Interpreting the efficacy findings in the CATIE study: what clinicians should know. CNS Spectrums 2006;11(suppl 7):14-24.
19. Kane JM. Review of treatments that can ameliorate nonadherence in patients with schizophrenia. J Clin Psychiatry 2006;67(suppl 5):9-14.
20. Leucht S, Kane JM, Kissling W, et al. What does the PANSS mean? Schizophr Res 2006;79:231-8.
21. Essock SM, Covell NH, Davis SM, et al. Effectiveness of switching antipsychotic medications. Am J Psychiatry 2006;163:2090-5.
22. Davis JM, Marder S, Tamminga CA. Switch or stay? Am J Psychiatry 2006;163:2032-3.
23. Tandon R, Targum SD, Nasrallah HA, et al. Strategies for maximizing clinical effectiveness in the treatment of schizophrenia. Journal of Psychiatric Practice 2006;12:348-63.
When treating chronic psychotic disorders, U.S. psychiatrists generally prefer second-generation antipsychotics (SGAs) to first-generation antipsychotics (FGAs) because of widely held views1,2 that SGAs:
- are more effective for negative and cognitive symptoms
- produce fewer troublesome side effects
- help patients realize a better quality of life.
These beliefs have been challenged by two large-scale, government-supported studies: the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) in the United States3-6 and more recently the Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study (CUtLASS) from the United Kingdom.7,8
CATIE and CUtLASS data suggest that the SGA advantage has been exaggerated, if in fact such an advantage exists. Other Current Psychiatry articles for the clinical practitioner have discussed the CATIE findings.9-11 This article addresses the CUtLASS results in the context of the trial’s methodology, using information from the primary publications7,8 and technical report.12
Cutlass study
Design. CUtLASS included 2 “bands” (Table 1):
- Band 1 compared the clinical usefulness and cost effectiveness of FGAs and SGAs in treating schizophrenia7
- Band 2 compared the effectiveness of clozapine versus other SGAs in treating refractory schizophrenia.8
CUtLASS Band 1 was not as extensive in scope as CATIE, and its design had some important differences (Table 2). Patients were referred for participation because their psychiatrists were considering a change in antipsychotic medication to address adverse effects or inadequate response. Fewer patients were recruited than expected—40% of the planned sample during 30 months of recruitment—but researchers considered the size sufficient to compare the effectiveness of FGAs and SGAs.
Patients were randomly assigned to treatment with an antipsychotic class, either:
- an FGA (1 of 11 options—including 5 depot formulations—chosen by the treating clinician)
- or an SGA (risperidone, olanzapine, quetiapine, or amisulpride, also chosen by the clinician).
Physicians and patients were not blinded to the medications used. They could choose medications within patients’ assigned classes and switch as needed in ways that mimicked clinical practice. Trained assessors, who were blinded to the medications being used, evaluated the patients after 12, 26, and 52 weeks.
Quality of life was the primary outcome measure.13 Secondary measures included symptoms, side effects, patient satisfaction, and cost of care.
Band 1 results. Patients assigned to the SGA or FGA classes showed no significant differences in quality of life measures or schizophrenia symptoms. If anything, the findings slightly favored the FGAs.
Patient satisfaction and overall cost of care were similar, and rates of extrapyramidal symptoms (EPS), tardive dyskinesia, and akathisia did not differ significantly.
Clozapine comparison. In CUtLASS band 2, a different sample of 136 schizophrenia patients who had responded poorly to ≥2 antipsychotics was randomly assigned to clozapine or one of the above four SGAs. During the 1-year comparison trial, clozapine:
- was found to be significantly more effective (P=0.01) in managing patients’ symptoms, as measured by total Positive and Negative Syndrome Scale (PANSS) score
- showed a trend (P=0.08) towards providing these treatment-resistant patients with a better quality of life.8
Table 1
Summary of CUtLASS trial design and results
Band 1
|
Band 2
|
| CUtLASS: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study |
| FGA: First-generation antipsychotic |
| PANSS: Positive and Negative Syndrome Scale |
| SGA: Second-generation antipsychotic |
Table 2
Comparing designs of the CUtLASS and CATIE schizophrenia trials
| CUtLASS | CATIE | |
|---|---|---|
| Trial duration | 12 months | 18 months |
| Clinical sites | 14 (United Kingdom) | 57 (United States) |
| Number of Subjects | 227 | 1,460 |
| Gender and age | 68% male; mean age 41 | 74% male; mean age 41 |
| Mental illness duration (mean) | 14 years | 16 years |
| Diagnosis | 75% schizophrenia | 100% schizophrenia |
| First-episode patients included? | Yes (13% of sample) | No |
| % of patients receiving antipsychotics at enrollment | 99% | 74% |
| Baseline PANSS score (mean) | 82% FGAs; 40% depot | 15% FGAs; <5% depot |
| Baseline PANSS score | 72.2 | 75.7 |
| Baseline EPS scores | Low | Low |
| Antipsychotic options in randomization | 2 classes (SGA or FGA) (50% of subjects assigned to an FGA) | 4 SGAs, 1 FGA (20% of subjects assigned to an FGA) |
| % of subjects given sulpiride | 49% | 0% |
| Administration methodology | Medication blinded to raters but not to patients and physicians | Medication blinded to patients and physicians |
| Primary outcome | Quality of life | Discontinuation of medication |
| Long-acting antipsychotic option? | Yes | No |
| Antipsychotic switching | All patients switched agents; 49% changed antipsychotic class | 15% stayed on some agent |
| CATIE: Clinical Antipsychotic Trials of Intervention Effectiveness | ||
| CUtLASS: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study | ||
| EPS: Extrapyramidal symptom | ||
| FGA: First-generation antipsychotic | ||
| PANSS: Positive and Negative Syndrome Scale | ||
| SGA: Second-generation antipsychotic | ||
Comparing catie, cutlass data
The CUtLASS findings are not identical to those of CATIE phase 114 but are remarkably similar: no differences in effectiveness were seen between FGAs and SGA when treating patients with chronic schizophrenia.15,16
CUtLASS investigators concluded that “in people with schizophrenia whose medication is changed for clinical reasons, there is no disadvantage across 1 year in terms of quality of life, symptoms, or associated costs of care in using FGAs rather than nonclozapine SGAs.”7
By confirming CATIE’s results, is CUtLASS the final word on antipsychotic treatment of chronic schizophrenia? Or is it just another piece of the puzzle? CATIE and CUtLASS add much to our knowledge, but methodologic “flies in the ointment” plague all clinical trials. We must consider potential biases and confounding factors to properly interpret and apply their findings.
Although the CUtLASS trial was well-constructed and executed, its conclusions—like those of CATIE—merit careful scrutiny. Its patient recruitment methods and study design involved choices and compromises that are appropriate to evaluate17,18 as we weigh CUtLASS’ contribution to the SGA/FGA debate (Table 3).
Table 3
‘Flies in the ointment’ of the CUtLASS trial design
| Who was studied |
|
| What was compared |
|
| Other Issues |
|
| CUtLASS: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study | |
| EPS: Extrapyramidal symptom | |
| FGA: First-generation antipsychotic | |
| SGA: Second-generation antipsychotic | |
Who was studied?
Selection questions. CUtLASS researchers had problems recruiting patients for their study, in part because clinicians were reluctant to expose their patients to a 50% probability of being assigned to an FGA. Only 40% of the targeted sample was recruited, and participating clinicians referred only 20% to 37% of their eligible patients to the study.12 Thus, one could ask:
- Were enrolled subjects truly representative of the population from which they were drawn?
- Or did selection bias result in a disproportionate inclusion of individuals with certain characteristics?
Is it possible, for example, that clinicians preferentially referred medication-noncompliant patients to CUtLASS because they believed the benefits of depot FGAs—such as more assured adherence—would compensate for the potential benefits of SGAs—better efficacy/tolerability?19
Treatment resistance. Although patients were randomly assigned to FGAs or SGAs, a significantly greater proportion of those whose antipsychotics were being changed because of treatment resistance were assigned to receive SGAs. Treatment resistance was one reason that 88% of subjects in the SGA arm were referred to the trial, compared with 70% of subjects in the FGA arm (P<0.01).12 The extent to which this differential assignment may have biased results against SGAs is unclear.
EPS risk. CUtLASS-1 patients had been ill a mean of 14 years and had low baseline EPS rates despite receiving long-term antipsychotics (primarily FGAs). Even so, FGAs and SGAs showed similar rates of akathisia and other EPS. Thus—as with the CATIE results—the extent to which CUtLASS-1 findings may apply beyond chronic schizophrenia patients at relatively low risk for EPS is unclear.11,17
Impact of switching. Although patients were referred to CUtLASS because of adverse effects or inadequate response to one or more antipsychotics, they were only moderately ill (mean PANSS total score 72)20 and probably were deriving some benefit from their baseline antipsychotics. Before randomization, 82% of patients were receiving an FGA and 19% an SGA. Consequently, a far larger percentage of patients in the SGA group had to switch to a different medication class as the trial began.
As observed in CATIE, switching antipsychotics often has short-term negative consequences for patients,21 although switching classes (as in CUtLASS) may have had a different impact than switching individual antipsychotics (as in CATIE). If unequal antipsychotic switching rates in the two arms differentially affected patients’ quality of life, we would expect to see this effect emerge at the 12-week assessment, which is precisely where the greatest difference in Quality of Life Scale (QLS)13 scores appeared.
The mean QLS score for patients in the SGA arm was 2.6 points lower than in the FGA group at 12 weeks. This difference disappeared and, in fact, reversed at 26 weeks, but this 12-week effect had a strong impact on results of the 52-week intent-to-treat analysis. CUtLASS—like CATIE—might exemplify the risks of switching patients from treatment with partially effective antipsychotics.22
What was compared?
Classes vs individual drugs. The decision in CUtLASS-1 to compare antipsychotic classes rather than individual agents makes it difficult to interpret its findings. Antipsychotics are not homogeneous; clear differences exist within both the SGA and FGA classes in terms of individual agents’ efficacy and tolerability, and each SGA has a reasonably well-established and different side-effect profile.23
Sulpiride was the most commonly used FGA in CUtLASS-1 (by 49% of FGA patients). Sulpiride has some unusual attributes—such as lower EPS liability—and is not available in the United States. Thus, including this agent might have affected how applicable CUtLASS findings are to clinical practice in the United States.
Oral vs depot delivery. Individuals assigned to an FGA could receive either oral or long-acting depot medication, whereas those assigned to an SGA could receive only oral medication. At baseline, 84 of 227 CUtLASS-1 participants were receiving a depot antipsychotic, which was discontinued during randomization in 72 patients. During the 1-year study, the number of patients receiving a depot antipsychotic tripled from 12 to 35, suggesting the usefulness of long-acting agents in this population.19
Cross-class switching. Although participating physicians and their patients were urged to stay within assigned antipsychotic classes at least for the first 12 weeks and ideally for 1 year, a high rate of cross-class switching occurred (Figure). At the 52-week assessment, 51 of 118 patients (43%) in the intent-to-treat FGA group were receiving SGAs instead.
The CUtLASS authors’ assert that the trial refutes the hypothesis that using SGAs is superior to using FGAs in improving quality of life. This conclusion is difficult to justify when so many patients assigned to the FGA class actually were receiving SGAs. The conclusion is further weakened if differential switching rates put SGAs at a disadvantage in the first 12 weeks of the trial.
A more accurate conclusion of the intent-to-treat comparison appears in the technical report: “There was no statistically significant difference in terms of quality of life or symptoms over 1 year in commencing [italics added] conventional antipsychotic drugs rather than new atypical drugs.”12
Figure CUtLASS-1: Did switching rate affect trial outcome?
The high rate of cross-class medication switching in CUtLASS-1 may have weakened the study’s conclusion that virtually no difference in effectiveness exists between first- and second-generation antipsychotics. At the 52-week assessment, 51 of 118 patients (43%) in the intent-to-treat FGA group were receiving SGAs instead. Not shown in the figure is that 4 of the total 55 patients who switched from FGAs to SGAs had switched back to FGAs by the 52-week assessment.
CUtLASS: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study
FGA: First-generation antipsychotic
SGA: Second-generation antipsychotic
Source: Adapted from reference 7, Figure 1
Clinical implications
Notwithstanding these cautionary notes, CUtLASS-1 findings add to the questions raised by CATIE about the relative effectiveness of SGAs and FGAs. At a minimum, the data indicate that the SGA advantage has been overstated or oversimplified and that FGAs may be suitable options for meeting the needs of some patients with psychosis (particularly those at low risk for EPS).
Depot antipsychotics. CUtLASS also suggests a wider role for long-acting antipsychotics in chronic psychotic disorders, beyond treating patients with severe nonadherence.19,23 The number of patients receiving long-acting agents tripled over the 1-year study.12
Clozapine. Both CATIE and CUtLASS-2 confirmed clozapine’s superior efficacy for patients with treatment-resistant psychotic illness (Table 4). CUtLASS-2 also reaffirmed the challenges of clozapine’s metabolic and other side effects, such as sedation, hypotension, and hypersalivation.
All-cause discontinuation was significantly higher (P<0.05) in patients taking clozapine (73%) than in those taking other SGAs (52%). Even so, clozapine-group patients achieved significantly greater symptom reduction and tended toward a higher quality of life than other SGA-group patients.
Table 4
Clinical ‘pearls’ from the CUtLASS trial data
|
| CUtLASS: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study |
| EPS: Extrapyramidal symptom |
| FGA: First-generation antipsychotic |
| SGA: Second-generation antipsychotic |
Overview. In conclusion, one can reasonably conclude from analyzing the CATIE and CUtLASS data that:
- FGA-SGA differences are not as great as previously thought.
- Substantial differences exist among agents within both antipsychotic classes, particularly in side effect profiles.
- Neither study disproves the following presumed benefit of SGAs: that compared with FGAs, SGAs provide an equivalent antipsychotic effect and pose a lower risk of problems related to unmitigated dopamine blockade—such as EPS, dysphoria, bradyphrenia, neuroleptic-induced deficit syndrome, and tardive dyskinesia.11
- To use antipsychotics effectively and optimize individual treatment, consider the CATIE and CUtLASS trials in the contexts of their designs and the results of other studies of patients with chronic schizophrenia.
Related resources
- Heres S, Davis J, Maino K, et al. Why olanzapine beats risperidone, risperidone beats quetiapine, and quetiapine beats olanzapine: An exploratory analysis of head-head comparison studies of second-generation antipsychotics. Am J Psychiatry 2006;163:185-94.
Drug brand names
- Clozapine • Clozaril
- Quetiapine • Seroquel
- Olanzapine • Zyprexa
- Risperidone • Risperdal
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
When treating chronic psychotic disorders, U.S. psychiatrists generally prefer second-generation antipsychotics (SGAs) to first-generation antipsychotics (FGAs) because of widely held views1,2 that SGAs:
- are more effective for negative and cognitive symptoms
- produce fewer troublesome side effects
- help patients realize a better quality of life.
These beliefs have been challenged by two large-scale, government-supported studies: the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) in the United States3-6 and more recently the Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study (CUtLASS) from the United Kingdom.7,8
CATIE and CUtLASS data suggest that the SGA advantage has been exaggerated, if in fact such an advantage exists. Other Current Psychiatry articles for the clinical practitioner have discussed the CATIE findings.9-11 This article addresses the CUtLASS results in the context of the trial’s methodology, using information from the primary publications7,8 and technical report.12
Cutlass study
Design. CUtLASS included 2 “bands” (Table 1):
- Band 1 compared the clinical usefulness and cost effectiveness of FGAs and SGAs in treating schizophrenia7
- Band 2 compared the effectiveness of clozapine versus other SGAs in treating refractory schizophrenia.8
CUtLASS Band 1 was not as extensive in scope as CATIE, and its design had some important differences (Table 2). Patients were referred for participation because their psychiatrists were considering a change in antipsychotic medication to address adverse effects or inadequate response. Fewer patients were recruited than expected—40% of the planned sample during 30 months of recruitment—but researchers considered the size sufficient to compare the effectiveness of FGAs and SGAs.
Patients were randomly assigned to treatment with an antipsychotic class, either:
- an FGA (1 of 11 options—including 5 depot formulations—chosen by the treating clinician)
- or an SGA (risperidone, olanzapine, quetiapine, or amisulpride, also chosen by the clinician).
Physicians and patients were not blinded to the medications used. They could choose medications within patients’ assigned classes and switch as needed in ways that mimicked clinical practice. Trained assessors, who were blinded to the medications being used, evaluated the patients after 12, 26, and 52 weeks.
Quality of life was the primary outcome measure.13 Secondary measures included symptoms, side effects, patient satisfaction, and cost of care.
Band 1 results. Patients assigned to the SGA or FGA classes showed no significant differences in quality of life measures or schizophrenia symptoms. If anything, the findings slightly favored the FGAs.
Patient satisfaction and overall cost of care were similar, and rates of extrapyramidal symptoms (EPS), tardive dyskinesia, and akathisia did not differ significantly.
Clozapine comparison. In CUtLASS band 2, a different sample of 136 schizophrenia patients who had responded poorly to ≥2 antipsychotics was randomly assigned to clozapine or one of the above four SGAs. During the 1-year comparison trial, clozapine:
- was found to be significantly more effective (P=0.01) in managing patients’ symptoms, as measured by total Positive and Negative Syndrome Scale (PANSS) score
- showed a trend (P=0.08) towards providing these treatment-resistant patients with a better quality of life.8
Table 1
Summary of CUtLASS trial design and results
Band 1
|
Band 2
|
| CUtLASS: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study |
| FGA: First-generation antipsychotic |
| PANSS: Positive and Negative Syndrome Scale |
| SGA: Second-generation antipsychotic |
Table 2
Comparing designs of the CUtLASS and CATIE schizophrenia trials
| CUtLASS | CATIE | |
|---|---|---|
| Trial duration | 12 months | 18 months |
| Clinical sites | 14 (United Kingdom) | 57 (United States) |
| Number of Subjects | 227 | 1,460 |
| Gender and age | 68% male; mean age 41 | 74% male; mean age 41 |
| Mental illness duration (mean) | 14 years | 16 years |
| Diagnosis | 75% schizophrenia | 100% schizophrenia |
| First-episode patients included? | Yes (13% of sample) | No |
| % of patients receiving antipsychotics at enrollment | 99% | 74% |
| Baseline PANSS score (mean) | 82% FGAs; 40% depot | 15% FGAs; <5% depot |
| Baseline PANSS score | 72.2 | 75.7 |
| Baseline EPS scores | Low | Low |
| Antipsychotic options in randomization | 2 classes (SGA or FGA) (50% of subjects assigned to an FGA) | 4 SGAs, 1 FGA (20% of subjects assigned to an FGA) |
| % of subjects given sulpiride | 49% | 0% |
| Administration methodology | Medication blinded to raters but not to patients and physicians | Medication blinded to patients and physicians |
| Primary outcome | Quality of life | Discontinuation of medication |
| Long-acting antipsychotic option? | Yes | No |
| Antipsychotic switching | All patients switched agents; 49% changed antipsychotic class | 15% stayed on some agent |
| CATIE: Clinical Antipsychotic Trials of Intervention Effectiveness | ||
| CUtLASS: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study | ||
| EPS: Extrapyramidal symptom | ||
| FGA: First-generation antipsychotic | ||
| PANSS: Positive and Negative Syndrome Scale | ||
| SGA: Second-generation antipsychotic | ||
Comparing catie, cutlass data
The CUtLASS findings are not identical to those of CATIE phase 114 but are remarkably similar: no differences in effectiveness were seen between FGAs and SGA when treating patients with chronic schizophrenia.15,16
CUtLASS investigators concluded that “in people with schizophrenia whose medication is changed for clinical reasons, there is no disadvantage across 1 year in terms of quality of life, symptoms, or associated costs of care in using FGAs rather than nonclozapine SGAs.”7
By confirming CATIE’s results, is CUtLASS the final word on antipsychotic treatment of chronic schizophrenia? Or is it just another piece of the puzzle? CATIE and CUtLASS add much to our knowledge, but methodologic “flies in the ointment” plague all clinical trials. We must consider potential biases and confounding factors to properly interpret and apply their findings.
Although the CUtLASS trial was well-constructed and executed, its conclusions—like those of CATIE—merit careful scrutiny. Its patient recruitment methods and study design involved choices and compromises that are appropriate to evaluate17,18 as we weigh CUtLASS’ contribution to the SGA/FGA debate (Table 3).
Table 3
‘Flies in the ointment’ of the CUtLASS trial design
| Who was studied |
|
| What was compared |
|
| Other Issues |
|
| CUtLASS: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study | |
| EPS: Extrapyramidal symptom | |
| FGA: First-generation antipsychotic | |
| SGA: Second-generation antipsychotic | |
Who was studied?
Selection questions. CUtLASS researchers had problems recruiting patients for their study, in part because clinicians were reluctant to expose their patients to a 50% probability of being assigned to an FGA. Only 40% of the targeted sample was recruited, and participating clinicians referred only 20% to 37% of their eligible patients to the study.12 Thus, one could ask:
- Were enrolled subjects truly representative of the population from which they were drawn?
- Or did selection bias result in a disproportionate inclusion of individuals with certain characteristics?
Is it possible, for example, that clinicians preferentially referred medication-noncompliant patients to CUtLASS because they believed the benefits of depot FGAs—such as more assured adherence—would compensate for the potential benefits of SGAs—better efficacy/tolerability?19
Treatment resistance. Although patients were randomly assigned to FGAs or SGAs, a significantly greater proportion of those whose antipsychotics were being changed because of treatment resistance were assigned to receive SGAs. Treatment resistance was one reason that 88% of subjects in the SGA arm were referred to the trial, compared with 70% of subjects in the FGA arm (P<0.01).12 The extent to which this differential assignment may have biased results against SGAs is unclear.
EPS risk. CUtLASS-1 patients had been ill a mean of 14 years and had low baseline EPS rates despite receiving long-term antipsychotics (primarily FGAs). Even so, FGAs and SGAs showed similar rates of akathisia and other EPS. Thus—as with the CATIE results—the extent to which CUtLASS-1 findings may apply beyond chronic schizophrenia patients at relatively low risk for EPS is unclear.11,17
Impact of switching. Although patients were referred to CUtLASS because of adverse effects or inadequate response to one or more antipsychotics, they were only moderately ill (mean PANSS total score 72)20 and probably were deriving some benefit from their baseline antipsychotics. Before randomization, 82% of patients were receiving an FGA and 19% an SGA. Consequently, a far larger percentage of patients in the SGA group had to switch to a different medication class as the trial began.
As observed in CATIE, switching antipsychotics often has short-term negative consequences for patients,21 although switching classes (as in CUtLASS) may have had a different impact than switching individual antipsychotics (as in CATIE). If unequal antipsychotic switching rates in the two arms differentially affected patients’ quality of life, we would expect to see this effect emerge at the 12-week assessment, which is precisely where the greatest difference in Quality of Life Scale (QLS)13 scores appeared.
The mean QLS score for patients in the SGA arm was 2.6 points lower than in the FGA group at 12 weeks. This difference disappeared and, in fact, reversed at 26 weeks, but this 12-week effect had a strong impact on results of the 52-week intent-to-treat analysis. CUtLASS—like CATIE—might exemplify the risks of switching patients from treatment with partially effective antipsychotics.22
What was compared?
Classes vs individual drugs. The decision in CUtLASS-1 to compare antipsychotic classes rather than individual agents makes it difficult to interpret its findings. Antipsychotics are not homogeneous; clear differences exist within both the SGA and FGA classes in terms of individual agents’ efficacy and tolerability, and each SGA has a reasonably well-established and different side-effect profile.23
Sulpiride was the most commonly used FGA in CUtLASS-1 (by 49% of FGA patients). Sulpiride has some unusual attributes—such as lower EPS liability—and is not available in the United States. Thus, including this agent might have affected how applicable CUtLASS findings are to clinical practice in the United States.
Oral vs depot delivery. Individuals assigned to an FGA could receive either oral or long-acting depot medication, whereas those assigned to an SGA could receive only oral medication. At baseline, 84 of 227 CUtLASS-1 participants were receiving a depot antipsychotic, which was discontinued during randomization in 72 patients. During the 1-year study, the number of patients receiving a depot antipsychotic tripled from 12 to 35, suggesting the usefulness of long-acting agents in this population.19
Cross-class switching. Although participating physicians and their patients were urged to stay within assigned antipsychotic classes at least for the first 12 weeks and ideally for 1 year, a high rate of cross-class switching occurred (Figure). At the 52-week assessment, 51 of 118 patients (43%) in the intent-to-treat FGA group were receiving SGAs instead.
The CUtLASS authors’ assert that the trial refutes the hypothesis that using SGAs is superior to using FGAs in improving quality of life. This conclusion is difficult to justify when so many patients assigned to the FGA class actually were receiving SGAs. The conclusion is further weakened if differential switching rates put SGAs at a disadvantage in the first 12 weeks of the trial.
A more accurate conclusion of the intent-to-treat comparison appears in the technical report: “There was no statistically significant difference in terms of quality of life or symptoms over 1 year in commencing [italics added] conventional antipsychotic drugs rather than new atypical drugs.”12
Figure CUtLASS-1: Did switching rate affect trial outcome?
The high rate of cross-class medication switching in CUtLASS-1 may have weakened the study’s conclusion that virtually no difference in effectiveness exists between first- and second-generation antipsychotics. At the 52-week assessment, 51 of 118 patients (43%) in the intent-to-treat FGA group were receiving SGAs instead. Not shown in the figure is that 4 of the total 55 patients who switched from FGAs to SGAs had switched back to FGAs by the 52-week assessment.
CUtLASS: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study
FGA: First-generation antipsychotic
SGA: Second-generation antipsychotic
Source: Adapted from reference 7, Figure 1
Clinical implications
Notwithstanding these cautionary notes, CUtLASS-1 findings add to the questions raised by CATIE about the relative effectiveness of SGAs and FGAs. At a minimum, the data indicate that the SGA advantage has been overstated or oversimplified and that FGAs may be suitable options for meeting the needs of some patients with psychosis (particularly those at low risk for EPS).
Depot antipsychotics. CUtLASS also suggests a wider role for long-acting antipsychotics in chronic psychotic disorders, beyond treating patients with severe nonadherence.19,23 The number of patients receiving long-acting agents tripled over the 1-year study.12
Clozapine. Both CATIE and CUtLASS-2 confirmed clozapine’s superior efficacy for patients with treatment-resistant psychotic illness (Table 4). CUtLASS-2 also reaffirmed the challenges of clozapine’s metabolic and other side effects, such as sedation, hypotension, and hypersalivation.
All-cause discontinuation was significantly higher (P<0.05) in patients taking clozapine (73%) than in those taking other SGAs (52%). Even so, clozapine-group patients achieved significantly greater symptom reduction and tended toward a higher quality of life than other SGA-group patients.
Table 4
Clinical ‘pearls’ from the CUtLASS trial data
|
| CUtLASS: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study |
| EPS: Extrapyramidal symptom |
| FGA: First-generation antipsychotic |
| SGA: Second-generation antipsychotic |
Overview. In conclusion, one can reasonably conclude from analyzing the CATIE and CUtLASS data that:
- FGA-SGA differences are not as great as previously thought.
- Substantial differences exist among agents within both antipsychotic classes, particularly in side effect profiles.
- Neither study disproves the following presumed benefit of SGAs: that compared with FGAs, SGAs provide an equivalent antipsychotic effect and pose a lower risk of problems related to unmitigated dopamine blockade—such as EPS, dysphoria, bradyphrenia, neuroleptic-induced deficit syndrome, and tardive dyskinesia.11
- To use antipsychotics effectively and optimize individual treatment, consider the CATIE and CUtLASS trials in the contexts of their designs and the results of other studies of patients with chronic schizophrenia.
Related resources
- Heres S, Davis J, Maino K, et al. Why olanzapine beats risperidone, risperidone beats quetiapine, and quetiapine beats olanzapine: An exploratory analysis of head-head comparison studies of second-generation antipsychotics. Am J Psychiatry 2006;163:185-94.
Drug brand names
- Clozapine • Clozaril
- Quetiapine • Seroquel
- Olanzapine • Zyprexa
- Risperidone • Risperdal
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Kane JM, Leucht S, Carpenter D, et al. Expert consensus guideline series: optimizing pharmacologic treatment of psychotic disorders. J Clin Psychiatry 2003;64(suppl 12):1-100.
2. Tandon R, Fleischhacker WW. Comparative efficacy of antipsychotics in the treatment of schizophrenia: a critical assessment. Schizophr Res 2005;79:145-55.
3. Lieberman JA, Stroup TS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med 2005;353:1209-23.
4. McEvoy JP, Lieberman JA, Stroup TS, et al. Effectiveness of clozapine versus olanzapine, quetiapine, and risperidone in patients with chronic schizophrenia who did not respond to prior antipsychotic treatment. Am J Psychiatry 2006;163:600-10.
5. Stroup TS, Lieberman JA, McEvoy JP, et al. Effectiveness of olanzapine, quetiapine, risperidone, and ziprasidone in patients with chronic schizophrenia following discontinuation of a previous atypical antipsychotic. Am J Psychiatry 2006;163:611-22.
6. Rosenheck RA, Leslie DL, Sindelar J, et al. Cost-effectiveness of second-generation antipsychotics and perphenazine in a randomized trial of treatment for chronic schizophrenia. Am J Psychiatry 2006;163:2080-9.
7. Jones PB, Barnes T, Davies L, et al. Randomized controlled trial of the effect on quality of life of second- vs first-generation antipsychotic drugs in schizophrenia: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study (CUtLASS). Arch Gen Psychiatry 2006;63:1079-87.
8. Lewis SW, Barnes TRE, Davies L, et al. Randomised controlled trial of effect of prescription of clozapine versus other second-generation antipsychotic drugs in resistant schizophrenia. Schizophr Bull 2006;32:715-23.
9. Nasrallah HA. CATIE’s surprises: in antipsychotics’ square-off, were there winners or losers? Current Psychiatry 2006;5(2):49-65.
10. Buckley PF. Which antipsychotic do I choose next? CATIE phase 2 offers insights on efficacy and tolerability. Current Psychiatry 2006;5(9):27-43.
11. Tandon R, Constantine R. Avoiding EPS is key to realizing ‘atypical’ benefits. Current Psychiatry 2006;5(11):35-45.
12. Lewis SW, Davies L, Jones PB, et al. Randomised controlled trials of conventional antipsychotic versus new atypical drugs, and new atypical drugs versus clozapine, in people with schizophrenia responding poorly to, or intolerant of, current drug treatment. Health Technology Assessment 2006;10(#17):1-182.Available at http://www.hta.ac.uk/project/1078.asp. Accessed January 3, 2007.
13. Heinrichs DW, Hanlon TE, Carpenter WT. The Quality of Life Scale: an instrument for assessing the schizophrenic deficit syndrome. Schizophr Bull 1984;10:388-98.
14. Tandon R, Davis JM, Carpenter WT. CATIE, CUtLASS, and the FGA-SGA debate (letter). Arch Gen Psychiatry 2007 (in press).
15. Lieberman J. Comparative effectiveness of antipsychotic drugs: a commentary on the Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study and Clinical Antipsychotic Trials of Intervention Effectiveness. Arch Gen Psychiatry 2006;63:1069-72.
16. Rosenheck RA. Outcomes, costs, and policy caution: a commentary on the Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study. Arch Gen Psychiatry 2006;63:1074-6.
17. Tandon R. Comparative effectiveness of antipsychotics in the treatment of schizophrenia: what CATIE tells us—Parts 1 and 2. International Drug Therapy Newsletter 2006;41(7,9):51-8,67-74.
18. Meltzer HY, Bobo WV. Interpreting the efficacy findings in the CATIE study: what clinicians should know. CNS Spectrums 2006;11(suppl 7):14-24.
19. Kane JM. Review of treatments that can ameliorate nonadherence in patients with schizophrenia. J Clin Psychiatry 2006;67(suppl 5):9-14.
20. Leucht S, Kane JM, Kissling W, et al. What does the PANSS mean? Schizophr Res 2006;79:231-8.
21. Essock SM, Covell NH, Davis SM, et al. Effectiveness of switching antipsychotic medications. Am J Psychiatry 2006;163:2090-5.
22. Davis JM, Marder S, Tamminga CA. Switch or stay? Am J Psychiatry 2006;163:2032-3.
23. Tandon R, Targum SD, Nasrallah HA, et al. Strategies for maximizing clinical effectiveness in the treatment of schizophrenia. Journal of Psychiatric Practice 2006;12:348-63.
1. Kane JM, Leucht S, Carpenter D, et al. Expert consensus guideline series: optimizing pharmacologic treatment of psychotic disorders. J Clin Psychiatry 2003;64(suppl 12):1-100.
2. Tandon R, Fleischhacker WW. Comparative efficacy of antipsychotics in the treatment of schizophrenia: a critical assessment. Schizophr Res 2005;79:145-55.
3. Lieberman JA, Stroup TS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med 2005;353:1209-23.
4. McEvoy JP, Lieberman JA, Stroup TS, et al. Effectiveness of clozapine versus olanzapine, quetiapine, and risperidone in patients with chronic schizophrenia who did not respond to prior antipsychotic treatment. Am J Psychiatry 2006;163:600-10.
5. Stroup TS, Lieberman JA, McEvoy JP, et al. Effectiveness of olanzapine, quetiapine, risperidone, and ziprasidone in patients with chronic schizophrenia following discontinuation of a previous atypical antipsychotic. Am J Psychiatry 2006;163:611-22.
6. Rosenheck RA, Leslie DL, Sindelar J, et al. Cost-effectiveness of second-generation antipsychotics and perphenazine in a randomized trial of treatment for chronic schizophrenia. Am J Psychiatry 2006;163:2080-9.
7. Jones PB, Barnes T, Davies L, et al. Randomized controlled trial of the effect on quality of life of second- vs first-generation antipsychotic drugs in schizophrenia: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study (CUtLASS). Arch Gen Psychiatry 2006;63:1079-87.
8. Lewis SW, Barnes TRE, Davies L, et al. Randomised controlled trial of effect of prescription of clozapine versus other second-generation antipsychotic drugs in resistant schizophrenia. Schizophr Bull 2006;32:715-23.
9. Nasrallah HA. CATIE’s surprises: in antipsychotics’ square-off, were there winners or losers? Current Psychiatry 2006;5(2):49-65.
10. Buckley PF. Which antipsychotic do I choose next? CATIE phase 2 offers insights on efficacy and tolerability. Current Psychiatry 2006;5(9):27-43.
11. Tandon R, Constantine R. Avoiding EPS is key to realizing ‘atypical’ benefits. Current Psychiatry 2006;5(11):35-45.
12. Lewis SW, Davies L, Jones PB, et al. Randomised controlled trials of conventional antipsychotic versus new atypical drugs, and new atypical drugs versus clozapine, in people with schizophrenia responding poorly to, or intolerant of, current drug treatment. Health Technology Assessment 2006;10(#17):1-182.Available at http://www.hta.ac.uk/project/1078.asp. Accessed January 3, 2007.
13. Heinrichs DW, Hanlon TE, Carpenter WT. The Quality of Life Scale: an instrument for assessing the schizophrenic deficit syndrome. Schizophr Bull 1984;10:388-98.
14. Tandon R, Davis JM, Carpenter WT. CATIE, CUtLASS, and the FGA-SGA debate (letter). Arch Gen Psychiatry 2007 (in press).
15. Lieberman J. Comparative effectiveness of antipsychotic drugs: a commentary on the Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study and Clinical Antipsychotic Trials of Intervention Effectiveness. Arch Gen Psychiatry 2006;63:1069-72.
16. Rosenheck RA. Outcomes, costs, and policy caution: a commentary on the Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study. Arch Gen Psychiatry 2006;63:1074-6.
17. Tandon R. Comparative effectiveness of antipsychotics in the treatment of schizophrenia: what CATIE tells us—Parts 1 and 2. International Drug Therapy Newsletter 2006;41(7,9):51-8,67-74.
18. Meltzer HY, Bobo WV. Interpreting the efficacy findings in the CATIE study: what clinicians should know. CNS Spectrums 2006;11(suppl 7):14-24.
19. Kane JM. Review of treatments that can ameliorate nonadherence in patients with schizophrenia. J Clin Psychiatry 2006;67(suppl 5):9-14.
20. Leucht S, Kane JM, Kissling W, et al. What does the PANSS mean? Schizophr Res 2006;79:231-8.
21. Essock SM, Covell NH, Davis SM, et al. Effectiveness of switching antipsychotic medications. Am J Psychiatry 2006;163:2090-5.
22. Davis JM, Marder S, Tamminga CA. Switch or stay? Am J Psychiatry 2006;163:2032-3.
23. Tandon R, Targum SD, Nasrallah HA, et al. Strategies for maximizing clinical effectiveness in the treatment of schizophrenia. Journal of Psychiatric Practice 2006;12:348-63.
Does marijuana contribute to psychotic illness?
Evidence grows that marijuana use can cause acute psychosis, bring forward in time a first schizophrenia episode, and worsen the prognosis of patients with psychotic disorders.
Roger, age 16, had been smoking marijuana on and off for about 2 years. His parents knew but believed this was a stage and not dangerous; they had tried marijuana in their youth without harm. Roger’s smoking had increased to several joints daily since he started a relationship with an older girl, who shared and encouraged his habit.
His parents became worried when Roger began making unusual comments, saying that food did not taste “right” and he thought someone was poisoning him. They brought Roger for psychiatric consultation at the recommendation of their family physician.
History and examination revealed that Roger had experienced vague persecutory ideas for several weeks but no systematized delusions or hallucinations. I told Roger and his parents he probably had a drug-induced psychosis and that symptoms would likely disappear without recurrence if he stopped using marijuana. At 2-weeks’ follow-up, he described no more psychotic experiences and said he now realized the danger for him of smoking marijuana. A review 1 month later showed Roger was doing well, and I discharged him after reinforcing the importance of abstinence. But his case didn’t end there.
The dopaminergic effect of cannabinoid receptors (such as CB1) may be one biologic mechanism, according to preliminary evidence. But the dopaminergic pathway might not be the most relevant mechanism, because the primary psychoactive constituent of marijuana—delta-9-tetrahydrocannabinol (delta-9-THC)—causes or increases psychotic symptoms in patients with schizophrenia despite treatment with dopamine receptor antagonists.2
Gene-environment interactions also appear to be relevant. A functional polymorphism in the catechol-O-methyltransferase (COMT) gene (COMT Val158 Met) moderates the influence of cannabis use on developing psychosis, according to a birth cohort study of 803 New Zealanders. COMT valine158 allele carriers were most likely to exhibit psychotic symptoms and develop schizophreniform disorder if they used cannabis during adolescence. This association did not apply to adult-onset cannabis use.3
Results were similar in a study in which 30 patients with a psychotic disorder, 12 relatives of patients with a psychotic disorder, and 32 healthy controls received delta-9-THC or placebo.4
Two years later, I received a request for information about Roger’s episode from an acute inpatient facility. Roger had been admitted after an incident at the local mall in which he screamed at people and accused bystanders of trying to harm him. Despite using marijuana only occasionally, his behavior had been deteriorating and was becoming increasingly bizarre. The attending psychiatrist believed Roger had schizophrenia.
Clinicians regularly deal with patients such as Roger who suffer from a psychotic disorder and use marijuana. This is hardly surprising because marijuana is the most widely used illicit drug. In 2006, 5% of 12th graders in the United States reported using marijuana daily during the previous month, and 42% had tried it at least once.1
Is psychotic patients’ use of marijuana a coincidence? Self-medication? Or could cannabis cause psychotic illness? This debate elicits strong views among community and professional groups. To help you provide up-to-date advice to patients and families, this review:
- describes the growing body of evidence on the mental health consequences of marijuana use
- seeks to help you detect and deal with the effects of marijuana use in clinical practice.
Marijuana and psychosis
Although the neurobiologic association is unclear (Box 1),2-4 up to 15% of users report psychotic phenomena after consuming marijuana.5 Naturalistic and experimental studies have confirmed that marijuana can induce short-lived psychotic experiences.
In two parallel trials, 22 healthy individuals6 and 13 stable, antipsychotic-treated schizophrenia patients7 were given 2.5 mg and 5 mg intravenously of delta-9-tetrahydrocannabinol (delta-9-THC)—the primary psychoactive constituent of marijuana. Both groups developed dose-related, transient, schizophrenia-like symptoms and altered perceptions:
- Healthy volunteers showed the full range of psychotic symptoms. One individual said, “I thought you were giving me THC through the blood pressure machine and the sheets.”2
- Schizophrenia patients tended to report increases in the symptoms of their specific conditions. Those with paranoid illnesses, for example, reported an escalation in persecutory ideas.
Transient psychotic phenomena are not equivalent to a psychotic illness, however. To meet diagnostic criteria for a psychotic disorder, symptoms must be persistent and impair psychosocial functioning.
Early reports. Anecdotal clinical reports that marijuana use could cause psychosis emerged in the 1960s but were largely ignored. Many clinicians assumed that psychotic individuals used marijuana to relieve troubling symptoms (self-medication).
A 15-year, longitudinal study examined the incidence of schizophrenia in >50,000 Swedish conscripts and concluded that marijuana use during adolescence increased the risk of schizophrenia.8 Skeptics questioned the validity of the diagnosis and the etiologic role of other drugs in this study and suggested that prodromal symptoms might have led to marijuana use, rather than marijuana triggering the psychosis.
Recent evidence. Better-designed studies have shown that marijuana use increases the risk of psychosis later in life.
Adolescents who used marijuana by age 15 were more likely to develop a schizophreniform disorder by age 26 than nonusers, according to data from 759 New Zealanders who took part in a prospective, longitudinal, general population study. Marijuana use by age 15 was associated with a higher risk than later use (by age 18).9
A 3-year, longitudinal, population-based study from the Netherlands found marijuana use associated with increased risk of psychosis in 4,045 previously psychosis-free individuals. More than 50% of psychosis diagnoses could be attributed to marijuana use.10
Data from the 21-year longitudinal Christchurch Health and Development Study in New Zealand showed elevated rates of psychotic symptoms in young people with cannabis dependence at ages 18 and 21. The associations remained even after adjustments were made for previous psychotic symptoms and other confounding factors.11
Follow-up analysis of data from the Swedish military conscripts study8 showed that the use of other psychoactive drugs or prodromal cases in the cohort did not explain the association between self-reported marijuana use and hospital admissions for schizophrenia and other psychoses.12
- Starting marijuana use in adolescence
- Using cannabis often (weekly or daily) or for long periods
- Unusual, psychotic-like experiences (such as fleeting persecutory ideas or ideas of reference) or displaying high “psychoticism” on the self-report Symptom Checklist-90-R
- Family history of psychosis
- Prior cannabis-induced psychotic episode
- Cannabis use increases the risk of developing psychosis and is estimated to double the risk for later schizophrenia (5 to 10 new cases per 10,000 person-years)
- The association is not an artifact of confounding factors such as prodromal symptoms or concurrent use of other substances (including amphetamines)
- The risk increases with the frequency and length of use (a dose-effect relationship)
- Self-medication is not the connection between cannabis use and schizophrenia, according to empiric evidence
Researchers in Israel cross-linked a cohort of 9,724 youths aged 16 to 17 screened by the Israeli Draft Board with a national registry of psychiatric hospital admissions for schizophrenia in the following 4 to 15 years. Self-reported drug abuse (mostly marijuana) was higher in adolescents who were later hospitalized for schizophrenia (12.4%) than in those not hospitalized (5.9%).13
Is the diagnosis worthwhile? Acute-phase cannabis-induced psychosis and schizophrenia have similar presentations, making differential diagnosis difficult. If their treatment also is similar, is it clinically meaningful to distinguish whether marijuana use or schizophrenia triggered psychotic symptoms? The answer is yes, because:
- schizophrenia has a worse course and prognosis
- many patients with cannabis-induced psychosis do not develop schizophrenia.
Diagnostic clues. Some clinicians believe cannabis-induced psychosis is more likely than schizophrenia to feature:
- expansive mood
- derealization or depersonalization experiences
- visual hallucinations
- less overall severity.
Consider the course. The only way to differentiate the two disorders is to consider the illness course. Cannabis-induced psychotic episodes occur during periods of intoxication or withdrawal, tend to be short-lived, and usually respond well to treatment if the person abstains.
Up to one-half of patients with a cannabis-induced psychosis develop a schizophrenia-spectrum disorder. Monitoring them (such as at 6-month intervals) is important, therefore, because schizophrenia onset often occurs >12 months after the cannabis-induced psychosis.
Summary. A review of these 5 studies concluded that evidence supports the hypothesis that marijuana use acts as a risk factor in schizophrenia onset.14 Although marijuana use is not a “necessary” causal factor in psychotic illness—most users do not develop the disorder, and many persons with schizophrenia do not use marijuana—strong evidence indicates that it is one of many factors that can cause a psychotic illness (Box 2).9-14
Who is at risk?
Can marijuana cause psychosis in any person or specifically in those at increased risk of psychosis? If the latter, then marijuana—rather than causing new, unanticipated cases—might bring forward schizophrenia onset in individuals who would have developed it later. This explanation is consistent with data showing that persons born in more-recent cohorts seem to have an earlier age of schizophrenia onset.15
Vulnerability for psychosis. Evidence strongly suggests that marijuana-induced psychotic symptoms are more prevalent among vulnerable or psychosis-prone individuals.
- When given 2.5 mg of delta-9-THC, 80% of 13 patients with well-controlled schizophrenia experienced high Positive and Negative Syndrome Scale scores, compared with 35% of 22 healthy controls.2
- Unusual perceptions or thought influence were more common following marijuana use in all participants in a naturalistic experiment, but much more so in “at risk” individuals who had previously described isolated psychotic symptoms.16
- Adolescents and young adults ages 14 to 24 who used marijuana and displayed high “psychoticism” scores at baseline had more than twice the risk of a psychosis outcome 4 years later than did those without high scores.17
Schizophrenia onset. Marijuana users who suffer a drug-induced psychosis are at very high risk of developing a psychotic illness later on. A ≥3-year follow-up study18 of 535 patients who had not been treated for psychotic problems before being diagnosed with marijuana-induced psychotic symptoms found that:
- marijuana-induced psychotic episodes often remitted quickly with minimal treatment
- about one-half of patients were diagnosed with a schizophrenia-spectrum disorder (mostly paranoid schizophrenia) at follow up
- the gap between the marijuana-induced episode and diagnosis of a schizophrenia-spectrum disorder was >1 year in 47% of cases.
- the first episode of schizophrenia in these patients occurred several years earlier than in schizophrenia patients without marijuana-induced psychosis.
Although these findings require replication, they challenge the belief that marijuana-induced psychosis is benign (Box 3).
Implications for treatment
Most psychiatric practitioners treat patients who have psychotic illness and use marijuana (Box 4). Compared with nonusers, these patients tend to have:
- earlier age of schizophrenia onset
- more psychotic symptoms
- worse prognosis because of poorer treatment adherence
- increased symptom severity and persistence
- higher relapse rates.19
Therefore, ask patients with psychotic disorders about their marijuana use, and treat both the marijuana use and the psychosis. Evidence to guide treatment is scarce, however. Nicotine, marijuana, and alcohol use are often intertwined. This suggests that treatments that target a variety of substances may be more efficient than targeted ones, even if the generic interventions are brief.20
A study of marijuana users with early psychosis showed, for example, that marijuana-focused treatment was not more effective than psychoeducation, although both resulted in reduced use.21 In nonpsychotic individuals, giving 90 adult patients incentive vouchers to exchange for retail items each time they provided a marijuana-negative urine specimen resulted in increased abstinence rates over a 12-month period (Box 5).22,23 Cognitive-behavioral therapy helped to sustain the vouchers’ positive effect on abstinence after the initial 14-week treatment.23
Efficacy. In voucher-based reinforcement therapy, patients receive vouchers or monetary incentives redeemable for goods and services, contingent on satisfying predetermined therapeutic goals. A meta-analysis22 showed this therapy model can produce better outcomes in substance use disorders, compared with control treatment.
Marijuana abstinence. A 12-month study of 90 cannabis-dependent adults23 found that voucher-based reinforcement therapy could extend marijuana abstinence. During the 14 weeks of active treatment, participants could redeem vouchers for goods or services—such as movie passes, sports/hobby equipment, work materials, or vocational classes.
- Participants earned a voucher worth $1.50 for the first negative specimen.
- Voucher values increased by $1.50 for each consecutive negative specimen.
- Two consecutive negative specimens earned a $10 bonus.
- Voucher values dropped back to $1.50 if participants provided a cannabinoid-positive specimen or failed to submit a scheduled specimen. Values then could re-escalate according to the same schedule.
Treatment with first-generation antipsychotics does not appear to decrease substance use. Several studies suggest that clozapine decreases the use of nicotine, alcohol, or other substances among patients with schizophrenia,24 though this does not necessarily apply to other second-generation antipsychotics (Box 6).
- Ask about marijuana use when evaluating all patients, particularly young ones
- Educate patients and, if appropriate, families about the risks of marijuana use. One way to do this without sounding judgmental or confrontational is to follow the principles of motivational interviewing
- Treat both the psychosis and the substance use
- Generic interventions that target drug use might be more effective than those specific to cannabis use because psychotic patients often abuse a variety of substances
- Psychoeducation might be as effective as cannabis-specific treatments
- Abstinence-based vouchers are a simple intervention with some evidence of effectiveness
- Clozapine, which seems to reduce relapse of substance use in these patients, might be the antipsychotic of choice
Implications for prevention
Psychiatric practitioners can play an important role in making young people aware of the mental health risks of using marijuana. Marijuana use fluctuates population-wide, depending in part on public perception of its harmfulness. Its use may diminish, therefore, as information on its mental health hazards percolates into high schools and the community at large. We also have the duty to make policy makers and legislators aware of this information.25
Related resources
- National Institute on Drug Abuse. https://www.drugabuse.gov/drugs-abuse/marijuana.
- Cannabis dependence. www.mentalhealth.com/dis/p20-sb03.html.
- Castle D, Murray R, eds. Marijuana and madness: psychiatry and neurobiology. Cambridge, UK: Cambridge University Press; 2004.
- Hall W, Pacula RL. Cannabis use and dependence: public health and public policy. Cambridge, UK: Cambridge University Press; 2003.
Drug brand names
- Clozapine • Clozaril
Disclosure
Dr. Rey reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Teen drug use continues down in 2006, particularly among older teens; but use of prescription-type drugs remains high. Ann Arbor, MI: University of Michigan News and Information Services; Dec. 21, 2006. Available at: http://monitoringthefuture.org. Accessed January 2, 2007.
2. D’Souza DC, Cho HS, Perry EB, Krystal JH. Cannabinoid ’model’ psychosis, dopamine-cannabinoid interactions and implications for schizophrenia. In: Castle D, Murray R, eds. Marijuana and madness: psychiatry and neurobiology. Cambridge, UK: Cambridge University Press; 2004:142-65.
3. Caspi A, Moffitt TE, Cannon M, et al. Moderation of the effect of adolescent-onset cannabis use on adult psychosis by a functional polymorphism in the catechol-O-methyltransferase gene: longitudinal evidence of a gene X environment interaction. Biol Psychiatry 2005;57(10):1117-27.
4. Henquet C, Rosa A, Krabbendam L, et al. An experimental study of catechol-O-methyltransferase Val158 Met moderation of Δ-9-tetrahydrocannabinol-induced effects on psychosis and cognition. Neuropsychopharmacol 2006;31:2748-57.
5. Thomas H. A community survey of adverse effects of cannabis use. Drug Alcohol Depend 1996;42(3):201-7.
6. D’Souza DC, Perry E, MacDougall L, et al. The psychotomimetic effects of intravenous delta-9-tetrahydrocannabinol in healthy individuals: implications for psychosis. Neuropsychopharmacology 2004;29:1558-72.
7. D’Souza DC, Abi-Saab WM, Madonick S, et al. Delta-9-tetrahydrocannabinol effects in schizophrenia: implications for cognition, psychosis, and addiction. Biol Psychiatry 2005;57:594-608.
8. Andreasson S, Allebeck P, Engstrom A, Rydberg U. Cannabis and schizophrenia. A longitudinal study of Swedish conscripts. Lancet 1987;2(8574):1483-6.
9. Arseneault L, Cannon M, Poulton R, et al. Cannabis use in adolescence and risk for adult psychosis: longitudinal prospective study. BMJ 2002;325(7374):1212-3.
10. van Os J, Bak M, Hanssen M, et al. Cannabis use and psychosis: a longitudinal population-based study. Am J Epidemiol 2002;156(4):319-27.
11. Fergusson DM, Horwood LJ, Swain-Campbell NR. Cannabis dependence and psychotic symptoms in young people. Psychol Med 2003;33(1):15-21.
12. Zammit S, Allebeck P, Andreasson S, et al. Self reported cannabis use as a risk factor for schizophrenia in Swedish conscripts of 1969: historical cohort study. BMJ 2002;325(7374):1199-201.
13. Weiser M, Knobler HY, Noy S, Kaplan Z. Clinical characteristics of adolescents later hospitalized for schizophrenia. Am J Med Genet 2002;114:949-55.
14. Smit F, Bolier L, Cuijpers P. Cannabis use and the risk of later schizophrenia: a review. Addiction 2004;99(4):425-30.
15. Di Maggio C, Martinez M, Menard JF, et al. Evidence of a cohort effect for age at onset of schizophrenia. Am J Psychiatry 2001;158(3):489-92.
16. Verdoux H, Gindre C, Sorbara F, et al. Effects of cannabis and psychosis vulnerability in daily life: an experience sampling test study. Psychol Med 2003;33(1):23-32.
17. Henquet C, Krabbendam L, Spauwen J, et al. Prospective cohort study of cannabis use, predisposition for psychosis, and psychotic symptoms in young people. BMJ 2005;330(7481):11-4.
18. Arendt M, Rosenberg R, Foldager L, et al. Cannabis-induced psychosis and subsequent schizophrenia-spectrum disorders: follow-up study of 535 incident cases. Br J Psychiatry 2005;187:510-5.
19. Pencer A, Addington J, Addington D. Outcome of a first episode of psychosis in adolescence: a 2-year follow-up. Psychiatry Res 2005;133(1):35-43.
20. McCambridge J, Strang J. The efficacy of single-session motivational interviewing in reducing drug consumption and perceptions of drug-related risk and harm among young people: results from a multi-site cluster randomized trial. Addiction 2004;99(1):39-52.
21. Edwards J, Elkins K, Hinton M, et al. Randomized controlled trial of a cannabis-focused intervention for young people with first-episode psychosis. Acta Psychiatr Scand 2006;114(2):109-17.
22. Lussier JP, Heil SH, Mongeon JA, et al. A meta-analysis of voucher-based reinforcement therapy for substance use disorders. Addiction 2006;101:192-203.
23. Budney AJ, Moore BA, Rocha HL, Higgins ST. Clinical trial of abstinence-based vouchers and cognitive-behavioral therapy for cannabis dependence. J Consult Clin Psychol 2006;74(2):307-16.
24. Brunette MF, Drake RE, Xie H, et al. Clozapine use and relapses of substance use disorder among patients with co-occurring schizophrenia and substance use disorders. Schizophr Bull 2006;32(4):637-43.
25. Hall W, Degenhardt L. What are the policy implications of the evidence on cannabis and psychosis? Can J Psychiatry 2006;51(9):566-74.
Evidence grows that marijuana use can cause acute psychosis, bring forward in time a first schizophrenia episode, and worsen the prognosis of patients with psychotic disorders.
Roger, age 16, had been smoking marijuana on and off for about 2 years. His parents knew but believed this was a stage and not dangerous; they had tried marijuana in their youth without harm. Roger’s smoking had increased to several joints daily since he started a relationship with an older girl, who shared and encouraged his habit.
His parents became worried when Roger began making unusual comments, saying that food did not taste “right” and he thought someone was poisoning him. They brought Roger for psychiatric consultation at the recommendation of their family physician.
History and examination revealed that Roger had experienced vague persecutory ideas for several weeks but no systematized delusions or hallucinations. I told Roger and his parents he probably had a drug-induced psychosis and that symptoms would likely disappear without recurrence if he stopped using marijuana. At 2-weeks’ follow-up, he described no more psychotic experiences and said he now realized the danger for him of smoking marijuana. A review 1 month later showed Roger was doing well, and I discharged him after reinforcing the importance of abstinence. But his case didn’t end there.
The dopaminergic effect of cannabinoid receptors (such as CB1) may be one biologic mechanism, according to preliminary evidence. But the dopaminergic pathway might not be the most relevant mechanism, because the primary psychoactive constituent of marijuana—delta-9-tetrahydrocannabinol (delta-9-THC)—causes or increases psychotic symptoms in patients with schizophrenia despite treatment with dopamine receptor antagonists.2
Gene-environment interactions also appear to be relevant. A functional polymorphism in the catechol-O-methyltransferase (COMT) gene (COMT Val158 Met) moderates the influence of cannabis use on developing psychosis, according to a birth cohort study of 803 New Zealanders. COMT valine158 allele carriers were most likely to exhibit psychotic symptoms and develop schizophreniform disorder if they used cannabis during adolescence. This association did not apply to adult-onset cannabis use.3
Results were similar in a study in which 30 patients with a psychotic disorder, 12 relatives of patients with a psychotic disorder, and 32 healthy controls received delta-9-THC or placebo.4
Two years later, I received a request for information about Roger’s episode from an acute inpatient facility. Roger had been admitted after an incident at the local mall in which he screamed at people and accused bystanders of trying to harm him. Despite using marijuana only occasionally, his behavior had been deteriorating and was becoming increasingly bizarre. The attending psychiatrist believed Roger had schizophrenia.
Clinicians regularly deal with patients such as Roger who suffer from a psychotic disorder and use marijuana. This is hardly surprising because marijuana is the most widely used illicit drug. In 2006, 5% of 12th graders in the United States reported using marijuana daily during the previous month, and 42% had tried it at least once.1
Is psychotic patients’ use of marijuana a coincidence? Self-medication? Or could cannabis cause psychotic illness? This debate elicits strong views among community and professional groups. To help you provide up-to-date advice to patients and families, this review:
- describes the growing body of evidence on the mental health consequences of marijuana use
- seeks to help you detect and deal with the effects of marijuana use in clinical practice.
Marijuana and psychosis
Although the neurobiologic association is unclear (Box 1),2-4 up to 15% of users report psychotic phenomena after consuming marijuana.5 Naturalistic and experimental studies have confirmed that marijuana can induce short-lived psychotic experiences.
In two parallel trials, 22 healthy individuals6 and 13 stable, antipsychotic-treated schizophrenia patients7 were given 2.5 mg and 5 mg intravenously of delta-9-tetrahydrocannabinol (delta-9-THC)—the primary psychoactive constituent of marijuana. Both groups developed dose-related, transient, schizophrenia-like symptoms and altered perceptions:
- Healthy volunteers showed the full range of psychotic symptoms. One individual said, “I thought you were giving me THC through the blood pressure machine and the sheets.”2
- Schizophrenia patients tended to report increases in the symptoms of their specific conditions. Those with paranoid illnesses, for example, reported an escalation in persecutory ideas.
Transient psychotic phenomena are not equivalent to a psychotic illness, however. To meet diagnostic criteria for a psychotic disorder, symptoms must be persistent and impair psychosocial functioning.
Early reports. Anecdotal clinical reports that marijuana use could cause psychosis emerged in the 1960s but were largely ignored. Many clinicians assumed that psychotic individuals used marijuana to relieve troubling symptoms (self-medication).
A 15-year, longitudinal study examined the incidence of schizophrenia in >50,000 Swedish conscripts and concluded that marijuana use during adolescence increased the risk of schizophrenia.8 Skeptics questioned the validity of the diagnosis and the etiologic role of other drugs in this study and suggested that prodromal symptoms might have led to marijuana use, rather than marijuana triggering the psychosis.
Recent evidence. Better-designed studies have shown that marijuana use increases the risk of psychosis later in life.
Adolescents who used marijuana by age 15 were more likely to develop a schizophreniform disorder by age 26 than nonusers, according to data from 759 New Zealanders who took part in a prospective, longitudinal, general population study. Marijuana use by age 15 was associated with a higher risk than later use (by age 18).9
A 3-year, longitudinal, population-based study from the Netherlands found marijuana use associated with increased risk of psychosis in 4,045 previously psychosis-free individuals. More than 50% of psychosis diagnoses could be attributed to marijuana use.10
Data from the 21-year longitudinal Christchurch Health and Development Study in New Zealand showed elevated rates of psychotic symptoms in young people with cannabis dependence at ages 18 and 21. The associations remained even after adjustments were made for previous psychotic symptoms and other confounding factors.11
Follow-up analysis of data from the Swedish military conscripts study8 showed that the use of other psychoactive drugs or prodromal cases in the cohort did not explain the association between self-reported marijuana use and hospital admissions for schizophrenia and other psychoses.12
- Starting marijuana use in adolescence
- Using cannabis often (weekly or daily) or for long periods
- Unusual, psychotic-like experiences (such as fleeting persecutory ideas or ideas of reference) or displaying high “psychoticism” on the self-report Symptom Checklist-90-R
- Family history of psychosis
- Prior cannabis-induced psychotic episode
- Cannabis use increases the risk of developing psychosis and is estimated to double the risk for later schizophrenia (5 to 10 new cases per 10,000 person-years)
- The association is not an artifact of confounding factors such as prodromal symptoms or concurrent use of other substances (including amphetamines)
- The risk increases with the frequency and length of use (a dose-effect relationship)
- Self-medication is not the connection between cannabis use and schizophrenia, according to empiric evidence
Researchers in Israel cross-linked a cohort of 9,724 youths aged 16 to 17 screened by the Israeli Draft Board with a national registry of psychiatric hospital admissions for schizophrenia in the following 4 to 15 years. Self-reported drug abuse (mostly marijuana) was higher in adolescents who were later hospitalized for schizophrenia (12.4%) than in those not hospitalized (5.9%).13
Is the diagnosis worthwhile? Acute-phase cannabis-induced psychosis and schizophrenia have similar presentations, making differential diagnosis difficult. If their treatment also is similar, is it clinically meaningful to distinguish whether marijuana use or schizophrenia triggered psychotic symptoms? The answer is yes, because:
- schizophrenia has a worse course and prognosis
- many patients with cannabis-induced psychosis do not develop schizophrenia.
Diagnostic clues. Some clinicians believe cannabis-induced psychosis is more likely than schizophrenia to feature:
- expansive mood
- derealization or depersonalization experiences
- visual hallucinations
- less overall severity.
Consider the course. The only way to differentiate the two disorders is to consider the illness course. Cannabis-induced psychotic episodes occur during periods of intoxication or withdrawal, tend to be short-lived, and usually respond well to treatment if the person abstains.
Up to one-half of patients with a cannabis-induced psychosis develop a schizophrenia-spectrum disorder. Monitoring them (such as at 6-month intervals) is important, therefore, because schizophrenia onset often occurs >12 months after the cannabis-induced psychosis.
Summary. A review of these 5 studies concluded that evidence supports the hypothesis that marijuana use acts as a risk factor in schizophrenia onset.14 Although marijuana use is not a “necessary” causal factor in psychotic illness—most users do not develop the disorder, and many persons with schizophrenia do not use marijuana—strong evidence indicates that it is one of many factors that can cause a psychotic illness (Box 2).9-14
Who is at risk?
Can marijuana cause psychosis in any person or specifically in those at increased risk of psychosis? If the latter, then marijuana—rather than causing new, unanticipated cases—might bring forward schizophrenia onset in individuals who would have developed it later. This explanation is consistent with data showing that persons born in more-recent cohorts seem to have an earlier age of schizophrenia onset.15
Vulnerability for psychosis. Evidence strongly suggests that marijuana-induced psychotic symptoms are more prevalent among vulnerable or psychosis-prone individuals.
- When given 2.5 mg of delta-9-THC, 80% of 13 patients with well-controlled schizophrenia experienced high Positive and Negative Syndrome Scale scores, compared with 35% of 22 healthy controls.2
- Unusual perceptions or thought influence were more common following marijuana use in all participants in a naturalistic experiment, but much more so in “at risk” individuals who had previously described isolated psychotic symptoms.16
- Adolescents and young adults ages 14 to 24 who used marijuana and displayed high “psychoticism” scores at baseline had more than twice the risk of a psychosis outcome 4 years later than did those without high scores.17
Schizophrenia onset. Marijuana users who suffer a drug-induced psychosis are at very high risk of developing a psychotic illness later on. A ≥3-year follow-up study18 of 535 patients who had not been treated for psychotic problems before being diagnosed with marijuana-induced psychotic symptoms found that:
- marijuana-induced psychotic episodes often remitted quickly with minimal treatment
- about one-half of patients were diagnosed with a schizophrenia-spectrum disorder (mostly paranoid schizophrenia) at follow up
- the gap between the marijuana-induced episode and diagnosis of a schizophrenia-spectrum disorder was >1 year in 47% of cases.
- the first episode of schizophrenia in these patients occurred several years earlier than in schizophrenia patients without marijuana-induced psychosis.
Although these findings require replication, they challenge the belief that marijuana-induced psychosis is benign (Box 3).
Implications for treatment
Most psychiatric practitioners treat patients who have psychotic illness and use marijuana (Box 4). Compared with nonusers, these patients tend to have:
- earlier age of schizophrenia onset
- more psychotic symptoms
- worse prognosis because of poorer treatment adherence
- increased symptom severity and persistence
- higher relapse rates.19
Therefore, ask patients with psychotic disorders about their marijuana use, and treat both the marijuana use and the psychosis. Evidence to guide treatment is scarce, however. Nicotine, marijuana, and alcohol use are often intertwined. This suggests that treatments that target a variety of substances may be more efficient than targeted ones, even if the generic interventions are brief.20
A study of marijuana users with early psychosis showed, for example, that marijuana-focused treatment was not more effective than psychoeducation, although both resulted in reduced use.21 In nonpsychotic individuals, giving 90 adult patients incentive vouchers to exchange for retail items each time they provided a marijuana-negative urine specimen resulted in increased abstinence rates over a 12-month period (Box 5).22,23 Cognitive-behavioral therapy helped to sustain the vouchers’ positive effect on abstinence after the initial 14-week treatment.23
Efficacy. In voucher-based reinforcement therapy, patients receive vouchers or monetary incentives redeemable for goods and services, contingent on satisfying predetermined therapeutic goals. A meta-analysis22 showed this therapy model can produce better outcomes in substance use disorders, compared with control treatment.
Marijuana abstinence. A 12-month study of 90 cannabis-dependent adults23 found that voucher-based reinforcement therapy could extend marijuana abstinence. During the 14 weeks of active treatment, participants could redeem vouchers for goods or services—such as movie passes, sports/hobby equipment, work materials, or vocational classes.
- Participants earned a voucher worth $1.50 for the first negative specimen.
- Voucher values increased by $1.50 for each consecutive negative specimen.
- Two consecutive negative specimens earned a $10 bonus.
- Voucher values dropped back to $1.50 if participants provided a cannabinoid-positive specimen or failed to submit a scheduled specimen. Values then could re-escalate according to the same schedule.
Treatment with first-generation antipsychotics does not appear to decrease substance use. Several studies suggest that clozapine decreases the use of nicotine, alcohol, or other substances among patients with schizophrenia,24 though this does not necessarily apply to other second-generation antipsychotics (Box 6).
- Ask about marijuana use when evaluating all patients, particularly young ones
- Educate patients and, if appropriate, families about the risks of marijuana use. One way to do this without sounding judgmental or confrontational is to follow the principles of motivational interviewing
- Treat both the psychosis and the substance use
- Generic interventions that target drug use might be more effective than those specific to cannabis use because psychotic patients often abuse a variety of substances
- Psychoeducation might be as effective as cannabis-specific treatments
- Abstinence-based vouchers are a simple intervention with some evidence of effectiveness
- Clozapine, which seems to reduce relapse of substance use in these patients, might be the antipsychotic of choice
Implications for prevention
Psychiatric practitioners can play an important role in making young people aware of the mental health risks of using marijuana. Marijuana use fluctuates population-wide, depending in part on public perception of its harmfulness. Its use may diminish, therefore, as information on its mental health hazards percolates into high schools and the community at large. We also have the duty to make policy makers and legislators aware of this information.25
Related resources
- National Institute on Drug Abuse. https://www.drugabuse.gov/drugs-abuse/marijuana.
- Cannabis dependence. www.mentalhealth.com/dis/p20-sb03.html.
- Castle D, Murray R, eds. Marijuana and madness: psychiatry and neurobiology. Cambridge, UK: Cambridge University Press; 2004.
- Hall W, Pacula RL. Cannabis use and dependence: public health and public policy. Cambridge, UK: Cambridge University Press; 2003.
Drug brand names
- Clozapine • Clozaril
Disclosure
Dr. Rey reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Evidence grows that marijuana use can cause acute psychosis, bring forward in time a first schizophrenia episode, and worsen the prognosis of patients with psychotic disorders.
Roger, age 16, had been smoking marijuana on and off for about 2 years. His parents knew but believed this was a stage and not dangerous; they had tried marijuana in their youth without harm. Roger’s smoking had increased to several joints daily since he started a relationship with an older girl, who shared and encouraged his habit.
His parents became worried when Roger began making unusual comments, saying that food did not taste “right” and he thought someone was poisoning him. They brought Roger for psychiatric consultation at the recommendation of their family physician.
History and examination revealed that Roger had experienced vague persecutory ideas for several weeks but no systematized delusions or hallucinations. I told Roger and his parents he probably had a drug-induced psychosis and that symptoms would likely disappear without recurrence if he stopped using marijuana. At 2-weeks’ follow-up, he described no more psychotic experiences and said he now realized the danger for him of smoking marijuana. A review 1 month later showed Roger was doing well, and I discharged him after reinforcing the importance of abstinence. But his case didn’t end there.
The dopaminergic effect of cannabinoid receptors (such as CB1) may be one biologic mechanism, according to preliminary evidence. But the dopaminergic pathway might not be the most relevant mechanism, because the primary psychoactive constituent of marijuana—delta-9-tetrahydrocannabinol (delta-9-THC)—causes or increases psychotic symptoms in patients with schizophrenia despite treatment with dopamine receptor antagonists.2
Gene-environment interactions also appear to be relevant. A functional polymorphism in the catechol-O-methyltransferase (COMT) gene (COMT Val158 Met) moderates the influence of cannabis use on developing psychosis, according to a birth cohort study of 803 New Zealanders. COMT valine158 allele carriers were most likely to exhibit psychotic symptoms and develop schizophreniform disorder if they used cannabis during adolescence. This association did not apply to adult-onset cannabis use.3
Results were similar in a study in which 30 patients with a psychotic disorder, 12 relatives of patients with a psychotic disorder, and 32 healthy controls received delta-9-THC or placebo.4
Two years later, I received a request for information about Roger’s episode from an acute inpatient facility. Roger had been admitted after an incident at the local mall in which he screamed at people and accused bystanders of trying to harm him. Despite using marijuana only occasionally, his behavior had been deteriorating and was becoming increasingly bizarre. The attending psychiatrist believed Roger had schizophrenia.
Clinicians regularly deal with patients such as Roger who suffer from a psychotic disorder and use marijuana. This is hardly surprising because marijuana is the most widely used illicit drug. In 2006, 5% of 12th graders in the United States reported using marijuana daily during the previous month, and 42% had tried it at least once.1
Is psychotic patients’ use of marijuana a coincidence? Self-medication? Or could cannabis cause psychotic illness? This debate elicits strong views among community and professional groups. To help you provide up-to-date advice to patients and families, this review:
- describes the growing body of evidence on the mental health consequences of marijuana use
- seeks to help you detect and deal with the effects of marijuana use in clinical practice.
Marijuana and psychosis
Although the neurobiologic association is unclear (Box 1),2-4 up to 15% of users report psychotic phenomena after consuming marijuana.5 Naturalistic and experimental studies have confirmed that marijuana can induce short-lived psychotic experiences.
In two parallel trials, 22 healthy individuals6 and 13 stable, antipsychotic-treated schizophrenia patients7 were given 2.5 mg and 5 mg intravenously of delta-9-tetrahydrocannabinol (delta-9-THC)—the primary psychoactive constituent of marijuana. Both groups developed dose-related, transient, schizophrenia-like symptoms and altered perceptions:
- Healthy volunteers showed the full range of psychotic symptoms. One individual said, “I thought you were giving me THC through the blood pressure machine and the sheets.”2
- Schizophrenia patients tended to report increases in the symptoms of their specific conditions. Those with paranoid illnesses, for example, reported an escalation in persecutory ideas.
Transient psychotic phenomena are not equivalent to a psychotic illness, however. To meet diagnostic criteria for a psychotic disorder, symptoms must be persistent and impair psychosocial functioning.
Early reports. Anecdotal clinical reports that marijuana use could cause psychosis emerged in the 1960s but were largely ignored. Many clinicians assumed that psychotic individuals used marijuana to relieve troubling symptoms (self-medication).
A 15-year, longitudinal study examined the incidence of schizophrenia in >50,000 Swedish conscripts and concluded that marijuana use during adolescence increased the risk of schizophrenia.8 Skeptics questioned the validity of the diagnosis and the etiologic role of other drugs in this study and suggested that prodromal symptoms might have led to marijuana use, rather than marijuana triggering the psychosis.
Recent evidence. Better-designed studies have shown that marijuana use increases the risk of psychosis later in life.
Adolescents who used marijuana by age 15 were more likely to develop a schizophreniform disorder by age 26 than nonusers, according to data from 759 New Zealanders who took part in a prospective, longitudinal, general population study. Marijuana use by age 15 was associated with a higher risk than later use (by age 18).9
A 3-year, longitudinal, population-based study from the Netherlands found marijuana use associated with increased risk of psychosis in 4,045 previously psychosis-free individuals. More than 50% of psychosis diagnoses could be attributed to marijuana use.10
Data from the 21-year longitudinal Christchurch Health and Development Study in New Zealand showed elevated rates of psychotic symptoms in young people with cannabis dependence at ages 18 and 21. The associations remained even after adjustments were made for previous psychotic symptoms and other confounding factors.11
Follow-up analysis of data from the Swedish military conscripts study8 showed that the use of other psychoactive drugs or prodromal cases in the cohort did not explain the association between self-reported marijuana use and hospital admissions for schizophrenia and other psychoses.12
- Starting marijuana use in adolescence
- Using cannabis often (weekly or daily) or for long periods
- Unusual, psychotic-like experiences (such as fleeting persecutory ideas or ideas of reference) or displaying high “psychoticism” on the self-report Symptom Checklist-90-R
- Family history of psychosis
- Prior cannabis-induced psychotic episode
- Cannabis use increases the risk of developing psychosis and is estimated to double the risk for later schizophrenia (5 to 10 new cases per 10,000 person-years)
- The association is not an artifact of confounding factors such as prodromal symptoms or concurrent use of other substances (including amphetamines)
- The risk increases with the frequency and length of use (a dose-effect relationship)
- Self-medication is not the connection between cannabis use and schizophrenia, according to empiric evidence
Researchers in Israel cross-linked a cohort of 9,724 youths aged 16 to 17 screened by the Israeli Draft Board with a national registry of psychiatric hospital admissions for schizophrenia in the following 4 to 15 years. Self-reported drug abuse (mostly marijuana) was higher in adolescents who were later hospitalized for schizophrenia (12.4%) than in those not hospitalized (5.9%).13
Is the diagnosis worthwhile? Acute-phase cannabis-induced psychosis and schizophrenia have similar presentations, making differential diagnosis difficult. If their treatment also is similar, is it clinically meaningful to distinguish whether marijuana use or schizophrenia triggered psychotic symptoms? The answer is yes, because:
- schizophrenia has a worse course and prognosis
- many patients with cannabis-induced psychosis do not develop schizophrenia.
Diagnostic clues. Some clinicians believe cannabis-induced psychosis is more likely than schizophrenia to feature:
- expansive mood
- derealization or depersonalization experiences
- visual hallucinations
- less overall severity.
Consider the course. The only way to differentiate the two disorders is to consider the illness course. Cannabis-induced psychotic episodes occur during periods of intoxication or withdrawal, tend to be short-lived, and usually respond well to treatment if the person abstains.
Up to one-half of patients with a cannabis-induced psychosis develop a schizophrenia-spectrum disorder. Monitoring them (such as at 6-month intervals) is important, therefore, because schizophrenia onset often occurs >12 months after the cannabis-induced psychosis.
Summary. A review of these 5 studies concluded that evidence supports the hypothesis that marijuana use acts as a risk factor in schizophrenia onset.14 Although marijuana use is not a “necessary” causal factor in psychotic illness—most users do not develop the disorder, and many persons with schizophrenia do not use marijuana—strong evidence indicates that it is one of many factors that can cause a psychotic illness (Box 2).9-14
Who is at risk?
Can marijuana cause psychosis in any person or specifically in those at increased risk of psychosis? If the latter, then marijuana—rather than causing new, unanticipated cases—might bring forward schizophrenia onset in individuals who would have developed it later. This explanation is consistent with data showing that persons born in more-recent cohorts seem to have an earlier age of schizophrenia onset.15
Vulnerability for psychosis. Evidence strongly suggests that marijuana-induced psychotic symptoms are more prevalent among vulnerable or psychosis-prone individuals.
- When given 2.5 mg of delta-9-THC, 80% of 13 patients with well-controlled schizophrenia experienced high Positive and Negative Syndrome Scale scores, compared with 35% of 22 healthy controls.2
- Unusual perceptions or thought influence were more common following marijuana use in all participants in a naturalistic experiment, but much more so in “at risk” individuals who had previously described isolated psychotic symptoms.16
- Adolescents and young adults ages 14 to 24 who used marijuana and displayed high “psychoticism” scores at baseline had more than twice the risk of a psychosis outcome 4 years later than did those without high scores.17
Schizophrenia onset. Marijuana users who suffer a drug-induced psychosis are at very high risk of developing a psychotic illness later on. A ≥3-year follow-up study18 of 535 patients who had not been treated for psychotic problems before being diagnosed with marijuana-induced psychotic symptoms found that:
- marijuana-induced psychotic episodes often remitted quickly with minimal treatment
- about one-half of patients were diagnosed with a schizophrenia-spectrum disorder (mostly paranoid schizophrenia) at follow up
- the gap between the marijuana-induced episode and diagnosis of a schizophrenia-spectrum disorder was >1 year in 47% of cases.
- the first episode of schizophrenia in these patients occurred several years earlier than in schizophrenia patients without marijuana-induced psychosis.
Although these findings require replication, they challenge the belief that marijuana-induced psychosis is benign (Box 3).
Implications for treatment
Most psychiatric practitioners treat patients who have psychotic illness and use marijuana (Box 4). Compared with nonusers, these patients tend to have:
- earlier age of schizophrenia onset
- more psychotic symptoms
- worse prognosis because of poorer treatment adherence
- increased symptom severity and persistence
- higher relapse rates.19
Therefore, ask patients with psychotic disorders about their marijuana use, and treat both the marijuana use and the psychosis. Evidence to guide treatment is scarce, however. Nicotine, marijuana, and alcohol use are often intertwined. This suggests that treatments that target a variety of substances may be more efficient than targeted ones, even if the generic interventions are brief.20
A study of marijuana users with early psychosis showed, for example, that marijuana-focused treatment was not more effective than psychoeducation, although both resulted in reduced use.21 In nonpsychotic individuals, giving 90 adult patients incentive vouchers to exchange for retail items each time they provided a marijuana-negative urine specimen resulted in increased abstinence rates over a 12-month period (Box 5).22,23 Cognitive-behavioral therapy helped to sustain the vouchers’ positive effect on abstinence after the initial 14-week treatment.23
Efficacy. In voucher-based reinforcement therapy, patients receive vouchers or monetary incentives redeemable for goods and services, contingent on satisfying predetermined therapeutic goals. A meta-analysis22 showed this therapy model can produce better outcomes in substance use disorders, compared with control treatment.
Marijuana abstinence. A 12-month study of 90 cannabis-dependent adults23 found that voucher-based reinforcement therapy could extend marijuana abstinence. During the 14 weeks of active treatment, participants could redeem vouchers for goods or services—such as movie passes, sports/hobby equipment, work materials, or vocational classes.
- Participants earned a voucher worth $1.50 for the first negative specimen.
- Voucher values increased by $1.50 for each consecutive negative specimen.
- Two consecutive negative specimens earned a $10 bonus.
- Voucher values dropped back to $1.50 if participants provided a cannabinoid-positive specimen or failed to submit a scheduled specimen. Values then could re-escalate according to the same schedule.
Treatment with first-generation antipsychotics does not appear to decrease substance use. Several studies suggest that clozapine decreases the use of nicotine, alcohol, or other substances among patients with schizophrenia,24 though this does not necessarily apply to other second-generation antipsychotics (Box 6).
- Ask about marijuana use when evaluating all patients, particularly young ones
- Educate patients and, if appropriate, families about the risks of marijuana use. One way to do this without sounding judgmental or confrontational is to follow the principles of motivational interviewing
- Treat both the psychosis and the substance use
- Generic interventions that target drug use might be more effective than those specific to cannabis use because psychotic patients often abuse a variety of substances
- Psychoeducation might be as effective as cannabis-specific treatments
- Abstinence-based vouchers are a simple intervention with some evidence of effectiveness
- Clozapine, which seems to reduce relapse of substance use in these patients, might be the antipsychotic of choice
Implications for prevention
Psychiatric practitioners can play an important role in making young people aware of the mental health risks of using marijuana. Marijuana use fluctuates population-wide, depending in part on public perception of its harmfulness. Its use may diminish, therefore, as information on its mental health hazards percolates into high schools and the community at large. We also have the duty to make policy makers and legislators aware of this information.25
Related resources
- National Institute on Drug Abuse. https://www.drugabuse.gov/drugs-abuse/marijuana.
- Cannabis dependence. www.mentalhealth.com/dis/p20-sb03.html.
- Castle D, Murray R, eds. Marijuana and madness: psychiatry and neurobiology. Cambridge, UK: Cambridge University Press; 2004.
- Hall W, Pacula RL. Cannabis use and dependence: public health and public policy. Cambridge, UK: Cambridge University Press; 2003.
Drug brand names
- Clozapine • Clozaril
Disclosure
Dr. Rey reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Teen drug use continues down in 2006, particularly among older teens; but use of prescription-type drugs remains high. Ann Arbor, MI: University of Michigan News and Information Services; Dec. 21, 2006. Available at: http://monitoringthefuture.org. Accessed January 2, 2007.
2. D’Souza DC, Cho HS, Perry EB, Krystal JH. Cannabinoid ’model’ psychosis, dopamine-cannabinoid interactions and implications for schizophrenia. In: Castle D, Murray R, eds. Marijuana and madness: psychiatry and neurobiology. Cambridge, UK: Cambridge University Press; 2004:142-65.
3. Caspi A, Moffitt TE, Cannon M, et al. Moderation of the effect of adolescent-onset cannabis use on adult psychosis by a functional polymorphism in the catechol-O-methyltransferase gene: longitudinal evidence of a gene X environment interaction. Biol Psychiatry 2005;57(10):1117-27.
4. Henquet C, Rosa A, Krabbendam L, et al. An experimental study of catechol-O-methyltransferase Val158 Met moderation of Δ-9-tetrahydrocannabinol-induced effects on psychosis and cognition. Neuropsychopharmacol 2006;31:2748-57.
5. Thomas H. A community survey of adverse effects of cannabis use. Drug Alcohol Depend 1996;42(3):201-7.
6. D’Souza DC, Perry E, MacDougall L, et al. The psychotomimetic effects of intravenous delta-9-tetrahydrocannabinol in healthy individuals: implications for psychosis. Neuropsychopharmacology 2004;29:1558-72.
7. D’Souza DC, Abi-Saab WM, Madonick S, et al. Delta-9-tetrahydrocannabinol effects in schizophrenia: implications for cognition, psychosis, and addiction. Biol Psychiatry 2005;57:594-608.
8. Andreasson S, Allebeck P, Engstrom A, Rydberg U. Cannabis and schizophrenia. A longitudinal study of Swedish conscripts. Lancet 1987;2(8574):1483-6.
9. Arseneault L, Cannon M, Poulton R, et al. Cannabis use in adolescence and risk for adult psychosis: longitudinal prospective study. BMJ 2002;325(7374):1212-3.
10. van Os J, Bak M, Hanssen M, et al. Cannabis use and psychosis: a longitudinal population-based study. Am J Epidemiol 2002;156(4):319-27.
11. Fergusson DM, Horwood LJ, Swain-Campbell NR. Cannabis dependence and psychotic symptoms in young people. Psychol Med 2003;33(1):15-21.
12. Zammit S, Allebeck P, Andreasson S, et al. Self reported cannabis use as a risk factor for schizophrenia in Swedish conscripts of 1969: historical cohort study. BMJ 2002;325(7374):1199-201.
13. Weiser M, Knobler HY, Noy S, Kaplan Z. Clinical characteristics of adolescents later hospitalized for schizophrenia. Am J Med Genet 2002;114:949-55.
14. Smit F, Bolier L, Cuijpers P. Cannabis use and the risk of later schizophrenia: a review. Addiction 2004;99(4):425-30.
15. Di Maggio C, Martinez M, Menard JF, et al. Evidence of a cohort effect for age at onset of schizophrenia. Am J Psychiatry 2001;158(3):489-92.
16. Verdoux H, Gindre C, Sorbara F, et al. Effects of cannabis and psychosis vulnerability in daily life: an experience sampling test study. Psychol Med 2003;33(1):23-32.
17. Henquet C, Krabbendam L, Spauwen J, et al. Prospective cohort study of cannabis use, predisposition for psychosis, and psychotic symptoms in young people. BMJ 2005;330(7481):11-4.
18. Arendt M, Rosenberg R, Foldager L, et al. Cannabis-induced psychosis and subsequent schizophrenia-spectrum disorders: follow-up study of 535 incident cases. Br J Psychiatry 2005;187:510-5.
19. Pencer A, Addington J, Addington D. Outcome of a first episode of psychosis in adolescence: a 2-year follow-up. Psychiatry Res 2005;133(1):35-43.
20. McCambridge J, Strang J. The efficacy of single-session motivational interviewing in reducing drug consumption and perceptions of drug-related risk and harm among young people: results from a multi-site cluster randomized trial. Addiction 2004;99(1):39-52.
21. Edwards J, Elkins K, Hinton M, et al. Randomized controlled trial of a cannabis-focused intervention for young people with first-episode psychosis. Acta Psychiatr Scand 2006;114(2):109-17.
22. Lussier JP, Heil SH, Mongeon JA, et al. A meta-analysis of voucher-based reinforcement therapy for substance use disorders. Addiction 2006;101:192-203.
23. Budney AJ, Moore BA, Rocha HL, Higgins ST. Clinical trial of abstinence-based vouchers and cognitive-behavioral therapy for cannabis dependence. J Consult Clin Psychol 2006;74(2):307-16.
24. Brunette MF, Drake RE, Xie H, et al. Clozapine use and relapses of substance use disorder among patients with co-occurring schizophrenia and substance use disorders. Schizophr Bull 2006;32(4):637-43.
25. Hall W, Degenhardt L. What are the policy implications of the evidence on cannabis and psychosis? Can J Psychiatry 2006;51(9):566-74.
1. Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Teen drug use continues down in 2006, particularly among older teens; but use of prescription-type drugs remains high. Ann Arbor, MI: University of Michigan News and Information Services; Dec. 21, 2006. Available at: http://monitoringthefuture.org. Accessed January 2, 2007.
2. D’Souza DC, Cho HS, Perry EB, Krystal JH. Cannabinoid ’model’ psychosis, dopamine-cannabinoid interactions and implications for schizophrenia. In: Castle D, Murray R, eds. Marijuana and madness: psychiatry and neurobiology. Cambridge, UK: Cambridge University Press; 2004:142-65.
3. Caspi A, Moffitt TE, Cannon M, et al. Moderation of the effect of adolescent-onset cannabis use on adult psychosis by a functional polymorphism in the catechol-O-methyltransferase gene: longitudinal evidence of a gene X environment interaction. Biol Psychiatry 2005;57(10):1117-27.
4. Henquet C, Rosa A, Krabbendam L, et al. An experimental study of catechol-O-methyltransferase Val158 Met moderation of Δ-9-tetrahydrocannabinol-induced effects on psychosis and cognition. Neuropsychopharmacol 2006;31:2748-57.
5. Thomas H. A community survey of adverse effects of cannabis use. Drug Alcohol Depend 1996;42(3):201-7.
6. D’Souza DC, Perry E, MacDougall L, et al. The psychotomimetic effects of intravenous delta-9-tetrahydrocannabinol in healthy individuals: implications for psychosis. Neuropsychopharmacology 2004;29:1558-72.
7. D’Souza DC, Abi-Saab WM, Madonick S, et al. Delta-9-tetrahydrocannabinol effects in schizophrenia: implications for cognition, psychosis, and addiction. Biol Psychiatry 2005;57:594-608.
8. Andreasson S, Allebeck P, Engstrom A, Rydberg U. Cannabis and schizophrenia. A longitudinal study of Swedish conscripts. Lancet 1987;2(8574):1483-6.
9. Arseneault L, Cannon M, Poulton R, et al. Cannabis use in adolescence and risk for adult psychosis: longitudinal prospective study. BMJ 2002;325(7374):1212-3.
10. van Os J, Bak M, Hanssen M, et al. Cannabis use and psychosis: a longitudinal population-based study. Am J Epidemiol 2002;156(4):319-27.
11. Fergusson DM, Horwood LJ, Swain-Campbell NR. Cannabis dependence and psychotic symptoms in young people. Psychol Med 2003;33(1):15-21.
12. Zammit S, Allebeck P, Andreasson S, et al. Self reported cannabis use as a risk factor for schizophrenia in Swedish conscripts of 1969: historical cohort study. BMJ 2002;325(7374):1199-201.
13. Weiser M, Knobler HY, Noy S, Kaplan Z. Clinical characteristics of adolescents later hospitalized for schizophrenia. Am J Med Genet 2002;114:949-55.
14. Smit F, Bolier L, Cuijpers P. Cannabis use and the risk of later schizophrenia: a review. Addiction 2004;99(4):425-30.
15. Di Maggio C, Martinez M, Menard JF, et al. Evidence of a cohort effect for age at onset of schizophrenia. Am J Psychiatry 2001;158(3):489-92.
16. Verdoux H, Gindre C, Sorbara F, et al. Effects of cannabis and psychosis vulnerability in daily life: an experience sampling test study. Psychol Med 2003;33(1):23-32.
17. Henquet C, Krabbendam L, Spauwen J, et al. Prospective cohort study of cannabis use, predisposition for psychosis, and psychotic symptoms in young people. BMJ 2005;330(7481):11-4.
18. Arendt M, Rosenberg R, Foldager L, et al. Cannabis-induced psychosis and subsequent schizophrenia-spectrum disorders: follow-up study of 535 incident cases. Br J Psychiatry 2005;187:510-5.
19. Pencer A, Addington J, Addington D. Outcome of a first episode of psychosis in adolescence: a 2-year follow-up. Psychiatry Res 2005;133(1):35-43.
20. McCambridge J, Strang J. The efficacy of single-session motivational interviewing in reducing drug consumption and perceptions of drug-related risk and harm among young people: results from a multi-site cluster randomized trial. Addiction 2004;99(1):39-52.
21. Edwards J, Elkins K, Hinton M, et al. Randomized controlled trial of a cannabis-focused intervention for young people with first-episode psychosis. Acta Psychiatr Scand 2006;114(2):109-17.
22. Lussier JP, Heil SH, Mongeon JA, et al. A meta-analysis of voucher-based reinforcement therapy for substance use disorders. Addiction 2006;101:192-203.
23. Budney AJ, Moore BA, Rocha HL, Higgins ST. Clinical trial of abstinence-based vouchers and cognitive-behavioral therapy for cannabis dependence. J Consult Clin Psychol 2006;74(2):307-16.
24. Brunette MF, Drake RE, Xie H, et al. Clozapine use and relapses of substance use disorder among patients with co-occurring schizophrenia and substance use disorders. Schizophr Bull 2006;32(4):637-43.
25. Hall W, Degenhardt L. What are the policy implications of the evidence on cannabis and psychosis? Can J Psychiatry 2006;51(9):566-74.
Malpractice distress: Help yourself and others survive
‘Immediately after the event I was a wreck. I vaguely remember talking to the family; I don’t know if I was much use to them. … That night I got drunk. It was the only way I could sleep. A sensitive colleague came and sat with me.”1
Besides being targets of malpractice suits, psychiatrists also serve as resources for colleagues who are sued. Specific actions can help you and those you counsel deal with the stress of an adverse event before and during litigation. Remember that:
- anticipation is the best defense
- knowledge is power
- action counters passivity
- a supportive environment is essential.
ANTICIPATING LITIGATION
What is the risk? No nationwide reporting system tracks the incidence of medical malpractice claims, but industry experts suggest a claim is leveled against 7% of psychiatrists each year.2 The risk is higher for other medical specialists: a recent survey by the American College of Obstetricians and Gynecologists found that 89% of practicing ObGyns had been sued at least once in their careers.3 Because a claim usually takes several years to resolve, a substantial number of physicians—including psychiatrists—are involved in litigation at any one time.
Successfully anticipating litigation begins with being familiar with your state’s statute of limitations—usually 2 to 3 years after discovery of the incident, with exceptions for children, the disabled, and designated special circumstances. If a plaintiff’s case is not filed within this time, a disputed outcome can never be the subject of a malpractice claim.
Adverse events. The severity of the outcome, the nature of your relationship with the patient, and the degree of your responsibility for an adverse event contribute to the intensity of your initial emotional response. If a mistake caused the event, your reaction may be even more severe.4-6 Whatever the event’s specifics, you may ruminate about your role and degree of responsibility (Table 1).
Table 1
Nagging questions after a ‘bad’ patient outcome
|
Expect that your view of the circumstances will generate a complex array of feelings: shock, anxiety, depression, shame, guilt, self-blame, disbelief, self-doubt and inadequacy, anger, and even relief from not having to work with a difficult patient anymore.
Patient suicide. More than one-half of psychiatrists and up to one-third of psychiatric residents experience a patient suicide.7-10 The Joint Commission on Accreditation of Healthcare Organizations reports that suicide is the most frequent sentinel event, representing 501 (13.1%) of the total 3,811 sentinel events reviewed since 1995.11 Professional Risk Management Services, a major medical malpractice insurer of psychiatrists, reports that suicide and attempted suicide are the most frequently identifiable causes of liability payments (Figure).
Figure 1 Psychiatric claims by cause of loss in the United States, 1998 to 2005
Almost all lawsuits assert multiple allegations of negligence, and “cause of loss” represents the main allegation made in the claim or lawsuit. Thus, the category of “incorrect treatment” may be alleged in a lawsuit based on a patient suicide, but the main or chief allegation/complaint is stated as “incorrect treatment.” The most frequent identifiable cause of loss is suicide and attempted suicide.
* “Other” includes administrative issues, abandonment, premises liability, Tarasoff, third parties (such as parents), retained object, libel/slander, boundary violation, deleted duplicate file, Fen-phen, lack of informed consent, forensic issues, and miscellaneous.
Source: Prepared by Professional Risk Management Services, Inc. Reprinted with permission.
Psychiatrists’ feelings of distress after a patient suicide mirror the personal sense of failure and inadequacy most physicians feel when they are unable to prevent a patient’s death or serious injury. At the same time, we must:
- deal with the event’s medical complications, with relevant notifications and disclosures (Table 2)
- address the emotional pain of the injured patient or family
- participate in mandated reviews
- recognize and manage our emotional disruption (Table 3).
Table 2
Recommended medical steps, notifications,
and disclosures after an adverse event
| MEDICAL STEPS Take necessary actions to limit further injury or disability Obtain appropriate consultations Review the medical record; anticipate the patient’s follow-up needs and make recommendations for further treatment |
| NOTIFICATIONS Follow the health care system’s and insurer’s guidelines for notifying the patient/family Inform the institution’s risk manager and your professional liability carrier as soon as possible Write a description of the event for the record and a narrative for your personal file (and your lawyer’s) in case a suit is filed later Do not talk with the media |
| DISCLOSURES Acknowledge your ethical obligation to be truthful Follow your institution’s and insurer’s disclosure guidelines Expect to feel intimidated and uneasy in discussing your role in the event Expect the patient/family to be angry and disappointed in you Convey an interest in the patient’s/family’s emotional state; express sorrow for their loss Tell the patient/family what you know for sure; don’t speculate about what is not known, and don’t make false promises or false reassurances Don’t hurry; give the patient/family time to ask questions Expect to feel better after a truthful exchange |
Table 3
Managing your emotions before and during litigation
| Anticipate having repeated thoughts and preoccupations about the event; work toward a realistic view of it |
| Recognize your feelings and work to understand their source |
| Talk with a trusted confidant (your spouse, colleague, etc.) about your feelings |
| Monitor your emotional and physical status and, if indicated, seek appropriate consultation |
| Avoid situations that generate anxiety and increase stress |
| Monitor and address changes in relationships with family, patients, colleagues, and staff |
| Be understanding of yourself and others; develop a realistic view of yourself as a ‘good doctor’ |
| Engage in active sports and take regular vacations unrelated to professional activities |
| Control what can be controlled |
Self-evaluation. To cope with distress when a patient dies, you could attend the funeral. If the death was by suicide, consider consulting with a therapist about your reactions or review the case with your supervisor. You also might:
- make changes in your practice that alert you to problem patients
- introduce a more structured approach to patients with particular clinical conditions, using practice guidelines as a resource12,13
- become more alert to patients who may benefit from consultation or referral.
Balance the time you devote to work and personal life. Schedule regular time for recreation and active sports, which can help you prepare for the prolonged stress that follows being sued. Engage a personal physician to monitor your physical and emotional health and to recommend appropriate referrals when indicated.
KNOWLEDGE IS POWER
What can I expect? A lawsuit generates a mixture of common emotions and exacerbates those felt at the time of the bad outcome: shock, outrage, anxiety, anguish, dread, depression, helplessness, hopelessness, feelings of being misunderstood, and the anger and vulnerability associated with a narcissistic injury. As one ObGyn stated, learning that a lawsuit was filed “just prolonged my misery.”14
Each of us reacts in our own way to a lawsuit—and differently to each lawsuit if we are sued more than once—because of:
- our personality traits and personal circumstances
- the specifics of each case
- our relationship with the patient
- the public nature of a lawsuit
- a range of other variables that makes each case unique.
Suddenly, we who perceive ourselves as caring, beneficent, well-meaning, and devoted to our patients are publicly accused of being careless and incompetent, of harming the patient by failing to meet our minimal obligations. Psychiatrists Richard Ferrell and Trevor Price15 capture the impact of these allegations:
"Here are the sense of assault and violation, the feelings of outrage and fear. Most painfully, here is the narcissistic injury, the astonishing wound to our understanding of ourselves as admirable, well-meaning people."
Litigation is a lengthy process with defined stages (Table 4). We have little control over a slow-paced process that involves an array of participants (lawyers, judges, jury, and experts) whose behavior is not predictable. This makes us feel dependent, vulnerable, and impotent.
Table 4
Stages of litigation: What happens in court
| Stage | Definitions |
|---|---|
| Summons | Notification that a suit has been filed |
| Complaint | The nature of the allegation in legal terms |
| Pleadings | The attorney begins to communicate with the court by filing motions, a request that the court do something |
| Discovery | A process designed to obtain information about the case:
|
| Summary judgment | A motion asking the court, after the facts have been established by discovery, to decide the validity of the case; if granted, the case is resolved without a trial by jury |
| Settlement | An agreement between parties that resolves their legal dispute |
| Trial | Case is presented to the judge or a judge and jury to determine culpability |
| Verdict | Decision reached by the deciding body |
| Post-trial | If the defendant receives an unfavorable verdict, motions may be offered to the court to void or appeal the verdict |
BE ACTIVE, NOT PASSIVE
What you can do. Contact your insurer and risk manager immediately. Inquire about the average length of litigation in your jurisdiction (might be 1 to 5 or more years, depending on locality, type of case, and severity of injury). Ask your lawyer to describe the steps in the process and your role as the case proceeds.
Take whatever steps are necessary to cover your clinical duties. If your initial emotional reaction is disruptive, obtain coverage or rearrange your schedule. Expect to change or limit your schedule before depositions and during trial to allow adequate time for preparation.
Accept the fact that you must play by rules far different from those of medical care. Litigation is time-consuming and frustrating. Delays and “continuances” are common in legal proceedings, so expect them. Consider adapting to your own situation strategies that other sued physicians have found useful in regaining control over their lives and work (Table 5).
Table 5
Regaining control: Managing your practice during litigation
| Learn as much as you can about the legal process |
| Introduce good risk management strategies, such as efficient record-keeping, into your practice |
| Clarify the responsibilities of office personnel and coverage responsibilities with associates |
| Rearrange office schedules during periods of increased stress |
| Re-evaluate your time commitments to work and family |
| Participate in relevant continuing education |
| Make sure your financial and estate planning is current |
| Cooperate with legal counsel |
| Devote sufficient time to deposition preparation and other demands of the case |
| Carefully evaluate the advice of legal and insurance counsel regarding a settlement |
| Do not try to “fit patients in” while on trial; trial is a full-time job |
GET NEEDED SUPPORT
Talking about the case. Sharing with responsible confidants your emotional reactions to being sued is healthy for you and others affected. Lawyers, however, may caution you not to “talk to anybody” about the case. They don’t want you to say anything that would suggest liability or jeopardize their defense of the case.
As psychiatrists, we know this is not good psychological advice. The support of others is a natural help during major life events that cause enormous stress and disruption.16 You can resolve this dilemma by accepting the discipline of talking about your feelings regarding the case without discussing the specifics of the case.
In addition to lawyers and claims representatives, you may talk with your spouse or another trusted person or colleague about your feelings. When other physicians or psychiatrists formally consult with you about their litigation experiences, you are protected by the confidentiality inherent in the doctor-patient relationship.
Trust issues. Trust lies at the core of psychotherapeutic work. After being sued, you may find it difficult to re-establish trusting and comfortable relationships with patients, especially those who are seriously ill.
Well-trained, competent physicians who keep current with standards of care and have good relationships with patients do not expect to be sued. Psychiatrists often feel unrealistically immune to litigation because we believe our training helps us understand our own psychology and relationships with others. A charge of negligence exposes our vulnerabilities and leaves us feeling hurt and betrayed. As one psychiatrist ruefully observed, “I lost my innocence.”14
Countertransference feelings may emerge. Most physicians acknowledge that after being sued their relationships with patients change17,18—a particularly distressing outcome for psychiatrists. We may feel uncomfortable and threatened when we need to “stretch the patient-doctor relationship in a paternalistic direction,” such as when a psychotic patient needs involuntary commitment.15
Feelings that you must change the way you practice and chronic anxiety about your work are barriers to good practice. You may contemplate changing practice circumstances or retiring early. Personal therapy may help if you remain uneasy or cannot resolve life choices that overshadow your work with patients.
Medical or psychiatric care. Be alert to the point at which you or others involved in litigation need a referral for medical or psychiatric consultation. Sued physicians, their families, or colleagues often experience diagnosable psychiatric conditions or other behavioral problems, such as:
- major depression
- adjustment disorders
- posttraumatic stress disorder
- worsening of a previously diagnosed psychiatric illness
- physical symptoms that require diagnosis and treatment
- alcohol and drug misuse or abuse
- anxiety and distress that interfere with work
- self-medication, especially for insomnia
- disturbances and dysfunctional behaviors that affect marital and family life.19,20
SUPPORT YOUR COLLEAGUES
When consulting with other physicians, be aware of litigation factors that may influence treatment.
Become familiar with the climate of litigation in the jurisdiction where the case was filed, including the incidence and outcome of cases. For example, does an attempted suicide case usually result in settlement or—if it goes to trial—take 2 to 5 or more years to resolve? More than 70% of cases filed nationwide result in no payment (no settlement) for the plaintiff. If cases go to trial, physicians win 80% of the time.21
Recognize that the source of the physician’s distress may be the trauma associated with the initial bad outcome, rather than the malpractice suit itself. As the case progresses and facts emerge, you may play a large role in helping your physician patient correct previous distortions of the event. Certain periods—during trial, for example—might require more-frequent visits, medication, and expressions of support.
You may harbor a bias about the case, but withhold judgment until it is resolved.
Related resources
- American College of Obstetricians and Gynecologists. From exam room to court room: navigating litigation and coping with stress (CD-ROM) http://sales.acog.com/acb/stores/1/product1.cfm?SID=1&Product_ID=589).
- Charles SC, Frisch PR. Adverse events, stress and litigation: a physician’s guide. New York: Oxford University Press; 2005.
- Physician Litigation Stress Resource Center. www.physicianlitigationstress.org.
Disclosure
Dr. Charles reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Anonymous. Looking back… BMJ 2000;320(7237):812.-
2. Martin G, Tracy JD. President and CEO, Professional Risk Management Services. Personal communication. October 20, 2006.
3. American College of Obstetricians and Gynecologists. ACOG 2006 Professional Liability Survey. Washington, DC; 2006. Available at: http://www.acog.org/departments/dept_notice.cfm?recno=4&bulletin=3963. Accessed January 16, 2007.
4. Christensen JF, Levinson W, Dunn PM. The heart of darkness: the impact of perceived mistakes on physicians. J Gen Intern Med 1992;7(4):424-31.
5. Wu AW. Medical error: the second victim. The doctor who makes the mistake needs help too. BMJ 2000;320(7237):726-7.
6. Aasland OG, Forde R. Impact of feeling responsible for adverse events on doctors’ personal and professional lives: the importance of being open to criticism from colleagues. Quality & Safety in Health Care 2005;14:13-7.
7. Alexander DA, Klein S, Grey NM, et al. Suicide by patients: questionnaire study of its effect on consultant psychiatrists. BMJ 2000;320:1571-4.
8. Chemtob CM, Hamada RS, Bauer G, et al. Patients’ suicides: frequency and impact on psychiatrists. Am J Psychiatry 1988;145:224-8.
9. Brown HN. The impact of suicide on therapists in training. Compr Psychiatry 1987;28:101-12.
10. Ellis TE, Dickey TO, Jones EC. Patient suicide in psychiatric residency programs: a national survey of training and postvention practices. Academic Psychiatry 1998;22:181-9.
11. Joint Commission on Accreditation of Healthcare Organizations. Sentinel event statistics. Available at: http://www.jointcommission.org/NR/rdonlyres/74540565-4D0F-4992-863E-8F9E949E6B56/0/se_stats_6_30_06.pdf. Accessed November 27, 2006.
12. Hendin H, Lipschitz A, Maltsberger JT, et al. Therapists’ reactions to patients’ suicides. Am J Psychiatry 2000;157(12):2022-7.
13. Practice guidelines for the treatment of psychiatric disorders (compendium 2006) Arlington, VA: American Psychiatric Publishing; 2006.
14. Charles SC, Frisch PR. Adverse events, stress and litigation: a physician’s guide. New York: Oxford University Press; 2005:94,120.
15. Ferrell RB, Price TRP. Effects of malpractice suits on physicians. In: Gold JH, Nemiah JC, eds. Beyond transference. Washington, DC: American Psychiatric Press; 1993:141-58.
16. Watson PJ, Friedman MJ, Gibson LE, et al. Early intervention in trauma-related problems. In: Ursano R, Norwood AE, eds. Trauma and disaster: responses and management. Review of psychiatry vol. 22. Washington, DC: American Psychiatric Press; 2003:100-1.
17. Charles SC, Psykoty CE, Nelson A. Physicians on trial—self-reported reactions to malpractice trials. West J Med 1988;148:358-60.
18. Charles SC. The doctor-patient relationship and medical malpractice litigation. Bull Menninger Clin 1993;57(2):195-207.
19. Charles SC, Wilbert JR, Franke KJ. Sued and non-sued physicians’ self-reported reactions to malpractice litigation. Am J Psychiatry 1985;142:437-40.
20. Martin CA, Wilson JA, Fiebelman ND, et al. Physicians’ psychologic reactions to malpractice litigation. South Med J 1991;84:1300-4.
21. Outcome of closed medical malpractice claims. National data (1985-2005). Physician Insurers Association of America (PIAA). Rockville, MD; 2006.
‘Immediately after the event I was a wreck. I vaguely remember talking to the family; I don’t know if I was much use to them. … That night I got drunk. It was the only way I could sleep. A sensitive colleague came and sat with me.”1
Besides being targets of malpractice suits, psychiatrists also serve as resources for colleagues who are sued. Specific actions can help you and those you counsel deal with the stress of an adverse event before and during litigation. Remember that:
- anticipation is the best defense
- knowledge is power
- action counters passivity
- a supportive environment is essential.
ANTICIPATING LITIGATION
What is the risk? No nationwide reporting system tracks the incidence of medical malpractice claims, but industry experts suggest a claim is leveled against 7% of psychiatrists each year.2 The risk is higher for other medical specialists: a recent survey by the American College of Obstetricians and Gynecologists found that 89% of practicing ObGyns had been sued at least once in their careers.3 Because a claim usually takes several years to resolve, a substantial number of physicians—including psychiatrists—are involved in litigation at any one time.
Successfully anticipating litigation begins with being familiar with your state’s statute of limitations—usually 2 to 3 years after discovery of the incident, with exceptions for children, the disabled, and designated special circumstances. If a plaintiff’s case is not filed within this time, a disputed outcome can never be the subject of a malpractice claim.
Adverse events. The severity of the outcome, the nature of your relationship with the patient, and the degree of your responsibility for an adverse event contribute to the intensity of your initial emotional response. If a mistake caused the event, your reaction may be even more severe.4-6 Whatever the event’s specifics, you may ruminate about your role and degree of responsibility (Table 1).
Table 1
Nagging questions after a ‘bad’ patient outcome
|
Expect that your view of the circumstances will generate a complex array of feelings: shock, anxiety, depression, shame, guilt, self-blame, disbelief, self-doubt and inadequacy, anger, and even relief from not having to work with a difficult patient anymore.
Patient suicide. More than one-half of psychiatrists and up to one-third of psychiatric residents experience a patient suicide.7-10 The Joint Commission on Accreditation of Healthcare Organizations reports that suicide is the most frequent sentinel event, representing 501 (13.1%) of the total 3,811 sentinel events reviewed since 1995.11 Professional Risk Management Services, a major medical malpractice insurer of psychiatrists, reports that suicide and attempted suicide are the most frequently identifiable causes of liability payments (Figure).
Figure 1 Psychiatric claims by cause of loss in the United States, 1998 to 2005
Almost all lawsuits assert multiple allegations of negligence, and “cause of loss” represents the main allegation made in the claim or lawsuit. Thus, the category of “incorrect treatment” may be alleged in a lawsuit based on a patient suicide, but the main or chief allegation/complaint is stated as “incorrect treatment.” The most frequent identifiable cause of loss is suicide and attempted suicide.
* “Other” includes administrative issues, abandonment, premises liability, Tarasoff, third parties (such as parents), retained object, libel/slander, boundary violation, deleted duplicate file, Fen-phen, lack of informed consent, forensic issues, and miscellaneous.
Source: Prepared by Professional Risk Management Services, Inc. Reprinted with permission.
Psychiatrists’ feelings of distress after a patient suicide mirror the personal sense of failure and inadequacy most physicians feel when they are unable to prevent a patient’s death or serious injury. At the same time, we must:
- deal with the event’s medical complications, with relevant notifications and disclosures (Table 2)
- address the emotional pain of the injured patient or family
- participate in mandated reviews
- recognize and manage our emotional disruption (Table 3).
Table 2
Recommended medical steps, notifications,
and disclosures after an adverse event
| MEDICAL STEPS Take necessary actions to limit further injury or disability Obtain appropriate consultations Review the medical record; anticipate the patient’s follow-up needs and make recommendations for further treatment |
| NOTIFICATIONS Follow the health care system’s and insurer’s guidelines for notifying the patient/family Inform the institution’s risk manager and your professional liability carrier as soon as possible Write a description of the event for the record and a narrative for your personal file (and your lawyer’s) in case a suit is filed later Do not talk with the media |
| DISCLOSURES Acknowledge your ethical obligation to be truthful Follow your institution’s and insurer’s disclosure guidelines Expect to feel intimidated and uneasy in discussing your role in the event Expect the patient/family to be angry and disappointed in you Convey an interest in the patient’s/family’s emotional state; express sorrow for their loss Tell the patient/family what you know for sure; don’t speculate about what is not known, and don’t make false promises or false reassurances Don’t hurry; give the patient/family time to ask questions Expect to feel better after a truthful exchange |
Table 3
Managing your emotions before and during litigation
| Anticipate having repeated thoughts and preoccupations about the event; work toward a realistic view of it |
| Recognize your feelings and work to understand their source |
| Talk with a trusted confidant (your spouse, colleague, etc.) about your feelings |
| Monitor your emotional and physical status and, if indicated, seek appropriate consultation |
| Avoid situations that generate anxiety and increase stress |
| Monitor and address changes in relationships with family, patients, colleagues, and staff |
| Be understanding of yourself and others; develop a realistic view of yourself as a ‘good doctor’ |
| Engage in active sports and take regular vacations unrelated to professional activities |
| Control what can be controlled |
Self-evaluation. To cope with distress when a patient dies, you could attend the funeral. If the death was by suicide, consider consulting with a therapist about your reactions or review the case with your supervisor. You also might:
- make changes in your practice that alert you to problem patients
- introduce a more structured approach to patients with particular clinical conditions, using practice guidelines as a resource12,13
- become more alert to patients who may benefit from consultation or referral.
Balance the time you devote to work and personal life. Schedule regular time for recreation and active sports, which can help you prepare for the prolonged stress that follows being sued. Engage a personal physician to monitor your physical and emotional health and to recommend appropriate referrals when indicated.
KNOWLEDGE IS POWER
What can I expect? A lawsuit generates a mixture of common emotions and exacerbates those felt at the time of the bad outcome: shock, outrage, anxiety, anguish, dread, depression, helplessness, hopelessness, feelings of being misunderstood, and the anger and vulnerability associated with a narcissistic injury. As one ObGyn stated, learning that a lawsuit was filed “just prolonged my misery.”14
Each of us reacts in our own way to a lawsuit—and differently to each lawsuit if we are sued more than once—because of:
- our personality traits and personal circumstances
- the specifics of each case
- our relationship with the patient
- the public nature of a lawsuit
- a range of other variables that makes each case unique.
Suddenly, we who perceive ourselves as caring, beneficent, well-meaning, and devoted to our patients are publicly accused of being careless and incompetent, of harming the patient by failing to meet our minimal obligations. Psychiatrists Richard Ferrell and Trevor Price15 capture the impact of these allegations:
"Here are the sense of assault and violation, the feelings of outrage and fear. Most painfully, here is the narcissistic injury, the astonishing wound to our understanding of ourselves as admirable, well-meaning people."
Litigation is a lengthy process with defined stages (Table 4). We have little control over a slow-paced process that involves an array of participants (lawyers, judges, jury, and experts) whose behavior is not predictable. This makes us feel dependent, vulnerable, and impotent.
Table 4
Stages of litigation: What happens in court
| Stage | Definitions |
|---|---|
| Summons | Notification that a suit has been filed |
| Complaint | The nature of the allegation in legal terms |
| Pleadings | The attorney begins to communicate with the court by filing motions, a request that the court do something |
| Discovery | A process designed to obtain information about the case:
|
| Summary judgment | A motion asking the court, after the facts have been established by discovery, to decide the validity of the case; if granted, the case is resolved without a trial by jury |
| Settlement | An agreement between parties that resolves their legal dispute |
| Trial | Case is presented to the judge or a judge and jury to determine culpability |
| Verdict | Decision reached by the deciding body |
| Post-trial | If the defendant receives an unfavorable verdict, motions may be offered to the court to void or appeal the verdict |
BE ACTIVE, NOT PASSIVE
What you can do. Contact your insurer and risk manager immediately. Inquire about the average length of litigation in your jurisdiction (might be 1 to 5 or more years, depending on locality, type of case, and severity of injury). Ask your lawyer to describe the steps in the process and your role as the case proceeds.
Take whatever steps are necessary to cover your clinical duties. If your initial emotional reaction is disruptive, obtain coverage or rearrange your schedule. Expect to change or limit your schedule before depositions and during trial to allow adequate time for preparation.
Accept the fact that you must play by rules far different from those of medical care. Litigation is time-consuming and frustrating. Delays and “continuances” are common in legal proceedings, so expect them. Consider adapting to your own situation strategies that other sued physicians have found useful in regaining control over their lives and work (Table 5).
Table 5
Regaining control: Managing your practice during litigation
| Learn as much as you can about the legal process |
| Introduce good risk management strategies, such as efficient record-keeping, into your practice |
| Clarify the responsibilities of office personnel and coverage responsibilities with associates |
| Rearrange office schedules during periods of increased stress |
| Re-evaluate your time commitments to work and family |
| Participate in relevant continuing education |
| Make sure your financial and estate planning is current |
| Cooperate with legal counsel |
| Devote sufficient time to deposition preparation and other demands of the case |
| Carefully evaluate the advice of legal and insurance counsel regarding a settlement |
| Do not try to “fit patients in” while on trial; trial is a full-time job |
GET NEEDED SUPPORT
Talking about the case. Sharing with responsible confidants your emotional reactions to being sued is healthy for you and others affected. Lawyers, however, may caution you not to “talk to anybody” about the case. They don’t want you to say anything that would suggest liability or jeopardize their defense of the case.
As psychiatrists, we know this is not good psychological advice. The support of others is a natural help during major life events that cause enormous stress and disruption.16 You can resolve this dilemma by accepting the discipline of talking about your feelings regarding the case without discussing the specifics of the case.
In addition to lawyers and claims representatives, you may talk with your spouse or another trusted person or colleague about your feelings. When other physicians or psychiatrists formally consult with you about their litigation experiences, you are protected by the confidentiality inherent in the doctor-patient relationship.
Trust issues. Trust lies at the core of psychotherapeutic work. After being sued, you may find it difficult to re-establish trusting and comfortable relationships with patients, especially those who are seriously ill.
Well-trained, competent physicians who keep current with standards of care and have good relationships with patients do not expect to be sued. Psychiatrists often feel unrealistically immune to litigation because we believe our training helps us understand our own psychology and relationships with others. A charge of negligence exposes our vulnerabilities and leaves us feeling hurt and betrayed. As one psychiatrist ruefully observed, “I lost my innocence.”14
Countertransference feelings may emerge. Most physicians acknowledge that after being sued their relationships with patients change17,18—a particularly distressing outcome for psychiatrists. We may feel uncomfortable and threatened when we need to “stretch the patient-doctor relationship in a paternalistic direction,” such as when a psychotic patient needs involuntary commitment.15
Feelings that you must change the way you practice and chronic anxiety about your work are barriers to good practice. You may contemplate changing practice circumstances or retiring early. Personal therapy may help if you remain uneasy or cannot resolve life choices that overshadow your work with patients.
Medical or psychiatric care. Be alert to the point at which you or others involved in litigation need a referral for medical or psychiatric consultation. Sued physicians, their families, or colleagues often experience diagnosable psychiatric conditions or other behavioral problems, such as:
- major depression
- adjustment disorders
- posttraumatic stress disorder
- worsening of a previously diagnosed psychiatric illness
- physical symptoms that require diagnosis and treatment
- alcohol and drug misuse or abuse
- anxiety and distress that interfere with work
- self-medication, especially for insomnia
- disturbances and dysfunctional behaviors that affect marital and family life.19,20
SUPPORT YOUR COLLEAGUES
When consulting with other physicians, be aware of litigation factors that may influence treatment.
Become familiar with the climate of litigation in the jurisdiction where the case was filed, including the incidence and outcome of cases. For example, does an attempted suicide case usually result in settlement or—if it goes to trial—take 2 to 5 or more years to resolve? More than 70% of cases filed nationwide result in no payment (no settlement) for the plaintiff. If cases go to trial, physicians win 80% of the time.21
Recognize that the source of the physician’s distress may be the trauma associated with the initial bad outcome, rather than the malpractice suit itself. As the case progresses and facts emerge, you may play a large role in helping your physician patient correct previous distortions of the event. Certain periods—during trial, for example—might require more-frequent visits, medication, and expressions of support.
You may harbor a bias about the case, but withhold judgment until it is resolved.
Related resources
- American College of Obstetricians and Gynecologists. From exam room to court room: navigating litigation and coping with stress (CD-ROM) http://sales.acog.com/acb/stores/1/product1.cfm?SID=1&Product_ID=589).
- Charles SC, Frisch PR. Adverse events, stress and litigation: a physician’s guide. New York: Oxford University Press; 2005.
- Physician Litigation Stress Resource Center. www.physicianlitigationstress.org.
Disclosure
Dr. Charles reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
‘Immediately after the event I was a wreck. I vaguely remember talking to the family; I don’t know if I was much use to them. … That night I got drunk. It was the only way I could sleep. A sensitive colleague came and sat with me.”1
Besides being targets of malpractice suits, psychiatrists also serve as resources for colleagues who are sued. Specific actions can help you and those you counsel deal with the stress of an adverse event before and during litigation. Remember that:
- anticipation is the best defense
- knowledge is power
- action counters passivity
- a supportive environment is essential.
ANTICIPATING LITIGATION
What is the risk? No nationwide reporting system tracks the incidence of medical malpractice claims, but industry experts suggest a claim is leveled against 7% of psychiatrists each year.2 The risk is higher for other medical specialists: a recent survey by the American College of Obstetricians and Gynecologists found that 89% of practicing ObGyns had been sued at least once in their careers.3 Because a claim usually takes several years to resolve, a substantial number of physicians—including psychiatrists—are involved in litigation at any one time.
Successfully anticipating litigation begins with being familiar with your state’s statute of limitations—usually 2 to 3 years after discovery of the incident, with exceptions for children, the disabled, and designated special circumstances. If a plaintiff’s case is not filed within this time, a disputed outcome can never be the subject of a malpractice claim.
Adverse events. The severity of the outcome, the nature of your relationship with the patient, and the degree of your responsibility for an adverse event contribute to the intensity of your initial emotional response. If a mistake caused the event, your reaction may be even more severe.4-6 Whatever the event’s specifics, you may ruminate about your role and degree of responsibility (Table 1).
Table 1
Nagging questions after a ‘bad’ patient outcome
|
Expect that your view of the circumstances will generate a complex array of feelings: shock, anxiety, depression, shame, guilt, self-blame, disbelief, self-doubt and inadequacy, anger, and even relief from not having to work with a difficult patient anymore.
Patient suicide. More than one-half of psychiatrists and up to one-third of psychiatric residents experience a patient suicide.7-10 The Joint Commission on Accreditation of Healthcare Organizations reports that suicide is the most frequent sentinel event, representing 501 (13.1%) of the total 3,811 sentinel events reviewed since 1995.11 Professional Risk Management Services, a major medical malpractice insurer of psychiatrists, reports that suicide and attempted suicide are the most frequently identifiable causes of liability payments (Figure).
Figure 1 Psychiatric claims by cause of loss in the United States, 1998 to 2005
Almost all lawsuits assert multiple allegations of negligence, and “cause of loss” represents the main allegation made in the claim or lawsuit. Thus, the category of “incorrect treatment” may be alleged in a lawsuit based on a patient suicide, but the main or chief allegation/complaint is stated as “incorrect treatment.” The most frequent identifiable cause of loss is suicide and attempted suicide.
* “Other” includes administrative issues, abandonment, premises liability, Tarasoff, third parties (such as parents), retained object, libel/slander, boundary violation, deleted duplicate file, Fen-phen, lack of informed consent, forensic issues, and miscellaneous.
Source: Prepared by Professional Risk Management Services, Inc. Reprinted with permission.
Psychiatrists’ feelings of distress after a patient suicide mirror the personal sense of failure and inadequacy most physicians feel when they are unable to prevent a patient’s death or serious injury. At the same time, we must:
- deal with the event’s medical complications, with relevant notifications and disclosures (Table 2)
- address the emotional pain of the injured patient or family
- participate in mandated reviews
- recognize and manage our emotional disruption (Table 3).
Table 2
Recommended medical steps, notifications,
and disclosures after an adverse event
| MEDICAL STEPS Take necessary actions to limit further injury or disability Obtain appropriate consultations Review the medical record; anticipate the patient’s follow-up needs and make recommendations for further treatment |
| NOTIFICATIONS Follow the health care system’s and insurer’s guidelines for notifying the patient/family Inform the institution’s risk manager and your professional liability carrier as soon as possible Write a description of the event for the record and a narrative for your personal file (and your lawyer’s) in case a suit is filed later Do not talk with the media |
| DISCLOSURES Acknowledge your ethical obligation to be truthful Follow your institution’s and insurer’s disclosure guidelines Expect to feel intimidated and uneasy in discussing your role in the event Expect the patient/family to be angry and disappointed in you Convey an interest in the patient’s/family’s emotional state; express sorrow for their loss Tell the patient/family what you know for sure; don’t speculate about what is not known, and don’t make false promises or false reassurances Don’t hurry; give the patient/family time to ask questions Expect to feel better after a truthful exchange |
Table 3
Managing your emotions before and during litigation
| Anticipate having repeated thoughts and preoccupations about the event; work toward a realistic view of it |
| Recognize your feelings and work to understand their source |
| Talk with a trusted confidant (your spouse, colleague, etc.) about your feelings |
| Monitor your emotional and physical status and, if indicated, seek appropriate consultation |
| Avoid situations that generate anxiety and increase stress |
| Monitor and address changes in relationships with family, patients, colleagues, and staff |
| Be understanding of yourself and others; develop a realistic view of yourself as a ‘good doctor’ |
| Engage in active sports and take regular vacations unrelated to professional activities |
| Control what can be controlled |
Self-evaluation. To cope with distress when a patient dies, you could attend the funeral. If the death was by suicide, consider consulting with a therapist about your reactions or review the case with your supervisor. You also might:
- make changes in your practice that alert you to problem patients
- introduce a more structured approach to patients with particular clinical conditions, using practice guidelines as a resource12,13
- become more alert to patients who may benefit from consultation or referral.
Balance the time you devote to work and personal life. Schedule regular time for recreation and active sports, which can help you prepare for the prolonged stress that follows being sued. Engage a personal physician to monitor your physical and emotional health and to recommend appropriate referrals when indicated.
KNOWLEDGE IS POWER
What can I expect? A lawsuit generates a mixture of common emotions and exacerbates those felt at the time of the bad outcome: shock, outrage, anxiety, anguish, dread, depression, helplessness, hopelessness, feelings of being misunderstood, and the anger and vulnerability associated with a narcissistic injury. As one ObGyn stated, learning that a lawsuit was filed “just prolonged my misery.”14
Each of us reacts in our own way to a lawsuit—and differently to each lawsuit if we are sued more than once—because of:
- our personality traits and personal circumstances
- the specifics of each case
- our relationship with the patient
- the public nature of a lawsuit
- a range of other variables that makes each case unique.
Suddenly, we who perceive ourselves as caring, beneficent, well-meaning, and devoted to our patients are publicly accused of being careless and incompetent, of harming the patient by failing to meet our minimal obligations. Psychiatrists Richard Ferrell and Trevor Price15 capture the impact of these allegations:
"Here are the sense of assault and violation, the feelings of outrage and fear. Most painfully, here is the narcissistic injury, the astonishing wound to our understanding of ourselves as admirable, well-meaning people."
Litigation is a lengthy process with defined stages (Table 4). We have little control over a slow-paced process that involves an array of participants (lawyers, judges, jury, and experts) whose behavior is not predictable. This makes us feel dependent, vulnerable, and impotent.
Table 4
Stages of litigation: What happens in court
| Stage | Definitions |
|---|---|
| Summons | Notification that a suit has been filed |
| Complaint | The nature of the allegation in legal terms |
| Pleadings | The attorney begins to communicate with the court by filing motions, a request that the court do something |
| Discovery | A process designed to obtain information about the case:
|
| Summary judgment | A motion asking the court, after the facts have been established by discovery, to decide the validity of the case; if granted, the case is resolved without a trial by jury |
| Settlement | An agreement between parties that resolves their legal dispute |
| Trial | Case is presented to the judge or a judge and jury to determine culpability |
| Verdict | Decision reached by the deciding body |
| Post-trial | If the defendant receives an unfavorable verdict, motions may be offered to the court to void or appeal the verdict |
BE ACTIVE, NOT PASSIVE
What you can do. Contact your insurer and risk manager immediately. Inquire about the average length of litigation in your jurisdiction (might be 1 to 5 or more years, depending on locality, type of case, and severity of injury). Ask your lawyer to describe the steps in the process and your role as the case proceeds.
Take whatever steps are necessary to cover your clinical duties. If your initial emotional reaction is disruptive, obtain coverage or rearrange your schedule. Expect to change or limit your schedule before depositions and during trial to allow adequate time for preparation.
Accept the fact that you must play by rules far different from those of medical care. Litigation is time-consuming and frustrating. Delays and “continuances” are common in legal proceedings, so expect them. Consider adapting to your own situation strategies that other sued physicians have found useful in regaining control over their lives and work (Table 5).
Table 5
Regaining control: Managing your practice during litigation
| Learn as much as you can about the legal process |
| Introduce good risk management strategies, such as efficient record-keeping, into your practice |
| Clarify the responsibilities of office personnel and coverage responsibilities with associates |
| Rearrange office schedules during periods of increased stress |
| Re-evaluate your time commitments to work and family |
| Participate in relevant continuing education |
| Make sure your financial and estate planning is current |
| Cooperate with legal counsel |
| Devote sufficient time to deposition preparation and other demands of the case |
| Carefully evaluate the advice of legal and insurance counsel regarding a settlement |
| Do not try to “fit patients in” while on trial; trial is a full-time job |
GET NEEDED SUPPORT
Talking about the case. Sharing with responsible confidants your emotional reactions to being sued is healthy for you and others affected. Lawyers, however, may caution you not to “talk to anybody” about the case. They don’t want you to say anything that would suggest liability or jeopardize their defense of the case.
As psychiatrists, we know this is not good psychological advice. The support of others is a natural help during major life events that cause enormous stress and disruption.16 You can resolve this dilemma by accepting the discipline of talking about your feelings regarding the case without discussing the specifics of the case.
In addition to lawyers and claims representatives, you may talk with your spouse or another trusted person or colleague about your feelings. When other physicians or psychiatrists formally consult with you about their litigation experiences, you are protected by the confidentiality inherent in the doctor-patient relationship.
Trust issues. Trust lies at the core of psychotherapeutic work. After being sued, you may find it difficult to re-establish trusting and comfortable relationships with patients, especially those who are seriously ill.
Well-trained, competent physicians who keep current with standards of care and have good relationships with patients do not expect to be sued. Psychiatrists often feel unrealistically immune to litigation because we believe our training helps us understand our own psychology and relationships with others. A charge of negligence exposes our vulnerabilities and leaves us feeling hurt and betrayed. As one psychiatrist ruefully observed, “I lost my innocence.”14
Countertransference feelings may emerge. Most physicians acknowledge that after being sued their relationships with patients change17,18—a particularly distressing outcome for psychiatrists. We may feel uncomfortable and threatened when we need to “stretch the patient-doctor relationship in a paternalistic direction,” such as when a psychotic patient needs involuntary commitment.15
Feelings that you must change the way you practice and chronic anxiety about your work are barriers to good practice. You may contemplate changing practice circumstances or retiring early. Personal therapy may help if you remain uneasy or cannot resolve life choices that overshadow your work with patients.
Medical or psychiatric care. Be alert to the point at which you or others involved in litigation need a referral for medical or psychiatric consultation. Sued physicians, their families, or colleagues often experience diagnosable psychiatric conditions or other behavioral problems, such as:
- major depression
- adjustment disorders
- posttraumatic stress disorder
- worsening of a previously diagnosed psychiatric illness
- physical symptoms that require diagnosis and treatment
- alcohol and drug misuse or abuse
- anxiety and distress that interfere with work
- self-medication, especially for insomnia
- disturbances and dysfunctional behaviors that affect marital and family life.19,20
SUPPORT YOUR COLLEAGUES
When consulting with other physicians, be aware of litigation factors that may influence treatment.
Become familiar with the climate of litigation in the jurisdiction where the case was filed, including the incidence and outcome of cases. For example, does an attempted suicide case usually result in settlement or—if it goes to trial—take 2 to 5 or more years to resolve? More than 70% of cases filed nationwide result in no payment (no settlement) for the plaintiff. If cases go to trial, physicians win 80% of the time.21
Recognize that the source of the physician’s distress may be the trauma associated with the initial bad outcome, rather than the malpractice suit itself. As the case progresses and facts emerge, you may play a large role in helping your physician patient correct previous distortions of the event. Certain periods—during trial, for example—might require more-frequent visits, medication, and expressions of support.
You may harbor a bias about the case, but withhold judgment until it is resolved.
Related resources
- American College of Obstetricians and Gynecologists. From exam room to court room: navigating litigation and coping with stress (CD-ROM) http://sales.acog.com/acb/stores/1/product1.cfm?SID=1&Product_ID=589).
- Charles SC, Frisch PR. Adverse events, stress and litigation: a physician’s guide. New York: Oxford University Press; 2005.
- Physician Litigation Stress Resource Center. www.physicianlitigationstress.org.
Disclosure
Dr. Charles reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Anonymous. Looking back… BMJ 2000;320(7237):812.-
2. Martin G, Tracy JD. President and CEO, Professional Risk Management Services. Personal communication. October 20, 2006.
3. American College of Obstetricians and Gynecologists. ACOG 2006 Professional Liability Survey. Washington, DC; 2006. Available at: http://www.acog.org/departments/dept_notice.cfm?recno=4&bulletin=3963. Accessed January 16, 2007.
4. Christensen JF, Levinson W, Dunn PM. The heart of darkness: the impact of perceived mistakes on physicians. J Gen Intern Med 1992;7(4):424-31.
5. Wu AW. Medical error: the second victim. The doctor who makes the mistake needs help too. BMJ 2000;320(7237):726-7.
6. Aasland OG, Forde R. Impact of feeling responsible for adverse events on doctors’ personal and professional lives: the importance of being open to criticism from colleagues. Quality & Safety in Health Care 2005;14:13-7.
7. Alexander DA, Klein S, Grey NM, et al. Suicide by patients: questionnaire study of its effect on consultant psychiatrists. BMJ 2000;320:1571-4.
8. Chemtob CM, Hamada RS, Bauer G, et al. Patients’ suicides: frequency and impact on psychiatrists. Am J Psychiatry 1988;145:224-8.
9. Brown HN. The impact of suicide on therapists in training. Compr Psychiatry 1987;28:101-12.
10. Ellis TE, Dickey TO, Jones EC. Patient suicide in psychiatric residency programs: a national survey of training and postvention practices. Academic Psychiatry 1998;22:181-9.
11. Joint Commission on Accreditation of Healthcare Organizations. Sentinel event statistics. Available at: http://www.jointcommission.org/NR/rdonlyres/74540565-4D0F-4992-863E-8F9E949E6B56/0/se_stats_6_30_06.pdf. Accessed November 27, 2006.
12. Hendin H, Lipschitz A, Maltsberger JT, et al. Therapists’ reactions to patients’ suicides. Am J Psychiatry 2000;157(12):2022-7.
13. Practice guidelines for the treatment of psychiatric disorders (compendium 2006) Arlington, VA: American Psychiatric Publishing; 2006.
14. Charles SC, Frisch PR. Adverse events, stress and litigation: a physician’s guide. New York: Oxford University Press; 2005:94,120.
15. Ferrell RB, Price TRP. Effects of malpractice suits on physicians. In: Gold JH, Nemiah JC, eds. Beyond transference. Washington, DC: American Psychiatric Press; 1993:141-58.
16. Watson PJ, Friedman MJ, Gibson LE, et al. Early intervention in trauma-related problems. In: Ursano R, Norwood AE, eds. Trauma and disaster: responses and management. Review of psychiatry vol. 22. Washington, DC: American Psychiatric Press; 2003:100-1.
17. Charles SC, Psykoty CE, Nelson A. Physicians on trial—self-reported reactions to malpractice trials. West J Med 1988;148:358-60.
18. Charles SC. The doctor-patient relationship and medical malpractice litigation. Bull Menninger Clin 1993;57(2):195-207.
19. Charles SC, Wilbert JR, Franke KJ. Sued and non-sued physicians’ self-reported reactions to malpractice litigation. Am J Psychiatry 1985;142:437-40.
20. Martin CA, Wilson JA, Fiebelman ND, et al. Physicians’ psychologic reactions to malpractice litigation. South Med J 1991;84:1300-4.
21. Outcome of closed medical malpractice claims. National data (1985-2005). Physician Insurers Association of America (PIAA). Rockville, MD; 2006.
1. Anonymous. Looking back… BMJ 2000;320(7237):812.-
2. Martin G, Tracy JD. President and CEO, Professional Risk Management Services. Personal communication. October 20, 2006.
3. American College of Obstetricians and Gynecologists. ACOG 2006 Professional Liability Survey. Washington, DC; 2006. Available at: http://www.acog.org/departments/dept_notice.cfm?recno=4&bulletin=3963. Accessed January 16, 2007.
4. Christensen JF, Levinson W, Dunn PM. The heart of darkness: the impact of perceived mistakes on physicians. J Gen Intern Med 1992;7(4):424-31.
5. Wu AW. Medical error: the second victim. The doctor who makes the mistake needs help too. BMJ 2000;320(7237):726-7.
6. Aasland OG, Forde R. Impact of feeling responsible for adverse events on doctors’ personal and professional lives: the importance of being open to criticism from colleagues. Quality & Safety in Health Care 2005;14:13-7.
7. Alexander DA, Klein S, Grey NM, et al. Suicide by patients: questionnaire study of its effect on consultant psychiatrists. BMJ 2000;320:1571-4.
8. Chemtob CM, Hamada RS, Bauer G, et al. Patients’ suicides: frequency and impact on psychiatrists. Am J Psychiatry 1988;145:224-8.
9. Brown HN. The impact of suicide on therapists in training. Compr Psychiatry 1987;28:101-12.
10. Ellis TE, Dickey TO, Jones EC. Patient suicide in psychiatric residency programs: a national survey of training and postvention practices. Academic Psychiatry 1998;22:181-9.
11. Joint Commission on Accreditation of Healthcare Organizations. Sentinel event statistics. Available at: http://www.jointcommission.org/NR/rdonlyres/74540565-4D0F-4992-863E-8F9E949E6B56/0/se_stats_6_30_06.pdf. Accessed November 27, 2006.
12. Hendin H, Lipschitz A, Maltsberger JT, et al. Therapists’ reactions to patients’ suicides. Am J Psychiatry 2000;157(12):2022-7.
13. Practice guidelines for the treatment of psychiatric disorders (compendium 2006) Arlington, VA: American Psychiatric Publishing; 2006.
14. Charles SC, Frisch PR. Adverse events, stress and litigation: a physician’s guide. New York: Oxford University Press; 2005:94,120.
15. Ferrell RB, Price TRP. Effects of malpractice suits on physicians. In: Gold JH, Nemiah JC, eds. Beyond transference. Washington, DC: American Psychiatric Press; 1993:141-58.
16. Watson PJ, Friedman MJ, Gibson LE, et al. Early intervention in trauma-related problems. In: Ursano R, Norwood AE, eds. Trauma and disaster: responses and management. Review of psychiatry vol. 22. Washington, DC: American Psychiatric Press; 2003:100-1.
17. Charles SC, Psykoty CE, Nelson A. Physicians on trial—self-reported reactions to malpractice trials. West J Med 1988;148:358-60.
18. Charles SC. The doctor-patient relationship and medical malpractice litigation. Bull Menninger Clin 1993;57(2):195-207.
19. Charles SC, Wilbert JR, Franke KJ. Sued and non-sued physicians’ self-reported reactions to malpractice litigation. Am J Psychiatry 1985;142:437-40.
20. Martin CA, Wilson JA, Fiebelman ND, et al. Physicians’ psychologic reactions to malpractice litigation. South Med J 1991;84:1300-4.
21. Outcome of closed medical malpractice claims. National data (1985-2005). Physician Insurers Association of America (PIAA). Rockville, MD; 2006.
Jump-starting depression treatment
The serendipitous discovery of medications that can improve mood transformed depression treatment more than 50 years ago.1 Most antidepressants produced since then could be called “me-too” medications because they all work by affecting the release of monoamines—serotonin, norepinephrine, and dopamine—which, in turn, modulate the activity of neurons that release glutamate.
Weeks may pass before antidepressants’ effect on monoamine-releasing neurons produces a therapeutic benefit, however, leaving many patients impaired or even suicidal. This delayed onset of action might be explained by antidepressants’ indirect blockade of glutamate. The route to more rapid results, therefore, might be to cut out the monoamine middlemen.
Glutamate clues
Glutamate, instead of monoamines, might offer a more direct means to affect mood and could be a new target for antidepressant treatment:2
- Positron-emission tomography of neuron function in depressed patients shows abnormal activity in neurons that release glutamate—so-called glutamate neurons.
- Approximately 60 % of neurons are glutamate neurons, the largest network of neurons in the brain.
- Increased glutamate activity is seen in depressed patients.
- Animal studies have shown that blocking the N-methyl-D-aspartate (NMDA) receptor—1 of 3 types of glutamate receptors—decreases depressive behavior.
- Chronic administration of antidepressant medication reduces the expression of NMDA receptors.
Rapid glutamate blockade
Prompted by evidence that glutamate may be involved in mood disorders, researchers at the National Institute of Mental Health designed a study to determine if blocking the NMDA receptor can produce a rapid antidepressant effect.3 They chose the agent ketamine for this study because of its potent affinity for the NMDA receptor.
Ketamine was developed in the 1960s as a general anaesthetic, and its use in the United States is limited almost exclusively to veterinary medicine. The drug’s propensity to induce perceptual disturbances limits its clinical use but enhances its illicit use.
Eighteen patients with treatment-resistant depression were enrolled in a randomized, placebo-controlled, double-blind, crossover study. After 2 weeks without medication, they received a single infusion of IV ketamine or placebo. One week later they received the alternate intervention. Changes in Hamilton Rating Scale for Depression scores were assessed after each infusion.
Figure Decrease in depressive symptoms with IV ketamine
* = P <0.05
Patients who received ketamine (blue) showed a marked reduction of depressive symptoms within 2 hours compared with those who received placebo (red).
Source: Reference 3Patients receiving ketamine showed a robust and sustained reduction in depressive symptoms compared with placebo within 110 minutes (Figure). “To our knowledge,” the authors wrote, “there has never been a report of any other drug or somatic treatment—such as sleep deprivation, thyrotropin-releasing hormone, antidepressant, dexamethasone, or electroconvulsive therapy—that results in such a dramatic rapid and prolonged response with a single administration.”
Seventy-one percent of patients responded to IV ketamine within 24 hours, which is comparable to reported response rates after 8 weeks with oral antidepressants such as bupropion (62%), selective serotonin reuptake inhibitors (63%), and venlafaxine (65%).4,5
Caution and caveats
Despite these “dramatic” results, we must be cautious about extrapolating too much from this small study. Glutamate blockers such as ketamine can have serious adverse effects—including psychosis—and patients may not tolerate long-term interventions. Likewise, oral administration of memantine—another NMDA blocker—in a double-blind study did not effectively treat depression.6 Finally, subjects in the ketamine trial had chronic, treatment-resistant depression, and the results might not apply to other forms of depression.
The results suggest the possibility of a new option for depression treatment, however. Specifically, this option could expedite response and “jump-start” treatment through a novel mechanism so that persons with depression can get back on their feet more rapidly.
Drug brand names
- Bupropion • Wellbutrin
- Ketamine • Ketalar
- Memantine • Namenda
- Venlafaxine • Effexor
1. Higgins ES, George MS. Neuroscientific foundations of clinical psychiatry. Philadelphia, PA: Lippincott Williams and Wilkins; 2007. In press.
2. Kugaya A, Sanacora G. Beyond monoamines: glutamatergic function in mood disorders. CNS Spectrums 2005;10(10):808-19.
3. Zarate CA, Jr, Singh JB, Carlson PJ, et al. A randomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depression. Arch Gen Psychiatry 2006;63(8):856-64.
4. Thase ME, Haight BR, Richard N, et al. Remission rates following antidepressant therapy with bupropion or selective serotonin reuptake inhibitors: a meta-analysis of original data from 7 randomized controlled trials. J Clin Psychiatry 2005;66(8):974-81.
5. Entsuah AR, Huang H, Thase ME. Response and remission rates in different subpopulations with major depressive disorder administered venlafaxine, selective serotonin reuptake inhibitors, or placebo. J Clin Psychiatry 2001;62(11):869-77.
6. Zarate CA, Jr, Singh JB, Quiroz JA, et al. A double-blind, placebo-controlled study of memantine in the treatment of major depression. Am J Psychiatry 2006;163(1):153-5.
The serendipitous discovery of medications that can improve mood transformed depression treatment more than 50 years ago.1 Most antidepressants produced since then could be called “me-too” medications because they all work by affecting the release of monoamines—serotonin, norepinephrine, and dopamine—which, in turn, modulate the activity of neurons that release glutamate.
Weeks may pass before antidepressants’ effect on monoamine-releasing neurons produces a therapeutic benefit, however, leaving many patients impaired or even suicidal. This delayed onset of action might be explained by antidepressants’ indirect blockade of glutamate. The route to more rapid results, therefore, might be to cut out the monoamine middlemen.
Glutamate clues
Glutamate, instead of monoamines, might offer a more direct means to affect mood and could be a new target for antidepressant treatment:2
- Positron-emission tomography of neuron function in depressed patients shows abnormal activity in neurons that release glutamate—so-called glutamate neurons.
- Approximately 60 % of neurons are glutamate neurons, the largest network of neurons in the brain.
- Increased glutamate activity is seen in depressed patients.
- Animal studies have shown that blocking the N-methyl-D-aspartate (NMDA) receptor—1 of 3 types of glutamate receptors—decreases depressive behavior.
- Chronic administration of antidepressant medication reduces the expression of NMDA receptors.
Rapid glutamate blockade
Prompted by evidence that glutamate may be involved in mood disorders, researchers at the National Institute of Mental Health designed a study to determine if blocking the NMDA receptor can produce a rapid antidepressant effect.3 They chose the agent ketamine for this study because of its potent affinity for the NMDA receptor.
Ketamine was developed in the 1960s as a general anaesthetic, and its use in the United States is limited almost exclusively to veterinary medicine. The drug’s propensity to induce perceptual disturbances limits its clinical use but enhances its illicit use.
Eighteen patients with treatment-resistant depression were enrolled in a randomized, placebo-controlled, double-blind, crossover study. After 2 weeks without medication, they received a single infusion of IV ketamine or placebo. One week later they received the alternate intervention. Changes in Hamilton Rating Scale for Depression scores were assessed after each infusion.
Figure Decrease in depressive symptoms with IV ketamine
* = P <0.05
Patients who received ketamine (blue) showed a marked reduction of depressive symptoms within 2 hours compared with those who received placebo (red).
Source: Reference 3Patients receiving ketamine showed a robust and sustained reduction in depressive symptoms compared with placebo within 110 minutes (Figure). “To our knowledge,” the authors wrote, “there has never been a report of any other drug or somatic treatment—such as sleep deprivation, thyrotropin-releasing hormone, antidepressant, dexamethasone, or electroconvulsive therapy—that results in such a dramatic rapid and prolonged response with a single administration.”
Seventy-one percent of patients responded to IV ketamine within 24 hours, which is comparable to reported response rates after 8 weeks with oral antidepressants such as bupropion (62%), selective serotonin reuptake inhibitors (63%), and venlafaxine (65%).4,5
Caution and caveats
Despite these “dramatic” results, we must be cautious about extrapolating too much from this small study. Glutamate blockers such as ketamine can have serious adverse effects—including psychosis—and patients may not tolerate long-term interventions. Likewise, oral administration of memantine—another NMDA blocker—in a double-blind study did not effectively treat depression.6 Finally, subjects in the ketamine trial had chronic, treatment-resistant depression, and the results might not apply to other forms of depression.
The results suggest the possibility of a new option for depression treatment, however. Specifically, this option could expedite response and “jump-start” treatment through a novel mechanism so that persons with depression can get back on their feet more rapidly.
Drug brand names
- Bupropion • Wellbutrin
- Ketamine • Ketalar
- Memantine • Namenda
- Venlafaxine • Effexor
The serendipitous discovery of medications that can improve mood transformed depression treatment more than 50 years ago.1 Most antidepressants produced since then could be called “me-too” medications because they all work by affecting the release of monoamines—serotonin, norepinephrine, and dopamine—which, in turn, modulate the activity of neurons that release glutamate.
Weeks may pass before antidepressants’ effect on monoamine-releasing neurons produces a therapeutic benefit, however, leaving many patients impaired or even suicidal. This delayed onset of action might be explained by antidepressants’ indirect blockade of glutamate. The route to more rapid results, therefore, might be to cut out the monoamine middlemen.
Glutamate clues
Glutamate, instead of monoamines, might offer a more direct means to affect mood and could be a new target for antidepressant treatment:2
- Positron-emission tomography of neuron function in depressed patients shows abnormal activity in neurons that release glutamate—so-called glutamate neurons.
- Approximately 60 % of neurons are glutamate neurons, the largest network of neurons in the brain.
- Increased glutamate activity is seen in depressed patients.
- Animal studies have shown that blocking the N-methyl-D-aspartate (NMDA) receptor—1 of 3 types of glutamate receptors—decreases depressive behavior.
- Chronic administration of antidepressant medication reduces the expression of NMDA receptors.
Rapid glutamate blockade
Prompted by evidence that glutamate may be involved in mood disorders, researchers at the National Institute of Mental Health designed a study to determine if blocking the NMDA receptor can produce a rapid antidepressant effect.3 They chose the agent ketamine for this study because of its potent affinity for the NMDA receptor.
Ketamine was developed in the 1960s as a general anaesthetic, and its use in the United States is limited almost exclusively to veterinary medicine. The drug’s propensity to induce perceptual disturbances limits its clinical use but enhances its illicit use.
Eighteen patients with treatment-resistant depression were enrolled in a randomized, placebo-controlled, double-blind, crossover study. After 2 weeks without medication, they received a single infusion of IV ketamine or placebo. One week later they received the alternate intervention. Changes in Hamilton Rating Scale for Depression scores were assessed after each infusion.
Figure Decrease in depressive symptoms with IV ketamine
* = P <0.05
Patients who received ketamine (blue) showed a marked reduction of depressive symptoms within 2 hours compared with those who received placebo (red).
Source: Reference 3Patients receiving ketamine showed a robust and sustained reduction in depressive symptoms compared with placebo within 110 minutes (Figure). “To our knowledge,” the authors wrote, “there has never been a report of any other drug or somatic treatment—such as sleep deprivation, thyrotropin-releasing hormone, antidepressant, dexamethasone, or electroconvulsive therapy—that results in such a dramatic rapid and prolonged response with a single administration.”
Seventy-one percent of patients responded to IV ketamine within 24 hours, which is comparable to reported response rates after 8 weeks with oral antidepressants such as bupropion (62%), selective serotonin reuptake inhibitors (63%), and venlafaxine (65%).4,5
Caution and caveats
Despite these “dramatic” results, we must be cautious about extrapolating too much from this small study. Glutamate blockers such as ketamine can have serious adverse effects—including psychosis—and patients may not tolerate long-term interventions. Likewise, oral administration of memantine—another NMDA blocker—in a double-blind study did not effectively treat depression.6 Finally, subjects in the ketamine trial had chronic, treatment-resistant depression, and the results might not apply to other forms of depression.
The results suggest the possibility of a new option for depression treatment, however. Specifically, this option could expedite response and “jump-start” treatment through a novel mechanism so that persons with depression can get back on their feet more rapidly.
Drug brand names
- Bupropion • Wellbutrin
- Ketamine • Ketalar
- Memantine • Namenda
- Venlafaxine • Effexor
1. Higgins ES, George MS. Neuroscientific foundations of clinical psychiatry. Philadelphia, PA: Lippincott Williams and Wilkins; 2007. In press.
2. Kugaya A, Sanacora G. Beyond monoamines: glutamatergic function in mood disorders. CNS Spectrums 2005;10(10):808-19.
3. Zarate CA, Jr, Singh JB, Carlson PJ, et al. A randomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depression. Arch Gen Psychiatry 2006;63(8):856-64.
4. Thase ME, Haight BR, Richard N, et al. Remission rates following antidepressant therapy with bupropion or selective serotonin reuptake inhibitors: a meta-analysis of original data from 7 randomized controlled trials. J Clin Psychiatry 2005;66(8):974-81.
5. Entsuah AR, Huang H, Thase ME. Response and remission rates in different subpopulations with major depressive disorder administered venlafaxine, selective serotonin reuptake inhibitors, or placebo. J Clin Psychiatry 2001;62(11):869-77.
6. Zarate CA, Jr, Singh JB, Quiroz JA, et al. A double-blind, placebo-controlled study of memantine in the treatment of major depression. Am J Psychiatry 2006;163(1):153-5.
1. Higgins ES, George MS. Neuroscientific foundations of clinical psychiatry. Philadelphia, PA: Lippincott Williams and Wilkins; 2007. In press.
2. Kugaya A, Sanacora G. Beyond monoamines: glutamatergic function in mood disorders. CNS Spectrums 2005;10(10):808-19.
3. Zarate CA, Jr, Singh JB, Carlson PJ, et al. A randomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depression. Arch Gen Psychiatry 2006;63(8):856-64.
4. Thase ME, Haight BR, Richard N, et al. Remission rates following antidepressant therapy with bupropion or selective serotonin reuptake inhibitors: a meta-analysis of original data from 7 randomized controlled trials. J Clin Psychiatry 2005;66(8):974-81.
5. Entsuah AR, Huang H, Thase ME. Response and remission rates in different subpopulations with major depressive disorder administered venlafaxine, selective serotonin reuptake inhibitors, or placebo. J Clin Psychiatry 2001;62(11):869-77.
6. Zarate CA, Jr, Singh JB, Quiroz JA, et al. A double-blind, placebo-controlled study of memantine in the treatment of major depression. Am J Psychiatry 2006;163(1):153-5.
Engage resistant patients in collaborative treatment
Whenever you feel you are doing more work than the patient and are more invested than he is, something has gone wrong in collaborative care.
With resistant or hostile patients, fight the urge to move quickly into clinical assessment and to prescribe what you think should be worked on and how. Instead, spend more time—especially when building the treatment alliance in the first 15 minutes (Box1)—exploring their ideas on how, when, and where they feel they can achieve what is most important to them (Table 12).
Resistant patients may have different agendas, but taking a pragmatic approach can merge their goals with yours.
More than 2,000 research publications in the last 30 years prove the clinical importance of the therapeutic alliance.1 When working with resistant patients, keep these points in mind:
Develop a strong alliance early in treatment. “Early” is relative to the length of therapy, but evidence suggests sessions 3 to 5 are a critical window.
The patient’s experience of being understood, supported, and provided with hope depends on the strength of the alliance early in therapy. His or her interpretation of what you do can be different from what you intend. You may be a great clinician but not necessarily for this particular individual at this time, doing the kind of work you do.
Progressively negotiate the quality of the relationship. The patient’s perception of the alliance—not yours—is most influential. Ask specifically if the treatment relationship is working for him or her.
Early in treatment, the alliance itself contributes more to outcomes than do therapeutic techniques and models. First develop a collaborative agreement on the goals and strategies to be used in the therapeutic work.
Table 1
How to merge the reluctant patient’s goals with clinical needs assessment
| Questions to prioritize patient goals | Questions for clinical needs assessment | Merging patient goals with assessed needs | |
|---|---|---|---|
| What? | What does the patient want the most? What undesired consequences will occur if s/he does not get help? | What does the clinical assessment indicate s/he needs? What obstacles/assets do you need to address to help her/him get what s/he wants? | What treatment contract will drive the treatment plan and organize treatment priorities? |
| Why? | Why did s/he seek help now? Has s/he realized or been told s/he is at risk to lose freedom, health, a relationship, or a job? How committed to change is s/he? | Why are the assessed obstacles and resources important to include in a treatment plan? What diagnostic, function, or severity problems do assessment data reveal? | Is the treatment plan linked to what s/he wants? Does s/he accept that the treatment priorities will help her/him get what s/he wants? |
| How? | How will s/he achieve the most important goal? Must you try her/his preferred treatment before s/he accepts methods you prescribe? | How will you develop patient buy-in and get her/him to accept the plan? | Does s/he believe your strategies will help get what s/he wants? Will s/he be actively invested or passively compliant in treatment? |
| Where? | Where is s/he willing to be treated? Does s/he have strong preferences (such as about group treatment or residential programs)? | Where is the appropriate setting for treatment? What is indicated by the placement criteria? | Refer her/him to the level of care that merges his/her preferences with what is clinically indicated and likely to be effective |
| When? | When does s/he want to begin treatment? Is s/he feeling pressure to start? How badly does s/he want treatment, or is s/he just complying? | When should treatment begin, based on your assessment? What are realistic expectations and milestones in the process? | How urgent is treatment? What is the process? What is expected from referral? |
| Source: Adapted from reference 2, Table 3. | |||
What does the patient want?
When a patient is difficult to engage, begin by listening for the most important concern that brought him to your office.
He may be depressed, anxious, or tired, but exploring why he decided to seek help now (“My wife said she would leave me if I didn’t get help”) reveals what is most important. The “treatment contract,” then, is helping this patient save his marriage.
Initial engagement
Collaborative treatment begins with a genuinely interested dialogue about what prompted the patient’s visit.
Therapist: “Thank you for choosing to work with me. How may I serve you? What is the most important thing you want me to help you with?”
Mr. L: “I didn’t choose you; they made me come.”
T: “I didn’t see anyone drag you in. What would happen if you had not come today?”
Mr. L: “I might lose my job. I came because my boss told me to.”
Focus on what the patient wants, not just what others have said he or she needs (treatment for substance abuse, angry outbursts, conflict at work). The patient may want to stay out of jail, keep his job or relationship, regain custody of his or her children, obtain housing, or get people to “leave me alone and quit locking me up against my will.” Although the patient’s problem may be obvious to us, he needs “discovery” work, not “recovery” work.
Why has the patient come now? What is his highest priority? Can we help him discover the link between his drinking or anger that affects his work performance?
Therapist: “So you want to get the boss off your back. You want people to leave you alone. You feel people treat you unfairly and want them to stop. But why did you come today and not last week or last month?”
Mr. L: “I came now because yesterday my boss said I could lose my job if I didn’t get some help.”
T: “So what you want most importantly is to keep your job, is that it?”
Mr. L: “Well yeah, but I don’t have a drinking problem or any problem with my temper. They’re just overreacting. It wasn’t as bad as they said.”
T: “OK, I am willing to work on helping you keep your job if that’s what is most important to you. Do you know what you are doing that makes them think you have a drinking or anger problem?
Mr. L: “All I did was come in late a couple of times and got into a little argument with a couple of people.”
T: “If we are going to help you keep your job, we could spend our time talking about how unfair your boss is and how she’s misjudging you. Or we could work to show her that she has you all wrong and that you are a productive worker who does not have a substance or anger problem.
“Let’s think together how we could gather the data that would prove you don’t have a substance problem. If all that data is squeaky clean, then I can write a very supportive letter to your boss and tell her all is well. If, however, we discover you do have a problem, I can still write a very supportive letter. But we’ll have to show her how you are taking care of any problems that interfere with your work performance.”
Reframe the presenting complaint
Few patients present fully ready to work on definitive behavioral health recovery. If patients at least attend sessions or talk with you, they must be motivated to do something. Otherwise, they would not show up.
Our task is help patients such as Mr. L get what they want, not what we think they should want. Eventually you will get to explore the patient’s substance use, impulse or parenting problems, mental health symptoms, or communication problems, but this discussion will be in the service of allying with his or her goals.
Rather than viewing patients as unmotivated or resistant, think of resistance as an interactional process. “If we are going to stop them from locking you up,” you might say, “let’s talk about what you are doing that makes you look like you are dangerous and out of control. And when you were not locked away, let’s think of how you kept ‘them’ off your back.”
Instead of interpreting resistance as pathology, view the behavior as an opportunity to understand and respond to the patient’s stage of readiness to change.
Stages of change
By being “difficult,” patients are often declaring that they are not invested in what you think the problem is or in working on that problem. Resistance thrives when we and the patient have not allied around a common goal and are at different stages of change. Think of the therapeutic alliance in the context of the widely-used and well-researched Transtheoretical Model’s stages of change:3,4
Precontemplation. A person at this stage is not considering the possibility of change, although others are aware of a problem. He or she will seldom appear for treatment without coercion. The person could benefit from nonthreatening information to raise awareness of a possible “problem” and possibilities for change.
Contemplation. The person is ambivalent, undecided, vacillating about whether he has a “problem.” He wants to change, but this desire exists simultaneously with resistance to change. Motivational strategies can be useful, but aggressive or premature confrontation could provoke strong resistance and defensive behaviors. Many persons at this stage have indefinite plans to take action in the next 6 months or so.
Preparation takes the person from the contemplation stage to specific steps to solve the problem in the action stage. He or she develops increasing confidence in the decision to change and takes the first steps on the road to action. Most people at this stage plan to take action within 1 month and are making final adjustments before beginning to change.
Action. The person takes specific actions intended to bring about change. This busiest stage of change is characterized by overt modification of behavior and surroundings and requires the greatest time and energy. Support and encouragement are crucial to prevent drop-out and regression in readiness to change.
Maintenance. Goals at this stage are to sustain the changes accomplished by previous action and to prevent relapse. Maintaining new behaviors requires different skills than were needed to initiate change. Gains are consolidated. “Maintenance” is not a static stage; it can last 6 months or up to a lifetime. The patient learns new coping and problem-solving strategies, replaces problem behaviors with a healthier life style, and works through emotional triggers of relapse.
Relapse/recycling can happen but is not inevitable. When setbacks occur, help the patient avoid becoming stuck, discouraged, or demoralized, and help him learn from relapse before committing to a new action cycle. Conduct a comprehensive, multidimensional assessment to explore all reasons for relapse.
Termination is the ultimate goal: to exit the cycle of change without fear of relapse. Certain problems may be terminated or merely kept in remission through maintenance strategies.
Match strategies with stages
Discovery planning. Engaging patients in collaborative care starts with honoring their stages of change and working with them and their families on different tasks for each stage of change.4-6 A patient such as Mr. L, for example—who is at an early stage of change and thinks he has an “unfair boss problem” (not an alcohol problem) or a “nagging wife problem” (not an anger or domestic violence problem)—needs a discovery, drop-out prevention plan.
The cause of the patient’s work or relationship problem may be obvious to you, but a patient in early stages of change resists that information and, if pressed, gets frustrated and leaves treatment. A “discovery” treatment plan embraces the patient’s views and could be focused, for example, on gathering data that would prove to the employer that there is not an alcohol problem.
If random breath alcohol testing, feedback from family, and review of past job losses all prove negative for alcohol problems, the patient would have data to support his or her view that he does not have an alcohol problem. If, however, this exploration reveals an alcohol problem, the patient “discovers” he has more of a problem than he thought. For this plan, the challenge is to keep Mr. L engaged long enough to discover the connection between his alcohol problems and his employment or marital problems.
Recovery planning. On the other hand, a person at the action stage who wants to avoid becoming depressed again or wishes to live a life of sobriety collaborates on a recovery, relapse prevention plan. This patient is committed to developing the knowledge and skills to prevent relapse and open to whatever will promote health and well-being.
The Transtheoretical Model’s 9 processes of change3,4 inform which interventions might be most effective at various stages of change (Table 2). For example, a patient might be proud of the fact that “I can hold my liquor and drink everyone under the table.” Consciousness-raising—such as by explaining that his high alcohol tolerance is a danger signal, not a beneficial ability—can enhance his change process. Even if he is not ready to commit to definitive change, at least exploring whether he has a problem may move him from precontemplation to a contemplation stage of change. Table 3 shows how other processes of change can help motivate patients in later stages of change.4,5
Table 2
Transtheoretical model’s 9 processes of change: What happens at each step
| Process of change | The person… |
|---|---|
| Conscious-raising | becomes aware of a problem from education, advice, self-awareness, or feedback from others |
| Social liberation | begins to think about change because external forces raise awareness (a ban on smoking in restaurants, for example, can heighten awareness that one has a smoking problem) |
| Emotional arousal | becomes more convinced of the need to change when faced with a strong and sudden emotional experience related to the problem (such as death of a loved one) |
| Self-reevaluation | examines his or her values to see whether or not the behavior conflicts with what is important to him or her |
| Commitment | accepts responsibility for changing and affirms to self and others the decision to change |
| Reward | uses self-praise, positive feedback from others, improved well-being or financial security, “natural highs,” and other reinforcing benefits to consolidate change |
| Countering | substitutes other responses to counter unhealthy choices and behavior (such as relaxation techniques to combat angry outbursts or urges to resume smoking) |
| Environmental control | changes surrounding people, places, or things to reduce the risk of continuing or resuming the problem behavior |
| Helping relationships | seeks assistance from trusted friends, professionals, spiritual advisors, or significant others to initiate and sustain the change process |
| Source: Adapted and reprinted with permission from reference 4. | |
Table 3
Strategies and interventions to motivate patients at each stage of change
| Stage of change | Most useful processes of change (see Table 2) | Goal of treatment | Strategies and interventions |
|---|---|---|---|
| Precontemplation | Consciousness-raising Social liberation | To raise doubt |
|
| Contemplation | Consciousness-raising Social liberation Emotional arousal Self-reevaluation | To tip the balance |
|
| Preparation | Social liberation Emotional arousal Self-reevaluation Commitment | To determine best course |
|
| Action | Social liberation Commitment Reward Countering Environment control Helping relationships | To take steps to change |
|
| Maintenance | Commitment Countering Environment control Helping relationships | To prevent relapse |
|
| Relapse/recycling | Depends on stage to which patient returned | To renew processes of change |
|
- Scott D. Miller, PhD. Institute for the Study of Therapeutic Change, Chicago, IL. (773) 404-5130; www.talkingcure.com.
- Miller WR, Rollnick S, Moyers TB. Motivational interviewing: professional training videotape series. Albuquerque, NM: University of New Mexico, 1998. Six videotapes (about $130 total); (505) 768-0279 or 0100.
- Miller WR, consensus panel chair. Treatment improvement protocol. Enhancing motivation for change in substance abuse treatment. Rockville, MD; Center for Substance Abuse Treatment, 1999. DHHS Publication 99-3354. Available from the National Clearinghouse for Alcohol/Drug Information, Rockville, MD; (800) 729-6686.
Dr. Mee-Lee is a board-certified psychiatrist and is certified by examination of the American Society of Addiction Medicine (ASAM). He is based in Davis, CA, and is involved in full-time training and consulting. For information, visit www.DMLMD.com.
1. Horvath AO, Bedi RP. The alliance. In: Norcross JC, ed. Psychotherapy relationships that work: therapist contributions and responsiveness to patients. New York: Oxford University Press; 2002.
2. Mee-Lee D. Treatment planning for dual disorders. Psychiatr Rehabil Skills 2001;5(1):52-79.
3. Prochaska JO, DiClemente CC, Norcross JC. In search of how people change: applications to addictive behaviors. Am Psychol 1992;47:1102-14.
4. Prochaska JO, Norcross JC, DiClemente CC. Changing for good. New York: Avon Books; 1994:54.
5. DiClemente CC. Conceptual models and applied research: the ongoing contribution of the transtheoretical model. J Addict Nurs 2005;16:5-12.
6. Miller WR, Rollnick S. Motivational interviewing: preparing people to change addictive behavior. New York: Guilford Press; 1991:18.
Whenever you feel you are doing more work than the patient and are more invested than he is, something has gone wrong in collaborative care.
With resistant or hostile patients, fight the urge to move quickly into clinical assessment and to prescribe what you think should be worked on and how. Instead, spend more time—especially when building the treatment alliance in the first 15 minutes (Box1)—exploring their ideas on how, when, and where they feel they can achieve what is most important to them (Table 12).
Resistant patients may have different agendas, but taking a pragmatic approach can merge their goals with yours.
More than 2,000 research publications in the last 30 years prove the clinical importance of the therapeutic alliance.1 When working with resistant patients, keep these points in mind:
Develop a strong alliance early in treatment. “Early” is relative to the length of therapy, but evidence suggests sessions 3 to 5 are a critical window.
The patient’s experience of being understood, supported, and provided with hope depends on the strength of the alliance early in therapy. His or her interpretation of what you do can be different from what you intend. You may be a great clinician but not necessarily for this particular individual at this time, doing the kind of work you do.
Progressively negotiate the quality of the relationship. The patient’s perception of the alliance—not yours—is most influential. Ask specifically if the treatment relationship is working for him or her.
Early in treatment, the alliance itself contributes more to outcomes than do therapeutic techniques and models. First develop a collaborative agreement on the goals and strategies to be used in the therapeutic work.
Table 1
How to merge the reluctant patient’s goals with clinical needs assessment
| Questions to prioritize patient goals | Questions for clinical needs assessment | Merging patient goals with assessed needs | |
|---|---|---|---|
| What? | What does the patient want the most? What undesired consequences will occur if s/he does not get help? | What does the clinical assessment indicate s/he needs? What obstacles/assets do you need to address to help her/him get what s/he wants? | What treatment contract will drive the treatment plan and organize treatment priorities? |
| Why? | Why did s/he seek help now? Has s/he realized or been told s/he is at risk to lose freedom, health, a relationship, or a job? How committed to change is s/he? | Why are the assessed obstacles and resources important to include in a treatment plan? What diagnostic, function, or severity problems do assessment data reveal? | Is the treatment plan linked to what s/he wants? Does s/he accept that the treatment priorities will help her/him get what s/he wants? |
| How? | How will s/he achieve the most important goal? Must you try her/his preferred treatment before s/he accepts methods you prescribe? | How will you develop patient buy-in and get her/him to accept the plan? | Does s/he believe your strategies will help get what s/he wants? Will s/he be actively invested or passively compliant in treatment? |
| Where? | Where is s/he willing to be treated? Does s/he have strong preferences (such as about group treatment or residential programs)? | Where is the appropriate setting for treatment? What is indicated by the placement criteria? | Refer her/him to the level of care that merges his/her preferences with what is clinically indicated and likely to be effective |
| When? | When does s/he want to begin treatment? Is s/he feeling pressure to start? How badly does s/he want treatment, or is s/he just complying? | When should treatment begin, based on your assessment? What are realistic expectations and milestones in the process? | How urgent is treatment? What is the process? What is expected from referral? |
| Source: Adapted from reference 2, Table 3. | |||
What does the patient want?
When a patient is difficult to engage, begin by listening for the most important concern that brought him to your office.
He may be depressed, anxious, or tired, but exploring why he decided to seek help now (“My wife said she would leave me if I didn’t get help”) reveals what is most important. The “treatment contract,” then, is helping this patient save his marriage.
Initial engagement
Collaborative treatment begins with a genuinely interested dialogue about what prompted the patient’s visit.
Therapist: “Thank you for choosing to work with me. How may I serve you? What is the most important thing you want me to help you with?”
Mr. L: “I didn’t choose you; they made me come.”
T: “I didn’t see anyone drag you in. What would happen if you had not come today?”
Mr. L: “I might lose my job. I came because my boss told me to.”
Focus on what the patient wants, not just what others have said he or she needs (treatment for substance abuse, angry outbursts, conflict at work). The patient may want to stay out of jail, keep his job or relationship, regain custody of his or her children, obtain housing, or get people to “leave me alone and quit locking me up against my will.” Although the patient’s problem may be obvious to us, he needs “discovery” work, not “recovery” work.
Why has the patient come now? What is his highest priority? Can we help him discover the link between his drinking or anger that affects his work performance?
Therapist: “So you want to get the boss off your back. You want people to leave you alone. You feel people treat you unfairly and want them to stop. But why did you come today and not last week or last month?”
Mr. L: “I came now because yesterday my boss said I could lose my job if I didn’t get some help.”
T: “So what you want most importantly is to keep your job, is that it?”
Mr. L: “Well yeah, but I don’t have a drinking problem or any problem with my temper. They’re just overreacting. It wasn’t as bad as they said.”
T: “OK, I am willing to work on helping you keep your job if that’s what is most important to you. Do you know what you are doing that makes them think you have a drinking or anger problem?
Mr. L: “All I did was come in late a couple of times and got into a little argument with a couple of people.”
T: “If we are going to help you keep your job, we could spend our time talking about how unfair your boss is and how she’s misjudging you. Or we could work to show her that she has you all wrong and that you are a productive worker who does not have a substance or anger problem.
“Let’s think together how we could gather the data that would prove you don’t have a substance problem. If all that data is squeaky clean, then I can write a very supportive letter to your boss and tell her all is well. If, however, we discover you do have a problem, I can still write a very supportive letter. But we’ll have to show her how you are taking care of any problems that interfere with your work performance.”
Reframe the presenting complaint
Few patients present fully ready to work on definitive behavioral health recovery. If patients at least attend sessions or talk with you, they must be motivated to do something. Otherwise, they would not show up.
Our task is help patients such as Mr. L get what they want, not what we think they should want. Eventually you will get to explore the patient’s substance use, impulse or parenting problems, mental health symptoms, or communication problems, but this discussion will be in the service of allying with his or her goals.
Rather than viewing patients as unmotivated or resistant, think of resistance as an interactional process. “If we are going to stop them from locking you up,” you might say, “let’s talk about what you are doing that makes you look like you are dangerous and out of control. And when you were not locked away, let’s think of how you kept ‘them’ off your back.”
Instead of interpreting resistance as pathology, view the behavior as an opportunity to understand and respond to the patient’s stage of readiness to change.
Stages of change
By being “difficult,” patients are often declaring that they are not invested in what you think the problem is or in working on that problem. Resistance thrives when we and the patient have not allied around a common goal and are at different stages of change. Think of the therapeutic alliance in the context of the widely-used and well-researched Transtheoretical Model’s stages of change:3,4
Precontemplation. A person at this stage is not considering the possibility of change, although others are aware of a problem. He or she will seldom appear for treatment without coercion. The person could benefit from nonthreatening information to raise awareness of a possible “problem” and possibilities for change.
Contemplation. The person is ambivalent, undecided, vacillating about whether he has a “problem.” He wants to change, but this desire exists simultaneously with resistance to change. Motivational strategies can be useful, but aggressive or premature confrontation could provoke strong resistance and defensive behaviors. Many persons at this stage have indefinite plans to take action in the next 6 months or so.
Preparation takes the person from the contemplation stage to specific steps to solve the problem in the action stage. He or she develops increasing confidence in the decision to change and takes the first steps on the road to action. Most people at this stage plan to take action within 1 month and are making final adjustments before beginning to change.
Action. The person takes specific actions intended to bring about change. This busiest stage of change is characterized by overt modification of behavior and surroundings and requires the greatest time and energy. Support and encouragement are crucial to prevent drop-out and regression in readiness to change.
Maintenance. Goals at this stage are to sustain the changes accomplished by previous action and to prevent relapse. Maintaining new behaviors requires different skills than were needed to initiate change. Gains are consolidated. “Maintenance” is not a static stage; it can last 6 months or up to a lifetime. The patient learns new coping and problem-solving strategies, replaces problem behaviors with a healthier life style, and works through emotional triggers of relapse.
Relapse/recycling can happen but is not inevitable. When setbacks occur, help the patient avoid becoming stuck, discouraged, or demoralized, and help him learn from relapse before committing to a new action cycle. Conduct a comprehensive, multidimensional assessment to explore all reasons for relapse.
Termination is the ultimate goal: to exit the cycle of change without fear of relapse. Certain problems may be terminated or merely kept in remission through maintenance strategies.
Match strategies with stages
Discovery planning. Engaging patients in collaborative care starts with honoring their stages of change and working with them and their families on different tasks for each stage of change.4-6 A patient such as Mr. L, for example—who is at an early stage of change and thinks he has an “unfair boss problem” (not an alcohol problem) or a “nagging wife problem” (not an anger or domestic violence problem)—needs a discovery, drop-out prevention plan.
The cause of the patient’s work or relationship problem may be obvious to you, but a patient in early stages of change resists that information and, if pressed, gets frustrated and leaves treatment. A “discovery” treatment plan embraces the patient’s views and could be focused, for example, on gathering data that would prove to the employer that there is not an alcohol problem.
If random breath alcohol testing, feedback from family, and review of past job losses all prove negative for alcohol problems, the patient would have data to support his or her view that he does not have an alcohol problem. If, however, this exploration reveals an alcohol problem, the patient “discovers” he has more of a problem than he thought. For this plan, the challenge is to keep Mr. L engaged long enough to discover the connection between his alcohol problems and his employment or marital problems.
Recovery planning. On the other hand, a person at the action stage who wants to avoid becoming depressed again or wishes to live a life of sobriety collaborates on a recovery, relapse prevention plan. This patient is committed to developing the knowledge and skills to prevent relapse and open to whatever will promote health and well-being.
The Transtheoretical Model’s 9 processes of change3,4 inform which interventions might be most effective at various stages of change (Table 2). For example, a patient might be proud of the fact that “I can hold my liquor and drink everyone under the table.” Consciousness-raising—such as by explaining that his high alcohol tolerance is a danger signal, not a beneficial ability—can enhance his change process. Even if he is not ready to commit to definitive change, at least exploring whether he has a problem may move him from precontemplation to a contemplation stage of change. Table 3 shows how other processes of change can help motivate patients in later stages of change.4,5
Table 2
Transtheoretical model’s 9 processes of change: What happens at each step
| Process of change | The person… |
|---|---|
| Conscious-raising | becomes aware of a problem from education, advice, self-awareness, or feedback from others |
| Social liberation | begins to think about change because external forces raise awareness (a ban on smoking in restaurants, for example, can heighten awareness that one has a smoking problem) |
| Emotional arousal | becomes more convinced of the need to change when faced with a strong and sudden emotional experience related to the problem (such as death of a loved one) |
| Self-reevaluation | examines his or her values to see whether or not the behavior conflicts with what is important to him or her |
| Commitment | accepts responsibility for changing and affirms to self and others the decision to change |
| Reward | uses self-praise, positive feedback from others, improved well-being or financial security, “natural highs,” and other reinforcing benefits to consolidate change |
| Countering | substitutes other responses to counter unhealthy choices and behavior (such as relaxation techniques to combat angry outbursts or urges to resume smoking) |
| Environmental control | changes surrounding people, places, or things to reduce the risk of continuing or resuming the problem behavior |
| Helping relationships | seeks assistance from trusted friends, professionals, spiritual advisors, or significant others to initiate and sustain the change process |
| Source: Adapted and reprinted with permission from reference 4. | |
Table 3
Strategies and interventions to motivate patients at each stage of change
| Stage of change | Most useful processes of change (see Table 2) | Goal of treatment | Strategies and interventions |
|---|---|---|---|
| Precontemplation | Consciousness-raising Social liberation | To raise doubt |
|
| Contemplation | Consciousness-raising Social liberation Emotional arousal Self-reevaluation | To tip the balance |
|
| Preparation | Social liberation Emotional arousal Self-reevaluation Commitment | To determine best course |
|
| Action | Social liberation Commitment Reward Countering Environment control Helping relationships | To take steps to change |
|
| Maintenance | Commitment Countering Environment control Helping relationships | To prevent relapse |
|
| Relapse/recycling | Depends on stage to which patient returned | To renew processes of change |
|
- Scott D. Miller, PhD. Institute for the Study of Therapeutic Change, Chicago, IL. (773) 404-5130; www.talkingcure.com.
- Miller WR, Rollnick S, Moyers TB. Motivational interviewing: professional training videotape series. Albuquerque, NM: University of New Mexico, 1998. Six videotapes (about $130 total); (505) 768-0279 or 0100.
- Miller WR, consensus panel chair. Treatment improvement protocol. Enhancing motivation for change in substance abuse treatment. Rockville, MD; Center for Substance Abuse Treatment, 1999. DHHS Publication 99-3354. Available from the National Clearinghouse for Alcohol/Drug Information, Rockville, MD; (800) 729-6686.
Dr. Mee-Lee is a board-certified psychiatrist and is certified by examination of the American Society of Addiction Medicine (ASAM). He is based in Davis, CA, and is involved in full-time training and consulting. For information, visit www.DMLMD.com.
Whenever you feel you are doing more work than the patient and are more invested than he is, something has gone wrong in collaborative care.
With resistant or hostile patients, fight the urge to move quickly into clinical assessment and to prescribe what you think should be worked on and how. Instead, spend more time—especially when building the treatment alliance in the first 15 minutes (Box1)—exploring their ideas on how, when, and where they feel they can achieve what is most important to them (Table 12).
Resistant patients may have different agendas, but taking a pragmatic approach can merge their goals with yours.
More than 2,000 research publications in the last 30 years prove the clinical importance of the therapeutic alliance.1 When working with resistant patients, keep these points in mind:
Develop a strong alliance early in treatment. “Early” is relative to the length of therapy, but evidence suggests sessions 3 to 5 are a critical window.
The patient’s experience of being understood, supported, and provided with hope depends on the strength of the alliance early in therapy. His or her interpretation of what you do can be different from what you intend. You may be a great clinician but not necessarily for this particular individual at this time, doing the kind of work you do.
Progressively negotiate the quality of the relationship. The patient’s perception of the alliance—not yours—is most influential. Ask specifically if the treatment relationship is working for him or her.
Early in treatment, the alliance itself contributes more to outcomes than do therapeutic techniques and models. First develop a collaborative agreement on the goals and strategies to be used in the therapeutic work.
Table 1
How to merge the reluctant patient’s goals with clinical needs assessment
| Questions to prioritize patient goals | Questions for clinical needs assessment | Merging patient goals with assessed needs | |
|---|---|---|---|
| What? | What does the patient want the most? What undesired consequences will occur if s/he does not get help? | What does the clinical assessment indicate s/he needs? What obstacles/assets do you need to address to help her/him get what s/he wants? | What treatment contract will drive the treatment plan and organize treatment priorities? |
| Why? | Why did s/he seek help now? Has s/he realized or been told s/he is at risk to lose freedom, health, a relationship, or a job? How committed to change is s/he? | Why are the assessed obstacles and resources important to include in a treatment plan? What diagnostic, function, or severity problems do assessment data reveal? | Is the treatment plan linked to what s/he wants? Does s/he accept that the treatment priorities will help her/him get what s/he wants? |
| How? | How will s/he achieve the most important goal? Must you try her/his preferred treatment before s/he accepts methods you prescribe? | How will you develop patient buy-in and get her/him to accept the plan? | Does s/he believe your strategies will help get what s/he wants? Will s/he be actively invested or passively compliant in treatment? |
| Where? | Where is s/he willing to be treated? Does s/he have strong preferences (such as about group treatment or residential programs)? | Where is the appropriate setting for treatment? What is indicated by the placement criteria? | Refer her/him to the level of care that merges his/her preferences with what is clinically indicated and likely to be effective |
| When? | When does s/he want to begin treatment? Is s/he feeling pressure to start? How badly does s/he want treatment, or is s/he just complying? | When should treatment begin, based on your assessment? What are realistic expectations and milestones in the process? | How urgent is treatment? What is the process? What is expected from referral? |
| Source: Adapted from reference 2, Table 3. | |||
What does the patient want?
When a patient is difficult to engage, begin by listening for the most important concern that brought him to your office.
He may be depressed, anxious, or tired, but exploring why he decided to seek help now (“My wife said she would leave me if I didn’t get help”) reveals what is most important. The “treatment contract,” then, is helping this patient save his marriage.
Initial engagement
Collaborative treatment begins with a genuinely interested dialogue about what prompted the patient’s visit.
Therapist: “Thank you for choosing to work with me. How may I serve you? What is the most important thing you want me to help you with?”
Mr. L: “I didn’t choose you; they made me come.”
T: “I didn’t see anyone drag you in. What would happen if you had not come today?”
Mr. L: “I might lose my job. I came because my boss told me to.”
Focus on what the patient wants, not just what others have said he or she needs (treatment for substance abuse, angry outbursts, conflict at work). The patient may want to stay out of jail, keep his job or relationship, regain custody of his or her children, obtain housing, or get people to “leave me alone and quit locking me up against my will.” Although the patient’s problem may be obvious to us, he needs “discovery” work, not “recovery” work.
Why has the patient come now? What is his highest priority? Can we help him discover the link between his drinking or anger that affects his work performance?
Therapist: “So you want to get the boss off your back. You want people to leave you alone. You feel people treat you unfairly and want them to stop. But why did you come today and not last week or last month?”
Mr. L: “I came now because yesterday my boss said I could lose my job if I didn’t get some help.”
T: “So what you want most importantly is to keep your job, is that it?”
Mr. L: “Well yeah, but I don’t have a drinking problem or any problem with my temper. They’re just overreacting. It wasn’t as bad as they said.”
T: “OK, I am willing to work on helping you keep your job if that’s what is most important to you. Do you know what you are doing that makes them think you have a drinking or anger problem?
Mr. L: “All I did was come in late a couple of times and got into a little argument with a couple of people.”
T: “If we are going to help you keep your job, we could spend our time talking about how unfair your boss is and how she’s misjudging you. Or we could work to show her that she has you all wrong and that you are a productive worker who does not have a substance or anger problem.
“Let’s think together how we could gather the data that would prove you don’t have a substance problem. If all that data is squeaky clean, then I can write a very supportive letter to your boss and tell her all is well. If, however, we discover you do have a problem, I can still write a very supportive letter. But we’ll have to show her how you are taking care of any problems that interfere with your work performance.”
Reframe the presenting complaint
Few patients present fully ready to work on definitive behavioral health recovery. If patients at least attend sessions or talk with you, they must be motivated to do something. Otherwise, they would not show up.
Our task is help patients such as Mr. L get what they want, not what we think they should want. Eventually you will get to explore the patient’s substance use, impulse or parenting problems, mental health symptoms, or communication problems, but this discussion will be in the service of allying with his or her goals.
Rather than viewing patients as unmotivated or resistant, think of resistance as an interactional process. “If we are going to stop them from locking you up,” you might say, “let’s talk about what you are doing that makes you look like you are dangerous and out of control. And when you were not locked away, let’s think of how you kept ‘them’ off your back.”
Instead of interpreting resistance as pathology, view the behavior as an opportunity to understand and respond to the patient’s stage of readiness to change.
Stages of change
By being “difficult,” patients are often declaring that they are not invested in what you think the problem is or in working on that problem. Resistance thrives when we and the patient have not allied around a common goal and are at different stages of change. Think of the therapeutic alliance in the context of the widely-used and well-researched Transtheoretical Model’s stages of change:3,4
Precontemplation. A person at this stage is not considering the possibility of change, although others are aware of a problem. He or she will seldom appear for treatment without coercion. The person could benefit from nonthreatening information to raise awareness of a possible “problem” and possibilities for change.
Contemplation. The person is ambivalent, undecided, vacillating about whether he has a “problem.” He wants to change, but this desire exists simultaneously with resistance to change. Motivational strategies can be useful, but aggressive or premature confrontation could provoke strong resistance and defensive behaviors. Many persons at this stage have indefinite plans to take action in the next 6 months or so.
Preparation takes the person from the contemplation stage to specific steps to solve the problem in the action stage. He or she develops increasing confidence in the decision to change and takes the first steps on the road to action. Most people at this stage plan to take action within 1 month and are making final adjustments before beginning to change.
Action. The person takes specific actions intended to bring about change. This busiest stage of change is characterized by overt modification of behavior and surroundings and requires the greatest time and energy. Support and encouragement are crucial to prevent drop-out and regression in readiness to change.
Maintenance. Goals at this stage are to sustain the changes accomplished by previous action and to prevent relapse. Maintaining new behaviors requires different skills than were needed to initiate change. Gains are consolidated. “Maintenance” is not a static stage; it can last 6 months or up to a lifetime. The patient learns new coping and problem-solving strategies, replaces problem behaviors with a healthier life style, and works through emotional triggers of relapse.
Relapse/recycling can happen but is not inevitable. When setbacks occur, help the patient avoid becoming stuck, discouraged, or demoralized, and help him learn from relapse before committing to a new action cycle. Conduct a comprehensive, multidimensional assessment to explore all reasons for relapse.
Termination is the ultimate goal: to exit the cycle of change without fear of relapse. Certain problems may be terminated or merely kept in remission through maintenance strategies.
Match strategies with stages
Discovery planning. Engaging patients in collaborative care starts with honoring their stages of change and working with them and their families on different tasks for each stage of change.4-6 A patient such as Mr. L, for example—who is at an early stage of change and thinks he has an “unfair boss problem” (not an alcohol problem) or a “nagging wife problem” (not an anger or domestic violence problem)—needs a discovery, drop-out prevention plan.
The cause of the patient’s work or relationship problem may be obvious to you, but a patient in early stages of change resists that information and, if pressed, gets frustrated and leaves treatment. A “discovery” treatment plan embraces the patient’s views and could be focused, for example, on gathering data that would prove to the employer that there is not an alcohol problem.
If random breath alcohol testing, feedback from family, and review of past job losses all prove negative for alcohol problems, the patient would have data to support his or her view that he does not have an alcohol problem. If, however, this exploration reveals an alcohol problem, the patient “discovers” he has more of a problem than he thought. For this plan, the challenge is to keep Mr. L engaged long enough to discover the connection between his alcohol problems and his employment or marital problems.
Recovery planning. On the other hand, a person at the action stage who wants to avoid becoming depressed again or wishes to live a life of sobriety collaborates on a recovery, relapse prevention plan. This patient is committed to developing the knowledge and skills to prevent relapse and open to whatever will promote health and well-being.
The Transtheoretical Model’s 9 processes of change3,4 inform which interventions might be most effective at various stages of change (Table 2). For example, a patient might be proud of the fact that “I can hold my liquor and drink everyone under the table.” Consciousness-raising—such as by explaining that his high alcohol tolerance is a danger signal, not a beneficial ability—can enhance his change process. Even if he is not ready to commit to definitive change, at least exploring whether he has a problem may move him from precontemplation to a contemplation stage of change. Table 3 shows how other processes of change can help motivate patients in later stages of change.4,5
Table 2
Transtheoretical model’s 9 processes of change: What happens at each step
| Process of change | The person… |
|---|---|
| Conscious-raising | becomes aware of a problem from education, advice, self-awareness, or feedback from others |
| Social liberation | begins to think about change because external forces raise awareness (a ban on smoking in restaurants, for example, can heighten awareness that one has a smoking problem) |
| Emotional arousal | becomes more convinced of the need to change when faced with a strong and sudden emotional experience related to the problem (such as death of a loved one) |
| Self-reevaluation | examines his or her values to see whether or not the behavior conflicts with what is important to him or her |
| Commitment | accepts responsibility for changing and affirms to self and others the decision to change |
| Reward | uses self-praise, positive feedback from others, improved well-being or financial security, “natural highs,” and other reinforcing benefits to consolidate change |
| Countering | substitutes other responses to counter unhealthy choices and behavior (such as relaxation techniques to combat angry outbursts or urges to resume smoking) |
| Environmental control | changes surrounding people, places, or things to reduce the risk of continuing or resuming the problem behavior |
| Helping relationships | seeks assistance from trusted friends, professionals, spiritual advisors, or significant others to initiate and sustain the change process |
| Source: Adapted and reprinted with permission from reference 4. | |
Table 3
Strategies and interventions to motivate patients at each stage of change
| Stage of change | Most useful processes of change (see Table 2) | Goal of treatment | Strategies and interventions |
|---|---|---|---|
| Precontemplation | Consciousness-raising Social liberation | To raise doubt |
|
| Contemplation | Consciousness-raising Social liberation Emotional arousal Self-reevaluation | To tip the balance |
|
| Preparation | Social liberation Emotional arousal Self-reevaluation Commitment | To determine best course |
|
| Action | Social liberation Commitment Reward Countering Environment control Helping relationships | To take steps to change |
|
| Maintenance | Commitment Countering Environment control Helping relationships | To prevent relapse |
|
| Relapse/recycling | Depends on stage to which patient returned | To renew processes of change |
|
- Scott D. Miller, PhD. Institute for the Study of Therapeutic Change, Chicago, IL. (773) 404-5130; www.talkingcure.com.
- Miller WR, Rollnick S, Moyers TB. Motivational interviewing: professional training videotape series. Albuquerque, NM: University of New Mexico, 1998. Six videotapes (about $130 total); (505) 768-0279 or 0100.
- Miller WR, consensus panel chair. Treatment improvement protocol. Enhancing motivation for change in substance abuse treatment. Rockville, MD; Center for Substance Abuse Treatment, 1999. DHHS Publication 99-3354. Available from the National Clearinghouse for Alcohol/Drug Information, Rockville, MD; (800) 729-6686.
Dr. Mee-Lee is a board-certified psychiatrist and is certified by examination of the American Society of Addiction Medicine (ASAM). He is based in Davis, CA, and is involved in full-time training and consulting. For information, visit www.DMLMD.com.
1. Horvath AO, Bedi RP. The alliance. In: Norcross JC, ed. Psychotherapy relationships that work: therapist contributions and responsiveness to patients. New York: Oxford University Press; 2002.
2. Mee-Lee D. Treatment planning for dual disorders. Psychiatr Rehabil Skills 2001;5(1):52-79.
3. Prochaska JO, DiClemente CC, Norcross JC. In search of how people change: applications to addictive behaviors. Am Psychol 1992;47:1102-14.
4. Prochaska JO, Norcross JC, DiClemente CC. Changing for good. New York: Avon Books; 1994:54.
5. DiClemente CC. Conceptual models and applied research: the ongoing contribution of the transtheoretical model. J Addict Nurs 2005;16:5-12.
6. Miller WR, Rollnick S. Motivational interviewing: preparing people to change addictive behavior. New York: Guilford Press; 1991:18.
1. Horvath AO, Bedi RP. The alliance. In: Norcross JC, ed. Psychotherapy relationships that work: therapist contributions and responsiveness to patients. New York: Oxford University Press; 2002.
2. Mee-Lee D. Treatment planning for dual disorders. Psychiatr Rehabil Skills 2001;5(1):52-79.
3. Prochaska JO, DiClemente CC, Norcross JC. In search of how people change: applications to addictive behaviors. Am Psychol 1992;47:1102-14.
4. Prochaska JO, Norcross JC, DiClemente CC. Changing for good. New York: Avon Books; 1994:54.
5. DiClemente CC. Conceptual models and applied research: the ongoing contribution of the transtheoretical model. J Addict Nurs 2005;16:5-12.
6. Miller WR, Rollnick S. Motivational interviewing: preparing people to change addictive behavior. New York: Guilford Press; 1991:18.
Dependent personality disorder: Effective time-limited therapy
Some dependent patients are needy, clingy, and insecure—unable to make the smallest decisions without inordinate advice and reassurance—whereas others are less easy to recognize. Dependency can be expressed in many different ways: obvious or subtle, maladaptive or adaptive.
Dependent psychotherapy patients are compliant and eager to please but can have difficulty terminating treatment. This article offers recommendations for clinical work with dependent adults to help you:
- assess and diagnose dependent personality disorder (DPD)
- distinguish unhealthy from healthy dependency
- provide effective psychotherapy for DPD in inpatient and outpatient settings.
What is a dependent personality?
DPD is diagnosed when an individual exhibits long-standing, inflexible dependency that creates difficulties in social, sexual, and occupational functioning, according to DSM-IV-TR.1 DPD’s essential feature is a pervasive and excessive need to be taken care of that leads to submissive and clinging behavior and fears of separation, beginning by early adulthood and present in a variety of contexts. To receive a DPD diagnosis, a patient must show 5 of 8 possible symptoms (Table 1).
Table 1
Symptoms of dependent personality disorder (DPD)*
| Difficulty making everyday decisions without excessive advice and reassurance |
| Needing others to assume responsibility for most major areas of life |
| Difficulty expressing disagreement because of a fear of disapproval |
| Difficulty initiating projects or doing things on one’s own |
| Going to excessive lengths to obtain nurturance and support from others |
| Feeling uncomfortable or helpless when alone |
| Urgently seeking another relationship as a source of care and support when a close relationship ends |
| Being unrealistically preoccupied with fears of being left to care for oneself |
| * 5 of 8 symptoms required for DPD |
| Source: Adapted from DSM-IV-TR |
Who has DPD? One of the more common Axis II disorders, DPD is not distributed equally across the population. No studies have assessed the impact of age on DPD risk, but variables that affect DPD prevalence include:
- gender (women are far more likely than men to receive a DPD diagnosis)
- practice setting (DPD is more prevalent in rehabilitation and psychiatric inpatient settings than in outpatient practices)
- race and ethnicity (dependency may be less prevalent in African-American than in Caucasian adults).3,4
Interpersonal, intrapsychic dynamics
DPD is viewed as having 4 related components:4,5
- Cognitive: A perception of oneself as powerless and ineffectual plus the belief that other people are comparatively confident and competent.
- Motivational: A strong desire to maintain close ties with protectors and caregivers.
- Emotional: Fear of abandonment or rejection; anxiety about evaluation by authority figures.
- Behavioral: A pattern of relationship-facilitating behavior designed to minimize the possibility of abandonment and rejection.
Interpersonal strategies. Dependent persons use interpersonal strategies to strengthen social ties and minimize the possibility of being rejected or abandoned (Table 2). Some strategies involve behavior that is active and assertive—even quite aggressive.8 Therefore, dependency does not necessarily equate with passivity.
Table 2
Self-presentation strategies
used by dependent persons to facilitate relationships
| Strategy | Goal | Typical behaviors |
|---|---|---|
| Supplication | Appear helpless and vulnerable | Submissiveness, self-deprecation |
| Ingratiation | Create indebtedness | Ego-bolstering, performing favors |
| Exemplification | Exploit others’ Guilt | Providing help, emphasizing effort and sacrifices |
| Self-promotion | Emphasize personal worth | Performance claims, exaggeration of accomplishments |
| Intimidation | Frighten and control others | Anger displays, breakdown threats |
What causes DPD?
Three theoretical frameworks have been used to explain the development and dynamics of DPD. Each suggests intervention techniques for dealing with dependency-related problems.
Psychodynamic. Psychodynamic theorists conceptualize problematic dependency in terms of dependency conflicts (such as conflicts between a desire to be cared for and an urge to dominate and compete). Ego defenses used to manage the affect associated with these conflicts (such as denial or projection) help determine the manner in which underlying dependency needs are expressed.9
Cognitive. Cognitive theorists regard problematic dependency as stemming from self-defeating thought patterns,10 including:
- helplessness-inducing automatic thoughts (reflexive thoughts that reflect the person’s lack of self-confidence)
- negative self-statements (self-deprecating internal monologues in which dependent persons reaffirm their perceived lack of competence and skill).
Diagnosis and assessment
Three principles guide the diagnosis of DPD.
- Dependency, as noted, is not always characterized by passivity. Dependent patients may use active, dramatic self-presentation strategies—such as breakdown threats or parasuicide attempts—to protect themselves from being abandoned.4,8
- Self-reports do not always give a true picture. Because dependency may be viewed as a sign of weakness and immaturity, many adults—especially men—are reluctant to acknowledge dependent thoughts and feelings.12 Interviewing knowledgeable informants can be enlightening.
- Dependency’s severity varies over time and across situations. Depressive episodes are associated with temporary increases in self-reported dependency. Even modest mood changes can amplify dependency.13,14
Questionnaires do not allow you to probe and follow-up, but paper-and-pencil tools are relatively inexpensive and efficient. They also avoid reliability problems that can occur with structured interviews. The 2 self-report instruments used most often to diagnose DPD are:
Differential diagnosis
DPD must be distinguished from Axis I and II syndromes with often-overlapping symptoms and similar presentations. These include:
- mood disorders, panic disorder, agoraphobia, and dependency arising from one or more general medical conditions
- borderline personality disorder, histrionic personality disorder, and avoidant personality disorder.1
Axis II comorbidity patterns likely reflect the generalized, nonspecific nature of personality pathology and the fact that patients may show personality disorder symptoms in one or more diagnostic categories.
DPD Treatment
Dependency is associated with patient cooperativeness and conscientiousness.3,4,16,17 Compared with nondependent patients, those with dependent personalities:
- delay less time before seeking treatment for psychological or medical symptoms
- adhere more conscientiously to psychotherapeutic and psychotropic regimens
- miss fewer therapy sessions
- show higher rates of treatment completion in outpatient individual and group therapy.
Psychotherapy. Traditional psychotherapies—psychodynamic, cognitive, behavioral—modestly improve DPD symptoms.19 Most effective has been psychotherapy that combines various modalities.2,4,20 Five interventions (Table 3) have been shown to:
- help the patient and therapist identify aspects of the patient’s environment that propagate dependent behavior
- provide the patient with coping skills needed to more effectively control dependency-related impulses.
Table 3
5 useful psychotherapeutic methods for dependent patients
| Explore key relationships from the patient’s past that reinforced dependent behavior; determine if similar patterns occur in present relationships |
| Examine his or her ‘helpless self-concept,’ dependency’s key cognitive component (Tip: Asking the patient to write a selfdescription can be useful) |
| Make explicit any self-denigrating statements that propagate the patient’s feelings of helplessness and vulnerability; challenge these statements when appropriate |
| Help the patient gain insight into the ways he or she expresses dependency needs in different situations (and more-flexible, adaptive ways he or she could express these needs) |
| Use in-session role play and betweensessions homework to help the patient build coping skills that will enable him or her to function more autonomously |
Limitations and caveats
Clinical work with DPD patients traditionally has focused on diminishing problematic dependency. Recent research suggests, however, that expressing dependency strivings in a flexible, situation-appropriate manner can strengthen interpersonal ties and facilitate adaptation and healthy psychological functioning.2,5 Thus, the most effective interventions emphasize replacing unhealthy, maladaptive dependency with flexible, adaptive dependency.
Beyond the strategies summarized in Table 3, several other considerations—such as setting limits—are important in managing DPD and in minimizing therapeutic obstacles and impasses.
Set firm limits on after-hours contact early in treatment. Unless you set firm limits at the outset of therapy, dependent patients tend to have a higher-than-average number of “pseudo-emergencies” and make frequent requests for between-sessions contact.
In inpatient settings, patients with DPD receive more consultations and psychotropic medications than do non-DPD patients with similar demographic and diagnostic profiles, and their treatment costs can become excessive.21
Shift responsibility. When you provide adequate structure early in treatment, the dependent patient will feel secure enough to open up and disclose troubling thoughts and feelings. Then, as therapy progresses, help the patient experience autonomy and competence within the therapeutic milieu by gradually requiring him or her to take on increasing responsibility for structuring treatment.10
Beware of countertransference. Many therapists infantilize dependent patients, and exploitation or abuse—financial or sexual—may follow. You must acknowledge and confront these problematic feelings when they occur, either in formal clinical supervision or in informal consultation with other mental health professionals.4,21
Two countertransference reactions are particularly common (and problematic) in therapeutic work with dependent patients:
- the fantasy of insatiability (believing that no matter how much support and reassurance the patient receives, it will never be enough)
- the fantasy of permanence (believing the patient will become so comfortable in therapy’s protective cocoon that he or she will never leave treatment).
Because some studies suggest that dependent patients may be at increased risk for suicide, monitor them continuously for negative indicators.8,9 Five danger signs (Table 4) suggest an increased risk of self-destructive behavior in dependent patients.
Table 4
5 warning signs of self-destructive behavior in dependent patients
| Recent relationship conflict or interpersonal loss |
| Excessive or unrealistic jealousy |
| Poor impulse control |
| Difficulty modulating negative emotions |
| Previous suicide attempts or suicidal gestures |
Because dependent persons often construct interpersonal milieus that foster and propagate their dependency, concurrent marital and/or family therapy may be warranted to disrupt entrenched dysfunctional patterns.16,17 Examine the rewards dependent patients obtain for behaving helpless and vulnerable and ways in which their dependency may reward friends, family members, and coworkers.
Related resources
- Baltes MM. The many faces of dependency in old age. Cambridge, UK: Cambridge University Press; 1996.
- Bornstein RF. The dependent personality: developmental, social, and clinical perspectives. Psychol Bull 1992;112(1):3-23.
- Millon T. Disorders of personality: DSM-IV and beyond. New York: Wiley; 1996.
The author reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Diagnostic and statistical manual of mental disorders. 4th ed, text revision. Washington, DC: American Psychiatric Association; 2000.
2. Bornstein RF, Languirand MA. Healthy dependency: leaning on others without losing yourself. New York, NY: Newmarket Press; 2003.
3. Bornstein RF. The dependent personality. New York: Guilford Press; 1993.
4. Bornstein RF. The dependent patient: a practitioner’s guide. Washington, DC: American Psychological Association; 2005.
5. Pincus AL, Wilson KR. Interpersonal variability in dependent personality. J Pers 2001;69(2):223-51.
6. Pincus AL, Gurtman MB. The three faces of interpersonal dependency: structural analysis of self-report dependency measures. J Pers Soc Psychol 1995;69(4):744-58.
7. Overholser JC. The dependent personality and interpersonal problems. J Nerv Ment Dis 1996;184(1)1:8-16.
8. Bornstein RF. The complex relationship between dependency and domestic violence: converging psychological factors and social forces. Am Psychol 2006;61(6):595-606.
9. Coen SJ. The misuse of persons: analyzing pathological dependency. Hillsdale, NJ: Analytic Press; 1992.
10. Overholser JC, Fine MA. Cognitive-behavioral treatment of excessive interpersonal dependency: a four-stage psychotherapy model. Journal of Cognitive Psychotherapy 1994;8(1):55-70.
11. Turkat ID. The personality disorders: a psychological approach to clinical management. New York, NY: Pergamon Press; 1990.
12. Bornstein RF. Criterion validity of objective and projective dependency tests: a meta-analytic assessment of behavioral prediction. Psychological Assessment 1999;11(1):48-57.
13. Birtchnell J. The measurement of dependence by questionnaire. Journal of Personality Disorders 1991;5(3):281-95.
14. Nietzel MT, Harris MJ. Relationship of dependency and achievement/autonomy to depression. Clinical Psychology Review 1990;10:279-97.
15. Bornstein RF. Dependent personality disorder in the DSM-IV and beyond. Clinical Psychology: Science and Practice 1997;4(2):175-87.
16. Ryder RD, Parry-Jones WL. Fears of dependence and its value in working with adolescents. J Adolesc 1982;5(1):71-8.
17. Tait M. Dependence: a means or an impediment to growth? British Journal of Guidance and Counselling. 1997;25(1):17-26.
18. Black DW, Monahan P, Wesner R, et al. The effects of fluvoxamine, cognitive therapy, and placebo on abnormal personality traits in 44 patients with panic disorder. Journal of Personality Disorders. 1996;10(2):185-94.
19. Rathus JH, Sanderson WC, Miller AL, Wetzler S. Impact of personality functioning on cognitive behavioral treatment of panic disorder: a preliminary report. Journal of Personality Disorders 1995;9(2):160-8.
20. Bornstein RF. Integrating cognitive and existential treatment strategies in psychotherapy with dependent patients. Journal of Contemporary Psychotherapy 2004;34(4):293-309.
21. Abramson PR, Cloud MY, Keese N, Keese R. How much is too much? Dependency in a psychotherapeutic relationship. Am J Psychother 1994;48(2):294-301.
Some dependent patients are needy, clingy, and insecure—unable to make the smallest decisions without inordinate advice and reassurance—whereas others are less easy to recognize. Dependency can be expressed in many different ways: obvious or subtle, maladaptive or adaptive.
Dependent psychotherapy patients are compliant and eager to please but can have difficulty terminating treatment. This article offers recommendations for clinical work with dependent adults to help you:
- assess and diagnose dependent personality disorder (DPD)
- distinguish unhealthy from healthy dependency
- provide effective psychotherapy for DPD in inpatient and outpatient settings.
What is a dependent personality?
DPD is diagnosed when an individual exhibits long-standing, inflexible dependency that creates difficulties in social, sexual, and occupational functioning, according to DSM-IV-TR.1 DPD’s essential feature is a pervasive and excessive need to be taken care of that leads to submissive and clinging behavior and fears of separation, beginning by early adulthood and present in a variety of contexts. To receive a DPD diagnosis, a patient must show 5 of 8 possible symptoms (Table 1).
Table 1
Symptoms of dependent personality disorder (DPD)*
| Difficulty making everyday decisions without excessive advice and reassurance |
| Needing others to assume responsibility for most major areas of life |
| Difficulty expressing disagreement because of a fear of disapproval |
| Difficulty initiating projects or doing things on one’s own |
| Going to excessive lengths to obtain nurturance and support from others |
| Feeling uncomfortable or helpless when alone |
| Urgently seeking another relationship as a source of care and support when a close relationship ends |
| Being unrealistically preoccupied with fears of being left to care for oneself |
| * 5 of 8 symptoms required for DPD |
| Source: Adapted from DSM-IV-TR |
Who has DPD? One of the more common Axis II disorders, DPD is not distributed equally across the population. No studies have assessed the impact of age on DPD risk, but variables that affect DPD prevalence include:
- gender (women are far more likely than men to receive a DPD diagnosis)
- practice setting (DPD is more prevalent in rehabilitation and psychiatric inpatient settings than in outpatient practices)
- race and ethnicity (dependency may be less prevalent in African-American than in Caucasian adults).3,4
Interpersonal, intrapsychic dynamics
DPD is viewed as having 4 related components:4,5
- Cognitive: A perception of oneself as powerless and ineffectual plus the belief that other people are comparatively confident and competent.
- Motivational: A strong desire to maintain close ties with protectors and caregivers.
- Emotional: Fear of abandonment or rejection; anxiety about evaluation by authority figures.
- Behavioral: A pattern of relationship-facilitating behavior designed to minimize the possibility of abandonment and rejection.
Interpersonal strategies. Dependent persons use interpersonal strategies to strengthen social ties and minimize the possibility of being rejected or abandoned (Table 2). Some strategies involve behavior that is active and assertive—even quite aggressive.8 Therefore, dependency does not necessarily equate with passivity.
Table 2
Self-presentation strategies
used by dependent persons to facilitate relationships
| Strategy | Goal | Typical behaviors |
|---|---|---|
| Supplication | Appear helpless and vulnerable | Submissiveness, self-deprecation |
| Ingratiation | Create indebtedness | Ego-bolstering, performing favors |
| Exemplification | Exploit others’ Guilt | Providing help, emphasizing effort and sacrifices |
| Self-promotion | Emphasize personal worth | Performance claims, exaggeration of accomplishments |
| Intimidation | Frighten and control others | Anger displays, breakdown threats |
What causes DPD?
Three theoretical frameworks have been used to explain the development and dynamics of DPD. Each suggests intervention techniques for dealing with dependency-related problems.
Psychodynamic. Psychodynamic theorists conceptualize problematic dependency in terms of dependency conflicts (such as conflicts between a desire to be cared for and an urge to dominate and compete). Ego defenses used to manage the affect associated with these conflicts (such as denial or projection) help determine the manner in which underlying dependency needs are expressed.9
Cognitive. Cognitive theorists regard problematic dependency as stemming from self-defeating thought patterns,10 including:
- helplessness-inducing automatic thoughts (reflexive thoughts that reflect the person’s lack of self-confidence)
- negative self-statements (self-deprecating internal monologues in which dependent persons reaffirm their perceived lack of competence and skill).
Diagnosis and assessment
Three principles guide the diagnosis of DPD.
- Dependency, as noted, is not always characterized by passivity. Dependent patients may use active, dramatic self-presentation strategies—such as breakdown threats or parasuicide attempts—to protect themselves from being abandoned.4,8
- Self-reports do not always give a true picture. Because dependency may be viewed as a sign of weakness and immaturity, many adults—especially men—are reluctant to acknowledge dependent thoughts and feelings.12 Interviewing knowledgeable informants can be enlightening.
- Dependency’s severity varies over time and across situations. Depressive episodes are associated with temporary increases in self-reported dependency. Even modest mood changes can amplify dependency.13,14
Questionnaires do not allow you to probe and follow-up, but paper-and-pencil tools are relatively inexpensive and efficient. They also avoid reliability problems that can occur with structured interviews. The 2 self-report instruments used most often to diagnose DPD are:
Differential diagnosis
DPD must be distinguished from Axis I and II syndromes with often-overlapping symptoms and similar presentations. These include:
- mood disorders, panic disorder, agoraphobia, and dependency arising from one or more general medical conditions
- borderline personality disorder, histrionic personality disorder, and avoidant personality disorder.1
Axis II comorbidity patterns likely reflect the generalized, nonspecific nature of personality pathology and the fact that patients may show personality disorder symptoms in one or more diagnostic categories.
DPD Treatment
Dependency is associated with patient cooperativeness and conscientiousness.3,4,16,17 Compared with nondependent patients, those with dependent personalities:
- delay less time before seeking treatment for psychological or medical symptoms
- adhere more conscientiously to psychotherapeutic and psychotropic regimens
- miss fewer therapy sessions
- show higher rates of treatment completion in outpatient individual and group therapy.
Psychotherapy. Traditional psychotherapies—psychodynamic, cognitive, behavioral—modestly improve DPD symptoms.19 Most effective has been psychotherapy that combines various modalities.2,4,20 Five interventions (Table 3) have been shown to:
- help the patient and therapist identify aspects of the patient’s environment that propagate dependent behavior
- provide the patient with coping skills needed to more effectively control dependency-related impulses.
Table 3
5 useful psychotherapeutic methods for dependent patients
| Explore key relationships from the patient’s past that reinforced dependent behavior; determine if similar patterns occur in present relationships |
| Examine his or her ‘helpless self-concept,’ dependency’s key cognitive component (Tip: Asking the patient to write a selfdescription can be useful) |
| Make explicit any self-denigrating statements that propagate the patient’s feelings of helplessness and vulnerability; challenge these statements when appropriate |
| Help the patient gain insight into the ways he or she expresses dependency needs in different situations (and more-flexible, adaptive ways he or she could express these needs) |
| Use in-session role play and betweensessions homework to help the patient build coping skills that will enable him or her to function more autonomously |
Limitations and caveats
Clinical work with DPD patients traditionally has focused on diminishing problematic dependency. Recent research suggests, however, that expressing dependency strivings in a flexible, situation-appropriate manner can strengthen interpersonal ties and facilitate adaptation and healthy psychological functioning.2,5 Thus, the most effective interventions emphasize replacing unhealthy, maladaptive dependency with flexible, adaptive dependency.
Beyond the strategies summarized in Table 3, several other considerations—such as setting limits—are important in managing DPD and in minimizing therapeutic obstacles and impasses.
Set firm limits on after-hours contact early in treatment. Unless you set firm limits at the outset of therapy, dependent patients tend to have a higher-than-average number of “pseudo-emergencies” and make frequent requests for between-sessions contact.
In inpatient settings, patients with DPD receive more consultations and psychotropic medications than do non-DPD patients with similar demographic and diagnostic profiles, and their treatment costs can become excessive.21
Shift responsibility. When you provide adequate structure early in treatment, the dependent patient will feel secure enough to open up and disclose troubling thoughts and feelings. Then, as therapy progresses, help the patient experience autonomy and competence within the therapeutic milieu by gradually requiring him or her to take on increasing responsibility for structuring treatment.10
Beware of countertransference. Many therapists infantilize dependent patients, and exploitation or abuse—financial or sexual—may follow. You must acknowledge and confront these problematic feelings when they occur, either in formal clinical supervision or in informal consultation with other mental health professionals.4,21
Two countertransference reactions are particularly common (and problematic) in therapeutic work with dependent patients:
- the fantasy of insatiability (believing that no matter how much support and reassurance the patient receives, it will never be enough)
- the fantasy of permanence (believing the patient will become so comfortable in therapy’s protective cocoon that he or she will never leave treatment).
Because some studies suggest that dependent patients may be at increased risk for suicide, monitor them continuously for negative indicators.8,9 Five danger signs (Table 4) suggest an increased risk of self-destructive behavior in dependent patients.
Table 4
5 warning signs of self-destructive behavior in dependent patients
| Recent relationship conflict or interpersonal loss |
| Excessive or unrealistic jealousy |
| Poor impulse control |
| Difficulty modulating negative emotions |
| Previous suicide attempts or suicidal gestures |
Because dependent persons often construct interpersonal milieus that foster and propagate their dependency, concurrent marital and/or family therapy may be warranted to disrupt entrenched dysfunctional patterns.16,17 Examine the rewards dependent patients obtain for behaving helpless and vulnerable and ways in which their dependency may reward friends, family members, and coworkers.
Related resources
- Baltes MM. The many faces of dependency in old age. Cambridge, UK: Cambridge University Press; 1996.
- Bornstein RF. The dependent personality: developmental, social, and clinical perspectives. Psychol Bull 1992;112(1):3-23.
- Millon T. Disorders of personality: DSM-IV and beyond. New York: Wiley; 1996.
The author reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Some dependent patients are needy, clingy, and insecure—unable to make the smallest decisions without inordinate advice and reassurance—whereas others are less easy to recognize. Dependency can be expressed in many different ways: obvious or subtle, maladaptive or adaptive.
Dependent psychotherapy patients are compliant and eager to please but can have difficulty terminating treatment. This article offers recommendations for clinical work with dependent adults to help you:
- assess and diagnose dependent personality disorder (DPD)
- distinguish unhealthy from healthy dependency
- provide effective psychotherapy for DPD in inpatient and outpatient settings.
What is a dependent personality?
DPD is diagnosed when an individual exhibits long-standing, inflexible dependency that creates difficulties in social, sexual, and occupational functioning, according to DSM-IV-TR.1 DPD’s essential feature is a pervasive and excessive need to be taken care of that leads to submissive and clinging behavior and fears of separation, beginning by early adulthood and present in a variety of contexts. To receive a DPD diagnosis, a patient must show 5 of 8 possible symptoms (Table 1).
Table 1
Symptoms of dependent personality disorder (DPD)*
| Difficulty making everyday decisions without excessive advice and reassurance |
| Needing others to assume responsibility for most major areas of life |
| Difficulty expressing disagreement because of a fear of disapproval |
| Difficulty initiating projects or doing things on one’s own |
| Going to excessive lengths to obtain nurturance and support from others |
| Feeling uncomfortable or helpless when alone |
| Urgently seeking another relationship as a source of care and support when a close relationship ends |
| Being unrealistically preoccupied with fears of being left to care for oneself |
| * 5 of 8 symptoms required for DPD |
| Source: Adapted from DSM-IV-TR |
Who has DPD? One of the more common Axis II disorders, DPD is not distributed equally across the population. No studies have assessed the impact of age on DPD risk, but variables that affect DPD prevalence include:
- gender (women are far more likely than men to receive a DPD diagnosis)
- practice setting (DPD is more prevalent in rehabilitation and psychiatric inpatient settings than in outpatient practices)
- race and ethnicity (dependency may be less prevalent in African-American than in Caucasian adults).3,4
Interpersonal, intrapsychic dynamics
DPD is viewed as having 4 related components:4,5
- Cognitive: A perception of oneself as powerless and ineffectual plus the belief that other people are comparatively confident and competent.
- Motivational: A strong desire to maintain close ties with protectors and caregivers.
- Emotional: Fear of abandonment or rejection; anxiety about evaluation by authority figures.
- Behavioral: A pattern of relationship-facilitating behavior designed to minimize the possibility of abandonment and rejection.
Interpersonal strategies. Dependent persons use interpersonal strategies to strengthen social ties and minimize the possibility of being rejected or abandoned (Table 2). Some strategies involve behavior that is active and assertive—even quite aggressive.8 Therefore, dependency does not necessarily equate with passivity.
Table 2
Self-presentation strategies
used by dependent persons to facilitate relationships
| Strategy | Goal | Typical behaviors |
|---|---|---|
| Supplication | Appear helpless and vulnerable | Submissiveness, self-deprecation |
| Ingratiation | Create indebtedness | Ego-bolstering, performing favors |
| Exemplification | Exploit others’ Guilt | Providing help, emphasizing effort and sacrifices |
| Self-promotion | Emphasize personal worth | Performance claims, exaggeration of accomplishments |
| Intimidation | Frighten and control others | Anger displays, breakdown threats |
What causes DPD?
Three theoretical frameworks have been used to explain the development and dynamics of DPD. Each suggests intervention techniques for dealing with dependency-related problems.
Psychodynamic. Psychodynamic theorists conceptualize problematic dependency in terms of dependency conflicts (such as conflicts between a desire to be cared for and an urge to dominate and compete). Ego defenses used to manage the affect associated with these conflicts (such as denial or projection) help determine the manner in which underlying dependency needs are expressed.9
Cognitive. Cognitive theorists regard problematic dependency as stemming from self-defeating thought patterns,10 including:
- helplessness-inducing automatic thoughts (reflexive thoughts that reflect the person’s lack of self-confidence)
- negative self-statements (self-deprecating internal monologues in which dependent persons reaffirm their perceived lack of competence and skill).
Diagnosis and assessment
Three principles guide the diagnosis of DPD.
- Dependency, as noted, is not always characterized by passivity. Dependent patients may use active, dramatic self-presentation strategies—such as breakdown threats or parasuicide attempts—to protect themselves from being abandoned.4,8
- Self-reports do not always give a true picture. Because dependency may be viewed as a sign of weakness and immaturity, many adults—especially men—are reluctant to acknowledge dependent thoughts and feelings.12 Interviewing knowledgeable informants can be enlightening.
- Dependency’s severity varies over time and across situations. Depressive episodes are associated with temporary increases in self-reported dependency. Even modest mood changes can amplify dependency.13,14
Questionnaires do not allow you to probe and follow-up, but paper-and-pencil tools are relatively inexpensive and efficient. They also avoid reliability problems that can occur with structured interviews. The 2 self-report instruments used most often to diagnose DPD are:
Differential diagnosis
DPD must be distinguished from Axis I and II syndromes with often-overlapping symptoms and similar presentations. These include:
- mood disorders, panic disorder, agoraphobia, and dependency arising from one or more general medical conditions
- borderline personality disorder, histrionic personality disorder, and avoidant personality disorder.1
Axis II comorbidity patterns likely reflect the generalized, nonspecific nature of personality pathology and the fact that patients may show personality disorder symptoms in one or more diagnostic categories.
DPD Treatment
Dependency is associated with patient cooperativeness and conscientiousness.3,4,16,17 Compared with nondependent patients, those with dependent personalities:
- delay less time before seeking treatment for psychological or medical symptoms
- adhere more conscientiously to psychotherapeutic and psychotropic regimens
- miss fewer therapy sessions
- show higher rates of treatment completion in outpatient individual and group therapy.
Psychotherapy. Traditional psychotherapies—psychodynamic, cognitive, behavioral—modestly improve DPD symptoms.19 Most effective has been psychotherapy that combines various modalities.2,4,20 Five interventions (Table 3) have been shown to:
- help the patient and therapist identify aspects of the patient’s environment that propagate dependent behavior
- provide the patient with coping skills needed to more effectively control dependency-related impulses.
Table 3
5 useful psychotherapeutic methods for dependent patients
| Explore key relationships from the patient’s past that reinforced dependent behavior; determine if similar patterns occur in present relationships |
| Examine his or her ‘helpless self-concept,’ dependency’s key cognitive component (Tip: Asking the patient to write a selfdescription can be useful) |
| Make explicit any self-denigrating statements that propagate the patient’s feelings of helplessness and vulnerability; challenge these statements when appropriate |
| Help the patient gain insight into the ways he or she expresses dependency needs in different situations (and more-flexible, adaptive ways he or she could express these needs) |
| Use in-session role play and betweensessions homework to help the patient build coping skills that will enable him or her to function more autonomously |
Limitations and caveats
Clinical work with DPD patients traditionally has focused on diminishing problematic dependency. Recent research suggests, however, that expressing dependency strivings in a flexible, situation-appropriate manner can strengthen interpersonal ties and facilitate adaptation and healthy psychological functioning.2,5 Thus, the most effective interventions emphasize replacing unhealthy, maladaptive dependency with flexible, adaptive dependency.
Beyond the strategies summarized in Table 3, several other considerations—such as setting limits—are important in managing DPD and in minimizing therapeutic obstacles and impasses.
Set firm limits on after-hours contact early in treatment. Unless you set firm limits at the outset of therapy, dependent patients tend to have a higher-than-average number of “pseudo-emergencies” and make frequent requests for between-sessions contact.
In inpatient settings, patients with DPD receive more consultations and psychotropic medications than do non-DPD patients with similar demographic and diagnostic profiles, and their treatment costs can become excessive.21
Shift responsibility. When you provide adequate structure early in treatment, the dependent patient will feel secure enough to open up and disclose troubling thoughts and feelings. Then, as therapy progresses, help the patient experience autonomy and competence within the therapeutic milieu by gradually requiring him or her to take on increasing responsibility for structuring treatment.10
Beware of countertransference. Many therapists infantilize dependent patients, and exploitation or abuse—financial or sexual—may follow. You must acknowledge and confront these problematic feelings when they occur, either in formal clinical supervision or in informal consultation with other mental health professionals.4,21
Two countertransference reactions are particularly common (and problematic) in therapeutic work with dependent patients:
- the fantasy of insatiability (believing that no matter how much support and reassurance the patient receives, it will never be enough)
- the fantasy of permanence (believing the patient will become so comfortable in therapy’s protective cocoon that he or she will never leave treatment).
Because some studies suggest that dependent patients may be at increased risk for suicide, monitor them continuously for negative indicators.8,9 Five danger signs (Table 4) suggest an increased risk of self-destructive behavior in dependent patients.
Table 4
5 warning signs of self-destructive behavior in dependent patients
| Recent relationship conflict or interpersonal loss |
| Excessive or unrealistic jealousy |
| Poor impulse control |
| Difficulty modulating negative emotions |
| Previous suicide attempts or suicidal gestures |
Because dependent persons often construct interpersonal milieus that foster and propagate their dependency, concurrent marital and/or family therapy may be warranted to disrupt entrenched dysfunctional patterns.16,17 Examine the rewards dependent patients obtain for behaving helpless and vulnerable and ways in which their dependency may reward friends, family members, and coworkers.
Related resources
- Baltes MM. The many faces of dependency in old age. Cambridge, UK: Cambridge University Press; 1996.
- Bornstein RF. The dependent personality: developmental, social, and clinical perspectives. Psychol Bull 1992;112(1):3-23.
- Millon T. Disorders of personality: DSM-IV and beyond. New York: Wiley; 1996.
The author reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Diagnostic and statistical manual of mental disorders. 4th ed, text revision. Washington, DC: American Psychiatric Association; 2000.
2. Bornstein RF, Languirand MA. Healthy dependency: leaning on others without losing yourself. New York, NY: Newmarket Press; 2003.
3. Bornstein RF. The dependent personality. New York: Guilford Press; 1993.
4. Bornstein RF. The dependent patient: a practitioner’s guide. Washington, DC: American Psychological Association; 2005.
5. Pincus AL, Wilson KR. Interpersonal variability in dependent personality. J Pers 2001;69(2):223-51.
6. Pincus AL, Gurtman MB. The three faces of interpersonal dependency: structural analysis of self-report dependency measures. J Pers Soc Psychol 1995;69(4):744-58.
7. Overholser JC. The dependent personality and interpersonal problems. J Nerv Ment Dis 1996;184(1)1:8-16.
8. Bornstein RF. The complex relationship between dependency and domestic violence: converging psychological factors and social forces. Am Psychol 2006;61(6):595-606.
9. Coen SJ. The misuse of persons: analyzing pathological dependency. Hillsdale, NJ: Analytic Press; 1992.
10. Overholser JC, Fine MA. Cognitive-behavioral treatment of excessive interpersonal dependency: a four-stage psychotherapy model. Journal of Cognitive Psychotherapy 1994;8(1):55-70.
11. Turkat ID. The personality disorders: a psychological approach to clinical management. New York, NY: Pergamon Press; 1990.
12. Bornstein RF. Criterion validity of objective and projective dependency tests: a meta-analytic assessment of behavioral prediction. Psychological Assessment 1999;11(1):48-57.
13. Birtchnell J. The measurement of dependence by questionnaire. Journal of Personality Disorders 1991;5(3):281-95.
14. Nietzel MT, Harris MJ. Relationship of dependency and achievement/autonomy to depression. Clinical Psychology Review 1990;10:279-97.
15. Bornstein RF. Dependent personality disorder in the DSM-IV and beyond. Clinical Psychology: Science and Practice 1997;4(2):175-87.
16. Ryder RD, Parry-Jones WL. Fears of dependence and its value in working with adolescents. J Adolesc 1982;5(1):71-8.
17. Tait M. Dependence: a means or an impediment to growth? British Journal of Guidance and Counselling. 1997;25(1):17-26.
18. Black DW, Monahan P, Wesner R, et al. The effects of fluvoxamine, cognitive therapy, and placebo on abnormal personality traits in 44 patients with panic disorder. Journal of Personality Disorders. 1996;10(2):185-94.
19. Rathus JH, Sanderson WC, Miller AL, Wetzler S. Impact of personality functioning on cognitive behavioral treatment of panic disorder: a preliminary report. Journal of Personality Disorders 1995;9(2):160-8.
20. Bornstein RF. Integrating cognitive and existential treatment strategies in psychotherapy with dependent patients. Journal of Contemporary Psychotherapy 2004;34(4):293-309.
21. Abramson PR, Cloud MY, Keese N, Keese R. How much is too much? Dependency in a psychotherapeutic relationship. Am J Psychother 1994;48(2):294-301.
1. Diagnostic and statistical manual of mental disorders. 4th ed, text revision. Washington, DC: American Psychiatric Association; 2000.
2. Bornstein RF, Languirand MA. Healthy dependency: leaning on others without losing yourself. New York, NY: Newmarket Press; 2003.
3. Bornstein RF. The dependent personality. New York: Guilford Press; 1993.
4. Bornstein RF. The dependent patient: a practitioner’s guide. Washington, DC: American Psychological Association; 2005.
5. Pincus AL, Wilson KR. Interpersonal variability in dependent personality. J Pers 2001;69(2):223-51.
6. Pincus AL, Gurtman MB. The three faces of interpersonal dependency: structural analysis of self-report dependency measures. J Pers Soc Psychol 1995;69(4):744-58.
7. Overholser JC. The dependent personality and interpersonal problems. J Nerv Ment Dis 1996;184(1)1:8-16.
8. Bornstein RF. The complex relationship between dependency and domestic violence: converging psychological factors and social forces. Am Psychol 2006;61(6):595-606.
9. Coen SJ. The misuse of persons: analyzing pathological dependency. Hillsdale, NJ: Analytic Press; 1992.
10. Overholser JC, Fine MA. Cognitive-behavioral treatment of excessive interpersonal dependency: a four-stage psychotherapy model. Journal of Cognitive Psychotherapy 1994;8(1):55-70.
11. Turkat ID. The personality disorders: a psychological approach to clinical management. New York, NY: Pergamon Press; 1990.
12. Bornstein RF. Criterion validity of objective and projective dependency tests: a meta-analytic assessment of behavioral prediction. Psychological Assessment 1999;11(1):48-57.
13. Birtchnell J. The measurement of dependence by questionnaire. Journal of Personality Disorders 1991;5(3):281-95.
14. Nietzel MT, Harris MJ. Relationship of dependency and achievement/autonomy to depression. Clinical Psychology Review 1990;10:279-97.
15. Bornstein RF. Dependent personality disorder in the DSM-IV and beyond. Clinical Psychology: Science and Practice 1997;4(2):175-87.
16. Ryder RD, Parry-Jones WL. Fears of dependence and its value in working with adolescents. J Adolesc 1982;5(1):71-8.
17. Tait M. Dependence: a means or an impediment to growth? British Journal of Guidance and Counselling. 1997;25(1):17-26.
18. Black DW, Monahan P, Wesner R, et al. The effects of fluvoxamine, cognitive therapy, and placebo on abnormal personality traits in 44 patients with panic disorder. Journal of Personality Disorders. 1996;10(2):185-94.
19. Rathus JH, Sanderson WC, Miller AL, Wetzler S. Impact of personality functioning on cognitive behavioral treatment of panic disorder: a preliminary report. Journal of Personality Disorders 1995;9(2):160-8.
20. Bornstein RF. Integrating cognitive and existential treatment strategies in psychotherapy with dependent patients. Journal of Contemporary Psychotherapy 2004;34(4):293-309.
21. Abramson PR, Cloud MY, Keese N, Keese R. How much is too much? Dependency in a psychotherapeutic relationship. Am J Psychother 1994;48(2):294-301.
7-point checkup: Defuse cardiovascular and psychiatric risks in schizophrenia outpatients
Mr. K, age 34, has been hospitalized 4 times in 5 years for acute exacerbations of schizophrenia caused by medication nonadherence. This time he reports he discontinued antipsychotic therapy because he was “tired of taking medications every day.”
He spent 2 weeks in the acute inpatient psychiatric unit and restarted olanzapine—titrated to 15 mg/d—to which he responded well. When he presented to our outpatient clinic for follow-up, Mr. K reported adhering to his medications and denied positive symptoms. He complained of mild daytime sedation but no other side effects.
Schizophrenia patients spend most of their lives stable, rather than hospitalized for acute psychotic episodes. While stable, they continue to require close attention, and medical issues are particularly important during this time. Outpatient maintenance—such as optimizing antipsychotic therapy, offering psychosocial interventions, and monitoring physical health and well-being—provides opportunities to improve the course of illness for patients such as Mr. K.
This article describes a 7-point checkup to keep schizophrenia outpatients stable. It can help you maintain or improve patients’ function, prevent relapse, and monitor for adverse effects (Table 1).
Table 1
7-point checkup for assessing the stable schizophrenia patient
| 1. | Evaluate positive, negative, and cognitive symptoms |
| 2. | Monitor level of adherence |
| 3. | Evaluate weight, cardiovascular risk factors, and other medical parameters |
| 4. | Examine for extrapyramidal symptoms or tardive dyskinesia |
| 5. | Evaluate for comorbid mood symptoms and substance use |
| 6. | Look for prodromal symptoms that may signal relapse |
| 7. | Evaluate psychosocial interventions |
1. Symptom clusters
For several years, Mr. K worked as a research technician in a university lab, maintained an apartment, and attended to activities of daily living while taking olanzapine, 15 mg nightly. After discontinuing his medication, he reported auditory hallucinations, paranoid delusions, ideas of reference, and grossly disorganized thinking and behavior. He also was using marijuana daily, which exacerbated his psychotic symptoms and paranoia.
Addressing schizophrenia’s symptom clusters (Table 2) is key to improving patients’ social and occupational function and quality of life. Mr. K no longer has hallucinations, delusions, or disorganized thinking or behavior, but our evaluation shows his improvements are limited to schizophrenia’s positive symptoms.
Table 2
Schizophrenia’s 4 symptom clusters*
| Positive symptoms | Delusions, hallucinations, disorganization |
| Negative symptoms | Blunted affect, alogia, avolition, anhedonia |
| Cognitive symptoms | Attention, memory, executive functions (such as abstraction) |
| Affective symptoms | Dysphoria, suicidality, hopelessness |
| * Interaction of symptoms contributes to social and occupational dysfunction and adversely affects work and interpersonal relationships and self-care. | |
Cognitive symptoms. Mr. K’s concentration, attention, and memory are impaired, which interferes with his work. His ability to abstract is not impaired.
Affective symptoms. Mr. K denies signs or symptoms of depression, mania, hopelessness, or thoughts of wanting to hurt himself or anyone else.
Because antipsychotics do not adequately treat negative and cognitive symptoms, we will address these symptom clusters with psychosocial interventions.
2. Adherence
Nonadherence to medication is the most common cause of relapse and rehospitalization for patients with schizophrenia.1 We find the following strategies helpful when encouraging, maintaining, and monitoring adherence to medications.
Normalize adherence and enlist patient participation.
We inform Mr. K that most patients have trouble taking medications every day and ask how he remembers. Brainstorming with patients on ways to remember to take medications increases their likelihood of participating.
Try reminder strategies. Recommend pillboxes, alarms, and other aids. Consider enlisting family members to help patients remember to take their medications every day.
Monitor prescriptions. We limit Mr. K’s prescription to 1 month so that we can assess the timeliness and consistency of refills.
Educate. Emphasize the link between adherence and wellness, and nonadherence and relapse-—which Mr. K has clearly demonstrated. We repeat this lesson on multiple visits and counsel any involved family members as well, so that everyone understands the importance of adherence to the patient’s continued well-being.
Look for signs of nonadherence. Because Mr. K discontinued his medications without telling his physician, we remain vigilant for signs of nonadherence—such as reemergence of hallucinations, delusions, paranoia, or ideas of reference—or sudden disappearance of a side effect—such as daytime sedation, which he has consistently reported with olanzapine.
Discontinuation rates in the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) suggest that many stable schizophrenia outpatients are dissatisfied with their medications. Most patients in all treatment groups changed their medications during the 18-month National Institute of Mental Health-sponsored trial.2
SGAs versus FGAs. Schizophrenia patients may be more likely to tolerate second-generation antipsychotics (SGAs) than first-generation antipsychotics (FGAs) because of FGAs’ higher risk of movement side effects such as akathisia. Some data suggest that patients find SGAs more tolerable overall, leading to lower discontinuation rates.3
Recent evidence, however, has cast doubt on the idea that SGAs are clinically superior to FGAs. The CUtLASS trial,4 for example, found no quality-of-life differences in patients using either class. Both FGAs and SGAs reduce the risk of relapse in stable patients, although SGAs may have an advantage over FGAs in preventing relapse. An analysis by Leucht et al5 found lower relapse/treatment failure rates in 6 placebo-controlled SGA trials (total 983 patients), compared with 11 FGA trials (total 2,032 patients).
Although the data comparing SGAs with FGAs are controversial, SGAs seem to have lower EPS potential. Regardless of the type of antipsychotic, however, studies have shown that patients who relapse while taking antipsychotics have less-severe episodes than those who relapse after discontinuing their medications.
For patients who frequently forget or incorrectly take oral medications, long-acting depot antipsychotics may increase adherence and decrease relapse rates during the stable phase.6
3. Weight gain, cardiovascular risk
Cardiovascular disease is the leading cause of death among persons with schizophrenia,7,8 whose life span is 10 to 20 years shorter than the population at large.9 Schizophrenia patients may be genetically predisposed to cardiovascular disease and metabolic syndrome (Table 3),10 exacerbated by typically sedentary lifestyles, high smoking rates, and poor diets. Certain SGAs add to the risk of weight gain and metabolic abnormalities.11
Table 3
Does your patient have metabolic syndrome?
| Metabolic syndrome is defined as having any 3 of these findings: | |
| Abdominal obesity | Waist circumference |
| >102 cm (40 in) in men | |
| >88 cm (35 in) in women | |
| Elevated triglycerides | ≥150 mg/dL |
| Low HDL | |
| Hypertension | ≥130/85 mm/Hg |
| Hyperglycemia | Fasting blood glucose ≥110 mg/dL |
| Source: National Cholesterol Education Program Adult Treatment Panel III guidelines, reference 10 | |
Table 4
Monitoring protocol for patients taking second-generation antipsychotics*
| Short-term | Long-term | ||||||
|---|---|---|---|---|---|---|---|
| Baseline | 4 wk | 8 wk | 12 wk | Quarterly | Annually | Every 5 yrs | |
| Personal/family history | X | X | |||||
| Weight (BMI) | X | X | X | X | X | ||
| Waist circumference | X | X | |||||
| Blood pressure | X | X | X | ||||
| Fasting plasma glucose | X | X | X | ||||
| Fasting lipid profile | X | X | X | ||||
| * More-frequent assessments may be warranted, based on clinical status. | |||||||
| BMI: body mass index | |||||||
| Source: Reference 12 | |||||||
- using treatments that do not increase the risk for cardiovascular disease
- switching to agents with less weight gain liability if a patient’s weight increases >7% or his or her body mass index (BMI) increases 1 unit during antipsychotic therapy.
Mr. K remained stable on olanzapine for several years, but his blood glucose, cholesterol, and triglycerides have risen dramatically and he has gained 40 lbs. Although we were concerned that he might not respond as well to another SGA, we reviewed the risks and benefits with specific concern about his cardiovascular health. As a result, we switched him to aripiprazole, 15 mg/d, with close monitoring and supervision for signs of relapse.
SGAs’ heterogeneity. The ADA/APA statement and multiple clinical trials support differential risks of weight gain and metabolic abnormalities with SGAs (Table 5). Patients in CATIE phase 1 who were randomly assigned to olanzapine experienced greater total weight gain and monthly weight gain (mean +2 lb/month) than patients taking any other antipsychotic.13 In an analysis of change from baseline to last observation, 30% of patients in the olanzapine group gained >7% of their baseline weight, compared with 7% to 16% of patients taking other antipsychotics.
Table 5
Differential risks of weigh gain and metabolic abnormalities with SGAs
| Risk | Antipsychotics |
|---|---|
| Highest | Clozapine, olanzapine |
| Intermediate/low | Risperidone, quetiapine |
| Lowest | Aripiprazole, ziprasidone |
| SGAs: Second-generation antipsychotics | |
Mr. K remains free of positive symptoms after taking aripiprazole for several months. He complains less of daytime sedation and has lost >10 lbs. We are awaiting repeat glucose, cholesterol, and triglyceride serum levels. We will continue to monitor his weight and metabolic values and ensure that he receives primary care follow-up.
4. Eps and tardive dyskinesia
Compared with FGAs, SGAs may be associated with a lower incidence of tardive dyskinesia (TD) and extrapyramidal symptoms (EPS). Even so, routine screening for EPS and TD remains necessary, according to the Mount Sinai consensus conference on physical health monitoring of patients with schizophrenia.16 At every visit, we observe Mr. K for:
- facial movements (excessive blinking, puckering, lip smacking, sucking, or grimacing)
- decreased arm swing while walking or choreoathetoid-like or writhing limb or trunk movements.
In addition to screening for metabolic syndrome, EPS, and movement disorders, the Mount Sinai consensus conference16 offers guidelines for monitoring prolactin, cardiac, and ocular changes in patients taking antipsychotics.
5. Mood disorders, substance abuse
Screen schizophrenia outpatients for signs of anxiety, depression, mania, and substance abuse at every visit. An antidepressant trial is recommended for depressive episodes even if antipsychotic therapy has adequately reduced positive psychotic symptoms.17 This strategy can prevent depressive relapses and might help prevent psychotic relapse as well.18 Also consider adjunctive therapy such as:
- mood stabilizers for affective instability
- benzodiazepines for short-term anxiety or agitation
- tricyclics or selective serotonin reuptake inhibitors for comorbid anxiety disorders such as obsessive-compulsive or panic disorder.19
Because of Mr. K’s history of marijuana abuse, we tell him we will use random urine toxicology screens. We also order urine toxicology if patients behave abnormally or appear impaired. We counsel patients and families about the link between substance use and psychotic decompensation, which Mr. K has demonstrated several times.
We emphasize that the goal of repeated questioning and screening is to ensure Mr. K’s well-being. If he is using substances, we will refer him to the help he needs.
6. Prodromal signs of relapse
Mr. K has reported decreased sleep, increased irritability, increased social isolation, and some agitation before his acute psychotic decompensations. These symptoms form his prodrome for relapse, which we routinely assess at follow-up visits.
We question him about sleep, social contacts, irritability, and agitation; assess psychotic symptoms; and observe thought processes and behaviors. If a patient endorses or displays prodromal signs of relapse, we consider:
- Is he taking the medication?
- Is he abusing substances?
- Does a change in dosage (actual or a cytochrome P450-mediated drug-drug interaction) explain a decrease in efficacy?
- Is he under stress and need an increased antipsychotic dosage?
- Might psychosocial interventions (support groups, cognitive-behavioral therapy, family involvement, etc.) help him deal with symptoms, decrease stress, or avoid an exacerbation?
- Has medication been optimized (correct dosing, long enough duration), or does the patient need an increased dosage or a different antipsychotic?
7. Psychosocial interventions
Combining medications with psychosocial programs is most effective for maintaining remission and improving patients’ social and occupational functioning.17 For Mr. K we recommend these interventions:
Social skills training. Mr. K now meets with other schizophrenia patients and a moderator to set long-term goals and smaller, attainable goals as homework assignments each week. Patients get feedback, positive reinforcement, and the opportunity to practice new skills. Mr. K is working on improving family relationships, furthering his career, and improving his interpersonal skills.
Family therapy and education. We have met with Mr. K’s mother several times, and she now visits him regularly and speaks with him on the phone at least once a week. She attends Support and Family Education and National Alliance on Mental Illness meetings to increase her understanding of her son’s illness.
Alcoholics Anonymous/Marijuana Anonymous. We refer Mr. K to AA/MA groups; he attends 2 to 3 times per week and has a sponsor. He is not sober yet but has dramatically cut back his substance use and continues to express motivation to quit.
Related resources
- Torrey EF. Surviving schizophrenia: a manual for families, patients, and providers, 5th ed. New York: Harper Collins; 2006.
- Mueser KT, Gingerich S. The complete family guide to schizophrenia: helping your loved one get the most out of life. New York: Guilford Press; 2006.
- National Alliance on Mental Illness. Resources for schizophrenia patients and their families. www.nami.org.
- Aripiprazole • Abilify
- Clozapine • Clozaril
- Haloperidol • Haldol
- Olanzapine • Zyprexa
- Perphenazine • Trilafon
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Thioridazine • Mellaril
- Ziprasidone • Geodon
Dr. Arey reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Marder receives research/grant support from Janssen Pharmaceutica and Eli Lilly and Co. and is a consultant or speaker for Bristol-Myers Squibb Co., Otsuka America Pharmaceutical, Pfizer, Solvay Pharmaceuticals, Merck and Co., and Roche.
1. Weiden P, Glazer M. Assessment and treatment selection for “revolving door” inpatients with schizophrenia. Psychiatr Q. 1997;68(4):377-92.
2. Lieberman JA, Stroup TS, McEvoy JP, et al. for the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) Investigators. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med 2005;22;353(12):1209-23.
3. Marder SR, Glynn SM, Wirshing WC, et al. Maintenance treatment of schizophrenia with risperidone or haloperidol: 2-year outcomes. Am J Psychiatry 2003;160:1405-12.
4. Jones PB, Barnes TRE, Davies L, et al. Randomized controlled trial of the effect on quality of life of second- vs first-generation antipsychotic drugs in schizophrenia: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study (CUtLASS 1). Arch Gen Psychiatry 2006;63:1079-87.
5. Leucht S, Barnes TR, Kissling W, et al. Relapse prevention in schizophrenia with new-generation antipsychotics: a systematic review and exploratory meta-analysis of randomized, controlled trials. Am J Psychiatry 2003;160:1209-22.
6. Davis JM, Kane JM, Marder SR, et al. Dose response of prophylactic antipsychotics. J Clin Psychiatry 1993;54(3, suppl):24-30.
7. Brown S. Excess mortality of schizophrenia. A meta-analysis. Br J Psychiatry 1997;171:502-8.
8. Harris EC, Barraclough B. Excess mortality of mental disorder. Br J Psychiatry 1998;173:11-53.
9. Colton CW, Manderscheid RW. Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Prev Chronic Dis [serial online] 2006 Apr [date cited]. Available from: http://www.cdc.gov/pcd/issues/2006/apr/05_0180.htm.
10. NCEP Expert Panel. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002;106(25):3143-421.
11. Newcomer JW, Haupt DW. The metabolic effects of antipsychotic medications. Can J Psychiatry 2006;51(8):480-91.
12. et al. American Diabetes Association, American Psychiatric Association, American Association of Clinical Endocrinologists Consensus development conference on antipsychotic drugs and obesity and diabetes. Diabetes Care 2004;27:596-601.
13. Lieberman JA, Stroup TS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med 2005;353:1209-23.
14. Stroup TS, Liberman JA, McEvoy JP, et al. for the CATIE Investigators. Effectiveness of olanzapine, quetiapine, risperidone, and ziprasidone in patients with chronic schizophrenia following discontinuation of a previous atypical antipsychotic. Am J Psychiatry 2006;163:4:611-22.
15. McQuade RD, Stock E, Marcus R, et al. A comparison of weight change during treatment with olanzapine or aripiprazole: results from a randomized, double-blind study. J Clin Psychiatry 2004;65(suppl 18):47-56.
16. Marder SR, Essock SM, Miller AL, et al. Physical health monitoring of patients with schizophrenia. Am J Psychiatry 2004;161:1334-49.
17. Lehman AF, Kreyenbuhl J, Buchanan RW, et al. The Schizophrenia Patient Outcomes Research Team (PORT): updated treatment recommendations 2003. Schizophr Bull 2004;30:193-217.
18. Siris SG, Morgan V, Fagerstrom R, et al. Adjunctive imipramine in the treatment of postpsychotic depression. Arch Gen Psychiatry 1987;44:533-9.
19. Braga RJ, Petrides G, Figueira I. Anxiety disorders in schizophrenia. Compr Psychiatry 2004;45(6):460-8.
Mr. K, age 34, has been hospitalized 4 times in 5 years for acute exacerbations of schizophrenia caused by medication nonadherence. This time he reports he discontinued antipsychotic therapy because he was “tired of taking medications every day.”
He spent 2 weeks in the acute inpatient psychiatric unit and restarted olanzapine—titrated to 15 mg/d—to which he responded well. When he presented to our outpatient clinic for follow-up, Mr. K reported adhering to his medications and denied positive symptoms. He complained of mild daytime sedation but no other side effects.
Schizophrenia patients spend most of their lives stable, rather than hospitalized for acute psychotic episodes. While stable, they continue to require close attention, and medical issues are particularly important during this time. Outpatient maintenance—such as optimizing antipsychotic therapy, offering psychosocial interventions, and monitoring physical health and well-being—provides opportunities to improve the course of illness for patients such as Mr. K.
This article describes a 7-point checkup to keep schizophrenia outpatients stable. It can help you maintain or improve patients’ function, prevent relapse, and monitor for adverse effects (Table 1).
Table 1
7-point checkup for assessing the stable schizophrenia patient
| 1. | Evaluate positive, negative, and cognitive symptoms |
| 2. | Monitor level of adherence |
| 3. | Evaluate weight, cardiovascular risk factors, and other medical parameters |
| 4. | Examine for extrapyramidal symptoms or tardive dyskinesia |
| 5. | Evaluate for comorbid mood symptoms and substance use |
| 6. | Look for prodromal symptoms that may signal relapse |
| 7. | Evaluate psychosocial interventions |
1. Symptom clusters
For several years, Mr. K worked as a research technician in a university lab, maintained an apartment, and attended to activities of daily living while taking olanzapine, 15 mg nightly. After discontinuing his medication, he reported auditory hallucinations, paranoid delusions, ideas of reference, and grossly disorganized thinking and behavior. He also was using marijuana daily, which exacerbated his psychotic symptoms and paranoia.
Addressing schizophrenia’s symptom clusters (Table 2) is key to improving patients’ social and occupational function and quality of life. Mr. K no longer has hallucinations, delusions, or disorganized thinking or behavior, but our evaluation shows his improvements are limited to schizophrenia’s positive symptoms.
Table 2
Schizophrenia’s 4 symptom clusters*
| Positive symptoms | Delusions, hallucinations, disorganization |
| Negative symptoms | Blunted affect, alogia, avolition, anhedonia |
| Cognitive symptoms | Attention, memory, executive functions (such as abstraction) |
| Affective symptoms | Dysphoria, suicidality, hopelessness |
| * Interaction of symptoms contributes to social and occupational dysfunction and adversely affects work and interpersonal relationships and self-care. | |
Cognitive symptoms. Mr. K’s concentration, attention, and memory are impaired, which interferes with his work. His ability to abstract is not impaired.
Affective symptoms. Mr. K denies signs or symptoms of depression, mania, hopelessness, or thoughts of wanting to hurt himself or anyone else.
Because antipsychotics do not adequately treat negative and cognitive symptoms, we will address these symptom clusters with psychosocial interventions.
2. Adherence
Nonadherence to medication is the most common cause of relapse and rehospitalization for patients with schizophrenia.1 We find the following strategies helpful when encouraging, maintaining, and monitoring adherence to medications.
Normalize adherence and enlist patient participation.
We inform Mr. K that most patients have trouble taking medications every day and ask how he remembers. Brainstorming with patients on ways to remember to take medications increases their likelihood of participating.
Try reminder strategies. Recommend pillboxes, alarms, and other aids. Consider enlisting family members to help patients remember to take their medications every day.
Monitor prescriptions. We limit Mr. K’s prescription to 1 month so that we can assess the timeliness and consistency of refills.
Educate. Emphasize the link between adherence and wellness, and nonadherence and relapse-—which Mr. K has clearly demonstrated. We repeat this lesson on multiple visits and counsel any involved family members as well, so that everyone understands the importance of adherence to the patient’s continued well-being.
Look for signs of nonadherence. Because Mr. K discontinued his medications without telling his physician, we remain vigilant for signs of nonadherence—such as reemergence of hallucinations, delusions, paranoia, or ideas of reference—or sudden disappearance of a side effect—such as daytime sedation, which he has consistently reported with olanzapine.
Discontinuation rates in the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) suggest that many stable schizophrenia outpatients are dissatisfied with their medications. Most patients in all treatment groups changed their medications during the 18-month National Institute of Mental Health-sponsored trial.2
SGAs versus FGAs. Schizophrenia patients may be more likely to tolerate second-generation antipsychotics (SGAs) than first-generation antipsychotics (FGAs) because of FGAs’ higher risk of movement side effects such as akathisia. Some data suggest that patients find SGAs more tolerable overall, leading to lower discontinuation rates.3
Recent evidence, however, has cast doubt on the idea that SGAs are clinically superior to FGAs. The CUtLASS trial,4 for example, found no quality-of-life differences in patients using either class. Both FGAs and SGAs reduce the risk of relapse in stable patients, although SGAs may have an advantage over FGAs in preventing relapse. An analysis by Leucht et al5 found lower relapse/treatment failure rates in 6 placebo-controlled SGA trials (total 983 patients), compared with 11 FGA trials (total 2,032 patients).
Although the data comparing SGAs with FGAs are controversial, SGAs seem to have lower EPS potential. Regardless of the type of antipsychotic, however, studies have shown that patients who relapse while taking antipsychotics have less-severe episodes than those who relapse after discontinuing their medications.
For patients who frequently forget or incorrectly take oral medications, long-acting depot antipsychotics may increase adherence and decrease relapse rates during the stable phase.6
3. Weight gain, cardiovascular risk
Cardiovascular disease is the leading cause of death among persons with schizophrenia,7,8 whose life span is 10 to 20 years shorter than the population at large.9 Schizophrenia patients may be genetically predisposed to cardiovascular disease and metabolic syndrome (Table 3),10 exacerbated by typically sedentary lifestyles, high smoking rates, and poor diets. Certain SGAs add to the risk of weight gain and metabolic abnormalities.11
Table 3
Does your patient have metabolic syndrome?
| Metabolic syndrome is defined as having any 3 of these findings: | |
| Abdominal obesity | Waist circumference |
| >102 cm (40 in) in men | |
| >88 cm (35 in) in women | |
| Elevated triglycerides | ≥150 mg/dL |
| Low HDL | |
| Hypertension | ≥130/85 mm/Hg |
| Hyperglycemia | Fasting blood glucose ≥110 mg/dL |
| Source: National Cholesterol Education Program Adult Treatment Panel III guidelines, reference 10 | |
Table 4
Monitoring protocol for patients taking second-generation antipsychotics*
| Short-term | Long-term | ||||||
|---|---|---|---|---|---|---|---|
| Baseline | 4 wk | 8 wk | 12 wk | Quarterly | Annually | Every 5 yrs | |
| Personal/family history | X | X | |||||
| Weight (BMI) | X | X | X | X | X | ||
| Waist circumference | X | X | |||||
| Blood pressure | X | X | X | ||||
| Fasting plasma glucose | X | X | X | ||||
| Fasting lipid profile | X | X | X | ||||
| * More-frequent assessments may be warranted, based on clinical status. | |||||||
| BMI: body mass index | |||||||
| Source: Reference 12 | |||||||
- using treatments that do not increase the risk for cardiovascular disease
- switching to agents with less weight gain liability if a patient’s weight increases >7% or his or her body mass index (BMI) increases 1 unit during antipsychotic therapy.
Mr. K remained stable on olanzapine for several years, but his blood glucose, cholesterol, and triglycerides have risen dramatically and he has gained 40 lbs. Although we were concerned that he might not respond as well to another SGA, we reviewed the risks and benefits with specific concern about his cardiovascular health. As a result, we switched him to aripiprazole, 15 mg/d, with close monitoring and supervision for signs of relapse.
SGAs’ heterogeneity. The ADA/APA statement and multiple clinical trials support differential risks of weight gain and metabolic abnormalities with SGAs (Table 5). Patients in CATIE phase 1 who were randomly assigned to olanzapine experienced greater total weight gain and monthly weight gain (mean +2 lb/month) than patients taking any other antipsychotic.13 In an analysis of change from baseline to last observation, 30% of patients in the olanzapine group gained >7% of their baseline weight, compared with 7% to 16% of patients taking other antipsychotics.
Table 5
Differential risks of weigh gain and metabolic abnormalities with SGAs
| Risk | Antipsychotics |
|---|---|
| Highest | Clozapine, olanzapine |
| Intermediate/low | Risperidone, quetiapine |
| Lowest | Aripiprazole, ziprasidone |
| SGAs: Second-generation antipsychotics | |
Mr. K remains free of positive symptoms after taking aripiprazole for several months. He complains less of daytime sedation and has lost >10 lbs. We are awaiting repeat glucose, cholesterol, and triglyceride serum levels. We will continue to monitor his weight and metabolic values and ensure that he receives primary care follow-up.
4. Eps and tardive dyskinesia
Compared with FGAs, SGAs may be associated with a lower incidence of tardive dyskinesia (TD) and extrapyramidal symptoms (EPS). Even so, routine screening for EPS and TD remains necessary, according to the Mount Sinai consensus conference on physical health monitoring of patients with schizophrenia.16 At every visit, we observe Mr. K for:
- facial movements (excessive blinking, puckering, lip smacking, sucking, or grimacing)
- decreased arm swing while walking or choreoathetoid-like or writhing limb or trunk movements.
In addition to screening for metabolic syndrome, EPS, and movement disorders, the Mount Sinai consensus conference16 offers guidelines for monitoring prolactin, cardiac, and ocular changes in patients taking antipsychotics.
5. Mood disorders, substance abuse
Screen schizophrenia outpatients for signs of anxiety, depression, mania, and substance abuse at every visit. An antidepressant trial is recommended for depressive episodes even if antipsychotic therapy has adequately reduced positive psychotic symptoms.17 This strategy can prevent depressive relapses and might help prevent psychotic relapse as well.18 Also consider adjunctive therapy such as:
- mood stabilizers for affective instability
- benzodiazepines for short-term anxiety or agitation
- tricyclics or selective serotonin reuptake inhibitors for comorbid anxiety disorders such as obsessive-compulsive or panic disorder.19
Because of Mr. K’s history of marijuana abuse, we tell him we will use random urine toxicology screens. We also order urine toxicology if patients behave abnormally or appear impaired. We counsel patients and families about the link between substance use and psychotic decompensation, which Mr. K has demonstrated several times.
We emphasize that the goal of repeated questioning and screening is to ensure Mr. K’s well-being. If he is using substances, we will refer him to the help he needs.
6. Prodromal signs of relapse
Mr. K has reported decreased sleep, increased irritability, increased social isolation, and some agitation before his acute psychotic decompensations. These symptoms form his prodrome for relapse, which we routinely assess at follow-up visits.
We question him about sleep, social contacts, irritability, and agitation; assess psychotic symptoms; and observe thought processes and behaviors. If a patient endorses or displays prodromal signs of relapse, we consider:
- Is he taking the medication?
- Is he abusing substances?
- Does a change in dosage (actual or a cytochrome P450-mediated drug-drug interaction) explain a decrease in efficacy?
- Is he under stress and need an increased antipsychotic dosage?
- Might psychosocial interventions (support groups, cognitive-behavioral therapy, family involvement, etc.) help him deal with symptoms, decrease stress, or avoid an exacerbation?
- Has medication been optimized (correct dosing, long enough duration), or does the patient need an increased dosage or a different antipsychotic?
7. Psychosocial interventions
Combining medications with psychosocial programs is most effective for maintaining remission and improving patients’ social and occupational functioning.17 For Mr. K we recommend these interventions:
Social skills training. Mr. K now meets with other schizophrenia patients and a moderator to set long-term goals and smaller, attainable goals as homework assignments each week. Patients get feedback, positive reinforcement, and the opportunity to practice new skills. Mr. K is working on improving family relationships, furthering his career, and improving his interpersonal skills.
Family therapy and education. We have met with Mr. K’s mother several times, and she now visits him regularly and speaks with him on the phone at least once a week. She attends Support and Family Education and National Alliance on Mental Illness meetings to increase her understanding of her son’s illness.
Alcoholics Anonymous/Marijuana Anonymous. We refer Mr. K to AA/MA groups; he attends 2 to 3 times per week and has a sponsor. He is not sober yet but has dramatically cut back his substance use and continues to express motivation to quit.
Related resources
- Torrey EF. Surviving schizophrenia: a manual for families, patients, and providers, 5th ed. New York: Harper Collins; 2006.
- Mueser KT, Gingerich S. The complete family guide to schizophrenia: helping your loved one get the most out of life. New York: Guilford Press; 2006.
- National Alliance on Mental Illness. Resources for schizophrenia patients and their families. www.nami.org.
- Aripiprazole • Abilify
- Clozapine • Clozaril
- Haloperidol • Haldol
- Olanzapine • Zyprexa
- Perphenazine • Trilafon
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Thioridazine • Mellaril
- Ziprasidone • Geodon
Dr. Arey reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Marder receives research/grant support from Janssen Pharmaceutica and Eli Lilly and Co. and is a consultant or speaker for Bristol-Myers Squibb Co., Otsuka America Pharmaceutical, Pfizer, Solvay Pharmaceuticals, Merck and Co., and Roche.
Mr. K, age 34, has been hospitalized 4 times in 5 years for acute exacerbations of schizophrenia caused by medication nonadherence. This time he reports he discontinued antipsychotic therapy because he was “tired of taking medications every day.”
He spent 2 weeks in the acute inpatient psychiatric unit and restarted olanzapine—titrated to 15 mg/d—to which he responded well. When he presented to our outpatient clinic for follow-up, Mr. K reported adhering to his medications and denied positive symptoms. He complained of mild daytime sedation but no other side effects.
Schizophrenia patients spend most of their lives stable, rather than hospitalized for acute psychotic episodes. While stable, they continue to require close attention, and medical issues are particularly important during this time. Outpatient maintenance—such as optimizing antipsychotic therapy, offering psychosocial interventions, and monitoring physical health and well-being—provides opportunities to improve the course of illness for patients such as Mr. K.
This article describes a 7-point checkup to keep schizophrenia outpatients stable. It can help you maintain or improve patients’ function, prevent relapse, and monitor for adverse effects (Table 1).
Table 1
7-point checkup for assessing the stable schizophrenia patient
| 1. | Evaluate positive, negative, and cognitive symptoms |
| 2. | Monitor level of adherence |
| 3. | Evaluate weight, cardiovascular risk factors, and other medical parameters |
| 4. | Examine for extrapyramidal symptoms or tardive dyskinesia |
| 5. | Evaluate for comorbid mood symptoms and substance use |
| 6. | Look for prodromal symptoms that may signal relapse |
| 7. | Evaluate psychosocial interventions |
1. Symptom clusters
For several years, Mr. K worked as a research technician in a university lab, maintained an apartment, and attended to activities of daily living while taking olanzapine, 15 mg nightly. After discontinuing his medication, he reported auditory hallucinations, paranoid delusions, ideas of reference, and grossly disorganized thinking and behavior. He also was using marijuana daily, which exacerbated his psychotic symptoms and paranoia.
Addressing schizophrenia’s symptom clusters (Table 2) is key to improving patients’ social and occupational function and quality of life. Mr. K no longer has hallucinations, delusions, or disorganized thinking or behavior, but our evaluation shows his improvements are limited to schizophrenia’s positive symptoms.
Table 2
Schizophrenia’s 4 symptom clusters*
| Positive symptoms | Delusions, hallucinations, disorganization |
| Negative symptoms | Blunted affect, alogia, avolition, anhedonia |
| Cognitive symptoms | Attention, memory, executive functions (such as abstraction) |
| Affective symptoms | Dysphoria, suicidality, hopelessness |
| * Interaction of symptoms contributes to social and occupational dysfunction and adversely affects work and interpersonal relationships and self-care. | |
Cognitive symptoms. Mr. K’s concentration, attention, and memory are impaired, which interferes with his work. His ability to abstract is not impaired.
Affective symptoms. Mr. K denies signs or symptoms of depression, mania, hopelessness, or thoughts of wanting to hurt himself or anyone else.
Because antipsychotics do not adequately treat negative and cognitive symptoms, we will address these symptom clusters with psychosocial interventions.
2. Adherence
Nonadherence to medication is the most common cause of relapse and rehospitalization for patients with schizophrenia.1 We find the following strategies helpful when encouraging, maintaining, and monitoring adherence to medications.
Normalize adherence and enlist patient participation.
We inform Mr. K that most patients have trouble taking medications every day and ask how he remembers. Brainstorming with patients on ways to remember to take medications increases their likelihood of participating.
Try reminder strategies. Recommend pillboxes, alarms, and other aids. Consider enlisting family members to help patients remember to take their medications every day.
Monitor prescriptions. We limit Mr. K’s prescription to 1 month so that we can assess the timeliness and consistency of refills.
Educate. Emphasize the link between adherence and wellness, and nonadherence and relapse-—which Mr. K has clearly demonstrated. We repeat this lesson on multiple visits and counsel any involved family members as well, so that everyone understands the importance of adherence to the patient’s continued well-being.
Look for signs of nonadherence. Because Mr. K discontinued his medications without telling his physician, we remain vigilant for signs of nonadherence—such as reemergence of hallucinations, delusions, paranoia, or ideas of reference—or sudden disappearance of a side effect—such as daytime sedation, which he has consistently reported with olanzapine.
Discontinuation rates in the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) suggest that many stable schizophrenia outpatients are dissatisfied with their medications. Most patients in all treatment groups changed their medications during the 18-month National Institute of Mental Health-sponsored trial.2
SGAs versus FGAs. Schizophrenia patients may be more likely to tolerate second-generation antipsychotics (SGAs) than first-generation antipsychotics (FGAs) because of FGAs’ higher risk of movement side effects such as akathisia. Some data suggest that patients find SGAs more tolerable overall, leading to lower discontinuation rates.3
Recent evidence, however, has cast doubt on the idea that SGAs are clinically superior to FGAs. The CUtLASS trial,4 for example, found no quality-of-life differences in patients using either class. Both FGAs and SGAs reduce the risk of relapse in stable patients, although SGAs may have an advantage over FGAs in preventing relapse. An analysis by Leucht et al5 found lower relapse/treatment failure rates in 6 placebo-controlled SGA trials (total 983 patients), compared with 11 FGA trials (total 2,032 patients).
Although the data comparing SGAs with FGAs are controversial, SGAs seem to have lower EPS potential. Regardless of the type of antipsychotic, however, studies have shown that patients who relapse while taking antipsychotics have less-severe episodes than those who relapse after discontinuing their medications.
For patients who frequently forget or incorrectly take oral medications, long-acting depot antipsychotics may increase adherence and decrease relapse rates during the stable phase.6
3. Weight gain, cardiovascular risk
Cardiovascular disease is the leading cause of death among persons with schizophrenia,7,8 whose life span is 10 to 20 years shorter than the population at large.9 Schizophrenia patients may be genetically predisposed to cardiovascular disease and metabolic syndrome (Table 3),10 exacerbated by typically sedentary lifestyles, high smoking rates, and poor diets. Certain SGAs add to the risk of weight gain and metabolic abnormalities.11
Table 3
Does your patient have metabolic syndrome?
| Metabolic syndrome is defined as having any 3 of these findings: | |
| Abdominal obesity | Waist circumference |
| >102 cm (40 in) in men | |
| >88 cm (35 in) in women | |
| Elevated triglycerides | ≥150 mg/dL |
| Low HDL | |
| Hypertension | ≥130/85 mm/Hg |
| Hyperglycemia | Fasting blood glucose ≥110 mg/dL |
| Source: National Cholesterol Education Program Adult Treatment Panel III guidelines, reference 10 | |
Table 4
Monitoring protocol for patients taking second-generation antipsychotics*
| Short-term | Long-term | ||||||
|---|---|---|---|---|---|---|---|
| Baseline | 4 wk | 8 wk | 12 wk | Quarterly | Annually | Every 5 yrs | |
| Personal/family history | X | X | |||||
| Weight (BMI) | X | X | X | X | X | ||
| Waist circumference | X | X | |||||
| Blood pressure | X | X | X | ||||
| Fasting plasma glucose | X | X | X | ||||
| Fasting lipid profile | X | X | X | ||||
| * More-frequent assessments may be warranted, based on clinical status. | |||||||
| BMI: body mass index | |||||||
| Source: Reference 12 | |||||||
- using treatments that do not increase the risk for cardiovascular disease
- switching to agents with less weight gain liability if a patient’s weight increases >7% or his or her body mass index (BMI) increases 1 unit during antipsychotic therapy.
Mr. K remained stable on olanzapine for several years, but his blood glucose, cholesterol, and triglycerides have risen dramatically and he has gained 40 lbs. Although we were concerned that he might not respond as well to another SGA, we reviewed the risks and benefits with specific concern about his cardiovascular health. As a result, we switched him to aripiprazole, 15 mg/d, with close monitoring and supervision for signs of relapse.
SGAs’ heterogeneity. The ADA/APA statement and multiple clinical trials support differential risks of weight gain and metabolic abnormalities with SGAs (Table 5). Patients in CATIE phase 1 who were randomly assigned to olanzapine experienced greater total weight gain and monthly weight gain (mean +2 lb/month) than patients taking any other antipsychotic.13 In an analysis of change from baseline to last observation, 30% of patients in the olanzapine group gained >7% of their baseline weight, compared with 7% to 16% of patients taking other antipsychotics.
Table 5
Differential risks of weigh gain and metabolic abnormalities with SGAs
| Risk | Antipsychotics |
|---|---|
| Highest | Clozapine, olanzapine |
| Intermediate/low | Risperidone, quetiapine |
| Lowest | Aripiprazole, ziprasidone |
| SGAs: Second-generation antipsychotics | |
Mr. K remains free of positive symptoms after taking aripiprazole for several months. He complains less of daytime sedation and has lost >10 lbs. We are awaiting repeat glucose, cholesterol, and triglyceride serum levels. We will continue to monitor his weight and metabolic values and ensure that he receives primary care follow-up.
4. Eps and tardive dyskinesia
Compared with FGAs, SGAs may be associated with a lower incidence of tardive dyskinesia (TD) and extrapyramidal symptoms (EPS). Even so, routine screening for EPS and TD remains necessary, according to the Mount Sinai consensus conference on physical health monitoring of patients with schizophrenia.16 At every visit, we observe Mr. K for:
- facial movements (excessive blinking, puckering, lip smacking, sucking, or grimacing)
- decreased arm swing while walking or choreoathetoid-like or writhing limb or trunk movements.
In addition to screening for metabolic syndrome, EPS, and movement disorders, the Mount Sinai consensus conference16 offers guidelines for monitoring prolactin, cardiac, and ocular changes in patients taking antipsychotics.
5. Mood disorders, substance abuse
Screen schizophrenia outpatients for signs of anxiety, depression, mania, and substance abuse at every visit. An antidepressant trial is recommended for depressive episodes even if antipsychotic therapy has adequately reduced positive psychotic symptoms.17 This strategy can prevent depressive relapses and might help prevent psychotic relapse as well.18 Also consider adjunctive therapy such as:
- mood stabilizers for affective instability
- benzodiazepines for short-term anxiety or agitation
- tricyclics or selective serotonin reuptake inhibitors for comorbid anxiety disorders such as obsessive-compulsive or panic disorder.19
Because of Mr. K’s history of marijuana abuse, we tell him we will use random urine toxicology screens. We also order urine toxicology if patients behave abnormally or appear impaired. We counsel patients and families about the link between substance use and psychotic decompensation, which Mr. K has demonstrated several times.
We emphasize that the goal of repeated questioning and screening is to ensure Mr. K’s well-being. If he is using substances, we will refer him to the help he needs.
6. Prodromal signs of relapse
Mr. K has reported decreased sleep, increased irritability, increased social isolation, and some agitation before his acute psychotic decompensations. These symptoms form his prodrome for relapse, which we routinely assess at follow-up visits.
We question him about sleep, social contacts, irritability, and agitation; assess psychotic symptoms; and observe thought processes and behaviors. If a patient endorses or displays prodromal signs of relapse, we consider:
- Is he taking the medication?
- Is he abusing substances?
- Does a change in dosage (actual or a cytochrome P450-mediated drug-drug interaction) explain a decrease in efficacy?
- Is he under stress and need an increased antipsychotic dosage?
- Might psychosocial interventions (support groups, cognitive-behavioral therapy, family involvement, etc.) help him deal with symptoms, decrease stress, or avoid an exacerbation?
- Has medication been optimized (correct dosing, long enough duration), or does the patient need an increased dosage or a different antipsychotic?
7. Psychosocial interventions
Combining medications with psychosocial programs is most effective for maintaining remission and improving patients’ social and occupational functioning.17 For Mr. K we recommend these interventions:
Social skills training. Mr. K now meets with other schizophrenia patients and a moderator to set long-term goals and smaller, attainable goals as homework assignments each week. Patients get feedback, positive reinforcement, and the opportunity to practice new skills. Mr. K is working on improving family relationships, furthering his career, and improving his interpersonal skills.
Family therapy and education. We have met with Mr. K’s mother several times, and she now visits him regularly and speaks with him on the phone at least once a week. She attends Support and Family Education and National Alliance on Mental Illness meetings to increase her understanding of her son’s illness.
Alcoholics Anonymous/Marijuana Anonymous. We refer Mr. K to AA/MA groups; he attends 2 to 3 times per week and has a sponsor. He is not sober yet but has dramatically cut back his substance use and continues to express motivation to quit.
Related resources
- Torrey EF. Surviving schizophrenia: a manual for families, patients, and providers, 5th ed. New York: Harper Collins; 2006.
- Mueser KT, Gingerich S. The complete family guide to schizophrenia: helping your loved one get the most out of life. New York: Guilford Press; 2006.
- National Alliance on Mental Illness. Resources for schizophrenia patients and their families. www.nami.org.
- Aripiprazole • Abilify
- Clozapine • Clozaril
- Haloperidol • Haldol
- Olanzapine • Zyprexa
- Perphenazine • Trilafon
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Thioridazine • Mellaril
- Ziprasidone • Geodon
Dr. Arey reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Marder receives research/grant support from Janssen Pharmaceutica and Eli Lilly and Co. and is a consultant or speaker for Bristol-Myers Squibb Co., Otsuka America Pharmaceutical, Pfizer, Solvay Pharmaceuticals, Merck and Co., and Roche.
1. Weiden P, Glazer M. Assessment and treatment selection for “revolving door” inpatients with schizophrenia. Psychiatr Q. 1997;68(4):377-92.
2. Lieberman JA, Stroup TS, McEvoy JP, et al. for the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) Investigators. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med 2005;22;353(12):1209-23.
3. Marder SR, Glynn SM, Wirshing WC, et al. Maintenance treatment of schizophrenia with risperidone or haloperidol: 2-year outcomes. Am J Psychiatry 2003;160:1405-12.
4. Jones PB, Barnes TRE, Davies L, et al. Randomized controlled trial of the effect on quality of life of second- vs first-generation antipsychotic drugs in schizophrenia: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study (CUtLASS 1). Arch Gen Psychiatry 2006;63:1079-87.
5. Leucht S, Barnes TR, Kissling W, et al. Relapse prevention in schizophrenia with new-generation antipsychotics: a systematic review and exploratory meta-analysis of randomized, controlled trials. Am J Psychiatry 2003;160:1209-22.
6. Davis JM, Kane JM, Marder SR, et al. Dose response of prophylactic antipsychotics. J Clin Psychiatry 1993;54(3, suppl):24-30.
7. Brown S. Excess mortality of schizophrenia. A meta-analysis. Br J Psychiatry 1997;171:502-8.
8. Harris EC, Barraclough B. Excess mortality of mental disorder. Br J Psychiatry 1998;173:11-53.
9. Colton CW, Manderscheid RW. Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Prev Chronic Dis [serial online] 2006 Apr [date cited]. Available from: http://www.cdc.gov/pcd/issues/2006/apr/05_0180.htm.
10. NCEP Expert Panel. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002;106(25):3143-421.
11. Newcomer JW, Haupt DW. The metabolic effects of antipsychotic medications. Can J Psychiatry 2006;51(8):480-91.
12. et al. American Diabetes Association, American Psychiatric Association, American Association of Clinical Endocrinologists Consensus development conference on antipsychotic drugs and obesity and diabetes. Diabetes Care 2004;27:596-601.
13. Lieberman JA, Stroup TS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med 2005;353:1209-23.
14. Stroup TS, Liberman JA, McEvoy JP, et al. for the CATIE Investigators. Effectiveness of olanzapine, quetiapine, risperidone, and ziprasidone in patients with chronic schizophrenia following discontinuation of a previous atypical antipsychotic. Am J Psychiatry 2006;163:4:611-22.
15. McQuade RD, Stock E, Marcus R, et al. A comparison of weight change during treatment with olanzapine or aripiprazole: results from a randomized, double-blind study. J Clin Psychiatry 2004;65(suppl 18):47-56.
16. Marder SR, Essock SM, Miller AL, et al. Physical health monitoring of patients with schizophrenia. Am J Psychiatry 2004;161:1334-49.
17. Lehman AF, Kreyenbuhl J, Buchanan RW, et al. The Schizophrenia Patient Outcomes Research Team (PORT): updated treatment recommendations 2003. Schizophr Bull 2004;30:193-217.
18. Siris SG, Morgan V, Fagerstrom R, et al. Adjunctive imipramine in the treatment of postpsychotic depression. Arch Gen Psychiatry 1987;44:533-9.
19. Braga RJ, Petrides G, Figueira I. Anxiety disorders in schizophrenia. Compr Psychiatry 2004;45(6):460-8.
1. Weiden P, Glazer M. Assessment and treatment selection for “revolving door” inpatients with schizophrenia. Psychiatr Q. 1997;68(4):377-92.
2. Lieberman JA, Stroup TS, McEvoy JP, et al. for the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) Investigators. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med 2005;22;353(12):1209-23.
3. Marder SR, Glynn SM, Wirshing WC, et al. Maintenance treatment of schizophrenia with risperidone or haloperidol: 2-year outcomes. Am J Psychiatry 2003;160:1405-12.
4. Jones PB, Barnes TRE, Davies L, et al. Randomized controlled trial of the effect on quality of life of second- vs first-generation antipsychotic drugs in schizophrenia: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study (CUtLASS 1). Arch Gen Psychiatry 2006;63:1079-87.
5. Leucht S, Barnes TR, Kissling W, et al. Relapse prevention in schizophrenia with new-generation antipsychotics: a systematic review and exploratory meta-analysis of randomized, controlled trials. Am J Psychiatry 2003;160:1209-22.
6. Davis JM, Kane JM, Marder SR, et al. Dose response of prophylactic antipsychotics. J Clin Psychiatry 1993;54(3, suppl):24-30.
7. Brown S. Excess mortality of schizophrenia. A meta-analysis. Br J Psychiatry 1997;171:502-8.
8. Harris EC, Barraclough B. Excess mortality of mental disorder. Br J Psychiatry 1998;173:11-53.
9. Colton CW, Manderscheid RW. Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Prev Chronic Dis [serial online] 2006 Apr [date cited]. Available from: http://www.cdc.gov/pcd/issues/2006/apr/05_0180.htm.
10. NCEP Expert Panel. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002;106(25):3143-421.
11. Newcomer JW, Haupt DW. The metabolic effects of antipsychotic medications. Can J Psychiatry 2006;51(8):480-91.
12. et al. American Diabetes Association, American Psychiatric Association, American Association of Clinical Endocrinologists Consensus development conference on antipsychotic drugs and obesity and diabetes. Diabetes Care 2004;27:596-601.
13. Lieberman JA, Stroup TS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med 2005;353:1209-23.
14. Stroup TS, Liberman JA, McEvoy JP, et al. for the CATIE Investigators. Effectiveness of olanzapine, quetiapine, risperidone, and ziprasidone in patients with chronic schizophrenia following discontinuation of a previous atypical antipsychotic. Am J Psychiatry 2006;163:4:611-22.
15. McQuade RD, Stock E, Marcus R, et al. A comparison of weight change during treatment with olanzapine or aripiprazole: results from a randomized, double-blind study. J Clin Psychiatry 2004;65(suppl 18):47-56.
16. Marder SR, Essock SM, Miller AL, et al. Physical health monitoring of patients with schizophrenia. Am J Psychiatry 2004;161:1334-49.
17. Lehman AF, Kreyenbuhl J, Buchanan RW, et al. The Schizophrenia Patient Outcomes Research Team (PORT): updated treatment recommendations 2003. Schizophr Bull 2004;30:193-217.
18. Siris SG, Morgan V, Fagerstrom R, et al. Adjunctive imipramine in the treatment of postpsychotic depression. Arch Gen Psychiatry 1987;44:533-9.
19. Braga RJ, Petrides G, Figueira I. Anxiety disorders in schizophrenia. Compr Psychiatry 2004;45(6):460-8.
Struggling not to nap: Causes of daytime sleepiness
Poor energy, hypersomnia, amotivation, irritability, and frustration can suggest depression or other psychiatric disorders to busy primary care physicians. As a result, psychiatrists often are referred patients with excessive daytime sleepiness (EDS) caused by undiagnosed primary sleep disorders.
Physicians may miss obstructive sleep apnea (OSA), restless legs syndrome, circadian rhythm disorders, or narcolepsy because:
- many have little training in sleep disorders and limited time to diagnose them1
- patients do not report sleepiness or recognize it as a legitimate medical concern
- definitive diagnostic tests are expensive and usually are not ordered.
Psychiatrists, therefore, need a clear understanding of the EDS differential diagnosis to determine whether a patient’s behavioral symptoms are a sleep or psychiatric issue.
How likely are you to doze off or fall asleep in the following situations, in contrast to feeling just tired? This refers to your usual way of life in recent times. Even if you have not done some of these things recently, try to work out how each situation would affect you now. Use the scale below to choose the most appropriate number for each situation:
0 no chance of dozing
1 slight chance of dozing
2 moderate chance of dozing
3 high chance of dozing
Chance of dozing Situation
Sitting and reading
Watching TV
Sitting inactive in a public place (such as in a theater or a meeting)
As a passenger in a car for an hour without a break
Lying down to rest in the afternoon when circumstances permit
Sitting and talking to someone
Sitting quietly after a lunch without alcohol
In a car, while stopped for a few minutes in traffic
Scoring key
1 to 6 Getting enough sleep
7 to 8 Average
>8 Seek a sleep specialist’s advice without delay
Assessing the sleepy patient
Sleepiness is an inability to stay awake at appropriate times. Fatigue, by comparison, does not involve sleepiness but very low energy associated with wakefulness. In general, sleepy patients get transient relief from napping, whereas fatigued patients report they cannot fall asleep.
Untreated EDS results in compromised quality of life, reduced productivity, and public safety concerns such as falling asleep while driving.2 Sleep complaints fall into three major categories:
- EDS
- insomnia (marked by distress because of poor sleep, but usually with minimal EDS)
- unusual nocturnal behaviors (ranging from arm waving to violent behaviors.
When you evaluate a patient with sleep complaints, valuable sources of data include observation, questionnaires, and screening devices. The most important may be common sense.
Observation. Observe the patient in the waiting room or office before starting the interview. Did he or she nod off while waiting to see you? Pay attention to anyone who appears sleepy—even those who deny having trouble staying awake. Over time, sleepy patients can lose their perspective on alertness. Some have had EDS so long that they no longer recall what it is like to feel fully awake.
Collateral history often is important because family members probably have observed the sleeping patient. The bed partner can provide information about snoring, irregular breathing, leg kicks, unplanned naps, and strained interpersonal relationships because of EDS. For the patient without a bed partner, consider interviewing a travel companion.
Questionnaires. Few useful screening tests exist for sleepiness; most are neither reliable nor valid. One of the better questionnaires—the Epworth Sleepiness Scale (Box 1)—helps confirm the presence of sleepiness with a score >8, differentiating the inability to stay awake from fatigue. This brief questionnaire also provides a useful measure of sleepiness severity.3
The Epworth scale’s value is limited because its questions of specific time and context might not represent a patient’s experiences. Additional validated surveys include the Pittsburgh Sleep Quality Inventory and several for sleep apnea.4
Screening. Electroencephalographic (EEG) monitoring can accurately measure the patient’s degree of sleep disruption. This information is key to understanding if a patient’s EDS is caused by a physiologic condition that prevents quality nocturnal sleep.
None of the widely used screening devices that assess leg kicks indicate the presence of possible periodic limb movements.
Overnight pulse oximetry has been used to screen for sleep-disordered breathing5 but also has limitations:
- Most pulse oximeters do not provide information about sleep stage or body position.
- Patients with sleep-disordered breathing can lack adequate oxygen desaturations but have frequent EEG arousals related to sleep issues. Because EEG data are not collected during arousals, pulse oximetry would generate a false-negative result in this scenario, which occurs most often in female and thin patients.
- Oximetry provides only oxygen saturation data and possibly heart rate, whereas other physiologic processes such as body movement or sleep architecture can be disrupted repetitively during sleep.
Common sense. The most productive tools for detecting sleep disorders are intuition and common sense. The Figure suggests sequential questions that might uncover specific sleep disorders. Then the decision whether to refer the patient to a sleep disorder center for diagnostic testing depends on the type of sleep disorder you detect.
Nasal continuous positive airway pressure
(CPAP) should be started in an observed setting so that the clinician can determine the optimal amount of positive pressure needed to keep the upper airway patent.
For some patients, CPAP is started in the second half of a “split-night” sleep study after a diagnosis of obstructive sleep apnea (OSA) is made. Other patients return a second night for a nasal CPAP trial. Those with severe OSA might notice improved sleep quality and reduced EDS after only a few hours of CPAP use. Some wish to start CPAP treatment immediately.
Advances in masks and equipment have improved patient adherence to CPAP. Innovations include auto-titrating machines, in which the pressure level can be varied depending on sleep state or body position. Many machines include a data microchip that allows the clinician to determine duration of usage, then use that information to counsel the patient about adherence, if necessary.
Patient education also can promote CPAP adherence. When patients are first told they might need to sleep each night wearing a nasal mask, they often voice well-founded concerns about comfort, claustrophobia, or sexual activity.
Obtaining the support of the bed partner by welcoming her or him to all appointments, including educational activities, is optimal. The bed partner’s concerns about the patient’s excessive snoring or apneas probably were the impetus for the appointment in the first place.
Medication. Some patients benefit from 1 to 2 weeks of a sleeping medication such as zolpidem or trazodone while they acclimate to using nasal CPAP.
Figure The sleepy patient: Possible medical and psychiatric explanations
* Supportive factors: Persuasive if present, but if absent do not exclude possible conditions
Obstructive sleep apnea
Because OSA affects at least 4% of men and 2% of women,6 you are virtually assured of seeing undiagnosed patients. OSA is caused by repeated collapse of the soft tissues surrounding the upper airway, decreasing airflow that is restored when the patient briefly awakens. Patients develop EDS because sleep is fragmented by frequent arousals.
Obese patients, because of their body habitus, are at higher risk for OSA than patients at normal weight. Carefully screen patients for OSA if they develop weight problems while taking psychotropics, such as antipsychotics.
Alcohol or sedatives used at bedtime can aggravate OSA. These substances promote muscle relaxation and increase the arousal threshold so that patients do not awaken readily when apneas occur.
Long-term complications of untreated OSA include sleepiness leading to accidents, hypertension, cerebrovascular disease, and progressive obesity. Data also associate OSA with cardiovascular complications such as arrhythmias, congestive heart failure, and myocardial infarction.7
Physical examination focuses on detecting:
- nasal obstruction (have patient sniff separately through each nostril)
- large neck
- crowded oropharynx (low-hanging palate, reddened uvula, enlarged tonsils, large tongue relative to oropharynx diameter)
- jaw structure (particularly a small, retrognathic mandible).
Sleep studies. Referral for nocturnal polysomnography might be the next step. A comprehensive sleep study collects data about respiratory, cardiovascular, and muscle activity at night, as well as the sounds the patient makes—such as snoring or coughing—when asleep. EEG monitoring also is performed. OSA may be diagnosed if repeated episodes of reduced airflow and oxygen desaturation (arousals) are observed as brief shifts in EEG frequency.
Treatment. First-line interventions for the patient with OSA include:
- no alcohol 1 to 2 hours before bedtime
- sleeping on the side instead of the back
- weight loss (ideally with exercise)
- nasal sprays for allergies.
If first-line treatments are ineffective, nasal continuous positive airway pressure (CPAP) works well for most patients who adhere to the regimen.8 CPAP requires the patient to wear a nasal mask that delivers room air, splinting open the nasopharynx and upper airway (Box 2).
Surgical options. The most common surgeries for OSA are uvulopalatopharyngoplasty and laser-assisted uvulopalatoplasty. Others include tongue reduction and mandibular advancement.
The response rate to surgery averages 50%, depending on patient characteristics and procedure.9 Positive outcomes are most likely for thin patients with obvious upper airway obstruction, including deviated nasal septum, large tonsils, low-hanging palate, and large uvula. Postsurgical complications include nasal regurgitation, voice change, pain, bleeding, infection, tongue numbness, and snoring without apnea (silent apnea).
Oral appliances open the oropharynx by moving the mandible and tongue out of way. Patients with mild to moderate OSA accept these devices well. Evidence suggests that oral appliances improve sleep and reduce EDS more effectively than nasal CPAP and are preferred by patients.10
Oral devices have drawbacks, however. In most settings, their effectiveness cannot be observed during a “split-night” laboratory sleep study because the patient has not yet purchased the device. Also, multiple visits sometimes are required to custom-fit the appliance; this can pose a hardship for patients who live a distance from the provider.
Restless legs syndrome
Patients with restless legs syndrome (RLS) typically report a restless, painful feeling in the limbs that occurs in the evening and at night, disrupting sleep. This condition—which affects 10% of the population—is associated with aging, blood loss, anemia, peripheral neuropathies, and pregnancy.11 Onset can occur in childhood, and in some cases there is a familial tendency.
Most patients with RLS have periodic limb movements (repetitive leg jerks or twitches). The clinical significance of periodic limb movements with no subjective disagreeable feelings in the limbs is controversial, and these cases usually are not treated.
The history usually confirms RLS. Order sleep studies only if you suspect a coexisting sleep problem or the diagnosis is unclear.
A suspected mechanism of restless legs is dopamine deficiency. Low serum ferritin levels have been associated with RLS—presumably because iron is a cofactor necessary for dopamine synthesis12—and may be diagnostically helpful.
The most common technique is to ask the patient to establish a consistent awakening time and a regular bedtime. Initially this could be unconventional by societal standards—such as bedtime at 5 AM and arising at 2 PM. After this pattern is in place, the patient gradually shifts the timing by 1 hour per day. Most patients find it easier to delay rather than advance the bedtime until it conforms to the desired time.
Reinforce this new sleep pattern with a structured daytime schedule that includes predictable mealtimes, regular exercise, social activities, and possibly bright light exposure. Provide reinforcement in the morning for patients with delayed sleep phase disorder and in the evening for advanced sleep phase disorder. These interventions take time and discipline.
Another approach is for the patient to skip sleep one night and, in a sleep-deprived state, establish a new bedtime at the desired time. Use the same modalities listed above to reinforce (“entrain”) this schedule; otherwise the patient will slip back into the previous abnormal sleep-wake rhythm.
Treatment can include iron repletion when indicated. Medications include dopaminergic agents, most notably pramipexole and levodopa/carbidopa. Other options include gabapentin, benzodiazepines, and narcotics.
Antidepressants have been suspected to worsen restless legs syndrome, but definitive studies are lacking.13
Circadian rhythm disorders
Instead of compromising the quality or quantity of sleep, circadian rhythm disorders cause sleep to occur at inappropriate times. These disorders are most common in adolescents and young adults.
Delayed sleep phase disorder—a persistent pattern of staying up late and “sleeping in”—is most common. Careful assessment will reveal that the patient is getting adequate sleep but at a socially unacceptable time, sometimes to the extreme that his or her nights and days are reversed.
Patients’ reluctance to acknowledge the severity of this problem can lead to inaccurate sleep diaries and interviews. A portable wrist actigraph can provide data about limb movement and is more objective than self-reports.
Delayed sleep phase disorder is highly comorbid with depressive disorders.14 The cause of this syndrome is unclear, but light exposure, social patterns, psychological issues, and possibly a genetic substrate are known to contribute.
Advanced sleep phase disorder—a less common circadian rhythm disorder—also can cause EDS. Patients have an inappropriately early time of sleep onset and then are fully awake in the middle of the night. A large family with a severe form of this disorder was found to have an abnormality on chromosome 2.15
Treatment. Relatively few treatments are effective for circadian rhythm disorders. Some patients elect not to pursue therapy, instead fitting activities around their unconventional sleep schedules.
Individuals with delayed sleep phase who cannot arrange their lives around their sleep schedules are at risk for poor early morning performance because of sleepiness. Their internal circadian clocks can be gradually readjusted with phototherapy or gradual shifting of the major sleep period (Box 3). Stimulants usually are not used, but hypnotics can sometimes help these patients fall asleep earlier.
Insufficient sleep syndrome
People attempting to “burn the candle at both ends” are at risk for developing insufficient sleep syndrome.16 In our 24/7 society, people trying to make do with less than the required 7.5 hours sleep per night may adversely affect their health. The problem is compounded for shift workers because of the difficulty in obtaining sufficient quality sleep during daylight hours.
Many patients do not seek treatment for fatigue or sleepiness because they are aware of their lifestyle choices. Still, they might develop psychological symptoms such as irritability, mood swings, and strained interpersonal relationships. These symptoms can prompt patients to request treatment.
Take a careful history that includes discussing the patient’s daily and weekly schedule. Avoid psychostimulants; instead, address the nonnegotiable need to get adequate sleep and challenge the patient to prioritize his or her activities around a full night’s sleep.
When to consider narcolepsy
Narcolepsy is a CNS disease characterized by abnormal regulation of REM sleep. EDS—the cardinal symptom—is often associated with cataplexy (75%), sleep paralysis (50%), vivid dreams, and insomnia, all of which interfere with REM phenomena. Narcolepsy affects 0.05% of the U.S. population and can lead to severe occupational, educational, and family disruption.
When you obtain a history that suggests narcolepsy, use the history, a sleep diary, or wrist actigraphy to document whether the patient is getting adequate sleep, with a consistent sleep/wake cycle. Next, consider referring the patient for polysomnography, primarily to rule out other causes of EDS such as sleep-disordered breathing. In some cases, REM latency on the overnight sleep study will be <20 minutes after sleep onset, which supports the diagnosis of narcolepsy.
A multiple sleep latency test (MSLT)—a diagnostic session in which the patient takes 4 to 5 daytime naps—is performed the following day. Narcolepsy is confirmed if the patient has a mean initial sleep latency of <10 minutes during these naps plus at least two REM episodes within 15 minutes after sleep onset.
The 4 most appropriate indications for an urgent sleep evaluation are:
- difficulty staying alert while driving
- nocturnal cardiac arrhythmias
- frequent observed apneas
- excessive daytime sleepiness (EDS) leading to academic or occupational problems.
Insurance companies usually cover a specialty sleep evaluation, particularly if the referring physician documents a suspicion of sleep-disordered breathing or EDS that jeopardizes safe driving.
Most patients with narcolepsy and cataplexy have undetectable cerebrospinal fluid levels of a neuropeptide called hypocretin or orexin.17 Hypocretin/orexin replacement therapy is a theoretical possibility, but for now treatment includes a combination of optimal sleep hygiene, psychostimulants, antidepressants, and hypnotics.
Other causes of EDS
EDS can also be caused by unrecognized alcohol dependence, inappropriate or excessive medication use, and depressive disorders. Overnight sleep studies are seldom indicated unless patients endorse the symptoms in the Figure.
Before pursuing polysomnography or an MSLT (Box 4), eliminate medications that might confound the results, such as:
- antidepressants, which alter the timing and duration of REM sleep
- sedating medications, which modify initial sleep latency and sleep efficiency and potentially aggravate sleep disordered breathing.
Initial REM latency provides a potential biologic marker of major depression but is used more often in research than in clinical psychiatry.
Primary insomnia is the distressing inability to sleep at night or nap during the day. It suggests a hyperarousal state—the opposite of EDS.18 In rare cases, however, patients who cannot sleep at night also have EDS. When evaluated, they typically endorse at least one symptom in the Figure. Sleep studies occasionally reveal OSA or restless legs syndrome.
Treating a patient with chronic insomnia may require several trials of behavioral interventions or sedating medications before you make a referral to a sleep disorder center. Patients can struggle with unrecognized primary sleep disorders for years, and many are given empiric trials of stimulating antidepressants. Antidepressants are unlikely to cause harm, but they might complicate diagnostic testing.
When you confirm coexisting depression and a primary sleep disorder, treatments that separately target each condition provide optimal management of the sleepy patient.
Medications to enhance wakefulness
Wake-promoting agents are a treatment option when EDS is contributing to compromised functioning. These drugs are no substitute for thoughtful evaluation of hypersomnolence, however. When you diagnose OSA or restless legs syndrome, first try treatments that target these conditions. If residual sleepiness persists, then consider augmenting with stimulating medications.
Modafinil is FDA-approved for residual sleepiness in patients with OSA and for shift work sleep disorder, a condition of circadian misalignment from frequent schedule changes. Evidence does not support its use for other circadian rhythm disorders, such as delayed sleep phase disorder.
Low-dose modafinil (such as 100 to 200 mg/d) is well tolerated, but its therapeutic effect as augmentation is modest.19 Increasing the dosage to >200 mg usually does not increase alertness.
Caffeine. Some patients report benefit from caffeine used in moderation and only in the morning. This practice is acceptable as long as patients do not use excessive amounts or experience insomnia, exacerbation of anxiety, or tachycardia.
Psychostimulants such as methylphenidate and amphetamines are less well-studied than modafinil for treating EDS in patients without narcolepsy. Monitor carefully for insomnia, exacerbation of anxiety, tachycardia, or hypertension and to prevent overuse of these habituating agents.
Related resources
- National Sleep Foundation. www.sleepfoundation.org.
- American Academy of Sleep Medicine. www.aasmnet.org.
- American Sleep Apnea Association. www.sleepapnea.org.
- Restless Legs Syndrome Foundation. www.rls.org.
- Association for the Study of Light Therapy and Biological Rhythms. www.sltbr.org.
Drug brand names
- Carbidopa/levodopa • Sinemet
- Gabapentin • Neurontin
- Modafinil • Provigil
- Pramipexole • Mirapex
- Trazodone • Desyrel
- Zolpidem • Ambien
Disclosure
Dr. Krahn reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgment
Dr. Krahn published the original version this article in the January 2002 issue of Current Psychiatry and has updated it for this issue.
1. Punjabi N, Haponik E. Ask about daytime sleepiness. J Amer Geriatr Soc 2000;48:228-9.
2. Ronald J, Delaive K, Roos L, et al. Health care utilization in the 10 years prior to diagnosis in obstructive sleep apnea syndrome patients. Sleep 1999;22(2):225-9.
3. Johns M. A new method for measuring daytime sleepiness: The Epworth Sleepiness Scale. Sleep 1991;14(6):540-5.
4. Rowley J, Aboussouan L, Badr M. The use of clinical prediction formulas in the evaluation of obstructive sleep apnea. Sleep 2000;23:929-38.
5. Yamashiro Y, Kryger M. Nocturnal oximetry: Is it a screening tool for sleep disorders? Sleep 1995;18:167-71.
6. Morrell M, Finn L, Kim H, et al. Sleep fragmentation, awake blood pressure, and sleep-disordered breathing in a population-based study. Am J Respir Critical Care Med 2000;162(6):2091-6.
7. Roux F, D’Ambrosio C, Mohsenin V. Sleep-related breathing disorders and cardiovascular disease. Am J Med. 2000;108:396-402.
8. Engleman H, Martin S, Deary I, Douglas N. Effect of continuous positive airway pressure treatment on daytime function in sleep apnoea/hypopnoea syndrome. Lancet 1994;343(8897):572-5.
9. Lojander J, Maasilta P, Partinen M, et al. Nasal-CPAP, surgery, and conservative management for treatment of obstructive sleep apnea syndrome. A randomized study. Chest. 1996;110(1):114-9.
10. Mehta A, Qian J, Petocz P, et al. A randomized, controlled study of a mandibular advancement splint for obstructive sleep apnea. Am J Respir Critical Care Med 2001;163(6):1457-61.
11. Chesson A, Wise M, Davila D, et al. Practice parameters for the treatment of restless legs syndrome and periodic limb movement disorder. An American Academy of Sleep Medicine Report. Standards of Practice Committee of the American Academy of Sleep Medicine. Sleep 1999;22(7):961-8.
12. Phillips B, Young T, Finn L, et al. Epidemiology of restless legs symptoms in adults. Arch Intern Med 2000;160(14):2137-41.
13. Thorpy M, Ehrenberg B, Hening W, et al. Restless legs syndrome: Detection and management in primary care. Amer Fam Phys 2000;62:108-14.
14. Regestein Q, Monk T. Delayed sleep phase syndrome: A review of its clinical aspects. Am J Psychiatry 1995;152:602-8.
15. Toh K, Jones C, He Y, et al. An hPer2 phosphorylation site mutation in familial advanced sleep phase syndrome. Science 2001;291(5506):1040-3.
16. Yoshikawa N, Suzuki S, Ishimoto T, et al. A case of insufficient sleep syndrome. Psychiatry Clin Neuro 1998;52(2):200-1.
17. Nishino S, Ripley B, Overeem S, et al. Hypocretin (orexin) deficiency in human narcolepsy. Lancet. 2000;355:39-40.
18. Hauri P, Esther M. Insomnia. Mayo Clin Proc 1990;65:869-82.
19. Schwartz JR. Modafinil: new indications for wake promotion. Expert Opin Pharmacother 2005;6(1):115-29.
Poor energy, hypersomnia, amotivation, irritability, and frustration can suggest depression or other psychiatric disorders to busy primary care physicians. As a result, psychiatrists often are referred patients with excessive daytime sleepiness (EDS) caused by undiagnosed primary sleep disorders.
Physicians may miss obstructive sleep apnea (OSA), restless legs syndrome, circadian rhythm disorders, or narcolepsy because:
- many have little training in sleep disorders and limited time to diagnose them1
- patients do not report sleepiness or recognize it as a legitimate medical concern
- definitive diagnostic tests are expensive and usually are not ordered.
Psychiatrists, therefore, need a clear understanding of the EDS differential diagnosis to determine whether a patient’s behavioral symptoms are a sleep or psychiatric issue.
How likely are you to doze off or fall asleep in the following situations, in contrast to feeling just tired? This refers to your usual way of life in recent times. Even if you have not done some of these things recently, try to work out how each situation would affect you now. Use the scale below to choose the most appropriate number for each situation:
0 no chance of dozing
1 slight chance of dozing
2 moderate chance of dozing
3 high chance of dozing
Chance of dozing Situation
Sitting and reading
Watching TV
Sitting inactive in a public place (such as in a theater or a meeting)
As a passenger in a car for an hour without a break
Lying down to rest in the afternoon when circumstances permit
Sitting and talking to someone
Sitting quietly after a lunch without alcohol
In a car, while stopped for a few minutes in traffic
Scoring key
1 to 6 Getting enough sleep
7 to 8 Average
>8 Seek a sleep specialist’s advice without delay
Assessing the sleepy patient
Sleepiness is an inability to stay awake at appropriate times. Fatigue, by comparison, does not involve sleepiness but very low energy associated with wakefulness. In general, sleepy patients get transient relief from napping, whereas fatigued patients report they cannot fall asleep.
Untreated EDS results in compromised quality of life, reduced productivity, and public safety concerns such as falling asleep while driving.2 Sleep complaints fall into three major categories:
- EDS
- insomnia (marked by distress because of poor sleep, but usually with minimal EDS)
- unusual nocturnal behaviors (ranging from arm waving to violent behaviors.
When you evaluate a patient with sleep complaints, valuable sources of data include observation, questionnaires, and screening devices. The most important may be common sense.
Observation. Observe the patient in the waiting room or office before starting the interview. Did he or she nod off while waiting to see you? Pay attention to anyone who appears sleepy—even those who deny having trouble staying awake. Over time, sleepy patients can lose their perspective on alertness. Some have had EDS so long that they no longer recall what it is like to feel fully awake.
Collateral history often is important because family members probably have observed the sleeping patient. The bed partner can provide information about snoring, irregular breathing, leg kicks, unplanned naps, and strained interpersonal relationships because of EDS. For the patient without a bed partner, consider interviewing a travel companion.
Questionnaires. Few useful screening tests exist for sleepiness; most are neither reliable nor valid. One of the better questionnaires—the Epworth Sleepiness Scale (Box 1)—helps confirm the presence of sleepiness with a score >8, differentiating the inability to stay awake from fatigue. This brief questionnaire also provides a useful measure of sleepiness severity.3
The Epworth scale’s value is limited because its questions of specific time and context might not represent a patient’s experiences. Additional validated surveys include the Pittsburgh Sleep Quality Inventory and several for sleep apnea.4
Screening. Electroencephalographic (EEG) monitoring can accurately measure the patient’s degree of sleep disruption. This information is key to understanding if a patient’s EDS is caused by a physiologic condition that prevents quality nocturnal sleep.
None of the widely used screening devices that assess leg kicks indicate the presence of possible periodic limb movements.
Overnight pulse oximetry has been used to screen for sleep-disordered breathing5 but also has limitations:
- Most pulse oximeters do not provide information about sleep stage or body position.
- Patients with sleep-disordered breathing can lack adequate oxygen desaturations but have frequent EEG arousals related to sleep issues. Because EEG data are not collected during arousals, pulse oximetry would generate a false-negative result in this scenario, which occurs most often in female and thin patients.
- Oximetry provides only oxygen saturation data and possibly heart rate, whereas other physiologic processes such as body movement or sleep architecture can be disrupted repetitively during sleep.
Common sense. The most productive tools for detecting sleep disorders are intuition and common sense. The Figure suggests sequential questions that might uncover specific sleep disorders. Then the decision whether to refer the patient to a sleep disorder center for diagnostic testing depends on the type of sleep disorder you detect.
Nasal continuous positive airway pressure
(CPAP) should be started in an observed setting so that the clinician can determine the optimal amount of positive pressure needed to keep the upper airway patent.
For some patients, CPAP is started in the second half of a “split-night” sleep study after a diagnosis of obstructive sleep apnea (OSA) is made. Other patients return a second night for a nasal CPAP trial. Those with severe OSA might notice improved sleep quality and reduced EDS after only a few hours of CPAP use. Some wish to start CPAP treatment immediately.
Advances in masks and equipment have improved patient adherence to CPAP. Innovations include auto-titrating machines, in which the pressure level can be varied depending on sleep state or body position. Many machines include a data microchip that allows the clinician to determine duration of usage, then use that information to counsel the patient about adherence, if necessary.
Patient education also can promote CPAP adherence. When patients are first told they might need to sleep each night wearing a nasal mask, they often voice well-founded concerns about comfort, claustrophobia, or sexual activity.
Obtaining the support of the bed partner by welcoming her or him to all appointments, including educational activities, is optimal. The bed partner’s concerns about the patient’s excessive snoring or apneas probably were the impetus for the appointment in the first place.
Medication. Some patients benefit from 1 to 2 weeks of a sleeping medication such as zolpidem or trazodone while they acclimate to using nasal CPAP.
Figure The sleepy patient: Possible medical and psychiatric explanations
* Supportive factors: Persuasive if present, but if absent do not exclude possible conditions
Obstructive sleep apnea
Because OSA affects at least 4% of men and 2% of women,6 you are virtually assured of seeing undiagnosed patients. OSA is caused by repeated collapse of the soft tissues surrounding the upper airway, decreasing airflow that is restored when the patient briefly awakens. Patients develop EDS because sleep is fragmented by frequent arousals.
Obese patients, because of their body habitus, are at higher risk for OSA than patients at normal weight. Carefully screen patients for OSA if they develop weight problems while taking psychotropics, such as antipsychotics.
Alcohol or sedatives used at bedtime can aggravate OSA. These substances promote muscle relaxation and increase the arousal threshold so that patients do not awaken readily when apneas occur.
Long-term complications of untreated OSA include sleepiness leading to accidents, hypertension, cerebrovascular disease, and progressive obesity. Data also associate OSA with cardiovascular complications such as arrhythmias, congestive heart failure, and myocardial infarction.7
Physical examination focuses on detecting:
- nasal obstruction (have patient sniff separately through each nostril)
- large neck
- crowded oropharynx (low-hanging palate, reddened uvula, enlarged tonsils, large tongue relative to oropharynx diameter)
- jaw structure (particularly a small, retrognathic mandible).
Sleep studies. Referral for nocturnal polysomnography might be the next step. A comprehensive sleep study collects data about respiratory, cardiovascular, and muscle activity at night, as well as the sounds the patient makes—such as snoring or coughing—when asleep. EEG monitoring also is performed. OSA may be diagnosed if repeated episodes of reduced airflow and oxygen desaturation (arousals) are observed as brief shifts in EEG frequency.
Treatment. First-line interventions for the patient with OSA include:
- no alcohol 1 to 2 hours before bedtime
- sleeping on the side instead of the back
- weight loss (ideally with exercise)
- nasal sprays for allergies.
If first-line treatments are ineffective, nasal continuous positive airway pressure (CPAP) works well for most patients who adhere to the regimen.8 CPAP requires the patient to wear a nasal mask that delivers room air, splinting open the nasopharynx and upper airway (Box 2).
Surgical options. The most common surgeries for OSA are uvulopalatopharyngoplasty and laser-assisted uvulopalatoplasty. Others include tongue reduction and mandibular advancement.
The response rate to surgery averages 50%, depending on patient characteristics and procedure.9 Positive outcomes are most likely for thin patients with obvious upper airway obstruction, including deviated nasal septum, large tonsils, low-hanging palate, and large uvula. Postsurgical complications include nasal regurgitation, voice change, pain, bleeding, infection, tongue numbness, and snoring without apnea (silent apnea).
Oral appliances open the oropharynx by moving the mandible and tongue out of way. Patients with mild to moderate OSA accept these devices well. Evidence suggests that oral appliances improve sleep and reduce EDS more effectively than nasal CPAP and are preferred by patients.10
Oral devices have drawbacks, however. In most settings, their effectiveness cannot be observed during a “split-night” laboratory sleep study because the patient has not yet purchased the device. Also, multiple visits sometimes are required to custom-fit the appliance; this can pose a hardship for patients who live a distance from the provider.
Restless legs syndrome
Patients with restless legs syndrome (RLS) typically report a restless, painful feeling in the limbs that occurs in the evening and at night, disrupting sleep. This condition—which affects 10% of the population—is associated with aging, blood loss, anemia, peripheral neuropathies, and pregnancy.11 Onset can occur in childhood, and in some cases there is a familial tendency.
Most patients with RLS have periodic limb movements (repetitive leg jerks or twitches). The clinical significance of periodic limb movements with no subjective disagreeable feelings in the limbs is controversial, and these cases usually are not treated.
The history usually confirms RLS. Order sleep studies only if you suspect a coexisting sleep problem or the diagnosis is unclear.
A suspected mechanism of restless legs is dopamine deficiency. Low serum ferritin levels have been associated with RLS—presumably because iron is a cofactor necessary for dopamine synthesis12—and may be diagnostically helpful.
The most common technique is to ask the patient to establish a consistent awakening time and a regular bedtime. Initially this could be unconventional by societal standards—such as bedtime at 5 AM and arising at 2 PM. After this pattern is in place, the patient gradually shifts the timing by 1 hour per day. Most patients find it easier to delay rather than advance the bedtime until it conforms to the desired time.
Reinforce this new sleep pattern with a structured daytime schedule that includes predictable mealtimes, regular exercise, social activities, and possibly bright light exposure. Provide reinforcement in the morning for patients with delayed sleep phase disorder and in the evening for advanced sleep phase disorder. These interventions take time and discipline.
Another approach is for the patient to skip sleep one night and, in a sleep-deprived state, establish a new bedtime at the desired time. Use the same modalities listed above to reinforce (“entrain”) this schedule; otherwise the patient will slip back into the previous abnormal sleep-wake rhythm.
Treatment can include iron repletion when indicated. Medications include dopaminergic agents, most notably pramipexole and levodopa/carbidopa. Other options include gabapentin, benzodiazepines, and narcotics.
Antidepressants have been suspected to worsen restless legs syndrome, but definitive studies are lacking.13
Circadian rhythm disorders
Instead of compromising the quality or quantity of sleep, circadian rhythm disorders cause sleep to occur at inappropriate times. These disorders are most common in adolescents and young adults.
Delayed sleep phase disorder—a persistent pattern of staying up late and “sleeping in”—is most common. Careful assessment will reveal that the patient is getting adequate sleep but at a socially unacceptable time, sometimes to the extreme that his or her nights and days are reversed.
Patients’ reluctance to acknowledge the severity of this problem can lead to inaccurate sleep diaries and interviews. A portable wrist actigraph can provide data about limb movement and is more objective than self-reports.
Delayed sleep phase disorder is highly comorbid with depressive disorders.14 The cause of this syndrome is unclear, but light exposure, social patterns, psychological issues, and possibly a genetic substrate are known to contribute.
Advanced sleep phase disorder—a less common circadian rhythm disorder—also can cause EDS. Patients have an inappropriately early time of sleep onset and then are fully awake in the middle of the night. A large family with a severe form of this disorder was found to have an abnormality on chromosome 2.15
Treatment. Relatively few treatments are effective for circadian rhythm disorders. Some patients elect not to pursue therapy, instead fitting activities around their unconventional sleep schedules.
Individuals with delayed sleep phase who cannot arrange their lives around their sleep schedules are at risk for poor early morning performance because of sleepiness. Their internal circadian clocks can be gradually readjusted with phototherapy or gradual shifting of the major sleep period (Box 3). Stimulants usually are not used, but hypnotics can sometimes help these patients fall asleep earlier.
Insufficient sleep syndrome
People attempting to “burn the candle at both ends” are at risk for developing insufficient sleep syndrome.16 In our 24/7 society, people trying to make do with less than the required 7.5 hours sleep per night may adversely affect their health. The problem is compounded for shift workers because of the difficulty in obtaining sufficient quality sleep during daylight hours.
Many patients do not seek treatment for fatigue or sleepiness because they are aware of their lifestyle choices. Still, they might develop psychological symptoms such as irritability, mood swings, and strained interpersonal relationships. These symptoms can prompt patients to request treatment.
Take a careful history that includes discussing the patient’s daily and weekly schedule. Avoid psychostimulants; instead, address the nonnegotiable need to get adequate sleep and challenge the patient to prioritize his or her activities around a full night’s sleep.
When to consider narcolepsy
Narcolepsy is a CNS disease characterized by abnormal regulation of REM sleep. EDS—the cardinal symptom—is often associated with cataplexy (75%), sleep paralysis (50%), vivid dreams, and insomnia, all of which interfere with REM phenomena. Narcolepsy affects 0.05% of the U.S. population and can lead to severe occupational, educational, and family disruption.
When you obtain a history that suggests narcolepsy, use the history, a sleep diary, or wrist actigraphy to document whether the patient is getting adequate sleep, with a consistent sleep/wake cycle. Next, consider referring the patient for polysomnography, primarily to rule out other causes of EDS such as sleep-disordered breathing. In some cases, REM latency on the overnight sleep study will be <20 minutes after sleep onset, which supports the diagnosis of narcolepsy.
A multiple sleep latency test (MSLT)—a diagnostic session in which the patient takes 4 to 5 daytime naps—is performed the following day. Narcolepsy is confirmed if the patient has a mean initial sleep latency of <10 minutes during these naps plus at least two REM episodes within 15 minutes after sleep onset.
The 4 most appropriate indications for an urgent sleep evaluation are:
- difficulty staying alert while driving
- nocturnal cardiac arrhythmias
- frequent observed apneas
- excessive daytime sleepiness (EDS) leading to academic or occupational problems.
Insurance companies usually cover a specialty sleep evaluation, particularly if the referring physician documents a suspicion of sleep-disordered breathing or EDS that jeopardizes safe driving.
Most patients with narcolepsy and cataplexy have undetectable cerebrospinal fluid levels of a neuropeptide called hypocretin or orexin.17 Hypocretin/orexin replacement therapy is a theoretical possibility, but for now treatment includes a combination of optimal sleep hygiene, psychostimulants, antidepressants, and hypnotics.
Other causes of EDS
EDS can also be caused by unrecognized alcohol dependence, inappropriate or excessive medication use, and depressive disorders. Overnight sleep studies are seldom indicated unless patients endorse the symptoms in the Figure.
Before pursuing polysomnography or an MSLT (Box 4), eliminate medications that might confound the results, such as:
- antidepressants, which alter the timing and duration of REM sleep
- sedating medications, which modify initial sleep latency and sleep efficiency and potentially aggravate sleep disordered breathing.
Initial REM latency provides a potential biologic marker of major depression but is used more often in research than in clinical psychiatry.
Primary insomnia is the distressing inability to sleep at night or nap during the day. It suggests a hyperarousal state—the opposite of EDS.18 In rare cases, however, patients who cannot sleep at night also have EDS. When evaluated, they typically endorse at least one symptom in the Figure. Sleep studies occasionally reveal OSA or restless legs syndrome.
Treating a patient with chronic insomnia may require several trials of behavioral interventions or sedating medications before you make a referral to a sleep disorder center. Patients can struggle with unrecognized primary sleep disorders for years, and many are given empiric trials of stimulating antidepressants. Antidepressants are unlikely to cause harm, but they might complicate diagnostic testing.
When you confirm coexisting depression and a primary sleep disorder, treatments that separately target each condition provide optimal management of the sleepy patient.
Medications to enhance wakefulness
Wake-promoting agents are a treatment option when EDS is contributing to compromised functioning. These drugs are no substitute for thoughtful evaluation of hypersomnolence, however. When you diagnose OSA or restless legs syndrome, first try treatments that target these conditions. If residual sleepiness persists, then consider augmenting with stimulating medications.
Modafinil is FDA-approved for residual sleepiness in patients with OSA and for shift work sleep disorder, a condition of circadian misalignment from frequent schedule changes. Evidence does not support its use for other circadian rhythm disorders, such as delayed sleep phase disorder.
Low-dose modafinil (such as 100 to 200 mg/d) is well tolerated, but its therapeutic effect as augmentation is modest.19 Increasing the dosage to >200 mg usually does not increase alertness.
Caffeine. Some patients report benefit from caffeine used in moderation and only in the morning. This practice is acceptable as long as patients do not use excessive amounts or experience insomnia, exacerbation of anxiety, or tachycardia.
Psychostimulants such as methylphenidate and amphetamines are less well-studied than modafinil for treating EDS in patients without narcolepsy. Monitor carefully for insomnia, exacerbation of anxiety, tachycardia, or hypertension and to prevent overuse of these habituating agents.
Related resources
- National Sleep Foundation. www.sleepfoundation.org.
- American Academy of Sleep Medicine. www.aasmnet.org.
- American Sleep Apnea Association. www.sleepapnea.org.
- Restless Legs Syndrome Foundation. www.rls.org.
- Association for the Study of Light Therapy and Biological Rhythms. www.sltbr.org.
Drug brand names
- Carbidopa/levodopa • Sinemet
- Gabapentin • Neurontin
- Modafinil • Provigil
- Pramipexole • Mirapex
- Trazodone • Desyrel
- Zolpidem • Ambien
Disclosure
Dr. Krahn reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgment
Dr. Krahn published the original version this article in the January 2002 issue of Current Psychiatry and has updated it for this issue.
Poor energy, hypersomnia, amotivation, irritability, and frustration can suggest depression or other psychiatric disorders to busy primary care physicians. As a result, psychiatrists often are referred patients with excessive daytime sleepiness (EDS) caused by undiagnosed primary sleep disorders.
Physicians may miss obstructive sleep apnea (OSA), restless legs syndrome, circadian rhythm disorders, or narcolepsy because:
- many have little training in sleep disorders and limited time to diagnose them1
- patients do not report sleepiness or recognize it as a legitimate medical concern
- definitive diagnostic tests are expensive and usually are not ordered.
Psychiatrists, therefore, need a clear understanding of the EDS differential diagnosis to determine whether a patient’s behavioral symptoms are a sleep or psychiatric issue.
How likely are you to doze off or fall asleep in the following situations, in contrast to feeling just tired? This refers to your usual way of life in recent times. Even if you have not done some of these things recently, try to work out how each situation would affect you now. Use the scale below to choose the most appropriate number for each situation:
0 no chance of dozing
1 slight chance of dozing
2 moderate chance of dozing
3 high chance of dozing
Chance of dozing Situation
Sitting and reading
Watching TV
Sitting inactive in a public place (such as in a theater or a meeting)
As a passenger in a car for an hour without a break
Lying down to rest in the afternoon when circumstances permit
Sitting and talking to someone
Sitting quietly after a lunch without alcohol
In a car, while stopped for a few minutes in traffic
Scoring key
1 to 6 Getting enough sleep
7 to 8 Average
>8 Seek a sleep specialist’s advice without delay
Assessing the sleepy patient
Sleepiness is an inability to stay awake at appropriate times. Fatigue, by comparison, does not involve sleepiness but very low energy associated with wakefulness. In general, sleepy patients get transient relief from napping, whereas fatigued patients report they cannot fall asleep.
Untreated EDS results in compromised quality of life, reduced productivity, and public safety concerns such as falling asleep while driving.2 Sleep complaints fall into three major categories:
- EDS
- insomnia (marked by distress because of poor sleep, but usually with minimal EDS)
- unusual nocturnal behaviors (ranging from arm waving to violent behaviors.
When you evaluate a patient with sleep complaints, valuable sources of data include observation, questionnaires, and screening devices. The most important may be common sense.
Observation. Observe the patient in the waiting room or office before starting the interview. Did he or she nod off while waiting to see you? Pay attention to anyone who appears sleepy—even those who deny having trouble staying awake. Over time, sleepy patients can lose their perspective on alertness. Some have had EDS so long that they no longer recall what it is like to feel fully awake.
Collateral history often is important because family members probably have observed the sleeping patient. The bed partner can provide information about snoring, irregular breathing, leg kicks, unplanned naps, and strained interpersonal relationships because of EDS. For the patient without a bed partner, consider interviewing a travel companion.
Questionnaires. Few useful screening tests exist for sleepiness; most are neither reliable nor valid. One of the better questionnaires—the Epworth Sleepiness Scale (Box 1)—helps confirm the presence of sleepiness with a score >8, differentiating the inability to stay awake from fatigue. This brief questionnaire also provides a useful measure of sleepiness severity.3
The Epworth scale’s value is limited because its questions of specific time and context might not represent a patient’s experiences. Additional validated surveys include the Pittsburgh Sleep Quality Inventory and several for sleep apnea.4
Screening. Electroencephalographic (EEG) monitoring can accurately measure the patient’s degree of sleep disruption. This information is key to understanding if a patient’s EDS is caused by a physiologic condition that prevents quality nocturnal sleep.
None of the widely used screening devices that assess leg kicks indicate the presence of possible periodic limb movements.
Overnight pulse oximetry has been used to screen for sleep-disordered breathing5 but also has limitations:
- Most pulse oximeters do not provide information about sleep stage or body position.
- Patients with sleep-disordered breathing can lack adequate oxygen desaturations but have frequent EEG arousals related to sleep issues. Because EEG data are not collected during arousals, pulse oximetry would generate a false-negative result in this scenario, which occurs most often in female and thin patients.
- Oximetry provides only oxygen saturation data and possibly heart rate, whereas other physiologic processes such as body movement or sleep architecture can be disrupted repetitively during sleep.
Common sense. The most productive tools for detecting sleep disorders are intuition and common sense. The Figure suggests sequential questions that might uncover specific sleep disorders. Then the decision whether to refer the patient to a sleep disorder center for diagnostic testing depends on the type of sleep disorder you detect.
Nasal continuous positive airway pressure
(CPAP) should be started in an observed setting so that the clinician can determine the optimal amount of positive pressure needed to keep the upper airway patent.
For some patients, CPAP is started in the second half of a “split-night” sleep study after a diagnosis of obstructive sleep apnea (OSA) is made. Other patients return a second night for a nasal CPAP trial. Those with severe OSA might notice improved sleep quality and reduced EDS after only a few hours of CPAP use. Some wish to start CPAP treatment immediately.
Advances in masks and equipment have improved patient adherence to CPAP. Innovations include auto-titrating machines, in which the pressure level can be varied depending on sleep state or body position. Many machines include a data microchip that allows the clinician to determine duration of usage, then use that information to counsel the patient about adherence, if necessary.
Patient education also can promote CPAP adherence. When patients are first told they might need to sleep each night wearing a nasal mask, they often voice well-founded concerns about comfort, claustrophobia, or sexual activity.
Obtaining the support of the bed partner by welcoming her or him to all appointments, including educational activities, is optimal. The bed partner’s concerns about the patient’s excessive snoring or apneas probably were the impetus for the appointment in the first place.
Medication. Some patients benefit from 1 to 2 weeks of a sleeping medication such as zolpidem or trazodone while they acclimate to using nasal CPAP.
Figure The sleepy patient: Possible medical and psychiatric explanations
* Supportive factors: Persuasive if present, but if absent do not exclude possible conditions
Obstructive sleep apnea
Because OSA affects at least 4% of men and 2% of women,6 you are virtually assured of seeing undiagnosed patients. OSA is caused by repeated collapse of the soft tissues surrounding the upper airway, decreasing airflow that is restored when the patient briefly awakens. Patients develop EDS because sleep is fragmented by frequent arousals.
Obese patients, because of their body habitus, are at higher risk for OSA than patients at normal weight. Carefully screen patients for OSA if they develop weight problems while taking psychotropics, such as antipsychotics.
Alcohol or sedatives used at bedtime can aggravate OSA. These substances promote muscle relaxation and increase the arousal threshold so that patients do not awaken readily when apneas occur.
Long-term complications of untreated OSA include sleepiness leading to accidents, hypertension, cerebrovascular disease, and progressive obesity. Data also associate OSA with cardiovascular complications such as arrhythmias, congestive heart failure, and myocardial infarction.7
Physical examination focuses on detecting:
- nasal obstruction (have patient sniff separately through each nostril)
- large neck
- crowded oropharynx (low-hanging palate, reddened uvula, enlarged tonsils, large tongue relative to oropharynx diameter)
- jaw structure (particularly a small, retrognathic mandible).
Sleep studies. Referral for nocturnal polysomnography might be the next step. A comprehensive sleep study collects data about respiratory, cardiovascular, and muscle activity at night, as well as the sounds the patient makes—such as snoring or coughing—when asleep. EEG monitoring also is performed. OSA may be diagnosed if repeated episodes of reduced airflow and oxygen desaturation (arousals) are observed as brief shifts in EEG frequency.
Treatment. First-line interventions for the patient with OSA include:
- no alcohol 1 to 2 hours before bedtime
- sleeping on the side instead of the back
- weight loss (ideally with exercise)
- nasal sprays for allergies.
If first-line treatments are ineffective, nasal continuous positive airway pressure (CPAP) works well for most patients who adhere to the regimen.8 CPAP requires the patient to wear a nasal mask that delivers room air, splinting open the nasopharynx and upper airway (Box 2).
Surgical options. The most common surgeries for OSA are uvulopalatopharyngoplasty and laser-assisted uvulopalatoplasty. Others include tongue reduction and mandibular advancement.
The response rate to surgery averages 50%, depending on patient characteristics and procedure.9 Positive outcomes are most likely for thin patients with obvious upper airway obstruction, including deviated nasal septum, large tonsils, low-hanging palate, and large uvula. Postsurgical complications include nasal regurgitation, voice change, pain, bleeding, infection, tongue numbness, and snoring without apnea (silent apnea).
Oral appliances open the oropharynx by moving the mandible and tongue out of way. Patients with mild to moderate OSA accept these devices well. Evidence suggests that oral appliances improve sleep and reduce EDS more effectively than nasal CPAP and are preferred by patients.10
Oral devices have drawbacks, however. In most settings, their effectiveness cannot be observed during a “split-night” laboratory sleep study because the patient has not yet purchased the device. Also, multiple visits sometimes are required to custom-fit the appliance; this can pose a hardship for patients who live a distance from the provider.
Restless legs syndrome
Patients with restless legs syndrome (RLS) typically report a restless, painful feeling in the limbs that occurs in the evening and at night, disrupting sleep. This condition—which affects 10% of the population—is associated with aging, blood loss, anemia, peripheral neuropathies, and pregnancy.11 Onset can occur in childhood, and in some cases there is a familial tendency.
Most patients with RLS have periodic limb movements (repetitive leg jerks or twitches). The clinical significance of periodic limb movements with no subjective disagreeable feelings in the limbs is controversial, and these cases usually are not treated.
The history usually confirms RLS. Order sleep studies only if you suspect a coexisting sleep problem or the diagnosis is unclear.
A suspected mechanism of restless legs is dopamine deficiency. Low serum ferritin levels have been associated with RLS—presumably because iron is a cofactor necessary for dopamine synthesis12—and may be diagnostically helpful.
The most common technique is to ask the patient to establish a consistent awakening time and a regular bedtime. Initially this could be unconventional by societal standards—such as bedtime at 5 AM and arising at 2 PM. After this pattern is in place, the patient gradually shifts the timing by 1 hour per day. Most patients find it easier to delay rather than advance the bedtime until it conforms to the desired time.
Reinforce this new sleep pattern with a structured daytime schedule that includes predictable mealtimes, regular exercise, social activities, and possibly bright light exposure. Provide reinforcement in the morning for patients with delayed sleep phase disorder and in the evening for advanced sleep phase disorder. These interventions take time and discipline.
Another approach is for the patient to skip sleep one night and, in a sleep-deprived state, establish a new bedtime at the desired time. Use the same modalities listed above to reinforce (“entrain”) this schedule; otherwise the patient will slip back into the previous abnormal sleep-wake rhythm.
Treatment can include iron repletion when indicated. Medications include dopaminergic agents, most notably pramipexole and levodopa/carbidopa. Other options include gabapentin, benzodiazepines, and narcotics.
Antidepressants have been suspected to worsen restless legs syndrome, but definitive studies are lacking.13
Circadian rhythm disorders
Instead of compromising the quality or quantity of sleep, circadian rhythm disorders cause sleep to occur at inappropriate times. These disorders are most common in adolescents and young adults.
Delayed sleep phase disorder—a persistent pattern of staying up late and “sleeping in”—is most common. Careful assessment will reveal that the patient is getting adequate sleep but at a socially unacceptable time, sometimes to the extreme that his or her nights and days are reversed.
Patients’ reluctance to acknowledge the severity of this problem can lead to inaccurate sleep diaries and interviews. A portable wrist actigraph can provide data about limb movement and is more objective than self-reports.
Delayed sleep phase disorder is highly comorbid with depressive disorders.14 The cause of this syndrome is unclear, but light exposure, social patterns, psychological issues, and possibly a genetic substrate are known to contribute.
Advanced sleep phase disorder—a less common circadian rhythm disorder—also can cause EDS. Patients have an inappropriately early time of sleep onset and then are fully awake in the middle of the night. A large family with a severe form of this disorder was found to have an abnormality on chromosome 2.15
Treatment. Relatively few treatments are effective for circadian rhythm disorders. Some patients elect not to pursue therapy, instead fitting activities around their unconventional sleep schedules.
Individuals with delayed sleep phase who cannot arrange their lives around their sleep schedules are at risk for poor early morning performance because of sleepiness. Their internal circadian clocks can be gradually readjusted with phototherapy or gradual shifting of the major sleep period (Box 3). Stimulants usually are not used, but hypnotics can sometimes help these patients fall asleep earlier.
Insufficient sleep syndrome
People attempting to “burn the candle at both ends” are at risk for developing insufficient sleep syndrome.16 In our 24/7 society, people trying to make do with less than the required 7.5 hours sleep per night may adversely affect their health. The problem is compounded for shift workers because of the difficulty in obtaining sufficient quality sleep during daylight hours.
Many patients do not seek treatment for fatigue or sleepiness because they are aware of their lifestyle choices. Still, they might develop psychological symptoms such as irritability, mood swings, and strained interpersonal relationships. These symptoms can prompt patients to request treatment.
Take a careful history that includes discussing the patient’s daily and weekly schedule. Avoid psychostimulants; instead, address the nonnegotiable need to get adequate sleep and challenge the patient to prioritize his or her activities around a full night’s sleep.
When to consider narcolepsy
Narcolepsy is a CNS disease characterized by abnormal regulation of REM sleep. EDS—the cardinal symptom—is often associated with cataplexy (75%), sleep paralysis (50%), vivid dreams, and insomnia, all of which interfere with REM phenomena. Narcolepsy affects 0.05% of the U.S. population and can lead to severe occupational, educational, and family disruption.
When you obtain a history that suggests narcolepsy, use the history, a sleep diary, or wrist actigraphy to document whether the patient is getting adequate sleep, with a consistent sleep/wake cycle. Next, consider referring the patient for polysomnography, primarily to rule out other causes of EDS such as sleep-disordered breathing. In some cases, REM latency on the overnight sleep study will be <20 minutes after sleep onset, which supports the diagnosis of narcolepsy.
A multiple sleep latency test (MSLT)—a diagnostic session in which the patient takes 4 to 5 daytime naps—is performed the following day. Narcolepsy is confirmed if the patient has a mean initial sleep latency of <10 minutes during these naps plus at least two REM episodes within 15 minutes after sleep onset.
The 4 most appropriate indications for an urgent sleep evaluation are:
- difficulty staying alert while driving
- nocturnal cardiac arrhythmias
- frequent observed apneas
- excessive daytime sleepiness (EDS) leading to academic or occupational problems.
Insurance companies usually cover a specialty sleep evaluation, particularly if the referring physician documents a suspicion of sleep-disordered breathing or EDS that jeopardizes safe driving.
Most patients with narcolepsy and cataplexy have undetectable cerebrospinal fluid levels of a neuropeptide called hypocretin or orexin.17 Hypocretin/orexin replacement therapy is a theoretical possibility, but for now treatment includes a combination of optimal sleep hygiene, psychostimulants, antidepressants, and hypnotics.
Other causes of EDS
EDS can also be caused by unrecognized alcohol dependence, inappropriate or excessive medication use, and depressive disorders. Overnight sleep studies are seldom indicated unless patients endorse the symptoms in the Figure.
Before pursuing polysomnography or an MSLT (Box 4), eliminate medications that might confound the results, such as:
- antidepressants, which alter the timing and duration of REM sleep
- sedating medications, which modify initial sleep latency and sleep efficiency and potentially aggravate sleep disordered breathing.
Initial REM latency provides a potential biologic marker of major depression but is used more often in research than in clinical psychiatry.
Primary insomnia is the distressing inability to sleep at night or nap during the day. It suggests a hyperarousal state—the opposite of EDS.18 In rare cases, however, patients who cannot sleep at night also have EDS. When evaluated, they typically endorse at least one symptom in the Figure. Sleep studies occasionally reveal OSA or restless legs syndrome.
Treating a patient with chronic insomnia may require several trials of behavioral interventions or sedating medications before you make a referral to a sleep disorder center. Patients can struggle with unrecognized primary sleep disorders for years, and many are given empiric trials of stimulating antidepressants. Antidepressants are unlikely to cause harm, but they might complicate diagnostic testing.
When you confirm coexisting depression and a primary sleep disorder, treatments that separately target each condition provide optimal management of the sleepy patient.
Medications to enhance wakefulness
Wake-promoting agents are a treatment option when EDS is contributing to compromised functioning. These drugs are no substitute for thoughtful evaluation of hypersomnolence, however. When you diagnose OSA or restless legs syndrome, first try treatments that target these conditions. If residual sleepiness persists, then consider augmenting with stimulating medications.
Modafinil is FDA-approved for residual sleepiness in patients with OSA and for shift work sleep disorder, a condition of circadian misalignment from frequent schedule changes. Evidence does not support its use for other circadian rhythm disorders, such as delayed sleep phase disorder.
Low-dose modafinil (such as 100 to 200 mg/d) is well tolerated, but its therapeutic effect as augmentation is modest.19 Increasing the dosage to >200 mg usually does not increase alertness.
Caffeine. Some patients report benefit from caffeine used in moderation and only in the morning. This practice is acceptable as long as patients do not use excessive amounts or experience insomnia, exacerbation of anxiety, or tachycardia.
Psychostimulants such as methylphenidate and amphetamines are less well-studied than modafinil for treating EDS in patients without narcolepsy. Monitor carefully for insomnia, exacerbation of anxiety, tachycardia, or hypertension and to prevent overuse of these habituating agents.
Related resources
- National Sleep Foundation. www.sleepfoundation.org.
- American Academy of Sleep Medicine. www.aasmnet.org.
- American Sleep Apnea Association. www.sleepapnea.org.
- Restless Legs Syndrome Foundation. www.rls.org.
- Association for the Study of Light Therapy and Biological Rhythms. www.sltbr.org.
Drug brand names
- Carbidopa/levodopa • Sinemet
- Gabapentin • Neurontin
- Modafinil • Provigil
- Pramipexole • Mirapex
- Trazodone • Desyrel
- Zolpidem • Ambien
Disclosure
Dr. Krahn reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgment
Dr. Krahn published the original version this article in the January 2002 issue of Current Psychiatry and has updated it for this issue.
1. Punjabi N, Haponik E. Ask about daytime sleepiness. J Amer Geriatr Soc 2000;48:228-9.
2. Ronald J, Delaive K, Roos L, et al. Health care utilization in the 10 years prior to diagnosis in obstructive sleep apnea syndrome patients. Sleep 1999;22(2):225-9.
3. Johns M. A new method for measuring daytime sleepiness: The Epworth Sleepiness Scale. Sleep 1991;14(6):540-5.
4. Rowley J, Aboussouan L, Badr M. The use of clinical prediction formulas in the evaluation of obstructive sleep apnea. Sleep 2000;23:929-38.
5. Yamashiro Y, Kryger M. Nocturnal oximetry: Is it a screening tool for sleep disorders? Sleep 1995;18:167-71.
6. Morrell M, Finn L, Kim H, et al. Sleep fragmentation, awake blood pressure, and sleep-disordered breathing in a population-based study. Am J Respir Critical Care Med 2000;162(6):2091-6.
7. Roux F, D’Ambrosio C, Mohsenin V. Sleep-related breathing disorders and cardiovascular disease. Am J Med. 2000;108:396-402.
8. Engleman H, Martin S, Deary I, Douglas N. Effect of continuous positive airway pressure treatment on daytime function in sleep apnoea/hypopnoea syndrome. Lancet 1994;343(8897):572-5.
9. Lojander J, Maasilta P, Partinen M, et al. Nasal-CPAP, surgery, and conservative management for treatment of obstructive sleep apnea syndrome. A randomized study. Chest. 1996;110(1):114-9.
10. Mehta A, Qian J, Petocz P, et al. A randomized, controlled study of a mandibular advancement splint for obstructive sleep apnea. Am J Respir Critical Care Med 2001;163(6):1457-61.
11. Chesson A, Wise M, Davila D, et al. Practice parameters for the treatment of restless legs syndrome and periodic limb movement disorder. An American Academy of Sleep Medicine Report. Standards of Practice Committee of the American Academy of Sleep Medicine. Sleep 1999;22(7):961-8.
12. Phillips B, Young T, Finn L, et al. Epidemiology of restless legs symptoms in adults. Arch Intern Med 2000;160(14):2137-41.
13. Thorpy M, Ehrenberg B, Hening W, et al. Restless legs syndrome: Detection and management in primary care. Amer Fam Phys 2000;62:108-14.
14. Regestein Q, Monk T. Delayed sleep phase syndrome: A review of its clinical aspects. Am J Psychiatry 1995;152:602-8.
15. Toh K, Jones C, He Y, et al. An hPer2 phosphorylation site mutation in familial advanced sleep phase syndrome. Science 2001;291(5506):1040-3.
16. Yoshikawa N, Suzuki S, Ishimoto T, et al. A case of insufficient sleep syndrome. Psychiatry Clin Neuro 1998;52(2):200-1.
17. Nishino S, Ripley B, Overeem S, et al. Hypocretin (orexin) deficiency in human narcolepsy. Lancet. 2000;355:39-40.
18. Hauri P, Esther M. Insomnia. Mayo Clin Proc 1990;65:869-82.
19. Schwartz JR. Modafinil: new indications for wake promotion. Expert Opin Pharmacother 2005;6(1):115-29.
1. Punjabi N, Haponik E. Ask about daytime sleepiness. J Amer Geriatr Soc 2000;48:228-9.
2. Ronald J, Delaive K, Roos L, et al. Health care utilization in the 10 years prior to diagnosis in obstructive sleep apnea syndrome patients. Sleep 1999;22(2):225-9.
3. Johns M. A new method for measuring daytime sleepiness: The Epworth Sleepiness Scale. Sleep 1991;14(6):540-5.
4. Rowley J, Aboussouan L, Badr M. The use of clinical prediction formulas in the evaluation of obstructive sleep apnea. Sleep 2000;23:929-38.
5. Yamashiro Y, Kryger M. Nocturnal oximetry: Is it a screening tool for sleep disorders? Sleep 1995;18:167-71.
6. Morrell M, Finn L, Kim H, et al. Sleep fragmentation, awake blood pressure, and sleep-disordered breathing in a population-based study. Am J Respir Critical Care Med 2000;162(6):2091-6.
7. Roux F, D’Ambrosio C, Mohsenin V. Sleep-related breathing disorders and cardiovascular disease. Am J Med. 2000;108:396-402.
8. Engleman H, Martin S, Deary I, Douglas N. Effect of continuous positive airway pressure treatment on daytime function in sleep apnoea/hypopnoea syndrome. Lancet 1994;343(8897):572-5.
9. Lojander J, Maasilta P, Partinen M, et al. Nasal-CPAP, surgery, and conservative management for treatment of obstructive sleep apnea syndrome. A randomized study. Chest. 1996;110(1):114-9.
10. Mehta A, Qian J, Petocz P, et al. A randomized, controlled study of a mandibular advancement splint for obstructive sleep apnea. Am J Respir Critical Care Med 2001;163(6):1457-61.
11. Chesson A, Wise M, Davila D, et al. Practice parameters for the treatment of restless legs syndrome and periodic limb movement disorder. An American Academy of Sleep Medicine Report. Standards of Practice Committee of the American Academy of Sleep Medicine. Sleep 1999;22(7):961-8.
12. Phillips B, Young T, Finn L, et al. Epidemiology of restless legs symptoms in adults. Arch Intern Med 2000;160(14):2137-41.
13. Thorpy M, Ehrenberg B, Hening W, et al. Restless legs syndrome: Detection and management in primary care. Amer Fam Phys 2000;62:108-14.
14. Regestein Q, Monk T. Delayed sleep phase syndrome: A review of its clinical aspects. Am J Psychiatry 1995;152:602-8.
15. Toh K, Jones C, He Y, et al. An hPer2 phosphorylation site mutation in familial advanced sleep phase syndrome. Science 2001;291(5506):1040-3.
16. Yoshikawa N, Suzuki S, Ishimoto T, et al. A case of insufficient sleep syndrome. Psychiatry Clin Neuro 1998;52(2):200-1.
17. Nishino S, Ripley B, Overeem S, et al. Hypocretin (orexin) deficiency in human narcolepsy. Lancet. 2000;355:39-40.
18. Hauri P, Esther M. Insomnia. Mayo Clin Proc 1990;65:869-82.
19. Schwartz JR. Modafinil: new indications for wake promotion. Expert Opin Pharmacother 2005;6(1):115-29.
Identifying hyperthyroidism’s psychiatric presentations
Ms. A experienced an anxiety attack while driving home from work, with cardiac palpitations, tingling of the face, and fear of impending doom. Over the following 3 months she endured a “living hell,” consisting of basal anxiety, intermittent panic attacks, and agoraphobia, with exceptional difficulty even going to the grocery store.
A high-functioning career woman in her 30s, Ms. A also developed insomnia, depressed mood, and intrusive ego-dystonic thoughts. These symptoms emerged 10 years after a subtotal thyroidectomy for hyperthyroidism (Graves’ disease).
Hyperthyroidism’s association with psychiatric-spectrum symptoms is well-recognized (Box 1).1-4 Hyperthyroid patients are significantly more likely than controls to report feelings of isolation, impaired social functioning, anxiety, and mood disturbances5 and are more likely to be hospitalized with an affective disorder.6
Other individuals with subclinical or overt biochemical hyperthyroidism self-report above-average mood and lower-than-average anxiety.7
Ms. A’s is the first of three cases presented here to help you screen for and identify thyrotoxicosis (thyroid and nonthyroid causes of excessive thyroid hormone). Cases include:
- recurrent Graves’ disease with panic disorder and residual obsessive-compulsive disorder (Ms. A)
- undetected Graves’ hyperthyroidism in a bipolar-like mood syndrome with severe anxiety and cognitive decline (Ms. B)
- occult hyperthyroidism with occult anxiety (Mr. C).
These cases show that even when biochemical euthyroidism is restored, many formerly hyperthyroid patients with severe mood, anxiety, and/or cognitive symptoms continue to have significant residual symptoms that require ongoing psychiatric attention.6
Ms. A: Anxiety and thyrotoxicosis
Ms. A was greatly troubled by her intrusive ego-dystonic thoughts, which involved:
- violence to her beloved young children (for example, what would happen if someone started shooting her children with a gun)
- bizarre sexual ideations (for example, during dinner with an elderly woman she could not stop imagining her naked)
- paranoid ideations (for example, “Is my husband poisoning me?”).
She consulted a psychologist who told her that she suffered from an anxiety disorder and recommended psychotherapy, which was not helpful. She then sought endocrine consultation, and tests showed low-grade overt hyperthyroidism, with unmeasurably low thyroid stimulating hormone (TSH) concentrations and marginally elevated total and free levothyroxine (T4). Her levothyroxine replacement dosage was reduced from 100 to 50 mcg/d, then discontinued.
Without thyroid supplementation or replacement, she became biochemically euthyroid, with TSH 1.47 mIU/L and triiodothyronine (T3) and T4 in mid-normal range. Her panic anxiety resolved and her mood and sleep normalized, but the bizarre thoughts remained. The endocrinologist referred her to a psychiatrist, who diagnosed obsessive-compulsive disorder. Ms. A was effectively treated with fluvoxamine, 125 mg/d.
Discussion. Many patients with hyperthyroidism suffer from anxiety syndromes,8-10 including generalized anxiety disorder and social phobia (Table 1). “Nervousness” (including “feelings of apprehension and inability to concentrate”) is almost invariably present in the thyrotoxicosis of Graves’ disease.11
Hyperthyroidism-related anxiety syndromes are typically complicated by major depression and cognitive decline, such as in memory and attention.9 Thus, a pituitary-thyroid workup is an important step in the psychiatric evaluation of any patient with clinically significant anxiety (Box 2).3
The brain has among the highest expression of thyroid hormone receptors of any organ,1,2 and neurons are often more sensitive to thyroid abnormalities—including overt or subclinical hyperthyroidism and thyrotoxicosis, thyroiditis, and hypothyroidism3—than are other tissues.
Hyperthyroidism is often associated with anxiety, depression, mixed mood disorders, a hypomanic-like picture, emotional lability, mood swings, irritability/edginess, or cognitive deterioration with concentration problems. It also can manifest as psychosis or delirium.
Hyperthyroidism affects approximately 2.5% of the U.S. population (~7.5 million persons), according to the National Health and Nutrition Examination Survey (NHANES III). One-half of those afflicted (1.3%) do not know they are hyperthyroid, including 0.5% with overt symptoms and 0.8% with subclinical disease.
NHANES III defined hyperthyroidism as thyroid-stimulating hormone (TSH) <0.1 mIU/L with total thyroxine (T4) levels either elevated (overt hyperthyroidism) or normal (subclinical hyperthyroidism). Women are at least 5 times more likely than men to be hyperthyroid.4
CNS hypersensitivity to low-grade hyperthyroidism can manifest as an anxiety disorder before other Graves’ disease stigmata emerge. Panic disorder, for example, has been reported to precede Graves’ hyperthyroidism by 4 to 5 years in some cases,12 although how frequently this occurs is not known. Therefore, re-evaluate the thyroid status of any patient with severe anxiety who is biochemically euthyroid. Check yearly, for example, if anxiety is incompletely resolved.
Table 1
Psychiatric symptoms seen with hyperthyroidism
| Anxiety |
| Apathy (more often seen in older patients) |
| Cognitive impairment |
| Delirium |
| Depression |
| Emotional lability |
| Fatigue |
| Hypomania or mania |
| Impaired concentration |
| Insomnia |
| Irritability |
| Mood swings |
| Psychomotor agitation |
| Psychosis |
Causes of hyperthyroidism
Approximately 20 causes of thyrotoxicosis and hyperthyroxinemia have been characterized (see Related resources).11,13-15 The most common causes of hyperthyroidism are Graves’ disease, toxic multinodular goiter, and toxic thyroid adenoma. Another is thyroiditis, such as from lithium or iodine excess (such as from the cardiac drug amiodarone). A TSH-secreting pituitary adenoma is a rare cause of hyperthyroidism.16
A drug-induced thyrotoxic state can be seen with excess administration of exogenous thyroid hormone. This condition usually occurs inadvertently but is sometimes intentional, as in factitious disorder or malingering.
Graves’ disease is an autoimmune disorder that occurs when antibodies (thyroid-stimulating hormone immunoglobulins) stimulate thyroid TSH receptors, increasing thyroid hormone synthesis and secretion. Graves’ disease—seen in 60% to 85% of patients with thyrotoxicosis—is the most common cause of hyperthyroidism.15
Patients most often are women of childbearing years to middle age. Exophthalmos and other eye changes are common, along with diffuse goiter. Encephalopathy can be seen in Graves’ disease and Hashimoto’s thyroiditis because the brain can become an antibody target in autoimmune disorders.
Toxic multinodular goiter consists of autonomously functioning, circumscribed thyroid nodules with an enlarged (goitrous) thyroid, that typically emerge at length from simple (nontoxic) goiter—characterized by enlarged thyroid but normal thyroid-related biochemistry. Onset is typically later in life than Graves’ disease.11,17
Thyrotoxicosis is often relatively mild in toxic multinodular goiter, with marginal elevations in T4 and/or T3. Unlike in Graves’ disease, ophthalmologic changes are unusual. Tachycardia and weakness are common (Table 2).
Table 2
Nonpsychiatric symptoms seen with hyperthyroidism
| Metabolic |
| Heat intolerance (cold tolerance) |
| Increased perspiration |
| Weight loss (despite good appetite) |
| Endocrinologic |
| Goiter (enlarged thyroid gland) |
| Ophthalmologic |
| Exophthalmos |
| Lid lag |
| Stare/infrequent blinking |
| Ophthalmoplegia |
| Neurologic |
| Tremor |
| Hyperreflexia |
| Motor restlessness |
| Proximal muscle weakness/myopathy |
| Cardiologic |
| Tachycardia |
| Palpitations |
| Arrhythmia |
| Worsening or precipitation of angina, heart failure |
| Sexual |
| Oligomenorrhea/amenorrhea |
| Rapid ejaculation |
| Dermatologic |
| Warm, moist skin |
| Fine hair |
| Velvety skin texture |
| Onycholysis |
| Myxedema/leg swelling |
| Ruddy or erythemic skin/facial flushing |
| Eyelash loss |
| Hair loss |
| Premature graying (Graves’ disease) |
| Pruritus |
| Gastrointestinal |
| Frequent bowel movements |
| Diarrhea |
| Nausea |
| Orthopedic |
| Osteopenia or osteoporosis |
Adenomas. Toxic thyroid adenoma is a hyperfunctioning (“toxic”) benign tumor of the thyroid follicular cell. A TSH-secreting pituitary adenoma is a rare cause of hyperthyroidism.16
Thyroid storm is a rare, life-threatening thyrotoxicosis, usually seen in medical or surgical patients. Symptoms include fever, tachycardia, hypotension, irritability and restlessness, nausea and vomiting, delirium, and possibly coma.
Psychiatrists rarely see these cases, but propranolol (40 mg initial dose), fluids, and swift transport to an emergency room or critical care unit are indicated. Antithyroid agents and glucocorticoids are the usual treatment.
Thyrotoxic symptoms from thyroid hormone therapy. Thyroid hormone has been used in psychiatric patients as an antidepressant supplement,18 with therapeutic benefit reported to range from highly valuable19 to modestly helpful or no effect.20 In some patients thyroid hormone causes thyrotoxic symptoms such as tachycardia, gross tremulousness, restlessness, anxiety, inability to sleep, and impaired concentration.
Patients newly diagnosed with hypothyroidism can be exquisitely sensitive to exogenous thyroid hormone and develop acute thyrotoxic symptoms. When this occurs, a more measured titration of thyroid dose is indicated, rather than discontinuing hormone therapy. For example, patients whose optimal maintenance levothyroxine dosage proves to be >100 mcg/d might do better by first adapting to 75 mcg/d.
Thyroid hormone replacement can increase demand on the adrenal glands of chronically hypothyroid patients. For those who develop thyrotoxic-like symptoms, a pulse of glucocorticoids—such as a single 20-mg dose of prednisone (2 to 3 times the typical daily glucocorticoid maintenance requirement)—is sometimes very helpful. Severe eye pain and periorbital edema has been reported to respond to prednisone doses of 120 mg/d.13
Serum TSH is a sensitive screen. Low (<0.1 mIU/mL) or immeasurably low (<0.05 mIU/mL) circulating TSH usually means hyperthyroidism. A TSH screen is not foolproof, however; very low TSH can be seen with low circulating thyroid hormones in central hypothyroidism or in cases of laboratory error.
The recommended routine initial screen of the pituitary-thyroid axis in psychiatric patients includes TSH, free T4, and possibly free T3.3 Suppressed TSH with high serum free T3 and/or free T4 (accompanied by high total T4 and/or T3) is diagnostic of frank biochemical hyperthyroidism. If circulating thyroid hormone concentrations are normal, hyperthyroidism is considered compensated or subclinical. Although only free thyroid hormones are active, total T4 and total T3 are of interest to grossly estimate thyroid hormone output.
When you identify a thyrotoxic state, refer the patient for an endocrinologic evaluation. Antithyroid antibodies are often positive in Graves’ disease, but anti-TSH antibodies (which can be routinely ordered) are particularly diagnostic. If thyroid dysfunction is present—especially if autoimmune-based—screening tests are indicated to rule out adrenal, gonadal, and pancreatic (glucose regulation) dysfunction.
Ms. B: Hyperthyroidism and mood
Ms. B, age 35, an energetic clerical worker and fitness devotee, developed severe insomnia. She slept no more than 1 hour per night, with irritability, verbal explosiveness, “hot flashes,” and depressed mood. “Everything pisses me off violently,” she said.
She consulted a psychiatrist and was diagnosed with major depression. Over a period of years, she was serially prescribed selective serotonin reuptake inhibitors, serotonin/norepinephrine reuptake inhibitors, and older-generation sedating agents including trazodone and amitriptyline. She tolerated none of these because of side effects, including dysphoric hyperarousal and cognitive disruption.
“They all made me stupid,” she complained.
Zolpidem, 20 mg at night, helped temporarily as a hypnotic, but insomnia recurred within weeks. Diazepam was effective at high dosages but also dulled her cognition. The psychiatrist did not suspect a thyroid abnormality and did not perform a pituitary-thyroid laboratory evaluation.
Ms. B consulted a gynecologist, who prescribed estrogen for borderline low estradiol levels and with the hope that Ms. B’s symptoms represented early menopause. This partially ameliorated her irritability, possibly because estradiol binding of circulating T4 reduced free thyroid hormone levels.
Ms. B tried to continue working and exercising, but within 4 years her symptoms progressed to severe depression with frequent crying spells, feelings of general malaise, excessive sweating, occasional panic attacks, fatigue, sleepiness, deteriorating vision, and cognitive impairment. She struggled to read printed words and eventually took sick leave while consulting with physicians.
Finally, a routine thyroid screen before minor surgery revealed an undetectable TSH concentration. Further testing showed elevated thyroxine consistent with thyrotoxicosis. Graves’ disease was diagnosed, and euthyroidism was established with antithyroid medication.
Residual mood and anxiety symptoms persisted 1 year after euthyroidism was restored, and Ms. B sought psychiatric consultation.
Discussion. Hyperthyroidism can trigger or present as a hypomania or manic-like state, characterized by increased energy, hyperactivity, racing thoughts, hair-trigger verbal explosiveness, and decreased need for sleep.
Hypertalkativeness is common, even without pressured speech, as is irritability. Mood may be elevated, depressed, mixed, or cycling. A hyperthyroidism-related mixed syndrome of depression and hypomania can be confounding.
Mr. C: Occult hyperthyroidism
Mr. C, age 26, was apparently healthy when he was admitted into a neuroendocrine research protocol as a volunteer. His job performance was excellent, and his interactions with others were good; he was in good general health and taking no medication.
Formal psychiatric screening found no history of psychiatric disorders in Mr. C nor his family. His mental status was within normal limits. Physical exam revealed no significant abnormality. He was afebrile, normotensive, and had a resting pulse of 81 bpm.
His neurologic status was unremarkable, and laboratory screening tests showed normal CBC, liver and renal profiles, glucose, platelets and clotting times. Tests during the study, however, showed frankly elevated T4, free thyroxine (FT4), and T3 concentrations, along with undetectable TSH. Mr. C was informed of these results and referred to an endocrinologist.
Graves’ disease was diagnosed, and Mr. C received partial thyroid ablation therapy. He later reported that he had never felt better. In retrospect, he realized he had been anxious before he was treated for hyperthyroidism because he felt much more relaxed and able to concentrate after treatment.
Discussion. Subjective well-being in a patient with occult biochemical thyrotoxicosis can be misleading. Mr. C was much less anxious and able to concentrate after his return to euthyroidism.
Treatment
Refer your hyperthyroid patients to an endocrinologist for further workup and, in most cases, management. Hyperthyroidism is usually easy to treat using a form of ablation (antithyroid drugs, radioactive iodine, or partial thyroidectomy).
Remain involved in the patient’s care when psychiatric symptoms are prominent, however, as they are likely to persist even after thyrotoxicosis is corrected.6 Reasonable interventions include:
- control of acute thyrotoxic symptoms such as palpitations and tremulousness with propranolol, 20 to 40 mg as needed, or a 20-mg bolus of prednisone (especially if thyroiditis is present)
- address mood cycling, depression, edginess, anxiety, lability, insomnia, and/or irritability with lithium3
- oversee smoking cessation in patients with Graves’ disease (smoking exacerbates the autoimmune pathology).
Address and correct hyperthyroidism that is artifactual (caused by overuse or secret use by a patient) or iatrogenic (related to excessive prescribed hormone dosages).
Subclinical hyperthyroidism can be transient and resolve without treatment. Lithium can be helpful when a mood disorder coexists with sub clinical hyperthyroidism. Start with 300 to 600 mg every evening with dinner. If the mood disorder is mild, even as little as 300 to 450 mg of lithium may elevate a depressed mood and remove edginess and irritability.
Lithium is antithyroid, decreases thyroid hormone output, and increases serum TSH within 24 hours of initiation, but it can provoke autoimmune hyperthyroidism in some individuals.21
- For comprehensive tables of hyperthyroidism’s causes, refer to Pearce EN. Diagnosis and management of thyrotoxicosis. BMJ 2006;332:1369-73, or Lazarus JH. Hyperthyroidism. Lancet 1997;349:339-43.
- Geracioti TD Jr. Identifying hypothyroidism’s psychiatric presentations. Current Psychiatry 2006;5(11):98-117.
- Bauer M, Heinz A, Whybrow PC. Thyroid hormones, serotonin and mood: of synergy and significance in the adult brain. Molecular Psychiatry 2002;7:140-56.
Drug brand names
- Fluvoxamine • Luvox
- Lithium • Lithobid, others
- Levothyroxine • Synthroid, others
- Prednisone • Various brands
- Propranolol • Inderal
- Zolpidem • Ambien
Disclosures
Dr. Geracioti reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Sakurai A, Nakai A, DeGroot LJ. Expression of three forms of thyroid hormone receptor in human tissues. Mol Endocrinol 1989;3:392-9.
2. Shahrara S, Drvota V, Sylven C. Organ specific expression of thyroid hormone receptor mRNA and protein in different human tissues. Biol Pharm Bull 1999;22:1027-33.
3. Geracioti TD, Jr. How to identify hypothyroidism’s psychiatric presentations. Current Psychiatry 2006;5(11):98-117.
4. Hollowell JG, Staehling NW, Flanders WD, et al. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab 2002;87:489-99.
5. Bianchi GP, Zaccheroni V, Vescini F, et al. Health-related quality of life in patients with thyroid disorders. Qual Life Res 2004;13:45-54.
6. Thomsen AF, Kvist TK, Andersen OK, Kessing LV. Increased risk of affective disorder following hospitalization with hyperthyroidism—a register-based study. Eur J Endocrinol 2005;152:535-43.
7. Grabe HJ, Volzke H, Ludermann J, et al. Mental and physical complaints in thyroid disorders in the general population. Acta Psychiatr Scand 2005;112:286-93.
8. Kathol RG, Delahunt JW. The relationship of anxiety and depression to symptoms of hyperthyroidism using operational criteria. Gen Hosp Psychiatry 1986;8:23-8.
9. Trzepacz PT, McCue M, Klein I, et al. A psychiatric and neuropsychological study of patients with untreated Graves’ disease. Gen Hosp Psychiatry 1988;10:49-55.
10. Bunevicius R, Velickiene D, Prange AJ, Jr. Mood and anxiety disorders in women with treated hyperthyroidism and ophthalmopathy caused by Graves’ disease. Gen Hosp Psychiatry 2005;27:133-9.
11. Larson PR, Davies TF, Hay ID. The thyroid gland. In: Wilson JD, Forster DW, Kronenberg HM, Larsen PR eds. Williams textbook of endocrinology. 9th ed. Philadelphia, PA: WB Saunders;1998:389-515.
12. Matsubayashi S, Tamai H, Matsumoto Y, et al. Graves’ disease after the onset of panic disorder. Psychother Psychosom 1996;65(5):277-80.
13. Lazarus JH. Hyperthyroidism. Lancet 1997;349:339-43.
14. Pearce EN. Diagnosis and management of thyrotoxicosis. BMJ 2006;332:1369-73.
15. Utiger RD. The thyroid: physiology, thyrotoxicosis, hypothyroidism, and the painful thyroid. In: Felig P, Frohman LA, eds. Endocrinology and metabolism, 4th ed. New York, NY: McGraw-Hill; 2001:261-347.
16. Beckers A, Abs R, Mahler C, et al. Thyrotropin-secreting pituitary adenomas: report of seven cases. J Clin Endocrinol Metab 1991;72:477-83.
17. Kinder BK, Burrow GN. The thyroid: nodules and neoplasiaIn: Felig P, Frohman LA eds. Endocrinology and metabolism, 4th ed New York, NY: McGraw-Hill; 2001:349-383.
18. Prange AJ, Jr, Wilson IC, Rabon AM, Lipton MA. Enhancement of imipramine antidepressant activity by thyroid hormone. Am J Psychiatry 1969;126:457-69.
19. Geracioti TD, Jr, Loosen PT, Gold PW, Kling MA. Cortisol, thyroid hormone, and mood in atypical depression: a longitudinal case study. Biol Psychiatry 1992;31:515-9.
20. Geracioti TD, Kling MA, Post R, Gold PW. Antithyroid antibody-linked symptoms in borderline personality disorder. Endocrine 2003;21:153-8.
21. Bocchetta A, Mossa P, Velluzzi F, et al. Ten-year follow-up of thyroid function in lithium patients. J Clin Psychopharmacol 2001;21:594-8.
Ms. A experienced an anxiety attack while driving home from work, with cardiac palpitations, tingling of the face, and fear of impending doom. Over the following 3 months she endured a “living hell,” consisting of basal anxiety, intermittent panic attacks, and agoraphobia, with exceptional difficulty even going to the grocery store.
A high-functioning career woman in her 30s, Ms. A also developed insomnia, depressed mood, and intrusive ego-dystonic thoughts. These symptoms emerged 10 years after a subtotal thyroidectomy for hyperthyroidism (Graves’ disease).
Hyperthyroidism’s association with psychiatric-spectrum symptoms is well-recognized (Box 1).1-4 Hyperthyroid patients are significantly more likely than controls to report feelings of isolation, impaired social functioning, anxiety, and mood disturbances5 and are more likely to be hospitalized with an affective disorder.6
Other individuals with subclinical or overt biochemical hyperthyroidism self-report above-average mood and lower-than-average anxiety.7
Ms. A’s is the first of three cases presented here to help you screen for and identify thyrotoxicosis (thyroid and nonthyroid causes of excessive thyroid hormone). Cases include:
- recurrent Graves’ disease with panic disorder and residual obsessive-compulsive disorder (Ms. A)
- undetected Graves’ hyperthyroidism in a bipolar-like mood syndrome with severe anxiety and cognitive decline (Ms. B)
- occult hyperthyroidism with occult anxiety (Mr. C).
These cases show that even when biochemical euthyroidism is restored, many formerly hyperthyroid patients with severe mood, anxiety, and/or cognitive symptoms continue to have significant residual symptoms that require ongoing psychiatric attention.6
Ms. A: Anxiety and thyrotoxicosis
Ms. A was greatly troubled by her intrusive ego-dystonic thoughts, which involved:
- violence to her beloved young children (for example, what would happen if someone started shooting her children with a gun)
- bizarre sexual ideations (for example, during dinner with an elderly woman she could not stop imagining her naked)
- paranoid ideations (for example, “Is my husband poisoning me?”).
She consulted a psychologist who told her that she suffered from an anxiety disorder and recommended psychotherapy, which was not helpful. She then sought endocrine consultation, and tests showed low-grade overt hyperthyroidism, with unmeasurably low thyroid stimulating hormone (TSH) concentrations and marginally elevated total and free levothyroxine (T4). Her levothyroxine replacement dosage was reduced from 100 to 50 mcg/d, then discontinued.
Without thyroid supplementation or replacement, she became biochemically euthyroid, with TSH 1.47 mIU/L and triiodothyronine (T3) and T4 in mid-normal range. Her panic anxiety resolved and her mood and sleep normalized, but the bizarre thoughts remained. The endocrinologist referred her to a psychiatrist, who diagnosed obsessive-compulsive disorder. Ms. A was effectively treated with fluvoxamine, 125 mg/d.
Discussion. Many patients with hyperthyroidism suffer from anxiety syndromes,8-10 including generalized anxiety disorder and social phobia (Table 1). “Nervousness” (including “feelings of apprehension and inability to concentrate”) is almost invariably present in the thyrotoxicosis of Graves’ disease.11
Hyperthyroidism-related anxiety syndromes are typically complicated by major depression and cognitive decline, such as in memory and attention.9 Thus, a pituitary-thyroid workup is an important step in the psychiatric evaluation of any patient with clinically significant anxiety (Box 2).3
The brain has among the highest expression of thyroid hormone receptors of any organ,1,2 and neurons are often more sensitive to thyroid abnormalities—including overt or subclinical hyperthyroidism and thyrotoxicosis, thyroiditis, and hypothyroidism3—than are other tissues.
Hyperthyroidism is often associated with anxiety, depression, mixed mood disorders, a hypomanic-like picture, emotional lability, mood swings, irritability/edginess, or cognitive deterioration with concentration problems. It also can manifest as psychosis or delirium.
Hyperthyroidism affects approximately 2.5% of the U.S. population (~7.5 million persons), according to the National Health and Nutrition Examination Survey (NHANES III). One-half of those afflicted (1.3%) do not know they are hyperthyroid, including 0.5% with overt symptoms and 0.8% with subclinical disease.
NHANES III defined hyperthyroidism as thyroid-stimulating hormone (TSH) <0.1 mIU/L with total thyroxine (T4) levels either elevated (overt hyperthyroidism) or normal (subclinical hyperthyroidism). Women are at least 5 times more likely than men to be hyperthyroid.4
CNS hypersensitivity to low-grade hyperthyroidism can manifest as an anxiety disorder before other Graves’ disease stigmata emerge. Panic disorder, for example, has been reported to precede Graves’ hyperthyroidism by 4 to 5 years in some cases,12 although how frequently this occurs is not known. Therefore, re-evaluate the thyroid status of any patient with severe anxiety who is biochemically euthyroid. Check yearly, for example, if anxiety is incompletely resolved.
Table 1
Psychiatric symptoms seen with hyperthyroidism
| Anxiety |
| Apathy (more often seen in older patients) |
| Cognitive impairment |
| Delirium |
| Depression |
| Emotional lability |
| Fatigue |
| Hypomania or mania |
| Impaired concentration |
| Insomnia |
| Irritability |
| Mood swings |
| Psychomotor agitation |
| Psychosis |
Causes of hyperthyroidism
Approximately 20 causes of thyrotoxicosis and hyperthyroxinemia have been characterized (see Related resources).11,13-15 The most common causes of hyperthyroidism are Graves’ disease, toxic multinodular goiter, and toxic thyroid adenoma. Another is thyroiditis, such as from lithium or iodine excess (such as from the cardiac drug amiodarone). A TSH-secreting pituitary adenoma is a rare cause of hyperthyroidism.16
A drug-induced thyrotoxic state can be seen with excess administration of exogenous thyroid hormone. This condition usually occurs inadvertently but is sometimes intentional, as in factitious disorder or malingering.
Graves’ disease is an autoimmune disorder that occurs when antibodies (thyroid-stimulating hormone immunoglobulins) stimulate thyroid TSH receptors, increasing thyroid hormone synthesis and secretion. Graves’ disease—seen in 60% to 85% of patients with thyrotoxicosis—is the most common cause of hyperthyroidism.15
Patients most often are women of childbearing years to middle age. Exophthalmos and other eye changes are common, along with diffuse goiter. Encephalopathy can be seen in Graves’ disease and Hashimoto’s thyroiditis because the brain can become an antibody target in autoimmune disorders.
Toxic multinodular goiter consists of autonomously functioning, circumscribed thyroid nodules with an enlarged (goitrous) thyroid, that typically emerge at length from simple (nontoxic) goiter—characterized by enlarged thyroid but normal thyroid-related biochemistry. Onset is typically later in life than Graves’ disease.11,17
Thyrotoxicosis is often relatively mild in toxic multinodular goiter, with marginal elevations in T4 and/or T3. Unlike in Graves’ disease, ophthalmologic changes are unusual. Tachycardia and weakness are common (Table 2).
Table 2
Nonpsychiatric symptoms seen with hyperthyroidism
| Metabolic |
| Heat intolerance (cold tolerance) |
| Increased perspiration |
| Weight loss (despite good appetite) |
| Endocrinologic |
| Goiter (enlarged thyroid gland) |
| Ophthalmologic |
| Exophthalmos |
| Lid lag |
| Stare/infrequent blinking |
| Ophthalmoplegia |
| Neurologic |
| Tremor |
| Hyperreflexia |
| Motor restlessness |
| Proximal muscle weakness/myopathy |
| Cardiologic |
| Tachycardia |
| Palpitations |
| Arrhythmia |
| Worsening or precipitation of angina, heart failure |
| Sexual |
| Oligomenorrhea/amenorrhea |
| Rapid ejaculation |
| Dermatologic |
| Warm, moist skin |
| Fine hair |
| Velvety skin texture |
| Onycholysis |
| Myxedema/leg swelling |
| Ruddy or erythemic skin/facial flushing |
| Eyelash loss |
| Hair loss |
| Premature graying (Graves’ disease) |
| Pruritus |
| Gastrointestinal |
| Frequent bowel movements |
| Diarrhea |
| Nausea |
| Orthopedic |
| Osteopenia or osteoporosis |
Adenomas. Toxic thyroid adenoma is a hyperfunctioning (“toxic”) benign tumor of the thyroid follicular cell. A TSH-secreting pituitary adenoma is a rare cause of hyperthyroidism.16
Thyroid storm is a rare, life-threatening thyrotoxicosis, usually seen in medical or surgical patients. Symptoms include fever, tachycardia, hypotension, irritability and restlessness, nausea and vomiting, delirium, and possibly coma.
Psychiatrists rarely see these cases, but propranolol (40 mg initial dose), fluids, and swift transport to an emergency room or critical care unit are indicated. Antithyroid agents and glucocorticoids are the usual treatment.
Thyrotoxic symptoms from thyroid hormone therapy. Thyroid hormone has been used in psychiatric patients as an antidepressant supplement,18 with therapeutic benefit reported to range from highly valuable19 to modestly helpful or no effect.20 In some patients thyroid hormone causes thyrotoxic symptoms such as tachycardia, gross tremulousness, restlessness, anxiety, inability to sleep, and impaired concentration.
Patients newly diagnosed with hypothyroidism can be exquisitely sensitive to exogenous thyroid hormone and develop acute thyrotoxic symptoms. When this occurs, a more measured titration of thyroid dose is indicated, rather than discontinuing hormone therapy. For example, patients whose optimal maintenance levothyroxine dosage proves to be >100 mcg/d might do better by first adapting to 75 mcg/d.
Thyroid hormone replacement can increase demand on the adrenal glands of chronically hypothyroid patients. For those who develop thyrotoxic-like symptoms, a pulse of glucocorticoids—such as a single 20-mg dose of prednisone (2 to 3 times the typical daily glucocorticoid maintenance requirement)—is sometimes very helpful. Severe eye pain and periorbital edema has been reported to respond to prednisone doses of 120 mg/d.13
Serum TSH is a sensitive screen. Low (<0.1 mIU/mL) or immeasurably low (<0.05 mIU/mL) circulating TSH usually means hyperthyroidism. A TSH screen is not foolproof, however; very low TSH can be seen with low circulating thyroid hormones in central hypothyroidism or in cases of laboratory error.
The recommended routine initial screen of the pituitary-thyroid axis in psychiatric patients includes TSH, free T4, and possibly free T3.3 Suppressed TSH with high serum free T3 and/or free T4 (accompanied by high total T4 and/or T3) is diagnostic of frank biochemical hyperthyroidism. If circulating thyroid hormone concentrations are normal, hyperthyroidism is considered compensated or subclinical. Although only free thyroid hormones are active, total T4 and total T3 are of interest to grossly estimate thyroid hormone output.
When you identify a thyrotoxic state, refer the patient for an endocrinologic evaluation. Antithyroid antibodies are often positive in Graves’ disease, but anti-TSH antibodies (which can be routinely ordered) are particularly diagnostic. If thyroid dysfunction is present—especially if autoimmune-based—screening tests are indicated to rule out adrenal, gonadal, and pancreatic (glucose regulation) dysfunction.
Ms. B: Hyperthyroidism and mood
Ms. B, age 35, an energetic clerical worker and fitness devotee, developed severe insomnia. She slept no more than 1 hour per night, with irritability, verbal explosiveness, “hot flashes,” and depressed mood. “Everything pisses me off violently,” she said.
She consulted a psychiatrist and was diagnosed with major depression. Over a period of years, she was serially prescribed selective serotonin reuptake inhibitors, serotonin/norepinephrine reuptake inhibitors, and older-generation sedating agents including trazodone and amitriptyline. She tolerated none of these because of side effects, including dysphoric hyperarousal and cognitive disruption.
“They all made me stupid,” she complained.
Zolpidem, 20 mg at night, helped temporarily as a hypnotic, but insomnia recurred within weeks. Diazepam was effective at high dosages but also dulled her cognition. The psychiatrist did not suspect a thyroid abnormality and did not perform a pituitary-thyroid laboratory evaluation.
Ms. B consulted a gynecologist, who prescribed estrogen for borderline low estradiol levels and with the hope that Ms. B’s symptoms represented early menopause. This partially ameliorated her irritability, possibly because estradiol binding of circulating T4 reduced free thyroid hormone levels.
Ms. B tried to continue working and exercising, but within 4 years her symptoms progressed to severe depression with frequent crying spells, feelings of general malaise, excessive sweating, occasional panic attacks, fatigue, sleepiness, deteriorating vision, and cognitive impairment. She struggled to read printed words and eventually took sick leave while consulting with physicians.
Finally, a routine thyroid screen before minor surgery revealed an undetectable TSH concentration. Further testing showed elevated thyroxine consistent with thyrotoxicosis. Graves’ disease was diagnosed, and euthyroidism was established with antithyroid medication.
Residual mood and anxiety symptoms persisted 1 year after euthyroidism was restored, and Ms. B sought psychiatric consultation.
Discussion. Hyperthyroidism can trigger or present as a hypomania or manic-like state, characterized by increased energy, hyperactivity, racing thoughts, hair-trigger verbal explosiveness, and decreased need for sleep.
Hypertalkativeness is common, even without pressured speech, as is irritability. Mood may be elevated, depressed, mixed, or cycling. A hyperthyroidism-related mixed syndrome of depression and hypomania can be confounding.
Mr. C: Occult hyperthyroidism
Mr. C, age 26, was apparently healthy when he was admitted into a neuroendocrine research protocol as a volunteer. His job performance was excellent, and his interactions with others were good; he was in good general health and taking no medication.
Formal psychiatric screening found no history of psychiatric disorders in Mr. C nor his family. His mental status was within normal limits. Physical exam revealed no significant abnormality. He was afebrile, normotensive, and had a resting pulse of 81 bpm.
His neurologic status was unremarkable, and laboratory screening tests showed normal CBC, liver and renal profiles, glucose, platelets and clotting times. Tests during the study, however, showed frankly elevated T4, free thyroxine (FT4), and T3 concentrations, along with undetectable TSH. Mr. C was informed of these results and referred to an endocrinologist.
Graves’ disease was diagnosed, and Mr. C received partial thyroid ablation therapy. He later reported that he had never felt better. In retrospect, he realized he had been anxious before he was treated for hyperthyroidism because he felt much more relaxed and able to concentrate after treatment.
Discussion. Subjective well-being in a patient with occult biochemical thyrotoxicosis can be misleading. Mr. C was much less anxious and able to concentrate after his return to euthyroidism.
Treatment
Refer your hyperthyroid patients to an endocrinologist for further workup and, in most cases, management. Hyperthyroidism is usually easy to treat using a form of ablation (antithyroid drugs, radioactive iodine, or partial thyroidectomy).
Remain involved in the patient’s care when psychiatric symptoms are prominent, however, as they are likely to persist even after thyrotoxicosis is corrected.6 Reasonable interventions include:
- control of acute thyrotoxic symptoms such as palpitations and tremulousness with propranolol, 20 to 40 mg as needed, or a 20-mg bolus of prednisone (especially if thyroiditis is present)
- address mood cycling, depression, edginess, anxiety, lability, insomnia, and/or irritability with lithium3
- oversee smoking cessation in patients with Graves’ disease (smoking exacerbates the autoimmune pathology).
Address and correct hyperthyroidism that is artifactual (caused by overuse or secret use by a patient) or iatrogenic (related to excessive prescribed hormone dosages).
Subclinical hyperthyroidism can be transient and resolve without treatment. Lithium can be helpful when a mood disorder coexists with sub clinical hyperthyroidism. Start with 300 to 600 mg every evening with dinner. If the mood disorder is mild, even as little as 300 to 450 mg of lithium may elevate a depressed mood and remove edginess and irritability.
Lithium is antithyroid, decreases thyroid hormone output, and increases serum TSH within 24 hours of initiation, but it can provoke autoimmune hyperthyroidism in some individuals.21
- For comprehensive tables of hyperthyroidism’s causes, refer to Pearce EN. Diagnosis and management of thyrotoxicosis. BMJ 2006;332:1369-73, or Lazarus JH. Hyperthyroidism. Lancet 1997;349:339-43.
- Geracioti TD Jr. Identifying hypothyroidism’s psychiatric presentations. Current Psychiatry 2006;5(11):98-117.
- Bauer M, Heinz A, Whybrow PC. Thyroid hormones, serotonin and mood: of synergy and significance in the adult brain. Molecular Psychiatry 2002;7:140-56.
Drug brand names
- Fluvoxamine • Luvox
- Lithium • Lithobid, others
- Levothyroxine • Synthroid, others
- Prednisone • Various brands
- Propranolol • Inderal
- Zolpidem • Ambien
Disclosures
Dr. Geracioti reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Ms. A experienced an anxiety attack while driving home from work, with cardiac palpitations, tingling of the face, and fear of impending doom. Over the following 3 months she endured a “living hell,” consisting of basal anxiety, intermittent panic attacks, and agoraphobia, with exceptional difficulty even going to the grocery store.
A high-functioning career woman in her 30s, Ms. A also developed insomnia, depressed mood, and intrusive ego-dystonic thoughts. These symptoms emerged 10 years after a subtotal thyroidectomy for hyperthyroidism (Graves’ disease).
Hyperthyroidism’s association with psychiatric-spectrum symptoms is well-recognized (Box 1).1-4 Hyperthyroid patients are significantly more likely than controls to report feelings of isolation, impaired social functioning, anxiety, and mood disturbances5 and are more likely to be hospitalized with an affective disorder.6
Other individuals with subclinical or overt biochemical hyperthyroidism self-report above-average mood and lower-than-average anxiety.7
Ms. A’s is the first of three cases presented here to help you screen for and identify thyrotoxicosis (thyroid and nonthyroid causes of excessive thyroid hormone). Cases include:
- recurrent Graves’ disease with panic disorder and residual obsessive-compulsive disorder (Ms. A)
- undetected Graves’ hyperthyroidism in a bipolar-like mood syndrome with severe anxiety and cognitive decline (Ms. B)
- occult hyperthyroidism with occult anxiety (Mr. C).
These cases show that even when biochemical euthyroidism is restored, many formerly hyperthyroid patients with severe mood, anxiety, and/or cognitive symptoms continue to have significant residual symptoms that require ongoing psychiatric attention.6
Ms. A: Anxiety and thyrotoxicosis
Ms. A was greatly troubled by her intrusive ego-dystonic thoughts, which involved:
- violence to her beloved young children (for example, what would happen if someone started shooting her children with a gun)
- bizarre sexual ideations (for example, during dinner with an elderly woman she could not stop imagining her naked)
- paranoid ideations (for example, “Is my husband poisoning me?”).
She consulted a psychologist who told her that she suffered from an anxiety disorder and recommended psychotherapy, which was not helpful. She then sought endocrine consultation, and tests showed low-grade overt hyperthyroidism, with unmeasurably low thyroid stimulating hormone (TSH) concentrations and marginally elevated total and free levothyroxine (T4). Her levothyroxine replacement dosage was reduced from 100 to 50 mcg/d, then discontinued.
Without thyroid supplementation or replacement, she became biochemically euthyroid, with TSH 1.47 mIU/L and triiodothyronine (T3) and T4 in mid-normal range. Her panic anxiety resolved and her mood and sleep normalized, but the bizarre thoughts remained. The endocrinologist referred her to a psychiatrist, who diagnosed obsessive-compulsive disorder. Ms. A was effectively treated with fluvoxamine, 125 mg/d.
Discussion. Many patients with hyperthyroidism suffer from anxiety syndromes,8-10 including generalized anxiety disorder and social phobia (Table 1). “Nervousness” (including “feelings of apprehension and inability to concentrate”) is almost invariably present in the thyrotoxicosis of Graves’ disease.11
Hyperthyroidism-related anxiety syndromes are typically complicated by major depression and cognitive decline, such as in memory and attention.9 Thus, a pituitary-thyroid workup is an important step in the psychiatric evaluation of any patient with clinically significant anxiety (Box 2).3
The brain has among the highest expression of thyroid hormone receptors of any organ,1,2 and neurons are often more sensitive to thyroid abnormalities—including overt or subclinical hyperthyroidism and thyrotoxicosis, thyroiditis, and hypothyroidism3—than are other tissues.
Hyperthyroidism is often associated with anxiety, depression, mixed mood disorders, a hypomanic-like picture, emotional lability, mood swings, irritability/edginess, or cognitive deterioration with concentration problems. It also can manifest as psychosis or delirium.
Hyperthyroidism affects approximately 2.5% of the U.S. population (~7.5 million persons), according to the National Health and Nutrition Examination Survey (NHANES III). One-half of those afflicted (1.3%) do not know they are hyperthyroid, including 0.5% with overt symptoms and 0.8% with subclinical disease.
NHANES III defined hyperthyroidism as thyroid-stimulating hormone (TSH) <0.1 mIU/L with total thyroxine (T4) levels either elevated (overt hyperthyroidism) or normal (subclinical hyperthyroidism). Women are at least 5 times more likely than men to be hyperthyroid.4
CNS hypersensitivity to low-grade hyperthyroidism can manifest as an anxiety disorder before other Graves’ disease stigmata emerge. Panic disorder, for example, has been reported to precede Graves’ hyperthyroidism by 4 to 5 years in some cases,12 although how frequently this occurs is not known. Therefore, re-evaluate the thyroid status of any patient with severe anxiety who is biochemically euthyroid. Check yearly, for example, if anxiety is incompletely resolved.
Table 1
Psychiatric symptoms seen with hyperthyroidism
| Anxiety |
| Apathy (more often seen in older patients) |
| Cognitive impairment |
| Delirium |
| Depression |
| Emotional lability |
| Fatigue |
| Hypomania or mania |
| Impaired concentration |
| Insomnia |
| Irritability |
| Mood swings |
| Psychomotor agitation |
| Psychosis |
Causes of hyperthyroidism
Approximately 20 causes of thyrotoxicosis and hyperthyroxinemia have been characterized (see Related resources).11,13-15 The most common causes of hyperthyroidism are Graves’ disease, toxic multinodular goiter, and toxic thyroid adenoma. Another is thyroiditis, such as from lithium or iodine excess (such as from the cardiac drug amiodarone). A TSH-secreting pituitary adenoma is a rare cause of hyperthyroidism.16
A drug-induced thyrotoxic state can be seen with excess administration of exogenous thyroid hormone. This condition usually occurs inadvertently but is sometimes intentional, as in factitious disorder or malingering.
Graves’ disease is an autoimmune disorder that occurs when antibodies (thyroid-stimulating hormone immunoglobulins) stimulate thyroid TSH receptors, increasing thyroid hormone synthesis and secretion. Graves’ disease—seen in 60% to 85% of patients with thyrotoxicosis—is the most common cause of hyperthyroidism.15
Patients most often are women of childbearing years to middle age. Exophthalmos and other eye changes are common, along with diffuse goiter. Encephalopathy can be seen in Graves’ disease and Hashimoto’s thyroiditis because the brain can become an antibody target in autoimmune disorders.
Toxic multinodular goiter consists of autonomously functioning, circumscribed thyroid nodules with an enlarged (goitrous) thyroid, that typically emerge at length from simple (nontoxic) goiter—characterized by enlarged thyroid but normal thyroid-related biochemistry. Onset is typically later in life than Graves’ disease.11,17
Thyrotoxicosis is often relatively mild in toxic multinodular goiter, with marginal elevations in T4 and/or T3. Unlike in Graves’ disease, ophthalmologic changes are unusual. Tachycardia and weakness are common (Table 2).
Table 2
Nonpsychiatric symptoms seen with hyperthyroidism
| Metabolic |
| Heat intolerance (cold tolerance) |
| Increased perspiration |
| Weight loss (despite good appetite) |
| Endocrinologic |
| Goiter (enlarged thyroid gland) |
| Ophthalmologic |
| Exophthalmos |
| Lid lag |
| Stare/infrequent blinking |
| Ophthalmoplegia |
| Neurologic |
| Tremor |
| Hyperreflexia |
| Motor restlessness |
| Proximal muscle weakness/myopathy |
| Cardiologic |
| Tachycardia |
| Palpitations |
| Arrhythmia |
| Worsening or precipitation of angina, heart failure |
| Sexual |
| Oligomenorrhea/amenorrhea |
| Rapid ejaculation |
| Dermatologic |
| Warm, moist skin |
| Fine hair |
| Velvety skin texture |
| Onycholysis |
| Myxedema/leg swelling |
| Ruddy or erythemic skin/facial flushing |
| Eyelash loss |
| Hair loss |
| Premature graying (Graves’ disease) |
| Pruritus |
| Gastrointestinal |
| Frequent bowel movements |
| Diarrhea |
| Nausea |
| Orthopedic |
| Osteopenia or osteoporosis |
Adenomas. Toxic thyroid adenoma is a hyperfunctioning (“toxic”) benign tumor of the thyroid follicular cell. A TSH-secreting pituitary adenoma is a rare cause of hyperthyroidism.16
Thyroid storm is a rare, life-threatening thyrotoxicosis, usually seen in medical or surgical patients. Symptoms include fever, tachycardia, hypotension, irritability and restlessness, nausea and vomiting, delirium, and possibly coma.
Psychiatrists rarely see these cases, but propranolol (40 mg initial dose), fluids, and swift transport to an emergency room or critical care unit are indicated. Antithyroid agents and glucocorticoids are the usual treatment.
Thyrotoxic symptoms from thyroid hormone therapy. Thyroid hormone has been used in psychiatric patients as an antidepressant supplement,18 with therapeutic benefit reported to range from highly valuable19 to modestly helpful or no effect.20 In some patients thyroid hormone causes thyrotoxic symptoms such as tachycardia, gross tremulousness, restlessness, anxiety, inability to sleep, and impaired concentration.
Patients newly diagnosed with hypothyroidism can be exquisitely sensitive to exogenous thyroid hormone and develop acute thyrotoxic symptoms. When this occurs, a more measured titration of thyroid dose is indicated, rather than discontinuing hormone therapy. For example, patients whose optimal maintenance levothyroxine dosage proves to be >100 mcg/d might do better by first adapting to 75 mcg/d.
Thyroid hormone replacement can increase demand on the adrenal glands of chronically hypothyroid patients. For those who develop thyrotoxic-like symptoms, a pulse of glucocorticoids—such as a single 20-mg dose of prednisone (2 to 3 times the typical daily glucocorticoid maintenance requirement)—is sometimes very helpful. Severe eye pain and periorbital edema has been reported to respond to prednisone doses of 120 mg/d.13
Serum TSH is a sensitive screen. Low (<0.1 mIU/mL) or immeasurably low (<0.05 mIU/mL) circulating TSH usually means hyperthyroidism. A TSH screen is not foolproof, however; very low TSH can be seen with low circulating thyroid hormones in central hypothyroidism or in cases of laboratory error.
The recommended routine initial screen of the pituitary-thyroid axis in psychiatric patients includes TSH, free T4, and possibly free T3.3 Suppressed TSH with high serum free T3 and/or free T4 (accompanied by high total T4 and/or T3) is diagnostic of frank biochemical hyperthyroidism. If circulating thyroid hormone concentrations are normal, hyperthyroidism is considered compensated or subclinical. Although only free thyroid hormones are active, total T4 and total T3 are of interest to grossly estimate thyroid hormone output.
When you identify a thyrotoxic state, refer the patient for an endocrinologic evaluation. Antithyroid antibodies are often positive in Graves’ disease, but anti-TSH antibodies (which can be routinely ordered) are particularly diagnostic. If thyroid dysfunction is present—especially if autoimmune-based—screening tests are indicated to rule out adrenal, gonadal, and pancreatic (glucose regulation) dysfunction.
Ms. B: Hyperthyroidism and mood
Ms. B, age 35, an energetic clerical worker and fitness devotee, developed severe insomnia. She slept no more than 1 hour per night, with irritability, verbal explosiveness, “hot flashes,” and depressed mood. “Everything pisses me off violently,” she said.
She consulted a psychiatrist and was diagnosed with major depression. Over a period of years, she was serially prescribed selective serotonin reuptake inhibitors, serotonin/norepinephrine reuptake inhibitors, and older-generation sedating agents including trazodone and amitriptyline. She tolerated none of these because of side effects, including dysphoric hyperarousal and cognitive disruption.
“They all made me stupid,” she complained.
Zolpidem, 20 mg at night, helped temporarily as a hypnotic, but insomnia recurred within weeks. Diazepam was effective at high dosages but also dulled her cognition. The psychiatrist did not suspect a thyroid abnormality and did not perform a pituitary-thyroid laboratory evaluation.
Ms. B consulted a gynecologist, who prescribed estrogen for borderline low estradiol levels and with the hope that Ms. B’s symptoms represented early menopause. This partially ameliorated her irritability, possibly because estradiol binding of circulating T4 reduced free thyroid hormone levels.
Ms. B tried to continue working and exercising, but within 4 years her symptoms progressed to severe depression with frequent crying spells, feelings of general malaise, excessive sweating, occasional panic attacks, fatigue, sleepiness, deteriorating vision, and cognitive impairment. She struggled to read printed words and eventually took sick leave while consulting with physicians.
Finally, a routine thyroid screen before minor surgery revealed an undetectable TSH concentration. Further testing showed elevated thyroxine consistent with thyrotoxicosis. Graves’ disease was diagnosed, and euthyroidism was established with antithyroid medication.
Residual mood and anxiety symptoms persisted 1 year after euthyroidism was restored, and Ms. B sought psychiatric consultation.
Discussion. Hyperthyroidism can trigger or present as a hypomania or manic-like state, characterized by increased energy, hyperactivity, racing thoughts, hair-trigger verbal explosiveness, and decreased need for sleep.
Hypertalkativeness is common, even without pressured speech, as is irritability. Mood may be elevated, depressed, mixed, or cycling. A hyperthyroidism-related mixed syndrome of depression and hypomania can be confounding.
Mr. C: Occult hyperthyroidism
Mr. C, age 26, was apparently healthy when he was admitted into a neuroendocrine research protocol as a volunteer. His job performance was excellent, and his interactions with others were good; he was in good general health and taking no medication.
Formal psychiatric screening found no history of psychiatric disorders in Mr. C nor his family. His mental status was within normal limits. Physical exam revealed no significant abnormality. He was afebrile, normotensive, and had a resting pulse of 81 bpm.
His neurologic status was unremarkable, and laboratory screening tests showed normal CBC, liver and renal profiles, glucose, platelets and clotting times. Tests during the study, however, showed frankly elevated T4, free thyroxine (FT4), and T3 concentrations, along with undetectable TSH. Mr. C was informed of these results and referred to an endocrinologist.
Graves’ disease was diagnosed, and Mr. C received partial thyroid ablation therapy. He later reported that he had never felt better. In retrospect, he realized he had been anxious before he was treated for hyperthyroidism because he felt much more relaxed and able to concentrate after treatment.
Discussion. Subjective well-being in a patient with occult biochemical thyrotoxicosis can be misleading. Mr. C was much less anxious and able to concentrate after his return to euthyroidism.
Treatment
Refer your hyperthyroid patients to an endocrinologist for further workup and, in most cases, management. Hyperthyroidism is usually easy to treat using a form of ablation (antithyroid drugs, radioactive iodine, or partial thyroidectomy).
Remain involved in the patient’s care when psychiatric symptoms are prominent, however, as they are likely to persist even after thyrotoxicosis is corrected.6 Reasonable interventions include:
- control of acute thyrotoxic symptoms such as palpitations and tremulousness with propranolol, 20 to 40 mg as needed, or a 20-mg bolus of prednisone (especially if thyroiditis is present)
- address mood cycling, depression, edginess, anxiety, lability, insomnia, and/or irritability with lithium3
- oversee smoking cessation in patients with Graves’ disease (smoking exacerbates the autoimmune pathology).
Address and correct hyperthyroidism that is artifactual (caused by overuse or secret use by a patient) or iatrogenic (related to excessive prescribed hormone dosages).
Subclinical hyperthyroidism can be transient and resolve without treatment. Lithium can be helpful when a mood disorder coexists with sub clinical hyperthyroidism. Start with 300 to 600 mg every evening with dinner. If the mood disorder is mild, even as little as 300 to 450 mg of lithium may elevate a depressed mood and remove edginess and irritability.
Lithium is antithyroid, decreases thyroid hormone output, and increases serum TSH within 24 hours of initiation, but it can provoke autoimmune hyperthyroidism in some individuals.21
- For comprehensive tables of hyperthyroidism’s causes, refer to Pearce EN. Diagnosis and management of thyrotoxicosis. BMJ 2006;332:1369-73, or Lazarus JH. Hyperthyroidism. Lancet 1997;349:339-43.
- Geracioti TD Jr. Identifying hypothyroidism’s psychiatric presentations. Current Psychiatry 2006;5(11):98-117.
- Bauer M, Heinz A, Whybrow PC. Thyroid hormones, serotonin and mood: of synergy and significance in the adult brain. Molecular Psychiatry 2002;7:140-56.
Drug brand names
- Fluvoxamine • Luvox
- Lithium • Lithobid, others
- Levothyroxine • Synthroid, others
- Prednisone • Various brands
- Propranolol • Inderal
- Zolpidem • Ambien
Disclosures
Dr. Geracioti reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Sakurai A, Nakai A, DeGroot LJ. Expression of three forms of thyroid hormone receptor in human tissues. Mol Endocrinol 1989;3:392-9.
2. Shahrara S, Drvota V, Sylven C. Organ specific expression of thyroid hormone receptor mRNA and protein in different human tissues. Biol Pharm Bull 1999;22:1027-33.
3. Geracioti TD, Jr. How to identify hypothyroidism’s psychiatric presentations. Current Psychiatry 2006;5(11):98-117.
4. Hollowell JG, Staehling NW, Flanders WD, et al. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab 2002;87:489-99.
5. Bianchi GP, Zaccheroni V, Vescini F, et al. Health-related quality of life in patients with thyroid disorders. Qual Life Res 2004;13:45-54.
6. Thomsen AF, Kvist TK, Andersen OK, Kessing LV. Increased risk of affective disorder following hospitalization with hyperthyroidism—a register-based study. Eur J Endocrinol 2005;152:535-43.
7. Grabe HJ, Volzke H, Ludermann J, et al. Mental and physical complaints in thyroid disorders in the general population. Acta Psychiatr Scand 2005;112:286-93.
8. Kathol RG, Delahunt JW. The relationship of anxiety and depression to symptoms of hyperthyroidism using operational criteria. Gen Hosp Psychiatry 1986;8:23-8.
9. Trzepacz PT, McCue M, Klein I, et al. A psychiatric and neuropsychological study of patients with untreated Graves’ disease. Gen Hosp Psychiatry 1988;10:49-55.
10. Bunevicius R, Velickiene D, Prange AJ, Jr. Mood and anxiety disorders in women with treated hyperthyroidism and ophthalmopathy caused by Graves’ disease. Gen Hosp Psychiatry 2005;27:133-9.
11. Larson PR, Davies TF, Hay ID. The thyroid gland. In: Wilson JD, Forster DW, Kronenberg HM, Larsen PR eds. Williams textbook of endocrinology. 9th ed. Philadelphia, PA: WB Saunders;1998:389-515.
12. Matsubayashi S, Tamai H, Matsumoto Y, et al. Graves’ disease after the onset of panic disorder. Psychother Psychosom 1996;65(5):277-80.
13. Lazarus JH. Hyperthyroidism. Lancet 1997;349:339-43.
14. Pearce EN. Diagnosis and management of thyrotoxicosis. BMJ 2006;332:1369-73.
15. Utiger RD. The thyroid: physiology, thyrotoxicosis, hypothyroidism, and the painful thyroid. In: Felig P, Frohman LA, eds. Endocrinology and metabolism, 4th ed. New York, NY: McGraw-Hill; 2001:261-347.
16. Beckers A, Abs R, Mahler C, et al. Thyrotropin-secreting pituitary adenomas: report of seven cases. J Clin Endocrinol Metab 1991;72:477-83.
17. Kinder BK, Burrow GN. The thyroid: nodules and neoplasiaIn: Felig P, Frohman LA eds. Endocrinology and metabolism, 4th ed New York, NY: McGraw-Hill; 2001:349-383.
18. Prange AJ, Jr, Wilson IC, Rabon AM, Lipton MA. Enhancement of imipramine antidepressant activity by thyroid hormone. Am J Psychiatry 1969;126:457-69.
19. Geracioti TD, Jr, Loosen PT, Gold PW, Kling MA. Cortisol, thyroid hormone, and mood in atypical depression: a longitudinal case study. Biol Psychiatry 1992;31:515-9.
20. Geracioti TD, Kling MA, Post R, Gold PW. Antithyroid antibody-linked symptoms in borderline personality disorder. Endocrine 2003;21:153-8.
21. Bocchetta A, Mossa P, Velluzzi F, et al. Ten-year follow-up of thyroid function in lithium patients. J Clin Psychopharmacol 2001;21:594-8.
1. Sakurai A, Nakai A, DeGroot LJ. Expression of three forms of thyroid hormone receptor in human tissues. Mol Endocrinol 1989;3:392-9.
2. Shahrara S, Drvota V, Sylven C. Organ specific expression of thyroid hormone receptor mRNA and protein in different human tissues. Biol Pharm Bull 1999;22:1027-33.
3. Geracioti TD, Jr. How to identify hypothyroidism’s psychiatric presentations. Current Psychiatry 2006;5(11):98-117.
4. Hollowell JG, Staehling NW, Flanders WD, et al. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab 2002;87:489-99.
5. Bianchi GP, Zaccheroni V, Vescini F, et al. Health-related quality of life in patients with thyroid disorders. Qual Life Res 2004;13:45-54.
6. Thomsen AF, Kvist TK, Andersen OK, Kessing LV. Increased risk of affective disorder following hospitalization with hyperthyroidism—a register-based study. Eur J Endocrinol 2005;152:535-43.
7. Grabe HJ, Volzke H, Ludermann J, et al. Mental and physical complaints in thyroid disorders in the general population. Acta Psychiatr Scand 2005;112:286-93.
8. Kathol RG, Delahunt JW. The relationship of anxiety and depression to symptoms of hyperthyroidism using operational criteria. Gen Hosp Psychiatry 1986;8:23-8.
9. Trzepacz PT, McCue M, Klein I, et al. A psychiatric and neuropsychological study of patients with untreated Graves’ disease. Gen Hosp Psychiatry 1988;10:49-55.
10. Bunevicius R, Velickiene D, Prange AJ, Jr. Mood and anxiety disorders in women with treated hyperthyroidism and ophthalmopathy caused by Graves’ disease. Gen Hosp Psychiatry 2005;27:133-9.
11. Larson PR, Davies TF, Hay ID. The thyroid gland. In: Wilson JD, Forster DW, Kronenberg HM, Larsen PR eds. Williams textbook of endocrinology. 9th ed. Philadelphia, PA: WB Saunders;1998:389-515.
12. Matsubayashi S, Tamai H, Matsumoto Y, et al. Graves’ disease after the onset of panic disorder. Psychother Psychosom 1996;65(5):277-80.
13. Lazarus JH. Hyperthyroidism. Lancet 1997;349:339-43.
14. Pearce EN. Diagnosis and management of thyrotoxicosis. BMJ 2006;332:1369-73.
15. Utiger RD. The thyroid: physiology, thyrotoxicosis, hypothyroidism, and the painful thyroid. In: Felig P, Frohman LA, eds. Endocrinology and metabolism, 4th ed. New York, NY: McGraw-Hill; 2001:261-347.
16. Beckers A, Abs R, Mahler C, et al. Thyrotropin-secreting pituitary adenomas: report of seven cases. J Clin Endocrinol Metab 1991;72:477-83.
17. Kinder BK, Burrow GN. The thyroid: nodules and neoplasiaIn: Felig P, Frohman LA eds. Endocrinology and metabolism, 4th ed New York, NY: McGraw-Hill; 2001:349-383.
18. Prange AJ, Jr, Wilson IC, Rabon AM, Lipton MA. Enhancement of imipramine antidepressant activity by thyroid hormone. Am J Psychiatry 1969;126:457-69.
19. Geracioti TD, Jr, Loosen PT, Gold PW, Kling MA. Cortisol, thyroid hormone, and mood in atypical depression: a longitudinal case study. Biol Psychiatry 1992;31:515-9.
20. Geracioti TD, Kling MA, Post R, Gold PW. Antithyroid antibody-linked symptoms in borderline personality disorder. Endocrine 2003;21:153-8.
21. Bocchetta A, Mossa P, Velluzzi F, et al. Ten-year follow-up of thyroid function in lithium patients. J Clin Psychopharmacol 2001;21:594-8.