User login
Perioperative statin associated with reduction in all-cause perioperative mortality in noncardiac surgery
CLINICAL QUESTION: Does perioperative statin use reduce 30-day mortality in noncardiac surgery?
BACKGROUND: Current perioperative guidelines focus on continuation of existing therapy in long-term statin users with weak recommendations of potential efficacy in reducing perioperative complications.
STUDY DESIGN: Retrospective, observational cohort analysis.
SYNOPSIS: Using the Veterans Affairs Surgical Quality Improvement Program database, 96,486 patients were studied who were undergoing elective or emergent noncardiac surgery (vascular, general, orthopedic, neurosurgery, otolaryngology, and urology). 96.3% were men. Patients who died the day of the surgery or the day after were excluded, as were patients with multiple surgeries during the assessment period. Statin exposure on the day of or the day after surgery was compared with no statin use. The primary outcome was 30-day mortality and the secondary outcomes were significant reduction in any other complication.
Statin exposure was associated with reduced 30-day all-cause mortality with a marginally favorable effect with longer-term statin use (6 months to 1 year before admission). For the secondary outcomes, there was significant risk reduction in cardiac, infectious, respiratory, and renal complications but no significant change in central nervous system or nonatherosclerotic thrombotic complications.
Statin exposure may be associated with adherence to medical treatment and follow-up thus causing a selection bias.
BOTTOM LINE: Perioperative statin use was associated with a reduction in 30-day mortality and other complications.
CITATIONS: London MJ, Schwartz GG, Hur K, Henderson WG. Association of perioperative statin use with mortality and morbidity after major noncardiac surgery. JAMA Intern Med. 2017 Feb 1;177(2):231-42.
Dr. Dietsche is a clinical instructor, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: Does perioperative statin use reduce 30-day mortality in noncardiac surgery?
BACKGROUND: Current perioperative guidelines focus on continuation of existing therapy in long-term statin users with weak recommendations of potential efficacy in reducing perioperative complications.
STUDY DESIGN: Retrospective, observational cohort analysis.
SYNOPSIS: Using the Veterans Affairs Surgical Quality Improvement Program database, 96,486 patients were studied who were undergoing elective or emergent noncardiac surgery (vascular, general, orthopedic, neurosurgery, otolaryngology, and urology). 96.3% were men. Patients who died the day of the surgery or the day after were excluded, as were patients with multiple surgeries during the assessment period. Statin exposure on the day of or the day after surgery was compared with no statin use. The primary outcome was 30-day mortality and the secondary outcomes were significant reduction in any other complication.
Statin exposure was associated with reduced 30-day all-cause mortality with a marginally favorable effect with longer-term statin use (6 months to 1 year before admission). For the secondary outcomes, there was significant risk reduction in cardiac, infectious, respiratory, and renal complications but no significant change in central nervous system or nonatherosclerotic thrombotic complications.
Statin exposure may be associated with adherence to medical treatment and follow-up thus causing a selection bias.
BOTTOM LINE: Perioperative statin use was associated with a reduction in 30-day mortality and other complications.
CITATIONS: London MJ, Schwartz GG, Hur K, Henderson WG. Association of perioperative statin use with mortality and morbidity after major noncardiac surgery. JAMA Intern Med. 2017 Feb 1;177(2):231-42.
Dr. Dietsche is a clinical instructor, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: Does perioperative statin use reduce 30-day mortality in noncardiac surgery?
BACKGROUND: Current perioperative guidelines focus on continuation of existing therapy in long-term statin users with weak recommendations of potential efficacy in reducing perioperative complications.
STUDY DESIGN: Retrospective, observational cohort analysis.
SYNOPSIS: Using the Veterans Affairs Surgical Quality Improvement Program database, 96,486 patients were studied who were undergoing elective or emergent noncardiac surgery (vascular, general, orthopedic, neurosurgery, otolaryngology, and urology). 96.3% were men. Patients who died the day of the surgery or the day after were excluded, as were patients with multiple surgeries during the assessment period. Statin exposure on the day of or the day after surgery was compared with no statin use. The primary outcome was 30-day mortality and the secondary outcomes were significant reduction in any other complication.
Statin exposure was associated with reduced 30-day all-cause mortality with a marginally favorable effect with longer-term statin use (6 months to 1 year before admission). For the secondary outcomes, there was significant risk reduction in cardiac, infectious, respiratory, and renal complications but no significant change in central nervous system or nonatherosclerotic thrombotic complications.
Statin exposure may be associated with adherence to medical treatment and follow-up thus causing a selection bias.
BOTTOM LINE: Perioperative statin use was associated with a reduction in 30-day mortality and other complications.
CITATIONS: London MJ, Schwartz GG, Hur K, Henderson WG. Association of perioperative statin use with mortality and morbidity after major noncardiac surgery. JAMA Intern Med. 2017 Feb 1;177(2):231-42.
Dr. Dietsche is a clinical instructor, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
Male vs. female hospitalists, a comparison in mortality and readmission rate for Medicare patients
CLINICAL QUESTION: Does physician sex affect hospitalized patient outcomes?
BACKGROUND: Previous studies had suggested different practice patterns between male and female physicians in process measure of quality. No prior evaluation of patient outcomes examining those differences was studied in the past.
STUDY DESIGN: Observational, cross-sectional study.
SYNOPSIS: This observational study assessed the difference in patients’ outcomes that were treated by a male or female physician. 30-days mortality rate was analyzed from 1,583,028 hospitalizations. The mortality rate of patients cared for by female physicians was lower and statistically significant: 11.07% vs. 11.49% (adjusted risk difference, –0.43%; 95% CI, –0.57% to –0.28%; P less than .001). The difference did not change after considering patient and physician characteristics as well as when looking at hospital fixed effects (that is, hospital indicators). In order to prevent one death, a female physician needs to treat 233 patients.
Also, 30-day readmission rate, after adjustment readmissions (from 1,540,797 hospitalizations) was 15.02% vs. 15.57% (adjusted risk difference, –0.55%; 95% confidence interval, –0.71% to 0.39%; P less than .001) showing that the care provided by a female physician can reduce one readmission when treating 182 patients.
BOTTOM LINE: Patients older than 65 years have lower 30-day mortality and readmission rates when receiving inpatient care from a female internist, compared with care by a male internist.
CITATIONS: Tsugawa Y, Jena AB, Figueroa JF, et al. Comparison of hospital mortality and readmission rates for Medicare patients treated by male vs. female physicians. JAMA Intern Med. 2017 Feb;177(2):206-13.
Dr. Orjuela is assistant professor of neurology at the University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: Does physician sex affect hospitalized patient outcomes?
BACKGROUND: Previous studies had suggested different practice patterns between male and female physicians in process measure of quality. No prior evaluation of patient outcomes examining those differences was studied in the past.
STUDY DESIGN: Observational, cross-sectional study.
SYNOPSIS: This observational study assessed the difference in patients’ outcomes that were treated by a male or female physician. 30-days mortality rate was analyzed from 1,583,028 hospitalizations. The mortality rate of patients cared for by female physicians was lower and statistically significant: 11.07% vs. 11.49% (adjusted risk difference, –0.43%; 95% CI, –0.57% to –0.28%; P less than .001). The difference did not change after considering patient and physician characteristics as well as when looking at hospital fixed effects (that is, hospital indicators). In order to prevent one death, a female physician needs to treat 233 patients.
Also, 30-day readmission rate, after adjustment readmissions (from 1,540,797 hospitalizations) was 15.02% vs. 15.57% (adjusted risk difference, –0.55%; 95% confidence interval, –0.71% to 0.39%; P less than .001) showing that the care provided by a female physician can reduce one readmission when treating 182 patients.
BOTTOM LINE: Patients older than 65 years have lower 30-day mortality and readmission rates when receiving inpatient care from a female internist, compared with care by a male internist.
CITATIONS: Tsugawa Y, Jena AB, Figueroa JF, et al. Comparison of hospital mortality and readmission rates for Medicare patients treated by male vs. female physicians. JAMA Intern Med. 2017 Feb;177(2):206-13.
Dr. Orjuela is assistant professor of neurology at the University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: Does physician sex affect hospitalized patient outcomes?
BACKGROUND: Previous studies had suggested different practice patterns between male and female physicians in process measure of quality. No prior evaluation of patient outcomes examining those differences was studied in the past.
STUDY DESIGN: Observational, cross-sectional study.
SYNOPSIS: This observational study assessed the difference in patients’ outcomes that were treated by a male or female physician. 30-days mortality rate was analyzed from 1,583,028 hospitalizations. The mortality rate of patients cared for by female physicians was lower and statistically significant: 11.07% vs. 11.49% (adjusted risk difference, –0.43%; 95% CI, –0.57% to –0.28%; P less than .001). The difference did not change after considering patient and physician characteristics as well as when looking at hospital fixed effects (that is, hospital indicators). In order to prevent one death, a female physician needs to treat 233 patients.
Also, 30-day readmission rate, after adjustment readmissions (from 1,540,797 hospitalizations) was 15.02% vs. 15.57% (adjusted risk difference, –0.55%; 95% confidence interval, –0.71% to 0.39%; P less than .001) showing that the care provided by a female physician can reduce one readmission when treating 182 patients.
BOTTOM LINE: Patients older than 65 years have lower 30-day mortality and readmission rates when receiving inpatient care from a female internist, compared with care by a male internist.
CITATIONS: Tsugawa Y, Jena AB, Figueroa JF, et al. Comparison of hospital mortality and readmission rates for Medicare patients treated by male vs. female physicians. JAMA Intern Med. 2017 Feb;177(2):206-13.
Dr. Orjuela is assistant professor of neurology at the University of Colorado School of Medicine, Aurora.
End-of-rotation resident transition in care and mortality among hospitalized patients
CLINICAL QUESTION: Are hospitalized patients experiencing an increased mortality risk at the end-rotation resident transition in care and is this association related to the Accreditation Council for Graduate Medical Education (ACGME) 2011 duty-hour regulations?
BACKGROUND: Prior studies of physicians’ transitions in care were associated with potential adverse patient events and outcomes. A higher mortality risk was suggested among patients with a complex hospital course or prolonged length of stay in association to house-staff transitions of care.
SETTING: 10 University-affiliated U.S. Veterans Health Administration hospitals.
SYNOPSIS: 230,701 patient discharges (mean age, 65.6 years; 95.8% male sex; median length of stay, 3 days) were included. The transition group included patients admitted at any time prior to an end-of-rotation who were either discharged or deceased within 7 days of transition. All other discharges were considered controls.
The primary outcome was in-hospital mortality rate; secondary outcomes included 30-day and 90-day mortality and readmission rates. An absolute increase of 1.5% to 1.9% in a unadjusted in-hospitality risk was found. The 30-day and 90-day mortality odds ratios were 1.10 and 1.21, respectively. A possible stronger association was found among interns’ transitions in care and the in-hospital and after-discharge mortality post-ACGME 2011 duty hour regulations. The latter raises questions about the interns’ inexperience and their amount of shift-to-shift handoffs. An adjusted analysis of the readmission rates at 30-day and 90-day was not significantly different between transition vs. control patients.
BOTTOM LINE: Elevated in-hospital mortality was seen among patients admitted to the inpatient medicine service at the end-of-rotation resident transitions in care. The association was stronger after the duty-hour ACGME (2011) regulations.
CITATIONS: Denson JL, Jensen A, Saag HS, et al. Association between end-of-rotation resident transition in care and mortality among hospitalized patients. JAMA. 2016 Dec 6;316(21):2204-13.
Dr. Orjuela is assistant professor of neurology at the University of Colorado School of Medicine, Aurora
CLINICAL QUESTION: Are hospitalized patients experiencing an increased mortality risk at the end-rotation resident transition in care and is this association related to the Accreditation Council for Graduate Medical Education (ACGME) 2011 duty-hour regulations?
BACKGROUND: Prior studies of physicians’ transitions in care were associated with potential adverse patient events and outcomes. A higher mortality risk was suggested among patients with a complex hospital course or prolonged length of stay in association to house-staff transitions of care.
SETTING: 10 University-affiliated U.S. Veterans Health Administration hospitals.
SYNOPSIS: 230,701 patient discharges (mean age, 65.6 years; 95.8% male sex; median length of stay, 3 days) were included. The transition group included patients admitted at any time prior to an end-of-rotation who were either discharged or deceased within 7 days of transition. All other discharges were considered controls.
The primary outcome was in-hospital mortality rate; secondary outcomes included 30-day and 90-day mortality and readmission rates. An absolute increase of 1.5% to 1.9% in a unadjusted in-hospitality risk was found. The 30-day and 90-day mortality odds ratios were 1.10 and 1.21, respectively. A possible stronger association was found among interns’ transitions in care and the in-hospital and after-discharge mortality post-ACGME 2011 duty hour regulations. The latter raises questions about the interns’ inexperience and their amount of shift-to-shift handoffs. An adjusted analysis of the readmission rates at 30-day and 90-day was not significantly different between transition vs. control patients.
BOTTOM LINE: Elevated in-hospital mortality was seen among patients admitted to the inpatient medicine service at the end-of-rotation resident transitions in care. The association was stronger after the duty-hour ACGME (2011) regulations.
CITATIONS: Denson JL, Jensen A, Saag HS, et al. Association between end-of-rotation resident transition in care and mortality among hospitalized patients. JAMA. 2016 Dec 6;316(21):2204-13.
Dr. Orjuela is assistant professor of neurology at the University of Colorado School of Medicine, Aurora
CLINICAL QUESTION: Are hospitalized patients experiencing an increased mortality risk at the end-rotation resident transition in care and is this association related to the Accreditation Council for Graduate Medical Education (ACGME) 2011 duty-hour regulations?
BACKGROUND: Prior studies of physicians’ transitions in care were associated with potential adverse patient events and outcomes. A higher mortality risk was suggested among patients with a complex hospital course or prolonged length of stay in association to house-staff transitions of care.
SETTING: 10 University-affiliated U.S. Veterans Health Administration hospitals.
SYNOPSIS: 230,701 patient discharges (mean age, 65.6 years; 95.8% male sex; median length of stay, 3 days) were included. The transition group included patients admitted at any time prior to an end-of-rotation who were either discharged or deceased within 7 days of transition. All other discharges were considered controls.
The primary outcome was in-hospital mortality rate; secondary outcomes included 30-day and 90-day mortality and readmission rates. An absolute increase of 1.5% to 1.9% in a unadjusted in-hospitality risk was found. The 30-day and 90-day mortality odds ratios were 1.10 and 1.21, respectively. A possible stronger association was found among interns’ transitions in care and the in-hospital and after-discharge mortality post-ACGME 2011 duty hour regulations. The latter raises questions about the interns’ inexperience and their amount of shift-to-shift handoffs. An adjusted analysis of the readmission rates at 30-day and 90-day was not significantly different between transition vs. control patients.
BOTTOM LINE: Elevated in-hospital mortality was seen among patients admitted to the inpatient medicine service at the end-of-rotation resident transitions in care. The association was stronger after the duty-hour ACGME (2011) regulations.
CITATIONS: Denson JL, Jensen A, Saag HS, et al. Association between end-of-rotation resident transition in care and mortality among hospitalized patients. JAMA. 2016 Dec 6;316(21):2204-13.
Dr. Orjuela is assistant professor of neurology at the University of Colorado School of Medicine, Aurora
Perioperative pharmacological thromboprophylaxis in patients with cancer: a systematic review and meta-analysis
CLINICAL QUESTION: What are the benefits and harms of perioperative pharmacological thromboprophylaxis in cancer patients undergoing surgery?
STUDY DESIGN: Systematic review and meta-analysis.
SYNOPSIS: Thirty-nine trials were deemed eligible for inclusion in the meta-analysis. Twenty-five of these were prospective and 14 were retrospective. The overall incidence of deep venous thrombosis (DVT) and pulmonary embolism was 0.9% (across 20 studies) and 0.3% (across 19 studies), respectively. Pharmacologic prophylaxis overall reduced DVT incidence (0.5% vs. 1.2%; relative risk, 0.51; P = .03). Subgroup analysis demonstrated this was significant for abdominal/pelvic surgeries and with low molecular weight heparin. Six studies compared duration of standard prophylaxis (10 days) with extended prophylaxis (4 weeks), with a lower VTE rate in the extended group. Bleeding events were noted in 13 studies and pharmacologic prophylaxis significantly increased bleeding risk (2.7% vs. 8%; RR, 2.51; P less than .0001).
BOTTOM LINE: Perioperative pharmacologic prophylaxis reduces DVT risk in patients with cancer, with greatest risk reduction seen in patients undergoing abdominal/pelvic surgeries. This comes at the cost of increased bleeding complications.
CITATIONS: Guo Q, Huang B, Zhao J, et al. Perioperative pharmacological thromboprophylaxis in patients with cancer: a systematic review and meta-analysis. Ann Surg. 2016 Nov. doi: 10.1097/SLA.0000000000002074.
Dr. Patil is a clinical instructor, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: What are the benefits and harms of perioperative pharmacological thromboprophylaxis in cancer patients undergoing surgery?
STUDY DESIGN: Systematic review and meta-analysis.
SYNOPSIS: Thirty-nine trials were deemed eligible for inclusion in the meta-analysis. Twenty-five of these were prospective and 14 were retrospective. The overall incidence of deep venous thrombosis (DVT) and pulmonary embolism was 0.9% (across 20 studies) and 0.3% (across 19 studies), respectively. Pharmacologic prophylaxis overall reduced DVT incidence (0.5% vs. 1.2%; relative risk, 0.51; P = .03). Subgroup analysis demonstrated this was significant for abdominal/pelvic surgeries and with low molecular weight heparin. Six studies compared duration of standard prophylaxis (10 days) with extended prophylaxis (4 weeks), with a lower VTE rate in the extended group. Bleeding events were noted in 13 studies and pharmacologic prophylaxis significantly increased bleeding risk (2.7% vs. 8%; RR, 2.51; P less than .0001).
BOTTOM LINE: Perioperative pharmacologic prophylaxis reduces DVT risk in patients with cancer, with greatest risk reduction seen in patients undergoing abdominal/pelvic surgeries. This comes at the cost of increased bleeding complications.
CITATIONS: Guo Q, Huang B, Zhao J, et al. Perioperative pharmacological thromboprophylaxis in patients with cancer: a systematic review and meta-analysis. Ann Surg. 2016 Nov. doi: 10.1097/SLA.0000000000002074.
Dr. Patil is a clinical instructor, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: What are the benefits and harms of perioperative pharmacological thromboprophylaxis in cancer patients undergoing surgery?
STUDY DESIGN: Systematic review and meta-analysis.
SYNOPSIS: Thirty-nine trials were deemed eligible for inclusion in the meta-analysis. Twenty-five of these were prospective and 14 were retrospective. The overall incidence of deep venous thrombosis (DVT) and pulmonary embolism was 0.9% (across 20 studies) and 0.3% (across 19 studies), respectively. Pharmacologic prophylaxis overall reduced DVT incidence (0.5% vs. 1.2%; relative risk, 0.51; P = .03). Subgroup analysis demonstrated this was significant for abdominal/pelvic surgeries and with low molecular weight heparin. Six studies compared duration of standard prophylaxis (10 days) with extended prophylaxis (4 weeks), with a lower VTE rate in the extended group. Bleeding events were noted in 13 studies and pharmacologic prophylaxis significantly increased bleeding risk (2.7% vs. 8%; RR, 2.51; P less than .0001).
BOTTOM LINE: Perioperative pharmacologic prophylaxis reduces DVT risk in patients with cancer, with greatest risk reduction seen in patients undergoing abdominal/pelvic surgeries. This comes at the cost of increased bleeding complications.
CITATIONS: Guo Q, Huang B, Zhao J, et al. Perioperative pharmacological thromboprophylaxis in patients with cancer: a systematic review and meta-analysis. Ann Surg. 2016 Nov. doi: 10.1097/SLA.0000000000002074.
Dr. Patil is a clinical instructor, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
Readmission rates after passage of the hospital readmissions reduction program
CLINICAL QUESTION: Did hospitals receiving the highest penalties for readmissions have accelerated improvement in this metric after passage of Medicare Hospital Readmissions Reduction Program (HRRP)?
BACKGROUND: Medicare passed the HRRP to incentivize reductions in readmission rates. The impact of penalties on relative hospital improvement rates remains unknown.
SETTING: Query of national Medicare Provider Analysis and Review files.
SYNOPSIS: 2,868 hospitals were identified as candidates for analysis and were stratified into four risk groups based on penalty size under HRRP: highest-performing, average-performing, low-performing, and lowest-performing. The primary outcomes were hospital-specific, 30-day, all-cause risk-standardized readmission rates (RSRRs) for patients discharged with acute MI, HF, or pneumonia. The investigators separated data into a pre-law period and post-law period. They fitted a logistic regression model to pre-law RSRRs and developed a piecewise linear model on post-law RSRRs with pre-law data as the dependent variable. All hospital groups had reductions in RSRRs, with the lowest quartile demonstrating greatest improvement.
BOTTOM LINE: HRRP has resulted in reductions in RSRRs with greatest improvement in hospitals with lowest pre-law performance.
CITATIONS: Wasfy JH, Zigler CM, Choirat C, et al. Readmission rates after passage of the hospital readmissions reduction program: a pre-post analysis. Ann Intern Med. 2017 Mar;166(5):324-31.
Dr. Patil is a clinical instructor, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: Did hospitals receiving the highest penalties for readmissions have accelerated improvement in this metric after passage of Medicare Hospital Readmissions Reduction Program (HRRP)?
BACKGROUND: Medicare passed the HRRP to incentivize reductions in readmission rates. The impact of penalties on relative hospital improvement rates remains unknown.
SETTING: Query of national Medicare Provider Analysis and Review files.
SYNOPSIS: 2,868 hospitals were identified as candidates for analysis and were stratified into four risk groups based on penalty size under HRRP: highest-performing, average-performing, low-performing, and lowest-performing. The primary outcomes were hospital-specific, 30-day, all-cause risk-standardized readmission rates (RSRRs) for patients discharged with acute MI, HF, or pneumonia. The investigators separated data into a pre-law period and post-law period. They fitted a logistic regression model to pre-law RSRRs and developed a piecewise linear model on post-law RSRRs with pre-law data as the dependent variable. All hospital groups had reductions in RSRRs, with the lowest quartile demonstrating greatest improvement.
BOTTOM LINE: HRRP has resulted in reductions in RSRRs with greatest improvement in hospitals with lowest pre-law performance.
CITATIONS: Wasfy JH, Zigler CM, Choirat C, et al. Readmission rates after passage of the hospital readmissions reduction program: a pre-post analysis. Ann Intern Med. 2017 Mar;166(5):324-31.
Dr. Patil is a clinical instructor, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: Did hospitals receiving the highest penalties for readmissions have accelerated improvement in this metric after passage of Medicare Hospital Readmissions Reduction Program (HRRP)?
BACKGROUND: Medicare passed the HRRP to incentivize reductions in readmission rates. The impact of penalties on relative hospital improvement rates remains unknown.
SETTING: Query of national Medicare Provider Analysis and Review files.
SYNOPSIS: 2,868 hospitals were identified as candidates for analysis and were stratified into four risk groups based on penalty size under HRRP: highest-performing, average-performing, low-performing, and lowest-performing. The primary outcomes were hospital-specific, 30-day, all-cause risk-standardized readmission rates (RSRRs) for patients discharged with acute MI, HF, or pneumonia. The investigators separated data into a pre-law period and post-law period. They fitted a logistic regression model to pre-law RSRRs and developed a piecewise linear model on post-law RSRRs with pre-law data as the dependent variable. All hospital groups had reductions in RSRRs, with the lowest quartile demonstrating greatest improvement.
BOTTOM LINE: HRRP has resulted in reductions in RSRRs with greatest improvement in hospitals with lowest pre-law performance.
CITATIONS: Wasfy JH, Zigler CM, Choirat C, et al. Readmission rates after passage of the hospital readmissions reduction program: a pre-post analysis. Ann Intern Med. 2017 Mar;166(5):324-31.
Dr. Patil is a clinical instructor, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
Assessment of goals of care in nursing home reduces hospitalization for patients with dementia
CLINICAL QUESTION: For patients with advanced dementia, does a goals-of-care intervention improve communication and care outcomes?
STUDY DESIGN: Single-blind cluster randomized trial.
SETTING: Twenty-two nursing homes in North Carolina.
SYNOPSIS: Three hundred and two patient/families enrolled. Intervention included video and print decision aids followed by a structured goals of care discussion with trained nursing home staff. Quality of communication results, the primary outcome, at 3 months were mixed. Family perception of communication with nursing home staff was better in the intervention. Family–health care provider concordance on primary goal of care and treatment consistent with preferences were not significantly different. By the end of the study at 9 months there was no difference in symptom control but some secondary outcomes were encouraging including greater completion of MOST advanced directives (35% vs. 16%; P = .05) and half as many hospital transfers. Multiple comparisons merits future verification of secondary outcome findings.
BOTTOM LINE: Goals of care discussions for patients with advanced dementia appears to reduce hospitalizations.
CITATIONS: Hanson LC, Zimmerman S, Song MK, et al. Effect of the goals of care intervention for advanced dementia: a randomized clinical trial. JAMA Intern Med. 2017 Jan;177:24-31.
Dr. Cumbler is the associate chief of hospital medicine, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: For patients with advanced dementia, does a goals-of-care intervention improve communication and care outcomes?
STUDY DESIGN: Single-blind cluster randomized trial.
SETTING: Twenty-two nursing homes in North Carolina.
SYNOPSIS: Three hundred and two patient/families enrolled. Intervention included video and print decision aids followed by a structured goals of care discussion with trained nursing home staff. Quality of communication results, the primary outcome, at 3 months were mixed. Family perception of communication with nursing home staff was better in the intervention. Family–health care provider concordance on primary goal of care and treatment consistent with preferences were not significantly different. By the end of the study at 9 months there was no difference in symptom control but some secondary outcomes were encouraging including greater completion of MOST advanced directives (35% vs. 16%; P = .05) and half as many hospital transfers. Multiple comparisons merits future verification of secondary outcome findings.
BOTTOM LINE: Goals of care discussions for patients with advanced dementia appears to reduce hospitalizations.
CITATIONS: Hanson LC, Zimmerman S, Song MK, et al. Effect of the goals of care intervention for advanced dementia: a randomized clinical trial. JAMA Intern Med. 2017 Jan;177:24-31.
Dr. Cumbler is the associate chief of hospital medicine, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: For patients with advanced dementia, does a goals-of-care intervention improve communication and care outcomes?
STUDY DESIGN: Single-blind cluster randomized trial.
SETTING: Twenty-two nursing homes in North Carolina.
SYNOPSIS: Three hundred and two patient/families enrolled. Intervention included video and print decision aids followed by a structured goals of care discussion with trained nursing home staff. Quality of communication results, the primary outcome, at 3 months were mixed. Family perception of communication with nursing home staff was better in the intervention. Family–health care provider concordance on primary goal of care and treatment consistent with preferences were not significantly different. By the end of the study at 9 months there was no difference in symptom control but some secondary outcomes were encouraging including greater completion of MOST advanced directives (35% vs. 16%; P = .05) and half as many hospital transfers. Multiple comparisons merits future verification of secondary outcome findings.
BOTTOM LINE: Goals of care discussions for patients with advanced dementia appears to reduce hospitalizations.
CITATIONS: Hanson LC, Zimmerman S, Song MK, et al. Effect of the goals of care intervention for advanced dementia: a randomized clinical trial. JAMA Intern Med. 2017 Jan;177:24-31.
Dr. Cumbler is the associate chief of hospital medicine, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
Antipsychotics ineffective for symptoms of delirium in palliative care
CLINICAL QUESTION: Do antipsychotics provide symptomatic benefit for delirium in palliative care?
BACKGROUND: Antipsychotics are frequently used for the treatment of delirium and guideline recommended for delirium-associated distress. However, a 2016 meta-analysis found antipsychotics are not associated with change in delirium duration or severity. Antipsychotics for palliative management of delirium at end of life is not well studied.
STUDY DESIGN: Double-blind randomized controlled trial with placebo, haloperidol, and risperidone arms.
SETTING: Eleven Australian inpatient hospice or palliative care services.
SYNOPSIS: 247 patients (mean age, 74.9 years; 88.3% with cancer) with advanced incurable disease and active delirium were studied. Most had mild-moderate severity delirium. All received nonpharmacological measures and plan to address reversible precipitants. Patients were randomized to placebo (84), haloperidol (81), or risperidone (82) for 72 hours. Dose titration was allowed based on delirium symptoms. In intention to treat analysis the delirium severity scores were statistically higher in haloperidol and risperidone arms, compared with placebo. This reached statistical significance although less than the minimum clinically significant difference. Mortality, use of rescue medicines, and extrapyramidal symptoms were higher in antipsychotic groups.
BOTTOM LINE: Antipsychotics cause side effects without efficacy in palliation of symptoms of delirium.
CITATIONS: Agar MR, Lawlor PG, Quinn S, et al. Efficacy of oral risperidone, haloperidol, or placebo for symptoms of delirium among patients in palliative care: a randomized clinical trial. JAMA Intern Med. 2017 Jan;177:34-42.
Dr. Cumbler is the associate chief of hospital medicine, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: Do antipsychotics provide symptomatic benefit for delirium in palliative care?
BACKGROUND: Antipsychotics are frequently used for the treatment of delirium and guideline recommended for delirium-associated distress. However, a 2016 meta-analysis found antipsychotics are not associated with change in delirium duration or severity. Antipsychotics for palliative management of delirium at end of life is not well studied.
STUDY DESIGN: Double-blind randomized controlled trial with placebo, haloperidol, and risperidone arms.
SETTING: Eleven Australian inpatient hospice or palliative care services.
SYNOPSIS: 247 patients (mean age, 74.9 years; 88.3% with cancer) with advanced incurable disease and active delirium were studied. Most had mild-moderate severity delirium. All received nonpharmacological measures and plan to address reversible precipitants. Patients were randomized to placebo (84), haloperidol (81), or risperidone (82) for 72 hours. Dose titration was allowed based on delirium symptoms. In intention to treat analysis the delirium severity scores were statistically higher in haloperidol and risperidone arms, compared with placebo. This reached statistical significance although less than the minimum clinically significant difference. Mortality, use of rescue medicines, and extrapyramidal symptoms were higher in antipsychotic groups.
BOTTOM LINE: Antipsychotics cause side effects without efficacy in palliation of symptoms of delirium.
CITATIONS: Agar MR, Lawlor PG, Quinn S, et al. Efficacy of oral risperidone, haloperidol, or placebo for symptoms of delirium among patients in palliative care: a randomized clinical trial. JAMA Intern Med. 2017 Jan;177:34-42.
Dr. Cumbler is the associate chief of hospital medicine, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: Do antipsychotics provide symptomatic benefit for delirium in palliative care?
BACKGROUND: Antipsychotics are frequently used for the treatment of delirium and guideline recommended for delirium-associated distress. However, a 2016 meta-analysis found antipsychotics are not associated with change in delirium duration or severity. Antipsychotics for palliative management of delirium at end of life is not well studied.
STUDY DESIGN: Double-blind randomized controlled trial with placebo, haloperidol, and risperidone arms.
SETTING: Eleven Australian inpatient hospice or palliative care services.
SYNOPSIS: 247 patients (mean age, 74.9 years; 88.3% with cancer) with advanced incurable disease and active delirium were studied. Most had mild-moderate severity delirium. All received nonpharmacological measures and plan to address reversible precipitants. Patients were randomized to placebo (84), haloperidol (81), or risperidone (82) for 72 hours. Dose titration was allowed based on delirium symptoms. In intention to treat analysis the delirium severity scores were statistically higher in haloperidol and risperidone arms, compared with placebo. This reached statistical significance although less than the minimum clinically significant difference. Mortality, use of rescue medicines, and extrapyramidal symptoms were higher in antipsychotic groups.
BOTTOM LINE: Antipsychotics cause side effects without efficacy in palliation of symptoms of delirium.
CITATIONS: Agar MR, Lawlor PG, Quinn S, et al. Efficacy of oral risperidone, haloperidol, or placebo for symptoms of delirium among patients in palliative care: a randomized clinical trial. JAMA Intern Med. 2017 Jan;177:34-42.
Dr. Cumbler is the associate chief of hospital medicine, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
Stump the Professor event entertains, educates
Gurpreet Dhaliwal, MD, professor of medicine at the University of California, San Francisco, joked that participating in a “Stump the Professor” event is “like taking an oral exam in front of 300 or 400 people.”
Dr. Dhaliwal passed his “exam” with flying colors on Wednesday at HM17, correctly making a diagnosis of a case of leptospirosis described by his co-presenter Daniel Brotman, MD, SFHM, professor of medicine and director of the hospitalist program at Johns Hopkins University, Baltimore.
While the format is intended to be fun and entertaining, he said that there is no doubt that learning is taking place – both by him and by the audience.
“The most important goal by far and away is to put our most important procedure on display, which is thinking,” he said. “We don’t always make our thinking explicit, and we don’t often open it to scrutiny. So the goal of this session is to do both.”
Talking through his uncertainty can be one of the most interesting aspects of the session, Dr. Dhaliwal told attendees.
“If I can’t say something insightful, let me try to capture my uncertainty and crystallize that for you so you recognize that as a real part of medicine,” he said.
The HM17 audience seemed to enjoy trying to solve the case and thinking through the clinical reasoning as Dr. Dhaliwal did the same. The diagnosis of leptospirosis in Wednesday’s case surprised the audience, many of whom shook their heads in amazement.
“I pick cases based on being dramatic and/or unusual enough to provide some clinical excitement and diagnostic challenge,” he said.
An “important bonus,” Dr. Dhaliwal said, is that the audience would learn something about the disease that’s being discussed.
“I suspect I learn the most, especially if I get the case wrong,” he told attendees. “After living it on stage, there’s a lot that I upload in my memory for the next time I see something like this in real life.”
He said he’s probably batting about 0.500 on getting the cases right.
“I’ve had plenty of experiences where I’ve pulled the rabbit out of the hat at the last minute, and it’s been glorious, and I’ve had plenty of experiences where I’ve fallen flat on my face, and I didn’t have a prayer of knowing it, either, because my thinking was off, my knowledge was deficient, or it was something I had never heard of before,” he said. “The one thing that’s always rewarding is that people are always very appreciative that I shared my thinking, whether it’s a flash of insight or a total stumble or an uncertainty that I have.”
It might seem that the event has more of a potential downside than upside: If he gets a case right, he’s doing what he should do; if he gets one wrong, it might be embarrassing. He doesn’t see it that way, he told the crowd.
“It’s a total joy to be up here,” Dr. Dhaliwal said. “There’s no doubt that standing in front of a crowd induces a little bit of anxiety, but it is a lot of fun to do. And I had mentors who did this, and then I started to learn it myself, and at some point, you get past the anxiety of being right or wrong, and you just enjoy being up there.”
Gurpreet Dhaliwal, MD, professor of medicine at the University of California, San Francisco, joked that participating in a “Stump the Professor” event is “like taking an oral exam in front of 300 or 400 people.”
Dr. Dhaliwal passed his “exam” with flying colors on Wednesday at HM17, correctly making a diagnosis of a case of leptospirosis described by his co-presenter Daniel Brotman, MD, SFHM, professor of medicine and director of the hospitalist program at Johns Hopkins University, Baltimore.
While the format is intended to be fun and entertaining, he said that there is no doubt that learning is taking place – both by him and by the audience.
“The most important goal by far and away is to put our most important procedure on display, which is thinking,” he said. “We don’t always make our thinking explicit, and we don’t often open it to scrutiny. So the goal of this session is to do both.”
Talking through his uncertainty can be one of the most interesting aspects of the session, Dr. Dhaliwal told attendees.
“If I can’t say something insightful, let me try to capture my uncertainty and crystallize that for you so you recognize that as a real part of medicine,” he said.
The HM17 audience seemed to enjoy trying to solve the case and thinking through the clinical reasoning as Dr. Dhaliwal did the same. The diagnosis of leptospirosis in Wednesday’s case surprised the audience, many of whom shook their heads in amazement.
“I pick cases based on being dramatic and/or unusual enough to provide some clinical excitement and diagnostic challenge,” he said.
An “important bonus,” Dr. Dhaliwal said, is that the audience would learn something about the disease that’s being discussed.
“I suspect I learn the most, especially if I get the case wrong,” he told attendees. “After living it on stage, there’s a lot that I upload in my memory for the next time I see something like this in real life.”
He said he’s probably batting about 0.500 on getting the cases right.
“I’ve had plenty of experiences where I’ve pulled the rabbit out of the hat at the last minute, and it’s been glorious, and I’ve had plenty of experiences where I’ve fallen flat on my face, and I didn’t have a prayer of knowing it, either, because my thinking was off, my knowledge was deficient, or it was something I had never heard of before,” he said. “The one thing that’s always rewarding is that people are always very appreciative that I shared my thinking, whether it’s a flash of insight or a total stumble or an uncertainty that I have.”
It might seem that the event has more of a potential downside than upside: If he gets a case right, he’s doing what he should do; if he gets one wrong, it might be embarrassing. He doesn’t see it that way, he told the crowd.
“It’s a total joy to be up here,” Dr. Dhaliwal said. “There’s no doubt that standing in front of a crowd induces a little bit of anxiety, but it is a lot of fun to do. And I had mentors who did this, and then I started to learn it myself, and at some point, you get past the anxiety of being right or wrong, and you just enjoy being up there.”
Gurpreet Dhaliwal, MD, professor of medicine at the University of California, San Francisco, joked that participating in a “Stump the Professor” event is “like taking an oral exam in front of 300 or 400 people.”
Dr. Dhaliwal passed his “exam” with flying colors on Wednesday at HM17, correctly making a diagnosis of a case of leptospirosis described by his co-presenter Daniel Brotman, MD, SFHM, professor of medicine and director of the hospitalist program at Johns Hopkins University, Baltimore.
While the format is intended to be fun and entertaining, he said that there is no doubt that learning is taking place – both by him and by the audience.
“The most important goal by far and away is to put our most important procedure on display, which is thinking,” he said. “We don’t always make our thinking explicit, and we don’t often open it to scrutiny. So the goal of this session is to do both.”
Talking through his uncertainty can be one of the most interesting aspects of the session, Dr. Dhaliwal told attendees.
“If I can’t say something insightful, let me try to capture my uncertainty and crystallize that for you so you recognize that as a real part of medicine,” he said.
The HM17 audience seemed to enjoy trying to solve the case and thinking through the clinical reasoning as Dr. Dhaliwal did the same. The diagnosis of leptospirosis in Wednesday’s case surprised the audience, many of whom shook their heads in amazement.
“I pick cases based on being dramatic and/or unusual enough to provide some clinical excitement and diagnostic challenge,” he said.
An “important bonus,” Dr. Dhaliwal said, is that the audience would learn something about the disease that’s being discussed.
“I suspect I learn the most, especially if I get the case wrong,” he told attendees. “After living it on stage, there’s a lot that I upload in my memory for the next time I see something like this in real life.”
He said he’s probably batting about 0.500 on getting the cases right.
“I’ve had plenty of experiences where I’ve pulled the rabbit out of the hat at the last minute, and it’s been glorious, and I’ve had plenty of experiences where I’ve fallen flat on my face, and I didn’t have a prayer of knowing it, either, because my thinking was off, my knowledge was deficient, or it was something I had never heard of before,” he said. “The one thing that’s always rewarding is that people are always very appreciative that I shared my thinking, whether it’s a flash of insight or a total stumble or an uncertainty that I have.”
It might seem that the event has more of a potential downside than upside: If he gets a case right, he’s doing what he should do; if he gets one wrong, it might be embarrassing. He doesn’t see it that way, he told the crowd.
“It’s a total joy to be up here,” Dr. Dhaliwal said. “There’s no doubt that standing in front of a crowd induces a little bit of anxiety, but it is a lot of fun to do. And I had mentors who did this, and then I started to learn it myself, and at some point, you get past the anxiety of being right or wrong, and you just enjoy being up there.”
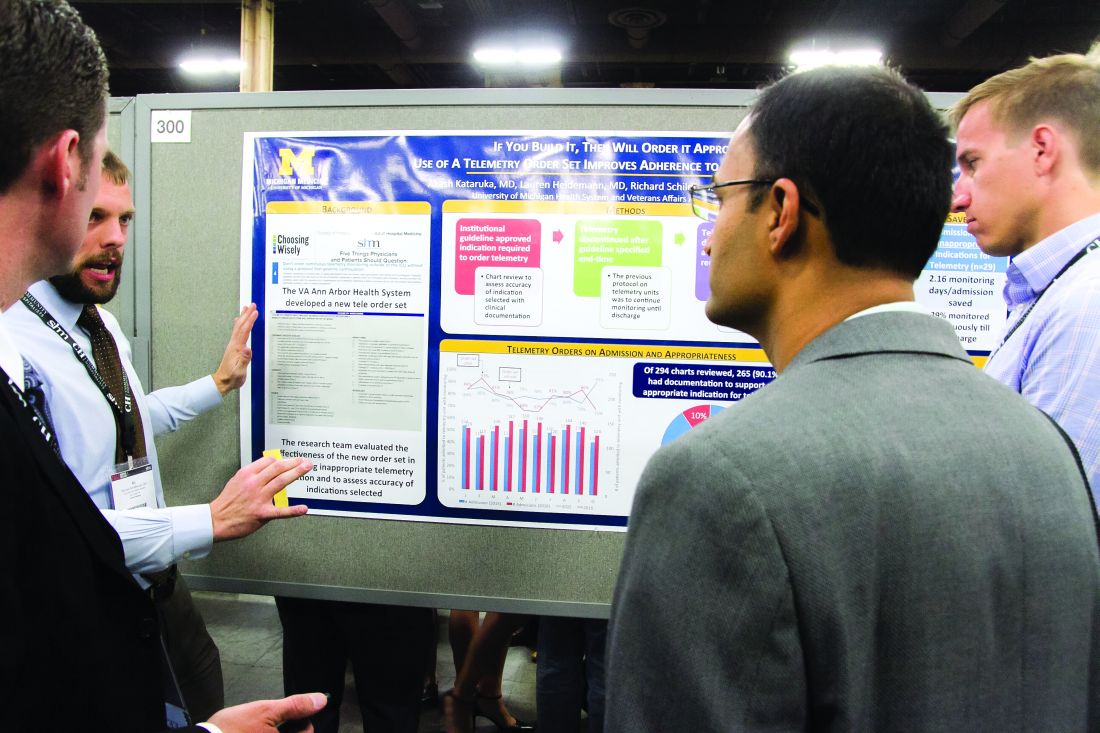
From idea to abstract, RIV posters highlight novel thinking
Masih Shinwa, MD, stood beside a half-circle of judges Tuesday night at SHM’s annual Research, Innovations and Clinical Vignettes (RIV) poster competition and argued why his entry, already a finalist, should win. And to think, his poster, “Please ‘THINK’ Before You Order: A Multidisciplinary Approach to Decreasing Overutilization of Daily Labs,” was born simply of a group of medical students who incredulously said they were amazed patients would be woken in the middle of the night for laboratory tests.
Eighteen months later, the poster drew hundreds of questions from passersby on how a team approach could help generate fewer labs and chemistry testing. Now, the work could serve as a potential guide for other hospitals seeking to reduce unnecessary tests, a focal point of SHM and the ABIM Foundation’s Choosing Wisely campaign.
“This is a way to make it national,” he said. “You may have affected the lives of the patients in your hospital, but unless you attend these types of national meetings, it’s hard to get that perspective across [the country].”
That level of personal and professional collaboration is the purpose of the RIV, one of the best-attended events of SHM’s annual meeting. The event has become so popular that submissions this year tallied 1,712, nearly triple the number of submissions at the 2010 event.
“One of the amazing things is everyone has their own poster. They are doing their work,” said Margaret Fang, MD, MPH, FHM, program chair for HM17’s scientific abstracts competition, the formal name for the poster contest. “But then they start up conversations with the people next to them. ... seeing the organic networking and the discussions that arise from that is really exciting. RIV really serves as a way of connecting people together who might not have known the other person was doing that kind of work.”
Dr. Shinwa said that the specialty’s focus on research is important. He said it positions the field to be leaders, not just for patient care, but for hospitals and institutions.
“We are physicians. Our role is taking care of patients,” he said. “[But] knowing that there are people who are not just focusing on taking care of specific patients, but are actually there to improve the entire system and the process, that is really gratifying.”
Masih Shinwa, MD, stood beside a half-circle of judges Tuesday night at SHM’s annual Research, Innovations and Clinical Vignettes (RIV) poster competition and argued why his entry, already a finalist, should win. And to think, his poster, “Please ‘THINK’ Before You Order: A Multidisciplinary Approach to Decreasing Overutilization of Daily Labs,” was born simply of a group of medical students who incredulously said they were amazed patients would be woken in the middle of the night for laboratory tests.
Eighteen months later, the poster drew hundreds of questions from passersby on how a team approach could help generate fewer labs and chemistry testing. Now, the work could serve as a potential guide for other hospitals seeking to reduce unnecessary tests, a focal point of SHM and the ABIM Foundation’s Choosing Wisely campaign.
“This is a way to make it national,” he said. “You may have affected the lives of the patients in your hospital, but unless you attend these types of national meetings, it’s hard to get that perspective across [the country].”
That level of personal and professional collaboration is the purpose of the RIV, one of the best-attended events of SHM’s annual meeting. The event has become so popular that submissions this year tallied 1,712, nearly triple the number of submissions at the 2010 event.
“One of the amazing things is everyone has their own poster. They are doing their work,” said Margaret Fang, MD, MPH, FHM, program chair for HM17’s scientific abstracts competition, the formal name for the poster contest. “But then they start up conversations with the people next to them. ... seeing the organic networking and the discussions that arise from that is really exciting. RIV really serves as a way of connecting people together who might not have known the other person was doing that kind of work.”
Dr. Shinwa said that the specialty’s focus on research is important. He said it positions the field to be leaders, not just for patient care, but for hospitals and institutions.
“We are physicians. Our role is taking care of patients,” he said. “[But] knowing that there are people who are not just focusing on taking care of specific patients, but are actually there to improve the entire system and the process, that is really gratifying.”
Masih Shinwa, MD, stood beside a half-circle of judges Tuesday night at SHM’s annual Research, Innovations and Clinical Vignettes (RIV) poster competition and argued why his entry, already a finalist, should win. And to think, his poster, “Please ‘THINK’ Before You Order: A Multidisciplinary Approach to Decreasing Overutilization of Daily Labs,” was born simply of a group of medical students who incredulously said they were amazed patients would be woken in the middle of the night for laboratory tests.
Eighteen months later, the poster drew hundreds of questions from passersby on how a team approach could help generate fewer labs and chemistry testing. Now, the work could serve as a potential guide for other hospitals seeking to reduce unnecessary tests, a focal point of SHM and the ABIM Foundation’s Choosing Wisely campaign.
“This is a way to make it national,” he said. “You may have affected the lives of the patients in your hospital, but unless you attend these types of national meetings, it’s hard to get that perspective across [the country].”
That level of personal and professional collaboration is the purpose of the RIV, one of the best-attended events of SHM’s annual meeting. The event has become so popular that submissions this year tallied 1,712, nearly triple the number of submissions at the 2010 event.
“One of the amazing things is everyone has their own poster. They are doing their work,” said Margaret Fang, MD, MPH, FHM, program chair for HM17’s scientific abstracts competition, the formal name for the poster contest. “But then they start up conversations with the people next to them. ... seeing the organic networking and the discussions that arise from that is really exciting. RIV really serves as a way of connecting people together who might not have known the other person was doing that kind of work.”
Dr. Shinwa said that the specialty’s focus on research is important. He said it positions the field to be leaders, not just for patient care, but for hospitals and institutions.
“We are physicians. Our role is taking care of patients,” he said. “[But] knowing that there are people who are not just focusing on taking care of specific patients, but are actually there to improve the entire system and the process, that is really gratifying.”
Proper UTI diagnosis, treatment relies on cautious approach
LAS VEGAS – Prudent use of catheters, cultures, and antibiotics are three keys to proper urinary tract diagnosis and management, according to a speaker at this year’s annual meeting of the Society of Hospital Medicine.
“We have not done very well with decreasing catheter-associated urinary tract infections,” said Jennifer Hanrahan, DO, an assistant professor of infectious disease medicine at Case Western Reserve University in Cleveland, Ohio, and an infectious disease physician at MetroHealth Medical Center, where she is the medical director for infection prevention. “The main reason is people don’t really think of i
The main way to reduce catheter-associated urinary tract infections is to avoid catheters, she said, noting “that’s obvious, but unnecessary catheters get put in all the time.”
Dr. Hanrahan recommended only putting them in when absolutely necessary, doing so in a sterile manner, and then continually monitoring whether the patient still needs the catheter.
Knowing when to obtain a urine culture is key to ensuring proper diagnosing and treatment for UTIs. A person who is asymptomatic does not need a culture, Dr. Hanrahan said during the well-attended, rapid-fire session. Those who do need a culture include septic patients with no apparent cause for their symptomatic presentation, despite a careful history taking and physical exam. Also, patients with pelvic pain, or flank tenderness for whom no cause can otherwise be determined should be cultured. It is also appropriate to screen for asymptomatic bacteriuria for pregnant patients, since it can be a sign of premature labor, and for patients about to undergo any invasive urologic procedure, Dr Hanrahan said.
“An awful lot of people have asymptomatic bacteriuria all the time,” she added, “and it doesn’t mean anything.”
Reasons to not culture include urine that smells “off” or that is cloudy or has sediment. “Anyone who has eaten asparagus knows that, after you eat it, your urine smells weird. It doesn’t mean you have a UTI,” she said.
She recommended against “pan culturing” in sepsis, and culturing “just because” when there is a clearly identifiable cause for the fever.
Once a diagnosis is made, Dr. Hanrahan urged physicians to avoid the overuse of antibiotics, suggesting that, whenever possible, the shortest possible course should be used. In order to help preserve antibiotic resistance, she also recommended using antibiotics that are not as prevalent, in order to help preserve antibiotic resistance. These could include nitrofurantoin and fosfomycin.
Dr. Hanrahan had no relevant financial disclosures.
[email protected]
On Twitter @whitneymcknight
LAS VEGAS – Prudent use of catheters, cultures, and antibiotics are three keys to proper urinary tract diagnosis and management, according to a speaker at this year’s annual meeting of the Society of Hospital Medicine.
“We have not done very well with decreasing catheter-associated urinary tract infections,” said Jennifer Hanrahan, DO, an assistant professor of infectious disease medicine at Case Western Reserve University in Cleveland, Ohio, and an infectious disease physician at MetroHealth Medical Center, where she is the medical director for infection prevention. “The main reason is people don’t really think of i
The main way to reduce catheter-associated urinary tract infections is to avoid catheters, she said, noting “that’s obvious, but unnecessary catheters get put in all the time.”
Dr. Hanrahan recommended only putting them in when absolutely necessary, doing so in a sterile manner, and then continually monitoring whether the patient still needs the catheter.
Knowing when to obtain a urine culture is key to ensuring proper diagnosing and treatment for UTIs. A person who is asymptomatic does not need a culture, Dr. Hanrahan said during the well-attended, rapid-fire session. Those who do need a culture include septic patients with no apparent cause for their symptomatic presentation, despite a careful history taking and physical exam. Also, patients with pelvic pain, or flank tenderness for whom no cause can otherwise be determined should be cultured. It is also appropriate to screen for asymptomatic bacteriuria for pregnant patients, since it can be a sign of premature labor, and for patients about to undergo any invasive urologic procedure, Dr Hanrahan said.
“An awful lot of people have asymptomatic bacteriuria all the time,” she added, “and it doesn’t mean anything.”
Reasons to not culture include urine that smells “off” or that is cloudy or has sediment. “Anyone who has eaten asparagus knows that, after you eat it, your urine smells weird. It doesn’t mean you have a UTI,” she said.
She recommended against “pan culturing” in sepsis, and culturing “just because” when there is a clearly identifiable cause for the fever.
Once a diagnosis is made, Dr. Hanrahan urged physicians to avoid the overuse of antibiotics, suggesting that, whenever possible, the shortest possible course should be used. In order to help preserve antibiotic resistance, she also recommended using antibiotics that are not as prevalent, in order to help preserve antibiotic resistance. These could include nitrofurantoin and fosfomycin.
Dr. Hanrahan had no relevant financial disclosures.
[email protected]
On Twitter @whitneymcknight
LAS VEGAS – Prudent use of catheters, cultures, and antibiotics are three keys to proper urinary tract diagnosis and management, according to a speaker at this year’s annual meeting of the Society of Hospital Medicine.
“We have not done very well with decreasing catheter-associated urinary tract infections,” said Jennifer Hanrahan, DO, an assistant professor of infectious disease medicine at Case Western Reserve University in Cleveland, Ohio, and an infectious disease physician at MetroHealth Medical Center, where she is the medical director for infection prevention. “The main reason is people don’t really think of i
The main way to reduce catheter-associated urinary tract infections is to avoid catheters, she said, noting “that’s obvious, but unnecessary catheters get put in all the time.”
Dr. Hanrahan recommended only putting them in when absolutely necessary, doing so in a sterile manner, and then continually monitoring whether the patient still needs the catheter.
Knowing when to obtain a urine culture is key to ensuring proper diagnosing and treatment for UTIs. A person who is asymptomatic does not need a culture, Dr. Hanrahan said during the well-attended, rapid-fire session. Those who do need a culture include septic patients with no apparent cause for their symptomatic presentation, despite a careful history taking and physical exam. Also, patients with pelvic pain, or flank tenderness for whom no cause can otherwise be determined should be cultured. It is also appropriate to screen for asymptomatic bacteriuria for pregnant patients, since it can be a sign of premature labor, and for patients about to undergo any invasive urologic procedure, Dr Hanrahan said.
“An awful lot of people have asymptomatic bacteriuria all the time,” she added, “and it doesn’t mean anything.”
Reasons to not culture include urine that smells “off” or that is cloudy or has sediment. “Anyone who has eaten asparagus knows that, after you eat it, your urine smells weird. It doesn’t mean you have a UTI,” she said.
She recommended against “pan culturing” in sepsis, and culturing “just because” when there is a clearly identifiable cause for the fever.
Once a diagnosis is made, Dr. Hanrahan urged physicians to avoid the overuse of antibiotics, suggesting that, whenever possible, the shortest possible course should be used. In order to help preserve antibiotic resistance, she also recommended using antibiotics that are not as prevalent, in order to help preserve antibiotic resistance. These could include nitrofurantoin and fosfomycin.
Dr. Hanrahan had no relevant financial disclosures.
[email protected]
On Twitter @whitneymcknight