User login
A Physical Therapist’s Role in Clinical Video Telehealth
Clinical video telehealth (CVT) uses live, interactive audio and video technology to connect patients with health care providers (HCPs) at remote facilities, allowing the patient to be examined and interviewed by a provider. An immediate evaluation of the patient is facilitated by the HCP’s ability to answer any questions, provide recommendations, and interact directly with the patient.
This article describes the VA’ s commitment to and uses of CVT, outlines various physical therapists’ roles in CVT, and details a specific physical therapist’s CVT practice.
The VA is recognized as a leader in this growing method of delivering direct patient care, combining the benefit of face-to-face interaction with the convenience of reduced travel. In 2013, the VA spent $500 million nationally on a telehealth expansion project to improve veteran access to health care. This expansion has continued, and telehealth capabilities have reached 152 VAMCs and clinics throughout the U.S.1 The VA was most recently recognized for its efforts in Hospitals & Health Networks, deeming VA as a “2014 most wired” U.S. hospital.2
Related: Helping Patients Set Goals for Better Health
To date, CVT has grown in the VA to include a multitude of specialty services. Clinical video telehealth fills an important niche in the VA community, providing flexible care to veterans when and where they need it. Providers use CVT to make diagnoses, manage care, perform checkups, and educate patients. It allows patients to come to many of the VA community-based outpatient clinics (CBOCs) and receive care from specialists or providers who may be located in the main facility, another state, or even across the country. Publications documenting successful video telehealth technology in the VHA include positive patient and provider satisfaction, accuracy of measuring physical function, merits in providing group weight loss programs, effective cognitive-behavioral and physical therapy group protocol, as well as a telehealth collaborative care program for persons with HIV in rural areas.3-7
Physical therapists (PTs) are making use of technology that brings care to the patient rather than the patient to the care. For instance, PTs have used this service for patients with spinal cord injuries for whom prolonged sitting during travel has the potential risk of worsening a sore or ulcer.6 By incorporating CVT into their practices, PTs can address current, evolving, and future health care needs.
PT’s Perspective
Yevgenia Gitlin-Nitti, PT, of the Miami VA Healthcare System (MVAHCS) works at the Key West CBOC, which consists of 1 primary care physician, 1 nurse practitioner, 2 registered nurses, 2 social workers, 1 psychiatrist, 1 PT, and 3 support staff. Over 160 miles from the Miami VA HCS where all the specialists are located, Key West CBOC needs remote services.
Working with 3 different clinics—spine, diabetes, and MOVE! (Management of Overweight and/or Obesity for Veterans Everywhere)—has allowed the PT to develop a thorough understanding of the need for telehealth services. Specifically, the spine clinic visits are designed to have a patient consult with a physical medicine and rehabilitation physician regarding any spine issues. The PT’s role in the spine clinic CVT is to serve as the extension of the evaluating physician’s hands. Physical therapists are trained to perform various orthopedic and neurologic tests and other vitals such as weight, blood pressure, and pulse. The PT is also trained to palpate and feel for soft tissue abnormalities, joint and quality of movement, and bony anomalies on behalf of the physician at the remote location.
Related: A Call to Action: Intensive Lifestyle Intervention Against Diabesity
The spine clinic typically meets for 1 hour, once a month, with 2 scheduled patients individually evaluated. The PT presents the patient to the physician via CVT and takes the patient through a comprehensive physical evaluation as per the physician’s requests. The Computerized Patient Record System allows both parties to view magnetic resonance images, X-rays, and other pertinent test results. The physician may then order additional tests, procedures, and/or consults with other specialty clinics.
The PT also leads a monthly diabetes CVT group session for Key West patients. A nutritionist and a certified diabetes educator nurse attend the session from the MVAHCS via CVT. The PT can be present in the room with the patient while the other specialty clinic provider is remote. The PT’s role is to educate the participants about exercise for better blood sugar control and to maintain foot care.
Related: Experiences of Veterans With Diabetes From Shared Medical Appointments
Oftentimes, the PT may make referrals to podiatry at the MVAHCS and may need to conduct a CVT session to help with the podiatry physical examination. Similarly, the PT also contributes to a weekly MOVE! class, which consists of Key West patients in a group appointment that includes a Miami-based nutritionist joining via CVT. Some MOVE! classes are set up with the PT educating patients remotely at other CBOCs on exercise and even performing exercises together via CVT. Other clinics are set up in Key West with the PT alongside the patient while another HCP observes via CVT. In the Key West CVT service, the PT educates patients on exercise with a focus on managing weight and staying healthy.
In fiscal year 2013, the PT successfully conducted over 120 CVT encounters in the diabetes and MOVE! CVT clinics and 9 CVT encounters in the spine clinic.
Conclusion
Multiple benefits have been observed from providing CVT clinics. Increasing the accessibility to these clinics makes it easier for veterans to keep their appointments. Also, CVT allows HCPs to reach patients who otherwise would likely not seek care because of the lack of access to specialists at the closest facility. This service can help patients who cannot physically travel great distances because of their conditions and who otherwise may not have been seen.1
Nonetheless, telehealth does have some drawbacks. There is the chance that the audio/video connection may be interrupted by severe weather.6 Equipment breakdown, other connectivity issues, and the HCP’s inability to touch and feel the patient during the evaluation are also limitations.
Ultimately, this personalized service can be recognized as convenient, cutting-edge, and most important, can improve the quality and timeliness of care to patients.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Fleisher C. At White River Junction VA, doctor is in—and on screen. Valley News. July 31, 2013. http://www.vnews.com/home/7851132-95/at-white-river-junction-va-doctor-is-in-and-on-screen. Accessed June 10, 2015.
2. Weinstock M, Hoppszallern S. 2014 most wired. Hospitals & Health Networks. July 9, 2014. http://www.hhnmag.com/Magazine/2014/Jul/mostwired-health-it-technology-data. Accessed June 10, 2015.
3. Wakefield BJ, Buresh KA, Flanagan JR, Kienzle MG. Interactive video specialty consultations in long-term care. J Am Geriatr Soc. 2004;52(5):789-793.
4. Hoenig H, Tate L, Dumbleton S, et al. A quality assurance study of the accuracy of measuring physical function under current conditions for use of clinical video telehealth. Arch Phys Med Rehabil. 2013;94(5):998-1002.
5. Ahrendt AD, Kattelmann KK, Rector TS, Maddox DA. The effectiveness of telemedicine for weight management in the MOVE! program. J Rural Health. 2014;30(1):113-119.
6. Palyo SA, Schopmeyer KA, McQuaid JR. Tele-pain management: use of videoconferencing technology in the delivery of an integrated cognitive-behavioral and physical therapy group intervention. Psychol Serv. 2012;9(2):200-202.
7. Ohl M, Dillon D, Moeckli J, et al. Mixed-methods evaluation of a telehealth collaborative care program for persons with HIV infection in a rural setting. J Gen Intern Med. 2013;28(9):1165-1173.
Clinical video telehealth (CVT) uses live, interactive audio and video technology to connect patients with health care providers (HCPs) at remote facilities, allowing the patient to be examined and interviewed by a provider. An immediate evaluation of the patient is facilitated by the HCP’s ability to answer any questions, provide recommendations, and interact directly with the patient.
This article describes the VA’ s commitment to and uses of CVT, outlines various physical therapists’ roles in CVT, and details a specific physical therapist’s CVT practice.
The VA is recognized as a leader in this growing method of delivering direct patient care, combining the benefit of face-to-face interaction with the convenience of reduced travel. In 2013, the VA spent $500 million nationally on a telehealth expansion project to improve veteran access to health care. This expansion has continued, and telehealth capabilities have reached 152 VAMCs and clinics throughout the U.S.1 The VA was most recently recognized for its efforts in Hospitals & Health Networks, deeming VA as a “2014 most wired” U.S. hospital.2
Related: Helping Patients Set Goals for Better Health
To date, CVT has grown in the VA to include a multitude of specialty services. Clinical video telehealth fills an important niche in the VA community, providing flexible care to veterans when and where they need it. Providers use CVT to make diagnoses, manage care, perform checkups, and educate patients. It allows patients to come to many of the VA community-based outpatient clinics (CBOCs) and receive care from specialists or providers who may be located in the main facility, another state, or even across the country. Publications documenting successful video telehealth technology in the VHA include positive patient and provider satisfaction, accuracy of measuring physical function, merits in providing group weight loss programs, effective cognitive-behavioral and physical therapy group protocol, as well as a telehealth collaborative care program for persons with HIV in rural areas.3-7
Physical therapists (PTs) are making use of technology that brings care to the patient rather than the patient to the care. For instance, PTs have used this service for patients with spinal cord injuries for whom prolonged sitting during travel has the potential risk of worsening a sore or ulcer.6 By incorporating CVT into their practices, PTs can address current, evolving, and future health care needs.
PT’s Perspective
Yevgenia Gitlin-Nitti, PT, of the Miami VA Healthcare System (MVAHCS) works at the Key West CBOC, which consists of 1 primary care physician, 1 nurse practitioner, 2 registered nurses, 2 social workers, 1 psychiatrist, 1 PT, and 3 support staff. Over 160 miles from the Miami VA HCS where all the specialists are located, Key West CBOC needs remote services.
Working with 3 different clinics—spine, diabetes, and MOVE! (Management of Overweight and/or Obesity for Veterans Everywhere)—has allowed the PT to develop a thorough understanding of the need for telehealth services. Specifically, the spine clinic visits are designed to have a patient consult with a physical medicine and rehabilitation physician regarding any spine issues. The PT’s role in the spine clinic CVT is to serve as the extension of the evaluating physician’s hands. Physical therapists are trained to perform various orthopedic and neurologic tests and other vitals such as weight, blood pressure, and pulse. The PT is also trained to palpate and feel for soft tissue abnormalities, joint and quality of movement, and bony anomalies on behalf of the physician at the remote location.
Related: A Call to Action: Intensive Lifestyle Intervention Against Diabesity
The spine clinic typically meets for 1 hour, once a month, with 2 scheduled patients individually evaluated. The PT presents the patient to the physician via CVT and takes the patient through a comprehensive physical evaluation as per the physician’s requests. The Computerized Patient Record System allows both parties to view magnetic resonance images, X-rays, and other pertinent test results. The physician may then order additional tests, procedures, and/or consults with other specialty clinics.
The PT also leads a monthly diabetes CVT group session for Key West patients. A nutritionist and a certified diabetes educator nurse attend the session from the MVAHCS via CVT. The PT can be present in the room with the patient while the other specialty clinic provider is remote. The PT’s role is to educate the participants about exercise for better blood sugar control and to maintain foot care.
Related: Experiences of Veterans With Diabetes From Shared Medical Appointments
Oftentimes, the PT may make referrals to podiatry at the MVAHCS and may need to conduct a CVT session to help with the podiatry physical examination. Similarly, the PT also contributes to a weekly MOVE! class, which consists of Key West patients in a group appointment that includes a Miami-based nutritionist joining via CVT. Some MOVE! classes are set up with the PT educating patients remotely at other CBOCs on exercise and even performing exercises together via CVT. Other clinics are set up in Key West with the PT alongside the patient while another HCP observes via CVT. In the Key West CVT service, the PT educates patients on exercise with a focus on managing weight and staying healthy.
In fiscal year 2013, the PT successfully conducted over 120 CVT encounters in the diabetes and MOVE! CVT clinics and 9 CVT encounters in the spine clinic.
Conclusion
Multiple benefits have been observed from providing CVT clinics. Increasing the accessibility to these clinics makes it easier for veterans to keep their appointments. Also, CVT allows HCPs to reach patients who otherwise would likely not seek care because of the lack of access to specialists at the closest facility. This service can help patients who cannot physically travel great distances because of their conditions and who otherwise may not have been seen.1
Nonetheless, telehealth does have some drawbacks. There is the chance that the audio/video connection may be interrupted by severe weather.6 Equipment breakdown, other connectivity issues, and the HCP’s inability to touch and feel the patient during the evaluation are also limitations.
Ultimately, this personalized service can be recognized as convenient, cutting-edge, and most important, can improve the quality and timeliness of care to patients.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Clinical video telehealth (CVT) uses live, interactive audio and video technology to connect patients with health care providers (HCPs) at remote facilities, allowing the patient to be examined and interviewed by a provider. An immediate evaluation of the patient is facilitated by the HCP’s ability to answer any questions, provide recommendations, and interact directly with the patient.
This article describes the VA’ s commitment to and uses of CVT, outlines various physical therapists’ roles in CVT, and details a specific physical therapist’s CVT practice.
The VA is recognized as a leader in this growing method of delivering direct patient care, combining the benefit of face-to-face interaction with the convenience of reduced travel. In 2013, the VA spent $500 million nationally on a telehealth expansion project to improve veteran access to health care. This expansion has continued, and telehealth capabilities have reached 152 VAMCs and clinics throughout the U.S.1 The VA was most recently recognized for its efforts in Hospitals & Health Networks, deeming VA as a “2014 most wired” U.S. hospital.2
Related: Helping Patients Set Goals for Better Health
To date, CVT has grown in the VA to include a multitude of specialty services. Clinical video telehealth fills an important niche in the VA community, providing flexible care to veterans when and where they need it. Providers use CVT to make diagnoses, manage care, perform checkups, and educate patients. It allows patients to come to many of the VA community-based outpatient clinics (CBOCs) and receive care from specialists or providers who may be located in the main facility, another state, or even across the country. Publications documenting successful video telehealth technology in the VHA include positive patient and provider satisfaction, accuracy of measuring physical function, merits in providing group weight loss programs, effective cognitive-behavioral and physical therapy group protocol, as well as a telehealth collaborative care program for persons with HIV in rural areas.3-7
Physical therapists (PTs) are making use of technology that brings care to the patient rather than the patient to the care. For instance, PTs have used this service for patients with spinal cord injuries for whom prolonged sitting during travel has the potential risk of worsening a sore or ulcer.6 By incorporating CVT into their practices, PTs can address current, evolving, and future health care needs.
PT’s Perspective
Yevgenia Gitlin-Nitti, PT, of the Miami VA Healthcare System (MVAHCS) works at the Key West CBOC, which consists of 1 primary care physician, 1 nurse practitioner, 2 registered nurses, 2 social workers, 1 psychiatrist, 1 PT, and 3 support staff. Over 160 miles from the Miami VA HCS where all the specialists are located, Key West CBOC needs remote services.
Working with 3 different clinics—spine, diabetes, and MOVE! (Management of Overweight and/or Obesity for Veterans Everywhere)—has allowed the PT to develop a thorough understanding of the need for telehealth services. Specifically, the spine clinic visits are designed to have a patient consult with a physical medicine and rehabilitation physician regarding any spine issues. The PT’s role in the spine clinic CVT is to serve as the extension of the evaluating physician’s hands. Physical therapists are trained to perform various orthopedic and neurologic tests and other vitals such as weight, blood pressure, and pulse. The PT is also trained to palpate and feel for soft tissue abnormalities, joint and quality of movement, and bony anomalies on behalf of the physician at the remote location.
Related: A Call to Action: Intensive Lifestyle Intervention Against Diabesity
The spine clinic typically meets for 1 hour, once a month, with 2 scheduled patients individually evaluated. The PT presents the patient to the physician via CVT and takes the patient through a comprehensive physical evaluation as per the physician’s requests. The Computerized Patient Record System allows both parties to view magnetic resonance images, X-rays, and other pertinent test results. The physician may then order additional tests, procedures, and/or consults with other specialty clinics.
The PT also leads a monthly diabetes CVT group session for Key West patients. A nutritionist and a certified diabetes educator nurse attend the session from the MVAHCS via CVT. The PT can be present in the room with the patient while the other specialty clinic provider is remote. The PT’s role is to educate the participants about exercise for better blood sugar control and to maintain foot care.
Related: Experiences of Veterans With Diabetes From Shared Medical Appointments
Oftentimes, the PT may make referrals to podiatry at the MVAHCS and may need to conduct a CVT session to help with the podiatry physical examination. Similarly, the PT also contributes to a weekly MOVE! class, which consists of Key West patients in a group appointment that includes a Miami-based nutritionist joining via CVT. Some MOVE! classes are set up with the PT educating patients remotely at other CBOCs on exercise and even performing exercises together via CVT. Other clinics are set up in Key West with the PT alongside the patient while another HCP observes via CVT. In the Key West CVT service, the PT educates patients on exercise with a focus on managing weight and staying healthy.
In fiscal year 2013, the PT successfully conducted over 120 CVT encounters in the diabetes and MOVE! CVT clinics and 9 CVT encounters in the spine clinic.
Conclusion
Multiple benefits have been observed from providing CVT clinics. Increasing the accessibility to these clinics makes it easier for veterans to keep their appointments. Also, CVT allows HCPs to reach patients who otherwise would likely not seek care because of the lack of access to specialists at the closest facility. This service can help patients who cannot physically travel great distances because of their conditions and who otherwise may not have been seen.1
Nonetheless, telehealth does have some drawbacks. There is the chance that the audio/video connection may be interrupted by severe weather.6 Equipment breakdown, other connectivity issues, and the HCP’s inability to touch and feel the patient during the evaluation are also limitations.
Ultimately, this personalized service can be recognized as convenient, cutting-edge, and most important, can improve the quality and timeliness of care to patients.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Fleisher C. At White River Junction VA, doctor is in—and on screen. Valley News. July 31, 2013. http://www.vnews.com/home/7851132-95/at-white-river-junction-va-doctor-is-in-and-on-screen. Accessed June 10, 2015.
2. Weinstock M, Hoppszallern S. 2014 most wired. Hospitals & Health Networks. July 9, 2014. http://www.hhnmag.com/Magazine/2014/Jul/mostwired-health-it-technology-data. Accessed June 10, 2015.
3. Wakefield BJ, Buresh KA, Flanagan JR, Kienzle MG. Interactive video specialty consultations in long-term care. J Am Geriatr Soc. 2004;52(5):789-793.
4. Hoenig H, Tate L, Dumbleton S, et al. A quality assurance study of the accuracy of measuring physical function under current conditions for use of clinical video telehealth. Arch Phys Med Rehabil. 2013;94(5):998-1002.
5. Ahrendt AD, Kattelmann KK, Rector TS, Maddox DA. The effectiveness of telemedicine for weight management in the MOVE! program. J Rural Health. 2014;30(1):113-119.
6. Palyo SA, Schopmeyer KA, McQuaid JR. Tele-pain management: use of videoconferencing technology in the delivery of an integrated cognitive-behavioral and physical therapy group intervention. Psychol Serv. 2012;9(2):200-202.
7. Ohl M, Dillon D, Moeckli J, et al. Mixed-methods evaluation of a telehealth collaborative care program for persons with HIV infection in a rural setting. J Gen Intern Med. 2013;28(9):1165-1173.
1. Fleisher C. At White River Junction VA, doctor is in—and on screen. Valley News. July 31, 2013. http://www.vnews.com/home/7851132-95/at-white-river-junction-va-doctor-is-in-and-on-screen. Accessed June 10, 2015.
2. Weinstock M, Hoppszallern S. 2014 most wired. Hospitals & Health Networks. July 9, 2014. http://www.hhnmag.com/Magazine/2014/Jul/mostwired-health-it-technology-data. Accessed June 10, 2015.
3. Wakefield BJ, Buresh KA, Flanagan JR, Kienzle MG. Interactive video specialty consultations in long-term care. J Am Geriatr Soc. 2004;52(5):789-793.
4. Hoenig H, Tate L, Dumbleton S, et al. A quality assurance study of the accuracy of measuring physical function under current conditions for use of clinical video telehealth. Arch Phys Med Rehabil. 2013;94(5):998-1002.
5. Ahrendt AD, Kattelmann KK, Rector TS, Maddox DA. The effectiveness of telemedicine for weight management in the MOVE! program. J Rural Health. 2014;30(1):113-119.
6. Palyo SA, Schopmeyer KA, McQuaid JR. Tele-pain management: use of videoconferencing technology in the delivery of an integrated cognitive-behavioral and physical therapy group intervention. Psychol Serv. 2012;9(2):200-202.
7. Ohl M, Dillon D, Moeckli J, et al. Mixed-methods evaluation of a telehealth collaborative care program for persons with HIV infection in a rural setting. J Gen Intern Med. 2013;28(9):1165-1173.
Using Life Stories to Connect Veterans and Providers
Anyone involved with the U.S. health care system has heard one or more of the following dispiriting comments. If you are a patient, you have heard or said, “I wish I felt like my provider understood me. He/she just doesn’t have the time.” If you are a provider, you have heard yourself or another provider say, “I wish I had more time to get to know my patients as people. I could do a better job or at least I could remember them without looking at the chart.” This article describes a novel program—My Life, My Story—instituted at the William S. Middleton Memorial Veterans Hospital (WSMMVH) in Madison, Wisconsin. The program uses personal narratives to foster a sense of connection between providers and their veteran patients.
Related: Infusing Gerontologic Practice Into PACT
My Life, My Story had its origins in a small performance improvement project aimed at helping psychiatric residents learn about their new outpatients during rotation. The clinic staff wanted residents to get to know their patients as people in addition to understanding the veterans’ medical conditions. The veterans were first offered the opportunity to come to writers’ workshops and create personal narratives that would be shared later with their clinicians. Unfortunately, only a few veterans were willing to take on this task.
A more patient-friendly approach for collecting and sharing the stories was developed and funded by the VHA Office of Patient-Centered Care and Cultural Transformation (OPCC&CT). Veterans who chose to participate worked with an interviewer/writer to create a personal narrative, which was then shared with their patient aligned care team (PACT). Another component of the interview process was the Personal Health Inventory (PHI), a questionnaire developed by the OPCC&CT that helps veterans articulate their goals and motivations for physical, social, psychological, and spiritual well-being.1 The PHI and personal narrative were paired, to give health care providers (HCPs) a sense of the veteran and their personal health goals.
Background
The health benefits of telling or writing the story of a difficult emotional event have been demonstrated by Pennebaker.2 In varied groups, from prisoners to patients with chronic pain, the writing or talking about experiences improved mood and lowered distress. In addition, studies of medically ill patients showed a decline in physician visits in the 2 to 6 months following the narrative process.3,4 Improved immune response was also shown for patients with hepatitis B, HIV, asthma, and rheumatoid arthritis in response to completing a narrative.5-7
Related: Experiences of Veterans With Diabetes From Shared Medical Appointments
But the writing task is difficult for many people, especially those with advanced illness. Interviewing these patients and writing their stories is a way to give them a voice that otherwise might go unheard.
Dignity therapy with terminally ill patients, a technique developed by Dr. H.M. Chochinov, used an expert to collect the story by bedside interview and to produce a dignity-enhancing life narrative.8-10 Wise and colleagues modified this process for patients with cancer stages III and IV by using telephone interviews, which showed reduced anger, depression, tension, and an increased sense of peace.11 Personal narratives in which patients tell their story and receive it in written form have been shown to reduce psychological distress, increase hope, and help the patient feel valued.10,12
Pennebaker hypothesized that several mechanisms account for these improvements in health measures.2 First, developing a narrative provides a contextual understanding of stressful events. Creating a personal narrative allows a patient to identify and give meaning to life’s struggles. Through this process, coping is hypothesized to occur.13-15 Second, storytelling connects the teller with a wider audience.16
Another study by Pennebaker and colleagues found an improvement in social connectedness in college students in the days following the disclosure of emotional stories.17 The study speculates that nondisclosure fosters isolation, whereas disclosure connects us with others, helping us to reach out to others and improving a sense of feeling understood.
Methods
Project staff were recruited to conduct the interviews and write the stories. Team members with varied backgrounds and experiences were selected: a nurse at the WSMMVH who served as an army interrogator in Afghanistan; a professional counselor with prior experience working for the VA; and a marriage and family therapist with a poetry MA.
Providers were recruited for participation in the project through (1) presentations to nursing staff on the inpatient units where stories were gathered; (2) compilations of de-identified stories from veterans on those units were distributed; (3) presentations on the project at outpatient clinics, where the narratives of veterans who were patients at those clinics were read aloud; and (4) discussions of the program at monthly hospital-wide meetings.
Related: Diabetes Patient-Centered Medical Home Approach
Patients were recruited from 2 inpatient units and 1 long-term rehabilitative care unit. Interviewers introduced themselves to the veterans, described the project, and gave each one a project brochure. Veterans were given the opportunity to be interviewed immediately, schedule a future interview, decide later, or not participate.
The majority of veterans who participated chose to be interviewed immediately. Scheduling interviews around procedures and discharges on busy inpatient units proved difficult. Overall participation rate was high: 60% of veterans who were told about the project eventually told their story.
Interview Process
Veterans signed a consent form before the interview, and the interviews were recorded on a digital audio recorder. They were informed they could choose to talk—or not talk—about any part of their life, the interviewer would write a draft of the story based on the interview and bring it back for their review, and the story would not be added to their patient record until they gave their approval. Spouses/partners were invited to participate if they desired.
Interviewers were encouraged to follow the lead of the veteran. Those who were clinicians were encouraged to “take off their clinician hat” during the interview. Unless guided otherwise by the veteran, the interview was semichronological and included the following subjects: birth and childhood, family, schooling, military service, relationships and/or marriage, children, career and employment, general health, and current hospital stay and presenting problem.
Interviews lasted about an hour, and 182 interviews were conducted. Interviews were frequently interrupted by HCPs who checked vitals, administering medications, rounding with residents, and so forth. If the HCP indicated that the patient could keep talking, the interview continued. If the patient had to leave the room for a procedure or medical appointment, the interviewer paused the recording and scheduled a time to come back and complete the interview.
After the interview, veterans were told that they could expect to see the first written draft of their story within 2 days. Veterans who were to be discharged the day of the interview or the following day were told that the story would be sent to them in the mail to review at home.
Personal Health Inventory
Interviewers introduced the PHI to veterans as an opportunity to identify their wellness goals and share these with the PACT. Veterans with late-stage cancer or in hospice care were given the option to skip the PHI. Of the 103 veterans who completed the PHI, 96 chose to have the interviewer read the questions and record their answers; only 7 chose to complete the PHI on their own.
One hundred eighty-two veterans completed personal narratives, and 103 completed the PHI. Incomplete PHIs occurred for the following reasons: hospice or end of life, 12; declined, 20; could not complete, 21; discharged, 19; lost to follow-up, 7.
Writing
The quality of the written stories was critical to the success of the project. Creativity was encouraged to produce stories that captured and brought to life the voice and spirit of the interview subject. The team identified the following features of a good story: (1) written in the first person; (2) nonjudgmental; (3) captures the voice of the veteran; (4) accurately reflects the content of the interview; and (5) nondiagnostic (not labeling).
A short story format was used to increase the likelihood that busy providers would read the narratives. Writers were encouraged to limit the length of the stories to 1 to 2 printed pages (650-1,300 words). Completed stories ranged from 95 words to 2,345 words with an average length of 1,053 words. Veterans wrote 3 and the interviewers wrote 178 narratives; 1 narrative was written by a team member who was not present during the interview but listened to the audio recording.
Editing Process
The first draft of the story was printed and given to the veteran to make any desired changes. Veterans reviewed and updated their stories in different ways. Some wrote their changes on the printed copy and had the writer return at a later time to pick it up. Others read through the story with the writer present and wrote their changes on the printed copy. Some had the writer read the story aloud and alerted the writer when an item needed changing.
Drafts were mailed to already discharged veterans, including a postage-paid return envelope to allow them to mail their changes to the team. After incorporating the veteran’s changes, the team member brought back a second draft of the story for the veteran to review. This process was repeated until the veteran gave final approval. Veterans could then approve whether to share their story with their PACT via the Computerized Patient Record System (CPRS).
Some participant attrition occurred at this point. Six veterans requested that their stories not go in the CPRS (although 3 of them requested printed copies). One veteran changed his mind after his story was added to the CPRS; the team then immediately removed it. Two veterans died shortly after being released from the hospital and before they could review their stories. The families of both these veterans requested that an audio file of the interview be mailed to them.
Sharing With Family and Providers
Veterans received a printed copy of the approved story and the option to have additional copies for family members. The average number of additional copies requested was 3. Family and friends responded positively to the interview process and stories. Spouses who sat in on the interviews always added something to the interview process, and some were active participants. Eight of the 182 stories were dual narratives that included the words of the veteran and his/her spouse.
Providers were alerted to the personal narratives and PHI via CPRS. The completed story was added to the veteran’s record with the title “My Story.” The story was then electronically cosigned to the veteran’s inpatient and outpatient PACT. Typically, this included 4 people: the inpatient resident and attending physician and the outpatient provider and nurse care manager. If other providers were directly involved in the care of the veteran (mental health, specialists, surgeons), they were also cosigned to the story. If a veteran received primary care outside WSMMVH, their PACT was notified of the presence of the story in CPRS (and given a copy) via encrypted e-mail, in the CPRS “Postings” section.
Program Feedback
The original interviewer/writer team members (2.5 full-time employee equivalent for 6 months) generated 182 stories. The corresponding My Story notes in the CPRS were cosigned to an average of 3.3 providers. The program received both formal (solicited) feedback and informal (unsolicited) feedback from veterans and providers.
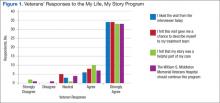
After gathering the first 80 stories, the team solicited participant satisfaction data from interviewed veterans, using a 5-point Likert-type scale. Veteran reaction was positive (Figure 1). The team polled VA providers with an online anonymous survey, using the same Likert-type scale to see whether the story and PHI were useful to providers in their clinical practice. The results suggested they were (Figure 2).
Perhaps the most enlightening and touching feedback were the following unsolicited e-mails and comments:
- I have so appreciated these stories, especially because they immediately become a source of connection with the veterans who come in (some for the first time) to see me about their heart failure. In the midst of a heavy “clinical” topic, knowing their stories has helped us form a stronger patient-provider relationship. It has provided moments of levity and a clear way to tell the patient that I am connecting with them and they are important. —VA employee
- I’m a veteran, and I love reading the real stories of veterans, told in their own words. For us, it’s always wonderful to feel like someone is listening. It’s good to feel like someone wants to hear what you’ve traveled through to get where you are. For those of us who put our lives, our health, our relationships, and our honor on the line for so many others, it’s great when someone will just take the time to listen and understand. It most definitely is very healing. —VA employee
- This is a great way to improve provider understanding and decrease bias and eliminate first impression issues, as people are generally ill and cranky when seeking medical care. —Veteran
- The My Story note was wonderful. I truly feel it has helped me to understand my patients better and to know where they are coming from. This is invaluable to the VA where experiences shape our patients in such a profound way. —VA employee
Recent developments at the WSMMVH suggest that veteran stories are becoming an accepted component of clinical care. The heart/lung transplant team requested that the My Story note be part of the transplant workup process for all new patients. The team also found that new HCPs who were assigned to a veteran regularly cosign that veteran’s My Story note to other providers on the care team. In addition, My Story referrals come from all types of HCPs and staff, both within the hospital and at primary care clinics.
Recent Developments
Two WSMMVH employees suggested using volunteers to gather stories and became the first volunteers: One was a housekeeper who had served in the U.S. Army during the Gulf War, and the other was a registered nurse; both had writing experience.
In 2014, staff trained 12 volunteers from the local community who have been trained to interview and write stories. The volunteers have varied professional backgrounds. All have a background and interest in writing or experience working in a health care setting; 2 are veterans. These volunteers are adding to the team at no additional cost. In development is a standardized training program and a method to look at story collection and writing fidelity, which will allow for further expansion of this program.
My Life, My Story continues to expand significantly. A total of 610 veterans have been interviewed, and 348 of these interviews were conducted by volunteers. The project now has 18 active volunteers with 4 more on a waiting list. A pilot has been launched at a WSMMVH outpatient clinic, which interviews VA primary care providers about their life stories and shares them with their veteran patients. There is now collaboration with the University of Wisconsin School of Medicine and Public Health in Madison to offer a 2-week My Story elective to fourth-year medical students in spring 2016. In March 2015, My Life, My Story expanded to 6 pilot facilities across the VA: Asheville, North Carolina; Bronx, New York; Iowa City, Iowa; Reno, Nevada; Topeka, Kansas; and White River Junction, Vermont.
Future Projects
- The team is currently analyzing the themes appearing in veteran stories, using grounded theory methodology
- The process for outpatients is being revised, using phone calls and telehealth modalities to collect stories
- The team members are examining relationships between themes in stories and health/wellness goals identified on the PHI
- Eventually, the team will study how this process might improve the veteran/provider relationship on measures of satisfaction with care, quality of care, and health outcomes. The authors will also assess the effects of this process on provider satisfaction and burnout
Conclusion
Veteran stories, when skillfully elicited and carefully crafted, give providers an opportunity to know their patients better, without impinging on their time. For veterans, the experience of being interviewed and the knowledge that their story will be shared with providers is an important recognition that they matter and have a voice in their health care. In a world of high-technology health care, where time is the only thing in short supply, My Life, My Story leverages the old-world technology of storytelling to bring providers and patients closer together.
Acknowledgments
The authors wish to acknowledge Amanda Hall and Jessica Jones who were interviewer/writers on the initial project. Both contributed immeasurably to the design and success of the project. The authors would also like to acknowledge Matt Spira who was our first volunteer interviewer and gave us the inspiration to recruit more volunteers. Volunteer Mary Johnston interviewed and wrote the sample veteran story in this article. We would also like to thank the nursing staff on 4A, 4B, and the community living center for their patience when we were in the way and for their support of the project. Last and most important, we would like to thank the veterans who were interviewed for this project. We have all learned more than we could have imagined from the stories that you shared with us. Your sacrifice, courage, and dedication both in the military and your personal lives are truly an inspiration. Thank you.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Veterans Health Administration, Office of Patient Centered Care and Cultural Transformation. My Story Personal Health Inventory, Revision 20. U.S. Department of Veterans Affairs Website. http://www .va.gov/patientcenteredcare/docs/va-opcc-personal -health-inventory-final-508.pdf. Revised October 7, 2013. Accessed May 11, 2015.
2. Pennebaker JW. Telling stories: the health benefits of narrative. Lit Med. 2000;19(1):3-18.
3. Greenberg MA, Stone AA. Writing about disclosed versus undisclosed traumas: immediate and long term effects on mood and health. J Pers Soc Psychol. 1992;63:75-84.
4. Pennebaker JW, Beall SK. Confronting a traumatic event: toward an understanding of inhibition and disease. J Abnorm Psychol. 1986;95(3):274-281.
5. Petrie KJ, Booth RJ, Pennebaker JW, Davidson KP, Thomas MG. Disclosure of trauma and immune response to hepatitis B vaccination program. J Consult Clin Psychol. 1995;63(5):787-792.
6. Petrie KJ, Fontanilla I, Thomas MG, Booth RJ, Pennebaker JW. Effect of written emotional expression on immune function in patients with human immunodeficiency virus infection: a randomized trial. Psychosom Med. 2004;66(2):272-275.
7. Smyth JM, Stone AA, Hurewitz A, Kaell A. Effects of writing about stressful experiences on symptom reduction in patients with asthma or rheumatoid arthritis. JAMA. 1999;281(14):1304-1309.
8. Chochinov HM. Dignity-conserving care—a new model for palliative care: helping the patient feel valued. JAMA. 2002;287(17):2253-2260.
9. Chochinov HM, Hack T, Hassard T, Kristjanson LJ, McClement S, Harlos M. Understanding the will to live in patients near death. Psychosom. 2005;46(1):7-10.
10. Chochinov HM, Kristjanson LJ, Breitbart W, et al. Effect of dignity therapy on distress and end-of-life experience in terminally ill patients: a randomised controlled trial. Lancet Oncol. 2011;12(8):753-762.
11. Wise M, Marchand L, Roberts LJ, Chih M. Existential suffering in advanced cancer: the buffering effects of narrative: a randomized control trial. Poster presented at: University of Washington School of Medicine 6th Annual Department Fair; April 8, 2015; Seattle, Washington.
12. Hall S, Goddard C, Opio D, Speck PW, Martin P, Higginson IJ. A novel approach to enhancing hope in patients with advanced cancer: a randomised phase II trial of dignity therapy. BMJ Support Palliat Care. 2011;1(3):315-321.
13. Heiney SP. The healing power of story. Oncol Nurs Forum. 1995;22(6):899-904.
14. Hyden L-C. Illness and narrative. Soc Health Illness. 1997;19(1):48-69.
15. Carlick A, Biley FC. Thoughts on the therapeutic use of narrative in the promotion of coping in cancer care. Eur J Cancer Care (Engl). 2004;13(4):308-317.
16. Niederhoffer KG, Pennebaker JW. Sharing one’s story: on the benefits of writing or talking about emotional experience. In: Snyder CR, Lopez SJ, eds. Handbook of Positive Psychology. New York, NY: Oxford University Press; 2001:573-583.
17. Pennebaker JW, Kiecolt-Glaser JK, Glaser R. Disclosure of traumas and immune function: health implications for psychotherapy. J Consult Clin Psychol. 1988:56(2):239-245.
Anyone involved with the U.S. health care system has heard one or more of the following dispiriting comments. If you are a patient, you have heard or said, “I wish I felt like my provider understood me. He/she just doesn’t have the time.” If you are a provider, you have heard yourself or another provider say, “I wish I had more time to get to know my patients as people. I could do a better job or at least I could remember them without looking at the chart.” This article describes a novel program—My Life, My Story—instituted at the William S. Middleton Memorial Veterans Hospital (WSMMVH) in Madison, Wisconsin. The program uses personal narratives to foster a sense of connection between providers and their veteran patients.
Related: Infusing Gerontologic Practice Into PACT
My Life, My Story had its origins in a small performance improvement project aimed at helping psychiatric residents learn about their new outpatients during rotation. The clinic staff wanted residents to get to know their patients as people in addition to understanding the veterans’ medical conditions. The veterans were first offered the opportunity to come to writers’ workshops and create personal narratives that would be shared later with their clinicians. Unfortunately, only a few veterans were willing to take on this task.
A more patient-friendly approach for collecting and sharing the stories was developed and funded by the VHA Office of Patient-Centered Care and Cultural Transformation (OPCC&CT). Veterans who chose to participate worked with an interviewer/writer to create a personal narrative, which was then shared with their patient aligned care team (PACT). Another component of the interview process was the Personal Health Inventory (PHI), a questionnaire developed by the OPCC&CT that helps veterans articulate their goals and motivations for physical, social, psychological, and spiritual well-being.1 The PHI and personal narrative were paired, to give health care providers (HCPs) a sense of the veteran and their personal health goals.
Background
The health benefits of telling or writing the story of a difficult emotional event have been demonstrated by Pennebaker.2 In varied groups, from prisoners to patients with chronic pain, the writing or talking about experiences improved mood and lowered distress. In addition, studies of medically ill patients showed a decline in physician visits in the 2 to 6 months following the narrative process.3,4 Improved immune response was also shown for patients with hepatitis B, HIV, asthma, and rheumatoid arthritis in response to completing a narrative.5-7
Related: Experiences of Veterans With Diabetes From Shared Medical Appointments
But the writing task is difficult for many people, especially those with advanced illness. Interviewing these patients and writing their stories is a way to give them a voice that otherwise might go unheard.
Dignity therapy with terminally ill patients, a technique developed by Dr. H.M. Chochinov, used an expert to collect the story by bedside interview and to produce a dignity-enhancing life narrative.8-10 Wise and colleagues modified this process for patients with cancer stages III and IV by using telephone interviews, which showed reduced anger, depression, tension, and an increased sense of peace.11 Personal narratives in which patients tell their story and receive it in written form have been shown to reduce psychological distress, increase hope, and help the patient feel valued.10,12
Pennebaker hypothesized that several mechanisms account for these improvements in health measures.2 First, developing a narrative provides a contextual understanding of stressful events. Creating a personal narrative allows a patient to identify and give meaning to life’s struggles. Through this process, coping is hypothesized to occur.13-15 Second, storytelling connects the teller with a wider audience.16
Another study by Pennebaker and colleagues found an improvement in social connectedness in college students in the days following the disclosure of emotional stories.17 The study speculates that nondisclosure fosters isolation, whereas disclosure connects us with others, helping us to reach out to others and improving a sense of feeling understood.
Methods
Project staff were recruited to conduct the interviews and write the stories. Team members with varied backgrounds and experiences were selected: a nurse at the WSMMVH who served as an army interrogator in Afghanistan; a professional counselor with prior experience working for the VA; and a marriage and family therapist with a poetry MA.
Providers were recruited for participation in the project through (1) presentations to nursing staff on the inpatient units where stories were gathered; (2) compilations of de-identified stories from veterans on those units were distributed; (3) presentations on the project at outpatient clinics, where the narratives of veterans who were patients at those clinics were read aloud; and (4) discussions of the program at monthly hospital-wide meetings.
Related: Diabetes Patient-Centered Medical Home Approach
Patients were recruited from 2 inpatient units and 1 long-term rehabilitative care unit. Interviewers introduced themselves to the veterans, described the project, and gave each one a project brochure. Veterans were given the opportunity to be interviewed immediately, schedule a future interview, decide later, or not participate.
The majority of veterans who participated chose to be interviewed immediately. Scheduling interviews around procedures and discharges on busy inpatient units proved difficult. Overall participation rate was high: 60% of veterans who were told about the project eventually told their story.
Interview Process
Veterans signed a consent form before the interview, and the interviews were recorded on a digital audio recorder. They were informed they could choose to talk—or not talk—about any part of their life, the interviewer would write a draft of the story based on the interview and bring it back for their review, and the story would not be added to their patient record until they gave their approval. Spouses/partners were invited to participate if they desired.
Interviewers were encouraged to follow the lead of the veteran. Those who were clinicians were encouraged to “take off their clinician hat” during the interview. Unless guided otherwise by the veteran, the interview was semichronological and included the following subjects: birth and childhood, family, schooling, military service, relationships and/or marriage, children, career and employment, general health, and current hospital stay and presenting problem.
Interviews lasted about an hour, and 182 interviews were conducted. Interviews were frequently interrupted by HCPs who checked vitals, administering medications, rounding with residents, and so forth. If the HCP indicated that the patient could keep talking, the interview continued. If the patient had to leave the room for a procedure or medical appointment, the interviewer paused the recording and scheduled a time to come back and complete the interview.
After the interview, veterans were told that they could expect to see the first written draft of their story within 2 days. Veterans who were to be discharged the day of the interview or the following day were told that the story would be sent to them in the mail to review at home.
Personal Health Inventory
Interviewers introduced the PHI to veterans as an opportunity to identify their wellness goals and share these with the PACT. Veterans with late-stage cancer or in hospice care were given the option to skip the PHI. Of the 103 veterans who completed the PHI, 96 chose to have the interviewer read the questions and record their answers; only 7 chose to complete the PHI on their own.
One hundred eighty-two veterans completed personal narratives, and 103 completed the PHI. Incomplete PHIs occurred for the following reasons: hospice or end of life, 12; declined, 20; could not complete, 21; discharged, 19; lost to follow-up, 7.
Writing
The quality of the written stories was critical to the success of the project. Creativity was encouraged to produce stories that captured and brought to life the voice and spirit of the interview subject. The team identified the following features of a good story: (1) written in the first person; (2) nonjudgmental; (3) captures the voice of the veteran; (4) accurately reflects the content of the interview; and (5) nondiagnostic (not labeling).
A short story format was used to increase the likelihood that busy providers would read the narratives. Writers were encouraged to limit the length of the stories to 1 to 2 printed pages (650-1,300 words). Completed stories ranged from 95 words to 2,345 words with an average length of 1,053 words. Veterans wrote 3 and the interviewers wrote 178 narratives; 1 narrative was written by a team member who was not present during the interview but listened to the audio recording.
Editing Process
The first draft of the story was printed and given to the veteran to make any desired changes. Veterans reviewed and updated their stories in different ways. Some wrote their changes on the printed copy and had the writer return at a later time to pick it up. Others read through the story with the writer present and wrote their changes on the printed copy. Some had the writer read the story aloud and alerted the writer when an item needed changing.
Drafts were mailed to already discharged veterans, including a postage-paid return envelope to allow them to mail their changes to the team. After incorporating the veteran’s changes, the team member brought back a second draft of the story for the veteran to review. This process was repeated until the veteran gave final approval. Veterans could then approve whether to share their story with their PACT via the Computerized Patient Record System (CPRS).
Some participant attrition occurred at this point. Six veterans requested that their stories not go in the CPRS (although 3 of them requested printed copies). One veteran changed his mind after his story was added to the CPRS; the team then immediately removed it. Two veterans died shortly after being released from the hospital and before they could review their stories. The families of both these veterans requested that an audio file of the interview be mailed to them.
Sharing With Family and Providers
Veterans received a printed copy of the approved story and the option to have additional copies for family members. The average number of additional copies requested was 3. Family and friends responded positively to the interview process and stories. Spouses who sat in on the interviews always added something to the interview process, and some were active participants. Eight of the 182 stories were dual narratives that included the words of the veteran and his/her spouse.
Providers were alerted to the personal narratives and PHI via CPRS. The completed story was added to the veteran’s record with the title “My Story.” The story was then electronically cosigned to the veteran’s inpatient and outpatient PACT. Typically, this included 4 people: the inpatient resident and attending physician and the outpatient provider and nurse care manager. If other providers were directly involved in the care of the veteran (mental health, specialists, surgeons), they were also cosigned to the story. If a veteran received primary care outside WSMMVH, their PACT was notified of the presence of the story in CPRS (and given a copy) via encrypted e-mail, in the CPRS “Postings” section.
Program Feedback
The original interviewer/writer team members (2.5 full-time employee equivalent for 6 months) generated 182 stories. The corresponding My Story notes in the CPRS were cosigned to an average of 3.3 providers. The program received both formal (solicited) feedback and informal (unsolicited) feedback from veterans and providers.
After gathering the first 80 stories, the team solicited participant satisfaction data from interviewed veterans, using a 5-point Likert-type scale. Veteran reaction was positive (Figure 1). The team polled VA providers with an online anonymous survey, using the same Likert-type scale to see whether the story and PHI were useful to providers in their clinical practice. The results suggested they were (Figure 2).
Perhaps the most enlightening and touching feedback were the following unsolicited e-mails and comments:
- I have so appreciated these stories, especially because they immediately become a source of connection with the veterans who come in (some for the first time) to see me about their heart failure. In the midst of a heavy “clinical” topic, knowing their stories has helped us form a stronger patient-provider relationship. It has provided moments of levity and a clear way to tell the patient that I am connecting with them and they are important. —VA employee
- I’m a veteran, and I love reading the real stories of veterans, told in their own words. For us, it’s always wonderful to feel like someone is listening. It’s good to feel like someone wants to hear what you’ve traveled through to get where you are. For those of us who put our lives, our health, our relationships, and our honor on the line for so many others, it’s great when someone will just take the time to listen and understand. It most definitely is very healing. —VA employee
- This is a great way to improve provider understanding and decrease bias and eliminate first impression issues, as people are generally ill and cranky when seeking medical care. —Veteran
- The My Story note was wonderful. I truly feel it has helped me to understand my patients better and to know where they are coming from. This is invaluable to the VA where experiences shape our patients in such a profound way. —VA employee
Recent developments at the WSMMVH suggest that veteran stories are becoming an accepted component of clinical care. The heart/lung transplant team requested that the My Story note be part of the transplant workup process for all new patients. The team also found that new HCPs who were assigned to a veteran regularly cosign that veteran’s My Story note to other providers on the care team. In addition, My Story referrals come from all types of HCPs and staff, both within the hospital and at primary care clinics.
Recent Developments
Two WSMMVH employees suggested using volunteers to gather stories and became the first volunteers: One was a housekeeper who had served in the U.S. Army during the Gulf War, and the other was a registered nurse; both had writing experience.
In 2014, staff trained 12 volunteers from the local community who have been trained to interview and write stories. The volunteers have varied professional backgrounds. All have a background and interest in writing or experience working in a health care setting; 2 are veterans. These volunteers are adding to the team at no additional cost. In development is a standardized training program and a method to look at story collection and writing fidelity, which will allow for further expansion of this program.
My Life, My Story continues to expand significantly. A total of 610 veterans have been interviewed, and 348 of these interviews were conducted by volunteers. The project now has 18 active volunteers with 4 more on a waiting list. A pilot has been launched at a WSMMVH outpatient clinic, which interviews VA primary care providers about their life stories and shares them with their veteran patients. There is now collaboration with the University of Wisconsin School of Medicine and Public Health in Madison to offer a 2-week My Story elective to fourth-year medical students in spring 2016. In March 2015, My Life, My Story expanded to 6 pilot facilities across the VA: Asheville, North Carolina; Bronx, New York; Iowa City, Iowa; Reno, Nevada; Topeka, Kansas; and White River Junction, Vermont.
Future Projects
- The team is currently analyzing the themes appearing in veteran stories, using grounded theory methodology
- The process for outpatients is being revised, using phone calls and telehealth modalities to collect stories
- The team members are examining relationships between themes in stories and health/wellness goals identified on the PHI
- Eventually, the team will study how this process might improve the veteran/provider relationship on measures of satisfaction with care, quality of care, and health outcomes. The authors will also assess the effects of this process on provider satisfaction and burnout
Conclusion
Veteran stories, when skillfully elicited and carefully crafted, give providers an opportunity to know their patients better, without impinging on their time. For veterans, the experience of being interviewed and the knowledge that their story will be shared with providers is an important recognition that they matter and have a voice in their health care. In a world of high-technology health care, where time is the only thing in short supply, My Life, My Story leverages the old-world technology of storytelling to bring providers and patients closer together.
Acknowledgments
The authors wish to acknowledge Amanda Hall and Jessica Jones who were interviewer/writers on the initial project. Both contributed immeasurably to the design and success of the project. The authors would also like to acknowledge Matt Spira who was our first volunteer interviewer and gave us the inspiration to recruit more volunteers. Volunteer Mary Johnston interviewed and wrote the sample veteran story in this article. We would also like to thank the nursing staff on 4A, 4B, and the community living center for their patience when we were in the way and for their support of the project. Last and most important, we would like to thank the veterans who were interviewed for this project. We have all learned more than we could have imagined from the stories that you shared with us. Your sacrifice, courage, and dedication both in the military and your personal lives are truly an inspiration. Thank you.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Anyone involved with the U.S. health care system has heard one or more of the following dispiriting comments. If you are a patient, you have heard or said, “I wish I felt like my provider understood me. He/she just doesn’t have the time.” If you are a provider, you have heard yourself or another provider say, “I wish I had more time to get to know my patients as people. I could do a better job or at least I could remember them without looking at the chart.” This article describes a novel program—My Life, My Story—instituted at the William S. Middleton Memorial Veterans Hospital (WSMMVH) in Madison, Wisconsin. The program uses personal narratives to foster a sense of connection between providers and their veteran patients.
Related: Infusing Gerontologic Practice Into PACT
My Life, My Story had its origins in a small performance improvement project aimed at helping psychiatric residents learn about their new outpatients during rotation. The clinic staff wanted residents to get to know their patients as people in addition to understanding the veterans’ medical conditions. The veterans were first offered the opportunity to come to writers’ workshops and create personal narratives that would be shared later with their clinicians. Unfortunately, only a few veterans were willing to take on this task.
A more patient-friendly approach for collecting and sharing the stories was developed and funded by the VHA Office of Patient-Centered Care and Cultural Transformation (OPCC&CT). Veterans who chose to participate worked with an interviewer/writer to create a personal narrative, which was then shared with their patient aligned care team (PACT). Another component of the interview process was the Personal Health Inventory (PHI), a questionnaire developed by the OPCC&CT that helps veterans articulate their goals and motivations for physical, social, psychological, and spiritual well-being.1 The PHI and personal narrative were paired, to give health care providers (HCPs) a sense of the veteran and their personal health goals.
Background
The health benefits of telling or writing the story of a difficult emotional event have been demonstrated by Pennebaker.2 In varied groups, from prisoners to patients with chronic pain, the writing or talking about experiences improved mood and lowered distress. In addition, studies of medically ill patients showed a decline in physician visits in the 2 to 6 months following the narrative process.3,4 Improved immune response was also shown for patients with hepatitis B, HIV, asthma, and rheumatoid arthritis in response to completing a narrative.5-7
Related: Experiences of Veterans With Diabetes From Shared Medical Appointments
But the writing task is difficult for many people, especially those with advanced illness. Interviewing these patients and writing their stories is a way to give them a voice that otherwise might go unheard.
Dignity therapy with terminally ill patients, a technique developed by Dr. H.M. Chochinov, used an expert to collect the story by bedside interview and to produce a dignity-enhancing life narrative.8-10 Wise and colleagues modified this process for patients with cancer stages III and IV by using telephone interviews, which showed reduced anger, depression, tension, and an increased sense of peace.11 Personal narratives in which patients tell their story and receive it in written form have been shown to reduce psychological distress, increase hope, and help the patient feel valued.10,12
Pennebaker hypothesized that several mechanisms account for these improvements in health measures.2 First, developing a narrative provides a contextual understanding of stressful events. Creating a personal narrative allows a patient to identify and give meaning to life’s struggles. Through this process, coping is hypothesized to occur.13-15 Second, storytelling connects the teller with a wider audience.16
Another study by Pennebaker and colleagues found an improvement in social connectedness in college students in the days following the disclosure of emotional stories.17 The study speculates that nondisclosure fosters isolation, whereas disclosure connects us with others, helping us to reach out to others and improving a sense of feeling understood.
Methods
Project staff were recruited to conduct the interviews and write the stories. Team members with varied backgrounds and experiences were selected: a nurse at the WSMMVH who served as an army interrogator in Afghanistan; a professional counselor with prior experience working for the VA; and a marriage and family therapist with a poetry MA.
Providers were recruited for participation in the project through (1) presentations to nursing staff on the inpatient units where stories were gathered; (2) compilations of de-identified stories from veterans on those units were distributed; (3) presentations on the project at outpatient clinics, where the narratives of veterans who were patients at those clinics were read aloud; and (4) discussions of the program at monthly hospital-wide meetings.
Related: Diabetes Patient-Centered Medical Home Approach
Patients were recruited from 2 inpatient units and 1 long-term rehabilitative care unit. Interviewers introduced themselves to the veterans, described the project, and gave each one a project brochure. Veterans were given the opportunity to be interviewed immediately, schedule a future interview, decide later, or not participate.
The majority of veterans who participated chose to be interviewed immediately. Scheduling interviews around procedures and discharges on busy inpatient units proved difficult. Overall participation rate was high: 60% of veterans who were told about the project eventually told their story.
Interview Process
Veterans signed a consent form before the interview, and the interviews were recorded on a digital audio recorder. They were informed they could choose to talk—or not talk—about any part of their life, the interviewer would write a draft of the story based on the interview and bring it back for their review, and the story would not be added to their patient record until they gave their approval. Spouses/partners were invited to participate if they desired.
Interviewers were encouraged to follow the lead of the veteran. Those who were clinicians were encouraged to “take off their clinician hat” during the interview. Unless guided otherwise by the veteran, the interview was semichronological and included the following subjects: birth and childhood, family, schooling, military service, relationships and/or marriage, children, career and employment, general health, and current hospital stay and presenting problem.
Interviews lasted about an hour, and 182 interviews were conducted. Interviews were frequently interrupted by HCPs who checked vitals, administering medications, rounding with residents, and so forth. If the HCP indicated that the patient could keep talking, the interview continued. If the patient had to leave the room for a procedure or medical appointment, the interviewer paused the recording and scheduled a time to come back and complete the interview.
After the interview, veterans were told that they could expect to see the first written draft of their story within 2 days. Veterans who were to be discharged the day of the interview or the following day were told that the story would be sent to them in the mail to review at home.
Personal Health Inventory
Interviewers introduced the PHI to veterans as an opportunity to identify their wellness goals and share these with the PACT. Veterans with late-stage cancer or in hospice care were given the option to skip the PHI. Of the 103 veterans who completed the PHI, 96 chose to have the interviewer read the questions and record their answers; only 7 chose to complete the PHI on their own.
One hundred eighty-two veterans completed personal narratives, and 103 completed the PHI. Incomplete PHIs occurred for the following reasons: hospice or end of life, 12; declined, 20; could not complete, 21; discharged, 19; lost to follow-up, 7.
Writing
The quality of the written stories was critical to the success of the project. Creativity was encouraged to produce stories that captured and brought to life the voice and spirit of the interview subject. The team identified the following features of a good story: (1) written in the first person; (2) nonjudgmental; (3) captures the voice of the veteran; (4) accurately reflects the content of the interview; and (5) nondiagnostic (not labeling).
A short story format was used to increase the likelihood that busy providers would read the narratives. Writers were encouraged to limit the length of the stories to 1 to 2 printed pages (650-1,300 words). Completed stories ranged from 95 words to 2,345 words with an average length of 1,053 words. Veterans wrote 3 and the interviewers wrote 178 narratives; 1 narrative was written by a team member who was not present during the interview but listened to the audio recording.
Editing Process
The first draft of the story was printed and given to the veteran to make any desired changes. Veterans reviewed and updated their stories in different ways. Some wrote their changes on the printed copy and had the writer return at a later time to pick it up. Others read through the story with the writer present and wrote their changes on the printed copy. Some had the writer read the story aloud and alerted the writer when an item needed changing.
Drafts were mailed to already discharged veterans, including a postage-paid return envelope to allow them to mail their changes to the team. After incorporating the veteran’s changes, the team member brought back a second draft of the story for the veteran to review. This process was repeated until the veteran gave final approval. Veterans could then approve whether to share their story with their PACT via the Computerized Patient Record System (CPRS).
Some participant attrition occurred at this point. Six veterans requested that their stories not go in the CPRS (although 3 of them requested printed copies). One veteran changed his mind after his story was added to the CPRS; the team then immediately removed it. Two veterans died shortly after being released from the hospital and before they could review their stories. The families of both these veterans requested that an audio file of the interview be mailed to them.
Sharing With Family and Providers
Veterans received a printed copy of the approved story and the option to have additional copies for family members. The average number of additional copies requested was 3. Family and friends responded positively to the interview process and stories. Spouses who sat in on the interviews always added something to the interview process, and some were active participants. Eight of the 182 stories were dual narratives that included the words of the veteran and his/her spouse.
Providers were alerted to the personal narratives and PHI via CPRS. The completed story was added to the veteran’s record with the title “My Story.” The story was then electronically cosigned to the veteran’s inpatient and outpatient PACT. Typically, this included 4 people: the inpatient resident and attending physician and the outpatient provider and nurse care manager. If other providers were directly involved in the care of the veteran (mental health, specialists, surgeons), they were also cosigned to the story. If a veteran received primary care outside WSMMVH, their PACT was notified of the presence of the story in CPRS (and given a copy) via encrypted e-mail, in the CPRS “Postings” section.
Program Feedback
The original interviewer/writer team members (2.5 full-time employee equivalent for 6 months) generated 182 stories. The corresponding My Story notes in the CPRS were cosigned to an average of 3.3 providers. The program received both formal (solicited) feedback and informal (unsolicited) feedback from veterans and providers.
After gathering the first 80 stories, the team solicited participant satisfaction data from interviewed veterans, using a 5-point Likert-type scale. Veteran reaction was positive (Figure 1). The team polled VA providers with an online anonymous survey, using the same Likert-type scale to see whether the story and PHI were useful to providers in their clinical practice. The results suggested they were (Figure 2).
Perhaps the most enlightening and touching feedback were the following unsolicited e-mails and comments:
- I have so appreciated these stories, especially because they immediately become a source of connection with the veterans who come in (some for the first time) to see me about their heart failure. In the midst of a heavy “clinical” topic, knowing their stories has helped us form a stronger patient-provider relationship. It has provided moments of levity and a clear way to tell the patient that I am connecting with them and they are important. —VA employee
- I’m a veteran, and I love reading the real stories of veterans, told in their own words. For us, it’s always wonderful to feel like someone is listening. It’s good to feel like someone wants to hear what you’ve traveled through to get where you are. For those of us who put our lives, our health, our relationships, and our honor on the line for so many others, it’s great when someone will just take the time to listen and understand. It most definitely is very healing. —VA employee
- This is a great way to improve provider understanding and decrease bias and eliminate first impression issues, as people are generally ill and cranky when seeking medical care. —Veteran
- The My Story note was wonderful. I truly feel it has helped me to understand my patients better and to know where they are coming from. This is invaluable to the VA where experiences shape our patients in such a profound way. —VA employee
Recent developments at the WSMMVH suggest that veteran stories are becoming an accepted component of clinical care. The heart/lung transplant team requested that the My Story note be part of the transplant workup process for all new patients. The team also found that new HCPs who were assigned to a veteran regularly cosign that veteran’s My Story note to other providers on the care team. In addition, My Story referrals come from all types of HCPs and staff, both within the hospital and at primary care clinics.
Recent Developments
Two WSMMVH employees suggested using volunteers to gather stories and became the first volunteers: One was a housekeeper who had served in the U.S. Army during the Gulf War, and the other was a registered nurse; both had writing experience.
In 2014, staff trained 12 volunteers from the local community who have been trained to interview and write stories. The volunteers have varied professional backgrounds. All have a background and interest in writing or experience working in a health care setting; 2 are veterans. These volunteers are adding to the team at no additional cost. In development is a standardized training program and a method to look at story collection and writing fidelity, which will allow for further expansion of this program.
My Life, My Story continues to expand significantly. A total of 610 veterans have been interviewed, and 348 of these interviews were conducted by volunteers. The project now has 18 active volunteers with 4 more on a waiting list. A pilot has been launched at a WSMMVH outpatient clinic, which interviews VA primary care providers about their life stories and shares them with their veteran patients. There is now collaboration with the University of Wisconsin School of Medicine and Public Health in Madison to offer a 2-week My Story elective to fourth-year medical students in spring 2016. In March 2015, My Life, My Story expanded to 6 pilot facilities across the VA: Asheville, North Carolina; Bronx, New York; Iowa City, Iowa; Reno, Nevada; Topeka, Kansas; and White River Junction, Vermont.
Future Projects
- The team is currently analyzing the themes appearing in veteran stories, using grounded theory methodology
- The process for outpatients is being revised, using phone calls and telehealth modalities to collect stories
- The team members are examining relationships between themes in stories and health/wellness goals identified on the PHI
- Eventually, the team will study how this process might improve the veteran/provider relationship on measures of satisfaction with care, quality of care, and health outcomes. The authors will also assess the effects of this process on provider satisfaction and burnout
Conclusion
Veteran stories, when skillfully elicited and carefully crafted, give providers an opportunity to know their patients better, without impinging on their time. For veterans, the experience of being interviewed and the knowledge that their story will be shared with providers is an important recognition that they matter and have a voice in their health care. In a world of high-technology health care, where time is the only thing in short supply, My Life, My Story leverages the old-world technology of storytelling to bring providers and patients closer together.
Acknowledgments
The authors wish to acknowledge Amanda Hall and Jessica Jones who were interviewer/writers on the initial project. Both contributed immeasurably to the design and success of the project. The authors would also like to acknowledge Matt Spira who was our first volunteer interviewer and gave us the inspiration to recruit more volunteers. Volunteer Mary Johnston interviewed and wrote the sample veteran story in this article. We would also like to thank the nursing staff on 4A, 4B, and the community living center for their patience when we were in the way and for their support of the project. Last and most important, we would like to thank the veterans who were interviewed for this project. We have all learned more than we could have imagined from the stories that you shared with us. Your sacrifice, courage, and dedication both in the military and your personal lives are truly an inspiration. Thank you.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Veterans Health Administration, Office of Patient Centered Care and Cultural Transformation. My Story Personal Health Inventory, Revision 20. U.S. Department of Veterans Affairs Website. http://www .va.gov/patientcenteredcare/docs/va-opcc-personal -health-inventory-final-508.pdf. Revised October 7, 2013. Accessed May 11, 2015.
2. Pennebaker JW. Telling stories: the health benefits of narrative. Lit Med. 2000;19(1):3-18.
3. Greenberg MA, Stone AA. Writing about disclosed versus undisclosed traumas: immediate and long term effects on mood and health. J Pers Soc Psychol. 1992;63:75-84.
4. Pennebaker JW, Beall SK. Confronting a traumatic event: toward an understanding of inhibition and disease. J Abnorm Psychol. 1986;95(3):274-281.
5. Petrie KJ, Booth RJ, Pennebaker JW, Davidson KP, Thomas MG. Disclosure of trauma and immune response to hepatitis B vaccination program. J Consult Clin Psychol. 1995;63(5):787-792.
6. Petrie KJ, Fontanilla I, Thomas MG, Booth RJ, Pennebaker JW. Effect of written emotional expression on immune function in patients with human immunodeficiency virus infection: a randomized trial. Psychosom Med. 2004;66(2):272-275.
7. Smyth JM, Stone AA, Hurewitz A, Kaell A. Effects of writing about stressful experiences on symptom reduction in patients with asthma or rheumatoid arthritis. JAMA. 1999;281(14):1304-1309.
8. Chochinov HM. Dignity-conserving care—a new model for palliative care: helping the patient feel valued. JAMA. 2002;287(17):2253-2260.
9. Chochinov HM, Hack T, Hassard T, Kristjanson LJ, McClement S, Harlos M. Understanding the will to live in patients near death. Psychosom. 2005;46(1):7-10.
10. Chochinov HM, Kristjanson LJ, Breitbart W, et al. Effect of dignity therapy on distress and end-of-life experience in terminally ill patients: a randomised controlled trial. Lancet Oncol. 2011;12(8):753-762.
11. Wise M, Marchand L, Roberts LJ, Chih M. Existential suffering in advanced cancer: the buffering effects of narrative: a randomized control trial. Poster presented at: University of Washington School of Medicine 6th Annual Department Fair; April 8, 2015; Seattle, Washington.
12. Hall S, Goddard C, Opio D, Speck PW, Martin P, Higginson IJ. A novel approach to enhancing hope in patients with advanced cancer: a randomised phase II trial of dignity therapy. BMJ Support Palliat Care. 2011;1(3):315-321.
13. Heiney SP. The healing power of story. Oncol Nurs Forum. 1995;22(6):899-904.
14. Hyden L-C. Illness and narrative. Soc Health Illness. 1997;19(1):48-69.
15. Carlick A, Biley FC. Thoughts on the therapeutic use of narrative in the promotion of coping in cancer care. Eur J Cancer Care (Engl). 2004;13(4):308-317.
16. Niederhoffer KG, Pennebaker JW. Sharing one’s story: on the benefits of writing or talking about emotional experience. In: Snyder CR, Lopez SJ, eds. Handbook of Positive Psychology. New York, NY: Oxford University Press; 2001:573-583.
17. Pennebaker JW, Kiecolt-Glaser JK, Glaser R. Disclosure of traumas and immune function: health implications for psychotherapy. J Consult Clin Psychol. 1988:56(2):239-245.
1. Veterans Health Administration, Office of Patient Centered Care and Cultural Transformation. My Story Personal Health Inventory, Revision 20. U.S. Department of Veterans Affairs Website. http://www .va.gov/patientcenteredcare/docs/va-opcc-personal -health-inventory-final-508.pdf. Revised October 7, 2013. Accessed May 11, 2015.
2. Pennebaker JW. Telling stories: the health benefits of narrative. Lit Med. 2000;19(1):3-18.
3. Greenberg MA, Stone AA. Writing about disclosed versus undisclosed traumas: immediate and long term effects on mood and health. J Pers Soc Psychol. 1992;63:75-84.
4. Pennebaker JW, Beall SK. Confronting a traumatic event: toward an understanding of inhibition and disease. J Abnorm Psychol. 1986;95(3):274-281.
5. Petrie KJ, Booth RJ, Pennebaker JW, Davidson KP, Thomas MG. Disclosure of trauma and immune response to hepatitis B vaccination program. J Consult Clin Psychol. 1995;63(5):787-792.
6. Petrie KJ, Fontanilla I, Thomas MG, Booth RJ, Pennebaker JW. Effect of written emotional expression on immune function in patients with human immunodeficiency virus infection: a randomized trial. Psychosom Med. 2004;66(2):272-275.
7. Smyth JM, Stone AA, Hurewitz A, Kaell A. Effects of writing about stressful experiences on symptom reduction in patients with asthma or rheumatoid arthritis. JAMA. 1999;281(14):1304-1309.
8. Chochinov HM. Dignity-conserving care—a new model for palliative care: helping the patient feel valued. JAMA. 2002;287(17):2253-2260.
9. Chochinov HM, Hack T, Hassard T, Kristjanson LJ, McClement S, Harlos M. Understanding the will to live in patients near death. Psychosom. 2005;46(1):7-10.
10. Chochinov HM, Kristjanson LJ, Breitbart W, et al. Effect of dignity therapy on distress and end-of-life experience in terminally ill patients: a randomised controlled trial. Lancet Oncol. 2011;12(8):753-762.
11. Wise M, Marchand L, Roberts LJ, Chih M. Existential suffering in advanced cancer: the buffering effects of narrative: a randomized control trial. Poster presented at: University of Washington School of Medicine 6th Annual Department Fair; April 8, 2015; Seattle, Washington.
12. Hall S, Goddard C, Opio D, Speck PW, Martin P, Higginson IJ. A novel approach to enhancing hope in patients with advanced cancer: a randomised phase II trial of dignity therapy. BMJ Support Palliat Care. 2011;1(3):315-321.
13. Heiney SP. The healing power of story. Oncol Nurs Forum. 1995;22(6):899-904.
14. Hyden L-C. Illness and narrative. Soc Health Illness. 1997;19(1):48-69.
15. Carlick A, Biley FC. Thoughts on the therapeutic use of narrative in the promotion of coping in cancer care. Eur J Cancer Care (Engl). 2004;13(4):308-317.
16. Niederhoffer KG, Pennebaker JW. Sharing one’s story: on the benefits of writing or talking about emotional experience. In: Snyder CR, Lopez SJ, eds. Handbook of Positive Psychology. New York, NY: Oxford University Press; 2001:573-583.
17. Pennebaker JW, Kiecolt-Glaser JK, Glaser R. Disclosure of traumas and immune function: health implications for psychotherapy. J Consult Clin Psychol. 1988:56(2):239-245.
The VA Geriatric Scholars Program
In 1973 the VA addressed the “age wave,” recognizing the need to advance geriatrics and gerontology in the U.S. by creating the Geriatric Research Education Clinical Centers (GRECCs) with its mission to improve health care for all older veterans. Twenty GRECCs were authorized, and as advances have moved from bench to bedside, the role of education has become increasingly important.
The Institute of Medicine observed the need to focus on training for the existing U.S. health care workforce, which lacks sufficient expertise in geriatrics. The VHA Office of Geriatrics and Extended Care (GEC) also noted that lack of training in the care of older adults is a serious problem in the VHA, because more than half the veterans who seek health care annually are aged > 65 years. The VHA also has fewer geriatricians per patient (1:11,515 patients) than the overall U.S. average (1:6,028 patients) (Kenneth Shay, DDS, MS, written communication, April 13, 2015).
About 2.4 million older veterans receive health care in primary care Patient Aligned Care Teams (PACTs), whereas only 87,000 older veterans receive specialty care in geriatrics. The lack of specialty care in geriatrics is even more problematic in rural areas, where there are fewer specialists and the patient population is older than in urban areas. Typically, rural-dwelling veterans are older, in poorer health, and have a higher incidence of mortality than do their urban counterparts.
Related: Infusing Gerontologic Practice Into PACT
To address this need, 10 of the 20 GRECC associate directors for education/evaluation have joined with the GEC and the VA Employee Education System (EES) to collaborate in a national longitudinal educational program to integrate state-of-the-art geriatric practices in primary care PACTs throughout the VA. The program targets primary care providers as well as associated health professionals who support the PACTs (pharmacists, psychologists, and social workers).
The VA Geriatric Scholars Program (GSP) is a longitudinal multimodal educational program designed on the principles of adult learning and continuous professional development, including a demonstration of skills. The VA Office of Rural Health and Primary Care Services fund the program. All learners are nominated by their respective VISNs and commit to implementing systematic changes in personal and clinic practices to improve the quality of care for older veterans.
Core Elements
The GSP consists of core elements and a broad variety of electives to meet learners’ individual goals for the development of new skills and competencies. There are 3 core elements: (1) a ≥ 35-hour CME/CEU intensive didactic course in geriatric medicine sponsored by leading universities; (2) an 8-hour CME/CEU course sponsored by the EES; and (3) a demonstration of how new knowledge is being applied through a quality improvement (QI) project in the PACT or clinic.
The GSP with the EES also developed specialized didactic courses for social workers and for psychologists when none previously existed. The optional learning components include clinical practicum experiences, online learning, audio conferences, and refresher courses. With evaluations of learners several times a year, new programs and educational materials are developed to meet the self-identified needs of VA clinicians. The program recently added advanced tracks in clinical leadership and management and in palliative care.
Since its inception as a pilot program in 2008, the GSP has continued to expand, adding components such as on-site team training at rural community-based outpatient clinics (CBOCs) and building infrastructure through online learning. The program has also spun off initiatives to provide high-quality geriatric education to rural CBOCs through its GRECC-CBOC Connection program, which offers case presentations and consultations through clinical video teleconferencing in 8 VISNs and a new virtual learning community at http//www.gerischolars.org.
Each of the 10 GRECCs has a unique and well-defined role in the collaboration. For example, the Nashville-based Tennessee Valley GRECC contributes its expertise in QI and is responsible for the curriculum design, training, approvals for QI projects (rather than research projects), and individualized coaching. The Bronx GRECC in New York pioneered the Rural Interdisciplinary Team Training (RITT) program, which provides education in geriatrics and clinical teamwork, combined with group activities to improve team function over the course of a year. The Palo Alto GRECC in California responded to requests from the field to develop a specialized course to enhance skills in geriatrics and gerontology for VHA psychologists. The Little Rock GRECC in Arkansas has taken a lead role in developing audio conferences to meet learner-defined educational needs, and the San Antonio GRECC in Texas is developing interactive online training modules.
Related: Home-Based Video Telehealth for Veterans With Dementia
The GRECCs offer unique, clinical practicum experiences for both groups and for individual scholars. These include late life issues in mental health and palliative care at the Boston, Massachusetts-based New England and Madison, Wisconsin GRECCs, dementia care at the Puget Sound GRECC in Washington, physical function and fitness at the Durham GRECC in North Carolina, and in alternating years, comprehensive functional assessment and integrative medicine at the Greater Los Angeles GRECC. The hub site for the program is at the Greater Los Angeles GRECC in California, which handles the administrative component and develops new components for social worker education, integrative health, and an online infrastructure to maintain and expand the didactic activities.
One of the GRECC missions is to export successful educational models. The GSP was adopted by the non-VA Western New York Medical Foundation and may be adapted as a VA Palliative Care Scholars Program. The VA Eastern Regional Rural Health Center has also explored implementing the model for training. The value of the program has also been recognized recently with 2 national awards. In 2012, the QI curriculum was recognized with the Duncan Neuhauser Award for Curricular Innovation in Healthcare Improvement by the Academy for Healthcare Improvement. More recently, Josea Kramer, PhD, program director, received the David M. Worthen Award for Educational Excellence from the VA Office of Academic Affiliations, in part based on the impact of the GSP enhancing geriatric skills and competencies in the VA primary care workforce.
Geriatric Scholars’ clinical teams in small rural CBOCs have made a difference with a focused local issue that could serve as a model for wide application throughout VHA. The projects have included improving access to oral and dental health to all clinic users; prioritization for community-based, long-term care options; identification and support for caregivers; documentation of end of life preferences; and follow-up after non-VA hospital discharges; other projects have reduced polypharmacy, falls, and clinic no-shows.
The impact of the GSP has been substantial, and learners represent every VISN. To date, the GSP has trained 1,901 VA clinicians at more than 360 facilities. The majority had no previous training in geriatrics, even during medical residency or associated health profession internships, yet today, older adults comprise an average 72% of their current patient panels.
Scholar Feedback
In testimonials, geriatric scholars have given positive feedback for many aspects of the program. Attending the program was “one of the best decisions of my life educationally and personally and opened my eyes to what is out there in geriatric care,” one scholar insisted. “This program has helped me with my day-to-day practices,” another attendee noted, “I feel more comfortable in my role. I can communicate better with my team and patients.”
Related: Using Facilitative Coaching to Support Patient Aligned Care Teams
One of the outcomes of the program was to standardize care for older veterans by teaching the state-of-the-art in geriatrics to clinicians who would teach-back the principles across disciplines and in their respective primary care settings. “I am using the [standardized brief cognitive instrument for] memory testing...that I have learned....The doctors really like it!” explained one attendee. “I went through the [GSP Learning Community] SharePoint site and picked out [a standardized brief cognitive instrument] CPRS template after our [RITT] training. I have already shared with our service line and got it approved,” added another scholar. The SharePoint site is open all VA employees.
Another outcome of the opportunity to teach-back has been preparing the interdisciplinary clinical team to interact efficiently within the environment of the patient-centered medical home or PACT. “The Geriatric Scholars Program showed how we should put veterans at the center, involve the entire team (nurses, pharmacy, etc.) in their care,” a scholar explained. “The Geriatric Scholars Program is a great tool to help roll out [PACT] at my CBOC,” another scholar reported. “I used the mentoring I got from the Geriatric Scholars Program to teach my clinic team.”
Through the GSP, an estimated 309,671 older veterans are now receiving care from clinicians who have developed additional skills in geriatrics. This fall, the GSP will be welcoming a new class of 60 learners, expanding the scope of the program and reaching veterans in more communities.
Acknowledgements
The Geriatric Scholars Program is a collaboration of 10 Geriatric Research Education and Clinical Centers (GRECCs) and the VA Office of Geriatrics and Extended Care (GEC). The contributions of all past and present collaborators are gratefully acknowledged, including Judith Howe, PhD (Bronx GRECC); Carol Callaway-Lane, DNP (Tennessee Valley GRECC); Terri Huh, PhD (Palo Alto GRECC); Steven Barzci, MD (Madison GRECC); Kathy Horvath, PhD, RN, and Scott Trudeau, PhD, PT (New England GRECC); Sandra Sanchez-Reilly, MD (San Antonio GRECC); Connie Bales, PhD, RD (Durham GRECC); Ronni Chernoff, PhD, RD, Kim Garner, MD, and Sheila Cox Sullivan, PhD, RN (Little Rock GRECC); Stephen Thielke, MD (Puget Sound GRECC); Nina Tumosa, PhD (currently at the U.S. Health Resources and Services Administration); and Kenneth Shay, DMD (Office GEC). We gratefully acknowledge and appreciate the staff at the VA Greater Los Angeles Healthcare System GRECC program hub site whose contributions “behind the scene” make this multi-faceted program possible: Luis Melendez, MPA, MS (program administrator); Joseph Douglas (special projects manager); Timothy Gardner, MBA (program analyst); Beth Creekmur, MA (budget analyst); and Diane Lee, MSW (program support staff).
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
In 1973 the VA addressed the “age wave,” recognizing the need to advance geriatrics and gerontology in the U.S. by creating the Geriatric Research Education Clinical Centers (GRECCs) with its mission to improve health care for all older veterans. Twenty GRECCs were authorized, and as advances have moved from bench to bedside, the role of education has become increasingly important.
The Institute of Medicine observed the need to focus on training for the existing U.S. health care workforce, which lacks sufficient expertise in geriatrics. The VHA Office of Geriatrics and Extended Care (GEC) also noted that lack of training in the care of older adults is a serious problem in the VHA, because more than half the veterans who seek health care annually are aged > 65 years. The VHA also has fewer geriatricians per patient (1:11,515 patients) than the overall U.S. average (1:6,028 patients) (Kenneth Shay, DDS, MS, written communication, April 13, 2015).
About 2.4 million older veterans receive health care in primary care Patient Aligned Care Teams (PACTs), whereas only 87,000 older veterans receive specialty care in geriatrics. The lack of specialty care in geriatrics is even more problematic in rural areas, where there are fewer specialists and the patient population is older than in urban areas. Typically, rural-dwelling veterans are older, in poorer health, and have a higher incidence of mortality than do their urban counterparts.
Related: Infusing Gerontologic Practice Into PACT
To address this need, 10 of the 20 GRECC associate directors for education/evaluation have joined with the GEC and the VA Employee Education System (EES) to collaborate in a national longitudinal educational program to integrate state-of-the-art geriatric practices in primary care PACTs throughout the VA. The program targets primary care providers as well as associated health professionals who support the PACTs (pharmacists, psychologists, and social workers).
The VA Geriatric Scholars Program (GSP) is a longitudinal multimodal educational program designed on the principles of adult learning and continuous professional development, including a demonstration of skills. The VA Office of Rural Health and Primary Care Services fund the program. All learners are nominated by their respective VISNs and commit to implementing systematic changes in personal and clinic practices to improve the quality of care for older veterans.
Core Elements
The GSP consists of core elements and a broad variety of electives to meet learners’ individual goals for the development of new skills and competencies. There are 3 core elements: (1) a ≥ 35-hour CME/CEU intensive didactic course in geriatric medicine sponsored by leading universities; (2) an 8-hour CME/CEU course sponsored by the EES; and (3) a demonstration of how new knowledge is being applied through a quality improvement (QI) project in the PACT or clinic.
The GSP with the EES also developed specialized didactic courses for social workers and for psychologists when none previously existed. The optional learning components include clinical practicum experiences, online learning, audio conferences, and refresher courses. With evaluations of learners several times a year, new programs and educational materials are developed to meet the self-identified needs of VA clinicians. The program recently added advanced tracks in clinical leadership and management and in palliative care.
Since its inception as a pilot program in 2008, the GSP has continued to expand, adding components such as on-site team training at rural community-based outpatient clinics (CBOCs) and building infrastructure through online learning. The program has also spun off initiatives to provide high-quality geriatric education to rural CBOCs through its GRECC-CBOC Connection program, which offers case presentations and consultations through clinical video teleconferencing in 8 VISNs and a new virtual learning community at http//www.gerischolars.org.
Each of the 10 GRECCs has a unique and well-defined role in the collaboration. For example, the Nashville-based Tennessee Valley GRECC contributes its expertise in QI and is responsible for the curriculum design, training, approvals for QI projects (rather than research projects), and individualized coaching. The Bronx GRECC in New York pioneered the Rural Interdisciplinary Team Training (RITT) program, which provides education in geriatrics and clinical teamwork, combined with group activities to improve team function over the course of a year. The Palo Alto GRECC in California responded to requests from the field to develop a specialized course to enhance skills in geriatrics and gerontology for VHA psychologists. The Little Rock GRECC in Arkansas has taken a lead role in developing audio conferences to meet learner-defined educational needs, and the San Antonio GRECC in Texas is developing interactive online training modules.
Related: Home-Based Video Telehealth for Veterans With Dementia
The GRECCs offer unique, clinical practicum experiences for both groups and for individual scholars. These include late life issues in mental health and palliative care at the Boston, Massachusetts-based New England and Madison, Wisconsin GRECCs, dementia care at the Puget Sound GRECC in Washington, physical function and fitness at the Durham GRECC in North Carolina, and in alternating years, comprehensive functional assessment and integrative medicine at the Greater Los Angeles GRECC. The hub site for the program is at the Greater Los Angeles GRECC in California, which handles the administrative component and develops new components for social worker education, integrative health, and an online infrastructure to maintain and expand the didactic activities.
One of the GRECC missions is to export successful educational models. The GSP was adopted by the non-VA Western New York Medical Foundation and may be adapted as a VA Palliative Care Scholars Program. The VA Eastern Regional Rural Health Center has also explored implementing the model for training. The value of the program has also been recognized recently with 2 national awards. In 2012, the QI curriculum was recognized with the Duncan Neuhauser Award for Curricular Innovation in Healthcare Improvement by the Academy for Healthcare Improvement. More recently, Josea Kramer, PhD, program director, received the David M. Worthen Award for Educational Excellence from the VA Office of Academic Affiliations, in part based on the impact of the GSP enhancing geriatric skills and competencies in the VA primary care workforce.
Geriatric Scholars’ clinical teams in small rural CBOCs have made a difference with a focused local issue that could serve as a model for wide application throughout VHA. The projects have included improving access to oral and dental health to all clinic users; prioritization for community-based, long-term care options; identification and support for caregivers; documentation of end of life preferences; and follow-up after non-VA hospital discharges; other projects have reduced polypharmacy, falls, and clinic no-shows.
The impact of the GSP has been substantial, and learners represent every VISN. To date, the GSP has trained 1,901 VA clinicians at more than 360 facilities. The majority had no previous training in geriatrics, even during medical residency or associated health profession internships, yet today, older adults comprise an average 72% of their current patient panels.
Scholar Feedback
In testimonials, geriatric scholars have given positive feedback for many aspects of the program. Attending the program was “one of the best decisions of my life educationally and personally and opened my eyes to what is out there in geriatric care,” one scholar insisted. “This program has helped me with my day-to-day practices,” another attendee noted, “I feel more comfortable in my role. I can communicate better with my team and patients.”
Related: Using Facilitative Coaching to Support Patient Aligned Care Teams
One of the outcomes of the program was to standardize care for older veterans by teaching the state-of-the-art in geriatrics to clinicians who would teach-back the principles across disciplines and in their respective primary care settings. “I am using the [standardized brief cognitive instrument for] memory testing...that I have learned....The doctors really like it!” explained one attendee. “I went through the [GSP Learning Community] SharePoint site and picked out [a standardized brief cognitive instrument] CPRS template after our [RITT] training. I have already shared with our service line and got it approved,” added another scholar. The SharePoint site is open all VA employees.
Another outcome of the opportunity to teach-back has been preparing the interdisciplinary clinical team to interact efficiently within the environment of the patient-centered medical home or PACT. “The Geriatric Scholars Program showed how we should put veterans at the center, involve the entire team (nurses, pharmacy, etc.) in their care,” a scholar explained. “The Geriatric Scholars Program is a great tool to help roll out [PACT] at my CBOC,” another scholar reported. “I used the mentoring I got from the Geriatric Scholars Program to teach my clinic team.”
Through the GSP, an estimated 309,671 older veterans are now receiving care from clinicians who have developed additional skills in geriatrics. This fall, the GSP will be welcoming a new class of 60 learners, expanding the scope of the program and reaching veterans in more communities.
Acknowledgements
The Geriatric Scholars Program is a collaboration of 10 Geriatric Research Education and Clinical Centers (GRECCs) and the VA Office of Geriatrics and Extended Care (GEC). The contributions of all past and present collaborators are gratefully acknowledged, including Judith Howe, PhD (Bronx GRECC); Carol Callaway-Lane, DNP (Tennessee Valley GRECC); Terri Huh, PhD (Palo Alto GRECC); Steven Barzci, MD (Madison GRECC); Kathy Horvath, PhD, RN, and Scott Trudeau, PhD, PT (New England GRECC); Sandra Sanchez-Reilly, MD (San Antonio GRECC); Connie Bales, PhD, RD (Durham GRECC); Ronni Chernoff, PhD, RD, Kim Garner, MD, and Sheila Cox Sullivan, PhD, RN (Little Rock GRECC); Stephen Thielke, MD (Puget Sound GRECC); Nina Tumosa, PhD (currently at the U.S. Health Resources and Services Administration); and Kenneth Shay, DMD (Office GEC). We gratefully acknowledge and appreciate the staff at the VA Greater Los Angeles Healthcare System GRECC program hub site whose contributions “behind the scene” make this multi-faceted program possible: Luis Melendez, MPA, MS (program administrator); Joseph Douglas (special projects manager); Timothy Gardner, MBA (program analyst); Beth Creekmur, MA (budget analyst); and Diane Lee, MSW (program support staff).
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
In 1973 the VA addressed the “age wave,” recognizing the need to advance geriatrics and gerontology in the U.S. by creating the Geriatric Research Education Clinical Centers (GRECCs) with its mission to improve health care for all older veterans. Twenty GRECCs were authorized, and as advances have moved from bench to bedside, the role of education has become increasingly important.
The Institute of Medicine observed the need to focus on training for the existing U.S. health care workforce, which lacks sufficient expertise in geriatrics. The VHA Office of Geriatrics and Extended Care (GEC) also noted that lack of training in the care of older adults is a serious problem in the VHA, because more than half the veterans who seek health care annually are aged > 65 years. The VHA also has fewer geriatricians per patient (1:11,515 patients) than the overall U.S. average (1:6,028 patients) (Kenneth Shay, DDS, MS, written communication, April 13, 2015).
About 2.4 million older veterans receive health care in primary care Patient Aligned Care Teams (PACTs), whereas only 87,000 older veterans receive specialty care in geriatrics. The lack of specialty care in geriatrics is even more problematic in rural areas, where there are fewer specialists and the patient population is older than in urban areas. Typically, rural-dwelling veterans are older, in poorer health, and have a higher incidence of mortality than do their urban counterparts.
Related: Infusing Gerontologic Practice Into PACT
To address this need, 10 of the 20 GRECC associate directors for education/evaluation have joined with the GEC and the VA Employee Education System (EES) to collaborate in a national longitudinal educational program to integrate state-of-the-art geriatric practices in primary care PACTs throughout the VA. The program targets primary care providers as well as associated health professionals who support the PACTs (pharmacists, psychologists, and social workers).
The VA Geriatric Scholars Program (GSP) is a longitudinal multimodal educational program designed on the principles of adult learning and continuous professional development, including a demonstration of skills. The VA Office of Rural Health and Primary Care Services fund the program. All learners are nominated by their respective VISNs and commit to implementing systematic changes in personal and clinic practices to improve the quality of care for older veterans.
Core Elements
The GSP consists of core elements and a broad variety of electives to meet learners’ individual goals for the development of new skills and competencies. There are 3 core elements: (1) a ≥ 35-hour CME/CEU intensive didactic course in geriatric medicine sponsored by leading universities; (2) an 8-hour CME/CEU course sponsored by the EES; and (3) a demonstration of how new knowledge is being applied through a quality improvement (QI) project in the PACT or clinic.
The GSP with the EES also developed specialized didactic courses for social workers and for psychologists when none previously existed. The optional learning components include clinical practicum experiences, online learning, audio conferences, and refresher courses. With evaluations of learners several times a year, new programs and educational materials are developed to meet the self-identified needs of VA clinicians. The program recently added advanced tracks in clinical leadership and management and in palliative care.
Since its inception as a pilot program in 2008, the GSP has continued to expand, adding components such as on-site team training at rural community-based outpatient clinics (CBOCs) and building infrastructure through online learning. The program has also spun off initiatives to provide high-quality geriatric education to rural CBOCs through its GRECC-CBOC Connection program, which offers case presentations and consultations through clinical video teleconferencing in 8 VISNs and a new virtual learning community at http//www.gerischolars.org.
Each of the 10 GRECCs has a unique and well-defined role in the collaboration. For example, the Nashville-based Tennessee Valley GRECC contributes its expertise in QI and is responsible for the curriculum design, training, approvals for QI projects (rather than research projects), and individualized coaching. The Bronx GRECC in New York pioneered the Rural Interdisciplinary Team Training (RITT) program, which provides education in geriatrics and clinical teamwork, combined with group activities to improve team function over the course of a year. The Palo Alto GRECC in California responded to requests from the field to develop a specialized course to enhance skills in geriatrics and gerontology for VHA psychologists. The Little Rock GRECC in Arkansas has taken a lead role in developing audio conferences to meet learner-defined educational needs, and the San Antonio GRECC in Texas is developing interactive online training modules.
Related: Home-Based Video Telehealth for Veterans With Dementia
The GRECCs offer unique, clinical practicum experiences for both groups and for individual scholars. These include late life issues in mental health and palliative care at the Boston, Massachusetts-based New England and Madison, Wisconsin GRECCs, dementia care at the Puget Sound GRECC in Washington, physical function and fitness at the Durham GRECC in North Carolina, and in alternating years, comprehensive functional assessment and integrative medicine at the Greater Los Angeles GRECC. The hub site for the program is at the Greater Los Angeles GRECC in California, which handles the administrative component and develops new components for social worker education, integrative health, and an online infrastructure to maintain and expand the didactic activities.
One of the GRECC missions is to export successful educational models. The GSP was adopted by the non-VA Western New York Medical Foundation and may be adapted as a VA Palliative Care Scholars Program. The VA Eastern Regional Rural Health Center has also explored implementing the model for training. The value of the program has also been recognized recently with 2 national awards. In 2012, the QI curriculum was recognized with the Duncan Neuhauser Award for Curricular Innovation in Healthcare Improvement by the Academy for Healthcare Improvement. More recently, Josea Kramer, PhD, program director, received the David M. Worthen Award for Educational Excellence from the VA Office of Academic Affiliations, in part based on the impact of the GSP enhancing geriatric skills and competencies in the VA primary care workforce.
Geriatric Scholars’ clinical teams in small rural CBOCs have made a difference with a focused local issue that could serve as a model for wide application throughout VHA. The projects have included improving access to oral and dental health to all clinic users; prioritization for community-based, long-term care options; identification and support for caregivers; documentation of end of life preferences; and follow-up after non-VA hospital discharges; other projects have reduced polypharmacy, falls, and clinic no-shows.
The impact of the GSP has been substantial, and learners represent every VISN. To date, the GSP has trained 1,901 VA clinicians at more than 360 facilities. The majority had no previous training in geriatrics, even during medical residency or associated health profession internships, yet today, older adults comprise an average 72% of their current patient panels.
Scholar Feedback
In testimonials, geriatric scholars have given positive feedback for many aspects of the program. Attending the program was “one of the best decisions of my life educationally and personally and opened my eyes to what is out there in geriatric care,” one scholar insisted. “This program has helped me with my day-to-day practices,” another attendee noted, “I feel more comfortable in my role. I can communicate better with my team and patients.”
Related: Using Facilitative Coaching to Support Patient Aligned Care Teams
One of the outcomes of the program was to standardize care for older veterans by teaching the state-of-the-art in geriatrics to clinicians who would teach-back the principles across disciplines and in their respective primary care settings. “I am using the [standardized brief cognitive instrument for] memory testing...that I have learned....The doctors really like it!” explained one attendee. “I went through the [GSP Learning Community] SharePoint site and picked out [a standardized brief cognitive instrument] CPRS template after our [RITT] training. I have already shared with our service line and got it approved,” added another scholar. The SharePoint site is open all VA employees.
Another outcome of the opportunity to teach-back has been preparing the interdisciplinary clinical team to interact efficiently within the environment of the patient-centered medical home or PACT. “The Geriatric Scholars Program showed how we should put veterans at the center, involve the entire team (nurses, pharmacy, etc.) in their care,” a scholar explained. “The Geriatric Scholars Program is a great tool to help roll out [PACT] at my CBOC,” another scholar reported. “I used the mentoring I got from the Geriatric Scholars Program to teach my clinic team.”
Through the GSP, an estimated 309,671 older veterans are now receiving care from clinicians who have developed additional skills in geriatrics. This fall, the GSP will be welcoming a new class of 60 learners, expanding the scope of the program and reaching veterans in more communities.
Acknowledgements
The Geriatric Scholars Program is a collaboration of 10 Geriatric Research Education and Clinical Centers (GRECCs) and the VA Office of Geriatrics and Extended Care (GEC). The contributions of all past and present collaborators are gratefully acknowledged, including Judith Howe, PhD (Bronx GRECC); Carol Callaway-Lane, DNP (Tennessee Valley GRECC); Terri Huh, PhD (Palo Alto GRECC); Steven Barzci, MD (Madison GRECC); Kathy Horvath, PhD, RN, and Scott Trudeau, PhD, PT (New England GRECC); Sandra Sanchez-Reilly, MD (San Antonio GRECC); Connie Bales, PhD, RD (Durham GRECC); Ronni Chernoff, PhD, RD, Kim Garner, MD, and Sheila Cox Sullivan, PhD, RN (Little Rock GRECC); Stephen Thielke, MD (Puget Sound GRECC); Nina Tumosa, PhD (currently at the U.S. Health Resources and Services Administration); and Kenneth Shay, DMD (Office GEC). We gratefully acknowledge and appreciate the staff at the VA Greater Los Angeles Healthcare System GRECC program hub site whose contributions “behind the scene” make this multi-faceted program possible: Luis Melendez, MPA, MS (program administrator); Joseph Douglas (special projects manager); Timothy Gardner, MBA (program analyst); Beth Creekmur, MA (budget analyst); and Diane Lee, MSW (program support staff).
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Redesign of a Screening Process for VA Homeless Housing
Homelessness is associated with disproportionate medical morbidity and mortality and use of nonpreventive health services.1 In fiscal year 2010, veterans experiencing homelessness were 4 times more likely to use VA emergency departments and had a greater 10-year mortality risk than did veterans who were housed.1 Veterans experiencing homelessness were more likely to be diagnosed with substance use disorder, schizophrenia, liver disease, and/or HIV/AIDS than were their housed counterparts.
Ending veteran homelessness is a federal priority, exemplified by the goal of President Obama to end veteran homelessness by 2015.2 Since the goal’s articulation, veteran homelessness has declined nationally by 33% (24,117 veterans) from 2009 to 2014 however, 49,933 veterans were identified as being homeless on a given night in January 2014.3
Related: Landmark Initiative Signed for Homeless Veterans
A crucial element needed to end veteran homelessness is veteran and health care provider knowledge of existing homeless services and mechanisms of access. In 2012, VHA launched a homelessness screening clinical reminder in the Computerized Patient Record System (CPRS), which prompts a discussion of housing status between the veteran and provider.4 The staff of the VA North Texas Health Care System (VANTHCS) Comprehensive Homeless Center Programs (CHCP) realized that homeless housing programs at the facility could be more accessible if staff from each program could screen for all available programs and if a single phone number existed for scheduling appointments. Therefore, VANTHCS transformed its homeless housing screening process to a standardized process through which veterans are screened for all CHCP housing programs during a single screening assessment, Universal Homeless Housing Screening (UHHS).
This article describes the creation of the UHHS, the screening tool, 3-month postimplementation findings, and recommendations based on initial VANTHCS staff experiences with this process. During the redesign of screening process for homeless housing, VANTHCS staff found a paucity of guidance regarding best practices. This article attempts to fill this gap and provide guidance to institutions that are considering standardizing their screening process for homeless housing across multiple programs at different locations.
Background
Established in 1990, VANTHCS CHCP is VA’ s first comprehensive homeless center. The CHCP provides both housing and vocational rehabilitation programs, including 13 housing programs in 6 different cities and long-standing partnerships between CHCP and 3 community agencies whose programs have specific housing for veterans.5 Screenings performed in Dallas, Texas, for CHCP housing programs are completed at 4 separate locations.
Prior to the inception of the UHHS process, access to housing programs was limited by veteran awareness of the programs and transportation to various program locations. To participate in these programs, veterans needed to complete a form for the VA Northeast Program Evaluation Center (NEPEC), which staff at the Healthcare for Homeless Veterans (HCHV) CHCP program could administer. This process created an admission bottleneck, because HCHV staff needed to evaluate veterans even if they were being admitted to non-HCHV programs.
UHHS Creation Process
In 2011, NEPEC launched the electronic Homeless Operations Management and Evaluation System (HOMES) to replace paper-based reporting.6 This tool allowed non-HCHV CHCP staff to complete NEPEC evaluation and allowed CHCP to meet its goal of designing a system where all CHCP housing programs could complete a screening assessment. This goal originated from the desire of then CHCP Director Teresa House-Hatfield to create a more efficient housing screening process and from similar feedback from veterans.
Furthermore, in 2009, then Secretary of Veterans Affairs Eric K. Shinseki described a “no wrong door” philosophy for ending veteran homelessness, which CHCP operationalized by screening veterans for any CHCP housing program regardless of initial point of contact within the CHCP system.2 Subsequently, in 2010, the VA Office of Mental Health Services contracted with Mathematica Policy Research, Inc., to conduct a quality review of VA Mental Health Residential Rehabilitation Treatment Programs. Notable among their recommendations was to create a one-stop screening process for these programs.
Related: Primary Care Medical Services for Homeless Veterans
In 2010, CHCP embarked on a process to transform the facility’s screening procedure to a one-stop assessment with standardized screening questions and create a systematic process to track outcomes across all CHCP housing programs. The new process allowed for a standardized appeal procedure when eligibility for a program was not met. It also improved the ease of communication by having 1 phone number for making appointments or informing about screening times. These changes were enacted without the addition of any new staff positions. Instead, in October 2011, Ms. House-Hatfield tasked Dina Hooshyar of the VANTHCS to champion and spearhead this transformation.
The challenge associated with the UHHS creation process was to balance individual program autonomy with standardized processes. This balance was achieved through weekly calls where Ms. House- Hatfield, Dr. Hooshyar, and CHCP program managers discussed how to design UHHS. The management of the CHCP also actively sought input from CHCP frontline staff. During the preimplementation phase, Dr. Hooshyar gave multiple UHHS trainings to CHCP staff who would become involved in UHHS process, another feedback mechanism.
Program managers retained their programs’ autonomy by picking screeners and the number of employees in that position for their program, screening location and time, and screening type (appointment, walk-in, telephone, and/or combination). Managers and staff also assisted in the creation of the UHHS tool by providing their program’s eligibility criteria and customary psychosocial assessment questions. The UHHS tool not only brought consistency to the screening process, but also removed any perceived biases by asking all veterans the same questions across all UHHS screening locations. Implemented on August 26, 2013, UHHS continues to be used.
UHHS Screening Tool
The UHHS tool is an assessment composed of 4 sections: (1) History; (2) Decision Tree; (3) Specific Program Eligibility Criteria; and (4) Plan. The sections exist as templates in the CPRS.
The History section asks about demographic information, diagnoses, alcohol and illicit drug use history, dependent status, outstanding legal issues, housing status, functional limitations, income and employment status, and potential benefit from and interest in psychosocial rehabilitation and care management. If the veteran would not benefit from and/or is not interested in participating in psychosocial rehabilitation and care management, the screener concludes the assessment, as these factors are eligibility requirements for all CHCP programs. Veterans can appeal their case to the screener’s program manager.
The Decision Tree template consists of 6 core eligibility criteria across programs that can serve to narrow the list of eligible programs: (1) Is the veteran currently homeless; (2) Has the veteran been homeless continuously for ≥ 1 year, or has the veteran had ≥ 4 separate occasions of homelessness in the past 3 years; (3) Does the veteran have a mental health or substance use diagnosis; (4) Can the veteran pay a program fee (9 of 16 UHHS-associated programs have no fees); (5) Is the veteran capable of self-administering medications; and (6) Can the veteran perform activities of daily living and does not need acute hospitalization?
Related: Using H-PACT to Overcome Treatment Obstacles for Homeless Veterans (audio)
Veterans are then asked in which town(s) they want to reside. The questions for the Specific Program Eligibility Criteria section are asked only for those programs for which the veteran is found to be tentatively eligible by the Decision Tree and has interest in participating.
The Plan section gives veterans the opportunity to appeal a UHHS finding to the specific program’s manager whose program they are not eligible to participate. Veterans also rank their preference for the programs for which they are interested and eligible. A shared folder contains all program census information. Through the screening tool, veterans devise a plan to contact the potential admitting program. Veterans are informed about the importance of keeping in contact with these programs, because programs will not hold openings for an indefinite time.
Completion of this screening assessment, which includes HOMES and the UHHS tool, generally takes 1.5 hours. After a veteran undergoes this assessment, a preadmission appointment is made with the first open program for which they are eligible and interested in participating. The main goal of this appointment varies by program, such as finalizing referral processes with associated community partners, performing a preliminary medical clearance, determining whether veterans have already used their program’s maximum allotted time, coordinating a Therapeutic Supported Employment Services assessment, or obtaining the required documents from veterans. If at the preadmission appointment, either the veteran declines participation or the program declines admittance, the veteran can follow up with other programs for which they met eligibility criteria and were interested in participating during the initial UHHS assessment instead of undergoing another housing screening.
Notification of Screening Results
The CHCP staff member who performs the screening is responsible for documenting the veteran’s name, phone number or means of contact, current residence, and housing outcome in a secure shared Microsoft Excel document called Housing Outcome. The Excel IF and VLOOKUP function link the original document to each program’s acceptance and petition documents. This linkage auto populates information entered in the Housing Outcome document to each program’s acceptance and petition documents if the veteran has a housing outcome associated with the program. CHCP staff members then look at their individual program’s acceptance and/or petition documents to see the list of veterans who have a housing outcome involving their program instead of having to sort through the Housing Outcome document. As a backup to the Housing Outcome document, screeners add the point of contact for the programs that the veteran had an associated housing outcome as additional signers to their CPRS screening note.
When UHHS was first implemented, the screeners had a daily call to discuss the screened veterans’ housing outcomes and screener experiences with the new system. Dr. Hooshyar also participated in this call as a means to answer screener questions and to get feedback. Within a month of UHHS implementation, these calls were cancelled, because the screeners felt comfortable with the UHHS process and the majority of housing programs were operating at full capacity.
UHHS Appointment Line
The UHHS appointment phone number uses an automatic call distributor, a call-center technology. Thus, 1 phone number can be answered by multiple people working in separate locations. The challenge was how to connect phones associated with offices located offsite from the VANTHCS campus. The solution was to use Internet phones in addition to existing staff phones.
Results
During the review period from August 26, 2013, to November 27, 2013 (65 workdays), 392 unique veterans attended a UHHS assessment. Four veterans who were screened twice were included only once in the analysis; outcomes from only their initial screenings were evaluated. Three hundred fifty-six veterans completed a UHHS assessment; 36 had an assessment but did not complete it. Rates of veterans not presenting for their scheduled appointments increased over time, from 24% in August 2013 to 50% in November 2013. To address the no-show rate, program managers decreased the number of offered scheduled appointments and increased the number of walk-in visits. Overall, the schedule distribution consisted of about twice as much time allotted for walk-in appointments compared with scheduled appointments. The UHHS appointment line received 873 calls, where the number decreased over time.
The typical screened veteran who completed a UHHS assessment was a non-Hispanic, African American male aged 51 years with no service connection or history of combat who served either in the Vietnam War era, post-Vietnam War era, or Persian Gulf War. He had accessed VANTHCS care in the year prior to screening; owned a working phone; and was staying in a shelter, a place not meant for human habitation, or a substance use treatment program the night prior to screening (Table 1). Only 20 veterans (5%) were ineligible for participation in all programs, because they did not meet core eligibility criteria as defined by the UHHS Decision Tree, their income surpassed the program limit, or they were not eligible for VA care (Table 2).
To determine the housing outcome of the veterans screened during the reviewed period, a 3-month follow-up from the end of the review period was used. During this time, 269 veterans (76%) who completed the UHHS process were housed, with 215 (60%) veterans housed in a UHHS-associated housing program (Table 3). Of the veterans who completed a UHHS assessment, 45 veterans (13%) did not complete the screening process; admitting program staff documented in CPRS unsuccessful attempts at reaching 12 veterans (3%), among whom 4 had no working phone at the time of their UHHS assessment. Time to admission depended on the program mission, openings, and the veteran’s UHHS engagement. Admission date indicates the date that programs housed veterans except in the case of the U.S. Department of Housing and Urban Development-VA Supportive Housing (HUD-VASH), where admission date indicates the date the veteran gave all required documents to HUD-VASH staff.
Discussion
Prior to the inception of UHHS, the staff of the CHCP housing program did not have a standardized process for communication across programs about veterans’ housing status and outcomes. Veterans went to multiple locations for screening if they were interested in > 1 program or if they were not admitted to the first program they approached. The UHHS process improved communication across CHCP housing programs, resulting in increased veteran accessibility to these programs as suggested by 3 CHCP housing programs having fewer days with openings post-UHHS implementation. Furthermore, a new screener position did not need to be created, because existing CHCP social workers were all capable screeners due to process standardization.
Fifty-five percent of the screened veterans were interested in and eligible for participation in > 1 housing program. They were eligible for 3 programs on average and were usually admitted to the housing program with the earliest opening. The need for screenings across all the CHCP housing programs was potentially decreased by ≥ one-third. This increased available time for the screeners to accomplish their other clinical responsibilities.
Limitations
A limitation of the review period evaluation is little information on noncompleters. The available data are confined to information documented in CPRS regarding why 45 veterans (13% of those who completed UHHS assessment) did not complete the screening process. For 12, admitting staff of the housing program documented in CPRS that they had been unable to reach the veteran; 9 of these veterans attended subsequent non-UHHS VANTHCS visits. To further improve the homeless housing delivery service, the creation of a CPRS-related process that informs VA clinicians that a housing program is attempting to contact a veteran is needed.
Challenges and Recommendations
Because the Housing Outcome document is a shared document, only 1 person at a time can save information in it. Facility staff have been unable to create a simple macro that closes the document automatically. Instead, screeners who need to save information when a document is already opened elsewhere must use a group e-mail list to alert others to close the document.
Streamlining the communication channel between the screeners and management evolved from the daily call, to e-mailing and program managers discussing topics with their staff, to Dr. Hooshyar facilitating a weekly call for screeners and program managers.
Optimizing the ratio of walk-in to scheduled appointments took time. Prior to the UHHS process, some CHCP housing programs offered scheduled appointments, whereas others had walk-in appointments. The decision to offer in-person scheduled appointments for veterans who preferred scheduled appointments or who commuted from a distance was made. Universal Homeless Housing Screening staff also offered scheduled telephone appointments for veterans who lacked transportation.
At times, admitting program staff was unable to reach veterans eligible for and interested in their program, despite screeners recommending to veterans that they should provide these programs with any changes in their contact information.
Recommendations for designing a screening process for homeless housing include:
- Have periodic retreats instead of weekly conference calls to quicken the pre-implementation process.
- Start with a pilot that includes some potential screeners to test the implementation process. The screeners involved in the pilot would train future screeners to expand the screener pool.
- Invest time in electronic tracking tools despite upfront and maintenance time requirements.
- Offer more walk-in than scheduled screening appointments.
- Embrace the idea that the pro-cess is always under development.
Conclusion
To ameliorate anxiety associated with changing the system, UHHS- associated staff redesigned the housing screening process through openness to stakeholder feedback and building on consensus. The staff also nurtured a culture that could change newly revised processes, depending on quality assurance findings. Without this method, the unknown likely would have propagated continued status quo. Universal Homeless Housing Screening processes improved veteran access to CHCP housing programs through instituting a one-stop housing screening assessment that also reduced the potential number of screenings by ≥ one-third.
Acknowledgments
The authors greatly appreciate the input of the many people involved in the creation of the UHHS process, in particular Daniel Anderson, Heather Arredondo, Tara Ayala, TiieShaiyon Banton, Melody Boyet, Amelia Bradley, Timothy Brown, Carnisha Campbell, Donald Capps, Burnell Carden Jr, Pushpi Chaudhary, Howard Cunningham, Rachael David, Marianna Demko, Derrick Evans, Steven Fisher, Kimberly Fite, Fatina Ford, Christi Godfrey, Gerald Goodwin, Melvin Haley, Tony Hall, Jessica Hennessey, Teresa House-Hatfield, Don Hubbard, Kathryn Jacob, Tonja King, Cecelia Knight, Janine Lenger-Gvist, Vickie Linden, Julia Long, Kristin Manley, Peggy Martin, Treva McDaniel, William McNair, Tammy Miller, Jeffery Milligan, Anhloan Nguyen, Tywanna Nichols, Cheryl Paul, Catherine Orsak, Dustin Perkins, Claudette Phillips, Joan Prescott, John Purkey, Martin Roback, Catriska Robertson, Charles Ross, Shanna Ruppert, Stephanie Saldivar, Linda Saucedo, Inga Sinclair-Henderson, John Smith, Zaire Smith, Cheryl Stringer, Valetta Ward, Carolyn Washington, Tammra Wood, and Skylar Woods-Nunley. They would also like to thank the veterans for their service and feedback.
Author disclosures
Dr. North discloses research support from National Institute on Alcohol Abuse and Alcoholism, National Institute of Diabetes and Digestive and Kidney Diseases, and VA and consultant fees from the University of Missouri-Columbia. Dr. Surís is Local Site Investigator for VA CSP #589 VIPSTAR-Veterans Individual Placement and Support Towards Advancing Recovery (PI Lori Davis, MD). She is co- investigator for VISN 17 grant Association of Myocardial Viability to Symptom Improvement post-CTO PCI (PI-Shuaib Abdullah, MD) and co-investigator for National Institutes on Drug Abuse grant Lidocaine Infusion as a Treatment for Cocaine Relapse and Craving (PI-Bryon Adinoff, MD). In addition, Dr. Surís is co-site-PI for the upcoming VA CSP #590 Lithium for Suicidal Behavior in Mood Disorders.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Tsai J, Doran KM, Rosenheck RA. When health insurance is not a factor: National comparison of homeless and nonhomeless US veterans who use Veterans Affairs emergency departments. Am J Public Health. 2013;103(suppl 2):S225-S231.
2. Secretary Shinseki Details Plan to End Homelessness for Veterans [news release]. U.S. Department of Veterans Affairs: Office of Public and Intergovernmental Affairs. http://www.va.gov/opa/pressrel/pressrelease.cfm?id=1807. Published November 3, 2009. Accessed March 3, 2014.
3. U.S. Department of Housing and Urban Development: Office of Community Planning and Development. The 2014 Annual Homeless Assessment Report (AHAR) to Congress. Part 1 Point-In-Time Estimates of Homelessness. https://www.hudexchange.info/resources/documents /2014-AHAR-Part1.pdf. Published October 2014. Accessed March 18, 2015.
4. Montgomery AE, Fargo JD, Byrne TH, Kane VR, Culhane DP. Universal screening for homelessness and risk for homelessness in the Veterans Health Administration. Am J Public Health. 2013;103(suppl 2):S210-S211.
5. Berman S, Barilich JE, Rosenheck R, Koerber G. The VA’s first comprehensive homeless center: A catalyst for public and private partnerships. Hosp Community Psychiatry. 1993;44(12):1183-1184.
6. U.S. Department of Veterans Affairs. Homeless Operations Management and Evaluation System (HOMES) User Manual–Phase 1. http://www.vfwsc.org/homes.pdf. Published April 19, 2011. Accessed March 3, 2014.
Homelessness is associated with disproportionate medical morbidity and mortality and use of nonpreventive health services.1 In fiscal year 2010, veterans experiencing homelessness were 4 times more likely to use VA emergency departments and had a greater 10-year mortality risk than did veterans who were housed.1 Veterans experiencing homelessness were more likely to be diagnosed with substance use disorder, schizophrenia, liver disease, and/or HIV/AIDS than were their housed counterparts.
Ending veteran homelessness is a federal priority, exemplified by the goal of President Obama to end veteran homelessness by 2015.2 Since the goal’s articulation, veteran homelessness has declined nationally by 33% (24,117 veterans) from 2009 to 2014 however, 49,933 veterans were identified as being homeless on a given night in January 2014.3
Related: Landmark Initiative Signed for Homeless Veterans
A crucial element needed to end veteran homelessness is veteran and health care provider knowledge of existing homeless services and mechanisms of access. In 2012, VHA launched a homelessness screening clinical reminder in the Computerized Patient Record System (CPRS), which prompts a discussion of housing status between the veteran and provider.4 The staff of the VA North Texas Health Care System (VANTHCS) Comprehensive Homeless Center Programs (CHCP) realized that homeless housing programs at the facility could be more accessible if staff from each program could screen for all available programs and if a single phone number existed for scheduling appointments. Therefore, VANTHCS transformed its homeless housing screening process to a standardized process through which veterans are screened for all CHCP housing programs during a single screening assessment, Universal Homeless Housing Screening (UHHS).
This article describes the creation of the UHHS, the screening tool, 3-month postimplementation findings, and recommendations based on initial VANTHCS staff experiences with this process. During the redesign of screening process for homeless housing, VANTHCS staff found a paucity of guidance regarding best practices. This article attempts to fill this gap and provide guidance to institutions that are considering standardizing their screening process for homeless housing across multiple programs at different locations.
Background
Established in 1990, VANTHCS CHCP is VA’ s first comprehensive homeless center. The CHCP provides both housing and vocational rehabilitation programs, including 13 housing programs in 6 different cities and long-standing partnerships between CHCP and 3 community agencies whose programs have specific housing for veterans.5 Screenings performed in Dallas, Texas, for CHCP housing programs are completed at 4 separate locations.
Prior to the inception of the UHHS process, access to housing programs was limited by veteran awareness of the programs and transportation to various program locations. To participate in these programs, veterans needed to complete a form for the VA Northeast Program Evaluation Center (NEPEC), which staff at the Healthcare for Homeless Veterans (HCHV) CHCP program could administer. This process created an admission bottleneck, because HCHV staff needed to evaluate veterans even if they were being admitted to non-HCHV programs.
UHHS Creation Process
In 2011, NEPEC launched the electronic Homeless Operations Management and Evaluation System (HOMES) to replace paper-based reporting.6 This tool allowed non-HCHV CHCP staff to complete NEPEC evaluation and allowed CHCP to meet its goal of designing a system where all CHCP housing programs could complete a screening assessment. This goal originated from the desire of then CHCP Director Teresa House-Hatfield to create a more efficient housing screening process and from similar feedback from veterans.
Furthermore, in 2009, then Secretary of Veterans Affairs Eric K. Shinseki described a “no wrong door” philosophy for ending veteran homelessness, which CHCP operationalized by screening veterans for any CHCP housing program regardless of initial point of contact within the CHCP system.2 Subsequently, in 2010, the VA Office of Mental Health Services contracted with Mathematica Policy Research, Inc., to conduct a quality review of VA Mental Health Residential Rehabilitation Treatment Programs. Notable among their recommendations was to create a one-stop screening process for these programs.
Related: Primary Care Medical Services for Homeless Veterans
In 2010, CHCP embarked on a process to transform the facility’s screening procedure to a one-stop assessment with standardized screening questions and create a systematic process to track outcomes across all CHCP housing programs. The new process allowed for a standardized appeal procedure when eligibility for a program was not met. It also improved the ease of communication by having 1 phone number for making appointments or informing about screening times. These changes were enacted without the addition of any new staff positions. Instead, in October 2011, Ms. House-Hatfield tasked Dina Hooshyar of the VANTHCS to champion and spearhead this transformation.
The challenge associated with the UHHS creation process was to balance individual program autonomy with standardized processes. This balance was achieved through weekly calls where Ms. House- Hatfield, Dr. Hooshyar, and CHCP program managers discussed how to design UHHS. The management of the CHCP also actively sought input from CHCP frontline staff. During the preimplementation phase, Dr. Hooshyar gave multiple UHHS trainings to CHCP staff who would become involved in UHHS process, another feedback mechanism.
Program managers retained their programs’ autonomy by picking screeners and the number of employees in that position for their program, screening location and time, and screening type (appointment, walk-in, telephone, and/or combination). Managers and staff also assisted in the creation of the UHHS tool by providing their program’s eligibility criteria and customary psychosocial assessment questions. The UHHS tool not only brought consistency to the screening process, but also removed any perceived biases by asking all veterans the same questions across all UHHS screening locations. Implemented on August 26, 2013, UHHS continues to be used.
UHHS Screening Tool
The UHHS tool is an assessment composed of 4 sections: (1) History; (2) Decision Tree; (3) Specific Program Eligibility Criteria; and (4) Plan. The sections exist as templates in the CPRS.
The History section asks about demographic information, diagnoses, alcohol and illicit drug use history, dependent status, outstanding legal issues, housing status, functional limitations, income and employment status, and potential benefit from and interest in psychosocial rehabilitation and care management. If the veteran would not benefit from and/or is not interested in participating in psychosocial rehabilitation and care management, the screener concludes the assessment, as these factors are eligibility requirements for all CHCP programs. Veterans can appeal their case to the screener’s program manager.
The Decision Tree template consists of 6 core eligibility criteria across programs that can serve to narrow the list of eligible programs: (1) Is the veteran currently homeless; (2) Has the veteran been homeless continuously for ≥ 1 year, or has the veteran had ≥ 4 separate occasions of homelessness in the past 3 years; (3) Does the veteran have a mental health or substance use diagnosis; (4) Can the veteran pay a program fee (9 of 16 UHHS-associated programs have no fees); (5) Is the veteran capable of self-administering medications; and (6) Can the veteran perform activities of daily living and does not need acute hospitalization?
Related: Using H-PACT to Overcome Treatment Obstacles for Homeless Veterans (audio)
Veterans are then asked in which town(s) they want to reside. The questions for the Specific Program Eligibility Criteria section are asked only for those programs for which the veteran is found to be tentatively eligible by the Decision Tree and has interest in participating.
The Plan section gives veterans the opportunity to appeal a UHHS finding to the specific program’s manager whose program they are not eligible to participate. Veterans also rank their preference for the programs for which they are interested and eligible. A shared folder contains all program census information. Through the screening tool, veterans devise a plan to contact the potential admitting program. Veterans are informed about the importance of keeping in contact with these programs, because programs will not hold openings for an indefinite time.
Completion of this screening assessment, which includes HOMES and the UHHS tool, generally takes 1.5 hours. After a veteran undergoes this assessment, a preadmission appointment is made with the first open program for which they are eligible and interested in participating. The main goal of this appointment varies by program, such as finalizing referral processes with associated community partners, performing a preliminary medical clearance, determining whether veterans have already used their program’s maximum allotted time, coordinating a Therapeutic Supported Employment Services assessment, or obtaining the required documents from veterans. If at the preadmission appointment, either the veteran declines participation or the program declines admittance, the veteran can follow up with other programs for which they met eligibility criteria and were interested in participating during the initial UHHS assessment instead of undergoing another housing screening.
Notification of Screening Results
The CHCP staff member who performs the screening is responsible for documenting the veteran’s name, phone number or means of contact, current residence, and housing outcome in a secure shared Microsoft Excel document called Housing Outcome. The Excel IF and VLOOKUP function link the original document to each program’s acceptance and petition documents. This linkage auto populates information entered in the Housing Outcome document to each program’s acceptance and petition documents if the veteran has a housing outcome associated with the program. CHCP staff members then look at their individual program’s acceptance and/or petition documents to see the list of veterans who have a housing outcome involving their program instead of having to sort through the Housing Outcome document. As a backup to the Housing Outcome document, screeners add the point of contact for the programs that the veteran had an associated housing outcome as additional signers to their CPRS screening note.
When UHHS was first implemented, the screeners had a daily call to discuss the screened veterans’ housing outcomes and screener experiences with the new system. Dr. Hooshyar also participated in this call as a means to answer screener questions and to get feedback. Within a month of UHHS implementation, these calls were cancelled, because the screeners felt comfortable with the UHHS process and the majority of housing programs were operating at full capacity.
UHHS Appointment Line
The UHHS appointment phone number uses an automatic call distributor, a call-center technology. Thus, 1 phone number can be answered by multiple people working in separate locations. The challenge was how to connect phones associated with offices located offsite from the VANTHCS campus. The solution was to use Internet phones in addition to existing staff phones.
Results
During the review period from August 26, 2013, to November 27, 2013 (65 workdays), 392 unique veterans attended a UHHS assessment. Four veterans who were screened twice were included only once in the analysis; outcomes from only their initial screenings were evaluated. Three hundred fifty-six veterans completed a UHHS assessment; 36 had an assessment but did not complete it. Rates of veterans not presenting for their scheduled appointments increased over time, from 24% in August 2013 to 50% in November 2013. To address the no-show rate, program managers decreased the number of offered scheduled appointments and increased the number of walk-in visits. Overall, the schedule distribution consisted of about twice as much time allotted for walk-in appointments compared with scheduled appointments. The UHHS appointment line received 873 calls, where the number decreased over time.
The typical screened veteran who completed a UHHS assessment was a non-Hispanic, African American male aged 51 years with no service connection or history of combat who served either in the Vietnam War era, post-Vietnam War era, or Persian Gulf War. He had accessed VANTHCS care in the year prior to screening; owned a working phone; and was staying in a shelter, a place not meant for human habitation, or a substance use treatment program the night prior to screening (Table 1). Only 20 veterans (5%) were ineligible for participation in all programs, because they did not meet core eligibility criteria as defined by the UHHS Decision Tree, their income surpassed the program limit, or they were not eligible for VA care (Table 2).
To determine the housing outcome of the veterans screened during the reviewed period, a 3-month follow-up from the end of the review period was used. During this time, 269 veterans (76%) who completed the UHHS process were housed, with 215 (60%) veterans housed in a UHHS-associated housing program (Table 3). Of the veterans who completed a UHHS assessment, 45 veterans (13%) did not complete the screening process; admitting program staff documented in CPRS unsuccessful attempts at reaching 12 veterans (3%), among whom 4 had no working phone at the time of their UHHS assessment. Time to admission depended on the program mission, openings, and the veteran’s UHHS engagement. Admission date indicates the date that programs housed veterans except in the case of the U.S. Department of Housing and Urban Development-VA Supportive Housing (HUD-VASH), where admission date indicates the date the veteran gave all required documents to HUD-VASH staff.
Discussion
Prior to the inception of UHHS, the staff of the CHCP housing program did not have a standardized process for communication across programs about veterans’ housing status and outcomes. Veterans went to multiple locations for screening if they were interested in > 1 program or if they were not admitted to the first program they approached. The UHHS process improved communication across CHCP housing programs, resulting in increased veteran accessibility to these programs as suggested by 3 CHCP housing programs having fewer days with openings post-UHHS implementation. Furthermore, a new screener position did not need to be created, because existing CHCP social workers were all capable screeners due to process standardization.
Fifty-five percent of the screened veterans were interested in and eligible for participation in > 1 housing program. They were eligible for 3 programs on average and were usually admitted to the housing program with the earliest opening. The need for screenings across all the CHCP housing programs was potentially decreased by ≥ one-third. This increased available time for the screeners to accomplish their other clinical responsibilities.
Limitations
A limitation of the review period evaluation is little information on noncompleters. The available data are confined to information documented in CPRS regarding why 45 veterans (13% of those who completed UHHS assessment) did not complete the screening process. For 12, admitting staff of the housing program documented in CPRS that they had been unable to reach the veteran; 9 of these veterans attended subsequent non-UHHS VANTHCS visits. To further improve the homeless housing delivery service, the creation of a CPRS-related process that informs VA clinicians that a housing program is attempting to contact a veteran is needed.
Challenges and Recommendations
Because the Housing Outcome document is a shared document, only 1 person at a time can save information in it. Facility staff have been unable to create a simple macro that closes the document automatically. Instead, screeners who need to save information when a document is already opened elsewhere must use a group e-mail list to alert others to close the document.
Streamlining the communication channel between the screeners and management evolved from the daily call, to e-mailing and program managers discussing topics with their staff, to Dr. Hooshyar facilitating a weekly call for screeners and program managers.
Optimizing the ratio of walk-in to scheduled appointments took time. Prior to the UHHS process, some CHCP housing programs offered scheduled appointments, whereas others had walk-in appointments. The decision to offer in-person scheduled appointments for veterans who preferred scheduled appointments or who commuted from a distance was made. Universal Homeless Housing Screening staff also offered scheduled telephone appointments for veterans who lacked transportation.
At times, admitting program staff was unable to reach veterans eligible for and interested in their program, despite screeners recommending to veterans that they should provide these programs with any changes in their contact information.
Recommendations for designing a screening process for homeless housing include:
- Have periodic retreats instead of weekly conference calls to quicken the pre-implementation process.
- Start with a pilot that includes some potential screeners to test the implementation process. The screeners involved in the pilot would train future screeners to expand the screener pool.
- Invest time in electronic tracking tools despite upfront and maintenance time requirements.
- Offer more walk-in than scheduled screening appointments.
- Embrace the idea that the pro-cess is always under development.
Conclusion
To ameliorate anxiety associated with changing the system, UHHS- associated staff redesigned the housing screening process through openness to stakeholder feedback and building on consensus. The staff also nurtured a culture that could change newly revised processes, depending on quality assurance findings. Without this method, the unknown likely would have propagated continued status quo. Universal Homeless Housing Screening processes improved veteran access to CHCP housing programs through instituting a one-stop housing screening assessment that also reduced the potential number of screenings by ≥ one-third.
Acknowledgments
The authors greatly appreciate the input of the many people involved in the creation of the UHHS process, in particular Daniel Anderson, Heather Arredondo, Tara Ayala, TiieShaiyon Banton, Melody Boyet, Amelia Bradley, Timothy Brown, Carnisha Campbell, Donald Capps, Burnell Carden Jr, Pushpi Chaudhary, Howard Cunningham, Rachael David, Marianna Demko, Derrick Evans, Steven Fisher, Kimberly Fite, Fatina Ford, Christi Godfrey, Gerald Goodwin, Melvin Haley, Tony Hall, Jessica Hennessey, Teresa House-Hatfield, Don Hubbard, Kathryn Jacob, Tonja King, Cecelia Knight, Janine Lenger-Gvist, Vickie Linden, Julia Long, Kristin Manley, Peggy Martin, Treva McDaniel, William McNair, Tammy Miller, Jeffery Milligan, Anhloan Nguyen, Tywanna Nichols, Cheryl Paul, Catherine Orsak, Dustin Perkins, Claudette Phillips, Joan Prescott, John Purkey, Martin Roback, Catriska Robertson, Charles Ross, Shanna Ruppert, Stephanie Saldivar, Linda Saucedo, Inga Sinclair-Henderson, John Smith, Zaire Smith, Cheryl Stringer, Valetta Ward, Carolyn Washington, Tammra Wood, and Skylar Woods-Nunley. They would also like to thank the veterans for their service and feedback.
Author disclosures
Dr. North discloses research support from National Institute on Alcohol Abuse and Alcoholism, National Institute of Diabetes and Digestive and Kidney Diseases, and VA and consultant fees from the University of Missouri-Columbia. Dr. Surís is Local Site Investigator for VA CSP #589 VIPSTAR-Veterans Individual Placement and Support Towards Advancing Recovery (PI Lori Davis, MD). She is co- investigator for VISN 17 grant Association of Myocardial Viability to Symptom Improvement post-CTO PCI (PI-Shuaib Abdullah, MD) and co-investigator for National Institutes on Drug Abuse grant Lidocaine Infusion as a Treatment for Cocaine Relapse and Craving (PI-Bryon Adinoff, MD). In addition, Dr. Surís is co-site-PI for the upcoming VA CSP #590 Lithium for Suicidal Behavior in Mood Disorders.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Homelessness is associated with disproportionate medical morbidity and mortality and use of nonpreventive health services.1 In fiscal year 2010, veterans experiencing homelessness were 4 times more likely to use VA emergency departments and had a greater 10-year mortality risk than did veterans who were housed.1 Veterans experiencing homelessness were more likely to be diagnosed with substance use disorder, schizophrenia, liver disease, and/or HIV/AIDS than were their housed counterparts.
Ending veteran homelessness is a federal priority, exemplified by the goal of President Obama to end veteran homelessness by 2015.2 Since the goal’s articulation, veteran homelessness has declined nationally by 33% (24,117 veterans) from 2009 to 2014 however, 49,933 veterans were identified as being homeless on a given night in January 2014.3
Related: Landmark Initiative Signed for Homeless Veterans
A crucial element needed to end veteran homelessness is veteran and health care provider knowledge of existing homeless services and mechanisms of access. In 2012, VHA launched a homelessness screening clinical reminder in the Computerized Patient Record System (CPRS), which prompts a discussion of housing status between the veteran and provider.4 The staff of the VA North Texas Health Care System (VANTHCS) Comprehensive Homeless Center Programs (CHCP) realized that homeless housing programs at the facility could be more accessible if staff from each program could screen for all available programs and if a single phone number existed for scheduling appointments. Therefore, VANTHCS transformed its homeless housing screening process to a standardized process through which veterans are screened for all CHCP housing programs during a single screening assessment, Universal Homeless Housing Screening (UHHS).
This article describes the creation of the UHHS, the screening tool, 3-month postimplementation findings, and recommendations based on initial VANTHCS staff experiences with this process. During the redesign of screening process for homeless housing, VANTHCS staff found a paucity of guidance regarding best practices. This article attempts to fill this gap and provide guidance to institutions that are considering standardizing their screening process for homeless housing across multiple programs at different locations.
Background
Established in 1990, VANTHCS CHCP is VA’ s first comprehensive homeless center. The CHCP provides both housing and vocational rehabilitation programs, including 13 housing programs in 6 different cities and long-standing partnerships between CHCP and 3 community agencies whose programs have specific housing for veterans.5 Screenings performed in Dallas, Texas, for CHCP housing programs are completed at 4 separate locations.
Prior to the inception of the UHHS process, access to housing programs was limited by veteran awareness of the programs and transportation to various program locations. To participate in these programs, veterans needed to complete a form for the VA Northeast Program Evaluation Center (NEPEC), which staff at the Healthcare for Homeless Veterans (HCHV) CHCP program could administer. This process created an admission bottleneck, because HCHV staff needed to evaluate veterans even if they were being admitted to non-HCHV programs.
UHHS Creation Process
In 2011, NEPEC launched the electronic Homeless Operations Management and Evaluation System (HOMES) to replace paper-based reporting.6 This tool allowed non-HCHV CHCP staff to complete NEPEC evaluation and allowed CHCP to meet its goal of designing a system where all CHCP housing programs could complete a screening assessment. This goal originated from the desire of then CHCP Director Teresa House-Hatfield to create a more efficient housing screening process and from similar feedback from veterans.
Furthermore, in 2009, then Secretary of Veterans Affairs Eric K. Shinseki described a “no wrong door” philosophy for ending veteran homelessness, which CHCP operationalized by screening veterans for any CHCP housing program regardless of initial point of contact within the CHCP system.2 Subsequently, in 2010, the VA Office of Mental Health Services contracted with Mathematica Policy Research, Inc., to conduct a quality review of VA Mental Health Residential Rehabilitation Treatment Programs. Notable among their recommendations was to create a one-stop screening process for these programs.
Related: Primary Care Medical Services for Homeless Veterans
In 2010, CHCP embarked on a process to transform the facility’s screening procedure to a one-stop assessment with standardized screening questions and create a systematic process to track outcomes across all CHCP housing programs. The new process allowed for a standardized appeal procedure when eligibility for a program was not met. It also improved the ease of communication by having 1 phone number for making appointments or informing about screening times. These changes were enacted without the addition of any new staff positions. Instead, in October 2011, Ms. House-Hatfield tasked Dina Hooshyar of the VANTHCS to champion and spearhead this transformation.
The challenge associated with the UHHS creation process was to balance individual program autonomy with standardized processes. This balance was achieved through weekly calls where Ms. House- Hatfield, Dr. Hooshyar, and CHCP program managers discussed how to design UHHS. The management of the CHCP also actively sought input from CHCP frontline staff. During the preimplementation phase, Dr. Hooshyar gave multiple UHHS trainings to CHCP staff who would become involved in UHHS process, another feedback mechanism.
Program managers retained their programs’ autonomy by picking screeners and the number of employees in that position for their program, screening location and time, and screening type (appointment, walk-in, telephone, and/or combination). Managers and staff also assisted in the creation of the UHHS tool by providing their program’s eligibility criteria and customary psychosocial assessment questions. The UHHS tool not only brought consistency to the screening process, but also removed any perceived biases by asking all veterans the same questions across all UHHS screening locations. Implemented on August 26, 2013, UHHS continues to be used.
UHHS Screening Tool
The UHHS tool is an assessment composed of 4 sections: (1) History; (2) Decision Tree; (3) Specific Program Eligibility Criteria; and (4) Plan. The sections exist as templates in the CPRS.
The History section asks about demographic information, diagnoses, alcohol and illicit drug use history, dependent status, outstanding legal issues, housing status, functional limitations, income and employment status, and potential benefit from and interest in psychosocial rehabilitation and care management. If the veteran would not benefit from and/or is not interested in participating in psychosocial rehabilitation and care management, the screener concludes the assessment, as these factors are eligibility requirements for all CHCP programs. Veterans can appeal their case to the screener’s program manager.
The Decision Tree template consists of 6 core eligibility criteria across programs that can serve to narrow the list of eligible programs: (1) Is the veteran currently homeless; (2) Has the veteran been homeless continuously for ≥ 1 year, or has the veteran had ≥ 4 separate occasions of homelessness in the past 3 years; (3) Does the veteran have a mental health or substance use diagnosis; (4) Can the veteran pay a program fee (9 of 16 UHHS-associated programs have no fees); (5) Is the veteran capable of self-administering medications; and (6) Can the veteran perform activities of daily living and does not need acute hospitalization?
Related: Using H-PACT to Overcome Treatment Obstacles for Homeless Veterans (audio)
Veterans are then asked in which town(s) they want to reside. The questions for the Specific Program Eligibility Criteria section are asked only for those programs for which the veteran is found to be tentatively eligible by the Decision Tree and has interest in participating.
The Plan section gives veterans the opportunity to appeal a UHHS finding to the specific program’s manager whose program they are not eligible to participate. Veterans also rank their preference for the programs for which they are interested and eligible. A shared folder contains all program census information. Through the screening tool, veterans devise a plan to contact the potential admitting program. Veterans are informed about the importance of keeping in contact with these programs, because programs will not hold openings for an indefinite time.
Completion of this screening assessment, which includes HOMES and the UHHS tool, generally takes 1.5 hours. After a veteran undergoes this assessment, a preadmission appointment is made with the first open program for which they are eligible and interested in participating. The main goal of this appointment varies by program, such as finalizing referral processes with associated community partners, performing a preliminary medical clearance, determining whether veterans have already used their program’s maximum allotted time, coordinating a Therapeutic Supported Employment Services assessment, or obtaining the required documents from veterans. If at the preadmission appointment, either the veteran declines participation or the program declines admittance, the veteran can follow up with other programs for which they met eligibility criteria and were interested in participating during the initial UHHS assessment instead of undergoing another housing screening.
Notification of Screening Results
The CHCP staff member who performs the screening is responsible for documenting the veteran’s name, phone number or means of contact, current residence, and housing outcome in a secure shared Microsoft Excel document called Housing Outcome. The Excel IF and VLOOKUP function link the original document to each program’s acceptance and petition documents. This linkage auto populates information entered in the Housing Outcome document to each program’s acceptance and petition documents if the veteran has a housing outcome associated with the program. CHCP staff members then look at their individual program’s acceptance and/or petition documents to see the list of veterans who have a housing outcome involving their program instead of having to sort through the Housing Outcome document. As a backup to the Housing Outcome document, screeners add the point of contact for the programs that the veteran had an associated housing outcome as additional signers to their CPRS screening note.
When UHHS was first implemented, the screeners had a daily call to discuss the screened veterans’ housing outcomes and screener experiences with the new system. Dr. Hooshyar also participated in this call as a means to answer screener questions and to get feedback. Within a month of UHHS implementation, these calls were cancelled, because the screeners felt comfortable with the UHHS process and the majority of housing programs were operating at full capacity.
UHHS Appointment Line
The UHHS appointment phone number uses an automatic call distributor, a call-center technology. Thus, 1 phone number can be answered by multiple people working in separate locations. The challenge was how to connect phones associated with offices located offsite from the VANTHCS campus. The solution was to use Internet phones in addition to existing staff phones.
Results
During the review period from August 26, 2013, to November 27, 2013 (65 workdays), 392 unique veterans attended a UHHS assessment. Four veterans who were screened twice were included only once in the analysis; outcomes from only their initial screenings were evaluated. Three hundred fifty-six veterans completed a UHHS assessment; 36 had an assessment but did not complete it. Rates of veterans not presenting for their scheduled appointments increased over time, from 24% in August 2013 to 50% in November 2013. To address the no-show rate, program managers decreased the number of offered scheduled appointments and increased the number of walk-in visits. Overall, the schedule distribution consisted of about twice as much time allotted for walk-in appointments compared with scheduled appointments. The UHHS appointment line received 873 calls, where the number decreased over time.
The typical screened veteran who completed a UHHS assessment was a non-Hispanic, African American male aged 51 years with no service connection or history of combat who served either in the Vietnam War era, post-Vietnam War era, or Persian Gulf War. He had accessed VANTHCS care in the year prior to screening; owned a working phone; and was staying in a shelter, a place not meant for human habitation, or a substance use treatment program the night prior to screening (Table 1). Only 20 veterans (5%) were ineligible for participation in all programs, because they did not meet core eligibility criteria as defined by the UHHS Decision Tree, their income surpassed the program limit, or they were not eligible for VA care (Table 2).
To determine the housing outcome of the veterans screened during the reviewed period, a 3-month follow-up from the end of the review period was used. During this time, 269 veterans (76%) who completed the UHHS process were housed, with 215 (60%) veterans housed in a UHHS-associated housing program (Table 3). Of the veterans who completed a UHHS assessment, 45 veterans (13%) did not complete the screening process; admitting program staff documented in CPRS unsuccessful attempts at reaching 12 veterans (3%), among whom 4 had no working phone at the time of their UHHS assessment. Time to admission depended on the program mission, openings, and the veteran’s UHHS engagement. Admission date indicates the date that programs housed veterans except in the case of the U.S. Department of Housing and Urban Development-VA Supportive Housing (HUD-VASH), where admission date indicates the date the veteran gave all required documents to HUD-VASH staff.
Discussion
Prior to the inception of UHHS, the staff of the CHCP housing program did not have a standardized process for communication across programs about veterans’ housing status and outcomes. Veterans went to multiple locations for screening if they were interested in > 1 program or if they were not admitted to the first program they approached. The UHHS process improved communication across CHCP housing programs, resulting in increased veteran accessibility to these programs as suggested by 3 CHCP housing programs having fewer days with openings post-UHHS implementation. Furthermore, a new screener position did not need to be created, because existing CHCP social workers were all capable screeners due to process standardization.
Fifty-five percent of the screened veterans were interested in and eligible for participation in > 1 housing program. They were eligible for 3 programs on average and were usually admitted to the housing program with the earliest opening. The need for screenings across all the CHCP housing programs was potentially decreased by ≥ one-third. This increased available time for the screeners to accomplish their other clinical responsibilities.
Limitations
A limitation of the review period evaluation is little information on noncompleters. The available data are confined to information documented in CPRS regarding why 45 veterans (13% of those who completed UHHS assessment) did not complete the screening process. For 12, admitting staff of the housing program documented in CPRS that they had been unable to reach the veteran; 9 of these veterans attended subsequent non-UHHS VANTHCS visits. To further improve the homeless housing delivery service, the creation of a CPRS-related process that informs VA clinicians that a housing program is attempting to contact a veteran is needed.
Challenges and Recommendations
Because the Housing Outcome document is a shared document, only 1 person at a time can save information in it. Facility staff have been unable to create a simple macro that closes the document automatically. Instead, screeners who need to save information when a document is already opened elsewhere must use a group e-mail list to alert others to close the document.
Streamlining the communication channel between the screeners and management evolved from the daily call, to e-mailing and program managers discussing topics with their staff, to Dr. Hooshyar facilitating a weekly call for screeners and program managers.
Optimizing the ratio of walk-in to scheduled appointments took time. Prior to the UHHS process, some CHCP housing programs offered scheduled appointments, whereas others had walk-in appointments. The decision to offer in-person scheduled appointments for veterans who preferred scheduled appointments or who commuted from a distance was made. Universal Homeless Housing Screening staff also offered scheduled telephone appointments for veterans who lacked transportation.
At times, admitting program staff was unable to reach veterans eligible for and interested in their program, despite screeners recommending to veterans that they should provide these programs with any changes in their contact information.
Recommendations for designing a screening process for homeless housing include:
- Have periodic retreats instead of weekly conference calls to quicken the pre-implementation process.
- Start with a pilot that includes some potential screeners to test the implementation process. The screeners involved in the pilot would train future screeners to expand the screener pool.
- Invest time in electronic tracking tools despite upfront and maintenance time requirements.
- Offer more walk-in than scheduled screening appointments.
- Embrace the idea that the pro-cess is always under development.
Conclusion
To ameliorate anxiety associated with changing the system, UHHS- associated staff redesigned the housing screening process through openness to stakeholder feedback and building on consensus. The staff also nurtured a culture that could change newly revised processes, depending on quality assurance findings. Without this method, the unknown likely would have propagated continued status quo. Universal Homeless Housing Screening processes improved veteran access to CHCP housing programs through instituting a one-stop housing screening assessment that also reduced the potential number of screenings by ≥ one-third.
Acknowledgments
The authors greatly appreciate the input of the many people involved in the creation of the UHHS process, in particular Daniel Anderson, Heather Arredondo, Tara Ayala, TiieShaiyon Banton, Melody Boyet, Amelia Bradley, Timothy Brown, Carnisha Campbell, Donald Capps, Burnell Carden Jr, Pushpi Chaudhary, Howard Cunningham, Rachael David, Marianna Demko, Derrick Evans, Steven Fisher, Kimberly Fite, Fatina Ford, Christi Godfrey, Gerald Goodwin, Melvin Haley, Tony Hall, Jessica Hennessey, Teresa House-Hatfield, Don Hubbard, Kathryn Jacob, Tonja King, Cecelia Knight, Janine Lenger-Gvist, Vickie Linden, Julia Long, Kristin Manley, Peggy Martin, Treva McDaniel, William McNair, Tammy Miller, Jeffery Milligan, Anhloan Nguyen, Tywanna Nichols, Cheryl Paul, Catherine Orsak, Dustin Perkins, Claudette Phillips, Joan Prescott, John Purkey, Martin Roback, Catriska Robertson, Charles Ross, Shanna Ruppert, Stephanie Saldivar, Linda Saucedo, Inga Sinclair-Henderson, John Smith, Zaire Smith, Cheryl Stringer, Valetta Ward, Carolyn Washington, Tammra Wood, and Skylar Woods-Nunley. They would also like to thank the veterans for their service and feedback.
Author disclosures
Dr. North discloses research support from National Institute on Alcohol Abuse and Alcoholism, National Institute of Diabetes and Digestive and Kidney Diseases, and VA and consultant fees from the University of Missouri-Columbia. Dr. Surís is Local Site Investigator for VA CSP #589 VIPSTAR-Veterans Individual Placement and Support Towards Advancing Recovery (PI Lori Davis, MD). She is co- investigator for VISN 17 grant Association of Myocardial Viability to Symptom Improvement post-CTO PCI (PI-Shuaib Abdullah, MD) and co-investigator for National Institutes on Drug Abuse grant Lidocaine Infusion as a Treatment for Cocaine Relapse and Craving (PI-Bryon Adinoff, MD). In addition, Dr. Surís is co-site-PI for the upcoming VA CSP #590 Lithium for Suicidal Behavior in Mood Disorders.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Tsai J, Doran KM, Rosenheck RA. When health insurance is not a factor: National comparison of homeless and nonhomeless US veterans who use Veterans Affairs emergency departments. Am J Public Health. 2013;103(suppl 2):S225-S231.
2. Secretary Shinseki Details Plan to End Homelessness for Veterans [news release]. U.S. Department of Veterans Affairs: Office of Public and Intergovernmental Affairs. http://www.va.gov/opa/pressrel/pressrelease.cfm?id=1807. Published November 3, 2009. Accessed March 3, 2014.
3. U.S. Department of Housing and Urban Development: Office of Community Planning and Development. The 2014 Annual Homeless Assessment Report (AHAR) to Congress. Part 1 Point-In-Time Estimates of Homelessness. https://www.hudexchange.info/resources/documents /2014-AHAR-Part1.pdf. Published October 2014. Accessed March 18, 2015.
4. Montgomery AE, Fargo JD, Byrne TH, Kane VR, Culhane DP. Universal screening for homelessness and risk for homelessness in the Veterans Health Administration. Am J Public Health. 2013;103(suppl 2):S210-S211.
5. Berman S, Barilich JE, Rosenheck R, Koerber G. The VA’s first comprehensive homeless center: A catalyst for public and private partnerships. Hosp Community Psychiatry. 1993;44(12):1183-1184.
6. U.S. Department of Veterans Affairs. Homeless Operations Management and Evaluation System (HOMES) User Manual–Phase 1. http://www.vfwsc.org/homes.pdf. Published April 19, 2011. Accessed March 3, 2014.
1. Tsai J, Doran KM, Rosenheck RA. When health insurance is not a factor: National comparison of homeless and nonhomeless US veterans who use Veterans Affairs emergency departments. Am J Public Health. 2013;103(suppl 2):S225-S231.
2. Secretary Shinseki Details Plan to End Homelessness for Veterans [news release]. U.S. Department of Veterans Affairs: Office of Public and Intergovernmental Affairs. http://www.va.gov/opa/pressrel/pressrelease.cfm?id=1807. Published November 3, 2009. Accessed March 3, 2014.
3. U.S. Department of Housing and Urban Development: Office of Community Planning and Development. The 2014 Annual Homeless Assessment Report (AHAR) to Congress. Part 1 Point-In-Time Estimates of Homelessness. https://www.hudexchange.info/resources/documents /2014-AHAR-Part1.pdf. Published October 2014. Accessed March 18, 2015.
4. Montgomery AE, Fargo JD, Byrne TH, Kane VR, Culhane DP. Universal screening for homelessness and risk for homelessness in the Veterans Health Administration. Am J Public Health. 2013;103(suppl 2):S210-S211.
5. Berman S, Barilich JE, Rosenheck R, Koerber G. The VA’s first comprehensive homeless center: A catalyst for public and private partnerships. Hosp Community Psychiatry. 1993;44(12):1183-1184.
6. U.S. Department of Veterans Affairs. Homeless Operations Management and Evaluation System (HOMES) User Manual–Phase 1. http://www.vfwsc.org/homes.pdf. Published April 19, 2011. Accessed March 3, 2014.
Development of a Multidisciplinary Stroke Program
Stroke is the fifth leading cause of death in the U.S. and a leading cause of long-term disability. About 15,000 military veterans are hospitalized for acute ischemic stroke each year, and $274 million was spent for their acute, postacute, and subsequent stroke-related care over the first 6 months following the stroke.1
The Durham VAMC (DVAMC) lies within the country’s “stroke belt,” an area of 8 contiguous southeastern states, and provides care to more than 200,000 veterans living in a 26-county area of central and eastern North Carolina. The stroke mortality rates in this region are up to 40% higher than that of the national average rate.2 The DVAMC sought to transform the organization of stroke care provided to hospitalized patients as an important step in optimizing their outcomes.
Background
The VHA is committed to providing high-quality, evidence-based health care and collects data reflecting its services, including care processes and outcomes. The 2009 Office of Quality and Performance report raised concerns about the delivery of stroke care within the VHA, based on an assessment of several quality indicators. This led to the 2011 VHA directive providing policies based on national standards for the management of acute ischemic stroke (AIS) in VHA medical facilities.3
The directive defined 3 types of VHA facilities: primary stroke centers, limited-hours stroke facilities, and supporting stroke facilities. The directive further required that “all VA medical facilities with inpatient acute care medical or surgical beds have a written policy guiding appropriate care to patients with AIS in place by January 1, 2012, and implemented no later than June 1, 2012,” which included “protocols or pathways for the rapid identification, evaluation, and treatment” of patients with acute stroke and monitoring of appropriate performance indicators. For many VHA facilities caring for patients with acute stroke, including the DVAMC, the directive necessitated the development of multidisciplinary teams, organized around the provision of stroke care.
DVAMC Stroke Program
A disease-specific program typically involves the coordination of multiple care components and aims to improve continuity of care. The approach is intended to reduce care fragmentation. Through an already existing program, many elements of stroke-specific care were being delivered at the DVAMC, but several gaps and no formal system existed for coordinating stroke-related care. Programmatic goals were developed to optimize adherence to national stroke-related process measures; minimize morbidity mortality, duration of hospitalization, postdischarge emergency department (ED) visits, and readmissions; and improve continuity of care.
The Team
The DVAMC is affiliated with Duke University School of Medicine and Duke University Medical Center. The Duke University Medical Center is a Joint Commission-certified Comprehensive Stroke Center, and its director also serves as the director of the Durham VAMC Stroke Program. Because of the time and clinical expertise required to develop and oversee the program, a critical initial step was to identify a dedicated stroke program coordinator (SPC) to integrate care services and manage its implementation and ongoing activities.
The specific responsibilities of the SPC vary, depending on a facility’s needs, goals, and resources. The SPC may serve primarily as the quality measure expert and data manager, have responsibilities for program implementation and maintenance, provide training for hospital staff, and help optimize communication and integration of neurologists, internal medicine teams, other consulting and treating services, and nursing and allied health providers. The SPC also may provide direct patient care, act as a case manager, and monitor longer-term outcomes.
The DVAMC SPC is a nurse practitioner (NP). The training was thought essential given an NP’s ability to work autonomously, manage all elements of care, conceptualize, collaborate, and provide medical management skills, as has been found beneficial in many other systems of care redesign.4 The DVAMC is a teaching hospital with much of the staff affiliated with Duke University Medical School and supervised by a team of expert attending physicians. The SPC’s roles at the DVAMC have been to facilitate program development, implementation, and maintenance and collect performance data and achieve quality metric goals.
Obtaining support and cooperation from all members of the health care team is necessary for success. Finding “champions”—selected staff with an interest in improving stroke care—is crucial to a multidisciplinary team approach. These staff members were identified and recruited to serve on work groups and task forces. The SPC served as the leader and as a resource for these teams.
Key Functions
The American Stroke Association’s Policy Recommendations for the Establishment of Stroke Systems of Care suggest that a stroke system should serve 3 critical functions: communication and collaboration, standardize care customized to the population, and include performance measures with a mechanism for evaluation.5
Communication/collaboration: Collaboration in the Durham VAMC occurs through multidisciplinary work groups, including all relevant disciplines. The SPC facilitated communication and integration of care. Communication with other SPCs and accessing community resources are invaluable.
Standardized care: Stroke policies and procedures ensure that care is not only evidence-based, but also consistent. Teams worked to develop policies, protocols, order sets, documentation templates, and standardized patient education materials. The SPC identified available resources, both within the hospital, as well as within the surrounding community and professional organizations to assist in developing these tools.
Performance measures and evaluation: Performance measures and program evaluations provide a means to evaluate the progress of already implemented strategies, assist in identifying further needs, and guide future plans. The DVAMC immediately began to monitor stroke care using a standardized set of metrics, and as the program developed further, additional performance measures were added, such as length of stay (LOS), postdischarge ED visits and readmissions, and stroke code treatment time goals.
Necessary Components
To ensure its comprehensiveness, the DVAMC Stroke Program was modeled after the American Heart Association (AHA) recommendations for necessary components of a stroke system: emergency medical system (EMS) response, acute in-hospital-based treatment, subacute and secondary prevention, rehabilitation, prevention and community education, and quality improvement initiatives.5 Although intended for larger community-integrated systems, the AHA model nonetheless provides a useful framework for the development of a hospital-based stroke program.
Emergency Medical Response
The establishment of collaborative networks with community partners is essential. The DVAMC staff worked closely with the local EMS providers, facilitating community collaboration. The hospital also maintains collaborative agreements with its medical affiliates for urgent and emergent treatments. The program director and program coordinator are involved in these relationships.
Acute Stroke Treatment
The first phase of system redesign for the DVAMC in response to the 2011 VHA directive included the formulation of an acute stroke medical center memorandum (MCM), or policy, which outlined the facility’s process for acute stroke evaluation and care. The DVAMC qualified as a limited-hours stroke facility (ie, a facility with the necessary personnel, infrastructure, expertise, and programs to diagnose and treat stroke patients emergently, including the administration of alteplase to appropriate candidates, limited to normal business hours).
Related: Stroke and Preventable Hospitalization: Who Is Most at Risk?
At the start of the Stroke Program, the DVAMC had only computed tomography (CT) services during daytime working hours and relied on on-call coverage during nonbusiness hours. There had been previous discussions regarding expansion of radiology CT services; however, development of the Stroke Program led to this expansion becoming a priority. Patients with symptoms of an acute stroke who might otherwise have been a candidate for treatment with IV alteplase or patients who had other symptoms warranting an emergent brain or other CT no longer needed to be transferred to another facility. Radiology Services worked with the Stroke Program, leading to the progressive expansion of CT availability to first include longer daytime coverage and in 2014, implementation of full 24/7 CT services, allowing the hospital to become a VHA primary stroke center.
In conjunction with the MCM, a stroke code team was also implemented. A stroke code facilitates the rapid evaluation and treatment of a patient with a suspected stroke who might be a candidate for acute revascularization by the neurology and critical care staff. Durham’s stroke code team consists of a neurologist, cardiac care unit resident and RN, SPC, escort services, CT technician, bed coordinator, and chaplain services. The SPC attends all stroke codes during normal working hours, collects real-time data, and obtains retrospective data from chart audits for codes occurring when the SPC is not available. By having protocols in place, the program is organized such that the SPC need not be present to facilitate care during each stroke code.
In the early stages of program development, a stroke code process was not used in the ED and was underused in the inpatient setting, making clear documentation and evaluation of acute stroke care and treatment times difficult, if not impossible. Throughout the first 15 months of the program implementation, monthly code activation use increased by 63%. The increase in stroke code team use led to improvements in acute stroke care and accurate determination of acute stroke treatment time goals.
The efforts of both the ED and radiology teams contributed to the improvements in “door-to-CT” and “door-to-CT results” times. Door-to-CT times are expected to improve further now that the facility has implemented CT services on a 24/7 basis. Currently, average door-to-CT time is 20.6 minutes, and door-to-CT results time is 42.4 minutes, both within the National Institute of Neurological Disorders and Stroke goals of < 25 minutes and < 45 minutes respectively.6 Time tracking was part of the program’s development, as this was not previously recorded. As a result, baseline door-to-CT times were not available, and a national benchmark for comparison was used. Part of the Stroke Program’s development was putting into place a process for tracking times.
Related: Does Stroke Hit Women Harder?
Standardized methods of acute stroke evaluation were implemented early in the program development and included the use of the National Institutes of Health Stroke Scale (NIHSS) and a bedside dysphagia screening process. Staff members responsible for these initial evaluations, specifically ED and intensive care unit nurses, were trained on the use of these tools, and electronic documentation templates were developed to facilitate the assessments. Comprehensive neurologic evaluation, including the essential elements of advanced stroke assessment, was also captured in standardized documentation templates for the neurology team.
The use of standardized practices and documentation templates helped the staff adhere to the requirements for the timely completion and documentation of the NIHSS to almost 100% consistently; however, it remains a challenge to consistently comply with the requirement to perform bedside dysphagia screens prior to oral intake (including medications). At the initiation of these measures, the dysphagia screen was performed for 58% of stroke patients; this rose to a fairly consistent 80% over time. Maintaining this percentage is a continual challenge that requires the SPC to work closely with the nursing staff, ED, and medicine teams.
Prior to and in the early phases of program implementation, the DVAMC effectively did not administer alteplase to patients with ischemic stroke, often because the requisite evaluations could not be completed in the required time frame. Since September of 2013, about 9 months after the program began, all 7 patients with AIS who qualified for treatment with alteplase were treated according to national guidelines. Continued work toward a goal of a < 60 minutes door-to-needle time is needed; but with notable progress, as door-to-needle time has decreased by 8% from the first alteplase administration to the most recent.
Overseen by the Simulations Department and the SPC, stroke code simulations (ie, mock stroke codes) are performed to aid in evaluating the acute stroke care process. Stroke simulation events should be an ongoing practice in any stroke program. It is an effective means to identify and address issues that may not otherwise be readily apparent.
Subacute Treatment
At DVAMC, postacute stroke care was identified as a priority. The SPC led a multidisciplinary team that was tasked with developing a postacute stroke care map, or integrated care pathway. Consistent care practices, a comprehensive tool to be used as a guide, can assist in improving outcomes, especially in a teaching facility with constantly changing medical and other clinical staff. The tool was developed using best practice guidelines from all disciplines. Staff members are encouraged to reference the pathway when caring for stroke patients, with necessary elements of care or performance measures in boldface to highlight their importance. Overall, DVAMC’s Best Care score (the percentage of patients whose care met all performance measures during the admission) rose from 57.1% to 78.6% over the course of the first year of the program.
Another key element of subacute stroke care is the provision of standardized patient stroke education. Before program initiation, stroke education at the DVAMC lacked consistency in both content and frequency. Secondary prevention should start at diagnosis, and education should be a continual process from admission to discharge. A patient booklet was developed that incorporated all required elements of stroke education per AHA guidelines: stroke risk factors, recognizing signs and symptoms, emergency activation, medications, and follow-up needs as well as other information, such as stroke pathophysiology, diet and activity, and managing lifestyle changes.7
Patient education templates were designed to facilitate documentation. Achieving this performance measure is a challenge not only for the DVAMC, but also for acute facilities nationwide. It requires involvement of the SPC as well as continual staff feedback and improvement challenges. Adherence to the patient education performance measure at the DVAMC improved from 0% meeting all 5 required elements at baseline to an average of 80% of patients.
A team of stroke champions representing each discipline involved in stroke care was recruited to be part of a postacute stroke team, led by the SPC. The team, consisting of neurologists, nurses, physical therapists, occupational therapists, speech therapists, nutritionists, social workers, and case managers, meets weekly for rounding on stroke patients, discussing patient care issues, assessing the effectiveness of the program, and addressing any system issues. This regular meeting facilitates collaboration and overall team building.
Rehabilitation and Follow-up
Routine physical, occupational, and speech therapy assessments are necessary to guide discharge planning. Although providing rehabilitation services is a priority, payer source can be a barrier to ideal rehabilitative care for DVAMC veterans. VA-based rehabilitation facilities are limited; therefore, community rehabilitation options, paid for by either VA funds or the patient’s insurance (if available), are used for the majority of stroke patients requiring these services. Efforts to increase access to stroke-specific rehabilitation options were undertaken by dedicated stroke champions at DVAMC; however, obtaining satisfactory payment agreements remains challenging.
Timely discharge is an element of care that the SPC also continually assesses. Discharge planning should begin on admission, and the SPC helps ensure that patient and caregiver needs are met and that all necessary follow-up and consultation visits have been scheduled. The LOS for stroke patients at the DVAMC had been on a steady upward trend from 6.39 days in 2005 to nearly 8 days in 2012. Over the course of 2013, the first year of the Stroke Program, stroke LOS decreased to just over 7 days (Figures 1 and 2).
Readmission rates are lower in high-risk populations when patients are seen for follow-up in the first 1 to 2 weeks postdischarge.8 Scheduling early visits can be challenging, especially in the current environment of an overburdened health care system. The DVAMC adopted the practice of Stroke Program follow-up phone calls, performed 7 to 10 days postdischarge. A standardized checklist of questions and dialogue was implemented that addressed common poststroke issues and education. Readmissions decreased from 21% in the first quarter of 2013, to 5% in the fourth quarter of 2013 after the implementation of this checklist follow-up. It is likely still too early to determine with any certainty whether the efforts aimed at improved patient education and early intervention are responsible for this decline.
Prevention and Education
Secondary prevention starts with stroke diagnosis and should include the patient and family/caregiver, when applicable. Inpatient stroke education was a priority early in the program. As the acute and postacute program developed, attention turned to community education and prevention.
Community education should emphasize early intervention. As elsewhere, the DVAMC found that the majority of patients present for care well outside the treatment window for alteplase administration. Based on national guidelines, IV alteplase must be initiated in selected patients within 4.5 hours of symptom onset. Many surveys confirm that patients are not able to accurately identify stroke symptoms or are not aware that stroke is a medical emergency. Challenges in stroke care lie in community education.9,10 The SPC met with primary care providers (PCPs) to coordinate educational and preventative efforts, recruiting them in primary and secondary prevention strategies and educating them on high-risk patients.
The SPC also collaborated with one of the outpatient clinic Patient Aligned Care Teams (PACT, or primary care team) on the development of a primary prevention program. The PACT initiated a risk reduction educational program after noting that many of their patients had suboptimal stroke risk factor management.
The project is still in the pilot stage but is showing promise regarding patient interest and participation. It is focused on addressing 4 major risk factors: hypertension, diabetes, hyperlipidemia, and tobacco use. Through a PACT report, patients were identified as having stroke risk factors that were not optimally controlled. The project aims to reduce the risk of stroke through education, goal setting, and lifestyle modification and saw a 25% rate of participation among those patients identified as candidates for the program. Of these participants, 100% completed all 4 sessions and rated the program highly favorable.
Quality Improvement Measures
Tracking performance measures should begin at program inception. “Measures improve fastest when they are being used. …Measurement and reporting with currently available data should begin immediately. …The implied message is this: since data will be impossible to ignore, we might as well make them better.”8 The VHA has a system for monitoring various quality measures, which include specific aspects of acute stroke care set forth by the VHA Stroke Directive: timely administration of alteplase, timely performance of NIHSS, and performance of a dysphagia screen prior to oral intake.
The DVAMC SPC began more comprehensive assessments of acute stroke care and evaluated elements of postacute stroke care, based on a nationally recognized set of performance measures. A system of tracking stroke performance data was initiated in the first month of the program and is based on the 10 stroke performance measures defined by the AHA and the Joint Commission. Data are currently analyzed independent of a national data management system that does not allow for national benchmarking; however, the analysis was a starting point to track facility progress and emphasized the need for consistent care. Along with collecting data on the 10 stroke-specific elements, the SPC began a system to follow duration of hospitalization, postdischarge ED visits, readmissions, and mortality rates, as well as stroke code and door-to-needle-time data. The data are shared with the DVAMC Critical Care Committee via monthly reports, program leadership via quarterly reports, facility leadership via annual reports, and facility staff through periodic e-mails and the all-employee share drive.
The first year of the program was associated with improvements in quality metrics across most areas of stroke care. Notably, 11 quality indicators that assess direct patient care measures have improved significantly from prior to program initiation in 2012 to after implementation of a comprehensive stroke care program at the conclusion of 2013. Those measures that were not already at goal of ≥ 85% achievement showed the most dramatic improvements (Figure 3).
Goals and Future Planning
The work of the DVAMC Stroke Program is far from over. Progress made is easily lost without continual monitoring and feedback. Challenges continue as well. Goals moving forward include improving door-to-needle times for IV alteplase therapy, more consistently performing swallow screens prior to oral intake, more consistently providing patient education, and increasing engagement with PCPs and the veteran community in providing stroke education and risk reduction.
A larger goal for future planning for the DVAMC is the need for a designated stroke care unit. Currently, stroke patients are admitted to the Critical Care Unit (CCU) for initial monitoring and treatment and when stable are moved to general medical wards. In some instances, this necessitates that the less acute patients occupy a CCU bed due to ward nursing limitations (ie, neuro checks every 2-hours is too great of a time demand for the ward nurses) or that the more neurologic acute patients are transferred to general medical wards when they would benefit from a more neurology-focused therapeutic environment. Stroke unit care has been associated with improved patient outcomes compared with care on general medical wards.11 The development of a designated stroke care unit is a long-range goal of the program.
Conclusion
The development of the Stroke Program, including an SPC, has improved the care of veterans with stroke at the DVAMC. The achievements of the DVAMC Stroke Program are the result of coordinated efforts of a team of dedicated health care professionals from all disciplines who sought to improve stroke care for veterans. The DVAMC continues to strive toward ever-improving outcomes, working with community partners and challenging itself to achieve a higher level of excellence. The lessons learned at the DVAMC may serve as a model for other VHA hospitals seeking to improve their stroke-related care programs.
Acknowledgements
The authors thank the executive leadership team and the chief of medicine of the DVAMC who recognized the need and potential for better stroke coordination and who have been fully supportive of the authors’ efforts to improve coordination, education, and care of their patients with strokes.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. QUERI—Quality Enhancement Research Initiative. Stroke QUERI. QUERI Website. http://www .queri.research.va.gov/str/default.cfm. Updated/Reviewed June 19, 2014. Accessed January 22, 2015.
2. Howard G, Evans GW, Pearce K, et al. Is the stroke belt disappearing? An analysis of racial, temporal, and age effects. Stroke. 1995;26(7):1153-1158.
3. Veterans Health Administration, U.S. Department of Veterans Affairs. Treatment of Acute Ischemic Stroke (AIS). VHA Directive 2011-038. U.S. Department of Veterans Affairs Website. http://www .va.gov/vhapublications/ViewPublication.asp?pub _ID=2458. Published November 2, 2011. Accessed January 22, 2015.
4. Green T, Newcommon N. Advancing nursing practice: The role of the nurse practitioner in an acute stroke program. J Neurosci Nurs. 2006;38(4 suppl):328-330.
5. Schwamm LH, Pancioli A, Acker JE III, et al; American Stroke Association’s Task Force on the Development of Stroke Systems. Recommendations for the establishment of stroke systems of care: Recommendations from the American Stroke Association’s Task Force on the Development of Stroke Systems. Stroke. 2005;36(3):690-703.
6. Bock BF. Response system for patients presenting with acute stroke. Paper presented at: Proceedings of a National Symposium on Rapid Identification and Treatment of Acute Stroke; December 12-13, 1996; Bethesda, MD. http://www.ninds.nih.gov/news_and _events/proceedings/stroke_proceedings/bock.htm.Published. Updated May 17, 2011. Accessed January 22, 2015.
7. American Heart Association, American Stroke Association. Stroke fact sheet. American Heart Association Website. http://www.heart.org/idc/groups/heart-public/@wcm/@private/@hcm/@gwtg/documents /downloadable/ucm_310976.pdf. Published April 2014. Accessed January 22, 2015.
8. Lee TH. Care redesign—A path forward for providers. N Engl J Med. 2012;367(5):466-472.
9. Kleindorfer D, Khoury J, Broderick JP, et al. Temporal trends in public awareness of stroke: Warning signs, risk factors, and treatment. Stroke. 2009;40(7):2502-2506.
10. Jauch EC, Saver JL, Adams HP Jr, et al; American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Perripheral Vascular Disease; Council on Clinical Cardiology. Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870-947.
11. How do stroke units improve patient outcomes? A collaborative systematic review of the randomized trials. Stroke Unit Trialists Collaboration. Stroke. 1997;28(11):2139-2144.
Stroke is the fifth leading cause of death in the U.S. and a leading cause of long-term disability. About 15,000 military veterans are hospitalized for acute ischemic stroke each year, and $274 million was spent for their acute, postacute, and subsequent stroke-related care over the first 6 months following the stroke.1
The Durham VAMC (DVAMC) lies within the country’s “stroke belt,” an area of 8 contiguous southeastern states, and provides care to more than 200,000 veterans living in a 26-county area of central and eastern North Carolina. The stroke mortality rates in this region are up to 40% higher than that of the national average rate.2 The DVAMC sought to transform the organization of stroke care provided to hospitalized patients as an important step in optimizing their outcomes.
Background
The VHA is committed to providing high-quality, evidence-based health care and collects data reflecting its services, including care processes and outcomes. The 2009 Office of Quality and Performance report raised concerns about the delivery of stroke care within the VHA, based on an assessment of several quality indicators. This led to the 2011 VHA directive providing policies based on national standards for the management of acute ischemic stroke (AIS) in VHA medical facilities.3
The directive defined 3 types of VHA facilities: primary stroke centers, limited-hours stroke facilities, and supporting stroke facilities. The directive further required that “all VA medical facilities with inpatient acute care medical or surgical beds have a written policy guiding appropriate care to patients with AIS in place by January 1, 2012, and implemented no later than June 1, 2012,” which included “protocols or pathways for the rapid identification, evaluation, and treatment” of patients with acute stroke and monitoring of appropriate performance indicators. For many VHA facilities caring for patients with acute stroke, including the DVAMC, the directive necessitated the development of multidisciplinary teams, organized around the provision of stroke care.
DVAMC Stroke Program
A disease-specific program typically involves the coordination of multiple care components and aims to improve continuity of care. The approach is intended to reduce care fragmentation. Through an already existing program, many elements of stroke-specific care were being delivered at the DVAMC, but several gaps and no formal system existed for coordinating stroke-related care. Programmatic goals were developed to optimize adherence to national stroke-related process measures; minimize morbidity mortality, duration of hospitalization, postdischarge emergency department (ED) visits, and readmissions; and improve continuity of care.
The Team
The DVAMC is affiliated with Duke University School of Medicine and Duke University Medical Center. The Duke University Medical Center is a Joint Commission-certified Comprehensive Stroke Center, and its director also serves as the director of the Durham VAMC Stroke Program. Because of the time and clinical expertise required to develop and oversee the program, a critical initial step was to identify a dedicated stroke program coordinator (SPC) to integrate care services and manage its implementation and ongoing activities.
The specific responsibilities of the SPC vary, depending on a facility’s needs, goals, and resources. The SPC may serve primarily as the quality measure expert and data manager, have responsibilities for program implementation and maintenance, provide training for hospital staff, and help optimize communication and integration of neurologists, internal medicine teams, other consulting and treating services, and nursing and allied health providers. The SPC also may provide direct patient care, act as a case manager, and monitor longer-term outcomes.
The DVAMC SPC is a nurse practitioner (NP). The training was thought essential given an NP’s ability to work autonomously, manage all elements of care, conceptualize, collaborate, and provide medical management skills, as has been found beneficial in many other systems of care redesign.4 The DVAMC is a teaching hospital with much of the staff affiliated with Duke University Medical School and supervised by a team of expert attending physicians. The SPC’s roles at the DVAMC have been to facilitate program development, implementation, and maintenance and collect performance data and achieve quality metric goals.
Obtaining support and cooperation from all members of the health care team is necessary for success. Finding “champions”—selected staff with an interest in improving stroke care—is crucial to a multidisciplinary team approach. These staff members were identified and recruited to serve on work groups and task forces. The SPC served as the leader and as a resource for these teams.
Key Functions
The American Stroke Association’s Policy Recommendations for the Establishment of Stroke Systems of Care suggest that a stroke system should serve 3 critical functions: communication and collaboration, standardize care customized to the population, and include performance measures with a mechanism for evaluation.5
Communication/collaboration: Collaboration in the Durham VAMC occurs through multidisciplinary work groups, including all relevant disciplines. The SPC facilitated communication and integration of care. Communication with other SPCs and accessing community resources are invaluable.
Standardized care: Stroke policies and procedures ensure that care is not only evidence-based, but also consistent. Teams worked to develop policies, protocols, order sets, documentation templates, and standardized patient education materials. The SPC identified available resources, both within the hospital, as well as within the surrounding community and professional organizations to assist in developing these tools.
Performance measures and evaluation: Performance measures and program evaluations provide a means to evaluate the progress of already implemented strategies, assist in identifying further needs, and guide future plans. The DVAMC immediately began to monitor stroke care using a standardized set of metrics, and as the program developed further, additional performance measures were added, such as length of stay (LOS), postdischarge ED visits and readmissions, and stroke code treatment time goals.
Necessary Components
To ensure its comprehensiveness, the DVAMC Stroke Program was modeled after the American Heart Association (AHA) recommendations for necessary components of a stroke system: emergency medical system (EMS) response, acute in-hospital-based treatment, subacute and secondary prevention, rehabilitation, prevention and community education, and quality improvement initiatives.5 Although intended for larger community-integrated systems, the AHA model nonetheless provides a useful framework for the development of a hospital-based stroke program.
Emergency Medical Response
The establishment of collaborative networks with community partners is essential. The DVAMC staff worked closely with the local EMS providers, facilitating community collaboration. The hospital also maintains collaborative agreements with its medical affiliates for urgent and emergent treatments. The program director and program coordinator are involved in these relationships.
Acute Stroke Treatment
The first phase of system redesign for the DVAMC in response to the 2011 VHA directive included the formulation of an acute stroke medical center memorandum (MCM), or policy, which outlined the facility’s process for acute stroke evaluation and care. The DVAMC qualified as a limited-hours stroke facility (ie, a facility with the necessary personnel, infrastructure, expertise, and programs to diagnose and treat stroke patients emergently, including the administration of alteplase to appropriate candidates, limited to normal business hours).
Related: Stroke and Preventable Hospitalization: Who Is Most at Risk?
At the start of the Stroke Program, the DVAMC had only computed tomography (CT) services during daytime working hours and relied on on-call coverage during nonbusiness hours. There had been previous discussions regarding expansion of radiology CT services; however, development of the Stroke Program led to this expansion becoming a priority. Patients with symptoms of an acute stroke who might otherwise have been a candidate for treatment with IV alteplase or patients who had other symptoms warranting an emergent brain or other CT no longer needed to be transferred to another facility. Radiology Services worked with the Stroke Program, leading to the progressive expansion of CT availability to first include longer daytime coverage and in 2014, implementation of full 24/7 CT services, allowing the hospital to become a VHA primary stroke center.
In conjunction with the MCM, a stroke code team was also implemented. A stroke code facilitates the rapid evaluation and treatment of a patient with a suspected stroke who might be a candidate for acute revascularization by the neurology and critical care staff. Durham’s stroke code team consists of a neurologist, cardiac care unit resident and RN, SPC, escort services, CT technician, bed coordinator, and chaplain services. The SPC attends all stroke codes during normal working hours, collects real-time data, and obtains retrospective data from chart audits for codes occurring when the SPC is not available. By having protocols in place, the program is organized such that the SPC need not be present to facilitate care during each stroke code.
In the early stages of program development, a stroke code process was not used in the ED and was underused in the inpatient setting, making clear documentation and evaluation of acute stroke care and treatment times difficult, if not impossible. Throughout the first 15 months of the program implementation, monthly code activation use increased by 63%. The increase in stroke code team use led to improvements in acute stroke care and accurate determination of acute stroke treatment time goals.
The efforts of both the ED and radiology teams contributed to the improvements in “door-to-CT” and “door-to-CT results” times. Door-to-CT times are expected to improve further now that the facility has implemented CT services on a 24/7 basis. Currently, average door-to-CT time is 20.6 minutes, and door-to-CT results time is 42.4 minutes, both within the National Institute of Neurological Disorders and Stroke goals of < 25 minutes and < 45 minutes respectively.6 Time tracking was part of the program’s development, as this was not previously recorded. As a result, baseline door-to-CT times were not available, and a national benchmark for comparison was used. Part of the Stroke Program’s development was putting into place a process for tracking times.
Related: Does Stroke Hit Women Harder?
Standardized methods of acute stroke evaluation were implemented early in the program development and included the use of the National Institutes of Health Stroke Scale (NIHSS) and a bedside dysphagia screening process. Staff members responsible for these initial evaluations, specifically ED and intensive care unit nurses, were trained on the use of these tools, and electronic documentation templates were developed to facilitate the assessments. Comprehensive neurologic evaluation, including the essential elements of advanced stroke assessment, was also captured in standardized documentation templates for the neurology team.
The use of standardized practices and documentation templates helped the staff adhere to the requirements for the timely completion and documentation of the NIHSS to almost 100% consistently; however, it remains a challenge to consistently comply with the requirement to perform bedside dysphagia screens prior to oral intake (including medications). At the initiation of these measures, the dysphagia screen was performed for 58% of stroke patients; this rose to a fairly consistent 80% over time. Maintaining this percentage is a continual challenge that requires the SPC to work closely with the nursing staff, ED, and medicine teams.
Prior to and in the early phases of program implementation, the DVAMC effectively did not administer alteplase to patients with ischemic stroke, often because the requisite evaluations could not be completed in the required time frame. Since September of 2013, about 9 months after the program began, all 7 patients with AIS who qualified for treatment with alteplase were treated according to national guidelines. Continued work toward a goal of a < 60 minutes door-to-needle time is needed; but with notable progress, as door-to-needle time has decreased by 8% from the first alteplase administration to the most recent.
Overseen by the Simulations Department and the SPC, stroke code simulations (ie, mock stroke codes) are performed to aid in evaluating the acute stroke care process. Stroke simulation events should be an ongoing practice in any stroke program. It is an effective means to identify and address issues that may not otherwise be readily apparent.
Subacute Treatment
At DVAMC, postacute stroke care was identified as a priority. The SPC led a multidisciplinary team that was tasked with developing a postacute stroke care map, or integrated care pathway. Consistent care practices, a comprehensive tool to be used as a guide, can assist in improving outcomes, especially in a teaching facility with constantly changing medical and other clinical staff. The tool was developed using best practice guidelines from all disciplines. Staff members are encouraged to reference the pathway when caring for stroke patients, with necessary elements of care or performance measures in boldface to highlight their importance. Overall, DVAMC’s Best Care score (the percentage of patients whose care met all performance measures during the admission) rose from 57.1% to 78.6% over the course of the first year of the program.
Another key element of subacute stroke care is the provision of standardized patient stroke education. Before program initiation, stroke education at the DVAMC lacked consistency in both content and frequency. Secondary prevention should start at diagnosis, and education should be a continual process from admission to discharge. A patient booklet was developed that incorporated all required elements of stroke education per AHA guidelines: stroke risk factors, recognizing signs and symptoms, emergency activation, medications, and follow-up needs as well as other information, such as stroke pathophysiology, diet and activity, and managing lifestyle changes.7
Patient education templates were designed to facilitate documentation. Achieving this performance measure is a challenge not only for the DVAMC, but also for acute facilities nationwide. It requires involvement of the SPC as well as continual staff feedback and improvement challenges. Adherence to the patient education performance measure at the DVAMC improved from 0% meeting all 5 required elements at baseline to an average of 80% of patients.
A team of stroke champions representing each discipline involved in stroke care was recruited to be part of a postacute stroke team, led by the SPC. The team, consisting of neurologists, nurses, physical therapists, occupational therapists, speech therapists, nutritionists, social workers, and case managers, meets weekly for rounding on stroke patients, discussing patient care issues, assessing the effectiveness of the program, and addressing any system issues. This regular meeting facilitates collaboration and overall team building.
Rehabilitation and Follow-up
Routine physical, occupational, and speech therapy assessments are necessary to guide discharge planning. Although providing rehabilitation services is a priority, payer source can be a barrier to ideal rehabilitative care for DVAMC veterans. VA-based rehabilitation facilities are limited; therefore, community rehabilitation options, paid for by either VA funds or the patient’s insurance (if available), are used for the majority of stroke patients requiring these services. Efforts to increase access to stroke-specific rehabilitation options were undertaken by dedicated stroke champions at DVAMC; however, obtaining satisfactory payment agreements remains challenging.
Timely discharge is an element of care that the SPC also continually assesses. Discharge planning should begin on admission, and the SPC helps ensure that patient and caregiver needs are met and that all necessary follow-up and consultation visits have been scheduled. The LOS for stroke patients at the DVAMC had been on a steady upward trend from 6.39 days in 2005 to nearly 8 days in 2012. Over the course of 2013, the first year of the Stroke Program, stroke LOS decreased to just over 7 days (Figures 1 and 2).
Readmission rates are lower in high-risk populations when patients are seen for follow-up in the first 1 to 2 weeks postdischarge.8 Scheduling early visits can be challenging, especially in the current environment of an overburdened health care system. The DVAMC adopted the practice of Stroke Program follow-up phone calls, performed 7 to 10 days postdischarge. A standardized checklist of questions and dialogue was implemented that addressed common poststroke issues and education. Readmissions decreased from 21% in the first quarter of 2013, to 5% in the fourth quarter of 2013 after the implementation of this checklist follow-up. It is likely still too early to determine with any certainty whether the efforts aimed at improved patient education and early intervention are responsible for this decline.
Prevention and Education
Secondary prevention starts with stroke diagnosis and should include the patient and family/caregiver, when applicable. Inpatient stroke education was a priority early in the program. As the acute and postacute program developed, attention turned to community education and prevention.
Community education should emphasize early intervention. As elsewhere, the DVAMC found that the majority of patients present for care well outside the treatment window for alteplase administration. Based on national guidelines, IV alteplase must be initiated in selected patients within 4.5 hours of symptom onset. Many surveys confirm that patients are not able to accurately identify stroke symptoms or are not aware that stroke is a medical emergency. Challenges in stroke care lie in community education.9,10 The SPC met with primary care providers (PCPs) to coordinate educational and preventative efforts, recruiting them in primary and secondary prevention strategies and educating them on high-risk patients.
The SPC also collaborated with one of the outpatient clinic Patient Aligned Care Teams (PACT, or primary care team) on the development of a primary prevention program. The PACT initiated a risk reduction educational program after noting that many of their patients had suboptimal stroke risk factor management.
The project is still in the pilot stage but is showing promise regarding patient interest and participation. It is focused on addressing 4 major risk factors: hypertension, diabetes, hyperlipidemia, and tobacco use. Through a PACT report, patients were identified as having stroke risk factors that were not optimally controlled. The project aims to reduce the risk of stroke through education, goal setting, and lifestyle modification and saw a 25% rate of participation among those patients identified as candidates for the program. Of these participants, 100% completed all 4 sessions and rated the program highly favorable.
Quality Improvement Measures
Tracking performance measures should begin at program inception. “Measures improve fastest when they are being used. …Measurement and reporting with currently available data should begin immediately. …The implied message is this: since data will be impossible to ignore, we might as well make them better.”8 The VHA has a system for monitoring various quality measures, which include specific aspects of acute stroke care set forth by the VHA Stroke Directive: timely administration of alteplase, timely performance of NIHSS, and performance of a dysphagia screen prior to oral intake.
The DVAMC SPC began more comprehensive assessments of acute stroke care and evaluated elements of postacute stroke care, based on a nationally recognized set of performance measures. A system of tracking stroke performance data was initiated in the first month of the program and is based on the 10 stroke performance measures defined by the AHA and the Joint Commission. Data are currently analyzed independent of a national data management system that does not allow for national benchmarking; however, the analysis was a starting point to track facility progress and emphasized the need for consistent care. Along with collecting data on the 10 stroke-specific elements, the SPC began a system to follow duration of hospitalization, postdischarge ED visits, readmissions, and mortality rates, as well as stroke code and door-to-needle-time data. The data are shared with the DVAMC Critical Care Committee via monthly reports, program leadership via quarterly reports, facility leadership via annual reports, and facility staff through periodic e-mails and the all-employee share drive.
The first year of the program was associated with improvements in quality metrics across most areas of stroke care. Notably, 11 quality indicators that assess direct patient care measures have improved significantly from prior to program initiation in 2012 to after implementation of a comprehensive stroke care program at the conclusion of 2013. Those measures that were not already at goal of ≥ 85% achievement showed the most dramatic improvements (Figure 3).
Goals and Future Planning
The work of the DVAMC Stroke Program is far from over. Progress made is easily lost without continual monitoring and feedback. Challenges continue as well. Goals moving forward include improving door-to-needle times for IV alteplase therapy, more consistently performing swallow screens prior to oral intake, more consistently providing patient education, and increasing engagement with PCPs and the veteran community in providing stroke education and risk reduction.
A larger goal for future planning for the DVAMC is the need for a designated stroke care unit. Currently, stroke patients are admitted to the Critical Care Unit (CCU) for initial monitoring and treatment and when stable are moved to general medical wards. In some instances, this necessitates that the less acute patients occupy a CCU bed due to ward nursing limitations (ie, neuro checks every 2-hours is too great of a time demand for the ward nurses) or that the more neurologic acute patients are transferred to general medical wards when they would benefit from a more neurology-focused therapeutic environment. Stroke unit care has been associated with improved patient outcomes compared with care on general medical wards.11 The development of a designated stroke care unit is a long-range goal of the program.
Conclusion
The development of the Stroke Program, including an SPC, has improved the care of veterans with stroke at the DVAMC. The achievements of the DVAMC Stroke Program are the result of coordinated efforts of a team of dedicated health care professionals from all disciplines who sought to improve stroke care for veterans. The DVAMC continues to strive toward ever-improving outcomes, working with community partners and challenging itself to achieve a higher level of excellence. The lessons learned at the DVAMC may serve as a model for other VHA hospitals seeking to improve their stroke-related care programs.
Acknowledgements
The authors thank the executive leadership team and the chief of medicine of the DVAMC who recognized the need and potential for better stroke coordination and who have been fully supportive of the authors’ efforts to improve coordination, education, and care of their patients with strokes.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Stroke is the fifth leading cause of death in the U.S. and a leading cause of long-term disability. About 15,000 military veterans are hospitalized for acute ischemic stroke each year, and $274 million was spent for their acute, postacute, and subsequent stroke-related care over the first 6 months following the stroke.1
The Durham VAMC (DVAMC) lies within the country’s “stroke belt,” an area of 8 contiguous southeastern states, and provides care to more than 200,000 veterans living in a 26-county area of central and eastern North Carolina. The stroke mortality rates in this region are up to 40% higher than that of the national average rate.2 The DVAMC sought to transform the organization of stroke care provided to hospitalized patients as an important step in optimizing their outcomes.
Background
The VHA is committed to providing high-quality, evidence-based health care and collects data reflecting its services, including care processes and outcomes. The 2009 Office of Quality and Performance report raised concerns about the delivery of stroke care within the VHA, based on an assessment of several quality indicators. This led to the 2011 VHA directive providing policies based on national standards for the management of acute ischemic stroke (AIS) in VHA medical facilities.3
The directive defined 3 types of VHA facilities: primary stroke centers, limited-hours stroke facilities, and supporting stroke facilities. The directive further required that “all VA medical facilities with inpatient acute care medical or surgical beds have a written policy guiding appropriate care to patients with AIS in place by January 1, 2012, and implemented no later than June 1, 2012,” which included “protocols or pathways for the rapid identification, evaluation, and treatment” of patients with acute stroke and monitoring of appropriate performance indicators. For many VHA facilities caring for patients with acute stroke, including the DVAMC, the directive necessitated the development of multidisciplinary teams, organized around the provision of stroke care.
DVAMC Stroke Program
A disease-specific program typically involves the coordination of multiple care components and aims to improve continuity of care. The approach is intended to reduce care fragmentation. Through an already existing program, many elements of stroke-specific care were being delivered at the DVAMC, but several gaps and no formal system existed for coordinating stroke-related care. Programmatic goals were developed to optimize adherence to national stroke-related process measures; minimize morbidity mortality, duration of hospitalization, postdischarge emergency department (ED) visits, and readmissions; and improve continuity of care.
The Team
The DVAMC is affiliated with Duke University School of Medicine and Duke University Medical Center. The Duke University Medical Center is a Joint Commission-certified Comprehensive Stroke Center, and its director also serves as the director of the Durham VAMC Stroke Program. Because of the time and clinical expertise required to develop and oversee the program, a critical initial step was to identify a dedicated stroke program coordinator (SPC) to integrate care services and manage its implementation and ongoing activities.
The specific responsibilities of the SPC vary, depending on a facility’s needs, goals, and resources. The SPC may serve primarily as the quality measure expert and data manager, have responsibilities for program implementation and maintenance, provide training for hospital staff, and help optimize communication and integration of neurologists, internal medicine teams, other consulting and treating services, and nursing and allied health providers. The SPC also may provide direct patient care, act as a case manager, and monitor longer-term outcomes.
The DVAMC SPC is a nurse practitioner (NP). The training was thought essential given an NP’s ability to work autonomously, manage all elements of care, conceptualize, collaborate, and provide medical management skills, as has been found beneficial in many other systems of care redesign.4 The DVAMC is a teaching hospital with much of the staff affiliated with Duke University Medical School and supervised by a team of expert attending physicians. The SPC’s roles at the DVAMC have been to facilitate program development, implementation, and maintenance and collect performance data and achieve quality metric goals.
Obtaining support and cooperation from all members of the health care team is necessary for success. Finding “champions”—selected staff with an interest in improving stroke care—is crucial to a multidisciplinary team approach. These staff members were identified and recruited to serve on work groups and task forces. The SPC served as the leader and as a resource for these teams.
Key Functions
The American Stroke Association’s Policy Recommendations for the Establishment of Stroke Systems of Care suggest that a stroke system should serve 3 critical functions: communication and collaboration, standardize care customized to the population, and include performance measures with a mechanism for evaluation.5
Communication/collaboration: Collaboration in the Durham VAMC occurs through multidisciplinary work groups, including all relevant disciplines. The SPC facilitated communication and integration of care. Communication with other SPCs and accessing community resources are invaluable.
Standardized care: Stroke policies and procedures ensure that care is not only evidence-based, but also consistent. Teams worked to develop policies, protocols, order sets, documentation templates, and standardized patient education materials. The SPC identified available resources, both within the hospital, as well as within the surrounding community and professional organizations to assist in developing these tools.
Performance measures and evaluation: Performance measures and program evaluations provide a means to evaluate the progress of already implemented strategies, assist in identifying further needs, and guide future plans. The DVAMC immediately began to monitor stroke care using a standardized set of metrics, and as the program developed further, additional performance measures were added, such as length of stay (LOS), postdischarge ED visits and readmissions, and stroke code treatment time goals.
Necessary Components
To ensure its comprehensiveness, the DVAMC Stroke Program was modeled after the American Heart Association (AHA) recommendations for necessary components of a stroke system: emergency medical system (EMS) response, acute in-hospital-based treatment, subacute and secondary prevention, rehabilitation, prevention and community education, and quality improvement initiatives.5 Although intended for larger community-integrated systems, the AHA model nonetheless provides a useful framework for the development of a hospital-based stroke program.
Emergency Medical Response
The establishment of collaborative networks with community partners is essential. The DVAMC staff worked closely with the local EMS providers, facilitating community collaboration. The hospital also maintains collaborative agreements with its medical affiliates for urgent and emergent treatments. The program director and program coordinator are involved in these relationships.
Acute Stroke Treatment
The first phase of system redesign for the DVAMC in response to the 2011 VHA directive included the formulation of an acute stroke medical center memorandum (MCM), or policy, which outlined the facility’s process for acute stroke evaluation and care. The DVAMC qualified as a limited-hours stroke facility (ie, a facility with the necessary personnel, infrastructure, expertise, and programs to diagnose and treat stroke patients emergently, including the administration of alteplase to appropriate candidates, limited to normal business hours).
Related: Stroke and Preventable Hospitalization: Who Is Most at Risk?
At the start of the Stroke Program, the DVAMC had only computed tomography (CT) services during daytime working hours and relied on on-call coverage during nonbusiness hours. There had been previous discussions regarding expansion of radiology CT services; however, development of the Stroke Program led to this expansion becoming a priority. Patients with symptoms of an acute stroke who might otherwise have been a candidate for treatment with IV alteplase or patients who had other symptoms warranting an emergent brain or other CT no longer needed to be transferred to another facility. Radiology Services worked with the Stroke Program, leading to the progressive expansion of CT availability to first include longer daytime coverage and in 2014, implementation of full 24/7 CT services, allowing the hospital to become a VHA primary stroke center.
In conjunction with the MCM, a stroke code team was also implemented. A stroke code facilitates the rapid evaluation and treatment of a patient with a suspected stroke who might be a candidate for acute revascularization by the neurology and critical care staff. Durham’s stroke code team consists of a neurologist, cardiac care unit resident and RN, SPC, escort services, CT technician, bed coordinator, and chaplain services. The SPC attends all stroke codes during normal working hours, collects real-time data, and obtains retrospective data from chart audits for codes occurring when the SPC is not available. By having protocols in place, the program is organized such that the SPC need not be present to facilitate care during each stroke code.
In the early stages of program development, a stroke code process was not used in the ED and was underused in the inpatient setting, making clear documentation and evaluation of acute stroke care and treatment times difficult, if not impossible. Throughout the first 15 months of the program implementation, monthly code activation use increased by 63%. The increase in stroke code team use led to improvements in acute stroke care and accurate determination of acute stroke treatment time goals.
The efforts of both the ED and radiology teams contributed to the improvements in “door-to-CT” and “door-to-CT results” times. Door-to-CT times are expected to improve further now that the facility has implemented CT services on a 24/7 basis. Currently, average door-to-CT time is 20.6 minutes, and door-to-CT results time is 42.4 minutes, both within the National Institute of Neurological Disorders and Stroke goals of < 25 minutes and < 45 minutes respectively.6 Time tracking was part of the program’s development, as this was not previously recorded. As a result, baseline door-to-CT times were not available, and a national benchmark for comparison was used. Part of the Stroke Program’s development was putting into place a process for tracking times.
Related: Does Stroke Hit Women Harder?
Standardized methods of acute stroke evaluation were implemented early in the program development and included the use of the National Institutes of Health Stroke Scale (NIHSS) and a bedside dysphagia screening process. Staff members responsible for these initial evaluations, specifically ED and intensive care unit nurses, were trained on the use of these tools, and electronic documentation templates were developed to facilitate the assessments. Comprehensive neurologic evaluation, including the essential elements of advanced stroke assessment, was also captured in standardized documentation templates for the neurology team.
The use of standardized practices and documentation templates helped the staff adhere to the requirements for the timely completion and documentation of the NIHSS to almost 100% consistently; however, it remains a challenge to consistently comply with the requirement to perform bedside dysphagia screens prior to oral intake (including medications). At the initiation of these measures, the dysphagia screen was performed for 58% of stroke patients; this rose to a fairly consistent 80% over time. Maintaining this percentage is a continual challenge that requires the SPC to work closely with the nursing staff, ED, and medicine teams.
Prior to and in the early phases of program implementation, the DVAMC effectively did not administer alteplase to patients with ischemic stroke, often because the requisite evaluations could not be completed in the required time frame. Since September of 2013, about 9 months after the program began, all 7 patients with AIS who qualified for treatment with alteplase were treated according to national guidelines. Continued work toward a goal of a < 60 minutes door-to-needle time is needed; but with notable progress, as door-to-needle time has decreased by 8% from the first alteplase administration to the most recent.
Overseen by the Simulations Department and the SPC, stroke code simulations (ie, mock stroke codes) are performed to aid in evaluating the acute stroke care process. Stroke simulation events should be an ongoing practice in any stroke program. It is an effective means to identify and address issues that may not otherwise be readily apparent.
Subacute Treatment
At DVAMC, postacute stroke care was identified as a priority. The SPC led a multidisciplinary team that was tasked with developing a postacute stroke care map, or integrated care pathway. Consistent care practices, a comprehensive tool to be used as a guide, can assist in improving outcomes, especially in a teaching facility with constantly changing medical and other clinical staff. The tool was developed using best practice guidelines from all disciplines. Staff members are encouraged to reference the pathway when caring for stroke patients, with necessary elements of care or performance measures in boldface to highlight their importance. Overall, DVAMC’s Best Care score (the percentage of patients whose care met all performance measures during the admission) rose from 57.1% to 78.6% over the course of the first year of the program.
Another key element of subacute stroke care is the provision of standardized patient stroke education. Before program initiation, stroke education at the DVAMC lacked consistency in both content and frequency. Secondary prevention should start at diagnosis, and education should be a continual process from admission to discharge. A patient booklet was developed that incorporated all required elements of stroke education per AHA guidelines: stroke risk factors, recognizing signs and symptoms, emergency activation, medications, and follow-up needs as well as other information, such as stroke pathophysiology, diet and activity, and managing lifestyle changes.7
Patient education templates were designed to facilitate documentation. Achieving this performance measure is a challenge not only for the DVAMC, but also for acute facilities nationwide. It requires involvement of the SPC as well as continual staff feedback and improvement challenges. Adherence to the patient education performance measure at the DVAMC improved from 0% meeting all 5 required elements at baseline to an average of 80% of patients.
A team of stroke champions representing each discipline involved in stroke care was recruited to be part of a postacute stroke team, led by the SPC. The team, consisting of neurologists, nurses, physical therapists, occupational therapists, speech therapists, nutritionists, social workers, and case managers, meets weekly for rounding on stroke patients, discussing patient care issues, assessing the effectiveness of the program, and addressing any system issues. This regular meeting facilitates collaboration and overall team building.
Rehabilitation and Follow-up
Routine physical, occupational, and speech therapy assessments are necessary to guide discharge planning. Although providing rehabilitation services is a priority, payer source can be a barrier to ideal rehabilitative care for DVAMC veterans. VA-based rehabilitation facilities are limited; therefore, community rehabilitation options, paid for by either VA funds or the patient’s insurance (if available), are used for the majority of stroke patients requiring these services. Efforts to increase access to stroke-specific rehabilitation options were undertaken by dedicated stroke champions at DVAMC; however, obtaining satisfactory payment agreements remains challenging.
Timely discharge is an element of care that the SPC also continually assesses. Discharge planning should begin on admission, and the SPC helps ensure that patient and caregiver needs are met and that all necessary follow-up and consultation visits have been scheduled. The LOS for stroke patients at the DVAMC had been on a steady upward trend from 6.39 days in 2005 to nearly 8 days in 2012. Over the course of 2013, the first year of the Stroke Program, stroke LOS decreased to just over 7 days (Figures 1 and 2).
Readmission rates are lower in high-risk populations when patients are seen for follow-up in the first 1 to 2 weeks postdischarge.8 Scheduling early visits can be challenging, especially in the current environment of an overburdened health care system. The DVAMC adopted the practice of Stroke Program follow-up phone calls, performed 7 to 10 days postdischarge. A standardized checklist of questions and dialogue was implemented that addressed common poststroke issues and education. Readmissions decreased from 21% in the first quarter of 2013, to 5% in the fourth quarter of 2013 after the implementation of this checklist follow-up. It is likely still too early to determine with any certainty whether the efforts aimed at improved patient education and early intervention are responsible for this decline.
Prevention and Education
Secondary prevention starts with stroke diagnosis and should include the patient and family/caregiver, when applicable. Inpatient stroke education was a priority early in the program. As the acute and postacute program developed, attention turned to community education and prevention.
Community education should emphasize early intervention. As elsewhere, the DVAMC found that the majority of patients present for care well outside the treatment window for alteplase administration. Based on national guidelines, IV alteplase must be initiated in selected patients within 4.5 hours of symptom onset. Many surveys confirm that patients are not able to accurately identify stroke symptoms or are not aware that stroke is a medical emergency. Challenges in stroke care lie in community education.9,10 The SPC met with primary care providers (PCPs) to coordinate educational and preventative efforts, recruiting them in primary and secondary prevention strategies and educating them on high-risk patients.
The SPC also collaborated with one of the outpatient clinic Patient Aligned Care Teams (PACT, or primary care team) on the development of a primary prevention program. The PACT initiated a risk reduction educational program after noting that many of their patients had suboptimal stroke risk factor management.
The project is still in the pilot stage but is showing promise regarding patient interest and participation. It is focused on addressing 4 major risk factors: hypertension, diabetes, hyperlipidemia, and tobacco use. Through a PACT report, patients were identified as having stroke risk factors that were not optimally controlled. The project aims to reduce the risk of stroke through education, goal setting, and lifestyle modification and saw a 25% rate of participation among those patients identified as candidates for the program. Of these participants, 100% completed all 4 sessions and rated the program highly favorable.
Quality Improvement Measures
Tracking performance measures should begin at program inception. “Measures improve fastest when they are being used. …Measurement and reporting with currently available data should begin immediately. …The implied message is this: since data will be impossible to ignore, we might as well make them better.”8 The VHA has a system for monitoring various quality measures, which include specific aspects of acute stroke care set forth by the VHA Stroke Directive: timely administration of alteplase, timely performance of NIHSS, and performance of a dysphagia screen prior to oral intake.
The DVAMC SPC began more comprehensive assessments of acute stroke care and evaluated elements of postacute stroke care, based on a nationally recognized set of performance measures. A system of tracking stroke performance data was initiated in the first month of the program and is based on the 10 stroke performance measures defined by the AHA and the Joint Commission. Data are currently analyzed independent of a national data management system that does not allow for national benchmarking; however, the analysis was a starting point to track facility progress and emphasized the need for consistent care. Along with collecting data on the 10 stroke-specific elements, the SPC began a system to follow duration of hospitalization, postdischarge ED visits, readmissions, and mortality rates, as well as stroke code and door-to-needle-time data. The data are shared with the DVAMC Critical Care Committee via monthly reports, program leadership via quarterly reports, facility leadership via annual reports, and facility staff through periodic e-mails and the all-employee share drive.
The first year of the program was associated with improvements in quality metrics across most areas of stroke care. Notably, 11 quality indicators that assess direct patient care measures have improved significantly from prior to program initiation in 2012 to after implementation of a comprehensive stroke care program at the conclusion of 2013. Those measures that were not already at goal of ≥ 85% achievement showed the most dramatic improvements (Figure 3).
Goals and Future Planning
The work of the DVAMC Stroke Program is far from over. Progress made is easily lost without continual monitoring and feedback. Challenges continue as well. Goals moving forward include improving door-to-needle times for IV alteplase therapy, more consistently performing swallow screens prior to oral intake, more consistently providing patient education, and increasing engagement with PCPs and the veteran community in providing stroke education and risk reduction.
A larger goal for future planning for the DVAMC is the need for a designated stroke care unit. Currently, stroke patients are admitted to the Critical Care Unit (CCU) for initial monitoring and treatment and when stable are moved to general medical wards. In some instances, this necessitates that the less acute patients occupy a CCU bed due to ward nursing limitations (ie, neuro checks every 2-hours is too great of a time demand for the ward nurses) or that the more neurologic acute patients are transferred to general medical wards when they would benefit from a more neurology-focused therapeutic environment. Stroke unit care has been associated with improved patient outcomes compared with care on general medical wards.11 The development of a designated stroke care unit is a long-range goal of the program.
Conclusion
The development of the Stroke Program, including an SPC, has improved the care of veterans with stroke at the DVAMC. The achievements of the DVAMC Stroke Program are the result of coordinated efforts of a team of dedicated health care professionals from all disciplines who sought to improve stroke care for veterans. The DVAMC continues to strive toward ever-improving outcomes, working with community partners and challenging itself to achieve a higher level of excellence. The lessons learned at the DVAMC may serve as a model for other VHA hospitals seeking to improve their stroke-related care programs.
Acknowledgements
The authors thank the executive leadership team and the chief of medicine of the DVAMC who recognized the need and potential for better stroke coordination and who have been fully supportive of the authors’ efforts to improve coordination, education, and care of their patients with strokes.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. QUERI—Quality Enhancement Research Initiative. Stroke QUERI. QUERI Website. http://www .queri.research.va.gov/str/default.cfm. Updated/Reviewed June 19, 2014. Accessed January 22, 2015.
2. Howard G, Evans GW, Pearce K, et al. Is the stroke belt disappearing? An analysis of racial, temporal, and age effects. Stroke. 1995;26(7):1153-1158.
3. Veterans Health Administration, U.S. Department of Veterans Affairs. Treatment of Acute Ischemic Stroke (AIS). VHA Directive 2011-038. U.S. Department of Veterans Affairs Website. http://www .va.gov/vhapublications/ViewPublication.asp?pub _ID=2458. Published November 2, 2011. Accessed January 22, 2015.
4. Green T, Newcommon N. Advancing nursing practice: The role of the nurse practitioner in an acute stroke program. J Neurosci Nurs. 2006;38(4 suppl):328-330.
5. Schwamm LH, Pancioli A, Acker JE III, et al; American Stroke Association’s Task Force on the Development of Stroke Systems. Recommendations for the establishment of stroke systems of care: Recommendations from the American Stroke Association’s Task Force on the Development of Stroke Systems. Stroke. 2005;36(3):690-703.
6. Bock BF. Response system for patients presenting with acute stroke. Paper presented at: Proceedings of a National Symposium on Rapid Identification and Treatment of Acute Stroke; December 12-13, 1996; Bethesda, MD. http://www.ninds.nih.gov/news_and _events/proceedings/stroke_proceedings/bock.htm.Published. Updated May 17, 2011. Accessed January 22, 2015.
7. American Heart Association, American Stroke Association. Stroke fact sheet. American Heart Association Website. http://www.heart.org/idc/groups/heart-public/@wcm/@private/@hcm/@gwtg/documents /downloadable/ucm_310976.pdf. Published April 2014. Accessed January 22, 2015.
8. Lee TH. Care redesign—A path forward for providers. N Engl J Med. 2012;367(5):466-472.
9. Kleindorfer D, Khoury J, Broderick JP, et al. Temporal trends in public awareness of stroke: Warning signs, risk factors, and treatment. Stroke. 2009;40(7):2502-2506.
10. Jauch EC, Saver JL, Adams HP Jr, et al; American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Perripheral Vascular Disease; Council on Clinical Cardiology. Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870-947.
11. How do stroke units improve patient outcomes? A collaborative systematic review of the randomized trials. Stroke Unit Trialists Collaboration. Stroke. 1997;28(11):2139-2144.
1. QUERI—Quality Enhancement Research Initiative. Stroke QUERI. QUERI Website. http://www .queri.research.va.gov/str/default.cfm. Updated/Reviewed June 19, 2014. Accessed January 22, 2015.
2. Howard G, Evans GW, Pearce K, et al. Is the stroke belt disappearing? An analysis of racial, temporal, and age effects. Stroke. 1995;26(7):1153-1158.
3. Veterans Health Administration, U.S. Department of Veterans Affairs. Treatment of Acute Ischemic Stroke (AIS). VHA Directive 2011-038. U.S. Department of Veterans Affairs Website. http://www .va.gov/vhapublications/ViewPublication.asp?pub _ID=2458. Published November 2, 2011. Accessed January 22, 2015.
4. Green T, Newcommon N. Advancing nursing practice: The role of the nurse practitioner in an acute stroke program. J Neurosci Nurs. 2006;38(4 suppl):328-330.
5. Schwamm LH, Pancioli A, Acker JE III, et al; American Stroke Association’s Task Force on the Development of Stroke Systems. Recommendations for the establishment of stroke systems of care: Recommendations from the American Stroke Association’s Task Force on the Development of Stroke Systems. Stroke. 2005;36(3):690-703.
6. Bock BF. Response system for patients presenting with acute stroke. Paper presented at: Proceedings of a National Symposium on Rapid Identification and Treatment of Acute Stroke; December 12-13, 1996; Bethesda, MD. http://www.ninds.nih.gov/news_and _events/proceedings/stroke_proceedings/bock.htm.Published. Updated May 17, 2011. Accessed January 22, 2015.
7. American Heart Association, American Stroke Association. Stroke fact sheet. American Heart Association Website. http://www.heart.org/idc/groups/heart-public/@wcm/@private/@hcm/@gwtg/documents /downloadable/ucm_310976.pdf. Published April 2014. Accessed January 22, 2015.
8. Lee TH. Care redesign—A path forward for providers. N Engl J Med. 2012;367(5):466-472.
9. Kleindorfer D, Khoury J, Broderick JP, et al. Temporal trends in public awareness of stroke: Warning signs, risk factors, and treatment. Stroke. 2009;40(7):2502-2506.
10. Jauch EC, Saver JL, Adams HP Jr, et al; American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Perripheral Vascular Disease; Council on Clinical Cardiology. Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870-947.
11. How do stroke units improve patient outcomes? A collaborative systematic review of the randomized trials. Stroke Unit Trialists Collaboration. Stroke. 1997;28(11):2139-2144.
Using Light to Manage Sleep-Wake Issues in Patients With Dementia
Care of patients with dementia requires dynamic, creative approaches. Given the high incidence of sleep-wake disturbances in this population and the concomitant caregiver stress and institutionalization, researchers at the Geriatric Research Education and Clinical Center (GRECC) at the Louis Stokes Cleveland (LSC) VAMC in Ohio are exploring light as a nonpharmacologic intervention to improve sleep-wake activity in veterans with dementia.1
Light has a powerful physiologic effect on human circadian rhythms, and those who live in northern latitudes or spend long periods inside buildings often have limited exposure to dramatic light-dark differences required for circadian entrainment to the solar day. This article is intended to give a brief overview of the relationship between light and human health and describe initial pilot studies in improving rest-activity patterns through lighting.
Light and the Aging Eye
Light is received at the back of the eye and absorbed by retinal cells, rods, and cones and by intrinsically photosensitive retinal ganglion cells that are specialized circadian light receptors. These specialized receptors respond most strongly to short-wavelength (blue) light. Nerve pathways lead from the retina to the suprachiasmatic nucleus, the circadian pacemaker, influencing the secretion and suppression of biomarkers, such as melatonin, cortisol, and hypocretin.2 Many hormonal systems, including the steroid axis, key on this 24-hour cycle that seems to be partially timed via the hormone melatonin.
Serum melatonin signals darkness and nighttime to the body. It rises in the early evening, peaks in the middle of the night, and is low during the daytime hours. Light exposure at night can suppress melatonin, which can in turn alter the timing of circadian rhythm peaks and troughs.
Related: Development and Evaluation of a Geriatric Mood Management Program
Normal aging of the eye can include good acuity. Most older adults retain 20/25 or better vision in 1 eye into their 70s and 80s. However, changes in the anatomy of the eye due to aging can reduce contrast sensitivity, color vision, and visual fields. Reduction of light to the retina due to these normal physiologic changes can impair the response to circadian light. By the eighth and ninth decades of life, the amount of circadian activating light reaching the retina is one-tenth that for a 10 year old; thus, brighter white light or more short-wavelength light is needed.3
In addition to the anatomic changes in the eye, a muted 24-hour light exposure pattern contributes to circadian disruption in older adults. For those with dementia, the circadian disruption is manifested in rest-activity disorders, such as sundowning and day-night disorientation. Yet patients with dementia residing at home or in nursing homes routinely are exposed to subdued light patterns. For example, according to the results of a study, nursing home residents in San Diego, California, had a median of 10.5 min/d of exposure to bright light (> 1,000 lux) and median illuminance was 52 lux during daylight hours.4
How can light levels be changed to make them optimal or even sufficient for health? The researchers considered this question when opting to study light and its possible effects on older patients with dementia.
Lighting interventions in nursing homes may be effective. For example, 2 hours of bright light exposure in the morning improved sleep efficiency (number of minutes sleeping divided by number of minutes in bed).5 Furthermore, 30 minutes of sunlight per day has been shown to reduce daytime napping.6 In an investigation of long-term exposure to bright light, participants in the experimental group had less than the expected decline of their Mini-Mental State Examination scores across 3.5 years, improved depression scores, and less functional decline in their activities of daily living.7 Thus, lighting may have therapeutic effects for institutionalized patients with dementia, particularly if there is prolonged exposure.
Although increasing light levels improves rest-activity patterns in those with dementia, implementation and adherence is a challenge due to discomfort and glare, difficulty maintaining the level of light exposure due to a person’s activity, and/or energy codes that restrict power consumption in nursing homes. Although many human studies have used mixed spectrum light at high light levels, evidence suggests that the circadian system is maximally sensitive to shorter wavelength blue light.8 Therefore, short-wavelength blue light can achieve the same clinical outcomes while using lower illuminations and obviating many of the issues with bright lights.
Dayroom Transformation
In “light” of this background, the LSC VAMC GRECC engaged in a transformation of a community living center (CLC) dayroom to introduce circadian lighting, determine its acceptance to patients and staff, and measure rest-activity measurements for 3 residents. The CLC ward specializes in the care of veterans with dementia and had recently undergone a cultural transformation into a neighborhood system with many activities still centered on the dayroom/dining room. Based on the research of colleagues at the Lighting Research Center (LRC) at Rensselaer Polytechnic Institute (RPI) in Troy, New York, scientists at General Electric (GE) Lighting division in Cleveland developed fluorescent lamps emitting light in the short-wavelength portion of the visible spectrum (lamps with correlated color temperature [CCT] of 14,000 kelvin [K]; typical commercial use lamps have a CCT of 3,000-5,000 K).
Related: Home-Based Videotelehealth for Veterans With Dementia
The 14,000 K lamp, which was perceived as bluish-white or “blue sky” light, was chosen for installation. According to the model of human circadian phototransduction (the process in which the retina converts light signals into neural signals for the circadian system), the 14,000 K lamp can affect the circadian system at light levels much lower than those used in previously published studies (400-500 lux compared with > 2,500 lux).9 Changes in lamp spectrum and total irradiance emitted offered an 8-fold increase in circadian stimulation over the existing lighting. The LSC Human Subjects Review Board approved the project.
Measurements in the CLC ward indicated that existing lighting in the halls and rooms was dim—between 75 lux and 100 lux. Although this level was similar to those reported in the literature and satisfactory for reading and general activities, it likely was not sufficient to stimulate residents’ circadian systems.4 The dayroom was selected for lamp installation, because it was used for dining and many daily activities, thus maximizing the number of veterans who could benefit from exposure to the new type of lighting.
The dayroom was large, 35 feet by 40 feet, and had windows on 3 sides. Illumination came from the windows, which had blinds and/or window air conditioning units, and 13 ceiling fluorescent light fixtures, each with 4 lamps. Using multiple light meter measurements, 14,000 K lamps were installed in 7 of 13 light fixtures to minimize significant engineering changes while maximizing the illumination.
The Table shows the illumination in lux in the dayroom with and without the 14,000 K lighting. Horizontal light levels, 3 feet above the floor and measured in a horizontal direction, increased from between 300 lux and 350 lux to 500 lux. The lamps added more light and contrast while not increasing glare or causing excessive brightness.
Five veterans with dementia consented (with family members involved), but due to actigraph malfunction, only 3 of the 5 participants completed the 2 data collection periods: 7 continuous days of rest/activity measurements under the regular ward lighting and experimental lighting plan with a 3-week adaptation period in between. Results were generally in the expected direction after exposure to new lighting: Sleep latency (time in bed until the first 20 minutes of sleep) improved, decreasing by 23%, and sleep efficiency increased by 6.6%. The new lighting was well received; there were no reports about heat or glare, and the staff frequently commented that the room looked as though it was in reflected sunlight. A new CLC building was subsequently built with excellent window access and lighting. Therefore, the lighting project was moved to the home of a test subject.
Home Lighting Projects
In a feasibility pilot, the light exposure and rest activity of an older veteran with dementia and his spouse was measured in their home.10,11 Neither were exposed to light > 400 lux for much of the 7 continuous days of measurement, and the majority of their waking hours was spent in light < 100 lux (insufficient for reading). Actigraphy data indicated fragmented nighttime sleep for both participants with the caregiver sleeping much less than the veteran.
Related: New Guidelines on Concussion and Sleep Disturbance
This pilot suggested that appropriate circadian lighting in the home could positively influence circadian sleep-wake cycles. Therefore, in collaboration with colleagues at the LRC at RPI and GE, the authors initiated a study funded by the National Institute on Aging (PI: Figueiro M) to install home lighting customized to the rooms used most during the day by veterans with dementia. In phase 1, the results showed that circadian disruption in those with dementia in winter months was significantly higher than in the summer months and that healthy older adults received more circadian light and were less disrupted than those with dementia.12 Phase 2 of the study, which is a pretest/posttest control group intervention of circadian lighting, is ongoing.
Conclusion
The research has not yet provided a definitive answer about whether circadian-active light can improve circadian synchrony and thereby benefit patients with dementia and their caregivers. Work in this area is translational and ongoing: The issues of dosing, timing, and delivery are still open questions for further research. The next steps related to testing light delivery and dose could include tailoring the daytime lighting in day care centers with blue lighting and/or testing the use of blue light goggles.
Acknowledgements
The work discussed in this paper was funded in part by the Cleveland VISN 10 GRECC and the National Institute on Aging (grant # R01AG034157; Figueiro PI). GE Lighting, Cleveland, OH, USA donated the lamps used in the study.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Vitiello MV, Borson S. Sleep disturbances in patients with Alzheimer’s disease: Epidemiology, pathophysiology and treatment. CNS Drugs. 2001;15(10):777-796.
2. Slats D, Claassen JA, Verbeek MM, Overeem S. Reciprocal interactions between sleep, circadian rhythms and Alzheimer’s disease: Focus on the role of hypocretin and melatonin. Ageing Res Rev. 2013;12(1):188-200.
3. Turner PL, Mainster MA. Circadian photoreception: Ageing and the eye’s important role in systemic health. Br J Ophthalmol. 2008;92(11):1439-1444.
4. Shochat T, Martin J, Marler M, Ancoli-Israel S. Illumination levels in nursing home patients: Effects on sleep and activity rhythms. J Sleep Res. 2000;9(4):373-379.
5. Fetveit A, Skjerve A, Bjorvatn B. Bright light treatment improves sleep in institutionalised elderly—an open trial. Int J Geriatr Psychiatry. 2003;18(6):520-526.
6. Alessi CA, Martin JL, Webber AP, Cynthia Kim E, Harker JO, Josephson KR. Randomized, controlled trial of a nonpharmacological intervention to improve abnormal sleep/wake patterns in nursing home residents. J Am Geriatr Soc. 2005;53(5):803-810.
7. Riemersma-van der Lek RF, Swaab DF, Twisk J, Hol EM, Hoogendijk WJ, Van Someren EJ. Effect of bright light and melatonin on cognitive and noncognitive function in elderly residents of group care facilities: A randomized controlled trial. JAMA. 2008;299(22):2642-2655.
8. Berson DM, Dunn FA, Takao M. Phototransduction by retinal ganglion cells that set the circadian clock. Science. 2002;295(5557):1070-1073.
9. Rea MS, Figueiro MG, Bullough JD, Bierman A. A model of phototransduction by the human circadian system. Brain Res Brain Res Rev. 2005;50(2):213-228.
10. Bierman A, Klein TR, Rea MS. The Daysimeter: A device for measuring optical radiation as a stimulus for the human circadian system. Meas Sci Technol. 2005;16(11):2292-2299.
11. Higgins PA, Hornick TR, Figueiro MG. Rest-activity and light exposure patterns in the home setting: A methodological case study. Am J Alzheimers Dis Other Demen. 2010;25(4):353-361.
12. Figueiro MG, Hamner R, Higgins P, Hornick T, Rea MS. Field measurements of light exposures and circadian disruption in two populations of older adults. J Alzheimers Dis. 2012;31(4):711-715.
Care of patients with dementia requires dynamic, creative approaches. Given the high incidence of sleep-wake disturbances in this population and the concomitant caregiver stress and institutionalization, researchers at the Geriatric Research Education and Clinical Center (GRECC) at the Louis Stokes Cleveland (LSC) VAMC in Ohio are exploring light as a nonpharmacologic intervention to improve sleep-wake activity in veterans with dementia.1
Light has a powerful physiologic effect on human circadian rhythms, and those who live in northern latitudes or spend long periods inside buildings often have limited exposure to dramatic light-dark differences required for circadian entrainment to the solar day. This article is intended to give a brief overview of the relationship between light and human health and describe initial pilot studies in improving rest-activity patterns through lighting.
Light and the Aging Eye
Light is received at the back of the eye and absorbed by retinal cells, rods, and cones and by intrinsically photosensitive retinal ganglion cells that are specialized circadian light receptors. These specialized receptors respond most strongly to short-wavelength (blue) light. Nerve pathways lead from the retina to the suprachiasmatic nucleus, the circadian pacemaker, influencing the secretion and suppression of biomarkers, such as melatonin, cortisol, and hypocretin.2 Many hormonal systems, including the steroid axis, key on this 24-hour cycle that seems to be partially timed via the hormone melatonin.
Serum melatonin signals darkness and nighttime to the body. It rises in the early evening, peaks in the middle of the night, and is low during the daytime hours. Light exposure at night can suppress melatonin, which can in turn alter the timing of circadian rhythm peaks and troughs.
Related: Development and Evaluation of a Geriatric Mood Management Program
Normal aging of the eye can include good acuity. Most older adults retain 20/25 or better vision in 1 eye into their 70s and 80s. However, changes in the anatomy of the eye due to aging can reduce contrast sensitivity, color vision, and visual fields. Reduction of light to the retina due to these normal physiologic changes can impair the response to circadian light. By the eighth and ninth decades of life, the amount of circadian activating light reaching the retina is one-tenth that for a 10 year old; thus, brighter white light or more short-wavelength light is needed.3
In addition to the anatomic changes in the eye, a muted 24-hour light exposure pattern contributes to circadian disruption in older adults. For those with dementia, the circadian disruption is manifested in rest-activity disorders, such as sundowning and day-night disorientation. Yet patients with dementia residing at home or in nursing homes routinely are exposed to subdued light patterns. For example, according to the results of a study, nursing home residents in San Diego, California, had a median of 10.5 min/d of exposure to bright light (> 1,000 lux) and median illuminance was 52 lux during daylight hours.4
How can light levels be changed to make them optimal or even sufficient for health? The researchers considered this question when opting to study light and its possible effects on older patients with dementia.
Lighting interventions in nursing homes may be effective. For example, 2 hours of bright light exposure in the morning improved sleep efficiency (number of minutes sleeping divided by number of minutes in bed).5 Furthermore, 30 minutes of sunlight per day has been shown to reduce daytime napping.6 In an investigation of long-term exposure to bright light, participants in the experimental group had less than the expected decline of their Mini-Mental State Examination scores across 3.5 years, improved depression scores, and less functional decline in their activities of daily living.7 Thus, lighting may have therapeutic effects for institutionalized patients with dementia, particularly if there is prolonged exposure.
Although increasing light levels improves rest-activity patterns in those with dementia, implementation and adherence is a challenge due to discomfort and glare, difficulty maintaining the level of light exposure due to a person’s activity, and/or energy codes that restrict power consumption in nursing homes. Although many human studies have used mixed spectrum light at high light levels, evidence suggests that the circadian system is maximally sensitive to shorter wavelength blue light.8 Therefore, short-wavelength blue light can achieve the same clinical outcomes while using lower illuminations and obviating many of the issues with bright lights.
Dayroom Transformation
In “light” of this background, the LSC VAMC GRECC engaged in a transformation of a community living center (CLC) dayroom to introduce circadian lighting, determine its acceptance to patients and staff, and measure rest-activity measurements for 3 residents. The CLC ward specializes in the care of veterans with dementia and had recently undergone a cultural transformation into a neighborhood system with many activities still centered on the dayroom/dining room. Based on the research of colleagues at the Lighting Research Center (LRC) at Rensselaer Polytechnic Institute (RPI) in Troy, New York, scientists at General Electric (GE) Lighting division in Cleveland developed fluorescent lamps emitting light in the short-wavelength portion of the visible spectrum (lamps with correlated color temperature [CCT] of 14,000 kelvin [K]; typical commercial use lamps have a CCT of 3,000-5,000 K).
Related: Home-Based Videotelehealth for Veterans With Dementia
The 14,000 K lamp, which was perceived as bluish-white or “blue sky” light, was chosen for installation. According to the model of human circadian phototransduction (the process in which the retina converts light signals into neural signals for the circadian system), the 14,000 K lamp can affect the circadian system at light levels much lower than those used in previously published studies (400-500 lux compared with > 2,500 lux).9 Changes in lamp spectrum and total irradiance emitted offered an 8-fold increase in circadian stimulation over the existing lighting. The LSC Human Subjects Review Board approved the project.
Measurements in the CLC ward indicated that existing lighting in the halls and rooms was dim—between 75 lux and 100 lux. Although this level was similar to those reported in the literature and satisfactory for reading and general activities, it likely was not sufficient to stimulate residents’ circadian systems.4 The dayroom was selected for lamp installation, because it was used for dining and many daily activities, thus maximizing the number of veterans who could benefit from exposure to the new type of lighting.
The dayroom was large, 35 feet by 40 feet, and had windows on 3 sides. Illumination came from the windows, which had blinds and/or window air conditioning units, and 13 ceiling fluorescent light fixtures, each with 4 lamps. Using multiple light meter measurements, 14,000 K lamps were installed in 7 of 13 light fixtures to minimize significant engineering changes while maximizing the illumination.
The Table shows the illumination in lux in the dayroom with and without the 14,000 K lighting. Horizontal light levels, 3 feet above the floor and measured in a horizontal direction, increased from between 300 lux and 350 lux to 500 lux. The lamps added more light and contrast while not increasing glare or causing excessive brightness.
Five veterans with dementia consented (with family members involved), but due to actigraph malfunction, only 3 of the 5 participants completed the 2 data collection periods: 7 continuous days of rest/activity measurements under the regular ward lighting and experimental lighting plan with a 3-week adaptation period in between. Results were generally in the expected direction after exposure to new lighting: Sleep latency (time in bed until the first 20 minutes of sleep) improved, decreasing by 23%, and sleep efficiency increased by 6.6%. The new lighting was well received; there were no reports about heat or glare, and the staff frequently commented that the room looked as though it was in reflected sunlight. A new CLC building was subsequently built with excellent window access and lighting. Therefore, the lighting project was moved to the home of a test subject.
Home Lighting Projects
In a feasibility pilot, the light exposure and rest activity of an older veteran with dementia and his spouse was measured in their home.10,11 Neither were exposed to light > 400 lux for much of the 7 continuous days of measurement, and the majority of their waking hours was spent in light < 100 lux (insufficient for reading). Actigraphy data indicated fragmented nighttime sleep for both participants with the caregiver sleeping much less than the veteran.
Related: New Guidelines on Concussion and Sleep Disturbance
This pilot suggested that appropriate circadian lighting in the home could positively influence circadian sleep-wake cycles. Therefore, in collaboration with colleagues at the LRC at RPI and GE, the authors initiated a study funded by the National Institute on Aging (PI: Figueiro M) to install home lighting customized to the rooms used most during the day by veterans with dementia. In phase 1, the results showed that circadian disruption in those with dementia in winter months was significantly higher than in the summer months and that healthy older adults received more circadian light and were less disrupted than those with dementia.12 Phase 2 of the study, which is a pretest/posttest control group intervention of circadian lighting, is ongoing.
Conclusion
The research has not yet provided a definitive answer about whether circadian-active light can improve circadian synchrony and thereby benefit patients with dementia and their caregivers. Work in this area is translational and ongoing: The issues of dosing, timing, and delivery are still open questions for further research. The next steps related to testing light delivery and dose could include tailoring the daytime lighting in day care centers with blue lighting and/or testing the use of blue light goggles.
Acknowledgements
The work discussed in this paper was funded in part by the Cleveland VISN 10 GRECC and the National Institute on Aging (grant # R01AG034157; Figueiro PI). GE Lighting, Cleveland, OH, USA donated the lamps used in the study.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Care of patients with dementia requires dynamic, creative approaches. Given the high incidence of sleep-wake disturbances in this population and the concomitant caregiver stress and institutionalization, researchers at the Geriatric Research Education and Clinical Center (GRECC) at the Louis Stokes Cleveland (LSC) VAMC in Ohio are exploring light as a nonpharmacologic intervention to improve sleep-wake activity in veterans with dementia.1
Light has a powerful physiologic effect on human circadian rhythms, and those who live in northern latitudes or spend long periods inside buildings often have limited exposure to dramatic light-dark differences required for circadian entrainment to the solar day. This article is intended to give a brief overview of the relationship between light and human health and describe initial pilot studies in improving rest-activity patterns through lighting.
Light and the Aging Eye
Light is received at the back of the eye and absorbed by retinal cells, rods, and cones and by intrinsically photosensitive retinal ganglion cells that are specialized circadian light receptors. These specialized receptors respond most strongly to short-wavelength (blue) light. Nerve pathways lead from the retina to the suprachiasmatic nucleus, the circadian pacemaker, influencing the secretion and suppression of biomarkers, such as melatonin, cortisol, and hypocretin.2 Many hormonal systems, including the steroid axis, key on this 24-hour cycle that seems to be partially timed via the hormone melatonin.
Serum melatonin signals darkness and nighttime to the body. It rises in the early evening, peaks in the middle of the night, and is low during the daytime hours. Light exposure at night can suppress melatonin, which can in turn alter the timing of circadian rhythm peaks and troughs.
Related: Development and Evaluation of a Geriatric Mood Management Program
Normal aging of the eye can include good acuity. Most older adults retain 20/25 or better vision in 1 eye into their 70s and 80s. However, changes in the anatomy of the eye due to aging can reduce contrast sensitivity, color vision, and visual fields. Reduction of light to the retina due to these normal physiologic changes can impair the response to circadian light. By the eighth and ninth decades of life, the amount of circadian activating light reaching the retina is one-tenth that for a 10 year old; thus, brighter white light or more short-wavelength light is needed.3
In addition to the anatomic changes in the eye, a muted 24-hour light exposure pattern contributes to circadian disruption in older adults. For those with dementia, the circadian disruption is manifested in rest-activity disorders, such as sundowning and day-night disorientation. Yet patients with dementia residing at home or in nursing homes routinely are exposed to subdued light patterns. For example, according to the results of a study, nursing home residents in San Diego, California, had a median of 10.5 min/d of exposure to bright light (> 1,000 lux) and median illuminance was 52 lux during daylight hours.4
How can light levels be changed to make them optimal or even sufficient for health? The researchers considered this question when opting to study light and its possible effects on older patients with dementia.
Lighting interventions in nursing homes may be effective. For example, 2 hours of bright light exposure in the morning improved sleep efficiency (number of minutes sleeping divided by number of minutes in bed).5 Furthermore, 30 minutes of sunlight per day has been shown to reduce daytime napping.6 In an investigation of long-term exposure to bright light, participants in the experimental group had less than the expected decline of their Mini-Mental State Examination scores across 3.5 years, improved depression scores, and less functional decline in their activities of daily living.7 Thus, lighting may have therapeutic effects for institutionalized patients with dementia, particularly if there is prolonged exposure.
Although increasing light levels improves rest-activity patterns in those with dementia, implementation and adherence is a challenge due to discomfort and glare, difficulty maintaining the level of light exposure due to a person’s activity, and/or energy codes that restrict power consumption in nursing homes. Although many human studies have used mixed spectrum light at high light levels, evidence suggests that the circadian system is maximally sensitive to shorter wavelength blue light.8 Therefore, short-wavelength blue light can achieve the same clinical outcomes while using lower illuminations and obviating many of the issues with bright lights.
Dayroom Transformation
In “light” of this background, the LSC VAMC GRECC engaged in a transformation of a community living center (CLC) dayroom to introduce circadian lighting, determine its acceptance to patients and staff, and measure rest-activity measurements for 3 residents. The CLC ward specializes in the care of veterans with dementia and had recently undergone a cultural transformation into a neighborhood system with many activities still centered on the dayroom/dining room. Based on the research of colleagues at the Lighting Research Center (LRC) at Rensselaer Polytechnic Institute (RPI) in Troy, New York, scientists at General Electric (GE) Lighting division in Cleveland developed fluorescent lamps emitting light in the short-wavelength portion of the visible spectrum (lamps with correlated color temperature [CCT] of 14,000 kelvin [K]; typical commercial use lamps have a CCT of 3,000-5,000 K).
Related: Home-Based Videotelehealth for Veterans With Dementia
The 14,000 K lamp, which was perceived as bluish-white or “blue sky” light, was chosen for installation. According to the model of human circadian phototransduction (the process in which the retina converts light signals into neural signals for the circadian system), the 14,000 K lamp can affect the circadian system at light levels much lower than those used in previously published studies (400-500 lux compared with > 2,500 lux).9 Changes in lamp spectrum and total irradiance emitted offered an 8-fold increase in circadian stimulation over the existing lighting. The LSC Human Subjects Review Board approved the project.
Measurements in the CLC ward indicated that existing lighting in the halls and rooms was dim—between 75 lux and 100 lux. Although this level was similar to those reported in the literature and satisfactory for reading and general activities, it likely was not sufficient to stimulate residents’ circadian systems.4 The dayroom was selected for lamp installation, because it was used for dining and many daily activities, thus maximizing the number of veterans who could benefit from exposure to the new type of lighting.
The dayroom was large, 35 feet by 40 feet, and had windows on 3 sides. Illumination came from the windows, which had blinds and/or window air conditioning units, and 13 ceiling fluorescent light fixtures, each with 4 lamps. Using multiple light meter measurements, 14,000 K lamps were installed in 7 of 13 light fixtures to minimize significant engineering changes while maximizing the illumination.
The Table shows the illumination in lux in the dayroom with and without the 14,000 K lighting. Horizontal light levels, 3 feet above the floor and measured in a horizontal direction, increased from between 300 lux and 350 lux to 500 lux. The lamps added more light and contrast while not increasing glare or causing excessive brightness.
Five veterans with dementia consented (with family members involved), but due to actigraph malfunction, only 3 of the 5 participants completed the 2 data collection periods: 7 continuous days of rest/activity measurements under the regular ward lighting and experimental lighting plan with a 3-week adaptation period in between. Results were generally in the expected direction after exposure to new lighting: Sleep latency (time in bed until the first 20 minutes of sleep) improved, decreasing by 23%, and sleep efficiency increased by 6.6%. The new lighting was well received; there were no reports about heat or glare, and the staff frequently commented that the room looked as though it was in reflected sunlight. A new CLC building was subsequently built with excellent window access and lighting. Therefore, the lighting project was moved to the home of a test subject.
Home Lighting Projects
In a feasibility pilot, the light exposure and rest activity of an older veteran with dementia and his spouse was measured in their home.10,11 Neither were exposed to light > 400 lux for much of the 7 continuous days of measurement, and the majority of their waking hours was spent in light < 100 lux (insufficient for reading). Actigraphy data indicated fragmented nighttime sleep for both participants with the caregiver sleeping much less than the veteran.
Related: New Guidelines on Concussion and Sleep Disturbance
This pilot suggested that appropriate circadian lighting in the home could positively influence circadian sleep-wake cycles. Therefore, in collaboration with colleagues at the LRC at RPI and GE, the authors initiated a study funded by the National Institute on Aging (PI: Figueiro M) to install home lighting customized to the rooms used most during the day by veterans with dementia. In phase 1, the results showed that circadian disruption in those with dementia in winter months was significantly higher than in the summer months and that healthy older adults received more circadian light and were less disrupted than those with dementia.12 Phase 2 of the study, which is a pretest/posttest control group intervention of circadian lighting, is ongoing.
Conclusion
The research has not yet provided a definitive answer about whether circadian-active light can improve circadian synchrony and thereby benefit patients with dementia and their caregivers. Work in this area is translational and ongoing: The issues of dosing, timing, and delivery are still open questions for further research. The next steps related to testing light delivery and dose could include tailoring the daytime lighting in day care centers with blue lighting and/or testing the use of blue light goggles.
Acknowledgements
The work discussed in this paper was funded in part by the Cleveland VISN 10 GRECC and the National Institute on Aging (grant # R01AG034157; Figueiro PI). GE Lighting, Cleveland, OH, USA donated the lamps used in the study.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Vitiello MV, Borson S. Sleep disturbances in patients with Alzheimer’s disease: Epidemiology, pathophysiology and treatment. CNS Drugs. 2001;15(10):777-796.
2. Slats D, Claassen JA, Verbeek MM, Overeem S. Reciprocal interactions between sleep, circadian rhythms and Alzheimer’s disease: Focus on the role of hypocretin and melatonin. Ageing Res Rev. 2013;12(1):188-200.
3. Turner PL, Mainster MA. Circadian photoreception: Ageing and the eye’s important role in systemic health. Br J Ophthalmol. 2008;92(11):1439-1444.
4. Shochat T, Martin J, Marler M, Ancoli-Israel S. Illumination levels in nursing home patients: Effects on sleep and activity rhythms. J Sleep Res. 2000;9(4):373-379.
5. Fetveit A, Skjerve A, Bjorvatn B. Bright light treatment improves sleep in institutionalised elderly—an open trial. Int J Geriatr Psychiatry. 2003;18(6):520-526.
6. Alessi CA, Martin JL, Webber AP, Cynthia Kim E, Harker JO, Josephson KR. Randomized, controlled trial of a nonpharmacological intervention to improve abnormal sleep/wake patterns in nursing home residents. J Am Geriatr Soc. 2005;53(5):803-810.
7. Riemersma-van der Lek RF, Swaab DF, Twisk J, Hol EM, Hoogendijk WJ, Van Someren EJ. Effect of bright light and melatonin on cognitive and noncognitive function in elderly residents of group care facilities: A randomized controlled trial. JAMA. 2008;299(22):2642-2655.
8. Berson DM, Dunn FA, Takao M. Phototransduction by retinal ganglion cells that set the circadian clock. Science. 2002;295(5557):1070-1073.
9. Rea MS, Figueiro MG, Bullough JD, Bierman A. A model of phototransduction by the human circadian system. Brain Res Brain Res Rev. 2005;50(2):213-228.
10. Bierman A, Klein TR, Rea MS. The Daysimeter: A device for measuring optical radiation as a stimulus for the human circadian system. Meas Sci Technol. 2005;16(11):2292-2299.
11. Higgins PA, Hornick TR, Figueiro MG. Rest-activity and light exposure patterns in the home setting: A methodological case study. Am J Alzheimers Dis Other Demen. 2010;25(4):353-361.
12. Figueiro MG, Hamner R, Higgins P, Hornick T, Rea MS. Field measurements of light exposures and circadian disruption in two populations of older adults. J Alzheimers Dis. 2012;31(4):711-715.
1. Vitiello MV, Borson S. Sleep disturbances in patients with Alzheimer’s disease: Epidemiology, pathophysiology and treatment. CNS Drugs. 2001;15(10):777-796.
2. Slats D, Claassen JA, Verbeek MM, Overeem S. Reciprocal interactions between sleep, circadian rhythms and Alzheimer’s disease: Focus on the role of hypocretin and melatonin. Ageing Res Rev. 2013;12(1):188-200.
3. Turner PL, Mainster MA. Circadian photoreception: Ageing and the eye’s important role in systemic health. Br J Ophthalmol. 2008;92(11):1439-1444.
4. Shochat T, Martin J, Marler M, Ancoli-Israel S. Illumination levels in nursing home patients: Effects on sleep and activity rhythms. J Sleep Res. 2000;9(4):373-379.
5. Fetveit A, Skjerve A, Bjorvatn B. Bright light treatment improves sleep in institutionalised elderly—an open trial. Int J Geriatr Psychiatry. 2003;18(6):520-526.
6. Alessi CA, Martin JL, Webber AP, Cynthia Kim E, Harker JO, Josephson KR. Randomized, controlled trial of a nonpharmacological intervention to improve abnormal sleep/wake patterns in nursing home residents. J Am Geriatr Soc. 2005;53(5):803-810.
7. Riemersma-van der Lek RF, Swaab DF, Twisk J, Hol EM, Hoogendijk WJ, Van Someren EJ. Effect of bright light and melatonin on cognitive and noncognitive function in elderly residents of group care facilities: A randomized controlled trial. JAMA. 2008;299(22):2642-2655.
8. Berson DM, Dunn FA, Takao M. Phototransduction by retinal ganglion cells that set the circadian clock. Science. 2002;295(5557):1070-1073.
9. Rea MS, Figueiro MG, Bullough JD, Bierman A. A model of phototransduction by the human circadian system. Brain Res Brain Res Rev. 2005;50(2):213-228.
10. Bierman A, Klein TR, Rea MS. The Daysimeter: A device for measuring optical radiation as a stimulus for the human circadian system. Meas Sci Technol. 2005;16(11):2292-2299.
11. Higgins PA, Hornick TR, Figueiro MG. Rest-activity and light exposure patterns in the home setting: A methodological case study. Am J Alzheimers Dis Other Demen. 2010;25(4):353-361.
12. Figueiro MG, Hamner R, Higgins P, Hornick T, Rea MS. Field measurements of light exposures and circadian disruption in two populations of older adults. J Alzheimers Dis. 2012;31(4):711-715.
Home-Based Video Telehealth for Veterans With Dementia
For nearly 4 decades, the unifying focus of the 2-site New England Geriatric Research Education and Clinical Center (GRECC) has been on dementia and related disorders. Veterans with dementia are an extremely vulnerable population with high rates of health care use that is projected to total > $203 billion in the U.S. in 2013.1 Their caregivers are also among the most burdened, having provided about 17.5 billion hours of unpaid care in 2012, which is valued at more than $216 billion.1 Additionally, spouses, who are the most common caregivers of persons with dementia, often experience poor health outcomes related to the experience of living with the afflicted spouse.2
Currently > 200,000 VA patients have dementia, and that number is expected to increase.3 Dementia is largely a disease of the elderly; thus, many veterans with dementia also have other medical and orthopedic conditions that increase their frailty and decrease their mobility. Behavioral and psychological symptoms are present in > 75% of people with dementia, contributing to the relative isolation of both those with dementia and their families.4
Disruption in routine and removal from familiar surroundings can cause many patients, particularly in the moderate stages of dementia, to become disoriented and agitated. For these patients, VA clinics can be unsettling and may reveal behavior that is not the same as the veterans’ behavior at home. For these reasons, veterans with dementia likely may benefit from remote access to health care via telehealth. However, current telehealth applications for this population are vastly underdeveloped.
Video Dementia Management
Many GRECCs and other VA geriatric programs provide video-based dementia evaluations and management at community-based outpatient clinics (CBOCs) affiliated with their medical centers. At this point, close to a dozen GRECC and geriatric programs nationally have geriatric psychiatrists, geriatricians, or neurologists conducting such visits from their office or clinic space with video links to a telehealth-enabled room in the corresponding CBOC.
The visits usually entail having the veteran and, when appropriate, a family member check in at the local CBOC for the appointment and receiving assistance throughout the video visit from the telehealth technician at the CBOC.
The technician assists with the technical aspects of the encounter, including establishing and maintaining the video link to the VA medical center (VAMC), and often is trained to administer a brief standardized mental status assessment. The telehealth technician also helps pass along the physician’s written recommendations to the veteran and family once the recommendation summary has been sent by e-mail or printed on the CBOC printer. These VAMC-CBOC video telehealth programs have been very popular with veterans, particularly those in rural settings, since traveling to the CBOC is usually more convenient.
Home-based Video Program
While CBOC-based video telehealth programs expand the population of veterans able to benefit from specialty dementia care, any travel out of the home can be challenging or disruptive for many veterans and their families. In addition, the performance and demeanor of a veteran with dementia in a clinic setting is sometimes different from that which the family describes as their more typical behavior at home.
A new in-home video telehealth program developed by the GRECC at the Edith Nourse Rogers Memorial Veterans Hospital in Bedford is addressing these issues. The Bedford site of the New England GRECC offers in-home clinical video telehealth services to community-dwelling veterans and caregivers as an extension of their Interdisciplinary Memory Assessment Continuity Clinic (IMACC). Currently, the percentage of IMACC veterans/caregivers who have voluntarily signed up for the program is nearly 30%. About 70% of the families that have enrolled to date have their video visits with their spouse caregivers.
Veterans participating in the home video telehealth program have had at least 1 in-person visit at the Bedford IMACC before being invited to join. Veterans and their caregivers are invited to participate in the GRECC home telehealth program either at the time of an in-person IMACC visit or afterward via a telephone call from either a provider or a member of the telehealth staff.
Telehealth visits are offered as a supplement to regularly scheduled in-person visits, not as a substitute. The frequency of telehealth visits is individualized, depending on the medical status of the veteran and preferences of the caregiver. Some participating families, finding the telehealth format much more convenient, have asked whether they could postpone upcoming in-person visits at the VAMC. Many patients are particularly interested in minimizing medical visits in the winter months in New England.
Case Example
A male World War II veteran with moderate stage dementia lived with his wife in an apartment down the street from his adult son and daughter-in-law. His son and daughter-in-law visited and helped with the veteran’s care most days, but his wife was his primary caregiver. However, due to her own mobility issues, she was unable to attend the veteran’s in-person IMACC initial evaluation or subsequent follow-up visit.
This family enthusiastically embraced the opportunity to participate in the home video telehealth program and had multiple telehealth visits. During these video encounters, the veteran, his wife, and his son and daughter-in-law were present. The clinician, communicating via computer from the Bedford VAMC, was able to hear from all the caregivers, observe the veteran as he interacted with each person, and watch as he walked within the comfort and familiarity of his home.
Based on these observations, the veteran was clearly at risk for falls. The clinician ordered a home safety consultation as a result. Thus the home video telehealth program allowed this veteran’s mobility-impaired wife to participate directly in his dementia care. It gave the clinician an opportunity to spot potential fall risks within the veteran’s home before a disabling fall and provided the entire family with additional, convenient dementia-related care beyond the standard in-person VAMC visits.
Establishing Home Video Links
Veterans must already have broadband Internet access and a home computer or laptop to participate in the program. To assess the connectivity status and computer comfort level of the family, a Bedford VAMC telehealth technician calls the caregiver to assess their computer, operating system, presence of a webcam, and Internet service provider.
In addition to assessing the equipment necessary for the telehealth visit, the Bedford VAMC telehealth team also determines whether or not the caregiver has had experience with videoconferencing. Based on this information, the proper level of support is given to the family for both the initial software and, when necessary, VA-provided webcam installation.
On a few occasions, program staff have visited the veteran’s home to install the software and camera. Thus the telehealth program is fit to the family needs and resources to ensure a successful visit. The Bedford VAMC telehealth team provides enrolled families with live phone-based support for download and installation of the VA-approved videoconferencing software and webcam. For each scheduled video telehealth visit, a telehealth technician is available via phone to assist the caregiver with initiating the video call to the clinician.
Next Steps
GRECC neurologist Lauren Moo, MD, is leading this telehealth initiative as a clinical demonstration project and is studying implementation of the service. Dr. Moo is collecting data on whether IMACC veterans/caregivers accept or decline enrollment and their reasons for declining. The goal is to empirically determine the degree to which age, Internet access, and other variables are barriers to wider adoption.
Dr. Moo predicts that the improved access to clinical care offered by home video telehealth will translate into reduced hotline calls, emergency department visits, and delay in community living center placement. Easier access should facilitate earlier intervention for common dementia-related issues, such as fall risk, behavioral symptoms, and disruption of circadian rhythm, thereby improving quality of life and reducing overall health care utilization for this growing population of veterans.
There is the perception that geriatric veterans are not “wired” for Internet-based communications or lack the technical proficiency to use current and evolving technologies. However, a recent national survey suggests that while only 34% of those aged > 75 years use the Internet, there has been a significant jump in the percentage of Americans aged ≥ 65 years that use the Internet or e-mail: from 40% in 2010 to 53% in 2012.5
Once online, 70% of adults aged ≥ 65 years use the Internet on a typical day, suggesting that when given the necessary tools and training, seniors are enthusiastic technology adopters.5 Thus, it is anticipated that the number of geriatric veterans interested in and able to take advantage of the in-home video visit format will grow rapidly in the near future. The initial enrollment rate at Bedford of 30% is expected to grow as families and providers become more familiar with this modality.
The Bedford VAMC is in an urban/suburban region with multiple Internet service providers, a relatively educated population, and comparatively low levels of poverty. As such, the Bedford VAMC veterans with dementia and their caregivers are likely a best-case scenario population in which to pilot this dementia home telehealth program. If the preliminary success of this pilot program is sustained, expansion to a broader range of home telehealth services, such as social work and home safety assessments, to more rural settings would be the logical next steps.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Thies W, Bleiler L; Alzheimer’s Association. 2013 Alzheimer’s disease facts and figures. Alzheimers Dement. 2013;9(2):208-245.
2. Kolanowski AM, Fick D, Waller JL, Shea D. Spouses of persons with dementia: Their healthcare problems, utilization, and costs. Res Nurs Health. 2004;27(5):296-306.
3. Veterans Health Administration Office of the Assistant Deputy Under Secretary for Health for Policy and Planning. Projections of the prevalence and incidence of dementias including Alzheimer’s Disease for the total, enrolled, and patient veteran populations age 65 or over. U.S. Department of Veterans Affairs Website. http://www4.va.gov/healthpolicyplanning/dementia/Dem022004.pdf. Published February 20, 2004. Accessed October 10, 2014.
4. Lyketsos CG, Lopez O, Jones B, Fitzpatrick AL, Breitner J, DeKosky S. Prevalence of neuropsychiatric symptoms in dementia and mild cognitive impairment: Results from the cardiovascular health study. JAMA. 2002;288(12):1475-1483.
5. Zickuhr K, Madden M. Older adults and Internet use. Pew Research Center’s Internet & American Life Project Website. http://pewinternet.org/Reports/2012/Older-adults-and-internet-use.aspx. Updated June 6, 2012. Accessed October 17, 2014.
For nearly 4 decades, the unifying focus of the 2-site New England Geriatric Research Education and Clinical Center (GRECC) has been on dementia and related disorders. Veterans with dementia are an extremely vulnerable population with high rates of health care use that is projected to total > $203 billion in the U.S. in 2013.1 Their caregivers are also among the most burdened, having provided about 17.5 billion hours of unpaid care in 2012, which is valued at more than $216 billion.1 Additionally, spouses, who are the most common caregivers of persons with dementia, often experience poor health outcomes related to the experience of living with the afflicted spouse.2
Currently > 200,000 VA patients have dementia, and that number is expected to increase.3 Dementia is largely a disease of the elderly; thus, many veterans with dementia also have other medical and orthopedic conditions that increase their frailty and decrease their mobility. Behavioral and psychological symptoms are present in > 75% of people with dementia, contributing to the relative isolation of both those with dementia and their families.4
Disruption in routine and removal from familiar surroundings can cause many patients, particularly in the moderate stages of dementia, to become disoriented and agitated. For these patients, VA clinics can be unsettling and may reveal behavior that is not the same as the veterans’ behavior at home. For these reasons, veterans with dementia likely may benefit from remote access to health care via telehealth. However, current telehealth applications for this population are vastly underdeveloped.
Video Dementia Management
Many GRECCs and other VA geriatric programs provide video-based dementia evaluations and management at community-based outpatient clinics (CBOCs) affiliated with their medical centers. At this point, close to a dozen GRECC and geriatric programs nationally have geriatric psychiatrists, geriatricians, or neurologists conducting such visits from their office or clinic space with video links to a telehealth-enabled room in the corresponding CBOC.
The visits usually entail having the veteran and, when appropriate, a family member check in at the local CBOC for the appointment and receiving assistance throughout the video visit from the telehealth technician at the CBOC.
The technician assists with the technical aspects of the encounter, including establishing and maintaining the video link to the VA medical center (VAMC), and often is trained to administer a brief standardized mental status assessment. The telehealth technician also helps pass along the physician’s written recommendations to the veteran and family once the recommendation summary has been sent by e-mail or printed on the CBOC printer. These VAMC-CBOC video telehealth programs have been very popular with veterans, particularly those in rural settings, since traveling to the CBOC is usually more convenient.
Home-based Video Program
While CBOC-based video telehealth programs expand the population of veterans able to benefit from specialty dementia care, any travel out of the home can be challenging or disruptive for many veterans and their families. In addition, the performance and demeanor of a veteran with dementia in a clinic setting is sometimes different from that which the family describes as their more typical behavior at home.
A new in-home video telehealth program developed by the GRECC at the Edith Nourse Rogers Memorial Veterans Hospital in Bedford is addressing these issues. The Bedford site of the New England GRECC offers in-home clinical video telehealth services to community-dwelling veterans and caregivers as an extension of their Interdisciplinary Memory Assessment Continuity Clinic (IMACC). Currently, the percentage of IMACC veterans/caregivers who have voluntarily signed up for the program is nearly 30%. About 70% of the families that have enrolled to date have their video visits with their spouse caregivers.
Veterans participating in the home video telehealth program have had at least 1 in-person visit at the Bedford IMACC before being invited to join. Veterans and their caregivers are invited to participate in the GRECC home telehealth program either at the time of an in-person IMACC visit or afterward via a telephone call from either a provider or a member of the telehealth staff.
Telehealth visits are offered as a supplement to regularly scheduled in-person visits, not as a substitute. The frequency of telehealth visits is individualized, depending on the medical status of the veteran and preferences of the caregiver. Some participating families, finding the telehealth format much more convenient, have asked whether they could postpone upcoming in-person visits at the VAMC. Many patients are particularly interested in minimizing medical visits in the winter months in New England.
Case Example
A male World War II veteran with moderate stage dementia lived with his wife in an apartment down the street from his adult son and daughter-in-law. His son and daughter-in-law visited and helped with the veteran’s care most days, but his wife was his primary caregiver. However, due to her own mobility issues, she was unable to attend the veteran’s in-person IMACC initial evaluation or subsequent follow-up visit.
This family enthusiastically embraced the opportunity to participate in the home video telehealth program and had multiple telehealth visits. During these video encounters, the veteran, his wife, and his son and daughter-in-law were present. The clinician, communicating via computer from the Bedford VAMC, was able to hear from all the caregivers, observe the veteran as he interacted with each person, and watch as he walked within the comfort and familiarity of his home.
Based on these observations, the veteran was clearly at risk for falls. The clinician ordered a home safety consultation as a result. Thus the home video telehealth program allowed this veteran’s mobility-impaired wife to participate directly in his dementia care. It gave the clinician an opportunity to spot potential fall risks within the veteran’s home before a disabling fall and provided the entire family with additional, convenient dementia-related care beyond the standard in-person VAMC visits.
Establishing Home Video Links
Veterans must already have broadband Internet access and a home computer or laptop to participate in the program. To assess the connectivity status and computer comfort level of the family, a Bedford VAMC telehealth technician calls the caregiver to assess their computer, operating system, presence of a webcam, and Internet service provider.
In addition to assessing the equipment necessary for the telehealth visit, the Bedford VAMC telehealth team also determines whether or not the caregiver has had experience with videoconferencing. Based on this information, the proper level of support is given to the family for both the initial software and, when necessary, VA-provided webcam installation.
On a few occasions, program staff have visited the veteran’s home to install the software and camera. Thus the telehealth program is fit to the family needs and resources to ensure a successful visit. The Bedford VAMC telehealth team provides enrolled families with live phone-based support for download and installation of the VA-approved videoconferencing software and webcam. For each scheduled video telehealth visit, a telehealth technician is available via phone to assist the caregiver with initiating the video call to the clinician.
Next Steps
GRECC neurologist Lauren Moo, MD, is leading this telehealth initiative as a clinical demonstration project and is studying implementation of the service. Dr. Moo is collecting data on whether IMACC veterans/caregivers accept or decline enrollment and their reasons for declining. The goal is to empirically determine the degree to which age, Internet access, and other variables are barriers to wider adoption.
Dr. Moo predicts that the improved access to clinical care offered by home video telehealth will translate into reduced hotline calls, emergency department visits, and delay in community living center placement. Easier access should facilitate earlier intervention for common dementia-related issues, such as fall risk, behavioral symptoms, and disruption of circadian rhythm, thereby improving quality of life and reducing overall health care utilization for this growing population of veterans.
There is the perception that geriatric veterans are not “wired” for Internet-based communications or lack the technical proficiency to use current and evolving technologies. However, a recent national survey suggests that while only 34% of those aged > 75 years use the Internet, there has been a significant jump in the percentage of Americans aged ≥ 65 years that use the Internet or e-mail: from 40% in 2010 to 53% in 2012.5
Once online, 70% of adults aged ≥ 65 years use the Internet on a typical day, suggesting that when given the necessary tools and training, seniors are enthusiastic technology adopters.5 Thus, it is anticipated that the number of geriatric veterans interested in and able to take advantage of the in-home video visit format will grow rapidly in the near future. The initial enrollment rate at Bedford of 30% is expected to grow as families and providers become more familiar with this modality.
The Bedford VAMC is in an urban/suburban region with multiple Internet service providers, a relatively educated population, and comparatively low levels of poverty. As such, the Bedford VAMC veterans with dementia and their caregivers are likely a best-case scenario population in which to pilot this dementia home telehealth program. If the preliminary success of this pilot program is sustained, expansion to a broader range of home telehealth services, such as social work and home safety assessments, to more rural settings would be the logical next steps.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
For nearly 4 decades, the unifying focus of the 2-site New England Geriatric Research Education and Clinical Center (GRECC) has been on dementia and related disorders. Veterans with dementia are an extremely vulnerable population with high rates of health care use that is projected to total > $203 billion in the U.S. in 2013.1 Their caregivers are also among the most burdened, having provided about 17.5 billion hours of unpaid care in 2012, which is valued at more than $216 billion.1 Additionally, spouses, who are the most common caregivers of persons with dementia, often experience poor health outcomes related to the experience of living with the afflicted spouse.2
Currently > 200,000 VA patients have dementia, and that number is expected to increase.3 Dementia is largely a disease of the elderly; thus, many veterans with dementia also have other medical and orthopedic conditions that increase their frailty and decrease their mobility. Behavioral and psychological symptoms are present in > 75% of people with dementia, contributing to the relative isolation of both those with dementia and their families.4
Disruption in routine and removal from familiar surroundings can cause many patients, particularly in the moderate stages of dementia, to become disoriented and agitated. For these patients, VA clinics can be unsettling and may reveal behavior that is not the same as the veterans’ behavior at home. For these reasons, veterans with dementia likely may benefit from remote access to health care via telehealth. However, current telehealth applications for this population are vastly underdeveloped.
Video Dementia Management
Many GRECCs and other VA geriatric programs provide video-based dementia evaluations and management at community-based outpatient clinics (CBOCs) affiliated with their medical centers. At this point, close to a dozen GRECC and geriatric programs nationally have geriatric psychiatrists, geriatricians, or neurologists conducting such visits from their office or clinic space with video links to a telehealth-enabled room in the corresponding CBOC.
The visits usually entail having the veteran and, when appropriate, a family member check in at the local CBOC for the appointment and receiving assistance throughout the video visit from the telehealth technician at the CBOC.
The technician assists with the technical aspects of the encounter, including establishing and maintaining the video link to the VA medical center (VAMC), and often is trained to administer a brief standardized mental status assessment. The telehealth technician also helps pass along the physician’s written recommendations to the veteran and family once the recommendation summary has been sent by e-mail or printed on the CBOC printer. These VAMC-CBOC video telehealth programs have been very popular with veterans, particularly those in rural settings, since traveling to the CBOC is usually more convenient.
Home-based Video Program
While CBOC-based video telehealth programs expand the population of veterans able to benefit from specialty dementia care, any travel out of the home can be challenging or disruptive for many veterans and their families. In addition, the performance and demeanor of a veteran with dementia in a clinic setting is sometimes different from that which the family describes as their more typical behavior at home.
A new in-home video telehealth program developed by the GRECC at the Edith Nourse Rogers Memorial Veterans Hospital in Bedford is addressing these issues. The Bedford site of the New England GRECC offers in-home clinical video telehealth services to community-dwelling veterans and caregivers as an extension of their Interdisciplinary Memory Assessment Continuity Clinic (IMACC). Currently, the percentage of IMACC veterans/caregivers who have voluntarily signed up for the program is nearly 30%. About 70% of the families that have enrolled to date have their video visits with their spouse caregivers.
Veterans participating in the home video telehealth program have had at least 1 in-person visit at the Bedford IMACC before being invited to join. Veterans and their caregivers are invited to participate in the GRECC home telehealth program either at the time of an in-person IMACC visit or afterward via a telephone call from either a provider or a member of the telehealth staff.
Telehealth visits are offered as a supplement to regularly scheduled in-person visits, not as a substitute. The frequency of telehealth visits is individualized, depending on the medical status of the veteran and preferences of the caregiver. Some participating families, finding the telehealth format much more convenient, have asked whether they could postpone upcoming in-person visits at the VAMC. Many patients are particularly interested in minimizing medical visits in the winter months in New England.
Case Example
A male World War II veteran with moderate stage dementia lived with his wife in an apartment down the street from his adult son and daughter-in-law. His son and daughter-in-law visited and helped with the veteran’s care most days, but his wife was his primary caregiver. However, due to her own mobility issues, she was unable to attend the veteran’s in-person IMACC initial evaluation or subsequent follow-up visit.
This family enthusiastically embraced the opportunity to participate in the home video telehealth program and had multiple telehealth visits. During these video encounters, the veteran, his wife, and his son and daughter-in-law were present. The clinician, communicating via computer from the Bedford VAMC, was able to hear from all the caregivers, observe the veteran as he interacted with each person, and watch as he walked within the comfort and familiarity of his home.
Based on these observations, the veteran was clearly at risk for falls. The clinician ordered a home safety consultation as a result. Thus the home video telehealth program allowed this veteran’s mobility-impaired wife to participate directly in his dementia care. It gave the clinician an opportunity to spot potential fall risks within the veteran’s home before a disabling fall and provided the entire family with additional, convenient dementia-related care beyond the standard in-person VAMC visits.
Establishing Home Video Links
Veterans must already have broadband Internet access and a home computer or laptop to participate in the program. To assess the connectivity status and computer comfort level of the family, a Bedford VAMC telehealth technician calls the caregiver to assess their computer, operating system, presence of a webcam, and Internet service provider.
In addition to assessing the equipment necessary for the telehealth visit, the Bedford VAMC telehealth team also determines whether or not the caregiver has had experience with videoconferencing. Based on this information, the proper level of support is given to the family for both the initial software and, when necessary, VA-provided webcam installation.
On a few occasions, program staff have visited the veteran’s home to install the software and camera. Thus the telehealth program is fit to the family needs and resources to ensure a successful visit. The Bedford VAMC telehealth team provides enrolled families with live phone-based support for download and installation of the VA-approved videoconferencing software and webcam. For each scheduled video telehealth visit, a telehealth technician is available via phone to assist the caregiver with initiating the video call to the clinician.
Next Steps
GRECC neurologist Lauren Moo, MD, is leading this telehealth initiative as a clinical demonstration project and is studying implementation of the service. Dr. Moo is collecting data on whether IMACC veterans/caregivers accept or decline enrollment and their reasons for declining. The goal is to empirically determine the degree to which age, Internet access, and other variables are barriers to wider adoption.
Dr. Moo predicts that the improved access to clinical care offered by home video telehealth will translate into reduced hotline calls, emergency department visits, and delay in community living center placement. Easier access should facilitate earlier intervention for common dementia-related issues, such as fall risk, behavioral symptoms, and disruption of circadian rhythm, thereby improving quality of life and reducing overall health care utilization for this growing population of veterans.
There is the perception that geriatric veterans are not “wired” for Internet-based communications or lack the technical proficiency to use current and evolving technologies. However, a recent national survey suggests that while only 34% of those aged > 75 years use the Internet, there has been a significant jump in the percentage of Americans aged ≥ 65 years that use the Internet or e-mail: from 40% in 2010 to 53% in 2012.5
Once online, 70% of adults aged ≥ 65 years use the Internet on a typical day, suggesting that when given the necessary tools and training, seniors are enthusiastic technology adopters.5 Thus, it is anticipated that the number of geriatric veterans interested in and able to take advantage of the in-home video visit format will grow rapidly in the near future. The initial enrollment rate at Bedford of 30% is expected to grow as families and providers become more familiar with this modality.
The Bedford VAMC is in an urban/suburban region with multiple Internet service providers, a relatively educated population, and comparatively low levels of poverty. As such, the Bedford VAMC veterans with dementia and their caregivers are likely a best-case scenario population in which to pilot this dementia home telehealth program. If the preliminary success of this pilot program is sustained, expansion to a broader range of home telehealth services, such as social work and home safety assessments, to more rural settings would be the logical next steps.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Thies W, Bleiler L; Alzheimer’s Association. 2013 Alzheimer’s disease facts and figures. Alzheimers Dement. 2013;9(2):208-245.
2. Kolanowski AM, Fick D, Waller JL, Shea D. Spouses of persons with dementia: Their healthcare problems, utilization, and costs. Res Nurs Health. 2004;27(5):296-306.
3. Veterans Health Administration Office of the Assistant Deputy Under Secretary for Health for Policy and Planning. Projections of the prevalence and incidence of dementias including Alzheimer’s Disease for the total, enrolled, and patient veteran populations age 65 or over. U.S. Department of Veterans Affairs Website. http://www4.va.gov/healthpolicyplanning/dementia/Dem022004.pdf. Published February 20, 2004. Accessed October 10, 2014.
4. Lyketsos CG, Lopez O, Jones B, Fitzpatrick AL, Breitner J, DeKosky S. Prevalence of neuropsychiatric symptoms in dementia and mild cognitive impairment: Results from the cardiovascular health study. JAMA. 2002;288(12):1475-1483.
5. Zickuhr K, Madden M. Older adults and Internet use. Pew Research Center’s Internet & American Life Project Website. http://pewinternet.org/Reports/2012/Older-adults-and-internet-use.aspx. Updated June 6, 2012. Accessed October 17, 2014.
1. Thies W, Bleiler L; Alzheimer’s Association. 2013 Alzheimer’s disease facts and figures. Alzheimers Dement. 2013;9(2):208-245.
2. Kolanowski AM, Fick D, Waller JL, Shea D. Spouses of persons with dementia: Their healthcare problems, utilization, and costs. Res Nurs Health. 2004;27(5):296-306.
3. Veterans Health Administration Office of the Assistant Deputy Under Secretary for Health for Policy and Planning. Projections of the prevalence and incidence of dementias including Alzheimer’s Disease for the total, enrolled, and patient veteran populations age 65 or over. U.S. Department of Veterans Affairs Website. http://www4.va.gov/healthpolicyplanning/dementia/Dem022004.pdf. Published February 20, 2004. Accessed October 10, 2014.
4. Lyketsos CG, Lopez O, Jones B, Fitzpatrick AL, Breitner J, DeKosky S. Prevalence of neuropsychiatric symptoms in dementia and mild cognitive impairment: Results from the cardiovascular health study. JAMA. 2002;288(12):1475-1483.
5. Zickuhr K, Madden M. Older adults and Internet use. Pew Research Center’s Internet & American Life Project Website. http://pewinternet.org/Reports/2012/Older-adults-and-internet-use.aspx. Updated June 6, 2012. Accessed October 17, 2014.
Primary Care Medical Services for Homeless Veterans
On a single night in 2012, 62,619 veterans experienced homelessness.1 With high rates of illness, as well as alcohol, tobacco, and other drug (ATOD) use among homeless adults, ending veteran homelessness is a signature initiative of the VA.2-4 However, despite increasing efforts to improve health care for homeless individuals, little is known about best practices in homeless-focused primary care.2,5
With an age-adjusted mortality that is 2 to 10 times higher than that of their housed counterparts, homeless veterans pose a formidable challenge for primary care providers (PCPs).6,7 The complexity of homeless persons’ primary care needs is compounded by poor social support and the need to navigate priorities (eg, shelter) that compete with medical care.6,8,9 Moreover, veterans may face unique vulnerabilities conferred by military-specific experiences.2,10
As of 2012, only 2 VA facilities had primary care clinics tailored to the needs of homeless veterans. McGuire and colleagues built a system of colocated primary care, mental health, and homeless services for mentally ill veterans in Los Angeles, California.11 Over 18 months, this clinic facilitated greater primary and preventive care delivery, though the population’s physical health status did not improve.11 More recently, O’Toole and colleagues implemented a homeless-focused primary care clinic in Providence, Rhode Island.6 Compared with a historical sample of homeless veterans in traditional VA primary care, veterans in this homeless-tailored clinic had greater improvements in some chronic disease outcomes.6 This clinic also decreased nonacute emergency department (ED) use and hospitalizations for general medical conditions.6
Despite these promising outcomes, the VA lacked a nationwide homeless-focused primary care initiative. In 2012 the VA Office of Homeless Programs and the Office of Primary Care Operations funded a national demonstration project to create Homeless Patient-Aligned Care Teams (HPACTs)—primary care medical clinics for homeless veterans—at 32 facilities. This demonstration project guided HPACTs to tailor clinical and social services to homeless veterans’ needs, establish processes to identify and refer appropriate veterans, and integrate distinct services.
There were no explicit instructions that detailed HPACT structure. Because new VA programs must fit local contextual factors, including infrastructure, space, personnel, and institutional/community resources, different models of homeless-focused primary care have evolved.
This article is a case study of HPACTs at 3 of the 32 participating VA facilities, each reflecting a distinct community and organizational context. In light of projected HPACT expansion and concerns that current services are better tailored to sheltered homeless veterans than to their unsheltered peers, there is particular importance to detailed clinic descriptions that vividly portray the intricate relationships between service design and populations served.1
METHODS
VA HPACTs established in May 2012 at 3 facilities were examined: Birmingham VAMC in Alabama (BIR), West Los Angeles VAMC in California (WLA), and VA Pittsburgh Healthcare System in Pennsylvania (PIT). Prior to this demonstration project, each facility offered a range of housing/social services and traditional primary care for veterans. These sites are a geographically diverse convenience sample that emerged from existing homeless-focused collaborations among the authors and represent geographically diverse HPACTs.
The national director of VA Homeless Programs formally determined that this comparison constitutes a VA operations activity that is not research.12 This activity was exempt from Institutional Review Board review.
Study Design
Timed at an early stage of HPACT implementation, this project had 3 aims: (1) To identify noteworthy similarities and/or differences among the initial HPACT clinic structures; (2) To compare and contrast the patient characteristics of veterans enrolled in each of these clinics; and (3) To use these data to inform ongoing HPACT service design.
HPACT program evaluation data are not presented. Rather, a nascent system of care is illustrated that contributes to the limited literature concerning the design and implementation of homeless-focused primary care. Such organizational profiles inform novel program delivery and hold particular utility for heterogeneous populations who are difficult to engage in care.13,14
Authors at each site independently developed lists of variables that fell within the 3 guiding principles of this demonstration project. These variables were compiled and iteratively reduced to a consolidated table that assessed each clinic, including location, operating hours, methods of patient identification and referral, and linkages to distinct services (eg, primary care, mental health, addiction, and social services).
This table also became a guide for HPACT directors to generate narrative clinic descriptions. Characteristics of VA medical homes that are embraced regardless of patients’ housing status (eg, patient-centered, team-based care) were also incorporated into these descriptions.15
Patient Characteristics
The VA electronic health record (EHR) was used to identify all patients enrolled in HPACTs at BIR, WLA, and PIT from May 1, 2012 (clinic inception), through September 30, 2012. Authors developed a standardized template for EHR review and coined the first HPACT record as the patient’s index visit. This record was used to code initial housing status, demographics, and acute medical conditions diagnosed/treated. If housing status was not recorded at the index visit, the first preceding informative record was used.
Records for 6 months preceding the index visit were used to identify the presence or absence of common medical conditions, psychiatric diagnoses, and ATOD abuse or dependence. Medical conditions were identified from a list of common outpatient diagnoses from the National Ambulatory Medical Care Survey, supplemented by common conditions among homeless men.16-18 The EHR problem list (a list of diagnoses, by patient) was used to obtain diagnoses, supplemented by notes from inpatient admissions/discharges, as well as ED, primary care, and subspecialty consultations within 6 months preceding the index visit. Prior VA health care use was ascertained from the EHR review of the same 6-month window, reflecting ED visits, inpatient admissions, primary care visits, subspecialty visits, and individual/group therapy for ATOD or other mental health problems. Data were used to generate site-specific descriptive statistics.
RESULTS
Like all VA hospital-based clinics, a universal EHR captured all medical and social service notes, orders, medications, and administrative records. All facilities had on-site EDs, medical/mental health specialty care, and pharmacies. Social services, including benefits counseling and housing services, were available on site. Table 1 summarizes the HPACT structures at BIR, WLA, and PIT.
Birmingham
The BIR HPACT was devised as a new homeless-focused team located within a VA primary care clinic where other providers continued to see primary care patients. Staff and space were reallocated for this HPACT, which recruited patients in 4 ways: (1) the facility’s primary homeless program, Healthcare for Homeless Veterans, referred patients who previously sought VA housing but who required primary care; (2) an outreach specialist sought homeless veterans in shelters and on the streets; (3) HPACT staff marketed the clinic with presentations and flyers to other VA services and non-VA community agencies; and (4) a referral mechanism within the EHR.
A nurse practitioner was the PCP at this site, supervised by an academic internist experienced in the care of underserved populations, and the HPACT director, a physician certified in internal and addiction medicine. Patients at the BIR HPACT also received care from a social worker, registered nurse, licensed practical nurse, and psychiatrist who received all or a portion of their salaries from this demonstration project. This clinic accommodated walk-in appointments during business hours. Clinicians discussed clinical cases daily, and the full clinical and administrative team met weekly. To promote service integration, HPACT staff attended meetings of the BIR general primary care and Healthcare for Homeless Veterans programs, and vice versa.
West Los Angeles
At WLA, a previously established Homeless Screening Clinic that offered integrated social and medical services for homeless veterans with mental illness was already available during business hours and located within the site’s mental health program.11 However, because ED use for homeless veterans peaked after hours, the new WLA HPACT was established within the WLA ED.
During WLA HPACT hours (3 weekday evenings/week), routine nursing triage occurred for all patients who presented to the ED. However, distinct from other times of day, veterans who were triaged with low-acuity and who were appropriate for outpatient care were given a self-administered, 4-item questionnaire to identify patients who were homeless or at risk for becoming homeless. Veterans who were identified with this screening tool were offered the choice of an ED or HPACT visit. Veterans who chose the latter were assigned to the queue for an HPACT primary care visit instead of the ED.
A physician led the clinical team, with additional services from a mental health clinical nurse specialist and clerks who worked with homeless and/or mental health patients during business hours and provided part-time HPACT coverage. When needed, additional services were provided from colocated ED nurses and social workers. Providers were chosen for their aptitude in culturally responsive communication.
Patients who chose to be seen in HPACT received a primary care visit that also addressed the reason for ED presentation. HPACT staff worked collaboratively, with interdisciplinary team huddles that preceded each clinic session and ended each patient visit. Referrals and social service needs were tracked and monitored by the PCP. Specialty care referrals were also tracked and facilitated when possible with direct communication between HPACT providers and specialty services. Meetings with daytime Homeless Screening Clinic and ED staff facilitated cross-departmental collaborations that helped veterans prepare for and retain housing.
Pittsburgh
The HPACT at PIT evolved from an existing PACT that provided primary care-based addiction services.2 That team included an internist credentialed in addiction medicine and experienced in homeless health care, nurse practitioner, nurse care manager, nursing assistant, and clerks. At this site, HPACT providers had subspecialty expertise in the assessment and treatment of ATOD use, certification to prescribe buprenorphine for outpatient opioid detoxification and/or maintenance, and experience engaging homeless and other vulnerable veterans. The existing colocated clinic included 2 additional addiction medicine clinicians and a physician assistant experienced in ATOD use. The PIT HPACT was not restricted to patients with ATOD use.
At PIT, HPACT care was provided during business hours in a flexible model that allowed for walk-in visits. Providers from the existing addiction-focused PACT identified and referred homeless veterans, as well as patients deemed at-risk for becoming homeless. In addition, other homeless veterans who did not have a PCP could be referred through e-consults placed by any VA staff member. If a referred homeless veteran was already enrolled on a PCP’s panel, HPACT facilitated reengagement with the existing provider. Near the end of this data collection period, a peer support specialist also began community outreach to engage both enrolled and potential HPACT patients.
Patient Characteristics
Table 2 presents the demographic and housing characteristics of enrolled HPACT patients at BIR, WLA, and PIT from May 1, 2012, to September 30, 2012. Each site had a similar number of patients (n = 35/47/43 at BIR/WLA/PIT, respectively). Across sites, most patients were male and African American or white. The majority of patients at each site were housed in VA transitional housing/residential rehabilitation programs (33%/32%/40% at BIR/WLA/PIT, respectively). Fewer patients were unsheltered (on the streets or other places not meant for sleeping), though WLA had the most unsheltered patients (26%) compared with BIR (6%) and PIT (2%). BIR had more patients from emergency shelters (14%) than did the other 2 sites (4% at WLA and 0% at PIT). PIT had the most domiciled patients in houses/apartments (26%, compared with 6% each at BIR and WLA), but who were at risk for homelessness.
Table 3 summarizes the diagnoses and VA health care use patterns of these cohorts. In the first week of HPACT care, WLA addressed the most acute medical conditions (81% of patients had≥ 1 common condition), followed by BIR (54%) and PIT (23%). Among chronic conditions, chronic pain was diagnosed in 51% of patients at BIR, 30% of patients at WLA, and 12% of patients at PIT. Hepatitis C diagnoses were most common at WLA (36%), similar at PIT (33%), and lower at BIR (17%). Overall, chronic medical diagnoses were most common among patients at BIR (91%), followed by WLA (85%), and PIT (60%).
Among mental health diagnoses, mood disorders were the most prevalent across sites (49%/55%/42% at BIR/WLA/PIT, respectively), followed by posttraumatic stress disorder (17%/21%/9% at BIR/WLA/PIT, respectively). WLA had more patients with psychosis (19%) than did the other 2 sites (7% at PIT and 0% at BIR). Overall, mental illness was common among HPACT patients across sites (60%/72%/72% at BIR/WLA/PIT, respectively).
Health care use in the 6 months before HPACT enrollment differed between sites. BIR and PIT had similar rates of ED/urgent care use (46% and 47% sought care over the prior 6 months, respectively), but WLA had the highest rate (62%). However, inpatient admission rates were lowest at WLA (13%) and again similar at BIR (23%) and PIT (26%). BIR patients had the most VA primary care exposure before HPACT entry (71% obtained primary care in the past 6 months), followed by WLA (38%) and PIT (18%). Mental health specialty care was also highest at BIR (60%), followed by PIT (56%), then WLA (39%)
Table 4 presents the prevalence of ATOD abuse or dependence among HPACT patients in the6 months before clinic enrollment. The most commonly misused substances were alcohol (60%/35%/44% at BIR/WLA/PIT, respectively), tobacco (71%/47%/40% at BIR/WLA/PIT, respectively), and cocaine (37%/19%/23% at BIR/WLA/PIT, respectively). PIT had the highest percentages of patients with opioid misuse (21%), followed by BIR (9%) and WLA (6%). Overall, these disorders were prevalent across sites, highest at BIR (94%) and similar at WLA (72%) and PIT (67%).
DISCUSSION
In this case report of early HPACT implementation, strikingly different models of homeless-focused primary care at the geographically distinct facilities were found. The lack of a gold standard primary care medical home for homeless persons—compounded by contrasting local contextual features—led to distinct clinic designs. BIR capitalized on primary care needs among veterans who previously sought housing and relied on the available space within an operating primary care clinic. As WLA already offered primary care for homeless veterans that was colocated with mental health services, the HPACT at this site was devised as an after-hours clinic colocated with the ED.11 At PIT, an existing primary care team with addiction expertise expanded its role to include a focus on homelessness, without needing new space or staff.
The initial HPACT patient cohorts likely reflected these contrasting clinic structures. That is, at WLA, the higher rates of unsheltered patients, prevalence of acute medical conditions and psychotic disorders, and greater ED use was likely driven by ED colocation. The physical location of this site’s HPACT may also speak to greater future decreases in ED use. At BIR, the use of a dedicated HPACT community outreach worker likely led to greater recruitment from emergency shelters. However, the clinic mainly recruited veterans who had previously engaged in VA mainstream primary care services and individuals with ATOD use. At PIT, higher rates of psychotherapy were likely facilitated by the HPACT’s placement within an addiction treatment setting, which may favor psychosocial rehabilitation. The distinctly higher rate of patients with opioid misuse at PIT likely paralleled the ATOD expertise of its providers and/or buprenorphine availability.
The more challenging questions surround the implementation of the current clinic models to address the needs of these patient cohorts and possible avenues to improve each clinic. High rates of chronic medical illness, mental illness, and ATOD use are well known in the homeless veteran and general populations.2,9 Within these 3 HPACTs, the high rates of medical/mental illness and ATOD use speak favorably about the clinics’ respective recruitment strategies; ie, normative homeless populations with high rates of illness are enrolling in these clinics. However, current service integration practices may be enhanced with the specific knowledge gained from this examination. For example, the very high rates of mood and anxiety disorders at each site suggest a role for an embedded mental health provider with prescribing privileges (the model adopted by BIR) as opposed to mental health referrals used at WLA and PIT. There may also be a role for cognitive behavioral therapy services within these clinics. Similarly, the high rates of ATOD (especially alcohol, tobacco, and cocaine) misuse suggest a role for addiction medicine training among the PCPs (the PIT model) as well as psychosocial rehabilitation for ATOD use within the HPACTs. High rates of chronic medical conditions, such as diabetes, hepatitis C, and hypertension elucidate possible roles for specialty care integration and/or chronic disease management programs tailored to the homeless.
Comparing the housing status of these cohorts can help in the design of future homeless-tailored primary care operations and improve these HPACTs. Most patients across sites lived in VA transitional housing/residential rehabilitation programs. As such, current referral practices at these 3 HPACTs proved sufficient in recruiting this subpopulation of homeless veterans. However, in light of national data showing that the count of unsheltered homeless veterans has not declined as rapidly as the count of homeless veterans overall, the higher numbers of veterans recruited from interim sheltering arrangements suggest a need for enhanced outreach to unsheltered individuals.1 WLA data suggest that linkages to EDs can advance this objective. BIR data show that targeted outreach in shelters can engage this high-risk, transiently sheltered subpopulation in primary care. At the time of this project, PIT just began using a peer support specialist for outreach to unsheltered veterans. It will be important to evaluate the outcomes of this new referral strategy.
Limitations
These exploratory findings—though from a small convenience sample within a nascent, growing program—generated critical and detailed information to guide ongoing policies and service design. However, these findings have limitations. First, though this research contributes to limited existing literature about the operational design of homeless-focused primary care, no outcome data were included. Although a comprehensive evaluation of all HPACT sites is a distinct and useful endeavor, this project instead offers a rapid, detailed illustration of 3 early-stage clinics. Though smaller in scope, this effort informs other facilities developing homeless-focused primary care initiatives and the larger demonstration project.
Second, a convenience sample of 3 urban facilities with strong academic ties and community commitment to providing services for homeless persons was presented. It may be difficult to translate these findings to communities with fewer resources.
Third, EHR review was used to determine patient demographics, diagnoses, and patterns of health care use. Though EHR review offers detailed information that is unavailable from administrative data, EHR is subject to variations in documentation patterns.
Last, differing characteristics of the homeless veteran population in each city may interact with contrasting HPACT structures to influence the characteristics of patients served. For example, though the data suggest that linkages with the ED may facilitate greater recruitment of unsheltered veterans in WLA, Los Angeles is known to have particularly high rates of unsheltered individuals.1
CONCLUSIONS
Clinicians, administrators, and researchers in the safety net may benefit from the experience implementing new clinics to recruit and engage homeless veterans in primary care. In a relatively nascent field with few accepted models of care, this paper offers detailed descriptions of newly developed homeless-focused primary care clinics at 3 VA facilities, which can inform other sites undertaking similar initiatives. This study highlights the wide range of approaches to building such clinics, with important variations in structural characteristics such as clinic location and operating hours, as well as within the intricacies of service integration patterns.
Within primary care clinics for homeless adults, this study suggests a role for embedded mental health (medication management and psychotherapy) and substance abuse services, chronic disease management programs tailored to this vulnerable population, and the role of linkages to the ED or community-based outreach to recruit unsheltered homeless patients. To pave a path toward identifying an evidence-based model of homeless-focused primary care, future studies are needed to study nationwide HPACT outcomes, including health status, patient satisfaction, quality of life, housing, and cost-effectiveness.
Acknowledgements
This work was undertaken in part by the VA’s PACT Demonstration Laboratory initiative, supporting and evaluating VA’s transition to a patient-centered medical home. Funding for the PACT Demonstration Laboratory initiative was provided by the VA Office of Patient Care Services. This project received support from the VISN 22 VA Assessment and Improvement Lab for Patient Centered Care (VAIL-PCC) (XVA 65-018; PI: Rubenstein).
Dr. Gabrielian was supported in part by the VA Office of Academic Affiliations, Advanced Fellowship Program in Mental Illness Research and Treatment. Drs. Gelberg and Andersen were supported in part by NIDA DA 022445. Dr. Andersen received additional support from the UCLA/DREW Project EXPORT, National Center on Minority Health and Health Disparities, P20MD000148/P20MD000182. Dr. Broyles was supported by a Career Development Award (CDA 10–014) from the VA Health Services Research & Development service. Dr. Kertesz was supported through funding of VISN 7.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Cortes A, Henry M, de la Cruz RJ, Brown S. The 2012 Point-in-Time Estimates of Homelessness: Volume I of the 2012 Annual Homeless Assessment Report. Washington, DC: The U.S. Department of Housing and Urban Development, Office of Community Planning and Development; 2012.
2. Balshem H, Christensen V, Tuepker A, Kansagara D. A Critical Review of the Literature Regarding Homelessness Among Veterans. U.S. Department of Veterans Affairs, Veterans Health Administration, Health Services Research & Development Service; 2011. VA-ESP Project #05-225.
3. O’Toole TP, Pirraglia PA, Dosa D, et al; Primary Care-Special Populations Treatment Team. Building care systems to improve access for high-risk and vulnerable veteran populations. J Gen Intern Med. 2011;26(suppl 2):683-688.
4. Opening Doors: Federal Strategic Plan to Prevent and End Homelessness. Washington, DC: The United States Interagency Council on Homelessness; 2010.
5. Nakashima J, McGuire J, Berman S, Daniels W. Developing programs for homeless veterans: Understanding driving forces in implementation. Soc Work Health Care. 2004;40(2):1-12.
6. O’Toole TP, Buckel L, Bourgault C, et al. Applying the chronic care model to homeless veterans: Effect of a population approach to primary care on utilization and clinical outcomes. Am J Public Health. 2010;100(12):2493-2499.
7. Desai MM, Rosenheck RA, Kasprow WJ. Determinants of receipt of ambulatory medical care in a national sample of mentally ill homeless veterans. Med Care. 2003;41(2):275-287.
8. Irene Wong YL, Stanhope V. Conceptualizing community: A comparison of neighborhood characteristics of supportive housing for persons with psychiatric and developmental disabilities. Soc Sci Med. 2009;68(8):1376-1387.
9. Gelberg L, Gallagher TC, Andersen RM, Koegel P. Competing priorities as a barrier to medical care among homeless adults in Los Angeles. Am J Public Health. 1997;87(2):217-220.
10. Hamilton AB, Poza I, Washington DL. “Homelessness and trauma go hand-in-hand”: Pathways to homelessness among women veterans. Womens Health Issues. 2011;21(suppl 4):S203-S209.
11. McGuire J, Gelberg L, Blue-Howells J, Rosenheck RA. Access to primary care for homeless veterans with serious mental illness or substance abuse: A follow-up evaluation of co-located primary care and homeless social services. Adm Policy Ment Health. 2009;36(4):255-264.
12. VHA Operations Activities That May Constitute Research. Washington, DC: U.S. Department of Veterans Affairs, Veterans Health Administration; 2011. VHA Handbook 1058.05.
13. Resnick SG, Armstrong M, Sperrazza M, Harkness L, Rosenheck RA. A model of consumer-provider partnership: Vet-to-Vet. Psychiatr Rehabil J. 2004;28(2):185-187.
14. Hogan TP, Wakefield B, Nazi KM, Houston TK, Weaver FM. Promoting access through complementary eHealth technologies: Recommendations for VA’s Home Telehealth and personal health record programs. J Gen Intern Med. 2011;26(suppl 2):628-635.
15. Rosland AM, Nelson K, Sun H, et al. The patient-centered medical home in the Veterans Health Administration. Am J Manag Care. 2013;19(7):e263-e272.
16. Hsiao CJ, Cherry DK, Beatty PC, Rechtsteiner EA. National Ambulatory Medical Care Survey: 2007 summary. Natl Health Stat Report. 2010;3(27):1-32.
17. Hwang SW, Orav EJ, O’Connell JJ, Lebow JM, Brennan TA. Causes of death in homeless adults in Boston. Ann Intern Med. 1997;126(8):625-628.
18. Hwang SW, Tolomiczenko G, Kouyoumdjian FG, Garner RE. Interventions to improve the health of the homeless: A systematic review. Am J Prev Med. 2005;29(4):311-319.
On a single night in 2012, 62,619 veterans experienced homelessness.1 With high rates of illness, as well as alcohol, tobacco, and other drug (ATOD) use among homeless adults, ending veteran homelessness is a signature initiative of the VA.2-4 However, despite increasing efforts to improve health care for homeless individuals, little is known about best practices in homeless-focused primary care.2,5
With an age-adjusted mortality that is 2 to 10 times higher than that of their housed counterparts, homeless veterans pose a formidable challenge for primary care providers (PCPs).6,7 The complexity of homeless persons’ primary care needs is compounded by poor social support and the need to navigate priorities (eg, shelter) that compete with medical care.6,8,9 Moreover, veterans may face unique vulnerabilities conferred by military-specific experiences.2,10
As of 2012, only 2 VA facilities had primary care clinics tailored to the needs of homeless veterans. McGuire and colleagues built a system of colocated primary care, mental health, and homeless services for mentally ill veterans in Los Angeles, California.11 Over 18 months, this clinic facilitated greater primary and preventive care delivery, though the population’s physical health status did not improve.11 More recently, O’Toole and colleagues implemented a homeless-focused primary care clinic in Providence, Rhode Island.6 Compared with a historical sample of homeless veterans in traditional VA primary care, veterans in this homeless-tailored clinic had greater improvements in some chronic disease outcomes.6 This clinic also decreased nonacute emergency department (ED) use and hospitalizations for general medical conditions.6
Despite these promising outcomes, the VA lacked a nationwide homeless-focused primary care initiative. In 2012 the VA Office of Homeless Programs and the Office of Primary Care Operations funded a national demonstration project to create Homeless Patient-Aligned Care Teams (HPACTs)—primary care medical clinics for homeless veterans—at 32 facilities. This demonstration project guided HPACTs to tailor clinical and social services to homeless veterans’ needs, establish processes to identify and refer appropriate veterans, and integrate distinct services.
There were no explicit instructions that detailed HPACT structure. Because new VA programs must fit local contextual factors, including infrastructure, space, personnel, and institutional/community resources, different models of homeless-focused primary care have evolved.
This article is a case study of HPACTs at 3 of the 32 participating VA facilities, each reflecting a distinct community and organizational context. In light of projected HPACT expansion and concerns that current services are better tailored to sheltered homeless veterans than to their unsheltered peers, there is particular importance to detailed clinic descriptions that vividly portray the intricate relationships between service design and populations served.1
METHODS
VA HPACTs established in May 2012 at 3 facilities were examined: Birmingham VAMC in Alabama (BIR), West Los Angeles VAMC in California (WLA), and VA Pittsburgh Healthcare System in Pennsylvania (PIT). Prior to this demonstration project, each facility offered a range of housing/social services and traditional primary care for veterans. These sites are a geographically diverse convenience sample that emerged from existing homeless-focused collaborations among the authors and represent geographically diverse HPACTs.
The national director of VA Homeless Programs formally determined that this comparison constitutes a VA operations activity that is not research.12 This activity was exempt from Institutional Review Board review.
Study Design
Timed at an early stage of HPACT implementation, this project had 3 aims: (1) To identify noteworthy similarities and/or differences among the initial HPACT clinic structures; (2) To compare and contrast the patient characteristics of veterans enrolled in each of these clinics; and (3) To use these data to inform ongoing HPACT service design.
HPACT program evaluation data are not presented. Rather, a nascent system of care is illustrated that contributes to the limited literature concerning the design and implementation of homeless-focused primary care. Such organizational profiles inform novel program delivery and hold particular utility for heterogeneous populations who are difficult to engage in care.13,14
Authors at each site independently developed lists of variables that fell within the 3 guiding principles of this demonstration project. These variables were compiled and iteratively reduced to a consolidated table that assessed each clinic, including location, operating hours, methods of patient identification and referral, and linkages to distinct services (eg, primary care, mental health, addiction, and social services).
This table also became a guide for HPACT directors to generate narrative clinic descriptions. Characteristics of VA medical homes that are embraced regardless of patients’ housing status (eg, patient-centered, team-based care) were also incorporated into these descriptions.15
Patient Characteristics
The VA electronic health record (EHR) was used to identify all patients enrolled in HPACTs at BIR, WLA, and PIT from May 1, 2012 (clinic inception), through September 30, 2012. Authors developed a standardized template for EHR review and coined the first HPACT record as the patient’s index visit. This record was used to code initial housing status, demographics, and acute medical conditions diagnosed/treated. If housing status was not recorded at the index visit, the first preceding informative record was used.
Records for 6 months preceding the index visit were used to identify the presence or absence of common medical conditions, psychiatric diagnoses, and ATOD abuse or dependence. Medical conditions were identified from a list of common outpatient diagnoses from the National Ambulatory Medical Care Survey, supplemented by common conditions among homeless men.16-18 The EHR problem list (a list of diagnoses, by patient) was used to obtain diagnoses, supplemented by notes from inpatient admissions/discharges, as well as ED, primary care, and subspecialty consultations within 6 months preceding the index visit. Prior VA health care use was ascertained from the EHR review of the same 6-month window, reflecting ED visits, inpatient admissions, primary care visits, subspecialty visits, and individual/group therapy for ATOD or other mental health problems. Data were used to generate site-specific descriptive statistics.
RESULTS
Like all VA hospital-based clinics, a universal EHR captured all medical and social service notes, orders, medications, and administrative records. All facilities had on-site EDs, medical/mental health specialty care, and pharmacies. Social services, including benefits counseling and housing services, were available on site. Table 1 summarizes the HPACT structures at BIR, WLA, and PIT.
Birmingham
The BIR HPACT was devised as a new homeless-focused team located within a VA primary care clinic where other providers continued to see primary care patients. Staff and space were reallocated for this HPACT, which recruited patients in 4 ways: (1) the facility’s primary homeless program, Healthcare for Homeless Veterans, referred patients who previously sought VA housing but who required primary care; (2) an outreach specialist sought homeless veterans in shelters and on the streets; (3) HPACT staff marketed the clinic with presentations and flyers to other VA services and non-VA community agencies; and (4) a referral mechanism within the EHR.
A nurse practitioner was the PCP at this site, supervised by an academic internist experienced in the care of underserved populations, and the HPACT director, a physician certified in internal and addiction medicine. Patients at the BIR HPACT also received care from a social worker, registered nurse, licensed practical nurse, and psychiatrist who received all or a portion of their salaries from this demonstration project. This clinic accommodated walk-in appointments during business hours. Clinicians discussed clinical cases daily, and the full clinical and administrative team met weekly. To promote service integration, HPACT staff attended meetings of the BIR general primary care and Healthcare for Homeless Veterans programs, and vice versa.
West Los Angeles
At WLA, a previously established Homeless Screening Clinic that offered integrated social and medical services for homeless veterans with mental illness was already available during business hours and located within the site’s mental health program.11 However, because ED use for homeless veterans peaked after hours, the new WLA HPACT was established within the WLA ED.
During WLA HPACT hours (3 weekday evenings/week), routine nursing triage occurred for all patients who presented to the ED. However, distinct from other times of day, veterans who were triaged with low-acuity and who were appropriate for outpatient care were given a self-administered, 4-item questionnaire to identify patients who were homeless or at risk for becoming homeless. Veterans who were identified with this screening tool were offered the choice of an ED or HPACT visit. Veterans who chose the latter were assigned to the queue for an HPACT primary care visit instead of the ED.
A physician led the clinical team, with additional services from a mental health clinical nurse specialist and clerks who worked with homeless and/or mental health patients during business hours and provided part-time HPACT coverage. When needed, additional services were provided from colocated ED nurses and social workers. Providers were chosen for their aptitude in culturally responsive communication.
Patients who chose to be seen in HPACT received a primary care visit that also addressed the reason for ED presentation. HPACT staff worked collaboratively, with interdisciplinary team huddles that preceded each clinic session and ended each patient visit. Referrals and social service needs were tracked and monitored by the PCP. Specialty care referrals were also tracked and facilitated when possible with direct communication between HPACT providers and specialty services. Meetings with daytime Homeless Screening Clinic and ED staff facilitated cross-departmental collaborations that helped veterans prepare for and retain housing.
Pittsburgh
The HPACT at PIT evolved from an existing PACT that provided primary care-based addiction services.2 That team included an internist credentialed in addiction medicine and experienced in homeless health care, nurse practitioner, nurse care manager, nursing assistant, and clerks. At this site, HPACT providers had subspecialty expertise in the assessment and treatment of ATOD use, certification to prescribe buprenorphine for outpatient opioid detoxification and/or maintenance, and experience engaging homeless and other vulnerable veterans. The existing colocated clinic included 2 additional addiction medicine clinicians and a physician assistant experienced in ATOD use. The PIT HPACT was not restricted to patients with ATOD use.
At PIT, HPACT care was provided during business hours in a flexible model that allowed for walk-in visits. Providers from the existing addiction-focused PACT identified and referred homeless veterans, as well as patients deemed at-risk for becoming homeless. In addition, other homeless veterans who did not have a PCP could be referred through e-consults placed by any VA staff member. If a referred homeless veteran was already enrolled on a PCP’s panel, HPACT facilitated reengagement with the existing provider. Near the end of this data collection period, a peer support specialist also began community outreach to engage both enrolled and potential HPACT patients.
Patient Characteristics
Table 2 presents the demographic and housing characteristics of enrolled HPACT patients at BIR, WLA, and PIT from May 1, 2012, to September 30, 2012. Each site had a similar number of patients (n = 35/47/43 at BIR/WLA/PIT, respectively). Across sites, most patients were male and African American or white. The majority of patients at each site were housed in VA transitional housing/residential rehabilitation programs (33%/32%/40% at BIR/WLA/PIT, respectively). Fewer patients were unsheltered (on the streets or other places not meant for sleeping), though WLA had the most unsheltered patients (26%) compared with BIR (6%) and PIT (2%). BIR had more patients from emergency shelters (14%) than did the other 2 sites (4% at WLA and 0% at PIT). PIT had the most domiciled patients in houses/apartments (26%, compared with 6% each at BIR and WLA), but who were at risk for homelessness.
Table 3 summarizes the diagnoses and VA health care use patterns of these cohorts. In the first week of HPACT care, WLA addressed the most acute medical conditions (81% of patients had≥ 1 common condition), followed by BIR (54%) and PIT (23%). Among chronic conditions, chronic pain was diagnosed in 51% of patients at BIR, 30% of patients at WLA, and 12% of patients at PIT. Hepatitis C diagnoses were most common at WLA (36%), similar at PIT (33%), and lower at BIR (17%). Overall, chronic medical diagnoses were most common among patients at BIR (91%), followed by WLA (85%), and PIT (60%).
Among mental health diagnoses, mood disorders were the most prevalent across sites (49%/55%/42% at BIR/WLA/PIT, respectively), followed by posttraumatic stress disorder (17%/21%/9% at BIR/WLA/PIT, respectively). WLA had more patients with psychosis (19%) than did the other 2 sites (7% at PIT and 0% at BIR). Overall, mental illness was common among HPACT patients across sites (60%/72%/72% at BIR/WLA/PIT, respectively).
Health care use in the 6 months before HPACT enrollment differed between sites. BIR and PIT had similar rates of ED/urgent care use (46% and 47% sought care over the prior 6 months, respectively), but WLA had the highest rate (62%). However, inpatient admission rates were lowest at WLA (13%) and again similar at BIR (23%) and PIT (26%). BIR patients had the most VA primary care exposure before HPACT entry (71% obtained primary care in the past 6 months), followed by WLA (38%) and PIT (18%). Mental health specialty care was also highest at BIR (60%), followed by PIT (56%), then WLA (39%)
Table 4 presents the prevalence of ATOD abuse or dependence among HPACT patients in the6 months before clinic enrollment. The most commonly misused substances were alcohol (60%/35%/44% at BIR/WLA/PIT, respectively), tobacco (71%/47%/40% at BIR/WLA/PIT, respectively), and cocaine (37%/19%/23% at BIR/WLA/PIT, respectively). PIT had the highest percentages of patients with opioid misuse (21%), followed by BIR (9%) and WLA (6%). Overall, these disorders were prevalent across sites, highest at BIR (94%) and similar at WLA (72%) and PIT (67%).
DISCUSSION
In this case report of early HPACT implementation, strikingly different models of homeless-focused primary care at the geographically distinct facilities were found. The lack of a gold standard primary care medical home for homeless persons—compounded by contrasting local contextual features—led to distinct clinic designs. BIR capitalized on primary care needs among veterans who previously sought housing and relied on the available space within an operating primary care clinic. As WLA already offered primary care for homeless veterans that was colocated with mental health services, the HPACT at this site was devised as an after-hours clinic colocated with the ED.11 At PIT, an existing primary care team with addiction expertise expanded its role to include a focus on homelessness, without needing new space or staff.
The initial HPACT patient cohorts likely reflected these contrasting clinic structures. That is, at WLA, the higher rates of unsheltered patients, prevalence of acute medical conditions and psychotic disorders, and greater ED use was likely driven by ED colocation. The physical location of this site’s HPACT may also speak to greater future decreases in ED use. At BIR, the use of a dedicated HPACT community outreach worker likely led to greater recruitment from emergency shelters. However, the clinic mainly recruited veterans who had previously engaged in VA mainstream primary care services and individuals with ATOD use. At PIT, higher rates of psychotherapy were likely facilitated by the HPACT’s placement within an addiction treatment setting, which may favor psychosocial rehabilitation. The distinctly higher rate of patients with opioid misuse at PIT likely paralleled the ATOD expertise of its providers and/or buprenorphine availability.
The more challenging questions surround the implementation of the current clinic models to address the needs of these patient cohorts and possible avenues to improve each clinic. High rates of chronic medical illness, mental illness, and ATOD use are well known in the homeless veteran and general populations.2,9 Within these 3 HPACTs, the high rates of medical/mental illness and ATOD use speak favorably about the clinics’ respective recruitment strategies; ie, normative homeless populations with high rates of illness are enrolling in these clinics. However, current service integration practices may be enhanced with the specific knowledge gained from this examination. For example, the very high rates of mood and anxiety disorders at each site suggest a role for an embedded mental health provider with prescribing privileges (the model adopted by BIR) as opposed to mental health referrals used at WLA and PIT. There may also be a role for cognitive behavioral therapy services within these clinics. Similarly, the high rates of ATOD (especially alcohol, tobacco, and cocaine) misuse suggest a role for addiction medicine training among the PCPs (the PIT model) as well as psychosocial rehabilitation for ATOD use within the HPACTs. High rates of chronic medical conditions, such as diabetes, hepatitis C, and hypertension elucidate possible roles for specialty care integration and/or chronic disease management programs tailored to the homeless.
Comparing the housing status of these cohorts can help in the design of future homeless-tailored primary care operations and improve these HPACTs. Most patients across sites lived in VA transitional housing/residential rehabilitation programs. As such, current referral practices at these 3 HPACTs proved sufficient in recruiting this subpopulation of homeless veterans. However, in light of national data showing that the count of unsheltered homeless veterans has not declined as rapidly as the count of homeless veterans overall, the higher numbers of veterans recruited from interim sheltering arrangements suggest a need for enhanced outreach to unsheltered individuals.1 WLA data suggest that linkages to EDs can advance this objective. BIR data show that targeted outreach in shelters can engage this high-risk, transiently sheltered subpopulation in primary care. At the time of this project, PIT just began using a peer support specialist for outreach to unsheltered veterans. It will be important to evaluate the outcomes of this new referral strategy.
Limitations
These exploratory findings—though from a small convenience sample within a nascent, growing program—generated critical and detailed information to guide ongoing policies and service design. However, these findings have limitations. First, though this research contributes to limited existing literature about the operational design of homeless-focused primary care, no outcome data were included. Although a comprehensive evaluation of all HPACT sites is a distinct and useful endeavor, this project instead offers a rapid, detailed illustration of 3 early-stage clinics. Though smaller in scope, this effort informs other facilities developing homeless-focused primary care initiatives and the larger demonstration project.
Second, a convenience sample of 3 urban facilities with strong academic ties and community commitment to providing services for homeless persons was presented. It may be difficult to translate these findings to communities with fewer resources.
Third, EHR review was used to determine patient demographics, diagnoses, and patterns of health care use. Though EHR review offers detailed information that is unavailable from administrative data, EHR is subject to variations in documentation patterns.
Last, differing characteristics of the homeless veteran population in each city may interact with contrasting HPACT structures to influence the characteristics of patients served. For example, though the data suggest that linkages with the ED may facilitate greater recruitment of unsheltered veterans in WLA, Los Angeles is known to have particularly high rates of unsheltered individuals.1
CONCLUSIONS
Clinicians, administrators, and researchers in the safety net may benefit from the experience implementing new clinics to recruit and engage homeless veterans in primary care. In a relatively nascent field with few accepted models of care, this paper offers detailed descriptions of newly developed homeless-focused primary care clinics at 3 VA facilities, which can inform other sites undertaking similar initiatives. This study highlights the wide range of approaches to building such clinics, with important variations in structural characteristics such as clinic location and operating hours, as well as within the intricacies of service integration patterns.
Within primary care clinics for homeless adults, this study suggests a role for embedded mental health (medication management and psychotherapy) and substance abuse services, chronic disease management programs tailored to this vulnerable population, and the role of linkages to the ED or community-based outreach to recruit unsheltered homeless patients. To pave a path toward identifying an evidence-based model of homeless-focused primary care, future studies are needed to study nationwide HPACT outcomes, including health status, patient satisfaction, quality of life, housing, and cost-effectiveness.
Acknowledgements
This work was undertaken in part by the VA’s PACT Demonstration Laboratory initiative, supporting and evaluating VA’s transition to a patient-centered medical home. Funding for the PACT Demonstration Laboratory initiative was provided by the VA Office of Patient Care Services. This project received support from the VISN 22 VA Assessment and Improvement Lab for Patient Centered Care (VAIL-PCC) (XVA 65-018; PI: Rubenstein).
Dr. Gabrielian was supported in part by the VA Office of Academic Affiliations, Advanced Fellowship Program in Mental Illness Research and Treatment. Drs. Gelberg and Andersen were supported in part by NIDA DA 022445. Dr. Andersen received additional support from the UCLA/DREW Project EXPORT, National Center on Minority Health and Health Disparities, P20MD000148/P20MD000182. Dr. Broyles was supported by a Career Development Award (CDA 10–014) from the VA Health Services Research & Development service. Dr. Kertesz was supported through funding of VISN 7.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
On a single night in 2012, 62,619 veterans experienced homelessness.1 With high rates of illness, as well as alcohol, tobacco, and other drug (ATOD) use among homeless adults, ending veteran homelessness is a signature initiative of the VA.2-4 However, despite increasing efforts to improve health care for homeless individuals, little is known about best practices in homeless-focused primary care.2,5
With an age-adjusted mortality that is 2 to 10 times higher than that of their housed counterparts, homeless veterans pose a formidable challenge for primary care providers (PCPs).6,7 The complexity of homeless persons’ primary care needs is compounded by poor social support and the need to navigate priorities (eg, shelter) that compete with medical care.6,8,9 Moreover, veterans may face unique vulnerabilities conferred by military-specific experiences.2,10
As of 2012, only 2 VA facilities had primary care clinics tailored to the needs of homeless veterans. McGuire and colleagues built a system of colocated primary care, mental health, and homeless services for mentally ill veterans in Los Angeles, California.11 Over 18 months, this clinic facilitated greater primary and preventive care delivery, though the population’s physical health status did not improve.11 More recently, O’Toole and colleagues implemented a homeless-focused primary care clinic in Providence, Rhode Island.6 Compared with a historical sample of homeless veterans in traditional VA primary care, veterans in this homeless-tailored clinic had greater improvements in some chronic disease outcomes.6 This clinic also decreased nonacute emergency department (ED) use and hospitalizations for general medical conditions.6
Despite these promising outcomes, the VA lacked a nationwide homeless-focused primary care initiative. In 2012 the VA Office of Homeless Programs and the Office of Primary Care Operations funded a national demonstration project to create Homeless Patient-Aligned Care Teams (HPACTs)—primary care medical clinics for homeless veterans—at 32 facilities. This demonstration project guided HPACTs to tailor clinical and social services to homeless veterans’ needs, establish processes to identify and refer appropriate veterans, and integrate distinct services.
There were no explicit instructions that detailed HPACT structure. Because new VA programs must fit local contextual factors, including infrastructure, space, personnel, and institutional/community resources, different models of homeless-focused primary care have evolved.
This article is a case study of HPACTs at 3 of the 32 participating VA facilities, each reflecting a distinct community and organizational context. In light of projected HPACT expansion and concerns that current services are better tailored to sheltered homeless veterans than to their unsheltered peers, there is particular importance to detailed clinic descriptions that vividly portray the intricate relationships between service design and populations served.1
METHODS
VA HPACTs established in May 2012 at 3 facilities were examined: Birmingham VAMC in Alabama (BIR), West Los Angeles VAMC in California (WLA), and VA Pittsburgh Healthcare System in Pennsylvania (PIT). Prior to this demonstration project, each facility offered a range of housing/social services and traditional primary care for veterans. These sites are a geographically diverse convenience sample that emerged from existing homeless-focused collaborations among the authors and represent geographically diverse HPACTs.
The national director of VA Homeless Programs formally determined that this comparison constitutes a VA operations activity that is not research.12 This activity was exempt from Institutional Review Board review.
Study Design
Timed at an early stage of HPACT implementation, this project had 3 aims: (1) To identify noteworthy similarities and/or differences among the initial HPACT clinic structures; (2) To compare and contrast the patient characteristics of veterans enrolled in each of these clinics; and (3) To use these data to inform ongoing HPACT service design.
HPACT program evaluation data are not presented. Rather, a nascent system of care is illustrated that contributes to the limited literature concerning the design and implementation of homeless-focused primary care. Such organizational profiles inform novel program delivery and hold particular utility for heterogeneous populations who are difficult to engage in care.13,14
Authors at each site independently developed lists of variables that fell within the 3 guiding principles of this demonstration project. These variables were compiled and iteratively reduced to a consolidated table that assessed each clinic, including location, operating hours, methods of patient identification and referral, and linkages to distinct services (eg, primary care, mental health, addiction, and social services).
This table also became a guide for HPACT directors to generate narrative clinic descriptions. Characteristics of VA medical homes that are embraced regardless of patients’ housing status (eg, patient-centered, team-based care) were also incorporated into these descriptions.15
Patient Characteristics
The VA electronic health record (EHR) was used to identify all patients enrolled in HPACTs at BIR, WLA, and PIT from May 1, 2012 (clinic inception), through September 30, 2012. Authors developed a standardized template for EHR review and coined the first HPACT record as the patient’s index visit. This record was used to code initial housing status, demographics, and acute medical conditions diagnosed/treated. If housing status was not recorded at the index visit, the first preceding informative record was used.
Records for 6 months preceding the index visit were used to identify the presence or absence of common medical conditions, psychiatric diagnoses, and ATOD abuse or dependence. Medical conditions were identified from a list of common outpatient diagnoses from the National Ambulatory Medical Care Survey, supplemented by common conditions among homeless men.16-18 The EHR problem list (a list of diagnoses, by patient) was used to obtain diagnoses, supplemented by notes from inpatient admissions/discharges, as well as ED, primary care, and subspecialty consultations within 6 months preceding the index visit. Prior VA health care use was ascertained from the EHR review of the same 6-month window, reflecting ED visits, inpatient admissions, primary care visits, subspecialty visits, and individual/group therapy for ATOD or other mental health problems. Data were used to generate site-specific descriptive statistics.
RESULTS
Like all VA hospital-based clinics, a universal EHR captured all medical and social service notes, orders, medications, and administrative records. All facilities had on-site EDs, medical/mental health specialty care, and pharmacies. Social services, including benefits counseling and housing services, were available on site. Table 1 summarizes the HPACT structures at BIR, WLA, and PIT.
Birmingham
The BIR HPACT was devised as a new homeless-focused team located within a VA primary care clinic where other providers continued to see primary care patients. Staff and space were reallocated for this HPACT, which recruited patients in 4 ways: (1) the facility’s primary homeless program, Healthcare for Homeless Veterans, referred patients who previously sought VA housing but who required primary care; (2) an outreach specialist sought homeless veterans in shelters and on the streets; (3) HPACT staff marketed the clinic with presentations and flyers to other VA services and non-VA community agencies; and (4) a referral mechanism within the EHR.
A nurse practitioner was the PCP at this site, supervised by an academic internist experienced in the care of underserved populations, and the HPACT director, a physician certified in internal and addiction medicine. Patients at the BIR HPACT also received care from a social worker, registered nurse, licensed practical nurse, and psychiatrist who received all or a portion of their salaries from this demonstration project. This clinic accommodated walk-in appointments during business hours. Clinicians discussed clinical cases daily, and the full clinical and administrative team met weekly. To promote service integration, HPACT staff attended meetings of the BIR general primary care and Healthcare for Homeless Veterans programs, and vice versa.
West Los Angeles
At WLA, a previously established Homeless Screening Clinic that offered integrated social and medical services for homeless veterans with mental illness was already available during business hours and located within the site’s mental health program.11 However, because ED use for homeless veterans peaked after hours, the new WLA HPACT was established within the WLA ED.
During WLA HPACT hours (3 weekday evenings/week), routine nursing triage occurred for all patients who presented to the ED. However, distinct from other times of day, veterans who were triaged with low-acuity and who were appropriate for outpatient care were given a self-administered, 4-item questionnaire to identify patients who were homeless or at risk for becoming homeless. Veterans who were identified with this screening tool were offered the choice of an ED or HPACT visit. Veterans who chose the latter were assigned to the queue for an HPACT primary care visit instead of the ED.
A physician led the clinical team, with additional services from a mental health clinical nurse specialist and clerks who worked with homeless and/or mental health patients during business hours and provided part-time HPACT coverage. When needed, additional services were provided from colocated ED nurses and social workers. Providers were chosen for their aptitude in culturally responsive communication.
Patients who chose to be seen in HPACT received a primary care visit that also addressed the reason for ED presentation. HPACT staff worked collaboratively, with interdisciplinary team huddles that preceded each clinic session and ended each patient visit. Referrals and social service needs were tracked and monitored by the PCP. Specialty care referrals were also tracked and facilitated when possible with direct communication between HPACT providers and specialty services. Meetings with daytime Homeless Screening Clinic and ED staff facilitated cross-departmental collaborations that helped veterans prepare for and retain housing.
Pittsburgh
The HPACT at PIT evolved from an existing PACT that provided primary care-based addiction services.2 That team included an internist credentialed in addiction medicine and experienced in homeless health care, nurse practitioner, nurse care manager, nursing assistant, and clerks. At this site, HPACT providers had subspecialty expertise in the assessment and treatment of ATOD use, certification to prescribe buprenorphine for outpatient opioid detoxification and/or maintenance, and experience engaging homeless and other vulnerable veterans. The existing colocated clinic included 2 additional addiction medicine clinicians and a physician assistant experienced in ATOD use. The PIT HPACT was not restricted to patients with ATOD use.
At PIT, HPACT care was provided during business hours in a flexible model that allowed for walk-in visits. Providers from the existing addiction-focused PACT identified and referred homeless veterans, as well as patients deemed at-risk for becoming homeless. In addition, other homeless veterans who did not have a PCP could be referred through e-consults placed by any VA staff member. If a referred homeless veteran was already enrolled on a PCP’s panel, HPACT facilitated reengagement with the existing provider. Near the end of this data collection period, a peer support specialist also began community outreach to engage both enrolled and potential HPACT patients.
Patient Characteristics
Table 2 presents the demographic and housing characteristics of enrolled HPACT patients at BIR, WLA, and PIT from May 1, 2012, to September 30, 2012. Each site had a similar number of patients (n = 35/47/43 at BIR/WLA/PIT, respectively). Across sites, most patients were male and African American or white. The majority of patients at each site were housed in VA transitional housing/residential rehabilitation programs (33%/32%/40% at BIR/WLA/PIT, respectively). Fewer patients were unsheltered (on the streets or other places not meant for sleeping), though WLA had the most unsheltered patients (26%) compared with BIR (6%) and PIT (2%). BIR had more patients from emergency shelters (14%) than did the other 2 sites (4% at WLA and 0% at PIT). PIT had the most domiciled patients in houses/apartments (26%, compared with 6% each at BIR and WLA), but who were at risk for homelessness.
Table 3 summarizes the diagnoses and VA health care use patterns of these cohorts. In the first week of HPACT care, WLA addressed the most acute medical conditions (81% of patients had≥ 1 common condition), followed by BIR (54%) and PIT (23%). Among chronic conditions, chronic pain was diagnosed in 51% of patients at BIR, 30% of patients at WLA, and 12% of patients at PIT. Hepatitis C diagnoses were most common at WLA (36%), similar at PIT (33%), and lower at BIR (17%). Overall, chronic medical diagnoses were most common among patients at BIR (91%), followed by WLA (85%), and PIT (60%).
Among mental health diagnoses, mood disorders were the most prevalent across sites (49%/55%/42% at BIR/WLA/PIT, respectively), followed by posttraumatic stress disorder (17%/21%/9% at BIR/WLA/PIT, respectively). WLA had more patients with psychosis (19%) than did the other 2 sites (7% at PIT and 0% at BIR). Overall, mental illness was common among HPACT patients across sites (60%/72%/72% at BIR/WLA/PIT, respectively).
Health care use in the 6 months before HPACT enrollment differed between sites. BIR and PIT had similar rates of ED/urgent care use (46% and 47% sought care over the prior 6 months, respectively), but WLA had the highest rate (62%). However, inpatient admission rates were lowest at WLA (13%) and again similar at BIR (23%) and PIT (26%). BIR patients had the most VA primary care exposure before HPACT entry (71% obtained primary care in the past 6 months), followed by WLA (38%) and PIT (18%). Mental health specialty care was also highest at BIR (60%), followed by PIT (56%), then WLA (39%)
Table 4 presents the prevalence of ATOD abuse or dependence among HPACT patients in the6 months before clinic enrollment. The most commonly misused substances were alcohol (60%/35%/44% at BIR/WLA/PIT, respectively), tobacco (71%/47%/40% at BIR/WLA/PIT, respectively), and cocaine (37%/19%/23% at BIR/WLA/PIT, respectively). PIT had the highest percentages of patients with opioid misuse (21%), followed by BIR (9%) and WLA (6%). Overall, these disorders were prevalent across sites, highest at BIR (94%) and similar at WLA (72%) and PIT (67%).
DISCUSSION
In this case report of early HPACT implementation, strikingly different models of homeless-focused primary care at the geographically distinct facilities were found. The lack of a gold standard primary care medical home for homeless persons—compounded by contrasting local contextual features—led to distinct clinic designs. BIR capitalized on primary care needs among veterans who previously sought housing and relied on the available space within an operating primary care clinic. As WLA already offered primary care for homeless veterans that was colocated with mental health services, the HPACT at this site was devised as an after-hours clinic colocated with the ED.11 At PIT, an existing primary care team with addiction expertise expanded its role to include a focus on homelessness, without needing new space or staff.
The initial HPACT patient cohorts likely reflected these contrasting clinic structures. That is, at WLA, the higher rates of unsheltered patients, prevalence of acute medical conditions and psychotic disorders, and greater ED use was likely driven by ED colocation. The physical location of this site’s HPACT may also speak to greater future decreases in ED use. At BIR, the use of a dedicated HPACT community outreach worker likely led to greater recruitment from emergency shelters. However, the clinic mainly recruited veterans who had previously engaged in VA mainstream primary care services and individuals with ATOD use. At PIT, higher rates of psychotherapy were likely facilitated by the HPACT’s placement within an addiction treatment setting, which may favor psychosocial rehabilitation. The distinctly higher rate of patients with opioid misuse at PIT likely paralleled the ATOD expertise of its providers and/or buprenorphine availability.
The more challenging questions surround the implementation of the current clinic models to address the needs of these patient cohorts and possible avenues to improve each clinic. High rates of chronic medical illness, mental illness, and ATOD use are well known in the homeless veteran and general populations.2,9 Within these 3 HPACTs, the high rates of medical/mental illness and ATOD use speak favorably about the clinics’ respective recruitment strategies; ie, normative homeless populations with high rates of illness are enrolling in these clinics. However, current service integration practices may be enhanced with the specific knowledge gained from this examination. For example, the very high rates of mood and anxiety disorders at each site suggest a role for an embedded mental health provider with prescribing privileges (the model adopted by BIR) as opposed to mental health referrals used at WLA and PIT. There may also be a role for cognitive behavioral therapy services within these clinics. Similarly, the high rates of ATOD (especially alcohol, tobacco, and cocaine) misuse suggest a role for addiction medicine training among the PCPs (the PIT model) as well as psychosocial rehabilitation for ATOD use within the HPACTs. High rates of chronic medical conditions, such as diabetes, hepatitis C, and hypertension elucidate possible roles for specialty care integration and/or chronic disease management programs tailored to the homeless.
Comparing the housing status of these cohorts can help in the design of future homeless-tailored primary care operations and improve these HPACTs. Most patients across sites lived in VA transitional housing/residential rehabilitation programs. As such, current referral practices at these 3 HPACTs proved sufficient in recruiting this subpopulation of homeless veterans. However, in light of national data showing that the count of unsheltered homeless veterans has not declined as rapidly as the count of homeless veterans overall, the higher numbers of veterans recruited from interim sheltering arrangements suggest a need for enhanced outreach to unsheltered individuals.1 WLA data suggest that linkages to EDs can advance this objective. BIR data show that targeted outreach in shelters can engage this high-risk, transiently sheltered subpopulation in primary care. At the time of this project, PIT just began using a peer support specialist for outreach to unsheltered veterans. It will be important to evaluate the outcomes of this new referral strategy.
Limitations
These exploratory findings—though from a small convenience sample within a nascent, growing program—generated critical and detailed information to guide ongoing policies and service design. However, these findings have limitations. First, though this research contributes to limited existing literature about the operational design of homeless-focused primary care, no outcome data were included. Although a comprehensive evaluation of all HPACT sites is a distinct and useful endeavor, this project instead offers a rapid, detailed illustration of 3 early-stage clinics. Though smaller in scope, this effort informs other facilities developing homeless-focused primary care initiatives and the larger demonstration project.
Second, a convenience sample of 3 urban facilities with strong academic ties and community commitment to providing services for homeless persons was presented. It may be difficult to translate these findings to communities with fewer resources.
Third, EHR review was used to determine patient demographics, diagnoses, and patterns of health care use. Though EHR review offers detailed information that is unavailable from administrative data, EHR is subject to variations in documentation patterns.
Last, differing characteristics of the homeless veteran population in each city may interact with contrasting HPACT structures to influence the characteristics of patients served. For example, though the data suggest that linkages with the ED may facilitate greater recruitment of unsheltered veterans in WLA, Los Angeles is known to have particularly high rates of unsheltered individuals.1
CONCLUSIONS
Clinicians, administrators, and researchers in the safety net may benefit from the experience implementing new clinics to recruit and engage homeless veterans in primary care. In a relatively nascent field with few accepted models of care, this paper offers detailed descriptions of newly developed homeless-focused primary care clinics at 3 VA facilities, which can inform other sites undertaking similar initiatives. This study highlights the wide range of approaches to building such clinics, with important variations in structural characteristics such as clinic location and operating hours, as well as within the intricacies of service integration patterns.
Within primary care clinics for homeless adults, this study suggests a role for embedded mental health (medication management and psychotherapy) and substance abuse services, chronic disease management programs tailored to this vulnerable population, and the role of linkages to the ED or community-based outreach to recruit unsheltered homeless patients. To pave a path toward identifying an evidence-based model of homeless-focused primary care, future studies are needed to study nationwide HPACT outcomes, including health status, patient satisfaction, quality of life, housing, and cost-effectiveness.
Acknowledgements
This work was undertaken in part by the VA’s PACT Demonstration Laboratory initiative, supporting and evaluating VA’s transition to a patient-centered medical home. Funding for the PACT Demonstration Laboratory initiative was provided by the VA Office of Patient Care Services. This project received support from the VISN 22 VA Assessment and Improvement Lab for Patient Centered Care (VAIL-PCC) (XVA 65-018; PI: Rubenstein).
Dr. Gabrielian was supported in part by the VA Office of Academic Affiliations, Advanced Fellowship Program in Mental Illness Research and Treatment. Drs. Gelberg and Andersen were supported in part by NIDA DA 022445. Dr. Andersen received additional support from the UCLA/DREW Project EXPORT, National Center on Minority Health and Health Disparities, P20MD000148/P20MD000182. Dr. Broyles was supported by a Career Development Award (CDA 10–014) from the VA Health Services Research & Development service. Dr. Kertesz was supported through funding of VISN 7.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Cortes A, Henry M, de la Cruz RJ, Brown S. The 2012 Point-in-Time Estimates of Homelessness: Volume I of the 2012 Annual Homeless Assessment Report. Washington, DC: The U.S. Department of Housing and Urban Development, Office of Community Planning and Development; 2012.
2. Balshem H, Christensen V, Tuepker A, Kansagara D. A Critical Review of the Literature Regarding Homelessness Among Veterans. U.S. Department of Veterans Affairs, Veterans Health Administration, Health Services Research & Development Service; 2011. VA-ESP Project #05-225.
3. O’Toole TP, Pirraglia PA, Dosa D, et al; Primary Care-Special Populations Treatment Team. Building care systems to improve access for high-risk and vulnerable veteran populations. J Gen Intern Med. 2011;26(suppl 2):683-688.
4. Opening Doors: Federal Strategic Plan to Prevent and End Homelessness. Washington, DC: The United States Interagency Council on Homelessness; 2010.
5. Nakashima J, McGuire J, Berman S, Daniels W. Developing programs for homeless veterans: Understanding driving forces in implementation. Soc Work Health Care. 2004;40(2):1-12.
6. O’Toole TP, Buckel L, Bourgault C, et al. Applying the chronic care model to homeless veterans: Effect of a population approach to primary care on utilization and clinical outcomes. Am J Public Health. 2010;100(12):2493-2499.
7. Desai MM, Rosenheck RA, Kasprow WJ. Determinants of receipt of ambulatory medical care in a national sample of mentally ill homeless veterans. Med Care. 2003;41(2):275-287.
8. Irene Wong YL, Stanhope V. Conceptualizing community: A comparison of neighborhood characteristics of supportive housing for persons with psychiatric and developmental disabilities. Soc Sci Med. 2009;68(8):1376-1387.
9. Gelberg L, Gallagher TC, Andersen RM, Koegel P. Competing priorities as a barrier to medical care among homeless adults in Los Angeles. Am J Public Health. 1997;87(2):217-220.
10. Hamilton AB, Poza I, Washington DL. “Homelessness and trauma go hand-in-hand”: Pathways to homelessness among women veterans. Womens Health Issues. 2011;21(suppl 4):S203-S209.
11. McGuire J, Gelberg L, Blue-Howells J, Rosenheck RA. Access to primary care for homeless veterans with serious mental illness or substance abuse: A follow-up evaluation of co-located primary care and homeless social services. Adm Policy Ment Health. 2009;36(4):255-264.
12. VHA Operations Activities That May Constitute Research. Washington, DC: U.S. Department of Veterans Affairs, Veterans Health Administration; 2011. VHA Handbook 1058.05.
13. Resnick SG, Armstrong M, Sperrazza M, Harkness L, Rosenheck RA. A model of consumer-provider partnership: Vet-to-Vet. Psychiatr Rehabil J. 2004;28(2):185-187.
14. Hogan TP, Wakefield B, Nazi KM, Houston TK, Weaver FM. Promoting access through complementary eHealth technologies: Recommendations for VA’s Home Telehealth and personal health record programs. J Gen Intern Med. 2011;26(suppl 2):628-635.
15. Rosland AM, Nelson K, Sun H, et al. The patient-centered medical home in the Veterans Health Administration. Am J Manag Care. 2013;19(7):e263-e272.
16. Hsiao CJ, Cherry DK, Beatty PC, Rechtsteiner EA. National Ambulatory Medical Care Survey: 2007 summary. Natl Health Stat Report. 2010;3(27):1-32.
17. Hwang SW, Orav EJ, O’Connell JJ, Lebow JM, Brennan TA. Causes of death in homeless adults in Boston. Ann Intern Med. 1997;126(8):625-628.
18. Hwang SW, Tolomiczenko G, Kouyoumdjian FG, Garner RE. Interventions to improve the health of the homeless: A systematic review. Am J Prev Med. 2005;29(4):311-319.
1. Cortes A, Henry M, de la Cruz RJ, Brown S. The 2012 Point-in-Time Estimates of Homelessness: Volume I of the 2012 Annual Homeless Assessment Report. Washington, DC: The U.S. Department of Housing and Urban Development, Office of Community Planning and Development; 2012.
2. Balshem H, Christensen V, Tuepker A, Kansagara D. A Critical Review of the Literature Regarding Homelessness Among Veterans. U.S. Department of Veterans Affairs, Veterans Health Administration, Health Services Research & Development Service; 2011. VA-ESP Project #05-225.
3. O’Toole TP, Pirraglia PA, Dosa D, et al; Primary Care-Special Populations Treatment Team. Building care systems to improve access for high-risk and vulnerable veteran populations. J Gen Intern Med. 2011;26(suppl 2):683-688.
4. Opening Doors: Federal Strategic Plan to Prevent and End Homelessness. Washington, DC: The United States Interagency Council on Homelessness; 2010.
5. Nakashima J, McGuire J, Berman S, Daniels W. Developing programs for homeless veterans: Understanding driving forces in implementation. Soc Work Health Care. 2004;40(2):1-12.
6. O’Toole TP, Buckel L, Bourgault C, et al. Applying the chronic care model to homeless veterans: Effect of a population approach to primary care on utilization and clinical outcomes. Am J Public Health. 2010;100(12):2493-2499.
7. Desai MM, Rosenheck RA, Kasprow WJ. Determinants of receipt of ambulatory medical care in a national sample of mentally ill homeless veterans. Med Care. 2003;41(2):275-287.
8. Irene Wong YL, Stanhope V. Conceptualizing community: A comparison of neighborhood characteristics of supportive housing for persons with psychiatric and developmental disabilities. Soc Sci Med. 2009;68(8):1376-1387.
9. Gelberg L, Gallagher TC, Andersen RM, Koegel P. Competing priorities as a barrier to medical care among homeless adults in Los Angeles. Am J Public Health. 1997;87(2):217-220.
10. Hamilton AB, Poza I, Washington DL. “Homelessness and trauma go hand-in-hand”: Pathways to homelessness among women veterans. Womens Health Issues. 2011;21(suppl 4):S203-S209.
11. McGuire J, Gelberg L, Blue-Howells J, Rosenheck RA. Access to primary care for homeless veterans with serious mental illness or substance abuse: A follow-up evaluation of co-located primary care and homeless social services. Adm Policy Ment Health. 2009;36(4):255-264.
12. VHA Operations Activities That May Constitute Research. Washington, DC: U.S. Department of Veterans Affairs, Veterans Health Administration; 2011. VHA Handbook 1058.05.
13. Resnick SG, Armstrong M, Sperrazza M, Harkness L, Rosenheck RA. A model of consumer-provider partnership: Vet-to-Vet. Psychiatr Rehabil J. 2004;28(2):185-187.
14. Hogan TP, Wakefield B, Nazi KM, Houston TK, Weaver FM. Promoting access through complementary eHealth technologies: Recommendations for VA’s Home Telehealth and personal health record programs. J Gen Intern Med. 2011;26(suppl 2):628-635.
15. Rosland AM, Nelson K, Sun H, et al. The patient-centered medical home in the Veterans Health Administration. Am J Manag Care. 2013;19(7):e263-e272.
16. Hsiao CJ, Cherry DK, Beatty PC, Rechtsteiner EA. National Ambulatory Medical Care Survey: 2007 summary. Natl Health Stat Report. 2010;3(27):1-32.
17. Hwang SW, Orav EJ, O’Connell JJ, Lebow JM, Brennan TA. Causes of death in homeless adults in Boston. Ann Intern Med. 1997;126(8):625-628.
18. Hwang SW, Tolomiczenko G, Kouyoumdjian FG, Garner RE. Interventions to improve the health of the homeless: A systematic review. Am J Prev Med. 2005;29(4):311-319.
BEST PRACTICES IN: Infant Feeding
Medical Education Library
A Best Practices Supplement to Pediatric News®. This supplement was sponsored by Perrigo Nutritionals.
Topics
- Introduction
- Store Brands and Advertised Brands
- FDA Regulation of Formula
- Formula Selection
- The Problem of Infant Formula Dilution
- Is Switching Formula Safe?
- Conclusion
Faculty/Faculty Disclosure
Joel R. Rosh, MD
Director, Pediatric
Gastroenterology
Goryeb Children’s
Hospital/Atlantic Health
Morristown, NJ
Professor of Pediatrics
Icahn School of Medicine
at Mount Sinai
New York, NY
Dr. Rosh discloses that he is on an advisory board for Perrigo Nutritionals.
Medical Education Library
A Best Practices Supplement to Pediatric News®. This supplement was sponsored by Perrigo Nutritionals.
Topics
- Introduction
- Store Brands and Advertised Brands
- FDA Regulation of Formula
- Formula Selection
- The Problem of Infant Formula Dilution
- Is Switching Formula Safe?
- Conclusion
Faculty/Faculty Disclosure
Joel R. Rosh, MD
Director, Pediatric
Gastroenterology
Goryeb Children’s
Hospital/Atlantic Health
Morristown, NJ
Professor of Pediatrics
Icahn School of Medicine
at Mount Sinai
New York, NY
Dr. Rosh discloses that he is on an advisory board for Perrigo Nutritionals.
Medical Education Library
A Best Practices Supplement to Pediatric News®. This supplement was sponsored by Perrigo Nutritionals.
Topics
- Introduction
- Store Brands and Advertised Brands
- FDA Regulation of Formula
- Formula Selection
- The Problem of Infant Formula Dilution
- Is Switching Formula Safe?
- Conclusion
Faculty/Faculty Disclosure
Joel R. Rosh, MD
Director, Pediatric
Gastroenterology
Goryeb Children’s
Hospital/Atlantic Health
Morristown, NJ
Professor of Pediatrics
Icahn School of Medicine
at Mount Sinai
New York, NY
Dr. Rosh discloses that he is on an advisory board for Perrigo Nutritionals.
The VALOR Program: Preparing Nursing Students to Care for Our Veterans
The VA Learning Opportunity Residency (VALOR) program is a prelicensure experience with a nurse preceptor for rising senior students enrolled in a bachelor of science in nursing program. Students must have a minimum 3.0 grade-point average to apply. The program provides 800 hours of paid learning experiences in diverse didactic and hands-on clinical situations. The first 400 hours of the program (10 weeks) occur over the summer, and the second 400 hours take place during the fall and spring semesters of the student’s last year of school.1 During the last 400 hours, students are placed in the areas they are interested in working as new graduate nurses.
The aim of the Salem VALOR program is to develop the next generation of VAMC nurses by recruiting new graduate nurses. The Salem VAMC structures the VALOR program to meet the needs of both the students and the facility. According to Glenda Fuller, the student programs manager for the VA, national VALOR retention rates from 2007 to 2011 have averaged 38%. However, more applicants apply for new graduate nurse positions than are available. Included in the VHA Directive 2011-039, facilities that hire a nurse with ≤ 1 year of experience must enroll them in a yearlong transition-to-practice program.2 Therefore, facilities may limit the number of new graduate nurse positions.
On entry into the VALOR program, participants write a journal entry regarding their fears and concerns about becoming a new graduate nurse. In addition, each student turns in a written reflection about their experiences each week and participates in daily group discussions with the program coordinator. The last day of the summer portion of the program, students again write about their fears and concerns about becoming a new graduate nurse. After reviewing the VALOR journals, conducting focus groups, and taking notes during the daily meetings, the authors describe the following VALOR experience from the summer of 2013 at the Salem VAMC.
Preparing New Graduates
Hospitals are under pressure to provide high-quality nursing care despite hiring new graduate nurses who are unfamiliar and inexperienced in caring for patients’ complex health care needs. New graduate nurses currently make up more than 10% of hospital nursing staff, and that number is expected to grow as baby boomers retire.3 Boswell and colleagues suggest that those new graduate nurses are unprepared for the registered nurse role.4 Identifying strategies to facilitate the transition from student to the new graduate nurse role will likely decrease attrition rates and increase the effectiveness and the quality of patient care. Nursing programs, such as the VALOR, can ease the transition from the classroom to the working environment.5
This result is evident when observing how VALOR students enhance their nursing skills after the 10-week summer program. VALOR participant Andrea King published her summer experience at the Salem VAMC in The Torch, the Virginia Nursing Students’ Association newsletter.6 “I had so much practice and eventually confidence in my nursing skills,” she wrote, “that I had the autonomy and independence to feel like I was working as an actual nurse.”6
The VALOR Experience
During the summer months, senior nursing students have the opportunity to go on rounds with the chaplain, work with nurse practitioners, attend outings with mental health patients, participate in home health visits, interact with patients in groups, and rotate to different hospital units. Students attend FranklinCovey classes (which specialize in employee performance improvement), participate in an evidence-based practice (EBP) project (which helps them to learn about teamwork), and collaborate with interdisciplinary health care professionals. At the end of the summer, students present their team EBP project to the nurse executive committee. Presentation experience assists students in acquiring public speaking skills. Students are nervous about presenting to a room full of executives. However, they learn to depend on one another and to strengthen weaknesses and build on strengths.
When high-performing students come together as one cohort, this dynamic poses challenges for the VALOR participants. One student described her vulnerability in relation to her VALOR peers as “the hardest hit to my self-confidence has been working with such intelligent and accomplished cohorts.” Another student found that even though she was at the top of her class, working with the other VALORs “challenged her self-confidence” because all the program participants were high-performing students. She found it pushed her to perform better. One person reflected, “I feel the VALOR experience has really given all of us the opportunity to unleash our full potential. I have no doubt that these students will become future health care leaders.”
Building Skills
Learning new skills and interacting with physicians are stressful experiences for new graduate nurses.7 A study by Casey and colleagues suggests that new graduate nurses feel inadequate and lack self-confidence.8 VALOR participants share these concerns. The initial journal entries revealed fears of making a mistake, harming patients, fitting in to the work culture, working with doctors, feeling anxious about patient interactions, and performing clinical skills competently.
Initially, students focused on needing extensive practice with nursing skills as evidenced by one student’s comments, “I’m honestly concerned about some of the procedures; I’ve only put in 3 IVs during nursing school, I am not confident walking in to a room and performing a procedure on my own. I would be overwhelmed.” When considering RN-to-MD communication, one student commented, “I’m nervous, doctors can be very hard on new nurses, I’ve witnessed this over and over.”
During the first weeks, the participants discussed the fear of being “on their own” without the benefit of their instructor once they graduate. One person noted this feeling as “The seed of fear grows as graduation approaches.” This lack of self-confidence and feeling scared is a consistent issue with all the VALOR students the first day of the program.
During the program, VALOR students developed nursing skills and became certified in advanced cardiac life support (ACLS). One student suggested that the ACLS class was a great team builder and instilled confidence among the VALOR participants. Another student shared, “We all agreed that attaining this certification was a culmination of our overall VA experience.” A student who was working in an acute care area applied the newly learned ACLS skills the following week when a patient coded. The student’s journal reflected how preparation makes a difference and described his experience and knowing how to react as “powerful.”
The Reality of Nursing
The VALOR program helps connect the academic environment with the realities of the workplace. Wilson found bridging the theory-practice gap between school and workplace improves learning opportunities for students.9 Wilson also suggests that having peers to identify with helps to bridge the theory-practice gap.9 Journal entries reflected “the perfect hospital” of textbooks was different from working every day and “almost being a nurse.” During the VALOR program, students immerse themselves in the realistic nursing environment of staff shortages, equipment unavailability, disgruntled patients, and peer-to-peer communication that is not always civil. The 40-hour workweek provides a realistic hands-on view of nursing and introduces students to socializing as a nurse and the nursing work culture.
After the 2013 summer portion of the program, students were able to differentiate between the realities of the world of health care and the academic view of the health care environment. As students progressed over the summer, a noticeable transformation took place. The student who wrote about needing more skills practice on day 1 found that she was comfortable with injections, hanging IVs, and providing patient care at the end of week 3. Students grew more comfortable collaborating with doctors and other interdisciplinary professionals. They also became competent with basic nursing skills and had a realistic view of the nursing world.
In addition, students became aware of the emotional aspects of nursing. One student discussed making a difference in a veteran’s life after participating in a substance abuse group. “While I was on my way home I started thinking about those vets and their stories, and I started getting emotional. I just felt bad that after doing the great deed of fighting for our country that they became victims of substance abuse,” the student explained. “That afternoon, as I departed the vets, I left hopeful and realized I could make a difference in the life of a veteran.” Another student perceived that doctors were discussing a veteran’s terminal lung cancer “nonchalantly” and reflected, “though I do recognize that a certain degree of disconnection must take place, a certain measure of empathy must remain at all times to effect positive outcomes in the patient’s health.”
VALOR students noted that the program gave them exposure to different areas of nursing. This experience assisted them in deciding on an area of nursing interest. One student who always wanted to be an emergency department nurse found that after that rotation, she was not “cut out to be an emergency department nurse.” Some students came into the program thinking they knew precisely what they wanted to do following graduation, but found a new interest.
Daily Debriefings
Through daily debriefing discussions, students learn about best practices, patient advocacy, nursing leadership, and communication skills. Some have said that it has helped them “get through the day” knowing they had an outlet to review their experiences with VALOR peers. Discussions focus on both the positive and negative aspects of their day.
Students found that group discussions bonded them as a team and allowed them to share their feelings openly. One student found, “What really impacted me was just the amount of learning I received from my VALOR friends.” The group discussions and projects allow students who may typically work in isolation to come together as a team, providing a safe outlet for reflection and self-expression. Meeting daily with peers to share personal experiences increases team cohesion. Research suggests that students learn from their peers.10,11 Working closely with these students, the benefit of peer-to-peer learning was obvious. Students support and teach one another in a nonthreatening environment, which enhances their learning process.
End of the Summer Journey
For the students’ final journal entry, they are asked to identify their greatest fear from week 1 and describe how that has changed by week 10. Journal entries indicated that the students were no longer afraid of being a new nurse, and doctors were “not so scary anymore.” Students already know that nursing is not “going to be peachy,” but participating in the VALOR program allayed their worst fears. One student wrote, “When I had the experiences of doctors, dieticians, and physical therapists asking me questions about my patient and taking what I said seriously, it really boosted my confidence.”
Students seemed less nervous taking on the new graduate nurse role, because they practiced skills and experienced the real life of a nurse. The student who was worried about starting IVs stated, “It is second nature now.” The student who was worried about talking to doctors is now paging and communicating with them in teams. “I feel that I’m more likely to converse with other members of the health care team because of this experience,” one student reported. Another student experienced being afraid of practicing clinical skills because of her lack of experience. “I had put in only 3 IVs previously. I had never seen a cardiac catheterization,” she related. “I had never run an electrocardiography (EKG), and I had never had an opportunity to see many of the things I have seen. I was afraid of taking a full patient load, and I was apprehensive about simple things such as hanging IV medications. I was unsure of myself, and desperately needed practice. I lacked confidence, and needed to gain experience. Now, looking back, those things seem silly.”
Coming out of this program, one student suggested, “I have found that my expectations were blown away.” The 2013 cohort walked away from the summer portion of the program with ACLS training, EKG classes, interdisciplinary team experiences, FranklinCovey personal development seminars, and most of all, hands-on experience that provided these future nurses with confidence in their abilities. Participants felt that after this summer they would be “a step ahead” of their peers when they returned to school in the fall. One student related, after returning to school, “My professor asked me to help teach an EKG class since I was ACLS certified.”
Conclusion
The goal of sharing the VALOR program and students’ experiences at the Salem VAMC is to highlight how students grow clinically and professionally. The program is not a single-person endeavor. The chief nurse executive, managers, interdisciplinary health care professionals, and nursing preceptors support the program. Gaining stakeholder buy-in for the program results in positive experiences for both students and veterans.
Taking top-performing students and grouping them as a cohort creates a learning experience for students and benefits the facility. Students develop essential nursing skills, which assist their transition to the new graduate nurse role. In the words of one student, “As this experience comes to a close, I find myself increasingly apprehensive of finishing. The VALOR position has been like a dream come true for me. I have developed as a person and a future nurse.” As the new generation of nurses, the VALORs provide the institution with fresh eyes and new ideas on how to improve the system and to care for our nation’s veterans.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Shipman D, Garrison M, Hooten J. VALOR: A win-win for VA medical centers and BSN students. Fed Pract. 2010;27(7):31-33.
2. U.S. Department of Veterans Affairs. VHA registered nurses (RN) transition-to-practice program. Veterans Health Administration Website.
http://www1.va.gov/vhapublications/ViewPublication.asp?pub_ID=2469. Published November 23, 2011. Accessed July 1, 2014.
3. Nursing Executive Center. Bridging the Preparation-Practice Gap. Vol. 1: Quantifying new graduate nurse improvement needs. Washington, DC: The Advisory Board Company; 2008. https://hci-portal.hci.utah.edu/sites/hch-nursing/staff-development/Shared%20Documents/Manager%20Tools/Published%20Articles/Bridging%20the%20Preparation%20Practice%20Gap.10.10.pdf. Published 2008. Accessed July 1, 2014.
4. Boswell S, Lowry LW, Wilhoit K. New nurses’ perceptions of nursing practice and quality patient care. J Nurs Care Qual. 2004;19(1):76-81.
5. Rhoads J, Sensenig K, Ruth-Sahd L, Thompson E. Nursing externship: A collaborative endeavor between nursing education and nursing administration. Dimens Crit Care Nurs. 2003;22(6):255-258.
6. King A. My summer externship experience. The Torch. Virginia Nursing Students’ Association Newsletter. Fall 2013. VNSA Website. http://www.vnsa.us/uploads/1/9/0/2/19025131/fall2013torch-final-1.pdf. Accessed July 1, 2014.
7. Oermann MH, Moffitt-Wolf A. New graduates’ perceptions of clinical practice. J Contin Educ Nurs. 1997;28(1):20-25.
8. Casey K, Fink R, Krugman M, Propst J. The graduate nurse experience. J Nurs Adm. 2004;34(6):303-311.
9. Wilson J. Bridging the theory practice gap. Aust Nurs J. 2008;16(4):25.
10. Etheridge SA. Learning to think like a nurse: Stories from new nurse graduates. J Contin Educ Nurs. 2007;38(1):24-30.
11. Roberts D. Friendship fosters learning: The importance of friendship in clinical practice. Nurse Educ Pract. 2009;9(6):367-371.
The VA Learning Opportunity Residency (VALOR) program is a prelicensure experience with a nurse preceptor for rising senior students enrolled in a bachelor of science in nursing program. Students must have a minimum 3.0 grade-point average to apply. The program provides 800 hours of paid learning experiences in diverse didactic and hands-on clinical situations. The first 400 hours of the program (10 weeks) occur over the summer, and the second 400 hours take place during the fall and spring semesters of the student’s last year of school.1 During the last 400 hours, students are placed in the areas they are interested in working as new graduate nurses.
The aim of the Salem VALOR program is to develop the next generation of VAMC nurses by recruiting new graduate nurses. The Salem VAMC structures the VALOR program to meet the needs of both the students and the facility. According to Glenda Fuller, the student programs manager for the VA, national VALOR retention rates from 2007 to 2011 have averaged 38%. However, more applicants apply for new graduate nurse positions than are available. Included in the VHA Directive 2011-039, facilities that hire a nurse with ≤ 1 year of experience must enroll them in a yearlong transition-to-practice program.2 Therefore, facilities may limit the number of new graduate nurse positions.
On entry into the VALOR program, participants write a journal entry regarding their fears and concerns about becoming a new graduate nurse. In addition, each student turns in a written reflection about their experiences each week and participates in daily group discussions with the program coordinator. The last day of the summer portion of the program, students again write about their fears and concerns about becoming a new graduate nurse. After reviewing the VALOR journals, conducting focus groups, and taking notes during the daily meetings, the authors describe the following VALOR experience from the summer of 2013 at the Salem VAMC.
Preparing New Graduates
Hospitals are under pressure to provide high-quality nursing care despite hiring new graduate nurses who are unfamiliar and inexperienced in caring for patients’ complex health care needs. New graduate nurses currently make up more than 10% of hospital nursing staff, and that number is expected to grow as baby boomers retire.3 Boswell and colleagues suggest that those new graduate nurses are unprepared for the registered nurse role.4 Identifying strategies to facilitate the transition from student to the new graduate nurse role will likely decrease attrition rates and increase the effectiveness and the quality of patient care. Nursing programs, such as the VALOR, can ease the transition from the classroom to the working environment.5
This result is evident when observing how VALOR students enhance their nursing skills after the 10-week summer program. VALOR participant Andrea King published her summer experience at the Salem VAMC in The Torch, the Virginia Nursing Students’ Association newsletter.6 “I had so much practice and eventually confidence in my nursing skills,” she wrote, “that I had the autonomy and independence to feel like I was working as an actual nurse.”6
The VALOR Experience
During the summer months, senior nursing students have the opportunity to go on rounds with the chaplain, work with nurse practitioners, attend outings with mental health patients, participate in home health visits, interact with patients in groups, and rotate to different hospital units. Students attend FranklinCovey classes (which specialize in employee performance improvement), participate in an evidence-based practice (EBP) project (which helps them to learn about teamwork), and collaborate with interdisciplinary health care professionals. At the end of the summer, students present their team EBP project to the nurse executive committee. Presentation experience assists students in acquiring public speaking skills. Students are nervous about presenting to a room full of executives. However, they learn to depend on one another and to strengthen weaknesses and build on strengths.
When high-performing students come together as one cohort, this dynamic poses challenges for the VALOR participants. One student described her vulnerability in relation to her VALOR peers as “the hardest hit to my self-confidence has been working with such intelligent and accomplished cohorts.” Another student found that even though she was at the top of her class, working with the other VALORs “challenged her self-confidence” because all the program participants were high-performing students. She found it pushed her to perform better. One person reflected, “I feel the VALOR experience has really given all of us the opportunity to unleash our full potential. I have no doubt that these students will become future health care leaders.”
Building Skills
Learning new skills and interacting with physicians are stressful experiences for new graduate nurses.7 A study by Casey and colleagues suggests that new graduate nurses feel inadequate and lack self-confidence.8 VALOR participants share these concerns. The initial journal entries revealed fears of making a mistake, harming patients, fitting in to the work culture, working with doctors, feeling anxious about patient interactions, and performing clinical skills competently.
Initially, students focused on needing extensive practice with nursing skills as evidenced by one student’s comments, “I’m honestly concerned about some of the procedures; I’ve only put in 3 IVs during nursing school, I am not confident walking in to a room and performing a procedure on my own. I would be overwhelmed.” When considering RN-to-MD communication, one student commented, “I’m nervous, doctors can be very hard on new nurses, I’ve witnessed this over and over.”
During the first weeks, the participants discussed the fear of being “on their own” without the benefit of their instructor once they graduate. One person noted this feeling as “The seed of fear grows as graduation approaches.” This lack of self-confidence and feeling scared is a consistent issue with all the VALOR students the first day of the program.
During the program, VALOR students developed nursing skills and became certified in advanced cardiac life support (ACLS). One student suggested that the ACLS class was a great team builder and instilled confidence among the VALOR participants. Another student shared, “We all agreed that attaining this certification was a culmination of our overall VA experience.” A student who was working in an acute care area applied the newly learned ACLS skills the following week when a patient coded. The student’s journal reflected how preparation makes a difference and described his experience and knowing how to react as “powerful.”
The Reality of Nursing
The VALOR program helps connect the academic environment with the realities of the workplace. Wilson found bridging the theory-practice gap between school and workplace improves learning opportunities for students.9 Wilson also suggests that having peers to identify with helps to bridge the theory-practice gap.9 Journal entries reflected “the perfect hospital” of textbooks was different from working every day and “almost being a nurse.” During the VALOR program, students immerse themselves in the realistic nursing environment of staff shortages, equipment unavailability, disgruntled patients, and peer-to-peer communication that is not always civil. The 40-hour workweek provides a realistic hands-on view of nursing and introduces students to socializing as a nurse and the nursing work culture.
After the 2013 summer portion of the program, students were able to differentiate between the realities of the world of health care and the academic view of the health care environment. As students progressed over the summer, a noticeable transformation took place. The student who wrote about needing more skills practice on day 1 found that she was comfortable with injections, hanging IVs, and providing patient care at the end of week 3. Students grew more comfortable collaborating with doctors and other interdisciplinary professionals. They also became competent with basic nursing skills and had a realistic view of the nursing world.
In addition, students became aware of the emotional aspects of nursing. One student discussed making a difference in a veteran’s life after participating in a substance abuse group. “While I was on my way home I started thinking about those vets and their stories, and I started getting emotional. I just felt bad that after doing the great deed of fighting for our country that they became victims of substance abuse,” the student explained. “That afternoon, as I departed the vets, I left hopeful and realized I could make a difference in the life of a veteran.” Another student perceived that doctors were discussing a veteran’s terminal lung cancer “nonchalantly” and reflected, “though I do recognize that a certain degree of disconnection must take place, a certain measure of empathy must remain at all times to effect positive outcomes in the patient’s health.”
VALOR students noted that the program gave them exposure to different areas of nursing. This experience assisted them in deciding on an area of nursing interest. One student who always wanted to be an emergency department nurse found that after that rotation, she was not “cut out to be an emergency department nurse.” Some students came into the program thinking they knew precisely what they wanted to do following graduation, but found a new interest.
Daily Debriefings
Through daily debriefing discussions, students learn about best practices, patient advocacy, nursing leadership, and communication skills. Some have said that it has helped them “get through the day” knowing they had an outlet to review their experiences with VALOR peers. Discussions focus on both the positive and negative aspects of their day.
Students found that group discussions bonded them as a team and allowed them to share their feelings openly. One student found, “What really impacted me was just the amount of learning I received from my VALOR friends.” The group discussions and projects allow students who may typically work in isolation to come together as a team, providing a safe outlet for reflection and self-expression. Meeting daily with peers to share personal experiences increases team cohesion. Research suggests that students learn from their peers.10,11 Working closely with these students, the benefit of peer-to-peer learning was obvious. Students support and teach one another in a nonthreatening environment, which enhances their learning process.
End of the Summer Journey
For the students’ final journal entry, they are asked to identify their greatest fear from week 1 and describe how that has changed by week 10. Journal entries indicated that the students were no longer afraid of being a new nurse, and doctors were “not so scary anymore.” Students already know that nursing is not “going to be peachy,” but participating in the VALOR program allayed their worst fears. One student wrote, “When I had the experiences of doctors, dieticians, and physical therapists asking me questions about my patient and taking what I said seriously, it really boosted my confidence.”
Students seemed less nervous taking on the new graduate nurse role, because they practiced skills and experienced the real life of a nurse. The student who was worried about starting IVs stated, “It is second nature now.” The student who was worried about talking to doctors is now paging and communicating with them in teams. “I feel that I’m more likely to converse with other members of the health care team because of this experience,” one student reported. Another student experienced being afraid of practicing clinical skills because of her lack of experience. “I had put in only 3 IVs previously. I had never seen a cardiac catheterization,” she related. “I had never run an electrocardiography (EKG), and I had never had an opportunity to see many of the things I have seen. I was afraid of taking a full patient load, and I was apprehensive about simple things such as hanging IV medications. I was unsure of myself, and desperately needed practice. I lacked confidence, and needed to gain experience. Now, looking back, those things seem silly.”
Coming out of this program, one student suggested, “I have found that my expectations were blown away.” The 2013 cohort walked away from the summer portion of the program with ACLS training, EKG classes, interdisciplinary team experiences, FranklinCovey personal development seminars, and most of all, hands-on experience that provided these future nurses with confidence in their abilities. Participants felt that after this summer they would be “a step ahead” of their peers when they returned to school in the fall. One student related, after returning to school, “My professor asked me to help teach an EKG class since I was ACLS certified.”
Conclusion
The goal of sharing the VALOR program and students’ experiences at the Salem VAMC is to highlight how students grow clinically and professionally. The program is not a single-person endeavor. The chief nurse executive, managers, interdisciplinary health care professionals, and nursing preceptors support the program. Gaining stakeholder buy-in for the program results in positive experiences for both students and veterans.
Taking top-performing students and grouping them as a cohort creates a learning experience for students and benefits the facility. Students develop essential nursing skills, which assist their transition to the new graduate nurse role. In the words of one student, “As this experience comes to a close, I find myself increasingly apprehensive of finishing. The VALOR position has been like a dream come true for me. I have developed as a person and a future nurse.” As the new generation of nurses, the VALORs provide the institution with fresh eyes and new ideas on how to improve the system and to care for our nation’s veterans.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
The VA Learning Opportunity Residency (VALOR) program is a prelicensure experience with a nurse preceptor for rising senior students enrolled in a bachelor of science in nursing program. Students must have a minimum 3.0 grade-point average to apply. The program provides 800 hours of paid learning experiences in diverse didactic and hands-on clinical situations. The first 400 hours of the program (10 weeks) occur over the summer, and the second 400 hours take place during the fall and spring semesters of the student’s last year of school.1 During the last 400 hours, students are placed in the areas they are interested in working as new graduate nurses.
The aim of the Salem VALOR program is to develop the next generation of VAMC nurses by recruiting new graduate nurses. The Salem VAMC structures the VALOR program to meet the needs of both the students and the facility. According to Glenda Fuller, the student programs manager for the VA, national VALOR retention rates from 2007 to 2011 have averaged 38%. However, more applicants apply for new graduate nurse positions than are available. Included in the VHA Directive 2011-039, facilities that hire a nurse with ≤ 1 year of experience must enroll them in a yearlong transition-to-practice program.2 Therefore, facilities may limit the number of new graduate nurse positions.
On entry into the VALOR program, participants write a journal entry regarding their fears and concerns about becoming a new graduate nurse. In addition, each student turns in a written reflection about their experiences each week and participates in daily group discussions with the program coordinator. The last day of the summer portion of the program, students again write about their fears and concerns about becoming a new graduate nurse. After reviewing the VALOR journals, conducting focus groups, and taking notes during the daily meetings, the authors describe the following VALOR experience from the summer of 2013 at the Salem VAMC.
Preparing New Graduates
Hospitals are under pressure to provide high-quality nursing care despite hiring new graduate nurses who are unfamiliar and inexperienced in caring for patients’ complex health care needs. New graduate nurses currently make up more than 10% of hospital nursing staff, and that number is expected to grow as baby boomers retire.3 Boswell and colleagues suggest that those new graduate nurses are unprepared for the registered nurse role.4 Identifying strategies to facilitate the transition from student to the new graduate nurse role will likely decrease attrition rates and increase the effectiveness and the quality of patient care. Nursing programs, such as the VALOR, can ease the transition from the classroom to the working environment.5
This result is evident when observing how VALOR students enhance their nursing skills after the 10-week summer program. VALOR participant Andrea King published her summer experience at the Salem VAMC in The Torch, the Virginia Nursing Students’ Association newsletter.6 “I had so much practice and eventually confidence in my nursing skills,” she wrote, “that I had the autonomy and independence to feel like I was working as an actual nurse.”6
The VALOR Experience
During the summer months, senior nursing students have the opportunity to go on rounds with the chaplain, work with nurse practitioners, attend outings with mental health patients, participate in home health visits, interact with patients in groups, and rotate to different hospital units. Students attend FranklinCovey classes (which specialize in employee performance improvement), participate in an evidence-based practice (EBP) project (which helps them to learn about teamwork), and collaborate with interdisciplinary health care professionals. At the end of the summer, students present their team EBP project to the nurse executive committee. Presentation experience assists students in acquiring public speaking skills. Students are nervous about presenting to a room full of executives. However, they learn to depend on one another and to strengthen weaknesses and build on strengths.
When high-performing students come together as one cohort, this dynamic poses challenges for the VALOR participants. One student described her vulnerability in relation to her VALOR peers as “the hardest hit to my self-confidence has been working with such intelligent and accomplished cohorts.” Another student found that even though she was at the top of her class, working with the other VALORs “challenged her self-confidence” because all the program participants were high-performing students. She found it pushed her to perform better. One person reflected, “I feel the VALOR experience has really given all of us the opportunity to unleash our full potential. I have no doubt that these students will become future health care leaders.”
Building Skills
Learning new skills and interacting with physicians are stressful experiences for new graduate nurses.7 A study by Casey and colleagues suggests that new graduate nurses feel inadequate and lack self-confidence.8 VALOR participants share these concerns. The initial journal entries revealed fears of making a mistake, harming patients, fitting in to the work culture, working with doctors, feeling anxious about patient interactions, and performing clinical skills competently.
Initially, students focused on needing extensive practice with nursing skills as evidenced by one student’s comments, “I’m honestly concerned about some of the procedures; I’ve only put in 3 IVs during nursing school, I am not confident walking in to a room and performing a procedure on my own. I would be overwhelmed.” When considering RN-to-MD communication, one student commented, “I’m nervous, doctors can be very hard on new nurses, I’ve witnessed this over and over.”
During the first weeks, the participants discussed the fear of being “on their own” without the benefit of their instructor once they graduate. One person noted this feeling as “The seed of fear grows as graduation approaches.” This lack of self-confidence and feeling scared is a consistent issue with all the VALOR students the first day of the program.
During the program, VALOR students developed nursing skills and became certified in advanced cardiac life support (ACLS). One student suggested that the ACLS class was a great team builder and instilled confidence among the VALOR participants. Another student shared, “We all agreed that attaining this certification was a culmination of our overall VA experience.” A student who was working in an acute care area applied the newly learned ACLS skills the following week when a patient coded. The student’s journal reflected how preparation makes a difference and described his experience and knowing how to react as “powerful.”
The Reality of Nursing
The VALOR program helps connect the academic environment with the realities of the workplace. Wilson found bridging the theory-practice gap between school and workplace improves learning opportunities for students.9 Wilson also suggests that having peers to identify with helps to bridge the theory-practice gap.9 Journal entries reflected “the perfect hospital” of textbooks was different from working every day and “almost being a nurse.” During the VALOR program, students immerse themselves in the realistic nursing environment of staff shortages, equipment unavailability, disgruntled patients, and peer-to-peer communication that is not always civil. The 40-hour workweek provides a realistic hands-on view of nursing and introduces students to socializing as a nurse and the nursing work culture.
After the 2013 summer portion of the program, students were able to differentiate between the realities of the world of health care and the academic view of the health care environment. As students progressed over the summer, a noticeable transformation took place. The student who wrote about needing more skills practice on day 1 found that she was comfortable with injections, hanging IVs, and providing patient care at the end of week 3. Students grew more comfortable collaborating with doctors and other interdisciplinary professionals. They also became competent with basic nursing skills and had a realistic view of the nursing world.
In addition, students became aware of the emotional aspects of nursing. One student discussed making a difference in a veteran’s life after participating in a substance abuse group. “While I was on my way home I started thinking about those vets and their stories, and I started getting emotional. I just felt bad that after doing the great deed of fighting for our country that they became victims of substance abuse,” the student explained. “That afternoon, as I departed the vets, I left hopeful and realized I could make a difference in the life of a veteran.” Another student perceived that doctors were discussing a veteran’s terminal lung cancer “nonchalantly” and reflected, “though I do recognize that a certain degree of disconnection must take place, a certain measure of empathy must remain at all times to effect positive outcomes in the patient’s health.”
VALOR students noted that the program gave them exposure to different areas of nursing. This experience assisted them in deciding on an area of nursing interest. One student who always wanted to be an emergency department nurse found that after that rotation, she was not “cut out to be an emergency department nurse.” Some students came into the program thinking they knew precisely what they wanted to do following graduation, but found a new interest.
Daily Debriefings
Through daily debriefing discussions, students learn about best practices, patient advocacy, nursing leadership, and communication skills. Some have said that it has helped them “get through the day” knowing they had an outlet to review their experiences with VALOR peers. Discussions focus on both the positive and negative aspects of their day.
Students found that group discussions bonded them as a team and allowed them to share their feelings openly. One student found, “What really impacted me was just the amount of learning I received from my VALOR friends.” The group discussions and projects allow students who may typically work in isolation to come together as a team, providing a safe outlet for reflection and self-expression. Meeting daily with peers to share personal experiences increases team cohesion. Research suggests that students learn from their peers.10,11 Working closely with these students, the benefit of peer-to-peer learning was obvious. Students support and teach one another in a nonthreatening environment, which enhances their learning process.
End of the Summer Journey
For the students’ final journal entry, they are asked to identify their greatest fear from week 1 and describe how that has changed by week 10. Journal entries indicated that the students were no longer afraid of being a new nurse, and doctors were “not so scary anymore.” Students already know that nursing is not “going to be peachy,” but participating in the VALOR program allayed their worst fears. One student wrote, “When I had the experiences of doctors, dieticians, and physical therapists asking me questions about my patient and taking what I said seriously, it really boosted my confidence.”
Students seemed less nervous taking on the new graduate nurse role, because they practiced skills and experienced the real life of a nurse. The student who was worried about starting IVs stated, “It is second nature now.” The student who was worried about talking to doctors is now paging and communicating with them in teams. “I feel that I’m more likely to converse with other members of the health care team because of this experience,” one student reported. Another student experienced being afraid of practicing clinical skills because of her lack of experience. “I had put in only 3 IVs previously. I had never seen a cardiac catheterization,” she related. “I had never run an electrocardiography (EKG), and I had never had an opportunity to see many of the things I have seen. I was afraid of taking a full patient load, and I was apprehensive about simple things such as hanging IV medications. I was unsure of myself, and desperately needed practice. I lacked confidence, and needed to gain experience. Now, looking back, those things seem silly.”
Coming out of this program, one student suggested, “I have found that my expectations were blown away.” The 2013 cohort walked away from the summer portion of the program with ACLS training, EKG classes, interdisciplinary team experiences, FranklinCovey personal development seminars, and most of all, hands-on experience that provided these future nurses with confidence in their abilities. Participants felt that after this summer they would be “a step ahead” of their peers when they returned to school in the fall. One student related, after returning to school, “My professor asked me to help teach an EKG class since I was ACLS certified.”
Conclusion
The goal of sharing the VALOR program and students’ experiences at the Salem VAMC is to highlight how students grow clinically and professionally. The program is not a single-person endeavor. The chief nurse executive, managers, interdisciplinary health care professionals, and nursing preceptors support the program. Gaining stakeholder buy-in for the program results in positive experiences for both students and veterans.
Taking top-performing students and grouping them as a cohort creates a learning experience for students and benefits the facility. Students develop essential nursing skills, which assist their transition to the new graduate nurse role. In the words of one student, “As this experience comes to a close, I find myself increasingly apprehensive of finishing. The VALOR position has been like a dream come true for me. I have developed as a person and a future nurse.” As the new generation of nurses, the VALORs provide the institution with fresh eyes and new ideas on how to improve the system and to care for our nation’s veterans.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Shipman D, Garrison M, Hooten J. VALOR: A win-win for VA medical centers and BSN students. Fed Pract. 2010;27(7):31-33.
2. U.S. Department of Veterans Affairs. VHA registered nurses (RN) transition-to-practice program. Veterans Health Administration Website.
http://www1.va.gov/vhapublications/ViewPublication.asp?pub_ID=2469. Published November 23, 2011. Accessed July 1, 2014.
3. Nursing Executive Center. Bridging the Preparation-Practice Gap. Vol. 1: Quantifying new graduate nurse improvement needs. Washington, DC: The Advisory Board Company; 2008. https://hci-portal.hci.utah.edu/sites/hch-nursing/staff-development/Shared%20Documents/Manager%20Tools/Published%20Articles/Bridging%20the%20Preparation%20Practice%20Gap.10.10.pdf. Published 2008. Accessed July 1, 2014.
4. Boswell S, Lowry LW, Wilhoit K. New nurses’ perceptions of nursing practice and quality patient care. J Nurs Care Qual. 2004;19(1):76-81.
5. Rhoads J, Sensenig K, Ruth-Sahd L, Thompson E. Nursing externship: A collaborative endeavor between nursing education and nursing administration. Dimens Crit Care Nurs. 2003;22(6):255-258.
6. King A. My summer externship experience. The Torch. Virginia Nursing Students’ Association Newsletter. Fall 2013. VNSA Website. http://www.vnsa.us/uploads/1/9/0/2/19025131/fall2013torch-final-1.pdf. Accessed July 1, 2014.
7. Oermann MH, Moffitt-Wolf A. New graduates’ perceptions of clinical practice. J Contin Educ Nurs. 1997;28(1):20-25.
8. Casey K, Fink R, Krugman M, Propst J. The graduate nurse experience. J Nurs Adm. 2004;34(6):303-311.
9. Wilson J. Bridging the theory practice gap. Aust Nurs J. 2008;16(4):25.
10. Etheridge SA. Learning to think like a nurse: Stories from new nurse graduates. J Contin Educ Nurs. 2007;38(1):24-30.
11. Roberts D. Friendship fosters learning: The importance of friendship in clinical practice. Nurse Educ Pract. 2009;9(6):367-371.
1. Shipman D, Garrison M, Hooten J. VALOR: A win-win for VA medical centers and BSN students. Fed Pract. 2010;27(7):31-33.
2. U.S. Department of Veterans Affairs. VHA registered nurses (RN) transition-to-practice program. Veterans Health Administration Website.
http://www1.va.gov/vhapublications/ViewPublication.asp?pub_ID=2469. Published November 23, 2011. Accessed July 1, 2014.
3. Nursing Executive Center. Bridging the Preparation-Practice Gap. Vol. 1: Quantifying new graduate nurse improvement needs. Washington, DC: The Advisory Board Company; 2008. https://hci-portal.hci.utah.edu/sites/hch-nursing/staff-development/Shared%20Documents/Manager%20Tools/Published%20Articles/Bridging%20the%20Preparation%20Practice%20Gap.10.10.pdf. Published 2008. Accessed July 1, 2014.
4. Boswell S, Lowry LW, Wilhoit K. New nurses’ perceptions of nursing practice and quality patient care. J Nurs Care Qual. 2004;19(1):76-81.
5. Rhoads J, Sensenig K, Ruth-Sahd L, Thompson E. Nursing externship: A collaborative endeavor between nursing education and nursing administration. Dimens Crit Care Nurs. 2003;22(6):255-258.
6. King A. My summer externship experience. The Torch. Virginia Nursing Students’ Association Newsletter. Fall 2013. VNSA Website. http://www.vnsa.us/uploads/1/9/0/2/19025131/fall2013torch-final-1.pdf. Accessed July 1, 2014.
7. Oermann MH, Moffitt-Wolf A. New graduates’ perceptions of clinical practice. J Contin Educ Nurs. 1997;28(1):20-25.
8. Casey K, Fink R, Krugman M, Propst J. The graduate nurse experience. J Nurs Adm. 2004;34(6):303-311.
9. Wilson J. Bridging the theory practice gap. Aust Nurs J. 2008;16(4):25.
10. Etheridge SA. Learning to think like a nurse: Stories from new nurse graduates. J Contin Educ Nurs. 2007;38(1):24-30.
11. Roberts D. Friendship fosters learning: The importance of friendship in clinical practice. Nurse Educ Pract. 2009;9(6):367-371.