User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'medstat-accordion-set article-series')]
More doctors used digital tools in 2019
The use of digital tools among physicians has markedly risen since 2016, with telehealth visits and remote patient monitoring making the greatest strides in usage, an American Medical Association report shows.
In 2019, 28% of physicians used televisits/virtual visits, up from 14% in 2016, while remote monitoring and management for improved care rose to 22% in 2019, an increase from 13% in 2016, according to the AMA report, released in February 2020. The report, which surveyed 1,359 doctors, includes responses from 672 primary care physicians and 687 specialists.
Remote monitoring for efficiency, meanwhile, grew to 16% in 2019 from 12% in 2016. Remote monitoring for efficiency pertains to smart versions of common clinical devices such as thermometers, blood pressure cuffs, and scales that automatically enter readings in the record. Remote monitoring for improved care refers to mobile applications and devices used for daily measurement of vital signs such as weight, blood pressure, blood glucose.
Adoption of other digital tools by physicians have also grown, including clinical decision support, which climbed to 37% in 2019 from 28% in 2016 and patient engagement tools, which rose to 33% in 2019, up from 26% in 2016. Clinical decision support tools pertain to modules used in conjunction with the electronic health record (EHR), or mobile applications integrated with an EHR that can signify changes in patient data, such as weight gain/loss, or change in blood chemistry. Patient engagement tools, meanwhile, refer to solutions that promote patient wellness and active patient participation in their care.
Tools that encompass use of point of care/workflow enhancement increased to 47% in 2019, from 42% in 2016. This area includes communication and sharing of electronic clinical data to consult with specialists, make referrals and/or transitions of care. Tools that address consumer access to their clinical data, meanwhile, rose to 58% in 2019 from 53% in 2016, the highest adoption rate among the digital health tool categories.
Overall, more physicians see an advantage to digital health solutions than did 3 years ago. More primary care physicians and specialists in 2019 reported a “definite advantage” to digital tools enhancing care of patients than in 2016. Doctors who see no advantage to such tools are trending downward and are concentrated to those age 50 and older, according to the report.
Solo-practice physicians are slowly increasing their use of digital health tools. In 2016, solo physicians reported using an average of 1.5 digital tools, which in 2019 increased to an average of 2.2 digital tools. Small practices with between one and three doctors used an average of 1.4 tools in 2016, which rose to an average of 2.2 tools in 2019, the report found. PCPs used slightly more digital tools, compared with specialists, in both 2016 and 2019.
Female doctors are slightly ahead of their male counterparts when it comes to digital health tools. In 2019, female physicians used an average of 2.6 digital tools, up from 1.9 in 2016. Male doctors used an average of 2.4 tools in 2019, compared with 1.9 tools in 2016.
For the physicians surveyed, the most important factor associated with usage was that digital tools were covered by malpractice insurance, followed by the importance of data privacy/security ensured by the EHR vendor, and that the tools were well integrated with the EHR. Other important factors included that data security was ensured by the practice or hospital, that doctors were reimbursed for their time spent using digital tools, and that the tools were supported by the EHR vendor.
Regarding the top motivator for doctors to use digital tools, 51% of physicians in 2019 said improved efficiency was “very important,” up from 48% in 2016. Other top motivators included that digital tools increased safety, improved diagnostic ability, and addressed physician burnout.
In 2019, the demonstration of safety and efficacy in peer-reviewed publications as it relates to digital tools also grew in importance. Of the physicians surveyed, 36% reported that safety and efficacy demonstrated in peer-reviewed publications was “very important,” an increase from 32% in 2016. Other “very important” factors for physicians are that digital tools used are proven to be as good/superior to traditional care, that they are intuitive/require no special training, that they align with the standard of care, and that their safety and efficacy is validated by the Food and Drug Administration.
“The rise of the digital-native physician will have a profound impact on health care and patient outcomes, and will place digital health technologies under pressure to perform according to higher expectations,” AMA board chair Jesse M. Ehrenfeld, MD, PhD, said in a statement. “The AMA survey provides deep insight into the emerging requirements that physicians expect from digital technologies and sets an industry guidepost for understanding what a growing number of physicians require to adopt new technology.”
The survey was derived from the same physician panel used in 2016, provided by WebMD. For the 2019 survey, the basic 2016 survey was followed in wording and question order, with a few variations to remove some questions no longer relevant. The 2019 sample used careful quotas to ensure a sample composition similar to that of 2016, according to the report.
SOURCE: AMA Digital Health Research: Physicians’ motivations and requirements for adopting digital health – Adoption and attitudinal shifts from 2016 to 2019. American Medical Association. February 2020.
The use of digital tools among physicians has markedly risen since 2016, with telehealth visits and remote patient monitoring making the greatest strides in usage, an American Medical Association report shows.
In 2019, 28% of physicians used televisits/virtual visits, up from 14% in 2016, while remote monitoring and management for improved care rose to 22% in 2019, an increase from 13% in 2016, according to the AMA report, released in February 2020. The report, which surveyed 1,359 doctors, includes responses from 672 primary care physicians and 687 specialists.
Remote monitoring for efficiency, meanwhile, grew to 16% in 2019 from 12% in 2016. Remote monitoring for efficiency pertains to smart versions of common clinical devices such as thermometers, blood pressure cuffs, and scales that automatically enter readings in the record. Remote monitoring for improved care refers to mobile applications and devices used for daily measurement of vital signs such as weight, blood pressure, blood glucose.
Adoption of other digital tools by physicians have also grown, including clinical decision support, which climbed to 37% in 2019 from 28% in 2016 and patient engagement tools, which rose to 33% in 2019, up from 26% in 2016. Clinical decision support tools pertain to modules used in conjunction with the electronic health record (EHR), or mobile applications integrated with an EHR that can signify changes in patient data, such as weight gain/loss, or change in blood chemistry. Patient engagement tools, meanwhile, refer to solutions that promote patient wellness and active patient participation in their care.
Tools that encompass use of point of care/workflow enhancement increased to 47% in 2019, from 42% in 2016. This area includes communication and sharing of electronic clinical data to consult with specialists, make referrals and/or transitions of care. Tools that address consumer access to their clinical data, meanwhile, rose to 58% in 2019 from 53% in 2016, the highest adoption rate among the digital health tool categories.
Overall, more physicians see an advantage to digital health solutions than did 3 years ago. More primary care physicians and specialists in 2019 reported a “definite advantage” to digital tools enhancing care of patients than in 2016. Doctors who see no advantage to such tools are trending downward and are concentrated to those age 50 and older, according to the report.
Solo-practice physicians are slowly increasing their use of digital health tools. In 2016, solo physicians reported using an average of 1.5 digital tools, which in 2019 increased to an average of 2.2 digital tools. Small practices with between one and three doctors used an average of 1.4 tools in 2016, which rose to an average of 2.2 tools in 2019, the report found. PCPs used slightly more digital tools, compared with specialists, in both 2016 and 2019.
Female doctors are slightly ahead of their male counterparts when it comes to digital health tools. In 2019, female physicians used an average of 2.6 digital tools, up from 1.9 in 2016. Male doctors used an average of 2.4 tools in 2019, compared with 1.9 tools in 2016.
For the physicians surveyed, the most important factor associated with usage was that digital tools were covered by malpractice insurance, followed by the importance of data privacy/security ensured by the EHR vendor, and that the tools were well integrated with the EHR. Other important factors included that data security was ensured by the practice or hospital, that doctors were reimbursed for their time spent using digital tools, and that the tools were supported by the EHR vendor.
Regarding the top motivator for doctors to use digital tools, 51% of physicians in 2019 said improved efficiency was “very important,” up from 48% in 2016. Other top motivators included that digital tools increased safety, improved diagnostic ability, and addressed physician burnout.
In 2019, the demonstration of safety and efficacy in peer-reviewed publications as it relates to digital tools also grew in importance. Of the physicians surveyed, 36% reported that safety and efficacy demonstrated in peer-reviewed publications was “very important,” an increase from 32% in 2016. Other “very important” factors for physicians are that digital tools used are proven to be as good/superior to traditional care, that they are intuitive/require no special training, that they align with the standard of care, and that their safety and efficacy is validated by the Food and Drug Administration.
“The rise of the digital-native physician will have a profound impact on health care and patient outcomes, and will place digital health technologies under pressure to perform according to higher expectations,” AMA board chair Jesse M. Ehrenfeld, MD, PhD, said in a statement. “The AMA survey provides deep insight into the emerging requirements that physicians expect from digital technologies and sets an industry guidepost for understanding what a growing number of physicians require to adopt new technology.”
The survey was derived from the same physician panel used in 2016, provided by WebMD. For the 2019 survey, the basic 2016 survey was followed in wording and question order, with a few variations to remove some questions no longer relevant. The 2019 sample used careful quotas to ensure a sample composition similar to that of 2016, according to the report.
SOURCE: AMA Digital Health Research: Physicians’ motivations and requirements for adopting digital health – Adoption and attitudinal shifts from 2016 to 2019. American Medical Association. February 2020.
The use of digital tools among physicians has markedly risen since 2016, with telehealth visits and remote patient monitoring making the greatest strides in usage, an American Medical Association report shows.
In 2019, 28% of physicians used televisits/virtual visits, up from 14% in 2016, while remote monitoring and management for improved care rose to 22% in 2019, an increase from 13% in 2016, according to the AMA report, released in February 2020. The report, which surveyed 1,359 doctors, includes responses from 672 primary care physicians and 687 specialists.
Remote monitoring for efficiency, meanwhile, grew to 16% in 2019 from 12% in 2016. Remote monitoring for efficiency pertains to smart versions of common clinical devices such as thermometers, blood pressure cuffs, and scales that automatically enter readings in the record. Remote monitoring for improved care refers to mobile applications and devices used for daily measurement of vital signs such as weight, blood pressure, blood glucose.
Adoption of other digital tools by physicians have also grown, including clinical decision support, which climbed to 37% in 2019 from 28% in 2016 and patient engagement tools, which rose to 33% in 2019, up from 26% in 2016. Clinical decision support tools pertain to modules used in conjunction with the electronic health record (EHR), or mobile applications integrated with an EHR that can signify changes in patient data, such as weight gain/loss, or change in blood chemistry. Patient engagement tools, meanwhile, refer to solutions that promote patient wellness and active patient participation in their care.
Tools that encompass use of point of care/workflow enhancement increased to 47% in 2019, from 42% in 2016. This area includes communication and sharing of electronic clinical data to consult with specialists, make referrals and/or transitions of care. Tools that address consumer access to their clinical data, meanwhile, rose to 58% in 2019 from 53% in 2016, the highest adoption rate among the digital health tool categories.
Overall, more physicians see an advantage to digital health solutions than did 3 years ago. More primary care physicians and specialists in 2019 reported a “definite advantage” to digital tools enhancing care of patients than in 2016. Doctors who see no advantage to such tools are trending downward and are concentrated to those age 50 and older, according to the report.
Solo-practice physicians are slowly increasing their use of digital health tools. In 2016, solo physicians reported using an average of 1.5 digital tools, which in 2019 increased to an average of 2.2 digital tools. Small practices with between one and three doctors used an average of 1.4 tools in 2016, which rose to an average of 2.2 tools in 2019, the report found. PCPs used slightly more digital tools, compared with specialists, in both 2016 and 2019.
Female doctors are slightly ahead of their male counterparts when it comes to digital health tools. In 2019, female physicians used an average of 2.6 digital tools, up from 1.9 in 2016. Male doctors used an average of 2.4 tools in 2019, compared with 1.9 tools in 2016.
For the physicians surveyed, the most important factor associated with usage was that digital tools were covered by malpractice insurance, followed by the importance of data privacy/security ensured by the EHR vendor, and that the tools were well integrated with the EHR. Other important factors included that data security was ensured by the practice or hospital, that doctors were reimbursed for their time spent using digital tools, and that the tools were supported by the EHR vendor.
Regarding the top motivator for doctors to use digital tools, 51% of physicians in 2019 said improved efficiency was “very important,” up from 48% in 2016. Other top motivators included that digital tools increased safety, improved diagnostic ability, and addressed physician burnout.
In 2019, the demonstration of safety and efficacy in peer-reviewed publications as it relates to digital tools also grew in importance. Of the physicians surveyed, 36% reported that safety and efficacy demonstrated in peer-reviewed publications was “very important,” an increase from 32% in 2016. Other “very important” factors for physicians are that digital tools used are proven to be as good/superior to traditional care, that they are intuitive/require no special training, that they align with the standard of care, and that their safety and efficacy is validated by the Food and Drug Administration.
“The rise of the digital-native physician will have a profound impact on health care and patient outcomes, and will place digital health technologies under pressure to perform according to higher expectations,” AMA board chair Jesse M. Ehrenfeld, MD, PhD, said in a statement. “The AMA survey provides deep insight into the emerging requirements that physicians expect from digital technologies and sets an industry guidepost for understanding what a growing number of physicians require to adopt new technology.”
The survey was derived from the same physician panel used in 2016, provided by WebMD. For the 2019 survey, the basic 2016 survey was followed in wording and question order, with a few variations to remove some questions no longer relevant. The 2019 sample used careful quotas to ensure a sample composition similar to that of 2016, according to the report.
SOURCE: AMA Digital Health Research: Physicians’ motivations and requirements for adopting digital health – Adoption and attitudinal shifts from 2016 to 2019. American Medical Association. February 2020.
COVID-19 spurs telemedicine, furloughs, retirement
The broad use of telemedicine has been a bright spot in the COVID-19 response, but the pandemic is also creating significant disruption as some physicians are furloughed and others consider practice changes.
A recent survey of physicians conducted by Merritt Hawkins and The Physicians Foundation examined how physicians are being affected by and responding to the pandemic. The findings are based on completed surveys from 842 physicians. About one-third of respondents are primary care physicians, while two-thirds are surgical, medical, and diagnostic specialists and subspecialists.
The survey shines a light on the rapid adoption of telemedicine, with 48% of physicians respondents reporting that they are now treating patients through telemedicine.
“I think that is purely explainable on the situation that COVID has led to with the desire to see patients remotely, still take care of them, and the fact that at the federal level this was recognized and doctors are being compensated for seeing patients remotely,” Gary Price, MD, a plastic surgeon and president of The Physicians Foundation, said in an interview.
“The Foundation does a study of the nation’s physicians every other year and in 2018, when we asked the same question, only 18% of physicians were using some form of telemedicine,” he added.
And Dr. Price said he thinks the shift to telemedicine is here to stay.
“I think that will be a lasting effect of the pandemic,” he said. “More physicians and more patients will be using telemedicine approaches, I think, from here on out. We will see a shift that persists. I think that’s a good thing. Physicians like it. Patients like it. It won’t replace all in-person visits, certainly, but there are a number of health care visits that could be taken care of quite well with a virtual visit and it saves the patients travel time, time away from work, and I think it can make the physicians’ practice more efficient as well.”
The key to sustainability, he said, will be that private insurers and the Centers for Medicare & Medicaid Services continue to pay for it.
“I think we will have had a good demonstration, not only that it can work, but that it does work and that it can be accomplished without any diminishment in the quality of care that’s delivered,” he said.
But the recent survey also identified a number of employment issues that have arisen during the COVID-19 pandemic. Overall, 18% of respondents who were treating COVID-19 patients and 30% of those not treating COVID-19 patients reported that they had been furloughed or experienced a pay cut. Among respondents, just 38.5% reported that they are seeing COVID-19 patients.
“It is unprecedented to my knowledge in the physician employment sphere,” Dr. Price said. “That was the most surprising thing to me. I think you might be able to explain that by the increasing number of physicians who are employees now of larger health systems and the fact that a big portion of those health systems too, in normal times, involves care that right now no one is able to get to or even wants to be seen for because of the risk, of course, of COVID-19.”
The survey also revealed that some respondents had or were planning a change in practice because of COVID-19: 14% said they had or would seek a different practice, 6% reported they had or would find a job without patient care, 7% said they had or would close their practice temporarily, 5% reported that they had or would retire, and 4% said they had or would leave private practice and seek employment at a hospital.
“The survey represents how they are feeling at the time and it doesn’t mean they will necessarily do that, but if even a portion of doctors did that all at once, we would really aggravate an access problem and what we know is a worsening physician shortage in the country,” he said. “So we are very concerned about that.”
Dr. Price also predicted there would be increased consolidation within the health care system as more smaller, independent practices feel the financial stress of the pandemic.
“I hope that I am wrong about that,” he said. “I think smaller practices offer a very cost-effective solution for high-quality care, and their competition in the marketplace for health care is a good and healthy thing.”
The broad use of telemedicine has been a bright spot in the COVID-19 response, but the pandemic is also creating significant disruption as some physicians are furloughed and others consider practice changes.
A recent survey of physicians conducted by Merritt Hawkins and The Physicians Foundation examined how physicians are being affected by and responding to the pandemic. The findings are based on completed surveys from 842 physicians. About one-third of respondents are primary care physicians, while two-thirds are surgical, medical, and diagnostic specialists and subspecialists.
The survey shines a light on the rapid adoption of telemedicine, with 48% of physicians respondents reporting that they are now treating patients through telemedicine.
“I think that is purely explainable on the situation that COVID has led to with the desire to see patients remotely, still take care of them, and the fact that at the federal level this was recognized and doctors are being compensated for seeing patients remotely,” Gary Price, MD, a plastic surgeon and president of The Physicians Foundation, said in an interview.
“The Foundation does a study of the nation’s physicians every other year and in 2018, when we asked the same question, only 18% of physicians were using some form of telemedicine,” he added.
And Dr. Price said he thinks the shift to telemedicine is here to stay.
“I think that will be a lasting effect of the pandemic,” he said. “More physicians and more patients will be using telemedicine approaches, I think, from here on out. We will see a shift that persists. I think that’s a good thing. Physicians like it. Patients like it. It won’t replace all in-person visits, certainly, but there are a number of health care visits that could be taken care of quite well with a virtual visit and it saves the patients travel time, time away from work, and I think it can make the physicians’ practice more efficient as well.”
The key to sustainability, he said, will be that private insurers and the Centers for Medicare & Medicaid Services continue to pay for it.
“I think we will have had a good demonstration, not only that it can work, but that it does work and that it can be accomplished without any diminishment in the quality of care that’s delivered,” he said.
But the recent survey also identified a number of employment issues that have arisen during the COVID-19 pandemic. Overall, 18% of respondents who were treating COVID-19 patients and 30% of those not treating COVID-19 patients reported that they had been furloughed or experienced a pay cut. Among respondents, just 38.5% reported that they are seeing COVID-19 patients.
“It is unprecedented to my knowledge in the physician employment sphere,” Dr. Price said. “That was the most surprising thing to me. I think you might be able to explain that by the increasing number of physicians who are employees now of larger health systems and the fact that a big portion of those health systems too, in normal times, involves care that right now no one is able to get to or even wants to be seen for because of the risk, of course, of COVID-19.”
The survey also revealed that some respondents had or were planning a change in practice because of COVID-19: 14% said they had or would seek a different practice, 6% reported they had or would find a job without patient care, 7% said they had or would close their practice temporarily, 5% reported that they had or would retire, and 4% said they had or would leave private practice and seek employment at a hospital.
“The survey represents how they are feeling at the time and it doesn’t mean they will necessarily do that, but if even a portion of doctors did that all at once, we would really aggravate an access problem and what we know is a worsening physician shortage in the country,” he said. “So we are very concerned about that.”
Dr. Price also predicted there would be increased consolidation within the health care system as more smaller, independent practices feel the financial stress of the pandemic.
“I hope that I am wrong about that,” he said. “I think smaller practices offer a very cost-effective solution for high-quality care, and their competition in the marketplace for health care is a good and healthy thing.”
The broad use of telemedicine has been a bright spot in the COVID-19 response, but the pandemic is also creating significant disruption as some physicians are furloughed and others consider practice changes.
A recent survey of physicians conducted by Merritt Hawkins and The Physicians Foundation examined how physicians are being affected by and responding to the pandemic. The findings are based on completed surveys from 842 physicians. About one-third of respondents are primary care physicians, while two-thirds are surgical, medical, and diagnostic specialists and subspecialists.
The survey shines a light on the rapid adoption of telemedicine, with 48% of physicians respondents reporting that they are now treating patients through telemedicine.
“I think that is purely explainable on the situation that COVID has led to with the desire to see patients remotely, still take care of them, and the fact that at the federal level this was recognized and doctors are being compensated for seeing patients remotely,” Gary Price, MD, a plastic surgeon and president of The Physicians Foundation, said in an interview.
“The Foundation does a study of the nation’s physicians every other year and in 2018, when we asked the same question, only 18% of physicians were using some form of telemedicine,” he added.
And Dr. Price said he thinks the shift to telemedicine is here to stay.
“I think that will be a lasting effect of the pandemic,” he said. “More physicians and more patients will be using telemedicine approaches, I think, from here on out. We will see a shift that persists. I think that’s a good thing. Physicians like it. Patients like it. It won’t replace all in-person visits, certainly, but there are a number of health care visits that could be taken care of quite well with a virtual visit and it saves the patients travel time, time away from work, and I think it can make the physicians’ practice more efficient as well.”
The key to sustainability, he said, will be that private insurers and the Centers for Medicare & Medicaid Services continue to pay for it.
“I think we will have had a good demonstration, not only that it can work, but that it does work and that it can be accomplished without any diminishment in the quality of care that’s delivered,” he said.
But the recent survey also identified a number of employment issues that have arisen during the COVID-19 pandemic. Overall, 18% of respondents who were treating COVID-19 patients and 30% of those not treating COVID-19 patients reported that they had been furloughed or experienced a pay cut. Among respondents, just 38.5% reported that they are seeing COVID-19 patients.
“It is unprecedented to my knowledge in the physician employment sphere,” Dr. Price said. “That was the most surprising thing to me. I think you might be able to explain that by the increasing number of physicians who are employees now of larger health systems and the fact that a big portion of those health systems too, in normal times, involves care that right now no one is able to get to or even wants to be seen for because of the risk, of course, of COVID-19.”
The survey also revealed that some respondents had or were planning a change in practice because of COVID-19: 14% said they had or would seek a different practice, 6% reported they had or would find a job without patient care, 7% said they had or would close their practice temporarily, 5% reported that they had or would retire, and 4% said they had or would leave private practice and seek employment at a hospital.
“The survey represents how they are feeling at the time and it doesn’t mean they will necessarily do that, but if even a portion of doctors did that all at once, we would really aggravate an access problem and what we know is a worsening physician shortage in the country,” he said. “So we are very concerned about that.”
Dr. Price also predicted there would be increased consolidation within the health care system as more smaller, independent practices feel the financial stress of the pandemic.
“I hope that I am wrong about that,” he said. “I think smaller practices offer a very cost-effective solution for high-quality care, and their competition in the marketplace for health care is a good and healthy thing.”
Will COVID-19 finally trigger action on health disparities?
Because of stark racial disparities in COVID-19 infection and mortality, the pandemic is being called a “sentinel” and “bellwether” event that should push the United States to finally come to grips with disparities in health care.
When it comes to COVID-19, the pattern is “irrefutable”: Blacks in the United States are being infected with SARS-CoV-2 and are dying of COVID-19 at higher rates than whites, Clyde W. Yancy, MD, Northwestern University, Chicago, wrote in a viewpoint article published online April 15 in JAMA.
According to one recent survey, he noted, the infection rate is threefold higher and the death rate is sixfold higher in predominantly black counties in the United States relative to predominantly white counties.
A sixfold increase in the rate of death for blacks due to a now ubiquitous virus should be deemed “unconscionable” and a moment of “ethical reckoning,” Dr. Yancy wrote.
“Why is this uniquely important to me? I am an academic cardiologist; I study health care disparities; and I am a black man,” he wrote.
The COVID-19 pandemic may be the “bellwether” event that the United States has needed to fully address disparities in health care, Dr. Yancy said.
“Public health is complicated and social reengineering is complex, but change of this magnitude does not happen without a new resolve,” he concluded. “The U.S. has needed a trigger to fully address health care disparities; COVID-19 may be that bellwether event. Certainly, within the broad and powerful economic and legislative engines of the U.S., there is room to definitively address a scourge even worse than COVID-19: health care disparities. It only takes will. It is time to end the refrain.”
The question is, he asks, will the nation finally “think differently, and, as has been done in response to other major diseases, declare that a civil society will no longer accept disproportionate suffering?”
Keith C. Ferdinand, MD, Tulane University, New Orleans, doesn’t think so.
In a related editorial published online April 17 in the Journal of the American College of Cardiology, he points out that the 1985 Heckler Report, from the Department of Health and Human Services, documented higher racial/ethnic mortality rates and the need to correct them. This was followed in 2002 by a report from the Institute of Medicine called Unequal Treatment that also underscored health disparities.
Despite some progress, the goal of reducing and eventually eliminating racial/ethnic disparities has not been realized, Dr. Ferdinand said. “I think baked into the consciousness of the American psyche is that there are some people who have and some who have not,” he said in an interview.
“To some extent, some societies at some point become immune. We would not like to think that America, with its sense of egalitarianism, would get to that point, but maybe we have,” said Dr. Ferdinand.
A ‘sentinel event’
He points out that black people are not genetically or biologically predisposed to COVID-19 but are socially prone to coronavirus exposure and are more likely to have comorbid conditions, such as hypertension, diabetes, obesity, and heart disease, that fuel complications.
The “tragic” higher COVID-19 mortality among African Americans and other racial/ethnic minorities confirms “inadequate” efforts on the part of society to eliminate disparities in cardiovascular disease (CVD) and is a “sentinel event,” Dr. Ferdinand wrote.
A sentinel event, as defined by the Joint Commission, is an unexpected occurrence that leads to death or serious physical or psychological injury or the risk thereof, he explained.
“Conventionally identified sentinel events, such as unintended retention of foreign objects and fall-related events, are used to evaluate quality in hospital care. Similarly, disparate [African American] COVID-19 mortality reflects long-standing, unacceptable U.S. racial/ethnic and socioeconomic CVD inequities and unmasks system failures and unacceptable care to be caught and mitigated,” Dr. Ferdinand concluded.
Dr. Yancy and Dr. Ferdinand have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Because of stark racial disparities in COVID-19 infection and mortality, the pandemic is being called a “sentinel” and “bellwether” event that should push the United States to finally come to grips with disparities in health care.
When it comes to COVID-19, the pattern is “irrefutable”: Blacks in the United States are being infected with SARS-CoV-2 and are dying of COVID-19 at higher rates than whites, Clyde W. Yancy, MD, Northwestern University, Chicago, wrote in a viewpoint article published online April 15 in JAMA.
According to one recent survey, he noted, the infection rate is threefold higher and the death rate is sixfold higher in predominantly black counties in the United States relative to predominantly white counties.
A sixfold increase in the rate of death for blacks due to a now ubiquitous virus should be deemed “unconscionable” and a moment of “ethical reckoning,” Dr. Yancy wrote.
“Why is this uniquely important to me? I am an academic cardiologist; I study health care disparities; and I am a black man,” he wrote.
The COVID-19 pandemic may be the “bellwether” event that the United States has needed to fully address disparities in health care, Dr. Yancy said.
“Public health is complicated and social reengineering is complex, but change of this magnitude does not happen without a new resolve,” he concluded. “The U.S. has needed a trigger to fully address health care disparities; COVID-19 may be that bellwether event. Certainly, within the broad and powerful economic and legislative engines of the U.S., there is room to definitively address a scourge even worse than COVID-19: health care disparities. It only takes will. It is time to end the refrain.”
The question is, he asks, will the nation finally “think differently, and, as has been done in response to other major diseases, declare that a civil society will no longer accept disproportionate suffering?”
Keith C. Ferdinand, MD, Tulane University, New Orleans, doesn’t think so.
In a related editorial published online April 17 in the Journal of the American College of Cardiology, he points out that the 1985 Heckler Report, from the Department of Health and Human Services, documented higher racial/ethnic mortality rates and the need to correct them. This was followed in 2002 by a report from the Institute of Medicine called Unequal Treatment that also underscored health disparities.
Despite some progress, the goal of reducing and eventually eliminating racial/ethnic disparities has not been realized, Dr. Ferdinand said. “I think baked into the consciousness of the American psyche is that there are some people who have and some who have not,” he said in an interview.
“To some extent, some societies at some point become immune. We would not like to think that America, with its sense of egalitarianism, would get to that point, but maybe we have,” said Dr. Ferdinand.
A ‘sentinel event’
He points out that black people are not genetically or biologically predisposed to COVID-19 but are socially prone to coronavirus exposure and are more likely to have comorbid conditions, such as hypertension, diabetes, obesity, and heart disease, that fuel complications.
The “tragic” higher COVID-19 mortality among African Americans and other racial/ethnic minorities confirms “inadequate” efforts on the part of society to eliminate disparities in cardiovascular disease (CVD) and is a “sentinel event,” Dr. Ferdinand wrote.
A sentinel event, as defined by the Joint Commission, is an unexpected occurrence that leads to death or serious physical or psychological injury or the risk thereof, he explained.
“Conventionally identified sentinel events, such as unintended retention of foreign objects and fall-related events, are used to evaluate quality in hospital care. Similarly, disparate [African American] COVID-19 mortality reflects long-standing, unacceptable U.S. racial/ethnic and socioeconomic CVD inequities and unmasks system failures and unacceptable care to be caught and mitigated,” Dr. Ferdinand concluded.
Dr. Yancy and Dr. Ferdinand have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Because of stark racial disparities in COVID-19 infection and mortality, the pandemic is being called a “sentinel” and “bellwether” event that should push the United States to finally come to grips with disparities in health care.
When it comes to COVID-19, the pattern is “irrefutable”: Blacks in the United States are being infected with SARS-CoV-2 and are dying of COVID-19 at higher rates than whites, Clyde W. Yancy, MD, Northwestern University, Chicago, wrote in a viewpoint article published online April 15 in JAMA.
According to one recent survey, he noted, the infection rate is threefold higher and the death rate is sixfold higher in predominantly black counties in the United States relative to predominantly white counties.
A sixfold increase in the rate of death for blacks due to a now ubiquitous virus should be deemed “unconscionable” and a moment of “ethical reckoning,” Dr. Yancy wrote.
“Why is this uniquely important to me? I am an academic cardiologist; I study health care disparities; and I am a black man,” he wrote.
The COVID-19 pandemic may be the “bellwether” event that the United States has needed to fully address disparities in health care, Dr. Yancy said.
“Public health is complicated and social reengineering is complex, but change of this magnitude does not happen without a new resolve,” he concluded. “The U.S. has needed a trigger to fully address health care disparities; COVID-19 may be that bellwether event. Certainly, within the broad and powerful economic and legislative engines of the U.S., there is room to definitively address a scourge even worse than COVID-19: health care disparities. It only takes will. It is time to end the refrain.”
The question is, he asks, will the nation finally “think differently, and, as has been done in response to other major diseases, declare that a civil society will no longer accept disproportionate suffering?”
Keith C. Ferdinand, MD, Tulane University, New Orleans, doesn’t think so.
In a related editorial published online April 17 in the Journal of the American College of Cardiology, he points out that the 1985 Heckler Report, from the Department of Health and Human Services, documented higher racial/ethnic mortality rates and the need to correct them. This was followed in 2002 by a report from the Institute of Medicine called Unequal Treatment that also underscored health disparities.
Despite some progress, the goal of reducing and eventually eliminating racial/ethnic disparities has not been realized, Dr. Ferdinand said. “I think baked into the consciousness of the American psyche is that there are some people who have and some who have not,” he said in an interview.
“To some extent, some societies at some point become immune. We would not like to think that America, with its sense of egalitarianism, would get to that point, but maybe we have,” said Dr. Ferdinand.
A ‘sentinel event’
He points out that black people are not genetically or biologically predisposed to COVID-19 but are socially prone to coronavirus exposure and are more likely to have comorbid conditions, such as hypertension, diabetes, obesity, and heart disease, that fuel complications.
The “tragic” higher COVID-19 mortality among African Americans and other racial/ethnic minorities confirms “inadequate” efforts on the part of society to eliminate disparities in cardiovascular disease (CVD) and is a “sentinel event,” Dr. Ferdinand wrote.
A sentinel event, as defined by the Joint Commission, is an unexpected occurrence that leads to death or serious physical or psychological injury or the risk thereof, he explained.
“Conventionally identified sentinel events, such as unintended retention of foreign objects and fall-related events, are used to evaluate quality in hospital care. Similarly, disparate [African American] COVID-19 mortality reflects long-standing, unacceptable U.S. racial/ethnic and socioeconomic CVD inequities and unmasks system failures and unacceptable care to be caught and mitigated,” Dr. Ferdinand concluded.
Dr. Yancy and Dr. Ferdinand have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Adalimumab serum levels and anti-drug antibodies fail to predict responses to other TNFi
Both antiadalimumab (Humira) antibodies and adalimumab serum levels fell short on predicting drug responses in rheumatoid arthritis patients who failed initial adalimumab therapy, based on a retrospective cohort study of 137 adults.
Biologic disease-modifying antirheumatic drugs (bDMARDs), notably adalimumab, are often prescribed for RA, but “approximately 41% of RA patients do not achieve good response after 6 months of treatment with adalimumab,” wrote Evy Ulijn of Sint Maartenskliniek, Nijmegen, the Netherlands, and colleagues. Preliminary studies have suggested that antiadalimumab antibodies (antidrug antibodies, ADA) and adalimumab serum levels (ADL) may predict the response to a second bDMARD in patients who fail initial adalimumab treatment, they said.
In a study published in Annals of the Rheumatic Diseases, the researchers examined data from 137 adult RA patients seen at the clinic during Jan. 2012–Jan. 2018 who failed to respond to adalimumab after at least 3 months of treatment and started another bDMARD. The average age of the patients was 64 years, and approximately 69% were women.
Overall, the presence of ADA was not a significant predictor of a European League Against Rheumatism good response in patients who switched to another TNFi (etanercept, golimumab, infliximab, or certolizumab pegol), with sensitivity of 18% and specificity of 75%. ADA also was not predictive of response to a non-TNFi bDMARD (rituximab, tocilizumab, or abatacept), with sensitivity and specificity of 33% and 70%, respectively.
Similarly, ADL levels in patients who switched to a TNFi or non-TNFi were not significant predictors of treatment response, with sensitivities and specificities of 50% and 52%, respectively, for TNFi and 32% and 69%, respectively, for non-TNFi.
The findings that neither ADA nor ADL showed predictive values contrast with previous studies, the researchers said.
“Not only did the results of this study show no predictive values, in some analyses a prediction is found in the opposite direction of what was expected,” they wrote.
The study findings were limited by several factors, including the random timing of sample collection, retrospective study design, and potential for misclassification of responders or nonresponders, the researchers noted.
However, the results were strengthened by the blinded choice of treatment and outcome assessment, larger sample size than previous studies, and focus on adalimumab in particular, they said.
“While counterintuitive, it is hard to find an explanation for the lack of a positive finding,” they concluded.
More research is needed to confirm the predictive value of ADA and ADL, they said. In the meantime, rheumatologists should base decisions to switch patients to TNFi or non-TNFi treatment after adalimumab failure based on factors including side effects, local protocol, economical aspects, and patient preferences, they said.
The study received no external funding. The researchers had no financial conflicts to disclose.
SOURCE: Ulijn E et al. Ann Rheum Dis. 2020 Apr 21. doi: 10.1136/annrheumdis-2020-216996.
Both antiadalimumab (Humira) antibodies and adalimumab serum levels fell short on predicting drug responses in rheumatoid arthritis patients who failed initial adalimumab therapy, based on a retrospective cohort study of 137 adults.
Biologic disease-modifying antirheumatic drugs (bDMARDs), notably adalimumab, are often prescribed for RA, but “approximately 41% of RA patients do not achieve good response after 6 months of treatment with adalimumab,” wrote Evy Ulijn of Sint Maartenskliniek, Nijmegen, the Netherlands, and colleagues. Preliminary studies have suggested that antiadalimumab antibodies (antidrug antibodies, ADA) and adalimumab serum levels (ADL) may predict the response to a second bDMARD in patients who fail initial adalimumab treatment, they said.
In a study published in Annals of the Rheumatic Diseases, the researchers examined data from 137 adult RA patients seen at the clinic during Jan. 2012–Jan. 2018 who failed to respond to adalimumab after at least 3 months of treatment and started another bDMARD. The average age of the patients was 64 years, and approximately 69% were women.
Overall, the presence of ADA was not a significant predictor of a European League Against Rheumatism good response in patients who switched to another TNFi (etanercept, golimumab, infliximab, or certolizumab pegol), with sensitivity of 18% and specificity of 75%. ADA also was not predictive of response to a non-TNFi bDMARD (rituximab, tocilizumab, or abatacept), with sensitivity and specificity of 33% and 70%, respectively.
Similarly, ADL levels in patients who switched to a TNFi or non-TNFi were not significant predictors of treatment response, with sensitivities and specificities of 50% and 52%, respectively, for TNFi and 32% and 69%, respectively, for non-TNFi.
The findings that neither ADA nor ADL showed predictive values contrast with previous studies, the researchers said.
“Not only did the results of this study show no predictive values, in some analyses a prediction is found in the opposite direction of what was expected,” they wrote.
The study findings were limited by several factors, including the random timing of sample collection, retrospective study design, and potential for misclassification of responders or nonresponders, the researchers noted.
However, the results were strengthened by the blinded choice of treatment and outcome assessment, larger sample size than previous studies, and focus on adalimumab in particular, they said.
“While counterintuitive, it is hard to find an explanation for the lack of a positive finding,” they concluded.
More research is needed to confirm the predictive value of ADA and ADL, they said. In the meantime, rheumatologists should base decisions to switch patients to TNFi or non-TNFi treatment after adalimumab failure based on factors including side effects, local protocol, economical aspects, and patient preferences, they said.
The study received no external funding. The researchers had no financial conflicts to disclose.
SOURCE: Ulijn E et al. Ann Rheum Dis. 2020 Apr 21. doi: 10.1136/annrheumdis-2020-216996.
Both antiadalimumab (Humira) antibodies and adalimumab serum levels fell short on predicting drug responses in rheumatoid arthritis patients who failed initial adalimumab therapy, based on a retrospective cohort study of 137 adults.
Biologic disease-modifying antirheumatic drugs (bDMARDs), notably adalimumab, are often prescribed for RA, but “approximately 41% of RA patients do not achieve good response after 6 months of treatment with adalimumab,” wrote Evy Ulijn of Sint Maartenskliniek, Nijmegen, the Netherlands, and colleagues. Preliminary studies have suggested that antiadalimumab antibodies (antidrug antibodies, ADA) and adalimumab serum levels (ADL) may predict the response to a second bDMARD in patients who fail initial adalimumab treatment, they said.
In a study published in Annals of the Rheumatic Diseases, the researchers examined data from 137 adult RA patients seen at the clinic during Jan. 2012–Jan. 2018 who failed to respond to adalimumab after at least 3 months of treatment and started another bDMARD. The average age of the patients was 64 years, and approximately 69% were women.
Overall, the presence of ADA was not a significant predictor of a European League Against Rheumatism good response in patients who switched to another TNFi (etanercept, golimumab, infliximab, or certolizumab pegol), with sensitivity of 18% and specificity of 75%. ADA also was not predictive of response to a non-TNFi bDMARD (rituximab, tocilizumab, or abatacept), with sensitivity and specificity of 33% and 70%, respectively.
Similarly, ADL levels in patients who switched to a TNFi or non-TNFi were not significant predictors of treatment response, with sensitivities and specificities of 50% and 52%, respectively, for TNFi and 32% and 69%, respectively, for non-TNFi.
The findings that neither ADA nor ADL showed predictive values contrast with previous studies, the researchers said.
“Not only did the results of this study show no predictive values, in some analyses a prediction is found in the opposite direction of what was expected,” they wrote.
The study findings were limited by several factors, including the random timing of sample collection, retrospective study design, and potential for misclassification of responders or nonresponders, the researchers noted.
However, the results were strengthened by the blinded choice of treatment and outcome assessment, larger sample size than previous studies, and focus on adalimumab in particular, they said.
“While counterintuitive, it is hard to find an explanation for the lack of a positive finding,” they concluded.
More research is needed to confirm the predictive value of ADA and ADL, they said. In the meantime, rheumatologists should base decisions to switch patients to TNFi or non-TNFi treatment after adalimumab failure based on factors including side effects, local protocol, economical aspects, and patient preferences, they said.
The study received no external funding. The researchers had no financial conflicts to disclose.
SOURCE: Ulijn E et al. Ann Rheum Dis. 2020 Apr 21. doi: 10.1136/annrheumdis-2020-216996.
FROM ANNALS OF THE RHEUMATIC DISEASES
Consensus recommendations on AMI management during COVID-19
A consensus statement from the American College of Cardiology (ACC), the American College of Emergency Physicians (ACEP), and the Society for Cardiovascular Angiography & Interventions (SCAI) outlines recommendations for a systematic approach for the care of patients with an acute myocardial infarction (AMI) during the COVID-19 pandemic.
The statement was published in the Journal of the American College of Cardiology.
During the COVID-19 pandemic, percutaneous coronary intervention (PCI) remains the standard of care for patients with ST-segment elevation MI (STEMI) at PCI-capable hospitals when it can be provided in a timely fashion in a dedicated cardiac catheterization laboratory with an expert care team wearing personal protection equipment (PPE), the writing group advised.
“A fibrinolysis-based strategy may be entertained at non-PCI capable referral hospitals or in specific situations where primary PCI cannot be executed or is not deemed the best option,” they said.
SCAI President Ehtisham Mahmud, MD, of the University of California, San Diego, and the writing group also said that clinicians should recognize that cardiovascular manifestations of COVID-19 are “complex” in patients presenting with AMI, myocarditis simulating a STEMI, stress cardiomyopathy, nonischemic cardiomyopathy, coronary spasm, or nonspecific myocardial injury.
A “broad differential diagnosis for ST elevations (including COVID-associated myocarditis) should be considered in the ED prior to choosing a reperfusion strategy,” they advised.
In the absence of hemodynamic instability or ongoing ischemic symptoms, non-STEMI patients with known or suspected COVID-19 are best managed with an initial medical stabilization strategy, the group said.
They also said it is “imperative that health care workers use appropriate PPE for all invasive procedures during this pandemic” and that new rapid COVID-19 testing be “expeditiously” disseminated to all hospitals that manage patients with AMI.
Major challenges are that the prevalence of the COVID-19 in the United States remains unknown and there is the risk for asymptomatic spread.
The writing group said it’s “critical” to “inform the public that we can minimize exposure to the coronavirus so they can continue to call the Emergency Medical System (EMS) for acute ischemic heart disease symptoms and therefore get the appropriate level of cardiac care that their presentation warrants.”
This research had no commercial funding. Dr. Mahmud reported receiving clinical trial research support from Corindus, Abbott Vascular, and CSI; consulting with Medtronic; and consulting and equity with Abiomed. A complete list of author disclosures is included with the original article.
A version of this article originally appeared on Medscape.com.
A consensus statement from the American College of Cardiology (ACC), the American College of Emergency Physicians (ACEP), and the Society for Cardiovascular Angiography & Interventions (SCAI) outlines recommendations for a systematic approach for the care of patients with an acute myocardial infarction (AMI) during the COVID-19 pandemic.
The statement was published in the Journal of the American College of Cardiology.
During the COVID-19 pandemic, percutaneous coronary intervention (PCI) remains the standard of care for patients with ST-segment elevation MI (STEMI) at PCI-capable hospitals when it can be provided in a timely fashion in a dedicated cardiac catheterization laboratory with an expert care team wearing personal protection equipment (PPE), the writing group advised.
“A fibrinolysis-based strategy may be entertained at non-PCI capable referral hospitals or in specific situations where primary PCI cannot be executed or is not deemed the best option,” they said.
SCAI President Ehtisham Mahmud, MD, of the University of California, San Diego, and the writing group also said that clinicians should recognize that cardiovascular manifestations of COVID-19 are “complex” in patients presenting with AMI, myocarditis simulating a STEMI, stress cardiomyopathy, nonischemic cardiomyopathy, coronary spasm, or nonspecific myocardial injury.
A “broad differential diagnosis for ST elevations (including COVID-associated myocarditis) should be considered in the ED prior to choosing a reperfusion strategy,” they advised.
In the absence of hemodynamic instability or ongoing ischemic symptoms, non-STEMI patients with known or suspected COVID-19 are best managed with an initial medical stabilization strategy, the group said.
They also said it is “imperative that health care workers use appropriate PPE for all invasive procedures during this pandemic” and that new rapid COVID-19 testing be “expeditiously” disseminated to all hospitals that manage patients with AMI.
Major challenges are that the prevalence of the COVID-19 in the United States remains unknown and there is the risk for asymptomatic spread.
The writing group said it’s “critical” to “inform the public that we can minimize exposure to the coronavirus so they can continue to call the Emergency Medical System (EMS) for acute ischemic heart disease symptoms and therefore get the appropriate level of cardiac care that their presentation warrants.”
This research had no commercial funding. Dr. Mahmud reported receiving clinical trial research support from Corindus, Abbott Vascular, and CSI; consulting with Medtronic; and consulting and equity with Abiomed. A complete list of author disclosures is included with the original article.
A version of this article originally appeared on Medscape.com.
A consensus statement from the American College of Cardiology (ACC), the American College of Emergency Physicians (ACEP), and the Society for Cardiovascular Angiography & Interventions (SCAI) outlines recommendations for a systematic approach for the care of patients with an acute myocardial infarction (AMI) during the COVID-19 pandemic.
The statement was published in the Journal of the American College of Cardiology.
During the COVID-19 pandemic, percutaneous coronary intervention (PCI) remains the standard of care for patients with ST-segment elevation MI (STEMI) at PCI-capable hospitals when it can be provided in a timely fashion in a dedicated cardiac catheterization laboratory with an expert care team wearing personal protection equipment (PPE), the writing group advised.
“A fibrinolysis-based strategy may be entertained at non-PCI capable referral hospitals or in specific situations where primary PCI cannot be executed or is not deemed the best option,” they said.
SCAI President Ehtisham Mahmud, MD, of the University of California, San Diego, and the writing group also said that clinicians should recognize that cardiovascular manifestations of COVID-19 are “complex” in patients presenting with AMI, myocarditis simulating a STEMI, stress cardiomyopathy, nonischemic cardiomyopathy, coronary spasm, or nonspecific myocardial injury.
A “broad differential diagnosis for ST elevations (including COVID-associated myocarditis) should be considered in the ED prior to choosing a reperfusion strategy,” they advised.
In the absence of hemodynamic instability or ongoing ischemic symptoms, non-STEMI patients with known or suspected COVID-19 are best managed with an initial medical stabilization strategy, the group said.
They also said it is “imperative that health care workers use appropriate PPE for all invasive procedures during this pandemic” and that new rapid COVID-19 testing be “expeditiously” disseminated to all hospitals that manage patients with AMI.
Major challenges are that the prevalence of the COVID-19 in the United States remains unknown and there is the risk for asymptomatic spread.
The writing group said it’s “critical” to “inform the public that we can minimize exposure to the coronavirus so they can continue to call the Emergency Medical System (EMS) for acute ischemic heart disease symptoms and therefore get the appropriate level of cardiac care that their presentation warrants.”
This research had no commercial funding. Dr. Mahmud reported receiving clinical trial research support from Corindus, Abbott Vascular, and CSI; consulting with Medtronic; and consulting and equity with Abiomed. A complete list of author disclosures is included with the original article.
A version of this article originally appeared on Medscape.com.
New advocacy group aims to give ‘every physician’ a voice
A new advocacy organization is launching on April 28 to give “every physician” a voice in decisions that affect their professional lives. But this group doesn’t intend to use the top-down approach to decision making seen in many medical societies.
Paul Teirstein, MD, chief of cardiology for Scripps Clinic in La Jolla, Calif., and founder of the new organization United Physicians, said in an interviewit is a nonprofit group that will operate through online participation.
He said
Projects would need the support of a two-thirds majority of United Physicians’ members to proceed with any proposals. Meetings will be held publicly online, Dr. Teirstein explained.
There is a need for a broad-based organization that will respond to the voice of practicing physicians rather than dictate legislative priorities from management ranks, he said.
Dr. Teirstein said he learned how challenging it is to bring physicians together on issues in 2014 in his battles against changes in maintenance of certification rules. The result of his efforts was the National Board of Physicians and Surgeons (NBPAS), set up to provide a means of certification different from the one offered by the American Board of Internal Medicine.
Dr. Teirstein has argued that the approach of ABIM unfairly burdened physicians with a stepped-up schedule of testing and relied on an outdated approach to the practice of medicine.
Physicians busy with their practices feel they lack a unified voice in contesting the growing administrative burden and unproductive federal and state policies, Dr. Teirstein said.
He cited the limited enrollment in the largest physician groups as evidence of how disenfranchised many clinicians feel. There are about 1 million professional active physicians in the United States, according to the nonprofit Kaiser Family Foundation. Yet, even the largest physician group, the American Medical Association, has about 250,000 members, according to its 2018 annual report
“Clearly, most physicians believe they have little voice when it comes to health care decisions,” Dr. Teirstein said. “Our physician associations are governed from the top down. The leaders set the agenda. There may be delegates, but does leadership really listen to the delegates? Do the delegates really listen to the physician community?”
On its website, AMA describes itself as “physicians’ powerful ally in patient care” that works with more than 190 state and specialty medical societies. In recent months, James L. Madara, MD, the group’s chief executive officer, has urged governors to remove obstacles for physicians who want to fill workforce gaps in COVID-19 hot spots, among other actions.
In its annual report, the AMA, which declined to comment for this article, said its membership rose by 3.4% in 2018, double the growth rate of the previous year, thanks to a membership drive.
“The campaign celebrates the powerful work of our physician members and showcases how their individual efforts – along with the AMA – are moving medicine forward,” wrote Dr. Madara and other organization leaders in the report.
What Dr. Teirstein proposes is an inversion of the structure used by other medical societies, in which he says leaders and delegates dictate priorities.
United Physicians will use meetings and votes held by members online to decide which projects to pursue. Fees would be kept nominal, likely about $10 a year, depending on the number of members. Fees would be subject to change on the basis of expenses. The AMA has a sliding fee schedule that tops out with annual dues for physicians in regular practice of $420.
“There are no delegates, no representatives, and no board of directors. We want every physician to join and every physician to vote on every issue,” Dr. Teirstein said.
He stressed that he sees United Physicians as being complementary to the AMA.
“We do not compete with other organizations. Ideally, other organizations will use the platform,” Dr. Teirstein said. “If the AMA is considering a new policy, it can use the United Physicians platform to measure physician support. For example, through online discussions, petitions, and voting, it might learn a proposed policy needs a few tweaks to be accepted by most physicians.”
No compensation
Dr. Teirstein is among physician leaders who in recent years have sought to rally their colleagues to fight back against growing administrative burdens.
In a 2015 article in JAMA that was written with Medscape’s editor in chief, Eric Topol, MD, Dr. Teirstein criticized the ABIM’s drive to have physicians complete tests every 2 years and participate in continuous certification instead of recertifying once a decade, as had been the practice.
Dr. Teirstein formed the NBPAS as an alternative path for certification, with Dr. Topol serving on the board for that organization. Dr. Topol also will serve as a member of the advisory board for Teirstein’s United Physicians.
Dr. Topol wrote an article that appeared in the New Yorker last August that argued for physicians to move beyond the confines of medical societies and seek a path for broad-based activism. He said he intended to challenge medical societies, which, for all the good they do, can sometimes lose focus on that core relationship in favor of the bottom line.
Dr. Topol said in an interview that his colleague’s new project is a “good idea for a democratized platform at a time when physician solidarity is needed more than ever.”
Dr. Teirstein plans to run United Physicians on a volunteer basis. This builds on the approach he has used for NBPAS. He and the directors of the NBPAS will receive no compensation, he said, as was confirmed by the NBPAS.
In contrast, Dr. Madara made about $2.5 million in total compensation for 2018, according to the organization’s Internal Revenue Service filing. Physicians who served as trustees and officials for the AMA that year received annual compensation that ranged from around $60,000 to $291,980, depending on their duties.
“Having volunteer leadership mitigates conflict of interest. It also ensures leadership has a ‘day job’ that keeps them in touch with issues impacting practicing physicians,” Dr. Teirstein said
Start-up costs for United Physicians will be supported by NBPAS, but it will function as a completely independent organization, he added.
In introducing the group, Dr. Teirstein outlined suggestions for proposals it might pursue. These include making hospitals secure adequate supplies of personal protective equipment ahead of health crises such as the COVID-19 pandemic.
His outline also includes suggestions for issues that likely will persist beyond the response to the pandemic.
Dr. Teirstein proposed a project for persuading insurance companies to provide online calendar appointments for peer-to-peer patient preauthorization. Failure of the insurer’s representative to attend would trigger approval of authorization under this proposal. He also suggested a lobbying effort for specific reimbursement for peer-to-peer, patient preauthorization phone calls.
Dr. Teirstein said he hopes most of the proposals will come from physicians who join United Physicians. Still, it is unclear whether United Physicians will succeed. An initial challenge could be in sorting through a barrage of competing ideas submitted to United Physicians.
But Dr. Teirstein appears hopeful about the changes for this experiment in online advocacy. He intends for United Physicians to be a pathway for clinicians to translate their complaints about policies into calls for action, with only a short investment of their time.
“Most of us have wonderful, engrossing jobs. It’s hard to beat helping a patient, and most of us get to do it every day,” Dr. .Teirstein said. “Will we take the 30 seconds required to sign up and become a United Physicians member? Will we spend a little time each week reviewing the issues and voting? I think it’s an experiment worth watching.”
A version of this article originally appeared on Medscape.com.
A new advocacy organization is launching on April 28 to give “every physician” a voice in decisions that affect their professional lives. But this group doesn’t intend to use the top-down approach to decision making seen in many medical societies.
Paul Teirstein, MD, chief of cardiology for Scripps Clinic in La Jolla, Calif., and founder of the new organization United Physicians, said in an interviewit is a nonprofit group that will operate through online participation.
He said
Projects would need the support of a two-thirds majority of United Physicians’ members to proceed with any proposals. Meetings will be held publicly online, Dr. Teirstein explained.
There is a need for a broad-based organization that will respond to the voice of practicing physicians rather than dictate legislative priorities from management ranks, he said.
Dr. Teirstein said he learned how challenging it is to bring physicians together on issues in 2014 in his battles against changes in maintenance of certification rules. The result of his efforts was the National Board of Physicians and Surgeons (NBPAS), set up to provide a means of certification different from the one offered by the American Board of Internal Medicine.
Dr. Teirstein has argued that the approach of ABIM unfairly burdened physicians with a stepped-up schedule of testing and relied on an outdated approach to the practice of medicine.
Physicians busy with their practices feel they lack a unified voice in contesting the growing administrative burden and unproductive federal and state policies, Dr. Teirstein said.
He cited the limited enrollment in the largest physician groups as evidence of how disenfranchised many clinicians feel. There are about 1 million professional active physicians in the United States, according to the nonprofit Kaiser Family Foundation. Yet, even the largest physician group, the American Medical Association, has about 250,000 members, according to its 2018 annual report
“Clearly, most physicians believe they have little voice when it comes to health care decisions,” Dr. Teirstein said. “Our physician associations are governed from the top down. The leaders set the agenda. There may be delegates, but does leadership really listen to the delegates? Do the delegates really listen to the physician community?”
On its website, AMA describes itself as “physicians’ powerful ally in patient care” that works with more than 190 state and specialty medical societies. In recent months, James L. Madara, MD, the group’s chief executive officer, has urged governors to remove obstacles for physicians who want to fill workforce gaps in COVID-19 hot spots, among other actions.
In its annual report, the AMA, which declined to comment for this article, said its membership rose by 3.4% in 2018, double the growth rate of the previous year, thanks to a membership drive.
“The campaign celebrates the powerful work of our physician members and showcases how their individual efforts – along with the AMA – are moving medicine forward,” wrote Dr. Madara and other organization leaders in the report.
What Dr. Teirstein proposes is an inversion of the structure used by other medical societies, in which he says leaders and delegates dictate priorities.
United Physicians will use meetings and votes held by members online to decide which projects to pursue. Fees would be kept nominal, likely about $10 a year, depending on the number of members. Fees would be subject to change on the basis of expenses. The AMA has a sliding fee schedule that tops out with annual dues for physicians in regular practice of $420.
“There are no delegates, no representatives, and no board of directors. We want every physician to join and every physician to vote on every issue,” Dr. Teirstein said.
He stressed that he sees United Physicians as being complementary to the AMA.
“We do not compete with other organizations. Ideally, other organizations will use the platform,” Dr. Teirstein said. “If the AMA is considering a new policy, it can use the United Physicians platform to measure physician support. For example, through online discussions, petitions, and voting, it might learn a proposed policy needs a few tweaks to be accepted by most physicians.”
No compensation
Dr. Teirstein is among physician leaders who in recent years have sought to rally their colleagues to fight back against growing administrative burdens.
In a 2015 article in JAMA that was written with Medscape’s editor in chief, Eric Topol, MD, Dr. Teirstein criticized the ABIM’s drive to have physicians complete tests every 2 years and participate in continuous certification instead of recertifying once a decade, as had been the practice.
Dr. Teirstein formed the NBPAS as an alternative path for certification, with Dr. Topol serving on the board for that organization. Dr. Topol also will serve as a member of the advisory board for Teirstein’s United Physicians.
Dr. Topol wrote an article that appeared in the New Yorker last August that argued for physicians to move beyond the confines of medical societies and seek a path for broad-based activism. He said he intended to challenge medical societies, which, for all the good they do, can sometimes lose focus on that core relationship in favor of the bottom line.
Dr. Topol said in an interview that his colleague’s new project is a “good idea for a democratized platform at a time when physician solidarity is needed more than ever.”
Dr. Teirstein plans to run United Physicians on a volunteer basis. This builds on the approach he has used for NBPAS. He and the directors of the NBPAS will receive no compensation, he said, as was confirmed by the NBPAS.
In contrast, Dr. Madara made about $2.5 million in total compensation for 2018, according to the organization’s Internal Revenue Service filing. Physicians who served as trustees and officials for the AMA that year received annual compensation that ranged from around $60,000 to $291,980, depending on their duties.
“Having volunteer leadership mitigates conflict of interest. It also ensures leadership has a ‘day job’ that keeps them in touch with issues impacting practicing physicians,” Dr. Teirstein said
Start-up costs for United Physicians will be supported by NBPAS, but it will function as a completely independent organization, he added.
In introducing the group, Dr. Teirstein outlined suggestions for proposals it might pursue. These include making hospitals secure adequate supplies of personal protective equipment ahead of health crises such as the COVID-19 pandemic.
His outline also includes suggestions for issues that likely will persist beyond the response to the pandemic.
Dr. Teirstein proposed a project for persuading insurance companies to provide online calendar appointments for peer-to-peer patient preauthorization. Failure of the insurer’s representative to attend would trigger approval of authorization under this proposal. He also suggested a lobbying effort for specific reimbursement for peer-to-peer, patient preauthorization phone calls.
Dr. Teirstein said he hopes most of the proposals will come from physicians who join United Physicians. Still, it is unclear whether United Physicians will succeed. An initial challenge could be in sorting through a barrage of competing ideas submitted to United Physicians.
But Dr. Teirstein appears hopeful about the changes for this experiment in online advocacy. He intends for United Physicians to be a pathway for clinicians to translate their complaints about policies into calls for action, with only a short investment of their time.
“Most of us have wonderful, engrossing jobs. It’s hard to beat helping a patient, and most of us get to do it every day,” Dr. .Teirstein said. “Will we take the 30 seconds required to sign up and become a United Physicians member? Will we spend a little time each week reviewing the issues and voting? I think it’s an experiment worth watching.”
A version of this article originally appeared on Medscape.com.
A new advocacy organization is launching on April 28 to give “every physician” a voice in decisions that affect their professional lives. But this group doesn’t intend to use the top-down approach to decision making seen in many medical societies.
Paul Teirstein, MD, chief of cardiology for Scripps Clinic in La Jolla, Calif., and founder of the new organization United Physicians, said in an interviewit is a nonprofit group that will operate through online participation.
He said
Projects would need the support of a two-thirds majority of United Physicians’ members to proceed with any proposals. Meetings will be held publicly online, Dr. Teirstein explained.
There is a need for a broad-based organization that will respond to the voice of practicing physicians rather than dictate legislative priorities from management ranks, he said.
Dr. Teirstein said he learned how challenging it is to bring physicians together on issues in 2014 in his battles against changes in maintenance of certification rules. The result of his efforts was the National Board of Physicians and Surgeons (NBPAS), set up to provide a means of certification different from the one offered by the American Board of Internal Medicine.
Dr. Teirstein has argued that the approach of ABIM unfairly burdened physicians with a stepped-up schedule of testing and relied on an outdated approach to the practice of medicine.
Physicians busy with their practices feel they lack a unified voice in contesting the growing administrative burden and unproductive federal and state policies, Dr. Teirstein said.
He cited the limited enrollment in the largest physician groups as evidence of how disenfranchised many clinicians feel. There are about 1 million professional active physicians in the United States, according to the nonprofit Kaiser Family Foundation. Yet, even the largest physician group, the American Medical Association, has about 250,000 members, according to its 2018 annual report
“Clearly, most physicians believe they have little voice when it comes to health care decisions,” Dr. Teirstein said. “Our physician associations are governed from the top down. The leaders set the agenda. There may be delegates, but does leadership really listen to the delegates? Do the delegates really listen to the physician community?”
On its website, AMA describes itself as “physicians’ powerful ally in patient care” that works with more than 190 state and specialty medical societies. In recent months, James L. Madara, MD, the group’s chief executive officer, has urged governors to remove obstacles for physicians who want to fill workforce gaps in COVID-19 hot spots, among other actions.
In its annual report, the AMA, which declined to comment for this article, said its membership rose by 3.4% in 2018, double the growth rate of the previous year, thanks to a membership drive.
“The campaign celebrates the powerful work of our physician members and showcases how their individual efforts – along with the AMA – are moving medicine forward,” wrote Dr. Madara and other organization leaders in the report.
What Dr. Teirstein proposes is an inversion of the structure used by other medical societies, in which he says leaders and delegates dictate priorities.
United Physicians will use meetings and votes held by members online to decide which projects to pursue. Fees would be kept nominal, likely about $10 a year, depending on the number of members. Fees would be subject to change on the basis of expenses. The AMA has a sliding fee schedule that tops out with annual dues for physicians in regular practice of $420.
“There are no delegates, no representatives, and no board of directors. We want every physician to join and every physician to vote on every issue,” Dr. Teirstein said.
He stressed that he sees United Physicians as being complementary to the AMA.
“We do not compete with other organizations. Ideally, other organizations will use the platform,” Dr. Teirstein said. “If the AMA is considering a new policy, it can use the United Physicians platform to measure physician support. For example, through online discussions, petitions, and voting, it might learn a proposed policy needs a few tweaks to be accepted by most physicians.”
No compensation
Dr. Teirstein is among physician leaders who in recent years have sought to rally their colleagues to fight back against growing administrative burdens.
In a 2015 article in JAMA that was written with Medscape’s editor in chief, Eric Topol, MD, Dr. Teirstein criticized the ABIM’s drive to have physicians complete tests every 2 years and participate in continuous certification instead of recertifying once a decade, as had been the practice.
Dr. Teirstein formed the NBPAS as an alternative path for certification, with Dr. Topol serving on the board for that organization. Dr. Topol also will serve as a member of the advisory board for Teirstein’s United Physicians.
Dr. Topol wrote an article that appeared in the New Yorker last August that argued for physicians to move beyond the confines of medical societies and seek a path for broad-based activism. He said he intended to challenge medical societies, which, for all the good they do, can sometimes lose focus on that core relationship in favor of the bottom line.
Dr. Topol said in an interview that his colleague’s new project is a “good idea for a democratized platform at a time when physician solidarity is needed more than ever.”
Dr. Teirstein plans to run United Physicians on a volunteer basis. This builds on the approach he has used for NBPAS. He and the directors of the NBPAS will receive no compensation, he said, as was confirmed by the NBPAS.
In contrast, Dr. Madara made about $2.5 million in total compensation for 2018, according to the organization’s Internal Revenue Service filing. Physicians who served as trustees and officials for the AMA that year received annual compensation that ranged from around $60,000 to $291,980, depending on their duties.
“Having volunteer leadership mitigates conflict of interest. It also ensures leadership has a ‘day job’ that keeps them in touch with issues impacting practicing physicians,” Dr. Teirstein said
Start-up costs for United Physicians will be supported by NBPAS, but it will function as a completely independent organization, he added.
In introducing the group, Dr. Teirstein outlined suggestions for proposals it might pursue. These include making hospitals secure adequate supplies of personal protective equipment ahead of health crises such as the COVID-19 pandemic.
His outline also includes suggestions for issues that likely will persist beyond the response to the pandemic.
Dr. Teirstein proposed a project for persuading insurance companies to provide online calendar appointments for peer-to-peer patient preauthorization. Failure of the insurer’s representative to attend would trigger approval of authorization under this proposal. He also suggested a lobbying effort for specific reimbursement for peer-to-peer, patient preauthorization phone calls.
Dr. Teirstein said he hopes most of the proposals will come from physicians who join United Physicians. Still, it is unclear whether United Physicians will succeed. An initial challenge could be in sorting through a barrage of competing ideas submitted to United Physicians.
But Dr. Teirstein appears hopeful about the changes for this experiment in online advocacy. He intends for United Physicians to be a pathway for clinicians to translate their complaints about policies into calls for action, with only a short investment of their time.
“Most of us have wonderful, engrossing jobs. It’s hard to beat helping a patient, and most of us get to do it every day,” Dr. .Teirstein said. “Will we take the 30 seconds required to sign up and become a United Physicians member? Will we spend a little time each week reviewing the issues and voting? I think it’s an experiment worth watching.”
A version of this article originally appeared on Medscape.com.
CMS suspends advance payment program to clinicians for COVID-19 relief
The Centers for Medicare & Medicaid Services will suspend its Medicare advance payment program for clinicians and is reevaluating how much to pay to hospitals going forward through particular COVID-19 relief initiatives. CMS announced the changes on April 26. Physicians and others who use the accelerated and advance Medicare payments program repay these advances, and they are typically given 1 year or less to repay the funding.
CMS said in a news release it will not accept new applications for the advanced Medicare payment, and it will be reevaluating all pending and new applications “in light of historical direct payments made available through the Department of Health & Human Services’ (HHS) Provider Relief Fund.”
The advance Medicare payment program predates COVID-19, although it previously was used on a much smaller scale. In the past 5 years, CMS approved about 100 total requests for advanced Medicare payment, with most being tied to natural disasters such as hurricanes.
CMS said it has approved, since March, more than 21,000 applications for advanced Medicare payment, totaling $59.6 billion, for hospitals and other organizations that bill its Part A program. In addition, CMS approved almost 24,000 applications for its Part B program, advancing $40.4 billion for physicians, other clinicians, and medical equipment suppliers.
CMS noted that Congress also has provided $175 billion in aid for the medical community that clinicians and medical organizations would not need to repay. The Coronavirus Aid, Relief, and Economic Security (CARES) Act enacted in March included $100 billion, and the Paycheck Protection Program and Health Care Enhancement Act, enacted March 24, includes another $75 billion.
A version of this article was originally published on Medscape.com.
The Centers for Medicare & Medicaid Services will suspend its Medicare advance payment program for clinicians and is reevaluating how much to pay to hospitals going forward through particular COVID-19 relief initiatives. CMS announced the changes on April 26. Physicians and others who use the accelerated and advance Medicare payments program repay these advances, and they are typically given 1 year or less to repay the funding.
CMS said in a news release it will not accept new applications for the advanced Medicare payment, and it will be reevaluating all pending and new applications “in light of historical direct payments made available through the Department of Health & Human Services’ (HHS) Provider Relief Fund.”
The advance Medicare payment program predates COVID-19, although it previously was used on a much smaller scale. In the past 5 years, CMS approved about 100 total requests for advanced Medicare payment, with most being tied to natural disasters such as hurricanes.
CMS said it has approved, since March, more than 21,000 applications for advanced Medicare payment, totaling $59.6 billion, for hospitals and other organizations that bill its Part A program. In addition, CMS approved almost 24,000 applications for its Part B program, advancing $40.4 billion for physicians, other clinicians, and medical equipment suppliers.
CMS noted that Congress also has provided $175 billion in aid for the medical community that clinicians and medical organizations would not need to repay. The Coronavirus Aid, Relief, and Economic Security (CARES) Act enacted in March included $100 billion, and the Paycheck Protection Program and Health Care Enhancement Act, enacted March 24, includes another $75 billion.
A version of this article was originally published on Medscape.com.
The Centers for Medicare & Medicaid Services will suspend its Medicare advance payment program for clinicians and is reevaluating how much to pay to hospitals going forward through particular COVID-19 relief initiatives. CMS announced the changes on April 26. Physicians and others who use the accelerated and advance Medicare payments program repay these advances, and they are typically given 1 year or less to repay the funding.
CMS said in a news release it will not accept new applications for the advanced Medicare payment, and it will be reevaluating all pending and new applications “in light of historical direct payments made available through the Department of Health & Human Services’ (HHS) Provider Relief Fund.”
The advance Medicare payment program predates COVID-19, although it previously was used on a much smaller scale. In the past 5 years, CMS approved about 100 total requests for advanced Medicare payment, with most being tied to natural disasters such as hurricanes.
CMS said it has approved, since March, more than 21,000 applications for advanced Medicare payment, totaling $59.6 billion, for hospitals and other organizations that bill its Part A program. In addition, CMS approved almost 24,000 applications for its Part B program, advancing $40.4 billion for physicians, other clinicians, and medical equipment suppliers.
CMS noted that Congress also has provided $175 billion in aid for the medical community that clinicians and medical organizations would not need to repay. The Coronavirus Aid, Relief, and Economic Security (CARES) Act enacted in March included $100 billion, and the Paycheck Protection Program and Health Care Enhancement Act, enacted March 24, includes another $75 billion.
A version of this article was originally published on Medscape.com.
Changing habits, sleep patterns, and home duties during the pandemic
Like you, I’m not sure when this weird Twilight Zone world of coronavirus will end. Even when it does, its effects will be with us for a long time to come.
But in some ways, they may be for the better. Hopefully some of these changes will stick. Like every new situation, I try to take away something of value from it.
As pithy as it sounds, I used to obsess (sort of) over the daily mail delivery. My secretary would check it mid-afternoon, and if it wasn’t there either she or I would run down again before we left. If it still wasn’t there I’d swing by the box when I came in early the next morning. On Saturdays, I’d sometimes drive in just to get the mail.
There certainly are things that come in that are important: payments, bills, medical records, legal cases to review ... but realistically a lot of mail is junk. Office-supply catalogs, CME or pharmaceutical ads, credit card promotions, and so on.
Now? I just don’t care. If I go several days without seeing patients at the office, the mail is at the back of my mind. It’s in a locked box and isn’t going anywhere. Why worry about it? Next time I’m there I can deal with it. It’s not worth thinking about, it’s just the mail. It’s not worth a special trip.
Sleep is another thing. For years my internal alarm has had me up around 4:00 a.m. (I don’t even bother to set one on my phone), and I get up and go in to get started on the day.
Now? I don’t think I’ve ever slept this much. If I have to go to my office, I’m much less rushed. Many days I don’t even have to do that. I walk down to my home office, call up my charts and the day’s video appointment schedule, and we’re off. Granted, once things return to speed, this will probably be back to normal.
My kids are all home from college, so I have the extra time at home to enjoy them and our dogs. My wife, an oncology infusion nurse, doesn’t get home until 6:00 each night, so for now I’ve become a stay-at-home dad. This is actually something I’ve always liked (in high school, I was voted “most likely to to be a house husband”). So I do the laundry and am in charge of dinner each night. I’m enjoying the last, as I get to pick things out, go through recipes, and cook. I won’t say I’m a great cook, but I’m learning and having fun. As strange as it sounds, being a house husband has always been something I wanted to do, so I’m appreciating the opportunity while it lasts.
I think all of us have come to accept this strange pause button that’s been pushed, and I’ll try to learn what I can from it and take that with me as I move forward.
Dr. Block has a solo neurology practice in Scottsdale, Ariz. He has no relevant disclosures.
Like you, I’m not sure when this weird Twilight Zone world of coronavirus will end. Even when it does, its effects will be with us for a long time to come.
But in some ways, they may be for the better. Hopefully some of these changes will stick. Like every new situation, I try to take away something of value from it.
As pithy as it sounds, I used to obsess (sort of) over the daily mail delivery. My secretary would check it mid-afternoon, and if it wasn’t there either she or I would run down again before we left. If it still wasn’t there I’d swing by the box when I came in early the next morning. On Saturdays, I’d sometimes drive in just to get the mail.
There certainly are things that come in that are important: payments, bills, medical records, legal cases to review ... but realistically a lot of mail is junk. Office-supply catalogs, CME or pharmaceutical ads, credit card promotions, and so on.
Now? I just don’t care. If I go several days without seeing patients at the office, the mail is at the back of my mind. It’s in a locked box and isn’t going anywhere. Why worry about it? Next time I’m there I can deal with it. It’s not worth thinking about, it’s just the mail. It’s not worth a special trip.
Sleep is another thing. For years my internal alarm has had me up around 4:00 a.m. (I don’t even bother to set one on my phone), and I get up and go in to get started on the day.
Now? I don’t think I’ve ever slept this much. If I have to go to my office, I’m much less rushed. Many days I don’t even have to do that. I walk down to my home office, call up my charts and the day’s video appointment schedule, and we’re off. Granted, once things return to speed, this will probably be back to normal.
My kids are all home from college, so I have the extra time at home to enjoy them and our dogs. My wife, an oncology infusion nurse, doesn’t get home until 6:00 each night, so for now I’ve become a stay-at-home dad. This is actually something I’ve always liked (in high school, I was voted “most likely to to be a house husband”). So I do the laundry and am in charge of dinner each night. I’m enjoying the last, as I get to pick things out, go through recipes, and cook. I won’t say I’m a great cook, but I’m learning and having fun. As strange as it sounds, being a house husband has always been something I wanted to do, so I’m appreciating the opportunity while it lasts.
I think all of us have come to accept this strange pause button that’s been pushed, and I’ll try to learn what I can from it and take that with me as I move forward.
Dr. Block has a solo neurology practice in Scottsdale, Ariz. He has no relevant disclosures.
Like you, I’m not sure when this weird Twilight Zone world of coronavirus will end. Even when it does, its effects will be with us for a long time to come.
But in some ways, they may be for the better. Hopefully some of these changes will stick. Like every new situation, I try to take away something of value from it.
As pithy as it sounds, I used to obsess (sort of) over the daily mail delivery. My secretary would check it mid-afternoon, and if it wasn’t there either she or I would run down again before we left. If it still wasn’t there I’d swing by the box when I came in early the next morning. On Saturdays, I’d sometimes drive in just to get the mail.
There certainly are things that come in that are important: payments, bills, medical records, legal cases to review ... but realistically a lot of mail is junk. Office-supply catalogs, CME or pharmaceutical ads, credit card promotions, and so on.
Now? I just don’t care. If I go several days without seeing patients at the office, the mail is at the back of my mind. It’s in a locked box and isn’t going anywhere. Why worry about it? Next time I’m there I can deal with it. It’s not worth thinking about, it’s just the mail. It’s not worth a special trip.
Sleep is another thing. For years my internal alarm has had me up around 4:00 a.m. (I don’t even bother to set one on my phone), and I get up and go in to get started on the day.
Now? I don’t think I’ve ever slept this much. If I have to go to my office, I’m much less rushed. Many days I don’t even have to do that. I walk down to my home office, call up my charts and the day’s video appointment schedule, and we’re off. Granted, once things return to speed, this will probably be back to normal.
My kids are all home from college, so I have the extra time at home to enjoy them and our dogs. My wife, an oncology infusion nurse, doesn’t get home until 6:00 each night, so for now I’ve become a stay-at-home dad. This is actually something I’ve always liked (in high school, I was voted “most likely to to be a house husband”). So I do the laundry and am in charge of dinner each night. I’m enjoying the last, as I get to pick things out, go through recipes, and cook. I won’t say I’m a great cook, but I’m learning and having fun. As strange as it sounds, being a house husband has always been something I wanted to do, so I’m appreciating the opportunity while it lasts.
I think all of us have come to accept this strange pause button that’s been pushed, and I’ll try to learn what I can from it and take that with me as I move forward.
Dr. Block has a solo neurology practice in Scottsdale, Ariz. He has no relevant disclosures.
Rural ICU capacity could be strained by COVID-19
The nonmetropolitan, largely rural, areas of the United States have fewer ICU beds than do urban areas, but their populations may be at higher risk for COVID-19 complications, according to the Kaiser Family Foundation.
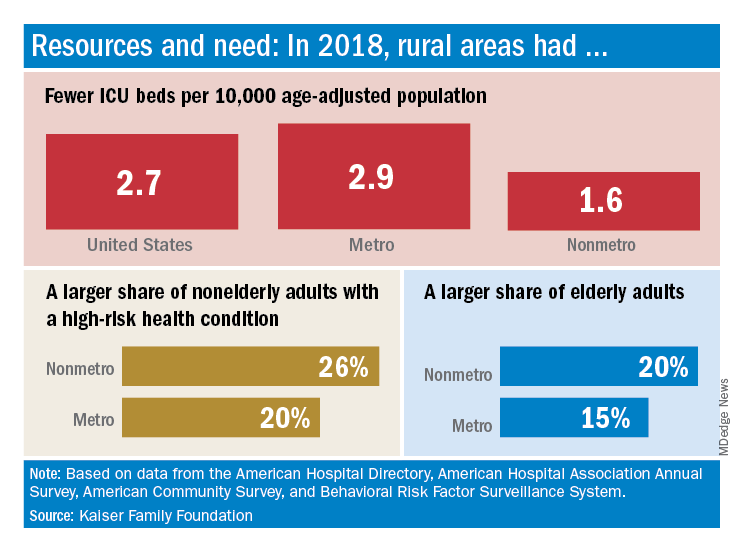
In 2018, the United States had 2.7 ICU beds per 10,000 age-adjusted population, but that number drops to 1.6 beds per 10,000 in nonmetro America and rises to 2.9 per 10,000 in metro areas. Counts for all hospital beds were much closer: 21.6 per 10,000 (rural) and 23.9 per 10,000 (urban), Kaiser investigators reported.
“The novel coronavirus was slower to spread to rural areas in the U.S., but that appears to be changing, with new outbreaks becoming evident in less densely populated parts of the country,” Kendal Orgera and associates said in a recent analysis.
Those rural areas have COVID-19 issues beyond ICU bed counts. Populations in nonmetro areas are less healthy – 26% of adults under age 65 years had a preexisting medical condition in 2018, compared with 20% in metro areas – and older – 20% of people are 65 and older, versus 15% in metro areas, they said.
“If coronavirus continues to spread in rural communities across the U.S., it is possible many [nonmetro] areas will face shortages of ICU beds with limited options to adapt. Patients in rural areas experiencing more severe illnesses may be transferred to hospitals with greater capacity, but if nearby urban areas are also overwhelmed, transfer may not be an option,” Ms. Orgera and associates wrote.
They defined nonmetro counties as those with rural towns of fewer than 2,500 people and/or “urban areas with populations ranging from 2,500 to 49,999 that are not part of larger labor market areas.” The Kaiser analysis involved 2018 data from the American Hospital Association, American Hospital Directory, American Community Survey, and the Behavioral Risk Factor Surveillance System.
The nonmetropolitan, largely rural, areas of the United States have fewer ICU beds than do urban areas, but their populations may be at higher risk for COVID-19 complications, according to the Kaiser Family Foundation.
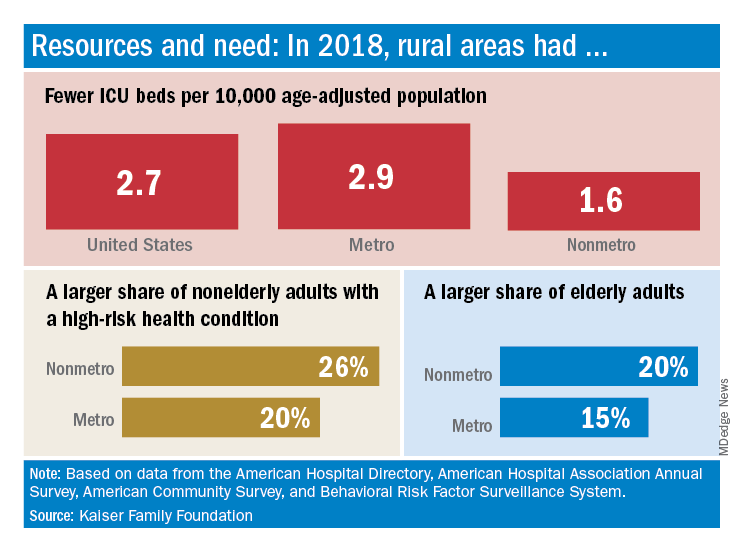
In 2018, the United States had 2.7 ICU beds per 10,000 age-adjusted population, but that number drops to 1.6 beds per 10,000 in nonmetro America and rises to 2.9 per 10,000 in metro areas. Counts for all hospital beds were much closer: 21.6 per 10,000 (rural) and 23.9 per 10,000 (urban), Kaiser investigators reported.
“The novel coronavirus was slower to spread to rural areas in the U.S., but that appears to be changing, with new outbreaks becoming evident in less densely populated parts of the country,” Kendal Orgera and associates said in a recent analysis.
Those rural areas have COVID-19 issues beyond ICU bed counts. Populations in nonmetro areas are less healthy – 26% of adults under age 65 years had a preexisting medical condition in 2018, compared with 20% in metro areas – and older – 20% of people are 65 and older, versus 15% in metro areas, they said.
“If coronavirus continues to spread in rural communities across the U.S., it is possible many [nonmetro] areas will face shortages of ICU beds with limited options to adapt. Patients in rural areas experiencing more severe illnesses may be transferred to hospitals with greater capacity, but if nearby urban areas are also overwhelmed, transfer may not be an option,” Ms. Orgera and associates wrote.
They defined nonmetro counties as those with rural towns of fewer than 2,500 people and/or “urban areas with populations ranging from 2,500 to 49,999 that are not part of larger labor market areas.” The Kaiser analysis involved 2018 data from the American Hospital Association, American Hospital Directory, American Community Survey, and the Behavioral Risk Factor Surveillance System.
The nonmetropolitan, largely rural, areas of the United States have fewer ICU beds than do urban areas, but their populations may be at higher risk for COVID-19 complications, according to the Kaiser Family Foundation.
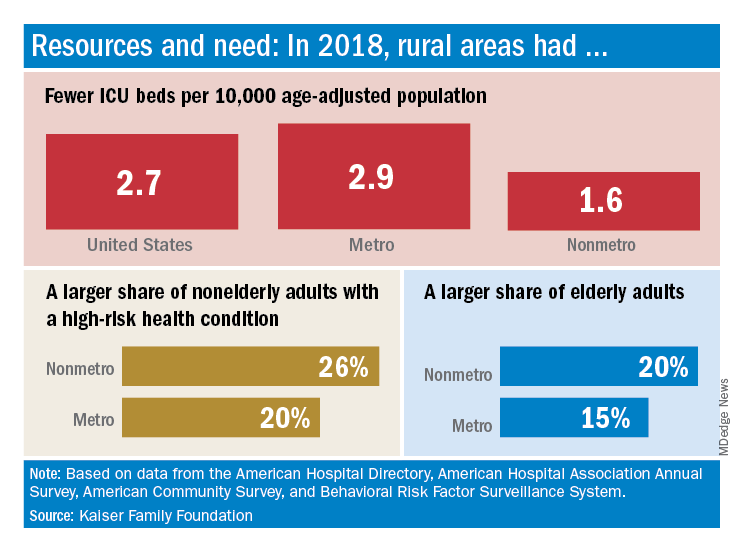
In 2018, the United States had 2.7 ICU beds per 10,000 age-adjusted population, but that number drops to 1.6 beds per 10,000 in nonmetro America and rises to 2.9 per 10,000 in metro areas. Counts for all hospital beds were much closer: 21.6 per 10,000 (rural) and 23.9 per 10,000 (urban), Kaiser investigators reported.
“The novel coronavirus was slower to spread to rural areas in the U.S., but that appears to be changing, with new outbreaks becoming evident in less densely populated parts of the country,” Kendal Orgera and associates said in a recent analysis.
Those rural areas have COVID-19 issues beyond ICU bed counts. Populations in nonmetro areas are less healthy – 26% of adults under age 65 years had a preexisting medical condition in 2018, compared with 20% in metro areas – and older – 20% of people are 65 and older, versus 15% in metro areas, they said.
“If coronavirus continues to spread in rural communities across the U.S., it is possible many [nonmetro] areas will face shortages of ICU beds with limited options to adapt. Patients in rural areas experiencing more severe illnesses may be transferred to hospitals with greater capacity, but if nearby urban areas are also overwhelmed, transfer may not be an option,” Ms. Orgera and associates wrote.
They defined nonmetro counties as those with rural towns of fewer than 2,500 people and/or “urban areas with populations ranging from 2,500 to 49,999 that are not part of larger labor market areas.” The Kaiser analysis involved 2018 data from the American Hospital Association, American Hospital Directory, American Community Survey, and the Behavioral Risk Factor Surveillance System.
Price increases for RA biologics keep out-of-pocket costs high for Medicare patients
Although the 2010 Patient Protection and Affordable Care Act attempted to close the coverage gap for prescription drugs, a new study has found that yearly price increases for expensive treatments like rheumatoid arthritis biologics have kept out-of-pocket spending high for patients enrolled in Medicare Part D.
“As the coverage gap is now considered closed, our results suggest a need for out-of-pocket maximums in the catastrophic phase to limit older Americans’ yearly financial burden and allow them to better estimate their annual drug costs,” wrote coauthors Alexandra Erath and Stacie B. Dusetzina, PhD, of Vanderbilt University in Nashville, Tenn. The study was published in JAMA Network Open.
To determine if closing the Medicare Part D coverage gap lowered out-of-pocket costs as anticipated, the researchers embarked on a cross-sectional study of Medicare data from the first quarter of each calendar year from 2010 to 2019. They analyzed the costs of 17 RA biologic drug and strength combinations, calculating the median point-of-sale price per fill for each drug and adjusting for medical inflation.
From 2010 to 2019, the median price per fill increased for all 17 drugs studied. With the exception of the 100-mg/1-mL golimumab (Simponi) autoinjector, every drug that had been on the market for 5 years or longer had a price increase of more than 20%. For the six drugs that have been on the market since 2010 – 200 mg of certolizumab pegol (Cimzia), 25 mg of etanercept (Enbrel), 50 mg of etanercept, 20 mg/0.4 mL of adalimumab (Humira), 40 mg/0.8 mL of adalimumab, and 50 mg/0.5 mL of golimumab – the median list price increased by a mean of 160% (standard deviation [SD], 17%; range, 136%-180%).
Mean (SD) annual out-of-pocket spending for those six drugs did decrease from $6,108 (SD, $234; range, $5,647-6,282) in 2010 to $4,801 (SD, $620; range, $3,594-$5,196) in 2019. However, the most significant decrease actually occurred between 2010 and 2011, when out-of-pocket spending dropped to $4,026 because the Affordable Care Act’s 50% manufacturer rebate for brand-name drugs filled in the coverage gap. This meant there was actually a mean increase of 19% in out-of-pocket costs from 2011 to 2019.
“This is the same story as the EpiPen,” said Maria Greenwald, MD, of Desert Medical Advances in Palm Desert, Calif., in an interview. “Patients have to have it, so you’re going to pay $600 even if you used to pay $50. Why do pharmaceutical companies keep raising their prices? Because they can. There’s no cap on list prices. And these drugs are miracles. They’re the difference between a high quality of life and being bound to a wheelchair. These patients don’t sleep without them. They’ll do whatever they can to pay for them, and so the prices continue to go up.”
This study reinforces the need for physicians to advocate for affordable biologics across the board, wrote Joel Lexchin, MD, of York University in Toronto in an accompanying editorial (doi: 10.1001/jamanetworkopen.2020.4753).
“Price increases for biologics do not only affect patients with rheumatologic conditions,” Dr. Lexchin noted, citing how the cost of multiple sclerosis therapies increased by thousands of dollars from the mid-1990s to 2013. In addition, although biologics make up a single-digit percentage of prescriptions in the United States, he highlighted that “they are responsible for $120 billion or 37% of net drug spending and, since 2014, for 93% of the overall growth in total spending.”
When it comes to potential solutions, he said that Medicare should negotiate directly with drug companies, that substitutions with biosimilars should become mandatory whenever possible, and that pharmaceutical companies should publicly validate their alleged research and development expenses. “Biologics can be transformational treatments,” he wrote, “but only if they are affordable at both the individual and societal levels.”
The authors shared their study’s potential limitations, including relying on list prices that do not factor in rebates and focusing on a single biologic filled every month rather than all treatments filled under Medicare, which could “result in our underestimating out-of-pocket spending by patients.” In addition, although a growing RA biosimilar market could increase price competition and lower costs, they added that progress in that area is limited by “aggressive litigation by the biologic manufacturers and an insufficient number of competitors to markedly affect price.”
The study was supported by the Commonwealth Fund and the Leukemia and Lymphoma Society. Dr. Dusetzina reported receiving grants from Arnold Ventures and personal fees from the Institute for Clinical and Economic Review.
SOURCE: Erath A et al. JAMA Netw Open. 2020 Apr 27. doi: 10.1001/jamanetworkopen.2020.3969.
Although the 2010 Patient Protection and Affordable Care Act attempted to close the coverage gap for prescription drugs, a new study has found that yearly price increases for expensive treatments like rheumatoid arthritis biologics have kept out-of-pocket spending high for patients enrolled in Medicare Part D.
“As the coverage gap is now considered closed, our results suggest a need for out-of-pocket maximums in the catastrophic phase to limit older Americans’ yearly financial burden and allow them to better estimate their annual drug costs,” wrote coauthors Alexandra Erath and Stacie B. Dusetzina, PhD, of Vanderbilt University in Nashville, Tenn. The study was published in JAMA Network Open.
To determine if closing the Medicare Part D coverage gap lowered out-of-pocket costs as anticipated, the researchers embarked on a cross-sectional study of Medicare data from the first quarter of each calendar year from 2010 to 2019. They analyzed the costs of 17 RA biologic drug and strength combinations, calculating the median point-of-sale price per fill for each drug and adjusting for medical inflation.
From 2010 to 2019, the median price per fill increased for all 17 drugs studied. With the exception of the 100-mg/1-mL golimumab (Simponi) autoinjector, every drug that had been on the market for 5 years or longer had a price increase of more than 20%. For the six drugs that have been on the market since 2010 – 200 mg of certolizumab pegol (Cimzia), 25 mg of etanercept (Enbrel), 50 mg of etanercept, 20 mg/0.4 mL of adalimumab (Humira), 40 mg/0.8 mL of adalimumab, and 50 mg/0.5 mL of golimumab – the median list price increased by a mean of 160% (standard deviation [SD], 17%; range, 136%-180%).
Mean (SD) annual out-of-pocket spending for those six drugs did decrease from $6,108 (SD, $234; range, $5,647-6,282) in 2010 to $4,801 (SD, $620; range, $3,594-$5,196) in 2019. However, the most significant decrease actually occurred between 2010 and 2011, when out-of-pocket spending dropped to $4,026 because the Affordable Care Act’s 50% manufacturer rebate for brand-name drugs filled in the coverage gap. This meant there was actually a mean increase of 19% in out-of-pocket costs from 2011 to 2019.
“This is the same story as the EpiPen,” said Maria Greenwald, MD, of Desert Medical Advances in Palm Desert, Calif., in an interview. “Patients have to have it, so you’re going to pay $600 even if you used to pay $50. Why do pharmaceutical companies keep raising their prices? Because they can. There’s no cap on list prices. And these drugs are miracles. They’re the difference between a high quality of life and being bound to a wheelchair. These patients don’t sleep without them. They’ll do whatever they can to pay for them, and so the prices continue to go up.”
This study reinforces the need for physicians to advocate for affordable biologics across the board, wrote Joel Lexchin, MD, of York University in Toronto in an accompanying editorial (doi: 10.1001/jamanetworkopen.2020.4753).
“Price increases for biologics do not only affect patients with rheumatologic conditions,” Dr. Lexchin noted, citing how the cost of multiple sclerosis therapies increased by thousands of dollars from the mid-1990s to 2013. In addition, although biologics make up a single-digit percentage of prescriptions in the United States, he highlighted that “they are responsible for $120 billion or 37% of net drug spending and, since 2014, for 93% of the overall growth in total spending.”
When it comes to potential solutions, he said that Medicare should negotiate directly with drug companies, that substitutions with biosimilars should become mandatory whenever possible, and that pharmaceutical companies should publicly validate their alleged research and development expenses. “Biologics can be transformational treatments,” he wrote, “but only if they are affordable at both the individual and societal levels.”
The authors shared their study’s potential limitations, including relying on list prices that do not factor in rebates and focusing on a single biologic filled every month rather than all treatments filled under Medicare, which could “result in our underestimating out-of-pocket spending by patients.” In addition, although a growing RA biosimilar market could increase price competition and lower costs, they added that progress in that area is limited by “aggressive litigation by the biologic manufacturers and an insufficient number of competitors to markedly affect price.”
The study was supported by the Commonwealth Fund and the Leukemia and Lymphoma Society. Dr. Dusetzina reported receiving grants from Arnold Ventures and personal fees from the Institute for Clinical and Economic Review.
SOURCE: Erath A et al. JAMA Netw Open. 2020 Apr 27. doi: 10.1001/jamanetworkopen.2020.3969.
Although the 2010 Patient Protection and Affordable Care Act attempted to close the coverage gap for prescription drugs, a new study has found that yearly price increases for expensive treatments like rheumatoid arthritis biologics have kept out-of-pocket spending high for patients enrolled in Medicare Part D.
“As the coverage gap is now considered closed, our results suggest a need for out-of-pocket maximums in the catastrophic phase to limit older Americans’ yearly financial burden and allow them to better estimate their annual drug costs,” wrote coauthors Alexandra Erath and Stacie B. Dusetzina, PhD, of Vanderbilt University in Nashville, Tenn. The study was published in JAMA Network Open.
To determine if closing the Medicare Part D coverage gap lowered out-of-pocket costs as anticipated, the researchers embarked on a cross-sectional study of Medicare data from the first quarter of each calendar year from 2010 to 2019. They analyzed the costs of 17 RA biologic drug and strength combinations, calculating the median point-of-sale price per fill for each drug and adjusting for medical inflation.
From 2010 to 2019, the median price per fill increased for all 17 drugs studied. With the exception of the 100-mg/1-mL golimumab (Simponi) autoinjector, every drug that had been on the market for 5 years or longer had a price increase of more than 20%. For the six drugs that have been on the market since 2010 – 200 mg of certolizumab pegol (Cimzia), 25 mg of etanercept (Enbrel), 50 mg of etanercept, 20 mg/0.4 mL of adalimumab (Humira), 40 mg/0.8 mL of adalimumab, and 50 mg/0.5 mL of golimumab – the median list price increased by a mean of 160% (standard deviation [SD], 17%; range, 136%-180%).
Mean (SD) annual out-of-pocket spending for those six drugs did decrease from $6,108 (SD, $234; range, $5,647-6,282) in 2010 to $4,801 (SD, $620; range, $3,594-$5,196) in 2019. However, the most significant decrease actually occurred between 2010 and 2011, when out-of-pocket spending dropped to $4,026 because the Affordable Care Act’s 50% manufacturer rebate for brand-name drugs filled in the coverage gap. This meant there was actually a mean increase of 19% in out-of-pocket costs from 2011 to 2019.
“This is the same story as the EpiPen,” said Maria Greenwald, MD, of Desert Medical Advances in Palm Desert, Calif., in an interview. “Patients have to have it, so you’re going to pay $600 even if you used to pay $50. Why do pharmaceutical companies keep raising their prices? Because they can. There’s no cap on list prices. And these drugs are miracles. They’re the difference between a high quality of life and being bound to a wheelchair. These patients don’t sleep without them. They’ll do whatever they can to pay for them, and so the prices continue to go up.”
This study reinforces the need for physicians to advocate for affordable biologics across the board, wrote Joel Lexchin, MD, of York University in Toronto in an accompanying editorial (doi: 10.1001/jamanetworkopen.2020.4753).
“Price increases for biologics do not only affect patients with rheumatologic conditions,” Dr. Lexchin noted, citing how the cost of multiple sclerosis therapies increased by thousands of dollars from the mid-1990s to 2013. In addition, although biologics make up a single-digit percentage of prescriptions in the United States, he highlighted that “they are responsible for $120 billion or 37% of net drug spending and, since 2014, for 93% of the overall growth in total spending.”
When it comes to potential solutions, he said that Medicare should negotiate directly with drug companies, that substitutions with biosimilars should become mandatory whenever possible, and that pharmaceutical companies should publicly validate their alleged research and development expenses. “Biologics can be transformational treatments,” he wrote, “but only if they are affordable at both the individual and societal levels.”
The authors shared their study’s potential limitations, including relying on list prices that do not factor in rebates and focusing on a single biologic filled every month rather than all treatments filled under Medicare, which could “result in our underestimating out-of-pocket spending by patients.” In addition, although a growing RA biosimilar market could increase price competition and lower costs, they added that progress in that area is limited by “aggressive litigation by the biologic manufacturers and an insufficient number of competitors to markedly affect price.”
The study was supported by the Commonwealth Fund and the Leukemia and Lymphoma Society. Dr. Dusetzina reported receiving grants from Arnold Ventures and personal fees from the Institute for Clinical and Economic Review.
SOURCE: Erath A et al. JAMA Netw Open. 2020 Apr 27. doi: 10.1001/jamanetworkopen.2020.3969.
FROM JAMA NETWORK OPEN



