User login
Severe anxiety and agitation
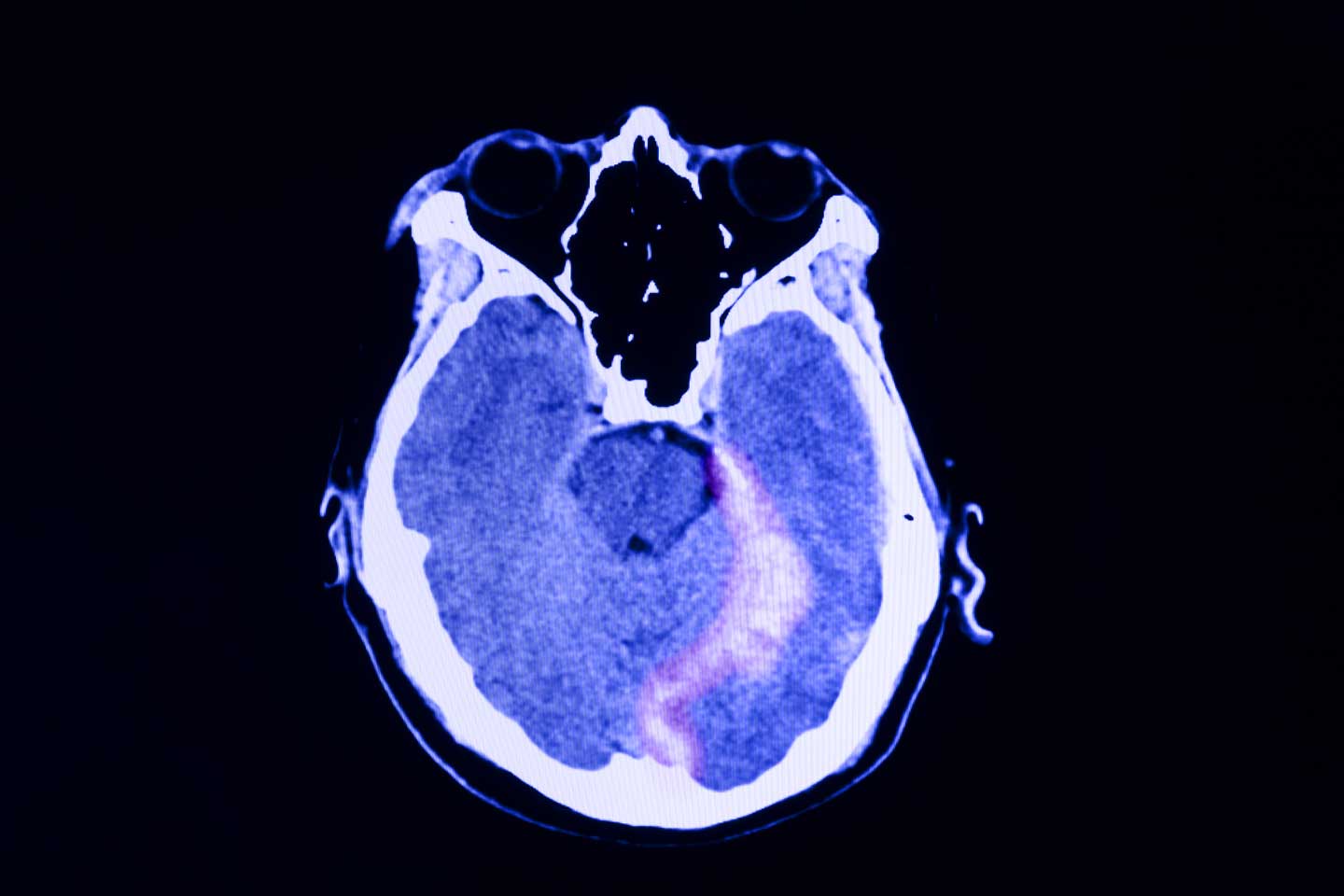
Posttraumatic stress disorder (PTSD) is the most likely diagnosis considering this patient’s symptoms of anxiety, hypervigilance, recurring nightmares, agitation, flashbacks, and violent outbursts. His experience of being robbed at gunpoint outside his gym seems to have been the triggering event for his PTSD, which may have also been influenced by his history of multiple concussions incurred in a fight setting in which he is forced to defend himself. His avoidance of continued training and appearing at scheduled fights further support this diagnosis. His CT scan, although not diagnostic for PTSD directly, does show evidence of minor brain injury, with the remaining hematomas.
Anxiety disorder may account for the patient’s severe anxiety, agitation, and headaches, but his symptoms are new and started after the robbery, which indicates PTSD and not a long-standing anxiety disorder.
Schizophrenia is an unlikely diagnosis for this patient. Although he is within the typical age range of symptom onset, has had violent outbursts, and is prone to vast changes in mood that come on quickly, he is not psychotic and does not experience any of the hallmark symptoms of schizophrenia: delusions, hallucinations, and disorganized speech/behavior, at least two of which would need to be present to support a diagnosis of schizophrenia.
Given this patient’s circumstances, post-traumatic epilepsy initially may be a potential diagnostic consideration. However, he is not experiencing seizures, but rather mood and behavioral disturbances, the onset of which occurred after a specific event. Additionally, posttraumatic epilepsy results from traumatic brain injury.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision, an update to the 2017 clinical treatment guidelines published by the American Psychiatric Association (APA), the diagnostic criteria for PTSD in an individual older than 6 years are:
1. Exposure to actual or threatened death, serious injury or sexual assault
2. The traumatic event is persistently re-experienced via flashbacks, nightmares, and intrusive thoughts that cause strong emotional reactions and psychological distress
3. Avoidance behaviors either in thoughts or conversations about the event or of people and places associated with the event
4. At least two examples of negative alterations in cognition and mood
5. At least two examples of hyperarousal
6. Duration of symptoms > 1 month
7. Significant distress or impairment in function because of these symptoms
Trauma-focused therapy is the gold standard of treatment for patients with PTSD. A recent review of current treatment strategies for PTSD found that cognitive processing therapy, cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing, all with a strong trauma focus, are the most effective treatments for PTSD.
The use of pharmacology to treat PTSD is controversial and varies by guideline. The APA and US Department of Veterans Affairs both recommend the use of antidepressants, particularly selective serotonin reuptake inhibitors, as a first-line treatment of PTSD. This is particularly important for patients who have psychiatric comorbid conditions, such as depression, who may not be able to effectively engage in cognitive- behavioral therapy. However, use of benzodiazepines or hypnotics should be strictly avoided in these patients because these drugs increase intrusive and avoidance symptoms over time. Medication should be continued for 6 to 12 months to help prevent relapse.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Posttraumatic stress disorder (PTSD) is the most likely diagnosis considering this patient’s symptoms of anxiety, hypervigilance, recurring nightmares, agitation, flashbacks, and violent outbursts. His experience of being robbed at gunpoint outside his gym seems to have been the triggering event for his PTSD, which may have also been influenced by his history of multiple concussions incurred in a fight setting in which he is forced to defend himself. His avoidance of continued training and appearing at scheduled fights further support this diagnosis. His CT scan, although not diagnostic for PTSD directly, does show evidence of minor brain injury, with the remaining hematomas.
Anxiety disorder may account for the patient’s severe anxiety, agitation, and headaches, but his symptoms are new and started after the robbery, which indicates PTSD and not a long-standing anxiety disorder.
Schizophrenia is an unlikely diagnosis for this patient. Although he is within the typical age range of symptom onset, has had violent outbursts, and is prone to vast changes in mood that come on quickly, he is not psychotic and does not experience any of the hallmark symptoms of schizophrenia: delusions, hallucinations, and disorganized speech/behavior, at least two of which would need to be present to support a diagnosis of schizophrenia.
Given this patient’s circumstances, post-traumatic epilepsy initially may be a potential diagnostic consideration. However, he is not experiencing seizures, but rather mood and behavioral disturbances, the onset of which occurred after a specific event. Additionally, posttraumatic epilepsy results from traumatic brain injury.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision, an update to the 2017 clinical treatment guidelines published by the American Psychiatric Association (APA), the diagnostic criteria for PTSD in an individual older than 6 years are:
1. Exposure to actual or threatened death, serious injury or sexual assault
2. The traumatic event is persistently re-experienced via flashbacks, nightmares, and intrusive thoughts that cause strong emotional reactions and psychological distress
3. Avoidance behaviors either in thoughts or conversations about the event or of people and places associated with the event
4. At least two examples of negative alterations in cognition and mood
5. At least two examples of hyperarousal
6. Duration of symptoms > 1 month
7. Significant distress or impairment in function because of these symptoms
Trauma-focused therapy is the gold standard of treatment for patients with PTSD. A recent review of current treatment strategies for PTSD found that cognitive processing therapy, cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing, all with a strong trauma focus, are the most effective treatments for PTSD.
The use of pharmacology to treat PTSD is controversial and varies by guideline. The APA and US Department of Veterans Affairs both recommend the use of antidepressants, particularly selective serotonin reuptake inhibitors, as a first-line treatment of PTSD. This is particularly important for patients who have psychiatric comorbid conditions, such as depression, who may not be able to effectively engage in cognitive- behavioral therapy. However, use of benzodiazepines or hypnotics should be strictly avoided in these patients because these drugs increase intrusive and avoidance symptoms over time. Medication should be continued for 6 to 12 months to help prevent relapse.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Posttraumatic stress disorder (PTSD) is the most likely diagnosis considering this patient’s symptoms of anxiety, hypervigilance, recurring nightmares, agitation, flashbacks, and violent outbursts. His experience of being robbed at gunpoint outside his gym seems to have been the triggering event for his PTSD, which may have also been influenced by his history of multiple concussions incurred in a fight setting in which he is forced to defend himself. His avoidance of continued training and appearing at scheduled fights further support this diagnosis. His CT scan, although not diagnostic for PTSD directly, does show evidence of minor brain injury, with the remaining hematomas.
Anxiety disorder may account for the patient’s severe anxiety, agitation, and headaches, but his symptoms are new and started after the robbery, which indicates PTSD and not a long-standing anxiety disorder.
Schizophrenia is an unlikely diagnosis for this patient. Although he is within the typical age range of symptom onset, has had violent outbursts, and is prone to vast changes in mood that come on quickly, he is not psychotic and does not experience any of the hallmark symptoms of schizophrenia: delusions, hallucinations, and disorganized speech/behavior, at least two of which would need to be present to support a diagnosis of schizophrenia.
Given this patient’s circumstances, post-traumatic epilepsy initially may be a potential diagnostic consideration. However, he is not experiencing seizures, but rather mood and behavioral disturbances, the onset of which occurred after a specific event. Additionally, posttraumatic epilepsy results from traumatic brain injury.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision, an update to the 2017 clinical treatment guidelines published by the American Psychiatric Association (APA), the diagnostic criteria for PTSD in an individual older than 6 years are:
1. Exposure to actual or threatened death, serious injury or sexual assault
2. The traumatic event is persistently re-experienced via flashbacks, nightmares, and intrusive thoughts that cause strong emotional reactions and psychological distress
3. Avoidance behaviors either in thoughts or conversations about the event or of people and places associated with the event
4. At least two examples of negative alterations in cognition and mood
5. At least two examples of hyperarousal
6. Duration of symptoms > 1 month
7. Significant distress or impairment in function because of these symptoms
Trauma-focused therapy is the gold standard of treatment for patients with PTSD. A recent review of current treatment strategies for PTSD found that cognitive processing therapy, cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing, all with a strong trauma focus, are the most effective treatments for PTSD.
The use of pharmacology to treat PTSD is controversial and varies by guideline. The APA and US Department of Veterans Affairs both recommend the use of antidepressants, particularly selective serotonin reuptake inhibitors, as a first-line treatment of PTSD. This is particularly important for patients who have psychiatric comorbid conditions, such as depression, who may not be able to effectively engage in cognitive- behavioral therapy. However, use of benzodiazepines or hypnotics should be strictly avoided in these patients because these drugs increase intrusive and avoidance symptoms over time. Medication should be continued for 6 to 12 months to help prevent relapse.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
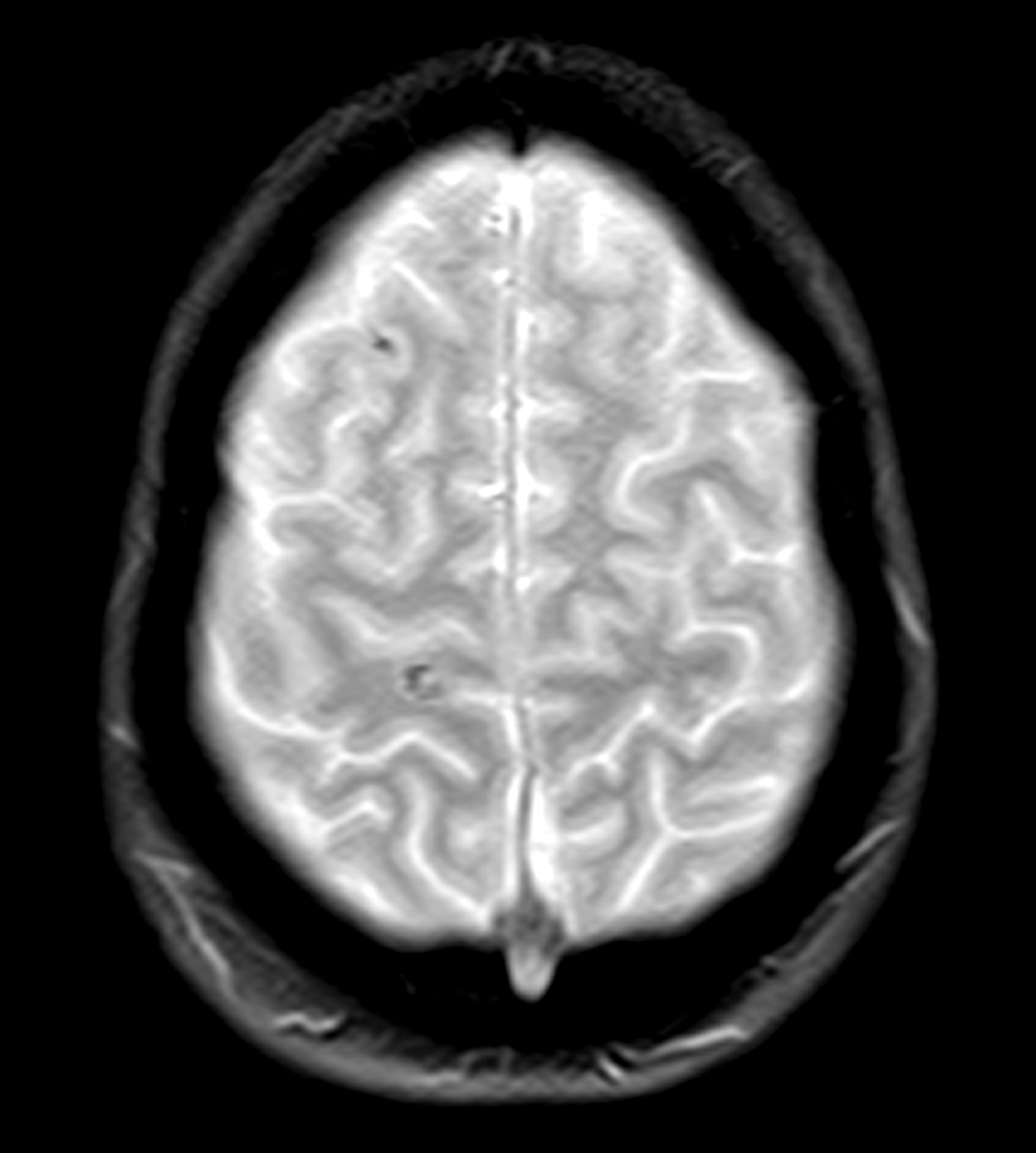
A 28-year-old professional boxer presents with severe anxiety, agitation, headaches, and insomnia with recurring nightmares and flashbacks. His symptoms began after he was robbed at gunpoint in the gym parking lot as he was getting into his car about 6 months ago. Since that time, he has had to postpone several fights because he is unable to maintain his training schedule and reports feeling depressed as a result. He is also at risk for suspension from his regular gym because he has gotten into several violent, unprovoked altercations with fellow boxers, and he has also had multiple violent outbursts outside of the gym. He has a history of concussion.
Physical exam reveals increased heart rate and hypervigilance. The patient is administered the Patient Health Questionnaire and has a score of 14 out of a possible 27. Zero to 4 indicates no depression, whereas 14 falls within the range of moderate depression. A brain CT scan (Figure) is ordered because of his history of concussion and his chronic symptoms. The scan reveals two subacute hematomas in the left hemisphere, one in the frontal lobe and the other in the temporal lobe. Additional tests are ordered: laboratory testing, to rule out organic or infectious causes of symptoms and electroencephalography, to assess for a possible seizure focus; both tests reveal nothing remarkable. The hematomas were noted at the time of a previous head injury 2 years ago.
PTSD Guidelines
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Flashbacks triggered by loud noises
Posttraumatic stress disorder (PTSD) is the most likely diagnosis given the patient's symptoms — recurrent nightmares, flashbacks, and anxiety triggered by trauma-related noises, all of which are classic indicators of the disorder. His history of witnessing traumatic events at work, including a fatal accident, further reinforces this diagnosis and strongly suggests PTSD as the most fitting explanation. Although the brain scan does not diagnose PTSD directly, it plays an important role in ruling out other potential causes, such as structural brain damage, that could be contributing to his symptoms. Thus, the patient's symptoms are more likely a result of PTSD rather than an underlying organic brain injury.
Although major depressive disorder could explain some of the patient's symptoms, such as impaired daily functioning and withdrawal, the presence of recurrent nightmares, flashbacks, and trauma-specific triggers are more indicative of PTSD.
Generalized anxiety disorder might account for the patient's heightened anxiety, but it typically involves chronic, pervasive worry rather than the trauma-specific symptoms seen here.
Chronic traumatic encephalopathy (CTE) is a possible concern given the patient's occupation and the findings on the CT scan. However, CTE generally presents with cognitive and behavioral changes over time, such as memory loss and aggression, rather than the distinctive trauma-related symptoms characteristic of PTSD.
Individuals with PTSD often display heightened emotional, cognitive, and behavioral responses when exposed to trauma-related cues; these responses include severe anxiety, dissociative episodes, flashbacks, and heightened reactivity. To manage their increased arousal, individuals with PTSD frequently engage in avoidance behaviors, which can result in emotional numbing, diminished interest in daily activities, and, in more severe cases, social withdrawal.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR), the diagnostic criteria for PTSD in individuals older than 6 years include (A) exposure to actual or threatened death, serious injury, or sexual violence; (B) the presence of one or more intrusion symptoms related to the trauma; (C) persistent avoidance of trauma-related stimuli; (D) negative changes in cognition and mood associated with the trauma; and (E) marked alterations in arousal and reactivity, with at least two specific symptoms.
Trauma-focused psychotherapy is generally recommended as the first-line treatment for most adults with PTSD, with exposure-based therapies often preferred over other therapeutic approaches or pharmacologic treatments, such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors. However, in patients with comorbid conditions such as depression or psychosis that hinder their ability to engage in trauma-focused therapy, initial pharmacologic management is recommended until symptoms stabilize, allowing for the later introduction of psychotherapy. Clinical trials and meta-analyses have demonstrated the effectiveness of various trauma-focused therapies, including trauma-focused cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing. Treatment selection should be made collaboratively, considering the patient's presentation and preferences and the therapist's expertise.
For effective management of PTSD, medication regimens should be maintained for at least 6 months to 1 year to prevent relapse or recurrence. Multiple clinical trials have shown that patients who continue SSRIs after acute treatment are less likely to experience a relapse than those who switch to placebo.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
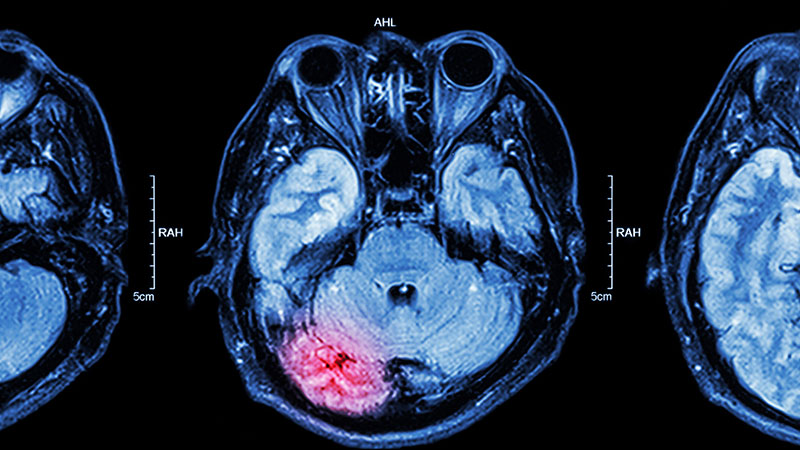
Posttraumatic stress disorder (PTSD) is the most likely diagnosis given the patient's symptoms — recurrent nightmares, flashbacks, and anxiety triggered by trauma-related noises, all of which are classic indicators of the disorder. His history of witnessing traumatic events at work, including a fatal accident, further reinforces this diagnosis and strongly suggests PTSD as the most fitting explanation. Although the brain scan does not diagnose PTSD directly, it plays an important role in ruling out other potential causes, such as structural brain damage, that could be contributing to his symptoms. Thus, the patient's symptoms are more likely a result of PTSD rather than an underlying organic brain injury.
Although major depressive disorder could explain some of the patient's symptoms, such as impaired daily functioning and withdrawal, the presence of recurrent nightmares, flashbacks, and trauma-specific triggers are more indicative of PTSD.
Generalized anxiety disorder might account for the patient's heightened anxiety, but it typically involves chronic, pervasive worry rather than the trauma-specific symptoms seen here.
Chronic traumatic encephalopathy (CTE) is a possible concern given the patient's occupation and the findings on the CT scan. However, CTE generally presents with cognitive and behavioral changes over time, such as memory loss and aggression, rather than the distinctive trauma-related symptoms characteristic of PTSD.
Individuals with PTSD often display heightened emotional, cognitive, and behavioral responses when exposed to trauma-related cues; these responses include severe anxiety, dissociative episodes, flashbacks, and heightened reactivity. To manage their increased arousal, individuals with PTSD frequently engage in avoidance behaviors, which can result in emotional numbing, diminished interest in daily activities, and, in more severe cases, social withdrawal.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR), the diagnostic criteria for PTSD in individuals older than 6 years include (A) exposure to actual or threatened death, serious injury, or sexual violence; (B) the presence of one or more intrusion symptoms related to the trauma; (C) persistent avoidance of trauma-related stimuli; (D) negative changes in cognition and mood associated with the trauma; and (E) marked alterations in arousal and reactivity, with at least two specific symptoms.
Trauma-focused psychotherapy is generally recommended as the first-line treatment for most adults with PTSD, with exposure-based therapies often preferred over other therapeutic approaches or pharmacologic treatments, such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors. However, in patients with comorbid conditions such as depression or psychosis that hinder their ability to engage in trauma-focused therapy, initial pharmacologic management is recommended until symptoms stabilize, allowing for the later introduction of psychotherapy. Clinical trials and meta-analyses have demonstrated the effectiveness of various trauma-focused therapies, including trauma-focused cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing. Treatment selection should be made collaboratively, considering the patient's presentation and preferences and the therapist's expertise.
For effective management of PTSD, medication regimens should be maintained for at least 6 months to 1 year to prevent relapse or recurrence. Multiple clinical trials have shown that patients who continue SSRIs after acute treatment are less likely to experience a relapse than those who switch to placebo.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Posttraumatic stress disorder (PTSD) is the most likely diagnosis given the patient's symptoms — recurrent nightmares, flashbacks, and anxiety triggered by trauma-related noises, all of which are classic indicators of the disorder. His history of witnessing traumatic events at work, including a fatal accident, further reinforces this diagnosis and strongly suggests PTSD as the most fitting explanation. Although the brain scan does not diagnose PTSD directly, it plays an important role in ruling out other potential causes, such as structural brain damage, that could be contributing to his symptoms. Thus, the patient's symptoms are more likely a result of PTSD rather than an underlying organic brain injury.
Although major depressive disorder could explain some of the patient's symptoms, such as impaired daily functioning and withdrawal, the presence of recurrent nightmares, flashbacks, and trauma-specific triggers are more indicative of PTSD.
Generalized anxiety disorder might account for the patient's heightened anxiety, but it typically involves chronic, pervasive worry rather than the trauma-specific symptoms seen here.
Chronic traumatic encephalopathy (CTE) is a possible concern given the patient's occupation and the findings on the CT scan. However, CTE generally presents with cognitive and behavioral changes over time, such as memory loss and aggression, rather than the distinctive trauma-related symptoms characteristic of PTSD.
Individuals with PTSD often display heightened emotional, cognitive, and behavioral responses when exposed to trauma-related cues; these responses include severe anxiety, dissociative episodes, flashbacks, and heightened reactivity. To manage their increased arousal, individuals with PTSD frequently engage in avoidance behaviors, which can result in emotional numbing, diminished interest in daily activities, and, in more severe cases, social withdrawal.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR), the diagnostic criteria for PTSD in individuals older than 6 years include (A) exposure to actual or threatened death, serious injury, or sexual violence; (B) the presence of one or more intrusion symptoms related to the trauma; (C) persistent avoidance of trauma-related stimuli; (D) negative changes in cognition and mood associated with the trauma; and (E) marked alterations in arousal and reactivity, with at least two specific symptoms.
Trauma-focused psychotherapy is generally recommended as the first-line treatment for most adults with PTSD, with exposure-based therapies often preferred over other therapeutic approaches or pharmacologic treatments, such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors. However, in patients with comorbid conditions such as depression or psychosis that hinder their ability to engage in trauma-focused therapy, initial pharmacologic management is recommended until symptoms stabilize, allowing for the later introduction of psychotherapy. Clinical trials and meta-analyses have demonstrated the effectiveness of various trauma-focused therapies, including trauma-focused cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing. Treatment selection should be made collaboratively, considering the patient's presentation and preferences and the therapist's expertise.
For effective management of PTSD, medication regimens should be maintained for at least 6 months to 1 year to prevent relapse or recurrence. Multiple clinical trials have shown that patients who continue SSRIs after acute treatment are less likely to experience a relapse than those who switch to placebo.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
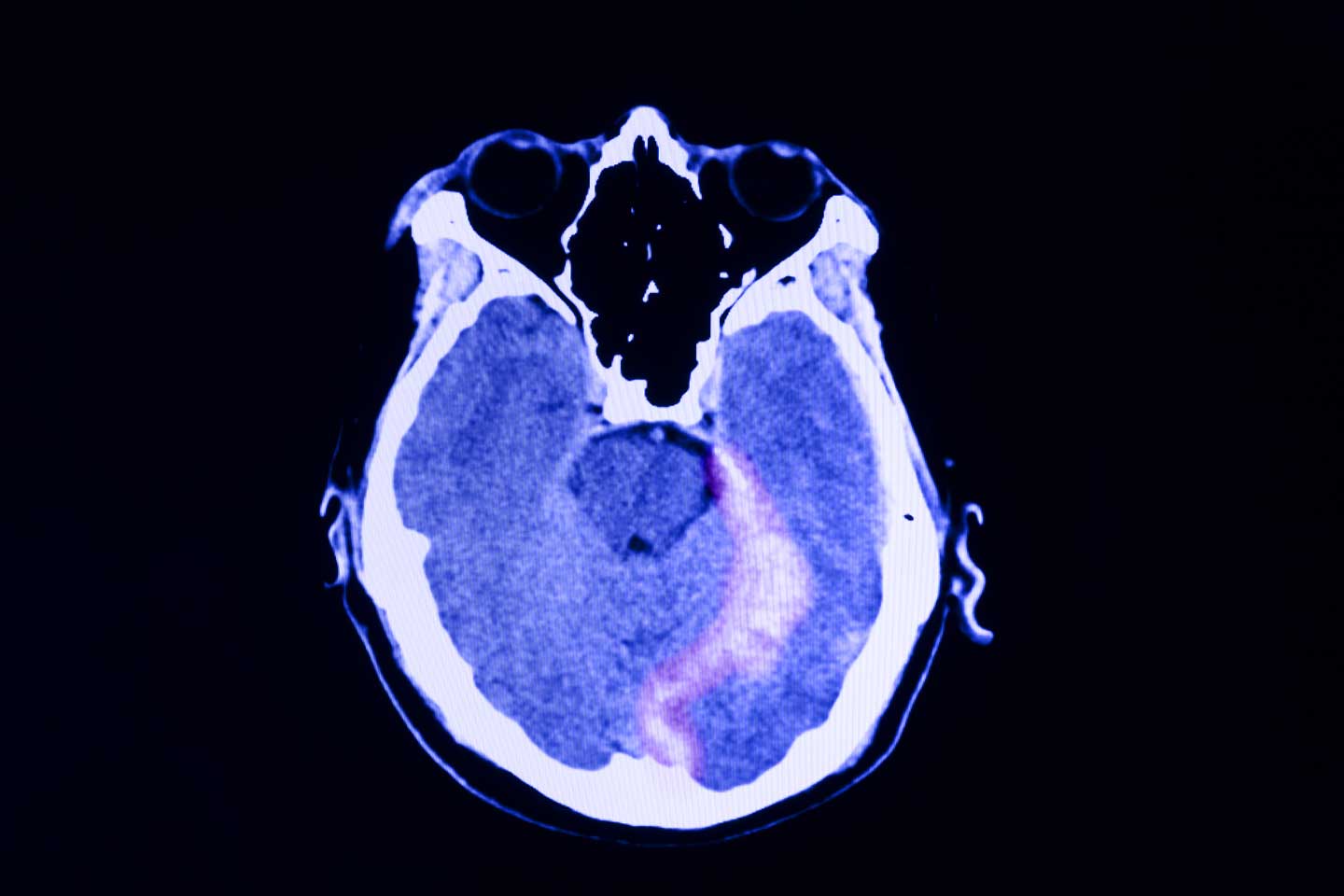
A 48-year-old male construction worker presented with worsening symptoms over the past year, including recurrent nightmares, heightened anxiety, and flashbacks triggered by loud noises such as those heard on job sites. These symptoms have begun to interfere with his daily functioning, particularly affecting his work and family life. The patient has a history of multiple traumatic experiences at work, including witnessing a fatal accident involving a coworker. On neurologic examination, he appeared highly agitated and displayed signs of hypervigilance. A brain CT scan (as shown in the image) was ordered because of the chronic nature of his symptoms and the potential for neurologic causes—such as traumatic brain injury—to contribute to his condition. The scan revealed an abnormality on the left side, prompting further investigation to determine whether the lesion is related to his symptoms or indicative of another underlying condition. Additional tests were ordered to further characterize the lesion: electroencephalography to assess for any associated seizure activity, and blood tests and a lumbar puncture to rule out infection or inflammatory processes. These additional tests came back negative, and the abnormality was later diagnosed as artifact.
PTSD in Children
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
PTSD Comorbidities
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Persistent headaches and nightmares
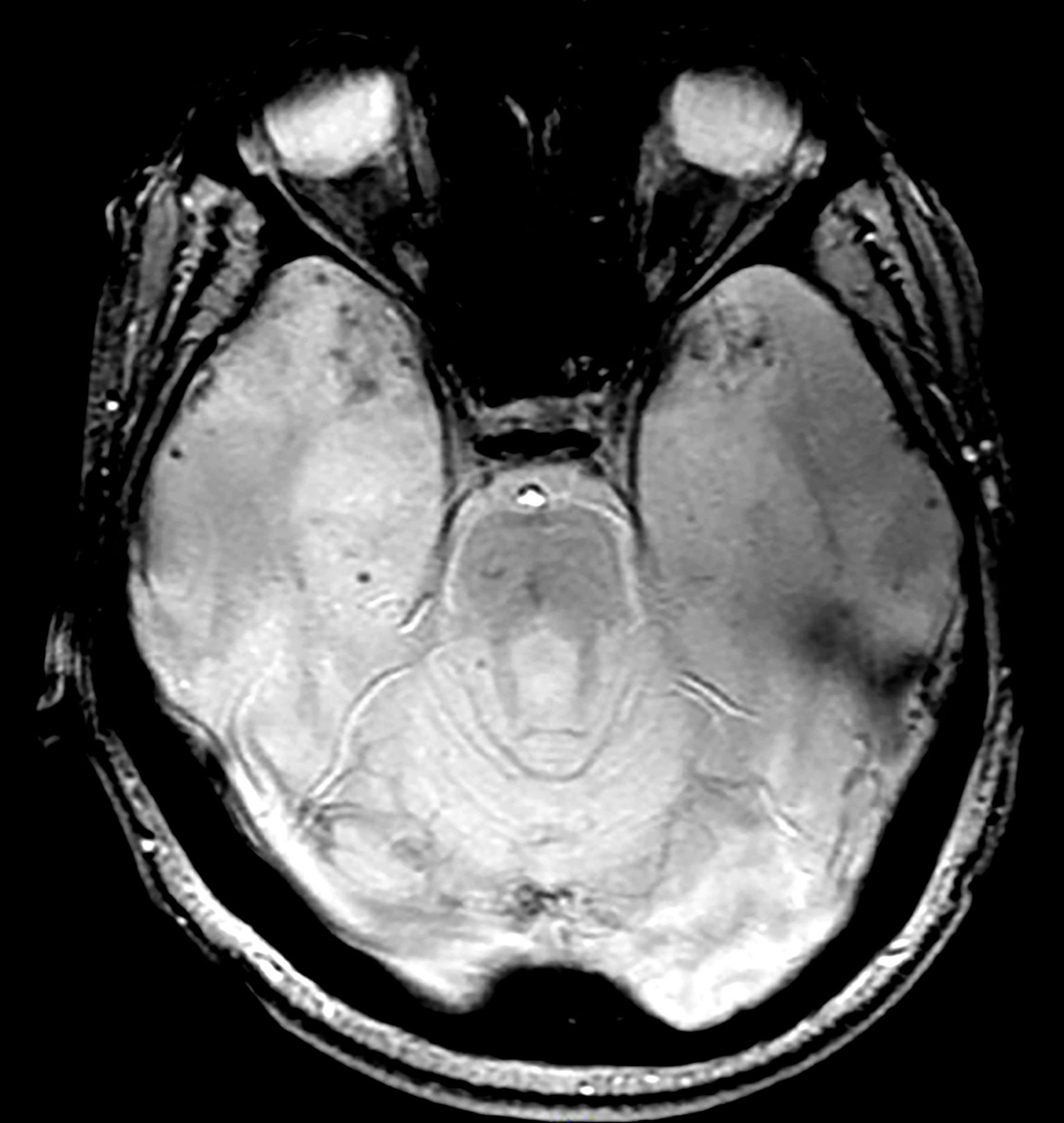
The correct diagnosis is adolescent posttraumatic stress disorder (PTSD), as the patient's symptoms — recurrent nightmares, flashbacks, hypervigilance, and avoidance behaviors — are closely linked to her recent traumatic experience, fitting the clinical profile of PTSD. The MRI finding, although abnormal, does not correlate with a neurologic cause for her symptoms and may be incidental.
Temporal lobe epilepsy can cause behavioral changes but does not explain the specific PTSD symptoms like flashbacks and nightmares.
Chronic migraine could explain the headaches but not the full spectrum of PTSD symptoms.
Major depressive disorder could account for some of the emotional and social symptoms but lacks the characteristic re-experiencing and avoidance behaviors typical of PTSD.
Adolescent PTSD is a significant public health concern, causing significant distress to a small portion of the youth population. By late adolescence, approximately two thirds of youths have been exposed to trauma, and 8% of these individuals meet the criteria for PTSD by age 18. The incidence is exceptionally high in cases of sexual abuse and assault, with rates reaching up to 40%. PTSD in adolescents is associated with severe psychological distress, reduced academic performance, and a high rate of comorbidities, including anxiety and depression. There are specific populations (including children who are evacuated from home, asylum seekers, etc.) that show higher rates of PTSD.
PTSD can lead to chronic impairments, comorbid psychiatric disorders, and an increased risk for suicide, with cases documented in toddlers as young as 1 year old. Thus, it is important to consider the individual's background and social history, as older children with PTSD may present with symptoms from early childhood trauma, often distant from the time of clinical evaluation.
Intrusion symptoms are a hallmark of PTSD, characterized by persistent and uncontrollable thoughts, dreams, and emotional reactions related to the traumatic event. These symptoms distinguish PTSD from other anxiety and mood disorders. Children with PTSD often experience involuntary, distressing thoughts and memories triggered by trauma cues, such as sights, sounds, or smells associated with the traumatic event. In younger children, these intrusive thoughts may manifest through repetitive play that re-enacts aspects of the trauma.
Nightmares are also common, although in children the content may not always directly relate to the traumatic event. Chronic nightmares contribute to sleep disturbances, exacerbating PTSD symptoms. Trauma reminders, which can be both internal (thoughts, memories) and external (places, sensory experiences), can provoke severe distress and physiologic reactions.
Avoidance symptoms often develop as a coping mechanism in response to distressing re-experiencing symptoms. Children may avoid thoughts, feelings, and memories of the traumatic event or people, places, and activities associated with the trauma. In young children, avoidance may manifest as restricted play or reduced exploration of their environment.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) outlines specific criteria for diagnosing PTSD in individuals over 6 years old, which includes exposure to actual or threatened death, serious injury, or sexual violence, and the presence of symptoms such as intrusion, avoidance, negative mood alterations, and heightened arousal. The DSM-5-TR provides tailored diagnostic criteria for developmental differences in symptom expression for children under 6.
Managing PTSD in children requires a patient-specific approach, with an emphasis on obtaining consent from both the patient and guardian. The American Academy of Child and Adolescent Psychiatry (AACAP) recommends psychotherapy as the first-line treatment for pediatric PTSD. However, patients with severe symptoms or comorbidities may initially be unable to engage in meaningful therapy and may require medication to stabilize symptoms before starting psychotherapy.
Trauma-focused psychotherapy, including cognitive-behavioral therapy (CBT), exposure-based therapy, and eye movement desensitization and reprocessing (EMDR) therapy, is the preferred treatment for PTSD. Clinical studies have shown that patients receiving trauma-focused psychotherapy experience more remarkable symptom improvement than those who do not receive treatment and, in children, psychotherapy generally yields better outcomes than pharmacotherapy.
While selective serotonin reuptake inhibitors like sertraline and paroxetine are FDA-approved for PTSD treatment in adults, their efficacy in children often produces outcomes similar to those of placebo. Medications are typically reserved for severe symptoms and are used as an off-label treatment in pediatric cases. Pharmacologic management may be necessary when the severity of symptoms prevents the use of trauma-focused psychotherapy or requires immediate stabilization.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The correct diagnosis is adolescent posttraumatic stress disorder (PTSD), as the patient's symptoms — recurrent nightmares, flashbacks, hypervigilance, and avoidance behaviors — are closely linked to her recent traumatic experience, fitting the clinical profile of PTSD. The MRI finding, although abnormal, does not correlate with a neurologic cause for her symptoms and may be incidental.
Temporal lobe epilepsy can cause behavioral changes but does not explain the specific PTSD symptoms like flashbacks and nightmares.
Chronic migraine could explain the headaches but not the full spectrum of PTSD symptoms.
Major depressive disorder could account for some of the emotional and social symptoms but lacks the characteristic re-experiencing and avoidance behaviors typical of PTSD.
Adolescent PTSD is a significant public health concern, causing significant distress to a small portion of the youth population. By late adolescence, approximately two thirds of youths have been exposed to trauma, and 8% of these individuals meet the criteria for PTSD by age 18. The incidence is exceptionally high in cases of sexual abuse and assault, with rates reaching up to 40%. PTSD in adolescents is associated with severe psychological distress, reduced academic performance, and a high rate of comorbidities, including anxiety and depression. There are specific populations (including children who are evacuated from home, asylum seekers, etc.) that show higher rates of PTSD.
PTSD can lead to chronic impairments, comorbid psychiatric disorders, and an increased risk for suicide, with cases documented in toddlers as young as 1 year old. Thus, it is important to consider the individual's background and social history, as older children with PTSD may present with symptoms from early childhood trauma, often distant from the time of clinical evaluation.
Intrusion symptoms are a hallmark of PTSD, characterized by persistent and uncontrollable thoughts, dreams, and emotional reactions related to the traumatic event. These symptoms distinguish PTSD from other anxiety and mood disorders. Children with PTSD often experience involuntary, distressing thoughts and memories triggered by trauma cues, such as sights, sounds, or smells associated with the traumatic event. In younger children, these intrusive thoughts may manifest through repetitive play that re-enacts aspects of the trauma.
Nightmares are also common, although in children the content may not always directly relate to the traumatic event. Chronic nightmares contribute to sleep disturbances, exacerbating PTSD symptoms. Trauma reminders, which can be both internal (thoughts, memories) and external (places, sensory experiences), can provoke severe distress and physiologic reactions.
Avoidance symptoms often develop as a coping mechanism in response to distressing re-experiencing symptoms. Children may avoid thoughts, feelings, and memories of the traumatic event or people, places, and activities associated with the trauma. In young children, avoidance may manifest as restricted play or reduced exploration of their environment.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) outlines specific criteria for diagnosing PTSD in individuals over 6 years old, which includes exposure to actual or threatened death, serious injury, or sexual violence, and the presence of symptoms such as intrusion, avoidance, negative mood alterations, and heightened arousal. The DSM-5-TR provides tailored diagnostic criteria for developmental differences in symptom expression for children under 6.
Managing PTSD in children requires a patient-specific approach, with an emphasis on obtaining consent from both the patient and guardian. The American Academy of Child and Adolescent Psychiatry (AACAP) recommends psychotherapy as the first-line treatment for pediatric PTSD. However, patients with severe symptoms or comorbidities may initially be unable to engage in meaningful therapy and may require medication to stabilize symptoms before starting psychotherapy.
Trauma-focused psychotherapy, including cognitive-behavioral therapy (CBT), exposure-based therapy, and eye movement desensitization and reprocessing (EMDR) therapy, is the preferred treatment for PTSD. Clinical studies have shown that patients receiving trauma-focused psychotherapy experience more remarkable symptom improvement than those who do not receive treatment and, in children, psychotherapy generally yields better outcomes than pharmacotherapy.
While selective serotonin reuptake inhibitors like sertraline and paroxetine are FDA-approved for PTSD treatment in adults, their efficacy in children often produces outcomes similar to those of placebo. Medications are typically reserved for severe symptoms and are used as an off-label treatment in pediatric cases. Pharmacologic management may be necessary when the severity of symptoms prevents the use of trauma-focused psychotherapy or requires immediate stabilization.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The correct diagnosis is adolescent posttraumatic stress disorder (PTSD), as the patient's symptoms — recurrent nightmares, flashbacks, hypervigilance, and avoidance behaviors — are closely linked to her recent traumatic experience, fitting the clinical profile of PTSD. The MRI finding, although abnormal, does not correlate with a neurologic cause for her symptoms and may be incidental.
Temporal lobe epilepsy can cause behavioral changes but does not explain the specific PTSD symptoms like flashbacks and nightmares.
Chronic migraine could explain the headaches but not the full spectrum of PTSD symptoms.
Major depressive disorder could account for some of the emotional and social symptoms but lacks the characteristic re-experiencing and avoidance behaviors typical of PTSD.
Adolescent PTSD is a significant public health concern, causing significant distress to a small portion of the youth population. By late adolescence, approximately two thirds of youths have been exposed to trauma, and 8% of these individuals meet the criteria for PTSD by age 18. The incidence is exceptionally high in cases of sexual abuse and assault, with rates reaching up to 40%. PTSD in adolescents is associated with severe psychological distress, reduced academic performance, and a high rate of comorbidities, including anxiety and depression. There are specific populations (including children who are evacuated from home, asylum seekers, etc.) that show higher rates of PTSD.
PTSD can lead to chronic impairments, comorbid psychiatric disorders, and an increased risk for suicide, with cases documented in toddlers as young as 1 year old. Thus, it is important to consider the individual's background and social history, as older children with PTSD may present with symptoms from early childhood trauma, often distant from the time of clinical evaluation.
Intrusion symptoms are a hallmark of PTSD, characterized by persistent and uncontrollable thoughts, dreams, and emotional reactions related to the traumatic event. These symptoms distinguish PTSD from other anxiety and mood disorders. Children with PTSD often experience involuntary, distressing thoughts and memories triggered by trauma cues, such as sights, sounds, or smells associated with the traumatic event. In younger children, these intrusive thoughts may manifest through repetitive play that re-enacts aspects of the trauma.
Nightmares are also common, although in children the content may not always directly relate to the traumatic event. Chronic nightmares contribute to sleep disturbances, exacerbating PTSD symptoms. Trauma reminders, which can be both internal (thoughts, memories) and external (places, sensory experiences), can provoke severe distress and physiologic reactions.
Avoidance symptoms often develop as a coping mechanism in response to distressing re-experiencing symptoms. Children may avoid thoughts, feelings, and memories of the traumatic event or people, places, and activities associated with the trauma. In young children, avoidance may manifest as restricted play or reduced exploration of their environment.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) outlines specific criteria for diagnosing PTSD in individuals over 6 years old, which includes exposure to actual or threatened death, serious injury, or sexual violence, and the presence of symptoms such as intrusion, avoidance, negative mood alterations, and heightened arousal. The DSM-5-TR provides tailored diagnostic criteria for developmental differences in symptom expression for children under 6.
Managing PTSD in children requires a patient-specific approach, with an emphasis on obtaining consent from both the patient and guardian. The American Academy of Child and Adolescent Psychiatry (AACAP) recommends psychotherapy as the first-line treatment for pediatric PTSD. However, patients with severe symptoms or comorbidities may initially be unable to engage in meaningful therapy and may require medication to stabilize symptoms before starting psychotherapy.
Trauma-focused psychotherapy, including cognitive-behavioral therapy (CBT), exposure-based therapy, and eye movement desensitization and reprocessing (EMDR) therapy, is the preferred treatment for PTSD. Clinical studies have shown that patients receiving trauma-focused psychotherapy experience more remarkable symptom improvement than those who do not receive treatment and, in children, psychotherapy generally yields better outcomes than pharmacotherapy.
While selective serotonin reuptake inhibitors like sertraline and paroxetine are FDA-approved for PTSD treatment in adults, their efficacy in children often produces outcomes similar to those of placebo. Medications are typically reserved for severe symptoms and are used as an off-label treatment in pediatric cases. Pharmacologic management may be necessary when the severity of symptoms prevents the use of trauma-focused psychotherapy or requires immediate stabilization.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
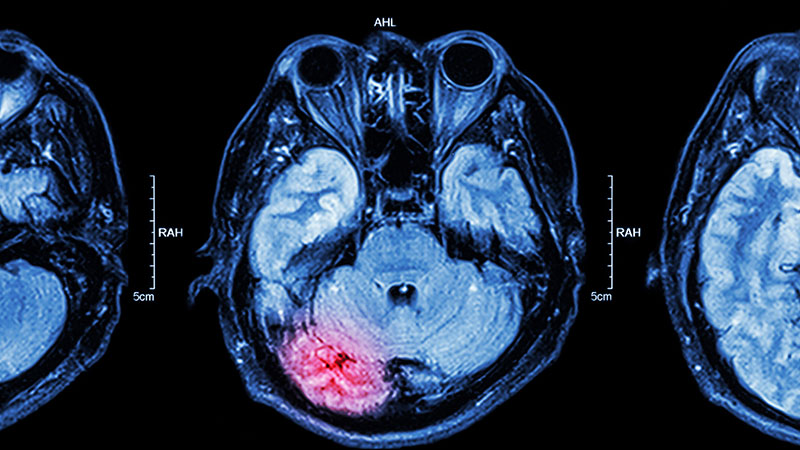
A 15-year-old girl presented to the emergency department with complaints of persistent headaches, nightmares, and difficulty concentrating in school over the past 3 months. The patient had recently experienced a traumatic event, a severe car accident in which a close friend was critically injured. Since the incident, the patient has been exhibiting increased irritability, avoidance of activities that she previously enjoyed, and a noticeable withdrawal from social interactions. Additionally, she reported recurrent flashbacks to the accident, often triggered by sounds resembling car engines. On physical examination, the patient appeared anxious and exhibited hypervigilance. An MRI of the brain was performed to rule out any organic causes of her symptoms, revealing an area of increased signal intensity in the left cerebellar hemisphere (as highlighted in the image).
Involuntary flashbacks
The correct diagnosis is posttraumatic stress disorder (PTSD). The patient's anxiety, irritability, sleep difficulties, and other symptoms are directly related to the recent traumatic event (car crash), and he has no significant physical injuries or neurologic abnormalities.
Generalized anxiety disorder is incorrect because it involves chronic worry about various life aspects for at least 6 months, unrelated to a specific trauma.
Postconcussion syndrome is not applicable because of the lack of concussion evidence and other symptoms, such as headaches or dizziness.
Acute stress disorder is similar to PTSD but is diagnosed when symptoms occur within 3 days to 1 month after a trauma. Because this patient's symptoms have persisted beyond 1 month, PTSD is the most likely diagnosis.
Patients with PTSD exhibit pronounced cognitive, affective, or behavioral responses to trauma reminders; these responses may include severe anxiety, dissociative episodes, flashbacks, and hyperreactive behaviors. The intensity of these symptoms and the resulting psychosocial impairment are more severe in individuals with PTSD compared with people who experience trauma without developing the disorder. To manage such heightened arousal, individuals with PTSD often engage in avoidance behaviors, leading to emotional numbing; reduced interest in daily activities; and, in severe cases, detachment from others.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) outlines specific criteria for diagnosing PTSD in individuals older than 6 years. These criteria include: (A) exposure to actual or threatened death, serious injury, or sexual violence; (B) the presence of one or more intrusion symptoms related to the traumatic event; (C) persistent avoidance of stimuli associated with the trauma; (D) negative alterations in cognitions and mood related to the trauma; and (E) marked alterations in arousal and reactivity, evidenced by two or more specific symptoms.
Early intervention is key in the treatment of PTSD to prevent the condition from becoming chronic. Although more empirical data are needed, especially regarding pharmacotherapy, early supportive interventions such as psychoeducation and case management have shown promise in acutely traumatized individuals.
Trauma-focused psychotherapy is recommended as the first-line treatment for most adults with PTSD. This approach, which includes exposure-based therapies, is generally preferred over other therapies or pharmacologic treatments, such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors. However, in patients with comorbid conditions (eg, depression, psychosis) that impair their ability to engage in trauma-focused therapy, initial pharmacologic management is advised until symptoms stabilize, after which psychotherapy can be introduced.
Clinical trials and meta-analyses have demonstrated the efficacy of various trauma-focused therapies, including trauma-focused cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing. The treatment choice should be collaborative, based on patient presentation, preference, and therapist expertise.
For individuals with PTSD experiencing significant sleep disturbances, particularly nightmares, prazosin is suggested. Clinical studies demonstrate that prazosin effectively reduces overall PTSD symptoms, nightmares, and sleep disturbances in approximately half of the patients treated.
Medication regimens effective for PTSD should be continued for at least 6 months to 1 year to prevent relapse or recurrence. Multiple clinical trials in patients with PTSD who completed acute treatment with SSRIs have demonstrated that those who continued with SSRIs were less likely to have relapse compared with those receiving placebo.
Jasvinder Chawla, MD, Professor of Neurology, Loyola University Medical Center, Maywood; Director, Clinical Neurophysiology Lab, Department of Neurology, Hines VA Hospital, Hines, IL.
Jasvinder Chawla, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The correct diagnosis is posttraumatic stress disorder (PTSD). The patient's anxiety, irritability, sleep difficulties, and other symptoms are directly related to the recent traumatic event (car crash), and he has no significant physical injuries or neurologic abnormalities.
Generalized anxiety disorder is incorrect because it involves chronic worry about various life aspects for at least 6 months, unrelated to a specific trauma.
Postconcussion syndrome is not applicable because of the lack of concussion evidence and other symptoms, such as headaches or dizziness.
Acute stress disorder is similar to PTSD but is diagnosed when symptoms occur within 3 days to 1 month after a trauma. Because this patient's symptoms have persisted beyond 1 month, PTSD is the most likely diagnosis.
Patients with PTSD exhibit pronounced cognitive, affective, or behavioral responses to trauma reminders; these responses may include severe anxiety, dissociative episodes, flashbacks, and hyperreactive behaviors. The intensity of these symptoms and the resulting psychosocial impairment are more severe in individuals with PTSD compared with people who experience trauma without developing the disorder. To manage such heightened arousal, individuals with PTSD often engage in avoidance behaviors, leading to emotional numbing; reduced interest in daily activities; and, in severe cases, detachment from others.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) outlines specific criteria for diagnosing PTSD in individuals older than 6 years. These criteria include: (A) exposure to actual or threatened death, serious injury, or sexual violence; (B) the presence of one or more intrusion symptoms related to the traumatic event; (C) persistent avoidance of stimuli associated with the trauma; (D) negative alterations in cognitions and mood related to the trauma; and (E) marked alterations in arousal and reactivity, evidenced by two or more specific symptoms.
Early intervention is key in the treatment of PTSD to prevent the condition from becoming chronic. Although more empirical data are needed, especially regarding pharmacotherapy, early supportive interventions such as psychoeducation and case management have shown promise in acutely traumatized individuals.
Trauma-focused psychotherapy is recommended as the first-line treatment for most adults with PTSD. This approach, which includes exposure-based therapies, is generally preferred over other therapies or pharmacologic treatments, such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors. However, in patients with comorbid conditions (eg, depression, psychosis) that impair their ability to engage in trauma-focused therapy, initial pharmacologic management is advised until symptoms stabilize, after which psychotherapy can be introduced.
Clinical trials and meta-analyses have demonstrated the efficacy of various trauma-focused therapies, including trauma-focused cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing. The treatment choice should be collaborative, based on patient presentation, preference, and therapist expertise.
For individuals with PTSD experiencing significant sleep disturbances, particularly nightmares, prazosin is suggested. Clinical studies demonstrate that prazosin effectively reduces overall PTSD symptoms, nightmares, and sleep disturbances in approximately half of the patients treated.
Medication regimens effective for PTSD should be continued for at least 6 months to 1 year to prevent relapse or recurrence. Multiple clinical trials in patients with PTSD who completed acute treatment with SSRIs have demonstrated that those who continued with SSRIs were less likely to have relapse compared with those receiving placebo.
Jasvinder Chawla, MD, Professor of Neurology, Loyola University Medical Center, Maywood; Director, Clinical Neurophysiology Lab, Department of Neurology, Hines VA Hospital, Hines, IL.
Jasvinder Chawla, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The correct diagnosis is posttraumatic stress disorder (PTSD). The patient's anxiety, irritability, sleep difficulties, and other symptoms are directly related to the recent traumatic event (car crash), and he has no significant physical injuries or neurologic abnormalities.
Generalized anxiety disorder is incorrect because it involves chronic worry about various life aspects for at least 6 months, unrelated to a specific trauma.
Postconcussion syndrome is not applicable because of the lack of concussion evidence and other symptoms, such as headaches or dizziness.
Acute stress disorder is similar to PTSD but is diagnosed when symptoms occur within 3 days to 1 month after a trauma. Because this patient's symptoms have persisted beyond 1 month, PTSD is the most likely diagnosis.
Patients with PTSD exhibit pronounced cognitive, affective, or behavioral responses to trauma reminders; these responses may include severe anxiety, dissociative episodes, flashbacks, and hyperreactive behaviors. The intensity of these symptoms and the resulting psychosocial impairment are more severe in individuals with PTSD compared with people who experience trauma without developing the disorder. To manage such heightened arousal, individuals with PTSD often engage in avoidance behaviors, leading to emotional numbing; reduced interest in daily activities; and, in severe cases, detachment from others.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) outlines specific criteria for diagnosing PTSD in individuals older than 6 years. These criteria include: (A) exposure to actual or threatened death, serious injury, or sexual violence; (B) the presence of one or more intrusion symptoms related to the traumatic event; (C) persistent avoidance of stimuli associated with the trauma; (D) negative alterations in cognitions and mood related to the trauma; and (E) marked alterations in arousal and reactivity, evidenced by two or more specific symptoms.
Early intervention is key in the treatment of PTSD to prevent the condition from becoming chronic. Although more empirical data are needed, especially regarding pharmacotherapy, early supportive interventions such as psychoeducation and case management have shown promise in acutely traumatized individuals.
Trauma-focused psychotherapy is recommended as the first-line treatment for most adults with PTSD. This approach, which includes exposure-based therapies, is generally preferred over other therapies or pharmacologic treatments, such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors. However, in patients with comorbid conditions (eg, depression, psychosis) that impair their ability to engage in trauma-focused therapy, initial pharmacologic management is advised until symptoms stabilize, after which psychotherapy can be introduced.
Clinical trials and meta-analyses have demonstrated the efficacy of various trauma-focused therapies, including trauma-focused cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing. The treatment choice should be collaborative, based on patient presentation, preference, and therapist expertise.
For individuals with PTSD experiencing significant sleep disturbances, particularly nightmares, prazosin is suggested. Clinical studies demonstrate that prazosin effectively reduces overall PTSD symptoms, nightmares, and sleep disturbances in approximately half of the patients treated.
Medication regimens effective for PTSD should be continued for at least 6 months to 1 year to prevent relapse or recurrence. Multiple clinical trials in patients with PTSD who completed acute treatment with SSRIs have demonstrated that those who continued with SSRIs were less likely to have relapse compared with those receiving placebo.
Jasvinder Chawla, MD, Professor of Neurology, Loyola University Medical Center, Maywood; Director, Clinical Neurophysiology Lab, Department of Neurology, Hines VA Hospital, Hines, IL.
Jasvinder Chawla, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
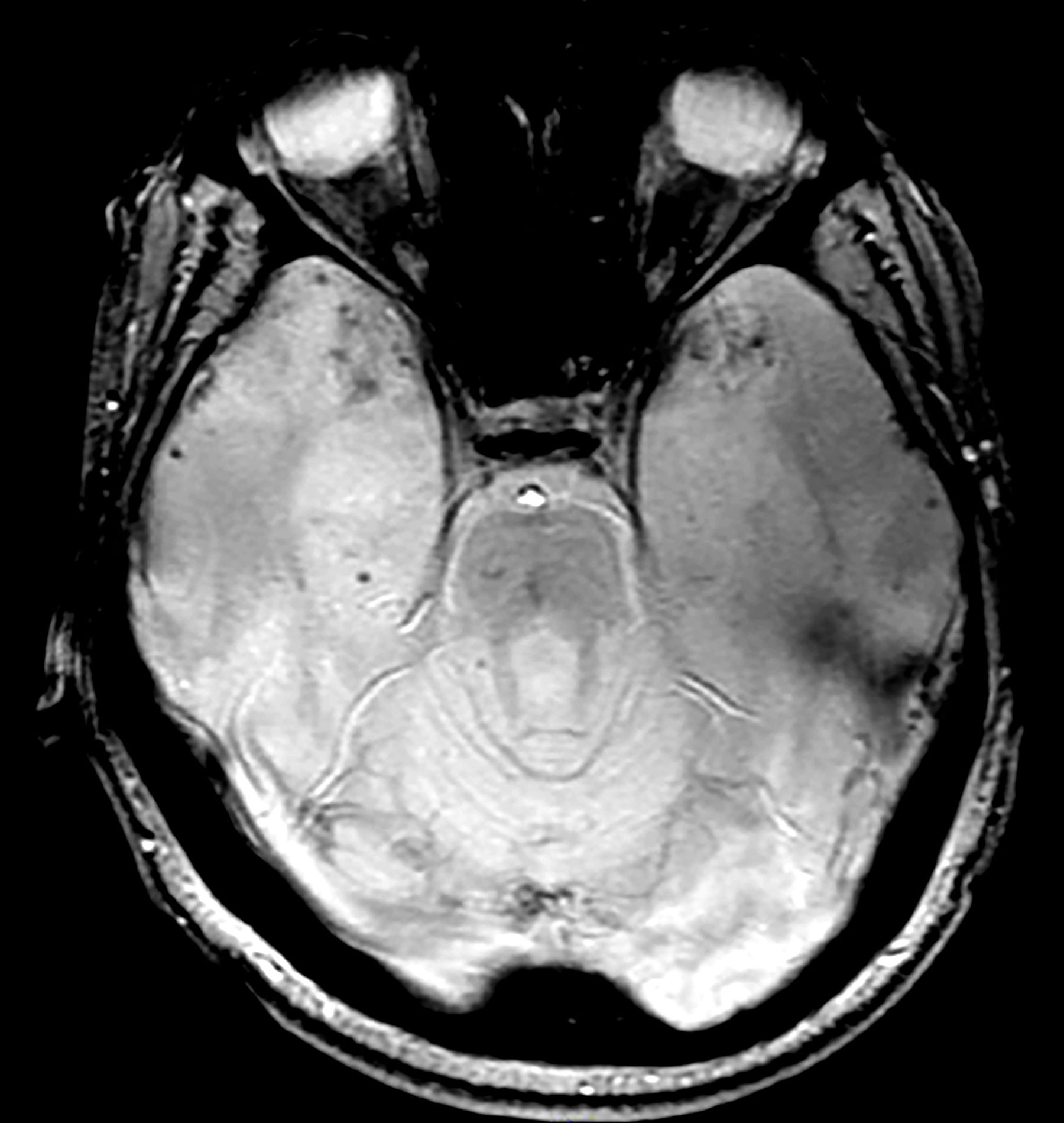
A 28-year-old man presented to the emergency department following a high-speed motor vehicle accident 2 months ago. He sustained no major physical injuries but had minor lacerations and bruising. The patient reported feeling unusually irritable and having difficulty sleeping since the accident, citing frequent flashbacks to the accident and occasional nightmares. He has started to feel more anxious and withdrawn, losing interest in hobbies such as swimming and biking that he previously enjoyed.
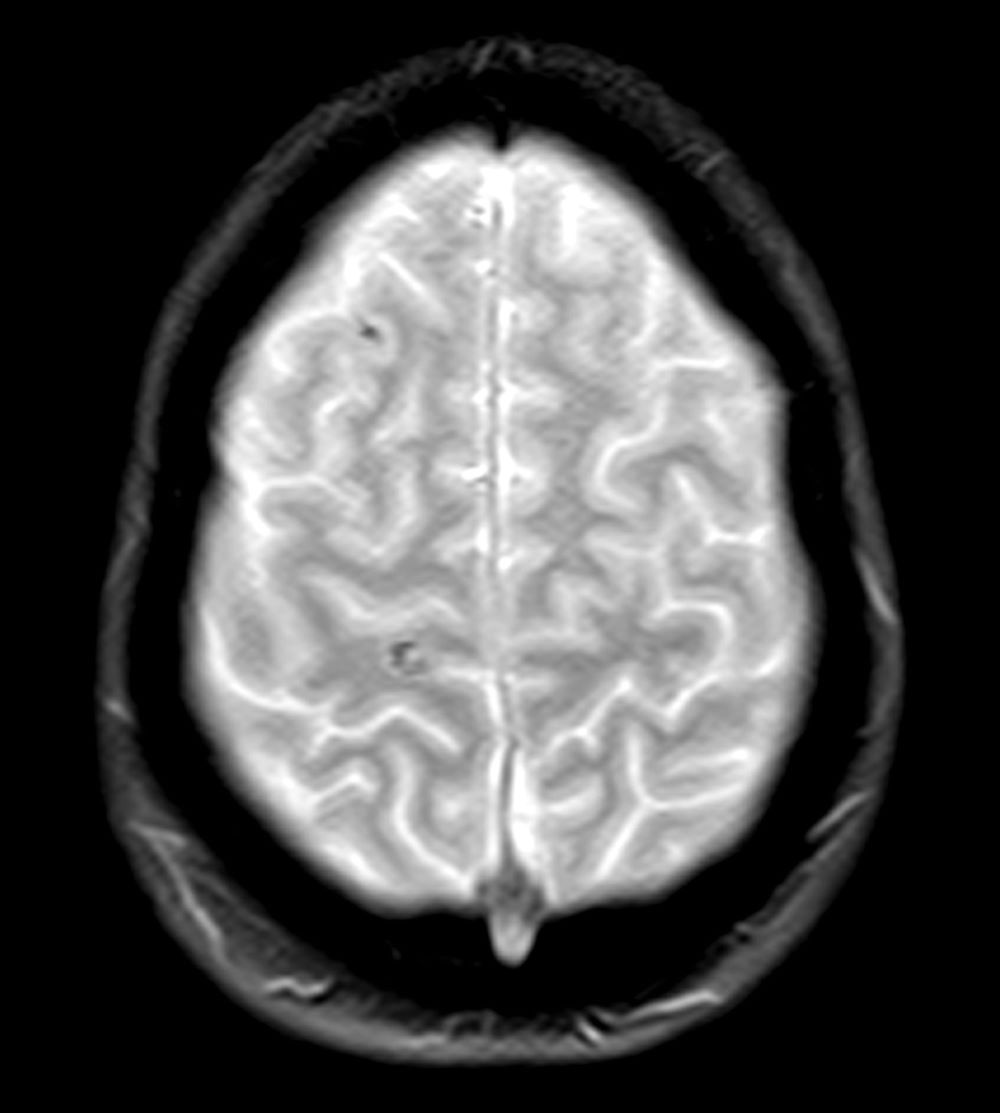
The patient's medical history is unremarkable, with no previous psychiatric or neurologic conditions. His neurologic examination was normal. An initial axial T2-weighted brain MRI demonstrated multiple small areas of hemorrhage, indicative of a diffuse axonal injury or shear-type injury. Despite the lack of significant physical injuries, the patient expressed ongoing distress related to the traumatic event.