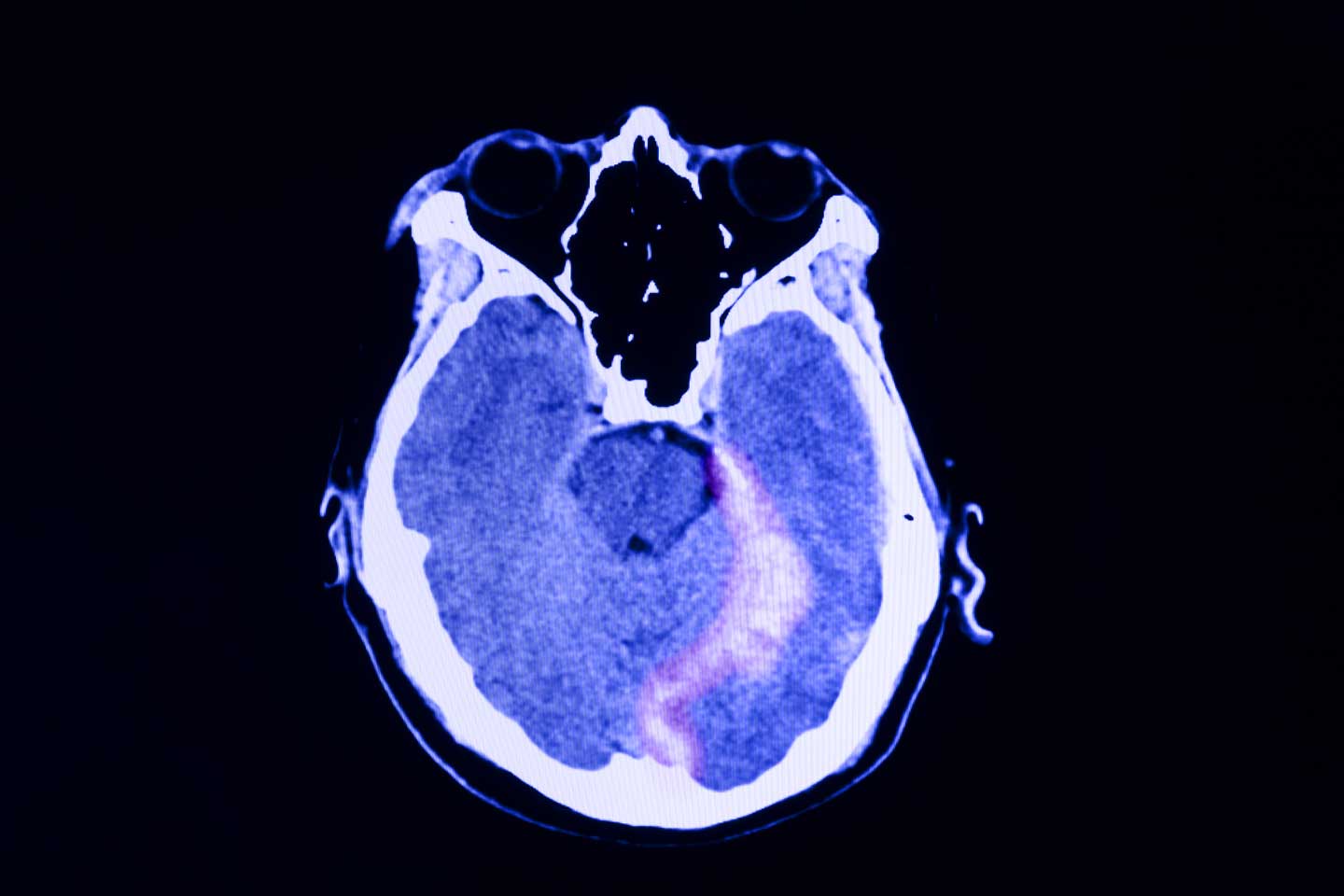
User login
Posttraumatic stress disorder (PTSD) is the most likely diagnosis given the patient's symptoms — recurrent nightmares, flashbacks, and anxiety triggered by trauma-related noises, all of which are classic indicators of the disorder. His history of witnessing traumatic events at work, including a fatal accident, further reinforces this diagnosis and strongly suggests PTSD as the most fitting explanation. Although the brain scan does not diagnose PTSD directly, it plays an important role in ruling out other potential causes, such as structural brain damage, that could be contributing to his symptoms. Thus, the patient's symptoms are more likely a result of PTSD rather than an underlying organic brain injury.
Although major depressive disorder could explain some of the patient's symptoms, such as impaired daily functioning and withdrawal, the presence of recurrent nightmares, flashbacks, and trauma-specific triggers are more indicative of PTSD.
Generalized anxiety disorder might account for the patient's heightened anxiety, but it typically involves chronic, pervasive worry rather than the trauma-specific symptoms seen here.
Chronic traumatic encephalopathy (CTE) is a possible concern given the patient's occupation and the findings on the CT scan. However, CTE generally presents with cognitive and behavioral changes over time, such as memory loss and aggression, rather than the distinctive trauma-related symptoms characteristic of PTSD.
Individuals with PTSD often display heightened emotional, cognitive, and behavioral responses when exposed to trauma-related cues; these responses include severe anxiety, dissociative episodes, flashbacks, and heightened reactivity. To manage their increased arousal, individuals with PTSD frequently engage in avoidance behaviors, which can result in emotional numbing, diminished interest in daily activities, and, in more severe cases, social withdrawal.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR), the diagnostic criteria for PTSD in individuals older than 6 years include (A) exposure to actual or threatened death, serious injury, or sexual violence; (B) the presence of one or more intrusion symptoms related to the trauma; (C) persistent avoidance of trauma-related stimuli; (D) negative changes in cognition and mood associated with the trauma; and (E) marked alterations in arousal and reactivity, with at least two specific symptoms.
Trauma-focused psychotherapy is generally recommended as the first-line treatment for most adults with PTSD, with exposure-based therapies often preferred over other therapeutic approaches or pharmacologic treatments, such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors. However, in patients with comorbid conditions such as depression or psychosis that hinder their ability to engage in trauma-focused therapy, initial pharmacologic management is recommended until symptoms stabilize, allowing for the later introduction of psychotherapy. Clinical trials and meta-analyses have demonstrated the effectiveness of various trauma-focused therapies, including trauma-focused cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing. Treatment selection should be made collaboratively, considering the patient's presentation and preferences and the therapist's expertise.
For effective management of PTSD, medication regimens should be maintained for at least 6 months to 1 year to prevent relapse or recurrence. Multiple clinical trials have shown that patients who continue SSRIs after acute treatment are less likely to experience a relapse than those who switch to placebo.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Posttraumatic stress disorder (PTSD) is the most likely diagnosis given the patient's symptoms — recurrent nightmares, flashbacks, and anxiety triggered by trauma-related noises, all of which are classic indicators of the disorder. His history of witnessing traumatic events at work, including a fatal accident, further reinforces this diagnosis and strongly suggests PTSD as the most fitting explanation. Although the brain scan does not diagnose PTSD directly, it plays an important role in ruling out other potential causes, such as structural brain damage, that could be contributing to his symptoms. Thus, the patient's symptoms are more likely a result of PTSD rather than an underlying organic brain injury.
Although major depressive disorder could explain some of the patient's symptoms, such as impaired daily functioning and withdrawal, the presence of recurrent nightmares, flashbacks, and trauma-specific triggers are more indicative of PTSD.
Generalized anxiety disorder might account for the patient's heightened anxiety, but it typically involves chronic, pervasive worry rather than the trauma-specific symptoms seen here.
Chronic traumatic encephalopathy (CTE) is a possible concern given the patient's occupation and the findings on the CT scan. However, CTE generally presents with cognitive and behavioral changes over time, such as memory loss and aggression, rather than the distinctive trauma-related symptoms characteristic of PTSD.
Individuals with PTSD often display heightened emotional, cognitive, and behavioral responses when exposed to trauma-related cues; these responses include severe anxiety, dissociative episodes, flashbacks, and heightened reactivity. To manage their increased arousal, individuals with PTSD frequently engage in avoidance behaviors, which can result in emotional numbing, diminished interest in daily activities, and, in more severe cases, social withdrawal.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR), the diagnostic criteria for PTSD in individuals older than 6 years include (A) exposure to actual or threatened death, serious injury, or sexual violence; (B) the presence of one or more intrusion symptoms related to the trauma; (C) persistent avoidance of trauma-related stimuli; (D) negative changes in cognition and mood associated with the trauma; and (E) marked alterations in arousal and reactivity, with at least two specific symptoms.
Trauma-focused psychotherapy is generally recommended as the first-line treatment for most adults with PTSD, with exposure-based therapies often preferred over other therapeutic approaches or pharmacologic treatments, such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors. However, in patients with comorbid conditions such as depression or psychosis that hinder their ability to engage in trauma-focused therapy, initial pharmacologic management is recommended until symptoms stabilize, allowing for the later introduction of psychotherapy. Clinical trials and meta-analyses have demonstrated the effectiveness of various trauma-focused therapies, including trauma-focused cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing. Treatment selection should be made collaboratively, considering the patient's presentation and preferences and the therapist's expertise.
For effective management of PTSD, medication regimens should be maintained for at least 6 months to 1 year to prevent relapse or recurrence. Multiple clinical trials have shown that patients who continue SSRIs after acute treatment are less likely to experience a relapse than those who switch to placebo.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Posttraumatic stress disorder (PTSD) is the most likely diagnosis given the patient's symptoms — recurrent nightmares, flashbacks, and anxiety triggered by trauma-related noises, all of which are classic indicators of the disorder. His history of witnessing traumatic events at work, including a fatal accident, further reinforces this diagnosis and strongly suggests PTSD as the most fitting explanation. Although the brain scan does not diagnose PTSD directly, it plays an important role in ruling out other potential causes, such as structural brain damage, that could be contributing to his symptoms. Thus, the patient's symptoms are more likely a result of PTSD rather than an underlying organic brain injury.
Although major depressive disorder could explain some of the patient's symptoms, such as impaired daily functioning and withdrawal, the presence of recurrent nightmares, flashbacks, and trauma-specific triggers are more indicative of PTSD.
Generalized anxiety disorder might account for the patient's heightened anxiety, but it typically involves chronic, pervasive worry rather than the trauma-specific symptoms seen here.
Chronic traumatic encephalopathy (CTE) is a possible concern given the patient's occupation and the findings on the CT scan. However, CTE generally presents with cognitive and behavioral changes over time, such as memory loss and aggression, rather than the distinctive trauma-related symptoms characteristic of PTSD.
Individuals with PTSD often display heightened emotional, cognitive, and behavioral responses when exposed to trauma-related cues; these responses include severe anxiety, dissociative episodes, flashbacks, and heightened reactivity. To manage their increased arousal, individuals with PTSD frequently engage in avoidance behaviors, which can result in emotional numbing, diminished interest in daily activities, and, in more severe cases, social withdrawal.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR), the diagnostic criteria for PTSD in individuals older than 6 years include (A) exposure to actual or threatened death, serious injury, or sexual violence; (B) the presence of one or more intrusion symptoms related to the trauma; (C) persistent avoidance of trauma-related stimuli; (D) negative changes in cognition and mood associated with the trauma; and (E) marked alterations in arousal and reactivity, with at least two specific symptoms.
Trauma-focused psychotherapy is generally recommended as the first-line treatment for most adults with PTSD, with exposure-based therapies often preferred over other therapeutic approaches or pharmacologic treatments, such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors. However, in patients with comorbid conditions such as depression or psychosis that hinder their ability to engage in trauma-focused therapy, initial pharmacologic management is recommended until symptoms stabilize, allowing for the later introduction of psychotherapy. Clinical trials and meta-analyses have demonstrated the effectiveness of various trauma-focused therapies, including trauma-focused cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing. Treatment selection should be made collaboratively, considering the patient's presentation and preferences and the therapist's expertise.
For effective management of PTSD, medication regimens should be maintained for at least 6 months to 1 year to prevent relapse or recurrence. Multiple clinical trials have shown that patients who continue SSRIs after acute treatment are less likely to experience a relapse than those who switch to placebo.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
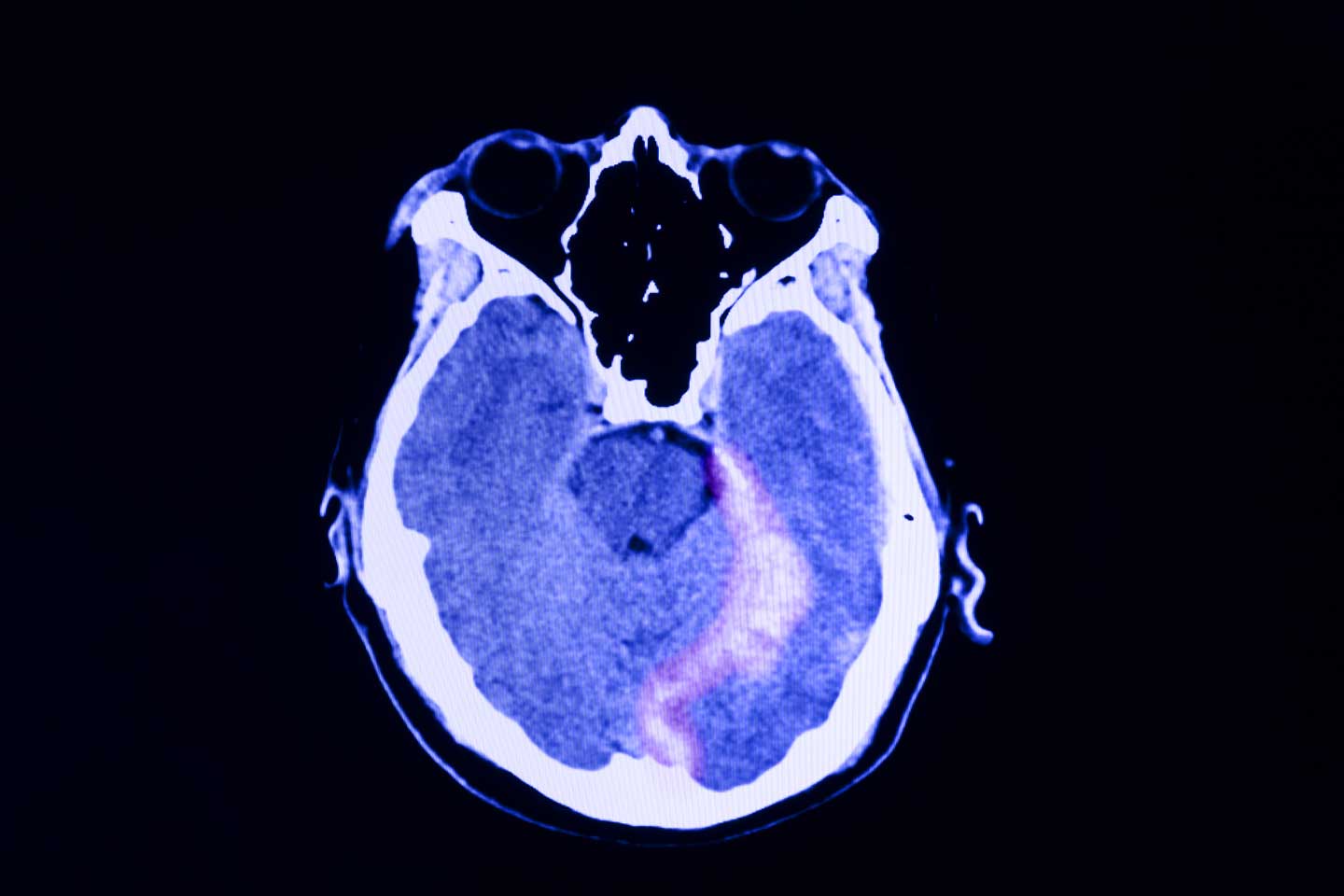
A 48-year-old male construction worker presented with worsening symptoms over the past year, including recurrent nightmares, heightened anxiety, and flashbacks triggered by loud noises such as those heard on job sites. These symptoms have begun to interfere with his daily functioning, particularly affecting his work and family life. The patient has a history of multiple traumatic experiences at work, including witnessing a fatal accident involving a coworker. On neurologic examination, he appeared highly agitated and displayed signs of hypervigilance. A brain CT scan (as shown in the image) was ordered because of the chronic nature of his symptoms and the potential for neurologic causes—such as traumatic brain injury—to contribute to his condition. The scan revealed an abnormality on the left side, prompting further investigation to determine whether the lesion is related to his symptoms or indicative of another underlying condition. Additional tests were ordered to further characterize the lesion: electroencephalography to assess for any associated seizure activity, and blood tests and a lumbar puncture to rule out infection or inflammatory processes. These additional tests came back negative, and the abnormality was later diagnosed as artifact.