User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Treatment augmentation strategies for OCD: A review of 8 studies
Obsessive-compulsive disorder (OCD) is a chronic, debilitating neuropsychiatric disorder that affects 1% to 3% of the population worldwide.1,2 Together, serotonin reuptake inhibitors (SRIs) and cognitive-behavior therapy (CBT) are considered the first-line treatment for OCD.3 In children and adults, CBT is considered at least as effective as pharmacotherapy.4 Despite being an effective treatment, CBT continues to have barriers to its widespread use, including limited availability of trained CBT therapists, delayed clinical response, and high costs.5
Only approximately one-half of patients with OCD respond to SRI therapy, and a considerable percentage (30% to 40%) show significant residual symptoms even after multiple trials of SRIs.6-8 In addition, SRIs may have adverse effects (eg, sexual dysfunction, gastrointestinal symptoms) that impair patient adherence to these medications.9 Therefore, finding better treatment options is important for managing patients with OCD.
Augmentation strategies are recommended for patients who show partial response to SRI treatment or poor response to multiple SRIs. Augmentation typically includes incorporating additional medications with the primary drug with the goal of boosting the therapeutic efficacy of the primary drug. Typically, these additional medications have different mechanisms of action. However, there are no large-scale randomized controlled trials (RCTs) to inform treatment augmentation after first-line treatments for OCD produce suboptimal outcomes. The available evidence is predominantly based on small-scale RCTs, open-label trials, and case series.
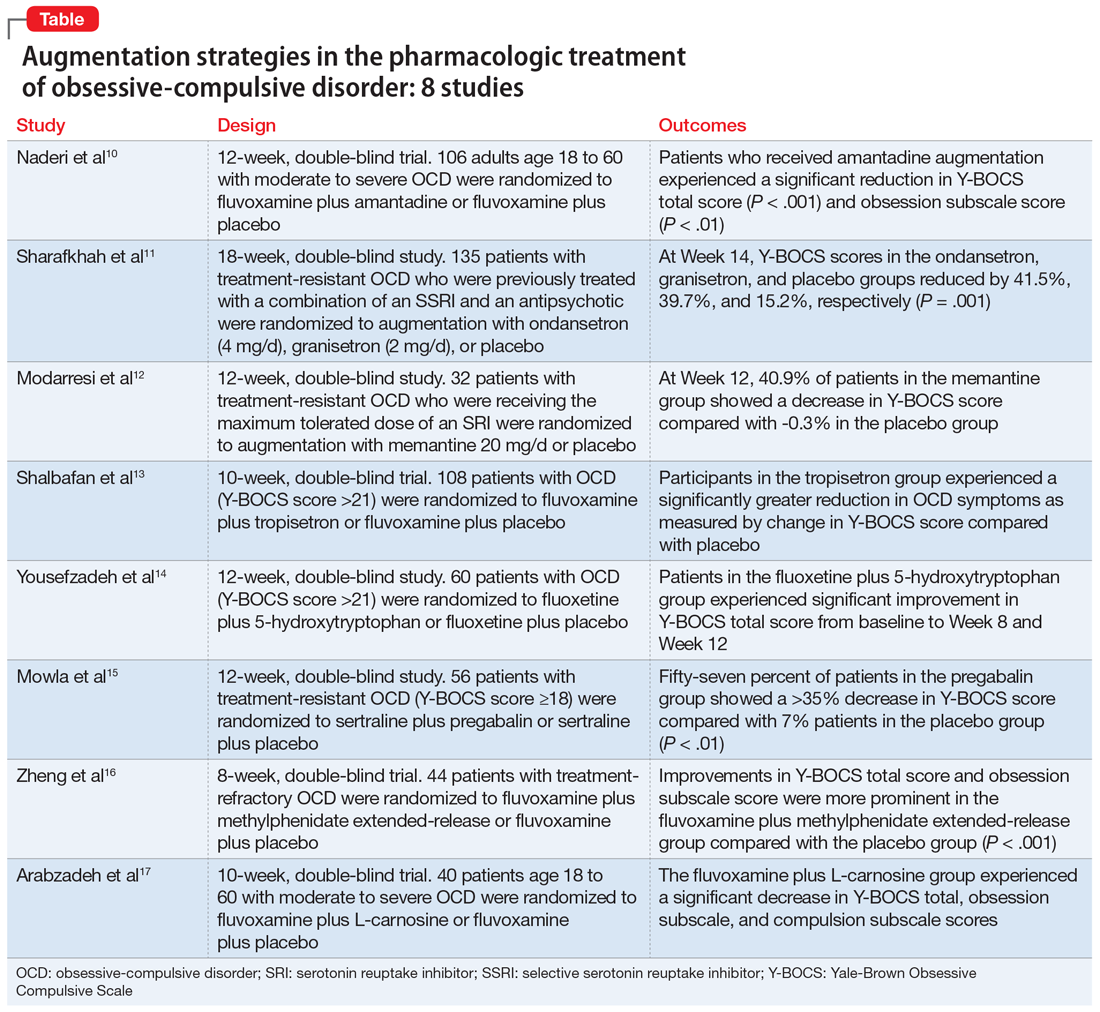
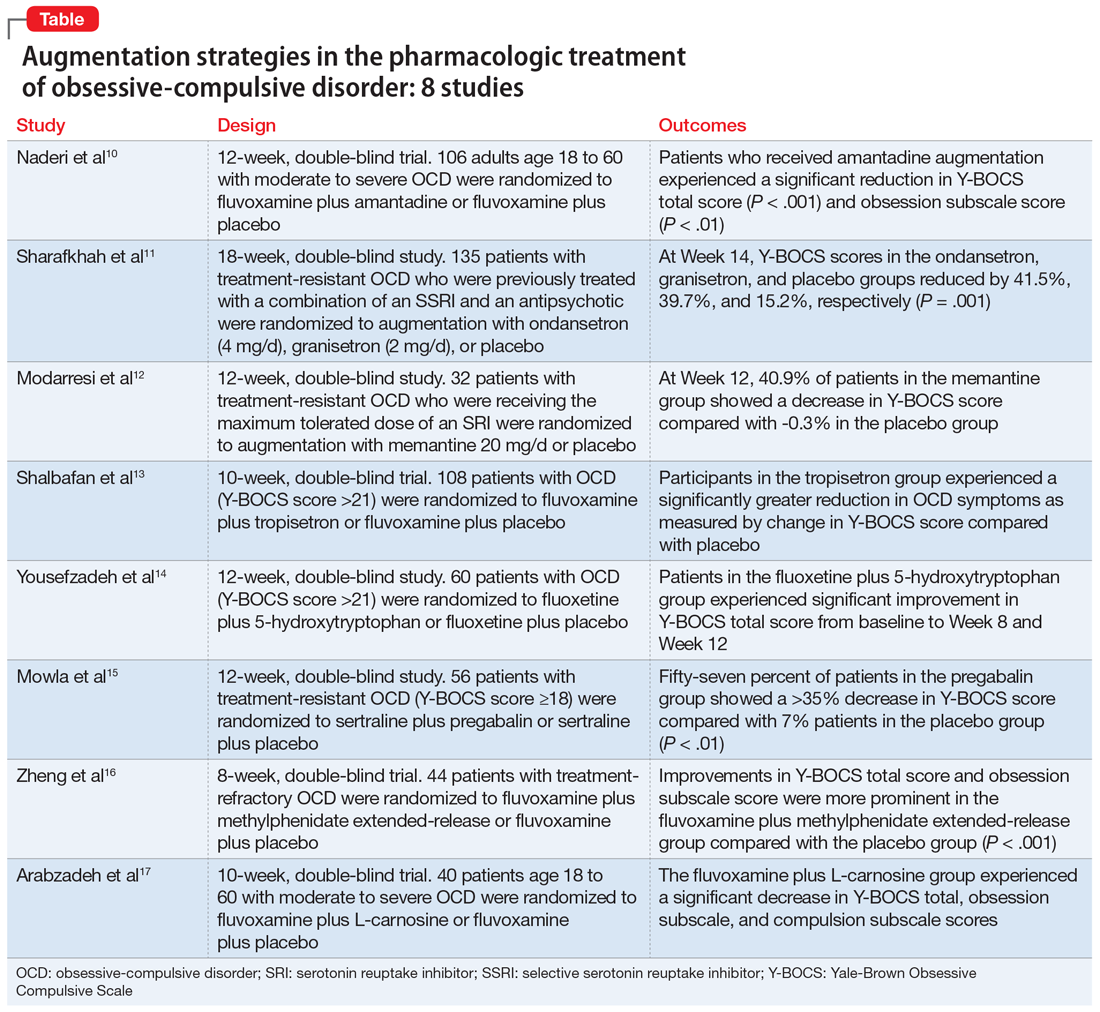
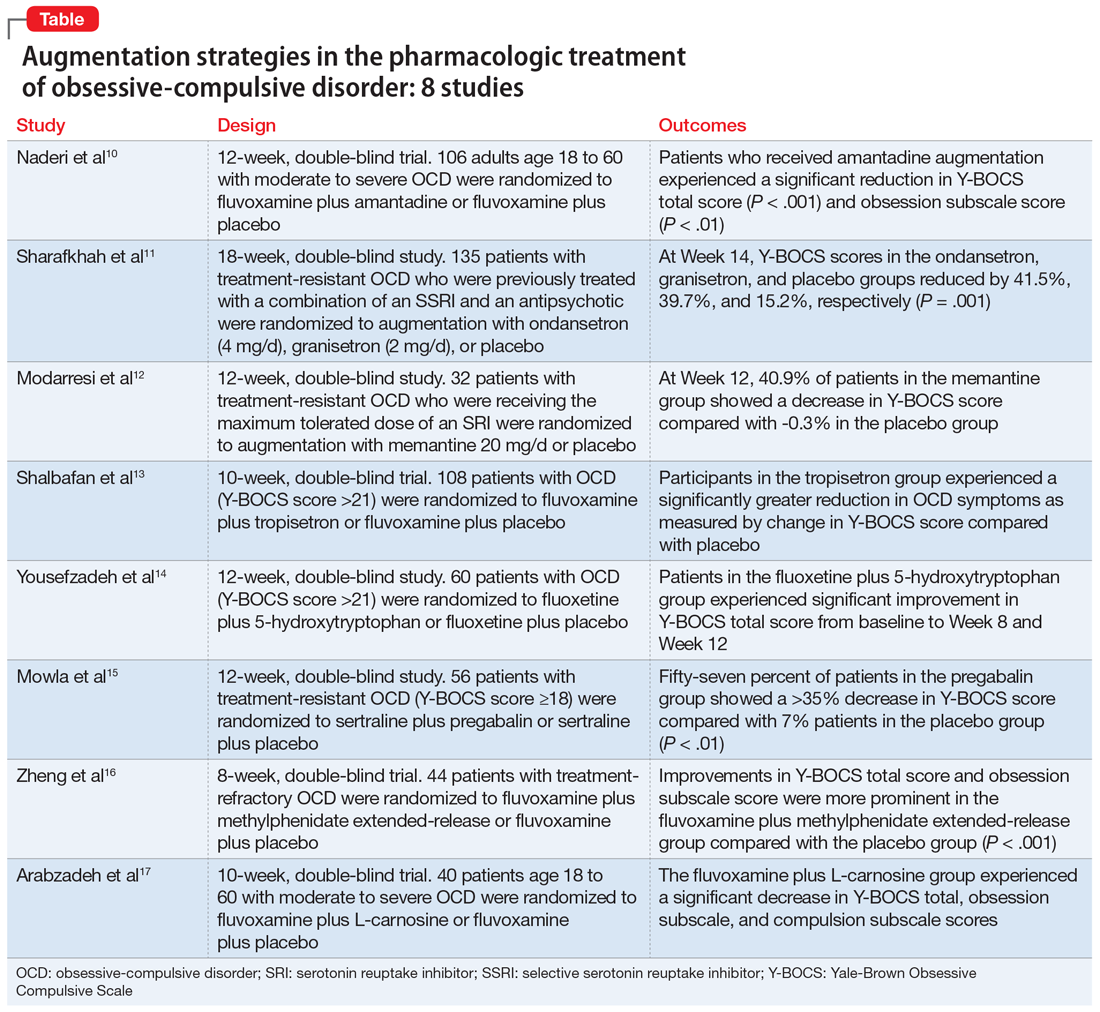
In this article, we review the evidence for treatment augmentation strategies for OCD and summarize 8 studies that show promising results (Table10-17). We focus only on pharmacologic agents and do not include other biological interventions, such as repetitive transcranial magnetic stimulation over supplementary motor area, ablative neurosurgery, or deep brain stimulation.
Continue to: Reference 1...
1. Naderi S, Faghih H , Aqamolaei A, et al. Amantadine as adjuvant therapy in the treatment of moderate to severe obsessivecompulsive disorder: a double-blind randomized trial with placebo control. Psychiatry Clin Neurosci. 2019;73(4):169-174. doi:10.1111/ pcn.12803
Numerous studies support the role of glutamate dysregulation in the pathophysiology of OCD. Cortico-striato-thalamo-cortical (CSTC) abnormalities play a major role in the pathophysiology of OCD as suggested by neuroimaging research studies that indicate glutamate is the fundamental neurotransmitter of the CSTC circuit. Dysregulation of glutamatergic signaling within this circuit has been linked to OCD. Patients with OCD have been found to have an increase of glutamate in the CSF. As a result, medications that affect glutamate levels can be used to treat patients with OCD who do not respond to first-line agents. In patients already taking SRIs, augmentation of glutamate-modulating medications can reduce OCD symptoms. As an uncompetitive antagonist of the N-methyl-
Naderi et al10 evaluated amantadine as augmentative therapy to fluvoxamine for treating patients with moderate to severe OCD.
Study design
- This 12-week, randomized, double-blind, placebo-controlled trial evaluated the efficacy and safety of amantadine as an augmentative agent to fluvoxamine in 106 patients age 18 to 60 with moderate to severe OCD.
- Participants met DSM-5 criteria for OCD and had a Yale-Brown Obsessive Compulsive Scale (Y-BOCS) score >21. Participants were excluded if they had any substance dependence; an IQ <70; any other Axis I mental disorder; any serious cardiac, renal, or hepatic disease; had received psychotropic medications during the last 6 weeks, were pregnant or breastfeeding, or had rising liver transaminases to 3 times the upper limit of normal or higher.
- Participants received fluvoxamine 100 mg twice daily plus amantadine 100 mg/d, or fluvoxamine 100 mg twice daily plus placebo. All patients received fluvoxamine 100 mg/d for 28 days followed by 200 mg/d for the remainder of the trial.
- The primary outcome measure was difference in Y-BOCS total scores between the amantadine and placebo groups. The secondary outcome was the difference in Y-BOCS obsession and compulsion subscale scores.
Outcomes
- Patients who received amantadine augmentation experienced a significant reduction in Y-BOCS total score (P < .001) and obsession subscale score (P < .01).
- The amantadine group showed good tolerability and safety. There were no clinically significant adverse effects.
- Amantadine is an effective adjuvant to fluvoxamine for reducing OCD symptoms.
Conclusion
- Ondansetron and granisetron can be beneficial as an augmentation strategy for patients with treatment-resistant OCD.
2. Sharafkhah M, Aghakarim Alamdar M, Massoudifar A, et al. Comparing the efficacy of ondansetron and granisetron augmentation in treatment-resistant obsessive-compulsive disorder: a randomized double-blind placebo-controlled study. Int Clin Psychopharmacol. 2019;34(5):222- 233. doi:10.1097/YIC.0000000000000267
Although selective serotonin reuptake inhibitors (SSRIs) are considered a first-line treatment when teamed with CBT and antipsychotic augmentation, symptom resolution is not always achieved, and treatment resistance is a common problem. Sharafkhah et al11 compared the efficacy of ondansetron and granisetron augmentation specifically for patients with treatment-resistant OCD.
Study Design
- In this 18-week, randomized, double-blind, placebo-controlled study, 135 patients with treatment-resistant OCD who were previously treated with a combination of an SSRI and an antipsychotic received augmentation with ondansetron (n = 45, 4 mg/d), granisetron (n = 45, 2 mg/d), or placebo.
- Patients were rated using Y-BOCS every 2 weeks during phase I (intervention period), which lasted 14 weeks. After completing the intervention, patients were followed for 4 more weeks during phase II (discontinuation period).
- The aim of this study was to determine the safety, efficacy, and tolerability of ondansetron vs granisetron as augmentation for patients with treatment-resistant OCD. A secondary aim was to determine the rate of relapse of OCD symptoms after discontinuing ondansetron as compared with granisetron at 4 weeks after intervention.
Outcomes
- At Week 14, the reductions in Y-BOCS scores in the ondansetron, granisetron, and placebo groups were 41.5%, 39.7%, and 15.2%, respectively (P = .001). The reduction in Y-BOCS score in the ondansetron and granisetron groups was significantly greater than placebo at all phase I visits.
- Complete response was higher in the ondansetron group compared with the granisetron group (P = .041).
- Y-BOCS scores increased in both the ondansetron and granisetron groups during the discontinuation phase, but OCD symptoms were not significantly exacerbated.
Conclusion
- Ondansetron and granisetron can be beneficial as an augmentation strategy for patients with treatment-resistant OCD.
3. Modarresi A, Sayyah M, Razooghi S, et al. Memantine augmentation improves symptoms in serotonin reuptake inhibitorrefractory obsessive-compulsive disorder: a randomized controlled trial. Pharmacopsychiatry. 2018;51(6):263-269. doi:10.1055/s-0043-120268
Increased glutamate levels in CSF, glutamatergic overactivity, and polymorphisms of genes coding the NMDA receptor have been shown to contribute to the occurrence of OCD. Memantine is a noncompetitive antagonist of the NMDA receptor. Various control trials have shown augmentation with memantine 5 mg/d to 20 mg/d significantly reduced symptom severity in patients with moderate to severe OCD. Modarresi et al12 evaluated memantine as a treatment option for patients with severe OCD who did not respond to SRI monotherapy.
Study design
- This 12-week, double-blind, randomized, placebo-controlled trial evaluated the efficacy of memantine augmentation in 32 patients age 18 to 40 who met DSM-5 criteria for OCD, had a Y-BOCS score ≥24, and no psychiatric comorbidity. Participants had not responded to ≥3 adequate trials (minimum 3 months) of SRI therapy, 1 of which was clomipramine.
- Individuals were excluded if they were undergoing CBT; had an additional anxiety disorder, mood disorder, or current drug or alcohol use disorder, or any systemic disorder; had a history of seizures; were pregnant or breastfeeding; or had a history of memantine use.
- Participants already receiving the maximum tolerated dose of an SRI received augmentation with memantine 20 mg/d or placebo.
- The primary outcome measure was change in Y-BOCS score from baseline. The secondary outcome was the number of individuals who achieved treatment response (defined as ≥35% reduction in Y-BOCS score).
Continue to: Outcomes...
Outcomes
- There was a statistically significant difference in Y-BOCS score in patients treated with memantine at Week 8 and Week 12 vs those who received placebo. By Week 8, 17.2% of patients in the memantine group showed a decrease in Y-BOCS score, compared with -0.8% patients in the placebo group. The difference became more significant by Week 12, with 40.9% in the memantine group showing a decrease in Y-BOCS score vs -0.3% in the placebo group. This resulted in 73.3% of patients achieving treatment response.
- Eight weeks of memantine augmentation was necessary to observe a significant improvement in OCD symptoms, and 12 weeks was needed for treatment response.
- The mean Y-BOCS total score decreased significantly in the memantine group from Week 4 to Week 8 (16.8%) and again from Week 8 to Week 12 (28.5%).
- The memantine group showed good tolerability and safety. There were no clinically significant adverse effects.
Conclusion
- Memantine augmentation in patients with severe OCD who do not respond to an SRI is effective and well-tolerated.
4. Shalbafan M, Malekpour F, Tadayon Najafabadi B, et al. Fluvoxamine combination therapy with tropisetron for obsessive-compulsive disorder patients: a placebo-controlled, randomized clinical trial. J Psychopharmacol. 2019;33(11):1407- 1414. doi:10.1177/0269881119878177
Studies have demonstrated the involvement of the amygdala, medial and lateral orbitofrontal cortex, and dorsal anterior cingulate cortex in OCD. Additionally, studies have also investigated the role of serotonin, dopamine, and glutamate system dysregulation in the pathology of OCD.
The 5-HT3 receptors are ligand-gated ion channels found in the prefrontal cortex, amygdala, and hippocampus. Studies of 5-HT3 receptor antagonists such as ondansetron and granisetron have shown beneficial results in augmentation with SSRIs for patients with OCD.11 Tropisetron, a 5-HT3 receptor antagonist, is highly lipophilic and able to cross the blood brain barrier. It also has dopamine-inhibiting properties that could have benefits in OCD management. Shalbafan et al13 evaluated the efficacy of tropisetron augmentation to fluvoxamine for patients with OCD.
Study design
- In a 10-week, randomized, double-blind, placebo-controlled, parallel-group trial, 108 individuals age 18 to 60 who met DSM-5 criteria for OCD and had a Y-BOCS score >21 received fluvoxamine plus tropisetron or fluvoxamine plus placebo. A total of 48 (44.4%) participants in each group completed the trial. Participants were evaluated using the Y-BOCS scale at baseline and at Week 4 and Week 10.
- The primary outcome was decrease in total Y-BOCS score from baseline to Week 10. The secondary outcome was the difference in change in Y-BOCS obsession and compulsion subscale scores between the groups.
Outcomes
- The Y-BOCS total score was not significantly different between the 2 groups (P = .975). Repeated measures analysis of variance determined a significant effect for time in both tropisetron and placebo groups (Greenhouse-Geisser F [2.72–2303.84] = 152.25, P < .001; and Greenhouse-Geisser F [1.37–1736.81] = 75.57, P < .001, respectively). At Week 10, 35 participants in the tropisetron group and 19 participants in the placebo group were complete responders.
- The baseline Y-BOCS obsession and compulsion subscales did not significantly differ between treatment groups.
Conclusion
- Compared with participants in the placebo group, those in the tropisetron group experienced a significantly greater reduction in OCD symptoms as measured by Y-BOCS score. More participants in the tropisetron group experienced complete response and remission.
- This study demonstrated that compared with placebo, when administered as augmentation with fluvoxamine, tropisetron can have beneficial effects for patients with OCD.
Continue to: Reference 5...
5. Yousefzadeh F, Sahebolzamani E, Sadri A, et al. 5-Hydroxytryptophan as adjuvant therapy in treatment of moderate to severe obsessive-compulsive disorder: a doubleblind randomized trial with placebo control. Int Clin Psychopharmacol. 2020;35(5):254- 262. doi:10.1097/YIC.0000000000000321
Nutraceuticals such as glycine, milk thistle, myoinositol, and serotonin (5-hydroxytryptophan) have been proposed as augmentation options for OCD. Yousefzadeh et al14 investigated the effectiveness of using 5-hydroxytryptophan in treating OCD.
Study design
- In a 12-week, randomized, double-blind study, 60 patients who met DSM-5 criteria for moderate to severe OCD (Y-BOCS score >21) were randomly assigned to receive fluoxetine plus 5-hydroxytryptophan 100 mg twice daily or fluoxetine plus placebo.
- All patients were administered fluoxetine 20 mg/d for the first 4 weeks of the study followed by fluoxetine 60 mg/d for the remainder of the trial.
- Symptoms were assessed using the Y-BOCS at baseline, Week 4, Week 8, and Week 12.
- The primary outcome measure was the difference between the 2 groups in change in Y-BOCS total score from baseline to the end of the trial. Secondary outcome measures were the differences in the Y-BOCS obsession and compulsion subscale scores from baseline to Week 12.
Outcomes
- Compared to the placebo group, the 5-hydroxytryptophan group experienced a statistically significant greater improvement in Y-BOCS total score from baseline to Week 8 (P = .002) and Week 12 (P < .001).
- General linear model repeated measure showed significant effects for time × treatment interaction on Y-BOCS total (F = 12.07, df = 2.29, P < .001), obsession subscale (F = 8.25, df = 1.91, P = .001), and compulsion subscale scores (F = 6.64, df = 2.01, P = .002).
- The 5-hydroxytryptophan group demonstrated higher partial and complete treatment response rates (P = .032 and P = .001, respectively) as determined by change in Y-BOCS total score.
- The 5-hydroxytryptophan group showed a significant improvement from baseline to Week 12 in Y-BOCS obsession subscale score (5.23 ± 2.33 vs 3.53 ± 2.13, P = .009).
- There was a significant change from baseline to the end of the trial in the Y-BOCS compulsion subscale score (3.88 ± 2.04 vs 2.30 ± 1.37, P = .002).
Conclusion
- This trial demonstrated the potential benefits of 5-hydroxytryptophan in combination with fluoxetine for patients with OCD.
6. Mowla A, Ghaedsharaf M. Pregabalin augmentation for resistant obsessive-compulsive disorder: a double-blind placebo-controlled clinical trial. CNS Spectr. 2020;25(4):552-556. doi:10.1017/S1092852919001500
Glutamatergic dysfunction has been identified as a potential cause of OCD. Studies have found elevated levels of glutamatergic transmission in the cortical-striatal-thalamic circuit of the brain and elevated glutamate concentration in the CSF in patients with OCD. Pregabalin has multiple mechanisms of action that inhibit the release of glutamate. Mowla et al15 evaluated pregabalin as an augmentation treatment for resistant OCD.
Study design
- This 12-week, double-blind, placebo-controlled clinical trial evaluated the efficacy of adjunctive pregabalin in 56 patients who met DSM-5 criteria for OCD and had not responded to ≥12 weeks of treatment with an adequate and stable dose of sertraline (baseline Y-BOCS score ≥18).
- Individuals who had other major psychiatric disorders, major medical problems, were pregnant, or had past substance or alcohol abuse were excluded.
- Participants were randomly assigned to receive sertraline plus pregabalin (n = 28) or sertraline plus placebo (n = 28). Mean sertraline dosage was 256.5 mg/d; range was 100 mg/d to 300 mg/d. Pregabalin was started at 75 mg/d and increased by 75 mg increments weekly. The mean dosage was 185.9 mg/d; range was 75 mg/d to 225 mg/d.
- The primary outcome measure was change in Y-BOCS score. A decrease >35% in Y-BOCS score was considered a significant response rate.
Outcomes
- There was a statistically significant decrease in Y-BOCS score in patients who received pregabalin. In the pregabalin group, 57.14% of patients (n = 16) showed a >35% decrease in Y-BOCS score compared with 7.14% of patients (n = 2) in the placebo group (P < .01).
- The pregabalin group showed good tolerability and safety. There were no clinically significant adverse effects.
Conclusion
- In patients with treatment-resistant OCD who did not respond to sertraline monotherapy, augmentation with pregabalin significantly decreases Y-BOCS scores compared with placebo.
Continue to: Reference 7...
7. Zheng H, Jia F, Han H, et al. Combined fluvoxamine and extended-release methylphenidate improved treatment response compared to fluvoxamine alone in patients with treatment-refractory obsessive-compulsive disorder: a randomized double-blind, placebocontrolled study. Eur Neuropsychopharmacol. 2019;29(3):397-404. doi:10.1016/j.euroneuro. 2018.12.010
Recent evidence suggests dysregulation of serotonin and dopamine in patients with OCD. Methylphenidate is a dopamine and norepinephrine inhibitor and releaser. A limited number of studies have suggested stimulants might be useful for OCD patients. Zheng et al16 conducted a pilot trial to determine whether methylphenidate augmentation may be of benefit in the management of outpatients with OCD.
Study design
- In an 8-week, double-blind, randomized, placebo-controlled trial, 44 patients (29 [66%] men, with a mean [SD] age of 24.7 [6]) with treatment-refractory OCD were randomized to receive fluvoxamine 250 mg/d plus methylphenidate extended-release (MPH-ER) 36 mg/d or fluvoxamine 250 mg/d plus placebo. The MPH-ER dose was 18 mg/d for the first 4 weeks and 36 mg/d for the rest of the trial.
- Biweekly assessments consisted of scores on the Y-BOCS, Hamilton Depression Rating Scale (HDRS), and Hamilton Anxiety Rating Scale (HAM-A).
- The primary outcomes were improvement in Y-BOCS score and the clinical response rate. Secondary outcomes included a change in score on the Y-BOCS subscales, HARS, and HAM-A. Data were analyzed with the intention-to-treat sample.
Outcomes
- Forty-one patients finished the trial. The baseline Y-BOCS total scores and subscale scores did not differ significantly between the 2 groups.
- Improvements in Y-BOCS total score and obsession subscale score were more prominent in the fluvoxamine plus MPH-ER group compared with the placebo group (P < .001).
- HDRS score decreased in both the placebo and MPH-ER groups. HAM-A scores decreased significantly in the MPH-ER plus fluvoxamine group compared with the placebo group.
Conclusion
- This study demonstrated that the combination of fluvoxamine and MPH-ER produces a higher and faster response rate than fluvoxamine plus placebo in patients with OCD.
8. Arabzadeh S, Shahhossenie M, Mesgarpour B, et al. L-carnosine as an adjuvant to fluvoxamine in treatment of obsessive compulsive disorder: a randomized double-blind study. Hum Psychopharmacol. 2017;32(4). doi:10.1002/hup.2584
Glutamate dysregulation is implicated in the pathogenesis of OCD. Glutamate-modulating agents have been used to treat OCD. Studies have shown L-carnosine has a neuroprotective role via its modulatory effect on glutamate. Arabzadeh et al17 evaluated the efficacy of L-carnosine as an adjuvant to fluvoxamine for treating OCD.
Study design
- This 10-week, randomized, double-blind, placebo-controlled trial evaluated the efficacy of adjunctive L-carnosine in 40 patients age 18 to 60 who met DSM-5 criteria for OCD and had moderate to severe OCD (Y-BOCS score ≥21).
- Individuals with any other DSM-5 major psychiatric disorders, serious medical or neurologic illness, substance dependence (other than caffeine or nicotine), mental retardation (based on clinical judgment), were pregnant or breastfeeding, had any contraindication for the use of L‐carnosine or fluvoxamine, or received any psychotropic drugs in the previous 6 weeks were excluded.
- Participants received fluvoxamine 100 mg/d for the first 4 weeks and 200 mg/d for the next 6 weeks plus either L-carnosine 500 mg twice daily or placebo. This dosage of L-carnosine was chosen because previously it had been tolerated and effective.
- The primary outcome measure was difference in Y-BOCS total scores. Secondary outcomes were differences in Y-BOCS obsession and compulsion subscale scores and differences in change in score on Y-BOCS total and subscale scores from baseline.
Outcomes
- The L-carnosine group experienced a significant decrease in Y-BOCS total score (P < .001), obsession subscale score (P < .01), and compulsion subscale score (P < .01).
- The group that received fluvoxamine plus L-carnosine also experienced a more complete response (P = .03).
- The L-carnosine group showed good tolerability and safety. There were no clinically significant adverse effects.
Conclusion
- L-carnosine significantly reduces OCD symptoms when used as an adjuvant to fluvoxamine.
1. Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593-602.
2. Ruscio AM, Stein DJ, Chiu WT, et al. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry. 2010;15(1):53-63.
3. Eddy KT, Dutra L, Bradley, R, et al. A multidimensional meta-analysis of psychotherapy and pharmacotherapy for obsessive-compulsive disorder. Clin Psychol Rev. 2004;24(8):1011-1030.
4. Franklin ME, Foa EB. Treatment of obsessive compulsive disorder. Annu Rev Clin Psychol. 2011;7:229-243.
5. Koran LM, Hanna GL, Hollander E, et al. Practice guideline for the treatment of patients with obsessive-compulsive disorder. Am J Psychiatry. 2007;164(7 Suppl):5-53.
6. Pittenger C, Bloch MH. Pharmacological treatment of obsessive-compulsive disorder. Psychiatr Clin North Am. 2014;37(3):375-391.
7. Pallanti S, Hollander E, Bienstock C, et al. Treatment non-response in OCD: methodological issues and operational definitions. Int J Neuropsychopharmacol. 2002;5(2):181-191.
8. Atmaca M. Treatment-refractory obsessive compulsive disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2016;70:127-133.
9. Barth M, Kriston L, Klostermann S, et al. Efficacy of selective serotonin reuptake inhibitors and adverse events: meta-regression and mediation analysis of placebo-controlled trials. Br J Psychiatry. 2016;208(2):114-119.
10. NaderiS, Faghih H, Aqamolaei A, et al. Amantadine as adjuvant therapy in the treatment of moderate to severe obsessive-compulsive disorder: a double-blind randomized trial with placebo control. Psychiatry Clin Neurosci. 2019;73(4):169-174. doi:10.1111/pcn.12803
11. SharafkhahM, Aghakarim Alamdar M, MassoudifarA, et al. Comparing the efficacy of ondansetron and granisetron augmentation in treatment-resistant obsessive-compulsive disorder: a randomized double-blind placebo-controlled study. Int Clin Psychopharmacol. 2019;34(5):222-233. doi:10.1097/YIC.0000000000000267
12. ModarresiA, Sayyah M, Razooghi S, et al. Memantine augmentation improves symptoms in serotonin reuptake inhibitor-refractory obsessive-compulsive disorder: a randomized controlled trial. Pharmacopsychiatry. 2018;51(6):263-269. doi:10.1055/s-0043-12026
13. Shalbafan M, Malekpour F, Tadayon Najafabadi B, et al. Fluvoxamine combination therapy with tropisetron for obsessive-compulsive disorder patients: a placebo-controlled, randomized clinical trial. J Psychopharmacol. 2019;33(11):1407-1414. doi:10.1177/0269881119878177
14. Yousefzadeh F, Sahebolzamani E, Sadri A, et al. 5-Hydroxytryptophan as adjuvant therapy in treatment of moderate to severe obsessive-compulsive disorder: a double-blind randomized trial with placebo control. Int Clin Psychopharmacol. 2020;35(5):254-262. doi:10.1097/YIC.0000000000000321
15. Mowla A, Ghaedsharaf M. Pregabalin augmentation for resistant obsessive-compulsive disorder: a double-blind placebo-controlled clinical trial. CNS Spectr. 2020;25(4):552-556. doi:10.1017/S1092852919001500
16. Zheng H, Jia F, Han H, et al.Combined fluvoxamine and extended-release methylphenidate improved treatment response compared to fluvoxamine alone in patients with treatment-refractory obsessive-compulsive disorder: a randomized double-blind, placebo-controlled study. Eur Neuropsychopharmacol. 2019;29(3):397-404. doi:10.1016/j.euroneuro.2018.12.010
17. Arabzadeh S, Shahhossenie M, Mesgarpour B, et al. L-carnosine as an adjuvant to fluvoxamine in treatment of obsessive compulsive disorder: a randomized double-blind study. Hum Psychopharmacol. 2017;32(4). doi:10.1002/hup.2584
Obsessive-compulsive disorder (OCD) is a chronic, debilitating neuropsychiatric disorder that affects 1% to 3% of the population worldwide.1,2 Together, serotonin reuptake inhibitors (SRIs) and cognitive-behavior therapy (CBT) are considered the first-line treatment for OCD.3 In children and adults, CBT is considered at least as effective as pharmacotherapy.4 Despite being an effective treatment, CBT continues to have barriers to its widespread use, including limited availability of trained CBT therapists, delayed clinical response, and high costs.5
Only approximately one-half of patients with OCD respond to SRI therapy, and a considerable percentage (30% to 40%) show significant residual symptoms even after multiple trials of SRIs.6-8 In addition, SRIs may have adverse effects (eg, sexual dysfunction, gastrointestinal symptoms) that impair patient adherence to these medications.9 Therefore, finding better treatment options is important for managing patients with OCD.
Augmentation strategies are recommended for patients who show partial response to SRI treatment or poor response to multiple SRIs. Augmentation typically includes incorporating additional medications with the primary drug with the goal of boosting the therapeutic efficacy of the primary drug. Typically, these additional medications have different mechanisms of action. However, there are no large-scale randomized controlled trials (RCTs) to inform treatment augmentation after first-line treatments for OCD produce suboptimal outcomes. The available evidence is predominantly based on small-scale RCTs, open-label trials, and case series.
In this article, we review the evidence for treatment augmentation strategies for OCD and summarize 8 studies that show promising results (Table10-17). We focus only on pharmacologic agents and do not include other biological interventions, such as repetitive transcranial magnetic stimulation over supplementary motor area, ablative neurosurgery, or deep brain stimulation.
Continue to: Reference 1...
1. Naderi S, Faghih H , Aqamolaei A, et al. Amantadine as adjuvant therapy in the treatment of moderate to severe obsessivecompulsive disorder: a double-blind randomized trial with placebo control. Psychiatry Clin Neurosci. 2019;73(4):169-174. doi:10.1111/ pcn.12803
Numerous studies support the role of glutamate dysregulation in the pathophysiology of OCD. Cortico-striato-thalamo-cortical (CSTC) abnormalities play a major role in the pathophysiology of OCD as suggested by neuroimaging research studies that indicate glutamate is the fundamental neurotransmitter of the CSTC circuit. Dysregulation of glutamatergic signaling within this circuit has been linked to OCD. Patients with OCD have been found to have an increase of glutamate in the CSF. As a result, medications that affect glutamate levels can be used to treat patients with OCD who do not respond to first-line agents. In patients already taking SRIs, augmentation of glutamate-modulating medications can reduce OCD symptoms. As an uncompetitive antagonist of the N-methyl-
Naderi et al10 evaluated amantadine as augmentative therapy to fluvoxamine for treating patients with moderate to severe OCD.
Study design
- This 12-week, randomized, double-blind, placebo-controlled trial evaluated the efficacy and safety of amantadine as an augmentative agent to fluvoxamine in 106 patients age 18 to 60 with moderate to severe OCD.
- Participants met DSM-5 criteria for OCD and had a Yale-Brown Obsessive Compulsive Scale (Y-BOCS) score >21. Participants were excluded if they had any substance dependence; an IQ <70; any other Axis I mental disorder; any serious cardiac, renal, or hepatic disease; had received psychotropic medications during the last 6 weeks, were pregnant or breastfeeding, or had rising liver transaminases to 3 times the upper limit of normal or higher.
- Participants received fluvoxamine 100 mg twice daily plus amantadine 100 mg/d, or fluvoxamine 100 mg twice daily plus placebo. All patients received fluvoxamine 100 mg/d for 28 days followed by 200 mg/d for the remainder of the trial.
- The primary outcome measure was difference in Y-BOCS total scores between the amantadine and placebo groups. The secondary outcome was the difference in Y-BOCS obsession and compulsion subscale scores.
Outcomes
- Patients who received amantadine augmentation experienced a significant reduction in Y-BOCS total score (P < .001) and obsession subscale score (P < .01).
- The amantadine group showed good tolerability and safety. There were no clinically significant adverse effects.
- Amantadine is an effective adjuvant to fluvoxamine for reducing OCD symptoms.
Conclusion
- Ondansetron and granisetron can be beneficial as an augmentation strategy for patients with treatment-resistant OCD.
2. Sharafkhah M, Aghakarim Alamdar M, Massoudifar A, et al. Comparing the efficacy of ondansetron and granisetron augmentation in treatment-resistant obsessive-compulsive disorder: a randomized double-blind placebo-controlled study. Int Clin Psychopharmacol. 2019;34(5):222- 233. doi:10.1097/YIC.0000000000000267
Although selective serotonin reuptake inhibitors (SSRIs) are considered a first-line treatment when teamed with CBT and antipsychotic augmentation, symptom resolution is not always achieved, and treatment resistance is a common problem. Sharafkhah et al11 compared the efficacy of ondansetron and granisetron augmentation specifically for patients with treatment-resistant OCD.
Study Design
- In this 18-week, randomized, double-blind, placebo-controlled study, 135 patients with treatment-resistant OCD who were previously treated with a combination of an SSRI and an antipsychotic received augmentation with ondansetron (n = 45, 4 mg/d), granisetron (n = 45, 2 mg/d), or placebo.
- Patients were rated using Y-BOCS every 2 weeks during phase I (intervention period), which lasted 14 weeks. After completing the intervention, patients were followed for 4 more weeks during phase II (discontinuation period).
- The aim of this study was to determine the safety, efficacy, and tolerability of ondansetron vs granisetron as augmentation for patients with treatment-resistant OCD. A secondary aim was to determine the rate of relapse of OCD symptoms after discontinuing ondansetron as compared with granisetron at 4 weeks after intervention.
Outcomes
- At Week 14, the reductions in Y-BOCS scores in the ondansetron, granisetron, and placebo groups were 41.5%, 39.7%, and 15.2%, respectively (P = .001). The reduction in Y-BOCS score in the ondansetron and granisetron groups was significantly greater than placebo at all phase I visits.
- Complete response was higher in the ondansetron group compared with the granisetron group (P = .041).
- Y-BOCS scores increased in both the ondansetron and granisetron groups during the discontinuation phase, but OCD symptoms were not significantly exacerbated.
Conclusion
- Ondansetron and granisetron can be beneficial as an augmentation strategy for patients with treatment-resistant OCD.
3. Modarresi A, Sayyah M, Razooghi S, et al. Memantine augmentation improves symptoms in serotonin reuptake inhibitorrefractory obsessive-compulsive disorder: a randomized controlled trial. Pharmacopsychiatry. 2018;51(6):263-269. doi:10.1055/s-0043-120268
Increased glutamate levels in CSF, glutamatergic overactivity, and polymorphisms of genes coding the NMDA receptor have been shown to contribute to the occurrence of OCD. Memantine is a noncompetitive antagonist of the NMDA receptor. Various control trials have shown augmentation with memantine 5 mg/d to 20 mg/d significantly reduced symptom severity in patients with moderate to severe OCD. Modarresi et al12 evaluated memantine as a treatment option for patients with severe OCD who did not respond to SRI monotherapy.
Study design
- This 12-week, double-blind, randomized, placebo-controlled trial evaluated the efficacy of memantine augmentation in 32 patients age 18 to 40 who met DSM-5 criteria for OCD, had a Y-BOCS score ≥24, and no psychiatric comorbidity. Participants had not responded to ≥3 adequate trials (minimum 3 months) of SRI therapy, 1 of which was clomipramine.
- Individuals were excluded if they were undergoing CBT; had an additional anxiety disorder, mood disorder, or current drug or alcohol use disorder, or any systemic disorder; had a history of seizures; were pregnant or breastfeeding; or had a history of memantine use.
- Participants already receiving the maximum tolerated dose of an SRI received augmentation with memantine 20 mg/d or placebo.
- The primary outcome measure was change in Y-BOCS score from baseline. The secondary outcome was the number of individuals who achieved treatment response (defined as ≥35% reduction in Y-BOCS score).
Continue to: Outcomes...
Outcomes
- There was a statistically significant difference in Y-BOCS score in patients treated with memantine at Week 8 and Week 12 vs those who received placebo. By Week 8, 17.2% of patients in the memantine group showed a decrease in Y-BOCS score, compared with -0.8% patients in the placebo group. The difference became more significant by Week 12, with 40.9% in the memantine group showing a decrease in Y-BOCS score vs -0.3% in the placebo group. This resulted in 73.3% of patients achieving treatment response.
- Eight weeks of memantine augmentation was necessary to observe a significant improvement in OCD symptoms, and 12 weeks was needed for treatment response.
- The mean Y-BOCS total score decreased significantly in the memantine group from Week 4 to Week 8 (16.8%) and again from Week 8 to Week 12 (28.5%).
- The memantine group showed good tolerability and safety. There were no clinically significant adverse effects.
Conclusion
- Memantine augmentation in patients with severe OCD who do not respond to an SRI is effective and well-tolerated.
4. Shalbafan M, Malekpour F, Tadayon Najafabadi B, et al. Fluvoxamine combination therapy with tropisetron for obsessive-compulsive disorder patients: a placebo-controlled, randomized clinical trial. J Psychopharmacol. 2019;33(11):1407- 1414. doi:10.1177/0269881119878177
Studies have demonstrated the involvement of the amygdala, medial and lateral orbitofrontal cortex, and dorsal anterior cingulate cortex in OCD. Additionally, studies have also investigated the role of serotonin, dopamine, and glutamate system dysregulation in the pathology of OCD.
The 5-HT3 receptors are ligand-gated ion channels found in the prefrontal cortex, amygdala, and hippocampus. Studies of 5-HT3 receptor antagonists such as ondansetron and granisetron have shown beneficial results in augmentation with SSRIs for patients with OCD.11 Tropisetron, a 5-HT3 receptor antagonist, is highly lipophilic and able to cross the blood brain barrier. It also has dopamine-inhibiting properties that could have benefits in OCD management. Shalbafan et al13 evaluated the efficacy of tropisetron augmentation to fluvoxamine for patients with OCD.
Study design
- In a 10-week, randomized, double-blind, placebo-controlled, parallel-group trial, 108 individuals age 18 to 60 who met DSM-5 criteria for OCD and had a Y-BOCS score >21 received fluvoxamine plus tropisetron or fluvoxamine plus placebo. A total of 48 (44.4%) participants in each group completed the trial. Participants were evaluated using the Y-BOCS scale at baseline and at Week 4 and Week 10.
- The primary outcome was decrease in total Y-BOCS score from baseline to Week 10. The secondary outcome was the difference in change in Y-BOCS obsession and compulsion subscale scores between the groups.
Outcomes
- The Y-BOCS total score was not significantly different between the 2 groups (P = .975). Repeated measures analysis of variance determined a significant effect for time in both tropisetron and placebo groups (Greenhouse-Geisser F [2.72–2303.84] = 152.25, P < .001; and Greenhouse-Geisser F [1.37–1736.81] = 75.57, P < .001, respectively). At Week 10, 35 participants in the tropisetron group and 19 participants in the placebo group were complete responders.
- The baseline Y-BOCS obsession and compulsion subscales did not significantly differ between treatment groups.
Conclusion
- Compared with participants in the placebo group, those in the tropisetron group experienced a significantly greater reduction in OCD symptoms as measured by Y-BOCS score. More participants in the tropisetron group experienced complete response and remission.
- This study demonstrated that compared with placebo, when administered as augmentation with fluvoxamine, tropisetron can have beneficial effects for patients with OCD.
Continue to: Reference 5...
5. Yousefzadeh F, Sahebolzamani E, Sadri A, et al. 5-Hydroxytryptophan as adjuvant therapy in treatment of moderate to severe obsessive-compulsive disorder: a doubleblind randomized trial with placebo control. Int Clin Psychopharmacol. 2020;35(5):254- 262. doi:10.1097/YIC.0000000000000321
Nutraceuticals such as glycine, milk thistle, myoinositol, and serotonin (5-hydroxytryptophan) have been proposed as augmentation options for OCD. Yousefzadeh et al14 investigated the effectiveness of using 5-hydroxytryptophan in treating OCD.
Study design
- In a 12-week, randomized, double-blind study, 60 patients who met DSM-5 criteria for moderate to severe OCD (Y-BOCS score >21) were randomly assigned to receive fluoxetine plus 5-hydroxytryptophan 100 mg twice daily or fluoxetine plus placebo.
- All patients were administered fluoxetine 20 mg/d for the first 4 weeks of the study followed by fluoxetine 60 mg/d for the remainder of the trial.
- Symptoms were assessed using the Y-BOCS at baseline, Week 4, Week 8, and Week 12.
- The primary outcome measure was the difference between the 2 groups in change in Y-BOCS total score from baseline to the end of the trial. Secondary outcome measures were the differences in the Y-BOCS obsession and compulsion subscale scores from baseline to Week 12.
Outcomes
- Compared to the placebo group, the 5-hydroxytryptophan group experienced a statistically significant greater improvement in Y-BOCS total score from baseline to Week 8 (P = .002) and Week 12 (P < .001).
- General linear model repeated measure showed significant effects for time × treatment interaction on Y-BOCS total (F = 12.07, df = 2.29, P < .001), obsession subscale (F = 8.25, df = 1.91, P = .001), and compulsion subscale scores (F = 6.64, df = 2.01, P = .002).
- The 5-hydroxytryptophan group demonstrated higher partial and complete treatment response rates (P = .032 and P = .001, respectively) as determined by change in Y-BOCS total score.
- The 5-hydroxytryptophan group showed a significant improvement from baseline to Week 12 in Y-BOCS obsession subscale score (5.23 ± 2.33 vs 3.53 ± 2.13, P = .009).
- There was a significant change from baseline to the end of the trial in the Y-BOCS compulsion subscale score (3.88 ± 2.04 vs 2.30 ± 1.37, P = .002).
Conclusion
- This trial demonstrated the potential benefits of 5-hydroxytryptophan in combination with fluoxetine for patients with OCD.
6. Mowla A, Ghaedsharaf M. Pregabalin augmentation for resistant obsessive-compulsive disorder: a double-blind placebo-controlled clinical trial. CNS Spectr. 2020;25(4):552-556. doi:10.1017/S1092852919001500
Glutamatergic dysfunction has been identified as a potential cause of OCD. Studies have found elevated levels of glutamatergic transmission in the cortical-striatal-thalamic circuit of the brain and elevated glutamate concentration in the CSF in patients with OCD. Pregabalin has multiple mechanisms of action that inhibit the release of glutamate. Mowla et al15 evaluated pregabalin as an augmentation treatment for resistant OCD.
Study design
- This 12-week, double-blind, placebo-controlled clinical trial evaluated the efficacy of adjunctive pregabalin in 56 patients who met DSM-5 criteria for OCD and had not responded to ≥12 weeks of treatment with an adequate and stable dose of sertraline (baseline Y-BOCS score ≥18).
- Individuals who had other major psychiatric disorders, major medical problems, were pregnant, or had past substance or alcohol abuse were excluded.
- Participants were randomly assigned to receive sertraline plus pregabalin (n = 28) or sertraline plus placebo (n = 28). Mean sertraline dosage was 256.5 mg/d; range was 100 mg/d to 300 mg/d. Pregabalin was started at 75 mg/d and increased by 75 mg increments weekly. The mean dosage was 185.9 mg/d; range was 75 mg/d to 225 mg/d.
- The primary outcome measure was change in Y-BOCS score. A decrease >35% in Y-BOCS score was considered a significant response rate.
Outcomes
- There was a statistically significant decrease in Y-BOCS score in patients who received pregabalin. In the pregabalin group, 57.14% of patients (n = 16) showed a >35% decrease in Y-BOCS score compared with 7.14% of patients (n = 2) in the placebo group (P < .01).
- The pregabalin group showed good tolerability and safety. There were no clinically significant adverse effects.
Conclusion
- In patients with treatment-resistant OCD who did not respond to sertraline monotherapy, augmentation with pregabalin significantly decreases Y-BOCS scores compared with placebo.
Continue to: Reference 7...
7. Zheng H, Jia F, Han H, et al. Combined fluvoxamine and extended-release methylphenidate improved treatment response compared to fluvoxamine alone in patients with treatment-refractory obsessive-compulsive disorder: a randomized double-blind, placebocontrolled study. Eur Neuropsychopharmacol. 2019;29(3):397-404. doi:10.1016/j.euroneuro. 2018.12.010
Recent evidence suggests dysregulation of serotonin and dopamine in patients with OCD. Methylphenidate is a dopamine and norepinephrine inhibitor and releaser. A limited number of studies have suggested stimulants might be useful for OCD patients. Zheng et al16 conducted a pilot trial to determine whether methylphenidate augmentation may be of benefit in the management of outpatients with OCD.
Study design
- In an 8-week, double-blind, randomized, placebo-controlled trial, 44 patients (29 [66%] men, with a mean [SD] age of 24.7 [6]) with treatment-refractory OCD were randomized to receive fluvoxamine 250 mg/d plus methylphenidate extended-release (MPH-ER) 36 mg/d or fluvoxamine 250 mg/d plus placebo. The MPH-ER dose was 18 mg/d for the first 4 weeks and 36 mg/d for the rest of the trial.
- Biweekly assessments consisted of scores on the Y-BOCS, Hamilton Depression Rating Scale (HDRS), and Hamilton Anxiety Rating Scale (HAM-A).
- The primary outcomes were improvement in Y-BOCS score and the clinical response rate. Secondary outcomes included a change in score on the Y-BOCS subscales, HARS, and HAM-A. Data were analyzed with the intention-to-treat sample.
Outcomes
- Forty-one patients finished the trial. The baseline Y-BOCS total scores and subscale scores did not differ significantly between the 2 groups.
- Improvements in Y-BOCS total score and obsession subscale score were more prominent in the fluvoxamine plus MPH-ER group compared with the placebo group (P < .001).
- HDRS score decreased in both the placebo and MPH-ER groups. HAM-A scores decreased significantly in the MPH-ER plus fluvoxamine group compared with the placebo group.
Conclusion
- This study demonstrated that the combination of fluvoxamine and MPH-ER produces a higher and faster response rate than fluvoxamine plus placebo in patients with OCD.
8. Arabzadeh S, Shahhossenie M, Mesgarpour B, et al. L-carnosine as an adjuvant to fluvoxamine in treatment of obsessive compulsive disorder: a randomized double-blind study. Hum Psychopharmacol. 2017;32(4). doi:10.1002/hup.2584
Glutamate dysregulation is implicated in the pathogenesis of OCD. Glutamate-modulating agents have been used to treat OCD. Studies have shown L-carnosine has a neuroprotective role via its modulatory effect on glutamate. Arabzadeh et al17 evaluated the efficacy of L-carnosine as an adjuvant to fluvoxamine for treating OCD.
Study design
- This 10-week, randomized, double-blind, placebo-controlled trial evaluated the efficacy of adjunctive L-carnosine in 40 patients age 18 to 60 who met DSM-5 criteria for OCD and had moderate to severe OCD (Y-BOCS score ≥21).
- Individuals with any other DSM-5 major psychiatric disorders, serious medical or neurologic illness, substance dependence (other than caffeine or nicotine), mental retardation (based on clinical judgment), were pregnant or breastfeeding, had any contraindication for the use of L‐carnosine or fluvoxamine, or received any psychotropic drugs in the previous 6 weeks were excluded.
- Participants received fluvoxamine 100 mg/d for the first 4 weeks and 200 mg/d for the next 6 weeks plus either L-carnosine 500 mg twice daily or placebo. This dosage of L-carnosine was chosen because previously it had been tolerated and effective.
- The primary outcome measure was difference in Y-BOCS total scores. Secondary outcomes were differences in Y-BOCS obsession and compulsion subscale scores and differences in change in score on Y-BOCS total and subscale scores from baseline.
Outcomes
- The L-carnosine group experienced a significant decrease in Y-BOCS total score (P < .001), obsession subscale score (P < .01), and compulsion subscale score (P < .01).
- The group that received fluvoxamine plus L-carnosine also experienced a more complete response (P = .03).
- The L-carnosine group showed good tolerability and safety. There were no clinically significant adverse effects.
Conclusion
- L-carnosine significantly reduces OCD symptoms when used as an adjuvant to fluvoxamine.
Obsessive-compulsive disorder (OCD) is a chronic, debilitating neuropsychiatric disorder that affects 1% to 3% of the population worldwide.1,2 Together, serotonin reuptake inhibitors (SRIs) and cognitive-behavior therapy (CBT) are considered the first-line treatment for OCD.3 In children and adults, CBT is considered at least as effective as pharmacotherapy.4 Despite being an effective treatment, CBT continues to have barriers to its widespread use, including limited availability of trained CBT therapists, delayed clinical response, and high costs.5
Only approximately one-half of patients with OCD respond to SRI therapy, and a considerable percentage (30% to 40%) show significant residual symptoms even after multiple trials of SRIs.6-8 In addition, SRIs may have adverse effects (eg, sexual dysfunction, gastrointestinal symptoms) that impair patient adherence to these medications.9 Therefore, finding better treatment options is important for managing patients with OCD.
Augmentation strategies are recommended for patients who show partial response to SRI treatment or poor response to multiple SRIs. Augmentation typically includes incorporating additional medications with the primary drug with the goal of boosting the therapeutic efficacy of the primary drug. Typically, these additional medications have different mechanisms of action. However, there are no large-scale randomized controlled trials (RCTs) to inform treatment augmentation after first-line treatments for OCD produce suboptimal outcomes. The available evidence is predominantly based on small-scale RCTs, open-label trials, and case series.
In this article, we review the evidence for treatment augmentation strategies for OCD and summarize 8 studies that show promising results (Table10-17). We focus only on pharmacologic agents and do not include other biological interventions, such as repetitive transcranial magnetic stimulation over supplementary motor area, ablative neurosurgery, or deep brain stimulation.
Continue to: Reference 1...
1. Naderi S, Faghih H , Aqamolaei A, et al. Amantadine as adjuvant therapy in the treatment of moderate to severe obsessivecompulsive disorder: a double-blind randomized trial with placebo control. Psychiatry Clin Neurosci. 2019;73(4):169-174. doi:10.1111/ pcn.12803
Numerous studies support the role of glutamate dysregulation in the pathophysiology of OCD. Cortico-striato-thalamo-cortical (CSTC) abnormalities play a major role in the pathophysiology of OCD as suggested by neuroimaging research studies that indicate glutamate is the fundamental neurotransmitter of the CSTC circuit. Dysregulation of glutamatergic signaling within this circuit has been linked to OCD. Patients with OCD have been found to have an increase of glutamate in the CSF. As a result, medications that affect glutamate levels can be used to treat patients with OCD who do not respond to first-line agents. In patients already taking SRIs, augmentation of glutamate-modulating medications can reduce OCD symptoms. As an uncompetitive antagonist of the N-methyl-
Naderi et al10 evaluated amantadine as augmentative therapy to fluvoxamine for treating patients with moderate to severe OCD.
Study design
- This 12-week, randomized, double-blind, placebo-controlled trial evaluated the efficacy and safety of amantadine as an augmentative agent to fluvoxamine in 106 patients age 18 to 60 with moderate to severe OCD.
- Participants met DSM-5 criteria for OCD and had a Yale-Brown Obsessive Compulsive Scale (Y-BOCS) score >21. Participants were excluded if they had any substance dependence; an IQ <70; any other Axis I mental disorder; any serious cardiac, renal, or hepatic disease; had received psychotropic medications during the last 6 weeks, were pregnant or breastfeeding, or had rising liver transaminases to 3 times the upper limit of normal or higher.
- Participants received fluvoxamine 100 mg twice daily plus amantadine 100 mg/d, or fluvoxamine 100 mg twice daily plus placebo. All patients received fluvoxamine 100 mg/d for 28 days followed by 200 mg/d for the remainder of the trial.
- The primary outcome measure was difference in Y-BOCS total scores between the amantadine and placebo groups. The secondary outcome was the difference in Y-BOCS obsession and compulsion subscale scores.
Outcomes
- Patients who received amantadine augmentation experienced a significant reduction in Y-BOCS total score (P < .001) and obsession subscale score (P < .01).
- The amantadine group showed good tolerability and safety. There were no clinically significant adverse effects.
- Amantadine is an effective adjuvant to fluvoxamine for reducing OCD symptoms.
Conclusion
- Ondansetron and granisetron can be beneficial as an augmentation strategy for patients with treatment-resistant OCD.
2. Sharafkhah M, Aghakarim Alamdar M, Massoudifar A, et al. Comparing the efficacy of ondansetron and granisetron augmentation in treatment-resistant obsessive-compulsive disorder: a randomized double-blind placebo-controlled study. Int Clin Psychopharmacol. 2019;34(5):222- 233. doi:10.1097/YIC.0000000000000267
Although selective serotonin reuptake inhibitors (SSRIs) are considered a first-line treatment when teamed with CBT and antipsychotic augmentation, symptom resolution is not always achieved, and treatment resistance is a common problem. Sharafkhah et al11 compared the efficacy of ondansetron and granisetron augmentation specifically for patients with treatment-resistant OCD.
Study Design
- In this 18-week, randomized, double-blind, placebo-controlled study, 135 patients with treatment-resistant OCD who were previously treated with a combination of an SSRI and an antipsychotic received augmentation with ondansetron (n = 45, 4 mg/d), granisetron (n = 45, 2 mg/d), or placebo.
- Patients were rated using Y-BOCS every 2 weeks during phase I (intervention period), which lasted 14 weeks. After completing the intervention, patients were followed for 4 more weeks during phase II (discontinuation period).
- The aim of this study was to determine the safety, efficacy, and tolerability of ondansetron vs granisetron as augmentation for patients with treatment-resistant OCD. A secondary aim was to determine the rate of relapse of OCD symptoms after discontinuing ondansetron as compared with granisetron at 4 weeks after intervention.
Outcomes
- At Week 14, the reductions in Y-BOCS scores in the ondansetron, granisetron, and placebo groups were 41.5%, 39.7%, and 15.2%, respectively (P = .001). The reduction in Y-BOCS score in the ondansetron and granisetron groups was significantly greater than placebo at all phase I visits.
- Complete response was higher in the ondansetron group compared with the granisetron group (P = .041).
- Y-BOCS scores increased in both the ondansetron and granisetron groups during the discontinuation phase, but OCD symptoms were not significantly exacerbated.
Conclusion
- Ondansetron and granisetron can be beneficial as an augmentation strategy for patients with treatment-resistant OCD.
3. Modarresi A, Sayyah M, Razooghi S, et al. Memantine augmentation improves symptoms in serotonin reuptake inhibitorrefractory obsessive-compulsive disorder: a randomized controlled trial. Pharmacopsychiatry. 2018;51(6):263-269. doi:10.1055/s-0043-120268
Increased glutamate levels in CSF, glutamatergic overactivity, and polymorphisms of genes coding the NMDA receptor have been shown to contribute to the occurrence of OCD. Memantine is a noncompetitive antagonist of the NMDA receptor. Various control trials have shown augmentation with memantine 5 mg/d to 20 mg/d significantly reduced symptom severity in patients with moderate to severe OCD. Modarresi et al12 evaluated memantine as a treatment option for patients with severe OCD who did not respond to SRI monotherapy.
Study design
- This 12-week, double-blind, randomized, placebo-controlled trial evaluated the efficacy of memantine augmentation in 32 patients age 18 to 40 who met DSM-5 criteria for OCD, had a Y-BOCS score ≥24, and no psychiatric comorbidity. Participants had not responded to ≥3 adequate trials (minimum 3 months) of SRI therapy, 1 of which was clomipramine.
- Individuals were excluded if they were undergoing CBT; had an additional anxiety disorder, mood disorder, or current drug or alcohol use disorder, or any systemic disorder; had a history of seizures; were pregnant or breastfeeding; or had a history of memantine use.
- Participants already receiving the maximum tolerated dose of an SRI received augmentation with memantine 20 mg/d or placebo.
- The primary outcome measure was change in Y-BOCS score from baseline. The secondary outcome was the number of individuals who achieved treatment response (defined as ≥35% reduction in Y-BOCS score).
Continue to: Outcomes...
Outcomes
- There was a statistically significant difference in Y-BOCS score in patients treated with memantine at Week 8 and Week 12 vs those who received placebo. By Week 8, 17.2% of patients in the memantine group showed a decrease in Y-BOCS score, compared with -0.8% patients in the placebo group. The difference became more significant by Week 12, with 40.9% in the memantine group showing a decrease in Y-BOCS score vs -0.3% in the placebo group. This resulted in 73.3% of patients achieving treatment response.
- Eight weeks of memantine augmentation was necessary to observe a significant improvement in OCD symptoms, and 12 weeks was needed for treatment response.
- The mean Y-BOCS total score decreased significantly in the memantine group from Week 4 to Week 8 (16.8%) and again from Week 8 to Week 12 (28.5%).
- The memantine group showed good tolerability and safety. There were no clinically significant adverse effects.
Conclusion
- Memantine augmentation in patients with severe OCD who do not respond to an SRI is effective and well-tolerated.
4. Shalbafan M, Malekpour F, Tadayon Najafabadi B, et al. Fluvoxamine combination therapy with tropisetron for obsessive-compulsive disorder patients: a placebo-controlled, randomized clinical trial. J Psychopharmacol. 2019;33(11):1407- 1414. doi:10.1177/0269881119878177
Studies have demonstrated the involvement of the amygdala, medial and lateral orbitofrontal cortex, and dorsal anterior cingulate cortex in OCD. Additionally, studies have also investigated the role of serotonin, dopamine, and glutamate system dysregulation in the pathology of OCD.
The 5-HT3 receptors are ligand-gated ion channels found in the prefrontal cortex, amygdala, and hippocampus. Studies of 5-HT3 receptor antagonists such as ondansetron and granisetron have shown beneficial results in augmentation with SSRIs for patients with OCD.11 Tropisetron, a 5-HT3 receptor antagonist, is highly lipophilic and able to cross the blood brain barrier. It also has dopamine-inhibiting properties that could have benefits in OCD management. Shalbafan et al13 evaluated the efficacy of tropisetron augmentation to fluvoxamine for patients with OCD.
Study design
- In a 10-week, randomized, double-blind, placebo-controlled, parallel-group trial, 108 individuals age 18 to 60 who met DSM-5 criteria for OCD and had a Y-BOCS score >21 received fluvoxamine plus tropisetron or fluvoxamine plus placebo. A total of 48 (44.4%) participants in each group completed the trial. Participants were evaluated using the Y-BOCS scale at baseline and at Week 4 and Week 10.
- The primary outcome was decrease in total Y-BOCS score from baseline to Week 10. The secondary outcome was the difference in change in Y-BOCS obsession and compulsion subscale scores between the groups.
Outcomes
- The Y-BOCS total score was not significantly different between the 2 groups (P = .975). Repeated measures analysis of variance determined a significant effect for time in both tropisetron and placebo groups (Greenhouse-Geisser F [2.72–2303.84] = 152.25, P < .001; and Greenhouse-Geisser F [1.37–1736.81] = 75.57, P < .001, respectively). At Week 10, 35 participants in the tropisetron group and 19 participants in the placebo group were complete responders.
- The baseline Y-BOCS obsession and compulsion subscales did not significantly differ between treatment groups.
Conclusion
- Compared with participants in the placebo group, those in the tropisetron group experienced a significantly greater reduction in OCD symptoms as measured by Y-BOCS score. More participants in the tropisetron group experienced complete response and remission.
- This study demonstrated that compared with placebo, when administered as augmentation with fluvoxamine, tropisetron can have beneficial effects for patients with OCD.
Continue to: Reference 5...
5. Yousefzadeh F, Sahebolzamani E, Sadri A, et al. 5-Hydroxytryptophan as adjuvant therapy in treatment of moderate to severe obsessive-compulsive disorder: a doubleblind randomized trial with placebo control. Int Clin Psychopharmacol. 2020;35(5):254- 262. doi:10.1097/YIC.0000000000000321
Nutraceuticals such as glycine, milk thistle, myoinositol, and serotonin (5-hydroxytryptophan) have been proposed as augmentation options for OCD. Yousefzadeh et al14 investigated the effectiveness of using 5-hydroxytryptophan in treating OCD.
Study design
- In a 12-week, randomized, double-blind study, 60 patients who met DSM-5 criteria for moderate to severe OCD (Y-BOCS score >21) were randomly assigned to receive fluoxetine plus 5-hydroxytryptophan 100 mg twice daily or fluoxetine plus placebo.
- All patients were administered fluoxetine 20 mg/d for the first 4 weeks of the study followed by fluoxetine 60 mg/d for the remainder of the trial.
- Symptoms were assessed using the Y-BOCS at baseline, Week 4, Week 8, and Week 12.
- The primary outcome measure was the difference between the 2 groups in change in Y-BOCS total score from baseline to the end of the trial. Secondary outcome measures were the differences in the Y-BOCS obsession and compulsion subscale scores from baseline to Week 12.
Outcomes
- Compared to the placebo group, the 5-hydroxytryptophan group experienced a statistically significant greater improvement in Y-BOCS total score from baseline to Week 8 (P = .002) and Week 12 (P < .001).
- General linear model repeated measure showed significant effects for time × treatment interaction on Y-BOCS total (F = 12.07, df = 2.29, P < .001), obsession subscale (F = 8.25, df = 1.91, P = .001), and compulsion subscale scores (F = 6.64, df = 2.01, P = .002).
- The 5-hydroxytryptophan group demonstrated higher partial and complete treatment response rates (P = .032 and P = .001, respectively) as determined by change in Y-BOCS total score.
- The 5-hydroxytryptophan group showed a significant improvement from baseline to Week 12 in Y-BOCS obsession subscale score (5.23 ± 2.33 vs 3.53 ± 2.13, P = .009).
- There was a significant change from baseline to the end of the trial in the Y-BOCS compulsion subscale score (3.88 ± 2.04 vs 2.30 ± 1.37, P = .002).
Conclusion
- This trial demonstrated the potential benefits of 5-hydroxytryptophan in combination with fluoxetine for patients with OCD.
6. Mowla A, Ghaedsharaf M. Pregabalin augmentation for resistant obsessive-compulsive disorder: a double-blind placebo-controlled clinical trial. CNS Spectr. 2020;25(4):552-556. doi:10.1017/S1092852919001500
Glutamatergic dysfunction has been identified as a potential cause of OCD. Studies have found elevated levels of glutamatergic transmission in the cortical-striatal-thalamic circuit of the brain and elevated glutamate concentration in the CSF in patients with OCD. Pregabalin has multiple mechanisms of action that inhibit the release of glutamate. Mowla et al15 evaluated pregabalin as an augmentation treatment for resistant OCD.
Study design
- This 12-week, double-blind, placebo-controlled clinical trial evaluated the efficacy of adjunctive pregabalin in 56 patients who met DSM-5 criteria for OCD and had not responded to ≥12 weeks of treatment with an adequate and stable dose of sertraline (baseline Y-BOCS score ≥18).
- Individuals who had other major psychiatric disorders, major medical problems, were pregnant, or had past substance or alcohol abuse were excluded.
- Participants were randomly assigned to receive sertraline plus pregabalin (n = 28) or sertraline plus placebo (n = 28). Mean sertraline dosage was 256.5 mg/d; range was 100 mg/d to 300 mg/d. Pregabalin was started at 75 mg/d and increased by 75 mg increments weekly. The mean dosage was 185.9 mg/d; range was 75 mg/d to 225 mg/d.
- The primary outcome measure was change in Y-BOCS score. A decrease >35% in Y-BOCS score was considered a significant response rate.
Outcomes
- There was a statistically significant decrease in Y-BOCS score in patients who received pregabalin. In the pregabalin group, 57.14% of patients (n = 16) showed a >35% decrease in Y-BOCS score compared with 7.14% of patients (n = 2) in the placebo group (P < .01).
- The pregabalin group showed good tolerability and safety. There were no clinically significant adverse effects.
Conclusion
- In patients with treatment-resistant OCD who did not respond to sertraline monotherapy, augmentation with pregabalin significantly decreases Y-BOCS scores compared with placebo.
Continue to: Reference 7...
7. Zheng H, Jia F, Han H, et al. Combined fluvoxamine and extended-release methylphenidate improved treatment response compared to fluvoxamine alone in patients with treatment-refractory obsessive-compulsive disorder: a randomized double-blind, placebocontrolled study. Eur Neuropsychopharmacol. 2019;29(3):397-404. doi:10.1016/j.euroneuro. 2018.12.010
Recent evidence suggests dysregulation of serotonin and dopamine in patients with OCD. Methylphenidate is a dopamine and norepinephrine inhibitor and releaser. A limited number of studies have suggested stimulants might be useful for OCD patients. Zheng et al16 conducted a pilot trial to determine whether methylphenidate augmentation may be of benefit in the management of outpatients with OCD.
Study design
- In an 8-week, double-blind, randomized, placebo-controlled trial, 44 patients (29 [66%] men, with a mean [SD] age of 24.7 [6]) with treatment-refractory OCD were randomized to receive fluvoxamine 250 mg/d plus methylphenidate extended-release (MPH-ER) 36 mg/d or fluvoxamine 250 mg/d plus placebo. The MPH-ER dose was 18 mg/d for the first 4 weeks and 36 mg/d for the rest of the trial.
- Biweekly assessments consisted of scores on the Y-BOCS, Hamilton Depression Rating Scale (HDRS), and Hamilton Anxiety Rating Scale (HAM-A).
- The primary outcomes were improvement in Y-BOCS score and the clinical response rate. Secondary outcomes included a change in score on the Y-BOCS subscales, HARS, and HAM-A. Data were analyzed with the intention-to-treat sample.
Outcomes
- Forty-one patients finished the trial. The baseline Y-BOCS total scores and subscale scores did not differ significantly between the 2 groups.
- Improvements in Y-BOCS total score and obsession subscale score were more prominent in the fluvoxamine plus MPH-ER group compared with the placebo group (P < .001).
- HDRS score decreased in both the placebo and MPH-ER groups. HAM-A scores decreased significantly in the MPH-ER plus fluvoxamine group compared with the placebo group.
Conclusion
- This study demonstrated that the combination of fluvoxamine and MPH-ER produces a higher and faster response rate than fluvoxamine plus placebo in patients with OCD.
8. Arabzadeh S, Shahhossenie M, Mesgarpour B, et al. L-carnosine as an adjuvant to fluvoxamine in treatment of obsessive compulsive disorder: a randomized double-blind study. Hum Psychopharmacol. 2017;32(4). doi:10.1002/hup.2584
Glutamate dysregulation is implicated in the pathogenesis of OCD. Glutamate-modulating agents have been used to treat OCD. Studies have shown L-carnosine has a neuroprotective role via its modulatory effect on glutamate. Arabzadeh et al17 evaluated the efficacy of L-carnosine as an adjuvant to fluvoxamine for treating OCD.
Study design
- This 10-week, randomized, double-blind, placebo-controlled trial evaluated the efficacy of adjunctive L-carnosine in 40 patients age 18 to 60 who met DSM-5 criteria for OCD and had moderate to severe OCD (Y-BOCS score ≥21).
- Individuals with any other DSM-5 major psychiatric disorders, serious medical or neurologic illness, substance dependence (other than caffeine or nicotine), mental retardation (based on clinical judgment), were pregnant or breastfeeding, had any contraindication for the use of L‐carnosine or fluvoxamine, or received any psychotropic drugs in the previous 6 weeks were excluded.
- Participants received fluvoxamine 100 mg/d for the first 4 weeks and 200 mg/d for the next 6 weeks plus either L-carnosine 500 mg twice daily or placebo. This dosage of L-carnosine was chosen because previously it had been tolerated and effective.
- The primary outcome measure was difference in Y-BOCS total scores. Secondary outcomes were differences in Y-BOCS obsession and compulsion subscale scores and differences in change in score on Y-BOCS total and subscale scores from baseline.
Outcomes
- The L-carnosine group experienced a significant decrease in Y-BOCS total score (P < .001), obsession subscale score (P < .01), and compulsion subscale score (P < .01).
- The group that received fluvoxamine plus L-carnosine also experienced a more complete response (P = .03).
- The L-carnosine group showed good tolerability and safety. There were no clinically significant adverse effects.
Conclusion
- L-carnosine significantly reduces OCD symptoms when used as an adjuvant to fluvoxamine.
1. Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593-602.
2. Ruscio AM, Stein DJ, Chiu WT, et al. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry. 2010;15(1):53-63.
3. Eddy KT, Dutra L, Bradley, R, et al. A multidimensional meta-analysis of psychotherapy and pharmacotherapy for obsessive-compulsive disorder. Clin Psychol Rev. 2004;24(8):1011-1030.
4. Franklin ME, Foa EB. Treatment of obsessive compulsive disorder. Annu Rev Clin Psychol. 2011;7:229-243.
5. Koran LM, Hanna GL, Hollander E, et al. Practice guideline for the treatment of patients with obsessive-compulsive disorder. Am J Psychiatry. 2007;164(7 Suppl):5-53.
6. Pittenger C, Bloch MH. Pharmacological treatment of obsessive-compulsive disorder. Psychiatr Clin North Am. 2014;37(3):375-391.
7. Pallanti S, Hollander E, Bienstock C, et al. Treatment non-response in OCD: methodological issues and operational definitions. Int J Neuropsychopharmacol. 2002;5(2):181-191.
8. Atmaca M. Treatment-refractory obsessive compulsive disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2016;70:127-133.
9. Barth M, Kriston L, Klostermann S, et al. Efficacy of selective serotonin reuptake inhibitors and adverse events: meta-regression and mediation analysis of placebo-controlled trials. Br J Psychiatry. 2016;208(2):114-119.
10. NaderiS, Faghih H, Aqamolaei A, et al. Amantadine as adjuvant therapy in the treatment of moderate to severe obsessive-compulsive disorder: a double-blind randomized trial with placebo control. Psychiatry Clin Neurosci. 2019;73(4):169-174. doi:10.1111/pcn.12803
11. SharafkhahM, Aghakarim Alamdar M, MassoudifarA, et al. Comparing the efficacy of ondansetron and granisetron augmentation in treatment-resistant obsessive-compulsive disorder: a randomized double-blind placebo-controlled study. Int Clin Psychopharmacol. 2019;34(5):222-233. doi:10.1097/YIC.0000000000000267
12. ModarresiA, Sayyah M, Razooghi S, et al. Memantine augmentation improves symptoms in serotonin reuptake inhibitor-refractory obsessive-compulsive disorder: a randomized controlled trial. Pharmacopsychiatry. 2018;51(6):263-269. doi:10.1055/s-0043-12026
13. Shalbafan M, Malekpour F, Tadayon Najafabadi B, et al. Fluvoxamine combination therapy with tropisetron for obsessive-compulsive disorder patients: a placebo-controlled, randomized clinical trial. J Psychopharmacol. 2019;33(11):1407-1414. doi:10.1177/0269881119878177
14. Yousefzadeh F, Sahebolzamani E, Sadri A, et al. 5-Hydroxytryptophan as adjuvant therapy in treatment of moderate to severe obsessive-compulsive disorder: a double-blind randomized trial with placebo control. Int Clin Psychopharmacol. 2020;35(5):254-262. doi:10.1097/YIC.0000000000000321
15. Mowla A, Ghaedsharaf M. Pregabalin augmentation for resistant obsessive-compulsive disorder: a double-blind placebo-controlled clinical trial. CNS Spectr. 2020;25(4):552-556. doi:10.1017/S1092852919001500
16. Zheng H, Jia F, Han H, et al.Combined fluvoxamine and extended-release methylphenidate improved treatment response compared to fluvoxamine alone in patients with treatment-refractory obsessive-compulsive disorder: a randomized double-blind, placebo-controlled study. Eur Neuropsychopharmacol. 2019;29(3):397-404. doi:10.1016/j.euroneuro.2018.12.010
17. Arabzadeh S, Shahhossenie M, Mesgarpour B, et al. L-carnosine as an adjuvant to fluvoxamine in treatment of obsessive compulsive disorder: a randomized double-blind study. Hum Psychopharmacol. 2017;32(4). doi:10.1002/hup.2584
1. Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593-602.
2. Ruscio AM, Stein DJ, Chiu WT, et al. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry. 2010;15(1):53-63.
3. Eddy KT, Dutra L, Bradley, R, et al. A multidimensional meta-analysis of psychotherapy and pharmacotherapy for obsessive-compulsive disorder. Clin Psychol Rev. 2004;24(8):1011-1030.
4. Franklin ME, Foa EB. Treatment of obsessive compulsive disorder. Annu Rev Clin Psychol. 2011;7:229-243.
5. Koran LM, Hanna GL, Hollander E, et al. Practice guideline for the treatment of patients with obsessive-compulsive disorder. Am J Psychiatry. 2007;164(7 Suppl):5-53.
6. Pittenger C, Bloch MH. Pharmacological treatment of obsessive-compulsive disorder. Psychiatr Clin North Am. 2014;37(3):375-391.
7. Pallanti S, Hollander E, Bienstock C, et al. Treatment non-response in OCD: methodological issues and operational definitions. Int J Neuropsychopharmacol. 2002;5(2):181-191.
8. Atmaca M. Treatment-refractory obsessive compulsive disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2016;70:127-133.
9. Barth M, Kriston L, Klostermann S, et al. Efficacy of selective serotonin reuptake inhibitors and adverse events: meta-regression and mediation analysis of placebo-controlled trials. Br J Psychiatry. 2016;208(2):114-119.
10. NaderiS, Faghih H, Aqamolaei A, et al. Amantadine as adjuvant therapy in the treatment of moderate to severe obsessive-compulsive disorder: a double-blind randomized trial with placebo control. Psychiatry Clin Neurosci. 2019;73(4):169-174. doi:10.1111/pcn.12803
11. SharafkhahM, Aghakarim Alamdar M, MassoudifarA, et al. Comparing the efficacy of ondansetron and granisetron augmentation in treatment-resistant obsessive-compulsive disorder: a randomized double-blind placebo-controlled study. Int Clin Psychopharmacol. 2019;34(5):222-233. doi:10.1097/YIC.0000000000000267
12. ModarresiA, Sayyah M, Razooghi S, et al. Memantine augmentation improves symptoms in serotonin reuptake inhibitor-refractory obsessive-compulsive disorder: a randomized controlled trial. Pharmacopsychiatry. 2018;51(6):263-269. doi:10.1055/s-0043-12026
13. Shalbafan M, Malekpour F, Tadayon Najafabadi B, et al. Fluvoxamine combination therapy with tropisetron for obsessive-compulsive disorder patients: a placebo-controlled, randomized clinical trial. J Psychopharmacol. 2019;33(11):1407-1414. doi:10.1177/0269881119878177
14. Yousefzadeh F, Sahebolzamani E, Sadri A, et al. 5-Hydroxytryptophan as adjuvant therapy in treatment of moderate to severe obsessive-compulsive disorder: a double-blind randomized trial with placebo control. Int Clin Psychopharmacol. 2020;35(5):254-262. doi:10.1097/YIC.0000000000000321
15. Mowla A, Ghaedsharaf M. Pregabalin augmentation for resistant obsessive-compulsive disorder: a double-blind placebo-controlled clinical trial. CNS Spectr. 2020;25(4):552-556. doi:10.1017/S1092852919001500
16. Zheng H, Jia F, Han H, et al.Combined fluvoxamine and extended-release methylphenidate improved treatment response compared to fluvoxamine alone in patients with treatment-refractory obsessive-compulsive disorder: a randomized double-blind, placebo-controlled study. Eur Neuropsychopharmacol. 2019;29(3):397-404. doi:10.1016/j.euroneuro.2018.12.010
17. Arabzadeh S, Shahhossenie M, Mesgarpour B, et al. L-carnosine as an adjuvant to fluvoxamine in treatment of obsessive compulsive disorder: a randomized double-blind study. Hum Psychopharmacol. 2017;32(4). doi:10.1002/hup.2584
Food for thought: Dangerous weight loss in an older adult
CASE Fixated on health and nutrition
At the insistence of her daughter, Ms. L, age 75, presents to the emergency department (ED) for self-neglect and severe weight loss, with a body mass index (BMI) of 13.5 kg/m2 (normal: 18.5 to 24.9 kg/m2). When asked why she is in the ED, Ms. L says she doesn’t know. She attributes her significant weight loss (approximately 20 pounds in the last few months) to gastroesophageal reflux disease (GERD). She constantly worries about her esophagus. She had been diagnosed with esophageal dysphagia 7 years ago after undergoing radiofrequency ablation for esophageal cancer. Ms. L fixates on the negative effects certain foods and ingredients might have on her stomach and esophagus.
Following transfer from the ED, Ms. L is involuntarily admitted to our inpatient unit. Although she acknowledges weight loss, she minimizes the severity of her illness and indicates she would like to gain weight, but only by eating healthy foods she is comfortable with, including kale, quinoa, and vegetables. Ms. L says that she has always been interested in “healthful foods” and that she “loves sugar,” but “it’s bad for you,” mentioning that “sugar fuels cancer.” She has daily thoughts about sugar causing cancer. Ms. L also mentions that she stopped eating flour, sugar, fried food, and oils because those foods affect her “stomach acid” and cause “pimples on my face and weight loss.” While in the inpatient unit, Ms. L requests a special diet and demands to know the origin and ingredients of the foods she is offered. She emphasizes that her esophageal cancer diagnosis and dysphagia exacerbate worries that certain foods cause cancer, and wants to continue her diet restrictions. Nonetheless, she says she wants to get healthy, and denies an intense fear of gaining weight or feeling fat.
HISTORY Multiple psychiatric diagnoses
Ms. L lives alone and enjoys spending time with her grandchildren, visiting museums, and listening to classical music. However, her family, social workers, and records from a previous psychiatric hospitalization reveal that Ms. L has a history of psychiatric illness and fears regarding certain types of foods for much of her adult life. Ms. L’s family also described a range of compulsive behaviors, including shoplifting, hoarding art, multiple plastic surgeries, and phases where Ms. L ate only frozen yogurt without sugar.
Ms. L’s daughter reported that Ms. L had seen a psychologist in the late 1990s for depression and had been diagnosed with obsessive-compulsive disorder (OCD) and attention deficit/hyperactivity disorder in the early 2000s. In 2006, during a depressive episode after her divorce, Ms. L had a suicide attempt with pills and alcohol, and was hospitalized. Records from that stay described a history of mood dysregulation with fears regarding food and nutrition. Ms. L was treated with aripiprazole 5 mg/d. A trial of trazodone 25 mg/d did not have any effect. When discharged, she was receiving lamotrigine 100 mg/d. However, her daughter believes she stopped taking all psychiatric medications shortly after discharge.
Her daughter says that in the past 2 years, Ms. L has seen multiple doctors for treatment of somatic gastrointestinal (GI) complaints. A 2018 note from a social worker indicated that Ms. L endorsed taking >80 supplements per day and constantly researched nutrition online. In the months leading to her current hospitalization, Ms. L suffered from severe self-neglect and fear regarding foods she felt were not healthy for her. She had stopped leaving her apartment.
Continue to: EVALUATION Poor insight, normal lab results...
EVALUATION Poor insight, normal lab results
During her evaluation, Ms. L appears cachectic and frail. She has a heavily constricted affect and is guarded, dismissive, and vague. Although her thought processes are linear and goal-directed, her insight into her condition is extremely poor and she appears surprised when clinicians inform her that her self-neglect would lead to death. Instead, Ms. L insists she is eating healthily and demonstrates severe anxiety in relation to her GI symptoms.
Ms. L is oriented to person, place, and time. She scores 27/30 on the Montreal Cognitive Assessment, indicating normal cognition. She denies any depressive symptoms or suicidal intent. She does not appear to be internally preoccupied and denies having auditory or visual hallucinations or manic symptoms.
A neurologic examination reveals that her cranial nerves are normal, and cerebellar function, strength, and sensory testing are intact. Her gait is steady and she walks without a walker. Despite her severely low BMI and recent history of self-neglect, Ms. L’s laboratory results are remarkably normal and show no liver, metabolic, or electrolyte abnormalities, no signs of infection, and normal vitamin B12 levels. She has slightly elevated creatinine and blood urea nitrogen levels, but a normal glomerular filtration rate.
Her medical history is significant for squamous cell esophageal cancer, treated with radiofrequency ablation. Although Ms. L is constantly worried about the recurrence of cancer, pathology reports demonstrate no esophageal dysplasia. However, she does show evidence of an approximately 1 cm × 1 cm mild, noncircumferential esophageal stenosis, likely resulting from radiofrequency ablation.
[polldaddy:11079394]
The authors’ observations
Several health- and physical symptom-related psychiatric disorders have overlapping features, which can complicate the differential diagnosis (Table 11). Ms. L presented to the ED with a severely low BMI of 13.5 kg/m2, obsessions regarding specific types of food, and preoccupations regarding her esophagus. Despite her extensive psychiatric history (including intense fears regarding food), we ruled out a primary psychotic disorder because she did not describe auditory or visual hallucinations and never appeared internally preoccupied. While her BMI and persistent minimization of the extent of her disease meet criteria for anorexia nervosa, she denied body dysmorphia and did not have any fear of gaining weight.
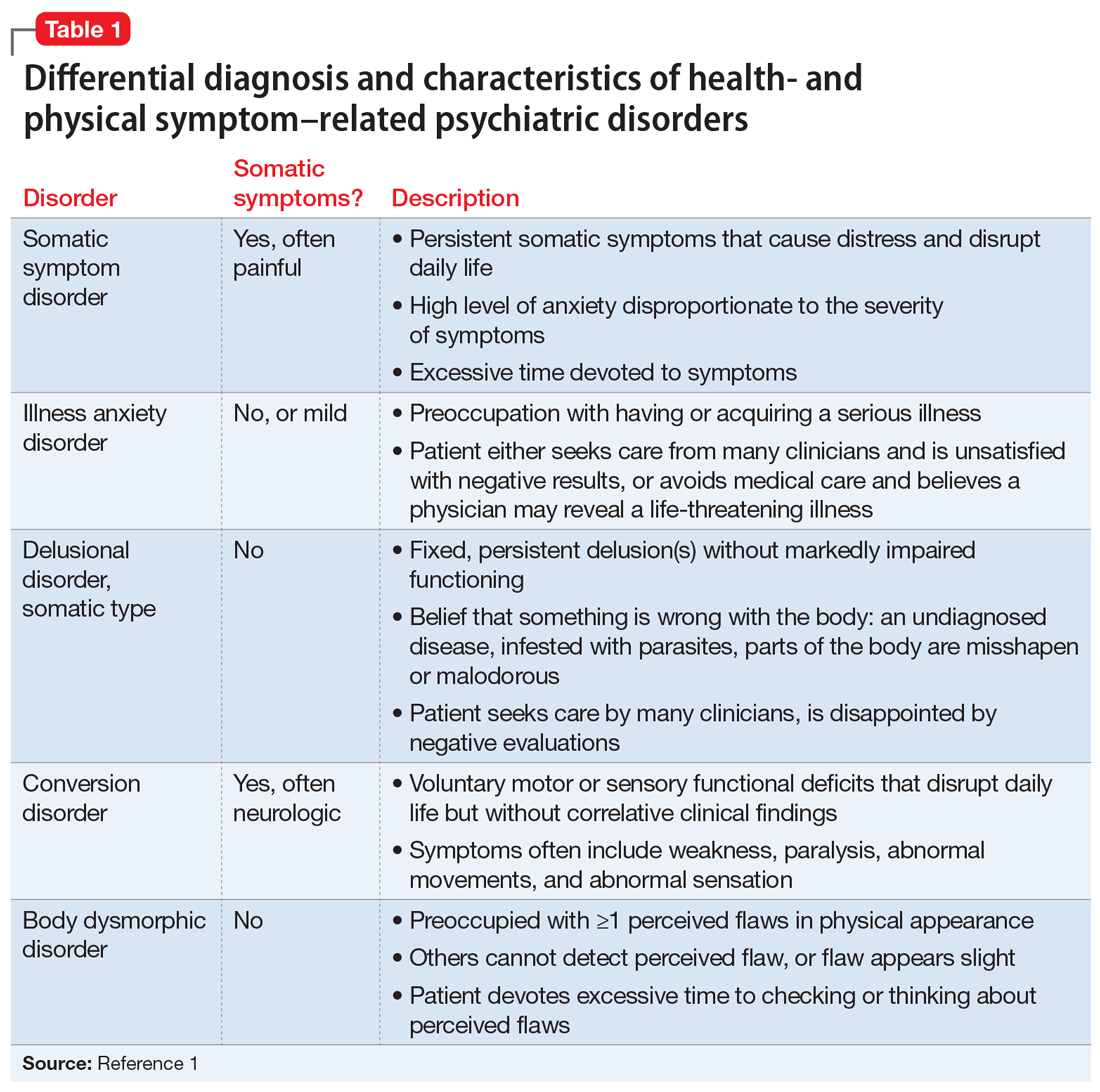
A central element of Ms. L’s presentation was her anxiety regarding how certain types of foods impact her health as well as her anxieties regarding her esophagus. While Ms. L was in remission from esophageal cancer and had a diagnosis of esophageal dysphagia, these preoccupations and obsessions regarding how certain types of foods affect her esophagus drove her to self-neglect and thus represent pathologic thought processes out of proportion to her symptoms. Illness anxiety disorder was considered because Ms. L met many of its criteria: preoccupation with having a serious illness, disproportionate preoccupation with somatic symptoms if they are present, extreme anxiety over health, and performance of health-related behaviors.1 However, illness anxiety disorder is a diagnosis of exclusion, and 1 criterion is that these symptoms cannot be explained by another mental disorder. We felt other diagnoses better fit Ms. L’s condition and ruled out illness anxiety disorder.
Ms. L’s long history of food and non-food–related obsessions and compulsions that interrupted her ability to perform daily activities were strongly suggestive for OCD. Additionally, her intense preoccupation, high level of anxiety, amount of time and energy spent seeking care for her esophagus and GERD symptoms, and the resulting significant disruption of daily life, met criteria for somatic symptom disorder (SSD). However, we did not believe that a diagnosis of OCD and SSD alone explained the entirety of Ms. L’s clinical picture. Despite ruling out anorexia nervosa, Ms. L nonetheless demonstrated disordered eating.
Avoidant/restrictive food intake disorder (ARFID) is an eating disorder in which patients restrict their diet and do not meet nutritional needs for any number of reasons, do not experience body dysmorphia, and do not fear weight gain.1 A common feature of ARFID is a fear of negative consequences from eating specific types of food.2 Table 21,2 summarizes additional clinical features of ARFID. Although ARFID is typically diagnosed in children and adolescents, particularly in individuals with autism with heightened sensory sensitivities, ARFID is also common among adult patients with GI disorders.3 In a retrospective chart review of 410 adults ages 18 to 90 (73% women) referred to a neurogastroenterology care center, 6.3% met the full criteria for ARFID and 17.3% had clinically significant avoidant or restrictive eating behaviors. Among patients with ARFID symptoms, 93% stated that a fear of GI symptoms was the driver of their avoidant or restrictive eating behaviors.2 Patients with GI diseases often develop dietary control and avoidance coping mechanisms to alleviate their symptoms.4 These strategies can exacerbate health anxieties and have a detrimental effect on mental health.5 Patients with GI disorders have a high degree of comorbidity with affective disorders, including anxiety disorders.6 These trends may arise from hypervigilance and the need to gain control over physical symptoms.7 Feeling a need for control, actions driven by anxiety and fear, and the need for compensatory behaviors are cardinal features of OCD and eating disorders.8 Multiple studies have demonstrated comorbidities between irritable bowel syndrome and eating disorders,9 SSD,10 and OCD.11 Taken together with observations that ARFID is also found in patients with GI disorders,2 these findings demonstrate that patients with a history of GI disease are at high risk of developing extreme health anxieties and behavioral coping strategies that can lead to disordered eating.
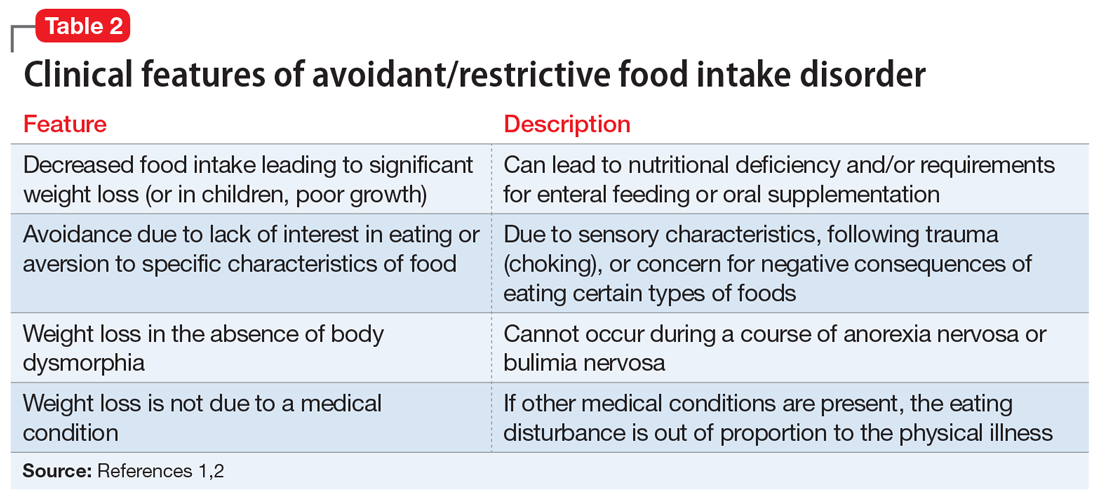
The rise in “healthy” eating materials online—particularly on social media—has created an atmosphere in which misinformation regarding diet and health is common and widespread. For patients with OCD and a predisposition to health anxiety, such as Ms. L, searching online for nutrition information and healthy living habits can exacerbate food-related anxieties and can lead to a pathological drive for purity and health.12Although not included in DSM-5, orthorexia nervosa was identified in 1997 as a proposed eating disorder best characterized as an obsession with healthy eating with associated restrictive behaviors.13 Patients with this disorder are rarely focused on losing weight, and orthorexic eating behaviors have been associated with both SSD and OCD.12,14 As in Ms. L’s case, patients with orthorexia nervosa demonstrate intrusive obsessions with nutrition, spend excessive amount of time researching nutrition, and fixate on food quality.12 Throughout Ms. L’s hospitalization, even as her food-related magical thinking symptoms improved, she constantly informed her care team that she had been “eating healthily” even though she was severely cachectic. Patients with SSD and OCD prone to health anxieties are at risk of developing pathologic food beliefs and dangerous eating behaviors. These patients may benefit from psychoeducation regarding nutrition and media literacy, which are components of effective eating disorder programs.15
[polldaddy:11079399]
Continue to: The authors' observations...
The authors’ observations
How do we approach the pharmacologic treatment of patients with co-occurring eating, somatic symptom, and anxiety disorders? Olanzapine facilitates recovery in children and adolescents with ARFID by promoting eating and weight gain, and decreasing symptoms of depression and anxiety.16 Patients with orthorexia nervosa also may benefit from treatment with olanzapine, which has decreased food-related fixations, magical thinking, and delusions regarding food.17 Further, orthorexic patients with ARFID have also been shown to respond to SSRIs due to those agents’ efficacy for treating intrusive thoughts, obsessions, and preoccupations from OCD and SSD.18,19 Thus, treating Ms. L’s symptoms with olanzapine and fluoxetine targeted the intersection of several diagnoses on our differential. Olanzapine’s propensity to cause weight gain is favorable in this population, particularly patients such as Ms. L, who do not exhibit body dysmorphia or fear of gaining weight.
OUTCOME Weight gain and fewer fears
Ms. L is prescribed olanzapine 5 mg/d and fluoxetine 20 mg/d. She gains 20.6 pounds in 4 weeks. Importantly, she endorses fewer fears related to foods and expands her palate to include foods she previously considered to be unhealthy, including white bread and farm-raised salmon. Further, she spends less time thinking about food and says she has less anxiety regarding the recurrence of GI symptoms.
1. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Association; 2013.
2. Murray HB, Bailey AP, Keshishian AC. Prevalence and characteristics of avoidant/restrictive food intake disorder in adult neurogastroenterology patients. Clin Gastroenterol Hepatol. 2020;18(9):1995-2002.e1.
3. Görmez A, Kılıç A, Kırpınar İ. Avoidant/restrictive food intake disorder: an adult case responding to cognitive behavioral therapy. Clinical Case Studies. 2018;17(6):443-452.
4. Reed-Knight B, Squires M, Chitkara DK, et al. Adolescents with irritable bowel syndrome report increased eating-associated symptoms, changes in dietary composition, and altered eating behaviors: a pilot comparison study to healthy adolescents. Neurogastroenterol Motil. 2016;28(12):1915-1920.
5. Melchior C, Desprez C, Riachi G, et al. Anxiety and depression profile is associated with eating disorders in patients with irritable bowel syndrome. Front Psychiatry. 2020;10:928.
6. Mayer EA, Craske M, Naliboff BD. Depression, anxiety, and the gastrointestinal system. J Clin Psychiatry. 2001;62 Suppl 8:28-37.
7. Abraham S, Kellow J. Exploring eating disorder quality of life and functional gastrointestinal disorders among eating disorder patients. J Psychosom Res. 2011;70(4):372-377.
8. Swinbourne JM, Touyz SW. The co-morbidity of eating disorders and anxiety disorders: a review. Eur Eat Disord Rev. 2007;15(4):253-274.
9. Perkins SJ, Keville S, Schmidt U, et al. Eating disorders and irritable bowel syndrome: is there a link? J Psychosom Res. 2005;59(2):57-64.
10. Hausteiner-Wiehle C, Henningsen P. Irritable bowel syndrome: relations with functional, mental, and somatoform disorders. World J Gastroenterol. 2014;20(2):6024-6030.
11. Masand PS, Keuthen NJ, Gupta S, et al. Prevalence of irritable bowel syndrome in obsessive-compulsive disorder. CNS Spectr. 2006;11(1):21-25.
12. Koven NS, Abry AW. The clinical basis of orthorexia nervosa: emerging perspectives. Neuropsychiatr Dis Treat. 2015;11:385-394.
13. Bratman S. Health food junkie. Yoga Journal. 1997;136:42-50.
14. Barthels F, Müller R, Schüth T, et al. Orthorexic eating behavior in patients with somatoform disorders. Eat Weight Disord. 2021;26(1):135-143.
15. Ciao AC, Loth K, Neumark-Sztainer D. Preventing eating disorder pathology: common and unique features of successful eating disorders prevention programs. Curr Psychiatry Rep. 2014;16(7):453.
16. Brewerton TD, D’Agostino M. Adjunctive use of olanzapine in the treatment of avoidant restrictive food intake disorder in children and adolescents in an eating disorders program. J Child Adolesc Psychopharmacol. 2017;27(10):920-922.
17. Moroze RM, Dunn TM, Craig Holland J, et al. Microthinking about micronutrients: a case of transition from obsessions about healthy eating to near-fatal “orthorexia nervosa” and proposed diagnostic criteria. Psychosomatics. 2015;56(4):397-403.
18. Spettigue W, Norris ML, Santos A, et al. Treatment of children and adolescents with avoidant/restrictive food intake disorder: a case series examining the feasibility of family therapy and adjunctive treatments. J Eat Disord. 2018;6:20.
19. Niedzielski A, Kaźmierczak-Wojtaś N. Prevalence of Orthorexia Nervosa and Its Diagnostic Tools-A Literature Review. Int J Environ Res Public Health. 2021;18(10):5488. Published 2021 May 20. doi:10.3390/ijerph18105488 Prevalence of orthorexia nervosa and its diagnostic tools-a literature review. Int J Environ Res Public Health. 2021;18(10):5488.
CASE Fixated on health and nutrition
At the insistence of her daughter, Ms. L, age 75, presents to the emergency department (ED) for self-neglect and severe weight loss, with a body mass index (BMI) of 13.5 kg/m2 (normal: 18.5 to 24.9 kg/m2). When asked why she is in the ED, Ms. L says she doesn’t know. She attributes her significant weight loss (approximately 20 pounds in the last few months) to gastroesophageal reflux disease (GERD). She constantly worries about her esophagus. She had been diagnosed with esophageal dysphagia 7 years ago after undergoing radiofrequency ablation for esophageal cancer. Ms. L fixates on the negative effects certain foods and ingredients might have on her stomach and esophagus.
Following transfer from the ED, Ms. L is involuntarily admitted to our inpatient unit. Although she acknowledges weight loss, she minimizes the severity of her illness and indicates she would like to gain weight, but only by eating healthy foods she is comfortable with, including kale, quinoa, and vegetables. Ms. L says that she has always been interested in “healthful foods” and that she “loves sugar,” but “it’s bad for you,” mentioning that “sugar fuels cancer.” She has daily thoughts about sugar causing cancer. Ms. L also mentions that she stopped eating flour, sugar, fried food, and oils because those foods affect her “stomach acid” and cause “pimples on my face and weight loss.” While in the inpatient unit, Ms. L requests a special diet and demands to know the origin and ingredients of the foods she is offered. She emphasizes that her esophageal cancer diagnosis and dysphagia exacerbate worries that certain foods cause cancer, and wants to continue her diet restrictions. Nonetheless, she says she wants to get healthy, and denies an intense fear of gaining weight or feeling fat.
HISTORY Multiple psychiatric diagnoses
Ms. L lives alone and enjoys spending time with her grandchildren, visiting museums, and listening to classical music. However, her family, social workers, and records from a previous psychiatric hospitalization reveal that Ms. L has a history of psychiatric illness and fears regarding certain types of foods for much of her adult life. Ms. L’s family also described a range of compulsive behaviors, including shoplifting, hoarding art, multiple plastic surgeries, and phases where Ms. L ate only frozen yogurt without sugar.
Ms. L’s daughter reported that Ms. L had seen a psychologist in the late 1990s for depression and had been diagnosed with obsessive-compulsive disorder (OCD) and attention deficit/hyperactivity disorder in the early 2000s. In 2006, during a depressive episode after her divorce, Ms. L had a suicide attempt with pills and alcohol, and was hospitalized. Records from that stay described a history of mood dysregulation with fears regarding food and nutrition. Ms. L was treated with aripiprazole 5 mg/d. A trial of trazodone 25 mg/d did not have any effect. When discharged, she was receiving lamotrigine 100 mg/d. However, her daughter believes she stopped taking all psychiatric medications shortly after discharge.
Her daughter says that in the past 2 years, Ms. L has seen multiple doctors for treatment of somatic gastrointestinal (GI) complaints. A 2018 note from a social worker indicated that Ms. L endorsed taking >80 supplements per day and constantly researched nutrition online. In the months leading to her current hospitalization, Ms. L suffered from severe self-neglect and fear regarding foods she felt were not healthy for her. She had stopped leaving her apartment.
Continue to: EVALUATION Poor insight, normal lab results...
EVALUATION Poor insight, normal lab results
During her evaluation, Ms. L appears cachectic and frail. She has a heavily constricted affect and is guarded, dismissive, and vague. Although her thought processes are linear and goal-directed, her insight into her condition is extremely poor and she appears surprised when clinicians inform her that her self-neglect would lead to death. Instead, Ms. L insists she is eating healthily and demonstrates severe anxiety in relation to her GI symptoms.
Ms. L is oriented to person, place, and time. She scores 27/30 on the Montreal Cognitive Assessment, indicating normal cognition. She denies any depressive symptoms or suicidal intent. She does not appear to be internally preoccupied and denies having auditory or visual hallucinations or manic symptoms.
A neurologic examination reveals that her cranial nerves are normal, and cerebellar function, strength, and sensory testing are intact. Her gait is steady and she walks without a walker. Despite her severely low BMI and recent history of self-neglect, Ms. L’s laboratory results are remarkably normal and show no liver, metabolic, or electrolyte abnormalities, no signs of infection, and normal vitamin B12 levels. She has slightly elevated creatinine and blood urea nitrogen levels, but a normal glomerular filtration rate.
Her medical history is significant for squamous cell esophageal cancer, treated with radiofrequency ablation. Although Ms. L is constantly worried about the recurrence of cancer, pathology reports demonstrate no esophageal dysplasia. However, she does show evidence of an approximately 1 cm × 1 cm mild, noncircumferential esophageal stenosis, likely resulting from radiofrequency ablation.
[polldaddy:11079394]
The authors’ observations
Several health- and physical symptom-related psychiatric disorders have overlapping features, which can complicate the differential diagnosis (Table 11). Ms. L presented to the ED with a severely low BMI of 13.5 kg/m2, obsessions regarding specific types of food, and preoccupations regarding her esophagus. Despite her extensive psychiatric history (including intense fears regarding food), we ruled out a primary psychotic disorder because she did not describe auditory or visual hallucinations and never appeared internally preoccupied. While her BMI and persistent minimization of the extent of her disease meet criteria for anorexia nervosa, she denied body dysmorphia and did not have any fear of gaining weight.
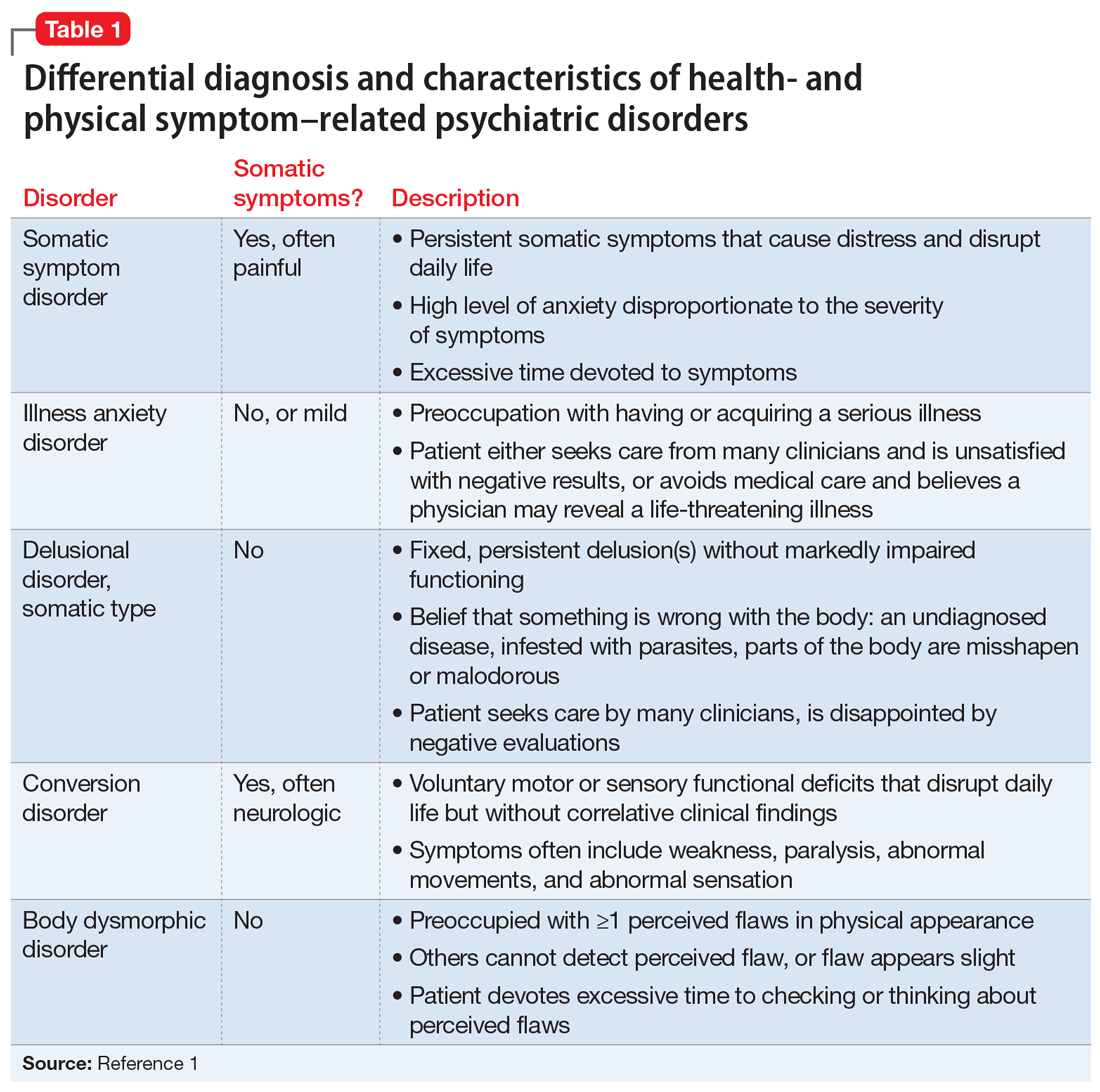
A central element of Ms. L’s presentation was her anxiety regarding how certain types of foods impact her health as well as her anxieties regarding her esophagus. While Ms. L was in remission from esophageal cancer and had a diagnosis of esophageal dysphagia, these preoccupations and obsessions regarding how certain types of foods affect her esophagus drove her to self-neglect and thus represent pathologic thought processes out of proportion to her symptoms. Illness anxiety disorder was considered because Ms. L met many of its criteria: preoccupation with having a serious illness, disproportionate preoccupation with somatic symptoms if they are present, extreme anxiety over health, and performance of health-related behaviors.1 However, illness anxiety disorder is a diagnosis of exclusion, and 1 criterion is that these symptoms cannot be explained by another mental disorder. We felt other diagnoses better fit Ms. L’s condition and ruled out illness anxiety disorder.
Ms. L’s long history of food and non-food–related obsessions and compulsions that interrupted her ability to perform daily activities were strongly suggestive for OCD. Additionally, her intense preoccupation, high level of anxiety, amount of time and energy spent seeking care for her esophagus and GERD symptoms, and the resulting significant disruption of daily life, met criteria for somatic symptom disorder (SSD). However, we did not believe that a diagnosis of OCD and SSD alone explained the entirety of Ms. L’s clinical picture. Despite ruling out anorexia nervosa, Ms. L nonetheless demonstrated disordered eating.
Avoidant/restrictive food intake disorder (ARFID) is an eating disorder in which patients restrict their diet and do not meet nutritional needs for any number of reasons, do not experience body dysmorphia, and do not fear weight gain.1 A common feature of ARFID is a fear of negative consequences from eating specific types of food.2 Table 21,2 summarizes additional clinical features of ARFID. Although ARFID is typically diagnosed in children and adolescents, particularly in individuals with autism with heightened sensory sensitivities, ARFID is also common among adult patients with GI disorders.3 In a retrospective chart review of 410 adults ages 18 to 90 (73% women) referred to a neurogastroenterology care center, 6.3% met the full criteria for ARFID and 17.3% had clinically significant avoidant or restrictive eating behaviors. Among patients with ARFID symptoms, 93% stated that a fear of GI symptoms was the driver of their avoidant or restrictive eating behaviors.2 Patients with GI diseases often develop dietary control and avoidance coping mechanisms to alleviate their symptoms.4 These strategies can exacerbate health anxieties and have a detrimental effect on mental health.5 Patients with GI disorders have a high degree of comorbidity with affective disorders, including anxiety disorders.6 These trends may arise from hypervigilance and the need to gain control over physical symptoms.7 Feeling a need for control, actions driven by anxiety and fear, and the need for compensatory behaviors are cardinal features of OCD and eating disorders.8 Multiple studies have demonstrated comorbidities between irritable bowel syndrome and eating disorders,9 SSD,10 and OCD.11 Taken together with observations that ARFID is also found in patients with GI disorders,2 these findings demonstrate that patients with a history of GI disease are at high risk of developing extreme health anxieties and behavioral coping strategies that can lead to disordered eating.
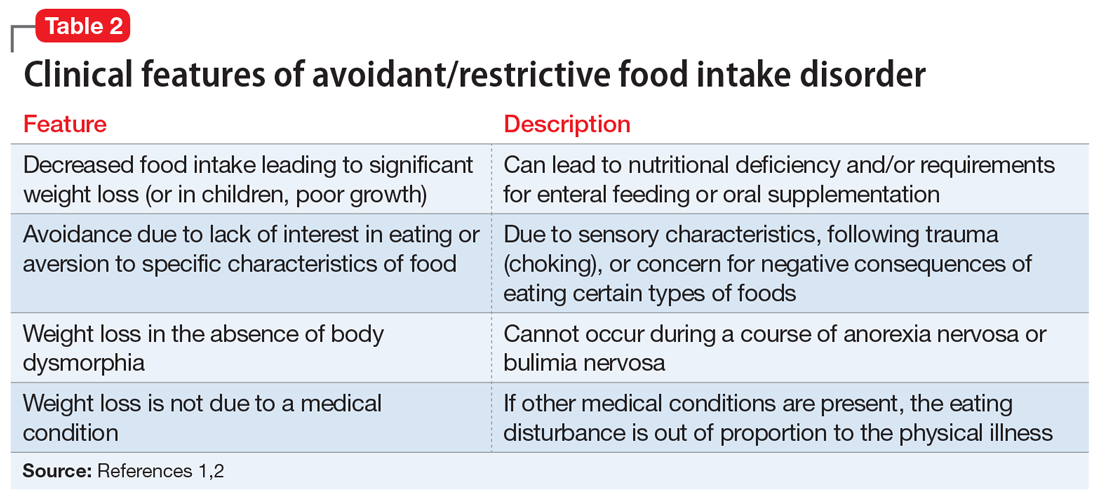
The rise in “healthy” eating materials online—particularly on social media—has created an atmosphere in which misinformation regarding diet and health is common and widespread. For patients with OCD and a predisposition to health anxiety, such as Ms. L, searching online for nutrition information and healthy living habits can exacerbate food-related anxieties and can lead to a pathological drive for purity and health.12Although not included in DSM-5, orthorexia nervosa was identified in 1997 as a proposed eating disorder best characterized as an obsession with healthy eating with associated restrictive behaviors.13 Patients with this disorder are rarely focused on losing weight, and orthorexic eating behaviors have been associated with both SSD and OCD.12,14 As in Ms. L’s case, patients with orthorexia nervosa demonstrate intrusive obsessions with nutrition, spend excessive amount of time researching nutrition, and fixate on food quality.12 Throughout Ms. L’s hospitalization, even as her food-related magical thinking symptoms improved, she constantly informed her care team that she had been “eating healthily” even though she was severely cachectic. Patients with SSD and OCD prone to health anxieties are at risk of developing pathologic food beliefs and dangerous eating behaviors. These patients may benefit from psychoeducation regarding nutrition and media literacy, which are components of effective eating disorder programs.15
[polldaddy:11079399]
Continue to: The authors' observations...
The authors’ observations
How do we approach the pharmacologic treatment of patients with co-occurring eating, somatic symptom, and anxiety disorders? Olanzapine facilitates recovery in children and adolescents with ARFID by promoting eating and weight gain, and decreasing symptoms of depression and anxiety.16 Patients with orthorexia nervosa also may benefit from treatment with olanzapine, which has decreased food-related fixations, magical thinking, and delusions regarding food.17 Further, orthorexic patients with ARFID have also been shown to respond to SSRIs due to those agents’ efficacy for treating intrusive thoughts, obsessions, and preoccupations from OCD and SSD.18,19 Thus, treating Ms. L’s symptoms with olanzapine and fluoxetine targeted the intersection of several diagnoses on our differential. Olanzapine’s propensity to cause weight gain is favorable in this population, particularly patients such as Ms. L, who do not exhibit body dysmorphia or fear of gaining weight.
OUTCOME Weight gain and fewer fears
Ms. L is prescribed olanzapine 5 mg/d and fluoxetine 20 mg/d. She gains 20.6 pounds in 4 weeks. Importantly, she endorses fewer fears related to foods and expands her palate to include foods she previously considered to be unhealthy, including white bread and farm-raised salmon. Further, she spends less time thinking about food and says she has less anxiety regarding the recurrence of GI symptoms.
CASE Fixated on health and nutrition
At the insistence of her daughter, Ms. L, age 75, presents to the emergency department (ED) for self-neglect and severe weight loss, with a body mass index (BMI) of 13.5 kg/m2 (normal: 18.5 to 24.9 kg/m2). When asked why she is in the ED, Ms. L says she doesn’t know. She attributes her significant weight loss (approximately 20 pounds in the last few months) to gastroesophageal reflux disease (GERD). She constantly worries about her esophagus. She had been diagnosed with esophageal dysphagia 7 years ago after undergoing radiofrequency ablation for esophageal cancer. Ms. L fixates on the negative effects certain foods and ingredients might have on her stomach and esophagus.
Following transfer from the ED, Ms. L is involuntarily admitted to our inpatient unit. Although she acknowledges weight loss, she minimizes the severity of her illness and indicates she would like to gain weight, but only by eating healthy foods she is comfortable with, including kale, quinoa, and vegetables. Ms. L says that she has always been interested in “healthful foods” and that she “loves sugar,” but “it’s bad for you,” mentioning that “sugar fuels cancer.” She has daily thoughts about sugar causing cancer. Ms. L also mentions that she stopped eating flour, sugar, fried food, and oils because those foods affect her “stomach acid” and cause “pimples on my face and weight loss.” While in the inpatient unit, Ms. L requests a special diet and demands to know the origin and ingredients of the foods she is offered. She emphasizes that her esophageal cancer diagnosis and dysphagia exacerbate worries that certain foods cause cancer, and wants to continue her diet restrictions. Nonetheless, she says she wants to get healthy, and denies an intense fear of gaining weight or feeling fat.
HISTORY Multiple psychiatric diagnoses
Ms. L lives alone and enjoys spending time with her grandchildren, visiting museums, and listening to classical music. However, her family, social workers, and records from a previous psychiatric hospitalization reveal that Ms. L has a history of psychiatric illness and fears regarding certain types of foods for much of her adult life. Ms. L’s family also described a range of compulsive behaviors, including shoplifting, hoarding art, multiple plastic surgeries, and phases where Ms. L ate only frozen yogurt without sugar.
Ms. L’s daughter reported that Ms. L had seen a psychologist in the late 1990s for depression and had been diagnosed with obsessive-compulsive disorder (OCD) and attention deficit/hyperactivity disorder in the early 2000s. In 2006, during a depressive episode after her divorce, Ms. L had a suicide attempt with pills and alcohol, and was hospitalized. Records from that stay described a history of mood dysregulation with fears regarding food and nutrition. Ms. L was treated with aripiprazole 5 mg/d. A trial of trazodone 25 mg/d did not have any effect. When discharged, she was receiving lamotrigine 100 mg/d. However, her daughter believes she stopped taking all psychiatric medications shortly after discharge.
Her daughter says that in the past 2 years, Ms. L has seen multiple doctors for treatment of somatic gastrointestinal (GI) complaints. A 2018 note from a social worker indicated that Ms. L endorsed taking >80 supplements per day and constantly researched nutrition online. In the months leading to her current hospitalization, Ms. L suffered from severe self-neglect and fear regarding foods she felt were not healthy for her. She had stopped leaving her apartment.
Continue to: EVALUATION Poor insight, normal lab results...
EVALUATION Poor insight, normal lab results
During her evaluation, Ms. L appears cachectic and frail. She has a heavily constricted affect and is guarded, dismissive, and vague. Although her thought processes are linear and goal-directed, her insight into her condition is extremely poor and she appears surprised when clinicians inform her that her self-neglect would lead to death. Instead, Ms. L insists she is eating healthily and demonstrates severe anxiety in relation to her GI symptoms.
Ms. L is oriented to person, place, and time. She scores 27/30 on the Montreal Cognitive Assessment, indicating normal cognition. She denies any depressive symptoms or suicidal intent. She does not appear to be internally preoccupied and denies having auditory or visual hallucinations or manic symptoms.
A neurologic examination reveals that her cranial nerves are normal, and cerebellar function, strength, and sensory testing are intact. Her gait is steady and she walks without a walker. Despite her severely low BMI and recent history of self-neglect, Ms. L’s laboratory results are remarkably normal and show no liver, metabolic, or electrolyte abnormalities, no signs of infection, and normal vitamin B12 levels. She has slightly elevated creatinine and blood urea nitrogen levels, but a normal glomerular filtration rate.
Her medical history is significant for squamous cell esophageal cancer, treated with radiofrequency ablation. Although Ms. L is constantly worried about the recurrence of cancer, pathology reports demonstrate no esophageal dysplasia. However, she does show evidence of an approximately 1 cm × 1 cm mild, noncircumferential esophageal stenosis, likely resulting from radiofrequency ablation.
[polldaddy:11079394]
The authors’ observations
Several health- and physical symptom-related psychiatric disorders have overlapping features, which can complicate the differential diagnosis (Table 11). Ms. L presented to the ED with a severely low BMI of 13.5 kg/m2, obsessions regarding specific types of food, and preoccupations regarding her esophagus. Despite her extensive psychiatric history (including intense fears regarding food), we ruled out a primary psychotic disorder because she did not describe auditory or visual hallucinations and never appeared internally preoccupied. While her BMI and persistent minimization of the extent of her disease meet criteria for anorexia nervosa, she denied body dysmorphia and did not have any fear of gaining weight.
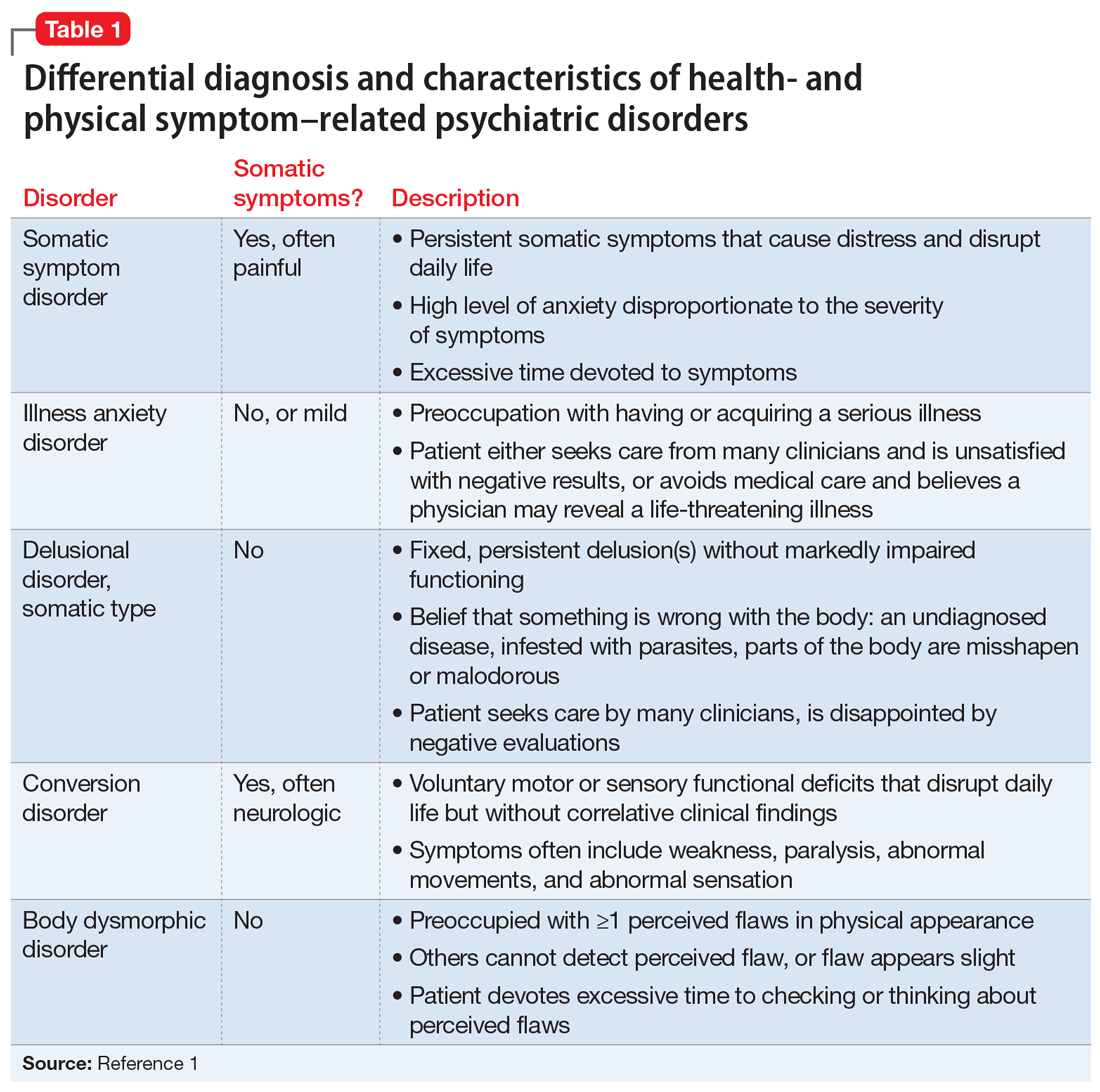
A central element of Ms. L’s presentation was her anxiety regarding how certain types of foods impact her health as well as her anxieties regarding her esophagus. While Ms. L was in remission from esophageal cancer and had a diagnosis of esophageal dysphagia, these preoccupations and obsessions regarding how certain types of foods affect her esophagus drove her to self-neglect and thus represent pathologic thought processes out of proportion to her symptoms. Illness anxiety disorder was considered because Ms. L met many of its criteria: preoccupation with having a serious illness, disproportionate preoccupation with somatic symptoms if they are present, extreme anxiety over health, and performance of health-related behaviors.1 However, illness anxiety disorder is a diagnosis of exclusion, and 1 criterion is that these symptoms cannot be explained by another mental disorder. We felt other diagnoses better fit Ms. L’s condition and ruled out illness anxiety disorder.
Ms. L’s long history of food and non-food–related obsessions and compulsions that interrupted her ability to perform daily activities were strongly suggestive for OCD. Additionally, her intense preoccupation, high level of anxiety, amount of time and energy spent seeking care for her esophagus and GERD symptoms, and the resulting significant disruption of daily life, met criteria for somatic symptom disorder (SSD). However, we did not believe that a diagnosis of OCD and SSD alone explained the entirety of Ms. L’s clinical picture. Despite ruling out anorexia nervosa, Ms. L nonetheless demonstrated disordered eating.
Avoidant/restrictive food intake disorder (ARFID) is an eating disorder in which patients restrict their diet and do not meet nutritional needs for any number of reasons, do not experience body dysmorphia, and do not fear weight gain.1 A common feature of ARFID is a fear of negative consequences from eating specific types of food.2 Table 21,2 summarizes additional clinical features of ARFID. Although ARFID is typically diagnosed in children and adolescents, particularly in individuals with autism with heightened sensory sensitivities, ARFID is also common among adult patients with GI disorders.3 In a retrospective chart review of 410 adults ages 18 to 90 (73% women) referred to a neurogastroenterology care center, 6.3% met the full criteria for ARFID and 17.3% had clinically significant avoidant or restrictive eating behaviors. Among patients with ARFID symptoms, 93% stated that a fear of GI symptoms was the driver of their avoidant or restrictive eating behaviors.2 Patients with GI diseases often develop dietary control and avoidance coping mechanisms to alleviate their symptoms.4 These strategies can exacerbate health anxieties and have a detrimental effect on mental health.5 Patients with GI disorders have a high degree of comorbidity with affective disorders, including anxiety disorders.6 These trends may arise from hypervigilance and the need to gain control over physical symptoms.7 Feeling a need for control, actions driven by anxiety and fear, and the need for compensatory behaviors are cardinal features of OCD and eating disorders.8 Multiple studies have demonstrated comorbidities between irritable bowel syndrome and eating disorders,9 SSD,10 and OCD.11 Taken together with observations that ARFID is also found in patients with GI disorders,2 these findings demonstrate that patients with a history of GI disease are at high risk of developing extreme health anxieties and behavioral coping strategies that can lead to disordered eating.
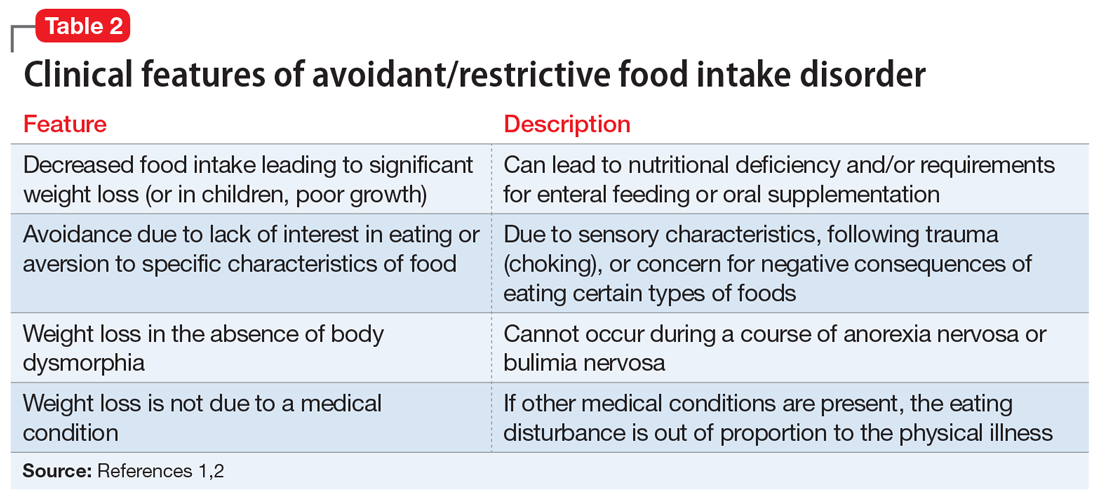
The rise in “healthy” eating materials online—particularly on social media—has created an atmosphere in which misinformation regarding diet and health is common and widespread. For patients with OCD and a predisposition to health anxiety, such as Ms. L, searching online for nutrition information and healthy living habits can exacerbate food-related anxieties and can lead to a pathological drive for purity and health.12Although not included in DSM-5, orthorexia nervosa was identified in 1997 as a proposed eating disorder best characterized as an obsession with healthy eating with associated restrictive behaviors.13 Patients with this disorder are rarely focused on losing weight, and orthorexic eating behaviors have been associated with both SSD and OCD.12,14 As in Ms. L’s case, patients with orthorexia nervosa demonstrate intrusive obsessions with nutrition, spend excessive amount of time researching nutrition, and fixate on food quality.12 Throughout Ms. L’s hospitalization, even as her food-related magical thinking symptoms improved, she constantly informed her care team that she had been “eating healthily” even though she was severely cachectic. Patients with SSD and OCD prone to health anxieties are at risk of developing pathologic food beliefs and dangerous eating behaviors. These patients may benefit from psychoeducation regarding nutrition and media literacy, which are components of effective eating disorder programs.15
[polldaddy:11079399]
Continue to: The authors' observations...
The authors’ observations
How do we approach the pharmacologic treatment of patients with co-occurring eating, somatic symptom, and anxiety disorders? Olanzapine facilitates recovery in children and adolescents with ARFID by promoting eating and weight gain, and decreasing symptoms of depression and anxiety.16 Patients with orthorexia nervosa also may benefit from treatment with olanzapine, which has decreased food-related fixations, magical thinking, and delusions regarding food.17 Further, orthorexic patients with ARFID have also been shown to respond to SSRIs due to those agents’ efficacy for treating intrusive thoughts, obsessions, and preoccupations from OCD and SSD.18,19 Thus, treating Ms. L’s symptoms with olanzapine and fluoxetine targeted the intersection of several diagnoses on our differential. Olanzapine’s propensity to cause weight gain is favorable in this population, particularly patients such as Ms. L, who do not exhibit body dysmorphia or fear of gaining weight.
OUTCOME Weight gain and fewer fears
Ms. L is prescribed olanzapine 5 mg/d and fluoxetine 20 mg/d. She gains 20.6 pounds in 4 weeks. Importantly, she endorses fewer fears related to foods and expands her palate to include foods she previously considered to be unhealthy, including white bread and farm-raised salmon. Further, she spends less time thinking about food and says she has less anxiety regarding the recurrence of GI symptoms.
1. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Association; 2013.
2. Murray HB, Bailey AP, Keshishian AC. Prevalence and characteristics of avoidant/restrictive food intake disorder in adult neurogastroenterology patients. Clin Gastroenterol Hepatol. 2020;18(9):1995-2002.e1.
3. Görmez A, Kılıç A, Kırpınar İ. Avoidant/restrictive food intake disorder: an adult case responding to cognitive behavioral therapy. Clinical Case Studies. 2018;17(6):443-452.
4. Reed-Knight B, Squires M, Chitkara DK, et al. Adolescents with irritable bowel syndrome report increased eating-associated symptoms, changes in dietary composition, and altered eating behaviors: a pilot comparison study to healthy adolescents. Neurogastroenterol Motil. 2016;28(12):1915-1920.
5. Melchior C, Desprez C, Riachi G, et al. Anxiety and depression profile is associated with eating disorders in patients with irritable bowel syndrome. Front Psychiatry. 2020;10:928.
6. Mayer EA, Craske M, Naliboff BD. Depression, anxiety, and the gastrointestinal system. J Clin Psychiatry. 2001;62 Suppl 8:28-37.
7. Abraham S, Kellow J. Exploring eating disorder quality of life and functional gastrointestinal disorders among eating disorder patients. J Psychosom Res. 2011;70(4):372-377.
8. Swinbourne JM, Touyz SW. The co-morbidity of eating disorders and anxiety disorders: a review. Eur Eat Disord Rev. 2007;15(4):253-274.
9. Perkins SJ, Keville S, Schmidt U, et al. Eating disorders and irritable bowel syndrome: is there a link? J Psychosom Res. 2005;59(2):57-64.
10. Hausteiner-Wiehle C, Henningsen P. Irritable bowel syndrome: relations with functional, mental, and somatoform disorders. World J Gastroenterol. 2014;20(2):6024-6030.
11. Masand PS, Keuthen NJ, Gupta S, et al. Prevalence of irritable bowel syndrome in obsessive-compulsive disorder. CNS Spectr. 2006;11(1):21-25.
12. Koven NS, Abry AW. The clinical basis of orthorexia nervosa: emerging perspectives. Neuropsychiatr Dis Treat. 2015;11:385-394.
13. Bratman S. Health food junkie. Yoga Journal. 1997;136:42-50.
14. Barthels F, Müller R, Schüth T, et al. Orthorexic eating behavior in patients with somatoform disorders. Eat Weight Disord. 2021;26(1):135-143.
15. Ciao AC, Loth K, Neumark-Sztainer D. Preventing eating disorder pathology: common and unique features of successful eating disorders prevention programs. Curr Psychiatry Rep. 2014;16(7):453.
16. Brewerton TD, D’Agostino M. Adjunctive use of olanzapine in the treatment of avoidant restrictive food intake disorder in children and adolescents in an eating disorders program. J Child Adolesc Psychopharmacol. 2017;27(10):920-922.
17. Moroze RM, Dunn TM, Craig Holland J, et al. Microthinking about micronutrients: a case of transition from obsessions about healthy eating to near-fatal “orthorexia nervosa” and proposed diagnostic criteria. Psychosomatics. 2015;56(4):397-403.
18. Spettigue W, Norris ML, Santos A, et al. Treatment of children and adolescents with avoidant/restrictive food intake disorder: a case series examining the feasibility of family therapy and adjunctive treatments. J Eat Disord. 2018;6:20.
19. Niedzielski A, Kaźmierczak-Wojtaś N. Prevalence of Orthorexia Nervosa and Its Diagnostic Tools-A Literature Review. Int J Environ Res Public Health. 2021;18(10):5488. Published 2021 May 20. doi:10.3390/ijerph18105488 Prevalence of orthorexia nervosa and its diagnostic tools-a literature review. Int J Environ Res Public Health. 2021;18(10):5488.
1. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Association; 2013.
2. Murray HB, Bailey AP, Keshishian AC. Prevalence and characteristics of avoidant/restrictive food intake disorder in adult neurogastroenterology patients. Clin Gastroenterol Hepatol. 2020;18(9):1995-2002.e1.
3. Görmez A, Kılıç A, Kırpınar İ. Avoidant/restrictive food intake disorder: an adult case responding to cognitive behavioral therapy. Clinical Case Studies. 2018;17(6):443-452.
4. Reed-Knight B, Squires M, Chitkara DK, et al. Adolescents with irritable bowel syndrome report increased eating-associated symptoms, changes in dietary composition, and altered eating behaviors: a pilot comparison study to healthy adolescents. Neurogastroenterol Motil. 2016;28(12):1915-1920.
5. Melchior C, Desprez C, Riachi G, et al. Anxiety and depression profile is associated with eating disorders in patients with irritable bowel syndrome. Front Psychiatry. 2020;10:928.
6. Mayer EA, Craske M, Naliboff BD. Depression, anxiety, and the gastrointestinal system. J Clin Psychiatry. 2001;62 Suppl 8:28-37.
7. Abraham S, Kellow J. Exploring eating disorder quality of life and functional gastrointestinal disorders among eating disorder patients. J Psychosom Res. 2011;70(4):372-377.
8. Swinbourne JM, Touyz SW. The co-morbidity of eating disorders and anxiety disorders: a review. Eur Eat Disord Rev. 2007;15(4):253-274.
9. Perkins SJ, Keville S, Schmidt U, et al. Eating disorders and irritable bowel syndrome: is there a link? J Psychosom Res. 2005;59(2):57-64.
10. Hausteiner-Wiehle C, Henningsen P. Irritable bowel syndrome: relations with functional, mental, and somatoform disorders. World J Gastroenterol. 2014;20(2):6024-6030.
11. Masand PS, Keuthen NJ, Gupta S, et al. Prevalence of irritable bowel syndrome in obsessive-compulsive disorder. CNS Spectr. 2006;11(1):21-25.
12. Koven NS, Abry AW. The clinical basis of orthorexia nervosa: emerging perspectives. Neuropsychiatr Dis Treat. 2015;11:385-394.
13. Bratman S. Health food junkie. Yoga Journal. 1997;136:42-50.
14. Barthels F, Müller R, Schüth T, et al. Orthorexic eating behavior in patients with somatoform disorders. Eat Weight Disord. 2021;26(1):135-143.
15. Ciao AC, Loth K, Neumark-Sztainer D. Preventing eating disorder pathology: common and unique features of successful eating disorders prevention programs. Curr Psychiatry Rep. 2014;16(7):453.
16. Brewerton TD, D’Agostino M. Adjunctive use of olanzapine in the treatment of avoidant restrictive food intake disorder in children and adolescents in an eating disorders program. J Child Adolesc Psychopharmacol. 2017;27(10):920-922.
17. Moroze RM, Dunn TM, Craig Holland J, et al. Microthinking about micronutrients: a case of transition from obsessions about healthy eating to near-fatal “orthorexia nervosa” and proposed diagnostic criteria. Psychosomatics. 2015;56(4):397-403.
18. Spettigue W, Norris ML, Santos A, et al. Treatment of children and adolescents with avoidant/restrictive food intake disorder: a case series examining the feasibility of family therapy and adjunctive treatments. J Eat Disord. 2018;6:20.
19. Niedzielski A, Kaźmierczak-Wojtaś N. Prevalence of Orthorexia Nervosa and Its Diagnostic Tools-A Literature Review. Int J Environ Res Public Health. 2021;18(10):5488. Published 2021 May 20. doi:10.3390/ijerph18105488 Prevalence of orthorexia nervosa and its diagnostic tools-a literature review. Int J Environ Res Public Health. 2021;18(10):5488.
I STEP: Recognizing cognitive distortions in posttraumatic stress disorder
Evidence-based cognitive-behavioral therapies for posttraumatic stress disorder (PTSD) may employ cognitive restructuring. This psychotherapeutic technique entails recognizing and correcting maladaptive, inaccurate thoughts that perpetuate illness.1 For example, a clinician helps a patient recognize that the negative thought “Nobody loves me” following a romantic breakup is an overgeneralization. The patient is taught to self-correct this to “While my ex-girlfriend doesn’t love me, others do. It only feels like nobody loves me.”2
We introduce the acronym I STEP to help clinicians recognize several common distorted thoughts in PTSD. These tend to occur within stereotyped themes in PTSD,3 as outlined and illustrated below. Recognizing distorted thoughts in these patients will help clinicians understand and address psychological distress following trauma.
Intimacy/In-touch. Intimacy involves comfort in relationships, including but not limited to sexual intimacy. This requires being in touch emotionally with self and others. In trauma involving loss, fear of further loss may impair intimacy with others. Difficulty with self-intimacy impairs commitment to life’s goals and prompts unhelpful avoidance behaviors, such as difficulty being alone or self-injurious use of drugs or alcohol. Comfort in spending some portion of time alone with one’s thoughts and emotions is a life skill necessary to attain optimum function. Patients who are unable to tolerate their own emotions without constant company might have excessive anxiety when social supports are otherwise occupied. Such patients might seek excessive and repeated reassurance rather than learning to tolerate their own emotions and thoughts. They would then find it difficult to engage successfully in solo activities.
Safety. After trauma, patients may view themselves and others as unsafe, and may overestimate risk. For example, a pedestrian who is struck by a vehicle may believe that crossing a street will again result in getting hit by a car without appreciating that people frequently cross streets without injury or that crossing cautiously is an essential life skill. Parents who have suffered from trauma may unduly believe that their children are in danger when engaging in an activity generally considered to be safe. This may create challenges in parenting and impede their children’s ability to develop a sense of independence.
Trust. Trauma victims may unfairly blame themselves, leading them to mistrust their own judgment. Such patients may have difficulty making decisions confidently and independently, such as choosing a job or a romantic partner. When traumatized by another person or people, it can be difficult to maintain positive views of others or to accept others’ positive behaviors as genuine. For example, a common reaction following rape may be a generalized mistrust of all men.
Esteem. Patients’ self-esteem may suffer following trauma due to irrational self-blame or believing the “just world hypothesis”—the idea that bad things only happen to bad people. For example, a patient who suffers an assault by an acquaintance might think “I must be stupid if I couldn’t figure out that my friend was dangerous.”
Power. Traumatic events usually occur outside of one’s control. Survivors of trauma may lose confidence in their ability to control any aspect of their lives. Conversely, they may attempt to gain control of all of life’s circumstances, including those that are beyond anyone’s control. Control can be applied to emotions, behaviors, or events. A driver struck by a vehicle may think “I can’t control other drivers, so I have no power to control my safety while driving,” and hence give up driving. While there are things that are beyond our control, this extreme thought ignores things that we can control, such as wearing seatbelts or having the vehicle’s brakes regularly serviced.
1. Wenzel A. Basic strategies of cognitive behavioral therapy. Psychiatr Clin North Am. 2017;40(4):597-609.
2. Beck J. Cognitive behavioral therapy: basics and beyond. 2nd ed. The Guilford Press; 2011.
3. Resick PA, Monson CM, Chard KM. Cognitive processing therapy for PTSD. A comprehensive manual. The Guilford Press; 2017.
Evidence-based cognitive-behavioral therapies for posttraumatic stress disorder (PTSD) may employ cognitive restructuring. This psychotherapeutic technique entails recognizing and correcting maladaptive, inaccurate thoughts that perpetuate illness.1 For example, a clinician helps a patient recognize that the negative thought “Nobody loves me” following a romantic breakup is an overgeneralization. The patient is taught to self-correct this to “While my ex-girlfriend doesn’t love me, others do. It only feels like nobody loves me.”2
We introduce the acronym I STEP to help clinicians recognize several common distorted thoughts in PTSD. These tend to occur within stereotyped themes in PTSD,3 as outlined and illustrated below. Recognizing distorted thoughts in these patients will help clinicians understand and address psychological distress following trauma.
Intimacy/In-touch. Intimacy involves comfort in relationships, including but not limited to sexual intimacy. This requires being in touch emotionally with self and others. In trauma involving loss, fear of further loss may impair intimacy with others. Difficulty with self-intimacy impairs commitment to life’s goals and prompts unhelpful avoidance behaviors, such as difficulty being alone or self-injurious use of drugs or alcohol. Comfort in spending some portion of time alone with one’s thoughts and emotions is a life skill necessary to attain optimum function. Patients who are unable to tolerate their own emotions without constant company might have excessive anxiety when social supports are otherwise occupied. Such patients might seek excessive and repeated reassurance rather than learning to tolerate their own emotions and thoughts. They would then find it difficult to engage successfully in solo activities.
Safety. After trauma, patients may view themselves and others as unsafe, and may overestimate risk. For example, a pedestrian who is struck by a vehicle may believe that crossing a street will again result in getting hit by a car without appreciating that people frequently cross streets without injury or that crossing cautiously is an essential life skill. Parents who have suffered from trauma may unduly believe that their children are in danger when engaging in an activity generally considered to be safe. This may create challenges in parenting and impede their children’s ability to develop a sense of independence.
Trust. Trauma victims may unfairly blame themselves, leading them to mistrust their own judgment. Such patients may have difficulty making decisions confidently and independently, such as choosing a job or a romantic partner. When traumatized by another person or people, it can be difficult to maintain positive views of others or to accept others’ positive behaviors as genuine. For example, a common reaction following rape may be a generalized mistrust of all men.
Esteem. Patients’ self-esteem may suffer following trauma due to irrational self-blame or believing the “just world hypothesis”—the idea that bad things only happen to bad people. For example, a patient who suffers an assault by an acquaintance might think “I must be stupid if I couldn’t figure out that my friend was dangerous.”
Power. Traumatic events usually occur outside of one’s control. Survivors of trauma may lose confidence in their ability to control any aspect of their lives. Conversely, they may attempt to gain control of all of life’s circumstances, including those that are beyond anyone’s control. Control can be applied to emotions, behaviors, or events. A driver struck by a vehicle may think “I can’t control other drivers, so I have no power to control my safety while driving,” and hence give up driving. While there are things that are beyond our control, this extreme thought ignores things that we can control, such as wearing seatbelts or having the vehicle’s brakes regularly serviced.
Evidence-based cognitive-behavioral therapies for posttraumatic stress disorder (PTSD) may employ cognitive restructuring. This psychotherapeutic technique entails recognizing and correcting maladaptive, inaccurate thoughts that perpetuate illness.1 For example, a clinician helps a patient recognize that the negative thought “Nobody loves me” following a romantic breakup is an overgeneralization. The patient is taught to self-correct this to “While my ex-girlfriend doesn’t love me, others do. It only feels like nobody loves me.”2
We introduce the acronym I STEP to help clinicians recognize several common distorted thoughts in PTSD. These tend to occur within stereotyped themes in PTSD,3 as outlined and illustrated below. Recognizing distorted thoughts in these patients will help clinicians understand and address psychological distress following trauma.
Intimacy/In-touch. Intimacy involves comfort in relationships, including but not limited to sexual intimacy. This requires being in touch emotionally with self and others. In trauma involving loss, fear of further loss may impair intimacy with others. Difficulty with self-intimacy impairs commitment to life’s goals and prompts unhelpful avoidance behaviors, such as difficulty being alone or self-injurious use of drugs or alcohol. Comfort in spending some portion of time alone with one’s thoughts and emotions is a life skill necessary to attain optimum function. Patients who are unable to tolerate their own emotions without constant company might have excessive anxiety when social supports are otherwise occupied. Such patients might seek excessive and repeated reassurance rather than learning to tolerate their own emotions and thoughts. They would then find it difficult to engage successfully in solo activities.
Safety. After trauma, patients may view themselves and others as unsafe, and may overestimate risk. For example, a pedestrian who is struck by a vehicle may believe that crossing a street will again result in getting hit by a car without appreciating that people frequently cross streets without injury or that crossing cautiously is an essential life skill. Parents who have suffered from trauma may unduly believe that their children are in danger when engaging in an activity generally considered to be safe. This may create challenges in parenting and impede their children’s ability to develop a sense of independence.
Trust. Trauma victims may unfairly blame themselves, leading them to mistrust their own judgment. Such patients may have difficulty making decisions confidently and independently, such as choosing a job or a romantic partner. When traumatized by another person or people, it can be difficult to maintain positive views of others or to accept others’ positive behaviors as genuine. For example, a common reaction following rape may be a generalized mistrust of all men.
Esteem. Patients’ self-esteem may suffer following trauma due to irrational self-blame or believing the “just world hypothesis”—the idea that bad things only happen to bad people. For example, a patient who suffers an assault by an acquaintance might think “I must be stupid if I couldn’t figure out that my friend was dangerous.”
Power. Traumatic events usually occur outside of one’s control. Survivors of trauma may lose confidence in their ability to control any aspect of their lives. Conversely, they may attempt to gain control of all of life’s circumstances, including those that are beyond anyone’s control. Control can be applied to emotions, behaviors, or events. A driver struck by a vehicle may think “I can’t control other drivers, so I have no power to control my safety while driving,” and hence give up driving. While there are things that are beyond our control, this extreme thought ignores things that we can control, such as wearing seatbelts or having the vehicle’s brakes regularly serviced.
1. Wenzel A. Basic strategies of cognitive behavioral therapy. Psychiatr Clin North Am. 2017;40(4):597-609.
2. Beck J. Cognitive behavioral therapy: basics and beyond. 2nd ed. The Guilford Press; 2011.
3. Resick PA, Monson CM, Chard KM. Cognitive processing therapy for PTSD. A comprehensive manual. The Guilford Press; 2017.
1. Wenzel A. Basic strategies of cognitive behavioral therapy. Psychiatr Clin North Am. 2017;40(4):597-609.
2. Beck J. Cognitive behavioral therapy: basics and beyond. 2nd ed. The Guilford Press; 2011.
3. Resick PA, Monson CM, Chard KM. Cognitive processing therapy for PTSD. A comprehensive manual. The Guilford Press; 2017.
Managing a COVID-19–positive psychiatric patient on a medical unit
With the COVID-19 pandemic turning the world on its head, we have seen more first-episode psychotic breaks and quick deterioration in previously stable patients. Early in the pandemic, care was particularly complicated for psychiatric patients who had been infected with the virus. Many of these patients required immediate psychiatric hospitalization. At that time, many community hospital psychiatric inpatient units did not have the capacity, staffing, or infrastructure to safely admit such patients, so they needed to be managed on a medical unit. Here, I discuss the case of a COVID-19–positive woman with psychiatric illness who we managed while she was in quarantine on a medical unit.
Case report
Early in the COVID-19 pandemic, Ms. B, a 35-year-old teacher with a history of depression, was evaluated in the emergency department for bizarre behavior and paranoid delusions regarding her family. Initial laboratory and imaging testing was negative for any potential medical causes of her psychiatric symptoms. Psychiatric hospitalization was recommended, but before Ms. B could be transferred to the psychiatric unit, she tested positive for COVID-19. At that time, our community hospital did not have a designated wing on our psychiatric unit for patients infected with COVID-19. Thus, Ms. B was admitted to the medical floor, where she was quarantined in her room. She would need to remain asymptomatic and test negative for COVID-19 before she could be transferred to the psychiatric unit.
Upon arriving at the medical unit, Ms. B was hostile and uncooperative. She frequently attempted to leave her room and required restraints throughout the day. Our consultation-liaison (CL) team was consulted to assist in managing her. During the initial interview, we noticed that she had covered all 4 walls of her room with papers filled with handwritten notes. Ms. B had cut her gown to expose her stomach and legs. She had pressured speech, tangential thinking, and was religiously preoccupied. She denied any visual and auditory hallucinations, but her persecutory delusions involving her family persisted. We believed that her signs and symptoms were consistent with a manic episode from underlying, and likely undiagnosed, bipolar I disorder that was precipitated by her COVID-19 infection.
We first addressed Ms. B’s and the staff’s safety by transferring her to a larger room with a vestibule at the end of the hallway so she had more room to walk and minimal exposure to the stimuli of the medical unit. We initiated one-on-one observation to redirect her and prevent elopement. We incentivized her cooperation with staff by providing her with paper, pencils, reading material, and phone privileges. We started oral risperidone 2 mg twice daily and lorazepam 2 mg 3 times daily for short-term behavioral control and acute treatment of her symptoms, with the goal of deferring additional treatment decisions to the inpatient psychiatry team after she was transferred to the psychiatric unit. Ms. B’s agitation and impulsivity improved. She began participating with the medical team and was eventually transferred out of our medical unit to a psychiatric unit at a different facility.
COVID-19 and psychiatric illness: Clinical concerns
While infection from COVID-19 and widespread social distancing of the general population have been linked to depression and anxiety, manic and psychotic symptoms secondary to the COVID-19 pandemic have not been well described. The association between influenza infection and psychosis has been reported since the Spanish Flu pandemic,1 but there is limited data on the association between COVID-19 and psychosis. A review of 14 studies found that 0.9% to 4% of people exposed to a virus during an epidemic or pandemic develop psychosis or psychotic symptoms.1 Psychosis was associated with viral exposure, treatments used to manage the infection (steroid therapy), and psychosocial stress. This study also found that treatment with low doses of antipsychotic medication—notably aripiprazole—seemed to have been effective.1
Nonetheless, it is important to keep in mind a thorough differential diagnosis and rule out any potential organic etiologies in a COVID-19–positive patient who presents with psychiatric symptoms.2 For Ms. B, we began by ruling out drug-induced psychosis and electrolyte imbalance, and obtained brain imaging to rule out malignancy. We considered an interictal behavior syndrome of temporal lobe epilepsy, a neuropsychiatric disorder characterized by alterations in sexual behavior, religiosity, and extensive and compulsive writing and drawing.3 Neurology was consulted to evaluate the patient and possibly use EEG to detect interictal spikes, a tall task given the patient’s restlessness and paranoia. Ultimately, we determined the patient was most likely exhibiting symptoms of previously undetected bipolar disorder.
Managing patients with psychiatric illness on a medical floor during a pandemic such as COVID-19 requires the psychiatrist to truly serve as a consultant and liaison between the patient and the treatment team.4 Clinical management should address both infection control and psychiatric symptoms.5 We visited with Ms. B frequently, provided psychoeducation, engaged her in treatment, and updated her on the treatment plan.
As the medical world continues to adjust to treating patients during the pandemic, CL psychiatrists may be tasked with managing patients with acute psychiatric illness on the medical unit while they await transfer to a psychiatric unit. A creative, multifaceted, and team-based approach is key to ensure effective care and safety for all involved.
1. Brown E, Gray R, Lo Monaco S, et al. The potential impact of COVID-19 on psychosis: a rapid review of contemporary epidemic and pandemic research. Schizophr Res. 2020;222:79-87. doi:10.1016/j.schres.2020.05.005
2. Byrne P. Managing the acute psychotic episode. BMJ. 2007;334(7595):686-692. doi:10.1136/bmj.39148.668160.80
3. Waxman SG, Geschwind N. The interictal behavior syndrome of temporal lobe epilepsy. Arch Gen Psychiatry. 1975;32(12):1580-1586. doi:10.1001/archpsyc.1975.01760300118011
4. Stern TA, Freudenreich O, Smith FA, et al. Psychotic patients. In: Massachusetts General Hospital: Handbook of General Hospital Psychiatry. Mosby; 1997:109-121.
5. Deshpande S, Livingstone A. First-onset psychosis in older adults: social isolation influence during COVID pandemic—a UK case series. Progress in Neurology and Psychiatry. 2021;25(1):14-18. doi:10.1002/pnp.692
With the COVID-19 pandemic turning the world on its head, we have seen more first-episode psychotic breaks and quick deterioration in previously stable patients. Early in the pandemic, care was particularly complicated for psychiatric patients who had been infected with the virus. Many of these patients required immediate psychiatric hospitalization. At that time, many community hospital psychiatric inpatient units did not have the capacity, staffing, or infrastructure to safely admit such patients, so they needed to be managed on a medical unit. Here, I discuss the case of a COVID-19–positive woman with psychiatric illness who we managed while she was in quarantine on a medical unit.
Case report
Early in the COVID-19 pandemic, Ms. B, a 35-year-old teacher with a history of depression, was evaluated in the emergency department for bizarre behavior and paranoid delusions regarding her family. Initial laboratory and imaging testing was negative for any potential medical causes of her psychiatric symptoms. Psychiatric hospitalization was recommended, but before Ms. B could be transferred to the psychiatric unit, she tested positive for COVID-19. At that time, our community hospital did not have a designated wing on our psychiatric unit for patients infected with COVID-19. Thus, Ms. B was admitted to the medical floor, where she was quarantined in her room. She would need to remain asymptomatic and test negative for COVID-19 before she could be transferred to the psychiatric unit.
Upon arriving at the medical unit, Ms. B was hostile and uncooperative. She frequently attempted to leave her room and required restraints throughout the day. Our consultation-liaison (CL) team was consulted to assist in managing her. During the initial interview, we noticed that she had covered all 4 walls of her room with papers filled with handwritten notes. Ms. B had cut her gown to expose her stomach and legs. She had pressured speech, tangential thinking, and was religiously preoccupied. She denied any visual and auditory hallucinations, but her persecutory delusions involving her family persisted. We believed that her signs and symptoms were consistent with a manic episode from underlying, and likely undiagnosed, bipolar I disorder that was precipitated by her COVID-19 infection.
We first addressed Ms. B’s and the staff’s safety by transferring her to a larger room with a vestibule at the end of the hallway so she had more room to walk and minimal exposure to the stimuli of the medical unit. We initiated one-on-one observation to redirect her and prevent elopement. We incentivized her cooperation with staff by providing her with paper, pencils, reading material, and phone privileges. We started oral risperidone 2 mg twice daily and lorazepam 2 mg 3 times daily for short-term behavioral control and acute treatment of her symptoms, with the goal of deferring additional treatment decisions to the inpatient psychiatry team after she was transferred to the psychiatric unit. Ms. B’s agitation and impulsivity improved. She began participating with the medical team and was eventually transferred out of our medical unit to a psychiatric unit at a different facility.
COVID-19 and psychiatric illness: Clinical concerns
While infection from COVID-19 and widespread social distancing of the general population have been linked to depression and anxiety, manic and psychotic symptoms secondary to the COVID-19 pandemic have not been well described. The association between influenza infection and psychosis has been reported since the Spanish Flu pandemic,1 but there is limited data on the association between COVID-19 and psychosis. A review of 14 studies found that 0.9% to 4% of people exposed to a virus during an epidemic or pandemic develop psychosis or psychotic symptoms.1 Psychosis was associated with viral exposure, treatments used to manage the infection (steroid therapy), and psychosocial stress. This study also found that treatment with low doses of antipsychotic medication—notably aripiprazole—seemed to have been effective.1
Nonetheless, it is important to keep in mind a thorough differential diagnosis and rule out any potential organic etiologies in a COVID-19–positive patient who presents with psychiatric symptoms.2 For Ms. B, we began by ruling out drug-induced psychosis and electrolyte imbalance, and obtained brain imaging to rule out malignancy. We considered an interictal behavior syndrome of temporal lobe epilepsy, a neuropsychiatric disorder characterized by alterations in sexual behavior, religiosity, and extensive and compulsive writing and drawing.3 Neurology was consulted to evaluate the patient and possibly use EEG to detect interictal spikes, a tall task given the patient’s restlessness and paranoia. Ultimately, we determined the patient was most likely exhibiting symptoms of previously undetected bipolar disorder.
Managing patients with psychiatric illness on a medical floor during a pandemic such as COVID-19 requires the psychiatrist to truly serve as a consultant and liaison between the patient and the treatment team.4 Clinical management should address both infection control and psychiatric symptoms.5 We visited with Ms. B frequently, provided psychoeducation, engaged her in treatment, and updated her on the treatment plan.
As the medical world continues to adjust to treating patients during the pandemic, CL psychiatrists may be tasked with managing patients with acute psychiatric illness on the medical unit while they await transfer to a psychiatric unit. A creative, multifaceted, and team-based approach is key to ensure effective care and safety for all involved.
With the COVID-19 pandemic turning the world on its head, we have seen more first-episode psychotic breaks and quick deterioration in previously stable patients. Early in the pandemic, care was particularly complicated for psychiatric patients who had been infected with the virus. Many of these patients required immediate psychiatric hospitalization. At that time, many community hospital psychiatric inpatient units did not have the capacity, staffing, or infrastructure to safely admit such patients, so they needed to be managed on a medical unit. Here, I discuss the case of a COVID-19–positive woman with psychiatric illness who we managed while she was in quarantine on a medical unit.
Case report
Early in the COVID-19 pandemic, Ms. B, a 35-year-old teacher with a history of depression, was evaluated in the emergency department for bizarre behavior and paranoid delusions regarding her family. Initial laboratory and imaging testing was negative for any potential medical causes of her psychiatric symptoms. Psychiatric hospitalization was recommended, but before Ms. B could be transferred to the psychiatric unit, she tested positive for COVID-19. At that time, our community hospital did not have a designated wing on our psychiatric unit for patients infected with COVID-19. Thus, Ms. B was admitted to the medical floor, where she was quarantined in her room. She would need to remain asymptomatic and test negative for COVID-19 before she could be transferred to the psychiatric unit.
Upon arriving at the medical unit, Ms. B was hostile and uncooperative. She frequently attempted to leave her room and required restraints throughout the day. Our consultation-liaison (CL) team was consulted to assist in managing her. During the initial interview, we noticed that she had covered all 4 walls of her room with papers filled with handwritten notes. Ms. B had cut her gown to expose her stomach and legs. She had pressured speech, tangential thinking, and was religiously preoccupied. She denied any visual and auditory hallucinations, but her persecutory delusions involving her family persisted. We believed that her signs and symptoms were consistent with a manic episode from underlying, and likely undiagnosed, bipolar I disorder that was precipitated by her COVID-19 infection.
We first addressed Ms. B’s and the staff’s safety by transferring her to a larger room with a vestibule at the end of the hallway so she had more room to walk and minimal exposure to the stimuli of the medical unit. We initiated one-on-one observation to redirect her and prevent elopement. We incentivized her cooperation with staff by providing her with paper, pencils, reading material, and phone privileges. We started oral risperidone 2 mg twice daily and lorazepam 2 mg 3 times daily for short-term behavioral control and acute treatment of her symptoms, with the goal of deferring additional treatment decisions to the inpatient psychiatry team after she was transferred to the psychiatric unit. Ms. B’s agitation and impulsivity improved. She began participating with the medical team and was eventually transferred out of our medical unit to a psychiatric unit at a different facility.
COVID-19 and psychiatric illness: Clinical concerns
While infection from COVID-19 and widespread social distancing of the general population have been linked to depression and anxiety, manic and psychotic symptoms secondary to the COVID-19 pandemic have not been well described. The association between influenza infection and psychosis has been reported since the Spanish Flu pandemic,1 but there is limited data on the association between COVID-19 and psychosis. A review of 14 studies found that 0.9% to 4% of people exposed to a virus during an epidemic or pandemic develop psychosis or psychotic symptoms.1 Psychosis was associated with viral exposure, treatments used to manage the infection (steroid therapy), and psychosocial stress. This study also found that treatment with low doses of antipsychotic medication—notably aripiprazole—seemed to have been effective.1
Nonetheless, it is important to keep in mind a thorough differential diagnosis and rule out any potential organic etiologies in a COVID-19–positive patient who presents with psychiatric symptoms.2 For Ms. B, we began by ruling out drug-induced psychosis and electrolyte imbalance, and obtained brain imaging to rule out malignancy. We considered an interictal behavior syndrome of temporal lobe epilepsy, a neuropsychiatric disorder characterized by alterations in sexual behavior, religiosity, and extensive and compulsive writing and drawing.3 Neurology was consulted to evaluate the patient and possibly use EEG to detect interictal spikes, a tall task given the patient’s restlessness and paranoia. Ultimately, we determined the patient was most likely exhibiting symptoms of previously undetected bipolar disorder.
Managing patients with psychiatric illness on a medical floor during a pandemic such as COVID-19 requires the psychiatrist to truly serve as a consultant and liaison between the patient and the treatment team.4 Clinical management should address both infection control and psychiatric symptoms.5 We visited with Ms. B frequently, provided psychoeducation, engaged her in treatment, and updated her on the treatment plan.
As the medical world continues to adjust to treating patients during the pandemic, CL psychiatrists may be tasked with managing patients with acute psychiatric illness on the medical unit while they await transfer to a psychiatric unit. A creative, multifaceted, and team-based approach is key to ensure effective care and safety for all involved.
1. Brown E, Gray R, Lo Monaco S, et al. The potential impact of COVID-19 on psychosis: a rapid review of contemporary epidemic and pandemic research. Schizophr Res. 2020;222:79-87. doi:10.1016/j.schres.2020.05.005
2. Byrne P. Managing the acute psychotic episode. BMJ. 2007;334(7595):686-692. doi:10.1136/bmj.39148.668160.80
3. Waxman SG, Geschwind N. The interictal behavior syndrome of temporal lobe epilepsy. Arch Gen Psychiatry. 1975;32(12):1580-1586. doi:10.1001/archpsyc.1975.01760300118011
4. Stern TA, Freudenreich O, Smith FA, et al. Psychotic patients. In: Massachusetts General Hospital: Handbook of General Hospital Psychiatry. Mosby; 1997:109-121.
5. Deshpande S, Livingstone A. First-onset psychosis in older adults: social isolation influence during COVID pandemic—a UK case series. Progress in Neurology and Psychiatry. 2021;25(1):14-18. doi:10.1002/pnp.692
1. Brown E, Gray R, Lo Monaco S, et al. The potential impact of COVID-19 on psychosis: a rapid review of contemporary epidemic and pandemic research. Schizophr Res. 2020;222:79-87. doi:10.1016/j.schres.2020.05.005
2. Byrne P. Managing the acute psychotic episode. BMJ. 2007;334(7595):686-692. doi:10.1136/bmj.39148.668160.80
3. Waxman SG, Geschwind N. The interictal behavior syndrome of temporal lobe epilepsy. Arch Gen Psychiatry. 1975;32(12):1580-1586. doi:10.1001/archpsyc.1975.01760300118011
4. Stern TA, Freudenreich O, Smith FA, et al. Psychotic patients. In: Massachusetts General Hospital: Handbook of General Hospital Psychiatry. Mosby; 1997:109-121.
5. Deshpande S, Livingstone A. First-onset psychosis in older adults: social isolation influence during COVID pandemic—a UK case series. Progress in Neurology and Psychiatry. 2021;25(1):14-18. doi:10.1002/pnp.692
Microdosing psychedelics: Untapped potential in psychiatry?
In her month-long memoir, A Really Good Day: How Microdosing Made a Mega Difference in My Mood, My Marriage, and My Life (Knopf, 2017), author Ayelet Waldman turns herself into a one-woman experiment.
Over a single month she takes one-tenth of a recreational dose of LSD every third day. She plots her emotions, her productivity, and her pain along the way. Ms. Waldman obtains the LSD in a single vial, enough for 10 doses, from a researcher, who is retiring. What she’s looking for, she tells the reader, is a really good day – something that has been elusive in her turbulent life.
Although psychedelics remain illegal for both recreational and therapeutic use, they are increasingly being studied at academic centers, and there is hope that they will offer something that our traditional medications might not. However, these are not “micro” doses, but full doses of psychedelic agents that induce clinically-monitored “trips” in order to treat conditions such as depression, anorexia nervosa, or for smoking cessation, to name just a few.
Yet
Because these drugs are illegal under most circumstances, many of the studies involve surveys of users in their natural environments who are already microdosing in an uncontrolled manner. In a 2019 study published in PLOS One, Vince Polito and Richard Stevenson, from Macquarie University, Sydney, gave daily surveys of psychological functioning to 98 microdosers over 6 weeks. Several participants were excluded for using doses that were too high or for concurrent use of other illicit substances.
Whereas the authors found that many people claimed to have positive experiences, there was an increase in neuroticism in some of the subjects. There was no control group and no uniformity to what the subject claimed to be ingesting with regard to dose, frequency, substance, or verification of the chemical content.
University of Chicago neuroscientist Harriet De Wit, PhD, leads one of the few laboratories that conducts controlled, double-blind studies looking at microdosing LSD.
“With microdosing there are expectations, and we don’t know if it’s the expectation or the agent that is making a difference,” she explained. And when asked who in her experience is experimenting with microdosing psychedelics, she expounded “Everybody under the sun!”
Dr. De Wit notes that people microdose to increase their creativity, productivity, focus, and energy, to heighten their spiritual awareness, improve empathy and social relational skills, and to improve their mood – all purported benefits of low-dose psychedelics.
Her group published a study in Addiction Biology, in which 39 subjects were administered low doses of LSD four times over 2 weeks. To address the issues of expectation, the subjects were not told they were participating in a study of hallucinogens specifically but were instead given a list of pharmaceuticals in different classes that they might be given. Microdoses of LSD did not improve either mood or performance, but they did appear to be safe, and they produced no adverse effects.
To date, studies on microdosing have looked at their effects on healthy populations, and the practice has been associated with “Silicon Valley techies” looking for performance enhancement. Ms. Waldman, however, is different.
She is open about her diagnosis of bipolar disorder, and her long history with therapy and medications. As she describes herself in the beginning of her book, she is emotionally uncomfortable, and both irritable and reactive to the point that her life is propelled by interpersonal chaos. In her uncontrolled ‘study,’ she is an N of 1, and she is pleased with the results. Microdosing, she believes, helped her become less irritable, more resilient, and in fact, have some very good days.
By the end of her memoir, she was looking for a way to continue microdosing but was unsure how to safely obtain more LSD and be certain of its purity. Her experience does raise the possibility that microdoses may have therapeutic benefits in people with certain psychiatric conditions, but this has yet to be studied.
J. Raymond DePaulo Jr., MD, is the chair of the National Network of Depression Centers and a distinguished service professor at Johns Hopkins Hospital, Baltimore. “Microdosing of psychedelics is very problematic for two equally serious reasons,” he cautioned. “There is no control over what it is that people are actually taking, it is completely unstudied scientifically, and there is no agreement on what a ‘micro’ dose is.”
He noted that one of his patients thought he was taking psilocybin. A chemical analysis was done that revealed the agent to contain a combination of THC, a stimulant, morphine, and fluoxetine. There wasn’t a trace of psilocybin. “Mislabeling is the rule, not the exception,” Dr. DePaulo has concluded.
He also believes the placebo effect has a powerful role with microdosing. “It’s not working because of what is in the pill, more likely it is working because of what is advertised to be in it.”
Ms. De Wit noted that when she started her study, she tried to find people who were elevated on measures of depression or anxiety, but she was not looking for a specific clinical population of patients with these clinical diagnoses. “We found a handful of people, and they improved, but so did those in the placebo group; they all got better.”
Psychedelic agents interact with antidepressants, so subjects in controlled studies need to go off their medications before enrolling – this is a limiting factor in studies of both macro- and microdosing. Ms. De Wit also notes that there are logistical and practical obstacles – it is difficult to get approval to use these agents, and the patients have to remain in the lab and be observed for several hours after they are administered, just as with standard doses.
As might be expected, data collection and anecdotal microdosing experiences are rampant on the internet. The social media forum Reddit alone boasts 192,000 members in its microdosing group, while Imperial College London invites microdosers to take part in surveys intended to add to the body of knowledge. But despite its popularity, there is little in the way of prospective, agent-verified, placebo-controlled research exploring whether or not microdosing is truly beneficial beyond just anecdotal evidence.
Perhaps microdosing is a fad, or perhaps it offers some benefits to some people. Given the current interest in the therapeutic uses of psychedelics, it would be useful to have controlled studies of lower doses that don’t carry the risk of “bad trips.”
Certainly, psychiatry could use more agents to address mental health issues, and society might benefit from the use of agents that are proven to be evidence-based options for improving creativity and productivity. Anything that has potential to reduce psychiatric suffering seems worthy of further study to delineate which populations could be helped or harmed.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins in Baltimore. Dr. Miller has no conflicts of interest.
A version of this article first appeared on Medscape.com.
In her month-long memoir, A Really Good Day: How Microdosing Made a Mega Difference in My Mood, My Marriage, and My Life (Knopf, 2017), author Ayelet Waldman turns herself into a one-woman experiment.
Over a single month she takes one-tenth of a recreational dose of LSD every third day. She plots her emotions, her productivity, and her pain along the way. Ms. Waldman obtains the LSD in a single vial, enough for 10 doses, from a researcher, who is retiring. What she’s looking for, she tells the reader, is a really good day – something that has been elusive in her turbulent life.
Although psychedelics remain illegal for both recreational and therapeutic use, they are increasingly being studied at academic centers, and there is hope that they will offer something that our traditional medications might not. However, these are not “micro” doses, but full doses of psychedelic agents that induce clinically-monitored “trips” in order to treat conditions such as depression, anorexia nervosa, or for smoking cessation, to name just a few.
Yet
Because these drugs are illegal under most circumstances, many of the studies involve surveys of users in their natural environments who are already microdosing in an uncontrolled manner. In a 2019 study published in PLOS One, Vince Polito and Richard Stevenson, from Macquarie University, Sydney, gave daily surveys of psychological functioning to 98 microdosers over 6 weeks. Several participants were excluded for using doses that were too high or for concurrent use of other illicit substances.
Whereas the authors found that many people claimed to have positive experiences, there was an increase in neuroticism in some of the subjects. There was no control group and no uniformity to what the subject claimed to be ingesting with regard to dose, frequency, substance, or verification of the chemical content.
University of Chicago neuroscientist Harriet De Wit, PhD, leads one of the few laboratories that conducts controlled, double-blind studies looking at microdosing LSD.
“With microdosing there are expectations, and we don’t know if it’s the expectation or the agent that is making a difference,” she explained. And when asked who in her experience is experimenting with microdosing psychedelics, she expounded “Everybody under the sun!”
Dr. De Wit notes that people microdose to increase their creativity, productivity, focus, and energy, to heighten their spiritual awareness, improve empathy and social relational skills, and to improve their mood – all purported benefits of low-dose psychedelics.
Her group published a study in Addiction Biology, in which 39 subjects were administered low doses of LSD four times over 2 weeks. To address the issues of expectation, the subjects were not told they were participating in a study of hallucinogens specifically but were instead given a list of pharmaceuticals in different classes that they might be given. Microdoses of LSD did not improve either mood or performance, but they did appear to be safe, and they produced no adverse effects.
To date, studies on microdosing have looked at their effects on healthy populations, and the practice has been associated with “Silicon Valley techies” looking for performance enhancement. Ms. Waldman, however, is different.
She is open about her diagnosis of bipolar disorder, and her long history with therapy and medications. As she describes herself in the beginning of her book, she is emotionally uncomfortable, and both irritable and reactive to the point that her life is propelled by interpersonal chaos. In her uncontrolled ‘study,’ she is an N of 1, and she is pleased with the results. Microdosing, she believes, helped her become less irritable, more resilient, and in fact, have some very good days.
By the end of her memoir, she was looking for a way to continue microdosing but was unsure how to safely obtain more LSD and be certain of its purity. Her experience does raise the possibility that microdoses may have therapeutic benefits in people with certain psychiatric conditions, but this has yet to be studied.
J. Raymond DePaulo Jr., MD, is the chair of the National Network of Depression Centers and a distinguished service professor at Johns Hopkins Hospital, Baltimore. “Microdosing of psychedelics is very problematic for two equally serious reasons,” he cautioned. “There is no control over what it is that people are actually taking, it is completely unstudied scientifically, and there is no agreement on what a ‘micro’ dose is.”
He noted that one of his patients thought he was taking psilocybin. A chemical analysis was done that revealed the agent to contain a combination of THC, a stimulant, morphine, and fluoxetine. There wasn’t a trace of psilocybin. “Mislabeling is the rule, not the exception,” Dr. DePaulo has concluded.
He also believes the placebo effect has a powerful role with microdosing. “It’s not working because of what is in the pill, more likely it is working because of what is advertised to be in it.”
Ms. De Wit noted that when she started her study, she tried to find people who were elevated on measures of depression or anxiety, but she was not looking for a specific clinical population of patients with these clinical diagnoses. “We found a handful of people, and they improved, but so did those in the placebo group; they all got better.”
Psychedelic agents interact with antidepressants, so subjects in controlled studies need to go off their medications before enrolling – this is a limiting factor in studies of both macro- and microdosing. Ms. De Wit also notes that there are logistical and practical obstacles – it is difficult to get approval to use these agents, and the patients have to remain in the lab and be observed for several hours after they are administered, just as with standard doses.
As might be expected, data collection and anecdotal microdosing experiences are rampant on the internet. The social media forum Reddit alone boasts 192,000 members in its microdosing group, while Imperial College London invites microdosers to take part in surveys intended to add to the body of knowledge. But despite its popularity, there is little in the way of prospective, agent-verified, placebo-controlled research exploring whether or not microdosing is truly beneficial beyond just anecdotal evidence.
Perhaps microdosing is a fad, or perhaps it offers some benefits to some people. Given the current interest in the therapeutic uses of psychedelics, it would be useful to have controlled studies of lower doses that don’t carry the risk of “bad trips.”
Certainly, psychiatry could use more agents to address mental health issues, and society might benefit from the use of agents that are proven to be evidence-based options for improving creativity and productivity. Anything that has potential to reduce psychiatric suffering seems worthy of further study to delineate which populations could be helped or harmed.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins in Baltimore. Dr. Miller has no conflicts of interest.
A version of this article first appeared on Medscape.com.
In her month-long memoir, A Really Good Day: How Microdosing Made a Mega Difference in My Mood, My Marriage, and My Life (Knopf, 2017), author Ayelet Waldman turns herself into a one-woman experiment.
Over a single month she takes one-tenth of a recreational dose of LSD every third day. She plots her emotions, her productivity, and her pain along the way. Ms. Waldman obtains the LSD in a single vial, enough for 10 doses, from a researcher, who is retiring. What she’s looking for, she tells the reader, is a really good day – something that has been elusive in her turbulent life.
Although psychedelics remain illegal for both recreational and therapeutic use, they are increasingly being studied at academic centers, and there is hope that they will offer something that our traditional medications might not. However, these are not “micro” doses, but full doses of psychedelic agents that induce clinically-monitored “trips” in order to treat conditions such as depression, anorexia nervosa, or for smoking cessation, to name just a few.
Yet
Because these drugs are illegal under most circumstances, many of the studies involve surveys of users in their natural environments who are already microdosing in an uncontrolled manner. In a 2019 study published in PLOS One, Vince Polito and Richard Stevenson, from Macquarie University, Sydney, gave daily surveys of psychological functioning to 98 microdosers over 6 weeks. Several participants were excluded for using doses that were too high or for concurrent use of other illicit substances.
Whereas the authors found that many people claimed to have positive experiences, there was an increase in neuroticism in some of the subjects. There was no control group and no uniformity to what the subject claimed to be ingesting with regard to dose, frequency, substance, or verification of the chemical content.
University of Chicago neuroscientist Harriet De Wit, PhD, leads one of the few laboratories that conducts controlled, double-blind studies looking at microdosing LSD.
“With microdosing there are expectations, and we don’t know if it’s the expectation or the agent that is making a difference,” she explained. And when asked who in her experience is experimenting with microdosing psychedelics, she expounded “Everybody under the sun!”
Dr. De Wit notes that people microdose to increase their creativity, productivity, focus, and energy, to heighten their spiritual awareness, improve empathy and social relational skills, and to improve their mood – all purported benefits of low-dose psychedelics.
Her group published a study in Addiction Biology, in which 39 subjects were administered low doses of LSD four times over 2 weeks. To address the issues of expectation, the subjects were not told they were participating in a study of hallucinogens specifically but were instead given a list of pharmaceuticals in different classes that they might be given. Microdoses of LSD did not improve either mood or performance, but they did appear to be safe, and they produced no adverse effects.
To date, studies on microdosing have looked at their effects on healthy populations, and the practice has been associated with “Silicon Valley techies” looking for performance enhancement. Ms. Waldman, however, is different.
She is open about her diagnosis of bipolar disorder, and her long history with therapy and medications. As she describes herself in the beginning of her book, she is emotionally uncomfortable, and both irritable and reactive to the point that her life is propelled by interpersonal chaos. In her uncontrolled ‘study,’ she is an N of 1, and she is pleased with the results. Microdosing, she believes, helped her become less irritable, more resilient, and in fact, have some very good days.
By the end of her memoir, she was looking for a way to continue microdosing but was unsure how to safely obtain more LSD and be certain of its purity. Her experience does raise the possibility that microdoses may have therapeutic benefits in people with certain psychiatric conditions, but this has yet to be studied.
J. Raymond DePaulo Jr., MD, is the chair of the National Network of Depression Centers and a distinguished service professor at Johns Hopkins Hospital, Baltimore. “Microdosing of psychedelics is very problematic for two equally serious reasons,” he cautioned. “There is no control over what it is that people are actually taking, it is completely unstudied scientifically, and there is no agreement on what a ‘micro’ dose is.”
He noted that one of his patients thought he was taking psilocybin. A chemical analysis was done that revealed the agent to contain a combination of THC, a stimulant, morphine, and fluoxetine. There wasn’t a trace of psilocybin. “Mislabeling is the rule, not the exception,” Dr. DePaulo has concluded.
He also believes the placebo effect has a powerful role with microdosing. “It’s not working because of what is in the pill, more likely it is working because of what is advertised to be in it.”
Ms. De Wit noted that when she started her study, she tried to find people who were elevated on measures of depression or anxiety, but she was not looking for a specific clinical population of patients with these clinical diagnoses. “We found a handful of people, and they improved, but so did those in the placebo group; they all got better.”
Psychedelic agents interact with antidepressants, so subjects in controlled studies need to go off their medications before enrolling – this is a limiting factor in studies of both macro- and microdosing. Ms. De Wit also notes that there are logistical and practical obstacles – it is difficult to get approval to use these agents, and the patients have to remain in the lab and be observed for several hours after they are administered, just as with standard doses.
As might be expected, data collection and anecdotal microdosing experiences are rampant on the internet. The social media forum Reddit alone boasts 192,000 members in its microdosing group, while Imperial College London invites microdosers to take part in surveys intended to add to the body of knowledge. But despite its popularity, there is little in the way of prospective, agent-verified, placebo-controlled research exploring whether or not microdosing is truly beneficial beyond just anecdotal evidence.
Perhaps microdosing is a fad, or perhaps it offers some benefits to some people. Given the current interest in the therapeutic uses of psychedelics, it would be useful to have controlled studies of lower doses that don’t carry the risk of “bad trips.”
Certainly, psychiatry could use more agents to address mental health issues, and society might benefit from the use of agents that are proven to be evidence-based options for improving creativity and productivity. Anything that has potential to reduce psychiatric suffering seems worthy of further study to delineate which populations could be helped or harmed.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins in Baltimore. Dr. Miller has no conflicts of interest.
A version of this article first appeared on Medscape.com.
‘Pre-death grief’ is a real, but overlooked, syndrome
When an individual develops a terminal illness, those closest to them often start to grieve long before the person dies. Although a common syndrome, it often goes unrecognized and unaddressed.
A new review proposes a way of defining this specific type of grief in the hope that better, more precise descriptive categories will inform therapeutic interventions to help those facing a life-changing loss.
, lead author Jonathan Singer, PhD, visiting assistant professor of clinical psychology, Texas Tech University, Lubbock, told this news organization.
“We proposed the overarching term ‘pre-death grief,’ with the two separate constructs under pre-death grief – anticipatory grief [AG] and illness-related grief [IRG],” he said. “These definitions provide the field with uniform constructs to advance the study of grief before the death of an individual with a life-limiting illness.
“Research examining grief experienced by family members prior to an individual’s death to a life-limiting illness revealed wide variation in the terminology used and characterization of such grief across studies,”
The study was published online Feb. 23 in Palliative Medicine.
‘Typical’ versus ‘impairing’ grief
“Most deaths worldwide are attributed to a chronic or life-limiting Illness,” the authors write. The experience of grief before the loss of a family member “has been studied frequently, but there have been conceptualization issues, which is problematic, as it hinders the potential advancement of the field in differentiating typical grief from more impairing grief before the death,” Dr. Singer said. “Further complicating the picture is the sheer number of terms used to describe grief before death.”
Dr. Singer said that when he started conducting research in this field, he “realized someone had to combine the articles that have been published in order to create definitions that will advance the field, so risk and protective factors could be identified and interventions could be tested.”
For the current study, the investigators searched six databases to find research that “evaluated family members’ or friends’ grief related to an individual currently living with a life-limiting illness.” They excluded studies that evaluated grief after death.
Of 9,568 records reviewed, the researchers selected 134 full-text articles that met inclusion criteria. Most studies (57.46%) were quantitative; 23.88% were qualitative, and 17.91% used mixed methods. Most studies were retrospective, although 14.93% were prospective, and 3% included both prospective and retrospective analyses.
Most participants reported that the family member/friend was diagnosed either with “late-stage dementia” or “advanced cancer.” The majority (58%) were adult children of the individual with the illness, followed by spouses/partners (28.1%) and other relatives/friends (13.9%) in studies that reported the relationship to the participant and the person with the illness.
Various scales were used in the studies to measure grief, particularly the Marwit-Meuser-Caregiver Grief Inventory (n = 28), the Anticipatory Grief Scale (n = 18), and the Prolonged Grief–12 (n = 13).
A new name
Owing to the large number of articles included in the review, the researchers limited the analysis to those in which a given term was used in ≥ 1 articles.
The researchers found 18 different terms used by family members/friends of individuals with life-limiting illness to describe grief, including AG (used in the most studies, n = 54); pre-death grief (n = 18), grief (n = 12), pre-loss grief (n = 6), caregiver grief (n = 5), and anticipatory mourning (n = 4). These 18 terms were associated with greater than or equal to 30 different definitions across all of the various studies.
“Definitions of these terms differed drastically,” and many studies used the term AG without defining it.
Nineteen studies used multiple terms within a single article, and the terms were “used interchangeably, with the same definition applied,” the researchers report.
For example, one study defined AG as “the process associated with grieving the eventual loss of a family member in advance of their inevitable death,” while another defined AG as “a series of losses based on a loved one’s progression of cognitive and physical decline.”
On the basis of this analysis, the researchers chose the term “pre-death grief,” which encompasses IRG and AG.
Dr. Singer explained that IRG is “present-oriented” and involves the “longing and yearning for the family member to be as they were before the illness.” AG is “future oriented” and is defined as “family members’ grief experience while the person with the life-limiting illness is alive but that is focused on feared or anticipated losses that will occur after the person’s death.”
The study was intended “to advance the field and provide the knowledge and definitions in order to create and test an evidence-based intervention,” Dr. Singer said.
He pointed to interventions (for example: behavioral activation, meaning-centered grief therapy) that could be tested to reduce pre-death grief or specific interventions that focus on addressing IRG or AG. “For example, cognitive behavior therapy might be used to challenge worry about life without the person, which would be classified as AG.”
Dr. Singer feels it is “vital” to reduce pre-death grief, insofar as numerous studies have shown that high rates of pre-death grief “result in higher rates of prolonged grief disorder.”
‘Paradoxical reality’
Francesca Falzarano, PhD, a postdoctoral associate in medicine, Weill Cornell Medicine, New York, called the article a “timely piece drawing much-needed attention to an all-too-often overlooked experience lived by those affected by terminal illnesses.”
Dr. Falzarano, who was not involved in the review, said that “from her own experience” as both a caregiver and behavioral scientist conducting research in this area, the concept of pre-death grief is a paradoxical reality – “how do we grieve someone we haven’t lost yet?”
The experience of pre-death grief is “quite distinct from grief after bereavement” because there is no end date. Rather, the person “cycles back and forth between preparing themselves for an impending death while also attending to whatever is happening in the current moment.” It’s also “unique in that both patients and caregivers individually and collectively grieve losses over the course of the illness,” she noted.
“We as researchers absolutely need to focus our attention on achieving consensus on an appropriate definition for pre-death grief that adequately encompasses its complexity and multidimensionality,” she said.
The authors and Dr. Falzarano report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
When an individual develops a terminal illness, those closest to them often start to grieve long before the person dies. Although a common syndrome, it often goes unrecognized and unaddressed.
A new review proposes a way of defining this specific type of grief in the hope that better, more precise descriptive categories will inform therapeutic interventions to help those facing a life-changing loss.
, lead author Jonathan Singer, PhD, visiting assistant professor of clinical psychology, Texas Tech University, Lubbock, told this news organization.
“We proposed the overarching term ‘pre-death grief,’ with the two separate constructs under pre-death grief – anticipatory grief [AG] and illness-related grief [IRG],” he said. “These definitions provide the field with uniform constructs to advance the study of grief before the death of an individual with a life-limiting illness.
“Research examining grief experienced by family members prior to an individual’s death to a life-limiting illness revealed wide variation in the terminology used and characterization of such grief across studies,”
The study was published online Feb. 23 in Palliative Medicine.
‘Typical’ versus ‘impairing’ grief
“Most deaths worldwide are attributed to a chronic or life-limiting Illness,” the authors write. The experience of grief before the loss of a family member “has been studied frequently, but there have been conceptualization issues, which is problematic, as it hinders the potential advancement of the field in differentiating typical grief from more impairing grief before the death,” Dr. Singer said. “Further complicating the picture is the sheer number of terms used to describe grief before death.”
Dr. Singer said that when he started conducting research in this field, he “realized someone had to combine the articles that have been published in order to create definitions that will advance the field, so risk and protective factors could be identified and interventions could be tested.”
For the current study, the investigators searched six databases to find research that “evaluated family members’ or friends’ grief related to an individual currently living with a life-limiting illness.” They excluded studies that evaluated grief after death.
Of 9,568 records reviewed, the researchers selected 134 full-text articles that met inclusion criteria. Most studies (57.46%) were quantitative; 23.88% were qualitative, and 17.91% used mixed methods. Most studies were retrospective, although 14.93% were prospective, and 3% included both prospective and retrospective analyses.
Most participants reported that the family member/friend was diagnosed either with “late-stage dementia” or “advanced cancer.” The majority (58%) were adult children of the individual with the illness, followed by spouses/partners (28.1%) and other relatives/friends (13.9%) in studies that reported the relationship to the participant and the person with the illness.
Various scales were used in the studies to measure grief, particularly the Marwit-Meuser-Caregiver Grief Inventory (n = 28), the Anticipatory Grief Scale (n = 18), and the Prolonged Grief–12 (n = 13).
A new name
Owing to the large number of articles included in the review, the researchers limited the analysis to those in which a given term was used in ≥ 1 articles.
The researchers found 18 different terms used by family members/friends of individuals with life-limiting illness to describe grief, including AG (used in the most studies, n = 54); pre-death grief (n = 18), grief (n = 12), pre-loss grief (n = 6), caregiver grief (n = 5), and anticipatory mourning (n = 4). These 18 terms were associated with greater than or equal to 30 different definitions across all of the various studies.
“Definitions of these terms differed drastically,” and many studies used the term AG without defining it.
Nineteen studies used multiple terms within a single article, and the terms were “used interchangeably, with the same definition applied,” the researchers report.
For example, one study defined AG as “the process associated with grieving the eventual loss of a family member in advance of their inevitable death,” while another defined AG as “a series of losses based on a loved one’s progression of cognitive and physical decline.”
On the basis of this analysis, the researchers chose the term “pre-death grief,” which encompasses IRG and AG.
Dr. Singer explained that IRG is “present-oriented” and involves the “longing and yearning for the family member to be as they were before the illness.” AG is “future oriented” and is defined as “family members’ grief experience while the person with the life-limiting illness is alive but that is focused on feared or anticipated losses that will occur after the person’s death.”
The study was intended “to advance the field and provide the knowledge and definitions in order to create and test an evidence-based intervention,” Dr. Singer said.
He pointed to interventions (for example: behavioral activation, meaning-centered grief therapy) that could be tested to reduce pre-death grief or specific interventions that focus on addressing IRG or AG. “For example, cognitive behavior therapy might be used to challenge worry about life without the person, which would be classified as AG.”
Dr. Singer feels it is “vital” to reduce pre-death grief, insofar as numerous studies have shown that high rates of pre-death grief “result in higher rates of prolonged grief disorder.”
‘Paradoxical reality’
Francesca Falzarano, PhD, a postdoctoral associate in medicine, Weill Cornell Medicine, New York, called the article a “timely piece drawing much-needed attention to an all-too-often overlooked experience lived by those affected by terminal illnesses.”
Dr. Falzarano, who was not involved in the review, said that “from her own experience” as both a caregiver and behavioral scientist conducting research in this area, the concept of pre-death grief is a paradoxical reality – “how do we grieve someone we haven’t lost yet?”
The experience of pre-death grief is “quite distinct from grief after bereavement” because there is no end date. Rather, the person “cycles back and forth between preparing themselves for an impending death while also attending to whatever is happening in the current moment.” It’s also “unique in that both patients and caregivers individually and collectively grieve losses over the course of the illness,” she noted.
“We as researchers absolutely need to focus our attention on achieving consensus on an appropriate definition for pre-death grief that adequately encompasses its complexity and multidimensionality,” she said.
The authors and Dr. Falzarano report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
When an individual develops a terminal illness, those closest to them often start to grieve long before the person dies. Although a common syndrome, it often goes unrecognized and unaddressed.
A new review proposes a way of defining this specific type of grief in the hope that better, more precise descriptive categories will inform therapeutic interventions to help those facing a life-changing loss.
, lead author Jonathan Singer, PhD, visiting assistant professor of clinical psychology, Texas Tech University, Lubbock, told this news organization.
“We proposed the overarching term ‘pre-death grief,’ with the two separate constructs under pre-death grief – anticipatory grief [AG] and illness-related grief [IRG],” he said. “These definitions provide the field with uniform constructs to advance the study of grief before the death of an individual with a life-limiting illness.
“Research examining grief experienced by family members prior to an individual’s death to a life-limiting illness revealed wide variation in the terminology used and characterization of such grief across studies,”
The study was published online Feb. 23 in Palliative Medicine.
‘Typical’ versus ‘impairing’ grief
“Most deaths worldwide are attributed to a chronic or life-limiting Illness,” the authors write. The experience of grief before the loss of a family member “has been studied frequently, but there have been conceptualization issues, which is problematic, as it hinders the potential advancement of the field in differentiating typical grief from more impairing grief before the death,” Dr. Singer said. “Further complicating the picture is the sheer number of terms used to describe grief before death.”
Dr. Singer said that when he started conducting research in this field, he “realized someone had to combine the articles that have been published in order to create definitions that will advance the field, so risk and protective factors could be identified and interventions could be tested.”
For the current study, the investigators searched six databases to find research that “evaluated family members’ or friends’ grief related to an individual currently living with a life-limiting illness.” They excluded studies that evaluated grief after death.
Of 9,568 records reviewed, the researchers selected 134 full-text articles that met inclusion criteria. Most studies (57.46%) were quantitative; 23.88% were qualitative, and 17.91% used mixed methods. Most studies were retrospective, although 14.93% were prospective, and 3% included both prospective and retrospective analyses.
Most participants reported that the family member/friend was diagnosed either with “late-stage dementia” or “advanced cancer.” The majority (58%) were adult children of the individual with the illness, followed by spouses/partners (28.1%) and other relatives/friends (13.9%) in studies that reported the relationship to the participant and the person with the illness.
Various scales were used in the studies to measure grief, particularly the Marwit-Meuser-Caregiver Grief Inventory (n = 28), the Anticipatory Grief Scale (n = 18), and the Prolonged Grief–12 (n = 13).
A new name
Owing to the large number of articles included in the review, the researchers limited the analysis to those in which a given term was used in ≥ 1 articles.
The researchers found 18 different terms used by family members/friends of individuals with life-limiting illness to describe grief, including AG (used in the most studies, n = 54); pre-death grief (n = 18), grief (n = 12), pre-loss grief (n = 6), caregiver grief (n = 5), and anticipatory mourning (n = 4). These 18 terms were associated with greater than or equal to 30 different definitions across all of the various studies.
“Definitions of these terms differed drastically,” and many studies used the term AG without defining it.
Nineteen studies used multiple terms within a single article, and the terms were “used interchangeably, with the same definition applied,” the researchers report.
For example, one study defined AG as “the process associated with grieving the eventual loss of a family member in advance of their inevitable death,” while another defined AG as “a series of losses based on a loved one’s progression of cognitive and physical decline.”
On the basis of this analysis, the researchers chose the term “pre-death grief,” which encompasses IRG and AG.
Dr. Singer explained that IRG is “present-oriented” and involves the “longing and yearning for the family member to be as they were before the illness.” AG is “future oriented” and is defined as “family members’ grief experience while the person with the life-limiting illness is alive but that is focused on feared or anticipated losses that will occur after the person’s death.”
The study was intended “to advance the field and provide the knowledge and definitions in order to create and test an evidence-based intervention,” Dr. Singer said.
He pointed to interventions (for example: behavioral activation, meaning-centered grief therapy) that could be tested to reduce pre-death grief or specific interventions that focus on addressing IRG or AG. “For example, cognitive behavior therapy might be used to challenge worry about life without the person, which would be classified as AG.”
Dr. Singer feels it is “vital” to reduce pre-death grief, insofar as numerous studies have shown that high rates of pre-death grief “result in higher rates of prolonged grief disorder.”
‘Paradoxical reality’
Francesca Falzarano, PhD, a postdoctoral associate in medicine, Weill Cornell Medicine, New York, called the article a “timely piece drawing much-needed attention to an all-too-often overlooked experience lived by those affected by terminal illnesses.”
Dr. Falzarano, who was not involved in the review, said that “from her own experience” as both a caregiver and behavioral scientist conducting research in this area, the concept of pre-death grief is a paradoxical reality – “how do we grieve someone we haven’t lost yet?”
The experience of pre-death grief is “quite distinct from grief after bereavement” because there is no end date. Rather, the person “cycles back and forth between preparing themselves for an impending death while also attending to whatever is happening in the current moment.” It’s also “unique in that both patients and caregivers individually and collectively grieve losses over the course of the illness,” she noted.
“We as researchers absolutely need to focus our attention on achieving consensus on an appropriate definition for pre-death grief that adequately encompasses its complexity and multidimensionality,” she said.
The authors and Dr. Falzarano report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Psychiatrist’s license revoked after alleged sexual assaults
after giving them ketamine and that he had an affair with the sister of another patient.
In its decision, the board stated that the psychiatrist, Cuyler Burns Goodwin, DO, committed gross negligence, violated ethical standards, departed from the standard of care, and was guilty of sexual misconduct.
“Even if one were to believe respondent’s denial of sexual assaults on Patient B and Patient C, his overall course of conduct in committing multiple other ethical violations and violations of the Medical Practice Act in connection with Patient A’s Sister, Patient B, and Patient C; his attitude toward and lack of insight into his offenses; and his lack of candor at hearing demonstrate that revocation of respondent’s license is required for protection of the public,” the board wrote in its March 8 order.
The board seeks to recover almost $65,000 in costs for the investigation, including for legal fees and expert testimony. The psychiatrist is not currently facing any criminal charges.
Family-run business
Dr. Goodwin received his medical license in 2013 and opened Sequoia Mind Health, a practice in Santa Rosa, Calif., soon after completing his residency at the University of California San Francisco, according to the board.
The allegations leading to the revocation of his license occurred at the Sequoia Mind Health practice, a family-run business that employed Dr. Goodwin’s mother as the office manager, his wife as the sole registered nurse, and his sister who worked reception for a time. Dr. Goodwin closed the practice in October 2019.
Until 2020, he worked as an emergency services psychiatrist for Sonoma County Behavioral Health. Other positions included stints at John George Psychiatric Pavilion in San Leandro, at Mendocino County Jail from 2018 to 2021, and at Lake County Jail from 2020 to 2021.
Since closing his practice, he also worked as a psychiatrist for Redwood Quality Management Company in Ukiah, Calif.
The board notified Dr. Goodwin in November 2020 that it was opening an investigation into his conduct.
Affair with patient’s sister
Patient A came to Dr. Goodwin in 2017 as an uninsured, homebound, 24-year-old with schizophrenia. He had not received previous mental health treatment and was entirely dependent on his family because of the severity of his symptoms.
Dr. Goodwin agreed to make home visits to provide medication management and psychotherapy and was paid in cash by the patient’s sister, who was a point of contact for the family.
The sister and Dr. Goodwin developed a friendship and, after commiserating about their troubled marriages, began a sexual relationship in 2018 and decided they would divorce their spouses and marry each other.
However, in November 2018, the sister became pregnant and, at her request, Dr. Goodwin prescribed misoprostol to induce an abortion. The affair and the abortion were later discovered by the sister’s family, who agreed to not file a complaint with the medical board in exchange for Dr. Goodwin’s agreeing to cease communications with the sister.
Nevertheless, the two continued the affair and in February 2019 the patient’s father and mother each separately complained to the medical board. The sister also sent a letter to the board urging against disciplinary action – but later acknowledged that the letter was prepared by Dr. Goodwin.
The family removed Patient A from Dr. Goodwin’s care in 2019. The sister’s relationship with Patient A and her family was damaged; she subsequently divorced her husband and moved out of state. She later told the board she regretted the relationship and knew it was wrong.
When Dr. Goodwin was initially interviewed in 2019 by the medical board, he refused to discuss the relationship or the misoprostol prescription. Then, at a later hearing, he said he did not see anything wrong with the relationship and did not believe it affected the care of Patient A.
The medical board’s expert witness said Dr. Goodwin’s behavior “showed he either had no knowledge of ethical boundaries or chose to ignore them, showing poor judgment and ‘cluelessness’ about the potential adverse effects of having a sexual relationship with Sister, which had the significant potential to compromise Patient A’s treatment.”
Sexual assault
Patient B came to Dr. Goodwin in 2017 to help taper her anxiety and depression medications. She informed him she had experienced multiple sexual assaults. He helped her taper off the drugs within a month and then hired her to work part-time at the practice’s reception desk.
After her symptoms worsened again after a traumatic event, Dr. Goodwin recommended the use of ketamine. Patient B received five ketamine treatments in a month with only Dr. Goodwin present in the room.
During one of those treatments he asked her questions about her sex life. Another night in the office he asked her to have a glass of wine with him and then allegedly sexually assaulted her.
Patient B soon quit the job via text, telling him his behavior was inappropriate. She told Dr. Goodwin she would not say anything about the assault but asked for a letter of recommendation for another job. Dr. Goodwin texted back that she was “100% right,” and he would give her a great recommendation, which he later did.
A year later, in 2019, Pamela Albro, PhD, a psychologist who provided therapy at Sequoia Mind Health, contacted Patient B to ask why she quit.
When Patient B told her about the assault, the therapist asked to share her name with Patient C, who had a similar experience. Patient B agreed and then submitted a police report and a complaint to the medical board in March 2019.
Dr. Goodwin denied Patient B’s allegations and “offered evasive and non-credible testimony” about Patient B’s text messages, the board said.
Another patient-employee
Patient C attended Dr. Goodwin’s clinic in May 2017 after a suicide attempt that required hospitalization. She told Dr. Goodwin she had experienced sexual trauma and assault in the past. Dr. Goodwin referred Patient C to Dr. Albro for therapy, managed her medications himself, and hired her to work at the clinic’s reception desk, even though she was still a patient.
Patient C worked 32 hours a week and took on other duties that included assisting in the administration of transcranial magnetic stimulation to clinic patients.
In late 2017, Dr. Goodwin recommended ketamine for Patient C and she received seven treatments from December 2017 through April 2019. There were no records of vital signs monitoring during the treatments, and Dr. Goodwin’s wife was present for only two sessions.
During the first treatment, where Patient C said she was feeling “out of it,” Dr. Goodwin allegedly sexually assaulted her.
Because of the ketamine, she told the medical board she was unable to speak or yell but said, “I screamed in my head.” After Dr. Goodwin left the room, she said she felt afraid, ashamed, and wanted to go home. Dr. Goodwin walked her to the lobby where her husband was waiting.
The patient did not tell her husband about the assault because she said she felt ashamed, and said she did not report Dr. Goodwin because it was not safe.
Disciplinary hearing
Patient C continued to work for Dr. Goodwin, calling it a confusing time in her life. She later learned about the affair with Patient A’s sister and about Patient B’s experience and resigned from the clinic in July 2019.
She still did not discuss the assault until early 2021 when the board contacted her again. She confided to her primary care physician, who noted that her PTSD symptoms had worsened.
Dr. Goodwin said in the disciplinary hearing that hiring Patient B and Patient C was “boundary crossing,” but he denied allegations of asking inappropriate questions or of sexual assault. The board, however, characterized the testimony of Patient B and Patient C as credible.
All of Dr. Goodwin’s other employers said at his disciplinary hearing that they believed he was a good psychiatrist and that they had never seen any unprofessional behavior.
The revocation of Dr. Goodwin’s license will be effective as of April 7. Dr. Goodwin’s attorney, Marvin H. Firestone, MD, JD, told this news organization he had “no comment” on the medical board’s decision or about his client.
A version of this article first appeared on Medscape.com.
after giving them ketamine and that he had an affair with the sister of another patient.
In its decision, the board stated that the psychiatrist, Cuyler Burns Goodwin, DO, committed gross negligence, violated ethical standards, departed from the standard of care, and was guilty of sexual misconduct.
“Even if one were to believe respondent’s denial of sexual assaults on Patient B and Patient C, his overall course of conduct in committing multiple other ethical violations and violations of the Medical Practice Act in connection with Patient A’s Sister, Patient B, and Patient C; his attitude toward and lack of insight into his offenses; and his lack of candor at hearing demonstrate that revocation of respondent’s license is required for protection of the public,” the board wrote in its March 8 order.
The board seeks to recover almost $65,000 in costs for the investigation, including for legal fees and expert testimony. The psychiatrist is not currently facing any criminal charges.
Family-run business
Dr. Goodwin received his medical license in 2013 and opened Sequoia Mind Health, a practice in Santa Rosa, Calif., soon after completing his residency at the University of California San Francisco, according to the board.
The allegations leading to the revocation of his license occurred at the Sequoia Mind Health practice, a family-run business that employed Dr. Goodwin’s mother as the office manager, his wife as the sole registered nurse, and his sister who worked reception for a time. Dr. Goodwin closed the practice in October 2019.
Until 2020, he worked as an emergency services psychiatrist for Sonoma County Behavioral Health. Other positions included stints at John George Psychiatric Pavilion in San Leandro, at Mendocino County Jail from 2018 to 2021, and at Lake County Jail from 2020 to 2021.
Since closing his practice, he also worked as a psychiatrist for Redwood Quality Management Company in Ukiah, Calif.
The board notified Dr. Goodwin in November 2020 that it was opening an investigation into his conduct.
Affair with patient’s sister
Patient A came to Dr. Goodwin in 2017 as an uninsured, homebound, 24-year-old with schizophrenia. He had not received previous mental health treatment and was entirely dependent on his family because of the severity of his symptoms.
Dr. Goodwin agreed to make home visits to provide medication management and psychotherapy and was paid in cash by the patient’s sister, who was a point of contact for the family.
The sister and Dr. Goodwin developed a friendship and, after commiserating about their troubled marriages, began a sexual relationship in 2018 and decided they would divorce their spouses and marry each other.
However, in November 2018, the sister became pregnant and, at her request, Dr. Goodwin prescribed misoprostol to induce an abortion. The affair and the abortion were later discovered by the sister’s family, who agreed to not file a complaint with the medical board in exchange for Dr. Goodwin’s agreeing to cease communications with the sister.
Nevertheless, the two continued the affair and in February 2019 the patient’s father and mother each separately complained to the medical board. The sister also sent a letter to the board urging against disciplinary action – but later acknowledged that the letter was prepared by Dr. Goodwin.
The family removed Patient A from Dr. Goodwin’s care in 2019. The sister’s relationship with Patient A and her family was damaged; she subsequently divorced her husband and moved out of state. She later told the board she regretted the relationship and knew it was wrong.
When Dr. Goodwin was initially interviewed in 2019 by the medical board, he refused to discuss the relationship or the misoprostol prescription. Then, at a later hearing, he said he did not see anything wrong with the relationship and did not believe it affected the care of Patient A.
The medical board’s expert witness said Dr. Goodwin’s behavior “showed he either had no knowledge of ethical boundaries or chose to ignore them, showing poor judgment and ‘cluelessness’ about the potential adverse effects of having a sexual relationship with Sister, which had the significant potential to compromise Patient A’s treatment.”
Sexual assault
Patient B came to Dr. Goodwin in 2017 to help taper her anxiety and depression medications. She informed him she had experienced multiple sexual assaults. He helped her taper off the drugs within a month and then hired her to work part-time at the practice’s reception desk.
After her symptoms worsened again after a traumatic event, Dr. Goodwin recommended the use of ketamine. Patient B received five ketamine treatments in a month with only Dr. Goodwin present in the room.
During one of those treatments he asked her questions about her sex life. Another night in the office he asked her to have a glass of wine with him and then allegedly sexually assaulted her.
Patient B soon quit the job via text, telling him his behavior was inappropriate. She told Dr. Goodwin she would not say anything about the assault but asked for a letter of recommendation for another job. Dr. Goodwin texted back that she was “100% right,” and he would give her a great recommendation, which he later did.
A year later, in 2019, Pamela Albro, PhD, a psychologist who provided therapy at Sequoia Mind Health, contacted Patient B to ask why she quit.
When Patient B told her about the assault, the therapist asked to share her name with Patient C, who had a similar experience. Patient B agreed and then submitted a police report and a complaint to the medical board in March 2019.
Dr. Goodwin denied Patient B’s allegations and “offered evasive and non-credible testimony” about Patient B’s text messages, the board said.
Another patient-employee
Patient C attended Dr. Goodwin’s clinic in May 2017 after a suicide attempt that required hospitalization. She told Dr. Goodwin she had experienced sexual trauma and assault in the past. Dr. Goodwin referred Patient C to Dr. Albro for therapy, managed her medications himself, and hired her to work at the clinic’s reception desk, even though she was still a patient.
Patient C worked 32 hours a week and took on other duties that included assisting in the administration of transcranial magnetic stimulation to clinic patients.
In late 2017, Dr. Goodwin recommended ketamine for Patient C and she received seven treatments from December 2017 through April 2019. There were no records of vital signs monitoring during the treatments, and Dr. Goodwin’s wife was present for only two sessions.
During the first treatment, where Patient C said she was feeling “out of it,” Dr. Goodwin allegedly sexually assaulted her.
Because of the ketamine, she told the medical board she was unable to speak or yell but said, “I screamed in my head.” After Dr. Goodwin left the room, she said she felt afraid, ashamed, and wanted to go home. Dr. Goodwin walked her to the lobby where her husband was waiting.
The patient did not tell her husband about the assault because she said she felt ashamed, and said she did not report Dr. Goodwin because it was not safe.
Disciplinary hearing
Patient C continued to work for Dr. Goodwin, calling it a confusing time in her life. She later learned about the affair with Patient A’s sister and about Patient B’s experience and resigned from the clinic in July 2019.
She still did not discuss the assault until early 2021 when the board contacted her again. She confided to her primary care physician, who noted that her PTSD symptoms had worsened.
Dr. Goodwin said in the disciplinary hearing that hiring Patient B and Patient C was “boundary crossing,” but he denied allegations of asking inappropriate questions or of sexual assault. The board, however, characterized the testimony of Patient B and Patient C as credible.
All of Dr. Goodwin’s other employers said at his disciplinary hearing that they believed he was a good psychiatrist and that they had never seen any unprofessional behavior.
The revocation of Dr. Goodwin’s license will be effective as of April 7. Dr. Goodwin’s attorney, Marvin H. Firestone, MD, JD, told this news organization he had “no comment” on the medical board’s decision or about his client.
A version of this article first appeared on Medscape.com.
after giving them ketamine and that he had an affair with the sister of another patient.
In its decision, the board stated that the psychiatrist, Cuyler Burns Goodwin, DO, committed gross negligence, violated ethical standards, departed from the standard of care, and was guilty of sexual misconduct.
“Even if one were to believe respondent’s denial of sexual assaults on Patient B and Patient C, his overall course of conduct in committing multiple other ethical violations and violations of the Medical Practice Act in connection with Patient A’s Sister, Patient B, and Patient C; his attitude toward and lack of insight into his offenses; and his lack of candor at hearing demonstrate that revocation of respondent’s license is required for protection of the public,” the board wrote in its March 8 order.
The board seeks to recover almost $65,000 in costs for the investigation, including for legal fees and expert testimony. The psychiatrist is not currently facing any criminal charges.
Family-run business
Dr. Goodwin received his medical license in 2013 and opened Sequoia Mind Health, a practice in Santa Rosa, Calif., soon after completing his residency at the University of California San Francisco, according to the board.
The allegations leading to the revocation of his license occurred at the Sequoia Mind Health practice, a family-run business that employed Dr. Goodwin’s mother as the office manager, his wife as the sole registered nurse, and his sister who worked reception for a time. Dr. Goodwin closed the practice in October 2019.
Until 2020, he worked as an emergency services psychiatrist for Sonoma County Behavioral Health. Other positions included stints at John George Psychiatric Pavilion in San Leandro, at Mendocino County Jail from 2018 to 2021, and at Lake County Jail from 2020 to 2021.
Since closing his practice, he also worked as a psychiatrist for Redwood Quality Management Company in Ukiah, Calif.
The board notified Dr. Goodwin in November 2020 that it was opening an investigation into his conduct.
Affair with patient’s sister
Patient A came to Dr. Goodwin in 2017 as an uninsured, homebound, 24-year-old with schizophrenia. He had not received previous mental health treatment and was entirely dependent on his family because of the severity of his symptoms.
Dr. Goodwin agreed to make home visits to provide medication management and psychotherapy and was paid in cash by the patient’s sister, who was a point of contact for the family.
The sister and Dr. Goodwin developed a friendship and, after commiserating about their troubled marriages, began a sexual relationship in 2018 and decided they would divorce their spouses and marry each other.
However, in November 2018, the sister became pregnant and, at her request, Dr. Goodwin prescribed misoprostol to induce an abortion. The affair and the abortion were later discovered by the sister’s family, who agreed to not file a complaint with the medical board in exchange for Dr. Goodwin’s agreeing to cease communications with the sister.
Nevertheless, the two continued the affair and in February 2019 the patient’s father and mother each separately complained to the medical board. The sister also sent a letter to the board urging against disciplinary action – but later acknowledged that the letter was prepared by Dr. Goodwin.
The family removed Patient A from Dr. Goodwin’s care in 2019. The sister’s relationship with Patient A and her family was damaged; she subsequently divorced her husband and moved out of state. She later told the board she regretted the relationship and knew it was wrong.
When Dr. Goodwin was initially interviewed in 2019 by the medical board, he refused to discuss the relationship or the misoprostol prescription. Then, at a later hearing, he said he did not see anything wrong with the relationship and did not believe it affected the care of Patient A.
The medical board’s expert witness said Dr. Goodwin’s behavior “showed he either had no knowledge of ethical boundaries or chose to ignore them, showing poor judgment and ‘cluelessness’ about the potential adverse effects of having a sexual relationship with Sister, which had the significant potential to compromise Patient A’s treatment.”
Sexual assault
Patient B came to Dr. Goodwin in 2017 to help taper her anxiety and depression medications. She informed him she had experienced multiple sexual assaults. He helped her taper off the drugs within a month and then hired her to work part-time at the practice’s reception desk.
After her symptoms worsened again after a traumatic event, Dr. Goodwin recommended the use of ketamine. Patient B received five ketamine treatments in a month with only Dr. Goodwin present in the room.
During one of those treatments he asked her questions about her sex life. Another night in the office he asked her to have a glass of wine with him and then allegedly sexually assaulted her.
Patient B soon quit the job via text, telling him his behavior was inappropriate. She told Dr. Goodwin she would not say anything about the assault but asked for a letter of recommendation for another job. Dr. Goodwin texted back that she was “100% right,” and he would give her a great recommendation, which he later did.
A year later, in 2019, Pamela Albro, PhD, a psychologist who provided therapy at Sequoia Mind Health, contacted Patient B to ask why she quit.
When Patient B told her about the assault, the therapist asked to share her name with Patient C, who had a similar experience. Patient B agreed and then submitted a police report and a complaint to the medical board in March 2019.
Dr. Goodwin denied Patient B’s allegations and “offered evasive and non-credible testimony” about Patient B’s text messages, the board said.
Another patient-employee
Patient C attended Dr. Goodwin’s clinic in May 2017 after a suicide attempt that required hospitalization. She told Dr. Goodwin she had experienced sexual trauma and assault in the past. Dr. Goodwin referred Patient C to Dr. Albro for therapy, managed her medications himself, and hired her to work at the clinic’s reception desk, even though she was still a patient.
Patient C worked 32 hours a week and took on other duties that included assisting in the administration of transcranial magnetic stimulation to clinic patients.
In late 2017, Dr. Goodwin recommended ketamine for Patient C and she received seven treatments from December 2017 through April 2019. There were no records of vital signs monitoring during the treatments, and Dr. Goodwin’s wife was present for only two sessions.
During the first treatment, where Patient C said she was feeling “out of it,” Dr. Goodwin allegedly sexually assaulted her.
Because of the ketamine, she told the medical board she was unable to speak or yell but said, “I screamed in my head.” After Dr. Goodwin left the room, she said she felt afraid, ashamed, and wanted to go home. Dr. Goodwin walked her to the lobby where her husband was waiting.
The patient did not tell her husband about the assault because she said she felt ashamed, and said she did not report Dr. Goodwin because it was not safe.
Disciplinary hearing
Patient C continued to work for Dr. Goodwin, calling it a confusing time in her life. She later learned about the affair with Patient A’s sister and about Patient B’s experience and resigned from the clinic in July 2019.
She still did not discuss the assault until early 2021 when the board contacted her again. She confided to her primary care physician, who noted that her PTSD symptoms had worsened.
Dr. Goodwin said in the disciplinary hearing that hiring Patient B and Patient C was “boundary crossing,” but he denied allegations of asking inappropriate questions or of sexual assault. The board, however, characterized the testimony of Patient B and Patient C as credible.
All of Dr. Goodwin’s other employers said at his disciplinary hearing that they believed he was a good psychiatrist and that they had never seen any unprofessional behavior.
The revocation of Dr. Goodwin’s license will be effective as of April 7. Dr. Goodwin’s attorney, Marvin H. Firestone, MD, JD, told this news organization he had “no comment” on the medical board’s decision or about his client.
A version of this article first appeared on Medscape.com.
Fingers take the fight to COVID-19
Pointing a finger at COVID-19
The battle against COVID-19 is seemingly never ending. It’s been 2 years and still we struggle against the virus. But now, a new hero rises against the eternal menace, a powerful weapon against this scourge of humanity. And that weapon? Finger length.
Before you break out the sad trombone, hear us out. One of the big questions around COVID-19 is the role testosterone plays in its severity: Does low testosterone increase or decrease the odds of contracting severe COVID-19? To help answer that question, English researchers have published a study analyzing finger length ratios in both COVID-19 patients and a healthy control group. That seems random, but high testosterone in the womb leads to longer ring fingers in adulthood, while high estrogen leads to longer index fingers.
According to the researchers, those who had significant left hand–right hand differences in the ratio between the second and fourth digits, as well as the third and fifth digits, were significantly more likely to have severe COVID-19 compared with those with more even ratios. Those with “feminized” short little fingers were also at risk. Those large ratio differences indicate low testosterone and high estrogen, which may explain why elderly men are at such high risk for severe COVID-19. Testosterone naturally falls off as men get older.
The results add credence to clinical trials looking to use testosterone-boosting drugs against COVID-19, the researchers said. It also gives credence to LOTME’s brand-new 12-step finger strength fitness routine and our branded finger weights. Now just $19.95! It’s the bargain of the century! Boost your testosterone naturally and protect yourself from COVID-19! We promise it’s not a scam.
Some emergencies need a superhero
Last week, we learned about the most boring person in the world. This week just happens to be opposite week, so we’re looking at a candidate for the most interesting person. Someone who can swoop down from the sky to save the injured and helpless. Someone who can go where helicopters fear to tread. Someone with jet engines for arms. Superhero-type stuff.
The Great North Air Ambulance Service (GNAAS), a charitable organization located in the United Kingdom, recently announced that one of its members has completed training on the Gravity Industries Jet Suit. The suit “has two engines on each arm and a larger engine on the back [that] provide up to 317 pounds of thrust,” Interesting Engineering explained.
GNAAS is putting the suit into operation in England’s Lake District National Park, which includes mountainous terrain that is not very hospitable to helicopter landings. A paramedic using the suit can reach hikers stranded on mountainsides much faster than rescuers who have to run or hike from the nearest helicopter landing site.
“Everyone looks at the wow factor and the fact we are the world’s first jet suit paramedics, but for us, it’s about delivering patient care,” GNAAS’ Andy Mawson told Interesting Engineering. Sounds like superhero-speak to us.
So if you’re in the Lake District and have taken a bit of a tumble, you can call a superhero on your cell phone or you can use this to summon one.
Why we’re rejecting food as medicine
Humans have been using food to treat ailments much longer than we’ve had the advances of modern medicine. So why have we rejected its worth in our treatment processes? And what can be done to change that? The Center for Food as Medicine and the Hunter College NYC Food Policy Center just released a 335-page report that answers those questions.
First, the why: Meals in health care settings are not medically designed to help with the specific needs of the patient. Produce-prescription and nutrition-incentive programs don’t have the government funds to fully support them. And a lot of medical schools don’t even require students to take a basic nutrition course. So there’s a lack of knowledge and a disconnect between health care providers and food as a resource.
Then there’s a lack of trust in the food industry and their validity. Social media uses food as a means of promoting “pseudoscientific alternative medicine” or spreading false info, pushing away legitimate providers. The food industry has had its fingers in food science studies and an almost mafia-esque chokehold on American dietary guidelines. No wonder food for medicine is getting the boot!
To change the situation, the report offers 10 key recommendations on how to advance the idea of incorporating food into medicine for treatment and prevention. They include boosting the funding for research, making hospitals more food-as-medicine focused, expanding federal programs, and improving public awareness on the role nutrition can play in medical treatment or prevention.
So maybe instead of rejecting food outright, we should be looking a little deeper at how we can use it to our advantage. Just a thought: Ice cream as an antidepressant.
Being rude is a good thing, apparently
If you’ve ever been called argumentative, stubborn, or unpleasant, then this LOTME is for you. Researchers at the University of Geneva have found that people who are more stubborn and hate to conform have brains that are more protected against Alzheimer’s disease. That type of personality seems to preserve the part of the brain that usually deteriorates as we grow older.
The original hypothesis that personality may have a protective effect against brain degeneration led the investigators to conduct cognitive and personality assessments of 65 elderly participants over a 5-year period. Researchers have been attempting to create vaccines to protect against Alzheimer’s disease, but these new findings offer a nonbiological way to help.
“For a long time, the brain is able to compensate by activating alternative networks; when the first clinical signs appear, however, it is unfortunately often too late. The identification of early biomarkers is therefore essential for … effective disease management,” lead author Panteleimon Giannakopoulos, MD, said in a Study Finds report.
You may be wondering how people with more agreeable and less confrontational personalities can seek help. Well, researchers are working on that, too. It’s a complex situation, but as always, we’re rooting for you, science!
At least now you can take solace in the fact that your elderly next-door neighbor who yells at you for stepping on his lawn is probably more protected against Alzheimer’s disease.
Pointing a finger at COVID-19
The battle against COVID-19 is seemingly never ending. It’s been 2 years and still we struggle against the virus. But now, a new hero rises against the eternal menace, a powerful weapon against this scourge of humanity. And that weapon? Finger length.
Before you break out the sad trombone, hear us out. One of the big questions around COVID-19 is the role testosterone plays in its severity: Does low testosterone increase or decrease the odds of contracting severe COVID-19? To help answer that question, English researchers have published a study analyzing finger length ratios in both COVID-19 patients and a healthy control group. That seems random, but high testosterone in the womb leads to longer ring fingers in adulthood, while high estrogen leads to longer index fingers.
According to the researchers, those who had significant left hand–right hand differences in the ratio between the second and fourth digits, as well as the third and fifth digits, were significantly more likely to have severe COVID-19 compared with those with more even ratios. Those with “feminized” short little fingers were also at risk. Those large ratio differences indicate low testosterone and high estrogen, which may explain why elderly men are at such high risk for severe COVID-19. Testosterone naturally falls off as men get older.
The results add credence to clinical trials looking to use testosterone-boosting drugs against COVID-19, the researchers said. It also gives credence to LOTME’s brand-new 12-step finger strength fitness routine and our branded finger weights. Now just $19.95! It’s the bargain of the century! Boost your testosterone naturally and protect yourself from COVID-19! We promise it’s not a scam.
Some emergencies need a superhero
Last week, we learned about the most boring person in the world. This week just happens to be opposite week, so we’re looking at a candidate for the most interesting person. Someone who can swoop down from the sky to save the injured and helpless. Someone who can go where helicopters fear to tread. Someone with jet engines for arms. Superhero-type stuff.
The Great North Air Ambulance Service (GNAAS), a charitable organization located in the United Kingdom, recently announced that one of its members has completed training on the Gravity Industries Jet Suit. The suit “has two engines on each arm and a larger engine on the back [that] provide up to 317 pounds of thrust,” Interesting Engineering explained.
GNAAS is putting the suit into operation in England’s Lake District National Park, which includes mountainous terrain that is not very hospitable to helicopter landings. A paramedic using the suit can reach hikers stranded on mountainsides much faster than rescuers who have to run or hike from the nearest helicopter landing site.
“Everyone looks at the wow factor and the fact we are the world’s first jet suit paramedics, but for us, it’s about delivering patient care,” GNAAS’ Andy Mawson told Interesting Engineering. Sounds like superhero-speak to us.
So if you’re in the Lake District and have taken a bit of a tumble, you can call a superhero on your cell phone or you can use this to summon one.
Why we’re rejecting food as medicine
Humans have been using food to treat ailments much longer than we’ve had the advances of modern medicine. So why have we rejected its worth in our treatment processes? And what can be done to change that? The Center for Food as Medicine and the Hunter College NYC Food Policy Center just released a 335-page report that answers those questions.
First, the why: Meals in health care settings are not medically designed to help with the specific needs of the patient. Produce-prescription and nutrition-incentive programs don’t have the government funds to fully support them. And a lot of medical schools don’t even require students to take a basic nutrition course. So there’s a lack of knowledge and a disconnect between health care providers and food as a resource.
Then there’s a lack of trust in the food industry and their validity. Social media uses food as a means of promoting “pseudoscientific alternative medicine” or spreading false info, pushing away legitimate providers. The food industry has had its fingers in food science studies and an almost mafia-esque chokehold on American dietary guidelines. No wonder food for medicine is getting the boot!
To change the situation, the report offers 10 key recommendations on how to advance the idea of incorporating food into medicine for treatment and prevention. They include boosting the funding for research, making hospitals more food-as-medicine focused, expanding federal programs, and improving public awareness on the role nutrition can play in medical treatment or prevention.
So maybe instead of rejecting food outright, we should be looking a little deeper at how we can use it to our advantage. Just a thought: Ice cream as an antidepressant.
Being rude is a good thing, apparently
If you’ve ever been called argumentative, stubborn, or unpleasant, then this LOTME is for you. Researchers at the University of Geneva have found that people who are more stubborn and hate to conform have brains that are more protected against Alzheimer’s disease. That type of personality seems to preserve the part of the brain that usually deteriorates as we grow older.
The original hypothesis that personality may have a protective effect against brain degeneration led the investigators to conduct cognitive and personality assessments of 65 elderly participants over a 5-year period. Researchers have been attempting to create vaccines to protect against Alzheimer’s disease, but these new findings offer a nonbiological way to help.
“For a long time, the brain is able to compensate by activating alternative networks; when the first clinical signs appear, however, it is unfortunately often too late. The identification of early biomarkers is therefore essential for … effective disease management,” lead author Panteleimon Giannakopoulos, MD, said in a Study Finds report.
You may be wondering how people with more agreeable and less confrontational personalities can seek help. Well, researchers are working on that, too. It’s a complex situation, but as always, we’re rooting for you, science!
At least now you can take solace in the fact that your elderly next-door neighbor who yells at you for stepping on his lawn is probably more protected against Alzheimer’s disease.
Pointing a finger at COVID-19
The battle against COVID-19 is seemingly never ending. It’s been 2 years and still we struggle against the virus. But now, a new hero rises against the eternal menace, a powerful weapon against this scourge of humanity. And that weapon? Finger length.
Before you break out the sad trombone, hear us out. One of the big questions around COVID-19 is the role testosterone plays in its severity: Does low testosterone increase or decrease the odds of contracting severe COVID-19? To help answer that question, English researchers have published a study analyzing finger length ratios in both COVID-19 patients and a healthy control group. That seems random, but high testosterone in the womb leads to longer ring fingers in adulthood, while high estrogen leads to longer index fingers.
According to the researchers, those who had significant left hand–right hand differences in the ratio between the second and fourth digits, as well as the third and fifth digits, were significantly more likely to have severe COVID-19 compared with those with more even ratios. Those with “feminized” short little fingers were also at risk. Those large ratio differences indicate low testosterone and high estrogen, which may explain why elderly men are at such high risk for severe COVID-19. Testosterone naturally falls off as men get older.
The results add credence to clinical trials looking to use testosterone-boosting drugs against COVID-19, the researchers said. It also gives credence to LOTME’s brand-new 12-step finger strength fitness routine and our branded finger weights. Now just $19.95! It’s the bargain of the century! Boost your testosterone naturally and protect yourself from COVID-19! We promise it’s not a scam.
Some emergencies need a superhero
Last week, we learned about the most boring person in the world. This week just happens to be opposite week, so we’re looking at a candidate for the most interesting person. Someone who can swoop down from the sky to save the injured and helpless. Someone who can go where helicopters fear to tread. Someone with jet engines for arms. Superhero-type stuff.
The Great North Air Ambulance Service (GNAAS), a charitable organization located in the United Kingdom, recently announced that one of its members has completed training on the Gravity Industries Jet Suit. The suit “has two engines on each arm and a larger engine on the back [that] provide up to 317 pounds of thrust,” Interesting Engineering explained.
GNAAS is putting the suit into operation in England’s Lake District National Park, which includes mountainous terrain that is not very hospitable to helicopter landings. A paramedic using the suit can reach hikers stranded on mountainsides much faster than rescuers who have to run or hike from the nearest helicopter landing site.
“Everyone looks at the wow factor and the fact we are the world’s first jet suit paramedics, but for us, it’s about delivering patient care,” GNAAS’ Andy Mawson told Interesting Engineering. Sounds like superhero-speak to us.
So if you’re in the Lake District and have taken a bit of a tumble, you can call a superhero on your cell phone or you can use this to summon one.
Why we’re rejecting food as medicine
Humans have been using food to treat ailments much longer than we’ve had the advances of modern medicine. So why have we rejected its worth in our treatment processes? And what can be done to change that? The Center for Food as Medicine and the Hunter College NYC Food Policy Center just released a 335-page report that answers those questions.
First, the why: Meals in health care settings are not medically designed to help with the specific needs of the patient. Produce-prescription and nutrition-incentive programs don’t have the government funds to fully support them. And a lot of medical schools don’t even require students to take a basic nutrition course. So there’s a lack of knowledge and a disconnect between health care providers and food as a resource.
Then there’s a lack of trust in the food industry and their validity. Social media uses food as a means of promoting “pseudoscientific alternative medicine” or spreading false info, pushing away legitimate providers. The food industry has had its fingers in food science studies and an almost mafia-esque chokehold on American dietary guidelines. No wonder food for medicine is getting the boot!
To change the situation, the report offers 10 key recommendations on how to advance the idea of incorporating food into medicine for treatment and prevention. They include boosting the funding for research, making hospitals more food-as-medicine focused, expanding federal programs, and improving public awareness on the role nutrition can play in medical treatment or prevention.
So maybe instead of rejecting food outright, we should be looking a little deeper at how we can use it to our advantage. Just a thought: Ice cream as an antidepressant.
Being rude is a good thing, apparently
If you’ve ever been called argumentative, stubborn, or unpleasant, then this LOTME is for you. Researchers at the University of Geneva have found that people who are more stubborn and hate to conform have brains that are more protected against Alzheimer’s disease. That type of personality seems to preserve the part of the brain that usually deteriorates as we grow older.
The original hypothesis that personality may have a protective effect against brain degeneration led the investigators to conduct cognitive and personality assessments of 65 elderly participants over a 5-year period. Researchers have been attempting to create vaccines to protect against Alzheimer’s disease, but these new findings offer a nonbiological way to help.
“For a long time, the brain is able to compensate by activating alternative networks; when the first clinical signs appear, however, it is unfortunately often too late. The identification of early biomarkers is therefore essential for … effective disease management,” lead author Panteleimon Giannakopoulos, MD, said in a Study Finds report.
You may be wondering how people with more agreeable and less confrontational personalities can seek help. Well, researchers are working on that, too. It’s a complex situation, but as always, we’re rooting for you, science!
At least now you can take solace in the fact that your elderly next-door neighbor who yells at you for stepping on his lawn is probably more protected against Alzheimer’s disease.
Science says this is the ‘most boring person in the world’
Apologies up front to anyone who spends their weekends bird-watching or doing math for fun. They are among the people expected to be boring, based on stereotypes about what they do for work or how they spend their spare time, new research reveals.
Researchers surveyed more than 500 people across five related experiments to identify what people perceive as the most boring jobs, traits, and hobbies. They also report how we could all be missing out by spending as little time as possible with our tax consultant, accountant, or financial adviser outside of work.
People who work in banking, finance, accounting, data analytics, and cleaning topped the most boring list in the study, published earlier this month in Personality and Social Psychology Bulletin.
Sleeping, religion, watching television, observing animals, and spending spare time on mathematics were the stereotypical most boring hobbies and activities. The “observing animals” group includes people who bird-watch or study ants.
On the flip side, the top five most exciting jobs, in order, were in the performing arts, science, journalism, health professions, and teaching.
The researchers also looked at the how likely people are to avoid spending time with stereotypical dullards.
“Are people who are stereotyped as being boring avoided, if possible? Our current research shows that this is likely,” says Wijnand A.P. Van Tilburg, PhD, one of the researchers who did the study.
Beyond specific traits and stereotypes, Dr. Van Tilburg and colleagues found that boring people are seen as lacking skills and warmth.
“To our surprise, it appears that they are seen as both unfriendly and incompetent,” says Dr. Van Tilburg, an experimental social psychologist at the University of Essex in the United Kingdom.
What qualities do people most often ascribe to boring people? Besides being “dull,” “dry,” “bland,” and “not interesting,” common stereotypes include thinking someone who is likely boring will have no sense of humor, lack opinions, or complain.
The people surveyed also were more likely to place boring people in towns and small cities rather than large metropolitan areas.
A vicious cycle?
What’s the possible harm of relying on boring stereotypes? If people are stereotyped as being boring solely based on professions and hobbies, “then that suggests that they will incur the negative consequences associated with being a stereotypically boring person -- even when others haven’t actually interacted with them,” Dr. Van Tilburg says.
“Having a stereotypically boring profession or hobby may come with the inability to prove the biased perceivers wrong,” he says.
So making distinctions between stereotypes and realities is important, Dr. Van Tilburg says. “Those who have hobbies or occupations that are stereotypically boring do, of course, not actually have to be boring.”
Mark Leary, PhD, a professor in the department of psychology and neuroscience at Duke University in Durham, N.C., agrees. “The research actually dealt with stereotypes about the kinds of people who hold certain jobs, have certain hobbies, and live in certain places -- and not about boring people per se,” he says.
Dr. Leary points out that few people encounter bankers, tax experts, and others perceived as most boring outside a professional setting.
“When we have interactions with data analysts, accountants, insurance agents, and bankers, for example, those interactions are often boring not because the people are boring, but rather because the context is not interesting.”
To get past the preconceptions, “the best advice might be to get people to try to separate people from their roles when forming impressions of them.”
“We need to recognize that many of our interactions with other people are tied up in particular roles and topics and, thus, don’t reveal much about the other people themselves,” Dr. Leary says. “Maybe my accountant is the life of the party in other contexts.”
Dollars to avoid the dull?
The researchers also found that as the perception of how boring a person is increased, people were more likely to say they would avoid them.
To find a way to measure this avoidance, they asked people in the study how much money they would have to be paid to pal around with a perceived bore for 1 to 7 days. The payments people said they would need varied by perceptions that their boredom would be low, intermediate, or high.
As an example, they would require an average of $50 to spend one day with a highly boring person. That amount would double to $100 to spend almost 4 days in their company, and up to $230 for the week.
Dr. Leary says boredom happens when people try to pay attention to an experience or event. This means boredom goes beyond simple disinterest or trying to pay attention to someone that is not “intrinsically captivating.” When it takes more brain power to pay attention, you’ll perceive the experience as even more boring.
“Perhaps the best way to see if other people are actually boring is to talk about interesting things and see how they respond,” Dr. Leary says. “But, be careful: The topics you think make interesting conversations may be boring to others.”
A version of this article first appeared on WebMD.com.
Apologies up front to anyone who spends their weekends bird-watching or doing math for fun. They are among the people expected to be boring, based on stereotypes about what they do for work or how they spend their spare time, new research reveals.
Researchers surveyed more than 500 people across five related experiments to identify what people perceive as the most boring jobs, traits, and hobbies. They also report how we could all be missing out by spending as little time as possible with our tax consultant, accountant, or financial adviser outside of work.
People who work in banking, finance, accounting, data analytics, and cleaning topped the most boring list in the study, published earlier this month in Personality and Social Psychology Bulletin.
Sleeping, religion, watching television, observing animals, and spending spare time on mathematics were the stereotypical most boring hobbies and activities. The “observing animals” group includes people who bird-watch or study ants.
On the flip side, the top five most exciting jobs, in order, were in the performing arts, science, journalism, health professions, and teaching.
The researchers also looked at the how likely people are to avoid spending time with stereotypical dullards.
“Are people who are stereotyped as being boring avoided, if possible? Our current research shows that this is likely,” says Wijnand A.P. Van Tilburg, PhD, one of the researchers who did the study.
Beyond specific traits and stereotypes, Dr. Van Tilburg and colleagues found that boring people are seen as lacking skills and warmth.
“To our surprise, it appears that they are seen as both unfriendly and incompetent,” says Dr. Van Tilburg, an experimental social psychologist at the University of Essex in the United Kingdom.
What qualities do people most often ascribe to boring people? Besides being “dull,” “dry,” “bland,” and “not interesting,” common stereotypes include thinking someone who is likely boring will have no sense of humor, lack opinions, or complain.
The people surveyed also were more likely to place boring people in towns and small cities rather than large metropolitan areas.
A vicious cycle?
What’s the possible harm of relying on boring stereotypes? If people are stereotyped as being boring solely based on professions and hobbies, “then that suggests that they will incur the negative consequences associated with being a stereotypically boring person -- even when others haven’t actually interacted with them,” Dr. Van Tilburg says.
“Having a stereotypically boring profession or hobby may come with the inability to prove the biased perceivers wrong,” he says.
So making distinctions between stereotypes and realities is important, Dr. Van Tilburg says. “Those who have hobbies or occupations that are stereotypically boring do, of course, not actually have to be boring.”
Mark Leary, PhD, a professor in the department of psychology and neuroscience at Duke University in Durham, N.C., agrees. “The research actually dealt with stereotypes about the kinds of people who hold certain jobs, have certain hobbies, and live in certain places -- and not about boring people per se,” he says.
Dr. Leary points out that few people encounter bankers, tax experts, and others perceived as most boring outside a professional setting.
“When we have interactions with data analysts, accountants, insurance agents, and bankers, for example, those interactions are often boring not because the people are boring, but rather because the context is not interesting.”
To get past the preconceptions, “the best advice might be to get people to try to separate people from their roles when forming impressions of them.”
“We need to recognize that many of our interactions with other people are tied up in particular roles and topics and, thus, don’t reveal much about the other people themselves,” Dr. Leary says. “Maybe my accountant is the life of the party in other contexts.”
Dollars to avoid the dull?
The researchers also found that as the perception of how boring a person is increased, people were more likely to say they would avoid them.
To find a way to measure this avoidance, they asked people in the study how much money they would have to be paid to pal around with a perceived bore for 1 to 7 days. The payments people said they would need varied by perceptions that their boredom would be low, intermediate, or high.
As an example, they would require an average of $50 to spend one day with a highly boring person. That amount would double to $100 to spend almost 4 days in their company, and up to $230 for the week.
Dr. Leary says boredom happens when people try to pay attention to an experience or event. This means boredom goes beyond simple disinterest or trying to pay attention to someone that is not “intrinsically captivating.” When it takes more brain power to pay attention, you’ll perceive the experience as even more boring.
“Perhaps the best way to see if other people are actually boring is to talk about interesting things and see how they respond,” Dr. Leary says. “But, be careful: The topics you think make interesting conversations may be boring to others.”
A version of this article first appeared on WebMD.com.
Apologies up front to anyone who spends their weekends bird-watching or doing math for fun. They are among the people expected to be boring, based on stereotypes about what they do for work or how they spend their spare time, new research reveals.
Researchers surveyed more than 500 people across five related experiments to identify what people perceive as the most boring jobs, traits, and hobbies. They also report how we could all be missing out by spending as little time as possible with our tax consultant, accountant, or financial adviser outside of work.
People who work in banking, finance, accounting, data analytics, and cleaning topped the most boring list in the study, published earlier this month in Personality and Social Psychology Bulletin.
Sleeping, religion, watching television, observing animals, and spending spare time on mathematics were the stereotypical most boring hobbies and activities. The “observing animals” group includes people who bird-watch or study ants.
On the flip side, the top five most exciting jobs, in order, were in the performing arts, science, journalism, health professions, and teaching.
The researchers also looked at the how likely people are to avoid spending time with stereotypical dullards.
“Are people who are stereotyped as being boring avoided, if possible? Our current research shows that this is likely,” says Wijnand A.P. Van Tilburg, PhD, one of the researchers who did the study.
Beyond specific traits and stereotypes, Dr. Van Tilburg and colleagues found that boring people are seen as lacking skills and warmth.
“To our surprise, it appears that they are seen as both unfriendly and incompetent,” says Dr. Van Tilburg, an experimental social psychologist at the University of Essex in the United Kingdom.
What qualities do people most often ascribe to boring people? Besides being “dull,” “dry,” “bland,” and “not interesting,” common stereotypes include thinking someone who is likely boring will have no sense of humor, lack opinions, or complain.
The people surveyed also were more likely to place boring people in towns and small cities rather than large metropolitan areas.
A vicious cycle?
What’s the possible harm of relying on boring stereotypes? If people are stereotyped as being boring solely based on professions and hobbies, “then that suggests that they will incur the negative consequences associated with being a stereotypically boring person -- even when others haven’t actually interacted with them,” Dr. Van Tilburg says.
“Having a stereotypically boring profession or hobby may come with the inability to prove the biased perceivers wrong,” he says.
So making distinctions between stereotypes and realities is important, Dr. Van Tilburg says. “Those who have hobbies or occupations that are stereotypically boring do, of course, not actually have to be boring.”
Mark Leary, PhD, a professor in the department of psychology and neuroscience at Duke University in Durham, N.C., agrees. “The research actually dealt with stereotypes about the kinds of people who hold certain jobs, have certain hobbies, and live in certain places -- and not about boring people per se,” he says.
Dr. Leary points out that few people encounter bankers, tax experts, and others perceived as most boring outside a professional setting.
“When we have interactions with data analysts, accountants, insurance agents, and bankers, for example, those interactions are often boring not because the people are boring, but rather because the context is not interesting.”
To get past the preconceptions, “the best advice might be to get people to try to separate people from their roles when forming impressions of them.”
“We need to recognize that many of our interactions with other people are tied up in particular roles and topics and, thus, don’t reveal much about the other people themselves,” Dr. Leary says. “Maybe my accountant is the life of the party in other contexts.”
Dollars to avoid the dull?
The researchers also found that as the perception of how boring a person is increased, people were more likely to say they would avoid them.
To find a way to measure this avoidance, they asked people in the study how much money they would have to be paid to pal around with a perceived bore for 1 to 7 days. The payments people said they would need varied by perceptions that their boredom would be low, intermediate, or high.
As an example, they would require an average of $50 to spend one day with a highly boring person. That amount would double to $100 to spend almost 4 days in their company, and up to $230 for the week.
Dr. Leary says boredom happens when people try to pay attention to an experience or event. This means boredom goes beyond simple disinterest or trying to pay attention to someone that is not “intrinsically captivating.” When it takes more brain power to pay attention, you’ll perceive the experience as even more boring.
“Perhaps the best way to see if other people are actually boring is to talk about interesting things and see how they respond,” Dr. Leary says. “But, be careful: The topics you think make interesting conversations may be boring to others.”
A version of this article first appeared on WebMD.com.
FROM PERSONALITY AND SOCIAL PSYCHOLOGY BULLETIN
Does evidence support benefits of omega-3 fatty acids?
Dietary supplements that contain omega-3 fatty acids have been widely consumed for years. Researchers have been investigating the benefits of such preparations for cardiovascular, neurologic, and psychological conditions. A recently published study on omega-3 fatty acids and depression inspired neurologist Hans-Christoph Diener, MD, PhD, of the Institute for Epidemiology at the University Duisburg-Essen (Germany), to examine scientific publications concerning omega-3 fatty acids or fish-oil capsules in more detail.
Prevention of depression
Dr. Diener told the story of how he stumbled upon an interesting article in JAMA in December 2021. It was about a placebo-controlled study that investigated whether omega-3 fatty acids can prevent incident depression.
As the study authors reported, treatment with omega-3 preparations in adults aged 50 years or older without clinically relevant symptoms of depression at study initiation was associated with a small but statistically significant increase in the risk for depression or clinically relevant symptoms of depression. There was no difference in mood scale value, however, over a median follow-up of 5.3 years. According to the study authors, these results did not support the administration of omega-3 preparations for the prevention of depression.
This study was, as Dr. Diener said, somewhat negative, but it did arouse his interest in questions such as what biological effects omega-3 fatty acids have and what is known “about this topic with regard to neurology,” he said. When reviewing the literature, he noticed that there “were association studies, i.e., studies that describe that the intake of omega-3 fatty acids may possibly be associated with a lower risk of certain diseases.”
Beginning with the Inuit
It all started “with observations of the Inuit [population] in Greenland and Alaska after World War II, because it was remarked upon that these people ate a lot of fish and seal meat and had a very low incidence of cardiovascular diseases.” Over the years, a large number of association studies have been published, which may have encouraged the assumption that omega-3 fatty acids have positive health effects on various conditions, such as cardiovascular diseases, hyperlipidemia, type 2 diabetes, various malignancies, cognitive impairments, Alzheimer’s disease, depression and anxiety disorders, heart failure, slipped disks, ADHD, symptoms of menopause, rheumatoid arthritis, asthma, periodontitis, epilepsy, chemotherapy tolerance, premenstrual syndrome, and nonalcoholic fatty liver disease.
Dr. Diener believes that the problem is that these are association studies. But association does not mean that there is a causal relationship.
Disappointing study results
On the contrary, the results from the randomized placebo-controlled studies are truly frustrating, according to the neurologist. A meta-analysis of the use of omega-3 fatty acids in cardiovascular diseases included 86 studies with over 162,000 patients. According to Dr. Diener, it did not reveal any benefit for overall and cardiovascular mortality, nor any benefit for the reduction of myocardial infarction and stroke.
The results did indicate a trend, however, for reduced mortality in coronary heart disease. Even so, the number needed to treat for this was 334, which means that 334 people would have to take omega-3 fatty acids for years to prevent one fatal cardiac event.
Aside from this study, Dr. Diener found six studies on Alzheimer’s disease and three studies on dementia with patient populations between 600 and 800. In these studies, too, a positive effect of omega-3 fatty acids could not be identified. Then he discovered another 31 placebo-controlled studies of omega-3 fatty acids for the treatment or prevention of depression and anxiety disorder. Despite including 50,000 patients, these studies also did not show any positive effect.
“I see a significant discrepancy between the promotion of omega-3 fatty acids, whether it’s on television, in the ‘yellow’ [journalism] press, or in advertisements, and the actual scientific evidence,” said Dr. Diener. “At least from a neurological perspective, there is no evidence that omega-3 fatty acids have any benefit. This is true for strokes, dementia, Alzheimer’s disease, depression, and anxiety disorders.”
Potential adverse effects
Omega-3 fatty acids also have potentially adverse effects. The VITAL Rhythm study recently provided evidence that, depending on the dose, preparations with omega-3 fatty acids may increase the risk for atrial fibrillation. As the authors wrote, the results do not support taking omega-3 fatty acids to prevent atrial fibrillation.
In 2019, the global market for omega-3 fatty acids reached a value of $4.1 billion. This value is expected to double by 2025, according to a comment by Gregory Curfman, MD, deputy editor of JAMA and lecturer in health care policy at Harvard Medical School, Boston.
As Dr. Curfman wrote, this impressive amount of expenditure shows how beloved these products are and how strongly many people believe that omega-3 fatty acids are beneficial for their health. It is therefore important to know the potential risks of such preparations. One such example for this would be the risk for atrial fibrillation.
According to Dr. Curfman, in the last 2 years, four randomized clinical studies have provided data on the risk for atrial fibrillation associated with omega-3 fatty acids. In the STRENGTH study, 13,078 high-risk patients with cardiovascular diseases were randomly assigned to one of two groups. The subjects received either a high dose (4 g/day) of a combination of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) or corn oil. After a median of 42 months, there was no significant difference between the two groups in the primary composite cardiovascular endpoint, but more frequent atrial fibrillation in the omega-3 fatty acid group, compared with the corn oil group (2.2% vs. 1.3%; hazard ratio, 1.69; 95% confidence interval, 1.29-2.21; P < .001).
In the REDUCE-IT study, 8179 subjects were randomly assigned to a high dose (4 g/day, as in STRENGTH) of an omega-3 fatty acid preparation consisting of a purified EPA (icosapent ethyl) or mineral oil. After a median observation period of 4.9 years, icosapent ethyl was associated with a relative reduction of the primary composite cardiovascular endpoint by 25%, compared with mineral oil. As in the STRENGTH study, this study found that the risk for atrial fibrillation associated with omega-3 fatty acids, compared with mineral oil, was significantly higher (5.3% vs. 3.9%; P = .003).
In a third study (OMEMI), as Dr. Curfman reported, 1027 elderly patients who had recently had a myocardial infarction were randomly assigned to receive either a median dose of 1.8 g/day of omega-3 fatty acids (a combination of EPA and DHA) or corn oil. After 2 years, there was no significant difference between the two groups in primary composite cardiovascular endpoints, but 7.2% of the patients taking omega-3 fatty acids developed atrial fibrillation. In the corn oil group, this proportion was 4% (HR, 1.84; 95% CI, 0.98-3.45; P = .06).
The data from the four studies together indicate a potential dose-dependent risk for atrial fibrillation associated with omega-3 fatty acids, according to Dr. Curfman. At a dose of 4.0 g/day, there is a highly significant risk increase (almost double). With a median dose of 1.8 g/day, the risk increase (HR, 1.84) did not reach statistical significance. At a daily standard dose of 840 mg/day, an increase in risk could not be determined.
Dr. Curfman’s recommendation is that patients who take, or want to take, preparations with omega-3 fatty acids be informed of the potential development of arrhythmia at higher dosages. These patients also should undergo cardiological monitoring.
A version of this article first appeared on Medscape.com.
Dietary supplements that contain omega-3 fatty acids have been widely consumed for years. Researchers have been investigating the benefits of such preparations for cardiovascular, neurologic, and psychological conditions. A recently published study on omega-3 fatty acids and depression inspired neurologist Hans-Christoph Diener, MD, PhD, of the Institute for Epidemiology at the University Duisburg-Essen (Germany), to examine scientific publications concerning omega-3 fatty acids or fish-oil capsules in more detail.
Prevention of depression
Dr. Diener told the story of how he stumbled upon an interesting article in JAMA in December 2021. It was about a placebo-controlled study that investigated whether omega-3 fatty acids can prevent incident depression.
As the study authors reported, treatment with omega-3 preparations in adults aged 50 years or older without clinically relevant symptoms of depression at study initiation was associated with a small but statistically significant increase in the risk for depression or clinically relevant symptoms of depression. There was no difference in mood scale value, however, over a median follow-up of 5.3 years. According to the study authors, these results did not support the administration of omega-3 preparations for the prevention of depression.
This study was, as Dr. Diener said, somewhat negative, but it did arouse his interest in questions such as what biological effects omega-3 fatty acids have and what is known “about this topic with regard to neurology,” he said. When reviewing the literature, he noticed that there “were association studies, i.e., studies that describe that the intake of omega-3 fatty acids may possibly be associated with a lower risk of certain diseases.”
Beginning with the Inuit
It all started “with observations of the Inuit [population] in Greenland and Alaska after World War II, because it was remarked upon that these people ate a lot of fish and seal meat and had a very low incidence of cardiovascular diseases.” Over the years, a large number of association studies have been published, which may have encouraged the assumption that omega-3 fatty acids have positive health effects on various conditions, such as cardiovascular diseases, hyperlipidemia, type 2 diabetes, various malignancies, cognitive impairments, Alzheimer’s disease, depression and anxiety disorders, heart failure, slipped disks, ADHD, symptoms of menopause, rheumatoid arthritis, asthma, periodontitis, epilepsy, chemotherapy tolerance, premenstrual syndrome, and nonalcoholic fatty liver disease.
Dr. Diener believes that the problem is that these are association studies. But association does not mean that there is a causal relationship.
Disappointing study results
On the contrary, the results from the randomized placebo-controlled studies are truly frustrating, according to the neurologist. A meta-analysis of the use of omega-3 fatty acids in cardiovascular diseases included 86 studies with over 162,000 patients. According to Dr. Diener, it did not reveal any benefit for overall and cardiovascular mortality, nor any benefit for the reduction of myocardial infarction and stroke.
The results did indicate a trend, however, for reduced mortality in coronary heart disease. Even so, the number needed to treat for this was 334, which means that 334 people would have to take omega-3 fatty acids for years to prevent one fatal cardiac event.
Aside from this study, Dr. Diener found six studies on Alzheimer’s disease and three studies on dementia with patient populations between 600 and 800. In these studies, too, a positive effect of omega-3 fatty acids could not be identified. Then he discovered another 31 placebo-controlled studies of omega-3 fatty acids for the treatment or prevention of depression and anxiety disorder. Despite including 50,000 patients, these studies also did not show any positive effect.
“I see a significant discrepancy between the promotion of omega-3 fatty acids, whether it’s on television, in the ‘yellow’ [journalism] press, or in advertisements, and the actual scientific evidence,” said Dr. Diener. “At least from a neurological perspective, there is no evidence that omega-3 fatty acids have any benefit. This is true for strokes, dementia, Alzheimer’s disease, depression, and anxiety disorders.”
Potential adverse effects
Omega-3 fatty acids also have potentially adverse effects. The VITAL Rhythm study recently provided evidence that, depending on the dose, preparations with omega-3 fatty acids may increase the risk for atrial fibrillation. As the authors wrote, the results do not support taking omega-3 fatty acids to prevent atrial fibrillation.
In 2019, the global market for omega-3 fatty acids reached a value of $4.1 billion. This value is expected to double by 2025, according to a comment by Gregory Curfman, MD, deputy editor of JAMA and lecturer in health care policy at Harvard Medical School, Boston.
As Dr. Curfman wrote, this impressive amount of expenditure shows how beloved these products are and how strongly many people believe that omega-3 fatty acids are beneficial for their health. It is therefore important to know the potential risks of such preparations. One such example for this would be the risk for atrial fibrillation.
According to Dr. Curfman, in the last 2 years, four randomized clinical studies have provided data on the risk for atrial fibrillation associated with omega-3 fatty acids. In the STRENGTH study, 13,078 high-risk patients with cardiovascular diseases were randomly assigned to one of two groups. The subjects received either a high dose (4 g/day) of a combination of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) or corn oil. After a median of 42 months, there was no significant difference between the two groups in the primary composite cardiovascular endpoint, but more frequent atrial fibrillation in the omega-3 fatty acid group, compared with the corn oil group (2.2% vs. 1.3%; hazard ratio, 1.69; 95% confidence interval, 1.29-2.21; P < .001).
In the REDUCE-IT study, 8179 subjects were randomly assigned to a high dose (4 g/day, as in STRENGTH) of an omega-3 fatty acid preparation consisting of a purified EPA (icosapent ethyl) or mineral oil. After a median observation period of 4.9 years, icosapent ethyl was associated with a relative reduction of the primary composite cardiovascular endpoint by 25%, compared with mineral oil. As in the STRENGTH study, this study found that the risk for atrial fibrillation associated with omega-3 fatty acids, compared with mineral oil, was significantly higher (5.3% vs. 3.9%; P = .003).
In a third study (OMEMI), as Dr. Curfman reported, 1027 elderly patients who had recently had a myocardial infarction were randomly assigned to receive either a median dose of 1.8 g/day of omega-3 fatty acids (a combination of EPA and DHA) or corn oil. After 2 years, there was no significant difference between the two groups in primary composite cardiovascular endpoints, but 7.2% of the patients taking omega-3 fatty acids developed atrial fibrillation. In the corn oil group, this proportion was 4% (HR, 1.84; 95% CI, 0.98-3.45; P = .06).
The data from the four studies together indicate a potential dose-dependent risk for atrial fibrillation associated with omega-3 fatty acids, according to Dr. Curfman. At a dose of 4.0 g/day, there is a highly significant risk increase (almost double). With a median dose of 1.8 g/day, the risk increase (HR, 1.84) did not reach statistical significance. At a daily standard dose of 840 mg/day, an increase in risk could not be determined.
Dr. Curfman’s recommendation is that patients who take, or want to take, preparations with omega-3 fatty acids be informed of the potential development of arrhythmia at higher dosages. These patients also should undergo cardiological monitoring.
A version of this article first appeared on Medscape.com.
Dietary supplements that contain omega-3 fatty acids have been widely consumed for years. Researchers have been investigating the benefits of such preparations for cardiovascular, neurologic, and psychological conditions. A recently published study on omega-3 fatty acids and depression inspired neurologist Hans-Christoph Diener, MD, PhD, of the Institute for Epidemiology at the University Duisburg-Essen (Germany), to examine scientific publications concerning omega-3 fatty acids or fish-oil capsules in more detail.
Prevention of depression
Dr. Diener told the story of how he stumbled upon an interesting article in JAMA in December 2021. It was about a placebo-controlled study that investigated whether omega-3 fatty acids can prevent incident depression.
As the study authors reported, treatment with omega-3 preparations in adults aged 50 years or older without clinically relevant symptoms of depression at study initiation was associated with a small but statistically significant increase in the risk for depression or clinically relevant symptoms of depression. There was no difference in mood scale value, however, over a median follow-up of 5.3 years. According to the study authors, these results did not support the administration of omega-3 preparations for the prevention of depression.
This study was, as Dr. Diener said, somewhat negative, but it did arouse his interest in questions such as what biological effects omega-3 fatty acids have and what is known “about this topic with regard to neurology,” he said. When reviewing the literature, he noticed that there “were association studies, i.e., studies that describe that the intake of omega-3 fatty acids may possibly be associated with a lower risk of certain diseases.”
Beginning with the Inuit
It all started “with observations of the Inuit [population] in Greenland and Alaska after World War II, because it was remarked upon that these people ate a lot of fish and seal meat and had a very low incidence of cardiovascular diseases.” Over the years, a large number of association studies have been published, which may have encouraged the assumption that omega-3 fatty acids have positive health effects on various conditions, such as cardiovascular diseases, hyperlipidemia, type 2 diabetes, various malignancies, cognitive impairments, Alzheimer’s disease, depression and anxiety disorders, heart failure, slipped disks, ADHD, symptoms of menopause, rheumatoid arthritis, asthma, periodontitis, epilepsy, chemotherapy tolerance, premenstrual syndrome, and nonalcoholic fatty liver disease.
Dr. Diener believes that the problem is that these are association studies. But association does not mean that there is a causal relationship.
Disappointing study results
On the contrary, the results from the randomized placebo-controlled studies are truly frustrating, according to the neurologist. A meta-analysis of the use of omega-3 fatty acids in cardiovascular diseases included 86 studies with over 162,000 patients. According to Dr. Diener, it did not reveal any benefit for overall and cardiovascular mortality, nor any benefit for the reduction of myocardial infarction and stroke.
The results did indicate a trend, however, for reduced mortality in coronary heart disease. Even so, the number needed to treat for this was 334, which means that 334 people would have to take omega-3 fatty acids for years to prevent one fatal cardiac event.
Aside from this study, Dr. Diener found six studies on Alzheimer’s disease and three studies on dementia with patient populations between 600 and 800. In these studies, too, a positive effect of omega-3 fatty acids could not be identified. Then he discovered another 31 placebo-controlled studies of omega-3 fatty acids for the treatment or prevention of depression and anxiety disorder. Despite including 50,000 patients, these studies also did not show any positive effect.
“I see a significant discrepancy between the promotion of omega-3 fatty acids, whether it’s on television, in the ‘yellow’ [journalism] press, or in advertisements, and the actual scientific evidence,” said Dr. Diener. “At least from a neurological perspective, there is no evidence that omega-3 fatty acids have any benefit. This is true for strokes, dementia, Alzheimer’s disease, depression, and anxiety disorders.”
Potential adverse effects
Omega-3 fatty acids also have potentially adverse effects. The VITAL Rhythm study recently provided evidence that, depending on the dose, preparations with omega-3 fatty acids may increase the risk for atrial fibrillation. As the authors wrote, the results do not support taking omega-3 fatty acids to prevent atrial fibrillation.
In 2019, the global market for omega-3 fatty acids reached a value of $4.1 billion. This value is expected to double by 2025, according to a comment by Gregory Curfman, MD, deputy editor of JAMA and lecturer in health care policy at Harvard Medical School, Boston.
As Dr. Curfman wrote, this impressive amount of expenditure shows how beloved these products are and how strongly many people believe that omega-3 fatty acids are beneficial for their health. It is therefore important to know the potential risks of such preparations. One such example for this would be the risk for atrial fibrillation.
According to Dr. Curfman, in the last 2 years, four randomized clinical studies have provided data on the risk for atrial fibrillation associated with omega-3 fatty acids. In the STRENGTH study, 13,078 high-risk patients with cardiovascular diseases were randomly assigned to one of two groups. The subjects received either a high dose (4 g/day) of a combination of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) or corn oil. After a median of 42 months, there was no significant difference between the two groups in the primary composite cardiovascular endpoint, but more frequent atrial fibrillation in the omega-3 fatty acid group, compared with the corn oil group (2.2% vs. 1.3%; hazard ratio, 1.69; 95% confidence interval, 1.29-2.21; P < .001).
In the REDUCE-IT study, 8179 subjects were randomly assigned to a high dose (4 g/day, as in STRENGTH) of an omega-3 fatty acid preparation consisting of a purified EPA (icosapent ethyl) or mineral oil. After a median observation period of 4.9 years, icosapent ethyl was associated with a relative reduction of the primary composite cardiovascular endpoint by 25%, compared with mineral oil. As in the STRENGTH study, this study found that the risk for atrial fibrillation associated with omega-3 fatty acids, compared with mineral oil, was significantly higher (5.3% vs. 3.9%; P = .003).
In a third study (OMEMI), as Dr. Curfman reported, 1027 elderly patients who had recently had a myocardial infarction were randomly assigned to receive either a median dose of 1.8 g/day of omega-3 fatty acids (a combination of EPA and DHA) or corn oil. After 2 years, there was no significant difference between the two groups in primary composite cardiovascular endpoints, but 7.2% of the patients taking omega-3 fatty acids developed atrial fibrillation. In the corn oil group, this proportion was 4% (HR, 1.84; 95% CI, 0.98-3.45; P = .06).
The data from the four studies together indicate a potential dose-dependent risk for atrial fibrillation associated with omega-3 fatty acids, according to Dr. Curfman. At a dose of 4.0 g/day, there is a highly significant risk increase (almost double). With a median dose of 1.8 g/day, the risk increase (HR, 1.84) did not reach statistical significance. At a daily standard dose of 840 mg/day, an increase in risk could not be determined.
Dr. Curfman’s recommendation is that patients who take, or want to take, preparations with omega-3 fatty acids be informed of the potential development of arrhythmia at higher dosages. These patients also should undergo cardiological monitoring.
A version of this article first appeared on Medscape.com.











