User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Charcoal could be the cure for the common high-fat diet
Charcoal won’t let high-fat diet weigh you down
Do you want to be the funniest person alive? Of course you do. It’s really simple too, just one joke can make you the greatest comedian of all time. All you have to do is go camping and cook food over a roaring campfire. When someone drops food into the fire (which they always will), get ready. Once they fish out the offending food, which is almost certainly coated in hot coals, tell them: “Ah, eat it anyway. A little texture never hurt!” Trust us, most hilarious and original gag of all time.
But before your hapless friend brushes off his hot dog and forces a laugh, consider this: Japanese researchers have found that a charcoal supplement can prevent weight gain in mice consuming a high-fat diet. Charcoal is actually quite the helpful substance, and not just for grilling. It’s been used as medicine for hundreds of years and even today is used as a treatment for drug overdose and excess gas and flatulence.
The study involved two groups of mice: One was fed a normal diet, the other a high-fat diet. After 12 weeks, the high-fat diet mice had gained weight. At that point, edible activated charcoal was added to their diet. From that point, weight gain was similar between the two groups, and the amount of bile acid, cholesterol, triglyceride, and fatty acid excreted by the high-fat mice increased by two to four times.
The researchers supported the notion that consuming an activated charcoal supplement before or while eating fatty food could prevent weight gain from said fatty food. Which works out well for the classic American barbecue, which is traditionally both high in fat and charcoal. All you have to do is buy some extra charcoal briquettes to pass around and munch on with your friends. Now that’s a party we can get behind.
There’s awake, and then there’s neurologically awake
Time to toss another urban legend onto the trash heap of history. Say goodbye to the benefits of uninterrupted sleep. It’s a fraud, a fake, a myth, a hit or myth, a swing and a myth, an old wives’ tale. You can stuff it and put it on a shelf next to Bigfoot, the Slender Man, and Twinkies.
We all thought we needed 8 hours of uninterrupted sleep every night, but guess who we forgot to tell? Our brains. They’ve been doing exactly the opposite all along, laughing at us the whole time. Smug SOBs.
To straighten out this mess, let’s bring in a scientist, Celia Kjaerby of the Center for Translational Neuromedicine at the University of Copenhagen: “You may think that sleep is a constant state that you are in, and then you wake up. But there is a lot more to sleep than meets the eye. We have learned that noradrenaline causes you to wake up more than 100 times a night. And that is during perfectly normal sleep.”
Those 100 or so sleep interruptions are so brief that we don’t even notice, but they are very important, according to a study conducted at the university. Those tiny little wake-up calls are “the essence for the part of sleep that makes us wake up rested and which enables us to remember what we learned the day before. ... The very short awakenings are created by waves of norepinephrine [and they] reset the brain so that it is ready to store memory when you dive back into sleep,” lead author Maiken Nedergaard, MD, explained.
The investigators compared the level of noradrenaline in sleeping mice with their electrical activity and found that the hormone constantly increased and decreased in a wavelike pattern. A high level meant that the animal was neurologically awake. Deeper valleys between the high points meant better sleep, and the mice with the “highest number of deep noradrenaline valleys were also the ones with the best memory,” the team said in their written statement.
Not just the best memory, they said, but “super memory.” That, of course, was enough to get the attention of Marvel Comics, so the next Disney superhero blockbuster will feature Nocturna, the queen of the night. Her power? Never forgets. Her archnemesis? The Insomniac. Her catchphrase? “Let me sleep on it.”
Words can hurt, literally
Growing up, we’re sure you heard the “sticks and stones” rhyme. Maybe you’ve even recited it once or twice to defend yourself. Well, forget it, because words can hurt and your brain knows it.
In a new study published in Frontiers in Communication, Marijn Struiksma, PhD, of Utrecht University, and colleagues incorporated the use of electroencephalography (EEG) and skin conductance on 79 women to see how words (specifically insults) actually affect the human body.
Each subject was asked to read three different types of statements: an insult, a compliment, and something factual but neutral. Half of the statements contained the subject’s name and half used somebody else’s. The participants were told that these statements were collected from three men.
Nobody interacted with each other, and the setting was completely clinical, yet the results were unmistakable. The EEG showed an effect in P2 amplitude with repetitive insults, no matter who it was about. Even though the insults weren’t real and the participants were aware of it, the brain still recognized them as hurtful, coming across as “mini slaps in the face,” Dr. Struiksma noted in a written statement.
The researchers noted that more needs to be done to better understand the long-term effects that insults can have and create a deeper understanding between words and emotion, but studying the effects of insults in a real-life setting is ethically tricky. This study is a start.
So, yeah, sticks and stones can break your bones, but words will actually hurt you.
This article was updated 7/21/22.
Charcoal won’t let high-fat diet weigh you down
Do you want to be the funniest person alive? Of course you do. It’s really simple too, just one joke can make you the greatest comedian of all time. All you have to do is go camping and cook food over a roaring campfire. When someone drops food into the fire (which they always will), get ready. Once they fish out the offending food, which is almost certainly coated in hot coals, tell them: “Ah, eat it anyway. A little texture never hurt!” Trust us, most hilarious and original gag of all time.
But before your hapless friend brushes off his hot dog and forces a laugh, consider this: Japanese researchers have found that a charcoal supplement can prevent weight gain in mice consuming a high-fat diet. Charcoal is actually quite the helpful substance, and not just for grilling. It’s been used as medicine for hundreds of years and even today is used as a treatment for drug overdose and excess gas and flatulence.
The study involved two groups of mice: One was fed a normal diet, the other a high-fat diet. After 12 weeks, the high-fat diet mice had gained weight. At that point, edible activated charcoal was added to their diet. From that point, weight gain was similar between the two groups, and the amount of bile acid, cholesterol, triglyceride, and fatty acid excreted by the high-fat mice increased by two to four times.
The researchers supported the notion that consuming an activated charcoal supplement before or while eating fatty food could prevent weight gain from said fatty food. Which works out well for the classic American barbecue, which is traditionally both high in fat and charcoal. All you have to do is buy some extra charcoal briquettes to pass around and munch on with your friends. Now that’s a party we can get behind.
There’s awake, and then there’s neurologically awake
Time to toss another urban legend onto the trash heap of history. Say goodbye to the benefits of uninterrupted sleep. It’s a fraud, a fake, a myth, a hit or myth, a swing and a myth, an old wives’ tale. You can stuff it and put it on a shelf next to Bigfoot, the Slender Man, and Twinkies.
We all thought we needed 8 hours of uninterrupted sleep every night, but guess who we forgot to tell? Our brains. They’ve been doing exactly the opposite all along, laughing at us the whole time. Smug SOBs.
To straighten out this mess, let’s bring in a scientist, Celia Kjaerby of the Center for Translational Neuromedicine at the University of Copenhagen: “You may think that sleep is a constant state that you are in, and then you wake up. But there is a lot more to sleep than meets the eye. We have learned that noradrenaline causes you to wake up more than 100 times a night. And that is during perfectly normal sleep.”
Those 100 or so sleep interruptions are so brief that we don’t even notice, but they are very important, according to a study conducted at the university. Those tiny little wake-up calls are “the essence for the part of sleep that makes us wake up rested and which enables us to remember what we learned the day before. ... The very short awakenings are created by waves of norepinephrine [and they] reset the brain so that it is ready to store memory when you dive back into sleep,” lead author Maiken Nedergaard, MD, explained.
The investigators compared the level of noradrenaline in sleeping mice with their electrical activity and found that the hormone constantly increased and decreased in a wavelike pattern. A high level meant that the animal was neurologically awake. Deeper valleys between the high points meant better sleep, and the mice with the “highest number of deep noradrenaline valleys were also the ones with the best memory,” the team said in their written statement.
Not just the best memory, they said, but “super memory.” That, of course, was enough to get the attention of Marvel Comics, so the next Disney superhero blockbuster will feature Nocturna, the queen of the night. Her power? Never forgets. Her archnemesis? The Insomniac. Her catchphrase? “Let me sleep on it.”
Words can hurt, literally
Growing up, we’re sure you heard the “sticks and stones” rhyme. Maybe you’ve even recited it once or twice to defend yourself. Well, forget it, because words can hurt and your brain knows it.
In a new study published in Frontiers in Communication, Marijn Struiksma, PhD, of Utrecht University, and colleagues incorporated the use of electroencephalography (EEG) and skin conductance on 79 women to see how words (specifically insults) actually affect the human body.
Each subject was asked to read three different types of statements: an insult, a compliment, and something factual but neutral. Half of the statements contained the subject’s name and half used somebody else’s. The participants were told that these statements were collected from three men.
Nobody interacted with each other, and the setting was completely clinical, yet the results were unmistakable. The EEG showed an effect in P2 amplitude with repetitive insults, no matter who it was about. Even though the insults weren’t real and the participants were aware of it, the brain still recognized them as hurtful, coming across as “mini slaps in the face,” Dr. Struiksma noted in a written statement.
The researchers noted that more needs to be done to better understand the long-term effects that insults can have and create a deeper understanding between words and emotion, but studying the effects of insults in a real-life setting is ethically tricky. This study is a start.
So, yeah, sticks and stones can break your bones, but words will actually hurt you.
This article was updated 7/21/22.
Charcoal won’t let high-fat diet weigh you down
Do you want to be the funniest person alive? Of course you do. It’s really simple too, just one joke can make you the greatest comedian of all time. All you have to do is go camping and cook food over a roaring campfire. When someone drops food into the fire (which they always will), get ready. Once they fish out the offending food, which is almost certainly coated in hot coals, tell them: “Ah, eat it anyway. A little texture never hurt!” Trust us, most hilarious and original gag of all time.
But before your hapless friend brushes off his hot dog and forces a laugh, consider this: Japanese researchers have found that a charcoal supplement can prevent weight gain in mice consuming a high-fat diet. Charcoal is actually quite the helpful substance, and not just for grilling. It’s been used as medicine for hundreds of years and even today is used as a treatment for drug overdose and excess gas and flatulence.
The study involved two groups of mice: One was fed a normal diet, the other a high-fat diet. After 12 weeks, the high-fat diet mice had gained weight. At that point, edible activated charcoal was added to their diet. From that point, weight gain was similar between the two groups, and the amount of bile acid, cholesterol, triglyceride, and fatty acid excreted by the high-fat mice increased by two to four times.
The researchers supported the notion that consuming an activated charcoal supplement before or while eating fatty food could prevent weight gain from said fatty food. Which works out well for the classic American barbecue, which is traditionally both high in fat and charcoal. All you have to do is buy some extra charcoal briquettes to pass around and munch on with your friends. Now that’s a party we can get behind.
There’s awake, and then there’s neurologically awake
Time to toss another urban legend onto the trash heap of history. Say goodbye to the benefits of uninterrupted sleep. It’s a fraud, a fake, a myth, a hit or myth, a swing and a myth, an old wives’ tale. You can stuff it and put it on a shelf next to Bigfoot, the Slender Man, and Twinkies.
We all thought we needed 8 hours of uninterrupted sleep every night, but guess who we forgot to tell? Our brains. They’ve been doing exactly the opposite all along, laughing at us the whole time. Smug SOBs.
To straighten out this mess, let’s bring in a scientist, Celia Kjaerby of the Center for Translational Neuromedicine at the University of Copenhagen: “You may think that sleep is a constant state that you are in, and then you wake up. But there is a lot more to sleep than meets the eye. We have learned that noradrenaline causes you to wake up more than 100 times a night. And that is during perfectly normal sleep.”
Those 100 or so sleep interruptions are so brief that we don’t even notice, but they are very important, according to a study conducted at the university. Those tiny little wake-up calls are “the essence for the part of sleep that makes us wake up rested and which enables us to remember what we learned the day before. ... The very short awakenings are created by waves of norepinephrine [and they] reset the brain so that it is ready to store memory when you dive back into sleep,” lead author Maiken Nedergaard, MD, explained.
The investigators compared the level of noradrenaline in sleeping mice with their electrical activity and found that the hormone constantly increased and decreased in a wavelike pattern. A high level meant that the animal was neurologically awake. Deeper valleys between the high points meant better sleep, and the mice with the “highest number of deep noradrenaline valleys were also the ones with the best memory,” the team said in their written statement.
Not just the best memory, they said, but “super memory.” That, of course, was enough to get the attention of Marvel Comics, so the next Disney superhero blockbuster will feature Nocturna, the queen of the night. Her power? Never forgets. Her archnemesis? The Insomniac. Her catchphrase? “Let me sleep on it.”
Words can hurt, literally
Growing up, we’re sure you heard the “sticks and stones” rhyme. Maybe you’ve even recited it once or twice to defend yourself. Well, forget it, because words can hurt and your brain knows it.
In a new study published in Frontiers in Communication, Marijn Struiksma, PhD, of Utrecht University, and colleagues incorporated the use of electroencephalography (EEG) and skin conductance on 79 women to see how words (specifically insults) actually affect the human body.
Each subject was asked to read three different types of statements: an insult, a compliment, and something factual but neutral. Half of the statements contained the subject’s name and half used somebody else’s. The participants were told that these statements were collected from three men.
Nobody interacted with each other, and the setting was completely clinical, yet the results were unmistakable. The EEG showed an effect in P2 amplitude with repetitive insults, no matter who it was about. Even though the insults weren’t real and the participants were aware of it, the brain still recognized them as hurtful, coming across as “mini slaps in the face,” Dr. Struiksma noted in a written statement.
The researchers noted that more needs to be done to better understand the long-term effects that insults can have and create a deeper understanding between words and emotion, but studying the effects of insults in a real-life setting is ethically tricky. This study is a start.
So, yeah, sticks and stones can break your bones, but words will actually hurt you.
This article was updated 7/21/22.
When and for whom is telehealth OCD treatment appropriate?
It is no secret that the COVID-19 pandemic resulted in widespread disruptions in health care services. While providers and resources were limited and many patients were apprehensive to present to health care settings out of concern of disease contraction, telehealth services did offer some relief.
Compared to other specialty care services, mental health care providers were well equipped to handle the expansion of telehealth services, as extensive treatment literature provides strong support for the use of psychotherapeutic interventions over telehealth mediums.1 This holds true in the context of obsessive-compulsive disorder (OCD), where an impressive literature supports the use of telehealth delivery for the gold-standard psychotherapeutic, exposure and response prevention (ERP).2,3,4
Through ERP, patients work with a clinician to systematically expose themselves to anxiety-providing triggers while actively resisting compulsive behaviors to learn the distress does go away with time and/or the distress is within their ability to cope. This intervention is conceptually similar to repeatedly watching a scary film, by which continued exposure results in less pronounced emotional reaction with subsequent viewings.
Fortunately for patients and providers, the expansion of telehealth ERP across different treatment settings has had many unintended benefits, including increased access to care, lower no-show rates due to the ease of attending appointments, and the ability to offer higher levels of care, including intensive outpatient programs, over telehealth mediums. Anecdotally, our clinic has been able to increase patient reach by providing telehealth ERP to those who historically would not have been able to access care due to geography. Even for those living within driving distance to our clinic, the ease of joining a video visit for a 45-minute appointment far outweighs driving into the clinic, in many circumstances. With these benefits, the delivery of ERP over telehealth appears likely to stay, although OCD providers delivering ERP will need to consider when and for whom this medium may not be appropriate.
To this end, we recently conducted a study examining ERP providers perceptions of telehealth and in-person ERP, patient characteristics best suited for telehealth services, and provider ability to identify and address factors that adversely impact the course of treatment (e.g., substance use, limited symptom insight, distractions during ERP, etc.).5 Providers reported lower feasibility ratings for telehealth compared to in-person ERP for younger patients (aged under 13 years), and patients with more severe OCD presentations. Providers also reported more difficulty identifying and addressing ERP interfering factors over telehealth relative to in-person. The findings from our research do not necessarily speak to the effectiveness of telehealth ERP, which has repeatedly been documented in treatment literature, but rather our findings highlight that ERP providers endorse reservations about the feasibility of ERP for certain OCD patient profiles, and that telehealth ERP may not be appropriate for all patients with OCD.
Mental health care providers, including those delivering ERP, should consider when telehealth is and is not appropriate. Importantly, telehealth offers a limited field of view compared to in-person, and providers can only observe what is captured by the camera. In the context of telehealth ERP, patients may engage in subtle avoidant behaviors that are more difficult to observe, which may prevent them from experiencing necessary anxiety during exposure practice. Many providers may have firsthand experience with this, or patients who appear distracted over telehealth mediums because of environmental factors that can be controlled for during in-person services.
As telehealth treatment options appear increasingly likely to stay, ERP providers and intervention researchers should continue identifying patient characteristics that are more and less appropriate for telehealth settings in order to maximize treatment outcomes. Providers should share concerns with patients when delivering telehealth ERP and work to address interfering factors impacting the course of treatment. In circumstances where this is not possible, such as when the patients age or symptom severity prevents effective telehealth ERP, or when treatment progress stalls, providers should speak with patients to determine if it would be beneficial to transition to in-person services.
Both in-person and telehealth ERP are fundamentally the same, however it does appear that subtle differences across these modalities may have differential impacts on treatment outcomes for certain OCD patient presentations. , however appropriate caution should be exhibited, and providers should use clinical judgment when offering telehealth services.
Dr. Wiese is a clinical psychologist in the department of psychiatry and behavioral sciences at Baylor College of Medicine, Houston, Texas. He is primarily focused on conducting research on OCD and related disorders and providing empirically supported treatments to individuals diagnosed with these conditions.
References
1. Fernandez E et al. Live psychotherapy by video versus in‐person: A meta‐analysis of efficacy and its relationship to types and targets of treatment. Clin Psychol Psychother. 2021 Nov;28(6):1535-49. doi: 10.1002/cpp.2594.
2. Storch EA et al. Preliminary investigation of web-camera delivered cognitive-behavioral therapy for youth with obsessive-compulsive disorder. Psychiatry Res. 2011 Oct 30;189(3):407-12. doi: 10.1016/j.psychres.2011.05.047.
3. Fletcher TL et al. A pilot open trial of video telehealth-delivered exposure and response prevention for obsessive-compulsive disorder in rural Veterans. Mil Psychol. 2021 Oct 28;34(1):83-90. doi: 10.1080/08995605.2021.1970983.
4. Wootton BM. Remote cognitive–behavior therapy for obsessive–compulsive symptoms: a meta-analysis. Clin Psychol Rev. 2016 Feb;43:103-13. doi: 10.1016/j.cpr.2015.10.001.
5. Wiese AD et al. Provider perceptions of telehealth and in-person exposure and response prevention for obsessive–compulsive disorder. Psychiatry Res. 2022 Jul;313:114610. doi: 10.1016/j.psychres.2022.114610.
It is no secret that the COVID-19 pandemic resulted in widespread disruptions in health care services. While providers and resources were limited and many patients were apprehensive to present to health care settings out of concern of disease contraction, telehealth services did offer some relief.
Compared to other specialty care services, mental health care providers were well equipped to handle the expansion of telehealth services, as extensive treatment literature provides strong support for the use of psychotherapeutic interventions over telehealth mediums.1 This holds true in the context of obsessive-compulsive disorder (OCD), where an impressive literature supports the use of telehealth delivery for the gold-standard psychotherapeutic, exposure and response prevention (ERP).2,3,4
Through ERP, patients work with a clinician to systematically expose themselves to anxiety-providing triggers while actively resisting compulsive behaviors to learn the distress does go away with time and/or the distress is within their ability to cope. This intervention is conceptually similar to repeatedly watching a scary film, by which continued exposure results in less pronounced emotional reaction with subsequent viewings.
Fortunately for patients and providers, the expansion of telehealth ERP across different treatment settings has had many unintended benefits, including increased access to care, lower no-show rates due to the ease of attending appointments, and the ability to offer higher levels of care, including intensive outpatient programs, over telehealth mediums. Anecdotally, our clinic has been able to increase patient reach by providing telehealth ERP to those who historically would not have been able to access care due to geography. Even for those living within driving distance to our clinic, the ease of joining a video visit for a 45-minute appointment far outweighs driving into the clinic, in many circumstances. With these benefits, the delivery of ERP over telehealth appears likely to stay, although OCD providers delivering ERP will need to consider when and for whom this medium may not be appropriate.
To this end, we recently conducted a study examining ERP providers perceptions of telehealth and in-person ERP, patient characteristics best suited for telehealth services, and provider ability to identify and address factors that adversely impact the course of treatment (e.g., substance use, limited symptom insight, distractions during ERP, etc.).5 Providers reported lower feasibility ratings for telehealth compared to in-person ERP for younger patients (aged under 13 years), and patients with more severe OCD presentations. Providers also reported more difficulty identifying and addressing ERP interfering factors over telehealth relative to in-person. The findings from our research do not necessarily speak to the effectiveness of telehealth ERP, which has repeatedly been documented in treatment literature, but rather our findings highlight that ERP providers endorse reservations about the feasibility of ERP for certain OCD patient profiles, and that telehealth ERP may not be appropriate for all patients with OCD.
Mental health care providers, including those delivering ERP, should consider when telehealth is and is not appropriate. Importantly, telehealth offers a limited field of view compared to in-person, and providers can only observe what is captured by the camera. In the context of telehealth ERP, patients may engage in subtle avoidant behaviors that are more difficult to observe, which may prevent them from experiencing necessary anxiety during exposure practice. Many providers may have firsthand experience with this, or patients who appear distracted over telehealth mediums because of environmental factors that can be controlled for during in-person services.
As telehealth treatment options appear increasingly likely to stay, ERP providers and intervention researchers should continue identifying patient characteristics that are more and less appropriate for telehealth settings in order to maximize treatment outcomes. Providers should share concerns with patients when delivering telehealth ERP and work to address interfering factors impacting the course of treatment. In circumstances where this is not possible, such as when the patients age or symptom severity prevents effective telehealth ERP, or when treatment progress stalls, providers should speak with patients to determine if it would be beneficial to transition to in-person services.
Both in-person and telehealth ERP are fundamentally the same, however it does appear that subtle differences across these modalities may have differential impacts on treatment outcomes for certain OCD patient presentations. , however appropriate caution should be exhibited, and providers should use clinical judgment when offering telehealth services.
Dr. Wiese is a clinical psychologist in the department of psychiatry and behavioral sciences at Baylor College of Medicine, Houston, Texas. He is primarily focused on conducting research on OCD and related disorders and providing empirically supported treatments to individuals diagnosed with these conditions.
References
1. Fernandez E et al. Live psychotherapy by video versus in‐person: A meta‐analysis of efficacy and its relationship to types and targets of treatment. Clin Psychol Psychother. 2021 Nov;28(6):1535-49. doi: 10.1002/cpp.2594.
2. Storch EA et al. Preliminary investigation of web-camera delivered cognitive-behavioral therapy for youth with obsessive-compulsive disorder. Psychiatry Res. 2011 Oct 30;189(3):407-12. doi: 10.1016/j.psychres.2011.05.047.
3. Fletcher TL et al. A pilot open trial of video telehealth-delivered exposure and response prevention for obsessive-compulsive disorder in rural Veterans. Mil Psychol. 2021 Oct 28;34(1):83-90. doi: 10.1080/08995605.2021.1970983.
4. Wootton BM. Remote cognitive–behavior therapy for obsessive–compulsive symptoms: a meta-analysis. Clin Psychol Rev. 2016 Feb;43:103-13. doi: 10.1016/j.cpr.2015.10.001.
5. Wiese AD et al. Provider perceptions of telehealth and in-person exposure and response prevention for obsessive–compulsive disorder. Psychiatry Res. 2022 Jul;313:114610. doi: 10.1016/j.psychres.2022.114610.
It is no secret that the COVID-19 pandemic resulted in widespread disruptions in health care services. While providers and resources were limited and many patients were apprehensive to present to health care settings out of concern of disease contraction, telehealth services did offer some relief.
Compared to other specialty care services, mental health care providers were well equipped to handle the expansion of telehealth services, as extensive treatment literature provides strong support for the use of psychotherapeutic interventions over telehealth mediums.1 This holds true in the context of obsessive-compulsive disorder (OCD), where an impressive literature supports the use of telehealth delivery for the gold-standard psychotherapeutic, exposure and response prevention (ERP).2,3,4
Through ERP, patients work with a clinician to systematically expose themselves to anxiety-providing triggers while actively resisting compulsive behaviors to learn the distress does go away with time and/or the distress is within their ability to cope. This intervention is conceptually similar to repeatedly watching a scary film, by which continued exposure results in less pronounced emotional reaction with subsequent viewings.
Fortunately for patients and providers, the expansion of telehealth ERP across different treatment settings has had many unintended benefits, including increased access to care, lower no-show rates due to the ease of attending appointments, and the ability to offer higher levels of care, including intensive outpatient programs, over telehealth mediums. Anecdotally, our clinic has been able to increase patient reach by providing telehealth ERP to those who historically would not have been able to access care due to geography. Even for those living within driving distance to our clinic, the ease of joining a video visit for a 45-minute appointment far outweighs driving into the clinic, in many circumstances. With these benefits, the delivery of ERP over telehealth appears likely to stay, although OCD providers delivering ERP will need to consider when and for whom this medium may not be appropriate.
To this end, we recently conducted a study examining ERP providers perceptions of telehealth and in-person ERP, patient characteristics best suited for telehealth services, and provider ability to identify and address factors that adversely impact the course of treatment (e.g., substance use, limited symptom insight, distractions during ERP, etc.).5 Providers reported lower feasibility ratings for telehealth compared to in-person ERP for younger patients (aged under 13 years), and patients with more severe OCD presentations. Providers also reported more difficulty identifying and addressing ERP interfering factors over telehealth relative to in-person. The findings from our research do not necessarily speak to the effectiveness of telehealth ERP, which has repeatedly been documented in treatment literature, but rather our findings highlight that ERP providers endorse reservations about the feasibility of ERP for certain OCD patient profiles, and that telehealth ERP may not be appropriate for all patients with OCD.
Mental health care providers, including those delivering ERP, should consider when telehealth is and is not appropriate. Importantly, telehealth offers a limited field of view compared to in-person, and providers can only observe what is captured by the camera. In the context of telehealth ERP, patients may engage in subtle avoidant behaviors that are more difficult to observe, which may prevent them from experiencing necessary anxiety during exposure practice. Many providers may have firsthand experience with this, or patients who appear distracted over telehealth mediums because of environmental factors that can be controlled for during in-person services.
As telehealth treatment options appear increasingly likely to stay, ERP providers and intervention researchers should continue identifying patient characteristics that are more and less appropriate for telehealth settings in order to maximize treatment outcomes. Providers should share concerns with patients when delivering telehealth ERP and work to address interfering factors impacting the course of treatment. In circumstances where this is not possible, such as when the patients age or symptom severity prevents effective telehealth ERP, or when treatment progress stalls, providers should speak with patients to determine if it would be beneficial to transition to in-person services.
Both in-person and telehealth ERP are fundamentally the same, however it does appear that subtle differences across these modalities may have differential impacts on treatment outcomes for certain OCD patient presentations. , however appropriate caution should be exhibited, and providers should use clinical judgment when offering telehealth services.
Dr. Wiese is a clinical psychologist in the department of psychiatry and behavioral sciences at Baylor College of Medicine, Houston, Texas. He is primarily focused on conducting research on OCD and related disorders and providing empirically supported treatments to individuals diagnosed with these conditions.
References
1. Fernandez E et al. Live psychotherapy by video versus in‐person: A meta‐analysis of efficacy and its relationship to types and targets of treatment. Clin Psychol Psychother. 2021 Nov;28(6):1535-49. doi: 10.1002/cpp.2594.
2. Storch EA et al. Preliminary investigation of web-camera delivered cognitive-behavioral therapy for youth with obsessive-compulsive disorder. Psychiatry Res. 2011 Oct 30;189(3):407-12. doi: 10.1016/j.psychres.2011.05.047.
3. Fletcher TL et al. A pilot open trial of video telehealth-delivered exposure and response prevention for obsessive-compulsive disorder in rural Veterans. Mil Psychol. 2021 Oct 28;34(1):83-90. doi: 10.1080/08995605.2021.1970983.
4. Wootton BM. Remote cognitive–behavior therapy for obsessive–compulsive symptoms: a meta-analysis. Clin Psychol Rev. 2016 Feb;43:103-13. doi: 10.1016/j.cpr.2015.10.001.
5. Wiese AD et al. Provider perceptions of telehealth and in-person exposure and response prevention for obsessive–compulsive disorder. Psychiatry Res. 2022 Jul;313:114610. doi: 10.1016/j.psychres.2022.114610.
No increase in overdose deaths with take-home methadone
new research shows.
Overdose deaths both with and without methadone rose sharply in March 2020, when the policy was announced. Of note, methadone-related deaths decreased in the following months, whereas deaths not involving methadone continued to increase.
“Coupled with research demonstrating improved patient satisfaction, treatment access, and engagement from these policies, these findings can inform decisions about permanently expanding take-home methadone,” the investigators wrote.
The study was published online in JAMA Psychiatry.
An essential tool
Before the pandemic, patients seeking methadone treatment for OUD in the United States had to visit a federally certified opioid treatment clinic every day to receive the medication.
In response to the pandemic, the Substance Abuse and Mental Health Services Administration instituted a new policy that allowed states to request exceptions to provide take-home methadone for up to 4 weeks for stable patients and up to 2 weeks for those who were less stable.
To determine the effect of this policy change on overdose death rates, researchers analyzed data on overdose deaths from January 2019 to August 2021.
Overall, the percentage of deaths involving methadone decreased from 4.5% in 2019 to 3.2% in 2021.
The investigators found a sharp increase in all overdose deaths in March 2020. Deaths that did not involve methadone increased by an average of 78.12 more each month before March 2020, increased by an average of 1,078.27 during March 2020, and then continued to increase by an average of 69.07 more each month after March 2020.
Overdose deaths involving methadone increased by a similar amount in March 2020, stabilized, and then decreased 0.05% per month.
Researchers attributed the increase in methadone-related deaths in March 2020 with the rise in overall drug overdose deaths driven by illicitly made fentanyl in the early months of the COVID-19 pandemic.
A study published in JAMA Network Open in March 2022 showed that methadone and other medications to treat OUD are widely underutilized.
That research cited concern over misuse as a key reason for clinicians’ reluctance to prescribe the drugs. The researchers of the current study hope that these new findings lay some of these fears to rest.
“Treatment is an essential tool to stop the addiction and overdose crises, but it is vastly underused,” Nora Volkow, MD, coinvestigator, and director of the National Institute on Drug Abuse, said in a press release. “This evidence adds significant weight to the argument that effective treatment for substance use disorders should be offered in an accessible and practical way that works for people who need it.”
The study was funded by the Centers for Disease Control and Prevention and the National Institutes of Health. The authors reported no relevant disclosures related to the study.
A version of this article first appeared on Medscape.com.
new research shows.
Overdose deaths both with and without methadone rose sharply in March 2020, when the policy was announced. Of note, methadone-related deaths decreased in the following months, whereas deaths not involving methadone continued to increase.
“Coupled with research demonstrating improved patient satisfaction, treatment access, and engagement from these policies, these findings can inform decisions about permanently expanding take-home methadone,” the investigators wrote.
The study was published online in JAMA Psychiatry.
An essential tool
Before the pandemic, patients seeking methadone treatment for OUD in the United States had to visit a federally certified opioid treatment clinic every day to receive the medication.
In response to the pandemic, the Substance Abuse and Mental Health Services Administration instituted a new policy that allowed states to request exceptions to provide take-home methadone for up to 4 weeks for stable patients and up to 2 weeks for those who were less stable.
To determine the effect of this policy change on overdose death rates, researchers analyzed data on overdose deaths from January 2019 to August 2021.
Overall, the percentage of deaths involving methadone decreased from 4.5% in 2019 to 3.2% in 2021.
The investigators found a sharp increase in all overdose deaths in March 2020. Deaths that did not involve methadone increased by an average of 78.12 more each month before March 2020, increased by an average of 1,078.27 during March 2020, and then continued to increase by an average of 69.07 more each month after March 2020.
Overdose deaths involving methadone increased by a similar amount in March 2020, stabilized, and then decreased 0.05% per month.
Researchers attributed the increase in methadone-related deaths in March 2020 with the rise in overall drug overdose deaths driven by illicitly made fentanyl in the early months of the COVID-19 pandemic.
A study published in JAMA Network Open in March 2022 showed that methadone and other medications to treat OUD are widely underutilized.
That research cited concern over misuse as a key reason for clinicians’ reluctance to prescribe the drugs. The researchers of the current study hope that these new findings lay some of these fears to rest.
“Treatment is an essential tool to stop the addiction and overdose crises, but it is vastly underused,” Nora Volkow, MD, coinvestigator, and director of the National Institute on Drug Abuse, said in a press release. “This evidence adds significant weight to the argument that effective treatment for substance use disorders should be offered in an accessible and practical way that works for people who need it.”
The study was funded by the Centers for Disease Control and Prevention and the National Institutes of Health. The authors reported no relevant disclosures related to the study.
A version of this article first appeared on Medscape.com.
new research shows.
Overdose deaths both with and without methadone rose sharply in March 2020, when the policy was announced. Of note, methadone-related deaths decreased in the following months, whereas deaths not involving methadone continued to increase.
“Coupled with research demonstrating improved patient satisfaction, treatment access, and engagement from these policies, these findings can inform decisions about permanently expanding take-home methadone,” the investigators wrote.
The study was published online in JAMA Psychiatry.
An essential tool
Before the pandemic, patients seeking methadone treatment for OUD in the United States had to visit a federally certified opioid treatment clinic every day to receive the medication.
In response to the pandemic, the Substance Abuse and Mental Health Services Administration instituted a new policy that allowed states to request exceptions to provide take-home methadone for up to 4 weeks for stable patients and up to 2 weeks for those who were less stable.
To determine the effect of this policy change on overdose death rates, researchers analyzed data on overdose deaths from January 2019 to August 2021.
Overall, the percentage of deaths involving methadone decreased from 4.5% in 2019 to 3.2% in 2021.
The investigators found a sharp increase in all overdose deaths in March 2020. Deaths that did not involve methadone increased by an average of 78.12 more each month before March 2020, increased by an average of 1,078.27 during March 2020, and then continued to increase by an average of 69.07 more each month after March 2020.
Overdose deaths involving methadone increased by a similar amount in March 2020, stabilized, and then decreased 0.05% per month.
Researchers attributed the increase in methadone-related deaths in March 2020 with the rise in overall drug overdose deaths driven by illicitly made fentanyl in the early months of the COVID-19 pandemic.
A study published in JAMA Network Open in March 2022 showed that methadone and other medications to treat OUD are widely underutilized.
That research cited concern over misuse as a key reason for clinicians’ reluctance to prescribe the drugs. The researchers of the current study hope that these new findings lay some of these fears to rest.
“Treatment is an essential tool to stop the addiction and overdose crises, but it is vastly underused,” Nora Volkow, MD, coinvestigator, and director of the National Institute on Drug Abuse, said in a press release. “This evidence adds significant weight to the argument that effective treatment for substance use disorders should be offered in an accessible and practical way that works for people who need it.”
The study was funded by the Centers for Disease Control and Prevention and the National Institutes of Health. The authors reported no relevant disclosures related to the study.
A version of this article first appeared on Medscape.com.
FROM JAMA PSYCHIATRY
Global data provide new insight into problem gambling
Across the globe few individuals at risk for gambling problems seek help for the issue, new research shows.
In the first study to examine global prevalence of help-seeking for problem gambling, the systematic review showed that
“Our findings suggest a considerable need for help among those experiencing problems related to their gambling,” Rimke Bijker, PhD, of the University of Auckland (New Zealand) and colleagues wrote.
The findings were published online in Addiction.
A public health concern
An increase in online gambling and stress and isolation during the COVID-19 pandemic led to experts sounding the alarm about gambling disorders. But despite its emergence as a public health concern, systematic investigation of help-seeking for problem gambling has been lacking, the investigators noted.
In their review, they included 24 studies conducted between 2010 and 2020 and involving a total of 188,234 individuals. More than 70% of the studies were conducted in Australia and New Zealand and 25% were conducted in the United States and Canada.
The overall prevalence of help-seeking for problem gambling among adults worldwide was 0.23% (95% confidence interval, 0.16-0.33).
Prevalence estimates were significantly higher in studies assessing lifetime help-seeking (0.50%; 95% CI, 0.35-0.71), compared with studies that examined current help-seeking (0.14%; 95% CI, 0.1-0.2, P < .001).
There were no significant differences in prevalence by gambling participation, region, type of help-seeking (professional only or mixed options), or year of data collection.
Gambling severity was measured by the Problem Gambling Severity Index as low risk, as moderate risk, or as problem gambling. Help-seeking was highest in the problem gambling and the moderate-risk groups, compared with the low-risk group (20.63%, 3.73%, and 0.27%, respectively; P < .001).
“A public health approach to gambling problems should be grounded in robust evidence on what people currently do to minimize and reduce their gambling harm and this should be inclusive of professional and nonprofessional support and self-help,” the investigators wrote.
Around 40% of individuals with problem gambling recover with or without professional oversight, they added.
Historically, gambling interventions have focused on those with more severe gambling problems. To truly address the issue, gambling reduction efforts should consider individuals with problems across the full continuum of risk, including those experiencing less severe problem gambling, the researchers wrote.
They added that those with more severe gambling issues “are likely to have comorbidities and may require more intensive interventions, guided by professionals,” such as general practitioners, psychiatrists, or psychologists.
Those with a less severe form “may prefer non-professional options and self-help strategies, which highlights the importance of information on such sources of help being promoted and easily accessible,” the investigators wrote.
No funding source for the study was reported. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Across the globe few individuals at risk for gambling problems seek help for the issue, new research shows.
In the first study to examine global prevalence of help-seeking for problem gambling, the systematic review showed that
“Our findings suggest a considerable need for help among those experiencing problems related to their gambling,” Rimke Bijker, PhD, of the University of Auckland (New Zealand) and colleagues wrote.
The findings were published online in Addiction.
A public health concern
An increase in online gambling and stress and isolation during the COVID-19 pandemic led to experts sounding the alarm about gambling disorders. But despite its emergence as a public health concern, systematic investigation of help-seeking for problem gambling has been lacking, the investigators noted.
In their review, they included 24 studies conducted between 2010 and 2020 and involving a total of 188,234 individuals. More than 70% of the studies were conducted in Australia and New Zealand and 25% were conducted in the United States and Canada.
The overall prevalence of help-seeking for problem gambling among adults worldwide was 0.23% (95% confidence interval, 0.16-0.33).
Prevalence estimates were significantly higher in studies assessing lifetime help-seeking (0.50%; 95% CI, 0.35-0.71), compared with studies that examined current help-seeking (0.14%; 95% CI, 0.1-0.2, P < .001).
There were no significant differences in prevalence by gambling participation, region, type of help-seeking (professional only or mixed options), or year of data collection.
Gambling severity was measured by the Problem Gambling Severity Index as low risk, as moderate risk, or as problem gambling. Help-seeking was highest in the problem gambling and the moderate-risk groups, compared with the low-risk group (20.63%, 3.73%, and 0.27%, respectively; P < .001).
“A public health approach to gambling problems should be grounded in robust evidence on what people currently do to minimize and reduce their gambling harm and this should be inclusive of professional and nonprofessional support and self-help,” the investigators wrote.
Around 40% of individuals with problem gambling recover with or without professional oversight, they added.
Historically, gambling interventions have focused on those with more severe gambling problems. To truly address the issue, gambling reduction efforts should consider individuals with problems across the full continuum of risk, including those experiencing less severe problem gambling, the researchers wrote.
They added that those with more severe gambling issues “are likely to have comorbidities and may require more intensive interventions, guided by professionals,” such as general practitioners, psychiatrists, or psychologists.
Those with a less severe form “may prefer non-professional options and self-help strategies, which highlights the importance of information on such sources of help being promoted and easily accessible,” the investigators wrote.
No funding source for the study was reported. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Across the globe few individuals at risk for gambling problems seek help for the issue, new research shows.
In the first study to examine global prevalence of help-seeking for problem gambling, the systematic review showed that
“Our findings suggest a considerable need for help among those experiencing problems related to their gambling,” Rimke Bijker, PhD, of the University of Auckland (New Zealand) and colleagues wrote.
The findings were published online in Addiction.
A public health concern
An increase in online gambling and stress and isolation during the COVID-19 pandemic led to experts sounding the alarm about gambling disorders. But despite its emergence as a public health concern, systematic investigation of help-seeking for problem gambling has been lacking, the investigators noted.
In their review, they included 24 studies conducted between 2010 and 2020 and involving a total of 188,234 individuals. More than 70% of the studies were conducted in Australia and New Zealand and 25% were conducted in the United States and Canada.
The overall prevalence of help-seeking for problem gambling among adults worldwide was 0.23% (95% confidence interval, 0.16-0.33).
Prevalence estimates were significantly higher in studies assessing lifetime help-seeking (0.50%; 95% CI, 0.35-0.71), compared with studies that examined current help-seeking (0.14%; 95% CI, 0.1-0.2, P < .001).
There were no significant differences in prevalence by gambling participation, region, type of help-seeking (professional only or mixed options), or year of data collection.
Gambling severity was measured by the Problem Gambling Severity Index as low risk, as moderate risk, or as problem gambling. Help-seeking was highest in the problem gambling and the moderate-risk groups, compared with the low-risk group (20.63%, 3.73%, and 0.27%, respectively; P < .001).
“A public health approach to gambling problems should be grounded in robust evidence on what people currently do to minimize and reduce their gambling harm and this should be inclusive of professional and nonprofessional support and self-help,” the investigators wrote.
Around 40% of individuals with problem gambling recover with or without professional oversight, they added.
Historically, gambling interventions have focused on those with more severe gambling problems. To truly address the issue, gambling reduction efforts should consider individuals with problems across the full continuum of risk, including those experiencing less severe problem gambling, the researchers wrote.
They added that those with more severe gambling issues “are likely to have comorbidities and may require more intensive interventions, guided by professionals,” such as general practitioners, psychiatrists, or psychologists.
Those with a less severe form “may prefer non-professional options and self-help strategies, which highlights the importance of information on such sources of help being promoted and easily accessible,” the investigators wrote.
No funding source for the study was reported. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ADDICTION
Electroacupuncture promising for depression-related insomnia
In a study of more than 200 adults with depression and comorbid insomnia, change from baseline to week 8 on the Pittsburgh Sleep Quality Index (PSQI) was 3 points greater in the group receiving EA versus a group receiving sham acupuncture (SA) plus standard care, and 5 points greater vs a control group receiving standard care only. The improvements were sustained during a 24-week postintervention follow-up.
The EA group also showed significant improvement in depression, insomnia, self-rated anxiety, and total sleep time – all of which were not found in the SA or control groups.
“Based on the results of our trial, we recommend patients with depression and insomnia seek the treatment of EA as an alternative and complementary therapy for better results,” study investigator Shifen Xu, PhD, Shanghai (China) Municipal Hospital of Traditional Chinese Medicine, Shanghai University of Traditional Chinese Medicine, told this news organization.
The findings were published online in JAMA Network Open.
Bidirectional relationship
“Sleep disturbance is the prominent symptom in patients with depression,” the investigators noted.
Depression and sleep issues have a bidirectional relationship, in that “poor sleep quality contributes to the development of depression, and having depression makes a person more likely to develop sleep issues,” they wrote.
Patients with co-occurring depression and sleep disorders are more difficult to treat and have a greater risk for relapse and recurrence of depression, they added.
Acupuncture may be an “effective drug-free approach to help treat mental illness and sleep disorders,” the researchers noted. A previous study suggested acupuncture may improve sleep efficacy and prolong total sleep in patients with primary insomnia.
“EA is the combination of traditional Chinese acupuncture with electric-impulse stimulation, and it can enhance the therapeutic effect of the acupoints throughout the needle retention time,” Dr. Xu said.
A previous pilot study of EA for depression-related insomnia showed significant improvements in sleep quality after EA treatment, but the sample size was small.
The current researchers, therefore, undertook the present study – with a larger sample size and comparison with SA and standard care. They divided 270 adults (mean age, 50.3 years; 71.9% women) at three tertiary hospitals in Shanghai into three groups, each consisting of 90 participants.
The EA plus standard care group and the SA plus standard care group received 30-minute treatments three times per week for 8 weeks. The control group received standard care only.
All participants had DSM-5–diagnosed depression; baseline PSQI scores greater than 7, with higher scores indicating worse sleep quality and a greater number or sleep disorders; and Hamilton Depression Rating Scales (HDRS-17) scores of 20-35, with higher scores indicating higher depression levels.
Patients with secondary depressive disorders caused by other conditions, medication, or psychotic disorders were excluded, as were patients with a history of alcohol abuse or drug dependence or those who had received acupuncture within the previous year.
Of the patients who completed the 8-week intervention, 83 were in the EA group, 81 in the SA group, and 83 in the control group. Almost all participants (91.5%) completed all outcome measurements by the end of the 24-week follow-up period (also known as week 32).
Calm mind, balanced mood
At the 8-week posttreatment assessment, which was the primary endpoint, the EA group had a mean reduction from baseline of 6.2 points (95% confidence interval, −6.9 to −5.6) in PSQI score.
There was a significant difference in PSQI score between the EA versus the SA group (−3.6 points; 95% CI, −4.4 to −2.8; P < .001) and vs the control group (−5.1 points; 95% CI, −6.0 to −4.2; P < .001).
The efficacy of EA in treating insomnia was sustained during the postintervention follow-up period when the EA group had a significantly greater reduction in PSQI score, compared with the SA group (−4.7; 95% CI, −5.4 to −3.9; P < .001) and the control group (−5.0; 95% CI, −5.8 to −4.1; P < .001).
Patients receiving EA also experienced significant (all P values < .001) improvement from baseline on secondary outcomes, including:
- Scores on the HDRS (−10.7; 95% CI, −11.8 to −9.7)
- Scores on the Insomnia Severity Index, (−7.6; 95% CI,−8.5 to −6.7)
- Scores on the Self-rated Anxiety Scale (−2.9; 95% CI, −4.1 to −1.7)
- Total sleep time, as recorded by sleep actigraphy (29.1 minutes; 95% CI, 21.5-36.7)
In addition, the EA group showed significant improvement in depression scores compared with the SA and control groups at both 8 and 32 weeks (all P values < .001).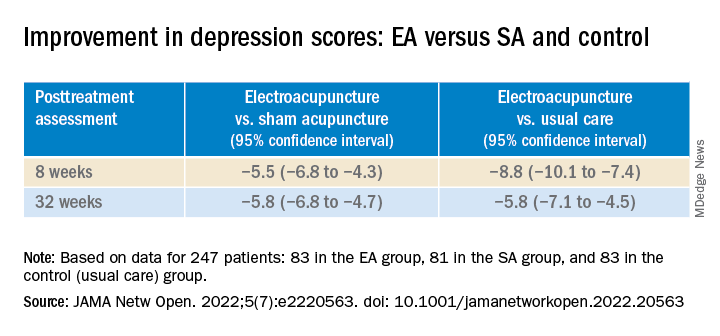
Participants in the EA group also had a 4.2% (95% CI, 2.6% - 5.8%) higher sleep efficiency score at week 8, compared with those in the SA group (P < .001).
In addition, they had lower scores on the Insomnia Severity Index and the Self-rated Anxiety Scale, and longer total sleep time, compared with the control group at week 8.
None of the participants reported any serious adverse events.
“Our findings constitute subjective and objective evidence of the efficacy and safety of EA with standard care in treating comorbid depression and insomnia compared with SA with standard care or standard care alone,” the investigators wrote.
“The acupoints we used in this trial mainly act on calming mind, relieving negative mood, and balancing the yin-yang,” Dr. Xu added.
Viable adjunctive treatment
Commenting on the study, Albert Yeung, MD, ScD, associate director of the Mass General Depression and Clinical Research Program and associate professor of psychiatry, Harvard Medical School, Boston, said that, with the evidence from this study, “acupuncture and/or electroacupuncture could be a viable adjunctive treatment for depressed patients who suffer from insomnia.”
Dr. Yeung, who was not involved with the study, is the coauthor of an accompanying editorial.
“More well-designed studies are warranted to provide evidence for integrating holistic treatment in medicine,” he said.
The study was funded by grants from the National Natural Science Foundation of China, and Shanghai Municipal Health. The investigators and Dr. Yeung reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a study of more than 200 adults with depression and comorbid insomnia, change from baseline to week 8 on the Pittsburgh Sleep Quality Index (PSQI) was 3 points greater in the group receiving EA versus a group receiving sham acupuncture (SA) plus standard care, and 5 points greater vs a control group receiving standard care only. The improvements were sustained during a 24-week postintervention follow-up.
The EA group also showed significant improvement in depression, insomnia, self-rated anxiety, and total sleep time – all of which were not found in the SA or control groups.
“Based on the results of our trial, we recommend patients with depression and insomnia seek the treatment of EA as an alternative and complementary therapy for better results,” study investigator Shifen Xu, PhD, Shanghai (China) Municipal Hospital of Traditional Chinese Medicine, Shanghai University of Traditional Chinese Medicine, told this news organization.
The findings were published online in JAMA Network Open.
Bidirectional relationship
“Sleep disturbance is the prominent symptom in patients with depression,” the investigators noted.
Depression and sleep issues have a bidirectional relationship, in that “poor sleep quality contributes to the development of depression, and having depression makes a person more likely to develop sleep issues,” they wrote.
Patients with co-occurring depression and sleep disorders are more difficult to treat and have a greater risk for relapse and recurrence of depression, they added.
Acupuncture may be an “effective drug-free approach to help treat mental illness and sleep disorders,” the researchers noted. A previous study suggested acupuncture may improve sleep efficacy and prolong total sleep in patients with primary insomnia.
“EA is the combination of traditional Chinese acupuncture with electric-impulse stimulation, and it can enhance the therapeutic effect of the acupoints throughout the needle retention time,” Dr. Xu said.
A previous pilot study of EA for depression-related insomnia showed significant improvements in sleep quality after EA treatment, but the sample size was small.
The current researchers, therefore, undertook the present study – with a larger sample size and comparison with SA and standard care. They divided 270 adults (mean age, 50.3 years; 71.9% women) at three tertiary hospitals in Shanghai into three groups, each consisting of 90 participants.
The EA plus standard care group and the SA plus standard care group received 30-minute treatments three times per week for 8 weeks. The control group received standard care only.
All participants had DSM-5–diagnosed depression; baseline PSQI scores greater than 7, with higher scores indicating worse sleep quality and a greater number or sleep disorders; and Hamilton Depression Rating Scales (HDRS-17) scores of 20-35, with higher scores indicating higher depression levels.
Patients with secondary depressive disorders caused by other conditions, medication, or psychotic disorders were excluded, as were patients with a history of alcohol abuse or drug dependence or those who had received acupuncture within the previous year.
Of the patients who completed the 8-week intervention, 83 were in the EA group, 81 in the SA group, and 83 in the control group. Almost all participants (91.5%) completed all outcome measurements by the end of the 24-week follow-up period (also known as week 32).
Calm mind, balanced mood
At the 8-week posttreatment assessment, which was the primary endpoint, the EA group had a mean reduction from baseline of 6.2 points (95% confidence interval, −6.9 to −5.6) in PSQI score.
There was a significant difference in PSQI score between the EA versus the SA group (−3.6 points; 95% CI, −4.4 to −2.8; P < .001) and vs the control group (−5.1 points; 95% CI, −6.0 to −4.2; P < .001).
The efficacy of EA in treating insomnia was sustained during the postintervention follow-up period when the EA group had a significantly greater reduction in PSQI score, compared with the SA group (−4.7; 95% CI, −5.4 to −3.9; P < .001) and the control group (−5.0; 95% CI, −5.8 to −4.1; P < .001).
Patients receiving EA also experienced significant (all P values < .001) improvement from baseline on secondary outcomes, including:
- Scores on the HDRS (−10.7; 95% CI, −11.8 to −9.7)
- Scores on the Insomnia Severity Index, (−7.6; 95% CI,−8.5 to −6.7)
- Scores on the Self-rated Anxiety Scale (−2.9; 95% CI, −4.1 to −1.7)
- Total sleep time, as recorded by sleep actigraphy (29.1 minutes; 95% CI, 21.5-36.7)
In addition, the EA group showed significant improvement in depression scores compared with the SA and control groups at both 8 and 32 weeks (all P values < .001).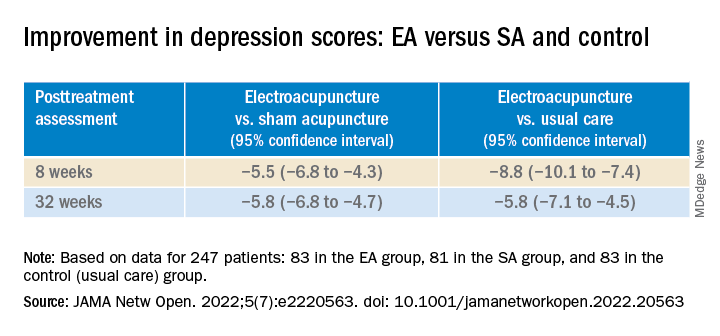
Participants in the EA group also had a 4.2% (95% CI, 2.6% - 5.8%) higher sleep efficiency score at week 8, compared with those in the SA group (P < .001).
In addition, they had lower scores on the Insomnia Severity Index and the Self-rated Anxiety Scale, and longer total sleep time, compared with the control group at week 8.
None of the participants reported any serious adverse events.
“Our findings constitute subjective and objective evidence of the efficacy and safety of EA with standard care in treating comorbid depression and insomnia compared with SA with standard care or standard care alone,” the investigators wrote.
“The acupoints we used in this trial mainly act on calming mind, relieving negative mood, and balancing the yin-yang,” Dr. Xu added.
Viable adjunctive treatment
Commenting on the study, Albert Yeung, MD, ScD, associate director of the Mass General Depression and Clinical Research Program and associate professor of psychiatry, Harvard Medical School, Boston, said that, with the evidence from this study, “acupuncture and/or electroacupuncture could be a viable adjunctive treatment for depressed patients who suffer from insomnia.”
Dr. Yeung, who was not involved with the study, is the coauthor of an accompanying editorial.
“More well-designed studies are warranted to provide evidence for integrating holistic treatment in medicine,” he said.
The study was funded by grants from the National Natural Science Foundation of China, and Shanghai Municipal Health. The investigators and Dr. Yeung reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a study of more than 200 adults with depression and comorbid insomnia, change from baseline to week 8 on the Pittsburgh Sleep Quality Index (PSQI) was 3 points greater in the group receiving EA versus a group receiving sham acupuncture (SA) plus standard care, and 5 points greater vs a control group receiving standard care only. The improvements were sustained during a 24-week postintervention follow-up.
The EA group also showed significant improvement in depression, insomnia, self-rated anxiety, and total sleep time – all of which were not found in the SA or control groups.
“Based on the results of our trial, we recommend patients with depression and insomnia seek the treatment of EA as an alternative and complementary therapy for better results,” study investigator Shifen Xu, PhD, Shanghai (China) Municipal Hospital of Traditional Chinese Medicine, Shanghai University of Traditional Chinese Medicine, told this news organization.
The findings were published online in JAMA Network Open.
Bidirectional relationship
“Sleep disturbance is the prominent symptom in patients with depression,” the investigators noted.
Depression and sleep issues have a bidirectional relationship, in that “poor sleep quality contributes to the development of depression, and having depression makes a person more likely to develop sleep issues,” they wrote.
Patients with co-occurring depression and sleep disorders are more difficult to treat and have a greater risk for relapse and recurrence of depression, they added.
Acupuncture may be an “effective drug-free approach to help treat mental illness and sleep disorders,” the researchers noted. A previous study suggested acupuncture may improve sleep efficacy and prolong total sleep in patients with primary insomnia.
“EA is the combination of traditional Chinese acupuncture with electric-impulse stimulation, and it can enhance the therapeutic effect of the acupoints throughout the needle retention time,” Dr. Xu said.
A previous pilot study of EA for depression-related insomnia showed significant improvements in sleep quality after EA treatment, but the sample size was small.
The current researchers, therefore, undertook the present study – with a larger sample size and comparison with SA and standard care. They divided 270 adults (mean age, 50.3 years; 71.9% women) at three tertiary hospitals in Shanghai into three groups, each consisting of 90 participants.
The EA plus standard care group and the SA plus standard care group received 30-minute treatments three times per week for 8 weeks. The control group received standard care only.
All participants had DSM-5–diagnosed depression; baseline PSQI scores greater than 7, with higher scores indicating worse sleep quality and a greater number or sleep disorders; and Hamilton Depression Rating Scales (HDRS-17) scores of 20-35, with higher scores indicating higher depression levels.
Patients with secondary depressive disorders caused by other conditions, medication, or psychotic disorders were excluded, as were patients with a history of alcohol abuse or drug dependence or those who had received acupuncture within the previous year.
Of the patients who completed the 8-week intervention, 83 were in the EA group, 81 in the SA group, and 83 in the control group. Almost all participants (91.5%) completed all outcome measurements by the end of the 24-week follow-up period (also known as week 32).
Calm mind, balanced mood
At the 8-week posttreatment assessment, which was the primary endpoint, the EA group had a mean reduction from baseline of 6.2 points (95% confidence interval, −6.9 to −5.6) in PSQI score.
There was a significant difference in PSQI score between the EA versus the SA group (−3.6 points; 95% CI, −4.4 to −2.8; P < .001) and vs the control group (−5.1 points; 95% CI, −6.0 to −4.2; P < .001).
The efficacy of EA in treating insomnia was sustained during the postintervention follow-up period when the EA group had a significantly greater reduction in PSQI score, compared with the SA group (−4.7; 95% CI, −5.4 to −3.9; P < .001) and the control group (−5.0; 95% CI, −5.8 to −4.1; P < .001).
Patients receiving EA also experienced significant (all P values < .001) improvement from baseline on secondary outcomes, including:
- Scores on the HDRS (−10.7; 95% CI, −11.8 to −9.7)
- Scores on the Insomnia Severity Index, (−7.6; 95% CI,−8.5 to −6.7)
- Scores on the Self-rated Anxiety Scale (−2.9; 95% CI, −4.1 to −1.7)
- Total sleep time, as recorded by sleep actigraphy (29.1 minutes; 95% CI, 21.5-36.7)
In addition, the EA group showed significant improvement in depression scores compared with the SA and control groups at both 8 and 32 weeks (all P values < .001).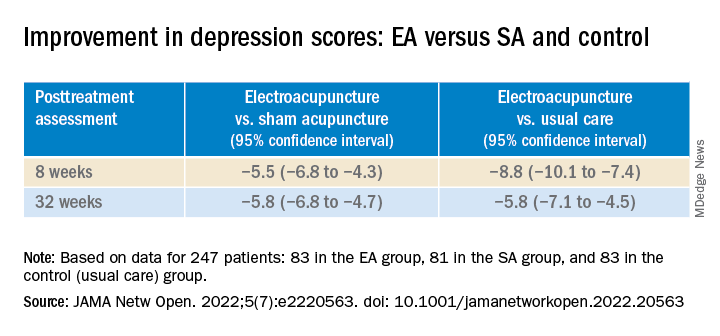
Participants in the EA group also had a 4.2% (95% CI, 2.6% - 5.8%) higher sleep efficiency score at week 8, compared with those in the SA group (P < .001).
In addition, they had lower scores on the Insomnia Severity Index and the Self-rated Anxiety Scale, and longer total sleep time, compared with the control group at week 8.
None of the participants reported any serious adverse events.
“Our findings constitute subjective and objective evidence of the efficacy and safety of EA with standard care in treating comorbid depression and insomnia compared with SA with standard care or standard care alone,” the investigators wrote.
“The acupoints we used in this trial mainly act on calming mind, relieving negative mood, and balancing the yin-yang,” Dr. Xu added.
Viable adjunctive treatment
Commenting on the study, Albert Yeung, MD, ScD, associate director of the Mass General Depression and Clinical Research Program and associate professor of psychiatry, Harvard Medical School, Boston, said that, with the evidence from this study, “acupuncture and/or electroacupuncture could be a viable adjunctive treatment for depressed patients who suffer from insomnia.”
Dr. Yeung, who was not involved with the study, is the coauthor of an accompanying editorial.
“More well-designed studies are warranted to provide evidence for integrating holistic treatment in medicine,” he said.
The study was funded by grants from the National Natural Science Foundation of China, and Shanghai Municipal Health. The investigators and Dr. Yeung reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Anxiety spreads from mother to daughter, father to son
The new findings suggest that children learn anxious behavior from their parents, study investigator Barbara Pavlova, PhD, clinical psychologist with Nova Scotia Health Authority, told this news organization.
“This means that transmission of anxiety from parents to children may be preventable,” said Dr. Pavlova, assistant professor, department of psychiatry, Dalhousie University, Halifax, Canada.
“Treating parents’ anxiety is not just important for their own health but also for the health of their children. This may be especially true if the child and the parent are the same sex,” Dr. Pavlova added.
The study was published online in JAMA Network Open.
Parental anxiety a disruptor
Anxiety disorders run in families. Both genes and environment are thought to be at play, but there are few data on sex-specific transmission from parent to child.
To investigate, the researchers conducted a cross-sectional study of 203 girls and 195 boys and their parents. The average age of the children was 11 years, and they had a familial risk for mood disorders.
Anxiety disorder in a same-sex parent was significantly associated with anxiety disorder in offspring (odds ratio, 2.85; 95% confidence interval, 1.52-5.34; P = .001) but not in an opposite-sex parent (OR, 1.51; 95% CI, 0.81-2.81; P = .20).
Living with a same-sex parent without anxiety was associated with lower rates of offspring anxiety (OR, 0.38; 95% CI, 0.22-0.67; P = .001).
Among all 398 children, 108 (27%) had been diagnosed with one or more anxiety disorders, including generalized anxiety disorder (7.8%), social anxiety disorder (6.3%), separation anxiety disorder (8.6%), specific phobia (8%), and anxiety disorder not otherwise specified (5%).
Rates of anxiety disorders in children increased with age, from 14% in those younger than 9 years to 52% in those older than 15 years. Anxiety disorders were similarly common among boys (24%) and girls (30%).
Rates of anxiety disorders were lowest (24%) in children of two parents without anxiety disorders and highest (41%) in cases in which both parents had anxiety disorders.
The findings point to the possible role of environmental factors, “such as modeling and vicarious learning,” in the transmission of anxiety from parents to their children, the researchers note.
“A child receives [a] similar amount of genetic information from each biological parent. A strong same-sex parent effect suggests children learn resilience by modeling the behavior of their same-sex parent. A parent’s anxiety disorder may disrupt this protective learning,” said Dr. Pavlova.
Early diagnosis, treatment essential
Reached for comment, Jill Emanuele, PhD, vice president of clinical training for the Child MIND Institute, New York, said that when it comes to anxiety, it’s important to assess and treat both the parent and the child.
“We know that both environment and genetics play a role in anxiety disorders. From a clinical perspective, if we see a parent with an anxiety disorder, we know that there is a chance that that is also going to affect the child – whether or not the child has an anxiety disorder,” Dr. Emanuele said in an interview.
“Anxiety disorders are the most common psychiatric disorders diagnosed. We also know that anxiety disorders emerge earlier than mood disorders and certainly can emerge in childhood. It’s important to address anxiety early because those same problems can continue into adulthood if left untreated,” Dr. Emanuele added.
The study was supported by the Canada Research Chairs Program, the Canadian Institutes of Health Research, the Brain & Behavior Research Foundation, the Nova Scotia Health Research Foundation, and the Dalhousie Medical Research Foundation. The authors have disclosed no relevant financial relationships. Dr. Emanuele is a board member with the Anxiety and Depression Association of America.
A version of this article first appeared on Medscape.com.
The new findings suggest that children learn anxious behavior from their parents, study investigator Barbara Pavlova, PhD, clinical psychologist with Nova Scotia Health Authority, told this news organization.
“This means that transmission of anxiety from parents to children may be preventable,” said Dr. Pavlova, assistant professor, department of psychiatry, Dalhousie University, Halifax, Canada.
“Treating parents’ anxiety is not just important for their own health but also for the health of their children. This may be especially true if the child and the parent are the same sex,” Dr. Pavlova added.
The study was published online in JAMA Network Open.
Parental anxiety a disruptor
Anxiety disorders run in families. Both genes and environment are thought to be at play, but there are few data on sex-specific transmission from parent to child.
To investigate, the researchers conducted a cross-sectional study of 203 girls and 195 boys and their parents. The average age of the children was 11 years, and they had a familial risk for mood disorders.
Anxiety disorder in a same-sex parent was significantly associated with anxiety disorder in offspring (odds ratio, 2.85; 95% confidence interval, 1.52-5.34; P = .001) but not in an opposite-sex parent (OR, 1.51; 95% CI, 0.81-2.81; P = .20).
Living with a same-sex parent without anxiety was associated with lower rates of offspring anxiety (OR, 0.38; 95% CI, 0.22-0.67; P = .001).
Among all 398 children, 108 (27%) had been diagnosed with one or more anxiety disorders, including generalized anxiety disorder (7.8%), social anxiety disorder (6.3%), separation anxiety disorder (8.6%), specific phobia (8%), and anxiety disorder not otherwise specified (5%).
Rates of anxiety disorders in children increased with age, from 14% in those younger than 9 years to 52% in those older than 15 years. Anxiety disorders were similarly common among boys (24%) and girls (30%).
Rates of anxiety disorders were lowest (24%) in children of two parents without anxiety disorders and highest (41%) in cases in which both parents had anxiety disorders.
The findings point to the possible role of environmental factors, “such as modeling and vicarious learning,” in the transmission of anxiety from parents to their children, the researchers note.
“A child receives [a] similar amount of genetic information from each biological parent. A strong same-sex parent effect suggests children learn resilience by modeling the behavior of their same-sex parent. A parent’s anxiety disorder may disrupt this protective learning,” said Dr. Pavlova.
Early diagnosis, treatment essential
Reached for comment, Jill Emanuele, PhD, vice president of clinical training for the Child MIND Institute, New York, said that when it comes to anxiety, it’s important to assess and treat both the parent and the child.
“We know that both environment and genetics play a role in anxiety disorders. From a clinical perspective, if we see a parent with an anxiety disorder, we know that there is a chance that that is also going to affect the child – whether or not the child has an anxiety disorder,” Dr. Emanuele said in an interview.
“Anxiety disorders are the most common psychiatric disorders diagnosed. We also know that anxiety disorders emerge earlier than mood disorders and certainly can emerge in childhood. It’s important to address anxiety early because those same problems can continue into adulthood if left untreated,” Dr. Emanuele added.
The study was supported by the Canada Research Chairs Program, the Canadian Institutes of Health Research, the Brain & Behavior Research Foundation, the Nova Scotia Health Research Foundation, and the Dalhousie Medical Research Foundation. The authors have disclosed no relevant financial relationships. Dr. Emanuele is a board member with the Anxiety and Depression Association of America.
A version of this article first appeared on Medscape.com.
The new findings suggest that children learn anxious behavior from their parents, study investigator Barbara Pavlova, PhD, clinical psychologist with Nova Scotia Health Authority, told this news organization.
“This means that transmission of anxiety from parents to children may be preventable,” said Dr. Pavlova, assistant professor, department of psychiatry, Dalhousie University, Halifax, Canada.
“Treating parents’ anxiety is not just important for their own health but also for the health of their children. This may be especially true if the child and the parent are the same sex,” Dr. Pavlova added.
The study was published online in JAMA Network Open.
Parental anxiety a disruptor
Anxiety disorders run in families. Both genes and environment are thought to be at play, but there are few data on sex-specific transmission from parent to child.
To investigate, the researchers conducted a cross-sectional study of 203 girls and 195 boys and their parents. The average age of the children was 11 years, and they had a familial risk for mood disorders.
Anxiety disorder in a same-sex parent was significantly associated with anxiety disorder in offspring (odds ratio, 2.85; 95% confidence interval, 1.52-5.34; P = .001) but not in an opposite-sex parent (OR, 1.51; 95% CI, 0.81-2.81; P = .20).
Living with a same-sex parent without anxiety was associated with lower rates of offspring anxiety (OR, 0.38; 95% CI, 0.22-0.67; P = .001).
Among all 398 children, 108 (27%) had been diagnosed with one or more anxiety disorders, including generalized anxiety disorder (7.8%), social anxiety disorder (6.3%), separation anxiety disorder (8.6%), specific phobia (8%), and anxiety disorder not otherwise specified (5%).
Rates of anxiety disorders in children increased with age, from 14% in those younger than 9 years to 52% in those older than 15 years. Anxiety disorders were similarly common among boys (24%) and girls (30%).
Rates of anxiety disorders were lowest (24%) in children of two parents without anxiety disorders and highest (41%) in cases in which both parents had anxiety disorders.
The findings point to the possible role of environmental factors, “such as modeling and vicarious learning,” in the transmission of anxiety from parents to their children, the researchers note.
“A child receives [a] similar amount of genetic information from each biological parent. A strong same-sex parent effect suggests children learn resilience by modeling the behavior of their same-sex parent. A parent’s anxiety disorder may disrupt this protective learning,” said Dr. Pavlova.
Early diagnosis, treatment essential
Reached for comment, Jill Emanuele, PhD, vice president of clinical training for the Child MIND Institute, New York, said that when it comes to anxiety, it’s important to assess and treat both the parent and the child.
“We know that both environment and genetics play a role in anxiety disorders. From a clinical perspective, if we see a parent with an anxiety disorder, we know that there is a chance that that is also going to affect the child – whether or not the child has an anxiety disorder,” Dr. Emanuele said in an interview.
“Anxiety disorders are the most common psychiatric disorders diagnosed. We also know that anxiety disorders emerge earlier than mood disorders and certainly can emerge in childhood. It’s important to address anxiety early because those same problems can continue into adulthood if left untreated,” Dr. Emanuele added.
The study was supported by the Canada Research Chairs Program, the Canadian Institutes of Health Research, the Brain & Behavior Research Foundation, the Nova Scotia Health Research Foundation, and the Dalhousie Medical Research Foundation. The authors have disclosed no relevant financial relationships. Dr. Emanuele is a board member with the Anxiety and Depression Association of America.
A version of this article first appeared on Medscape.com.
Americans’ biggest source of anxiety? Hint: It’s not COVID-19
, results from a new national report from the American Psychiatric Association show.
“The economy seems to have supplanted COVID as a major factor in Americans’ day-to-day anxiety,” APA President Rebecca W. Brendel, MD, JD, said in a news release.
“Knowing that so many Americans are concerned about finances is important because it can prepare clinicians to be ready to approach the subject, which is one that people are often reluctant or ashamed to raise on their own,” Dr. Brendel told this news organization.
What’s the best way to bring up the sensitive topic of money?
“In general, it’s best to start with open-ended questions to allow individuals in therapy to share what is on their minds, explore their concerns, and develop strategies to address these issues. Once a patient raises a concern, that is a good time to ask more about the issues they’ve raised and to explore other potential sources of anxiety or stress,” said Dr. Brendel.
The latest APA poll was conducted by Morning Consult, June 18-20, 2022, among a nationally representative sample of 2,210 adults.
In addition to an uptick in worry about inflation, the poll shows that more than half (51%) of adults are worried about a potential loss of income.
Hispanic adults (66%), mothers (65%), millennials (63%), and genZers (62%) are among the groups most likely to be concerned about income loss.
“Stress is not good for health, mental or physical. So, while it’s a reality that Americans are faced with finding ways of making ends meet, it’s more important than ever to make sure that we are all accessing the care that we need,” said Dr. Brendel.
“People should be aware that there may be low- or no-cost options such as community mental health centers or employer-sponsored resources to address mental health concerns,” she added.
Coping with traumatic events
The latest poll also shows that about one-third of adults are worried about gun violence (35% overall, 47% among genZers) or a natural disaster (29%) personally affecting them.
Climate change anxiety is also up slightly in June, compared with May (+4%).
The same goes for mid-term election-related anxiety (+3%) – particularly among Democrats (54% vs. 59%) compared with Republicans (48% vs. 48%).
The latest poll provides insight how Americans would cope after a traumatic event. More adults report they will turn to family and friends for support (60%) than practice self-care (42%), speak openly about their feelings (37%), or seek help from a professional (31%). Nearly one-third (30%) say they will move on from it and not dwell on their feelings.
GenZers are the least likely to say they will speak openly about their feelings (29%) and are less likely than millennials to say they would speak to a health professional (28% vs. 38%).
“While many people show resilience, it’s troubling that most Americans wouldn’t speak openly about their feelings after a traumatic event,” APA CEO and Medical Director Saul Levin, MD, said in the news release.
“In many ways, naming feelings is the most important step toward healing, and this reluctance to air our thoughts may indicate that mental health stigma is still a powerful force in our society,” Dr. Levin said.
After a traumatic current event, 41% of Americans say they consume more news and 30% say they take in more social media, but the majority say this does not impact their mental health, the poll shows.
Two in five adults (43%) say the news of a traumatic event makes them feel more informed, 32% say it makes them feel more anxious, and about one-quarter say it makes them feel overwhelmed (27%) or discouraged (24%).
Dr. Brendel noted that, after a traumatic event, “it’s expected that people may experience anxiety or other symptoms for brief periods of time. However, no two people experience things the same way. If symptoms don’t go away, are overwhelming, or get worse over time, for example, it’s critical to seek help right away.”
The June poll shows that 50% of Americans are anxious about the future of reproductive rights but the poll was conducted before the Dobbs ruling.
Anxiety around COVID-19 continues to ease, with about 47% of Americans saying they are concerned about the pandemic, down 2% among all Americans and 16% among Black Americans since May.
The APA’s Healthy Minds Monthly tracks timely mental health issues throughout the year. The APA also releases its annual Healthy Minds Poll each May in conjunction with Mental Health Awareness Month.
A version of this article first appeared on Medscape.com.
, results from a new national report from the American Psychiatric Association show.
“The economy seems to have supplanted COVID as a major factor in Americans’ day-to-day anxiety,” APA President Rebecca W. Brendel, MD, JD, said in a news release.
“Knowing that so many Americans are concerned about finances is important because it can prepare clinicians to be ready to approach the subject, which is one that people are often reluctant or ashamed to raise on their own,” Dr. Brendel told this news organization.
What’s the best way to bring up the sensitive topic of money?
“In general, it’s best to start with open-ended questions to allow individuals in therapy to share what is on their minds, explore their concerns, and develop strategies to address these issues. Once a patient raises a concern, that is a good time to ask more about the issues they’ve raised and to explore other potential sources of anxiety or stress,” said Dr. Brendel.
The latest APA poll was conducted by Morning Consult, June 18-20, 2022, among a nationally representative sample of 2,210 adults.
In addition to an uptick in worry about inflation, the poll shows that more than half (51%) of adults are worried about a potential loss of income.
Hispanic adults (66%), mothers (65%), millennials (63%), and genZers (62%) are among the groups most likely to be concerned about income loss.
“Stress is not good for health, mental or physical. So, while it’s a reality that Americans are faced with finding ways of making ends meet, it’s more important than ever to make sure that we are all accessing the care that we need,” said Dr. Brendel.
“People should be aware that there may be low- or no-cost options such as community mental health centers or employer-sponsored resources to address mental health concerns,” she added.
Coping with traumatic events
The latest poll also shows that about one-third of adults are worried about gun violence (35% overall, 47% among genZers) or a natural disaster (29%) personally affecting them.
Climate change anxiety is also up slightly in June, compared with May (+4%).
The same goes for mid-term election-related anxiety (+3%) – particularly among Democrats (54% vs. 59%) compared with Republicans (48% vs. 48%).
The latest poll provides insight how Americans would cope after a traumatic event. More adults report they will turn to family and friends for support (60%) than practice self-care (42%), speak openly about their feelings (37%), or seek help from a professional (31%). Nearly one-third (30%) say they will move on from it and not dwell on their feelings.
GenZers are the least likely to say they will speak openly about their feelings (29%) and are less likely than millennials to say they would speak to a health professional (28% vs. 38%).
“While many people show resilience, it’s troubling that most Americans wouldn’t speak openly about their feelings after a traumatic event,” APA CEO and Medical Director Saul Levin, MD, said in the news release.
“In many ways, naming feelings is the most important step toward healing, and this reluctance to air our thoughts may indicate that mental health stigma is still a powerful force in our society,” Dr. Levin said.
After a traumatic current event, 41% of Americans say they consume more news and 30% say they take in more social media, but the majority say this does not impact their mental health, the poll shows.
Two in five adults (43%) say the news of a traumatic event makes them feel more informed, 32% say it makes them feel more anxious, and about one-quarter say it makes them feel overwhelmed (27%) or discouraged (24%).
Dr. Brendel noted that, after a traumatic event, “it’s expected that people may experience anxiety or other symptoms for brief periods of time. However, no two people experience things the same way. If symptoms don’t go away, are overwhelming, or get worse over time, for example, it’s critical to seek help right away.”
The June poll shows that 50% of Americans are anxious about the future of reproductive rights but the poll was conducted before the Dobbs ruling.
Anxiety around COVID-19 continues to ease, with about 47% of Americans saying they are concerned about the pandemic, down 2% among all Americans and 16% among Black Americans since May.
The APA’s Healthy Minds Monthly tracks timely mental health issues throughout the year. The APA also releases its annual Healthy Minds Poll each May in conjunction with Mental Health Awareness Month.
A version of this article first appeared on Medscape.com.
, results from a new national report from the American Psychiatric Association show.
“The economy seems to have supplanted COVID as a major factor in Americans’ day-to-day anxiety,” APA President Rebecca W. Brendel, MD, JD, said in a news release.
“Knowing that so many Americans are concerned about finances is important because it can prepare clinicians to be ready to approach the subject, which is one that people are often reluctant or ashamed to raise on their own,” Dr. Brendel told this news organization.
What’s the best way to bring up the sensitive topic of money?
“In general, it’s best to start with open-ended questions to allow individuals in therapy to share what is on their minds, explore their concerns, and develop strategies to address these issues. Once a patient raises a concern, that is a good time to ask more about the issues they’ve raised and to explore other potential sources of anxiety or stress,” said Dr. Brendel.
The latest APA poll was conducted by Morning Consult, June 18-20, 2022, among a nationally representative sample of 2,210 adults.
In addition to an uptick in worry about inflation, the poll shows that more than half (51%) of adults are worried about a potential loss of income.
Hispanic adults (66%), mothers (65%), millennials (63%), and genZers (62%) are among the groups most likely to be concerned about income loss.
“Stress is not good for health, mental or physical. So, while it’s a reality that Americans are faced with finding ways of making ends meet, it’s more important than ever to make sure that we are all accessing the care that we need,” said Dr. Brendel.
“People should be aware that there may be low- or no-cost options such as community mental health centers or employer-sponsored resources to address mental health concerns,” she added.
Coping with traumatic events
The latest poll also shows that about one-third of adults are worried about gun violence (35% overall, 47% among genZers) or a natural disaster (29%) personally affecting them.
Climate change anxiety is also up slightly in June, compared with May (+4%).
The same goes for mid-term election-related anxiety (+3%) – particularly among Democrats (54% vs. 59%) compared with Republicans (48% vs. 48%).
The latest poll provides insight how Americans would cope after a traumatic event. More adults report they will turn to family and friends for support (60%) than practice self-care (42%), speak openly about their feelings (37%), or seek help from a professional (31%). Nearly one-third (30%) say they will move on from it and not dwell on their feelings.
GenZers are the least likely to say they will speak openly about their feelings (29%) and are less likely than millennials to say they would speak to a health professional (28% vs. 38%).
“While many people show resilience, it’s troubling that most Americans wouldn’t speak openly about their feelings after a traumatic event,” APA CEO and Medical Director Saul Levin, MD, said in the news release.
“In many ways, naming feelings is the most important step toward healing, and this reluctance to air our thoughts may indicate that mental health stigma is still a powerful force in our society,” Dr. Levin said.
After a traumatic current event, 41% of Americans say they consume more news and 30% say they take in more social media, but the majority say this does not impact their mental health, the poll shows.
Two in five adults (43%) say the news of a traumatic event makes them feel more informed, 32% say it makes them feel more anxious, and about one-quarter say it makes them feel overwhelmed (27%) or discouraged (24%).
Dr. Brendel noted that, after a traumatic event, “it’s expected that people may experience anxiety or other symptoms for brief periods of time. However, no two people experience things the same way. If symptoms don’t go away, are overwhelming, or get worse over time, for example, it’s critical to seek help right away.”
The June poll shows that 50% of Americans are anxious about the future of reproductive rights but the poll was conducted before the Dobbs ruling.
Anxiety around COVID-19 continues to ease, with about 47% of Americans saying they are concerned about the pandemic, down 2% among all Americans and 16% among Black Americans since May.
The APA’s Healthy Minds Monthly tracks timely mental health issues throughout the year. The APA also releases its annual Healthy Minds Poll each May in conjunction with Mental Health Awareness Month.
A version of this article first appeared on Medscape.com.
Red Flag: Suicide risk
How AI is helping prevent suicide in veterans

Medically reviewed by Jennifer Casarella, MD
Dan Miller has parked his Nissan Altima on the side of the road near a field outside Chicago and is holding a gun to his head.
Haunted for years by the compounded trauma of tours of duty in the Middle East and his work as a police officer in Chicago, at that moment, Dr. Miller saw no reason to live. And there were troubles at home with his wife and children, who had grown fearful of his behavior.
“My whole world was falling apart,” he says of that dark night in 2014. “It left a hole I didn’t know how to fill.”
He chose not to pull the trigger after a brochure on the passenger seat of his car gave him an unexpected perspective – and launched him on a path to help others in his situation.
Had Mr. Miller taken his life that night, he would have joined thousands of other veterans who died by suicide. About 17 U.S. veterans lose their lives this way each day, on average, according to the Department of Veterans Affairs. In 2019, the last year for which records are available, 6,261 veterans took their own lives – and the suicide rate for veterans was 52% higher than for nonveterans, the agency’s records show.
The problem has become so severe that
But that wasn’t available when Dan Miller’s life was unraveling.
In the years leading up to his near-suicide, his wife had pushed him to get help. “She said, ‘You’re not the same person you were when you left. The kids are scared of you. The pets are scared of you,” he recalls.
He resisted, even when his wife threatened divorce. Rising through the ranks of the Marines, Mr. Miller had become more emotionally isolated. He feared losing his job and the respect of others if he let anyone know what he was going through.
Finally, he gave the VHA a chance. He went in for an initial consultation in 2010 and didn’t find it helpful. He didn’t like being told what to do. So he stopped. He turned to obsessive exercise and excessive drinking.
That day in 2014, Mr. Miller’s wife told him she was taking the kids out for a playdate. After she left, he was served with divorce papers. Less than an hour later, he was parked in his car with his gun, ready to end his life.
But if it all had happened just a few years later, things might never have gotten to that point.
Scanning for suicide risk
In 2017, the VHA piloted its AI program, called REACH VET, that aims to help prevent veterans from dying by suicide.
Every month, a computer scans the electronic health records of all VHA patients who’ve had a health care visit for any reason in the last 2 years. It checks more than 140 variables and weights them to estimate someone’s overall suicide risk at that moment in time.
To build the risk algorithm, a computer combed through the medical records of 6,360 veterans confirmed to have died by suicide between 2009 and 2011. (The VHA continually updates the list of variables from the health records of VHA patients, including those who have died by suicide since then and others.)
Some variables are things you’d expect:
- A past suicide attempt.
- A diagnosis of depression or other mental illness.
- A diagnosis of a terminal illness.
Others are more surprising. For example, a diagnosis of arthritis or diabetes adds weight.
REACH VET flags the riskiest cases – the top 0.1% – for a mental health or primary care provider to review. They reach out to the patient to tell them how and why their record was flagged, discuss any recommended treatment changes, and ask them to come in for a visit.
“It’s an opportunity to talk about their risk factors, which is designed to lead to a conversation about safety planning,” says clinical psychologist Matthew Miller, PhD, national director of the U.S. Department of Veterans Affairs’ Suicide Prevention Program. He’s not related to Dan Miller.
Making a suicide safety plan
A safety plan is a document that outlines how a person can help prevent their own suicide in a crisis.
The plan may include:
- A list of personal triggers or warning signs.
- What’s helped them in the past.
- Names of people or organizations who can support them.
- Plans to remove means of suicide, such as guns, from their environment.
- Their reasons for living.
In people at risk for suicide, research shows that having a safety plan reduces suicidal thoughts and attempts, lowers rates of depression and hopelessness, and boosts veterans’ engagement with the health care system. It may also help people manage things that trigger their suicidal thoughts.
Getting the call
What if REACH VET had been around when Dan Miller was in crisis – and he’d gotten a call from the VHA?
“It absolutely, positively would have helped because one of the biggest things on that day when I got served was feeling completely alone and that I had no one to turn to,” Mr. Miller says. He’s now a speaker for the Wounded Warrior Project, a nonprofit that serves veterans and active-duty service people.
Vets’ reactions to the unexpected VHA phone call, psychologist Dr. Miller says, “run the gamut from ‘Thank you for contacting me. Let’s talk,’ to ‘What are you talking about? Leave me alone!’ ”
Nothing stops all suicides. But REACH VET is having an impact. In a clinical trial, vets contacted through REACH VET had more doctor visits, were more likely to have a written suicide prevention safety plan, and had fewer hospital admissions for mental health, ER visits, and suicide attempts.
An assist from AI
Even simple outreach can make a big difference. And there’s research to prove it.
One study included 4,730 veterans recently discharged from psychiatric care at the VHA, a group considered at high risk for suicide.
Half of them got 13 caring emails from hospital staff in the weeks after leaving the hospital. The emails mentioned personal things the patient had shared, like a love of hiking, and wished them well. The other veterans got routine follow-up but no emails.
Two years later, those who got the caring emails were less likely to have died by suicide than the other vets. The study was published in 2014 in Contemporary Clinical Trials.
Researchers have done studies like this many times: with handwritten notes from the primary care doctor, postcards from the ER, and so forth. The results never vary: The notes reduce suicide risk.
“If we could use AI to identify people to receive notes or phone calls, it would be a very effective and inexpensive way to guide follow-up care,” says Rebecca Bernert, PhD, director and founder of the Suicide Prevention Research Laboratory at Stanford (Calif.) University.
AI doesn’t replace clinical judgment.
“AI can capture data that we miss due to the limits of our humanity,” psychologist Dr. Miller says. “There’s suicide prevention processes founded on big data and AI, and there are processes founded in clinical intuition and acumen.”
AI is only as good as the data it’s based on. If that data lacks diversity, it may miss things. And variables that apply to veterans may differ in civilians.
Stopping suicidal thoughts
Google is putting AI to work against suicide, too. Its MUM (Multitask Unified Model) technology seeks to understand the intent behind what we google.
MUM powers Google Search. It can often tell the difference between a search for information about suicide for someone writing a research paper on the topic and a search for information on how or where to carry out a suicide.
When Google Search detects that someone in the United States might be in crisis and at risk of suicide, the first search results that person gets are the number for the National Suicide Prevention Lifeline and other resources for people in crisis.
Google Home Assistant works in the same way. When a user makes a query that signals a suicide-related crisis, the gadget serves up resources that offer help.
MUM is working to understand the nuances of crisis language in 75 languages so that Google Search can provide people in crisis with hotlines or other resources in many countries.
“We want to find partners that are accessible to users in terms of hours of operation. We have a strong preference for finding partners that promise confidentiality and privacy to the extent that those are permitted [in that country],” says Anne Merritt, MD, a product manager at Google Search.
Other companies are working on apps that use AI to spot suicide risk in other ways, including voice technology that may notice subtle changes in the voice of someone who’s depressed and may be thinking of suicide. Those are still in development but show promise. Keep in mind that apps do not require government approval, so if you try one, be sure to let your health care provider know.
Changing the channel
Seeing a hotline number on your phone or computer screen can help, Dan Miller says. “If I happened to be online, searching maybe for a bridge to jump off of ... and suddenly that pops up on the screen, it’s like it changes the channel.”
It may not work for everyone, he says, but that search result could interrupt someone’s suicidal train of thought.
That’s crucial, psychologist Dr. Miller says, because most suicide attempts escalate from first thought to potentially fatal action in just 1 hour. That’s how fast it happened for Dan Miller in 2014.
“When you’re able to put time and space between the suicidal thought and the access to the method to act on that thought, you save lives,” Dr. Bernert says.
Making a different choice
An interruption in Mr. Miller’s thinking is what had saved his life.
Holding the gun to his head, Mr. Miller looked over at the passenger seat at a brochure from Wounded Warrior Project, which he had just learned about. Mr. Miller noticed a photo of a man in a wheelchair, a veteran like him, who had no legs. He thought that the man looked worse off than him but hadn’t given up.
Mr. Miller put down his gun and decided to get help.
Recovering from a near suicide attempt, he says, is a journey. It doesn’t happen overnight. Now, 8 years later, Mr. Miller is planning a brief break from the speaker circuit. He plans to spend 2 weeks in an outpatient counseling program for posttraumatic stress disorder and traumatic brain injury.
“Telling my story to strangers – part of it is healing me in a way, but I’m learning that repeating the story over and over again is also keeping me from letting it go. And I’m still healing.”
A version of this article first appeared on WebMD.com.
How AI is helping prevent suicide in veterans
How AI is helping prevent suicide in veterans

Medically reviewed by Jennifer Casarella, MD
Dan Miller has parked his Nissan Altima on the side of the road near a field outside Chicago and is holding a gun to his head.
Haunted for years by the compounded trauma of tours of duty in the Middle East and his work as a police officer in Chicago, at that moment, Dr. Miller saw no reason to live. And there were troubles at home with his wife and children, who had grown fearful of his behavior.
“My whole world was falling apart,” he says of that dark night in 2014. “It left a hole I didn’t know how to fill.”
He chose not to pull the trigger after a brochure on the passenger seat of his car gave him an unexpected perspective – and launched him on a path to help others in his situation.
Had Mr. Miller taken his life that night, he would have joined thousands of other veterans who died by suicide. About 17 U.S. veterans lose their lives this way each day, on average, according to the Department of Veterans Affairs. In 2019, the last year for which records are available, 6,261 veterans took their own lives – and the suicide rate for veterans was 52% higher than for nonveterans, the agency’s records show.
The problem has become so severe that
But that wasn’t available when Dan Miller’s life was unraveling.
In the years leading up to his near-suicide, his wife had pushed him to get help. “She said, ‘You’re not the same person you were when you left. The kids are scared of you. The pets are scared of you,” he recalls.
He resisted, even when his wife threatened divorce. Rising through the ranks of the Marines, Mr. Miller had become more emotionally isolated. He feared losing his job and the respect of others if he let anyone know what he was going through.
Finally, he gave the VHA a chance. He went in for an initial consultation in 2010 and didn’t find it helpful. He didn’t like being told what to do. So he stopped. He turned to obsessive exercise and excessive drinking.
That day in 2014, Mr. Miller’s wife told him she was taking the kids out for a playdate. After she left, he was served with divorce papers. Less than an hour later, he was parked in his car with his gun, ready to end his life.
But if it all had happened just a few years later, things might never have gotten to that point.
Scanning for suicide risk
In 2017, the VHA piloted its AI program, called REACH VET, that aims to help prevent veterans from dying by suicide.
Every month, a computer scans the electronic health records of all VHA patients who’ve had a health care visit for any reason in the last 2 years. It checks more than 140 variables and weights them to estimate someone’s overall suicide risk at that moment in time.
To build the risk algorithm, a computer combed through the medical records of 6,360 veterans confirmed to have died by suicide between 2009 and 2011. (The VHA continually updates the list of variables from the health records of VHA patients, including those who have died by suicide since then and others.)
Some variables are things you’d expect:
- A past suicide attempt.
- A diagnosis of depression or other mental illness.
- A diagnosis of a terminal illness.
Others are more surprising. For example, a diagnosis of arthritis or diabetes adds weight.
REACH VET flags the riskiest cases – the top 0.1% – for a mental health or primary care provider to review. They reach out to the patient to tell them how and why their record was flagged, discuss any recommended treatment changes, and ask them to come in for a visit.
“It’s an opportunity to talk about their risk factors, which is designed to lead to a conversation about safety planning,” says clinical psychologist Matthew Miller, PhD, national director of the U.S. Department of Veterans Affairs’ Suicide Prevention Program. He’s not related to Dan Miller.
Making a suicide safety plan
A safety plan is a document that outlines how a person can help prevent their own suicide in a crisis.
The plan may include:
- A list of personal triggers or warning signs.
- What’s helped them in the past.
- Names of people or organizations who can support them.
- Plans to remove means of suicide, such as guns, from their environment.
- Their reasons for living.
In people at risk for suicide, research shows that having a safety plan reduces suicidal thoughts and attempts, lowers rates of depression and hopelessness, and boosts veterans’ engagement with the health care system. It may also help people manage things that trigger their suicidal thoughts.
Getting the call
What if REACH VET had been around when Dan Miller was in crisis – and he’d gotten a call from the VHA?
“It absolutely, positively would have helped because one of the biggest things on that day when I got served was feeling completely alone and that I had no one to turn to,” Mr. Miller says. He’s now a speaker for the Wounded Warrior Project, a nonprofit that serves veterans and active-duty service people.
Vets’ reactions to the unexpected VHA phone call, psychologist Dr. Miller says, “run the gamut from ‘Thank you for contacting me. Let’s talk,’ to ‘What are you talking about? Leave me alone!’ ”
Nothing stops all suicides. But REACH VET is having an impact. In a clinical trial, vets contacted through REACH VET had more doctor visits, were more likely to have a written suicide prevention safety plan, and had fewer hospital admissions for mental health, ER visits, and suicide attempts.
An assist from AI
Even simple outreach can make a big difference. And there’s research to prove it.
One study included 4,730 veterans recently discharged from psychiatric care at the VHA, a group considered at high risk for suicide.
Half of them got 13 caring emails from hospital staff in the weeks after leaving the hospital. The emails mentioned personal things the patient had shared, like a love of hiking, and wished them well. The other veterans got routine follow-up but no emails.
Two years later, those who got the caring emails were less likely to have died by suicide than the other vets. The study was published in 2014 in Contemporary Clinical Trials.
Researchers have done studies like this many times: with handwritten notes from the primary care doctor, postcards from the ER, and so forth. The results never vary: The notes reduce suicide risk.
“If we could use AI to identify people to receive notes or phone calls, it would be a very effective and inexpensive way to guide follow-up care,” says Rebecca Bernert, PhD, director and founder of the Suicide Prevention Research Laboratory at Stanford (Calif.) University.
AI doesn’t replace clinical judgment.
“AI can capture data that we miss due to the limits of our humanity,” psychologist Dr. Miller says. “There’s suicide prevention processes founded on big data and AI, and there are processes founded in clinical intuition and acumen.”
AI is only as good as the data it’s based on. If that data lacks diversity, it may miss things. And variables that apply to veterans may differ in civilians.
Stopping suicidal thoughts
Google is putting AI to work against suicide, too. Its MUM (Multitask Unified Model) technology seeks to understand the intent behind what we google.
MUM powers Google Search. It can often tell the difference between a search for information about suicide for someone writing a research paper on the topic and a search for information on how or where to carry out a suicide.
When Google Search detects that someone in the United States might be in crisis and at risk of suicide, the first search results that person gets are the number for the National Suicide Prevention Lifeline and other resources for people in crisis.
Google Home Assistant works in the same way. When a user makes a query that signals a suicide-related crisis, the gadget serves up resources that offer help.
MUM is working to understand the nuances of crisis language in 75 languages so that Google Search can provide people in crisis with hotlines or other resources in many countries.
“We want to find partners that are accessible to users in terms of hours of operation. We have a strong preference for finding partners that promise confidentiality and privacy to the extent that those are permitted [in that country],” says Anne Merritt, MD, a product manager at Google Search.
Other companies are working on apps that use AI to spot suicide risk in other ways, including voice technology that may notice subtle changes in the voice of someone who’s depressed and may be thinking of suicide. Those are still in development but show promise. Keep in mind that apps do not require government approval, so if you try one, be sure to let your health care provider know.
Changing the channel
Seeing a hotline number on your phone or computer screen can help, Dan Miller says. “If I happened to be online, searching maybe for a bridge to jump off of ... and suddenly that pops up on the screen, it’s like it changes the channel.”
It may not work for everyone, he says, but that search result could interrupt someone’s suicidal train of thought.
That’s crucial, psychologist Dr. Miller says, because most suicide attempts escalate from first thought to potentially fatal action in just 1 hour. That’s how fast it happened for Dan Miller in 2014.
“When you’re able to put time and space between the suicidal thought and the access to the method to act on that thought, you save lives,” Dr. Bernert says.
Making a different choice
An interruption in Mr. Miller’s thinking is what had saved his life.
Holding the gun to his head, Mr. Miller looked over at the passenger seat at a brochure from Wounded Warrior Project, which he had just learned about. Mr. Miller noticed a photo of a man in a wheelchair, a veteran like him, who had no legs. He thought that the man looked worse off than him but hadn’t given up.
Mr. Miller put down his gun and decided to get help.
Recovering from a near suicide attempt, he says, is a journey. It doesn’t happen overnight. Now, 8 years later, Mr. Miller is planning a brief break from the speaker circuit. He plans to spend 2 weeks in an outpatient counseling program for posttraumatic stress disorder and traumatic brain injury.
“Telling my story to strangers – part of it is healing me in a way, but I’m learning that repeating the story over and over again is also keeping me from letting it go. And I’m still healing.”
A version of this article first appeared on WebMD.com.

Medically reviewed by Jennifer Casarella, MD
Dan Miller has parked his Nissan Altima on the side of the road near a field outside Chicago and is holding a gun to his head.
Haunted for years by the compounded trauma of tours of duty in the Middle East and his work as a police officer in Chicago, at that moment, Dr. Miller saw no reason to live. And there were troubles at home with his wife and children, who had grown fearful of his behavior.
“My whole world was falling apart,” he says of that dark night in 2014. “It left a hole I didn’t know how to fill.”
He chose not to pull the trigger after a brochure on the passenger seat of his car gave him an unexpected perspective – and launched him on a path to help others in his situation.
Had Mr. Miller taken his life that night, he would have joined thousands of other veterans who died by suicide. About 17 U.S. veterans lose their lives this way each day, on average, according to the Department of Veterans Affairs. In 2019, the last year for which records are available, 6,261 veterans took their own lives – and the suicide rate for veterans was 52% higher than for nonveterans, the agency’s records show.
The problem has become so severe that
But that wasn’t available when Dan Miller’s life was unraveling.
In the years leading up to his near-suicide, his wife had pushed him to get help. “She said, ‘You’re not the same person you were when you left. The kids are scared of you. The pets are scared of you,” he recalls.
He resisted, even when his wife threatened divorce. Rising through the ranks of the Marines, Mr. Miller had become more emotionally isolated. He feared losing his job and the respect of others if he let anyone know what he was going through.
Finally, he gave the VHA a chance. He went in for an initial consultation in 2010 and didn’t find it helpful. He didn’t like being told what to do. So he stopped. He turned to obsessive exercise and excessive drinking.
That day in 2014, Mr. Miller’s wife told him she was taking the kids out for a playdate. After she left, he was served with divorce papers. Less than an hour later, he was parked in his car with his gun, ready to end his life.
But if it all had happened just a few years later, things might never have gotten to that point.
Scanning for suicide risk
In 2017, the VHA piloted its AI program, called REACH VET, that aims to help prevent veterans from dying by suicide.
Every month, a computer scans the electronic health records of all VHA patients who’ve had a health care visit for any reason in the last 2 years. It checks more than 140 variables and weights them to estimate someone’s overall suicide risk at that moment in time.
To build the risk algorithm, a computer combed through the medical records of 6,360 veterans confirmed to have died by suicide between 2009 and 2011. (The VHA continually updates the list of variables from the health records of VHA patients, including those who have died by suicide since then and others.)
Some variables are things you’d expect:
- A past suicide attempt.
- A diagnosis of depression or other mental illness.
- A diagnosis of a terminal illness.
Others are more surprising. For example, a diagnosis of arthritis or diabetes adds weight.
REACH VET flags the riskiest cases – the top 0.1% – for a mental health or primary care provider to review. They reach out to the patient to tell them how and why their record was flagged, discuss any recommended treatment changes, and ask them to come in for a visit.
“It’s an opportunity to talk about their risk factors, which is designed to lead to a conversation about safety planning,” says clinical psychologist Matthew Miller, PhD, national director of the U.S. Department of Veterans Affairs’ Suicide Prevention Program. He’s not related to Dan Miller.
Making a suicide safety plan
A safety plan is a document that outlines how a person can help prevent their own suicide in a crisis.
The plan may include:
- A list of personal triggers or warning signs.
- What’s helped them in the past.
- Names of people or organizations who can support them.
- Plans to remove means of suicide, such as guns, from their environment.
- Their reasons for living.
In people at risk for suicide, research shows that having a safety plan reduces suicidal thoughts and attempts, lowers rates of depression and hopelessness, and boosts veterans’ engagement with the health care system. It may also help people manage things that trigger their suicidal thoughts.
Getting the call
What if REACH VET had been around when Dan Miller was in crisis – and he’d gotten a call from the VHA?
“It absolutely, positively would have helped because one of the biggest things on that day when I got served was feeling completely alone and that I had no one to turn to,” Mr. Miller says. He’s now a speaker for the Wounded Warrior Project, a nonprofit that serves veterans and active-duty service people.
Vets’ reactions to the unexpected VHA phone call, psychologist Dr. Miller says, “run the gamut from ‘Thank you for contacting me. Let’s talk,’ to ‘What are you talking about? Leave me alone!’ ”
Nothing stops all suicides. But REACH VET is having an impact. In a clinical trial, vets contacted through REACH VET had more doctor visits, were more likely to have a written suicide prevention safety plan, and had fewer hospital admissions for mental health, ER visits, and suicide attempts.
An assist from AI
Even simple outreach can make a big difference. And there’s research to prove it.
One study included 4,730 veterans recently discharged from psychiatric care at the VHA, a group considered at high risk for suicide.
Half of them got 13 caring emails from hospital staff in the weeks after leaving the hospital. The emails mentioned personal things the patient had shared, like a love of hiking, and wished them well. The other veterans got routine follow-up but no emails.
Two years later, those who got the caring emails were less likely to have died by suicide than the other vets. The study was published in 2014 in Contemporary Clinical Trials.
Researchers have done studies like this many times: with handwritten notes from the primary care doctor, postcards from the ER, and so forth. The results never vary: The notes reduce suicide risk.
“If we could use AI to identify people to receive notes or phone calls, it would be a very effective and inexpensive way to guide follow-up care,” says Rebecca Bernert, PhD, director and founder of the Suicide Prevention Research Laboratory at Stanford (Calif.) University.
AI doesn’t replace clinical judgment.
“AI can capture data that we miss due to the limits of our humanity,” psychologist Dr. Miller says. “There’s suicide prevention processes founded on big data and AI, and there are processes founded in clinical intuition and acumen.”
AI is only as good as the data it’s based on. If that data lacks diversity, it may miss things. And variables that apply to veterans may differ in civilians.
Stopping suicidal thoughts
Google is putting AI to work against suicide, too. Its MUM (Multitask Unified Model) technology seeks to understand the intent behind what we google.
MUM powers Google Search. It can often tell the difference between a search for information about suicide for someone writing a research paper on the topic and a search for information on how or where to carry out a suicide.
When Google Search detects that someone in the United States might be in crisis and at risk of suicide, the first search results that person gets are the number for the National Suicide Prevention Lifeline and other resources for people in crisis.
Google Home Assistant works in the same way. When a user makes a query that signals a suicide-related crisis, the gadget serves up resources that offer help.
MUM is working to understand the nuances of crisis language in 75 languages so that Google Search can provide people in crisis with hotlines or other resources in many countries.
“We want to find partners that are accessible to users in terms of hours of operation. We have a strong preference for finding partners that promise confidentiality and privacy to the extent that those are permitted [in that country],” says Anne Merritt, MD, a product manager at Google Search.
Other companies are working on apps that use AI to spot suicide risk in other ways, including voice technology that may notice subtle changes in the voice of someone who’s depressed and may be thinking of suicide. Those are still in development but show promise. Keep in mind that apps do not require government approval, so if you try one, be sure to let your health care provider know.
Changing the channel
Seeing a hotline number on your phone or computer screen can help, Dan Miller says. “If I happened to be online, searching maybe for a bridge to jump off of ... and suddenly that pops up on the screen, it’s like it changes the channel.”
It may not work for everyone, he says, but that search result could interrupt someone’s suicidal train of thought.
That’s crucial, psychologist Dr. Miller says, because most suicide attempts escalate from first thought to potentially fatal action in just 1 hour. That’s how fast it happened for Dan Miller in 2014.
“When you’re able to put time and space between the suicidal thought and the access to the method to act on that thought, you save lives,” Dr. Bernert says.
Making a different choice
An interruption in Mr. Miller’s thinking is what had saved his life.
Holding the gun to his head, Mr. Miller looked over at the passenger seat at a brochure from Wounded Warrior Project, which he had just learned about. Mr. Miller noticed a photo of a man in a wheelchair, a veteran like him, who had no legs. He thought that the man looked worse off than him but hadn’t given up.
Mr. Miller put down his gun and decided to get help.
Recovering from a near suicide attempt, he says, is a journey. It doesn’t happen overnight. Now, 8 years later, Mr. Miller is planning a brief break from the speaker circuit. He plans to spend 2 weeks in an outpatient counseling program for posttraumatic stress disorder and traumatic brain injury.
“Telling my story to strangers – part of it is healing me in a way, but I’m learning that repeating the story over and over again is also keeping me from letting it go. And I’m still healing.”
A version of this article first appeared on WebMD.com.
Alcohol’s detrimental impact on the brain explained?
Results of a large observational study suggest brain iron accumulation is a “plausible pathway” through which alcohol negatively affects cognition, study Anya Topiwala, MD, PhD, senior clinical researcher, Nuffield Department of Population Health, University of Oxford, England, said in an interview.
Study participants who drank 56 grams of alcohol a week had higher brain iron levels. The U.K. guideline for “low risk” alcohol consumption is less than 14 units weekly, or 112 grams.
“We are finding harmful associations with iron within those low-risk alcohol intake guidelines,” said Dr. Topiwala.
The study was published online in PLOS Medicine.
Early intervention opportunity?
Previous research suggests higher brain iron may be involved in the pathophysiology of Alzheimer’s and Parkinson’s diseases. However, it’s unclear whether deposition plays a role in alcohol’s effect on the brain and if it does, whether this could present an opportunity for early intervention with, for example, chelating agents.
The study included 20,729 participants in the UK Biobank study, which recruited volunteers from 2006 to 2010. Participants had a mean age of 54.8 years, and 48.6% were female.
Participants self-identified as current, never, or previous alcohol consumers. For current drinkers, researchers calculated the total weekly number of U.K. units of alcohol consumed. One unit is 8 grams. A standard drink in the United States is 14 grams. They categorized weekly consumption into quintiles and used the lowest quintile as the reference category.
Participants underwent MRI to determine brain iron levels. Areas of interest were deep brain structures in the basal ganglia.
Mean weekly alcohol consumption was 17.7 units, which is higher than U.K. guidelines for low-risk consumption. “Half of the sample were drinking above what is recommended,” said Dr. Topiwala.
Alcohol consumption was associated with markers of higher iron in the bilateral putamen (beta, 0.08 standard deviation; 95% confidence interval, 0.06-0.09; P < .001), caudate (beta, 0.05; 95% CI, 0.04-0.07; P < .001), and substantia nigra (beta, 0.03; 95% CI; 0.02-0.05; P < .001).
Poorer performance
Drinking more than 7 units (56 grams) weekly was associated with higher susceptibility for all brain regions, except the thalamus.
Controlling for menopause status did not alter associations between alcohol and susceptibility for any brain region. This was also the case when excluding blood pressure and cholesterol as covariates.
There were significant interactions with age in the bilateral putamen and caudate but not with sex, smoking, or Townsend Deprivation Index, which includes such factors as unemployment and living conditions.
To gather data on liver iron levels, participants underwent abdominal imaging at the same time as brain imaging. Dr. Topiwala explained that the liver is a primary storage center for iron, so it was used as “a kind of surrogate marker” of iron in the body.
The researchers showed an indirect effect of alcohol through systemic iron. A 1 SD increase in weekly alcohol consumption was associated with a 0.05 mg/g (95% CI, 0.02-0.07; P < .001) increase in liver iron. In addition, a 1 mg/g increase in liver iron was associated with a 0.44 (95% CI, 0.35-0.52; P < .001) SD increase in left putamen susceptibility.
In this sample, 32% (95% CI, 22-49; P < .001) of alcohol’s total effect on left putamen susceptibility was mediated via higher systemic iron levels.
To minimize the impact of other factors influencing the association between alcohol consumption and brain iron – and the possibility that people with more brain iron drink more – researchers used Mendelian randomization that considers genetically predicted alcohol intake. This analysis supported findings of associations between alcohol consumption and brain iron.
Participants completed a cognitive battery, which included trail-making tests that reflect executive function, puzzle tests that assess fluid intelligence or logic and reasoning, and task-based tests using the “Snap” card game to measure reaction time.
Investigators found the more iron that was present in certain brain regions, the poorer participants’ cognitive performance.
Patients should know about the risks of moderate alcohol intake so they can make decisions about drinking, said Dr. Topiwala. “They should be aware that 14 units of alcohol per week is not a zero risk.”
Novel research
Commenting for this news organization, Heather Snyder, PhD, vice president of medical and scientific relations, Alzheimer’s Association, noted the study’s large size as a strength of the research.
She noted previous research has shown an association between higher iron levels and alcohol dependence and worse cognitive function, but the potential connection of brain iron levels, moderate alcohol consumption, and cognition has not been studied to date.
“This paper aims to look at whether there is a potential biological link between moderate alcohol consumption and cognition through iron-related pathways.”
The authors suggest more work is needed to understand whether alcohol consumption impacts iron-related biologies to affect downstream cognition, said Dr. Snyder. “Although this study does not answer that question, it does highlight some important questions.”
Study authors received funding from Wellcome Trust, UK Medical Research Council, National Institute for Health Research (NIHR) Oxford Biomedical Research Centre, BHF Centre of Research Excellence, British Heart Foundation, NIHR Cambridge Biomedical Research Centre, U.S. Department of Veterans Affairs, China Scholarship Council, and Li Ka Shing Centre for Health Information and Discovery. Dr. Topiwala has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results of a large observational study suggest brain iron accumulation is a “plausible pathway” through which alcohol negatively affects cognition, study Anya Topiwala, MD, PhD, senior clinical researcher, Nuffield Department of Population Health, University of Oxford, England, said in an interview.
Study participants who drank 56 grams of alcohol a week had higher brain iron levels. The U.K. guideline for “low risk” alcohol consumption is less than 14 units weekly, or 112 grams.
“We are finding harmful associations with iron within those low-risk alcohol intake guidelines,” said Dr. Topiwala.
The study was published online in PLOS Medicine.
Early intervention opportunity?
Previous research suggests higher brain iron may be involved in the pathophysiology of Alzheimer’s and Parkinson’s diseases. However, it’s unclear whether deposition plays a role in alcohol’s effect on the brain and if it does, whether this could present an opportunity for early intervention with, for example, chelating agents.
The study included 20,729 participants in the UK Biobank study, which recruited volunteers from 2006 to 2010. Participants had a mean age of 54.8 years, and 48.6% were female.
Participants self-identified as current, never, or previous alcohol consumers. For current drinkers, researchers calculated the total weekly number of U.K. units of alcohol consumed. One unit is 8 grams. A standard drink in the United States is 14 grams. They categorized weekly consumption into quintiles and used the lowest quintile as the reference category.
Participants underwent MRI to determine brain iron levels. Areas of interest were deep brain structures in the basal ganglia.
Mean weekly alcohol consumption was 17.7 units, which is higher than U.K. guidelines for low-risk consumption. “Half of the sample were drinking above what is recommended,” said Dr. Topiwala.
Alcohol consumption was associated with markers of higher iron in the bilateral putamen (beta, 0.08 standard deviation; 95% confidence interval, 0.06-0.09; P < .001), caudate (beta, 0.05; 95% CI, 0.04-0.07; P < .001), and substantia nigra (beta, 0.03; 95% CI; 0.02-0.05; P < .001).
Poorer performance
Drinking more than 7 units (56 grams) weekly was associated with higher susceptibility for all brain regions, except the thalamus.
Controlling for menopause status did not alter associations between alcohol and susceptibility for any brain region. This was also the case when excluding blood pressure and cholesterol as covariates.
There were significant interactions with age in the bilateral putamen and caudate but not with sex, smoking, or Townsend Deprivation Index, which includes such factors as unemployment and living conditions.
To gather data on liver iron levels, participants underwent abdominal imaging at the same time as brain imaging. Dr. Topiwala explained that the liver is a primary storage center for iron, so it was used as “a kind of surrogate marker” of iron in the body.
The researchers showed an indirect effect of alcohol through systemic iron. A 1 SD increase in weekly alcohol consumption was associated with a 0.05 mg/g (95% CI, 0.02-0.07; P < .001) increase in liver iron. In addition, a 1 mg/g increase in liver iron was associated with a 0.44 (95% CI, 0.35-0.52; P < .001) SD increase in left putamen susceptibility.
In this sample, 32% (95% CI, 22-49; P < .001) of alcohol’s total effect on left putamen susceptibility was mediated via higher systemic iron levels.
To minimize the impact of other factors influencing the association between alcohol consumption and brain iron – and the possibility that people with more brain iron drink more – researchers used Mendelian randomization that considers genetically predicted alcohol intake. This analysis supported findings of associations between alcohol consumption and brain iron.
Participants completed a cognitive battery, which included trail-making tests that reflect executive function, puzzle tests that assess fluid intelligence or logic and reasoning, and task-based tests using the “Snap” card game to measure reaction time.
Investigators found the more iron that was present in certain brain regions, the poorer participants’ cognitive performance.
Patients should know about the risks of moderate alcohol intake so they can make decisions about drinking, said Dr. Topiwala. “They should be aware that 14 units of alcohol per week is not a zero risk.”
Novel research
Commenting for this news organization, Heather Snyder, PhD, vice president of medical and scientific relations, Alzheimer’s Association, noted the study’s large size as a strength of the research.
She noted previous research has shown an association between higher iron levels and alcohol dependence and worse cognitive function, but the potential connection of brain iron levels, moderate alcohol consumption, and cognition has not been studied to date.
“This paper aims to look at whether there is a potential biological link between moderate alcohol consumption and cognition through iron-related pathways.”
The authors suggest more work is needed to understand whether alcohol consumption impacts iron-related biologies to affect downstream cognition, said Dr. Snyder. “Although this study does not answer that question, it does highlight some important questions.”
Study authors received funding from Wellcome Trust, UK Medical Research Council, National Institute for Health Research (NIHR) Oxford Biomedical Research Centre, BHF Centre of Research Excellence, British Heart Foundation, NIHR Cambridge Biomedical Research Centre, U.S. Department of Veterans Affairs, China Scholarship Council, and Li Ka Shing Centre for Health Information and Discovery. Dr. Topiwala has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results of a large observational study suggest brain iron accumulation is a “plausible pathway” through which alcohol negatively affects cognition, study Anya Topiwala, MD, PhD, senior clinical researcher, Nuffield Department of Population Health, University of Oxford, England, said in an interview.
Study participants who drank 56 grams of alcohol a week had higher brain iron levels. The U.K. guideline for “low risk” alcohol consumption is less than 14 units weekly, or 112 grams.
“We are finding harmful associations with iron within those low-risk alcohol intake guidelines,” said Dr. Topiwala.
The study was published online in PLOS Medicine.
Early intervention opportunity?
Previous research suggests higher brain iron may be involved in the pathophysiology of Alzheimer’s and Parkinson’s diseases. However, it’s unclear whether deposition plays a role in alcohol’s effect on the brain and if it does, whether this could present an opportunity for early intervention with, for example, chelating agents.
The study included 20,729 participants in the UK Biobank study, which recruited volunteers from 2006 to 2010. Participants had a mean age of 54.8 years, and 48.6% were female.
Participants self-identified as current, never, or previous alcohol consumers. For current drinkers, researchers calculated the total weekly number of U.K. units of alcohol consumed. One unit is 8 grams. A standard drink in the United States is 14 grams. They categorized weekly consumption into quintiles and used the lowest quintile as the reference category.
Participants underwent MRI to determine brain iron levels. Areas of interest were deep brain structures in the basal ganglia.
Mean weekly alcohol consumption was 17.7 units, which is higher than U.K. guidelines for low-risk consumption. “Half of the sample were drinking above what is recommended,” said Dr. Topiwala.
Alcohol consumption was associated with markers of higher iron in the bilateral putamen (beta, 0.08 standard deviation; 95% confidence interval, 0.06-0.09; P < .001), caudate (beta, 0.05; 95% CI, 0.04-0.07; P < .001), and substantia nigra (beta, 0.03; 95% CI; 0.02-0.05; P < .001).
Poorer performance
Drinking more than 7 units (56 grams) weekly was associated with higher susceptibility for all brain regions, except the thalamus.
Controlling for menopause status did not alter associations between alcohol and susceptibility for any brain region. This was also the case when excluding blood pressure and cholesterol as covariates.
There were significant interactions with age in the bilateral putamen and caudate but not with sex, smoking, or Townsend Deprivation Index, which includes such factors as unemployment and living conditions.
To gather data on liver iron levels, participants underwent abdominal imaging at the same time as brain imaging. Dr. Topiwala explained that the liver is a primary storage center for iron, so it was used as “a kind of surrogate marker” of iron in the body.
The researchers showed an indirect effect of alcohol through systemic iron. A 1 SD increase in weekly alcohol consumption was associated with a 0.05 mg/g (95% CI, 0.02-0.07; P < .001) increase in liver iron. In addition, a 1 mg/g increase in liver iron was associated with a 0.44 (95% CI, 0.35-0.52; P < .001) SD increase in left putamen susceptibility.
In this sample, 32% (95% CI, 22-49; P < .001) of alcohol’s total effect on left putamen susceptibility was mediated via higher systemic iron levels.
To minimize the impact of other factors influencing the association between alcohol consumption and brain iron – and the possibility that people with more brain iron drink more – researchers used Mendelian randomization that considers genetically predicted alcohol intake. This analysis supported findings of associations between alcohol consumption and brain iron.
Participants completed a cognitive battery, which included trail-making tests that reflect executive function, puzzle tests that assess fluid intelligence or logic and reasoning, and task-based tests using the “Snap” card game to measure reaction time.
Investigators found the more iron that was present in certain brain regions, the poorer participants’ cognitive performance.
Patients should know about the risks of moderate alcohol intake so they can make decisions about drinking, said Dr. Topiwala. “They should be aware that 14 units of alcohol per week is not a zero risk.”
Novel research
Commenting for this news organization, Heather Snyder, PhD, vice president of medical and scientific relations, Alzheimer’s Association, noted the study’s large size as a strength of the research.
She noted previous research has shown an association between higher iron levels and alcohol dependence and worse cognitive function, but the potential connection of brain iron levels, moderate alcohol consumption, and cognition has not been studied to date.
“This paper aims to look at whether there is a potential biological link between moderate alcohol consumption and cognition through iron-related pathways.”
The authors suggest more work is needed to understand whether alcohol consumption impacts iron-related biologies to affect downstream cognition, said Dr. Snyder. “Although this study does not answer that question, it does highlight some important questions.”
Study authors received funding from Wellcome Trust, UK Medical Research Council, National Institute for Health Research (NIHR) Oxford Biomedical Research Centre, BHF Centre of Research Excellence, British Heart Foundation, NIHR Cambridge Biomedical Research Centre, U.S. Department of Veterans Affairs, China Scholarship Council, and Li Ka Shing Centre for Health Information and Discovery. Dr. Topiwala has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM PLOS MEDICINE
Best meds for insomnia identified?
In a comprehensive comparative-effectiveness analysis, lemborexant and eszopiclone showed the best efficacy, acceptability, and tolerability for acute and long-term insomnia treatment.
However, eszopiclone may cause substantial side effects – and safety data on lemborexant were inconclusive, the researchers note.
Not surprisingly, short-acting, intermediate-acting, and long-acting benzodiazepines were effective in the acute treatment of insomnia, but they have unfavorable tolerability and safety profiles, and there are no long-term data on these issues.
For many insomnia medications, there is a “striking” and “appalling” lack of long-term data, study investigator Andrea Cipriani, MD, PhD, professor of psychiatry, University of Oxford, United Kingdom, noted during a press briefing.
“This is a call for regulators to raise the bar and ask for long-term data when companies submit an application for licensing insomnia drugs,” Dr. Cipriani said.
The findings were published online in The Lancet.
Prevalent, debilitating
Insomnia is highly prevalent, affecting up to 1 in 5 adults, and can have a profound impact on health, well-being, and productivity.
Sleep hygiene and cognitive-behavioral therapy for insomnia (CBT-I) are recommended first-line treatments, but they are often unavailable, which often leads patients and clinicians to turn to medications.
However, “insomnia drugs are not all created equal. Even within the same drug class there are differences,” Dr. Cipriani said.
In a large-scale systematic review and network meta-analysis, the researchers analyzed data from 154 double-blind, randomized controlled trials of medications (licensed or not) used for acute and long-term treatment of insomnia in 44,089 adults (mean age, 51.7 years; 63% women).
Results showed, for the acute treatment of insomnia, benzodiazepines, doxylamine, eszopiclone, lemborexant, seltorexant, zolpidem, and zopiclone were more effective than placebo (standardized mean difference range, 0.36-0.83; high-to-moderate certainty of evidence).
In addition, benzodiazepines, eszopiclone, zolpidem, and zopiclone were more effective than melatonin, ramelteon, and zaleplon (SMD, 0.27-0.71; moderate-to-very low certainty of evidence).
“Our results show that the melatonergic drugs melatonin and ramelteon are not really effective. The data do not support the regular use of these drugs,” co-investigator Phil Cowen, PhD, professor of psychopharmacology, University of Oxford, said at the briefing.
Best available evidence
What little long-term data is available suggest eszopiclone and lemborexant are more effective than placebo. Plus, eszopiclone is more effective than ramelteon and zolpidem but with “very low” certainty of evidence, the researchers report.
“There was insufficient evidence to support the prescription of benzodiazepines and zolpidem in long-term treatment,” they write.
Another problem was lack of data on other important outcomes, they add.
“We wanted to look at hangover effects, daytime sleepiness, [and] rebound effect, but often there was no data reported in trials. We need to collect data about these outcomes because they matter to clinicians and patients,” Dr. Cipriani said.
Summing up, the researchers note the current findings represent the “best available evidence base to guide the choice about pharmacological treatment for insomnia disorder in adults and will assist in shared decisionmaking between patients, carers, and their clinicians, as well as policy makers.”
They caution, however, that all statements comparing the merits of one drug with another “should be tempered by the potential limitations of the current analysis, the quality of the available evidence, the characteristics of the patient populations, and the uncertainties that might result from choice of dose or treatment setting.”
In addition, it is important to also consider nonpharmacologic treatments for insomnia disorder, as they are supported by “high-quality evidence and recommended as first-line treatment by guidelines,” the investigator write.
Shared decisionmaking
In an accompanying editorial, Myrto Samara, MD, University of Thessaly, Larissa, Greece, agrees with the researchers that discussion with patients is key.
“For insomnia treatment, patient-physician shared decisionmaking is crucial to decide when a pharmacological intervention is deemed necessary and which drug [is] to be given by considering the trade-offs for efficacy and side effects,” Dr. Samara writes.
The study was funded by the UK National Institute for Health Research (NIHR) Oxford Health Biomedical Research Center. Dr. Cipriani has received research and consultancy fees from the Italian Network for Pediatric Trials, CARIPLO Foundation, and Angelini Pharma, and is the chief and principal investigator of two trials of seltorexant in depression that are sponsored by Janssen. Dr. Samara has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a comprehensive comparative-effectiveness analysis, lemborexant and eszopiclone showed the best efficacy, acceptability, and tolerability for acute and long-term insomnia treatment.
However, eszopiclone may cause substantial side effects – and safety data on lemborexant were inconclusive, the researchers note.
Not surprisingly, short-acting, intermediate-acting, and long-acting benzodiazepines were effective in the acute treatment of insomnia, but they have unfavorable tolerability and safety profiles, and there are no long-term data on these issues.
For many insomnia medications, there is a “striking” and “appalling” lack of long-term data, study investigator Andrea Cipriani, MD, PhD, professor of psychiatry, University of Oxford, United Kingdom, noted during a press briefing.
“This is a call for regulators to raise the bar and ask for long-term data when companies submit an application for licensing insomnia drugs,” Dr. Cipriani said.
The findings were published online in The Lancet.
Prevalent, debilitating
Insomnia is highly prevalent, affecting up to 1 in 5 adults, and can have a profound impact on health, well-being, and productivity.
Sleep hygiene and cognitive-behavioral therapy for insomnia (CBT-I) are recommended first-line treatments, but they are often unavailable, which often leads patients and clinicians to turn to medications.
However, “insomnia drugs are not all created equal. Even within the same drug class there are differences,” Dr. Cipriani said.
In a large-scale systematic review and network meta-analysis, the researchers analyzed data from 154 double-blind, randomized controlled trials of medications (licensed or not) used for acute and long-term treatment of insomnia in 44,089 adults (mean age, 51.7 years; 63% women).
Results showed, for the acute treatment of insomnia, benzodiazepines, doxylamine, eszopiclone, lemborexant, seltorexant, zolpidem, and zopiclone were more effective than placebo (standardized mean difference range, 0.36-0.83; high-to-moderate certainty of evidence).
In addition, benzodiazepines, eszopiclone, zolpidem, and zopiclone were more effective than melatonin, ramelteon, and zaleplon (SMD, 0.27-0.71; moderate-to-very low certainty of evidence).
“Our results show that the melatonergic drugs melatonin and ramelteon are not really effective. The data do not support the regular use of these drugs,” co-investigator Phil Cowen, PhD, professor of psychopharmacology, University of Oxford, said at the briefing.
Best available evidence
What little long-term data is available suggest eszopiclone and lemborexant are more effective than placebo. Plus, eszopiclone is more effective than ramelteon and zolpidem but with “very low” certainty of evidence, the researchers report.
“There was insufficient evidence to support the prescription of benzodiazepines and zolpidem in long-term treatment,” they write.
Another problem was lack of data on other important outcomes, they add.
“We wanted to look at hangover effects, daytime sleepiness, [and] rebound effect, but often there was no data reported in trials. We need to collect data about these outcomes because they matter to clinicians and patients,” Dr. Cipriani said.
Summing up, the researchers note the current findings represent the “best available evidence base to guide the choice about pharmacological treatment for insomnia disorder in adults and will assist in shared decisionmaking between patients, carers, and their clinicians, as well as policy makers.”
They caution, however, that all statements comparing the merits of one drug with another “should be tempered by the potential limitations of the current analysis, the quality of the available evidence, the characteristics of the patient populations, and the uncertainties that might result from choice of dose or treatment setting.”
In addition, it is important to also consider nonpharmacologic treatments for insomnia disorder, as they are supported by “high-quality evidence and recommended as first-line treatment by guidelines,” the investigator write.
Shared decisionmaking
In an accompanying editorial, Myrto Samara, MD, University of Thessaly, Larissa, Greece, agrees with the researchers that discussion with patients is key.
“For insomnia treatment, patient-physician shared decisionmaking is crucial to decide when a pharmacological intervention is deemed necessary and which drug [is] to be given by considering the trade-offs for efficacy and side effects,” Dr. Samara writes.
The study was funded by the UK National Institute for Health Research (NIHR) Oxford Health Biomedical Research Center. Dr. Cipriani has received research and consultancy fees from the Italian Network for Pediatric Trials, CARIPLO Foundation, and Angelini Pharma, and is the chief and principal investigator of two trials of seltorexant in depression that are sponsored by Janssen. Dr. Samara has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a comprehensive comparative-effectiveness analysis, lemborexant and eszopiclone showed the best efficacy, acceptability, and tolerability for acute and long-term insomnia treatment.
However, eszopiclone may cause substantial side effects – and safety data on lemborexant were inconclusive, the researchers note.
Not surprisingly, short-acting, intermediate-acting, and long-acting benzodiazepines were effective in the acute treatment of insomnia, but they have unfavorable tolerability and safety profiles, and there are no long-term data on these issues.
For many insomnia medications, there is a “striking” and “appalling” lack of long-term data, study investigator Andrea Cipriani, MD, PhD, professor of psychiatry, University of Oxford, United Kingdom, noted during a press briefing.
“This is a call for regulators to raise the bar and ask for long-term data when companies submit an application for licensing insomnia drugs,” Dr. Cipriani said.
The findings were published online in The Lancet.
Prevalent, debilitating
Insomnia is highly prevalent, affecting up to 1 in 5 adults, and can have a profound impact on health, well-being, and productivity.
Sleep hygiene and cognitive-behavioral therapy for insomnia (CBT-I) are recommended first-line treatments, but they are often unavailable, which often leads patients and clinicians to turn to medications.
However, “insomnia drugs are not all created equal. Even within the same drug class there are differences,” Dr. Cipriani said.
In a large-scale systematic review and network meta-analysis, the researchers analyzed data from 154 double-blind, randomized controlled trials of medications (licensed or not) used for acute and long-term treatment of insomnia in 44,089 adults (mean age, 51.7 years; 63% women).
Results showed, for the acute treatment of insomnia, benzodiazepines, doxylamine, eszopiclone, lemborexant, seltorexant, zolpidem, and zopiclone were more effective than placebo (standardized mean difference range, 0.36-0.83; high-to-moderate certainty of evidence).
In addition, benzodiazepines, eszopiclone, zolpidem, and zopiclone were more effective than melatonin, ramelteon, and zaleplon (SMD, 0.27-0.71; moderate-to-very low certainty of evidence).
“Our results show that the melatonergic drugs melatonin and ramelteon are not really effective. The data do not support the regular use of these drugs,” co-investigator Phil Cowen, PhD, professor of psychopharmacology, University of Oxford, said at the briefing.
Best available evidence
What little long-term data is available suggest eszopiclone and lemborexant are more effective than placebo. Plus, eszopiclone is more effective than ramelteon and zolpidem but with “very low” certainty of evidence, the researchers report.
“There was insufficient evidence to support the prescription of benzodiazepines and zolpidem in long-term treatment,” they write.
Another problem was lack of data on other important outcomes, they add.
“We wanted to look at hangover effects, daytime sleepiness, [and] rebound effect, but often there was no data reported in trials. We need to collect data about these outcomes because they matter to clinicians and patients,” Dr. Cipriani said.
Summing up, the researchers note the current findings represent the “best available evidence base to guide the choice about pharmacological treatment for insomnia disorder in adults and will assist in shared decisionmaking between patients, carers, and their clinicians, as well as policy makers.”
They caution, however, that all statements comparing the merits of one drug with another “should be tempered by the potential limitations of the current analysis, the quality of the available evidence, the characteristics of the patient populations, and the uncertainties that might result from choice of dose or treatment setting.”
In addition, it is important to also consider nonpharmacologic treatments for insomnia disorder, as they are supported by “high-quality evidence and recommended as first-line treatment by guidelines,” the investigator write.
Shared decisionmaking
In an accompanying editorial, Myrto Samara, MD, University of Thessaly, Larissa, Greece, agrees with the researchers that discussion with patients is key.
“For insomnia treatment, patient-physician shared decisionmaking is crucial to decide when a pharmacological intervention is deemed necessary and which drug [is] to be given by considering the trade-offs for efficacy and side effects,” Dr. Samara writes.
The study was funded by the UK National Institute for Health Research (NIHR) Oxford Health Biomedical Research Center. Dr. Cipriani has received research and consultancy fees from the Italian Network for Pediatric Trials, CARIPLO Foundation, and Angelini Pharma, and is the chief and principal investigator of two trials of seltorexant in depression that are sponsored by Janssen. Dr. Samara has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE LANCET













