User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Surgeons, intensivists earn more than do colleagues from private insurance
General and orthopedic surgeons and intensivists earn the highest net reimbursements from private U.S. insurers, a new report estimates.
On average in 2021, they were paid $5.8 million, $4.9 million, and $3.3 million, respectively, according to figures compiled by AMN Healthcare, a Dallas-based health staffing company.
None of 15 other physician specialties topped $3 million in net reimbursement on average, and three – dermatology, pediatrics, and family medicine – didn’t reach $1 million.
The report doesn’t include data about reimbursement from Medicare and Medicaid, and its numbers assume that 50% of insurance claims are denied. Denial rates differ from practice to practice.
Still, the findings offer a “benchmark tool” to help clinicians understand how they rank against their peers, Linda Murphy, president of AMN Healthcare’s Revenue Cycle Solutions division, said in an interview.
This is the first year that the company has calculated physician reimbursement levels by using claim and clearinghouse data, Ms. Murphy said. Previously, a division of the firm compiled data by surveying chief financial officers from hospitals.
The report’s estimate that insurers deny 50% of claims is “conservative,” Ms. Murphy said. Miscoding is a significant factor behind that number.
The estimated 2021 net private insurance reimbursements by specialty for direct services, assuming a 50% denial rate:
- Anesthesiology: $1,665,510
- Cardiology: $1,703,013
- Critical Care (intensivist): $3,338,656
- Dermatology: $729,107
- Family medicine: $697,094
- Gastroenterology: $2,765,110
- Internal medicine: $1,297,200
- Neurology: $1,390,181
- Obstetrician/gynecology: $1,880,888
- Otolaryngology: $2,095,277
- Pediatrics: $661,552
- Psychiatry: $1,348,730
- Pulmonology: $1,561,617
- Radiology: $1,015,750
- Rheumatology: $1,705,140
- General surgery: $5,834,508
- Orthopedic surgery: $4,904,757
- Urology: $2,943,381
Among 18 physician specialties overall, the report estimated that the average net reimbursement in 2021 was $1.9 million.
The report also estimated that the net reimbursement amounts at $875,140 for certified registered nurse anesthetists and $388,696 for nurse practitioners.
Surprisingly, Ms. Murphy said, there’s “a really large swing” among reimbursement levels for individual specialties. The quartile of cardiologists with the lowest level of reimbursement, for example, submitted $2.1 million in claims in 2021, netting about $1 million at a 50% denial rate versus the $7.3 million made by those in the highest quartile, netting about $3.6 million.
The gap seems to be due to regional variations, she said, adding that a rural cardiologist will have different billing practices than does one practicing in New York City.
The quartile of general surgeons with the highest reimbursement levels billed for $21.1 million on average in 2021, making about $10.5 million at a 50% denial rate. The lowest quartile billed for $5.5 million, making about $2.7 million at a 50% denial rate.
The report noted that primary care physicians – that is, family medicine, internal medicine, and pediatrics specialists – have much lower levels of reimbursement, compared with most other specialties. But the work of primary care physicians “may lead to considerable ‘downstream revenue’ through the hospital admissions, tests and treatment they order.”
A previous analysis by a division of AMN Healthcare found that primary care physicians, on average, generate $2,113,273 a year in net annual revenue for their affiliated hospitals, nearing the $2,446,429 in net annual hospital revenue generated by specialists.
AMN Healthcare is preparing another report that will examine Medicare reimbursements, Ms. Murphy said. According to the new report, payments by nonprivate insurers amount to about one-third of the total amount of reimbursement by commercial insurers.
A version of this article originally appeared on Medscape.com.
General and orthopedic surgeons and intensivists earn the highest net reimbursements from private U.S. insurers, a new report estimates.
On average in 2021, they were paid $5.8 million, $4.9 million, and $3.3 million, respectively, according to figures compiled by AMN Healthcare, a Dallas-based health staffing company.
None of 15 other physician specialties topped $3 million in net reimbursement on average, and three – dermatology, pediatrics, and family medicine – didn’t reach $1 million.
The report doesn’t include data about reimbursement from Medicare and Medicaid, and its numbers assume that 50% of insurance claims are denied. Denial rates differ from practice to practice.
Still, the findings offer a “benchmark tool” to help clinicians understand how they rank against their peers, Linda Murphy, president of AMN Healthcare’s Revenue Cycle Solutions division, said in an interview.
This is the first year that the company has calculated physician reimbursement levels by using claim and clearinghouse data, Ms. Murphy said. Previously, a division of the firm compiled data by surveying chief financial officers from hospitals.
The report’s estimate that insurers deny 50% of claims is “conservative,” Ms. Murphy said. Miscoding is a significant factor behind that number.
The estimated 2021 net private insurance reimbursements by specialty for direct services, assuming a 50% denial rate:
- Anesthesiology: $1,665,510
- Cardiology: $1,703,013
- Critical Care (intensivist): $3,338,656
- Dermatology: $729,107
- Family medicine: $697,094
- Gastroenterology: $2,765,110
- Internal medicine: $1,297,200
- Neurology: $1,390,181
- Obstetrician/gynecology: $1,880,888
- Otolaryngology: $2,095,277
- Pediatrics: $661,552
- Psychiatry: $1,348,730
- Pulmonology: $1,561,617
- Radiology: $1,015,750
- Rheumatology: $1,705,140
- General surgery: $5,834,508
- Orthopedic surgery: $4,904,757
- Urology: $2,943,381
Among 18 physician specialties overall, the report estimated that the average net reimbursement in 2021 was $1.9 million.
The report also estimated that the net reimbursement amounts at $875,140 for certified registered nurse anesthetists and $388,696 for nurse practitioners.
Surprisingly, Ms. Murphy said, there’s “a really large swing” among reimbursement levels for individual specialties. The quartile of cardiologists with the lowest level of reimbursement, for example, submitted $2.1 million in claims in 2021, netting about $1 million at a 50% denial rate versus the $7.3 million made by those in the highest quartile, netting about $3.6 million.
The gap seems to be due to regional variations, she said, adding that a rural cardiologist will have different billing practices than does one practicing in New York City.
The quartile of general surgeons with the highest reimbursement levels billed for $21.1 million on average in 2021, making about $10.5 million at a 50% denial rate. The lowest quartile billed for $5.5 million, making about $2.7 million at a 50% denial rate.
The report noted that primary care physicians – that is, family medicine, internal medicine, and pediatrics specialists – have much lower levels of reimbursement, compared with most other specialties. But the work of primary care physicians “may lead to considerable ‘downstream revenue’ through the hospital admissions, tests and treatment they order.”
A previous analysis by a division of AMN Healthcare found that primary care physicians, on average, generate $2,113,273 a year in net annual revenue for their affiliated hospitals, nearing the $2,446,429 in net annual hospital revenue generated by specialists.
AMN Healthcare is preparing another report that will examine Medicare reimbursements, Ms. Murphy said. According to the new report, payments by nonprivate insurers amount to about one-third of the total amount of reimbursement by commercial insurers.
A version of this article originally appeared on Medscape.com.
General and orthopedic surgeons and intensivists earn the highest net reimbursements from private U.S. insurers, a new report estimates.
On average in 2021, they were paid $5.8 million, $4.9 million, and $3.3 million, respectively, according to figures compiled by AMN Healthcare, a Dallas-based health staffing company.
None of 15 other physician specialties topped $3 million in net reimbursement on average, and three – dermatology, pediatrics, and family medicine – didn’t reach $1 million.
The report doesn’t include data about reimbursement from Medicare and Medicaid, and its numbers assume that 50% of insurance claims are denied. Denial rates differ from practice to practice.
Still, the findings offer a “benchmark tool” to help clinicians understand how they rank against their peers, Linda Murphy, president of AMN Healthcare’s Revenue Cycle Solutions division, said in an interview.
This is the first year that the company has calculated physician reimbursement levels by using claim and clearinghouse data, Ms. Murphy said. Previously, a division of the firm compiled data by surveying chief financial officers from hospitals.
The report’s estimate that insurers deny 50% of claims is “conservative,” Ms. Murphy said. Miscoding is a significant factor behind that number.
The estimated 2021 net private insurance reimbursements by specialty for direct services, assuming a 50% denial rate:
- Anesthesiology: $1,665,510
- Cardiology: $1,703,013
- Critical Care (intensivist): $3,338,656
- Dermatology: $729,107
- Family medicine: $697,094
- Gastroenterology: $2,765,110
- Internal medicine: $1,297,200
- Neurology: $1,390,181
- Obstetrician/gynecology: $1,880,888
- Otolaryngology: $2,095,277
- Pediatrics: $661,552
- Psychiatry: $1,348,730
- Pulmonology: $1,561,617
- Radiology: $1,015,750
- Rheumatology: $1,705,140
- General surgery: $5,834,508
- Orthopedic surgery: $4,904,757
- Urology: $2,943,381
Among 18 physician specialties overall, the report estimated that the average net reimbursement in 2021 was $1.9 million.
The report also estimated that the net reimbursement amounts at $875,140 for certified registered nurse anesthetists and $388,696 for nurse practitioners.
Surprisingly, Ms. Murphy said, there’s “a really large swing” among reimbursement levels for individual specialties. The quartile of cardiologists with the lowest level of reimbursement, for example, submitted $2.1 million in claims in 2021, netting about $1 million at a 50% denial rate versus the $7.3 million made by those in the highest quartile, netting about $3.6 million.
The gap seems to be due to regional variations, she said, adding that a rural cardiologist will have different billing practices than does one practicing in New York City.
The quartile of general surgeons with the highest reimbursement levels billed for $21.1 million on average in 2021, making about $10.5 million at a 50% denial rate. The lowest quartile billed for $5.5 million, making about $2.7 million at a 50% denial rate.
The report noted that primary care physicians – that is, family medicine, internal medicine, and pediatrics specialists – have much lower levels of reimbursement, compared with most other specialties. But the work of primary care physicians “may lead to considerable ‘downstream revenue’ through the hospital admissions, tests and treatment they order.”
A previous analysis by a division of AMN Healthcare found that primary care physicians, on average, generate $2,113,273 a year in net annual revenue for their affiliated hospitals, nearing the $2,446,429 in net annual hospital revenue generated by specialists.
AMN Healthcare is preparing another report that will examine Medicare reimbursements, Ms. Murphy said. According to the new report, payments by nonprivate insurers amount to about one-third of the total amount of reimbursement by commercial insurers.
A version of this article originally appeared on Medscape.com.
Steep rise in cannabis-related suicide attempts
The increases were notable both during and after the pandemic and were highest among children and female persons.
Investigators examined closed cases of cannabis-related human exposures that were coded as intentional-suspected suicidal.
Of note, there was a statistically significant increase in cannabis poisonings in young children (5-13 years) in 2021, during the pandemic, compared with 2019, a prepandemic year (3.1% vs. 1.3%; P < .001), the researchers report.
“This may speak to both increased access to cannabis as well as poor mental health status during the pandemic period,” study investigator Tracy Klein, PhD, assistant director, Center for Cannabis Policy, Research and Outreach, Washington State University Vancouver, Mount Vista, said in an interview.
The study was published online in JAMA Network Open.
Reports of intentional poisonings with cannabis increased by roughly 17% annually over the study period. Most cases occurred in recent years and involved individuals aged 14-64 years. Nearly all (96.5%) cases involved more than one substance.
“The resemblance of cannabis edibles, implicated in the majority of poisonings to candy, vitamins, and food products, is a risk to patients across the life span who may not fully understand what they are consuming or how potent it is,” Dr. Klein said in an interview.
Overall, nearly 1 in 10 exposures resulted in death or other major outcomes (life-threatening outcomes or outcomes involving major residual disability or disfigurement). For older adults, 19.4% of exposures led to death or other major harm.
“Elderly patients may also have comorbid conditions and polypharmacy, which contributes to their much more serious outcomes from cannabis poisoning,” Dr. Klein said.
The researchers caution that, owing to the cross-sectional nature of the data, they could not identify a causal association between cannabis use and suicide attempt.
With more states legalizing cannabis use by adults, increases in cannabis use will likely persist.
“It is important to further examine the suspected association between cannabis use and suicidal behaviors and how risks can be prevented or mitigated,” the researchers note.
Dr. Klein encourages health care providers to ask patients whether they are using cannabis and how they obtain and store it.
“As with all medications and substances, storage is a key safety issue that is elicited during a careful history,” said Dr. Klein.
Support for the study was provided in part by funds provided for medical and biological research by the State of Washington Initiative Measure No. 171. Dr. Klein has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The increases were notable both during and after the pandemic and were highest among children and female persons.
Investigators examined closed cases of cannabis-related human exposures that were coded as intentional-suspected suicidal.
Of note, there was a statistically significant increase in cannabis poisonings in young children (5-13 years) in 2021, during the pandemic, compared with 2019, a prepandemic year (3.1% vs. 1.3%; P < .001), the researchers report.
“This may speak to both increased access to cannabis as well as poor mental health status during the pandemic period,” study investigator Tracy Klein, PhD, assistant director, Center for Cannabis Policy, Research and Outreach, Washington State University Vancouver, Mount Vista, said in an interview.
The study was published online in JAMA Network Open.
Reports of intentional poisonings with cannabis increased by roughly 17% annually over the study period. Most cases occurred in recent years and involved individuals aged 14-64 years. Nearly all (96.5%) cases involved more than one substance.
“The resemblance of cannabis edibles, implicated in the majority of poisonings to candy, vitamins, and food products, is a risk to patients across the life span who may not fully understand what they are consuming or how potent it is,” Dr. Klein said in an interview.
Overall, nearly 1 in 10 exposures resulted in death or other major outcomes (life-threatening outcomes or outcomes involving major residual disability or disfigurement). For older adults, 19.4% of exposures led to death or other major harm.
“Elderly patients may also have comorbid conditions and polypharmacy, which contributes to their much more serious outcomes from cannabis poisoning,” Dr. Klein said.
The researchers caution that, owing to the cross-sectional nature of the data, they could not identify a causal association between cannabis use and suicide attempt.
With more states legalizing cannabis use by adults, increases in cannabis use will likely persist.
“It is important to further examine the suspected association between cannabis use and suicidal behaviors and how risks can be prevented or mitigated,” the researchers note.
Dr. Klein encourages health care providers to ask patients whether they are using cannabis and how they obtain and store it.
“As with all medications and substances, storage is a key safety issue that is elicited during a careful history,” said Dr. Klein.
Support for the study was provided in part by funds provided for medical and biological research by the State of Washington Initiative Measure No. 171. Dr. Klein has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The increases were notable both during and after the pandemic and were highest among children and female persons.
Investigators examined closed cases of cannabis-related human exposures that were coded as intentional-suspected suicidal.
Of note, there was a statistically significant increase in cannabis poisonings in young children (5-13 years) in 2021, during the pandemic, compared with 2019, a prepandemic year (3.1% vs. 1.3%; P < .001), the researchers report.
“This may speak to both increased access to cannabis as well as poor mental health status during the pandemic period,” study investigator Tracy Klein, PhD, assistant director, Center for Cannabis Policy, Research and Outreach, Washington State University Vancouver, Mount Vista, said in an interview.
The study was published online in JAMA Network Open.
Reports of intentional poisonings with cannabis increased by roughly 17% annually over the study period. Most cases occurred in recent years and involved individuals aged 14-64 years. Nearly all (96.5%) cases involved more than one substance.
“The resemblance of cannabis edibles, implicated in the majority of poisonings to candy, vitamins, and food products, is a risk to patients across the life span who may not fully understand what they are consuming or how potent it is,” Dr. Klein said in an interview.
Overall, nearly 1 in 10 exposures resulted in death or other major outcomes (life-threatening outcomes or outcomes involving major residual disability or disfigurement). For older adults, 19.4% of exposures led to death or other major harm.
“Elderly patients may also have comorbid conditions and polypharmacy, which contributes to their much more serious outcomes from cannabis poisoning,” Dr. Klein said.
The researchers caution that, owing to the cross-sectional nature of the data, they could not identify a causal association between cannabis use and suicide attempt.
With more states legalizing cannabis use by adults, increases in cannabis use will likely persist.
“It is important to further examine the suspected association between cannabis use and suicidal behaviors and how risks can be prevented or mitigated,” the researchers note.
Dr. Klein encourages health care providers to ask patients whether they are using cannabis and how they obtain and store it.
“As with all medications and substances, storage is a key safety issue that is elicited during a careful history,” said Dr. Klein.
Support for the study was provided in part by funds provided for medical and biological research by the State of Washington Initiative Measure No. 171. Dr. Klein has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Telehealth suicide prevention program safe, acceptable
WASHINGTON –
Skeptics had worried that participating in the program through telehealth would exacerbate safety and other issues veterans had about discussing suicide in a group setting, study investigator Sarah Sullivan, PhD student, Health Psychology & Clinical Science, City University of New York, told this news organization.
“But that for us was not really true. People opened up about their suicidal thoughts and triggers even on this telehealth format, and that’s really important for providers to know,” she said.
The findings were presented as part of the Anxiety and Depression Association of America Anxiety & Depression conference.
Trial run
Suicide is a major public health issue, particularly for veterans. Recent data from the Veterans Administration show 17 veterans die by suicide every day.
The current study included 15 male and 2 female veterans (29.4% White, 70.6% Hispanic) from New York City and Philadelphia. Participants had an average age of 50 and all were either deemed by a clinician to be at extremely high risk for suicide or were hospitalized for this reason.
The individuals completed an online version of the Project Life Force (PLF) program, which uses dialectical behavioral therapy and psychoeducational approaches. The program includes the brief Safety Planning intervention (SPI), aimed at reducing short-term suicide risk.
Considered a best practice, the SPI includes a written list of personal suicide warning signs or triggers, internal coping strategies, social contacts who offer support and distraction from suicidal thoughts, contact information for professionals, a suicide crisis hotline, and nearby emergency services.
In addition to these steps, the PLF program focuses on sleep, exercise, and making the safety plan accessible.
The telehealth platform for the program was WebEx software. Participants were offered a “trial run” to orient them to the technology, said Ms. Sullivan.
Group sessions were held once weekly for 10 weeks, with optional “booster” sessions if needed. Each session included about five participants.
To ensure privacy, participants were provided with headphones and laptops. This was especially important for those sharing a living space, including spouses and children, said Ms. Sullivan.
High ratings
Participants completed the Acceptability of Intervention Measure (AIM), Intervention Appropriateness Measure (IAM), and Feasibility of Intervention Measure (FIM). Each of these yields scores from four items rated on a Likert scale of 1-5, for a total score ranging from 5 to 20, with higher scores indicating higher ratings.
Veterans rated PLF-T as highly acceptable (mean AIM, 17.50), appropriate (mean IAM, 17.25), and feasible (mean FIM, 18).
Study participants reported the program was convenient and noted that it decreased the burden of traveling to sessions, especially during the COVID-19 pandemic.
They also reported the program was less likely to compete with other demands such as childcare and other appointments, said Ms. Sullivan.
In addition, it helped those with comorbidities such as posttraumatic stress disorder, she added. She noted veterans with PTSD may be triggered on subways or buses when traveling to in-person treatment sessions.
“That can take away from addressing the suicidal triggers,” said Ms. Sullivan. “So, this program allows them to fully concentrate on the safety plan.”
Results showed that study participants “enjoyed the group and would recommend it to others,” said Ms. Sullivan. “I think that signifies the group was effective in its goal of mitigating loneliness, which was exacerbated during the COVID-19 pandemic, and creating a socially supportive environment, especially for the vets living alone.”
Veterans also reported that the program helped them understand the connection between depression or PTSD and suicidal thoughts, urges, and plans. In addition, they appreciated the group dynamics, where they felt connected to other veterans experiencing similar challenges.
Hopeful results
Commenting on the study, Paul E. Holtzheimer, MD, deputy director for research at the National Center for PTSD, praised the study for focusing on a very high-risk group.
“This gets you closer to the population you’re probably going to have an impact on in terms of preventing suicide,” said Dr. Holtzheimer, a professor of psychiatry and surgery at Dartmouth College’s Geisel School of Medicine, Hanover, N.H.
The fact that many of the participants had attempted suicide in the last year underlines that this was a very high-risk population, said Dr. Holtzheimer. “Not only are they thinking about suicide, but almost two-thirds had actually attempted or tried something.”
This kind of program “would be great for rural environments where people may be living like four hours away from the VA or a clinic,” said Dr. Holtzheimer, noting that many veterans are often quite isolated.
“One of the very positive outcomes of the COVID-19 pandemic was helping us strengthen our ability to do telehealth,” he said.
However, Dr. Holtzheimer noted the study was small and qualitative. “The next step ideally would be a controlled trial looking at not just ideation but at risky behavior or clear suicide attempts or preparation, like buying a gun or hoarding medication, to help determine efficacy.”
The researchers and Dr. Holtzheimer report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
WASHINGTON –
Skeptics had worried that participating in the program through telehealth would exacerbate safety and other issues veterans had about discussing suicide in a group setting, study investigator Sarah Sullivan, PhD student, Health Psychology & Clinical Science, City University of New York, told this news organization.
“But that for us was not really true. People opened up about their suicidal thoughts and triggers even on this telehealth format, and that’s really important for providers to know,” she said.
The findings were presented as part of the Anxiety and Depression Association of America Anxiety & Depression conference.
Trial run
Suicide is a major public health issue, particularly for veterans. Recent data from the Veterans Administration show 17 veterans die by suicide every day.
The current study included 15 male and 2 female veterans (29.4% White, 70.6% Hispanic) from New York City and Philadelphia. Participants had an average age of 50 and all were either deemed by a clinician to be at extremely high risk for suicide or were hospitalized for this reason.
The individuals completed an online version of the Project Life Force (PLF) program, which uses dialectical behavioral therapy and psychoeducational approaches. The program includes the brief Safety Planning intervention (SPI), aimed at reducing short-term suicide risk.
Considered a best practice, the SPI includes a written list of personal suicide warning signs or triggers, internal coping strategies, social contacts who offer support and distraction from suicidal thoughts, contact information for professionals, a suicide crisis hotline, and nearby emergency services.
In addition to these steps, the PLF program focuses on sleep, exercise, and making the safety plan accessible.
The telehealth platform for the program was WebEx software. Participants were offered a “trial run” to orient them to the technology, said Ms. Sullivan.
Group sessions were held once weekly for 10 weeks, with optional “booster” sessions if needed. Each session included about five participants.
To ensure privacy, participants were provided with headphones and laptops. This was especially important for those sharing a living space, including spouses and children, said Ms. Sullivan.
High ratings
Participants completed the Acceptability of Intervention Measure (AIM), Intervention Appropriateness Measure (IAM), and Feasibility of Intervention Measure (FIM). Each of these yields scores from four items rated on a Likert scale of 1-5, for a total score ranging from 5 to 20, with higher scores indicating higher ratings.
Veterans rated PLF-T as highly acceptable (mean AIM, 17.50), appropriate (mean IAM, 17.25), and feasible (mean FIM, 18).
Study participants reported the program was convenient and noted that it decreased the burden of traveling to sessions, especially during the COVID-19 pandemic.
They also reported the program was less likely to compete with other demands such as childcare and other appointments, said Ms. Sullivan.
In addition, it helped those with comorbidities such as posttraumatic stress disorder, she added. She noted veterans with PTSD may be triggered on subways or buses when traveling to in-person treatment sessions.
“That can take away from addressing the suicidal triggers,” said Ms. Sullivan. “So, this program allows them to fully concentrate on the safety plan.”
Results showed that study participants “enjoyed the group and would recommend it to others,” said Ms. Sullivan. “I think that signifies the group was effective in its goal of mitigating loneliness, which was exacerbated during the COVID-19 pandemic, and creating a socially supportive environment, especially for the vets living alone.”
Veterans also reported that the program helped them understand the connection between depression or PTSD and suicidal thoughts, urges, and plans. In addition, they appreciated the group dynamics, where they felt connected to other veterans experiencing similar challenges.
Hopeful results
Commenting on the study, Paul E. Holtzheimer, MD, deputy director for research at the National Center for PTSD, praised the study for focusing on a very high-risk group.
“This gets you closer to the population you’re probably going to have an impact on in terms of preventing suicide,” said Dr. Holtzheimer, a professor of psychiatry and surgery at Dartmouth College’s Geisel School of Medicine, Hanover, N.H.
The fact that many of the participants had attempted suicide in the last year underlines that this was a very high-risk population, said Dr. Holtzheimer. “Not only are they thinking about suicide, but almost two-thirds had actually attempted or tried something.”
This kind of program “would be great for rural environments where people may be living like four hours away from the VA or a clinic,” said Dr. Holtzheimer, noting that many veterans are often quite isolated.
“One of the very positive outcomes of the COVID-19 pandemic was helping us strengthen our ability to do telehealth,” he said.
However, Dr. Holtzheimer noted the study was small and qualitative. “The next step ideally would be a controlled trial looking at not just ideation but at risky behavior or clear suicide attempts or preparation, like buying a gun or hoarding medication, to help determine efficacy.”
The researchers and Dr. Holtzheimer report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
WASHINGTON –
Skeptics had worried that participating in the program through telehealth would exacerbate safety and other issues veterans had about discussing suicide in a group setting, study investigator Sarah Sullivan, PhD student, Health Psychology & Clinical Science, City University of New York, told this news organization.
“But that for us was not really true. People opened up about their suicidal thoughts and triggers even on this telehealth format, and that’s really important for providers to know,” she said.
The findings were presented as part of the Anxiety and Depression Association of America Anxiety & Depression conference.
Trial run
Suicide is a major public health issue, particularly for veterans. Recent data from the Veterans Administration show 17 veterans die by suicide every day.
The current study included 15 male and 2 female veterans (29.4% White, 70.6% Hispanic) from New York City and Philadelphia. Participants had an average age of 50 and all were either deemed by a clinician to be at extremely high risk for suicide or were hospitalized for this reason.
The individuals completed an online version of the Project Life Force (PLF) program, which uses dialectical behavioral therapy and psychoeducational approaches. The program includes the brief Safety Planning intervention (SPI), aimed at reducing short-term suicide risk.
Considered a best practice, the SPI includes a written list of personal suicide warning signs or triggers, internal coping strategies, social contacts who offer support and distraction from suicidal thoughts, contact information for professionals, a suicide crisis hotline, and nearby emergency services.
In addition to these steps, the PLF program focuses on sleep, exercise, and making the safety plan accessible.
The telehealth platform for the program was WebEx software. Participants were offered a “trial run” to orient them to the technology, said Ms. Sullivan.
Group sessions were held once weekly for 10 weeks, with optional “booster” sessions if needed. Each session included about five participants.
To ensure privacy, participants were provided with headphones and laptops. This was especially important for those sharing a living space, including spouses and children, said Ms. Sullivan.
High ratings
Participants completed the Acceptability of Intervention Measure (AIM), Intervention Appropriateness Measure (IAM), and Feasibility of Intervention Measure (FIM). Each of these yields scores from four items rated on a Likert scale of 1-5, for a total score ranging from 5 to 20, with higher scores indicating higher ratings.
Veterans rated PLF-T as highly acceptable (mean AIM, 17.50), appropriate (mean IAM, 17.25), and feasible (mean FIM, 18).
Study participants reported the program was convenient and noted that it decreased the burden of traveling to sessions, especially during the COVID-19 pandemic.
They also reported the program was less likely to compete with other demands such as childcare and other appointments, said Ms. Sullivan.
In addition, it helped those with comorbidities such as posttraumatic stress disorder, she added. She noted veterans with PTSD may be triggered on subways or buses when traveling to in-person treatment sessions.
“That can take away from addressing the suicidal triggers,” said Ms. Sullivan. “So, this program allows them to fully concentrate on the safety plan.”
Results showed that study participants “enjoyed the group and would recommend it to others,” said Ms. Sullivan. “I think that signifies the group was effective in its goal of mitigating loneliness, which was exacerbated during the COVID-19 pandemic, and creating a socially supportive environment, especially for the vets living alone.”
Veterans also reported that the program helped them understand the connection between depression or PTSD and suicidal thoughts, urges, and plans. In addition, they appreciated the group dynamics, where they felt connected to other veterans experiencing similar challenges.
Hopeful results
Commenting on the study, Paul E. Holtzheimer, MD, deputy director for research at the National Center for PTSD, praised the study for focusing on a very high-risk group.
“This gets you closer to the population you’re probably going to have an impact on in terms of preventing suicide,” said Dr. Holtzheimer, a professor of psychiatry and surgery at Dartmouth College’s Geisel School of Medicine, Hanover, N.H.
The fact that many of the participants had attempted suicide in the last year underlines that this was a very high-risk population, said Dr. Holtzheimer. “Not only are they thinking about suicide, but almost two-thirds had actually attempted or tried something.”
This kind of program “would be great for rural environments where people may be living like four hours away from the VA or a clinic,” said Dr. Holtzheimer, noting that many veterans are often quite isolated.
“One of the very positive outcomes of the COVID-19 pandemic was helping us strengthen our ability to do telehealth,” he said.
However, Dr. Holtzheimer noted the study was small and qualitative. “The next step ideally would be a controlled trial looking at not just ideation but at risky behavior or clear suicide attempts or preparation, like buying a gun or hoarding medication, to help determine efficacy.”
The researchers and Dr. Holtzheimer report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ADAA 2023
CMS inpatient payment rule for 2024: Key takeaways
The Centers for Medicare & Medicaid Services (CMS) released its annual update to the inpatient prospective payment system (IPPS) and long-term care hospital (LTCH) PPS on April 10, with many changes centered around improving health equity and quality as well as alleviating rural clinician shortages.
“This proposed rule reflects our person-centric approach to better measure health care quality and safety in hospitals to reduce preventable harm and our commitment to ensure that people with Medicare in rural and underserved areas have improved access to high-quality health care,” said CMS Administrator Chiquita Brooks-LaSure said in a statement.
Here are 14 things to know about the fiscal year (FY) 2024 proposal:
1. New payment rate: Acute-care hospitals that report inpatient quality data and participate in the EHR Meaningful Use program will receive a 2.8% net increase in payment rates. The rate adjustment will send approximately $3.3 billion more funding to hospitals compared with 2023.
2. LTCH payments: CMS projects that the LTCH standard payment rate will increase by 2.9%, whereas discharge payments will decrease by 2.5% or $59 million.
3. Disproportionate share hospital payments: Medicare disproportionate share hospital payments and Medicare uncompensated care payments will decrease by about $115 million for FY 2024.
4. Health equity categories: CMS proposes adding 15 new health equity hospital categorizations for IPPS payments to advance the goals of its Framework for Health Equity initiative.
5. Social determinants of health codes: To reflect increased resource utilization, the severity designation for the three International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) diagnosis codes describing homelessness will change from noncomplication or comorbidity to complication or comorbidity.
6. Rural emergency hospitals: The proposed rule will allow designated rural emergency hospitals to serve as training sites and receive Medicare graduate medical education payments to address concerns over rural hospital closures.
7. COVID treatment add-on payments: If the public health emergency ends in May, add-on payments for discharges involving eligible products like convalescent plasma and nirmatrelvir-ritonavir will expire on Sept. 30.
8. Technology add-on payments: Requests for new technology add-on payments must include a complete, active Food and Drug Administration market authorization application. Beginning with FY 2025 applications, the FDA approval deadline will move from July 1 to May 1.
9. Physician-owned hospitals: To receive Medicare payment for services referred by a physician owner or investor, the hospital must satisfy all requirements of the whole hospital exception or the rural provider exception to the Stark Law. In either case, a hospital may not increase the aggregate number of operating rooms, procedure rooms, or beds above the level it was licensed for on March 23, 2010, unless CMS grants an exception.
10. Electronic clinical quality measures: The new rule will remove and modify several existing electronic clinical quality measures and add three new ones: hospital harm, pressure injury; hospital harm, acute kidney injury; and excessive radiation dose or inadequate image quality for diagnostic CT in adult inpatients.
11. HCAHPS survey: Beginning Jan. 1, 2025, modifications to the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey will extend the data collection period from 42 to 49 days, limit supplemental survey items to 12, and require an official Spanish translation for patients.
12. Safety-net hospitals request for information: CMS seeks public input about the unique challenges faced by safety-net hospitals and potential solutions to ensure that uninsured, underinsured, and other vulnerable populations have access to essential services.
13. LTCH quality reporting: CMS proposes several quality-measure updates, including a functional discharge score measure beginning in FY 2025 and reporting the percentage of patients current with Centers for Disease Control and Prevention–recommended COVID vaccinations starting in FY 2026.
14. Commenting period: CMS will accept comments on the proposed rule through June 9.
A version of this article originally appeared on Medscape.com.
The Centers for Medicare & Medicaid Services (CMS) released its annual update to the inpatient prospective payment system (IPPS) and long-term care hospital (LTCH) PPS on April 10, with many changes centered around improving health equity and quality as well as alleviating rural clinician shortages.
“This proposed rule reflects our person-centric approach to better measure health care quality and safety in hospitals to reduce preventable harm and our commitment to ensure that people with Medicare in rural and underserved areas have improved access to high-quality health care,” said CMS Administrator Chiquita Brooks-LaSure said in a statement.
Here are 14 things to know about the fiscal year (FY) 2024 proposal:
1. New payment rate: Acute-care hospitals that report inpatient quality data and participate in the EHR Meaningful Use program will receive a 2.8% net increase in payment rates. The rate adjustment will send approximately $3.3 billion more funding to hospitals compared with 2023.
2. LTCH payments: CMS projects that the LTCH standard payment rate will increase by 2.9%, whereas discharge payments will decrease by 2.5% or $59 million.
3. Disproportionate share hospital payments: Medicare disproportionate share hospital payments and Medicare uncompensated care payments will decrease by about $115 million for FY 2024.
4. Health equity categories: CMS proposes adding 15 new health equity hospital categorizations for IPPS payments to advance the goals of its Framework for Health Equity initiative.
5. Social determinants of health codes: To reflect increased resource utilization, the severity designation for the three International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) diagnosis codes describing homelessness will change from noncomplication or comorbidity to complication or comorbidity.
6. Rural emergency hospitals: The proposed rule will allow designated rural emergency hospitals to serve as training sites and receive Medicare graduate medical education payments to address concerns over rural hospital closures.
7. COVID treatment add-on payments: If the public health emergency ends in May, add-on payments for discharges involving eligible products like convalescent plasma and nirmatrelvir-ritonavir will expire on Sept. 30.
8. Technology add-on payments: Requests for new technology add-on payments must include a complete, active Food and Drug Administration market authorization application. Beginning with FY 2025 applications, the FDA approval deadline will move from July 1 to May 1.
9. Physician-owned hospitals: To receive Medicare payment for services referred by a physician owner or investor, the hospital must satisfy all requirements of the whole hospital exception or the rural provider exception to the Stark Law. In either case, a hospital may not increase the aggregate number of operating rooms, procedure rooms, or beds above the level it was licensed for on March 23, 2010, unless CMS grants an exception.
10. Electronic clinical quality measures: The new rule will remove and modify several existing electronic clinical quality measures and add three new ones: hospital harm, pressure injury; hospital harm, acute kidney injury; and excessive radiation dose or inadequate image quality for diagnostic CT in adult inpatients.
11. HCAHPS survey: Beginning Jan. 1, 2025, modifications to the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey will extend the data collection period from 42 to 49 days, limit supplemental survey items to 12, and require an official Spanish translation for patients.
12. Safety-net hospitals request for information: CMS seeks public input about the unique challenges faced by safety-net hospitals and potential solutions to ensure that uninsured, underinsured, and other vulnerable populations have access to essential services.
13. LTCH quality reporting: CMS proposes several quality-measure updates, including a functional discharge score measure beginning in FY 2025 and reporting the percentage of patients current with Centers for Disease Control and Prevention–recommended COVID vaccinations starting in FY 2026.
14. Commenting period: CMS will accept comments on the proposed rule through June 9.
A version of this article originally appeared on Medscape.com.
The Centers for Medicare & Medicaid Services (CMS) released its annual update to the inpatient prospective payment system (IPPS) and long-term care hospital (LTCH) PPS on April 10, with many changes centered around improving health equity and quality as well as alleviating rural clinician shortages.
“This proposed rule reflects our person-centric approach to better measure health care quality and safety in hospitals to reduce preventable harm and our commitment to ensure that people with Medicare in rural and underserved areas have improved access to high-quality health care,” said CMS Administrator Chiquita Brooks-LaSure said in a statement.
Here are 14 things to know about the fiscal year (FY) 2024 proposal:
1. New payment rate: Acute-care hospitals that report inpatient quality data and participate in the EHR Meaningful Use program will receive a 2.8% net increase in payment rates. The rate adjustment will send approximately $3.3 billion more funding to hospitals compared with 2023.
2. LTCH payments: CMS projects that the LTCH standard payment rate will increase by 2.9%, whereas discharge payments will decrease by 2.5% or $59 million.
3. Disproportionate share hospital payments: Medicare disproportionate share hospital payments and Medicare uncompensated care payments will decrease by about $115 million for FY 2024.
4. Health equity categories: CMS proposes adding 15 new health equity hospital categorizations for IPPS payments to advance the goals of its Framework for Health Equity initiative.
5. Social determinants of health codes: To reflect increased resource utilization, the severity designation for the three International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) diagnosis codes describing homelessness will change from noncomplication or comorbidity to complication or comorbidity.
6. Rural emergency hospitals: The proposed rule will allow designated rural emergency hospitals to serve as training sites and receive Medicare graduate medical education payments to address concerns over rural hospital closures.
7. COVID treatment add-on payments: If the public health emergency ends in May, add-on payments for discharges involving eligible products like convalescent plasma and nirmatrelvir-ritonavir will expire on Sept. 30.
8. Technology add-on payments: Requests for new technology add-on payments must include a complete, active Food and Drug Administration market authorization application. Beginning with FY 2025 applications, the FDA approval deadline will move from July 1 to May 1.
9. Physician-owned hospitals: To receive Medicare payment for services referred by a physician owner or investor, the hospital must satisfy all requirements of the whole hospital exception or the rural provider exception to the Stark Law. In either case, a hospital may not increase the aggregate number of operating rooms, procedure rooms, or beds above the level it was licensed for on March 23, 2010, unless CMS grants an exception.
10. Electronic clinical quality measures: The new rule will remove and modify several existing electronic clinical quality measures and add three new ones: hospital harm, pressure injury; hospital harm, acute kidney injury; and excessive radiation dose or inadequate image quality for diagnostic CT in adult inpatients.
11. HCAHPS survey: Beginning Jan. 1, 2025, modifications to the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey will extend the data collection period from 42 to 49 days, limit supplemental survey items to 12, and require an official Spanish translation for patients.
12. Safety-net hospitals request for information: CMS seeks public input about the unique challenges faced by safety-net hospitals and potential solutions to ensure that uninsured, underinsured, and other vulnerable populations have access to essential services.
13. LTCH quality reporting: CMS proposes several quality-measure updates, including a functional discharge score measure beginning in FY 2025 and reporting the percentage of patients current with Centers for Disease Control and Prevention–recommended COVID vaccinations starting in FY 2026.
14. Commenting period: CMS will accept comments on the proposed rule through June 9.
A version of this article originally appeared on Medscape.com.
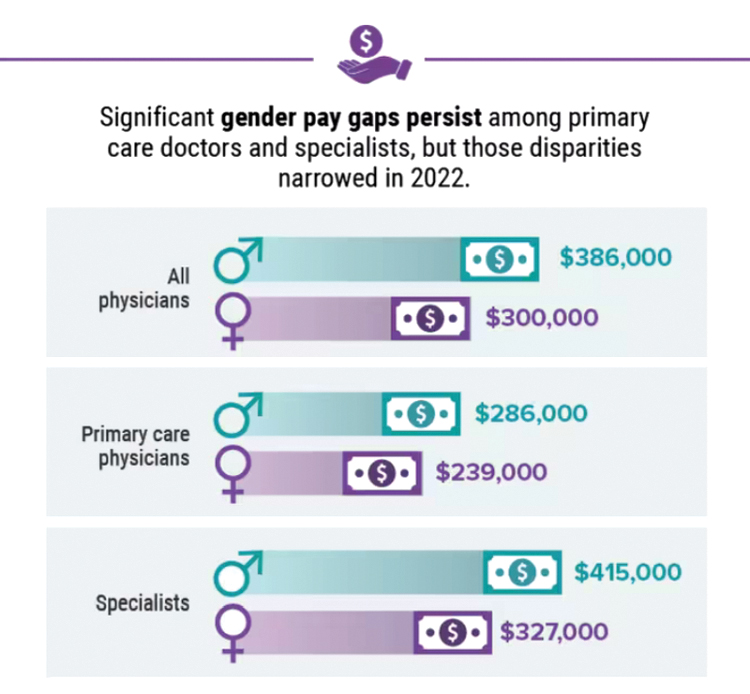
Infographic: Is your compensation rising as fast as your peers?
Did doctors’ salaries continue their zesty postpandemic rise in 2022? Are female physicians making pay gains versus their male counterparts that spark optimism for the future?
reveals which medical specialties pay better than others, and evaluates the current gender pay gap in medicine. If you’re interested in delving deeper into the data, check out Your Income vs. Your Peers’: Physician Compensation Report 2023.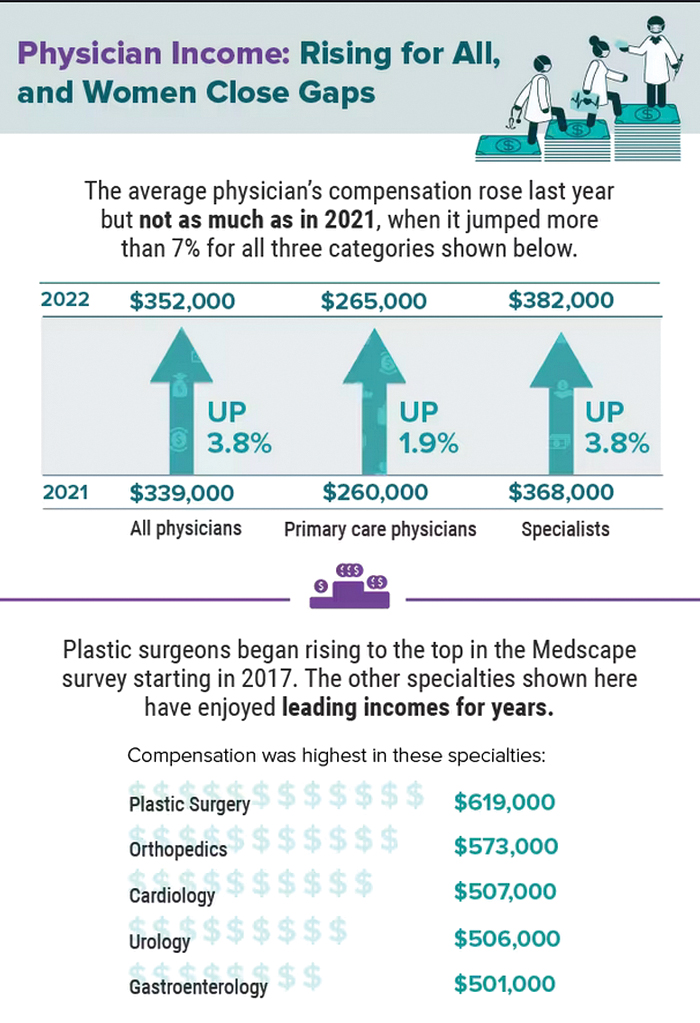
A version of this article first appeared on Medscape.com.
Did doctors’ salaries continue their zesty postpandemic rise in 2022? Are female physicians making pay gains versus their male counterparts that spark optimism for the future?
reveals which medical specialties pay better than others, and evaluates the current gender pay gap in medicine. If you’re interested in delving deeper into the data, check out Your Income vs. Your Peers’: Physician Compensation Report 2023.
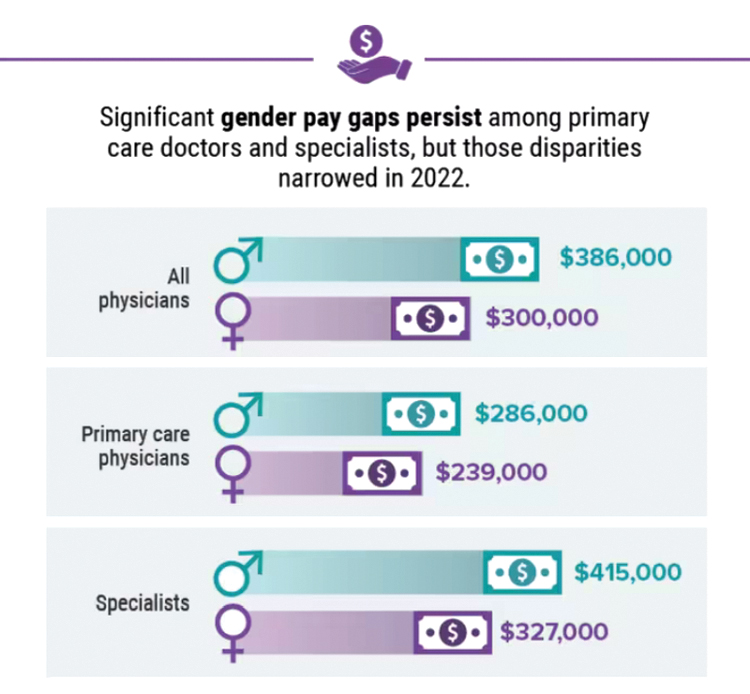
A version of this article first appeared on Medscape.com.
Did doctors’ salaries continue their zesty postpandemic rise in 2022? Are female physicians making pay gains versus their male counterparts that spark optimism for the future?
reveals which medical specialties pay better than others, and evaluates the current gender pay gap in medicine. If you’re interested in delving deeper into the data, check out Your Income vs. Your Peers’: Physician Compensation Report 2023.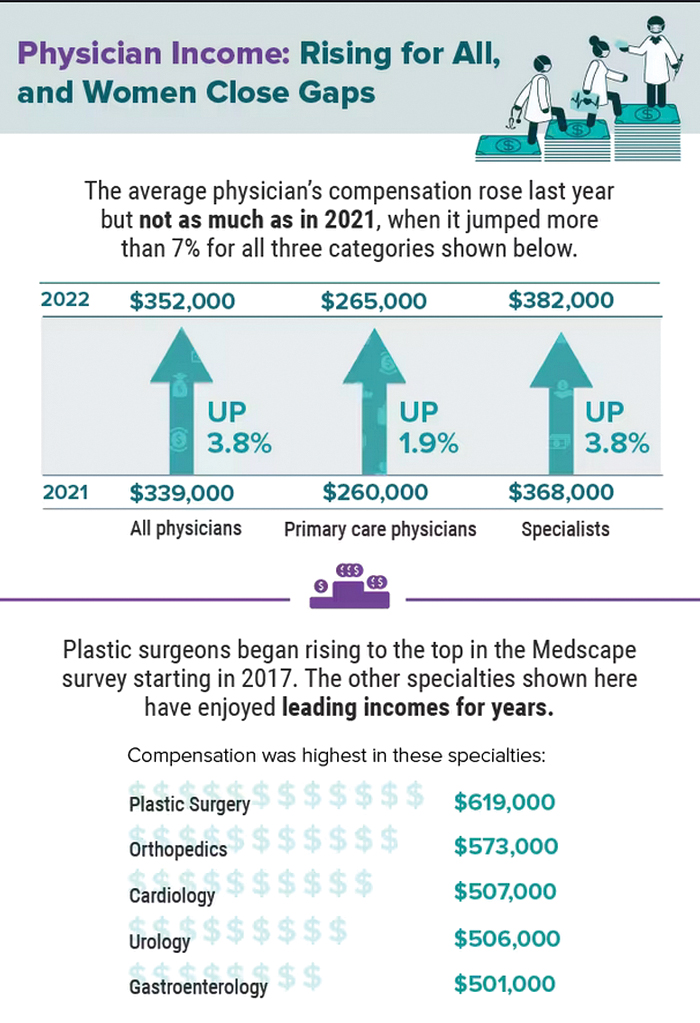
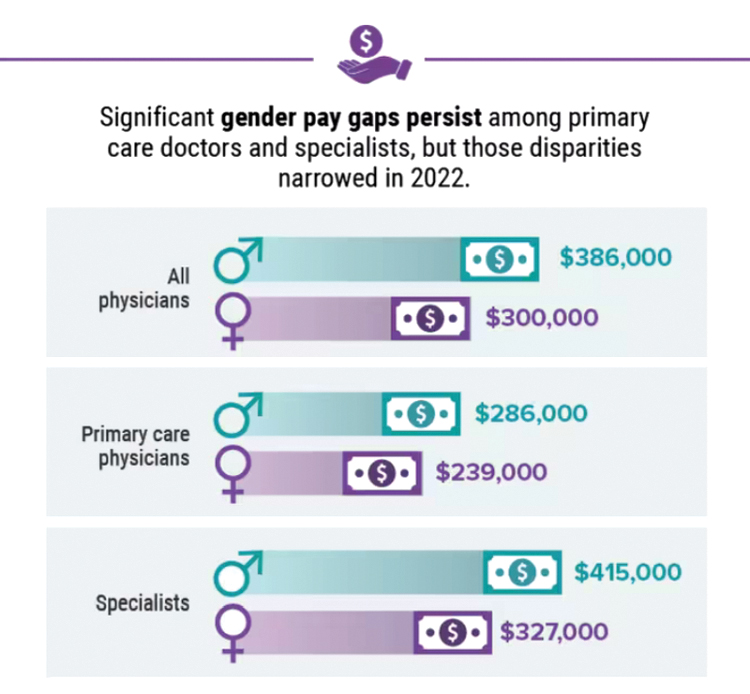
A version of this article first appeared on Medscape.com.
Five chronic mistakes that can sabotage your medical practice
A physician who in the past has led medical groups as both chief medical officer and president, Gerda Maissel, MD, president of My MD Advisor, a private patient advocacy group, has seen the good, bad, and ugly of practice administration. There’s a spectrum of infractions: Anything from doctors making inappropriate jokes with staff or patients, to failing to establish key relationships with other critical entities, says Dr. Maissel.
“Being a good physician who provides value is important in building a practice,” explained Dr. Maissel. “But it is not the be-all and end-all.”
While the number of physician-owned practices is declining, just under 50% are still in private practice, according to the American Medical Association’s 2020 survey. There’s also a continuing trend toward larger practices. Whatever the size, the physicians are responsible for strategy, marketing, building the practice, and maintaining profitability.
Catherine Lightfoot, CPA, CHBC, president of the National Society of Certified Healthcare Business Consultants (NSCHBC), has her finger on the pulse of what’s right and what’s wrong when it comes to running a medical practice. Although she says there are no hard and fast rules on how to run a thriving medical group, there are common mistakes that physicians often don’t recognize.
Here are the five key mistakes that commonly crop up, and the experts’ thoughts on how to prevent or fix them.
1. Failing to engage in outreach activities and community efforts to build your practice.
Yes, physicians earn good reputations through dedicated work, and that often precedes them when it comes to building a practice. But assuming that hanging a shingle backed by strong credentials is all it takes for success is akin to building a website and assuming people will find it organically. Maybe there was a time, in a small community, where this was good enough. But no longer.
It’s important to plan to get your practice and your name known to potential patients. “Most physicians think that means advertising, but that’s not the complete case,” Dr. Maissel said.
Much of the equation involves ensuring availability. This means setting office hours that work for your target audience of patients, and then ensuring you stick to those hours. This extends beyond scheduling your current patients and into referral patients, too. And it’s particularly true while in the building phase of a new practice.
“If one of your colleagues calls with a referral patient, and they consider the matter urgent, you need to heed that,” explained Dr. Maissel. “So have a breadth of availability for these referral cases.” Through word of mouth, you’ll get a good reputation for patient care and availability, and that will go a long way toward helping to grow your practice.
Establishing a culture that doesn’t involve canceling and rescheduling patients is part of the scheduling equation, too. “I’ve seen the full gamut of cancellation policies, ranging from a month’s notice on changes to 3 months’ notice,” said Dr. Maissel. “It all gets at the same issue, which is failing to set up a culture where doctors don’t change their schedules and leave patients hanging.”
In the end, wonky scheduling, cancellations, and a lack of respect for the urgency of referrals can cost a practice. Forge a reputation in reliability and word will get around, in all the right ways.
2. Not having enough oversight of your outsourced billing service
Billing is one of the biggest pieces of running a successful and profitable practice, yet too many practices ignore it once they’ve handed it off to a billing company. That can cost you in more ways than one, said Ms. Lightfoot. “Billing changes all the time, and if you’re not monitoring your billing partner, you don’t know what you’re getting,” she said.
Ms. Lightfoot said that a decade ago, billing was much more straightforward – essentially, you did the work and received payment. Today’s complex insurance, Medicare, and Medicaid environment have changed the landscape. “Now you have to fight for every dollar you’re billing,” said Ms. Lightfoot. “Rates get cut all the time, you might miss out on a claim, and the rules are constantly changing.”
The solution for many practices is to outsource billing, which Ms. Lightfoot supports. “They specialize in this, and that’s a great start,” she said. “But it’s not as simple as handing it off and forgetting it.”
Instead, ensure your internal staff is up to date on all things coding and billing so that they can catch what your outsourced billing partner doesn’t. Your internal staff should be prepared to carry out coding, check coding, and stay on top of the billing company if they aren’t processing claims quickly enough. For instance: If there’s a denial, how many times will the billing company go after that money?
Other questions to ask when entering a billing relationship: What does the billing company expect from your practice? Do they communicate what needs to be worked on or fixed? Are they providing you with monthly reports? “You want to make sure you’re getting those reports every month and reading them over carefully,” said Ms. Lightfoot.
This means that if you have a large practice, you should have a point person within your billing department to handle the relationship with your billing partner. If it’s a smaller practice, the task will likely fall to the office manager. The ‘who’ isn’t important, but having someone on the case is.
Another important aspect of this billing relationship is understanding what you’re receiving for your payment. “Sometimes going with the cheapest offer amounts to a billing partner who isn’t working on those claims and denials as much as they should,” said Ms. Lightfoot. “I’ve seen fees anywhere from 4% to 9%, and the lower end can mean you’ll need to chase down every penny.”
3. Neglecting to forge the right relationships in the community.
Another common mistake physicians make is failing to develop the professional relationships that will help you thrive. Successful practices need to establish relationships with the right people and organizations. While the occasional afternoon of golf used to serve this purpose, today outreach must go beyond that, said Dr. Maissel. “You need to create relationships with hospitals and hospital-based practices because you may have value to them,” she said. “You should also get into some sort of relationship with your local ACO (Accountable Care Organization) or PHO (Physician Hospital Organization). Identify the leaders there and let them know you exist.”
Establishing these relationships goes beyond that first step of introducing yourself, or you risk losing their benefits. You must also nurture and “fertilize” these relationships in an ongoing fashion. “For years, as the head of employee practice, I had a competitor who would go out of his way to invite me to lunch regularly,” said Dr. Maissel. “When there were opportunities for his group, I would connect him. I wouldn’t have done that had he not worked on our relationship over time.”
The adage of “it’s not what you know but who you know” holds up here. If you don’t do the reach out to the right people and organizations in your community, you will have a harder time succeeding as a practice.
4. Hiring the wrong person/a family member for the job.
When starting a new practice, or if you’re running a small practice, it can be tempting to look for affordable or reliable staffing from among family members or friends. That’s fine if your family member or friend is also qualified for the job. If they aren’t, however, you might be setting up for failure.
“When you hire someone without the right qualifications, you need to be willing to train them for the job,” said Ms. Lightfoot. “Doctors don’t have that kind of time.”
Too often, Ms. Lightfoot said, a doctor will have a position like officer manager open and fill it with an in-law, whether he or she is experienced or not. “Now you have someone in the role who is unqualified, and the rest of the office can’t speak up about that because it’s a relative to the lead physician,” she said. “That doesn’t create a good environment for anyone.”
Also, a setup for failure is hiring someone who might be qualified, but not possessing the right personality for the role. A front desk position, for instance, should be held by someone who’s a bit upbeat and able to multitask. “You can’t put a shy, quiet person in that job,” said Ms. Lightfoot. “So, if you see a person with 10 years’ experience in a medical practice, but they’re reserved, what will happen? You must think about this when hiring.”
One PA recalled a small family practice in which the lead physician’s wife was the office manager. To save money, the wife removed lights from the staff restroom and staff lunchroom and declined staff requests for earned vacation. The staff felt unable to speak up, and they – and all new office staff members – ultimately left the practice.
5. Overlooking the importance of acting like a professional and respecting your staff.
This one might seem obvious, but many physicians get a bit too comfortable in the office environment, said Dr. Maissel. This can encompass a whole host of bad behaviors, from making inappropriate jokes to staff and patients, to trash-talking colleagues. None of this behavior is acceptable and can set you up for things to go wrong, especially when good labor is hard to come by. “Your staff is made up of people for whom 50 cents an hour is meaningful,” she said. “If they don’t have a warm, supportive office, they will look elsewhere.”
This is especially true of younger people now entering the workforce – they are less tolerant than generations past of egregious behavior. Try to establish a professional, yet nurturing environment for your staff. “Inquire about things that matter to them,” said Dr. Maissel. “Small talk can go a long way. See them as human beings, not cogs in the wheel.”
Inappropriate and uncaring behaviors will give physician leaders a reputation, one that sticks. “The medical community is pretty connected, and if you behave inappropriately enough times, it will circle back to you,” said Dr. Maissel.
Launching, and sustaining, a successful medical practice is never a given, but mistakes are. With the right approach, however, you can avoid these common – and impactful – errors and set your practice up for success.
A version of this article first appeared on Medscape.com.
A physician who in the past has led medical groups as both chief medical officer and president, Gerda Maissel, MD, president of My MD Advisor, a private patient advocacy group, has seen the good, bad, and ugly of practice administration. There’s a spectrum of infractions: Anything from doctors making inappropriate jokes with staff or patients, to failing to establish key relationships with other critical entities, says Dr. Maissel.
“Being a good physician who provides value is important in building a practice,” explained Dr. Maissel. “But it is not the be-all and end-all.”
While the number of physician-owned practices is declining, just under 50% are still in private practice, according to the American Medical Association’s 2020 survey. There’s also a continuing trend toward larger practices. Whatever the size, the physicians are responsible for strategy, marketing, building the practice, and maintaining profitability.
Catherine Lightfoot, CPA, CHBC, president of the National Society of Certified Healthcare Business Consultants (NSCHBC), has her finger on the pulse of what’s right and what’s wrong when it comes to running a medical practice. Although she says there are no hard and fast rules on how to run a thriving medical group, there are common mistakes that physicians often don’t recognize.
Here are the five key mistakes that commonly crop up, and the experts’ thoughts on how to prevent or fix them.
1. Failing to engage in outreach activities and community efforts to build your practice.
Yes, physicians earn good reputations through dedicated work, and that often precedes them when it comes to building a practice. But assuming that hanging a shingle backed by strong credentials is all it takes for success is akin to building a website and assuming people will find it organically. Maybe there was a time, in a small community, where this was good enough. But no longer.
It’s important to plan to get your practice and your name known to potential patients. “Most physicians think that means advertising, but that’s not the complete case,” Dr. Maissel said.
Much of the equation involves ensuring availability. This means setting office hours that work for your target audience of patients, and then ensuring you stick to those hours. This extends beyond scheduling your current patients and into referral patients, too. And it’s particularly true while in the building phase of a new practice.
“If one of your colleagues calls with a referral patient, and they consider the matter urgent, you need to heed that,” explained Dr. Maissel. “So have a breadth of availability for these referral cases.” Through word of mouth, you’ll get a good reputation for patient care and availability, and that will go a long way toward helping to grow your practice.
Establishing a culture that doesn’t involve canceling and rescheduling patients is part of the scheduling equation, too. “I’ve seen the full gamut of cancellation policies, ranging from a month’s notice on changes to 3 months’ notice,” said Dr. Maissel. “It all gets at the same issue, which is failing to set up a culture where doctors don’t change their schedules and leave patients hanging.”
In the end, wonky scheduling, cancellations, and a lack of respect for the urgency of referrals can cost a practice. Forge a reputation in reliability and word will get around, in all the right ways.
2. Not having enough oversight of your outsourced billing service
Billing is one of the biggest pieces of running a successful and profitable practice, yet too many practices ignore it once they’ve handed it off to a billing company. That can cost you in more ways than one, said Ms. Lightfoot. “Billing changes all the time, and if you’re not monitoring your billing partner, you don’t know what you’re getting,” she said.
Ms. Lightfoot said that a decade ago, billing was much more straightforward – essentially, you did the work and received payment. Today’s complex insurance, Medicare, and Medicaid environment have changed the landscape. “Now you have to fight for every dollar you’re billing,” said Ms. Lightfoot. “Rates get cut all the time, you might miss out on a claim, and the rules are constantly changing.”
The solution for many practices is to outsource billing, which Ms. Lightfoot supports. “They specialize in this, and that’s a great start,” she said. “But it’s not as simple as handing it off and forgetting it.”
Instead, ensure your internal staff is up to date on all things coding and billing so that they can catch what your outsourced billing partner doesn’t. Your internal staff should be prepared to carry out coding, check coding, and stay on top of the billing company if they aren’t processing claims quickly enough. For instance: If there’s a denial, how many times will the billing company go after that money?
Other questions to ask when entering a billing relationship: What does the billing company expect from your practice? Do they communicate what needs to be worked on or fixed? Are they providing you with monthly reports? “You want to make sure you’re getting those reports every month and reading them over carefully,” said Ms. Lightfoot.
This means that if you have a large practice, you should have a point person within your billing department to handle the relationship with your billing partner. If it’s a smaller practice, the task will likely fall to the office manager. The ‘who’ isn’t important, but having someone on the case is.
Another important aspect of this billing relationship is understanding what you’re receiving for your payment. “Sometimes going with the cheapest offer amounts to a billing partner who isn’t working on those claims and denials as much as they should,” said Ms. Lightfoot. “I’ve seen fees anywhere from 4% to 9%, and the lower end can mean you’ll need to chase down every penny.”
3. Neglecting to forge the right relationships in the community.
Another common mistake physicians make is failing to develop the professional relationships that will help you thrive. Successful practices need to establish relationships with the right people and organizations. While the occasional afternoon of golf used to serve this purpose, today outreach must go beyond that, said Dr. Maissel. “You need to create relationships with hospitals and hospital-based practices because you may have value to them,” she said. “You should also get into some sort of relationship with your local ACO (Accountable Care Organization) or PHO (Physician Hospital Organization). Identify the leaders there and let them know you exist.”
Establishing these relationships goes beyond that first step of introducing yourself, or you risk losing their benefits. You must also nurture and “fertilize” these relationships in an ongoing fashion. “For years, as the head of employee practice, I had a competitor who would go out of his way to invite me to lunch regularly,” said Dr. Maissel. “When there were opportunities for his group, I would connect him. I wouldn’t have done that had he not worked on our relationship over time.”
The adage of “it’s not what you know but who you know” holds up here. If you don’t do the reach out to the right people and organizations in your community, you will have a harder time succeeding as a practice.
4. Hiring the wrong person/a family member for the job.
When starting a new practice, or if you’re running a small practice, it can be tempting to look for affordable or reliable staffing from among family members or friends. That’s fine if your family member or friend is also qualified for the job. If they aren’t, however, you might be setting up for failure.
“When you hire someone without the right qualifications, you need to be willing to train them for the job,” said Ms. Lightfoot. “Doctors don’t have that kind of time.”
Too often, Ms. Lightfoot said, a doctor will have a position like officer manager open and fill it with an in-law, whether he or she is experienced or not. “Now you have someone in the role who is unqualified, and the rest of the office can’t speak up about that because it’s a relative to the lead physician,” she said. “That doesn’t create a good environment for anyone.”
Also, a setup for failure is hiring someone who might be qualified, but not possessing the right personality for the role. A front desk position, for instance, should be held by someone who’s a bit upbeat and able to multitask. “You can’t put a shy, quiet person in that job,” said Ms. Lightfoot. “So, if you see a person with 10 years’ experience in a medical practice, but they’re reserved, what will happen? You must think about this when hiring.”
One PA recalled a small family practice in which the lead physician’s wife was the office manager. To save money, the wife removed lights from the staff restroom and staff lunchroom and declined staff requests for earned vacation. The staff felt unable to speak up, and they – and all new office staff members – ultimately left the practice.
5. Overlooking the importance of acting like a professional and respecting your staff.
This one might seem obvious, but many physicians get a bit too comfortable in the office environment, said Dr. Maissel. This can encompass a whole host of bad behaviors, from making inappropriate jokes to staff and patients, to trash-talking colleagues. None of this behavior is acceptable and can set you up for things to go wrong, especially when good labor is hard to come by. “Your staff is made up of people for whom 50 cents an hour is meaningful,” she said. “If they don’t have a warm, supportive office, they will look elsewhere.”
This is especially true of younger people now entering the workforce – they are less tolerant than generations past of egregious behavior. Try to establish a professional, yet nurturing environment for your staff. “Inquire about things that matter to them,” said Dr. Maissel. “Small talk can go a long way. See them as human beings, not cogs in the wheel.”
Inappropriate and uncaring behaviors will give physician leaders a reputation, one that sticks. “The medical community is pretty connected, and if you behave inappropriately enough times, it will circle back to you,” said Dr. Maissel.
Launching, and sustaining, a successful medical practice is never a given, but mistakes are. With the right approach, however, you can avoid these common – and impactful – errors and set your practice up for success.
A version of this article first appeared on Medscape.com.
A physician who in the past has led medical groups as both chief medical officer and president, Gerda Maissel, MD, president of My MD Advisor, a private patient advocacy group, has seen the good, bad, and ugly of practice administration. There’s a spectrum of infractions: Anything from doctors making inappropriate jokes with staff or patients, to failing to establish key relationships with other critical entities, says Dr. Maissel.
“Being a good physician who provides value is important in building a practice,” explained Dr. Maissel. “But it is not the be-all and end-all.”
While the number of physician-owned practices is declining, just under 50% are still in private practice, according to the American Medical Association’s 2020 survey. There’s also a continuing trend toward larger practices. Whatever the size, the physicians are responsible for strategy, marketing, building the practice, and maintaining profitability.
Catherine Lightfoot, CPA, CHBC, president of the National Society of Certified Healthcare Business Consultants (NSCHBC), has her finger on the pulse of what’s right and what’s wrong when it comes to running a medical practice. Although she says there are no hard and fast rules on how to run a thriving medical group, there are common mistakes that physicians often don’t recognize.
Here are the five key mistakes that commonly crop up, and the experts’ thoughts on how to prevent or fix them.
1. Failing to engage in outreach activities and community efforts to build your practice.
Yes, physicians earn good reputations through dedicated work, and that often precedes them when it comes to building a practice. But assuming that hanging a shingle backed by strong credentials is all it takes for success is akin to building a website and assuming people will find it organically. Maybe there was a time, in a small community, where this was good enough. But no longer.
It’s important to plan to get your practice and your name known to potential patients. “Most physicians think that means advertising, but that’s not the complete case,” Dr. Maissel said.
Much of the equation involves ensuring availability. This means setting office hours that work for your target audience of patients, and then ensuring you stick to those hours. This extends beyond scheduling your current patients and into referral patients, too. And it’s particularly true while in the building phase of a new practice.
“If one of your colleagues calls with a referral patient, and they consider the matter urgent, you need to heed that,” explained Dr. Maissel. “So have a breadth of availability for these referral cases.” Through word of mouth, you’ll get a good reputation for patient care and availability, and that will go a long way toward helping to grow your practice.
Establishing a culture that doesn’t involve canceling and rescheduling patients is part of the scheduling equation, too. “I’ve seen the full gamut of cancellation policies, ranging from a month’s notice on changes to 3 months’ notice,” said Dr. Maissel. “It all gets at the same issue, which is failing to set up a culture where doctors don’t change their schedules and leave patients hanging.”
In the end, wonky scheduling, cancellations, and a lack of respect for the urgency of referrals can cost a practice. Forge a reputation in reliability and word will get around, in all the right ways.
2. Not having enough oversight of your outsourced billing service
Billing is one of the biggest pieces of running a successful and profitable practice, yet too many practices ignore it once they’ve handed it off to a billing company. That can cost you in more ways than one, said Ms. Lightfoot. “Billing changes all the time, and if you’re not monitoring your billing partner, you don’t know what you’re getting,” she said.
Ms. Lightfoot said that a decade ago, billing was much more straightforward – essentially, you did the work and received payment. Today’s complex insurance, Medicare, and Medicaid environment have changed the landscape. “Now you have to fight for every dollar you’re billing,” said Ms. Lightfoot. “Rates get cut all the time, you might miss out on a claim, and the rules are constantly changing.”
The solution for many practices is to outsource billing, which Ms. Lightfoot supports. “They specialize in this, and that’s a great start,” she said. “But it’s not as simple as handing it off and forgetting it.”
Instead, ensure your internal staff is up to date on all things coding and billing so that they can catch what your outsourced billing partner doesn’t. Your internal staff should be prepared to carry out coding, check coding, and stay on top of the billing company if they aren’t processing claims quickly enough. For instance: If there’s a denial, how many times will the billing company go after that money?
Other questions to ask when entering a billing relationship: What does the billing company expect from your practice? Do they communicate what needs to be worked on or fixed? Are they providing you with monthly reports? “You want to make sure you’re getting those reports every month and reading them over carefully,” said Ms. Lightfoot.
This means that if you have a large practice, you should have a point person within your billing department to handle the relationship with your billing partner. If it’s a smaller practice, the task will likely fall to the office manager. The ‘who’ isn’t important, but having someone on the case is.
Another important aspect of this billing relationship is understanding what you’re receiving for your payment. “Sometimes going with the cheapest offer amounts to a billing partner who isn’t working on those claims and denials as much as they should,” said Ms. Lightfoot. “I’ve seen fees anywhere from 4% to 9%, and the lower end can mean you’ll need to chase down every penny.”
3. Neglecting to forge the right relationships in the community.
Another common mistake physicians make is failing to develop the professional relationships that will help you thrive. Successful practices need to establish relationships with the right people and organizations. While the occasional afternoon of golf used to serve this purpose, today outreach must go beyond that, said Dr. Maissel. “You need to create relationships with hospitals and hospital-based practices because you may have value to them,” she said. “You should also get into some sort of relationship with your local ACO (Accountable Care Organization) or PHO (Physician Hospital Organization). Identify the leaders there and let them know you exist.”
Establishing these relationships goes beyond that first step of introducing yourself, or you risk losing their benefits. You must also nurture and “fertilize” these relationships in an ongoing fashion. “For years, as the head of employee practice, I had a competitor who would go out of his way to invite me to lunch regularly,” said Dr. Maissel. “When there were opportunities for his group, I would connect him. I wouldn’t have done that had he not worked on our relationship over time.”
The adage of “it’s not what you know but who you know” holds up here. If you don’t do the reach out to the right people and organizations in your community, you will have a harder time succeeding as a practice.
4. Hiring the wrong person/a family member for the job.
When starting a new practice, or if you’re running a small practice, it can be tempting to look for affordable or reliable staffing from among family members or friends. That’s fine if your family member or friend is also qualified for the job. If they aren’t, however, you might be setting up for failure.
“When you hire someone without the right qualifications, you need to be willing to train them for the job,” said Ms. Lightfoot. “Doctors don’t have that kind of time.”
Too often, Ms. Lightfoot said, a doctor will have a position like officer manager open and fill it with an in-law, whether he or she is experienced or not. “Now you have someone in the role who is unqualified, and the rest of the office can’t speak up about that because it’s a relative to the lead physician,” she said. “That doesn’t create a good environment for anyone.”
Also, a setup for failure is hiring someone who might be qualified, but not possessing the right personality for the role. A front desk position, for instance, should be held by someone who’s a bit upbeat and able to multitask. “You can’t put a shy, quiet person in that job,” said Ms. Lightfoot. “So, if you see a person with 10 years’ experience in a medical practice, but they’re reserved, what will happen? You must think about this when hiring.”
One PA recalled a small family practice in which the lead physician’s wife was the office manager. To save money, the wife removed lights from the staff restroom and staff lunchroom and declined staff requests for earned vacation. The staff felt unable to speak up, and they – and all new office staff members – ultimately left the practice.
5. Overlooking the importance of acting like a professional and respecting your staff.
This one might seem obvious, but many physicians get a bit too comfortable in the office environment, said Dr. Maissel. This can encompass a whole host of bad behaviors, from making inappropriate jokes to staff and patients, to trash-talking colleagues. None of this behavior is acceptable and can set you up for things to go wrong, especially when good labor is hard to come by. “Your staff is made up of people for whom 50 cents an hour is meaningful,” she said. “If they don’t have a warm, supportive office, they will look elsewhere.”
This is especially true of younger people now entering the workforce – they are less tolerant than generations past of egregious behavior. Try to establish a professional, yet nurturing environment for your staff. “Inquire about things that matter to them,” said Dr. Maissel. “Small talk can go a long way. See them as human beings, not cogs in the wheel.”
Inappropriate and uncaring behaviors will give physician leaders a reputation, one that sticks. “The medical community is pretty connected, and if you behave inappropriately enough times, it will circle back to you,” said Dr. Maissel.
Launching, and sustaining, a successful medical practice is never a given, but mistakes are. With the right approach, however, you can avoid these common – and impactful – errors and set your practice up for success.
A version of this article first appeared on Medscape.com.
Living the introvert’s dream: Alone for 500 days, but never lonely
Beating the allegory of the cave
When Beatriz Flamini spoke with reporters on April 14, she knew nothing of the previous 18 months. The Russian invasion of Ukraine? Nope. The death of Queen Elizabeth? Also no. But before you make fun of her, she has an excuse. She’s been living under a rock.
As part of an experiment to test how social isolation and disorientation affect a person’s mind, sense of time, and sleeping patterns, Ms. Flamini lived in a 70-meter-deep cave in southern Spain for 500 days, starting in November 2021. Alone. No outside communication with the outside world in any way, though she was constantly monitored by a team of researchers. She also had multiple cameras filming her for an upcoming documentary.
This is a massive step up from the previous record for time spent underground for science: A team of 15 spent 50 days underground in 2021 to similar study of isolation and how it affected circadian rhythms. It’s also almost certainly a world record for time spent underground.
All that time alone certainly sounds like some sort of medieval torture, but Ms. Flamini had access to food, water, and a library of books. Which she made liberal use of, reading at least 60 books during her stay. She also had a panic button in case the isolation became too much or an emergency developed, but she never considered using it.
She lost track of time after 2 months, flies invaded the cave on occasion, and maintaining coherence was occasionally a struggle, but she kept things together very well. In fact, she didn’t even want to leave when her team came for her. She wasn’t even finished with her 61st book.
When she spoke with gathered reporters after the ordeal, words were obviously difficult to come by for her, having not spoken in nearly 18 months, but her mind was clearly still sharp and she had a very important question for everyone gathered around her.
Who’s buying the beer?
We approve of this request.
Staphylococcus and the speed of evolution
Bacteria, we know, are tough little buggers that are hard to see and even harder to get rid of. So hard, actually, that human bodies eventually gave up on the task and decided to just incorporate them into our organ systems. But why are bacteria so hard to eliminate?
Two words: rapid evolution. How rapid? For the first time, scientists have directly observed adaptive evolution by Staphylococcus aureus in a single person’s skin microbiome. That’s how rapid.
For their study, the researchers collected samples from the nostrils, backs of knees, insides of elbows, and forearms of 23 children with eczema. They eventually cultured almost 1,500 unique colonies of S. aureus cells from those samples and sequenced the cells’ genomes.
All that sampling and culturing and sequencing showed that it was rare for a new S. aureus strain to come in and replace the existing strain. “Despite the stability at the lineage level, we see a lot of dynamics at the whole genome level, where new mutations are constantly arising in these bacteria and then spreading throughout the entire body,” Tami D. Lieberman, PhD, of the Massachusetts Institute of Technology, Cambridge, said in a written statement from MIT.
One frequent mutation involved a gene called capD, which encodes an enzyme necessary for synthesizing the capsular polysaccharide – a coating that protects S. aureus from recognition by immune cells. In one patient, four different mutations of capD arose independently in different samples before one variant became dominant and spread over the entire microbiome, MIT reported.
The mutation, which actually results in the loss of the polysaccharide capsule, may allow cells to grow faster than those without the mutation because they have more fuel to power their own growth, the researchers suggested. It’s also possible that loss of the capsule allows S. aureus cells to stick to the skin better because proteins that allow them to adhere to the skin are more exposed.
Dr. Lieberman and her associates hope that these variant-containing cells could be a new target for eczema treatments, but we’re never optimistic when it comes to bacteria. That’s because some of us are old enough to remember evolutionary biologist Stephen Jay Gould, who wrote in his book “Full House”: “Our planet has always been in the ‘Age of Bacteria,’ ever since the first fossils – bacteria, of course – were entombed in rocks more than 3 billion years ago. On any possible, reasonable or fair criterion, bacteria are – and always have been – the dominant forms of life on Earth.”
In the distant future, long after humans have left the scene, the bacteria will be laughing at the last rats and cockroaches scurrying across the landscape. Wanna bet?
The height of genetic prediction
Genetics are practically a DNA Scrabble bag. Traits like eye color and hair texture are chosen in the same fashion, based on what gets pulled from our own genetic bag of letters, but what about height? Researchers may now have a way to predict adult height and make it more than just an educated guess.
How? By looking at the genes in our growth plates. The cartilage on the ends of our bones hardens as we age, eventually deciding an individual’s stature. In a recently published study, a research team looked at 600 million cartilage cells linked to maturation and cell growth in mice. Because everything starts with rodents.
After that search identified 145 genes linked to growth plate maturation and formation of the bones, they compared the mouse genes with data from genome-wide association studies (GWAS) of human height to look for hotspots where the height genes exist in human DNA.
The results showed which genes play a role in deciding height, and the GWAS data also suggested that genetic changes affecting cartilage cell maturation may strongly influence adult height, said the investigators, who hope that earlier interventions can improve outcomes in patients with conditions such as skeletal dysplasia.
So, yeah, you may want to be a little taller or shorter, but the outcome of that particular Scrabble game was determined when your parents, you know, dropped the letters in the bag.
Beating the allegory of the cave
When Beatriz Flamini spoke with reporters on April 14, she knew nothing of the previous 18 months. The Russian invasion of Ukraine? Nope. The death of Queen Elizabeth? Also no. But before you make fun of her, she has an excuse. She’s been living under a rock.
As part of an experiment to test how social isolation and disorientation affect a person’s mind, sense of time, and sleeping patterns, Ms. Flamini lived in a 70-meter-deep cave in southern Spain for 500 days, starting in November 2021. Alone. No outside communication with the outside world in any way, though she was constantly monitored by a team of researchers. She also had multiple cameras filming her for an upcoming documentary.
This is a massive step up from the previous record for time spent underground for science: A team of 15 spent 50 days underground in 2021 to similar study of isolation and how it affected circadian rhythms. It’s also almost certainly a world record for time spent underground.
All that time alone certainly sounds like some sort of medieval torture, but Ms. Flamini had access to food, water, and a library of books. Which she made liberal use of, reading at least 60 books during her stay. She also had a panic button in case the isolation became too much or an emergency developed, but she never considered using it.
She lost track of time after 2 months, flies invaded the cave on occasion, and maintaining coherence was occasionally a struggle, but she kept things together very well. In fact, she didn’t even want to leave when her team came for her. She wasn’t even finished with her 61st book.
When she spoke with gathered reporters after the ordeal, words were obviously difficult to come by for her, having not spoken in nearly 18 months, but her mind was clearly still sharp and she had a very important question for everyone gathered around her.
Who’s buying the beer?
We approve of this request.
Staphylococcus and the speed of evolution
Bacteria, we know, are tough little buggers that are hard to see and even harder to get rid of. So hard, actually, that human bodies eventually gave up on the task and decided to just incorporate them into our organ systems. But why are bacteria so hard to eliminate?
Two words: rapid evolution. How rapid? For the first time, scientists have directly observed adaptive evolution by Staphylococcus aureus in a single person’s skin microbiome. That’s how rapid.
For their study, the researchers collected samples from the nostrils, backs of knees, insides of elbows, and forearms of 23 children with eczema. They eventually cultured almost 1,500 unique colonies of S. aureus cells from those samples and sequenced the cells’ genomes.
All that sampling and culturing and sequencing showed that it was rare for a new S. aureus strain to come in and replace the existing strain. “Despite the stability at the lineage level, we see a lot of dynamics at the whole genome level, where new mutations are constantly arising in these bacteria and then spreading throughout the entire body,” Tami D. Lieberman, PhD, of the Massachusetts Institute of Technology, Cambridge, said in a written statement from MIT.
One frequent mutation involved a gene called capD, which encodes an enzyme necessary for synthesizing the capsular polysaccharide – a coating that protects S. aureus from recognition by immune cells. In one patient, four different mutations of capD arose independently in different samples before one variant became dominant and spread over the entire microbiome, MIT reported.
The mutation, which actually results in the loss of the polysaccharide capsule, may allow cells to grow faster than those without the mutation because they have more fuel to power their own growth, the researchers suggested. It’s also possible that loss of the capsule allows S. aureus cells to stick to the skin better because proteins that allow them to adhere to the skin are more exposed.
Dr. Lieberman and her associates hope that these variant-containing cells could be a new target for eczema treatments, but we’re never optimistic when it comes to bacteria. That’s because some of us are old enough to remember evolutionary biologist Stephen Jay Gould, who wrote in his book “Full House”: “Our planet has always been in the ‘Age of Bacteria,’ ever since the first fossils – bacteria, of course – were entombed in rocks more than 3 billion years ago. On any possible, reasonable or fair criterion, bacteria are – and always have been – the dominant forms of life on Earth.”
In the distant future, long after humans have left the scene, the bacteria will be laughing at the last rats and cockroaches scurrying across the landscape. Wanna bet?
The height of genetic prediction
Genetics are practically a DNA Scrabble bag. Traits like eye color and hair texture are chosen in the same fashion, based on what gets pulled from our own genetic bag of letters, but what about height? Researchers may now have a way to predict adult height and make it more than just an educated guess.
How? By looking at the genes in our growth plates. The cartilage on the ends of our bones hardens as we age, eventually deciding an individual’s stature. In a recently published study, a research team looked at 600 million cartilage cells linked to maturation and cell growth in mice. Because everything starts with rodents.
After that search identified 145 genes linked to growth plate maturation and formation of the bones, they compared the mouse genes with data from genome-wide association studies (GWAS) of human height to look for hotspots where the height genes exist in human DNA.
The results showed which genes play a role in deciding height, and the GWAS data also suggested that genetic changes affecting cartilage cell maturation may strongly influence adult height, said the investigators, who hope that earlier interventions can improve outcomes in patients with conditions such as skeletal dysplasia.
So, yeah, you may want to be a little taller or shorter, but the outcome of that particular Scrabble game was determined when your parents, you know, dropped the letters in the bag.
Beating the allegory of the cave
When Beatriz Flamini spoke with reporters on April 14, she knew nothing of the previous 18 months. The Russian invasion of Ukraine? Nope. The death of Queen Elizabeth? Also no. But before you make fun of her, she has an excuse. She’s been living under a rock.
As part of an experiment to test how social isolation and disorientation affect a person’s mind, sense of time, and sleeping patterns, Ms. Flamini lived in a 70-meter-deep cave in southern Spain for 500 days, starting in November 2021. Alone. No outside communication with the outside world in any way, though she was constantly monitored by a team of researchers. She also had multiple cameras filming her for an upcoming documentary.
This is a massive step up from the previous record for time spent underground for science: A team of 15 spent 50 days underground in 2021 to similar study of isolation and how it affected circadian rhythms. It’s also almost certainly a world record for time spent underground.
All that time alone certainly sounds like some sort of medieval torture, but Ms. Flamini had access to food, water, and a library of books. Which she made liberal use of, reading at least 60 books during her stay. She also had a panic button in case the isolation became too much or an emergency developed, but she never considered using it.
She lost track of time after 2 months, flies invaded the cave on occasion, and maintaining coherence was occasionally a struggle, but she kept things together very well. In fact, she didn’t even want to leave when her team came for her. She wasn’t even finished with her 61st book.
When she spoke with gathered reporters after the ordeal, words were obviously difficult to come by for her, having not spoken in nearly 18 months, but her mind was clearly still sharp and she had a very important question for everyone gathered around her.
Who’s buying the beer?
We approve of this request.
Staphylococcus and the speed of evolution
Bacteria, we know, are tough little buggers that are hard to see and even harder to get rid of. So hard, actually, that human bodies eventually gave up on the task and decided to just incorporate them into our organ systems. But why are bacteria so hard to eliminate?
Two words: rapid evolution. How rapid? For the first time, scientists have directly observed adaptive evolution by Staphylococcus aureus in a single person’s skin microbiome. That’s how rapid.
For their study, the researchers collected samples from the nostrils, backs of knees, insides of elbows, and forearms of 23 children with eczema. They eventually cultured almost 1,500 unique colonies of S. aureus cells from those samples and sequenced the cells’ genomes.
All that sampling and culturing and sequencing showed that it was rare for a new S. aureus strain to come in and replace the existing strain. “Despite the stability at the lineage level, we see a lot of dynamics at the whole genome level, where new mutations are constantly arising in these bacteria and then spreading throughout the entire body,” Tami D. Lieberman, PhD, of the Massachusetts Institute of Technology, Cambridge, said in a written statement from MIT.
One frequent mutation involved a gene called capD, which encodes an enzyme necessary for synthesizing the capsular polysaccharide – a coating that protects S. aureus from recognition by immune cells. In one patient, four different mutations of capD arose independently in different samples before one variant became dominant and spread over the entire microbiome, MIT reported.
The mutation, which actually results in the loss of the polysaccharide capsule, may allow cells to grow faster than those without the mutation because they have more fuel to power their own growth, the researchers suggested. It’s also possible that loss of the capsule allows S. aureus cells to stick to the skin better because proteins that allow them to adhere to the skin are more exposed.
Dr. Lieberman and her associates hope that these variant-containing cells could be a new target for eczema treatments, but we’re never optimistic when it comes to bacteria. That’s because some of us are old enough to remember evolutionary biologist Stephen Jay Gould, who wrote in his book “Full House”: “Our planet has always been in the ‘Age of Bacteria,’ ever since the first fossils – bacteria, of course – were entombed in rocks more than 3 billion years ago. On any possible, reasonable or fair criterion, bacteria are – and always have been – the dominant forms of life on Earth.”
In the distant future, long after humans have left the scene, the bacteria will be laughing at the last rats and cockroaches scurrying across the landscape. Wanna bet?
The height of genetic prediction
Genetics are practically a DNA Scrabble bag. Traits like eye color and hair texture are chosen in the same fashion, based on what gets pulled from our own genetic bag of letters, but what about height? Researchers may now have a way to predict adult height and make it more than just an educated guess.
How? By looking at the genes in our growth plates. The cartilage on the ends of our bones hardens as we age, eventually deciding an individual’s stature. In a recently published study, a research team looked at 600 million cartilage cells linked to maturation and cell growth in mice. Because everything starts with rodents.
After that search identified 145 genes linked to growth plate maturation and formation of the bones, they compared the mouse genes with data from genome-wide association studies (GWAS) of human height to look for hotspots where the height genes exist in human DNA.
The results showed which genes play a role in deciding height, and the GWAS data also suggested that genetic changes affecting cartilage cell maturation may strongly influence adult height, said the investigators, who hope that earlier interventions can improve outcomes in patients with conditions such as skeletal dysplasia.
So, yeah, you may want to be a little taller or shorter, but the outcome of that particular Scrabble game was determined when your parents, you know, dropped the letters in the bag.
Obstructive sleep apnea linked to early cognitive decline
In a pilot study out of King’s College London, participants with severe OSA experienced worse executive functioning as well as social and emotional recognition versus healthy controls.
Major risk factors for OSA include obesity, high blood pressure, smoking, high cholesterol, and being middle-aged or older. Because some researchers have hypothesized that cognitive deficits could be driven by such comorbidities, the study investigators recruited middle-aged men with no medical comorbidities.
“Traditionally, we were more concerned with sleep apnea’s metabolic and cardiovascular comorbidities, and indeed, when cognitive deficits were demonstrated, most were attributed to them, and yet, our patients and their partners/families commonly tell us differently,” lead investigator Ivana Rosenzweig, MD, PhD, of King’s College London, who is also a consultant in sleep medicine and neuropsychiatry at Guy’s and St Thomas’ Hospital, London, said in an interview.
“Our findings provide a very important first step towards challenging the long-standing dogma that sleep apnea has little to do with the brain – apart from causing sleepiness – and that it is a predominantly nonneuro/psychiatric illness,” added Dr. Rosenzweig.
The findings were published online in Frontiers in Sleep.
Brain changes
The researchers wanted to understand how OSA may be linked to cognitive decline in the absence of cardiovascular and metabolic conditions.
To accomplish this, the investigators studied 27 men between the ages of 35 and 70 with a new diagnosis of mild to severe OSA without any comorbidities (16 with mild OSA and 11 with severe OSA). They also studied a control group of seven men matched for age, body mass index, and education level.
The team tested participants’ cognitive performance using the Cambridge Neuropsychological Test Automated Battery and found that the most significant deficits for the OSA group, compared with controls, were in areas of visual matching ability (P < .0001), short-term visual recognition memory, nonverbal patterns, executive functioning and attentional set-shifting (P < .001), psychomotor functioning, and social cognition and emotional recognition (P < .05).
On the latter two tests, impaired participants were less likely to accurately identify the emotion on computer-generated faces. Those with mild OSA performed better than those with severe OSA on these tasks, but rarely worse than controls.
Dr. Rosenzweig noted that the findings were one-of-a-kind because of the recruitment of patients with OSA who were otherwise healthy and nonobese, “something one rarely sees in the sleep clinic, where we commonly encounter patients with already developed comorbidities.
“In order to truly revolutionize the treatment for our patients, it is important to understand how much the accompanying comorbidities, such as systemic hypertension, obesity, diabetes, hyperlipidemia, and other various serious cardiovascular and metabolic diseases and how much the illness itself may shape the demonstrated cognitive deficits,” she said.
She also said that “it is widely agreed that medical problems in middle age may predispose to increased prevalence of dementia in later years.
Moreover, the very link between sleep apnea and Alzheimer’s, vascular and mixed dementia is increasingly demonstrated,” said Dr. Rosenzweig.
Although women typically have a lower prevalence of OSA than men, Dr. Rosenzweig said women were not included in the study “because we are too complex. As a lifelong feminist it pains me to say this, but to get any authoritative answer on our physiology, we need decent funding in place so that we can take into account all the intricacies of the changes of our sleep, physiology, and metabolism.
“While there is always lots of noise about how important it is to answer these questions, there are only very limited funds available for the sleep research,” she added.
Dr. Rosenzweig’s future research will focus on the potential link between OSA and neuroinflammation.
In a comment, Liza Ashbrook, MD, associate professor of neurology at the University of California, San Francisco, said the findings “add to the growing list of negative health consequences associated with sleep apnea.”
She said that, if the cognitive changes found in the study are, in fact, caused by OSA, it is unclear whether they are the beginning of long-term cognitive changes or a symptom of fragmented sleep that may be reversible.
Dr. Ashbrook said she would be interested in seeing research on understanding the effect of OSA treatment on the affected cognitive domains.
The study was funded by the Wellcome Trust. No relevant financial relationships were reported.
A version of this article originally appeared on Medscape.com.
In a pilot study out of King’s College London, participants with severe OSA experienced worse executive functioning as well as social and emotional recognition versus healthy controls.
Major risk factors for OSA include obesity, high blood pressure, smoking, high cholesterol, and being middle-aged or older. Because some researchers have hypothesized that cognitive deficits could be driven by such comorbidities, the study investigators recruited middle-aged men with no medical comorbidities.
“Traditionally, we were more concerned with sleep apnea’s metabolic and cardiovascular comorbidities, and indeed, when cognitive deficits were demonstrated, most were attributed to them, and yet, our patients and their partners/families commonly tell us differently,” lead investigator Ivana Rosenzweig, MD, PhD, of King’s College London, who is also a consultant in sleep medicine and neuropsychiatry at Guy’s and St Thomas’ Hospital, London, said in an interview.
“Our findings provide a very important first step towards challenging the long-standing dogma that sleep apnea has little to do with the brain – apart from causing sleepiness – and that it is a predominantly nonneuro/psychiatric illness,” added Dr. Rosenzweig.
The findings were published online in Frontiers in Sleep.
Brain changes
The researchers wanted to understand how OSA may be linked to cognitive decline in the absence of cardiovascular and metabolic conditions.
To accomplish this, the investigators studied 27 men between the ages of 35 and 70 with a new diagnosis of mild to severe OSA without any comorbidities (16 with mild OSA and 11 with severe OSA). They also studied a control group of seven men matched for age, body mass index, and education level.
The team tested participants’ cognitive performance using the Cambridge Neuropsychological Test Automated Battery and found that the most significant deficits for the OSA group, compared with controls, were in areas of visual matching ability (P < .0001), short-term visual recognition memory, nonverbal patterns, executive functioning and attentional set-shifting (P < .001), psychomotor functioning, and social cognition and emotional recognition (P < .05).
On the latter two tests, impaired participants were less likely to accurately identify the emotion on computer-generated faces. Those with mild OSA performed better than those with severe OSA on these tasks, but rarely worse than controls.
Dr. Rosenzweig noted that the findings were one-of-a-kind because of the recruitment of patients with OSA who were otherwise healthy and nonobese, “something one rarely sees in the sleep clinic, where we commonly encounter patients with already developed comorbidities.
“In order to truly revolutionize the treatment for our patients, it is important to understand how much the accompanying comorbidities, such as systemic hypertension, obesity, diabetes, hyperlipidemia, and other various serious cardiovascular and metabolic diseases and how much the illness itself may shape the demonstrated cognitive deficits,” she said.
She also said that “it is widely agreed that medical problems in middle age may predispose to increased prevalence of dementia in later years.
Moreover, the very link between sleep apnea and Alzheimer’s, vascular and mixed dementia is increasingly demonstrated,” said Dr. Rosenzweig.
Although women typically have a lower prevalence of OSA than men, Dr. Rosenzweig said women were not included in the study “because we are too complex. As a lifelong feminist it pains me to say this, but to get any authoritative answer on our physiology, we need decent funding in place so that we can take into account all the intricacies of the changes of our sleep, physiology, and metabolism.
“While there is always lots of noise about how important it is to answer these questions, there are only very limited funds available for the sleep research,” she added.
Dr. Rosenzweig’s future research will focus on the potential link between OSA and neuroinflammation.
In a comment, Liza Ashbrook, MD, associate professor of neurology at the University of California, San Francisco, said the findings “add to the growing list of negative health consequences associated with sleep apnea.”
She said that, if the cognitive changes found in the study are, in fact, caused by OSA, it is unclear whether they are the beginning of long-term cognitive changes or a symptom of fragmented sleep that may be reversible.
Dr. Ashbrook said she would be interested in seeing research on understanding the effect of OSA treatment on the affected cognitive domains.
The study was funded by the Wellcome Trust. No relevant financial relationships were reported.
A version of this article originally appeared on Medscape.com.
In a pilot study out of King’s College London, participants with severe OSA experienced worse executive functioning as well as social and emotional recognition versus healthy controls.
Major risk factors for OSA include obesity, high blood pressure, smoking, high cholesterol, and being middle-aged or older. Because some researchers have hypothesized that cognitive deficits could be driven by such comorbidities, the study investigators recruited middle-aged men with no medical comorbidities.
“Traditionally, we were more concerned with sleep apnea’s metabolic and cardiovascular comorbidities, and indeed, when cognitive deficits were demonstrated, most were attributed to them, and yet, our patients and their partners/families commonly tell us differently,” lead investigator Ivana Rosenzweig, MD, PhD, of King’s College London, who is also a consultant in sleep medicine and neuropsychiatry at Guy’s and St Thomas’ Hospital, London, said in an interview.
“Our findings provide a very important first step towards challenging the long-standing dogma that sleep apnea has little to do with the brain – apart from causing sleepiness – and that it is a predominantly nonneuro/psychiatric illness,” added Dr. Rosenzweig.
The findings were published online in Frontiers in Sleep.
Brain changes
The researchers wanted to understand how OSA may be linked to cognitive decline in the absence of cardiovascular and metabolic conditions.
To accomplish this, the investigators studied 27 men between the ages of 35 and 70 with a new diagnosis of mild to severe OSA without any comorbidities (16 with mild OSA and 11 with severe OSA). They also studied a control group of seven men matched for age, body mass index, and education level.
The team tested participants’ cognitive performance using the Cambridge Neuropsychological Test Automated Battery and found that the most significant deficits for the OSA group, compared with controls, were in areas of visual matching ability (P < .0001), short-term visual recognition memory, nonverbal patterns, executive functioning and attentional set-shifting (P < .001), psychomotor functioning, and social cognition and emotional recognition (P < .05).
On the latter two tests, impaired participants were less likely to accurately identify the emotion on computer-generated faces. Those with mild OSA performed better than those with severe OSA on these tasks, but rarely worse than controls.
Dr. Rosenzweig noted that the findings were one-of-a-kind because of the recruitment of patients with OSA who were otherwise healthy and nonobese, “something one rarely sees in the sleep clinic, where we commonly encounter patients with already developed comorbidities.
“In order to truly revolutionize the treatment for our patients, it is important to understand how much the accompanying comorbidities, such as systemic hypertension, obesity, diabetes, hyperlipidemia, and other various serious cardiovascular and metabolic diseases and how much the illness itself may shape the demonstrated cognitive deficits,” she said.
She also said that “it is widely agreed that medical problems in middle age may predispose to increased prevalence of dementia in later years.
Moreover, the very link between sleep apnea and Alzheimer’s, vascular and mixed dementia is increasingly demonstrated,” said Dr. Rosenzweig.
Although women typically have a lower prevalence of OSA than men, Dr. Rosenzweig said women were not included in the study “because we are too complex. As a lifelong feminist it pains me to say this, but to get any authoritative answer on our physiology, we need decent funding in place so that we can take into account all the intricacies of the changes of our sleep, physiology, and metabolism.
“While there is always lots of noise about how important it is to answer these questions, there are only very limited funds available for the sleep research,” she added.
Dr. Rosenzweig’s future research will focus on the potential link between OSA and neuroinflammation.
In a comment, Liza Ashbrook, MD, associate professor of neurology at the University of California, San Francisco, said the findings “add to the growing list of negative health consequences associated with sleep apnea.”
She said that, if the cognitive changes found in the study are, in fact, caused by OSA, it is unclear whether they are the beginning of long-term cognitive changes or a symptom of fragmented sleep that may be reversible.
Dr. Ashbrook said she would be interested in seeing research on understanding the effect of OSA treatment on the affected cognitive domains.
The study was funded by the Wellcome Trust. No relevant financial relationships were reported.
A version of this article originally appeared on Medscape.com.
FROM FRONTIERS IN SLEEP
Physicians may retire en masse soon. What does that mean for medicine?
The double whammy of pandemic burnout and the aging of baby boomer physicians has, indeed, the makings of some scary headlines. A recent survey by Elsevier Health predicts that up to 75% of health care workers will leave the profession by 2025. And a 2020 study conducted by the Association of American Medical Colleges (AAMC) projected a shortfall of up to 139,000 physicians by 2033.
“We’ve paid a lot of attention to physician retirement,” says Michael Dill, AAMC’s director of workforce studies. “It’s a significant concern in terms of whether we have an adequate supply of physicians in the U.S. to meet our nation’s medical care needs. Anyone who thinks otherwise is incorrect.”
To Mr. Dill,
“The physician workforce as a whole is aging,” he said. “Close to a quarter of the physicians in the U.S. are 65 and over. So, you don’t need any extraordinary events driving retirement in order for retirement to be a real phenomenon of which we should all be concerned.”
And, although Mr. Dill said there aren’t any data to suggest that doctors in rural or urban areas are retiring faster than in the suburbs, that doesn’t mean retirement will have the same impact depending on where patients live.
“If you live in a rural area with one small practice in town and that physician retires, there goes the entirety of the physician supply,” he said. “In a major metro area, that’s not as big a deal.”
Why younger doctors are fast-tracking retirement
Fernando Mendoza, MD, 54, a pediatric emergency department physician in Miami, worries that physicians are getting so bogged down by paperwork that this may lead to even more doctors, at younger ages, leaving the profession.
“I love taking care of kids, but there’s going to be a cost to doing your work when you’re spending as much time as we need to spend on charts, pharmacy requests, and making sure all of the Medicare and Medicaid compliance issues are worked out.”
These stressors may compel some younger doctors to consider carving out a second career or fast-track younger physicians toward retirement.
“A medical degree carries a lot of weight, which helps when pivoting,” said Dr. Mendoza, who launched Scrivas, a Miami-based medical scribe agency, to help reduce the paperwork workload for physicians. “It might be that a doctor wants to get involved in the acquisition of medical equipment, or maybe they can focus on their investments. Either way, by leaving medicine, they’re not dealing with the hassle and churn-and-burn of seeing patients.”
What this means for patients
The time is now to stem the upcoming tide of retirement, said Mr. Dill. But the challenges remain daunting. For starters, the country needs more physicians trained now – but it will take years to replace those baby boomer doctors ready to hang up their white coats.
The medical profession also needs to find ways to support physicians who spend their days juggling an endless array of responsibilities, he said.
The AAMC study found that patients already feel the physician shortfall. Their public opinion research in 2019 said 35% of patients had trouble finding a physician over the past 2 or 3 years, up 10 percentage points since they asked the question in 2015.
Moreover, according to the report, the over-65 population is expected to grow by 45.1%, leaving a specialty care gap because older people generally have more complicated health cases that require specialists. In addition, physician burnout may lead more physicians under 65 to retire much earlier than expected.
Changes in how medicine is practiced, telemedicine care, and medical education – such as disruption of classes or clinical rotations, regulatory changes, and a lack of interest in certain specialties – could also be affected by a mass physician retirement.
What can we do about mass retirement?
The AAMC reports in “The Complexities of Physician Supply and Demand: Projections From 2019 to 2034” that federally funded GME support is in the works to train 15,000 physicians per year, with 3,000 new residency slots added per year over 5 years. The proposed model will add 3,750 new physicians each year beginning in 2026.
Other efforts include increasing use of APRNs and PAs, whose population is estimated to more than double by 2034, improve population health through preventive care, increase equity in health outcomes, and improve access and affordable care.
Removing licensing barriers for immigrant doctors can also help alleviate the shortage.
“We need to find better ways to leverage the entirety of the health care team so that not as much falls on physicians,” Mr. Dill said. “It’s also imperative that we focus on ways to support physician wellness and allow physicians to remain active in the field, but at a reduced rate.”
That’s precisely what Marie Brown, MD, director of practice redesign at the American Medical Association, is seeing nationwide. Cutting back their hours is not only trending, but it’s also helping doctors cope with burnout.
“We’re seeing physicians take a 20% or more cut in salary in order to decrease their burden,” she said. “They’ll spend 4 days on clinical time with patients so that on that fifth ‘day off,’ they’re doing the paperwork and documentation they need to do so they don’t compromise care on the other 4 days of the week.”
And this may only be a Band-Aid solution, she fears.
“If a physician is spending 3 hours a day doing unnecessary work that could be done by another team member, that’s contributing to burnout,” Dr. Brown said. “It’s no surprise that they’ll want to escape and retire if they’re in a financial situation to do so.”
“I advocate negotiating within your organization so you’re doing more of what you like, such as mentoring or running a residency, and less of what you don’t, while cutting back from full-time to something less than full-time while maintaining benefits,” said Joel Greenwald, MD, a certified financial planner in Minneapolis, who specializes in helping physicians manage their financial affairs.
“Falling into the ‘like less’ bucket are usually things like working weekends and taking calls,” he said.
“This benefits everyone on a large scale because those doctors who find things they enjoy are generally working to a later age but working less hard,” he said. “Remaining comfortably and happily gainfully employed for a longer period, even if you’re not working full-time, has a very powerful effect on your financial planning, and you’ll avoid the risk of running out of money.”
A version of this article first appeared on Medscape.com.
The double whammy of pandemic burnout and the aging of baby boomer physicians has, indeed, the makings of some scary headlines. A recent survey by Elsevier Health predicts that up to 75% of health care workers will leave the profession by 2025. And a 2020 study conducted by the Association of American Medical Colleges (AAMC) projected a shortfall of up to 139,000 physicians by 2033.
“We’ve paid a lot of attention to physician retirement,” says Michael Dill, AAMC’s director of workforce studies. “It’s a significant concern in terms of whether we have an adequate supply of physicians in the U.S. to meet our nation’s medical care needs. Anyone who thinks otherwise is incorrect.”
To Mr. Dill,
“The physician workforce as a whole is aging,” he said. “Close to a quarter of the physicians in the U.S. are 65 and over. So, you don’t need any extraordinary events driving retirement in order for retirement to be a real phenomenon of which we should all be concerned.”
And, although Mr. Dill said there aren’t any data to suggest that doctors in rural or urban areas are retiring faster than in the suburbs, that doesn’t mean retirement will have the same impact depending on where patients live.
“If you live in a rural area with one small practice in town and that physician retires, there goes the entirety of the physician supply,” he said. “In a major metro area, that’s not as big a deal.”
Why younger doctors are fast-tracking retirement
Fernando Mendoza, MD, 54, a pediatric emergency department physician in Miami, worries that physicians are getting so bogged down by paperwork that this may lead to even more doctors, at younger ages, leaving the profession.
“I love taking care of kids, but there’s going to be a cost to doing your work when you’re spending as much time as we need to spend on charts, pharmacy requests, and making sure all of the Medicare and Medicaid compliance issues are worked out.”
These stressors may compel some younger doctors to consider carving out a second career or fast-track younger physicians toward retirement.
“A medical degree carries a lot of weight, which helps when pivoting,” said Dr. Mendoza, who launched Scrivas, a Miami-based medical scribe agency, to help reduce the paperwork workload for physicians. “It might be that a doctor wants to get involved in the acquisition of medical equipment, or maybe they can focus on their investments. Either way, by leaving medicine, they’re not dealing with the hassle and churn-and-burn of seeing patients.”
What this means for patients
The time is now to stem the upcoming tide of retirement, said Mr. Dill. But the challenges remain daunting. For starters, the country needs more physicians trained now – but it will take years to replace those baby boomer doctors ready to hang up their white coats.
The medical profession also needs to find ways to support physicians who spend their days juggling an endless array of responsibilities, he said.
The AAMC study found that patients already feel the physician shortfall. Their public opinion research in 2019 said 35% of patients had trouble finding a physician over the past 2 or 3 years, up 10 percentage points since they asked the question in 2015.
Moreover, according to the report, the over-65 population is expected to grow by 45.1%, leaving a specialty care gap because older people generally have more complicated health cases that require specialists. In addition, physician burnout may lead more physicians under 65 to retire much earlier than expected.
Changes in how medicine is practiced, telemedicine care, and medical education – such as disruption of classes or clinical rotations, regulatory changes, and a lack of interest in certain specialties – could also be affected by a mass physician retirement.
What can we do about mass retirement?
The AAMC reports in “The Complexities of Physician Supply and Demand: Projections From 2019 to 2034” that federally funded GME support is in the works to train 15,000 physicians per year, with 3,000 new residency slots added per year over 5 years. The proposed model will add 3,750 new physicians each year beginning in 2026.
Other efforts include increasing use of APRNs and PAs, whose population is estimated to more than double by 2034, improve population health through preventive care, increase equity in health outcomes, and improve access and affordable care.
Removing licensing barriers for immigrant doctors can also help alleviate the shortage.
“We need to find better ways to leverage the entirety of the health care team so that not as much falls on physicians,” Mr. Dill said. “It’s also imperative that we focus on ways to support physician wellness and allow physicians to remain active in the field, but at a reduced rate.”
That’s precisely what Marie Brown, MD, director of practice redesign at the American Medical Association, is seeing nationwide. Cutting back their hours is not only trending, but it’s also helping doctors cope with burnout.
“We’re seeing physicians take a 20% or more cut in salary in order to decrease their burden,” she said. “They’ll spend 4 days on clinical time with patients so that on that fifth ‘day off,’ they’re doing the paperwork and documentation they need to do so they don’t compromise care on the other 4 days of the week.”
And this may only be a Band-Aid solution, she fears.
“If a physician is spending 3 hours a day doing unnecessary work that could be done by another team member, that’s contributing to burnout,” Dr. Brown said. “It’s no surprise that they’ll want to escape and retire if they’re in a financial situation to do so.”
“I advocate negotiating within your organization so you’re doing more of what you like, such as mentoring or running a residency, and less of what you don’t, while cutting back from full-time to something less than full-time while maintaining benefits,” said Joel Greenwald, MD, a certified financial planner in Minneapolis, who specializes in helping physicians manage their financial affairs.
“Falling into the ‘like less’ bucket are usually things like working weekends and taking calls,” he said.
“This benefits everyone on a large scale because those doctors who find things they enjoy are generally working to a later age but working less hard,” he said. “Remaining comfortably and happily gainfully employed for a longer period, even if you’re not working full-time, has a very powerful effect on your financial planning, and you’ll avoid the risk of running out of money.”
A version of this article first appeared on Medscape.com.
The double whammy of pandemic burnout and the aging of baby boomer physicians has, indeed, the makings of some scary headlines. A recent survey by Elsevier Health predicts that up to 75% of health care workers will leave the profession by 2025. And a 2020 study conducted by the Association of American Medical Colleges (AAMC) projected a shortfall of up to 139,000 physicians by 2033.
“We’ve paid a lot of attention to physician retirement,” says Michael Dill, AAMC’s director of workforce studies. “It’s a significant concern in terms of whether we have an adequate supply of physicians in the U.S. to meet our nation’s medical care needs. Anyone who thinks otherwise is incorrect.”
To Mr. Dill,
“The physician workforce as a whole is aging,” he said. “Close to a quarter of the physicians in the U.S. are 65 and over. So, you don’t need any extraordinary events driving retirement in order for retirement to be a real phenomenon of which we should all be concerned.”
And, although Mr. Dill said there aren’t any data to suggest that doctors in rural or urban areas are retiring faster than in the suburbs, that doesn’t mean retirement will have the same impact depending on where patients live.
“If you live in a rural area with one small practice in town and that physician retires, there goes the entirety of the physician supply,” he said. “In a major metro area, that’s not as big a deal.”
Why younger doctors are fast-tracking retirement
Fernando Mendoza, MD, 54, a pediatric emergency department physician in Miami, worries that physicians are getting so bogged down by paperwork that this may lead to even more doctors, at younger ages, leaving the profession.
“I love taking care of kids, but there’s going to be a cost to doing your work when you’re spending as much time as we need to spend on charts, pharmacy requests, and making sure all of the Medicare and Medicaid compliance issues are worked out.”
These stressors may compel some younger doctors to consider carving out a second career or fast-track younger physicians toward retirement.
“A medical degree carries a lot of weight, which helps when pivoting,” said Dr. Mendoza, who launched Scrivas, a Miami-based medical scribe agency, to help reduce the paperwork workload for physicians. “It might be that a doctor wants to get involved in the acquisition of medical equipment, or maybe they can focus on their investments. Either way, by leaving medicine, they’re not dealing with the hassle and churn-and-burn of seeing patients.”
What this means for patients
The time is now to stem the upcoming tide of retirement, said Mr. Dill. But the challenges remain daunting. For starters, the country needs more physicians trained now – but it will take years to replace those baby boomer doctors ready to hang up their white coats.
The medical profession also needs to find ways to support physicians who spend their days juggling an endless array of responsibilities, he said.
The AAMC study found that patients already feel the physician shortfall. Their public opinion research in 2019 said 35% of patients had trouble finding a physician over the past 2 or 3 years, up 10 percentage points since they asked the question in 2015.
Moreover, according to the report, the over-65 population is expected to grow by 45.1%, leaving a specialty care gap because older people generally have more complicated health cases that require specialists. In addition, physician burnout may lead more physicians under 65 to retire much earlier than expected.
Changes in how medicine is practiced, telemedicine care, and medical education – such as disruption of classes or clinical rotations, regulatory changes, and a lack of interest in certain specialties – could also be affected by a mass physician retirement.
What can we do about mass retirement?
The AAMC reports in “The Complexities of Physician Supply and Demand: Projections From 2019 to 2034” that federally funded GME support is in the works to train 15,000 physicians per year, with 3,000 new residency slots added per year over 5 years. The proposed model will add 3,750 new physicians each year beginning in 2026.
Other efforts include increasing use of APRNs and PAs, whose population is estimated to more than double by 2034, improve population health through preventive care, increase equity in health outcomes, and improve access and affordable care.
Removing licensing barriers for immigrant doctors can also help alleviate the shortage.
“We need to find better ways to leverage the entirety of the health care team so that not as much falls on physicians,” Mr. Dill said. “It’s also imperative that we focus on ways to support physician wellness and allow physicians to remain active in the field, but at a reduced rate.”
That’s precisely what Marie Brown, MD, director of practice redesign at the American Medical Association, is seeing nationwide. Cutting back their hours is not only trending, but it’s also helping doctors cope with burnout.
“We’re seeing physicians take a 20% or more cut in salary in order to decrease their burden,” she said. “They’ll spend 4 days on clinical time with patients so that on that fifth ‘day off,’ they’re doing the paperwork and documentation they need to do so they don’t compromise care on the other 4 days of the week.”
And this may only be a Band-Aid solution, she fears.
“If a physician is spending 3 hours a day doing unnecessary work that could be done by another team member, that’s contributing to burnout,” Dr. Brown said. “It’s no surprise that they’ll want to escape and retire if they’re in a financial situation to do so.”
“I advocate negotiating within your organization so you’re doing more of what you like, such as mentoring or running a residency, and less of what you don’t, while cutting back from full-time to something less than full-time while maintaining benefits,” said Joel Greenwald, MD, a certified financial planner in Minneapolis, who specializes in helping physicians manage their financial affairs.
“Falling into the ‘like less’ bucket are usually things like working weekends and taking calls,” he said.
“This benefits everyone on a large scale because those doctors who find things they enjoy are generally working to a later age but working less hard,” he said. “Remaining comfortably and happily gainfully employed for a longer period, even if you’re not working full-time, has a very powerful effect on your financial planning, and you’ll avoid the risk of running out of money.”
A version of this article first appeared on Medscape.com.
Physician compensation continues to climb amid postpandemic change
In addition, gender-based pay disparity among primary care physicians shrank, and the number of physicians who declined to take new Medicare patients rose.
The annual report is based on a survey of more than 10,000 physicians in over 29 specialties who answered questions about their income, workload, challenges, and level of satisfaction.
Average compensation across specialties rose to $352,000 – up nearly 17% from the 2018 average of $299,000. Fallout from the COVID-19 public health emergency continued to affect both physician compensation and job satisfaction, including Medicare reimbursements and staffing shortages due to burnout or retirement.
“Many physicians reevaluated what drove them to be a physician,” says Marc Adam, a recruiter at MASC Medical, a Florida physician recruiting firm.
Adam cites telehealth as an example. “An overwhelming majority of physicians prefer telehealth because of the convenience, but some really did not want to do it long term. They miss the patient interaction.”
The report also revealed that the gender-based pay gap in primary physicians fell, with men earning 19% more – down from 25% more in recent years. Among specialists, the gender gap was 27% on average, down from 31% last year. One reason may be an increase in compensation transparency, which Mr. Adam says should be the norm.
Income increases will likely continue, owing in large part to the growing disparity between physician supply and demand.
The projected physician shortage is expected to grow to 124,000 by 2034, according to the American Association of Medical Colleges. Federal lawmakers are considering passing the Resident Physician Shortage Reduction Act of 2023, which would add 14,000 Medicare-funded residency positions to help alleviate shortages.
Patient needs, Medicare rules continue to shift
Specialties with the biggest increases in compensation include oncology, anesthesiology, gastroenterology, radiology, critical care, and urology. Many procedure-related specialties saw more volume post pandemic.
Some respondents identified Medicare cuts and low reimbursement rates as a factor in tamping down compensation hikes. The number of physicians who expect to continue to take new Medicare patients is 65%, down from 71% 5 years ago.
For example, Medicare reimbursements for telehealth are expected to scale down in May, when the COVID-19 Public Health Emergency, which expanded telehealth services for Medicare patients, winds down.
“Telehealth will still exist,” says Mr. Adam, “but certain requirements will shape it going forward.”
Medicare isn’t viewed negatively across the board, however. Florida is among the top-earning states for physicians – along with Indiana, Connecticut, and Missouri. One reason is Florida’s unique health care environment, explains Mr. Adam, whose Florida-based firm places physicians nationwide.
“Florida is very progressive in terms of health care. For one thing, we have a large aging population and a large Medicare population.” Several growing organizations that focus on quality-based care are based in Florida, including ChenMed and Cano Health. Add to that the fact that owners of Florida’s health care organizations don’t have to be physicians, he explains, and the stage is set for experimentation.
“Being able to segment tasks frees up physicians to be more focused on medicine and provide better care while other people focus on the business and innovation.”
If Florida’s high compensation ranking continues, it may help employers there fulfill a growing need. The state is among those expected to experience the largest physician shortages in 2030, along with California, Texas, Arizona, and Georgia.
Side gigs up, satisfaction (slightly) down
In general, physicians aren’t fazed by these challenges. Many reported taking side gigs, some for additional income. Even so, 73% say they would still choose medicine, and more than 90% of physicians in 10 specialties would choose their specialty again. Still, burnout and stressors have led some to stop practicing altogether.
More and more organizations are hiring “travel physicians,” Mr. Adam says, and more physicians are choosing to take contract work (“locum tenens”) and practice in many different regions. Contract physicians typically help meet patient demand or provide coverage during the hiring process as well as while staff are on vacation or maternity leave.
Says Mr. Adam, “There’s no security, but there’s higher income and more flexibility.”
According to CHG Healthcare, locum tenens staffing is rising – approximately 7% of U.S. physicians (around 50,000) filled assignments in 2022, up 88% from 2015. In 2022, 56% of locum tenens employers reported a reduction in staff burnout, up from 30% in 2020.
The report indicates that more than half of physicians are satisfied with their income, down slightly from 55% 5 years ago (prepandemic). Physicians in some of the lower-paying specialties are among those most satisfied with their income. It’s not very surprising to Mr. Adam: “Higher earners generally suffer the most from burnout.
“They’re overworked, they have the largest number of patients, and they’re performing in high-stress situations doing challenging procedures on a daily basis – and they probably have worse work-life balance.” These physicians know going in that they need to be paid more to deal with such burdens. “That’s the feedback I get when I speak to high earners,” says Mr. Adam.
“The experienced ones are very clear about their [compensation] expectations.”
A version of this article first appeared on Medscape.com.
In addition, gender-based pay disparity among primary care physicians shrank, and the number of physicians who declined to take new Medicare patients rose.
The annual report is based on a survey of more than 10,000 physicians in over 29 specialties who answered questions about their income, workload, challenges, and level of satisfaction.
Average compensation across specialties rose to $352,000 – up nearly 17% from the 2018 average of $299,000. Fallout from the COVID-19 public health emergency continued to affect both physician compensation and job satisfaction, including Medicare reimbursements and staffing shortages due to burnout or retirement.
“Many physicians reevaluated what drove them to be a physician,” says Marc Adam, a recruiter at MASC Medical, a Florida physician recruiting firm.
Adam cites telehealth as an example. “An overwhelming majority of physicians prefer telehealth because of the convenience, but some really did not want to do it long term. They miss the patient interaction.”
The report also revealed that the gender-based pay gap in primary physicians fell, with men earning 19% more – down from 25% more in recent years. Among specialists, the gender gap was 27% on average, down from 31% last year. One reason may be an increase in compensation transparency, which Mr. Adam says should be the norm.
Income increases will likely continue, owing in large part to the growing disparity between physician supply and demand.
The projected physician shortage is expected to grow to 124,000 by 2034, according to the American Association of Medical Colleges. Federal lawmakers are considering passing the Resident Physician Shortage Reduction Act of 2023, which would add 14,000 Medicare-funded residency positions to help alleviate shortages.
Patient needs, Medicare rules continue to shift
Specialties with the biggest increases in compensation include oncology, anesthesiology, gastroenterology, radiology, critical care, and urology. Many procedure-related specialties saw more volume post pandemic.
Some respondents identified Medicare cuts and low reimbursement rates as a factor in tamping down compensation hikes. The number of physicians who expect to continue to take new Medicare patients is 65%, down from 71% 5 years ago.
For example, Medicare reimbursements for telehealth are expected to scale down in May, when the COVID-19 Public Health Emergency, which expanded telehealth services for Medicare patients, winds down.
“Telehealth will still exist,” says Mr. Adam, “but certain requirements will shape it going forward.”
Medicare isn’t viewed negatively across the board, however. Florida is among the top-earning states for physicians – along with Indiana, Connecticut, and Missouri. One reason is Florida’s unique health care environment, explains Mr. Adam, whose Florida-based firm places physicians nationwide.
“Florida is very progressive in terms of health care. For one thing, we have a large aging population and a large Medicare population.” Several growing organizations that focus on quality-based care are based in Florida, including ChenMed and Cano Health. Add to that the fact that owners of Florida’s health care organizations don’t have to be physicians, he explains, and the stage is set for experimentation.
“Being able to segment tasks frees up physicians to be more focused on medicine and provide better care while other people focus on the business and innovation.”
If Florida’s high compensation ranking continues, it may help employers there fulfill a growing need. The state is among those expected to experience the largest physician shortages in 2030, along with California, Texas, Arizona, and Georgia.
Side gigs up, satisfaction (slightly) down
In general, physicians aren’t fazed by these challenges. Many reported taking side gigs, some for additional income. Even so, 73% say they would still choose medicine, and more than 90% of physicians in 10 specialties would choose their specialty again. Still, burnout and stressors have led some to stop practicing altogether.
More and more organizations are hiring “travel physicians,” Mr. Adam says, and more physicians are choosing to take contract work (“locum tenens”) and practice in many different regions. Contract physicians typically help meet patient demand or provide coverage during the hiring process as well as while staff are on vacation or maternity leave.
Says Mr. Adam, “There’s no security, but there’s higher income and more flexibility.”
According to CHG Healthcare, locum tenens staffing is rising – approximately 7% of U.S. physicians (around 50,000) filled assignments in 2022, up 88% from 2015. In 2022, 56% of locum tenens employers reported a reduction in staff burnout, up from 30% in 2020.
The report indicates that more than half of physicians are satisfied with their income, down slightly from 55% 5 years ago (prepandemic). Physicians in some of the lower-paying specialties are among those most satisfied with their income. It’s not very surprising to Mr. Adam: “Higher earners generally suffer the most from burnout.
“They’re overworked, they have the largest number of patients, and they’re performing in high-stress situations doing challenging procedures on a daily basis – and they probably have worse work-life balance.” These physicians know going in that they need to be paid more to deal with such burdens. “That’s the feedback I get when I speak to high earners,” says Mr. Adam.
“The experienced ones are very clear about their [compensation] expectations.”
A version of this article first appeared on Medscape.com.
In addition, gender-based pay disparity among primary care physicians shrank, and the number of physicians who declined to take new Medicare patients rose.
The annual report is based on a survey of more than 10,000 physicians in over 29 specialties who answered questions about their income, workload, challenges, and level of satisfaction.
Average compensation across specialties rose to $352,000 – up nearly 17% from the 2018 average of $299,000. Fallout from the COVID-19 public health emergency continued to affect both physician compensation and job satisfaction, including Medicare reimbursements and staffing shortages due to burnout or retirement.
“Many physicians reevaluated what drove them to be a physician,” says Marc Adam, a recruiter at MASC Medical, a Florida physician recruiting firm.
Adam cites telehealth as an example. “An overwhelming majority of physicians prefer telehealth because of the convenience, but some really did not want to do it long term. They miss the patient interaction.”
The report also revealed that the gender-based pay gap in primary physicians fell, with men earning 19% more – down from 25% more in recent years. Among specialists, the gender gap was 27% on average, down from 31% last year. One reason may be an increase in compensation transparency, which Mr. Adam says should be the norm.
Income increases will likely continue, owing in large part to the growing disparity between physician supply and demand.
The projected physician shortage is expected to grow to 124,000 by 2034, according to the American Association of Medical Colleges. Federal lawmakers are considering passing the Resident Physician Shortage Reduction Act of 2023, which would add 14,000 Medicare-funded residency positions to help alleviate shortages.
Patient needs, Medicare rules continue to shift
Specialties with the biggest increases in compensation include oncology, anesthesiology, gastroenterology, radiology, critical care, and urology. Many procedure-related specialties saw more volume post pandemic.
Some respondents identified Medicare cuts and low reimbursement rates as a factor in tamping down compensation hikes. The number of physicians who expect to continue to take new Medicare patients is 65%, down from 71% 5 years ago.
For example, Medicare reimbursements for telehealth are expected to scale down in May, when the COVID-19 Public Health Emergency, which expanded telehealth services for Medicare patients, winds down.
“Telehealth will still exist,” says Mr. Adam, “but certain requirements will shape it going forward.”
Medicare isn’t viewed negatively across the board, however. Florida is among the top-earning states for physicians – along with Indiana, Connecticut, and Missouri. One reason is Florida’s unique health care environment, explains Mr. Adam, whose Florida-based firm places physicians nationwide.
“Florida is very progressive in terms of health care. For one thing, we have a large aging population and a large Medicare population.” Several growing organizations that focus on quality-based care are based in Florida, including ChenMed and Cano Health. Add to that the fact that owners of Florida’s health care organizations don’t have to be physicians, he explains, and the stage is set for experimentation.
“Being able to segment tasks frees up physicians to be more focused on medicine and provide better care while other people focus on the business and innovation.”
If Florida’s high compensation ranking continues, it may help employers there fulfill a growing need. The state is among those expected to experience the largest physician shortages in 2030, along with California, Texas, Arizona, and Georgia.
Side gigs up, satisfaction (slightly) down
In general, physicians aren’t fazed by these challenges. Many reported taking side gigs, some for additional income. Even so, 73% say they would still choose medicine, and more than 90% of physicians in 10 specialties would choose their specialty again. Still, burnout and stressors have led some to stop practicing altogether.
More and more organizations are hiring “travel physicians,” Mr. Adam says, and more physicians are choosing to take contract work (“locum tenens”) and practice in many different regions. Contract physicians typically help meet patient demand or provide coverage during the hiring process as well as while staff are on vacation or maternity leave.
Says Mr. Adam, “There’s no security, but there’s higher income and more flexibility.”
According to CHG Healthcare, locum tenens staffing is rising – approximately 7% of U.S. physicians (around 50,000) filled assignments in 2022, up 88% from 2015. In 2022, 56% of locum tenens employers reported a reduction in staff burnout, up from 30% in 2020.
The report indicates that more than half of physicians are satisfied with their income, down slightly from 55% 5 years ago (prepandemic). Physicians in some of the lower-paying specialties are among those most satisfied with their income. It’s not very surprising to Mr. Adam: “Higher earners generally suffer the most from burnout.
“They’re overworked, they have the largest number of patients, and they’re performing in high-stress situations doing challenging procedures on a daily basis – and they probably have worse work-life balance.” These physicians know going in that they need to be paid more to deal with such burdens. “That’s the feedback I get when I speak to high earners,” says Mr. Adam.
“The experienced ones are very clear about their [compensation] expectations.”
A version of this article first appeared on Medscape.com.