User login
News and Views that Matter to Pediatricians
The leading independent newspaper covering news and commentary in pediatrics.
FDA to review PDE4-inhibitor roflumilast for psoriasis
The , according to a statement from the manufacturer.
Roflumilast cream (also known as ARQ-151) is a small molecule inhibitor of PDE4, an enzyme that increases proinflammatory mediators and decreases anti-inflammatory mediators. PDE4 is an established treatment target in dermatology: The FDA approved PDE-4 inhibitor crisaborole (Eucrisa) as a topical treatment for mild to moderate atopic dermatitis in 2016, and an oral PDE-4 inhibitor, orismilast, is being studied for the treatment of plaque psoriasis.
Topical roflumilast, if approved, would be the first topical PDE4 inhibitor for psoriasis in particular, according to the Arcutis Biotherapeutics statement. The cream is designed for use on the entire body, including the face and sensitive intertriginous areas.
The NDA is based on data from a pair of phase 3 randomized, double-blind 8-week studies known as DERMIS 1 and DERMIS 2 (Trials of PDE4 Inhibition with Roflumilast for the Management of Plaque Psoriasis” One and Two) and a long-term phase 2b open-label study.
DERMIS 1 and DERMIS 2 were identical multinational, multicenter studies designed to assess the safety and efficacy of 0.3% roflumilast cream. In the studies, roflumilast met its primary endpoint and patients treated with it demonstrated an Investigator Global Assessment (IGA) success rate of 42.4% compared with 6.1% for the vehicle control (P < .0001), and 37.5% compared with 6.9% for the vehicle control (P < .0001), in the DERMIS 1 and 2 trials, respectively, according to Arcutis.
In the phase 2b study, the treatment effect lasted for 52-64 weeks. Roflumilast was well tolerated across the three studies.
Overall, the most common adverse events reported in the studies were diarrhea (3%), headache (2%), insomnia (1%), nausea (1%), upper respiratory tract infections (1%), and urinary tract infections (1%).
Roflumilast also showed statistically significant improvement compared to a vehicle on secondary endpoints including Intertriginous IGA (I-IGA) Success, Psoriasis Area Severity Index-75 (PASI-75), reductions in itch as measured by the Worst Itch-Numerical Rating Scale (WI-NRS), and patient perceptions of symptoms based on the Psoriasis Symptoms Diary (PSD).
The FDA has set a Prescription Drug User Fee Act (PDUFA) target action date of July 29, 2022, according to the manufacturer’s statement. An oral formulation of roflumilast was approved by the FDA in 2011, for reducing the risk of exacerbations of chronic obstructive pulmonary disease (COPD) in patients with severe COPD.
The , according to a statement from the manufacturer.
Roflumilast cream (also known as ARQ-151) is a small molecule inhibitor of PDE4, an enzyme that increases proinflammatory mediators and decreases anti-inflammatory mediators. PDE4 is an established treatment target in dermatology: The FDA approved PDE-4 inhibitor crisaborole (Eucrisa) as a topical treatment for mild to moderate atopic dermatitis in 2016, and an oral PDE-4 inhibitor, orismilast, is being studied for the treatment of plaque psoriasis.
Topical roflumilast, if approved, would be the first topical PDE4 inhibitor for psoriasis in particular, according to the Arcutis Biotherapeutics statement. The cream is designed for use on the entire body, including the face and sensitive intertriginous areas.
The NDA is based on data from a pair of phase 3 randomized, double-blind 8-week studies known as DERMIS 1 and DERMIS 2 (Trials of PDE4 Inhibition with Roflumilast for the Management of Plaque Psoriasis” One and Two) and a long-term phase 2b open-label study.
DERMIS 1 and DERMIS 2 were identical multinational, multicenter studies designed to assess the safety and efficacy of 0.3% roflumilast cream. In the studies, roflumilast met its primary endpoint and patients treated with it demonstrated an Investigator Global Assessment (IGA) success rate of 42.4% compared with 6.1% for the vehicle control (P < .0001), and 37.5% compared with 6.9% for the vehicle control (P < .0001), in the DERMIS 1 and 2 trials, respectively, according to Arcutis.
In the phase 2b study, the treatment effect lasted for 52-64 weeks. Roflumilast was well tolerated across the three studies.
Overall, the most common adverse events reported in the studies were diarrhea (3%), headache (2%), insomnia (1%), nausea (1%), upper respiratory tract infections (1%), and urinary tract infections (1%).
Roflumilast also showed statistically significant improvement compared to a vehicle on secondary endpoints including Intertriginous IGA (I-IGA) Success, Psoriasis Area Severity Index-75 (PASI-75), reductions in itch as measured by the Worst Itch-Numerical Rating Scale (WI-NRS), and patient perceptions of symptoms based on the Psoriasis Symptoms Diary (PSD).
The FDA has set a Prescription Drug User Fee Act (PDUFA) target action date of July 29, 2022, according to the manufacturer’s statement. An oral formulation of roflumilast was approved by the FDA in 2011, for reducing the risk of exacerbations of chronic obstructive pulmonary disease (COPD) in patients with severe COPD.
The , according to a statement from the manufacturer.
Roflumilast cream (also known as ARQ-151) is a small molecule inhibitor of PDE4, an enzyme that increases proinflammatory mediators and decreases anti-inflammatory mediators. PDE4 is an established treatment target in dermatology: The FDA approved PDE-4 inhibitor crisaborole (Eucrisa) as a topical treatment for mild to moderate atopic dermatitis in 2016, and an oral PDE-4 inhibitor, orismilast, is being studied for the treatment of plaque psoriasis.
Topical roflumilast, if approved, would be the first topical PDE4 inhibitor for psoriasis in particular, according to the Arcutis Biotherapeutics statement. The cream is designed for use on the entire body, including the face and sensitive intertriginous areas.
The NDA is based on data from a pair of phase 3 randomized, double-blind 8-week studies known as DERMIS 1 and DERMIS 2 (Trials of PDE4 Inhibition with Roflumilast for the Management of Plaque Psoriasis” One and Two) and a long-term phase 2b open-label study.
DERMIS 1 and DERMIS 2 were identical multinational, multicenter studies designed to assess the safety and efficacy of 0.3% roflumilast cream. In the studies, roflumilast met its primary endpoint and patients treated with it demonstrated an Investigator Global Assessment (IGA) success rate of 42.4% compared with 6.1% for the vehicle control (P < .0001), and 37.5% compared with 6.9% for the vehicle control (P < .0001), in the DERMIS 1 and 2 trials, respectively, according to Arcutis.
In the phase 2b study, the treatment effect lasted for 52-64 weeks. Roflumilast was well tolerated across the three studies.
Overall, the most common adverse events reported in the studies were diarrhea (3%), headache (2%), insomnia (1%), nausea (1%), upper respiratory tract infections (1%), and urinary tract infections (1%).
Roflumilast also showed statistically significant improvement compared to a vehicle on secondary endpoints including Intertriginous IGA (I-IGA) Success, Psoriasis Area Severity Index-75 (PASI-75), reductions in itch as measured by the Worst Itch-Numerical Rating Scale (WI-NRS), and patient perceptions of symptoms based on the Psoriasis Symptoms Diary (PSD).
The FDA has set a Prescription Drug User Fee Act (PDUFA) target action date of July 29, 2022, according to the manufacturer’s statement. An oral formulation of roflumilast was approved by the FDA in 2011, for reducing the risk of exacerbations of chronic obstructive pulmonary disease (COPD) in patients with severe COPD.
COVID-19, sure, but what else will we remember 2021 for?
who answered a recent Medscape Medical News poll. Perhaps no surprise there.
Coming in distant second, at 26%, was the new law requiring that patients be granted electronic access to clinical notes. The controversial Food and Drug Administration approval of aducanumab (Aduhelm, Biogen/Eisai) to treat Alzheimer’s disease was next, cited by almost 16% when asked what they would remember most about 2021.
Coming in at 10% or less were the permanent end to the Step 2 Clinical Skills test, the JAMA deputy editor resignation over controversial comments, and an “other” option that allowed for write-in responses.
It should be noted respondents could choose up to three answers to this and other questions in this survey, except for questions about profession and specialty.
Exciting news in 2021
Widespread availability of COVID-19 vaccines was the No. 1 response – chosen by 85% – when asked what medical news or events excited them in 2021.
FDA clearance of a 5-minute test for early dementia was selected by 22%, followed by almost 16% citing approval in October 2021 of abemaciclib (Verzenio, Lilly) “described as the first advance for early breast cancer in 20 years.”
The resignation of JAMA editors over a podcast on race rounded out the list of exciting medical news or events – coming in fourth at 11%. A total 5% of readers chose “other” and were asked to specify what news or events excited them in 2021.
A frustrating year?
Medscape also asked readers what medical news or events frustrated them in 2021. A majority, 81%, chose COVID-19 vaccine hesitancy or refusal. Almost one-third, 31%, chose the effect of climate change on health worldwide.
Some of the most memorable news or events of 2021 were also selected as frustrating by readers. For example, 22% were frustrated by the law requiring that patients be granted electronic access to clinical notes, followed by 19% who referred to the aducanumab approval in June. Furthermore, about 12% selected the JAMA resignations.
A shocking survey question
Asked what medical news or event from 2021 shocked readers, COVID-19 vaccine hesitancy or refusal was the most common answer, at 69%.
The U.S. Preventive Services Task Force ruling out aspirin in people over age 60 for primary prevention of cardiovascular disease shocked 36% of respondents.
Coming in third and fourth on the survey were the two JAMA editors resigning after a podcast on race, chosen by 19%, and the demise of the Step 2 Clinical Skills test, selected by 18%.
Interestingly, almost 96% of respondents were physicians. Less than 1% were residents, physician assistants, or nurses. Respondents also represented a wide range of specialties. From a list of 29 possible specialties, including “other,” family medicine, internal medicine, and psychiatry were the most common.
For more on the year that was 2021, see the Medscape Year in Medicine 2021: News That Made a Difference slideshow. Read Medscape’s full Year in Medicine report.
Wondering what stood out most to our readers in 2020? Here is a story about the results of a similar survey 1 year ago.
A version of this article first appeared on Medscape.com.
who answered a recent Medscape Medical News poll. Perhaps no surprise there.
Coming in distant second, at 26%, was the new law requiring that patients be granted electronic access to clinical notes. The controversial Food and Drug Administration approval of aducanumab (Aduhelm, Biogen/Eisai) to treat Alzheimer’s disease was next, cited by almost 16% when asked what they would remember most about 2021.
Coming in at 10% or less were the permanent end to the Step 2 Clinical Skills test, the JAMA deputy editor resignation over controversial comments, and an “other” option that allowed for write-in responses.
It should be noted respondents could choose up to three answers to this and other questions in this survey, except for questions about profession and specialty.
Exciting news in 2021
Widespread availability of COVID-19 vaccines was the No. 1 response – chosen by 85% – when asked what medical news or events excited them in 2021.
FDA clearance of a 5-minute test for early dementia was selected by 22%, followed by almost 16% citing approval in October 2021 of abemaciclib (Verzenio, Lilly) “described as the first advance for early breast cancer in 20 years.”
The resignation of JAMA editors over a podcast on race rounded out the list of exciting medical news or events – coming in fourth at 11%. A total 5% of readers chose “other” and were asked to specify what news or events excited them in 2021.
A frustrating year?
Medscape also asked readers what medical news or events frustrated them in 2021. A majority, 81%, chose COVID-19 vaccine hesitancy or refusal. Almost one-third, 31%, chose the effect of climate change on health worldwide.
Some of the most memorable news or events of 2021 were also selected as frustrating by readers. For example, 22% were frustrated by the law requiring that patients be granted electronic access to clinical notes, followed by 19% who referred to the aducanumab approval in June. Furthermore, about 12% selected the JAMA resignations.
A shocking survey question
Asked what medical news or event from 2021 shocked readers, COVID-19 vaccine hesitancy or refusal was the most common answer, at 69%.
The U.S. Preventive Services Task Force ruling out aspirin in people over age 60 for primary prevention of cardiovascular disease shocked 36% of respondents.
Coming in third and fourth on the survey were the two JAMA editors resigning after a podcast on race, chosen by 19%, and the demise of the Step 2 Clinical Skills test, selected by 18%.
Interestingly, almost 96% of respondents were physicians. Less than 1% were residents, physician assistants, or nurses. Respondents also represented a wide range of specialties. From a list of 29 possible specialties, including “other,” family medicine, internal medicine, and psychiatry were the most common.
For more on the year that was 2021, see the Medscape Year in Medicine 2021: News That Made a Difference slideshow. Read Medscape’s full Year in Medicine report.
Wondering what stood out most to our readers in 2020? Here is a story about the results of a similar survey 1 year ago.
A version of this article first appeared on Medscape.com.
who answered a recent Medscape Medical News poll. Perhaps no surprise there.
Coming in distant second, at 26%, was the new law requiring that patients be granted electronic access to clinical notes. The controversial Food and Drug Administration approval of aducanumab (Aduhelm, Biogen/Eisai) to treat Alzheimer’s disease was next, cited by almost 16% when asked what they would remember most about 2021.
Coming in at 10% or less were the permanent end to the Step 2 Clinical Skills test, the JAMA deputy editor resignation over controversial comments, and an “other” option that allowed for write-in responses.
It should be noted respondents could choose up to three answers to this and other questions in this survey, except for questions about profession and specialty.
Exciting news in 2021
Widespread availability of COVID-19 vaccines was the No. 1 response – chosen by 85% – when asked what medical news or events excited them in 2021.
FDA clearance of a 5-minute test for early dementia was selected by 22%, followed by almost 16% citing approval in October 2021 of abemaciclib (Verzenio, Lilly) “described as the first advance for early breast cancer in 20 years.”
The resignation of JAMA editors over a podcast on race rounded out the list of exciting medical news or events – coming in fourth at 11%. A total 5% of readers chose “other” and were asked to specify what news or events excited them in 2021.
A frustrating year?
Medscape also asked readers what medical news or events frustrated them in 2021. A majority, 81%, chose COVID-19 vaccine hesitancy or refusal. Almost one-third, 31%, chose the effect of climate change on health worldwide.
Some of the most memorable news or events of 2021 were also selected as frustrating by readers. For example, 22% were frustrated by the law requiring that patients be granted electronic access to clinical notes, followed by 19% who referred to the aducanumab approval in June. Furthermore, about 12% selected the JAMA resignations.
A shocking survey question
Asked what medical news or event from 2021 shocked readers, COVID-19 vaccine hesitancy or refusal was the most common answer, at 69%.
The U.S. Preventive Services Task Force ruling out aspirin in people over age 60 for primary prevention of cardiovascular disease shocked 36% of respondents.
Coming in third and fourth on the survey were the two JAMA editors resigning after a podcast on race, chosen by 19%, and the demise of the Step 2 Clinical Skills test, selected by 18%.
Interestingly, almost 96% of respondents were physicians. Less than 1% were residents, physician assistants, or nurses. Respondents also represented a wide range of specialties. From a list of 29 possible specialties, including “other,” family medicine, internal medicine, and psychiatry were the most common.
For more on the year that was 2021, see the Medscape Year in Medicine 2021: News That Made a Difference slideshow. Read Medscape’s full Year in Medicine report.
Wondering what stood out most to our readers in 2020? Here is a story about the results of a similar survey 1 year ago.
A version of this article first appeared on Medscape.com.
Why patients should ditch cloth masks
Are you still wearing a cloth face mask?
Amid the rapidly spreading Omicron variant, experts stress that we all should swap cloth masks for N95 respirators or 3-ply surgical masks.
For background: N95 respirators are tightly fitting masks that cover your mouth and nose and help prevent contact with droplets and tiny particles in the air from people talking, coughing, sneezing, and spreading in other ways. Usually worn by health care workers and first responders, these masks can filter up to 95% of air droplets and particles, according to the CDC.
KN95 and KN94 masks are similar but are designed to meet international standards, unlike N95s that are approved by the Centers for Disease Control and Prevention’s National Institute for Occupational Safety and Health.
Meanwhile, a 3-ply surgical mask is a looser-fitting mask that can help prevent contact with infected droplets in the air.
But recommendations to opt for N95 and 3-ply surgical masks over cloth masks are nothing new, says Leana Wen, MD, an emergency doctor and public health professor at George Washington University, Washington.
In fact, public health experts have been urging stronger mask protection for months.
“It’s not just with Omicron that we need better masks, it was with Delta, it was with Alpha before that,” Dr. Wen said. “We have known for many months that COVID-19 is airborne, and therefore, a simple cloth mask is not going to cut it.”
Here’s what to know about these protective masks.
They’re necessary
Omicron is spreading much faster than previous COVID-19 variants. As it’s up to three times as likely to spread as the Delta variant, mask-wearing is paramount right now, says Anita Gupta, DO, an adjunct assistant professor of anesthesiology and critical care medicine and pain medicine at Johns Hopkins University, Baltimore.
The quality of a mask also matters a lot, said Dr. Wen.
“Double masking, including a well-fitting cloth mask on top of a surgical mask, adds additional protection,” she said. “Ideally, though, people should be wearing an N95, KN95, or KF94 when in indoor settings around other people with unknown vaccination status.”
If wearing an N95 mask causes extreme discomfort, wear it in high-risk settings where there are lots of people, like crowded restaurants and busy commuter trains, says Dr. Wen. “If you’re in a grocery store, there’s plenty of space and ventilation. You may not need an N95. I recommend that people obtain different masks and practice with them in low-risk settings before they go out in public in a high-risk setting.”
But people should wear a 3-ply surgical mask at the very least.
Three-ply surgical and N95 mask qualities
With 3-ply surgical masks, the fit of the mask is often more of an issue than its comfort, Dr. Wen said. But there are ways to adjust these masks, especially for those who have smaller heads.
“You can put a rubber band around the ear loops and make them a bit tighter,” said Dr. Wen. “Some people have found that using pins in their hair, that’s another way of keeping the loops in place.”
Another important tip on 3-ply surgical masks and N95s: These masks are reusable.
But how many times you should use them varies, Dr. Wen said. “As an example, if you are sweating a lot, and the mask is now really damp. Or putting it in your purse or backpack, and now it’s misshapen, and you cannot get it back to fit on your face, then it’s time to throw it away.”
Protection first
For some, cloth masks became somewhat of a statement, with people sporting logos of their favorite NFL team, or maybe even a fun animal print.
But you should always keep in mind the purpose of wearing a mask, Dr. Wen said. “Mask wearing is very functional and is about reducing your likelihood of contracting COVID. People should also use whatever methods inspire them, too, but for me, it’s purely a functional exercise.”
Mask wearing is not always enjoyable, but it remains critical in keeping people safe from COVID-19, especially the elderly and other high-risk people, Gupta says.
“There is lots of research and experts working hard to stop COVID-19,” she says. “It is important for all of us to remember that wearing a mask alone doesn’t make us safe.”
“We all need to keep washing our hands frequently and maintaining a distance from people, as well.”
For more information on where to find 3-ply surgical masks and N95s, check here or here to start.
A version of this article first appeared on WebMD.com.
Are you still wearing a cloth face mask?
Amid the rapidly spreading Omicron variant, experts stress that we all should swap cloth masks for N95 respirators or 3-ply surgical masks.
For background: N95 respirators are tightly fitting masks that cover your mouth and nose and help prevent contact with droplets and tiny particles in the air from people talking, coughing, sneezing, and spreading in other ways. Usually worn by health care workers and first responders, these masks can filter up to 95% of air droplets and particles, according to the CDC.
KN95 and KN94 masks are similar but are designed to meet international standards, unlike N95s that are approved by the Centers for Disease Control and Prevention’s National Institute for Occupational Safety and Health.
Meanwhile, a 3-ply surgical mask is a looser-fitting mask that can help prevent contact with infected droplets in the air.
But recommendations to opt for N95 and 3-ply surgical masks over cloth masks are nothing new, says Leana Wen, MD, an emergency doctor and public health professor at George Washington University, Washington.
In fact, public health experts have been urging stronger mask protection for months.
“It’s not just with Omicron that we need better masks, it was with Delta, it was with Alpha before that,” Dr. Wen said. “We have known for many months that COVID-19 is airborne, and therefore, a simple cloth mask is not going to cut it.”
Here’s what to know about these protective masks.
They’re necessary
Omicron is spreading much faster than previous COVID-19 variants. As it’s up to three times as likely to spread as the Delta variant, mask-wearing is paramount right now, says Anita Gupta, DO, an adjunct assistant professor of anesthesiology and critical care medicine and pain medicine at Johns Hopkins University, Baltimore.
The quality of a mask also matters a lot, said Dr. Wen.
“Double masking, including a well-fitting cloth mask on top of a surgical mask, adds additional protection,” she said. “Ideally, though, people should be wearing an N95, KN95, or KF94 when in indoor settings around other people with unknown vaccination status.”
If wearing an N95 mask causes extreme discomfort, wear it in high-risk settings where there are lots of people, like crowded restaurants and busy commuter trains, says Dr. Wen. “If you’re in a grocery store, there’s plenty of space and ventilation. You may not need an N95. I recommend that people obtain different masks and practice with them in low-risk settings before they go out in public in a high-risk setting.”
But people should wear a 3-ply surgical mask at the very least.
Three-ply surgical and N95 mask qualities
With 3-ply surgical masks, the fit of the mask is often more of an issue than its comfort, Dr. Wen said. But there are ways to adjust these masks, especially for those who have smaller heads.
“You can put a rubber band around the ear loops and make them a bit tighter,” said Dr. Wen. “Some people have found that using pins in their hair, that’s another way of keeping the loops in place.”
Another important tip on 3-ply surgical masks and N95s: These masks are reusable.
But how many times you should use them varies, Dr. Wen said. “As an example, if you are sweating a lot, and the mask is now really damp. Or putting it in your purse or backpack, and now it’s misshapen, and you cannot get it back to fit on your face, then it’s time to throw it away.”
Protection first
For some, cloth masks became somewhat of a statement, with people sporting logos of their favorite NFL team, or maybe even a fun animal print.
But you should always keep in mind the purpose of wearing a mask, Dr. Wen said. “Mask wearing is very functional and is about reducing your likelihood of contracting COVID. People should also use whatever methods inspire them, too, but for me, it’s purely a functional exercise.”
Mask wearing is not always enjoyable, but it remains critical in keeping people safe from COVID-19, especially the elderly and other high-risk people, Gupta says.
“There is lots of research and experts working hard to stop COVID-19,” she says. “It is important for all of us to remember that wearing a mask alone doesn’t make us safe.”
“We all need to keep washing our hands frequently and maintaining a distance from people, as well.”
For more information on where to find 3-ply surgical masks and N95s, check here or here to start.
A version of this article first appeared on WebMD.com.
Are you still wearing a cloth face mask?
Amid the rapidly spreading Omicron variant, experts stress that we all should swap cloth masks for N95 respirators or 3-ply surgical masks.
For background: N95 respirators are tightly fitting masks that cover your mouth and nose and help prevent contact with droplets and tiny particles in the air from people talking, coughing, sneezing, and spreading in other ways. Usually worn by health care workers and first responders, these masks can filter up to 95% of air droplets and particles, according to the CDC.
KN95 and KN94 masks are similar but are designed to meet international standards, unlike N95s that are approved by the Centers for Disease Control and Prevention’s National Institute for Occupational Safety and Health.
Meanwhile, a 3-ply surgical mask is a looser-fitting mask that can help prevent contact with infected droplets in the air.
But recommendations to opt for N95 and 3-ply surgical masks over cloth masks are nothing new, says Leana Wen, MD, an emergency doctor and public health professor at George Washington University, Washington.
In fact, public health experts have been urging stronger mask protection for months.
“It’s not just with Omicron that we need better masks, it was with Delta, it was with Alpha before that,” Dr. Wen said. “We have known for many months that COVID-19 is airborne, and therefore, a simple cloth mask is not going to cut it.”
Here’s what to know about these protective masks.
They’re necessary
Omicron is spreading much faster than previous COVID-19 variants. As it’s up to three times as likely to spread as the Delta variant, mask-wearing is paramount right now, says Anita Gupta, DO, an adjunct assistant professor of anesthesiology and critical care medicine and pain medicine at Johns Hopkins University, Baltimore.
The quality of a mask also matters a lot, said Dr. Wen.
“Double masking, including a well-fitting cloth mask on top of a surgical mask, adds additional protection,” she said. “Ideally, though, people should be wearing an N95, KN95, or KF94 when in indoor settings around other people with unknown vaccination status.”
If wearing an N95 mask causes extreme discomfort, wear it in high-risk settings where there are lots of people, like crowded restaurants and busy commuter trains, says Dr. Wen. “If you’re in a grocery store, there’s plenty of space and ventilation. You may not need an N95. I recommend that people obtain different masks and practice with them in low-risk settings before they go out in public in a high-risk setting.”
But people should wear a 3-ply surgical mask at the very least.
Three-ply surgical and N95 mask qualities
With 3-ply surgical masks, the fit of the mask is often more of an issue than its comfort, Dr. Wen said. But there are ways to adjust these masks, especially for those who have smaller heads.
“You can put a rubber band around the ear loops and make them a bit tighter,” said Dr. Wen. “Some people have found that using pins in their hair, that’s another way of keeping the loops in place.”
Another important tip on 3-ply surgical masks and N95s: These masks are reusable.
But how many times you should use them varies, Dr. Wen said. “As an example, if you are sweating a lot, and the mask is now really damp. Or putting it in your purse or backpack, and now it’s misshapen, and you cannot get it back to fit on your face, then it’s time to throw it away.”
Protection first
For some, cloth masks became somewhat of a statement, with people sporting logos of their favorite NFL team, or maybe even a fun animal print.
But you should always keep in mind the purpose of wearing a mask, Dr. Wen said. “Mask wearing is very functional and is about reducing your likelihood of contracting COVID. People should also use whatever methods inspire them, too, but for me, it’s purely a functional exercise.”
Mask wearing is not always enjoyable, but it remains critical in keeping people safe from COVID-19, especially the elderly and other high-risk people, Gupta says.
“There is lots of research and experts working hard to stop COVID-19,” she says. “It is important for all of us to remember that wearing a mask alone doesn’t make us safe.”
“We all need to keep washing our hands frequently and maintaining a distance from people, as well.”
For more information on where to find 3-ply surgical masks and N95s, check here or here to start.
A version of this article first appeared on WebMD.com.
COVID-19–positive or exposed? What to do next
With new cases of COVID-19 skyrocketing to more than 240,000 a day recently in the U.S., many people are facing the same situation: A family member or friend tests positive or was exposed to someone who did, and the holiday gathering, visit, or return to work is just days or hours away. Now what?
New guidance issued Dec. 27 by the Centers for Disease Control and Prevention shortens the recommended isolation and quarantine period for the general population, coming after the agency shortened the isolation period for health care workers.
This news organization reached out to two infectious disease specialists to get answers to questions that are frequently asked in these situations.
If you have tested positive for COVID-19, what do you do next?
“If you have tested positive, you are infected. At the moment, you are [either] symptomatically affected or presymptomatically infected,’’ said Paul A. Offit, MD, director of the Vaccine Education Center and professor of pediatrics at Children’s Hospital of Philadelphia. At that point, you need to isolate for 5 days, according to the new CDC guidance. (That period has been shortened from 10 days.)
Isolation means separating the infected person from others. Quarantine refers to things you should do if you’re exposed to the virus or you have a close contact infected with COVID-19.
Under the new CDC guidelines, after the 5-day isolation, if the infected person then has no symptoms, he or she can leave isolation and then wear a mask for 5 days.
Those who test positive also need to tell their close contacts they are positive, said Amesh Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security.
According to the CDC, the change to a shortened quarantine time is motivated by science ‘’demonstrating that the majority of SARS-CoV-2 transmission occurs early in the course of the illness, generally in the 1-2 days prior to onset of symptoms and the 2-3 days after.”
If you have been exposed to someone with COVID-19, what do you do next?
“If they are vaccinated and boosted, the guidance says there is no need to quarantine,” Dr. Adalja said. But the CDC guidance does recommend these people wear a well-fitting mask at all times when around others for 10 days after exposure.
For everyone else, including the unvaccinated and those who are more than 6 months out from their second Pfizer or Moderna vaccine dose, or more than 2 months from their J&J dose, the CDC recommends a quarantine for 5 days – and wearing a mask for the 5 days after that.
On a practical level, Dr. Adalja said he thinks those who are vaccinated but not boosted could also skip the quarantine and wear a mask for 10 days. Dr. Offit agrees. Because many people exposed have trouble quarantining, Dr. Offit advises those exposed who can’t follow that guidance to be sure to wear a mask for 10 days when indoors. The CDC guidance also offers that as another strategy – that if a 5-day quarantine is not feasible, the exposed person should wear a mask for 10 days when around others.
But if someone who was exposed gets symptoms, that person then enters the infected category and follows that guidance, Dr. Offit said.
When should the person who has been exposed get tested?
After the exposure, ‘’you should probably wait 2-3 days,” Dr. Offit said. “The virus has to reproduce itself.”
Testing should be done by those exposed at least once, Dr. Adalja said.
“But there’s data to support daily testing to guide their activities, but this is not CDC guidance. Home tests are sufficient for this purpose.”
At what point can the infected person mingle safely with others?
“Technically, if asymptomatic, 10 days without a mask, 5 days with a mask,” said Dr. Adalja. “I think this could also be guided with home test negativity being a gauge [as to whether to mingle].”
A version of this article first appeared on WebMD.com.
With new cases of COVID-19 skyrocketing to more than 240,000 a day recently in the U.S., many people are facing the same situation: A family member or friend tests positive or was exposed to someone who did, and the holiday gathering, visit, or return to work is just days or hours away. Now what?
New guidance issued Dec. 27 by the Centers for Disease Control and Prevention shortens the recommended isolation and quarantine period for the general population, coming after the agency shortened the isolation period for health care workers.
This news organization reached out to two infectious disease specialists to get answers to questions that are frequently asked in these situations.
If you have tested positive for COVID-19, what do you do next?
“If you have tested positive, you are infected. At the moment, you are [either] symptomatically affected or presymptomatically infected,’’ said Paul A. Offit, MD, director of the Vaccine Education Center and professor of pediatrics at Children’s Hospital of Philadelphia. At that point, you need to isolate for 5 days, according to the new CDC guidance. (That period has been shortened from 10 days.)
Isolation means separating the infected person from others. Quarantine refers to things you should do if you’re exposed to the virus or you have a close contact infected with COVID-19.
Under the new CDC guidelines, after the 5-day isolation, if the infected person then has no symptoms, he or she can leave isolation and then wear a mask for 5 days.
Those who test positive also need to tell their close contacts they are positive, said Amesh Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security.
According to the CDC, the change to a shortened quarantine time is motivated by science ‘’demonstrating that the majority of SARS-CoV-2 transmission occurs early in the course of the illness, generally in the 1-2 days prior to onset of symptoms and the 2-3 days after.”
If you have been exposed to someone with COVID-19, what do you do next?
“If they are vaccinated and boosted, the guidance says there is no need to quarantine,” Dr. Adalja said. But the CDC guidance does recommend these people wear a well-fitting mask at all times when around others for 10 days after exposure.
For everyone else, including the unvaccinated and those who are more than 6 months out from their second Pfizer or Moderna vaccine dose, or more than 2 months from their J&J dose, the CDC recommends a quarantine for 5 days – and wearing a mask for the 5 days after that.
On a practical level, Dr. Adalja said he thinks those who are vaccinated but not boosted could also skip the quarantine and wear a mask for 10 days. Dr. Offit agrees. Because many people exposed have trouble quarantining, Dr. Offit advises those exposed who can’t follow that guidance to be sure to wear a mask for 10 days when indoors. The CDC guidance also offers that as another strategy – that if a 5-day quarantine is not feasible, the exposed person should wear a mask for 10 days when around others.
But if someone who was exposed gets symptoms, that person then enters the infected category and follows that guidance, Dr. Offit said.
When should the person who has been exposed get tested?
After the exposure, ‘’you should probably wait 2-3 days,” Dr. Offit said. “The virus has to reproduce itself.”
Testing should be done by those exposed at least once, Dr. Adalja said.
“But there’s data to support daily testing to guide their activities, but this is not CDC guidance. Home tests are sufficient for this purpose.”
At what point can the infected person mingle safely with others?
“Technically, if asymptomatic, 10 days without a mask, 5 days with a mask,” said Dr. Adalja. “I think this could also be guided with home test negativity being a gauge [as to whether to mingle].”
A version of this article first appeared on WebMD.com.
With new cases of COVID-19 skyrocketing to more than 240,000 a day recently in the U.S., many people are facing the same situation: A family member or friend tests positive or was exposed to someone who did, and the holiday gathering, visit, or return to work is just days or hours away. Now what?
New guidance issued Dec. 27 by the Centers for Disease Control and Prevention shortens the recommended isolation and quarantine period for the general population, coming after the agency shortened the isolation period for health care workers.
This news organization reached out to two infectious disease specialists to get answers to questions that are frequently asked in these situations.
If you have tested positive for COVID-19, what do you do next?
“If you have tested positive, you are infected. At the moment, you are [either] symptomatically affected or presymptomatically infected,’’ said Paul A. Offit, MD, director of the Vaccine Education Center and professor of pediatrics at Children’s Hospital of Philadelphia. At that point, you need to isolate for 5 days, according to the new CDC guidance. (That period has been shortened from 10 days.)
Isolation means separating the infected person from others. Quarantine refers to things you should do if you’re exposed to the virus or you have a close contact infected with COVID-19.
Under the new CDC guidelines, after the 5-day isolation, if the infected person then has no symptoms, he or she can leave isolation and then wear a mask for 5 days.
Those who test positive also need to tell their close contacts they are positive, said Amesh Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security.
According to the CDC, the change to a shortened quarantine time is motivated by science ‘’demonstrating that the majority of SARS-CoV-2 transmission occurs early in the course of the illness, generally in the 1-2 days prior to onset of symptoms and the 2-3 days after.”
If you have been exposed to someone with COVID-19, what do you do next?
“If they are vaccinated and boosted, the guidance says there is no need to quarantine,” Dr. Adalja said. But the CDC guidance does recommend these people wear a well-fitting mask at all times when around others for 10 days after exposure.
For everyone else, including the unvaccinated and those who are more than 6 months out from their second Pfizer or Moderna vaccine dose, or more than 2 months from their J&J dose, the CDC recommends a quarantine for 5 days – and wearing a mask for the 5 days after that.
On a practical level, Dr. Adalja said he thinks those who are vaccinated but not boosted could also skip the quarantine and wear a mask for 10 days. Dr. Offit agrees. Because many people exposed have trouble quarantining, Dr. Offit advises those exposed who can’t follow that guidance to be sure to wear a mask for 10 days when indoors. The CDC guidance also offers that as another strategy – that if a 5-day quarantine is not feasible, the exposed person should wear a mask for 10 days when around others.
But if someone who was exposed gets symptoms, that person then enters the infected category and follows that guidance, Dr. Offit said.
When should the person who has been exposed get tested?
After the exposure, ‘’you should probably wait 2-3 days,” Dr. Offit said. “The virus has to reproduce itself.”
Testing should be done by those exposed at least once, Dr. Adalja said.
“But there’s data to support daily testing to guide their activities, but this is not CDC guidance. Home tests are sufficient for this purpose.”
At what point can the infected person mingle safely with others?
“Technically, if asymptomatic, 10 days without a mask, 5 days with a mask,” said Dr. Adalja. “I think this could also be guided with home test negativity being a gauge [as to whether to mingle].”
A version of this article first appeared on WebMD.com.
COVID-19 antigen tests may be less sensitive to Omicron: FDA
Rapid antigen tests for COVID-19 might be less effective at detecting the Omicron variant that is spreading rapidly across the United States, according to the Food and Drug Administration.
Early data suggest that COVID-19 antigen tests “do detect the Omicron variant but may have reduced sensitivity,” the FDA said in a statement posted Dec. 28 on its website.
The FDA is working with the National Institutes of Health’s Rapid Acceleration of Diagnostics (RADx) initiative to assess the performance of antigen tests with patient samples that have the Omicron variant.
The potential for antigen tests to be less sensitive for the Omicron variant emerged in tests using patient samples containing live virus, “which represents the best way to evaluate true test performance in the short term,” the FDA said.
Initial laboratory tests using heat-activated (killed) virus samples found that antigen tests were able to detect the Omicron variant.
“It is important to note that these laboratory data are not a replacement for clinical study evaluations using patient samples with live virus, which are ongoing. The FDA and RADx are continuing to further evaluate the performance of antigen tests using patient samples with live virus,” the FDA said.
Testing still important
The agency continues to recommend use of antigen tests as directed in the authorized labeling and in accordance with the instructions included with the tests.
They note that antigen tests are generally less sensitive and less likely to pick up very early infections, compared with molecular tests.
The FDA continues to recommend that an individual with a negative antigen test who has symptoms or a high likelihood of infection because of exposure follow-up with a molecular test to determine if they have COVID-19.
An individual with a positive antigen test should self-isolate and seek follow-up care with a health care provider to determine the next steps.
The FDA, with partners and test developers, are continuing to evaluate test sensitivity, as well as the best timing and frequency of antigen testing.
The agency said that it will provide updated information and any needed recommendations when appropriate.
A version of this article first appeared on Medscape.com.
Rapid antigen tests for COVID-19 might be less effective at detecting the Omicron variant that is spreading rapidly across the United States, according to the Food and Drug Administration.
Early data suggest that COVID-19 antigen tests “do detect the Omicron variant but may have reduced sensitivity,” the FDA said in a statement posted Dec. 28 on its website.
The FDA is working with the National Institutes of Health’s Rapid Acceleration of Diagnostics (RADx) initiative to assess the performance of antigen tests with patient samples that have the Omicron variant.
The potential for antigen tests to be less sensitive for the Omicron variant emerged in tests using patient samples containing live virus, “which represents the best way to evaluate true test performance in the short term,” the FDA said.
Initial laboratory tests using heat-activated (killed) virus samples found that antigen tests were able to detect the Omicron variant.
“It is important to note that these laboratory data are not a replacement for clinical study evaluations using patient samples with live virus, which are ongoing. The FDA and RADx are continuing to further evaluate the performance of antigen tests using patient samples with live virus,” the FDA said.
Testing still important
The agency continues to recommend use of antigen tests as directed in the authorized labeling and in accordance with the instructions included with the tests.
They note that antigen tests are generally less sensitive and less likely to pick up very early infections, compared with molecular tests.
The FDA continues to recommend that an individual with a negative antigen test who has symptoms or a high likelihood of infection because of exposure follow-up with a molecular test to determine if they have COVID-19.
An individual with a positive antigen test should self-isolate and seek follow-up care with a health care provider to determine the next steps.
The FDA, with partners and test developers, are continuing to evaluate test sensitivity, as well as the best timing and frequency of antigen testing.
The agency said that it will provide updated information and any needed recommendations when appropriate.
A version of this article first appeared on Medscape.com.
Rapid antigen tests for COVID-19 might be less effective at detecting the Omicron variant that is spreading rapidly across the United States, according to the Food and Drug Administration.
Early data suggest that COVID-19 antigen tests “do detect the Omicron variant but may have reduced sensitivity,” the FDA said in a statement posted Dec. 28 on its website.
The FDA is working with the National Institutes of Health’s Rapid Acceleration of Diagnostics (RADx) initiative to assess the performance of antigen tests with patient samples that have the Omicron variant.
The potential for antigen tests to be less sensitive for the Omicron variant emerged in tests using patient samples containing live virus, “which represents the best way to evaluate true test performance in the short term,” the FDA said.
Initial laboratory tests using heat-activated (killed) virus samples found that antigen tests were able to detect the Omicron variant.
“It is important to note that these laboratory data are not a replacement for clinical study evaluations using patient samples with live virus, which are ongoing. The FDA and RADx are continuing to further evaluate the performance of antigen tests using patient samples with live virus,” the FDA said.
Testing still important
The agency continues to recommend use of antigen tests as directed in the authorized labeling and in accordance with the instructions included with the tests.
They note that antigen tests are generally less sensitive and less likely to pick up very early infections, compared with molecular tests.
The FDA continues to recommend that an individual with a negative antigen test who has symptoms or a high likelihood of infection because of exposure follow-up with a molecular test to determine if they have COVID-19.
An individual with a positive antigen test should self-isolate and seek follow-up care with a health care provider to determine the next steps.
The FDA, with partners and test developers, are continuing to evaluate test sensitivity, as well as the best timing and frequency of antigen testing.
The agency said that it will provide updated information and any needed recommendations when appropriate.
A version of this article first appeared on Medscape.com.
Coronavirus can spread to heart, brain days after infection
The coronavirus that causes COVID-19 can spread to the heart and brain within days of infection and can survive for months in organs, according to a new study by the National Institutes of Health.
The virus can spread to almost every organ system in the body, which could contribute to the ongoing symptoms seen in “long COVID” patients, the study authors wrote. The study is considered one of the most comprehensive reviews of how the virus replicates in human cells and persists in the human body. It is under review for publication in the journal Nature.
“This is remarkably important work,” Ziyad Al-Aly, MD, director of the Clinical Epidemiology Center at the Veterans Affairs St. Louis Health Care System, told Bloomberg News. Dr. Al-Aly wasn’t involved with the NIH study but has researched the long-term effects of COVID-19.
“For a long time now, we have been scratching our heads and asking why long COVID seems to affect so many organ systems,” he said. “This paper sheds some light and may help explain why long COVID can occur even in people who had mild or asymptomatic acute disease.”
The NIH researchers sampled and analyzed tissues from autopsies on 44 patients who died after contracting the coronavirus during the first year of the pandemic. They found persistent virus particles in multiple parts of the body, including the heart and brain, for as long as 230 days after symptoms began. This could represent infection with defective virus particles, they said, which has also been seen in persistent infections among measles patients.
“We don’t yet know what burden of chronic illness will result in years to come,” Raina MacIntyre, PhD, a professor of global biosecurity at the University of New South Wales, Sydney, told Bloomberg News.
“Will we see young-onset cardiac failure in survivors or early-onset dementia?” she asked. “These are unanswered questions which call for a precautionary public health approach to mitigation of the spread of this virus.”
Unlike other COVID-19 autopsy research, the NIH team had a more comprehensive postmortem tissue collection process, which typically occurred within a day of the patient’s death, Bloomberg News reported. The researchers also used a variety of ways to preserve tissue to figure out viral levels. They were able to grow the virus collected from several tissues, including the heart, lungs, small intestine, and adrenal glands.
“Our results collectively show that, while the highest burden of SARS-CoV-2 is in the airways and lung, the virus can disseminate early during infection and infect cells throughout the entire body, including widely throughout the brain,” the study authors wrote.
A version of this article first appeared on WebMD.com.
The coronavirus that causes COVID-19 can spread to the heart and brain within days of infection and can survive for months in organs, according to a new study by the National Institutes of Health.
The virus can spread to almost every organ system in the body, which could contribute to the ongoing symptoms seen in “long COVID” patients, the study authors wrote. The study is considered one of the most comprehensive reviews of how the virus replicates in human cells and persists in the human body. It is under review for publication in the journal Nature.
“This is remarkably important work,” Ziyad Al-Aly, MD, director of the Clinical Epidemiology Center at the Veterans Affairs St. Louis Health Care System, told Bloomberg News. Dr. Al-Aly wasn’t involved with the NIH study but has researched the long-term effects of COVID-19.
“For a long time now, we have been scratching our heads and asking why long COVID seems to affect so many organ systems,” he said. “This paper sheds some light and may help explain why long COVID can occur even in people who had mild or asymptomatic acute disease.”
The NIH researchers sampled and analyzed tissues from autopsies on 44 patients who died after contracting the coronavirus during the first year of the pandemic. They found persistent virus particles in multiple parts of the body, including the heart and brain, for as long as 230 days after symptoms began. This could represent infection with defective virus particles, they said, which has also been seen in persistent infections among measles patients.
“We don’t yet know what burden of chronic illness will result in years to come,” Raina MacIntyre, PhD, a professor of global biosecurity at the University of New South Wales, Sydney, told Bloomberg News.
“Will we see young-onset cardiac failure in survivors or early-onset dementia?” she asked. “These are unanswered questions which call for a precautionary public health approach to mitigation of the spread of this virus.”
Unlike other COVID-19 autopsy research, the NIH team had a more comprehensive postmortem tissue collection process, which typically occurred within a day of the patient’s death, Bloomberg News reported. The researchers also used a variety of ways to preserve tissue to figure out viral levels. They were able to grow the virus collected from several tissues, including the heart, lungs, small intestine, and adrenal glands.
“Our results collectively show that, while the highest burden of SARS-CoV-2 is in the airways and lung, the virus can disseminate early during infection and infect cells throughout the entire body, including widely throughout the brain,” the study authors wrote.
A version of this article first appeared on WebMD.com.
The coronavirus that causes COVID-19 can spread to the heart and brain within days of infection and can survive for months in organs, according to a new study by the National Institutes of Health.
The virus can spread to almost every organ system in the body, which could contribute to the ongoing symptoms seen in “long COVID” patients, the study authors wrote. The study is considered one of the most comprehensive reviews of how the virus replicates in human cells and persists in the human body. It is under review for publication in the journal Nature.
“This is remarkably important work,” Ziyad Al-Aly, MD, director of the Clinical Epidemiology Center at the Veterans Affairs St. Louis Health Care System, told Bloomberg News. Dr. Al-Aly wasn’t involved with the NIH study but has researched the long-term effects of COVID-19.
“For a long time now, we have been scratching our heads and asking why long COVID seems to affect so many organ systems,” he said. “This paper sheds some light and may help explain why long COVID can occur even in people who had mild or asymptomatic acute disease.”
The NIH researchers sampled and analyzed tissues from autopsies on 44 patients who died after contracting the coronavirus during the first year of the pandemic. They found persistent virus particles in multiple parts of the body, including the heart and brain, for as long as 230 days after symptoms began. This could represent infection with defective virus particles, they said, which has also been seen in persistent infections among measles patients.
“We don’t yet know what burden of chronic illness will result in years to come,” Raina MacIntyre, PhD, a professor of global biosecurity at the University of New South Wales, Sydney, told Bloomberg News.
“Will we see young-onset cardiac failure in survivors or early-onset dementia?” she asked. “These are unanswered questions which call for a precautionary public health approach to mitigation of the spread of this virus.”
Unlike other COVID-19 autopsy research, the NIH team had a more comprehensive postmortem tissue collection process, which typically occurred within a day of the patient’s death, Bloomberg News reported. The researchers also used a variety of ways to preserve tissue to figure out viral levels. They were able to grow the virus collected from several tissues, including the heart, lungs, small intestine, and adrenal glands.
“Our results collectively show that, while the highest burden of SARS-CoV-2 is in the airways and lung, the virus can disseminate early during infection and infect cells throughout the entire body, including widely throughout the brain,” the study authors wrote.
A version of this article first appeared on WebMD.com.
Children and COVID: Nearly 200,000 new cases reported in 1 week
, according to the American Academy of Pediatrics and the Children’s Hospital Association.
Available state data show that 198,551 child COVID cases were added during the week of Dec. 17-23 – up by 16.8% from the nearly 170,000 new cases reported the previous week and the highest 7-day figure since Sept. 17-23, when 207,000 cases were reported, the AAP and the CHA said in their weekly COVID report. Since Oct. 22-28, when the weekly count dropped to a seasonal low, the weekly count has nearly doubled.
The largest shares of the nearly 199,000 new cases were divided pretty equally between the Northeast and the South, while the West had just a small bump in cases and the Midwest was in the middle. The largest statewide percent increases came in the New England states, along with New Jersey, the District of Columbia, and Puerto Rico. New York State does not report age ranges for COVID cases, the AAP/CHA report noted.
Emergency department visits and hospital admissions are following a similar trend, as both have risen considerably over the last 2 months, data from the Centers for Disease Control and Prevention show.
COVID-related ED visits for children aged 0-11 years – measured as a proportion of all ED visits – are nearing the pandemic high of 4.1% set in late August, while visits in 12- to 15-year-olds have risen from 1.4% in early November to 5.6% on Dec. 24 and 16- to 17-year-olds have gone from 1.5% to 6% over the same period of time, the CDC reported on its COVID Data Tracker.
As for hospital admissions in children aged 0-17 years, the rate was down to 0.19 per 100,000 population on Nov. 11 but had risen to 0.38 per 100,000 as of Dec. 24. The highest point reached in children during the pandemic was 0.46 per 100,000 in early September, the CDC said.
On Dec. 23, 367 children were admitted to hospitals in the United States, the highest number since Sept. 7, when 374 were hospitalized. The highest 1-day total over the course of the pandemic, 394, came just a week before that, Aug. 31, according to the Department of Health & Human Services.
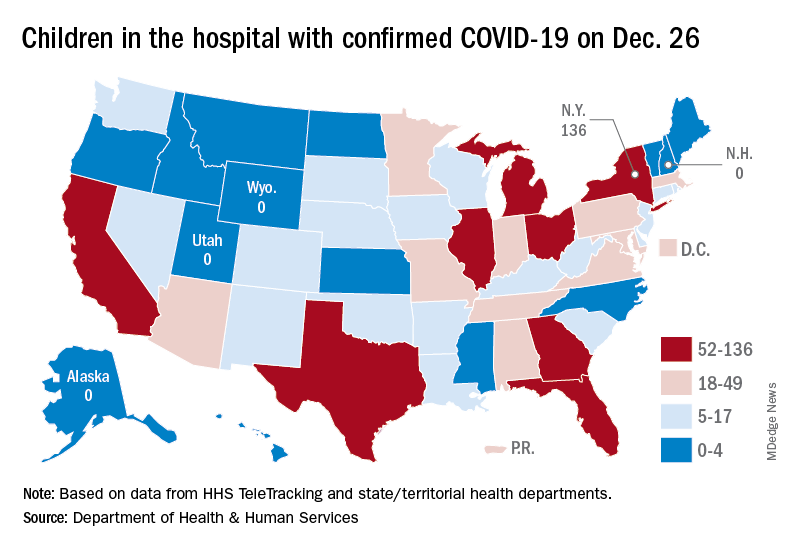
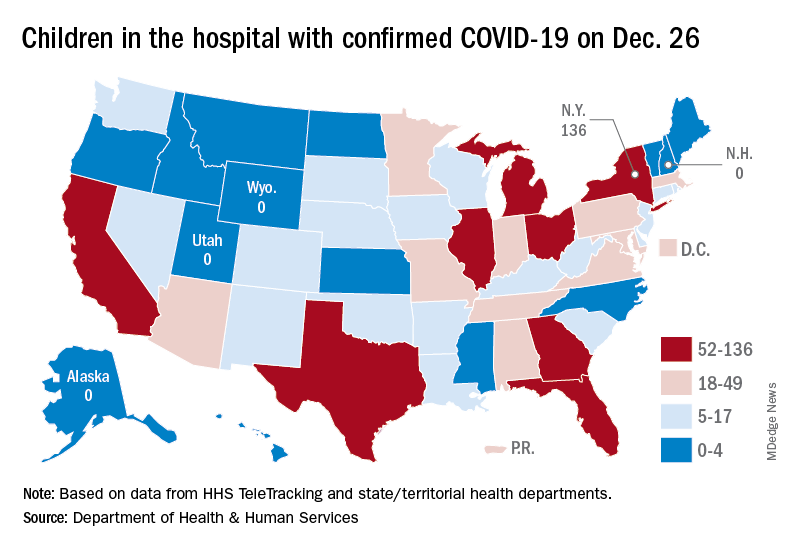
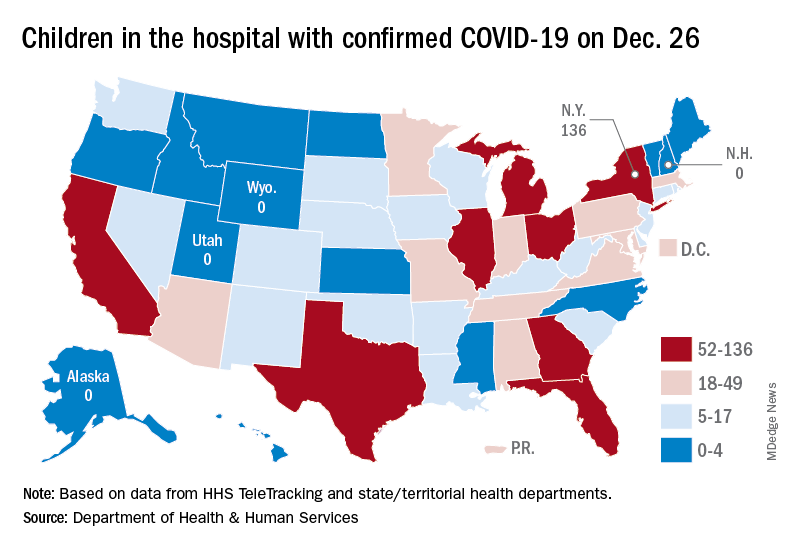
A look at the most recent HHS data shows that 1,161 children were being hospitalized in pediatric inpatient beds with confirmed COVID-19 on Dec. 26. The highest number by state was in New York (136), followed by Texas (90) and Illinois and Ohio, both with 83. There were four states – Alaska, New Hampshire, Utah, and Wyoming – with no hospitalized children, the HHS said. Puerto Rico, meanwhile, had 28 children in the hospital with COVID, more than 38 states.
, according to the American Academy of Pediatrics and the Children’s Hospital Association.
Available state data show that 198,551 child COVID cases were added during the week of Dec. 17-23 – up by 16.8% from the nearly 170,000 new cases reported the previous week and the highest 7-day figure since Sept. 17-23, when 207,000 cases were reported, the AAP and the CHA said in their weekly COVID report. Since Oct. 22-28, when the weekly count dropped to a seasonal low, the weekly count has nearly doubled.
The largest shares of the nearly 199,000 new cases were divided pretty equally between the Northeast and the South, while the West had just a small bump in cases and the Midwest was in the middle. The largest statewide percent increases came in the New England states, along with New Jersey, the District of Columbia, and Puerto Rico. New York State does not report age ranges for COVID cases, the AAP/CHA report noted.
Emergency department visits and hospital admissions are following a similar trend, as both have risen considerably over the last 2 months, data from the Centers for Disease Control and Prevention show.
COVID-related ED visits for children aged 0-11 years – measured as a proportion of all ED visits – are nearing the pandemic high of 4.1% set in late August, while visits in 12- to 15-year-olds have risen from 1.4% in early November to 5.6% on Dec. 24 and 16- to 17-year-olds have gone from 1.5% to 6% over the same period of time, the CDC reported on its COVID Data Tracker.
As for hospital admissions in children aged 0-17 years, the rate was down to 0.19 per 100,000 population on Nov. 11 but had risen to 0.38 per 100,000 as of Dec. 24. The highest point reached in children during the pandemic was 0.46 per 100,000 in early September, the CDC said.
On Dec. 23, 367 children were admitted to hospitals in the United States, the highest number since Sept. 7, when 374 were hospitalized. The highest 1-day total over the course of the pandemic, 394, came just a week before that, Aug. 31, according to the Department of Health & Human Services.
A look at the most recent HHS data shows that 1,161 children were being hospitalized in pediatric inpatient beds with confirmed COVID-19 on Dec. 26. The highest number by state was in New York (136), followed by Texas (90) and Illinois and Ohio, both with 83. There were four states – Alaska, New Hampshire, Utah, and Wyoming – with no hospitalized children, the HHS said. Puerto Rico, meanwhile, had 28 children in the hospital with COVID, more than 38 states.
, according to the American Academy of Pediatrics and the Children’s Hospital Association.
Available state data show that 198,551 child COVID cases were added during the week of Dec. 17-23 – up by 16.8% from the nearly 170,000 new cases reported the previous week and the highest 7-day figure since Sept. 17-23, when 207,000 cases were reported, the AAP and the CHA said in their weekly COVID report. Since Oct. 22-28, when the weekly count dropped to a seasonal low, the weekly count has nearly doubled.
The largest shares of the nearly 199,000 new cases were divided pretty equally between the Northeast and the South, while the West had just a small bump in cases and the Midwest was in the middle. The largest statewide percent increases came in the New England states, along with New Jersey, the District of Columbia, and Puerto Rico. New York State does not report age ranges for COVID cases, the AAP/CHA report noted.
Emergency department visits and hospital admissions are following a similar trend, as both have risen considerably over the last 2 months, data from the Centers for Disease Control and Prevention show.
COVID-related ED visits for children aged 0-11 years – measured as a proportion of all ED visits – are nearing the pandemic high of 4.1% set in late August, while visits in 12- to 15-year-olds have risen from 1.4% in early November to 5.6% on Dec. 24 and 16- to 17-year-olds have gone from 1.5% to 6% over the same period of time, the CDC reported on its COVID Data Tracker.
As for hospital admissions in children aged 0-17 years, the rate was down to 0.19 per 100,000 population on Nov. 11 but had risen to 0.38 per 100,000 as of Dec. 24. The highest point reached in children during the pandemic was 0.46 per 100,000 in early September, the CDC said.
On Dec. 23, 367 children were admitted to hospitals in the United States, the highest number since Sept. 7, when 374 were hospitalized. The highest 1-day total over the course of the pandemic, 394, came just a week before that, Aug. 31, according to the Department of Health & Human Services.
A look at the most recent HHS data shows that 1,161 children were being hospitalized in pediatric inpatient beds with confirmed COVID-19 on Dec. 26. The highest number by state was in New York (136), followed by Texas (90) and Illinois and Ohio, both with 83. There were four states – Alaska, New Hampshire, Utah, and Wyoming – with no hospitalized children, the HHS said. Puerto Rico, meanwhile, had 28 children in the hospital with COVID, more than 38 states.
COVID booster protection may wane in about 10 weeks, new data show
, according to new data from Britain.
U.K. health officials shared the data just before Christmas and noted that there haven’t been enough severe cases of the Omicron variant to calculate how well boosters protect against severe disease. But they believe the extra shots provide significant protection against hospitalization and death.
“It will be a few weeks before effectiveness against severe disease with Omicron can be estimated,” U.K. Health Security Agency officials wrote in the report. “However, based on experience with previous variants, this is likely to be substantially higher than the estimates against symptomatic disease.”
Since countries began reporting Omicron cases in November, multiple studies have suggested the variant is better at escaping antibodies from vaccination and previous infection, according to the New York Times. The U.K. report adds to that, noting that both the initial vaccine series and booster doses were less effective and faded faster against the Omicron variant than the Delta variant.
Among those who received two doses of the AstraZeneca vaccine, a booster of the Pfizer or Moderna vaccine was 60% effective at preventing symptomatic disease 2 to 4 weeks after the shot. But after 10 weeks, the Pfizer booster was 35% effective, and the Moderna booster was 45% effective. (The AstraZeneca vaccine is not authorized in the United States, but the Johnson & Johnson shot uses a similar technology, the New York Times reported.)
Among those who received three Pfizer doses, vaccine effectiveness was 70% about a week after the booster but dropped to 45% after 10 weeks. At the same time, those who received an initial two-dose series of the Pfizer vaccine and then a Moderna booster seemed to have 75% effectiveness up to 9 weeks.
The report was based on an analysis of 148,000 Delta cases and 68,000 Omicron cases in the United Kingdom through Dec. 20. So far, the U.K. health officials wrote, Omicron infections appear to be less severe and less likely to lead to hospitalization than Delta infections. At that time, 132 people with lab-confirmed Omicron had been admitted to hospitals, and 14 deaths had been reported among ages 52-96.
“This analysis is preliminary because of the small numbers of Omicron cases currently in hospital and the limited spread of Omicron into older age groups as yet,” the report said.
The reinfection rate has also increased for the Omicron variant, the report found. Among the 116,000 people who had an Omicron infection, about 11,000 -- or 9.5% -- were linked to a previously confirmed infection, which is likely an undercount of reinfections. In the data analyzed, 69 Omicron cases were a third episode of COVID-19 infection, and 290 cases occurred 60-89 days after a first infection.
A version of this article first appeared on WebMD.com.
, according to new data from Britain.
U.K. health officials shared the data just before Christmas and noted that there haven’t been enough severe cases of the Omicron variant to calculate how well boosters protect against severe disease. But they believe the extra shots provide significant protection against hospitalization and death.
“It will be a few weeks before effectiveness against severe disease with Omicron can be estimated,” U.K. Health Security Agency officials wrote in the report. “However, based on experience with previous variants, this is likely to be substantially higher than the estimates against symptomatic disease.”
Since countries began reporting Omicron cases in November, multiple studies have suggested the variant is better at escaping antibodies from vaccination and previous infection, according to the New York Times. The U.K. report adds to that, noting that both the initial vaccine series and booster doses were less effective and faded faster against the Omicron variant than the Delta variant.
Among those who received two doses of the AstraZeneca vaccine, a booster of the Pfizer or Moderna vaccine was 60% effective at preventing symptomatic disease 2 to 4 weeks after the shot. But after 10 weeks, the Pfizer booster was 35% effective, and the Moderna booster was 45% effective. (The AstraZeneca vaccine is not authorized in the United States, but the Johnson & Johnson shot uses a similar technology, the New York Times reported.)
Among those who received three Pfizer doses, vaccine effectiveness was 70% about a week after the booster but dropped to 45% after 10 weeks. At the same time, those who received an initial two-dose series of the Pfizer vaccine and then a Moderna booster seemed to have 75% effectiveness up to 9 weeks.
The report was based on an analysis of 148,000 Delta cases and 68,000 Omicron cases in the United Kingdom through Dec. 20. So far, the U.K. health officials wrote, Omicron infections appear to be less severe and less likely to lead to hospitalization than Delta infections. At that time, 132 people with lab-confirmed Omicron had been admitted to hospitals, and 14 deaths had been reported among ages 52-96.
“This analysis is preliminary because of the small numbers of Omicron cases currently in hospital and the limited spread of Omicron into older age groups as yet,” the report said.
The reinfection rate has also increased for the Omicron variant, the report found. Among the 116,000 people who had an Omicron infection, about 11,000 -- or 9.5% -- were linked to a previously confirmed infection, which is likely an undercount of reinfections. In the data analyzed, 69 Omicron cases were a third episode of COVID-19 infection, and 290 cases occurred 60-89 days after a first infection.
A version of this article first appeared on WebMD.com.
, according to new data from Britain.
U.K. health officials shared the data just before Christmas and noted that there haven’t been enough severe cases of the Omicron variant to calculate how well boosters protect against severe disease. But they believe the extra shots provide significant protection against hospitalization and death.
“It will be a few weeks before effectiveness against severe disease with Omicron can be estimated,” U.K. Health Security Agency officials wrote in the report. “However, based on experience with previous variants, this is likely to be substantially higher than the estimates against symptomatic disease.”
Since countries began reporting Omicron cases in November, multiple studies have suggested the variant is better at escaping antibodies from vaccination and previous infection, according to the New York Times. The U.K. report adds to that, noting that both the initial vaccine series and booster doses were less effective and faded faster against the Omicron variant than the Delta variant.
Among those who received two doses of the AstraZeneca vaccine, a booster of the Pfizer or Moderna vaccine was 60% effective at preventing symptomatic disease 2 to 4 weeks after the shot. But after 10 weeks, the Pfizer booster was 35% effective, and the Moderna booster was 45% effective. (The AstraZeneca vaccine is not authorized in the United States, but the Johnson & Johnson shot uses a similar technology, the New York Times reported.)
Among those who received three Pfizer doses, vaccine effectiveness was 70% about a week after the booster but dropped to 45% after 10 weeks. At the same time, those who received an initial two-dose series of the Pfizer vaccine and then a Moderna booster seemed to have 75% effectiveness up to 9 weeks.
The report was based on an analysis of 148,000 Delta cases and 68,000 Omicron cases in the United Kingdom through Dec. 20. So far, the U.K. health officials wrote, Omicron infections appear to be less severe and less likely to lead to hospitalization than Delta infections. At that time, 132 people with lab-confirmed Omicron had been admitted to hospitals, and 14 deaths had been reported among ages 52-96.
“This analysis is preliminary because of the small numbers of Omicron cases currently in hospital and the limited spread of Omicron into older age groups as yet,” the report said.
The reinfection rate has also increased for the Omicron variant, the report found. Among the 116,000 people who had an Omicron infection, about 11,000 -- or 9.5% -- were linked to a previously confirmed infection, which is likely an undercount of reinfections. In the data analyzed, 69 Omicron cases were a third episode of COVID-19 infection, and 290 cases occurred 60-89 days after a first infection.
A version of this article first appeared on WebMD.com.
Remdesivir may keep unvaccinated out of the hospital: Study
The antiviral remdesivir, an intravenous drug given mostly to seriously ill COVID-19 patients in hospitals, could keep unvaccinated people who become infected out of the hospital if given on an outpatient basis, a new study says.
Researchers studied 562 unvaccinated people from September 2020 to April 2021, according to the study published in the New England Journal of Medicine. The study determined the risk of hospitalization or death was 87% lower in study participants who were given remdesivir than participants who received a placebo.
All participants were at high risk of developing severe COVID-19 because of their age – they were over 60 – or because they had an underlying medical condition such as diabetes or obesity.
An important caveat: The findings are based on data collected before the Delta variant surged in the summer of 2021 or the Omicron variant surged late in the year, the Washington Post reported.
The new study says the drug could be helpful in keeping vaccinated as well as unvaccinated people out of the hospital – an important factor as the Omicron surge threatens to overwhelm health systems around the world.
Remdesivir could be a boon for COVID-19 patients in parts of the world that don’t have vaccines or for patients with immunocompromised systems.
“These data provide evidence that a 3-day course of remdesivir could play a critical role in helping COVID-19 patients stay out of the hospital,” Robert L. Gottlieb, MD, PhD, the therapeutic lead for COVID-19 research at Baylor Scott & White Health in Dallas, said in a news release from Gilead Pharmaceuticals. “While our hospitals are ready to assist patients in need, prevention and early intervention are preferable to reduce the risk of disease progression and allow patients not requiring oxygen to recover from home when appropriate.”
Remdesivir was the first antiviral for COVID-19 authorized by the Food and Drug Administration. It was given to then-President Donald Trump when he was hospitalized with COVID-19 in October 2020.
Gilead released the study findings in September.
A version of this article first appeared on WebMD.com.
The antiviral remdesivir, an intravenous drug given mostly to seriously ill COVID-19 patients in hospitals, could keep unvaccinated people who become infected out of the hospital if given on an outpatient basis, a new study says.
Researchers studied 562 unvaccinated people from September 2020 to April 2021, according to the study published in the New England Journal of Medicine. The study determined the risk of hospitalization or death was 87% lower in study participants who were given remdesivir than participants who received a placebo.
All participants were at high risk of developing severe COVID-19 because of their age – they were over 60 – or because they had an underlying medical condition such as diabetes or obesity.
An important caveat: The findings are based on data collected before the Delta variant surged in the summer of 2021 or the Omicron variant surged late in the year, the Washington Post reported.
The new study says the drug could be helpful in keeping vaccinated as well as unvaccinated people out of the hospital – an important factor as the Omicron surge threatens to overwhelm health systems around the world.
Remdesivir could be a boon for COVID-19 patients in parts of the world that don’t have vaccines or for patients with immunocompromised systems.
“These data provide evidence that a 3-day course of remdesivir could play a critical role in helping COVID-19 patients stay out of the hospital,” Robert L. Gottlieb, MD, PhD, the therapeutic lead for COVID-19 research at Baylor Scott & White Health in Dallas, said in a news release from Gilead Pharmaceuticals. “While our hospitals are ready to assist patients in need, prevention and early intervention are preferable to reduce the risk of disease progression and allow patients not requiring oxygen to recover from home when appropriate.”
Remdesivir was the first antiviral for COVID-19 authorized by the Food and Drug Administration. It was given to then-President Donald Trump when he was hospitalized with COVID-19 in October 2020.
Gilead released the study findings in September.
A version of this article first appeared on WebMD.com.
The antiviral remdesivir, an intravenous drug given mostly to seriously ill COVID-19 patients in hospitals, could keep unvaccinated people who become infected out of the hospital if given on an outpatient basis, a new study says.
Researchers studied 562 unvaccinated people from September 2020 to April 2021, according to the study published in the New England Journal of Medicine. The study determined the risk of hospitalization or death was 87% lower in study participants who were given remdesivir than participants who received a placebo.
All participants were at high risk of developing severe COVID-19 because of their age – they were over 60 – or because they had an underlying medical condition such as diabetes or obesity.
An important caveat: The findings are based on data collected before the Delta variant surged in the summer of 2021 or the Omicron variant surged late in the year, the Washington Post reported.
The new study says the drug could be helpful in keeping vaccinated as well as unvaccinated people out of the hospital – an important factor as the Omicron surge threatens to overwhelm health systems around the world.
Remdesivir could be a boon for COVID-19 patients in parts of the world that don’t have vaccines or for patients with immunocompromised systems.
“These data provide evidence that a 3-day course of remdesivir could play a critical role in helping COVID-19 patients stay out of the hospital,” Robert L. Gottlieb, MD, PhD, the therapeutic lead for COVID-19 research at Baylor Scott & White Health in Dallas, said in a news release from Gilead Pharmaceuticals. “While our hospitals are ready to assist patients in need, prevention and early intervention are preferable to reduce the risk of disease progression and allow patients not requiring oxygen to recover from home when appropriate.”
Remdesivir was the first antiviral for COVID-19 authorized by the Food and Drug Administration. It was given to then-President Donald Trump when he was hospitalized with COVID-19 in October 2020.
Gilead released the study findings in September.
A version of this article first appeared on WebMD.com.
Tap of the brakes on gender-affirming care
In the November 2021 issue of Pediatric News are two stories that on the surface present viewpoints that couldn’t be more divergent. On page 1 under the headline “Gender dysphoria” you will read about a position statement by the Royal Australian and New Zealand College of Psychiatrists (RANZCP) in which they strongly recommend a mental health evaluation for any child or adolescent with gender dysphoria “before any firm decisions are made on whether to prescribe hormonal treatments to transition, or perform surgeries.”
On page 6 is another story titled “Gender-affirming care ‘can save lives’ new research shows” that reports on a research study in which transgender and binary young people who received a year of gender-affirming care experienced less depression and fewer suicidal thoughts. Dr. David J. Inwards-Breland, chief of adolescent and young adult medicine at Rady Children’s Hospital in San Diego and one of the authors of the study is quoted as saying “The younger we can provide gender-affirming care, the less likely [our patients are] to have depression and then negative outcomes.” One can’t avoid the impression that he is in favor of moving ahead without delay in prescribing gender-affirming care.
Where does the new recommendation by the RANZCP fit in with this sense of urgency? Does requiring a mental health evaluation constitute a delay in the institution of gender-affirming care that could increase the risk of negative mental health outcomes for gender dysphoric patients?
In one of the final paragraphs in the Pediatric News article one learns that Dr. Inwards-Breland would agree with the folks of RANZCP. He acknowledges that his study relied on screening and not diagnostic testing and says that “future studies should look at a mental health evaluation and diagnosis by a mental health provider.”
When we drill into the details there are two issues that demand clarification. First, what kind of time course are we talking about for a mental health evaluation? Are we talking weeks, or months, hopefully not years? This of course depends on the availability of mental health services for the specific patient and the depth of the evaluation required. How long a delay is acceptable?
Second, will the evaluation be performed by a provider free of bias? Can it be performed without creating the impression that the patient needs to see a mental health provider because there is something wrong with being trans and we can fix it? One would hope these evaluations would be performed in the spirit of wanting to learn more about the patient with the goal of making the process go more smoothly.
Listening to neighborhood discussions around the fire pit I find that the RANZCP plea for a broader and deeper look at each gender-dysphoric child strikes a chord with the general population. More and more people are realizing that gender-dysphoria happens and that for too long it was closeted with unfortunate consequences. However, there is a feeling, in fact one in which I share, that the rapid rise in its prevalence contains an element of social contagion. And, some irreversible decisions are being made without sufficient consideration. This may or not be a valid concern but it seems to me a thorough and sensitively done mental health evaluation might minimize the collateral damage from some gender-affirming care and at least help those patients for whom it is prescribed transition more smoothly.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
In the November 2021 issue of Pediatric News are two stories that on the surface present viewpoints that couldn’t be more divergent. On page 1 under the headline “Gender dysphoria” you will read about a position statement by the Royal Australian and New Zealand College of Psychiatrists (RANZCP) in which they strongly recommend a mental health evaluation for any child or adolescent with gender dysphoria “before any firm decisions are made on whether to prescribe hormonal treatments to transition, or perform surgeries.”
On page 6 is another story titled “Gender-affirming care ‘can save lives’ new research shows” that reports on a research study in which transgender and binary young people who received a year of gender-affirming care experienced less depression and fewer suicidal thoughts. Dr. David J. Inwards-Breland, chief of adolescent and young adult medicine at Rady Children’s Hospital in San Diego and one of the authors of the study is quoted as saying “The younger we can provide gender-affirming care, the less likely [our patients are] to have depression and then negative outcomes.” One can’t avoid the impression that he is in favor of moving ahead without delay in prescribing gender-affirming care.
Where does the new recommendation by the RANZCP fit in with this sense of urgency? Does requiring a mental health evaluation constitute a delay in the institution of gender-affirming care that could increase the risk of negative mental health outcomes for gender dysphoric patients?
In one of the final paragraphs in the Pediatric News article one learns that Dr. Inwards-Breland would agree with the folks of RANZCP. He acknowledges that his study relied on screening and not diagnostic testing and says that “future studies should look at a mental health evaluation and diagnosis by a mental health provider.”
When we drill into the details there are two issues that demand clarification. First, what kind of time course are we talking about for a mental health evaluation? Are we talking weeks, or months, hopefully not years? This of course depends on the availability of mental health services for the specific patient and the depth of the evaluation required. How long a delay is acceptable?
Second, will the evaluation be performed by a provider free of bias? Can it be performed without creating the impression that the patient needs to see a mental health provider because there is something wrong with being trans and we can fix it? One would hope these evaluations would be performed in the spirit of wanting to learn more about the patient with the goal of making the process go more smoothly.
Listening to neighborhood discussions around the fire pit I find that the RANZCP plea for a broader and deeper look at each gender-dysphoric child strikes a chord with the general population. More and more people are realizing that gender-dysphoria happens and that for too long it was closeted with unfortunate consequences. However, there is a feeling, in fact one in which I share, that the rapid rise in its prevalence contains an element of social contagion. And, some irreversible decisions are being made without sufficient consideration. This may or not be a valid concern but it seems to me a thorough and sensitively done mental health evaluation might minimize the collateral damage from some gender-affirming care and at least help those patients for whom it is prescribed transition more smoothly.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
In the November 2021 issue of Pediatric News are two stories that on the surface present viewpoints that couldn’t be more divergent. On page 1 under the headline “Gender dysphoria” you will read about a position statement by the Royal Australian and New Zealand College of Psychiatrists (RANZCP) in which they strongly recommend a mental health evaluation for any child or adolescent with gender dysphoria “before any firm decisions are made on whether to prescribe hormonal treatments to transition, or perform surgeries.”
On page 6 is another story titled “Gender-affirming care ‘can save lives’ new research shows” that reports on a research study in which transgender and binary young people who received a year of gender-affirming care experienced less depression and fewer suicidal thoughts. Dr. David J. Inwards-Breland, chief of adolescent and young adult medicine at Rady Children’s Hospital in San Diego and one of the authors of the study is quoted as saying “The younger we can provide gender-affirming care, the less likely [our patients are] to have depression and then negative outcomes.” One can’t avoid the impression that he is in favor of moving ahead without delay in prescribing gender-affirming care.
Where does the new recommendation by the RANZCP fit in with this sense of urgency? Does requiring a mental health evaluation constitute a delay in the institution of gender-affirming care that could increase the risk of negative mental health outcomes for gender dysphoric patients?
In one of the final paragraphs in the Pediatric News article one learns that Dr. Inwards-Breland would agree with the folks of RANZCP. He acknowledges that his study relied on screening and not diagnostic testing and says that “future studies should look at a mental health evaluation and diagnosis by a mental health provider.”
When we drill into the details there are two issues that demand clarification. First, what kind of time course are we talking about for a mental health evaluation? Are we talking weeks, or months, hopefully not years? This of course depends on the availability of mental health services for the specific patient and the depth of the evaluation required. How long a delay is acceptable?
Second, will the evaluation be performed by a provider free of bias? Can it be performed without creating the impression that the patient needs to see a mental health provider because there is something wrong with being trans and we can fix it? One would hope these evaluations would be performed in the spirit of wanting to learn more about the patient with the goal of making the process go more smoothly.
Listening to neighborhood discussions around the fire pit I find that the RANZCP plea for a broader and deeper look at each gender-dysphoric child strikes a chord with the general population. More and more people are realizing that gender-dysphoria happens and that for too long it was closeted with unfortunate consequences. However, there is a feeling, in fact one in which I share, that the rapid rise in its prevalence contains an element of social contagion. And, some irreversible decisions are being made without sufficient consideration. This may or not be a valid concern but it seems to me a thorough and sensitively done mental health evaluation might minimize the collateral damage from some gender-affirming care and at least help those patients for whom it is prescribed transition more smoothly.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].

