User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Has the time come to bury BMI in favor of other screening measures?
In 1832, Belgian statistician Adolphe Quetelet introduced the concept of body mass index (BMI) – one’s weight (in kilograms) divided by the square of one’s height (in meters) as a measurement of ideal body weight. Approximately 140 years later, nutritional epidemiologist Ancel Keys proposed the use of BMI as a surrogate marker for evaluating body fat percentage within a population.
For the past 50 years, the scientific and medical communities have relied on BMI as a research and study tool to categorize patients’ weight (that is, severely underweight, underweight, normal weight, overweight, and obesity). The World Health Organization, National Institutes of Health, and U.S. Centers for Disease Control and Prevention use the following BMI weight classifications for adult patients:
- Underweight: BMI < 18.5
- Normal weight: BMI ≥ 18.5 to 24.9
- Overweight: BMI ≥ 25 to 29.9
- Obesity: BMI ≥ 30
Of note, BMI categories for children and adolescents (aged 2-19 years) are based on sex- and age-specific percentiles and will not be addressed in this article.
BMI appears to be a straightforward, easy, and cost-effective way to identify “healthy” weight and assess a patient’s risk for related conditions. For example, studies show that a BMI ≥ 35 kg/m2 correlates to higher prevalence of type 2 diabetes, hypertension, dyslipidemia, and decreased lifespan. At least 13 types of cancer have been linked to obesity, regardless of dietary or physical activity behaviors. While the health dangers associated with BMI ≥ 35 are substantial and difficult to dispute, concerns arise when BMI alone is used to determine healthy weight and disease risk in patients with a BMI of 25-35.
BMI limitations
There are troubling limitations to using BMI alone to assess a patient’s weight and health status. BMI only takes into account a patient’s height and weight, neither of which are sole determinants of health. Moreover, BMI measurements do not distinguish between fat mass and fat-free mass, each of which has very distinct effects on health. High fat mass is associated with an increased risk for disease and mortality, while higher lean body mass correlates with increased physical fitness and longevity. BMI also does not consider age, sex, race, ethnicity, or types of adipose tissue, all of which tremendously influence disease risk across all BMI categories.
Body composition and adipose tissue
Body composition and type of excess adipose tissue better correlate disease risk than does BMI. The World Health Organization defines obesity as having a body fat percentage > 25% for men and > 35% for women. Body composition can be measured by skin-fold thickness, bioelectrical impedance, dual-energy x-ray absorptiometry (DXA), CT, or MRI.
A cross-sectional study by Shah and colleagues) comparing BMI and DXA found that BMI underestimated obesity prevalence. In the study, BMI characterized 26% of participants as obese while DXA (a direct measurement of fat) characterized 64%. Further, 39% of patients categorized as nonobese based on BMI were found to be obese on DXA. Also, BMI misclassified 25% of men and 48% of women in the study. These findings and those of other studies suggest that BMI has a high specificity but low sensitivity for diagnosing obesity, questioning its reliability as a clinical screening tool.
Current guideline recommendations on pharmacologic and surgical treatment options for patients with overweight or obesity, including those of the American Association of Clinical Endocrinology and American College of Endocrinology (AACE/ACE) and the American College of Cardiology/American Heart Association and The Obesity Society (ACC/AHA/TOS), rely on BMI, diminishing their utilization. For example, a recent literature search by Li and associates found that Asian American patients with lower BMIs and BMIs of 25 or 27 are at increased risk for metabolic disease. On the basis of study findings, some organizations recommend considering pharmacotherapy at a lower BMI cutoff of ≥ 25.0 or ≥ 27.5 for Asian people to ensure early treatment intervention in this patient population because guidelines do not recommend pharmacologic treatment unless the BMI is 27 with weight-related complications or 30. Under the current guidelines, a patient of Asian descent has greater disease severity with potentially more complications by the time pharmacotherapy is initiated.
As previously noted, body composition, which requires the use of special equipment (skinfold calipers, DXA, CT, MRI, body impedance scale), best captures the ratio of fat mass to fat-free mass. DXA is frequently used in research studies looking at body composition because of its lower cost, faster time to obtain the study, and ability to measure bone density. MRI has been found to be as accurate as CT for assessing visceral adipose tissue (VAT), skeletal muscle mass, and organ mass, and does not expose patients to ionizing radiation like CT does. MRI clinical use, however, is limited because of its high cost, and it may be problematic for patients with claustrophobia or who are unable to remain immobile for an extended period.
Patients with a high VAT mass, compared with subcutaneous adipose tissue (SAT), are at increased risk for metabolic syndrome, nonalcoholic fatty liver disease, and cardiovascular disease regardless of BMI, underscoring the clinical usefulness of measuring visceral adiposity over BMI.
One of the barriers to implementing VAT assessment in clinical practice is the cost of imaging studies. Fortunately, data suggest that waist circumference and/or waist-to-hip ratio measurements can be a valuable surrogate for VAT measurement. A waist circumference greater than 35 inches (88 cm) or a waist-to-hip ratio greater than 0.8 for women, and greater than 40 inches (102 cm) or a waist-to-hip ratio greater than 0.95 for men, increases metabolic disease risk. Obtaining these measurements requires a tape measure and a few extra minutes and offers more potent data than BMI alone. For example, a large cardiometabolic study found that within each BMI category, increasing gender-specific waist circumferences were associated with significantly higher VAT, liver fat, and a more harmful cardiometabolic risk profile. Men and women with a lower or normal BMI and a high waist circumference are at greatest relative health risk, compared with those with low waist circumference values. Yet, using the BMI alone in these patients would not raise any clinical concern, which is a missed opportunity for cardiometabolic risk reduction.
Biomarkers
Specific biomarkers are closely related to obesity. Leptin and resistin protein levels increase with adipose mass, while adiponectin decreases, probably contributing to insulin resistance. The higher levels of tumor necrosis factor–alpha and interleukin-6 from obesity contribute to chronic inflammation. The combined effect of chronic inflammation and insulin resistance allows greater bioavailability of insulinlike growth factor-1 (IGF-1), which has a role in initiating type 2 diabetes, cardiovascular disease, and cancer. Ideally, measuring these biomarkers could provide more advantageous information than BMI. Unfortunately, for now, the lack of standardized assays and imperfect knowledge of exactly how these biomarkers elicit disease prevents clinical use.
Obesity is a common, highly complex, chronic, and relapsing disease. Thankfully, a number of effective treatments and interventions are available. Although an accurate diagnosis of obesity is essential, underdiagnosed cases and missed opportunities for metabolic disease risk reduction persist. Overdiagnosing obesity, however, has the potential to incur unnecessary health care costs and result in weight bias and stigma.
While BMI is a quick and inexpensive means to assess obesity, by itself it lacks the necessary components for an accurate diagnosis. Particularly for individuals with a normal BMI or less severe overweight/obesity (BMI 27-34.9), other factors must be accounted for, including age, gender, and race. At a minimum, waist circumference should be measured to best risk-stratify and determine treatment intensity. Body composition analysis with BMI calculation refines the diagnosis of obesity.
Finally, clinicians may find best practices by using BMI delta change models. As with so many other clinical measurements, the trajectory tells the most astute story. For example, a patient whose BMI decreased from 45 to 35 may warrant less intensive treatment than a patient whose BMI increased from 26 to 31. Any change in BMI warrants clinical attention. A rapidly or consistently increasing BMI, even within normal range, should prompt clinicians to assess other factors related to obesity and metabolic disease risk (for example, lifestyle factors, waist circumference, blood pressure, cholesterol, diabetes screening) and initiate a conversation about weight management. Similarly, a consistently or rapidly decreasing BMI – even in elevated ranges and particularly with unintentional weight loss – should prompt evaluation.
Although BMI continues to be useful in clinical practice, epidemiology, and research, it should be used in combination with other clinical factors to provide the utmost quality of care.
Dr. Bartfield is assistant professor, obesity medicine specialist, Wake Forest Baptists Medical Center/Atrium Health Weight Management Center, Greensboro, N.C. She has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
In 1832, Belgian statistician Adolphe Quetelet introduced the concept of body mass index (BMI) – one’s weight (in kilograms) divided by the square of one’s height (in meters) as a measurement of ideal body weight. Approximately 140 years later, nutritional epidemiologist Ancel Keys proposed the use of BMI as a surrogate marker for evaluating body fat percentage within a population.
For the past 50 years, the scientific and medical communities have relied on BMI as a research and study tool to categorize patients’ weight (that is, severely underweight, underweight, normal weight, overweight, and obesity). The World Health Organization, National Institutes of Health, and U.S. Centers for Disease Control and Prevention use the following BMI weight classifications for adult patients:
- Underweight: BMI < 18.5
- Normal weight: BMI ≥ 18.5 to 24.9
- Overweight: BMI ≥ 25 to 29.9
- Obesity: BMI ≥ 30
Of note, BMI categories for children and adolescents (aged 2-19 years) are based on sex- and age-specific percentiles and will not be addressed in this article.
BMI appears to be a straightforward, easy, and cost-effective way to identify “healthy” weight and assess a patient’s risk for related conditions. For example, studies show that a BMI ≥ 35 kg/m2 correlates to higher prevalence of type 2 diabetes, hypertension, dyslipidemia, and decreased lifespan. At least 13 types of cancer have been linked to obesity, regardless of dietary or physical activity behaviors. While the health dangers associated with BMI ≥ 35 are substantial and difficult to dispute, concerns arise when BMI alone is used to determine healthy weight and disease risk in patients with a BMI of 25-35.
BMI limitations
There are troubling limitations to using BMI alone to assess a patient’s weight and health status. BMI only takes into account a patient’s height and weight, neither of which are sole determinants of health. Moreover, BMI measurements do not distinguish between fat mass and fat-free mass, each of which has very distinct effects on health. High fat mass is associated with an increased risk for disease and mortality, while higher lean body mass correlates with increased physical fitness and longevity. BMI also does not consider age, sex, race, ethnicity, or types of adipose tissue, all of which tremendously influence disease risk across all BMI categories.
Body composition and adipose tissue
Body composition and type of excess adipose tissue better correlate disease risk than does BMI. The World Health Organization defines obesity as having a body fat percentage > 25% for men and > 35% for women. Body composition can be measured by skin-fold thickness, bioelectrical impedance, dual-energy x-ray absorptiometry (DXA), CT, or MRI.
A cross-sectional study by Shah and colleagues) comparing BMI and DXA found that BMI underestimated obesity prevalence. In the study, BMI characterized 26% of participants as obese while DXA (a direct measurement of fat) characterized 64%. Further, 39% of patients categorized as nonobese based on BMI were found to be obese on DXA. Also, BMI misclassified 25% of men and 48% of women in the study. These findings and those of other studies suggest that BMI has a high specificity but low sensitivity for diagnosing obesity, questioning its reliability as a clinical screening tool.
Current guideline recommendations on pharmacologic and surgical treatment options for patients with overweight or obesity, including those of the American Association of Clinical Endocrinology and American College of Endocrinology (AACE/ACE) and the American College of Cardiology/American Heart Association and The Obesity Society (ACC/AHA/TOS), rely on BMI, diminishing their utilization. For example, a recent literature search by Li and associates found that Asian American patients with lower BMIs and BMIs of 25 or 27 are at increased risk for metabolic disease. On the basis of study findings, some organizations recommend considering pharmacotherapy at a lower BMI cutoff of ≥ 25.0 or ≥ 27.5 for Asian people to ensure early treatment intervention in this patient population because guidelines do not recommend pharmacologic treatment unless the BMI is 27 with weight-related complications or 30. Under the current guidelines, a patient of Asian descent has greater disease severity with potentially more complications by the time pharmacotherapy is initiated.
As previously noted, body composition, which requires the use of special equipment (skinfold calipers, DXA, CT, MRI, body impedance scale), best captures the ratio of fat mass to fat-free mass. DXA is frequently used in research studies looking at body composition because of its lower cost, faster time to obtain the study, and ability to measure bone density. MRI has been found to be as accurate as CT for assessing visceral adipose tissue (VAT), skeletal muscle mass, and organ mass, and does not expose patients to ionizing radiation like CT does. MRI clinical use, however, is limited because of its high cost, and it may be problematic for patients with claustrophobia or who are unable to remain immobile for an extended period.
Patients with a high VAT mass, compared with subcutaneous adipose tissue (SAT), are at increased risk for metabolic syndrome, nonalcoholic fatty liver disease, and cardiovascular disease regardless of BMI, underscoring the clinical usefulness of measuring visceral adiposity over BMI.
One of the barriers to implementing VAT assessment in clinical practice is the cost of imaging studies. Fortunately, data suggest that waist circumference and/or waist-to-hip ratio measurements can be a valuable surrogate for VAT measurement. A waist circumference greater than 35 inches (88 cm) or a waist-to-hip ratio greater than 0.8 for women, and greater than 40 inches (102 cm) or a waist-to-hip ratio greater than 0.95 for men, increases metabolic disease risk. Obtaining these measurements requires a tape measure and a few extra minutes and offers more potent data than BMI alone. For example, a large cardiometabolic study found that within each BMI category, increasing gender-specific waist circumferences were associated with significantly higher VAT, liver fat, and a more harmful cardiometabolic risk profile. Men and women with a lower or normal BMI and a high waist circumference are at greatest relative health risk, compared with those with low waist circumference values. Yet, using the BMI alone in these patients would not raise any clinical concern, which is a missed opportunity for cardiometabolic risk reduction.
Biomarkers
Specific biomarkers are closely related to obesity. Leptin and resistin protein levels increase with adipose mass, while adiponectin decreases, probably contributing to insulin resistance. The higher levels of tumor necrosis factor–alpha and interleukin-6 from obesity contribute to chronic inflammation. The combined effect of chronic inflammation and insulin resistance allows greater bioavailability of insulinlike growth factor-1 (IGF-1), which has a role in initiating type 2 diabetes, cardiovascular disease, and cancer. Ideally, measuring these biomarkers could provide more advantageous information than BMI. Unfortunately, for now, the lack of standardized assays and imperfect knowledge of exactly how these biomarkers elicit disease prevents clinical use.
Obesity is a common, highly complex, chronic, and relapsing disease. Thankfully, a number of effective treatments and interventions are available. Although an accurate diagnosis of obesity is essential, underdiagnosed cases and missed opportunities for metabolic disease risk reduction persist. Overdiagnosing obesity, however, has the potential to incur unnecessary health care costs and result in weight bias and stigma.
While BMI is a quick and inexpensive means to assess obesity, by itself it lacks the necessary components for an accurate diagnosis. Particularly for individuals with a normal BMI or less severe overweight/obesity (BMI 27-34.9), other factors must be accounted for, including age, gender, and race. At a minimum, waist circumference should be measured to best risk-stratify and determine treatment intensity. Body composition analysis with BMI calculation refines the diagnosis of obesity.
Finally, clinicians may find best practices by using BMI delta change models. As with so many other clinical measurements, the trajectory tells the most astute story. For example, a patient whose BMI decreased from 45 to 35 may warrant less intensive treatment than a patient whose BMI increased from 26 to 31. Any change in BMI warrants clinical attention. A rapidly or consistently increasing BMI, even within normal range, should prompt clinicians to assess other factors related to obesity and metabolic disease risk (for example, lifestyle factors, waist circumference, blood pressure, cholesterol, diabetes screening) and initiate a conversation about weight management. Similarly, a consistently or rapidly decreasing BMI – even in elevated ranges and particularly with unintentional weight loss – should prompt evaluation.
Although BMI continues to be useful in clinical practice, epidemiology, and research, it should be used in combination with other clinical factors to provide the utmost quality of care.
Dr. Bartfield is assistant professor, obesity medicine specialist, Wake Forest Baptists Medical Center/Atrium Health Weight Management Center, Greensboro, N.C. She has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
In 1832, Belgian statistician Adolphe Quetelet introduced the concept of body mass index (BMI) – one’s weight (in kilograms) divided by the square of one’s height (in meters) as a measurement of ideal body weight. Approximately 140 years later, nutritional epidemiologist Ancel Keys proposed the use of BMI as a surrogate marker for evaluating body fat percentage within a population.
For the past 50 years, the scientific and medical communities have relied on BMI as a research and study tool to categorize patients’ weight (that is, severely underweight, underweight, normal weight, overweight, and obesity). The World Health Organization, National Institutes of Health, and U.S. Centers for Disease Control and Prevention use the following BMI weight classifications for adult patients:
- Underweight: BMI < 18.5
- Normal weight: BMI ≥ 18.5 to 24.9
- Overweight: BMI ≥ 25 to 29.9
- Obesity: BMI ≥ 30
Of note, BMI categories for children and adolescents (aged 2-19 years) are based on sex- and age-specific percentiles and will not be addressed in this article.
BMI appears to be a straightforward, easy, and cost-effective way to identify “healthy” weight and assess a patient’s risk for related conditions. For example, studies show that a BMI ≥ 35 kg/m2 correlates to higher prevalence of type 2 diabetes, hypertension, dyslipidemia, and decreased lifespan. At least 13 types of cancer have been linked to obesity, regardless of dietary or physical activity behaviors. While the health dangers associated with BMI ≥ 35 are substantial and difficult to dispute, concerns arise when BMI alone is used to determine healthy weight and disease risk in patients with a BMI of 25-35.
BMI limitations
There are troubling limitations to using BMI alone to assess a patient’s weight and health status. BMI only takes into account a patient’s height and weight, neither of which are sole determinants of health. Moreover, BMI measurements do not distinguish between fat mass and fat-free mass, each of which has very distinct effects on health. High fat mass is associated with an increased risk for disease and mortality, while higher lean body mass correlates with increased physical fitness and longevity. BMI also does not consider age, sex, race, ethnicity, or types of adipose tissue, all of which tremendously influence disease risk across all BMI categories.
Body composition and adipose tissue
Body composition and type of excess adipose tissue better correlate disease risk than does BMI. The World Health Organization defines obesity as having a body fat percentage > 25% for men and > 35% for women. Body composition can be measured by skin-fold thickness, bioelectrical impedance, dual-energy x-ray absorptiometry (DXA), CT, or MRI.
A cross-sectional study by Shah and colleagues) comparing BMI and DXA found that BMI underestimated obesity prevalence. In the study, BMI characterized 26% of participants as obese while DXA (a direct measurement of fat) characterized 64%. Further, 39% of patients categorized as nonobese based on BMI were found to be obese on DXA. Also, BMI misclassified 25% of men and 48% of women in the study. These findings and those of other studies suggest that BMI has a high specificity but low sensitivity for diagnosing obesity, questioning its reliability as a clinical screening tool.
Current guideline recommendations on pharmacologic and surgical treatment options for patients with overweight or obesity, including those of the American Association of Clinical Endocrinology and American College of Endocrinology (AACE/ACE) and the American College of Cardiology/American Heart Association and The Obesity Society (ACC/AHA/TOS), rely on BMI, diminishing their utilization. For example, a recent literature search by Li and associates found that Asian American patients with lower BMIs and BMIs of 25 or 27 are at increased risk for metabolic disease. On the basis of study findings, some organizations recommend considering pharmacotherapy at a lower BMI cutoff of ≥ 25.0 or ≥ 27.5 for Asian people to ensure early treatment intervention in this patient population because guidelines do not recommend pharmacologic treatment unless the BMI is 27 with weight-related complications or 30. Under the current guidelines, a patient of Asian descent has greater disease severity with potentially more complications by the time pharmacotherapy is initiated.
As previously noted, body composition, which requires the use of special equipment (skinfold calipers, DXA, CT, MRI, body impedance scale), best captures the ratio of fat mass to fat-free mass. DXA is frequently used in research studies looking at body composition because of its lower cost, faster time to obtain the study, and ability to measure bone density. MRI has been found to be as accurate as CT for assessing visceral adipose tissue (VAT), skeletal muscle mass, and organ mass, and does not expose patients to ionizing radiation like CT does. MRI clinical use, however, is limited because of its high cost, and it may be problematic for patients with claustrophobia or who are unable to remain immobile for an extended period.
Patients with a high VAT mass, compared with subcutaneous adipose tissue (SAT), are at increased risk for metabolic syndrome, nonalcoholic fatty liver disease, and cardiovascular disease regardless of BMI, underscoring the clinical usefulness of measuring visceral adiposity over BMI.
One of the barriers to implementing VAT assessment in clinical practice is the cost of imaging studies. Fortunately, data suggest that waist circumference and/or waist-to-hip ratio measurements can be a valuable surrogate for VAT measurement. A waist circumference greater than 35 inches (88 cm) or a waist-to-hip ratio greater than 0.8 for women, and greater than 40 inches (102 cm) or a waist-to-hip ratio greater than 0.95 for men, increases metabolic disease risk. Obtaining these measurements requires a tape measure and a few extra minutes and offers more potent data than BMI alone. For example, a large cardiometabolic study found that within each BMI category, increasing gender-specific waist circumferences were associated with significantly higher VAT, liver fat, and a more harmful cardiometabolic risk profile. Men and women with a lower or normal BMI and a high waist circumference are at greatest relative health risk, compared with those with low waist circumference values. Yet, using the BMI alone in these patients would not raise any clinical concern, which is a missed opportunity for cardiometabolic risk reduction.
Biomarkers
Specific biomarkers are closely related to obesity. Leptin and resistin protein levels increase with adipose mass, while adiponectin decreases, probably contributing to insulin resistance. The higher levels of tumor necrosis factor–alpha and interleukin-6 from obesity contribute to chronic inflammation. The combined effect of chronic inflammation and insulin resistance allows greater bioavailability of insulinlike growth factor-1 (IGF-1), which has a role in initiating type 2 diabetes, cardiovascular disease, and cancer. Ideally, measuring these biomarkers could provide more advantageous information than BMI. Unfortunately, for now, the lack of standardized assays and imperfect knowledge of exactly how these biomarkers elicit disease prevents clinical use.
Obesity is a common, highly complex, chronic, and relapsing disease. Thankfully, a number of effective treatments and interventions are available. Although an accurate diagnosis of obesity is essential, underdiagnosed cases and missed opportunities for metabolic disease risk reduction persist. Overdiagnosing obesity, however, has the potential to incur unnecessary health care costs and result in weight bias and stigma.
While BMI is a quick and inexpensive means to assess obesity, by itself it lacks the necessary components for an accurate diagnosis. Particularly for individuals with a normal BMI or less severe overweight/obesity (BMI 27-34.9), other factors must be accounted for, including age, gender, and race. At a minimum, waist circumference should be measured to best risk-stratify and determine treatment intensity. Body composition analysis with BMI calculation refines the diagnosis of obesity.
Finally, clinicians may find best practices by using BMI delta change models. As with so many other clinical measurements, the trajectory tells the most astute story. For example, a patient whose BMI decreased from 45 to 35 may warrant less intensive treatment than a patient whose BMI increased from 26 to 31. Any change in BMI warrants clinical attention. A rapidly or consistently increasing BMI, even within normal range, should prompt clinicians to assess other factors related to obesity and metabolic disease risk (for example, lifestyle factors, waist circumference, blood pressure, cholesterol, diabetes screening) and initiate a conversation about weight management. Similarly, a consistently or rapidly decreasing BMI – even in elevated ranges and particularly with unintentional weight loss – should prompt evaluation.
Although BMI continues to be useful in clinical practice, epidemiology, and research, it should be used in combination with other clinical factors to provide the utmost quality of care.
Dr. Bartfield is assistant professor, obesity medicine specialist, Wake Forest Baptists Medical Center/Atrium Health Weight Management Center, Greensboro, N.C. She has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
FDA approves first over-the-counter birth control pill
The Food and Drug Administration’s approval today of the first birth control pill for women to be available without a prescription is being hailed by many as a long-needed development, but there remain questions to be resolved, including how much the drug will cost and how it will be used.
The drug, Opill, is expected to be available early next year, and its maker has yet to reveal a retail price. It is the same birth control pill that has been available by prescription for 50 years. But for the first time, women will be able to buy the contraception at a local pharmacy, other retail locations, or online without having to see a doctor first.
Likely to drive debate
Contraception in the United States is not without controversy. The FDA’s approval spurred reactions both for and against making hormonal birth control for women available without a prescription.
“It’s an exciting time, especially right now when reproductive rights are being curtailed in a lot of states. Giving people an additional option for contraception will change people’s lives,” said Beverly Gray, MD, division director of Women’s Community and Population Health at Duke University Medical Center in Durham, N.C.
“It’s a huge win for patients who need better access to contraception,” said Dr. Gray, who is also a spokesperson for the American College of Obstetricians and Gynecologists.
Women who want hormonal birth control but live in areas without convenient access to a doctor, women who cannot easily take time off of work to see a doctor and get a prescription filled, and women without insurance are examples of people who will benefit, she said.
The Catholic Medical Association, in contrast, expressed “deep concern and disappointment” after an FDA advisory committee’s unanimous vote on May 11 recommending the drug be available over the counter. In a statement after the vote, the group cited “extensive medical studies demonstrating the risks and adverse effects of hormonal contraceptives,” adding that “the social impact of [full approval] would be dramatic.”
But doctors largely disagreed.
“It is definitely a huge win for reproductive autonomy. I’m glad that the FDA is prioritizing patient safety and well-being over politics,” said Catherine Cansino, MD, MPH, an ob.gyn. and clinical professor in the University of California Davis department of obstetrics and gynecology. She said the FDA approved the over-the-counter version because the medication is safe.
While opponents like the Catholic Medical Association cite safety concerns and believe doctors should screen all women before prescribing hormonal contraception, Dr. Gray disagreed. “There’s a lot of evidence that patients can figure out if a progestin-only pill is right for them and safe for them. Medical professionals don’t have to be the gatekeepers for contraception,” she said.
Pricing unknown
Whether insurance companies will pay for Opill now that it will be available without a prescription remains unknown. For some medications, paying a copay through insurance can be less expensive than buying at a retail price.
“Although pricing issues will be relevant, the FDA’s decision will enhance women’s access to hormonal birth control,” said Andrew M. Kaunitz, MD, a professor and associate chairman in the department of obstetrics and gynecology at the University of Florida College of Medicine in Jacksonville.
The drugmaker, Perrigo, based in Ireland, has not yet announced how much the pill will cost. The price tag could affect how widely available this form of birth control is. The drug has been shown to be as much as 93% effective for pregnancy prevention. Perrigo says it plans to make the pill available at low or no cost to some women.
Caveats to consider
There are some women for whom hormonal contraceptives have always carried greater risks. For example, women who have breast cancer or a history of breast cancer should not use hormonal contraceptives, the FDA said in a news release announcing the approval. Women with other types of cancer should check with their doctors first, the agency noted.
Women who smoke, who take some medications to lower blood pressure, or who have migraines should also take caution, Dr. Cansino said. “People with migraines may not be suitable for over-the-counter oral contraceptives. But a simple screening through a provider can identify whether you are truly eligible or not.”
Irregular bleeding, headaches, dizziness, nausea, increased appetite, belly pain, cramps, or bloating are the most common side effects of Opill, the FDA said.
The Opill is a progestin-only birth control pill. Similar pills have been available in the United Kingdiom for about 2 years, often referred to as “mini pills” because they contain a single hormone. In contrast, prescription birth control pills in the United States and elsewhere contain more than one hormone, estrogen and progestin, to prevent pregnancy.
Prescription pill packs for combination contraception often feature a week of placebo pills without an active ingredient. While skipping a placebo pill might not make a difference in pregnancy prevention, Opill is different. Every pill in the packet will contain medication, Gray said. “So it’s important to take the pill the same time every day for it to be most effective.”
Even though this may mean one less visit to your doctor, Dr. Kaunitz hopes women will stay up to date on their other medical checkups. “One of our challenges as providers of care to women will be to encourage them to continue to receive important services, including cancer screening and vaccinations, even while they can initiate and continue hormonal contraception without contact with a provider.”
Just the beginning?
The American Medical Association hopes this approval signals more to come.
“While we applaud this move, the AMA continues to urge the FDA and HHS to consider a variety of oral contraceptive options for over-the-counter use,” the association, which has more than 250,000 doctor members, said in a statement. “It is important patients have options when choosing which type of birth control works best for them,”
The American College of Obstetricians and Gynecologists said the FDA’s decision will help many women. “We are glad that more patients will now be empowered to choose when and where they obtain a safe method of contraception without having to wait for a medical appointment or for a prescription to be filled,” Verda J. Hicks, MD, the group’s president, and Christopher M. Zahn, MD, interim chief executive officer, said in a statement.
“Allowing individuals to access birth control at their local pharmacy or drug store will eliminate some barriers,” they said.
A version of this article first appeared on WebMD.com.
This article was updated 7/13/23.
The Food and Drug Administration’s approval today of the first birth control pill for women to be available without a prescription is being hailed by many as a long-needed development, but there remain questions to be resolved, including how much the drug will cost and how it will be used.
The drug, Opill, is expected to be available early next year, and its maker has yet to reveal a retail price. It is the same birth control pill that has been available by prescription for 50 years. But for the first time, women will be able to buy the contraception at a local pharmacy, other retail locations, or online without having to see a doctor first.
Likely to drive debate
Contraception in the United States is not without controversy. The FDA’s approval spurred reactions both for and against making hormonal birth control for women available without a prescription.
“It’s an exciting time, especially right now when reproductive rights are being curtailed in a lot of states. Giving people an additional option for contraception will change people’s lives,” said Beverly Gray, MD, division director of Women’s Community and Population Health at Duke University Medical Center in Durham, N.C.
“It’s a huge win for patients who need better access to contraception,” said Dr. Gray, who is also a spokesperson for the American College of Obstetricians and Gynecologists.
Women who want hormonal birth control but live in areas without convenient access to a doctor, women who cannot easily take time off of work to see a doctor and get a prescription filled, and women without insurance are examples of people who will benefit, she said.
The Catholic Medical Association, in contrast, expressed “deep concern and disappointment” after an FDA advisory committee’s unanimous vote on May 11 recommending the drug be available over the counter. In a statement after the vote, the group cited “extensive medical studies demonstrating the risks and adverse effects of hormonal contraceptives,” adding that “the social impact of [full approval] would be dramatic.”
But doctors largely disagreed.
“It is definitely a huge win for reproductive autonomy. I’m glad that the FDA is prioritizing patient safety and well-being over politics,” said Catherine Cansino, MD, MPH, an ob.gyn. and clinical professor in the University of California Davis department of obstetrics and gynecology. She said the FDA approved the over-the-counter version because the medication is safe.
While opponents like the Catholic Medical Association cite safety concerns and believe doctors should screen all women before prescribing hormonal contraception, Dr. Gray disagreed. “There’s a lot of evidence that patients can figure out if a progestin-only pill is right for them and safe for them. Medical professionals don’t have to be the gatekeepers for contraception,” she said.
Pricing unknown
Whether insurance companies will pay for Opill now that it will be available without a prescription remains unknown. For some medications, paying a copay through insurance can be less expensive than buying at a retail price.
“Although pricing issues will be relevant, the FDA’s decision will enhance women’s access to hormonal birth control,” said Andrew M. Kaunitz, MD, a professor and associate chairman in the department of obstetrics and gynecology at the University of Florida College of Medicine in Jacksonville.
The drugmaker, Perrigo, based in Ireland, has not yet announced how much the pill will cost. The price tag could affect how widely available this form of birth control is. The drug has been shown to be as much as 93% effective for pregnancy prevention. Perrigo says it plans to make the pill available at low or no cost to some women.
Caveats to consider
There are some women for whom hormonal contraceptives have always carried greater risks. For example, women who have breast cancer or a history of breast cancer should not use hormonal contraceptives, the FDA said in a news release announcing the approval. Women with other types of cancer should check with their doctors first, the agency noted.
Women who smoke, who take some medications to lower blood pressure, or who have migraines should also take caution, Dr. Cansino said. “People with migraines may not be suitable for over-the-counter oral contraceptives. But a simple screening through a provider can identify whether you are truly eligible or not.”
Irregular bleeding, headaches, dizziness, nausea, increased appetite, belly pain, cramps, or bloating are the most common side effects of Opill, the FDA said.
The Opill is a progestin-only birth control pill. Similar pills have been available in the United Kingdiom for about 2 years, often referred to as “mini pills” because they contain a single hormone. In contrast, prescription birth control pills in the United States and elsewhere contain more than one hormone, estrogen and progestin, to prevent pregnancy.
Prescription pill packs for combination contraception often feature a week of placebo pills without an active ingredient. While skipping a placebo pill might not make a difference in pregnancy prevention, Opill is different. Every pill in the packet will contain medication, Gray said. “So it’s important to take the pill the same time every day for it to be most effective.”
Even though this may mean one less visit to your doctor, Dr. Kaunitz hopes women will stay up to date on their other medical checkups. “One of our challenges as providers of care to women will be to encourage them to continue to receive important services, including cancer screening and vaccinations, even while they can initiate and continue hormonal contraception without contact with a provider.”
Just the beginning?
The American Medical Association hopes this approval signals more to come.
“While we applaud this move, the AMA continues to urge the FDA and HHS to consider a variety of oral contraceptive options for over-the-counter use,” the association, which has more than 250,000 doctor members, said in a statement. “It is important patients have options when choosing which type of birth control works best for them,”
The American College of Obstetricians and Gynecologists said the FDA’s decision will help many women. “We are glad that more patients will now be empowered to choose when and where they obtain a safe method of contraception without having to wait for a medical appointment or for a prescription to be filled,” Verda J. Hicks, MD, the group’s president, and Christopher M. Zahn, MD, interim chief executive officer, said in a statement.
“Allowing individuals to access birth control at their local pharmacy or drug store will eliminate some barriers,” they said.
A version of this article first appeared on WebMD.com.
This article was updated 7/13/23.
The Food and Drug Administration’s approval today of the first birth control pill for women to be available without a prescription is being hailed by many as a long-needed development, but there remain questions to be resolved, including how much the drug will cost and how it will be used.
The drug, Opill, is expected to be available early next year, and its maker has yet to reveal a retail price. It is the same birth control pill that has been available by prescription for 50 years. But for the first time, women will be able to buy the contraception at a local pharmacy, other retail locations, or online without having to see a doctor first.
Likely to drive debate
Contraception in the United States is not without controversy. The FDA’s approval spurred reactions both for and against making hormonal birth control for women available without a prescription.
“It’s an exciting time, especially right now when reproductive rights are being curtailed in a lot of states. Giving people an additional option for contraception will change people’s lives,” said Beverly Gray, MD, division director of Women’s Community and Population Health at Duke University Medical Center in Durham, N.C.
“It’s a huge win for patients who need better access to contraception,” said Dr. Gray, who is also a spokesperson for the American College of Obstetricians and Gynecologists.
Women who want hormonal birth control but live in areas without convenient access to a doctor, women who cannot easily take time off of work to see a doctor and get a prescription filled, and women without insurance are examples of people who will benefit, she said.
The Catholic Medical Association, in contrast, expressed “deep concern and disappointment” after an FDA advisory committee’s unanimous vote on May 11 recommending the drug be available over the counter. In a statement after the vote, the group cited “extensive medical studies demonstrating the risks and adverse effects of hormonal contraceptives,” adding that “the social impact of [full approval] would be dramatic.”
But doctors largely disagreed.
“It is definitely a huge win for reproductive autonomy. I’m glad that the FDA is prioritizing patient safety and well-being over politics,” said Catherine Cansino, MD, MPH, an ob.gyn. and clinical professor in the University of California Davis department of obstetrics and gynecology. She said the FDA approved the over-the-counter version because the medication is safe.
While opponents like the Catholic Medical Association cite safety concerns and believe doctors should screen all women before prescribing hormonal contraception, Dr. Gray disagreed. “There’s a lot of evidence that patients can figure out if a progestin-only pill is right for them and safe for them. Medical professionals don’t have to be the gatekeepers for contraception,” she said.
Pricing unknown
Whether insurance companies will pay for Opill now that it will be available without a prescription remains unknown. For some medications, paying a copay through insurance can be less expensive than buying at a retail price.
“Although pricing issues will be relevant, the FDA’s decision will enhance women’s access to hormonal birth control,” said Andrew M. Kaunitz, MD, a professor and associate chairman in the department of obstetrics and gynecology at the University of Florida College of Medicine in Jacksonville.
The drugmaker, Perrigo, based in Ireland, has not yet announced how much the pill will cost. The price tag could affect how widely available this form of birth control is. The drug has been shown to be as much as 93% effective for pregnancy prevention. Perrigo says it plans to make the pill available at low or no cost to some women.
Caveats to consider
There are some women for whom hormonal contraceptives have always carried greater risks. For example, women who have breast cancer or a history of breast cancer should not use hormonal contraceptives, the FDA said in a news release announcing the approval. Women with other types of cancer should check with their doctors first, the agency noted.
Women who smoke, who take some medications to lower blood pressure, or who have migraines should also take caution, Dr. Cansino said. “People with migraines may not be suitable for over-the-counter oral contraceptives. But a simple screening through a provider can identify whether you are truly eligible or not.”
Irregular bleeding, headaches, dizziness, nausea, increased appetite, belly pain, cramps, or bloating are the most common side effects of Opill, the FDA said.
The Opill is a progestin-only birth control pill. Similar pills have been available in the United Kingdiom for about 2 years, often referred to as “mini pills” because they contain a single hormone. In contrast, prescription birth control pills in the United States and elsewhere contain more than one hormone, estrogen and progestin, to prevent pregnancy.
Prescription pill packs for combination contraception often feature a week of placebo pills without an active ingredient. While skipping a placebo pill might not make a difference in pregnancy prevention, Opill is different. Every pill in the packet will contain medication, Gray said. “So it’s important to take the pill the same time every day for it to be most effective.”
Even though this may mean one less visit to your doctor, Dr. Kaunitz hopes women will stay up to date on their other medical checkups. “One of our challenges as providers of care to women will be to encourage them to continue to receive important services, including cancer screening and vaccinations, even while they can initiate and continue hormonal contraception without contact with a provider.”
Just the beginning?
The American Medical Association hopes this approval signals more to come.
“While we applaud this move, the AMA continues to urge the FDA and HHS to consider a variety of oral contraceptive options for over-the-counter use,” the association, which has more than 250,000 doctor members, said in a statement. “It is important patients have options when choosing which type of birth control works best for them,”
The American College of Obstetricians and Gynecologists said the FDA’s decision will help many women. “We are glad that more patients will now be empowered to choose when and where they obtain a safe method of contraception without having to wait for a medical appointment or for a prescription to be filled,” Verda J. Hicks, MD, the group’s president, and Christopher M. Zahn, MD, interim chief executive officer, said in a statement.
“Allowing individuals to access birth control at their local pharmacy or drug store will eliminate some barriers,” they said.
A version of this article first appeared on WebMD.com.
This article was updated 7/13/23.
Higher risk of death with endocrine therapy nonadherence
TOPLINE:
a new systematic review found.
METHODOLOGY:
- The investigators conducted a systematic literature search of five databases, looking for studies involving patients with nonmetastatic hormone receptor–positive breast cancer that were published between 2010 and 2020.
- Adequate adherence was defined as a medical possession ratio – the percentage of days the prescribed treatment dose of adjuvant endocrine therapy was available to the patient – of at least 80%.
- Medication nonpersistence was defined as a period in which no new adjuvant endocrine therapy prescriptions were filled before the scheduled end of treatment of 90-180 days, depending on the study.
- The impact of both parameters on event-free survival, which included breast cancer recurrence, disease-free survival, breast cancer–specific survival, and overall survival cancer was calculated.
- Of 2,026 articles retrieved, 14 studies, with sample sizes ranging from 857 to 30,573 patients, met the eligibility and quality criteria; 11 examined patient adherence, and 6 examined patient persistence.
TAKEAWAY:
- Of 10 studies that assessed event-free survival, 7 showed significantly worse survival for nonadherent or nonpersistent patients, at hazard ratios of 1.39-2.44.
- Of nine studies that examined overall survival, seven demonstrated a significantly higher risk for mortality in the groups with nonadherence and nonpersistence, at HRs of 1.26-2.18.
- The largest study, which included data on more than 30,000 patients in Taiwan, found that nonadherence and nonpersistence were associated with a significantly increased risk for mortality, at HRs of 1.98 and 2.18, respectively.
IN PRACTICE:
“The available data highlight the dangers of nonadherence and nonpersistence, showing an up to twofold higher risk of relapse or death for patients who do not use endocrine treatment as prescribed,” the researchers said. “Importantly, improving adherence and persistence represents a low-hanging fruit for increasing survival in luminal breast cancer.”
SOURCE:
The study, led by Finn Magnus Eliassen, MD, department of surgery, Stavanger (Norway) University Hospital, was published online on July 4 in BMC Cancer.
LIMITATIONS:
- The review is limited by the relatively small number of studies that met the eligibility criteria and by their heterogeneity, which ruled out a meta-analysis.
- There are no gold-standard definitions of adherence and persistence.
DISCLOSURES:
- No funding was declared. No relevant financial relationships were declared.
- A version of this article first appeared on Medscape.com.
TOPLINE:
a new systematic review found.
METHODOLOGY:
- The investigators conducted a systematic literature search of five databases, looking for studies involving patients with nonmetastatic hormone receptor–positive breast cancer that were published between 2010 and 2020.
- Adequate adherence was defined as a medical possession ratio – the percentage of days the prescribed treatment dose of adjuvant endocrine therapy was available to the patient – of at least 80%.
- Medication nonpersistence was defined as a period in which no new adjuvant endocrine therapy prescriptions were filled before the scheduled end of treatment of 90-180 days, depending on the study.
- The impact of both parameters on event-free survival, which included breast cancer recurrence, disease-free survival, breast cancer–specific survival, and overall survival cancer was calculated.
- Of 2,026 articles retrieved, 14 studies, with sample sizes ranging from 857 to 30,573 patients, met the eligibility and quality criteria; 11 examined patient adherence, and 6 examined patient persistence.
TAKEAWAY:
- Of 10 studies that assessed event-free survival, 7 showed significantly worse survival for nonadherent or nonpersistent patients, at hazard ratios of 1.39-2.44.
- Of nine studies that examined overall survival, seven demonstrated a significantly higher risk for mortality in the groups with nonadherence and nonpersistence, at HRs of 1.26-2.18.
- The largest study, which included data on more than 30,000 patients in Taiwan, found that nonadherence and nonpersistence were associated with a significantly increased risk for mortality, at HRs of 1.98 and 2.18, respectively.
IN PRACTICE:
“The available data highlight the dangers of nonadherence and nonpersistence, showing an up to twofold higher risk of relapse or death for patients who do not use endocrine treatment as prescribed,” the researchers said. “Importantly, improving adherence and persistence represents a low-hanging fruit for increasing survival in luminal breast cancer.”
SOURCE:
The study, led by Finn Magnus Eliassen, MD, department of surgery, Stavanger (Norway) University Hospital, was published online on July 4 in BMC Cancer.
LIMITATIONS:
- The review is limited by the relatively small number of studies that met the eligibility criteria and by their heterogeneity, which ruled out a meta-analysis.
- There are no gold-standard definitions of adherence and persistence.
DISCLOSURES:
- No funding was declared. No relevant financial relationships were declared.
- A version of this article first appeared on Medscape.com.
TOPLINE:
a new systematic review found.
METHODOLOGY:
- The investigators conducted a systematic literature search of five databases, looking for studies involving patients with nonmetastatic hormone receptor–positive breast cancer that were published between 2010 and 2020.
- Adequate adherence was defined as a medical possession ratio – the percentage of days the prescribed treatment dose of adjuvant endocrine therapy was available to the patient – of at least 80%.
- Medication nonpersistence was defined as a period in which no new adjuvant endocrine therapy prescriptions were filled before the scheduled end of treatment of 90-180 days, depending on the study.
- The impact of both parameters on event-free survival, which included breast cancer recurrence, disease-free survival, breast cancer–specific survival, and overall survival cancer was calculated.
- Of 2,026 articles retrieved, 14 studies, with sample sizes ranging from 857 to 30,573 patients, met the eligibility and quality criteria; 11 examined patient adherence, and 6 examined patient persistence.
TAKEAWAY:
- Of 10 studies that assessed event-free survival, 7 showed significantly worse survival for nonadherent or nonpersistent patients, at hazard ratios of 1.39-2.44.
- Of nine studies that examined overall survival, seven demonstrated a significantly higher risk for mortality in the groups with nonadherence and nonpersistence, at HRs of 1.26-2.18.
- The largest study, which included data on more than 30,000 patients in Taiwan, found that nonadherence and nonpersistence were associated with a significantly increased risk for mortality, at HRs of 1.98 and 2.18, respectively.
IN PRACTICE:
“The available data highlight the dangers of nonadherence and nonpersistence, showing an up to twofold higher risk of relapse or death for patients who do not use endocrine treatment as prescribed,” the researchers said. “Importantly, improving adherence and persistence represents a low-hanging fruit for increasing survival in luminal breast cancer.”
SOURCE:
The study, led by Finn Magnus Eliassen, MD, department of surgery, Stavanger (Norway) University Hospital, was published online on July 4 in BMC Cancer.
LIMITATIONS:
- The review is limited by the relatively small number of studies that met the eligibility criteria and by their heterogeneity, which ruled out a meta-analysis.
- There are no gold-standard definitions of adherence and persistence.
DISCLOSURES:
- No funding was declared. No relevant financial relationships were declared.
- A version of this article first appeared on Medscape.com.
Is there a link between body image concerns and polycystic ovary syndrome?
This transcript has been edited for clarity.
At ENDO 2023, I presented our systematic review and meta-analysis related to body image concerns in women and individuals with polycystic ovary syndrome (PCOS). PCOS is the most common endocrine condition affecting women worldwide. It’s as common as 10%-15%.
Previously thought to be a benign condition affecting a small proportion of women of reproductive age, it’s changed now. It affects women of all ages, all ethnicities, and throughout the world. Body image concern is an area where one feels uncomfortable with how they look and how they feel. Someone might wonder, why worry about body image concerns? When people have body image concerns, it leads to low self-esteem.
Low self-esteem can lead to depression and anxiety, eventually making you a not-so-productive member of society. Several studies have also shown that body image concerns can lead to eating disorders such as anorexia and bulimia, which can be life threatening. Several studies in the past have shown there is a link between PCOS and body image concerns, but what exactly is the link? We don’t know. How big is the problem? We didn’t know until now.
To answer this, we looked at everything published about PCOS and body image concerns together, be it a randomized study, a cluster study, or any kind of study. We put them all into one place and studied them for evidence. The second objective of our work was that we wanted to share any evidence with the international PCOS guidelines group, who are currently reviewing and revising the guidelines for 2023.
We looked at all the major scientific databases, such as PubMed, PubMed Central, and Medline, for any study that’s been published for polycystic ovary syndrome and body image concerns where they specifically used a validated questionnaire – that’s important, and I’ll come back to that later.
We found 6,221 articles on an initial search. After meticulously looking through all of them, we narrowed it down to 9 articles that were relevant to our work. That’s going from 6,221 articles to 9, which were reviewed by 2 independent researchers. If there was any conflict between them, a third independent researcher resolved the conflict.
We found some studies had used the same questionnaires and some had their own questionnaire. We combined the studies where they used the same questionnaire and we did what we call a meta-analysis. We used their data and combined them to find an additional analysis, which is a combination of the two.
The two most commonly used questionnaires were the Multidimensional Body-Self Relations Questionnaire (MBSRQ) survey and the Body-Esteem Scale for Adolescents and Adults (BESAA). I’m not going into detail, but in simplest terms, the MBSRQ has 69 questions, which breaks down into 5 subscales, and BESAA has 3 subscales, which has 23 questions.
When we combined the results in the MBSRQ questionnaire, women with PCOS fared worse in all the subscales, showing there is a concern about body image in women with PCOS when compared with their colleagues who are healthy and do not have PCOS.
With BESAA, we found a little bit of a mixed picture. There was still a significant difference about weight perception, but how they felt and how they attributed, there was no significant difference. Probably the main reason was that only two studies used it and there was a smaller number of people involved in the study.
Why is this important? We feel that by identifying or diagnosing body image concerns, we will be addressing patient concerns. That is important because we clinicians have our own thoughts of what we need to do to help women with PCOS to prevent long-term risk, but it’s also important to talk to the person sitting in front of you right now. What is their concern?
There’s also been a generational shift where women with PCOS used say, “Oh, I’m worried that I can’t have a kid,” to now say, “I’m worried that I don’t feel well about myself.” We need to address that.
When we shared these findings with the international PCOS guidelines, they said we should probably approach this on an individual case-by-case basis because it will mean that the length of consultation might increase if we spend time with body image concerns.
This is where questionnaires come into play. With a validated questionnaire, a person can complete that before they come into the consultation, thereby minimizing the amount of time spent. If they’re not scoring high on the questionnaire, we don’t need to address that. If they are scoring high, then it can be picked up as a topic to discuss.
As I mentioned, there are a couple of limitations, one being the fewer studies and lower numbers of people in the studies. We need to address this in the future.
Long story short, at the moment, there is evidence to say that body image concerns are quite significantly high in women and individuals with PCOS. This is something we need to address as soon as possible.
We are planning future work to understand how social media comes into play, how society influences body image, and how health care professionals across the world are addressing PCOS and body image concerns. Hopefully, we will be able to share these findings in the near future. Thank you.
Dr. Kempegowda is assistant professor in endocrinology, diabetes, and general medicine at the Institute of Applied Health Research, University of Birmingham, and a consultant in endocrinology, diabetes and acute medicine, Queen Elizabeth Hospital, Birmingham, England, and disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
At ENDO 2023, I presented our systematic review and meta-analysis related to body image concerns in women and individuals with polycystic ovary syndrome (PCOS). PCOS is the most common endocrine condition affecting women worldwide. It’s as common as 10%-15%.
Previously thought to be a benign condition affecting a small proportion of women of reproductive age, it’s changed now. It affects women of all ages, all ethnicities, and throughout the world. Body image concern is an area where one feels uncomfortable with how they look and how they feel. Someone might wonder, why worry about body image concerns? When people have body image concerns, it leads to low self-esteem.
Low self-esteem can lead to depression and anxiety, eventually making you a not-so-productive member of society. Several studies have also shown that body image concerns can lead to eating disorders such as anorexia and bulimia, which can be life threatening. Several studies in the past have shown there is a link between PCOS and body image concerns, but what exactly is the link? We don’t know. How big is the problem? We didn’t know until now.
To answer this, we looked at everything published about PCOS and body image concerns together, be it a randomized study, a cluster study, or any kind of study. We put them all into one place and studied them for evidence. The second objective of our work was that we wanted to share any evidence with the international PCOS guidelines group, who are currently reviewing and revising the guidelines for 2023.
We looked at all the major scientific databases, such as PubMed, PubMed Central, and Medline, for any study that’s been published for polycystic ovary syndrome and body image concerns where they specifically used a validated questionnaire – that’s important, and I’ll come back to that later.
We found 6,221 articles on an initial search. After meticulously looking through all of them, we narrowed it down to 9 articles that were relevant to our work. That’s going from 6,221 articles to 9, which were reviewed by 2 independent researchers. If there was any conflict between them, a third independent researcher resolved the conflict.
We found some studies had used the same questionnaires and some had their own questionnaire. We combined the studies where they used the same questionnaire and we did what we call a meta-analysis. We used their data and combined them to find an additional analysis, which is a combination of the two.
The two most commonly used questionnaires were the Multidimensional Body-Self Relations Questionnaire (MBSRQ) survey and the Body-Esteem Scale for Adolescents and Adults (BESAA). I’m not going into detail, but in simplest terms, the MBSRQ has 69 questions, which breaks down into 5 subscales, and BESAA has 3 subscales, which has 23 questions.
When we combined the results in the MBSRQ questionnaire, women with PCOS fared worse in all the subscales, showing there is a concern about body image in women with PCOS when compared with their colleagues who are healthy and do not have PCOS.
With BESAA, we found a little bit of a mixed picture. There was still a significant difference about weight perception, but how they felt and how they attributed, there was no significant difference. Probably the main reason was that only two studies used it and there was a smaller number of people involved in the study.
Why is this important? We feel that by identifying or diagnosing body image concerns, we will be addressing patient concerns. That is important because we clinicians have our own thoughts of what we need to do to help women with PCOS to prevent long-term risk, but it’s also important to talk to the person sitting in front of you right now. What is their concern?
There’s also been a generational shift where women with PCOS used say, “Oh, I’m worried that I can’t have a kid,” to now say, “I’m worried that I don’t feel well about myself.” We need to address that.
When we shared these findings with the international PCOS guidelines, they said we should probably approach this on an individual case-by-case basis because it will mean that the length of consultation might increase if we spend time with body image concerns.
This is where questionnaires come into play. With a validated questionnaire, a person can complete that before they come into the consultation, thereby minimizing the amount of time spent. If they’re not scoring high on the questionnaire, we don’t need to address that. If they are scoring high, then it can be picked up as a topic to discuss.
As I mentioned, there are a couple of limitations, one being the fewer studies and lower numbers of people in the studies. We need to address this in the future.
Long story short, at the moment, there is evidence to say that body image concerns are quite significantly high in women and individuals with PCOS. This is something we need to address as soon as possible.
We are planning future work to understand how social media comes into play, how society influences body image, and how health care professionals across the world are addressing PCOS and body image concerns. Hopefully, we will be able to share these findings in the near future. Thank you.
Dr. Kempegowda is assistant professor in endocrinology, diabetes, and general medicine at the Institute of Applied Health Research, University of Birmingham, and a consultant in endocrinology, diabetes and acute medicine, Queen Elizabeth Hospital, Birmingham, England, and disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
At ENDO 2023, I presented our systematic review and meta-analysis related to body image concerns in women and individuals with polycystic ovary syndrome (PCOS). PCOS is the most common endocrine condition affecting women worldwide. It’s as common as 10%-15%.
Previously thought to be a benign condition affecting a small proportion of women of reproductive age, it’s changed now. It affects women of all ages, all ethnicities, and throughout the world. Body image concern is an area where one feels uncomfortable with how they look and how they feel. Someone might wonder, why worry about body image concerns? When people have body image concerns, it leads to low self-esteem.
Low self-esteem can lead to depression and anxiety, eventually making you a not-so-productive member of society. Several studies have also shown that body image concerns can lead to eating disorders such as anorexia and bulimia, which can be life threatening. Several studies in the past have shown there is a link between PCOS and body image concerns, but what exactly is the link? We don’t know. How big is the problem? We didn’t know until now.
To answer this, we looked at everything published about PCOS and body image concerns together, be it a randomized study, a cluster study, or any kind of study. We put them all into one place and studied them for evidence. The second objective of our work was that we wanted to share any evidence with the international PCOS guidelines group, who are currently reviewing and revising the guidelines for 2023.
We looked at all the major scientific databases, such as PubMed, PubMed Central, and Medline, for any study that’s been published for polycystic ovary syndrome and body image concerns where they specifically used a validated questionnaire – that’s important, and I’ll come back to that later.
We found 6,221 articles on an initial search. After meticulously looking through all of them, we narrowed it down to 9 articles that were relevant to our work. That’s going from 6,221 articles to 9, which were reviewed by 2 independent researchers. If there was any conflict between them, a third independent researcher resolved the conflict.
We found some studies had used the same questionnaires and some had their own questionnaire. We combined the studies where they used the same questionnaire and we did what we call a meta-analysis. We used their data and combined them to find an additional analysis, which is a combination of the two.
The two most commonly used questionnaires were the Multidimensional Body-Self Relations Questionnaire (MBSRQ) survey and the Body-Esteem Scale for Adolescents and Adults (BESAA). I’m not going into detail, but in simplest terms, the MBSRQ has 69 questions, which breaks down into 5 subscales, and BESAA has 3 subscales, which has 23 questions.
When we combined the results in the MBSRQ questionnaire, women with PCOS fared worse in all the subscales, showing there is a concern about body image in women with PCOS when compared with their colleagues who are healthy and do not have PCOS.
With BESAA, we found a little bit of a mixed picture. There was still a significant difference about weight perception, but how they felt and how they attributed, there was no significant difference. Probably the main reason was that only two studies used it and there was a smaller number of people involved in the study.
Why is this important? We feel that by identifying or diagnosing body image concerns, we will be addressing patient concerns. That is important because we clinicians have our own thoughts of what we need to do to help women with PCOS to prevent long-term risk, but it’s also important to talk to the person sitting in front of you right now. What is their concern?
There’s also been a generational shift where women with PCOS used say, “Oh, I’m worried that I can’t have a kid,” to now say, “I’m worried that I don’t feel well about myself.” We need to address that.
When we shared these findings with the international PCOS guidelines, they said we should probably approach this on an individual case-by-case basis because it will mean that the length of consultation might increase if we spend time with body image concerns.
This is where questionnaires come into play. With a validated questionnaire, a person can complete that before they come into the consultation, thereby minimizing the amount of time spent. If they’re not scoring high on the questionnaire, we don’t need to address that. If they are scoring high, then it can be picked up as a topic to discuss.
As I mentioned, there are a couple of limitations, one being the fewer studies and lower numbers of people in the studies. We need to address this in the future.
Long story short, at the moment, there is evidence to say that body image concerns are quite significantly high in women and individuals with PCOS. This is something we need to address as soon as possible.
We are planning future work to understand how social media comes into play, how society influences body image, and how health care professionals across the world are addressing PCOS and body image concerns. Hopefully, we will be able to share these findings in the near future. Thank you.
Dr. Kempegowda is assistant professor in endocrinology, diabetes, and general medicine at the Institute of Applied Health Research, University of Birmingham, and a consultant in endocrinology, diabetes and acute medicine, Queen Elizabeth Hospital, Birmingham, England, and disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Heart-protective diet in PURE study allows whole-fat dairy
Most of the protective food categories are in line with standard dietary guidelines for good health, but one that may be heart-protective is not usually included in such recommendations.
The food categories that were found to be protective include fruit, vegetables, nuts, legumes, and fish but also dairy, “mainly whole-fat,” in an analysis based on the international Prospective Urban and Rural Epidemiological (PURE) study and data from five other international trials that encompassed more than 240,000 people.
A healthy diet scoring system was derived from dietary patterns and clinical events observed in the PURE study and was applied to the populations of the other trials. Higher scores, corresponding to greater consumption of the six food categories, tracked with significantly reduced risks for death, myocardial infarction (MI), and stroke.
Reductions in mortality and CV-disease risk that were linked to the higher scores were especially pronounced in lower-income countries in the study published onlinein the European Heart Journal with lead author Andrew Mente, PhD, Population Health Research Institute, McMaster University, Hamilton, Ont.
The study in part refutes the frequent preference for low-fat or no-fat dairy foods over whole-fat dairy in healthy-diet recommendations. But it is consistent with earlier findings from PURE of reduced mortality risk with increased consumption of dietary fat, including saturated fat.
Whereas healthy-diet recommendations tend to emphasize reduced intake of fat, especially saturated fat, the report notes that “there are almost no national or international strategies and policies to increase a number of protective foods,” such as nuts, fish, and dairy.
“Therefore, while the findings from PURE are largely consistent with the nutrition science and modern dietary recommendations to focus on protective foods, the public’s understanding of healthy eating and relevant global policies have not yet caught up to this science,” it states.
“Guidelines and policy actions need to be updated with this newer evidence,” Dr. Mente said in an interview. “For example, the World Health Organization remains mainly focused on reducing certain nutrients, such as fat, saturated fat, added sugar, and salt,” he said. “These recommendations are echoed by government policy actions and industry, as evident by the continued focus on the usual nutrients in food labels of many countries.”
The current findings, Dr. Mente said, “can be used to ensure that the public’s understanding of healthy eating and relevant global policies are able to catch up to the science.”
Healthy diet score
PURE investigators developed their healthy diet score using data from 147,642 people from the general population in 21 countries. The investigators compared self-reported dietary intakes with long-term clinical outcomes.
The scoring system assigned a value of 1 for each of the six health-food categories when individuals’ intake exceeded the entire cohort’s median intake. It assigned a 0 when intake was below the median. The total PURE healthy diet score consisted of the sum of the six values, with higher scores corresponding to a healthier diet. The mean score for cohort was 2.95.
There were 15,707 deaths and 40,764 CV events during a median follow-up of 9.3 years. A score of at least 5 points, compared with 0 or 1 point, was associated with significantly reduced hazard ratios for mortality, MI, and stroke in multivariable analysis:
- Mortality: HR, 0.70 (95% CI, 0.63-0.77; P < .0001).
- Major CV disease: HR, 0.82 (95% CI, 0.75-0.91; P < .0001).
- MI: HR, 0.86 (95% CI, 0.75-0.99; P = .0014).
- Stroke: HR, 0.81 (95% CI, 0.71-0.93; P = .0034).
The healthy diet score’s relationship to clinical outcomes was explored in five other large independent studies, including three prospective trials of patients with CV disease that spanned 50 countries, a case-control study with MI patients in 52 countries, and a case-control study with stroke patients in 33 countries.
In the three prospective trials, higher scores were associated with reduced mortality, CV disease events, and MI:
- Mortality: HR, 0.73 (95% CI, 0.66-0.81).
- Major CV disease: HR, 0.79 (95% CI, 0.72-0.87).
- MI: HR, 0.85 (95% CI, 0.71-0.99).
In the two case-control studies, a higher diet score was associated with reduced odds ratios for first MI and for stroke:
- MI: OR, 0.72 (95% CI, 0.65-0.80).
- Stroke: OR, 0.57 (95% CI, 0.50-0.65).
In an analysis based on the PURE cohort, incorporation of unprocessed red meat or whole grains into the health diet score produced similar results, suggesting that a “modest amount” of meat or whole grains can be part of a healthy diet, the authors contend.
The results were similar in a combined analysis of all the prospective studies. In particular, improvement in diet score by one quintile was associated with significantly reduced risks for the following:
- Mortality: HR, 0.92 (95% CI, 0.90-0.93).
- Major CV disease: HR, 0.94 (95% CI, 0.93-0.95).
- MI: HR, 0.94 (95% CI, 0.92-0.96).
- Stroke: HR, 0.94 (95% CI, 0.89-0.99).
- Death or CV disease: HR, 0.93 (95% CI, 0.92-0.94).
“This strongly indicates that the take-home message for patients is the same as for general populations,” Dr. Mente said. “Eat plenty of fruits, vegetables, nuts, legumes, and a moderate amount of fish and whole-fat dairy to lower risk of CV disease and mortality.”
Dairy foods are not widely consumed in some cultures, he said, “but availability and cost are also factors in determining consumption.” Nonetheless, a high-quality diet can be achieved without including or excluding dairy foods. Context-specific policies and priorities are needed for different populations, “rather than a one-size-fits-all global policy.”
Food labels in many countries mainly focus on “reducing certain nutrients as the end-all, be-all,” Dr. Mente observed. “Our findings can be used as a basis for recommendations regarding what a healthy diet should be globally and then modified for each region based on the specific types of foods that are available and affordable in each region.”
Moreover, he said, “targeted food policies are needed to increase the availability and affordability of healthy foods, especially in lower-income countries where intakes are low.”
Common human biology
The current results from PURE “confirm prior observations from mostly Western nations that low intakes of fruits, vegetables, nuts, legumes, and fish are major risk factors for poor health,” observes Dariush Mozaffarian, MD, DrPH, MPH, Tufts University, Boston, in an accompanying editorial. “This suggests that common human biology, not merely confounding, explains these observed diet–disease relationships, strengthening causal inference on the power of nutrition.”
Moreover, “These findings provide further support that dairy foods, including whole-fat dairy, can be part of a healthy diet,” Dr. Mozaffarian writes. “The new results in PURE, in combination with prior reports, call for a re-evaluation of unrelenting guidelines to avoid whole-fat dairy products.”
Such studies “remind us of the continuing and devastating rise in diet-related chronic diseases globally, and of the power of protective foods to help address these burdens,” the editorial continues. “It is time for national nutrition guidelines, private sector innovations, government tax policy and agricultural incentives, food procurement policies, labeling and other regulatory priorities, and food-based health care interventions to catch up to the science.”
Not automatically superior
“I do not believe guidelines should be changed based on this single study,” contends Howard D. Sesso, ScD, MPH, associate director of the division of preventive medicine at Brigham and Women’s Hospital, Boston, who isn’t part of PURE. “But I welcome the scientific dialog that should come out of any study that challenges what we think we know,” he told this news organization.
“Many other dietary patterns have been identified over the years that also do a great job in predicting disease risk in observational studies,” observed Dr. Sesso. “Is PURE that much better? Maybe, maybe not. But not enough to dismiss other dietary patterns that are already the basis of dietary recommendations in the U.S., Europe, and worldwide.”
The PURE healthy diet score, he said, “appears to work well within the confines of their large pooling of studies around the world, but that doesn’t automatically make it superior to other dietary patterns.” The score “was only modestly, but not greatly, better than existing dietary patterns evaluated.”
Randomized controlled trials are needed, Dr. Sesso said, to “delve into more specific dietary components,” including unprocessed red meat, whole grains, and high-fat dairy foods. And, he said, more observational studies are needed to examine the score’s association with other cardiometabolic outcomes.
The PURE study is funded by the Population Health Research Institute, the Hamilton Health Sciences Research Institute, the Canadian Institutes of Health Research, the Heart and Stroke Foundation of Ontario; with support from Canadian Institutes of Health Research’s Strategy for Patient Oriented Research through the Ontario SPOR Support Unit, as well as the Ontario Ministry of Health and Long-Term Care; and through unrestricted grants from several pharmaceutical companies, with major contributions from AstraZeneca, Sanofi-Aventis, Boehringer Ingelheim, Servier, and GlaxoSmithKline. Additional contributions are from Novartis and King Pharma. Dr. Mente, Dr. Mozaffarian, and Dr. Sesso have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Most of the protective food categories are in line with standard dietary guidelines for good health, but one that may be heart-protective is not usually included in such recommendations.
The food categories that were found to be protective include fruit, vegetables, nuts, legumes, and fish but also dairy, “mainly whole-fat,” in an analysis based on the international Prospective Urban and Rural Epidemiological (PURE) study and data from five other international trials that encompassed more than 240,000 people.
A healthy diet scoring system was derived from dietary patterns and clinical events observed in the PURE study and was applied to the populations of the other trials. Higher scores, corresponding to greater consumption of the six food categories, tracked with significantly reduced risks for death, myocardial infarction (MI), and stroke.
Reductions in mortality and CV-disease risk that were linked to the higher scores were especially pronounced in lower-income countries in the study published onlinein the European Heart Journal with lead author Andrew Mente, PhD, Population Health Research Institute, McMaster University, Hamilton, Ont.
The study in part refutes the frequent preference for low-fat or no-fat dairy foods over whole-fat dairy in healthy-diet recommendations. But it is consistent with earlier findings from PURE of reduced mortality risk with increased consumption of dietary fat, including saturated fat.
Whereas healthy-diet recommendations tend to emphasize reduced intake of fat, especially saturated fat, the report notes that “there are almost no national or international strategies and policies to increase a number of protective foods,” such as nuts, fish, and dairy.
“Therefore, while the findings from PURE are largely consistent with the nutrition science and modern dietary recommendations to focus on protective foods, the public’s understanding of healthy eating and relevant global policies have not yet caught up to this science,” it states.
“Guidelines and policy actions need to be updated with this newer evidence,” Dr. Mente said in an interview. “For example, the World Health Organization remains mainly focused on reducing certain nutrients, such as fat, saturated fat, added sugar, and salt,” he said. “These recommendations are echoed by government policy actions and industry, as evident by the continued focus on the usual nutrients in food labels of many countries.”
The current findings, Dr. Mente said, “can be used to ensure that the public’s understanding of healthy eating and relevant global policies are able to catch up to the science.”
Healthy diet score
PURE investigators developed their healthy diet score using data from 147,642 people from the general population in 21 countries. The investigators compared self-reported dietary intakes with long-term clinical outcomes.
The scoring system assigned a value of 1 for each of the six health-food categories when individuals’ intake exceeded the entire cohort’s median intake. It assigned a 0 when intake was below the median. The total PURE healthy diet score consisted of the sum of the six values, with higher scores corresponding to a healthier diet. The mean score for cohort was 2.95.
There were 15,707 deaths and 40,764 CV events during a median follow-up of 9.3 years. A score of at least 5 points, compared with 0 or 1 point, was associated with significantly reduced hazard ratios for mortality, MI, and stroke in multivariable analysis:
- Mortality: HR, 0.70 (95% CI, 0.63-0.77; P < .0001).
- Major CV disease: HR, 0.82 (95% CI, 0.75-0.91; P < .0001).
- MI: HR, 0.86 (95% CI, 0.75-0.99; P = .0014).
- Stroke: HR, 0.81 (95% CI, 0.71-0.93; P = .0034).
The healthy diet score’s relationship to clinical outcomes was explored in five other large independent studies, including three prospective trials of patients with CV disease that spanned 50 countries, a case-control study with MI patients in 52 countries, and a case-control study with stroke patients in 33 countries.
In the three prospective trials, higher scores were associated with reduced mortality, CV disease events, and MI:
- Mortality: HR, 0.73 (95% CI, 0.66-0.81).
- Major CV disease: HR, 0.79 (95% CI, 0.72-0.87).
- MI: HR, 0.85 (95% CI, 0.71-0.99).
In the two case-control studies, a higher diet score was associated with reduced odds ratios for first MI and for stroke:
- MI: OR, 0.72 (95% CI, 0.65-0.80).
- Stroke: OR, 0.57 (95% CI, 0.50-0.65).
In an analysis based on the PURE cohort, incorporation of unprocessed red meat or whole grains into the health diet score produced similar results, suggesting that a “modest amount” of meat or whole grains can be part of a healthy diet, the authors contend.
The results were similar in a combined analysis of all the prospective studies. In particular, improvement in diet score by one quintile was associated with significantly reduced risks for the following:
- Mortality: HR, 0.92 (95% CI, 0.90-0.93).
- Major CV disease: HR, 0.94 (95% CI, 0.93-0.95).
- MI: HR, 0.94 (95% CI, 0.92-0.96).
- Stroke: HR, 0.94 (95% CI, 0.89-0.99).
- Death or CV disease: HR, 0.93 (95% CI, 0.92-0.94).
“This strongly indicates that the take-home message for patients is the same as for general populations,” Dr. Mente said. “Eat plenty of fruits, vegetables, nuts, legumes, and a moderate amount of fish and whole-fat dairy to lower risk of CV disease and mortality.”
Dairy foods are not widely consumed in some cultures, he said, “but availability and cost are also factors in determining consumption.” Nonetheless, a high-quality diet can be achieved without including or excluding dairy foods. Context-specific policies and priorities are needed for different populations, “rather than a one-size-fits-all global policy.”
Food labels in many countries mainly focus on “reducing certain nutrients as the end-all, be-all,” Dr. Mente observed. “Our findings can be used as a basis for recommendations regarding what a healthy diet should be globally and then modified for each region based on the specific types of foods that are available and affordable in each region.”
Moreover, he said, “targeted food policies are needed to increase the availability and affordability of healthy foods, especially in lower-income countries where intakes are low.”
Common human biology
The current results from PURE “confirm prior observations from mostly Western nations that low intakes of fruits, vegetables, nuts, legumes, and fish are major risk factors for poor health,” observes Dariush Mozaffarian, MD, DrPH, MPH, Tufts University, Boston, in an accompanying editorial. “This suggests that common human biology, not merely confounding, explains these observed diet–disease relationships, strengthening causal inference on the power of nutrition.”
Moreover, “These findings provide further support that dairy foods, including whole-fat dairy, can be part of a healthy diet,” Dr. Mozaffarian writes. “The new results in PURE, in combination with prior reports, call for a re-evaluation of unrelenting guidelines to avoid whole-fat dairy products.”
Such studies “remind us of the continuing and devastating rise in diet-related chronic diseases globally, and of the power of protective foods to help address these burdens,” the editorial continues. “It is time for national nutrition guidelines, private sector innovations, government tax policy and agricultural incentives, food procurement policies, labeling and other regulatory priorities, and food-based health care interventions to catch up to the science.”
Not automatically superior
“I do not believe guidelines should be changed based on this single study,” contends Howard D. Sesso, ScD, MPH, associate director of the division of preventive medicine at Brigham and Women’s Hospital, Boston, who isn’t part of PURE. “But I welcome the scientific dialog that should come out of any study that challenges what we think we know,” he told this news organization.
“Many other dietary patterns have been identified over the years that also do a great job in predicting disease risk in observational studies,” observed Dr. Sesso. “Is PURE that much better? Maybe, maybe not. But not enough to dismiss other dietary patterns that are already the basis of dietary recommendations in the U.S., Europe, and worldwide.”
The PURE healthy diet score, he said, “appears to work well within the confines of their large pooling of studies around the world, but that doesn’t automatically make it superior to other dietary patterns.” The score “was only modestly, but not greatly, better than existing dietary patterns evaluated.”
Randomized controlled trials are needed, Dr. Sesso said, to “delve into more specific dietary components,” including unprocessed red meat, whole grains, and high-fat dairy foods. And, he said, more observational studies are needed to examine the score’s association with other cardiometabolic outcomes.
The PURE study is funded by the Population Health Research Institute, the Hamilton Health Sciences Research Institute, the Canadian Institutes of Health Research, the Heart and Stroke Foundation of Ontario; with support from Canadian Institutes of Health Research’s Strategy for Patient Oriented Research through the Ontario SPOR Support Unit, as well as the Ontario Ministry of Health and Long-Term Care; and through unrestricted grants from several pharmaceutical companies, with major contributions from AstraZeneca, Sanofi-Aventis, Boehringer Ingelheim, Servier, and GlaxoSmithKline. Additional contributions are from Novartis and King Pharma. Dr. Mente, Dr. Mozaffarian, and Dr. Sesso have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Most of the protective food categories are in line with standard dietary guidelines for good health, but one that may be heart-protective is not usually included in such recommendations.
The food categories that were found to be protective include fruit, vegetables, nuts, legumes, and fish but also dairy, “mainly whole-fat,” in an analysis based on the international Prospective Urban and Rural Epidemiological (PURE) study and data from five other international trials that encompassed more than 240,000 people.
A healthy diet scoring system was derived from dietary patterns and clinical events observed in the PURE study and was applied to the populations of the other trials. Higher scores, corresponding to greater consumption of the six food categories, tracked with significantly reduced risks for death, myocardial infarction (MI), and stroke.
Reductions in mortality and CV-disease risk that were linked to the higher scores were especially pronounced in lower-income countries in the study published onlinein the European Heart Journal with lead author Andrew Mente, PhD, Population Health Research Institute, McMaster University, Hamilton, Ont.
The study in part refutes the frequent preference for low-fat or no-fat dairy foods over whole-fat dairy in healthy-diet recommendations. But it is consistent with earlier findings from PURE of reduced mortality risk with increased consumption of dietary fat, including saturated fat.
Whereas healthy-diet recommendations tend to emphasize reduced intake of fat, especially saturated fat, the report notes that “there are almost no national or international strategies and policies to increase a number of protective foods,” such as nuts, fish, and dairy.
“Therefore, while the findings from PURE are largely consistent with the nutrition science and modern dietary recommendations to focus on protective foods, the public’s understanding of healthy eating and relevant global policies have not yet caught up to this science,” it states.
“Guidelines and policy actions need to be updated with this newer evidence,” Dr. Mente said in an interview. “For example, the World Health Organization remains mainly focused on reducing certain nutrients, such as fat, saturated fat, added sugar, and salt,” he said. “These recommendations are echoed by government policy actions and industry, as evident by the continued focus on the usual nutrients in food labels of many countries.”
The current findings, Dr. Mente said, “can be used to ensure that the public’s understanding of healthy eating and relevant global policies are able to catch up to the science.”
Healthy diet score
PURE investigators developed their healthy diet score using data from 147,642 people from the general population in 21 countries. The investigators compared self-reported dietary intakes with long-term clinical outcomes.
The scoring system assigned a value of 1 for each of the six health-food categories when individuals’ intake exceeded the entire cohort’s median intake. It assigned a 0 when intake was below the median. The total PURE healthy diet score consisted of the sum of the six values, with higher scores corresponding to a healthier diet. The mean score for cohort was 2.95.
There were 15,707 deaths and 40,764 CV events during a median follow-up of 9.3 years. A score of at least 5 points, compared with 0 or 1 point, was associated with significantly reduced hazard ratios for mortality, MI, and stroke in multivariable analysis:
- Mortality: HR, 0.70 (95% CI, 0.63-0.77; P < .0001).
- Major CV disease: HR, 0.82 (95% CI, 0.75-0.91; P < .0001).
- MI: HR, 0.86 (95% CI, 0.75-0.99; P = .0014).
- Stroke: HR, 0.81 (95% CI, 0.71-0.93; P = .0034).
The healthy diet score’s relationship to clinical outcomes was explored in five other large independent studies, including three prospective trials of patients with CV disease that spanned 50 countries, a case-control study with MI patients in 52 countries, and a case-control study with stroke patients in 33 countries.
In the three prospective trials, higher scores were associated with reduced mortality, CV disease events, and MI:
- Mortality: HR, 0.73 (95% CI, 0.66-0.81).
- Major CV disease: HR, 0.79 (95% CI, 0.72-0.87).
- MI: HR, 0.85 (95% CI, 0.71-0.99).
In the two case-control studies, a higher diet score was associated with reduced odds ratios for first MI and for stroke:
- MI: OR, 0.72 (95% CI, 0.65-0.80).
- Stroke: OR, 0.57 (95% CI, 0.50-0.65).
In an analysis based on the PURE cohort, incorporation of unprocessed red meat or whole grains into the health diet score produced similar results, suggesting that a “modest amount” of meat or whole grains can be part of a healthy diet, the authors contend.
The results were similar in a combined analysis of all the prospective studies. In particular, improvement in diet score by one quintile was associated with significantly reduced risks for the following:
- Mortality: HR, 0.92 (95% CI, 0.90-0.93).
- Major CV disease: HR, 0.94 (95% CI, 0.93-0.95).
- MI: HR, 0.94 (95% CI, 0.92-0.96).
- Stroke: HR, 0.94 (95% CI, 0.89-0.99).
- Death or CV disease: HR, 0.93 (95% CI, 0.92-0.94).
“This strongly indicates that the take-home message for patients is the same as for general populations,” Dr. Mente said. “Eat plenty of fruits, vegetables, nuts, legumes, and a moderate amount of fish and whole-fat dairy to lower risk of CV disease and mortality.”
Dairy foods are not widely consumed in some cultures, he said, “but availability and cost are also factors in determining consumption.” Nonetheless, a high-quality diet can be achieved without including or excluding dairy foods. Context-specific policies and priorities are needed for different populations, “rather than a one-size-fits-all global policy.”
Food labels in many countries mainly focus on “reducing certain nutrients as the end-all, be-all,” Dr. Mente observed. “Our findings can be used as a basis for recommendations regarding what a healthy diet should be globally and then modified for each region based on the specific types of foods that are available and affordable in each region.”
Moreover, he said, “targeted food policies are needed to increase the availability and affordability of healthy foods, especially in lower-income countries where intakes are low.”
Common human biology
The current results from PURE “confirm prior observations from mostly Western nations that low intakes of fruits, vegetables, nuts, legumes, and fish are major risk factors for poor health,” observes Dariush Mozaffarian, MD, DrPH, MPH, Tufts University, Boston, in an accompanying editorial. “This suggests that common human biology, not merely confounding, explains these observed diet–disease relationships, strengthening causal inference on the power of nutrition.”
Moreover, “These findings provide further support that dairy foods, including whole-fat dairy, can be part of a healthy diet,” Dr. Mozaffarian writes. “The new results in PURE, in combination with prior reports, call for a re-evaluation of unrelenting guidelines to avoid whole-fat dairy products.”
Such studies “remind us of the continuing and devastating rise in diet-related chronic diseases globally, and of the power of protective foods to help address these burdens,” the editorial continues. “It is time for national nutrition guidelines, private sector innovations, government tax policy and agricultural incentives, food procurement policies, labeling and other regulatory priorities, and food-based health care interventions to catch up to the science.”
Not automatically superior
“I do not believe guidelines should be changed based on this single study,” contends Howard D. Sesso, ScD, MPH, associate director of the division of preventive medicine at Brigham and Women’s Hospital, Boston, who isn’t part of PURE. “But I welcome the scientific dialog that should come out of any study that challenges what we think we know,” he told this news organization.
“Many other dietary patterns have been identified over the years that also do a great job in predicting disease risk in observational studies,” observed Dr. Sesso. “Is PURE that much better? Maybe, maybe not. But not enough to dismiss other dietary patterns that are already the basis of dietary recommendations in the U.S., Europe, and worldwide.”
The PURE healthy diet score, he said, “appears to work well within the confines of their large pooling of studies around the world, but that doesn’t automatically make it superior to other dietary patterns.” The score “was only modestly, but not greatly, better than existing dietary patterns evaluated.”
Randomized controlled trials are needed, Dr. Sesso said, to “delve into more specific dietary components,” including unprocessed red meat, whole grains, and high-fat dairy foods. And, he said, more observational studies are needed to examine the score’s association with other cardiometabolic outcomes.
The PURE study is funded by the Population Health Research Institute, the Hamilton Health Sciences Research Institute, the Canadian Institutes of Health Research, the Heart and Stroke Foundation of Ontario; with support from Canadian Institutes of Health Research’s Strategy for Patient Oriented Research through the Ontario SPOR Support Unit, as well as the Ontario Ministry of Health and Long-Term Care; and through unrestricted grants from several pharmaceutical companies, with major contributions from AstraZeneca, Sanofi-Aventis, Boehringer Ingelheim, Servier, and GlaxoSmithKline. Additional contributions are from Novartis and King Pharma. Dr. Mente, Dr. Mozaffarian, and Dr. Sesso have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM EUROPEAN HEART CENTER
The surprising occupations with higher-than-expected ovarian cancer rates
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study.
Basically, all cancers are caused by a mix of genetic and environmental factors, with some cancers driven more strongly by one or the other. When it comes to ovarian cancer, which kills more than 13,000 women per year in the United States, genetic factors like the BRCA gene mutations are well described.
Other risk factors, like early menarche and nulliparity, are difficult to modify. The only slam-dunk environmental toxin to be linked to ovarian cancer is asbestos. Still, the vast majority of women who develop ovarian cancer do not have a known high-risk gene or asbestos exposure, so other triggers may be out there. How do we find them? The answer may just be good old-fashioned epidemiology.
That’s just what researchers, led by Anita Koushik at the University of Montreal, did in a new study appearing in the journal Occupational and Environmental Medicine.
They identified 497 women in Montreal who had recently been diagnosed with ovarian cancer. They then matched those women to 897 women without ovarian cancer, based on age and address. (This approach would not work well in the United States, as diagnosis of ovarian cancer might depend on access to medical care, which is not universal here. In Canada, however, it’s safer to assume that anyone who could have gotten ovarian cancer in Montreal would have been detected.)
Cases and controls identified, the researchers took a detailed occupational history for each participant: every job they ever worked, and when, and for how long. Each occupation was mapped to a standardized set of industries and, interestingly, to a set of environmental exposures ranging from cosmetic talc to cooking fumes to cotton dust, in what is known as a job-exposure matrix. Of course, they also collected data on other ovarian cancer risk factors.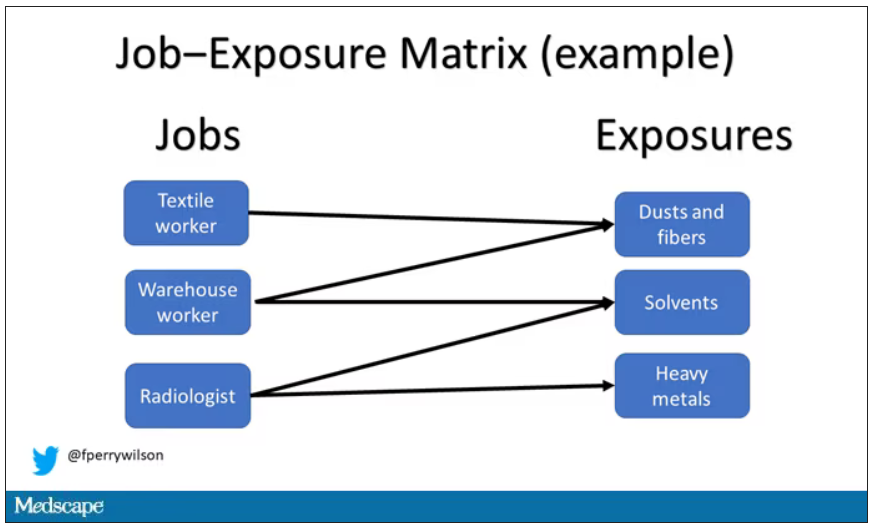
After that, it’s a simple matter of looking at the rate of ovarian cancer by occupation and occupation-associated exposures, accounting for differences in things like pregnancy rates.
A brief aside here. I was at dinner with my wife the other night and telling her about this study, and I asked, “What do you think the occupation with the highest rate of ovarian cancer is?” And without missing a beat, she said: “Hairdressers.” Which blew my mind because of how random that was, but she was also – as usual – 100% correct.
Hairdressers, at least those who had been in the industry for more than 10 years, had a threefold higher risk for ovarian cancer than matched controls who had never been hairdressers.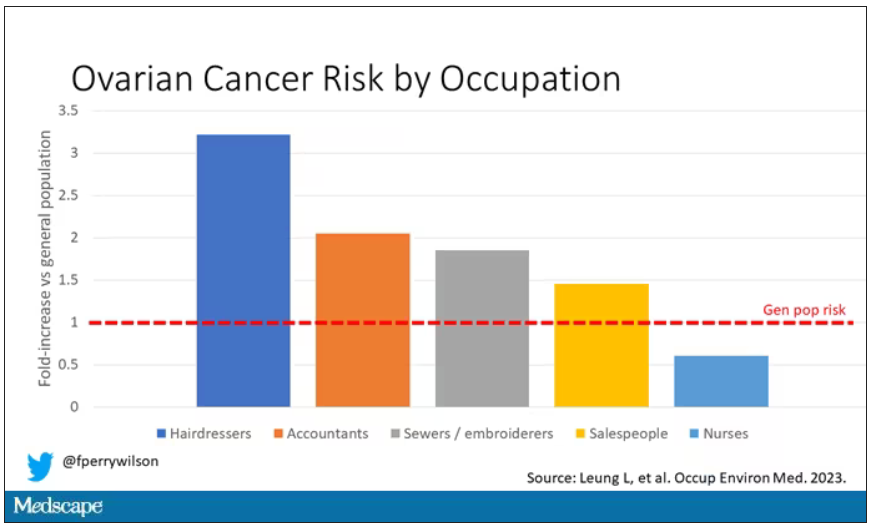
Of course, my wife is a cancer surgeon, so she has a bit of a leg up on me here. Many of you may also know that there is actually a decent body of literature showing higher rates of various cancers among hairdressers, presumably due to the variety of chemicals they are exposed to on a continuous basis.
The No. 2 highest-risk profession on the list? Accountants, with about a twofold higher risk. That one is more of a puzzler. It could be a false positive; after all, there were multiple occupations checked and random error might give a few hits that are meaningless. But there are certainly some occupational factors unique to accountants that might bear further investigation – maybe exposure to volatile organic compounds from office printers, or just a particularly sedentary office environment.
In terms of specific exposures, there were high risks seen with mononuclear aromatic hydrocarbons, bleaches, ethanol, and fluorocarbons, among others, but we have to be a bit more careful here. These exposures were not directly measured. Rather, based on the job category a woman described, the exposures were imputed based on the job-exposure matrix. As such, the correlations between the job and the particular exposure are really quite high, making it essentially impossible to tease out whether it is, for example, being a hairdresser, or being exposed to fluorocarbons as a hairdresser, or being exposed to something else as a hairdresser, that is the problem.
This is how these types of studies work; they tend to raise more questions than they answer. But in a world where a cancer diagnosis can seem to come completely out of the blue, they provide the starting point that someday may lead to a more definitive culprit agent or group of agents. Until then, it might be wise for hairdressers to make sure their workplace is well ventilated.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale University’s Clinical and Translational Research Accelerator in New Haven, Conn. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study.
Basically, all cancers are caused by a mix of genetic and environmental factors, with some cancers driven more strongly by one or the other. When it comes to ovarian cancer, which kills more than 13,000 women per year in the United States, genetic factors like the BRCA gene mutations are well described.
Other risk factors, like early menarche and nulliparity, are difficult to modify. The only slam-dunk environmental toxin to be linked to ovarian cancer is asbestos. Still, the vast majority of women who develop ovarian cancer do not have a known high-risk gene or asbestos exposure, so other triggers may be out there. How do we find them? The answer may just be good old-fashioned epidemiology.
That’s just what researchers, led by Anita Koushik at the University of Montreal, did in a new study appearing in the journal Occupational and Environmental Medicine.
They identified 497 women in Montreal who had recently been diagnosed with ovarian cancer. They then matched those women to 897 women without ovarian cancer, based on age and address. (This approach would not work well in the United States, as diagnosis of ovarian cancer might depend on access to medical care, which is not universal here. In Canada, however, it’s safer to assume that anyone who could have gotten ovarian cancer in Montreal would have been detected.)
Cases and controls identified, the researchers took a detailed occupational history for each participant: every job they ever worked, and when, and for how long. Each occupation was mapped to a standardized set of industries and, interestingly, to a set of environmental exposures ranging from cosmetic talc to cooking fumes to cotton dust, in what is known as a job-exposure matrix. Of course, they also collected data on other ovarian cancer risk factors.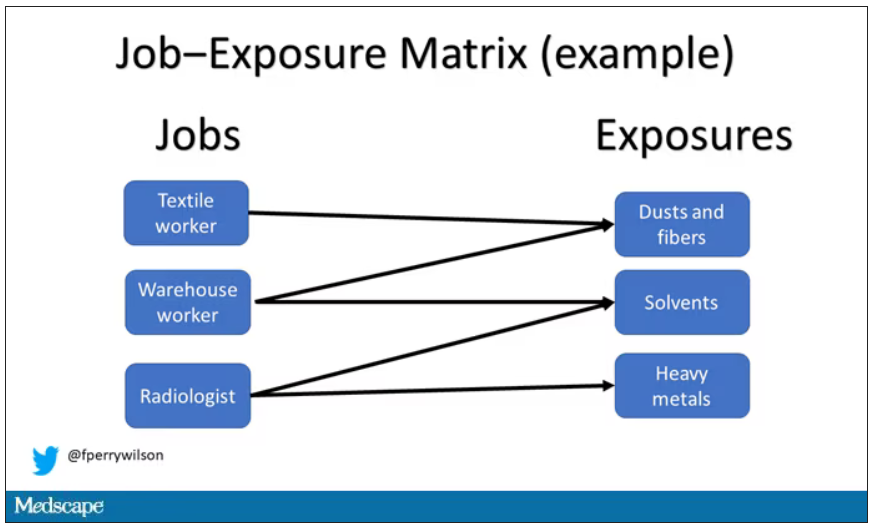
After that, it’s a simple matter of looking at the rate of ovarian cancer by occupation and occupation-associated exposures, accounting for differences in things like pregnancy rates.
A brief aside here. I was at dinner with my wife the other night and telling her about this study, and I asked, “What do you think the occupation with the highest rate of ovarian cancer is?” And without missing a beat, she said: “Hairdressers.” Which blew my mind because of how random that was, but she was also – as usual – 100% correct.
Hairdressers, at least those who had been in the industry for more than 10 years, had a threefold higher risk for ovarian cancer than matched controls who had never been hairdressers.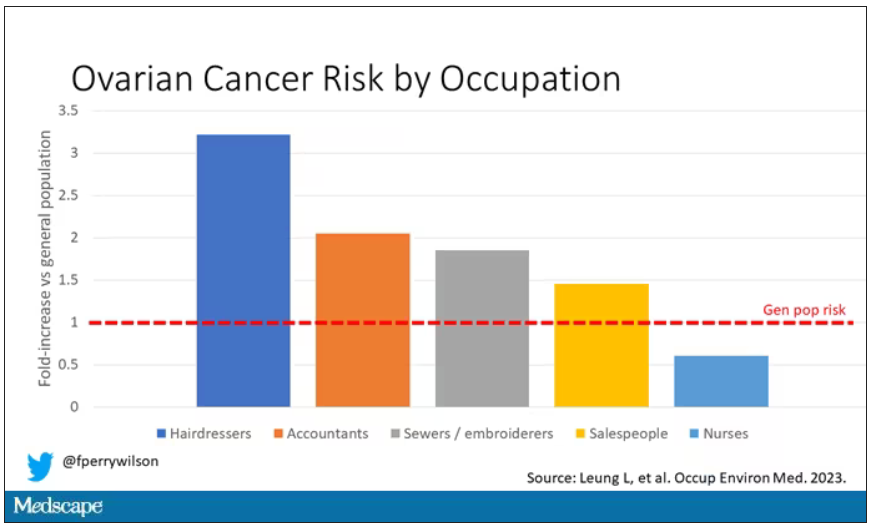
Of course, my wife is a cancer surgeon, so she has a bit of a leg up on me here. Many of you may also know that there is actually a decent body of literature showing higher rates of various cancers among hairdressers, presumably due to the variety of chemicals they are exposed to on a continuous basis.
The No. 2 highest-risk profession on the list? Accountants, with about a twofold higher risk. That one is more of a puzzler. It could be a false positive; after all, there were multiple occupations checked and random error might give a few hits that are meaningless. But there are certainly some occupational factors unique to accountants that might bear further investigation – maybe exposure to volatile organic compounds from office printers, or just a particularly sedentary office environment.
In terms of specific exposures, there were high risks seen with mononuclear aromatic hydrocarbons, bleaches, ethanol, and fluorocarbons, among others, but we have to be a bit more careful here. These exposures were not directly measured. Rather, based on the job category a woman described, the exposures were imputed based on the job-exposure matrix. As such, the correlations between the job and the particular exposure are really quite high, making it essentially impossible to tease out whether it is, for example, being a hairdresser, or being exposed to fluorocarbons as a hairdresser, or being exposed to something else as a hairdresser, that is the problem.
This is how these types of studies work; they tend to raise more questions than they answer. But in a world where a cancer diagnosis can seem to come completely out of the blue, they provide the starting point that someday may lead to a more definitive culprit agent or group of agents. Until then, it might be wise for hairdressers to make sure their workplace is well ventilated.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale University’s Clinical and Translational Research Accelerator in New Haven, Conn. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study.
Basically, all cancers are caused by a mix of genetic and environmental factors, with some cancers driven more strongly by one or the other. When it comes to ovarian cancer, which kills more than 13,000 women per year in the United States, genetic factors like the BRCA gene mutations are well described.
Other risk factors, like early menarche and nulliparity, are difficult to modify. The only slam-dunk environmental toxin to be linked to ovarian cancer is asbestos. Still, the vast majority of women who develop ovarian cancer do not have a known high-risk gene or asbestos exposure, so other triggers may be out there. How do we find them? The answer may just be good old-fashioned epidemiology.
That’s just what researchers, led by Anita Koushik at the University of Montreal, did in a new study appearing in the journal Occupational and Environmental Medicine.
They identified 497 women in Montreal who had recently been diagnosed with ovarian cancer. They then matched those women to 897 women without ovarian cancer, based on age and address. (This approach would not work well in the United States, as diagnosis of ovarian cancer might depend on access to medical care, which is not universal here. In Canada, however, it’s safer to assume that anyone who could have gotten ovarian cancer in Montreal would have been detected.)
Cases and controls identified, the researchers took a detailed occupational history for each participant: every job they ever worked, and when, and for how long. Each occupation was mapped to a standardized set of industries and, interestingly, to a set of environmental exposures ranging from cosmetic talc to cooking fumes to cotton dust, in what is known as a job-exposure matrix. Of course, they also collected data on other ovarian cancer risk factors.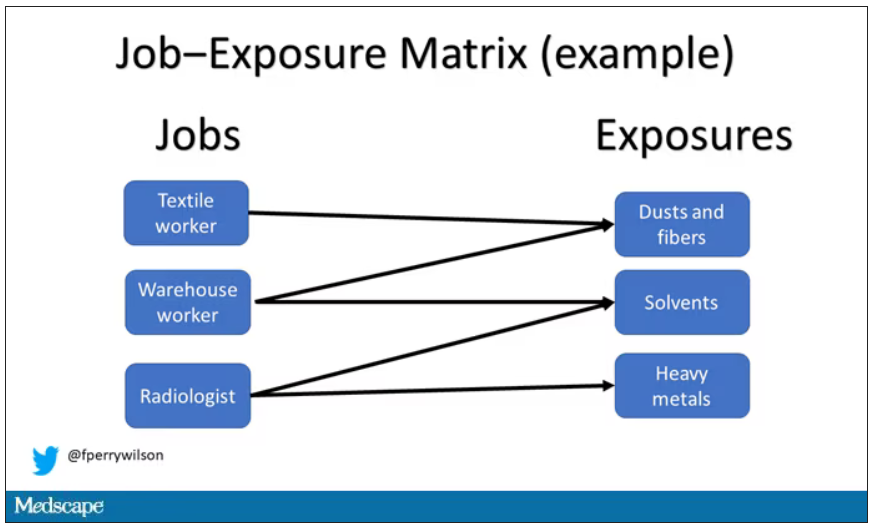
After that, it’s a simple matter of looking at the rate of ovarian cancer by occupation and occupation-associated exposures, accounting for differences in things like pregnancy rates.
A brief aside here. I was at dinner with my wife the other night and telling her about this study, and I asked, “What do you think the occupation with the highest rate of ovarian cancer is?” And without missing a beat, she said: “Hairdressers.” Which blew my mind because of how random that was, but she was also – as usual – 100% correct.
Hairdressers, at least those who had been in the industry for more than 10 years, had a threefold higher risk for ovarian cancer than matched controls who had never been hairdressers.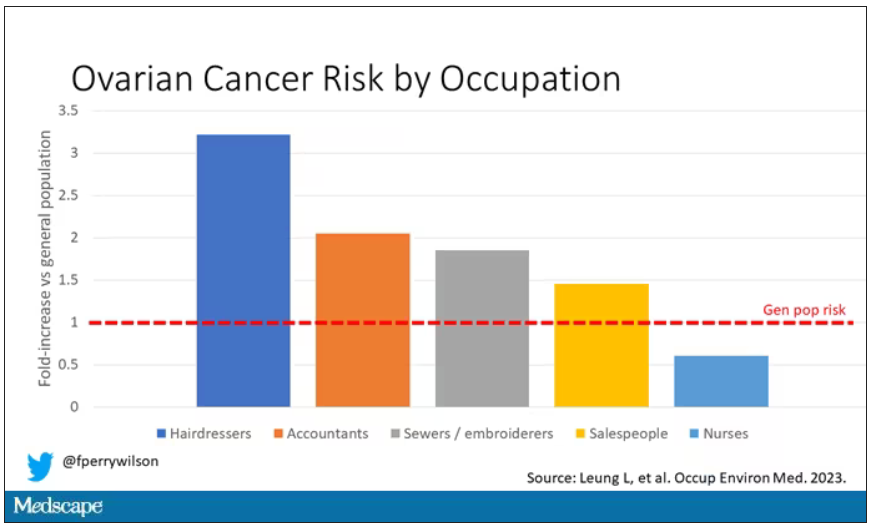
Of course, my wife is a cancer surgeon, so she has a bit of a leg up on me here. Many of you may also know that there is actually a decent body of literature showing higher rates of various cancers among hairdressers, presumably due to the variety of chemicals they are exposed to on a continuous basis.
The No. 2 highest-risk profession on the list? Accountants, with about a twofold higher risk. That one is more of a puzzler. It could be a false positive; after all, there were multiple occupations checked and random error might give a few hits that are meaningless. But there are certainly some occupational factors unique to accountants that might bear further investigation – maybe exposure to volatile organic compounds from office printers, or just a particularly sedentary office environment.
In terms of specific exposures, there were high risks seen with mononuclear aromatic hydrocarbons, bleaches, ethanol, and fluorocarbons, among others, but we have to be a bit more careful here. These exposures were not directly measured. Rather, based on the job category a woman described, the exposures were imputed based on the job-exposure matrix. As such, the correlations between the job and the particular exposure are really quite high, making it essentially impossible to tease out whether it is, for example, being a hairdresser, or being exposed to fluorocarbons as a hairdresser, or being exposed to something else as a hairdresser, that is the problem.
This is how these types of studies work; they tend to raise more questions than they answer. But in a world where a cancer diagnosis can seem to come completely out of the blue, they provide the starting point that someday may lead to a more definitive culprit agent or group of agents. Until then, it might be wise for hairdressers to make sure their workplace is well ventilated.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale University’s Clinical and Translational Research Accelerator in New Haven, Conn. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Surgeon in the C-suite

“If you don’t have a seat at the table, you are probably on the menu.” I first heard this quote in 2013, and it launched my interest in health care leadership and influenced me countless times over the last 10 years.
As Chief of Staff at Cleveland Clinic, I oversee nearly 5,000 physicians and scientists across the globe. I am involved in the physician life cycle: recruiting, hiring, privileging and credentialing, talent development, promotion, professionalism, and career transitions. I also sit at the intersection of medical care and the business of medicine. This means leading 18 clinical service lines responsible for 5.6 million visits, 161,000 surgeries, and billions of dollars in operating revenue per year. How I spend most of my time is a far cry from what I spent 11 years’ training to do—gynecologic surgery. This shift in my career was not because I changed my mind about caring for patients or that I tired of being a full-time surgeon. Nothing could be further from the truth. Women’s health remains my “why,” and my leadership journey has taught me that it is critical to have a seat at the table for the sake of ObGyns and women everywhere.
Women’s health on the menu
I will start with a concrete example of when we, as women and ObGyns, were on the menu. In late 2019, the Ohio state House of Representatives introduced a bill that subjected doctors to potential murder charges if they did not try everything to save the life of a mother and fetus, “including attempting to reimplant an ectopic pregnancy into the woman’s uterus.”1 This bill was based on 2 case reports—one from 1915 and one from 1980—which were both low quality, and the latter case was deemed to be fraudulent.2 How did this happen?
An Ohio state representative developed the bill with help from a lobbyist and without input from physicians or content experts. When asked, the representative shared that “he never researched whether re-implanting an ectopic pregnancy into a woman’s uterus was a viable medical procedure before including it in the bill.”3 He added, “I heard about it over the years. I never questioned it or gave it a lot of thought.”3
This example resonates deeply with many of us; it inspires us to speak up and act. As ObGyns, we clearly understand the consequences of legal and regulatory change in women’s health and how it directly impacts our patients and each of us as physicians. Let’s shift to something that you may feel less passion about, but I believe is equally important. This is where obstetrician-gynecologists sit in the intersection of medical care and business. This is the space where I spend most of my time, and from this vantage point, I worry about our field.
The business of medicine
Starting at the macroeconomic level, let’s think about how we as physicians are reimbursed and who makes these decisions. Looking at the national health care expenditure data, Medicare and Medicaid spending makes up nearly 40% of the total spend, and it is growing.4 Additionally, private health insurance tends to follow Centers for Medicare and Medicaid Services (CMS) decision making, further compounding its influence.4 In simple terms, CMS decides what is covered and how much we are paid. Whether you are in a solo private practice, an employer health care organization, or an academic medical center, physician reimbursement is declining.
In fact, Congress passed its year-end omnibus legislation in the final days of 2022, including a 2% Medicare physician payment cut for 2023,5 at a time when expenses to practice medicine, including nonphysician staff and supplies, are at an all-time high and we are living in a 6% inflationary state. This translates into being asked to serve more patients and cut costs. Our day-to-day feels much tighter, and this is why: Medicare physician pay increased just 11% over the past 20 years6 (2001–2021) in comparison to the cost of running a medical practice, which increased nearly 40% during that time. In other words, adjusting for inflation in practice costs, Medicare physician payment has fallen 22% over the last 20 years.7
Depending on your employment model, you may feel insulated from these changes as increases in reimbursement have occurred in other areas, such as hospitals and ambulatory surgery centers.8 In the short term, these increases help, as organizations will see additional funds. But there are 2 main issues: First, it is not nearly enough when you consider the soaring costs of running a hospital. And second, looking at our national population, we rely tremendously on self-employed doctors to serve our patients.
More than 80% of US counties lack adequate health care infrastructure.9 More than a third of the US population has less-than-adequate access to pharmacies, primary care physicians, hospitals, trauma centers, and low-cost health centers.9 To put things into perspective, more than 20% of counties in the United States are hospital deserts, where most people must drive more than 30 minutes to reach the closest hospital.9
There is good reason for this. Operating a hospital is a challenging endeavor. Even before the COVID-19 pandemic and the most recent health care financial challenges, most health care systems and large hospitals operated with very low operating margins (2%–3%). Businesses with similar margins include grocery stores and car dealerships. These low-margin businesses, including health care, rely on high volume for sustainability. High patient volumes distribute expensive hospital costs over many encounters. If physicians cannot sustain practices across the country, it is challenging to have sufficient admission and surgical volumes to justify the cost base of hospitals.
To tie this together, we have very little influence on what we are paid for our services. Reimbursement is declining, which makes it hard to have financially sustainable practices. As hospitals struggle, there is more pressure to prioritize highly profitable service lines, like orthopedics and urology, which are associated with favorable technical revenue. As hospitals are threatened, health care deserts widen, which leaves our entire health care system in jeopardy. Not surprisingly, this most likely affects those who face additional barriers to access, such as those with lower income, limited internet access, and lack of insurance. Together, these barriers further widen disparities in health care outcomes, including outcomes for women. Additionally, this death by a thousand cuts has eroded morale and increased physician burnout.
Transforming how we practice medicine is the only viable solution. I have good news: You are the leaders you have been waiting for.
Continue to: Physicians make good managers...
Physicians make good managers
To successfully transform how we practice medicine, it is critical that those leading the transformation deeply understand how medicine is practiced. The level of understanding required can be achieved only through years of medical practice, as a doctor. We understand how medical teams interact and that different sectors of our health care system are interdependent. Also, because physicians drive patient activity and ultimately reimbursement, having a seat at the table is crucial.
Some health care systems are run by businesspeople—people with finance backgrounds—and others are led by physicians. In 2017, Becker’s Hospital Review listed the chief executive officers (CEOs) of 183 nonprofit hospital and health systems.10 Of these, only 25% were led by individuals with an MD. Looking at the 115 largest hospitals in the United States, 30% are physician led.10 Considering the top 10 hospitals ranked by U.S. News & World Report for 2022, 8 of 10 have a physician at the helm.
Beyond raters and rankers, physician-led hospitals do better. Goodall compared CEOs in the top 100 best hospitals in U.S. News & World Report in 3 key medical specialties: cancer, digestive disorders, and cardiac care.11 The study explored the question: “Are hospitals’ quality ranked more highly when they are led by a medically trained doctor or non-MD professional managers?”11 Analysis revealed that hospital quality scores are about 25% higher in physician-run hospitals than in manager-run hospitals.11 Additional research shows that good management practices correlate with hospital performance, and that “the proportion of managers with a clinical degree has the largest positive effect.”12
Several theories exist as to why doctors make good managers in the health care setting.13,14 Doctors may create a more sympathetic and productive work environment for other clinicians because they are one of them. They have peer-to-peer credibility—because they have walked the walk, they have insight and perspective into how medicine is practiced.
Physicians serve as effective change agents for their organizations in several ways:
- First, physicians take a clinical approach in their leadership roles13 and focus on patient care at the center of their decisions. We see the people behind the numbers. Simply put, we humanize the operational side of health care.
- As physicians, we understand the interconnectivity in the practice of medicine. While closing certain service lines may be financially beneficial, these services are often closely linked to profitable service lines.
- Beyond physicians taking a clinical approach to leadership, we emphasize quality.13 Because we all have experienced complications and lived through bad outcomes alongside our patients, we understand deeply how important patient safety and quality is, and we are not willing to sacrifice that for financial gain. For us, this is personal. We don’t see our solution to health care challenges as an “or” situation, instead we view it as an “and” situation.
- Physician leaders often can improve medical staff engagement.13 A 2018 national survey of physicians found that those who are satisfied with their leadership are more engaged at work, have greater job satisfaction, and are less likely to experience signs of burnout.15 Physician administrators add value here.
Continue to: Surgeons as leaders...
Surgeons as leaders
What do we know about surgeons as physician leaders? Looking at the previously mentioned lists of physician leaders, surgeons are relatively absent. In the Becker’s Hospital Review study of nonprofit hospitals, only 9% of CEOs were surgeons.10 In addition, when reviewing data that associated physician leaders and hospital performance, only 3 of the CEOs were surgeons.11 Given that surgeons make up approximately 19% of US physicians, we are underrepresented.
The omission of surgeons as leaders seems inappropriate given that most hospitals are financially reliant on revenue related to surgical care and optimizing this space is an enormous opportunity. Berger and colleagues offered 3 theories as to why there are fewer surgeon leaders16:
- The relative pay of surgeons exceeds that of most other specialties, and there may be less incentive to accept the challenges presented by leadership roles. (I will add that surgeon leadership is more costly to a system.)
- The craftsmanship nature of surgery discourages the development of other career interests beginning at the trainee level.
- Surgeons have been perceived stereotypically to exhibit arrogance, a characteristic that others may not warm to.
This last observation stings. Successful leadership takes social skill and teamwork.14 Although medical care is one of the few disciplines in which lack of teamwork might cost lives, physicians are not trained to be team players. We recognize how our training has led us to be lone wolves or gunners, situations where we as individuals had to beat others to secure our spot. We have been trained in command-and-control environments, in stepping up as a leader in highly stressful situations. This part of surgical culture may handicap surgeons in their quest to be health care leaders.
Other traits, however, make us particularly great leaders in health care. Our desire to succeed, willingness to push ourselves to extremes, ability to laser focus on a task, acceptance of delayed gratification, and aptitude for making timely decisions on limited data help us succeed in leadership roles. Seven years of surgical training helped me develop the grit I use every day in the C-suite.
We need more physician and surgeon leadership to thrive in the challenging health care landscape. Berger and colleagues proposed 3 potential solutions to increase the number of surgeons in hospital leadership positions16:
Nurture future surgical leaders through exposure to management training. Given the contribution to both expense in support services and resources and revenue related to surgical care, each organization needs a content expert to guide these decisions.
Recognize the important contributions that surgeons already make regarding quality, safety, and operational efficiency. An excellent example of this is the American College of Surgeons National Surgical Quality Improvement Program. Because surgeons are content experts in this area, we are primed to lead.
Hospitals, medical schools, and academic departments of surgery should recognize administrative efforts as an important part of the overall academic mission. As the adage states, “No margin, no mission.” We need bright minds to preserve and grow our margins so that we can further invest in our missions.
This is not easy. Given the barriers, this will not happen organically. Charan and colleagues provided an outline for a leadership pathway adapted for physicians (FIGURE).17,18 It starts with the individual practitioner who is a practicing physician and spends most of their time focused on patient care. As a physician becomes more interested in leadership, they develop new skills and take on more and more responsibility. As they increase in leadership responsibility, they tend to reduce clinical time and increase time spent on strategic and business management. This framework creates a pipeline so that physicians and surgeons can be developed strategically and given increasing responsibility as they develop their capabilities and expand their skill sets.
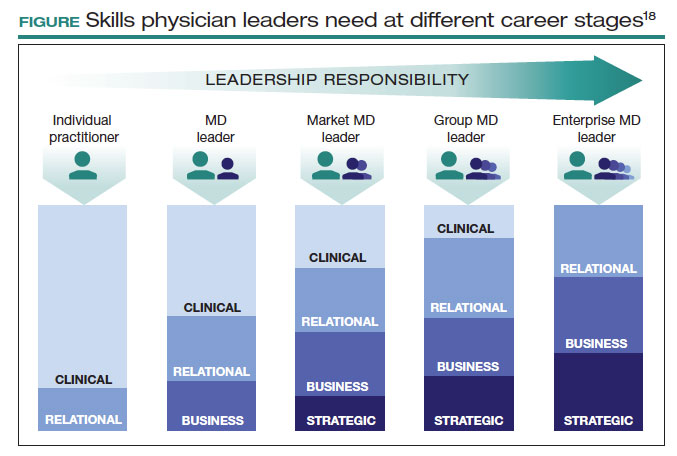
The leadership challenge
To thrive, we must transform health care by changing how we practice medicine. As ObGyns, we are the leaders we have been waiting for. As you ponder your future, think of your current career and the opportunities you might have. Do you have a seat at the table? What table is that? How are you using your knowledge, expertise, and privilege to advance health care and medicine? I challenge you to critically evaluate this—and lead. ●
- Law T. Ohio bill suggests doctors who perform abortions could face jail, unless they perform a non-existent treatment. December 1, 2019. Time. Accessed June 12, 2023. https://time.com/5742053 /ectopic-pregnancy-ohio-abortion-bill/
- Grossman D. Ohio abortion, ectopic pregnancy bill: ‘it’s both bad medicine and bad law-making.’ May 21, 2019. Cincinnati.com–The Enquirer. Accessed June 12, 2023. https://www .cincinnati.com/story/opinion/2019/05/21/ohio-abortion-bill -john-becker-daniel-grossman-ectopic-pregnancy-false-medicine /3753610002/
- Lobbyist had hand in bill sparking ectopic pregnancy flap. December 11, 2019. Associated Press. Accessed June 12, 2023. https://apnews .com/article/03216e44405fa184ae0ab80fa85089f8
- NHE fact sheet. CMS.gov. Updated February 17, 2023. Accessed June 12, 2023. https://www.cms.gov/research-statistics-data-and -systems/statistics-trends-and-reports/nationalhealthexpenddata /nhe-fact-sheet
- Senate passes omnibus spending bill with health provisions. December 23, 2022. American Hospital Association. Accessed June 12, 2023. https://www.aha.org/special-bulletin/2022-12-20-appropriations -committees-release-omnibus-spending-bill-health-provisions
- Medicare updates compared to inflation (2001-2021). October 2021. American Medical Association. Accessed June 12, 2023. https://www .ama-assn.org/system/files/medicare-pay-chart-2021.pdf
- Resneck Jr J. Medicare physician payment reform is long overdue. October 3, 2022. American Medical Association. Accessed June 7, 2023. https://www.ama-assn.org/about/leadership /medicare-physician-payment-reform-long-overdue
- Isenberg M. The stark reality of physician reimbursement. August 24, 2022. Zotec Partners. Accessed June 13, 2023. https://zotecpartners. com/advocacy-zpac/test-1/
- Nguyen A. Mapping healthcare deserts: 80% of the country lacks adequate access to healthcare. September 9, 2021. GoodRx Health. Accessed June 13, 2023. https://www.goodrx.com/healthcare -access/research/healthcare-deserts-80-percent-of-country-lacks -adequate-healthcare-access
- 183 nonprofit hospital and health system CEOs to know–2017. Updated June 20, 2018. Becker’s Hospital Review. Accessed June 7, 2023. https://www.beckershospitalreview.com/lists/188-nonprofit -hospital-and-health-system-ceos-to-know-2017.html
- Goodall AH. Physician-leaders and hospital performance: is there an association? Soc Sci Med. 2011;73:535-539. doi:10.1016 /j.socscimed.2011.06.025
- Bloom N, Sadun R, Van Reenen J. Does Management Matter in Healthcare? Center for Economic Performance and Harvard Business School; 2014.
- Turner J. Why healthcare C-suites should include physicians. September 3, 2019. Managed Healthcare Executive. Accessed June 13, 2023. https://www.managedhealthcareexecutive.com /view/why-healthcare-c-suites-should-include-physicians
- Stoller JK, Goodall A, Baker A. Why the best hospitals are managed by doctors. December 27, 2016. Harvard Business Review. Accessed June 13, 2023. https://hbr.org/2016/12/why-the-best-hospitals -are-managed-by-doctors
- Hayhurst C. Data confirms: leaders, physician burnout is on you. April 3, 2019. Aetnahealth. Accessed June 13, 2023. https://www .athenahealth.com/knowledge-hub/practice-management /research-confirms-leaders-burnout-you
- Berger DH, Goodall A, Tsai AY. The importance of increasing surgeon participation in hospital leadership. JAMA Surg. 2019;154:281-282. doi:10.1001/jamasurg.2018.5080
- Charan R, Drotter S, Noel J. The Leadership Pipeline: How to Build the Leadership-Powered Company. Jossey-Bass; 2001.
- Perry J, Mobley F, Brubaker M. Most doctors have little or no management training, and that’s a problem. December 15, 2017. Harvard Business Review. Accessed June 7, 2023. https://hbr.org/2017/12 /most-doctors-have-little-or-no-management-training-and-thats -a-problem

“If you don’t have a seat at the table, you are probably on the menu.” I first heard this quote in 2013, and it launched my interest in health care leadership and influenced me countless times over the last 10 years.
As Chief of Staff at Cleveland Clinic, I oversee nearly 5,000 physicians and scientists across the globe. I am involved in the physician life cycle: recruiting, hiring, privileging and credentialing, talent development, promotion, professionalism, and career transitions. I also sit at the intersection of medical care and the business of medicine. This means leading 18 clinical service lines responsible for 5.6 million visits, 161,000 surgeries, and billions of dollars in operating revenue per year. How I spend most of my time is a far cry from what I spent 11 years’ training to do—gynecologic surgery. This shift in my career was not because I changed my mind about caring for patients or that I tired of being a full-time surgeon. Nothing could be further from the truth. Women’s health remains my “why,” and my leadership journey has taught me that it is critical to have a seat at the table for the sake of ObGyns and women everywhere.
Women’s health on the menu
I will start with a concrete example of when we, as women and ObGyns, were on the menu. In late 2019, the Ohio state House of Representatives introduced a bill that subjected doctors to potential murder charges if they did not try everything to save the life of a mother and fetus, “including attempting to reimplant an ectopic pregnancy into the woman’s uterus.”1 This bill was based on 2 case reports—one from 1915 and one from 1980—which were both low quality, and the latter case was deemed to be fraudulent.2 How did this happen?
An Ohio state representative developed the bill with help from a lobbyist and without input from physicians or content experts. When asked, the representative shared that “he never researched whether re-implanting an ectopic pregnancy into a woman’s uterus was a viable medical procedure before including it in the bill.”3 He added, “I heard about it over the years. I never questioned it or gave it a lot of thought.”3
This example resonates deeply with many of us; it inspires us to speak up and act. As ObGyns, we clearly understand the consequences of legal and regulatory change in women’s health and how it directly impacts our patients and each of us as physicians. Let’s shift to something that you may feel less passion about, but I believe is equally important. This is where obstetrician-gynecologists sit in the intersection of medical care and business. This is the space where I spend most of my time, and from this vantage point, I worry about our field.
The business of medicine
Starting at the macroeconomic level, let’s think about how we as physicians are reimbursed and who makes these decisions. Looking at the national health care expenditure data, Medicare and Medicaid spending makes up nearly 40% of the total spend, and it is growing.4 Additionally, private health insurance tends to follow Centers for Medicare and Medicaid Services (CMS) decision making, further compounding its influence.4 In simple terms, CMS decides what is covered and how much we are paid. Whether you are in a solo private practice, an employer health care organization, or an academic medical center, physician reimbursement is declining.
In fact, Congress passed its year-end omnibus legislation in the final days of 2022, including a 2% Medicare physician payment cut for 2023,5 at a time when expenses to practice medicine, including nonphysician staff and supplies, are at an all-time high and we are living in a 6% inflationary state. This translates into being asked to serve more patients and cut costs. Our day-to-day feels much tighter, and this is why: Medicare physician pay increased just 11% over the past 20 years6 (2001–2021) in comparison to the cost of running a medical practice, which increased nearly 40% during that time. In other words, adjusting for inflation in practice costs, Medicare physician payment has fallen 22% over the last 20 years.7
Depending on your employment model, you may feel insulated from these changes as increases in reimbursement have occurred in other areas, such as hospitals and ambulatory surgery centers.8 In the short term, these increases help, as organizations will see additional funds. But there are 2 main issues: First, it is not nearly enough when you consider the soaring costs of running a hospital. And second, looking at our national population, we rely tremendously on self-employed doctors to serve our patients.
More than 80% of US counties lack adequate health care infrastructure.9 More than a third of the US population has less-than-adequate access to pharmacies, primary care physicians, hospitals, trauma centers, and low-cost health centers.9 To put things into perspective, more than 20% of counties in the United States are hospital deserts, where most people must drive more than 30 minutes to reach the closest hospital.9
There is good reason for this. Operating a hospital is a challenging endeavor. Even before the COVID-19 pandemic and the most recent health care financial challenges, most health care systems and large hospitals operated with very low operating margins (2%–3%). Businesses with similar margins include grocery stores and car dealerships. These low-margin businesses, including health care, rely on high volume for sustainability. High patient volumes distribute expensive hospital costs over many encounters. If physicians cannot sustain practices across the country, it is challenging to have sufficient admission and surgical volumes to justify the cost base of hospitals.
To tie this together, we have very little influence on what we are paid for our services. Reimbursement is declining, which makes it hard to have financially sustainable practices. As hospitals struggle, there is more pressure to prioritize highly profitable service lines, like orthopedics and urology, which are associated with favorable technical revenue. As hospitals are threatened, health care deserts widen, which leaves our entire health care system in jeopardy. Not surprisingly, this most likely affects those who face additional barriers to access, such as those with lower income, limited internet access, and lack of insurance. Together, these barriers further widen disparities in health care outcomes, including outcomes for women. Additionally, this death by a thousand cuts has eroded morale and increased physician burnout.
Transforming how we practice medicine is the only viable solution. I have good news: You are the leaders you have been waiting for.
Continue to: Physicians make good managers...
Physicians make good managers
To successfully transform how we practice medicine, it is critical that those leading the transformation deeply understand how medicine is practiced. The level of understanding required can be achieved only through years of medical practice, as a doctor. We understand how medical teams interact and that different sectors of our health care system are interdependent. Also, because physicians drive patient activity and ultimately reimbursement, having a seat at the table is crucial.
Some health care systems are run by businesspeople—people with finance backgrounds—and others are led by physicians. In 2017, Becker’s Hospital Review listed the chief executive officers (CEOs) of 183 nonprofit hospital and health systems.10 Of these, only 25% were led by individuals with an MD. Looking at the 115 largest hospitals in the United States, 30% are physician led.10 Considering the top 10 hospitals ranked by U.S. News & World Report for 2022, 8 of 10 have a physician at the helm.
Beyond raters and rankers, physician-led hospitals do better. Goodall compared CEOs in the top 100 best hospitals in U.S. News & World Report in 3 key medical specialties: cancer, digestive disorders, and cardiac care.11 The study explored the question: “Are hospitals’ quality ranked more highly when they are led by a medically trained doctor or non-MD professional managers?”11 Analysis revealed that hospital quality scores are about 25% higher in physician-run hospitals than in manager-run hospitals.11 Additional research shows that good management practices correlate with hospital performance, and that “the proportion of managers with a clinical degree has the largest positive effect.”12
Several theories exist as to why doctors make good managers in the health care setting.13,14 Doctors may create a more sympathetic and productive work environment for other clinicians because they are one of them. They have peer-to-peer credibility—because they have walked the walk, they have insight and perspective into how medicine is practiced.
Physicians serve as effective change agents for their organizations in several ways:
- First, physicians take a clinical approach in their leadership roles13 and focus on patient care at the center of their decisions. We see the people behind the numbers. Simply put, we humanize the operational side of health care.
- As physicians, we understand the interconnectivity in the practice of medicine. While closing certain service lines may be financially beneficial, these services are often closely linked to profitable service lines.
- Beyond physicians taking a clinical approach to leadership, we emphasize quality.13 Because we all have experienced complications and lived through bad outcomes alongside our patients, we understand deeply how important patient safety and quality is, and we are not willing to sacrifice that for financial gain. For us, this is personal. We don’t see our solution to health care challenges as an “or” situation, instead we view it as an “and” situation.
- Physician leaders often can improve medical staff engagement.13 A 2018 national survey of physicians found that those who are satisfied with their leadership are more engaged at work, have greater job satisfaction, and are less likely to experience signs of burnout.15 Physician administrators add value here.
Continue to: Surgeons as leaders...
Surgeons as leaders
What do we know about surgeons as physician leaders? Looking at the previously mentioned lists of physician leaders, surgeons are relatively absent. In the Becker’s Hospital Review study of nonprofit hospitals, only 9% of CEOs were surgeons.10 In addition, when reviewing data that associated physician leaders and hospital performance, only 3 of the CEOs were surgeons.11 Given that surgeons make up approximately 19% of US physicians, we are underrepresented.
The omission of surgeons as leaders seems inappropriate given that most hospitals are financially reliant on revenue related to surgical care and optimizing this space is an enormous opportunity. Berger and colleagues offered 3 theories as to why there are fewer surgeon leaders16:
- The relative pay of surgeons exceeds that of most other specialties, and there may be less incentive to accept the challenges presented by leadership roles. (I will add that surgeon leadership is more costly to a system.)
- The craftsmanship nature of surgery discourages the development of other career interests beginning at the trainee level.
- Surgeons have been perceived stereotypically to exhibit arrogance, a characteristic that others may not warm to.
This last observation stings. Successful leadership takes social skill and teamwork.14 Although medical care is one of the few disciplines in which lack of teamwork might cost lives, physicians are not trained to be team players. We recognize how our training has led us to be lone wolves or gunners, situations where we as individuals had to beat others to secure our spot. We have been trained in command-and-control environments, in stepping up as a leader in highly stressful situations. This part of surgical culture may handicap surgeons in their quest to be health care leaders.
Other traits, however, make us particularly great leaders in health care. Our desire to succeed, willingness to push ourselves to extremes, ability to laser focus on a task, acceptance of delayed gratification, and aptitude for making timely decisions on limited data help us succeed in leadership roles. Seven years of surgical training helped me develop the grit I use every day in the C-suite.
We need more physician and surgeon leadership to thrive in the challenging health care landscape. Berger and colleagues proposed 3 potential solutions to increase the number of surgeons in hospital leadership positions16:
Nurture future surgical leaders through exposure to management training. Given the contribution to both expense in support services and resources and revenue related to surgical care, each organization needs a content expert to guide these decisions.
Recognize the important contributions that surgeons already make regarding quality, safety, and operational efficiency. An excellent example of this is the American College of Surgeons National Surgical Quality Improvement Program. Because surgeons are content experts in this area, we are primed to lead.
Hospitals, medical schools, and academic departments of surgery should recognize administrative efforts as an important part of the overall academic mission. As the adage states, “No margin, no mission.” We need bright minds to preserve and grow our margins so that we can further invest in our missions.
This is not easy. Given the barriers, this will not happen organically. Charan and colleagues provided an outline for a leadership pathway adapted for physicians (FIGURE).17,18 It starts with the individual practitioner who is a practicing physician and spends most of their time focused on patient care. As a physician becomes more interested in leadership, they develop new skills and take on more and more responsibility. As they increase in leadership responsibility, they tend to reduce clinical time and increase time spent on strategic and business management. This framework creates a pipeline so that physicians and surgeons can be developed strategically and given increasing responsibility as they develop their capabilities and expand their skill sets.
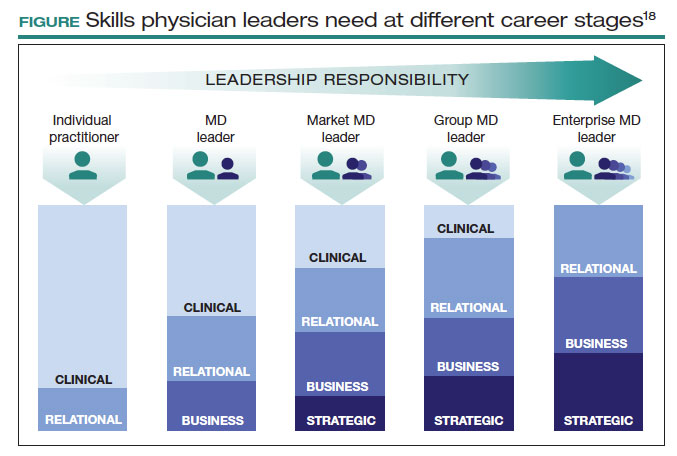
The leadership challenge
To thrive, we must transform health care by changing how we practice medicine. As ObGyns, we are the leaders we have been waiting for. As you ponder your future, think of your current career and the opportunities you might have. Do you have a seat at the table? What table is that? How are you using your knowledge, expertise, and privilege to advance health care and medicine? I challenge you to critically evaluate this—and lead. ●

“If you don’t have a seat at the table, you are probably on the menu.” I first heard this quote in 2013, and it launched my interest in health care leadership and influenced me countless times over the last 10 years.
As Chief of Staff at Cleveland Clinic, I oversee nearly 5,000 physicians and scientists across the globe. I am involved in the physician life cycle: recruiting, hiring, privileging and credentialing, talent development, promotion, professionalism, and career transitions. I also sit at the intersection of medical care and the business of medicine. This means leading 18 clinical service lines responsible for 5.6 million visits, 161,000 surgeries, and billions of dollars in operating revenue per year. How I spend most of my time is a far cry from what I spent 11 years’ training to do—gynecologic surgery. This shift in my career was not because I changed my mind about caring for patients or that I tired of being a full-time surgeon. Nothing could be further from the truth. Women’s health remains my “why,” and my leadership journey has taught me that it is critical to have a seat at the table for the sake of ObGyns and women everywhere.
Women’s health on the menu
I will start with a concrete example of when we, as women and ObGyns, were on the menu. In late 2019, the Ohio state House of Representatives introduced a bill that subjected doctors to potential murder charges if they did not try everything to save the life of a mother and fetus, “including attempting to reimplant an ectopic pregnancy into the woman’s uterus.”1 This bill was based on 2 case reports—one from 1915 and one from 1980—which were both low quality, and the latter case was deemed to be fraudulent.2 How did this happen?
An Ohio state representative developed the bill with help from a lobbyist and without input from physicians or content experts. When asked, the representative shared that “he never researched whether re-implanting an ectopic pregnancy into a woman’s uterus was a viable medical procedure before including it in the bill.”3 He added, “I heard about it over the years. I never questioned it or gave it a lot of thought.”3
This example resonates deeply with many of us; it inspires us to speak up and act. As ObGyns, we clearly understand the consequences of legal and regulatory change in women’s health and how it directly impacts our patients and each of us as physicians. Let’s shift to something that you may feel less passion about, but I believe is equally important. This is where obstetrician-gynecologists sit in the intersection of medical care and business. This is the space where I spend most of my time, and from this vantage point, I worry about our field.
The business of medicine
Starting at the macroeconomic level, let’s think about how we as physicians are reimbursed and who makes these decisions. Looking at the national health care expenditure data, Medicare and Medicaid spending makes up nearly 40% of the total spend, and it is growing.4 Additionally, private health insurance tends to follow Centers for Medicare and Medicaid Services (CMS) decision making, further compounding its influence.4 In simple terms, CMS decides what is covered and how much we are paid. Whether you are in a solo private practice, an employer health care organization, or an academic medical center, physician reimbursement is declining.
In fact, Congress passed its year-end omnibus legislation in the final days of 2022, including a 2% Medicare physician payment cut for 2023,5 at a time when expenses to practice medicine, including nonphysician staff and supplies, are at an all-time high and we are living in a 6% inflationary state. This translates into being asked to serve more patients and cut costs. Our day-to-day feels much tighter, and this is why: Medicare physician pay increased just 11% over the past 20 years6 (2001–2021) in comparison to the cost of running a medical practice, which increased nearly 40% during that time. In other words, adjusting for inflation in practice costs, Medicare physician payment has fallen 22% over the last 20 years.7
Depending on your employment model, you may feel insulated from these changes as increases in reimbursement have occurred in other areas, such as hospitals and ambulatory surgery centers.8 In the short term, these increases help, as organizations will see additional funds. But there are 2 main issues: First, it is not nearly enough when you consider the soaring costs of running a hospital. And second, looking at our national population, we rely tremendously on self-employed doctors to serve our patients.
More than 80% of US counties lack adequate health care infrastructure.9 More than a third of the US population has less-than-adequate access to pharmacies, primary care physicians, hospitals, trauma centers, and low-cost health centers.9 To put things into perspective, more than 20% of counties in the United States are hospital deserts, where most people must drive more than 30 minutes to reach the closest hospital.9
There is good reason for this. Operating a hospital is a challenging endeavor. Even before the COVID-19 pandemic and the most recent health care financial challenges, most health care systems and large hospitals operated with very low operating margins (2%–3%). Businesses with similar margins include grocery stores and car dealerships. These low-margin businesses, including health care, rely on high volume for sustainability. High patient volumes distribute expensive hospital costs over many encounters. If physicians cannot sustain practices across the country, it is challenging to have sufficient admission and surgical volumes to justify the cost base of hospitals.
To tie this together, we have very little influence on what we are paid for our services. Reimbursement is declining, which makes it hard to have financially sustainable practices. As hospitals struggle, there is more pressure to prioritize highly profitable service lines, like orthopedics and urology, which are associated with favorable technical revenue. As hospitals are threatened, health care deserts widen, which leaves our entire health care system in jeopardy. Not surprisingly, this most likely affects those who face additional barriers to access, such as those with lower income, limited internet access, and lack of insurance. Together, these barriers further widen disparities in health care outcomes, including outcomes for women. Additionally, this death by a thousand cuts has eroded morale and increased physician burnout.
Transforming how we practice medicine is the only viable solution. I have good news: You are the leaders you have been waiting for.
Continue to: Physicians make good managers...
Physicians make good managers
To successfully transform how we practice medicine, it is critical that those leading the transformation deeply understand how medicine is practiced. The level of understanding required can be achieved only through years of medical practice, as a doctor. We understand how medical teams interact and that different sectors of our health care system are interdependent. Also, because physicians drive patient activity and ultimately reimbursement, having a seat at the table is crucial.
Some health care systems are run by businesspeople—people with finance backgrounds—and others are led by physicians. In 2017, Becker’s Hospital Review listed the chief executive officers (CEOs) of 183 nonprofit hospital and health systems.10 Of these, only 25% were led by individuals with an MD. Looking at the 115 largest hospitals in the United States, 30% are physician led.10 Considering the top 10 hospitals ranked by U.S. News & World Report for 2022, 8 of 10 have a physician at the helm.
Beyond raters and rankers, physician-led hospitals do better. Goodall compared CEOs in the top 100 best hospitals in U.S. News & World Report in 3 key medical specialties: cancer, digestive disorders, and cardiac care.11 The study explored the question: “Are hospitals’ quality ranked more highly when they are led by a medically trained doctor or non-MD professional managers?”11 Analysis revealed that hospital quality scores are about 25% higher in physician-run hospitals than in manager-run hospitals.11 Additional research shows that good management practices correlate with hospital performance, and that “the proportion of managers with a clinical degree has the largest positive effect.”12
Several theories exist as to why doctors make good managers in the health care setting.13,14 Doctors may create a more sympathetic and productive work environment for other clinicians because they are one of them. They have peer-to-peer credibility—because they have walked the walk, they have insight and perspective into how medicine is practiced.
Physicians serve as effective change agents for their organizations in several ways:
- First, physicians take a clinical approach in their leadership roles13 and focus on patient care at the center of their decisions. We see the people behind the numbers. Simply put, we humanize the operational side of health care.
- As physicians, we understand the interconnectivity in the practice of medicine. While closing certain service lines may be financially beneficial, these services are often closely linked to profitable service lines.
- Beyond physicians taking a clinical approach to leadership, we emphasize quality.13 Because we all have experienced complications and lived through bad outcomes alongside our patients, we understand deeply how important patient safety and quality is, and we are not willing to sacrifice that for financial gain. For us, this is personal. We don’t see our solution to health care challenges as an “or” situation, instead we view it as an “and” situation.
- Physician leaders often can improve medical staff engagement.13 A 2018 national survey of physicians found that those who are satisfied with their leadership are more engaged at work, have greater job satisfaction, and are less likely to experience signs of burnout.15 Physician administrators add value here.
Continue to: Surgeons as leaders...
Surgeons as leaders
What do we know about surgeons as physician leaders? Looking at the previously mentioned lists of physician leaders, surgeons are relatively absent. In the Becker’s Hospital Review study of nonprofit hospitals, only 9% of CEOs were surgeons.10 In addition, when reviewing data that associated physician leaders and hospital performance, only 3 of the CEOs were surgeons.11 Given that surgeons make up approximately 19% of US physicians, we are underrepresented.
The omission of surgeons as leaders seems inappropriate given that most hospitals are financially reliant on revenue related to surgical care and optimizing this space is an enormous opportunity. Berger and colleagues offered 3 theories as to why there are fewer surgeon leaders16:
- The relative pay of surgeons exceeds that of most other specialties, and there may be less incentive to accept the challenges presented by leadership roles. (I will add that surgeon leadership is more costly to a system.)
- The craftsmanship nature of surgery discourages the development of other career interests beginning at the trainee level.
- Surgeons have been perceived stereotypically to exhibit arrogance, a characteristic that others may not warm to.
This last observation stings. Successful leadership takes social skill and teamwork.14 Although medical care is one of the few disciplines in which lack of teamwork might cost lives, physicians are not trained to be team players. We recognize how our training has led us to be lone wolves or gunners, situations where we as individuals had to beat others to secure our spot. We have been trained in command-and-control environments, in stepping up as a leader in highly stressful situations. This part of surgical culture may handicap surgeons in their quest to be health care leaders.
Other traits, however, make us particularly great leaders in health care. Our desire to succeed, willingness to push ourselves to extremes, ability to laser focus on a task, acceptance of delayed gratification, and aptitude for making timely decisions on limited data help us succeed in leadership roles. Seven years of surgical training helped me develop the grit I use every day in the C-suite.
We need more physician and surgeon leadership to thrive in the challenging health care landscape. Berger and colleagues proposed 3 potential solutions to increase the number of surgeons in hospital leadership positions16:
Nurture future surgical leaders through exposure to management training. Given the contribution to both expense in support services and resources and revenue related to surgical care, each organization needs a content expert to guide these decisions.
Recognize the important contributions that surgeons already make regarding quality, safety, and operational efficiency. An excellent example of this is the American College of Surgeons National Surgical Quality Improvement Program. Because surgeons are content experts in this area, we are primed to lead.
Hospitals, medical schools, and academic departments of surgery should recognize administrative efforts as an important part of the overall academic mission. As the adage states, “No margin, no mission.” We need bright minds to preserve and grow our margins so that we can further invest in our missions.
This is not easy. Given the barriers, this will not happen organically. Charan and colleagues provided an outline for a leadership pathway adapted for physicians (FIGURE).17,18 It starts with the individual practitioner who is a practicing physician and spends most of their time focused on patient care. As a physician becomes more interested in leadership, they develop new skills and take on more and more responsibility. As they increase in leadership responsibility, they tend to reduce clinical time and increase time spent on strategic and business management. This framework creates a pipeline so that physicians and surgeons can be developed strategically and given increasing responsibility as they develop their capabilities and expand their skill sets.
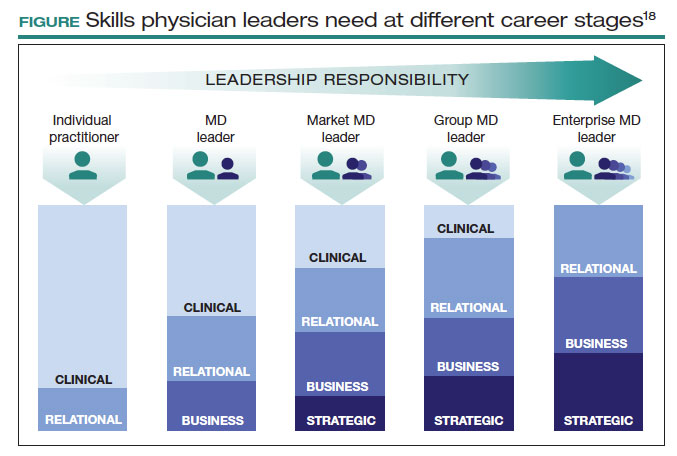
The leadership challenge
To thrive, we must transform health care by changing how we practice medicine. As ObGyns, we are the leaders we have been waiting for. As you ponder your future, think of your current career and the opportunities you might have. Do you have a seat at the table? What table is that? How are you using your knowledge, expertise, and privilege to advance health care and medicine? I challenge you to critically evaluate this—and lead. ●
- Law T. Ohio bill suggests doctors who perform abortions could face jail, unless they perform a non-existent treatment. December 1, 2019. Time. Accessed June 12, 2023. https://time.com/5742053 /ectopic-pregnancy-ohio-abortion-bill/
- Grossman D. Ohio abortion, ectopic pregnancy bill: ‘it’s both bad medicine and bad law-making.’ May 21, 2019. Cincinnati.com–The Enquirer. Accessed June 12, 2023. https://www .cincinnati.com/story/opinion/2019/05/21/ohio-abortion-bill -john-becker-daniel-grossman-ectopic-pregnancy-false-medicine /3753610002/
- Lobbyist had hand in bill sparking ectopic pregnancy flap. December 11, 2019. Associated Press. Accessed June 12, 2023. https://apnews .com/article/03216e44405fa184ae0ab80fa85089f8
- NHE fact sheet. CMS.gov. Updated February 17, 2023. Accessed June 12, 2023. https://www.cms.gov/research-statistics-data-and -systems/statistics-trends-and-reports/nationalhealthexpenddata /nhe-fact-sheet
- Senate passes omnibus spending bill with health provisions. December 23, 2022. American Hospital Association. Accessed June 12, 2023. https://www.aha.org/special-bulletin/2022-12-20-appropriations -committees-release-omnibus-spending-bill-health-provisions
- Medicare updates compared to inflation (2001-2021). October 2021. American Medical Association. Accessed June 12, 2023. https://www .ama-assn.org/system/files/medicare-pay-chart-2021.pdf
- Resneck Jr J. Medicare physician payment reform is long overdue. October 3, 2022. American Medical Association. Accessed June 7, 2023. https://www.ama-assn.org/about/leadership /medicare-physician-payment-reform-long-overdue
- Isenberg M. The stark reality of physician reimbursement. August 24, 2022. Zotec Partners. Accessed June 13, 2023. https://zotecpartners. com/advocacy-zpac/test-1/
- Nguyen A. Mapping healthcare deserts: 80% of the country lacks adequate access to healthcare. September 9, 2021. GoodRx Health. Accessed June 13, 2023. https://www.goodrx.com/healthcare -access/research/healthcare-deserts-80-percent-of-country-lacks -adequate-healthcare-access
- 183 nonprofit hospital and health system CEOs to know–2017. Updated June 20, 2018. Becker’s Hospital Review. Accessed June 7, 2023. https://www.beckershospitalreview.com/lists/188-nonprofit -hospital-and-health-system-ceos-to-know-2017.html
- Goodall AH. Physician-leaders and hospital performance: is there an association? Soc Sci Med. 2011;73:535-539. doi:10.1016 /j.socscimed.2011.06.025
- Bloom N, Sadun R, Van Reenen J. Does Management Matter in Healthcare? Center for Economic Performance and Harvard Business School; 2014.
- Turner J. Why healthcare C-suites should include physicians. September 3, 2019. Managed Healthcare Executive. Accessed June 13, 2023. https://www.managedhealthcareexecutive.com /view/why-healthcare-c-suites-should-include-physicians
- Stoller JK, Goodall A, Baker A. Why the best hospitals are managed by doctors. December 27, 2016. Harvard Business Review. Accessed June 13, 2023. https://hbr.org/2016/12/why-the-best-hospitals -are-managed-by-doctors
- Hayhurst C. Data confirms: leaders, physician burnout is on you. April 3, 2019. Aetnahealth. Accessed June 13, 2023. https://www .athenahealth.com/knowledge-hub/practice-management /research-confirms-leaders-burnout-you
- Berger DH, Goodall A, Tsai AY. The importance of increasing surgeon participation in hospital leadership. JAMA Surg. 2019;154:281-282. doi:10.1001/jamasurg.2018.5080
- Charan R, Drotter S, Noel J. The Leadership Pipeline: How to Build the Leadership-Powered Company. Jossey-Bass; 2001.
- Perry J, Mobley F, Brubaker M. Most doctors have little or no management training, and that’s a problem. December 15, 2017. Harvard Business Review. Accessed June 7, 2023. https://hbr.org/2017/12 /most-doctors-have-little-or-no-management-training-and-thats -a-problem
- Law T. Ohio bill suggests doctors who perform abortions could face jail, unless they perform a non-existent treatment. December 1, 2019. Time. Accessed June 12, 2023. https://time.com/5742053 /ectopic-pregnancy-ohio-abortion-bill/
- Grossman D. Ohio abortion, ectopic pregnancy bill: ‘it’s both bad medicine and bad law-making.’ May 21, 2019. Cincinnati.com–The Enquirer. Accessed June 12, 2023. https://www .cincinnati.com/story/opinion/2019/05/21/ohio-abortion-bill -john-becker-daniel-grossman-ectopic-pregnancy-false-medicine /3753610002/
- Lobbyist had hand in bill sparking ectopic pregnancy flap. December 11, 2019. Associated Press. Accessed June 12, 2023. https://apnews .com/article/03216e44405fa184ae0ab80fa85089f8
- NHE fact sheet. CMS.gov. Updated February 17, 2023. Accessed June 12, 2023. https://www.cms.gov/research-statistics-data-and -systems/statistics-trends-and-reports/nationalhealthexpenddata /nhe-fact-sheet
- Senate passes omnibus spending bill with health provisions. December 23, 2022. American Hospital Association. Accessed June 12, 2023. https://www.aha.org/special-bulletin/2022-12-20-appropriations -committees-release-omnibus-spending-bill-health-provisions
- Medicare updates compared to inflation (2001-2021). October 2021. American Medical Association. Accessed June 12, 2023. https://www .ama-assn.org/system/files/medicare-pay-chart-2021.pdf
- Resneck Jr J. Medicare physician payment reform is long overdue. October 3, 2022. American Medical Association. Accessed June 7, 2023. https://www.ama-assn.org/about/leadership /medicare-physician-payment-reform-long-overdue
- Isenberg M. The stark reality of physician reimbursement. August 24, 2022. Zotec Partners. Accessed June 13, 2023. https://zotecpartners. com/advocacy-zpac/test-1/
- Nguyen A. Mapping healthcare deserts: 80% of the country lacks adequate access to healthcare. September 9, 2021. GoodRx Health. Accessed June 13, 2023. https://www.goodrx.com/healthcare -access/research/healthcare-deserts-80-percent-of-country-lacks -adequate-healthcare-access
- 183 nonprofit hospital and health system CEOs to know–2017. Updated June 20, 2018. Becker’s Hospital Review. Accessed June 7, 2023. https://www.beckershospitalreview.com/lists/188-nonprofit -hospital-and-health-system-ceos-to-know-2017.html
- Goodall AH. Physician-leaders and hospital performance: is there an association? Soc Sci Med. 2011;73:535-539. doi:10.1016 /j.socscimed.2011.06.025
- Bloom N, Sadun R, Van Reenen J. Does Management Matter in Healthcare? Center for Economic Performance and Harvard Business School; 2014.
- Turner J. Why healthcare C-suites should include physicians. September 3, 2019. Managed Healthcare Executive. Accessed June 13, 2023. https://www.managedhealthcareexecutive.com /view/why-healthcare-c-suites-should-include-physicians
- Stoller JK, Goodall A, Baker A. Why the best hospitals are managed by doctors. December 27, 2016. Harvard Business Review. Accessed June 13, 2023. https://hbr.org/2016/12/why-the-best-hospitals -are-managed-by-doctors
- Hayhurst C. Data confirms: leaders, physician burnout is on you. April 3, 2019. Aetnahealth. Accessed June 13, 2023. https://www .athenahealth.com/knowledge-hub/practice-management /research-confirms-leaders-burnout-you
- Berger DH, Goodall A, Tsai AY. The importance of increasing surgeon participation in hospital leadership. JAMA Surg. 2019;154:281-282. doi:10.1001/jamasurg.2018.5080
- Charan R, Drotter S, Noel J. The Leadership Pipeline: How to Build the Leadership-Powered Company. Jossey-Bass; 2001.
- Perry J, Mobley F, Brubaker M. Most doctors have little or no management training, and that’s a problem. December 15, 2017. Harvard Business Review. Accessed June 7, 2023. https://hbr.org/2017/12 /most-doctors-have-little-or-no-management-training-and-thats -a-problem
Surgical volume and outcomes for gynecologic surgery: Is more always better?
Over the last 3 decades, abundant evidence has demonstrated the association between surgical volume and outcomes. Patients operated on by high-volume surgeons and at high-volume hospitals have superior outcomes.
Surgical volume in gynecology
The association between both hospital and surgeon volume and outcomes has been explored across a number of gynecologic procedures.3 A meta-analysis that included 741,000 patients found that low-volume surgeons had an increased rate of complications overall, a higher rate of intraoperative complications, and a higher rate of postoperative complications compared with high-volume surgeons. While there was no association between volume and mortality overall, when limited to gynecologic oncology studies, low surgeon volume was associated with increased perioperative mortality.3
While these studies demonstrated a statistically significant association between surgeon volume and perioperative outcomes, the magnitude of the effect is modest compared with other higher-risk procedures associated with greater perioperative morbidity. For example, in a large study that examined oncologic and cardiovascular surgery, perioperative mortality in patients who underwent pancreatic resection was reduced from 15% for low-volume surgeons to 5% for high-volume surgeons.1 By contrast, for gynecologic surgery, complications occurred in 97 per 1,000 patients operated on by high-volume surgeons compared with between 114 and 137 per 1,000 for low-volume surgeons. Thus, to avoid 1 in-hospital complication, 30 surgeries performed by low-volume surgeons would need to be moved to high-volume surgeons. For intraoperative complications, 38 patients would need to be moved from low- to high-volume surgeons to prevent 1 such complication.3 In addition to morbidity and mortality, higher surgeon volume is associated with greater use of minimally invasive surgery, a lower likelihood of conversion to laparotomy, and lower costs.3
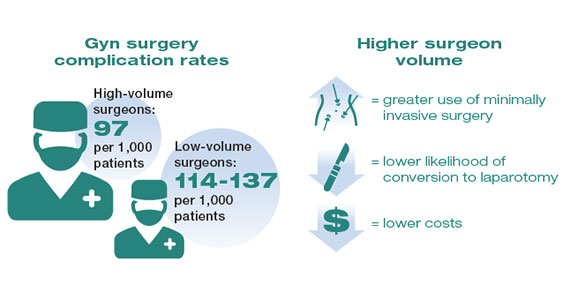
Similarly, hospital volume also has been associated with outcomes for gynecologic surgery.4 In a report of patients who underwent laparoscopic hysterectomy, the authors found that the complication rate was 18% lower for patients at high- versus low-volume hospitals. In addition, cost was lower at the high-volume centers.4 Like surgeon volume, the magnitude of the differential in outcomes between high- and low-volume hospitals is often modest.4
While most studies have focused on short-term outcomes, surgical volume appears also to be associated with longer-term outcomes. For gynecologic cancer, studies have demonstrated an association between hospital volume and survival for ovarian and cervical cancer.5-7 A large report of centers across the United States found that the 5-year survival rate increased from 39% for patients treated at low-volume centers to 51% at the highest-volume hospitals.5 In urogynecology, surgeon volume has been associated with midurethral sling revision. One study noted that after an individual surgeon performed 50 procedures a year, each additional case was associated with a decline in the rate of sling revision.8 One could argue that these longer-term end points may be the measures that matter most to patients.
Although the magnitude of the association between surgical volume and outcomes in gynecology appears to be relatively modest, outcomes for very-low-volume (VLV) surgeons are substantially worse. An analysis of more than 430,000 patients who underwent hysterectomy compared outcomes between VLV surgeons (characterized as surgeons who performed only 1 hysterectomy in the prior year) and other gynecologic surgeons. The overall complication rate was 32% in VLV surgeons compared with 10% among other surgeons, while the perioperative mortality rate was 2.5% versus 0.2% in the 2 groups, respectively. Likely reflecting changing practice patterns in gynecology, a sizable number of surgeons were classified as VLV physicians.9
Continue to: Public health applications of gynecologic surgical volume...
Public health applications of gynecologic surgical volume
The large body of literature on volume and outcomes has led to a number of public health initiatives aimed at reducing perioperative morbidity and mortality. Broadly, these efforts focus on regionalization of care, targeted quality improvement, and the development of minimum volume standards. Each strategy holds promise but also the potential to lead to unwanted consequences.
Regionalization of care
Recognition of the volume-outcomes paradigm has led to efforts to regionalize care for complex procedures to high-volume surgeons and centers.10 A cohort study of surgical patterns of care for Medicare recipients who underwent cancer resections or abdominal aortic aneurysm repair from 1999 to 2008 demonstrated these shifting practice patterns. For example, in 1999–2000, pancreatectomy was performed in 1,308 hospitals, with a median case volume of 5 procedures per year. By 2007–2008, the number of hospitals in which pancreatectomy was performed declined to 978, and the median case volume rose to 16 procedures per year. Importantly, over this time period, risk-adjusted mortality for pancreatectomy declined by 19%, and increased hospital volume was responsible for more than two-thirds of the decline in mortality.10
There has similarly been a gradual concentration of some gynecologic procedures to higher-volume surgeons and centers.11,12 Among patients undergoing hysterectomy for endometrial cancer in New York State, 845 surgeons with a mean case volume of 3 procedures per year treated patients in 2000. By 2014, the number of surgeons who performed these operations declined to 317 while mean annual case volume rose to 10 procedures per year. The number of hospitals in which women with endometrial cancer were treated declined from 182 to 98 over the same time period.11 Similar trends were noted for patients undergoing ovarian cancer resection.12 While patterns of gynecologic care for some surgical procedures have clearly changed, it has been more difficult to link these changes to improvements in outcomes.11,12
Despite the intuitive appeal of regionalization of surgical care, such a strategy has a number of limitations and practical challenges. Not surprisingly, limiting the number of surgeons and hospitals that perform a given procedure necessitates that patients travel a greater distance to obtain necessary surgical care.13,14 An analysis of endometrial cancer patients in New York State stratified patients based on their area of residence into 10 hospital referral regions (HRRs), which represent health care markets for tertiary medical care. From 2000 to 2014, the distance patients traveled to receive their surgical care increased in all of the HRRs studied. This was most pronounced in 1 of the HRRs in which the median travel distance rose by 47 miles over the 15-year period (FIGURE 1; FIGURE 2).14
Whether patients are willing to travel for care remains a matter of debate and depends on the disease, the surgical procedure, and the anticipated benefit associated with a longer travel distance.15,16 In a discrete choice experiment, 100 participants were given a hypothetical scenario in which they had potentially resectable pancreatic cancer; they were queried on their willingness to travel for care based on varying differences in mortality between a local and regional hospital.15 When mortality at the local hospital was double that of the regional hospital (6% vs 3%), 45% of patients chose to remain at the local hospital. When the differential increased to a 4 times greater mortality at the local hospital (12% vs 3%), 23% of patients still chose to remain at the local hospital.15
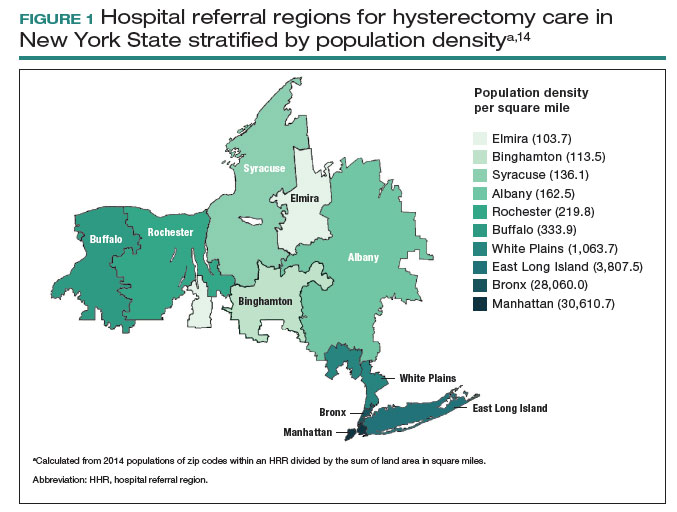
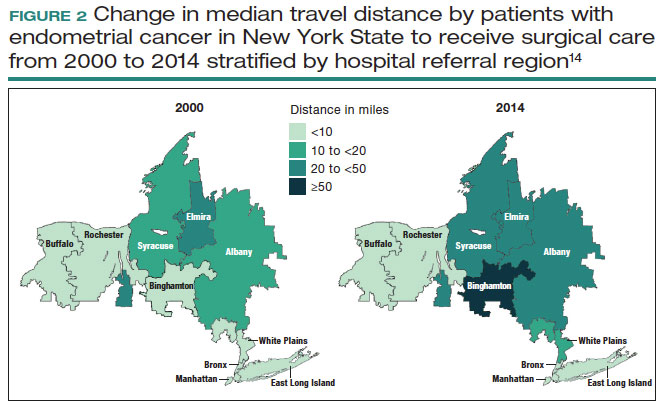
A similar study asked patients with ovarian neoplasms whether they would travel 50 miles to a regional center for surgery based on some degree of increased 5-year survival.16 Overall, 79% of patients would travel for a 4% improvement in survival while 97% would travel for a 12% improvement in survival.16
Lastly, a number of studies have shown that regionalization of surgical care disproportionately affects Black and Hispanic patients and those with low socioeconomic status.12,13,17 A simulation study on the effect of regionalizing care for pancreatectomy noted that using a hospital volume threshold of 20 procedures per year, a higher percentage of Black and Hispanic patients than White patients would be required to travel to a higher-volume center.13 Similarly, Medicaid recipients were more likely to be affected.13 Despite the inequities in who must travel for regionalized care, prior work has suggested that regionalization of cancer care to high-volume centers may reduce racial and socioeconomic disparities in survival for some cancers.18
Targeted quality improvement
Realizing the practical limitations of regionalization of care, an alternative strategy is to improve the quality of care at low-volume hospitals.5,19 Quality of care and surgical volume often are correlated, and the delivery of high-quality care can mitigate some of the influence of surgical volume on outcomes.
These principles were demonstrated in a study of more than 100,000 patients with ovarian cancer that stratified treating hospitals into volume quintiles.5 As expected, survival (both 2- and 5-year) was highest in the highest-volume quintile hospitals (FIGURE 3).5 Similarly, quality of care, measured through adherence to various process measures, was also highest in the highest-volume quintile hospitals. Interestingly, in the second-fourth volume quintile hospitals, there was substantial variation in adherence to quality metrics. Among hospitals with higher quality care, an improved survival was noted compared with lower quality care hospitals within the same volume quintile. Survival at high-quality, intermediate-volume hospitals approached that of the high-volume quintile hospitals.5
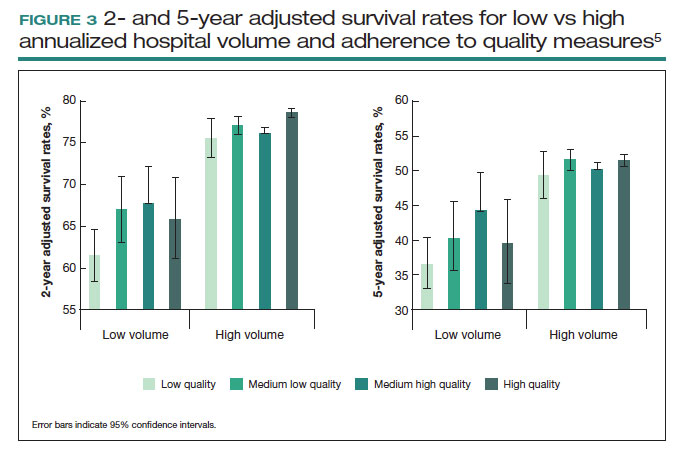
These findings highlight the importance of quality of care as well as the complex interplay of surgical volume and other factors.20 Many have argued that it may be more appropriate to measure quality of care and past performance and outcomes rather than surgical volume.21
Continue to: Minimum volume standards...
Minimum volume standards
While efforts to regionalize surgical care have gradually evolved, calls have been growing to formalize policies that limit the performance of some procedures to surgeons and centers that meet a minimum volume threshold or standard.21 One such effort, based on consensus from 3 academic hospital systems, was a campaign for hospitals to “Take the Volume Pledge.”21 The campaign’s goal is to encourage health care systems to restrict the performance of 10 procedures to surgeons and hospitals within their systems that meet a minimum volume standard for the given operations.21 In essence, procedures would be restricted for low-volume providers and centers and triaged to higher-volume surgeons and hospitals within a given health care system.21
Proponents of the Volume Pledge argue that it is a relatively straightforward way to align patients and providers to optimize outcomes. The Volume Pledge focuses on larger hospital systems and encourages referral within the given system, thus mitigating competitive and financial concerns about referring patients to outside providers. Those who have argued against the Volume Pledge point out that the volume cut points chosen are somewhat arbitrary, that these policies have the potential to negatively impact rural hospitals and those serving smaller communities, and that quality is a more appropriate metric than volume.22 The Volume Pledge does not include any gynecologic procedures, and to date it has met with only limited success.23
Perhaps more directly applicable to gynecologic surgeons are ongoing national trends to base hospital credentialing on surgical volume. In essence, individual surgeons must demonstrate that they have performed a minimum number of procedures to obtain or retain privileges.24,25 While there is strong evidence of the association between volume and outcomes for some complex surgical procedures, linking volume to credentialing has a number of potential pitfalls. Studies of surgical outcomes based on volume represent average performance, and many low-volume providers have better-than-expected outcomes. Volume measures typically represent recent performance; it is difficult to measure the overall experience of individual surgeons. Similarly, surgical outcomes depend on both the surgeon and the system in which the surgeon operates. It is difficult, if not impossible, to account for differences in the environment in which a surgeon works.25
A study of gynecologic surgeons who performed hysterectomy in New York State demonstrates many of the complexities of volume-based credentialing.26 In a cohort of more than55,000 patients who underwent abdominal hysterectomy, there was a strong association between low surgeon volume and a higher-than-expected rate of complications. If one were to consider limiting privileges to even the lowest-volume providers, there would be a significant impact on the surgical workforce. In this cohort, limiting credentialing to the lowest-volume providers, those who performed only 1 abdominal hysterectomy in the prior year would restrict the privileges of 17.5% of the surgeons in the cohort. Further, in this low-volume cohort that performed only 1 abdominal hysterectomy in the prior year, 69% of the surgeons actually had outcomes that were better than predicted.26 These data highlight not only the difficulty of applying averages to individual surgeons but also the profound impact that policy changes could have on the practice of gynecologic surgery.
Volume-outcomes paradigm discussions continue
The association between higher surgeon and hospital procedural volume for gynecologic surgeries and improved outcomes now has been convincingly demonstrated. With this knowledge, over the last decade the patterns of care for patients undergoing gynecologic surgery have clearly shifted, and these operations are now more commonly being performed by a smaller number of physicians and at fewer hospitals.
While efforts to improve quality are clearly important, many policy interventions, such as regionalization of care, have untoward consequences that must be considered. As we move forward, it will be essential to ensure that there is a robust debate among patients, providers, and policymakers on the merits of public health policies based on the volume-outcomes paradigm. ●
- Birkmeyer JD, Stukel TA, Siewers AE, et al. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003;349:2117-2127.
- Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346:11281137.
- Mowat A, Maher C, Ballard E. Surgical outcomes for low-volume vs high-volume surgeons in gynecology surgery: a systematic review and meta-analysis. Am J Obstet Gynecol. 2016;215:21-33.
- Wallenstein MR, Ananth CV, Kim JH, et al. Effect of surgical volume on outcomes for laparoscopic hysterectomy for benign indications. Obstet Gynecol. 2012;119:709-716.
- Wright JD, Chen L, Hou JY, et al. Association of hospital volume and quality of care with survival for ovarian cancer. Obstet Gynecol. 2017;130:545-553.
- Cliby WA, Powell MA, Al-Hammadi N, et al. Ovarian cancer in the United States: contemporary patterns of care associated with improved survival. Gynecol Oncol. 2015;136:11-17.
- Matsuo K, Shimada M, Yamaguchi S, et al. Association of radical hysterectomy surgical volume and survival for early-stage cervical cancer. Obstet Gynecol. 2019;133:1086-1098.
- Brennand EA, Quan H. Evaluation of the effect of surgeon’s operative volume and specialty on likelihood of revision after mesh midurethral sling placement. Obstet Gynecol. 2019;133:1099-1108.
- Ruiz MP, Chen L, Hou JY, et al. Outcomes of hysterectomy performed by very low-volume surgeons. Obstet Gynecol. 2018;131:981-990.
- Finks JF, Osborne NH, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med. 2011;364:21282137.
- Wright JD, Ruiz MP, Chen L, et al. Changes in surgical volume and outcomes over time for women undergoing hysterectomy for endometrial cancer. Obstet Gynecol. 2018;132:59-69.
- Wright JD, Chen L, Buskwofie A, et al. Regionalization of care for women with ovarian cancer. Gynecol Oncol. 2019;154:394-400.
- Fong ZV, Hashimoto DA, Jin G, et al. Simulated volume-based regionalization of complex procedures: impact on spatial access to care. Ann Surg. 2021;274:312-318.
- Knisely A, Huang Y, Melamed A, et al. Effect of regionalization of endometrial cancer care on site of care and patient travel. Am J Obstet Gynecol. 2020;222:58.e1-58.e10.
- Finlayson SR, Birkmeyer JD, Tosteson AN, et al. Patient preferences for location of care: implications for regionalization. Med Care. 1999;37:204-209.
- Shalowitz DI, Nivasch E, Burger RA, et al. Are patients willing to travel for better ovarian cancer care? Gynecol Oncol. 2018;148:42-48.
- Rehmani SS, Liu B, Al-Ayoubi AM, et al. Racial disparity in utilization of high-volume hospitals for surgical treatment of esophageal cancer. Ann Thorac Surg. 2018;106:346-353.
- Nattinger AB, Rademacher N, McGinley EL, et al. Can regionalization of care reduce socioeconomic disparities in breast cancer survival? Med Care. 2021;59:77-81.
- Auerbach AD, Hilton JF, Maselli J, et al. Shop for quality or volume? Volume, quality, and outcomes of coronary artery bypass surgery. Ann Intern Med. 2009;150:696-704.
- Kurlansky PA, Argenziano M, Dunton R, et al. Quality, not volume, determines outcome of coronary artery bypass surgery in a university-based community hospital network. J Thorac Cardiovasc Surg. 2012;143:287-293.
- Urbach DR. Pledging to eliminate low-volume surgery. N Engl J Med. 2015;373:1388-1390.
- Blanco BA, Kothari AN, Blackwell RH, et al. “Take the Volume Pledge” may result in disparity in access to care. Surgery. 2017;161:837-845.
- Farjah F, Grau-Sepulveda MV, Gaissert H, et al. Volume Pledge is not associated with better short-term outcomes after lung cancer resection. J Clin Oncol. 2020;38:3518-3527.
- Tracy EE, Zephyrin LC, Rosman DA, et al. Credentialing based on surgical volume, physician workforce challenges, and patient access. Obstet Gynecol. 2013;122:947-951.
- Statement on credentialing and privileging and volume performance issues. April 1, 2018. American College of Surgeons. Accessed April 10, 2023. https://facs.org/about-acs/statements/credentialing-andprivileging-and-volume-performance-issues/
- Ruiz MP, Chen L, Hou JY, et al. Effect of minimum-volume standards on patient outcomes and surgical practice patterns for hysterectomy. Obstet Gynecol. 2018;132:1229-1237.
Over the last 3 decades, abundant evidence has demonstrated the association between surgical volume and outcomes. Patients operated on by high-volume surgeons and at high-volume hospitals have superior outcomes.
Surgical volume in gynecology
The association between both hospital and surgeon volume and outcomes has been explored across a number of gynecologic procedures.3 A meta-analysis that included 741,000 patients found that low-volume surgeons had an increased rate of complications overall, a higher rate of intraoperative complications, and a higher rate of postoperative complications compared with high-volume surgeons. While there was no association between volume and mortality overall, when limited to gynecologic oncology studies, low surgeon volume was associated with increased perioperative mortality.3
While these studies demonstrated a statistically significant association between surgeon volume and perioperative outcomes, the magnitude of the effect is modest compared with other higher-risk procedures associated with greater perioperative morbidity. For example, in a large study that examined oncologic and cardiovascular surgery, perioperative mortality in patients who underwent pancreatic resection was reduced from 15% for low-volume surgeons to 5% for high-volume surgeons.1 By contrast, for gynecologic surgery, complications occurred in 97 per 1,000 patients operated on by high-volume surgeons compared with between 114 and 137 per 1,000 for low-volume surgeons. Thus, to avoid 1 in-hospital complication, 30 surgeries performed by low-volume surgeons would need to be moved to high-volume surgeons. For intraoperative complications, 38 patients would need to be moved from low- to high-volume surgeons to prevent 1 such complication.3 In addition to morbidity and mortality, higher surgeon volume is associated with greater use of minimally invasive surgery, a lower likelihood of conversion to laparotomy, and lower costs.3
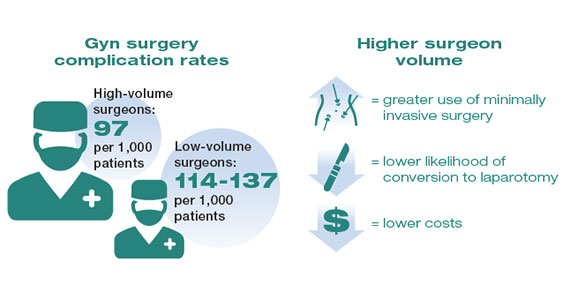
Similarly, hospital volume also has been associated with outcomes for gynecologic surgery.4 In a report of patients who underwent laparoscopic hysterectomy, the authors found that the complication rate was 18% lower for patients at high- versus low-volume hospitals. In addition, cost was lower at the high-volume centers.4 Like surgeon volume, the magnitude of the differential in outcomes between high- and low-volume hospitals is often modest.4
While most studies have focused on short-term outcomes, surgical volume appears also to be associated with longer-term outcomes. For gynecologic cancer, studies have demonstrated an association between hospital volume and survival for ovarian and cervical cancer.5-7 A large report of centers across the United States found that the 5-year survival rate increased from 39% for patients treated at low-volume centers to 51% at the highest-volume hospitals.5 In urogynecology, surgeon volume has been associated with midurethral sling revision. One study noted that after an individual surgeon performed 50 procedures a year, each additional case was associated with a decline in the rate of sling revision.8 One could argue that these longer-term end points may be the measures that matter most to patients.
Although the magnitude of the association between surgical volume and outcomes in gynecology appears to be relatively modest, outcomes for very-low-volume (VLV) surgeons are substantially worse. An analysis of more than 430,000 patients who underwent hysterectomy compared outcomes between VLV surgeons (characterized as surgeons who performed only 1 hysterectomy in the prior year) and other gynecologic surgeons. The overall complication rate was 32% in VLV surgeons compared with 10% among other surgeons, while the perioperative mortality rate was 2.5% versus 0.2% in the 2 groups, respectively. Likely reflecting changing practice patterns in gynecology, a sizable number of surgeons were classified as VLV physicians.9
Continue to: Public health applications of gynecologic surgical volume...
Public health applications of gynecologic surgical volume
The large body of literature on volume and outcomes has led to a number of public health initiatives aimed at reducing perioperative morbidity and mortality. Broadly, these efforts focus on regionalization of care, targeted quality improvement, and the development of minimum volume standards. Each strategy holds promise but also the potential to lead to unwanted consequences.
Regionalization of care
Recognition of the volume-outcomes paradigm has led to efforts to regionalize care for complex procedures to high-volume surgeons and centers.10 A cohort study of surgical patterns of care for Medicare recipients who underwent cancer resections or abdominal aortic aneurysm repair from 1999 to 2008 demonstrated these shifting practice patterns. For example, in 1999–2000, pancreatectomy was performed in 1,308 hospitals, with a median case volume of 5 procedures per year. By 2007–2008, the number of hospitals in which pancreatectomy was performed declined to 978, and the median case volume rose to 16 procedures per year. Importantly, over this time period, risk-adjusted mortality for pancreatectomy declined by 19%, and increased hospital volume was responsible for more than two-thirds of the decline in mortality.10
There has similarly been a gradual concentration of some gynecologic procedures to higher-volume surgeons and centers.11,12 Among patients undergoing hysterectomy for endometrial cancer in New York State, 845 surgeons with a mean case volume of 3 procedures per year treated patients in 2000. By 2014, the number of surgeons who performed these operations declined to 317 while mean annual case volume rose to 10 procedures per year. The number of hospitals in which women with endometrial cancer were treated declined from 182 to 98 over the same time period.11 Similar trends were noted for patients undergoing ovarian cancer resection.12 While patterns of gynecologic care for some surgical procedures have clearly changed, it has been more difficult to link these changes to improvements in outcomes.11,12
Despite the intuitive appeal of regionalization of surgical care, such a strategy has a number of limitations and practical challenges. Not surprisingly, limiting the number of surgeons and hospitals that perform a given procedure necessitates that patients travel a greater distance to obtain necessary surgical care.13,14 An analysis of endometrial cancer patients in New York State stratified patients based on their area of residence into 10 hospital referral regions (HRRs), which represent health care markets for tertiary medical care. From 2000 to 2014, the distance patients traveled to receive their surgical care increased in all of the HRRs studied. This was most pronounced in 1 of the HRRs in which the median travel distance rose by 47 miles over the 15-year period (FIGURE 1; FIGURE 2).14
Whether patients are willing to travel for care remains a matter of debate and depends on the disease, the surgical procedure, and the anticipated benefit associated with a longer travel distance.15,16 In a discrete choice experiment, 100 participants were given a hypothetical scenario in which they had potentially resectable pancreatic cancer; they were queried on their willingness to travel for care based on varying differences in mortality between a local and regional hospital.15 When mortality at the local hospital was double that of the regional hospital (6% vs 3%), 45% of patients chose to remain at the local hospital. When the differential increased to a 4 times greater mortality at the local hospital (12% vs 3%), 23% of patients still chose to remain at the local hospital.15
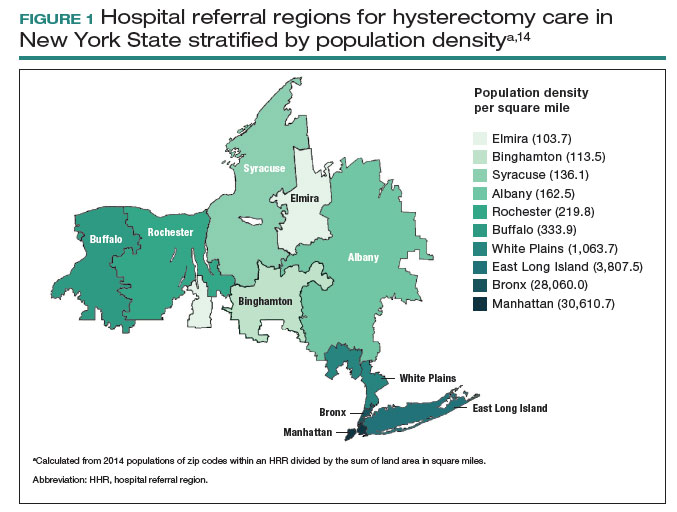
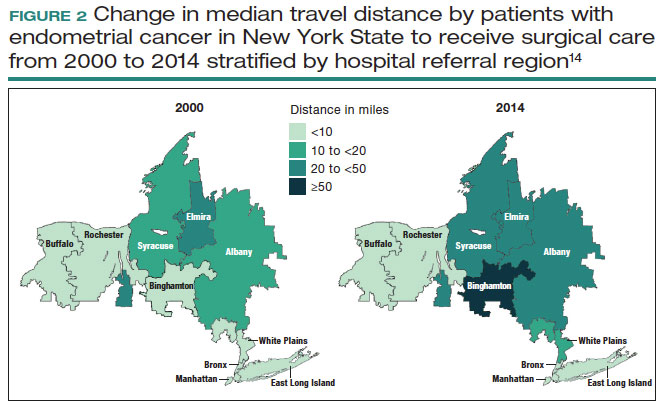
A similar study asked patients with ovarian neoplasms whether they would travel 50 miles to a regional center for surgery based on some degree of increased 5-year survival.16 Overall, 79% of patients would travel for a 4% improvement in survival while 97% would travel for a 12% improvement in survival.16
Lastly, a number of studies have shown that regionalization of surgical care disproportionately affects Black and Hispanic patients and those with low socioeconomic status.12,13,17 A simulation study on the effect of regionalizing care for pancreatectomy noted that using a hospital volume threshold of 20 procedures per year, a higher percentage of Black and Hispanic patients than White patients would be required to travel to a higher-volume center.13 Similarly, Medicaid recipients were more likely to be affected.13 Despite the inequities in who must travel for regionalized care, prior work has suggested that regionalization of cancer care to high-volume centers may reduce racial and socioeconomic disparities in survival for some cancers.18
Targeted quality improvement
Realizing the practical limitations of regionalization of care, an alternative strategy is to improve the quality of care at low-volume hospitals.5,19 Quality of care and surgical volume often are correlated, and the delivery of high-quality care can mitigate some of the influence of surgical volume on outcomes.
These principles were demonstrated in a study of more than 100,000 patients with ovarian cancer that stratified treating hospitals into volume quintiles.5 As expected, survival (both 2- and 5-year) was highest in the highest-volume quintile hospitals (FIGURE 3).5 Similarly, quality of care, measured through adherence to various process measures, was also highest in the highest-volume quintile hospitals. Interestingly, in the second-fourth volume quintile hospitals, there was substantial variation in adherence to quality metrics. Among hospitals with higher quality care, an improved survival was noted compared with lower quality care hospitals within the same volume quintile. Survival at high-quality, intermediate-volume hospitals approached that of the high-volume quintile hospitals.5
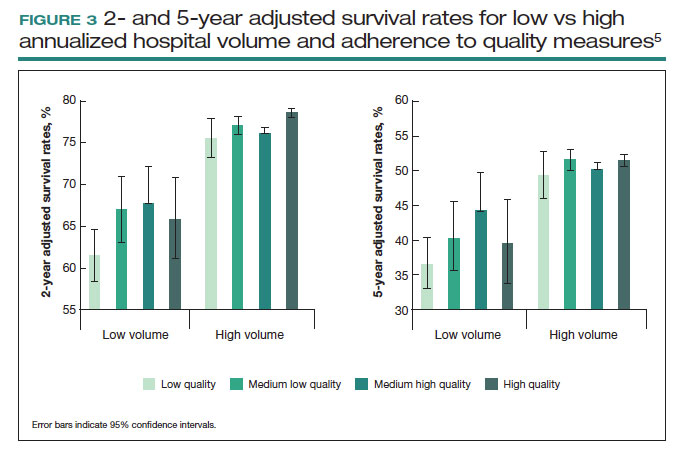
These findings highlight the importance of quality of care as well as the complex interplay of surgical volume and other factors.20 Many have argued that it may be more appropriate to measure quality of care and past performance and outcomes rather than surgical volume.21
Continue to: Minimum volume standards...
Minimum volume standards
While efforts to regionalize surgical care have gradually evolved, calls have been growing to formalize policies that limit the performance of some procedures to surgeons and centers that meet a minimum volume threshold or standard.21 One such effort, based on consensus from 3 academic hospital systems, was a campaign for hospitals to “Take the Volume Pledge.”21 The campaign’s goal is to encourage health care systems to restrict the performance of 10 procedures to surgeons and hospitals within their systems that meet a minimum volume standard for the given operations.21 In essence, procedures would be restricted for low-volume providers and centers and triaged to higher-volume surgeons and hospitals within a given health care system.21
Proponents of the Volume Pledge argue that it is a relatively straightforward way to align patients and providers to optimize outcomes. The Volume Pledge focuses on larger hospital systems and encourages referral within the given system, thus mitigating competitive and financial concerns about referring patients to outside providers. Those who have argued against the Volume Pledge point out that the volume cut points chosen are somewhat arbitrary, that these policies have the potential to negatively impact rural hospitals and those serving smaller communities, and that quality is a more appropriate metric than volume.22 The Volume Pledge does not include any gynecologic procedures, and to date it has met with only limited success.23
Perhaps more directly applicable to gynecologic surgeons are ongoing national trends to base hospital credentialing on surgical volume. In essence, individual surgeons must demonstrate that they have performed a minimum number of procedures to obtain or retain privileges.24,25 While there is strong evidence of the association between volume and outcomes for some complex surgical procedures, linking volume to credentialing has a number of potential pitfalls. Studies of surgical outcomes based on volume represent average performance, and many low-volume providers have better-than-expected outcomes. Volume measures typically represent recent performance; it is difficult to measure the overall experience of individual surgeons. Similarly, surgical outcomes depend on both the surgeon and the system in which the surgeon operates. It is difficult, if not impossible, to account for differences in the environment in which a surgeon works.25
A study of gynecologic surgeons who performed hysterectomy in New York State demonstrates many of the complexities of volume-based credentialing.26 In a cohort of more than55,000 patients who underwent abdominal hysterectomy, there was a strong association between low surgeon volume and a higher-than-expected rate of complications. If one were to consider limiting privileges to even the lowest-volume providers, there would be a significant impact on the surgical workforce. In this cohort, limiting credentialing to the lowest-volume providers, those who performed only 1 abdominal hysterectomy in the prior year would restrict the privileges of 17.5% of the surgeons in the cohort. Further, in this low-volume cohort that performed only 1 abdominal hysterectomy in the prior year, 69% of the surgeons actually had outcomes that were better than predicted.26 These data highlight not only the difficulty of applying averages to individual surgeons but also the profound impact that policy changes could have on the practice of gynecologic surgery.
Volume-outcomes paradigm discussions continue
The association between higher surgeon and hospital procedural volume for gynecologic surgeries and improved outcomes now has been convincingly demonstrated. With this knowledge, over the last decade the patterns of care for patients undergoing gynecologic surgery have clearly shifted, and these operations are now more commonly being performed by a smaller number of physicians and at fewer hospitals.
While efforts to improve quality are clearly important, many policy interventions, such as regionalization of care, have untoward consequences that must be considered. As we move forward, it will be essential to ensure that there is a robust debate among patients, providers, and policymakers on the merits of public health policies based on the volume-outcomes paradigm. ●
Over the last 3 decades, abundant evidence has demonstrated the association between surgical volume and outcomes. Patients operated on by high-volume surgeons and at high-volume hospitals have superior outcomes.
Surgical volume in gynecology
The association between both hospital and surgeon volume and outcomes has been explored across a number of gynecologic procedures.3 A meta-analysis that included 741,000 patients found that low-volume surgeons had an increased rate of complications overall, a higher rate of intraoperative complications, and a higher rate of postoperative complications compared with high-volume surgeons. While there was no association between volume and mortality overall, when limited to gynecologic oncology studies, low surgeon volume was associated with increased perioperative mortality.3
While these studies demonstrated a statistically significant association between surgeon volume and perioperative outcomes, the magnitude of the effect is modest compared with other higher-risk procedures associated with greater perioperative morbidity. For example, in a large study that examined oncologic and cardiovascular surgery, perioperative mortality in patients who underwent pancreatic resection was reduced from 15% for low-volume surgeons to 5% for high-volume surgeons.1 By contrast, for gynecologic surgery, complications occurred in 97 per 1,000 patients operated on by high-volume surgeons compared with between 114 and 137 per 1,000 for low-volume surgeons. Thus, to avoid 1 in-hospital complication, 30 surgeries performed by low-volume surgeons would need to be moved to high-volume surgeons. For intraoperative complications, 38 patients would need to be moved from low- to high-volume surgeons to prevent 1 such complication.3 In addition to morbidity and mortality, higher surgeon volume is associated with greater use of minimally invasive surgery, a lower likelihood of conversion to laparotomy, and lower costs.3
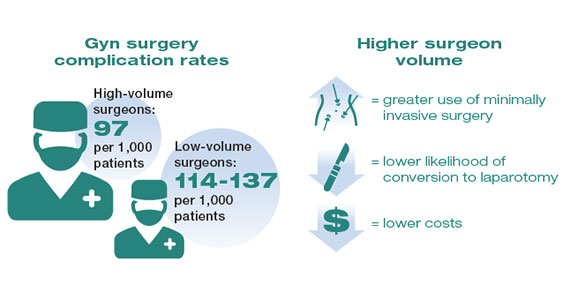
Similarly, hospital volume also has been associated with outcomes for gynecologic surgery.4 In a report of patients who underwent laparoscopic hysterectomy, the authors found that the complication rate was 18% lower for patients at high- versus low-volume hospitals. In addition, cost was lower at the high-volume centers.4 Like surgeon volume, the magnitude of the differential in outcomes between high- and low-volume hospitals is often modest.4
While most studies have focused on short-term outcomes, surgical volume appears also to be associated with longer-term outcomes. For gynecologic cancer, studies have demonstrated an association between hospital volume and survival for ovarian and cervical cancer.5-7 A large report of centers across the United States found that the 5-year survival rate increased from 39% for patients treated at low-volume centers to 51% at the highest-volume hospitals.5 In urogynecology, surgeon volume has been associated with midurethral sling revision. One study noted that after an individual surgeon performed 50 procedures a year, each additional case was associated with a decline in the rate of sling revision.8 One could argue that these longer-term end points may be the measures that matter most to patients.
Although the magnitude of the association between surgical volume and outcomes in gynecology appears to be relatively modest, outcomes for very-low-volume (VLV) surgeons are substantially worse. An analysis of more than 430,000 patients who underwent hysterectomy compared outcomes between VLV surgeons (characterized as surgeons who performed only 1 hysterectomy in the prior year) and other gynecologic surgeons. The overall complication rate was 32% in VLV surgeons compared with 10% among other surgeons, while the perioperative mortality rate was 2.5% versus 0.2% in the 2 groups, respectively. Likely reflecting changing practice patterns in gynecology, a sizable number of surgeons were classified as VLV physicians.9
Continue to: Public health applications of gynecologic surgical volume...
Public health applications of gynecologic surgical volume
The large body of literature on volume and outcomes has led to a number of public health initiatives aimed at reducing perioperative morbidity and mortality. Broadly, these efforts focus on regionalization of care, targeted quality improvement, and the development of minimum volume standards. Each strategy holds promise but also the potential to lead to unwanted consequences.
Regionalization of care
Recognition of the volume-outcomes paradigm has led to efforts to regionalize care for complex procedures to high-volume surgeons and centers.10 A cohort study of surgical patterns of care for Medicare recipients who underwent cancer resections or abdominal aortic aneurysm repair from 1999 to 2008 demonstrated these shifting practice patterns. For example, in 1999–2000, pancreatectomy was performed in 1,308 hospitals, with a median case volume of 5 procedures per year. By 2007–2008, the number of hospitals in which pancreatectomy was performed declined to 978, and the median case volume rose to 16 procedures per year. Importantly, over this time period, risk-adjusted mortality for pancreatectomy declined by 19%, and increased hospital volume was responsible for more than two-thirds of the decline in mortality.10
There has similarly been a gradual concentration of some gynecologic procedures to higher-volume surgeons and centers.11,12 Among patients undergoing hysterectomy for endometrial cancer in New York State, 845 surgeons with a mean case volume of 3 procedures per year treated patients in 2000. By 2014, the number of surgeons who performed these operations declined to 317 while mean annual case volume rose to 10 procedures per year. The number of hospitals in which women with endometrial cancer were treated declined from 182 to 98 over the same time period.11 Similar trends were noted for patients undergoing ovarian cancer resection.12 While patterns of gynecologic care for some surgical procedures have clearly changed, it has been more difficult to link these changes to improvements in outcomes.11,12
Despite the intuitive appeal of regionalization of surgical care, such a strategy has a number of limitations and practical challenges. Not surprisingly, limiting the number of surgeons and hospitals that perform a given procedure necessitates that patients travel a greater distance to obtain necessary surgical care.13,14 An analysis of endometrial cancer patients in New York State stratified patients based on their area of residence into 10 hospital referral regions (HRRs), which represent health care markets for tertiary medical care. From 2000 to 2014, the distance patients traveled to receive their surgical care increased in all of the HRRs studied. This was most pronounced in 1 of the HRRs in which the median travel distance rose by 47 miles over the 15-year period (FIGURE 1; FIGURE 2).14
Whether patients are willing to travel for care remains a matter of debate and depends on the disease, the surgical procedure, and the anticipated benefit associated with a longer travel distance.15,16 In a discrete choice experiment, 100 participants were given a hypothetical scenario in which they had potentially resectable pancreatic cancer; they were queried on their willingness to travel for care based on varying differences in mortality between a local and regional hospital.15 When mortality at the local hospital was double that of the regional hospital (6% vs 3%), 45% of patients chose to remain at the local hospital. When the differential increased to a 4 times greater mortality at the local hospital (12% vs 3%), 23% of patients still chose to remain at the local hospital.15
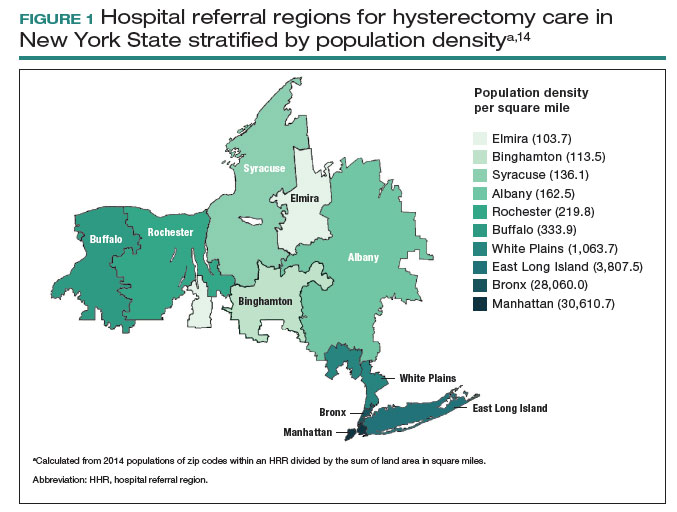
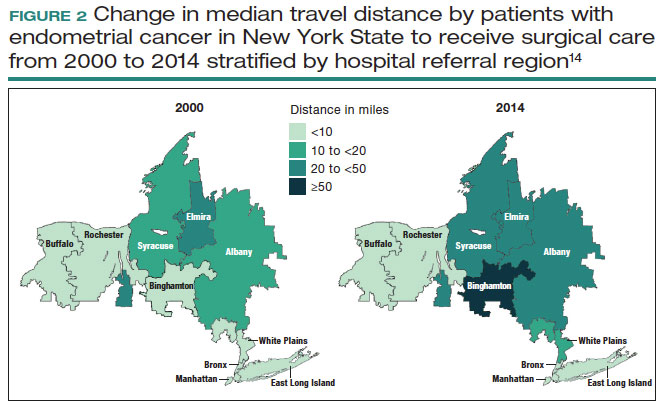
A similar study asked patients with ovarian neoplasms whether they would travel 50 miles to a regional center for surgery based on some degree of increased 5-year survival.16 Overall, 79% of patients would travel for a 4% improvement in survival while 97% would travel for a 12% improvement in survival.16
Lastly, a number of studies have shown that regionalization of surgical care disproportionately affects Black and Hispanic patients and those with low socioeconomic status.12,13,17 A simulation study on the effect of regionalizing care for pancreatectomy noted that using a hospital volume threshold of 20 procedures per year, a higher percentage of Black and Hispanic patients than White patients would be required to travel to a higher-volume center.13 Similarly, Medicaid recipients were more likely to be affected.13 Despite the inequities in who must travel for regionalized care, prior work has suggested that regionalization of cancer care to high-volume centers may reduce racial and socioeconomic disparities in survival for some cancers.18
Targeted quality improvement
Realizing the practical limitations of regionalization of care, an alternative strategy is to improve the quality of care at low-volume hospitals.5,19 Quality of care and surgical volume often are correlated, and the delivery of high-quality care can mitigate some of the influence of surgical volume on outcomes.
These principles were demonstrated in a study of more than 100,000 patients with ovarian cancer that stratified treating hospitals into volume quintiles.5 As expected, survival (both 2- and 5-year) was highest in the highest-volume quintile hospitals (FIGURE 3).5 Similarly, quality of care, measured through adherence to various process measures, was also highest in the highest-volume quintile hospitals. Interestingly, in the second-fourth volume quintile hospitals, there was substantial variation in adherence to quality metrics. Among hospitals with higher quality care, an improved survival was noted compared with lower quality care hospitals within the same volume quintile. Survival at high-quality, intermediate-volume hospitals approached that of the high-volume quintile hospitals.5
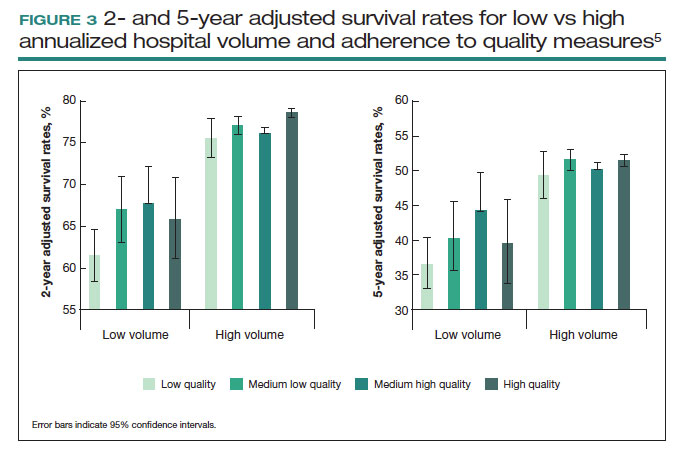
These findings highlight the importance of quality of care as well as the complex interplay of surgical volume and other factors.20 Many have argued that it may be more appropriate to measure quality of care and past performance and outcomes rather than surgical volume.21
Continue to: Minimum volume standards...
Minimum volume standards
While efforts to regionalize surgical care have gradually evolved, calls have been growing to formalize policies that limit the performance of some procedures to surgeons and centers that meet a minimum volume threshold or standard.21 One such effort, based on consensus from 3 academic hospital systems, was a campaign for hospitals to “Take the Volume Pledge.”21 The campaign’s goal is to encourage health care systems to restrict the performance of 10 procedures to surgeons and hospitals within their systems that meet a minimum volume standard for the given operations.21 In essence, procedures would be restricted for low-volume providers and centers and triaged to higher-volume surgeons and hospitals within a given health care system.21
Proponents of the Volume Pledge argue that it is a relatively straightforward way to align patients and providers to optimize outcomes. The Volume Pledge focuses on larger hospital systems and encourages referral within the given system, thus mitigating competitive and financial concerns about referring patients to outside providers. Those who have argued against the Volume Pledge point out that the volume cut points chosen are somewhat arbitrary, that these policies have the potential to negatively impact rural hospitals and those serving smaller communities, and that quality is a more appropriate metric than volume.22 The Volume Pledge does not include any gynecologic procedures, and to date it has met with only limited success.23
Perhaps more directly applicable to gynecologic surgeons are ongoing national trends to base hospital credentialing on surgical volume. In essence, individual surgeons must demonstrate that they have performed a minimum number of procedures to obtain or retain privileges.24,25 While there is strong evidence of the association between volume and outcomes for some complex surgical procedures, linking volume to credentialing has a number of potential pitfalls. Studies of surgical outcomes based on volume represent average performance, and many low-volume providers have better-than-expected outcomes. Volume measures typically represent recent performance; it is difficult to measure the overall experience of individual surgeons. Similarly, surgical outcomes depend on both the surgeon and the system in which the surgeon operates. It is difficult, if not impossible, to account for differences in the environment in which a surgeon works.25
A study of gynecologic surgeons who performed hysterectomy in New York State demonstrates many of the complexities of volume-based credentialing.26 In a cohort of more than55,000 patients who underwent abdominal hysterectomy, there was a strong association between low surgeon volume and a higher-than-expected rate of complications. If one were to consider limiting privileges to even the lowest-volume providers, there would be a significant impact on the surgical workforce. In this cohort, limiting credentialing to the lowest-volume providers, those who performed only 1 abdominal hysterectomy in the prior year would restrict the privileges of 17.5% of the surgeons in the cohort. Further, in this low-volume cohort that performed only 1 abdominal hysterectomy in the prior year, 69% of the surgeons actually had outcomes that were better than predicted.26 These data highlight not only the difficulty of applying averages to individual surgeons but also the profound impact that policy changes could have on the practice of gynecologic surgery.
Volume-outcomes paradigm discussions continue
The association between higher surgeon and hospital procedural volume for gynecologic surgeries and improved outcomes now has been convincingly demonstrated. With this knowledge, over the last decade the patterns of care for patients undergoing gynecologic surgery have clearly shifted, and these operations are now more commonly being performed by a smaller number of physicians and at fewer hospitals.
While efforts to improve quality are clearly important, many policy interventions, such as regionalization of care, have untoward consequences that must be considered. As we move forward, it will be essential to ensure that there is a robust debate among patients, providers, and policymakers on the merits of public health policies based on the volume-outcomes paradigm. ●
- Birkmeyer JD, Stukel TA, Siewers AE, et al. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003;349:2117-2127.
- Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346:11281137.
- Mowat A, Maher C, Ballard E. Surgical outcomes for low-volume vs high-volume surgeons in gynecology surgery: a systematic review and meta-analysis. Am J Obstet Gynecol. 2016;215:21-33.
- Wallenstein MR, Ananth CV, Kim JH, et al. Effect of surgical volume on outcomes for laparoscopic hysterectomy for benign indications. Obstet Gynecol. 2012;119:709-716.
- Wright JD, Chen L, Hou JY, et al. Association of hospital volume and quality of care with survival for ovarian cancer. Obstet Gynecol. 2017;130:545-553.
- Cliby WA, Powell MA, Al-Hammadi N, et al. Ovarian cancer in the United States: contemporary patterns of care associated with improved survival. Gynecol Oncol. 2015;136:11-17.
- Matsuo K, Shimada M, Yamaguchi S, et al. Association of radical hysterectomy surgical volume and survival for early-stage cervical cancer. Obstet Gynecol. 2019;133:1086-1098.
- Brennand EA, Quan H. Evaluation of the effect of surgeon’s operative volume and specialty on likelihood of revision after mesh midurethral sling placement. Obstet Gynecol. 2019;133:1099-1108.
- Ruiz MP, Chen L, Hou JY, et al. Outcomes of hysterectomy performed by very low-volume surgeons. Obstet Gynecol. 2018;131:981-990.
- Finks JF, Osborne NH, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med. 2011;364:21282137.
- Wright JD, Ruiz MP, Chen L, et al. Changes in surgical volume and outcomes over time for women undergoing hysterectomy for endometrial cancer. Obstet Gynecol. 2018;132:59-69.
- Wright JD, Chen L, Buskwofie A, et al. Regionalization of care for women with ovarian cancer. Gynecol Oncol. 2019;154:394-400.
- Fong ZV, Hashimoto DA, Jin G, et al. Simulated volume-based regionalization of complex procedures: impact on spatial access to care. Ann Surg. 2021;274:312-318.
- Knisely A, Huang Y, Melamed A, et al. Effect of regionalization of endometrial cancer care on site of care and patient travel. Am J Obstet Gynecol. 2020;222:58.e1-58.e10.
- Finlayson SR, Birkmeyer JD, Tosteson AN, et al. Patient preferences for location of care: implications for regionalization. Med Care. 1999;37:204-209.
- Shalowitz DI, Nivasch E, Burger RA, et al. Are patients willing to travel for better ovarian cancer care? Gynecol Oncol. 2018;148:42-48.
- Rehmani SS, Liu B, Al-Ayoubi AM, et al. Racial disparity in utilization of high-volume hospitals for surgical treatment of esophageal cancer. Ann Thorac Surg. 2018;106:346-353.
- Nattinger AB, Rademacher N, McGinley EL, et al. Can regionalization of care reduce socioeconomic disparities in breast cancer survival? Med Care. 2021;59:77-81.
- Auerbach AD, Hilton JF, Maselli J, et al. Shop for quality or volume? Volume, quality, and outcomes of coronary artery bypass surgery. Ann Intern Med. 2009;150:696-704.
- Kurlansky PA, Argenziano M, Dunton R, et al. Quality, not volume, determines outcome of coronary artery bypass surgery in a university-based community hospital network. J Thorac Cardiovasc Surg. 2012;143:287-293.
- Urbach DR. Pledging to eliminate low-volume surgery. N Engl J Med. 2015;373:1388-1390.
- Blanco BA, Kothari AN, Blackwell RH, et al. “Take the Volume Pledge” may result in disparity in access to care. Surgery. 2017;161:837-845.
- Farjah F, Grau-Sepulveda MV, Gaissert H, et al. Volume Pledge is not associated with better short-term outcomes after lung cancer resection. J Clin Oncol. 2020;38:3518-3527.
- Tracy EE, Zephyrin LC, Rosman DA, et al. Credentialing based on surgical volume, physician workforce challenges, and patient access. Obstet Gynecol. 2013;122:947-951.
- Statement on credentialing and privileging and volume performance issues. April 1, 2018. American College of Surgeons. Accessed April 10, 2023. https://facs.org/about-acs/statements/credentialing-andprivileging-and-volume-performance-issues/
- Ruiz MP, Chen L, Hou JY, et al. Effect of minimum-volume standards on patient outcomes and surgical practice patterns for hysterectomy. Obstet Gynecol. 2018;132:1229-1237.
- Birkmeyer JD, Stukel TA, Siewers AE, et al. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003;349:2117-2127.
- Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346:11281137.
- Mowat A, Maher C, Ballard E. Surgical outcomes for low-volume vs high-volume surgeons in gynecology surgery: a systematic review and meta-analysis. Am J Obstet Gynecol. 2016;215:21-33.
- Wallenstein MR, Ananth CV, Kim JH, et al. Effect of surgical volume on outcomes for laparoscopic hysterectomy for benign indications. Obstet Gynecol. 2012;119:709-716.
- Wright JD, Chen L, Hou JY, et al. Association of hospital volume and quality of care with survival for ovarian cancer. Obstet Gynecol. 2017;130:545-553.
- Cliby WA, Powell MA, Al-Hammadi N, et al. Ovarian cancer in the United States: contemporary patterns of care associated with improved survival. Gynecol Oncol. 2015;136:11-17.
- Matsuo K, Shimada M, Yamaguchi S, et al. Association of radical hysterectomy surgical volume and survival for early-stage cervical cancer. Obstet Gynecol. 2019;133:1086-1098.
- Brennand EA, Quan H. Evaluation of the effect of surgeon’s operative volume and specialty on likelihood of revision after mesh midurethral sling placement. Obstet Gynecol. 2019;133:1099-1108.
- Ruiz MP, Chen L, Hou JY, et al. Outcomes of hysterectomy performed by very low-volume surgeons. Obstet Gynecol. 2018;131:981-990.
- Finks JF, Osborne NH, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med. 2011;364:21282137.
- Wright JD, Ruiz MP, Chen L, et al. Changes in surgical volume and outcomes over time for women undergoing hysterectomy for endometrial cancer. Obstet Gynecol. 2018;132:59-69.
- Wright JD, Chen L, Buskwofie A, et al. Regionalization of care for women with ovarian cancer. Gynecol Oncol. 2019;154:394-400.
- Fong ZV, Hashimoto DA, Jin G, et al. Simulated volume-based regionalization of complex procedures: impact on spatial access to care. Ann Surg. 2021;274:312-318.
- Knisely A, Huang Y, Melamed A, et al. Effect of regionalization of endometrial cancer care on site of care and patient travel. Am J Obstet Gynecol. 2020;222:58.e1-58.e10.
- Finlayson SR, Birkmeyer JD, Tosteson AN, et al. Patient preferences for location of care: implications for regionalization. Med Care. 1999;37:204-209.
- Shalowitz DI, Nivasch E, Burger RA, et al. Are patients willing to travel for better ovarian cancer care? Gynecol Oncol. 2018;148:42-48.
- Rehmani SS, Liu B, Al-Ayoubi AM, et al. Racial disparity in utilization of high-volume hospitals for surgical treatment of esophageal cancer. Ann Thorac Surg. 2018;106:346-353.
- Nattinger AB, Rademacher N, McGinley EL, et al. Can regionalization of care reduce socioeconomic disparities in breast cancer survival? Med Care. 2021;59:77-81.
- Auerbach AD, Hilton JF, Maselli J, et al. Shop for quality or volume? Volume, quality, and outcomes of coronary artery bypass surgery. Ann Intern Med. 2009;150:696-704.
- Kurlansky PA, Argenziano M, Dunton R, et al. Quality, not volume, determines outcome of coronary artery bypass surgery in a university-based community hospital network. J Thorac Cardiovasc Surg. 2012;143:287-293.
- Urbach DR. Pledging to eliminate low-volume surgery. N Engl J Med. 2015;373:1388-1390.
- Blanco BA, Kothari AN, Blackwell RH, et al. “Take the Volume Pledge” may result in disparity in access to care. Surgery. 2017;161:837-845.
- Farjah F, Grau-Sepulveda MV, Gaissert H, et al. Volume Pledge is not associated with better short-term outcomes after lung cancer resection. J Clin Oncol. 2020;38:3518-3527.
- Tracy EE, Zephyrin LC, Rosman DA, et al. Credentialing based on surgical volume, physician workforce challenges, and patient access. Obstet Gynecol. 2013;122:947-951.
- Statement on credentialing and privileging and volume performance issues. April 1, 2018. American College of Surgeons. Accessed April 10, 2023. https://facs.org/about-acs/statements/credentialing-andprivileging-and-volume-performance-issues/
- Ruiz MP, Chen L, Hou JY, et al. Effect of minimum-volume standards on patient outcomes and surgical practice patterns for hysterectomy. Obstet Gynecol. 2018;132:1229-1237.
Mental health questions cut from MD licensing applications in 21 states
Since May, physicians in 21 states are no longer being asked broad mental health or substance abuse questions when they apply for a medical license. That’s a major shift that could ease doctors’ concerns about seeking treatment, according to the Dr. Lorna Breen Heroes› Foundation, a physician burnout prevention group that tracks such changes.
The foundation was named in honor of Lorna Breen, MD, an emergency medicine physician in New York City who died by suicide in April 2020 as the pandemic unfolded. The rate of suicide among physicians is twice that of the general population.
“The issue is not whether a physician may have had a serious or a mild mental illness ... but whether they have any disabilities that may affect their current work,” said Peter Yellowlees, MD, distinguished professor of psychiatry at the University of California, Davis. “Asking about any past mental illness episodes, which may have occurred years previously ... is simply discriminatory and is an example of the stigma associated with mental disorders.”
The Breen Foundation has been working with state medical boards and hospitals to remove stigmatizing mental health and substance abuse questions from licensing and credentialing applications.
Dr. Breen had told her sister and brother-in-law shortly before her suicide that she was afraid she could lose her license and the career she loved if the medical board found out that she had received inpatient mental health treatment, said J. Corey Feist, JD, MBA, her brother-in-law and cofounder and president of the foundation.
She wasn’t aware that New York was a state that didn’t ask physicians questions about their mental health, said Mr. Feist.
“That’s why we want to make it very clear to physicians which states continue to ask these questions and which ones don’t,” Mr. Feist said.
Many physicians share Dr. Breen’s concern about professional consequences.
Four in 10 physicians said that they did not seek help for burnout or depression because they worried that their employer or state medical board would find out, according to the Medscape ‘I Cry but No One Cares’: Physician Burnout & Depression Report 2023.
One Oregon emergency department physician said that informing her state medical board about an episode of mania resulted in public disclosures, a 4-month long investigation, lost income, and poorer work evaluations. Looking back on her decision to be transparent with the board, Susan Haney, MD, said that she was naive. “The board is not your friend.”
Fearing for her career, now-retired ob.gyn. Robyn Alley-Hay, MD, never disclosed on licensing applications that in the 1990s, she had been hospitalized and treated for depression. She stopped practicing medicine in 2014 and now works as a life coach.
“I hated those questions because I felt I could never tell the whole truth,” Dr. Alley-Hay said. “But I could always truthfully answer ‘no’ to questions about impairment. That was a line that I wouldn’t cross – if you’re impaired, you shouldn’t be practicing.”
Does the focus on current impairment protect the public?
New York, Texas, California, Montana, Illinois, and North Carolina are among the 21 states that either ask no health-related questions or ask only a single question to address physical and mental health, said Mr. Feist.
Most of these changes align with the 2018 Federation of State Medical Boards recommendations, said Joe Knickrehm, FSMB vice president of communications. “Application questions must focus only on current impairment and not on illness, diagnosis, or previous treatment in order to be compliant with the Americans With Disabilities Act,” states the FSMB.
Mental health questions were often added to licensing and credentialing applications out of a “misplaced desire to protect patients and families from clinicians who might not be fit to give care. Yet there is no evidence they serve that function,” said Mr. Feist.
Marian Hollingsworth, a patient safety advocate in California, says medical boards have a responsibility to ensure that doctors pose no risk or a negligible risk to the public. She questioned whether the medical boards can adequately protect the public if they only ask about medical conditions rather than mental illness or substance abuse.
“There’s a fine line between privacy and right to know for public protection. I would want to see the approving medical board have assurance from a treating professional that this physician is stable and is doing well with continued treatment,” said Ms. Hollingsworth.
Legislation requires that mental health questions be removed
In March, Virginia became the first state to enact a law that requires all health care profession regulatory boards, including medical boards, to remove or replace mental health questions on licensing, certification, and registration applications.
The law requires that boards use the following wording if they replace mental health questions: “Do you have any reason to believe you would pose a risk to the safety or well-being of patients?” “Are you able to perform the essential functions of your job with or without reasonable accommodations?”
The Illinois General Assembly passed a more limited bill in May that requires medical boards to remove or replace mental health questions on its licensing applications. Gov. J. B. Pritzker (D) is expected to sign the bill.
The Virginia Healthcare and Hospital Association, which represents more than 100 hospitals and health systems in the state, partnered with the Medical Society of Virginia and the Virginia Nurses Association to advocate for the new legislation.
“The reason that the Virginia coalition pushed for the law was because the state’s medical boards weren’t acting quickly enough. Although state laws vary about what medical boards can do, legislation isn’t necessary in most states to change licensing questions,” said Mr. Feist.
Virginia hospitals began working last year with the foundation to change their mental health questions on credentialing applications. About 20% of Virginia’s hospitals have completed the process, including four large health systems: Inova, UVA Health, Centerra, and Children’s Hospitals of King’s Daughters, said Mr. Feist.
The foundation also challenged Lisa MacLean, MD, a psychiatrist and chief clinical wellness officer at the Henry Ford Medical Group in Detroit, to review their credentialing application for any stigmatizing mental health questions.
Dr. MacLean told the American Medical Association that she had found one question that needed to be changed but that it took time to get through the hospital›s approval process. Ultimately, the wording was changed from “a diagnosis or treatment of a physical, mental, chemical dependency or emotional condition” to “a diagnosis or treatment of any condition which could impair your ability to practice medicine.”
National medical organizations back changes
The Joint Commission, which accredits hospitals, has emphasized since 2020 that it doesn’t require hospitals to ask about an applicant’s mental health history.
“We strongly encourage organizations to not ask about past history of mental health conditions or treatment,” the Commission said in a statement. “It is critical that we ensure health care workers can feel free to access mental health resources.”
The Joint Commission said it supports the FSMB recommendations and the AMA’s recommendation that questions about clinicians’ mental health be limited to “conditions that currently impair the clinicians’ ability to perform their job.”
More than 40 professional medical organizations, including the American Academy of Family Physicians and the American Psychiatric Association, signed a joint statement in 2020 calling for changes in disclosure rules about mental health.
“The backing of major organizations is helpful because it’s changing the conversation that occurs within and outside the house of medicine,” said Mr. Feist.
Should doctors answer mental health questions?
Many states continue to ask questions about hospitalization and mental health diagnoses or treatment on their licensing and credentialing applications.
Yellowlees advises doctors to “be honest and not lie or deny past mental health problems, as medical boards tend to take a very serious view of physicians who do not tell the truth.”
However, the questions asked by medical boards can vary by state. “If it’s possible, physicians can give accurate but minimal information while trying to focus mainly on their current work capacity,” said Dr. Yellowlees.
He also suggested that physicians who are uncertain about how to respond to mental health questions consider obtaining advice from lawyers accustomed to working with the relevant medical boards.
Physicians who want to get involved in removing licensing and credentialing barriers to mental health care can find resources here and here.
A version of this article first appeared on Medscape.com.
Since May, physicians in 21 states are no longer being asked broad mental health or substance abuse questions when they apply for a medical license. That’s a major shift that could ease doctors’ concerns about seeking treatment, according to the Dr. Lorna Breen Heroes› Foundation, a physician burnout prevention group that tracks such changes.
The foundation was named in honor of Lorna Breen, MD, an emergency medicine physician in New York City who died by suicide in April 2020 as the pandemic unfolded. The rate of suicide among physicians is twice that of the general population.
“The issue is not whether a physician may have had a serious or a mild mental illness ... but whether they have any disabilities that may affect their current work,” said Peter Yellowlees, MD, distinguished professor of psychiatry at the University of California, Davis. “Asking about any past mental illness episodes, which may have occurred years previously ... is simply discriminatory and is an example of the stigma associated with mental disorders.”
The Breen Foundation has been working with state medical boards and hospitals to remove stigmatizing mental health and substance abuse questions from licensing and credentialing applications.
Dr. Breen had told her sister and brother-in-law shortly before her suicide that she was afraid she could lose her license and the career she loved if the medical board found out that she had received inpatient mental health treatment, said J. Corey Feist, JD, MBA, her brother-in-law and cofounder and president of the foundation.
She wasn’t aware that New York was a state that didn’t ask physicians questions about their mental health, said Mr. Feist.
“That’s why we want to make it very clear to physicians which states continue to ask these questions and which ones don’t,” Mr. Feist said.
Many physicians share Dr. Breen’s concern about professional consequences.
Four in 10 physicians said that they did not seek help for burnout or depression because they worried that their employer or state medical board would find out, according to the Medscape ‘I Cry but No One Cares’: Physician Burnout & Depression Report 2023.
One Oregon emergency department physician said that informing her state medical board about an episode of mania resulted in public disclosures, a 4-month long investigation, lost income, and poorer work evaluations. Looking back on her decision to be transparent with the board, Susan Haney, MD, said that she was naive. “The board is not your friend.”
Fearing for her career, now-retired ob.gyn. Robyn Alley-Hay, MD, never disclosed on licensing applications that in the 1990s, she had been hospitalized and treated for depression. She stopped practicing medicine in 2014 and now works as a life coach.
“I hated those questions because I felt I could never tell the whole truth,” Dr. Alley-Hay said. “But I could always truthfully answer ‘no’ to questions about impairment. That was a line that I wouldn’t cross – if you’re impaired, you shouldn’t be practicing.”
Does the focus on current impairment protect the public?
New York, Texas, California, Montana, Illinois, and North Carolina are among the 21 states that either ask no health-related questions or ask only a single question to address physical and mental health, said Mr. Feist.
Most of these changes align with the 2018 Federation of State Medical Boards recommendations, said Joe Knickrehm, FSMB vice president of communications. “Application questions must focus only on current impairment and not on illness, diagnosis, or previous treatment in order to be compliant with the Americans With Disabilities Act,” states the FSMB.
Mental health questions were often added to licensing and credentialing applications out of a “misplaced desire to protect patients and families from clinicians who might not be fit to give care. Yet there is no evidence they serve that function,” said Mr. Feist.
Marian Hollingsworth, a patient safety advocate in California, says medical boards have a responsibility to ensure that doctors pose no risk or a negligible risk to the public. She questioned whether the medical boards can adequately protect the public if they only ask about medical conditions rather than mental illness or substance abuse.
“There’s a fine line between privacy and right to know for public protection. I would want to see the approving medical board have assurance from a treating professional that this physician is stable and is doing well with continued treatment,” said Ms. Hollingsworth.
Legislation requires that mental health questions be removed
In March, Virginia became the first state to enact a law that requires all health care profession regulatory boards, including medical boards, to remove or replace mental health questions on licensing, certification, and registration applications.
The law requires that boards use the following wording if they replace mental health questions: “Do you have any reason to believe you would pose a risk to the safety or well-being of patients?” “Are you able to perform the essential functions of your job with or without reasonable accommodations?”
The Illinois General Assembly passed a more limited bill in May that requires medical boards to remove or replace mental health questions on its licensing applications. Gov. J. B. Pritzker (D) is expected to sign the bill.
The Virginia Healthcare and Hospital Association, which represents more than 100 hospitals and health systems in the state, partnered with the Medical Society of Virginia and the Virginia Nurses Association to advocate for the new legislation.
“The reason that the Virginia coalition pushed for the law was because the state’s medical boards weren’t acting quickly enough. Although state laws vary about what medical boards can do, legislation isn’t necessary in most states to change licensing questions,” said Mr. Feist.
Virginia hospitals began working last year with the foundation to change their mental health questions on credentialing applications. About 20% of Virginia’s hospitals have completed the process, including four large health systems: Inova, UVA Health, Centerra, and Children’s Hospitals of King’s Daughters, said Mr. Feist.
The foundation also challenged Lisa MacLean, MD, a psychiatrist and chief clinical wellness officer at the Henry Ford Medical Group in Detroit, to review their credentialing application for any stigmatizing mental health questions.
Dr. MacLean told the American Medical Association that she had found one question that needed to be changed but that it took time to get through the hospital›s approval process. Ultimately, the wording was changed from “a diagnosis or treatment of a physical, mental, chemical dependency or emotional condition” to “a diagnosis or treatment of any condition which could impair your ability to practice medicine.”
National medical organizations back changes
The Joint Commission, which accredits hospitals, has emphasized since 2020 that it doesn’t require hospitals to ask about an applicant’s mental health history.
“We strongly encourage organizations to not ask about past history of mental health conditions or treatment,” the Commission said in a statement. “It is critical that we ensure health care workers can feel free to access mental health resources.”
The Joint Commission said it supports the FSMB recommendations and the AMA’s recommendation that questions about clinicians’ mental health be limited to “conditions that currently impair the clinicians’ ability to perform their job.”
More than 40 professional medical organizations, including the American Academy of Family Physicians and the American Psychiatric Association, signed a joint statement in 2020 calling for changes in disclosure rules about mental health.
“The backing of major organizations is helpful because it’s changing the conversation that occurs within and outside the house of medicine,” said Mr. Feist.
Should doctors answer mental health questions?
Many states continue to ask questions about hospitalization and mental health diagnoses or treatment on their licensing and credentialing applications.
Yellowlees advises doctors to “be honest and not lie or deny past mental health problems, as medical boards tend to take a very serious view of physicians who do not tell the truth.”
However, the questions asked by medical boards can vary by state. “If it’s possible, physicians can give accurate but minimal information while trying to focus mainly on their current work capacity,” said Dr. Yellowlees.
He also suggested that physicians who are uncertain about how to respond to mental health questions consider obtaining advice from lawyers accustomed to working with the relevant medical boards.
Physicians who want to get involved in removing licensing and credentialing barriers to mental health care can find resources here and here.
A version of this article first appeared on Medscape.com.
Since May, physicians in 21 states are no longer being asked broad mental health or substance abuse questions when they apply for a medical license. That’s a major shift that could ease doctors’ concerns about seeking treatment, according to the Dr. Lorna Breen Heroes› Foundation, a physician burnout prevention group that tracks such changes.
The foundation was named in honor of Lorna Breen, MD, an emergency medicine physician in New York City who died by suicide in April 2020 as the pandemic unfolded. The rate of suicide among physicians is twice that of the general population.
“The issue is not whether a physician may have had a serious or a mild mental illness ... but whether they have any disabilities that may affect their current work,” said Peter Yellowlees, MD, distinguished professor of psychiatry at the University of California, Davis. “Asking about any past mental illness episodes, which may have occurred years previously ... is simply discriminatory and is an example of the stigma associated with mental disorders.”
The Breen Foundation has been working with state medical boards and hospitals to remove stigmatizing mental health and substance abuse questions from licensing and credentialing applications.
Dr. Breen had told her sister and brother-in-law shortly before her suicide that she was afraid she could lose her license and the career she loved if the medical board found out that she had received inpatient mental health treatment, said J. Corey Feist, JD, MBA, her brother-in-law and cofounder and president of the foundation.
She wasn’t aware that New York was a state that didn’t ask physicians questions about their mental health, said Mr. Feist.
“That’s why we want to make it very clear to physicians which states continue to ask these questions and which ones don’t,” Mr. Feist said.
Many physicians share Dr. Breen’s concern about professional consequences.
Four in 10 physicians said that they did not seek help for burnout or depression because they worried that their employer or state medical board would find out, according to the Medscape ‘I Cry but No One Cares’: Physician Burnout & Depression Report 2023.
One Oregon emergency department physician said that informing her state medical board about an episode of mania resulted in public disclosures, a 4-month long investigation, lost income, and poorer work evaluations. Looking back on her decision to be transparent with the board, Susan Haney, MD, said that she was naive. “The board is not your friend.”
Fearing for her career, now-retired ob.gyn. Robyn Alley-Hay, MD, never disclosed on licensing applications that in the 1990s, she had been hospitalized and treated for depression. She stopped practicing medicine in 2014 and now works as a life coach.
“I hated those questions because I felt I could never tell the whole truth,” Dr. Alley-Hay said. “But I could always truthfully answer ‘no’ to questions about impairment. That was a line that I wouldn’t cross – if you’re impaired, you shouldn’t be practicing.”
Does the focus on current impairment protect the public?
New York, Texas, California, Montana, Illinois, and North Carolina are among the 21 states that either ask no health-related questions or ask only a single question to address physical and mental health, said Mr. Feist.
Most of these changes align with the 2018 Federation of State Medical Boards recommendations, said Joe Knickrehm, FSMB vice president of communications. “Application questions must focus only on current impairment and not on illness, diagnosis, or previous treatment in order to be compliant with the Americans With Disabilities Act,” states the FSMB.
Mental health questions were often added to licensing and credentialing applications out of a “misplaced desire to protect patients and families from clinicians who might not be fit to give care. Yet there is no evidence they serve that function,” said Mr. Feist.
Marian Hollingsworth, a patient safety advocate in California, says medical boards have a responsibility to ensure that doctors pose no risk or a negligible risk to the public. She questioned whether the medical boards can adequately protect the public if they only ask about medical conditions rather than mental illness or substance abuse.
“There’s a fine line between privacy and right to know for public protection. I would want to see the approving medical board have assurance from a treating professional that this physician is stable and is doing well with continued treatment,” said Ms. Hollingsworth.
Legislation requires that mental health questions be removed
In March, Virginia became the first state to enact a law that requires all health care profession regulatory boards, including medical boards, to remove or replace mental health questions on licensing, certification, and registration applications.
The law requires that boards use the following wording if they replace mental health questions: “Do you have any reason to believe you would pose a risk to the safety or well-being of patients?” “Are you able to perform the essential functions of your job with or without reasonable accommodations?”
The Illinois General Assembly passed a more limited bill in May that requires medical boards to remove or replace mental health questions on its licensing applications. Gov. J. B. Pritzker (D) is expected to sign the bill.
The Virginia Healthcare and Hospital Association, which represents more than 100 hospitals and health systems in the state, partnered with the Medical Society of Virginia and the Virginia Nurses Association to advocate for the new legislation.
“The reason that the Virginia coalition pushed for the law was because the state’s medical boards weren’t acting quickly enough. Although state laws vary about what medical boards can do, legislation isn’t necessary in most states to change licensing questions,” said Mr. Feist.
Virginia hospitals began working last year with the foundation to change their mental health questions on credentialing applications. About 20% of Virginia’s hospitals have completed the process, including four large health systems: Inova, UVA Health, Centerra, and Children’s Hospitals of King’s Daughters, said Mr. Feist.
The foundation also challenged Lisa MacLean, MD, a psychiatrist and chief clinical wellness officer at the Henry Ford Medical Group in Detroit, to review their credentialing application for any stigmatizing mental health questions.
Dr. MacLean told the American Medical Association that she had found one question that needed to be changed but that it took time to get through the hospital›s approval process. Ultimately, the wording was changed from “a diagnosis or treatment of a physical, mental, chemical dependency or emotional condition” to “a diagnosis or treatment of any condition which could impair your ability to practice medicine.”
National medical organizations back changes
The Joint Commission, which accredits hospitals, has emphasized since 2020 that it doesn’t require hospitals to ask about an applicant’s mental health history.
“We strongly encourage organizations to not ask about past history of mental health conditions or treatment,” the Commission said in a statement. “It is critical that we ensure health care workers can feel free to access mental health resources.”
The Joint Commission said it supports the FSMB recommendations and the AMA’s recommendation that questions about clinicians’ mental health be limited to “conditions that currently impair the clinicians’ ability to perform their job.”
More than 40 professional medical organizations, including the American Academy of Family Physicians and the American Psychiatric Association, signed a joint statement in 2020 calling for changes in disclosure rules about mental health.
“The backing of major organizations is helpful because it’s changing the conversation that occurs within and outside the house of medicine,” said Mr. Feist.
Should doctors answer mental health questions?
Many states continue to ask questions about hospitalization and mental health diagnoses or treatment on their licensing and credentialing applications.
Yellowlees advises doctors to “be honest and not lie or deny past mental health problems, as medical boards tend to take a very serious view of physicians who do not tell the truth.”
However, the questions asked by medical boards can vary by state. “If it’s possible, physicians can give accurate but minimal information while trying to focus mainly on their current work capacity,” said Dr. Yellowlees.
He also suggested that physicians who are uncertain about how to respond to mental health questions consider obtaining advice from lawyers accustomed to working with the relevant medical boards.
Physicians who want to get involved in removing licensing and credentialing barriers to mental health care can find resources here and here.
A version of this article first appeared on Medscape.com.
Catch-up HPV screenings help detect cancer in women over 65
The findings, published in PLOS Medicine, included women between ages 65 and 69 years in Denmark who had no record of cervical cancer screening or an HPV test in the previous 5 years.
“It may be valuable to get women above the current screening age to get this one-time catch-up HPV test if they haven’t had one before,” said Mette Tranberg, PhD, a cancer epidemiologist and researcher at Randers Regional Hospital in Denmark and lead author of the study. “That is valuable knowledge for health care providers and policy makers.”
Cervical cancer in the United States is most often diagnosed in women aged 35-44 years, according to the American Cancer Society, with the average age at diagnosis of 50 years. The cancer rarely occurs in women who have undergone regular screenings.
Though current guidelines recommend that clinicians stop screening women for cervical cancer at age 65 years if their previous screening results have been normal, Dr. Tranberg said that many women do not get screened as they get closer to age 65 years.
A study from researchers at the University of California, Davis, found several factors contribute to older women not receiving adequate screening. Some women may think that they no longer need Pap smears after going through menopause, or they might have received a hysterectomy and think that they no longer require screening. And although Pap tests have built-in HPV screenings, these tend to be less accurate in postmenopausal women.
But women older than 65 years account for about 20% of new cervical cancer cases.
According to the Centers for Disease Control and Prevention, until women reach age 80 years, they are as likely to get cervical cancer as are younger women. Jack Cuzick, PhD, professor of epidemiology at Queen Mary University of London, said that the new data should inform patient care and public health efforts.
“People often don’t realize HPV can last even if people haven’t been sexually active,” Dr. Cuzick said. “Even if somebody is nearing 70, it’s probably still worth getting an exit test.”
The intervention group
Study participants were assigned to two groups, one of which was invited to participate in a free HPV screening, either with their general practitioner or by ordering a vaginal self-sampling kit. The control group received standard care, which in Denmark, includes having the opportunity to undergo routine cervical cytology.
Dr. Tranberg and her colleagues found that among women in the intervention group, 62.2% were screened within 1 year. Among the control group, 2.2% had a Pap test. The rate of diagnosed cervical intraepithelial neoplasia grade 2 or worse was 3.9 cases per 1,000 eligible women in the intervention group and 0.3 cases per 1,000 eligible women in the control group (P < .001).
The study also found that women who had been insufficiently screened between ages 50 and 64 years had a higher prevalence of HPV, with more grade 2 cervical intraepithelial neoplasia lesions or worse, than did those who were sufficiently screened.
High-risk HPV tests are replacing the Pap smear as the primary cervical cancer screening test because of superior sensitivity, according to Dr. Tranberg. Though Pap smears detect abnormal cells on the cervix that can lead to cervical cancer, HPV tests specifically look for certain high-risk types of HPV on the cervix.
In the United States, patient histories of screenings, diagnosis, and treatment of HPV are often unavailable because electronic health records between health systems are often not linked, according to Cosette Wheeler, PhD, professor at the University of New Mexico Comprehensive Cancer Center in Albuquerque, and founding director of the New Mexico HPV Pap Registry. Clinicians may not know whether a patient needs a screening.
HPV tests usually have a high threshold of detection in an effort to produce fewer false positives, according to Dr. Wheeler, who was not involved in the latest study. But fewer false positives means that the test could produce more false negatives. Older women could benefit from more sensitive screening, such as the high-risk test that the Danish researchers used, according to Dr. Wheeler.
Dr. Tranberg said that she was surprised and pleased by the high percentage of women who accepted the screening tests in the intervention group, especially those who received at-home tests and followed up with a clinician.
“Female life expectancy is really increasing and therefore the number of cervical cancers in women over the age of 65 is expected to rise,” Dr. Tranberg said. “That’s a big reason to rethink whether or not we should do something for these older women.”
The HPV test kits in the intervention region were provided by Roche Diagnostics. According to the contract between Roche and Randers Regional Hospital, Roche had no influence on the scientific process and no editorial rights pertaining to this manuscript.
A version of this article first appeared on Medscape.com.
The findings, published in PLOS Medicine, included women between ages 65 and 69 years in Denmark who had no record of cervical cancer screening or an HPV test in the previous 5 years.
“It may be valuable to get women above the current screening age to get this one-time catch-up HPV test if they haven’t had one before,” said Mette Tranberg, PhD, a cancer epidemiologist and researcher at Randers Regional Hospital in Denmark and lead author of the study. “That is valuable knowledge for health care providers and policy makers.”
Cervical cancer in the United States is most often diagnosed in women aged 35-44 years, according to the American Cancer Society, with the average age at diagnosis of 50 years. The cancer rarely occurs in women who have undergone regular screenings.
Though current guidelines recommend that clinicians stop screening women for cervical cancer at age 65 years if their previous screening results have been normal, Dr. Tranberg said that many women do not get screened as they get closer to age 65 years.
A study from researchers at the University of California, Davis, found several factors contribute to older women not receiving adequate screening. Some women may think that they no longer need Pap smears after going through menopause, or they might have received a hysterectomy and think that they no longer require screening. And although Pap tests have built-in HPV screenings, these tend to be less accurate in postmenopausal women.
But women older than 65 years account for about 20% of new cervical cancer cases.
According to the Centers for Disease Control and Prevention, until women reach age 80 years, they are as likely to get cervical cancer as are younger women. Jack Cuzick, PhD, professor of epidemiology at Queen Mary University of London, said that the new data should inform patient care and public health efforts.
“People often don’t realize HPV can last even if people haven’t been sexually active,” Dr. Cuzick said. “Even if somebody is nearing 70, it’s probably still worth getting an exit test.”
The intervention group
Study participants were assigned to two groups, one of which was invited to participate in a free HPV screening, either with their general practitioner or by ordering a vaginal self-sampling kit. The control group received standard care, which in Denmark, includes having the opportunity to undergo routine cervical cytology.
Dr. Tranberg and her colleagues found that among women in the intervention group, 62.2% were screened within 1 year. Among the control group, 2.2% had a Pap test. The rate of diagnosed cervical intraepithelial neoplasia grade 2 or worse was 3.9 cases per 1,000 eligible women in the intervention group and 0.3 cases per 1,000 eligible women in the control group (P < .001).
The study also found that women who had been insufficiently screened between ages 50 and 64 years had a higher prevalence of HPV, with more grade 2 cervical intraepithelial neoplasia lesions or worse, than did those who were sufficiently screened.
High-risk HPV tests are replacing the Pap smear as the primary cervical cancer screening test because of superior sensitivity, according to Dr. Tranberg. Though Pap smears detect abnormal cells on the cervix that can lead to cervical cancer, HPV tests specifically look for certain high-risk types of HPV on the cervix.
In the United States, patient histories of screenings, diagnosis, and treatment of HPV are often unavailable because electronic health records between health systems are often not linked, according to Cosette Wheeler, PhD, professor at the University of New Mexico Comprehensive Cancer Center in Albuquerque, and founding director of the New Mexico HPV Pap Registry. Clinicians may not know whether a patient needs a screening.
HPV tests usually have a high threshold of detection in an effort to produce fewer false positives, according to Dr. Wheeler, who was not involved in the latest study. But fewer false positives means that the test could produce more false negatives. Older women could benefit from more sensitive screening, such as the high-risk test that the Danish researchers used, according to Dr. Wheeler.
Dr. Tranberg said that she was surprised and pleased by the high percentage of women who accepted the screening tests in the intervention group, especially those who received at-home tests and followed up with a clinician.
“Female life expectancy is really increasing and therefore the number of cervical cancers in women over the age of 65 is expected to rise,” Dr. Tranberg said. “That’s a big reason to rethink whether or not we should do something for these older women.”
The HPV test kits in the intervention region were provided by Roche Diagnostics. According to the contract between Roche and Randers Regional Hospital, Roche had no influence on the scientific process and no editorial rights pertaining to this manuscript.
A version of this article first appeared on Medscape.com.
The findings, published in PLOS Medicine, included women between ages 65 and 69 years in Denmark who had no record of cervical cancer screening or an HPV test in the previous 5 years.
“It may be valuable to get women above the current screening age to get this one-time catch-up HPV test if they haven’t had one before,” said Mette Tranberg, PhD, a cancer epidemiologist and researcher at Randers Regional Hospital in Denmark and lead author of the study. “That is valuable knowledge for health care providers and policy makers.”
Cervical cancer in the United States is most often diagnosed in women aged 35-44 years, according to the American Cancer Society, with the average age at diagnosis of 50 years. The cancer rarely occurs in women who have undergone regular screenings.
Though current guidelines recommend that clinicians stop screening women for cervical cancer at age 65 years if their previous screening results have been normal, Dr. Tranberg said that many women do not get screened as they get closer to age 65 years.
A study from researchers at the University of California, Davis, found several factors contribute to older women not receiving adequate screening. Some women may think that they no longer need Pap smears after going through menopause, or they might have received a hysterectomy and think that they no longer require screening. And although Pap tests have built-in HPV screenings, these tend to be less accurate in postmenopausal women.
But women older than 65 years account for about 20% of new cervical cancer cases.
According to the Centers for Disease Control and Prevention, until women reach age 80 years, they are as likely to get cervical cancer as are younger women. Jack Cuzick, PhD, professor of epidemiology at Queen Mary University of London, said that the new data should inform patient care and public health efforts.
“People often don’t realize HPV can last even if people haven’t been sexually active,” Dr. Cuzick said. “Even if somebody is nearing 70, it’s probably still worth getting an exit test.”
The intervention group
Study participants were assigned to two groups, one of which was invited to participate in a free HPV screening, either with their general practitioner or by ordering a vaginal self-sampling kit. The control group received standard care, which in Denmark, includes having the opportunity to undergo routine cervical cytology.
Dr. Tranberg and her colleagues found that among women in the intervention group, 62.2% were screened within 1 year. Among the control group, 2.2% had a Pap test. The rate of diagnosed cervical intraepithelial neoplasia grade 2 or worse was 3.9 cases per 1,000 eligible women in the intervention group and 0.3 cases per 1,000 eligible women in the control group (P < .001).
The study also found that women who had been insufficiently screened between ages 50 and 64 years had a higher prevalence of HPV, with more grade 2 cervical intraepithelial neoplasia lesions or worse, than did those who were sufficiently screened.
High-risk HPV tests are replacing the Pap smear as the primary cervical cancer screening test because of superior sensitivity, according to Dr. Tranberg. Though Pap smears detect abnormal cells on the cervix that can lead to cervical cancer, HPV tests specifically look for certain high-risk types of HPV on the cervix.
In the United States, patient histories of screenings, diagnosis, and treatment of HPV are often unavailable because electronic health records between health systems are often not linked, according to Cosette Wheeler, PhD, professor at the University of New Mexico Comprehensive Cancer Center in Albuquerque, and founding director of the New Mexico HPV Pap Registry. Clinicians may not know whether a patient needs a screening.
HPV tests usually have a high threshold of detection in an effort to produce fewer false positives, according to Dr. Wheeler, who was not involved in the latest study. But fewer false positives means that the test could produce more false negatives. Older women could benefit from more sensitive screening, such as the high-risk test that the Danish researchers used, according to Dr. Wheeler.
Dr. Tranberg said that she was surprised and pleased by the high percentage of women who accepted the screening tests in the intervention group, especially those who received at-home tests and followed up with a clinician.
“Female life expectancy is really increasing and therefore the number of cervical cancers in women over the age of 65 is expected to rise,” Dr. Tranberg said. “That’s a big reason to rethink whether or not we should do something for these older women.”
The HPV test kits in the intervention region were provided by Roche Diagnostics. According to the contract between Roche and Randers Regional Hospital, Roche had no influence on the scientific process and no editorial rights pertaining to this manuscript.
A version of this article first appeared on Medscape.com.
FROM PLOS MEDICINE