User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
How 100 years of insulin have changed pregnancy for women with type 1 diabetes
Mark B. Landon, MD: The discovery of insulin in 1921 by Dr. Frederick Banting and Dr. Charles Best and its introduction into clinical practice may well be the most significant achievement in the care of pregnant women with diabetes mellitus in the last century. Why was this advance so monumental?
Steven G. Gabbe, MD: Insulin is the single most important drug we use in taking care of diabetes in pregnancy. It is required not only by all patients with type 1 diabetes, but also by the majority of patients with type 2 diabetes. Moreover, at least a third of our patients with gestational diabetes require more than lifestyle change. The American College of Obstetricians and Gynecologists and the American Diabetes Association recommend that insulin be considered as the first-line pharmacologic therapy.
Before insulin, the most prudent option for women who had glucose in their urine early in pregnancy, which was called “true diabetes,” was deemed to be termination of the pregnancy. The chances of surviving a pregnancy, and of having a surviving infant, were low.
Pregnancies were a rarity to begin with because most women of reproductive age died within a year or two of the onset of their illness. Moreover, most women with what we now know as type 1 diabetes were amenorrheic and infertile. In fact, before insulin, there were few cases of pregnancy complicated by diabetes reported in the literature. A summary of the world literature published in 1909 in the American Journal of the Medical Sciences reported: 66 pregnancies in 43 women; 50% maternal mortality (27% immediate; 23% in next 2 years); and a 41% pregnancy loss (Obstet Gynecol. 1992;79:295-9, Cited Am J Med Sci. 1909;137:1).
The first injection of insulin was administered in 1922 to a 13-year-old Canadian boy, and for several years the focus was on children. (Some of them had been kept alive with 450 calories/day long enough to benefit from the new treatment.)
For women with what we now know as type 1 diabetes, insulin kept them alive, restored their fertility, and enabled them to survive a pregnancy. Maternal mortality dropped dramatically, down to a few percent, once pregnant women became beneficiaries of insulin therapy.
Perinatal outcomes remained poor, however. In the early years of insulin therapy, more than half of the babies died. Some were stillbirths, which had been the primary cause of perinatal deaths in the pre-insulin era. Others were spontaneous preterm births, and still others were delivered prematurely in order to avert a stillbirth, and subsequently died.
Dr. Landon: A significant improvement in perinatal outcomes was eventually realized about two decades after insulin was introduced. By then Dr. Priscilla White of the Joslin Clinic had recorded that women who had so-called ‘normal hormonal balance’ – basically good glucose control – had very low rates of fetal demise and fetal loss compared with those who did not have good control. You had the opportunity to work alongside Dr. White. How did she achieve these results without all the tools we have today?
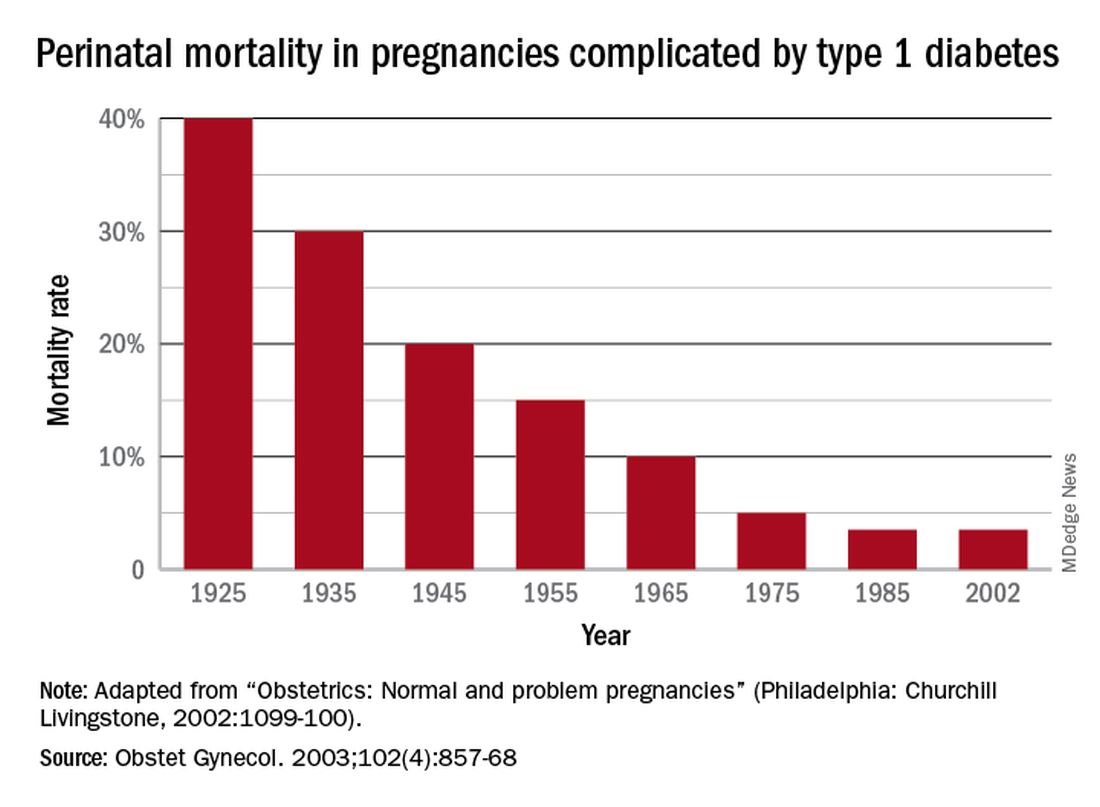
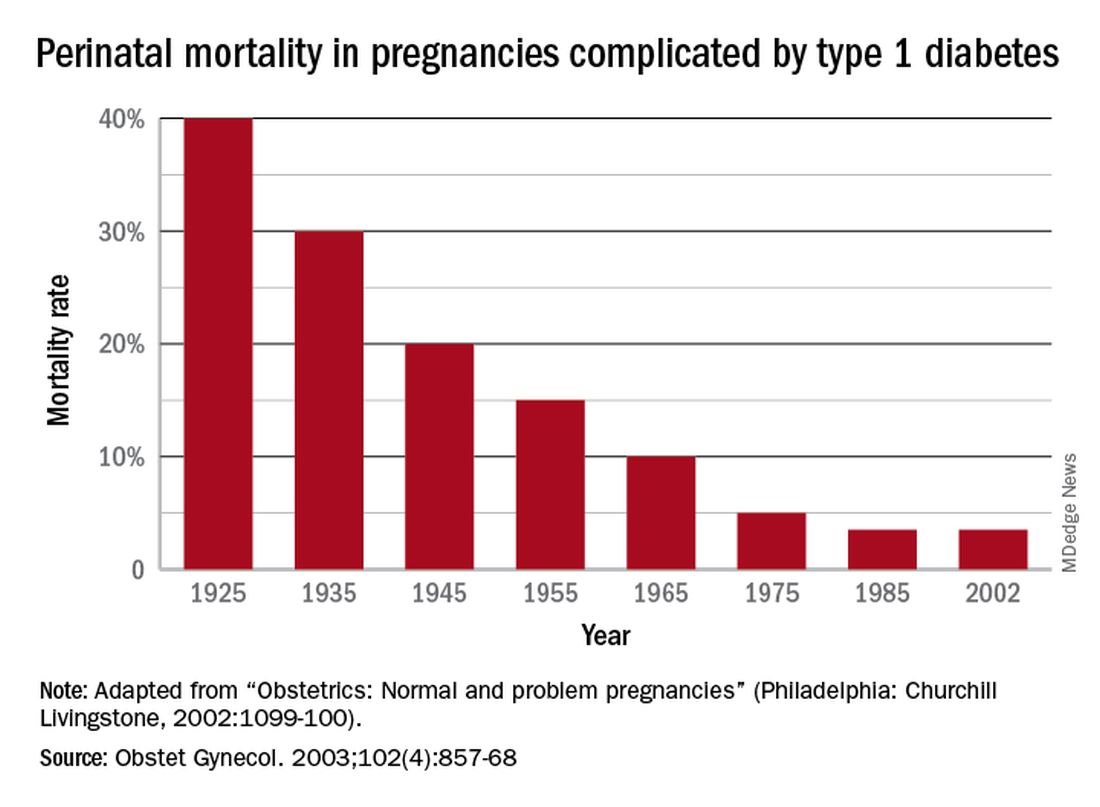
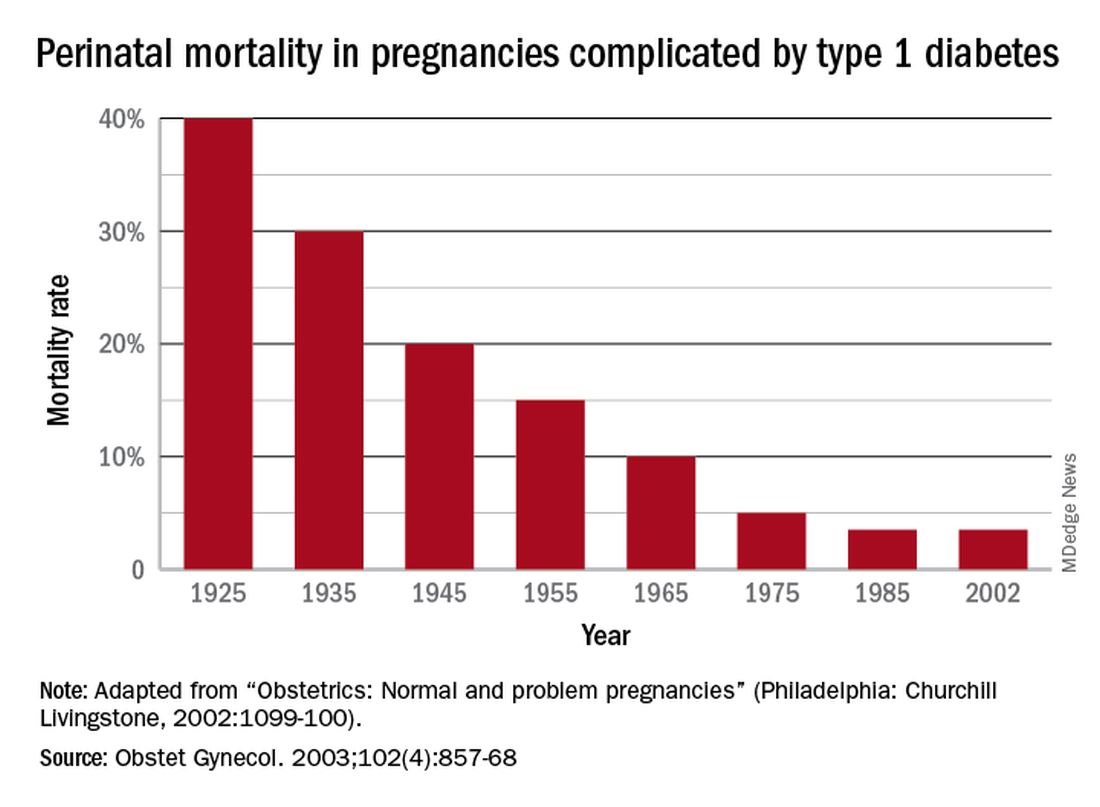
Dr. Gabbe: In 1925, the perinatal mortality in pregnancies complicated by type 1 diabetes was about 40%. By 1965 it was 10%, and when I began my residency at the Joslin Clinic and Boston Hospital for Women in 1972 it was closer to 5%
In those days we didn’t have accurate methods for dating pregnancies or assessing fetal size or well-being. We didn’t have tools to monitor blood glucose levels, and our insulins were limited to regular insulins and NPH (neutral protamine Hagedorn) as a basal insulin.
Dr. White had concluded early on, and wrote in a 1928 paper, that controlling diabetes was essential to fetal welfare and that the “high glucose content of placental blood” was probably linked to excessive fetal growth. She also wrote about the importance of “close and persistent supervision” of the patient by both an internist and obstetrician.
When I began working with her in the 1970s, her program involved antepartum visits every week or two and a team approach. Patients would be seen by Dr. White and other diabetologists, by head obstetrician Dr. Luke Gillespie, and by nurses and nutritionists. At the end of each day, after all the patients had been seen, we’d gather in Dr. White’s office and look at each patient’s single morning blood glucose measurement and the histories we’d obtained, and we’d make adjustments to their insulin regimens.
Dr. White’s solution to the problem of monitoring blood glucose was a program of hospitalization throughout pregnancy. Patients were hospitalized for a week initially to achieve blood glucose control, and then again around 20 weeks of gestation for monitoring and improvement. Hospitalizations later in the pregnancy were timed according to her classification of obstetric diabetes, which had been published in a landmark paper in 1949. In that paper Dr. Priscilla White wrote: “It is evident that age at onset of diabetes, duration, severity, and degree of maternal vascular disease all influence the fetal survival unfavorably”(Obstet Gynecol. 1992;79:295-9 / Am J Med. 1949;7:609-16).
The classification system considered age of onset, duration of diabetes, need for insulin, and presence of vascular disease. Women in higher classes and at greater risk for intrauterine death were admitted at 32 weeks, while those at less risk could wait until about 34 weeks. The timing of delivery was somewhat arbitrary, but the goal was to choose a time at which the fetus could survive in the nursery and, as Dr. White had written, “before the dreaded late intrauterine accident could occur.” (In the early ’70s, approximately half of newborns admitted to [newborn intensive care unites] at 32 weeks would survive.)
We did measure estriol levels through 24-hour urine collections as a marker for fetal and placental well-being, but as we subsequently learned, a sharp drop was often too late an indicator that something was wrong.
Dr. Landon: Dr. White and others trying to manage diabetes in pregnancy during the initial decades after insulin’s discovery were indeed significantly handicapped by a lack of tools for assessing glucose control. However, the 1970s then ushered in a “Golden Era” of fetal testing. How did advances in antepartum fetal monitoring complement the use of insulin?
Dr. Gabbe: By the mid-1970s, researchers had recognized that fetal heart rate decelerations in labor signaled fetal hypoxemia, and Dr. Roger Freeman had applied these findings to the antepartum setting, pioneering development of the contraction stress test, or oxytocin stress test. The absence of late decelerations during 10 minutes of contractions meant that the fetus was unlikely to be compromised.
When the test was administered to high-risk patients at Los Angeles County Women’s Hospital, including women with diabetes, a negative result predicted that a baby would not die within the next week. The contraction stress test was a major breakthrough. It was the first biophysical test for fetal compromise and was important for pregnancies complicated by diabetes. However, it had to be done on the labor and delivery floor, it could take hours, and it might not be definitive if one couldn’t produce enough contractions.
In the mid-1970s, the nonstress test, which relied on the presence of fetal heart rate accelerations in response to fetal movement, was found to be as reliable as the contraction stress test. It became another important tool for prolonging gestation in women with type 1 diabetes.
Even more predictive and reliable was the biophysical profile described several years later. It combined the nonstress test with an assessment using real-time fetal ultrasound of fetal movements, fetal tone and breathing movements, and amniotic fluid.
So, in a relatively short period of time, antepartum surveillance progressed from the contraction stress test to the nonstress test to the biophysical profile. These advances, along with advances in neonatal intensive care, all contributed to the continued decline in perinatal mortality.
Dr. Landon: You have taught for many years that the principal benefit of these tests of fetal surveillance is not necessarily the results identifying a fetus at risk, but the reassuring normal results that allow further maturation of the fetus that is not at risk in the pregnancy complicated by type 1 diabetes.
You also taught – as I experienced some 40 years ago when training with you at the University of Pennsylvania – that hospitalization later in pregnancy allowed for valuable optimization of our patients’ insulin regimens prior to their scheduled deliveries. This optimization helped to reduce complications such as neonatal hypoglycemia.
The introduction of the first reflectance meters to the antepartum unit eliminated the need for so many blood draws. Subsequently, came portable self-monitoring blood glucose units, which I’d argue were the second greatest achievement after the introduction of insulin because they eliminated the need for routine antepartum admissions. What are your thoughts?
Dr. Gabbe: The reflectance meters as first developed were in-hospital devices. They needed frequent calibration, and readings took several minutes. Once introduced, however, there was rapid advancement in their accuracy, size, and speed of providing results.
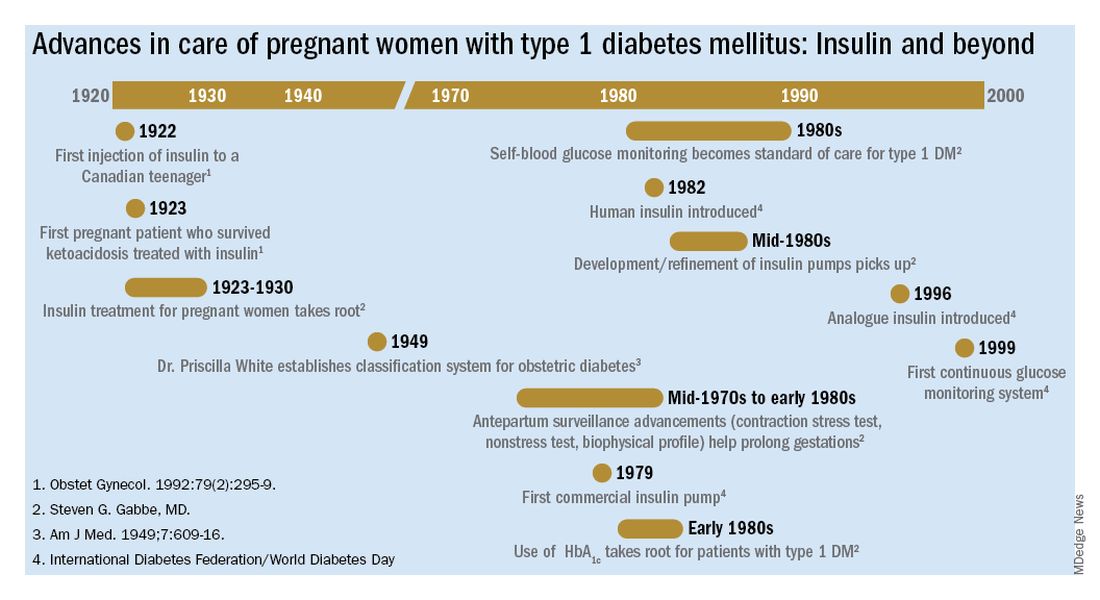
Other important advances were the development of rapid-acting insulins and new basal insulins and, in the late 1980s and early 1990s, the development of insulin pumps. At Penn, we studied an early pump that we called the “blue brick” because of its size. Today, of course, smaller and safer pumps paired with continuous glucose monitors are making an enormous difference for our patients with type 1 diabetes, providing them with much better outcomes.
Dr. Landon: A century after the discovery of insulin, congenital malformations remain a problem. We have seen a reduction overall, but recent data here and in Sweden show that the rate of malformations in pregnancy complicated by diabetes still is several-fold greater than in the general population.
The data also support what we’ve known for decades – that the level of glucose control during the periconceptual period is directly correlated with the risk of malformations. Can you speak to our efforts, which have been somewhat, but not completely, successful?
Dr. Gabbe: This is one of our remaining challenges. Malformations are now the leading cause of perinatal mortality in pregnancies involving type 1 and type 2 diabetes. We’ve seen these tragic outcomes over the years. While there were always questions about what caused malformations, our concerns focused on hyperglycemia early in pregnancy as a risk factor.
Knowing now that it is an abnormal intrauterine milieu during the period of organogenesis that leads to the malformations, we have improved by having patients come to us before pregnancy. Studies have shown that we can reduce malformations to a level comparable to the general population, or perhaps a bit higher, through intensive control as a result of prepregnancy care.
The challenge is that many obstetric patients don’t have a planned pregnancy. Our efforts to improve glucose control don’t always go the way we’d like them to. Still, considering where we’ve come from since the introduction of insulin to the modern management of diabetes in pregnancy, our progress has been truly remarkable.
Mark B. Landon, MD: The discovery of insulin in 1921 by Dr. Frederick Banting and Dr. Charles Best and its introduction into clinical practice may well be the most significant achievement in the care of pregnant women with diabetes mellitus in the last century. Why was this advance so monumental?
Steven G. Gabbe, MD: Insulin is the single most important drug we use in taking care of diabetes in pregnancy. It is required not only by all patients with type 1 diabetes, but also by the majority of patients with type 2 diabetes. Moreover, at least a third of our patients with gestational diabetes require more than lifestyle change. The American College of Obstetricians and Gynecologists and the American Diabetes Association recommend that insulin be considered as the first-line pharmacologic therapy.
Before insulin, the most prudent option for women who had glucose in their urine early in pregnancy, which was called “true diabetes,” was deemed to be termination of the pregnancy. The chances of surviving a pregnancy, and of having a surviving infant, were low.
Pregnancies were a rarity to begin with because most women of reproductive age died within a year or two of the onset of their illness. Moreover, most women with what we now know as type 1 diabetes were amenorrheic and infertile. In fact, before insulin, there were few cases of pregnancy complicated by diabetes reported in the literature. A summary of the world literature published in 1909 in the American Journal of the Medical Sciences reported: 66 pregnancies in 43 women; 50% maternal mortality (27% immediate; 23% in next 2 years); and a 41% pregnancy loss (Obstet Gynecol. 1992;79:295-9, Cited Am J Med Sci. 1909;137:1).
The first injection of insulin was administered in 1922 to a 13-year-old Canadian boy, and for several years the focus was on children. (Some of them had been kept alive with 450 calories/day long enough to benefit from the new treatment.)
For women with what we now know as type 1 diabetes, insulin kept them alive, restored their fertility, and enabled them to survive a pregnancy. Maternal mortality dropped dramatically, down to a few percent, once pregnant women became beneficiaries of insulin therapy.
Perinatal outcomes remained poor, however. In the early years of insulin therapy, more than half of the babies died. Some were stillbirths, which had been the primary cause of perinatal deaths in the pre-insulin era. Others were spontaneous preterm births, and still others were delivered prematurely in order to avert a stillbirth, and subsequently died.
Dr. Landon: A significant improvement in perinatal outcomes was eventually realized about two decades after insulin was introduced. By then Dr. Priscilla White of the Joslin Clinic had recorded that women who had so-called ‘normal hormonal balance’ – basically good glucose control – had very low rates of fetal demise and fetal loss compared with those who did not have good control. You had the opportunity to work alongside Dr. White. How did she achieve these results without all the tools we have today?
Dr. Gabbe: In 1925, the perinatal mortality in pregnancies complicated by type 1 diabetes was about 40%. By 1965 it was 10%, and when I began my residency at the Joslin Clinic and Boston Hospital for Women in 1972 it was closer to 5%
In those days we didn’t have accurate methods for dating pregnancies or assessing fetal size or well-being. We didn’t have tools to monitor blood glucose levels, and our insulins were limited to regular insulins and NPH (neutral protamine Hagedorn) as a basal insulin.
Dr. White had concluded early on, and wrote in a 1928 paper, that controlling diabetes was essential to fetal welfare and that the “high glucose content of placental blood” was probably linked to excessive fetal growth. She also wrote about the importance of “close and persistent supervision” of the patient by both an internist and obstetrician.
When I began working with her in the 1970s, her program involved antepartum visits every week or two and a team approach. Patients would be seen by Dr. White and other diabetologists, by head obstetrician Dr. Luke Gillespie, and by nurses and nutritionists. At the end of each day, after all the patients had been seen, we’d gather in Dr. White’s office and look at each patient’s single morning blood glucose measurement and the histories we’d obtained, and we’d make adjustments to their insulin regimens.
Dr. White’s solution to the problem of monitoring blood glucose was a program of hospitalization throughout pregnancy. Patients were hospitalized for a week initially to achieve blood glucose control, and then again around 20 weeks of gestation for monitoring and improvement. Hospitalizations later in the pregnancy were timed according to her classification of obstetric diabetes, which had been published in a landmark paper in 1949. In that paper Dr. Priscilla White wrote: “It is evident that age at onset of diabetes, duration, severity, and degree of maternal vascular disease all influence the fetal survival unfavorably”(Obstet Gynecol. 1992;79:295-9 / Am J Med. 1949;7:609-16).
The classification system considered age of onset, duration of diabetes, need for insulin, and presence of vascular disease. Women in higher classes and at greater risk for intrauterine death were admitted at 32 weeks, while those at less risk could wait until about 34 weeks. The timing of delivery was somewhat arbitrary, but the goal was to choose a time at which the fetus could survive in the nursery and, as Dr. White had written, “before the dreaded late intrauterine accident could occur.” (In the early ’70s, approximately half of newborns admitted to [newborn intensive care unites] at 32 weeks would survive.)
We did measure estriol levels through 24-hour urine collections as a marker for fetal and placental well-being, but as we subsequently learned, a sharp drop was often too late an indicator that something was wrong.
Dr. Landon: Dr. White and others trying to manage diabetes in pregnancy during the initial decades after insulin’s discovery were indeed significantly handicapped by a lack of tools for assessing glucose control. However, the 1970s then ushered in a “Golden Era” of fetal testing. How did advances in antepartum fetal monitoring complement the use of insulin?
Dr. Gabbe: By the mid-1970s, researchers had recognized that fetal heart rate decelerations in labor signaled fetal hypoxemia, and Dr. Roger Freeman had applied these findings to the antepartum setting, pioneering development of the contraction stress test, or oxytocin stress test. The absence of late decelerations during 10 minutes of contractions meant that the fetus was unlikely to be compromised.
When the test was administered to high-risk patients at Los Angeles County Women’s Hospital, including women with diabetes, a negative result predicted that a baby would not die within the next week. The contraction stress test was a major breakthrough. It was the first biophysical test for fetal compromise and was important for pregnancies complicated by diabetes. However, it had to be done on the labor and delivery floor, it could take hours, and it might not be definitive if one couldn’t produce enough contractions.
In the mid-1970s, the nonstress test, which relied on the presence of fetal heart rate accelerations in response to fetal movement, was found to be as reliable as the contraction stress test. It became another important tool for prolonging gestation in women with type 1 diabetes.
Even more predictive and reliable was the biophysical profile described several years later. It combined the nonstress test with an assessment using real-time fetal ultrasound of fetal movements, fetal tone and breathing movements, and amniotic fluid.
So, in a relatively short period of time, antepartum surveillance progressed from the contraction stress test to the nonstress test to the biophysical profile. These advances, along with advances in neonatal intensive care, all contributed to the continued decline in perinatal mortality.
Dr. Landon: You have taught for many years that the principal benefit of these tests of fetal surveillance is not necessarily the results identifying a fetus at risk, but the reassuring normal results that allow further maturation of the fetus that is not at risk in the pregnancy complicated by type 1 diabetes.
You also taught – as I experienced some 40 years ago when training with you at the University of Pennsylvania – that hospitalization later in pregnancy allowed for valuable optimization of our patients’ insulin regimens prior to their scheduled deliveries. This optimization helped to reduce complications such as neonatal hypoglycemia.
The introduction of the first reflectance meters to the antepartum unit eliminated the need for so many blood draws. Subsequently, came portable self-monitoring blood glucose units, which I’d argue were the second greatest achievement after the introduction of insulin because they eliminated the need for routine antepartum admissions. What are your thoughts?
Dr. Gabbe: The reflectance meters as first developed were in-hospital devices. They needed frequent calibration, and readings took several minutes. Once introduced, however, there was rapid advancement in their accuracy, size, and speed of providing results.
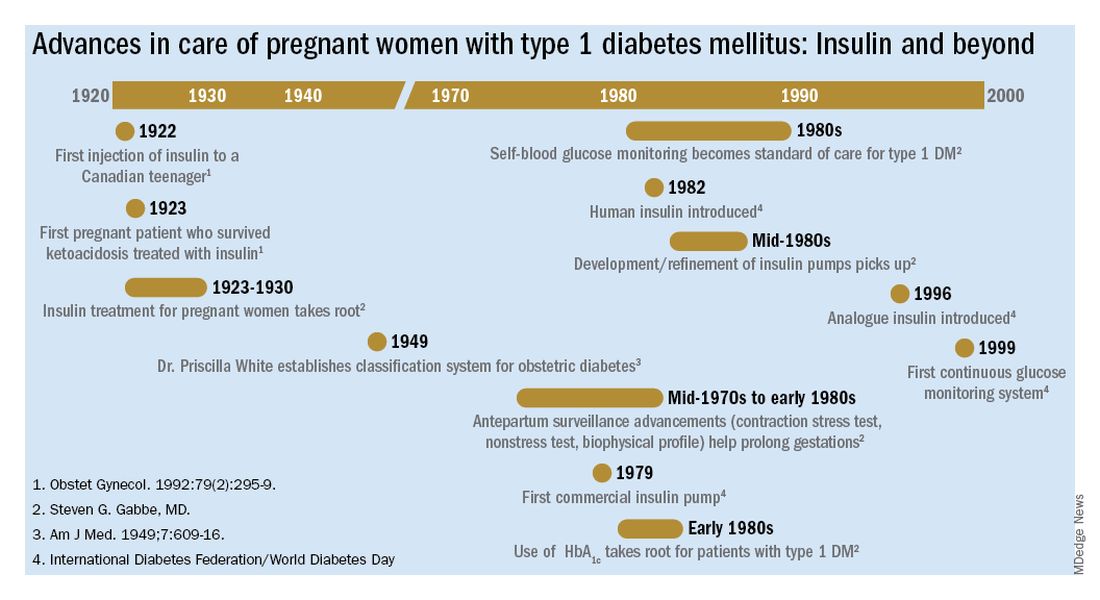
Other important advances were the development of rapid-acting insulins and new basal insulins and, in the late 1980s and early 1990s, the development of insulin pumps. At Penn, we studied an early pump that we called the “blue brick” because of its size. Today, of course, smaller and safer pumps paired with continuous glucose monitors are making an enormous difference for our patients with type 1 diabetes, providing them with much better outcomes.
Dr. Landon: A century after the discovery of insulin, congenital malformations remain a problem. We have seen a reduction overall, but recent data here and in Sweden show that the rate of malformations in pregnancy complicated by diabetes still is several-fold greater than in the general population.
The data also support what we’ve known for decades – that the level of glucose control during the periconceptual period is directly correlated with the risk of malformations. Can you speak to our efforts, which have been somewhat, but not completely, successful?
Dr. Gabbe: This is one of our remaining challenges. Malformations are now the leading cause of perinatal mortality in pregnancies involving type 1 and type 2 diabetes. We’ve seen these tragic outcomes over the years. While there were always questions about what caused malformations, our concerns focused on hyperglycemia early in pregnancy as a risk factor.
Knowing now that it is an abnormal intrauterine milieu during the period of organogenesis that leads to the malformations, we have improved by having patients come to us before pregnancy. Studies have shown that we can reduce malformations to a level comparable to the general population, or perhaps a bit higher, through intensive control as a result of prepregnancy care.
The challenge is that many obstetric patients don’t have a planned pregnancy. Our efforts to improve glucose control don’t always go the way we’d like them to. Still, considering where we’ve come from since the introduction of insulin to the modern management of diabetes in pregnancy, our progress has been truly remarkable.
Mark B. Landon, MD: The discovery of insulin in 1921 by Dr. Frederick Banting and Dr. Charles Best and its introduction into clinical practice may well be the most significant achievement in the care of pregnant women with diabetes mellitus in the last century. Why was this advance so monumental?
Steven G. Gabbe, MD: Insulin is the single most important drug we use in taking care of diabetes in pregnancy. It is required not only by all patients with type 1 diabetes, but also by the majority of patients with type 2 diabetes. Moreover, at least a third of our patients with gestational diabetes require more than lifestyle change. The American College of Obstetricians and Gynecologists and the American Diabetes Association recommend that insulin be considered as the first-line pharmacologic therapy.
Before insulin, the most prudent option for women who had glucose in their urine early in pregnancy, which was called “true diabetes,” was deemed to be termination of the pregnancy. The chances of surviving a pregnancy, and of having a surviving infant, were low.
Pregnancies were a rarity to begin with because most women of reproductive age died within a year or two of the onset of their illness. Moreover, most women with what we now know as type 1 diabetes were amenorrheic and infertile. In fact, before insulin, there were few cases of pregnancy complicated by diabetes reported in the literature. A summary of the world literature published in 1909 in the American Journal of the Medical Sciences reported: 66 pregnancies in 43 women; 50% maternal mortality (27% immediate; 23% in next 2 years); and a 41% pregnancy loss (Obstet Gynecol. 1992;79:295-9, Cited Am J Med Sci. 1909;137:1).
The first injection of insulin was administered in 1922 to a 13-year-old Canadian boy, and for several years the focus was on children. (Some of them had been kept alive with 450 calories/day long enough to benefit from the new treatment.)
For women with what we now know as type 1 diabetes, insulin kept them alive, restored their fertility, and enabled them to survive a pregnancy. Maternal mortality dropped dramatically, down to a few percent, once pregnant women became beneficiaries of insulin therapy.
Perinatal outcomes remained poor, however. In the early years of insulin therapy, more than half of the babies died. Some were stillbirths, which had been the primary cause of perinatal deaths in the pre-insulin era. Others were spontaneous preterm births, and still others were delivered prematurely in order to avert a stillbirth, and subsequently died.
Dr. Landon: A significant improvement in perinatal outcomes was eventually realized about two decades after insulin was introduced. By then Dr. Priscilla White of the Joslin Clinic had recorded that women who had so-called ‘normal hormonal balance’ – basically good glucose control – had very low rates of fetal demise and fetal loss compared with those who did not have good control. You had the opportunity to work alongside Dr. White. How did she achieve these results without all the tools we have today?
Dr. Gabbe: In 1925, the perinatal mortality in pregnancies complicated by type 1 diabetes was about 40%. By 1965 it was 10%, and when I began my residency at the Joslin Clinic and Boston Hospital for Women in 1972 it was closer to 5%
In those days we didn’t have accurate methods for dating pregnancies or assessing fetal size or well-being. We didn’t have tools to monitor blood glucose levels, and our insulins were limited to regular insulins and NPH (neutral protamine Hagedorn) as a basal insulin.
Dr. White had concluded early on, and wrote in a 1928 paper, that controlling diabetes was essential to fetal welfare and that the “high glucose content of placental blood” was probably linked to excessive fetal growth. She also wrote about the importance of “close and persistent supervision” of the patient by both an internist and obstetrician.
When I began working with her in the 1970s, her program involved antepartum visits every week or two and a team approach. Patients would be seen by Dr. White and other diabetologists, by head obstetrician Dr. Luke Gillespie, and by nurses and nutritionists. At the end of each day, after all the patients had been seen, we’d gather in Dr. White’s office and look at each patient’s single morning blood glucose measurement and the histories we’d obtained, and we’d make adjustments to their insulin regimens.
Dr. White’s solution to the problem of monitoring blood glucose was a program of hospitalization throughout pregnancy. Patients were hospitalized for a week initially to achieve blood glucose control, and then again around 20 weeks of gestation for monitoring and improvement. Hospitalizations later in the pregnancy were timed according to her classification of obstetric diabetes, which had been published in a landmark paper in 1949. In that paper Dr. Priscilla White wrote: “It is evident that age at onset of diabetes, duration, severity, and degree of maternal vascular disease all influence the fetal survival unfavorably”(Obstet Gynecol. 1992;79:295-9 / Am J Med. 1949;7:609-16).
The classification system considered age of onset, duration of diabetes, need for insulin, and presence of vascular disease. Women in higher classes and at greater risk for intrauterine death were admitted at 32 weeks, while those at less risk could wait until about 34 weeks. The timing of delivery was somewhat arbitrary, but the goal was to choose a time at which the fetus could survive in the nursery and, as Dr. White had written, “before the dreaded late intrauterine accident could occur.” (In the early ’70s, approximately half of newborns admitted to [newborn intensive care unites] at 32 weeks would survive.)
We did measure estriol levels through 24-hour urine collections as a marker for fetal and placental well-being, but as we subsequently learned, a sharp drop was often too late an indicator that something was wrong.
Dr. Landon: Dr. White and others trying to manage diabetes in pregnancy during the initial decades after insulin’s discovery were indeed significantly handicapped by a lack of tools for assessing glucose control. However, the 1970s then ushered in a “Golden Era” of fetal testing. How did advances in antepartum fetal monitoring complement the use of insulin?
Dr. Gabbe: By the mid-1970s, researchers had recognized that fetal heart rate decelerations in labor signaled fetal hypoxemia, and Dr. Roger Freeman had applied these findings to the antepartum setting, pioneering development of the contraction stress test, or oxytocin stress test. The absence of late decelerations during 10 minutes of contractions meant that the fetus was unlikely to be compromised.
When the test was administered to high-risk patients at Los Angeles County Women’s Hospital, including women with diabetes, a negative result predicted that a baby would not die within the next week. The contraction stress test was a major breakthrough. It was the first biophysical test for fetal compromise and was important for pregnancies complicated by diabetes. However, it had to be done on the labor and delivery floor, it could take hours, and it might not be definitive if one couldn’t produce enough contractions.
In the mid-1970s, the nonstress test, which relied on the presence of fetal heart rate accelerations in response to fetal movement, was found to be as reliable as the contraction stress test. It became another important tool for prolonging gestation in women with type 1 diabetes.
Even more predictive and reliable was the biophysical profile described several years later. It combined the nonstress test with an assessment using real-time fetal ultrasound of fetal movements, fetal tone and breathing movements, and amniotic fluid.
So, in a relatively short period of time, antepartum surveillance progressed from the contraction stress test to the nonstress test to the biophysical profile. These advances, along with advances in neonatal intensive care, all contributed to the continued decline in perinatal mortality.
Dr. Landon: You have taught for many years that the principal benefit of these tests of fetal surveillance is not necessarily the results identifying a fetus at risk, but the reassuring normal results that allow further maturation of the fetus that is not at risk in the pregnancy complicated by type 1 diabetes.
You also taught – as I experienced some 40 years ago when training with you at the University of Pennsylvania – that hospitalization later in pregnancy allowed for valuable optimization of our patients’ insulin regimens prior to their scheduled deliveries. This optimization helped to reduce complications such as neonatal hypoglycemia.
The introduction of the first reflectance meters to the antepartum unit eliminated the need for so many blood draws. Subsequently, came portable self-monitoring blood glucose units, which I’d argue were the second greatest achievement after the introduction of insulin because they eliminated the need for routine antepartum admissions. What are your thoughts?
Dr. Gabbe: The reflectance meters as first developed were in-hospital devices. They needed frequent calibration, and readings took several minutes. Once introduced, however, there was rapid advancement in their accuracy, size, and speed of providing results.
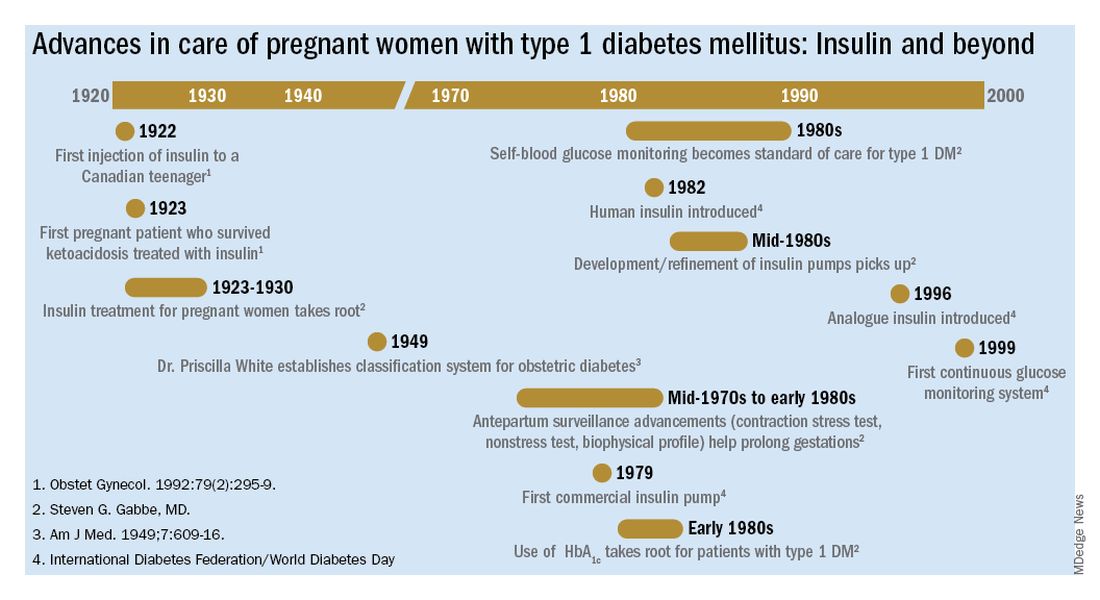
Other important advances were the development of rapid-acting insulins and new basal insulins and, in the late 1980s and early 1990s, the development of insulin pumps. At Penn, we studied an early pump that we called the “blue brick” because of its size. Today, of course, smaller and safer pumps paired with continuous glucose monitors are making an enormous difference for our patients with type 1 diabetes, providing them with much better outcomes.
Dr. Landon: A century after the discovery of insulin, congenital malformations remain a problem. We have seen a reduction overall, but recent data here and in Sweden show that the rate of malformations in pregnancy complicated by diabetes still is several-fold greater than in the general population.
The data also support what we’ve known for decades – that the level of glucose control during the periconceptual period is directly correlated with the risk of malformations. Can you speak to our efforts, which have been somewhat, but not completely, successful?
Dr. Gabbe: This is one of our remaining challenges. Malformations are now the leading cause of perinatal mortality in pregnancies involving type 1 and type 2 diabetes. We’ve seen these tragic outcomes over the years. While there were always questions about what caused malformations, our concerns focused on hyperglycemia early in pregnancy as a risk factor.
Knowing now that it is an abnormal intrauterine milieu during the period of organogenesis that leads to the malformations, we have improved by having patients come to us before pregnancy. Studies have shown that we can reduce malformations to a level comparable to the general population, or perhaps a bit higher, through intensive control as a result of prepregnancy care.
The challenge is that many obstetric patients don’t have a planned pregnancy. Our efforts to improve glucose control don’t always go the way we’d like them to. Still, considering where we’ve come from since the introduction of insulin to the modern management of diabetes in pregnancy, our progress has been truly remarkable.
Insulin in pregnancy: A look back at history for Diabetes Awareness Month
Each November, Diabetes Awareness Month, we commemorate the myriad advances that have made living with diabetes possible. This year is especially auspicious as it marks the 100th anniversary of the discovery of insulin by Frederick Banting, MD, and Charles Best, MD. The miracle of insulin cannot be overstated. In the preinsulin era, life expectancy after a diabetes diagnosis was 4-7 years for a 30-year-old patient. Within 3 years after the introduction of insulin, life expectancy after diagnosis jumped to about 17 years, a 167% increase.1
For ob.gyns. and their patients, insulin was a godsend. In the early 1920s, patients with pre-existing diabetes and pregnancy (recall that gestational diabetes mellitus would not be recognized as a unique condition until the 1960s)2 were advised to terminate the pregnancy; those who did not do so faced almost certain death for the fetus and, sometimes, themselves.3 By 1935, approximately 10 years after the introduction of insulin into practice, perinatal mortality dropped by 25%. By 1955, it had dropped by nearly 63%.4
The advent of technologies such as continuous glucose monitors, mobile phone–based health applications, and the artificial pancreas, have further transformed diabetes care.5 In addition, studies using animal models of diabetic pregnancy have revealed the molecular mechanisms responsible for hyperglycemia-induced birth defects – including alterations in lipid metabolism, excess generation of free radicals, and aberrant cell death – and uncovered potential strategies for prevention.6
To reflect on the herculean accomplishments in ob.gyn. since the discovery of insulin, we have invited two pillars of the diabetes in pregnancy research and clinical care communities: Steven G. Gabbe, MD, current professor of ob.gyn. at The Ohio State University (OSU) College of Medicine, former chair of ob.gyn. at OSU and University of Washington Medical Center, former senior vice president for health sciences and CEO of the OSU Medical Center, and former dean of Vanderbilt University School of Medicine; and Mark B. Landon, MD, the Richard L. Meiling professor and chair of ob.gyn. at OSU.
Dr. Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He has no relevant financial disclosures. Contact him at [email protected].
References
1. Brostoff JM et al. Diabetologia. 2007;50(6):1351-3.
2. Panaitescu AM and Peltecu G. Acta Endocrinol (Buchar). 2016;12(3):331-4.
3. Joslin EP. Boston Med Surg J 1915;173:841-9.
4. Gabbe SG and Graves CR. Obstet Gynecol. 2003;102(4):857-68.
5. Crimmins SD et al. Clin Diabetes. 2020;38(5):486-94.
6. Gabbay-Benziv R et al. World J Diabetes. 2015;6(3):481-8.
Each November, Diabetes Awareness Month, we commemorate the myriad advances that have made living with diabetes possible. This year is especially auspicious as it marks the 100th anniversary of the discovery of insulin by Frederick Banting, MD, and Charles Best, MD. The miracle of insulin cannot be overstated. In the preinsulin era, life expectancy after a diabetes diagnosis was 4-7 years for a 30-year-old patient. Within 3 years after the introduction of insulin, life expectancy after diagnosis jumped to about 17 years, a 167% increase.1
For ob.gyns. and their patients, insulin was a godsend. In the early 1920s, patients with pre-existing diabetes and pregnancy (recall that gestational diabetes mellitus would not be recognized as a unique condition until the 1960s)2 were advised to terminate the pregnancy; those who did not do so faced almost certain death for the fetus and, sometimes, themselves.3 By 1935, approximately 10 years after the introduction of insulin into practice, perinatal mortality dropped by 25%. By 1955, it had dropped by nearly 63%.4
The advent of technologies such as continuous glucose monitors, mobile phone–based health applications, and the artificial pancreas, have further transformed diabetes care.5 In addition, studies using animal models of diabetic pregnancy have revealed the molecular mechanisms responsible for hyperglycemia-induced birth defects – including alterations in lipid metabolism, excess generation of free radicals, and aberrant cell death – and uncovered potential strategies for prevention.6
To reflect on the herculean accomplishments in ob.gyn. since the discovery of insulin, we have invited two pillars of the diabetes in pregnancy research and clinical care communities: Steven G. Gabbe, MD, current professor of ob.gyn. at The Ohio State University (OSU) College of Medicine, former chair of ob.gyn. at OSU and University of Washington Medical Center, former senior vice president for health sciences and CEO of the OSU Medical Center, and former dean of Vanderbilt University School of Medicine; and Mark B. Landon, MD, the Richard L. Meiling professor and chair of ob.gyn. at OSU.
Dr. Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He has no relevant financial disclosures. Contact him at [email protected].
References
1. Brostoff JM et al. Diabetologia. 2007;50(6):1351-3.
2. Panaitescu AM and Peltecu G. Acta Endocrinol (Buchar). 2016;12(3):331-4.
3. Joslin EP. Boston Med Surg J 1915;173:841-9.
4. Gabbe SG and Graves CR. Obstet Gynecol. 2003;102(4):857-68.
5. Crimmins SD et al. Clin Diabetes. 2020;38(5):486-94.
6. Gabbay-Benziv R et al. World J Diabetes. 2015;6(3):481-8.
Each November, Diabetes Awareness Month, we commemorate the myriad advances that have made living with diabetes possible. This year is especially auspicious as it marks the 100th anniversary of the discovery of insulin by Frederick Banting, MD, and Charles Best, MD. The miracle of insulin cannot be overstated. In the preinsulin era, life expectancy after a diabetes diagnosis was 4-7 years for a 30-year-old patient. Within 3 years after the introduction of insulin, life expectancy after diagnosis jumped to about 17 years, a 167% increase.1
For ob.gyns. and their patients, insulin was a godsend. In the early 1920s, patients with pre-existing diabetes and pregnancy (recall that gestational diabetes mellitus would not be recognized as a unique condition until the 1960s)2 were advised to terminate the pregnancy; those who did not do so faced almost certain death for the fetus and, sometimes, themselves.3 By 1935, approximately 10 years after the introduction of insulin into practice, perinatal mortality dropped by 25%. By 1955, it had dropped by nearly 63%.4
The advent of technologies such as continuous glucose monitors, mobile phone–based health applications, and the artificial pancreas, have further transformed diabetes care.5 In addition, studies using animal models of diabetic pregnancy have revealed the molecular mechanisms responsible for hyperglycemia-induced birth defects – including alterations in lipid metabolism, excess generation of free radicals, and aberrant cell death – and uncovered potential strategies for prevention.6
To reflect on the herculean accomplishments in ob.gyn. since the discovery of insulin, we have invited two pillars of the diabetes in pregnancy research and clinical care communities: Steven G. Gabbe, MD, current professor of ob.gyn. at The Ohio State University (OSU) College of Medicine, former chair of ob.gyn. at OSU and University of Washington Medical Center, former senior vice president for health sciences and CEO of the OSU Medical Center, and former dean of Vanderbilt University School of Medicine; and Mark B. Landon, MD, the Richard L. Meiling professor and chair of ob.gyn. at OSU.
Dr. Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He has no relevant financial disclosures. Contact him at [email protected].
References
1. Brostoff JM et al. Diabetologia. 2007;50(6):1351-3.
2. Panaitescu AM and Peltecu G. Acta Endocrinol (Buchar). 2016;12(3):331-4.
3. Joslin EP. Boston Med Surg J 1915;173:841-9.
4. Gabbe SG and Graves CR. Obstet Gynecol. 2003;102(4):857-68.
5. Crimmins SD et al. Clin Diabetes. 2020;38(5):486-94.
6. Gabbay-Benziv R et al. World J Diabetes. 2015;6(3):481-8.
Your patient’s medication label lacks human safety information: What now?
Nearly 9 in 10 U.S. women take a medication at some point in their pregnancy, with approximately 50% of women taking at least one prescription medication.1 These medications may be prescribed without the benefit of knowledge gained through clinical trials. Knowledge is gained after market, often after multiple years, and potentially following widespread use. The situation is similar for vaccines, as was recently seen with the SARS-CoV2 pandemic. Early in the pandemic, evidence emerged that pregnancy increased the risk for severe illness from COVID-19, yet pregnant people and their providers were forced to make a difficult decision of risk/benefit with little data to guide them.
The FDA product label provides a summary and narrative of animal and human safety studies relating to pregnancy. But what if that label contains little to no information, or reports studies with conflicting results? Perhaps the product is new on the market or is infrequently used during pregnancy. Regardless, health care providers and pregnant patients still need to make decisions about medication use. The following list outlines information that can be found, and strategies to support providers and patients in making informed choices for a treatment plan.
Taking stock of the available information:
- If possible, connect with the specialist who prescribed the patient’s medication in question. They may have already assembled information regarding use of that medication in pregnancy.
- The sponsor may have published useful information from the phase 3 trials, including the outcomes of enrolled patients who inadvertently became pregnant.
- Review the animal data in the product label. Regulators require the careful selection of animal models, and this data can present a source of adjunct information regarding the medication’s effects on pregnancy, reproduction, and development. Negative results can be as revealing as positive results.
- Pharmacologic data in the label can also be informative. Although most labels have pharmacologic data based on trials in healthy nonpregnant individuals, understanding pregnancy physiology and the patient’s preexisting or pregnancy-specific condition(s) can provide insights.2 Close patient monitoring and follow-up are of key importance.
- Consider viable alternatives that may address the patient’s needs. There may be effective alternatives that have been better studied and shown to have low reproductive toxicity.
- Consider the risks to the patient as well as the developing fetus if the preexisting or pregnancy-specific condition is uncontrolled.
- Consult a teratogen specialist who can provide information to both patients and health care providers on the reproductive hazards or safety of many exposures, even those with limited data regarding use in pregnancy. For example, MotherToBaby provides a network of teratogen specialists.
Understanding perceptions of risk, decision-making, and strategies to support informed choices:
- Perceptions of risk: Each person perceives risk and benefit differently. The few studies that have attempted to investigate perception of teratogenic risk have found that many pregnant people overestimate the magnitude of teratogenic risk associated with a particular exposure.3 Alternatively, a medication’s benefit in controlling the maternal condition is often not considered sufficiently. Health care providers may have their own distorted perceptions of risk, even in the presence of evidence.
- Decision-making: Most teratogen data inherently involve uncertainty; it is rare to have completely nonconflicting data with which to make a decision. This makes decisions about whether or not to utilize a particular medication or other agent in pregnancy very difficult. For example, a patient would prefer to be told a black and white answer such as vaccines are either 100% safe or 100% harmful. However, no medical treatment is held to that standard of certainty. Even though it may be more comfortable to avoid an action and “just let things happen,” the lack of a decision is still a decision. The decision to not take medication may have risks inherent in not treating a condition and may result in adverse outcomes in the developing fetus. Lastly, presenting teratogen information often involves challenges in portraying and interpreting numerical risk. For example, when considering data presented in fraction format, patients and some health care providers may focus on the numerator or count of adverse events, while ignoring the magnitude of the denominator.
- Strategies: Health literacy “best practice” strategies are useful whether there is a lot of data or very little. These include the of use plain language and messages delivered in a clear and respectful voice, the use of visual aids, and the use effective teaching methods such as asking open-ended questions to assess understanding. Other strategies include using caution in framing information: for example, discussing a 1% increase in risk for a baby to have a medication-associated birth defect should also be presented as a 99% chance the medication will not cause a birth defect. Numeracy challenges can also be addressed by using natural numbers rather than fractions or percentages: for example, if there were 100 women in this room, one would have a baby with a birth defect after taking this medication in pregnancy, but 99 of these women would not.
In today’s medical world, shared decision-making is the preferred approach to choices. Communicating and appropriately utilizing information to make choices about medication safety in pregnancy are vital undertakings. An important provider responsibility is helping patients understand that science is built on evidence that amasses and changes over time and that it represents rich shades of gray rather than “black and white” options.
Contributing to evidence: A pregnancy exposure registry is a study that collects health information from women who take prescription medicines or vaccines when they are pregnant. Information is also collected on the neonate. This information is compared with women who have not taken medicine during pregnancy. Enrolling in a pregnancy exposure registry can help improve safety information for medication used during pregnancy and can be used to update drug labeling. Please consult the Food and Drug Administration listing below to learn if there is an ongoing registry for the patient’s medication in question. If there is and the patient is eligible, provide her with the information. If she is interested and willing, help her enroll. It’s a great step toward building the scientific evidence on medication safety in pregnancy.
For further information about health literacy, consult:
https://www.cdc.gov/pregnancy/meds/treatingfortwo/index.html
https://www.cdc.gov/ncbddd/birthdefects/index.html
https://mothertobaby.org
The MotherToBaby web page has hundreds of fact sheets written in a way that patients can understand, and available in English and Spanish. MotherToBaby coordinates research studies on specific agents. The toll-free number is 866-626-6847.
For a listing of pregnancy registries, consult:
https://www.fda.gov/science-research/womens-health-research/pregnancy-registries
Dr. Hardy is executive director, head of pharmacoepidemiology, Biohaven Pharmaceuticals. She serves as a member of Council for the Society for Birth Defects Research and Prevention (BDRP), represents the BDRP on the Coalition to Advance Maternal Therapeutics, and is a member of the North American Board for Amandla Development, South Africa. Dr. Conover is the director of Nebraska MotherToBaby. She is assistant professor at the Munroe Meyer Institute, University of Nebraska Medical Center.
References
1. Mitchell AA et al. Am J Obstet Gynecol. 2011;205(1):51:e1-e8.
2. Feghali M et al. Semin Perinatol 2015;39:512-9.
3. Conover EA, Polifka JE. Am J Med Genet Part C Semin Med Genet 2011;157:227-33.
Nearly 9 in 10 U.S. women take a medication at some point in their pregnancy, with approximately 50% of women taking at least one prescription medication.1 These medications may be prescribed without the benefit of knowledge gained through clinical trials. Knowledge is gained after market, often after multiple years, and potentially following widespread use. The situation is similar for vaccines, as was recently seen with the SARS-CoV2 pandemic. Early in the pandemic, evidence emerged that pregnancy increased the risk for severe illness from COVID-19, yet pregnant people and their providers were forced to make a difficult decision of risk/benefit with little data to guide them.
The FDA product label provides a summary and narrative of animal and human safety studies relating to pregnancy. But what if that label contains little to no information, or reports studies with conflicting results? Perhaps the product is new on the market or is infrequently used during pregnancy. Regardless, health care providers and pregnant patients still need to make decisions about medication use. The following list outlines information that can be found, and strategies to support providers and patients in making informed choices for a treatment plan.
Taking stock of the available information:
- If possible, connect with the specialist who prescribed the patient’s medication in question. They may have already assembled information regarding use of that medication in pregnancy.
- The sponsor may have published useful information from the phase 3 trials, including the outcomes of enrolled patients who inadvertently became pregnant.
- Review the animal data in the product label. Regulators require the careful selection of animal models, and this data can present a source of adjunct information regarding the medication’s effects on pregnancy, reproduction, and development. Negative results can be as revealing as positive results.
- Pharmacologic data in the label can also be informative. Although most labels have pharmacologic data based on trials in healthy nonpregnant individuals, understanding pregnancy physiology and the patient’s preexisting or pregnancy-specific condition(s) can provide insights.2 Close patient monitoring and follow-up are of key importance.
- Consider viable alternatives that may address the patient’s needs. There may be effective alternatives that have been better studied and shown to have low reproductive toxicity.
- Consider the risks to the patient as well as the developing fetus if the preexisting or pregnancy-specific condition is uncontrolled.
- Consult a teratogen specialist who can provide information to both patients and health care providers on the reproductive hazards or safety of many exposures, even those with limited data regarding use in pregnancy. For example, MotherToBaby provides a network of teratogen specialists.
Understanding perceptions of risk, decision-making, and strategies to support informed choices:
- Perceptions of risk: Each person perceives risk and benefit differently. The few studies that have attempted to investigate perception of teratogenic risk have found that many pregnant people overestimate the magnitude of teratogenic risk associated with a particular exposure.3 Alternatively, a medication’s benefit in controlling the maternal condition is often not considered sufficiently. Health care providers may have their own distorted perceptions of risk, even in the presence of evidence.
- Decision-making: Most teratogen data inherently involve uncertainty; it is rare to have completely nonconflicting data with which to make a decision. This makes decisions about whether or not to utilize a particular medication or other agent in pregnancy very difficult. For example, a patient would prefer to be told a black and white answer such as vaccines are either 100% safe or 100% harmful. However, no medical treatment is held to that standard of certainty. Even though it may be more comfortable to avoid an action and “just let things happen,” the lack of a decision is still a decision. The decision to not take medication may have risks inherent in not treating a condition and may result in adverse outcomes in the developing fetus. Lastly, presenting teratogen information often involves challenges in portraying and interpreting numerical risk. For example, when considering data presented in fraction format, patients and some health care providers may focus on the numerator or count of adverse events, while ignoring the magnitude of the denominator.
- Strategies: Health literacy “best practice” strategies are useful whether there is a lot of data or very little. These include the of use plain language and messages delivered in a clear and respectful voice, the use of visual aids, and the use effective teaching methods such as asking open-ended questions to assess understanding. Other strategies include using caution in framing information: for example, discussing a 1% increase in risk for a baby to have a medication-associated birth defect should also be presented as a 99% chance the medication will not cause a birth defect. Numeracy challenges can also be addressed by using natural numbers rather than fractions or percentages: for example, if there were 100 women in this room, one would have a baby with a birth defect after taking this medication in pregnancy, but 99 of these women would not.
In today’s medical world, shared decision-making is the preferred approach to choices. Communicating and appropriately utilizing information to make choices about medication safety in pregnancy are vital undertakings. An important provider responsibility is helping patients understand that science is built on evidence that amasses and changes over time and that it represents rich shades of gray rather than “black and white” options.
Contributing to evidence: A pregnancy exposure registry is a study that collects health information from women who take prescription medicines or vaccines when they are pregnant. Information is also collected on the neonate. This information is compared with women who have not taken medicine during pregnancy. Enrolling in a pregnancy exposure registry can help improve safety information for medication used during pregnancy and can be used to update drug labeling. Please consult the Food and Drug Administration listing below to learn if there is an ongoing registry for the patient’s medication in question. If there is and the patient is eligible, provide her with the information. If she is interested and willing, help her enroll. It’s a great step toward building the scientific evidence on medication safety in pregnancy.
For further information about health literacy, consult:
https://www.cdc.gov/pregnancy/meds/treatingfortwo/index.html
https://www.cdc.gov/ncbddd/birthdefects/index.html
https://mothertobaby.org
The MotherToBaby web page has hundreds of fact sheets written in a way that patients can understand, and available in English and Spanish. MotherToBaby coordinates research studies on specific agents. The toll-free number is 866-626-6847.
For a listing of pregnancy registries, consult:
https://www.fda.gov/science-research/womens-health-research/pregnancy-registries
Dr. Hardy is executive director, head of pharmacoepidemiology, Biohaven Pharmaceuticals. She serves as a member of Council for the Society for Birth Defects Research and Prevention (BDRP), represents the BDRP on the Coalition to Advance Maternal Therapeutics, and is a member of the North American Board for Amandla Development, South Africa. Dr. Conover is the director of Nebraska MotherToBaby. She is assistant professor at the Munroe Meyer Institute, University of Nebraska Medical Center.
References
1. Mitchell AA et al. Am J Obstet Gynecol. 2011;205(1):51:e1-e8.
2. Feghali M et al. Semin Perinatol 2015;39:512-9.
3. Conover EA, Polifka JE. Am J Med Genet Part C Semin Med Genet 2011;157:227-33.
Nearly 9 in 10 U.S. women take a medication at some point in their pregnancy, with approximately 50% of women taking at least one prescription medication.1 These medications may be prescribed without the benefit of knowledge gained through clinical trials. Knowledge is gained after market, often after multiple years, and potentially following widespread use. The situation is similar for vaccines, as was recently seen with the SARS-CoV2 pandemic. Early in the pandemic, evidence emerged that pregnancy increased the risk for severe illness from COVID-19, yet pregnant people and their providers were forced to make a difficult decision of risk/benefit with little data to guide them.
The FDA product label provides a summary and narrative of animal and human safety studies relating to pregnancy. But what if that label contains little to no information, or reports studies with conflicting results? Perhaps the product is new on the market or is infrequently used during pregnancy. Regardless, health care providers and pregnant patients still need to make decisions about medication use. The following list outlines information that can be found, and strategies to support providers and patients in making informed choices for a treatment plan.
Taking stock of the available information:
- If possible, connect with the specialist who prescribed the patient’s medication in question. They may have already assembled information regarding use of that medication in pregnancy.
- The sponsor may have published useful information from the phase 3 trials, including the outcomes of enrolled patients who inadvertently became pregnant.
- Review the animal data in the product label. Regulators require the careful selection of animal models, and this data can present a source of adjunct information regarding the medication’s effects on pregnancy, reproduction, and development. Negative results can be as revealing as positive results.
- Pharmacologic data in the label can also be informative. Although most labels have pharmacologic data based on trials in healthy nonpregnant individuals, understanding pregnancy physiology and the patient’s preexisting or pregnancy-specific condition(s) can provide insights.2 Close patient monitoring and follow-up are of key importance.
- Consider viable alternatives that may address the patient’s needs. There may be effective alternatives that have been better studied and shown to have low reproductive toxicity.
- Consider the risks to the patient as well as the developing fetus if the preexisting or pregnancy-specific condition is uncontrolled.
- Consult a teratogen specialist who can provide information to both patients and health care providers on the reproductive hazards or safety of many exposures, even those with limited data regarding use in pregnancy. For example, MotherToBaby provides a network of teratogen specialists.
Understanding perceptions of risk, decision-making, and strategies to support informed choices:
- Perceptions of risk: Each person perceives risk and benefit differently. The few studies that have attempted to investigate perception of teratogenic risk have found that many pregnant people overestimate the magnitude of teratogenic risk associated with a particular exposure.3 Alternatively, a medication’s benefit in controlling the maternal condition is often not considered sufficiently. Health care providers may have their own distorted perceptions of risk, even in the presence of evidence.
- Decision-making: Most teratogen data inherently involve uncertainty; it is rare to have completely nonconflicting data with which to make a decision. This makes decisions about whether or not to utilize a particular medication or other agent in pregnancy very difficult. For example, a patient would prefer to be told a black and white answer such as vaccines are either 100% safe or 100% harmful. However, no medical treatment is held to that standard of certainty. Even though it may be more comfortable to avoid an action and “just let things happen,” the lack of a decision is still a decision. The decision to not take medication may have risks inherent in not treating a condition and may result in adverse outcomes in the developing fetus. Lastly, presenting teratogen information often involves challenges in portraying and interpreting numerical risk. For example, when considering data presented in fraction format, patients and some health care providers may focus on the numerator or count of adverse events, while ignoring the magnitude of the denominator.
- Strategies: Health literacy “best practice” strategies are useful whether there is a lot of data or very little. These include the of use plain language and messages delivered in a clear and respectful voice, the use of visual aids, and the use effective teaching methods such as asking open-ended questions to assess understanding. Other strategies include using caution in framing information: for example, discussing a 1% increase in risk for a baby to have a medication-associated birth defect should also be presented as a 99% chance the medication will not cause a birth defect. Numeracy challenges can also be addressed by using natural numbers rather than fractions or percentages: for example, if there were 100 women in this room, one would have a baby with a birth defect after taking this medication in pregnancy, but 99 of these women would not.
In today’s medical world, shared decision-making is the preferred approach to choices. Communicating and appropriately utilizing information to make choices about medication safety in pregnancy are vital undertakings. An important provider responsibility is helping patients understand that science is built on evidence that amasses and changes over time and that it represents rich shades of gray rather than “black and white” options.
Contributing to evidence: A pregnancy exposure registry is a study that collects health information from women who take prescription medicines or vaccines when they are pregnant. Information is also collected on the neonate. This information is compared with women who have not taken medicine during pregnancy. Enrolling in a pregnancy exposure registry can help improve safety information for medication used during pregnancy and can be used to update drug labeling. Please consult the Food and Drug Administration listing below to learn if there is an ongoing registry for the patient’s medication in question. If there is and the patient is eligible, provide her with the information. If she is interested and willing, help her enroll. It’s a great step toward building the scientific evidence on medication safety in pregnancy.
For further information about health literacy, consult:
https://www.cdc.gov/pregnancy/meds/treatingfortwo/index.html
https://www.cdc.gov/ncbddd/birthdefects/index.html
https://mothertobaby.org
The MotherToBaby web page has hundreds of fact sheets written in a way that patients can understand, and available in English and Spanish. MotherToBaby coordinates research studies on specific agents. The toll-free number is 866-626-6847.
For a listing of pregnancy registries, consult:
https://www.fda.gov/science-research/womens-health-research/pregnancy-registries
Dr. Hardy is executive director, head of pharmacoepidemiology, Biohaven Pharmaceuticals. She serves as a member of Council for the Society for Birth Defects Research and Prevention (BDRP), represents the BDRP on the Coalition to Advance Maternal Therapeutics, and is a member of the North American Board for Amandla Development, South Africa. Dr. Conover is the director of Nebraska MotherToBaby. She is assistant professor at the Munroe Meyer Institute, University of Nebraska Medical Center.
References
1. Mitchell AA et al. Am J Obstet Gynecol. 2011;205(1):51:e1-e8.
2. Feghali M et al. Semin Perinatol 2015;39:512-9.
3. Conover EA, Polifka JE. Am J Med Genet Part C Semin Med Genet 2011;157:227-33.
Overview of guidelines for patients seeking gender-affirmation surgery
Gender-affirmation surgery refers to a collection of procedures by which a transgender individual physically alters characteristics to align with their gender identity. While not all patients who identify as transgender will choose to undergo surgery, the surgeries are considered medically necessary and lead to significant improvements in emotional and psychological well-being.1 With increasing insurance coverage and improved access to care, more and more patients are seeking gender-affirming surgery, and it is incumbent for providers to familiarize themselves with preoperative recommendations and requirements.
Ob.gyns. play a key role in patients seeking surgical treatment as patients may inquire about available procedures and what steps are necessary prior to scheduling a visit with the appropriate surgeon. The World Professional Association of Transgender Health has established standards of care that provide multidisciplinary, evidence-based guidance for patients seeking a variety of gender-affirming services ranging from mental health, hormone therapy, and surgery.
Basic preoperative surgical prerequisites set forth by WPATH include being a patient with well-documented gender dysphoria, being the age of majority, and having the ability to provide informed consent.1
As with any surgical candidate, it is also equally important for a patient to have well-controlled medical and psychiatric comorbidities, which should also include smoking cessation. A variety of surgical procedures are available to patients and include breast/chest surgery, genital (bottom) surgery, and nongenital surgery (facial feminization, pectoral implant placement, thyroid chondroplasty, lipofilling/liposuction, body contouring, and voice modification). Patients may choose to undergo chest/breast surgery and/or bottom surgery or forgo surgical procedures altogether.
For transmasculine patients, breast/chest surgery, otherwise known as top surgery, is the most common and desired procedure. According to a recent survey, approximately 97% of transmasculine patients had or wanted masculinizing chest surgery.2 In addition to patients meeting the basic requirements set forth by WPATH, one referral from a mental health provider specializing in gender-affirming care is also needed prior to this procedure. It is also important to note that testosterone use is no longer a needed prior to masculinizing chest surgery.
Transmasculine bottom surgery, which includes hysterectomy, bilateral salpingo-oophorectomy, metoidioplasty, vaginectomy, scrotoplasty, testicular implant placement, and/or phalloplasty have additional nuances. Compared with transmasculine individuals seeking top surgery, the number of patients who have had or desire metoidioplasty and phalloplasty is much lower, which is mainly because of the high complication rates of these procedures. In the same survey, only 4% of patients had undergone a metoidioplasty procedure and 2% of patients had undergone a phalloplasty.2
In evaluating rates of hysterectomy with or without salpingo-oophorectomy, approximately 21% of transgender men underwent hysterectomy, with 58% desiring it in the future.2 Unlike patients pursuing top surgery, patients who desire any form of bottom surgery need to be on 12 months of continuous hormone therapy.1 They also must provide two letters from two different mental health providers, one of whom must have either an MD/DO or PhD. In cases in which a patient requests a hysterectomy for reasons other than gender dysphoria, such as pelvic pain or abnormal uterine bleeding, these criteria do not apply.
For transfeminine individuals, augmentation mammoplasty is performed following 12 months of continuous hormone therapy. This is to allow maximum breast growth, which occurs approximately 2-3 months after hormone initiation and peaks at 1-2 years.3 Rates of transfeminine individuals seeking augmentation mammoplasty is similar to that of their transmasculine counterparts at 74%.2 One referral letter from a mental health provider is also needed prior to augmentation mammoplasty.
Transfeminine patients who desire bottom surgery, which can involve an orchiectomy or vaginoplasty (single-stage penile inversion, peritoneal, or colonic interposition), have the same additional requirements as transmasculine individuals seeking bottom surgery. Furthermore, it is interesting to note that 25% of transfeminine individuals had already undergone orchiectomy and 87% had either undergone or desired a vaginoplasty in the future.2 This is in stark contrast to transmasculine patients and rates of bottom surgery.
Unless there is a specific medical contraindication to hormone therapy, emphasis is placed on 12 months of continuous hormone usage. Additional emphasis is placed on patients seeking bottom surgery to live for a minimum of 12 months in their congruent gender role. This also allows patients to further explore their gender identity and make appropriate preparations for surgery.
As with any surgical procedure, obtaining informed consent and reviewing patient expectations are key. In my clinical practice, I discuss with patients that the general surgical goals are to achieve both function and good aesthetic outcome but that their results are also tailored to their individual bodies. Assessing a patient’s support system and social factors is also equally important in the preoperative planning period. As this field continues to grow, it is essential for providers to understand the evolving distinctions in surgical care to improve access to patients.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa. She has no conflicts. Email her at [email protected].
References
1. The World Professional Association for Transgender Health. Standards of Care for the Health of Transsexual, Transgender, and Gender Nonconforming People. https://www.wpath.org/publications/soc.
2. James SE et al. The report of the 2015 U.S. Transgender survey. Washington, D.C.: National Center for Transgender Equality. 2016.
3. Thomas TN. Overview of surgery for transgender patients, in “Comprehensive care for the transgender patient.” Philadelphia: Elsevier, 2020. pp. 48-53.
Gender-affirmation surgery refers to a collection of procedures by which a transgender individual physically alters characteristics to align with their gender identity. While not all patients who identify as transgender will choose to undergo surgery, the surgeries are considered medically necessary and lead to significant improvements in emotional and psychological well-being.1 With increasing insurance coverage and improved access to care, more and more patients are seeking gender-affirming surgery, and it is incumbent for providers to familiarize themselves with preoperative recommendations and requirements.
Ob.gyns. play a key role in patients seeking surgical treatment as patients may inquire about available procedures and what steps are necessary prior to scheduling a visit with the appropriate surgeon. The World Professional Association of Transgender Health has established standards of care that provide multidisciplinary, evidence-based guidance for patients seeking a variety of gender-affirming services ranging from mental health, hormone therapy, and surgery.
Basic preoperative surgical prerequisites set forth by WPATH include being a patient with well-documented gender dysphoria, being the age of majority, and having the ability to provide informed consent.1
As with any surgical candidate, it is also equally important for a patient to have well-controlled medical and psychiatric comorbidities, which should also include smoking cessation. A variety of surgical procedures are available to patients and include breast/chest surgery, genital (bottom) surgery, and nongenital surgery (facial feminization, pectoral implant placement, thyroid chondroplasty, lipofilling/liposuction, body contouring, and voice modification). Patients may choose to undergo chest/breast surgery and/or bottom surgery or forgo surgical procedures altogether.
For transmasculine patients, breast/chest surgery, otherwise known as top surgery, is the most common and desired procedure. According to a recent survey, approximately 97% of transmasculine patients had or wanted masculinizing chest surgery.2 In addition to patients meeting the basic requirements set forth by WPATH, one referral from a mental health provider specializing in gender-affirming care is also needed prior to this procedure. It is also important to note that testosterone use is no longer a needed prior to masculinizing chest surgery.
Transmasculine bottom surgery, which includes hysterectomy, bilateral salpingo-oophorectomy, metoidioplasty, vaginectomy, scrotoplasty, testicular implant placement, and/or phalloplasty have additional nuances. Compared with transmasculine individuals seeking top surgery, the number of patients who have had or desire metoidioplasty and phalloplasty is much lower, which is mainly because of the high complication rates of these procedures. In the same survey, only 4% of patients had undergone a metoidioplasty procedure and 2% of patients had undergone a phalloplasty.2
In evaluating rates of hysterectomy with or without salpingo-oophorectomy, approximately 21% of transgender men underwent hysterectomy, with 58% desiring it in the future.2 Unlike patients pursuing top surgery, patients who desire any form of bottom surgery need to be on 12 months of continuous hormone therapy.1 They also must provide two letters from two different mental health providers, one of whom must have either an MD/DO or PhD. In cases in which a patient requests a hysterectomy for reasons other than gender dysphoria, such as pelvic pain or abnormal uterine bleeding, these criteria do not apply.
For transfeminine individuals, augmentation mammoplasty is performed following 12 months of continuous hormone therapy. This is to allow maximum breast growth, which occurs approximately 2-3 months after hormone initiation and peaks at 1-2 years.3 Rates of transfeminine individuals seeking augmentation mammoplasty is similar to that of their transmasculine counterparts at 74%.2 One referral letter from a mental health provider is also needed prior to augmentation mammoplasty.
Transfeminine patients who desire bottom surgery, which can involve an orchiectomy or vaginoplasty (single-stage penile inversion, peritoneal, or colonic interposition), have the same additional requirements as transmasculine individuals seeking bottom surgery. Furthermore, it is interesting to note that 25% of transfeminine individuals had already undergone orchiectomy and 87% had either undergone or desired a vaginoplasty in the future.2 This is in stark contrast to transmasculine patients and rates of bottom surgery.
Unless there is a specific medical contraindication to hormone therapy, emphasis is placed on 12 months of continuous hormone usage. Additional emphasis is placed on patients seeking bottom surgery to live for a minimum of 12 months in their congruent gender role. This also allows patients to further explore their gender identity and make appropriate preparations for surgery.
As with any surgical procedure, obtaining informed consent and reviewing patient expectations are key. In my clinical practice, I discuss with patients that the general surgical goals are to achieve both function and good aesthetic outcome but that their results are also tailored to their individual bodies. Assessing a patient’s support system and social factors is also equally important in the preoperative planning period. As this field continues to grow, it is essential for providers to understand the evolving distinctions in surgical care to improve access to patients.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa. She has no conflicts. Email her at [email protected].
References
1. The World Professional Association for Transgender Health. Standards of Care for the Health of Transsexual, Transgender, and Gender Nonconforming People. https://www.wpath.org/publications/soc.
2. James SE et al. The report of the 2015 U.S. Transgender survey. Washington, D.C.: National Center for Transgender Equality. 2016.
3. Thomas TN. Overview of surgery for transgender patients, in “Comprehensive care for the transgender patient.” Philadelphia: Elsevier, 2020. pp. 48-53.
Gender-affirmation surgery refers to a collection of procedures by which a transgender individual physically alters characteristics to align with their gender identity. While not all patients who identify as transgender will choose to undergo surgery, the surgeries are considered medically necessary and lead to significant improvements in emotional and psychological well-being.1 With increasing insurance coverage and improved access to care, more and more patients are seeking gender-affirming surgery, and it is incumbent for providers to familiarize themselves with preoperative recommendations and requirements.
Ob.gyns. play a key role in patients seeking surgical treatment as patients may inquire about available procedures and what steps are necessary prior to scheduling a visit with the appropriate surgeon. The World Professional Association of Transgender Health has established standards of care that provide multidisciplinary, evidence-based guidance for patients seeking a variety of gender-affirming services ranging from mental health, hormone therapy, and surgery.
Basic preoperative surgical prerequisites set forth by WPATH include being a patient with well-documented gender dysphoria, being the age of majority, and having the ability to provide informed consent.1
As with any surgical candidate, it is also equally important for a patient to have well-controlled medical and psychiatric comorbidities, which should also include smoking cessation. A variety of surgical procedures are available to patients and include breast/chest surgery, genital (bottom) surgery, and nongenital surgery (facial feminization, pectoral implant placement, thyroid chondroplasty, lipofilling/liposuction, body contouring, and voice modification). Patients may choose to undergo chest/breast surgery and/or bottom surgery or forgo surgical procedures altogether.
For transmasculine patients, breast/chest surgery, otherwise known as top surgery, is the most common and desired procedure. According to a recent survey, approximately 97% of transmasculine patients had or wanted masculinizing chest surgery.2 In addition to patients meeting the basic requirements set forth by WPATH, one referral from a mental health provider specializing in gender-affirming care is also needed prior to this procedure. It is also important to note that testosterone use is no longer a needed prior to masculinizing chest surgery.
Transmasculine bottom surgery, which includes hysterectomy, bilateral salpingo-oophorectomy, metoidioplasty, vaginectomy, scrotoplasty, testicular implant placement, and/or phalloplasty have additional nuances. Compared with transmasculine individuals seeking top surgery, the number of patients who have had or desire metoidioplasty and phalloplasty is much lower, which is mainly because of the high complication rates of these procedures. In the same survey, only 4% of patients had undergone a metoidioplasty procedure and 2% of patients had undergone a phalloplasty.2
In evaluating rates of hysterectomy with or without salpingo-oophorectomy, approximately 21% of transgender men underwent hysterectomy, with 58% desiring it in the future.2 Unlike patients pursuing top surgery, patients who desire any form of bottom surgery need to be on 12 months of continuous hormone therapy.1 They also must provide two letters from two different mental health providers, one of whom must have either an MD/DO or PhD. In cases in which a patient requests a hysterectomy for reasons other than gender dysphoria, such as pelvic pain or abnormal uterine bleeding, these criteria do not apply.
For transfeminine individuals, augmentation mammoplasty is performed following 12 months of continuous hormone therapy. This is to allow maximum breast growth, which occurs approximately 2-3 months after hormone initiation and peaks at 1-2 years.3 Rates of transfeminine individuals seeking augmentation mammoplasty is similar to that of their transmasculine counterparts at 74%.2 One referral letter from a mental health provider is also needed prior to augmentation mammoplasty.
Transfeminine patients who desire bottom surgery, which can involve an orchiectomy or vaginoplasty (single-stage penile inversion, peritoneal, or colonic interposition), have the same additional requirements as transmasculine individuals seeking bottom surgery. Furthermore, it is interesting to note that 25% of transfeminine individuals had already undergone orchiectomy and 87% had either undergone or desired a vaginoplasty in the future.2 This is in stark contrast to transmasculine patients and rates of bottom surgery.
Unless there is a specific medical contraindication to hormone therapy, emphasis is placed on 12 months of continuous hormone usage. Additional emphasis is placed on patients seeking bottom surgery to live for a minimum of 12 months in their congruent gender role. This also allows patients to further explore their gender identity and make appropriate preparations for surgery.
As with any surgical procedure, obtaining informed consent and reviewing patient expectations are key. In my clinical practice, I discuss with patients that the general surgical goals are to achieve both function and good aesthetic outcome but that their results are also tailored to their individual bodies. Assessing a patient’s support system and social factors is also equally important in the preoperative planning period. As this field continues to grow, it is essential for providers to understand the evolving distinctions in surgical care to improve access to patients.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa. She has no conflicts. Email her at [email protected].
References
1. The World Professional Association for Transgender Health. Standards of Care for the Health of Transsexual, Transgender, and Gender Nonconforming People. https://www.wpath.org/publications/soc.
2. James SE et al. The report of the 2015 U.S. Transgender survey. Washington, D.C.: National Center for Transgender Equality. 2016.
3. Thomas TN. Overview of surgery for transgender patients, in “Comprehensive care for the transgender patient.” Philadelphia: Elsevier, 2020. pp. 48-53.
The male biological clock – How to tell the time
For decades, we have recognized the age-related natural decline in female fecundity (the ability to reproduce) after the age of 30 (Maturitas 1988;[Suppl]1:15-22). Advanced maternal age (AMA) has also been demonstrated to increase miscarriage and pregnancies with chromosomal abnormalities, presumably from the increased rate of oocyte aneuploidy. There has been a sixfold increase in the rate of first birth in women aged 35-39 years (NCHS Data Brief 2014;152:1-8). Consequently, over the last decade, women, often before they reach AMA, have turned to elective oocyte cryopreservation for fertility preservation.
Ovarian aging
Ovarian aging occurs through the decline in quality and quantity of oocytes. The former is a reflection of the woman’s chronologic age. Markers of female ovarian aging have been utilized, for the past 3 decades, most commonly by basal follicle stimulating hormone. Currently, to assess the quantity of ovarian follicles, antimüllerian hormone (AMH) and transvaginal ultrasound for ovarian antral follicle count (AFC) are the most accurate indicators (J Clin Endocrinol Metab 2004:89:2977-81). While ovarian age testing, particularly AMH, has been widely used to assess a woman’s “fertility potential,” it does not reflect her natural fecundity. In a prospective cohort study, AMH levels (ng/mL) divided into < 0.7, 0.7-8.4, and > 8.4, did not affect natural conception in women aged 30-44 who were divided into the categories of <35, 35-37, or 38-44 years (JAMA 2017;318:1367-76). Although AMH does reduce success with IVF, its main value is the inverse correlation when prescribing gonadotropin dosage for controlled ovarian stimulation.
Despite the familiarity with ovarian aging effects on fertility, the male biological clock remains less studied and understood. Over the last 4 decades, paternal age has increased an average of 3.5 years presumably due to delayed child rearing from professional or personal reasons, improved contraception as well as increased divorce, remarriage, and life expectancy (Hum Reprod. 2017;32:2110-6). Nevertheless, we have little data to definitively counsel men on the effects of advanced paternal age (APA) and no consensus on an actual defined age of designation. This month’s article will summarize the current literature on male age and its impact on fertility.
Testicular aging
Men older than 45 years require approximately five times longer to achieve a pregnancy as men less than 25 after adjustment for female age (Fertil Steril. 2003;79:1520-7). The most likely parameter to assess male fertility, other than pregnancy rates, would be the sperm. Sperm counts, beginning at age 41, may decline but concentrations have been shown to increase in older men apparently because of declining semen volume (Ageing Res Rev. 2015;19:22-33). Sperm motility, but not morphology, also declines while genetic alterations of sperm increase with age. The issue of chromosomal abnormalities in sperm from men of advanced age appears to be similar to that in the oocytes of women with AMA. Consequently, both sexes may contribute to embryo aneuploidy resulting in declining fertility and increasing miscarriage.
For all ages, studies have suggested that elevated male body mass index as well as alcohol consumption and cigarette smoking, including e-cigarettes, can lead to impaired sperm production (Hum Reprod Update 2013;19:221-31).
Fertility treatment outcomes
A mainstay of fertility treatment, particularly in men with mild to moderate impairments in semen parameters, is ovulation induction with intrauterine insemination. Male age has been shown to be a significant indicator for pregnancy rates, including those with normal semen parameters (J Obstet Gynaecol. 2011;31:420-3). Men above age 45 contributed to lower pregnancy rates and higher miscarriages during IUI treatment cycles (Reprod BioMed Online 2008;17:392-7).
During IVF cycles, the sperm of men with APA often undergo ICSI (intracytoplasmic sperm injection) due to higher fertilization rates compared with standard insemination. However, APA sperm appear to have lower fertilization rates and decreased embryo development to the blastocyst stage during cycles using donor oocytes, although pregnancy outcomes are inconsistent (Trans Androl Urol. 2019;8[Suppl 1]:S22-S30; Fertil Steril. 2008;90:97-103).
Perinatal and children’s health
The offspring from APA men appear to have higher rates of stillbirth, low birth weight, and preterm birth, as well as birth defects. Men older than 40-45 years have twice the risk of an autistic child and three times the risk of schizophrenia in their offspring (Transl Psychiatry 2017;7:e1019; Am J Psychiatry 2002;159:1528-33).
Conclusions
Most of the literature supports negative effects on sperm and reproduction from men with APA. The challenge in deciphering the true role of APA on fertility is that the partner is often of AMA. A consideration to avoid this effect would be sperm cryopreservation at a younger age, similar to the common trend among women. Preimplantation genetic testing of embryos from men with APA is also a potential option to reduce miscarriage and avoid a chromosomally abnormal pregnancy. Ethicists have pondered the impact of APA on parenthood and the detrimental effect of early paternal death on the child. Nevertheless, the effect of APA in reproduction is a vital area to study with the same fervor as AMA (Fertil Steril 2009;92:1772-5).
Dr. Trolice is director of Fertility CARE – The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando. He has no conflicts. Email him at [email protected].
For decades, we have recognized the age-related natural decline in female fecundity (the ability to reproduce) after the age of 30 (Maturitas 1988;[Suppl]1:15-22). Advanced maternal age (AMA) has also been demonstrated to increase miscarriage and pregnancies with chromosomal abnormalities, presumably from the increased rate of oocyte aneuploidy. There has been a sixfold increase in the rate of first birth in women aged 35-39 years (NCHS Data Brief 2014;152:1-8). Consequently, over the last decade, women, often before they reach AMA, have turned to elective oocyte cryopreservation for fertility preservation.
Ovarian aging
Ovarian aging occurs through the decline in quality and quantity of oocytes. The former is a reflection of the woman’s chronologic age. Markers of female ovarian aging have been utilized, for the past 3 decades, most commonly by basal follicle stimulating hormone. Currently, to assess the quantity of ovarian follicles, antimüllerian hormone (AMH) and transvaginal ultrasound for ovarian antral follicle count (AFC) are the most accurate indicators (J Clin Endocrinol Metab 2004:89:2977-81). While ovarian age testing, particularly AMH, has been widely used to assess a woman’s “fertility potential,” it does not reflect her natural fecundity. In a prospective cohort study, AMH levels (ng/mL) divided into < 0.7, 0.7-8.4, and > 8.4, did not affect natural conception in women aged 30-44 who were divided into the categories of <35, 35-37, or 38-44 years (JAMA 2017;318:1367-76). Although AMH does reduce success with IVF, its main value is the inverse correlation when prescribing gonadotropin dosage for controlled ovarian stimulation.
Despite the familiarity with ovarian aging effects on fertility, the male biological clock remains less studied and understood. Over the last 4 decades, paternal age has increased an average of 3.5 years presumably due to delayed child rearing from professional or personal reasons, improved contraception as well as increased divorce, remarriage, and life expectancy (Hum Reprod. 2017;32:2110-6). Nevertheless, we have little data to definitively counsel men on the effects of advanced paternal age (APA) and no consensus on an actual defined age of designation. This month’s article will summarize the current literature on male age and its impact on fertility.
Testicular aging
Men older than 45 years require approximately five times longer to achieve a pregnancy as men less than 25 after adjustment for female age (Fertil Steril. 2003;79:1520-7). The most likely parameter to assess male fertility, other than pregnancy rates, would be the sperm. Sperm counts, beginning at age 41, may decline but concentrations have been shown to increase in older men apparently because of declining semen volume (Ageing Res Rev. 2015;19:22-33). Sperm motility, but not morphology, also declines while genetic alterations of sperm increase with age. The issue of chromosomal abnormalities in sperm from men of advanced age appears to be similar to that in the oocytes of women with AMA. Consequently, both sexes may contribute to embryo aneuploidy resulting in declining fertility and increasing miscarriage.
For all ages, studies have suggested that elevated male body mass index as well as alcohol consumption and cigarette smoking, including e-cigarettes, can lead to impaired sperm production (Hum Reprod Update 2013;19:221-31).
Fertility treatment outcomes
A mainstay of fertility treatment, particularly in men with mild to moderate impairments in semen parameters, is ovulation induction with intrauterine insemination. Male age has been shown to be a significant indicator for pregnancy rates, including those with normal semen parameters (J Obstet Gynaecol. 2011;31:420-3). Men above age 45 contributed to lower pregnancy rates and higher miscarriages during IUI treatment cycles (Reprod BioMed Online 2008;17:392-7).
During IVF cycles, the sperm of men with APA often undergo ICSI (intracytoplasmic sperm injection) due to higher fertilization rates compared with standard insemination. However, APA sperm appear to have lower fertilization rates and decreased embryo development to the blastocyst stage during cycles using donor oocytes, although pregnancy outcomes are inconsistent (Trans Androl Urol. 2019;8[Suppl 1]:S22-S30; Fertil Steril. 2008;90:97-103).
Perinatal and children’s health
The offspring from APA men appear to have higher rates of stillbirth, low birth weight, and preterm birth, as well as birth defects. Men older than 40-45 years have twice the risk of an autistic child and three times the risk of schizophrenia in their offspring (Transl Psychiatry 2017;7:e1019; Am J Psychiatry 2002;159:1528-33).
Conclusions
Most of the literature supports negative effects on sperm and reproduction from men with APA. The challenge in deciphering the true role of APA on fertility is that the partner is often of AMA. A consideration to avoid this effect would be sperm cryopreservation at a younger age, similar to the common trend among women. Preimplantation genetic testing of embryos from men with APA is also a potential option to reduce miscarriage and avoid a chromosomally abnormal pregnancy. Ethicists have pondered the impact of APA on parenthood and the detrimental effect of early paternal death on the child. Nevertheless, the effect of APA in reproduction is a vital area to study with the same fervor as AMA (Fertil Steril 2009;92:1772-5).
Dr. Trolice is director of Fertility CARE – The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando. He has no conflicts. Email him at [email protected].
For decades, we have recognized the age-related natural decline in female fecundity (the ability to reproduce) after the age of 30 (Maturitas 1988;[Suppl]1:15-22). Advanced maternal age (AMA) has also been demonstrated to increase miscarriage and pregnancies with chromosomal abnormalities, presumably from the increased rate of oocyte aneuploidy. There has been a sixfold increase in the rate of first birth in women aged 35-39 years (NCHS Data Brief 2014;152:1-8). Consequently, over the last decade, women, often before they reach AMA, have turned to elective oocyte cryopreservation for fertility preservation.
Ovarian aging
Ovarian aging occurs through the decline in quality and quantity of oocytes. The former is a reflection of the woman’s chronologic age. Markers of female ovarian aging have been utilized, for the past 3 decades, most commonly by basal follicle stimulating hormone. Currently, to assess the quantity of ovarian follicles, antimüllerian hormone (AMH) and transvaginal ultrasound for ovarian antral follicle count (AFC) are the most accurate indicators (J Clin Endocrinol Metab 2004:89:2977-81). While ovarian age testing, particularly AMH, has been widely used to assess a woman’s “fertility potential,” it does not reflect her natural fecundity. In a prospective cohort study, AMH levels (ng/mL) divided into < 0.7, 0.7-8.4, and > 8.4, did not affect natural conception in women aged 30-44 who were divided into the categories of <35, 35-37, or 38-44 years (JAMA 2017;318:1367-76). Although AMH does reduce success with IVF, its main value is the inverse correlation when prescribing gonadotropin dosage for controlled ovarian stimulation.
Despite the familiarity with ovarian aging effects on fertility, the male biological clock remains less studied and understood. Over the last 4 decades, paternal age has increased an average of 3.5 years presumably due to delayed child rearing from professional or personal reasons, improved contraception as well as increased divorce, remarriage, and life expectancy (Hum Reprod. 2017;32:2110-6). Nevertheless, we have little data to definitively counsel men on the effects of advanced paternal age (APA) and no consensus on an actual defined age of designation. This month’s article will summarize the current literature on male age and its impact on fertility.
Testicular aging
Men older than 45 years require approximately five times longer to achieve a pregnancy as men less than 25 after adjustment for female age (Fertil Steril. 2003;79:1520-7). The most likely parameter to assess male fertility, other than pregnancy rates, would be the sperm. Sperm counts, beginning at age 41, may decline but concentrations have been shown to increase in older men apparently because of declining semen volume (Ageing Res Rev. 2015;19:22-33). Sperm motility, but not morphology, also declines while genetic alterations of sperm increase with age. The issue of chromosomal abnormalities in sperm from men of advanced age appears to be similar to that in the oocytes of women with AMA. Consequently, both sexes may contribute to embryo aneuploidy resulting in declining fertility and increasing miscarriage.
For all ages, studies have suggested that elevated male body mass index as well as alcohol consumption and cigarette smoking, including e-cigarettes, can lead to impaired sperm production (Hum Reprod Update 2013;19:221-31).
Fertility treatment outcomes
A mainstay of fertility treatment, particularly in men with mild to moderate impairments in semen parameters, is ovulation induction with intrauterine insemination. Male age has been shown to be a significant indicator for pregnancy rates, including those with normal semen parameters (J Obstet Gynaecol. 2011;31:420-3). Men above age 45 contributed to lower pregnancy rates and higher miscarriages during IUI treatment cycles (Reprod BioMed Online 2008;17:392-7).
During IVF cycles, the sperm of men with APA often undergo ICSI (intracytoplasmic sperm injection) due to higher fertilization rates compared with standard insemination. However, APA sperm appear to have lower fertilization rates and decreased embryo development to the blastocyst stage during cycles using donor oocytes, although pregnancy outcomes are inconsistent (Trans Androl Urol. 2019;8[Suppl 1]:S22-S30; Fertil Steril. 2008;90:97-103).
Perinatal and children’s health
The offspring from APA men appear to have higher rates of stillbirth, low birth weight, and preterm birth, as well as birth defects. Men older than 40-45 years have twice the risk of an autistic child and three times the risk of schizophrenia in their offspring (Transl Psychiatry 2017;7:e1019; Am J Psychiatry 2002;159:1528-33).
Conclusions
Most of the literature supports negative effects on sperm and reproduction from men with APA. The challenge in deciphering the true role of APA on fertility is that the partner is often of AMA. A consideration to avoid this effect would be sperm cryopreservation at a younger age, similar to the common trend among women. Preimplantation genetic testing of embryos from men with APA is also a potential option to reduce miscarriage and avoid a chromosomally abnormal pregnancy. Ethicists have pondered the impact of APA on parenthood and the detrimental effect of early paternal death on the child. Nevertheless, the effect of APA in reproduction is a vital area to study with the same fervor as AMA (Fertil Steril 2009;92:1772-5).
Dr. Trolice is director of Fertility CARE – The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando. He has no conflicts. Email him at [email protected].
What if your patient refuses to disrobe?
Sterling Ransone Jr., MD, a family physician in Deltaville, Va., knocked on the exam room door and entered to find the patient, a 28-year-old woman, seated on the examination table. She was complaining about a fever, sore throat, and congestion.
Dr. Ransone asked if it was okay for him to lift her shirt and listen to her heart. She shook her head slightly. He decided to listen without removing the clothing, but when he put one hand on her shoulder and the stethoscope on her back, she flinched.
Instead of proceeding with the examination, Dr. Ransone, who is president-elect of the American Academy of Family Physicians, asked the patient whether everything was okay. It turned out that she had been the victim of a sexual assault and did not want a male to remove any clothing or touch her chest or back. Fortunately, Dr. Ransone’s practice had a female partner, who came in and listened to the patient’s chest.
“I’m glad I asked the patient what was going on for her because otherwise, I wouldn’t have known what she was going through,” Dr. Ransone said. “The patient felt respected and safe, and the therapeutic relationship was enhanced instead of compromised.”
Patient dignity is one of Dr. Ransone’s most important professional values. He recounts that during rounds in medical school, the attending and several interns and students crowded into the semiprivate room of an elderly woman who was lying in bed. The attending pulled off the bed covers, leaving the patient exposed while he discussed her case.
“I was mortified for her, and I learned a lot from watching this unfold, just seeing this woman lying naked in front all of these strangers and God,” said Dr. Ransone, physician practice director at Riverside Fishing Bay Family Practice, Deltaville, and assistant clinical professor of family medicine and population health at Virginia Commonwealth University, in Richmond. “I’ve been in practice for 25 years, and making sure the patient feels comfortable and respected is one of my priorities that dates back to that very first encounter.”
Trauma-informed care
Trauma is a common reason why patients feel reluctant to remove their clothing, according to Lauren Radziejewski, DNP, ANP-BC, clinical program manager, Mount Sinai Center for Transgender Medicine and Surgery, New York.
“We teach and endorse trauma-informed care for any type of procedure that is potentially triggering, and I would certainly put any type of care where people have to take off their clothes as potentially triggering,” she said.
Trauma can be caused by many factors. “Traumas of a sexual nature – having been subjected to sexual violence, for example – are the most obvious that come to mind, but any trauma that involves violation and disempowerment, even a nonsexual one, can make people more reluctant to be in a sensitive situation that can be perceived as invasive or disempowering,” Dr. Radziejewski said.
Talk before you touch
There are other reasons, often multiple intersecting reasons, why patients are reluctant to disrobe, according to Alicia Arbaje, MD, MPH, PhD, associate professor of medicine and director of transitional care research at the Center for Transformative Geriatrics Research, division of geriatric medicine and gerontology, Johns Hopkins University, Baltimore. These include culture and religion, generational sensitivities, and body discomfort associated with transitional times in life (e.g., teen or menopausal years).
Some general approaches apply, regardless of the reason for the patient’s discomfort. Others are specific to the patient’s particular problem or concern, Dr. Arbaje said.
“So much of medicine in this day and age is to quickly get down to business, hurry, and move on to the next patient,” said Dr. Arbaje, who also serves as chair of the American Geriatric Society’s Public Education Committee. “But establishing a little bit of a relationship is crucial before beginning the physical exam with any patient, especially with seniors or other patients who might have particular discomforts.”
She advises practitioners to “spend time talking before touching.” In other words, “Find a way to create some kind of meeting, even very briefly, and establish rapport before the patient changes into a gown and before you touch the patient to examine him or her.”
She acknowledged this might be difficult to do in certain clinical settings, but “to whatever extent you can, try to build this extra time and extra step into your workflow.”
She suggested that physicians first meet with the patient in the office or examining room to hear about his or her concerns. If a gown is necessary, the patient can change into one after the physician leaves the room. This builds trust and rapport.
Choice of language is important, especially when talking with older individuals. “Address the patient by their title until you are told not to – Ms. or Mrs. Smith, or Mr. Jones – or ask, ‘How would you like to be addressed?’ And don’t use terms of endearment, like ‘dear’ or ‘sweetie,’ or the plural, such as ‘How are we feeling today?’ “ These are “infantilizing and patronizing” and can impact the patient’s level of comfort with the entire appointment, including undressing and being examined.
Regarding transgender people, “many have experienced sexual violence and inappropriate touching, but even those fortunate enough to have escaped that type of common problem typically have still undergone traumatic experiences just by being transgender, having been socialized incorrectly, misunderstood, or having the ‘wrong’ genitalia,” said Dr. Radziejewski.
Particularly when dealing with a transgender patient, “you have to assume that there may be a history of trauma. Be sensitive to the patient’s discomforts about disrobing, recognize the examination itself as a potential trigger, and take appropriate measures to mitigate the trauma.”
To do this, Dr. Radziejewski gives her patients a “menu of options,” because “when people are navigating the world after trauma, including marginalized identity, they often have a complete loss of control, so the key is to give them as much control as possible every step of the way.”
For example, Dr. Radziejewski might tell a transgender masculine patient, “I’m looking through your chart and see no documented Pap test.” She acknowledges that after explaining why the test is recommended, the patient might be uncomfortable with it. She then makes a series of suggestions that range from being completely noninvasive to more invasive.
“You can say you don’t want it at all, or you can take a swab that I will give you and do it in the bathroom yourself. If you’re more comfortable with a man performing it, I can arrange that, or if you’re more comfortable with someone other than myself – your regular provider – I can arrange that, too.” By the end of the interaction, most patients are comfortable with Dr. Radziejewski performing the exam.
Regarding invasive exams, she recommends setting up an appointment specifically dedicated to that exam, rather than trying to cram a sensitive process into the time allotted for a patent visit, when other topics are also being discussed. “This also reinforces a sense of control,” she said.
This approach is relevant not only for transgender patients but also for any patient who has experienced trauma or some type of shame associated with the body, she said.
Dr. Ransone asks transgender patients what pronoun they would like him to use when he addresses them.
Prior to the examination, talking about what will be done and why further enhances trust, comfort, and rapport.
Who should be present?
Dr. Arbaje suggested that the pre-examination conversation should include a discussion of who the patient would like to have present during the exam. This is particularly relevant with a geriatric patient who might have been brought in by a family member or caregiver.
Similarly, adolescents may not feel comfortable with a parent being present for an examination. To protect the teen’s privacy, Dr. Ransone asks parents to step out. “There are also subjects that adolescents won’t bring up if their parents are there,” he said.
A question that is relevant in many clinical settings is whether the presence of a chaperone enhances or detracts from the patient’s comfort. Although the use of chaperones is recommended by many societies, it is a judgment call whether a chaperone should be present during all examinations – unless the state in which one practices requires it. Seven states mandate the presence of a chaperone during an intimate exam: Alabama, Delaware, Georgia, Montana, New Jersey, Ohio, and Tennessee.
Dr. Ransone utilizes a medical scribe to take notes on patient visits. The nurse or medical assistant who escorts the patient into the exam room informs the patient that a scribe will be in the room but that the patient should feel free to say whether he or she wants to talk about something privately, in which case the scribe will leave.
Dr. Ransone’s scribe is female and serves as the chaperone during an intimate exam of a female patient. “I have assumed, and my established patients know, that there will be a chaperone present, but my patients also know they can ask for the chaperone to step out,” he said. “When that happens, I document the discussion in the patient’s chart for my own legal protection.”
He recommended that practices consider posting signage or including information about chaperones in the practice’s informational brochures regarding policies and procedures.
Armin Brott, MBA, senior editor of Talking About Men’s Health , said that having a chaperone in the room when a female practitioner is examining a male patient – even if the chaperone is male – would be “extremely uncomfortable, weird, and even voyeuristic for the male patient.”
He noted that typically, male physicians use a chaperone when examining a female patient “for their own legal self-protection and maybe to make the female patient more comfortable, but female physicians are typically less concerned about potentially being accused of violating a male patient and typically do not have chaperones.”
Men face unique challenges
Men have “unique needs and challenges” when it comes to healthcare, said Mr. Brott, an advisory board member of the Men’s Health Network.
Mr. Brott cited research showing that men do not seek healthcare as frequently as women do. “So it’s already hard to get men in the door of a doctor, no matter what the provider’s gender is,” he said. Notably, men are even less likely to seek medical care when the clinician is female, owing to discomfort at having to undergo an intimate exam.
“I think that many men have issues about sexuality and of becoming aroused during an exam if it’s a female practitioner doing the exam,” said Mr. Brott. “I’m sure this is something physicians and nurses are accustomed to, but for the patient, it’s extremely embarrassing. The man may worry that he’ll be perceived as making unwanted sexual overtures to the practitioner.”
The way to mitigate these concerns is through communication, according to Mr. Brott. He recalled his own experience during a catherization conducted by a female practitioner he had never met. “She came in and started dealing with me as if I wasn’t even a person. She didn’t say much. It would have helped if she had created some type of human connection and talked to me – something like, ‘I’ve done this a thousand times and here’s what you’ll be feeling,’ or, “Would you like me to describe what I’m doing, or just do it as quickly as possible?’ ”
On another occasion, Mr. Brott underwent a procedure that was performed by two female practitioners, who were more communicative and even brought some light humor to the encounter, “which set me at ease,” he said.
If a man does become aroused, reassurance would be helpful, Mr. Brott said. “You can say something like, ‘Don’t worry, it’s perfectly natural, it happens all the time. Let’s finish up, and I’ll be out of your way as soon as I can.’ ”
Explain at every step of the way
All the experts emphasize the critical importance of continuing to offer explanations throughout the exam, even if the exam has been discussed beforehand.
“During the exam, it’s key to explain what you’re doing each step of the way – especially with seniors, but with other patients too,” said Arbaje. “For example, ‘I’d like you to remove your arms from your shirt so I can examine the joint better.’ Often there’s apprehension about what you’re going to do next. You can also ask, ‘Is there anything I should know before I examine this part of you? How are you doing?’ “ She advised asking the patient for “ongoing feedback. ‘Is this okay? Is this too rough?’ “
This is especially important when conducting a pelvic exam or palpating the patient’s abdomen, which is a more personal area than, say, the knee. Only the body part that is being examined should be uncovered, and it should be re-covered after the exam of that body part is complete and a different body part is to then be examined.
Asking for feedback is especially important, because many older patients have been acculturated not to question physicians and other medical authorities and may suffer a sense of humiliation silently.
Dr. Arbaje noted that feedback can be nonverbal: “For example, wincing or flinching are signs of discomfort you should ask the patient about or empathetically acknowledge.”
Rapport building doesn’t end after the examination
Dr. Arbaje advises physicians to “spend a little more time with the patient after the examination and not just walk out the door, leaving the person as they are, half undressed or in a gown.”
In the case of an older person, this might involve helping patients get their shoes and socks on or helping them get off the table. “Spend some time closing the encounter, not just doing what you need to do and then leaving or leaving it for someone else or family to do, which can be very dehumanizing,” she said. Even a few minutes of human contact beyond the examination can enhance rapport and help the patient feel respected and more comfortable.
Setting the stage: Create a conducive office environment
Setting patients at ease begins well before the patient enters the examination room, experts say. The overall atmosphere of the practice – the professionalism, courtesy, and friendliness of the staff – contributes to a sense of safety that will set the stage for the patient to feel more comfortable disrobing, if necessary, and being examined.
Mr. Brott pointed out that most medical offices tend to be more “female-friendly” in decor, utilizing pastel colors and flower motifs, for example, and displaying women’s magazines in the waiting room. Gender-neutral decor and different types of reading materials might set men at ease. Receptionists and medical staff are often female, and it is helpful for practices to employ male staff to bring the patient into the examination room or check vital signs. “This would go a long way toward making a man feel welcome and comfortable, even if the physician is female,” he said.
Dr. Radziejewski agreed: “If possible, having male and female support staff available will set patients of any gender at their ease.”
The setup of the examination room may contribute to a patient’s level of comfort. In Dr. Ransone’s examination room, the patient faces the door when on the table, and the door is locked during the exam so that no one can enter.
“I think that if patients are facing away from the door, they may feel claustrophobic or trapped, and I don’t want to position myself between the patient and an exit,” Dr. Ransone said. “My exam room happens to have no windows, but I’ve seen situations where the patient is lying on the table, exposed in front of the window, which can feel vulnerable, even if the office is on a high floor and no one can see into the window.”
Dr. Ransone positions the scribe or chaperone to the side, where the patient can see them, but not directly in front, where the examination might be visible to them. “I think it would be more uncomfortable and anxiety provoking knowing that someone is standing behind me and I can’t see them,” he said.
Choosing the best gown ... when necessary
Is it necessary for patients to disrobe and put on a gown — especially in light of the fact that research suggests that wearing a gown can induce psychological distress?
Danielle Ofri, MD, PhD, clinical professor, department of medicine, NYU Grossman School of Medicine, New York, said that in her practice, patients wear street clothes unless the patient is to undergo a full physical exam.
Even an abdominal exam can be conducted by loosening and slightly lowering the pants. Dr. Ofri stresses that patients should retain full control over how much to expose: “The patient should always take the lead in adjusting or opening clothing for a focused physical exam. And, of course, we always need to ask permission before starting any part of the exam.”
A gown is more conducive for certain exams, such as pelvic or breast exams. Dr. Ransone said that cloth gowns are preferable to paper gowns, which can tear more easily and so lead to unnecessary exposure. Gowns that hang open at the back should be avoided. If that’s the only type available, a second gown can be provided so as to cover the backside.
This is especially important if the examination involves walking across the room – for example, to evaluate gait – or standing on the scale. Alternatively, the patient can be given a sheet to drape over the gown, which can be moved around during the examination.
Dr. Ransome’s own practice uses gowns that fully wrap around the person. “I’ve seen too many people in gowns that are too small, so I make sure the patient has an appropriately sized gown. The extra material also leaves room for draping, while exposing only the part of the body that’s necessary,” he said.
Numerous types of modest gowns are now available, including kimono-type gowns with ties and snaps that allow partial exposure. All the experts encouraged utilizing these or similar types of gowns if possible.
Cultural and religious considerations
It is important for clinicians to be sensitive to cultural and religious factors that might affect patients’ attitudes toward attire and opposite-sex practitioners, said Dr. Ofri, an internist at Bellevue Hospital, New York.
For example, in Islamic and ultra-Orthodox Jewish traditions, certain parts of the body may not be exposed in the presence of a man who is unrelated by blood or marriage. Studies have shown that Hispanic and Asian women have avoided mammography because of embarrassment.
Dr. Arbaje described a 90-year-old patient whose physician ordered a pelvic ultrasound. The ultrasound department conducted the test transvaginally. “The patient, a widow, came from a Catholic background and regarded this as tantamount to ‘cheating’ on her deceased husband, and she felt violated and ashamed,” Dr. Arbaje said.
Dr. Ofri, who is the author of Medicine in Translation: Journeys With My Patients, said that she has Muslim and Orthodox Jewish male patients who allow her to examine their knees but won’t shake her hand because of the prohibition against touching an unrelated woman. Muslim female patients are willing to unsnap their veils because Dr. Ofri is female, but they would be uncomfortable with a male practitioner.
Whenever possible, gender-concordant care should be provided. If that is not possible, patients should be offered the option of not undergoing the examination, unless it’s an emergent situation, Dr. Ofri said. It may be necessary to reschedule the appointment to a time when a same-sex practitioner is available or to refer the patient to another practitioner.
Keeping cultural and religious considerations in mind is important, but there are variations in any given culture or religion. Practitioners should take cues directly from the patient, the experts advise.
Meeting the needs of cognitively impaired patients
Patients who are cognitively impaired have particular needs, Dr. Arbaje says. Many such patients are seniors with dementia, although developmental disabilities, neurodegenerative diseases, and other problems that affect cognition can occur among patients of any age and stage of life.
“People with dementia don’t necessarily understand what you’re doing and why you’re touching them. Even people with advanced dementia often retain a sense of modesty and may feel humiliated by an examination,” Dr. Arbaje said.
Dr. Arbaje encourages offering clear explanations of what is being done. The language one uses should be respectful and nonpatronizing, even if the patient does not understand what is being said. However, the bulk of one’s communication should be nonverbal. “Convey gentleness, safety, and reassurance through your tone and touch,” Dr. Arbaje said.
For cognitively impaired patient, it is helpful for a trusted family member or caregiver to be present during the examination, rather than a stranger. Depending on the degree of impairment, it might also be helpful for them to have a familiar object, perhaps a blanket; the odor and texture can convey familiarity and reassurance.
Nonclinical touch can also be reassuring. “We’re often scared of touching a patient because we don’t want to be considered inappropriate, but people who have dementia in later life are often understimulated, in terms of loving and caring touch,” she said. “For people in that situation, touch is typically of a practical or clinical nature – like bathing the person or taking their blood pressure. Providing reassuring touch or having someone else present to do so can help ease the patient’s fear and can be very healing.”
Making your patient’s eyes light up
“I can’t even count how many times I’ve had patients thank me for just explaining things clearly and giving them the right to opt out of wearing a gown or having an examination or procedure,” Dr. Radziejewski said.
“Obviously, I express recommendations, strong recommendations, but people like to know this is a place where they’ll be acknowledged for who they are, where they can feel safe and their dignity will be preserved. That should be the environment for any patient, whatever their culture, religion, age, background, or sexual identity. Offering that type of venue makes their eyes light up and makes all the difference in adherence to my recommendations and feeling empowered to truly care for their health,” she said.
A version of this article first appeared on Medscape.com.
Sterling Ransone Jr., MD, a family physician in Deltaville, Va., knocked on the exam room door and entered to find the patient, a 28-year-old woman, seated on the examination table. She was complaining about a fever, sore throat, and congestion.
Dr. Ransone asked if it was okay for him to lift her shirt and listen to her heart. She shook her head slightly. He decided to listen without removing the clothing, but when he put one hand on her shoulder and the stethoscope on her back, she flinched.
Instead of proceeding with the examination, Dr. Ransone, who is president-elect of the American Academy of Family Physicians, asked the patient whether everything was okay. It turned out that she had been the victim of a sexual assault and did not want a male to remove any clothing or touch her chest or back. Fortunately, Dr. Ransone’s practice had a female partner, who came in and listened to the patient’s chest.
“I’m glad I asked the patient what was going on for her because otherwise, I wouldn’t have known what she was going through,” Dr. Ransone said. “The patient felt respected and safe, and the therapeutic relationship was enhanced instead of compromised.”
Patient dignity is one of Dr. Ransone’s most important professional values. He recounts that during rounds in medical school, the attending and several interns and students crowded into the semiprivate room of an elderly woman who was lying in bed. The attending pulled off the bed covers, leaving the patient exposed while he discussed her case.
“I was mortified for her, and I learned a lot from watching this unfold, just seeing this woman lying naked in front all of these strangers and God,” said Dr. Ransone, physician practice director at Riverside Fishing Bay Family Practice, Deltaville, and assistant clinical professor of family medicine and population health at Virginia Commonwealth University, in Richmond. “I’ve been in practice for 25 years, and making sure the patient feels comfortable and respected is one of my priorities that dates back to that very first encounter.”
Trauma-informed care
Trauma is a common reason why patients feel reluctant to remove their clothing, according to Lauren Radziejewski, DNP, ANP-BC, clinical program manager, Mount Sinai Center for Transgender Medicine and Surgery, New York.
“We teach and endorse trauma-informed care for any type of procedure that is potentially triggering, and I would certainly put any type of care where people have to take off their clothes as potentially triggering,” she said.
Trauma can be caused by many factors. “Traumas of a sexual nature – having been subjected to sexual violence, for example – are the most obvious that come to mind, but any trauma that involves violation and disempowerment, even a nonsexual one, can make people more reluctant to be in a sensitive situation that can be perceived as invasive or disempowering,” Dr. Radziejewski said.
Talk before you touch
There are other reasons, often multiple intersecting reasons, why patients are reluctant to disrobe, according to Alicia Arbaje, MD, MPH, PhD, associate professor of medicine and director of transitional care research at the Center for Transformative Geriatrics Research, division of geriatric medicine and gerontology, Johns Hopkins University, Baltimore. These include culture and religion, generational sensitivities, and body discomfort associated with transitional times in life (e.g., teen or menopausal years).
Some general approaches apply, regardless of the reason for the patient’s discomfort. Others are specific to the patient’s particular problem or concern, Dr. Arbaje said.
“So much of medicine in this day and age is to quickly get down to business, hurry, and move on to the next patient,” said Dr. Arbaje, who also serves as chair of the American Geriatric Society’s Public Education Committee. “But establishing a little bit of a relationship is crucial before beginning the physical exam with any patient, especially with seniors or other patients who might have particular discomforts.”
She advises practitioners to “spend time talking before touching.” In other words, “Find a way to create some kind of meeting, even very briefly, and establish rapport before the patient changes into a gown and before you touch the patient to examine him or her.”
She acknowledged this might be difficult to do in certain clinical settings, but “to whatever extent you can, try to build this extra time and extra step into your workflow.”
She suggested that physicians first meet with the patient in the office or examining room to hear about his or her concerns. If a gown is necessary, the patient can change into one after the physician leaves the room. This builds trust and rapport.
Choice of language is important, especially when talking with older individuals. “Address the patient by their title until you are told not to – Ms. or Mrs. Smith, or Mr. Jones – or ask, ‘How would you like to be addressed?’ And don’t use terms of endearment, like ‘dear’ or ‘sweetie,’ or the plural, such as ‘How are we feeling today?’ “ These are “infantilizing and patronizing” and can impact the patient’s level of comfort with the entire appointment, including undressing and being examined.
Regarding transgender people, “many have experienced sexual violence and inappropriate touching, but even those fortunate enough to have escaped that type of common problem typically have still undergone traumatic experiences just by being transgender, having been socialized incorrectly, misunderstood, or having the ‘wrong’ genitalia,” said Dr. Radziejewski.
Particularly when dealing with a transgender patient, “you have to assume that there may be a history of trauma. Be sensitive to the patient’s discomforts about disrobing, recognize the examination itself as a potential trigger, and take appropriate measures to mitigate the trauma.”
To do this, Dr. Radziejewski gives her patients a “menu of options,” because “when people are navigating the world after trauma, including marginalized identity, they often have a complete loss of control, so the key is to give them as much control as possible every step of the way.”
For example, Dr. Radziejewski might tell a transgender masculine patient, “I’m looking through your chart and see no documented Pap test.” She acknowledges that after explaining why the test is recommended, the patient might be uncomfortable with it. She then makes a series of suggestions that range from being completely noninvasive to more invasive.
“You can say you don’t want it at all, or you can take a swab that I will give you and do it in the bathroom yourself. If you’re more comfortable with a man performing it, I can arrange that, or if you’re more comfortable with someone other than myself – your regular provider – I can arrange that, too.” By the end of the interaction, most patients are comfortable with Dr. Radziejewski performing the exam.
Regarding invasive exams, she recommends setting up an appointment specifically dedicated to that exam, rather than trying to cram a sensitive process into the time allotted for a patent visit, when other topics are also being discussed. “This also reinforces a sense of control,” she said.
This approach is relevant not only for transgender patients but also for any patient who has experienced trauma or some type of shame associated with the body, she said.
Dr. Ransone asks transgender patients what pronoun they would like him to use when he addresses them.
Prior to the examination, talking about what will be done and why further enhances trust, comfort, and rapport.
Who should be present?
Dr. Arbaje suggested that the pre-examination conversation should include a discussion of who the patient would like to have present during the exam. This is particularly relevant with a geriatric patient who might have been brought in by a family member or caregiver.
Similarly, adolescents may not feel comfortable with a parent being present for an examination. To protect the teen’s privacy, Dr. Ransone asks parents to step out. “There are also subjects that adolescents won’t bring up if their parents are there,” he said.
A question that is relevant in many clinical settings is whether the presence of a chaperone enhances or detracts from the patient’s comfort. Although the use of chaperones is recommended by many societies, it is a judgment call whether a chaperone should be present during all examinations – unless the state in which one practices requires it. Seven states mandate the presence of a chaperone during an intimate exam: Alabama, Delaware, Georgia, Montana, New Jersey, Ohio, and Tennessee.
Dr. Ransone utilizes a medical scribe to take notes on patient visits. The nurse or medical assistant who escorts the patient into the exam room informs the patient that a scribe will be in the room but that the patient should feel free to say whether he or she wants to talk about something privately, in which case the scribe will leave.
Dr. Ransone’s scribe is female and serves as the chaperone during an intimate exam of a female patient. “I have assumed, and my established patients know, that there will be a chaperone present, but my patients also know they can ask for the chaperone to step out,” he said. “When that happens, I document the discussion in the patient’s chart for my own legal protection.”
He recommended that practices consider posting signage or including information about chaperones in the practice’s informational brochures regarding policies and procedures.
Armin Brott, MBA, senior editor of Talking About Men’s Health , said that having a chaperone in the room when a female practitioner is examining a male patient – even if the chaperone is male – would be “extremely uncomfortable, weird, and even voyeuristic for the male patient.”
He noted that typically, male physicians use a chaperone when examining a female patient “for their own legal self-protection and maybe to make the female patient more comfortable, but female physicians are typically less concerned about potentially being accused of violating a male patient and typically do not have chaperones.”
Men face unique challenges
Men have “unique needs and challenges” when it comes to healthcare, said Mr. Brott, an advisory board member of the Men’s Health Network.
Mr. Brott cited research showing that men do not seek healthcare as frequently as women do. “So it’s already hard to get men in the door of a doctor, no matter what the provider’s gender is,” he said. Notably, men are even less likely to seek medical care when the clinician is female, owing to discomfort at having to undergo an intimate exam.
“I think that many men have issues about sexuality and of becoming aroused during an exam if it’s a female practitioner doing the exam,” said Mr. Brott. “I’m sure this is something physicians and nurses are accustomed to, but for the patient, it’s extremely embarrassing. The man may worry that he’ll be perceived as making unwanted sexual overtures to the practitioner.”
The way to mitigate these concerns is through communication, according to Mr. Brott. He recalled his own experience during a catherization conducted by a female practitioner he had never met. “She came in and started dealing with me as if I wasn’t even a person. She didn’t say much. It would have helped if she had created some type of human connection and talked to me – something like, ‘I’ve done this a thousand times and here’s what you’ll be feeling,’ or, “Would you like me to describe what I’m doing, or just do it as quickly as possible?’ ”
On another occasion, Mr. Brott underwent a procedure that was performed by two female practitioners, who were more communicative and even brought some light humor to the encounter, “which set me at ease,” he said.
If a man does become aroused, reassurance would be helpful, Mr. Brott said. “You can say something like, ‘Don’t worry, it’s perfectly natural, it happens all the time. Let’s finish up, and I’ll be out of your way as soon as I can.’ ”
Explain at every step of the way
All the experts emphasize the critical importance of continuing to offer explanations throughout the exam, even if the exam has been discussed beforehand.
“During the exam, it’s key to explain what you’re doing each step of the way – especially with seniors, but with other patients too,” said Arbaje. “For example, ‘I’d like you to remove your arms from your shirt so I can examine the joint better.’ Often there’s apprehension about what you’re going to do next. You can also ask, ‘Is there anything I should know before I examine this part of you? How are you doing?’ “ She advised asking the patient for “ongoing feedback. ‘Is this okay? Is this too rough?’ “
This is especially important when conducting a pelvic exam or palpating the patient’s abdomen, which is a more personal area than, say, the knee. Only the body part that is being examined should be uncovered, and it should be re-covered after the exam of that body part is complete and a different body part is to then be examined.
Asking for feedback is especially important, because many older patients have been acculturated not to question physicians and other medical authorities and may suffer a sense of humiliation silently.
Dr. Arbaje noted that feedback can be nonverbal: “For example, wincing or flinching are signs of discomfort you should ask the patient about or empathetically acknowledge.”
Rapport building doesn’t end after the examination
Dr. Arbaje advises physicians to “spend a little more time with the patient after the examination and not just walk out the door, leaving the person as they are, half undressed or in a gown.”
In the case of an older person, this might involve helping patients get their shoes and socks on or helping them get off the table. “Spend some time closing the encounter, not just doing what you need to do and then leaving or leaving it for someone else or family to do, which can be very dehumanizing,” she said. Even a few minutes of human contact beyond the examination can enhance rapport and help the patient feel respected and more comfortable.
Setting the stage: Create a conducive office environment
Setting patients at ease begins well before the patient enters the examination room, experts say. The overall atmosphere of the practice – the professionalism, courtesy, and friendliness of the staff – contributes to a sense of safety that will set the stage for the patient to feel more comfortable disrobing, if necessary, and being examined.
Mr. Brott pointed out that most medical offices tend to be more “female-friendly” in decor, utilizing pastel colors and flower motifs, for example, and displaying women’s magazines in the waiting room. Gender-neutral decor and different types of reading materials might set men at ease. Receptionists and medical staff are often female, and it is helpful for practices to employ male staff to bring the patient into the examination room or check vital signs. “This would go a long way toward making a man feel welcome and comfortable, even if the physician is female,” he said.
Dr. Radziejewski agreed: “If possible, having male and female support staff available will set patients of any gender at their ease.”
The setup of the examination room may contribute to a patient’s level of comfort. In Dr. Ransone’s examination room, the patient faces the door when on the table, and the door is locked during the exam so that no one can enter.
“I think that if patients are facing away from the door, they may feel claustrophobic or trapped, and I don’t want to position myself between the patient and an exit,” Dr. Ransone said. “My exam room happens to have no windows, but I’ve seen situations where the patient is lying on the table, exposed in front of the window, which can feel vulnerable, even if the office is on a high floor and no one can see into the window.”
Dr. Ransone positions the scribe or chaperone to the side, where the patient can see them, but not directly in front, where the examination might be visible to them. “I think it would be more uncomfortable and anxiety provoking knowing that someone is standing behind me and I can’t see them,” he said.
Choosing the best gown ... when necessary
Is it necessary for patients to disrobe and put on a gown — especially in light of the fact that research suggests that wearing a gown can induce psychological distress?
Danielle Ofri, MD, PhD, clinical professor, department of medicine, NYU Grossman School of Medicine, New York, said that in her practice, patients wear street clothes unless the patient is to undergo a full physical exam.
Even an abdominal exam can be conducted by loosening and slightly lowering the pants. Dr. Ofri stresses that patients should retain full control over how much to expose: “The patient should always take the lead in adjusting or opening clothing for a focused physical exam. And, of course, we always need to ask permission before starting any part of the exam.”
A gown is more conducive for certain exams, such as pelvic or breast exams. Dr. Ransone said that cloth gowns are preferable to paper gowns, which can tear more easily and so lead to unnecessary exposure. Gowns that hang open at the back should be avoided. If that’s the only type available, a second gown can be provided so as to cover the backside.
This is especially important if the examination involves walking across the room – for example, to evaluate gait – or standing on the scale. Alternatively, the patient can be given a sheet to drape over the gown, which can be moved around during the examination.
Dr. Ransome’s own practice uses gowns that fully wrap around the person. “I’ve seen too many people in gowns that are too small, so I make sure the patient has an appropriately sized gown. The extra material also leaves room for draping, while exposing only the part of the body that’s necessary,” he said.
Numerous types of modest gowns are now available, including kimono-type gowns with ties and snaps that allow partial exposure. All the experts encouraged utilizing these or similar types of gowns if possible.
Cultural and religious considerations
It is important for clinicians to be sensitive to cultural and religious factors that might affect patients’ attitudes toward attire and opposite-sex practitioners, said Dr. Ofri, an internist at Bellevue Hospital, New York.
For example, in Islamic and ultra-Orthodox Jewish traditions, certain parts of the body may not be exposed in the presence of a man who is unrelated by blood or marriage. Studies have shown that Hispanic and Asian women have avoided mammography because of embarrassment.
Dr. Arbaje described a 90-year-old patient whose physician ordered a pelvic ultrasound. The ultrasound department conducted the test transvaginally. “The patient, a widow, came from a Catholic background and regarded this as tantamount to ‘cheating’ on her deceased husband, and she felt violated and ashamed,” Dr. Arbaje said.
Dr. Ofri, who is the author of Medicine in Translation: Journeys With My Patients, said that she has Muslim and Orthodox Jewish male patients who allow her to examine their knees but won’t shake her hand because of the prohibition against touching an unrelated woman. Muslim female patients are willing to unsnap their veils because Dr. Ofri is female, but they would be uncomfortable with a male practitioner.
Whenever possible, gender-concordant care should be provided. If that is not possible, patients should be offered the option of not undergoing the examination, unless it’s an emergent situation, Dr. Ofri said. It may be necessary to reschedule the appointment to a time when a same-sex practitioner is available or to refer the patient to another practitioner.
Keeping cultural and religious considerations in mind is important, but there are variations in any given culture or religion. Practitioners should take cues directly from the patient, the experts advise.
Meeting the needs of cognitively impaired patients
Patients who are cognitively impaired have particular needs, Dr. Arbaje says. Many such patients are seniors with dementia, although developmental disabilities, neurodegenerative diseases, and other problems that affect cognition can occur among patients of any age and stage of life.
“People with dementia don’t necessarily understand what you’re doing and why you’re touching them. Even people with advanced dementia often retain a sense of modesty and may feel humiliated by an examination,” Dr. Arbaje said.
Dr. Arbaje encourages offering clear explanations of what is being done. The language one uses should be respectful and nonpatronizing, even if the patient does not understand what is being said. However, the bulk of one’s communication should be nonverbal. “Convey gentleness, safety, and reassurance through your tone and touch,” Dr. Arbaje said.
For cognitively impaired patient, it is helpful for a trusted family member or caregiver to be present during the examination, rather than a stranger. Depending on the degree of impairment, it might also be helpful for them to have a familiar object, perhaps a blanket; the odor and texture can convey familiarity and reassurance.
Nonclinical touch can also be reassuring. “We’re often scared of touching a patient because we don’t want to be considered inappropriate, but people who have dementia in later life are often understimulated, in terms of loving and caring touch,” she said. “For people in that situation, touch is typically of a practical or clinical nature – like bathing the person or taking their blood pressure. Providing reassuring touch or having someone else present to do so can help ease the patient’s fear and can be very healing.”
Making your patient’s eyes light up
“I can’t even count how many times I’ve had patients thank me for just explaining things clearly and giving them the right to opt out of wearing a gown or having an examination or procedure,” Dr. Radziejewski said.
“Obviously, I express recommendations, strong recommendations, but people like to know this is a place where they’ll be acknowledged for who they are, where they can feel safe and their dignity will be preserved. That should be the environment for any patient, whatever their culture, religion, age, background, or sexual identity. Offering that type of venue makes their eyes light up and makes all the difference in adherence to my recommendations and feeling empowered to truly care for their health,” she said.
A version of this article first appeared on Medscape.com.
Sterling Ransone Jr., MD, a family physician in Deltaville, Va., knocked on the exam room door and entered to find the patient, a 28-year-old woman, seated on the examination table. She was complaining about a fever, sore throat, and congestion.
Dr. Ransone asked if it was okay for him to lift her shirt and listen to her heart. She shook her head slightly. He decided to listen without removing the clothing, but when he put one hand on her shoulder and the stethoscope on her back, she flinched.
Instead of proceeding with the examination, Dr. Ransone, who is president-elect of the American Academy of Family Physicians, asked the patient whether everything was okay. It turned out that she had been the victim of a sexual assault and did not want a male to remove any clothing or touch her chest or back. Fortunately, Dr. Ransone’s practice had a female partner, who came in and listened to the patient’s chest.
“I’m glad I asked the patient what was going on for her because otherwise, I wouldn’t have known what she was going through,” Dr. Ransone said. “The patient felt respected and safe, and the therapeutic relationship was enhanced instead of compromised.”
Patient dignity is one of Dr. Ransone’s most important professional values. He recounts that during rounds in medical school, the attending and several interns and students crowded into the semiprivate room of an elderly woman who was lying in bed. The attending pulled off the bed covers, leaving the patient exposed while he discussed her case.
“I was mortified for her, and I learned a lot from watching this unfold, just seeing this woman lying naked in front all of these strangers and God,” said Dr. Ransone, physician practice director at Riverside Fishing Bay Family Practice, Deltaville, and assistant clinical professor of family medicine and population health at Virginia Commonwealth University, in Richmond. “I’ve been in practice for 25 years, and making sure the patient feels comfortable and respected is one of my priorities that dates back to that very first encounter.”
Trauma-informed care
Trauma is a common reason why patients feel reluctant to remove their clothing, according to Lauren Radziejewski, DNP, ANP-BC, clinical program manager, Mount Sinai Center for Transgender Medicine and Surgery, New York.
“We teach and endorse trauma-informed care for any type of procedure that is potentially triggering, and I would certainly put any type of care where people have to take off their clothes as potentially triggering,” she said.
Trauma can be caused by many factors. “Traumas of a sexual nature – having been subjected to sexual violence, for example – are the most obvious that come to mind, but any trauma that involves violation and disempowerment, even a nonsexual one, can make people more reluctant to be in a sensitive situation that can be perceived as invasive or disempowering,” Dr. Radziejewski said.
Talk before you touch
There are other reasons, often multiple intersecting reasons, why patients are reluctant to disrobe, according to Alicia Arbaje, MD, MPH, PhD, associate professor of medicine and director of transitional care research at the Center for Transformative Geriatrics Research, division of geriatric medicine and gerontology, Johns Hopkins University, Baltimore. These include culture and religion, generational sensitivities, and body discomfort associated with transitional times in life (e.g., teen or menopausal years).
Some general approaches apply, regardless of the reason for the patient’s discomfort. Others are specific to the patient’s particular problem or concern, Dr. Arbaje said.
“So much of medicine in this day and age is to quickly get down to business, hurry, and move on to the next patient,” said Dr. Arbaje, who also serves as chair of the American Geriatric Society’s Public Education Committee. “But establishing a little bit of a relationship is crucial before beginning the physical exam with any patient, especially with seniors or other patients who might have particular discomforts.”
She advises practitioners to “spend time talking before touching.” In other words, “Find a way to create some kind of meeting, even very briefly, and establish rapport before the patient changes into a gown and before you touch the patient to examine him or her.”
She acknowledged this might be difficult to do in certain clinical settings, but “to whatever extent you can, try to build this extra time and extra step into your workflow.”
She suggested that physicians first meet with the patient in the office or examining room to hear about his or her concerns. If a gown is necessary, the patient can change into one after the physician leaves the room. This builds trust and rapport.
Choice of language is important, especially when talking with older individuals. “Address the patient by their title until you are told not to – Ms. or Mrs. Smith, or Mr. Jones – or ask, ‘How would you like to be addressed?’ And don’t use terms of endearment, like ‘dear’ or ‘sweetie,’ or the plural, such as ‘How are we feeling today?’ “ These are “infantilizing and patronizing” and can impact the patient’s level of comfort with the entire appointment, including undressing and being examined.
Regarding transgender people, “many have experienced sexual violence and inappropriate touching, but even those fortunate enough to have escaped that type of common problem typically have still undergone traumatic experiences just by being transgender, having been socialized incorrectly, misunderstood, or having the ‘wrong’ genitalia,” said Dr. Radziejewski.
Particularly when dealing with a transgender patient, “you have to assume that there may be a history of trauma. Be sensitive to the patient’s discomforts about disrobing, recognize the examination itself as a potential trigger, and take appropriate measures to mitigate the trauma.”
To do this, Dr. Radziejewski gives her patients a “menu of options,” because “when people are navigating the world after trauma, including marginalized identity, they often have a complete loss of control, so the key is to give them as much control as possible every step of the way.”
For example, Dr. Radziejewski might tell a transgender masculine patient, “I’m looking through your chart and see no documented Pap test.” She acknowledges that after explaining why the test is recommended, the patient might be uncomfortable with it. She then makes a series of suggestions that range from being completely noninvasive to more invasive.
“You can say you don’t want it at all, or you can take a swab that I will give you and do it in the bathroom yourself. If you’re more comfortable with a man performing it, I can arrange that, or if you’re more comfortable with someone other than myself – your regular provider – I can arrange that, too.” By the end of the interaction, most patients are comfortable with Dr. Radziejewski performing the exam.
Regarding invasive exams, she recommends setting up an appointment specifically dedicated to that exam, rather than trying to cram a sensitive process into the time allotted for a patent visit, when other topics are also being discussed. “This also reinforces a sense of control,” she said.
This approach is relevant not only for transgender patients but also for any patient who has experienced trauma or some type of shame associated with the body, she said.
Dr. Ransone asks transgender patients what pronoun they would like him to use when he addresses them.
Prior to the examination, talking about what will be done and why further enhances trust, comfort, and rapport.
Who should be present?
Dr. Arbaje suggested that the pre-examination conversation should include a discussion of who the patient would like to have present during the exam. This is particularly relevant with a geriatric patient who might have been brought in by a family member or caregiver.
Similarly, adolescents may not feel comfortable with a parent being present for an examination. To protect the teen’s privacy, Dr. Ransone asks parents to step out. “There are also subjects that adolescents won’t bring up if their parents are there,” he said.
A question that is relevant in many clinical settings is whether the presence of a chaperone enhances or detracts from the patient’s comfort. Although the use of chaperones is recommended by many societies, it is a judgment call whether a chaperone should be present during all examinations – unless the state in which one practices requires it. Seven states mandate the presence of a chaperone during an intimate exam: Alabama, Delaware, Georgia, Montana, New Jersey, Ohio, and Tennessee.
Dr. Ransone utilizes a medical scribe to take notes on patient visits. The nurse or medical assistant who escorts the patient into the exam room informs the patient that a scribe will be in the room but that the patient should feel free to say whether he or she wants to talk about something privately, in which case the scribe will leave.
Dr. Ransone’s scribe is female and serves as the chaperone during an intimate exam of a female patient. “I have assumed, and my established patients know, that there will be a chaperone present, but my patients also know they can ask for the chaperone to step out,” he said. “When that happens, I document the discussion in the patient’s chart for my own legal protection.”
He recommended that practices consider posting signage or including information about chaperones in the practice’s informational brochures regarding policies and procedures.
Armin Brott, MBA, senior editor of Talking About Men’s Health , said that having a chaperone in the room when a female practitioner is examining a male patient – even if the chaperone is male – would be “extremely uncomfortable, weird, and even voyeuristic for the male patient.”
He noted that typically, male physicians use a chaperone when examining a female patient “for their own legal self-protection and maybe to make the female patient more comfortable, but female physicians are typically less concerned about potentially being accused of violating a male patient and typically do not have chaperones.”
Men face unique challenges
Men have “unique needs and challenges” when it comes to healthcare, said Mr. Brott, an advisory board member of the Men’s Health Network.
Mr. Brott cited research showing that men do not seek healthcare as frequently as women do. “So it’s already hard to get men in the door of a doctor, no matter what the provider’s gender is,” he said. Notably, men are even less likely to seek medical care when the clinician is female, owing to discomfort at having to undergo an intimate exam.
“I think that many men have issues about sexuality and of becoming aroused during an exam if it’s a female practitioner doing the exam,” said Mr. Brott. “I’m sure this is something physicians and nurses are accustomed to, but for the patient, it’s extremely embarrassing. The man may worry that he’ll be perceived as making unwanted sexual overtures to the practitioner.”
The way to mitigate these concerns is through communication, according to Mr. Brott. He recalled his own experience during a catherization conducted by a female practitioner he had never met. “She came in and started dealing with me as if I wasn’t even a person. She didn’t say much. It would have helped if she had created some type of human connection and talked to me – something like, ‘I’ve done this a thousand times and here’s what you’ll be feeling,’ or, “Would you like me to describe what I’m doing, or just do it as quickly as possible?’ ”
On another occasion, Mr. Brott underwent a procedure that was performed by two female practitioners, who were more communicative and even brought some light humor to the encounter, “which set me at ease,” he said.
If a man does become aroused, reassurance would be helpful, Mr. Brott said. “You can say something like, ‘Don’t worry, it’s perfectly natural, it happens all the time. Let’s finish up, and I’ll be out of your way as soon as I can.’ ”
Explain at every step of the way
All the experts emphasize the critical importance of continuing to offer explanations throughout the exam, even if the exam has been discussed beforehand.
“During the exam, it’s key to explain what you’re doing each step of the way – especially with seniors, but with other patients too,” said Arbaje. “For example, ‘I’d like you to remove your arms from your shirt so I can examine the joint better.’ Often there’s apprehension about what you’re going to do next. You can also ask, ‘Is there anything I should know before I examine this part of you? How are you doing?’ “ She advised asking the patient for “ongoing feedback. ‘Is this okay? Is this too rough?’ “
This is especially important when conducting a pelvic exam or palpating the patient’s abdomen, which is a more personal area than, say, the knee. Only the body part that is being examined should be uncovered, and it should be re-covered after the exam of that body part is complete and a different body part is to then be examined.
Asking for feedback is especially important, because many older patients have been acculturated not to question physicians and other medical authorities and may suffer a sense of humiliation silently.
Dr. Arbaje noted that feedback can be nonverbal: “For example, wincing or flinching are signs of discomfort you should ask the patient about or empathetically acknowledge.”
Rapport building doesn’t end after the examination
Dr. Arbaje advises physicians to “spend a little more time with the patient after the examination and not just walk out the door, leaving the person as they are, half undressed or in a gown.”
In the case of an older person, this might involve helping patients get their shoes and socks on or helping them get off the table. “Spend some time closing the encounter, not just doing what you need to do and then leaving or leaving it for someone else or family to do, which can be very dehumanizing,” she said. Even a few minutes of human contact beyond the examination can enhance rapport and help the patient feel respected and more comfortable.
Setting the stage: Create a conducive office environment
Setting patients at ease begins well before the patient enters the examination room, experts say. The overall atmosphere of the practice – the professionalism, courtesy, and friendliness of the staff – contributes to a sense of safety that will set the stage for the patient to feel more comfortable disrobing, if necessary, and being examined.
Mr. Brott pointed out that most medical offices tend to be more “female-friendly” in decor, utilizing pastel colors and flower motifs, for example, and displaying women’s magazines in the waiting room. Gender-neutral decor and different types of reading materials might set men at ease. Receptionists and medical staff are often female, and it is helpful for practices to employ male staff to bring the patient into the examination room or check vital signs. “This would go a long way toward making a man feel welcome and comfortable, even if the physician is female,” he said.
Dr. Radziejewski agreed: “If possible, having male and female support staff available will set patients of any gender at their ease.”
The setup of the examination room may contribute to a patient’s level of comfort. In Dr. Ransone’s examination room, the patient faces the door when on the table, and the door is locked during the exam so that no one can enter.
“I think that if patients are facing away from the door, they may feel claustrophobic or trapped, and I don’t want to position myself between the patient and an exit,” Dr. Ransone said. “My exam room happens to have no windows, but I’ve seen situations where the patient is lying on the table, exposed in front of the window, which can feel vulnerable, even if the office is on a high floor and no one can see into the window.”
Dr. Ransone positions the scribe or chaperone to the side, where the patient can see them, but not directly in front, where the examination might be visible to them. “I think it would be more uncomfortable and anxiety provoking knowing that someone is standing behind me and I can’t see them,” he said.
Choosing the best gown ... when necessary
Is it necessary for patients to disrobe and put on a gown — especially in light of the fact that research suggests that wearing a gown can induce psychological distress?
Danielle Ofri, MD, PhD, clinical professor, department of medicine, NYU Grossman School of Medicine, New York, said that in her practice, patients wear street clothes unless the patient is to undergo a full physical exam.
Even an abdominal exam can be conducted by loosening and slightly lowering the pants. Dr. Ofri stresses that patients should retain full control over how much to expose: “The patient should always take the lead in adjusting or opening clothing for a focused physical exam. And, of course, we always need to ask permission before starting any part of the exam.”
A gown is more conducive for certain exams, such as pelvic or breast exams. Dr. Ransone said that cloth gowns are preferable to paper gowns, which can tear more easily and so lead to unnecessary exposure. Gowns that hang open at the back should be avoided. If that’s the only type available, a second gown can be provided so as to cover the backside.
This is especially important if the examination involves walking across the room – for example, to evaluate gait – or standing on the scale. Alternatively, the patient can be given a sheet to drape over the gown, which can be moved around during the examination.
Dr. Ransome’s own practice uses gowns that fully wrap around the person. “I’ve seen too many people in gowns that are too small, so I make sure the patient has an appropriately sized gown. The extra material also leaves room for draping, while exposing only the part of the body that’s necessary,” he said.
Numerous types of modest gowns are now available, including kimono-type gowns with ties and snaps that allow partial exposure. All the experts encouraged utilizing these or similar types of gowns if possible.
Cultural and religious considerations
It is important for clinicians to be sensitive to cultural and religious factors that might affect patients’ attitudes toward attire and opposite-sex practitioners, said Dr. Ofri, an internist at Bellevue Hospital, New York.
For example, in Islamic and ultra-Orthodox Jewish traditions, certain parts of the body may not be exposed in the presence of a man who is unrelated by blood or marriage. Studies have shown that Hispanic and Asian women have avoided mammography because of embarrassment.
Dr. Arbaje described a 90-year-old patient whose physician ordered a pelvic ultrasound. The ultrasound department conducted the test transvaginally. “The patient, a widow, came from a Catholic background and regarded this as tantamount to ‘cheating’ on her deceased husband, and she felt violated and ashamed,” Dr. Arbaje said.
Dr. Ofri, who is the author of Medicine in Translation: Journeys With My Patients, said that she has Muslim and Orthodox Jewish male patients who allow her to examine their knees but won’t shake her hand because of the prohibition against touching an unrelated woman. Muslim female patients are willing to unsnap their veils because Dr. Ofri is female, but they would be uncomfortable with a male practitioner.
Whenever possible, gender-concordant care should be provided. If that is not possible, patients should be offered the option of not undergoing the examination, unless it’s an emergent situation, Dr. Ofri said. It may be necessary to reschedule the appointment to a time when a same-sex practitioner is available or to refer the patient to another practitioner.
Keeping cultural and religious considerations in mind is important, but there are variations in any given culture or religion. Practitioners should take cues directly from the patient, the experts advise.
Meeting the needs of cognitively impaired patients
Patients who are cognitively impaired have particular needs, Dr. Arbaje says. Many such patients are seniors with dementia, although developmental disabilities, neurodegenerative diseases, and other problems that affect cognition can occur among patients of any age and stage of life.
“People with dementia don’t necessarily understand what you’re doing and why you’re touching them. Even people with advanced dementia often retain a sense of modesty and may feel humiliated by an examination,” Dr. Arbaje said.
Dr. Arbaje encourages offering clear explanations of what is being done. The language one uses should be respectful and nonpatronizing, even if the patient does not understand what is being said. However, the bulk of one’s communication should be nonverbal. “Convey gentleness, safety, and reassurance through your tone and touch,” Dr. Arbaje said.
For cognitively impaired patient, it is helpful for a trusted family member or caregiver to be present during the examination, rather than a stranger. Depending on the degree of impairment, it might also be helpful for them to have a familiar object, perhaps a blanket; the odor and texture can convey familiarity and reassurance.
Nonclinical touch can also be reassuring. “We’re often scared of touching a patient because we don’t want to be considered inappropriate, but people who have dementia in later life are often understimulated, in terms of loving and caring touch,” she said. “For people in that situation, touch is typically of a practical or clinical nature – like bathing the person or taking their blood pressure. Providing reassuring touch or having someone else present to do so can help ease the patient’s fear and can be very healing.”
Making your patient’s eyes light up
“I can’t even count how many times I’ve had patients thank me for just explaining things clearly and giving them the right to opt out of wearing a gown or having an examination or procedure,” Dr. Radziejewski said.
“Obviously, I express recommendations, strong recommendations, but people like to know this is a place where they’ll be acknowledged for who they are, where they can feel safe and their dignity will be preserved. That should be the environment for any patient, whatever their culture, religion, age, background, or sexual identity. Offering that type of venue makes their eyes light up and makes all the difference in adherence to my recommendations and feeling empowered to truly care for their health,” she said.
A version of this article first appeared on Medscape.com.
CDC panel backs COVID-19 boosters for nearly all adults
Editor’s note: This story was updated with the CDC director’s endorsement.
Centers for Disease Control and Prevention (CDC) Director Rochelle Walensky, MD, has signed off on an advisory panel’s earlier unanimous vote to recommend boosters for the Moderna and Johnson and Johnson COVID vaccines.
The decision now means that millions of Americans are eligible to get a booster shot for either the Pfizer, Moderna, or J&J COVID vaccines.
“The evidence shows that all three COVID-19 vaccines authorized in the United States are safe – as demonstrated by the over 400 million vaccine doses already given. And, they are all highly effective in reducing the risk of severe disease, hospitalization, and death, even in the midst of the widely circulating Delta variant,” Dr. Walensky said in a CDC news release.
She also signed off on the panel’s suggestion that individuals can mix or match the booster from any one of the three available COVID-19 vaccines.
The Advisory Committee on Immunization Practices (ACIP) recommended in a late afternoon 15-0 vote that everyone over age 18 who are at least 2 months past their Johnson & Johnson vaccine should get a booster, an endorsement that affects an estimated 13 million Americans.
Those eligible for a booster at least 6 months after their last Moderna shot are the same groups who can get a Pfizer booster.
They are:
- Anyone over age 65.
- Those over age 18 with an underlying health condition that puts them at risk of severe COVID-19.
- Those over age 18 who may be at higher risk of a COVID-19 infection because they live or work in a risky setting.
These recommendations are in line with the Food and Drug Administration’s Oct. 20 authorization of the boosters, along with the ability to mix-and-match vaccines.
There are an estimated 47 million Pfizer recipients and 39 million people vaccinated with Moderna who are now eligible for a booster dose, according to data presented by the CDC.
Questions, concerns
Before voting, some committee members expressed discomfort in broadly recommending boosters, stressing that there is very little evidence supporting the need for boosters in people younger than age 50.
“I can’t say that I am comfortable that anybody under 50 – an otherwise healthy individual – needs a booster vaccine at this time with either Moderna or Pfizer,” said ACIP member Sarah Long, MD, professor of pediatrics at Drexel University in Philadelphia.
She said she would try to mitigate any potential harm by having some kind of age restriction on the otherwise worried well.
“We don’t usually have the vaccines [for] the worried well. We give it because we have a need that’s worth the risk, and there’s a burden of severity of disease,” Dr. Long said.
The evidence to date shows that all the vaccines authorized for use in the U.S. continue to protect people well against severe COVID-19 outcomes, including hospitalization and death.
But breakthrough infections are on the rise, especially for people who initially received the Johnson and Johnson one-dose vaccine.
On Oct. 21, Pfizer released data from a study of more than 10,000 fully vaccinated people. Half were randomly assigned to get a booster of their Comirnaty vaccine, the other half were given a placebo.
Over the ensuing 2.5 months, there were 5 COVID-19 cases in the boosted group, and 109 in the group that got a placebo.
The data were posted in a press release and have not yet been peer reviewed, but are the first to show clinical effectiveness of boosters at preventing COVID-19 infections.
Data recently considered by the FDA and CDC for booster doses come from studies that were mostly shorter and smaller. These studies looked at biomarkers of immunity like the concentration of antibodies in a person’s blood and the percentage of study participants who saw a boost to those antibodies.
The studies demonstrated that boosters indeed restore high levels of antibodies, but unlike the newest Pfizer data they were not able to show that these antibodies prevented COVID-19.
These studies also weren’t powered to pick up on any less common safety problems that might arise after another dose of the shots.
“Real world” recommendations
In the end, however, the panel felt it was more important to be permissive in allowing boosters so that individuals and their doctors could be free to make their own decisions.
“The decision made by the FDA and the ACIP recommendations, I think, reflects the real world. The public is going to do what they feel driven to do. This at least adds a scientific review of the currently available data,” said Jay Varkey, MD, an infectious disease physician and associate professor at Emory University in Atlanta, who was not involved in the ACIP’s deliberations.
Dr. Varkey said he would recommend that anyone who is younger than 65, and who has no underlying medical conditions such as diabetes or obesity, speak with their doctor about their individual benefits and risks before getting a booster.
The CDC is planning to release a detailed suite of clinical considerations to help people weigh the risks and benefits of getting a booster.
Safety updates presented at the meeting show that serious adverse events after vaccination are extremely rare, but in some cases, they may rise above the risk for those problems generally seen in the population.
Those rare events include the disabling autoimmune condition Guillain-Barré syndrome and the platelet disorder thrombosis with thrombocytopenia (TTS), which causes blood clots along with the risk of excess bleeding because of a low platelet count.
Both can occur after the J&J vaccine. Out of 15.3 million doses of the vaccine given to date, there have been 47 cases of TTS and five deaths. These events are more common in younger women.
The mRNA vaccines, such as those from Pfizer and Moderna, can cause heart inflammation called myocarditis or pericarditis. This side effect is more common in men 18-24 years old. The reported rate of myocarditis after vaccination is 39 cases for every 1 million doses.
In voting to permit boosters, committee member Wilbur Chen, MD, professor at the University of Maryland’s Center for Vaccine Development, said he hoped boosters wouldn’t give Americans false confidence.
Dr. Chen stressed that ending the pandemic would depend on “a multilayered approach” that includes masking, social distancing, avoiding large crowds indoors, and convincing more Americans to take their first doses of the vaccines.
“We’re not just going to vaccinate ourselves out of this situation,” Dr. Chen said.
A version of this article first appeared on WebMD.com.
Editor’s note: This story was updated with the CDC director’s endorsement.
Centers for Disease Control and Prevention (CDC) Director Rochelle Walensky, MD, has signed off on an advisory panel’s earlier unanimous vote to recommend boosters for the Moderna and Johnson and Johnson COVID vaccines.
The decision now means that millions of Americans are eligible to get a booster shot for either the Pfizer, Moderna, or J&J COVID vaccines.
“The evidence shows that all three COVID-19 vaccines authorized in the United States are safe – as demonstrated by the over 400 million vaccine doses already given. And, they are all highly effective in reducing the risk of severe disease, hospitalization, and death, even in the midst of the widely circulating Delta variant,” Dr. Walensky said in a CDC news release.
She also signed off on the panel’s suggestion that individuals can mix or match the booster from any one of the three available COVID-19 vaccines.
The Advisory Committee on Immunization Practices (ACIP) recommended in a late afternoon 15-0 vote that everyone over age 18 who are at least 2 months past their Johnson & Johnson vaccine should get a booster, an endorsement that affects an estimated 13 million Americans.
Those eligible for a booster at least 6 months after their last Moderna shot are the same groups who can get a Pfizer booster.
They are:
- Anyone over age 65.
- Those over age 18 with an underlying health condition that puts them at risk of severe COVID-19.
- Those over age 18 who may be at higher risk of a COVID-19 infection because they live or work in a risky setting.
These recommendations are in line with the Food and Drug Administration’s Oct. 20 authorization of the boosters, along with the ability to mix-and-match vaccines.
There are an estimated 47 million Pfizer recipients and 39 million people vaccinated with Moderna who are now eligible for a booster dose, according to data presented by the CDC.
Questions, concerns
Before voting, some committee members expressed discomfort in broadly recommending boosters, stressing that there is very little evidence supporting the need for boosters in people younger than age 50.
“I can’t say that I am comfortable that anybody under 50 – an otherwise healthy individual – needs a booster vaccine at this time with either Moderna or Pfizer,” said ACIP member Sarah Long, MD, professor of pediatrics at Drexel University in Philadelphia.
She said she would try to mitigate any potential harm by having some kind of age restriction on the otherwise worried well.
“We don’t usually have the vaccines [for] the worried well. We give it because we have a need that’s worth the risk, and there’s a burden of severity of disease,” Dr. Long said.
The evidence to date shows that all the vaccines authorized for use in the U.S. continue to protect people well against severe COVID-19 outcomes, including hospitalization and death.
But breakthrough infections are on the rise, especially for people who initially received the Johnson and Johnson one-dose vaccine.
On Oct. 21, Pfizer released data from a study of more than 10,000 fully vaccinated people. Half were randomly assigned to get a booster of their Comirnaty vaccine, the other half were given a placebo.
Over the ensuing 2.5 months, there were 5 COVID-19 cases in the boosted group, and 109 in the group that got a placebo.
The data were posted in a press release and have not yet been peer reviewed, but are the first to show clinical effectiveness of boosters at preventing COVID-19 infections.
Data recently considered by the FDA and CDC for booster doses come from studies that were mostly shorter and smaller. These studies looked at biomarkers of immunity like the concentration of antibodies in a person’s blood and the percentage of study participants who saw a boost to those antibodies.
The studies demonstrated that boosters indeed restore high levels of antibodies, but unlike the newest Pfizer data they were not able to show that these antibodies prevented COVID-19.
These studies also weren’t powered to pick up on any less common safety problems that might arise after another dose of the shots.
“Real world” recommendations
In the end, however, the panel felt it was more important to be permissive in allowing boosters so that individuals and their doctors could be free to make their own decisions.
“The decision made by the FDA and the ACIP recommendations, I think, reflects the real world. The public is going to do what they feel driven to do. This at least adds a scientific review of the currently available data,” said Jay Varkey, MD, an infectious disease physician and associate professor at Emory University in Atlanta, who was not involved in the ACIP’s deliberations.
Dr. Varkey said he would recommend that anyone who is younger than 65, and who has no underlying medical conditions such as diabetes or obesity, speak with their doctor about their individual benefits and risks before getting a booster.
The CDC is planning to release a detailed suite of clinical considerations to help people weigh the risks and benefits of getting a booster.
Safety updates presented at the meeting show that serious adverse events after vaccination are extremely rare, but in some cases, they may rise above the risk for those problems generally seen in the population.
Those rare events include the disabling autoimmune condition Guillain-Barré syndrome and the platelet disorder thrombosis with thrombocytopenia (TTS), which causes blood clots along with the risk of excess bleeding because of a low platelet count.
Both can occur after the J&J vaccine. Out of 15.3 million doses of the vaccine given to date, there have been 47 cases of TTS and five deaths. These events are more common in younger women.
The mRNA vaccines, such as those from Pfizer and Moderna, can cause heart inflammation called myocarditis or pericarditis. This side effect is more common in men 18-24 years old. The reported rate of myocarditis after vaccination is 39 cases for every 1 million doses.
In voting to permit boosters, committee member Wilbur Chen, MD, professor at the University of Maryland’s Center for Vaccine Development, said he hoped boosters wouldn’t give Americans false confidence.
Dr. Chen stressed that ending the pandemic would depend on “a multilayered approach” that includes masking, social distancing, avoiding large crowds indoors, and convincing more Americans to take their first doses of the vaccines.
“We’re not just going to vaccinate ourselves out of this situation,” Dr. Chen said.
A version of this article first appeared on WebMD.com.
Editor’s note: This story was updated with the CDC director’s endorsement.
Centers for Disease Control and Prevention (CDC) Director Rochelle Walensky, MD, has signed off on an advisory panel’s earlier unanimous vote to recommend boosters for the Moderna and Johnson and Johnson COVID vaccines.
The decision now means that millions of Americans are eligible to get a booster shot for either the Pfizer, Moderna, or J&J COVID vaccines.
“The evidence shows that all three COVID-19 vaccines authorized in the United States are safe – as demonstrated by the over 400 million vaccine doses already given. And, they are all highly effective in reducing the risk of severe disease, hospitalization, and death, even in the midst of the widely circulating Delta variant,” Dr. Walensky said in a CDC news release.
She also signed off on the panel’s suggestion that individuals can mix or match the booster from any one of the three available COVID-19 vaccines.
The Advisory Committee on Immunization Practices (ACIP) recommended in a late afternoon 15-0 vote that everyone over age 18 who are at least 2 months past their Johnson & Johnson vaccine should get a booster, an endorsement that affects an estimated 13 million Americans.
Those eligible for a booster at least 6 months after their last Moderna shot are the same groups who can get a Pfizer booster.
They are:
- Anyone over age 65.
- Those over age 18 with an underlying health condition that puts them at risk of severe COVID-19.
- Those over age 18 who may be at higher risk of a COVID-19 infection because they live or work in a risky setting.
These recommendations are in line with the Food and Drug Administration’s Oct. 20 authorization of the boosters, along with the ability to mix-and-match vaccines.
There are an estimated 47 million Pfizer recipients and 39 million people vaccinated with Moderna who are now eligible for a booster dose, according to data presented by the CDC.
Questions, concerns
Before voting, some committee members expressed discomfort in broadly recommending boosters, stressing that there is very little evidence supporting the need for boosters in people younger than age 50.
“I can’t say that I am comfortable that anybody under 50 – an otherwise healthy individual – needs a booster vaccine at this time with either Moderna or Pfizer,” said ACIP member Sarah Long, MD, professor of pediatrics at Drexel University in Philadelphia.
She said she would try to mitigate any potential harm by having some kind of age restriction on the otherwise worried well.
“We don’t usually have the vaccines [for] the worried well. We give it because we have a need that’s worth the risk, and there’s a burden of severity of disease,” Dr. Long said.
The evidence to date shows that all the vaccines authorized for use in the U.S. continue to protect people well against severe COVID-19 outcomes, including hospitalization and death.
But breakthrough infections are on the rise, especially for people who initially received the Johnson and Johnson one-dose vaccine.
On Oct. 21, Pfizer released data from a study of more than 10,000 fully vaccinated people. Half were randomly assigned to get a booster of their Comirnaty vaccine, the other half were given a placebo.
Over the ensuing 2.5 months, there were 5 COVID-19 cases in the boosted group, and 109 in the group that got a placebo.
The data were posted in a press release and have not yet been peer reviewed, but are the first to show clinical effectiveness of boosters at preventing COVID-19 infections.
Data recently considered by the FDA and CDC for booster doses come from studies that were mostly shorter and smaller. These studies looked at biomarkers of immunity like the concentration of antibodies in a person’s blood and the percentage of study participants who saw a boost to those antibodies.
The studies demonstrated that boosters indeed restore high levels of antibodies, but unlike the newest Pfizer data they were not able to show that these antibodies prevented COVID-19.
These studies also weren’t powered to pick up on any less common safety problems that might arise after another dose of the shots.
“Real world” recommendations
In the end, however, the panel felt it was more important to be permissive in allowing boosters so that individuals and their doctors could be free to make their own decisions.
“The decision made by the FDA and the ACIP recommendations, I think, reflects the real world. The public is going to do what they feel driven to do. This at least adds a scientific review of the currently available data,” said Jay Varkey, MD, an infectious disease physician and associate professor at Emory University in Atlanta, who was not involved in the ACIP’s deliberations.
Dr. Varkey said he would recommend that anyone who is younger than 65, and who has no underlying medical conditions such as diabetes or obesity, speak with their doctor about their individual benefits and risks before getting a booster.
The CDC is planning to release a detailed suite of clinical considerations to help people weigh the risks and benefits of getting a booster.
Safety updates presented at the meeting show that serious adverse events after vaccination are extremely rare, but in some cases, they may rise above the risk for those problems generally seen in the population.
Those rare events include the disabling autoimmune condition Guillain-Barré syndrome and the platelet disorder thrombosis with thrombocytopenia (TTS), which causes blood clots along with the risk of excess bleeding because of a low platelet count.
Both can occur after the J&J vaccine. Out of 15.3 million doses of the vaccine given to date, there have been 47 cases of TTS and five deaths. These events are more common in younger women.
The mRNA vaccines, such as those from Pfizer and Moderna, can cause heart inflammation called myocarditis or pericarditis. This side effect is more common in men 18-24 years old. The reported rate of myocarditis after vaccination is 39 cases for every 1 million doses.
In voting to permit boosters, committee member Wilbur Chen, MD, professor at the University of Maryland’s Center for Vaccine Development, said he hoped boosters wouldn’t give Americans false confidence.
Dr. Chen stressed that ending the pandemic would depend on “a multilayered approach” that includes masking, social distancing, avoiding large crowds indoors, and convincing more Americans to take their first doses of the vaccines.
“We’re not just going to vaccinate ourselves out of this situation,” Dr. Chen said.
A version of this article first appeared on WebMD.com.
COVID-19 pandemic affects menstrual cycles, presenting challenges for conception
A survey of more than 12,000 women of reproductive age found that one in three had experienced changes to their menstrual cycles and symptoms during the COVID-19 pandemic. Noticeably higher stress levels than prepandemic benchmarks could be affecting menstruation.
This has implications for women trying to conceive or struggling with infertility, said Shannon M. Malloy, a research and data associate with Ovia Health, a women’s and family health technology company in Boston. Ms. Malloy presented this study at the American Society of Reproductive Medicine’s 2021 meeting.
COVID-19 has introduced new psychosocial, interpersonal, and environmental stressors. The pandemic is “one of the most stressful, collectively experienced disasters modern society has ever seen,” said Ms. Malloy. Once imagined as an explicit event in time, COVID-19 has ingrained itself into daily life for the foreseeable future.
Research has shown that chronic, long-term stress produces high cortisol levels, which can alter endocrinology and regulation of menstrual cycles. This can make family building even more challenging, said Ms. Malloy. Physicians and other providers have always taken stress into account when managing patients, but never at this level of chronic, episodic stress, she said.
Survey examines impact on ART
Ovia Health decided to investigate the relationship between perceived stress and menstrual cycle and symptom changes during the COVID-19 pandemic, to see how it might affect assisted reproductive technology (ART).
From March 2020 to April 2021, users of Ovia Health’s Fertility mobile application in the United States took part in a survey. Items captured changes in menstruation pattern and symptomatology and included the Perceived Stress Scale 4-item version (PSS-4). A paired t-test evaluated differences between groups (menstrual changes versus no menstrual changes). The survey asked participants what changes they noticed in their menstrual cycle and why they thought cycle patterns or symptoms changed.
One-third report changes in cycle, symptoms
Among 12,302 respondents, 1 in 3 (36%) reported changes in cycle or symptoms. Eighty-seven percent said that their cycle started early or late. Twenty-nine percent reported stronger symptoms during menstruation such as low back pain, cramping, or discharge changes, and 27% said bleeding was heavier during periods.
These results are similar to other studies investigating the affect of episodic stress on menstruation, said Ms. Malloy.
Those who reported menstrual cycle or symptom changes scored higher on average on the PSS-4 compared with those who didn’t report any changes (8.5 v. 8.3, respectively, P < .05). PSS-4 scores across the board were notably higher in all respondents, regardless of cycle/symptom irregularity, compared with prepandemic benchmarking in similar populations.
Slightly more than half (55%) thought stress contributed to their menstrual cycle pattern and/or symptom changes, whereas 33% pointed to changes in mental health, such as depression or anxiety. “Interestingly, many users believed the COVID-19 vaccine impacted their menstrual cycle symptom changes,” said Ms. Malloy.
No definitive link between vaccine, menstruation
While known side effects of the vaccine include sore arm, fever, fatigue, and myalgia, some women have reported changes in their menstrual cycle, Mark P. Trolice, MD, professor of obstetrics and gynecology at the University of Central Florida and director of the IVF Center in Orlando, said in an interview.
“Vaccination reaction from the immune response rather than the vaccine may be the implicating factor,” said Dr. Trolice, who was not involved in the study.
Currently, there’s no direct link between the vaccine and subsequent effects on menstruation, he continued. “Most women experience resumption of normal intervals 1 month following vaccination. Further, there is no credible evidence that links the vaccine to infertility.
“Nevertheless, research in this area is vital and underway,” he added.
Physicians can help with stress
Menstrual cycle disruption is especially frustrating for women trying to build a family, said Ms. Malloy. Providers may be observing more menstrual irregularity in their patient populations, and seeing more patients struggle to conceive on their own, turning to ART.
Providers can’t make COVID-19 go away, but they could help patients by doing a better job of integrating mental health screening, connecting patients to treatments that optimize conception and fertility treatment outcomes, said Ms. Malloy.
The survey was limited in that its questions didn’t consider proper diagnostic criteria for irregularity, versus self-reported changes. But it does highlight the need for more research on the pandemic’s affect on menstruation and the vaccine on menstruation, said Ms. Malloy. “The National Institutes of Health in August committed $1.6 million to explore this connection. We’re looking forward to seeing what their results are.”
Dr. Trolice and Ms. Malloy had no disclosures.
A survey of more than 12,000 women of reproductive age found that one in three had experienced changes to their menstrual cycles and symptoms during the COVID-19 pandemic. Noticeably higher stress levels than prepandemic benchmarks could be affecting menstruation.
This has implications for women trying to conceive or struggling with infertility, said Shannon M. Malloy, a research and data associate with Ovia Health, a women’s and family health technology company in Boston. Ms. Malloy presented this study at the American Society of Reproductive Medicine’s 2021 meeting.
COVID-19 has introduced new psychosocial, interpersonal, and environmental stressors. The pandemic is “one of the most stressful, collectively experienced disasters modern society has ever seen,” said Ms. Malloy. Once imagined as an explicit event in time, COVID-19 has ingrained itself into daily life for the foreseeable future.
Research has shown that chronic, long-term stress produces high cortisol levels, which can alter endocrinology and regulation of menstrual cycles. This can make family building even more challenging, said Ms. Malloy. Physicians and other providers have always taken stress into account when managing patients, but never at this level of chronic, episodic stress, she said.
Survey examines impact on ART
Ovia Health decided to investigate the relationship between perceived stress and menstrual cycle and symptom changes during the COVID-19 pandemic, to see how it might affect assisted reproductive technology (ART).
From March 2020 to April 2021, users of Ovia Health’s Fertility mobile application in the United States took part in a survey. Items captured changes in menstruation pattern and symptomatology and included the Perceived Stress Scale 4-item version (PSS-4). A paired t-test evaluated differences between groups (menstrual changes versus no menstrual changes). The survey asked participants what changes they noticed in their menstrual cycle and why they thought cycle patterns or symptoms changed.
One-third report changes in cycle, symptoms
Among 12,302 respondents, 1 in 3 (36%) reported changes in cycle or symptoms. Eighty-seven percent said that their cycle started early or late. Twenty-nine percent reported stronger symptoms during menstruation such as low back pain, cramping, or discharge changes, and 27% said bleeding was heavier during periods.
These results are similar to other studies investigating the affect of episodic stress on menstruation, said Ms. Malloy.
Those who reported menstrual cycle or symptom changes scored higher on average on the PSS-4 compared with those who didn’t report any changes (8.5 v. 8.3, respectively, P < .05). PSS-4 scores across the board were notably higher in all respondents, regardless of cycle/symptom irregularity, compared with prepandemic benchmarking in similar populations.
Slightly more than half (55%) thought stress contributed to their menstrual cycle pattern and/or symptom changes, whereas 33% pointed to changes in mental health, such as depression or anxiety. “Interestingly, many users believed the COVID-19 vaccine impacted their menstrual cycle symptom changes,” said Ms. Malloy.
No definitive link between vaccine, menstruation
While known side effects of the vaccine include sore arm, fever, fatigue, and myalgia, some women have reported changes in their menstrual cycle, Mark P. Trolice, MD, professor of obstetrics and gynecology at the University of Central Florida and director of the IVF Center in Orlando, said in an interview.
“Vaccination reaction from the immune response rather than the vaccine may be the implicating factor,” said Dr. Trolice, who was not involved in the study.
Currently, there’s no direct link between the vaccine and subsequent effects on menstruation, he continued. “Most women experience resumption of normal intervals 1 month following vaccination. Further, there is no credible evidence that links the vaccine to infertility.
“Nevertheless, research in this area is vital and underway,” he added.
Physicians can help with stress
Menstrual cycle disruption is especially frustrating for women trying to build a family, said Ms. Malloy. Providers may be observing more menstrual irregularity in their patient populations, and seeing more patients struggle to conceive on their own, turning to ART.
Providers can’t make COVID-19 go away, but they could help patients by doing a better job of integrating mental health screening, connecting patients to treatments that optimize conception and fertility treatment outcomes, said Ms. Malloy.
The survey was limited in that its questions didn’t consider proper diagnostic criteria for irregularity, versus self-reported changes. But it does highlight the need for more research on the pandemic’s affect on menstruation and the vaccine on menstruation, said Ms. Malloy. “The National Institutes of Health in August committed $1.6 million to explore this connection. We’re looking forward to seeing what their results are.”
Dr. Trolice and Ms. Malloy had no disclosures.
A survey of more than 12,000 women of reproductive age found that one in three had experienced changes to their menstrual cycles and symptoms during the COVID-19 pandemic. Noticeably higher stress levels than prepandemic benchmarks could be affecting menstruation.
This has implications for women trying to conceive or struggling with infertility, said Shannon M. Malloy, a research and data associate with Ovia Health, a women’s and family health technology company in Boston. Ms. Malloy presented this study at the American Society of Reproductive Medicine’s 2021 meeting.
COVID-19 has introduced new psychosocial, interpersonal, and environmental stressors. The pandemic is “one of the most stressful, collectively experienced disasters modern society has ever seen,” said Ms. Malloy. Once imagined as an explicit event in time, COVID-19 has ingrained itself into daily life for the foreseeable future.
Research has shown that chronic, long-term stress produces high cortisol levels, which can alter endocrinology and regulation of menstrual cycles. This can make family building even more challenging, said Ms. Malloy. Physicians and other providers have always taken stress into account when managing patients, but never at this level of chronic, episodic stress, she said.
Survey examines impact on ART
Ovia Health decided to investigate the relationship between perceived stress and menstrual cycle and symptom changes during the COVID-19 pandemic, to see how it might affect assisted reproductive technology (ART).
From March 2020 to April 2021, users of Ovia Health’s Fertility mobile application in the United States took part in a survey. Items captured changes in menstruation pattern and symptomatology and included the Perceived Stress Scale 4-item version (PSS-4). A paired t-test evaluated differences between groups (menstrual changes versus no menstrual changes). The survey asked participants what changes they noticed in their menstrual cycle and why they thought cycle patterns or symptoms changed.
One-third report changes in cycle, symptoms
Among 12,302 respondents, 1 in 3 (36%) reported changes in cycle or symptoms. Eighty-seven percent said that their cycle started early or late. Twenty-nine percent reported stronger symptoms during menstruation such as low back pain, cramping, or discharge changes, and 27% said bleeding was heavier during periods.
These results are similar to other studies investigating the affect of episodic stress on menstruation, said Ms. Malloy.
Those who reported menstrual cycle or symptom changes scored higher on average on the PSS-4 compared with those who didn’t report any changes (8.5 v. 8.3, respectively, P < .05). PSS-4 scores across the board were notably higher in all respondents, regardless of cycle/symptom irregularity, compared with prepandemic benchmarking in similar populations.
Slightly more than half (55%) thought stress contributed to their menstrual cycle pattern and/or symptom changes, whereas 33% pointed to changes in mental health, such as depression or anxiety. “Interestingly, many users believed the COVID-19 vaccine impacted their menstrual cycle symptom changes,” said Ms. Malloy.
No definitive link between vaccine, menstruation
While known side effects of the vaccine include sore arm, fever, fatigue, and myalgia, some women have reported changes in their menstrual cycle, Mark P. Trolice, MD, professor of obstetrics and gynecology at the University of Central Florida and director of the IVF Center in Orlando, said in an interview.
“Vaccination reaction from the immune response rather than the vaccine may be the implicating factor,” said Dr. Trolice, who was not involved in the study.
Currently, there’s no direct link between the vaccine and subsequent effects on menstruation, he continued. “Most women experience resumption of normal intervals 1 month following vaccination. Further, there is no credible evidence that links the vaccine to infertility.
“Nevertheless, research in this area is vital and underway,” he added.
Physicians can help with stress
Menstrual cycle disruption is especially frustrating for women trying to build a family, said Ms. Malloy. Providers may be observing more menstrual irregularity in their patient populations, and seeing more patients struggle to conceive on their own, turning to ART.
Providers can’t make COVID-19 go away, but they could help patients by doing a better job of integrating mental health screening, connecting patients to treatments that optimize conception and fertility treatment outcomes, said Ms. Malloy.
The survey was limited in that its questions didn’t consider proper diagnostic criteria for irregularity, versus self-reported changes. But it does highlight the need for more research on the pandemic’s affect on menstruation and the vaccine on menstruation, said Ms. Malloy. “The National Institutes of Health in August committed $1.6 million to explore this connection. We’re looking forward to seeing what their results are.”
Dr. Trolice and Ms. Malloy had no disclosures.
FROM ASRM 2021
Patients seeking infertility care report infrequent counseling on weight loss
Physicians could be doing a better job of counseling patients with obesity and overweight on weight loss and fertility. A study of 48 women seeking infertility care at a large academic center found that less than half received advice on weight loss from their primary ob.gyn. prior to referral for infertility treatment.
Patients are thinking about this – many attempt to lose weight independently of support from their health care providers, said lead study author Margaret R. O’Neill, MD, a resident at the University of Massachusetts Medical Center in Worcester. Dr. O’Neill discussed these results at the American Society of Reproductive Medicine’s 2021 meeting.
Nearly half of all U.S. women of reproductive age have overweight or obesity, with a body mass index of >25 kg/m2. Menstrual irregularity, ovulatory dysfunction, reduced fecundity, and lower efficacy of infertility treatment are some of the consequences of obesity on fertility, said Dr. O’Neill. Obesity also affects the health of expectant mothers and fetuses, increasing the likelihood of gestational diabetes, preterm delivery, and preeclampsia, and increased incidence of fetal anomalies.
“Unfortunately, even though the prevalence of obesity has been increasing substantially in our country, there’s not excellent rates of this being addressed by physicians,” said Dr. O’Neill. BMI is often left out of documentation and rates of referrals to weight loss specialists are also low.
Conversations have been taking place about IVF centers instituting different BMI cutoffs for certain types of assisted reproductive technology, she noted.
Dr. O’Neill and her colleagues undertook a survey to see what advice community providers were dispensing about weight management on fertility.
Infertility specialists offer the most guidance
The prospective study included 48 nonpregnant women of reproductive age women presenting for IVF who needed an anesthesia consultation because of elevated BMI (> 35) prior to initiation of IVF. Mean age was 36 years and mean BMI was 38.5. More than 70% of the patients were White and they were predominantly English speakers.
All participants had attempted weight loss, including an attempt in the last year, and 93.8% reported trying to lose weight in the last year. On average, patients weighed about 20 pounds less than their heaviest adult weight. Nineteen percent of the participants were at their heaviest adult weight.
While 60% said they’d received weight loss/infertility counseling by any health care provider, just 41.7% reported that their primary ob.gyn. counseled them about weight loss before referring them for treatment. Infertility specialists seem to provide the most assistance: Nearly 70% of the respondents said they’ve been counseled by these providers.
Women with a higher-than-average BMI (39) were more likely to report a referral to weight loss counseling compared with women not referred (37.9, P = .2).
Investigators also asked patients about their knowledge of obesity and its relationship to other health conditions. About 90% understood that infertility and excess weight were related. Overall, they were less sure about the link between obesity and still birth, breast cancer, and birth defects. Only 37% were able to identify a normal BMI range.
Avoiding a touchy subject
BMI is a highly sensitive area for many women, despite its detrimental effect on fertility, Mark P. Trolice, MD, professor of obstetrics and gynecology at the University of Central Florida and director of the IVF Center in Orlando, said in an interview.
“By the time their journey has led them to an infertility specialist, most women are very anxious to begin treatment,” said Dr. Trolice, who was not involved in the survey. These patients, however, could interpret any medical advice to achieve a more optimal BMI and healthier lifestyle as a negative judgment that could delay their goal of having a healthy child, he said.
Physicians in turn may avoid these conversations because they don’t want to encourage the ire of patients and/or risk a negative online rating review, he added.
Don’t say ‘just lose weight’
When asked what type of counseling works best, many said that nonspecific recommendations such as “you need to lose weight” or “exercise more” were the least helpful. Targeted advice such as “avoid eating at night and take walks every day,” works more effectively. “Any kind of referral to a bariatrics team or weight loss program was seen as helpful by patients,” said Dr. O’Neill.
Suggestions that considered the difficulty of this process, such as seeking therapy, were also helpful. “Patients appreciated empathy, compassion, and encouragement” from their physicians, she said.
The role of physicians in weight loss
Physicians can make a difference. Studies show that patients who received weight loss counseling were more likely to attempt weight loss and report clinically significant weight loss.
The American College of Obstetricians and Gynecologists and ASRM recommend counseling patients with overweight and obesity to lose weight before getting pregnant. A modest weight loss of 10% is associated with improved ovulatory function and higher pregnancy rates, said Dr. O’Neill.
“Appropriately, the infertility specialist should strongly recommend [that women who are obese] obtain a more optimal BMI prior to fertility treatment. While there is no guarantee of decreased infertility and decreased pregnancy complications following weight loss, a lower BMI improves outcomes,” said Dr. Trolice.
Future research should address the fertility outcomes of women who have been counseled by their providers to lose weight and the most effective method of counseling, noted Dr. O’Neill. “We have to find the best ways to address this at each fertility institution.”
The study had limited generalizability because of its narrow patient population and regional differences in access to insurance and weight loss specialists. COVID-19 also reduced the sample size, said Dr. O’Neill. She noted that patient perceptions might not equate with actual counseling delivered.
Dr. O’Neill and Dr. Trolice had no disclosures.
Physicians could be doing a better job of counseling patients with obesity and overweight on weight loss and fertility. A study of 48 women seeking infertility care at a large academic center found that less than half received advice on weight loss from their primary ob.gyn. prior to referral for infertility treatment.
Patients are thinking about this – many attempt to lose weight independently of support from their health care providers, said lead study author Margaret R. O’Neill, MD, a resident at the University of Massachusetts Medical Center in Worcester. Dr. O’Neill discussed these results at the American Society of Reproductive Medicine’s 2021 meeting.
Nearly half of all U.S. women of reproductive age have overweight or obesity, with a body mass index of >25 kg/m2. Menstrual irregularity, ovulatory dysfunction, reduced fecundity, and lower efficacy of infertility treatment are some of the consequences of obesity on fertility, said Dr. O’Neill. Obesity also affects the health of expectant mothers and fetuses, increasing the likelihood of gestational diabetes, preterm delivery, and preeclampsia, and increased incidence of fetal anomalies.
“Unfortunately, even though the prevalence of obesity has been increasing substantially in our country, there’s not excellent rates of this being addressed by physicians,” said Dr. O’Neill. BMI is often left out of documentation and rates of referrals to weight loss specialists are also low.
Conversations have been taking place about IVF centers instituting different BMI cutoffs for certain types of assisted reproductive technology, she noted.
Dr. O’Neill and her colleagues undertook a survey to see what advice community providers were dispensing about weight management on fertility.
Infertility specialists offer the most guidance
The prospective study included 48 nonpregnant women of reproductive age women presenting for IVF who needed an anesthesia consultation because of elevated BMI (> 35) prior to initiation of IVF. Mean age was 36 years and mean BMI was 38.5. More than 70% of the patients were White and they were predominantly English speakers.
All participants had attempted weight loss, including an attempt in the last year, and 93.8% reported trying to lose weight in the last year. On average, patients weighed about 20 pounds less than their heaviest adult weight. Nineteen percent of the participants were at their heaviest adult weight.
While 60% said they’d received weight loss/infertility counseling by any health care provider, just 41.7% reported that their primary ob.gyn. counseled them about weight loss before referring them for treatment. Infertility specialists seem to provide the most assistance: Nearly 70% of the respondents said they’ve been counseled by these providers.
Women with a higher-than-average BMI (39) were more likely to report a referral to weight loss counseling compared with women not referred (37.9, P = .2).
Investigators also asked patients about their knowledge of obesity and its relationship to other health conditions. About 90% understood that infertility and excess weight were related. Overall, they were less sure about the link between obesity and still birth, breast cancer, and birth defects. Only 37% were able to identify a normal BMI range.
Avoiding a touchy subject
BMI is a highly sensitive area for many women, despite its detrimental effect on fertility, Mark P. Trolice, MD, professor of obstetrics and gynecology at the University of Central Florida and director of the IVF Center in Orlando, said in an interview.
“By the time their journey has led them to an infertility specialist, most women are very anxious to begin treatment,” said Dr. Trolice, who was not involved in the survey. These patients, however, could interpret any medical advice to achieve a more optimal BMI and healthier lifestyle as a negative judgment that could delay their goal of having a healthy child, he said.
Physicians in turn may avoid these conversations because they don’t want to encourage the ire of patients and/or risk a negative online rating review, he added.
Don’t say ‘just lose weight’
When asked what type of counseling works best, many said that nonspecific recommendations such as “you need to lose weight” or “exercise more” were the least helpful. Targeted advice such as “avoid eating at night and take walks every day,” works more effectively. “Any kind of referral to a bariatrics team or weight loss program was seen as helpful by patients,” said Dr. O’Neill.
Suggestions that considered the difficulty of this process, such as seeking therapy, were also helpful. “Patients appreciated empathy, compassion, and encouragement” from their physicians, she said.
The role of physicians in weight loss
Physicians can make a difference. Studies show that patients who received weight loss counseling were more likely to attempt weight loss and report clinically significant weight loss.
The American College of Obstetricians and Gynecologists and ASRM recommend counseling patients with overweight and obesity to lose weight before getting pregnant. A modest weight loss of 10% is associated with improved ovulatory function and higher pregnancy rates, said Dr. O’Neill.
“Appropriately, the infertility specialist should strongly recommend [that women who are obese] obtain a more optimal BMI prior to fertility treatment. While there is no guarantee of decreased infertility and decreased pregnancy complications following weight loss, a lower BMI improves outcomes,” said Dr. Trolice.
Future research should address the fertility outcomes of women who have been counseled by their providers to lose weight and the most effective method of counseling, noted Dr. O’Neill. “We have to find the best ways to address this at each fertility institution.”
The study had limited generalizability because of its narrow patient population and regional differences in access to insurance and weight loss specialists. COVID-19 also reduced the sample size, said Dr. O’Neill. She noted that patient perceptions might not equate with actual counseling delivered.
Dr. O’Neill and Dr. Trolice had no disclosures.
Physicians could be doing a better job of counseling patients with obesity and overweight on weight loss and fertility. A study of 48 women seeking infertility care at a large academic center found that less than half received advice on weight loss from their primary ob.gyn. prior to referral for infertility treatment.
Patients are thinking about this – many attempt to lose weight independently of support from their health care providers, said lead study author Margaret R. O’Neill, MD, a resident at the University of Massachusetts Medical Center in Worcester. Dr. O’Neill discussed these results at the American Society of Reproductive Medicine’s 2021 meeting.
Nearly half of all U.S. women of reproductive age have overweight or obesity, with a body mass index of >25 kg/m2. Menstrual irregularity, ovulatory dysfunction, reduced fecundity, and lower efficacy of infertility treatment are some of the consequences of obesity on fertility, said Dr. O’Neill. Obesity also affects the health of expectant mothers and fetuses, increasing the likelihood of gestational diabetes, preterm delivery, and preeclampsia, and increased incidence of fetal anomalies.
“Unfortunately, even though the prevalence of obesity has been increasing substantially in our country, there’s not excellent rates of this being addressed by physicians,” said Dr. O’Neill. BMI is often left out of documentation and rates of referrals to weight loss specialists are also low.
Conversations have been taking place about IVF centers instituting different BMI cutoffs for certain types of assisted reproductive technology, she noted.
Dr. O’Neill and her colleagues undertook a survey to see what advice community providers were dispensing about weight management on fertility.
Infertility specialists offer the most guidance
The prospective study included 48 nonpregnant women of reproductive age women presenting for IVF who needed an anesthesia consultation because of elevated BMI (> 35) prior to initiation of IVF. Mean age was 36 years and mean BMI was 38.5. More than 70% of the patients were White and they were predominantly English speakers.
All participants had attempted weight loss, including an attempt in the last year, and 93.8% reported trying to lose weight in the last year. On average, patients weighed about 20 pounds less than their heaviest adult weight. Nineteen percent of the participants were at their heaviest adult weight.
While 60% said they’d received weight loss/infertility counseling by any health care provider, just 41.7% reported that their primary ob.gyn. counseled them about weight loss before referring them for treatment. Infertility specialists seem to provide the most assistance: Nearly 70% of the respondents said they’ve been counseled by these providers.
Women with a higher-than-average BMI (39) were more likely to report a referral to weight loss counseling compared with women not referred (37.9, P = .2).
Investigators also asked patients about their knowledge of obesity and its relationship to other health conditions. About 90% understood that infertility and excess weight were related. Overall, they were less sure about the link between obesity and still birth, breast cancer, and birth defects. Only 37% were able to identify a normal BMI range.
Avoiding a touchy subject
BMI is a highly sensitive area for many women, despite its detrimental effect on fertility, Mark P. Trolice, MD, professor of obstetrics and gynecology at the University of Central Florida and director of the IVF Center in Orlando, said in an interview.
“By the time their journey has led them to an infertility specialist, most women are very anxious to begin treatment,” said Dr. Trolice, who was not involved in the survey. These patients, however, could interpret any medical advice to achieve a more optimal BMI and healthier lifestyle as a negative judgment that could delay their goal of having a healthy child, he said.
Physicians in turn may avoid these conversations because they don’t want to encourage the ire of patients and/or risk a negative online rating review, he added.
Don’t say ‘just lose weight’
When asked what type of counseling works best, many said that nonspecific recommendations such as “you need to lose weight” or “exercise more” were the least helpful. Targeted advice such as “avoid eating at night and take walks every day,” works more effectively. “Any kind of referral to a bariatrics team or weight loss program was seen as helpful by patients,” said Dr. O’Neill.
Suggestions that considered the difficulty of this process, such as seeking therapy, were also helpful. “Patients appreciated empathy, compassion, and encouragement” from their physicians, she said.
The role of physicians in weight loss
Physicians can make a difference. Studies show that patients who received weight loss counseling were more likely to attempt weight loss and report clinically significant weight loss.
The American College of Obstetricians and Gynecologists and ASRM recommend counseling patients with overweight and obesity to lose weight before getting pregnant. A modest weight loss of 10% is associated with improved ovulatory function and higher pregnancy rates, said Dr. O’Neill.
“Appropriately, the infertility specialist should strongly recommend [that women who are obese] obtain a more optimal BMI prior to fertility treatment. While there is no guarantee of decreased infertility and decreased pregnancy complications following weight loss, a lower BMI improves outcomes,” said Dr. Trolice.
Future research should address the fertility outcomes of women who have been counseled by their providers to lose weight and the most effective method of counseling, noted Dr. O’Neill. “We have to find the best ways to address this at each fertility institution.”
The study had limited generalizability because of its narrow patient population and regional differences in access to insurance and weight loss specialists. COVID-19 also reduced the sample size, said Dr. O’Neill. She noted that patient perceptions might not equate with actual counseling delivered.
Dr. O’Neill and Dr. Trolice had no disclosures.
FROM ASRM 2021
The compass that points toward food
The new breakfast of champions
We love a good ranking system here at LOTME world headquarters, especially the food-based ones. Luckily for us (and our readers), a new study published in Nature Food offers a food-based ranking system.
Sadly, unlike the last food-related ranking we covered, the Food Compass doesn’t tell you how much life you gain or lose from each food you eat down to the precise minute. Instead, it favors a more simple rating system from 1 to 100, with healthier foods scoring higher, and even incorporates mixed foods, not just single ingredients. This makes it better at assessing and comparing food combinations, rather than trying to mix and match the many ingredients that go into even relatively simple recipes.
The top and bottom of the rankings contain the usual suspects. Legumes and nuts, at 78.6, had the highest average score among the broad food groups, followed by fruits and then vegetables. Rounding out the bottom were sweets and savory snacks at 16.4. Among the individual foods, there were perfect scores in both directions: 100 for raw raspberries, while instant noodle soup and nonchocolate, ready-to-eat, nonfat pudding (very specific there) each earned a 1.
There are a few surprises in between. Nonfat cappuccino received a green light from the investigators, great news for the coffee drinkers out there. A serving of sweet potato chips scored better than a simple grilled chicken breast, and a slice of pizza, loaded up with extra meat and a thick crust, is still more nutritious than a bowl of corn flakes.
Neither is good for you, of course, but we’re still going to take this as a sign that pizza is the ideal breakfast food. Add that to your morning coffee, and you’re ready to start the day. Move over Wheaties, there’s a new breakfast of champions.
COVID-19 resisters, please step forward
Some people have all the luck with good genes, both inside and out.
Genetically speaking, humans are 99.9% the same, but that 0.1% is where things get interesting. Because of that 0.1% difference, some people are more likely to contract diseases such as HIV, while others might be more resistant. These small differences in genetic code could be the key to finding treatments for COVID-19.
“The introduction of SARS-CoV-2 to a naive population, on a global scale, has provided yet another demonstration of the remarkable clinical variability between individuals in the course of infection, ranging from asymptomatic infections to life-threatening disease,” the researchers said in Nature Immunology.
The investigators have been scouring the world to find people who might be resistant to SARS-CoV-2 and have enrolled over 400 individuals in a “dedicated resistance study cohort,” according to ScienceAlert.
The investigators are looking at households in which families were infected but one member did not show severe symptoms, or for individuals who have been around the virus multiple times and haven’t contracted it. They are also looking at blood types.
Enrollment is ongoing, so if you’ve been in contact with COVID-19 multiple times and have not gotten sick, scientists would like to hear from you.
Better living through parasitization
How would you like to triple your life span, while maintaining a youthful appearance and gaining special social standing and privileges?
Sounds pretty good, right, so what’s the catch? Well, you have to be infected with a tapeworm ... and you have to be an ant.
If you are an ant, here’s the deal: Workers of the species Temnothorax nylanderi that have tapeworms live much longer than uninfected workers, and while living out those longer lives they do less work and receive gifts of food.
In a study conducted at Johannes Gutenberg University in Mainz, Germany, infected ants’ metabolic rates and lipid levels were similar to those of younger ants, and they appeared to remain in a permanent juvenile stage as a result of the infection, the investigators reported.
They tracked Temnothorax colonies for 3 years, at which point 95% of the uninfected workers had died but over half of the infected ants were still alive. Pretty great, right? Wrong. There was no joy in antville, for the uninfected workers had struck out. “Strained by the additional burden of their wormed-up nestmates, they seemed to be shunting care away from their queen. They were dying sooner than they might have if the colonies had remained parasite-free,” according to an article in the Atlantic.
Does this situation seem just a wee bit familiar? A small group lives longer, healthier lives and enjoys special privileges while the majority of that society works harder to support them? We’ll put it into the form of a chicken-and-egg argument: Which came first, the tapeworms or the one-percenters?
Laughing the pandemic stress away
Doomscrolling on social media has become one of the world’s favorite pastimes during the pandemic, but research shows that those memes about COVID-19 might combat the doom and gloom of the outside world.
A study recently published in Psychology of Popular Media showed that viewing memes, specifically those that were COVID-19 related, actually lessened the stress of the pandemic.
The researchers conducted a survey of 748 people aged 18-88 years. Each participant viewed three memes with text or three memes with text but no images. All three memes had similar cuteness levels (baby or adult), subject (animal or human), and caption (COVID-19–related or not). The participants were then asked to report on their stress levels and feelings before and after the memes.
The people who looked at memes felt less stressed and a higher humor level, especially the participants who received the COVID-19 memes. Study Finds said that they had more “pandemic-coping confidence” than those who got regular memes.
“While the World Health Organization recommended that people avoid too much COVID-related media for the benefit of their mental health, our research reveals that memes about COVID-19 could help people feel more confident in their ability to deal with the pandemic,” lead author Jessica Gall Myrick, PhD, said in a written statement. “The positive emotions associated with this type of content may make people feel psychologically safer and therefore better able to pay attention to the underlying messages related to health threats.”
So if you think you’ve been wasting time looking at memes during this pandemic, think again. It actually might keep you sane. Keep on scrolling!
Giving the gift of stress reduction
It’s a big week here at LOTME. You’ve just read our 100th edition, and to help celebrate that milestone – along with Count Your Buttons Day, Celebration of the Mind Day, and the International Day of the Nacho – we’re presenting an extra-special bonus feature, courtesy of Sad and Useless: The most depressive humor site on the Internet.
We hope you’ll stop your doomscrolling long enough to enjoy this stress-reducing meme. Thanks for reading!
The new breakfast of champions
We love a good ranking system here at LOTME world headquarters, especially the food-based ones. Luckily for us (and our readers), a new study published in Nature Food offers a food-based ranking system.
Sadly, unlike the last food-related ranking we covered, the Food Compass doesn’t tell you how much life you gain or lose from each food you eat down to the precise minute. Instead, it favors a more simple rating system from 1 to 100, with healthier foods scoring higher, and even incorporates mixed foods, not just single ingredients. This makes it better at assessing and comparing food combinations, rather than trying to mix and match the many ingredients that go into even relatively simple recipes.
The top and bottom of the rankings contain the usual suspects. Legumes and nuts, at 78.6, had the highest average score among the broad food groups, followed by fruits and then vegetables. Rounding out the bottom were sweets and savory snacks at 16.4. Among the individual foods, there were perfect scores in both directions: 100 for raw raspberries, while instant noodle soup and nonchocolate, ready-to-eat, nonfat pudding (very specific there) each earned a 1.
There are a few surprises in between. Nonfat cappuccino received a green light from the investigators, great news for the coffee drinkers out there. A serving of sweet potato chips scored better than a simple grilled chicken breast, and a slice of pizza, loaded up with extra meat and a thick crust, is still more nutritious than a bowl of corn flakes.
Neither is good for you, of course, but we’re still going to take this as a sign that pizza is the ideal breakfast food. Add that to your morning coffee, and you’re ready to start the day. Move over Wheaties, there’s a new breakfast of champions.
COVID-19 resisters, please step forward
Some people have all the luck with good genes, both inside and out.
Genetically speaking, humans are 99.9% the same, but that 0.1% is where things get interesting. Because of that 0.1% difference, some people are more likely to contract diseases such as HIV, while others might be more resistant. These small differences in genetic code could be the key to finding treatments for COVID-19.
“The introduction of SARS-CoV-2 to a naive population, on a global scale, has provided yet another demonstration of the remarkable clinical variability between individuals in the course of infection, ranging from asymptomatic infections to life-threatening disease,” the researchers said in Nature Immunology.
The investigators have been scouring the world to find people who might be resistant to SARS-CoV-2 and have enrolled over 400 individuals in a “dedicated resistance study cohort,” according to ScienceAlert.
The investigators are looking at households in which families were infected but one member did not show severe symptoms, or for individuals who have been around the virus multiple times and haven’t contracted it. They are also looking at blood types.
Enrollment is ongoing, so if you’ve been in contact with COVID-19 multiple times and have not gotten sick, scientists would like to hear from you.
Better living through parasitization
How would you like to triple your life span, while maintaining a youthful appearance and gaining special social standing and privileges?
Sounds pretty good, right, so what’s the catch? Well, you have to be infected with a tapeworm ... and you have to be an ant.
If you are an ant, here’s the deal: Workers of the species Temnothorax nylanderi that have tapeworms live much longer than uninfected workers, and while living out those longer lives they do less work and receive gifts of food.
In a study conducted at Johannes Gutenberg University in Mainz, Germany, infected ants’ metabolic rates and lipid levels were similar to those of younger ants, and they appeared to remain in a permanent juvenile stage as a result of the infection, the investigators reported.
They tracked Temnothorax colonies for 3 years, at which point 95% of the uninfected workers had died but over half of the infected ants were still alive. Pretty great, right? Wrong. There was no joy in antville, for the uninfected workers had struck out. “Strained by the additional burden of their wormed-up nestmates, they seemed to be shunting care away from their queen. They were dying sooner than they might have if the colonies had remained parasite-free,” according to an article in the Atlantic.
Does this situation seem just a wee bit familiar? A small group lives longer, healthier lives and enjoys special privileges while the majority of that society works harder to support them? We’ll put it into the form of a chicken-and-egg argument: Which came first, the tapeworms or the one-percenters?
Laughing the pandemic stress away
Doomscrolling on social media has become one of the world’s favorite pastimes during the pandemic, but research shows that those memes about COVID-19 might combat the doom and gloom of the outside world.
A study recently published in Psychology of Popular Media showed that viewing memes, specifically those that were COVID-19 related, actually lessened the stress of the pandemic.
The researchers conducted a survey of 748 people aged 18-88 years. Each participant viewed three memes with text or three memes with text but no images. All three memes had similar cuteness levels (baby or adult), subject (animal or human), and caption (COVID-19–related or not). The participants were then asked to report on their stress levels and feelings before and after the memes.
The people who looked at memes felt less stressed and a higher humor level, especially the participants who received the COVID-19 memes. Study Finds said that they had more “pandemic-coping confidence” than those who got regular memes.
“While the World Health Organization recommended that people avoid too much COVID-related media for the benefit of their mental health, our research reveals that memes about COVID-19 could help people feel more confident in their ability to deal with the pandemic,” lead author Jessica Gall Myrick, PhD, said in a written statement. “The positive emotions associated with this type of content may make people feel psychologically safer and therefore better able to pay attention to the underlying messages related to health threats.”
So if you think you’ve been wasting time looking at memes during this pandemic, think again. It actually might keep you sane. Keep on scrolling!
Giving the gift of stress reduction
It’s a big week here at LOTME. You’ve just read our 100th edition, and to help celebrate that milestone – along with Count Your Buttons Day, Celebration of the Mind Day, and the International Day of the Nacho – we’re presenting an extra-special bonus feature, courtesy of Sad and Useless: The most depressive humor site on the Internet.
We hope you’ll stop your doomscrolling long enough to enjoy this stress-reducing meme. Thanks for reading!
The new breakfast of champions
We love a good ranking system here at LOTME world headquarters, especially the food-based ones. Luckily for us (and our readers), a new study published in Nature Food offers a food-based ranking system.
Sadly, unlike the last food-related ranking we covered, the Food Compass doesn’t tell you how much life you gain or lose from each food you eat down to the precise minute. Instead, it favors a more simple rating system from 1 to 100, with healthier foods scoring higher, and even incorporates mixed foods, not just single ingredients. This makes it better at assessing and comparing food combinations, rather than trying to mix and match the many ingredients that go into even relatively simple recipes.
The top and bottom of the rankings contain the usual suspects. Legumes and nuts, at 78.6, had the highest average score among the broad food groups, followed by fruits and then vegetables. Rounding out the bottom were sweets and savory snacks at 16.4. Among the individual foods, there were perfect scores in both directions: 100 for raw raspberries, while instant noodle soup and nonchocolate, ready-to-eat, nonfat pudding (very specific there) each earned a 1.
There are a few surprises in between. Nonfat cappuccino received a green light from the investigators, great news for the coffee drinkers out there. A serving of sweet potato chips scored better than a simple grilled chicken breast, and a slice of pizza, loaded up with extra meat and a thick crust, is still more nutritious than a bowl of corn flakes.
Neither is good for you, of course, but we’re still going to take this as a sign that pizza is the ideal breakfast food. Add that to your morning coffee, and you’re ready to start the day. Move over Wheaties, there’s a new breakfast of champions.
COVID-19 resisters, please step forward
Some people have all the luck with good genes, both inside and out.
Genetically speaking, humans are 99.9% the same, but that 0.1% is where things get interesting. Because of that 0.1% difference, some people are more likely to contract diseases such as HIV, while others might be more resistant. These small differences in genetic code could be the key to finding treatments for COVID-19.
“The introduction of SARS-CoV-2 to a naive population, on a global scale, has provided yet another demonstration of the remarkable clinical variability between individuals in the course of infection, ranging from asymptomatic infections to life-threatening disease,” the researchers said in Nature Immunology.
The investigators have been scouring the world to find people who might be resistant to SARS-CoV-2 and have enrolled over 400 individuals in a “dedicated resistance study cohort,” according to ScienceAlert.
The investigators are looking at households in which families were infected but one member did not show severe symptoms, or for individuals who have been around the virus multiple times and haven’t contracted it. They are also looking at blood types.
Enrollment is ongoing, so if you’ve been in contact with COVID-19 multiple times and have not gotten sick, scientists would like to hear from you.
Better living through parasitization
How would you like to triple your life span, while maintaining a youthful appearance and gaining special social standing and privileges?
Sounds pretty good, right, so what’s the catch? Well, you have to be infected with a tapeworm ... and you have to be an ant.
If you are an ant, here’s the deal: Workers of the species Temnothorax nylanderi that have tapeworms live much longer than uninfected workers, and while living out those longer lives they do less work and receive gifts of food.
In a study conducted at Johannes Gutenberg University in Mainz, Germany, infected ants’ metabolic rates and lipid levels were similar to those of younger ants, and they appeared to remain in a permanent juvenile stage as a result of the infection, the investigators reported.
They tracked Temnothorax colonies for 3 years, at which point 95% of the uninfected workers had died but over half of the infected ants were still alive. Pretty great, right? Wrong. There was no joy in antville, for the uninfected workers had struck out. “Strained by the additional burden of their wormed-up nestmates, they seemed to be shunting care away from their queen. They were dying sooner than they might have if the colonies had remained parasite-free,” according to an article in the Atlantic.
Does this situation seem just a wee bit familiar? A small group lives longer, healthier lives and enjoys special privileges while the majority of that society works harder to support them? We’ll put it into the form of a chicken-and-egg argument: Which came first, the tapeworms or the one-percenters?
Laughing the pandemic stress away
Doomscrolling on social media has become one of the world’s favorite pastimes during the pandemic, but research shows that those memes about COVID-19 might combat the doom and gloom of the outside world.
A study recently published in Psychology of Popular Media showed that viewing memes, specifically those that were COVID-19 related, actually lessened the stress of the pandemic.
The researchers conducted a survey of 748 people aged 18-88 years. Each participant viewed three memes with text or three memes with text but no images. All three memes had similar cuteness levels (baby or adult), subject (animal or human), and caption (COVID-19–related or not). The participants were then asked to report on their stress levels and feelings before and after the memes.
The people who looked at memes felt less stressed and a higher humor level, especially the participants who received the COVID-19 memes. Study Finds said that they had more “pandemic-coping confidence” than those who got regular memes.
“While the World Health Organization recommended that people avoid too much COVID-related media for the benefit of their mental health, our research reveals that memes about COVID-19 could help people feel more confident in their ability to deal with the pandemic,” lead author Jessica Gall Myrick, PhD, said in a written statement. “The positive emotions associated with this type of content may make people feel psychologically safer and therefore better able to pay attention to the underlying messages related to health threats.”
So if you think you’ve been wasting time looking at memes during this pandemic, think again. It actually might keep you sane. Keep on scrolling!
Giving the gift of stress reduction
It’s a big week here at LOTME. You’ve just read our 100th edition, and to help celebrate that milestone – along with Count Your Buttons Day, Celebration of the Mind Day, and the International Day of the Nacho – we’re presenting an extra-special bonus feature, courtesy of Sad and Useless: The most depressive humor site on the Internet.
We hope you’ll stop your doomscrolling long enough to enjoy this stress-reducing meme. Thanks for reading!