User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
High response rates with T-DXd in early HER2-low breast cancer
SAN Antonio – How do you shoot at an invisible target? It seems counterintuitive, but
In the investigator-initiated TRIO-US B-12 TALENT study looking at neoadjuvant T-DXd either alone or in combination with the hormone therapy anastrazole, the objective response rate (ORR) with T-DXd alone was 68%, compared with 58% for T-DXd plus anastrazole, reported Aditya Bardia, MD, MPH, a medical oncologist with Massachusetts General Hospital Cancer Center in Boston. He recently presented the study findings at the 2022 San Antonio Breast Cancer Symposium.
“The study provides a rich platform for additional translational research to evaluate more sensitive methods of HER2 detection, develop predictive biomarkers, and understand mechanisms of resistance in residual disease which would guide subsequent therapeutic strategies, including combination therapy,” he said in an oral abstract session at the meeting.
Not-so-innocent bystander
In an interview, Dr. Bardia explained that the T-DXd may have efficacy in HER2-low cancers because of a bystander effect.
“With these antibody drug conjugates, if you have the antigen, the ADC binds to the antigen, gets internalized, and releases the payload, but the payload has a bystander effect ... it’s membrane permeable, so it can go outside and affect other cells that do not express the antigen. So for HER2-low tumors, even if there is HER2 heterogeneity or if there are some cells that do not express HER2, this would work because of the bystander effect,” he said.
Although neoadjuvant chemotherapy with an anthracycline and taxane is often used to treat patients with high-risk localized HR-positive breast cancer, the therapy is associated with low pathologic complete response (pCR) rates, radiological response rates of around 50%, and significant toxicities, including myelosuppression, neuropathy, cardiomyopathy, and leukemia risk, Dr. Bardia said.
At cross purposes
The trial included both a T-DXd monotherapy arm and a second arm containing the antibody drug conjugate (ADC) with endocrine therapy. The rationale for the latter is that there is documented “cross-talk” between the estrogen receptor (ER) and HER2.
“In tumors that become endocrine resistant, you see an increase in the HER2 pathway, and if you block ER, you see that HER2 goes up and vice versa. If you just block HER2 alone, the expression of ER can go up, and if you block the PI3 kinase alone, the expression of ER goes up,” he said.
Dual blockade can be effective with antibody-based therapy or with tyrosine kinase inhibitors, but with an ADC, the dual blockade strategy may be less effective, Dr. Bardia said, “because if you have an ADC, you need HER2, the ADC binds to HER2, then gives the payload to the cancer cells and essentially kills the cancer cells,” Dr. Bardia explained in a media briefing held prior to his presentation.
In fact, the T-DXd–anastrozole combination was associated with a lower overall response rate in the study than T-DXd alone, but Dr. Bardia cautioned about overinterpreting these results, as the study included only 39 patients.
Study details
The investigators enrolled 58 patients – 56 pre- and postmenopausal women and 2 men – with HR+/HER2-low tumors determined by local and/or central review, and operable stage II or III cancers.
After stratification by HER2 expression level and menopausal status, the patients were randomized to receive either T-DXd alone at a dose of 5.4 mg/kg, or with T-DXd at the same dose plus anastrozole, with men and premenopausal women also receiving a gonadotropin-releasing hormone analog.
The protocol originally called for six cycles of therapy, but was amended in February 2022 to increase the number to eight for newly enrolled participants and patients who were already on study treatment but had not yet had surgery.
The majority of patients in each arm had invasive ductal cancers, and most had HER2 expression on immunohistochemistry (IHC) of 1+, which is generally considered to be HER2-negative. However, there was only modest concordance between local and central review in determining HER2 expression levels, Dr. Bardia noted. Indeed, the entire question of HER2-low cancers, whether they compose a separate clinical entity from other cancers and how to standardize testing, was the subject of a special session at this year’s SABCS.
Results
Overall response rate, the primary endpoint, was 68% in the T-DXd arm and 58% in the T-DXd plus anastrazole arm.
Although the low response rate with the combination suggests that endocrine therapy may not be helpful in this patient population, it’s still too early to say so conclusively, Dr. Bardia said.
Looking at the change in HER2 expression by IHC from baseline to surgery, they found that 48.6% of patients had a change in HER2 IHC expression after T-DXd treatment, and that nearly 90% of these patients had a decrease in expression levels.
Among 42 patients with available data on residual cancer burden (RCB) at the time of data cutoff, one patient in the T-DXd alone arm with stage 3A disease had an RCB of 0, equivalent to a pathologic complete response (pCR). There were no other RCB 0 tumors after surgery in either study arm. The rate of combined RCB and RCB 1 (near pCR) was about 15% in each arm.
In all, 3 of the 58 patients in the study (5.2%) required dose reductions because of adverse events. There were no cases of grade 3 or greater pneumonitis, and no cases of either cardiomyopathy or neuropathy.
Way better than chemotherapy?
“It was very exciting when we got the DESTINY-Breast04 results showing this impressive activity of trastuzumab deruxtecan in this HER2-low entity, and now we know that hormone-positive [tumors], the majority of them are HER2-low. It was really encouraging, it was practice changing, but we were left wondering about this HER2-low entity, and can we act on it in the earlier setting,” commented Jason A. Mouabbi, MD, from the University of Texas MD Anderson Cancer Center in Houston.
“The beauty of the TRIO-US B-12 TALENT study is that it looked at the neoadjuvant setting where we know those patients who are hormone-positive usually do not respond well to chemotherapy,” he said in an interview.
He said that although the study didn’t compare T-DXd to chemotherapy, “it’s an excellent first start.”
An overall response rate near 70% “is something amazing. I’m really excited to see it against chemo. I think it’s going to do way better,” Dr. Mouabbi said.
The study was conducted by the Translational Research In Oncology (TRIO)-US network. Funding was provided by Daiichi Sankyo, the maker of trastuzumab deruxtecan (Enhertu). Dr. Bardia serves as a consultant or advisory board member for Pfizer, Novartis, Genentech, Merck, Radius Health, Immunomedics/Gilead Sciences, Sanofi, Daiichi Sankyo, AstraZeneca, and Eli Lilly, and has received research funding from Genentech, Novartis, Pfizer, Merck, Sanofi, Radius Health, Immunomedics/Gilead Sciences, Daiichi Sankyo, AstraZeneca, and Eli Lilly.
Dr. Mouabbi disclosed honoraria from BostonGene, Cardinal Health, Napo Pharmaceuticals, and Fresenius Kabi.
SAN Antonio – How do you shoot at an invisible target? It seems counterintuitive, but
In the investigator-initiated TRIO-US B-12 TALENT study looking at neoadjuvant T-DXd either alone or in combination with the hormone therapy anastrazole, the objective response rate (ORR) with T-DXd alone was 68%, compared with 58% for T-DXd plus anastrazole, reported Aditya Bardia, MD, MPH, a medical oncologist with Massachusetts General Hospital Cancer Center in Boston. He recently presented the study findings at the 2022 San Antonio Breast Cancer Symposium.
“The study provides a rich platform for additional translational research to evaluate more sensitive methods of HER2 detection, develop predictive biomarkers, and understand mechanisms of resistance in residual disease which would guide subsequent therapeutic strategies, including combination therapy,” he said in an oral abstract session at the meeting.
Not-so-innocent bystander
In an interview, Dr. Bardia explained that the T-DXd may have efficacy in HER2-low cancers because of a bystander effect.
“With these antibody drug conjugates, if you have the antigen, the ADC binds to the antigen, gets internalized, and releases the payload, but the payload has a bystander effect ... it’s membrane permeable, so it can go outside and affect other cells that do not express the antigen. So for HER2-low tumors, even if there is HER2 heterogeneity or if there are some cells that do not express HER2, this would work because of the bystander effect,” he said.
Although neoadjuvant chemotherapy with an anthracycline and taxane is often used to treat patients with high-risk localized HR-positive breast cancer, the therapy is associated with low pathologic complete response (pCR) rates, radiological response rates of around 50%, and significant toxicities, including myelosuppression, neuropathy, cardiomyopathy, and leukemia risk, Dr. Bardia said.
At cross purposes
The trial included both a T-DXd monotherapy arm and a second arm containing the antibody drug conjugate (ADC) with endocrine therapy. The rationale for the latter is that there is documented “cross-talk” between the estrogen receptor (ER) and HER2.
“In tumors that become endocrine resistant, you see an increase in the HER2 pathway, and if you block ER, you see that HER2 goes up and vice versa. If you just block HER2 alone, the expression of ER can go up, and if you block the PI3 kinase alone, the expression of ER goes up,” he said.
Dual blockade can be effective with antibody-based therapy or with tyrosine kinase inhibitors, but with an ADC, the dual blockade strategy may be less effective, Dr. Bardia said, “because if you have an ADC, you need HER2, the ADC binds to HER2, then gives the payload to the cancer cells and essentially kills the cancer cells,” Dr. Bardia explained in a media briefing held prior to his presentation.
In fact, the T-DXd–anastrozole combination was associated with a lower overall response rate in the study than T-DXd alone, but Dr. Bardia cautioned about overinterpreting these results, as the study included only 39 patients.
Study details
The investigators enrolled 58 patients – 56 pre- and postmenopausal women and 2 men – with HR+/HER2-low tumors determined by local and/or central review, and operable stage II or III cancers.
After stratification by HER2 expression level and menopausal status, the patients were randomized to receive either T-DXd alone at a dose of 5.4 mg/kg, or with T-DXd at the same dose plus anastrozole, with men and premenopausal women also receiving a gonadotropin-releasing hormone analog.
The protocol originally called for six cycles of therapy, but was amended in February 2022 to increase the number to eight for newly enrolled participants and patients who were already on study treatment but had not yet had surgery.
The majority of patients in each arm had invasive ductal cancers, and most had HER2 expression on immunohistochemistry (IHC) of 1+, which is generally considered to be HER2-negative. However, there was only modest concordance between local and central review in determining HER2 expression levels, Dr. Bardia noted. Indeed, the entire question of HER2-low cancers, whether they compose a separate clinical entity from other cancers and how to standardize testing, was the subject of a special session at this year’s SABCS.
Results
Overall response rate, the primary endpoint, was 68% in the T-DXd arm and 58% in the T-DXd plus anastrazole arm.
Although the low response rate with the combination suggests that endocrine therapy may not be helpful in this patient population, it’s still too early to say so conclusively, Dr. Bardia said.
Looking at the change in HER2 expression by IHC from baseline to surgery, they found that 48.6% of patients had a change in HER2 IHC expression after T-DXd treatment, and that nearly 90% of these patients had a decrease in expression levels.
Among 42 patients with available data on residual cancer burden (RCB) at the time of data cutoff, one patient in the T-DXd alone arm with stage 3A disease had an RCB of 0, equivalent to a pathologic complete response (pCR). There were no other RCB 0 tumors after surgery in either study arm. The rate of combined RCB and RCB 1 (near pCR) was about 15% in each arm.
In all, 3 of the 58 patients in the study (5.2%) required dose reductions because of adverse events. There were no cases of grade 3 or greater pneumonitis, and no cases of either cardiomyopathy or neuropathy.
Way better than chemotherapy?
“It was very exciting when we got the DESTINY-Breast04 results showing this impressive activity of trastuzumab deruxtecan in this HER2-low entity, and now we know that hormone-positive [tumors], the majority of them are HER2-low. It was really encouraging, it was practice changing, but we were left wondering about this HER2-low entity, and can we act on it in the earlier setting,” commented Jason A. Mouabbi, MD, from the University of Texas MD Anderson Cancer Center in Houston.
“The beauty of the TRIO-US B-12 TALENT study is that it looked at the neoadjuvant setting where we know those patients who are hormone-positive usually do not respond well to chemotherapy,” he said in an interview.
He said that although the study didn’t compare T-DXd to chemotherapy, “it’s an excellent first start.”
An overall response rate near 70% “is something amazing. I’m really excited to see it against chemo. I think it’s going to do way better,” Dr. Mouabbi said.
The study was conducted by the Translational Research In Oncology (TRIO)-US network. Funding was provided by Daiichi Sankyo, the maker of trastuzumab deruxtecan (Enhertu). Dr. Bardia serves as a consultant or advisory board member for Pfizer, Novartis, Genentech, Merck, Radius Health, Immunomedics/Gilead Sciences, Sanofi, Daiichi Sankyo, AstraZeneca, and Eli Lilly, and has received research funding from Genentech, Novartis, Pfizer, Merck, Sanofi, Radius Health, Immunomedics/Gilead Sciences, Daiichi Sankyo, AstraZeneca, and Eli Lilly.
Dr. Mouabbi disclosed honoraria from BostonGene, Cardinal Health, Napo Pharmaceuticals, and Fresenius Kabi.
SAN Antonio – How do you shoot at an invisible target? It seems counterintuitive, but
In the investigator-initiated TRIO-US B-12 TALENT study looking at neoadjuvant T-DXd either alone or in combination with the hormone therapy anastrazole, the objective response rate (ORR) with T-DXd alone was 68%, compared with 58% for T-DXd plus anastrazole, reported Aditya Bardia, MD, MPH, a medical oncologist with Massachusetts General Hospital Cancer Center in Boston. He recently presented the study findings at the 2022 San Antonio Breast Cancer Symposium.
“The study provides a rich platform for additional translational research to evaluate more sensitive methods of HER2 detection, develop predictive biomarkers, and understand mechanisms of resistance in residual disease which would guide subsequent therapeutic strategies, including combination therapy,” he said in an oral abstract session at the meeting.
Not-so-innocent bystander
In an interview, Dr. Bardia explained that the T-DXd may have efficacy in HER2-low cancers because of a bystander effect.
“With these antibody drug conjugates, if you have the antigen, the ADC binds to the antigen, gets internalized, and releases the payload, but the payload has a bystander effect ... it’s membrane permeable, so it can go outside and affect other cells that do not express the antigen. So for HER2-low tumors, even if there is HER2 heterogeneity or if there are some cells that do not express HER2, this would work because of the bystander effect,” he said.
Although neoadjuvant chemotherapy with an anthracycline and taxane is often used to treat patients with high-risk localized HR-positive breast cancer, the therapy is associated with low pathologic complete response (pCR) rates, radiological response rates of around 50%, and significant toxicities, including myelosuppression, neuropathy, cardiomyopathy, and leukemia risk, Dr. Bardia said.
At cross purposes
The trial included both a T-DXd monotherapy arm and a second arm containing the antibody drug conjugate (ADC) with endocrine therapy. The rationale for the latter is that there is documented “cross-talk” between the estrogen receptor (ER) and HER2.
“In tumors that become endocrine resistant, you see an increase in the HER2 pathway, and if you block ER, you see that HER2 goes up and vice versa. If you just block HER2 alone, the expression of ER can go up, and if you block the PI3 kinase alone, the expression of ER goes up,” he said.
Dual blockade can be effective with antibody-based therapy or with tyrosine kinase inhibitors, but with an ADC, the dual blockade strategy may be less effective, Dr. Bardia said, “because if you have an ADC, you need HER2, the ADC binds to HER2, then gives the payload to the cancer cells and essentially kills the cancer cells,” Dr. Bardia explained in a media briefing held prior to his presentation.
In fact, the T-DXd–anastrozole combination was associated with a lower overall response rate in the study than T-DXd alone, but Dr. Bardia cautioned about overinterpreting these results, as the study included only 39 patients.
Study details
The investigators enrolled 58 patients – 56 pre- and postmenopausal women and 2 men – with HR+/HER2-low tumors determined by local and/or central review, and operable stage II or III cancers.
After stratification by HER2 expression level and menopausal status, the patients were randomized to receive either T-DXd alone at a dose of 5.4 mg/kg, or with T-DXd at the same dose plus anastrozole, with men and premenopausal women also receiving a gonadotropin-releasing hormone analog.
The protocol originally called for six cycles of therapy, but was amended in February 2022 to increase the number to eight for newly enrolled participants and patients who were already on study treatment but had not yet had surgery.
The majority of patients in each arm had invasive ductal cancers, and most had HER2 expression on immunohistochemistry (IHC) of 1+, which is generally considered to be HER2-negative. However, there was only modest concordance between local and central review in determining HER2 expression levels, Dr. Bardia noted. Indeed, the entire question of HER2-low cancers, whether they compose a separate clinical entity from other cancers and how to standardize testing, was the subject of a special session at this year’s SABCS.
Results
Overall response rate, the primary endpoint, was 68% in the T-DXd arm and 58% in the T-DXd plus anastrazole arm.
Although the low response rate with the combination suggests that endocrine therapy may not be helpful in this patient population, it’s still too early to say so conclusively, Dr. Bardia said.
Looking at the change in HER2 expression by IHC from baseline to surgery, they found that 48.6% of patients had a change in HER2 IHC expression after T-DXd treatment, and that nearly 90% of these patients had a decrease in expression levels.
Among 42 patients with available data on residual cancer burden (RCB) at the time of data cutoff, one patient in the T-DXd alone arm with stage 3A disease had an RCB of 0, equivalent to a pathologic complete response (pCR). There were no other RCB 0 tumors after surgery in either study arm. The rate of combined RCB and RCB 1 (near pCR) was about 15% in each arm.
In all, 3 of the 58 patients in the study (5.2%) required dose reductions because of adverse events. There were no cases of grade 3 or greater pneumonitis, and no cases of either cardiomyopathy or neuropathy.
Way better than chemotherapy?
“It was very exciting when we got the DESTINY-Breast04 results showing this impressive activity of trastuzumab deruxtecan in this HER2-low entity, and now we know that hormone-positive [tumors], the majority of them are HER2-low. It was really encouraging, it was practice changing, but we were left wondering about this HER2-low entity, and can we act on it in the earlier setting,” commented Jason A. Mouabbi, MD, from the University of Texas MD Anderson Cancer Center in Houston.
“The beauty of the TRIO-US B-12 TALENT study is that it looked at the neoadjuvant setting where we know those patients who are hormone-positive usually do not respond well to chemotherapy,” he said in an interview.
He said that although the study didn’t compare T-DXd to chemotherapy, “it’s an excellent first start.”
An overall response rate near 70% “is something amazing. I’m really excited to see it against chemo. I think it’s going to do way better,” Dr. Mouabbi said.
The study was conducted by the Translational Research In Oncology (TRIO)-US network. Funding was provided by Daiichi Sankyo, the maker of trastuzumab deruxtecan (Enhertu). Dr. Bardia serves as a consultant or advisory board member for Pfizer, Novartis, Genentech, Merck, Radius Health, Immunomedics/Gilead Sciences, Sanofi, Daiichi Sankyo, AstraZeneca, and Eli Lilly, and has received research funding from Genentech, Novartis, Pfizer, Merck, Sanofi, Radius Health, Immunomedics/Gilead Sciences, Daiichi Sankyo, AstraZeneca, and Eli Lilly.
Dr. Mouabbi disclosed honoraria from BostonGene, Cardinal Health, Napo Pharmaceuticals, and Fresenius Kabi.
AT SABCS 2022
Incorporating medication abortion into your ObGyn practice: Why and how
The Supreme Court’s Dobbs decision on June 24, 2022, which nullified the federal protections of Roe v Wade, resulted in the swift and devastating dissolution of access to abortion care for hundreds of thousands of patients in the United States.1 Within days of the decision, 11 states in the South and Midwest implemented complete or 6-week abortion bans that, in part, led to the closure of over half the abortion clinics in these states.2 Abortion bans, severe restrictions, and clinic closures affect all patients and magnify existing health care inequities.
Medication abortion is becoming increasingly popular; as of 2020, approximately 50% of US abortions were performed using this method.3 Through a combination of mifepristone and misoprostol, medication abortion induces the physiologic process and symptoms similar to those of a miscarriage. Notably, this regimen is also the most effective medical management method for a missed abortion in the first trimester, and therefore, should already be incorporated into any general ObGyn practice.4
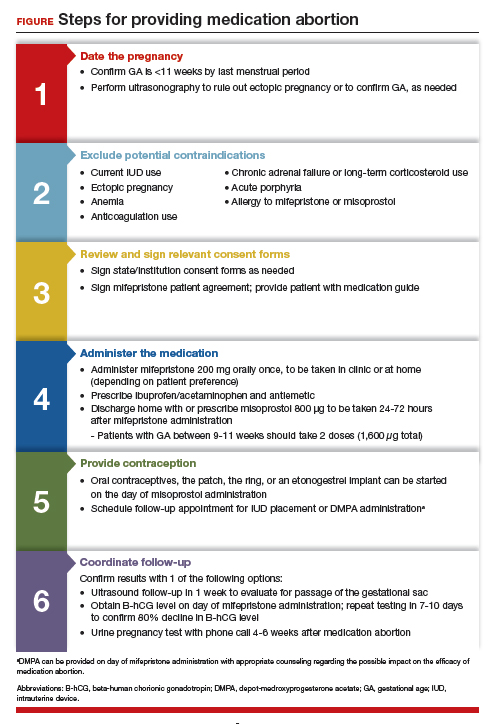
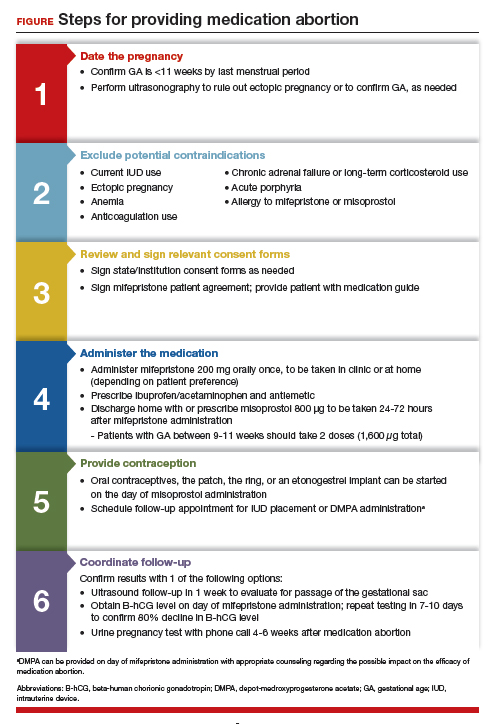
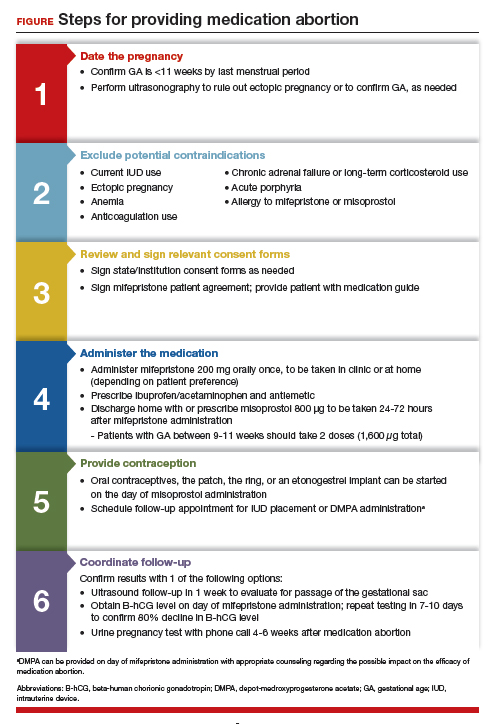
Although a recent study found that 97% of ObGyn physicians report encountering patients who seek an abortion, only 15% to 25% of them reported providing abortion services.5,6 Given our expertise, ObGyns are well-positioned to incorporate medication abortion into our practices. For those ObGyn providers who practice in states without extreme abortion bans, this article provides guidance on how to incorporate medication abortion into your practice (FIGURE). Several states now have early gestational limits on abortion, and the abortion-dedicated clinics that remain open are over capacity. Therefore, by incorporating medication abortion into your practice you can contribute to timely abortion access for your patients.
Medication abortion: The process
Determine your ability and patient’s eligibility
Abortion-specific laws for your state have now become the first determinant of your ability to provide medication abortion to your patients. The Guttmacher Institute is one reliable source of specific state laws that your practice can reference and is updated regularly.7
From a practice perspective, most ObGyn physicians already have the technical capabilities in place to provide medication abortion. First, you must be able to accurately determine the patient’s gestational age by their last menstrual period, which is often confirmed through ultrasonography.
Medication abortion is safe and routinely used in many practices up to 77 days, or 11 weeks, of gestation. Authors of a recent retrospective cohort study found that medication abortion also may be initiated for a pregnancy of unknown location in patients who are asymptomatic and determined to have low risk for an ectopic pregnancy. In this study, initiation of medication abortion on the day of presentation, with concurrent evaluation for ectopic pregnancy, was associated with a shorter time to a completed abortion, but a lower rate of successful medication abortion when compared with patients who delayed the initiation of medication abortion until a clear intrauterine pregnancy was diagnosed.8
Few medical contraindications exist for patients who seek a medication abortion. These contraindications include allergy to or medication interaction with mifepristone or misoprostol, chronic adrenal failure or long-term corticosteroid therapy, acute porphyria, anemia or the use of anticoagulation therapy, or current intrauterine device (IUD) use.
Continue to: Gather consents and administer treatment...
Gather consents and administer treatment
Historically, mifepristone has been dispensed directly at an ObGyn physician’s office. However, the US Food and Drug Administration (FDA) regulations requiring this were lifted during the COVID-19 pandemic, and as of December 2021, the inperson dispensing requirement was permanently removed.9 To provide mifepristone in a medical practice under current guidelines, a confidential prescriber agreement must be completed once by one person on behalf of the practice. Then each patient must read the manufacturer’s medication guide and sign the patient agreement form as part of the consent process (available on the FDA’s website).10 These agreement forms must be filled out by a physician and each patient if your practice uses mifepristone for any pregnancy indication, including induction of labor or medical management of miscarriage. Given the multiple evidence-based indications for mifepristone in pregnancy, it is hoped that these agreement forms will become a routine part of most ObGyn practices. Other consent requirements vary by state.
After signing consent forms, patients receive and often immediately take mifepristone 200 mg orally. Mifepristone is a progesterone receptor antagonist that sensitizes the uterine myometrium to the effects of prostaglandin.11 Rarely, patients may experience symptoms of bleeding or cramping after mifepristone administration alone.
Patients are discharged home with ibuprofen and an antiemetic for symptom relief to be taken around the time of administration of misoprostol. Misoprostol is a synthetic prostaglandin that causes uterine cramping and expulsion of the pregnancy typically within 4 hours of administration. Patients leave with the pills of misoprostol 800 μg (4 tablets, 200 µg each), which they self-administer buccally 24-48 hours after mifepristone administration. A prescription for misoprostol can be given instead of the actual pills, but geographic distance to the pharmacy and other potential barriers should be considered when evaluating the feasibility and convenience of providing pharmacy-dispensed misoprostol.
We instruct patients to place 2 tablets buccally between each gum and cheek, dosing all 4 tablets at the same time. Patients are instructed to let the tablets dissolve buccally and, after 30 minutes, to swallow the tablets with water. Administration of an automatic second dose of misoprostol 3-6 hours after the first dose for pregnancies between 9-11 weeks of gestation is recommended to increase success rate at these later gestational ages.12,13 Several different routes of administration, including buccal, vaginal, and sublingual, have been used for first trimester medication abortion with misoprostol.
Follow up and confirm the results
Patients can safely follow up after their medication abortion in several ways. In our practice, patients are offered 3 possible options.
- The first is ultrasound follow-up, whereby the patient returns to the clinic 1 week after their medication abortion for a pelvic ultrasound to confirm the gestational sac has passed.
- The second method is to test beta-human chorionic gonadotropin (B-hCG) levels. Patients interested in this option have a baseline B-hCG drawn on the day of presentation and follow up 7-10 days later for a repeat B-hCG test. An 80% drop in B-hCG level is consistent with a successful medication abortion.
- The third option, a phone checklist that is usually combined with a urine pregnancy test 4-6 weeks after a medication abortion, is an effective patient-centered approach. The COVID-19 pandemic and the subsequent compulsory shift to providing medical care via telemedicine highlighted the safety, acceptability, and patient preference for the provision of medication abortion using telehealth platforms.14
Outcomes and complications
Medication abortion using a combined regimen of mifepristone followed by misoprostol is approximately 95% effective at complete expulsion of the pregnancy.15,16 Complications after a first trimester medication abortion are rare. In a retrospective cohort study of 54,911 abortions, the most common complication was incomplete abortion.17 Symptoms concerning for incomplete abortion included persistent heavy vaginal bleeding and pelvic cramping. An incomplete or failed abortion should be managed with an additional dose of misoprostol or dilation and evacuation. Other possible complications such as infection are also rare, and prophylactic antibiotics are not encouraged.18
Future fertility and pregnancy implications
Patients should be counseled that a medication abortion is not associated with infertility or increased risk for adverse outcomes in future pregnancies.19 Contraceptive counseling should be provided to all interested patients at the time of a medication abortion and ideally provided to the patient on the day of their visit. Oral contraceptives, the patch, and the ring can be started on the day of misoprostol administration.20 The optimal timing of IUD insertion has been examined in 2 randomized control trials. Results indicated a higher uptake in the group of patients who received their IUD approximately 1 week after medication abortion versus delaying placement for several weeks, with no difference in IUD expulsion rates.21,22 Patients interested in depot-medroxyprogesterone acetate (DMPA) injection should be counseled on the theoretical decreased efficacy of medication abortion in the setting of concurrent DMPA administration. If possible, a follow-up plan should be made so that the patient can receive DMPA, if desired, at a later date.23 The etonogestrel implant (Nexplanon), however, can be placed on the day of mifepristone administration and does not affect the efficacy of a medication abortion.24,25
Summary
During this critical time for reproductive health care, it is essential that ObGyns consider how their professional position and expertise can assist with the provision of medication abortions. Most ObGyn practices already have the resources in place to effectively care for patients before, during, and after a medication abortion. Integrating abortion health care into your practice promotes patient-centered care, continuity, and patient satisfaction. Furthermore, by improving abortion referrals or offering information on safe, self-procured abortion, you can contribute to destigmatizing abortion care, while playing an integral role in connecting your patients with the care they need and desire. ●
- Jones RK, Philbin J, Kirstein M, et al. Long-term decline in US abortions reverses, showing rising need for abortion as Supreme Court is poised to overturn Roe v. Wade. Guttmacher Institute. August 30, 2022. https://www.gut. Accessed November 2, 2022. tmacher.org/article/2022/06 /long-term-decline-us-abortions-reverses-showing-rising -need-abortion-supreme-court.
- Kirstein M, Jones RK, Philbin J. One month post-roe: at least 43 abortion clinics across 11 states have stopped offering abortion care. Guttmacher Institute. September 5, 2022. https://www.guttmacher.org/article/2022/07/one-month -post-roe-least-43-abortion-clinics-across-11-states-have -stopped-offering. Accessed November 2, 2022.
- Jones RK, Nash E, Cross L, et al. Medication abortion now accounts for more than half of all US abortions. Guttmacher Institute. September 12, 2022. https://www.guttmacher.org /article/2022/02/medication-abortion-now-accounts-more-half-all-us-abortions. Accessed November 2, 2022.
- Schreiber CA, Creinin MD, Atrio J, et al. Mifepristone pretreatment for the medical management of early pregnancy loss. N Engl J Med. 2018;378:2161-2170. doi:10.1056/ nejmoa1715726.
- Stulberg DB, Dude AM, Dahlquist I, Curlin, FA. Abortion provision among practicing obstetrician-gynecologists. Obstet Gynecol. 2011;118:609-614. doi:10.1097/aog.0b013e31822ad973.
- Daniel S, Schulkin J, Grossman D. Obstetrician-gynecologist willingness to provide medication abortion with removal of the in-person dispensing requirement for mifepristone. Contraception. 2021;104:73-76. doi:10.1016/j. contraception.2021.03.026.
- Guttmacher Institute. State legislation tracker. Updated October 31, 2022. https://www.guttmacher.org/state-policy. Accessed November 2, 2022.
- Goldberg AB, Fulcher IR, Fortin J, et al. Mifepristone and misoprostol for undesired pregnancy of unknown location. Obstet Gynecol. 2022;139:771-780. doi:10.1097/ aog.0000000000004756.
- The American College of Obstetricians and Gynecologists. Understanding the practical implications of the FDA’s December 2021 mifepristone REMS decision: a Q&A with Dr. Nisha Verma and Vanessa Wellbery. March 28, 2022. https:// www.acog.org/news/news-articles/2022/03/understanding -the-practical-implications-of-the-fdas-december-2021 -mifepristone-rems-decision. Accessed November 2, 2022.
- US Food and Drug Administration. Mifeprex (mifepristone) information. December 16, 2021. https://www.fda.gov/ drugs/postmarket-drug-safety-information-patients-and-providers/ifeprex-mifepristone-information. Accessed November 2, 2022.
- Cadepond F, Ulmann A, Baulieu EE. Ru486 (mifepristone): mechanisms of action and clinical uses. Annu Rev Med. 1997;48:129-156. doi:10.1146/annurev.med.48.1.129.
- Ashok PW, Templeton A, Wagaarachchi PT, Flett GMM. Factors affecting the outcome of early medical abortion: a review of 4132 consecutive cases. BJOG. 2002;109:1281-1289. doi:10.1046/j.1471-0528.2002.02156.x.
- Coyaji K, Krishna U, Ambardekar S, et al. Are two doses of misoprostol after mifepristone for early abortion better than one? BJOG. 2007;114:271-278. doi:10.1111/j.14710528.2006.01208.x.
- Aiken A, Lohr PA, Lord J, et al. Effectiveness, safety and acceptability of no‐test medical abortion (termination of pregnancy) provided via telemedicine: a national cohort study. BJOG. 2021;128:1464-1474. doi:10.1111/14710528.16668.
- Schaff EA, Eisinger SH, Stadalius LS, et al. Low-dose mifepristone 200 mg and vaginal misoprostol for abortion. Contraception. 1999;59:1-6. doi:10.1016/s00107824(98)00150-4.
- Schaff EA, Fielding SL, Westhoff C. Randomized trial of oral versus vaginal misoprostol at one day after mifepristone for early medical abortion. Contraception. 2001;64:81-85. doi:10.1016/s0010-7824(01)00229-3.
- Upadhyay UD, Desai S, Zlidar V, et al. Incidence of emergency department visits and complications after abortion. Obstet Gynecol. 2015;125:175-183. doi:10.1097/ aog.0000000000000603.
- Shannon C, Brothers LP, Philip NM, Winikoff B. Infection after medical abortion: a review of the literature. Contraception. 2004;70:183-190. doi:10.1016/j.contraception.2004.04.009.
- Virk J, Zhang J, Olsen J. Medical abortion and the risk of subsequent adverse pregnancy outcomes. N Engl J Med. 2007;357:648-653. doi:10.1056/nejmoa070445.
- Mittal S. Contraception after medical abortion. Contraception. 2006;74:56-60. doi:10.1016/j.contraception.2006.03.006.
- Shimoni N, Davis A, Ramos ME, et al. Timing of copper intrauterine device insertion after medical abortion. Obstet Gynecol. 2011;118:623-628. doi:10.1097/aog.0b013e31822ade67.
- Sääv I, Stephansson O, Gemzell-Danielsson K. Early versus delayed insertion of intrauterine contraception after medical abortion—a randomized controlled trial. PloS ONE. 2012;7:e48948. doi:10.1371/journal.pone.0048948.
- Raymond EG, Weaver MA, Louie KS, et al. Effects of depot medroxyprogesterone acetate injection timing on medical abortion efficacy and repeat pregnancy: a randomized controlled trial. Obstet Gynecol. 2016;128:739-745. doi:10.1097/aog.0000000000001627.
- Hognert H, Kopp Kallner H, Cameron S, et al. Immediate versus delayed insertion of an etonogestrel releasing implant at medical abortion—a randomized controlled equivalence trial. Hum Reprod. 2016;31:2484-2490. doi:10.1093/humrep/ dew238.
- Raymond EG, Weaver MA, Tan Y-L, et al. Effect of immediate compared with delayed insertion of etonogestrel implants on medical abortion efficacy and repeat pregnancy. Obstet Gynecol. 2016;127:306-312. doi:10.1097/ aog.0000000000001274.
The Supreme Court’s Dobbs decision on June 24, 2022, which nullified the federal protections of Roe v Wade, resulted in the swift and devastating dissolution of access to abortion care for hundreds of thousands of patients in the United States.1 Within days of the decision, 11 states in the South and Midwest implemented complete or 6-week abortion bans that, in part, led to the closure of over half the abortion clinics in these states.2 Abortion bans, severe restrictions, and clinic closures affect all patients and magnify existing health care inequities.
Medication abortion is becoming increasingly popular; as of 2020, approximately 50% of US abortions were performed using this method.3 Through a combination of mifepristone and misoprostol, medication abortion induces the physiologic process and symptoms similar to those of a miscarriage. Notably, this regimen is also the most effective medical management method for a missed abortion in the first trimester, and therefore, should already be incorporated into any general ObGyn practice.4
Although a recent study found that 97% of ObGyn physicians report encountering patients who seek an abortion, only 15% to 25% of them reported providing abortion services.5,6 Given our expertise, ObGyns are well-positioned to incorporate medication abortion into our practices. For those ObGyn providers who practice in states without extreme abortion bans, this article provides guidance on how to incorporate medication abortion into your practice (FIGURE). Several states now have early gestational limits on abortion, and the abortion-dedicated clinics that remain open are over capacity. Therefore, by incorporating medication abortion into your practice you can contribute to timely abortion access for your patients.
Medication abortion: The process
Determine your ability and patient’s eligibility
Abortion-specific laws for your state have now become the first determinant of your ability to provide medication abortion to your patients. The Guttmacher Institute is one reliable source of specific state laws that your practice can reference and is updated regularly.7
From a practice perspective, most ObGyn physicians already have the technical capabilities in place to provide medication abortion. First, you must be able to accurately determine the patient’s gestational age by their last menstrual period, which is often confirmed through ultrasonography.
Medication abortion is safe and routinely used in many practices up to 77 days, or 11 weeks, of gestation. Authors of a recent retrospective cohort study found that medication abortion also may be initiated for a pregnancy of unknown location in patients who are asymptomatic and determined to have low risk for an ectopic pregnancy. In this study, initiation of medication abortion on the day of presentation, with concurrent evaluation for ectopic pregnancy, was associated with a shorter time to a completed abortion, but a lower rate of successful medication abortion when compared with patients who delayed the initiation of medication abortion until a clear intrauterine pregnancy was diagnosed.8
Few medical contraindications exist for patients who seek a medication abortion. These contraindications include allergy to or medication interaction with mifepristone or misoprostol, chronic adrenal failure or long-term corticosteroid therapy, acute porphyria, anemia or the use of anticoagulation therapy, or current intrauterine device (IUD) use.
Continue to: Gather consents and administer treatment...
Gather consents and administer treatment
Historically, mifepristone has been dispensed directly at an ObGyn physician’s office. However, the US Food and Drug Administration (FDA) regulations requiring this were lifted during the COVID-19 pandemic, and as of December 2021, the inperson dispensing requirement was permanently removed.9 To provide mifepristone in a medical practice under current guidelines, a confidential prescriber agreement must be completed once by one person on behalf of the practice. Then each patient must read the manufacturer’s medication guide and sign the patient agreement form as part of the consent process (available on the FDA’s website).10 These agreement forms must be filled out by a physician and each patient if your practice uses mifepristone for any pregnancy indication, including induction of labor or medical management of miscarriage. Given the multiple evidence-based indications for mifepristone in pregnancy, it is hoped that these agreement forms will become a routine part of most ObGyn practices. Other consent requirements vary by state.
After signing consent forms, patients receive and often immediately take mifepristone 200 mg orally. Mifepristone is a progesterone receptor antagonist that sensitizes the uterine myometrium to the effects of prostaglandin.11 Rarely, patients may experience symptoms of bleeding or cramping after mifepristone administration alone.
Patients are discharged home with ibuprofen and an antiemetic for symptom relief to be taken around the time of administration of misoprostol. Misoprostol is a synthetic prostaglandin that causes uterine cramping and expulsion of the pregnancy typically within 4 hours of administration. Patients leave with the pills of misoprostol 800 μg (4 tablets, 200 µg each), which they self-administer buccally 24-48 hours after mifepristone administration. A prescription for misoprostol can be given instead of the actual pills, but geographic distance to the pharmacy and other potential barriers should be considered when evaluating the feasibility and convenience of providing pharmacy-dispensed misoprostol.
We instruct patients to place 2 tablets buccally between each gum and cheek, dosing all 4 tablets at the same time. Patients are instructed to let the tablets dissolve buccally and, after 30 minutes, to swallow the tablets with water. Administration of an automatic second dose of misoprostol 3-6 hours after the first dose for pregnancies between 9-11 weeks of gestation is recommended to increase success rate at these later gestational ages.12,13 Several different routes of administration, including buccal, vaginal, and sublingual, have been used for first trimester medication abortion with misoprostol.
Follow up and confirm the results
Patients can safely follow up after their medication abortion in several ways. In our practice, patients are offered 3 possible options.
- The first is ultrasound follow-up, whereby the patient returns to the clinic 1 week after their medication abortion for a pelvic ultrasound to confirm the gestational sac has passed.
- The second method is to test beta-human chorionic gonadotropin (B-hCG) levels. Patients interested in this option have a baseline B-hCG drawn on the day of presentation and follow up 7-10 days later for a repeat B-hCG test. An 80% drop in B-hCG level is consistent with a successful medication abortion.
- The third option, a phone checklist that is usually combined with a urine pregnancy test 4-6 weeks after a medication abortion, is an effective patient-centered approach. The COVID-19 pandemic and the subsequent compulsory shift to providing medical care via telemedicine highlighted the safety, acceptability, and patient preference for the provision of medication abortion using telehealth platforms.14
Outcomes and complications
Medication abortion using a combined regimen of mifepristone followed by misoprostol is approximately 95% effective at complete expulsion of the pregnancy.15,16 Complications after a first trimester medication abortion are rare. In a retrospective cohort study of 54,911 abortions, the most common complication was incomplete abortion.17 Symptoms concerning for incomplete abortion included persistent heavy vaginal bleeding and pelvic cramping. An incomplete or failed abortion should be managed with an additional dose of misoprostol or dilation and evacuation. Other possible complications such as infection are also rare, and prophylactic antibiotics are not encouraged.18
Future fertility and pregnancy implications
Patients should be counseled that a medication abortion is not associated with infertility or increased risk for adverse outcomes in future pregnancies.19 Contraceptive counseling should be provided to all interested patients at the time of a medication abortion and ideally provided to the patient on the day of their visit. Oral contraceptives, the patch, and the ring can be started on the day of misoprostol administration.20 The optimal timing of IUD insertion has been examined in 2 randomized control trials. Results indicated a higher uptake in the group of patients who received their IUD approximately 1 week after medication abortion versus delaying placement for several weeks, with no difference in IUD expulsion rates.21,22 Patients interested in depot-medroxyprogesterone acetate (DMPA) injection should be counseled on the theoretical decreased efficacy of medication abortion in the setting of concurrent DMPA administration. If possible, a follow-up plan should be made so that the patient can receive DMPA, if desired, at a later date.23 The etonogestrel implant (Nexplanon), however, can be placed on the day of mifepristone administration and does not affect the efficacy of a medication abortion.24,25
Summary
During this critical time for reproductive health care, it is essential that ObGyns consider how their professional position and expertise can assist with the provision of medication abortions. Most ObGyn practices already have the resources in place to effectively care for patients before, during, and after a medication abortion. Integrating abortion health care into your practice promotes patient-centered care, continuity, and patient satisfaction. Furthermore, by improving abortion referrals or offering information on safe, self-procured abortion, you can contribute to destigmatizing abortion care, while playing an integral role in connecting your patients with the care they need and desire. ●
The Supreme Court’s Dobbs decision on June 24, 2022, which nullified the federal protections of Roe v Wade, resulted in the swift and devastating dissolution of access to abortion care for hundreds of thousands of patients in the United States.1 Within days of the decision, 11 states in the South and Midwest implemented complete or 6-week abortion bans that, in part, led to the closure of over half the abortion clinics in these states.2 Abortion bans, severe restrictions, and clinic closures affect all patients and magnify existing health care inequities.
Medication abortion is becoming increasingly popular; as of 2020, approximately 50% of US abortions were performed using this method.3 Through a combination of mifepristone and misoprostol, medication abortion induces the physiologic process and symptoms similar to those of a miscarriage. Notably, this regimen is also the most effective medical management method for a missed abortion in the first trimester, and therefore, should already be incorporated into any general ObGyn practice.4
Although a recent study found that 97% of ObGyn physicians report encountering patients who seek an abortion, only 15% to 25% of them reported providing abortion services.5,6 Given our expertise, ObGyns are well-positioned to incorporate medication abortion into our practices. For those ObGyn providers who practice in states without extreme abortion bans, this article provides guidance on how to incorporate medication abortion into your practice (FIGURE). Several states now have early gestational limits on abortion, and the abortion-dedicated clinics that remain open are over capacity. Therefore, by incorporating medication abortion into your practice you can contribute to timely abortion access for your patients.
Medication abortion: The process
Determine your ability and patient’s eligibility
Abortion-specific laws for your state have now become the first determinant of your ability to provide medication abortion to your patients. The Guttmacher Institute is one reliable source of specific state laws that your practice can reference and is updated regularly.7
From a practice perspective, most ObGyn physicians already have the technical capabilities in place to provide medication abortion. First, you must be able to accurately determine the patient’s gestational age by their last menstrual period, which is often confirmed through ultrasonography.
Medication abortion is safe and routinely used in many practices up to 77 days, or 11 weeks, of gestation. Authors of a recent retrospective cohort study found that medication abortion also may be initiated for a pregnancy of unknown location in patients who are asymptomatic and determined to have low risk for an ectopic pregnancy. In this study, initiation of medication abortion on the day of presentation, with concurrent evaluation for ectopic pregnancy, was associated with a shorter time to a completed abortion, but a lower rate of successful medication abortion when compared with patients who delayed the initiation of medication abortion until a clear intrauterine pregnancy was diagnosed.8
Few medical contraindications exist for patients who seek a medication abortion. These contraindications include allergy to or medication interaction with mifepristone or misoprostol, chronic adrenal failure or long-term corticosteroid therapy, acute porphyria, anemia or the use of anticoagulation therapy, or current intrauterine device (IUD) use.
Continue to: Gather consents and administer treatment...
Gather consents and administer treatment
Historically, mifepristone has been dispensed directly at an ObGyn physician’s office. However, the US Food and Drug Administration (FDA) regulations requiring this were lifted during the COVID-19 pandemic, and as of December 2021, the inperson dispensing requirement was permanently removed.9 To provide mifepristone in a medical practice under current guidelines, a confidential prescriber agreement must be completed once by one person on behalf of the practice. Then each patient must read the manufacturer’s medication guide and sign the patient agreement form as part of the consent process (available on the FDA’s website).10 These agreement forms must be filled out by a physician and each patient if your practice uses mifepristone for any pregnancy indication, including induction of labor or medical management of miscarriage. Given the multiple evidence-based indications for mifepristone in pregnancy, it is hoped that these agreement forms will become a routine part of most ObGyn practices. Other consent requirements vary by state.
After signing consent forms, patients receive and often immediately take mifepristone 200 mg orally. Mifepristone is a progesterone receptor antagonist that sensitizes the uterine myometrium to the effects of prostaglandin.11 Rarely, patients may experience symptoms of bleeding or cramping after mifepristone administration alone.
Patients are discharged home with ibuprofen and an antiemetic for symptom relief to be taken around the time of administration of misoprostol. Misoprostol is a synthetic prostaglandin that causes uterine cramping and expulsion of the pregnancy typically within 4 hours of administration. Patients leave with the pills of misoprostol 800 μg (4 tablets, 200 µg each), which they self-administer buccally 24-48 hours after mifepristone administration. A prescription for misoprostol can be given instead of the actual pills, but geographic distance to the pharmacy and other potential barriers should be considered when evaluating the feasibility and convenience of providing pharmacy-dispensed misoprostol.
We instruct patients to place 2 tablets buccally between each gum and cheek, dosing all 4 tablets at the same time. Patients are instructed to let the tablets dissolve buccally and, after 30 minutes, to swallow the tablets with water. Administration of an automatic second dose of misoprostol 3-6 hours after the first dose for pregnancies between 9-11 weeks of gestation is recommended to increase success rate at these later gestational ages.12,13 Several different routes of administration, including buccal, vaginal, and sublingual, have been used for first trimester medication abortion with misoprostol.
Follow up and confirm the results
Patients can safely follow up after their medication abortion in several ways. In our practice, patients are offered 3 possible options.
- The first is ultrasound follow-up, whereby the patient returns to the clinic 1 week after their medication abortion for a pelvic ultrasound to confirm the gestational sac has passed.
- The second method is to test beta-human chorionic gonadotropin (B-hCG) levels. Patients interested in this option have a baseline B-hCG drawn on the day of presentation and follow up 7-10 days later for a repeat B-hCG test. An 80% drop in B-hCG level is consistent with a successful medication abortion.
- The third option, a phone checklist that is usually combined with a urine pregnancy test 4-6 weeks after a medication abortion, is an effective patient-centered approach. The COVID-19 pandemic and the subsequent compulsory shift to providing medical care via telemedicine highlighted the safety, acceptability, and patient preference for the provision of medication abortion using telehealth platforms.14
Outcomes and complications
Medication abortion using a combined regimen of mifepristone followed by misoprostol is approximately 95% effective at complete expulsion of the pregnancy.15,16 Complications after a first trimester medication abortion are rare. In a retrospective cohort study of 54,911 abortions, the most common complication was incomplete abortion.17 Symptoms concerning for incomplete abortion included persistent heavy vaginal bleeding and pelvic cramping. An incomplete or failed abortion should be managed with an additional dose of misoprostol or dilation and evacuation. Other possible complications such as infection are also rare, and prophylactic antibiotics are not encouraged.18
Future fertility and pregnancy implications
Patients should be counseled that a medication abortion is not associated with infertility or increased risk for adverse outcomes in future pregnancies.19 Contraceptive counseling should be provided to all interested patients at the time of a medication abortion and ideally provided to the patient on the day of their visit. Oral contraceptives, the patch, and the ring can be started on the day of misoprostol administration.20 The optimal timing of IUD insertion has been examined in 2 randomized control trials. Results indicated a higher uptake in the group of patients who received their IUD approximately 1 week after medication abortion versus delaying placement for several weeks, with no difference in IUD expulsion rates.21,22 Patients interested in depot-medroxyprogesterone acetate (DMPA) injection should be counseled on the theoretical decreased efficacy of medication abortion in the setting of concurrent DMPA administration. If possible, a follow-up plan should be made so that the patient can receive DMPA, if desired, at a later date.23 The etonogestrel implant (Nexplanon), however, can be placed on the day of mifepristone administration and does not affect the efficacy of a medication abortion.24,25
Summary
During this critical time for reproductive health care, it is essential that ObGyns consider how their professional position and expertise can assist with the provision of medication abortions. Most ObGyn practices already have the resources in place to effectively care for patients before, during, and after a medication abortion. Integrating abortion health care into your practice promotes patient-centered care, continuity, and patient satisfaction. Furthermore, by improving abortion referrals or offering information on safe, self-procured abortion, you can contribute to destigmatizing abortion care, while playing an integral role in connecting your patients with the care they need and desire. ●
- Jones RK, Philbin J, Kirstein M, et al. Long-term decline in US abortions reverses, showing rising need for abortion as Supreme Court is poised to overturn Roe v. Wade. Guttmacher Institute. August 30, 2022. https://www.gut. Accessed November 2, 2022. tmacher.org/article/2022/06 /long-term-decline-us-abortions-reverses-showing-rising -need-abortion-supreme-court.
- Kirstein M, Jones RK, Philbin J. One month post-roe: at least 43 abortion clinics across 11 states have stopped offering abortion care. Guttmacher Institute. September 5, 2022. https://www.guttmacher.org/article/2022/07/one-month -post-roe-least-43-abortion-clinics-across-11-states-have -stopped-offering. Accessed November 2, 2022.
- Jones RK, Nash E, Cross L, et al. Medication abortion now accounts for more than half of all US abortions. Guttmacher Institute. September 12, 2022. https://www.guttmacher.org /article/2022/02/medication-abortion-now-accounts-more-half-all-us-abortions. Accessed November 2, 2022.
- Schreiber CA, Creinin MD, Atrio J, et al. Mifepristone pretreatment for the medical management of early pregnancy loss. N Engl J Med. 2018;378:2161-2170. doi:10.1056/ nejmoa1715726.
- Stulberg DB, Dude AM, Dahlquist I, Curlin, FA. Abortion provision among practicing obstetrician-gynecologists. Obstet Gynecol. 2011;118:609-614. doi:10.1097/aog.0b013e31822ad973.
- Daniel S, Schulkin J, Grossman D. Obstetrician-gynecologist willingness to provide medication abortion with removal of the in-person dispensing requirement for mifepristone. Contraception. 2021;104:73-76. doi:10.1016/j. contraception.2021.03.026.
- Guttmacher Institute. State legislation tracker. Updated October 31, 2022. https://www.guttmacher.org/state-policy. Accessed November 2, 2022.
- Goldberg AB, Fulcher IR, Fortin J, et al. Mifepristone and misoprostol for undesired pregnancy of unknown location. Obstet Gynecol. 2022;139:771-780. doi:10.1097/ aog.0000000000004756.
- The American College of Obstetricians and Gynecologists. Understanding the practical implications of the FDA’s December 2021 mifepristone REMS decision: a Q&A with Dr. Nisha Verma and Vanessa Wellbery. March 28, 2022. https:// www.acog.org/news/news-articles/2022/03/understanding -the-practical-implications-of-the-fdas-december-2021 -mifepristone-rems-decision. Accessed November 2, 2022.
- US Food and Drug Administration. Mifeprex (mifepristone) information. December 16, 2021. https://www.fda.gov/ drugs/postmarket-drug-safety-information-patients-and-providers/ifeprex-mifepristone-information. Accessed November 2, 2022.
- Cadepond F, Ulmann A, Baulieu EE. Ru486 (mifepristone): mechanisms of action and clinical uses. Annu Rev Med. 1997;48:129-156. doi:10.1146/annurev.med.48.1.129.
- Ashok PW, Templeton A, Wagaarachchi PT, Flett GMM. Factors affecting the outcome of early medical abortion: a review of 4132 consecutive cases. BJOG. 2002;109:1281-1289. doi:10.1046/j.1471-0528.2002.02156.x.
- Coyaji K, Krishna U, Ambardekar S, et al. Are two doses of misoprostol after mifepristone for early abortion better than one? BJOG. 2007;114:271-278. doi:10.1111/j.14710528.2006.01208.x.
- Aiken A, Lohr PA, Lord J, et al. Effectiveness, safety and acceptability of no‐test medical abortion (termination of pregnancy) provided via telemedicine: a national cohort study. BJOG. 2021;128:1464-1474. doi:10.1111/14710528.16668.
- Schaff EA, Eisinger SH, Stadalius LS, et al. Low-dose mifepristone 200 mg and vaginal misoprostol for abortion. Contraception. 1999;59:1-6. doi:10.1016/s00107824(98)00150-4.
- Schaff EA, Fielding SL, Westhoff C. Randomized trial of oral versus vaginal misoprostol at one day after mifepristone for early medical abortion. Contraception. 2001;64:81-85. doi:10.1016/s0010-7824(01)00229-3.
- Upadhyay UD, Desai S, Zlidar V, et al. Incidence of emergency department visits and complications after abortion. Obstet Gynecol. 2015;125:175-183. doi:10.1097/ aog.0000000000000603.
- Shannon C, Brothers LP, Philip NM, Winikoff B. Infection after medical abortion: a review of the literature. Contraception. 2004;70:183-190. doi:10.1016/j.contraception.2004.04.009.
- Virk J, Zhang J, Olsen J. Medical abortion and the risk of subsequent adverse pregnancy outcomes. N Engl J Med. 2007;357:648-653. doi:10.1056/nejmoa070445.
- Mittal S. Contraception after medical abortion. Contraception. 2006;74:56-60. doi:10.1016/j.contraception.2006.03.006.
- Shimoni N, Davis A, Ramos ME, et al. Timing of copper intrauterine device insertion after medical abortion. Obstet Gynecol. 2011;118:623-628. doi:10.1097/aog.0b013e31822ade67.
- Sääv I, Stephansson O, Gemzell-Danielsson K. Early versus delayed insertion of intrauterine contraception after medical abortion—a randomized controlled trial. PloS ONE. 2012;7:e48948. doi:10.1371/journal.pone.0048948.
- Raymond EG, Weaver MA, Louie KS, et al. Effects of depot medroxyprogesterone acetate injection timing on medical abortion efficacy and repeat pregnancy: a randomized controlled trial. Obstet Gynecol. 2016;128:739-745. doi:10.1097/aog.0000000000001627.
- Hognert H, Kopp Kallner H, Cameron S, et al. Immediate versus delayed insertion of an etonogestrel releasing implant at medical abortion—a randomized controlled equivalence trial. Hum Reprod. 2016;31:2484-2490. doi:10.1093/humrep/ dew238.
- Raymond EG, Weaver MA, Tan Y-L, et al. Effect of immediate compared with delayed insertion of etonogestrel implants on medical abortion efficacy and repeat pregnancy. Obstet Gynecol. 2016;127:306-312. doi:10.1097/ aog.0000000000001274.
- Jones RK, Philbin J, Kirstein M, et al. Long-term decline in US abortions reverses, showing rising need for abortion as Supreme Court is poised to overturn Roe v. Wade. Guttmacher Institute. August 30, 2022. https://www.gut. Accessed November 2, 2022. tmacher.org/article/2022/06 /long-term-decline-us-abortions-reverses-showing-rising -need-abortion-supreme-court.
- Kirstein M, Jones RK, Philbin J. One month post-roe: at least 43 abortion clinics across 11 states have stopped offering abortion care. Guttmacher Institute. September 5, 2022. https://www.guttmacher.org/article/2022/07/one-month -post-roe-least-43-abortion-clinics-across-11-states-have -stopped-offering. Accessed November 2, 2022.
- Jones RK, Nash E, Cross L, et al. Medication abortion now accounts for more than half of all US abortions. Guttmacher Institute. September 12, 2022. https://www.guttmacher.org /article/2022/02/medication-abortion-now-accounts-more-half-all-us-abortions. Accessed November 2, 2022.
- Schreiber CA, Creinin MD, Atrio J, et al. Mifepristone pretreatment for the medical management of early pregnancy loss. N Engl J Med. 2018;378:2161-2170. doi:10.1056/ nejmoa1715726.
- Stulberg DB, Dude AM, Dahlquist I, Curlin, FA. Abortion provision among practicing obstetrician-gynecologists. Obstet Gynecol. 2011;118:609-614. doi:10.1097/aog.0b013e31822ad973.
- Daniel S, Schulkin J, Grossman D. Obstetrician-gynecologist willingness to provide medication abortion with removal of the in-person dispensing requirement for mifepristone. Contraception. 2021;104:73-76. doi:10.1016/j. contraception.2021.03.026.
- Guttmacher Institute. State legislation tracker. Updated October 31, 2022. https://www.guttmacher.org/state-policy. Accessed November 2, 2022.
- Goldberg AB, Fulcher IR, Fortin J, et al. Mifepristone and misoprostol for undesired pregnancy of unknown location. Obstet Gynecol. 2022;139:771-780. doi:10.1097/ aog.0000000000004756.
- The American College of Obstetricians and Gynecologists. Understanding the practical implications of the FDA’s December 2021 mifepristone REMS decision: a Q&A with Dr. Nisha Verma and Vanessa Wellbery. March 28, 2022. https:// www.acog.org/news/news-articles/2022/03/understanding -the-practical-implications-of-the-fdas-december-2021 -mifepristone-rems-decision. Accessed November 2, 2022.
- US Food and Drug Administration. Mifeprex (mifepristone) information. December 16, 2021. https://www.fda.gov/ drugs/postmarket-drug-safety-information-patients-and-providers/ifeprex-mifepristone-information. Accessed November 2, 2022.
- Cadepond F, Ulmann A, Baulieu EE. Ru486 (mifepristone): mechanisms of action and clinical uses. Annu Rev Med. 1997;48:129-156. doi:10.1146/annurev.med.48.1.129.
- Ashok PW, Templeton A, Wagaarachchi PT, Flett GMM. Factors affecting the outcome of early medical abortion: a review of 4132 consecutive cases. BJOG. 2002;109:1281-1289. doi:10.1046/j.1471-0528.2002.02156.x.
- Coyaji K, Krishna U, Ambardekar S, et al. Are two doses of misoprostol after mifepristone for early abortion better than one? BJOG. 2007;114:271-278. doi:10.1111/j.14710528.2006.01208.x.
- Aiken A, Lohr PA, Lord J, et al. Effectiveness, safety and acceptability of no‐test medical abortion (termination of pregnancy) provided via telemedicine: a national cohort study. BJOG. 2021;128:1464-1474. doi:10.1111/14710528.16668.
- Schaff EA, Eisinger SH, Stadalius LS, et al. Low-dose mifepristone 200 mg and vaginal misoprostol for abortion. Contraception. 1999;59:1-6. doi:10.1016/s00107824(98)00150-4.
- Schaff EA, Fielding SL, Westhoff C. Randomized trial of oral versus vaginal misoprostol at one day after mifepristone for early medical abortion. Contraception. 2001;64:81-85. doi:10.1016/s0010-7824(01)00229-3.
- Upadhyay UD, Desai S, Zlidar V, et al. Incidence of emergency department visits and complications after abortion. Obstet Gynecol. 2015;125:175-183. doi:10.1097/ aog.0000000000000603.
- Shannon C, Brothers LP, Philip NM, Winikoff B. Infection after medical abortion: a review of the literature. Contraception. 2004;70:183-190. doi:10.1016/j.contraception.2004.04.009.
- Virk J, Zhang J, Olsen J. Medical abortion and the risk of subsequent adverse pregnancy outcomes. N Engl J Med. 2007;357:648-653. doi:10.1056/nejmoa070445.
- Mittal S. Contraception after medical abortion. Contraception. 2006;74:56-60. doi:10.1016/j.contraception.2006.03.006.
- Shimoni N, Davis A, Ramos ME, et al. Timing of copper intrauterine device insertion after medical abortion. Obstet Gynecol. 2011;118:623-628. doi:10.1097/aog.0b013e31822ade67.
- Sääv I, Stephansson O, Gemzell-Danielsson K. Early versus delayed insertion of intrauterine contraception after medical abortion—a randomized controlled trial. PloS ONE. 2012;7:e48948. doi:10.1371/journal.pone.0048948.
- Raymond EG, Weaver MA, Louie KS, et al. Effects of depot medroxyprogesterone acetate injection timing on medical abortion efficacy and repeat pregnancy: a randomized controlled trial. Obstet Gynecol. 2016;128:739-745. doi:10.1097/aog.0000000000001627.
- Hognert H, Kopp Kallner H, Cameron S, et al. Immediate versus delayed insertion of an etonogestrel releasing implant at medical abortion—a randomized controlled equivalence trial. Hum Reprod. 2016;31:2484-2490. doi:10.1093/humrep/ dew238.
- Raymond EG, Weaver MA, Tan Y-L, et al. Effect of immediate compared with delayed insertion of etonogestrel implants on medical abortion efficacy and repeat pregnancy. Obstet Gynecol. 2016;127:306-312. doi:10.1097/ aog.0000000000001274.
More states to consider extending postpartum Medicaid coverage beyond 2 months
Lawmakers in several conservative-led states – including Montana, Wyoming, Missouri, and Mississippi – are expected to consider proposals to provide a year of continuous health coverage to new mothers enrolled in Medicaid.
Medicaid beneficiaries nationwide are guaranteed continuous postpartum coverage during the ongoing covid-19 public health emergency. But momentum has been building for states to extend the default 60-day required coverage period ahead of the emergency’s eventual end. Approximately 42% of births nationwide are covered under Medicaid, the federal-state health insurance program for low-income people, and extending postpartum coverage aims to reduce the risk of pregnancy-related deaths and illnesses by ensuring that new mothers’ medical care isn’t interrupted.
The push comes as a provision in the American Rescue Plan Act makes extending postpartum Medicaid coverage easier because states no longer need to apply for a waiver. A renewed focus on maternal health amid high U.S. maternal mortality rates also is driving the proposals, as is the expectation that more women will need postpartum care as state abortion bans proliferate in the wake of the U.S. Supreme Court’s decision to eliminate federal protections.
Thirty-five states and Washington have already extended, or plan to extend, postpartum eligibility in their Medicaid programs. That number includes Texas and Wisconsin, which did not implement the ARPA provision but have proposed limited extensions of 6 months and 90 days, respectively.
The 15 states that limit postpartum Medicaid eligibility to 60 days are predominantly a swath of Republican-led states that stretch from the Mountain West to the South. But that could change when legislative sessions start in the new year.
In Montana, Republican Gov. Greg Gianforte and Department of Public Health and Human Services Director Charlie Brereton included 12-month postpartum eligibility in the governor’s proposed state budget. It would cost $9.2 million in federal and state funding over the next 2 years, according to the proposal, with the federal government covering nearly 70%.
A 2021 U.S. Department of Health and Human Services report estimated about 2,000 women in Montana would benefit from the change. State health department spokesperson Jon Ebelt said state officials’ estimate is half that number. The reason for the disparity was not immediately clear.
Mr. Brereton considers the “extension of coverage for new mothers to be a pro-life, pro-family reform,” Mr. Ebelt said.
To become law, the proposal must be approved by state lawmakers once the legislative session begins in January. It has already received enthusiastic support from the senior Democrat on the committee that oversees the health department’s budget. “Continuous eligibility for women after they have a baby is really important,” said state Rep. Mary Caferro during the Children’s Legislative Forum in Helena on Nov. 30.
The top Republican on the committee, state Rep.-elect Bob Keenan, said he hasn’t dug in on the governor’s budget proposal but added that he plans to survey his fellow lawmakers and health care providers on the postpartum extension. “I wouldn’t dare venture a guess as to its acceptance,” he said.
Nationwide, more than 1 in 5 mothers whose pregnancies were covered by Medicaid lose their insurance within 6 months of giving birth, and 1 in 3 pregnancy-related deaths happen between a week and a year after a birth occurs, according to federal health officials.
The United States had the highest overall maternal mortality rate, by far, among wealthy nations in 2020, at 23.8 deaths per 100,000 births, according to a report by the Commonwealth Fund, a foundation that supports research focused on health care issues. The rate for Black women in the United States is even higher, 55.3 deaths.
“Many maternal deaths result from missed or delayed opportunities for treatment,” the report said.
The maternal mortality rate in Montana is not publicly available because the Centers for Disease Control and Prevention suppressed the state data in 2020 “due to reliability and confidentiality restrictions.” Mr. Ebelt, the state health department spokesperson, could not provide a rate before this article’s publication.
Annie Glover, a senior research scientist for the University of Montana’s Rural Institute for Inclusive Communities, said the governor’s proposal to extend postpartum Medicaid coverage could make a significant difference in improving overall maternal health in Montana. The university was awarded a federal grant this year for such efforts, particularly to lower the mortality rate among Native Americans, and Ms. Glover said the state measure could further reduce rates.
“The reason really has to do with maintaining access to care during this very critical period,” Ms. Glover said. That goes for helping mothers with postpartum depression, as well as medical conditions like high blood pressure that require follow-ups with a physician well after delivery, she said.
In Wyoming, a legislative committee voted 6-5 in August to introduce a bill in the next session; dissenters cited the cost and their reluctance to further entangle the state in federal government programs.
About a third of Wyoming births are covered by Medicaid, and state officials estimate about 1,250 women would benefit from the change.
Postpartum eligibility bills are also expected to be taken up by legislators in Missouri and Mississippi, two states that have previously grappled with the issue. Both states have outlawed most abortions since the U.S. Supreme Court lifted federal protections in June, and Mississippi leaders have said additional postpartum care is needed because of the thousands of additional births expected as a result of the state’s ban.
A proposed coverage expansion died in the Mississippi House last session, but Lt. Gov. Delbert Hosemann said the Senate will revive the measure, according to Mississippi Today.
Last year, federal officials approved a Medicaid waiver for Missouri that allows the state to extend postpartum eligibility. But state officials delayed implementing the change to determine how enrollment would be affected by Missouri voters’ decision in August 2020 to expand Medicaid eligibility to more people. The delay prompted a bill to be filed last session that would have extended postpartum coverage by a year. That measure died, but a state lawmaker has pre-filed a bill that will bring back the debate in the upcoming session.
In Idaho, a children’s advocacy group said it will press lawmakers to approve a postpartum eligibility extension, among other measures, after the state banned nearly all abortions this year.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Lawmakers in several conservative-led states – including Montana, Wyoming, Missouri, and Mississippi – are expected to consider proposals to provide a year of continuous health coverage to new mothers enrolled in Medicaid.
Medicaid beneficiaries nationwide are guaranteed continuous postpartum coverage during the ongoing covid-19 public health emergency. But momentum has been building for states to extend the default 60-day required coverage period ahead of the emergency’s eventual end. Approximately 42% of births nationwide are covered under Medicaid, the federal-state health insurance program for low-income people, and extending postpartum coverage aims to reduce the risk of pregnancy-related deaths and illnesses by ensuring that new mothers’ medical care isn’t interrupted.
The push comes as a provision in the American Rescue Plan Act makes extending postpartum Medicaid coverage easier because states no longer need to apply for a waiver. A renewed focus on maternal health amid high U.S. maternal mortality rates also is driving the proposals, as is the expectation that more women will need postpartum care as state abortion bans proliferate in the wake of the U.S. Supreme Court’s decision to eliminate federal protections.
Thirty-five states and Washington have already extended, or plan to extend, postpartum eligibility in their Medicaid programs. That number includes Texas and Wisconsin, which did not implement the ARPA provision but have proposed limited extensions of 6 months and 90 days, respectively.
The 15 states that limit postpartum Medicaid eligibility to 60 days are predominantly a swath of Republican-led states that stretch from the Mountain West to the South. But that could change when legislative sessions start in the new year.
In Montana, Republican Gov. Greg Gianforte and Department of Public Health and Human Services Director Charlie Brereton included 12-month postpartum eligibility in the governor’s proposed state budget. It would cost $9.2 million in federal and state funding over the next 2 years, according to the proposal, with the federal government covering nearly 70%.
A 2021 U.S. Department of Health and Human Services report estimated about 2,000 women in Montana would benefit from the change. State health department spokesperson Jon Ebelt said state officials’ estimate is half that number. The reason for the disparity was not immediately clear.
Mr. Brereton considers the “extension of coverage for new mothers to be a pro-life, pro-family reform,” Mr. Ebelt said.
To become law, the proposal must be approved by state lawmakers once the legislative session begins in January. It has already received enthusiastic support from the senior Democrat on the committee that oversees the health department’s budget. “Continuous eligibility for women after they have a baby is really important,” said state Rep. Mary Caferro during the Children’s Legislative Forum in Helena on Nov. 30.
The top Republican on the committee, state Rep.-elect Bob Keenan, said he hasn’t dug in on the governor’s budget proposal but added that he plans to survey his fellow lawmakers and health care providers on the postpartum extension. “I wouldn’t dare venture a guess as to its acceptance,” he said.
Nationwide, more than 1 in 5 mothers whose pregnancies were covered by Medicaid lose their insurance within 6 months of giving birth, and 1 in 3 pregnancy-related deaths happen between a week and a year after a birth occurs, according to federal health officials.
The United States had the highest overall maternal mortality rate, by far, among wealthy nations in 2020, at 23.8 deaths per 100,000 births, according to a report by the Commonwealth Fund, a foundation that supports research focused on health care issues. The rate for Black women in the United States is even higher, 55.3 deaths.
“Many maternal deaths result from missed or delayed opportunities for treatment,” the report said.
The maternal mortality rate in Montana is not publicly available because the Centers for Disease Control and Prevention suppressed the state data in 2020 “due to reliability and confidentiality restrictions.” Mr. Ebelt, the state health department spokesperson, could not provide a rate before this article’s publication.
Annie Glover, a senior research scientist for the University of Montana’s Rural Institute for Inclusive Communities, said the governor’s proposal to extend postpartum Medicaid coverage could make a significant difference in improving overall maternal health in Montana. The university was awarded a federal grant this year for such efforts, particularly to lower the mortality rate among Native Americans, and Ms. Glover said the state measure could further reduce rates.
“The reason really has to do with maintaining access to care during this very critical period,” Ms. Glover said. That goes for helping mothers with postpartum depression, as well as medical conditions like high blood pressure that require follow-ups with a physician well after delivery, she said.
In Wyoming, a legislative committee voted 6-5 in August to introduce a bill in the next session; dissenters cited the cost and their reluctance to further entangle the state in federal government programs.
About a third of Wyoming births are covered by Medicaid, and state officials estimate about 1,250 women would benefit from the change.
Postpartum eligibility bills are also expected to be taken up by legislators in Missouri and Mississippi, two states that have previously grappled with the issue. Both states have outlawed most abortions since the U.S. Supreme Court lifted federal protections in June, and Mississippi leaders have said additional postpartum care is needed because of the thousands of additional births expected as a result of the state’s ban.
A proposed coverage expansion died in the Mississippi House last session, but Lt. Gov. Delbert Hosemann said the Senate will revive the measure, according to Mississippi Today.
Last year, federal officials approved a Medicaid waiver for Missouri that allows the state to extend postpartum eligibility. But state officials delayed implementing the change to determine how enrollment would be affected by Missouri voters’ decision in August 2020 to expand Medicaid eligibility to more people. The delay prompted a bill to be filed last session that would have extended postpartum coverage by a year. That measure died, but a state lawmaker has pre-filed a bill that will bring back the debate in the upcoming session.
In Idaho, a children’s advocacy group said it will press lawmakers to approve a postpartum eligibility extension, among other measures, after the state banned nearly all abortions this year.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Lawmakers in several conservative-led states – including Montana, Wyoming, Missouri, and Mississippi – are expected to consider proposals to provide a year of continuous health coverage to new mothers enrolled in Medicaid.
Medicaid beneficiaries nationwide are guaranteed continuous postpartum coverage during the ongoing covid-19 public health emergency. But momentum has been building for states to extend the default 60-day required coverage period ahead of the emergency’s eventual end. Approximately 42% of births nationwide are covered under Medicaid, the federal-state health insurance program for low-income people, and extending postpartum coverage aims to reduce the risk of pregnancy-related deaths and illnesses by ensuring that new mothers’ medical care isn’t interrupted.
The push comes as a provision in the American Rescue Plan Act makes extending postpartum Medicaid coverage easier because states no longer need to apply for a waiver. A renewed focus on maternal health amid high U.S. maternal mortality rates also is driving the proposals, as is the expectation that more women will need postpartum care as state abortion bans proliferate in the wake of the U.S. Supreme Court’s decision to eliminate federal protections.
Thirty-five states and Washington have already extended, or plan to extend, postpartum eligibility in their Medicaid programs. That number includes Texas and Wisconsin, which did not implement the ARPA provision but have proposed limited extensions of 6 months and 90 days, respectively.
The 15 states that limit postpartum Medicaid eligibility to 60 days are predominantly a swath of Republican-led states that stretch from the Mountain West to the South. But that could change when legislative sessions start in the new year.
In Montana, Republican Gov. Greg Gianforte and Department of Public Health and Human Services Director Charlie Brereton included 12-month postpartum eligibility in the governor’s proposed state budget. It would cost $9.2 million in federal and state funding over the next 2 years, according to the proposal, with the federal government covering nearly 70%.
A 2021 U.S. Department of Health and Human Services report estimated about 2,000 women in Montana would benefit from the change. State health department spokesperson Jon Ebelt said state officials’ estimate is half that number. The reason for the disparity was not immediately clear.
Mr. Brereton considers the “extension of coverage for new mothers to be a pro-life, pro-family reform,” Mr. Ebelt said.
To become law, the proposal must be approved by state lawmakers once the legislative session begins in January. It has already received enthusiastic support from the senior Democrat on the committee that oversees the health department’s budget. “Continuous eligibility for women after they have a baby is really important,” said state Rep. Mary Caferro during the Children’s Legislative Forum in Helena on Nov. 30.
The top Republican on the committee, state Rep.-elect Bob Keenan, said he hasn’t dug in on the governor’s budget proposal but added that he plans to survey his fellow lawmakers and health care providers on the postpartum extension. “I wouldn’t dare venture a guess as to its acceptance,” he said.
Nationwide, more than 1 in 5 mothers whose pregnancies were covered by Medicaid lose their insurance within 6 months of giving birth, and 1 in 3 pregnancy-related deaths happen between a week and a year after a birth occurs, according to federal health officials.
The United States had the highest overall maternal mortality rate, by far, among wealthy nations in 2020, at 23.8 deaths per 100,000 births, according to a report by the Commonwealth Fund, a foundation that supports research focused on health care issues. The rate for Black women in the United States is even higher, 55.3 deaths.
“Many maternal deaths result from missed or delayed opportunities for treatment,” the report said.
The maternal mortality rate in Montana is not publicly available because the Centers for Disease Control and Prevention suppressed the state data in 2020 “due to reliability and confidentiality restrictions.” Mr. Ebelt, the state health department spokesperson, could not provide a rate before this article’s publication.
Annie Glover, a senior research scientist for the University of Montana’s Rural Institute for Inclusive Communities, said the governor’s proposal to extend postpartum Medicaid coverage could make a significant difference in improving overall maternal health in Montana. The university was awarded a federal grant this year for such efforts, particularly to lower the mortality rate among Native Americans, and Ms. Glover said the state measure could further reduce rates.
“The reason really has to do with maintaining access to care during this very critical period,” Ms. Glover said. That goes for helping mothers with postpartum depression, as well as medical conditions like high blood pressure that require follow-ups with a physician well after delivery, she said.
In Wyoming, a legislative committee voted 6-5 in August to introduce a bill in the next session; dissenters cited the cost and their reluctance to further entangle the state in federal government programs.
About a third of Wyoming births are covered by Medicaid, and state officials estimate about 1,250 women would benefit from the change.
Postpartum eligibility bills are also expected to be taken up by legislators in Missouri and Mississippi, two states that have previously grappled with the issue. Both states have outlawed most abortions since the U.S. Supreme Court lifted federal protections in June, and Mississippi leaders have said additional postpartum care is needed because of the thousands of additional births expected as a result of the state’s ban.
A proposed coverage expansion died in the Mississippi House last session, but Lt. Gov. Delbert Hosemann said the Senate will revive the measure, according to Mississippi Today.
Last year, federal officials approved a Medicaid waiver for Missouri that allows the state to extend postpartum eligibility. But state officials delayed implementing the change to determine how enrollment would be affected by Missouri voters’ decision in August 2020 to expand Medicaid eligibility to more people. The delay prompted a bill to be filed last session that would have extended postpartum coverage by a year. That measure died, but a state lawmaker has pre-filed a bill that will bring back the debate in the upcoming session.
In Idaho, a children’s advocacy group said it will press lawmakers to approve a postpartum eligibility extension, among other measures, after the state banned nearly all abortions this year.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
No, you can’t see a different doctor: We need zero tolerance of patient bias
It was 1970. I was in my second year of medical school. I can remember the hurt and embarrassment as if it were yesterday.
Coming from the Deep South, I was very familiar with racial bias, but I did not expect it at that level and in that environment. From that point on, I was anxious at each patient encounter, concerned that this might happen again. And it did several times during my residency and fellowship.
The Occupational Safety and Health Administration defines workplace violence as “any act or threat of physical violence, harassment, intimidation, or other threatening disruptive behavior that occurs at the work site. It ranges from threats and verbal abuse to physical assaults.”
There is considerable media focus on incidents of physical violence against health care workers, but when patients, their families, or visitors openly display bias and request a different doctor, nurse, or technician for nonmedical reasons, the impact is profound. This is extremely hurtful to a professional who has worked long and hard to acquire skills and expertise. And, while speech may not constitute violence in the strictest sense of the word, there is growing evidence that it can be physically harmful through its effect on the nervous system, even if no physical contact is involved.
Incidents of bias occur regularly and are clearly on the rise. In most cases the request for a different health care worker is granted to honor the rights of the patient. The healthcare worker is left alone and emotionally wounded; the healthcare institutions are complicit.
This bias is mostly racial but can also be based on religion, sexual orientation, age, disability, body size, accent, or gender.
An entire issue of the American Medical Association Journal of Ethics was devoted to this topic. From recognizing that there are limits to what clinicians should be expected to tolerate when patients’ preferences express unjust bias, the issue also explored where those limits should be placed, why, and who is obliged to enforce them.
The newly adopted Mass General Patient Code of Conduct is evidence that health care systems are beginning to recognize this problem and that such behavior will not be tolerated.
But having a zero-tolerance policy is not enough. We must have procedures in place to discourage and mitigate the impact of patient bias.
A clear definition of what constitutes a bias incident is essential. All team members must be made aware of the procedures for reporting such incidents and the chain of command for escalation. Reporting should be encouraged, and resources must be made available to impacted team members. Surveillance, monitoring, and review are also essential as is clarification on when patient preferences should be honored.
The Mayo Clinic 5 Step Plan is an excellent example of a protocol to deal with patient bias against health care workers and is based on a thoughtful analysis of what constitutes an unreasonable request for a different clinician. I’m pleased to report that my health care system (Inova Health) is developing a similar protocol.
The health care setting should be a bias-free zone for both patients and health care workers. I have been a strong advocate of patients’ rights and worked hard to guard against bias and eliminate disparities in care, but health care workers have rights as well.
We should expect to be treated with respect.
The views expressed by the author are those of the author alone and do not represent the views of the Inova Health System. Dr. Francis is a cardiologist at Inova Heart and Vascular Institute, McLean, Va. He disclosed no conflicts of interest.
A version of this article first appeared on Medscape.com.
It was 1970. I was in my second year of medical school. I can remember the hurt and embarrassment as if it were yesterday.
Coming from the Deep South, I was very familiar with racial bias, but I did not expect it at that level and in that environment. From that point on, I was anxious at each patient encounter, concerned that this might happen again. And it did several times during my residency and fellowship.
The Occupational Safety and Health Administration defines workplace violence as “any act or threat of physical violence, harassment, intimidation, or other threatening disruptive behavior that occurs at the work site. It ranges from threats and verbal abuse to physical assaults.”
There is considerable media focus on incidents of physical violence against health care workers, but when patients, their families, or visitors openly display bias and request a different doctor, nurse, or technician for nonmedical reasons, the impact is profound. This is extremely hurtful to a professional who has worked long and hard to acquire skills and expertise. And, while speech may not constitute violence in the strictest sense of the word, there is growing evidence that it can be physically harmful through its effect on the nervous system, even if no physical contact is involved.
Incidents of bias occur regularly and are clearly on the rise. In most cases the request for a different health care worker is granted to honor the rights of the patient. The healthcare worker is left alone and emotionally wounded; the healthcare institutions are complicit.
This bias is mostly racial but can also be based on religion, sexual orientation, age, disability, body size, accent, or gender.
An entire issue of the American Medical Association Journal of Ethics was devoted to this topic. From recognizing that there are limits to what clinicians should be expected to tolerate when patients’ preferences express unjust bias, the issue also explored where those limits should be placed, why, and who is obliged to enforce them.
The newly adopted Mass General Patient Code of Conduct is evidence that health care systems are beginning to recognize this problem and that such behavior will not be tolerated.
But having a zero-tolerance policy is not enough. We must have procedures in place to discourage and mitigate the impact of patient bias.
A clear definition of what constitutes a bias incident is essential. All team members must be made aware of the procedures for reporting such incidents and the chain of command for escalation. Reporting should be encouraged, and resources must be made available to impacted team members. Surveillance, monitoring, and review are also essential as is clarification on when patient preferences should be honored.
The Mayo Clinic 5 Step Plan is an excellent example of a protocol to deal with patient bias against health care workers and is based on a thoughtful analysis of what constitutes an unreasonable request for a different clinician. I’m pleased to report that my health care system (Inova Health) is developing a similar protocol.
The health care setting should be a bias-free zone for both patients and health care workers. I have been a strong advocate of patients’ rights and worked hard to guard against bias and eliminate disparities in care, but health care workers have rights as well.
We should expect to be treated with respect.
The views expressed by the author are those of the author alone and do not represent the views of the Inova Health System. Dr. Francis is a cardiologist at Inova Heart and Vascular Institute, McLean, Va. He disclosed no conflicts of interest.
A version of this article first appeared on Medscape.com.
It was 1970. I was in my second year of medical school. I can remember the hurt and embarrassment as if it were yesterday.
Coming from the Deep South, I was very familiar with racial bias, but I did not expect it at that level and in that environment. From that point on, I was anxious at each patient encounter, concerned that this might happen again. And it did several times during my residency and fellowship.
The Occupational Safety and Health Administration defines workplace violence as “any act or threat of physical violence, harassment, intimidation, or other threatening disruptive behavior that occurs at the work site. It ranges from threats and verbal abuse to physical assaults.”
There is considerable media focus on incidents of physical violence against health care workers, but when patients, their families, or visitors openly display bias and request a different doctor, nurse, or technician for nonmedical reasons, the impact is profound. This is extremely hurtful to a professional who has worked long and hard to acquire skills and expertise. And, while speech may not constitute violence in the strictest sense of the word, there is growing evidence that it can be physically harmful through its effect on the nervous system, even if no physical contact is involved.
Incidents of bias occur regularly and are clearly on the rise. In most cases the request for a different health care worker is granted to honor the rights of the patient. The healthcare worker is left alone and emotionally wounded; the healthcare institutions are complicit.
This bias is mostly racial but can also be based on religion, sexual orientation, age, disability, body size, accent, or gender.
An entire issue of the American Medical Association Journal of Ethics was devoted to this topic. From recognizing that there are limits to what clinicians should be expected to tolerate when patients’ preferences express unjust bias, the issue also explored where those limits should be placed, why, and who is obliged to enforce them.
The newly adopted Mass General Patient Code of Conduct is evidence that health care systems are beginning to recognize this problem and that such behavior will not be tolerated.
But having a zero-tolerance policy is not enough. We must have procedures in place to discourage and mitigate the impact of patient bias.
A clear definition of what constitutes a bias incident is essential. All team members must be made aware of the procedures for reporting such incidents and the chain of command for escalation. Reporting should be encouraged, and resources must be made available to impacted team members. Surveillance, monitoring, and review are also essential as is clarification on when patient preferences should be honored.
The Mayo Clinic 5 Step Plan is an excellent example of a protocol to deal with patient bias against health care workers and is based on a thoughtful analysis of what constitutes an unreasonable request for a different clinician. I’m pleased to report that my health care system (Inova Health) is developing a similar protocol.
The health care setting should be a bias-free zone for both patients and health care workers. I have been a strong advocate of patients’ rights and worked hard to guard against bias and eliminate disparities in care, but health care workers have rights as well.
We should expect to be treated with respect.
The views expressed by the author are those of the author alone and do not represent the views of the Inova Health System. Dr. Francis is a cardiologist at Inova Heart and Vascular Institute, McLean, Va. He disclosed no conflicts of interest.
A version of this article first appeared on Medscape.com.
States cracking down harder on docs who sexually abuse patients
It’s the latest example of states taking doctor sexual misconduct more seriously after longstanding criticism that medical boards have been too lenient.
The law, which takes effect in January 2023, requires the state’s medical board to permanently revoke these doctors’ licenses instead of allowing them to petition the board for reinstatement after 3 years.
“Physician licenses should not be reinstated after egregious sexual misconduct with patients. The doctor-patient relationship has to remain sacrosanct and trusted,” said Peter Yellowlees, MD, a professor of psychiatry at the University of California, Davis.
Although the vast majority of the nation’s estimated 1 million doctors don’t sexually abuse patients, the problem is a national one.
The Federation of State Medical Boards defines sexual misconduct as the exploitation of the physician-patient relationship in a sexual way. The exploitation may be verbal or physical and can occur in person or virtually.
The FSMB conducted a 2-year review of how medical boards handled cases of sexual misconduct, issuing a report in 2020 that contained 38 recommended actions.
Four states in addition to California have enacted laws that incorporate some FSMB recommendations. These include revoking doctors’ licenses after a single egregious act of sexual misconduct (including sexual assault), regardless of whether the physician was charged or convicted; increased reporting by hospitals and doctors of sexual misconduct; and training of physicians to recognize and report sexual misconduct.
The four state laws are:
- Georgia’s HB 458. It was signed into law in May 2021, and it authorizes the medical board to revoke or suspend a license if a physician is found guilty of sexually assaulting a patient in a criminal case. Doctors are required to report other doctors who have sexually abused patients and to take continuing medical education (CME) units on sexual misconduct.
- Florida’s SB 1934. This legislation was signed into law in June 2021, and it bars physicians charged with serious crimes such as sexual assault, sexual misconduct against patients, or possession of child pornography from seeing patients until those charges are resolved by the legal system.
- West Virginia’s SB 603. Signed into law in March 2022 it prohibits the medical board from issuing a license to a physician who engaged in sexual activity or misconduct with a patient whose license was revoked in another state or was involved in other violations.
- Tennessee HB 1045. It was signed into law in May 2021, and authorizes the medical board, upon learning of an indictment against a physician for a controlled substance violation or sexual offense, to immediately suspend the doctor’s ability to prescribe controlled substances until the doctor’s case is resolved.
A published study identified a total of 1,721 reports of physician sexual misconduct that were submitted to the National Practitioner Data Bank between 2000 and 2019. The annual incidence of sexual misconduct reports averaged 10.8 per 100,000 U.S. physician licensees, said the researchers.
In a groundbreaking 2016 investigation, the Atlanta Journal-Constitution reviewed thousands of documents and found more than 2,400 doctors whose sexual misconduct cases clearly involved patients since 1999.
Physician sexual misconduct is likely underreported
The actual incidence of physician-patient sexual misconduct is likely higher as a result of underreporting, according to the researchers.
Because a substantial power differential exists between patients and their physicians, the researchers noted, it follows that patient victims, like other sexual assault victims, may be unwilling or unable to report the incident in question.
Many violations involving physician sexual misconduct of patients never came to the attention of state regulators, according to the Journal-Constitution investigation. Reporting showed that hospitals, clinics, and fellow doctors fail to report sexual misconduct to regulators, despite laws in most states requiring them to do so.
Media investigations highlight medical board shortcomings
Public pressure on the California Medical Board increased after the Los Angeles Times investigated what happened to doctors who surrendered or had their licenses revoked after being reported for sexual abuse with patients. The Times revealed in 2021 that the board reinstated 10 of 17 doctors who petitioned for reinstatement.
They include Esmail Nadjmabadi, MD, of Bakersfield, Calif., who had sexually abused six female patients, including one in her mid-teens. The Times reported that, in 2009, he pleaded no contest to a criminal charge that he sexually exploited two or more women and surrendered his medical license the following year.
Five years later, Dr. Nadjmabadi petitioned the medical board to be reinstated and the board approved his request.
The California board has also reinstated several doctors who underwent sex offender rehabilitation. Board members rely heavily on a doctor’s evidence of rehabilitation, usually with the testimony of therapists hired by the doctor, and no input from the patients who were harmed, according to the Times’ investigation.
High-profile sexual misconduct or abuse cases involving Larry Nassar, MD, and Robert Anderson, MD, in Michigan; Richard Strauss, MD, in Ohio; and Ricardo Cruciani, MD, in New York, added to the mounting criticism that medical boards were too lenient in their handling of complaints of sexual misconduct.
Another state tackles sexual misconduct
Ohio’s medical board created an administrative rule stating that licensed physicians have a legal and ethical duty to report colleagues for sexual misconduct with patients and to complete a 1-hour CME training. Failure to report sexual misconduct complaints can lead to a doctor being permanently stripped of his license.
This happened to Robert S. Geiger, MD, in 2016 after not reporting his colleague James Bressi, MD, to the medical board after receiving complaints that Dr. Bressi was sexually abusing female patients at their pain clinic.
Dr. Bressi was convicted of sexual misconduct with a patient, stripped of his medical license, and sentenced to 59 days in prison.
“I think all of these reforms are a step in the right direction and will help to deter doctors from committing sexual misconduct to some extent,” said California activist Marian Hollingsworth, cofounder of the Patient Safety League.
But there’s room for improvement, she said, since “most states fall short in not requiring medical boards to notify law enforcement when they get a complaint of doctor sexual misconduct so the public can be aware of it.”
A version of this article first appeared on Medscape.com.
It’s the latest example of states taking doctor sexual misconduct more seriously after longstanding criticism that medical boards have been too lenient.
The law, which takes effect in January 2023, requires the state’s medical board to permanently revoke these doctors’ licenses instead of allowing them to petition the board for reinstatement after 3 years.
“Physician licenses should not be reinstated after egregious sexual misconduct with patients. The doctor-patient relationship has to remain sacrosanct and trusted,” said Peter Yellowlees, MD, a professor of psychiatry at the University of California, Davis.
Although the vast majority of the nation’s estimated 1 million doctors don’t sexually abuse patients, the problem is a national one.
The Federation of State Medical Boards defines sexual misconduct as the exploitation of the physician-patient relationship in a sexual way. The exploitation may be verbal or physical and can occur in person or virtually.
The FSMB conducted a 2-year review of how medical boards handled cases of sexual misconduct, issuing a report in 2020 that contained 38 recommended actions.
Four states in addition to California have enacted laws that incorporate some FSMB recommendations. These include revoking doctors’ licenses after a single egregious act of sexual misconduct (including sexual assault), regardless of whether the physician was charged or convicted; increased reporting by hospitals and doctors of sexual misconduct; and training of physicians to recognize and report sexual misconduct.
The four state laws are:
- Georgia’s HB 458. It was signed into law in May 2021, and it authorizes the medical board to revoke or suspend a license if a physician is found guilty of sexually assaulting a patient in a criminal case. Doctors are required to report other doctors who have sexually abused patients and to take continuing medical education (CME) units on sexual misconduct.
- Florida’s SB 1934. This legislation was signed into law in June 2021, and it bars physicians charged with serious crimes such as sexual assault, sexual misconduct against patients, or possession of child pornography from seeing patients until those charges are resolved by the legal system.
- West Virginia’s SB 603. Signed into law in March 2022 it prohibits the medical board from issuing a license to a physician who engaged in sexual activity or misconduct with a patient whose license was revoked in another state or was involved in other violations.
- Tennessee HB 1045. It was signed into law in May 2021, and authorizes the medical board, upon learning of an indictment against a physician for a controlled substance violation or sexual offense, to immediately suspend the doctor’s ability to prescribe controlled substances until the doctor’s case is resolved.
A published study identified a total of 1,721 reports of physician sexual misconduct that were submitted to the National Practitioner Data Bank between 2000 and 2019. The annual incidence of sexual misconduct reports averaged 10.8 per 100,000 U.S. physician licensees, said the researchers.
In a groundbreaking 2016 investigation, the Atlanta Journal-Constitution reviewed thousands of documents and found more than 2,400 doctors whose sexual misconduct cases clearly involved patients since 1999.
Physician sexual misconduct is likely underreported
The actual incidence of physician-patient sexual misconduct is likely higher as a result of underreporting, according to the researchers.
Because a substantial power differential exists between patients and their physicians, the researchers noted, it follows that patient victims, like other sexual assault victims, may be unwilling or unable to report the incident in question.
Many violations involving physician sexual misconduct of patients never came to the attention of state regulators, according to the Journal-Constitution investigation. Reporting showed that hospitals, clinics, and fellow doctors fail to report sexual misconduct to regulators, despite laws in most states requiring them to do so.
Media investigations highlight medical board shortcomings
Public pressure on the California Medical Board increased after the Los Angeles Times investigated what happened to doctors who surrendered or had their licenses revoked after being reported for sexual abuse with patients. The Times revealed in 2021 that the board reinstated 10 of 17 doctors who petitioned for reinstatement.
They include Esmail Nadjmabadi, MD, of Bakersfield, Calif., who had sexually abused six female patients, including one in her mid-teens. The Times reported that, in 2009, he pleaded no contest to a criminal charge that he sexually exploited two or more women and surrendered his medical license the following year.
Five years later, Dr. Nadjmabadi petitioned the medical board to be reinstated and the board approved his request.
The California board has also reinstated several doctors who underwent sex offender rehabilitation. Board members rely heavily on a doctor’s evidence of rehabilitation, usually with the testimony of therapists hired by the doctor, and no input from the patients who were harmed, according to the Times’ investigation.
High-profile sexual misconduct or abuse cases involving Larry Nassar, MD, and Robert Anderson, MD, in Michigan; Richard Strauss, MD, in Ohio; and Ricardo Cruciani, MD, in New York, added to the mounting criticism that medical boards were too lenient in their handling of complaints of sexual misconduct.
Another state tackles sexual misconduct
Ohio’s medical board created an administrative rule stating that licensed physicians have a legal and ethical duty to report colleagues for sexual misconduct with patients and to complete a 1-hour CME training. Failure to report sexual misconduct complaints can lead to a doctor being permanently stripped of his license.
This happened to Robert S. Geiger, MD, in 2016 after not reporting his colleague James Bressi, MD, to the medical board after receiving complaints that Dr. Bressi was sexually abusing female patients at their pain clinic.
Dr. Bressi was convicted of sexual misconduct with a patient, stripped of his medical license, and sentenced to 59 days in prison.
“I think all of these reforms are a step in the right direction and will help to deter doctors from committing sexual misconduct to some extent,” said California activist Marian Hollingsworth, cofounder of the Patient Safety League.
But there’s room for improvement, she said, since “most states fall short in not requiring medical boards to notify law enforcement when they get a complaint of doctor sexual misconduct so the public can be aware of it.”
A version of this article first appeared on Medscape.com.
It’s the latest example of states taking doctor sexual misconduct more seriously after longstanding criticism that medical boards have been too lenient.
The law, which takes effect in January 2023, requires the state’s medical board to permanently revoke these doctors’ licenses instead of allowing them to petition the board for reinstatement after 3 years.
“Physician licenses should not be reinstated after egregious sexual misconduct with patients. The doctor-patient relationship has to remain sacrosanct and trusted,” said Peter Yellowlees, MD, a professor of psychiatry at the University of California, Davis.
Although the vast majority of the nation’s estimated 1 million doctors don’t sexually abuse patients, the problem is a national one.
The Federation of State Medical Boards defines sexual misconduct as the exploitation of the physician-patient relationship in a sexual way. The exploitation may be verbal or physical and can occur in person or virtually.
The FSMB conducted a 2-year review of how medical boards handled cases of sexual misconduct, issuing a report in 2020 that contained 38 recommended actions.
Four states in addition to California have enacted laws that incorporate some FSMB recommendations. These include revoking doctors’ licenses after a single egregious act of sexual misconduct (including sexual assault), regardless of whether the physician was charged or convicted; increased reporting by hospitals and doctors of sexual misconduct; and training of physicians to recognize and report sexual misconduct.
The four state laws are:
- Georgia’s HB 458. It was signed into law in May 2021, and it authorizes the medical board to revoke or suspend a license if a physician is found guilty of sexually assaulting a patient in a criminal case. Doctors are required to report other doctors who have sexually abused patients and to take continuing medical education (CME) units on sexual misconduct.
- Florida’s SB 1934. This legislation was signed into law in June 2021, and it bars physicians charged with serious crimes such as sexual assault, sexual misconduct against patients, or possession of child pornography from seeing patients until those charges are resolved by the legal system.
- West Virginia’s SB 603. Signed into law in March 2022 it prohibits the medical board from issuing a license to a physician who engaged in sexual activity or misconduct with a patient whose license was revoked in another state or was involved in other violations.
- Tennessee HB 1045. It was signed into law in May 2021, and authorizes the medical board, upon learning of an indictment against a physician for a controlled substance violation or sexual offense, to immediately suspend the doctor’s ability to prescribe controlled substances until the doctor’s case is resolved.
A published study identified a total of 1,721 reports of physician sexual misconduct that were submitted to the National Practitioner Data Bank between 2000 and 2019. The annual incidence of sexual misconduct reports averaged 10.8 per 100,000 U.S. physician licensees, said the researchers.
In a groundbreaking 2016 investigation, the Atlanta Journal-Constitution reviewed thousands of documents and found more than 2,400 doctors whose sexual misconduct cases clearly involved patients since 1999.
Physician sexual misconduct is likely underreported
The actual incidence of physician-patient sexual misconduct is likely higher as a result of underreporting, according to the researchers.
Because a substantial power differential exists between patients and their physicians, the researchers noted, it follows that patient victims, like other sexual assault victims, may be unwilling or unable to report the incident in question.
Many violations involving physician sexual misconduct of patients never came to the attention of state regulators, according to the Journal-Constitution investigation. Reporting showed that hospitals, clinics, and fellow doctors fail to report sexual misconduct to regulators, despite laws in most states requiring them to do so.
Media investigations highlight medical board shortcomings
Public pressure on the California Medical Board increased after the Los Angeles Times investigated what happened to doctors who surrendered or had their licenses revoked after being reported for sexual abuse with patients. The Times revealed in 2021 that the board reinstated 10 of 17 doctors who petitioned for reinstatement.
They include Esmail Nadjmabadi, MD, of Bakersfield, Calif., who had sexually abused six female patients, including one in her mid-teens. The Times reported that, in 2009, he pleaded no contest to a criminal charge that he sexually exploited two or more women and surrendered his medical license the following year.
Five years later, Dr. Nadjmabadi petitioned the medical board to be reinstated and the board approved his request.
The California board has also reinstated several doctors who underwent sex offender rehabilitation. Board members rely heavily on a doctor’s evidence of rehabilitation, usually with the testimony of therapists hired by the doctor, and no input from the patients who were harmed, according to the Times’ investigation.
High-profile sexual misconduct or abuse cases involving Larry Nassar, MD, and Robert Anderson, MD, in Michigan; Richard Strauss, MD, in Ohio; and Ricardo Cruciani, MD, in New York, added to the mounting criticism that medical boards were too lenient in their handling of complaints of sexual misconduct.
Another state tackles sexual misconduct
Ohio’s medical board created an administrative rule stating that licensed physicians have a legal and ethical duty to report colleagues for sexual misconduct with patients and to complete a 1-hour CME training. Failure to report sexual misconduct complaints can lead to a doctor being permanently stripped of his license.
This happened to Robert S. Geiger, MD, in 2016 after not reporting his colleague James Bressi, MD, to the medical board after receiving complaints that Dr. Bressi was sexually abusing female patients at their pain clinic.
Dr. Bressi was convicted of sexual misconduct with a patient, stripped of his medical license, and sentenced to 59 days in prison.
“I think all of these reforms are a step in the right direction and will help to deter doctors from committing sexual misconduct to some extent,” said California activist Marian Hollingsworth, cofounder of the Patient Safety League.
But there’s room for improvement, she said, since “most states fall short in not requiring medical boards to notify law enforcement when they get a complaint of doctor sexual misconduct so the public can be aware of it.”
A version of this article first appeared on Medscape.com.
Postpartum hemorrhage rates and risk factors rising
The rate of postpartum hemorrhage for hospital deliveries in the United States increased significantly over a 20-year period, according to data from more than 76 million delivery hospitalizations from the National Inpatient Sample.
Postpartum hemorrhage remains the leading cause of maternal morbidity and mortality worldwide, and many clinical and patient-level risk factors appear to be on the rise, wrote Chiara M. Corbetta-Rastelli, MD, of the University of California, San Francisco, and colleagues.
Although practice changes have been introduced to reduce postpartum hemorrhage, recent trends in postpartum hemorrhage risk and outcomes in the context of such changes as hemorrhage safety bundles have not been examined, they said.
In a study published in Obstetrics & Gynecology, the researchers reviewed data from hospitalizations for females aged 15-54 years for deliveries between 2000 and 2019 using the National Inpatient Sample. They used a regression analysis to estimate average annual percentage changes (AAPC). Their objectives were to characterize trends and also to assess the association between risk factors and the occurrence of postpartum hemorrhage and related interventions. Demographics, clinical factors, and hospital characteristics were mainly similar between the group of patients with postpartum hemorrhage and those with no postpartum hemorrhage.
Approximately 3% (2.3 million) of 76.7 million hospitalizations for delivery were complicated by postpartum hemorrhage during the study period, and the annual rate increased from 2.7% to 4.3%.
Overall, 21.4% of individuals with delivery hospitalizations complicated by postpartum hemorrhage had one postpartum risk factor, and 1.4% had two or more risk factors. The number of individuals with at least one risk factor for postpartum hemorrhage increased significantly, from 18.6% to 26.9%, during the study period, with an annual percentage change of 1.9%.
Compared with deliveries in individuals without risk factors, individuals with one risk factor had slightly higher odds of postpartum hemorrhage (odds ratio, 1.14), but those with two or more risk factors were more than twice as likely to experience postpartum hemorrhage as those with no risk factors (OR, 2.31).
The researchers also examined the association of specific risk factors and interventions related to hemorrhage, notably blood transfusion and peripartum hysterectomy. Blood transfusions in individuals with postpartum hemorrhage increased from 5.4% to 16.7% between 2000 and 2011, (AAPC, 10.2%) then decreased from 16.7% to 12.6% from 2011 to 2019 (AAPC, –3.9%).
Peripartum hysterectomy in the study population increased from 1.4% to 2.4% from 2000 to 2009 (AAPC 5.0%), remained steady from 2009 to 2016, and then decreased from 2.1% to 0.9% from 2016 to 2019 (AAPC –27%).
Other risk factors associated with postpartum hemorrhage itself and with blood transfusion and hysterectomy in the setting of postpartum hemorrhage included prior cesarean delivery with placenta previa or accreta, placenta previa without prior cesarean delivery, and antepartum hemorrhage or placental abruption, the researchers noted.
“In addition to placental abnormalities, risk factors such as preeclampsia with severe features, polyhydramnios, and uterine leiomyomas demonstrated the highest rates of increase in our data,” they wrote in their discussion. These trends may lead to continuing increases in postpartum hemorrhage risk, which was not fully explained by the increase in risk factors seen in the current study, the researchers said.
The study findings were limited by several factors, including the use of billing codes that could lead to misclassification of diagnoses, as well as possible differences in the definition and coding for postpartum hemorrhage among hospitals, the researchers noted. Other limitations were the exclusion of cases of readmission for postpartum hemorrhage and lack of clinical details involving use of medications or nonoperative interventions, they said.
Notably, the study finding of stable to decreasing peripartum hysterectomy rates in hospitalized patients with postpartum hemorrhage conflicts with another recent study showing an increase in peripartum hysterectomy from 2009 to 2020, but this difference may reflect changes in billing, indications for hysterectomy, or study modeling, they said.
The current study was strengthened by the use of a large database to analyze population trends, a contemporary study period, and the inclusion of meaningful outcomes such as peripartum hysterectomy, the researchers wrote.
The shift in blood transfusion and peripartum hysterectomy may reflect the implementation of protocols to promote early intervention and identification of postpartum hemorrhage, they concluded.
Interventions can have an effect
“Hemorrhage remains a leading cause of maternal mortality in the United States and blood transfusion is the most common severe maternal morbidity,” Catherine M. Albright, MD, MS, associate professor of maternal-fetal medicine at the University of Washington, Seattle, said in an interview. “It is important to understand the current state, especially given that many hospitals have implemented policies and procedures to better identify and treat postpartum hemorrhage,” she said.
Dr. Albright said, “I was pleased to see that they did not just look at a diagnosis of postpartum hemorrhage but rather also looked at complications arising from postpartum hemorrhage, such as blood transfusion or hysterectomy.”
Postpartum hemorrhage is often a clinical diagnosis that uses estimated blood loss, a notoriously inaccurate measure, said Dr. Albright. “Additionally, the definitions of postpartum hemorrhage, as well as the ICD codes, changed during the time period of the study,” she noted. “These factors all could lead to both underreporting and overreporting of the true incidence of postpartum hemorrhage. Blood transfusion and hysterectomy are more objective outcomes and demonstrate true morbidity,” she said.
“Most of the risk factors that are listed in the article are not modifiable during that pregnancy,” said Dr. Albright. For example, a history of a prior cesarean or having a twin pregnancy is not something that can be changed, she said. “Many of the other risk factors or associated clinical factors, such as obesity, chronic hypertension, and pregestational diabetes, are modifiable, but before pregnancy. Universal and easy access to primary medical care prior to and between pregnancies may help to mitigate some of these factors,” she noted.
Looking ahead, “It would be helpful to ensure that these types of data are available at the state and hospital level; this will allow for local evaluation of programs that are in place to reduce postpartum hemorrhage risk and improve identification and treatment,” Dr. Albright said.
The study received no outside funding. Dr. Corbetta-Rastelli and Dr. Albright had no financial conflicts to disclose.
The rate of postpartum hemorrhage for hospital deliveries in the United States increased significantly over a 20-year period, according to data from more than 76 million delivery hospitalizations from the National Inpatient Sample.
Postpartum hemorrhage remains the leading cause of maternal morbidity and mortality worldwide, and many clinical and patient-level risk factors appear to be on the rise, wrote Chiara M. Corbetta-Rastelli, MD, of the University of California, San Francisco, and colleagues.
Although practice changes have been introduced to reduce postpartum hemorrhage, recent trends in postpartum hemorrhage risk and outcomes in the context of such changes as hemorrhage safety bundles have not been examined, they said.
In a study published in Obstetrics & Gynecology, the researchers reviewed data from hospitalizations for females aged 15-54 years for deliveries between 2000 and 2019 using the National Inpatient Sample. They used a regression analysis to estimate average annual percentage changes (AAPC). Their objectives were to characterize trends and also to assess the association between risk factors and the occurrence of postpartum hemorrhage and related interventions. Demographics, clinical factors, and hospital characteristics were mainly similar between the group of patients with postpartum hemorrhage and those with no postpartum hemorrhage.
Approximately 3% (2.3 million) of 76.7 million hospitalizations for delivery were complicated by postpartum hemorrhage during the study period, and the annual rate increased from 2.7% to 4.3%.
Overall, 21.4% of individuals with delivery hospitalizations complicated by postpartum hemorrhage had one postpartum risk factor, and 1.4% had two or more risk factors. The number of individuals with at least one risk factor for postpartum hemorrhage increased significantly, from 18.6% to 26.9%, during the study period, with an annual percentage change of 1.9%.
Compared with deliveries in individuals without risk factors, individuals with one risk factor had slightly higher odds of postpartum hemorrhage (odds ratio, 1.14), but those with two or more risk factors were more than twice as likely to experience postpartum hemorrhage as those with no risk factors (OR, 2.31).
The researchers also examined the association of specific risk factors and interventions related to hemorrhage, notably blood transfusion and peripartum hysterectomy. Blood transfusions in individuals with postpartum hemorrhage increased from 5.4% to 16.7% between 2000 and 2011, (AAPC, 10.2%) then decreased from 16.7% to 12.6% from 2011 to 2019 (AAPC, –3.9%).
Peripartum hysterectomy in the study population increased from 1.4% to 2.4% from 2000 to 2009 (AAPC 5.0%), remained steady from 2009 to 2016, and then decreased from 2.1% to 0.9% from 2016 to 2019 (AAPC –27%).
Other risk factors associated with postpartum hemorrhage itself and with blood transfusion and hysterectomy in the setting of postpartum hemorrhage included prior cesarean delivery with placenta previa or accreta, placenta previa without prior cesarean delivery, and antepartum hemorrhage or placental abruption, the researchers noted.
“In addition to placental abnormalities, risk factors such as preeclampsia with severe features, polyhydramnios, and uterine leiomyomas demonstrated the highest rates of increase in our data,” they wrote in their discussion. These trends may lead to continuing increases in postpartum hemorrhage risk, which was not fully explained by the increase in risk factors seen in the current study, the researchers said.
The study findings were limited by several factors, including the use of billing codes that could lead to misclassification of diagnoses, as well as possible differences in the definition and coding for postpartum hemorrhage among hospitals, the researchers noted. Other limitations were the exclusion of cases of readmission for postpartum hemorrhage and lack of clinical details involving use of medications or nonoperative interventions, they said.
Notably, the study finding of stable to decreasing peripartum hysterectomy rates in hospitalized patients with postpartum hemorrhage conflicts with another recent study showing an increase in peripartum hysterectomy from 2009 to 2020, but this difference may reflect changes in billing, indications for hysterectomy, or study modeling, they said.
The current study was strengthened by the use of a large database to analyze population trends, a contemporary study period, and the inclusion of meaningful outcomes such as peripartum hysterectomy, the researchers wrote.
The shift in blood transfusion and peripartum hysterectomy may reflect the implementation of protocols to promote early intervention and identification of postpartum hemorrhage, they concluded.
Interventions can have an effect
“Hemorrhage remains a leading cause of maternal mortality in the United States and blood transfusion is the most common severe maternal morbidity,” Catherine M. Albright, MD, MS, associate professor of maternal-fetal medicine at the University of Washington, Seattle, said in an interview. “It is important to understand the current state, especially given that many hospitals have implemented policies and procedures to better identify and treat postpartum hemorrhage,” she said.
Dr. Albright said, “I was pleased to see that they did not just look at a diagnosis of postpartum hemorrhage but rather also looked at complications arising from postpartum hemorrhage, such as blood transfusion or hysterectomy.”
Postpartum hemorrhage is often a clinical diagnosis that uses estimated blood loss, a notoriously inaccurate measure, said Dr. Albright. “Additionally, the definitions of postpartum hemorrhage, as well as the ICD codes, changed during the time period of the study,” she noted. “These factors all could lead to both underreporting and overreporting of the true incidence of postpartum hemorrhage. Blood transfusion and hysterectomy are more objective outcomes and demonstrate true morbidity,” she said.
“Most of the risk factors that are listed in the article are not modifiable during that pregnancy,” said Dr. Albright. For example, a history of a prior cesarean or having a twin pregnancy is not something that can be changed, she said. “Many of the other risk factors or associated clinical factors, such as obesity, chronic hypertension, and pregestational diabetes, are modifiable, but before pregnancy. Universal and easy access to primary medical care prior to and between pregnancies may help to mitigate some of these factors,” she noted.
Looking ahead, “It would be helpful to ensure that these types of data are available at the state and hospital level; this will allow for local evaluation of programs that are in place to reduce postpartum hemorrhage risk and improve identification and treatment,” Dr. Albright said.
The study received no outside funding. Dr. Corbetta-Rastelli and Dr. Albright had no financial conflicts to disclose.
The rate of postpartum hemorrhage for hospital deliveries in the United States increased significantly over a 20-year period, according to data from more than 76 million delivery hospitalizations from the National Inpatient Sample.
Postpartum hemorrhage remains the leading cause of maternal morbidity and mortality worldwide, and many clinical and patient-level risk factors appear to be on the rise, wrote Chiara M. Corbetta-Rastelli, MD, of the University of California, San Francisco, and colleagues.
Although practice changes have been introduced to reduce postpartum hemorrhage, recent trends in postpartum hemorrhage risk and outcomes in the context of such changes as hemorrhage safety bundles have not been examined, they said.
In a study published in Obstetrics & Gynecology, the researchers reviewed data from hospitalizations for females aged 15-54 years for deliveries between 2000 and 2019 using the National Inpatient Sample. They used a regression analysis to estimate average annual percentage changes (AAPC). Their objectives were to characterize trends and also to assess the association between risk factors and the occurrence of postpartum hemorrhage and related interventions. Demographics, clinical factors, and hospital characteristics were mainly similar between the group of patients with postpartum hemorrhage and those with no postpartum hemorrhage.
Approximately 3% (2.3 million) of 76.7 million hospitalizations for delivery were complicated by postpartum hemorrhage during the study period, and the annual rate increased from 2.7% to 4.3%.
Overall, 21.4% of individuals with delivery hospitalizations complicated by postpartum hemorrhage had one postpartum risk factor, and 1.4% had two or more risk factors. The number of individuals with at least one risk factor for postpartum hemorrhage increased significantly, from 18.6% to 26.9%, during the study period, with an annual percentage change of 1.9%.
Compared with deliveries in individuals without risk factors, individuals with one risk factor had slightly higher odds of postpartum hemorrhage (odds ratio, 1.14), but those with two or more risk factors were more than twice as likely to experience postpartum hemorrhage as those with no risk factors (OR, 2.31).
The researchers also examined the association of specific risk factors and interventions related to hemorrhage, notably blood transfusion and peripartum hysterectomy. Blood transfusions in individuals with postpartum hemorrhage increased from 5.4% to 16.7% between 2000 and 2011, (AAPC, 10.2%) then decreased from 16.7% to 12.6% from 2011 to 2019 (AAPC, –3.9%).
Peripartum hysterectomy in the study population increased from 1.4% to 2.4% from 2000 to 2009 (AAPC 5.0%), remained steady from 2009 to 2016, and then decreased from 2.1% to 0.9% from 2016 to 2019 (AAPC –27%).
Other risk factors associated with postpartum hemorrhage itself and with blood transfusion and hysterectomy in the setting of postpartum hemorrhage included prior cesarean delivery with placenta previa or accreta, placenta previa without prior cesarean delivery, and antepartum hemorrhage or placental abruption, the researchers noted.
“In addition to placental abnormalities, risk factors such as preeclampsia with severe features, polyhydramnios, and uterine leiomyomas demonstrated the highest rates of increase in our data,” they wrote in their discussion. These trends may lead to continuing increases in postpartum hemorrhage risk, which was not fully explained by the increase in risk factors seen in the current study, the researchers said.
The study findings were limited by several factors, including the use of billing codes that could lead to misclassification of diagnoses, as well as possible differences in the definition and coding for postpartum hemorrhage among hospitals, the researchers noted. Other limitations were the exclusion of cases of readmission for postpartum hemorrhage and lack of clinical details involving use of medications or nonoperative interventions, they said.
Notably, the study finding of stable to decreasing peripartum hysterectomy rates in hospitalized patients with postpartum hemorrhage conflicts with another recent study showing an increase in peripartum hysterectomy from 2009 to 2020, but this difference may reflect changes in billing, indications for hysterectomy, or study modeling, they said.
The current study was strengthened by the use of a large database to analyze population trends, a contemporary study period, and the inclusion of meaningful outcomes such as peripartum hysterectomy, the researchers wrote.
The shift in blood transfusion and peripartum hysterectomy may reflect the implementation of protocols to promote early intervention and identification of postpartum hemorrhage, they concluded.
Interventions can have an effect
“Hemorrhage remains a leading cause of maternal mortality in the United States and blood transfusion is the most common severe maternal morbidity,” Catherine M. Albright, MD, MS, associate professor of maternal-fetal medicine at the University of Washington, Seattle, said in an interview. “It is important to understand the current state, especially given that many hospitals have implemented policies and procedures to better identify and treat postpartum hemorrhage,” she said.
Dr. Albright said, “I was pleased to see that they did not just look at a diagnosis of postpartum hemorrhage but rather also looked at complications arising from postpartum hemorrhage, such as blood transfusion or hysterectomy.”
Postpartum hemorrhage is often a clinical diagnosis that uses estimated blood loss, a notoriously inaccurate measure, said Dr. Albright. “Additionally, the definitions of postpartum hemorrhage, as well as the ICD codes, changed during the time period of the study,” she noted. “These factors all could lead to both underreporting and overreporting of the true incidence of postpartum hemorrhage. Blood transfusion and hysterectomy are more objective outcomes and demonstrate true morbidity,” she said.
“Most of the risk factors that are listed in the article are not modifiable during that pregnancy,” said Dr. Albright. For example, a history of a prior cesarean or having a twin pregnancy is not something that can be changed, she said. “Many of the other risk factors or associated clinical factors, such as obesity, chronic hypertension, and pregestational diabetes, are modifiable, but before pregnancy. Universal and easy access to primary medical care prior to and between pregnancies may help to mitigate some of these factors,” she noted.
Looking ahead, “It would be helpful to ensure that these types of data are available at the state and hospital level; this will allow for local evaluation of programs that are in place to reduce postpartum hemorrhage risk and improve identification and treatment,” Dr. Albright said.
The study received no outside funding. Dr. Corbetta-Rastelli and Dr. Albright had no financial conflicts to disclose.
FROM OBSTETRICS & GYNECOLOGY
Oral SERD camizestrant prolongs PFS vs. fulvestrant in breast cancer
SAN ANTONIO – compared with the first-generation SERD fulvestrant Faslodex, in the SERENA-2 trial, shows a study recently presented at the San Antonio Breast Cancer Symposium.
Among 180 postmenopausal women with ER+/HER2– breast cancers that had recurred or progressed following at least one line of endocrine therapy, the median progression-free survival (PFS) after a median follow-up of 16.6-17.4 months was 7.2 months for patients treated at a 75-mg dose of camizestrant and 7.7 months for those treated at a 150-mg dose, compared with 3.7 months for patients who received fulvestrant, reported Mafalda Oliveira, MD, PhD, from Vall d’Hebron University Hospital in Barcelona.
Oral agent
Camizestrant is a next-generation oral SERD and pure estrogen receptor antagonist that was shown in the SERENA-1 trial to be safe and to have clinical activity against ER+ breast cancers.
SERENA-2 pitted camizestrant at doses of 75 mg, 150 mg, or 300 mg against standard-dose fulvestrant, although the 300-mg dose was dropped in a protocol amendment after 20 patients had been assigned to that arm. (Currently planned studies with camizestrant will be conducted with the 75-mg dose.)
The investigators enrolled women with ER+/HER2– advanced breast cancer who had not previously received fulvestrant or an oral SERD. Eligible patients were limited to no more than one prior line of endocrine and one prior line of chemotherapy for advanced breast cancers. The study included patients with both measurable and unmeasurable disease.
The median patient age was about 60 years. Approximately 59% of patients in each arm had either lung or liver metastases. Patients with recurrence in bone only comprised 14.9%-19.4%.
Mutations in ESR1, a gene associated with hormonal resistance, were detectable in 29.7%-47.9% of patients.
Better PFS
As noted before, the primary endpoint of investigator-assessed median PFS favored camizestrant in both the 75-mg arm (7.2 months) and the 150-mg arm (7.7 months), with respective adjusted hazard ratios for progression versus fulvestrant of 0.58 (P = .0124) and 0.67 (P = .0161).
Camizestrant at the 75-mg dose was also superior to fulvestrant among patients who had previously received a cyclin-dependent kinase 4/6 inhibitor, with median PFS of 5.5 months and 3.8 months for the 75-mg and 150-mg doses, respectively, compared with 2.1 months.
The adjusted HR for progression with camizestrant with the 75-mg dose was 0.49, with a 90% confidence interval indicating significance. The 150-mg dose was not significantly superior to fulvestrant, however.
Both camizestrant doses were also superior for prolonging PFS versus fulvestrant among patients with lung and/or liver metastases, with median PFS of 7.2 months, 5.6 months, and 2.0 months, respectively.
The experimental SERD also outperformed fulvestrant in an analysis looking at PFS by ESR1 mutational status and ER-driven disease. Among patients with ESR1 wild type, however, median PFS rates with camizestrant 75 mg and fulvestrant were the same (7.2 months).
The 24-week objective response rates were 15.7% in the 75-mg camizestrant arm, 20% in the 150-mg arm, and 11.8% in the fulvestrant arm. The respective clinical benefit rates, including all patients with responses or stable disease, were 47.3%, 49.3%, and 38.4%. The camizestrant clinical benefit rates did not differ significantly from those with fulvestrant, however.
Treatment-related adverse events of grade 3 or greater occurred in only five patients, and only two patients, both in the 75-mg camizestrant arm, discontinued therapy because of adverse events. There were no treatment-related deaths.
Adverse events that occurred only with camizestrant included photopsia (flashing lights or floaters in the field of vision) and sinus bradycardia.
Promising, but early
Carlos Artega, MD, codirector of SABCS and director of the Simmons Comprehensive Cancer Center at UT Southwestern Medical Center, Dallas, who was not involved in the study, said the data look promising in comparison with fulvestrant.
“There is a clear suggestion that this might be better,” he said. “[Camizestrant] seems to be better at reducing the titer in plasma of the ESR1 mutation, and there is very strong basic science that supports that.”
He noted that the study numbers were relatively small, however.
Dr. Arteaga was speaking at a media briefing held immediately prior to the presentation of the data in an oral abstract session.
Fabrice Andre, MD, from Gustave Roussy in Villejuif, France, the invited discussant for the oral session, noted that, in patients with ESR1 wild type, where fulvestrant shows some efficacy, camizestrant appears to be equally effective, and that the latter agent may be more synergistic with targeted therapies than fulvestrant.
Given high patient dropout rates with currently available SERDs, there is a need for SERDs used in the adjuvant setting that are effective at minimally bioactive doses for patients who are predicted to poorly adherent, Dr. Andre said.
The study was funded by AstraZeneca. Dr. Oliveira has received personal funding from AstraZeneca, Guardant Health, Roche, Merck Sharp & Dohme, Pfizer, Seagen, iTeos Therapeutics, Eisai, Novartis, Relay Therapeutics, and Gilead. Dr. Arteaga is a scientific adviser to AstraZeneca and others, and has received grant support from Pfizer Lilly and Takeda. Dr. Andre disclosed fees to his hospital on his behalf from AstraZeneca, Daiichi Sankyo, Sanofi, Pfizer, Lilly, and Roche.
SAN ANTONIO – compared with the first-generation SERD fulvestrant Faslodex, in the SERENA-2 trial, shows a study recently presented at the San Antonio Breast Cancer Symposium.
Among 180 postmenopausal women with ER+/HER2– breast cancers that had recurred or progressed following at least one line of endocrine therapy, the median progression-free survival (PFS) after a median follow-up of 16.6-17.4 months was 7.2 months for patients treated at a 75-mg dose of camizestrant and 7.7 months for those treated at a 150-mg dose, compared with 3.7 months for patients who received fulvestrant, reported Mafalda Oliveira, MD, PhD, from Vall d’Hebron University Hospital in Barcelona.
Oral agent
Camizestrant is a next-generation oral SERD and pure estrogen receptor antagonist that was shown in the SERENA-1 trial to be safe and to have clinical activity against ER+ breast cancers.
SERENA-2 pitted camizestrant at doses of 75 mg, 150 mg, or 300 mg against standard-dose fulvestrant, although the 300-mg dose was dropped in a protocol amendment after 20 patients had been assigned to that arm. (Currently planned studies with camizestrant will be conducted with the 75-mg dose.)
The investigators enrolled women with ER+/HER2– advanced breast cancer who had not previously received fulvestrant or an oral SERD. Eligible patients were limited to no more than one prior line of endocrine and one prior line of chemotherapy for advanced breast cancers. The study included patients with both measurable and unmeasurable disease.
The median patient age was about 60 years. Approximately 59% of patients in each arm had either lung or liver metastases. Patients with recurrence in bone only comprised 14.9%-19.4%.
Mutations in ESR1, a gene associated with hormonal resistance, were detectable in 29.7%-47.9% of patients.
Better PFS
As noted before, the primary endpoint of investigator-assessed median PFS favored camizestrant in both the 75-mg arm (7.2 months) and the 150-mg arm (7.7 months), with respective adjusted hazard ratios for progression versus fulvestrant of 0.58 (P = .0124) and 0.67 (P = .0161).
Camizestrant at the 75-mg dose was also superior to fulvestrant among patients who had previously received a cyclin-dependent kinase 4/6 inhibitor, with median PFS of 5.5 months and 3.8 months for the 75-mg and 150-mg doses, respectively, compared with 2.1 months.
The adjusted HR for progression with camizestrant with the 75-mg dose was 0.49, with a 90% confidence interval indicating significance. The 150-mg dose was not significantly superior to fulvestrant, however.
Both camizestrant doses were also superior for prolonging PFS versus fulvestrant among patients with lung and/or liver metastases, with median PFS of 7.2 months, 5.6 months, and 2.0 months, respectively.
The experimental SERD also outperformed fulvestrant in an analysis looking at PFS by ESR1 mutational status and ER-driven disease. Among patients with ESR1 wild type, however, median PFS rates with camizestrant 75 mg and fulvestrant were the same (7.2 months).
The 24-week objective response rates were 15.7% in the 75-mg camizestrant arm, 20% in the 150-mg arm, and 11.8% in the fulvestrant arm. The respective clinical benefit rates, including all patients with responses or stable disease, were 47.3%, 49.3%, and 38.4%. The camizestrant clinical benefit rates did not differ significantly from those with fulvestrant, however.
Treatment-related adverse events of grade 3 or greater occurred in only five patients, and only two patients, both in the 75-mg camizestrant arm, discontinued therapy because of adverse events. There were no treatment-related deaths.
Adverse events that occurred only with camizestrant included photopsia (flashing lights or floaters in the field of vision) and sinus bradycardia.
Promising, but early
Carlos Artega, MD, codirector of SABCS and director of the Simmons Comprehensive Cancer Center at UT Southwestern Medical Center, Dallas, who was not involved in the study, said the data look promising in comparison with fulvestrant.
“There is a clear suggestion that this might be better,” he said. “[Camizestrant] seems to be better at reducing the titer in plasma of the ESR1 mutation, and there is very strong basic science that supports that.”
He noted that the study numbers were relatively small, however.
Dr. Arteaga was speaking at a media briefing held immediately prior to the presentation of the data in an oral abstract session.
Fabrice Andre, MD, from Gustave Roussy in Villejuif, France, the invited discussant for the oral session, noted that, in patients with ESR1 wild type, where fulvestrant shows some efficacy, camizestrant appears to be equally effective, and that the latter agent may be more synergistic with targeted therapies than fulvestrant.
Given high patient dropout rates with currently available SERDs, there is a need for SERDs used in the adjuvant setting that are effective at minimally bioactive doses for patients who are predicted to poorly adherent, Dr. Andre said.
The study was funded by AstraZeneca. Dr. Oliveira has received personal funding from AstraZeneca, Guardant Health, Roche, Merck Sharp & Dohme, Pfizer, Seagen, iTeos Therapeutics, Eisai, Novartis, Relay Therapeutics, and Gilead. Dr. Arteaga is a scientific adviser to AstraZeneca and others, and has received grant support from Pfizer Lilly and Takeda. Dr. Andre disclosed fees to his hospital on his behalf from AstraZeneca, Daiichi Sankyo, Sanofi, Pfizer, Lilly, and Roche.
SAN ANTONIO – compared with the first-generation SERD fulvestrant Faslodex, in the SERENA-2 trial, shows a study recently presented at the San Antonio Breast Cancer Symposium.
Among 180 postmenopausal women with ER+/HER2– breast cancers that had recurred or progressed following at least one line of endocrine therapy, the median progression-free survival (PFS) after a median follow-up of 16.6-17.4 months was 7.2 months for patients treated at a 75-mg dose of camizestrant and 7.7 months for those treated at a 150-mg dose, compared with 3.7 months for patients who received fulvestrant, reported Mafalda Oliveira, MD, PhD, from Vall d’Hebron University Hospital in Barcelona.
Oral agent
Camizestrant is a next-generation oral SERD and pure estrogen receptor antagonist that was shown in the SERENA-1 trial to be safe and to have clinical activity against ER+ breast cancers.
SERENA-2 pitted camizestrant at doses of 75 mg, 150 mg, or 300 mg against standard-dose fulvestrant, although the 300-mg dose was dropped in a protocol amendment after 20 patients had been assigned to that arm. (Currently planned studies with camizestrant will be conducted with the 75-mg dose.)
The investigators enrolled women with ER+/HER2– advanced breast cancer who had not previously received fulvestrant or an oral SERD. Eligible patients were limited to no more than one prior line of endocrine and one prior line of chemotherapy for advanced breast cancers. The study included patients with both measurable and unmeasurable disease.
The median patient age was about 60 years. Approximately 59% of patients in each arm had either lung or liver metastases. Patients with recurrence in bone only comprised 14.9%-19.4%.
Mutations in ESR1, a gene associated with hormonal resistance, were detectable in 29.7%-47.9% of patients.
Better PFS
As noted before, the primary endpoint of investigator-assessed median PFS favored camizestrant in both the 75-mg arm (7.2 months) and the 150-mg arm (7.7 months), with respective adjusted hazard ratios for progression versus fulvestrant of 0.58 (P = .0124) and 0.67 (P = .0161).
Camizestrant at the 75-mg dose was also superior to fulvestrant among patients who had previously received a cyclin-dependent kinase 4/6 inhibitor, with median PFS of 5.5 months and 3.8 months for the 75-mg and 150-mg doses, respectively, compared with 2.1 months.
The adjusted HR for progression with camizestrant with the 75-mg dose was 0.49, with a 90% confidence interval indicating significance. The 150-mg dose was not significantly superior to fulvestrant, however.
Both camizestrant doses were also superior for prolonging PFS versus fulvestrant among patients with lung and/or liver metastases, with median PFS of 7.2 months, 5.6 months, and 2.0 months, respectively.
The experimental SERD also outperformed fulvestrant in an analysis looking at PFS by ESR1 mutational status and ER-driven disease. Among patients with ESR1 wild type, however, median PFS rates with camizestrant 75 mg and fulvestrant were the same (7.2 months).
The 24-week objective response rates were 15.7% in the 75-mg camizestrant arm, 20% in the 150-mg arm, and 11.8% in the fulvestrant arm. The respective clinical benefit rates, including all patients with responses or stable disease, were 47.3%, 49.3%, and 38.4%. The camizestrant clinical benefit rates did not differ significantly from those with fulvestrant, however.
Treatment-related adverse events of grade 3 or greater occurred in only five patients, and only two patients, both in the 75-mg camizestrant arm, discontinued therapy because of adverse events. There were no treatment-related deaths.
Adverse events that occurred only with camizestrant included photopsia (flashing lights or floaters in the field of vision) and sinus bradycardia.
Promising, but early
Carlos Artega, MD, codirector of SABCS and director of the Simmons Comprehensive Cancer Center at UT Southwestern Medical Center, Dallas, who was not involved in the study, said the data look promising in comparison with fulvestrant.
“There is a clear suggestion that this might be better,” he said. “[Camizestrant] seems to be better at reducing the titer in plasma of the ESR1 mutation, and there is very strong basic science that supports that.”
He noted that the study numbers were relatively small, however.
Dr. Arteaga was speaking at a media briefing held immediately prior to the presentation of the data in an oral abstract session.
Fabrice Andre, MD, from Gustave Roussy in Villejuif, France, the invited discussant for the oral session, noted that, in patients with ESR1 wild type, where fulvestrant shows some efficacy, camizestrant appears to be equally effective, and that the latter agent may be more synergistic with targeted therapies than fulvestrant.
Given high patient dropout rates with currently available SERDs, there is a need for SERDs used in the adjuvant setting that are effective at minimally bioactive doses for patients who are predicted to poorly adherent, Dr. Andre said.
The study was funded by AstraZeneca. Dr. Oliveira has received personal funding from AstraZeneca, Guardant Health, Roche, Merck Sharp & Dohme, Pfizer, Seagen, iTeos Therapeutics, Eisai, Novartis, Relay Therapeutics, and Gilead. Dr. Arteaga is a scientific adviser to AstraZeneca and others, and has received grant support from Pfizer Lilly and Takeda. Dr. Andre disclosed fees to his hospital on his behalf from AstraZeneca, Daiichi Sankyo, Sanofi, Pfizer, Lilly, and Roche.
AT SABCS 2022
Potential cause of worse outcomes among Black breast cancer patients found
SAN ANTONIO – compared with White women, a discovery that may at least partially explain racial differences in breast cancer outcomes, investigators say.
The finding, which comes from a retrospective study comparing differences in tumor microenvironment of metastasis (TMEM) “doorways” between Black and White women suggest that tumors in Black women may have a stronger prometastatic response to neoadjuvant chemotherapy than tumors in White women, reported Maja H. Oktay, MD, PhD, of Montefiore Einstein Cancer Center, Albert Einstein College of Medicine, New York, at the San Antonio Breast Cancer Symposium.
“Looking forward ... we propose to use TMEM doorway density as a prognostic marker for distant recurrence-free survival as a marker of dissemination, and also as a predictive marker of response to drugs that can block TMEM doorways,” she said at a briefing held prior to the presentation of data in an oral abstract session.
Entry points
As their name implies, TMEM doorways are transient entry points or portals that allow cancer cells to disseminate to distant sites. TMEM doorways are composed of tumor cells, macrophages, and endothelial cells that come into direct contact and together create temporary vascular openings that allow tumor cells to cross cell walls into circulation, where they can then hitch a ride and travel to distant organ sites.
Previous studies have shown that TMEM doorway density is a prognostic marker of metastasis in breast cancer patients treated with adjuvant chemotherapy. And as Dr. Oktay and colleagues showed in the current study, TMEM doorway density, as measured by a TMEM doorway score, is a prognostic marker for distant metastatic recurrence of ER+/HER2– breast cancer following neoadjuvant chemotherapy.
They also showed that neoadjuvant chemotherapy may increase the TMEM doorway score and lead to a pro–metastatic tumor microenvironment in some women.
Doorway scores
The investigators measured TMEM doorway scores from residual breast cancers in women who had undergone standard neoadjuvant chemotherapy. The cohort consisted of 96 Black women, 43 of whom had ER+/HER2– breast cancer and 37 of whom had triple-negative breast cancer (TNBC), and 87 White women, 50 with ER+/HER2– cancer and 22 with TNBC. The remaining patients had other breast cancer subtypes.
They found that TNBCs had higher TMEM doorway density score and higher macrophage density scores, which may explain why patients with TNBC often have early recurrence of disease.
They also found that, compared with White patients, Black patients with ER+/HER2– tumors, but not TNBC tumors, had higher TMEM doorway density scores. Similarly, Black patients with ER+/HER– cancers, but not TNBC, had higher macrophage levels than White women, a finding that may explain racial disparity in ER+/HER2– disease, Dr. Oktay said.
For the entire cohort, patients with high TMEM doorway density scores had significantly worse distant recurrence–free survival than patients with intermediate or low scores (P = .008), and there was a trend toward worse DRFS among all patients with ER+/HER2– who were in the highest third of scores, but this did not quite reach statistical significance.
High versus low TMEM doorway density score was also an independent prognostic factor for worse outcomes among the entire cohort (P = .01).
There was no significant difference in TMEM density scores among patients with TNBC.
Neither high macrophage counts nor microvascular density alone were significantly associated with inferior DRFS. TMEM doorway score was the only factor significantly prognostic for worse outcomes among patients in the entire cohort.
Hypothesis needs further testing
Invited discussant Lori Pierce, MD, a radiation oncologist with Michigan Medicine, University of Michigan, Ann Arbor, said it’s unclear whether TMEM doorway density changed following neoadjuvant chemotherapy as there were no prechemotherapy scores available in this study.
“But I think the key part is that, if we think neoadjuvant chemotherapy promotes metastasis, then there should be an inferior outcome compared to adjuvant chemotherapy, but that’s not what we see. Well-powered randomized trials show equivalent outcomes with neoadjuvant chemotherapy as well as adjuvant,” she said.
She noted that a 2018 meta-analysis of individual patient data from 10 randomized trials comparing neoadjuvant with adjuvant chemotherapy in early breast cancer showed no differences in long-term distant recurrences, breast cancer–specific mortality, or all-cause mortality between the two modalities.
“While I think these data are very provocative, I certainly wouldn’t want Black women or any women who need neoadjuvant therapy to be discouraged because of these data. We need these data to be tested rigorously, so I look forward to the clinical trials that will test this question and can really give us more information about this very interesting hypothesis,” Dr. Pierce said.
The study was funded by the National Institutes of Health, New York State Department of Health Peter T. Rowley Breast Cancer Scientific Research Projects, Helen & Irving Spatz Family Foundation, Evelyn Gruss Lipper Charitable Foundation, and the Gruss-Lipper Biophotonics Center and the integrated imaging program at the Albert Einstein College of Medicine. Dr. Oktay reported no conflicts of interests.
SAN ANTONIO – compared with White women, a discovery that may at least partially explain racial differences in breast cancer outcomes, investigators say.
The finding, which comes from a retrospective study comparing differences in tumor microenvironment of metastasis (TMEM) “doorways” between Black and White women suggest that tumors in Black women may have a stronger prometastatic response to neoadjuvant chemotherapy than tumors in White women, reported Maja H. Oktay, MD, PhD, of Montefiore Einstein Cancer Center, Albert Einstein College of Medicine, New York, at the San Antonio Breast Cancer Symposium.
“Looking forward ... we propose to use TMEM doorway density as a prognostic marker for distant recurrence-free survival as a marker of dissemination, and also as a predictive marker of response to drugs that can block TMEM doorways,” she said at a briefing held prior to the presentation of data in an oral abstract session.
Entry points
As their name implies, TMEM doorways are transient entry points or portals that allow cancer cells to disseminate to distant sites. TMEM doorways are composed of tumor cells, macrophages, and endothelial cells that come into direct contact and together create temporary vascular openings that allow tumor cells to cross cell walls into circulation, where they can then hitch a ride and travel to distant organ sites.
Previous studies have shown that TMEM doorway density is a prognostic marker of metastasis in breast cancer patients treated with adjuvant chemotherapy. And as Dr. Oktay and colleagues showed in the current study, TMEM doorway density, as measured by a TMEM doorway score, is a prognostic marker for distant metastatic recurrence of ER+/HER2– breast cancer following neoadjuvant chemotherapy.
They also showed that neoadjuvant chemotherapy may increase the TMEM doorway score and lead to a pro–metastatic tumor microenvironment in some women.
Doorway scores
The investigators measured TMEM doorway scores from residual breast cancers in women who had undergone standard neoadjuvant chemotherapy. The cohort consisted of 96 Black women, 43 of whom had ER+/HER2– breast cancer and 37 of whom had triple-negative breast cancer (TNBC), and 87 White women, 50 with ER+/HER2– cancer and 22 with TNBC. The remaining patients had other breast cancer subtypes.
They found that TNBCs had higher TMEM doorway density score and higher macrophage density scores, which may explain why patients with TNBC often have early recurrence of disease.
They also found that, compared with White patients, Black patients with ER+/HER2– tumors, but not TNBC tumors, had higher TMEM doorway density scores. Similarly, Black patients with ER+/HER– cancers, but not TNBC, had higher macrophage levels than White women, a finding that may explain racial disparity in ER+/HER2– disease, Dr. Oktay said.
For the entire cohort, patients with high TMEM doorway density scores had significantly worse distant recurrence–free survival than patients with intermediate or low scores (P = .008), and there was a trend toward worse DRFS among all patients with ER+/HER2– who were in the highest third of scores, but this did not quite reach statistical significance.
High versus low TMEM doorway density score was also an independent prognostic factor for worse outcomes among the entire cohort (P = .01).
There was no significant difference in TMEM density scores among patients with TNBC.
Neither high macrophage counts nor microvascular density alone were significantly associated with inferior DRFS. TMEM doorway score was the only factor significantly prognostic for worse outcomes among patients in the entire cohort.
Hypothesis needs further testing
Invited discussant Lori Pierce, MD, a radiation oncologist with Michigan Medicine, University of Michigan, Ann Arbor, said it’s unclear whether TMEM doorway density changed following neoadjuvant chemotherapy as there were no prechemotherapy scores available in this study.
“But I think the key part is that, if we think neoadjuvant chemotherapy promotes metastasis, then there should be an inferior outcome compared to adjuvant chemotherapy, but that’s not what we see. Well-powered randomized trials show equivalent outcomes with neoadjuvant chemotherapy as well as adjuvant,” she said.
She noted that a 2018 meta-analysis of individual patient data from 10 randomized trials comparing neoadjuvant with adjuvant chemotherapy in early breast cancer showed no differences in long-term distant recurrences, breast cancer–specific mortality, or all-cause mortality between the two modalities.
“While I think these data are very provocative, I certainly wouldn’t want Black women or any women who need neoadjuvant therapy to be discouraged because of these data. We need these data to be tested rigorously, so I look forward to the clinical trials that will test this question and can really give us more information about this very interesting hypothesis,” Dr. Pierce said.
The study was funded by the National Institutes of Health, New York State Department of Health Peter T. Rowley Breast Cancer Scientific Research Projects, Helen & Irving Spatz Family Foundation, Evelyn Gruss Lipper Charitable Foundation, and the Gruss-Lipper Biophotonics Center and the integrated imaging program at the Albert Einstein College of Medicine. Dr. Oktay reported no conflicts of interests.
SAN ANTONIO – compared with White women, a discovery that may at least partially explain racial differences in breast cancer outcomes, investigators say.
The finding, which comes from a retrospective study comparing differences in tumor microenvironment of metastasis (TMEM) “doorways” between Black and White women suggest that tumors in Black women may have a stronger prometastatic response to neoadjuvant chemotherapy than tumors in White women, reported Maja H. Oktay, MD, PhD, of Montefiore Einstein Cancer Center, Albert Einstein College of Medicine, New York, at the San Antonio Breast Cancer Symposium.
“Looking forward ... we propose to use TMEM doorway density as a prognostic marker for distant recurrence-free survival as a marker of dissemination, and also as a predictive marker of response to drugs that can block TMEM doorways,” she said at a briefing held prior to the presentation of data in an oral abstract session.
Entry points
As their name implies, TMEM doorways are transient entry points or portals that allow cancer cells to disseminate to distant sites. TMEM doorways are composed of tumor cells, macrophages, and endothelial cells that come into direct contact and together create temporary vascular openings that allow tumor cells to cross cell walls into circulation, where they can then hitch a ride and travel to distant organ sites.
Previous studies have shown that TMEM doorway density is a prognostic marker of metastasis in breast cancer patients treated with adjuvant chemotherapy. And as Dr. Oktay and colleagues showed in the current study, TMEM doorway density, as measured by a TMEM doorway score, is a prognostic marker for distant metastatic recurrence of ER+/HER2– breast cancer following neoadjuvant chemotherapy.
They also showed that neoadjuvant chemotherapy may increase the TMEM doorway score and lead to a pro–metastatic tumor microenvironment in some women.
Doorway scores
The investigators measured TMEM doorway scores from residual breast cancers in women who had undergone standard neoadjuvant chemotherapy. The cohort consisted of 96 Black women, 43 of whom had ER+/HER2– breast cancer and 37 of whom had triple-negative breast cancer (TNBC), and 87 White women, 50 with ER+/HER2– cancer and 22 with TNBC. The remaining patients had other breast cancer subtypes.
They found that TNBCs had higher TMEM doorway density score and higher macrophage density scores, which may explain why patients with TNBC often have early recurrence of disease.
They also found that, compared with White patients, Black patients with ER+/HER2– tumors, but not TNBC tumors, had higher TMEM doorway density scores. Similarly, Black patients with ER+/HER– cancers, but not TNBC, had higher macrophage levels than White women, a finding that may explain racial disparity in ER+/HER2– disease, Dr. Oktay said.
For the entire cohort, patients with high TMEM doorway density scores had significantly worse distant recurrence–free survival than patients with intermediate or low scores (P = .008), and there was a trend toward worse DRFS among all patients with ER+/HER2– who were in the highest third of scores, but this did not quite reach statistical significance.
High versus low TMEM doorway density score was also an independent prognostic factor for worse outcomes among the entire cohort (P = .01).
There was no significant difference in TMEM density scores among patients with TNBC.
Neither high macrophage counts nor microvascular density alone were significantly associated with inferior DRFS. TMEM doorway score was the only factor significantly prognostic for worse outcomes among patients in the entire cohort.
Hypothesis needs further testing
Invited discussant Lori Pierce, MD, a radiation oncologist with Michigan Medicine, University of Michigan, Ann Arbor, said it’s unclear whether TMEM doorway density changed following neoadjuvant chemotherapy as there were no prechemotherapy scores available in this study.
“But I think the key part is that, if we think neoadjuvant chemotherapy promotes metastasis, then there should be an inferior outcome compared to adjuvant chemotherapy, but that’s not what we see. Well-powered randomized trials show equivalent outcomes with neoadjuvant chemotherapy as well as adjuvant,” she said.
She noted that a 2018 meta-analysis of individual patient data from 10 randomized trials comparing neoadjuvant with adjuvant chemotherapy in early breast cancer showed no differences in long-term distant recurrences, breast cancer–specific mortality, or all-cause mortality between the two modalities.
“While I think these data are very provocative, I certainly wouldn’t want Black women or any women who need neoadjuvant therapy to be discouraged because of these data. We need these data to be tested rigorously, so I look forward to the clinical trials that will test this question and can really give us more information about this very interesting hypothesis,” Dr. Pierce said.
The study was funded by the National Institutes of Health, New York State Department of Health Peter T. Rowley Breast Cancer Scientific Research Projects, Helen & Irving Spatz Family Foundation, Evelyn Gruss Lipper Charitable Foundation, and the Gruss-Lipper Biophotonics Center and the integrated imaging program at the Albert Einstein College of Medicine. Dr. Oktay reported no conflicts of interests.
AT SABCS 2022
They trusted their prenatal test. They didn’t know the industry is an unregulated ‘Wild West.’
Amanda wanted to warn someone. In June 2021, her daughter – the one she and her husband had tried for 3 years to conceive – had died after only 28 hours. With an underdeveloped nose, she had battled for every breath.
Nobody knew why. Later, an autopsy report revealed their daughter had an extra 13th chromosome. The condition is nearly always fatal.
“But didn’t we test for that?” Amanda recalled asking herself. “That was kind of where the light bulb clicked.”
Through her doctor, Amanda had gotten a popular prenatal screening from a lab company. It had come back “negative.”
For three major conditions, including the one her baby had, the report gave the impression of near certainty. The likelihood that she would be born without them was “greater than 99%.”
As she recovered from a cesarean section, Amanda found herself facing a long maternity leave without a child. She shut the door to the empty nursery and began spending what seemed like endless hours of that hazy summer learning about the test.
It’s a simple blood draw designed to check for an array of genetic anomalies. But Amanda, a science researcher, read academic articles showing there was a higher risk of inaccurate results than she had realized. (She asked to be identified by only her first name to protect her privacy.)
On Reddit, she found other women reporting problems with the tests, too. She thought Labcorp, the company that made her test, would want to know about the screening that failed her. Maybe by alerting them, she could help other families. Maybe it would help her understand what happened.
“I was trying to gain answers,” said Amanda, now 32. She tried calling Labcorp’s customer service line, but she said she was passed along from one person to another. “It was just a circle,” she remembered.
She phoned Labcorp a second time. The call ended when an employee hung up on her.
Amanda was baffled. Why didn’t the company seem interested in her experience? Why, she wondered, wouldn’t it want to collect this data? Why wasn’t there someone who could answer her questions about how often this happens, and why?
If she had taken any number of other common commercial tests – including certain tests for COVID-19 or, say, pregnancy – the company would have been required to inform the U.S. Food and Drug Administration about reports of so-called adverse events.
But the test Amanda had falls into a regulatory void. No federal agency checks to make sure these prenatal screenings work the way they claim before they’re sold to health care providers. The FDA doesn’t ensure that marketing claims are backed up by evidence before screenings reach patients. And companies aren’t required to publicly report instances of when the tests get it wrong – sometimes catastrophically.
The broader lab testing industry and its lobbyists have successfully fought for years to keep it this way, cowing regulators into staying on the sidelines.
Worried about a growing variety of tests escaping scrutiny, the FDA was on the cusp of stepping in 6 years ago. But then it backed down.
Peter Lurie, then a top agency official, was at the meetings where the FDA tabled its plans. Not pushing harder, he told ProPublica, “remains one of my greatest regrets.”
The risk of false positives from prenatal screenings, in particular, has been known for years.
In 2014, the New England Center for Investigative Reporting detailed how some companies gave a misleading impression of the precision of the prenatal screenings. Women often didn’t understand they needed diagnostic testing to confirm the results. Some had gotten abortions based on false positive results, the story said. Earlier this year, the New York Times reported how companies sell optional extra screenings that are “usually wrong” when they predict a disorder.
Despite these stories and calls for reform by patient advocates, the government has done little to improve oversight of prenatal screenings. ProPublica set out to examine the forces that led to this inertia and left patients like Amanda feeling misled. Interviews with more than three dozen women revealed ongoing confusion about the screenings – and anger when their reliability proved to be overblown.
“This is a Wild West scenario where everybody is on their own,” said Lawrence Gostin, a Georgetown University, Washington, law professor specializing in bioethics.
The stakes for families are increasing. Upward of half of all pregnant people now receive one of these prenatal screenings. And with many states banning abortions or limiting them to early in pregnancies, the need for fast, accurate information has become more urgent.
The FDA itself acknowledges the problem. In correspondence with ProPublica, a spokesperson cited an “outdated policy” regarding the lack of vetting of many lab tests that the agency has “spent the better part of the last 2 decades trying to address.”
The screening industry, meanwhile, continues to expand, proving lucrative for those who lead it. The chief executive of Natera, which claims about 40% of the market share of prenatal screenings, received a $23 million compensation package last year, the highest of any executive at a publicly traded lab company.
Testing companies told ProPublica that, even without the FDA, there is significant oversight. Labs must abide by state regulations, and another federal agency, the Centers for Medicare and Medicaid Services, is charged with monitoring quality standards. It does not, however, check whether the tests the labs perform are clinically valid.
Companies also said the screenings offer important guidance to expectant families. Echoing others in the field, Labcorp said in a statement that the screenings, when used properly, “provide vital information about the presence of increased risk, but do not provide a definitive diagnosis.” (It declined to discuss the specifics of Amanda’s experience.)
Natera pointed out that its materials tell patients that “this test does not make a final diagnosis.” It reports results as “high-risk” or “low-risk,” not positive or negative.
Companies have stressed that, ultimately, it’s the responsibility of health care providers, who order the tests, to inform patients about the limits of screenings.
For all that, the statistical nuances of the test aren’t easy to parse for patients and even some doctors and nurses. For example, the test for trisomy 13, which doomed Amanda’s baby, is actually less likely to correctly predict the condition than other tests in the standard bundle of screenings offered to every patient.
When ProPublica asked readers to share their experiences with noninvasive prenatal screening tests, often referred to as NIPTs or NIPS, more than a thousand responded. Many said the tests had given them peace of mind. Some said they had provided an early warning about problems.
But others had more questions than answers. None more so than Amanda.
“What are these tests?” she wondered. “And how did mine end up in the margin of error?”
‘They started using it on humans, and then they went back and said: “Was our test accurate?” ’
Scientists have long tried to find ways to help parents and doctors understand what’s happening inside the womb. Amniocentesis was first used to reveal genetic anomalies in the late 1960s. But it didn’t become more popular until it began to be paired with ultrasound to precisely guide the procedure.
In the 1980s, doctors started using chorionic villus sampling, or CVS, an analysis of placental tissue that offers a diagnosis earlier in pregnancy. But, like amniocentesis, it is an invasive test that involves some risk to the fetus, though experts say it’s exceptionally low.
A breakthrough came in the late 1990s, when a scientist recognized that free-floating placental DNA could be detected in the mother’s blood. This meant that the fetus’s chromosomes could be examined by collecting a blood sample as soon as 9 weeks into pregnancy. This also provides an early opportunity to learn the likely fetal sex – a particularly popular feature.
Champions of the new science celebrated the arrival of a simple technique for patients that was particularly precise, at least for some conditions. Many favored it over other noninvasive options. But the industry that developed around NIPT has been marred by controversy from the beginning.
Dr. Ronald Wapner, director of reproductive genetics at Columbia University, described that time as “very chaotic.”
The tests had not been appropriately evaluated in clinical practice, said Dr. Wapner, whose research has sometimes been funded by testing companies. Because of this, he said, the industry “had very incomplete data on how well it worked.”
That didn’t stop the excitement. The chief executive of Sequenom, a biotechnology company that planned to release the first NIPT for Down syndrome, championed the company as the “Google of Molecular Diagnostics.” Its stock price soared.
Then, about 2 months before an expected launch in 2009, Sequenom killed the plan. The company’s research director, it turned out, had manipulated testing data and made misleading claims about how well the screening worked.
The U.S. Securities and Exchange Commission and Federal Bureau of Investigation opened investigations. Top executives were fired, and the research director pleaded guilty to conspiracy to commit securities fraud. Sequenom still managed to commercialize the test in 2011. (Labcorp, which later acquired Sequenom, said it uses a different kind of test.)
Other companies soon debuted their own tests. Still, there was little data on their clinical performance, researchers said.
As Megan Allyse, a bioethicist at the Mayo Clinic, put it, the companies “launched the test, they started using it on humans, and then they went back and said, ‘Was our test accurate?’ ” She also questioned the lack of attention to the ethics of how tests are presented to patients.
Despite missteps by the industry, the FDA didn’t scrutinize the screenings because they were considered lab-developed tests, which means they are created by the same laboratory that conducts them.
In 1976, Congress revamped oversight over medical devices. Since then, the FDA has effectively exempted such “home-brew” tests from key regulatory requirements. The idea was that when, say, a hospital lab wanted to create a simple test for its own patients, it was spared the time, money, and hassle of getting approval from Washington bureaucrats.
Today, lab-developed tests are vastly more numerous and complex. Because they aren’t registered with the federal government, nobody knows how many exist.
The distinction between tests the FDA actively regulates and those they don’t can seem nonsensical. It isn’t based on the complexity of the tests, or how people use them. It’s simply a matter of where the test is made.
The prenatal genetic screening industry took off almost immediately, powered by an army of aggressive sales representatives.
“At the very beginning, obstetricians in practice were being just completely inundated with visits from the sales reps,” said Dr. John Williams, director of reproductive health at Cedars-Sinai Medical Center in Los Angeles. The push left many ob.gyns. and patients thinking the screenings were accurate enough to substitute for diagnostic tests, such as amniocentesis or CVS.
In some cases, sales tactics escalated into lawbreaking.
Former Sequenom executives who exited during the fraud scandal created a new company that became Progenity, which also offered prenatal screening. Shortly after the company went public in 2020, it finalized a $49 million settlement with federal and state governments, where it admitted to falsifying insurance claims and giving kickbacks to physicians and their staff. According to a legal filing, one sales rep spent $65,658 on meals and alcohol for physicians in 1 year.
Now called Biora Therapeutics, the company said in a statement it no longer does any laboratory testing, including prenatal screenings.
Industry revenue continues to grow, but some testing companies are still fighting to make a profit, and competition to survive is fierce. “There’s a multibillion-dollar market, and they all want a piece of it,” said a former Progenity sales rep who quit in disgust after 5 months in 2016.
The rep, who requested anonymity because she continues to work in the field, said she still sees competitors from NIPT companies visiting medical practices “every week, buying breakfast or dinner, or taking them out for happy hour.”
Over time, companies pointed to new peer-reviewed studies, research the industry itself funded, to earn the confidence of doctors and other stakeholders. They showed that two tests – for Down syndrome and trisomy 18 – often performed better than other screening methods.
This research was valid, said Dr. Mary Norton, a perinatologist and clinical geneticist at the University of California, San Francisco, Medical Center’s prenatal diagnostic center. Considered a leading researcher in the field, she was an author of many of these key industry-funded studies.
But, she said, when research findings were presented publicly, the companies sometimes downplayed “inconvenient truths,” such as the exclusion of inconclusive results from accuracy estimates. Crucial caveats were also glossed over by some companies when they translated research into promotional copy aimed at health care providers and patients. Those materials didn’t always mention the many factors that can limit the performance of the screenings, including high body weight, the rarity of the condition tested, and younger maternal age.
Testing companies said they try to help patients understand the screenings through online resources and other materials. Some offer genetic counseling services.
The younger a person is, the lower the test’s positive predictive value – that is, the probability that a positive screening result will turn out to be correct – will be for some conditions. For instance, because Down syndrome is less prevalent in younger people’s pregnancies, a positive screening test is more likely to be a false positive for them.
Kristina was 30 years old in 2016, when her Progenity test came back positive for Down syndrome. She and her husband, who asked not to be fully named to protect their privacy, said they didn’t plan to carry a pregnancy with this condition to term.
But waiting to get an amniocentesis, and then waiting for the results, took 5 agonizing weeks, she said. It showed her son did not have Down syndrome.
Kristina, who lives in Texas, is still troubled by what she describes as a traumatic experience.
“I researched both late-term abortion providers and cemeteries,” she said. They even picked out a burial place, near their house.
She bought a blue baby blanket she intended to bury the baby’s tiny body in. She still has it. Her son, now 5, sleeps with it every night.
‘I can’t believe I didn’t say more’
As lab-developed tests became a bigger business, moving well past their home-brew origins, regulators looked for a way to assert oversight. In 2014, after years of study and debate, the time seemed right.
The FDA released plans proposing to regulate the tests, prioritizing those used to make major medical decisions. The agency has pointed to NIPTs as 1 of 20 concerning tests.
But, over the next 2 years, a coalition of power players urged the FDA to back off. Professional associations issued statements and hosted webinars devoted to the issue. Some created polished websites featuring sample letters to send to Washington.
Academic medical centers and pathology departments joined the fight, too. Scientists from 23 of them put it bluntly in a letter to the Office of Management and Budget: “FDA regulation of LDTs would be contrary to the public health,” it said, using a common acronym for the tests.
“Critical testing would be unavailable in the ‘lag time’ between development of new tests and FDA authorizing them,” the authors of the letter wrote, “and subsequent improvements on existing tests would slow significantly under the rigid, inflexible, and duplicative FDA regulatory scheme.”
This could delay essential care for patients. What’s more, opponents argued, existing lab reviews by the Centers for Medicare and Medicaid Services are sufficiently rigorous. Some have suggested modernizing the CMS review process to improve oversight.
An FDA spokesperson told ProPublica that the agency encountered “continued, negative feedback,” including a 25-page paper written by two legal heavyweights hired by the American Clinical Laboratory Association: Paul Clement, President George W. Bush’s former solicitor general, and Laurence Tribe, law professor at Harvard University.
Mr. Clement has reportedly commanded rates of $1,350 per hour. He and Mr. Tribe did not respond to ProPublica’s queries about their work.
Their brief argued that the FDA “lacked legal authority” to regulate lab-developed tests because they are properly seen as the practice of medicine: a service, rather than a product.
However, as lawyers representing the American Association of Bioanalysts countered, the FDA would vet tests before they reach the market, not control how doctors use them. The government proposal, they wrote, is “similar to imposing requirements to screen blood or label drugs.”
After the election of President Donald Trump, but before he took office, a handful of FDA officials discussed their battered proposal. It had represented a breakthrough in the decades of excruciating back-and-forth with industry. But now, with an incoming administration bent on deregulation, their efforts seemed futile.
The regulators feared anything they enacted would be undone by Congress – and, under the Congressional Review Act, they might not be able to reissue anything “substantially similar” in the future. So the FDA published a white paper instead, summarizing the issue “for further public discussion.”
After the meeting where officials made this call, Mr. Lurie, then the FDA’s associate commissioner, recalled a colleague approaching him: “I can’t believe you didn’t say more.”
“And I was like, ‘Yeah, actually, I can’t believe I didn’t say more either,’ ” Mr. Lurie later told ProPublica. (After leaving the agency, Mr. Lurie went on to lead the Center for Science in the Public Interest, a consumer advocacy nonprofit, which has pushed the FDA to finally assert oversight over lab-developed tests.)
Nancy Stade, an attorney and senior policy official who left the FDA in 2015, said the agency often moves slowly as it seeks to get buy-in from industry and professional groups. In her work on regulatory policy, she saw it happen with lab-developed tests.
The agency is “always testing the waters,” she said, “and always coming out with something a little bit softer.”
In 2020, the influential American College of Obstetricians and Gynecologists and Society for Maternal-Fetal Medicine, representing doctors who handle pregnancies, gave the screening industry another huge boost.
In a bulletin updating their advice on the tests, the two groups described growing research on the performance of some of the standard tests and said people have the right to information about their pregnancies, so the tests should be offered to all patients. Previously, they recommended this only for those facing higher risk of genetic anomalies.
The bulletin said the coauthors had disclosed no conflicts of interest. But two of the four coauthors, including Mary Norton, had disclosed in prior publications that test-makers had provided funding for their research. A company had provided a third coauthor with laboratory services needed to run tests, according to that researcher, a connection she also disclosed in past papers.
ACOG, in a statement to ProPublica, said the organization “identified no conflicts because research funding is provided to academic institutions with institutional review boards, not to individual investigators.” Two of the three researchers responded to questions from ProPublica and said they maintained independence over their work.
One test-maker, Illumina, celebrated the ACOG guidance in a tweet, saying it “recognizes the superior performance of #NIPT and the benefit it provides expectant families.” Natera’s share prices doubled in 5 months. UnitedHealthcare, the nation’s largest private insurer and long a target of industry lobbying, told ProPublica it changed its stance to cover screenings for all patients, regardless of risk, because of the recommendation.
In a recent shareholder report, Natera stated that prenatal genetic and carrier screenings “represent the significant majority of our revenues,” which totaled $625.5 million in 2021. The company expects more growth to come.
“The NIPT market is still very underpenetrated, compared to the 4 to 5 million pregnancies in the U.S.,” Natera’s chief executive said on a 2021 earnings call, “so there’s a long way to go.”
But even Dr. Norton, who coauthored the ACOG recommendation and favors NIPTs for patients 40 and over, has concerns about screenings becoming widespread among those who are younger. In most cases, she prefers other screening methods that catch the nongenetic problems younger moms are more likely to face. Negative results from an NIPT, she said, can be “falsely reassuring.”
In the years after the FDA set aside its regulatory proposal, the agency has assisted members of Congress on a proposed legislative solution. That effort, dubbed the VALID Act, aims to end any debate over the agency’s authority over lab-developed tests. An FDA press officer said the legislation would ensure the prenatal screening tests and others are “accurate and reliable.”
But, as in the past, intense lobbying followed the proposal. The VALID Act was a rider to a funding reauthorization bill, but in September the House and Senate agreed to remove it. Advocates now hope to attach it to proposed end-of-year legislation.
Meanwhile, earlier this year, 4 months after the New York Times story on the usefulness of some screenings, the FDA took a step toward more public awareness about prenatal genetic screening. It issued its first safety communication on them, noting the potential for false results.
It cautioned patients about making “critical health care decisions based on results from these screening tests alone.”
Cara Tenenbaum, a former FDA policy advisor, was pleased to see the statement. Still, she said, it was long overdue.
“This has been known – known, or should have been known – for 10 years,” she said.
‘It had me so messed up’
With the demise of Roe v. Wade, restrictive and ever-changing abortion laws can pressure people to act quickly with limited information, heightening the stakes of prenatal screening.
Julia, a mom from Mississippi’s Gulf Coast, knows what it’s like to face harrowing consequences while navigating state-imposed time limits – and doing so with little guidance. Last fall, she was pregnant with her fourth child when, she said, a nurse practitioner suggested prenatal genetic screening.
At 33, Julia had no risk factors. Her previous pregnancies hadn’t been screened with an NIPT. But with three sons and 18 nephews, she and her husband were curious about the baby’s sex. And the screening seemed like it had no downside.
Julia figured it would only be offered if it was reliable, so her nurse practitioner ordered her both the basic bundle of screenings and the extra tests. (The medical practice didn’t respond to interview requests. Julia is a family nickname that’s used here to protect her privacy.)
The screenings showed the baby was a girl – but the extra tests also detected trisomy 16, a condition caused by an extra chromosome that is so rare, the nurse didn’t know what it was, Julia recalled.
The nurse borrowed Julia’s phone, using it to search online and read aloud what she found. Julia was stunned to hear trisomy 16 was incompatible with life.
“I was utterly devastated,” she said. “I made it out of my doctor’s office but completely broke down in the car.”
But ACOG does not recommend the trisomy 16 screening, saying “its accuracy with regard to detection and the false-positive rate is not established.” Julia wasn’t informed of this, she said, and she’s not sure if her health care providers knew it either.
The lab report recommended diagnostic testing to confirm the results, but time was short. She had her amniocentesis at 17 weeks. It could take up to 4 more weeks to receive results.
That would be too late for a legal abortion in Mississippi. So she made an appointment for one in Florida, where the cutoff was 24 weeks. (It’s now 15 weeks in Florida, while Mississippi went from 15 weeks for legal procedures to a ban on nearly all abortions.)
The wait was excruciating. Julia was driving twice a week to New Orleans for specialized care. With work and child care, it was too hard. She quit the teaching job she loved.
One winter night, she felt the fetus move for the first time – ordinarily a milestone, but now, facing a fatal prognosis, she didn’t want to get attached. “It had me so messed up,” she said.
On the way to the amniocentesis, Julia and her husband chose a name. Drawing from a language conjured by J.R.R. Tolkien in the fantasy novels they love, it means “hope.”
More than halfway through her pregnancy, the amnio results arrived. The prenatal screening had given a false positive. The baby would be fine. In May, Julia gave birth to a healthy daughter.
Julia and her husband are upset about the needless anguish brought on by the screening. “They like to have it both ways,” said Julia’s husband. “They say they are 99% accurate, but when there’s a false positive, they say, ‘Well, we’re not diagnostic.’ ”
Believing the prenatal screening was likely accurate, they had seriously considered canceling the amniocentesis, saving their limited funds for an abortion in Florida, hundreds of miles away.
Their dilemma points to a longtime concern: ending pregnancies based on false positives. The FDA cited it as a risk as far back as 2015. Now, those with positive results are facing an even tighter time crunch. They must consider whether waiting for a definitive test, and possibly traveling to another state for an abortion later in pregnancy, is worth it.
In their promotional material, some companies not only sidestep the variability of the standard tests, they fail to distinguish them from the least reliable ones – those for exceptionally rare conditions. They tout the extra screenings as “premium,” “plus,” or “advanced” options.
“Going to greater lengths for the answers that matter most,” says a brochure aimed at health care providers from test-maker Illumina. Elsewhere it states that the “expanded” panel of tests provides “confident results” and “the additional insights you need.”
But the companies themselves know the accuracy of some of their tests has yet to be established in the research. Natera acknowledged in a recent shareholder report that many insurers won’t pay for screenings for missing chromosomal fragments, known as microdeletions, in part because there isn’t enough published data behind them.
The company, responding to ProPublica, stressed the quality of the data over the quantity, saying the research so far has been favorable. “Natera’s microdeletion testing was thoroughly validated with results published in peer-reviewed publications,” it said in a statement.
Natera pointed to a recent study that looked at DiGeorge syndrome, one of several chromosomal anomalies it checks for with its microdeletion screenings. Researchers found the positive predictive value (PPV) of the test to be 52.6%, meaning that nearly half of positive results are false positives. (For many patients, PPVs for more common conditions can exceed 90%.)
Natera said the performance of the diGeorge syndrome test “is excellent and not considered a low PPV,” because of the condition being extremely rare.
Companies also play up the danger of diagnostic tests like amnio. They “can cause miscarriages,” warns the marketing from Labcorp, which made Amanda’s screening, while its test “does not cause miscarriages.” But medical experts emphasize that diagnostic tests, such as amniocentesis, are more accurate and, in fact, carry little risk to the pregnancy.
Labcorp, in a statement, said the company “acknowledges the well-documented risk associated with amniocentesis and CVS in our literature. It is the patient’s prerogative to decide which risks they are willing or unwilling to take.”
Marketing claims also sometimes skate over the nuances in the guidance from the leading professional societies. On a webpage targeting health care providers, for example, a Labcorp chart said groups such as ACOG “endorse and/or recognize” prenatal screenings as an option for all pregnancies. But the chart listed screenings ACOG does not recommend, including trisomy 16.
When asked about it, Labcorp said in a statement that ACOG “endorses NIPS for all pregnancies.” In fact, the guidance is not so sweeping. It says only that the basic bundle of tests should be offered to all, alongside other screening options. It explicitly advises providers to not offer patients the extra tests.
Soon after ProPublica’s query, the Labcorp webpage was updated to remove any mention of the professional societies.
Patients say they often don’t know where to turn for informed and unbiased information. That’s why the r/NIPT Reddit page became such a robust community. Facing difficult news, Julia turned to it for counsel from other prospective parents. Kristina in Texas found the same community. Amanda, too.
‘The margin of error is a human life’
On a warm and cloudy day this past June, on what would have been their daughter’s first birthday, Amanda and her husband visited her grave. They brought a unicorn balloon and vanilla cake, which they ate nearby on the grass. Her husband read a poem.
To them, their baby had been perfect. She had fingers and toes. A thatch of dark hair. While in intensive care, peering up at her parents, she grabbed for her mother’s hand.
Had her condition been known, they would’ve spared her futile medical interventions, as doctors tried to save her life. Their family priest would have been able to baptize her. As it was, they never got to hold their child while she was alive.
These days, when Amanda and her husband say grace before dinner, they give thanks for the 28 hours of their daughter’s life.
They’re also thinking about making comfort boxes the hospital could give to other parents who lose a child. It might include books on grief. Softer tissues. Something that says, as Amanda puts it, “This is to help you get through.”
Amid their grief, they had a prayer answered: Amanda is pregnant again.
It’s frightening to go through this again. She barely sleeps the night before visiting the doctor. It feels like she never stopped being pregnant. It will feel that way, she said, until she brings a baby home – one who lives past the first 2 nights.
Amanda planned to get another genetic screening test. At first she couldn’t bear it, wasn’t sure she could trust it. “The margin of error is a human life,” Amanda said.
The 10-week appointment passed. Then the 12-week appointment. After her 13th week, she took the plunge. The test she was given was from Labcorp.
Around this time, more than a year after Amanda had desperately tried to alert the company about what had happened to her and her first baby, she finally heard back. Labcorp’s vice president of genetic counseling and services reached out – after ProPublica contacted the company and shared Amanda’s story.
The executive would only speak to Amanda without a reporter present.
Amanda said that during the call, the executive told her that prenatal genetic tests are evolving, and doctors should be clear about what the screenings can and cannot do. By the end of the conversation, the executive offered Amanda her cell number.
Amanda said she appreciated the call. “I feel better. I feel like I got something.”
The same day, her screening results came back. They were negative.
This story was originally published on ProPublica. ProPublica is a nonprofit newsroom that investigates abuses of power. Sign up to receive their biggest stories as soon as they’re published.
Amanda wanted to warn someone. In June 2021, her daughter – the one she and her husband had tried for 3 years to conceive – had died after only 28 hours. With an underdeveloped nose, she had battled for every breath.
Nobody knew why. Later, an autopsy report revealed their daughter had an extra 13th chromosome. The condition is nearly always fatal.
“But didn’t we test for that?” Amanda recalled asking herself. “That was kind of where the light bulb clicked.”
Through her doctor, Amanda had gotten a popular prenatal screening from a lab company. It had come back “negative.”
For three major conditions, including the one her baby had, the report gave the impression of near certainty. The likelihood that she would be born without them was “greater than 99%.”
As she recovered from a cesarean section, Amanda found herself facing a long maternity leave without a child. She shut the door to the empty nursery and began spending what seemed like endless hours of that hazy summer learning about the test.
It’s a simple blood draw designed to check for an array of genetic anomalies. But Amanda, a science researcher, read academic articles showing there was a higher risk of inaccurate results than she had realized. (She asked to be identified by only her first name to protect her privacy.)
On Reddit, she found other women reporting problems with the tests, too. She thought Labcorp, the company that made her test, would want to know about the screening that failed her. Maybe by alerting them, she could help other families. Maybe it would help her understand what happened.
“I was trying to gain answers,” said Amanda, now 32. She tried calling Labcorp’s customer service line, but she said she was passed along from one person to another. “It was just a circle,” she remembered.
She phoned Labcorp a second time. The call ended when an employee hung up on her.
Amanda was baffled. Why didn’t the company seem interested in her experience? Why, she wondered, wouldn’t it want to collect this data? Why wasn’t there someone who could answer her questions about how often this happens, and why?
If she had taken any number of other common commercial tests – including certain tests for COVID-19 or, say, pregnancy – the company would have been required to inform the U.S. Food and Drug Administration about reports of so-called adverse events.
But the test Amanda had falls into a regulatory void. No federal agency checks to make sure these prenatal screenings work the way they claim before they’re sold to health care providers. The FDA doesn’t ensure that marketing claims are backed up by evidence before screenings reach patients. And companies aren’t required to publicly report instances of when the tests get it wrong – sometimes catastrophically.
The broader lab testing industry and its lobbyists have successfully fought for years to keep it this way, cowing regulators into staying on the sidelines.
Worried about a growing variety of tests escaping scrutiny, the FDA was on the cusp of stepping in 6 years ago. But then it backed down.
Peter Lurie, then a top agency official, was at the meetings where the FDA tabled its plans. Not pushing harder, he told ProPublica, “remains one of my greatest regrets.”
The risk of false positives from prenatal screenings, in particular, has been known for years.
In 2014, the New England Center for Investigative Reporting detailed how some companies gave a misleading impression of the precision of the prenatal screenings. Women often didn’t understand they needed diagnostic testing to confirm the results. Some had gotten abortions based on false positive results, the story said. Earlier this year, the New York Times reported how companies sell optional extra screenings that are “usually wrong” when they predict a disorder.
Despite these stories and calls for reform by patient advocates, the government has done little to improve oversight of prenatal screenings. ProPublica set out to examine the forces that led to this inertia and left patients like Amanda feeling misled. Interviews with more than three dozen women revealed ongoing confusion about the screenings – and anger when their reliability proved to be overblown.
“This is a Wild West scenario where everybody is on their own,” said Lawrence Gostin, a Georgetown University, Washington, law professor specializing in bioethics.
The stakes for families are increasing. Upward of half of all pregnant people now receive one of these prenatal screenings. And with many states banning abortions or limiting them to early in pregnancies, the need for fast, accurate information has become more urgent.
The FDA itself acknowledges the problem. In correspondence with ProPublica, a spokesperson cited an “outdated policy” regarding the lack of vetting of many lab tests that the agency has “spent the better part of the last 2 decades trying to address.”
The screening industry, meanwhile, continues to expand, proving lucrative for those who lead it. The chief executive of Natera, which claims about 40% of the market share of prenatal screenings, received a $23 million compensation package last year, the highest of any executive at a publicly traded lab company.
Testing companies told ProPublica that, even without the FDA, there is significant oversight. Labs must abide by state regulations, and another federal agency, the Centers for Medicare and Medicaid Services, is charged with monitoring quality standards. It does not, however, check whether the tests the labs perform are clinically valid.
Companies also said the screenings offer important guidance to expectant families. Echoing others in the field, Labcorp said in a statement that the screenings, when used properly, “provide vital information about the presence of increased risk, but do not provide a definitive diagnosis.” (It declined to discuss the specifics of Amanda’s experience.)
Natera pointed out that its materials tell patients that “this test does not make a final diagnosis.” It reports results as “high-risk” or “low-risk,” not positive or negative.
Companies have stressed that, ultimately, it’s the responsibility of health care providers, who order the tests, to inform patients about the limits of screenings.
For all that, the statistical nuances of the test aren’t easy to parse for patients and even some doctors and nurses. For example, the test for trisomy 13, which doomed Amanda’s baby, is actually less likely to correctly predict the condition than other tests in the standard bundle of screenings offered to every patient.
When ProPublica asked readers to share their experiences with noninvasive prenatal screening tests, often referred to as NIPTs or NIPS, more than a thousand responded. Many said the tests had given them peace of mind. Some said they had provided an early warning about problems.
But others had more questions than answers. None more so than Amanda.
“What are these tests?” she wondered. “And how did mine end up in the margin of error?”
‘They started using it on humans, and then they went back and said: “Was our test accurate?” ’
Scientists have long tried to find ways to help parents and doctors understand what’s happening inside the womb. Amniocentesis was first used to reveal genetic anomalies in the late 1960s. But it didn’t become more popular until it began to be paired with ultrasound to precisely guide the procedure.
In the 1980s, doctors started using chorionic villus sampling, or CVS, an analysis of placental tissue that offers a diagnosis earlier in pregnancy. But, like amniocentesis, it is an invasive test that involves some risk to the fetus, though experts say it’s exceptionally low.
A breakthrough came in the late 1990s, when a scientist recognized that free-floating placental DNA could be detected in the mother’s blood. This meant that the fetus’s chromosomes could be examined by collecting a blood sample as soon as 9 weeks into pregnancy. This also provides an early opportunity to learn the likely fetal sex – a particularly popular feature.
Champions of the new science celebrated the arrival of a simple technique for patients that was particularly precise, at least for some conditions. Many favored it over other noninvasive options. But the industry that developed around NIPT has been marred by controversy from the beginning.
Dr. Ronald Wapner, director of reproductive genetics at Columbia University, described that time as “very chaotic.”
The tests had not been appropriately evaluated in clinical practice, said Dr. Wapner, whose research has sometimes been funded by testing companies. Because of this, he said, the industry “had very incomplete data on how well it worked.”
That didn’t stop the excitement. The chief executive of Sequenom, a biotechnology company that planned to release the first NIPT for Down syndrome, championed the company as the “Google of Molecular Diagnostics.” Its stock price soared.
Then, about 2 months before an expected launch in 2009, Sequenom killed the plan. The company’s research director, it turned out, had manipulated testing data and made misleading claims about how well the screening worked.
The U.S. Securities and Exchange Commission and Federal Bureau of Investigation opened investigations. Top executives were fired, and the research director pleaded guilty to conspiracy to commit securities fraud. Sequenom still managed to commercialize the test in 2011. (Labcorp, which later acquired Sequenom, said it uses a different kind of test.)
Other companies soon debuted their own tests. Still, there was little data on their clinical performance, researchers said.
As Megan Allyse, a bioethicist at the Mayo Clinic, put it, the companies “launched the test, they started using it on humans, and then they went back and said, ‘Was our test accurate?’ ” She also questioned the lack of attention to the ethics of how tests are presented to patients.
Despite missteps by the industry, the FDA didn’t scrutinize the screenings because they were considered lab-developed tests, which means they are created by the same laboratory that conducts them.
In 1976, Congress revamped oversight over medical devices. Since then, the FDA has effectively exempted such “home-brew” tests from key regulatory requirements. The idea was that when, say, a hospital lab wanted to create a simple test for its own patients, it was spared the time, money, and hassle of getting approval from Washington bureaucrats.
Today, lab-developed tests are vastly more numerous and complex. Because they aren’t registered with the federal government, nobody knows how many exist.
The distinction between tests the FDA actively regulates and those they don’t can seem nonsensical. It isn’t based on the complexity of the tests, or how people use them. It’s simply a matter of where the test is made.
The prenatal genetic screening industry took off almost immediately, powered by an army of aggressive sales representatives.
“At the very beginning, obstetricians in practice were being just completely inundated with visits from the sales reps,” said Dr. John Williams, director of reproductive health at Cedars-Sinai Medical Center in Los Angeles. The push left many ob.gyns. and patients thinking the screenings were accurate enough to substitute for diagnostic tests, such as amniocentesis or CVS.
In some cases, sales tactics escalated into lawbreaking.
Former Sequenom executives who exited during the fraud scandal created a new company that became Progenity, which also offered prenatal screening. Shortly after the company went public in 2020, it finalized a $49 million settlement with federal and state governments, where it admitted to falsifying insurance claims and giving kickbacks to physicians and their staff. According to a legal filing, one sales rep spent $65,658 on meals and alcohol for physicians in 1 year.
Now called Biora Therapeutics, the company said in a statement it no longer does any laboratory testing, including prenatal screenings.
Industry revenue continues to grow, but some testing companies are still fighting to make a profit, and competition to survive is fierce. “There’s a multibillion-dollar market, and they all want a piece of it,” said a former Progenity sales rep who quit in disgust after 5 months in 2016.
The rep, who requested anonymity because she continues to work in the field, said she still sees competitors from NIPT companies visiting medical practices “every week, buying breakfast or dinner, or taking them out for happy hour.”
Over time, companies pointed to new peer-reviewed studies, research the industry itself funded, to earn the confidence of doctors and other stakeholders. They showed that two tests – for Down syndrome and trisomy 18 – often performed better than other screening methods.
This research was valid, said Dr. Mary Norton, a perinatologist and clinical geneticist at the University of California, San Francisco, Medical Center’s prenatal diagnostic center. Considered a leading researcher in the field, she was an author of many of these key industry-funded studies.
But, she said, when research findings were presented publicly, the companies sometimes downplayed “inconvenient truths,” such as the exclusion of inconclusive results from accuracy estimates. Crucial caveats were also glossed over by some companies when they translated research into promotional copy aimed at health care providers and patients. Those materials didn’t always mention the many factors that can limit the performance of the screenings, including high body weight, the rarity of the condition tested, and younger maternal age.
Testing companies said they try to help patients understand the screenings through online resources and other materials. Some offer genetic counseling services.
The younger a person is, the lower the test’s positive predictive value – that is, the probability that a positive screening result will turn out to be correct – will be for some conditions. For instance, because Down syndrome is less prevalent in younger people’s pregnancies, a positive screening test is more likely to be a false positive for them.
Kristina was 30 years old in 2016, when her Progenity test came back positive for Down syndrome. She and her husband, who asked not to be fully named to protect their privacy, said they didn’t plan to carry a pregnancy with this condition to term.
But waiting to get an amniocentesis, and then waiting for the results, took 5 agonizing weeks, she said. It showed her son did not have Down syndrome.
Kristina, who lives in Texas, is still troubled by what she describes as a traumatic experience.
“I researched both late-term abortion providers and cemeteries,” she said. They even picked out a burial place, near their house.
She bought a blue baby blanket she intended to bury the baby’s tiny body in. She still has it. Her son, now 5, sleeps with it every night.
‘I can’t believe I didn’t say more’
As lab-developed tests became a bigger business, moving well past their home-brew origins, regulators looked for a way to assert oversight. In 2014, after years of study and debate, the time seemed right.
The FDA released plans proposing to regulate the tests, prioritizing those used to make major medical decisions. The agency has pointed to NIPTs as 1 of 20 concerning tests.
But, over the next 2 years, a coalition of power players urged the FDA to back off. Professional associations issued statements and hosted webinars devoted to the issue. Some created polished websites featuring sample letters to send to Washington.
Academic medical centers and pathology departments joined the fight, too. Scientists from 23 of them put it bluntly in a letter to the Office of Management and Budget: “FDA regulation of LDTs would be contrary to the public health,” it said, using a common acronym for the tests.
“Critical testing would be unavailable in the ‘lag time’ between development of new tests and FDA authorizing them,” the authors of the letter wrote, “and subsequent improvements on existing tests would slow significantly under the rigid, inflexible, and duplicative FDA regulatory scheme.”
This could delay essential care for patients. What’s more, opponents argued, existing lab reviews by the Centers for Medicare and Medicaid Services are sufficiently rigorous. Some have suggested modernizing the CMS review process to improve oversight.
An FDA spokesperson told ProPublica that the agency encountered “continued, negative feedback,” including a 25-page paper written by two legal heavyweights hired by the American Clinical Laboratory Association: Paul Clement, President George W. Bush’s former solicitor general, and Laurence Tribe, law professor at Harvard University.
Mr. Clement has reportedly commanded rates of $1,350 per hour. He and Mr. Tribe did not respond to ProPublica’s queries about their work.
Their brief argued that the FDA “lacked legal authority” to regulate lab-developed tests because they are properly seen as the practice of medicine: a service, rather than a product.
However, as lawyers representing the American Association of Bioanalysts countered, the FDA would vet tests before they reach the market, not control how doctors use them. The government proposal, they wrote, is “similar to imposing requirements to screen blood or label drugs.”
After the election of President Donald Trump, but before he took office, a handful of FDA officials discussed their battered proposal. It had represented a breakthrough in the decades of excruciating back-and-forth with industry. But now, with an incoming administration bent on deregulation, their efforts seemed futile.
The regulators feared anything they enacted would be undone by Congress – and, under the Congressional Review Act, they might not be able to reissue anything “substantially similar” in the future. So the FDA published a white paper instead, summarizing the issue “for further public discussion.”
After the meeting where officials made this call, Mr. Lurie, then the FDA’s associate commissioner, recalled a colleague approaching him: “I can’t believe you didn’t say more.”
“And I was like, ‘Yeah, actually, I can’t believe I didn’t say more either,’ ” Mr. Lurie later told ProPublica. (After leaving the agency, Mr. Lurie went on to lead the Center for Science in the Public Interest, a consumer advocacy nonprofit, which has pushed the FDA to finally assert oversight over lab-developed tests.)
Nancy Stade, an attorney and senior policy official who left the FDA in 2015, said the agency often moves slowly as it seeks to get buy-in from industry and professional groups. In her work on regulatory policy, she saw it happen with lab-developed tests.
The agency is “always testing the waters,” she said, “and always coming out with something a little bit softer.”
In 2020, the influential American College of Obstetricians and Gynecologists and Society for Maternal-Fetal Medicine, representing doctors who handle pregnancies, gave the screening industry another huge boost.
In a bulletin updating their advice on the tests, the two groups described growing research on the performance of some of the standard tests and said people have the right to information about their pregnancies, so the tests should be offered to all patients. Previously, they recommended this only for those facing higher risk of genetic anomalies.
The bulletin said the coauthors had disclosed no conflicts of interest. But two of the four coauthors, including Mary Norton, had disclosed in prior publications that test-makers had provided funding for their research. A company had provided a third coauthor with laboratory services needed to run tests, according to that researcher, a connection she also disclosed in past papers.
ACOG, in a statement to ProPublica, said the organization “identified no conflicts because research funding is provided to academic institutions with institutional review boards, not to individual investigators.” Two of the three researchers responded to questions from ProPublica and said they maintained independence over their work.
One test-maker, Illumina, celebrated the ACOG guidance in a tweet, saying it “recognizes the superior performance of #NIPT and the benefit it provides expectant families.” Natera’s share prices doubled in 5 months. UnitedHealthcare, the nation’s largest private insurer and long a target of industry lobbying, told ProPublica it changed its stance to cover screenings for all patients, regardless of risk, because of the recommendation.
In a recent shareholder report, Natera stated that prenatal genetic and carrier screenings “represent the significant majority of our revenues,” which totaled $625.5 million in 2021. The company expects more growth to come.
“The NIPT market is still very underpenetrated, compared to the 4 to 5 million pregnancies in the U.S.,” Natera’s chief executive said on a 2021 earnings call, “so there’s a long way to go.”
But even Dr. Norton, who coauthored the ACOG recommendation and favors NIPTs for patients 40 and over, has concerns about screenings becoming widespread among those who are younger. In most cases, she prefers other screening methods that catch the nongenetic problems younger moms are more likely to face. Negative results from an NIPT, she said, can be “falsely reassuring.”
In the years after the FDA set aside its regulatory proposal, the agency has assisted members of Congress on a proposed legislative solution. That effort, dubbed the VALID Act, aims to end any debate over the agency’s authority over lab-developed tests. An FDA press officer said the legislation would ensure the prenatal screening tests and others are “accurate and reliable.”
But, as in the past, intense lobbying followed the proposal. The VALID Act was a rider to a funding reauthorization bill, but in September the House and Senate agreed to remove it. Advocates now hope to attach it to proposed end-of-year legislation.
Meanwhile, earlier this year, 4 months after the New York Times story on the usefulness of some screenings, the FDA took a step toward more public awareness about prenatal genetic screening. It issued its first safety communication on them, noting the potential for false results.
It cautioned patients about making “critical health care decisions based on results from these screening tests alone.”
Cara Tenenbaum, a former FDA policy advisor, was pleased to see the statement. Still, she said, it was long overdue.
“This has been known – known, or should have been known – for 10 years,” she said.
‘It had me so messed up’
With the demise of Roe v. Wade, restrictive and ever-changing abortion laws can pressure people to act quickly with limited information, heightening the stakes of prenatal screening.
Julia, a mom from Mississippi’s Gulf Coast, knows what it’s like to face harrowing consequences while navigating state-imposed time limits – and doing so with little guidance. Last fall, she was pregnant with her fourth child when, she said, a nurse practitioner suggested prenatal genetic screening.
At 33, Julia had no risk factors. Her previous pregnancies hadn’t been screened with an NIPT. But with three sons and 18 nephews, she and her husband were curious about the baby’s sex. And the screening seemed like it had no downside.
Julia figured it would only be offered if it was reliable, so her nurse practitioner ordered her both the basic bundle of screenings and the extra tests. (The medical practice didn’t respond to interview requests. Julia is a family nickname that’s used here to protect her privacy.)
The screenings showed the baby was a girl – but the extra tests also detected trisomy 16, a condition caused by an extra chromosome that is so rare, the nurse didn’t know what it was, Julia recalled.
The nurse borrowed Julia’s phone, using it to search online and read aloud what she found. Julia was stunned to hear trisomy 16 was incompatible with life.
“I was utterly devastated,” she said. “I made it out of my doctor’s office but completely broke down in the car.”
But ACOG does not recommend the trisomy 16 screening, saying “its accuracy with regard to detection and the false-positive rate is not established.” Julia wasn’t informed of this, she said, and she’s not sure if her health care providers knew it either.
The lab report recommended diagnostic testing to confirm the results, but time was short. She had her amniocentesis at 17 weeks. It could take up to 4 more weeks to receive results.
That would be too late for a legal abortion in Mississippi. So she made an appointment for one in Florida, where the cutoff was 24 weeks. (It’s now 15 weeks in Florida, while Mississippi went from 15 weeks for legal procedures to a ban on nearly all abortions.)
The wait was excruciating. Julia was driving twice a week to New Orleans for specialized care. With work and child care, it was too hard. She quit the teaching job she loved.
One winter night, she felt the fetus move for the first time – ordinarily a milestone, but now, facing a fatal prognosis, she didn’t want to get attached. “It had me so messed up,” she said.
On the way to the amniocentesis, Julia and her husband chose a name. Drawing from a language conjured by J.R.R. Tolkien in the fantasy novels they love, it means “hope.”
More than halfway through her pregnancy, the amnio results arrived. The prenatal screening had given a false positive. The baby would be fine. In May, Julia gave birth to a healthy daughter.
Julia and her husband are upset about the needless anguish brought on by the screening. “They like to have it both ways,” said Julia’s husband. “They say they are 99% accurate, but when there’s a false positive, they say, ‘Well, we’re not diagnostic.’ ”
Believing the prenatal screening was likely accurate, they had seriously considered canceling the amniocentesis, saving their limited funds for an abortion in Florida, hundreds of miles away.
Their dilemma points to a longtime concern: ending pregnancies based on false positives. The FDA cited it as a risk as far back as 2015. Now, those with positive results are facing an even tighter time crunch. They must consider whether waiting for a definitive test, and possibly traveling to another state for an abortion later in pregnancy, is worth it.
In their promotional material, some companies not only sidestep the variability of the standard tests, they fail to distinguish them from the least reliable ones – those for exceptionally rare conditions. They tout the extra screenings as “premium,” “plus,” or “advanced” options.
“Going to greater lengths for the answers that matter most,” says a brochure aimed at health care providers from test-maker Illumina. Elsewhere it states that the “expanded” panel of tests provides “confident results” and “the additional insights you need.”
But the companies themselves know the accuracy of some of their tests has yet to be established in the research. Natera acknowledged in a recent shareholder report that many insurers won’t pay for screenings for missing chromosomal fragments, known as microdeletions, in part because there isn’t enough published data behind them.
The company, responding to ProPublica, stressed the quality of the data over the quantity, saying the research so far has been favorable. “Natera’s microdeletion testing was thoroughly validated with results published in peer-reviewed publications,” it said in a statement.
Natera pointed to a recent study that looked at DiGeorge syndrome, one of several chromosomal anomalies it checks for with its microdeletion screenings. Researchers found the positive predictive value (PPV) of the test to be 52.6%, meaning that nearly half of positive results are false positives. (For many patients, PPVs for more common conditions can exceed 90%.)
Natera said the performance of the diGeorge syndrome test “is excellent and not considered a low PPV,” because of the condition being extremely rare.
Companies also play up the danger of diagnostic tests like amnio. They “can cause miscarriages,” warns the marketing from Labcorp, which made Amanda’s screening, while its test “does not cause miscarriages.” But medical experts emphasize that diagnostic tests, such as amniocentesis, are more accurate and, in fact, carry little risk to the pregnancy.
Labcorp, in a statement, said the company “acknowledges the well-documented risk associated with amniocentesis and CVS in our literature. It is the patient’s prerogative to decide which risks they are willing or unwilling to take.”
Marketing claims also sometimes skate over the nuances in the guidance from the leading professional societies. On a webpage targeting health care providers, for example, a Labcorp chart said groups such as ACOG “endorse and/or recognize” prenatal screenings as an option for all pregnancies. But the chart listed screenings ACOG does not recommend, including trisomy 16.
When asked about it, Labcorp said in a statement that ACOG “endorses NIPS for all pregnancies.” In fact, the guidance is not so sweeping. It says only that the basic bundle of tests should be offered to all, alongside other screening options. It explicitly advises providers to not offer patients the extra tests.
Soon after ProPublica’s query, the Labcorp webpage was updated to remove any mention of the professional societies.
Patients say they often don’t know where to turn for informed and unbiased information. That’s why the r/NIPT Reddit page became such a robust community. Facing difficult news, Julia turned to it for counsel from other prospective parents. Kristina in Texas found the same community. Amanda, too.
‘The margin of error is a human life’
On a warm and cloudy day this past June, on what would have been their daughter’s first birthday, Amanda and her husband visited her grave. They brought a unicorn balloon and vanilla cake, which they ate nearby on the grass. Her husband read a poem.
To them, their baby had been perfect. She had fingers and toes. A thatch of dark hair. While in intensive care, peering up at her parents, she grabbed for her mother’s hand.
Had her condition been known, they would’ve spared her futile medical interventions, as doctors tried to save her life. Their family priest would have been able to baptize her. As it was, they never got to hold their child while she was alive.
These days, when Amanda and her husband say grace before dinner, they give thanks for the 28 hours of their daughter’s life.
They’re also thinking about making comfort boxes the hospital could give to other parents who lose a child. It might include books on grief. Softer tissues. Something that says, as Amanda puts it, “This is to help you get through.”
Amid their grief, they had a prayer answered: Amanda is pregnant again.
It’s frightening to go through this again. She barely sleeps the night before visiting the doctor. It feels like she never stopped being pregnant. It will feel that way, she said, until she brings a baby home – one who lives past the first 2 nights.
Amanda planned to get another genetic screening test. At first she couldn’t bear it, wasn’t sure she could trust it. “The margin of error is a human life,” Amanda said.
The 10-week appointment passed. Then the 12-week appointment. After her 13th week, she took the plunge. The test she was given was from Labcorp.
Around this time, more than a year after Amanda had desperately tried to alert the company about what had happened to her and her first baby, she finally heard back. Labcorp’s vice president of genetic counseling and services reached out – after ProPublica contacted the company and shared Amanda’s story.
The executive would only speak to Amanda without a reporter present.
Amanda said that during the call, the executive told her that prenatal genetic tests are evolving, and doctors should be clear about what the screenings can and cannot do. By the end of the conversation, the executive offered Amanda her cell number.
Amanda said she appreciated the call. “I feel better. I feel like I got something.”
The same day, her screening results came back. They were negative.
This story was originally published on ProPublica. ProPublica is a nonprofit newsroom that investigates abuses of power. Sign up to receive their biggest stories as soon as they’re published.
Amanda wanted to warn someone. In June 2021, her daughter – the one she and her husband had tried for 3 years to conceive – had died after only 28 hours. With an underdeveloped nose, she had battled for every breath.
Nobody knew why. Later, an autopsy report revealed their daughter had an extra 13th chromosome. The condition is nearly always fatal.
“But didn’t we test for that?” Amanda recalled asking herself. “That was kind of where the light bulb clicked.”
Through her doctor, Amanda had gotten a popular prenatal screening from a lab company. It had come back “negative.”
For three major conditions, including the one her baby had, the report gave the impression of near certainty. The likelihood that she would be born without them was “greater than 99%.”
As she recovered from a cesarean section, Amanda found herself facing a long maternity leave without a child. She shut the door to the empty nursery and began spending what seemed like endless hours of that hazy summer learning about the test.
It’s a simple blood draw designed to check for an array of genetic anomalies. But Amanda, a science researcher, read academic articles showing there was a higher risk of inaccurate results than she had realized. (She asked to be identified by only her first name to protect her privacy.)
On Reddit, she found other women reporting problems with the tests, too. She thought Labcorp, the company that made her test, would want to know about the screening that failed her. Maybe by alerting them, she could help other families. Maybe it would help her understand what happened.
“I was trying to gain answers,” said Amanda, now 32. She tried calling Labcorp’s customer service line, but she said she was passed along from one person to another. “It was just a circle,” she remembered.
She phoned Labcorp a second time. The call ended when an employee hung up on her.
Amanda was baffled. Why didn’t the company seem interested in her experience? Why, she wondered, wouldn’t it want to collect this data? Why wasn’t there someone who could answer her questions about how often this happens, and why?
If she had taken any number of other common commercial tests – including certain tests for COVID-19 or, say, pregnancy – the company would have been required to inform the U.S. Food and Drug Administration about reports of so-called adverse events.
But the test Amanda had falls into a regulatory void. No federal agency checks to make sure these prenatal screenings work the way they claim before they’re sold to health care providers. The FDA doesn’t ensure that marketing claims are backed up by evidence before screenings reach patients. And companies aren’t required to publicly report instances of when the tests get it wrong – sometimes catastrophically.
The broader lab testing industry and its lobbyists have successfully fought for years to keep it this way, cowing regulators into staying on the sidelines.
Worried about a growing variety of tests escaping scrutiny, the FDA was on the cusp of stepping in 6 years ago. But then it backed down.
Peter Lurie, then a top agency official, was at the meetings where the FDA tabled its plans. Not pushing harder, he told ProPublica, “remains one of my greatest regrets.”
The risk of false positives from prenatal screenings, in particular, has been known for years.
In 2014, the New England Center for Investigative Reporting detailed how some companies gave a misleading impression of the precision of the prenatal screenings. Women often didn’t understand they needed diagnostic testing to confirm the results. Some had gotten abortions based on false positive results, the story said. Earlier this year, the New York Times reported how companies sell optional extra screenings that are “usually wrong” when they predict a disorder.
Despite these stories and calls for reform by patient advocates, the government has done little to improve oversight of prenatal screenings. ProPublica set out to examine the forces that led to this inertia and left patients like Amanda feeling misled. Interviews with more than three dozen women revealed ongoing confusion about the screenings – and anger when their reliability proved to be overblown.
“This is a Wild West scenario where everybody is on their own,” said Lawrence Gostin, a Georgetown University, Washington, law professor specializing in bioethics.
The stakes for families are increasing. Upward of half of all pregnant people now receive one of these prenatal screenings. And with many states banning abortions or limiting them to early in pregnancies, the need for fast, accurate information has become more urgent.
The FDA itself acknowledges the problem. In correspondence with ProPublica, a spokesperson cited an “outdated policy” regarding the lack of vetting of many lab tests that the agency has “spent the better part of the last 2 decades trying to address.”
The screening industry, meanwhile, continues to expand, proving lucrative for those who lead it. The chief executive of Natera, which claims about 40% of the market share of prenatal screenings, received a $23 million compensation package last year, the highest of any executive at a publicly traded lab company.
Testing companies told ProPublica that, even without the FDA, there is significant oversight. Labs must abide by state regulations, and another federal agency, the Centers for Medicare and Medicaid Services, is charged with monitoring quality standards. It does not, however, check whether the tests the labs perform are clinically valid.
Companies also said the screenings offer important guidance to expectant families. Echoing others in the field, Labcorp said in a statement that the screenings, when used properly, “provide vital information about the presence of increased risk, but do not provide a definitive diagnosis.” (It declined to discuss the specifics of Amanda’s experience.)
Natera pointed out that its materials tell patients that “this test does not make a final diagnosis.” It reports results as “high-risk” or “low-risk,” not positive or negative.
Companies have stressed that, ultimately, it’s the responsibility of health care providers, who order the tests, to inform patients about the limits of screenings.
For all that, the statistical nuances of the test aren’t easy to parse for patients and even some doctors and nurses. For example, the test for trisomy 13, which doomed Amanda’s baby, is actually less likely to correctly predict the condition than other tests in the standard bundle of screenings offered to every patient.
When ProPublica asked readers to share their experiences with noninvasive prenatal screening tests, often referred to as NIPTs or NIPS, more than a thousand responded. Many said the tests had given them peace of mind. Some said they had provided an early warning about problems.
But others had more questions than answers. None more so than Amanda.
“What are these tests?” she wondered. “And how did mine end up in the margin of error?”
‘They started using it on humans, and then they went back and said: “Was our test accurate?” ’
Scientists have long tried to find ways to help parents and doctors understand what’s happening inside the womb. Amniocentesis was first used to reveal genetic anomalies in the late 1960s. But it didn’t become more popular until it began to be paired with ultrasound to precisely guide the procedure.
In the 1980s, doctors started using chorionic villus sampling, or CVS, an analysis of placental tissue that offers a diagnosis earlier in pregnancy. But, like amniocentesis, it is an invasive test that involves some risk to the fetus, though experts say it’s exceptionally low.
A breakthrough came in the late 1990s, when a scientist recognized that free-floating placental DNA could be detected in the mother’s blood. This meant that the fetus’s chromosomes could be examined by collecting a blood sample as soon as 9 weeks into pregnancy. This also provides an early opportunity to learn the likely fetal sex – a particularly popular feature.
Champions of the new science celebrated the arrival of a simple technique for patients that was particularly precise, at least for some conditions. Many favored it over other noninvasive options. But the industry that developed around NIPT has been marred by controversy from the beginning.
Dr. Ronald Wapner, director of reproductive genetics at Columbia University, described that time as “very chaotic.”
The tests had not been appropriately evaluated in clinical practice, said Dr. Wapner, whose research has sometimes been funded by testing companies. Because of this, he said, the industry “had very incomplete data on how well it worked.”
That didn’t stop the excitement. The chief executive of Sequenom, a biotechnology company that planned to release the first NIPT for Down syndrome, championed the company as the “Google of Molecular Diagnostics.” Its stock price soared.
Then, about 2 months before an expected launch in 2009, Sequenom killed the plan. The company’s research director, it turned out, had manipulated testing data and made misleading claims about how well the screening worked.
The U.S. Securities and Exchange Commission and Federal Bureau of Investigation opened investigations. Top executives were fired, and the research director pleaded guilty to conspiracy to commit securities fraud. Sequenom still managed to commercialize the test in 2011. (Labcorp, which later acquired Sequenom, said it uses a different kind of test.)
Other companies soon debuted their own tests. Still, there was little data on their clinical performance, researchers said.
As Megan Allyse, a bioethicist at the Mayo Clinic, put it, the companies “launched the test, they started using it on humans, and then they went back and said, ‘Was our test accurate?’ ” She also questioned the lack of attention to the ethics of how tests are presented to patients.
Despite missteps by the industry, the FDA didn’t scrutinize the screenings because they were considered lab-developed tests, which means they are created by the same laboratory that conducts them.
In 1976, Congress revamped oversight over medical devices. Since then, the FDA has effectively exempted such “home-brew” tests from key regulatory requirements. The idea was that when, say, a hospital lab wanted to create a simple test for its own patients, it was spared the time, money, and hassle of getting approval from Washington bureaucrats.
Today, lab-developed tests are vastly more numerous and complex. Because they aren’t registered with the federal government, nobody knows how many exist.
The distinction between tests the FDA actively regulates and those they don’t can seem nonsensical. It isn’t based on the complexity of the tests, or how people use them. It’s simply a matter of where the test is made.
The prenatal genetic screening industry took off almost immediately, powered by an army of aggressive sales representatives.
“At the very beginning, obstetricians in practice were being just completely inundated with visits from the sales reps,” said Dr. John Williams, director of reproductive health at Cedars-Sinai Medical Center in Los Angeles. The push left many ob.gyns. and patients thinking the screenings were accurate enough to substitute for diagnostic tests, such as amniocentesis or CVS.
In some cases, sales tactics escalated into lawbreaking.
Former Sequenom executives who exited during the fraud scandal created a new company that became Progenity, which also offered prenatal screening. Shortly after the company went public in 2020, it finalized a $49 million settlement with federal and state governments, where it admitted to falsifying insurance claims and giving kickbacks to physicians and their staff. According to a legal filing, one sales rep spent $65,658 on meals and alcohol for physicians in 1 year.
Now called Biora Therapeutics, the company said in a statement it no longer does any laboratory testing, including prenatal screenings.
Industry revenue continues to grow, but some testing companies are still fighting to make a profit, and competition to survive is fierce. “There’s a multibillion-dollar market, and they all want a piece of it,” said a former Progenity sales rep who quit in disgust after 5 months in 2016.
The rep, who requested anonymity because she continues to work in the field, said she still sees competitors from NIPT companies visiting medical practices “every week, buying breakfast or dinner, or taking them out for happy hour.”
Over time, companies pointed to new peer-reviewed studies, research the industry itself funded, to earn the confidence of doctors and other stakeholders. They showed that two tests – for Down syndrome and trisomy 18 – often performed better than other screening methods.
This research was valid, said Dr. Mary Norton, a perinatologist and clinical geneticist at the University of California, San Francisco, Medical Center’s prenatal diagnostic center. Considered a leading researcher in the field, she was an author of many of these key industry-funded studies.
But, she said, when research findings were presented publicly, the companies sometimes downplayed “inconvenient truths,” such as the exclusion of inconclusive results from accuracy estimates. Crucial caveats were also glossed over by some companies when they translated research into promotional copy aimed at health care providers and patients. Those materials didn’t always mention the many factors that can limit the performance of the screenings, including high body weight, the rarity of the condition tested, and younger maternal age.
Testing companies said they try to help patients understand the screenings through online resources and other materials. Some offer genetic counseling services.
The younger a person is, the lower the test’s positive predictive value – that is, the probability that a positive screening result will turn out to be correct – will be for some conditions. For instance, because Down syndrome is less prevalent in younger people’s pregnancies, a positive screening test is more likely to be a false positive for them.
Kristina was 30 years old in 2016, when her Progenity test came back positive for Down syndrome. She and her husband, who asked not to be fully named to protect their privacy, said they didn’t plan to carry a pregnancy with this condition to term.
But waiting to get an amniocentesis, and then waiting for the results, took 5 agonizing weeks, she said. It showed her son did not have Down syndrome.
Kristina, who lives in Texas, is still troubled by what she describes as a traumatic experience.
“I researched both late-term abortion providers and cemeteries,” she said. They even picked out a burial place, near their house.
She bought a blue baby blanket she intended to bury the baby’s tiny body in. She still has it. Her son, now 5, sleeps with it every night.
‘I can’t believe I didn’t say more’
As lab-developed tests became a bigger business, moving well past their home-brew origins, regulators looked for a way to assert oversight. In 2014, after years of study and debate, the time seemed right.
The FDA released plans proposing to regulate the tests, prioritizing those used to make major medical decisions. The agency has pointed to NIPTs as 1 of 20 concerning tests.
But, over the next 2 years, a coalition of power players urged the FDA to back off. Professional associations issued statements and hosted webinars devoted to the issue. Some created polished websites featuring sample letters to send to Washington.
Academic medical centers and pathology departments joined the fight, too. Scientists from 23 of them put it bluntly in a letter to the Office of Management and Budget: “FDA regulation of LDTs would be contrary to the public health,” it said, using a common acronym for the tests.
“Critical testing would be unavailable in the ‘lag time’ between development of new tests and FDA authorizing them,” the authors of the letter wrote, “and subsequent improvements on existing tests would slow significantly under the rigid, inflexible, and duplicative FDA regulatory scheme.”
This could delay essential care for patients. What’s more, opponents argued, existing lab reviews by the Centers for Medicare and Medicaid Services are sufficiently rigorous. Some have suggested modernizing the CMS review process to improve oversight.
An FDA spokesperson told ProPublica that the agency encountered “continued, negative feedback,” including a 25-page paper written by two legal heavyweights hired by the American Clinical Laboratory Association: Paul Clement, President George W. Bush’s former solicitor general, and Laurence Tribe, law professor at Harvard University.
Mr. Clement has reportedly commanded rates of $1,350 per hour. He and Mr. Tribe did not respond to ProPublica’s queries about their work.
Their brief argued that the FDA “lacked legal authority” to regulate lab-developed tests because they are properly seen as the practice of medicine: a service, rather than a product.
However, as lawyers representing the American Association of Bioanalysts countered, the FDA would vet tests before they reach the market, not control how doctors use them. The government proposal, they wrote, is “similar to imposing requirements to screen blood or label drugs.”
After the election of President Donald Trump, but before he took office, a handful of FDA officials discussed their battered proposal. It had represented a breakthrough in the decades of excruciating back-and-forth with industry. But now, with an incoming administration bent on deregulation, their efforts seemed futile.
The regulators feared anything they enacted would be undone by Congress – and, under the Congressional Review Act, they might not be able to reissue anything “substantially similar” in the future. So the FDA published a white paper instead, summarizing the issue “for further public discussion.”
After the meeting where officials made this call, Mr. Lurie, then the FDA’s associate commissioner, recalled a colleague approaching him: “I can’t believe you didn’t say more.”
“And I was like, ‘Yeah, actually, I can’t believe I didn’t say more either,’ ” Mr. Lurie later told ProPublica. (After leaving the agency, Mr. Lurie went on to lead the Center for Science in the Public Interest, a consumer advocacy nonprofit, which has pushed the FDA to finally assert oversight over lab-developed tests.)
Nancy Stade, an attorney and senior policy official who left the FDA in 2015, said the agency often moves slowly as it seeks to get buy-in from industry and professional groups. In her work on regulatory policy, she saw it happen with lab-developed tests.
The agency is “always testing the waters,” she said, “and always coming out with something a little bit softer.”
In 2020, the influential American College of Obstetricians and Gynecologists and Society for Maternal-Fetal Medicine, representing doctors who handle pregnancies, gave the screening industry another huge boost.
In a bulletin updating their advice on the tests, the two groups described growing research on the performance of some of the standard tests and said people have the right to information about their pregnancies, so the tests should be offered to all patients. Previously, they recommended this only for those facing higher risk of genetic anomalies.
The bulletin said the coauthors had disclosed no conflicts of interest. But two of the four coauthors, including Mary Norton, had disclosed in prior publications that test-makers had provided funding for their research. A company had provided a third coauthor with laboratory services needed to run tests, according to that researcher, a connection she also disclosed in past papers.
ACOG, in a statement to ProPublica, said the organization “identified no conflicts because research funding is provided to academic institutions with institutional review boards, not to individual investigators.” Two of the three researchers responded to questions from ProPublica and said they maintained independence over their work.
One test-maker, Illumina, celebrated the ACOG guidance in a tweet, saying it “recognizes the superior performance of #NIPT and the benefit it provides expectant families.” Natera’s share prices doubled in 5 months. UnitedHealthcare, the nation’s largest private insurer and long a target of industry lobbying, told ProPublica it changed its stance to cover screenings for all patients, regardless of risk, because of the recommendation.
In a recent shareholder report, Natera stated that prenatal genetic and carrier screenings “represent the significant majority of our revenues,” which totaled $625.5 million in 2021. The company expects more growth to come.
“The NIPT market is still very underpenetrated, compared to the 4 to 5 million pregnancies in the U.S.,” Natera’s chief executive said on a 2021 earnings call, “so there’s a long way to go.”
But even Dr. Norton, who coauthored the ACOG recommendation and favors NIPTs for patients 40 and over, has concerns about screenings becoming widespread among those who are younger. In most cases, she prefers other screening methods that catch the nongenetic problems younger moms are more likely to face. Negative results from an NIPT, she said, can be “falsely reassuring.”
In the years after the FDA set aside its regulatory proposal, the agency has assisted members of Congress on a proposed legislative solution. That effort, dubbed the VALID Act, aims to end any debate over the agency’s authority over lab-developed tests. An FDA press officer said the legislation would ensure the prenatal screening tests and others are “accurate and reliable.”
But, as in the past, intense lobbying followed the proposal. The VALID Act was a rider to a funding reauthorization bill, but in September the House and Senate agreed to remove it. Advocates now hope to attach it to proposed end-of-year legislation.
Meanwhile, earlier this year, 4 months after the New York Times story on the usefulness of some screenings, the FDA took a step toward more public awareness about prenatal genetic screening. It issued its first safety communication on them, noting the potential for false results.
It cautioned patients about making “critical health care decisions based on results from these screening tests alone.”
Cara Tenenbaum, a former FDA policy advisor, was pleased to see the statement. Still, she said, it was long overdue.
“This has been known – known, or should have been known – for 10 years,” she said.
‘It had me so messed up’
With the demise of Roe v. Wade, restrictive and ever-changing abortion laws can pressure people to act quickly with limited information, heightening the stakes of prenatal screening.
Julia, a mom from Mississippi’s Gulf Coast, knows what it’s like to face harrowing consequences while navigating state-imposed time limits – and doing so with little guidance. Last fall, she was pregnant with her fourth child when, she said, a nurse practitioner suggested prenatal genetic screening.
At 33, Julia had no risk factors. Her previous pregnancies hadn’t been screened with an NIPT. But with three sons and 18 nephews, she and her husband were curious about the baby’s sex. And the screening seemed like it had no downside.
Julia figured it would only be offered if it was reliable, so her nurse practitioner ordered her both the basic bundle of screenings and the extra tests. (The medical practice didn’t respond to interview requests. Julia is a family nickname that’s used here to protect her privacy.)
The screenings showed the baby was a girl – but the extra tests also detected trisomy 16, a condition caused by an extra chromosome that is so rare, the nurse didn’t know what it was, Julia recalled.
The nurse borrowed Julia’s phone, using it to search online and read aloud what she found. Julia was stunned to hear trisomy 16 was incompatible with life.
“I was utterly devastated,” she said. “I made it out of my doctor’s office but completely broke down in the car.”
But ACOG does not recommend the trisomy 16 screening, saying “its accuracy with regard to detection and the false-positive rate is not established.” Julia wasn’t informed of this, she said, and she’s not sure if her health care providers knew it either.
The lab report recommended diagnostic testing to confirm the results, but time was short. She had her amniocentesis at 17 weeks. It could take up to 4 more weeks to receive results.
That would be too late for a legal abortion in Mississippi. So she made an appointment for one in Florida, where the cutoff was 24 weeks. (It’s now 15 weeks in Florida, while Mississippi went from 15 weeks for legal procedures to a ban on nearly all abortions.)
The wait was excruciating. Julia was driving twice a week to New Orleans for specialized care. With work and child care, it was too hard. She quit the teaching job she loved.
One winter night, she felt the fetus move for the first time – ordinarily a milestone, but now, facing a fatal prognosis, she didn’t want to get attached. “It had me so messed up,” she said.
On the way to the amniocentesis, Julia and her husband chose a name. Drawing from a language conjured by J.R.R. Tolkien in the fantasy novels they love, it means “hope.”
More than halfway through her pregnancy, the amnio results arrived. The prenatal screening had given a false positive. The baby would be fine. In May, Julia gave birth to a healthy daughter.
Julia and her husband are upset about the needless anguish brought on by the screening. “They like to have it both ways,” said Julia’s husband. “They say they are 99% accurate, but when there’s a false positive, they say, ‘Well, we’re not diagnostic.’ ”
Believing the prenatal screening was likely accurate, they had seriously considered canceling the amniocentesis, saving their limited funds for an abortion in Florida, hundreds of miles away.
Their dilemma points to a longtime concern: ending pregnancies based on false positives. The FDA cited it as a risk as far back as 2015. Now, those with positive results are facing an even tighter time crunch. They must consider whether waiting for a definitive test, and possibly traveling to another state for an abortion later in pregnancy, is worth it.
In their promotional material, some companies not only sidestep the variability of the standard tests, they fail to distinguish them from the least reliable ones – those for exceptionally rare conditions. They tout the extra screenings as “premium,” “plus,” or “advanced” options.
“Going to greater lengths for the answers that matter most,” says a brochure aimed at health care providers from test-maker Illumina. Elsewhere it states that the “expanded” panel of tests provides “confident results” and “the additional insights you need.”
But the companies themselves know the accuracy of some of their tests has yet to be established in the research. Natera acknowledged in a recent shareholder report that many insurers won’t pay for screenings for missing chromosomal fragments, known as microdeletions, in part because there isn’t enough published data behind them.
The company, responding to ProPublica, stressed the quality of the data over the quantity, saying the research so far has been favorable. “Natera’s microdeletion testing was thoroughly validated with results published in peer-reviewed publications,” it said in a statement.
Natera pointed to a recent study that looked at DiGeorge syndrome, one of several chromosomal anomalies it checks for with its microdeletion screenings. Researchers found the positive predictive value (PPV) of the test to be 52.6%, meaning that nearly half of positive results are false positives. (For many patients, PPVs for more common conditions can exceed 90%.)
Natera said the performance of the diGeorge syndrome test “is excellent and not considered a low PPV,” because of the condition being extremely rare.
Companies also play up the danger of diagnostic tests like amnio. They “can cause miscarriages,” warns the marketing from Labcorp, which made Amanda’s screening, while its test “does not cause miscarriages.” But medical experts emphasize that diagnostic tests, such as amniocentesis, are more accurate and, in fact, carry little risk to the pregnancy.
Labcorp, in a statement, said the company “acknowledges the well-documented risk associated with amniocentesis and CVS in our literature. It is the patient’s prerogative to decide which risks they are willing or unwilling to take.”
Marketing claims also sometimes skate over the nuances in the guidance from the leading professional societies. On a webpage targeting health care providers, for example, a Labcorp chart said groups such as ACOG “endorse and/or recognize” prenatal screenings as an option for all pregnancies. But the chart listed screenings ACOG does not recommend, including trisomy 16.
When asked about it, Labcorp said in a statement that ACOG “endorses NIPS for all pregnancies.” In fact, the guidance is not so sweeping. It says only that the basic bundle of tests should be offered to all, alongside other screening options. It explicitly advises providers to not offer patients the extra tests.
Soon after ProPublica’s query, the Labcorp webpage was updated to remove any mention of the professional societies.
Patients say they often don’t know where to turn for informed and unbiased information. That’s why the r/NIPT Reddit page became such a robust community. Facing difficult news, Julia turned to it for counsel from other prospective parents. Kristina in Texas found the same community. Amanda, too.
‘The margin of error is a human life’
On a warm and cloudy day this past June, on what would have been their daughter’s first birthday, Amanda and her husband visited her grave. They brought a unicorn balloon and vanilla cake, which they ate nearby on the grass. Her husband read a poem.
To them, their baby had been perfect. She had fingers and toes. A thatch of dark hair. While in intensive care, peering up at her parents, she grabbed for her mother’s hand.
Had her condition been known, they would’ve spared her futile medical interventions, as doctors tried to save her life. Their family priest would have been able to baptize her. As it was, they never got to hold their child while she was alive.
These days, when Amanda and her husband say grace before dinner, they give thanks for the 28 hours of their daughter’s life.
They’re also thinking about making comfort boxes the hospital could give to other parents who lose a child. It might include books on grief. Softer tissues. Something that says, as Amanda puts it, “This is to help you get through.”
Amid their grief, they had a prayer answered: Amanda is pregnant again.
It’s frightening to go through this again. She barely sleeps the night before visiting the doctor. It feels like she never stopped being pregnant. It will feel that way, she said, until she brings a baby home – one who lives past the first 2 nights.
Amanda planned to get another genetic screening test. At first she couldn’t bear it, wasn’t sure she could trust it. “The margin of error is a human life,” Amanda said.
The 10-week appointment passed. Then the 12-week appointment. After her 13th week, she took the plunge. The test she was given was from Labcorp.
Around this time, more than a year after Amanda had desperately tried to alert the company about what had happened to her and her first baby, she finally heard back. Labcorp’s vice president of genetic counseling and services reached out – after ProPublica contacted the company and shared Amanda’s story.
The executive would only speak to Amanda without a reporter present.
Amanda said that during the call, the executive told her that prenatal genetic tests are evolving, and doctors should be clear about what the screenings can and cannot do. By the end of the conversation, the executive offered Amanda her cell number.
Amanda said she appreciated the call. “I feel better. I feel like I got something.”
The same day, her screening results came back. They were negative.
This story was originally published on ProPublica. ProPublica is a nonprofit newsroom that investigates abuses of power. Sign up to receive their biggest stories as soon as they’re published.
More evidence in utero exposure to antiseizure meds safe for children’s cognition
NASHVILLE, TENN. – There is no negative impact of in utero exposure to antiseizure medications on children’s creativity, new research shows.
The results of this study, along with other research, suggest the risk for cognitive problems “is fairly low” overall for children of women with epilepsy taking lamotrigine or levetiracetam, study investigator, Kimford J. Meador, MD, professor, department of neurology & neurological sciences, Stanford (Calif.) University School of Medicine, told this news organization.
“This is another encouraging piece that’s showing these new drugs are safe with regard to cognition.”
The findings were presented at the annual meeting of the American Epilepsy Society.
Capturing creativity
Fetal exposure to antiseizure medications can produce adverse neurodevelopmental effects. These are typically assessed using measures such as general intelligence, verbal/nonverbal abilities, or additional educational needs.
However, these measures don’t capture creativity, which “is related to intelligence but not completely,” said Dr. Meador. “I have seen wonderful examples of creativity in people who have a lot of cognitive impairment.”
He referred to one of his patients with epilepsy who is “spectacularly good” at painting with watercolors, even though she has significant cognitive impairment.
The new analysis is part of the MONEAD study, a prospective, observational multicenter study examining pregnancy outcomes for both mother and child. It included pregnant women who were enrolled at under 20 weeks’ gestational age.
The women with epilepsy in the study were primarily on monotherapy (73%), and of these, 82% were on lamotrigine or levetiracetam. About 22% were on polytherapy, of which 42% were on dual therapy with lamotrigine and levetiracetam.
Fluency, originality
Researchers assessed the children of these women at age 4½ years using the Torrance Test of Creative Thinking-Figural (TTCT-F). This is a standardized assessment of creative thinking with index scores measuring such things as fluency, originality, abstractness, and elaboration.
Dr. Meador noted the research team used a shorter version of the test battery “so as to not wear out the families and kids.”
During the test, children were given lines of different shapes and asked to draw a picture using these lines. Dr. Meador pointed out the drawings ranged from quite basic to more intricate.
One child cleverly turned a few squiggly lines into a car. “I can look at this and say this kid’s going to do very well,” said Dr. Meador.
Investigators compared scores between 241 children of women with epilepsy (WWE) and 65 children of healthy women (HW). They adjusted for the mother’s IQ, education level, age at enrollment, gestation age at enrollment, post-birth average anxiety score, and the child’s ethnicity and sex.
Investigators found the mean TTCT-F scores did not differ significantly between the two groups: adjusted least squares mean of 89.5 (95% confidence interval, 86.7-92.3) for children of WWE, compared with adjusted least square mean of 92.0 (95% CI, 86.4-97.6) for children of HW.
Balancing act
The researchers haven’t looked at a dose effect in this current study, but Dr. Meador said it’s always “a balancing act” between giving enough of the drug to keep mothers from seizing, which affect both the mother and fetus, and giving as low a dose as possible to protect the fetus.
In addition, as medication levels change during pregnancy, he said he recommends that drug levels are monitored monthly so that medication can be adjusted as necessary.
Looking at what factors might predict creativity scores, researchers found children did less well creatively if their mother didn’t have a college degree (estimate –9.5; 95% CI, –17.9 to –1.2; P = .025).
“It looks like being in a home where the mother has had more education is going to have an impact on the kid’s thinking and creativity,” said Dr. Meador.
These new findings are consistent with a lack of differences in other cognitive abilities that Dr. Meador and his team found when the children were younger.
“At age 3, we did not find an overall difference in cognitive and verbal abilities and intelligence between the children of mothers with epilepsy and those of healthy women,” he said.
The researchers aim to assess cognitive and behavioral outcomes in these children when they are 6 years old.
Helpful information
Commenting on the findings, Stéphane Auvin, MD, PhD, chair of the department of pediatric neurology at the University of Paris, who co-moderated a platform session featuring the research, said the study “is an interesting measure of the impact of being exposed to antiseizure medications.”
Creativity is “complex,” he said. “It’s not only cognition; it could be things like behavior and impulsivity.”
The new information is “very helpful.” Focusing on something broader than just IQ “gives you a better picture of what’s going on.”
The study received funding from NIH, NINDS, and NICH. Dr. Meador has received grants from NIH/NINDS, NIH/NICHD, Veterans Administration, and Eisai. He has been a consultant for Epilepsy Consortium, Novartis, Supernus, Upsher Smith Labs, and UCB Pharma. Dr. Auvin reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
NASHVILLE, TENN. – There is no negative impact of in utero exposure to antiseizure medications on children’s creativity, new research shows.
The results of this study, along with other research, suggest the risk for cognitive problems “is fairly low” overall for children of women with epilepsy taking lamotrigine or levetiracetam, study investigator, Kimford J. Meador, MD, professor, department of neurology & neurological sciences, Stanford (Calif.) University School of Medicine, told this news organization.
“This is another encouraging piece that’s showing these new drugs are safe with regard to cognition.”
The findings were presented at the annual meeting of the American Epilepsy Society.
Capturing creativity
Fetal exposure to antiseizure medications can produce adverse neurodevelopmental effects. These are typically assessed using measures such as general intelligence, verbal/nonverbal abilities, or additional educational needs.
However, these measures don’t capture creativity, which “is related to intelligence but not completely,” said Dr. Meador. “I have seen wonderful examples of creativity in people who have a lot of cognitive impairment.”
He referred to one of his patients with epilepsy who is “spectacularly good” at painting with watercolors, even though she has significant cognitive impairment.
The new analysis is part of the MONEAD study, a prospective, observational multicenter study examining pregnancy outcomes for both mother and child. It included pregnant women who were enrolled at under 20 weeks’ gestational age.
The women with epilepsy in the study were primarily on monotherapy (73%), and of these, 82% were on lamotrigine or levetiracetam. About 22% were on polytherapy, of which 42% were on dual therapy with lamotrigine and levetiracetam.
Fluency, originality
Researchers assessed the children of these women at age 4½ years using the Torrance Test of Creative Thinking-Figural (TTCT-F). This is a standardized assessment of creative thinking with index scores measuring such things as fluency, originality, abstractness, and elaboration.
Dr. Meador noted the research team used a shorter version of the test battery “so as to not wear out the families and kids.”
During the test, children were given lines of different shapes and asked to draw a picture using these lines. Dr. Meador pointed out the drawings ranged from quite basic to more intricate.
One child cleverly turned a few squiggly lines into a car. “I can look at this and say this kid’s going to do very well,” said Dr. Meador.
Investigators compared scores between 241 children of women with epilepsy (WWE) and 65 children of healthy women (HW). They adjusted for the mother’s IQ, education level, age at enrollment, gestation age at enrollment, post-birth average anxiety score, and the child’s ethnicity and sex.
Investigators found the mean TTCT-F scores did not differ significantly between the two groups: adjusted least squares mean of 89.5 (95% confidence interval, 86.7-92.3) for children of WWE, compared with adjusted least square mean of 92.0 (95% CI, 86.4-97.6) for children of HW.
Balancing act
The researchers haven’t looked at a dose effect in this current study, but Dr. Meador said it’s always “a balancing act” between giving enough of the drug to keep mothers from seizing, which affect both the mother and fetus, and giving as low a dose as possible to protect the fetus.
In addition, as medication levels change during pregnancy, he said he recommends that drug levels are monitored monthly so that medication can be adjusted as necessary.
Looking at what factors might predict creativity scores, researchers found children did less well creatively if their mother didn’t have a college degree (estimate –9.5; 95% CI, –17.9 to –1.2; P = .025).
“It looks like being in a home where the mother has had more education is going to have an impact on the kid’s thinking and creativity,” said Dr. Meador.
These new findings are consistent with a lack of differences in other cognitive abilities that Dr. Meador and his team found when the children were younger.
“At age 3, we did not find an overall difference in cognitive and verbal abilities and intelligence between the children of mothers with epilepsy and those of healthy women,” he said.
The researchers aim to assess cognitive and behavioral outcomes in these children when they are 6 years old.
Helpful information
Commenting on the findings, Stéphane Auvin, MD, PhD, chair of the department of pediatric neurology at the University of Paris, who co-moderated a platform session featuring the research, said the study “is an interesting measure of the impact of being exposed to antiseizure medications.”
Creativity is “complex,” he said. “It’s not only cognition; it could be things like behavior and impulsivity.”
The new information is “very helpful.” Focusing on something broader than just IQ “gives you a better picture of what’s going on.”
The study received funding from NIH, NINDS, and NICH. Dr. Meador has received grants from NIH/NINDS, NIH/NICHD, Veterans Administration, and Eisai. He has been a consultant for Epilepsy Consortium, Novartis, Supernus, Upsher Smith Labs, and UCB Pharma. Dr. Auvin reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
NASHVILLE, TENN. – There is no negative impact of in utero exposure to antiseizure medications on children’s creativity, new research shows.
The results of this study, along with other research, suggest the risk for cognitive problems “is fairly low” overall for children of women with epilepsy taking lamotrigine or levetiracetam, study investigator, Kimford J. Meador, MD, professor, department of neurology & neurological sciences, Stanford (Calif.) University School of Medicine, told this news organization.
“This is another encouraging piece that’s showing these new drugs are safe with regard to cognition.”
The findings were presented at the annual meeting of the American Epilepsy Society.
Capturing creativity
Fetal exposure to antiseizure medications can produce adverse neurodevelopmental effects. These are typically assessed using measures such as general intelligence, verbal/nonverbal abilities, or additional educational needs.
However, these measures don’t capture creativity, which “is related to intelligence but not completely,” said Dr. Meador. “I have seen wonderful examples of creativity in people who have a lot of cognitive impairment.”
He referred to one of his patients with epilepsy who is “spectacularly good” at painting with watercolors, even though she has significant cognitive impairment.
The new analysis is part of the MONEAD study, a prospective, observational multicenter study examining pregnancy outcomes for both mother and child. It included pregnant women who were enrolled at under 20 weeks’ gestational age.
The women with epilepsy in the study were primarily on monotherapy (73%), and of these, 82% were on lamotrigine or levetiracetam. About 22% were on polytherapy, of which 42% were on dual therapy with lamotrigine and levetiracetam.
Fluency, originality
Researchers assessed the children of these women at age 4½ years using the Torrance Test of Creative Thinking-Figural (TTCT-F). This is a standardized assessment of creative thinking with index scores measuring such things as fluency, originality, abstractness, and elaboration.
Dr. Meador noted the research team used a shorter version of the test battery “so as to not wear out the families and kids.”
During the test, children were given lines of different shapes and asked to draw a picture using these lines. Dr. Meador pointed out the drawings ranged from quite basic to more intricate.
One child cleverly turned a few squiggly lines into a car. “I can look at this and say this kid’s going to do very well,” said Dr. Meador.
Investigators compared scores between 241 children of women with epilepsy (WWE) and 65 children of healthy women (HW). They adjusted for the mother’s IQ, education level, age at enrollment, gestation age at enrollment, post-birth average anxiety score, and the child’s ethnicity and sex.
Investigators found the mean TTCT-F scores did not differ significantly between the two groups: adjusted least squares mean of 89.5 (95% confidence interval, 86.7-92.3) for children of WWE, compared with adjusted least square mean of 92.0 (95% CI, 86.4-97.6) for children of HW.
Balancing act
The researchers haven’t looked at a dose effect in this current study, but Dr. Meador said it’s always “a balancing act” between giving enough of the drug to keep mothers from seizing, which affect both the mother and fetus, and giving as low a dose as possible to protect the fetus.
In addition, as medication levels change during pregnancy, he said he recommends that drug levels are monitored monthly so that medication can be adjusted as necessary.
Looking at what factors might predict creativity scores, researchers found children did less well creatively if their mother didn’t have a college degree (estimate –9.5; 95% CI, –17.9 to –1.2; P = .025).
“It looks like being in a home where the mother has had more education is going to have an impact on the kid’s thinking and creativity,” said Dr. Meador.
These new findings are consistent with a lack of differences in other cognitive abilities that Dr. Meador and his team found when the children were younger.
“At age 3, we did not find an overall difference in cognitive and verbal abilities and intelligence between the children of mothers with epilepsy and those of healthy women,” he said.
The researchers aim to assess cognitive and behavioral outcomes in these children when they are 6 years old.
Helpful information
Commenting on the findings, Stéphane Auvin, MD, PhD, chair of the department of pediatric neurology at the University of Paris, who co-moderated a platform session featuring the research, said the study “is an interesting measure of the impact of being exposed to antiseizure medications.”
Creativity is “complex,” he said. “It’s not only cognition; it could be things like behavior and impulsivity.”
The new information is “very helpful.” Focusing on something broader than just IQ “gives you a better picture of what’s going on.”
The study received funding from NIH, NINDS, and NICH. Dr. Meador has received grants from NIH/NINDS, NIH/NICHD, Veterans Administration, and Eisai. He has been a consultant for Epilepsy Consortium, Novartis, Supernus, Upsher Smith Labs, and UCB Pharma. Dr. Auvin reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AES 2022







