User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
ObGyn’s steady progress toward going green in the OR—but gaps persist
Have you ever looked at the operating room (OR) trash bin at the end of a case and wondered if all that waste is necessary? Since I started my residency, not a day goes by that I have not asked myself this question.
In the mid-1990s, John Elkington introduced the concept of the triple bottom line—that is, people, planet, and profit—for implementation and measurement of sustainability in businesses.1 The health care sector is no exception when it comes to the bottom line! However, “people” remain the priority. What is our role, as ObGyns, in protecting the “planet” while keeping the “people” safe?
According to the World Health Organization (WHO), climate change remains the single biggest health threat to humanity.2 The health care system is both the victim and the culprit. Studies suggest that the health care system, second to the food industry, is the biggest contributor to waste production in the United States. This sector generates more than 6,000 metric tons of waste each day and nearly 4 million tons (3.6 million metric tons) of solid waste each year.3 The health care system is responsible for an estimated 8% to 10% of total greenhouse gas emissions in the United States; the US health care system alone contributes to more than one-fourth of the global health care carbon footprint. If it were a country, the US health care system would rank 13th among all countries in emissions.4In turn, pollution produced by the health sector negatively impacts population health, further burdening the health care system. According to 2013 study data, the annual health damage caused by health care pollution was comparable to that of the deaths caused by preventable medical error.4
Aside from the environmental aspects, hospital waste disposal is expensive; reducing this cost is a potential area of interest for institutions.
As ObGyns, what is our role in reducing our waste generation and carbon footprint while keeping patients safe?
Defining health care waste, and disposal considerations
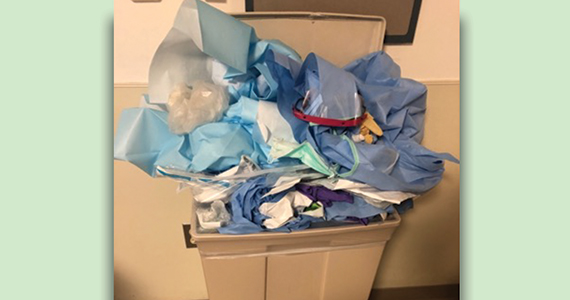
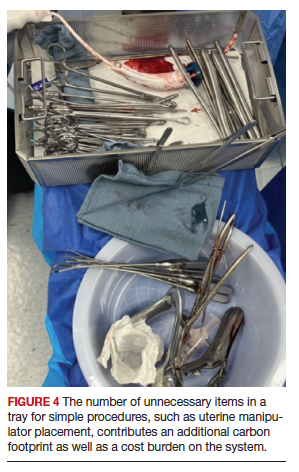
The WHO defines health care waste as including “the waste generated by health-care establishments, research facilities, and laboratories” as well as waste from scattered sources such as home dialysis and insulin injections.5 Despite representing a relatively small physical area of hospitals, labor and delivery units combined with ORs account for approximately 70% of all hospital waste.3 Operating room waste consists of disposable surgical supplies, personal protective equipment, drapes, plastic wrappers, sterile blue wraps, glass, cardboard, packaging material, medications, fluids, and other materials (FIGURE 1).
The WHO also notes that of all the waste generated by health care activities, about 85% is general, nonhazardous waste that is comparable to domestic waste.6 Hazardous waste is any material that poses a health risk, including potentially infectious materials, such as blood-soaked gauze, sharps, pharmaceuticals, or radioactive materials.6
Disposal of hazardous waste is expensiveand energy consuming as it is typically incinerated rather than disposed of in a landfill. This process produces substantial greenhouse gases, about 3 kg of carbon dioxide for every 1 kg of hazardous waste.7
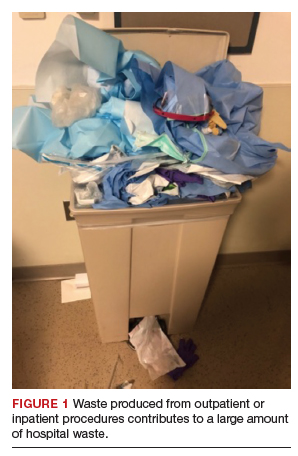
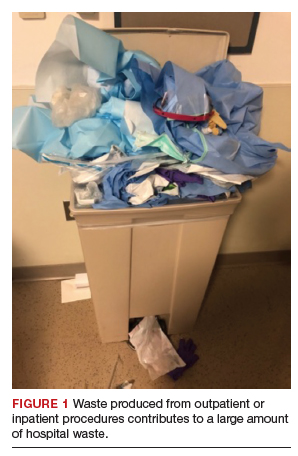
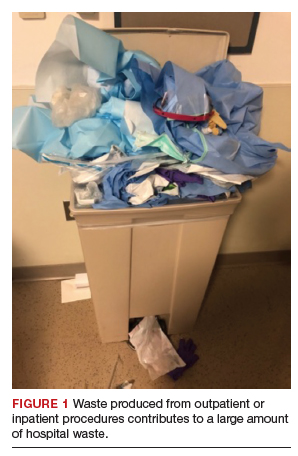
Red bags are used for hazardous waste disposal, while clear bags are used for general waste. Operating rooms produce about two-thirds of the hospital red-bag waste.8 Waste segregation unfortunately is not accurate, and as much as 90% of OR general waste is improperly designated as hazardous waste.3 Drapes and uncontaminated, needleless syringes, for example, should be disposed of in clear bags, but often they are instead directed to the red-bag and sharps container (FIGURE 2).
Obstetrics and gynecology has an important role to play in accurate waste segregation given the specialty’s frequent interaction with bodily fluids. Clinicians and other staff need to recognize and appropriately separate hazardous waste from general waste. For instance, not all fabrics involved in a case should be disposed of in the red bin, only those saturated with blood or body fluids. Educating health care staff and placing instruction posters on the red trash bins potentially could aid in accurate waste segregation and reduce regulated waste while decreasing disposal costs.
Recycling in the OR
Recycling has become an established practice in many health care facilities and ORs. Studies suggest that introducing recycling programs in ORs not only reduces carbon footprints but also reduces costs.3 One study reported that US academic medical centers consume 2 million lb ($15 million) each year of recoverable medical supplies.9
Single-stream recycling, a system in which all recyclable material—including plastics, paper, metal, and glass—are placed in a single bin without segregation at the collection site, has gained in popularity. Recycling can be implemented both in ORs and in other perioperative areas where regular trash bins are located.
In a study done at Oxford University Hospitals in the United Kingdom, introducing recycling bins in every OR, as well as in recovery and staff rest areas, helped improve waste segregation such that approximately 22% of OR waste was recycled.10 Studies show that recycling programs not only decrease the health care carbon footprint but also have a considerable financial impact. Albert and colleagues demonstrated that introducing a single-stream recycling program to a 9-OR day (or ambulatory) surgery center could redirect more than 4 tons of waste each month and saved thousands of dollars.11
Despite continued improvement in recycling programs, the segregation process is still far from optimal. In a survey done at the Mayo Clinic by Azouz and colleagues, more than half of the staff reported being unclear about which OR items are recyclable and nearly half reported that lack of knowledge was the barrier to proper recycling.12 That study also showed that after implementation of a recycling education program, costs decreased 10% relative to the same time period in prior years.12
Blue wraps. One example of recycling optimization is blue wraps, the polypropylene (No. 5 plastic) material used for wrapping surgical instruments. Blue wraps account for approximately 19% of OR waste and 5% of all hospital waste.11 Blue wraps are not biodegradable and also are not widely recycled. In recent years, a resale market has emerged for blue wraps, as they can be used for production of other No. 5 plastic items.9 By reselling blue wraps, revenue can be generated by recycling a necessary packing material that would otherwise require payment for disposal.
Sterility considerations. While recycling in ORs may raise concern due to the absolute sterility required in procedural settings, technologic developments have been promising in advancing safe recycling to reduce carbon footprints and health care costs without compromising patients’ safety. Segregation of waste from recyclable packaging material prior to the case, as well as directing trash to the correct bin (regular vs red bin), is one example. Moreover, because about 80% of all OR waste is generated during the set up before the patient arrives in the OR, it is not contaminated and can be safely recycled.13
Continue to: Packaging material...
Packaging material
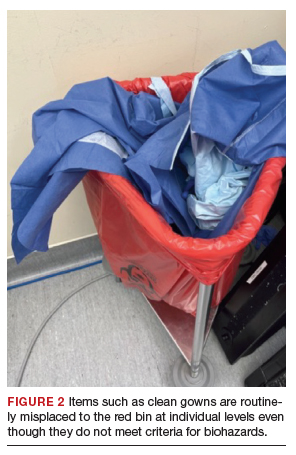
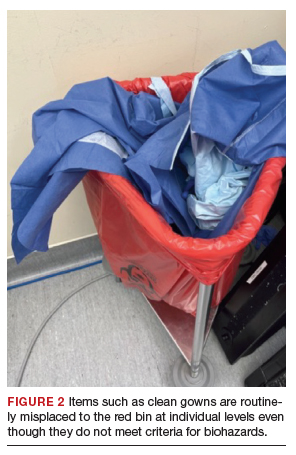
A substantial part of OR waste consists of packaging material; of all OR waste, 26% consists of plastics and 7%, paper and cartons.14 Increasing use of disposable or “single use” medical products in ORs, along with the intention to safeguard sterility, contributes significantly to the generation of medical waste in operating units. Containers, wraps and overwraps, cardboard, and plastic packaging are all composed of materials that when clean, can be recycled; however, these items often end up in the landfill (FIGURE 3).
Although the segregation of packaging material to recycling versus regular trash versus red bin is of paramount importance, packaging design plays a significant role as well. In 2018, Boston Scientific introduced a new packaging design for ureteral stents that reduced plastic use in packaging by 120,000 lb each year.15 Despite the advances in the medical packaging industry to increase sustainability while safeguarding sterility for medical devices, there is still room for innovation in this area.
Reducing overage by judicious selection of surgical devices, instruments, and supplies
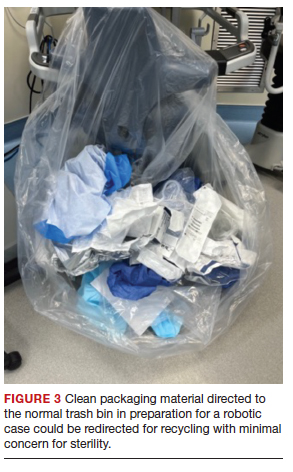
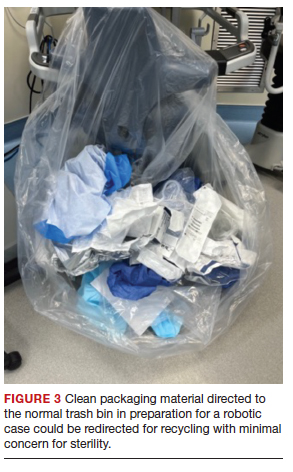
Overage is the term used to describe surgical inventory that is opened and prepared for surgery but ultimately not used and therefore discarded. Design of surgical carts and instrument and supply selection requires direct input from ObGyns. Opening only the needed instruments while ensuring ready availability of potentially needed supplies can significantly reduce OR waste generation as well as decrease chemical pollution generated by instrument sterilization. Decreasing OR overage reduces overall costs as well (FIGURE 4).
In a pilot study at the University of Massachusetts, Albert and colleagues examined the sets of disposable items and instruments designated for common plastic and hand surgery procedures.11 They identified the supplies and instruments that are routinely opened and wasted, based on surgeons’ interview responses, and redesigned the sets. Fifteen items were removed from disposable plastic surgery packs and 7 items from hand surgery packs. The authors reported saving thousands of dollars per year with these changes alone, as well as reducing waste.11 This same concept easily could be implemented in obstetrics and gynecology. We must ask ourselves: Do we always need, for example, a complete dilation and curettage kit to place the uterine manipulator prior to a minimally invasive hysterectomy?
In another pilot study, Greenberg and colleagues investigated whether cesarean deliveries consistently could be performed in a safe manner with only 20 instruments in the surgical kit.16 Obstetricians rated the 20-instrument kit an 8.7 out of 10 for performing cesarean deliveries safely.16
In addition to instrument selection, surgeons have a role in other supply use and waste generation: for instance, opening multiple pairs of surgical gloves and surgical gowns in advance when most of them will not be used during the case. Furthermore, many ObGyn surgeons routinely change gloves or even gowns during gynecologic procedures when they go back and forth between the vaginal and abdominal fields. Is the perineum “dirty” after application of a surgical prep solution?
In an observational study, Shockley and colleagues investigated the type and quantity of bacteria found intraoperatively on the abdomen, vagina, surgical gloves, instrument tips, and uterus at distinct time points during total laparoscopic hysterectomy.17 They showed that in 98.9% of cultures, the overall bacterial concentrations did not exceed the threshold for infection. There was no bacterial growth from vaginal cultures, and the only samples with some bacterial growth belonged to the surgeon’s gloves after specimen extraction; about one-third of samples showed growth after specimen extraction, but only 1 sample had a bacterial load above the infectious threshold of 5,000 colony-forming units per mL. The authors therefore suggested that if a surgeon changes gloves, doing so after specimen extraction and before turning attention back to the abdomen for vaginal cuff closure may be most effective in reducing bacterial load.17
Surgical site infection contributes to medical cost and likely medical waste as well. For example, surgical site infection may require prolonged treatments, tests, and medical instruments. In severe cases with abscesses, treatment entails hospitalization with prolonged antibiotic therapy with or without procedures to drain the collections. Further research therefore is warranted to investigate safe and environmentally friendly practices.
Myriad products are introduced to the medical system each day, some of which replace conventional tools. For instance, low-density polyethylene, or LDPE, transfer sheet is advertised for lateral patient transfer from the OR table to the bed or stretcher. This No. 4–coded plastic, while recyclable, is routinely discarded as trash in ORs. One ergonomic study found that reusable slide boards are as effective for reducing friction and staff muscle activities and are noninferior to the plastic sheets.18
Steps to making an impact
Operating rooms and labor and delivery units are responsible for a large proportion of hospital waste, and therefore they are of paramount importance in reducing waste and carbon footprint at the individual and institutional level. Reduction of OR waste not only is environmentally conscious but also decreases cost. Steps as small as individual practices to as big as changing infrastructures can make an impact. For instance:
- redesigning surgical carts
- reformulating surgeon-specific supply lists
- raising awareness about surgical overage
- encouraging recycling through education and audit
- optimizing surgical waste segregation through educational posters.
These are all simple steps that could significantly reduce waste and carbon footprint.
Bottom line
Although waste reduction is the responsibility of all health care providers, as leaders in their workplace physicians can serve as role models by implementing “green” practices in procedural units. Raising awareness and using a team approach is critical to succeed in our endeavors to move toward an environmentally friendly future. ●
- Elkington J. Towards the sustainable corporation: win-winwin business strategies for sustainable development. Calif Manage Rev. 1994;36:90-100.
- Climate change and health. October 30, 2021. World Health Organization. Accessed October 10, 2022. https://www.who .int/news-room/fact-sheets/detail/climate-change-and -health
- Kwakye G, Brat GA, Makary MA. Green surgical practices for health care. Arch Surg. 2011;146:131-136.
- Eckelman MJ, Sherman J. Environmental impacts of the US health care system and effects on public health. PloS One. 2016;11:e0157014.
- Pruss A, Giroult E, Rushbrook P. Safe management of wastes from health-care activities. World Health Organization; 1999.
- Health-care waste. February 8, 2018. World Health Organization. Accessed October 4, 2022. https://www.who. int/news-room/fact-sheets/detail/health-care-waste2
- Southorn T, Norrish AR, Gardner K, et al. Reducing the carbon footprint of the operating theatre: a multicentre quality improvement report. J Perioper Pract. 2013;23:144-146.
- Greening the OR. Practice Greenhealth. Accessed October 24, 2022. https://practicegreenhealth.org/topics/greening -operating-room/greening-or
- Babu MA, Dalenberg AK, Goodsell G, et al. Greening the operating room: results of a scalable initiative to reduce waste and recover supply costs. Neurosurgery. 2019;85:432-437.
- Oxford University Hospitals NHS Trust. Introducing recycling into the operating theatres. Mapping Greener Healthcare. Accessed October 14, 2022. https://map .sustainablehealthcare.org.uk/oxford-radcliffe-hospitals -nhs-trust/introducing-recycling-operating-theatres
- Albert MG, Rothkopf DM. Operating room waste reduction in plastic and hand surgery. Plast Surg. 2015;23:235-238.
- Azouz S, Boyll P, Swanson M, et al. Managing barriers to recycling in the operating room. Am J Surg. 2019;217:634-638.
- Wyssusek KH, Keys MT, van Zundert AAJ. Operating room greening initiatives—the old, the new, and the way forward: a narrative review. Waste Manag Res. 2019;37:3-19.
- Tieszen ME, Gruenberg JC. A quantitative, qualitative, and critical assessment of surgical waste: surgeons venture through the trash can. JAMA. 1992;267:2765-2768.
- Boston Scientific 2018 Performance Report. Boston Scientific. Accessed November 19, 2022. https://www.bostonscientific. com/content/dam/bostonscientific/corporate/citizenship /sustainability/Boston_Scientific_Performance _Report_2018.pdf
- Greenberg JA, Wylie B, Robinson JN. A pilot study to assess the adequacy of the Brigham 20 Kit for cesarean delivery. Int J Gynaecol Obstet. 2012;117:157-159.
- Shockley ME, Beran B, Nutting H, et al. Sterility of selected operative sites during total laparoscopic hysterectomy. J Minim Invasive Gynecol. 2017;24:990-997.
- Al-Qaisi SK, El Tannir A, Younan LA, et al. An ergonomic assessment of using laterally-tilting operating room tables and friction reducing devices for patient lateral transfers. Appl Ergon. 2020;87:103122.
Have you ever looked at the operating room (OR) trash bin at the end of a case and wondered if all that waste is necessary? Since I started my residency, not a day goes by that I have not asked myself this question.
In the mid-1990s, John Elkington introduced the concept of the triple bottom line—that is, people, planet, and profit—for implementation and measurement of sustainability in businesses.1 The health care sector is no exception when it comes to the bottom line! However, “people” remain the priority. What is our role, as ObGyns, in protecting the “planet” while keeping the “people” safe?
According to the World Health Organization (WHO), climate change remains the single biggest health threat to humanity.2 The health care system is both the victim and the culprit. Studies suggest that the health care system, second to the food industry, is the biggest contributor to waste production in the United States. This sector generates more than 6,000 metric tons of waste each day and nearly 4 million tons (3.6 million metric tons) of solid waste each year.3 The health care system is responsible for an estimated 8% to 10% of total greenhouse gas emissions in the United States; the US health care system alone contributes to more than one-fourth of the global health care carbon footprint. If it were a country, the US health care system would rank 13th among all countries in emissions.4In turn, pollution produced by the health sector negatively impacts population health, further burdening the health care system. According to 2013 study data, the annual health damage caused by health care pollution was comparable to that of the deaths caused by preventable medical error.4
Aside from the environmental aspects, hospital waste disposal is expensive; reducing this cost is a potential area of interest for institutions.
As ObGyns, what is our role in reducing our waste generation and carbon footprint while keeping patients safe?
Defining health care waste, and disposal considerations
The WHO defines health care waste as including “the waste generated by health-care establishments, research facilities, and laboratories” as well as waste from scattered sources such as home dialysis and insulin injections.5 Despite representing a relatively small physical area of hospitals, labor and delivery units combined with ORs account for approximately 70% of all hospital waste.3 Operating room waste consists of disposable surgical supplies, personal protective equipment, drapes, plastic wrappers, sterile blue wraps, glass, cardboard, packaging material, medications, fluids, and other materials (FIGURE 1).
The WHO also notes that of all the waste generated by health care activities, about 85% is general, nonhazardous waste that is comparable to domestic waste.6 Hazardous waste is any material that poses a health risk, including potentially infectious materials, such as blood-soaked gauze, sharps, pharmaceuticals, or radioactive materials.6
Disposal of hazardous waste is expensiveand energy consuming as it is typically incinerated rather than disposed of in a landfill. This process produces substantial greenhouse gases, about 3 kg of carbon dioxide for every 1 kg of hazardous waste.7
Red bags are used for hazardous waste disposal, while clear bags are used for general waste. Operating rooms produce about two-thirds of the hospital red-bag waste.8 Waste segregation unfortunately is not accurate, and as much as 90% of OR general waste is improperly designated as hazardous waste.3 Drapes and uncontaminated, needleless syringes, for example, should be disposed of in clear bags, but often they are instead directed to the red-bag and sharps container (FIGURE 2).
Obstetrics and gynecology has an important role to play in accurate waste segregation given the specialty’s frequent interaction with bodily fluids. Clinicians and other staff need to recognize and appropriately separate hazardous waste from general waste. For instance, not all fabrics involved in a case should be disposed of in the red bin, only those saturated with blood or body fluids. Educating health care staff and placing instruction posters on the red trash bins potentially could aid in accurate waste segregation and reduce regulated waste while decreasing disposal costs.
Recycling in the OR
Recycling has become an established practice in many health care facilities and ORs. Studies suggest that introducing recycling programs in ORs not only reduces carbon footprints but also reduces costs.3 One study reported that US academic medical centers consume 2 million lb ($15 million) each year of recoverable medical supplies.9
Single-stream recycling, a system in which all recyclable material—including plastics, paper, metal, and glass—are placed in a single bin without segregation at the collection site, has gained in popularity. Recycling can be implemented both in ORs and in other perioperative areas where regular trash bins are located.
In a study done at Oxford University Hospitals in the United Kingdom, introducing recycling bins in every OR, as well as in recovery and staff rest areas, helped improve waste segregation such that approximately 22% of OR waste was recycled.10 Studies show that recycling programs not only decrease the health care carbon footprint but also have a considerable financial impact. Albert and colleagues demonstrated that introducing a single-stream recycling program to a 9-OR day (or ambulatory) surgery center could redirect more than 4 tons of waste each month and saved thousands of dollars.11
Despite continued improvement in recycling programs, the segregation process is still far from optimal. In a survey done at the Mayo Clinic by Azouz and colleagues, more than half of the staff reported being unclear about which OR items are recyclable and nearly half reported that lack of knowledge was the barrier to proper recycling.12 That study also showed that after implementation of a recycling education program, costs decreased 10% relative to the same time period in prior years.12
Blue wraps. One example of recycling optimization is blue wraps, the polypropylene (No. 5 plastic) material used for wrapping surgical instruments. Blue wraps account for approximately 19% of OR waste and 5% of all hospital waste.11 Blue wraps are not biodegradable and also are not widely recycled. In recent years, a resale market has emerged for blue wraps, as they can be used for production of other No. 5 plastic items.9 By reselling blue wraps, revenue can be generated by recycling a necessary packing material that would otherwise require payment for disposal.
Sterility considerations. While recycling in ORs may raise concern due to the absolute sterility required in procedural settings, technologic developments have been promising in advancing safe recycling to reduce carbon footprints and health care costs without compromising patients’ safety. Segregation of waste from recyclable packaging material prior to the case, as well as directing trash to the correct bin (regular vs red bin), is one example. Moreover, because about 80% of all OR waste is generated during the set up before the patient arrives in the OR, it is not contaminated and can be safely recycled.13
Continue to: Packaging material...
Packaging material
A substantial part of OR waste consists of packaging material; of all OR waste, 26% consists of plastics and 7%, paper and cartons.14 Increasing use of disposable or “single use” medical products in ORs, along with the intention to safeguard sterility, contributes significantly to the generation of medical waste in operating units. Containers, wraps and overwraps, cardboard, and plastic packaging are all composed of materials that when clean, can be recycled; however, these items often end up in the landfill (FIGURE 3).
Although the segregation of packaging material to recycling versus regular trash versus red bin is of paramount importance, packaging design plays a significant role as well. In 2018, Boston Scientific introduced a new packaging design for ureteral stents that reduced plastic use in packaging by 120,000 lb each year.15 Despite the advances in the medical packaging industry to increase sustainability while safeguarding sterility for medical devices, there is still room for innovation in this area.
Reducing overage by judicious selection of surgical devices, instruments, and supplies
Overage is the term used to describe surgical inventory that is opened and prepared for surgery but ultimately not used and therefore discarded. Design of surgical carts and instrument and supply selection requires direct input from ObGyns. Opening only the needed instruments while ensuring ready availability of potentially needed supplies can significantly reduce OR waste generation as well as decrease chemical pollution generated by instrument sterilization. Decreasing OR overage reduces overall costs as well (FIGURE 4).
In a pilot study at the University of Massachusetts, Albert and colleagues examined the sets of disposable items and instruments designated for common plastic and hand surgery procedures.11 They identified the supplies and instruments that are routinely opened and wasted, based on surgeons’ interview responses, and redesigned the sets. Fifteen items were removed from disposable plastic surgery packs and 7 items from hand surgery packs. The authors reported saving thousands of dollars per year with these changes alone, as well as reducing waste.11 This same concept easily could be implemented in obstetrics and gynecology. We must ask ourselves: Do we always need, for example, a complete dilation and curettage kit to place the uterine manipulator prior to a minimally invasive hysterectomy?
In another pilot study, Greenberg and colleagues investigated whether cesarean deliveries consistently could be performed in a safe manner with only 20 instruments in the surgical kit.16 Obstetricians rated the 20-instrument kit an 8.7 out of 10 for performing cesarean deliveries safely.16
In addition to instrument selection, surgeons have a role in other supply use and waste generation: for instance, opening multiple pairs of surgical gloves and surgical gowns in advance when most of them will not be used during the case. Furthermore, many ObGyn surgeons routinely change gloves or even gowns during gynecologic procedures when they go back and forth between the vaginal and abdominal fields. Is the perineum “dirty” after application of a surgical prep solution?
In an observational study, Shockley and colleagues investigated the type and quantity of bacteria found intraoperatively on the abdomen, vagina, surgical gloves, instrument tips, and uterus at distinct time points during total laparoscopic hysterectomy.17 They showed that in 98.9% of cultures, the overall bacterial concentrations did not exceed the threshold for infection. There was no bacterial growth from vaginal cultures, and the only samples with some bacterial growth belonged to the surgeon’s gloves after specimen extraction; about one-third of samples showed growth after specimen extraction, but only 1 sample had a bacterial load above the infectious threshold of 5,000 colony-forming units per mL. The authors therefore suggested that if a surgeon changes gloves, doing so after specimen extraction and before turning attention back to the abdomen for vaginal cuff closure may be most effective in reducing bacterial load.17
Surgical site infection contributes to medical cost and likely medical waste as well. For example, surgical site infection may require prolonged treatments, tests, and medical instruments. In severe cases with abscesses, treatment entails hospitalization with prolonged antibiotic therapy with or without procedures to drain the collections. Further research therefore is warranted to investigate safe and environmentally friendly practices.
Myriad products are introduced to the medical system each day, some of which replace conventional tools. For instance, low-density polyethylene, or LDPE, transfer sheet is advertised for lateral patient transfer from the OR table to the bed or stretcher. This No. 4–coded plastic, while recyclable, is routinely discarded as trash in ORs. One ergonomic study found that reusable slide boards are as effective for reducing friction and staff muscle activities and are noninferior to the plastic sheets.18
Steps to making an impact
Operating rooms and labor and delivery units are responsible for a large proportion of hospital waste, and therefore they are of paramount importance in reducing waste and carbon footprint at the individual and institutional level. Reduction of OR waste not only is environmentally conscious but also decreases cost. Steps as small as individual practices to as big as changing infrastructures can make an impact. For instance:
- redesigning surgical carts
- reformulating surgeon-specific supply lists
- raising awareness about surgical overage
- encouraging recycling through education and audit
- optimizing surgical waste segregation through educational posters.
These are all simple steps that could significantly reduce waste and carbon footprint.
Bottom line
Although waste reduction is the responsibility of all health care providers, as leaders in their workplace physicians can serve as role models by implementing “green” practices in procedural units. Raising awareness and using a team approach is critical to succeed in our endeavors to move toward an environmentally friendly future. ●
Have you ever looked at the operating room (OR) trash bin at the end of a case and wondered if all that waste is necessary? Since I started my residency, not a day goes by that I have not asked myself this question.
In the mid-1990s, John Elkington introduced the concept of the triple bottom line—that is, people, planet, and profit—for implementation and measurement of sustainability in businesses.1 The health care sector is no exception when it comes to the bottom line! However, “people” remain the priority. What is our role, as ObGyns, in protecting the “planet” while keeping the “people” safe?
According to the World Health Organization (WHO), climate change remains the single biggest health threat to humanity.2 The health care system is both the victim and the culprit. Studies suggest that the health care system, second to the food industry, is the biggest contributor to waste production in the United States. This sector generates more than 6,000 metric tons of waste each day and nearly 4 million tons (3.6 million metric tons) of solid waste each year.3 The health care system is responsible for an estimated 8% to 10% of total greenhouse gas emissions in the United States; the US health care system alone contributes to more than one-fourth of the global health care carbon footprint. If it were a country, the US health care system would rank 13th among all countries in emissions.4In turn, pollution produced by the health sector negatively impacts population health, further burdening the health care system. According to 2013 study data, the annual health damage caused by health care pollution was comparable to that of the deaths caused by preventable medical error.4
Aside from the environmental aspects, hospital waste disposal is expensive; reducing this cost is a potential area of interest for institutions.
As ObGyns, what is our role in reducing our waste generation and carbon footprint while keeping patients safe?
Defining health care waste, and disposal considerations
The WHO defines health care waste as including “the waste generated by health-care establishments, research facilities, and laboratories” as well as waste from scattered sources such as home dialysis and insulin injections.5 Despite representing a relatively small physical area of hospitals, labor and delivery units combined with ORs account for approximately 70% of all hospital waste.3 Operating room waste consists of disposable surgical supplies, personal protective equipment, drapes, plastic wrappers, sterile blue wraps, glass, cardboard, packaging material, medications, fluids, and other materials (FIGURE 1).
The WHO also notes that of all the waste generated by health care activities, about 85% is general, nonhazardous waste that is comparable to domestic waste.6 Hazardous waste is any material that poses a health risk, including potentially infectious materials, such as blood-soaked gauze, sharps, pharmaceuticals, or radioactive materials.6
Disposal of hazardous waste is expensiveand energy consuming as it is typically incinerated rather than disposed of in a landfill. This process produces substantial greenhouse gases, about 3 kg of carbon dioxide for every 1 kg of hazardous waste.7
Red bags are used for hazardous waste disposal, while clear bags are used for general waste. Operating rooms produce about two-thirds of the hospital red-bag waste.8 Waste segregation unfortunately is not accurate, and as much as 90% of OR general waste is improperly designated as hazardous waste.3 Drapes and uncontaminated, needleless syringes, for example, should be disposed of in clear bags, but often they are instead directed to the red-bag and sharps container (FIGURE 2).
Obstetrics and gynecology has an important role to play in accurate waste segregation given the specialty’s frequent interaction with bodily fluids. Clinicians and other staff need to recognize and appropriately separate hazardous waste from general waste. For instance, not all fabrics involved in a case should be disposed of in the red bin, only those saturated with blood or body fluids. Educating health care staff and placing instruction posters on the red trash bins potentially could aid in accurate waste segregation and reduce regulated waste while decreasing disposal costs.
Recycling in the OR
Recycling has become an established practice in many health care facilities and ORs. Studies suggest that introducing recycling programs in ORs not only reduces carbon footprints but also reduces costs.3 One study reported that US academic medical centers consume 2 million lb ($15 million) each year of recoverable medical supplies.9
Single-stream recycling, a system in which all recyclable material—including plastics, paper, metal, and glass—are placed in a single bin without segregation at the collection site, has gained in popularity. Recycling can be implemented both in ORs and in other perioperative areas where regular trash bins are located.
In a study done at Oxford University Hospitals in the United Kingdom, introducing recycling bins in every OR, as well as in recovery and staff rest areas, helped improve waste segregation such that approximately 22% of OR waste was recycled.10 Studies show that recycling programs not only decrease the health care carbon footprint but also have a considerable financial impact. Albert and colleagues demonstrated that introducing a single-stream recycling program to a 9-OR day (or ambulatory) surgery center could redirect more than 4 tons of waste each month and saved thousands of dollars.11
Despite continued improvement in recycling programs, the segregation process is still far from optimal. In a survey done at the Mayo Clinic by Azouz and colleagues, more than half of the staff reported being unclear about which OR items are recyclable and nearly half reported that lack of knowledge was the barrier to proper recycling.12 That study also showed that after implementation of a recycling education program, costs decreased 10% relative to the same time period in prior years.12
Blue wraps. One example of recycling optimization is blue wraps, the polypropylene (No. 5 plastic) material used for wrapping surgical instruments. Blue wraps account for approximately 19% of OR waste and 5% of all hospital waste.11 Blue wraps are not biodegradable and also are not widely recycled. In recent years, a resale market has emerged for blue wraps, as they can be used for production of other No. 5 plastic items.9 By reselling blue wraps, revenue can be generated by recycling a necessary packing material that would otherwise require payment for disposal.
Sterility considerations. While recycling in ORs may raise concern due to the absolute sterility required in procedural settings, technologic developments have been promising in advancing safe recycling to reduce carbon footprints and health care costs without compromising patients’ safety. Segregation of waste from recyclable packaging material prior to the case, as well as directing trash to the correct bin (regular vs red bin), is one example. Moreover, because about 80% of all OR waste is generated during the set up before the patient arrives in the OR, it is not contaminated and can be safely recycled.13
Continue to: Packaging material...
Packaging material
A substantial part of OR waste consists of packaging material; of all OR waste, 26% consists of plastics and 7%, paper and cartons.14 Increasing use of disposable or “single use” medical products in ORs, along with the intention to safeguard sterility, contributes significantly to the generation of medical waste in operating units. Containers, wraps and overwraps, cardboard, and plastic packaging are all composed of materials that when clean, can be recycled; however, these items often end up in the landfill (FIGURE 3).
Although the segregation of packaging material to recycling versus regular trash versus red bin is of paramount importance, packaging design plays a significant role as well. In 2018, Boston Scientific introduced a new packaging design for ureteral stents that reduced plastic use in packaging by 120,000 lb each year.15 Despite the advances in the medical packaging industry to increase sustainability while safeguarding sterility for medical devices, there is still room for innovation in this area.
Reducing overage by judicious selection of surgical devices, instruments, and supplies
Overage is the term used to describe surgical inventory that is opened and prepared for surgery but ultimately not used and therefore discarded. Design of surgical carts and instrument and supply selection requires direct input from ObGyns. Opening only the needed instruments while ensuring ready availability of potentially needed supplies can significantly reduce OR waste generation as well as decrease chemical pollution generated by instrument sterilization. Decreasing OR overage reduces overall costs as well (FIGURE 4).
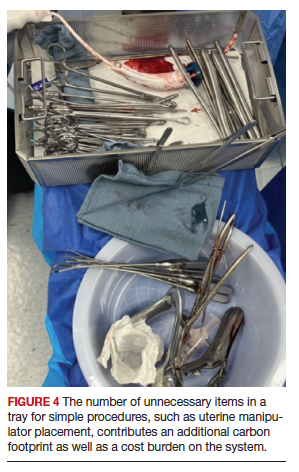
In a pilot study at the University of Massachusetts, Albert and colleagues examined the sets of disposable items and instruments designated for common plastic and hand surgery procedures.11 They identified the supplies and instruments that are routinely opened and wasted, based on surgeons’ interview responses, and redesigned the sets. Fifteen items were removed from disposable plastic surgery packs and 7 items from hand surgery packs. The authors reported saving thousands of dollars per year with these changes alone, as well as reducing waste.11 This same concept easily could be implemented in obstetrics and gynecology. We must ask ourselves: Do we always need, for example, a complete dilation and curettage kit to place the uterine manipulator prior to a minimally invasive hysterectomy?
In another pilot study, Greenberg and colleagues investigated whether cesarean deliveries consistently could be performed in a safe manner with only 20 instruments in the surgical kit.16 Obstetricians rated the 20-instrument kit an 8.7 out of 10 for performing cesarean deliveries safely.16
In addition to instrument selection, surgeons have a role in other supply use and waste generation: for instance, opening multiple pairs of surgical gloves and surgical gowns in advance when most of them will not be used during the case. Furthermore, many ObGyn surgeons routinely change gloves or even gowns during gynecologic procedures when they go back and forth between the vaginal and abdominal fields. Is the perineum “dirty” after application of a surgical prep solution?
In an observational study, Shockley and colleagues investigated the type and quantity of bacteria found intraoperatively on the abdomen, vagina, surgical gloves, instrument tips, and uterus at distinct time points during total laparoscopic hysterectomy.17 They showed that in 98.9% of cultures, the overall bacterial concentrations did not exceed the threshold for infection. There was no bacterial growth from vaginal cultures, and the only samples with some bacterial growth belonged to the surgeon’s gloves after specimen extraction; about one-third of samples showed growth after specimen extraction, but only 1 sample had a bacterial load above the infectious threshold of 5,000 colony-forming units per mL. The authors therefore suggested that if a surgeon changes gloves, doing so after specimen extraction and before turning attention back to the abdomen for vaginal cuff closure may be most effective in reducing bacterial load.17
Surgical site infection contributes to medical cost and likely medical waste as well. For example, surgical site infection may require prolonged treatments, tests, and medical instruments. In severe cases with abscesses, treatment entails hospitalization with prolonged antibiotic therapy with or without procedures to drain the collections. Further research therefore is warranted to investigate safe and environmentally friendly practices.
Myriad products are introduced to the medical system each day, some of which replace conventional tools. For instance, low-density polyethylene, or LDPE, transfer sheet is advertised for lateral patient transfer from the OR table to the bed or stretcher. This No. 4–coded plastic, while recyclable, is routinely discarded as trash in ORs. One ergonomic study found that reusable slide boards are as effective for reducing friction and staff muscle activities and are noninferior to the plastic sheets.18
Steps to making an impact
Operating rooms and labor and delivery units are responsible for a large proportion of hospital waste, and therefore they are of paramount importance in reducing waste and carbon footprint at the individual and institutional level. Reduction of OR waste not only is environmentally conscious but also decreases cost. Steps as small as individual practices to as big as changing infrastructures can make an impact. For instance:
- redesigning surgical carts
- reformulating surgeon-specific supply lists
- raising awareness about surgical overage
- encouraging recycling through education and audit
- optimizing surgical waste segregation through educational posters.
These are all simple steps that could significantly reduce waste and carbon footprint.
Bottom line
Although waste reduction is the responsibility of all health care providers, as leaders in their workplace physicians can serve as role models by implementing “green” practices in procedural units. Raising awareness and using a team approach is critical to succeed in our endeavors to move toward an environmentally friendly future. ●
- Elkington J. Towards the sustainable corporation: win-winwin business strategies for sustainable development. Calif Manage Rev. 1994;36:90-100.
- Climate change and health. October 30, 2021. World Health Organization. Accessed October 10, 2022. https://www.who .int/news-room/fact-sheets/detail/climate-change-and -health
- Kwakye G, Brat GA, Makary MA. Green surgical practices for health care. Arch Surg. 2011;146:131-136.
- Eckelman MJ, Sherman J. Environmental impacts of the US health care system and effects on public health. PloS One. 2016;11:e0157014.
- Pruss A, Giroult E, Rushbrook P. Safe management of wastes from health-care activities. World Health Organization; 1999.
- Health-care waste. February 8, 2018. World Health Organization. Accessed October 4, 2022. https://www.who. int/news-room/fact-sheets/detail/health-care-waste2
- Southorn T, Norrish AR, Gardner K, et al. Reducing the carbon footprint of the operating theatre: a multicentre quality improvement report. J Perioper Pract. 2013;23:144-146.
- Greening the OR. Practice Greenhealth. Accessed October 24, 2022. https://practicegreenhealth.org/topics/greening -operating-room/greening-or
- Babu MA, Dalenberg AK, Goodsell G, et al. Greening the operating room: results of a scalable initiative to reduce waste and recover supply costs. Neurosurgery. 2019;85:432-437.
- Oxford University Hospitals NHS Trust. Introducing recycling into the operating theatres. Mapping Greener Healthcare. Accessed October 14, 2022. https://map .sustainablehealthcare.org.uk/oxford-radcliffe-hospitals -nhs-trust/introducing-recycling-operating-theatres
- Albert MG, Rothkopf DM. Operating room waste reduction in plastic and hand surgery. Plast Surg. 2015;23:235-238.
- Azouz S, Boyll P, Swanson M, et al. Managing barriers to recycling in the operating room. Am J Surg. 2019;217:634-638.
- Wyssusek KH, Keys MT, van Zundert AAJ. Operating room greening initiatives—the old, the new, and the way forward: a narrative review. Waste Manag Res. 2019;37:3-19.
- Tieszen ME, Gruenberg JC. A quantitative, qualitative, and critical assessment of surgical waste: surgeons venture through the trash can. JAMA. 1992;267:2765-2768.
- Boston Scientific 2018 Performance Report. Boston Scientific. Accessed November 19, 2022. https://www.bostonscientific. com/content/dam/bostonscientific/corporate/citizenship /sustainability/Boston_Scientific_Performance _Report_2018.pdf
- Greenberg JA, Wylie B, Robinson JN. A pilot study to assess the adequacy of the Brigham 20 Kit for cesarean delivery. Int J Gynaecol Obstet. 2012;117:157-159.
- Shockley ME, Beran B, Nutting H, et al. Sterility of selected operative sites during total laparoscopic hysterectomy. J Minim Invasive Gynecol. 2017;24:990-997.
- Al-Qaisi SK, El Tannir A, Younan LA, et al. An ergonomic assessment of using laterally-tilting operating room tables and friction reducing devices for patient lateral transfers. Appl Ergon. 2020;87:103122.
- Elkington J. Towards the sustainable corporation: win-winwin business strategies for sustainable development. Calif Manage Rev. 1994;36:90-100.
- Climate change and health. October 30, 2021. World Health Organization. Accessed October 10, 2022. https://www.who .int/news-room/fact-sheets/detail/climate-change-and -health
- Kwakye G, Brat GA, Makary MA. Green surgical practices for health care. Arch Surg. 2011;146:131-136.
- Eckelman MJ, Sherman J. Environmental impacts of the US health care system and effects on public health. PloS One. 2016;11:e0157014.
- Pruss A, Giroult E, Rushbrook P. Safe management of wastes from health-care activities. World Health Organization; 1999.
- Health-care waste. February 8, 2018. World Health Organization. Accessed October 4, 2022. https://www.who. int/news-room/fact-sheets/detail/health-care-waste2
- Southorn T, Norrish AR, Gardner K, et al. Reducing the carbon footprint of the operating theatre: a multicentre quality improvement report. J Perioper Pract. 2013;23:144-146.
- Greening the OR. Practice Greenhealth. Accessed October 24, 2022. https://practicegreenhealth.org/topics/greening -operating-room/greening-or
- Babu MA, Dalenberg AK, Goodsell G, et al. Greening the operating room: results of a scalable initiative to reduce waste and recover supply costs. Neurosurgery. 2019;85:432-437.
- Oxford University Hospitals NHS Trust. Introducing recycling into the operating theatres. Mapping Greener Healthcare. Accessed October 14, 2022. https://map .sustainablehealthcare.org.uk/oxford-radcliffe-hospitals -nhs-trust/introducing-recycling-operating-theatres
- Albert MG, Rothkopf DM. Operating room waste reduction in plastic and hand surgery. Plast Surg. 2015;23:235-238.
- Azouz S, Boyll P, Swanson M, et al. Managing barriers to recycling in the operating room. Am J Surg. 2019;217:634-638.
- Wyssusek KH, Keys MT, van Zundert AAJ. Operating room greening initiatives—the old, the new, and the way forward: a narrative review. Waste Manag Res. 2019;37:3-19.
- Tieszen ME, Gruenberg JC. A quantitative, qualitative, and critical assessment of surgical waste: surgeons venture through the trash can. JAMA. 1992;267:2765-2768.
- Boston Scientific 2018 Performance Report. Boston Scientific. Accessed November 19, 2022. https://www.bostonscientific. com/content/dam/bostonscientific/corporate/citizenship /sustainability/Boston_Scientific_Performance _Report_2018.pdf
- Greenberg JA, Wylie B, Robinson JN. A pilot study to assess the adequacy of the Brigham 20 Kit for cesarean delivery. Int J Gynaecol Obstet. 2012;117:157-159.
- Shockley ME, Beran B, Nutting H, et al. Sterility of selected operative sites during total laparoscopic hysterectomy. J Minim Invasive Gynecol. 2017;24:990-997.
- Al-Qaisi SK, El Tannir A, Younan LA, et al. An ergonomic assessment of using laterally-tilting operating room tables and friction reducing devices for patient lateral transfers. Appl Ergon. 2020;87:103122.
Understanding clinic-reported IVF success rates
The field of assisted reproductive technologies (ART) continues to evolve from its first successful birth in 1978 in England, and then in 1981 in the United States. Over the last 6 years, the total number of cycles in the U.S. has increased by 44% to nearly 370,000.
SART membership consists of more than 350 clinics throughout the United States, representing 80% of ART clinics. Over 95% of ART cycles in 2021 in the United States were performed in SART-member clinics.
SART is an invaluable resource for both patients and physicians. Their website includes a “Predict My Success” calculator that allows patients and physicians to enter individualized data to calculate the chance of having a baby over one or more complete cycles of IVF. To help us understand the pregnancy outcome data from ART – cycles per clinic along with national results – I posed the questions below to Amy Sparks, PhD, HCLD, director of the IVF and Andrology Laboratories and the Center for Advanced Reproductive Care at University of Iowa Hospitals and Clinics, Iowa City. Dr. Sparks is past president of SART and former chairperson of the SART Registry committee when the current Clinic Summary Report format was initially released.
Question: The Fertility Clinic Success Rate and Certification Act (FCSRCA) of 1992 mandated that all ART clinics report success rate data to the federal government, through the Centers for Disease Control and Prevention, in a standardized manner. As ART is the only field in medicine to be required to annually report their patient outcomes, that is, all initiated cycles and live births, why do you believe this law was enacted and is limited to reproductive medicine?
Answer: The FCSRCA of 1992 was enacted in response to the lack of open and reliable pregnancy success rate information for patients seeking infertility care using assisted reproductive technologies. Success rates of 25%-50% were being advertised by independent clinics when, nationally, fewer than 15% of ART procedures led to live births. The Federal Trade Commission said such claims were deceptive and filed charges against five clinics, saying they misrepresented their success in helping women become pregnant. The government won one case by court order and the other four cases were settled out of court.
This field of medicine was in the spotlight as the majority of patients lacked insurance coverage for their ART cycles, and there was a strong desire to protect consumers paying out of pocket for relatively low success. Recognizing that the FTC’s mission is to ensure truth in advertising and not regulate medical care, Congress passed the FCSRCA, mandating that all centers providing ART services report all initiated cycles and their outcomes. The CDC was appointed as the agency responsible for collecting cycle data and reporting outcomes. Centers not reporting their cycles are listed as nonreporting centers.
This act also established standards for accreditation of embryology laboratories including personnel and traditional clinical laboratory management requirements. These standards serve as the foundation for embryology laboratory accrediting agencies.
Q: Why have live-birth rates on SART appeared to be focused on “per IVF cycle” as opposed to the CDC reporting of live births “per embryo transfer?”
A: An ART cycle “start” is defined as the initiation of ovarian stimulation with medication that may or may not include administration of exogenous gonadotropins, followed by oocyte retrieval and embryo transfer. Not every patient beginning a cycle will undergo an oocyte retrieval and not all patients who undergo oocyte retrieval have an embryo transfer. The live-birth rates (LBR) for each of these steps of progression in the ART process are available in the SART and CDC reports.
In 2016, SART recognized that practices were foregoing fresh embryo transfer after oocyte retrieval, opting to cryopreserve all embryos to either accommodate genetic testing of the embryos prior to transfer or to avoid embryo transfer to an unfavorable uterine environment. In response to changes in practice and in an effort to deemphasize live birth per transfer, thereby alleviating a potential motivator or pressure for practitioners to transfer multiple embryos, SART moved to a report that displays the cumulative live-birth rate per cycle start for oocyte retrieval. The cumulative live-birth rate per cycle start for oocyte retrieval is the chance of live birth from transfers of embryos derived from the oocyte retrieval and performed within 1 year of the oocyte retrieval.
This change in reporting further reduced the pressure to transfer multiple embryos and encouraged elective, single-embryo transfer. The outcome per transfer is no longer the report’s primary focus.
Q: The latest pregnancy outcomes statistics are from the year 2020 and are finalized by the CDC. Why does the SART website have this same year labeled “preliminary” outcomes?
A: Shortly after the 2016 SART report change, the CDC made similar changes to their report. The difference is that SART provides a “preliminary” report of outcomes within the year of the cycle start for oocyte retrieval. The cumulative outcome is not “finalized” until the following year as transfers may be performed as late as 12 months after the oocyte retrieval.
SART has opted to report both the “preliminary” or interim outcome and the “final” outcome a year later. The CDC has opted to limit their report to “final” outcomes. I’m happy to report that SART recently released the final report for 2021 cycles.
Q: Have national success rates in the United States continued to rise or have they plateaued?
A: It appears that success rates have plateaued; however, we find ourselves at another point where practice patterns and patients’ approach to using ART for family building have changed.
Recognizing the impact of maternal aging on reproductive potential, patients are opting to undergo multiple ART cycles to cryopreserve embryos for family building before they attempt to get pregnant. This family-building path reduces the value of measuring the LBR per cycle start as we may not know the outcome for many years. SART leaders are deliberating intently as to how to best represent this growing patient population in outcome reporting.
Q: Can you comment on the reduction of multiple gestations with the increasing use of single-embryo transfer?
A: The reduction in emphasis on live births per transfer, emphasis on singleton live-birth rates in both the SART and CDC reports, and American Society for Reproductive Medicine practice committee guidelines strongly supporting single embryo transfer have significantly reduced the rate of multiple gestations.
A decade ago, only a third of the transfers were single-embryo transfers and over 25% of live births resulted in a multiple birth. Today, the majority of embryo transfers are elective, single-embryo transfers, and the multiple birth rate has been reduced by nearly 80%. In 2020, 93% of live births from IVF were singletons.
Q: SART offers an online IVF calculator so both patients and physicians can plug in data for an approximate cumulative success rate for up to three IVF cycles. The calculator pools data from all U.S.-reporting IVF centers. Can you explain what an “IVF cycle” is and what patient information is required? Why do success rates increase over time?
A: Each “IVF cycle” is a cycle start for an oocyte retrieval and all transfers of embryos from that cycle within a year of the oocyte retrieval. If the first cycle and subsequent transfers do not lead to a live birth, patients still have a chance to achieve a live birth with a second or third cycle. The success rate increases over time as it reflects the chance of success for a population of patients, with some achieving a live birth after the first cycle and additional patients who achieve success following their third cycle.
Q: The SART IVF calculator can be used with no prior IVF cycles or following an unsuccessful cycle. Are there data to support an estimation of outcome following two or even more unsuccessful cycles?
A: The variables in the SART IVF calculator are based upon the cycle-specific data from patients seeking care at SART member clinics. The current predictor was built with data from cycles performed in 2015-2016. SART is adjusting the predictor and developing a calculator that will be routinely updated, accordingly.
Q: Only approximately 40% of states have some form of infertility coverage law in place; however the number of IVF cycles in the United States continues to increase on an annual basis. What do you think are the driving factors behind this?
A: Advocacy efforts to improve patients’ access to infertility care have included giving patients tools to encourage their employers to include infertility care in their health care benefits package. More recently, the “Great Resignation” has led to the “Great Recruitment” and employers are recognizing that the addition of infertility care to health care benefits is a powerful recruitment tool.
Dr. Trolice is director of The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando.
The field of assisted reproductive technologies (ART) continues to evolve from its first successful birth in 1978 in England, and then in 1981 in the United States. Over the last 6 years, the total number of cycles in the U.S. has increased by 44% to nearly 370,000.
SART membership consists of more than 350 clinics throughout the United States, representing 80% of ART clinics. Over 95% of ART cycles in 2021 in the United States were performed in SART-member clinics.
SART is an invaluable resource for both patients and physicians. Their website includes a “Predict My Success” calculator that allows patients and physicians to enter individualized data to calculate the chance of having a baby over one or more complete cycles of IVF. To help us understand the pregnancy outcome data from ART – cycles per clinic along with national results – I posed the questions below to Amy Sparks, PhD, HCLD, director of the IVF and Andrology Laboratories and the Center for Advanced Reproductive Care at University of Iowa Hospitals and Clinics, Iowa City. Dr. Sparks is past president of SART and former chairperson of the SART Registry committee when the current Clinic Summary Report format was initially released.
Question: The Fertility Clinic Success Rate and Certification Act (FCSRCA) of 1992 mandated that all ART clinics report success rate data to the federal government, through the Centers for Disease Control and Prevention, in a standardized manner. As ART is the only field in medicine to be required to annually report their patient outcomes, that is, all initiated cycles and live births, why do you believe this law was enacted and is limited to reproductive medicine?
Answer: The FCSRCA of 1992 was enacted in response to the lack of open and reliable pregnancy success rate information for patients seeking infertility care using assisted reproductive technologies. Success rates of 25%-50% were being advertised by independent clinics when, nationally, fewer than 15% of ART procedures led to live births. The Federal Trade Commission said such claims were deceptive and filed charges against five clinics, saying they misrepresented their success in helping women become pregnant. The government won one case by court order and the other four cases were settled out of court.
This field of medicine was in the spotlight as the majority of patients lacked insurance coverage for their ART cycles, and there was a strong desire to protect consumers paying out of pocket for relatively low success. Recognizing that the FTC’s mission is to ensure truth in advertising and not regulate medical care, Congress passed the FCSRCA, mandating that all centers providing ART services report all initiated cycles and their outcomes. The CDC was appointed as the agency responsible for collecting cycle data and reporting outcomes. Centers not reporting their cycles are listed as nonreporting centers.
This act also established standards for accreditation of embryology laboratories including personnel and traditional clinical laboratory management requirements. These standards serve as the foundation for embryology laboratory accrediting agencies.
Q: Why have live-birth rates on SART appeared to be focused on “per IVF cycle” as opposed to the CDC reporting of live births “per embryo transfer?”
A: An ART cycle “start” is defined as the initiation of ovarian stimulation with medication that may or may not include administration of exogenous gonadotropins, followed by oocyte retrieval and embryo transfer. Not every patient beginning a cycle will undergo an oocyte retrieval and not all patients who undergo oocyte retrieval have an embryo transfer. The live-birth rates (LBR) for each of these steps of progression in the ART process are available in the SART and CDC reports.
In 2016, SART recognized that practices were foregoing fresh embryo transfer after oocyte retrieval, opting to cryopreserve all embryos to either accommodate genetic testing of the embryos prior to transfer or to avoid embryo transfer to an unfavorable uterine environment. In response to changes in practice and in an effort to deemphasize live birth per transfer, thereby alleviating a potential motivator or pressure for practitioners to transfer multiple embryos, SART moved to a report that displays the cumulative live-birth rate per cycle start for oocyte retrieval. The cumulative live-birth rate per cycle start for oocyte retrieval is the chance of live birth from transfers of embryos derived from the oocyte retrieval and performed within 1 year of the oocyte retrieval.
This change in reporting further reduced the pressure to transfer multiple embryos and encouraged elective, single-embryo transfer. The outcome per transfer is no longer the report’s primary focus.
Q: The latest pregnancy outcomes statistics are from the year 2020 and are finalized by the CDC. Why does the SART website have this same year labeled “preliminary” outcomes?
A: Shortly after the 2016 SART report change, the CDC made similar changes to their report. The difference is that SART provides a “preliminary” report of outcomes within the year of the cycle start for oocyte retrieval. The cumulative outcome is not “finalized” until the following year as transfers may be performed as late as 12 months after the oocyte retrieval.
SART has opted to report both the “preliminary” or interim outcome and the “final” outcome a year later. The CDC has opted to limit their report to “final” outcomes. I’m happy to report that SART recently released the final report for 2021 cycles.
Q: Have national success rates in the United States continued to rise or have they plateaued?
A: It appears that success rates have plateaued; however, we find ourselves at another point where practice patterns and patients’ approach to using ART for family building have changed.
Recognizing the impact of maternal aging on reproductive potential, patients are opting to undergo multiple ART cycles to cryopreserve embryos for family building before they attempt to get pregnant. This family-building path reduces the value of measuring the LBR per cycle start as we may not know the outcome for many years. SART leaders are deliberating intently as to how to best represent this growing patient population in outcome reporting.
Q: Can you comment on the reduction of multiple gestations with the increasing use of single-embryo transfer?
A: The reduction in emphasis on live births per transfer, emphasis on singleton live-birth rates in both the SART and CDC reports, and American Society for Reproductive Medicine practice committee guidelines strongly supporting single embryo transfer have significantly reduced the rate of multiple gestations.
A decade ago, only a third of the transfers were single-embryo transfers and over 25% of live births resulted in a multiple birth. Today, the majority of embryo transfers are elective, single-embryo transfers, and the multiple birth rate has been reduced by nearly 80%. In 2020, 93% of live births from IVF were singletons.
Q: SART offers an online IVF calculator so both patients and physicians can plug in data for an approximate cumulative success rate for up to three IVF cycles. The calculator pools data from all U.S.-reporting IVF centers. Can you explain what an “IVF cycle” is and what patient information is required? Why do success rates increase over time?
A: Each “IVF cycle” is a cycle start for an oocyte retrieval and all transfers of embryos from that cycle within a year of the oocyte retrieval. If the first cycle and subsequent transfers do not lead to a live birth, patients still have a chance to achieve a live birth with a second or third cycle. The success rate increases over time as it reflects the chance of success for a population of patients, with some achieving a live birth after the first cycle and additional patients who achieve success following their third cycle.
Q: The SART IVF calculator can be used with no prior IVF cycles or following an unsuccessful cycle. Are there data to support an estimation of outcome following two or even more unsuccessful cycles?
A: The variables in the SART IVF calculator are based upon the cycle-specific data from patients seeking care at SART member clinics. The current predictor was built with data from cycles performed in 2015-2016. SART is adjusting the predictor and developing a calculator that will be routinely updated, accordingly.
Q: Only approximately 40% of states have some form of infertility coverage law in place; however the number of IVF cycles in the United States continues to increase on an annual basis. What do you think are the driving factors behind this?
A: Advocacy efforts to improve patients’ access to infertility care have included giving patients tools to encourage their employers to include infertility care in their health care benefits package. More recently, the “Great Resignation” has led to the “Great Recruitment” and employers are recognizing that the addition of infertility care to health care benefits is a powerful recruitment tool.
Dr. Trolice is director of The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando.
The field of assisted reproductive technologies (ART) continues to evolve from its first successful birth in 1978 in England, and then in 1981 in the United States. Over the last 6 years, the total number of cycles in the U.S. has increased by 44% to nearly 370,000.
SART membership consists of more than 350 clinics throughout the United States, representing 80% of ART clinics. Over 95% of ART cycles in 2021 in the United States were performed in SART-member clinics.
SART is an invaluable resource for both patients and physicians. Their website includes a “Predict My Success” calculator that allows patients and physicians to enter individualized data to calculate the chance of having a baby over one or more complete cycles of IVF. To help us understand the pregnancy outcome data from ART – cycles per clinic along with national results – I posed the questions below to Amy Sparks, PhD, HCLD, director of the IVF and Andrology Laboratories and the Center for Advanced Reproductive Care at University of Iowa Hospitals and Clinics, Iowa City. Dr. Sparks is past president of SART and former chairperson of the SART Registry committee when the current Clinic Summary Report format was initially released.
Question: The Fertility Clinic Success Rate and Certification Act (FCSRCA) of 1992 mandated that all ART clinics report success rate data to the federal government, through the Centers for Disease Control and Prevention, in a standardized manner. As ART is the only field in medicine to be required to annually report their patient outcomes, that is, all initiated cycles and live births, why do you believe this law was enacted and is limited to reproductive medicine?
Answer: The FCSRCA of 1992 was enacted in response to the lack of open and reliable pregnancy success rate information for patients seeking infertility care using assisted reproductive technologies. Success rates of 25%-50% were being advertised by independent clinics when, nationally, fewer than 15% of ART procedures led to live births. The Federal Trade Commission said such claims were deceptive and filed charges against five clinics, saying they misrepresented their success in helping women become pregnant. The government won one case by court order and the other four cases were settled out of court.
This field of medicine was in the spotlight as the majority of patients lacked insurance coverage for their ART cycles, and there was a strong desire to protect consumers paying out of pocket for relatively low success. Recognizing that the FTC’s mission is to ensure truth in advertising and not regulate medical care, Congress passed the FCSRCA, mandating that all centers providing ART services report all initiated cycles and their outcomes. The CDC was appointed as the agency responsible for collecting cycle data and reporting outcomes. Centers not reporting their cycles are listed as nonreporting centers.
This act also established standards for accreditation of embryology laboratories including personnel and traditional clinical laboratory management requirements. These standards serve as the foundation for embryology laboratory accrediting agencies.
Q: Why have live-birth rates on SART appeared to be focused on “per IVF cycle” as opposed to the CDC reporting of live births “per embryo transfer?”
A: An ART cycle “start” is defined as the initiation of ovarian stimulation with medication that may or may not include administration of exogenous gonadotropins, followed by oocyte retrieval and embryo transfer. Not every patient beginning a cycle will undergo an oocyte retrieval and not all patients who undergo oocyte retrieval have an embryo transfer. The live-birth rates (LBR) for each of these steps of progression in the ART process are available in the SART and CDC reports.
In 2016, SART recognized that practices were foregoing fresh embryo transfer after oocyte retrieval, opting to cryopreserve all embryos to either accommodate genetic testing of the embryos prior to transfer or to avoid embryo transfer to an unfavorable uterine environment. In response to changes in practice and in an effort to deemphasize live birth per transfer, thereby alleviating a potential motivator or pressure for practitioners to transfer multiple embryos, SART moved to a report that displays the cumulative live-birth rate per cycle start for oocyte retrieval. The cumulative live-birth rate per cycle start for oocyte retrieval is the chance of live birth from transfers of embryos derived from the oocyte retrieval and performed within 1 year of the oocyte retrieval.
This change in reporting further reduced the pressure to transfer multiple embryos and encouraged elective, single-embryo transfer. The outcome per transfer is no longer the report’s primary focus.
Q: The latest pregnancy outcomes statistics are from the year 2020 and are finalized by the CDC. Why does the SART website have this same year labeled “preliminary” outcomes?
A: Shortly after the 2016 SART report change, the CDC made similar changes to their report. The difference is that SART provides a “preliminary” report of outcomes within the year of the cycle start for oocyte retrieval. The cumulative outcome is not “finalized” until the following year as transfers may be performed as late as 12 months after the oocyte retrieval.
SART has opted to report both the “preliminary” or interim outcome and the “final” outcome a year later. The CDC has opted to limit their report to “final” outcomes. I’m happy to report that SART recently released the final report for 2021 cycles.
Q: Have national success rates in the United States continued to rise or have they plateaued?
A: It appears that success rates have plateaued; however, we find ourselves at another point where practice patterns and patients’ approach to using ART for family building have changed.
Recognizing the impact of maternal aging on reproductive potential, patients are opting to undergo multiple ART cycles to cryopreserve embryos for family building before they attempt to get pregnant. This family-building path reduces the value of measuring the LBR per cycle start as we may not know the outcome for many years. SART leaders are deliberating intently as to how to best represent this growing patient population in outcome reporting.
Q: Can you comment on the reduction of multiple gestations with the increasing use of single-embryo transfer?
A: The reduction in emphasis on live births per transfer, emphasis on singleton live-birth rates in both the SART and CDC reports, and American Society for Reproductive Medicine practice committee guidelines strongly supporting single embryo transfer have significantly reduced the rate of multiple gestations.
A decade ago, only a third of the transfers were single-embryo transfers and over 25% of live births resulted in a multiple birth. Today, the majority of embryo transfers are elective, single-embryo transfers, and the multiple birth rate has been reduced by nearly 80%. In 2020, 93% of live births from IVF were singletons.
Q: SART offers an online IVF calculator so both patients and physicians can plug in data for an approximate cumulative success rate for up to three IVF cycles. The calculator pools data from all U.S.-reporting IVF centers. Can you explain what an “IVF cycle” is and what patient information is required? Why do success rates increase over time?
A: Each “IVF cycle” is a cycle start for an oocyte retrieval and all transfers of embryos from that cycle within a year of the oocyte retrieval. If the first cycle and subsequent transfers do not lead to a live birth, patients still have a chance to achieve a live birth with a second or third cycle. The success rate increases over time as it reflects the chance of success for a population of patients, with some achieving a live birth after the first cycle and additional patients who achieve success following their third cycle.
Q: The SART IVF calculator can be used with no prior IVF cycles or following an unsuccessful cycle. Are there data to support an estimation of outcome following two or even more unsuccessful cycles?
A: The variables in the SART IVF calculator are based upon the cycle-specific data from patients seeking care at SART member clinics. The current predictor was built with data from cycles performed in 2015-2016. SART is adjusting the predictor and developing a calculator that will be routinely updated, accordingly.
Q: Only approximately 40% of states have some form of infertility coverage law in place; however the number of IVF cycles in the United States continues to increase on an annual basis. What do you think are the driving factors behind this?
A: Advocacy efforts to improve patients’ access to infertility care have included giving patients tools to encourage their employers to include infertility care in their health care benefits package. More recently, the “Great Resignation” has led to the “Great Recruitment” and employers are recognizing that the addition of infertility care to health care benefits is a powerful recruitment tool.
Dr. Trolice is director of The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando.
Remote weight monitoring minimizes office visits for newborns
WASHINGTON, D.C. – according to a new study presented at the Pediatric Academic Societies annual meeting.
The pilot trial compared the frequency of office visits for healthy babies born at 37 weeks’ gestation or later. One group of 20 infants had their weight monitored at home by parents, and another group of 20 infants received usual care, which included two in-person office visits over the first 6 weeks of life.
Researchers found that visits for infants in the intervention group decreased by 25% after the first week of life and by 23% after the second week.
The remote method can help alert physicians earlier to insufficient weight because parents report gains or losses three times a week over the 6 weeks, resulting in more data for providers.
“You’re going to see fewer visits with people who have scales because the docs are getting the information they need, which is: ‘Is this baby doing okay or not?’ ” said Diane DiTomasso, PhD, RN, a professor at the University of Rhode Island, South Kingstown, who was not involved with the study. “I think it’s a very necessary study because, to my knowledge, nobody has done a randomized controlled trial on this topic.”
Keeping infants at home can also protect babies from infections they might catch in the clinic.
“There are a lot of other kids in an office setting, and kids like touching things,” said Anirudha Das, MD, MPH, a neonatologist at Cleveland Clinic Children’s and the lead author of the study. “When there are a lot of other kids, there are a lot of viruses. It’s a very dangerous environment.”
Parents in the intervention group were given scales and asked to enter their infant’s weight into a patient portal app three times per week for 6 weeks. Physicians then determined if in-office visits were necessary.
The benefits of home weight checks can include helping to allow for breastfeeding for a longer duration.
Weight is more closely monitored for breastfed infants. Waiting weeks for office checks can heighten parental anxiety and lead to prematurely stopping breastfeeding. With regular at-home checks, parents receive up-to-date information from physicians that can alleviate concerns and empower them with more control over the process, according to Dr. DiTomasso.
Breastfeeding is associated with a lower risk for cardiovascular disease, diabetes, obesity, cancer in later life, and a lower risk of breast cancer for breastfeeding parents.
Office weight checks can also alleviate a significant and unnecessary burden for parents, Dr. Das said.
“You shouldn’t have to put your baby in a car, possibly in freezing temperatures, hire someone to take care of your other kids, drive to the hospital, pay for parking, and walk to the office for a weight check,” Dr. Das said.
Dr. Das noted that, because of technical errors, parents weren’t able to use remote monitoring and had in-person visits during the first 5 days of life. The intervention group had more visits during that period than the usual-care group.
The study was funded by the American Academy of Pediatrics. The authors and Dr. Das reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
WASHINGTON, D.C. – according to a new study presented at the Pediatric Academic Societies annual meeting.
The pilot trial compared the frequency of office visits for healthy babies born at 37 weeks’ gestation or later. One group of 20 infants had their weight monitored at home by parents, and another group of 20 infants received usual care, which included two in-person office visits over the first 6 weeks of life.
Researchers found that visits for infants in the intervention group decreased by 25% after the first week of life and by 23% after the second week.
The remote method can help alert physicians earlier to insufficient weight because parents report gains or losses three times a week over the 6 weeks, resulting in more data for providers.
“You’re going to see fewer visits with people who have scales because the docs are getting the information they need, which is: ‘Is this baby doing okay or not?’ ” said Diane DiTomasso, PhD, RN, a professor at the University of Rhode Island, South Kingstown, who was not involved with the study. “I think it’s a very necessary study because, to my knowledge, nobody has done a randomized controlled trial on this topic.”
Keeping infants at home can also protect babies from infections they might catch in the clinic.
“There are a lot of other kids in an office setting, and kids like touching things,” said Anirudha Das, MD, MPH, a neonatologist at Cleveland Clinic Children’s and the lead author of the study. “When there are a lot of other kids, there are a lot of viruses. It’s a very dangerous environment.”
Parents in the intervention group were given scales and asked to enter their infant’s weight into a patient portal app three times per week for 6 weeks. Physicians then determined if in-office visits were necessary.
The benefits of home weight checks can include helping to allow for breastfeeding for a longer duration.
Weight is more closely monitored for breastfed infants. Waiting weeks for office checks can heighten parental anxiety and lead to prematurely stopping breastfeeding. With regular at-home checks, parents receive up-to-date information from physicians that can alleviate concerns and empower them with more control over the process, according to Dr. DiTomasso.
Breastfeeding is associated with a lower risk for cardiovascular disease, diabetes, obesity, cancer in later life, and a lower risk of breast cancer for breastfeeding parents.
Office weight checks can also alleviate a significant and unnecessary burden for parents, Dr. Das said.
“You shouldn’t have to put your baby in a car, possibly in freezing temperatures, hire someone to take care of your other kids, drive to the hospital, pay for parking, and walk to the office for a weight check,” Dr. Das said.
Dr. Das noted that, because of technical errors, parents weren’t able to use remote monitoring and had in-person visits during the first 5 days of life. The intervention group had more visits during that period than the usual-care group.
The study was funded by the American Academy of Pediatrics. The authors and Dr. Das reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
WASHINGTON, D.C. – according to a new study presented at the Pediatric Academic Societies annual meeting.
The pilot trial compared the frequency of office visits for healthy babies born at 37 weeks’ gestation or later. One group of 20 infants had their weight monitored at home by parents, and another group of 20 infants received usual care, which included two in-person office visits over the first 6 weeks of life.
Researchers found that visits for infants in the intervention group decreased by 25% after the first week of life and by 23% after the second week.
The remote method can help alert physicians earlier to insufficient weight because parents report gains or losses three times a week over the 6 weeks, resulting in more data for providers.
“You’re going to see fewer visits with people who have scales because the docs are getting the information they need, which is: ‘Is this baby doing okay or not?’ ” said Diane DiTomasso, PhD, RN, a professor at the University of Rhode Island, South Kingstown, who was not involved with the study. “I think it’s a very necessary study because, to my knowledge, nobody has done a randomized controlled trial on this topic.”
Keeping infants at home can also protect babies from infections they might catch in the clinic.
“There are a lot of other kids in an office setting, and kids like touching things,” said Anirudha Das, MD, MPH, a neonatologist at Cleveland Clinic Children’s and the lead author of the study. “When there are a lot of other kids, there are a lot of viruses. It’s a very dangerous environment.”
Parents in the intervention group were given scales and asked to enter their infant’s weight into a patient portal app three times per week for 6 weeks. Physicians then determined if in-office visits were necessary.
The benefits of home weight checks can include helping to allow for breastfeeding for a longer duration.
Weight is more closely monitored for breastfed infants. Waiting weeks for office checks can heighten parental anxiety and lead to prematurely stopping breastfeeding. With regular at-home checks, parents receive up-to-date information from physicians that can alleviate concerns and empower them with more control over the process, according to Dr. DiTomasso.
Breastfeeding is associated with a lower risk for cardiovascular disease, diabetes, obesity, cancer in later life, and a lower risk of breast cancer for breastfeeding parents.
Office weight checks can also alleviate a significant and unnecessary burden for parents, Dr. Das said.
“You shouldn’t have to put your baby in a car, possibly in freezing temperatures, hire someone to take care of your other kids, drive to the hospital, pay for parking, and walk to the office for a weight check,” Dr. Das said.
Dr. Das noted that, because of technical errors, parents weren’t able to use remote monitoring and had in-person visits during the first 5 days of life. The intervention group had more visits during that period than the usual-care group.
The study was funded by the American Academy of Pediatrics. The authors and Dr. Das reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
AT PAS 2023
Osteoporosis and osteopenia: Latest treatment recommendations
This transcript has been edited for clarity.
I’m Dr. Neil Skolnik. Today’s topic is the new osteoporosis treatment guidelines issued by the American College of Physicians (ACP). The focus of the guidelines is treatment of osteoporosis. But first, I want to discuss screening.
In its 2018 statement, the U.S. Preventive Services Task Force (USPSTF) says that osteoporosis should be screened for in women older than 65 years of age, and those who are younger who are at increased risk based on a risk assessment tool (usually the FRAX tool). There is not enough evidence to weigh in for or against screening men. The other large organization that weighs in on screening is the Bone Health & Osteoporosis Foundation, which agrees with the USPSTF, but in addition says that we should be screening men over age 70 and men who are younger (age 50 to 69) who have risk factors. We should also screen anyone who has a fracture after low impact or no trauma.
Let’s now go on to the ACP treatment guidelines. Osteoporosis is defined as bone mineral density at the femoral neck or the lumbar spine, or both, with a T score less than -2.5.
For postmenopausal women with osteoporosis, you should use a bisphosphonate as first-line treatment to reduce the risk for future fractures. This is given a strong recommendation based on a high certainty of evidence. Bisphosphonates vs. placebo over 3 years leads to one fewer hip fracture per 150 patients treated and one fewer vertebral fracture per 50 people treated.
All the other recommendations in the guidelines are considered “conditional recommendations” that are correct for most people. But whether they make sense for an individual patient depends upon other details, as well as their values and preferences. For instance, treatment of osteoporosis in men is given a conditional recommendation, not because the evidence suggests that it’s not as effective, but because there is not as much evidence. Initial treatment for a man with osteoporosis is with bisphosphonates. Men do get osteoporosis and account for about 30% of hip fractures. This is not a surprise to anyone who takes care of older adults.
For postmenopausal women or men who you would want to treat but who can’t tolerate a bisphosphonate, then the recommendation is to use a RANK ligand inhibitor. Denosumab can be used as second-line treatment to reduce the risk for fractures. Remember, bisphosphonates and denosumab are antiresorptive drugs, meaning they slow the progression of osteoporosis. The anabolic drugs, on the other hand, such as the sclerostin inhibitor romosozumab and recombinant human parathyroid hormone (PTH) teriparatide, increase bone density. The anabolic agents should be used only in women with primary osteoporosis who are at very high risk for fractures, and use of these agents always needs to be followed by an antiresorptive agent, because otherwise there’s a risk for rebound osteoporosis and an increased risk for vertebral fractures.
Now, how about osteopenia? The guidelines recommend that for women over 65 with osteopenia, use an individualized approach influenced by the level of risk for fracture, including increased age, low body weight, current smoking, hip fracture in a parent, fall risk, and a personal history of fracture. The guidelines note that increasing the duration of bisphosphonate therapy beyond 3-5 years does reduce the risk for new vertebral fractures, but it doesn’t reduce the risk for other fractures and it increases the risk for osteonecrosis of the jaw and atypical hip fractures. Therefore, the guidelines say that we should use bisphosphonates only for 3-5 years unless someone is at extremely high risk. It’s also important to note that there’s a fivefold higher risk for atypical femoral fractures among Asian women.
Don’t forget about adequate vitamin D and calcium. And most importantly, don’t forget about exercise, particularly exercise aimed at improving balance and quadriceps strength, which helps prevent falls.
Dr. Skolnik is professor, department of family medicine, Sidney Kimmel Medical College of Thomas Jefferson University, Philadelphia, and associate director, department of family medicine, Abington (Pa.) Jefferson Health. He disclosed ties with AstraZeneca, Bayer, Boehringer Ingelheim, Eli Lilly, GlaxoSmithKline, Merck, Sanofi, Sanofi Pasteur, and Teva.
A version of this article originally appeared on Medscape.com.
This transcript has been edited for clarity.
I’m Dr. Neil Skolnik. Today’s topic is the new osteoporosis treatment guidelines issued by the American College of Physicians (ACP). The focus of the guidelines is treatment of osteoporosis. But first, I want to discuss screening.
In its 2018 statement, the U.S. Preventive Services Task Force (USPSTF) says that osteoporosis should be screened for in women older than 65 years of age, and those who are younger who are at increased risk based on a risk assessment tool (usually the FRAX tool). There is not enough evidence to weigh in for or against screening men. The other large organization that weighs in on screening is the Bone Health & Osteoporosis Foundation, which agrees with the USPSTF, but in addition says that we should be screening men over age 70 and men who are younger (age 50 to 69) who have risk factors. We should also screen anyone who has a fracture after low impact or no trauma.
Let’s now go on to the ACP treatment guidelines. Osteoporosis is defined as bone mineral density at the femoral neck or the lumbar spine, or both, with a T score less than -2.5.
For postmenopausal women with osteoporosis, you should use a bisphosphonate as first-line treatment to reduce the risk for future fractures. This is given a strong recommendation based on a high certainty of evidence. Bisphosphonates vs. placebo over 3 years leads to one fewer hip fracture per 150 patients treated and one fewer vertebral fracture per 50 people treated.
All the other recommendations in the guidelines are considered “conditional recommendations” that are correct for most people. But whether they make sense for an individual patient depends upon other details, as well as their values and preferences. For instance, treatment of osteoporosis in men is given a conditional recommendation, not because the evidence suggests that it’s not as effective, but because there is not as much evidence. Initial treatment for a man with osteoporosis is with bisphosphonates. Men do get osteoporosis and account for about 30% of hip fractures. This is not a surprise to anyone who takes care of older adults.
For postmenopausal women or men who you would want to treat but who can’t tolerate a bisphosphonate, then the recommendation is to use a RANK ligand inhibitor. Denosumab can be used as second-line treatment to reduce the risk for fractures. Remember, bisphosphonates and denosumab are antiresorptive drugs, meaning they slow the progression of osteoporosis. The anabolic drugs, on the other hand, such as the sclerostin inhibitor romosozumab and recombinant human parathyroid hormone (PTH) teriparatide, increase bone density. The anabolic agents should be used only in women with primary osteoporosis who are at very high risk for fractures, and use of these agents always needs to be followed by an antiresorptive agent, because otherwise there’s a risk for rebound osteoporosis and an increased risk for vertebral fractures.
Now, how about osteopenia? The guidelines recommend that for women over 65 with osteopenia, use an individualized approach influenced by the level of risk for fracture, including increased age, low body weight, current smoking, hip fracture in a parent, fall risk, and a personal history of fracture. The guidelines note that increasing the duration of bisphosphonate therapy beyond 3-5 years does reduce the risk for new vertebral fractures, but it doesn’t reduce the risk for other fractures and it increases the risk for osteonecrosis of the jaw and atypical hip fractures. Therefore, the guidelines say that we should use bisphosphonates only for 3-5 years unless someone is at extremely high risk. It’s also important to note that there’s a fivefold higher risk for atypical femoral fractures among Asian women.
Don’t forget about adequate vitamin D and calcium. And most importantly, don’t forget about exercise, particularly exercise aimed at improving balance and quadriceps strength, which helps prevent falls.
Dr. Skolnik is professor, department of family medicine, Sidney Kimmel Medical College of Thomas Jefferson University, Philadelphia, and associate director, department of family medicine, Abington (Pa.) Jefferson Health. He disclosed ties with AstraZeneca, Bayer, Boehringer Ingelheim, Eli Lilly, GlaxoSmithKline, Merck, Sanofi, Sanofi Pasteur, and Teva.
A version of this article originally appeared on Medscape.com.
This transcript has been edited for clarity.
I’m Dr. Neil Skolnik. Today’s topic is the new osteoporosis treatment guidelines issued by the American College of Physicians (ACP). The focus of the guidelines is treatment of osteoporosis. But first, I want to discuss screening.
In its 2018 statement, the U.S. Preventive Services Task Force (USPSTF) says that osteoporosis should be screened for in women older than 65 years of age, and those who are younger who are at increased risk based on a risk assessment tool (usually the FRAX tool). There is not enough evidence to weigh in for or against screening men. The other large organization that weighs in on screening is the Bone Health & Osteoporosis Foundation, which agrees with the USPSTF, but in addition says that we should be screening men over age 70 and men who are younger (age 50 to 69) who have risk factors. We should also screen anyone who has a fracture after low impact or no trauma.
Let’s now go on to the ACP treatment guidelines. Osteoporosis is defined as bone mineral density at the femoral neck or the lumbar spine, or both, with a T score less than -2.5.
For postmenopausal women with osteoporosis, you should use a bisphosphonate as first-line treatment to reduce the risk for future fractures. This is given a strong recommendation based on a high certainty of evidence. Bisphosphonates vs. placebo over 3 years leads to one fewer hip fracture per 150 patients treated and one fewer vertebral fracture per 50 people treated.
All the other recommendations in the guidelines are considered “conditional recommendations” that are correct for most people. But whether they make sense for an individual patient depends upon other details, as well as their values and preferences. For instance, treatment of osteoporosis in men is given a conditional recommendation, not because the evidence suggests that it’s not as effective, but because there is not as much evidence. Initial treatment for a man with osteoporosis is with bisphosphonates. Men do get osteoporosis and account for about 30% of hip fractures. This is not a surprise to anyone who takes care of older adults.
For postmenopausal women or men who you would want to treat but who can’t tolerate a bisphosphonate, then the recommendation is to use a RANK ligand inhibitor. Denosumab can be used as second-line treatment to reduce the risk for fractures. Remember, bisphosphonates and denosumab are antiresorptive drugs, meaning they slow the progression of osteoporosis. The anabolic drugs, on the other hand, such as the sclerostin inhibitor romosozumab and recombinant human parathyroid hormone (PTH) teriparatide, increase bone density. The anabolic agents should be used only in women with primary osteoporosis who are at very high risk for fractures, and use of these agents always needs to be followed by an antiresorptive agent, because otherwise there’s a risk for rebound osteoporosis and an increased risk for vertebral fractures.
Now, how about osteopenia? The guidelines recommend that for women over 65 with osteopenia, use an individualized approach influenced by the level of risk for fracture, including increased age, low body weight, current smoking, hip fracture in a parent, fall risk, and a personal history of fracture. The guidelines note that increasing the duration of bisphosphonate therapy beyond 3-5 years does reduce the risk for new vertebral fractures, but it doesn’t reduce the risk for other fractures and it increases the risk for osteonecrosis of the jaw and atypical hip fractures. Therefore, the guidelines say that we should use bisphosphonates only for 3-5 years unless someone is at extremely high risk. It’s also important to note that there’s a fivefold higher risk for atypical femoral fractures among Asian women.
Don’t forget about adequate vitamin D and calcium. And most importantly, don’t forget about exercise, particularly exercise aimed at improving balance and quadriceps strength, which helps prevent falls.
Dr. Skolnik is professor, department of family medicine, Sidney Kimmel Medical College of Thomas Jefferson University, Philadelphia, and associate director, department of family medicine, Abington (Pa.) Jefferson Health. He disclosed ties with AstraZeneca, Bayer, Boehringer Ingelheim, Eli Lilly, GlaxoSmithKline, Merck, Sanofi, Sanofi Pasteur, and Teva.
A version of this article originally appeared on Medscape.com.
Liver disease does not worsen IVF outcomes
Having chronic liver disease does not affect outcomes for women who undergo in vitro fertilization (IVF), new research suggests.
The study, published online in the American Journal of Gastroenterology, compared women with and those without chronic liver disease who had normal ovarian reserve and who underwent assisted reproductive technology (ART) treatment in a high-volume fertility practice from 2002 to 2021.
“IVF treatment and pregnancy outcomes were not significantly different compared to controls,” the researchers wrote.
Women with liver disease may experience impaired fertility. For example, women with chronic liver disease, such as hepatitis C virus infection, may have premature ovarian insufficiency, while women with advanced liver disease, cirrhosis, and hepatic decompensation are known to have abnormally low gonadotropin levels.
leading to “an immediate need for the clinical assessment of reproductive potential in women with chronic liver disease,” the authors wrote.
The literature about ART treatment outcomes for women with liver disease was limited and may not reflect current therapy protocols, researchers found.
“To the best of our knowledge, this study is the largest to date to evaluate IVF efficacy in women with liver disease,” they wrote.
Similar outcomes
Researchers identified 295 women with liver disease (mean age, 37.8 ± 5.2 years) who underwent 1,033 contemporary, standard ART treatment cycles. Six patients (2%) had cirrhosis, eight (2.7%) had undergone liver transplantation, and 281 (95.3%) had chronic liver disease, of which viral hepatitis B and C infections were the most prevalent. The final study population consisted of 115 women who underwent 186 IVF cycles, as well as embryo biopsy for genetic testing.
The control group consisted of all the women at the treatment center without liver disease who received contemporary, standard ART treatment because of male factor infertility, which served as an indication that the women had normal ovarian reserve and were considered fertile. These 624 patients underwent 868 IVF cycles with embryo biopsy.
The mean age of the patients with liver disease was significantly higher than that of the control participants. Mean body mass index was also significantly higher for the patients with liver disease, and there were differences in baseline levels of selected hormones, compared with control participants. In addition, among those with liver disease, the number of oocytes retrieved was significantly lower (12.3 ± 7.6 vs. 16.5 ± 8.2; P < .05), as were the number of mature oocytes (9.1 ± 6.2 vs. 12.6 ± 6.7; P < .05), the number of fertilized embryos (7.0 ± 5.2 vs. 9.9 ± 5.9; P < .05), the number of embryos for which biopsy was performed (3.4 ± 2.2 vs. 5.1 ± 3.5; P < .05), and the number of euploid embryos (1.6 ± 1.4 vs. 2.7 ± 2.4; P < .05), compared with control participants.
Among the two groups, there were no statistically significant differences in mature oocyte rate (an indicator of response to controlled ovarian stimulation), fertilization per mature oocyte rate (an indicator of oocyte quality and ability to be fertilized), or embryo ploidy rate (an indicator of genetically normal embryos), as determined by embryo biopsy, the researchers write.
A subanalysis of women who went on to have a single thawed euploid (chromosomally normal) embryo transfer to achieve pregnancy found no statistically significant differences in rates of clinical pregnancy, clinical pregnancy loss, or live births between the liver disease group and the control group.
“Overall, women with chronic liver disease can be counseled that IVF treatment will not significantly differ in response to controlled ovarian stimulation, embryo fertilization rate, or ploidy outcome compared to women without liver disease,” the researchers wrote.
Data for patient counseling
The results could change the current common thinking among clinicians that IVF should not be conducted until liver disease is under optimal control, first author Jessica Lee, BS, a student at Icahn School of Medicine at Mount Sinai, New York, said.
“There was a knowledge gap for studies in the United States, and we hope this study will not only help patients with liver disease but also providers with counseling,” she said.
The findings suggest that “even if you have chronic liver disease and it’s not fully optimized, that should not interfere with pursuing IVF,” said principal investigator Tatyana Kushner, MD, an associate professor of medicine in liver diseases at the Icahn School.
Women with liver disease whose fertility is impaired should receive counseling about fertility preservation options earlier to help access fertility care, the researchers write.
The study’s findings are “encouraging,” said Monika Sarkar, MD, associate professor of medicine in gastroenterology at the University of California, San Francisco.
“With rising numbers of young adults with liver disease, it is encouraging to see dedicated studies that address a topic of importance to our patients – namely, their reproductive health,” she said. “The current study nicely expands beyond previous data to include a control population without liver disease.”
Differences in oocyte numbers
Although there were no differences in the success rate of embryo transfer, the researchers did see differences in the number of oocytes. Only 37 mature oocytes made it to transfer in the liver disease group, compared with 609 in the control group, noted Dr. Sarkar, who was not involved with the study.
“The challenge of ART is less at the level of embryo transfer, which is very successful once a euploid embryo is achieved, but rather at the earlier step of retrieval of mature oocytes,” Dr. Sarkar said. “Here, the authors found that patients with liver disease had a significantly lower number of oocytes retrieved, number of mature oocytes, and lower number of fertilized embryos.”
The data suggest that fewer eggs are retrieved per cycle from patients with liver disease, “which ultimately will lower the success per cycle,” Dr. Sarkar said.
“This suggests that referring women with chronic liver disease to ART sooner may help to optimize outcomes,” she added. “Larger data evaluating ability to achieve mature oocytes and subsequent fertilization will also be key for determining whether ART success differs by presence, severity, and type of liver disease.”
As more research on ART outcomes in women with liver disease is conducted, subspecialists in gastrointestinal and liver disease may gain confidence in counseling patients, Dr. Sarkar said.
Ms. Lee, Dr. Kushner, and Dr. Sarkar report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Having chronic liver disease does not affect outcomes for women who undergo in vitro fertilization (IVF), new research suggests.
The study, published online in the American Journal of Gastroenterology, compared women with and those without chronic liver disease who had normal ovarian reserve and who underwent assisted reproductive technology (ART) treatment in a high-volume fertility practice from 2002 to 2021.
“IVF treatment and pregnancy outcomes were not significantly different compared to controls,” the researchers wrote.
Women with liver disease may experience impaired fertility. For example, women with chronic liver disease, such as hepatitis C virus infection, may have premature ovarian insufficiency, while women with advanced liver disease, cirrhosis, and hepatic decompensation are known to have abnormally low gonadotropin levels.
leading to “an immediate need for the clinical assessment of reproductive potential in women with chronic liver disease,” the authors wrote.
The literature about ART treatment outcomes for women with liver disease was limited and may not reflect current therapy protocols, researchers found.
“To the best of our knowledge, this study is the largest to date to evaluate IVF efficacy in women with liver disease,” they wrote.
Similar outcomes
Researchers identified 295 women with liver disease (mean age, 37.8 ± 5.2 years) who underwent 1,033 contemporary, standard ART treatment cycles. Six patients (2%) had cirrhosis, eight (2.7%) had undergone liver transplantation, and 281 (95.3%) had chronic liver disease, of which viral hepatitis B and C infections were the most prevalent. The final study population consisted of 115 women who underwent 186 IVF cycles, as well as embryo biopsy for genetic testing.
The control group consisted of all the women at the treatment center without liver disease who received contemporary, standard ART treatment because of male factor infertility, which served as an indication that the women had normal ovarian reserve and were considered fertile. These 624 patients underwent 868 IVF cycles with embryo biopsy.
The mean age of the patients with liver disease was significantly higher than that of the control participants. Mean body mass index was also significantly higher for the patients with liver disease, and there were differences in baseline levels of selected hormones, compared with control participants. In addition, among those with liver disease, the number of oocytes retrieved was significantly lower (12.3 ± 7.6 vs. 16.5 ± 8.2; P < .05), as were the number of mature oocytes (9.1 ± 6.2 vs. 12.6 ± 6.7; P < .05), the number of fertilized embryos (7.0 ± 5.2 vs. 9.9 ± 5.9; P < .05), the number of embryos for which biopsy was performed (3.4 ± 2.2 vs. 5.1 ± 3.5; P < .05), and the number of euploid embryos (1.6 ± 1.4 vs. 2.7 ± 2.4; P < .05), compared with control participants.
Among the two groups, there were no statistically significant differences in mature oocyte rate (an indicator of response to controlled ovarian stimulation), fertilization per mature oocyte rate (an indicator of oocyte quality and ability to be fertilized), or embryo ploidy rate (an indicator of genetically normal embryos), as determined by embryo biopsy, the researchers write.
A subanalysis of women who went on to have a single thawed euploid (chromosomally normal) embryo transfer to achieve pregnancy found no statistically significant differences in rates of clinical pregnancy, clinical pregnancy loss, or live births between the liver disease group and the control group.
“Overall, women with chronic liver disease can be counseled that IVF treatment will not significantly differ in response to controlled ovarian stimulation, embryo fertilization rate, or ploidy outcome compared to women without liver disease,” the researchers wrote.
Data for patient counseling
The results could change the current common thinking among clinicians that IVF should not be conducted until liver disease is under optimal control, first author Jessica Lee, BS, a student at Icahn School of Medicine at Mount Sinai, New York, said.
“There was a knowledge gap for studies in the United States, and we hope this study will not only help patients with liver disease but also providers with counseling,” she said.
The findings suggest that “even if you have chronic liver disease and it’s not fully optimized, that should not interfere with pursuing IVF,” said principal investigator Tatyana Kushner, MD, an associate professor of medicine in liver diseases at the Icahn School.
Women with liver disease whose fertility is impaired should receive counseling about fertility preservation options earlier to help access fertility care, the researchers write.
The study’s findings are “encouraging,” said Monika Sarkar, MD, associate professor of medicine in gastroenterology at the University of California, San Francisco.
“With rising numbers of young adults with liver disease, it is encouraging to see dedicated studies that address a topic of importance to our patients – namely, their reproductive health,” she said. “The current study nicely expands beyond previous data to include a control population without liver disease.”
Differences in oocyte numbers
Although there were no differences in the success rate of embryo transfer, the researchers did see differences in the number of oocytes. Only 37 mature oocytes made it to transfer in the liver disease group, compared with 609 in the control group, noted Dr. Sarkar, who was not involved with the study.
“The challenge of ART is less at the level of embryo transfer, which is very successful once a euploid embryo is achieved, but rather at the earlier step of retrieval of mature oocytes,” Dr. Sarkar said. “Here, the authors found that patients with liver disease had a significantly lower number of oocytes retrieved, number of mature oocytes, and lower number of fertilized embryos.”
The data suggest that fewer eggs are retrieved per cycle from patients with liver disease, “which ultimately will lower the success per cycle,” Dr. Sarkar said.
“This suggests that referring women with chronic liver disease to ART sooner may help to optimize outcomes,” she added. “Larger data evaluating ability to achieve mature oocytes and subsequent fertilization will also be key for determining whether ART success differs by presence, severity, and type of liver disease.”
As more research on ART outcomes in women with liver disease is conducted, subspecialists in gastrointestinal and liver disease may gain confidence in counseling patients, Dr. Sarkar said.
Ms. Lee, Dr. Kushner, and Dr. Sarkar report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Having chronic liver disease does not affect outcomes for women who undergo in vitro fertilization (IVF), new research suggests.
The study, published online in the American Journal of Gastroenterology, compared women with and those without chronic liver disease who had normal ovarian reserve and who underwent assisted reproductive technology (ART) treatment in a high-volume fertility practice from 2002 to 2021.
“IVF treatment and pregnancy outcomes were not significantly different compared to controls,” the researchers wrote.
Women with liver disease may experience impaired fertility. For example, women with chronic liver disease, such as hepatitis C virus infection, may have premature ovarian insufficiency, while women with advanced liver disease, cirrhosis, and hepatic decompensation are known to have abnormally low gonadotropin levels.
leading to “an immediate need for the clinical assessment of reproductive potential in women with chronic liver disease,” the authors wrote.
The literature about ART treatment outcomes for women with liver disease was limited and may not reflect current therapy protocols, researchers found.
“To the best of our knowledge, this study is the largest to date to evaluate IVF efficacy in women with liver disease,” they wrote.
Similar outcomes
Researchers identified 295 women with liver disease (mean age, 37.8 ± 5.2 years) who underwent 1,033 contemporary, standard ART treatment cycles. Six patients (2%) had cirrhosis, eight (2.7%) had undergone liver transplantation, and 281 (95.3%) had chronic liver disease, of which viral hepatitis B and C infections were the most prevalent. The final study population consisted of 115 women who underwent 186 IVF cycles, as well as embryo biopsy for genetic testing.
The control group consisted of all the women at the treatment center without liver disease who received contemporary, standard ART treatment because of male factor infertility, which served as an indication that the women had normal ovarian reserve and were considered fertile. These 624 patients underwent 868 IVF cycles with embryo biopsy.
The mean age of the patients with liver disease was significantly higher than that of the control participants. Mean body mass index was also significantly higher for the patients with liver disease, and there were differences in baseline levels of selected hormones, compared with control participants. In addition, among those with liver disease, the number of oocytes retrieved was significantly lower (12.3 ± 7.6 vs. 16.5 ± 8.2; P < .05), as were the number of mature oocytes (9.1 ± 6.2 vs. 12.6 ± 6.7; P < .05), the number of fertilized embryos (7.0 ± 5.2 vs. 9.9 ± 5.9; P < .05), the number of embryos for which biopsy was performed (3.4 ± 2.2 vs. 5.1 ± 3.5; P < .05), and the number of euploid embryos (1.6 ± 1.4 vs. 2.7 ± 2.4; P < .05), compared with control participants.
Among the two groups, there were no statistically significant differences in mature oocyte rate (an indicator of response to controlled ovarian stimulation), fertilization per mature oocyte rate (an indicator of oocyte quality and ability to be fertilized), or embryo ploidy rate (an indicator of genetically normal embryos), as determined by embryo biopsy, the researchers write.
A subanalysis of women who went on to have a single thawed euploid (chromosomally normal) embryo transfer to achieve pregnancy found no statistically significant differences in rates of clinical pregnancy, clinical pregnancy loss, or live births between the liver disease group and the control group.
“Overall, women with chronic liver disease can be counseled that IVF treatment will not significantly differ in response to controlled ovarian stimulation, embryo fertilization rate, or ploidy outcome compared to women without liver disease,” the researchers wrote.
Data for patient counseling
The results could change the current common thinking among clinicians that IVF should not be conducted until liver disease is under optimal control, first author Jessica Lee, BS, a student at Icahn School of Medicine at Mount Sinai, New York, said.
“There was a knowledge gap for studies in the United States, and we hope this study will not only help patients with liver disease but also providers with counseling,” she said.
The findings suggest that “even if you have chronic liver disease and it’s not fully optimized, that should not interfere with pursuing IVF,” said principal investigator Tatyana Kushner, MD, an associate professor of medicine in liver diseases at the Icahn School.
Women with liver disease whose fertility is impaired should receive counseling about fertility preservation options earlier to help access fertility care, the researchers write.
The study’s findings are “encouraging,” said Monika Sarkar, MD, associate professor of medicine in gastroenterology at the University of California, San Francisco.
“With rising numbers of young adults with liver disease, it is encouraging to see dedicated studies that address a topic of importance to our patients – namely, their reproductive health,” she said. “The current study nicely expands beyond previous data to include a control population without liver disease.”
Differences in oocyte numbers
Although there were no differences in the success rate of embryo transfer, the researchers did see differences in the number of oocytes. Only 37 mature oocytes made it to transfer in the liver disease group, compared with 609 in the control group, noted Dr. Sarkar, who was not involved with the study.
“The challenge of ART is less at the level of embryo transfer, which is very successful once a euploid embryo is achieved, but rather at the earlier step of retrieval of mature oocytes,” Dr. Sarkar said. “Here, the authors found that patients with liver disease had a significantly lower number of oocytes retrieved, number of mature oocytes, and lower number of fertilized embryos.”
The data suggest that fewer eggs are retrieved per cycle from patients with liver disease, “which ultimately will lower the success per cycle,” Dr. Sarkar said.
“This suggests that referring women with chronic liver disease to ART sooner may help to optimize outcomes,” she added. “Larger data evaluating ability to achieve mature oocytes and subsequent fertilization will also be key for determining whether ART success differs by presence, severity, and type of liver disease.”
As more research on ART outcomes in women with liver disease is conducted, subspecialists in gastrointestinal and liver disease may gain confidence in counseling patients, Dr. Sarkar said.
Ms. Lee, Dr. Kushner, and Dr. Sarkar report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF GASTROENTEROLOGY
Drive, chip, and putt your way to osteoarthritis relief
Taking a swing against arthritis
Osteoarthritis is a tough disease to manage. Exercise helps ease the stiffness and pain of the joints, but at the same time, the disease makes it difficult to do that beneficial exercise. Even a relatively simple activity like jogging can hurt more than it helps. If only there were a low-impact exercise that was incredibly popular among the generally older population who are likely to have arthritis.
We love a good golf study here at LOTME, and a group of Australian and U.K. researchers have provided. Osteoarthritis affects 2 million people in the land down under, making it the most common source of disability there. In that population, only 64% reported their physical health to be good, very good, or excellent. Among the 459 golfers with OA that the study authors surveyed, however, the percentage reporting good health rose to more than 90%.
A similar story emerged when they looked at mental health. Nearly a quarter of nongolfers with OA reported high or very high levels of psychological distress, compared with just 8% of golfers. This pattern of improved physical and mental health remained when the researchers looked at the general, non-OA population.
This isn’t the first time golf’s been connected with improved health, and previous studies have shown golf to reduce the risks of cardiovascular disease, diabetes, and obesity, among other things. Just walking one 18-hole round significantly exceeds the CDC’s recommended 150 minutes of physical activity per week. Go out multiple times a week – leaving the cart and beer at home, American golfers – and you’ll be fit for a lifetime.
The golfers on our staff, however, are still waiting for those mental health benefits to kick in. Because when we’re adding up our scorecard after that string of four double bogeys to end the round, we’re most definitely thinking: “Yes, this sport is reducing my psychological distress. I am having fun right now.”
Battle of the sexes’ intestines
There are, we’re sure you’ve noticed, some differences between males and females. Females, for one thing, have longer small intestines than males. Everybody knows that, right? You didn’t know? Really? … Really?
Well, then, we’re guessing you haven’t read “Hidden diversity: Comparative functional morphology of humans and other species” by Erin A. McKenney, PhD, of North Carolina State University, Raleigh, and associates, which just appeared in PeerJ. We couldn’t put it down, even in the shower – a real page-turner/scroller. (It’s a great way to clean a phone, for those who also like to scroll, text, or talk on the toilet.)
The researchers got out their rulers, calipers, and string and took many measurements of the digestive systems of 45 human cadavers (21 female and 24 male), which were compared with data from 10 rats, 10 pigs, and 10 bullfrogs, which had been collected (the measurements, not the animals) by undergraduate students enrolled in a comparative anatomy laboratory course at the university.
There was little intestinal-length variation among the four-legged subjects, but when it comes to humans, females have “consistently and significantly longer small intestines than males,” the investigators noted.
The women’s small intestines, almost 14 feet long on average, were about a foot longer than the men’s, which suggests that women are better able to extract nutrients from food and “supports the canalization hypothesis, which posits that women are better able to survive during periods of stress,” coauthor Amanda Hale said in a written statement from the school. The way to a man’s heart may be through his stomach, but the way to a woman’s heart is through her duodenum, it seems.
Fascinating stuff, to be sure, but the thing that really caught our eye in the PeerJ article was the authors’ suggestion “that organs behave independently of one another, both within and across species.” Organs behaving independently? A somewhat ominous concept, no doubt, but it does explain a lot of the sounds we hear coming from our guts, which can get pretty frightening, especially on chili night.
Dog walking is dangerous business
Yes, you did read that right. A lot of strange things can send you to the emergency department. Go ahead and add dog walking onto that list.
Investigators from Johns Hopkins University estimate that over 422,000 adults presented to U.S. emergency departments with leash-dependent dog walking-related injuries between 2001 and 2020.
With almost 53% of U.S. households owning at least one dog in 2021-2022 in the wake of the COVID pet boom, this kind of occurrence is becoming more common than you think. The annual number of dog-walking injuries more than quadrupled from 7,300 to 32,000 over the course of the study, and the researchers link that spike to the promotion of dog walking for fitness, along with the boost of ownership itself.
The most common injuries listed in the National Electronic Injury Surveillance System database were finger fracture, traumatic brain injury, and shoulder sprain or strain. These mostly involved falls from being pulled, tripped, or tangled up in the leash while walking. For those aged 65 years and older, traumatic brain injury and hip fracture were the most common.
Women were 50% more likely to sustain a fracture than were men, and dog owners aged 65 and older were three times as likely to fall, twice as likely to get a fracture, and 60% more likely to have brain injury than were younger people. Now, that’s not to say younger people don’t also get hurt. After all, dogs aren’t ageists. The researchers have that data but it’s coming out later.
Meanwhile, the pitfalls involved with just trying to get our daily steps in while letting Muffin do her business have us on the lookout for random squirrels.
Taking a swing against arthritis
Osteoarthritis is a tough disease to manage. Exercise helps ease the stiffness and pain of the joints, but at the same time, the disease makes it difficult to do that beneficial exercise. Even a relatively simple activity like jogging can hurt more than it helps. If only there were a low-impact exercise that was incredibly popular among the generally older population who are likely to have arthritis.
We love a good golf study here at LOTME, and a group of Australian and U.K. researchers have provided. Osteoarthritis affects 2 million people in the land down under, making it the most common source of disability there. In that population, only 64% reported their physical health to be good, very good, or excellent. Among the 459 golfers with OA that the study authors surveyed, however, the percentage reporting good health rose to more than 90%.
A similar story emerged when they looked at mental health. Nearly a quarter of nongolfers with OA reported high or very high levels of psychological distress, compared with just 8% of golfers. This pattern of improved physical and mental health remained when the researchers looked at the general, non-OA population.
This isn’t the first time golf’s been connected with improved health, and previous studies have shown golf to reduce the risks of cardiovascular disease, diabetes, and obesity, among other things. Just walking one 18-hole round significantly exceeds the CDC’s recommended 150 minutes of physical activity per week. Go out multiple times a week – leaving the cart and beer at home, American golfers – and you’ll be fit for a lifetime.
The golfers on our staff, however, are still waiting for those mental health benefits to kick in. Because when we’re adding up our scorecard after that string of four double bogeys to end the round, we’re most definitely thinking: “Yes, this sport is reducing my psychological distress. I am having fun right now.”
Battle of the sexes’ intestines
There are, we’re sure you’ve noticed, some differences between males and females. Females, for one thing, have longer small intestines than males. Everybody knows that, right? You didn’t know? Really? … Really?
Well, then, we’re guessing you haven’t read “Hidden diversity: Comparative functional morphology of humans and other species” by Erin A. McKenney, PhD, of North Carolina State University, Raleigh, and associates, which just appeared in PeerJ. We couldn’t put it down, even in the shower – a real page-turner/scroller. (It’s a great way to clean a phone, for those who also like to scroll, text, or talk on the toilet.)
The researchers got out their rulers, calipers, and string and took many measurements of the digestive systems of 45 human cadavers (21 female and 24 male), which were compared with data from 10 rats, 10 pigs, and 10 bullfrogs, which had been collected (the measurements, not the animals) by undergraduate students enrolled in a comparative anatomy laboratory course at the university.
There was little intestinal-length variation among the four-legged subjects, but when it comes to humans, females have “consistently and significantly longer small intestines than males,” the investigators noted.
The women’s small intestines, almost 14 feet long on average, were about a foot longer than the men’s, which suggests that women are better able to extract nutrients from food and “supports the canalization hypothesis, which posits that women are better able to survive during periods of stress,” coauthor Amanda Hale said in a written statement from the school. The way to a man’s heart may be through his stomach, but the way to a woman’s heart is through her duodenum, it seems.
Fascinating stuff, to be sure, but the thing that really caught our eye in the PeerJ article was the authors’ suggestion “that organs behave independently of one another, both within and across species.” Organs behaving independently? A somewhat ominous concept, no doubt, but it does explain a lot of the sounds we hear coming from our guts, which can get pretty frightening, especially on chili night.
Dog walking is dangerous business
Yes, you did read that right. A lot of strange things can send you to the emergency department. Go ahead and add dog walking onto that list.
Investigators from Johns Hopkins University estimate that over 422,000 adults presented to U.S. emergency departments with leash-dependent dog walking-related injuries between 2001 and 2020.
With almost 53% of U.S. households owning at least one dog in 2021-2022 in the wake of the COVID pet boom, this kind of occurrence is becoming more common than you think. The annual number of dog-walking injuries more than quadrupled from 7,300 to 32,000 over the course of the study, and the researchers link that spike to the promotion of dog walking for fitness, along with the boost of ownership itself.
The most common injuries listed in the National Electronic Injury Surveillance System database were finger fracture, traumatic brain injury, and shoulder sprain or strain. These mostly involved falls from being pulled, tripped, or tangled up in the leash while walking. For those aged 65 years and older, traumatic brain injury and hip fracture were the most common.
Women were 50% more likely to sustain a fracture than were men, and dog owners aged 65 and older were three times as likely to fall, twice as likely to get a fracture, and 60% more likely to have brain injury than were younger people. Now, that’s not to say younger people don’t also get hurt. After all, dogs aren’t ageists. The researchers have that data but it’s coming out later.
Meanwhile, the pitfalls involved with just trying to get our daily steps in while letting Muffin do her business have us on the lookout for random squirrels.
Taking a swing against arthritis
Osteoarthritis is a tough disease to manage. Exercise helps ease the stiffness and pain of the joints, but at the same time, the disease makes it difficult to do that beneficial exercise. Even a relatively simple activity like jogging can hurt more than it helps. If only there were a low-impact exercise that was incredibly popular among the generally older population who are likely to have arthritis.
We love a good golf study here at LOTME, and a group of Australian and U.K. researchers have provided. Osteoarthritis affects 2 million people in the land down under, making it the most common source of disability there. In that population, only 64% reported their physical health to be good, very good, or excellent. Among the 459 golfers with OA that the study authors surveyed, however, the percentage reporting good health rose to more than 90%.
A similar story emerged when they looked at mental health. Nearly a quarter of nongolfers with OA reported high or very high levels of psychological distress, compared with just 8% of golfers. This pattern of improved physical and mental health remained when the researchers looked at the general, non-OA population.
This isn’t the first time golf’s been connected with improved health, and previous studies have shown golf to reduce the risks of cardiovascular disease, diabetes, and obesity, among other things. Just walking one 18-hole round significantly exceeds the CDC’s recommended 150 minutes of physical activity per week. Go out multiple times a week – leaving the cart and beer at home, American golfers – and you’ll be fit for a lifetime.
The golfers on our staff, however, are still waiting for those mental health benefits to kick in. Because when we’re adding up our scorecard after that string of four double bogeys to end the round, we’re most definitely thinking: “Yes, this sport is reducing my psychological distress. I am having fun right now.”
Battle of the sexes’ intestines
There are, we’re sure you’ve noticed, some differences between males and females. Females, for one thing, have longer small intestines than males. Everybody knows that, right? You didn’t know? Really? … Really?
Well, then, we’re guessing you haven’t read “Hidden diversity: Comparative functional morphology of humans and other species” by Erin A. McKenney, PhD, of North Carolina State University, Raleigh, and associates, which just appeared in PeerJ. We couldn’t put it down, even in the shower – a real page-turner/scroller. (It’s a great way to clean a phone, for those who also like to scroll, text, or talk on the toilet.)
The researchers got out their rulers, calipers, and string and took many measurements of the digestive systems of 45 human cadavers (21 female and 24 male), which were compared with data from 10 rats, 10 pigs, and 10 bullfrogs, which had been collected (the measurements, not the animals) by undergraduate students enrolled in a comparative anatomy laboratory course at the university.
There was little intestinal-length variation among the four-legged subjects, but when it comes to humans, females have “consistently and significantly longer small intestines than males,” the investigators noted.
The women’s small intestines, almost 14 feet long on average, were about a foot longer than the men’s, which suggests that women are better able to extract nutrients from food and “supports the canalization hypothesis, which posits that women are better able to survive during periods of stress,” coauthor Amanda Hale said in a written statement from the school. The way to a man’s heart may be through his stomach, but the way to a woman’s heart is through her duodenum, it seems.
Fascinating stuff, to be sure, but the thing that really caught our eye in the PeerJ article was the authors’ suggestion “that organs behave independently of one another, both within and across species.” Organs behaving independently? A somewhat ominous concept, no doubt, but it does explain a lot of the sounds we hear coming from our guts, which can get pretty frightening, especially on chili night.
Dog walking is dangerous business
Yes, you did read that right. A lot of strange things can send you to the emergency department. Go ahead and add dog walking onto that list.
Investigators from Johns Hopkins University estimate that over 422,000 adults presented to U.S. emergency departments with leash-dependent dog walking-related injuries between 2001 and 2020.
With almost 53% of U.S. households owning at least one dog in 2021-2022 in the wake of the COVID pet boom, this kind of occurrence is becoming more common than you think. The annual number of dog-walking injuries more than quadrupled from 7,300 to 32,000 over the course of the study, and the researchers link that spike to the promotion of dog walking for fitness, along with the boost of ownership itself.
The most common injuries listed in the National Electronic Injury Surveillance System database were finger fracture, traumatic brain injury, and shoulder sprain or strain. These mostly involved falls from being pulled, tripped, or tangled up in the leash while walking. For those aged 65 years and older, traumatic brain injury and hip fracture were the most common.
Women were 50% more likely to sustain a fracture than were men, and dog owners aged 65 and older were three times as likely to fall, twice as likely to get a fracture, and 60% more likely to have brain injury than were younger people. Now, that’s not to say younger people don’t also get hurt. After all, dogs aren’t ageists. The researchers have that data but it’s coming out later.
Meanwhile, the pitfalls involved with just trying to get our daily steps in while letting Muffin do her business have us on the lookout for random squirrels.
‘Shocking’ data on what’s really in melatonin gummies
New data may explain the recent massive jump in pediatric hospitalizations.
Thenvestigators found that consuming some products as directed could expose consumers, including children, to doses that are 40-130 times greater than what’s recommended.
“The results were quite shocking,” lead researcher Pieter Cohen, MD, with Harvard Medical School, Boston, and Cambridge Health Alliance, Somerville, Mass., said in an interview.
“Melatonin gummies contained up to 347% more melatonin than what was listed on the label, and some products also contained cannabidiol; in one brand of melatonin gummies, there was zero melatonin, just CBD,” Dr. Cohen said.
The study was published online in JAMA.
530% jump in pediatric hospitalizations
Melatonin products are not approved by the Food and Drug Administration but are sold over the counter or online.
Previous research from JAMA has shown the use of melatonin has increased over the past 2 decades among people of all ages.
With increased use has come a spike in reports of melatonin overdose, calls to poison control centers, and related ED visits for children.
Federal data show the number of U.S. children who unintentionally ingested melatonin supplements jumped 530% from 2012 to 2021. More than 4,000 of the reported ingestions led to a hospital stay; 287 children required intensive care, and two children died.
It was unclear why melatonin supplements were causing these harms, which led Dr. Cohen’s team to analyze 25 unique brands of “melatonin” gummies purchased online.
One product didn’t contain any melatonin but did contain 31.3 mg of CBD.
In the remaining products, the quantity of melatonin ranged from 1.3 mg to 13.1 mg per serving. The actual quantity of melatonin ranged from 74% to 347% of the labeled quantity, the researchers found.
They note that for a young adult who takes as little as 0.1-0.3 mg of melatonin, plasma concentrations can increase into the normal night-time range.
Of the 25 products (88%) analyzed, 22 were inaccurately labeled, and only 3 (12%) contained a quantity of melatonin that was within 10% (plus or minus) of the declared quantity.
Five products listed CBD as an ingredient. The listed quantity ranged from 10.6 mg to 31.3 mg per serving, although the actual quantity of CBD ranged from 104% to 118% of the labeled quantity.
Inquire about use in kids
A limitation of the study is that only one sample of each brand was analyzed, and only gummies were analyzed. It is not known whether the results are generalizable to melatonin products sold as tablets and capsules in the United States or whether the quantity of melatonin within an individual brand may vary from batch to batch.
A recent study from Canada showed similar results. In an analysis of 16 Canadian melatonin brands, the actual dose of melatonin ranged from 17% to 478% of the declared quantity.
It’s estimated that more than 1% of all U.S. children use melatonin supplements, most commonly for sleep, stress, and relaxation.
“Given new research as to the excessive quantities of melatonin in gummies, caution should be used if considering their use,” said Dr. Cohen.
“It’s important to inquire about melatonin use when caring for children, particularly when parents express concerns about their child’s sleep,” he added.
The American Academy of Sleep Medicine recently issued a health advisory encouraging parents to talk to a health care professional before giving melatonin or any supplement to children.
Children don’t need melatonin
Commenting on the study, Michael Breus, PhD, clinical psychologist and founder of TheSleepDoctor.com, agreed that analyzing only one sample of each brand is a key limitation “because supplements are made in batches, and gummies in particular are difficult to distribute the active ingredient evenly.
“But even with that being said, 88% of them were labeled incorrectly, so even if there were a few single-sample issues, I kind of doubt its all of them,” Dr. Breus said.
“Kids as a general rule do not need melatonin. Their brains make almost four times the necessary amount already. If you start giving kids pills to help them sleep, then they start to have a pill problem, causing another issue,” Dr. Breus added.
“Most children’s falling asleep and staying sleep issues can be treated with behavioral measures like cognitive-behavioral therapy for insomnia,” he said.
The study had no specific funding. Dr. Cohen has received research support from Consumers Union and PEW Charitable Trusts and royalties from UptoDate. Dr. Breus disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New data may explain the recent massive jump in pediatric hospitalizations.
Thenvestigators found that consuming some products as directed could expose consumers, including children, to doses that are 40-130 times greater than what’s recommended.
“The results were quite shocking,” lead researcher Pieter Cohen, MD, with Harvard Medical School, Boston, and Cambridge Health Alliance, Somerville, Mass., said in an interview.
“Melatonin gummies contained up to 347% more melatonin than what was listed on the label, and some products also contained cannabidiol; in one brand of melatonin gummies, there was zero melatonin, just CBD,” Dr. Cohen said.
The study was published online in JAMA.
530% jump in pediatric hospitalizations
Melatonin products are not approved by the Food and Drug Administration but are sold over the counter or online.
Previous research from JAMA has shown the use of melatonin has increased over the past 2 decades among people of all ages.
With increased use has come a spike in reports of melatonin overdose, calls to poison control centers, and related ED visits for children.
Federal data show the number of U.S. children who unintentionally ingested melatonin supplements jumped 530% from 2012 to 2021. More than 4,000 of the reported ingestions led to a hospital stay; 287 children required intensive care, and two children died.
It was unclear why melatonin supplements were causing these harms, which led Dr. Cohen’s team to analyze 25 unique brands of “melatonin” gummies purchased online.
One product didn’t contain any melatonin but did contain 31.3 mg of CBD.
In the remaining products, the quantity of melatonin ranged from 1.3 mg to 13.1 mg per serving. The actual quantity of melatonin ranged from 74% to 347% of the labeled quantity, the researchers found.
They note that for a young adult who takes as little as 0.1-0.3 mg of melatonin, plasma concentrations can increase into the normal night-time range.
Of the 25 products (88%) analyzed, 22 were inaccurately labeled, and only 3 (12%) contained a quantity of melatonin that was within 10% (plus or minus) of the declared quantity.
Five products listed CBD as an ingredient. The listed quantity ranged from 10.6 mg to 31.3 mg per serving, although the actual quantity of CBD ranged from 104% to 118% of the labeled quantity.
Inquire about use in kids
A limitation of the study is that only one sample of each brand was analyzed, and only gummies were analyzed. It is not known whether the results are generalizable to melatonin products sold as tablets and capsules in the United States or whether the quantity of melatonin within an individual brand may vary from batch to batch.
A recent study from Canada showed similar results. In an analysis of 16 Canadian melatonin brands, the actual dose of melatonin ranged from 17% to 478% of the declared quantity.
It’s estimated that more than 1% of all U.S. children use melatonin supplements, most commonly for sleep, stress, and relaxation.
“Given new research as to the excessive quantities of melatonin in gummies, caution should be used if considering their use,” said Dr. Cohen.
“It’s important to inquire about melatonin use when caring for children, particularly when parents express concerns about their child’s sleep,” he added.
The American Academy of Sleep Medicine recently issued a health advisory encouraging parents to talk to a health care professional before giving melatonin or any supplement to children.
Children don’t need melatonin
Commenting on the study, Michael Breus, PhD, clinical psychologist and founder of TheSleepDoctor.com, agreed that analyzing only one sample of each brand is a key limitation “because supplements are made in batches, and gummies in particular are difficult to distribute the active ingredient evenly.
“But even with that being said, 88% of them were labeled incorrectly, so even if there were a few single-sample issues, I kind of doubt its all of them,” Dr. Breus said.
“Kids as a general rule do not need melatonin. Their brains make almost four times the necessary amount already. If you start giving kids pills to help them sleep, then they start to have a pill problem, causing another issue,” Dr. Breus added.
“Most children’s falling asleep and staying sleep issues can be treated with behavioral measures like cognitive-behavioral therapy for insomnia,” he said.
The study had no specific funding. Dr. Cohen has received research support from Consumers Union and PEW Charitable Trusts and royalties from UptoDate. Dr. Breus disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New data may explain the recent massive jump in pediatric hospitalizations.
Thenvestigators found that consuming some products as directed could expose consumers, including children, to doses that are 40-130 times greater than what’s recommended.
“The results were quite shocking,” lead researcher Pieter Cohen, MD, with Harvard Medical School, Boston, and Cambridge Health Alliance, Somerville, Mass., said in an interview.
“Melatonin gummies contained up to 347% more melatonin than what was listed on the label, and some products also contained cannabidiol; in one brand of melatonin gummies, there was zero melatonin, just CBD,” Dr. Cohen said.
The study was published online in JAMA.
530% jump in pediatric hospitalizations
Melatonin products are not approved by the Food and Drug Administration but are sold over the counter or online.
Previous research from JAMA has shown the use of melatonin has increased over the past 2 decades among people of all ages.
With increased use has come a spike in reports of melatonin overdose, calls to poison control centers, and related ED visits for children.
Federal data show the number of U.S. children who unintentionally ingested melatonin supplements jumped 530% from 2012 to 2021. More than 4,000 of the reported ingestions led to a hospital stay; 287 children required intensive care, and two children died.
It was unclear why melatonin supplements were causing these harms, which led Dr. Cohen’s team to analyze 25 unique brands of “melatonin” gummies purchased online.
One product didn’t contain any melatonin but did contain 31.3 mg of CBD.
In the remaining products, the quantity of melatonin ranged from 1.3 mg to 13.1 mg per serving. The actual quantity of melatonin ranged from 74% to 347% of the labeled quantity, the researchers found.
They note that for a young adult who takes as little as 0.1-0.3 mg of melatonin, plasma concentrations can increase into the normal night-time range.
Of the 25 products (88%) analyzed, 22 were inaccurately labeled, and only 3 (12%) contained a quantity of melatonin that was within 10% (plus or minus) of the declared quantity.
Five products listed CBD as an ingredient. The listed quantity ranged from 10.6 mg to 31.3 mg per serving, although the actual quantity of CBD ranged from 104% to 118% of the labeled quantity.
Inquire about use in kids
A limitation of the study is that only one sample of each brand was analyzed, and only gummies were analyzed. It is not known whether the results are generalizable to melatonin products sold as tablets and capsules in the United States or whether the quantity of melatonin within an individual brand may vary from batch to batch.
A recent study from Canada showed similar results. In an analysis of 16 Canadian melatonin brands, the actual dose of melatonin ranged from 17% to 478% of the declared quantity.
It’s estimated that more than 1% of all U.S. children use melatonin supplements, most commonly for sleep, stress, and relaxation.
“Given new research as to the excessive quantities of melatonin in gummies, caution should be used if considering their use,” said Dr. Cohen.
“It’s important to inquire about melatonin use when caring for children, particularly when parents express concerns about their child’s sleep,” he added.
The American Academy of Sleep Medicine recently issued a health advisory encouraging parents to talk to a health care professional before giving melatonin or any supplement to children.
Children don’t need melatonin
Commenting on the study, Michael Breus, PhD, clinical psychologist and founder of TheSleepDoctor.com, agreed that analyzing only one sample of each brand is a key limitation “because supplements are made in batches, and gummies in particular are difficult to distribute the active ingredient evenly.
“But even with that being said, 88% of them were labeled incorrectly, so even if there were a few single-sample issues, I kind of doubt its all of them,” Dr. Breus said.
“Kids as a general rule do not need melatonin. Their brains make almost four times the necessary amount already. If you start giving kids pills to help them sleep, then they start to have a pill problem, causing another issue,” Dr. Breus added.
“Most children’s falling asleep and staying sleep issues can be treated with behavioral measures like cognitive-behavioral therapy for insomnia,” he said.
The study had no specific funding. Dr. Cohen has received research support from Consumers Union and PEW Charitable Trusts and royalties from UptoDate. Dr. Breus disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA
New ABIM fees to stay listed as ‘board certified’ irk physicians
Abdul Moiz Hafiz, MD, was flabbergasted when he received a phone call from his institution’s credentialing office telling him that he was not certified for interventional cardiology – even though he had passed that exam in 2016.
Dr. Hafiz, who directs the Advanced Structural Heart Disease Program at Southern Illinois University, phoned the American Board of Internal Medicine (ABIM), where he learned that to restore his credentials, he would need to pay $1,225 in maintenance of certification (MOC) fees.
Like Dr. Hafiz,
Even doctors who are participating in mandatory continuing education outside the ABIM’s auspices are finding themselves listed as “not certified.” Some physicians learned of the policy change only after applying for hospital privileges or for jobs that require ABIM certification.
Now that increasing numbers of physicians are employed by hospitals and health care organizations that require ABIM certification, many doctors have no option but to pony up the fees if they want to continue to practice medicine.
“We have no say in the matter,” said Dr. Hafiz, “and there’s no appeal process.”
The change affects nearly 330,000 physicians. Responses to the policy on Twitter included accusations of extortion and denunciations of the ABIM’s “money grab policies.”
Sunil Rao, MD, director of interventional cardiology at NYU Langone Health and president of the Society for Cardiovascular Angiography and Interventions (SCAI), has heard from many SCAI members who had experiences similar to Dr. Hafiz’s. While Dr. Rao describes some of the Twitter outrage as “emotional,” he does acknowledge that the ABIM’s moves appear to be financially motivated.
“The issue here was that as soon as they paid the fee, all of a sudden, ABIM flipped the switch and said they were certified,” he said. “It certainly sounds like a purely financial kind of structure.”
Richard Baron, MD, president and CEO of the ABIM, said doctors are misunderstanding the policy change.
“No doctor loses certification solely for failure to pay fees,” Dr. Baron told this news organization. “What caused them to be reported as not certified was that we didn’t have evidence that they had met program requirements. They could say, ‘But I did meet program requirements, you just didn’t know it.’ To which our answer would be, for us to know it, we have to process them. And our policy is that we don’t process them unless you are current on your fees.”
This is not the first time ABIM policies have alienated physicians.
Last year, the ABIM raised its MOC fees from $165 to $220. That also prompted a wave of outrage. Other grievances go further back. At one time, being board certified was a lifetime credential. However, in 1990 the ABIM made periodic recertification mandatory.
The process, which came to be known as “maintenance of certification,” had to be completed every 10 years, and fees were charged for each certification. At that point, said Dr. Baron, the relationship between the ABIM and physicians changed from a one-time interaction to a career-long relationship. He advises doctors to check in periodically on their portal page at the ABIM or download the app so they will always know their status.
Many physicians would prefer not to be bound to a lifetime relationship with the ABIM. There is an alternative licensing board, the National Board of Physicians and Surgeons (NBPAS), but it is accepted by only a limited number of hospitals.
“Until the NBPAS gains wide recognition,” said Dr. Hafiz, “the ABIM is going to continue to have basically a monopoly over the market.”
The value of MOC itself has been called into question. “There are no direct data supporting the value of the MOC process in either improving care, making patient care safer, or making patient care higher quality,” said Dr. Rao. This feeds frustration in a clinical community already dealing with onerous training requirements and expensive board certification exams and adds to the perception that it is a purely financial transaction, he said. (Studies examining whether the MOC system improves patient care have shown mixed results.)
The true value of the ABIM to physicians, Dr. Baron contends, is that the organization is an independent third party that differentiates those doctors from people who don’t have their skills, training, and expertise. “In these days, where anyone can be an ‘expert’ on the Internet, that’s more valuable than ever before,” he said.
A version of this article first appeared on Medscape.com.
Abdul Moiz Hafiz, MD, was flabbergasted when he received a phone call from his institution’s credentialing office telling him that he was not certified for interventional cardiology – even though he had passed that exam in 2016.
Dr. Hafiz, who directs the Advanced Structural Heart Disease Program at Southern Illinois University, phoned the American Board of Internal Medicine (ABIM), where he learned that to restore his credentials, he would need to pay $1,225 in maintenance of certification (MOC) fees.
Like Dr. Hafiz,
Even doctors who are participating in mandatory continuing education outside the ABIM’s auspices are finding themselves listed as “not certified.” Some physicians learned of the policy change only after applying for hospital privileges or for jobs that require ABIM certification.
Now that increasing numbers of physicians are employed by hospitals and health care organizations that require ABIM certification, many doctors have no option but to pony up the fees if they want to continue to practice medicine.
“We have no say in the matter,” said Dr. Hafiz, “and there’s no appeal process.”
The change affects nearly 330,000 physicians. Responses to the policy on Twitter included accusations of extortion and denunciations of the ABIM’s “money grab policies.”
Sunil Rao, MD, director of interventional cardiology at NYU Langone Health and president of the Society for Cardiovascular Angiography and Interventions (SCAI), has heard from many SCAI members who had experiences similar to Dr. Hafiz’s. While Dr. Rao describes some of the Twitter outrage as “emotional,” he does acknowledge that the ABIM’s moves appear to be financially motivated.
“The issue here was that as soon as they paid the fee, all of a sudden, ABIM flipped the switch and said they were certified,” he said. “It certainly sounds like a purely financial kind of structure.”
Richard Baron, MD, president and CEO of the ABIM, said doctors are misunderstanding the policy change.
“No doctor loses certification solely for failure to pay fees,” Dr. Baron told this news organization. “What caused them to be reported as not certified was that we didn’t have evidence that they had met program requirements. They could say, ‘But I did meet program requirements, you just didn’t know it.’ To which our answer would be, for us to know it, we have to process them. And our policy is that we don’t process them unless you are current on your fees.”
This is not the first time ABIM policies have alienated physicians.
Last year, the ABIM raised its MOC fees from $165 to $220. That also prompted a wave of outrage. Other grievances go further back. At one time, being board certified was a lifetime credential. However, in 1990 the ABIM made periodic recertification mandatory.
The process, which came to be known as “maintenance of certification,” had to be completed every 10 years, and fees were charged for each certification. At that point, said Dr. Baron, the relationship between the ABIM and physicians changed from a one-time interaction to a career-long relationship. He advises doctors to check in periodically on their portal page at the ABIM or download the app so they will always know their status.
Many physicians would prefer not to be bound to a lifetime relationship with the ABIM. There is an alternative licensing board, the National Board of Physicians and Surgeons (NBPAS), but it is accepted by only a limited number of hospitals.
“Until the NBPAS gains wide recognition,” said Dr. Hafiz, “the ABIM is going to continue to have basically a monopoly over the market.”
The value of MOC itself has been called into question. “There are no direct data supporting the value of the MOC process in either improving care, making patient care safer, or making patient care higher quality,” said Dr. Rao. This feeds frustration in a clinical community already dealing with onerous training requirements and expensive board certification exams and adds to the perception that it is a purely financial transaction, he said. (Studies examining whether the MOC system improves patient care have shown mixed results.)
The true value of the ABIM to physicians, Dr. Baron contends, is that the organization is an independent third party that differentiates those doctors from people who don’t have their skills, training, and expertise. “In these days, where anyone can be an ‘expert’ on the Internet, that’s more valuable than ever before,” he said.
A version of this article first appeared on Medscape.com.
Abdul Moiz Hafiz, MD, was flabbergasted when he received a phone call from his institution’s credentialing office telling him that he was not certified for interventional cardiology – even though he had passed that exam in 2016.
Dr. Hafiz, who directs the Advanced Structural Heart Disease Program at Southern Illinois University, phoned the American Board of Internal Medicine (ABIM), where he learned that to restore his credentials, he would need to pay $1,225 in maintenance of certification (MOC) fees.
Like Dr. Hafiz,
Even doctors who are participating in mandatory continuing education outside the ABIM’s auspices are finding themselves listed as “not certified.” Some physicians learned of the policy change only after applying for hospital privileges or for jobs that require ABIM certification.
Now that increasing numbers of physicians are employed by hospitals and health care organizations that require ABIM certification, many doctors have no option but to pony up the fees if they want to continue to practice medicine.
“We have no say in the matter,” said Dr. Hafiz, “and there’s no appeal process.”
The change affects nearly 330,000 physicians. Responses to the policy on Twitter included accusations of extortion and denunciations of the ABIM’s “money grab policies.”
Sunil Rao, MD, director of interventional cardiology at NYU Langone Health and president of the Society for Cardiovascular Angiography and Interventions (SCAI), has heard from many SCAI members who had experiences similar to Dr. Hafiz’s. While Dr. Rao describes some of the Twitter outrage as “emotional,” he does acknowledge that the ABIM’s moves appear to be financially motivated.
“The issue here was that as soon as they paid the fee, all of a sudden, ABIM flipped the switch and said they were certified,” he said. “It certainly sounds like a purely financial kind of structure.”
Richard Baron, MD, president and CEO of the ABIM, said doctors are misunderstanding the policy change.
“No doctor loses certification solely for failure to pay fees,” Dr. Baron told this news organization. “What caused them to be reported as not certified was that we didn’t have evidence that they had met program requirements. They could say, ‘But I did meet program requirements, you just didn’t know it.’ To which our answer would be, for us to know it, we have to process them. And our policy is that we don’t process them unless you are current on your fees.”
This is not the first time ABIM policies have alienated physicians.
Last year, the ABIM raised its MOC fees from $165 to $220. That also prompted a wave of outrage. Other grievances go further back. At one time, being board certified was a lifetime credential. However, in 1990 the ABIM made periodic recertification mandatory.
The process, which came to be known as “maintenance of certification,” had to be completed every 10 years, and fees were charged for each certification. At that point, said Dr. Baron, the relationship between the ABIM and physicians changed from a one-time interaction to a career-long relationship. He advises doctors to check in periodically on their portal page at the ABIM or download the app so they will always know their status.
Many physicians would prefer not to be bound to a lifetime relationship with the ABIM. There is an alternative licensing board, the National Board of Physicians and Surgeons (NBPAS), but it is accepted by only a limited number of hospitals.
“Until the NBPAS gains wide recognition,” said Dr. Hafiz, “the ABIM is going to continue to have basically a monopoly over the market.”
The value of MOC itself has been called into question. “There are no direct data supporting the value of the MOC process in either improving care, making patient care safer, or making patient care higher quality,” said Dr. Rao. This feeds frustration in a clinical community already dealing with onerous training requirements and expensive board certification exams and adds to the perception that it is a purely financial transaction, he said. (Studies examining whether the MOC system improves patient care have shown mixed results.)
The true value of the ABIM to physicians, Dr. Baron contends, is that the organization is an independent third party that differentiates those doctors from people who don’t have their skills, training, and expertise. “In these days, where anyone can be an ‘expert’ on the Internet, that’s more valuable than ever before,” he said.
A version of this article first appeared on Medscape.com.
BMI is a flawed measure of obesity. What are alternatives?
“BMI is trash. Full stop.” This controversial tweet, which received thousands of likes and retweets, was cited in a recent article by one doctor on when physicians might stop using body mass index (BMI) to diagnose obesity.
BMI has for years been the consensus default method for assessing whether a person is overweight or has obesity, and is still widely used as the gatekeeper metric for treatment eligibility for certain weight-loss agents and bariatric surgery.
an important determinant of the cardiometabolic consequences of fat.
Alternative metrics include waist circumference and/or waist-to-height ratio (WHtR); imaging methods such as CT, MRI, and dual-energy x-ray absorptiometry (DXA); and bioelectrical impedance to assess fat volume and location. All have made some inroads on the tight grip BMI has had on obesity assessment.
Chances are, however, that BMI will not fade away anytime soon given how entrenched it has become in clinical practice and for insurance coverage, as well as its relative simplicity and precision.
“BMI is embedded in a wide range of guidelines on the use of medications and surgery. It’s embedded in Food and Drug Administration regulations and for billing and insurance coverage. It would take extremely strong data and years of work to undo the infrastructure built around BMI and replace it with something else. I don’t see that happening [anytime soon],” commented Daniel H. Bessesen, MD, a professor at the University of Colorado at Denver, Aurora, and chief of endocrinology for Denver Health.
“It would be almost impossible to replace all the studies that have used BMI with investigations using some other measure,” he said.
BMI Is ‘imperfect’
The entrenched position of BMI as the go-to metric doesn’t keep detractors from weighing in. As noted in a commentary on current clinical challenges surrounding obesity recently published in Annals of Internal Medicine, the journal’s editor-in-chief, Christine Laine, MD, and senior deputy editor Christina C. Wee, MD, listed six top issues clinicians must deal with, one of which, they say, is the need for a better measure of obesity than BMI.
“Unfortunately, BMI is an imperfect measure of body composition that differs with ethnicity, sex, body frame, and muscle mass,” noted Dr. Laine and Dr. Wee.
BMI is based on a person’s weight in kilograms divided by the square of their height in meters. A “healthy” BMI is between 18.5 and 24.9 kg/m2, overweight is 25-29.9, and 30 or greater is considered to represent obesity. However, certain ethnic groups have lower cutoffs for overweight or obesity because of evidence that such individuals can be at higher risk of obesity-related comorbidities at lower BMIs.
“BMI was chosen as the initial screening tool [for obesity] not because anyone thought it was perfect or the best measure but because of its simplicity. All you need is height, weight, and a calculator,” Dr. Wee said in an interview.
Numerous online calculators are available, including one from the Centers for Disease Control and Prevention where height in feet and inches and weight in pounds can be entered to generate the BMI.
BMI is also inherently limited by being “a proxy for adiposity” and not a direct measure, added Dr. Wee, who is also director of the Obesity Research Program of Beth Israel Deaconess Medical Center, Boston.
As such, BMI can’t distinguish between fat and muscle because it relies on weight only to gauge adiposity, noted Tiffany Powell-Wiley, MD, an obesity researcher at the National Heart, Lung, and Blood Institute in Bethesda, Md. Another shortcoming of BMI is that it “is good for distinguishing population-level risk for cardiovascular disease and other chronic diseases, but it does not help as much for distinguishing risk at an individual level,” she said in an interview.
These and other drawbacks have prompted researchers to look for other useful metrics. WHtR, for example, has recently made headway as a potential BMI alternative or complement.
The case for WHtR
Concern about overreliance on BMI despite its limitations is not new. In 2015, an American Heart Association scientific statement from the group’s Obesity Committee concluded that “BMI alone, even with lower thresholds, is a useful but not an ideal tool for identification of obesity or assessment of cardiovascular risk,” especially for people from Asian, Black, Hispanic, and Pacific Islander populations.
The writing panel also recommended that clinicians measure waist circumference annually and use that information along with BMI “to better gauge cardiovascular risk in diverse populations.”
Momentum for moving beyond BMI alone has continued to build following the AHA statement.
In September 2022, the National Institute for Health and Care Excellence, which sets policies for the United Kingdom’s National Health Service, revised its guidancefor assessment and management of people with obesity. The updated guidance recommends that when clinicians assess “adults with BMI below 35 kg/m2, measure and use their WHtR, as well as their BMI, as a practical estimate of central adiposity and use these measurements to help to assess and predict health risks.”
NICE released an extensive literature review with the revision, and based on the evidence, said that “using waist-to-height ratio as well as BMI would help give a practical estimate of central adiposity in adults with BMI under 35 kg/m2. This would in turn help professionals assess and predict health risks.”
However, the review added that, “because people with a BMI over 35 kg/m2 are always likely to have a high WHtR, the committee recognized that it may not be a useful addition for predicting health risks in this group.” The 2022 NICE review also said that it is “important to estimate central adiposity when assessing future health risks, including for people whose BMI is in the healthy-weight category.”
This new emphasis by NICE on measuring and using WHtR as part of obesity assessment “represents an important change in population health policy,” commented Dr. Powell-Wiley. “I expect more professional organizations will endorse use of waist circumference or waist-to-height ratio now that NICE has taken this step,” she predicted.
Waist circumference and WHtR may become standard measures of adiposity in clinical practice over the next 5-10 years.
The recent move by NICE to highlight a complementary role for WHtR “is another acknowledgment that BMI is an imperfect tool for stratifying cardiometabolic risk in a diverse population, especially in people with lower BMIs” because of its variability, commented Jamie Almandoz, MD, medical director of the weight wellness program at UT Southwestern Medical Center, Dallas.
WHtR vs. BMI
Another recent step forward for WHtR came with the publication of a post hoc analysis of data collected in the PARADIGM-HF trial, a study that had the primary purpose of comparing two medications for improving outcomes in more than 8,000 patients with heart failure with reduced ejection fraction.
The new analysis showed that “two indices that incorporate waist circumference and height, but not weight, showed a clearer association between greater adiposity and a higher risk of heart failure hospitalization,” compared with BMI.
WHtR was one of the two indices identified as being a better correlate for the adverse effect of excess adiposity compared with BMI.
The authors of the post hoc analysis did not design their analysis to compare WHtR with BMI. Instead, their goal was to better understand what’s known as the “obesity paradox” in people with heart failure with reduced ejection fraction: The recurring observation that, when these patients with heart failure have lower BMIs they fare worse, with higher rates of mortality and adverse cardiovascular outcomes, compared with patients with higher BMIs.
The new analysis showed that this paradox disappeared when WHtR was substituted for BMI as the obesity metric.
This “provides meaningful data about the superiority of WHtR, compared with BMI, for predicting heart failure outcomes,” said Dr. Powell-Wiley, although she cautioned that the analysis was limited by scant data in diverse populations and did not look at other important cardiovascular disease outcomes. While Dr. Powell-Wiley does not think that WHtR needs assessment in a prospective, controlled trial, she called for analysis of pooled prospective studies with more diverse populations to better document the advantages of WHtR over BMI.
The PARADIGM-HF post hoc analysis shows again how flawed BMI is for health assessment and the relative importance of an individualized understanding of a person’s body composition, Dr. Almandoz said in an interview. “As we collect more data, there is increasing awareness of how imperfect BMI is.”
Measuring waist circumference is tricky
Although WHtR looks promising as a substitute for or add-on to BMI, it has its own limitations, particularly the challenge of accurately measuring waist circumference.
Measuring waist circumference “not only takes more time but requires the assessor to be well trained about where to put the tape measure and making sure it’s measured at the same place each time,” even when different people take serial measurements from individual patients, noted Dr. Wee. Determining waist circumference can also be technically difficult when done on larger people, she added, and collectively these challenges make waist circumference “less reproducible from measurement to measurement.”
“It’s relatively clear how to standardize measurement of weight and height, but there is a huge amount of variability when the waist is measured,” agreed Dr. Almandoz. “And waist circumference also differs by ethnicity, race, sex, and body frame. There are significant differences in waist circumference levels that associate with increased health risks” between, for example, White and South Asian people.
Another limitation of waist circumference and WHtR is that they “cannot differentiate between visceral and abdominal subcutaneous adipose tissue, which are vastly different regarding cardiometabolic risk, commented Ian Neeland, MD, director of cardiovascular prevention at the University Hospitals Harrington Heart & Vascular Institute, Cleveland.
The imaging option
“Waist-to-height ratio is not the ultimate answer,” Dr. Neeland said in an interview. He instead endorsed “advanced imaging for body fat distribution,” such as CT or MRI scans, as his pick for what should be the standard obesity metric, “given that it is much more specific and actionable for both risk assessment and response to therapy. I expect slow but steady advancements that move away from BMI cutoffs, for example for bariatric surgery, given that BMI is an imprecise and crude tool.”
But although imaging with methods like CT and MRI may provide the best accuracy and precision for tracking the volume of a person’s cardiometabolically dangerous fat, they are also hampered by relatively high cost and, for CT and DXA, the issue of radiation exposure.
“CT, MRI, and DXA scans give more in-depth assessment of body composition, but should we expose people to the radiation and the cost?” Dr. Almandoz wondered.
“Height, weight, and waist circumference cost nothing to obtain,” creating a big relative disadvantage for imaging, said Naveed Sattar, MD, professor of metabolic medicine at the University of Glasgow.
“Data would need to show that imaging gives clinicians substantially more information about future risk” to justify its price, Dr. Sattar emphasized.
BMI’s limits mean adding on
Regardless of whichever alternatives to BMI end up getting used most, experts generally agree that BMI alone is looking increasingly inadequate.
“Over the next 5 years, BMI will come to be seen as a screening tool that categorizes people into general risk groups” that also needs “other metrics and variables, such as age, race, ethnicity, family history, blood glucose, and blood pressure to better describe health risk in an individual,” predicted Dr. Bessesen.
The endorsement of WHtR by NICE “will lead to more research into how to incorporate WHtR into routine practice. We need more evidence to translate what NICE said into practice,” said Dr. Sattar. “I don’t think we’ll see a shift away from BMI, but we’ll add alternative measures that are particularly useful in certain patients.”
“Because we live in diverse societies, we need to individualize risk assessment and couple that with technology that makes analysis of body composition more accessible,” agreed Dr. Almandoz. He noted that the UT Southwestern weight wellness program where he practices has, for about the past decade, routinely collected waist circumference and bioelectrical impedance data as well as BMI on all people seen in the practice for obesity concerns. Making these additional measurements on a routine basis also helps strengthen patient engagement.
“We get into trouble when we make rigid health policy and clinical decisions based on BMI alone without looking at the patient holistically,” said Dr. Wee. “Patients are more than arbitrary numbers, and clinicians should make clinical decisions based on the totality of evidence for each individual patient.”
Dr. Bessesen, Dr. Wee, Dr. Powell-Wiley, and Dr. Almandoz reported no relevant financial relationships. Dr. Neeland has reported being a consultant for Merck. Dr. Sattar has reported being a consultant or speaker for Abbott Laboratories, Afimmune, Amgen, AstraZeneca, Boehringer Ingelheim, Eli Lilly, Hanmi Pharmaceuticals, Janssen, MSD, Novartis, Novo Nordisk, Pfizer, Roche Diagnostics, and Sanofi.
A version of this article originally appeared on Medscape.com.
“BMI is trash. Full stop.” This controversial tweet, which received thousands of likes and retweets, was cited in a recent article by one doctor on when physicians might stop using body mass index (BMI) to diagnose obesity.
BMI has for years been the consensus default method for assessing whether a person is overweight or has obesity, and is still widely used as the gatekeeper metric for treatment eligibility for certain weight-loss agents and bariatric surgery.
an important determinant of the cardiometabolic consequences of fat.
Alternative metrics include waist circumference and/or waist-to-height ratio (WHtR); imaging methods such as CT, MRI, and dual-energy x-ray absorptiometry (DXA); and bioelectrical impedance to assess fat volume and location. All have made some inroads on the tight grip BMI has had on obesity assessment.
Chances are, however, that BMI will not fade away anytime soon given how entrenched it has become in clinical practice and for insurance coverage, as well as its relative simplicity and precision.
“BMI is embedded in a wide range of guidelines on the use of medications and surgery. It’s embedded in Food and Drug Administration regulations and for billing and insurance coverage. It would take extremely strong data and years of work to undo the infrastructure built around BMI and replace it with something else. I don’t see that happening [anytime soon],” commented Daniel H. Bessesen, MD, a professor at the University of Colorado at Denver, Aurora, and chief of endocrinology for Denver Health.
“It would be almost impossible to replace all the studies that have used BMI with investigations using some other measure,” he said.
BMI Is ‘imperfect’
The entrenched position of BMI as the go-to metric doesn’t keep detractors from weighing in. As noted in a commentary on current clinical challenges surrounding obesity recently published in Annals of Internal Medicine, the journal’s editor-in-chief, Christine Laine, MD, and senior deputy editor Christina C. Wee, MD, listed six top issues clinicians must deal with, one of which, they say, is the need for a better measure of obesity than BMI.
“Unfortunately, BMI is an imperfect measure of body composition that differs with ethnicity, sex, body frame, and muscle mass,” noted Dr. Laine and Dr. Wee.
BMI is based on a person’s weight in kilograms divided by the square of their height in meters. A “healthy” BMI is between 18.5 and 24.9 kg/m2, overweight is 25-29.9, and 30 or greater is considered to represent obesity. However, certain ethnic groups have lower cutoffs for overweight or obesity because of evidence that such individuals can be at higher risk of obesity-related comorbidities at lower BMIs.
“BMI was chosen as the initial screening tool [for obesity] not because anyone thought it was perfect or the best measure but because of its simplicity. All you need is height, weight, and a calculator,” Dr. Wee said in an interview.
Numerous online calculators are available, including one from the Centers for Disease Control and Prevention where height in feet and inches and weight in pounds can be entered to generate the BMI.
BMI is also inherently limited by being “a proxy for adiposity” and not a direct measure, added Dr. Wee, who is also director of the Obesity Research Program of Beth Israel Deaconess Medical Center, Boston.
As such, BMI can’t distinguish between fat and muscle because it relies on weight only to gauge adiposity, noted Tiffany Powell-Wiley, MD, an obesity researcher at the National Heart, Lung, and Blood Institute in Bethesda, Md. Another shortcoming of BMI is that it “is good for distinguishing population-level risk for cardiovascular disease and other chronic diseases, but it does not help as much for distinguishing risk at an individual level,” she said in an interview.
These and other drawbacks have prompted researchers to look for other useful metrics. WHtR, for example, has recently made headway as a potential BMI alternative or complement.
The case for WHtR
Concern about overreliance on BMI despite its limitations is not new. In 2015, an American Heart Association scientific statement from the group’s Obesity Committee concluded that “BMI alone, even with lower thresholds, is a useful but not an ideal tool for identification of obesity or assessment of cardiovascular risk,” especially for people from Asian, Black, Hispanic, and Pacific Islander populations.
The writing panel also recommended that clinicians measure waist circumference annually and use that information along with BMI “to better gauge cardiovascular risk in diverse populations.”
Momentum for moving beyond BMI alone has continued to build following the AHA statement.
In September 2022, the National Institute for Health and Care Excellence, which sets policies for the United Kingdom’s National Health Service, revised its guidancefor assessment and management of people with obesity. The updated guidance recommends that when clinicians assess “adults with BMI below 35 kg/m2, measure and use their WHtR, as well as their BMI, as a practical estimate of central adiposity and use these measurements to help to assess and predict health risks.”
NICE released an extensive literature review with the revision, and based on the evidence, said that “using waist-to-height ratio as well as BMI would help give a practical estimate of central adiposity in adults with BMI under 35 kg/m2. This would in turn help professionals assess and predict health risks.”
However, the review added that, “because people with a BMI over 35 kg/m2 are always likely to have a high WHtR, the committee recognized that it may not be a useful addition for predicting health risks in this group.” The 2022 NICE review also said that it is “important to estimate central adiposity when assessing future health risks, including for people whose BMI is in the healthy-weight category.”
This new emphasis by NICE on measuring and using WHtR as part of obesity assessment “represents an important change in population health policy,” commented Dr. Powell-Wiley. “I expect more professional organizations will endorse use of waist circumference or waist-to-height ratio now that NICE has taken this step,” she predicted.
Waist circumference and WHtR may become standard measures of adiposity in clinical practice over the next 5-10 years.
The recent move by NICE to highlight a complementary role for WHtR “is another acknowledgment that BMI is an imperfect tool for stratifying cardiometabolic risk in a diverse population, especially in people with lower BMIs” because of its variability, commented Jamie Almandoz, MD, medical director of the weight wellness program at UT Southwestern Medical Center, Dallas.
WHtR vs. BMI
Another recent step forward for WHtR came with the publication of a post hoc analysis of data collected in the PARADIGM-HF trial, a study that had the primary purpose of comparing two medications for improving outcomes in more than 8,000 patients with heart failure with reduced ejection fraction.
The new analysis showed that “two indices that incorporate waist circumference and height, but not weight, showed a clearer association between greater adiposity and a higher risk of heart failure hospitalization,” compared with BMI.
WHtR was one of the two indices identified as being a better correlate for the adverse effect of excess adiposity compared with BMI.
The authors of the post hoc analysis did not design their analysis to compare WHtR with BMI. Instead, their goal was to better understand what’s known as the “obesity paradox” in people with heart failure with reduced ejection fraction: The recurring observation that, when these patients with heart failure have lower BMIs they fare worse, with higher rates of mortality and adverse cardiovascular outcomes, compared with patients with higher BMIs.
The new analysis showed that this paradox disappeared when WHtR was substituted for BMI as the obesity metric.
This “provides meaningful data about the superiority of WHtR, compared with BMI, for predicting heart failure outcomes,” said Dr. Powell-Wiley, although she cautioned that the analysis was limited by scant data in diverse populations and did not look at other important cardiovascular disease outcomes. While Dr. Powell-Wiley does not think that WHtR needs assessment in a prospective, controlled trial, she called for analysis of pooled prospective studies with more diverse populations to better document the advantages of WHtR over BMI.
The PARADIGM-HF post hoc analysis shows again how flawed BMI is for health assessment and the relative importance of an individualized understanding of a person’s body composition, Dr. Almandoz said in an interview. “As we collect more data, there is increasing awareness of how imperfect BMI is.”
Measuring waist circumference is tricky
Although WHtR looks promising as a substitute for or add-on to BMI, it has its own limitations, particularly the challenge of accurately measuring waist circumference.
Measuring waist circumference “not only takes more time but requires the assessor to be well trained about where to put the tape measure and making sure it’s measured at the same place each time,” even when different people take serial measurements from individual patients, noted Dr. Wee. Determining waist circumference can also be technically difficult when done on larger people, she added, and collectively these challenges make waist circumference “less reproducible from measurement to measurement.”
“It’s relatively clear how to standardize measurement of weight and height, but there is a huge amount of variability when the waist is measured,” agreed Dr. Almandoz. “And waist circumference also differs by ethnicity, race, sex, and body frame. There are significant differences in waist circumference levels that associate with increased health risks” between, for example, White and South Asian people.
Another limitation of waist circumference and WHtR is that they “cannot differentiate between visceral and abdominal subcutaneous adipose tissue, which are vastly different regarding cardiometabolic risk, commented Ian Neeland, MD, director of cardiovascular prevention at the University Hospitals Harrington Heart & Vascular Institute, Cleveland.
The imaging option
“Waist-to-height ratio is not the ultimate answer,” Dr. Neeland said in an interview. He instead endorsed “advanced imaging for body fat distribution,” such as CT or MRI scans, as his pick for what should be the standard obesity metric, “given that it is much more specific and actionable for both risk assessment and response to therapy. I expect slow but steady advancements that move away from BMI cutoffs, for example for bariatric surgery, given that BMI is an imprecise and crude tool.”
But although imaging with methods like CT and MRI may provide the best accuracy and precision for tracking the volume of a person’s cardiometabolically dangerous fat, they are also hampered by relatively high cost and, for CT and DXA, the issue of radiation exposure.
“CT, MRI, and DXA scans give more in-depth assessment of body composition, but should we expose people to the radiation and the cost?” Dr. Almandoz wondered.
“Height, weight, and waist circumference cost nothing to obtain,” creating a big relative disadvantage for imaging, said Naveed Sattar, MD, professor of metabolic medicine at the University of Glasgow.
“Data would need to show that imaging gives clinicians substantially more information about future risk” to justify its price, Dr. Sattar emphasized.
BMI’s limits mean adding on
Regardless of whichever alternatives to BMI end up getting used most, experts generally agree that BMI alone is looking increasingly inadequate.
“Over the next 5 years, BMI will come to be seen as a screening tool that categorizes people into general risk groups” that also needs “other metrics and variables, such as age, race, ethnicity, family history, blood glucose, and blood pressure to better describe health risk in an individual,” predicted Dr. Bessesen.
The endorsement of WHtR by NICE “will lead to more research into how to incorporate WHtR into routine practice. We need more evidence to translate what NICE said into practice,” said Dr. Sattar. “I don’t think we’ll see a shift away from BMI, but we’ll add alternative measures that are particularly useful in certain patients.”
“Because we live in diverse societies, we need to individualize risk assessment and couple that with technology that makes analysis of body composition more accessible,” agreed Dr. Almandoz. He noted that the UT Southwestern weight wellness program where he practices has, for about the past decade, routinely collected waist circumference and bioelectrical impedance data as well as BMI on all people seen in the practice for obesity concerns. Making these additional measurements on a routine basis also helps strengthen patient engagement.
“We get into trouble when we make rigid health policy and clinical decisions based on BMI alone without looking at the patient holistically,” said Dr. Wee. “Patients are more than arbitrary numbers, and clinicians should make clinical decisions based on the totality of evidence for each individual patient.”
Dr. Bessesen, Dr. Wee, Dr. Powell-Wiley, and Dr. Almandoz reported no relevant financial relationships. Dr. Neeland has reported being a consultant for Merck. Dr. Sattar has reported being a consultant or speaker for Abbott Laboratories, Afimmune, Amgen, AstraZeneca, Boehringer Ingelheim, Eli Lilly, Hanmi Pharmaceuticals, Janssen, MSD, Novartis, Novo Nordisk, Pfizer, Roche Diagnostics, and Sanofi.
A version of this article originally appeared on Medscape.com.
“BMI is trash. Full stop.” This controversial tweet, which received thousands of likes and retweets, was cited in a recent article by one doctor on when physicians might stop using body mass index (BMI) to diagnose obesity.
BMI has for years been the consensus default method for assessing whether a person is overweight or has obesity, and is still widely used as the gatekeeper metric for treatment eligibility for certain weight-loss agents and bariatric surgery.
an important determinant of the cardiometabolic consequences of fat.
Alternative metrics include waist circumference and/or waist-to-height ratio (WHtR); imaging methods such as CT, MRI, and dual-energy x-ray absorptiometry (DXA); and bioelectrical impedance to assess fat volume and location. All have made some inroads on the tight grip BMI has had on obesity assessment.
Chances are, however, that BMI will not fade away anytime soon given how entrenched it has become in clinical practice and for insurance coverage, as well as its relative simplicity and precision.
“BMI is embedded in a wide range of guidelines on the use of medications and surgery. It’s embedded in Food and Drug Administration regulations and for billing and insurance coverage. It would take extremely strong data and years of work to undo the infrastructure built around BMI and replace it with something else. I don’t see that happening [anytime soon],” commented Daniel H. Bessesen, MD, a professor at the University of Colorado at Denver, Aurora, and chief of endocrinology for Denver Health.
“It would be almost impossible to replace all the studies that have used BMI with investigations using some other measure,” he said.
BMI Is ‘imperfect’
The entrenched position of BMI as the go-to metric doesn’t keep detractors from weighing in. As noted in a commentary on current clinical challenges surrounding obesity recently published in Annals of Internal Medicine, the journal’s editor-in-chief, Christine Laine, MD, and senior deputy editor Christina C. Wee, MD, listed six top issues clinicians must deal with, one of which, they say, is the need for a better measure of obesity than BMI.
“Unfortunately, BMI is an imperfect measure of body composition that differs with ethnicity, sex, body frame, and muscle mass,” noted Dr. Laine and Dr. Wee.
BMI is based on a person’s weight in kilograms divided by the square of their height in meters. A “healthy” BMI is between 18.5 and 24.9 kg/m2, overweight is 25-29.9, and 30 or greater is considered to represent obesity. However, certain ethnic groups have lower cutoffs for overweight or obesity because of evidence that such individuals can be at higher risk of obesity-related comorbidities at lower BMIs.
“BMI was chosen as the initial screening tool [for obesity] not because anyone thought it was perfect or the best measure but because of its simplicity. All you need is height, weight, and a calculator,” Dr. Wee said in an interview.
Numerous online calculators are available, including one from the Centers for Disease Control and Prevention where height in feet and inches and weight in pounds can be entered to generate the BMI.
BMI is also inherently limited by being “a proxy for adiposity” and not a direct measure, added Dr. Wee, who is also director of the Obesity Research Program of Beth Israel Deaconess Medical Center, Boston.
As such, BMI can’t distinguish between fat and muscle because it relies on weight only to gauge adiposity, noted Tiffany Powell-Wiley, MD, an obesity researcher at the National Heart, Lung, and Blood Institute in Bethesda, Md. Another shortcoming of BMI is that it “is good for distinguishing population-level risk for cardiovascular disease and other chronic diseases, but it does not help as much for distinguishing risk at an individual level,” she said in an interview.
These and other drawbacks have prompted researchers to look for other useful metrics. WHtR, for example, has recently made headway as a potential BMI alternative or complement.
The case for WHtR
Concern about overreliance on BMI despite its limitations is not new. In 2015, an American Heart Association scientific statement from the group’s Obesity Committee concluded that “BMI alone, even with lower thresholds, is a useful but not an ideal tool for identification of obesity or assessment of cardiovascular risk,” especially for people from Asian, Black, Hispanic, and Pacific Islander populations.
The writing panel also recommended that clinicians measure waist circumference annually and use that information along with BMI “to better gauge cardiovascular risk in diverse populations.”
Momentum for moving beyond BMI alone has continued to build following the AHA statement.
In September 2022, the National Institute for Health and Care Excellence, which sets policies for the United Kingdom’s National Health Service, revised its guidancefor assessment and management of people with obesity. The updated guidance recommends that when clinicians assess “adults with BMI below 35 kg/m2, measure and use their WHtR, as well as their BMI, as a practical estimate of central adiposity and use these measurements to help to assess and predict health risks.”
NICE released an extensive literature review with the revision, and based on the evidence, said that “using waist-to-height ratio as well as BMI would help give a practical estimate of central adiposity in adults with BMI under 35 kg/m2. This would in turn help professionals assess and predict health risks.”
However, the review added that, “because people with a BMI over 35 kg/m2 are always likely to have a high WHtR, the committee recognized that it may not be a useful addition for predicting health risks in this group.” The 2022 NICE review also said that it is “important to estimate central adiposity when assessing future health risks, including for people whose BMI is in the healthy-weight category.”
This new emphasis by NICE on measuring and using WHtR as part of obesity assessment “represents an important change in population health policy,” commented Dr. Powell-Wiley. “I expect more professional organizations will endorse use of waist circumference or waist-to-height ratio now that NICE has taken this step,” she predicted.
Waist circumference and WHtR may become standard measures of adiposity in clinical practice over the next 5-10 years.
The recent move by NICE to highlight a complementary role for WHtR “is another acknowledgment that BMI is an imperfect tool for stratifying cardiometabolic risk in a diverse population, especially in people with lower BMIs” because of its variability, commented Jamie Almandoz, MD, medical director of the weight wellness program at UT Southwestern Medical Center, Dallas.
WHtR vs. BMI
Another recent step forward for WHtR came with the publication of a post hoc analysis of data collected in the PARADIGM-HF trial, a study that had the primary purpose of comparing two medications for improving outcomes in more than 8,000 patients with heart failure with reduced ejection fraction.
The new analysis showed that “two indices that incorporate waist circumference and height, but not weight, showed a clearer association between greater adiposity and a higher risk of heart failure hospitalization,” compared with BMI.
WHtR was one of the two indices identified as being a better correlate for the adverse effect of excess adiposity compared with BMI.
The authors of the post hoc analysis did not design their analysis to compare WHtR with BMI. Instead, their goal was to better understand what’s known as the “obesity paradox” in people with heart failure with reduced ejection fraction: The recurring observation that, when these patients with heart failure have lower BMIs they fare worse, with higher rates of mortality and adverse cardiovascular outcomes, compared with patients with higher BMIs.
The new analysis showed that this paradox disappeared when WHtR was substituted for BMI as the obesity metric.
This “provides meaningful data about the superiority of WHtR, compared with BMI, for predicting heart failure outcomes,” said Dr. Powell-Wiley, although she cautioned that the analysis was limited by scant data in diverse populations and did not look at other important cardiovascular disease outcomes. While Dr. Powell-Wiley does not think that WHtR needs assessment in a prospective, controlled trial, she called for analysis of pooled prospective studies with more diverse populations to better document the advantages of WHtR over BMI.
The PARADIGM-HF post hoc analysis shows again how flawed BMI is for health assessment and the relative importance of an individualized understanding of a person’s body composition, Dr. Almandoz said in an interview. “As we collect more data, there is increasing awareness of how imperfect BMI is.”
Measuring waist circumference is tricky
Although WHtR looks promising as a substitute for or add-on to BMI, it has its own limitations, particularly the challenge of accurately measuring waist circumference.
Measuring waist circumference “not only takes more time but requires the assessor to be well trained about where to put the tape measure and making sure it’s measured at the same place each time,” even when different people take serial measurements from individual patients, noted Dr. Wee. Determining waist circumference can also be technically difficult when done on larger people, she added, and collectively these challenges make waist circumference “less reproducible from measurement to measurement.”
“It’s relatively clear how to standardize measurement of weight and height, but there is a huge amount of variability when the waist is measured,” agreed Dr. Almandoz. “And waist circumference also differs by ethnicity, race, sex, and body frame. There are significant differences in waist circumference levels that associate with increased health risks” between, for example, White and South Asian people.
Another limitation of waist circumference and WHtR is that they “cannot differentiate between visceral and abdominal subcutaneous adipose tissue, which are vastly different regarding cardiometabolic risk, commented Ian Neeland, MD, director of cardiovascular prevention at the University Hospitals Harrington Heart & Vascular Institute, Cleveland.
The imaging option
“Waist-to-height ratio is not the ultimate answer,” Dr. Neeland said in an interview. He instead endorsed “advanced imaging for body fat distribution,” such as CT or MRI scans, as his pick for what should be the standard obesity metric, “given that it is much more specific and actionable for both risk assessment and response to therapy. I expect slow but steady advancements that move away from BMI cutoffs, for example for bariatric surgery, given that BMI is an imprecise and crude tool.”
But although imaging with methods like CT and MRI may provide the best accuracy and precision for tracking the volume of a person’s cardiometabolically dangerous fat, they are also hampered by relatively high cost and, for CT and DXA, the issue of radiation exposure.
“CT, MRI, and DXA scans give more in-depth assessment of body composition, but should we expose people to the radiation and the cost?” Dr. Almandoz wondered.
“Height, weight, and waist circumference cost nothing to obtain,” creating a big relative disadvantage for imaging, said Naveed Sattar, MD, professor of metabolic medicine at the University of Glasgow.
“Data would need to show that imaging gives clinicians substantially more information about future risk” to justify its price, Dr. Sattar emphasized.
BMI’s limits mean adding on
Regardless of whichever alternatives to BMI end up getting used most, experts generally agree that BMI alone is looking increasingly inadequate.
“Over the next 5 years, BMI will come to be seen as a screening tool that categorizes people into general risk groups” that also needs “other metrics and variables, such as age, race, ethnicity, family history, blood glucose, and blood pressure to better describe health risk in an individual,” predicted Dr. Bessesen.
The endorsement of WHtR by NICE “will lead to more research into how to incorporate WHtR into routine practice. We need more evidence to translate what NICE said into practice,” said Dr. Sattar. “I don’t think we’ll see a shift away from BMI, but we’ll add alternative measures that are particularly useful in certain patients.”
“Because we live in diverse societies, we need to individualize risk assessment and couple that with technology that makes analysis of body composition more accessible,” agreed Dr. Almandoz. He noted that the UT Southwestern weight wellness program where he practices has, for about the past decade, routinely collected waist circumference and bioelectrical impedance data as well as BMI on all people seen in the practice for obesity concerns. Making these additional measurements on a routine basis also helps strengthen patient engagement.
“We get into trouble when we make rigid health policy and clinical decisions based on BMI alone without looking at the patient holistically,” said Dr. Wee. “Patients are more than arbitrary numbers, and clinicians should make clinical decisions based on the totality of evidence for each individual patient.”
Dr. Bessesen, Dr. Wee, Dr. Powell-Wiley, and Dr. Almandoz reported no relevant financial relationships. Dr. Neeland has reported being a consultant for Merck. Dr. Sattar has reported being a consultant or speaker for Abbott Laboratories, Afimmune, Amgen, AstraZeneca, Boehringer Ingelheim, Eli Lilly, Hanmi Pharmaceuticals, Janssen, MSD, Novartis, Novo Nordisk, Pfizer, Roche Diagnostics, and Sanofi.
A version of this article originally appeared on Medscape.com.
Walnuts linked to improved attention, psychological maturity in teens
, new research shows. Adolescents who consumed walnuts for at least 100 days showed improved sustained attention and fluid intelligence as well as a reduction in symptoms of attension deficit hyperactivity disorder, compared with matched controls who did not consume the nuts. However, there were no statistically significant changes between the groups in other parameters, such as working memory and executive function.
Clinicians should advise adolescents “to eat a handful of walnuts three times a week for the rest of their lives. They may have a healthier brain with better cognitive function,” said senior investigator Jordi Julvez, PhD, group leader at the Institute of Health Research Pere Virgili, Barcelona, and associated researcher at the Barcelona Institute for Global Health.
The study was published online in eClinicalMedicine.
Rich source of omega-3s
Adolescence is “a period of refinement of brain connectivity and complex behaviors,” the investigators noted.
Previous research suggests polyunsaturated fatty acids are key in central nervous system architecture and function during times of neural development, with three specific PUFAs playing an “essential developmental role.”
Two omega-3 fatty acids – docosahexaenoic acid and eicosapentaenoic acid – are PUFAs that must be obtained through diet, mainly from seafood. Walnuts are “among the richest sources” of plant-derived omega-3 fatty acids, particularly alpha-linolenic acid (ALA), a precursor for longer-chain EPA and DHA.
ALA independently “has positive effects on brain function and plasticity,” the authors wrote. In addition, walnut constituents – particularly polyphenols and other bioactive compounds – “may act synergistically with ALA to foster brain health.”
Earlier small studies have found positive associations between walnut consumption and cognitive function in children, adolescents, and young adults, but to date, no randomized controlled trial has focused on the effect of walnut consumption on adolescent neuropsychological function.
The researchers studied 771 healthy adolescents (aged 11-16 years, mean age 14) drawn from 12 Spanish high schools. Participants were instructed to follow healthy eating recommendations and were randomly assigned 1:1 to the intervention (n = 386) or the control group (n = 385).
At baseline and after 6 months, they completed neuropsychological tests and behavioral rating scales. The Attention Network Test assessed attention, and the N-back test was used to assess working memory. The Tests of Primary Mental Abilities assessed fluid intelligence. Risky decision-making was tested using the Roulettes Task.
Fruit and nuts
Participants also completed the Strengths and Difficulties Questionnaire, which provided a total score of problem behavior. Teachers filled out the ADHD DSM-IV form list to provide additional information about ADHD behaviors.
The intervention group received 30 grams/day of raw California walnut kernels to incorporate into their daily diet. It is estimated that this walnut contains about 9 g of ALA per 100 g.
All participants received a seasonal fruit calendar and were asked to eat at least one piece of seasonal fruit daily.
Parents reported their child’s daily walnut consumption, with adherence defined as 100 or more days of eating walnuts during the 6-month period.
All main analyses were based on an intention-to-treat method (participants were analyzed according to their original group assignment, regardless of their adherence to the intervention).
The researchers also conducted a secondary per-protocol analysis, comparing the intervention and control groups to estimate the effect if all participants had adhered to their assigned intervention. They censored data for participants who reported eating walnuts for less than 100 days during the 6-month trial period.
Secondary outcomes included changes in height, weight, waist circumference, and BMI, as well as red blood cell proportions of omega-3 fatty acids (DHA, EPA, and ALA) at baseline and after 6 months.
Adherence counts
Most participants had “medium” or “high” levels of adherence to the Mediterranean diet, with “no meaningful differences” at baseline between the intervention and control groups in lifestyle characteristics or mean scores in all primary endpoints.
In the ITT analysis, there were no statistically significant differences in primary outcomes between the groups following the intervention. As for secondary outcomes, the RBC ALA significantly increased in the walnuts group but not the control group (coefficient, 0.04%; 95% confidence interval, 0.03%-0.06%; P < .0001).
However, there were differences in primary outcomes between the groups in the per-protocol analysis: The adherence-adjusted effect on improvement in attention score was −11.26 ms; 95% CI, −19.92 to −2.60; P = .011) for the intervention versus the control group.
The per-protocol analysis showed other differences: an improvement in fluid intelligence score (1.78; 95% CI, 0.90 - 2.67; P < .0001) and a reduction in ADHD symptom score (−2.18; 95% CI, −3.70 to −0.67; P = .0050).
“Overall, no significant differences were found in the intervention group in relation to the control group,” Dr. Julvez said in a news release. “But if the adherence factor is considered, then positive results are observed, since participants who most closely followed the guidelines – in terms of the recommended dose of walnuts and the number of days of consumption – did show improvements in the neuropsychological functions evaluated.”
Adolescence “is a time of great biological changes. Hormonal transformation occurs, which in turn is responsible for stimulating the synaptic growth of the frontal lobe,” he continued, adding that this brain region “enables neuropsychological maturation of more complex emotional and cognitive functions.”
“Neurons that are well nourished with these types of fatty acids will be able to grow and form new, stronger synapses,” he said.
Food as medicine
Uma Naidoo, MD, director of nutritional and lifestyle psychiatry at Massachusetts General Hospital, Boston, “commends” the researchers for conducting an RCT with a “robust” sample size and said she is “excited to see research like this furthering functional nutrition for mental health,” as she believes that “food is medicine.”
Dr. Naidoo, a professional chef, nutritional biologist, and author of the book “This Is Your Brain on Food,” said the findings “align” with her own approach to nutritional psychiatry and are also “in line” with her clinical practice.
However, although these results are “promising,” more research is needed across more diverse populations to “make sure these results are truly generalizable,” said Dr. Naidoo, a faculty member at Harvard Medical School, Boston, who was not involved with the study.
She “envisions a future where the research is so advanced that we can ‘dose’ these healthy whole foods for specific psychiatric symptoms and conditions.”
This study was supported by Instituto de Salud Carlos III (co-funded by European Union Regional Development Fund “A way to make Europe”). The California Walnut Commission has given support by supplying the walnuts for free for the Walnuts Smart Snack Dietary Intervention Trial. Dr. Julvez holds a Miguel Servet-II contract awarded by the Instituto de Salud Carlos III (co-funded by European Union Social Fund). The other authors’ disclosures are listed in the original article. Dr. Naidoo reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research shows. Adolescents who consumed walnuts for at least 100 days showed improved sustained attention and fluid intelligence as well as a reduction in symptoms of attension deficit hyperactivity disorder, compared with matched controls who did not consume the nuts. However, there were no statistically significant changes between the groups in other parameters, such as working memory and executive function.
Clinicians should advise adolescents “to eat a handful of walnuts three times a week for the rest of their lives. They may have a healthier brain with better cognitive function,” said senior investigator Jordi Julvez, PhD, group leader at the Institute of Health Research Pere Virgili, Barcelona, and associated researcher at the Barcelona Institute for Global Health.
The study was published online in eClinicalMedicine.
Rich source of omega-3s
Adolescence is “a period of refinement of brain connectivity and complex behaviors,” the investigators noted.
Previous research suggests polyunsaturated fatty acids are key in central nervous system architecture and function during times of neural development, with three specific PUFAs playing an “essential developmental role.”
Two omega-3 fatty acids – docosahexaenoic acid and eicosapentaenoic acid – are PUFAs that must be obtained through diet, mainly from seafood. Walnuts are “among the richest sources” of plant-derived omega-3 fatty acids, particularly alpha-linolenic acid (ALA), a precursor for longer-chain EPA and DHA.
ALA independently “has positive effects on brain function and plasticity,” the authors wrote. In addition, walnut constituents – particularly polyphenols and other bioactive compounds – “may act synergistically with ALA to foster brain health.”
Earlier small studies have found positive associations between walnut consumption and cognitive function in children, adolescents, and young adults, but to date, no randomized controlled trial has focused on the effect of walnut consumption on adolescent neuropsychological function.
The researchers studied 771 healthy adolescents (aged 11-16 years, mean age 14) drawn from 12 Spanish high schools. Participants were instructed to follow healthy eating recommendations and were randomly assigned 1:1 to the intervention (n = 386) or the control group (n = 385).
At baseline and after 6 months, they completed neuropsychological tests and behavioral rating scales. The Attention Network Test assessed attention, and the N-back test was used to assess working memory. The Tests of Primary Mental Abilities assessed fluid intelligence. Risky decision-making was tested using the Roulettes Task.
Fruit and nuts
Participants also completed the Strengths and Difficulties Questionnaire, which provided a total score of problem behavior. Teachers filled out the ADHD DSM-IV form list to provide additional information about ADHD behaviors.
The intervention group received 30 grams/day of raw California walnut kernels to incorporate into their daily diet. It is estimated that this walnut contains about 9 g of ALA per 100 g.
All participants received a seasonal fruit calendar and were asked to eat at least one piece of seasonal fruit daily.
Parents reported their child’s daily walnut consumption, with adherence defined as 100 or more days of eating walnuts during the 6-month period.
All main analyses were based on an intention-to-treat method (participants were analyzed according to their original group assignment, regardless of their adherence to the intervention).
The researchers also conducted a secondary per-protocol analysis, comparing the intervention and control groups to estimate the effect if all participants had adhered to their assigned intervention. They censored data for participants who reported eating walnuts for less than 100 days during the 6-month trial period.
Secondary outcomes included changes in height, weight, waist circumference, and BMI, as well as red blood cell proportions of omega-3 fatty acids (DHA, EPA, and ALA) at baseline and after 6 months.
Adherence counts
Most participants had “medium” or “high” levels of adherence to the Mediterranean diet, with “no meaningful differences” at baseline between the intervention and control groups in lifestyle characteristics or mean scores in all primary endpoints.
In the ITT analysis, there were no statistically significant differences in primary outcomes between the groups following the intervention. As for secondary outcomes, the RBC ALA significantly increased in the walnuts group but not the control group (coefficient, 0.04%; 95% confidence interval, 0.03%-0.06%; P < .0001).
However, there were differences in primary outcomes between the groups in the per-protocol analysis: The adherence-adjusted effect on improvement in attention score was −11.26 ms; 95% CI, −19.92 to −2.60; P = .011) for the intervention versus the control group.
The per-protocol analysis showed other differences: an improvement in fluid intelligence score (1.78; 95% CI, 0.90 - 2.67; P < .0001) and a reduction in ADHD symptom score (−2.18; 95% CI, −3.70 to −0.67; P = .0050).
“Overall, no significant differences were found in the intervention group in relation to the control group,” Dr. Julvez said in a news release. “But if the adherence factor is considered, then positive results are observed, since participants who most closely followed the guidelines – in terms of the recommended dose of walnuts and the number of days of consumption – did show improvements in the neuropsychological functions evaluated.”
Adolescence “is a time of great biological changes. Hormonal transformation occurs, which in turn is responsible for stimulating the synaptic growth of the frontal lobe,” he continued, adding that this brain region “enables neuropsychological maturation of more complex emotional and cognitive functions.”
“Neurons that are well nourished with these types of fatty acids will be able to grow and form new, stronger synapses,” he said.
Food as medicine
Uma Naidoo, MD, director of nutritional and lifestyle psychiatry at Massachusetts General Hospital, Boston, “commends” the researchers for conducting an RCT with a “robust” sample size and said she is “excited to see research like this furthering functional nutrition for mental health,” as she believes that “food is medicine.”
Dr. Naidoo, a professional chef, nutritional biologist, and author of the book “This Is Your Brain on Food,” said the findings “align” with her own approach to nutritional psychiatry and are also “in line” with her clinical practice.
However, although these results are “promising,” more research is needed across more diverse populations to “make sure these results are truly generalizable,” said Dr. Naidoo, a faculty member at Harvard Medical School, Boston, who was not involved with the study.
She “envisions a future where the research is so advanced that we can ‘dose’ these healthy whole foods for specific psychiatric symptoms and conditions.”
This study was supported by Instituto de Salud Carlos III (co-funded by European Union Regional Development Fund “A way to make Europe”). The California Walnut Commission has given support by supplying the walnuts for free for the Walnuts Smart Snack Dietary Intervention Trial. Dr. Julvez holds a Miguel Servet-II contract awarded by the Instituto de Salud Carlos III (co-funded by European Union Social Fund). The other authors’ disclosures are listed in the original article. Dr. Naidoo reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research shows. Adolescents who consumed walnuts for at least 100 days showed improved sustained attention and fluid intelligence as well as a reduction in symptoms of attension deficit hyperactivity disorder, compared with matched controls who did not consume the nuts. However, there were no statistically significant changes between the groups in other parameters, such as working memory and executive function.
Clinicians should advise adolescents “to eat a handful of walnuts three times a week for the rest of their lives. They may have a healthier brain with better cognitive function,” said senior investigator Jordi Julvez, PhD, group leader at the Institute of Health Research Pere Virgili, Barcelona, and associated researcher at the Barcelona Institute for Global Health.
The study was published online in eClinicalMedicine.
Rich source of omega-3s
Adolescence is “a period of refinement of brain connectivity and complex behaviors,” the investigators noted.
Previous research suggests polyunsaturated fatty acids are key in central nervous system architecture and function during times of neural development, with three specific PUFAs playing an “essential developmental role.”
Two omega-3 fatty acids – docosahexaenoic acid and eicosapentaenoic acid – are PUFAs that must be obtained through diet, mainly from seafood. Walnuts are “among the richest sources” of plant-derived omega-3 fatty acids, particularly alpha-linolenic acid (ALA), a precursor for longer-chain EPA and DHA.
ALA independently “has positive effects on brain function and plasticity,” the authors wrote. In addition, walnut constituents – particularly polyphenols and other bioactive compounds – “may act synergistically with ALA to foster brain health.”
Earlier small studies have found positive associations between walnut consumption and cognitive function in children, adolescents, and young adults, but to date, no randomized controlled trial has focused on the effect of walnut consumption on adolescent neuropsychological function.
The researchers studied 771 healthy adolescents (aged 11-16 years, mean age 14) drawn from 12 Spanish high schools. Participants were instructed to follow healthy eating recommendations and were randomly assigned 1:1 to the intervention (n = 386) or the control group (n = 385).
At baseline and after 6 months, they completed neuropsychological tests and behavioral rating scales. The Attention Network Test assessed attention, and the N-back test was used to assess working memory. The Tests of Primary Mental Abilities assessed fluid intelligence. Risky decision-making was tested using the Roulettes Task.
Fruit and nuts
Participants also completed the Strengths and Difficulties Questionnaire, which provided a total score of problem behavior. Teachers filled out the ADHD DSM-IV form list to provide additional information about ADHD behaviors.
The intervention group received 30 grams/day of raw California walnut kernels to incorporate into their daily diet. It is estimated that this walnut contains about 9 g of ALA per 100 g.
All participants received a seasonal fruit calendar and were asked to eat at least one piece of seasonal fruit daily.
Parents reported their child’s daily walnut consumption, with adherence defined as 100 or more days of eating walnuts during the 6-month period.
All main analyses were based on an intention-to-treat method (participants were analyzed according to their original group assignment, regardless of their adherence to the intervention).
The researchers also conducted a secondary per-protocol analysis, comparing the intervention and control groups to estimate the effect if all participants had adhered to their assigned intervention. They censored data for participants who reported eating walnuts for less than 100 days during the 6-month trial period.
Secondary outcomes included changes in height, weight, waist circumference, and BMI, as well as red blood cell proportions of omega-3 fatty acids (DHA, EPA, and ALA) at baseline and after 6 months.
Adherence counts
Most participants had “medium” or “high” levels of adherence to the Mediterranean diet, with “no meaningful differences” at baseline between the intervention and control groups in lifestyle characteristics or mean scores in all primary endpoints.
In the ITT analysis, there were no statistically significant differences in primary outcomes between the groups following the intervention. As for secondary outcomes, the RBC ALA significantly increased in the walnuts group but not the control group (coefficient, 0.04%; 95% confidence interval, 0.03%-0.06%; P < .0001).
However, there were differences in primary outcomes between the groups in the per-protocol analysis: The adherence-adjusted effect on improvement in attention score was −11.26 ms; 95% CI, −19.92 to −2.60; P = .011) for the intervention versus the control group.
The per-protocol analysis showed other differences: an improvement in fluid intelligence score (1.78; 95% CI, 0.90 - 2.67; P < .0001) and a reduction in ADHD symptom score (−2.18; 95% CI, −3.70 to −0.67; P = .0050).
“Overall, no significant differences were found in the intervention group in relation to the control group,” Dr. Julvez said in a news release. “But if the adherence factor is considered, then positive results are observed, since participants who most closely followed the guidelines – in terms of the recommended dose of walnuts and the number of days of consumption – did show improvements in the neuropsychological functions evaluated.”
Adolescence “is a time of great biological changes. Hormonal transformation occurs, which in turn is responsible for stimulating the synaptic growth of the frontal lobe,” he continued, adding that this brain region “enables neuropsychological maturation of more complex emotional and cognitive functions.”
“Neurons that are well nourished with these types of fatty acids will be able to grow and form new, stronger synapses,” he said.
Food as medicine
Uma Naidoo, MD, director of nutritional and lifestyle psychiatry at Massachusetts General Hospital, Boston, “commends” the researchers for conducting an RCT with a “robust” sample size and said she is “excited to see research like this furthering functional nutrition for mental health,” as she believes that “food is medicine.”
Dr. Naidoo, a professional chef, nutritional biologist, and author of the book “This Is Your Brain on Food,” said the findings “align” with her own approach to nutritional psychiatry and are also “in line” with her clinical practice.
However, although these results are “promising,” more research is needed across more diverse populations to “make sure these results are truly generalizable,” said Dr. Naidoo, a faculty member at Harvard Medical School, Boston, who was not involved with the study.
She “envisions a future where the research is so advanced that we can ‘dose’ these healthy whole foods for specific psychiatric symptoms and conditions.”
This study was supported by Instituto de Salud Carlos III (co-funded by European Union Regional Development Fund “A way to make Europe”). The California Walnut Commission has given support by supplying the walnuts for free for the Walnuts Smart Snack Dietary Intervention Trial. Dr. Julvez holds a Miguel Servet-II contract awarded by the Instituto de Salud Carlos III (co-funded by European Union Social Fund). The other authors’ disclosures are listed in the original article. Dr. Naidoo reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ECLINICALMEDICINE