User login
Keto/paleo diets ‘lower quality than others,’ and bad for planet
suggests a new analysis that reveals meat-based, as well as keto and paleo diets, to be the worst on both measures.
The research was published online in The American Journal of Clinical Nutrition.
To obtain a real-world view on the environmental and health impact of diets as consumed by U.S. adults, the team examined a nationally representative survey of the 1-day eating habits of more than 16,000 individuals.
This revealed that the best quality diet was pescatarian, followed by vegetarian and vegan diets. Omnivore diets, although less healthy, tended to score better than keto and paleo diets, which were the lowest ranked.
Both keto and paleo diets tend to be higher in animal foods and lower in plant foods than other popular diets, the researchers explain in their study, and they both have been associated with negative effects on blood lipids, specifically increased LDL cholesterol, raising concern about the long-term health outcomes associated with these diets.”
Analysis of the environmental impact of the different eating patterns showed that the vegan diet had the lowest carbon footprint, followed by the vegetarian and pescatarian diets. The omnivore, paleo, and keto diets had a far higher carbon footprint, with that of the keto diet more than four times greater than that for a vegan diet.
“Climate change is arguably one of the most pressing problems of our time, and a lot of people are interested in moving to a plant-based diet,” said senior author Diego Rose, PhD, MPH, RD, in a press release.
“Based on our results, that would reduce your footprint and be generally healthy,” noted Dr. Rose, nutrition program director, Tulane University, New Orleans.
To determine the carbon footprint and quality of popular diets as they are consumed by U.S. adults, Keelia O’Malley, PhD, MPH, Amelia Willits-Smith, PhD, MSc, and Dr. Rose, all with Tulane University, studied 24-hour recall data from the ongoing, nationally representative National Health and Nutrition Examination Survey (NHANES) for the years 2005-2010.
The data, which was captured by trained interviewers using a validated tool, was matched with the U.S. Department of Agriculture Food Patterns Equivalents Database to categorize the participants into one of six mutually exclusive categories: vegan, vegetarian, pescatarian, keto, paleo, or omnivore.
The omnivore category included anyone who did not fit into any of the preceding categories.
The environmental impact of the diets was then calculated by matching the established greenhouse gas emissions (GHGE) of over 300 commodities to foods listed on the NHANES, which was then summarized for each individual to give a carbon footprint for their 1-day diet.
Finally, the quality of their diet was estimated using the 2010 versions of the Healthy Eating Index and the Alternate Healthy Eating Index, both of which award a score to food components based on their impact on health.
Overall, 16,412 individuals were included in the analysis, of whom 52.1% were female.
The most common diet was omnivore, which was followed by 83.6% of respondents, followed by vegetarian (7.5%), pescatarian (4.7%), vegan (0.7%), keto (0.4%), and paleo diets (0.3%).
The lowest carbon footprint was seen with a vegan diet, at an average of 0.69 kg of carbon dioxide equivalents per 1,000 kcal consumed, followed by a vegetarian diet (1.16 kg of carbon dioxide equivalents per 1,000 kcal) and pescatarian diet (1.66 kg of carbon dioxide equivalents per 1,000 kcal).
The highest carbon footprints were observed with the omnivore (2.23 kg of carbon dioxide equivalents per 1,000 kcal), paleo (2.62 kg of carbon dioxide equivalents per 1,000 kcal), and keto diets (2.91 kg of carbon dioxide equivalents per 1,000 kcal).
In terms of diet quality, the pescatarian diet was ranked the highest on both eating index scores, followed by the vegetarian, then vegan, diets. The order of the three lowest scores depended on the index used, with either the keto or paleo diet deemed to be the worst quality.
Analysis of individuals following an omnivore diet suggested that those who ate in line with the DASH or Mediterranean diets had higher diet quality, as well as a lower environmental impact, than other people within the group.
Hence, Dr. Rose observed, “Our research ... shows there is a way to improve your health and footprint without giving up meat entirely.”
The researchers acknowledge that the use of 1-day diets has limitations, including that whatever individuals may have eaten during those 24 hours may not correspond to their overall day-in, day-out diet.
The study was supported by the Wellcome Trust. Dr. Rose declares relationships with the Center for Biological Diversity, the NCI, and the Health Resources and Services Administration. Dr. Willits-Smith has received funding from CBD and NCI. Dr. O’Malley has received funding from HRSA.
A version of this article first appeared on Medscape.com.
suggests a new analysis that reveals meat-based, as well as keto and paleo diets, to be the worst on both measures.
The research was published online in The American Journal of Clinical Nutrition.
To obtain a real-world view on the environmental and health impact of diets as consumed by U.S. adults, the team examined a nationally representative survey of the 1-day eating habits of more than 16,000 individuals.
This revealed that the best quality diet was pescatarian, followed by vegetarian and vegan diets. Omnivore diets, although less healthy, tended to score better than keto and paleo diets, which were the lowest ranked.
Both keto and paleo diets tend to be higher in animal foods and lower in plant foods than other popular diets, the researchers explain in their study, and they both have been associated with negative effects on blood lipids, specifically increased LDL cholesterol, raising concern about the long-term health outcomes associated with these diets.”
Analysis of the environmental impact of the different eating patterns showed that the vegan diet had the lowest carbon footprint, followed by the vegetarian and pescatarian diets. The omnivore, paleo, and keto diets had a far higher carbon footprint, with that of the keto diet more than four times greater than that for a vegan diet.
“Climate change is arguably one of the most pressing problems of our time, and a lot of people are interested in moving to a plant-based diet,” said senior author Diego Rose, PhD, MPH, RD, in a press release.
“Based on our results, that would reduce your footprint and be generally healthy,” noted Dr. Rose, nutrition program director, Tulane University, New Orleans.
To determine the carbon footprint and quality of popular diets as they are consumed by U.S. adults, Keelia O’Malley, PhD, MPH, Amelia Willits-Smith, PhD, MSc, and Dr. Rose, all with Tulane University, studied 24-hour recall data from the ongoing, nationally representative National Health and Nutrition Examination Survey (NHANES) for the years 2005-2010.
The data, which was captured by trained interviewers using a validated tool, was matched with the U.S. Department of Agriculture Food Patterns Equivalents Database to categorize the participants into one of six mutually exclusive categories: vegan, vegetarian, pescatarian, keto, paleo, or omnivore.
The omnivore category included anyone who did not fit into any of the preceding categories.
The environmental impact of the diets was then calculated by matching the established greenhouse gas emissions (GHGE) of over 300 commodities to foods listed on the NHANES, which was then summarized for each individual to give a carbon footprint for their 1-day diet.
Finally, the quality of their diet was estimated using the 2010 versions of the Healthy Eating Index and the Alternate Healthy Eating Index, both of which award a score to food components based on their impact on health.
Overall, 16,412 individuals were included in the analysis, of whom 52.1% were female.
The most common diet was omnivore, which was followed by 83.6% of respondents, followed by vegetarian (7.5%), pescatarian (4.7%), vegan (0.7%), keto (0.4%), and paleo diets (0.3%).
The lowest carbon footprint was seen with a vegan diet, at an average of 0.69 kg of carbon dioxide equivalents per 1,000 kcal consumed, followed by a vegetarian diet (1.16 kg of carbon dioxide equivalents per 1,000 kcal) and pescatarian diet (1.66 kg of carbon dioxide equivalents per 1,000 kcal).
The highest carbon footprints were observed with the omnivore (2.23 kg of carbon dioxide equivalents per 1,000 kcal), paleo (2.62 kg of carbon dioxide equivalents per 1,000 kcal), and keto diets (2.91 kg of carbon dioxide equivalents per 1,000 kcal).
In terms of diet quality, the pescatarian diet was ranked the highest on both eating index scores, followed by the vegetarian, then vegan, diets. The order of the three lowest scores depended on the index used, with either the keto or paleo diet deemed to be the worst quality.
Analysis of individuals following an omnivore diet suggested that those who ate in line with the DASH or Mediterranean diets had higher diet quality, as well as a lower environmental impact, than other people within the group.
Hence, Dr. Rose observed, “Our research ... shows there is a way to improve your health and footprint without giving up meat entirely.”
The researchers acknowledge that the use of 1-day diets has limitations, including that whatever individuals may have eaten during those 24 hours may not correspond to their overall day-in, day-out diet.
The study was supported by the Wellcome Trust. Dr. Rose declares relationships with the Center for Biological Diversity, the NCI, and the Health Resources and Services Administration. Dr. Willits-Smith has received funding from CBD and NCI. Dr. O’Malley has received funding from HRSA.
A version of this article first appeared on Medscape.com.
suggests a new analysis that reveals meat-based, as well as keto and paleo diets, to be the worst on both measures.
The research was published online in The American Journal of Clinical Nutrition.
To obtain a real-world view on the environmental and health impact of diets as consumed by U.S. adults, the team examined a nationally representative survey of the 1-day eating habits of more than 16,000 individuals.
This revealed that the best quality diet was pescatarian, followed by vegetarian and vegan diets. Omnivore diets, although less healthy, tended to score better than keto and paleo diets, which were the lowest ranked.
Both keto and paleo diets tend to be higher in animal foods and lower in plant foods than other popular diets, the researchers explain in their study, and they both have been associated with negative effects on blood lipids, specifically increased LDL cholesterol, raising concern about the long-term health outcomes associated with these diets.”
Analysis of the environmental impact of the different eating patterns showed that the vegan diet had the lowest carbon footprint, followed by the vegetarian and pescatarian diets. The omnivore, paleo, and keto diets had a far higher carbon footprint, with that of the keto diet more than four times greater than that for a vegan diet.
“Climate change is arguably one of the most pressing problems of our time, and a lot of people are interested in moving to a plant-based diet,” said senior author Diego Rose, PhD, MPH, RD, in a press release.
“Based on our results, that would reduce your footprint and be generally healthy,” noted Dr. Rose, nutrition program director, Tulane University, New Orleans.
To determine the carbon footprint and quality of popular diets as they are consumed by U.S. adults, Keelia O’Malley, PhD, MPH, Amelia Willits-Smith, PhD, MSc, and Dr. Rose, all with Tulane University, studied 24-hour recall data from the ongoing, nationally representative National Health and Nutrition Examination Survey (NHANES) for the years 2005-2010.
The data, which was captured by trained interviewers using a validated tool, was matched with the U.S. Department of Agriculture Food Patterns Equivalents Database to categorize the participants into one of six mutually exclusive categories: vegan, vegetarian, pescatarian, keto, paleo, or omnivore.
The omnivore category included anyone who did not fit into any of the preceding categories.
The environmental impact of the diets was then calculated by matching the established greenhouse gas emissions (GHGE) of over 300 commodities to foods listed on the NHANES, which was then summarized for each individual to give a carbon footprint for their 1-day diet.
Finally, the quality of their diet was estimated using the 2010 versions of the Healthy Eating Index and the Alternate Healthy Eating Index, both of which award a score to food components based on their impact on health.
Overall, 16,412 individuals were included in the analysis, of whom 52.1% were female.
The most common diet was omnivore, which was followed by 83.6% of respondents, followed by vegetarian (7.5%), pescatarian (4.7%), vegan (0.7%), keto (0.4%), and paleo diets (0.3%).
The lowest carbon footprint was seen with a vegan diet, at an average of 0.69 kg of carbon dioxide equivalents per 1,000 kcal consumed, followed by a vegetarian diet (1.16 kg of carbon dioxide equivalents per 1,000 kcal) and pescatarian diet (1.66 kg of carbon dioxide equivalents per 1,000 kcal).
The highest carbon footprints were observed with the omnivore (2.23 kg of carbon dioxide equivalents per 1,000 kcal), paleo (2.62 kg of carbon dioxide equivalents per 1,000 kcal), and keto diets (2.91 kg of carbon dioxide equivalents per 1,000 kcal).
In terms of diet quality, the pescatarian diet was ranked the highest on both eating index scores, followed by the vegetarian, then vegan, diets. The order of the three lowest scores depended on the index used, with either the keto or paleo diet deemed to be the worst quality.
Analysis of individuals following an omnivore diet suggested that those who ate in line with the DASH or Mediterranean diets had higher diet quality, as well as a lower environmental impact, than other people within the group.
Hence, Dr. Rose observed, “Our research ... shows there is a way to improve your health and footprint without giving up meat entirely.”
The researchers acknowledge that the use of 1-day diets has limitations, including that whatever individuals may have eaten during those 24 hours may not correspond to their overall day-in, day-out diet.
The study was supported by the Wellcome Trust. Dr. Rose declares relationships with the Center for Biological Diversity, the NCI, and the Health Resources and Services Administration. Dr. Willits-Smith has received funding from CBD and NCI. Dr. O’Malley has received funding from HRSA.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF CLINICAL NUTRITION
Do artificial sweeteners alter postmeal glucose, hunger hormones?
Drinking a sugar-sweetened beverage (SSB), however, had a different effect on postprandial levels of glucose and the hormones insulin, glucagonlike peptide–1 (GLP-1), gastric inhibitory polypeptide (GIP), peptide YY (PYY), ghrelin, leptin, and glucagon.
These findings are from a new meta-analysis by Roselyn Zhang and colleagues, supported by the nonprofit organization Institute for the Advancement of Food and Nutrition Sciences. The study was published recently in Nutrients.
“Nonnutritive sweeteners have no acute metabolic or endocrine effects and they are similar to water in that respect, and they show a different response from caloric sweeteners,” study author Tauseef Khan, MBBS, PhD, summarized in an interview following a press briefing from the IAFNS.
“Our study supports that nonnutritive sweeteners are a healthier alternative to sugar-sweetened beverages or caloric beverages,” said Dr. Khan, an epidemiologist in the department of nutritional sciences, University of Toronto.
Most participants in the 36 trials included in the meta-analysis were healthy, he noted. However, for certain types of NNS beverages, “we had enough studies for type 2 diabetes to also assess that separately, and the results were the same: Nonnutritive sweeteners were no different from water; however, they were different from caloric sweeteners.”
Of note, none of the studies included erythritol – a sugar alcohol (polyol) increasingly used as an artificial sweetener in keto and other types of foods – which was associated with a risk for adverse cardiac events in a paper in Nature Medicine.
Are these NNS drinks largely inert?
“This [meta-analysis] implies that sweeteners are largely inert,” in terms of acute postprandial glucose and hormone response, but the review did not include newer reports that differ, Duane Mellor, PhD, RD, RNutr, who was not involved with the research, noted in an email.
“This is possibly,” he said, because the study “only reviewed the literature up until January 2022 and therefore it missed the World Health Organization review ‘Health Effects of the Use of Non-Sugar Sweeteners’ published in April [2022], and a study published in August 2022 in the journal Cell suggesting that some nonnutritive sweeteners may have a minor effect on gut microbiome and glucose response.
“Although there is a place of nonnutritive sweeteners as a way to reduce sugar intake, they are a small part of dietary pattern and lifestyle which can help reduce risk of disease,” said Dr. Mellor, a registered dietitian and senior teaching fellow at Aston University, Birmingham, England.
“So, although we are clear we need to reduce our intake of sugar-sweetened beverages, switching to non-nutritive sweetened beverages (such as diet sodas) is not necessarily the healthiest option, as unlike water, it seems that some nonnutritive sweeteners may influence glucose responses and levels of related hormones in more recent studies.”
NNS beverages ‘are similar to water’
Dr. Khan pointed out that the meta-analysis addressed two major concerns about NNS beverages.
First, the “sweet uncoupling hypothesis” proposes that low-calorie sweeteners affect sweet taste by separating sweet taste from calories. “The body is confused, and then there is hormonal change. Our study shows that actually that’s not true, and [NNS beverages] are similar to water.”
Second, when no-calorie or low-calorie sweeteners are taken with calories (coupling), a concern is that “then you eat more somehow, or your response is different. However, the results [in this meta-analysis] also show that that is not the case for glucose response, insulin response, and other hormonal markers.”
“The strength is not that low-calorie sweeteners have some benefit per se,” he elaborated. “The advantage is that they replace caloric beverages.
“We are not saying that anybody who is not taking low-calorie sweeteners should start taking [them],” he continued. “What we are saying is somebody who is taking sugar-sweetened beverages and has a problem of taking excess calories, if you replace those calories with low-calorie sweetener, replacement of calories itself may be beneficial, and also they should not be concerned of any [acute] issues with a moderate amount of low-calorie sweeteners.”
Postprandial effect of NNS beverages, SSBs, water
Eight NNS are currently approved by the Food and Drug Administration: aspartame, acesulfame potassium (ace-K), luo han guo (monkfruit) extract, neotame, saccharin, stevia, sucralose, and advantame, the researchers noted.
Ms. Zhang and colleagues searched the literature up until Jan. 15, 2022, for studies of NNS beverages and acute postprandial glycemic and endocrine responses.
Trials were excluded if they involved sugar alcohols (eg, erythritol) or rare sugars (eg, allulose), or if they were shorter than 2 hours, lacked a comparator arm, or did not provide suitable endpoint data.
They identified 36 randomized and nonrandomized clinical trials of 472 predominantly healthy participants: 21 trials (15 reports, n = 266) with NNS consumed alone (uncoupled), 3 trials (3 reports, n = 27) with NNS consumed in a solution containing a carbohydrate (coupled), and 12 trials (7 reports, n = 179) with NNS consumed up to 15 minutes before oral glucose carbohydrate load (delayed coupling).
The four types of beverages were single NNS (ace-K, aspartame, cyclamate, saccharin, stevia, and sucralose), NNS blends (ace-K + aspartame; ace-K + sucralose; ace-K + aspartame + cyclamate; and ace-K + aspartame + sucralose), SSBs (glucose, sucrose, and fructose), and water (control).
In the uncoupled interventions, NNS beverages (single or blends) had no effect on postprandial glucose, insulin, GLP-1, GIP, PYY, ghrelin, and glucagon, with responses similar to water.
In the uncoupled interventions, SSBs sweetened with caloric sugars (glucose and sucrose) increased postprandial glucose, insulin, GLP-1, and GIP responses, with no differences in postprandial ghrelin and glucagon responses.
In the coupled and delayed coupling interventions, NNS beverages had no postprandial glucose and endocrine effects, with responses similar to water.
The studies generally had low to moderate confidence.
The study was supported by an unrestricted grant from IAFNS. Dr. Khan has received research support from the Canadian Institutes of Health Research, the International Life Sciences Institute, and the National Honey Board. He has received honorariums for lectures from the International Food Information Council and the IAFNS. Dr. Mellor has no disclosures.
A version of this article first appeared on Medscape.com.
Drinking a sugar-sweetened beverage (SSB), however, had a different effect on postprandial levels of glucose and the hormones insulin, glucagonlike peptide–1 (GLP-1), gastric inhibitory polypeptide (GIP), peptide YY (PYY), ghrelin, leptin, and glucagon.
These findings are from a new meta-analysis by Roselyn Zhang and colleagues, supported by the nonprofit organization Institute for the Advancement of Food and Nutrition Sciences. The study was published recently in Nutrients.
“Nonnutritive sweeteners have no acute metabolic or endocrine effects and they are similar to water in that respect, and they show a different response from caloric sweeteners,” study author Tauseef Khan, MBBS, PhD, summarized in an interview following a press briefing from the IAFNS.
“Our study supports that nonnutritive sweeteners are a healthier alternative to sugar-sweetened beverages or caloric beverages,” said Dr. Khan, an epidemiologist in the department of nutritional sciences, University of Toronto.
Most participants in the 36 trials included in the meta-analysis were healthy, he noted. However, for certain types of NNS beverages, “we had enough studies for type 2 diabetes to also assess that separately, and the results were the same: Nonnutritive sweeteners were no different from water; however, they were different from caloric sweeteners.”
Of note, none of the studies included erythritol – a sugar alcohol (polyol) increasingly used as an artificial sweetener in keto and other types of foods – which was associated with a risk for adverse cardiac events in a paper in Nature Medicine.
Are these NNS drinks largely inert?
“This [meta-analysis] implies that sweeteners are largely inert,” in terms of acute postprandial glucose and hormone response, but the review did not include newer reports that differ, Duane Mellor, PhD, RD, RNutr, who was not involved with the research, noted in an email.
“This is possibly,” he said, because the study “only reviewed the literature up until January 2022 and therefore it missed the World Health Organization review ‘Health Effects of the Use of Non-Sugar Sweeteners’ published in April [2022], and a study published in August 2022 in the journal Cell suggesting that some nonnutritive sweeteners may have a minor effect on gut microbiome and glucose response.
“Although there is a place of nonnutritive sweeteners as a way to reduce sugar intake, they are a small part of dietary pattern and lifestyle which can help reduce risk of disease,” said Dr. Mellor, a registered dietitian and senior teaching fellow at Aston University, Birmingham, England.
“So, although we are clear we need to reduce our intake of sugar-sweetened beverages, switching to non-nutritive sweetened beverages (such as diet sodas) is not necessarily the healthiest option, as unlike water, it seems that some nonnutritive sweeteners may influence glucose responses and levels of related hormones in more recent studies.”
NNS beverages ‘are similar to water’
Dr. Khan pointed out that the meta-analysis addressed two major concerns about NNS beverages.
First, the “sweet uncoupling hypothesis” proposes that low-calorie sweeteners affect sweet taste by separating sweet taste from calories. “The body is confused, and then there is hormonal change. Our study shows that actually that’s not true, and [NNS beverages] are similar to water.”
Second, when no-calorie or low-calorie sweeteners are taken with calories (coupling), a concern is that “then you eat more somehow, or your response is different. However, the results [in this meta-analysis] also show that that is not the case for glucose response, insulin response, and other hormonal markers.”
“The strength is not that low-calorie sweeteners have some benefit per se,” he elaborated. “The advantage is that they replace caloric beverages.
“We are not saying that anybody who is not taking low-calorie sweeteners should start taking [them],” he continued. “What we are saying is somebody who is taking sugar-sweetened beverages and has a problem of taking excess calories, if you replace those calories with low-calorie sweetener, replacement of calories itself may be beneficial, and also they should not be concerned of any [acute] issues with a moderate amount of low-calorie sweeteners.”
Postprandial effect of NNS beverages, SSBs, water
Eight NNS are currently approved by the Food and Drug Administration: aspartame, acesulfame potassium (ace-K), luo han guo (monkfruit) extract, neotame, saccharin, stevia, sucralose, and advantame, the researchers noted.
Ms. Zhang and colleagues searched the literature up until Jan. 15, 2022, for studies of NNS beverages and acute postprandial glycemic and endocrine responses.
Trials were excluded if they involved sugar alcohols (eg, erythritol) or rare sugars (eg, allulose), or if they were shorter than 2 hours, lacked a comparator arm, or did not provide suitable endpoint data.
They identified 36 randomized and nonrandomized clinical trials of 472 predominantly healthy participants: 21 trials (15 reports, n = 266) with NNS consumed alone (uncoupled), 3 trials (3 reports, n = 27) with NNS consumed in a solution containing a carbohydrate (coupled), and 12 trials (7 reports, n = 179) with NNS consumed up to 15 minutes before oral glucose carbohydrate load (delayed coupling).
The four types of beverages were single NNS (ace-K, aspartame, cyclamate, saccharin, stevia, and sucralose), NNS blends (ace-K + aspartame; ace-K + sucralose; ace-K + aspartame + cyclamate; and ace-K + aspartame + sucralose), SSBs (glucose, sucrose, and fructose), and water (control).
In the uncoupled interventions, NNS beverages (single or blends) had no effect on postprandial glucose, insulin, GLP-1, GIP, PYY, ghrelin, and glucagon, with responses similar to water.
In the uncoupled interventions, SSBs sweetened with caloric sugars (glucose and sucrose) increased postprandial glucose, insulin, GLP-1, and GIP responses, with no differences in postprandial ghrelin and glucagon responses.
In the coupled and delayed coupling interventions, NNS beverages had no postprandial glucose and endocrine effects, with responses similar to water.
The studies generally had low to moderate confidence.
The study was supported by an unrestricted grant from IAFNS. Dr. Khan has received research support from the Canadian Institutes of Health Research, the International Life Sciences Institute, and the National Honey Board. He has received honorariums for lectures from the International Food Information Council and the IAFNS. Dr. Mellor has no disclosures.
A version of this article first appeared on Medscape.com.
Drinking a sugar-sweetened beverage (SSB), however, had a different effect on postprandial levels of glucose and the hormones insulin, glucagonlike peptide–1 (GLP-1), gastric inhibitory polypeptide (GIP), peptide YY (PYY), ghrelin, leptin, and glucagon.
These findings are from a new meta-analysis by Roselyn Zhang and colleagues, supported by the nonprofit organization Institute for the Advancement of Food and Nutrition Sciences. The study was published recently in Nutrients.
“Nonnutritive sweeteners have no acute metabolic or endocrine effects and they are similar to water in that respect, and they show a different response from caloric sweeteners,” study author Tauseef Khan, MBBS, PhD, summarized in an interview following a press briefing from the IAFNS.
“Our study supports that nonnutritive sweeteners are a healthier alternative to sugar-sweetened beverages or caloric beverages,” said Dr. Khan, an epidemiologist in the department of nutritional sciences, University of Toronto.
Most participants in the 36 trials included in the meta-analysis were healthy, he noted. However, for certain types of NNS beverages, “we had enough studies for type 2 diabetes to also assess that separately, and the results were the same: Nonnutritive sweeteners were no different from water; however, they were different from caloric sweeteners.”
Of note, none of the studies included erythritol – a sugar alcohol (polyol) increasingly used as an artificial sweetener in keto and other types of foods – which was associated with a risk for adverse cardiac events in a paper in Nature Medicine.
Are these NNS drinks largely inert?
“This [meta-analysis] implies that sweeteners are largely inert,” in terms of acute postprandial glucose and hormone response, but the review did not include newer reports that differ, Duane Mellor, PhD, RD, RNutr, who was not involved with the research, noted in an email.
“This is possibly,” he said, because the study “only reviewed the literature up until January 2022 and therefore it missed the World Health Organization review ‘Health Effects of the Use of Non-Sugar Sweeteners’ published in April [2022], and a study published in August 2022 in the journal Cell suggesting that some nonnutritive sweeteners may have a minor effect on gut microbiome and glucose response.
“Although there is a place of nonnutritive sweeteners as a way to reduce sugar intake, they are a small part of dietary pattern and lifestyle which can help reduce risk of disease,” said Dr. Mellor, a registered dietitian and senior teaching fellow at Aston University, Birmingham, England.
“So, although we are clear we need to reduce our intake of sugar-sweetened beverages, switching to non-nutritive sweetened beverages (such as diet sodas) is not necessarily the healthiest option, as unlike water, it seems that some nonnutritive sweeteners may influence glucose responses and levels of related hormones in more recent studies.”
NNS beverages ‘are similar to water’
Dr. Khan pointed out that the meta-analysis addressed two major concerns about NNS beverages.
First, the “sweet uncoupling hypothesis” proposes that low-calorie sweeteners affect sweet taste by separating sweet taste from calories. “The body is confused, and then there is hormonal change. Our study shows that actually that’s not true, and [NNS beverages] are similar to water.”
Second, when no-calorie or low-calorie sweeteners are taken with calories (coupling), a concern is that “then you eat more somehow, or your response is different. However, the results [in this meta-analysis] also show that that is not the case for glucose response, insulin response, and other hormonal markers.”
“The strength is not that low-calorie sweeteners have some benefit per se,” he elaborated. “The advantage is that they replace caloric beverages.
“We are not saying that anybody who is not taking low-calorie sweeteners should start taking [them],” he continued. “What we are saying is somebody who is taking sugar-sweetened beverages and has a problem of taking excess calories, if you replace those calories with low-calorie sweetener, replacement of calories itself may be beneficial, and also they should not be concerned of any [acute] issues with a moderate amount of low-calorie sweeteners.”
Postprandial effect of NNS beverages, SSBs, water
Eight NNS are currently approved by the Food and Drug Administration: aspartame, acesulfame potassium (ace-K), luo han guo (monkfruit) extract, neotame, saccharin, stevia, sucralose, and advantame, the researchers noted.
Ms. Zhang and colleagues searched the literature up until Jan. 15, 2022, for studies of NNS beverages and acute postprandial glycemic and endocrine responses.
Trials were excluded if they involved sugar alcohols (eg, erythritol) or rare sugars (eg, allulose), or if they were shorter than 2 hours, lacked a comparator arm, or did not provide suitable endpoint data.
They identified 36 randomized and nonrandomized clinical trials of 472 predominantly healthy participants: 21 trials (15 reports, n = 266) with NNS consumed alone (uncoupled), 3 trials (3 reports, n = 27) with NNS consumed in a solution containing a carbohydrate (coupled), and 12 trials (7 reports, n = 179) with NNS consumed up to 15 minutes before oral glucose carbohydrate load (delayed coupling).
The four types of beverages were single NNS (ace-K, aspartame, cyclamate, saccharin, stevia, and sucralose), NNS blends (ace-K + aspartame; ace-K + sucralose; ace-K + aspartame + cyclamate; and ace-K + aspartame + sucralose), SSBs (glucose, sucrose, and fructose), and water (control).
In the uncoupled interventions, NNS beverages (single or blends) had no effect on postprandial glucose, insulin, GLP-1, GIP, PYY, ghrelin, and glucagon, with responses similar to water.
In the uncoupled interventions, SSBs sweetened with caloric sugars (glucose and sucrose) increased postprandial glucose, insulin, GLP-1, and GIP responses, with no differences in postprandial ghrelin and glucagon responses.
In the coupled and delayed coupling interventions, NNS beverages had no postprandial glucose and endocrine effects, with responses similar to water.
The studies generally had low to moderate confidence.
The study was supported by an unrestricted grant from IAFNS. Dr. Khan has received research support from the Canadian Institutes of Health Research, the International Life Sciences Institute, and the National Honey Board. He has received honorariums for lectures from the International Food Information Council and the IAFNS. Dr. Mellor has no disclosures.
A version of this article first appeared on Medscape.com.
FROM NUTRIENTS
High CV risk factor burden in young adults a ‘smoldering’ crisis
New data show a high and rising burden of most cardiovascular (CV) risk factors among young adults aged 20-44 years in the United States.
In this age group, over the past 10 years, there has been an increase in the prevalence of diabetes and obesity, no improvement in the prevalence of hypertension, and a decrease in the prevalence of hyperlipidemia.
Yet medical treatment rates for CV risk factors are “surprisingly” low among young adults, study investigator Rishi Wadhera, MD, with Beth Israel Deaconess Medical Center and Harvard Medical School, both in Boston, told this news organization.
The findings are “extremely concerning. We’re witnessing a smoldering public health crisis. The onset of these risk factors earlier in life is associated with a higher lifetime risk of heart disease and potentially life-threatening,” Dr. Wadhera added.
The study was presented March 5 at the joint scientific sessions of the American College of Cardiology and the World Heart Federation and was simultaneously published in JAMA.
The burden of CV risk factors among young adults is “unacceptably high and increasing,” write the co-authors of a JAMA editorial.
“The time is now for aggressive preventive measures in young adults. Without immediate action there will continue to be a rise in heart disease and the burden it places on patients, families, and communities,” say Norrina Allen, PhD, and John Wilkins, MD, with Northwestern University, Chicago.
Preventing a tsunami of heart disease
The findings stem from a cross-sectional study of 12,294 U.S. adults aged 20-44 years (mean age, 32; 51% women) who participated in National Health and Nutrition Examination Survey (NHANES) cycles for 2009-2010 to 2017-2020.
Overall, the prevalence of hypertension was 9.3% in 2009-2010 and increased to 11.5% in 2017-2020. The prevalence of diabetes rose from 3.0% to 4.1%, and the prevalence of obesity rose from 32.7% to 40.9%. The prevalence of hyperlipidemia decreased from 40.5% to 36.1%.
Black adults consistently had high rates of hypertension during the study period – 16.2% in 2009-2010 and 20.1% in 2017-2020 – and significant increases in hypertension occurred among Mexican American adults (from 6.5% to 9.5%) and other Hispanic adults (from 4.4% to 10.5%), while Mexican American adults had a significant uptick in diabetes (from 4.3% to 7.5%).
Equally concerning, said Dr. Wadhera, is the fact that only about 55% of young adults with hypertension were receiving antihypertensive medication, and just 1 in 2 young adults with diabetes were receiving treatment. “These low rates were driven, in part, by many young adults not being aware of their diagnosis,” he noted.
The NHANES data also show that the percentage of young adults who were treated for hypertension and who achieved blood pressure control did not change significantly over the study period (65.0% in 2009-2010 and 74.8% in 2017-2020). Blood sugar control among young adults being treated for diabetes remained suboptimal throughout the study period (45.5% in 2009-2010 and 56.6% in 2017-2020).
“The fact that blood pressure control and glycemic control are so poor is really worrisome,” Jeffrey Berger, MD, director of the Center for the Prevention of Cardiovascular Disease at NYU Langone Heart, who wasn’t involved in the study, told this news organization.
“Even in the lipid control, while it did get a little bit better, it’s still only around 30%-40%. So, I think we have ways to go as a society,” Dr. Berger noted.
Double down on screening
Dr. Wadhera said “we need to double down on efforts to screen for and treat cardiovascular risk factors like high blood pressure and diabetes in young adults. We need to intensify clinical and public health interventions focused on primordial and primary prevention in young adults now so that we can avoid a tsunami of cardiovascular disease in the long term.”
“It’s critically important that young adults speak with their health care provider about whether – and when – they should undergo screening for high blood pressure, diabetes, and high cholesterol,” Dr. Wadhera added.
Dr. Berger said one problem is that younger people often have a “superman or superwoman” view and don’t comprehend that they are at risk for some of these conditions. Studies such as this “reinforce the idea that it’s never too young to be checked out.”
As a cardiologist who specializes in cardiovascular prevention, Dr. Berger said he sometimes hears patients say things like, “I don’t ever want to need a cardiologist,” or “I hope I never need a cardiologist.”
“My response is, ‘There are many different types of cardiologists,’ and I think it would really be helpful for many people to see a prevention-focused cardiologist way before they have problems,” he said in an interview.
“As a system, medicine has become very good at treating patients with different diseases. I think we need to get better in terms of preventing some of these problems,” Dr. Berger added.
In their editorial, Dr. Allen and Dr. Wilkins say the “foundation of cardiovascular health begins early in life. These worsening trends in risk factors highlight the importance of focusing on prevention in adolescence and young adulthood in order to promote cardiovascular health across the lifetime.”
The study was funded by a grant from the National Heart, Lung, and Blood Institute. Dr. Wadhera has served as a consultant for Abbott and CVS Health. Dr. Wilkins has received personal fees from 3M. Dr. Berger has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New data show a high and rising burden of most cardiovascular (CV) risk factors among young adults aged 20-44 years in the United States.
In this age group, over the past 10 years, there has been an increase in the prevalence of diabetes and obesity, no improvement in the prevalence of hypertension, and a decrease in the prevalence of hyperlipidemia.
Yet medical treatment rates for CV risk factors are “surprisingly” low among young adults, study investigator Rishi Wadhera, MD, with Beth Israel Deaconess Medical Center and Harvard Medical School, both in Boston, told this news organization.
The findings are “extremely concerning. We’re witnessing a smoldering public health crisis. The onset of these risk factors earlier in life is associated with a higher lifetime risk of heart disease and potentially life-threatening,” Dr. Wadhera added.
The study was presented March 5 at the joint scientific sessions of the American College of Cardiology and the World Heart Federation and was simultaneously published in JAMA.
The burden of CV risk factors among young adults is “unacceptably high and increasing,” write the co-authors of a JAMA editorial.
“The time is now for aggressive preventive measures in young adults. Without immediate action there will continue to be a rise in heart disease and the burden it places on patients, families, and communities,” say Norrina Allen, PhD, and John Wilkins, MD, with Northwestern University, Chicago.
Preventing a tsunami of heart disease
The findings stem from a cross-sectional study of 12,294 U.S. adults aged 20-44 years (mean age, 32; 51% women) who participated in National Health and Nutrition Examination Survey (NHANES) cycles for 2009-2010 to 2017-2020.
Overall, the prevalence of hypertension was 9.3% in 2009-2010 and increased to 11.5% in 2017-2020. The prevalence of diabetes rose from 3.0% to 4.1%, and the prevalence of obesity rose from 32.7% to 40.9%. The prevalence of hyperlipidemia decreased from 40.5% to 36.1%.
Black adults consistently had high rates of hypertension during the study period – 16.2% in 2009-2010 and 20.1% in 2017-2020 – and significant increases in hypertension occurred among Mexican American adults (from 6.5% to 9.5%) and other Hispanic adults (from 4.4% to 10.5%), while Mexican American adults had a significant uptick in diabetes (from 4.3% to 7.5%).
Equally concerning, said Dr. Wadhera, is the fact that only about 55% of young adults with hypertension were receiving antihypertensive medication, and just 1 in 2 young adults with diabetes were receiving treatment. “These low rates were driven, in part, by many young adults not being aware of their diagnosis,” he noted.
The NHANES data also show that the percentage of young adults who were treated for hypertension and who achieved blood pressure control did not change significantly over the study period (65.0% in 2009-2010 and 74.8% in 2017-2020). Blood sugar control among young adults being treated for diabetes remained suboptimal throughout the study period (45.5% in 2009-2010 and 56.6% in 2017-2020).
“The fact that blood pressure control and glycemic control are so poor is really worrisome,” Jeffrey Berger, MD, director of the Center for the Prevention of Cardiovascular Disease at NYU Langone Heart, who wasn’t involved in the study, told this news organization.
“Even in the lipid control, while it did get a little bit better, it’s still only around 30%-40%. So, I think we have ways to go as a society,” Dr. Berger noted.
Double down on screening
Dr. Wadhera said “we need to double down on efforts to screen for and treat cardiovascular risk factors like high blood pressure and diabetes in young adults. We need to intensify clinical and public health interventions focused on primordial and primary prevention in young adults now so that we can avoid a tsunami of cardiovascular disease in the long term.”
“It’s critically important that young adults speak with their health care provider about whether – and when – they should undergo screening for high blood pressure, diabetes, and high cholesterol,” Dr. Wadhera added.
Dr. Berger said one problem is that younger people often have a “superman or superwoman” view and don’t comprehend that they are at risk for some of these conditions. Studies such as this “reinforce the idea that it’s never too young to be checked out.”
As a cardiologist who specializes in cardiovascular prevention, Dr. Berger said he sometimes hears patients say things like, “I don’t ever want to need a cardiologist,” or “I hope I never need a cardiologist.”
“My response is, ‘There are many different types of cardiologists,’ and I think it would really be helpful for many people to see a prevention-focused cardiologist way before they have problems,” he said in an interview.
“As a system, medicine has become very good at treating patients with different diseases. I think we need to get better in terms of preventing some of these problems,” Dr. Berger added.
In their editorial, Dr. Allen and Dr. Wilkins say the “foundation of cardiovascular health begins early in life. These worsening trends in risk factors highlight the importance of focusing on prevention in adolescence and young adulthood in order to promote cardiovascular health across the lifetime.”
The study was funded by a grant from the National Heart, Lung, and Blood Institute. Dr. Wadhera has served as a consultant for Abbott and CVS Health. Dr. Wilkins has received personal fees from 3M. Dr. Berger has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New data show a high and rising burden of most cardiovascular (CV) risk factors among young adults aged 20-44 years in the United States.
In this age group, over the past 10 years, there has been an increase in the prevalence of diabetes and obesity, no improvement in the prevalence of hypertension, and a decrease in the prevalence of hyperlipidemia.
Yet medical treatment rates for CV risk factors are “surprisingly” low among young adults, study investigator Rishi Wadhera, MD, with Beth Israel Deaconess Medical Center and Harvard Medical School, both in Boston, told this news organization.
The findings are “extremely concerning. We’re witnessing a smoldering public health crisis. The onset of these risk factors earlier in life is associated with a higher lifetime risk of heart disease and potentially life-threatening,” Dr. Wadhera added.
The study was presented March 5 at the joint scientific sessions of the American College of Cardiology and the World Heart Federation and was simultaneously published in JAMA.
The burden of CV risk factors among young adults is “unacceptably high and increasing,” write the co-authors of a JAMA editorial.
“The time is now for aggressive preventive measures in young adults. Without immediate action there will continue to be a rise in heart disease and the burden it places on patients, families, and communities,” say Norrina Allen, PhD, and John Wilkins, MD, with Northwestern University, Chicago.
Preventing a tsunami of heart disease
The findings stem from a cross-sectional study of 12,294 U.S. adults aged 20-44 years (mean age, 32; 51% women) who participated in National Health and Nutrition Examination Survey (NHANES) cycles for 2009-2010 to 2017-2020.
Overall, the prevalence of hypertension was 9.3% in 2009-2010 and increased to 11.5% in 2017-2020. The prevalence of diabetes rose from 3.0% to 4.1%, and the prevalence of obesity rose from 32.7% to 40.9%. The prevalence of hyperlipidemia decreased from 40.5% to 36.1%.
Black adults consistently had high rates of hypertension during the study period – 16.2% in 2009-2010 and 20.1% in 2017-2020 – and significant increases in hypertension occurred among Mexican American adults (from 6.5% to 9.5%) and other Hispanic adults (from 4.4% to 10.5%), while Mexican American adults had a significant uptick in diabetes (from 4.3% to 7.5%).
Equally concerning, said Dr. Wadhera, is the fact that only about 55% of young adults with hypertension were receiving antihypertensive medication, and just 1 in 2 young adults with diabetes were receiving treatment. “These low rates were driven, in part, by many young adults not being aware of their diagnosis,” he noted.
The NHANES data also show that the percentage of young adults who were treated for hypertension and who achieved blood pressure control did not change significantly over the study period (65.0% in 2009-2010 and 74.8% in 2017-2020). Blood sugar control among young adults being treated for diabetes remained suboptimal throughout the study period (45.5% in 2009-2010 and 56.6% in 2017-2020).
“The fact that blood pressure control and glycemic control are so poor is really worrisome,” Jeffrey Berger, MD, director of the Center for the Prevention of Cardiovascular Disease at NYU Langone Heart, who wasn’t involved in the study, told this news organization.
“Even in the lipid control, while it did get a little bit better, it’s still only around 30%-40%. So, I think we have ways to go as a society,” Dr. Berger noted.
Double down on screening
Dr. Wadhera said “we need to double down on efforts to screen for and treat cardiovascular risk factors like high blood pressure and diabetes in young adults. We need to intensify clinical and public health interventions focused on primordial and primary prevention in young adults now so that we can avoid a tsunami of cardiovascular disease in the long term.”
“It’s critically important that young adults speak with their health care provider about whether – and when – they should undergo screening for high blood pressure, diabetes, and high cholesterol,” Dr. Wadhera added.
Dr. Berger said one problem is that younger people often have a “superman or superwoman” view and don’t comprehend that they are at risk for some of these conditions. Studies such as this “reinforce the idea that it’s never too young to be checked out.”
As a cardiologist who specializes in cardiovascular prevention, Dr. Berger said he sometimes hears patients say things like, “I don’t ever want to need a cardiologist,” or “I hope I never need a cardiologist.”
“My response is, ‘There are many different types of cardiologists,’ and I think it would really be helpful for many people to see a prevention-focused cardiologist way before they have problems,” he said in an interview.
“As a system, medicine has become very good at treating patients with different diseases. I think we need to get better in terms of preventing some of these problems,” Dr. Berger added.
In their editorial, Dr. Allen and Dr. Wilkins say the “foundation of cardiovascular health begins early in life. These worsening trends in risk factors highlight the importance of focusing on prevention in adolescence and young adulthood in order to promote cardiovascular health across the lifetime.”
The study was funded by a grant from the National Heart, Lung, and Blood Institute. Dr. Wadhera has served as a consultant for Abbott and CVS Health. Dr. Wilkins has received personal fees from 3M. Dr. Berger has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ACC 2023
OTC budesonide-formoterol for asthma could save lives, money
, according to a computer modeling study presented at the American Academy of Allergy, Asthma, and Immunology 2023 annual meeting in San Antonio.
Asthma affects 25 million people, about 1 in 13, in the United States. About 28% are uninsured or underinsured, and 70% have mild asthma. Many are using a $30 inhaled epinephrine product (Primatene Mist) – the only FDA-approved asthma inhaler available without a prescription, said Marcus Shaker, MD, MS, professor of pediatrics and medicine at Geisel School of Medicine at Dartmouth, and clinician at Dartmouth Health Children’s, N.H.
A new version of Primatene Mist was reintroduced on the market in 2018 after the product was pulled for containing chlorofluorocarbons in 2011, but it is not recommended by professional medical societies because of safety concerns over epinephrine’s adverse effects, such as increased heart rate and blood pressure.
Drugs in its class (bronchodilators) have long been associated with a higher risk for death or near-death.
Meanwhile, research more than 2 decades ago linked regular use of low-dose inhaled corticosteroids with reduced risk for asthma death.
More recently, two large studies (SYGMA 1 and SYGMA 2) compared maintenance therapy with a low-dose inhaled corticosteroid (budesonide) vs. on-demand treatment with an inhaler containing both a corticosteroid (budesonide) and a long-acting bronchodilator (formoterol).
“Using as-needed budesonide-formoterol led to outcomes that are almost as good as taking a maintenance budesonide dose every day,” said Dr. Shaker.
The Global Initiative for Asthma guidelines now recommend this approach – as-needed inhaled corticosteroids (ICS) plus long-acting bronchodilators – for adults with mild asthma. In the United States, however, the National Heart, Lung, and Blood Institute still suggests daily ICS plus quick-relief therapy as needed.
Dr. Shaker and colleagues used computer modeling to compare the cost-effectiveness of as-needed budesonide-formoterol vs. over-the-counter inhaled epinephrine in underinsured U.S. adults who were self-managing their mild asthma. The study randomly assigned these individuals into three groups: OTC inhaled epinephrine (current reality), OTC budesonide-formoterol (not yet available), or no OTC option. The model assumed that patients treated for an exacerbation were referred to a health care provider and started a regimen of ICS plus as-needed rescue therapy.
In this analysis, which has been submitted for publication, the OTC budesonide-formoterol strategy was associated with 12,495 fewer deaths, prevented nearly 14 million severe asthma exacerbations, and saved more than $68 billion. And “when we looked at OTC budesonide-formoterol vs. having no OTC option at all, budesonide-formoterol was similarly cost-effective,” said Dr. Shaker, who presented the results at an AAAAI oral abstract session.
The cost savings emerged even though in the United States asthma controller therapies (for example, fluticasone) cost about 10 times more than rescue therapies (for instance, salbutamol, OTC epinephrine).
Nevertheless, the results make sense. “If you’re using Primatene Mist, your health costs are predicted to be much greater because you’re going to be in the hospital more. Your asthma is not going to be well-controlled,” Thanai Pongdee, MD, an allergist-immunologist with the Mayo Clinic in Rochester, Minn., told this news organization. “It’s not only the cost of your ER visit but also the cost of loss of work or school, and loss of daily productivity. There are all these associated costs.”
The analysis “is certainly something policy makers could take a look at,” he said.
He noted that current use of budesonide-formoterol is stymied by difficulties with insurance coverage. The difficulties stem from a mismatch between the updated recommendation for as-needed use and the description printed on the brand-name product (Symbicort).
“On the product label, it says Symbicort should be used on a daily basis,” Dr. Pongdee said. “But if a prescription comes through and says you’re going to use this ‘as needed,’ the health plan may say that’s not appropriate because that’s not on the product label.”
Given these access challenges with the all-in-one inhaler, other researchers have developed a workaround – asking patients to continue their usual care (that is, using a rescue inhaler as needed) but to also administer a controller medication after each rescue. When tested in Black and Latino patients with moderate to severe asthma, this easy strategy (patient activated reliever-triggered inhaled corticosteroid, or PARTICS) reduced severe asthma exacerbations about as well as the all-in-one inhaler.
If the all-in-one budesonide-formoterol does become available OTC, Dr. Shaker stressed that it “would not be a substitute for seeing an allergist and getting appropriate medical care and an evaluation and all the rest. But it’s better than the status quo. It’s the sort of thing where the perfect is not the enemy of the good,” he said.
Dr. Shaker is the AAAAI cochair of the Joint Task Force on Practice Parameters and serves as an editorial board member of the Journal of Allergy and Clinical Immunology in Practice. He is also an associate editor of the Annals of Allergy, Asthma, and Immunology. Dr. Pongdee serves as an at-large director on the AAAAI board of directors. He receives grant funding from GlaxoSmithKline, and Mayo Clinic is a trial site for GlaxoSmithKline and AstraZeneca.
A version of this article first appeared on Medscape.com.
, according to a computer modeling study presented at the American Academy of Allergy, Asthma, and Immunology 2023 annual meeting in San Antonio.
Asthma affects 25 million people, about 1 in 13, in the United States. About 28% are uninsured or underinsured, and 70% have mild asthma. Many are using a $30 inhaled epinephrine product (Primatene Mist) – the only FDA-approved asthma inhaler available without a prescription, said Marcus Shaker, MD, MS, professor of pediatrics and medicine at Geisel School of Medicine at Dartmouth, and clinician at Dartmouth Health Children’s, N.H.
A new version of Primatene Mist was reintroduced on the market in 2018 after the product was pulled for containing chlorofluorocarbons in 2011, but it is not recommended by professional medical societies because of safety concerns over epinephrine’s adverse effects, such as increased heart rate and blood pressure.
Drugs in its class (bronchodilators) have long been associated with a higher risk for death or near-death.
Meanwhile, research more than 2 decades ago linked regular use of low-dose inhaled corticosteroids with reduced risk for asthma death.
More recently, two large studies (SYGMA 1 and SYGMA 2) compared maintenance therapy with a low-dose inhaled corticosteroid (budesonide) vs. on-demand treatment with an inhaler containing both a corticosteroid (budesonide) and a long-acting bronchodilator (formoterol).
“Using as-needed budesonide-formoterol led to outcomes that are almost as good as taking a maintenance budesonide dose every day,” said Dr. Shaker.
The Global Initiative for Asthma guidelines now recommend this approach – as-needed inhaled corticosteroids (ICS) plus long-acting bronchodilators – for adults with mild asthma. In the United States, however, the National Heart, Lung, and Blood Institute still suggests daily ICS plus quick-relief therapy as needed.
Dr. Shaker and colleagues used computer modeling to compare the cost-effectiveness of as-needed budesonide-formoterol vs. over-the-counter inhaled epinephrine in underinsured U.S. adults who were self-managing their mild asthma. The study randomly assigned these individuals into three groups: OTC inhaled epinephrine (current reality), OTC budesonide-formoterol (not yet available), or no OTC option. The model assumed that patients treated for an exacerbation were referred to a health care provider and started a regimen of ICS plus as-needed rescue therapy.
In this analysis, which has been submitted for publication, the OTC budesonide-formoterol strategy was associated with 12,495 fewer deaths, prevented nearly 14 million severe asthma exacerbations, and saved more than $68 billion. And “when we looked at OTC budesonide-formoterol vs. having no OTC option at all, budesonide-formoterol was similarly cost-effective,” said Dr. Shaker, who presented the results at an AAAAI oral abstract session.
The cost savings emerged even though in the United States asthma controller therapies (for example, fluticasone) cost about 10 times more than rescue therapies (for instance, salbutamol, OTC epinephrine).
Nevertheless, the results make sense. “If you’re using Primatene Mist, your health costs are predicted to be much greater because you’re going to be in the hospital more. Your asthma is not going to be well-controlled,” Thanai Pongdee, MD, an allergist-immunologist with the Mayo Clinic in Rochester, Minn., told this news organization. “It’s not only the cost of your ER visit but also the cost of loss of work or school, and loss of daily productivity. There are all these associated costs.”
The analysis “is certainly something policy makers could take a look at,” he said.
He noted that current use of budesonide-formoterol is stymied by difficulties with insurance coverage. The difficulties stem from a mismatch between the updated recommendation for as-needed use and the description printed on the brand-name product (Symbicort).
“On the product label, it says Symbicort should be used on a daily basis,” Dr. Pongdee said. “But if a prescription comes through and says you’re going to use this ‘as needed,’ the health plan may say that’s not appropriate because that’s not on the product label.”
Given these access challenges with the all-in-one inhaler, other researchers have developed a workaround – asking patients to continue their usual care (that is, using a rescue inhaler as needed) but to also administer a controller medication after each rescue. When tested in Black and Latino patients with moderate to severe asthma, this easy strategy (patient activated reliever-triggered inhaled corticosteroid, or PARTICS) reduced severe asthma exacerbations about as well as the all-in-one inhaler.
If the all-in-one budesonide-formoterol does become available OTC, Dr. Shaker stressed that it “would not be a substitute for seeing an allergist and getting appropriate medical care and an evaluation and all the rest. But it’s better than the status quo. It’s the sort of thing where the perfect is not the enemy of the good,” he said.
Dr. Shaker is the AAAAI cochair of the Joint Task Force on Practice Parameters and serves as an editorial board member of the Journal of Allergy and Clinical Immunology in Practice. He is also an associate editor of the Annals of Allergy, Asthma, and Immunology. Dr. Pongdee serves as an at-large director on the AAAAI board of directors. He receives grant funding from GlaxoSmithKline, and Mayo Clinic is a trial site for GlaxoSmithKline and AstraZeneca.
A version of this article first appeared on Medscape.com.
, according to a computer modeling study presented at the American Academy of Allergy, Asthma, and Immunology 2023 annual meeting in San Antonio.
Asthma affects 25 million people, about 1 in 13, in the United States. About 28% are uninsured or underinsured, and 70% have mild asthma. Many are using a $30 inhaled epinephrine product (Primatene Mist) – the only FDA-approved asthma inhaler available without a prescription, said Marcus Shaker, MD, MS, professor of pediatrics and medicine at Geisel School of Medicine at Dartmouth, and clinician at Dartmouth Health Children’s, N.H.
A new version of Primatene Mist was reintroduced on the market in 2018 after the product was pulled for containing chlorofluorocarbons in 2011, but it is not recommended by professional medical societies because of safety concerns over epinephrine’s adverse effects, such as increased heart rate and blood pressure.
Drugs in its class (bronchodilators) have long been associated with a higher risk for death or near-death.
Meanwhile, research more than 2 decades ago linked regular use of low-dose inhaled corticosteroids with reduced risk for asthma death.
More recently, two large studies (SYGMA 1 and SYGMA 2) compared maintenance therapy with a low-dose inhaled corticosteroid (budesonide) vs. on-demand treatment with an inhaler containing both a corticosteroid (budesonide) and a long-acting bronchodilator (formoterol).
“Using as-needed budesonide-formoterol led to outcomes that are almost as good as taking a maintenance budesonide dose every day,” said Dr. Shaker.
The Global Initiative for Asthma guidelines now recommend this approach – as-needed inhaled corticosteroids (ICS) plus long-acting bronchodilators – for adults with mild asthma. In the United States, however, the National Heart, Lung, and Blood Institute still suggests daily ICS plus quick-relief therapy as needed.
Dr. Shaker and colleagues used computer modeling to compare the cost-effectiveness of as-needed budesonide-formoterol vs. over-the-counter inhaled epinephrine in underinsured U.S. adults who were self-managing their mild asthma. The study randomly assigned these individuals into three groups: OTC inhaled epinephrine (current reality), OTC budesonide-formoterol (not yet available), or no OTC option. The model assumed that patients treated for an exacerbation were referred to a health care provider and started a regimen of ICS plus as-needed rescue therapy.
In this analysis, which has been submitted for publication, the OTC budesonide-formoterol strategy was associated with 12,495 fewer deaths, prevented nearly 14 million severe asthma exacerbations, and saved more than $68 billion. And “when we looked at OTC budesonide-formoterol vs. having no OTC option at all, budesonide-formoterol was similarly cost-effective,” said Dr. Shaker, who presented the results at an AAAAI oral abstract session.
The cost savings emerged even though in the United States asthma controller therapies (for example, fluticasone) cost about 10 times more than rescue therapies (for instance, salbutamol, OTC epinephrine).
Nevertheless, the results make sense. “If you’re using Primatene Mist, your health costs are predicted to be much greater because you’re going to be in the hospital more. Your asthma is not going to be well-controlled,” Thanai Pongdee, MD, an allergist-immunologist with the Mayo Clinic in Rochester, Minn., told this news organization. “It’s not only the cost of your ER visit but also the cost of loss of work or school, and loss of daily productivity. There are all these associated costs.”
The analysis “is certainly something policy makers could take a look at,” he said.
He noted that current use of budesonide-formoterol is stymied by difficulties with insurance coverage. The difficulties stem from a mismatch between the updated recommendation for as-needed use and the description printed on the brand-name product (Symbicort).
“On the product label, it says Symbicort should be used on a daily basis,” Dr. Pongdee said. “But if a prescription comes through and says you’re going to use this ‘as needed,’ the health plan may say that’s not appropriate because that’s not on the product label.”
Given these access challenges with the all-in-one inhaler, other researchers have developed a workaround – asking patients to continue their usual care (that is, using a rescue inhaler as needed) but to also administer a controller medication after each rescue. When tested in Black and Latino patients with moderate to severe asthma, this easy strategy (patient activated reliever-triggered inhaled corticosteroid, or PARTICS) reduced severe asthma exacerbations about as well as the all-in-one inhaler.
If the all-in-one budesonide-formoterol does become available OTC, Dr. Shaker stressed that it “would not be a substitute for seeing an allergist and getting appropriate medical care and an evaluation and all the rest. But it’s better than the status quo. It’s the sort of thing where the perfect is not the enemy of the good,” he said.
Dr. Shaker is the AAAAI cochair of the Joint Task Force on Practice Parameters and serves as an editorial board member of the Journal of Allergy and Clinical Immunology in Practice. He is also an associate editor of the Annals of Allergy, Asthma, and Immunology. Dr. Pongdee serves as an at-large director on the AAAAI board of directors. He receives grant funding from GlaxoSmithKline, and Mayo Clinic is a trial site for GlaxoSmithKline and AstraZeneca.
A version of this article first appeared on Medscape.com.
FROM AAAAI 2023
What impact do carbs have on bone health?
I am often asked about the impact of dietary nutrients on bone health, particularly as many patients with low bone density, many with a history of multiple fractures, are referred to me. Many factors affect bone density, an important predictor of fracture risk, including genetics, body weight and muscle mass, bone loading exercise, menstrual status, other hormonal factors, nutritional status, optimal absorption of dietary nutrients, and medication use.
Dietary nutrients include macronutrients (carbohydrates, proteins, fat, and fiber) and micronutrients (such as dietary minerals and vitamins). The importance of micronutrients such as calcium, phosphorus, magnesium, and vitamins C, D, and K in optimizing bone mineralization and bone formation has been well documented.
The impact of protein intake on bone health is slightly more controversial, with some studies suggesting that increased protein intake may be deleterious to bone by increasing acid load, which in turn, increases calcium loss in urine. Overall data analysis from multiple studies support the finding that a higher protein intake is modestly beneficial for bone at certain sites, such as the spine.
Though data regarding the impact of dietary carbohydrates on bone are not as robust, it’s important to understand these effects given the increasing knowledge of the deleterious impact of processed carbohydrates on weight and cardiometabolic outcomes. This leads to the growing recommendations to limit carbohydrates in diet.
Quality and quantity of carbs affect bone health
Available studies suggest that both the quality and quantity of carbohydrates that are in a diet as well as the glycemic index of food may affect bone outcomes. Glycemic index refers to the extent of blood glucose elevation that occurs after the intake of any specific food. Foods with a higher glycemic index cause a rapid increase in blood glucose, whereas those with a low glycemic index result in a slower and more gradual increase. Examples of high–glycemic index food include processed and baked foods (such as breakfast cereals [unless whole grain], pretzels, cookies, doughnuts, pastries, cake, white bread, bagels, croissants, and corn chips), sugar-sweetened beverages, white rice, fast food (such as pizza and burgers), and potatoes. Examples of low glycemic index foods include vegetables, fruits, legumes, dairy and dairy products (without added sugar), whole-grain foods (such as oat porridge), and nuts.
A high–glycemic index diet has been associated with a greater risk for obesity and cardiovascular disease, and with lower bone density, an increased risk for fracture. This has been attributed to acute increases in glucose and insulin levels after consumption of high–glycemic index food, which causes increased oxidative stress and secretion of inflammatory cytokines, such as interleukin 6 and tumor necrosis factor alpha, that activate cells in bone that increase bone loss.
Higher blood glucose concentrations induced by a higher dietary glycemic index can have deleterious effects on osteoblasts, the cells important for bone formation, and increase bone loss through production of advanced glycation end products that affect the cross linking of collagen in bone (important for bone strength), as well as calcium loss in urine. This was recently reported in a study by Garcia-Gavilan and others, in which the authors showed that high dietary glycemic index and dietary glucose load are associated with a higher risk for osteoporosis-related fractures in an older Mediterranean population who are at high risk for cardiovascular events. Similar data were reported by Nouri and coauthors in a study from Iran.
The quantity and quality of dietary carbohydrates may also have an impact on bone. The quality of carbohydrates has been assessed using the carbohydrate quality index (CQI) and the low carbohydrate diet score (LCDS). The CQI takes into account dietary fiber intake, glycemic index, intake of processed vs. whole grain, and solid vs. total carbohydrates in diet. A higher CQI diet is associated with reduced cardiovascular risk. Higher LCDS reflects lower carbohydrate and higher fat and protein intake.
Diets that are rich in refined or processed carbohydrates with added sugar are proinflammatory and increase oxidative stress, which may lead to increased bone loss, low bone density, and increased fracture risk. These foods also have a high glycemic index.
In contrast, diets that are rich in whole grains, legumes, fruits, vegetables, nuts, and olive oil have a lower glycemic index and are beneficial to bone. These diets have a higher CQI and LCDS (as reported by Nouri and coauthors) and provide a rich source of antioxidants, vitamins, minerals, and other nutrients (such as calcium, magnesium, and vitamins B, C, and K), which are all beneficial to bone. Gao and others have reported that implementing a low glycemic index pulse-based diet (lentils, peas, beans) is superior to a regular hospital diet in preventing the increase in bone loss that typically occurs during hospitalization with enforced bed rest.
Most reports of the impact of carbohydrates on bone health are from observational studies. In an interventional study, Dalskov and coauthors randomly assigned children aged 5-18 years who had parents with overweight to one of five diets (high protein/low glycemic index, high protein/high glycemic index, low protein/low glycemic index, low protein/high glycemic index, or regular) for 6 months.
Contrasting with our understanding that protein intake is overall good for bone, this study found that among patients receiving a high–glycemic index diet, those who were on a high-protein diet had greater reductions in a bone formation marker than did those on a low-protein diet, with no major changes observed with the other diets. This suggests the influence of associated dietary nutrients on bone outcomes and that protein intake may modify the effects of dietary carbohydrates on bone formation. Similarly, the fat content of food can alter the glycemic index and thus may modify the impact of dietary carbohydrates on bone.
In summary, available data suggest that the quantity and quality of carbohydrates, including the glycemic index of food, may affect bone health and that it is important to exercise moderation in the consumption of such foods. However, there are only a few studies that have examined these associations, and more studies are necessary to further clarify the impact of dietary carbohydrates on bone as well as any modifications of these effects by other associated food groups. These studies will allow us to refine our recommendations to our patients as we advance our understanding of the impact of the combined effects of various dietary nutrients on bone.
Madhusmita Misra, MD, MPH, is chief of the division of pediatric endocrinology, Mass General for Children, Boston, and serves or has served as a director, officer, partner, employee, advisor, consultant, or trustee for AbbVie, Sanofi, and Ipsen.
A version of this article first appeared on Medscape.com.
I am often asked about the impact of dietary nutrients on bone health, particularly as many patients with low bone density, many with a history of multiple fractures, are referred to me. Many factors affect bone density, an important predictor of fracture risk, including genetics, body weight and muscle mass, bone loading exercise, menstrual status, other hormonal factors, nutritional status, optimal absorption of dietary nutrients, and medication use.
Dietary nutrients include macronutrients (carbohydrates, proteins, fat, and fiber) and micronutrients (such as dietary minerals and vitamins). The importance of micronutrients such as calcium, phosphorus, magnesium, and vitamins C, D, and K in optimizing bone mineralization and bone formation has been well documented.
The impact of protein intake on bone health is slightly more controversial, with some studies suggesting that increased protein intake may be deleterious to bone by increasing acid load, which in turn, increases calcium loss in urine. Overall data analysis from multiple studies support the finding that a higher protein intake is modestly beneficial for bone at certain sites, such as the spine.
Though data regarding the impact of dietary carbohydrates on bone are not as robust, it’s important to understand these effects given the increasing knowledge of the deleterious impact of processed carbohydrates on weight and cardiometabolic outcomes. This leads to the growing recommendations to limit carbohydrates in diet.
Quality and quantity of carbs affect bone health
Available studies suggest that both the quality and quantity of carbohydrates that are in a diet as well as the glycemic index of food may affect bone outcomes. Glycemic index refers to the extent of blood glucose elevation that occurs after the intake of any specific food. Foods with a higher glycemic index cause a rapid increase in blood glucose, whereas those with a low glycemic index result in a slower and more gradual increase. Examples of high–glycemic index food include processed and baked foods (such as breakfast cereals [unless whole grain], pretzels, cookies, doughnuts, pastries, cake, white bread, bagels, croissants, and corn chips), sugar-sweetened beverages, white rice, fast food (such as pizza and burgers), and potatoes. Examples of low glycemic index foods include vegetables, fruits, legumes, dairy and dairy products (without added sugar), whole-grain foods (such as oat porridge), and nuts.
A high–glycemic index diet has been associated with a greater risk for obesity and cardiovascular disease, and with lower bone density, an increased risk for fracture. This has been attributed to acute increases in glucose and insulin levels after consumption of high–glycemic index food, which causes increased oxidative stress and secretion of inflammatory cytokines, such as interleukin 6 and tumor necrosis factor alpha, that activate cells in bone that increase bone loss.
Higher blood glucose concentrations induced by a higher dietary glycemic index can have deleterious effects on osteoblasts, the cells important for bone formation, and increase bone loss through production of advanced glycation end products that affect the cross linking of collagen in bone (important for bone strength), as well as calcium loss in urine. This was recently reported in a study by Garcia-Gavilan and others, in which the authors showed that high dietary glycemic index and dietary glucose load are associated with a higher risk for osteoporosis-related fractures in an older Mediterranean population who are at high risk for cardiovascular events. Similar data were reported by Nouri and coauthors in a study from Iran.
The quantity and quality of dietary carbohydrates may also have an impact on bone. The quality of carbohydrates has been assessed using the carbohydrate quality index (CQI) and the low carbohydrate diet score (LCDS). The CQI takes into account dietary fiber intake, glycemic index, intake of processed vs. whole grain, and solid vs. total carbohydrates in diet. A higher CQI diet is associated with reduced cardiovascular risk. Higher LCDS reflects lower carbohydrate and higher fat and protein intake.
Diets that are rich in refined or processed carbohydrates with added sugar are proinflammatory and increase oxidative stress, which may lead to increased bone loss, low bone density, and increased fracture risk. These foods also have a high glycemic index.
In contrast, diets that are rich in whole grains, legumes, fruits, vegetables, nuts, and olive oil have a lower glycemic index and are beneficial to bone. These diets have a higher CQI and LCDS (as reported by Nouri and coauthors) and provide a rich source of antioxidants, vitamins, minerals, and other nutrients (such as calcium, magnesium, and vitamins B, C, and K), which are all beneficial to bone. Gao and others have reported that implementing a low glycemic index pulse-based diet (lentils, peas, beans) is superior to a regular hospital diet in preventing the increase in bone loss that typically occurs during hospitalization with enforced bed rest.
Most reports of the impact of carbohydrates on bone health are from observational studies. In an interventional study, Dalskov and coauthors randomly assigned children aged 5-18 years who had parents with overweight to one of five diets (high protein/low glycemic index, high protein/high glycemic index, low protein/low glycemic index, low protein/high glycemic index, or regular) for 6 months.
Contrasting with our understanding that protein intake is overall good for bone, this study found that among patients receiving a high–glycemic index diet, those who were on a high-protein diet had greater reductions in a bone formation marker than did those on a low-protein diet, with no major changes observed with the other diets. This suggests the influence of associated dietary nutrients on bone outcomes and that protein intake may modify the effects of dietary carbohydrates on bone formation. Similarly, the fat content of food can alter the glycemic index and thus may modify the impact of dietary carbohydrates on bone.
In summary, available data suggest that the quantity and quality of carbohydrates, including the glycemic index of food, may affect bone health and that it is important to exercise moderation in the consumption of such foods. However, there are only a few studies that have examined these associations, and more studies are necessary to further clarify the impact of dietary carbohydrates on bone as well as any modifications of these effects by other associated food groups. These studies will allow us to refine our recommendations to our patients as we advance our understanding of the impact of the combined effects of various dietary nutrients on bone.
Madhusmita Misra, MD, MPH, is chief of the division of pediatric endocrinology, Mass General for Children, Boston, and serves or has served as a director, officer, partner, employee, advisor, consultant, or trustee for AbbVie, Sanofi, and Ipsen.
A version of this article first appeared on Medscape.com.
I am often asked about the impact of dietary nutrients on bone health, particularly as many patients with low bone density, many with a history of multiple fractures, are referred to me. Many factors affect bone density, an important predictor of fracture risk, including genetics, body weight and muscle mass, bone loading exercise, menstrual status, other hormonal factors, nutritional status, optimal absorption of dietary nutrients, and medication use.
Dietary nutrients include macronutrients (carbohydrates, proteins, fat, and fiber) and micronutrients (such as dietary minerals and vitamins). The importance of micronutrients such as calcium, phosphorus, magnesium, and vitamins C, D, and K in optimizing bone mineralization and bone formation has been well documented.
The impact of protein intake on bone health is slightly more controversial, with some studies suggesting that increased protein intake may be deleterious to bone by increasing acid load, which in turn, increases calcium loss in urine. Overall data analysis from multiple studies support the finding that a higher protein intake is modestly beneficial for bone at certain sites, such as the spine.
Though data regarding the impact of dietary carbohydrates on bone are not as robust, it’s important to understand these effects given the increasing knowledge of the deleterious impact of processed carbohydrates on weight and cardiometabolic outcomes. This leads to the growing recommendations to limit carbohydrates in diet.
Quality and quantity of carbs affect bone health
Available studies suggest that both the quality and quantity of carbohydrates that are in a diet as well as the glycemic index of food may affect bone outcomes. Glycemic index refers to the extent of blood glucose elevation that occurs after the intake of any specific food. Foods with a higher glycemic index cause a rapid increase in blood glucose, whereas those with a low glycemic index result in a slower and more gradual increase. Examples of high–glycemic index food include processed and baked foods (such as breakfast cereals [unless whole grain], pretzels, cookies, doughnuts, pastries, cake, white bread, bagels, croissants, and corn chips), sugar-sweetened beverages, white rice, fast food (such as pizza and burgers), and potatoes. Examples of low glycemic index foods include vegetables, fruits, legumes, dairy and dairy products (without added sugar), whole-grain foods (such as oat porridge), and nuts.
A high–glycemic index diet has been associated with a greater risk for obesity and cardiovascular disease, and with lower bone density, an increased risk for fracture. This has been attributed to acute increases in glucose and insulin levels after consumption of high–glycemic index food, which causes increased oxidative stress and secretion of inflammatory cytokines, such as interleukin 6 and tumor necrosis factor alpha, that activate cells in bone that increase bone loss.
Higher blood glucose concentrations induced by a higher dietary glycemic index can have deleterious effects on osteoblasts, the cells important for bone formation, and increase bone loss through production of advanced glycation end products that affect the cross linking of collagen in bone (important for bone strength), as well as calcium loss in urine. This was recently reported in a study by Garcia-Gavilan and others, in which the authors showed that high dietary glycemic index and dietary glucose load are associated with a higher risk for osteoporosis-related fractures in an older Mediterranean population who are at high risk for cardiovascular events. Similar data were reported by Nouri and coauthors in a study from Iran.
The quantity and quality of dietary carbohydrates may also have an impact on bone. The quality of carbohydrates has been assessed using the carbohydrate quality index (CQI) and the low carbohydrate diet score (LCDS). The CQI takes into account dietary fiber intake, glycemic index, intake of processed vs. whole grain, and solid vs. total carbohydrates in diet. A higher CQI diet is associated with reduced cardiovascular risk. Higher LCDS reflects lower carbohydrate and higher fat and protein intake.
Diets that are rich in refined or processed carbohydrates with added sugar are proinflammatory and increase oxidative stress, which may lead to increased bone loss, low bone density, and increased fracture risk. These foods also have a high glycemic index.
In contrast, diets that are rich in whole grains, legumes, fruits, vegetables, nuts, and olive oil have a lower glycemic index and are beneficial to bone. These diets have a higher CQI and LCDS (as reported by Nouri and coauthors) and provide a rich source of antioxidants, vitamins, minerals, and other nutrients (such as calcium, magnesium, and vitamins B, C, and K), which are all beneficial to bone. Gao and others have reported that implementing a low glycemic index pulse-based diet (lentils, peas, beans) is superior to a regular hospital diet in preventing the increase in bone loss that typically occurs during hospitalization with enforced bed rest.
Most reports of the impact of carbohydrates on bone health are from observational studies. In an interventional study, Dalskov and coauthors randomly assigned children aged 5-18 years who had parents with overweight to one of five diets (high protein/low glycemic index, high protein/high glycemic index, low protein/low glycemic index, low protein/high glycemic index, or regular) for 6 months.
Contrasting with our understanding that protein intake is overall good for bone, this study found that among patients receiving a high–glycemic index diet, those who were on a high-protein diet had greater reductions in a bone formation marker than did those on a low-protein diet, with no major changes observed with the other diets. This suggests the influence of associated dietary nutrients on bone outcomes and that protein intake may modify the effects of dietary carbohydrates on bone formation. Similarly, the fat content of food can alter the glycemic index and thus may modify the impact of dietary carbohydrates on bone.
In summary, available data suggest that the quantity and quality of carbohydrates, including the glycemic index of food, may affect bone health and that it is important to exercise moderation in the consumption of such foods. However, there are only a few studies that have examined these associations, and more studies are necessary to further clarify the impact of dietary carbohydrates on bone as well as any modifications of these effects by other associated food groups. These studies will allow us to refine our recommendations to our patients as we advance our understanding of the impact of the combined effects of various dietary nutrients on bone.
Madhusmita Misra, MD, MPH, is chief of the division of pediatric endocrinology, Mass General for Children, Boston, and serves or has served as a director, officer, partner, employee, advisor, consultant, or trustee for AbbVie, Sanofi, and Ipsen.
A version of this article first appeared on Medscape.com.
Pembrolizumab before and after melanoma surgery boosts outcomes
, show results from the phase 2 SWOG S1801 trial.
The trial involved 319 patients with operable stage IIIB to stage IV melanoma. The investigators found that patients who received pembrolizumab both before and after surgery (i.e., neoadjuvant and adjuvant therapy) fared better than those who received the drug only after surgery: The 2-year event-free survival rates were 72% vs. 49%, respectively.
The research was published in the New England Journal of Medicine, but similar results had already been presented at the European Society for Medical Oncology 2022 annual Meeting.
“It’s not just what you give; it’s when you give it,” said lead author Sapna Patel, MD, in a press release issued by the University of Texas MD Anderson Cancer Center, echoing comments she gave at ESMO 2022.
The study, she continued, “demonstrates the same treatment for resectable melanoma given before surgery can generate better outcomes.”
On the basis of their findings, Dr. Patel, who is associate professor of melanoma medical oncology at the University of Texas MD Anderson Cancer Center, Houston, said that patients with high-risk melanoma “should start immunotherapy prior to surgery to generate an immune response while the bulk of the melanoma and the anti-tumor T cells are intact.”
The mechanism of action of PD-1 blockade “relies on the presence of preexisting anti-tumor T cells attempting to attack cancer cells,” with the immunotherapy allowing the anti-tumor cells to proliferate and mediate clinical responses.
Resection of the bulk of the tumor is therefore “likely to take away some or even most of the potential anti-tumor T cells that would proliferate after PD-1 blockade,” they write.
Likely to apply also to nivolumab
Approached for comment, Jeffrey S. Weber, MD, PhD, professor of medicine, NYU Langone Medical Center, New York, said that outside of trials, both pembrolizumab and ipilimumab (Yervoy)/nivolumab (Opdivo) are already being used neoadjuvantly.
He thinks that the findings for neoadjuvant and adjuvant pembrolizumab could also apply to nivolumab because “the drugs are quite similar in efficacy.”
Dr. Weber told this news organization that, “even though the S1801 trial was not accepted as a registration trial by the FDA, I think that its results could very well change practice and confirm it for others who already use neoadjuvant therapy for palpable stage III melanoma.”
One question that is being addressed to an extent in the NADINA trial is whether adjuvant immunotherapy can be avoided all together and patients receive only neoadjuvant therapy, although Dr. Weber said, “I doubt that will be the case.”
Study details
In this study, patients were randomly assigned to either surgery followed by 18 doses of adjuvant pembrolizumab, or to receive 3 doses of neoadjuvant pembrolizumab followed by surgery and then 15 additional doses of adjuvant pembrolizumab.
After a median duration of follow-up of 14.7 months, there were 38 events in the neoadjuvant-adjuvant group and 67 in the adjuvant-only group.
“Events” were defined as disease progression, toxic effects, or complications that precluded surgery or the initiation of adjuvant therapy within 84 days of surgery, as well as the inability to fully resect the gross disease, melanoma recurrence, and death.
The team calculated that event-free survival was significantly longer in the neoadjuvant-adjuvant group (P = .004), with 2-year event-free survival at 72% vs. 49% in the adjuvant-only group.
“The benefit of neoadjuvant pembrolizumab was seen across all subgroups of patients,” the investigators note.
At the data cut-off, there were 14 deaths in the neoadjuvant-adjuvant group vs. 22 in the adjuvant-only group, which the researchers say is too few to allow “definitive comparison” in terms of overall survival.
Definitive surgery had been performed in 88% of neoadjuvant-adjuvant patients and in 95% of those assigned to adjuvant-only pembrolizumab. The most common reason for not undergoing surgery was disease progression.
Among the patients for whom safety data were available, 7% in the neoadjuvant-adjuvant group had at least one grade 3 or 4 adverse event related to pembrolizumab, whereas 7% had at least one grade 3 or 4 adverse event related to surgery.
In the adjuvant-only arm, 4% of patients had at least one grade 3 adverse event related to surgery, with no grade 4 adverse events reported.
The rates of grade 3 or 4 adverse events during adjuvant therapy were similar in the two groups, at 12% in patients assigned to neoadjuvant-adjuvant therapy and 14% in those given adjuvant-only pembrolizumab.
“Future studies can explore deescalation strategies for both surgery and adjuvant therapy, as well as approaches for patients whose melanoma does not respond to neoadjuvant therapy,” the researchers commented.
The study was funded by the National Cancer Institute and Merck Sharp and Dohme.
Dr. Patel reports numerous relationships with industry, including with Merck, manufacturer of pembrolizumab; other coauthors also have numerous relationships with industry. Dr. Weber is a regular columnist for this news organization and lists his disclosures in his Weber on Oncology column.
A version of this article first appeared on Medscape.com.
, show results from the phase 2 SWOG S1801 trial.
The trial involved 319 patients with operable stage IIIB to stage IV melanoma. The investigators found that patients who received pembrolizumab both before and after surgery (i.e., neoadjuvant and adjuvant therapy) fared better than those who received the drug only after surgery: The 2-year event-free survival rates were 72% vs. 49%, respectively.
The research was published in the New England Journal of Medicine, but similar results had already been presented at the European Society for Medical Oncology 2022 annual Meeting.
“It’s not just what you give; it’s when you give it,” said lead author Sapna Patel, MD, in a press release issued by the University of Texas MD Anderson Cancer Center, echoing comments she gave at ESMO 2022.
The study, she continued, “demonstrates the same treatment for resectable melanoma given before surgery can generate better outcomes.”
On the basis of their findings, Dr. Patel, who is associate professor of melanoma medical oncology at the University of Texas MD Anderson Cancer Center, Houston, said that patients with high-risk melanoma “should start immunotherapy prior to surgery to generate an immune response while the bulk of the melanoma and the anti-tumor T cells are intact.”
The mechanism of action of PD-1 blockade “relies on the presence of preexisting anti-tumor T cells attempting to attack cancer cells,” with the immunotherapy allowing the anti-tumor cells to proliferate and mediate clinical responses.
Resection of the bulk of the tumor is therefore “likely to take away some or even most of the potential anti-tumor T cells that would proliferate after PD-1 blockade,” they write.
Likely to apply also to nivolumab
Approached for comment, Jeffrey S. Weber, MD, PhD, professor of medicine, NYU Langone Medical Center, New York, said that outside of trials, both pembrolizumab and ipilimumab (Yervoy)/nivolumab (Opdivo) are already being used neoadjuvantly.
He thinks that the findings for neoadjuvant and adjuvant pembrolizumab could also apply to nivolumab because “the drugs are quite similar in efficacy.”
Dr. Weber told this news organization that, “even though the S1801 trial was not accepted as a registration trial by the FDA, I think that its results could very well change practice and confirm it for others who already use neoadjuvant therapy for palpable stage III melanoma.”
One question that is being addressed to an extent in the NADINA trial is whether adjuvant immunotherapy can be avoided all together and patients receive only neoadjuvant therapy, although Dr. Weber said, “I doubt that will be the case.”
Study details
In this study, patients were randomly assigned to either surgery followed by 18 doses of adjuvant pembrolizumab, or to receive 3 doses of neoadjuvant pembrolizumab followed by surgery and then 15 additional doses of adjuvant pembrolizumab.
After a median duration of follow-up of 14.7 months, there were 38 events in the neoadjuvant-adjuvant group and 67 in the adjuvant-only group.
“Events” were defined as disease progression, toxic effects, or complications that precluded surgery or the initiation of adjuvant therapy within 84 days of surgery, as well as the inability to fully resect the gross disease, melanoma recurrence, and death.
The team calculated that event-free survival was significantly longer in the neoadjuvant-adjuvant group (P = .004), with 2-year event-free survival at 72% vs. 49% in the adjuvant-only group.
“The benefit of neoadjuvant pembrolizumab was seen across all subgroups of patients,” the investigators note.
At the data cut-off, there were 14 deaths in the neoadjuvant-adjuvant group vs. 22 in the adjuvant-only group, which the researchers say is too few to allow “definitive comparison” in terms of overall survival.
Definitive surgery had been performed in 88% of neoadjuvant-adjuvant patients and in 95% of those assigned to adjuvant-only pembrolizumab. The most common reason for not undergoing surgery was disease progression.
Among the patients for whom safety data were available, 7% in the neoadjuvant-adjuvant group had at least one grade 3 or 4 adverse event related to pembrolizumab, whereas 7% had at least one grade 3 or 4 adverse event related to surgery.
In the adjuvant-only arm, 4% of patients had at least one grade 3 adverse event related to surgery, with no grade 4 adverse events reported.
The rates of grade 3 or 4 adverse events during adjuvant therapy were similar in the two groups, at 12% in patients assigned to neoadjuvant-adjuvant therapy and 14% in those given adjuvant-only pembrolizumab.
“Future studies can explore deescalation strategies for both surgery and adjuvant therapy, as well as approaches for patients whose melanoma does not respond to neoadjuvant therapy,” the researchers commented.
The study was funded by the National Cancer Institute and Merck Sharp and Dohme.
Dr. Patel reports numerous relationships with industry, including with Merck, manufacturer of pembrolizumab; other coauthors also have numerous relationships with industry. Dr. Weber is a regular columnist for this news organization and lists his disclosures in his Weber on Oncology column.
A version of this article first appeared on Medscape.com.
, show results from the phase 2 SWOG S1801 trial.
The trial involved 319 patients with operable stage IIIB to stage IV melanoma. The investigators found that patients who received pembrolizumab both before and after surgery (i.e., neoadjuvant and adjuvant therapy) fared better than those who received the drug only after surgery: The 2-year event-free survival rates were 72% vs. 49%, respectively.
The research was published in the New England Journal of Medicine, but similar results had already been presented at the European Society for Medical Oncology 2022 annual Meeting.
“It’s not just what you give; it’s when you give it,” said lead author Sapna Patel, MD, in a press release issued by the University of Texas MD Anderson Cancer Center, echoing comments she gave at ESMO 2022.
The study, she continued, “demonstrates the same treatment for resectable melanoma given before surgery can generate better outcomes.”
On the basis of their findings, Dr. Patel, who is associate professor of melanoma medical oncology at the University of Texas MD Anderson Cancer Center, Houston, said that patients with high-risk melanoma “should start immunotherapy prior to surgery to generate an immune response while the bulk of the melanoma and the anti-tumor T cells are intact.”
The mechanism of action of PD-1 blockade “relies on the presence of preexisting anti-tumor T cells attempting to attack cancer cells,” with the immunotherapy allowing the anti-tumor cells to proliferate and mediate clinical responses.
Resection of the bulk of the tumor is therefore “likely to take away some or even most of the potential anti-tumor T cells that would proliferate after PD-1 blockade,” they write.
Likely to apply also to nivolumab
Approached for comment, Jeffrey S. Weber, MD, PhD, professor of medicine, NYU Langone Medical Center, New York, said that outside of trials, both pembrolizumab and ipilimumab (Yervoy)/nivolumab (Opdivo) are already being used neoadjuvantly.
He thinks that the findings for neoadjuvant and adjuvant pembrolizumab could also apply to nivolumab because “the drugs are quite similar in efficacy.”
Dr. Weber told this news organization that, “even though the S1801 trial was not accepted as a registration trial by the FDA, I think that its results could very well change practice and confirm it for others who already use neoadjuvant therapy for palpable stage III melanoma.”
One question that is being addressed to an extent in the NADINA trial is whether adjuvant immunotherapy can be avoided all together and patients receive only neoadjuvant therapy, although Dr. Weber said, “I doubt that will be the case.”
Study details
In this study, patients were randomly assigned to either surgery followed by 18 doses of adjuvant pembrolizumab, or to receive 3 doses of neoadjuvant pembrolizumab followed by surgery and then 15 additional doses of adjuvant pembrolizumab.
After a median duration of follow-up of 14.7 months, there were 38 events in the neoadjuvant-adjuvant group and 67 in the adjuvant-only group.
“Events” were defined as disease progression, toxic effects, or complications that precluded surgery or the initiation of adjuvant therapy within 84 days of surgery, as well as the inability to fully resect the gross disease, melanoma recurrence, and death.
The team calculated that event-free survival was significantly longer in the neoadjuvant-adjuvant group (P = .004), with 2-year event-free survival at 72% vs. 49% in the adjuvant-only group.
“The benefit of neoadjuvant pembrolizumab was seen across all subgroups of patients,” the investigators note.
At the data cut-off, there were 14 deaths in the neoadjuvant-adjuvant group vs. 22 in the adjuvant-only group, which the researchers say is too few to allow “definitive comparison” in terms of overall survival.
Definitive surgery had been performed in 88% of neoadjuvant-adjuvant patients and in 95% of those assigned to adjuvant-only pembrolizumab. The most common reason for not undergoing surgery was disease progression.
Among the patients for whom safety data were available, 7% in the neoadjuvant-adjuvant group had at least one grade 3 or 4 adverse event related to pembrolizumab, whereas 7% had at least one grade 3 or 4 adverse event related to surgery.
In the adjuvant-only arm, 4% of patients had at least one grade 3 adverse event related to surgery, with no grade 4 adverse events reported.
The rates of grade 3 or 4 adverse events during adjuvant therapy were similar in the two groups, at 12% in patients assigned to neoadjuvant-adjuvant therapy and 14% in those given adjuvant-only pembrolizumab.
“Future studies can explore deescalation strategies for both surgery and adjuvant therapy, as well as approaches for patients whose melanoma does not respond to neoadjuvant therapy,” the researchers commented.
The study was funded by the National Cancer Institute and Merck Sharp and Dohme.
Dr. Patel reports numerous relationships with industry, including with Merck, manufacturer of pembrolizumab; other coauthors also have numerous relationships with industry. Dr. Weber is a regular columnist for this news organization and lists his disclosures in his Weber on Oncology column.
A version of this article first appeared on Medscape.com.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Daily socialization may extend lifespan in elderly
Sometimes more is more.
Correlations between socializing and survival were detected regardless of baseline health status, suggesting that physicians should be recommending daily socialization for all elderly patients, lead author Ziqiong Wang, MD, of Sichuan University West China Hospital, Chengdu, China, and colleagues reported.
These findings align with an array of prior studies reporting physical and mental health benefits from socialization, and negative impacts from isolation, the investigators wrote in the Journal of Epidemiology & Community Health. Not all studies have yielded the same picture, however, and most research has been conducted in Western countries, leading to uncertainty about whether different outcomes would be seen in populations in other parts of the world. Furthermore, the authors added that few studies have explored the amount of socialization needed to derive a positive benefit.
To address this knowledge gap, the investigators analyzed survival data from 28,563 participants in the Chinese Longitudinal Healthy Longevity Survey with a median age of 89 years at baseline.
“[This analysis] is from a highly respected ongoing longitudinal study of aging in China, which includes a large number of subjects and employs very strong research design and statistical analytical methods, so it has credibility,” John W. Rowe, MD, Julius B. Richmond Professor of Health Policy and Aging at Columbia University, New York, said in a written comment.
The investigators stratified frequency of socialization into five tiers: never, not monthly but sometimes, not weekly but at least once per month, not daily but at least once per week, and almost every day.
Survival proportions were calculated using the Kaplan-Meier method after accounting for a range of individual characteristics, including age, sex, household income, smoking status, diabetes, self-rated health, and others. Comparative findings were described in terms of time ratios using multivariable parametric accelerated failure time (AFT) models.
“The AFT model estimates the time ratio (TR), which is interpreted as the expected time to events in one category relative to the reference group,” the investigators wrote. “Unlike the interpretation of proportional hazard model results where hazard ratios larger than 1 are equal to higher risk, a TR of greater than 1 is considered to have a longer time to events, compared with the reference group.”
From baseline to 5 years, each socialization tier was significantly associated with prolonged survival, suggesting a general benefit. Compared with no socialization, socializing sometimes but not monthly was associated with 42% longer survival, at least monthly socialization was associated with 48% longer survival, at least weekly was associated with 110% longer survival, and socializing almost every day was associated with 87% longer survival.
The outsized benefit of daily socialization became clear in a long-term survival analysis, which spanned 5 years through the end of follow-up. Compared with no socialization, daily socialization tripled survival (TR, 3.04; P < .001), compared with prolongations ranging from 5% to 64% for less socialization, with just one of these lower tiers achieving statistical significance (P = .046).
Of note, the benefit of daily socialization was detected regardless of a person’s health status at baseline.
“No matter if elderly participants had chronic diseases or not, [and] no matter if older people had good self-rated health or not, the survival benefits of frequently participating in social activity were the same,” said principal author Sen He, MD, of Sichuan University, in a written comment.
“Socializing almost every day seems to be the most beneficial for a long life,” Dr. Sen added, noting that more research is needed to determine if there is an optimal type of social activity.
Dr. Rowe pointed out two key findings from the study. The first was that it confirmed “prior studies that have identified a beneficial effect of social activity on life expectancy.
“We have known that engagement is essential for successful aging and that isolation is toxic. While this finding is not novel, it is nice to see this confirmation of what we thought we knew,” he wrote.
Secondly, the study has identified “a threshold effect”, which is that “the long-term benefit on life expectancy was only seen in the presence of fairly intense social interactions, essentially daily,” he said.
According to Preeti Malani, MD, professor of medicine and geriatrician at the University of Michigan, Ann Arbor, the findings are also helpful because they offer data from another part of the world, adding confidence in findings from Western countries.
“This [study] happens to focus on older adults in China, which is helpful since aging is not the same everywhere in the world,” Dr. Malani said. “While the numbers here may not be precise, it’s fair to say that socialization is good for your health – for everyone but especially for older adults.”
Considering the body of evidence now spanning a range of populations, Dr. Malani said physicians should be screening for, and recommending, socialization for all elderly patients, particularly because many aren’t getting enough of it.
“Work that my colleagues and I have done (with the National Poll on Healthy Aging) suggests that there is a portion of older adults that have very little to no social contact,” Dr. Malani said. “A physician may not know this unless they are asking routinely about socialization the way we might ask about diet and exercise. How much is enough? No one knows, but anything is better than nothing and likely more is better.”
She also suggested that personalization is key.
“Physical and emotional health may limit the ability to socialize, so not everyone can engage all the time,” Dr. Malani said. “Also, socialization can look different for different people. Technology allows for socialization even if an individual has trouble leaving their home. I especially worry about this issue for older adults that are also caregivers. Those individuals also need time for themselves” and on way to fulfill that need is by socializing with others.
The study was supported by Sichuan (China) Science and Technology Program, the National Key R&D Program of China, and the National Natural Science Foundation of China. The investigators, Dr. Rowe, and Dr. Malani disclosed no relevant conflicts of interest.
Sometimes more is more.
Correlations between socializing and survival were detected regardless of baseline health status, suggesting that physicians should be recommending daily socialization for all elderly patients, lead author Ziqiong Wang, MD, of Sichuan University West China Hospital, Chengdu, China, and colleagues reported.
These findings align with an array of prior studies reporting physical and mental health benefits from socialization, and negative impacts from isolation, the investigators wrote in the Journal of Epidemiology & Community Health. Not all studies have yielded the same picture, however, and most research has been conducted in Western countries, leading to uncertainty about whether different outcomes would be seen in populations in other parts of the world. Furthermore, the authors added that few studies have explored the amount of socialization needed to derive a positive benefit.
To address this knowledge gap, the investigators analyzed survival data from 28,563 participants in the Chinese Longitudinal Healthy Longevity Survey with a median age of 89 years at baseline.
“[This analysis] is from a highly respected ongoing longitudinal study of aging in China, which includes a large number of subjects and employs very strong research design and statistical analytical methods, so it has credibility,” John W. Rowe, MD, Julius B. Richmond Professor of Health Policy and Aging at Columbia University, New York, said in a written comment.
The investigators stratified frequency of socialization into five tiers: never, not monthly but sometimes, not weekly but at least once per month, not daily but at least once per week, and almost every day.
Survival proportions were calculated using the Kaplan-Meier method after accounting for a range of individual characteristics, including age, sex, household income, smoking status, diabetes, self-rated health, and others. Comparative findings were described in terms of time ratios using multivariable parametric accelerated failure time (AFT) models.
“The AFT model estimates the time ratio (TR), which is interpreted as the expected time to events in one category relative to the reference group,” the investigators wrote. “Unlike the interpretation of proportional hazard model results where hazard ratios larger than 1 are equal to higher risk, a TR of greater than 1 is considered to have a longer time to events, compared with the reference group.”
From baseline to 5 years, each socialization tier was significantly associated with prolonged survival, suggesting a general benefit. Compared with no socialization, socializing sometimes but not monthly was associated with 42% longer survival, at least monthly socialization was associated with 48% longer survival, at least weekly was associated with 110% longer survival, and socializing almost every day was associated with 87% longer survival.
The outsized benefit of daily socialization became clear in a long-term survival analysis, which spanned 5 years through the end of follow-up. Compared with no socialization, daily socialization tripled survival (TR, 3.04; P < .001), compared with prolongations ranging from 5% to 64% for less socialization, with just one of these lower tiers achieving statistical significance (P = .046).
Of note, the benefit of daily socialization was detected regardless of a person’s health status at baseline.
“No matter if elderly participants had chronic diseases or not, [and] no matter if older people had good self-rated health or not, the survival benefits of frequently participating in social activity were the same,” said principal author Sen He, MD, of Sichuan University, in a written comment.
“Socializing almost every day seems to be the most beneficial for a long life,” Dr. Sen added, noting that more research is needed to determine if there is an optimal type of social activity.
Dr. Rowe pointed out two key findings from the study. The first was that it confirmed “prior studies that have identified a beneficial effect of social activity on life expectancy.
“We have known that engagement is essential for successful aging and that isolation is toxic. While this finding is not novel, it is nice to see this confirmation of what we thought we knew,” he wrote.
Secondly, the study has identified “a threshold effect”, which is that “the long-term benefit on life expectancy was only seen in the presence of fairly intense social interactions, essentially daily,” he said.
According to Preeti Malani, MD, professor of medicine and geriatrician at the University of Michigan, Ann Arbor, the findings are also helpful because they offer data from another part of the world, adding confidence in findings from Western countries.
“This [study] happens to focus on older adults in China, which is helpful since aging is not the same everywhere in the world,” Dr. Malani said. “While the numbers here may not be precise, it’s fair to say that socialization is good for your health – for everyone but especially for older adults.”
Considering the body of evidence now spanning a range of populations, Dr. Malani said physicians should be screening for, and recommending, socialization for all elderly patients, particularly because many aren’t getting enough of it.
“Work that my colleagues and I have done (with the National Poll on Healthy Aging) suggests that there is a portion of older adults that have very little to no social contact,” Dr. Malani said. “A physician may not know this unless they are asking routinely about socialization the way we might ask about diet and exercise. How much is enough? No one knows, but anything is better than nothing and likely more is better.”
She also suggested that personalization is key.
“Physical and emotional health may limit the ability to socialize, so not everyone can engage all the time,” Dr. Malani said. “Also, socialization can look different for different people. Technology allows for socialization even if an individual has trouble leaving their home. I especially worry about this issue for older adults that are also caregivers. Those individuals also need time for themselves” and on way to fulfill that need is by socializing with others.
The study was supported by Sichuan (China) Science and Technology Program, the National Key R&D Program of China, and the National Natural Science Foundation of China. The investigators, Dr. Rowe, and Dr. Malani disclosed no relevant conflicts of interest.
Sometimes more is more.
Correlations between socializing and survival were detected regardless of baseline health status, suggesting that physicians should be recommending daily socialization for all elderly patients, lead author Ziqiong Wang, MD, of Sichuan University West China Hospital, Chengdu, China, and colleagues reported.
These findings align with an array of prior studies reporting physical and mental health benefits from socialization, and negative impacts from isolation, the investigators wrote in the Journal of Epidemiology & Community Health. Not all studies have yielded the same picture, however, and most research has been conducted in Western countries, leading to uncertainty about whether different outcomes would be seen in populations in other parts of the world. Furthermore, the authors added that few studies have explored the amount of socialization needed to derive a positive benefit.
To address this knowledge gap, the investigators analyzed survival data from 28,563 participants in the Chinese Longitudinal Healthy Longevity Survey with a median age of 89 years at baseline.
“[This analysis] is from a highly respected ongoing longitudinal study of aging in China, which includes a large number of subjects and employs very strong research design and statistical analytical methods, so it has credibility,” John W. Rowe, MD, Julius B. Richmond Professor of Health Policy and Aging at Columbia University, New York, said in a written comment.
The investigators stratified frequency of socialization into five tiers: never, not monthly but sometimes, not weekly but at least once per month, not daily but at least once per week, and almost every day.
Survival proportions were calculated using the Kaplan-Meier method after accounting for a range of individual characteristics, including age, sex, household income, smoking status, diabetes, self-rated health, and others. Comparative findings were described in terms of time ratios using multivariable parametric accelerated failure time (AFT) models.
“The AFT model estimates the time ratio (TR), which is interpreted as the expected time to events in one category relative to the reference group,” the investigators wrote. “Unlike the interpretation of proportional hazard model results where hazard ratios larger than 1 are equal to higher risk, a TR of greater than 1 is considered to have a longer time to events, compared with the reference group.”
From baseline to 5 years, each socialization tier was significantly associated with prolonged survival, suggesting a general benefit. Compared with no socialization, socializing sometimes but not monthly was associated with 42% longer survival, at least monthly socialization was associated with 48% longer survival, at least weekly was associated with 110% longer survival, and socializing almost every day was associated with 87% longer survival.
The outsized benefit of daily socialization became clear in a long-term survival analysis, which spanned 5 years through the end of follow-up. Compared with no socialization, daily socialization tripled survival (TR, 3.04; P < .001), compared with prolongations ranging from 5% to 64% for less socialization, with just one of these lower tiers achieving statistical significance (P = .046).
Of note, the benefit of daily socialization was detected regardless of a person’s health status at baseline.
“No matter if elderly participants had chronic diseases or not, [and] no matter if older people had good self-rated health or not, the survival benefits of frequently participating in social activity were the same,” said principal author Sen He, MD, of Sichuan University, in a written comment.
“Socializing almost every day seems to be the most beneficial for a long life,” Dr. Sen added, noting that more research is needed to determine if there is an optimal type of social activity.
Dr. Rowe pointed out two key findings from the study. The first was that it confirmed “prior studies that have identified a beneficial effect of social activity on life expectancy.
“We have known that engagement is essential for successful aging and that isolation is toxic. While this finding is not novel, it is nice to see this confirmation of what we thought we knew,” he wrote.
Secondly, the study has identified “a threshold effect”, which is that “the long-term benefit on life expectancy was only seen in the presence of fairly intense social interactions, essentially daily,” he said.
According to Preeti Malani, MD, professor of medicine and geriatrician at the University of Michigan, Ann Arbor, the findings are also helpful because they offer data from another part of the world, adding confidence in findings from Western countries.
“This [study] happens to focus on older adults in China, which is helpful since aging is not the same everywhere in the world,” Dr. Malani said. “While the numbers here may not be precise, it’s fair to say that socialization is good for your health – for everyone but especially for older adults.”
Considering the body of evidence now spanning a range of populations, Dr. Malani said physicians should be screening for, and recommending, socialization for all elderly patients, particularly because many aren’t getting enough of it.
“Work that my colleagues and I have done (with the National Poll on Healthy Aging) suggests that there is a portion of older adults that have very little to no social contact,” Dr. Malani said. “A physician may not know this unless they are asking routinely about socialization the way we might ask about diet and exercise. How much is enough? No one knows, but anything is better than nothing and likely more is better.”
She also suggested that personalization is key.
“Physical and emotional health may limit the ability to socialize, so not everyone can engage all the time,” Dr. Malani said. “Also, socialization can look different for different people. Technology allows for socialization even if an individual has trouble leaving their home. I especially worry about this issue for older adults that are also caregivers. Those individuals also need time for themselves” and on way to fulfill that need is by socializing with others.
The study was supported by Sichuan (China) Science and Technology Program, the National Key R&D Program of China, and the National Natural Science Foundation of China. The investigators, Dr. Rowe, and Dr. Malani disclosed no relevant conflicts of interest.
FROM THE JOURNAL OF EPIDEMIOLOGY & COMMUNITY HEALTH
Be vigilant about suspected cases of measles, expert advises
HONOLULU – .
“Measles is one of the most contagious of human viruses, and we are seeing a resurgence,” Adelaide A. Hebert, MD, professor of dermatology and pediatrics, and chief of pediatric dermatology at the Universtiy of Texas, Houston, said at the Hawaii Dermatology Seminar provided by MedscapeLIVE! “This is a re-emerging viral infection that dermatologists must recognize. Measles often starts behind the ears, and the eruption can look a lot like a drug eruption,” she noted. “Many of my pediatric colleagues have never seen a case of measles before because we have had a vaccine since 1963. Measles can almost entirely be prevented with vaccination. You get herd immunity if both doses have been administered to 95% of the population.”
In 2021, the World Health Organization estimated that 25 million children worldwide missed the measles vaccine. This caused 9 million cases of measles and 128,000 deaths in 22 countries, mainly from viral pneumonia, secondary bacterial pneumonia, and postviral encephalitis. According to the Centers for Disease Control and Prevention, 1,274 measles cases occurred in 31 states in 2019, mostly in individuals who were not vaccinated against it. Reported cases fell to 13 in 2020 but rose to 49 cases in 2021 and to 121 cases in 2022. As of Feb. 28, 2023, three cases have been reported in the United States.
“Measles spreads through direct contact with an infected person and through airborne transmission,” said Dr. Hebert, who recommended an article published in The Lancet for background on the topic. “Unlike COVID-19, measles has not mutated, so the original measles vaccine will work very well.”
Common clinical signs of measles include a generalized, maculopapular eruption lasting for 3 days or more, a temperature above 101° F plus cough, coryza, or conjunctivitis. Confirmation of measles can be made by PCR for viral RNA. Clinicians can also send a blood draw to the state public health lab for analysis. The serologic standard is a fourfold rise or fall in IgG titer with a paired sample sent 10-14 days after the initial collection.
“You can administer immune globulin up to 6 days after exposure to potentially prevent measles or decrease severity [in] immunocompromised hosts not previously vaccinated,” she said. The recommended intramuscular dose is 0.5 mL/kg, up to a dose of 15 mL/kg. Treatment is supportive and focused on relieving common symptoms and providing nutritional support. Administration of vitamin A is currently recommended for all children with acute measles.
Vitamin A supplements are available either as capsules (50,000 IU; 100,000 IU; 200,000 IU) or in liquid form. Parenteral formulations are also available. “Capsules need to be cut open and the contents squeezed into the mouths of children younger than 2 years,” Dr. Hebert said. “Capsules have the advantage that they can be given to mothers for administration at home.”
The recommended dosage of vitamin A in children is as follows, she said:
- Aged 12 months or older: 200,000 IU daily for 2 days.
- Aged 6 to 11 months: 100,000 IU daily for 2 days.
- Aged 6 months or younger: 50,000 IU daily for 2 days.
The American Academy of Pediatrics recommends a third dose given 2-4 weeks later to children with clinical signs and symptoms of vitamin A deficiency.
In an interview following the meeting, Moise L. Levy, MD, professor of internal medicine and pediatrics at the University of Texas, Austin, emphasized that when clinicians evaluate pediatric patients with viral symptoms such as fever, cough, and skin eruption, “measles should be in the differential diagnosis.” The 2022 uptick in measles cases “would be another reason to engage in regular vaccinations.”
Dr. Hebert disclosed that she is a consultant or advisor for AbbVie, Almirall, Amryt Pharma, Arcutis Biotherapeutics, Beiersdorf, Dermavant Sciences, Galderma Laboratories, L’Oreal, Novan, Ortho Dermatologics, Pfizer, and Verrica.
Dr. Levy disclosed that he is consultant or advisor for Abeona, Castle Creek, Dusa Pharma, Krystal Bio, Novan, Regeneron, and Sanofi-Genzyme.
MedscapeLIVE! and this news organization are owned by the same parent company.
HONOLULU – .
“Measles is one of the most contagious of human viruses, and we are seeing a resurgence,” Adelaide A. Hebert, MD, professor of dermatology and pediatrics, and chief of pediatric dermatology at the Universtiy of Texas, Houston, said at the Hawaii Dermatology Seminar provided by MedscapeLIVE! “This is a re-emerging viral infection that dermatologists must recognize. Measles often starts behind the ears, and the eruption can look a lot like a drug eruption,” she noted. “Many of my pediatric colleagues have never seen a case of measles before because we have had a vaccine since 1963. Measles can almost entirely be prevented with vaccination. You get herd immunity if both doses have been administered to 95% of the population.”
In 2021, the World Health Organization estimated that 25 million children worldwide missed the measles vaccine. This caused 9 million cases of measles and 128,000 deaths in 22 countries, mainly from viral pneumonia, secondary bacterial pneumonia, and postviral encephalitis. According to the Centers for Disease Control and Prevention, 1,274 measles cases occurred in 31 states in 2019, mostly in individuals who were not vaccinated against it. Reported cases fell to 13 in 2020 but rose to 49 cases in 2021 and to 121 cases in 2022. As of Feb. 28, 2023, three cases have been reported in the United States.
“Measles spreads through direct contact with an infected person and through airborne transmission,” said Dr. Hebert, who recommended an article published in The Lancet for background on the topic. “Unlike COVID-19, measles has not mutated, so the original measles vaccine will work very well.”
Common clinical signs of measles include a generalized, maculopapular eruption lasting for 3 days or more, a temperature above 101° F plus cough, coryza, or conjunctivitis. Confirmation of measles can be made by PCR for viral RNA. Clinicians can also send a blood draw to the state public health lab for analysis. The serologic standard is a fourfold rise or fall in IgG titer with a paired sample sent 10-14 days after the initial collection.
“You can administer immune globulin up to 6 days after exposure to potentially prevent measles or decrease severity [in] immunocompromised hosts not previously vaccinated,” she said. The recommended intramuscular dose is 0.5 mL/kg, up to a dose of 15 mL/kg. Treatment is supportive and focused on relieving common symptoms and providing nutritional support. Administration of vitamin A is currently recommended for all children with acute measles.
Vitamin A supplements are available either as capsules (50,000 IU; 100,000 IU; 200,000 IU) or in liquid form. Parenteral formulations are also available. “Capsules need to be cut open and the contents squeezed into the mouths of children younger than 2 years,” Dr. Hebert said. “Capsules have the advantage that they can be given to mothers for administration at home.”
The recommended dosage of vitamin A in children is as follows, she said:
- Aged 12 months or older: 200,000 IU daily for 2 days.
- Aged 6 to 11 months: 100,000 IU daily for 2 days.
- Aged 6 months or younger: 50,000 IU daily for 2 days.
The American Academy of Pediatrics recommends a third dose given 2-4 weeks later to children with clinical signs and symptoms of vitamin A deficiency.
In an interview following the meeting, Moise L. Levy, MD, professor of internal medicine and pediatrics at the University of Texas, Austin, emphasized that when clinicians evaluate pediatric patients with viral symptoms such as fever, cough, and skin eruption, “measles should be in the differential diagnosis.” The 2022 uptick in measles cases “would be another reason to engage in regular vaccinations.”
Dr. Hebert disclosed that she is a consultant or advisor for AbbVie, Almirall, Amryt Pharma, Arcutis Biotherapeutics, Beiersdorf, Dermavant Sciences, Galderma Laboratories, L’Oreal, Novan, Ortho Dermatologics, Pfizer, and Verrica.
Dr. Levy disclosed that he is consultant or advisor for Abeona, Castle Creek, Dusa Pharma, Krystal Bio, Novan, Regeneron, and Sanofi-Genzyme.
MedscapeLIVE! and this news organization are owned by the same parent company.
HONOLULU – .
“Measles is one of the most contagious of human viruses, and we are seeing a resurgence,” Adelaide A. Hebert, MD, professor of dermatology and pediatrics, and chief of pediatric dermatology at the Universtiy of Texas, Houston, said at the Hawaii Dermatology Seminar provided by MedscapeLIVE! “This is a re-emerging viral infection that dermatologists must recognize. Measles often starts behind the ears, and the eruption can look a lot like a drug eruption,” she noted. “Many of my pediatric colleagues have never seen a case of measles before because we have had a vaccine since 1963. Measles can almost entirely be prevented with vaccination. You get herd immunity if both doses have been administered to 95% of the population.”
In 2021, the World Health Organization estimated that 25 million children worldwide missed the measles vaccine. This caused 9 million cases of measles and 128,000 deaths in 22 countries, mainly from viral pneumonia, secondary bacterial pneumonia, and postviral encephalitis. According to the Centers for Disease Control and Prevention, 1,274 measles cases occurred in 31 states in 2019, mostly in individuals who were not vaccinated against it. Reported cases fell to 13 in 2020 but rose to 49 cases in 2021 and to 121 cases in 2022. As of Feb. 28, 2023, three cases have been reported in the United States.
“Measles spreads through direct contact with an infected person and through airborne transmission,” said Dr. Hebert, who recommended an article published in The Lancet for background on the topic. “Unlike COVID-19, measles has not mutated, so the original measles vaccine will work very well.”
Common clinical signs of measles include a generalized, maculopapular eruption lasting for 3 days or more, a temperature above 101° F plus cough, coryza, or conjunctivitis. Confirmation of measles can be made by PCR for viral RNA. Clinicians can also send a blood draw to the state public health lab for analysis. The serologic standard is a fourfold rise or fall in IgG titer with a paired sample sent 10-14 days after the initial collection.
“You can administer immune globulin up to 6 days after exposure to potentially prevent measles or decrease severity [in] immunocompromised hosts not previously vaccinated,” she said. The recommended intramuscular dose is 0.5 mL/kg, up to a dose of 15 mL/kg. Treatment is supportive and focused on relieving common symptoms and providing nutritional support. Administration of vitamin A is currently recommended for all children with acute measles.
Vitamin A supplements are available either as capsules (50,000 IU; 100,000 IU; 200,000 IU) or in liquid form. Parenteral formulations are also available. “Capsules need to be cut open and the contents squeezed into the mouths of children younger than 2 years,” Dr. Hebert said. “Capsules have the advantage that they can be given to mothers for administration at home.”
The recommended dosage of vitamin A in children is as follows, she said:
- Aged 12 months or older: 200,000 IU daily for 2 days.
- Aged 6 to 11 months: 100,000 IU daily for 2 days.
- Aged 6 months or younger: 50,000 IU daily for 2 days.
The American Academy of Pediatrics recommends a third dose given 2-4 weeks later to children with clinical signs and symptoms of vitamin A deficiency.
In an interview following the meeting, Moise L. Levy, MD, professor of internal medicine and pediatrics at the University of Texas, Austin, emphasized that when clinicians evaluate pediatric patients with viral symptoms such as fever, cough, and skin eruption, “measles should be in the differential diagnosis.” The 2022 uptick in measles cases “would be another reason to engage in regular vaccinations.”
Dr. Hebert disclosed that she is a consultant or advisor for AbbVie, Almirall, Amryt Pharma, Arcutis Biotherapeutics, Beiersdorf, Dermavant Sciences, Galderma Laboratories, L’Oreal, Novan, Ortho Dermatologics, Pfizer, and Verrica.
Dr. Levy disclosed that he is consultant or advisor for Abeona, Castle Creek, Dusa Pharma, Krystal Bio, Novan, Regeneron, and Sanofi-Genzyme.
MedscapeLIVE! and this news organization are owned by the same parent company.
AT THE MEDSCAPELIVE! HAWAII DERMATOLOGY SEMINAR
Catheterized urine color change
Physical examination revealed an older man whose vital signs were normal and who had a regular heart rate and rhythm. He denied any pain, and his abdomen was soft and nontender with normal bowel sounds. There was no suprapubic or costovertebral angle tenderness, and his urinary catheter was correctly placed. His urine output was within normal limits, but the urine in the catheter and collection bag was purple.
The patient’s medical history was remarkable for mild cognitive impairment, BPH, and hypertension. A urine culture was significant for > 100,000 CFU/mL pan-sensitive Pseudomonas aeruginosa.
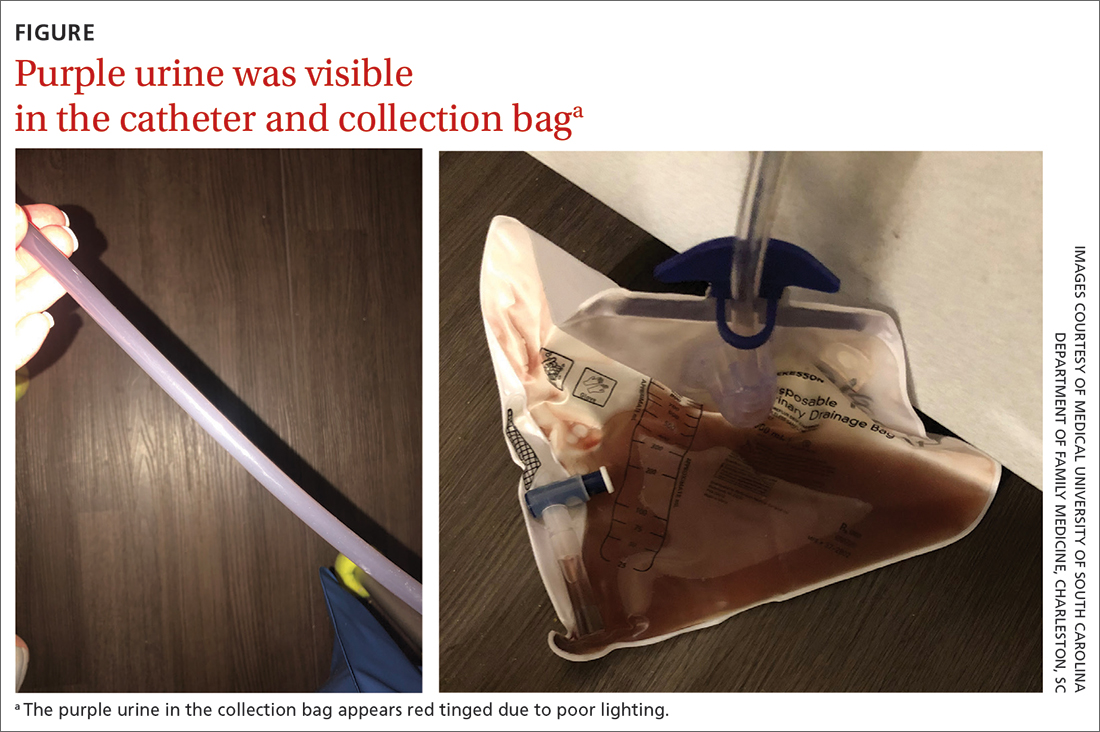
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Purple urine bag syndrome
The diagnosis of purple urine bag syndrome (PUBS) was made based on the patient’s clinical presentation and medical history. PUBS is generally a benign condition that can occur in patients who have urinary catheters for prolonged periods of time and urinary tract infections (UTIs), often with constipation.1
PUBS was first described in the literature in 1978.2 Its prevalence has been estimated to be 9.8% in long-term wards and higher in patients with chronic catheters.3-5 PUBS is reported more often in institutionalized older women, although it has been documented in men as well.1 Risk factors include having a chronic indwelling urinary catheter; alkaline urine; the use of plastic, polyvinylchloride urine bags3; chronic constipation6; renal failure4,5; and dementia.1 In many cases, patients with PUBS have been found to have stable vitals and lack systemic symptoms, such as fever, that could indicate an infection.1,5
The pathogenesis of PUBS has been associated with tryptophan.3 Gut bacteria metabolize tryptophan to indole, which is converted to indoxyl sulfate in the liver.3,7 Then certain bacteria associated with UTIs, including Pseudomonas, Escherichia coli, Proteus mirabilis, Providencia spp, Enterococcus faecalis, and Klebsiella,5-7 which contain indoxyl phosphatase and sulfatase enzymes, can convert indoxyl sulfate into indirubin (red) and indigo (blue) compounds; this results in a purple hue in the urine seen in a Foley catheter and bag.
Differential is generally limited to medication and food consumption
Clinical presentation and a detailed history and review of medication and/or food ingestion may distinguish PUBS from other conditions.
Medications and foods, such as rifampicin or beets, may discolor urine and need to be ruled out as a cause with a thorough history.3
Cyanide toxicity in those taking vitamin B12 can result in purple-tinged urine.8 Signs and symptoms can also include reddening of the skin, dyspnea, nausea, headache, erythema at the injection site, and a modest increase in blood pressure.8
Identify the infection and treat as needed
There have been some case reports regarding the progression of PUBS to Fournier gangrene,4 but such cases are rare and associated with immunocompromised patients.9 PUBS is generally a benign condition associated with UTIs. Management involves identifying the underlying infection, treating with antibiotics if indicated (ie, patient is symptomatic or immunocompromised),3 providing proper treatment of constipation if needed, and replacing the Foley catheter.4 Some studies suggest that simply exchanging the catheter may resolve PUBS, particularly in asymptomatic patients.5
In light of his complicated urologic history, our patient was treated with a 10-day course of renally dosed intravenous cefepime (500 mg every 24 hours based on calculated creatine clearance of 21 mL/min) and Foley exchange. The patient’s urine color returned to normal after Foley exchange and 24 hours of antibiotics. His kidney function continued to improve and normalized by the time he was discharged from the facility approximately 2 weeks later.
1. Goyal A, Vikas G, Jindal J. Purple urine bag syndrome: series of nine cases and review of literature. J Clin Diagn Res. 2018;12:PR01-PR03. doi: 10.7860/JCDR/2018/34951.12202
2. Barlow GB, Dickson JAS. Purple urine bags. Lancet. 1978;28:220-221. doi: 10.1016/S0140-6736(78)90667-0
3. Richardson-May J. Single case of purple urine bag syndrome in an elderly woman with stroke. BMJ Case Rep. 2016;2016:bcr2016215465. doi: 10.1136/bcr-2016-215465
4. Khan F, Chaudhry MA, Qureshi N, et al. Purple urine bag syndrome: an alarming hue? A brief review of the literature. Int J Nephrol. 2011;2011:419213. doi: 10.4061/2011/419213
5. Ben-Chetrit E, Munter G. Purple urine. JAMA. 2012;307:193-194. doi: 10.1001/jama.2011.1997
6. Al Montasir A, Al Mustaque A. Purple urine bag syndrome. J Family Med Prim Care. 2013;2:104-105. doi: 10.4103/2249-4863.109970
7. Dealler SF, Hawkey PM, Millar MR. Enzymatic degradation of urinary indoxyl sulfate by Providencia stuartii and Klebsiella pneumoniae causes the purple urine bag syndrome. J Clin Microbiol. 1988;26:2152-2156. doi: 10.1128/jcm.26.10.2152-2156.1988
8. Hudson M, Cashin BV, Matlock AG, et al. A man with purple urine. Hydroxocobalamin-induced chromaturia. Clin Toxicol (Phila). 2012;50:77. doi: 10.3109/15563650.2011.626782
9. Tasi Y-M, Huang M-S, Yang C-J, et al. Purple urine bag syndrome, not always a benign process. Am J Emerg Med. 2009;27:895-897. doi: 10.1016/j.ajem.2009.01.030
Physical examination revealed an older man whose vital signs were normal and who had a regular heart rate and rhythm. He denied any pain, and his abdomen was soft and nontender with normal bowel sounds. There was no suprapubic or costovertebral angle tenderness, and his urinary catheter was correctly placed. His urine output was within normal limits, but the urine in the catheter and collection bag was purple.
The patient’s medical history was remarkable for mild cognitive impairment, BPH, and hypertension. A urine culture was significant for > 100,000 CFU/mL pan-sensitive Pseudomonas aeruginosa.
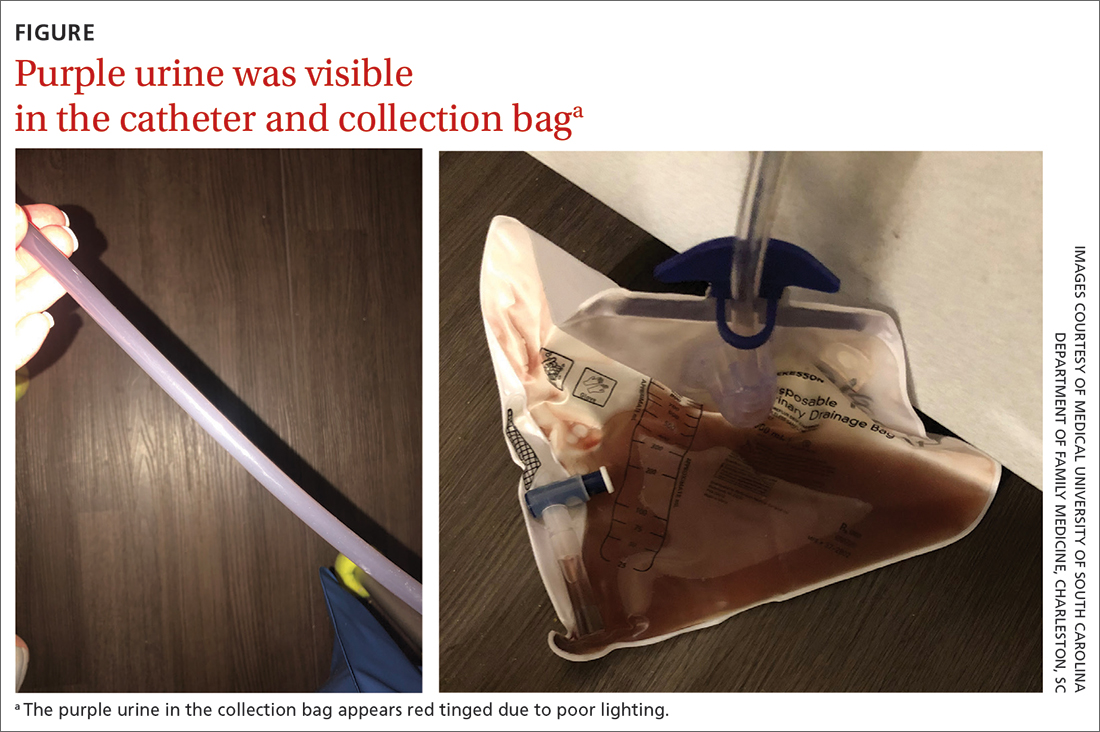
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Purple urine bag syndrome
The diagnosis of purple urine bag syndrome (PUBS) was made based on the patient’s clinical presentation and medical history. PUBS is generally a benign condition that can occur in patients who have urinary catheters for prolonged periods of time and urinary tract infections (UTIs), often with constipation.1
PUBS was first described in the literature in 1978.2 Its prevalence has been estimated to be 9.8% in long-term wards and higher in patients with chronic catheters.3-5 PUBS is reported more often in institutionalized older women, although it has been documented in men as well.1 Risk factors include having a chronic indwelling urinary catheter; alkaline urine; the use of plastic, polyvinylchloride urine bags3; chronic constipation6; renal failure4,5; and dementia.1 In many cases, patients with PUBS have been found to have stable vitals and lack systemic symptoms, such as fever, that could indicate an infection.1,5
The pathogenesis of PUBS has been associated with tryptophan.3 Gut bacteria metabolize tryptophan to indole, which is converted to indoxyl sulfate in the liver.3,7 Then certain bacteria associated with UTIs, including Pseudomonas, Escherichia coli, Proteus mirabilis, Providencia spp, Enterococcus faecalis, and Klebsiella,5-7 which contain indoxyl phosphatase and sulfatase enzymes, can convert indoxyl sulfate into indirubin (red) and indigo (blue) compounds; this results in a purple hue in the urine seen in a Foley catheter and bag.
Differential is generally limited to medication and food consumption
Clinical presentation and a detailed history and review of medication and/or food ingestion may distinguish PUBS from other conditions.
Medications and foods, such as rifampicin or beets, may discolor urine and need to be ruled out as a cause with a thorough history.3
Cyanide toxicity in those taking vitamin B12 can result in purple-tinged urine.8 Signs and symptoms can also include reddening of the skin, dyspnea, nausea, headache, erythema at the injection site, and a modest increase in blood pressure.8
Identify the infection and treat as needed
There have been some case reports regarding the progression of PUBS to Fournier gangrene,4 but such cases are rare and associated with immunocompromised patients.9 PUBS is generally a benign condition associated with UTIs. Management involves identifying the underlying infection, treating with antibiotics if indicated (ie, patient is symptomatic or immunocompromised),3 providing proper treatment of constipation if needed, and replacing the Foley catheter.4 Some studies suggest that simply exchanging the catheter may resolve PUBS, particularly in asymptomatic patients.5
In light of his complicated urologic history, our patient was treated with a 10-day course of renally dosed intravenous cefepime (500 mg every 24 hours based on calculated creatine clearance of 21 mL/min) and Foley exchange. The patient’s urine color returned to normal after Foley exchange and 24 hours of antibiotics. His kidney function continued to improve and normalized by the time he was discharged from the facility approximately 2 weeks later.
Physical examination revealed an older man whose vital signs were normal and who had a regular heart rate and rhythm. He denied any pain, and his abdomen was soft and nontender with normal bowel sounds. There was no suprapubic or costovertebral angle tenderness, and his urinary catheter was correctly placed. His urine output was within normal limits, but the urine in the catheter and collection bag was purple.
The patient’s medical history was remarkable for mild cognitive impairment, BPH, and hypertension. A urine culture was significant for > 100,000 CFU/mL pan-sensitive Pseudomonas aeruginosa.
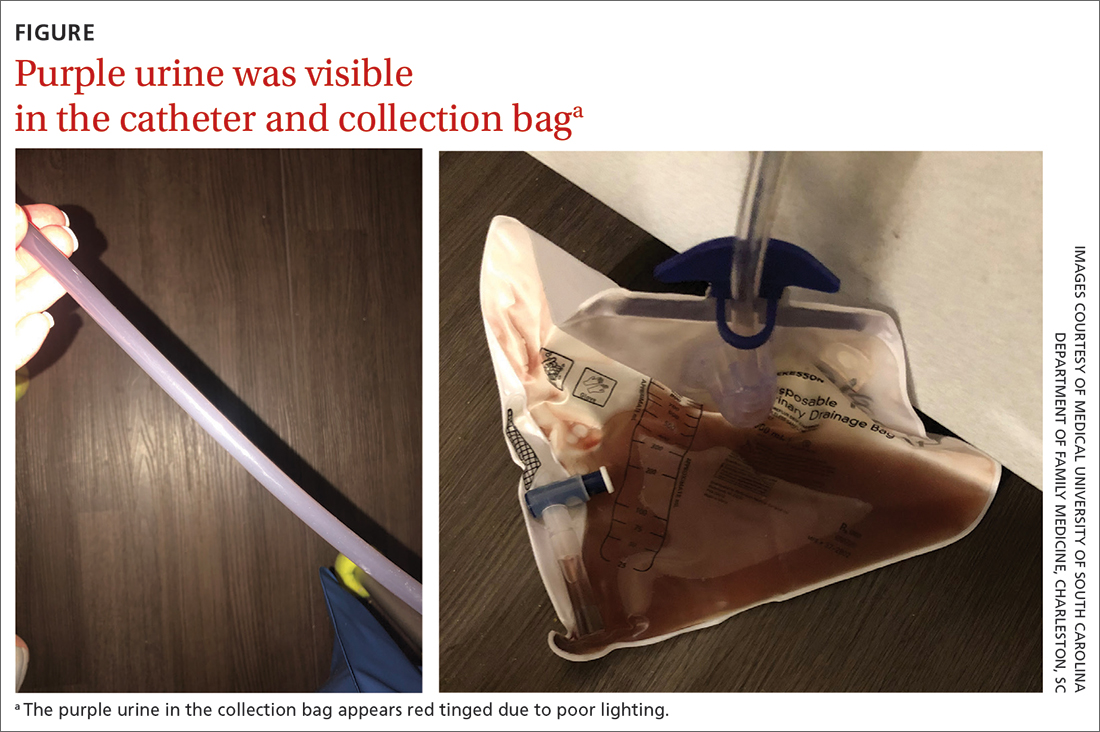
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Purple urine bag syndrome
The diagnosis of purple urine bag syndrome (PUBS) was made based on the patient’s clinical presentation and medical history. PUBS is generally a benign condition that can occur in patients who have urinary catheters for prolonged periods of time and urinary tract infections (UTIs), often with constipation.1
PUBS was first described in the literature in 1978.2 Its prevalence has been estimated to be 9.8% in long-term wards and higher in patients with chronic catheters.3-5 PUBS is reported more often in institutionalized older women, although it has been documented in men as well.1 Risk factors include having a chronic indwelling urinary catheter; alkaline urine; the use of plastic, polyvinylchloride urine bags3; chronic constipation6; renal failure4,5; and dementia.1 In many cases, patients with PUBS have been found to have stable vitals and lack systemic symptoms, such as fever, that could indicate an infection.1,5
The pathogenesis of PUBS has been associated with tryptophan.3 Gut bacteria metabolize tryptophan to indole, which is converted to indoxyl sulfate in the liver.3,7 Then certain bacteria associated with UTIs, including Pseudomonas, Escherichia coli, Proteus mirabilis, Providencia spp, Enterococcus faecalis, and Klebsiella,5-7 which contain indoxyl phosphatase and sulfatase enzymes, can convert indoxyl sulfate into indirubin (red) and indigo (blue) compounds; this results in a purple hue in the urine seen in a Foley catheter and bag.
Differential is generally limited to medication and food consumption
Clinical presentation and a detailed history and review of medication and/or food ingestion may distinguish PUBS from other conditions.
Medications and foods, such as rifampicin or beets, may discolor urine and need to be ruled out as a cause with a thorough history.3
Cyanide toxicity in those taking vitamin B12 can result in purple-tinged urine.8 Signs and symptoms can also include reddening of the skin, dyspnea, nausea, headache, erythema at the injection site, and a modest increase in blood pressure.8
Identify the infection and treat as needed
There have been some case reports regarding the progression of PUBS to Fournier gangrene,4 but such cases are rare and associated with immunocompromised patients.9 PUBS is generally a benign condition associated with UTIs. Management involves identifying the underlying infection, treating with antibiotics if indicated (ie, patient is symptomatic or immunocompromised),3 providing proper treatment of constipation if needed, and replacing the Foley catheter.4 Some studies suggest that simply exchanging the catheter may resolve PUBS, particularly in asymptomatic patients.5
In light of his complicated urologic history, our patient was treated with a 10-day course of renally dosed intravenous cefepime (500 mg every 24 hours based on calculated creatine clearance of 21 mL/min) and Foley exchange. The patient’s urine color returned to normal after Foley exchange and 24 hours of antibiotics. His kidney function continued to improve and normalized by the time he was discharged from the facility approximately 2 weeks later.
1. Goyal A, Vikas G, Jindal J. Purple urine bag syndrome: series of nine cases and review of literature. J Clin Diagn Res. 2018;12:PR01-PR03. doi: 10.7860/JCDR/2018/34951.12202
2. Barlow GB, Dickson JAS. Purple urine bags. Lancet. 1978;28:220-221. doi: 10.1016/S0140-6736(78)90667-0
3. Richardson-May J. Single case of purple urine bag syndrome in an elderly woman with stroke. BMJ Case Rep. 2016;2016:bcr2016215465. doi: 10.1136/bcr-2016-215465
4. Khan F, Chaudhry MA, Qureshi N, et al. Purple urine bag syndrome: an alarming hue? A brief review of the literature. Int J Nephrol. 2011;2011:419213. doi: 10.4061/2011/419213
5. Ben-Chetrit E, Munter G. Purple urine. JAMA. 2012;307:193-194. doi: 10.1001/jama.2011.1997
6. Al Montasir A, Al Mustaque A. Purple urine bag syndrome. J Family Med Prim Care. 2013;2:104-105. doi: 10.4103/2249-4863.109970
7. Dealler SF, Hawkey PM, Millar MR. Enzymatic degradation of urinary indoxyl sulfate by Providencia stuartii and Klebsiella pneumoniae causes the purple urine bag syndrome. J Clin Microbiol. 1988;26:2152-2156. doi: 10.1128/jcm.26.10.2152-2156.1988
8. Hudson M, Cashin BV, Matlock AG, et al. A man with purple urine. Hydroxocobalamin-induced chromaturia. Clin Toxicol (Phila). 2012;50:77. doi: 10.3109/15563650.2011.626782
9. Tasi Y-M, Huang M-S, Yang C-J, et al. Purple urine bag syndrome, not always a benign process. Am J Emerg Med. 2009;27:895-897. doi: 10.1016/j.ajem.2009.01.030
1. Goyal A, Vikas G, Jindal J. Purple urine bag syndrome: series of nine cases and review of literature. J Clin Diagn Res. 2018;12:PR01-PR03. doi: 10.7860/JCDR/2018/34951.12202
2. Barlow GB, Dickson JAS. Purple urine bags. Lancet. 1978;28:220-221. doi: 10.1016/S0140-6736(78)90667-0
3. Richardson-May J. Single case of purple urine bag syndrome in an elderly woman with stroke. BMJ Case Rep. 2016;2016:bcr2016215465. doi: 10.1136/bcr-2016-215465
4. Khan F, Chaudhry MA, Qureshi N, et al. Purple urine bag syndrome: an alarming hue? A brief review of the literature. Int J Nephrol. 2011;2011:419213. doi: 10.4061/2011/419213
5. Ben-Chetrit E, Munter G. Purple urine. JAMA. 2012;307:193-194. doi: 10.1001/jama.2011.1997
6. Al Montasir A, Al Mustaque A. Purple urine bag syndrome. J Family Med Prim Care. 2013;2:104-105. doi: 10.4103/2249-4863.109970
7. Dealler SF, Hawkey PM, Millar MR. Enzymatic degradation of urinary indoxyl sulfate by Providencia stuartii and Klebsiella pneumoniae causes the purple urine bag syndrome. J Clin Microbiol. 1988;26:2152-2156. doi: 10.1128/jcm.26.10.2152-2156.1988
8. Hudson M, Cashin BV, Matlock AG, et al. A man with purple urine. Hydroxocobalamin-induced chromaturia. Clin Toxicol (Phila). 2012;50:77. doi: 10.3109/15563650.2011.626782
9. Tasi Y-M, Huang M-S, Yang C-J, et al. Purple urine bag syndrome, not always a benign process. Am J Emerg Med. 2009;27:895-897. doi: 10.1016/j.ajem.2009.01.030
44-year-old man • elevated total cholesterol • chest pains • ketogenic diet • Dx?
THE CASE
A 44-year-old man with a history of morbid obesity reestablished care in our clinic. He had been treated in our health care system about 5 years previously, and prior lab testing showed a total cholesterol of 203 mg/dL; triglycerides, 191 mg/dL; high-density lipoprotein (HDL), 56 mg/dL; and low-density lipoprotein (LDL), 109 mg/dL. At that time, he weighed 299 lbs (BMI, 39.4). He then started a strict ketogenic diet and a regular exercise program (running ~ 16 miles per week and lifting weights), which he maintained for several years. He had experienced remarkable weight loss; upon reestablishing care, he weighed 199 lbs (BMI, 26.33).
However, lipid testing revealed a severely elevated total cholesterol of 334 mg/dL; LDL, 248 mg/dL; HDL, 67 mg/dL; and triglycerides, 95 mg/dL. He was advised to start statin therapy and to stop his ketogenic diet, but he was hesitant to take either step. He elected to have his lab work reevaluated in 6 months.
About 4 months later, he presented with new and increasing burning pain in his mid chest and upper abdomen. He rated the pain 6/10 in severity and said it occurred during exertion or at night when lying down. Resting would relieve the pain. Reduced intake of spicy foods and caffeine had also helped. He denied dyspnea, diaphoresis, palpitations, or nausea.
The patient was a nonsmoker but did have a strong family history of cardiovascular disease. His vital signs and physical examination were unremarkable, apart from mild epigastric and periumbilical tenderness on palpation.
THE DIAGNOSIS
The patient’s chest pain had features of both gastroesophageal reflux disease (GERD) and coronary artery disease (CAD) with exertional angina. His high-fat diet, nightly symptoms, and the partial relief he achieved by cutting back on spicy foods and caffeine suggested GERD, but the exertional nature of the chest pain and gradual relief with rest was highly suggestive of angina, so an outpatient electrocardiogram treadmill stress test was ordered.
The stress test was markedly abnormal, showing worsening ST depressions and T-wave inversions with exertion, and he experienced chest pain during testing. An urgent left heart catheterization was performed, showing severe multivessel CAD. He subsequently underwent 3-vessel coronary artery bypass grafting. A familial hypercholesterolemia panel failed to reveal any significant variants.
As a result of these findings, the patient received a diagnosis of severe ketogenic diet–associated hypercholesterolemia and early-onset CAD.
Continue to: DISCUSSION
DISCUSSION
Low-carbohydrate (low-carb) and ketogenic diets have grown in popularity throughout the United States over the past decade, particularly for weight loss, and the diet has entered the popular consciousness with several celebrities publicly supporting it.1 Simultaneously, there also has been a growing interest in these diets for the treatment of chronic diseases, such as type 2 diabetes.2 However, the long-term cardiovascular effects of low-carb diets are not well studied, and there is significant heterogeneity among these diets.
Low-carb vs low-fat. Multiple meta-analyses comparing low-carb diets to low-fat diets have found that those following low-carb diets have significantly higher total cholesterol and LDL levels.3,4,5 The National Lipid Association’s review of evidence determined that LDL and total cholesterol responses vary in individuals following a low-carb diet, but that increasing LDL levels in particular were concerning enough to warrant lipid monitoring of patients on low-carb diets.6 Another meta-analysis evaluated the difference in estimated atherosclerotic cardiovascular disease (ASCVD) risk between low-carb and low-fat diets, finding those following a low-carb diet to have a lower estimated ASCVD risk but higher LDL levels.7
Weighing the benefits and harms. Since our patient’s dramatic weight loss and greatly increased exercise level would be expected to lower his LDL levels, the severe worsening of his LDL levels was likely related to his ketogenic diet and was a factor in the early onset of CAD. The benefits of low-carb diets for weight loss, contrasted with the consistent worsening of LDL levels, has prompted a debate about which parameters should be considered in estimating the long-term risk of these diets for patients. Diamond et al8 posit that these diets have beneficial effects on “the most reliable [cardiovascular disease] risk factors,” but long-term, patient-oriented outcome data are lacking, and these diets may not be appropriate for certain patients, as our case demonstrates.
A reasonable strategy for patients contemplating a low-carb diet specifically for weight loss would be to use such a diet for 3 to 6 months to achieve initial and rapid results, then continue with a heart-healthy diet and increased exercise levels to maintain weight loss and reduce long-term cardiovascular risk.
Our patient was started on a postoperative medication regimen of aspirin 81 mg/d, evolocumab 140 mg every 14 days, metoprolol tartrate 25 mg bid, and rosuvastatin 10 mg/d. A year later, he was able to resume a high level of physical activity (6-mile runs) without chest pain. His follow-up lipid panel showed a total cholesterol of 153 mg/dL; LDL, 53 mg/dL; HDL, 89 mg/dL; and triglycerides, 55 mg/dL. He had also switched to a regular diet and had been able to maintain his weight loss.
THE TAKEAWAY
Growing evidence suggests that low-carb diets may have a significant and detrimental effect on LDL levels. The long-term safety of these diets hasn’t been well studied, particularly regarding cardiovascular outcomes. At a minimum, patients who initiate low-carb diets should be counseled on general dietary recommendations regarding saturated fat and cholesterol intake, and they should have a follow-up lipid screening to evaluate for any significant worsening in total cholesterol and LDL levels.
CORRESPONDENCE
Samuel Dickmann, MD, 13611 NW 1st Lane, Suite 200, Newberry, FL 32669; [email protected]
1. Gorin A. What is the keto diet – and is it right for you? NBC News BETTER. February 22, 2018. Accessed February 3, 2023. www.nbcnews.com/better/health/what-keto-diet-it-right-you-ncna847256
2. Tinguely D, Gross J, Kosinski, C. Efficacy of ketogenic diets on type 2 diabetes: a systematic review. Current Diabetes Reports. 2021;21:32. doi: 10.1007/s11892-021-01399-z
3. Mansoor N, Vinknes KJ, Veierod MB, et al. Effects of low-carbohydrate diets v. low-fat diets on body weight and cardiovascular risk factors a meta-analysis of randomised controlled trials. Br J Nutr. 2016;115:466-479. doi: 10.1017/S0007114515004699
4. Bueno NB, de Melo ISV, de Oliveira SL, et al. Very-low-carbohydrate ketogenic diet v. low-fat diet for long-term weight loss: a meta-analysis of randomised controlled trials. Br J Nutr. 2013;110:1178-1187. doi: 10.1017/S0007114513000548
5. Chawla S, Tessarolo Silva F, Amaral Medeiros S, et al. The effect of low-fat and low-carbohydrate diets on weight loss and lipid levels: a systematic review and meta-analysis. Nutrients. 2020;12:3774. doi: 10.3390/nu12123774
6. Kirkpatrick CF, Bolick JP, Kris-Etherton PM, et al. Review of current evidence and clinical recommendations on the effects of low-carbohydrate and very-low-carbohydrate (including ketogenic) diets for the management of body weight and other cardiometabolic risk factors: a scientific statement from the National Lipid Association Nutrition and Lifestyle Task Force. J Clin Lipidol. 2019;13:689-711.e1. doi: 10.1016/j.jacl.2019.08.003
7. Sackner-Bernstein J, Kanter D, Kaul S. Dietary intervention for overweight and obese adults: comparison of low-carbohydrate and low-fat diets. a meta-analysis. PLoS One. 2015;10:e0139817. doi: 10.1371/journal.pone.0139817
8. Diamond DM, O’Neill BJ, Volek JS. Low carbohydrate diet: are concerns with saturated fat, lipids, and cardiovascular disease risk justified? Curr Opin Endocrinol Diabetes Obes. 2020;27:291-300. doi: 10.1097/MED.0000000000000568
THE CASE
A 44-year-old man with a history of morbid obesity reestablished care in our clinic. He had been treated in our health care system about 5 years previously, and prior lab testing showed a total cholesterol of 203 mg/dL; triglycerides, 191 mg/dL; high-density lipoprotein (HDL), 56 mg/dL; and low-density lipoprotein (LDL), 109 mg/dL. At that time, he weighed 299 lbs (BMI, 39.4). He then started a strict ketogenic diet and a regular exercise program (running ~ 16 miles per week and lifting weights), which he maintained for several years. He had experienced remarkable weight loss; upon reestablishing care, he weighed 199 lbs (BMI, 26.33).
However, lipid testing revealed a severely elevated total cholesterol of 334 mg/dL; LDL, 248 mg/dL; HDL, 67 mg/dL; and triglycerides, 95 mg/dL. He was advised to start statin therapy and to stop his ketogenic diet, but he was hesitant to take either step. He elected to have his lab work reevaluated in 6 months.
About 4 months later, he presented with new and increasing burning pain in his mid chest and upper abdomen. He rated the pain 6/10 in severity and said it occurred during exertion or at night when lying down. Resting would relieve the pain. Reduced intake of spicy foods and caffeine had also helped. He denied dyspnea, diaphoresis, palpitations, or nausea.
The patient was a nonsmoker but did have a strong family history of cardiovascular disease. His vital signs and physical examination were unremarkable, apart from mild epigastric and periumbilical tenderness on palpation.
THE DIAGNOSIS
The patient’s chest pain had features of both gastroesophageal reflux disease (GERD) and coronary artery disease (CAD) with exertional angina. His high-fat diet, nightly symptoms, and the partial relief he achieved by cutting back on spicy foods and caffeine suggested GERD, but the exertional nature of the chest pain and gradual relief with rest was highly suggestive of angina, so an outpatient electrocardiogram treadmill stress test was ordered.
The stress test was markedly abnormal, showing worsening ST depressions and T-wave inversions with exertion, and he experienced chest pain during testing. An urgent left heart catheterization was performed, showing severe multivessel CAD. He subsequently underwent 3-vessel coronary artery bypass grafting. A familial hypercholesterolemia panel failed to reveal any significant variants.
As a result of these findings, the patient received a diagnosis of severe ketogenic diet–associated hypercholesterolemia and early-onset CAD.
Continue to: DISCUSSION
DISCUSSION
Low-carbohydrate (low-carb) and ketogenic diets have grown in popularity throughout the United States over the past decade, particularly for weight loss, and the diet has entered the popular consciousness with several celebrities publicly supporting it.1 Simultaneously, there also has been a growing interest in these diets for the treatment of chronic diseases, such as type 2 diabetes.2 However, the long-term cardiovascular effects of low-carb diets are not well studied, and there is significant heterogeneity among these diets.
Low-carb vs low-fat. Multiple meta-analyses comparing low-carb diets to low-fat diets have found that those following low-carb diets have significantly higher total cholesterol and LDL levels.3,4,5 The National Lipid Association’s review of evidence determined that LDL and total cholesterol responses vary in individuals following a low-carb diet, but that increasing LDL levels in particular were concerning enough to warrant lipid monitoring of patients on low-carb diets.6 Another meta-analysis evaluated the difference in estimated atherosclerotic cardiovascular disease (ASCVD) risk between low-carb and low-fat diets, finding those following a low-carb diet to have a lower estimated ASCVD risk but higher LDL levels.7
Weighing the benefits and harms. Since our patient’s dramatic weight loss and greatly increased exercise level would be expected to lower his LDL levels, the severe worsening of his LDL levels was likely related to his ketogenic diet and was a factor in the early onset of CAD. The benefits of low-carb diets for weight loss, contrasted with the consistent worsening of LDL levels, has prompted a debate about which parameters should be considered in estimating the long-term risk of these diets for patients. Diamond et al8 posit that these diets have beneficial effects on “the most reliable [cardiovascular disease] risk factors,” but long-term, patient-oriented outcome data are lacking, and these diets may not be appropriate for certain patients, as our case demonstrates.
A reasonable strategy for patients contemplating a low-carb diet specifically for weight loss would be to use such a diet for 3 to 6 months to achieve initial and rapid results, then continue with a heart-healthy diet and increased exercise levels to maintain weight loss and reduce long-term cardiovascular risk.
Our patient was started on a postoperative medication regimen of aspirin 81 mg/d, evolocumab 140 mg every 14 days, metoprolol tartrate 25 mg bid, and rosuvastatin 10 mg/d. A year later, he was able to resume a high level of physical activity (6-mile runs) without chest pain. His follow-up lipid panel showed a total cholesterol of 153 mg/dL; LDL, 53 mg/dL; HDL, 89 mg/dL; and triglycerides, 55 mg/dL. He had also switched to a regular diet and had been able to maintain his weight loss.
THE TAKEAWAY
Growing evidence suggests that low-carb diets may have a significant and detrimental effect on LDL levels. The long-term safety of these diets hasn’t been well studied, particularly regarding cardiovascular outcomes. At a minimum, patients who initiate low-carb diets should be counseled on general dietary recommendations regarding saturated fat and cholesterol intake, and they should have a follow-up lipid screening to evaluate for any significant worsening in total cholesterol and LDL levels.
CORRESPONDENCE
Samuel Dickmann, MD, 13611 NW 1st Lane, Suite 200, Newberry, FL 32669; [email protected]
THE CASE
A 44-year-old man with a history of morbid obesity reestablished care in our clinic. He had been treated in our health care system about 5 years previously, and prior lab testing showed a total cholesterol of 203 mg/dL; triglycerides, 191 mg/dL; high-density lipoprotein (HDL), 56 mg/dL; and low-density lipoprotein (LDL), 109 mg/dL. At that time, he weighed 299 lbs (BMI, 39.4). He then started a strict ketogenic diet and a regular exercise program (running ~ 16 miles per week and lifting weights), which he maintained for several years. He had experienced remarkable weight loss; upon reestablishing care, he weighed 199 lbs (BMI, 26.33).
However, lipid testing revealed a severely elevated total cholesterol of 334 mg/dL; LDL, 248 mg/dL; HDL, 67 mg/dL; and triglycerides, 95 mg/dL. He was advised to start statin therapy and to stop his ketogenic diet, but he was hesitant to take either step. He elected to have his lab work reevaluated in 6 months.
About 4 months later, he presented with new and increasing burning pain in his mid chest and upper abdomen. He rated the pain 6/10 in severity and said it occurred during exertion or at night when lying down. Resting would relieve the pain. Reduced intake of spicy foods and caffeine had also helped. He denied dyspnea, diaphoresis, palpitations, or nausea.
The patient was a nonsmoker but did have a strong family history of cardiovascular disease. His vital signs and physical examination were unremarkable, apart from mild epigastric and periumbilical tenderness on palpation.
THE DIAGNOSIS
The patient’s chest pain had features of both gastroesophageal reflux disease (GERD) and coronary artery disease (CAD) with exertional angina. His high-fat diet, nightly symptoms, and the partial relief he achieved by cutting back on spicy foods and caffeine suggested GERD, but the exertional nature of the chest pain and gradual relief with rest was highly suggestive of angina, so an outpatient electrocardiogram treadmill stress test was ordered.
The stress test was markedly abnormal, showing worsening ST depressions and T-wave inversions with exertion, and he experienced chest pain during testing. An urgent left heart catheterization was performed, showing severe multivessel CAD. He subsequently underwent 3-vessel coronary artery bypass grafting. A familial hypercholesterolemia panel failed to reveal any significant variants.
As a result of these findings, the patient received a diagnosis of severe ketogenic diet–associated hypercholesterolemia and early-onset CAD.
Continue to: DISCUSSION
DISCUSSION
Low-carbohydrate (low-carb) and ketogenic diets have grown in popularity throughout the United States over the past decade, particularly for weight loss, and the diet has entered the popular consciousness with several celebrities publicly supporting it.1 Simultaneously, there also has been a growing interest in these diets for the treatment of chronic diseases, such as type 2 diabetes.2 However, the long-term cardiovascular effects of low-carb diets are not well studied, and there is significant heterogeneity among these diets.
Low-carb vs low-fat. Multiple meta-analyses comparing low-carb diets to low-fat diets have found that those following low-carb diets have significantly higher total cholesterol and LDL levels.3,4,5 The National Lipid Association’s review of evidence determined that LDL and total cholesterol responses vary in individuals following a low-carb diet, but that increasing LDL levels in particular were concerning enough to warrant lipid monitoring of patients on low-carb diets.6 Another meta-analysis evaluated the difference in estimated atherosclerotic cardiovascular disease (ASCVD) risk between low-carb and low-fat diets, finding those following a low-carb diet to have a lower estimated ASCVD risk but higher LDL levels.7
Weighing the benefits and harms. Since our patient’s dramatic weight loss and greatly increased exercise level would be expected to lower his LDL levels, the severe worsening of his LDL levels was likely related to his ketogenic diet and was a factor in the early onset of CAD. The benefits of low-carb diets for weight loss, contrasted with the consistent worsening of LDL levels, has prompted a debate about which parameters should be considered in estimating the long-term risk of these diets for patients. Diamond et al8 posit that these diets have beneficial effects on “the most reliable [cardiovascular disease] risk factors,” but long-term, patient-oriented outcome data are lacking, and these diets may not be appropriate for certain patients, as our case demonstrates.
A reasonable strategy for patients contemplating a low-carb diet specifically for weight loss would be to use such a diet for 3 to 6 months to achieve initial and rapid results, then continue with a heart-healthy diet and increased exercise levels to maintain weight loss and reduce long-term cardiovascular risk.
Our patient was started on a postoperative medication regimen of aspirin 81 mg/d, evolocumab 140 mg every 14 days, metoprolol tartrate 25 mg bid, and rosuvastatin 10 mg/d. A year later, he was able to resume a high level of physical activity (6-mile runs) without chest pain. His follow-up lipid panel showed a total cholesterol of 153 mg/dL; LDL, 53 mg/dL; HDL, 89 mg/dL; and triglycerides, 55 mg/dL. He had also switched to a regular diet and had been able to maintain his weight loss.
THE TAKEAWAY
Growing evidence suggests that low-carb diets may have a significant and detrimental effect on LDL levels. The long-term safety of these diets hasn’t been well studied, particularly regarding cardiovascular outcomes. At a minimum, patients who initiate low-carb diets should be counseled on general dietary recommendations regarding saturated fat and cholesterol intake, and they should have a follow-up lipid screening to evaluate for any significant worsening in total cholesterol and LDL levels.
CORRESPONDENCE
Samuel Dickmann, MD, 13611 NW 1st Lane, Suite 200, Newberry, FL 32669; [email protected]
1. Gorin A. What is the keto diet – and is it right for you? NBC News BETTER. February 22, 2018. Accessed February 3, 2023. www.nbcnews.com/better/health/what-keto-diet-it-right-you-ncna847256
2. Tinguely D, Gross J, Kosinski, C. Efficacy of ketogenic diets on type 2 diabetes: a systematic review. Current Diabetes Reports. 2021;21:32. doi: 10.1007/s11892-021-01399-z
3. Mansoor N, Vinknes KJ, Veierod MB, et al. Effects of low-carbohydrate diets v. low-fat diets on body weight and cardiovascular risk factors a meta-analysis of randomised controlled trials. Br J Nutr. 2016;115:466-479. doi: 10.1017/S0007114515004699
4. Bueno NB, de Melo ISV, de Oliveira SL, et al. Very-low-carbohydrate ketogenic diet v. low-fat diet for long-term weight loss: a meta-analysis of randomised controlled trials. Br J Nutr. 2013;110:1178-1187. doi: 10.1017/S0007114513000548
5. Chawla S, Tessarolo Silva F, Amaral Medeiros S, et al. The effect of low-fat and low-carbohydrate diets on weight loss and lipid levels: a systematic review and meta-analysis. Nutrients. 2020;12:3774. doi: 10.3390/nu12123774
6. Kirkpatrick CF, Bolick JP, Kris-Etherton PM, et al. Review of current evidence and clinical recommendations on the effects of low-carbohydrate and very-low-carbohydrate (including ketogenic) diets for the management of body weight and other cardiometabolic risk factors: a scientific statement from the National Lipid Association Nutrition and Lifestyle Task Force. J Clin Lipidol. 2019;13:689-711.e1. doi: 10.1016/j.jacl.2019.08.003
7. Sackner-Bernstein J, Kanter D, Kaul S. Dietary intervention for overweight and obese adults: comparison of low-carbohydrate and low-fat diets. a meta-analysis. PLoS One. 2015;10:e0139817. doi: 10.1371/journal.pone.0139817
8. Diamond DM, O’Neill BJ, Volek JS. Low carbohydrate diet: are concerns with saturated fat, lipids, and cardiovascular disease risk justified? Curr Opin Endocrinol Diabetes Obes. 2020;27:291-300. doi: 10.1097/MED.0000000000000568
1. Gorin A. What is the keto diet – and is it right for you? NBC News BETTER. February 22, 2018. Accessed February 3, 2023. www.nbcnews.com/better/health/what-keto-diet-it-right-you-ncna847256
2. Tinguely D, Gross J, Kosinski, C. Efficacy of ketogenic diets on type 2 diabetes: a systematic review. Current Diabetes Reports. 2021;21:32. doi: 10.1007/s11892-021-01399-z
3. Mansoor N, Vinknes KJ, Veierod MB, et al. Effects of low-carbohydrate diets v. low-fat diets on body weight and cardiovascular risk factors a meta-analysis of randomised controlled trials. Br J Nutr. 2016;115:466-479. doi: 10.1017/S0007114515004699
4. Bueno NB, de Melo ISV, de Oliveira SL, et al. Very-low-carbohydrate ketogenic diet v. low-fat diet for long-term weight loss: a meta-analysis of randomised controlled trials. Br J Nutr. 2013;110:1178-1187. doi: 10.1017/S0007114513000548
5. Chawla S, Tessarolo Silva F, Amaral Medeiros S, et al. The effect of low-fat and low-carbohydrate diets on weight loss and lipid levels: a systematic review and meta-analysis. Nutrients. 2020;12:3774. doi: 10.3390/nu12123774
6. Kirkpatrick CF, Bolick JP, Kris-Etherton PM, et al. Review of current evidence and clinical recommendations on the effects of low-carbohydrate and very-low-carbohydrate (including ketogenic) diets for the management of body weight and other cardiometabolic risk factors: a scientific statement from the National Lipid Association Nutrition and Lifestyle Task Force. J Clin Lipidol. 2019;13:689-711.e1. doi: 10.1016/j.jacl.2019.08.003
7. Sackner-Bernstein J, Kanter D, Kaul S. Dietary intervention for overweight and obese adults: comparison of low-carbohydrate and low-fat diets. a meta-analysis. PLoS One. 2015;10:e0139817. doi: 10.1371/journal.pone.0139817
8. Diamond DM, O’Neill BJ, Volek JS. Low carbohydrate diet: are concerns with saturated fat, lipids, and cardiovascular disease risk justified? Curr Opin Endocrinol Diabetes Obes. 2020;27:291-300. doi: 10.1097/MED.0000000000000568









