User login
GERD in the School-Age Child
General pediatricians can take care of a great number of children with reflux disease. I recommend a step-up approach employing lifestyle modifications and/or medication prior to specialist referral in most cases. When symptoms become more troublesome or there is no response to therapeutic interventions, consultation with a pediatric gastroenterologist may be appropriate.
Begin with a thorough patient history, which is instrumental to distinguishing gastroesophageal reflux disease (GERD) from other conditions. Family medical and medication history also are important because of compelling evidence demonstrating a family link with GERD.
Advise school-age children with GERD to eat smaller meals throughout the day and not to eat too close to bedtime. Tomato-containing products, caffeine-containing products, citrus, and—believe it or not—chocolate are commonly implicated as evoking or exacerbating symptoms of GERD. Foods with high-fat content also are associated with the disorder, as they delay the ability of the stomach to empty quickly, thus potentially worsening GERD.
Sleep disturbances may be the sole symptom for a lot of older children with reflux. Microburps or microaspirations that occur when children are supine at night wake some; they do not wake others, so keep in mind that some children might be unaware of their GERD. A good question to ask is how many pillows they sleep on at night; some children already self-manage their symptoms by elevating their upper torso at night without realizing why.
Early morning nausea also can occur after a night of continuous reflux. Therefore, the presentation of a child who says he or she routinely does not want to eat in the morning, particularly if he or she complains of nausea, raises clinical suspicion for GERD. Also, some children can report regurgitating and re-swallowing all day as they sit in class.
In addition to lifestyle changes, a trial of acid-suppressing medication, such as an H2 blocker or a proton pump inhibitor, can be tried. Limit initial treatment to 6-8 weeks for most children. If a child reports respiratory symptoms associated with GERD, consider a longer course of acid suppression therapy. It is important to discuss the specific GERD-related symptoms you expect the medication to resolve prior to initiation of therapy.
A referral to a pediatric gastroenterologist is warranted after lifestyle modifications and pharmacotherapy fail, or if symptoms return after therapy is discontinued. Sometimes patients do not improve with these interventions or they get better but you cannot get patients off the medication without symptoms returning. Also, other warning signs or symptoms such as anemia or occult blood in the stool or vomit require a referral.
Frequently, children, particularly those of school age, with GERD complain of a stomachache. However, GERD is more of a burning pain versus a cramping pain. Pain that is associated with GERD or due to another “organic” cause tends to be pain that localizes away from the belly button and is more epigastric, versus periumbilical pain, which tends to be more functional. In addition, abdominal pain that awakens children at night tends to be more organic in nature. Some children with GERD are misdiagnosed and actually have a functional GI disorder or vice versa. Definitions of pediatric functional GI disorders can aid in the differential diagnosis; these are outlined in Rome III criteria (www.romecriteria.org
There is no diagnostic test that is 100% accurate for the diagnosis of GERD. Thus, it is important to avoid too much testing or inappropriate treatment. For example, pediatricians tend to do an upper gastrointestinal series using barium and x-ray fluoroscopy, which is not good for ruling GERD in or out, but can be beneficial in identifying upper GI anatomic abnormalities. Nuclear scintigraphy can be employed to assess gastric emptying and aspiration of reflux contents.
Pediatricians can order a pH probe to ascertain the degree of acid exposure to the esophagus, although some centers require a GI consultation first. Endoscopic studies require a referral to a specialist. Specialists also may perform a newer modality called multichannel intraluminal impedance, which, when combined with the pH probe, can measure both acid reflux and nonacid or weakly acid reflux.
In a survey of 6,000 American Academy of Pediatrics members, 82% of the 1,245 responding pediatricians and pediatric specialists said they treat GERD based on clinical suspicion (J. Pediatr. Gastroenterol. Nutr. 2007;45:56-64). Such empiric therapy is still appropriate in the pediatric patient. However, there is a need for future research on the optimal therapy type, dose, and duration in these patients with clinically suspected GERD.
To promote a more standardized approach to pediatric GERD, I participated on an international committee that released an evidence-based set of definitions for reflux and GERD in the pediatric population (Am. J. Gastroenterol. 2009;104:1278-95). Additional guidance on GERD is available from the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (www.naspghan.orgwww.cdhnf.org
General pediatricians can take care of a great number of children with reflux disease. I recommend a step-up approach employing lifestyle modifications and/or medication prior to specialist referral in most cases. When symptoms become more troublesome or there is no response to therapeutic interventions, consultation with a pediatric gastroenterologist may be appropriate.
Begin with a thorough patient history, which is instrumental to distinguishing gastroesophageal reflux disease (GERD) from other conditions. Family medical and medication history also are important because of compelling evidence demonstrating a family link with GERD.
Advise school-age children with GERD to eat smaller meals throughout the day and not to eat too close to bedtime. Tomato-containing products, caffeine-containing products, citrus, and—believe it or not—chocolate are commonly implicated as evoking or exacerbating symptoms of GERD. Foods with high-fat content also are associated with the disorder, as they delay the ability of the stomach to empty quickly, thus potentially worsening GERD.
Sleep disturbances may be the sole symptom for a lot of older children with reflux. Microburps or microaspirations that occur when children are supine at night wake some; they do not wake others, so keep in mind that some children might be unaware of their GERD. A good question to ask is how many pillows they sleep on at night; some children already self-manage their symptoms by elevating their upper torso at night without realizing why.
Early morning nausea also can occur after a night of continuous reflux. Therefore, the presentation of a child who says he or she routinely does not want to eat in the morning, particularly if he or she complains of nausea, raises clinical suspicion for GERD. Also, some children can report regurgitating and re-swallowing all day as they sit in class.
In addition to lifestyle changes, a trial of acid-suppressing medication, such as an H2 blocker or a proton pump inhibitor, can be tried. Limit initial treatment to 6-8 weeks for most children. If a child reports respiratory symptoms associated with GERD, consider a longer course of acid suppression therapy. It is important to discuss the specific GERD-related symptoms you expect the medication to resolve prior to initiation of therapy.
A referral to a pediatric gastroenterologist is warranted after lifestyle modifications and pharmacotherapy fail, or if symptoms return after therapy is discontinued. Sometimes patients do not improve with these interventions or they get better but you cannot get patients off the medication without symptoms returning. Also, other warning signs or symptoms such as anemia or occult blood in the stool or vomit require a referral.
Frequently, children, particularly those of school age, with GERD complain of a stomachache. However, GERD is more of a burning pain versus a cramping pain. Pain that is associated with GERD or due to another “organic” cause tends to be pain that localizes away from the belly button and is more epigastric, versus periumbilical pain, which tends to be more functional. In addition, abdominal pain that awakens children at night tends to be more organic in nature. Some children with GERD are misdiagnosed and actually have a functional GI disorder or vice versa. Definitions of pediatric functional GI disorders can aid in the differential diagnosis; these are outlined in Rome III criteria (www.romecriteria.org
There is no diagnostic test that is 100% accurate for the diagnosis of GERD. Thus, it is important to avoid too much testing or inappropriate treatment. For example, pediatricians tend to do an upper gastrointestinal series using barium and x-ray fluoroscopy, which is not good for ruling GERD in or out, but can be beneficial in identifying upper GI anatomic abnormalities. Nuclear scintigraphy can be employed to assess gastric emptying and aspiration of reflux contents.
Pediatricians can order a pH probe to ascertain the degree of acid exposure to the esophagus, although some centers require a GI consultation first. Endoscopic studies require a referral to a specialist. Specialists also may perform a newer modality called multichannel intraluminal impedance, which, when combined with the pH probe, can measure both acid reflux and nonacid or weakly acid reflux.
In a survey of 6,000 American Academy of Pediatrics members, 82% of the 1,245 responding pediatricians and pediatric specialists said they treat GERD based on clinical suspicion (J. Pediatr. Gastroenterol. Nutr. 2007;45:56-64). Such empiric therapy is still appropriate in the pediatric patient. However, there is a need for future research on the optimal therapy type, dose, and duration in these patients with clinically suspected GERD.
To promote a more standardized approach to pediatric GERD, I participated on an international committee that released an evidence-based set of definitions for reflux and GERD in the pediatric population (Am. J. Gastroenterol. 2009;104:1278-95). Additional guidance on GERD is available from the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (www.naspghan.orgwww.cdhnf.org
General pediatricians can take care of a great number of children with reflux disease. I recommend a step-up approach employing lifestyle modifications and/or medication prior to specialist referral in most cases. When symptoms become more troublesome or there is no response to therapeutic interventions, consultation with a pediatric gastroenterologist may be appropriate.
Begin with a thorough patient history, which is instrumental to distinguishing gastroesophageal reflux disease (GERD) from other conditions. Family medical and medication history also are important because of compelling evidence demonstrating a family link with GERD.
Advise school-age children with GERD to eat smaller meals throughout the day and not to eat too close to bedtime. Tomato-containing products, caffeine-containing products, citrus, and—believe it or not—chocolate are commonly implicated as evoking or exacerbating symptoms of GERD. Foods with high-fat content also are associated with the disorder, as they delay the ability of the stomach to empty quickly, thus potentially worsening GERD.
Sleep disturbances may be the sole symptom for a lot of older children with reflux. Microburps or microaspirations that occur when children are supine at night wake some; they do not wake others, so keep in mind that some children might be unaware of their GERD. A good question to ask is how many pillows they sleep on at night; some children already self-manage their symptoms by elevating their upper torso at night without realizing why.
Early morning nausea also can occur after a night of continuous reflux. Therefore, the presentation of a child who says he or she routinely does not want to eat in the morning, particularly if he or she complains of nausea, raises clinical suspicion for GERD. Also, some children can report regurgitating and re-swallowing all day as they sit in class.
In addition to lifestyle changes, a trial of acid-suppressing medication, such as an H2 blocker or a proton pump inhibitor, can be tried. Limit initial treatment to 6-8 weeks for most children. If a child reports respiratory symptoms associated with GERD, consider a longer course of acid suppression therapy. It is important to discuss the specific GERD-related symptoms you expect the medication to resolve prior to initiation of therapy.
A referral to a pediatric gastroenterologist is warranted after lifestyle modifications and pharmacotherapy fail, or if symptoms return after therapy is discontinued. Sometimes patients do not improve with these interventions or they get better but you cannot get patients off the medication without symptoms returning. Also, other warning signs or symptoms such as anemia or occult blood in the stool or vomit require a referral.
Frequently, children, particularly those of school age, with GERD complain of a stomachache. However, GERD is more of a burning pain versus a cramping pain. Pain that is associated with GERD or due to another “organic” cause tends to be pain that localizes away from the belly button and is more epigastric, versus periumbilical pain, which tends to be more functional. In addition, abdominal pain that awakens children at night tends to be more organic in nature. Some children with GERD are misdiagnosed and actually have a functional GI disorder or vice versa. Definitions of pediatric functional GI disorders can aid in the differential diagnosis; these are outlined in Rome III criteria (www.romecriteria.org
There is no diagnostic test that is 100% accurate for the diagnosis of GERD. Thus, it is important to avoid too much testing or inappropriate treatment. For example, pediatricians tend to do an upper gastrointestinal series using barium and x-ray fluoroscopy, which is not good for ruling GERD in or out, but can be beneficial in identifying upper GI anatomic abnormalities. Nuclear scintigraphy can be employed to assess gastric emptying and aspiration of reflux contents.
Pediatricians can order a pH probe to ascertain the degree of acid exposure to the esophagus, although some centers require a GI consultation first. Endoscopic studies require a referral to a specialist. Specialists also may perform a newer modality called multichannel intraluminal impedance, which, when combined with the pH probe, can measure both acid reflux and nonacid or weakly acid reflux.
In a survey of 6,000 American Academy of Pediatrics members, 82% of the 1,245 responding pediatricians and pediatric specialists said they treat GERD based on clinical suspicion (J. Pediatr. Gastroenterol. Nutr. 2007;45:56-64). Such empiric therapy is still appropriate in the pediatric patient. However, there is a need for future research on the optimal therapy type, dose, and duration in these patients with clinically suspected GERD.
To promote a more standardized approach to pediatric GERD, I participated on an international committee that released an evidence-based set of definitions for reflux and GERD in the pediatric population (Am. J. Gastroenterol. 2009;104:1278-95). Additional guidance on GERD is available from the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (www.naspghan.orgwww.cdhnf.org
HM's Watershed Moment
John Nelson, MD, FACP, FHM, hasn't taken a medical test in more than 20 years. So when news began to spread last week that the American Board of Internal Medicine (ABIM) soon will be offering a Recognition of Focused Practice (RFP) in Hospital Medicine certification, he started to get a little nervous.
"I will lose sleep the week before I take this test," says Dr. Nelson, co-founder and past president of SHM, and a principal in the practice management firm Nelson Flores Hospital Medicine Consultants. "This exam will help identify those who see this as a career. … Boy, there is nothing like a test to demonstrate professional centeredness."
The exam, likely to be available in the fall of 2010, will identify physicians who have "maintained their internal medicine certification focused in hospital medicine," according to the ABIM Web site.
"For those individuals [whose certificate] will be expiring in 2010 or 2011, this is a viable pathway for re-certification," says Eric Holmbloe, MD, senior vice president and chief medical officer at ABIM. "Interested diplomats should be able to begin the application process in early 2010. We are feverishly working to complete the test and build the technology infrastructure. We should have more information available in about six weeks."
HM pioneers like Dr. Nelson consider the RFP designation a validation of decades-long efforts to carve a niche in medicine. The test will symbolize dedication to the specialty and provide HM physicians with professional self-regulation.
Scott Flanders, MD, FHM, president of SHM, terms the announcement a "watershed moment" for the field.
"I think this is a major, major moment for HM," says Dr. Flanders, who practices at the University of Michigan Medical Center in Ann Arbor. "We've been looking at this for a long time. This validates the field, and the belief that HM is a positive [for the field of medicine]."
Dr. Nelson couldn't agree more. "This test is the first way hospitalists will be able to show their competence," he says. "I think it's a great opportunity. This will help people take our field more seriously."
John Nelson, MD, FACP, FHM, hasn't taken a medical test in more than 20 years. So when news began to spread last week that the American Board of Internal Medicine (ABIM) soon will be offering a Recognition of Focused Practice (RFP) in Hospital Medicine certification, he started to get a little nervous.
"I will lose sleep the week before I take this test," says Dr. Nelson, co-founder and past president of SHM, and a principal in the practice management firm Nelson Flores Hospital Medicine Consultants. "This exam will help identify those who see this as a career. … Boy, there is nothing like a test to demonstrate professional centeredness."
The exam, likely to be available in the fall of 2010, will identify physicians who have "maintained their internal medicine certification focused in hospital medicine," according to the ABIM Web site.
"For those individuals [whose certificate] will be expiring in 2010 or 2011, this is a viable pathway for re-certification," says Eric Holmbloe, MD, senior vice president and chief medical officer at ABIM. "Interested diplomats should be able to begin the application process in early 2010. We are feverishly working to complete the test and build the technology infrastructure. We should have more information available in about six weeks."
HM pioneers like Dr. Nelson consider the RFP designation a validation of decades-long efforts to carve a niche in medicine. The test will symbolize dedication to the specialty and provide HM physicians with professional self-regulation.
Scott Flanders, MD, FHM, president of SHM, terms the announcement a "watershed moment" for the field.
"I think this is a major, major moment for HM," says Dr. Flanders, who practices at the University of Michigan Medical Center in Ann Arbor. "We've been looking at this for a long time. This validates the field, and the belief that HM is a positive [for the field of medicine]."
Dr. Nelson couldn't agree more. "This test is the first way hospitalists will be able to show their competence," he says. "I think it's a great opportunity. This will help people take our field more seriously."
John Nelson, MD, FACP, FHM, hasn't taken a medical test in more than 20 years. So when news began to spread last week that the American Board of Internal Medicine (ABIM) soon will be offering a Recognition of Focused Practice (RFP) in Hospital Medicine certification, he started to get a little nervous.
"I will lose sleep the week before I take this test," says Dr. Nelson, co-founder and past president of SHM, and a principal in the practice management firm Nelson Flores Hospital Medicine Consultants. "This exam will help identify those who see this as a career. … Boy, there is nothing like a test to demonstrate professional centeredness."
The exam, likely to be available in the fall of 2010, will identify physicians who have "maintained their internal medicine certification focused in hospital medicine," according to the ABIM Web site.
"For those individuals [whose certificate] will be expiring in 2010 or 2011, this is a viable pathway for re-certification," says Eric Holmbloe, MD, senior vice president and chief medical officer at ABIM. "Interested diplomats should be able to begin the application process in early 2010. We are feverishly working to complete the test and build the technology infrastructure. We should have more information available in about six weeks."
HM pioneers like Dr. Nelson consider the RFP designation a validation of decades-long efforts to carve a niche in medicine. The test will symbolize dedication to the specialty and provide HM physicians with professional self-regulation.
Scott Flanders, MD, FHM, president of SHM, terms the announcement a "watershed moment" for the field.
"I think this is a major, major moment for HM," says Dr. Flanders, who practices at the University of Michigan Medical Center in Ann Arbor. "We've been looking at this for a long time. This validates the field, and the belief that HM is a positive [for the field of medicine]."
Dr. Nelson couldn't agree more. "This test is the first way hospitalists will be able to show their competence," he says. "I think it's a great opportunity. This will help people take our field more seriously."
Social Distortion?
A presentation at last week's 13th annual Management of the Hospitalized Patient conference in San Francisco described various ways that hospitals, hospitalists, and HM groups can incorporate new social media into their practice routines.
Hospitalist Russell Cucina, MD, MS, associate medical director of information technology at the University of California at San Francisco, says some physicians mistakenly disclose unprofessional content through social networks. He points to a recent article in the Journal of the American Medical Association (2009;302(12):1309-1315), which shows some physicians inadvertently violate Health Insurance Portability and Accountability Act privacy rules by accepting e-mails from patients that contain protected personal health information.
But in many cases, hospitals and physicians use blogs, Twitter, Facebook, LinkedIn, and other networking sites to exchange information with colleagues, promote their practice in their communities, or recruit new physicians. Such organizations as the Mayo Clinic and SHM use Facebook to reach targeted audiences, while the Centers for Disease Control and Prevention (CDC) uses Twitter to quickly disseminate influenza updates. Dr. Cucina says he knows of 167 U.S. hospitals using the much-hyped Twitter, but he could not find an HM group that uses the quick-hit network. He also reports that Ozmosis and Sermo, networking sites reserved for physicians, have yet to catch on in a big way.
Christine Roed, MD, a hospitalist at El Camino Hospital in Mountain View, Calif., says she sees great potential for communicating within her small medical group and for tapping into public health information. "I also feel it might be quite overwhelming. I think we have to look quite carefully at which information sources are reliable and, in turn, advise the public," Dr. Roed says. "I think a lot of physicians don't really have time to sit down and figure out what they're going to do with these things."
A presentation at last week's 13th annual Management of the Hospitalized Patient conference in San Francisco described various ways that hospitals, hospitalists, and HM groups can incorporate new social media into their practice routines.
Hospitalist Russell Cucina, MD, MS, associate medical director of information technology at the University of California at San Francisco, says some physicians mistakenly disclose unprofessional content through social networks. He points to a recent article in the Journal of the American Medical Association (2009;302(12):1309-1315), which shows some physicians inadvertently violate Health Insurance Portability and Accountability Act privacy rules by accepting e-mails from patients that contain protected personal health information.
But in many cases, hospitals and physicians use blogs, Twitter, Facebook, LinkedIn, and other networking sites to exchange information with colleagues, promote their practice in their communities, or recruit new physicians. Such organizations as the Mayo Clinic and SHM use Facebook to reach targeted audiences, while the Centers for Disease Control and Prevention (CDC) uses Twitter to quickly disseminate influenza updates. Dr. Cucina says he knows of 167 U.S. hospitals using the much-hyped Twitter, but he could not find an HM group that uses the quick-hit network. He also reports that Ozmosis and Sermo, networking sites reserved for physicians, have yet to catch on in a big way.
Christine Roed, MD, a hospitalist at El Camino Hospital in Mountain View, Calif., says she sees great potential for communicating within her small medical group and for tapping into public health information. "I also feel it might be quite overwhelming. I think we have to look quite carefully at which information sources are reliable and, in turn, advise the public," Dr. Roed says. "I think a lot of physicians don't really have time to sit down and figure out what they're going to do with these things."
A presentation at last week's 13th annual Management of the Hospitalized Patient conference in San Francisco described various ways that hospitals, hospitalists, and HM groups can incorporate new social media into their practice routines.
Hospitalist Russell Cucina, MD, MS, associate medical director of information technology at the University of California at San Francisco, says some physicians mistakenly disclose unprofessional content through social networks. He points to a recent article in the Journal of the American Medical Association (2009;302(12):1309-1315), which shows some physicians inadvertently violate Health Insurance Portability and Accountability Act privacy rules by accepting e-mails from patients that contain protected personal health information.
But in many cases, hospitals and physicians use blogs, Twitter, Facebook, LinkedIn, and other networking sites to exchange information with colleagues, promote their practice in their communities, or recruit new physicians. Such organizations as the Mayo Clinic and SHM use Facebook to reach targeted audiences, while the Centers for Disease Control and Prevention (CDC) uses Twitter to quickly disseminate influenza updates. Dr. Cucina says he knows of 167 U.S. hospitals using the much-hyped Twitter, but he could not find an HM group that uses the quick-hit network. He also reports that Ozmosis and Sermo, networking sites reserved for physicians, have yet to catch on in a big way.
Christine Roed, MD, a hospitalist at El Camino Hospital in Mountain View, Calif., says she sees great potential for communicating within her small medical group and for tapping into public health information. "I also feel it might be quite overwhelming. I think we have to look quite carefully at which information sources are reliable and, in turn, advise the public," Dr. Roed says. "I think a lot of physicians don't really have time to sit down and figure out what they're going to do with these things."
Baucus Plan Lends Clarity to Healthcare Debate
Last week’s release of the “chairman’s mark” of the America’s Healthy Future Act from Senate Finance Committee Chairman Max Baucus (D-Mont.) opened the latest chapter in the debate over healthcare reform. Beyond the hot-button issues, several Medicare-related proposals could directly impact hospitalists. Here’s a look at four of them, with observations from Eric Siegal, MD, FHM, chair of SHM’s Public Policy Committee.
Addition of a hospital value-based purchasing (VBP) program to Medicare beginning in 2012. The program would tie incentive payments to performance on quality measures related to such conditions as heart failure, pneumonia, surgical care, and patient perceptions of care. So far, the program’s rough outlines have been well received. “We fundamentally support hospital value-based purchasing,” Dr. Siegal says. “We think it’s a necessary step in the evolution to higher-value health care in general.”
Expansion of the Physician’s Quality Reporting Initiative, with a 1% payment penalty by 2012 for nonparticipants. The bill also would direct the Centers for Medicare and Medicaid Services (CMS) to improve the appeals process and feedback mechanism. Although the Baucus plan’s “mark” doesn’t discuss transitioning to pay-for-performance, Dr. Siegal says the shift likely is inevitable. In the meantime, pay-for-reporting can encourage better outcomes through a public reporting mechanism and “grease the skids” for a pay-for-performance initiative.
Creation of a CMS Payment Innovation Center “authorized to test, evaluate, and expand different payment structures and methodologies,” with a goal of improving quality and reducing Medicare costs. Dr. Siegal says the proposal is consistent with SHM’s aims. “We have for a long time advocated for a robust capability to test new payment models and to figure out what works better than what we have right now,” he says.
Establishment of a three-year Medicare pilot called the Community Care Transitions Program. The program would spend $500 million over 10 years on efforts to reduce preventable rehospitalizations. SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions) likely would qualify. “We’re very positive about that,” Dr. Siegal says. “I think there is a huge amount of scrutiny now on avoidable rehospitalizations. We think BOOST is a step in the right direction, and we’d love to see greater funding to roll this out on a much larger basis.”
For more information on the current healthcare reform debate, visit SHM’s advocacy portal.
Last week’s release of the “chairman’s mark” of the America’s Healthy Future Act from Senate Finance Committee Chairman Max Baucus (D-Mont.) opened the latest chapter in the debate over healthcare reform. Beyond the hot-button issues, several Medicare-related proposals could directly impact hospitalists. Here’s a look at four of them, with observations from Eric Siegal, MD, FHM, chair of SHM’s Public Policy Committee.
Addition of a hospital value-based purchasing (VBP) program to Medicare beginning in 2012. The program would tie incentive payments to performance on quality measures related to such conditions as heart failure, pneumonia, surgical care, and patient perceptions of care. So far, the program’s rough outlines have been well received. “We fundamentally support hospital value-based purchasing,” Dr. Siegal says. “We think it’s a necessary step in the evolution to higher-value health care in general.”
Expansion of the Physician’s Quality Reporting Initiative, with a 1% payment penalty by 2012 for nonparticipants. The bill also would direct the Centers for Medicare and Medicaid Services (CMS) to improve the appeals process and feedback mechanism. Although the Baucus plan’s “mark” doesn’t discuss transitioning to pay-for-performance, Dr. Siegal says the shift likely is inevitable. In the meantime, pay-for-reporting can encourage better outcomes through a public reporting mechanism and “grease the skids” for a pay-for-performance initiative.
Creation of a CMS Payment Innovation Center “authorized to test, evaluate, and expand different payment structures and methodologies,” with a goal of improving quality and reducing Medicare costs. Dr. Siegal says the proposal is consistent with SHM’s aims. “We have for a long time advocated for a robust capability to test new payment models and to figure out what works better than what we have right now,” he says.
Establishment of a three-year Medicare pilot called the Community Care Transitions Program. The program would spend $500 million over 10 years on efforts to reduce preventable rehospitalizations. SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions) likely would qualify. “We’re very positive about that,” Dr. Siegal says. “I think there is a huge amount of scrutiny now on avoidable rehospitalizations. We think BOOST is a step in the right direction, and we’d love to see greater funding to roll this out on a much larger basis.”
For more information on the current healthcare reform debate, visit SHM’s advocacy portal.
Last week’s release of the “chairman’s mark” of the America’s Healthy Future Act from Senate Finance Committee Chairman Max Baucus (D-Mont.) opened the latest chapter in the debate over healthcare reform. Beyond the hot-button issues, several Medicare-related proposals could directly impact hospitalists. Here’s a look at four of them, with observations from Eric Siegal, MD, FHM, chair of SHM’s Public Policy Committee.
Addition of a hospital value-based purchasing (VBP) program to Medicare beginning in 2012. The program would tie incentive payments to performance on quality measures related to such conditions as heart failure, pneumonia, surgical care, and patient perceptions of care. So far, the program’s rough outlines have been well received. “We fundamentally support hospital value-based purchasing,” Dr. Siegal says. “We think it’s a necessary step in the evolution to higher-value health care in general.”
Expansion of the Physician’s Quality Reporting Initiative, with a 1% payment penalty by 2012 for nonparticipants. The bill also would direct the Centers for Medicare and Medicaid Services (CMS) to improve the appeals process and feedback mechanism. Although the Baucus plan’s “mark” doesn’t discuss transitioning to pay-for-performance, Dr. Siegal says the shift likely is inevitable. In the meantime, pay-for-reporting can encourage better outcomes through a public reporting mechanism and “grease the skids” for a pay-for-performance initiative.
Creation of a CMS Payment Innovation Center “authorized to test, evaluate, and expand different payment structures and methodologies,” with a goal of improving quality and reducing Medicare costs. Dr. Siegal says the proposal is consistent with SHM’s aims. “We have for a long time advocated for a robust capability to test new payment models and to figure out what works better than what we have right now,” he says.
Establishment of a three-year Medicare pilot called the Community Care Transitions Program. The program would spend $500 million over 10 years on efforts to reduce preventable rehospitalizations. SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions) likely would qualify. “We’re very positive about that,” Dr. Siegal says. “I think there is a huge amount of scrutiny now on avoidable rehospitalizations. We think BOOST is a step in the right direction, and we’d love to see greater funding to roll this out on a much larger basis.”
For more information on the current healthcare reform debate, visit SHM’s advocacy portal.
1,200 Satisfied Customers and Counting
Another SHM Leadership Academy just ended, with introductory and advanced courses presented at the Fontainebleau resort, complete with the backdrop of Miami Beach. These four-day courses are aimed at hospitalist leaders, and have trained more than 1,200 participants to date. The faculty includes nationally recognized experts in their respective fields, as well as experienced HM leaders.
Level I courses are designed to help new leaders in HM, and focus on communication skills, hospital business drivers, leadership, strategic planning, and conflict resolution. Harjit Bhogal, MD, a hospitalist at Johns Hopkins University School of Medicine in Baltimore, found the Level I course addressed many of the roles she has as a new hospitalist. “The session on strategic planning was interactive and extremely informative,” Dr. Bhogal says. She also says the academy is an ideal place for networking, as attendees have access to more than 100 practicing hospitalist leaders with whom to connect.
Level II takes concepts introduced in Level I and refines them. Communication and negotiation, “meta-leadership,” financial storytelling, and a leadership roundtable help more advanced leaders tackle more complex issues. The session on meta-leadership was “terrific,” according to hospitalist Darlene Tad-y, MD, of Johns Hopkins. “One of the best days I have spent as an adult learner,” she says. “Lenny [Marcus] was absolutely amazing; his walk-in-the-woods approach was a terrific method to discuss leadership.”
Many see hospitalists as the future leaders of the hospital and throughout healthcare. “In addition to helping train leaders for hospital medicine, we believe that SHM has the obligation to train hospitalists to be the next hospital CMOs and CEOs,” says Larry Wellikson, MD, FHM, CEO of SHM.
Apparently, 1,200 academy graduates agree with him.
Another SHM Leadership Academy just ended, with introductory and advanced courses presented at the Fontainebleau resort, complete with the backdrop of Miami Beach. These four-day courses are aimed at hospitalist leaders, and have trained more than 1,200 participants to date. The faculty includes nationally recognized experts in their respective fields, as well as experienced HM leaders.
Level I courses are designed to help new leaders in HM, and focus on communication skills, hospital business drivers, leadership, strategic planning, and conflict resolution. Harjit Bhogal, MD, a hospitalist at Johns Hopkins University School of Medicine in Baltimore, found the Level I course addressed many of the roles she has as a new hospitalist. “The session on strategic planning was interactive and extremely informative,” Dr. Bhogal says. She also says the academy is an ideal place for networking, as attendees have access to more than 100 practicing hospitalist leaders with whom to connect.
Level II takes concepts introduced in Level I and refines them. Communication and negotiation, “meta-leadership,” financial storytelling, and a leadership roundtable help more advanced leaders tackle more complex issues. The session on meta-leadership was “terrific,” according to hospitalist Darlene Tad-y, MD, of Johns Hopkins. “One of the best days I have spent as an adult learner,” she says. “Lenny [Marcus] was absolutely amazing; his walk-in-the-woods approach was a terrific method to discuss leadership.”
Many see hospitalists as the future leaders of the hospital and throughout healthcare. “In addition to helping train leaders for hospital medicine, we believe that SHM has the obligation to train hospitalists to be the next hospital CMOs and CEOs,” says Larry Wellikson, MD, FHM, CEO of SHM.
Apparently, 1,200 academy graduates agree with him.
Another SHM Leadership Academy just ended, with introductory and advanced courses presented at the Fontainebleau resort, complete with the backdrop of Miami Beach. These four-day courses are aimed at hospitalist leaders, and have trained more than 1,200 participants to date. The faculty includes nationally recognized experts in their respective fields, as well as experienced HM leaders.
Level I courses are designed to help new leaders in HM, and focus on communication skills, hospital business drivers, leadership, strategic planning, and conflict resolution. Harjit Bhogal, MD, a hospitalist at Johns Hopkins University School of Medicine in Baltimore, found the Level I course addressed many of the roles she has as a new hospitalist. “The session on strategic planning was interactive and extremely informative,” Dr. Bhogal says. She also says the academy is an ideal place for networking, as attendees have access to more than 100 practicing hospitalist leaders with whom to connect.
Level II takes concepts introduced in Level I and refines them. Communication and negotiation, “meta-leadership,” financial storytelling, and a leadership roundtable help more advanced leaders tackle more complex issues. The session on meta-leadership was “terrific,” according to hospitalist Darlene Tad-y, MD, of Johns Hopkins. “One of the best days I have spent as an adult learner,” she says. “Lenny [Marcus] was absolutely amazing; his walk-in-the-woods approach was a terrific method to discuss leadership.”
Many see hospitalists as the future leaders of the hospital and throughout healthcare. “In addition to helping train leaders for hospital medicine, we believe that SHM has the obligation to train hospitalists to be the next hospital CMOs and CEOs,” says Larry Wellikson, MD, FHM, CEO of SHM.
Apparently, 1,200 academy graduates agree with him.
Sleep Disruptions and Sedative Use
Adequate sleep is important for health, yet the hospital environment commonly disrupts sleep.13 Sleep improves after several days in the hospital.3, 4 Sleep deprivation increases cortisol levels5 and sleep loss of greater than 4 hours may be hyperalgesic.6 Even a few days' suppression of slow‐wave sleep worsens glucose tolerance.7 Sleep disruption may cause irritability and aggressiveness,8 impaired memory consolidation, and delirium.2
Noise may disrupt sleep. The World Health Organization recommends a maximum of 30 to 40 dBA in patients' rooms at night.9, 10 Normal conversation occurs at 60 dBA. Medical equipment alarms are about 80 dBA.
Sedative use is common in the hospital.3 Sedatives typically shorten sleep latency and suppress rapid eye movement (REM) sleep. However, some sedatives cause delirium, falls, amnesia, and confusion, particularly in the elderly.1113
Most research on sleep in hospitalized patients has been done in the critical care setting, often in sedated ventilated patients, where sleep disruption is well‐described.1416 Only a few small studies have assessed the sleep of hospitalized patients outside critical care.17, 18
A single blinded interventional trial assessed sedative use, but was a nonrandomized study.19, 20 As‐needed sedative use was measured among hospitalized elderly patients as a secondary endpoint. The intervention, known as the Hospital Elder Life Program (HELP), included a protocol with noise reduction, massage, music, and warm drinks, as well as rescheduling of medications and procedures; it resulted in a 24% reduction in as‐needed sedative use. Another trial decreased noise and reduced overnight X‐rays on a surgical unit, then measured staff and patient attitudes.21 Two interventional studies in nursing homes reduced noise and light, and/or increased daytime activity and found no effect on most objective measures of sleep.22, 23 One descriptive study found most sleep disturbances in medical‐surgical patients came from noise and sleeping in an unfamiliar bed.4
We hypothesized that an intervention designed to improve patient sleep through changes in staff behavior would decrease sedative use among unselected patients in a medical‐surgical unit. We measured sedative use as our primary endpoint as a marker for effective sleep, and because decreased sedative use is desirable. We also hypothesized that the intervention would lead to improved sleep experiences, as measured by a questionnaire and Verran Snyder‐Halpern (VSH) sleep scores as secondary endpoints.24
Materials And Methods
Study Design
This was a pre‐post study assessing the effect of the intervention on as‐needed sedative use, questionnaire responses, and sleep quality. It was an intention‐to‐treat analysis, and was blinded in terms of measurement of sedative use. The Institutional Review Board of Cambridge Health Alliance approved the study.
Setting and Patients
The site was the only medical‐surgical unit of Somerville Hospital, a small urban community teaching hospital that is part of Cambridge Health Alliance. The hospital unit was chosen for its architectural characteristics, and is organized spatially as 3 U‐shaped pods surrounding nursing workstations. Hence, patient rooms were nearly equidistant from the nurses' stations, unlike a hallway design where distant rooms are quieter. Six rooms were private; 11 were semiprivate. Most of the unit's 28 beds are used for medical patients covered by the hospitalist service. Residents see a minority of patients. A hospitalist is available around the clock. Few agency nurses are used.
Preintervention patients were recruited between April and August 2007. The intervention was planned and implemented from September 2007 to January 2008. Intervention patients were recruited between February and June 2008. The most common principle diagnoses on the unit were chest pain (11%), pneumonia (8%), congestive heart failure (CHF) (5.1%), and chronic obstructive pulmonary disease (COPD) flare (3%). Exclusion criteria ensured that no patient was ill enough to require intensive care unit (ICU)‐level care or was actively dying. All consecutive hospitalized patients on the unit on Tuesdays through Fridays were potentially eligible and invited to participate unless they met exclusion criteria. The limited days of the week ensured that technical support would be available during the intervention phase.
Exclusion criteria were: known sleep disorders; language other than English, Spanish, Portuguese, or Haitian Creole; surgery the prior day; arrival on the floor after 10 PM the prior evening; residence on the unit for more than 4 days; alcohol or drug withdrawal; end‐of‐life morphine drip; significant hearing loss; and blindness.
Study Protocol
A single investigator surveyed patients in the morning about the prior night's sleep experience. The surveys consisted of the VSH sleep scale, as well as an 8‐item questionnaire developed from informal pilot interviews with about 18 patients conducted by 1 of the investigators (M.B.) (Supporting Information Figure 1). The VSH scale is a visual analog scale using a 100‐cm line,24 which we modified with a 100‐mm line to make it easier to collect data. The questionnaire and VSH scores of patients with cognitive impairment were not included in the final analysis. Cognitive impairment was determined by diagnoses present in chart review. Surveys and consent forms were available in 4 languages and trained interpreters were used as needed. Nurses, providers, and patients were blinded to the measurement of as‐needed sedative use, and staff were unaware of which patients were study subjects.
Measurements
Nighttime administration of any medication ordered prn sleep or insomnia was measured using the pharmacy dispensing equipment (Pyxis; Cardinal Health, Dublin, OH), then verified by reviewing the patients' medication administration records. VSH sleep scores were created by measuring the distance in millimeters from the lower end of the scale (0) to the location marked.
We also tracked adherence to some aspects of the intervention. The questionnaire recorded door closing. Chart audits measured the numbers of different prescribers, and the frequency of medication orders using flexible timing.
Data Analysis
Medication use was analyzed as any as‐needed sedative use vs. none. The proportions of patients who used sedatives preintervention and postintervention were compared using a 2‐sample Z statistic, as were survey items. Mean VSH scores were compared with 2‐sample t tests. The study had greater than 80% power to detect a difference in proportion of at least 0.14 at alpha = 0.05.
Design and Implementation of the Intervention
Preintervention, routine vital signs were taken every 8 hours: 8 AM, 4 PM, and midnight. Night nurses arrived at 11 PM, and typically turned off the hallway lights, but the practice was variable and occurred at no set time.
Patients in our informal pilot interviews identified vital signs, medication administration, noise, and evening diuretic administration as disrupting their sleep. After the preintervention phase, we spent 4 months designing and implementing the intervention. We solicited opinions from staff, who identified inflexible timing of medications as disruptive. The plan was discussed at routine staff meetings of all shifts.
The intervention, called the Somerville Protocol (Figure 1) created an 8‐hour Quiet Time from 10 PM to 6 AM, when disruptions were minimized. Vital signs were taken 2 hours earlier (6 AM, 2 PM, and 10 PM); routine medication administration was avoided; and noise was reduced. As before, telemetry patients required vital signs every 4 hours. At 10 PM, hallway lights were turned off by a timer while the Lullaby by Brahms played overhead, signaling the start of Quiet Time to staff and patients. Inexpensive sound meters were installed in each nursing area. They flashed warning lights when 60 dBA was exceeded.
A physician and nurse served as champions. Educational signs were posted in the hospitalists' call room and in the nursing areas. The champions used e‐mail and detailed the intervention to staff. Because the staff played an active role in intervention planning, implementation went smoothly.
Results
During the preintervention phase, 334 patients were screened, 294 were eligible, and 54.7% of eligible subjects were enrolled (n = 161). During the intervention phase, 211 patients were screened, 188 were eligible, and 56.3% of eligible patients were enrolled (n = 106). The mean patient age was 60.6 years. The preintervention and intervention groups did not differ significantly in enrollment rate, age, gender, cognitive impairment, surgical status, or hearing deficiencies (Table 1). Over 93% of patients were nonsurgical.
| Preintervention Patients (n = 161) | Intervention Patients (n = 106) | P Values for Difference | |
|---|---|---|---|
| Mean age (years) | 59.1 | 62.95 | P = 0.146 |
| Males, n (%) | 79 (49.1%) | 46 (43.4%) | P = 0.38 |
| Hard of hearing, n (%) (self‐report) | 33/157 (21.0%) | 14/103 (13.6%) | P = 0.128 |
| English‐speaking, n (%) | 134 (83%) | 83 (78.3%) | P = 0.34 |
| Cognitive impairment, n (%) | 4 (2.5%) | 3 (2.8%) | P = 0.88 |
| Surgical patients, n (%) | 10 (6.2%) | 2 (1.8%) | P = 0.089 |
Sedative Use
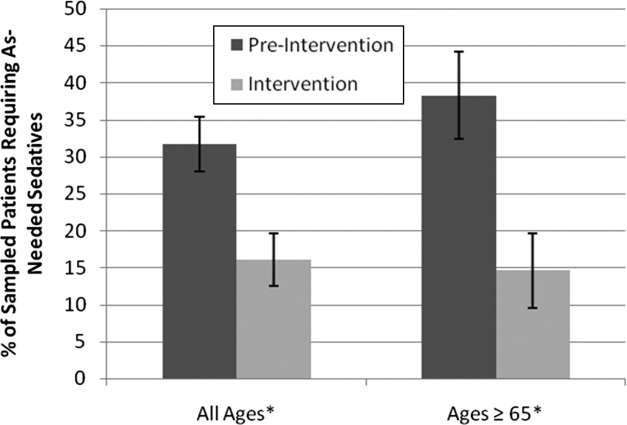
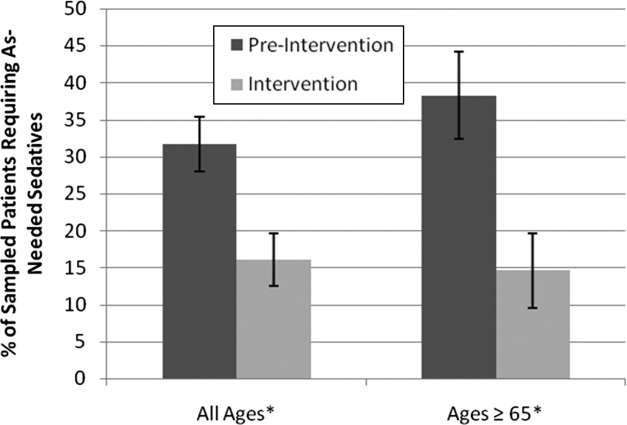
Preintervention, 31.7% of patients received nighttime as‐needed sedatives, versus 16.0% of the intervention group, a 49.4% reduction (P = 0.0041; 95% confidence interval [CI]: 0.056‐0.26) (Figure 2). In patients aged 65 years or older, 38.2% received nighttime as‐needed sedatives preintervention, and 14.6% did postintervention, a 61.2% reduction (P = 0.0054; 95% CI: 0.084‐0.39).
Questionnaire Results
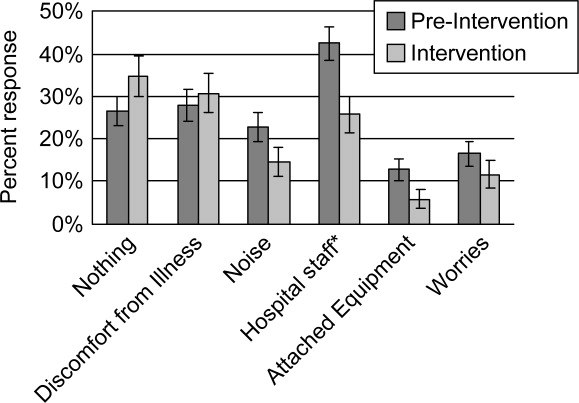
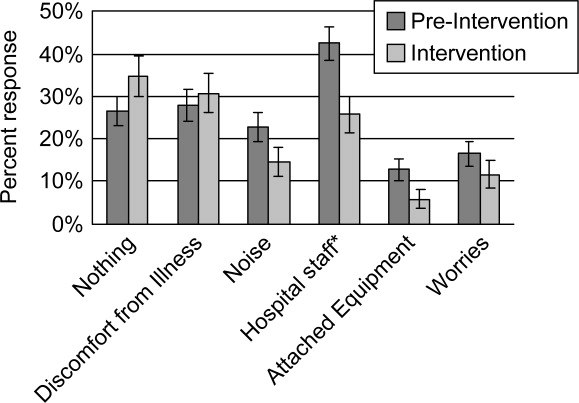
Preintervention, hospital staff was by far the biggest factor keeping patients awake, with 42.4% of patients reporting it (Figure 3). This dropped to only 25.7% with the intervention, a 39.3% decrease (P = 0.009; 95% CI: 0.0452‐0.2765). Preintervention, 19.2% of patients selected voices as the noise most likely to bother them at night, and this dropped to 9.9% with the intervention, a 48% decrease (P = 0.045; 95% CI: 0.0074‐0.1787). No other significant differences were found.
VSH Sleep Score Results
We found no improvement in any measure of the VSH sleep scale. However, 75% of our patients were unable to use the modified VSH scale, generally because they felt too ill, and were then prompted by the surveyor to choose a number between 1 and 10 that reflected their experience.
Protocol Adherence
Changes in unit routines resulted in complete adherence to the new vital signs schedule and avoidance of routine evening diuretics. The closing of patients' doors did not change. An audit of 40 charts found that the percentage of medication orders written with appropriate flexible timing increased from 82% (n = 228) to 95.5% (n = 200) (P = 0.001; 95% CI: 0.077‐0.192). From 20 to 30 different providers wrote orders during each phase.
Discussion
Our trial found that hospital staff was the factor most responsible for patient sleep disruption, and that behavioral interventions on hospital staff can reduce use of as‐needed sedatives. The only previously reported intervention to reduce sedative use, the HELP strategy, involved a complex intervention requiring extra staff, with adherence ranging from 10% to 75%.19, 20, 25 In contrast, our protocol can be easily replicated at minimal cost.
Our results are consistent with those of Freedman et al.,26 who found that noise was not the primary factor responsible for sleep disruption in ICU patients, and that staff activities were at least as important a factor. The study is also consistent with the nursing home studies in which decreases in noise and light did not improve sleep.22, 23 It refutes the study that showed that most sleep disturbance in medical‐surgical patients comes from noise and sleeping in an unfamiliar bed.4 Our results call into question the use of the VSH scale in hospitalized patients, which was designed for use in healthy subjects.
Limitations of this study were as follows: moderate size, lack of refined measures of disease severity, and, as in previous studies,19, 2123 the lack of randomized concurrent controls. Evaluation of secondary endpoints was limited by lack of validation of the questionnaire with objective observations, and inability to use the modified VSH scale. Self‐reports of sleep may correlate imperfectly with objective measures, such as polysomnography.27
A larger concurrent trial randomizing similar units at multiple hospitals would be ideal. Future research is needed to determine whether improving sleep in the hospital improves other outcomes, such as recovery times, delirium, falls, or cost.
The need to reduce as‐needed sedatives is an important safety issue and similar interventions in other hospitals may be helpful. Simple changes in staff routines and provider prescribing habits can yield significant reductions in sedative use.
Acknowledgements
The authors thank Gertrude Gavin, Steffie Woolhandler, MD, Linda Borodkin, John Brusch, MD, Patricia Crombie, Priscilla Dasse, Glen Dawson, Ben Davenny, Linda Kasten, Judith Krempin, Mark Letzeisen, Carmen Mohan, and Arun Mohan. Linda Kasten, Timothy Schmidt, and Glen Dawson provided statistical analysis. The sound meters (Yacker Trackers, Creative Toys of Colorado) were donated by John Brusch, who has no financial conflict of interest.
- ,,,.Sleep in hospitalized medical patients, Part 1: Factors affecting sleep.J Hosp Med.2008;3:473–482.
- ,.Sleep‐dependent learning and memory consolidation.Neuron.2004;44:121–133.
- ,,,,,.An assessment of quality of sleep and the use of drugs with sedating properties in hospitalized adult patients.Health Qual Life Outcomes.2004;2:17.
- ,,,.The sleep experience of medical and surgical patients.Clin Nurs Res.2003;12:159–173.
- .Metabolic and endocrine effects of sleep deprivation.Essent Psychopharmacol.2005;6:341–347.
- ,,,,.Sleep loss and REM sleep loss are hyperalgesic.Sleep.2006;29:145–151.
- ,,,.Slow‐wave sleep and the risk of type 2 diabetes in humans.Proc Natl Acad Sci USA.2008;105:1044–1049.
- .Sleep inquiry: a look with fresh eyes.Image J Nurs Sch.1993;25:249–256.
- Berglund B, Lindvall T, Schwela D, eds.Guidelines for Community Noise.World Health Organization;1999:47.
- ,,,,,.Noise levels in Johns Hopkins Hospital.J Acoust Soc Am.2005;118:3629–3645.
- .Explicit criteria for determining potentially inappropriate medication use by the elderly. An update.Arch Intern Med.1997;157:1531–1536.
- .Delirium in older persons.N Engl J Med.2006;354:1157–1165.
- ,,,,.Sedative hypnotics in older people with insomnia: meta‐analysis of risks and benefits.BMJ.2005;331:1169.
- .Sleep in acute care units.Sleep Breath.2006;10:6–15.
- ,,,,.Quantity and quality of sleep in the surgical intensive care unit: are our patients sleeping?J Trauma.2007;63:1210–1214.
- ,.Sleep in the critically ill patient.Sleep.2006;29:707–716.
- ,,.Sleep quality in hospitalized patients.J Clin Nurs.2005;14:107–113.
- ,.Interactive relationships between hospital patients' noise‐induced stress and other stress with sleep.Heart Lung.2001;30:237–243.
- ,,, et al.A multicomponent intervention to prevent delirium in hospitalized older patients.N Engl J Med.1999;340:669–676.
- ,,,,.The Hospital Elder Life Program: a model of care to prevent cognitive and functional decline in older hospitalized patients. Hospital Elder Life Program.J Am Geriatr Soc.2000;48:1697–1706.
- ,,,,.Noise control: a nursing team's approach to sleep promotion.Am J Nurs.2004;104:40–48; quiz 48‐49.
- ,,,,,.A nonpharmacological intervention to improve sleep in nursing home patients: results of a controlled clinical trial.J Am Geriatr Soc.2006;54:38–47.
- ,,,,.The nursing home at night: effects of an intervention on noise, light, and sleep.J Am Geriatr Soc.1999;47:430–438.
- ,.Instrumentation to describe subjective sleep characteristics in healthy subjects.Res Nurs Health.1987;10:155–163.
- ,,,,.The role of adherence on the effectiveness of nonpharmacologic interventions: evidence from the delirium prevention trial.Arch Intern Med.2003;163:958–964.
- ,,.Patient perception of sleep quality and etiology of sleep disruption in the intensive care unit.Am J Respir Crit Care Med.1999;159:1155–1162.
- ,,.When sleep is perceived as wakefulness: an experimental study on state perception during physiological sleep.J Sleep Res.2007;16:346–353.
Adequate sleep is important for health, yet the hospital environment commonly disrupts sleep.13 Sleep improves after several days in the hospital.3, 4 Sleep deprivation increases cortisol levels5 and sleep loss of greater than 4 hours may be hyperalgesic.6 Even a few days' suppression of slow‐wave sleep worsens glucose tolerance.7 Sleep disruption may cause irritability and aggressiveness,8 impaired memory consolidation, and delirium.2
Noise may disrupt sleep. The World Health Organization recommends a maximum of 30 to 40 dBA in patients' rooms at night.9, 10 Normal conversation occurs at 60 dBA. Medical equipment alarms are about 80 dBA.
Sedative use is common in the hospital.3 Sedatives typically shorten sleep latency and suppress rapid eye movement (REM) sleep. However, some sedatives cause delirium, falls, amnesia, and confusion, particularly in the elderly.1113
Most research on sleep in hospitalized patients has been done in the critical care setting, often in sedated ventilated patients, where sleep disruption is well‐described.1416 Only a few small studies have assessed the sleep of hospitalized patients outside critical care.17, 18
A single blinded interventional trial assessed sedative use, but was a nonrandomized study.19, 20 As‐needed sedative use was measured among hospitalized elderly patients as a secondary endpoint. The intervention, known as the Hospital Elder Life Program (HELP), included a protocol with noise reduction, massage, music, and warm drinks, as well as rescheduling of medications and procedures; it resulted in a 24% reduction in as‐needed sedative use. Another trial decreased noise and reduced overnight X‐rays on a surgical unit, then measured staff and patient attitudes.21 Two interventional studies in nursing homes reduced noise and light, and/or increased daytime activity and found no effect on most objective measures of sleep.22, 23 One descriptive study found most sleep disturbances in medical‐surgical patients came from noise and sleeping in an unfamiliar bed.4
We hypothesized that an intervention designed to improve patient sleep through changes in staff behavior would decrease sedative use among unselected patients in a medical‐surgical unit. We measured sedative use as our primary endpoint as a marker for effective sleep, and because decreased sedative use is desirable. We also hypothesized that the intervention would lead to improved sleep experiences, as measured by a questionnaire and Verran Snyder‐Halpern (VSH) sleep scores as secondary endpoints.24
Materials And Methods
Study Design
This was a pre‐post study assessing the effect of the intervention on as‐needed sedative use, questionnaire responses, and sleep quality. It was an intention‐to‐treat analysis, and was blinded in terms of measurement of sedative use. The Institutional Review Board of Cambridge Health Alliance approved the study.
Setting and Patients
The site was the only medical‐surgical unit of Somerville Hospital, a small urban community teaching hospital that is part of Cambridge Health Alliance. The hospital unit was chosen for its architectural characteristics, and is organized spatially as 3 U‐shaped pods surrounding nursing workstations. Hence, patient rooms were nearly equidistant from the nurses' stations, unlike a hallway design where distant rooms are quieter. Six rooms were private; 11 were semiprivate. Most of the unit's 28 beds are used for medical patients covered by the hospitalist service. Residents see a minority of patients. A hospitalist is available around the clock. Few agency nurses are used.
Preintervention patients were recruited between April and August 2007. The intervention was planned and implemented from September 2007 to January 2008. Intervention patients were recruited between February and June 2008. The most common principle diagnoses on the unit were chest pain (11%), pneumonia (8%), congestive heart failure (CHF) (5.1%), and chronic obstructive pulmonary disease (COPD) flare (3%). Exclusion criteria ensured that no patient was ill enough to require intensive care unit (ICU)‐level care or was actively dying. All consecutive hospitalized patients on the unit on Tuesdays through Fridays were potentially eligible and invited to participate unless they met exclusion criteria. The limited days of the week ensured that technical support would be available during the intervention phase.
Exclusion criteria were: known sleep disorders; language other than English, Spanish, Portuguese, or Haitian Creole; surgery the prior day; arrival on the floor after 10 PM the prior evening; residence on the unit for more than 4 days; alcohol or drug withdrawal; end‐of‐life morphine drip; significant hearing loss; and blindness.
Study Protocol
A single investigator surveyed patients in the morning about the prior night's sleep experience. The surveys consisted of the VSH sleep scale, as well as an 8‐item questionnaire developed from informal pilot interviews with about 18 patients conducted by 1 of the investigators (M.B.) (Supporting Information Figure 1). The VSH scale is a visual analog scale using a 100‐cm line,24 which we modified with a 100‐mm line to make it easier to collect data. The questionnaire and VSH scores of patients with cognitive impairment were not included in the final analysis. Cognitive impairment was determined by diagnoses present in chart review. Surveys and consent forms were available in 4 languages and trained interpreters were used as needed. Nurses, providers, and patients were blinded to the measurement of as‐needed sedative use, and staff were unaware of which patients were study subjects.
Measurements
Nighttime administration of any medication ordered prn sleep or insomnia was measured using the pharmacy dispensing equipment (Pyxis; Cardinal Health, Dublin, OH), then verified by reviewing the patients' medication administration records. VSH sleep scores were created by measuring the distance in millimeters from the lower end of the scale (0) to the location marked.
We also tracked adherence to some aspects of the intervention. The questionnaire recorded door closing. Chart audits measured the numbers of different prescribers, and the frequency of medication orders using flexible timing.
Data Analysis
Medication use was analyzed as any as‐needed sedative use vs. none. The proportions of patients who used sedatives preintervention and postintervention were compared using a 2‐sample Z statistic, as were survey items. Mean VSH scores were compared with 2‐sample t tests. The study had greater than 80% power to detect a difference in proportion of at least 0.14 at alpha = 0.05.
Design and Implementation of the Intervention
Preintervention, routine vital signs were taken every 8 hours: 8 AM, 4 PM, and midnight. Night nurses arrived at 11 PM, and typically turned off the hallway lights, but the practice was variable and occurred at no set time.
Patients in our informal pilot interviews identified vital signs, medication administration, noise, and evening diuretic administration as disrupting their sleep. After the preintervention phase, we spent 4 months designing and implementing the intervention. We solicited opinions from staff, who identified inflexible timing of medications as disruptive. The plan was discussed at routine staff meetings of all shifts.
The intervention, called the Somerville Protocol (Figure 1) created an 8‐hour Quiet Time from 10 PM to 6 AM, when disruptions were minimized. Vital signs were taken 2 hours earlier (6 AM, 2 PM, and 10 PM); routine medication administration was avoided; and noise was reduced. As before, telemetry patients required vital signs every 4 hours. At 10 PM, hallway lights were turned off by a timer while the Lullaby by Brahms played overhead, signaling the start of Quiet Time to staff and patients. Inexpensive sound meters were installed in each nursing area. They flashed warning lights when 60 dBA was exceeded.
A physician and nurse served as champions. Educational signs were posted in the hospitalists' call room and in the nursing areas. The champions used e‐mail and detailed the intervention to staff. Because the staff played an active role in intervention planning, implementation went smoothly.
Results
During the preintervention phase, 334 patients were screened, 294 were eligible, and 54.7% of eligible subjects were enrolled (n = 161). During the intervention phase, 211 patients were screened, 188 were eligible, and 56.3% of eligible patients were enrolled (n = 106). The mean patient age was 60.6 years. The preintervention and intervention groups did not differ significantly in enrollment rate, age, gender, cognitive impairment, surgical status, or hearing deficiencies (Table 1). Over 93% of patients were nonsurgical.
| Preintervention Patients (n = 161) | Intervention Patients (n = 106) | P Values for Difference | |
|---|---|---|---|
| Mean age (years) | 59.1 | 62.95 | P = 0.146 |
| Males, n (%) | 79 (49.1%) | 46 (43.4%) | P = 0.38 |
| Hard of hearing, n (%) (self‐report) | 33/157 (21.0%) | 14/103 (13.6%) | P = 0.128 |
| English‐speaking, n (%) | 134 (83%) | 83 (78.3%) | P = 0.34 |
| Cognitive impairment, n (%) | 4 (2.5%) | 3 (2.8%) | P = 0.88 |
| Surgical patients, n (%) | 10 (6.2%) | 2 (1.8%) | P = 0.089 |
Sedative Use
Preintervention, 31.7% of patients received nighttime as‐needed sedatives, versus 16.0% of the intervention group, a 49.4% reduction (P = 0.0041; 95% confidence interval [CI]: 0.056‐0.26) (Figure 2). In patients aged 65 years or older, 38.2% received nighttime as‐needed sedatives preintervention, and 14.6% did postintervention, a 61.2% reduction (P = 0.0054; 95% CI: 0.084‐0.39).
Questionnaire Results
Preintervention, hospital staff was by far the biggest factor keeping patients awake, with 42.4% of patients reporting it (Figure 3). This dropped to only 25.7% with the intervention, a 39.3% decrease (P = 0.009; 95% CI: 0.0452‐0.2765). Preintervention, 19.2% of patients selected voices as the noise most likely to bother them at night, and this dropped to 9.9% with the intervention, a 48% decrease (P = 0.045; 95% CI: 0.0074‐0.1787). No other significant differences were found.
VSH Sleep Score Results
We found no improvement in any measure of the VSH sleep scale. However, 75% of our patients were unable to use the modified VSH scale, generally because they felt too ill, and were then prompted by the surveyor to choose a number between 1 and 10 that reflected their experience.
Protocol Adherence
Changes in unit routines resulted in complete adherence to the new vital signs schedule and avoidance of routine evening diuretics. The closing of patients' doors did not change. An audit of 40 charts found that the percentage of medication orders written with appropriate flexible timing increased from 82% (n = 228) to 95.5% (n = 200) (P = 0.001; 95% CI: 0.077‐0.192). From 20 to 30 different providers wrote orders during each phase.
Discussion
Our trial found that hospital staff was the factor most responsible for patient sleep disruption, and that behavioral interventions on hospital staff can reduce use of as‐needed sedatives. The only previously reported intervention to reduce sedative use, the HELP strategy, involved a complex intervention requiring extra staff, with adherence ranging from 10% to 75%.19, 20, 25 In contrast, our protocol can be easily replicated at minimal cost.
Our results are consistent with those of Freedman et al.,26 who found that noise was not the primary factor responsible for sleep disruption in ICU patients, and that staff activities were at least as important a factor. The study is also consistent with the nursing home studies in which decreases in noise and light did not improve sleep.22, 23 It refutes the study that showed that most sleep disturbance in medical‐surgical patients comes from noise and sleeping in an unfamiliar bed.4 Our results call into question the use of the VSH scale in hospitalized patients, which was designed for use in healthy subjects.
Limitations of this study were as follows: moderate size, lack of refined measures of disease severity, and, as in previous studies,19, 2123 the lack of randomized concurrent controls. Evaluation of secondary endpoints was limited by lack of validation of the questionnaire with objective observations, and inability to use the modified VSH scale. Self‐reports of sleep may correlate imperfectly with objective measures, such as polysomnography.27
A larger concurrent trial randomizing similar units at multiple hospitals would be ideal. Future research is needed to determine whether improving sleep in the hospital improves other outcomes, such as recovery times, delirium, falls, or cost.
The need to reduce as‐needed sedatives is an important safety issue and similar interventions in other hospitals may be helpful. Simple changes in staff routines and provider prescribing habits can yield significant reductions in sedative use.
Acknowledgements
The authors thank Gertrude Gavin, Steffie Woolhandler, MD, Linda Borodkin, John Brusch, MD, Patricia Crombie, Priscilla Dasse, Glen Dawson, Ben Davenny, Linda Kasten, Judith Krempin, Mark Letzeisen, Carmen Mohan, and Arun Mohan. Linda Kasten, Timothy Schmidt, and Glen Dawson provided statistical analysis. The sound meters (Yacker Trackers, Creative Toys of Colorado) were donated by John Brusch, who has no financial conflict of interest.
Adequate sleep is important for health, yet the hospital environment commonly disrupts sleep.13 Sleep improves after several days in the hospital.3, 4 Sleep deprivation increases cortisol levels5 and sleep loss of greater than 4 hours may be hyperalgesic.6 Even a few days' suppression of slow‐wave sleep worsens glucose tolerance.7 Sleep disruption may cause irritability and aggressiveness,8 impaired memory consolidation, and delirium.2
Noise may disrupt sleep. The World Health Organization recommends a maximum of 30 to 40 dBA in patients' rooms at night.9, 10 Normal conversation occurs at 60 dBA. Medical equipment alarms are about 80 dBA.
Sedative use is common in the hospital.3 Sedatives typically shorten sleep latency and suppress rapid eye movement (REM) sleep. However, some sedatives cause delirium, falls, amnesia, and confusion, particularly in the elderly.1113
Most research on sleep in hospitalized patients has been done in the critical care setting, often in sedated ventilated patients, where sleep disruption is well‐described.1416 Only a few small studies have assessed the sleep of hospitalized patients outside critical care.17, 18
A single blinded interventional trial assessed sedative use, but was a nonrandomized study.19, 20 As‐needed sedative use was measured among hospitalized elderly patients as a secondary endpoint. The intervention, known as the Hospital Elder Life Program (HELP), included a protocol with noise reduction, massage, music, and warm drinks, as well as rescheduling of medications and procedures; it resulted in a 24% reduction in as‐needed sedative use. Another trial decreased noise and reduced overnight X‐rays on a surgical unit, then measured staff and patient attitudes.21 Two interventional studies in nursing homes reduced noise and light, and/or increased daytime activity and found no effect on most objective measures of sleep.22, 23 One descriptive study found most sleep disturbances in medical‐surgical patients came from noise and sleeping in an unfamiliar bed.4
We hypothesized that an intervention designed to improve patient sleep through changes in staff behavior would decrease sedative use among unselected patients in a medical‐surgical unit. We measured sedative use as our primary endpoint as a marker for effective sleep, and because decreased sedative use is desirable. We also hypothesized that the intervention would lead to improved sleep experiences, as measured by a questionnaire and Verran Snyder‐Halpern (VSH) sleep scores as secondary endpoints.24
Materials And Methods
Study Design
This was a pre‐post study assessing the effect of the intervention on as‐needed sedative use, questionnaire responses, and sleep quality. It was an intention‐to‐treat analysis, and was blinded in terms of measurement of sedative use. The Institutional Review Board of Cambridge Health Alliance approved the study.
Setting and Patients
The site was the only medical‐surgical unit of Somerville Hospital, a small urban community teaching hospital that is part of Cambridge Health Alliance. The hospital unit was chosen for its architectural characteristics, and is organized spatially as 3 U‐shaped pods surrounding nursing workstations. Hence, patient rooms were nearly equidistant from the nurses' stations, unlike a hallway design where distant rooms are quieter. Six rooms were private; 11 were semiprivate. Most of the unit's 28 beds are used for medical patients covered by the hospitalist service. Residents see a minority of patients. A hospitalist is available around the clock. Few agency nurses are used.
Preintervention patients were recruited between April and August 2007. The intervention was planned and implemented from September 2007 to January 2008. Intervention patients were recruited between February and June 2008. The most common principle diagnoses on the unit were chest pain (11%), pneumonia (8%), congestive heart failure (CHF) (5.1%), and chronic obstructive pulmonary disease (COPD) flare (3%). Exclusion criteria ensured that no patient was ill enough to require intensive care unit (ICU)‐level care or was actively dying. All consecutive hospitalized patients on the unit on Tuesdays through Fridays were potentially eligible and invited to participate unless they met exclusion criteria. The limited days of the week ensured that technical support would be available during the intervention phase.
Exclusion criteria were: known sleep disorders; language other than English, Spanish, Portuguese, or Haitian Creole; surgery the prior day; arrival on the floor after 10 PM the prior evening; residence on the unit for more than 4 days; alcohol or drug withdrawal; end‐of‐life morphine drip; significant hearing loss; and blindness.
Study Protocol
A single investigator surveyed patients in the morning about the prior night's sleep experience. The surveys consisted of the VSH sleep scale, as well as an 8‐item questionnaire developed from informal pilot interviews with about 18 patients conducted by 1 of the investigators (M.B.) (Supporting Information Figure 1). The VSH scale is a visual analog scale using a 100‐cm line,24 which we modified with a 100‐mm line to make it easier to collect data. The questionnaire and VSH scores of patients with cognitive impairment were not included in the final analysis. Cognitive impairment was determined by diagnoses present in chart review. Surveys and consent forms were available in 4 languages and trained interpreters were used as needed. Nurses, providers, and patients were blinded to the measurement of as‐needed sedative use, and staff were unaware of which patients were study subjects.
Measurements
Nighttime administration of any medication ordered prn sleep or insomnia was measured using the pharmacy dispensing equipment (Pyxis; Cardinal Health, Dublin, OH), then verified by reviewing the patients' medication administration records. VSH sleep scores were created by measuring the distance in millimeters from the lower end of the scale (0) to the location marked.
We also tracked adherence to some aspects of the intervention. The questionnaire recorded door closing. Chart audits measured the numbers of different prescribers, and the frequency of medication orders using flexible timing.
Data Analysis
Medication use was analyzed as any as‐needed sedative use vs. none. The proportions of patients who used sedatives preintervention and postintervention were compared using a 2‐sample Z statistic, as were survey items. Mean VSH scores were compared with 2‐sample t tests. The study had greater than 80% power to detect a difference in proportion of at least 0.14 at alpha = 0.05.
Design and Implementation of the Intervention
Preintervention, routine vital signs were taken every 8 hours: 8 AM, 4 PM, and midnight. Night nurses arrived at 11 PM, and typically turned off the hallway lights, but the practice was variable and occurred at no set time.
Patients in our informal pilot interviews identified vital signs, medication administration, noise, and evening diuretic administration as disrupting their sleep. After the preintervention phase, we spent 4 months designing and implementing the intervention. We solicited opinions from staff, who identified inflexible timing of medications as disruptive. The plan was discussed at routine staff meetings of all shifts.
The intervention, called the Somerville Protocol (Figure 1) created an 8‐hour Quiet Time from 10 PM to 6 AM, when disruptions were minimized. Vital signs were taken 2 hours earlier (6 AM, 2 PM, and 10 PM); routine medication administration was avoided; and noise was reduced. As before, telemetry patients required vital signs every 4 hours. At 10 PM, hallway lights were turned off by a timer while the Lullaby by Brahms played overhead, signaling the start of Quiet Time to staff and patients. Inexpensive sound meters were installed in each nursing area. They flashed warning lights when 60 dBA was exceeded.
A physician and nurse served as champions. Educational signs were posted in the hospitalists' call room and in the nursing areas. The champions used e‐mail and detailed the intervention to staff. Because the staff played an active role in intervention planning, implementation went smoothly.
Results
During the preintervention phase, 334 patients were screened, 294 were eligible, and 54.7% of eligible subjects were enrolled (n = 161). During the intervention phase, 211 patients were screened, 188 were eligible, and 56.3% of eligible patients were enrolled (n = 106). The mean patient age was 60.6 years. The preintervention and intervention groups did not differ significantly in enrollment rate, age, gender, cognitive impairment, surgical status, or hearing deficiencies (Table 1). Over 93% of patients were nonsurgical.
| Preintervention Patients (n = 161) | Intervention Patients (n = 106) | P Values for Difference | |
|---|---|---|---|
| Mean age (years) | 59.1 | 62.95 | P = 0.146 |
| Males, n (%) | 79 (49.1%) | 46 (43.4%) | P = 0.38 |
| Hard of hearing, n (%) (self‐report) | 33/157 (21.0%) | 14/103 (13.6%) | P = 0.128 |
| English‐speaking, n (%) | 134 (83%) | 83 (78.3%) | P = 0.34 |
| Cognitive impairment, n (%) | 4 (2.5%) | 3 (2.8%) | P = 0.88 |
| Surgical patients, n (%) | 10 (6.2%) | 2 (1.8%) | P = 0.089 |
Sedative Use
Preintervention, 31.7% of patients received nighttime as‐needed sedatives, versus 16.0% of the intervention group, a 49.4% reduction (P = 0.0041; 95% confidence interval [CI]: 0.056‐0.26) (Figure 2). In patients aged 65 years or older, 38.2% received nighttime as‐needed sedatives preintervention, and 14.6% did postintervention, a 61.2% reduction (P = 0.0054; 95% CI: 0.084‐0.39).
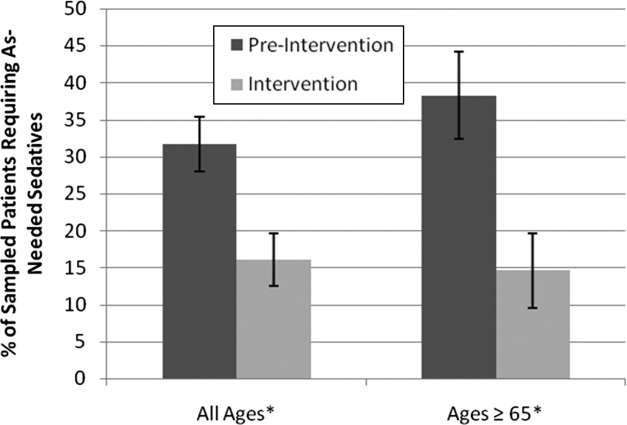
Questionnaire Results
Preintervention, hospital staff was by far the biggest factor keeping patients awake, with 42.4% of patients reporting it (Figure 3). This dropped to only 25.7% with the intervention, a 39.3% decrease (P = 0.009; 95% CI: 0.0452‐0.2765). Preintervention, 19.2% of patients selected voices as the noise most likely to bother them at night, and this dropped to 9.9% with the intervention, a 48% decrease (P = 0.045; 95% CI: 0.0074‐0.1787). No other significant differences were found.
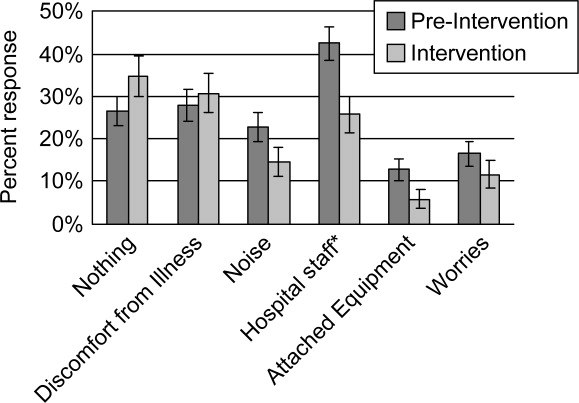
VSH Sleep Score Results
We found no improvement in any measure of the VSH sleep scale. However, 75% of our patients were unable to use the modified VSH scale, generally because they felt too ill, and were then prompted by the surveyor to choose a number between 1 and 10 that reflected their experience.
Protocol Adherence
Changes in unit routines resulted in complete adherence to the new vital signs schedule and avoidance of routine evening diuretics. The closing of patients' doors did not change. An audit of 40 charts found that the percentage of medication orders written with appropriate flexible timing increased from 82% (n = 228) to 95.5% (n = 200) (P = 0.001; 95% CI: 0.077‐0.192). From 20 to 30 different providers wrote orders during each phase.
Discussion
Our trial found that hospital staff was the factor most responsible for patient sleep disruption, and that behavioral interventions on hospital staff can reduce use of as‐needed sedatives. The only previously reported intervention to reduce sedative use, the HELP strategy, involved a complex intervention requiring extra staff, with adherence ranging from 10% to 75%.19, 20, 25 In contrast, our protocol can be easily replicated at minimal cost.
Our results are consistent with those of Freedman et al.,26 who found that noise was not the primary factor responsible for sleep disruption in ICU patients, and that staff activities were at least as important a factor. The study is also consistent with the nursing home studies in which decreases in noise and light did not improve sleep.22, 23 It refutes the study that showed that most sleep disturbance in medical‐surgical patients comes from noise and sleeping in an unfamiliar bed.4 Our results call into question the use of the VSH scale in hospitalized patients, which was designed for use in healthy subjects.
Limitations of this study were as follows: moderate size, lack of refined measures of disease severity, and, as in previous studies,19, 2123 the lack of randomized concurrent controls. Evaluation of secondary endpoints was limited by lack of validation of the questionnaire with objective observations, and inability to use the modified VSH scale. Self‐reports of sleep may correlate imperfectly with objective measures, such as polysomnography.27
A larger concurrent trial randomizing similar units at multiple hospitals would be ideal. Future research is needed to determine whether improving sleep in the hospital improves other outcomes, such as recovery times, delirium, falls, or cost.
The need to reduce as‐needed sedatives is an important safety issue and similar interventions in other hospitals may be helpful. Simple changes in staff routines and provider prescribing habits can yield significant reductions in sedative use.
Acknowledgements
The authors thank Gertrude Gavin, Steffie Woolhandler, MD, Linda Borodkin, John Brusch, MD, Patricia Crombie, Priscilla Dasse, Glen Dawson, Ben Davenny, Linda Kasten, Judith Krempin, Mark Letzeisen, Carmen Mohan, and Arun Mohan. Linda Kasten, Timothy Schmidt, and Glen Dawson provided statistical analysis. The sound meters (Yacker Trackers, Creative Toys of Colorado) were donated by John Brusch, who has no financial conflict of interest.
- ,,,.Sleep in hospitalized medical patients, Part 1: Factors affecting sleep.J Hosp Med.2008;3:473–482.
- ,.Sleep‐dependent learning and memory consolidation.Neuron.2004;44:121–133.
- ,,,,,.An assessment of quality of sleep and the use of drugs with sedating properties in hospitalized adult patients.Health Qual Life Outcomes.2004;2:17.
- ,,,.The sleep experience of medical and surgical patients.Clin Nurs Res.2003;12:159–173.
- .Metabolic and endocrine effects of sleep deprivation.Essent Psychopharmacol.2005;6:341–347.
- ,,,,.Sleep loss and REM sleep loss are hyperalgesic.Sleep.2006;29:145–151.
- ,,,.Slow‐wave sleep and the risk of type 2 diabetes in humans.Proc Natl Acad Sci USA.2008;105:1044–1049.
- .Sleep inquiry: a look with fresh eyes.Image J Nurs Sch.1993;25:249–256.
- Berglund B, Lindvall T, Schwela D, eds.Guidelines for Community Noise.World Health Organization;1999:47.
- ,,,,,.Noise levels in Johns Hopkins Hospital.J Acoust Soc Am.2005;118:3629–3645.
- .Explicit criteria for determining potentially inappropriate medication use by the elderly. An update.Arch Intern Med.1997;157:1531–1536.
- .Delirium in older persons.N Engl J Med.2006;354:1157–1165.
- ,,,,.Sedative hypnotics in older people with insomnia: meta‐analysis of risks and benefits.BMJ.2005;331:1169.
- .Sleep in acute care units.Sleep Breath.2006;10:6–15.
- ,,,,.Quantity and quality of sleep in the surgical intensive care unit: are our patients sleeping?J Trauma.2007;63:1210–1214.
- ,.Sleep in the critically ill patient.Sleep.2006;29:707–716.
- ,,.Sleep quality in hospitalized patients.J Clin Nurs.2005;14:107–113.
- ,.Interactive relationships between hospital patients' noise‐induced stress and other stress with sleep.Heart Lung.2001;30:237–243.
- ,,, et al.A multicomponent intervention to prevent delirium in hospitalized older patients.N Engl J Med.1999;340:669–676.
- ,,,,.The Hospital Elder Life Program: a model of care to prevent cognitive and functional decline in older hospitalized patients. Hospital Elder Life Program.J Am Geriatr Soc.2000;48:1697–1706.
- ,,,,.Noise control: a nursing team's approach to sleep promotion.Am J Nurs.2004;104:40–48; quiz 48‐49.
- ,,,,,.A nonpharmacological intervention to improve sleep in nursing home patients: results of a controlled clinical trial.J Am Geriatr Soc.2006;54:38–47.
- ,,,,.The nursing home at night: effects of an intervention on noise, light, and sleep.J Am Geriatr Soc.1999;47:430–438.
- ,.Instrumentation to describe subjective sleep characteristics in healthy subjects.Res Nurs Health.1987;10:155–163.
- ,,,,.The role of adherence on the effectiveness of nonpharmacologic interventions: evidence from the delirium prevention trial.Arch Intern Med.2003;163:958–964.
- ,,.Patient perception of sleep quality and etiology of sleep disruption in the intensive care unit.Am J Respir Crit Care Med.1999;159:1155–1162.
- ,,.When sleep is perceived as wakefulness: an experimental study on state perception during physiological sleep.J Sleep Res.2007;16:346–353.
- ,,,.Sleep in hospitalized medical patients, Part 1: Factors affecting sleep.J Hosp Med.2008;3:473–482.
- ,.Sleep‐dependent learning and memory consolidation.Neuron.2004;44:121–133.
- ,,,,,.An assessment of quality of sleep and the use of drugs with sedating properties in hospitalized adult patients.Health Qual Life Outcomes.2004;2:17.
- ,,,.The sleep experience of medical and surgical patients.Clin Nurs Res.2003;12:159–173.
- .Metabolic and endocrine effects of sleep deprivation.Essent Psychopharmacol.2005;6:341–347.
- ,,,,.Sleep loss and REM sleep loss are hyperalgesic.Sleep.2006;29:145–151.
- ,,,.Slow‐wave sleep and the risk of type 2 diabetes in humans.Proc Natl Acad Sci USA.2008;105:1044–1049.
- .Sleep inquiry: a look with fresh eyes.Image J Nurs Sch.1993;25:249–256.
- Berglund B, Lindvall T, Schwela D, eds.Guidelines for Community Noise.World Health Organization;1999:47.
- ,,,,,.Noise levels in Johns Hopkins Hospital.J Acoust Soc Am.2005;118:3629–3645.
- .Explicit criteria for determining potentially inappropriate medication use by the elderly. An update.Arch Intern Med.1997;157:1531–1536.
- .Delirium in older persons.N Engl J Med.2006;354:1157–1165.
- ,,,,.Sedative hypnotics in older people with insomnia: meta‐analysis of risks and benefits.BMJ.2005;331:1169.
- .Sleep in acute care units.Sleep Breath.2006;10:6–15.
- ,,,,.Quantity and quality of sleep in the surgical intensive care unit: are our patients sleeping?J Trauma.2007;63:1210–1214.
- ,.Sleep in the critically ill patient.Sleep.2006;29:707–716.
- ,,.Sleep quality in hospitalized patients.J Clin Nurs.2005;14:107–113.
- ,.Interactive relationships between hospital patients' noise‐induced stress and other stress with sleep.Heart Lung.2001;30:237–243.
- ,,, et al.A multicomponent intervention to prevent delirium in hospitalized older patients.N Engl J Med.1999;340:669–676.
- ,,,,.The Hospital Elder Life Program: a model of care to prevent cognitive and functional decline in older hospitalized patients. Hospital Elder Life Program.J Am Geriatr Soc.2000;48:1697–1706.
- ,,,,.Noise control: a nursing team's approach to sleep promotion.Am J Nurs.2004;104:40–48; quiz 48‐49.
- ,,,,,.A nonpharmacological intervention to improve sleep in nursing home patients: results of a controlled clinical trial.J Am Geriatr Soc.2006;54:38–47.
- ,,,,.The nursing home at night: effects of an intervention on noise, light, and sleep.J Am Geriatr Soc.1999;47:430–438.
- ,.Instrumentation to describe subjective sleep characteristics in healthy subjects.Res Nurs Health.1987;10:155–163.
- ,,,,.The role of adherence on the effectiveness of nonpharmacologic interventions: evidence from the delirium prevention trial.Arch Intern Med.2003;163:958–964.
- ,,.Patient perception of sleep quality and etiology of sleep disruption in the intensive care unit.Am J Respir Crit Care Med.1999;159:1155–1162.
- ,,.When sleep is perceived as wakefulness: an experimental study on state perception during physiological sleep.J Sleep Res.2007;16:346–353.
New Jersey Cracks Down on Never Events
A landmark New Jersey law that increases public disclosure of major preventable medical errors and prohibits charges for certain medical expenses related to those mistakes has hospitalists poised to take a leadership role in patient-safety efforts.
The legislation allows the state to release hospital-specific data on 14 medical mistakes considered by the federal government to be most preventable. It also bans hospitals from charging patients or insurers for follow-up medical costs related to the errors, including pressure ulcers, DVT, and catheter-associated urinary tract infections.
“It’s hard to argue the New Jersey legislation doesn’t make sense,” says hospitalist Niraj Sehgal, MD, MPH, associate chair for quality and safety in the Department of Medicine at the University of California at San Francisco. “After all, if I had the wrong limb operated on, I certainly wouldn’t expect to pay for the subsequent care needs, and nor should our system.”
Dr. Sehgal expects more states to follow New Jersey’s lead, a likely outcome given the fact the AARP is calling the Garden State measure “a national landmark.” The legislation also dovetails with the “no pay for errors” initiative from the Centers for Medicare & Medicaid Services.
Many hospitalists think HM groups are best positioned to spearhead quality and patient-safety efforts tied to the legislation. Hospitalist Vincent Barba, MD, FACP, FHM, medical director for quality improvement with University of Medicine and Dentistry of New Jersey in Newark, says HM leaders just have to seize the opportunity.
“Be the home team,” Dr. Barba says. “Step up. Take a leading role.”
A landmark New Jersey law that increases public disclosure of major preventable medical errors and prohibits charges for certain medical expenses related to those mistakes has hospitalists poised to take a leadership role in patient-safety efforts.
The legislation allows the state to release hospital-specific data on 14 medical mistakes considered by the federal government to be most preventable. It also bans hospitals from charging patients or insurers for follow-up medical costs related to the errors, including pressure ulcers, DVT, and catheter-associated urinary tract infections.
“It’s hard to argue the New Jersey legislation doesn’t make sense,” says hospitalist Niraj Sehgal, MD, MPH, associate chair for quality and safety in the Department of Medicine at the University of California at San Francisco. “After all, if I had the wrong limb operated on, I certainly wouldn’t expect to pay for the subsequent care needs, and nor should our system.”
Dr. Sehgal expects more states to follow New Jersey’s lead, a likely outcome given the fact the AARP is calling the Garden State measure “a national landmark.” The legislation also dovetails with the “no pay for errors” initiative from the Centers for Medicare & Medicaid Services.
Many hospitalists think HM groups are best positioned to spearhead quality and patient-safety efforts tied to the legislation. Hospitalist Vincent Barba, MD, FACP, FHM, medical director for quality improvement with University of Medicine and Dentistry of New Jersey in Newark, says HM leaders just have to seize the opportunity.
“Be the home team,” Dr. Barba says. “Step up. Take a leading role.”
A landmark New Jersey law that increases public disclosure of major preventable medical errors and prohibits charges for certain medical expenses related to those mistakes has hospitalists poised to take a leadership role in patient-safety efforts.
The legislation allows the state to release hospital-specific data on 14 medical mistakes considered by the federal government to be most preventable. It also bans hospitals from charging patients or insurers for follow-up medical costs related to the errors, including pressure ulcers, DVT, and catheter-associated urinary tract infections.
“It’s hard to argue the New Jersey legislation doesn’t make sense,” says hospitalist Niraj Sehgal, MD, MPH, associate chair for quality and safety in the Department of Medicine at the University of California at San Francisco. “After all, if I had the wrong limb operated on, I certainly wouldn’t expect to pay for the subsequent care needs, and nor should our system.”
Dr. Sehgal expects more states to follow New Jersey’s lead, a likely outcome given the fact the AARP is calling the Garden State measure “a national landmark.” The legislation also dovetails with the “no pay for errors” initiative from the Centers for Medicare & Medicaid Services.
Many hospitalists think HM groups are best positioned to spearhead quality and patient-safety efforts tied to the legislation. Hospitalist Vincent Barba, MD, FACP, FHM, medical director for quality improvement with University of Medicine and Dentistry of New Jersey in Newark, says HM leaders just have to seize the opportunity.
“Be the home team,” Dr. Barba says. “Step up. Take a leading role.”
In the Literature: Research You Need to Know
Clinical question: Does aspirin prevent cardiovascular events in patients with peripheral artery disease (PAD)?
Background: Evidence that aspirin decreases risk of cardiovascular events in patients with symptomatic coronary artery disease and cerebrovascular disease has led to a recommendation of aspirin as secondary prevention in PAD. Evidence for its efficacy in this context is not established.
Study design: Meta-analysis.
Setting: Multiple study sites.
Synopsis: The investigators looked at 18 randomized controlled trials involving 5,269 participants, 2,823 of whom received aspirin, including 1,516 as monotherapy and 2,446 controls. The primary endpoint investigated was cardiovascular events.
This meta-analysis did not show a statistical benefit in cardiovascular event reduction (8.9% vs. 11%) in aspirin therapy in patients with peripheral artery disease, but it did show a decrease in the secondary endpoint of nonfatal strokes. A subset analysis of aspirin monotherapy versus placebo showed a nonsignificant decrease in the primary endpoint.
The studies had a short timeline with few cardiovascular events, so conclusions cannot be drawn about longer timeframes. Furthermore, some of the included studies were not designed to measure cardiovascular events. Finally, the study was not powered to detect differences less than 25%.
Bottom line: In patients with PAD, aspirin might not decrease the incidence of cardiovascular events.
Citation: Berger JT, Krantz MJ, Kittelson JM, Hiatt WR. Aspirin for the prevention of cardiovascular events in patients with peripheral artery disease: a meta-analysis of randomized trials. JAMA. 2009;301(18):1909-1919.
—Reviewed for The Hospitalist by Steven Deitelzweig, MD, MMM, FHM; Frank Wharton, MD, FACP; Renee Meadows, MD, FHM; Srinivas Vuppala, MD; Kevin Hude, MD; Doris Lin, MD; Damodar Kumbala, MD, Department of Hospital Medicine, Ochsner Medical Center, New Orleans
Clinical question: Does aspirin prevent cardiovascular events in patients with peripheral artery disease (PAD)?
Background: Evidence that aspirin decreases risk of cardiovascular events in patients with symptomatic coronary artery disease and cerebrovascular disease has led to a recommendation of aspirin as secondary prevention in PAD. Evidence for its efficacy in this context is not established.
Study design: Meta-analysis.
Setting: Multiple study sites.
Synopsis: The investigators looked at 18 randomized controlled trials involving 5,269 participants, 2,823 of whom received aspirin, including 1,516 as monotherapy and 2,446 controls. The primary endpoint investigated was cardiovascular events.
This meta-analysis did not show a statistical benefit in cardiovascular event reduction (8.9% vs. 11%) in aspirin therapy in patients with peripheral artery disease, but it did show a decrease in the secondary endpoint of nonfatal strokes. A subset analysis of aspirin monotherapy versus placebo showed a nonsignificant decrease in the primary endpoint.
The studies had a short timeline with few cardiovascular events, so conclusions cannot be drawn about longer timeframes. Furthermore, some of the included studies were not designed to measure cardiovascular events. Finally, the study was not powered to detect differences less than 25%.
Bottom line: In patients with PAD, aspirin might not decrease the incidence of cardiovascular events.
Citation: Berger JT, Krantz MJ, Kittelson JM, Hiatt WR. Aspirin for the prevention of cardiovascular events in patients with peripheral artery disease: a meta-analysis of randomized trials. JAMA. 2009;301(18):1909-1919.
—Reviewed for The Hospitalist by Steven Deitelzweig, MD, MMM, FHM; Frank Wharton, MD, FACP; Renee Meadows, MD, FHM; Srinivas Vuppala, MD; Kevin Hude, MD; Doris Lin, MD; Damodar Kumbala, MD, Department of Hospital Medicine, Ochsner Medical Center, New Orleans
Clinical question: Does aspirin prevent cardiovascular events in patients with peripheral artery disease (PAD)?
Background: Evidence that aspirin decreases risk of cardiovascular events in patients with symptomatic coronary artery disease and cerebrovascular disease has led to a recommendation of aspirin as secondary prevention in PAD. Evidence for its efficacy in this context is not established.
Study design: Meta-analysis.
Setting: Multiple study sites.
Synopsis: The investigators looked at 18 randomized controlled trials involving 5,269 participants, 2,823 of whom received aspirin, including 1,516 as monotherapy and 2,446 controls. The primary endpoint investigated was cardiovascular events.
This meta-analysis did not show a statistical benefit in cardiovascular event reduction (8.9% vs. 11%) in aspirin therapy in patients with peripheral artery disease, but it did show a decrease in the secondary endpoint of nonfatal strokes. A subset analysis of aspirin monotherapy versus placebo showed a nonsignificant decrease in the primary endpoint.
The studies had a short timeline with few cardiovascular events, so conclusions cannot be drawn about longer timeframes. Furthermore, some of the included studies were not designed to measure cardiovascular events. Finally, the study was not powered to detect differences less than 25%.
Bottom line: In patients with PAD, aspirin might not decrease the incidence of cardiovascular events.
Citation: Berger JT, Krantz MJ, Kittelson JM, Hiatt WR. Aspirin for the prevention of cardiovascular events in patients with peripheral artery disease: a meta-analysis of randomized trials. JAMA. 2009;301(18):1909-1919.
—Reviewed for The Hospitalist by Steven Deitelzweig, MD, MMM, FHM; Frank Wharton, MD, FACP; Renee Meadows, MD, FHM; Srinivas Vuppala, MD; Kevin Hude, MD; Doris Lin, MD; Damodar Kumbala, MD, Department of Hospital Medicine, Ochsner Medical Center, New Orleans
Progesterone use in management of secondary amenorrhea
An e-newsletter focusing on challenging case studies
Progesterone use in management of secondary amenorrhea
Read the following case study and earn
FREE 0.5 CME/CE CREDIT
Expiration date: July 31, 2009
Estimated time to complete activity: 0.5 hour
Target: Physicians, physician assistants and nurse practitioners
Supported by an educational grant from Solvay Pharmaceuticals, Inc.
Sponsored by the American Society for Reproductive Medicine.
Click here to take the FREE CME/CE test online for 0.5 credits
Nicole is 27 years old, gravida 0, with a long history of obesity and great difficulty losing weight. She reports having irregular menstrual cycles ranging from 45 days to 6 months apart. Her last menstrual period was 5 months ago, when she had a heavy menses that lasted 2 weeks. Her body mass index is 42 kg/m2, which is considered morbid obesity. Nicole has a large abdominal pannus and normal blood pressure. She has scattered acne lesions on her face and upper back and acanthosis nigricans, a dark pigmentation around the neck and the axilla. Acanthosis nigricans is a biomarker for insulin resistance and high circulating insulin levels.
Nicole’s pelvic exam showed a normal vagina and cervix, but it was not possible to palpate her uterus or ovaries because of her abdominal girth. Transvaginal ultrasound found an endometrial thickness of 22 mm. Her ovaries appeared to be multicystic but had normal ovarian volumes. We performed an endometrial biopsy because of concerns about the long duration of unopposed estrogen exposure. The biopsy revealed complex hyperplasia with no atypia.
A lipid profile demonstrated cholesterol 245 mg/dL low-density lipoprotein cholesterol of 180 mg/dL and triglyceride levels of 259 mg/dL. This patient demonstrates many features we see with increasing frequency in reproductive-aged women as we deal with the obesity epidemic.
A complicated diagnosis
Nicole’s abdominal obesity, high triglycerides, and evidence of insulin-resistance constituted metabolic syndrome. Although there are many different criteria for this, we used those of the National Cholesterol Education Program (TABLE).1
| Components of Metabolic Syndrome Related to Cardiovascular Disease
Source: Grundy SM, et al. Circulation. 2002;106:3143-3421. |
Long-term prognosis?
If she is not treated, Nicole would be unable to achieve pregnancy because she does not ovulate and she may have an increased risk of endometrial cancer. Her obesity would eventually cause increasing insulin levels, exhaustion of her pancreatic insulin secretion, and type 2 diabetes. Her obesity might also result in osteoarthritis and difficulty with mobility. Her lipid levels confer increased risk of hypertension and cardiovascular events.
Selecting a treatment strategy: Considerations
If this patient does not desire pregnancy, short-term treatment for endometrial hyperplasia involves administration of progesterone or progestins for at least 2 weeks per month for 3 months, with a follow-up endometrial biopsy.
Nicole also needs protection against endometrial hyperplasia even after this episode is addressed. Oral contraceptives are frequently used for long-term treatment, although there might be concern about the risk of deep vein thrombosis (DVT), particularly in obese or morbidly obese patients and older patients who smoke.
If this patient were not a candidate for oral contraceptives, progesterone or a progestin would typically be administered for approximately 2 weeks each month to prevent recurrence of the hyperplasia. Patients who do not desire a monthly withdrawal bleed can take progesterone every 2 to 3 months. Patients who are being treated with a progestogen for amenorrhea and hyperplasia may occasionally ovulate. They should be counseled that an alternative form of contraception, such as condoms, is needed to avoid pregnancy.
An intrauterine device (IUD) for this patient could also be considered for this patient. We have individual patients using a levonorgestrel-containing IUD. One challenge we have faced with some of our obese patients is difficultly accessing the cervix for placement.
Case study follow-up
Nicole received norethindrone,2,3 5 mg, a strong progestin, for 2 weeks and had a withdrawal flow for 3 months in a row. Her repeat endometrial biopsy showed a normal endometrium. She still did not ovulate, and since she was not sexually active at that time, she elected to use progesterone, 200 mg, for 14 days every 2 months. We treated her acne with topical clindamycin gel and she joined our supervised diet and exercise program. She is considering bariatric surgery but must participate in the lifestyle program for at least 6 months in order to qualify.
| Click here to take the FREE CME/CE test online for 0.5 credits References 1. Grundy SM, Becker D, Clark LT, et al, for the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation.2002;106:3143-3421. 2. King RJ, Whitehead MI. Assessment of the potency of orally administered progestins in women. Fertil Steril.1986;46(6):1062-1066. 3. Whitehead MI, Hillard TC, Crook D. The role and use of progestogens. Obstet Gynecol.1990;75(4)suppl):59S-76S. Additional newsletters with free CME/CE: Progesterone use in assisted reproductive technology Sexuality, Reproduction & Menopause © 2009 Quadrant HealthCom Inc. |
An e-newsletter focusing on challenging case studies
Progesterone use in management of secondary amenorrhea
Read the following case study and earn
FREE 0.5 CME/CE CREDIT
Expiration date: July 31, 2009
Estimated time to complete activity: 0.5 hour
Target: Physicians, physician assistants and nurse practitioners
Supported by an educational grant from Solvay Pharmaceuticals, Inc.
Sponsored by the American Society for Reproductive Medicine.
Click here to take the FREE CME/CE test online for 0.5 credits
Nicole is 27 years old, gravida 0, with a long history of obesity and great difficulty losing weight. She reports having irregular menstrual cycles ranging from 45 days to 6 months apart. Her last menstrual period was 5 months ago, when she had a heavy menses that lasted 2 weeks. Her body mass index is 42 kg/m2, which is considered morbid obesity. Nicole has a large abdominal pannus and normal blood pressure. She has scattered acne lesions on her face and upper back and acanthosis nigricans, a dark pigmentation around the neck and the axilla. Acanthosis nigricans is a biomarker for insulin resistance and high circulating insulin levels.
Nicole’s pelvic exam showed a normal vagina and cervix, but it was not possible to palpate her uterus or ovaries because of her abdominal girth. Transvaginal ultrasound found an endometrial thickness of 22 mm. Her ovaries appeared to be multicystic but had normal ovarian volumes. We performed an endometrial biopsy because of concerns about the long duration of unopposed estrogen exposure. The biopsy revealed complex hyperplasia with no atypia.
A lipid profile demonstrated cholesterol 245 mg/dL low-density lipoprotein cholesterol of 180 mg/dL and triglyceride levels of 259 mg/dL. This patient demonstrates many features we see with increasing frequency in reproductive-aged women as we deal with the obesity epidemic.
A complicated diagnosis
Nicole’s abdominal obesity, high triglycerides, and evidence of insulin-resistance constituted metabolic syndrome. Although there are many different criteria for this, we used those of the National Cholesterol Education Program (TABLE).1
| Components of Metabolic Syndrome Related to Cardiovascular Disease
Source: Grundy SM, et al. Circulation. 2002;106:3143-3421. |
Long-term prognosis?
If she is not treated, Nicole would be unable to achieve pregnancy because she does not ovulate and she may have an increased risk of endometrial cancer. Her obesity would eventually cause increasing insulin levels, exhaustion of her pancreatic insulin secretion, and type 2 diabetes. Her obesity might also result in osteoarthritis and difficulty with mobility. Her lipid levels confer increased risk of hypertension and cardiovascular events.
Selecting a treatment strategy: Considerations
If this patient does not desire pregnancy, short-term treatment for endometrial hyperplasia involves administration of progesterone or progestins for at least 2 weeks per month for 3 months, with a follow-up endometrial biopsy.
Nicole also needs protection against endometrial hyperplasia even after this episode is addressed. Oral contraceptives are frequently used for long-term treatment, although there might be concern about the risk of deep vein thrombosis (DVT), particularly in obese or morbidly obese patients and older patients who smoke.
If this patient were not a candidate for oral contraceptives, progesterone or a progestin would typically be administered for approximately 2 weeks each month to prevent recurrence of the hyperplasia. Patients who do not desire a monthly withdrawal bleed can take progesterone every 2 to 3 months. Patients who are being treated with a progestogen for amenorrhea and hyperplasia may occasionally ovulate. They should be counseled that an alternative form of contraception, such as condoms, is needed to avoid pregnancy.
An intrauterine device (IUD) for this patient could also be considered for this patient. We have individual patients using a levonorgestrel-containing IUD. One challenge we have faced with some of our obese patients is difficultly accessing the cervix for placement.
Case study follow-up
Nicole received norethindrone,2,3 5 mg, a strong progestin, for 2 weeks and had a withdrawal flow for 3 months in a row. Her repeat endometrial biopsy showed a normal endometrium. She still did not ovulate, and since she was not sexually active at that time, she elected to use progesterone, 200 mg, for 14 days every 2 months. We treated her acne with topical clindamycin gel and she joined our supervised diet and exercise program. She is considering bariatric surgery but must participate in the lifestyle program for at least 6 months in order to qualify.
| Click here to take the FREE CME/CE test online for 0.5 credits References 1. Grundy SM, Becker D, Clark LT, et al, for the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation.2002;106:3143-3421. 2. King RJ, Whitehead MI. Assessment of the potency of orally administered progestins in women. Fertil Steril.1986;46(6):1062-1066. 3. Whitehead MI, Hillard TC, Crook D. The role and use of progestogens. Obstet Gynecol.1990;75(4)suppl):59S-76S. Additional newsletters with free CME/CE: Progesterone use in assisted reproductive technology Sexuality, Reproduction & Menopause © 2009 Quadrant HealthCom Inc. |
An e-newsletter focusing on challenging case studies
Progesterone use in management of secondary amenorrhea
Read the following case study and earn
FREE 0.5 CME/CE CREDIT
Expiration date: July 31, 2009
Estimated time to complete activity: 0.5 hour
Target: Physicians, physician assistants and nurse practitioners
Supported by an educational grant from Solvay Pharmaceuticals, Inc.
Sponsored by the American Society for Reproductive Medicine.
Click here to take the FREE CME/CE test online for 0.5 credits
Nicole is 27 years old, gravida 0, with a long history of obesity and great difficulty losing weight. She reports having irregular menstrual cycles ranging from 45 days to 6 months apart. Her last menstrual period was 5 months ago, when she had a heavy menses that lasted 2 weeks. Her body mass index is 42 kg/m2, which is considered morbid obesity. Nicole has a large abdominal pannus and normal blood pressure. She has scattered acne lesions on her face and upper back and acanthosis nigricans, a dark pigmentation around the neck and the axilla. Acanthosis nigricans is a biomarker for insulin resistance and high circulating insulin levels.
Nicole’s pelvic exam showed a normal vagina and cervix, but it was not possible to palpate her uterus or ovaries because of her abdominal girth. Transvaginal ultrasound found an endometrial thickness of 22 mm. Her ovaries appeared to be multicystic but had normal ovarian volumes. We performed an endometrial biopsy because of concerns about the long duration of unopposed estrogen exposure. The biopsy revealed complex hyperplasia with no atypia.
A lipid profile demonstrated cholesterol 245 mg/dL low-density lipoprotein cholesterol of 180 mg/dL and triglyceride levels of 259 mg/dL. This patient demonstrates many features we see with increasing frequency in reproductive-aged women as we deal with the obesity epidemic.
A complicated diagnosis
Nicole’s abdominal obesity, high triglycerides, and evidence of insulin-resistance constituted metabolic syndrome. Although there are many different criteria for this, we used those of the National Cholesterol Education Program (TABLE).1
| Components of Metabolic Syndrome Related to Cardiovascular Disease
Source: Grundy SM, et al. Circulation. 2002;106:3143-3421. |
Long-term prognosis?
If she is not treated, Nicole would be unable to achieve pregnancy because she does not ovulate and she may have an increased risk of endometrial cancer. Her obesity would eventually cause increasing insulin levels, exhaustion of her pancreatic insulin secretion, and type 2 diabetes. Her obesity might also result in osteoarthritis and difficulty with mobility. Her lipid levels confer increased risk of hypertension and cardiovascular events.
Selecting a treatment strategy: Considerations
If this patient does not desire pregnancy, short-term treatment for endometrial hyperplasia involves administration of progesterone or progestins for at least 2 weeks per month for 3 months, with a follow-up endometrial biopsy.
Nicole also needs protection against endometrial hyperplasia even after this episode is addressed. Oral contraceptives are frequently used for long-term treatment, although there might be concern about the risk of deep vein thrombosis (DVT), particularly in obese or morbidly obese patients and older patients who smoke.
If this patient were not a candidate for oral contraceptives, progesterone or a progestin would typically be administered for approximately 2 weeks each month to prevent recurrence of the hyperplasia. Patients who do not desire a monthly withdrawal bleed can take progesterone every 2 to 3 months. Patients who are being treated with a progestogen for amenorrhea and hyperplasia may occasionally ovulate. They should be counseled that an alternative form of contraception, such as condoms, is needed to avoid pregnancy.
An intrauterine device (IUD) for this patient could also be considered for this patient. We have individual patients using a levonorgestrel-containing IUD. One challenge we have faced with some of our obese patients is difficultly accessing the cervix for placement.
Case study follow-up
Nicole received norethindrone,2,3 5 mg, a strong progestin, for 2 weeks and had a withdrawal flow for 3 months in a row. Her repeat endometrial biopsy showed a normal endometrium. She still did not ovulate, and since she was not sexually active at that time, she elected to use progesterone, 200 mg, for 14 days every 2 months. We treated her acne with topical clindamycin gel and she joined our supervised diet and exercise program. She is considering bariatric surgery but must participate in the lifestyle program for at least 6 months in order to qualify.
| Click here to take the FREE CME/CE test online for 0.5 credits References 1. Grundy SM, Becker D, Clark LT, et al, for the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation.2002;106:3143-3421. 2. King RJ, Whitehead MI. Assessment of the potency of orally administered progestins in women. Fertil Steril.1986;46(6):1062-1066. 3. Whitehead MI, Hillard TC, Crook D. The role and use of progestogens. Obstet Gynecol.1990;75(4)suppl):59S-76S. Additional newsletters with free CME/CE: Progesterone use in assisted reproductive technology Sexuality, Reproduction & Menopause © 2009 Quadrant HealthCom Inc. |
Trivialization of Diagnosis
Historically, diagnosis has been central to patient care. Making the correct diagnosis serves as a guide to the choice of treatment, permits assessment of prognosis, and indicates what complications to expect. Arriving at the correct diagnosis has been a major goalthe Holy Grail, as it were. Accurate diagnosis continues to be a major focus of medical practice, and accurate diagnoses are routinely made every day. Still, many experienced clinicians have the impression that in recent years the primacy of diagnosis has been coming under attack from several sources.
A decade ago, Thomas Szasz pointed out that disease is a fact of nature, while diagnosis is man made.1 The noun diagnosis is derived from the Greek verb diagignoskeinindicating knowledge attained through analysis. As defined in Merriam‐Webster's Collegiate Dictionary, the diagnosis essentially means the conclusion arrived at by the art of identifying a disease. It is the product of an intellectual effort of a particular analytic type. The response to the question What is the diagnosis? has been the name of the specific disease entity with which the patient is afflicted.
Disease entities represent coherent, organizing concepts.2 A specific disease is a condition with characteristic manifestationsclinical, histologic, or pathophysiologic. If untreated, it results in dysfunction or, in some cases, death. Differentiation of one disease from another is enhanced when there is some sort of understanding, even if incomplete, of the specific pathophysiology at play. Admittedly, concepts of what constitute specific disease entities are not fixed; they evolve with time. Not all diseases have been identified. The underlying etiology may or may not be known. Nonetheless, diseases are recognized as specific entities, distinct from other diseases. Thus, anemia is not regarded as a disease, while pernicious anemia and iron deficiency anemia are diseases. Fever is not a disease, while typhoid fever is. Arthritis is not a disease, while gonococcal arthritis is.
Billable Terms Are Replacing Traditional Medical Diagnoses
The term diagnosis has been redefined to comply with the need to enter a diagnosis for billing purposes. Use of this term for this purpose has confused the issue. Diagnoses entered for such purposes are largely derived from International Classification of Diseases (ICD) lists.3 However, the ICD was not intended to definitively identify underlying diseases, nor to serve as a guide to management and prognostication. The 6th revision of the ICD in 1948, the first revision to be widely employed, was designed for epidemiologic purposes and achieved widespread use to obtain mortality and morbidity statistics.4 It was subsequently also used as a tool to index hospital medical records.
Significantly, it was also employed for billing purposes, with far‐reaching pernicious consequences. Although the ICD purports to be a list of diseases, it actually includes symptoms and signs. Consequently, in the billing context, diagnosis no longer necessarily refers to specific disease states; it now refers to billable termsoften the manifestation that was responsible for the patient seeking medical assistance. Far from being the product of an intellectual effort, it is often merely a justification for submitting a bill. Examples of such diagnoses are shown in Table 1. Many of them represent symptoms, signs, or laboratory abnormalities. The importance of accurate medical diagnosis has been cheapened by this change. The effect is to devalue diagnosisto lessen its status as the Holy Grail.
| Abdominal pain | General symptoms | Special symptom |
| Abnormal blood test | Immune disorders | Splenomegaly |
| Back disorder | Joint disorder | Throat pain |
| Coagulation defects | Myoneural disorder | Urinary symptoms |
| Diseases of esophagus | Otalgia | Visual disturbance |
| Eye disorders | Pain in joint | Vomiting |
| Fluid/electrolyte disorders | Right lower quadrant mass | Wheezing |
The effect of this on trainees is invidious, and predictable. The traditional meaning of diagnosis is being replaced in our minds. Physicians in training are tempted to deceive themselves into believing that they have arrived at an understanding of what they are dealing with when they enter such a diagnosis. After all, have they not responded to the question: what is the diagnosis?
We do not mean to imply that physicians are doing anything wrong by entering ICD terms for billing purposes. What must be done for billing purposes must be done. It is important to be aware, however, and to continually remind ourselves, that what has been entered for this purpose is often not a true medical diagnosis.
Further, when the diagnosis is not yet known, it is not possible to enter a true diagnosis. There is no way to say I don't know. It would be preferable to simply admit that the diagnosis is not yet established, as a medical resident has recently emphasized.5
Diagnosis Often Gets Short Shrift Because of the Perceived Urgency of Discharge
The emphasis on diagnosis several generations ago may have resulted, at least in part, from the relative paucity of effective therapeutic interventions before the 1930s. Things have changed; therapeutic capabilities are much more powerful now. Making the correct diagnosis seems to have lost its urgency. Instead of the major question being what is the diagnosis? it now is often what do we do now? The diagnosis is often an afterthought. Indeed, it is sometimes not even mentioned in discharge summaries, where, not uncommonly, one sees nondiagnoses such as blood in stool or polyarthritis.
In addition, we are under pressure to shorten the inpatient stay of hospitalized patients. At least a portion of the public is aware of this; thus, it has been noted in the New York Times that: The pressure to get patients out of the hospital rapidly can focus medical attention on treatment rather than diagnosis.6 We commonly seek to ameliorate the patients' status to permit discharge before (or often without) learning what we are dealing with. Sometimes one senses that the primary question has become how soon can we discharge this patient?
A price is paid for this. In the absence of a valid diagnosis, patients may be subjected to a broad array of nonessential investigations and therapeutic interventions, each with its own possible complications. Patients are often discharged without a diagnosis having been made, presenting a serious challenge to outpatient physicians who are left to manage them without a clear idea of what they are dealing with. It often falls to the outpatient physicians to make the diagnosis. This is somewhat problematic, since they themselves are under harsh time pressure. Patients often require rehospitalization for the same as‐yet‐undiagnosed condition.
The Problem‐Oriented Record Poses Problems
The widespread use of the problem‐oriented record, originated by Lawrence Weed,7 has led to problems of its own.8 It has evolved, away from its original intent. In practice, its major emphasis often seems to be on identification of problems and tracking their progress, rather than on synthesis. This often leads to muddy rather than clear diagnostic thinking. Assessments and progress notes frequently consist of lists of symptoms, organs, abnormal laboratory findings, or even medical specialties. The net effect is often fragmented thinkingas Weed7 put it, failure to integrate findings into a single entity. Synthesizing diverse findings into a single entity, when possible, is necessary to define a diagnosis. Failure to do so may have serious consequences. In a recent study of diagnostic errors in internal medicine, cognitive errors were frequently found to contribute to such errors.9 The most common cognitive problem was faulty synthesis. How much worse than faulty synthesis is failure to synthesize at all!
Presumptive Diagnoses, Even if Incorrect, Metamorphose into Established Diagnoses
We must often treat empirically. When there is no firm diagnosis, presumptive diagnoses must be made and acted upon. Unfortunately, there are not always mechanisms for the physician to make it clear that his or her diagnosis is only presumptive. (A common example is acute viral syndrome, generally an educated guess.) All too often, presumptive diagnoses are entered, without qualification, as definitive diagnoses, and then achieve immortality. Thus, if a patient is incorrectly diagnosed as having rheumatoid arthritis, all subsequent presentations will start: A so‐and‐so year‐old woman with rheumatoid arthritis for many years Presumptive diagnoses are frequently not questioned. It is easier to assume that they were arrived at after due consideration. Once entered in the medical record, they may be difficult to remove.
It is true that the need to arrive at a precise diagnosis is less pressing for some medical specialties than for others. Emergency physicians, critical care physicians, and frequently, surgeons, must commonly act on the basis of presumptive diagnoses. In contrast, internists, family physicians, psychiatrists, and indeed all physicians who care for patients with chronic illnesses can, with time, be expected to sort out accurate from inaccurate presumptive diagnoses.
A specific example of the problem of presumptive diagnosis is of interest. It is not uncommon, following a first encounter, for a diagnosis to be entered based on the patient's history alone. While such diagnoses are frequently correct, they are not invariably correct. The patient may have arrived at the conclusion herself; she may have misunderstood what she was told by her physician, or her physician may have been in error. Such inaccurate diagnoses also often achieve immortality in the medical record.
Apparent Disparaging of the Importance of Diagnosis
Further trivialization has come from a number of publications expressing concerns about the importance of diagnosis. Thus we read that there are negative consequences of emphasis on diagnosis. When we know what is wrong, we focus less on the individual and more on the disease.10 In his recent book Our Present Complaint. American Medicine, Then and Now, the scholar C.E. Rosenberg11 includes a chapter with the provocative title The Tyranny of Diagnosis. He points out that even a century ago the fear was expressed that burgeoning scientific medicine would lead to denigration of physicians' holistic and intuitive skills.11 Other authors maintain that firm diagnoses may be misleading, since many diseases are a matter of degree in a continuuma spectrumthat are best defined employing a statistical model of risk prediction.12 The suggestion is made that the usefulness of diagnostic tests should not be related to the presence or absence of a disease, but rather to whether they influence outcome.13
Scientific medicine is focused on diagnosis. Denigration of diagnosis has often come, as a philosophical posture, from opponents of reductionist thinking. As Rosenberg11 points out: It has become fashionable among humanistic and social science‐oriented commentators to dwell on the distinction between illness and disease, between the patient's felt experience and the constructions placed on that experience by the world of medicine. Their opposition, he feels, reflects the value‐laden mutual incompatibility (real or apparent) of art and science, of holism and reductionism.2
It is true that medicine is more than just biology. There is a great deal to be said for the view that scientific medicine tends to deemphasize the humanistic, holistic aspects of medical practice. However, despite all these concerns, most physiciansand, to be fair, most criticsagree that making an accurate diagnosis is important. Thus, though the title of his relevant chapter is The Tyranny of Diagnosis, Rosenberg11 states: I might just as well have used the term indispensability. Indeed, the opening words of that chapter are: Diagnosis has always played a pivotal role in medicine.11 Other authors cited above issue this disclaimer: We are not against diagnosis. Diagnosis does and always will play a central role in clinical medicine.12
The importance of diagnosis is underscored by the vigorous debate about how to assess diagnostic tests;14 apparently, diagnosis does indeed matter. While it is true that diagnoses are not always precise, objective, and quantifiable,10 abundant evidence points to the unavoidable conclusion that identifying the patient's disease is heuristically useful; that is, it works.2 The track record of modern scientific medicine in improving mortality and morbidity speaks for itself. It hardly seems necessary to defend it. In addition to representing a valuable intellectual challenge in its own right, diagnosis is pivotal to the scientific mission of medicine.
What Can Be Done?
The net effect of all these forces: the use of billable terms as diagnoses, the pressures of managed care, fragmented problem lists, persistence of incorrect presumptive diagnoses in medical records, and antireductionist criticisms is to encourage sloppy diagnostic thinking in some physicians. What can be done to emphasize the proper use of differential diagnosis in arriving at a definitive diagnosis? What can be done to underscore the importance of differentiating between presumptive and definitive diagnoses? Most importantly, how can we instill the respect for the intellectual honesty necessary to acquire and retain these skills?
Above all, we should relentlessly impress on our students and trainees the importance of arriving at an accurate definitive diagnosis. They should be aware that the job is only half done if the diagnosis has not been made. We should do this repeatedly, both by word and by example. We ourselves must display intellectual honesty.
In addition, we ought to be able to enter diagnosis uncertain, so coded, or to append the phrase cause unknown after the manifestation of concern, when we don't really know what is going on. We should routinely indicate when a diagnosis is merely presumptive. Perhaps we need a way to indicate: This diagnosis is definitive or to indicate the specific evidence that led to the diagnosis (eg, biopsy, laboratory result, radiographic finding). Finally, we need to correct the current confusion between diseases and billable terms, to differentiate the disease from the symptom, perhaps by labeling ICD‐9‐CM codes simply as billing codes, with a separate entry for actual medical diagnoses.
Although powerful historical forces have brought us to this state, we believe that arriving at the correct diagnosis is at least as important now as it has been in the past, and that its primacy should be recognized, celebrated, and fought for. We owe our patients no less.
Acknowledgements
The authors thank Drs. James Pile, Neal Dawson, and David Samols for their helpful suggestions.
- .What counts as disease? Rationales and rationalizations for treatment.Forsch Komplementarmed.1998;5(suppl S1):40–46.
- .What is disease? In memory of Owsei Temkin.Bull Hist Med.2003;77:491–505.
- World Health Organization (WHO). International Classification of Diseases (ICD). Available at: http://www.who.int/classifications/icd/en. Accessed June2009.
- World Health Organization (WHO). History of the development of the ICD. Available at: http://www.who.int/classifications/icd/en/HistoryOfICD. pdf. Accessed June2009.
- .Living unlabeled—diagnosis and disorder.N Engl J Med.2008;359:1650–1653.
- . Poison Pill. New York Times Magazine. 2008: 24–26. Available at: http://www.nytimes.com/2008/04/13/magazine/13wwln‐diagnosis‐t.html. Accessed June2009.
- .Medical records that guide and teach.N Engl J Med.1968;278:593–600.
- .Clear writing, clear thinking and the disappearing art of the problem list.J Hosp Med.2007;2:199–202.
- , , .Diagnostic error in internal medicine.Arch Intern Med.2005;165:1493–1499.
- . The Tyranny of Diagnosis. New York Times. Available at: http://www.nytimes.com/2008/09/19/health/chen9‐18.html?partner=rssnyt2007.
- , , .Against diagnosis.Ann Intern Med.2008;149:200–203.
- , , .A philosophical perspective supports the need for patient‐outcome studies in diagnostic test evaluation.J Clin Epidemiol.2009;62:58–61.
- , .Evidence based diagnostics.BMJ.2005;330:724–726.
Historically, diagnosis has been central to patient care. Making the correct diagnosis serves as a guide to the choice of treatment, permits assessment of prognosis, and indicates what complications to expect. Arriving at the correct diagnosis has been a major goalthe Holy Grail, as it were. Accurate diagnosis continues to be a major focus of medical practice, and accurate diagnoses are routinely made every day. Still, many experienced clinicians have the impression that in recent years the primacy of diagnosis has been coming under attack from several sources.
A decade ago, Thomas Szasz pointed out that disease is a fact of nature, while diagnosis is man made.1 The noun diagnosis is derived from the Greek verb diagignoskeinindicating knowledge attained through analysis. As defined in Merriam‐Webster's Collegiate Dictionary, the diagnosis essentially means the conclusion arrived at by the art of identifying a disease. It is the product of an intellectual effort of a particular analytic type. The response to the question What is the diagnosis? has been the name of the specific disease entity with which the patient is afflicted.
Disease entities represent coherent, organizing concepts.2 A specific disease is a condition with characteristic manifestationsclinical, histologic, or pathophysiologic. If untreated, it results in dysfunction or, in some cases, death. Differentiation of one disease from another is enhanced when there is some sort of understanding, even if incomplete, of the specific pathophysiology at play. Admittedly, concepts of what constitute specific disease entities are not fixed; they evolve with time. Not all diseases have been identified. The underlying etiology may or may not be known. Nonetheless, diseases are recognized as specific entities, distinct from other diseases. Thus, anemia is not regarded as a disease, while pernicious anemia and iron deficiency anemia are diseases. Fever is not a disease, while typhoid fever is. Arthritis is not a disease, while gonococcal arthritis is.
Billable Terms Are Replacing Traditional Medical Diagnoses
The term diagnosis has been redefined to comply with the need to enter a diagnosis for billing purposes. Use of this term for this purpose has confused the issue. Diagnoses entered for such purposes are largely derived from International Classification of Diseases (ICD) lists.3 However, the ICD was not intended to definitively identify underlying diseases, nor to serve as a guide to management and prognostication. The 6th revision of the ICD in 1948, the first revision to be widely employed, was designed for epidemiologic purposes and achieved widespread use to obtain mortality and morbidity statistics.4 It was subsequently also used as a tool to index hospital medical records.
Significantly, it was also employed for billing purposes, with far‐reaching pernicious consequences. Although the ICD purports to be a list of diseases, it actually includes symptoms and signs. Consequently, in the billing context, diagnosis no longer necessarily refers to specific disease states; it now refers to billable termsoften the manifestation that was responsible for the patient seeking medical assistance. Far from being the product of an intellectual effort, it is often merely a justification for submitting a bill. Examples of such diagnoses are shown in Table 1. Many of them represent symptoms, signs, or laboratory abnormalities. The importance of accurate medical diagnosis has been cheapened by this change. The effect is to devalue diagnosisto lessen its status as the Holy Grail.
| Abdominal pain | General symptoms | Special symptom |
| Abnormal blood test | Immune disorders | Splenomegaly |
| Back disorder | Joint disorder | Throat pain |
| Coagulation defects | Myoneural disorder | Urinary symptoms |
| Diseases of esophagus | Otalgia | Visual disturbance |
| Eye disorders | Pain in joint | Vomiting |
| Fluid/electrolyte disorders | Right lower quadrant mass | Wheezing |
The effect of this on trainees is invidious, and predictable. The traditional meaning of diagnosis is being replaced in our minds. Physicians in training are tempted to deceive themselves into believing that they have arrived at an understanding of what they are dealing with when they enter such a diagnosis. After all, have they not responded to the question: what is the diagnosis?
We do not mean to imply that physicians are doing anything wrong by entering ICD terms for billing purposes. What must be done for billing purposes must be done. It is important to be aware, however, and to continually remind ourselves, that what has been entered for this purpose is often not a true medical diagnosis.
Further, when the diagnosis is not yet known, it is not possible to enter a true diagnosis. There is no way to say I don't know. It would be preferable to simply admit that the diagnosis is not yet established, as a medical resident has recently emphasized.5
Diagnosis Often Gets Short Shrift Because of the Perceived Urgency of Discharge
The emphasis on diagnosis several generations ago may have resulted, at least in part, from the relative paucity of effective therapeutic interventions before the 1930s. Things have changed; therapeutic capabilities are much more powerful now. Making the correct diagnosis seems to have lost its urgency. Instead of the major question being what is the diagnosis? it now is often what do we do now? The diagnosis is often an afterthought. Indeed, it is sometimes not even mentioned in discharge summaries, where, not uncommonly, one sees nondiagnoses such as blood in stool or polyarthritis.
In addition, we are under pressure to shorten the inpatient stay of hospitalized patients. At least a portion of the public is aware of this; thus, it has been noted in the New York Times that: The pressure to get patients out of the hospital rapidly can focus medical attention on treatment rather than diagnosis.6 We commonly seek to ameliorate the patients' status to permit discharge before (or often without) learning what we are dealing with. Sometimes one senses that the primary question has become how soon can we discharge this patient?
A price is paid for this. In the absence of a valid diagnosis, patients may be subjected to a broad array of nonessential investigations and therapeutic interventions, each with its own possible complications. Patients are often discharged without a diagnosis having been made, presenting a serious challenge to outpatient physicians who are left to manage them without a clear idea of what they are dealing with. It often falls to the outpatient physicians to make the diagnosis. This is somewhat problematic, since they themselves are under harsh time pressure. Patients often require rehospitalization for the same as‐yet‐undiagnosed condition.
The Problem‐Oriented Record Poses Problems
The widespread use of the problem‐oriented record, originated by Lawrence Weed,7 has led to problems of its own.8 It has evolved, away from its original intent. In practice, its major emphasis often seems to be on identification of problems and tracking their progress, rather than on synthesis. This often leads to muddy rather than clear diagnostic thinking. Assessments and progress notes frequently consist of lists of symptoms, organs, abnormal laboratory findings, or even medical specialties. The net effect is often fragmented thinkingas Weed7 put it, failure to integrate findings into a single entity. Synthesizing diverse findings into a single entity, when possible, is necessary to define a diagnosis. Failure to do so may have serious consequences. In a recent study of diagnostic errors in internal medicine, cognitive errors were frequently found to contribute to such errors.9 The most common cognitive problem was faulty synthesis. How much worse than faulty synthesis is failure to synthesize at all!
Presumptive Diagnoses, Even if Incorrect, Metamorphose into Established Diagnoses
We must often treat empirically. When there is no firm diagnosis, presumptive diagnoses must be made and acted upon. Unfortunately, there are not always mechanisms for the physician to make it clear that his or her diagnosis is only presumptive. (A common example is acute viral syndrome, generally an educated guess.) All too often, presumptive diagnoses are entered, without qualification, as definitive diagnoses, and then achieve immortality. Thus, if a patient is incorrectly diagnosed as having rheumatoid arthritis, all subsequent presentations will start: A so‐and‐so year‐old woman with rheumatoid arthritis for many years Presumptive diagnoses are frequently not questioned. It is easier to assume that they were arrived at after due consideration. Once entered in the medical record, they may be difficult to remove.
It is true that the need to arrive at a precise diagnosis is less pressing for some medical specialties than for others. Emergency physicians, critical care physicians, and frequently, surgeons, must commonly act on the basis of presumptive diagnoses. In contrast, internists, family physicians, psychiatrists, and indeed all physicians who care for patients with chronic illnesses can, with time, be expected to sort out accurate from inaccurate presumptive diagnoses.
A specific example of the problem of presumptive diagnosis is of interest. It is not uncommon, following a first encounter, for a diagnosis to be entered based on the patient's history alone. While such diagnoses are frequently correct, they are not invariably correct. The patient may have arrived at the conclusion herself; she may have misunderstood what she was told by her physician, or her physician may have been in error. Such inaccurate diagnoses also often achieve immortality in the medical record.
Apparent Disparaging of the Importance of Diagnosis
Further trivialization has come from a number of publications expressing concerns about the importance of diagnosis. Thus we read that there are negative consequences of emphasis on diagnosis. When we know what is wrong, we focus less on the individual and more on the disease.10 In his recent book Our Present Complaint. American Medicine, Then and Now, the scholar C.E. Rosenberg11 includes a chapter with the provocative title The Tyranny of Diagnosis. He points out that even a century ago the fear was expressed that burgeoning scientific medicine would lead to denigration of physicians' holistic and intuitive skills.11 Other authors maintain that firm diagnoses may be misleading, since many diseases are a matter of degree in a continuuma spectrumthat are best defined employing a statistical model of risk prediction.12 The suggestion is made that the usefulness of diagnostic tests should not be related to the presence or absence of a disease, but rather to whether they influence outcome.13
Scientific medicine is focused on diagnosis. Denigration of diagnosis has often come, as a philosophical posture, from opponents of reductionist thinking. As Rosenberg11 points out: It has become fashionable among humanistic and social science‐oriented commentators to dwell on the distinction between illness and disease, between the patient's felt experience and the constructions placed on that experience by the world of medicine. Their opposition, he feels, reflects the value‐laden mutual incompatibility (real or apparent) of art and science, of holism and reductionism.2
It is true that medicine is more than just biology. There is a great deal to be said for the view that scientific medicine tends to deemphasize the humanistic, holistic aspects of medical practice. However, despite all these concerns, most physiciansand, to be fair, most criticsagree that making an accurate diagnosis is important. Thus, though the title of his relevant chapter is The Tyranny of Diagnosis, Rosenberg11 states: I might just as well have used the term indispensability. Indeed, the opening words of that chapter are: Diagnosis has always played a pivotal role in medicine.11 Other authors cited above issue this disclaimer: We are not against diagnosis. Diagnosis does and always will play a central role in clinical medicine.12
The importance of diagnosis is underscored by the vigorous debate about how to assess diagnostic tests;14 apparently, diagnosis does indeed matter. While it is true that diagnoses are not always precise, objective, and quantifiable,10 abundant evidence points to the unavoidable conclusion that identifying the patient's disease is heuristically useful; that is, it works.2 The track record of modern scientific medicine in improving mortality and morbidity speaks for itself. It hardly seems necessary to defend it. In addition to representing a valuable intellectual challenge in its own right, diagnosis is pivotal to the scientific mission of medicine.
What Can Be Done?
The net effect of all these forces: the use of billable terms as diagnoses, the pressures of managed care, fragmented problem lists, persistence of incorrect presumptive diagnoses in medical records, and antireductionist criticisms is to encourage sloppy diagnostic thinking in some physicians. What can be done to emphasize the proper use of differential diagnosis in arriving at a definitive diagnosis? What can be done to underscore the importance of differentiating between presumptive and definitive diagnoses? Most importantly, how can we instill the respect for the intellectual honesty necessary to acquire and retain these skills?
Above all, we should relentlessly impress on our students and trainees the importance of arriving at an accurate definitive diagnosis. They should be aware that the job is only half done if the diagnosis has not been made. We should do this repeatedly, both by word and by example. We ourselves must display intellectual honesty.
In addition, we ought to be able to enter diagnosis uncertain, so coded, or to append the phrase cause unknown after the manifestation of concern, when we don't really know what is going on. We should routinely indicate when a diagnosis is merely presumptive. Perhaps we need a way to indicate: This diagnosis is definitive or to indicate the specific evidence that led to the diagnosis (eg, biopsy, laboratory result, radiographic finding). Finally, we need to correct the current confusion between diseases and billable terms, to differentiate the disease from the symptom, perhaps by labeling ICD‐9‐CM codes simply as billing codes, with a separate entry for actual medical diagnoses.
Although powerful historical forces have brought us to this state, we believe that arriving at the correct diagnosis is at least as important now as it has been in the past, and that its primacy should be recognized, celebrated, and fought for. We owe our patients no less.
Acknowledgements
The authors thank Drs. James Pile, Neal Dawson, and David Samols for their helpful suggestions.
Historically, diagnosis has been central to patient care. Making the correct diagnosis serves as a guide to the choice of treatment, permits assessment of prognosis, and indicates what complications to expect. Arriving at the correct diagnosis has been a major goalthe Holy Grail, as it were. Accurate diagnosis continues to be a major focus of medical practice, and accurate diagnoses are routinely made every day. Still, many experienced clinicians have the impression that in recent years the primacy of diagnosis has been coming under attack from several sources.
A decade ago, Thomas Szasz pointed out that disease is a fact of nature, while diagnosis is man made.1 The noun diagnosis is derived from the Greek verb diagignoskeinindicating knowledge attained through analysis. As defined in Merriam‐Webster's Collegiate Dictionary, the diagnosis essentially means the conclusion arrived at by the art of identifying a disease. It is the product of an intellectual effort of a particular analytic type. The response to the question What is the diagnosis? has been the name of the specific disease entity with which the patient is afflicted.
Disease entities represent coherent, organizing concepts.2 A specific disease is a condition with characteristic manifestationsclinical, histologic, or pathophysiologic. If untreated, it results in dysfunction or, in some cases, death. Differentiation of one disease from another is enhanced when there is some sort of understanding, even if incomplete, of the specific pathophysiology at play. Admittedly, concepts of what constitute specific disease entities are not fixed; they evolve with time. Not all diseases have been identified. The underlying etiology may or may not be known. Nonetheless, diseases are recognized as specific entities, distinct from other diseases. Thus, anemia is not regarded as a disease, while pernicious anemia and iron deficiency anemia are diseases. Fever is not a disease, while typhoid fever is. Arthritis is not a disease, while gonococcal arthritis is.
Billable Terms Are Replacing Traditional Medical Diagnoses
The term diagnosis has been redefined to comply with the need to enter a diagnosis for billing purposes. Use of this term for this purpose has confused the issue. Diagnoses entered for such purposes are largely derived from International Classification of Diseases (ICD) lists.3 However, the ICD was not intended to definitively identify underlying diseases, nor to serve as a guide to management and prognostication. The 6th revision of the ICD in 1948, the first revision to be widely employed, was designed for epidemiologic purposes and achieved widespread use to obtain mortality and morbidity statistics.4 It was subsequently also used as a tool to index hospital medical records.
Significantly, it was also employed for billing purposes, with far‐reaching pernicious consequences. Although the ICD purports to be a list of diseases, it actually includes symptoms and signs. Consequently, in the billing context, diagnosis no longer necessarily refers to specific disease states; it now refers to billable termsoften the manifestation that was responsible for the patient seeking medical assistance. Far from being the product of an intellectual effort, it is often merely a justification for submitting a bill. Examples of such diagnoses are shown in Table 1. Many of them represent symptoms, signs, or laboratory abnormalities. The importance of accurate medical diagnosis has been cheapened by this change. The effect is to devalue diagnosisto lessen its status as the Holy Grail.
| Abdominal pain | General symptoms | Special symptom |
| Abnormal blood test | Immune disorders | Splenomegaly |
| Back disorder | Joint disorder | Throat pain |
| Coagulation defects | Myoneural disorder | Urinary symptoms |
| Diseases of esophagus | Otalgia | Visual disturbance |
| Eye disorders | Pain in joint | Vomiting |
| Fluid/electrolyte disorders | Right lower quadrant mass | Wheezing |
The effect of this on trainees is invidious, and predictable. The traditional meaning of diagnosis is being replaced in our minds. Physicians in training are tempted to deceive themselves into believing that they have arrived at an understanding of what they are dealing with when they enter such a diagnosis. After all, have they not responded to the question: what is the diagnosis?
We do not mean to imply that physicians are doing anything wrong by entering ICD terms for billing purposes. What must be done for billing purposes must be done. It is important to be aware, however, and to continually remind ourselves, that what has been entered for this purpose is often not a true medical diagnosis.
Further, when the diagnosis is not yet known, it is not possible to enter a true diagnosis. There is no way to say I don't know. It would be preferable to simply admit that the diagnosis is not yet established, as a medical resident has recently emphasized.5
Diagnosis Often Gets Short Shrift Because of the Perceived Urgency of Discharge
The emphasis on diagnosis several generations ago may have resulted, at least in part, from the relative paucity of effective therapeutic interventions before the 1930s. Things have changed; therapeutic capabilities are much more powerful now. Making the correct diagnosis seems to have lost its urgency. Instead of the major question being what is the diagnosis? it now is often what do we do now? The diagnosis is often an afterthought. Indeed, it is sometimes not even mentioned in discharge summaries, where, not uncommonly, one sees nondiagnoses such as blood in stool or polyarthritis.
In addition, we are under pressure to shorten the inpatient stay of hospitalized patients. At least a portion of the public is aware of this; thus, it has been noted in the New York Times that: The pressure to get patients out of the hospital rapidly can focus medical attention on treatment rather than diagnosis.6 We commonly seek to ameliorate the patients' status to permit discharge before (or often without) learning what we are dealing with. Sometimes one senses that the primary question has become how soon can we discharge this patient?
A price is paid for this. In the absence of a valid diagnosis, patients may be subjected to a broad array of nonessential investigations and therapeutic interventions, each with its own possible complications. Patients are often discharged without a diagnosis having been made, presenting a serious challenge to outpatient physicians who are left to manage them without a clear idea of what they are dealing with. It often falls to the outpatient physicians to make the diagnosis. This is somewhat problematic, since they themselves are under harsh time pressure. Patients often require rehospitalization for the same as‐yet‐undiagnosed condition.
The Problem‐Oriented Record Poses Problems
The widespread use of the problem‐oriented record, originated by Lawrence Weed,7 has led to problems of its own.8 It has evolved, away from its original intent. In practice, its major emphasis often seems to be on identification of problems and tracking their progress, rather than on synthesis. This often leads to muddy rather than clear diagnostic thinking. Assessments and progress notes frequently consist of lists of symptoms, organs, abnormal laboratory findings, or even medical specialties. The net effect is often fragmented thinkingas Weed7 put it, failure to integrate findings into a single entity. Synthesizing diverse findings into a single entity, when possible, is necessary to define a diagnosis. Failure to do so may have serious consequences. In a recent study of diagnostic errors in internal medicine, cognitive errors were frequently found to contribute to such errors.9 The most common cognitive problem was faulty synthesis. How much worse than faulty synthesis is failure to synthesize at all!
Presumptive Diagnoses, Even if Incorrect, Metamorphose into Established Diagnoses
We must often treat empirically. When there is no firm diagnosis, presumptive diagnoses must be made and acted upon. Unfortunately, there are not always mechanisms for the physician to make it clear that his or her diagnosis is only presumptive. (A common example is acute viral syndrome, generally an educated guess.) All too often, presumptive diagnoses are entered, without qualification, as definitive diagnoses, and then achieve immortality. Thus, if a patient is incorrectly diagnosed as having rheumatoid arthritis, all subsequent presentations will start: A so‐and‐so year‐old woman with rheumatoid arthritis for many years Presumptive diagnoses are frequently not questioned. It is easier to assume that they were arrived at after due consideration. Once entered in the medical record, they may be difficult to remove.
It is true that the need to arrive at a precise diagnosis is less pressing for some medical specialties than for others. Emergency physicians, critical care physicians, and frequently, surgeons, must commonly act on the basis of presumptive diagnoses. In contrast, internists, family physicians, psychiatrists, and indeed all physicians who care for patients with chronic illnesses can, with time, be expected to sort out accurate from inaccurate presumptive diagnoses.
A specific example of the problem of presumptive diagnosis is of interest. It is not uncommon, following a first encounter, for a diagnosis to be entered based on the patient's history alone. While such diagnoses are frequently correct, they are not invariably correct. The patient may have arrived at the conclusion herself; she may have misunderstood what she was told by her physician, or her physician may have been in error. Such inaccurate diagnoses also often achieve immortality in the medical record.
Apparent Disparaging of the Importance of Diagnosis
Further trivialization has come from a number of publications expressing concerns about the importance of diagnosis. Thus we read that there are negative consequences of emphasis on diagnosis. When we know what is wrong, we focus less on the individual and more on the disease.10 In his recent book Our Present Complaint. American Medicine, Then and Now, the scholar C.E. Rosenberg11 includes a chapter with the provocative title The Tyranny of Diagnosis. He points out that even a century ago the fear was expressed that burgeoning scientific medicine would lead to denigration of physicians' holistic and intuitive skills.11 Other authors maintain that firm diagnoses may be misleading, since many diseases are a matter of degree in a continuuma spectrumthat are best defined employing a statistical model of risk prediction.12 The suggestion is made that the usefulness of diagnostic tests should not be related to the presence or absence of a disease, but rather to whether they influence outcome.13
Scientific medicine is focused on diagnosis. Denigration of diagnosis has often come, as a philosophical posture, from opponents of reductionist thinking. As Rosenberg11 points out: It has become fashionable among humanistic and social science‐oriented commentators to dwell on the distinction between illness and disease, between the patient's felt experience and the constructions placed on that experience by the world of medicine. Their opposition, he feels, reflects the value‐laden mutual incompatibility (real or apparent) of art and science, of holism and reductionism.2
It is true that medicine is more than just biology. There is a great deal to be said for the view that scientific medicine tends to deemphasize the humanistic, holistic aspects of medical practice. However, despite all these concerns, most physiciansand, to be fair, most criticsagree that making an accurate diagnosis is important. Thus, though the title of his relevant chapter is The Tyranny of Diagnosis, Rosenberg11 states: I might just as well have used the term indispensability. Indeed, the opening words of that chapter are: Diagnosis has always played a pivotal role in medicine.11 Other authors cited above issue this disclaimer: We are not against diagnosis. Diagnosis does and always will play a central role in clinical medicine.12
The importance of diagnosis is underscored by the vigorous debate about how to assess diagnostic tests;14 apparently, diagnosis does indeed matter. While it is true that diagnoses are not always precise, objective, and quantifiable,10 abundant evidence points to the unavoidable conclusion that identifying the patient's disease is heuristically useful; that is, it works.2 The track record of modern scientific medicine in improving mortality and morbidity speaks for itself. It hardly seems necessary to defend it. In addition to representing a valuable intellectual challenge in its own right, diagnosis is pivotal to the scientific mission of medicine.
What Can Be Done?
The net effect of all these forces: the use of billable terms as diagnoses, the pressures of managed care, fragmented problem lists, persistence of incorrect presumptive diagnoses in medical records, and antireductionist criticisms is to encourage sloppy diagnostic thinking in some physicians. What can be done to emphasize the proper use of differential diagnosis in arriving at a definitive diagnosis? What can be done to underscore the importance of differentiating between presumptive and definitive diagnoses? Most importantly, how can we instill the respect for the intellectual honesty necessary to acquire and retain these skills?
Above all, we should relentlessly impress on our students and trainees the importance of arriving at an accurate definitive diagnosis. They should be aware that the job is only half done if the diagnosis has not been made. We should do this repeatedly, both by word and by example. We ourselves must display intellectual honesty.
In addition, we ought to be able to enter diagnosis uncertain, so coded, or to append the phrase cause unknown after the manifestation of concern, when we don't really know what is going on. We should routinely indicate when a diagnosis is merely presumptive. Perhaps we need a way to indicate: This diagnosis is definitive or to indicate the specific evidence that led to the diagnosis (eg, biopsy, laboratory result, radiographic finding). Finally, we need to correct the current confusion between diseases and billable terms, to differentiate the disease from the symptom, perhaps by labeling ICD‐9‐CM codes simply as billing codes, with a separate entry for actual medical diagnoses.
Although powerful historical forces have brought us to this state, we believe that arriving at the correct diagnosis is at least as important now as it has been in the past, and that its primacy should be recognized, celebrated, and fought for. We owe our patients no less.
Acknowledgements
The authors thank Drs. James Pile, Neal Dawson, and David Samols for their helpful suggestions.
- .What counts as disease? Rationales and rationalizations for treatment.Forsch Komplementarmed.1998;5(suppl S1):40–46.
- .What is disease? In memory of Owsei Temkin.Bull Hist Med.2003;77:491–505.
- World Health Organization (WHO). International Classification of Diseases (ICD). Available at: http://www.who.int/classifications/icd/en. Accessed June2009.
- World Health Organization (WHO). History of the development of the ICD. Available at: http://www.who.int/classifications/icd/en/HistoryOfICD. pdf. Accessed June2009.
- .Living unlabeled—diagnosis and disorder.N Engl J Med.2008;359:1650–1653.
- . Poison Pill. New York Times Magazine. 2008: 24–26. Available at: http://www.nytimes.com/2008/04/13/magazine/13wwln‐diagnosis‐t.html. Accessed June2009.
- .Medical records that guide and teach.N Engl J Med.1968;278:593–600.
- .Clear writing, clear thinking and the disappearing art of the problem list.J Hosp Med.2007;2:199–202.
- , , .Diagnostic error in internal medicine.Arch Intern Med.2005;165:1493–1499.
- . The Tyranny of Diagnosis. New York Times. Available at: http://www.nytimes.com/2008/09/19/health/chen9‐18.html?partner=rssnyt2007.
- , , .Against diagnosis.Ann Intern Med.2008;149:200–203.
- , , .A philosophical perspective supports the need for patient‐outcome studies in diagnostic test evaluation.J Clin Epidemiol.2009;62:58–61.
- , .Evidence based diagnostics.BMJ.2005;330:724–726.
- .What counts as disease? Rationales and rationalizations for treatment.Forsch Komplementarmed.1998;5(suppl S1):40–46.
- .What is disease? In memory of Owsei Temkin.Bull Hist Med.2003;77:491–505.
- World Health Organization (WHO). International Classification of Diseases (ICD). Available at: http://www.who.int/classifications/icd/en. Accessed June2009.
- World Health Organization (WHO). History of the development of the ICD. Available at: http://www.who.int/classifications/icd/en/HistoryOfICD. pdf. Accessed June2009.
- .Living unlabeled—diagnosis and disorder.N Engl J Med.2008;359:1650–1653.
- . Poison Pill. New York Times Magazine. 2008: 24–26. Available at: http://www.nytimes.com/2008/04/13/magazine/13wwln‐diagnosis‐t.html. Accessed June2009.
- .Medical records that guide and teach.N Engl J Med.1968;278:593–600.
- .Clear writing, clear thinking and the disappearing art of the problem list.J Hosp Med.2007;2:199–202.
- , , .Diagnostic error in internal medicine.Arch Intern Med.2005;165:1493–1499.
- . The Tyranny of Diagnosis. New York Times. Available at: http://www.nytimes.com/2008/09/19/health/chen9‐18.html?partner=rssnyt2007.
- , , .Against diagnosis.Ann Intern Med.2008;149:200–203.
- , , .A philosophical perspective supports the need for patient‐outcome studies in diagnostic test evaluation.J Clin Epidemiol.2009;62:58–61.
- , .Evidence based diagnostics.BMJ.2005;330:724–726.