User login
Dust mite immunotherapy may help some with eczema
, but improvement in the primary outcome was not significant, new data show.
Results of the small, randomized, double-blind, placebo-controlled trial were published recently in The Journal of Allergy and Clinical Immunology: In Practice.
Lead author Sarah Sella Langer, MD, of the department of medicine, Ribeirão Preto (Brazil) Medical School, University of São Paulo, and colleagues said their results suggest HDM SLIT is safe and effective as an add-on treatment.
The dust mite extract therapy had no major side effects after 18 months of treatment, the authors reported.
The researchers included data from 66 patients who completed the study. The participants were at least 3 years old, registered at least 15 on the SCORing Atopic Dermatitis (SCORAD) measure, and had a skin prick test and/or immunoglobulin E (IgE) test for sensitization to dust mites.
Patients were grouped by age (younger than 12 years or 12 years and older) to receive HDM SLIT (n = 35) or placebo (n = 31) 3 days a week for the study period – between May 2018 and June 2020 – at the Clinical Research Unit of Ribeirão Preto Medical School Hospital.
At baseline, the mean SCORAD was 46.9 (range, 17-87).
After 18 months, 74.2% and 58% of patients in HDM SLIT and placebo groups, respectively, showed at least a15-point decrease in SCORAD (relative risk, 1.28; 95% confidence interval, 0.89-1.83). However, those primary outcome results did not reach statistical significance.
On the other hand, some secondary outcomes did show significant results.
At 95% CI, the researchers reported significant objective-SCORAD decreases of 56.8% and 34.9% in HDM SLIT and placebo groups (average difference, 21.3). Significantly more patients had a score of 0 or 1 on the 5-point Investigator’s Global Assessment scale in the intervention group than in the placebo group (14/35 vs. 5/31; RR, 2.63).
There were no significant changes in the Eczema Area and Severity Index, the visual analogue scale for symptoms, the pruritus scale, or the Dermatology Life Quality Index.
Patients in the trial, most of whom had moderate to severe disease, continued to be treated with usual, individualized therapy for AD, in accordance with current guidelines and experts’ recommendations.
Tina Sindher, MD, an allergist with the Sean N. Parker Center for Allergy and Asthma Research at Stanford (Calif.) University, , told this news organization that the results are not robust enough to recommend the immunotherapy widely.
She pointed out that even in the placebo group, more than half the patients met the primary endpoint.
However, she did say HDM SLIT could be considered as an add-on treatment for the right patients, especially since risk for an allergic reaction or other adverse condition is small. The most common adverse effects were headache and abdominal pain, and they were reported in both the treatment and placebo groups.
With AD, she said, “there is no one drug that’s right for everyone,” because genetics and environment make the kind of symptoms and severity and duration different for each patient.
It all comes down to risk and benefits, she said.
She said if she had a patient with an environmental allergy who’s trying to manage nasal congestion and also happened to have eczema, “I think they’re a great candidate for sublingual dust mite therapy because then not only am I treating their nasal congestions, their other symptoms, it may also help their eczema,” Dr. Sindher said.
Without those concurrent conditions, she said, the benefits of dust mite immunotherapy would not outweigh the risks or the potential burden on the patient of having to take the SLIT.
She said she would present the choice to the patient, and if other treatments haven’t been successful and the patient wants to try it, she would be open to a trial period.
The study was supported by the Brazilian National Council for Scientific and Technological Development, the Institute of Investigation in Immunology, the National Institutes of Science and Technology, the Brazilian National Council for Scientific and Technological Development, and the São Paulo Research Foundation. The mite extract for immunotherapy was provided by the laboratory IPI-ASAC Brasil/ASAC Pharma Brasil. Dr. Langer received a doctoral scholarship from the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES). Dr. Sindher reported no relevant financial relationships.
Commentary by Lawrence F. Eichenfield, MD
Environmental triggers of atopic dermatitis (AD) may be difficult to assess, especially as children with AD commonly develop “overlap” conditions of allergic rhinitis, food allergy, and asthma. The place of immunotherapy in treatment of AD has been controversial over the years, with mixed results from studies on its effect on eczema in different subpopulations. However, a holistic view of allergy care makes consideration of environmental allergies reasonable. The study by Dr. Langer and colleagues was a well-designed double-blind placebo-controlled trial of house dust mite sublingual immunotherapy in mite-sensitized AD patients aged 3 and older with at least mild AD, though the mean eczema severity was severe. After 18 months, there was an impressive 74% decrease in eczema score (SCORAD), but also a 58% decrease in the placebo group. While the primary outcome measure wasn’t statistically significant, some secondary ones were. I agree with the commentary in the article that the data doesn’t support immunotherapy being advised to everyone, while its use as an add-on treatment for certain patients in whom the eczema may overlap with other allergic manifestations is reasonable. For several years at Rady Children’s Hospital, San Diego, we have run a multidisciplinary atopic dermatitis program where patients are comanaged by dermatology and allergy. We have learned to appreciate that a broad perspective on managing comorbid conditions in children with AD really helps the patients and families to understand the many effects of inflammatory and allergic conditions, with improved outcomes and quality of life.
Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children's Hospital-San Diego. He is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego. He disclosed that he has served as an investigator and/or consultant to AbbVie, Lilly, Pfizer, Regeneron, Sanofi-Genzyme, and Verrica.
A version of this article first appeared on Medscape.com.
This article was updated 6/18/22.
, but improvement in the primary outcome was not significant, new data show.
Results of the small, randomized, double-blind, placebo-controlled trial were published recently in The Journal of Allergy and Clinical Immunology: In Practice.
Lead author Sarah Sella Langer, MD, of the department of medicine, Ribeirão Preto (Brazil) Medical School, University of São Paulo, and colleagues said their results suggest HDM SLIT is safe and effective as an add-on treatment.
The dust mite extract therapy had no major side effects after 18 months of treatment, the authors reported.
The researchers included data from 66 patients who completed the study. The participants were at least 3 years old, registered at least 15 on the SCORing Atopic Dermatitis (SCORAD) measure, and had a skin prick test and/or immunoglobulin E (IgE) test for sensitization to dust mites.
Patients were grouped by age (younger than 12 years or 12 years and older) to receive HDM SLIT (n = 35) or placebo (n = 31) 3 days a week for the study period – between May 2018 and June 2020 – at the Clinical Research Unit of Ribeirão Preto Medical School Hospital.
At baseline, the mean SCORAD was 46.9 (range, 17-87).
After 18 months, 74.2% and 58% of patients in HDM SLIT and placebo groups, respectively, showed at least a15-point decrease in SCORAD (relative risk, 1.28; 95% confidence interval, 0.89-1.83). However, those primary outcome results did not reach statistical significance.
On the other hand, some secondary outcomes did show significant results.
At 95% CI, the researchers reported significant objective-SCORAD decreases of 56.8% and 34.9% in HDM SLIT and placebo groups (average difference, 21.3). Significantly more patients had a score of 0 or 1 on the 5-point Investigator’s Global Assessment scale in the intervention group than in the placebo group (14/35 vs. 5/31; RR, 2.63).
There were no significant changes in the Eczema Area and Severity Index, the visual analogue scale for symptoms, the pruritus scale, or the Dermatology Life Quality Index.
Patients in the trial, most of whom had moderate to severe disease, continued to be treated with usual, individualized therapy for AD, in accordance with current guidelines and experts’ recommendations.
Tina Sindher, MD, an allergist with the Sean N. Parker Center for Allergy and Asthma Research at Stanford (Calif.) University, , told this news organization that the results are not robust enough to recommend the immunotherapy widely.
She pointed out that even in the placebo group, more than half the patients met the primary endpoint.
However, she did say HDM SLIT could be considered as an add-on treatment for the right patients, especially since risk for an allergic reaction or other adverse condition is small. The most common adverse effects were headache and abdominal pain, and they were reported in both the treatment and placebo groups.
With AD, she said, “there is no one drug that’s right for everyone,” because genetics and environment make the kind of symptoms and severity and duration different for each patient.
It all comes down to risk and benefits, she said.
She said if she had a patient with an environmental allergy who’s trying to manage nasal congestion and also happened to have eczema, “I think they’re a great candidate for sublingual dust mite therapy because then not only am I treating their nasal congestions, their other symptoms, it may also help their eczema,” Dr. Sindher said.
Without those concurrent conditions, she said, the benefits of dust mite immunotherapy would not outweigh the risks or the potential burden on the patient of having to take the SLIT.
She said she would present the choice to the patient, and if other treatments haven’t been successful and the patient wants to try it, she would be open to a trial period.
The study was supported by the Brazilian National Council for Scientific and Technological Development, the Institute of Investigation in Immunology, the National Institutes of Science and Technology, the Brazilian National Council for Scientific and Technological Development, and the São Paulo Research Foundation. The mite extract for immunotherapy was provided by the laboratory IPI-ASAC Brasil/ASAC Pharma Brasil. Dr. Langer received a doctoral scholarship from the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES). Dr. Sindher reported no relevant financial relationships.
Commentary by Lawrence F. Eichenfield, MD
Environmental triggers of atopic dermatitis (AD) may be difficult to assess, especially as children with AD commonly develop “overlap” conditions of allergic rhinitis, food allergy, and asthma. The place of immunotherapy in treatment of AD has been controversial over the years, with mixed results from studies on its effect on eczema in different subpopulations. However, a holistic view of allergy care makes consideration of environmental allergies reasonable. The study by Dr. Langer and colleagues was a well-designed double-blind placebo-controlled trial of house dust mite sublingual immunotherapy in mite-sensitized AD patients aged 3 and older with at least mild AD, though the mean eczema severity was severe. After 18 months, there was an impressive 74% decrease in eczema score (SCORAD), but also a 58% decrease in the placebo group. While the primary outcome measure wasn’t statistically significant, some secondary ones were. I agree with the commentary in the article that the data doesn’t support immunotherapy being advised to everyone, while its use as an add-on treatment for certain patients in whom the eczema may overlap with other allergic manifestations is reasonable. For several years at Rady Children’s Hospital, San Diego, we have run a multidisciplinary atopic dermatitis program where patients are comanaged by dermatology and allergy. We have learned to appreciate that a broad perspective on managing comorbid conditions in children with AD really helps the patients and families to understand the many effects of inflammatory and allergic conditions, with improved outcomes and quality of life.
Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children's Hospital-San Diego. He is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego. He disclosed that he has served as an investigator and/or consultant to AbbVie, Lilly, Pfizer, Regeneron, Sanofi-Genzyme, and Verrica.
A version of this article first appeared on Medscape.com.
This article was updated 6/18/22.
, but improvement in the primary outcome was not significant, new data show.
Results of the small, randomized, double-blind, placebo-controlled trial were published recently in The Journal of Allergy and Clinical Immunology: In Practice.
Lead author Sarah Sella Langer, MD, of the department of medicine, Ribeirão Preto (Brazil) Medical School, University of São Paulo, and colleagues said their results suggest HDM SLIT is safe and effective as an add-on treatment.
The dust mite extract therapy had no major side effects after 18 months of treatment, the authors reported.
The researchers included data from 66 patients who completed the study. The participants were at least 3 years old, registered at least 15 on the SCORing Atopic Dermatitis (SCORAD) measure, and had a skin prick test and/or immunoglobulin E (IgE) test for sensitization to dust mites.
Patients were grouped by age (younger than 12 years or 12 years and older) to receive HDM SLIT (n = 35) or placebo (n = 31) 3 days a week for the study period – between May 2018 and June 2020 – at the Clinical Research Unit of Ribeirão Preto Medical School Hospital.
At baseline, the mean SCORAD was 46.9 (range, 17-87).
After 18 months, 74.2% and 58% of patients in HDM SLIT and placebo groups, respectively, showed at least a15-point decrease in SCORAD (relative risk, 1.28; 95% confidence interval, 0.89-1.83). However, those primary outcome results did not reach statistical significance.
On the other hand, some secondary outcomes did show significant results.
At 95% CI, the researchers reported significant objective-SCORAD decreases of 56.8% and 34.9% in HDM SLIT and placebo groups (average difference, 21.3). Significantly more patients had a score of 0 or 1 on the 5-point Investigator’s Global Assessment scale in the intervention group than in the placebo group (14/35 vs. 5/31; RR, 2.63).
There were no significant changes in the Eczema Area and Severity Index, the visual analogue scale for symptoms, the pruritus scale, or the Dermatology Life Quality Index.
Patients in the trial, most of whom had moderate to severe disease, continued to be treated with usual, individualized therapy for AD, in accordance with current guidelines and experts’ recommendations.
Tina Sindher, MD, an allergist with the Sean N. Parker Center for Allergy and Asthma Research at Stanford (Calif.) University, , told this news organization that the results are not robust enough to recommend the immunotherapy widely.
She pointed out that even in the placebo group, more than half the patients met the primary endpoint.
However, she did say HDM SLIT could be considered as an add-on treatment for the right patients, especially since risk for an allergic reaction or other adverse condition is small. The most common adverse effects were headache and abdominal pain, and they were reported in both the treatment and placebo groups.
With AD, she said, “there is no one drug that’s right for everyone,” because genetics and environment make the kind of symptoms and severity and duration different for each patient.
It all comes down to risk and benefits, she said.
She said if she had a patient with an environmental allergy who’s trying to manage nasal congestion and also happened to have eczema, “I think they’re a great candidate for sublingual dust mite therapy because then not only am I treating their nasal congestions, their other symptoms, it may also help their eczema,” Dr. Sindher said.
Without those concurrent conditions, she said, the benefits of dust mite immunotherapy would not outweigh the risks or the potential burden on the patient of having to take the SLIT.
She said she would present the choice to the patient, and if other treatments haven’t been successful and the patient wants to try it, she would be open to a trial period.
The study was supported by the Brazilian National Council for Scientific and Technological Development, the Institute of Investigation in Immunology, the National Institutes of Science and Technology, the Brazilian National Council for Scientific and Technological Development, and the São Paulo Research Foundation. The mite extract for immunotherapy was provided by the laboratory IPI-ASAC Brasil/ASAC Pharma Brasil. Dr. Langer received a doctoral scholarship from the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES). Dr. Sindher reported no relevant financial relationships.
Commentary by Lawrence F. Eichenfield, MD
Environmental triggers of atopic dermatitis (AD) may be difficult to assess, especially as children with AD commonly develop “overlap” conditions of allergic rhinitis, food allergy, and asthma. The place of immunotherapy in treatment of AD has been controversial over the years, with mixed results from studies on its effect on eczema in different subpopulations. However, a holistic view of allergy care makes consideration of environmental allergies reasonable. The study by Dr. Langer and colleagues was a well-designed double-blind placebo-controlled trial of house dust mite sublingual immunotherapy in mite-sensitized AD patients aged 3 and older with at least mild AD, though the mean eczema severity was severe. After 18 months, there was an impressive 74% decrease in eczema score (SCORAD), but also a 58% decrease in the placebo group. While the primary outcome measure wasn’t statistically significant, some secondary ones were. I agree with the commentary in the article that the data doesn’t support immunotherapy being advised to everyone, while its use as an add-on treatment for certain patients in whom the eczema may overlap with other allergic manifestations is reasonable. For several years at Rady Children’s Hospital, San Diego, we have run a multidisciplinary atopic dermatitis program where patients are comanaged by dermatology and allergy. We have learned to appreciate that a broad perspective on managing comorbid conditions in children with AD really helps the patients and families to understand the many effects of inflammatory and allergic conditions, with improved outcomes and quality of life.
Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children's Hospital-San Diego. He is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego. He disclosed that he has served as an investigator and/or consultant to AbbVie, Lilly, Pfizer, Regeneron, Sanofi-Genzyme, and Verrica.
A version of this article first appeared on Medscape.com.
This article was updated 6/18/22.
The road less traveled in gastroenterology and hepatology: Becoming a medical educator
How did you realize medical education was the pathway for you?
Near the end of medical school, I recall my friends and I casting predictions about what each person would be doing in twenty years. The projections offered up about my ultimate landing place were unanimous: a clinical researcher leading a gastroenterology division. I was excited when they said this to me. It made sense, as I had already done over 3 years of clinical research on inflammatory bowel disease at the time. But as I began leading various clinical research projects during my internal medicine residency, I realized that they were not generating a strong sense of fulfillment or passion for me. I greatly enjoyed the process of research and writing, but there still was something missing; I could no longer see the role of a funded clinical researcher sustaining me for the length of my medical and academic career.
Thus, at the end of my 2nd year of residency, I began to self-reflect more on the various aspects of my medical journey to elucidate my path forward. This process was jump-started by a humbling recognition from that year’s graduating class of medical students for my contributions to their education over the past 3 years. I had served as a teaching assistant for their pathophysiology course and then subsequently worked alongside many of them on their medicine rotations. I realized that helping foster their growth as physicians in a longitudinal way was unquestionably the most rewarding experience that I had had to date. With further reflection, I recognized that, amid the chaos of a busy call day, I most looked forward to the moments when I could teach the interns and students about the nuances of the patients being admitted. It never felt like an obligation but rather always left me feeling revitalized. So, by the beginning of my 3rd year of residency, I knew that I wanted to pursue a career within medical education.
Once you decided to become a medical educator, what were your next steps?
As I began to vocalize this change in career trajectory, I did not always encounter enthusiastic support. Because the medical educator pathway is more typical amongst the general medicine community, some faculty members advised me to avoid solely focusing on medical education as a specialist because academic success would be difficult to attain. But I had just recognized this could be my vocation within medicine, so I could not turn back now. Thus, I began to seek the mentorship of educators at my institution, and many of them wisely advised me to consider pursuing additional training in medical education to accrue the skill sets needed to lay the groundwork for a lifelong career. So, I participated in a 1-year medical education fellowship in conjunction with my chief residency year. This training was profoundly formative; I learned about the various theories on adult learning, as well as how to create curricula, how to teach effectively in a clinical environment, and how to deliver meaningful feedback to learners. But perhaps most importantly, I learned how to generate tangible evidence of productivity within medical education to allow for advancement in academia. This included rigorously studying the impact of educational interventions. It became clear to me by the end of this year that the pathways of medical education and researcher were not incongruent but could actually be quite complementary. In light of this, I designed and implemented a mandatory inpatient hepatology curriculum for internal medicine residents, for which I studied its immediate and long-term effects throughout my gastroenterology and hepatology fellowships as well as during my time as an attending. Currently, I am also investigating medical students’ exposure to liver disease through a multicenter assessment. Projects such as these would not have been feasible without dedicated mentorship, but as alluded to above, in contrast to the traditional clinical research paradigm, my mentors have often been from outside the fields of gastroenterology and hepatology.
What advice would you offer a junior faculty member interested in a career in medical education within gastroenterology and hepatology?
1. Just before I completed fellowship, I asked Holly Humphrey, MD, the former dean of the Pritzker School of Medicine at the University of Chicago, this same question. Her answer was simple and is worth sharing: “In the beginning, just focus on becoming the best clinician possible. The rest will fall into place with time.” So, I did exactly this. I continually tried to push the limits of my knowledge, always questioning standard clinical practices to understand the evidence behind (or not behind) them. This knowledge then naturally became the content of my teaching for trainees in the clinical environment so that eventually patient care and teaching were seamlessly integrated into the same day-to-day workflow. The more I taught trainees, the more my commitment to education was recognized by my institution.
2. Meet with leadership of your medical school, internal medicine residency program, and gastroenterology and hepatology fellowships early in the course of your career to assert your desire to contribute to their respective educational missions.
3. Create a teaching philosophy that clearly communicates “your fundamental beliefs about teaching and learning, why you hold those values and beliefs, and how you translate these claims into practice.”1 This document will act as a guiding force in your career by highlighting the themes and principles that you have already incorporated and will continue to incorporate into your teaching practices and educational activities. For example, it can provide clarity when you are in doubt of how to address a difficult learning environment or whether to accept a certain position.
4. Because of No. 1 and No. 2, you will start to be offered opportunities to formally become involved in curricula within undergraduate (UME) and graduate medical education (GME). It will likely begin with requests to lecture or precept small group sessions. Use these smaller opportunities not only to refine your teaching skills but to explore whether your career aspirations better align with UME or GME. With hard work and perseverance, the opportunities can progress to invitations to become a course director, join a curriculum committee, or become an associate program director for a residency or fellowship program (which at this point is why you want to know if you prefer working in UME, GME, or both).
5. Seek feedback often from your learners. It is the only way you will continue to improve your teaching skills and the learning environment you create. Furthermore, formal evaluations can be used in the promotion process.
6. Collaborate with and seek mentorship from fellow medical educators both at your own institution and at others. As previously mentioned, these relationships do not need to be (and are often not) with other gastroenterologists or hepatologists.
7. Seek out national opportunities related to medical education. Most of the gastroenterology and hepatology societies have one or more committees focused on medical training. The AGA Academy of Educators is a fantastic community of education-focused individuals within our specialty that provides opportunities for networking, funding, and career development. Furthermore, other general societies (for example, the Association of American Medical Colleges, American College of Physicians) may be interested in including subspecialty members in their educational committees and activities.
Dr. Mikolajczyk is an assistant professor of medicine and an associate program director for the Internal Medicine Residency Program at the University of Illinois Chicago. He is the lead faculty adviser for the Liver Fellow Network. He has no conflicts of interest to disclose.
How did you realize medical education was the pathway for you?
Near the end of medical school, I recall my friends and I casting predictions about what each person would be doing in twenty years. The projections offered up about my ultimate landing place were unanimous: a clinical researcher leading a gastroenterology division. I was excited when they said this to me. It made sense, as I had already done over 3 years of clinical research on inflammatory bowel disease at the time. But as I began leading various clinical research projects during my internal medicine residency, I realized that they were not generating a strong sense of fulfillment or passion for me. I greatly enjoyed the process of research and writing, but there still was something missing; I could no longer see the role of a funded clinical researcher sustaining me for the length of my medical and academic career.
Thus, at the end of my 2nd year of residency, I began to self-reflect more on the various aspects of my medical journey to elucidate my path forward. This process was jump-started by a humbling recognition from that year’s graduating class of medical students for my contributions to their education over the past 3 years. I had served as a teaching assistant for their pathophysiology course and then subsequently worked alongside many of them on their medicine rotations. I realized that helping foster their growth as physicians in a longitudinal way was unquestionably the most rewarding experience that I had had to date. With further reflection, I recognized that, amid the chaos of a busy call day, I most looked forward to the moments when I could teach the interns and students about the nuances of the patients being admitted. It never felt like an obligation but rather always left me feeling revitalized. So, by the beginning of my 3rd year of residency, I knew that I wanted to pursue a career within medical education.
Once you decided to become a medical educator, what were your next steps?
As I began to vocalize this change in career trajectory, I did not always encounter enthusiastic support. Because the medical educator pathway is more typical amongst the general medicine community, some faculty members advised me to avoid solely focusing on medical education as a specialist because academic success would be difficult to attain. But I had just recognized this could be my vocation within medicine, so I could not turn back now. Thus, I began to seek the mentorship of educators at my institution, and many of them wisely advised me to consider pursuing additional training in medical education to accrue the skill sets needed to lay the groundwork for a lifelong career. So, I participated in a 1-year medical education fellowship in conjunction with my chief residency year. This training was profoundly formative; I learned about the various theories on adult learning, as well as how to create curricula, how to teach effectively in a clinical environment, and how to deliver meaningful feedback to learners. But perhaps most importantly, I learned how to generate tangible evidence of productivity within medical education to allow for advancement in academia. This included rigorously studying the impact of educational interventions. It became clear to me by the end of this year that the pathways of medical education and researcher were not incongruent but could actually be quite complementary. In light of this, I designed and implemented a mandatory inpatient hepatology curriculum for internal medicine residents, for which I studied its immediate and long-term effects throughout my gastroenterology and hepatology fellowships as well as during my time as an attending. Currently, I am also investigating medical students’ exposure to liver disease through a multicenter assessment. Projects such as these would not have been feasible without dedicated mentorship, but as alluded to above, in contrast to the traditional clinical research paradigm, my mentors have often been from outside the fields of gastroenterology and hepatology.
What advice would you offer a junior faculty member interested in a career in medical education within gastroenterology and hepatology?
1. Just before I completed fellowship, I asked Holly Humphrey, MD, the former dean of the Pritzker School of Medicine at the University of Chicago, this same question. Her answer was simple and is worth sharing: “In the beginning, just focus on becoming the best clinician possible. The rest will fall into place with time.” So, I did exactly this. I continually tried to push the limits of my knowledge, always questioning standard clinical practices to understand the evidence behind (or not behind) them. This knowledge then naturally became the content of my teaching for trainees in the clinical environment so that eventually patient care and teaching were seamlessly integrated into the same day-to-day workflow. The more I taught trainees, the more my commitment to education was recognized by my institution.
2. Meet with leadership of your medical school, internal medicine residency program, and gastroenterology and hepatology fellowships early in the course of your career to assert your desire to contribute to their respective educational missions.
3. Create a teaching philosophy that clearly communicates “your fundamental beliefs about teaching and learning, why you hold those values and beliefs, and how you translate these claims into practice.”1 This document will act as a guiding force in your career by highlighting the themes and principles that you have already incorporated and will continue to incorporate into your teaching practices and educational activities. For example, it can provide clarity when you are in doubt of how to address a difficult learning environment or whether to accept a certain position.
4. Because of No. 1 and No. 2, you will start to be offered opportunities to formally become involved in curricula within undergraduate (UME) and graduate medical education (GME). It will likely begin with requests to lecture or precept small group sessions. Use these smaller opportunities not only to refine your teaching skills but to explore whether your career aspirations better align with UME or GME. With hard work and perseverance, the opportunities can progress to invitations to become a course director, join a curriculum committee, or become an associate program director for a residency or fellowship program (which at this point is why you want to know if you prefer working in UME, GME, or both).
5. Seek feedback often from your learners. It is the only way you will continue to improve your teaching skills and the learning environment you create. Furthermore, formal evaluations can be used in the promotion process.
6. Collaborate with and seek mentorship from fellow medical educators both at your own institution and at others. As previously mentioned, these relationships do not need to be (and are often not) with other gastroenterologists or hepatologists.
7. Seek out national opportunities related to medical education. Most of the gastroenterology and hepatology societies have one or more committees focused on medical training. The AGA Academy of Educators is a fantastic community of education-focused individuals within our specialty that provides opportunities for networking, funding, and career development. Furthermore, other general societies (for example, the Association of American Medical Colleges, American College of Physicians) may be interested in including subspecialty members in their educational committees and activities.
Dr. Mikolajczyk is an assistant professor of medicine and an associate program director for the Internal Medicine Residency Program at the University of Illinois Chicago. He is the lead faculty adviser for the Liver Fellow Network. He has no conflicts of interest to disclose.
How did you realize medical education was the pathway for you?
Near the end of medical school, I recall my friends and I casting predictions about what each person would be doing in twenty years. The projections offered up about my ultimate landing place were unanimous: a clinical researcher leading a gastroenterology division. I was excited when they said this to me. It made sense, as I had already done over 3 years of clinical research on inflammatory bowel disease at the time. But as I began leading various clinical research projects during my internal medicine residency, I realized that they were not generating a strong sense of fulfillment or passion for me. I greatly enjoyed the process of research and writing, but there still was something missing; I could no longer see the role of a funded clinical researcher sustaining me for the length of my medical and academic career.
Thus, at the end of my 2nd year of residency, I began to self-reflect more on the various aspects of my medical journey to elucidate my path forward. This process was jump-started by a humbling recognition from that year’s graduating class of medical students for my contributions to their education over the past 3 years. I had served as a teaching assistant for their pathophysiology course and then subsequently worked alongside many of them on their medicine rotations. I realized that helping foster their growth as physicians in a longitudinal way was unquestionably the most rewarding experience that I had had to date. With further reflection, I recognized that, amid the chaos of a busy call day, I most looked forward to the moments when I could teach the interns and students about the nuances of the patients being admitted. It never felt like an obligation but rather always left me feeling revitalized. So, by the beginning of my 3rd year of residency, I knew that I wanted to pursue a career within medical education.
Once you decided to become a medical educator, what were your next steps?
As I began to vocalize this change in career trajectory, I did not always encounter enthusiastic support. Because the medical educator pathway is more typical amongst the general medicine community, some faculty members advised me to avoid solely focusing on medical education as a specialist because academic success would be difficult to attain. But I had just recognized this could be my vocation within medicine, so I could not turn back now. Thus, I began to seek the mentorship of educators at my institution, and many of them wisely advised me to consider pursuing additional training in medical education to accrue the skill sets needed to lay the groundwork for a lifelong career. So, I participated in a 1-year medical education fellowship in conjunction with my chief residency year. This training was profoundly formative; I learned about the various theories on adult learning, as well as how to create curricula, how to teach effectively in a clinical environment, and how to deliver meaningful feedback to learners. But perhaps most importantly, I learned how to generate tangible evidence of productivity within medical education to allow for advancement in academia. This included rigorously studying the impact of educational interventions. It became clear to me by the end of this year that the pathways of medical education and researcher were not incongruent but could actually be quite complementary. In light of this, I designed and implemented a mandatory inpatient hepatology curriculum for internal medicine residents, for which I studied its immediate and long-term effects throughout my gastroenterology and hepatology fellowships as well as during my time as an attending. Currently, I am also investigating medical students’ exposure to liver disease through a multicenter assessment. Projects such as these would not have been feasible without dedicated mentorship, but as alluded to above, in contrast to the traditional clinical research paradigm, my mentors have often been from outside the fields of gastroenterology and hepatology.
What advice would you offer a junior faculty member interested in a career in medical education within gastroenterology and hepatology?
1. Just before I completed fellowship, I asked Holly Humphrey, MD, the former dean of the Pritzker School of Medicine at the University of Chicago, this same question. Her answer was simple and is worth sharing: “In the beginning, just focus on becoming the best clinician possible. The rest will fall into place with time.” So, I did exactly this. I continually tried to push the limits of my knowledge, always questioning standard clinical practices to understand the evidence behind (or not behind) them. This knowledge then naturally became the content of my teaching for trainees in the clinical environment so that eventually patient care and teaching were seamlessly integrated into the same day-to-day workflow. The more I taught trainees, the more my commitment to education was recognized by my institution.
2. Meet with leadership of your medical school, internal medicine residency program, and gastroenterology and hepatology fellowships early in the course of your career to assert your desire to contribute to their respective educational missions.
3. Create a teaching philosophy that clearly communicates “your fundamental beliefs about teaching and learning, why you hold those values and beliefs, and how you translate these claims into practice.”1 This document will act as a guiding force in your career by highlighting the themes and principles that you have already incorporated and will continue to incorporate into your teaching practices and educational activities. For example, it can provide clarity when you are in doubt of how to address a difficult learning environment or whether to accept a certain position.
4. Because of No. 1 and No. 2, you will start to be offered opportunities to formally become involved in curricula within undergraduate (UME) and graduate medical education (GME). It will likely begin with requests to lecture or precept small group sessions. Use these smaller opportunities not only to refine your teaching skills but to explore whether your career aspirations better align with UME or GME. With hard work and perseverance, the opportunities can progress to invitations to become a course director, join a curriculum committee, or become an associate program director for a residency or fellowship program (which at this point is why you want to know if you prefer working in UME, GME, or both).
5. Seek feedback often from your learners. It is the only way you will continue to improve your teaching skills and the learning environment you create. Furthermore, formal evaluations can be used in the promotion process.
6. Collaborate with and seek mentorship from fellow medical educators both at your own institution and at others. As previously mentioned, these relationships do not need to be (and are often not) with other gastroenterologists or hepatologists.
7. Seek out national opportunities related to medical education. Most of the gastroenterology and hepatology societies have one or more committees focused on medical training. The AGA Academy of Educators is a fantastic community of education-focused individuals within our specialty that provides opportunities for networking, funding, and career development. Furthermore, other general societies (for example, the Association of American Medical Colleges, American College of Physicians) may be interested in including subspecialty members in their educational committees and activities.
Dr. Mikolajczyk is an assistant professor of medicine and an associate program director for the Internal Medicine Residency Program at the University of Illinois Chicago. He is the lead faculty adviser for the Liver Fellow Network. He has no conflicts of interest to disclose.
Specialists think it’s up to the PCP to recommend flu vaccines. But many patients don’t see a PCP every year
A new survey from the National Foundation for Infectious Diseases shows that, despite the recommendation that patients who have chronic illnesses receive annual flu vaccines, only 45% of these patients do get them. People with chronic diseases are at increased risk for serious flu-related complications, including hospitalization and death.
The survey looked at physicians’ practices toward flu vaccination and communication between health care providers (HCP) and their adult patients with chronic health conditions.
Overall, less than a third of HCPs (31%) said they recommend annual flu vaccination to all of their patients with chronic health conditions. There were some surprising differences between subspecialists. For example, 72% of patients with a heart problem who saw a cardiologist said that physician recommended the flu vaccine. The recommendation rate dropped to 32% of lung patients seeing a pulmonary physician and only 10% of people with diabetes who saw an endocrinologist.
There is quite a large gap between what physicians and patients say about their interactions. Fully 77% of HCPs who recommend annual flu vaccination say they tell patients when they are at higher risk of complications from influenza. Yet only 48% of patients say they have been given such information.
Although it is critically important information for patients to learn, their risk of influenza is often missing from the discussion. For example, patients with heart disease are six times more likely to have a heart attack within 7 days of flu infection. People with diabetes are six times more likely to be hospitalized from flu and three times more likely to die. Similarly, those with asthma or chronic obstructive pulmonary disorder are at a much higher risk of complications.
One problem is that Yet only 65% of patients with one of these chronic illnesses report seeing their primary care physician at least annually.
Much of the disparity between the patient’s perception of what they were told and the physician’s is “how the ‘recommendation’ is actually made,” William Schaffner, MD, NFID’s medical director and professor of medicine at Vanderbilt University, Nashville, Tenn., told this news organization. Dr. Schaffner offered the following example: At the end of the visit, the doctor might say: “It’s that time of the year again – you want to think about getting your flu shot.”
“The doctor thinks they’ve recommended that, but the doctor really has opened the door for you to think about it and leave [yourself] unvaccinated.”
Dr. Schaffner’s alternative? Tell the patient: “‘You’ll get your flu vaccine on the way out. Tom or Sally will give it to you.’ That’s a very different kind of recommendation. And it’s a much greater assurance of providing the vaccine.”
Another major problem, Dr. Schaffner said, is that many specialists “don’t think of vaccination as something that’s included with their routine care” even though they do direct much of the patient’s care. He said that physicians should be more “directive” in their care and that immunizations should be better integrated into routine practice.
Jody Lanard, MD, a retired risk communication consultant who spent many years working with the World Health Organization on disease outbreak communications, said in an interview that this disconnect between physician and patient reports “was really jarring. And it’s actionable!”
She offered several practical suggestions. For one, she said, “the messaging to the specialists has to be very, very empathic. We know you’re already overburdened. And here we’re asking you to do something that you think of as somebody else’s job.” But if your patient gets flu, then your job as the cardiologist or endocrinologist will become more complicated and time-consuming. So getting the patients vaccinated will be a good investment and will make your job easier.
Because of the disparity in patient and physician reports, Dr. Lanard suggested implementing a “feedback mechanism where they [the health care providers] give out the prescription, and then the office calls [the patient] to see if they’ve gotten the shot or not. Because that way it will help correct the mismatch between them thinking that they told the patient and the patient not hearing it.”
Asked about why there might be a big gap between what physicians report they said and what patients heard, Dr. Lanard explained that “physicians often communicate in [a manner] sort of like a checklist. And the patients are focused on one or two things that are high in their minds. And the physician was mentioning some things that are on a separate topic that are not on a patient’s list and it goes right past them.”
Dr. Lanard recommended brief storytelling instead of checklists. For example: “I’ve been treating your diabetes for 10 years. During this last flu season, several of my diabetic patients had a really hard time when they caught the flu. So now I’m trying harder to remember to remind you to get your flu shots.”
She urged HCPs to “make it more personal ... but it can still be scripted in advance as part of something that [you’re] remembering to do during the check.” She added that their professional associations may be able to send them suggested language they can adapt.
Finally, Dr. Lanard cautioned about vaccine myths. “The word myth is so insulting. It’s basically a word that sends the signal that you’re an idiot.”
She advised specialists to avoid the word “myth,” which will make the person defensive. Instead, say something like, “A lot of people, even some of my own family members, think the flu vaccine gives you the flu. ... But it doesn’t. And then you go into the reality.”
Dr. Lanard suggested that specialists implement the follow-up calls and close the feedback loop, saying: “If they did the survey a few years later, I bet that gap would narrow.”
Dr. Schaffner and Dr. Lanard disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new survey from the National Foundation for Infectious Diseases shows that, despite the recommendation that patients who have chronic illnesses receive annual flu vaccines, only 45% of these patients do get them. People with chronic diseases are at increased risk for serious flu-related complications, including hospitalization and death.
The survey looked at physicians’ practices toward flu vaccination and communication between health care providers (HCP) and their adult patients with chronic health conditions.
Overall, less than a third of HCPs (31%) said they recommend annual flu vaccination to all of their patients with chronic health conditions. There were some surprising differences between subspecialists. For example, 72% of patients with a heart problem who saw a cardiologist said that physician recommended the flu vaccine. The recommendation rate dropped to 32% of lung patients seeing a pulmonary physician and only 10% of people with diabetes who saw an endocrinologist.
There is quite a large gap between what physicians and patients say about their interactions. Fully 77% of HCPs who recommend annual flu vaccination say they tell patients when they are at higher risk of complications from influenza. Yet only 48% of patients say they have been given such information.
Although it is critically important information for patients to learn, their risk of influenza is often missing from the discussion. For example, patients with heart disease are six times more likely to have a heart attack within 7 days of flu infection. People with diabetes are six times more likely to be hospitalized from flu and three times more likely to die. Similarly, those with asthma or chronic obstructive pulmonary disorder are at a much higher risk of complications.
One problem is that Yet only 65% of patients with one of these chronic illnesses report seeing their primary care physician at least annually.
Much of the disparity between the patient’s perception of what they were told and the physician’s is “how the ‘recommendation’ is actually made,” William Schaffner, MD, NFID’s medical director and professor of medicine at Vanderbilt University, Nashville, Tenn., told this news organization. Dr. Schaffner offered the following example: At the end of the visit, the doctor might say: “It’s that time of the year again – you want to think about getting your flu shot.”
“The doctor thinks they’ve recommended that, but the doctor really has opened the door for you to think about it and leave [yourself] unvaccinated.”
Dr. Schaffner’s alternative? Tell the patient: “‘You’ll get your flu vaccine on the way out. Tom or Sally will give it to you.’ That’s a very different kind of recommendation. And it’s a much greater assurance of providing the vaccine.”
Another major problem, Dr. Schaffner said, is that many specialists “don’t think of vaccination as something that’s included with their routine care” even though they do direct much of the patient’s care. He said that physicians should be more “directive” in their care and that immunizations should be better integrated into routine practice.
Jody Lanard, MD, a retired risk communication consultant who spent many years working with the World Health Organization on disease outbreak communications, said in an interview that this disconnect between physician and patient reports “was really jarring. And it’s actionable!”
She offered several practical suggestions. For one, she said, “the messaging to the specialists has to be very, very empathic. We know you’re already overburdened. And here we’re asking you to do something that you think of as somebody else’s job.” But if your patient gets flu, then your job as the cardiologist or endocrinologist will become more complicated and time-consuming. So getting the patients vaccinated will be a good investment and will make your job easier.
Because of the disparity in patient and physician reports, Dr. Lanard suggested implementing a “feedback mechanism where they [the health care providers] give out the prescription, and then the office calls [the patient] to see if they’ve gotten the shot or not. Because that way it will help correct the mismatch between them thinking that they told the patient and the patient not hearing it.”
Asked about why there might be a big gap between what physicians report they said and what patients heard, Dr. Lanard explained that “physicians often communicate in [a manner] sort of like a checklist. And the patients are focused on one or two things that are high in their minds. And the physician was mentioning some things that are on a separate topic that are not on a patient’s list and it goes right past them.”
Dr. Lanard recommended brief storytelling instead of checklists. For example: “I’ve been treating your diabetes for 10 years. During this last flu season, several of my diabetic patients had a really hard time when they caught the flu. So now I’m trying harder to remember to remind you to get your flu shots.”
She urged HCPs to “make it more personal ... but it can still be scripted in advance as part of something that [you’re] remembering to do during the check.” She added that their professional associations may be able to send them suggested language they can adapt.
Finally, Dr. Lanard cautioned about vaccine myths. “The word myth is so insulting. It’s basically a word that sends the signal that you’re an idiot.”
She advised specialists to avoid the word “myth,” which will make the person defensive. Instead, say something like, “A lot of people, even some of my own family members, think the flu vaccine gives you the flu. ... But it doesn’t. And then you go into the reality.”
Dr. Lanard suggested that specialists implement the follow-up calls and close the feedback loop, saying: “If they did the survey a few years later, I bet that gap would narrow.”
Dr. Schaffner and Dr. Lanard disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new survey from the National Foundation for Infectious Diseases shows that, despite the recommendation that patients who have chronic illnesses receive annual flu vaccines, only 45% of these patients do get them. People with chronic diseases are at increased risk for serious flu-related complications, including hospitalization and death.
The survey looked at physicians’ practices toward flu vaccination and communication between health care providers (HCP) and their adult patients with chronic health conditions.
Overall, less than a third of HCPs (31%) said they recommend annual flu vaccination to all of their patients with chronic health conditions. There were some surprising differences between subspecialists. For example, 72% of patients with a heart problem who saw a cardiologist said that physician recommended the flu vaccine. The recommendation rate dropped to 32% of lung patients seeing a pulmonary physician and only 10% of people with diabetes who saw an endocrinologist.
There is quite a large gap between what physicians and patients say about their interactions. Fully 77% of HCPs who recommend annual flu vaccination say they tell patients when they are at higher risk of complications from influenza. Yet only 48% of patients say they have been given such information.
Although it is critically important information for patients to learn, their risk of influenza is often missing from the discussion. For example, patients with heart disease are six times more likely to have a heart attack within 7 days of flu infection. People with diabetes are six times more likely to be hospitalized from flu and three times more likely to die. Similarly, those with asthma or chronic obstructive pulmonary disorder are at a much higher risk of complications.
One problem is that Yet only 65% of patients with one of these chronic illnesses report seeing their primary care physician at least annually.
Much of the disparity between the patient’s perception of what they were told and the physician’s is “how the ‘recommendation’ is actually made,” William Schaffner, MD, NFID’s medical director and professor of medicine at Vanderbilt University, Nashville, Tenn., told this news organization. Dr. Schaffner offered the following example: At the end of the visit, the doctor might say: “It’s that time of the year again – you want to think about getting your flu shot.”
“The doctor thinks they’ve recommended that, but the doctor really has opened the door for you to think about it and leave [yourself] unvaccinated.”
Dr. Schaffner’s alternative? Tell the patient: “‘You’ll get your flu vaccine on the way out. Tom or Sally will give it to you.’ That’s a very different kind of recommendation. And it’s a much greater assurance of providing the vaccine.”
Another major problem, Dr. Schaffner said, is that many specialists “don’t think of vaccination as something that’s included with their routine care” even though they do direct much of the patient’s care. He said that physicians should be more “directive” in their care and that immunizations should be better integrated into routine practice.
Jody Lanard, MD, a retired risk communication consultant who spent many years working with the World Health Organization on disease outbreak communications, said in an interview that this disconnect between physician and patient reports “was really jarring. And it’s actionable!”
She offered several practical suggestions. For one, she said, “the messaging to the specialists has to be very, very empathic. We know you’re already overburdened. And here we’re asking you to do something that you think of as somebody else’s job.” But if your patient gets flu, then your job as the cardiologist or endocrinologist will become more complicated and time-consuming. So getting the patients vaccinated will be a good investment and will make your job easier.
Because of the disparity in patient and physician reports, Dr. Lanard suggested implementing a “feedback mechanism where they [the health care providers] give out the prescription, and then the office calls [the patient] to see if they’ve gotten the shot or not. Because that way it will help correct the mismatch between them thinking that they told the patient and the patient not hearing it.”
Asked about why there might be a big gap between what physicians report they said and what patients heard, Dr. Lanard explained that “physicians often communicate in [a manner] sort of like a checklist. And the patients are focused on one or two things that are high in their minds. And the physician was mentioning some things that are on a separate topic that are not on a patient’s list and it goes right past them.”
Dr. Lanard recommended brief storytelling instead of checklists. For example: “I’ve been treating your diabetes for 10 years. During this last flu season, several of my diabetic patients had a really hard time when they caught the flu. So now I’m trying harder to remember to remind you to get your flu shots.”
She urged HCPs to “make it more personal ... but it can still be scripted in advance as part of something that [you’re] remembering to do during the check.” She added that their professional associations may be able to send them suggested language they can adapt.
Finally, Dr. Lanard cautioned about vaccine myths. “The word myth is so insulting. It’s basically a word that sends the signal that you’re an idiot.”
She advised specialists to avoid the word “myth,” which will make the person defensive. Instead, say something like, “A lot of people, even some of my own family members, think the flu vaccine gives you the flu. ... But it doesn’t. And then you go into the reality.”
Dr. Lanard suggested that specialists implement the follow-up calls and close the feedback loop, saying: “If they did the survey a few years later, I bet that gap would narrow.”
Dr. Schaffner and Dr. Lanard disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Compression therapy prevents recurrence of cellulitis
Background: Recurrent cellulitis is a common condition in patients with lower-extremity edema. Although some clinicians recommend compression garments as a preventative treatment, there are no data evaluating their efficacy for this purpose.
Study design: Participants were randomized to receive either education alone or education plus compression therapy. Neither the participants nor the assessors were blinded to the treatment arm.
Setting: Single-center study in Australia.
Synopsis: Participants with cellulitis who also had at least two previous episodes of cellulitis in the previous 2 years and had lower-extremity edema were enrolled. Of participants, 84 were randomized. Both groups received education regarding skin care, body weight, and exercise, while the compression therapy group also received compression garments and instructions for their use. The primary outcome was recurrent cellulitis. Patients in the control group were allowed to cross over after an episode of cellulitis. The trial was stopped early for efficacy. At the time the trial was halted, 17 of 43 (40%) participants in the control group had recurrent cellulitis, compared with only 6 of 41 (15%) in the intervention (hazard ratio, 0.23; 95% CI, 0.09-0.59; P = .002). Limitations include the lack of blinding, which could have introduced bias, although the diagnosis of recurrent cellulitis was made by clinicians external to the trial. This study supports the use of compression garments in preventing recurrent cellulitis in patients with lower-extremity edema.
Bottom line: Compression garments can be used to prevent recurrent cellulitis in patients with edema.
Citation: Webb E et al. Compression therapy to prevent recurrent cellulitis of the leg. N Engl J Med. 2020;383(7):630-9. doi:10.1056/NEJMoa1917197.
Dr. Herscher is a hospitalist in the Division of Hospital Medicine, Mount Sinai Health System, New York.
Background: Recurrent cellulitis is a common condition in patients with lower-extremity edema. Although some clinicians recommend compression garments as a preventative treatment, there are no data evaluating their efficacy for this purpose.
Study design: Participants were randomized to receive either education alone or education plus compression therapy. Neither the participants nor the assessors were blinded to the treatment arm.
Setting: Single-center study in Australia.
Synopsis: Participants with cellulitis who also had at least two previous episodes of cellulitis in the previous 2 years and had lower-extremity edema were enrolled. Of participants, 84 were randomized. Both groups received education regarding skin care, body weight, and exercise, while the compression therapy group also received compression garments and instructions for their use. The primary outcome was recurrent cellulitis. Patients in the control group were allowed to cross over after an episode of cellulitis. The trial was stopped early for efficacy. At the time the trial was halted, 17 of 43 (40%) participants in the control group had recurrent cellulitis, compared with only 6 of 41 (15%) in the intervention (hazard ratio, 0.23; 95% CI, 0.09-0.59; P = .002). Limitations include the lack of blinding, which could have introduced bias, although the diagnosis of recurrent cellulitis was made by clinicians external to the trial. This study supports the use of compression garments in preventing recurrent cellulitis in patients with lower-extremity edema.
Bottom line: Compression garments can be used to prevent recurrent cellulitis in patients with edema.
Citation: Webb E et al. Compression therapy to prevent recurrent cellulitis of the leg. N Engl J Med. 2020;383(7):630-9. doi:10.1056/NEJMoa1917197.
Dr. Herscher is a hospitalist in the Division of Hospital Medicine, Mount Sinai Health System, New York.
Background: Recurrent cellulitis is a common condition in patients with lower-extremity edema. Although some clinicians recommend compression garments as a preventative treatment, there are no data evaluating their efficacy for this purpose.
Study design: Participants were randomized to receive either education alone or education plus compression therapy. Neither the participants nor the assessors were blinded to the treatment arm.
Setting: Single-center study in Australia.
Synopsis: Participants with cellulitis who also had at least two previous episodes of cellulitis in the previous 2 years and had lower-extremity edema were enrolled. Of participants, 84 were randomized. Both groups received education regarding skin care, body weight, and exercise, while the compression therapy group also received compression garments and instructions for their use. The primary outcome was recurrent cellulitis. Patients in the control group were allowed to cross over after an episode of cellulitis. The trial was stopped early for efficacy. At the time the trial was halted, 17 of 43 (40%) participants in the control group had recurrent cellulitis, compared with only 6 of 41 (15%) in the intervention (hazard ratio, 0.23; 95% CI, 0.09-0.59; P = .002). Limitations include the lack of blinding, which could have introduced bias, although the diagnosis of recurrent cellulitis was made by clinicians external to the trial. This study supports the use of compression garments in preventing recurrent cellulitis in patients with lower-extremity edema.
Bottom line: Compression garments can be used to prevent recurrent cellulitis in patients with edema.
Citation: Webb E et al. Compression therapy to prevent recurrent cellulitis of the leg. N Engl J Med. 2020;383(7):630-9. doi:10.1056/NEJMoa1917197.
Dr. Herscher is a hospitalist in the Division of Hospital Medicine, Mount Sinai Health System, New York.
Online reviews most important factor in choosing a doctor: Survey
from Press Ganey, a provider of patient satisfaction surveys. According to the data, this online information is more important to consumers in selecting a physician than another doctor’s referral and is more than twice as important when choosing a primary care physician.
In fact, 83% of respondents said they went online to read reviews of a physician after receiving a referral from another provider.
The online research trend reflects not only the increased familiarity of all generations with the internet but also the growing consumerization of health care, Thomas Jeffrey, president of the Sullivan/Luallin Group, a patient experience consulting firm, told this news organization.
“According to patient satisfaction surveys, people are becoming health care consumers more than in the past,” he noted. “Historically, we didn’t look at health care as a consumer product. But, with high deductibles and copays, doctor visits can represent a pretty significant out-of-pocket expense. As it begins to hit folks’ pocketbooks, they become more savvy shoppers.”
Digital preferences for providers were gaining “positive momentum” even before the COVID-19 pandemic, but the crisis “drove upticks in some consumer digital behaviors,” the Press Ganey report pointed out.
Mr. Jeffrey agreed, noting that this finding matches what Sullivan/Luallin has discovered in its research. “I think the pandemic pushed people to engage more online,” he said. “The highest net promoter score [likelihood to recommend in market surveys] for a pharmacy is the Amazon pharmacy, which is an online-based delivery service. Then you have telehealth visits, which are more convenient in many ways.”
How patients search online
In choosing a new primary care doctor, 51.1% go on the web first, 23.8% seek a referral from another health care provider, and 4.4% get information from an insurer or a benefits manager, according to the survey.
The factors that matter most to consumers when they pick any provider, in order, are online ratings and reviews of the physician, referral from a current doctor, ratings and reviews of the facility, and the quality and completeness of a doctor’s profile on a website or online directory. The doctor’s online presence and the quality of their website are also important.
According to Press Ganey, search engines like Google are the most used digital resources, with 65.4% of consumers employing them to find a doctor. However, consumers now use an average of 2.7 sites in their search. The leading destinations are a hospital or a clinic site, WebMD, Healthgrades, and Facebook. (This news organization is owned by WebMD.)
Compared with 2019, the report said, there has been a 22.8% decline in the use of search engines for seeking a doctor and a 53.7% increase in the use of health care review sites such as Healthgrades and Vitals.
When reading provider reviews, consumers look for more recent reviews and want the reviews to be “authentic and informative.” They also value the star ratings. About 84%of respondents said they wouldn’t book an appointment with a referred provider that had a rating of less than four stars.
Overall, the top reasons why people are deterred from making an appointment are difficulty contacting the office, the poor quality of online reviews, and an average online rating of less than four stars.
The vast majority of respondents (77%) said they believe internet reviews reflect their own experience with a provider organization, and only 2.6% said the reviews were inaccurate. Another finding of the survey indicates that this attention of patients to reviews of their own provider doesn’t represent idle curiosity: About 57% of Baby Boomers and 45% of millennials/Gen Z’ers said they’d written online reviews of a doctor or a hospital.
Factors in patient loyalty
The Press Ganey survey asked which of several factors, besides excellent care, patients weighed when giving a five-star review to a health care provider.
Quality of customer service was rated first by 70.8% of respondents, followed by cleanliness of facilities (67.5%), communication (63.4%), the provider’s bedside manner (63%), ease of appointment booking (58.8%), ease of patient intake/registration (52.3%), quality and accuracy of information (40.1%), availability of telehealth services (21.7%), and waiting room amenities (21.8%).
The report explained that “quality of customer service” means “demeanor, attentiveness, and helpfulness of staff and practitioners.” “Communication” refers to things like follow-up appointment reminders and annual checkup reminders.
According to Mr. Jeffrey, these factors were considered more important than a doctor’s bedside manner because of the team care approach in most physician offices. “We see a lot more folks derive their notion of quality from continuity of care. And if they feel the physician they love is being supported by a less than competent team, that can impact significantly their sense of the quality of care,” he said.
Online appointment booking is a must
To win over the online consumer, Press Ganey emphasized, practices should ensure that provider listings are accurate and complete. In addition, offering online appointment booking can avoid the top challenge in making a new appointment, which is getting through to the office.
Mr. Jeffrey concurred, although he notes that practices have to be careful about how they enable patients to select appointment slots online. He suggests that an appointment request form on a patient portal first ask what the purpose of the visit is and that it offer five or so options. If the request fits into a routine visit category, the provider’s calendar pops up and the patient can select a convenient time slot. If it’s something else, an appointment scheduler calls the patient back.
“There needs to be greater access to standard appointments online,” he said. “While privacy is an issue, you can use the patient portal that most EHRs have to provide online booking. If you want to succeed going forward, that’s going to be a major plus.”
Of course, to do any of this, including reading provider reviews, a consumer needs a good internet connection and a mobile or desktop device. While broadband internet access is still not available in some communities, the breakdown of the survey respondents by demographics shows that low-income people were included.
Mr. Jeffrey doesn’t believe that a lack of internet access or digital devices prevents many Americans from going online today. “Even in poor communities, most people have internet access through their smartphones. Even baby boomers are familiar with smartphones. I haven’t seen internet access be a big barrier for low-income households, because they all have access to phones.”
A version of this article first appeared on Medscape.com.
from Press Ganey, a provider of patient satisfaction surveys. According to the data, this online information is more important to consumers in selecting a physician than another doctor’s referral and is more than twice as important when choosing a primary care physician.
In fact, 83% of respondents said they went online to read reviews of a physician after receiving a referral from another provider.
The online research trend reflects not only the increased familiarity of all generations with the internet but also the growing consumerization of health care, Thomas Jeffrey, president of the Sullivan/Luallin Group, a patient experience consulting firm, told this news organization.
“According to patient satisfaction surveys, people are becoming health care consumers more than in the past,” he noted. “Historically, we didn’t look at health care as a consumer product. But, with high deductibles and copays, doctor visits can represent a pretty significant out-of-pocket expense. As it begins to hit folks’ pocketbooks, they become more savvy shoppers.”
Digital preferences for providers were gaining “positive momentum” even before the COVID-19 pandemic, but the crisis “drove upticks in some consumer digital behaviors,” the Press Ganey report pointed out.
Mr. Jeffrey agreed, noting that this finding matches what Sullivan/Luallin has discovered in its research. “I think the pandemic pushed people to engage more online,” he said. “The highest net promoter score [likelihood to recommend in market surveys] for a pharmacy is the Amazon pharmacy, which is an online-based delivery service. Then you have telehealth visits, which are more convenient in many ways.”
How patients search online
In choosing a new primary care doctor, 51.1% go on the web first, 23.8% seek a referral from another health care provider, and 4.4% get information from an insurer or a benefits manager, according to the survey.
The factors that matter most to consumers when they pick any provider, in order, are online ratings and reviews of the physician, referral from a current doctor, ratings and reviews of the facility, and the quality and completeness of a doctor’s profile on a website or online directory. The doctor’s online presence and the quality of their website are also important.
According to Press Ganey, search engines like Google are the most used digital resources, with 65.4% of consumers employing them to find a doctor. However, consumers now use an average of 2.7 sites in their search. The leading destinations are a hospital or a clinic site, WebMD, Healthgrades, and Facebook. (This news organization is owned by WebMD.)
Compared with 2019, the report said, there has been a 22.8% decline in the use of search engines for seeking a doctor and a 53.7% increase in the use of health care review sites such as Healthgrades and Vitals.
When reading provider reviews, consumers look for more recent reviews and want the reviews to be “authentic and informative.” They also value the star ratings. About 84%of respondents said they wouldn’t book an appointment with a referred provider that had a rating of less than four stars.
Overall, the top reasons why people are deterred from making an appointment are difficulty contacting the office, the poor quality of online reviews, and an average online rating of less than four stars.
The vast majority of respondents (77%) said they believe internet reviews reflect their own experience with a provider organization, and only 2.6% said the reviews were inaccurate. Another finding of the survey indicates that this attention of patients to reviews of their own provider doesn’t represent idle curiosity: About 57% of Baby Boomers and 45% of millennials/Gen Z’ers said they’d written online reviews of a doctor or a hospital.
Factors in patient loyalty
The Press Ganey survey asked which of several factors, besides excellent care, patients weighed when giving a five-star review to a health care provider.
Quality of customer service was rated first by 70.8% of respondents, followed by cleanliness of facilities (67.5%), communication (63.4%), the provider’s bedside manner (63%), ease of appointment booking (58.8%), ease of patient intake/registration (52.3%), quality and accuracy of information (40.1%), availability of telehealth services (21.7%), and waiting room amenities (21.8%).
The report explained that “quality of customer service” means “demeanor, attentiveness, and helpfulness of staff and practitioners.” “Communication” refers to things like follow-up appointment reminders and annual checkup reminders.
According to Mr. Jeffrey, these factors were considered more important than a doctor’s bedside manner because of the team care approach in most physician offices. “We see a lot more folks derive their notion of quality from continuity of care. And if they feel the physician they love is being supported by a less than competent team, that can impact significantly their sense of the quality of care,” he said.
Online appointment booking is a must
To win over the online consumer, Press Ganey emphasized, practices should ensure that provider listings are accurate and complete. In addition, offering online appointment booking can avoid the top challenge in making a new appointment, which is getting through to the office.
Mr. Jeffrey concurred, although he notes that practices have to be careful about how they enable patients to select appointment slots online. He suggests that an appointment request form on a patient portal first ask what the purpose of the visit is and that it offer five or so options. If the request fits into a routine visit category, the provider’s calendar pops up and the patient can select a convenient time slot. If it’s something else, an appointment scheduler calls the patient back.
“There needs to be greater access to standard appointments online,” he said. “While privacy is an issue, you can use the patient portal that most EHRs have to provide online booking. If you want to succeed going forward, that’s going to be a major plus.”
Of course, to do any of this, including reading provider reviews, a consumer needs a good internet connection and a mobile or desktop device. While broadband internet access is still not available in some communities, the breakdown of the survey respondents by demographics shows that low-income people were included.
Mr. Jeffrey doesn’t believe that a lack of internet access or digital devices prevents many Americans from going online today. “Even in poor communities, most people have internet access through their smartphones. Even baby boomers are familiar with smartphones. I haven’t seen internet access be a big barrier for low-income households, because they all have access to phones.”
A version of this article first appeared on Medscape.com.
from Press Ganey, a provider of patient satisfaction surveys. According to the data, this online information is more important to consumers in selecting a physician than another doctor’s referral and is more than twice as important when choosing a primary care physician.
In fact, 83% of respondents said they went online to read reviews of a physician after receiving a referral from another provider.
The online research trend reflects not only the increased familiarity of all generations with the internet but also the growing consumerization of health care, Thomas Jeffrey, president of the Sullivan/Luallin Group, a patient experience consulting firm, told this news organization.
“According to patient satisfaction surveys, people are becoming health care consumers more than in the past,” he noted. “Historically, we didn’t look at health care as a consumer product. But, with high deductibles and copays, doctor visits can represent a pretty significant out-of-pocket expense. As it begins to hit folks’ pocketbooks, they become more savvy shoppers.”
Digital preferences for providers were gaining “positive momentum” even before the COVID-19 pandemic, but the crisis “drove upticks in some consumer digital behaviors,” the Press Ganey report pointed out.
Mr. Jeffrey agreed, noting that this finding matches what Sullivan/Luallin has discovered in its research. “I think the pandemic pushed people to engage more online,” he said. “The highest net promoter score [likelihood to recommend in market surveys] for a pharmacy is the Amazon pharmacy, which is an online-based delivery service. Then you have telehealth visits, which are more convenient in many ways.”
How patients search online
In choosing a new primary care doctor, 51.1% go on the web first, 23.8% seek a referral from another health care provider, and 4.4% get information from an insurer or a benefits manager, according to the survey.
The factors that matter most to consumers when they pick any provider, in order, are online ratings and reviews of the physician, referral from a current doctor, ratings and reviews of the facility, and the quality and completeness of a doctor’s profile on a website or online directory. The doctor’s online presence and the quality of their website are also important.
According to Press Ganey, search engines like Google are the most used digital resources, with 65.4% of consumers employing them to find a doctor. However, consumers now use an average of 2.7 sites in their search. The leading destinations are a hospital or a clinic site, WebMD, Healthgrades, and Facebook. (This news organization is owned by WebMD.)
Compared with 2019, the report said, there has been a 22.8% decline in the use of search engines for seeking a doctor and a 53.7% increase in the use of health care review sites such as Healthgrades and Vitals.
When reading provider reviews, consumers look for more recent reviews and want the reviews to be “authentic and informative.” They also value the star ratings. About 84%of respondents said they wouldn’t book an appointment with a referred provider that had a rating of less than four stars.
Overall, the top reasons why people are deterred from making an appointment are difficulty contacting the office, the poor quality of online reviews, and an average online rating of less than four stars.
The vast majority of respondents (77%) said they believe internet reviews reflect their own experience with a provider organization, and only 2.6% said the reviews were inaccurate. Another finding of the survey indicates that this attention of patients to reviews of their own provider doesn’t represent idle curiosity: About 57% of Baby Boomers and 45% of millennials/Gen Z’ers said they’d written online reviews of a doctor or a hospital.
Factors in patient loyalty
The Press Ganey survey asked which of several factors, besides excellent care, patients weighed when giving a five-star review to a health care provider.
Quality of customer service was rated first by 70.8% of respondents, followed by cleanliness of facilities (67.5%), communication (63.4%), the provider’s bedside manner (63%), ease of appointment booking (58.8%), ease of patient intake/registration (52.3%), quality and accuracy of information (40.1%), availability of telehealth services (21.7%), and waiting room amenities (21.8%).
The report explained that “quality of customer service” means “demeanor, attentiveness, and helpfulness of staff and practitioners.” “Communication” refers to things like follow-up appointment reminders and annual checkup reminders.
According to Mr. Jeffrey, these factors were considered more important than a doctor’s bedside manner because of the team care approach in most physician offices. “We see a lot more folks derive their notion of quality from continuity of care. And if they feel the physician they love is being supported by a less than competent team, that can impact significantly their sense of the quality of care,” he said.
Online appointment booking is a must
To win over the online consumer, Press Ganey emphasized, practices should ensure that provider listings are accurate and complete. In addition, offering online appointment booking can avoid the top challenge in making a new appointment, which is getting through to the office.
Mr. Jeffrey concurred, although he notes that practices have to be careful about how they enable patients to select appointment slots online. He suggests that an appointment request form on a patient portal first ask what the purpose of the visit is and that it offer five or so options. If the request fits into a routine visit category, the provider’s calendar pops up and the patient can select a convenient time slot. If it’s something else, an appointment scheduler calls the patient back.
“There needs to be greater access to standard appointments online,” he said. “While privacy is an issue, you can use the patient portal that most EHRs have to provide online booking. If you want to succeed going forward, that’s going to be a major plus.”
Of course, to do any of this, including reading provider reviews, a consumer needs a good internet connection and a mobile or desktop device. While broadband internet access is still not available in some communities, the breakdown of the survey respondents by demographics shows that low-income people were included.
Mr. Jeffrey doesn’t believe that a lack of internet access or digital devices prevents many Americans from going online today. “Even in poor communities, most people have internet access through their smartphones. Even baby boomers are familiar with smartphones. I haven’t seen internet access be a big barrier for low-income households, because they all have access to phones.”
A version of this article first appeared on Medscape.com.
Metabolites implicated in CHD development in African Americans
Selected metabolic biomarkers may influence disease risk and progression in African American and White persons in different ways, a cohort study of the landmark Jackson Heart Study has found.
The investigators identified 22 specific metabolites that seem to influence incident CHD risk in African American patients – 13 metabolites that were also replicated in a multiethnic population and 9 novel metabolites that include N-acylamides and leucine, a branched-chain amino acid.
“To our knowledge, this is the first time that an N-acylamide as a class of molecule has been shown to be associated with incident coronary heart disease,” lead study author Daniel E. Cruz, MD, an instructor at Harvard Medical School in the division of cardiovascular medicine at Beth Israel Deaconess Medical Center in Boston, said in an interview.
The researchers analyzed targeted plasma metabolomic profiles of 2,346 participants in the Jackson Heart Study, a prospective population-based cohort study in the Mississippi city that included 5,306 African American patients evaluated over 15 years. They then performed a replication analysis of CHD-associated metabolites among 1,588 multiethnic participants in the Women’s Health Initiative, another population-based cohort study that included 161,808 postmenopausal women, also over 15 years. In all, the study, published in JAMA Cardiology, identified 46 metabolites that were associated with incident CHD up to 16 years before the incident event
Dr. Cruz said the “most interesting” findings were the roles of the N-acylamide linoleoyl ethanolamide and leucine. The former is of interest “because it is a lipid-signaling molecule that has been shown to have anti-inflammatory effects on macrophages; the influence and effects on macrophages are of particular interest because of macrophages’ central role in atherosclerosis and coronary heart disease,” he said.
Leucine draws interest because, in this study population, it was linked to a reduced risk of incident CHD. The researchers cited four previous studies in predominantly non-Hispanic White populations that found no association between branched-chain amino acids and incident CHD in Circulation, Stroke Circulation: Genomic and Precision Medicine, and Atherosclerosis. Other branched-amino acids included in the analysis trended toward a decreased risk of CHD, but those didn’t achieve the same statistical significance as that of leucine, Dr. Cruz said.
“In some of the analyses we did, there was a subset of metabolites that the associations with CHD appeared to be different between self-identified African Americans in the Jackson cohort vs. self-identified non-Hispanic Whites, and leucine was one of them,” Dr. Cruz said.
He emphasized that this study “is not a genetic analysis” because the participants self-identified their race. “So our next step is to figure out why this difference appears between these self-identified groups,” Dr. Cruz said. “We suspect environmental factors play a role – psychological stress, diet, income level, to name a few – but we are also interested to see if there are genetic causes.”
The results “are not clinically applicable,” Dr. Cruz said, but they do point to a need for more ethnically and racially diverse study populations. “The big picture is that, before we go implementing novel biomarkers into clinical practice, we need to make sure that they are accurate across different populations of people,” he said. “The only way to do this is to study different groups with the same rigor and vigor and thoughtfulness as any other group.”
These findings fall in line with other studies that found other nonmetabolomic biomarkers have countervailing effects on CHD risk in African Americans and non-Hispanic Whites, said Christie M. Ballantyne, MD, chief of cardiology at Baylor College of Medicine in Houston. For example, African Americans have been found to have lower triglyceride and HDL cholesterol levels than those of Whites.
The study “points out that there may be important biological differences in the metabolic pathways and abnormalities in the development of CHD between races,” Dr. Ballantyne said. “This further emphasizes both the importance and challenge of testing therapies in multiple racial/ethnic groups and with more even representation between men and women.”
Combining metabolomic profiling along with other biomarkers and possibly genetics may be helpful to “personalize” therapies in the future, he added.
Dr. Cruz and Dr. Ballantyne have no relevant relationships to disclose.
Selected metabolic biomarkers may influence disease risk and progression in African American and White persons in different ways, a cohort study of the landmark Jackson Heart Study has found.
The investigators identified 22 specific metabolites that seem to influence incident CHD risk in African American patients – 13 metabolites that were also replicated in a multiethnic population and 9 novel metabolites that include N-acylamides and leucine, a branched-chain amino acid.
“To our knowledge, this is the first time that an N-acylamide as a class of molecule has been shown to be associated with incident coronary heart disease,” lead study author Daniel E. Cruz, MD, an instructor at Harvard Medical School in the division of cardiovascular medicine at Beth Israel Deaconess Medical Center in Boston, said in an interview.
The researchers analyzed targeted plasma metabolomic profiles of 2,346 participants in the Jackson Heart Study, a prospective population-based cohort study in the Mississippi city that included 5,306 African American patients evaluated over 15 years. They then performed a replication analysis of CHD-associated metabolites among 1,588 multiethnic participants in the Women’s Health Initiative, another population-based cohort study that included 161,808 postmenopausal women, also over 15 years. In all, the study, published in JAMA Cardiology, identified 46 metabolites that were associated with incident CHD up to 16 years before the incident event
Dr. Cruz said the “most interesting” findings were the roles of the N-acylamide linoleoyl ethanolamide and leucine. The former is of interest “because it is a lipid-signaling molecule that has been shown to have anti-inflammatory effects on macrophages; the influence and effects on macrophages are of particular interest because of macrophages’ central role in atherosclerosis and coronary heart disease,” he said.
Leucine draws interest because, in this study population, it was linked to a reduced risk of incident CHD. The researchers cited four previous studies in predominantly non-Hispanic White populations that found no association between branched-chain amino acids and incident CHD in Circulation, Stroke Circulation: Genomic and Precision Medicine, and Atherosclerosis. Other branched-amino acids included in the analysis trended toward a decreased risk of CHD, but those didn’t achieve the same statistical significance as that of leucine, Dr. Cruz said.
“In some of the analyses we did, there was a subset of metabolites that the associations with CHD appeared to be different between self-identified African Americans in the Jackson cohort vs. self-identified non-Hispanic Whites, and leucine was one of them,” Dr. Cruz said.
He emphasized that this study “is not a genetic analysis” because the participants self-identified their race. “So our next step is to figure out why this difference appears between these self-identified groups,” Dr. Cruz said. “We suspect environmental factors play a role – psychological stress, diet, income level, to name a few – but we are also interested to see if there are genetic causes.”
The results “are not clinically applicable,” Dr. Cruz said, but they do point to a need for more ethnically and racially diverse study populations. “The big picture is that, before we go implementing novel biomarkers into clinical practice, we need to make sure that they are accurate across different populations of people,” he said. “The only way to do this is to study different groups with the same rigor and vigor and thoughtfulness as any other group.”
These findings fall in line with other studies that found other nonmetabolomic biomarkers have countervailing effects on CHD risk in African Americans and non-Hispanic Whites, said Christie M. Ballantyne, MD, chief of cardiology at Baylor College of Medicine in Houston. For example, African Americans have been found to have lower triglyceride and HDL cholesterol levels than those of Whites.
The study “points out that there may be important biological differences in the metabolic pathways and abnormalities in the development of CHD between races,” Dr. Ballantyne said. “This further emphasizes both the importance and challenge of testing therapies in multiple racial/ethnic groups and with more even representation between men and women.”
Combining metabolomic profiling along with other biomarkers and possibly genetics may be helpful to “personalize” therapies in the future, he added.
Dr. Cruz and Dr. Ballantyne have no relevant relationships to disclose.
Selected metabolic biomarkers may influence disease risk and progression in African American and White persons in different ways, a cohort study of the landmark Jackson Heart Study has found.
The investigators identified 22 specific metabolites that seem to influence incident CHD risk in African American patients – 13 metabolites that were also replicated in a multiethnic population and 9 novel metabolites that include N-acylamides and leucine, a branched-chain amino acid.
“To our knowledge, this is the first time that an N-acylamide as a class of molecule has been shown to be associated with incident coronary heart disease,” lead study author Daniel E. Cruz, MD, an instructor at Harvard Medical School in the division of cardiovascular medicine at Beth Israel Deaconess Medical Center in Boston, said in an interview.
The researchers analyzed targeted plasma metabolomic profiles of 2,346 participants in the Jackson Heart Study, a prospective population-based cohort study in the Mississippi city that included 5,306 African American patients evaluated over 15 years. They then performed a replication analysis of CHD-associated metabolites among 1,588 multiethnic participants in the Women’s Health Initiative, another population-based cohort study that included 161,808 postmenopausal women, also over 15 years. In all, the study, published in JAMA Cardiology, identified 46 metabolites that were associated with incident CHD up to 16 years before the incident event
Dr. Cruz said the “most interesting” findings were the roles of the N-acylamide linoleoyl ethanolamide and leucine. The former is of interest “because it is a lipid-signaling molecule that has been shown to have anti-inflammatory effects on macrophages; the influence and effects on macrophages are of particular interest because of macrophages’ central role in atherosclerosis and coronary heart disease,” he said.
Leucine draws interest because, in this study population, it was linked to a reduced risk of incident CHD. The researchers cited four previous studies in predominantly non-Hispanic White populations that found no association between branched-chain amino acids and incident CHD in Circulation, Stroke Circulation: Genomic and Precision Medicine, and Atherosclerosis. Other branched-amino acids included in the analysis trended toward a decreased risk of CHD, but those didn’t achieve the same statistical significance as that of leucine, Dr. Cruz said.
“In some of the analyses we did, there was a subset of metabolites that the associations with CHD appeared to be different between self-identified African Americans in the Jackson cohort vs. self-identified non-Hispanic Whites, and leucine was one of them,” Dr. Cruz said.
He emphasized that this study “is not a genetic analysis” because the participants self-identified their race. “So our next step is to figure out why this difference appears between these self-identified groups,” Dr. Cruz said. “We suspect environmental factors play a role – psychological stress, diet, income level, to name a few – but we are also interested to see if there are genetic causes.”
The results “are not clinically applicable,” Dr. Cruz said, but they do point to a need for more ethnically and racially diverse study populations. “The big picture is that, before we go implementing novel biomarkers into clinical practice, we need to make sure that they are accurate across different populations of people,” he said. “The only way to do this is to study different groups with the same rigor and vigor and thoughtfulness as any other group.”
These findings fall in line with other studies that found other nonmetabolomic biomarkers have countervailing effects on CHD risk in African Americans and non-Hispanic Whites, said Christie M. Ballantyne, MD, chief of cardiology at Baylor College of Medicine in Houston. For example, African Americans have been found to have lower triglyceride and HDL cholesterol levels than those of Whites.
The study “points out that there may be important biological differences in the metabolic pathways and abnormalities in the development of CHD between races,” Dr. Ballantyne said. “This further emphasizes both the importance and challenge of testing therapies in multiple racial/ethnic groups and with more even representation between men and women.”
Combining metabolomic profiling along with other biomarkers and possibly genetics may be helpful to “personalize” therapies in the future, he added.
Dr. Cruz and Dr. Ballantyne have no relevant relationships to disclose.
FROM JAMA CARDIOLOGY
Treating ALL: Asparaginase enzyme levels linked to toxicities
Key toxicities related to treating acute lymphoblastic leukemia (ALL) with asparaginase, specifically pancreatitis and osteonecrosis, are associated with increases in asparaginase enzyme activity, suggesting that patients at risk for those toxicities would benefit from therapeutic drug monitoring, according to new research.
In the study, published Oct. 8 in Blood Advances, increased asparaginase enzyme activity was not significantly associated with overall asparaginase toxicity. However,“ the authors concluded.
“The [findings are] new, and we have included patients from a quite big cohort, which is unique,” coauthor Birgitte Klug Albertsen, MD, PhD, associate clinical professor with Aarhus (Denmark) University Hospital, told this news organization.
Therapeutic drug monitoring already is widely used during treatment with asparaginase, the standard of care treatment for ALL; however, the focus of this monitoring has typically been on clinical effectiveness, as levels of asparaginase enzyme activity can indicate hypersensitivity reactions, while the absence of such activity can suggest inferior outcomes.
Meanwhile, drug monitoring is not normally used to assess the risk of treatment-related toxicities. This has been due to a lack of evidence regarding asparaginase enzyme activity and toxicity risk, which, if severe enough, can prevent further treatment.
To investigate the relationship with toxicities, Dr. Albertsen and colleagues evaluated data from seven countries in Europe on 1,155 children between the ages of 1 and 17.9 who were diagnosed with ALL and treated with asparaginase, according to the Nordic Society of Paediatric Haematology and Oncology (NOPHO) ALL2008 protocol between July 2008 and March 2016.
Blood samples drawn approximately 14 days after asparaginase administration showed that some level of asparaginase enzyme activity was measurable in 955 patients (82.7%), while 200 patients (17.3%) had asparaginase inactivation. Overall, there were 159 asparaginase-associated toxicities of pancreatitis, thromboembolism, or osteonecrosis among the 955 patients with measurable asparaginase enzyme activity.
There were no significant differences in median asparaginase enzyme activity levels between those who did and did not experience toxicities (224 IU/L vs. 221 IU/L, respectively; P = .1), and the results did not change after adjustment for age and sex. However, the risk of pancreatitis was found to increase with a hazard ratio (HR) of 1.40 for each 100 IU/L increase in the median asparaginase enzyme activity level (P = .002).
Likewise, an increase in risk was observed for osteonecrosis (HR 1.36; P = .02) per 100 IU/L increase in median asparaginase enzyme activity. However, the HR for the risk of thromboembolism, the most common of asparaginase-related toxicities, was not significant (HR 0.99; P = .96).
Dr. Albertsen said the etiology behind the occurrence of osteonecrosis is not well understood.
“We know that steroids, especially dexamethasone, are a risk factor,” she said. “We believe that asparaginase may play a role too, but a clear association has not been demonstrated.”
In the NOPHO ALL2008 protocol used in the study, dexamethasone is used in the same time periods as PEG-asparaginase treatment for patients receiving 15 doses.
The finding of only a nonsignificant trend between asparaginase enzyme activity with overall toxicities may have reflected the low dose that was used, Dr. Albertsen added.
“In the NOPHO ALL2008 protocol, we used quite a low dose of PEG-asparaginase, and the risk may be higher in protocols using higher doses,” she said.
Relapse reduction
Notably, the study showed that asparaginase enzyme elevations were, in fact, not significantly associated with a reduction in the risk of leukemic relapse (HR .88 per 100 IU/L increase; P = .35).
Those findings suggest that measurable asparaginase enzyme activity levels, and thus asparaginase depletion, “may be sufficient to ensure an antileukemic effect,” the authors noted.
“Therapeutic drug monitoring of asparaginase enzyme activity is indicated mainly to detect inactivation, but [it] may be further explored for dose reduction to reduce some specific toxicities,” they concluded.
Dr. Albertsen disclosed being sponsor of the investigator-initiatied NOR-GRASPALL 2016 trial.
Key toxicities related to treating acute lymphoblastic leukemia (ALL) with asparaginase, specifically pancreatitis and osteonecrosis, are associated with increases in asparaginase enzyme activity, suggesting that patients at risk for those toxicities would benefit from therapeutic drug monitoring, according to new research.
In the study, published Oct. 8 in Blood Advances, increased asparaginase enzyme activity was not significantly associated with overall asparaginase toxicity. However,“ the authors concluded.
“The [findings are] new, and we have included patients from a quite big cohort, which is unique,” coauthor Birgitte Klug Albertsen, MD, PhD, associate clinical professor with Aarhus (Denmark) University Hospital, told this news organization.
Therapeutic drug monitoring already is widely used during treatment with asparaginase, the standard of care treatment for ALL; however, the focus of this monitoring has typically been on clinical effectiveness, as levels of asparaginase enzyme activity can indicate hypersensitivity reactions, while the absence of such activity can suggest inferior outcomes.
Meanwhile, drug monitoring is not normally used to assess the risk of treatment-related toxicities. This has been due to a lack of evidence regarding asparaginase enzyme activity and toxicity risk, which, if severe enough, can prevent further treatment.
To investigate the relationship with toxicities, Dr. Albertsen and colleagues evaluated data from seven countries in Europe on 1,155 children between the ages of 1 and 17.9 who were diagnosed with ALL and treated with asparaginase, according to the Nordic Society of Paediatric Haematology and Oncology (NOPHO) ALL2008 protocol between July 2008 and March 2016.
Blood samples drawn approximately 14 days after asparaginase administration showed that some level of asparaginase enzyme activity was measurable in 955 patients (82.7%), while 200 patients (17.3%) had asparaginase inactivation. Overall, there were 159 asparaginase-associated toxicities of pancreatitis, thromboembolism, or osteonecrosis among the 955 patients with measurable asparaginase enzyme activity.
There were no significant differences in median asparaginase enzyme activity levels between those who did and did not experience toxicities (224 IU/L vs. 221 IU/L, respectively; P = .1), and the results did not change after adjustment for age and sex. However, the risk of pancreatitis was found to increase with a hazard ratio (HR) of 1.40 for each 100 IU/L increase in the median asparaginase enzyme activity level (P = .002).
Likewise, an increase in risk was observed for osteonecrosis (HR 1.36; P = .02) per 100 IU/L increase in median asparaginase enzyme activity. However, the HR for the risk of thromboembolism, the most common of asparaginase-related toxicities, was not significant (HR 0.99; P = .96).
Dr. Albertsen said the etiology behind the occurrence of osteonecrosis is not well understood.
“We know that steroids, especially dexamethasone, are a risk factor,” she said. “We believe that asparaginase may play a role too, but a clear association has not been demonstrated.”
In the NOPHO ALL2008 protocol used in the study, dexamethasone is used in the same time periods as PEG-asparaginase treatment for patients receiving 15 doses.
The finding of only a nonsignificant trend between asparaginase enzyme activity with overall toxicities may have reflected the low dose that was used, Dr. Albertsen added.
“In the NOPHO ALL2008 protocol, we used quite a low dose of PEG-asparaginase, and the risk may be higher in protocols using higher doses,” she said.
Relapse reduction
Notably, the study showed that asparaginase enzyme elevations were, in fact, not significantly associated with a reduction in the risk of leukemic relapse (HR .88 per 100 IU/L increase; P = .35).
Those findings suggest that measurable asparaginase enzyme activity levels, and thus asparaginase depletion, “may be sufficient to ensure an antileukemic effect,” the authors noted.
“Therapeutic drug monitoring of asparaginase enzyme activity is indicated mainly to detect inactivation, but [it] may be further explored for dose reduction to reduce some specific toxicities,” they concluded.
Dr. Albertsen disclosed being sponsor of the investigator-initiatied NOR-GRASPALL 2016 trial.
Key toxicities related to treating acute lymphoblastic leukemia (ALL) with asparaginase, specifically pancreatitis and osteonecrosis, are associated with increases in asparaginase enzyme activity, suggesting that patients at risk for those toxicities would benefit from therapeutic drug monitoring, according to new research.
In the study, published Oct. 8 in Blood Advances, increased asparaginase enzyme activity was not significantly associated with overall asparaginase toxicity. However,“ the authors concluded.
“The [findings are] new, and we have included patients from a quite big cohort, which is unique,” coauthor Birgitte Klug Albertsen, MD, PhD, associate clinical professor with Aarhus (Denmark) University Hospital, told this news organization.
Therapeutic drug monitoring already is widely used during treatment with asparaginase, the standard of care treatment for ALL; however, the focus of this monitoring has typically been on clinical effectiveness, as levels of asparaginase enzyme activity can indicate hypersensitivity reactions, while the absence of such activity can suggest inferior outcomes.
Meanwhile, drug monitoring is not normally used to assess the risk of treatment-related toxicities. This has been due to a lack of evidence regarding asparaginase enzyme activity and toxicity risk, which, if severe enough, can prevent further treatment.
To investigate the relationship with toxicities, Dr. Albertsen and colleagues evaluated data from seven countries in Europe on 1,155 children between the ages of 1 and 17.9 who were diagnosed with ALL and treated with asparaginase, according to the Nordic Society of Paediatric Haematology and Oncology (NOPHO) ALL2008 protocol between July 2008 and March 2016.
Blood samples drawn approximately 14 days after asparaginase administration showed that some level of asparaginase enzyme activity was measurable in 955 patients (82.7%), while 200 patients (17.3%) had asparaginase inactivation. Overall, there were 159 asparaginase-associated toxicities of pancreatitis, thromboembolism, or osteonecrosis among the 955 patients with measurable asparaginase enzyme activity.
There were no significant differences in median asparaginase enzyme activity levels between those who did and did not experience toxicities (224 IU/L vs. 221 IU/L, respectively; P = .1), and the results did not change after adjustment for age and sex. However, the risk of pancreatitis was found to increase with a hazard ratio (HR) of 1.40 for each 100 IU/L increase in the median asparaginase enzyme activity level (P = .002).
Likewise, an increase in risk was observed for osteonecrosis (HR 1.36; P = .02) per 100 IU/L increase in median asparaginase enzyme activity. However, the HR for the risk of thromboembolism, the most common of asparaginase-related toxicities, was not significant (HR 0.99; P = .96).
Dr. Albertsen said the etiology behind the occurrence of osteonecrosis is not well understood.
“We know that steroids, especially dexamethasone, are a risk factor,” she said. “We believe that asparaginase may play a role too, but a clear association has not been demonstrated.”
In the NOPHO ALL2008 protocol used in the study, dexamethasone is used in the same time periods as PEG-asparaginase treatment for patients receiving 15 doses.
The finding of only a nonsignificant trend between asparaginase enzyme activity with overall toxicities may have reflected the low dose that was used, Dr. Albertsen added.
“In the NOPHO ALL2008 protocol, we used quite a low dose of PEG-asparaginase, and the risk may be higher in protocols using higher doses,” she said.
Relapse reduction
Notably, the study showed that asparaginase enzyme elevations were, in fact, not significantly associated with a reduction in the risk of leukemic relapse (HR .88 per 100 IU/L increase; P = .35).
Those findings suggest that measurable asparaginase enzyme activity levels, and thus asparaginase depletion, “may be sufficient to ensure an antileukemic effect,” the authors noted.
“Therapeutic drug monitoring of asparaginase enzyme activity is indicated mainly to detect inactivation, but [it] may be further explored for dose reduction to reduce some specific toxicities,” they concluded.
Dr. Albertsen disclosed being sponsor of the investigator-initiatied NOR-GRASPALL 2016 trial.
New AKI risk score for PCI patients passes validation
A pair of updated scoring models for estimating a patient’s risk for contrast-associated acute kidney injury during and immediately after percutaneous coronary intervention worked better than a widely used prior version in initial validation testing using data collected at a single U.S. tertiary-care hospital.
While the two new risk scores looked promising, they need further, external validation with additional, diverse patient cohorts, Roxana Mehran, MD, cautioned at the American Heart Association scientific sessions.
“Don’t change anything until we externally validate this,” urged Dr. Mehran, professor and director of the Center for Interventional Cardiovascular Research and Clinical Trials at Icahn School of Medicine at Mount Sinai in New York. External validation of the two new risk scores is in progress with planned reporting of the results in 2022, she said in an interview.
One of the two new algorithms, which both predict a patient’s risk for developing acute kidney injury (AKI) as a result of receiving iodinated contrast media within 48 hours of a percutaneous coronary intervention (PCI), relies on eight easily available variables taken from a patient’s medical record just prior to undergoing PCI: age, type of coronary disease (ranging from asymptomatic or stable angina to ST-segment elevation MI), estimated glomerular filtration rate, left ventricular ejection fraction, diabetes, hemoglobin, basal glucose, and heart failure.
This risk score accounted for 72% (a C-statistic of 0.72) of the observed AKI episodes during the derivation phase, which used data from 14,616 consecutive Mount Sinai patients who underwent PCI during January 2012–December 2017.
Internal validation using data from 5,606 consecutive Mount Sinai patients who underwent PCI during January 2018–December 2020 showed that the eight-item formula accounted for 84% of all incident AKI events occurring during or within 48 hours of a PCI procedure.
Accounting for periprocedural variables
A second risk score included the eight preprocedural variables plus four additional periprocedural variables: complex PCI anatomy, contrast volume during the procedure, development of a periprocedural bleed, and having slow or no reflow into affected coronaries (less than TIMI grade 3 flow) immediately after the procedure. The second model produced a C-statistic of 0.74 during derivation and accounted for 86% of incident AKI events in the validation analysis.
The data Dr. Mehran reported appeared in The Lancet .
She and her coauthors designed these two new algorithms to replace a “widely used” and externally validated risk score that Dr. Mehran and associates introduced in 2004. Despite its merits, the 17-year-old scoring formula has limitations including “low discrimination” with a C-statistic of 0.67, derivation from data that’s now 20 years old, and exclusion of patients with ST-elevation MIs, the authors said in the new report.
Dr. Mehran encouraged interventional cardiologists to use both new risk scores (once externally validated) when possible.
The eight-item preprocedural model “gives clinicians an idea about a patient’s risk [for incident AKI] before they go into the catheterization laboratory,” and then they can further refine the risk assessment during the procedure based on the four periprocedural risk factors, she explained. The goal is to target “tailored preventive strategies” to patients identified by the scoring algorithms as being at high risk for AKI.
A role for preventive measures
Preventive strategies to consider for higher-risk patients include limiting the administered volume of iodinated contrast media, increasing hydration, and avoiding nephrotoxic agents, Dr. Mehran said. The two new risk-assessment tools will “allow for better evaluation of PCI patients” when testing “innovative strategies and treatments” designed to help avoid contrast-associated AKI.
“The focus to date has been on measures to protect renal function from contrast media, based on indirect data,” Estelle C. Nijssen, MSc, and Joachim E. Wildberger, MD, wrote in an editorial that accompanied the published report. “The effect of prophylactic measures on longer-term averse outcomes is still unclear,” they noted. “Perhaps our focus should shift from contrast and renal function to the heart, the role of which has probably been undervalued in this setting,” wrote Ms. Nijssen, a researcher at Maastricht (The Netherlands) University, and Dr. Wildberger, professor and chairman of the department of radiology at Maastricht University.
The editorial’s authors noted that the two new risk scores have the advantage of relying on variables that are “readily available in clinical practice.” But they also noted several limitations, such as the model’s development from largely low-risk patients who had a low, roughly 30% prevalence of chronic kidney disease. During 9 full years studied, 2012-2020, the annual incidence of AKI showed a downward trend, with an incidence of just over 3% in 2020.
Dr. Mehran attributed this decline in AKI to “great work identifying high-risk patients” and using the prophylactic measures she cited. But even when occurring at relatively low incidence, “AKI is still an important complication that is associated with mortality post PCI,” she stressed.
Establishing a safe contrast dose
“The study is great, and helps reinforce the risk factors that are most important to consider when risk stratifying patients prior to PCI,” said Neal Yuan, MD, a cardiologist at the University of California, San Francisco, who has studied contrast-associated AKI in patients who undergo PCI. The report from Dr. Mehran also “confirms in a large cohort the association between contrast-associated AKI and death,” and describes “an easy method for calculating risk,” he said in an interview.
Dr. Yuan agreed on the need for external validation, and once adequately validated he called for incorporation of the risk score into EHRs. Another important issue for future study is “how much [AKI] risk is too much risk,” he said.
The risk factors identified in Dr. Mehran’s report “are some of the same ones identified in previous studies. Even though this was a more contemporary dataset, there is not a ton of new [findings]; it mainly strengthens findings from prior studies.”
Results published by Dr. Yuan and his associates in 2020 used data from more than 20,000 U.S. patients who underwent PCI to try to identify a generally safe upper limit for the dose of iodinated contrast.
The main purpose for performing AKI risk stratification on PCI patients is to “identify high-risk patients and use preventive strategies when treating these patients.” Current AKI preventive strategies “mainly fall into intravascular volume expansion, and reduced contrast.” What’s less clear is “how to operationalize reduced contrast,” he said.
The report by Dr. Yuan showed that “about 10% of PCI patients were at very high risk” for contrast-associated AKI “no matter what is done.” In contrast, about two-thirds of PCI patients “could receive lots of contrast and still be very unlikely to develop AKI,” Dr. Yuan said.
He voiced some skepticism about the willingness of many clinicians to routinely use a formal risk score to assess their patients scheduled for PCI.
Most operators “approximate AKI risk based on variables such as age and creatinine level, but few take time to put the variables into a calculator to get an exact risk number.” In a “small survey” he ran, he found that these rough approximations often ignore important risk factors like hemoglobin level. This inertia by clinicians against routinely using a risk score could be addressed, at least in part, by integrating the risk score into an EHR for automatic calculation, Dr. Yuan suggested.
Dr. Mehran noted that the risk score that she introduced in 2004 is used “in many EHRs to identify high-risk patients.”
The current study received no commercial or external funding. Dr. Mehran has been a consultant to Boston Scientific, Cine-Med Research, CIRM, and Janssen, and she holds equity in Applied Therapeutics, Elixir Medical, and STEL. Dr. Wildberger had no relevant disclosures. Ms. Nijssen and Dr. Yuan had no disclosures.
A pair of updated scoring models for estimating a patient’s risk for contrast-associated acute kidney injury during and immediately after percutaneous coronary intervention worked better than a widely used prior version in initial validation testing using data collected at a single U.S. tertiary-care hospital.
While the two new risk scores looked promising, they need further, external validation with additional, diverse patient cohorts, Roxana Mehran, MD, cautioned at the American Heart Association scientific sessions.
“Don’t change anything until we externally validate this,” urged Dr. Mehran, professor and director of the Center for Interventional Cardiovascular Research and Clinical Trials at Icahn School of Medicine at Mount Sinai in New York. External validation of the two new risk scores is in progress with planned reporting of the results in 2022, she said in an interview.
One of the two new algorithms, which both predict a patient’s risk for developing acute kidney injury (AKI) as a result of receiving iodinated contrast media within 48 hours of a percutaneous coronary intervention (PCI), relies on eight easily available variables taken from a patient’s medical record just prior to undergoing PCI: age, type of coronary disease (ranging from asymptomatic or stable angina to ST-segment elevation MI), estimated glomerular filtration rate, left ventricular ejection fraction, diabetes, hemoglobin, basal glucose, and heart failure.
This risk score accounted for 72% (a C-statistic of 0.72) of the observed AKI episodes during the derivation phase, which used data from 14,616 consecutive Mount Sinai patients who underwent PCI during January 2012–December 2017.
Internal validation using data from 5,606 consecutive Mount Sinai patients who underwent PCI during January 2018–December 2020 showed that the eight-item formula accounted for 84% of all incident AKI events occurring during or within 48 hours of a PCI procedure.
Accounting for periprocedural variables
A second risk score included the eight preprocedural variables plus four additional periprocedural variables: complex PCI anatomy, contrast volume during the procedure, development of a periprocedural bleed, and having slow or no reflow into affected coronaries (less than TIMI grade 3 flow) immediately after the procedure. The second model produced a C-statistic of 0.74 during derivation and accounted for 86% of incident AKI events in the validation analysis.
The data Dr. Mehran reported appeared in The Lancet .
She and her coauthors designed these two new algorithms to replace a “widely used” and externally validated risk score that Dr. Mehran and associates introduced in 2004. Despite its merits, the 17-year-old scoring formula has limitations including “low discrimination” with a C-statistic of 0.67, derivation from data that’s now 20 years old, and exclusion of patients with ST-elevation MIs, the authors said in the new report.
Dr. Mehran encouraged interventional cardiologists to use both new risk scores (once externally validated) when possible.
The eight-item preprocedural model “gives clinicians an idea about a patient’s risk [for incident AKI] before they go into the catheterization laboratory,” and then they can further refine the risk assessment during the procedure based on the four periprocedural risk factors, she explained. The goal is to target “tailored preventive strategies” to patients identified by the scoring algorithms as being at high risk for AKI.
A role for preventive measures
Preventive strategies to consider for higher-risk patients include limiting the administered volume of iodinated contrast media, increasing hydration, and avoiding nephrotoxic agents, Dr. Mehran said. The two new risk-assessment tools will “allow for better evaluation of PCI patients” when testing “innovative strategies and treatments” designed to help avoid contrast-associated AKI.
“The focus to date has been on measures to protect renal function from contrast media, based on indirect data,” Estelle C. Nijssen, MSc, and Joachim E. Wildberger, MD, wrote in an editorial that accompanied the published report. “The effect of prophylactic measures on longer-term averse outcomes is still unclear,” they noted. “Perhaps our focus should shift from contrast and renal function to the heart, the role of which has probably been undervalued in this setting,” wrote Ms. Nijssen, a researcher at Maastricht (The Netherlands) University, and Dr. Wildberger, professor and chairman of the department of radiology at Maastricht University.
The editorial’s authors noted that the two new risk scores have the advantage of relying on variables that are “readily available in clinical practice.” But they also noted several limitations, such as the model’s development from largely low-risk patients who had a low, roughly 30% prevalence of chronic kidney disease. During 9 full years studied, 2012-2020, the annual incidence of AKI showed a downward trend, with an incidence of just over 3% in 2020.
Dr. Mehran attributed this decline in AKI to “great work identifying high-risk patients” and using the prophylactic measures she cited. But even when occurring at relatively low incidence, “AKI is still an important complication that is associated with mortality post PCI,” she stressed.
Establishing a safe contrast dose
“The study is great, and helps reinforce the risk factors that are most important to consider when risk stratifying patients prior to PCI,” said Neal Yuan, MD, a cardiologist at the University of California, San Francisco, who has studied contrast-associated AKI in patients who undergo PCI. The report from Dr. Mehran also “confirms in a large cohort the association between contrast-associated AKI and death,” and describes “an easy method for calculating risk,” he said in an interview.
Dr. Yuan agreed on the need for external validation, and once adequately validated he called for incorporation of the risk score into EHRs. Another important issue for future study is “how much [AKI] risk is too much risk,” he said.
The risk factors identified in Dr. Mehran’s report “are some of the same ones identified in previous studies. Even though this was a more contemporary dataset, there is not a ton of new [findings]; it mainly strengthens findings from prior studies.”
Results published by Dr. Yuan and his associates in 2020 used data from more than 20,000 U.S. patients who underwent PCI to try to identify a generally safe upper limit for the dose of iodinated contrast.
The main purpose for performing AKI risk stratification on PCI patients is to “identify high-risk patients and use preventive strategies when treating these patients.” Current AKI preventive strategies “mainly fall into intravascular volume expansion, and reduced contrast.” What’s less clear is “how to operationalize reduced contrast,” he said.
The report by Dr. Yuan showed that “about 10% of PCI patients were at very high risk” for contrast-associated AKI “no matter what is done.” In contrast, about two-thirds of PCI patients “could receive lots of contrast and still be very unlikely to develop AKI,” Dr. Yuan said.
He voiced some skepticism about the willingness of many clinicians to routinely use a formal risk score to assess their patients scheduled for PCI.
Most operators “approximate AKI risk based on variables such as age and creatinine level, but few take time to put the variables into a calculator to get an exact risk number.” In a “small survey” he ran, he found that these rough approximations often ignore important risk factors like hemoglobin level. This inertia by clinicians against routinely using a risk score could be addressed, at least in part, by integrating the risk score into an EHR for automatic calculation, Dr. Yuan suggested.
Dr. Mehran noted that the risk score that she introduced in 2004 is used “in many EHRs to identify high-risk patients.”
The current study received no commercial or external funding. Dr. Mehran has been a consultant to Boston Scientific, Cine-Med Research, CIRM, and Janssen, and she holds equity in Applied Therapeutics, Elixir Medical, and STEL. Dr. Wildberger had no relevant disclosures. Ms. Nijssen and Dr. Yuan had no disclosures.
A pair of updated scoring models for estimating a patient’s risk for contrast-associated acute kidney injury during and immediately after percutaneous coronary intervention worked better than a widely used prior version in initial validation testing using data collected at a single U.S. tertiary-care hospital.
While the two new risk scores looked promising, they need further, external validation with additional, diverse patient cohorts, Roxana Mehran, MD, cautioned at the American Heart Association scientific sessions.
“Don’t change anything until we externally validate this,” urged Dr. Mehran, professor and director of the Center for Interventional Cardiovascular Research and Clinical Trials at Icahn School of Medicine at Mount Sinai in New York. External validation of the two new risk scores is in progress with planned reporting of the results in 2022, she said in an interview.
One of the two new algorithms, which both predict a patient’s risk for developing acute kidney injury (AKI) as a result of receiving iodinated contrast media within 48 hours of a percutaneous coronary intervention (PCI), relies on eight easily available variables taken from a patient’s medical record just prior to undergoing PCI: age, type of coronary disease (ranging from asymptomatic or stable angina to ST-segment elevation MI), estimated glomerular filtration rate, left ventricular ejection fraction, diabetes, hemoglobin, basal glucose, and heart failure.
This risk score accounted for 72% (a C-statistic of 0.72) of the observed AKI episodes during the derivation phase, which used data from 14,616 consecutive Mount Sinai patients who underwent PCI during January 2012–December 2017.
Internal validation using data from 5,606 consecutive Mount Sinai patients who underwent PCI during January 2018–December 2020 showed that the eight-item formula accounted for 84% of all incident AKI events occurring during or within 48 hours of a PCI procedure.
Accounting for periprocedural variables
A second risk score included the eight preprocedural variables plus four additional periprocedural variables: complex PCI anatomy, contrast volume during the procedure, development of a periprocedural bleed, and having slow or no reflow into affected coronaries (less than TIMI grade 3 flow) immediately after the procedure. The second model produced a C-statistic of 0.74 during derivation and accounted for 86% of incident AKI events in the validation analysis.
The data Dr. Mehran reported appeared in The Lancet .
She and her coauthors designed these two new algorithms to replace a “widely used” and externally validated risk score that Dr. Mehran and associates introduced in 2004. Despite its merits, the 17-year-old scoring formula has limitations including “low discrimination” with a C-statistic of 0.67, derivation from data that’s now 20 years old, and exclusion of patients with ST-elevation MIs, the authors said in the new report.
Dr. Mehran encouraged interventional cardiologists to use both new risk scores (once externally validated) when possible.
The eight-item preprocedural model “gives clinicians an idea about a patient’s risk [for incident AKI] before they go into the catheterization laboratory,” and then they can further refine the risk assessment during the procedure based on the four periprocedural risk factors, she explained. The goal is to target “tailored preventive strategies” to patients identified by the scoring algorithms as being at high risk for AKI.
A role for preventive measures
Preventive strategies to consider for higher-risk patients include limiting the administered volume of iodinated contrast media, increasing hydration, and avoiding nephrotoxic agents, Dr. Mehran said. The two new risk-assessment tools will “allow for better evaluation of PCI patients” when testing “innovative strategies and treatments” designed to help avoid contrast-associated AKI.
“The focus to date has been on measures to protect renal function from contrast media, based on indirect data,” Estelle C. Nijssen, MSc, and Joachim E. Wildberger, MD, wrote in an editorial that accompanied the published report. “The effect of prophylactic measures on longer-term averse outcomes is still unclear,” they noted. “Perhaps our focus should shift from contrast and renal function to the heart, the role of which has probably been undervalued in this setting,” wrote Ms. Nijssen, a researcher at Maastricht (The Netherlands) University, and Dr. Wildberger, professor and chairman of the department of radiology at Maastricht University.
The editorial’s authors noted that the two new risk scores have the advantage of relying on variables that are “readily available in clinical practice.” But they also noted several limitations, such as the model’s development from largely low-risk patients who had a low, roughly 30% prevalence of chronic kidney disease. During 9 full years studied, 2012-2020, the annual incidence of AKI showed a downward trend, with an incidence of just over 3% in 2020.
Dr. Mehran attributed this decline in AKI to “great work identifying high-risk patients” and using the prophylactic measures she cited. But even when occurring at relatively low incidence, “AKI is still an important complication that is associated with mortality post PCI,” she stressed.
Establishing a safe contrast dose
“The study is great, and helps reinforce the risk factors that are most important to consider when risk stratifying patients prior to PCI,” said Neal Yuan, MD, a cardiologist at the University of California, San Francisco, who has studied contrast-associated AKI in patients who undergo PCI. The report from Dr. Mehran also “confirms in a large cohort the association between contrast-associated AKI and death,” and describes “an easy method for calculating risk,” he said in an interview.
Dr. Yuan agreed on the need for external validation, and once adequately validated he called for incorporation of the risk score into EHRs. Another important issue for future study is “how much [AKI] risk is too much risk,” he said.
The risk factors identified in Dr. Mehran’s report “are some of the same ones identified in previous studies. Even though this was a more contemporary dataset, there is not a ton of new [findings]; it mainly strengthens findings from prior studies.”
Results published by Dr. Yuan and his associates in 2020 used data from more than 20,000 U.S. patients who underwent PCI to try to identify a generally safe upper limit for the dose of iodinated contrast.
The main purpose for performing AKI risk stratification on PCI patients is to “identify high-risk patients and use preventive strategies when treating these patients.” Current AKI preventive strategies “mainly fall into intravascular volume expansion, and reduced contrast.” What’s less clear is “how to operationalize reduced contrast,” he said.
The report by Dr. Yuan showed that “about 10% of PCI patients were at very high risk” for contrast-associated AKI “no matter what is done.” In contrast, about two-thirds of PCI patients “could receive lots of contrast and still be very unlikely to develop AKI,” Dr. Yuan said.
He voiced some skepticism about the willingness of many clinicians to routinely use a formal risk score to assess their patients scheduled for PCI.
Most operators “approximate AKI risk based on variables such as age and creatinine level, but few take time to put the variables into a calculator to get an exact risk number.” In a “small survey” he ran, he found that these rough approximations often ignore important risk factors like hemoglobin level. This inertia by clinicians against routinely using a risk score could be addressed, at least in part, by integrating the risk score into an EHR for automatic calculation, Dr. Yuan suggested.
Dr. Mehran noted that the risk score that she introduced in 2004 is used “in many EHRs to identify high-risk patients.”
The current study received no commercial or external funding. Dr. Mehran has been a consultant to Boston Scientific, Cine-Med Research, CIRM, and Janssen, and she holds equity in Applied Therapeutics, Elixir Medical, and STEL. Dr. Wildberger had no relevant disclosures. Ms. Nijssen and Dr. Yuan had no disclosures.
FROM AHA 2021
Peripheral manifestations make mark on spondyloarthritis trajectory
Peripheral manifestations contribute significantly to disease activity in adults with spondyloarthritis (SpA), point toward a generally worse prognosis, and play a big role in defining the phenotypic clustering of the heterogenous disease, according to findings from what researchers called the first prospective study “to comprehensively describe the prevalence, clinical patterns, and prognostic implications of peripheral manifestations across the entire SpA spectrum.”
The stratification of patients in the study based on the presence of peripheral manifestations (arthritis, enthesitis, and/or dactylitis) led to the identification of an endotype with unfavorable outcomes, which not only has prognostic value but supports the need for an endotype-based treatment approach rather than one centered on C-reactive protein (CRP) and the Ankylosing Spondylitis Disease Activity Score (ASDAS).
The findings “advocate strongly for the presence of a distinct SpA endotype, based on potentially different immunopathological mechanisms and characterized by high disease activity at initial presentation with lack of substantial improvement upon follow-up,” first author Ann-Sophie De Craemer, MD, of Ghent, Belgium, and colleagues wrote.
Because the diagnostic and prognostic value of peripheral manifestations has not been well studied in SpA in general and in newly diagnosed patients in particular, Dr. De Craemer and associates decided to analyze their impact in 367 patients in the Be-Giant (BelGian Inflammatory Arthritis and spoNdylitis cohorT) cohort, a multicenter, prospective, observational cohort of newly diagnosed patients with SpA in Belgium. The study was published in Rheumatology.
The study population included 257 (70%) patients with axial-predominant SpA (axSpA) as classified by Assessment of Spondyloarthritis International Society criteria and 110 (30%) with peripheral-predominant SpA (pSpA) as defined by ASAS criteria. A total of 52 patients with axSpA had peripheral manifestations at baseline. The mean age of the patients was 34 years, and 52% were male.
The 162 patients with peripheral manifestations included 143 with arthritis, 52 with enthesitis, and 55 with dactylitis.
Two patient clusters emerge from data
In a cluster analysis that used baseline clinical features, the researchers divided the patients into cluster A (of which 242 of 248 were patients with axSpA) and cluster B (of which 104 of 119 were patients with pSpA). Most of the patients with peripheral manifestations were in cluster B (117 of 162 [72%]), compared with cluster A (45 of 162 [28%]).
A longitudinal analysis included 195 patients who completed a minimum 2-year follow-up. The longitudinal analysis identified high- and low-disease activity trajectories in each cluster.
In axSpA-predominant cluster A, patients with “high” trajectory had high disease activity levels at baseline (mean ASDAS-CRP, 3.2) that remained relatively stable, while those in the low-trajectory group (62%) had less disease activity at baseline (mean ASDAS-CRP, 2.0), which then further declined during follow-up.
Patients in the high trajectory in cluster A were more often affected by peripheral manifestations, “which remained a significant predictor in multivariate analysis,” with an odds ratio of 2.4, the researchers noted. In addition, patients with peripheral manifestations were significantly more likely to have persistent high disease activity despite starting biologics earlier than patients without peripheral manifestations (hazard ratio, 2.1).
Patients in pSpA-predominant cluster B showed differences that were similar to those seen in cluster A in terms of high– and low–disease activity trajectories (mean ASDAS-CRP of 3.6 and 2.8, respectively), but among these patients, a high level of disease activity was significantly associated with elevated CRP, rather than with peripheral disease, the researchers said.
The study findings were limited by several factors, including the exclusion of patients who did not complete the follow-up, which reduced the sample size for longitudinal analysis. However, the results were strengthened by the inclusion of patients from the full SpA spectrum, a geographically spread-out patient population, and a study design that mirrored clinical practice, the researchers noted.
The Be-Giant cohort was supported by an unrestricted grant from AbbVie. Several authors reported financial relationships with AbbVie and other pharmaceutical companies.
Peripheral manifestations contribute significantly to disease activity in adults with spondyloarthritis (SpA), point toward a generally worse prognosis, and play a big role in defining the phenotypic clustering of the heterogenous disease, according to findings from what researchers called the first prospective study “to comprehensively describe the prevalence, clinical patterns, and prognostic implications of peripheral manifestations across the entire SpA spectrum.”
The stratification of patients in the study based on the presence of peripheral manifestations (arthritis, enthesitis, and/or dactylitis) led to the identification of an endotype with unfavorable outcomes, which not only has prognostic value but supports the need for an endotype-based treatment approach rather than one centered on C-reactive protein (CRP) and the Ankylosing Spondylitis Disease Activity Score (ASDAS).
The findings “advocate strongly for the presence of a distinct SpA endotype, based on potentially different immunopathological mechanisms and characterized by high disease activity at initial presentation with lack of substantial improvement upon follow-up,” first author Ann-Sophie De Craemer, MD, of Ghent, Belgium, and colleagues wrote.
Because the diagnostic and prognostic value of peripheral manifestations has not been well studied in SpA in general and in newly diagnosed patients in particular, Dr. De Craemer and associates decided to analyze their impact in 367 patients in the Be-Giant (BelGian Inflammatory Arthritis and spoNdylitis cohorT) cohort, a multicenter, prospective, observational cohort of newly diagnosed patients with SpA in Belgium. The study was published in Rheumatology.
The study population included 257 (70%) patients with axial-predominant SpA (axSpA) as classified by Assessment of Spondyloarthritis International Society criteria and 110 (30%) with peripheral-predominant SpA (pSpA) as defined by ASAS criteria. A total of 52 patients with axSpA had peripheral manifestations at baseline. The mean age of the patients was 34 years, and 52% were male.
The 162 patients with peripheral manifestations included 143 with arthritis, 52 with enthesitis, and 55 with dactylitis.
Two patient clusters emerge from data
In a cluster analysis that used baseline clinical features, the researchers divided the patients into cluster A (of which 242 of 248 were patients with axSpA) and cluster B (of which 104 of 119 were patients with pSpA). Most of the patients with peripheral manifestations were in cluster B (117 of 162 [72%]), compared with cluster A (45 of 162 [28%]).
A longitudinal analysis included 195 patients who completed a minimum 2-year follow-up. The longitudinal analysis identified high- and low-disease activity trajectories in each cluster.
In axSpA-predominant cluster A, patients with “high” trajectory had high disease activity levels at baseline (mean ASDAS-CRP, 3.2) that remained relatively stable, while those in the low-trajectory group (62%) had less disease activity at baseline (mean ASDAS-CRP, 2.0), which then further declined during follow-up.
Patients in the high trajectory in cluster A were more often affected by peripheral manifestations, “which remained a significant predictor in multivariate analysis,” with an odds ratio of 2.4, the researchers noted. In addition, patients with peripheral manifestations were significantly more likely to have persistent high disease activity despite starting biologics earlier than patients without peripheral manifestations (hazard ratio, 2.1).
Patients in pSpA-predominant cluster B showed differences that were similar to those seen in cluster A in terms of high– and low–disease activity trajectories (mean ASDAS-CRP of 3.6 and 2.8, respectively), but among these patients, a high level of disease activity was significantly associated with elevated CRP, rather than with peripheral disease, the researchers said.
The study findings were limited by several factors, including the exclusion of patients who did not complete the follow-up, which reduced the sample size for longitudinal analysis. However, the results were strengthened by the inclusion of patients from the full SpA spectrum, a geographically spread-out patient population, and a study design that mirrored clinical practice, the researchers noted.
The Be-Giant cohort was supported by an unrestricted grant from AbbVie. Several authors reported financial relationships with AbbVie and other pharmaceutical companies.
Peripheral manifestations contribute significantly to disease activity in adults with spondyloarthritis (SpA), point toward a generally worse prognosis, and play a big role in defining the phenotypic clustering of the heterogenous disease, according to findings from what researchers called the first prospective study “to comprehensively describe the prevalence, clinical patterns, and prognostic implications of peripheral manifestations across the entire SpA spectrum.”
The stratification of patients in the study based on the presence of peripheral manifestations (arthritis, enthesitis, and/or dactylitis) led to the identification of an endotype with unfavorable outcomes, which not only has prognostic value but supports the need for an endotype-based treatment approach rather than one centered on C-reactive protein (CRP) and the Ankylosing Spondylitis Disease Activity Score (ASDAS).
The findings “advocate strongly for the presence of a distinct SpA endotype, based on potentially different immunopathological mechanisms and characterized by high disease activity at initial presentation with lack of substantial improvement upon follow-up,” first author Ann-Sophie De Craemer, MD, of Ghent, Belgium, and colleagues wrote.
Because the diagnostic and prognostic value of peripheral manifestations has not been well studied in SpA in general and in newly diagnosed patients in particular, Dr. De Craemer and associates decided to analyze their impact in 367 patients in the Be-Giant (BelGian Inflammatory Arthritis and spoNdylitis cohorT) cohort, a multicenter, prospective, observational cohort of newly diagnosed patients with SpA in Belgium. The study was published in Rheumatology.
The study population included 257 (70%) patients with axial-predominant SpA (axSpA) as classified by Assessment of Spondyloarthritis International Society criteria and 110 (30%) with peripheral-predominant SpA (pSpA) as defined by ASAS criteria. A total of 52 patients with axSpA had peripheral manifestations at baseline. The mean age of the patients was 34 years, and 52% were male.
The 162 patients with peripheral manifestations included 143 with arthritis, 52 with enthesitis, and 55 with dactylitis.
Two patient clusters emerge from data
In a cluster analysis that used baseline clinical features, the researchers divided the patients into cluster A (of which 242 of 248 were patients with axSpA) and cluster B (of which 104 of 119 were patients with pSpA). Most of the patients with peripheral manifestations were in cluster B (117 of 162 [72%]), compared with cluster A (45 of 162 [28%]).
A longitudinal analysis included 195 patients who completed a minimum 2-year follow-up. The longitudinal analysis identified high- and low-disease activity trajectories in each cluster.
In axSpA-predominant cluster A, patients with “high” trajectory had high disease activity levels at baseline (mean ASDAS-CRP, 3.2) that remained relatively stable, while those in the low-trajectory group (62%) had less disease activity at baseline (mean ASDAS-CRP, 2.0), which then further declined during follow-up.
Patients in the high trajectory in cluster A were more often affected by peripheral manifestations, “which remained a significant predictor in multivariate analysis,” with an odds ratio of 2.4, the researchers noted. In addition, patients with peripheral manifestations were significantly more likely to have persistent high disease activity despite starting biologics earlier than patients without peripheral manifestations (hazard ratio, 2.1).
Patients in pSpA-predominant cluster B showed differences that were similar to those seen in cluster A in terms of high– and low–disease activity trajectories (mean ASDAS-CRP of 3.6 and 2.8, respectively), but among these patients, a high level of disease activity was significantly associated with elevated CRP, rather than with peripheral disease, the researchers said.
The study findings were limited by several factors, including the exclusion of patients who did not complete the follow-up, which reduced the sample size for longitudinal analysis. However, the results were strengthened by the inclusion of patients from the full SpA spectrum, a geographically spread-out patient population, and a study design that mirrored clinical practice, the researchers noted.
The Be-Giant cohort was supported by an unrestricted grant from AbbVie. Several authors reported financial relationships with AbbVie and other pharmaceutical companies.
FROM RHEUMATOLOGY
‘Best Hospitals for Maternity’ offers national perspective
“The Best Hospitals for Maternity” looked at data for 2019 and covered uncomplicated but not high-risk pregnancies. “All families deserve to be informed on how hospitals perform on key indicators of quality, which is why U.S. News has compiled and published a trove of maternal health data from hospitals across the country,” Ben Harder, managing editor and chief of health analysis at U.S. News, said in a written statement.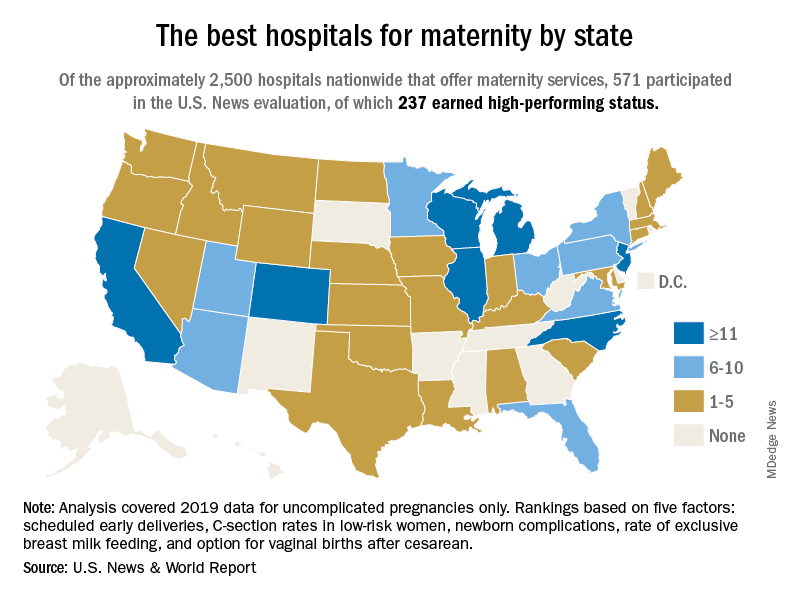
The 237 best performers were selected from an overall pool of 571 hospitals that participated in the analysis, representing every state except Alaska, Arkansas, and Vermont, U.S. News said, noting that about 2,700 hospitals in the United States offer maternity services.
California has the highest number of best performers, 33, followed by Illinois and New Jersey, both with 15. Colorado is home to 14 best-performing hospitals, Michigan has 12, and North Carolina and Wisconsin each have 12. “Hospitals that performed well had fewer newborn complications, fewer early deliveries and fewer C-sections, compared to other hospitals across the nation,” Mr. Harder said.
The composite score constructed by U.S. News involved five quality measures: nulliparous, term, singleton, and vertex cesarean delivery rates; early elective delivery rates; unexpected newborn complications rates; routine vaginal birth after cesarean (VBAC) delivery availability; and exclusive breast milk–feeding rates. The composite score averaged 80.0 for high performers and 54.9 for the other participating hospitals, U.S. News reported.
Averages for the high performers on each of the five measures looked like this:
- C-section rate, 21.1%.
- Early elective delivery rate, 1.3%.
- Overall unexpected newborn complication rates, 2.38%
- Exclusive breast milk–feeding rate, 58.6%.
- VBAC availability, 92.4%.
Data for four measures were collected from the hospitals via online survey over a 4-month window that began on April 29, 2021. Rates of early elective delivery came from the Centers for Medicare & Medicaid Services Care Compare.
“The Best Hospitals for Maternity” looked at data for 2019 and covered uncomplicated but not high-risk pregnancies. “All families deserve to be informed on how hospitals perform on key indicators of quality, which is why U.S. News has compiled and published a trove of maternal health data from hospitals across the country,” Ben Harder, managing editor and chief of health analysis at U.S. News, said in a written statement.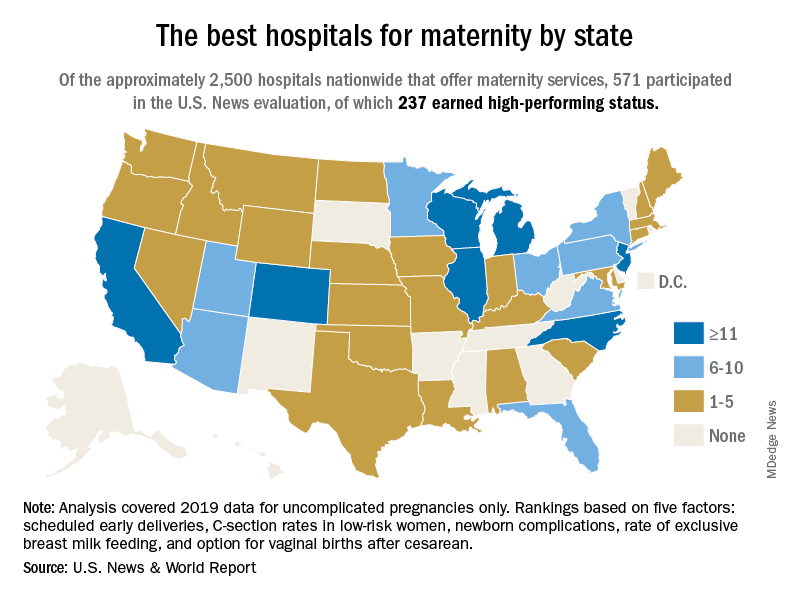
The 237 best performers were selected from an overall pool of 571 hospitals that participated in the analysis, representing every state except Alaska, Arkansas, and Vermont, U.S. News said, noting that about 2,700 hospitals in the United States offer maternity services.
California has the highest number of best performers, 33, followed by Illinois and New Jersey, both with 15. Colorado is home to 14 best-performing hospitals, Michigan has 12, and North Carolina and Wisconsin each have 12. “Hospitals that performed well had fewer newborn complications, fewer early deliveries and fewer C-sections, compared to other hospitals across the nation,” Mr. Harder said.
The composite score constructed by U.S. News involved five quality measures: nulliparous, term, singleton, and vertex cesarean delivery rates; early elective delivery rates; unexpected newborn complications rates; routine vaginal birth after cesarean (VBAC) delivery availability; and exclusive breast milk–feeding rates. The composite score averaged 80.0 for high performers and 54.9 for the other participating hospitals, U.S. News reported.
Averages for the high performers on each of the five measures looked like this:
- C-section rate, 21.1%.
- Early elective delivery rate, 1.3%.
- Overall unexpected newborn complication rates, 2.38%
- Exclusive breast milk–feeding rate, 58.6%.
- VBAC availability, 92.4%.
Data for four measures were collected from the hospitals via online survey over a 4-month window that began on April 29, 2021. Rates of early elective delivery came from the Centers for Medicare & Medicaid Services Care Compare.
“The Best Hospitals for Maternity” looked at data for 2019 and covered uncomplicated but not high-risk pregnancies. “All families deserve to be informed on how hospitals perform on key indicators of quality, which is why U.S. News has compiled and published a trove of maternal health data from hospitals across the country,” Ben Harder, managing editor and chief of health analysis at U.S. News, said in a written statement.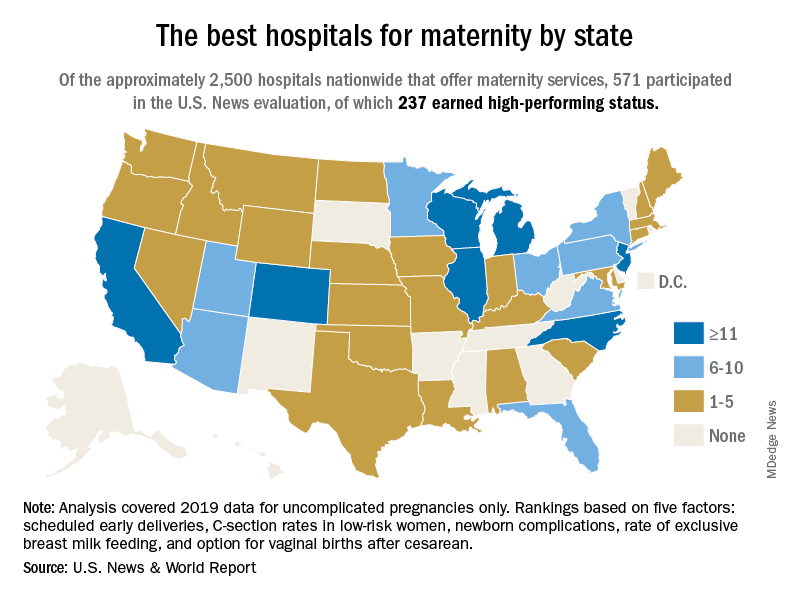
The 237 best performers were selected from an overall pool of 571 hospitals that participated in the analysis, representing every state except Alaska, Arkansas, and Vermont, U.S. News said, noting that about 2,700 hospitals in the United States offer maternity services.
California has the highest number of best performers, 33, followed by Illinois and New Jersey, both with 15. Colorado is home to 14 best-performing hospitals, Michigan has 12, and North Carolina and Wisconsin each have 12. “Hospitals that performed well had fewer newborn complications, fewer early deliveries and fewer C-sections, compared to other hospitals across the nation,” Mr. Harder said.
The composite score constructed by U.S. News involved five quality measures: nulliparous, term, singleton, and vertex cesarean delivery rates; early elective delivery rates; unexpected newborn complications rates; routine vaginal birth after cesarean (VBAC) delivery availability; and exclusive breast milk–feeding rates. The composite score averaged 80.0 for high performers and 54.9 for the other participating hospitals, U.S. News reported.
Averages for the high performers on each of the five measures looked like this:
- C-section rate, 21.1%.
- Early elective delivery rate, 1.3%.
- Overall unexpected newborn complication rates, 2.38%
- Exclusive breast milk–feeding rate, 58.6%.
- VBAC availability, 92.4%.
Data for four measures were collected from the hospitals via online survey over a 4-month window that began on April 29, 2021. Rates of early elective delivery came from the Centers for Medicare & Medicaid Services Care Compare.












