User login
Gastroenteritis Deaths Soar, Largely Due to C. difficile, Norovirus
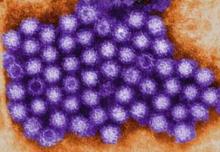
ATLANTA – The incidence of gastroenteritis-related deaths in the United States more than doubled from 1997 to 2007, largely because of Clostridium difficile and norovirus infections, mortality data from the National Center for Health Statistics show.
The apparent increase in C. difficile identified in this study is likely caused in part to increased recognition – and improved coding by physicians, but it also is likely because of a real increase resulting from the emergence of a hypervirulent and fluoroquinolone-resistant strain, Aron J. Hall, DVM, said at the International Conference on Emerging Infectious Diseases.
The elderly are disproportionately affected by these deadly infections, with those aged 65 years and older accounting for 83% of the gastroenteritis deaths during the study period, said Dr. Hall of the Centers for Disease Control and Prevention’s Viral Gastroenteritis Team.
"The mortality rate increases with increasing age, even within this older age group." These findings could help guide clinical management and development of candidate vaccines.
Between 1997 and 2007, all-cause gastroenteritis mortality increased from 25/1,000,000 person-years, to 57/1,000,000, which equates to an increase from about 7,000 to about 17,000 gastroenteritis-related deaths per year. The rate among those aged 65 years and older in 2007 was 259/1,000,000 person-years, Dr. Hall noted.
C. difficile was the leading cause of gastroenteritis-related death, and the incidence of C. difficile infection increased fivefold, from 10/1,000,000 in 1999-2000 to 48/1,000,000 in 2006-2007 – or from about 2,700 to 14,500 deaths per year.
Further, this study is the first to demonstrate that norovirus is likely the second leading infectious cause, Dr. Hall said.
On average, norovirus contributed to nearly 800 deaths per year during the study period (3/1,000,000 person-years), but mortality rates surged about every 3 years by up to 50%; these surges coincided with outbreaks associated with emergent viral strains, he explained.
As with C. difficile–related gastroenteritis deaths, most of these were in the elderly. However, a "small, but perhaps important" fraction of deaths occurred among children younger than age 5 years, Dr. Hall noted.
Seasonal variations also were apparent in this study, with C. difficile–associated deaths occurring most often during the spring months of March through May, and with norovirus-related deaths peaking in the winter months of December through February.
C. difficile and norovirus have emerged in recent years and are recognized as important contributors to gastroenteritis, but there have been limited data on deaths, Dr. Hall explained, adding that this is due in part to limited availability and/or sensitivity of clinical diagnostic assays, and also because deaths have historically not been coded specifically as being associated with a particular pathogen.
In fact, half of the gastroenteritis deaths included in the National Center for Health Statistics multiple cause of death mortality data are uncoded.
For this study, deaths with gastroenteritis listed as an underlying or contributing cause were included in the analysis, and an indirect attribution model was used to estimate the proportion of cause-unspecified gastroenteritis deaths that likely were due to specific causes. C. difficile, using this model, accounted for nearly 70% of gastroenteritis deaths.
The estimates of norovirus-associated gastroenteritis deaths in this study represent a 40% higher incidence than previously estimated based on extrapolation from community studies and studies from other industrialized countries, he added.
Gastroenteritis has long been recognized as an important contributor to mortality among children in developing countries, but less has been known about gastroenteritis-related mortality among adults and about the contributions of specific pathogens. These findings provide the first comprehensive analysis of data in more than 2 decades to characterize gastroenteritis deaths across all aged, he said.
The disease burden and seasonal patterns identified in this study could be helpful for the development of clinical management strategies, he said, adding that the mortality burden of these pathogens – particularly in the elderly – underscores the need for judicious use of antibiotics and proper infection control, as well as the need for effective interventions.
Dr. Hall noted that candidate vaccines are currently in development for both C. difficile and norovirus.
He reported having no relevant conflicts of interest.
ATLANTA – The incidence of gastroenteritis-related deaths in the United States more than doubled from 1997 to 2007, largely because of Clostridium difficile and norovirus infections, mortality data from the National Center for Health Statistics show.
The apparent increase in C. difficile identified in this study is likely caused in part to increased recognition – and improved coding by physicians, but it also is likely because of a real increase resulting from the emergence of a hypervirulent and fluoroquinolone-resistant strain, Aron J. Hall, DVM, said at the International Conference on Emerging Infectious Diseases.
The elderly are disproportionately affected by these deadly infections, with those aged 65 years and older accounting for 83% of the gastroenteritis deaths during the study period, said Dr. Hall of the Centers for Disease Control and Prevention’s Viral Gastroenteritis Team.
"The mortality rate increases with increasing age, even within this older age group." These findings could help guide clinical management and development of candidate vaccines.
Between 1997 and 2007, all-cause gastroenteritis mortality increased from 25/1,000,000 person-years, to 57/1,000,000, which equates to an increase from about 7,000 to about 17,000 gastroenteritis-related deaths per year. The rate among those aged 65 years and older in 2007 was 259/1,000,000 person-years, Dr. Hall noted.
C. difficile was the leading cause of gastroenteritis-related death, and the incidence of C. difficile infection increased fivefold, from 10/1,000,000 in 1999-2000 to 48/1,000,000 in 2006-2007 – or from about 2,700 to 14,500 deaths per year.
Further, this study is the first to demonstrate that norovirus is likely the second leading infectious cause, Dr. Hall said.
On average, norovirus contributed to nearly 800 deaths per year during the study period (3/1,000,000 person-years), but mortality rates surged about every 3 years by up to 50%; these surges coincided with outbreaks associated with emergent viral strains, he explained.
As with C. difficile–related gastroenteritis deaths, most of these were in the elderly. However, a "small, but perhaps important" fraction of deaths occurred among children younger than age 5 years, Dr. Hall noted.
Seasonal variations also were apparent in this study, with C. difficile–associated deaths occurring most often during the spring months of March through May, and with norovirus-related deaths peaking in the winter months of December through February.
C. difficile and norovirus have emerged in recent years and are recognized as important contributors to gastroenteritis, but there have been limited data on deaths, Dr. Hall explained, adding that this is due in part to limited availability and/or sensitivity of clinical diagnostic assays, and also because deaths have historically not been coded specifically as being associated with a particular pathogen.
In fact, half of the gastroenteritis deaths included in the National Center for Health Statistics multiple cause of death mortality data are uncoded.
For this study, deaths with gastroenteritis listed as an underlying or contributing cause were included in the analysis, and an indirect attribution model was used to estimate the proportion of cause-unspecified gastroenteritis deaths that likely were due to specific causes. C. difficile, using this model, accounted for nearly 70% of gastroenteritis deaths.
The estimates of norovirus-associated gastroenteritis deaths in this study represent a 40% higher incidence than previously estimated based on extrapolation from community studies and studies from other industrialized countries, he added.
Gastroenteritis has long been recognized as an important contributor to mortality among children in developing countries, but less has been known about gastroenteritis-related mortality among adults and about the contributions of specific pathogens. These findings provide the first comprehensive analysis of data in more than 2 decades to characterize gastroenteritis deaths across all aged, he said.
The disease burden and seasonal patterns identified in this study could be helpful for the development of clinical management strategies, he said, adding that the mortality burden of these pathogens – particularly in the elderly – underscores the need for judicious use of antibiotics and proper infection control, as well as the need for effective interventions.
Dr. Hall noted that candidate vaccines are currently in development for both C. difficile and norovirus.
He reported having no relevant conflicts of interest.
ATLANTA – The incidence of gastroenteritis-related deaths in the United States more than doubled from 1997 to 2007, largely because of Clostridium difficile and norovirus infections, mortality data from the National Center for Health Statistics show.
The apparent increase in C. difficile identified in this study is likely caused in part to increased recognition – and improved coding by physicians, but it also is likely because of a real increase resulting from the emergence of a hypervirulent and fluoroquinolone-resistant strain, Aron J. Hall, DVM, said at the International Conference on Emerging Infectious Diseases.
The elderly are disproportionately affected by these deadly infections, with those aged 65 years and older accounting for 83% of the gastroenteritis deaths during the study period, said Dr. Hall of the Centers for Disease Control and Prevention’s Viral Gastroenteritis Team.
"The mortality rate increases with increasing age, even within this older age group." These findings could help guide clinical management and development of candidate vaccines.
Between 1997 and 2007, all-cause gastroenteritis mortality increased from 25/1,000,000 person-years, to 57/1,000,000, which equates to an increase from about 7,000 to about 17,000 gastroenteritis-related deaths per year. The rate among those aged 65 years and older in 2007 was 259/1,000,000 person-years, Dr. Hall noted.
C. difficile was the leading cause of gastroenteritis-related death, and the incidence of C. difficile infection increased fivefold, from 10/1,000,000 in 1999-2000 to 48/1,000,000 in 2006-2007 – or from about 2,700 to 14,500 deaths per year.
Further, this study is the first to demonstrate that norovirus is likely the second leading infectious cause, Dr. Hall said.
On average, norovirus contributed to nearly 800 deaths per year during the study period (3/1,000,000 person-years), but mortality rates surged about every 3 years by up to 50%; these surges coincided with outbreaks associated with emergent viral strains, he explained.
As with C. difficile–related gastroenteritis deaths, most of these were in the elderly. However, a "small, but perhaps important" fraction of deaths occurred among children younger than age 5 years, Dr. Hall noted.
Seasonal variations also were apparent in this study, with C. difficile–associated deaths occurring most often during the spring months of March through May, and with norovirus-related deaths peaking in the winter months of December through February.
C. difficile and norovirus have emerged in recent years and are recognized as important contributors to gastroenteritis, but there have been limited data on deaths, Dr. Hall explained, adding that this is due in part to limited availability and/or sensitivity of clinical diagnostic assays, and also because deaths have historically not been coded specifically as being associated with a particular pathogen.
In fact, half of the gastroenteritis deaths included in the National Center for Health Statistics multiple cause of death mortality data are uncoded.
For this study, deaths with gastroenteritis listed as an underlying or contributing cause were included in the analysis, and an indirect attribution model was used to estimate the proportion of cause-unspecified gastroenteritis deaths that likely were due to specific causes. C. difficile, using this model, accounted for nearly 70% of gastroenteritis deaths.
The estimates of norovirus-associated gastroenteritis deaths in this study represent a 40% higher incidence than previously estimated based on extrapolation from community studies and studies from other industrialized countries, he added.
Gastroenteritis has long been recognized as an important contributor to mortality among children in developing countries, but less has been known about gastroenteritis-related mortality among adults and about the contributions of specific pathogens. These findings provide the first comprehensive analysis of data in more than 2 decades to characterize gastroenteritis deaths across all aged, he said.
The disease burden and seasonal patterns identified in this study could be helpful for the development of clinical management strategies, he said, adding that the mortality burden of these pathogens – particularly in the elderly – underscores the need for judicious use of antibiotics and proper infection control, as well as the need for effective interventions.
Dr. Hall noted that candidate vaccines are currently in development for both C. difficile and norovirus.
He reported having no relevant conflicts of interest.
FROM THE INTERNATIONAL CONFERENCE ON EMERGING INFECTIOUS DISEASES
Major Finding: Between 1997 and 2007, all-cause gastroenteritis mortality increased from 25/1,000,000 person-years, to 57/1,000,000, which equates to an increase from about 7,000 to about 17,000 gastroenteritis-related deaths per year. The rate among those aged 65 years and older in 2007 was 259/1,000,000 person-years.
Data Source: An analysis of data from the National Center for Health Statistics. An indirect attribution model was used to estimate the proportion of cause-unspecified gastroenteritis deaths that likely were from specific causes.
Disclosures: Dr. Hall had no disclosures to report.
Lyme Disease Presents Differently in Men and Women
ATLANTA – Women with Lyme disease display more clinical symptoms than do men with the disease and also are less likely to seroconvert following treatment, according to findings from a prospective cohort study involving 77 patients.
Numerous symptoms were reported more often by the 37 women in the study than by the 40 men. For example, significantly more women than men reported joint pain, muscle pain, headache, back pain, heart palpitations, nausea, vomiting, anxiety, numbness and tingling, and changes in vision during at least one of six preplanned study visits with a physician, Lauren A. Crowder, M.P.H. reported in a poster at the International Conference on Emerging Infectious Diseases.
Joint pain, heart palpitations, nausea, vomiting, and changes in vision were reported significantly more often by women at two of the six visits, and headache was reported significantly more often by women at four of the six visits.
"The second preliminary finding we observed in our cohort of patients was that women were less likely to seroconvert on the antibody tests for serodiagnosis of Lyme disease," Ms. Crowder of the Lyme Disease Research Foundation, Lutherville, Md., said in an interview.
At the initial study visit, a similar proportion of men and women (about 60% of each) tested negative for Lyme disease using the Centers for Disease Control and Prevention’s recommended two-tier testing criteria for serodiagnosis. However, at the second visit, which was performed immediately post treatment, 70% of women who tested negative at the first visit remained negative, compared with only 35% of the men who initially tested negative.
Additionally, polychromatic flow cytometry performed on patient samples indicated that women had significantly higher frequency of CD4+CCR5+ T-cells prior to treatment than did men (mean of 9.82% vs. 5.96%).
"These findings suggest to us that there may be a difference between how men and women respond to infection with Lyme disease. One hypothesis for these differences is that there may be an immunological variation in response to Borrelia burgdorferi, the bacterial infection that causes Lyme disease, between men and women," Ms. Crowder said.
Study participants had early, untreated erythema migrans and clinically confirmed Lyme disease. At the first of the six study visits, they were tested using the CDC criteria by a commercial laboratory. All were treated with 3-week course of doxycycline and were then followed for up to 2 years. At each study visit, participants underwent a physical examination and interval history, reported clinical symptoms and completed self-administered surveys, and underwent repeat laboratory evaluations.
The findings highlight a need for additional research on sex-based differences in the effects of early Lyme disease. Such differences have been seen in other infectious disease, but have not been thoroughly explored in early Lyme disease, Ms. Crowder noted.
Such study is important given that Lyme disease is the most common vector-borne infectious disease in the United States. Although most patients recover from acute infection with proper antibiotic treatment, a subset of patients develop Post-Treatment Lyme Disease Syndrome. The CDC defines this syndrome as involving lingering symptoms of fatigue, pain, or joint and muscle aches. In some cases, these can last for more than 6 months.
"We will continue to explore these suggested differences both in this cohort and in future research studies," she said.
Ms. Crowder also stressed the importance of encouraging patients to look for ticks if they live in Lyme endemic areas.
This study was supported by the Lyme Disease Research Foundation. Ms. Crowder had no disclosures to report.
ATLANTA – Women with Lyme disease display more clinical symptoms than do men with the disease and also are less likely to seroconvert following treatment, according to findings from a prospective cohort study involving 77 patients.
Numerous symptoms were reported more often by the 37 women in the study than by the 40 men. For example, significantly more women than men reported joint pain, muscle pain, headache, back pain, heart palpitations, nausea, vomiting, anxiety, numbness and tingling, and changes in vision during at least one of six preplanned study visits with a physician, Lauren A. Crowder, M.P.H. reported in a poster at the International Conference on Emerging Infectious Diseases.
Joint pain, heart palpitations, nausea, vomiting, and changes in vision were reported significantly more often by women at two of the six visits, and headache was reported significantly more often by women at four of the six visits.
"The second preliminary finding we observed in our cohort of patients was that women were less likely to seroconvert on the antibody tests for serodiagnosis of Lyme disease," Ms. Crowder of the Lyme Disease Research Foundation, Lutherville, Md., said in an interview.
At the initial study visit, a similar proportion of men and women (about 60% of each) tested negative for Lyme disease using the Centers for Disease Control and Prevention’s recommended two-tier testing criteria for serodiagnosis. However, at the second visit, which was performed immediately post treatment, 70% of women who tested negative at the first visit remained negative, compared with only 35% of the men who initially tested negative.
Additionally, polychromatic flow cytometry performed on patient samples indicated that women had significantly higher frequency of CD4+CCR5+ T-cells prior to treatment than did men (mean of 9.82% vs. 5.96%).
"These findings suggest to us that there may be a difference between how men and women respond to infection with Lyme disease. One hypothesis for these differences is that there may be an immunological variation in response to Borrelia burgdorferi, the bacterial infection that causes Lyme disease, between men and women," Ms. Crowder said.
Study participants had early, untreated erythema migrans and clinically confirmed Lyme disease. At the first of the six study visits, they were tested using the CDC criteria by a commercial laboratory. All were treated with 3-week course of doxycycline and were then followed for up to 2 years. At each study visit, participants underwent a physical examination and interval history, reported clinical symptoms and completed self-administered surveys, and underwent repeat laboratory evaluations.
The findings highlight a need for additional research on sex-based differences in the effects of early Lyme disease. Such differences have been seen in other infectious disease, but have not been thoroughly explored in early Lyme disease, Ms. Crowder noted.
Such study is important given that Lyme disease is the most common vector-borne infectious disease in the United States. Although most patients recover from acute infection with proper antibiotic treatment, a subset of patients develop Post-Treatment Lyme Disease Syndrome. The CDC defines this syndrome as involving lingering symptoms of fatigue, pain, or joint and muscle aches. In some cases, these can last for more than 6 months.
"We will continue to explore these suggested differences both in this cohort and in future research studies," she said.
Ms. Crowder also stressed the importance of encouraging patients to look for ticks if they live in Lyme endemic areas.
This study was supported by the Lyme Disease Research Foundation. Ms. Crowder had no disclosures to report.
ATLANTA – Women with Lyme disease display more clinical symptoms than do men with the disease and also are less likely to seroconvert following treatment, according to findings from a prospective cohort study involving 77 patients.
Numerous symptoms were reported more often by the 37 women in the study than by the 40 men. For example, significantly more women than men reported joint pain, muscle pain, headache, back pain, heart palpitations, nausea, vomiting, anxiety, numbness and tingling, and changes in vision during at least one of six preplanned study visits with a physician, Lauren A. Crowder, M.P.H. reported in a poster at the International Conference on Emerging Infectious Diseases.
Joint pain, heart palpitations, nausea, vomiting, and changes in vision were reported significantly more often by women at two of the six visits, and headache was reported significantly more often by women at four of the six visits.
"The second preliminary finding we observed in our cohort of patients was that women were less likely to seroconvert on the antibody tests for serodiagnosis of Lyme disease," Ms. Crowder of the Lyme Disease Research Foundation, Lutherville, Md., said in an interview.
At the initial study visit, a similar proportion of men and women (about 60% of each) tested negative for Lyme disease using the Centers for Disease Control and Prevention’s recommended two-tier testing criteria for serodiagnosis. However, at the second visit, which was performed immediately post treatment, 70% of women who tested negative at the first visit remained negative, compared with only 35% of the men who initially tested negative.
Additionally, polychromatic flow cytometry performed on patient samples indicated that women had significantly higher frequency of CD4+CCR5+ T-cells prior to treatment than did men (mean of 9.82% vs. 5.96%).
"These findings suggest to us that there may be a difference between how men and women respond to infection with Lyme disease. One hypothesis for these differences is that there may be an immunological variation in response to Borrelia burgdorferi, the bacterial infection that causes Lyme disease, between men and women," Ms. Crowder said.
Study participants had early, untreated erythema migrans and clinically confirmed Lyme disease. At the first of the six study visits, they were tested using the CDC criteria by a commercial laboratory. All were treated with 3-week course of doxycycline and were then followed for up to 2 years. At each study visit, participants underwent a physical examination and interval history, reported clinical symptoms and completed self-administered surveys, and underwent repeat laboratory evaluations.
The findings highlight a need for additional research on sex-based differences in the effects of early Lyme disease. Such differences have been seen in other infectious disease, but have not been thoroughly explored in early Lyme disease, Ms. Crowder noted.
Such study is important given that Lyme disease is the most common vector-borne infectious disease in the United States. Although most patients recover from acute infection with proper antibiotic treatment, a subset of patients develop Post-Treatment Lyme Disease Syndrome. The CDC defines this syndrome as involving lingering symptoms of fatigue, pain, or joint and muscle aches. In some cases, these can last for more than 6 months.
"We will continue to explore these suggested differences both in this cohort and in future research studies," she said.
Ms. Crowder also stressed the importance of encouraging patients to look for ticks if they live in Lyme endemic areas.
This study was supported by the Lyme Disease Research Foundation. Ms. Crowder had no disclosures to report.
FROM THE INTERNATIONAL CONFERENCE ON EMERGING INFECTIOUS DISEASES
Major Finding: Significantly more women than men with Lyme disease reported joint pain, muscle pain, headache, back pain, heart palpitations, nausea, vomiting, anxiety, numbness and tingling, and changes in vision during at least one of six preplanned study visits with a physician.
Data Source: Findings were from a prospective cohort study.
Disclosures: This study was supported by the Lyme Disease Research Foundation. Ms. Crowder had no disclosures to report.
WBCs Help Identify More Severe Pertussis in Infants
ATLANTA – Infants with more-severe pertussis infections are more likely to have higher white blood cell counts and more-rapid increases in those counts than are infants with less-severe infections, according to findings from a California study of 31 infants.
These 31 infants, aged 90 days or younger, were admitted to the pediatric ICU at one of five participating centers in California following a 2010 Bordetella pertussis epidemic in the state, during which 10 infants died from the infection. The findings have implications for identifying infants with potentially severe infections early in the course of their illness, to allow for more rapid implementation of interventions such as exchange transfusion that may improve outcomes, Dr. James D. Cherry reported at the International Conference on Emerging Infectious Diseases.
Of the 31 infants who were admitted between September 1, 2009, and June 30, 2011, at a median age of 36 days, 8 had more-severe infections (defined by the presence of pulmonary hypertension or by infection-related mortality). Seven had pulmonary hypertension, and four of the eight infants died.
Compared with the 23 infants who had less-severe infections, the 8 with more-severe infections had significantly higher peak WBC counts (72.8 vs. 26.3 x 103/mcL), their WBC count exceeded 30.0 more rapidly following onset of illness (5.1 vs. 14.6 days), and they were more likely to have a 50% increase in their WBC count within 24 hours of illness onset (50% vs. 0%), said Dr. Cherry, a pediatric infectious disease specialist with Mattel Children’s Hospital at the University of California, Los Angeles.
Those with more severe infection also were significantly more likely to receive an exchange transfusion (75% vs. 0%), to be diagnosed with pneumonia (100% vs. 43%), and to be intubated (75% vs. 9%), he noted.
The more-severe and less-severe patient groups were similar with respect to sex, ethnicity, and median age at onset. Overall, 54% were girls and 94% were Hispanic.
This study is unique in that all patients in the pediatric ICU were younger than 3 months of age, Dr. Cherry said, noting that based on earlier data, it was assumed that this differences in outcomes among infants with pertussis was associated with delays in getting appropriate care.
"But after seeing [these new] data, I think it’s a lot more complicated than that," he said, explaining that no differences were seen between the groups in demographic factors that are health care indicators.
The findings suggest that it is imperative in these very young babies to assess WBC immediately so the trajectory can be tracked. Those at risk for a more-severe course should be considered for exchange transfusion, he concluded.
Dr. Cherry said he had no relevant financial disclosures.
ATLANTA – Infants with more-severe pertussis infections are more likely to have higher white blood cell counts and more-rapid increases in those counts than are infants with less-severe infections, according to findings from a California study of 31 infants.
These 31 infants, aged 90 days or younger, were admitted to the pediatric ICU at one of five participating centers in California following a 2010 Bordetella pertussis epidemic in the state, during which 10 infants died from the infection. The findings have implications for identifying infants with potentially severe infections early in the course of their illness, to allow for more rapid implementation of interventions such as exchange transfusion that may improve outcomes, Dr. James D. Cherry reported at the International Conference on Emerging Infectious Diseases.
Of the 31 infants who were admitted between September 1, 2009, and June 30, 2011, at a median age of 36 days, 8 had more-severe infections (defined by the presence of pulmonary hypertension or by infection-related mortality). Seven had pulmonary hypertension, and four of the eight infants died.
Compared with the 23 infants who had less-severe infections, the 8 with more-severe infections had significantly higher peak WBC counts (72.8 vs. 26.3 x 103/mcL), their WBC count exceeded 30.0 more rapidly following onset of illness (5.1 vs. 14.6 days), and they were more likely to have a 50% increase in their WBC count within 24 hours of illness onset (50% vs. 0%), said Dr. Cherry, a pediatric infectious disease specialist with Mattel Children’s Hospital at the University of California, Los Angeles.
Those with more severe infection also were significantly more likely to receive an exchange transfusion (75% vs. 0%), to be diagnosed with pneumonia (100% vs. 43%), and to be intubated (75% vs. 9%), he noted.
The more-severe and less-severe patient groups were similar with respect to sex, ethnicity, and median age at onset. Overall, 54% were girls and 94% were Hispanic.
This study is unique in that all patients in the pediatric ICU were younger than 3 months of age, Dr. Cherry said, noting that based on earlier data, it was assumed that this differences in outcomes among infants with pertussis was associated with delays in getting appropriate care.
"But after seeing [these new] data, I think it’s a lot more complicated than that," he said, explaining that no differences were seen between the groups in demographic factors that are health care indicators.
The findings suggest that it is imperative in these very young babies to assess WBC immediately so the trajectory can be tracked. Those at risk for a more-severe course should be considered for exchange transfusion, he concluded.
Dr. Cherry said he had no relevant financial disclosures.
ATLANTA – Infants with more-severe pertussis infections are more likely to have higher white blood cell counts and more-rapid increases in those counts than are infants with less-severe infections, according to findings from a California study of 31 infants.
These 31 infants, aged 90 days or younger, were admitted to the pediatric ICU at one of five participating centers in California following a 2010 Bordetella pertussis epidemic in the state, during which 10 infants died from the infection. The findings have implications for identifying infants with potentially severe infections early in the course of their illness, to allow for more rapid implementation of interventions such as exchange transfusion that may improve outcomes, Dr. James D. Cherry reported at the International Conference on Emerging Infectious Diseases.
Of the 31 infants who were admitted between September 1, 2009, and June 30, 2011, at a median age of 36 days, 8 had more-severe infections (defined by the presence of pulmonary hypertension or by infection-related mortality). Seven had pulmonary hypertension, and four of the eight infants died.
Compared with the 23 infants who had less-severe infections, the 8 with more-severe infections had significantly higher peak WBC counts (72.8 vs. 26.3 x 103/mcL), their WBC count exceeded 30.0 more rapidly following onset of illness (5.1 vs. 14.6 days), and they were more likely to have a 50% increase in their WBC count within 24 hours of illness onset (50% vs. 0%), said Dr. Cherry, a pediatric infectious disease specialist with Mattel Children’s Hospital at the University of California, Los Angeles.
Those with more severe infection also were significantly more likely to receive an exchange transfusion (75% vs. 0%), to be diagnosed with pneumonia (100% vs. 43%), and to be intubated (75% vs. 9%), he noted.
The more-severe and less-severe patient groups were similar with respect to sex, ethnicity, and median age at onset. Overall, 54% were girls and 94% were Hispanic.
This study is unique in that all patients in the pediatric ICU were younger than 3 months of age, Dr. Cherry said, noting that based on earlier data, it was assumed that this differences in outcomes among infants with pertussis was associated with delays in getting appropriate care.
"But after seeing [these new] data, I think it’s a lot more complicated than that," he said, explaining that no differences were seen between the groups in demographic factors that are health care indicators.
The findings suggest that it is imperative in these very young babies to assess WBC immediately so the trajectory can be tracked. Those at risk for a more-severe course should be considered for exchange transfusion, he concluded.
Dr. Cherry said he had no relevant financial disclosures.
FROM THE INTERNATIONAL CONFERENCE ON EMERGING INFECTIOUS DISEASES
Major Finding: Compared with 23 infants with less-severe infections, the 8 with more-severe infections had significantly higher peak WBC counts (72.8 vs. 26.3 x 103/mcL), their WBC count exceeded 30.0 more rapidly following onset of illness (5.1 vs. 14.6 days), and they were more likely to have a 50% increase in their WBC count within 24 hours of illness onset (50% vs. 0%).
Data Source: Data are from an observational study of 31 infants looking at characteristics of infants with severe pertussis infection.
Disclosures: Dr. Cherry said he had no relevant financial disclosures.
Connecticut Sees Overall Decline in MRSA Infections
ATLANTA – The overall incidence of methicillin-resistant Staphylococcus aureus infection has been declining in Connecticut since 2007, due entirely to decreases in infections caused by health care–related strains, according to laboratory reports on invasive MRSA isolates from across the state.
From 2001 to 2010, the overall incidence of MRSA infections declined significantly from 26.0 to 22.1 per 100,000 population. The incidence of health care–related MRSA infections declined significantly from 14.4 to 13.8 per 100,000 population, and the incidence of hospital-onset MRSA infections declined significantly from 10.0 to 5.2 per 100,000 population, which together were enough to offset a significant increase in the incidence of community-acquired MRSA infection during the same time period from 1.4 to 3.1 per 100,000 population, Dr. James Hadler reported during a poster session at the International Conference on Emerging Infectious Diseases.
The improvements in the health care–related strains of MRSA coincided with increased public, public health, and hospital attention to the problem of MRSA infections, said Dr. Hadler of the Connecticut and Yale Emerging Infections Program, Yale School of Public Health, New Haven, Conn.
MRSA has posed two distinct problems over the years, including hospital-onset bloodstream infections associated with highly-resistant strains, and community-onset infections, which mostly involve skin and soft-tissue infections caused by less resistant community MRSA strains. These started to increase in the 1980s and 1990s, respectively. Now hospital strains are causing infection in the community, and community strains are causing infections in the hospital, Dr. Hadler said.
Laboratory reporting for invasive MRSA became mandatory in Connecticut in 2001, and legislative initiatives in Connecticut in 2006 resulted in laws requiring reporting of hospital-related infection. In 2007, national attention was called to MRSA in a publication by the Emerging Infections Program that highlighted the magnitude of the problem, and the passing of legislation in Connecticut and other states mandating reporting of hospital infections.
From 2001 to 2007, the incidence of MRSA in Connecticut was either increasing or stable, but after 2007 the incidence began to decline, he explained.
Furthermore, an examination of incidence trends in three time periods (2001-2003, 2004-2006, and 2007-2010) showed that the trends for decline did indeed occur only from 2007 to 2010 for the overall, health care–associated, and hospital-onset cases. The increase in community-acquired disease occurred from 2004 to 2006.
Between 2007 and 2010, the overall incidence decreased 18.8%, the hospital-onset incidence decreased by 33.2%, and health care–associated infections decreased by 12.8%. After the initial increase from 2004 to 2006, the incidence of community-acquired cases decreased by 12.7%.
MRSA cases in this study were defined as those with MRSA isolated from normally sterile body sites. Cases were classified, based on a medical record review, as being a hospital-onset case (with MRSA isolated greater than 2 days after admission), a community-onset case, or a health care–associated case (with MRSA acquired during hospitalization, surgery, dialysis, or a stay in a long-term care facility in the past year, or central line at diagnosis).
The findings are encouraging, although continued monitoring to assess the sustainability of these apparent improvements in MRSA prevention is needed, according to Dr. Hadler.
"It looks like we’re making real progress with MRSA-related hospital- and health care–associated infections, but bigger improvements have been dampened by the community MRSA strains," he said in an interview.
The findings in Connecticut may reflect those of other areas in the United States, because Connecticut, which serves as one of seven MRSA surveillance areas that are part of the Centers for Disease Control and Prevention’s Emerging Infections Programs, is demographically diverse and representative of the larger U.S. population, he added.
Dr. Hadler said he had no relevant financial disclosures.
ATLANTA – The overall incidence of methicillin-resistant Staphylococcus aureus infection has been declining in Connecticut since 2007, due entirely to decreases in infections caused by health care–related strains, according to laboratory reports on invasive MRSA isolates from across the state.
From 2001 to 2010, the overall incidence of MRSA infections declined significantly from 26.0 to 22.1 per 100,000 population. The incidence of health care–related MRSA infections declined significantly from 14.4 to 13.8 per 100,000 population, and the incidence of hospital-onset MRSA infections declined significantly from 10.0 to 5.2 per 100,000 population, which together were enough to offset a significant increase in the incidence of community-acquired MRSA infection during the same time period from 1.4 to 3.1 per 100,000 population, Dr. James Hadler reported during a poster session at the International Conference on Emerging Infectious Diseases.
The improvements in the health care–related strains of MRSA coincided with increased public, public health, and hospital attention to the problem of MRSA infections, said Dr. Hadler of the Connecticut and Yale Emerging Infections Program, Yale School of Public Health, New Haven, Conn.
MRSA has posed two distinct problems over the years, including hospital-onset bloodstream infections associated with highly-resistant strains, and community-onset infections, which mostly involve skin and soft-tissue infections caused by less resistant community MRSA strains. These started to increase in the 1980s and 1990s, respectively. Now hospital strains are causing infection in the community, and community strains are causing infections in the hospital, Dr. Hadler said.
Laboratory reporting for invasive MRSA became mandatory in Connecticut in 2001, and legislative initiatives in Connecticut in 2006 resulted in laws requiring reporting of hospital-related infection. In 2007, national attention was called to MRSA in a publication by the Emerging Infections Program that highlighted the magnitude of the problem, and the passing of legislation in Connecticut and other states mandating reporting of hospital infections.
From 2001 to 2007, the incidence of MRSA in Connecticut was either increasing or stable, but after 2007 the incidence began to decline, he explained.
Furthermore, an examination of incidence trends in three time periods (2001-2003, 2004-2006, and 2007-2010) showed that the trends for decline did indeed occur only from 2007 to 2010 for the overall, health care–associated, and hospital-onset cases. The increase in community-acquired disease occurred from 2004 to 2006.
Between 2007 and 2010, the overall incidence decreased 18.8%, the hospital-onset incidence decreased by 33.2%, and health care–associated infections decreased by 12.8%. After the initial increase from 2004 to 2006, the incidence of community-acquired cases decreased by 12.7%.
MRSA cases in this study were defined as those with MRSA isolated from normally sterile body sites. Cases were classified, based on a medical record review, as being a hospital-onset case (with MRSA isolated greater than 2 days after admission), a community-onset case, or a health care–associated case (with MRSA acquired during hospitalization, surgery, dialysis, or a stay in a long-term care facility in the past year, or central line at diagnosis).
The findings are encouraging, although continued monitoring to assess the sustainability of these apparent improvements in MRSA prevention is needed, according to Dr. Hadler.
"It looks like we’re making real progress with MRSA-related hospital- and health care–associated infections, but bigger improvements have been dampened by the community MRSA strains," he said in an interview.
The findings in Connecticut may reflect those of other areas in the United States, because Connecticut, which serves as one of seven MRSA surveillance areas that are part of the Centers for Disease Control and Prevention’s Emerging Infections Programs, is demographically diverse and representative of the larger U.S. population, he added.
Dr. Hadler said he had no relevant financial disclosures.
ATLANTA – The overall incidence of methicillin-resistant Staphylococcus aureus infection has been declining in Connecticut since 2007, due entirely to decreases in infections caused by health care–related strains, according to laboratory reports on invasive MRSA isolates from across the state.
From 2001 to 2010, the overall incidence of MRSA infections declined significantly from 26.0 to 22.1 per 100,000 population. The incidence of health care–related MRSA infections declined significantly from 14.4 to 13.8 per 100,000 population, and the incidence of hospital-onset MRSA infections declined significantly from 10.0 to 5.2 per 100,000 population, which together were enough to offset a significant increase in the incidence of community-acquired MRSA infection during the same time period from 1.4 to 3.1 per 100,000 population, Dr. James Hadler reported during a poster session at the International Conference on Emerging Infectious Diseases.
The improvements in the health care–related strains of MRSA coincided with increased public, public health, and hospital attention to the problem of MRSA infections, said Dr. Hadler of the Connecticut and Yale Emerging Infections Program, Yale School of Public Health, New Haven, Conn.
MRSA has posed two distinct problems over the years, including hospital-onset bloodstream infections associated with highly-resistant strains, and community-onset infections, which mostly involve skin and soft-tissue infections caused by less resistant community MRSA strains. These started to increase in the 1980s and 1990s, respectively. Now hospital strains are causing infection in the community, and community strains are causing infections in the hospital, Dr. Hadler said.
Laboratory reporting for invasive MRSA became mandatory in Connecticut in 2001, and legislative initiatives in Connecticut in 2006 resulted in laws requiring reporting of hospital-related infection. In 2007, national attention was called to MRSA in a publication by the Emerging Infections Program that highlighted the magnitude of the problem, and the passing of legislation in Connecticut and other states mandating reporting of hospital infections.
From 2001 to 2007, the incidence of MRSA in Connecticut was either increasing or stable, but after 2007 the incidence began to decline, he explained.
Furthermore, an examination of incidence trends in three time periods (2001-2003, 2004-2006, and 2007-2010) showed that the trends for decline did indeed occur only from 2007 to 2010 for the overall, health care–associated, and hospital-onset cases. The increase in community-acquired disease occurred from 2004 to 2006.
Between 2007 and 2010, the overall incidence decreased 18.8%, the hospital-onset incidence decreased by 33.2%, and health care–associated infections decreased by 12.8%. After the initial increase from 2004 to 2006, the incidence of community-acquired cases decreased by 12.7%.
MRSA cases in this study were defined as those with MRSA isolated from normally sterile body sites. Cases were classified, based on a medical record review, as being a hospital-onset case (with MRSA isolated greater than 2 days after admission), a community-onset case, or a health care–associated case (with MRSA acquired during hospitalization, surgery, dialysis, or a stay in a long-term care facility in the past year, or central line at diagnosis).
The findings are encouraging, although continued monitoring to assess the sustainability of these apparent improvements in MRSA prevention is needed, according to Dr. Hadler.
"It looks like we’re making real progress with MRSA-related hospital- and health care–associated infections, but bigger improvements have been dampened by the community MRSA strains," he said in an interview.
The findings in Connecticut may reflect those of other areas in the United States, because Connecticut, which serves as one of seven MRSA surveillance areas that are part of the Centers for Disease Control and Prevention’s Emerging Infections Programs, is demographically diverse and representative of the larger U.S. population, he added.
Dr. Hadler said he had no relevant financial disclosures.
FROM THE INTERNATIONAL CONFERENCE ON EMERGING INFECTIOUS DISEASES
Major Finding: The incidence of health care–related MRSA infections declined significantly from 14.4 to 13.8 per 100,000 population, and the incidence of hospital-onset MRSA infections declined significantly from 10.0 to 5.2 per 100,000 population, which together were enough to offset a significant increase in the incidence of community-acquired MRSA infection during the same time period from 1.4 to 3.1 per 100,000 population.
Data Source: Surveillance data/statewide lab reports from 2001 to 2010 were studied.
Disclosures: Dr. Hadler said he had no relevant financial disclosures.
Hepatitis C Infection Increasing Among Adolescents, Young Adults
ATLANTA – The incidence of hepatitis C infection is increasing among adolescents and young adults in Pennsylvania, just as it has in other areas in the United States, according to surveillance data for 2003 through 2010.
During that 7-year period, the number of reports of newly recognized confirmed or probable cases of hepatitis C past or present infection among those aged 15-34 years increased from 1,384 to 2,393, representing a near doubling of the rate of cases (from 43 to 72) per 100,000 population, Dr. Sameh W. Boktor reported in a poster at the International Conference on Emerging Infectious Diseases.
The rates in other age groups, however, declined during this time period.
For example, the overall rate of newly reported cases for all age groups combined declined from 85 to 72 per 100,000 population, and the rate of cases among those aged 45-64 years declined from 185 to 142 per 100,000 population, said Dr. Boktor of the Pennsylvania Department of Health, Harrisburg.
The increases in the adolescent and young adult age groups are likely caused by high-risk behaviors, such as intravenous drug use and unprotected sex between men – and, to a lesser degree – unprotected heterosexual sex.
"We know high-risk behaviors are common in this age group," Dr. Boktor said, noting that evidence suggests such high-risk behaviors are increasing among residents in rural areas, and the increases in cases of hepatitis C among adolescents and young adults in this study were greater in rural areas, compared with two large urban centers.
This finding, however, should be interpreted with caution because of the small population in rural counties; targeted studies may shed more light on this apparent trend.
The data for this study were derived mainly from laboratories via electronic reporting. Age-specific rates of reported cases were calculated and compared over time, as were demographic and spatial characteristic, Dr. Boktor said.
The findings, which are similar to those from Massachusetts and other areas, are of concern, because hepatitis C infection is the leading cause of advanced liver cirrhosis and liver cancer in the United States. They indicate a need for increased attention to prevention in the adolescent and young adult population.
"We need to work more on characterizing risk factors, and we need to work more on developing effective prevention strategies in this very productive age group," Dr. Boktor said.
He noted that these findings "almost certainly underestimate the real impact of viral hepatitis," because they reflect only those patients with access to testing, and whose results are reported.
Dr. Boktor said he had no relevant financial disclosures.
ATLANTA – The incidence of hepatitis C infection is increasing among adolescents and young adults in Pennsylvania, just as it has in other areas in the United States, according to surveillance data for 2003 through 2010.
During that 7-year period, the number of reports of newly recognized confirmed or probable cases of hepatitis C past or present infection among those aged 15-34 years increased from 1,384 to 2,393, representing a near doubling of the rate of cases (from 43 to 72) per 100,000 population, Dr. Sameh W. Boktor reported in a poster at the International Conference on Emerging Infectious Diseases.
The rates in other age groups, however, declined during this time period.
For example, the overall rate of newly reported cases for all age groups combined declined from 85 to 72 per 100,000 population, and the rate of cases among those aged 45-64 years declined from 185 to 142 per 100,000 population, said Dr. Boktor of the Pennsylvania Department of Health, Harrisburg.
The increases in the adolescent and young adult age groups are likely caused by high-risk behaviors, such as intravenous drug use and unprotected sex between men – and, to a lesser degree – unprotected heterosexual sex.
"We know high-risk behaviors are common in this age group," Dr. Boktor said, noting that evidence suggests such high-risk behaviors are increasing among residents in rural areas, and the increases in cases of hepatitis C among adolescents and young adults in this study were greater in rural areas, compared with two large urban centers.
This finding, however, should be interpreted with caution because of the small population in rural counties; targeted studies may shed more light on this apparent trend.
The data for this study were derived mainly from laboratories via electronic reporting. Age-specific rates of reported cases were calculated and compared over time, as were demographic and spatial characteristic, Dr. Boktor said.
The findings, which are similar to those from Massachusetts and other areas, are of concern, because hepatitis C infection is the leading cause of advanced liver cirrhosis and liver cancer in the United States. They indicate a need for increased attention to prevention in the adolescent and young adult population.
"We need to work more on characterizing risk factors, and we need to work more on developing effective prevention strategies in this very productive age group," Dr. Boktor said.
He noted that these findings "almost certainly underestimate the real impact of viral hepatitis," because they reflect only those patients with access to testing, and whose results are reported.
Dr. Boktor said he had no relevant financial disclosures.
ATLANTA – The incidence of hepatitis C infection is increasing among adolescents and young adults in Pennsylvania, just as it has in other areas in the United States, according to surveillance data for 2003 through 2010.
During that 7-year period, the number of reports of newly recognized confirmed or probable cases of hepatitis C past or present infection among those aged 15-34 years increased from 1,384 to 2,393, representing a near doubling of the rate of cases (from 43 to 72) per 100,000 population, Dr. Sameh W. Boktor reported in a poster at the International Conference on Emerging Infectious Diseases.
The rates in other age groups, however, declined during this time period.
For example, the overall rate of newly reported cases for all age groups combined declined from 85 to 72 per 100,000 population, and the rate of cases among those aged 45-64 years declined from 185 to 142 per 100,000 population, said Dr. Boktor of the Pennsylvania Department of Health, Harrisburg.
The increases in the adolescent and young adult age groups are likely caused by high-risk behaviors, such as intravenous drug use and unprotected sex between men – and, to a lesser degree – unprotected heterosexual sex.
"We know high-risk behaviors are common in this age group," Dr. Boktor said, noting that evidence suggests such high-risk behaviors are increasing among residents in rural areas, and the increases in cases of hepatitis C among adolescents and young adults in this study were greater in rural areas, compared with two large urban centers.
This finding, however, should be interpreted with caution because of the small population in rural counties; targeted studies may shed more light on this apparent trend.
The data for this study were derived mainly from laboratories via electronic reporting. Age-specific rates of reported cases were calculated and compared over time, as were demographic and spatial characteristic, Dr. Boktor said.
The findings, which are similar to those from Massachusetts and other areas, are of concern, because hepatitis C infection is the leading cause of advanced liver cirrhosis and liver cancer in the United States. They indicate a need for increased attention to prevention in the adolescent and young adult population.
"We need to work more on characterizing risk factors, and we need to work more on developing effective prevention strategies in this very productive age group," Dr. Boktor said.
He noted that these findings "almost certainly underestimate the real impact of viral hepatitis," because they reflect only those patients with access to testing, and whose results are reported.
Dr. Boktor said he had no relevant financial disclosures.
FROM THE INTERNATIONAL CONFERENCE ON EMERGING INFECTIOUS DISEASES
Major Finding: The number of reports of newly recognized confirmed or probable cases of hepatitis C past or present infection among those aged 15-34 years increased from 1,384 to 2,393 from 2003 to 2010, representing a near doubling of the rate of cases (from 43 to 72) per 100,000 population.
Data Source: A review of surveillance data from 2003 to 2010.
Disclosures: Dr. Boktor said he had no relevant financial disclosures.