User login
EBUS Equals Mediastinoscopy for NSCLC Staging
PHILADELPHIA – Endobronchial ultrasound–guided biopsy of mediastinal lymph nodes in patients with operable non–small cell lung cancer worked as effectively for staging as did the standard approach – mediastinoscopy – in the first head-to-head comparison of the two methods.
"Our results showed that EBUS-TBNA [endobronchial ultrasound–guided transbronchial needle aspiration], when performed as in this study, can replace mediastinoscopy for accurate staging of the mediastinum in potentially resectable lung cancer," Dr. Kazuhiro Yasufuku said at the annual meeting of the American Association for Thoracic Surgery.
Based on these results, which were obtained in 153 patients treated by any one of seven surgeons working at Toronto General Hospital, Dr. Yasufuku and his colleagues now routinely use EBUS-TBNA as their initial approach for staging patients with inoperable non–small cell lung cancer (NSCLC), who account for about 70% of all NSCLC patients they treat. As long as they can collect adequate cell specimens for cytologic analysis from the lymph node stations they routinely assess, they rely exclusively on EBUS-TBNA for staging, which allows them to avoid mediastinoscopy for most of their patients, Dr. Yasufuku said in an interview.
"We knew that EBUS-TBNA was good, but [until now] we never knew how it compared with the gold standard, mediastinoscopy," he said. The major limiting factor is lymph node size, he noted. Surgeons find it challenging to routinely obtain an adequate cell specimen from nodes smaller than 5 mm in diameter, Dr. Yasufuku said. "The smaller the node, the harder it is to put a needle into it."
The Toronto group uses rapid, onsite cytologic evaluation, which means that a cytologist attends the procedure in the combined surgical and endoscopy suite. In the study, and also in routine practice, "we can make repeated needle passes until we obtain good specimens. The surgeon can learn how to place the needle by getting immediate feedback" on the specimens, he said.
The specimens obtained allow for a tissue diagnosis, and typically provide enough material to assess cells for the presence of epidermal growth factor receptor mutations, he added.
EBUS-TBNA uses local rather than general anesthesia, is less invasive, and has fewer complications compared with mediastinoscopy, said Dr. Yasufuku, a thoracic surgeon and director of the interventional thoracic surgery program at Toronto General and the University of Toronto.
The study enrolled adults with NSCLC who required mediastinoscopy as part of their staging to determine their suitability for lung cancer resection. The study excluded patients who were not fit for definitive surgical resection, because the researchers used the status of the surgically excised lymph nodes as the basis for judging the diagnostic accuracy of both techniques.
During July 2006–August 2010, they enrolled 153 patients with an average age of 69 years. The most common NSCLC histologic subtype was adenocarcinoma (59%), followed by squamous cell carcinoma (25%). Staging by ultrasound imaging identified 57% of the patients with stage I or II disease, and 39% with stage IIIA disease. The remaining 4% had stage IIIB or stage IV disease.
All patients underwent general anesthesia. A surgeon first performed EBUS-TBNA on each patient, followed immediately by mediastinoscopy. All patients then underwent surgical lymph node resection to definitively assess their nodes if EBUS-TBNA, mediastinoscopy, or both did not show signs of metastatic disease.
The surgeons attempted biopsies at five lymph node stations in each patient: stations 2R, 2L, 4R, 4L, and 7. They successfully biopsied an average of three stations per patient using EBUSTBNA, with an inadequate specimen obtained on an average of one station per patient. Average lymph node diameter on the short axis was 7 mm, and the procedure averaged a total of 20 minutes per patient. Overall, EBUS-TBNA identified 78 biopsies as malignant. During mediastinoscopy, surgeons successfully biopsied an average of 4 nodes per patient, with inadequate specimens obtained from 10 nodes, an average of fewer than 0.1 inadequate specimen per patient. Mediastinoscopy retrieved 79 biopsies that were identified as malignant.
The surgeons reached an identical and correct diagnosis using both modalities in 136 patients (89%). Neither modality produced the correct diagnosis in four patients (3%), which meant that overall EBUS-TBNA and mediastinoscopy agreed 92% of the time. EBUS-TBNA was correct and mediastinoscopy incorrect in seven patients, and mediastinoscopy was correct and EBUS-TBNA incorrect in six patients.
These outcomes meant that EBUS-TBNA had 81% sensitivity, 91% negative predictive value, and 93% diagnostic accuracy. Mediastinoscopy led to 79% sensitivity, 90% negative predictive value, and 93% accuracy. Both methods had a specificity and positive predictive value of 100%, Dr. Yasufuku said.
No complications occurred after EBUS-TBNA, but there were four minor complications following subsequent mediastinoscopy: Two patients had a hematoma, one had a recurrent nerve injury, and one had a wound infection.
"It was a very clean study, showing that in the hands of a trained surgeon in our setting, EBUS-TBNA works very well. We clearly showed that the diagnostic yield is similar, and that patients who require mediastinoscopy as part of their staging can undergo EBUS-TBNA as their initial modality. Depending on what you find, you want to also do mediastinoscopy," he added.
"I’m convinced that [Dr. Yasufuku has] demonstrated equivalent ability to stage the mediastinum with EBUS-TBNA and with mediastinoscopy," commented Dr. Joel D. Cooper, professor of surgery and chief of thoracic surgery at the University of Pennsylvania in Philadelphia.
The study was supported by Olympus Medical Systems, a company that markets an EBUS-TBNA system. Dr. Yasufuku said that he has received research support from Olympus. Dr. Cooper said that he had no relevant disclosures.
PHILADELPHIA – Endobronchial ultrasound–guided biopsy of mediastinal lymph nodes in patients with operable non–small cell lung cancer worked as effectively for staging as did the standard approach – mediastinoscopy – in the first head-to-head comparison of the two methods.
"Our results showed that EBUS-TBNA [endobronchial ultrasound–guided transbronchial needle aspiration], when performed as in this study, can replace mediastinoscopy for accurate staging of the mediastinum in potentially resectable lung cancer," Dr. Kazuhiro Yasufuku said at the annual meeting of the American Association for Thoracic Surgery.
Based on these results, which were obtained in 153 patients treated by any one of seven surgeons working at Toronto General Hospital, Dr. Yasufuku and his colleagues now routinely use EBUS-TBNA as their initial approach for staging patients with inoperable non–small cell lung cancer (NSCLC), who account for about 70% of all NSCLC patients they treat. As long as they can collect adequate cell specimens for cytologic analysis from the lymph node stations they routinely assess, they rely exclusively on EBUS-TBNA for staging, which allows them to avoid mediastinoscopy for most of their patients, Dr. Yasufuku said in an interview.
"We knew that EBUS-TBNA was good, but [until now] we never knew how it compared with the gold standard, mediastinoscopy," he said. The major limiting factor is lymph node size, he noted. Surgeons find it challenging to routinely obtain an adequate cell specimen from nodes smaller than 5 mm in diameter, Dr. Yasufuku said. "The smaller the node, the harder it is to put a needle into it."
The Toronto group uses rapid, onsite cytologic evaluation, which means that a cytologist attends the procedure in the combined surgical and endoscopy suite. In the study, and also in routine practice, "we can make repeated needle passes until we obtain good specimens. The surgeon can learn how to place the needle by getting immediate feedback" on the specimens, he said.
The specimens obtained allow for a tissue diagnosis, and typically provide enough material to assess cells for the presence of epidermal growth factor receptor mutations, he added.
EBUS-TBNA uses local rather than general anesthesia, is less invasive, and has fewer complications compared with mediastinoscopy, said Dr. Yasufuku, a thoracic surgeon and director of the interventional thoracic surgery program at Toronto General and the University of Toronto.
The study enrolled adults with NSCLC who required mediastinoscopy as part of their staging to determine their suitability for lung cancer resection. The study excluded patients who were not fit for definitive surgical resection, because the researchers used the status of the surgically excised lymph nodes as the basis for judging the diagnostic accuracy of both techniques.
During July 2006–August 2010, they enrolled 153 patients with an average age of 69 years. The most common NSCLC histologic subtype was adenocarcinoma (59%), followed by squamous cell carcinoma (25%). Staging by ultrasound imaging identified 57% of the patients with stage I or II disease, and 39% with stage IIIA disease. The remaining 4% had stage IIIB or stage IV disease.
All patients underwent general anesthesia. A surgeon first performed EBUS-TBNA on each patient, followed immediately by mediastinoscopy. All patients then underwent surgical lymph node resection to definitively assess their nodes if EBUS-TBNA, mediastinoscopy, or both did not show signs of metastatic disease.
The surgeons attempted biopsies at five lymph node stations in each patient: stations 2R, 2L, 4R, 4L, and 7. They successfully biopsied an average of three stations per patient using EBUSTBNA, with an inadequate specimen obtained on an average of one station per patient. Average lymph node diameter on the short axis was 7 mm, and the procedure averaged a total of 20 minutes per patient. Overall, EBUS-TBNA identified 78 biopsies as malignant. During mediastinoscopy, surgeons successfully biopsied an average of 4 nodes per patient, with inadequate specimens obtained from 10 nodes, an average of fewer than 0.1 inadequate specimen per patient. Mediastinoscopy retrieved 79 biopsies that were identified as malignant.
The surgeons reached an identical and correct diagnosis using both modalities in 136 patients (89%). Neither modality produced the correct diagnosis in four patients (3%), which meant that overall EBUS-TBNA and mediastinoscopy agreed 92% of the time. EBUS-TBNA was correct and mediastinoscopy incorrect in seven patients, and mediastinoscopy was correct and EBUS-TBNA incorrect in six patients.
These outcomes meant that EBUS-TBNA had 81% sensitivity, 91% negative predictive value, and 93% diagnostic accuracy. Mediastinoscopy led to 79% sensitivity, 90% negative predictive value, and 93% accuracy. Both methods had a specificity and positive predictive value of 100%, Dr. Yasufuku said.
No complications occurred after EBUS-TBNA, but there were four minor complications following subsequent mediastinoscopy: Two patients had a hematoma, one had a recurrent nerve injury, and one had a wound infection.
"It was a very clean study, showing that in the hands of a trained surgeon in our setting, EBUS-TBNA works very well. We clearly showed that the diagnostic yield is similar, and that patients who require mediastinoscopy as part of their staging can undergo EBUS-TBNA as their initial modality. Depending on what you find, you want to also do mediastinoscopy," he added.
"I’m convinced that [Dr. Yasufuku has] demonstrated equivalent ability to stage the mediastinum with EBUS-TBNA and with mediastinoscopy," commented Dr. Joel D. Cooper, professor of surgery and chief of thoracic surgery at the University of Pennsylvania in Philadelphia.
The study was supported by Olympus Medical Systems, a company that markets an EBUS-TBNA system. Dr. Yasufuku said that he has received research support from Olympus. Dr. Cooper said that he had no relevant disclosures.
PHILADELPHIA – Endobronchial ultrasound–guided biopsy of mediastinal lymph nodes in patients with operable non–small cell lung cancer worked as effectively for staging as did the standard approach – mediastinoscopy – in the first head-to-head comparison of the two methods.
"Our results showed that EBUS-TBNA [endobronchial ultrasound–guided transbronchial needle aspiration], when performed as in this study, can replace mediastinoscopy for accurate staging of the mediastinum in potentially resectable lung cancer," Dr. Kazuhiro Yasufuku said at the annual meeting of the American Association for Thoracic Surgery.
Based on these results, which were obtained in 153 patients treated by any one of seven surgeons working at Toronto General Hospital, Dr. Yasufuku and his colleagues now routinely use EBUS-TBNA as their initial approach for staging patients with inoperable non–small cell lung cancer (NSCLC), who account for about 70% of all NSCLC patients they treat. As long as they can collect adequate cell specimens for cytologic analysis from the lymph node stations they routinely assess, they rely exclusively on EBUS-TBNA for staging, which allows them to avoid mediastinoscopy for most of their patients, Dr. Yasufuku said in an interview.
"We knew that EBUS-TBNA was good, but [until now] we never knew how it compared with the gold standard, mediastinoscopy," he said. The major limiting factor is lymph node size, he noted. Surgeons find it challenging to routinely obtain an adequate cell specimen from nodes smaller than 5 mm in diameter, Dr. Yasufuku said. "The smaller the node, the harder it is to put a needle into it."
The Toronto group uses rapid, onsite cytologic evaluation, which means that a cytologist attends the procedure in the combined surgical and endoscopy suite. In the study, and also in routine practice, "we can make repeated needle passes until we obtain good specimens. The surgeon can learn how to place the needle by getting immediate feedback" on the specimens, he said.
The specimens obtained allow for a tissue diagnosis, and typically provide enough material to assess cells for the presence of epidermal growth factor receptor mutations, he added.
EBUS-TBNA uses local rather than general anesthesia, is less invasive, and has fewer complications compared with mediastinoscopy, said Dr. Yasufuku, a thoracic surgeon and director of the interventional thoracic surgery program at Toronto General and the University of Toronto.
The study enrolled adults with NSCLC who required mediastinoscopy as part of their staging to determine their suitability for lung cancer resection. The study excluded patients who were not fit for definitive surgical resection, because the researchers used the status of the surgically excised lymph nodes as the basis for judging the diagnostic accuracy of both techniques.
During July 2006–August 2010, they enrolled 153 patients with an average age of 69 years. The most common NSCLC histologic subtype was adenocarcinoma (59%), followed by squamous cell carcinoma (25%). Staging by ultrasound imaging identified 57% of the patients with stage I or II disease, and 39% with stage IIIA disease. The remaining 4% had stage IIIB or stage IV disease.
All patients underwent general anesthesia. A surgeon first performed EBUS-TBNA on each patient, followed immediately by mediastinoscopy. All patients then underwent surgical lymph node resection to definitively assess their nodes if EBUS-TBNA, mediastinoscopy, or both did not show signs of metastatic disease.
The surgeons attempted biopsies at five lymph node stations in each patient: stations 2R, 2L, 4R, 4L, and 7. They successfully biopsied an average of three stations per patient using EBUSTBNA, with an inadequate specimen obtained on an average of one station per patient. Average lymph node diameter on the short axis was 7 mm, and the procedure averaged a total of 20 minutes per patient. Overall, EBUS-TBNA identified 78 biopsies as malignant. During mediastinoscopy, surgeons successfully biopsied an average of 4 nodes per patient, with inadequate specimens obtained from 10 nodes, an average of fewer than 0.1 inadequate specimen per patient. Mediastinoscopy retrieved 79 biopsies that were identified as malignant.
The surgeons reached an identical and correct diagnosis using both modalities in 136 patients (89%). Neither modality produced the correct diagnosis in four patients (3%), which meant that overall EBUS-TBNA and mediastinoscopy agreed 92% of the time. EBUS-TBNA was correct and mediastinoscopy incorrect in seven patients, and mediastinoscopy was correct and EBUS-TBNA incorrect in six patients.
These outcomes meant that EBUS-TBNA had 81% sensitivity, 91% negative predictive value, and 93% diagnostic accuracy. Mediastinoscopy led to 79% sensitivity, 90% negative predictive value, and 93% accuracy. Both methods had a specificity and positive predictive value of 100%, Dr. Yasufuku said.
No complications occurred after EBUS-TBNA, but there were four minor complications following subsequent mediastinoscopy: Two patients had a hematoma, one had a recurrent nerve injury, and one had a wound infection.
"It was a very clean study, showing that in the hands of a trained surgeon in our setting, EBUS-TBNA works very well. We clearly showed that the diagnostic yield is similar, and that patients who require mediastinoscopy as part of their staging can undergo EBUS-TBNA as their initial modality. Depending on what you find, you want to also do mediastinoscopy," he added.
"I’m convinced that [Dr. Yasufuku has] demonstrated equivalent ability to stage the mediastinum with EBUS-TBNA and with mediastinoscopy," commented Dr. Joel D. Cooper, professor of surgery and chief of thoracic surgery at the University of Pennsylvania in Philadelphia.
The study was supported by Olympus Medical Systems, a company that markets an EBUS-TBNA system. Dr. Yasufuku said that he has received research support from Olympus. Dr. Cooper said that he had no relevant disclosures.
FROM THE AMERICAN ASSOCIATION FOR THORACIC SURGERY ANNUAL MEETING
Major Finding: EBUS-TBNA proved similar to mediastinoscopy for lymph node staging of patients with operable NSCLC. EBUS-TBNA had a sensitivity of 81%, a negative predictive value of 91%, and 93% accuracy, compared with comparable values of 79%, 90%, and 93%, respectively, for mediastinoscopy when surgeons performed the two methods sequentially in each patient.
Data Source: A single-center study that included 153 patients who were staged by one of seven participating surgeons.
Disclosures: The study was supported by Olympus Medical Systems, a company that markets an EBUS-TBNA system. Dr. Yasufuku said that he has received research support from Olympus. Dr. Cooper said that he had no relevant disclosures.
CABG Outcomes Support More Liberal Blood Glucose Range
PHILADELPHIA – A blood glucose target of 121-180 mg/dL for patients following isolated coronary bypass surgery was as clinically effective as was a stricter glucose target and was easier to maintain in a randomized study with 189 patients.
Based on these results, the cardiac surgery program that ran the study switched its blood glucose range for postoperative patients from 90-120 mg/dL to the more liberal range of 121-180 mg/dL, Dr. Shalin P. Desai said at the annual meeting of the American Association for Thoracic Surgery.
"We believe that maintaining patients at a blood glucose level less than 180 mg/dL is safe and effective, and therefore should be considered for patients undergoing coronary artery bypass grafting surgery," said Dr. Desai, a cardiac surgeon at Inova Heart and Vascular Institute in Falls Church, Va.
"We know that a glucose level of less than 180 mg/dL is good, but does it need to be so strict that it’s almost normoglycemic, or can it be more liberal when we know the glucose levels will rise with the stress of surgery and illness? A range of 121-180 mg/dL is probably sufficient," Dr. Desai said in an interview. At that level, "we used less insulin, fewer finger sticks, and fewer resources" than when the target range aims for lower blood glucose levels, he said.
Dr. Desai and his associates enrolled patients undergoing first-time, isolated CABG who had diabetes or required insulin treatment following surgery based on having three consecutive blood glucose readings of at least 150 mg/dL, or one reading of at least 200 mg/dL. The researchers used a bedside, computerized device that regularly assessed blood glucose levels and adjusted the insulin infusion accordingly. The patients averaged 62 years of age, and about 43% had diabetes.
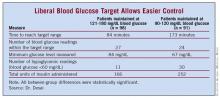
Among the 98 patients maintained on the 121-180 mg/dL regimen, the average time needed to reach the target blood glucose range was 84 minutes – significantly shorter than the average 173 minutes needed for the 91 patients on the strict regimen.
Patients maintained on the liberal target also fared significantly better in their average number of readings within their target range, minimum glucose level, number of hypoglycemic readings, and total insulin dose received (see table).
Assessment of clinical outcomes – renal failure, atrial fibrillation, pneumonia, deep sternal wound infections, prolonged ventilation, prolonged hospitalization, and operative mortality – showed that the liberal range was not inferior to the strict range for preventing these complications in the primary, intention-to-treat analysis. In the as-treated and per-protocol analyses, the liberal-range patients had outcomes that were noninferior to those of the strict control patients for all parameters except for atrial fibrillation. The liberal-range patients showed a small excess of atrial fibrillations in these two additional analyses.
Future studies should look at the same issue in patients undergoing other types of cardiac surgery, such as valve repair or replacement, or a maze procedure, he said.
Dr. Desai said that he had no relevant financial disclosures.
My associates and I recently reported similar results from a randomized study of 82 patients with diabetes who underwent coronary artery bypass grafting surgery. We also compared a target blood glucose range of 90-120 mg/dL with a range of 121-180 mg/dL. Like the current study, we found no difference in the 30-day rates of death, myocardial infarction, neurologic complications, deep sternal wound infections, or atrial fibrillation incidence. The patients maintained with more aggressive glucose control had a higher rate of hypoglycemic events, but this did not result in increased neurologic complications.
Why did tighter glycemic control not produce better outcomes? One possible explanation is that cardiac surgery patients often receive good treatment with cardioprotective drugs, including aspirin, statins, beta-blockers, and angiotensin-converting enzyme inhibitors. Also, the more liberal regimens still produce good glucose control. In our study, the average blood glucose level in the more liberal group was 135 mg/dL.
Tight glucose control may provide long-term benefits that have not yet been identified in these studies. For example, it may improve long-term graft patency and reduce long-term ischemic events. In our studies, we see that more aggressive glucose control results in lower levels of free fatty acids, a marker of inflammation.
Moderate glycemic control produces a significant reduction in morbidity and mortality in cardiac surgery patients that may be hard to improve upon with more aggressive control. I agree that the optimal glucose range following cardiac surgery appears to be 120-180 mg/dL. While the exact level for optimal control remains unknown, the importance of perioperative glycemic control by continuous insulin infusion is now well established.
Dr. Harold L. Lazar is a thoracic surgeon at Boston Medical Center. He said that he has received research support from Eli Lilly to study the effects of glycemic control during cardiac surgery.
My associates and I recently reported similar results from a randomized study of 82 patients with diabetes who underwent coronary artery bypass grafting surgery. We also compared a target blood glucose range of 90-120 mg/dL with a range of 121-180 mg/dL. Like the current study, we found no difference in the 30-day rates of death, myocardial infarction, neurologic complications, deep sternal wound infections, or atrial fibrillation incidence. The patients maintained with more aggressive glucose control had a higher rate of hypoglycemic events, but this did not result in increased neurologic complications.
Why did tighter glycemic control not produce better outcomes? One possible explanation is that cardiac surgery patients often receive good treatment with cardioprotective drugs, including aspirin, statins, beta-blockers, and angiotensin-converting enzyme inhibitors. Also, the more liberal regimens still produce good glucose control. In our study, the average blood glucose level in the more liberal group was 135 mg/dL.
Tight glucose control may provide long-term benefits that have not yet been identified in these studies. For example, it may improve long-term graft patency and reduce long-term ischemic events. In our studies, we see that more aggressive glucose control results in lower levels of free fatty acids, a marker of inflammation.
Moderate glycemic control produces a significant reduction in morbidity and mortality in cardiac surgery patients that may be hard to improve upon with more aggressive control. I agree that the optimal glucose range following cardiac surgery appears to be 120-180 mg/dL. While the exact level for optimal control remains unknown, the importance of perioperative glycemic control by continuous insulin infusion is now well established.
Dr. Harold L. Lazar is a thoracic surgeon at Boston Medical Center. He said that he has received research support from Eli Lilly to study the effects of glycemic control during cardiac surgery.
My associates and I recently reported similar results from a randomized study of 82 patients with diabetes who underwent coronary artery bypass grafting surgery. We also compared a target blood glucose range of 90-120 mg/dL with a range of 121-180 mg/dL. Like the current study, we found no difference in the 30-day rates of death, myocardial infarction, neurologic complications, deep sternal wound infections, or atrial fibrillation incidence. The patients maintained with more aggressive glucose control had a higher rate of hypoglycemic events, but this did not result in increased neurologic complications.
Why did tighter glycemic control not produce better outcomes? One possible explanation is that cardiac surgery patients often receive good treatment with cardioprotective drugs, including aspirin, statins, beta-blockers, and angiotensin-converting enzyme inhibitors. Also, the more liberal regimens still produce good glucose control. In our study, the average blood glucose level in the more liberal group was 135 mg/dL.
Tight glucose control may provide long-term benefits that have not yet been identified in these studies. For example, it may improve long-term graft patency and reduce long-term ischemic events. In our studies, we see that more aggressive glucose control results in lower levels of free fatty acids, a marker of inflammation.
Moderate glycemic control produces a significant reduction in morbidity and mortality in cardiac surgery patients that may be hard to improve upon with more aggressive control. I agree that the optimal glucose range following cardiac surgery appears to be 120-180 mg/dL. While the exact level for optimal control remains unknown, the importance of perioperative glycemic control by continuous insulin infusion is now well established.
Dr. Harold L. Lazar is a thoracic surgeon at Boston Medical Center. He said that he has received research support from Eli Lilly to study the effects of glycemic control during cardiac surgery.
PHILADELPHIA – A blood glucose target of 121-180 mg/dL for patients following isolated coronary bypass surgery was as clinically effective as was a stricter glucose target and was easier to maintain in a randomized study with 189 patients.
Based on these results, the cardiac surgery program that ran the study switched its blood glucose range for postoperative patients from 90-120 mg/dL to the more liberal range of 121-180 mg/dL, Dr. Shalin P. Desai said at the annual meeting of the American Association for Thoracic Surgery.
"We believe that maintaining patients at a blood glucose level less than 180 mg/dL is safe and effective, and therefore should be considered for patients undergoing coronary artery bypass grafting surgery," said Dr. Desai, a cardiac surgeon at Inova Heart and Vascular Institute in Falls Church, Va.
"We know that a glucose level of less than 180 mg/dL is good, but does it need to be so strict that it’s almost normoglycemic, or can it be more liberal when we know the glucose levels will rise with the stress of surgery and illness? A range of 121-180 mg/dL is probably sufficient," Dr. Desai said in an interview. At that level, "we used less insulin, fewer finger sticks, and fewer resources" than when the target range aims for lower blood glucose levels, he said.
Dr. Desai and his associates enrolled patients undergoing first-time, isolated CABG who had diabetes or required insulin treatment following surgery based on having three consecutive blood glucose readings of at least 150 mg/dL, or one reading of at least 200 mg/dL. The researchers used a bedside, computerized device that regularly assessed blood glucose levels and adjusted the insulin infusion accordingly. The patients averaged 62 years of age, and about 43% had diabetes.
Among the 98 patients maintained on the 121-180 mg/dL regimen, the average time needed to reach the target blood glucose range was 84 minutes – significantly shorter than the average 173 minutes needed for the 91 patients on the strict regimen.
Patients maintained on the liberal target also fared significantly better in their average number of readings within their target range, minimum glucose level, number of hypoglycemic readings, and total insulin dose received (see table).
Assessment of clinical outcomes – renal failure, atrial fibrillation, pneumonia, deep sternal wound infections, prolonged ventilation, prolonged hospitalization, and operative mortality – showed that the liberal range was not inferior to the strict range for preventing these complications in the primary, intention-to-treat analysis. In the as-treated and per-protocol analyses, the liberal-range patients had outcomes that were noninferior to those of the strict control patients for all parameters except for atrial fibrillation. The liberal-range patients showed a small excess of atrial fibrillations in these two additional analyses.
Future studies should look at the same issue in patients undergoing other types of cardiac surgery, such as valve repair or replacement, or a maze procedure, he said.
Dr. Desai said that he had no relevant financial disclosures.
PHILADELPHIA – A blood glucose target of 121-180 mg/dL for patients following isolated coronary bypass surgery was as clinically effective as was a stricter glucose target and was easier to maintain in a randomized study with 189 patients.
Based on these results, the cardiac surgery program that ran the study switched its blood glucose range for postoperative patients from 90-120 mg/dL to the more liberal range of 121-180 mg/dL, Dr. Shalin P. Desai said at the annual meeting of the American Association for Thoracic Surgery.
"We believe that maintaining patients at a blood glucose level less than 180 mg/dL is safe and effective, and therefore should be considered for patients undergoing coronary artery bypass grafting surgery," said Dr. Desai, a cardiac surgeon at Inova Heart and Vascular Institute in Falls Church, Va.
"We know that a glucose level of less than 180 mg/dL is good, but does it need to be so strict that it’s almost normoglycemic, or can it be more liberal when we know the glucose levels will rise with the stress of surgery and illness? A range of 121-180 mg/dL is probably sufficient," Dr. Desai said in an interview. At that level, "we used less insulin, fewer finger sticks, and fewer resources" than when the target range aims for lower blood glucose levels, he said.
Dr. Desai and his associates enrolled patients undergoing first-time, isolated CABG who had diabetes or required insulin treatment following surgery based on having three consecutive blood glucose readings of at least 150 mg/dL, or one reading of at least 200 mg/dL. The researchers used a bedside, computerized device that regularly assessed blood glucose levels and adjusted the insulin infusion accordingly. The patients averaged 62 years of age, and about 43% had diabetes.
Among the 98 patients maintained on the 121-180 mg/dL regimen, the average time needed to reach the target blood glucose range was 84 minutes – significantly shorter than the average 173 minutes needed for the 91 patients on the strict regimen.
Patients maintained on the liberal target also fared significantly better in their average number of readings within their target range, minimum glucose level, number of hypoglycemic readings, and total insulin dose received (see table).
Assessment of clinical outcomes – renal failure, atrial fibrillation, pneumonia, deep sternal wound infections, prolonged ventilation, prolonged hospitalization, and operative mortality – showed that the liberal range was not inferior to the strict range for preventing these complications in the primary, intention-to-treat analysis. In the as-treated and per-protocol analyses, the liberal-range patients had outcomes that were noninferior to those of the strict control patients for all parameters except for atrial fibrillation. The liberal-range patients showed a small excess of atrial fibrillations in these two additional analyses.
Future studies should look at the same issue in patients undergoing other types of cardiac surgery, such as valve repair or replacement, or a maze procedure, he said.
Dr. Desai said that he had no relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE AMERICAN ASSOCIATION FOR THORACIC SURGERY
CABG Outcomes Support More Liberal Blood Glucose Range
PHILADELPHIA – A blood glucose target of 121-180 mg/dL for patients following isolated coronary bypass surgery was as clinically effective as was a stricter glucose target and was easier to maintain in a randomized study with 189 patients.
Based on these results, the cardiac surgery program that ran the study switched its blood glucose range for postoperative patients from 90-120 mg/dL to the more liberal range of 121-180 mg/dL, Dr. Shalin P. Desai said at the annual meeting of the American Association for Thoracic Surgery.
"We believe that maintaining patients at a blood glucose level less than 180 mg/dL is safe and effective, and therefore should be considered for patients undergoing coronary artery bypass grafting surgery," said Dr. Desai, a cardiac surgeon at Inova Heart and Vascular Institute in Falls Church, Va.
"We know that a glucose level of less than 180 mg/dL is good, but does it need to be so strict that it’s almost normoglycemic, or can it be more liberal when we know the glucose levels will rise with the stress of surgery and illness? A range of 121-180 mg/dL is probably sufficient," Dr. Desai said in an interview. At that level, "we used less insulin, fewer finger sticks, and fewer resources" than when the target range aims for lower blood glucose levels, he said.
Dr. Desai and his associates enrolled patients undergoing first-time, isolated CABG who had diabetes or required insulin treatment following surgery based on having three consecutive blood glucose readings of at least 150 mg/dL, or one reading of at least 200 mg/dL. The researchers used a bedside, computerized device that regularly assessed blood glucose levels and adjusted the insulin infusion accordingly. The patients averaged 62 years of age, and about 43% had diabetes.
Among the 98 patients maintained on the 121-180 mg/dL regimen, the average time needed to reach the target blood glucose range was 84 minutes – significantly shorter than the average 173 minutes needed for the 91 patients on the strict regimen.
Patients maintained on the liberal target also fared significantly better in their average number of readings within their target range, minimum glucose level, number of hypoglycemic readings, and total insulin dose received (see table).
Assessment of clinical outcomes – renal failure, atrial fibrillation, pneumonia, deep sternal wound infections, prolonged ventilation, prolonged hospitalization, and operative mortality – showed that the liberal range was not inferior to the strict range for preventing these complications in the primary, intention-to-treat analysis. In the as-treated and per-protocol analyses, the liberal-range patients had outcomes that were noninferior to those of the strict control patients for all parameters except for atrial fibrillation. The liberal-range patients showed a small excess of atrial fibrillations in these two additional analyses.
Future studies should look at the same issue in patients undergoing other types of cardiac surgery, such as valve repair or replacement, or a maze procedure, he said.
Dr. Desai said that he had no relevant financial disclosures.
My associates and I recently reported similar results from a randomized study of 82 patients with diabetes who underwent coronary artery bypass grafting surgery. We also compared a target blood glucose range of 90-120 mg/dL with a range of 121-180 mg/dL. Like the current study, we found no difference in the 30-day rates of death, myocardial infarction, neurologic complications, deep sternal wound infections, or atrial fibrillation incidence. The patients maintained with more aggressive glucose control had a higher rate of hypoglycemic events, but this did not result in increased neurologic complications.
Why did tighter glycemic control not produce better outcomes? One possible explanation is that cardiac surgery patients often receive good treatment with cardioprotective drugs, including aspirin, statins, beta-blockers, and angiotensin-converting enzyme inhibitors. Also, the more liberal regimens still produce good glucose control. In our study, the average blood glucose level in the more liberal group was 135 mg/dL.
Tight glucose control may provide long-term benefits that have not yet been identified in these studies. For example, it may improve long-term graft patency and reduce long-term ischemic events. In our studies, we see that more aggressive glucose control results in lower levels of free fatty acids, a marker of inflammation.
Moderate glycemic control produces a significant reduction in morbidity and mortality in cardiac surgery patients that may be hard to improve upon with more aggressive control. I agree that the optimal glucose range following cardiac surgery appears to be 120-180 mg/dL. While the exact level for optimal control remains unknown, the importance of perioperative glycemic control by continuous insulin infusion is now well established.
Dr. Harold L. Lazar is a thoracic surgeon at Boston Medical Center. He said that he has received research support from Eli Lilly to study the effects of glycemic control during cardiac surgery.
My associates and I recently reported similar results from a randomized study of 82 patients with diabetes who underwent coronary artery bypass grafting surgery. We also compared a target blood glucose range of 90-120 mg/dL with a range of 121-180 mg/dL. Like the current study, we found no difference in the 30-day rates of death, myocardial infarction, neurologic complications, deep sternal wound infections, or atrial fibrillation incidence. The patients maintained with more aggressive glucose control had a higher rate of hypoglycemic events, but this did not result in increased neurologic complications.
Why did tighter glycemic control not produce better outcomes? One possible explanation is that cardiac surgery patients often receive good treatment with cardioprotective drugs, including aspirin, statins, beta-blockers, and angiotensin-converting enzyme inhibitors. Also, the more liberal regimens still produce good glucose control. In our study, the average blood glucose level in the more liberal group was 135 mg/dL.
Tight glucose control may provide long-term benefits that have not yet been identified in these studies. For example, it may improve long-term graft patency and reduce long-term ischemic events. In our studies, we see that more aggressive glucose control results in lower levels of free fatty acids, a marker of inflammation.
Moderate glycemic control produces a significant reduction in morbidity and mortality in cardiac surgery patients that may be hard to improve upon with more aggressive control. I agree that the optimal glucose range following cardiac surgery appears to be 120-180 mg/dL. While the exact level for optimal control remains unknown, the importance of perioperative glycemic control by continuous insulin infusion is now well established.
Dr. Harold L. Lazar is a thoracic surgeon at Boston Medical Center. He said that he has received research support from Eli Lilly to study the effects of glycemic control during cardiac surgery.
My associates and I recently reported similar results from a randomized study of 82 patients with diabetes who underwent coronary artery bypass grafting surgery. We also compared a target blood glucose range of 90-120 mg/dL with a range of 121-180 mg/dL. Like the current study, we found no difference in the 30-day rates of death, myocardial infarction, neurologic complications, deep sternal wound infections, or atrial fibrillation incidence. The patients maintained with more aggressive glucose control had a higher rate of hypoglycemic events, but this did not result in increased neurologic complications.
Why did tighter glycemic control not produce better outcomes? One possible explanation is that cardiac surgery patients often receive good treatment with cardioprotective drugs, including aspirin, statins, beta-blockers, and angiotensin-converting enzyme inhibitors. Also, the more liberal regimens still produce good glucose control. In our study, the average blood glucose level in the more liberal group was 135 mg/dL.
Tight glucose control may provide long-term benefits that have not yet been identified in these studies. For example, it may improve long-term graft patency and reduce long-term ischemic events. In our studies, we see that more aggressive glucose control results in lower levels of free fatty acids, a marker of inflammation.
Moderate glycemic control produces a significant reduction in morbidity and mortality in cardiac surgery patients that may be hard to improve upon with more aggressive control. I agree that the optimal glucose range following cardiac surgery appears to be 120-180 mg/dL. While the exact level for optimal control remains unknown, the importance of perioperative glycemic control by continuous insulin infusion is now well established.
Dr. Harold L. Lazar is a thoracic surgeon at Boston Medical Center. He said that he has received research support from Eli Lilly to study the effects of glycemic control during cardiac surgery.
PHILADELPHIA – A blood glucose target of 121-180 mg/dL for patients following isolated coronary bypass surgery was as clinically effective as was a stricter glucose target and was easier to maintain in a randomized study with 189 patients.
Based on these results, the cardiac surgery program that ran the study switched its blood glucose range for postoperative patients from 90-120 mg/dL to the more liberal range of 121-180 mg/dL, Dr. Shalin P. Desai said at the annual meeting of the American Association for Thoracic Surgery.
"We believe that maintaining patients at a blood glucose level less than 180 mg/dL is safe and effective, and therefore should be considered for patients undergoing coronary artery bypass grafting surgery," said Dr. Desai, a cardiac surgeon at Inova Heart and Vascular Institute in Falls Church, Va.
"We know that a glucose level of less than 180 mg/dL is good, but does it need to be so strict that it’s almost normoglycemic, or can it be more liberal when we know the glucose levels will rise with the stress of surgery and illness? A range of 121-180 mg/dL is probably sufficient," Dr. Desai said in an interview. At that level, "we used less insulin, fewer finger sticks, and fewer resources" than when the target range aims for lower blood glucose levels, he said.
Dr. Desai and his associates enrolled patients undergoing first-time, isolated CABG who had diabetes or required insulin treatment following surgery based on having three consecutive blood glucose readings of at least 150 mg/dL, or one reading of at least 200 mg/dL. The researchers used a bedside, computerized device that regularly assessed blood glucose levels and adjusted the insulin infusion accordingly. The patients averaged 62 years of age, and about 43% had diabetes.
Among the 98 patients maintained on the 121-180 mg/dL regimen, the average time needed to reach the target blood glucose range was 84 minutes – significantly shorter than the average 173 minutes needed for the 91 patients on the strict regimen.
Patients maintained on the liberal target also fared significantly better in their average number of readings within their target range, minimum glucose level, number of hypoglycemic readings, and total insulin dose received (see table).
Assessment of clinical outcomes – renal failure, atrial fibrillation, pneumonia, deep sternal wound infections, prolonged ventilation, prolonged hospitalization, and operative mortality – showed that the liberal range was not inferior to the strict range for preventing these complications in the primary, intention-to-treat analysis. In the as-treated and per-protocol analyses, the liberal-range patients had outcomes that were noninferior to those of the strict control patients for all parameters except for atrial fibrillation. The liberal-range patients showed a small excess of atrial fibrillations in these two additional analyses.
Future studies should look at the same issue in patients undergoing other types of cardiac surgery, such as valve repair or replacement, or a maze procedure, he said.
Dr. Desai said that he had no relevant financial disclosures.
PHILADELPHIA – A blood glucose target of 121-180 mg/dL for patients following isolated coronary bypass surgery was as clinically effective as was a stricter glucose target and was easier to maintain in a randomized study with 189 patients.
Based on these results, the cardiac surgery program that ran the study switched its blood glucose range for postoperative patients from 90-120 mg/dL to the more liberal range of 121-180 mg/dL, Dr. Shalin P. Desai said at the annual meeting of the American Association for Thoracic Surgery.
"We believe that maintaining patients at a blood glucose level less than 180 mg/dL is safe and effective, and therefore should be considered for patients undergoing coronary artery bypass grafting surgery," said Dr. Desai, a cardiac surgeon at Inova Heart and Vascular Institute in Falls Church, Va.
"We know that a glucose level of less than 180 mg/dL is good, but does it need to be so strict that it’s almost normoglycemic, or can it be more liberal when we know the glucose levels will rise with the stress of surgery and illness? A range of 121-180 mg/dL is probably sufficient," Dr. Desai said in an interview. At that level, "we used less insulin, fewer finger sticks, and fewer resources" than when the target range aims for lower blood glucose levels, he said.
Dr. Desai and his associates enrolled patients undergoing first-time, isolated CABG who had diabetes or required insulin treatment following surgery based on having three consecutive blood glucose readings of at least 150 mg/dL, or one reading of at least 200 mg/dL. The researchers used a bedside, computerized device that regularly assessed blood glucose levels and adjusted the insulin infusion accordingly. The patients averaged 62 years of age, and about 43% had diabetes.
Among the 98 patients maintained on the 121-180 mg/dL regimen, the average time needed to reach the target blood glucose range was 84 minutes – significantly shorter than the average 173 minutes needed for the 91 patients on the strict regimen.
Patients maintained on the liberal target also fared significantly better in their average number of readings within their target range, minimum glucose level, number of hypoglycemic readings, and total insulin dose received (see table).
Assessment of clinical outcomes – renal failure, atrial fibrillation, pneumonia, deep sternal wound infections, prolonged ventilation, prolonged hospitalization, and operative mortality – showed that the liberal range was not inferior to the strict range for preventing these complications in the primary, intention-to-treat analysis. In the as-treated and per-protocol analyses, the liberal-range patients had outcomes that were noninferior to those of the strict control patients for all parameters except for atrial fibrillation. The liberal-range patients showed a small excess of atrial fibrillations in these two additional analyses.
Future studies should look at the same issue in patients undergoing other types of cardiac surgery, such as valve repair or replacement, or a maze procedure, he said.
Dr. Desai said that he had no relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE AMERICAN ASSOCIATION FOR THORACIC SURGERY
Major Finding: A postoperative blood glucose target range of 121-180 mg/dL led to similar clinical outcomes and proved more practical than did a target range of 90-120 mg/dL in patients undergoing first-time, isolated coronary artery bypass grafting surgery.
Data Source: Single-center, randomized trial with 189 patients.
Disclosures: Dr. Desai said he had no relevant financial disclosures.
CABG Outcomes Support More Liberal Blood Glucose Range
PHILADELPHIA – A blood glucose target of 121-180 mg/dL for patients following isolated coronary bypass surgery was as clinically effective as was a stricter glucose target and was easier to maintain in a randomized study with 189 patients.
Based on these results, the cardiac surgery program that ran the study switched its blood glucose range for postoperative patients from 90-120 mg/dL to the more liberal range of 121-180 mg/dL, Dr. Shalin P. Desai said at the annual meeting of the American Association for Thoracic Surgery.
"We believe that maintaining patients at a blood glucose level less than 180 mg/dL is safe and effective, and therefore should be considered for patients undergoing coronary artery bypass grafting surgery," said Dr. Desai, a cardiac surgeon at Inova Heart and Vascular Institute in Falls Church, Va.
"We know that a glucose level of less than 180 mg/dL is good, but does it need to be so strict that it’s almost normoglycemic, or can it be more liberal when we know the glucose levels will rise with the stress of surgery and illness? A range of 121-180 mg/dL is probably sufficient," Dr. Desai said in an interview. At that level, "we used less insulin, fewer finger sticks, and fewer resources" than when the target range aims for lower blood glucose levels, he said.
Dr. Desai and his associates enrolled patients undergoing first-time, isolated CABG who had diabetes or required insulin treatment following surgery based on having three consecutive blood glucose readings of at least 150 mg/dL, or one reading of at least 200 mg/dL. The researchers used a bedside, computerized device that regularly assessed blood glucose levels and adjusted the insulin infusion accordingly. The patients averaged 62 years of age, and about 43% had diabetes.
Among the 98 patients maintained on the 121-180 mg/dL regimen, the average time needed to reach the target blood glucose range was 84 minutes – significantly shorter than the average 173 minutes needed for the 91 patients on the strict regimen.
Patients maintained on the liberal target also fared significantly better in their average number of readings within their target range, minimum glucose level, number of hypoglycemic readings, and total insulin dose received (see table).
Assessment of clinical outcomes – renal failure, atrial fibrillation, pneumonia, deep sternal wound infections, prolonged ventilation, prolonged hospitalization, and operative mortality – showed that the liberal range was not inferior to the strict range for preventing these complications in the primary, intention-to-treat analysis. In the as-treated and per-protocol analyses, the liberal-range patients had outcomes that were noninferior to those of the strict control patients for all parameters except for atrial fibrillation. The liberal-range patients showed a small excess of atrial fibrillations in these two additional analyses.
Future studies should look at the same issue in patients undergoing other types of cardiac surgery, such as valve repair or replacement, or a maze procedure, he said.
Dr. Desai said that he had no relevant financial disclosures.
My associates and I recently reported similar results from a randomized study of 82 patients with diabetes who underwent coronary artery bypass grafting surgery. We also compared a target blood glucose range of 90-120 mg/dL with a range of 121-180 mg/dL. Like the current study, we found no difference in the 30-day rates of death, myocardial infarction, neurologic complications, deep sternal wound infections, or atrial fibrillation incidence. The patients maintained with more aggressive glucose control had a higher rate of hypoglycemic events, but this did not result in increased neurologic complications.
Why did tighter glycemic control not produce better outcomes? One possible explanation is that cardiac surgery patients often receive good treatment with cardioprotective drugs, including aspirin, statins, beta-blockers, and angiotensin-converting enzyme inhibitors. Also, the more liberal regimens still produce good glucose control. In our study, the average blood glucose level in the more liberal group was 135 mg/dL.
Tight glucose control may provide long-term benefits that have not yet been identified in these studies. For example, it may improve long-term graft patency and reduce long-term ischemic events. In our studies, we see that more aggressive glucose control results in lower levels of free fatty acids, a marker of inflammation.
Moderate glycemic control produces a significant reduction in morbidity and mortality in cardiac surgery patients that may be hard to improve upon with more aggressive control. I agree that the optimal glucose range following cardiac surgery appears to be 120-180 mg/dL. While the exact level for optimal control remains unknown, the importance of perioperative glycemic control by continuous insulin infusion is now well established.
Dr. Harold L. Lazar is a thoracic surgeon at Boston Medical Center. He said that he has received research support from Eli Lilly to study the effects of glycemic control during cardiac surgery.
My associates and I recently reported similar results from a randomized study of 82 patients with diabetes who underwent coronary artery bypass grafting surgery. We also compared a target blood glucose range of 90-120 mg/dL with a range of 121-180 mg/dL. Like the current study, we found no difference in the 30-day rates of death, myocardial infarction, neurologic complications, deep sternal wound infections, or atrial fibrillation incidence. The patients maintained with more aggressive glucose control had a higher rate of hypoglycemic events, but this did not result in increased neurologic complications.
Why did tighter glycemic control not produce better outcomes? One possible explanation is that cardiac surgery patients often receive good treatment with cardioprotective drugs, including aspirin, statins, beta-blockers, and angiotensin-converting enzyme inhibitors. Also, the more liberal regimens still produce good glucose control. In our study, the average blood glucose level in the more liberal group was 135 mg/dL.
Tight glucose control may provide long-term benefits that have not yet been identified in these studies. For example, it may improve long-term graft patency and reduce long-term ischemic events. In our studies, we see that more aggressive glucose control results in lower levels of free fatty acids, a marker of inflammation.
Moderate glycemic control produces a significant reduction in morbidity and mortality in cardiac surgery patients that may be hard to improve upon with more aggressive control. I agree that the optimal glucose range following cardiac surgery appears to be 120-180 mg/dL. While the exact level for optimal control remains unknown, the importance of perioperative glycemic control by continuous insulin infusion is now well established.
Dr. Harold L. Lazar is a thoracic surgeon at Boston Medical Center. He said that he has received research support from Eli Lilly to study the effects of glycemic control during cardiac surgery.
My associates and I recently reported similar results from a randomized study of 82 patients with diabetes who underwent coronary artery bypass grafting surgery. We also compared a target blood glucose range of 90-120 mg/dL with a range of 121-180 mg/dL. Like the current study, we found no difference in the 30-day rates of death, myocardial infarction, neurologic complications, deep sternal wound infections, or atrial fibrillation incidence. The patients maintained with more aggressive glucose control had a higher rate of hypoglycemic events, but this did not result in increased neurologic complications.
Why did tighter glycemic control not produce better outcomes? One possible explanation is that cardiac surgery patients often receive good treatment with cardioprotective drugs, including aspirin, statins, beta-blockers, and angiotensin-converting enzyme inhibitors. Also, the more liberal regimens still produce good glucose control. In our study, the average blood glucose level in the more liberal group was 135 mg/dL.
Tight glucose control may provide long-term benefits that have not yet been identified in these studies. For example, it may improve long-term graft patency and reduce long-term ischemic events. In our studies, we see that more aggressive glucose control results in lower levels of free fatty acids, a marker of inflammation.
Moderate glycemic control produces a significant reduction in morbidity and mortality in cardiac surgery patients that may be hard to improve upon with more aggressive control. I agree that the optimal glucose range following cardiac surgery appears to be 120-180 mg/dL. While the exact level for optimal control remains unknown, the importance of perioperative glycemic control by continuous insulin infusion is now well established.
Dr. Harold L. Lazar is a thoracic surgeon at Boston Medical Center. He said that he has received research support from Eli Lilly to study the effects of glycemic control during cardiac surgery.
PHILADELPHIA – A blood glucose target of 121-180 mg/dL for patients following isolated coronary bypass surgery was as clinically effective as was a stricter glucose target and was easier to maintain in a randomized study with 189 patients.
Based on these results, the cardiac surgery program that ran the study switched its blood glucose range for postoperative patients from 90-120 mg/dL to the more liberal range of 121-180 mg/dL, Dr. Shalin P. Desai said at the annual meeting of the American Association for Thoracic Surgery.
"We believe that maintaining patients at a blood glucose level less than 180 mg/dL is safe and effective, and therefore should be considered for patients undergoing coronary artery bypass grafting surgery," said Dr. Desai, a cardiac surgeon at Inova Heart and Vascular Institute in Falls Church, Va.
"We know that a glucose level of less than 180 mg/dL is good, but does it need to be so strict that it’s almost normoglycemic, or can it be more liberal when we know the glucose levels will rise with the stress of surgery and illness? A range of 121-180 mg/dL is probably sufficient," Dr. Desai said in an interview. At that level, "we used less insulin, fewer finger sticks, and fewer resources" than when the target range aims for lower blood glucose levels, he said.
Dr. Desai and his associates enrolled patients undergoing first-time, isolated CABG who had diabetes or required insulin treatment following surgery based on having three consecutive blood glucose readings of at least 150 mg/dL, or one reading of at least 200 mg/dL. The researchers used a bedside, computerized device that regularly assessed blood glucose levels and adjusted the insulin infusion accordingly. The patients averaged 62 years of age, and about 43% had diabetes.
Among the 98 patients maintained on the 121-180 mg/dL regimen, the average time needed to reach the target blood glucose range was 84 minutes – significantly shorter than the average 173 minutes needed for the 91 patients on the strict regimen.
Patients maintained on the liberal target also fared significantly better in their average number of readings within their target range, minimum glucose level, number of hypoglycemic readings, and total insulin dose received (see table).
Assessment of clinical outcomes – renal failure, atrial fibrillation, pneumonia, deep sternal wound infections, prolonged ventilation, prolonged hospitalization, and operative mortality – showed that the liberal range was not inferior to the strict range for preventing these complications in the primary, intention-to-treat analysis. In the as-treated and per-protocol analyses, the liberal-range patients had outcomes that were noninferior to those of the strict control patients for all parameters except for atrial fibrillation. The liberal-range patients showed a small excess of atrial fibrillations in these two additional analyses.
Future studies should look at the same issue in patients undergoing other types of cardiac surgery, such as valve repair or replacement, or a maze procedure, he said.
Dr. Desai said that he had no relevant financial disclosures.
PHILADELPHIA – A blood glucose target of 121-180 mg/dL for patients following isolated coronary bypass surgery was as clinically effective as was a stricter glucose target and was easier to maintain in a randomized study with 189 patients.
Based on these results, the cardiac surgery program that ran the study switched its blood glucose range for postoperative patients from 90-120 mg/dL to the more liberal range of 121-180 mg/dL, Dr. Shalin P. Desai said at the annual meeting of the American Association for Thoracic Surgery.
"We believe that maintaining patients at a blood glucose level less than 180 mg/dL is safe and effective, and therefore should be considered for patients undergoing coronary artery bypass grafting surgery," said Dr. Desai, a cardiac surgeon at Inova Heart and Vascular Institute in Falls Church, Va.
"We know that a glucose level of less than 180 mg/dL is good, but does it need to be so strict that it’s almost normoglycemic, or can it be more liberal when we know the glucose levels will rise with the stress of surgery and illness? A range of 121-180 mg/dL is probably sufficient," Dr. Desai said in an interview. At that level, "we used less insulin, fewer finger sticks, and fewer resources" than when the target range aims for lower blood glucose levels, he said.
Dr. Desai and his associates enrolled patients undergoing first-time, isolated CABG who had diabetes or required insulin treatment following surgery based on having three consecutive blood glucose readings of at least 150 mg/dL, or one reading of at least 200 mg/dL. The researchers used a bedside, computerized device that regularly assessed blood glucose levels and adjusted the insulin infusion accordingly. The patients averaged 62 years of age, and about 43% had diabetes.
Among the 98 patients maintained on the 121-180 mg/dL regimen, the average time needed to reach the target blood glucose range was 84 minutes – significantly shorter than the average 173 minutes needed for the 91 patients on the strict regimen.
Patients maintained on the liberal target also fared significantly better in their average number of readings within their target range, minimum glucose level, number of hypoglycemic readings, and total insulin dose received (see table).
Assessment of clinical outcomes – renal failure, atrial fibrillation, pneumonia, deep sternal wound infections, prolonged ventilation, prolonged hospitalization, and operative mortality – showed that the liberal range was not inferior to the strict range for preventing these complications in the primary, intention-to-treat analysis. In the as-treated and per-protocol analyses, the liberal-range patients had outcomes that were noninferior to those of the strict control patients for all parameters except for atrial fibrillation. The liberal-range patients showed a small excess of atrial fibrillations in these two additional analyses.
Future studies should look at the same issue in patients undergoing other types of cardiac surgery, such as valve repair or replacement, or a maze procedure, he said.
Dr. Desai said that he had no relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE AMERICAN ASSOCIATION FOR THORACIC SURGERY
Major Finding: A postoperative blood glucose target range of 121-180 mg/dL led to similar clinical outcomes and proved more practical than did a target range of 90-120 mg/dL in patients undergoing first-time, isolated coronary artery bypass grafting surgery.
Data Source: Single-center, randomized trial with 189 patients.
Disclosures: Dr. Desai said he had no relevant financial disclosures.
TEVAR Edges Open Surgical Repair in Smaller U.S. Hospitals
PHILADELPHIA – Endovascular repair may be better than open surgery for emergency treatment of patients with a thoracic aortic aneurysm rupture who receive care at smaller U.S. hospitals, based on an analysis of more than 900 patients treated during 2006-2008.
Investigators found that emergency thoracic endovascular aneurysm repair (TEVAR) led to a nearly 80% reduction in complications, compared with open surgical aneurysm repair, in patients who were treated at smaller U.S. hospitals. At larger hospitals, TEVAR and open repair produced similar outcomes, Dr. Raja R. Gopaldas said at the annual meeting of the American Association for Thoracic Surgery.
"TEVAR is an ideal alternative when transfer to a larger facility is not feasible," said Dr. Gopaldas, a cardiothoracic surgeon at the University of Missouri in Columbia.
"We were surprised when we saw that smaller hospitals had better outcomes with TEVAR, but it makes sense. A lot of hospitals lack expertise in open thoracic aortic repair because it requires a highly skilled surgeon, whereas a lot of small hospitals have a cardiac catheterization lab and a cardiologist or vascular surgeon available," he said in an interview. He added that open repair was more successful when performed at larger hospitals, but when TEVAR was used, results were similar.
Widespread availability of TEVAR catheter systems began in 2005. During 2006-2008, TEVAR was used in 40% of emergency thoracic aortic aneurysm repairs. Because these were the first 3 years after U.S. approval, such a high level of TEVAR use, especially in emergency circumstances, fell beyond Dr. Gopaldas’s expectations. "Forty percent is a huge number," he said.
The findings also suggested a role for "TEVAR first" in the emergency repair of ruptured thoracic aortic aneurysms, because the operative team often can intervene more quickly with an endovascular approach than with open surgical repair.
"I think there will be a lot of push to use the endovascular approach more frequently, because it is probably a lot quicker to set up your team," Dr. Gopaldas said. ""It’s quicker to get a TEVAR stent deployed than to cut open a patient’s chest. The endovascular team is probably geared to respond more quickly [than is] the open-heart surgical team in smaller hospitals. In bigger hospitals, there may not be as much of a difference."
The study used data collected by the Nationwide Inpatient Sample, an annual sampling of slightly more than 1,000 U.S. hospitals – about 20% of all U.S. patient discharge records – done by the Agency for Healthcare Research and Quality. Using data for 2006-2008, Dr. Gopaldas and his associates identified 923 patients who underwent emergency repair of a thoracic aortic aneurysm at one of 107 hospitals that performed these repairs. Among those hospitals, 41 (38%) performed TEVAR.
The analysis also divided hospitals into smaller and larger hospitals based on bed numbers. The definition of "smaller" differed based on U.S. geographical region (Northeast, Midwest, South, or West), rural vs. urban, and teaching vs. nonteaching hospitals. The bed sizes of smaller hospitals ranged from 1 to 449 (an urban teaching hospital in the Southern region). Larger hospitals included any center with a bed number larger than the study definition of smaller. Among the 107 hospitals that performed TEVAR during the study period, 27 (25%) were smaller hospitals.
In a risk-adjusted analysis, patients who underwent open surgical repair at a smaller hospital had a threefold increased risk for a subsequent complication, compared with patients treated by surgery at a larger hospital. But among the patients treated with TEVAR, the outcomes at smaller hospitals matched those that were achieved at larger hospitals. A comparison of open surgery and TEVAR outcomes within smaller hospitals showed that TEVAR led to a 79% lower complication rate, Dr. Gopaldas reported. In larger hospitals, outcomes were similar for patients treated with open surgery vs. TEVAR.
The risk-adjusted analysis also showed that once patients developed complications, they fared worse in smaller hospitals regardless of the type of aneurysm repair they received. Smaller hospitals had a failure-to-rescue rate that was nearly fourfold higher than that of larger hospitals. By lowering complication rates, TEVAR proved especially advantageous in smaller hospitals, Dr. Gopaldas said. He did these analyses in collaboration with researchers from Baylor College of Medicine and the Texas Heart Institute, also in Houston.
Dr. Gopaldas said that he had no relevant financial disclosures.
PHILADELPHIA – Endovascular repair may be better than open surgery for emergency treatment of patients with a thoracic aortic aneurysm rupture who receive care at smaller U.S. hospitals, based on an analysis of more than 900 patients treated during 2006-2008.
Investigators found that emergency thoracic endovascular aneurysm repair (TEVAR) led to a nearly 80% reduction in complications, compared with open surgical aneurysm repair, in patients who were treated at smaller U.S. hospitals. At larger hospitals, TEVAR and open repair produced similar outcomes, Dr. Raja R. Gopaldas said at the annual meeting of the American Association for Thoracic Surgery.
"TEVAR is an ideal alternative when transfer to a larger facility is not feasible," said Dr. Gopaldas, a cardiothoracic surgeon at the University of Missouri in Columbia.
"We were surprised when we saw that smaller hospitals had better outcomes with TEVAR, but it makes sense. A lot of hospitals lack expertise in open thoracic aortic repair because it requires a highly skilled surgeon, whereas a lot of small hospitals have a cardiac catheterization lab and a cardiologist or vascular surgeon available," he said in an interview. He added that open repair was more successful when performed at larger hospitals, but when TEVAR was used, results were similar.
Widespread availability of TEVAR catheter systems began in 2005. During 2006-2008, TEVAR was used in 40% of emergency thoracic aortic aneurysm repairs. Because these were the first 3 years after U.S. approval, such a high level of TEVAR use, especially in emergency circumstances, fell beyond Dr. Gopaldas’s expectations. "Forty percent is a huge number," he said.
The findings also suggested a role for "TEVAR first" in the emergency repair of ruptured thoracic aortic aneurysms, because the operative team often can intervene more quickly with an endovascular approach than with open surgical repair.
"I think there will be a lot of push to use the endovascular approach more frequently, because it is probably a lot quicker to set up your team," Dr. Gopaldas said. ""It’s quicker to get a TEVAR stent deployed than to cut open a patient’s chest. The endovascular team is probably geared to respond more quickly [than is] the open-heart surgical team in smaller hospitals. In bigger hospitals, there may not be as much of a difference."
The study used data collected by the Nationwide Inpatient Sample, an annual sampling of slightly more than 1,000 U.S. hospitals – about 20% of all U.S. patient discharge records – done by the Agency for Healthcare Research and Quality. Using data for 2006-2008, Dr. Gopaldas and his associates identified 923 patients who underwent emergency repair of a thoracic aortic aneurysm at one of 107 hospitals that performed these repairs. Among those hospitals, 41 (38%) performed TEVAR.
The analysis also divided hospitals into smaller and larger hospitals based on bed numbers. The definition of "smaller" differed based on U.S. geographical region (Northeast, Midwest, South, or West), rural vs. urban, and teaching vs. nonteaching hospitals. The bed sizes of smaller hospitals ranged from 1 to 449 (an urban teaching hospital in the Southern region). Larger hospitals included any center with a bed number larger than the study definition of smaller. Among the 107 hospitals that performed TEVAR during the study period, 27 (25%) were smaller hospitals.
In a risk-adjusted analysis, patients who underwent open surgical repair at a smaller hospital had a threefold increased risk for a subsequent complication, compared with patients treated by surgery at a larger hospital. But among the patients treated with TEVAR, the outcomes at smaller hospitals matched those that were achieved at larger hospitals. A comparison of open surgery and TEVAR outcomes within smaller hospitals showed that TEVAR led to a 79% lower complication rate, Dr. Gopaldas reported. In larger hospitals, outcomes were similar for patients treated with open surgery vs. TEVAR.
The risk-adjusted analysis also showed that once patients developed complications, they fared worse in smaller hospitals regardless of the type of aneurysm repair they received. Smaller hospitals had a failure-to-rescue rate that was nearly fourfold higher than that of larger hospitals. By lowering complication rates, TEVAR proved especially advantageous in smaller hospitals, Dr. Gopaldas said. He did these analyses in collaboration with researchers from Baylor College of Medicine and the Texas Heart Institute, also in Houston.
Dr. Gopaldas said that he had no relevant financial disclosures.
PHILADELPHIA – Endovascular repair may be better than open surgery for emergency treatment of patients with a thoracic aortic aneurysm rupture who receive care at smaller U.S. hospitals, based on an analysis of more than 900 patients treated during 2006-2008.
Investigators found that emergency thoracic endovascular aneurysm repair (TEVAR) led to a nearly 80% reduction in complications, compared with open surgical aneurysm repair, in patients who were treated at smaller U.S. hospitals. At larger hospitals, TEVAR and open repair produced similar outcomes, Dr. Raja R. Gopaldas said at the annual meeting of the American Association for Thoracic Surgery.
"TEVAR is an ideal alternative when transfer to a larger facility is not feasible," said Dr. Gopaldas, a cardiothoracic surgeon at the University of Missouri in Columbia.
"We were surprised when we saw that smaller hospitals had better outcomes with TEVAR, but it makes sense. A lot of hospitals lack expertise in open thoracic aortic repair because it requires a highly skilled surgeon, whereas a lot of small hospitals have a cardiac catheterization lab and a cardiologist or vascular surgeon available," he said in an interview. He added that open repair was more successful when performed at larger hospitals, but when TEVAR was used, results were similar.
Widespread availability of TEVAR catheter systems began in 2005. During 2006-2008, TEVAR was used in 40% of emergency thoracic aortic aneurysm repairs. Because these were the first 3 years after U.S. approval, such a high level of TEVAR use, especially in emergency circumstances, fell beyond Dr. Gopaldas’s expectations. "Forty percent is a huge number," he said.
The findings also suggested a role for "TEVAR first" in the emergency repair of ruptured thoracic aortic aneurysms, because the operative team often can intervene more quickly with an endovascular approach than with open surgical repair.
"I think there will be a lot of push to use the endovascular approach more frequently, because it is probably a lot quicker to set up your team," Dr. Gopaldas said. ""It’s quicker to get a TEVAR stent deployed than to cut open a patient’s chest. The endovascular team is probably geared to respond more quickly [than is] the open-heart surgical team in smaller hospitals. In bigger hospitals, there may not be as much of a difference."
The study used data collected by the Nationwide Inpatient Sample, an annual sampling of slightly more than 1,000 U.S. hospitals – about 20% of all U.S. patient discharge records – done by the Agency for Healthcare Research and Quality. Using data for 2006-2008, Dr. Gopaldas and his associates identified 923 patients who underwent emergency repair of a thoracic aortic aneurysm at one of 107 hospitals that performed these repairs. Among those hospitals, 41 (38%) performed TEVAR.
The analysis also divided hospitals into smaller and larger hospitals based on bed numbers. The definition of "smaller" differed based on U.S. geographical region (Northeast, Midwest, South, or West), rural vs. urban, and teaching vs. nonteaching hospitals. The bed sizes of smaller hospitals ranged from 1 to 449 (an urban teaching hospital in the Southern region). Larger hospitals included any center with a bed number larger than the study definition of smaller. Among the 107 hospitals that performed TEVAR during the study period, 27 (25%) were smaller hospitals.
In a risk-adjusted analysis, patients who underwent open surgical repair at a smaller hospital had a threefold increased risk for a subsequent complication, compared with patients treated by surgery at a larger hospital. But among the patients treated with TEVAR, the outcomes at smaller hospitals matched those that were achieved at larger hospitals. A comparison of open surgery and TEVAR outcomes within smaller hospitals showed that TEVAR led to a 79% lower complication rate, Dr. Gopaldas reported. In larger hospitals, outcomes were similar for patients treated with open surgery vs. TEVAR.
The risk-adjusted analysis also showed that once patients developed complications, they fared worse in smaller hospitals regardless of the type of aneurysm repair they received. Smaller hospitals had a failure-to-rescue rate that was nearly fourfold higher than that of larger hospitals. By lowering complication rates, TEVAR proved especially advantageous in smaller hospitals, Dr. Gopaldas said. He did these analyses in collaboration with researchers from Baylor College of Medicine and the Texas Heart Institute, also in Houston.
Dr. Gopaldas said that he had no relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE AMERICAN ASSOCIATION FOR THORACIC SURGERY
TEVAR Edges Open Surgical Repair in Smaller U.S. Hospitals
PHILADELPHIA – Endovascular repair may be better than open surgery for emergency treatment of patients with a thoracic aortic aneurysm rupture who receive care at smaller U.S. hospitals, based on an analysis of more than 900 patients treated during 2006-2008.
Investigators found that emergency thoracic endovascular aneurysm repair (TEVAR) led to a nearly 80% reduction in complications, compared with open surgical aneurysm repair, in patients who were treated at smaller U.S. hospitals. At larger hospitals, TEVAR and open repair produced similar outcomes, Dr. Raja R. Gopaldas said at the annual meeting of the American Association for Thoracic Surgery.
"TEVAR is an ideal alternative when transfer to a larger facility is not feasible," said Dr. Gopaldas, a cardiothoracic surgeon at the University of Missouri in Columbia.
"We were surprised when we saw that smaller hospitals had better outcomes with TEVAR, but it makes sense. A lot of hospitals lack expertise in open thoracic aortic repair because it requires a highly skilled surgeon, whereas a lot of small hospitals have a cardiac catheterization lab and a cardiologist or vascular surgeon available," he said in an interview. He added that open repair was more successful when performed at larger hospitals, but when TEVAR was used, results were similar.
Widespread availability of TEVAR catheter systems began in 2005. During 2006-2008, TEVAR was used in 40% of emergency thoracic aortic aneurysm repairs. Because these were the first 3 years after U.S. approval, such a high level of TEVAR use, especially in emergency circumstances, fell beyond Dr. Gopaldas’s expectations. "Forty percent is a huge number," he said.
The findings also suggested a role for "TEVAR first" in the emergency repair of ruptured thoracic aortic aneurysms, because the operative team often can intervene more quickly with an endovascular approach than with open surgical repair.
"I think there will be a lot of push to use the endovascular approach more frequently, because it is probably a lot quicker to set up your team," Dr. Gopaldas said. ""It’s quicker to get a TEVAR stent deployed than to cut open a patient’s chest. The endovascular team is probably geared to respond more quickly [than is] the open-heart surgical team in smaller hospitals. In bigger hospitals, there may not be as much of a difference."
The study used data collected by the Nationwide Inpatient Sample, an annual sampling of slightly more than 1,000 U.S. hospitals – about 20% of all U.S. patient discharge records – done by the Agency for Healthcare Research and Quality. Using data for 2006-2008, Dr. Gopaldas and his associates identified 923 patients who underwent emergency repair of a thoracic aortic aneurysm at one of 107 hospitals that performed these repairs. Among those hospitals, 41 (38%) performed TEVAR.
The analysis also divided hospitals into smaller and larger hospitals based on bed numbers. The definition of "smaller" differed based on U.S. geographical region (Northeast, Midwest, South, or West), rural vs. urban, and teaching vs. nonteaching hospitals. The bed sizes of smaller hospitals ranged from 1 to 449 (an urban teaching hospital in the Southern region). Larger hospitals included any center with a bed number larger than the study definition of smaller. Among the 107 hospitals that performed TEVAR during the study period, 27 (25%) were smaller hospitals.
In a risk-adjusted analysis, patients who underwent open surgical repair at a smaller hospital had a threefold increased risk for a subsequent complication, compared with patients treated by surgery at a larger hospital. But among the patients treated with TEVAR, the outcomes at smaller hospitals matched those that were achieved at larger hospitals. A comparison of open surgery and TEVAR outcomes within smaller hospitals showed that TEVAR led to a 79% lower complication rate, Dr. Gopaldas reported. In larger hospitals, outcomes were similar for patients treated with open surgery vs. TEVAR.
The risk-adjusted analysis also showed that once patients developed complications, they fared worse in smaller hospitals regardless of the type of aneurysm repair they received. Smaller hospitals had a failure-to-rescue rate that was nearly fourfold higher than that of larger hospitals. By lowering complication rates, TEVAR proved especially advantageous in smaller hospitals, Dr. Gopaldas said. He did these analyses in collaboration with researchers from Baylor College of Medicine and the Texas Heart Institute, also in Houston.
Dr. Gopaldas said that he had no relevant financial disclosures.
PHILADELPHIA – Endovascular repair may be better than open surgery for emergency treatment of patients with a thoracic aortic aneurysm rupture who receive care at smaller U.S. hospitals, based on an analysis of more than 900 patients treated during 2006-2008.
Investigators found that emergency thoracic endovascular aneurysm repair (TEVAR) led to a nearly 80% reduction in complications, compared with open surgical aneurysm repair, in patients who were treated at smaller U.S. hospitals. At larger hospitals, TEVAR and open repair produced similar outcomes, Dr. Raja R. Gopaldas said at the annual meeting of the American Association for Thoracic Surgery.
"TEVAR is an ideal alternative when transfer to a larger facility is not feasible," said Dr. Gopaldas, a cardiothoracic surgeon at the University of Missouri in Columbia.
"We were surprised when we saw that smaller hospitals had better outcomes with TEVAR, but it makes sense. A lot of hospitals lack expertise in open thoracic aortic repair because it requires a highly skilled surgeon, whereas a lot of small hospitals have a cardiac catheterization lab and a cardiologist or vascular surgeon available," he said in an interview. He added that open repair was more successful when performed at larger hospitals, but when TEVAR was used, results were similar.
Widespread availability of TEVAR catheter systems began in 2005. During 2006-2008, TEVAR was used in 40% of emergency thoracic aortic aneurysm repairs. Because these were the first 3 years after U.S. approval, such a high level of TEVAR use, especially in emergency circumstances, fell beyond Dr. Gopaldas’s expectations. "Forty percent is a huge number," he said.
The findings also suggested a role for "TEVAR first" in the emergency repair of ruptured thoracic aortic aneurysms, because the operative team often can intervene more quickly with an endovascular approach than with open surgical repair.
"I think there will be a lot of push to use the endovascular approach more frequently, because it is probably a lot quicker to set up your team," Dr. Gopaldas said. ""It’s quicker to get a TEVAR stent deployed than to cut open a patient’s chest. The endovascular team is probably geared to respond more quickly [than is] the open-heart surgical team in smaller hospitals. In bigger hospitals, there may not be as much of a difference."
The study used data collected by the Nationwide Inpatient Sample, an annual sampling of slightly more than 1,000 U.S. hospitals – about 20% of all U.S. patient discharge records – done by the Agency for Healthcare Research and Quality. Using data for 2006-2008, Dr. Gopaldas and his associates identified 923 patients who underwent emergency repair of a thoracic aortic aneurysm at one of 107 hospitals that performed these repairs. Among those hospitals, 41 (38%) performed TEVAR.
The analysis also divided hospitals into smaller and larger hospitals based on bed numbers. The definition of "smaller" differed based on U.S. geographical region (Northeast, Midwest, South, or West), rural vs. urban, and teaching vs. nonteaching hospitals. The bed sizes of smaller hospitals ranged from 1 to 449 (an urban teaching hospital in the Southern region). Larger hospitals included any center with a bed number larger than the study definition of smaller. Among the 107 hospitals that performed TEVAR during the study period, 27 (25%) were smaller hospitals.
In a risk-adjusted analysis, patients who underwent open surgical repair at a smaller hospital had a threefold increased risk for a subsequent complication, compared with patients treated by surgery at a larger hospital. But among the patients treated with TEVAR, the outcomes at smaller hospitals matched those that were achieved at larger hospitals. A comparison of open surgery and TEVAR outcomes within smaller hospitals showed that TEVAR led to a 79% lower complication rate, Dr. Gopaldas reported. In larger hospitals, outcomes were similar for patients treated with open surgery vs. TEVAR.
The risk-adjusted analysis also showed that once patients developed complications, they fared worse in smaller hospitals regardless of the type of aneurysm repair they received. Smaller hospitals had a failure-to-rescue rate that was nearly fourfold higher than that of larger hospitals. By lowering complication rates, TEVAR proved especially advantageous in smaller hospitals, Dr. Gopaldas said. He did these analyses in collaboration with researchers from Baylor College of Medicine and the Texas Heart Institute, also in Houston.
Dr. Gopaldas said that he had no relevant financial disclosures.
PHILADELPHIA – Endovascular repair may be better than open surgery for emergency treatment of patients with a thoracic aortic aneurysm rupture who receive care at smaller U.S. hospitals, based on an analysis of more than 900 patients treated during 2006-2008.
Investigators found that emergency thoracic endovascular aneurysm repair (TEVAR) led to a nearly 80% reduction in complications, compared with open surgical aneurysm repair, in patients who were treated at smaller U.S. hospitals. At larger hospitals, TEVAR and open repair produced similar outcomes, Dr. Raja R. Gopaldas said at the annual meeting of the American Association for Thoracic Surgery.
"TEVAR is an ideal alternative when transfer to a larger facility is not feasible," said Dr. Gopaldas, a cardiothoracic surgeon at the University of Missouri in Columbia.
"We were surprised when we saw that smaller hospitals had better outcomes with TEVAR, but it makes sense. A lot of hospitals lack expertise in open thoracic aortic repair because it requires a highly skilled surgeon, whereas a lot of small hospitals have a cardiac catheterization lab and a cardiologist or vascular surgeon available," he said in an interview. He added that open repair was more successful when performed at larger hospitals, but when TEVAR was used, results were similar.
Widespread availability of TEVAR catheter systems began in 2005. During 2006-2008, TEVAR was used in 40% of emergency thoracic aortic aneurysm repairs. Because these were the first 3 years after U.S. approval, such a high level of TEVAR use, especially in emergency circumstances, fell beyond Dr. Gopaldas’s expectations. "Forty percent is a huge number," he said.
The findings also suggested a role for "TEVAR first" in the emergency repair of ruptured thoracic aortic aneurysms, because the operative team often can intervene more quickly with an endovascular approach than with open surgical repair.
"I think there will be a lot of push to use the endovascular approach more frequently, because it is probably a lot quicker to set up your team," Dr. Gopaldas said. ""It’s quicker to get a TEVAR stent deployed than to cut open a patient’s chest. The endovascular team is probably geared to respond more quickly [than is] the open-heart surgical team in smaller hospitals. In bigger hospitals, there may not be as much of a difference."
The study used data collected by the Nationwide Inpatient Sample, an annual sampling of slightly more than 1,000 U.S. hospitals – about 20% of all U.S. patient discharge records – done by the Agency for Healthcare Research and Quality. Using data for 2006-2008, Dr. Gopaldas and his associates identified 923 patients who underwent emergency repair of a thoracic aortic aneurysm at one of 107 hospitals that performed these repairs. Among those hospitals, 41 (38%) performed TEVAR.
The analysis also divided hospitals into smaller and larger hospitals based on bed numbers. The definition of "smaller" differed based on U.S. geographical region (Northeast, Midwest, South, or West), rural vs. urban, and teaching vs. nonteaching hospitals. The bed sizes of smaller hospitals ranged from 1 to 449 (an urban teaching hospital in the Southern region). Larger hospitals included any center with a bed number larger than the study definition of smaller. Among the 107 hospitals that performed TEVAR during the study period, 27 (25%) were smaller hospitals.
In a risk-adjusted analysis, patients who underwent open surgical repair at a smaller hospital had a threefold increased risk for a subsequent complication, compared with patients treated by surgery at a larger hospital. But among the patients treated with TEVAR, the outcomes at smaller hospitals matched those that were achieved at larger hospitals. A comparison of open surgery and TEVAR outcomes within smaller hospitals showed that TEVAR led to a 79% lower complication rate, Dr. Gopaldas reported. In larger hospitals, outcomes were similar for patients treated with open surgery vs. TEVAR.
The risk-adjusted analysis also showed that once patients developed complications, they fared worse in smaller hospitals regardless of the type of aneurysm repair they received. Smaller hospitals had a failure-to-rescue rate that was nearly fourfold higher than that of larger hospitals. By lowering complication rates, TEVAR proved especially advantageous in smaller hospitals, Dr. Gopaldas said. He did these analyses in collaboration with researchers from Baylor College of Medicine and the Texas Heart Institute, also in Houston.
Dr. Gopaldas said that he had no relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE AMERICAN ASSOCIATION FOR THORACIC SURGERY
Major Finding: In smaller U.S. hospitals, among patients who required emergency repair of a ruptured thoracic aortic aneurysm, TEVAR led to a 79% reduced complication rate, compared with patients undergoing open surgical repair. In larger U.S. hospitals, the two repair methods led to similar outcomes.
Data Source: An analysis of 923 patients who were treated for emergency repair of a ruptured thoracic aortic aneurysm at 107 U.S. hospitals during 2006-2008.
Disclosures: Dr. Gopaldas said that he had no relevant financial disclosures.
CABG Track Record Improved in Past Decade
PHILADELPHIA – U.S. cardiac surgeons increasingly performed coronary artery bypass surgery on more complex patients during 2000-2009, yet significant drops in the rates of perioperative deaths and strokes were seen during those years, according to a review of more than 1.4 million procedures.
"The major implication of this study is that we are operating on a more complex cohort of patients, and we’re doing a better job, with less death and stroke than [was the case] not too long ago. This has implications for how we stratify patients for revascularization therapy," said Dr. Andrew W. ElBardissi at the annual meeting of the American Association for Thoracic Surgery.
"A lot of the patterns that we are seeing reflect the results from some of the more rigorous prospective studies that have dictated practice. We have seen improvements in process and surgical decision making, including more optimal medical management when patients go to surgery – not just in the operating room, but throughout the perioperative period (preop, op, and the ICU). Not only have outcomes improved, but we seem to be operating on the correct cohort of patients," said Dr. ElBardissi, a cardiac surgeon at Brigham and Women’s Hospital in Boston.
"These outcomes appear to reflect improvements in perioperative surgical care as they continue to be significant after adjustment for patient risk," he added.
Dr. T. Bruce Ferguson Jr. concurred with Dr. ElBardissi’s assessment. "This study clearly documented continued improvement in CABG [coronary artery bypass grafting], particularly in the CABG-PCI [percutaneous coronary intervention] era of the last decade. These are clearly more technically difficult operations, with increased rates of prior PCI, left main disease, and distal anastomoses," said Dr. Ferguson, professor of surgery and chairman of cardiovascular sciences at East Carolina University in Greenville, N.C.
Dr. ElBardissi’s analysis used data that were collected on more than 1.4 million patients who underwent first-time, isolated CABG surgery at a hospital participating in the Society of Thoracic Surgeons’ adult cardiac surgery database. The data he presented compared 136,513 patients who underwent CABG in 2000 vs. 160,905 patients who had this surgery in 2009.
Major shifts during those years included a statistically significant drop in the prevalence of recent smoking (from 60% in 2000 to 30% in 2009), but significant increases in the prevalence of patients with hypercholesterolemia (84% in 2009 vs. 60% in 2000), hypertension (85% vs. 71%), and chronic obstructive pulmonary disease (23% vs. 16%). The percentage of patients who were previously treated by PCI also jumped to 26% in 2009, compared with 19% in 2000.
Significant rises in the rate of preoperative treatment with cardioprotective drugs were also seen, notably in the use of aspirin, beta-blockers, ACE inhibitors, and statins. Beta-blocker use jumped from 61% of patients in 2000 to 81% in 2009.
The prevalence of left main coronary artery stenosis rose from 23% of patients in 2000 to 32% in 2009.
The statistics also documented meaningful changes in how CABG occurred. Use of an internal mammary artery graft rose from 84% of cases in 2000 to 95% in 2009, and off-pump surgery increased from 14% of cases to 21%.
Elective procedures dropped from 58% in 2000 to 41% in 2009. The largest subgroup of patients shifted to urgent cases, which rose from 38% of patients in 2000 to 54% in 2009.
Mortality during 30-day follow-up fell significantly, from 2.4% in 2000 to 1.9% in 2009 – a 24% relative rate reduction after adjustment for differences in patient risk. Among elective and urgent cases, 30-day mortality fell from 2.1% in 2000 to 1.6% in 2009.
The rate of 30-day stoke in all patients dropped from 1.6% in 2000 to 1.2% in 2009, a statistically significant decline. The risk-adjusted analysis showed this as a 26% relative fall in stroke rates. In elective and urgent cases, the rate declined from 1.6% to 1.1%.
The 30-day outcome results also showed significant declines in deep sternal wound rates (from 0.55% in 2000 to 0.37% in 2009), and in the need for reoperations because of bleeding (2.5% vs. 2.2%). The statistics showed no significant changes in the rates of postoperative renal failure or new-onset atrial fibrillation.
Dr. ElBardissi and Dr. Ferguson said they had no disclosures.
PHILADELPHIA – U.S. cardiac surgeons increasingly performed coronary artery bypass surgery on more complex patients during 2000-2009, yet significant drops in the rates of perioperative deaths and strokes were seen during those years, according to a review of more than 1.4 million procedures.
"The major implication of this study is that we are operating on a more complex cohort of patients, and we’re doing a better job, with less death and stroke than [was the case] not too long ago. This has implications for how we stratify patients for revascularization therapy," said Dr. Andrew W. ElBardissi at the annual meeting of the American Association for Thoracic Surgery.
"A lot of the patterns that we are seeing reflect the results from some of the more rigorous prospective studies that have dictated practice. We have seen improvements in process and surgical decision making, including more optimal medical management when patients go to surgery – not just in the operating room, but throughout the perioperative period (preop, op, and the ICU). Not only have outcomes improved, but we seem to be operating on the correct cohort of patients," said Dr. ElBardissi, a cardiac surgeon at Brigham and Women’s Hospital in Boston.
"These outcomes appear to reflect improvements in perioperative surgical care as they continue to be significant after adjustment for patient risk," he added.
Dr. T. Bruce Ferguson Jr. concurred with Dr. ElBardissi’s assessment. "This study clearly documented continued improvement in CABG [coronary artery bypass grafting], particularly in the CABG-PCI [percutaneous coronary intervention] era of the last decade. These are clearly more technically difficult operations, with increased rates of prior PCI, left main disease, and distal anastomoses," said Dr. Ferguson, professor of surgery and chairman of cardiovascular sciences at East Carolina University in Greenville, N.C.
Dr. ElBardissi’s analysis used data that were collected on more than 1.4 million patients who underwent first-time, isolated CABG surgery at a hospital participating in the Society of Thoracic Surgeons’ adult cardiac surgery database. The data he presented compared 136,513 patients who underwent CABG in 2000 vs. 160,905 patients who had this surgery in 2009.
Major shifts during those years included a statistically significant drop in the prevalence of recent smoking (from 60% in 2000 to 30% in 2009), but significant increases in the prevalence of patients with hypercholesterolemia (84% in 2009 vs. 60% in 2000), hypertension (85% vs. 71%), and chronic obstructive pulmonary disease (23% vs. 16%). The percentage of patients who were previously treated by PCI also jumped to 26% in 2009, compared with 19% in 2000.
Significant rises in the rate of preoperative treatment with cardioprotective drugs were also seen, notably in the use of aspirin, beta-blockers, ACE inhibitors, and statins. Beta-blocker use jumped from 61% of patients in 2000 to 81% in 2009.
The prevalence of left main coronary artery stenosis rose from 23% of patients in 2000 to 32% in 2009.
The statistics also documented meaningful changes in how CABG occurred. Use of an internal mammary artery graft rose from 84% of cases in 2000 to 95% in 2009, and off-pump surgery increased from 14% of cases to 21%.
Elective procedures dropped from 58% in 2000 to 41% in 2009. The largest subgroup of patients shifted to urgent cases, which rose from 38% of patients in 2000 to 54% in 2009.
Mortality during 30-day follow-up fell significantly, from 2.4% in 2000 to 1.9% in 2009 – a 24% relative rate reduction after adjustment for differences in patient risk. Among elective and urgent cases, 30-day mortality fell from 2.1% in 2000 to 1.6% in 2009.
The rate of 30-day stoke in all patients dropped from 1.6% in 2000 to 1.2% in 2009, a statistically significant decline. The risk-adjusted analysis showed this as a 26% relative fall in stroke rates. In elective and urgent cases, the rate declined from 1.6% to 1.1%.
The 30-day outcome results also showed significant declines in deep sternal wound rates (from 0.55% in 2000 to 0.37% in 2009), and in the need for reoperations because of bleeding (2.5% vs. 2.2%). The statistics showed no significant changes in the rates of postoperative renal failure or new-onset atrial fibrillation.
Dr. ElBardissi and Dr. Ferguson said they had no disclosures.
PHILADELPHIA – U.S. cardiac surgeons increasingly performed coronary artery bypass surgery on more complex patients during 2000-2009, yet significant drops in the rates of perioperative deaths and strokes were seen during those years, according to a review of more than 1.4 million procedures.
"The major implication of this study is that we are operating on a more complex cohort of patients, and we’re doing a better job, with less death and stroke than [was the case] not too long ago. This has implications for how we stratify patients for revascularization therapy," said Dr. Andrew W. ElBardissi at the annual meeting of the American Association for Thoracic Surgery.
"A lot of the patterns that we are seeing reflect the results from some of the more rigorous prospective studies that have dictated practice. We have seen improvements in process and surgical decision making, including more optimal medical management when patients go to surgery – not just in the operating room, but throughout the perioperative period (preop, op, and the ICU). Not only have outcomes improved, but we seem to be operating on the correct cohort of patients," said Dr. ElBardissi, a cardiac surgeon at Brigham and Women’s Hospital in Boston.
"These outcomes appear to reflect improvements in perioperative surgical care as they continue to be significant after adjustment for patient risk," he added.
Dr. T. Bruce Ferguson Jr. concurred with Dr. ElBardissi’s assessment. "This study clearly documented continued improvement in CABG [coronary artery bypass grafting], particularly in the CABG-PCI [percutaneous coronary intervention] era of the last decade. These are clearly more technically difficult operations, with increased rates of prior PCI, left main disease, and distal anastomoses," said Dr. Ferguson, professor of surgery and chairman of cardiovascular sciences at East Carolina University in Greenville, N.C.
Dr. ElBardissi’s analysis used data that were collected on more than 1.4 million patients who underwent first-time, isolated CABG surgery at a hospital participating in the Society of Thoracic Surgeons’ adult cardiac surgery database. The data he presented compared 136,513 patients who underwent CABG in 2000 vs. 160,905 patients who had this surgery in 2009.
Major shifts during those years included a statistically significant drop in the prevalence of recent smoking (from 60% in 2000 to 30% in 2009), but significant increases in the prevalence of patients with hypercholesterolemia (84% in 2009 vs. 60% in 2000), hypertension (85% vs. 71%), and chronic obstructive pulmonary disease (23% vs. 16%). The percentage of patients who were previously treated by PCI also jumped to 26% in 2009, compared with 19% in 2000.
Significant rises in the rate of preoperative treatment with cardioprotective drugs were also seen, notably in the use of aspirin, beta-blockers, ACE inhibitors, and statins. Beta-blocker use jumped from 61% of patients in 2000 to 81% in 2009.
The prevalence of left main coronary artery stenosis rose from 23% of patients in 2000 to 32% in 2009.
The statistics also documented meaningful changes in how CABG occurred. Use of an internal mammary artery graft rose from 84% of cases in 2000 to 95% in 2009, and off-pump surgery increased from 14% of cases to 21%.
Elective procedures dropped from 58% in 2000 to 41% in 2009. The largest subgroup of patients shifted to urgent cases, which rose from 38% of patients in 2000 to 54% in 2009.
Mortality during 30-day follow-up fell significantly, from 2.4% in 2000 to 1.9% in 2009 – a 24% relative rate reduction after adjustment for differences in patient risk. Among elective and urgent cases, 30-day mortality fell from 2.1% in 2000 to 1.6% in 2009.
The rate of 30-day stoke in all patients dropped from 1.6% in 2000 to 1.2% in 2009, a statistically significant decline. The risk-adjusted analysis showed this as a 26% relative fall in stroke rates. In elective and urgent cases, the rate declined from 1.6% to 1.1%.
The 30-day outcome results also showed significant declines in deep sternal wound rates (from 0.55% in 2000 to 0.37% in 2009), and in the need for reoperations because of bleeding (2.5% vs. 2.2%). The statistics showed no significant changes in the rates of postoperative renal failure or new-onset atrial fibrillation.
Dr. ElBardissi and Dr. Ferguson said they had no disclosures.
FROM THE ANNUAL MEETING OF THE AMERICAN ASSOCIATION FOR THORACIC SURGERY
CABG Track Record Improved in Past Decade
PHILADELPHIA – U.S. cardiac surgeons increasingly performed coronary artery bypass surgery on more complex patients during 2000-2009, yet significant drops in the rates of perioperative deaths and strokes were seen during those years, according to a review of more than 1.4 million procedures.
"The major implication of this study is that we are operating on a more complex cohort of patients, and we’re doing a better job, with less death and stroke than [was the case] not too long ago. This has implications for how we stratify patients for revascularization therapy," said Dr. Andrew W. ElBardissi at the annual meeting of the American Association for Thoracic Surgery.
"A lot of the patterns that we are seeing reflect the results from some of the more rigorous prospective studies that have dictated practice. We have seen improvements in process and surgical decision making, including more optimal medical management when patients go to surgery – not just in the operating room, but throughout the perioperative period (preop, op, and the ICU). Not only have outcomes improved, but we seem to be operating on the correct cohort of patients," said Dr. ElBardissi, a cardiac surgeon at Brigham and Women’s Hospital in Boston.
"These outcomes appear to reflect improvements in perioperative surgical care as they continue to be significant after adjustment for patient risk," he added.
Dr. T. Bruce Ferguson Jr. concurred with Dr. ElBardissi’s assessment. "This study clearly documented continued improvement in CABG [coronary artery bypass grafting], particularly in the CABG-PCI [percutaneous coronary intervention] era of the last decade. These are clearly more technically difficult operations, with increased rates of prior PCI, left main disease, and distal anastomoses," said Dr. Ferguson, professor of surgery and chairman of cardiovascular sciences at East Carolina University in Greenville, N.C.
Dr. ElBardissi’s analysis used data that were collected on more than 1.4 million patients who underwent first-time, isolated CABG surgery at a hospital participating in the Society of Thoracic Surgeons’ adult cardiac surgery database. The data he presented compared 136,513 patients who underwent CABG in 2000 vs. 160,905 patients who had this surgery in 2009.
Major shifts during those years included a statistically significant drop in the prevalence of recent smoking (from 60% in 2000 to 30% in 2009), but significant increases in the prevalence of patients with hypercholesterolemia (84% in 2009 vs. 60% in 2000), hypertension (85% vs. 71%), and chronic obstructive pulmonary disease (23% vs. 16%). The percentage of patients who were previously treated by PCI also jumped to 26% in 2009, compared with 19% in 2000.
Significant rises in the rate of preoperative treatment with cardioprotective drugs were also seen, notably in the use of aspirin, beta-blockers, ACE inhibitors, and statins. Beta-blocker use jumped from 61% of patients in 2000 to 81% in 2009.
The prevalence of left main coronary artery stenosis rose from 23% of patients in 2000 to 32% in 2009.
The statistics also documented meaningful changes in how CABG occurred. Use of an internal mammary artery graft rose from 84% of cases in 2000 to 95% in 2009, and off-pump surgery increased from 14% of cases to 21%.
Elective procedures dropped from 58% in 2000 to 41% in 2009. The largest subgroup of patients shifted to urgent cases, which rose from 38% of patients in 2000 to 54% in 2009.
Mortality during 30-day follow-up fell significantly, from 2.4% in 2000 to 1.9% in 2009 – a 24% relative rate reduction after adjustment for differences in patient risk. Among elective and urgent cases, 30-day mortality fell from 2.1% in 2000 to 1.6% in 2009.
The rate of 30-day stoke in all patients dropped from 1.6% in 2000 to 1.2% in 2009, a statistically significant decline. The risk-adjusted analysis showed this as a 26% relative fall in stroke rates. In elective and urgent cases, the rate declined from 1.6% to 1.1%.
The 30-day outcome results also showed significant declines in deep sternal wound rates (from 0.55% in 2000 to 0.37% in 2009), and in the need for reoperations because of bleeding (2.5% vs. 2.2%). The statistics showed no significant changes in the rates of postoperative renal failure or new-onset atrial fibrillation.
Dr. ElBardissi and Dr. Ferguson said they had no disclosures.
PHILADELPHIA – U.S. cardiac surgeons increasingly performed coronary artery bypass surgery on more complex patients during 2000-2009, yet significant drops in the rates of perioperative deaths and strokes were seen during those years, according to a review of more than 1.4 million procedures.
"The major implication of this study is that we are operating on a more complex cohort of patients, and we’re doing a better job, with less death and stroke than [was the case] not too long ago. This has implications for how we stratify patients for revascularization therapy," said Dr. Andrew W. ElBardissi at the annual meeting of the American Association for Thoracic Surgery.
"A lot of the patterns that we are seeing reflect the results from some of the more rigorous prospective studies that have dictated practice. We have seen improvements in process and surgical decision making, including more optimal medical management when patients go to surgery – not just in the operating room, but throughout the perioperative period (preop, op, and the ICU). Not only have outcomes improved, but we seem to be operating on the correct cohort of patients," said Dr. ElBardissi, a cardiac surgeon at Brigham and Women’s Hospital in Boston.
"These outcomes appear to reflect improvements in perioperative surgical care as they continue to be significant after adjustment for patient risk," he added.
Dr. T. Bruce Ferguson Jr. concurred with Dr. ElBardissi’s assessment. "This study clearly documented continued improvement in CABG [coronary artery bypass grafting], particularly in the CABG-PCI [percutaneous coronary intervention] era of the last decade. These are clearly more technically difficult operations, with increased rates of prior PCI, left main disease, and distal anastomoses," said Dr. Ferguson, professor of surgery and chairman of cardiovascular sciences at East Carolina University in Greenville, N.C.
Dr. ElBardissi’s analysis used data that were collected on more than 1.4 million patients who underwent first-time, isolated CABG surgery at a hospital participating in the Society of Thoracic Surgeons’ adult cardiac surgery database. The data he presented compared 136,513 patients who underwent CABG in 2000 vs. 160,905 patients who had this surgery in 2009.
Major shifts during those years included a statistically significant drop in the prevalence of recent smoking (from 60% in 2000 to 30% in 2009), but significant increases in the prevalence of patients with hypercholesterolemia (84% in 2009 vs. 60% in 2000), hypertension (85% vs. 71%), and chronic obstructive pulmonary disease (23% vs. 16%). The percentage of patients who were previously treated by PCI also jumped to 26% in 2009, compared with 19% in 2000.
Significant rises in the rate of preoperative treatment with cardioprotective drugs were also seen, notably in the use of aspirin, beta-blockers, ACE inhibitors, and statins. Beta-blocker use jumped from 61% of patients in 2000 to 81% in 2009.
The prevalence of left main coronary artery stenosis rose from 23% of patients in 2000 to 32% in 2009.
The statistics also documented meaningful changes in how CABG occurred. Use of an internal mammary artery graft rose from 84% of cases in 2000 to 95% in 2009, and off-pump surgery increased from 14% of cases to 21%.
Elective procedures dropped from 58% in 2000 to 41% in 2009. The largest subgroup of patients shifted to urgent cases, which rose from 38% of patients in 2000 to 54% in 2009.
Mortality during 30-day follow-up fell significantly, from 2.4% in 2000 to 1.9% in 2009 – a 24% relative rate reduction after adjustment for differences in patient risk. Among elective and urgent cases, 30-day mortality fell from 2.1% in 2000 to 1.6% in 2009.
The rate of 30-day stoke in all patients dropped from 1.6% in 2000 to 1.2% in 2009, a statistically significant decline. The risk-adjusted analysis showed this as a 26% relative fall in stroke rates. In elective and urgent cases, the rate declined from 1.6% to 1.1%.
The 30-day outcome results also showed significant declines in deep sternal wound rates (from 0.55% in 2000 to 0.37% in 2009), and in the need for reoperations because of bleeding (2.5% vs. 2.2%). The statistics showed no significant changes in the rates of postoperative renal failure or new-onset atrial fibrillation.
Dr. ElBardissi and Dr. Ferguson said they had no disclosures.
PHILADELPHIA – U.S. cardiac surgeons increasingly performed coronary artery bypass surgery on more complex patients during 2000-2009, yet significant drops in the rates of perioperative deaths and strokes were seen during those years, according to a review of more than 1.4 million procedures.
"The major implication of this study is that we are operating on a more complex cohort of patients, and we’re doing a better job, with less death and stroke than [was the case] not too long ago. This has implications for how we stratify patients for revascularization therapy," said Dr. Andrew W. ElBardissi at the annual meeting of the American Association for Thoracic Surgery.
"A lot of the patterns that we are seeing reflect the results from some of the more rigorous prospective studies that have dictated practice. We have seen improvements in process and surgical decision making, including more optimal medical management when patients go to surgery – not just in the operating room, but throughout the perioperative period (preop, op, and the ICU). Not only have outcomes improved, but we seem to be operating on the correct cohort of patients," said Dr. ElBardissi, a cardiac surgeon at Brigham and Women’s Hospital in Boston.
"These outcomes appear to reflect improvements in perioperative surgical care as they continue to be significant after adjustment for patient risk," he added.
Dr. T. Bruce Ferguson Jr. concurred with Dr. ElBardissi’s assessment. "This study clearly documented continued improvement in CABG [coronary artery bypass grafting], particularly in the CABG-PCI [percutaneous coronary intervention] era of the last decade. These are clearly more technically difficult operations, with increased rates of prior PCI, left main disease, and distal anastomoses," said Dr. Ferguson, professor of surgery and chairman of cardiovascular sciences at East Carolina University in Greenville, N.C.
Dr. ElBardissi’s analysis used data that were collected on more than 1.4 million patients who underwent first-time, isolated CABG surgery at a hospital participating in the Society of Thoracic Surgeons’ adult cardiac surgery database. The data he presented compared 136,513 patients who underwent CABG in 2000 vs. 160,905 patients who had this surgery in 2009.
Major shifts during those years included a statistically significant drop in the prevalence of recent smoking (from 60% in 2000 to 30% in 2009), but significant increases in the prevalence of patients with hypercholesterolemia (84% in 2009 vs. 60% in 2000), hypertension (85% vs. 71%), and chronic obstructive pulmonary disease (23% vs. 16%). The percentage of patients who were previously treated by PCI also jumped to 26% in 2009, compared with 19% in 2000.
Significant rises in the rate of preoperative treatment with cardioprotective drugs were also seen, notably in the use of aspirin, beta-blockers, ACE inhibitors, and statins. Beta-blocker use jumped from 61% of patients in 2000 to 81% in 2009.
The prevalence of left main coronary artery stenosis rose from 23% of patients in 2000 to 32% in 2009.
The statistics also documented meaningful changes in how CABG occurred. Use of an internal mammary artery graft rose from 84% of cases in 2000 to 95% in 2009, and off-pump surgery increased from 14% of cases to 21%.
Elective procedures dropped from 58% in 2000 to 41% in 2009. The largest subgroup of patients shifted to urgent cases, which rose from 38% of patients in 2000 to 54% in 2009.
Mortality during 30-day follow-up fell significantly, from 2.4% in 2000 to 1.9% in 2009 – a 24% relative rate reduction after adjustment for differences in patient risk. Among elective and urgent cases, 30-day mortality fell from 2.1% in 2000 to 1.6% in 2009.
The rate of 30-day stoke in all patients dropped from 1.6% in 2000 to 1.2% in 2009, a statistically significant decline. The risk-adjusted analysis showed this as a 26% relative fall in stroke rates. In elective and urgent cases, the rate declined from 1.6% to 1.1%.
The 30-day outcome results also showed significant declines in deep sternal wound rates (from 0.55% in 2000 to 0.37% in 2009), and in the need for reoperations because of bleeding (2.5% vs. 2.2%). The statistics showed no significant changes in the rates of postoperative renal failure or new-onset atrial fibrillation.
Dr. ElBardissi and Dr. Ferguson said they had no disclosures.
FROM THE ANNUAL MEETING OF THE AMERICAN ASSOCIATION FOR THORACIC SURGERY
Major Finding: In 2009, U.S. patients who underwent first-time, isolated CABG surgery had a 1.9% perioperative mortality rate and a 1.2% stroke rate, significant declines compared with the 2.4% mortality rate and 1.6% stroke rate during 2000.
Data Source: Review of records for 1.4 million U.S. patients in the Society of Thoracic Surgeons’ national adult cardiac surgery database.
Disclosures: Dr. ElBardissi and Dr. Ferguson said they had no disclosures.
CABG Track Record Improved in Past Decade
PHILADELPHIA – U.S. cardiac surgeons increasingly performed coronary artery bypass surgery on more complex patients during 2000-2009, yet significant drops in the rates of perioperative deaths and strokes were seen during those years, according to a review of more than 1.4 million procedures.
"The major implication of this study is that we are operating on a more complex cohort of patients, and we’re doing a better job, with less death and stroke than [was the case] not too long ago. This has implications for how we stratify patients for revascularization therapy," said Dr. Andrew W. ElBardissi at the annual meeting of the American Association for Thoracic Surgery.
"A lot of the patterns that we are seeing reflect the results from some of the more rigorous prospective studies that have dictated practice. We have seen improvements in process and surgical decision making, including more optimal medical management when patients go to surgery – not just in the operating room, but throughout the perioperative period (preop, op, and the ICU). Not only have outcomes improved, but we seem to be operating on the correct cohort of patients," said Dr. ElBardissi, a cardiac surgeon at Brigham and Women’s Hospital in Boston.
"These outcomes appear to reflect improvements in perioperative surgical care as they continue to be significant after adjustment for patient risk," he added.
Dr. T. Bruce Ferguson Jr. concurred with Dr. ElBardissi’s assessment. "This study clearly documented continued improvement in CABG [coronary artery bypass grafting], particularly in the CABG-PCI [percutaneous coronary intervention] era of the last decade. These are clearly more technically difficult operations, with increased rates of prior PCI, left main disease, and distal anastomoses," said Dr. Ferguson, professor of surgery and chairman of cardiovascular sciences at East Carolina University in Greenville, N.C.
Dr. ElBardissi’s analysis used data that were collected on more than 1.4 million patients who underwent first-time, isolated CABG surgery at a hospital participating in the Society of Thoracic Surgeons’ adult cardiac surgery database. The data he presented compared 136,513 patients who underwent CABG in 2000 vs. 160,905 patients who had this surgery in 2009.
Major shifts during those years included a statistically significant drop in the prevalence of recent smoking (from 60% in 2000 to 30% in 2009), but significant increases in the prevalence of patients with hypercholesterolemia (84% in 2009 vs. 60% in 2000), hypertension (85% vs. 71%), and chronic obstructive pulmonary disease (23% vs. 16%). The percentage of patients who were previously treated by PCI also jumped to 26% in 2009, compared with 19% in 2000.
Significant rises in the rate of preoperative treatment with cardioprotective drugs were also seen, notably in the use of aspirin, beta-blockers, ACE inhibitors, and statins. Beta-blocker use jumped from 61% of patients in 2000 to 81% in 2009.
The prevalence of left main coronary artery stenosis rose from 23% of patients in 2000 to 32% in 2009.
The statistics also documented meaningful changes in how CABG occurred. Use of an internal mammary artery graft rose from 84% of cases in 2000 to 95% in 2009, and off-pump surgery increased from 14% of cases to 21%.
Elective procedures dropped from 58% in 2000 to 41% in 2009. The largest subgroup of patients shifted to urgent cases, which rose from 38% of patients in 2000 to 54% in 2009.
Mortality during 30-day follow-up fell significantly, from 2.4% in 2000 to 1.9% in 2009 – a 24% relative rate reduction after adjustment for differences in patient risk. Among elective and urgent cases, 30-day mortality fell from 2.1% in 2000 to 1.6% in 2009.
The rate of 30-day stoke in all patients dropped from 1.6% in 2000 to 1.2% in 2009, a statistically significant decline. The risk-adjusted analysis showed this as a 26% relative fall in stroke rates. In elective and urgent cases, the rate declined from 1.6% to 1.1%.
The 30-day outcome results also showed significant declines in deep sternal wound rates (from 0.55% in 2000 to 0.37% in 2009), and in the need for reoperations because of bleeding (2.5% vs. 2.2%). The statistics showed no significant changes in the rates of postoperative renal failure or new-onset atrial fibrillation.
Dr. ElBardissi and Dr. Ferguson said they had no disclosures.
PHILADELPHIA – U.S. cardiac surgeons increasingly performed coronary artery bypass surgery on more complex patients during 2000-2009, yet significant drops in the rates of perioperative deaths and strokes were seen during those years, according to a review of more than 1.4 million procedures.
"The major implication of this study is that we are operating on a more complex cohort of patients, and we’re doing a better job, with less death and stroke than [was the case] not too long ago. This has implications for how we stratify patients for revascularization therapy," said Dr. Andrew W. ElBardissi at the annual meeting of the American Association for Thoracic Surgery.
"A lot of the patterns that we are seeing reflect the results from some of the more rigorous prospective studies that have dictated practice. We have seen improvements in process and surgical decision making, including more optimal medical management when patients go to surgery – not just in the operating room, but throughout the perioperative period (preop, op, and the ICU). Not only have outcomes improved, but we seem to be operating on the correct cohort of patients," said Dr. ElBardissi, a cardiac surgeon at Brigham and Women’s Hospital in Boston.
"These outcomes appear to reflect improvements in perioperative surgical care as they continue to be significant after adjustment for patient risk," he added.
Dr. T. Bruce Ferguson Jr. concurred with Dr. ElBardissi’s assessment. "This study clearly documented continued improvement in CABG [coronary artery bypass grafting], particularly in the CABG-PCI [percutaneous coronary intervention] era of the last decade. These are clearly more technically difficult operations, with increased rates of prior PCI, left main disease, and distal anastomoses," said Dr. Ferguson, professor of surgery and chairman of cardiovascular sciences at East Carolina University in Greenville, N.C.
Dr. ElBardissi’s analysis used data that were collected on more than 1.4 million patients who underwent first-time, isolated CABG surgery at a hospital participating in the Society of Thoracic Surgeons’ adult cardiac surgery database. The data he presented compared 136,513 patients who underwent CABG in 2000 vs. 160,905 patients who had this surgery in 2009.
Major shifts during those years included a statistically significant drop in the prevalence of recent smoking (from 60% in 2000 to 30% in 2009), but significant increases in the prevalence of patients with hypercholesterolemia (84% in 2009 vs. 60% in 2000), hypertension (85% vs. 71%), and chronic obstructive pulmonary disease (23% vs. 16%). The percentage of patients who were previously treated by PCI also jumped to 26% in 2009, compared with 19% in 2000.
Significant rises in the rate of preoperative treatment with cardioprotective drugs were also seen, notably in the use of aspirin, beta-blockers, ACE inhibitors, and statins. Beta-blocker use jumped from 61% of patients in 2000 to 81% in 2009.
The prevalence of left main coronary artery stenosis rose from 23% of patients in 2000 to 32% in 2009.
The statistics also documented meaningful changes in how CABG occurred. Use of an internal mammary artery graft rose from 84% of cases in 2000 to 95% in 2009, and off-pump surgery increased from 14% of cases to 21%.
Elective procedures dropped from 58% in 2000 to 41% in 2009. The largest subgroup of patients shifted to urgent cases, which rose from 38% of patients in 2000 to 54% in 2009.
Mortality during 30-day follow-up fell significantly, from 2.4% in 2000 to 1.9% in 2009 – a 24% relative rate reduction after adjustment for differences in patient risk. Among elective and urgent cases, 30-day mortality fell from 2.1% in 2000 to 1.6% in 2009.
The rate of 30-day stoke in all patients dropped from 1.6% in 2000 to 1.2% in 2009, a statistically significant decline. The risk-adjusted analysis showed this as a 26% relative fall in stroke rates. In elective and urgent cases, the rate declined from 1.6% to 1.1%.
The 30-day outcome results also showed significant declines in deep sternal wound rates (from 0.55% in 2000 to 0.37% in 2009), and in the need for reoperations because of bleeding (2.5% vs. 2.2%). The statistics showed no significant changes in the rates of postoperative renal failure or new-onset atrial fibrillation.
Dr. ElBardissi and Dr. Ferguson said they had no disclosures.
PHILADELPHIA – U.S. cardiac surgeons increasingly performed coronary artery bypass surgery on more complex patients during 2000-2009, yet significant drops in the rates of perioperative deaths and strokes were seen during those years, according to a review of more than 1.4 million procedures.
"The major implication of this study is that we are operating on a more complex cohort of patients, and we’re doing a better job, with less death and stroke than [was the case] not too long ago. This has implications for how we stratify patients for revascularization therapy," said Dr. Andrew W. ElBardissi at the annual meeting of the American Association for Thoracic Surgery.
"A lot of the patterns that we are seeing reflect the results from some of the more rigorous prospective studies that have dictated practice. We have seen improvements in process and surgical decision making, including more optimal medical management when patients go to surgery – not just in the operating room, but throughout the perioperative period (preop, op, and the ICU). Not only have outcomes improved, but we seem to be operating on the correct cohort of patients," said Dr. ElBardissi, a cardiac surgeon at Brigham and Women’s Hospital in Boston.
"These outcomes appear to reflect improvements in perioperative surgical care as they continue to be significant after adjustment for patient risk," he added.
Dr. T. Bruce Ferguson Jr. concurred with Dr. ElBardissi’s assessment. "This study clearly documented continued improvement in CABG [coronary artery bypass grafting], particularly in the CABG-PCI [percutaneous coronary intervention] era of the last decade. These are clearly more technically difficult operations, with increased rates of prior PCI, left main disease, and distal anastomoses," said Dr. Ferguson, professor of surgery and chairman of cardiovascular sciences at East Carolina University in Greenville, N.C.
Dr. ElBardissi’s analysis used data that were collected on more than 1.4 million patients who underwent first-time, isolated CABG surgery at a hospital participating in the Society of Thoracic Surgeons’ adult cardiac surgery database. The data he presented compared 136,513 patients who underwent CABG in 2000 vs. 160,905 patients who had this surgery in 2009.
Major shifts during those years included a statistically significant drop in the prevalence of recent smoking (from 60% in 2000 to 30% in 2009), but significant increases in the prevalence of patients with hypercholesterolemia (84% in 2009 vs. 60% in 2000), hypertension (85% vs. 71%), and chronic obstructive pulmonary disease (23% vs. 16%). The percentage of patients who were previously treated by PCI also jumped to 26% in 2009, compared with 19% in 2000.
Significant rises in the rate of preoperative treatment with cardioprotective drugs were also seen, notably in the use of aspirin, beta-blockers, ACE inhibitors, and statins. Beta-blocker use jumped from 61% of patients in 2000 to 81% in 2009.
The prevalence of left main coronary artery stenosis rose from 23% of patients in 2000 to 32% in 2009.
The statistics also documented meaningful changes in how CABG occurred. Use of an internal mammary artery graft rose from 84% of cases in 2000 to 95% in 2009, and off-pump surgery increased from 14% of cases to 21%.
Elective procedures dropped from 58% in 2000 to 41% in 2009. The largest subgroup of patients shifted to urgent cases, which rose from 38% of patients in 2000 to 54% in 2009.
Mortality during 30-day follow-up fell significantly, from 2.4% in 2000 to 1.9% in 2009 – a 24% relative rate reduction after adjustment for differences in patient risk. Among elective and urgent cases, 30-day mortality fell from 2.1% in 2000 to 1.6% in 2009.
The rate of 30-day stoke in all patients dropped from 1.6% in 2000 to 1.2% in 2009, a statistically significant decline. The risk-adjusted analysis showed this as a 26% relative fall in stroke rates. In elective and urgent cases, the rate declined from 1.6% to 1.1%.
The 30-day outcome results also showed significant declines in deep sternal wound rates (from 0.55% in 2000 to 0.37% in 2009), and in the need for reoperations because of bleeding (2.5% vs. 2.2%). The statistics showed no significant changes in the rates of postoperative renal failure or new-onset atrial fibrillation.
Dr. ElBardissi and Dr. Ferguson said they had no disclosures.
FROM THE ANNUAL MEETING OF THE AMERICAN ASSOCIATION FOR THORACIC SURGERY
Major Finding: In 2009, U.S. patients who underwent first-time, isolated CABG surgery had a 1.9% perioperative mortality rate and a 1.2% stroke rate, significant declines compared with the 2.4% mortality rate and 1.6% stroke rate during 2000.
Data Source: Review of records for 1.4 million U.S. patients in the Society of Thoracic Surgeons’ national adult cardiac surgery database.
Disclosures: Dr. ElBardissi and Dr. Ferguson said they had no disclosures.
Blood Transfusions Linked to Increased Deaths in CABG Patients
PHILADELPHIA – Blood transfusions can kill surgery patients, a finding that puts the onus on surgeons to administer transfusions only when absolutely necessary, according to Dr. Gaetano Paone.
An analysis of more than 31,000 patients who underwent isolated coronary artery bypass grafting (CABG) surgery in Michigan during January 2006–June 2010 showed that receiving one or more blood transfusions conferred a nearly threefold increased risk of operative mortality, compared with not receiving a transfusion, Dr. Paone reported at the annual meeting of the American Association for Thoracic Surgery.*
The propensity analysis, which controlled for 17 significant clinical and demographic variables, confirms that "patients who get transfusions don’t do as well as those who don’t. I can’t say unequivocably that it’s the blood transfusions that cause these worse outcomes, but this is a reason to – whenever possible – avoid giving blood transfusions," Dr. Paone said in an interview.
"There is great variability in the rates of transfusions across institutions," noted Dr. Paone, a cardiac surgeon at Henry Ford Hospital in Detroit. In some places, the transfusion rates of isolated CABG patients are 15%, and other places have rates of more than 90%. "That suggests it’s quite discretionary."
Surgeons "have different opinions on the necessary blood level, and the appropriate hematocrit level. It’s hard to see an almost fivefold range of differences in transfusion rates and not have that somehow based on individual preferences rather than on science," he added.
Dr. Paone suggested that surgeons who believe that it is often necessary to give transfusions should strive to make it less necessary. "It’s not just on the basis of this study," he noted. "This study looked at the situation from a somewhat different perspective, but it reached the same conclusion as many others."
Dr. Paone and his associates examined data on 31,818 patients who underwent isolated CABG during the study period at any one of the 33 Michigan hospitals that perform cardiac surgery. The data came from records maintained by the Michigan Society of Thoracic and Cardiovascular Surgeons Quality Collaborative.
The researchers calculated the mortality risk faced by each patient using the STS-PROM (Society of Thoracic Surgeons Predicted Risk of Mortality) model, which takes into account 30 preoperative patient variables. They stratified the patients into four risk groups based on their scores, which represent the percent risk for 30-day perioperative mortality (less than 2%, 2%-5%, 6%-10%, and more than 10%). The percentage of study patients in each ascending risk stratum were 69%, 21%, 7%, and 3%, respectively. The analysis also divided patients into the 55% who received transfusions and the 45% who did not receive any blood. Overall operative mortality among the patients studied was 2%.
As expected, operative mortality was higher among patients who received a transfusion (3.3%), compared with those who did not get blood (0.6%) – a statistically significant sixfold difference in death rates.
The analysis also showed that the significant link between increased mortality and transfusion remained fairly constant across all four risk strata in the study, ranging from a twofold increased risk among patients with an STS-PROM score of 2%-5%, to a fourfold increased risk among patients with a score of more than 10%. The researchers found no statistically significant differences in the increased rate of death among the transfusion recipients across the four preoperative risk strata, Dr. Paone said.
In a further analysis aimed at teasing apart the mortality risk from transfusion and the patients’ background mortality risk based on their disease severity, the researchers performed a propensity score analysis that controlled for 17 significant preoperative risk determinants, including age, sex, weight, race, hypertension, smoking status, need for dialysis, and chronic obstructive pulmonary disease. This analysis showed that patients who received a transfusion had a 2.88-fold increased risk for operative death, compared with patients who did not receive a transfusion, Dr. Paone said.
Dr. Paone said that he had no disclosures.
* Correction, 5/26/2011: An earlier version of this story incorrectly identified the name of the American Association for Thoracic Surgery.
PHILADELPHIA – Blood transfusions can kill surgery patients, a finding that puts the onus on surgeons to administer transfusions only when absolutely necessary, according to Dr. Gaetano Paone.
An analysis of more than 31,000 patients who underwent isolated coronary artery bypass grafting (CABG) surgery in Michigan during January 2006–June 2010 showed that receiving one or more blood transfusions conferred a nearly threefold increased risk of operative mortality, compared with not receiving a transfusion, Dr. Paone reported at the annual meeting of the American Association for Thoracic Surgery.*
The propensity analysis, which controlled for 17 significant clinical and demographic variables, confirms that "patients who get transfusions don’t do as well as those who don’t. I can’t say unequivocably that it’s the blood transfusions that cause these worse outcomes, but this is a reason to – whenever possible – avoid giving blood transfusions," Dr. Paone said in an interview.
"There is great variability in the rates of transfusions across institutions," noted Dr. Paone, a cardiac surgeon at Henry Ford Hospital in Detroit. In some places, the transfusion rates of isolated CABG patients are 15%, and other places have rates of more than 90%. "That suggests it’s quite discretionary."
Surgeons "have different opinions on the necessary blood level, and the appropriate hematocrit level. It’s hard to see an almost fivefold range of differences in transfusion rates and not have that somehow based on individual preferences rather than on science," he added.
Dr. Paone suggested that surgeons who believe that it is often necessary to give transfusions should strive to make it less necessary. "It’s not just on the basis of this study," he noted. "This study looked at the situation from a somewhat different perspective, but it reached the same conclusion as many others."
Dr. Paone and his associates examined data on 31,818 patients who underwent isolated CABG during the study period at any one of the 33 Michigan hospitals that perform cardiac surgery. The data came from records maintained by the Michigan Society of Thoracic and Cardiovascular Surgeons Quality Collaborative.
The researchers calculated the mortality risk faced by each patient using the STS-PROM (Society of Thoracic Surgeons Predicted Risk of Mortality) model, which takes into account 30 preoperative patient variables. They stratified the patients into four risk groups based on their scores, which represent the percent risk for 30-day perioperative mortality (less than 2%, 2%-5%, 6%-10%, and more than 10%). The percentage of study patients in each ascending risk stratum were 69%, 21%, 7%, and 3%, respectively. The analysis also divided patients into the 55% who received transfusions and the 45% who did not receive any blood. Overall operative mortality among the patients studied was 2%.
As expected, operative mortality was higher among patients who received a transfusion (3.3%), compared with those who did not get blood (0.6%) – a statistically significant sixfold difference in death rates.
The analysis also showed that the significant link between increased mortality and transfusion remained fairly constant across all four risk strata in the study, ranging from a twofold increased risk among patients with an STS-PROM score of 2%-5%, to a fourfold increased risk among patients with a score of more than 10%. The researchers found no statistically significant differences in the increased rate of death among the transfusion recipients across the four preoperative risk strata, Dr. Paone said.
In a further analysis aimed at teasing apart the mortality risk from transfusion and the patients’ background mortality risk based on their disease severity, the researchers performed a propensity score analysis that controlled for 17 significant preoperative risk determinants, including age, sex, weight, race, hypertension, smoking status, need for dialysis, and chronic obstructive pulmonary disease. This analysis showed that patients who received a transfusion had a 2.88-fold increased risk for operative death, compared with patients who did not receive a transfusion, Dr. Paone said.
Dr. Paone said that he had no disclosures.
* Correction, 5/26/2011: An earlier version of this story incorrectly identified the name of the American Association for Thoracic Surgery.
PHILADELPHIA – Blood transfusions can kill surgery patients, a finding that puts the onus on surgeons to administer transfusions only when absolutely necessary, according to Dr. Gaetano Paone.
An analysis of more than 31,000 patients who underwent isolated coronary artery bypass grafting (CABG) surgery in Michigan during January 2006–June 2010 showed that receiving one or more blood transfusions conferred a nearly threefold increased risk of operative mortality, compared with not receiving a transfusion, Dr. Paone reported at the annual meeting of the American Association for Thoracic Surgery.*
The propensity analysis, which controlled for 17 significant clinical and demographic variables, confirms that "patients who get transfusions don’t do as well as those who don’t. I can’t say unequivocably that it’s the blood transfusions that cause these worse outcomes, but this is a reason to – whenever possible – avoid giving blood transfusions," Dr. Paone said in an interview.
"There is great variability in the rates of transfusions across institutions," noted Dr. Paone, a cardiac surgeon at Henry Ford Hospital in Detroit. In some places, the transfusion rates of isolated CABG patients are 15%, and other places have rates of more than 90%. "That suggests it’s quite discretionary."
Surgeons "have different opinions on the necessary blood level, and the appropriate hematocrit level. It’s hard to see an almost fivefold range of differences in transfusion rates and not have that somehow based on individual preferences rather than on science," he added.
Dr. Paone suggested that surgeons who believe that it is often necessary to give transfusions should strive to make it less necessary. "It’s not just on the basis of this study," he noted. "This study looked at the situation from a somewhat different perspective, but it reached the same conclusion as many others."
Dr. Paone and his associates examined data on 31,818 patients who underwent isolated CABG during the study period at any one of the 33 Michigan hospitals that perform cardiac surgery. The data came from records maintained by the Michigan Society of Thoracic and Cardiovascular Surgeons Quality Collaborative.
The researchers calculated the mortality risk faced by each patient using the STS-PROM (Society of Thoracic Surgeons Predicted Risk of Mortality) model, which takes into account 30 preoperative patient variables. They stratified the patients into four risk groups based on their scores, which represent the percent risk for 30-day perioperative mortality (less than 2%, 2%-5%, 6%-10%, and more than 10%). The percentage of study patients in each ascending risk stratum were 69%, 21%, 7%, and 3%, respectively. The analysis also divided patients into the 55% who received transfusions and the 45% who did not receive any blood. Overall operative mortality among the patients studied was 2%.
As expected, operative mortality was higher among patients who received a transfusion (3.3%), compared with those who did not get blood (0.6%) – a statistically significant sixfold difference in death rates.
The analysis also showed that the significant link between increased mortality and transfusion remained fairly constant across all four risk strata in the study, ranging from a twofold increased risk among patients with an STS-PROM score of 2%-5%, to a fourfold increased risk among patients with a score of more than 10%. The researchers found no statistically significant differences in the increased rate of death among the transfusion recipients across the four preoperative risk strata, Dr. Paone said.
In a further analysis aimed at teasing apart the mortality risk from transfusion and the patients’ background mortality risk based on their disease severity, the researchers performed a propensity score analysis that controlled for 17 significant preoperative risk determinants, including age, sex, weight, race, hypertension, smoking status, need for dialysis, and chronic obstructive pulmonary disease. This analysis showed that patients who received a transfusion had a 2.88-fold increased risk for operative death, compared with patients who did not receive a transfusion, Dr. Paone said.
Dr. Paone said that he had no disclosures.
* Correction, 5/26/2011: An earlier version of this story incorrectly identified the name of the American Association for Thoracic Surgery.
FROM THE ANNUAL MEETING OF THE AMERICAN ASSOCIATION FOR THORACIC SURGERY
Major Finding: Patients undergoing isolated CABG surgery had a 2.88-fold increased risk of operative mortality, compared with patients who did not receive a transfusion, in a propensity score analysis that controlled for 17 demographic and clinical variables.
Data Source: Review of data on 31,818 patients who underwent CABG surgery at any of 33 Michigan hospitals during January 2006–June 2010.
Disclosures: Dr. Paone said he had no disclosures.