User login
The Journal of Clinical Outcomes Management® is an independent, peer-reviewed journal offering evidence-based, practical information for improving the quality, safety, and value of health care.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Pandemic strains blood supply for COVID-19 and noninfected patients
The COVID-19 pandemic is putting a strain on the blood supply and could be putting people – including those who normally get transfusions, such as patients with sickle cell disease and cancer – at risk.
“Around the beginning of March, the hematology community got wind of what was going on because the blood banks were saying think about your patients and begin to restrict blood usage because we are expecting an increase in usage for COVID-positive ICU patients,” Ifeyinwa (Ify) Osunkwo, MD, a specialist in hematology and sickle cell disease at Levine Cancer Institute in Charlotte, N.C., said in an interview.
“I think that was the first call to arms around hematology ... you don’t want to shortchange somebody who is well and who is being sustained by life-giving transfusions and cut out their transfusion therapy because you are hoping to use the blood for people who are coming in with COVID-19,” she continued. “That is an ethical dilemma that no doctor wants to have to go through. But the reality is we have to do something to make it work for everybody.”
And the timing of the social restrictions due to the pandemic has added additional strain on the blood supply.
“Over the winter, traditionally, blood drives slow down because of the flu and different viruses,” she noted. “The spring and the summer are when we see the biggest recruitment and uptake of blood donation. COVID-19 hit [and] a lot of the blood drives that were traditionally scheduled to supply blood for the country have been canceled because of the new guidance for social distancing.”
Another big source of blood are health care professionals themselves and they may not be able to donate because of the extra hours being worked because of the pandemic.
In speaking about the needs for traditional patients such as those who are dealing with cancer or leukemia or sickle cell diseases as well as those who are being treated for COVID-19 in North Carolina, “we are not at the critical point, but I am a little bit nervous that we may get there because they are not going to up the usual blood drives anytime this summer. We project [sometime] in the fall, but maybe not even then. So there needs to be a significant call-out for people to make every effort to donate blood,” said Dr. Osunkwo. She added that in places such as New York City that are hot spots for the COVID-19 outbreak, the need is likely a lot greater.
She recalled a recent incident at a New York hospital that highlighted how those managing blood supplies are being restrictive and how this could be harming patients.
“A sickle cell patient came in with COVID-19 and the treatment recommendation was do a red blood cell exchange but the blood bank was nervous about getting enough blood to supply for that exchange transfusion,” she said, noting that the doctor still went to bat for that patient to get the needed treatment. “We gave her the supporting evidence that when you are on treatment for sickle cell disease, you tend to do better if you get COVID-19 or any other viral infection. The symptoms of COVID-19 in sickle cell disease is acute chest syndrome, for which the treatment is red blood cell exchange. Not doing that for [these patients] is really not giving them the optimal way of managing their disease, and managing their disease in the setting of COVID-19.”
To that end, Dr. Osunkwo stressed that doctors need to be doing all they can to get the word out that blood is needed and that the American Red Cross and other donation organizations are making it safe for people to donate. She has been using social media to highlight when her fellow doctors and others make donations as a way to motivate individuals.
“Everybody can do something during this pandemic,” she said. “Don’t feel like you are not working, that you are not a frontline worker, that you have nothing to contribute. You can donate blood. Your cousin can donate blood. You can tell your friends, your neighbors, your relatives, your enemies to go donate. We will take every kind of blood we can get because people are needing it more now. Even though we canceled elective surgeries, my patients when they get COVID-19, they need more blood ... than they usually do during their regular sickle cell admission. It is going to be the same for people who have other blood disorders like cancer and leukemia. We can’t stop life-saving treatments just because we have the COVID pandemic.”
Dr. Osunkwo also praised recent actions taken by the Food and Drug Administration to lessen some of the deferral periods for when an individual can donate.
The FDA on April 2 issued three sets of revised recommendations aimed at getting more people eligible to donate blood. All of the revised recommendations will remain in effect after the COVID-19 health emergency is declared over.
The first revised recommendation makes changes to December 2015 guidance.
For male blood donors who would have been deferred for having sex with another male partner, the deferral period has been reduced from 12 months to 3 months. That deferral period change also applies to female donors who had sex with a man who had sex with another man as well as for those with recent tattoos and piercings.
The second recommendation revises guidance from August 2013 and relates to the risk of transfusion-transmitted malaria.
Under the new recommendations, for those who traveled to malaria-endemic areas (and are residents of malaria non-endemic countries), the FDA is lowering the recommended deferral period from 12 months to 3 months, and also provides notices of an alternate procedure that permits donations without a deferral period provided the blood components are pathogen-reduced using an FDA-approved pathogen reduction device.
The third recommendation finalizes draft guidance from January that eliminates the referral period for donors who spent time in certain European countries or were on military bases in Europe and were previously considered to have been exposed to a potential risk of transmission of Creutzfeldt-Jakob Disease or Variant Creutzfeldt-Jakob Disease.
Dr. Osunkwo reports consultancy and being on the speakers bureau and participating in the advisory board for Novartis, and relationships with a variety of other pharmaceutical companies. She is the editor-in-chief for Hematology News.
The COVID-19 pandemic is putting a strain on the blood supply and could be putting people – including those who normally get transfusions, such as patients with sickle cell disease and cancer – at risk.
“Around the beginning of March, the hematology community got wind of what was going on because the blood banks were saying think about your patients and begin to restrict blood usage because we are expecting an increase in usage for COVID-positive ICU patients,” Ifeyinwa (Ify) Osunkwo, MD, a specialist in hematology and sickle cell disease at Levine Cancer Institute in Charlotte, N.C., said in an interview.
“I think that was the first call to arms around hematology ... you don’t want to shortchange somebody who is well and who is being sustained by life-giving transfusions and cut out their transfusion therapy because you are hoping to use the blood for people who are coming in with COVID-19,” she continued. “That is an ethical dilemma that no doctor wants to have to go through. But the reality is we have to do something to make it work for everybody.”
And the timing of the social restrictions due to the pandemic has added additional strain on the blood supply.
“Over the winter, traditionally, blood drives slow down because of the flu and different viruses,” she noted. “The spring and the summer are when we see the biggest recruitment and uptake of blood donation. COVID-19 hit [and] a lot of the blood drives that were traditionally scheduled to supply blood for the country have been canceled because of the new guidance for social distancing.”
Another big source of blood are health care professionals themselves and they may not be able to donate because of the extra hours being worked because of the pandemic.
In speaking about the needs for traditional patients such as those who are dealing with cancer or leukemia or sickle cell diseases as well as those who are being treated for COVID-19 in North Carolina, “we are not at the critical point, but I am a little bit nervous that we may get there because they are not going to up the usual blood drives anytime this summer. We project [sometime] in the fall, but maybe not even then. So there needs to be a significant call-out for people to make every effort to donate blood,” said Dr. Osunkwo. She added that in places such as New York City that are hot spots for the COVID-19 outbreak, the need is likely a lot greater.
She recalled a recent incident at a New York hospital that highlighted how those managing blood supplies are being restrictive and how this could be harming patients.
“A sickle cell patient came in with COVID-19 and the treatment recommendation was do a red blood cell exchange but the blood bank was nervous about getting enough blood to supply for that exchange transfusion,” she said, noting that the doctor still went to bat for that patient to get the needed treatment. “We gave her the supporting evidence that when you are on treatment for sickle cell disease, you tend to do better if you get COVID-19 or any other viral infection. The symptoms of COVID-19 in sickle cell disease is acute chest syndrome, for which the treatment is red blood cell exchange. Not doing that for [these patients] is really not giving them the optimal way of managing their disease, and managing their disease in the setting of COVID-19.”
To that end, Dr. Osunkwo stressed that doctors need to be doing all they can to get the word out that blood is needed and that the American Red Cross and other donation organizations are making it safe for people to donate. She has been using social media to highlight when her fellow doctors and others make donations as a way to motivate individuals.
“Everybody can do something during this pandemic,” she said. “Don’t feel like you are not working, that you are not a frontline worker, that you have nothing to contribute. You can donate blood. Your cousin can donate blood. You can tell your friends, your neighbors, your relatives, your enemies to go donate. We will take every kind of blood we can get because people are needing it more now. Even though we canceled elective surgeries, my patients when they get COVID-19, they need more blood ... than they usually do during their regular sickle cell admission. It is going to be the same for people who have other blood disorders like cancer and leukemia. We can’t stop life-saving treatments just because we have the COVID pandemic.”
Dr. Osunkwo also praised recent actions taken by the Food and Drug Administration to lessen some of the deferral periods for when an individual can donate.
The FDA on April 2 issued three sets of revised recommendations aimed at getting more people eligible to donate blood. All of the revised recommendations will remain in effect after the COVID-19 health emergency is declared over.
The first revised recommendation makes changes to December 2015 guidance.
For male blood donors who would have been deferred for having sex with another male partner, the deferral period has been reduced from 12 months to 3 months. That deferral period change also applies to female donors who had sex with a man who had sex with another man as well as for those with recent tattoos and piercings.
The second recommendation revises guidance from August 2013 and relates to the risk of transfusion-transmitted malaria.
Under the new recommendations, for those who traveled to malaria-endemic areas (and are residents of malaria non-endemic countries), the FDA is lowering the recommended deferral period from 12 months to 3 months, and also provides notices of an alternate procedure that permits donations without a deferral period provided the blood components are pathogen-reduced using an FDA-approved pathogen reduction device.
The third recommendation finalizes draft guidance from January that eliminates the referral period for donors who spent time in certain European countries or were on military bases in Europe and were previously considered to have been exposed to a potential risk of transmission of Creutzfeldt-Jakob Disease or Variant Creutzfeldt-Jakob Disease.
Dr. Osunkwo reports consultancy and being on the speakers bureau and participating in the advisory board for Novartis, and relationships with a variety of other pharmaceutical companies. She is the editor-in-chief for Hematology News.
The COVID-19 pandemic is putting a strain on the blood supply and could be putting people – including those who normally get transfusions, such as patients with sickle cell disease and cancer – at risk.
“Around the beginning of March, the hematology community got wind of what was going on because the blood banks were saying think about your patients and begin to restrict blood usage because we are expecting an increase in usage for COVID-positive ICU patients,” Ifeyinwa (Ify) Osunkwo, MD, a specialist in hematology and sickle cell disease at Levine Cancer Institute in Charlotte, N.C., said in an interview.
“I think that was the first call to arms around hematology ... you don’t want to shortchange somebody who is well and who is being sustained by life-giving transfusions and cut out their transfusion therapy because you are hoping to use the blood for people who are coming in with COVID-19,” she continued. “That is an ethical dilemma that no doctor wants to have to go through. But the reality is we have to do something to make it work for everybody.”
And the timing of the social restrictions due to the pandemic has added additional strain on the blood supply.
“Over the winter, traditionally, blood drives slow down because of the flu and different viruses,” she noted. “The spring and the summer are when we see the biggest recruitment and uptake of blood donation. COVID-19 hit [and] a lot of the blood drives that were traditionally scheduled to supply blood for the country have been canceled because of the new guidance for social distancing.”
Another big source of blood are health care professionals themselves and they may not be able to donate because of the extra hours being worked because of the pandemic.
In speaking about the needs for traditional patients such as those who are dealing with cancer or leukemia or sickle cell diseases as well as those who are being treated for COVID-19 in North Carolina, “we are not at the critical point, but I am a little bit nervous that we may get there because they are not going to up the usual blood drives anytime this summer. We project [sometime] in the fall, but maybe not even then. So there needs to be a significant call-out for people to make every effort to donate blood,” said Dr. Osunkwo. She added that in places such as New York City that are hot spots for the COVID-19 outbreak, the need is likely a lot greater.
She recalled a recent incident at a New York hospital that highlighted how those managing blood supplies are being restrictive and how this could be harming patients.
“A sickle cell patient came in with COVID-19 and the treatment recommendation was do a red blood cell exchange but the blood bank was nervous about getting enough blood to supply for that exchange transfusion,” she said, noting that the doctor still went to bat for that patient to get the needed treatment. “We gave her the supporting evidence that when you are on treatment for sickle cell disease, you tend to do better if you get COVID-19 or any other viral infection. The symptoms of COVID-19 in sickle cell disease is acute chest syndrome, for which the treatment is red blood cell exchange. Not doing that for [these patients] is really not giving them the optimal way of managing their disease, and managing their disease in the setting of COVID-19.”
To that end, Dr. Osunkwo stressed that doctors need to be doing all they can to get the word out that blood is needed and that the American Red Cross and other donation organizations are making it safe for people to donate. She has been using social media to highlight when her fellow doctors and others make donations as a way to motivate individuals.
“Everybody can do something during this pandemic,” she said. “Don’t feel like you are not working, that you are not a frontline worker, that you have nothing to contribute. You can donate blood. Your cousin can donate blood. You can tell your friends, your neighbors, your relatives, your enemies to go donate. We will take every kind of blood we can get because people are needing it more now. Even though we canceled elective surgeries, my patients when they get COVID-19, they need more blood ... than they usually do during their regular sickle cell admission. It is going to be the same for people who have other blood disorders like cancer and leukemia. We can’t stop life-saving treatments just because we have the COVID pandemic.”
Dr. Osunkwo also praised recent actions taken by the Food and Drug Administration to lessen some of the deferral periods for when an individual can donate.
The FDA on April 2 issued three sets of revised recommendations aimed at getting more people eligible to donate blood. All of the revised recommendations will remain in effect after the COVID-19 health emergency is declared over.
The first revised recommendation makes changes to December 2015 guidance.
For male blood donors who would have been deferred for having sex with another male partner, the deferral period has been reduced from 12 months to 3 months. That deferral period change also applies to female donors who had sex with a man who had sex with another man as well as for those with recent tattoos and piercings.
The second recommendation revises guidance from August 2013 and relates to the risk of transfusion-transmitted malaria.
Under the new recommendations, for those who traveled to malaria-endemic areas (and are residents of malaria non-endemic countries), the FDA is lowering the recommended deferral period from 12 months to 3 months, and also provides notices of an alternate procedure that permits donations without a deferral period provided the blood components are pathogen-reduced using an FDA-approved pathogen reduction device.
The third recommendation finalizes draft guidance from January that eliminates the referral period for donors who spent time in certain European countries or were on military bases in Europe and were previously considered to have been exposed to a potential risk of transmission of Creutzfeldt-Jakob Disease or Variant Creutzfeldt-Jakob Disease.
Dr. Osunkwo reports consultancy and being on the speakers bureau and participating in the advisory board for Novartis, and relationships with a variety of other pharmaceutical companies. She is the editor-in-chief for Hematology News.
COVID-19 PPE-related skin effects described in survey of Chinese doctors, nurses
Almost 75% of doctors and nurses in and around Wuhan, China, where the outbreak first emerged, reported skin problems during a single week in early February 2020, in a survey of health care workers (HCW) caring for COVID-19 patients at five university and five regional hospitals. Hands, cheeks, and the nasal bridge were the most commonly affected areas, with skin dryness, maceration, papules, and erythema the most common problems, according to research published in the British Journal of Dermatology.
In New York City, masks in particular are “really an issue,” said Ellen Marmur, MD, a dermatologist in private practice and an associate clinical professor at the Mount Sinai School of Medicine, New York.
She’s dealing with patients who have abrasions and skin infections at the tip of the nose, bruising from the metal strap that goes across the bridge of the nose, and skin irritation from the straps. “Rosacea is [also] definitely flaring up, [and] people’s acne is definitely flaring up, not only because of the stress, but because of the sweat and humidity” that builds up under the masks, she said.
“It’s not a life-threatening thing, but it’s definitely something we’ve been helping people with,” she said. This includes her husband, a cardiologist pulling 12-hour shifts in a New York City hospital wearing an N95 mask; when he comes home, the tip of his nose is red and abraded.
Treatment entails first aid skin care: a dab of a gentle ointment like Aquaphor to prevent abrasions while the mask is on and to help them heal after it’s off, and bacitracin if infection is a worry. For acne and rosacea flares, a course of minocycline or topical clindamycin might help, Dr. Marmur said.
Although almost 75% of the doctors and nurses in the Chinese study reported skin problems, the response rate was low, just 376 of the 1,000 surveyed (37.6%). That might have tilted the results to providers who actually ran into problems, wrote the investigators, led by Ping Lin of the department of dermatology and venereology at Peking University First Hospital, Beijing.
Still, 280 (74.5%) reported adverse skin reactions from caring for COVID-19 patients. “Of note, this rate was much higher than the rate of occupational contact dermatitis (31.5%) in HCWs under normal working condition[s], and that of adverse skin reactions (21.4%-35.5%)” during the outbreak of another coronavirus in 2003, severe acute respiratory syndrome, they wrote.
Most providers in the study washed their hands more than 10 times a day, but only about 22% applied hand cream afterwards, they reported.
On multivariate analysis, working in hospitals harder hit by the pandemic (odds ratio, 2.41; P = .001), working on inpatient wards (OR, 2.44; P = .003), wearing full-body personal protective equipment over 6 hours (OR, 4.26; P < .001), and female sex (OR, 1.87; P = .038) increased the risk of adverse skin reactions. The team suggested moisturizers would help to protect against hand dermatitis, and alcohol-based products instead of soaps “as the former show high antimicrobial activity and low risks of skin damage.” Also, “restricting duration of wearing” of protection gear “to no more than 6 hours would help.”
The study investigators reported that they had no conflicts of interest.
SOURCE: Lin P et al. Br J Dermatol. 2020 Apr 7. doi: 10.1111/bjd.19089.
Almost 75% of doctors and nurses in and around Wuhan, China, where the outbreak first emerged, reported skin problems during a single week in early February 2020, in a survey of health care workers (HCW) caring for COVID-19 patients at five university and five regional hospitals. Hands, cheeks, and the nasal bridge were the most commonly affected areas, with skin dryness, maceration, papules, and erythema the most common problems, according to research published in the British Journal of Dermatology.
In New York City, masks in particular are “really an issue,” said Ellen Marmur, MD, a dermatologist in private practice and an associate clinical professor at the Mount Sinai School of Medicine, New York.
She’s dealing with patients who have abrasions and skin infections at the tip of the nose, bruising from the metal strap that goes across the bridge of the nose, and skin irritation from the straps. “Rosacea is [also] definitely flaring up, [and] people’s acne is definitely flaring up, not only because of the stress, but because of the sweat and humidity” that builds up under the masks, she said.
“It’s not a life-threatening thing, but it’s definitely something we’ve been helping people with,” she said. This includes her husband, a cardiologist pulling 12-hour shifts in a New York City hospital wearing an N95 mask; when he comes home, the tip of his nose is red and abraded.
Treatment entails first aid skin care: a dab of a gentle ointment like Aquaphor to prevent abrasions while the mask is on and to help them heal after it’s off, and bacitracin if infection is a worry. For acne and rosacea flares, a course of minocycline or topical clindamycin might help, Dr. Marmur said.
Although almost 75% of the doctors and nurses in the Chinese study reported skin problems, the response rate was low, just 376 of the 1,000 surveyed (37.6%). That might have tilted the results to providers who actually ran into problems, wrote the investigators, led by Ping Lin of the department of dermatology and venereology at Peking University First Hospital, Beijing.
Still, 280 (74.5%) reported adverse skin reactions from caring for COVID-19 patients. “Of note, this rate was much higher than the rate of occupational contact dermatitis (31.5%) in HCWs under normal working condition[s], and that of adverse skin reactions (21.4%-35.5%)” during the outbreak of another coronavirus in 2003, severe acute respiratory syndrome, they wrote.
Most providers in the study washed their hands more than 10 times a day, but only about 22% applied hand cream afterwards, they reported.
On multivariate analysis, working in hospitals harder hit by the pandemic (odds ratio, 2.41; P = .001), working on inpatient wards (OR, 2.44; P = .003), wearing full-body personal protective equipment over 6 hours (OR, 4.26; P < .001), and female sex (OR, 1.87; P = .038) increased the risk of adverse skin reactions. The team suggested moisturizers would help to protect against hand dermatitis, and alcohol-based products instead of soaps “as the former show high antimicrobial activity and low risks of skin damage.” Also, “restricting duration of wearing” of protection gear “to no more than 6 hours would help.”
The study investigators reported that they had no conflicts of interest.
SOURCE: Lin P et al. Br J Dermatol. 2020 Apr 7. doi: 10.1111/bjd.19089.
Almost 75% of doctors and nurses in and around Wuhan, China, where the outbreak first emerged, reported skin problems during a single week in early February 2020, in a survey of health care workers (HCW) caring for COVID-19 patients at five university and five regional hospitals. Hands, cheeks, and the nasal bridge were the most commonly affected areas, with skin dryness, maceration, papules, and erythema the most common problems, according to research published in the British Journal of Dermatology.
In New York City, masks in particular are “really an issue,” said Ellen Marmur, MD, a dermatologist in private practice and an associate clinical professor at the Mount Sinai School of Medicine, New York.
She’s dealing with patients who have abrasions and skin infections at the tip of the nose, bruising from the metal strap that goes across the bridge of the nose, and skin irritation from the straps. “Rosacea is [also] definitely flaring up, [and] people’s acne is definitely flaring up, not only because of the stress, but because of the sweat and humidity” that builds up under the masks, she said.
“It’s not a life-threatening thing, but it’s definitely something we’ve been helping people with,” she said. This includes her husband, a cardiologist pulling 12-hour shifts in a New York City hospital wearing an N95 mask; when he comes home, the tip of his nose is red and abraded.
Treatment entails first aid skin care: a dab of a gentle ointment like Aquaphor to prevent abrasions while the mask is on and to help them heal after it’s off, and bacitracin if infection is a worry. For acne and rosacea flares, a course of minocycline or topical clindamycin might help, Dr. Marmur said.
Although almost 75% of the doctors and nurses in the Chinese study reported skin problems, the response rate was low, just 376 of the 1,000 surveyed (37.6%). That might have tilted the results to providers who actually ran into problems, wrote the investigators, led by Ping Lin of the department of dermatology and venereology at Peking University First Hospital, Beijing.
Still, 280 (74.5%) reported adverse skin reactions from caring for COVID-19 patients. “Of note, this rate was much higher than the rate of occupational contact dermatitis (31.5%) in HCWs under normal working condition[s], and that of adverse skin reactions (21.4%-35.5%)” during the outbreak of another coronavirus in 2003, severe acute respiratory syndrome, they wrote.
Most providers in the study washed their hands more than 10 times a day, but only about 22% applied hand cream afterwards, they reported.
On multivariate analysis, working in hospitals harder hit by the pandemic (odds ratio, 2.41; P = .001), working on inpatient wards (OR, 2.44; P = .003), wearing full-body personal protective equipment over 6 hours (OR, 4.26; P < .001), and female sex (OR, 1.87; P = .038) increased the risk of adverse skin reactions. The team suggested moisturizers would help to protect against hand dermatitis, and alcohol-based products instead of soaps “as the former show high antimicrobial activity and low risks of skin damage.” Also, “restricting duration of wearing” of protection gear “to no more than 6 hours would help.”
The study investigators reported that they had no conflicts of interest.
SOURCE: Lin P et al. Br J Dermatol. 2020 Apr 7. doi: 10.1111/bjd.19089.
FROM THE BRITISH JOURNAL OF DERMATOLOGY
Bone density slow to rebound after lactation in women with HIV
Women with HIV had more bone mobilization during lactation, and attenuated skeletal recovery after lactation, compared with HIV-negative women, according to research presented during the Conference on Retroviruses & Opportunistic Infections, which was presented online this year. CROI organizers chose to hold a virtual meeting because of concerns about the spread of COVID-19.
The study “demonstrated that there were reductions as expected in BMD during breastfeeding, and there was recovery at the end of breastfeeding, which was higher among women who were not HIV-infected compared to HIV-infected women,” said Mary Glenn Fowler, MD, speaking in a video presentation during the virtual conference. The differences between women who had HIV and the HIV-negative reference group were statistically significant (P = .003 for lumbar spine and P less than .001 for whole-body aBMD).
“We also saw that for whole-body BMD, there was recovery at the end of breastfeeding for women who were not HIV infected, but a dampened response of recovery for BMD for HIV-infected women,” she went on, adding: “These findings held after adjustment for parity, age, body mass, breastfeeding practices, duration of breastfeeding, use of [injectable medroxyprogesterone acetate], and resumption of menses.”
Dr. Fowler presented the study’s results on behalf of lead author Florence Nabwire, PhD, an investigator scientist in the nutrition and bone health group of the United Kingdom’s Medical Research Council (Cambridge).
Although it’s known that antiretroviral therapy (ART) is associated with bone loss, Dr. Fowler explained that there are only limited data in HIV-positive women who are lactating. It’s important to see what happens during lactation for this group of women because of the potential sequelae later in life of insufficient recovery from the physiological bone mobilization that occurs during lactation. The study looked at changes in areal bone mineral density (aBMD) both during and after lactation for women with HIV living in Uganda who were taking Option B+ ART, a regimen that includes tenofovir, 3TC, and efavirenz. These women were compared with a reference group of HIV-negative women.
In all, 95 women with HIV and 96 HIV negative women were recruited into the study during pregnancy. Participants were followed postpartum at weeks 2, 14, and 26, and at a final visit that occurred 14 weeks after lactation stopped.
In addition to lumbar spine, total hip, and femoral neck aBMD measurements, the investigators also obtained whole body-less-head reading.
For total hip and femoral neck aBMD, the nadir of density was seen at 26 postpartum, when a drop of about 6% was seen from baseline readings. By the final post-lactation visit, women without HIV had recovered to their baseline; for women with HIV, some recovery also occurred, but the effect was dampened, with a persistent bone density deficit of about 3% from baseline. The differences between HIV-positive and HIV-negative women in these measurements were also statistically significant, at P less than .001 for total hip aBMD differences and P = .0008 for femoral neck differences. Again, correction for multiple confounders didn’t attenuate the results, said Dr. Fowler.
“In conclusion, these data showed accentuated mobilization of hip and whole body aBMD during lactation,” said Dr. Fowler, who also noted “slower skeletal recovery post lactation for HIV-infected women.” Clinical implications of these findings aren’t currently known, she said. Further ongoing studies are aiming to tease out both mechanisms and longer-term consequences for the bone health of HIV-infected women and their children, who may also see differences in bone mineral accretion and growth.
Session moderator Risa Hoffman, MD, in introductory remarks, set the findings in some context. “As we know, HIV-positive adults have low bone mineral density, and this appears to be a result of interactions of HIV, traditional risk factors for loss of bone density, and antiretroviral therapy,” said Dr. Hoffman, director of the global health program at the University of California, Los Angeles. She added that previous work had shown that “middle-aged HIV-positive women have higher 10-year fracture incidence compared to their HIV-negative counterparts.” The current study, she said, “has both short- and long-term implications for women as they go through multiple pregnancies and multiple periods of breastfeeding.”
The study was funded by the United Kingdom’s Medical Research Council and Department for International Development as well as the Alborada Trust and the Gates Cambridge Scholarship. The authors reported no conflicts of interest.
SOURCE: Nabwire F et al. CROI 2020, Abstract 768.
Women with HIV had more bone mobilization during lactation, and attenuated skeletal recovery after lactation, compared with HIV-negative women, according to research presented during the Conference on Retroviruses & Opportunistic Infections, which was presented online this year. CROI organizers chose to hold a virtual meeting because of concerns about the spread of COVID-19.
The study “demonstrated that there were reductions as expected in BMD during breastfeeding, and there was recovery at the end of breastfeeding, which was higher among women who were not HIV-infected compared to HIV-infected women,” said Mary Glenn Fowler, MD, speaking in a video presentation during the virtual conference. The differences between women who had HIV and the HIV-negative reference group were statistically significant (P = .003 for lumbar spine and P less than .001 for whole-body aBMD).
“We also saw that for whole-body BMD, there was recovery at the end of breastfeeding for women who were not HIV infected, but a dampened response of recovery for BMD for HIV-infected women,” she went on, adding: “These findings held after adjustment for parity, age, body mass, breastfeeding practices, duration of breastfeeding, use of [injectable medroxyprogesterone acetate], and resumption of menses.”
Dr. Fowler presented the study’s results on behalf of lead author Florence Nabwire, PhD, an investigator scientist in the nutrition and bone health group of the United Kingdom’s Medical Research Council (Cambridge).
Although it’s known that antiretroviral therapy (ART) is associated with bone loss, Dr. Fowler explained that there are only limited data in HIV-positive women who are lactating. It’s important to see what happens during lactation for this group of women because of the potential sequelae later in life of insufficient recovery from the physiological bone mobilization that occurs during lactation. The study looked at changes in areal bone mineral density (aBMD) both during and after lactation for women with HIV living in Uganda who were taking Option B+ ART, a regimen that includes tenofovir, 3TC, and efavirenz. These women were compared with a reference group of HIV-negative women.
In all, 95 women with HIV and 96 HIV negative women were recruited into the study during pregnancy. Participants were followed postpartum at weeks 2, 14, and 26, and at a final visit that occurred 14 weeks after lactation stopped.
In addition to lumbar spine, total hip, and femoral neck aBMD measurements, the investigators also obtained whole body-less-head reading.
For total hip and femoral neck aBMD, the nadir of density was seen at 26 postpartum, when a drop of about 6% was seen from baseline readings. By the final post-lactation visit, women without HIV had recovered to their baseline; for women with HIV, some recovery also occurred, but the effect was dampened, with a persistent bone density deficit of about 3% from baseline. The differences between HIV-positive and HIV-negative women in these measurements were also statistically significant, at P less than .001 for total hip aBMD differences and P = .0008 for femoral neck differences. Again, correction for multiple confounders didn’t attenuate the results, said Dr. Fowler.
“In conclusion, these data showed accentuated mobilization of hip and whole body aBMD during lactation,” said Dr. Fowler, who also noted “slower skeletal recovery post lactation for HIV-infected women.” Clinical implications of these findings aren’t currently known, she said. Further ongoing studies are aiming to tease out both mechanisms and longer-term consequences for the bone health of HIV-infected women and their children, who may also see differences in bone mineral accretion and growth.
Session moderator Risa Hoffman, MD, in introductory remarks, set the findings in some context. “As we know, HIV-positive adults have low bone mineral density, and this appears to be a result of interactions of HIV, traditional risk factors for loss of bone density, and antiretroviral therapy,” said Dr. Hoffman, director of the global health program at the University of California, Los Angeles. She added that previous work had shown that “middle-aged HIV-positive women have higher 10-year fracture incidence compared to their HIV-negative counterparts.” The current study, she said, “has both short- and long-term implications for women as they go through multiple pregnancies and multiple periods of breastfeeding.”
The study was funded by the United Kingdom’s Medical Research Council and Department for International Development as well as the Alborada Trust and the Gates Cambridge Scholarship. The authors reported no conflicts of interest.
SOURCE: Nabwire F et al. CROI 2020, Abstract 768.
Women with HIV had more bone mobilization during lactation, and attenuated skeletal recovery after lactation, compared with HIV-negative women, according to research presented during the Conference on Retroviruses & Opportunistic Infections, which was presented online this year. CROI organizers chose to hold a virtual meeting because of concerns about the spread of COVID-19.
The study “demonstrated that there were reductions as expected in BMD during breastfeeding, and there was recovery at the end of breastfeeding, which was higher among women who were not HIV-infected compared to HIV-infected women,” said Mary Glenn Fowler, MD, speaking in a video presentation during the virtual conference. The differences between women who had HIV and the HIV-negative reference group were statistically significant (P = .003 for lumbar spine and P less than .001 for whole-body aBMD).
“We also saw that for whole-body BMD, there was recovery at the end of breastfeeding for women who were not HIV infected, but a dampened response of recovery for BMD for HIV-infected women,” she went on, adding: “These findings held after adjustment for parity, age, body mass, breastfeeding practices, duration of breastfeeding, use of [injectable medroxyprogesterone acetate], and resumption of menses.”
Dr. Fowler presented the study’s results on behalf of lead author Florence Nabwire, PhD, an investigator scientist in the nutrition and bone health group of the United Kingdom’s Medical Research Council (Cambridge).
Although it’s known that antiretroviral therapy (ART) is associated with bone loss, Dr. Fowler explained that there are only limited data in HIV-positive women who are lactating. It’s important to see what happens during lactation for this group of women because of the potential sequelae later in life of insufficient recovery from the physiological bone mobilization that occurs during lactation. The study looked at changes in areal bone mineral density (aBMD) both during and after lactation for women with HIV living in Uganda who were taking Option B+ ART, a regimen that includes tenofovir, 3TC, and efavirenz. These women were compared with a reference group of HIV-negative women.
In all, 95 women with HIV and 96 HIV negative women were recruited into the study during pregnancy. Participants were followed postpartum at weeks 2, 14, and 26, and at a final visit that occurred 14 weeks after lactation stopped.
In addition to lumbar spine, total hip, and femoral neck aBMD measurements, the investigators also obtained whole body-less-head reading.
For total hip and femoral neck aBMD, the nadir of density was seen at 26 postpartum, when a drop of about 6% was seen from baseline readings. By the final post-lactation visit, women without HIV had recovered to their baseline; for women with HIV, some recovery also occurred, but the effect was dampened, with a persistent bone density deficit of about 3% from baseline. The differences between HIV-positive and HIV-negative women in these measurements were also statistically significant, at P less than .001 for total hip aBMD differences and P = .0008 for femoral neck differences. Again, correction for multiple confounders didn’t attenuate the results, said Dr. Fowler.
“In conclusion, these data showed accentuated mobilization of hip and whole body aBMD during lactation,” said Dr. Fowler, who also noted “slower skeletal recovery post lactation for HIV-infected women.” Clinical implications of these findings aren’t currently known, she said. Further ongoing studies are aiming to tease out both mechanisms and longer-term consequences for the bone health of HIV-infected women and their children, who may also see differences in bone mineral accretion and growth.
Session moderator Risa Hoffman, MD, in introductory remarks, set the findings in some context. “As we know, HIV-positive adults have low bone mineral density, and this appears to be a result of interactions of HIV, traditional risk factors for loss of bone density, and antiretroviral therapy,” said Dr. Hoffman, director of the global health program at the University of California, Los Angeles. She added that previous work had shown that “middle-aged HIV-positive women have higher 10-year fracture incidence compared to their HIV-negative counterparts.” The current study, she said, “has both short- and long-term implications for women as they go through multiple pregnancies and multiple periods of breastfeeding.”
The study was funded by the United Kingdom’s Medical Research Council and Department for International Development as well as the Alborada Trust and the Gates Cambridge Scholarship. The authors reported no conflicts of interest.
SOURCE: Nabwire F et al. CROI 2020, Abstract 768.
FROM CROI 2020
Making something ordinary out of the extraordinary
These are tough times for families, children, and practices. In this case, the entire world is going through it at the same time, leaving no escape. There are so many new things each of us needs to do, and for some of the challenges, we are completely thwarted by safety restrictions from doing anything. Adults and children alike are trying to work or learn at home in new ways. This also means that old daily routines have been broken. The sense of disorientation is pervasive. Although it is only one part of what is needed, reestablishing routines can go a long way toward restoring a sense of control and meaning that you can institute for yourself and recommend to your patients.
Examples of such change include natural disasters such as COVID-19, deaths, or separations from loved ones, but also moving, job loss, or new financial instability. Many families and many doctors and staff are experiencing several of these at once these days.
Evidence from studies of times of major disruption such as divorce, a death, war, and natural disasters show that parenting tends to shift to being less organized, with less overall discipline or more arbitrary punishment, and, in some cases, less parent-child connection. Children, on their part, also tend to act differently under these conditions. They are more irritable, upset, anxious, clingy, and aggressive, and also tend to regress in recent developmental achievements such as maintaining toileting and sleep patterns. Parents often do not see the connection to the stress and react to these behaviors in ways that may make things worse by scolding or punishing.
I was really surprised to hear Daniel Kahneman, PhD, Nobel laureate in economics, talk about how even he has trouble judging risk based on mathematical probability. Instead, he recognizes that adults decide about risk based on the behavior of the people around them – when others act worried or agitated, the person does too. Children, even more than adults, must decide if they are safe based on the behavior of the adults around them. When parents maintain routines as closely as possible after a major disruption, children feel reassured that they can expect continuity of their relationship – their most important lifeboat. If their parents keep doing the things they are used to, children basically feel safe.
Simple aspects of sameness important to children are very familiar to pediatricians: always wanting the same spoon, the sandwich cut the same way, only chicken nuggets from a certain store. This tends to be true in typically developing toddlers, preschool, and some school-aged children. The desire to have the same story read to them multiple times – until parents are ready to scream! – is another sign of the importance of predictable routines to children. All of these are best accommodated during times of stress rather than trying to “avoid making a bad habit.” All disruptions of routine are even more disorienting for children with intellectual disabilities or those on the autism spectrum who are generally less able to understand or control their world. Children and adults with preexisting anxiety disorders also are more likely to have more severe reactions to major disruptions and need extra understanding.
Routines for eating at least something at regular times – even if the food is not as interesting as prior fare – provide a sense of security, as well as stabilizing blood sugar and bowel patterns. Keeping patterns of washing hands, sitting together as a family, and interacting in conversation, rather than watching TV news, allow an oasis of respite from ongoing stresses. Family meals are also known to promote learning, vocabulary growth, and better behavior.
Setting a schedule for schooling, play, hygiene, and exercise may seem silly when parents and children are home all day, but it instills a sense of meaning to the day. Making a visual schedule for younger children or a written or online one for older children can be a shared activity in itself. I remember hearing about how important changing clothes and cleaning teeth were to prisoners of war during World War II in maintaining a sense of normalcy in that time of chaos.
Exercise is particularly important to set as a routine as it directly reduces stress – even if it may need to take new forms. While there are lots of online exercise programs for adults, it is better for everyone to go outside if they can manage adequate personal spacing. There they can experience the orderly changing of the seasons and the weather, as well as soak up some sunshine. Interactive parent-child play serves multiple purposes of stress relief, seeing each other more relaxed, interacting, and having fun!
Routines for sleep are especially important. To fall asleep under normal circumstances requires a sense of safety, perhaps for evolutionary reasons because of the vulnerability of the paralysis that is part of REM sleep stages. Fear at bedtime is common in young children, as is disorientation in the elderly. Both respond to reassuring bedtime routines done the same way every night, such as brushing teeth, changing clothes, washing up, reading or being read to, and praying – if these were the previous habit. When there has been a major disruption, these routines take on added importance, even if some modifications need to be made in sleep location, privacy, etc. Keeping schedules for naps, bedtime, and wake time as stable as possible makes sleep onset easier and sleep maintenance more likely. It also increases the chances of adequate sleep duration. Getting enough sleep stabilizes mood, reduces irritability, and improves daytime concentration and problem-solving skills. These all are especially needed by adults as well as children when there are major disruptions.
Maintaining chores at times of disruption can be extra difficult, plus this may seem to parents like an added stress for their already-stressed child. But in fact, children are reassured by adults’ continuing these requirements. Not only is an expectation that chores be done a signal that life can be expected to proceed normally, but having children do things to help – such as cleaning up, restocking soap and towels, or emptying trash – gives them an active role and hence some sense of control.
Discipline is, in essence, also a routine. Maintaining standards for kindness to others and following rules can be especially difficult when life has been disrupted because emotional lability is more likely in both adults and children when severely stressed. It is important for parents to consider the source of the misbehavior as possibly stress related and to interrupt it in a gentle and understanding way. A parent might say: “I know you are upset by all the changes. It is even more important now than ever to be kind to your brother.” Under stressful conditions, it is especially important to ask how the child was feeling when acting up, but also to “speak for them” about possible stress-related reasons for their behavior. While parents may correctly say that their child will “take advantage of this excuse,” it is still a teaching opportunity. Children have little insight into these connections to their feelings and actions, but they can learn.
Times when old patterns are disrupted also are times for making new habits. The main new habit I recommend for stress relief and overall mental health are the practices of mindfulness or meditation. Mindfulness may be easier to teach children as it involves paying close attention to one’s thoughts, feelings, and sensations, but doing this without judgment. Children often are naturally better at this than adults, who have layered on more experiences to their thoughts. We pediatricians, as well as the parents we serve, can benefit – especially in stressful times – from sharing in the simple ways children experience the world.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. Email her at [email protected].
These are tough times for families, children, and practices. In this case, the entire world is going through it at the same time, leaving no escape. There are so many new things each of us needs to do, and for some of the challenges, we are completely thwarted by safety restrictions from doing anything. Adults and children alike are trying to work or learn at home in new ways. This also means that old daily routines have been broken. The sense of disorientation is pervasive. Although it is only one part of what is needed, reestablishing routines can go a long way toward restoring a sense of control and meaning that you can institute for yourself and recommend to your patients.
Examples of such change include natural disasters such as COVID-19, deaths, or separations from loved ones, but also moving, job loss, or new financial instability. Many families and many doctors and staff are experiencing several of these at once these days.
Evidence from studies of times of major disruption such as divorce, a death, war, and natural disasters show that parenting tends to shift to being less organized, with less overall discipline or more arbitrary punishment, and, in some cases, less parent-child connection. Children, on their part, also tend to act differently under these conditions. They are more irritable, upset, anxious, clingy, and aggressive, and also tend to regress in recent developmental achievements such as maintaining toileting and sleep patterns. Parents often do not see the connection to the stress and react to these behaviors in ways that may make things worse by scolding or punishing.
I was really surprised to hear Daniel Kahneman, PhD, Nobel laureate in economics, talk about how even he has trouble judging risk based on mathematical probability. Instead, he recognizes that adults decide about risk based on the behavior of the people around them – when others act worried or agitated, the person does too. Children, even more than adults, must decide if they are safe based on the behavior of the adults around them. When parents maintain routines as closely as possible after a major disruption, children feel reassured that they can expect continuity of their relationship – their most important lifeboat. If their parents keep doing the things they are used to, children basically feel safe.
Simple aspects of sameness important to children are very familiar to pediatricians: always wanting the same spoon, the sandwich cut the same way, only chicken nuggets from a certain store. This tends to be true in typically developing toddlers, preschool, and some school-aged children. The desire to have the same story read to them multiple times – until parents are ready to scream! – is another sign of the importance of predictable routines to children. All of these are best accommodated during times of stress rather than trying to “avoid making a bad habit.” All disruptions of routine are even more disorienting for children with intellectual disabilities or those on the autism spectrum who are generally less able to understand or control their world. Children and adults with preexisting anxiety disorders also are more likely to have more severe reactions to major disruptions and need extra understanding.
Routines for eating at least something at regular times – even if the food is not as interesting as prior fare – provide a sense of security, as well as stabilizing blood sugar and bowel patterns. Keeping patterns of washing hands, sitting together as a family, and interacting in conversation, rather than watching TV news, allow an oasis of respite from ongoing stresses. Family meals are also known to promote learning, vocabulary growth, and better behavior.
Setting a schedule for schooling, play, hygiene, and exercise may seem silly when parents and children are home all day, but it instills a sense of meaning to the day. Making a visual schedule for younger children or a written or online one for older children can be a shared activity in itself. I remember hearing about how important changing clothes and cleaning teeth were to prisoners of war during World War II in maintaining a sense of normalcy in that time of chaos.
Exercise is particularly important to set as a routine as it directly reduces stress – even if it may need to take new forms. While there are lots of online exercise programs for adults, it is better for everyone to go outside if they can manage adequate personal spacing. There they can experience the orderly changing of the seasons and the weather, as well as soak up some sunshine. Interactive parent-child play serves multiple purposes of stress relief, seeing each other more relaxed, interacting, and having fun!
Routines for sleep are especially important. To fall asleep under normal circumstances requires a sense of safety, perhaps for evolutionary reasons because of the vulnerability of the paralysis that is part of REM sleep stages. Fear at bedtime is common in young children, as is disorientation in the elderly. Both respond to reassuring bedtime routines done the same way every night, such as brushing teeth, changing clothes, washing up, reading or being read to, and praying – if these were the previous habit. When there has been a major disruption, these routines take on added importance, even if some modifications need to be made in sleep location, privacy, etc. Keeping schedules for naps, bedtime, and wake time as stable as possible makes sleep onset easier and sleep maintenance more likely. It also increases the chances of adequate sleep duration. Getting enough sleep stabilizes mood, reduces irritability, and improves daytime concentration and problem-solving skills. These all are especially needed by adults as well as children when there are major disruptions.
Maintaining chores at times of disruption can be extra difficult, plus this may seem to parents like an added stress for their already-stressed child. But in fact, children are reassured by adults’ continuing these requirements. Not only is an expectation that chores be done a signal that life can be expected to proceed normally, but having children do things to help – such as cleaning up, restocking soap and towels, or emptying trash – gives them an active role and hence some sense of control.
Discipline is, in essence, also a routine. Maintaining standards for kindness to others and following rules can be especially difficult when life has been disrupted because emotional lability is more likely in both adults and children when severely stressed. It is important for parents to consider the source of the misbehavior as possibly stress related and to interrupt it in a gentle and understanding way. A parent might say: “I know you are upset by all the changes. It is even more important now than ever to be kind to your brother.” Under stressful conditions, it is especially important to ask how the child was feeling when acting up, but also to “speak for them” about possible stress-related reasons for their behavior. While parents may correctly say that their child will “take advantage of this excuse,” it is still a teaching opportunity. Children have little insight into these connections to their feelings and actions, but they can learn.
Times when old patterns are disrupted also are times for making new habits. The main new habit I recommend for stress relief and overall mental health are the practices of mindfulness or meditation. Mindfulness may be easier to teach children as it involves paying close attention to one’s thoughts, feelings, and sensations, but doing this without judgment. Children often are naturally better at this than adults, who have layered on more experiences to their thoughts. We pediatricians, as well as the parents we serve, can benefit – especially in stressful times – from sharing in the simple ways children experience the world.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. Email her at [email protected].
These are tough times for families, children, and practices. In this case, the entire world is going through it at the same time, leaving no escape. There are so many new things each of us needs to do, and for some of the challenges, we are completely thwarted by safety restrictions from doing anything. Adults and children alike are trying to work or learn at home in new ways. This also means that old daily routines have been broken. The sense of disorientation is pervasive. Although it is only one part of what is needed, reestablishing routines can go a long way toward restoring a sense of control and meaning that you can institute for yourself and recommend to your patients.
Examples of such change include natural disasters such as COVID-19, deaths, or separations from loved ones, but also moving, job loss, or new financial instability. Many families and many doctors and staff are experiencing several of these at once these days.
Evidence from studies of times of major disruption such as divorce, a death, war, and natural disasters show that parenting tends to shift to being less organized, with less overall discipline or more arbitrary punishment, and, in some cases, less parent-child connection. Children, on their part, also tend to act differently under these conditions. They are more irritable, upset, anxious, clingy, and aggressive, and also tend to regress in recent developmental achievements such as maintaining toileting and sleep patterns. Parents often do not see the connection to the stress and react to these behaviors in ways that may make things worse by scolding or punishing.
I was really surprised to hear Daniel Kahneman, PhD, Nobel laureate in economics, talk about how even he has trouble judging risk based on mathematical probability. Instead, he recognizes that adults decide about risk based on the behavior of the people around them – when others act worried or agitated, the person does too. Children, even more than adults, must decide if they are safe based on the behavior of the adults around them. When parents maintain routines as closely as possible after a major disruption, children feel reassured that they can expect continuity of their relationship – their most important lifeboat. If their parents keep doing the things they are used to, children basically feel safe.
Simple aspects of sameness important to children are very familiar to pediatricians: always wanting the same spoon, the sandwich cut the same way, only chicken nuggets from a certain store. This tends to be true in typically developing toddlers, preschool, and some school-aged children. The desire to have the same story read to them multiple times – until parents are ready to scream! – is another sign of the importance of predictable routines to children. All of these are best accommodated during times of stress rather than trying to “avoid making a bad habit.” All disruptions of routine are even more disorienting for children with intellectual disabilities or those on the autism spectrum who are generally less able to understand or control their world. Children and adults with preexisting anxiety disorders also are more likely to have more severe reactions to major disruptions and need extra understanding.
Routines for eating at least something at regular times – even if the food is not as interesting as prior fare – provide a sense of security, as well as stabilizing blood sugar and bowel patterns. Keeping patterns of washing hands, sitting together as a family, and interacting in conversation, rather than watching TV news, allow an oasis of respite from ongoing stresses. Family meals are also known to promote learning, vocabulary growth, and better behavior.
Setting a schedule for schooling, play, hygiene, and exercise may seem silly when parents and children are home all day, but it instills a sense of meaning to the day. Making a visual schedule for younger children or a written or online one for older children can be a shared activity in itself. I remember hearing about how important changing clothes and cleaning teeth were to prisoners of war during World War II in maintaining a sense of normalcy in that time of chaos.
Exercise is particularly important to set as a routine as it directly reduces stress – even if it may need to take new forms. While there are lots of online exercise programs for adults, it is better for everyone to go outside if they can manage adequate personal spacing. There they can experience the orderly changing of the seasons and the weather, as well as soak up some sunshine. Interactive parent-child play serves multiple purposes of stress relief, seeing each other more relaxed, interacting, and having fun!
Routines for sleep are especially important. To fall asleep under normal circumstances requires a sense of safety, perhaps for evolutionary reasons because of the vulnerability of the paralysis that is part of REM sleep stages. Fear at bedtime is common in young children, as is disorientation in the elderly. Both respond to reassuring bedtime routines done the same way every night, such as brushing teeth, changing clothes, washing up, reading or being read to, and praying – if these were the previous habit. When there has been a major disruption, these routines take on added importance, even if some modifications need to be made in sleep location, privacy, etc. Keeping schedules for naps, bedtime, and wake time as stable as possible makes sleep onset easier and sleep maintenance more likely. It also increases the chances of adequate sleep duration. Getting enough sleep stabilizes mood, reduces irritability, and improves daytime concentration and problem-solving skills. These all are especially needed by adults as well as children when there are major disruptions.
Maintaining chores at times of disruption can be extra difficult, plus this may seem to parents like an added stress for their already-stressed child. But in fact, children are reassured by adults’ continuing these requirements. Not only is an expectation that chores be done a signal that life can be expected to proceed normally, but having children do things to help – such as cleaning up, restocking soap and towels, or emptying trash – gives them an active role and hence some sense of control.
Discipline is, in essence, also a routine. Maintaining standards for kindness to others and following rules can be especially difficult when life has been disrupted because emotional lability is more likely in both adults and children when severely stressed. It is important for parents to consider the source of the misbehavior as possibly stress related and to interrupt it in a gentle and understanding way. A parent might say: “I know you are upset by all the changes. It is even more important now than ever to be kind to your brother.” Under stressful conditions, it is especially important to ask how the child was feeling when acting up, but also to “speak for them” about possible stress-related reasons for their behavior. While parents may correctly say that their child will “take advantage of this excuse,” it is still a teaching opportunity. Children have little insight into these connections to their feelings and actions, but they can learn.
Times when old patterns are disrupted also are times for making new habits. The main new habit I recommend for stress relief and overall mental health are the practices of mindfulness or meditation. Mindfulness may be easier to teach children as it involves paying close attention to one’s thoughts, feelings, and sensations, but doing this without judgment. Children often are naturally better at this than adults, who have layered on more experiences to their thoughts. We pediatricians, as well as the parents we serve, can benefit – especially in stressful times – from sharing in the simple ways children experience the world.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. Email her at [email protected].
Metformin use linked to improved surgery outcomes
Patients with type 2 diabetes who take metformin may have lower risk-adjusted mortality and readmission rates after surgery than do those who don’t take metformin, findings from a large retrospective cohort study suggest.
Of 10,088 individuals with diabetes who underwent a major surgery requiring hospital admission between January 1, 2010, and January 1, 2016, a total of 5,962 (59%) had received a prescription for metformin in the 180 days before surgery, and 5,460 of those patients were propensity score–matched to controls who did not receive a metformin prescription.
The study participants had a mean age of 67.7 years and underwent surgery requiring general anesthesia and postoperative admission at any of 15 hospitals in a single Pennsylvania health system. In addition to being prescribed metformin within 180 days before surgery, they also had metformin on their list of active medications at their most recent preoperative encounter before the surgery. The were followed until December 18, 2018.
In all, the 90-day and 5-year mortality hazards were reduced by 28% and 26%, respectively, in the metformin prescription recipients, compared with the propensity score–matched controls (hazard ratios, 0.72 and 0.74, respectively), Katherine M. Reitz, MD, and colleagues at the University of Pittsburgh reported in JAMA Surgery.
The readmission hazard – with mortality as a competing risk – was reduced by 16% at 30 days and 14% at 90 days (sub-HRs, 0.84 and 0.86, respectively), the researchers found.
“Hospital readmissions among those with preoperative metformin prescriptions were observed by postdischarge days 30 and 90 (304 [11%] and 538 [20.1%], respectively), whereas among those without prescriptions, 361 readmissions (13%) occurred by day 30 and 614 (23%) by day 90,” they wrote.
The investigators also noted that inflammation was reduced in patients who received a metformin prescription, compared with those who did not (mean preoperative neutrophil to leukocyte ratio, 4.5 vs. 5.0, respectively).
“In the full cohort, multivariable regression analysis similarly demonstrated that metformin was associated with a reduced hazard for both 90-day and 5-year mortality (adjusted HRs, 0.77 and 0.80, respectively) and for 30-day and 90-day readmission (aHR, 0.83 and 0.86), with mortality as a competing risk,” they added.
The findings support those from previous studies showing a decrease in all-cause mortality among diabetes patients taking metformin, said the researchers, noting that those patients had fewer age-related chronic diseases.
“These associations may reflect the anti-aging properties of metformin against the onset of disease or diabetes-associated complications. This study extends these finding by demonstrating that preoperative metformin prescriptions were associated with a reduction in postoperative mortality and readmission, a surrogate for postoperative complications, and with long-term mortality,” they wrote.
The study was limited by a number of factors, such as the potential for residual confounding inherent in retrospective analyses and a lack of adequate power to evaluate the association between metformin use and outcomes for individual surgical procedures. But the authors added that the findings are of note, because adults with comorbidities, such as diabetes, have less physiological reserve and an increased postoperative mortality and readmission rate. The results, therefore, warrant investigation with a prospective randomized clinical trial, they concluded.
In an accompanying editorial, Elizabeth L. George, MD, and Sherry M. Wren, MD, of Stanford (Calif.) University wrote that the study “demonstrates how variables, besides coexisting medical diseases, can affect surgical outcomes.”
“Metformin now joins beta-blockers, statins, and immunonutrition as preoperative agents associated with improved surgical outcomes,” they wrote, adding that future studies should factor in statin use and whether those and other medications should be continued postoperatively because metformin is often held after surgery owing to concerns about contrast agent interactions, whereas statin continuation is recommended.
Future studies of metformin in this setting should exclude patients who are taking statins, or look at possible interactions between the two agents, they said, adding that they would be “interested in seeing a subanalysis of this data set that excludes patients who were prescribed statins.”
“Those data would further solidify the role of metformin as a possible modifiable perioperative factor,” they wrote.
The study was funded by the University of Pittsburgh Medical Center and by grants from the National Heart, Lung, and Blood Institute and the National Institutes of Health. Dr. Reitz reported having no disclosures. Dr. George and Dr. Wren also reported having no disclosures.
SOURCE: Reitz K et al. JAMA Surg. 2020 Apr 8. doi: 10.1001/jamasurg.2020.0416.
Patients with type 2 diabetes who take metformin may have lower risk-adjusted mortality and readmission rates after surgery than do those who don’t take metformin, findings from a large retrospective cohort study suggest.
Of 10,088 individuals with diabetes who underwent a major surgery requiring hospital admission between January 1, 2010, and January 1, 2016, a total of 5,962 (59%) had received a prescription for metformin in the 180 days before surgery, and 5,460 of those patients were propensity score–matched to controls who did not receive a metformin prescription.
The study participants had a mean age of 67.7 years and underwent surgery requiring general anesthesia and postoperative admission at any of 15 hospitals in a single Pennsylvania health system. In addition to being prescribed metformin within 180 days before surgery, they also had metformin on their list of active medications at their most recent preoperative encounter before the surgery. The were followed until December 18, 2018.
In all, the 90-day and 5-year mortality hazards were reduced by 28% and 26%, respectively, in the metformin prescription recipients, compared with the propensity score–matched controls (hazard ratios, 0.72 and 0.74, respectively), Katherine M. Reitz, MD, and colleagues at the University of Pittsburgh reported in JAMA Surgery.
The readmission hazard – with mortality as a competing risk – was reduced by 16% at 30 days and 14% at 90 days (sub-HRs, 0.84 and 0.86, respectively), the researchers found.
“Hospital readmissions among those with preoperative metformin prescriptions were observed by postdischarge days 30 and 90 (304 [11%] and 538 [20.1%], respectively), whereas among those without prescriptions, 361 readmissions (13%) occurred by day 30 and 614 (23%) by day 90,” they wrote.
The investigators also noted that inflammation was reduced in patients who received a metformin prescription, compared with those who did not (mean preoperative neutrophil to leukocyte ratio, 4.5 vs. 5.0, respectively).
“In the full cohort, multivariable regression analysis similarly demonstrated that metformin was associated with a reduced hazard for both 90-day and 5-year mortality (adjusted HRs, 0.77 and 0.80, respectively) and for 30-day and 90-day readmission (aHR, 0.83 and 0.86), with mortality as a competing risk,” they added.
The findings support those from previous studies showing a decrease in all-cause mortality among diabetes patients taking metformin, said the researchers, noting that those patients had fewer age-related chronic diseases.
“These associations may reflect the anti-aging properties of metformin against the onset of disease or diabetes-associated complications. This study extends these finding by demonstrating that preoperative metformin prescriptions were associated with a reduction in postoperative mortality and readmission, a surrogate for postoperative complications, and with long-term mortality,” they wrote.
The study was limited by a number of factors, such as the potential for residual confounding inherent in retrospective analyses and a lack of adequate power to evaluate the association between metformin use and outcomes for individual surgical procedures. But the authors added that the findings are of note, because adults with comorbidities, such as diabetes, have less physiological reserve and an increased postoperative mortality and readmission rate. The results, therefore, warrant investigation with a prospective randomized clinical trial, they concluded.
In an accompanying editorial, Elizabeth L. George, MD, and Sherry M. Wren, MD, of Stanford (Calif.) University wrote that the study “demonstrates how variables, besides coexisting medical diseases, can affect surgical outcomes.”
“Metformin now joins beta-blockers, statins, and immunonutrition as preoperative agents associated with improved surgical outcomes,” they wrote, adding that future studies should factor in statin use and whether those and other medications should be continued postoperatively because metformin is often held after surgery owing to concerns about contrast agent interactions, whereas statin continuation is recommended.
Future studies of metformin in this setting should exclude patients who are taking statins, or look at possible interactions between the two agents, they said, adding that they would be “interested in seeing a subanalysis of this data set that excludes patients who were prescribed statins.”
“Those data would further solidify the role of metformin as a possible modifiable perioperative factor,” they wrote.
The study was funded by the University of Pittsburgh Medical Center and by grants from the National Heart, Lung, and Blood Institute and the National Institutes of Health. Dr. Reitz reported having no disclosures. Dr. George and Dr. Wren also reported having no disclosures.
SOURCE: Reitz K et al. JAMA Surg. 2020 Apr 8. doi: 10.1001/jamasurg.2020.0416.
Patients with type 2 diabetes who take metformin may have lower risk-adjusted mortality and readmission rates after surgery than do those who don’t take metformin, findings from a large retrospective cohort study suggest.
Of 10,088 individuals with diabetes who underwent a major surgery requiring hospital admission between January 1, 2010, and January 1, 2016, a total of 5,962 (59%) had received a prescription for metformin in the 180 days before surgery, and 5,460 of those patients were propensity score–matched to controls who did not receive a metformin prescription.
The study participants had a mean age of 67.7 years and underwent surgery requiring general anesthesia and postoperative admission at any of 15 hospitals in a single Pennsylvania health system. In addition to being prescribed metformin within 180 days before surgery, they also had metformin on their list of active medications at their most recent preoperative encounter before the surgery. The were followed until December 18, 2018.
In all, the 90-day and 5-year mortality hazards were reduced by 28% and 26%, respectively, in the metformin prescription recipients, compared with the propensity score–matched controls (hazard ratios, 0.72 and 0.74, respectively), Katherine M. Reitz, MD, and colleagues at the University of Pittsburgh reported in JAMA Surgery.
The readmission hazard – with mortality as a competing risk – was reduced by 16% at 30 days and 14% at 90 days (sub-HRs, 0.84 and 0.86, respectively), the researchers found.
“Hospital readmissions among those with preoperative metformin prescriptions were observed by postdischarge days 30 and 90 (304 [11%] and 538 [20.1%], respectively), whereas among those without prescriptions, 361 readmissions (13%) occurred by day 30 and 614 (23%) by day 90,” they wrote.
The investigators also noted that inflammation was reduced in patients who received a metformin prescription, compared with those who did not (mean preoperative neutrophil to leukocyte ratio, 4.5 vs. 5.0, respectively).
“In the full cohort, multivariable regression analysis similarly demonstrated that metformin was associated with a reduced hazard for both 90-day and 5-year mortality (adjusted HRs, 0.77 and 0.80, respectively) and for 30-day and 90-day readmission (aHR, 0.83 and 0.86), with mortality as a competing risk,” they added.
The findings support those from previous studies showing a decrease in all-cause mortality among diabetes patients taking metformin, said the researchers, noting that those patients had fewer age-related chronic diseases.
“These associations may reflect the anti-aging properties of metformin against the onset of disease or diabetes-associated complications. This study extends these finding by demonstrating that preoperative metformin prescriptions were associated with a reduction in postoperative mortality and readmission, a surrogate for postoperative complications, and with long-term mortality,” they wrote.
The study was limited by a number of factors, such as the potential for residual confounding inherent in retrospective analyses and a lack of adequate power to evaluate the association between metformin use and outcomes for individual surgical procedures. But the authors added that the findings are of note, because adults with comorbidities, such as diabetes, have less physiological reserve and an increased postoperative mortality and readmission rate. The results, therefore, warrant investigation with a prospective randomized clinical trial, they concluded.
In an accompanying editorial, Elizabeth L. George, MD, and Sherry M. Wren, MD, of Stanford (Calif.) University wrote that the study “demonstrates how variables, besides coexisting medical diseases, can affect surgical outcomes.”
“Metformin now joins beta-blockers, statins, and immunonutrition as preoperative agents associated with improved surgical outcomes,” they wrote, adding that future studies should factor in statin use and whether those and other medications should be continued postoperatively because metformin is often held after surgery owing to concerns about contrast agent interactions, whereas statin continuation is recommended.
Future studies of metformin in this setting should exclude patients who are taking statins, or look at possible interactions between the two agents, they said, adding that they would be “interested in seeing a subanalysis of this data set that excludes patients who were prescribed statins.”
“Those data would further solidify the role of metformin as a possible modifiable perioperative factor,” they wrote.
The study was funded by the University of Pittsburgh Medical Center and by grants from the National Heart, Lung, and Blood Institute and the National Institutes of Health. Dr. Reitz reported having no disclosures. Dr. George and Dr. Wren also reported having no disclosures.
SOURCE: Reitz K et al. JAMA Surg. 2020 Apr 8. doi: 10.1001/jamasurg.2020.0416.
FROM JAMA SURGERY
COVID-19: When health care personnel become patients
according to the Centers for Disease Control and Prevention.
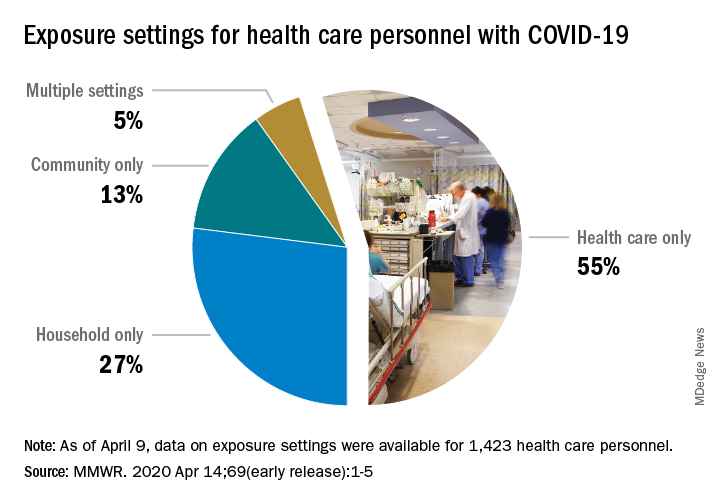
That number, however, is probably an underestimation because health care personnel (HCP) status was available for just over 49,000 of the 315,000 COVID-19 cases reported to the CDC as of April 9. Of the cases with known HCP status, 9,282 (19%) were health care personnel, Matthew J. Stuckey, PhD, and the CDC’s COVID-19 Response Team said.
“The number of cases in HCP reported here must be considered a lower bound because additional cases likely have gone unidentified or unreported,” they said.
The median age of the nearly 9,300 HCP with COVID-19 was 42 years, and the majority (55%) were aged 16-44 years; another 21% were 45-54, 18% were 55-64, and 6% were age 65 and over. The oldest group, however, represented 10 of the 27 known HCP deaths, the investigators reported in the Morbidity and Mortality Weekly Report.
The majority of infected HCP (55%) reported exposure to a COVID-19 patient in the health care setting, but “there were also known exposures in households and in the community, highlighting the potential for exposure in multiple settings, especially as community transmission increases,” the response team said.
Since “contact tracing after recognized occupational exposures likely will fail to identify many HCP at risk for developing COVID-19,” other measures will probably be needed to “reduce the risk for infected HCP transmitting the virus to colleagues and patients,” they added.
HCP with COVID-19 were less likely to be hospitalized (8%-10%) than the overall population (21%-31%), which “might reflect the younger median age … of HCP patients, compared with that of reported COVID-19 patients overall, as well as prioritization of HCP for testing, which might identify less-severe illness,” the investigators suggested.
The prevalence of underlying conditions in HCP patients, 38%, was the same as all patients with COVID-19, and 92% of the HCP patients presented with fever, cough, or shortness of breath. Two-thirds of all HCP reported muscle aches, and 65% reported headache, the CDC response team noted.
“It is critical to make every effort to ensure the health and safety of this essential national workforce of approximately 18 million HCP, both at work and in the community,” they wrote.
SOURCE: Stuckey MJ et al. MMWR. Apr 14;69(early release):1-5.
according to the Centers for Disease Control and Prevention.
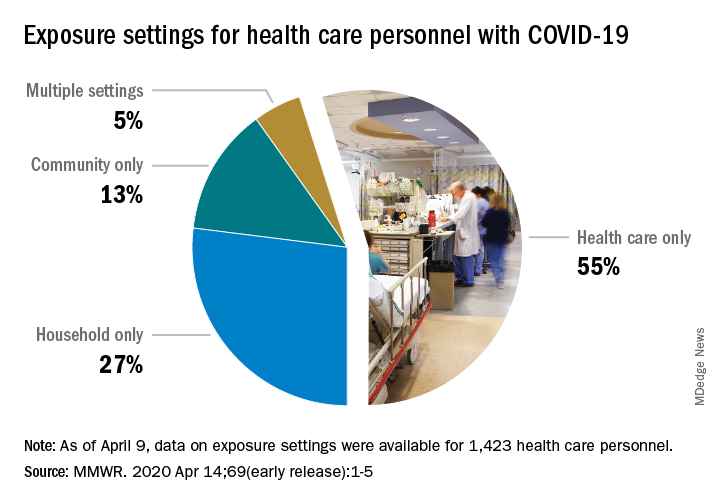
That number, however, is probably an underestimation because health care personnel (HCP) status was available for just over 49,000 of the 315,000 COVID-19 cases reported to the CDC as of April 9. Of the cases with known HCP status, 9,282 (19%) were health care personnel, Matthew J. Stuckey, PhD, and the CDC’s COVID-19 Response Team said.
“The number of cases in HCP reported here must be considered a lower bound because additional cases likely have gone unidentified or unreported,” they said.
The median age of the nearly 9,300 HCP with COVID-19 was 42 years, and the majority (55%) were aged 16-44 years; another 21% were 45-54, 18% were 55-64, and 6% were age 65 and over. The oldest group, however, represented 10 of the 27 known HCP deaths, the investigators reported in the Morbidity and Mortality Weekly Report.
The majority of infected HCP (55%) reported exposure to a COVID-19 patient in the health care setting, but “there were also known exposures in households and in the community, highlighting the potential for exposure in multiple settings, especially as community transmission increases,” the response team said.
Since “contact tracing after recognized occupational exposures likely will fail to identify many HCP at risk for developing COVID-19,” other measures will probably be needed to “reduce the risk for infected HCP transmitting the virus to colleagues and patients,” they added.
HCP with COVID-19 were less likely to be hospitalized (8%-10%) than the overall population (21%-31%), which “might reflect the younger median age … of HCP patients, compared with that of reported COVID-19 patients overall, as well as prioritization of HCP for testing, which might identify less-severe illness,” the investigators suggested.
The prevalence of underlying conditions in HCP patients, 38%, was the same as all patients with COVID-19, and 92% of the HCP patients presented with fever, cough, or shortness of breath. Two-thirds of all HCP reported muscle aches, and 65% reported headache, the CDC response team noted.
“It is critical to make every effort to ensure the health and safety of this essential national workforce of approximately 18 million HCP, both at work and in the community,” they wrote.
SOURCE: Stuckey MJ et al. MMWR. Apr 14;69(early release):1-5.
according to the Centers for Disease Control and Prevention.
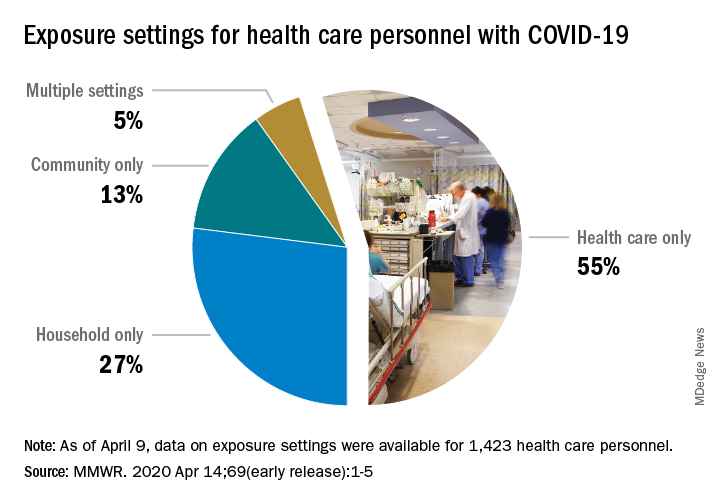
That number, however, is probably an underestimation because health care personnel (HCP) status was available for just over 49,000 of the 315,000 COVID-19 cases reported to the CDC as of April 9. Of the cases with known HCP status, 9,282 (19%) were health care personnel, Matthew J. Stuckey, PhD, and the CDC’s COVID-19 Response Team said.
“The number of cases in HCP reported here must be considered a lower bound because additional cases likely have gone unidentified or unreported,” they said.
The median age of the nearly 9,300 HCP with COVID-19 was 42 years, and the majority (55%) were aged 16-44 years; another 21% were 45-54, 18% were 55-64, and 6% were age 65 and over. The oldest group, however, represented 10 of the 27 known HCP deaths, the investigators reported in the Morbidity and Mortality Weekly Report.
The majority of infected HCP (55%) reported exposure to a COVID-19 patient in the health care setting, but “there were also known exposures in households and in the community, highlighting the potential for exposure in multiple settings, especially as community transmission increases,” the response team said.
Since “contact tracing after recognized occupational exposures likely will fail to identify many HCP at risk for developing COVID-19,” other measures will probably be needed to “reduce the risk for infected HCP transmitting the virus to colleagues and patients,” they added.
HCP with COVID-19 were less likely to be hospitalized (8%-10%) than the overall population (21%-31%), which “might reflect the younger median age … of HCP patients, compared with that of reported COVID-19 patients overall, as well as prioritization of HCP for testing, which might identify less-severe illness,” the investigators suggested.
The prevalence of underlying conditions in HCP patients, 38%, was the same as all patients with COVID-19, and 92% of the HCP patients presented with fever, cough, or shortness of breath. Two-thirds of all HCP reported muscle aches, and 65% reported headache, the CDC response team noted.
“It is critical to make every effort to ensure the health and safety of this essential national workforce of approximately 18 million HCP, both at work and in the community,” they wrote.
SOURCE: Stuckey MJ et al. MMWR. Apr 14;69(early release):1-5.
FROM THE MMWR
FDA approves emergency use of saliva test to detect COVID-19
As the race to develop rapid testing for COVID-19 expands, the Food and Drug Administration has granted emergency approval for an approach that uses saliva as the primary test biomaterial.
According to a document provided to the FDA, the Rutgers Clinical Genomics Laboratory TaqPath SARS-CoV-2 Assay is intended for the qualitative detection of nucleic acid from SARS-CoV-2 in oropharyngeal (throat) swab, nasopharyngeal swab, anterior nasal swab, mid-turbinate nasal swab from individuals suspected of COVID-19 by their health care clinicians. To expand on this assay, Rutgers University–based RUCDR Infinite Biologics developed a saliva collection method in partnership with Spectrum Solutions and Accurate Diagnostic Labs.
The document states that Samples are transported for RNA extraction and are tested within 48 hours of collection. In saliva samples obtained from 60 patients evaluated by the researchers, all were in agreement with the presence of COVID-19.
“If shown to be as accurate as nasopharyngeal and oropharyngeal samples, saliva as a biomatrix offers the advantage of not generating aerosols or creating as many respiratory droplets during specimen procurement, therefore decreasing the risk of transmission to the health care worker doing the testing,” said Matthew P. Cheng, MDCM, of the division of infectious diseases at McGill University Health Centre, Montreal, who was not involved in development of the test but who has written about diagnostic testing for the virus.
“Also, it may be easy enough for patients to do saliva self-collection at home. However, it is important to note that SARS-CoV-2 tests on saliva have not yet undergone the more rigorous evaluation of full FDA authorization, and saliva is not a preferred specimen type of the FDA nor the [Centers for Disease Control and Prevention] for respiratory virus testing.”
In a prepared statement, Andrew I. Brooks, PhD, chief operating officer at RUCDR Infinite Biologics, said the saliva collection method enables clinicians to preserve personal protective equipment for use in patient care instead of testing. “We can significantly increase the number of people tested each and every day as self-collection of saliva is quicker and more scalable than swab collections,” he said. “All of this combined will have a tremendous impact on testing in New Jersey and across the United States.”
The tests are currently available to the RWJBarnabas Health network, based in West Orange, N.J., which has partnered with Rutgers University.
As the race to develop rapid testing for COVID-19 expands, the Food and Drug Administration has granted emergency approval for an approach that uses saliva as the primary test biomaterial.
According to a document provided to the FDA, the Rutgers Clinical Genomics Laboratory TaqPath SARS-CoV-2 Assay is intended for the qualitative detection of nucleic acid from SARS-CoV-2 in oropharyngeal (throat) swab, nasopharyngeal swab, anterior nasal swab, mid-turbinate nasal swab from individuals suspected of COVID-19 by their health care clinicians. To expand on this assay, Rutgers University–based RUCDR Infinite Biologics developed a saliva collection method in partnership with Spectrum Solutions and Accurate Diagnostic Labs.
The document states that Samples are transported for RNA extraction and are tested within 48 hours of collection. In saliva samples obtained from 60 patients evaluated by the researchers, all were in agreement with the presence of COVID-19.
“If shown to be as accurate as nasopharyngeal and oropharyngeal samples, saliva as a biomatrix offers the advantage of not generating aerosols or creating as many respiratory droplets during specimen procurement, therefore decreasing the risk of transmission to the health care worker doing the testing,” said Matthew P. Cheng, MDCM, of the division of infectious diseases at McGill University Health Centre, Montreal, who was not involved in development of the test but who has written about diagnostic testing for the virus.
“Also, it may be easy enough for patients to do saliva self-collection at home. However, it is important to note that SARS-CoV-2 tests on saliva have not yet undergone the more rigorous evaluation of full FDA authorization, and saliva is not a preferred specimen type of the FDA nor the [Centers for Disease Control and Prevention] for respiratory virus testing.”
In a prepared statement, Andrew I. Brooks, PhD, chief operating officer at RUCDR Infinite Biologics, said the saliva collection method enables clinicians to preserve personal protective equipment for use in patient care instead of testing. “We can significantly increase the number of people tested each and every day as self-collection of saliva is quicker and more scalable than swab collections,” he said. “All of this combined will have a tremendous impact on testing in New Jersey and across the United States.”
The tests are currently available to the RWJBarnabas Health network, based in West Orange, N.J., which has partnered with Rutgers University.
As the race to develop rapid testing for COVID-19 expands, the Food and Drug Administration has granted emergency approval for an approach that uses saliva as the primary test biomaterial.
According to a document provided to the FDA, the Rutgers Clinical Genomics Laboratory TaqPath SARS-CoV-2 Assay is intended for the qualitative detection of nucleic acid from SARS-CoV-2 in oropharyngeal (throat) swab, nasopharyngeal swab, anterior nasal swab, mid-turbinate nasal swab from individuals suspected of COVID-19 by their health care clinicians. To expand on this assay, Rutgers University–based RUCDR Infinite Biologics developed a saliva collection method in partnership with Spectrum Solutions and Accurate Diagnostic Labs.
The document states that Samples are transported for RNA extraction and are tested within 48 hours of collection. In saliva samples obtained from 60 patients evaluated by the researchers, all were in agreement with the presence of COVID-19.
“If shown to be as accurate as nasopharyngeal and oropharyngeal samples, saliva as a biomatrix offers the advantage of not generating aerosols or creating as many respiratory droplets during specimen procurement, therefore decreasing the risk of transmission to the health care worker doing the testing,” said Matthew P. Cheng, MDCM, of the division of infectious diseases at McGill University Health Centre, Montreal, who was not involved in development of the test but who has written about diagnostic testing for the virus.
“Also, it may be easy enough for patients to do saliva self-collection at home. However, it is important to note that SARS-CoV-2 tests on saliva have not yet undergone the more rigorous evaluation of full FDA authorization, and saliva is not a preferred specimen type of the FDA nor the [Centers for Disease Control and Prevention] for respiratory virus testing.”
In a prepared statement, Andrew I. Brooks, PhD, chief operating officer at RUCDR Infinite Biologics, said the saliva collection method enables clinicians to preserve personal protective equipment for use in patient care instead of testing. “We can significantly increase the number of people tested each and every day as self-collection of saliva is quicker and more scalable than swab collections,” he said. “All of this combined will have a tremendous impact on testing in New Jersey and across the United States.”
The tests are currently available to the RWJBarnabas Health network, based in West Orange, N.J., which has partnered with Rutgers University.
Learning about the curve
Empty shelves that once cradled toilet paper rolls; lines of shoppers, some with masks; waiting 6 feet or at least a shopping cart length apart to get into grocery stores; hazmat-suited workers loading body bags into makeshift mortuaries ... These are the images we have come to associate with the COVID-19 pandemic. But then there also are the graphs and charts, none of them bearing good news. Some are difficult to interpret because they may be missing a key ingredient, such as a scale. Day to day fluctuations in the timeliness of the data points can make valid comparisons impossible. In most cases, it is too early to look at the graphs and hope for the big picture. Whether you are concerned about the stock market or the number of new cases of the virus in your county, you are hoping to see some graphic depiction of a favorable trend.
We have suddenly learned about the urgency of a process called “flattening the curve.” Are we doing as good a job of flattening as we could be? Are we doing better than France or Spain? Or are we heading toward an Italianesque apocalypse? Who is going to tell us when the flattening is for real and not just a 2- or 3-day statistical aberration?
The curves we are obsessed with today are those showing us new cases and new deaths. But And we won’t be seeing this curve in four-color graphics on the front page of our newspapers. It is the learning curve, and we want it to be as steep as we can make it without any hint of flattening in the foreseeable future.
We need to learn more about corona-like viruses. Why are some of us more vulnerable? We need to learn more about contagion. Does the 6-foot guideline make any sense? How long are viral particles floating in the air capable of initiating disease? What about air flow and dilution? Can we build a cruise ship or airplane that will be less of a health hazard?
More importantly, we need to learn to be better prepared. Even before the pandemic there have been shortages in intravenous solutions and drugs of critical importance to common diseases. Can we learn how to create reliable and affordable supply chains that allow researchers and developers to make a reasonable profit? Can we relearn to value science? Can we learn to invest more heavily in epidemiology and make it a specialty that attracts our best thinkers and communicators? Then can we elect officials who will share our trust in their recommendations?
Can we do a better job of resolving the tension between those who believe in a strong federal government and those who believe in local autonomy because we are seeing every day that this is an issue of survival, not just coexistence? Can we learn that the globalization that has allowed this viral spread can also be leveraged to beat it into submission?
Over the last half century there has been an unfortunate flattening of the learning curve. Ironically we have seen exponential growth among hi-tech industries that have forced us to keep abreast of new developments. But along with this has been a growing skepticism about value of scientific investigation. It is time we climbed back on that steep learning curve. The view gets better the higher we climb.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Empty shelves that once cradled toilet paper rolls; lines of shoppers, some with masks; waiting 6 feet or at least a shopping cart length apart to get into grocery stores; hazmat-suited workers loading body bags into makeshift mortuaries ... These are the images we have come to associate with the COVID-19 pandemic. But then there also are the graphs and charts, none of them bearing good news. Some are difficult to interpret because they may be missing a key ingredient, such as a scale. Day to day fluctuations in the timeliness of the data points can make valid comparisons impossible. In most cases, it is too early to look at the graphs and hope for the big picture. Whether you are concerned about the stock market or the number of new cases of the virus in your county, you are hoping to see some graphic depiction of a favorable trend.
We have suddenly learned about the urgency of a process called “flattening the curve.” Are we doing as good a job of flattening as we could be? Are we doing better than France or Spain? Or are we heading toward an Italianesque apocalypse? Who is going to tell us when the flattening is for real and not just a 2- or 3-day statistical aberration?
The curves we are obsessed with today are those showing us new cases and new deaths. But And we won’t be seeing this curve in four-color graphics on the front page of our newspapers. It is the learning curve, and we want it to be as steep as we can make it without any hint of flattening in the foreseeable future.
We need to learn more about corona-like viruses. Why are some of us more vulnerable? We need to learn more about contagion. Does the 6-foot guideline make any sense? How long are viral particles floating in the air capable of initiating disease? What about air flow and dilution? Can we build a cruise ship or airplane that will be less of a health hazard?
More importantly, we need to learn to be better prepared. Even before the pandemic there have been shortages in intravenous solutions and drugs of critical importance to common diseases. Can we learn how to create reliable and affordable supply chains that allow researchers and developers to make a reasonable profit? Can we relearn to value science? Can we learn to invest more heavily in epidemiology and make it a specialty that attracts our best thinkers and communicators? Then can we elect officials who will share our trust in their recommendations?
Can we do a better job of resolving the tension between those who believe in a strong federal government and those who believe in local autonomy because we are seeing every day that this is an issue of survival, not just coexistence? Can we learn that the globalization that has allowed this viral spread can also be leveraged to beat it into submission?
Over the last half century there has been an unfortunate flattening of the learning curve. Ironically we have seen exponential growth among hi-tech industries that have forced us to keep abreast of new developments. But along with this has been a growing skepticism about value of scientific investigation. It is time we climbed back on that steep learning curve. The view gets better the higher we climb.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Empty shelves that once cradled toilet paper rolls; lines of shoppers, some with masks; waiting 6 feet or at least a shopping cart length apart to get into grocery stores; hazmat-suited workers loading body bags into makeshift mortuaries ... These are the images we have come to associate with the COVID-19 pandemic. But then there also are the graphs and charts, none of them bearing good news. Some are difficult to interpret because they may be missing a key ingredient, such as a scale. Day to day fluctuations in the timeliness of the data points can make valid comparisons impossible. In most cases, it is too early to look at the graphs and hope for the big picture. Whether you are concerned about the stock market or the number of new cases of the virus in your county, you are hoping to see some graphic depiction of a favorable trend.
We have suddenly learned about the urgency of a process called “flattening the curve.” Are we doing as good a job of flattening as we could be? Are we doing better than France or Spain? Or are we heading toward an Italianesque apocalypse? Who is going to tell us when the flattening is for real and not just a 2- or 3-day statistical aberration?
The curves we are obsessed with today are those showing us new cases and new deaths. But And we won’t be seeing this curve in four-color graphics on the front page of our newspapers. It is the learning curve, and we want it to be as steep as we can make it without any hint of flattening in the foreseeable future.
We need to learn more about corona-like viruses. Why are some of us more vulnerable? We need to learn more about contagion. Does the 6-foot guideline make any sense? How long are viral particles floating in the air capable of initiating disease? What about air flow and dilution? Can we build a cruise ship or airplane that will be less of a health hazard?
More importantly, we need to learn to be better prepared. Even before the pandemic there have been shortages in intravenous solutions and drugs of critical importance to common diseases. Can we learn how to create reliable and affordable supply chains that allow researchers and developers to make a reasonable profit? Can we relearn to value science? Can we learn to invest more heavily in epidemiology and make it a specialty that attracts our best thinkers and communicators? Then can we elect officials who will share our trust in their recommendations?
Can we do a better job of resolving the tension between those who believe in a strong federal government and those who believe in local autonomy because we are seeing every day that this is an issue of survival, not just coexistence? Can we learn that the globalization that has allowed this viral spread can also be leveraged to beat it into submission?
Over the last half century there has been an unfortunate flattening of the learning curve. Ironically we have seen exponential growth among hi-tech industries that have forced us to keep abreast of new developments. But along with this has been a growing skepticism about value of scientific investigation. It is time we climbed back on that steep learning curve. The view gets better the higher we climb.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Social distancing comes to the medicine wards
As the coronavirus pandemic has swept across America, so have advisories for social distancing. As of April 2, stay-at-home orders had been given in 38 states and parts of 7 more, affecting about 300 million people. Most of these people have been asked to maintain 6 feet of separation to anyone outside their immediate family and to avoid all avoidable contacts.
Typical hospital medicine patients at an academic hospital, however, traditionally receive visits from their hospitalist, an intern, a resident, and sometimes several medical students, pharmacists, and case managers. At University of California, San Diego, Health, many of these visits would occur during Focused Interdisciplinary Team rounds, with providers moving together in close proximity.
Asymptomatic and presymptomatic spread of coronavirus have been documented, which means distancing is a good idea for everyone. The risks of traditional patient visits during the coronavirus pandemic include spread to both patients (at high risk of complications) and staff (taken out of the workforce during surge times). Even if coronavirus were not a risk, visits to isolation rooms consume PPE, which is in short supply.
In response to the pandemic, UCSD Hospital Medicine drafted guidelines for the reduction of patient contacts. Our slide presentations and written guidelines were then distributed to physicians, nurses, pharmacists, and other staff by our pandemic response command center. Key points include the following:
- Target one in-person MD visit per day for stable patients. This means that attending reexaminations of patients seen by residents, nurse practitioners, physician assistants, and so on would not be done for billing or teaching purposes, only when clinically necessary.
- Use phone or video conferencing for follow-up discussions unless direct patient contact is needed.
- Consider skipping daily exams on patients who do not require them, such as patients awaiting placement or stably receiving long courses of antibiotics. Interview them remotely or from the door instead.
- Conduct team rounds, patient discussions, and handoffs with all members 6 feet apart or by telephone or video. Avoid shared work rooms. Substitute video conferences for in-person meetings. Use EMR embedded messaging to reduce face-to-face discussions.
- Check if a patient is ready for a visit before donning PPE to avoid waste.
- Explain to patients that distancing is being conducted to protect them. In our experience, when patients are asked about distancing, they welcome the changes.
We have also considered that most patient visits are generated by nurses and assistants. To increase distancing and reduce PPE waste, we have encouraged nurses and pharmacists to maximize their use of remote communication with patients and to suggest changes to care plans and come up with creative solutions to reduce traffic. We specifically suggested the following changes to routine care:
- Reduce frequency of taking vital signs, such as just daily or as needed, in stable patients (for example, those awaiting placement).
- Reduce checks for alcohol withdrawal and neurologic status as soon as possible, and stop fingersticks in patients with well-controlled diabetes not receiving insulin.
- Substitute less frequently administered medications where appropriate if doing so would reduce room traffic (such as enoxaparin for heparin, ceftriaxone for cefazolin, naproxen for ibuprofen, or patient-controlled analgesia for as needed morphine).
- Place intravenous pumps in halls if needed – luckily, our situation has not required these measures in San Diego.
- Explore the possibility of increased patient self-management (self-dosed insulin or inhalers) where medically appropriate.
- Eliminate food service and janitorial trips to isolation rooms unless requested by registered nurse.
There are clear downsides to medical distancing for hospital medicine patients. Patients might have delayed diagnosis of new conditions or inadequate management of conditions requiring frequent assessment, such as alcohol withdrawal. Opportunities for miscommunication (either patient-provider or provider-provider) may be increased with distancing. Isolation also comes with emotional costs such as stress and feelings of isolation or abandonment. Given the dynamic nature of the pandemic response, we are continually reevaluating our distancing guidelines to administer the safest and most effective hospital care possible as we approach California’s expected peak coronavirus infection period.
Dr. Jenkins is professor and chair of the Patient Safety Committee in the Division of Hospital Medicine at UCSD. Dr. Seymann is clinical professor and vice chief for academic affairs, UCSD division of hospital medicine. Dr. Horman and Dr. Bell are hospitalists and associate professors of medicine at UC San Diego Health.
As the coronavirus pandemic has swept across America, so have advisories for social distancing. As of April 2, stay-at-home orders had been given in 38 states and parts of 7 more, affecting about 300 million people. Most of these people have been asked to maintain 6 feet of separation to anyone outside their immediate family and to avoid all avoidable contacts.
Typical hospital medicine patients at an academic hospital, however, traditionally receive visits from their hospitalist, an intern, a resident, and sometimes several medical students, pharmacists, and case managers. At University of California, San Diego, Health, many of these visits would occur during Focused Interdisciplinary Team rounds, with providers moving together in close proximity.
Asymptomatic and presymptomatic spread of coronavirus have been documented, which means distancing is a good idea for everyone. The risks of traditional patient visits during the coronavirus pandemic include spread to both patients (at high risk of complications) and staff (taken out of the workforce during surge times). Even if coronavirus were not a risk, visits to isolation rooms consume PPE, which is in short supply.
In response to the pandemic, UCSD Hospital Medicine drafted guidelines for the reduction of patient contacts. Our slide presentations and written guidelines were then distributed to physicians, nurses, pharmacists, and other staff by our pandemic response command center. Key points include the following:
- Target one in-person MD visit per day for stable patients. This means that attending reexaminations of patients seen by residents, nurse practitioners, physician assistants, and so on would not be done for billing or teaching purposes, only when clinically necessary.
- Use phone or video conferencing for follow-up discussions unless direct patient contact is needed.
- Consider skipping daily exams on patients who do not require them, such as patients awaiting placement or stably receiving long courses of antibiotics. Interview them remotely or from the door instead.
- Conduct team rounds, patient discussions, and handoffs with all members 6 feet apart or by telephone or video. Avoid shared work rooms. Substitute video conferences for in-person meetings. Use EMR embedded messaging to reduce face-to-face discussions.
- Check if a patient is ready for a visit before donning PPE to avoid waste.
- Explain to patients that distancing is being conducted to protect them. In our experience, when patients are asked about distancing, they welcome the changes.
We have also considered that most patient visits are generated by nurses and assistants. To increase distancing and reduce PPE waste, we have encouraged nurses and pharmacists to maximize their use of remote communication with patients and to suggest changes to care plans and come up with creative solutions to reduce traffic. We specifically suggested the following changes to routine care:
- Reduce frequency of taking vital signs, such as just daily or as needed, in stable patients (for example, those awaiting placement).
- Reduce checks for alcohol withdrawal and neurologic status as soon as possible, and stop fingersticks in patients with well-controlled diabetes not receiving insulin.
- Substitute less frequently administered medications where appropriate if doing so would reduce room traffic (such as enoxaparin for heparin, ceftriaxone for cefazolin, naproxen for ibuprofen, or patient-controlled analgesia for as needed morphine).
- Place intravenous pumps in halls if needed – luckily, our situation has not required these measures in San Diego.
- Explore the possibility of increased patient self-management (self-dosed insulin or inhalers) where medically appropriate.
- Eliminate food service and janitorial trips to isolation rooms unless requested by registered nurse.
There are clear downsides to medical distancing for hospital medicine patients. Patients might have delayed diagnosis of new conditions or inadequate management of conditions requiring frequent assessment, such as alcohol withdrawal. Opportunities for miscommunication (either patient-provider or provider-provider) may be increased with distancing. Isolation also comes with emotional costs such as stress and feelings of isolation or abandonment. Given the dynamic nature of the pandemic response, we are continually reevaluating our distancing guidelines to administer the safest and most effective hospital care possible as we approach California’s expected peak coronavirus infection period.
Dr. Jenkins is professor and chair of the Patient Safety Committee in the Division of Hospital Medicine at UCSD. Dr. Seymann is clinical professor and vice chief for academic affairs, UCSD division of hospital medicine. Dr. Horman and Dr. Bell are hospitalists and associate professors of medicine at UC San Diego Health.
As the coronavirus pandemic has swept across America, so have advisories for social distancing. As of April 2, stay-at-home orders had been given in 38 states and parts of 7 more, affecting about 300 million people. Most of these people have been asked to maintain 6 feet of separation to anyone outside their immediate family and to avoid all avoidable contacts.
Typical hospital medicine patients at an academic hospital, however, traditionally receive visits from their hospitalist, an intern, a resident, and sometimes several medical students, pharmacists, and case managers. At University of California, San Diego, Health, many of these visits would occur during Focused Interdisciplinary Team rounds, with providers moving together in close proximity.
Asymptomatic and presymptomatic spread of coronavirus have been documented, which means distancing is a good idea for everyone. The risks of traditional patient visits during the coronavirus pandemic include spread to both patients (at high risk of complications) and staff (taken out of the workforce during surge times). Even if coronavirus were not a risk, visits to isolation rooms consume PPE, which is in short supply.
In response to the pandemic, UCSD Hospital Medicine drafted guidelines for the reduction of patient contacts. Our slide presentations and written guidelines were then distributed to physicians, nurses, pharmacists, and other staff by our pandemic response command center. Key points include the following:
- Target one in-person MD visit per day for stable patients. This means that attending reexaminations of patients seen by residents, nurse practitioners, physician assistants, and so on would not be done for billing or teaching purposes, only when clinically necessary.
- Use phone or video conferencing for follow-up discussions unless direct patient contact is needed.
- Consider skipping daily exams on patients who do not require them, such as patients awaiting placement or stably receiving long courses of antibiotics. Interview them remotely or from the door instead.
- Conduct team rounds, patient discussions, and handoffs with all members 6 feet apart or by telephone or video. Avoid shared work rooms. Substitute video conferences for in-person meetings. Use EMR embedded messaging to reduce face-to-face discussions.
- Check if a patient is ready for a visit before donning PPE to avoid waste.
- Explain to patients that distancing is being conducted to protect them. In our experience, when patients are asked about distancing, they welcome the changes.
We have also considered that most patient visits are generated by nurses and assistants. To increase distancing and reduce PPE waste, we have encouraged nurses and pharmacists to maximize their use of remote communication with patients and to suggest changes to care plans and come up with creative solutions to reduce traffic. We specifically suggested the following changes to routine care:
- Reduce frequency of taking vital signs, such as just daily or as needed, in stable patients (for example, those awaiting placement).
- Reduce checks for alcohol withdrawal and neurologic status as soon as possible, and stop fingersticks in patients with well-controlled diabetes not receiving insulin.
- Substitute less frequently administered medications where appropriate if doing so would reduce room traffic (such as enoxaparin for heparin, ceftriaxone for cefazolin, naproxen for ibuprofen, or patient-controlled analgesia for as needed morphine).
- Place intravenous pumps in halls if needed – luckily, our situation has not required these measures in San Diego.
- Explore the possibility of increased patient self-management (self-dosed insulin or inhalers) where medically appropriate.
- Eliminate food service and janitorial trips to isolation rooms unless requested by registered nurse.
There are clear downsides to medical distancing for hospital medicine patients. Patients might have delayed diagnosis of new conditions or inadequate management of conditions requiring frequent assessment, such as alcohol withdrawal. Opportunities for miscommunication (either patient-provider or provider-provider) may be increased with distancing. Isolation also comes with emotional costs such as stress and feelings of isolation or abandonment. Given the dynamic nature of the pandemic response, we are continually reevaluating our distancing guidelines to administer the safest and most effective hospital care possible as we approach California’s expected peak coronavirus infection period.
Dr. Jenkins is professor and chair of the Patient Safety Committee in the Division of Hospital Medicine at UCSD. Dr. Seymann is clinical professor and vice chief for academic affairs, UCSD division of hospital medicine. Dr. Horman and Dr. Bell are hospitalists and associate professors of medicine at UC San Diego Health.
Most e-consults not followed by specialist visit
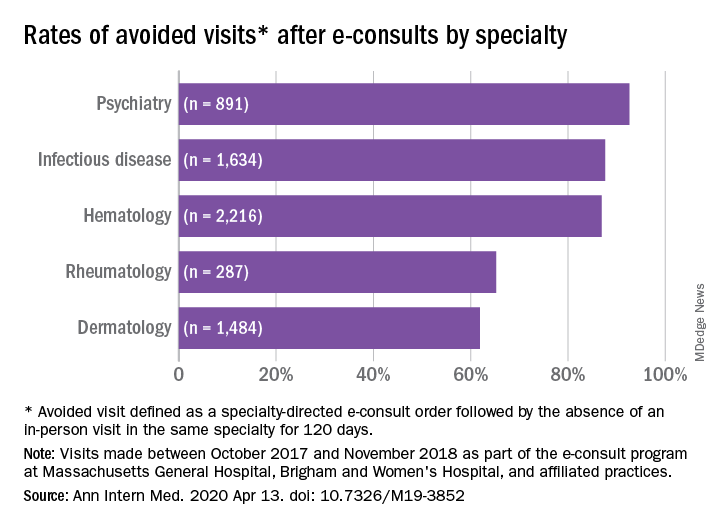
Studies have shown that e-consults increase access to specialist care and primary care physician (PCP) education, according to research published in the Annals of Internal Medicine (2020. Apr 14. doi: 10.7326/M19-3852) by Salman Ahmed, MD, and colleagues.
These resources are already being frequently used by physicians, but more often by general internists and hospitalists than by subspecialists, according to a recent survey by the American College of Physicians. That survey found that 42% of its respondents are using e-consults and that subspecialists’ use is less common primarily because of the lack of access to e-consult technology.
What hasn’t been widely researched are the effects of large-scale e-consult programs, said Dr. Ahmed, who is associate physician in the renal division at Brigham and Women’s Hospital, Boston, in an interview.
For frontline providers such as PCPs, e-consults are a way to quickly seek out answers to clinical questions from specialists. In turn, the specialist can help a wider pool of participants, he noted.
The findings of Dr. Ahmed’s study, which included several academic centers and hospitals affiliated with Partners HealthCare System, a nonprofit network in eastern Massachusetts that includes Brigham and Women’s Hospital, used several metrics to analyze the appropriateness and utility of e-consults across a range of specialties. An e-consult was considered useful if it resulted in the avoidance of a visit to a specialist, which was defined as the absence of an in-person visit to the type of specialist consulted electronically for 120 days. An e-consult was considered appropriate if it met the following four criteria.
- It could not be answered by referring to society guidelines or widely available, evidence-based summary sources.
- It did not seek logistic information, such as where to have a specific laboratory test done.
- It did not include a question of high urgency.
- The medical complexity of the clinical situation was not substantial enough to warrant an in-person consultation.
The investigators examined e-consult inquiries to mostly physician health care providers in five specialties – hematology, infectious disease, dermatology, rheumatology, and psychiatry – over a year.
High rates of appropriateness
The search spanned 6,512 eligible e-consults from 1,096 referring providers to 121 specialist consultants. Narrowing their search to 741 records with complete data, the investigators found that 70.2% of these consults met the criteria for appropriateness. In an analysis of four reviewers blinded to each other’s results, raters agreed on the appropriateness of 94% of e-consults.
Across specialties, more than 81% of e-consults were associated with avoided in-person visits.
The reasons for most e-consults were to seek answers to questions about diagnosis, therapeutics, or patient inquiries, or to request further education by PCPs.
“Across all specialties, the most common reasons an e-consult was not considered appropriate were failing the point-of-care resource test and asking a question of inappropriately high complexity,” the authors summarized.
Physicians and PCPs from tertiary care practices made up the majority of referring providers, with turnaround time for consults averaging 24 hours across specialties.
Rates of appropriateness, content, patient demographics, and timeliness of e-consult responses varied among the four specialties. Those with high avoidance of visits rates tended to have high appropriateness rates, indicating that some specialties may be more conducive to e-consults than others, the authors noted. Psychiatry and hematology had the highest proportion of appropriate e-consults (77.9% and 73.3% respectively). Rheumatology had the lowest proportion of appropriate e-consults and one of the lowest rates of avoided in-person visits, and dermatology had the lowest rate of avoided in-person visits, at 61.9%.
The majority (93%) of e-consults sought in psychiatry were therapy related, whereas 88.4% of the e-consult questions in rheumatology related to diagnosis.
“Questions about diagnosis were less likely to be answerable via e-consult, which suggests that to provide diagnoses, consultants may wish to engage with the patient directly,” Dr. Ahmed said in an interview.
Infectious disease specialists seemed to be the fastest responders, with nearly 90% of their consultations having been answered within a day. Dermatology specialists had the distinction of having the youngest e-consult patients (mean age, 38.6 years).
PCPs weigh in on results
Physicians said in interviews that the study data reflects their own positive experiences with e-consults.
“Although I don’t always think [an e-consult] is able to fully prevent the specialist visit, it does allow the specialist to provide recommendations for work-up that can be done prior to the specialist visit,” said Santina Wheat MD, a family physician at Erie Family Health Center in Chicago. This reduces the time in which the consult is placed to when effective treatment can take place.
Patients who may have to wait months or even years to see a specialty doctor, benefit from e-consults, said Dr. Wheat, who is also a member of the editorial advisory board of Family Practice News. “As part of an organization that does e-consults to another hospital with a different electronic medical record, the e-consult increases the likelihood that all of the clinical information reaches the specialists and prevents tests from being repeated.”
Starting an e-consult may also increase the likelihood that the patient quickly sees a specialist at the contracted hospital, she added.
Sarah G. Candler, MD, said in an interview that she also sees e-consults as an essential tool. “When patients present with rare, complex, or atypical pictures, I find it helpful to have specialists weigh in. The e-consult helps me ensure that I work to the top of my abilities as an internist,” said Dr. Candler, who is practice medical director and physician director of academic relations at Iora Primary Care, Northside Clinic, Houston. However, she did not agree with the study’s avoided in-person visits metric for assessing utility.
“In some cases, the end result of an e-consult is a referral for an in-person evaluation, and the role of the e-consult is to ensure that I have done my due diligence as a primary care doctor asking the correct questions, getting the appropriate work-up completed, and referring to the appropriate specialty for next steps, when necessary,” noted Dr. Candler, who also serves on the editorial advisory board of Internal Medicine News.
Financial considerations
The study’s authors suggested taking a closer look at standardizing payment for the use of e-consults and developing appropriateness criteria for them.
Health systems could use such criteria to study what makes an e-consult useful and how to best utilize this tool, Dr. Ahmed said in an interview.
“Compensation models that promote high-quality, effective, and efficient e-consults are needed to reinforce the ability of health systems to optimize the mix of e-consults and in-person visits,” Dr. Ahmed and colleagues suggested.
Because not all patient care requires e-consults, the model makes the most sense in practices that already participate in value-based payment programs. In these types of programs, the cost can be shared according to the variable risk and patient need for the service, Dr. Candler explained.
“I have been fortunate to work in two different systems that function in this way, which means that e-consults have been readily available and encouraged-both to improve patient care and decrease overall cost by decreasing unnecessary testing or specialist referral,” she said.
Dr. Wheat said that the managed care organization affiliated with her practice seems to be saving money with e-consults, as it decreases the need to pay for specialist visits in some instances and for repeated work-ups.
Future studies
The study’s cohort represented just one large health care system with a shared electronic health record. “Single-system descriptive studies, such as that of Ahmed and colleagues, are particularly useful for local evaluation and quality improvement efforts,” Varsha G. Vimalananda, MD, and B. Graeme Fincke, MD, both of the Center for Healthcare Organization and Implementation Research at Bedford (Mass.) Veterans Affairs Hospital, wrote in a related editorial.
“However, we need innovative approaches to evaluation that estimate the effect of e-consults on quality and cost of care across health care systems and over time. Implementation studies can help to identify key contributors to success,” the editorialists wrote.
One of the study authors, reported receiving personal fees from Bayer outside the submitted work. The other authors of the paper and the authors of the editorial reported no conflicts of interest. Dr. Candler said her employer contracts with an e-consult service, but that she is not compensated for use of the service. She is also a coeditor of Annals of Internal Medicine’s blog, “Fresh Look.”
SOURCE: Ahmed S et al. Ann Intern Med. 2020 Apr 14. doi: 10.7326/M19-3852.
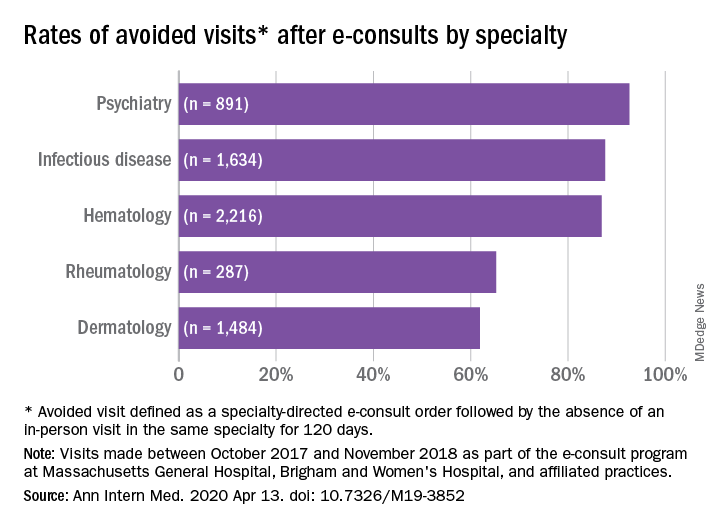
Studies have shown that e-consults increase access to specialist care and primary care physician (PCP) education, according to research published in the Annals of Internal Medicine (2020. Apr 14. doi: 10.7326/M19-3852) by Salman Ahmed, MD, and colleagues.
These resources are already being frequently used by physicians, but more often by general internists and hospitalists than by subspecialists, according to a recent survey by the American College of Physicians. That survey found that 42% of its respondents are using e-consults and that subspecialists’ use is less common primarily because of the lack of access to e-consult technology.
What hasn’t been widely researched are the effects of large-scale e-consult programs, said Dr. Ahmed, who is associate physician in the renal division at Brigham and Women’s Hospital, Boston, in an interview.
For frontline providers such as PCPs, e-consults are a way to quickly seek out answers to clinical questions from specialists. In turn, the specialist can help a wider pool of participants, he noted.
The findings of Dr. Ahmed’s study, which included several academic centers and hospitals affiliated with Partners HealthCare System, a nonprofit network in eastern Massachusetts that includes Brigham and Women’s Hospital, used several metrics to analyze the appropriateness and utility of e-consults across a range of specialties. An e-consult was considered useful if it resulted in the avoidance of a visit to a specialist, which was defined as the absence of an in-person visit to the type of specialist consulted electronically for 120 days. An e-consult was considered appropriate if it met the following four criteria.
- It could not be answered by referring to society guidelines or widely available, evidence-based summary sources.
- It did not seek logistic information, such as where to have a specific laboratory test done.
- It did not include a question of high urgency.
- The medical complexity of the clinical situation was not substantial enough to warrant an in-person consultation.
The investigators examined e-consult inquiries to mostly physician health care providers in five specialties – hematology, infectious disease, dermatology, rheumatology, and psychiatry – over a year.
High rates of appropriateness
The search spanned 6,512 eligible e-consults from 1,096 referring providers to 121 specialist consultants. Narrowing their search to 741 records with complete data, the investigators found that 70.2% of these consults met the criteria for appropriateness. In an analysis of four reviewers blinded to each other’s results, raters agreed on the appropriateness of 94% of e-consults.
Across specialties, more than 81% of e-consults were associated with avoided in-person visits.
The reasons for most e-consults were to seek answers to questions about diagnosis, therapeutics, or patient inquiries, or to request further education by PCPs.
“Across all specialties, the most common reasons an e-consult was not considered appropriate were failing the point-of-care resource test and asking a question of inappropriately high complexity,” the authors summarized.
Physicians and PCPs from tertiary care practices made up the majority of referring providers, with turnaround time for consults averaging 24 hours across specialties.
Rates of appropriateness, content, patient demographics, and timeliness of e-consult responses varied among the four specialties. Those with high avoidance of visits rates tended to have high appropriateness rates, indicating that some specialties may be more conducive to e-consults than others, the authors noted. Psychiatry and hematology had the highest proportion of appropriate e-consults (77.9% and 73.3% respectively). Rheumatology had the lowest proportion of appropriate e-consults and one of the lowest rates of avoided in-person visits, and dermatology had the lowest rate of avoided in-person visits, at 61.9%.
The majority (93%) of e-consults sought in psychiatry were therapy related, whereas 88.4% of the e-consult questions in rheumatology related to diagnosis.
“Questions about diagnosis were less likely to be answerable via e-consult, which suggests that to provide diagnoses, consultants may wish to engage with the patient directly,” Dr. Ahmed said in an interview.
Infectious disease specialists seemed to be the fastest responders, with nearly 90% of their consultations having been answered within a day. Dermatology specialists had the distinction of having the youngest e-consult patients (mean age, 38.6 years).
PCPs weigh in on results
Physicians said in interviews that the study data reflects their own positive experiences with e-consults.
“Although I don’t always think [an e-consult] is able to fully prevent the specialist visit, it does allow the specialist to provide recommendations for work-up that can be done prior to the specialist visit,” said Santina Wheat MD, a family physician at Erie Family Health Center in Chicago. This reduces the time in which the consult is placed to when effective treatment can take place.
Patients who may have to wait months or even years to see a specialty doctor, benefit from e-consults, said Dr. Wheat, who is also a member of the editorial advisory board of Family Practice News. “As part of an organization that does e-consults to another hospital with a different electronic medical record, the e-consult increases the likelihood that all of the clinical information reaches the specialists and prevents tests from being repeated.”
Starting an e-consult may also increase the likelihood that the patient quickly sees a specialist at the contracted hospital, she added.
Sarah G. Candler, MD, said in an interview that she also sees e-consults as an essential tool. “When patients present with rare, complex, or atypical pictures, I find it helpful to have specialists weigh in. The e-consult helps me ensure that I work to the top of my abilities as an internist,” said Dr. Candler, who is practice medical director and physician director of academic relations at Iora Primary Care, Northside Clinic, Houston. However, she did not agree with the study’s avoided in-person visits metric for assessing utility.
“In some cases, the end result of an e-consult is a referral for an in-person evaluation, and the role of the e-consult is to ensure that I have done my due diligence as a primary care doctor asking the correct questions, getting the appropriate work-up completed, and referring to the appropriate specialty for next steps, when necessary,” noted Dr. Candler, who also serves on the editorial advisory board of Internal Medicine News.
Financial considerations
The study’s authors suggested taking a closer look at standardizing payment for the use of e-consults and developing appropriateness criteria for them.
Health systems could use such criteria to study what makes an e-consult useful and how to best utilize this tool, Dr. Ahmed said in an interview.
“Compensation models that promote high-quality, effective, and efficient e-consults are needed to reinforce the ability of health systems to optimize the mix of e-consults and in-person visits,” Dr. Ahmed and colleagues suggested.
Because not all patient care requires e-consults, the model makes the most sense in practices that already participate in value-based payment programs. In these types of programs, the cost can be shared according to the variable risk and patient need for the service, Dr. Candler explained.
“I have been fortunate to work in two different systems that function in this way, which means that e-consults have been readily available and encouraged-both to improve patient care and decrease overall cost by decreasing unnecessary testing or specialist referral,” she said.
Dr. Wheat said that the managed care organization affiliated with her practice seems to be saving money with e-consults, as it decreases the need to pay for specialist visits in some instances and for repeated work-ups.
Future studies
The study’s cohort represented just one large health care system with a shared electronic health record. “Single-system descriptive studies, such as that of Ahmed and colleagues, are particularly useful for local evaluation and quality improvement efforts,” Varsha G. Vimalananda, MD, and B. Graeme Fincke, MD, both of the Center for Healthcare Organization and Implementation Research at Bedford (Mass.) Veterans Affairs Hospital, wrote in a related editorial.
“However, we need innovative approaches to evaluation that estimate the effect of e-consults on quality and cost of care across health care systems and over time. Implementation studies can help to identify key contributors to success,” the editorialists wrote.
One of the study authors, reported receiving personal fees from Bayer outside the submitted work. The other authors of the paper and the authors of the editorial reported no conflicts of interest. Dr. Candler said her employer contracts with an e-consult service, but that she is not compensated for use of the service. She is also a coeditor of Annals of Internal Medicine’s blog, “Fresh Look.”
SOURCE: Ahmed S et al. Ann Intern Med. 2020 Apr 14. doi: 10.7326/M19-3852.
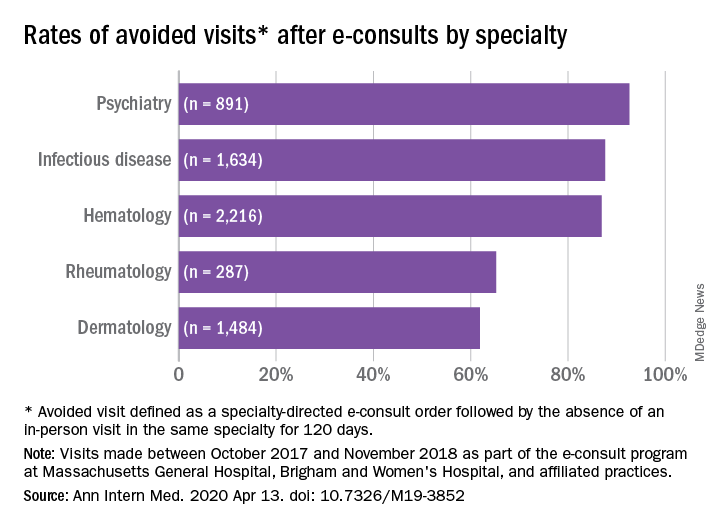
Studies have shown that e-consults increase access to specialist care and primary care physician (PCP) education, according to research published in the Annals of Internal Medicine (2020. Apr 14. doi: 10.7326/M19-3852) by Salman Ahmed, MD, and colleagues.
These resources are already being frequently used by physicians, but more often by general internists and hospitalists than by subspecialists, according to a recent survey by the American College of Physicians. That survey found that 42% of its respondents are using e-consults and that subspecialists’ use is less common primarily because of the lack of access to e-consult technology.
What hasn’t been widely researched are the effects of large-scale e-consult programs, said Dr. Ahmed, who is associate physician in the renal division at Brigham and Women’s Hospital, Boston, in an interview.
For frontline providers such as PCPs, e-consults are a way to quickly seek out answers to clinical questions from specialists. In turn, the specialist can help a wider pool of participants, he noted.
The findings of Dr. Ahmed’s study, which included several academic centers and hospitals affiliated with Partners HealthCare System, a nonprofit network in eastern Massachusetts that includes Brigham and Women’s Hospital, used several metrics to analyze the appropriateness and utility of e-consults across a range of specialties. An e-consult was considered useful if it resulted in the avoidance of a visit to a specialist, which was defined as the absence of an in-person visit to the type of specialist consulted electronically for 120 days. An e-consult was considered appropriate if it met the following four criteria.
- It could not be answered by referring to society guidelines or widely available, evidence-based summary sources.
- It did not seek logistic information, such as where to have a specific laboratory test done.
- It did not include a question of high urgency.
- The medical complexity of the clinical situation was not substantial enough to warrant an in-person consultation.
The investigators examined e-consult inquiries to mostly physician health care providers in five specialties – hematology, infectious disease, dermatology, rheumatology, and psychiatry – over a year.
High rates of appropriateness
The search spanned 6,512 eligible e-consults from 1,096 referring providers to 121 specialist consultants. Narrowing their search to 741 records with complete data, the investigators found that 70.2% of these consults met the criteria for appropriateness. In an analysis of four reviewers blinded to each other’s results, raters agreed on the appropriateness of 94% of e-consults.
Across specialties, more than 81% of e-consults were associated with avoided in-person visits.
The reasons for most e-consults were to seek answers to questions about diagnosis, therapeutics, or patient inquiries, or to request further education by PCPs.
“Across all specialties, the most common reasons an e-consult was not considered appropriate were failing the point-of-care resource test and asking a question of inappropriately high complexity,” the authors summarized.
Physicians and PCPs from tertiary care practices made up the majority of referring providers, with turnaround time for consults averaging 24 hours across specialties.
Rates of appropriateness, content, patient demographics, and timeliness of e-consult responses varied among the four specialties. Those with high avoidance of visits rates tended to have high appropriateness rates, indicating that some specialties may be more conducive to e-consults than others, the authors noted. Psychiatry and hematology had the highest proportion of appropriate e-consults (77.9% and 73.3% respectively). Rheumatology had the lowest proportion of appropriate e-consults and one of the lowest rates of avoided in-person visits, and dermatology had the lowest rate of avoided in-person visits, at 61.9%.
The majority (93%) of e-consults sought in psychiatry were therapy related, whereas 88.4% of the e-consult questions in rheumatology related to diagnosis.
“Questions about diagnosis were less likely to be answerable via e-consult, which suggests that to provide diagnoses, consultants may wish to engage with the patient directly,” Dr. Ahmed said in an interview.
Infectious disease specialists seemed to be the fastest responders, with nearly 90% of their consultations having been answered within a day. Dermatology specialists had the distinction of having the youngest e-consult patients (mean age, 38.6 years).
PCPs weigh in on results
Physicians said in interviews that the study data reflects their own positive experiences with e-consults.
“Although I don’t always think [an e-consult] is able to fully prevent the specialist visit, it does allow the specialist to provide recommendations for work-up that can be done prior to the specialist visit,” said Santina Wheat MD, a family physician at Erie Family Health Center in Chicago. This reduces the time in which the consult is placed to when effective treatment can take place.
Patients who may have to wait months or even years to see a specialty doctor, benefit from e-consults, said Dr. Wheat, who is also a member of the editorial advisory board of Family Practice News. “As part of an organization that does e-consults to another hospital with a different electronic medical record, the e-consult increases the likelihood that all of the clinical information reaches the specialists and prevents tests from being repeated.”
Starting an e-consult may also increase the likelihood that the patient quickly sees a specialist at the contracted hospital, she added.
Sarah G. Candler, MD, said in an interview that she also sees e-consults as an essential tool. “When patients present with rare, complex, or atypical pictures, I find it helpful to have specialists weigh in. The e-consult helps me ensure that I work to the top of my abilities as an internist,” said Dr. Candler, who is practice medical director and physician director of academic relations at Iora Primary Care, Northside Clinic, Houston. However, she did not agree with the study’s avoided in-person visits metric for assessing utility.
“In some cases, the end result of an e-consult is a referral for an in-person evaluation, and the role of the e-consult is to ensure that I have done my due diligence as a primary care doctor asking the correct questions, getting the appropriate work-up completed, and referring to the appropriate specialty for next steps, when necessary,” noted Dr. Candler, who also serves on the editorial advisory board of Internal Medicine News.
Financial considerations
The study’s authors suggested taking a closer look at standardizing payment for the use of e-consults and developing appropriateness criteria for them.
Health systems could use such criteria to study what makes an e-consult useful and how to best utilize this tool, Dr. Ahmed said in an interview.
“Compensation models that promote high-quality, effective, and efficient e-consults are needed to reinforce the ability of health systems to optimize the mix of e-consults and in-person visits,” Dr. Ahmed and colleagues suggested.
Because not all patient care requires e-consults, the model makes the most sense in practices that already participate in value-based payment programs. In these types of programs, the cost can be shared according to the variable risk and patient need for the service, Dr. Candler explained.
“I have been fortunate to work in two different systems that function in this way, which means that e-consults have been readily available and encouraged-both to improve patient care and decrease overall cost by decreasing unnecessary testing or specialist referral,” she said.
Dr. Wheat said that the managed care organization affiliated with her practice seems to be saving money with e-consults, as it decreases the need to pay for specialist visits in some instances and for repeated work-ups.
Future studies
The study’s cohort represented just one large health care system with a shared electronic health record. “Single-system descriptive studies, such as that of Ahmed and colleagues, are particularly useful for local evaluation and quality improvement efforts,” Varsha G. Vimalananda, MD, and B. Graeme Fincke, MD, both of the Center for Healthcare Organization and Implementation Research at Bedford (Mass.) Veterans Affairs Hospital, wrote in a related editorial.
“However, we need innovative approaches to evaluation that estimate the effect of e-consults on quality and cost of care across health care systems and over time. Implementation studies can help to identify key contributors to success,” the editorialists wrote.
One of the study authors, reported receiving personal fees from Bayer outside the submitted work. The other authors of the paper and the authors of the editorial reported no conflicts of interest. Dr. Candler said her employer contracts with an e-consult service, but that she is not compensated for use of the service. She is also a coeditor of Annals of Internal Medicine’s blog, “Fresh Look.”
SOURCE: Ahmed S et al. Ann Intern Med. 2020 Apr 14. doi: 10.7326/M19-3852.
FROM ANNALS OF INTERNAL MEDICINE


















