User login
Red eyes with a brown spot
A 32-year-old woman came to the rescue mission clinic with her 2 sons because she had red eyes and a runny nose. Her sons both had symptoms highly suggestive of viral upper respiratory infection. They lived in a homeless shelter.
The patient stated she did not use contact lenses or have any eye trauma, itching, photophobia, loss or change of vision, eye pain, eye discharge, or previous episodes of pinkeye. She had no other medical problems or history of allergies.
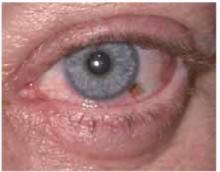
On physical exam, her vital signs were normal. She had conjunctival injection, without purulent discharge or limbal blush (Figures 1 and 2). Eyelids were mildly erythematous with no cobble-stoning. Pupils were equal, round, and reactive to light. The anterior chamber by flashlight exam from the side did not show a narrow angle. Visual acuity was normal by Snellen exam. She had clear nasal discharge and bilateral preauricular lymphadenopathy.
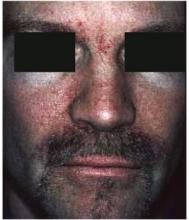
In addition, she had a brown macule under the left iris on the conjunctiva. The patient said this had been present since childhood and it had not changed.
FIGURE 1
Red eyes
FIGURE 2
Brown macule
What is the differential iagnosis?
What about the brown macule?
Are any diagnostic tests Necessary for either condition?
Differential diagnosis
The differential diagnosis of a red eye includes:
- Conjunctivitis
- Uveitis
- Acute glaucoma
- Corneal disease or foreign body trauma
- Scleritis and episcleritis.1
For this patient, conjunctivitis is the most likely diagnosis. The absence of eye pain or loss of vision makes uveitis, acute glaucoma, or corneal disease (including foreign-body trauma) less likely. The round shape of the pupil and the absence of the limbal blush also make uveitis less likely. The pattern of injection does not match the wedge-shaped inflammation of episcleritis or the depth of scleritis.
Diagnosis: viral conjunctivitis
This patient has viral conjunctivitis. Conjunctivitis can be infectious, allergic, chemical/irritative, or autoimmune in origin. The most common infectious agents are viral—specifically, the adenoviruses. Other infectious agents include bacteria (Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria gonorrhoeae), chlamydia, and herpes simplex virus.
Both infectious and allergic conjunctivitis are common. In this patient, the presence of nasal discharge, preauricular lymphadenopathy, and the lack of pruritus make viral infection more likely than allergic. Conjunctivitis that is bilateral without purulent discharge is more likely to be viral than bacterial.
What about the brown macule?
This patient also had a brown macule on her conjunctiva. The differential diagnosis of pigmented areas on the conjunctiva includes nevus, racial melanosis, primary acquired melanosis, secondary pigmentary deposition, and ocular melanoma.2 These conditions (besides ocular melanoma) are benign.
Although ocular melanoma is the most common primary intraocular malignancy in adults, and the second most likely location for primary melanoma after the skin, it is still exceedingly rare. In the Causasian population, it has an average annual incidence of 6 cases per million, with approximately 1200 cases diagnosed each year. Ocular melanoma occurs in the uvea much more commonly than in the conjunctiva, at a ratio of 35:1. Conjunctival melanomas have a propensity for regional spread to the lymph nodes analogous to cutaneous disease, with 10-year survival rates of more than 80%.3
In this case, the patient had this dark spot since childhood and had noted no growth or change. It was consistent with a conjunctival nevus and did not need biopsy.
Diagnostic tests: only for cases that do not respond
When viral conjunctivitis is suspected, no laboratory tests are routinely recommended. Bacterial and viral cultures may be helpful to establish the diagnosis in cases that do not resolve or when patients have recurrent episodes. Infections that do not respond to empiric treatment should be cultured for the suspected organisms (bacteria, chlamydia, or herpes simplex). When chlamydial conjunctivitis is suspected, the diagnosis should be confirmed by means of an immunodiagnostic test (direct fluorescent antibody [DFA]) or culture (level of evidence [LOE]=1a).4
A fluorescein exam is helpful in cases with a question of corneal involvement from foreign-body trauma, herpes simplex, or epidemic kerato-conjunctivitis. Herpes simplex infections have a dendritic pattern of ulceration, and epidemic keratoconjunctivitis infections cause multiple small areas of increased fluorescein uptake.
Management: conjunctivitis usually self-limiting
Typical viral conjunctivitis caused by the adenoviruses or other common viruses (not herpes) does not require medication. Warm compresses may be recommended to reduce discomfort. Infectious conjunctivitis caused by bacteria are also usually self-limiting; however, a recent meta-analysis indicates that treatment with antibiotics can shorten the clinical duration (LOE=1a).5
Appropriate medications for bacterial conjunctivitis include 0.3% tobramycin or gentamycin, 10% sodium sulfacetamide, or erythromycin ophthalmic ointment. If herpetic keratoconjuntivitis is suspected, prompt ophthalmologic referral is indicated.1
Patient’s treatment and outcome
This patient was managed with reassurance and symptomatic treatment of her viral respiratory illness. Her red eyes and upper respiratory infection both resolved spontaneously within 1 week.
As her nevus had not changed in many years, she was instructed to continue to watch the nevus and report any changes to a physician for evaluation. If the lesion changed in the future, she should be referred to an ophthalmologist.
- Erythromycin (ophthalmic) • Ilotycin
- Gentamycin (ophthalmic) • Garamycin, Genoptic Liquifilm, Genoptic SOP, Gentacidin, Gentafair, Gentak, Ocu-Mycin, Spectro-Genta
- Sulfacetamide (ophthalmic) • AK-Sulf, Bleph-10, Cetamide, Isopto Cetamide, Ocusulf-10, Sodium Sulamyd, Sulf-10
- Tobramycin (ophthalmic) • AKTob, Tobrex
Correspondence
Richard P. Usatine, Editor, Photo Rounds, University of Texas Health Sciences Center at San Antonio, Dept of Family and Community Medicine, MC 7794, 7703 Floyd Curl Drive, San Antonio, TX 78229-3900. E-mail: [email protected].
1. Ricketson CW. Conjunctivitis in 5-minute clinical consult. Dambro, MR (ed). InfoRetriever [electronic database]. Charlottesville, Va: InfoPOEMs, Inc; 2004.
2. Shields CL, Shields JA. Tumors of the conjunctiva and cornea. Surv Ophthalmol 2004;49:3-24.
3. Hurst EA, Harbour JW, Cornelius LA. Ocular melanoma: a review and the relationship to cutaneous melanoma. Arch Dermatol 2003;139:1067-1073.
4. American Academy of Ophthalmology. Preferred Practice Patterns. Conjunctivitis. Available at: www.aao.org/aao/education/library/ppp/index.cfm. Accessed on February 3, 2004.
5. Sheikh A, Hurwitz B, Cave J. Antibiotics versus placebo for acute bacterial conjunctivitis (Cochrane Review). In: The Cochrane Library, Issue 4, 2003.
A 32-year-old woman came to the rescue mission clinic with her 2 sons because she had red eyes and a runny nose. Her sons both had symptoms highly suggestive of viral upper respiratory infection. They lived in a homeless shelter.
The patient stated she did not use contact lenses or have any eye trauma, itching, photophobia, loss or change of vision, eye pain, eye discharge, or previous episodes of pinkeye. She had no other medical problems or history of allergies.
On physical exam, her vital signs were normal. She had conjunctival injection, without purulent discharge or limbal blush (Figures 1 and 2). Eyelids were mildly erythematous with no cobble-stoning. Pupils were equal, round, and reactive to light. The anterior chamber by flashlight exam from the side did not show a narrow angle. Visual acuity was normal by Snellen exam. She had clear nasal discharge and bilateral preauricular lymphadenopathy.
In addition, she had a brown macule under the left iris on the conjunctiva. The patient said this had been present since childhood and it had not changed.
FIGURE 1
Red eyes
FIGURE 2
Brown macule
What is the differential iagnosis?
What about the brown macule?
Are any diagnostic tests Necessary for either condition?
Differential diagnosis
The differential diagnosis of a red eye includes:
- Conjunctivitis
- Uveitis
- Acute glaucoma
- Corneal disease or foreign body trauma
- Scleritis and episcleritis.1
For this patient, conjunctivitis is the most likely diagnosis. The absence of eye pain or loss of vision makes uveitis, acute glaucoma, or corneal disease (including foreign-body trauma) less likely. The round shape of the pupil and the absence of the limbal blush also make uveitis less likely. The pattern of injection does not match the wedge-shaped inflammation of episcleritis or the depth of scleritis.
Diagnosis: viral conjunctivitis
This patient has viral conjunctivitis. Conjunctivitis can be infectious, allergic, chemical/irritative, or autoimmune in origin. The most common infectious agents are viral—specifically, the adenoviruses. Other infectious agents include bacteria (Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria gonorrhoeae), chlamydia, and herpes simplex virus.
Both infectious and allergic conjunctivitis are common. In this patient, the presence of nasal discharge, preauricular lymphadenopathy, and the lack of pruritus make viral infection more likely than allergic. Conjunctivitis that is bilateral without purulent discharge is more likely to be viral than bacterial.
What about the brown macule?
This patient also had a brown macule on her conjunctiva. The differential diagnosis of pigmented areas on the conjunctiva includes nevus, racial melanosis, primary acquired melanosis, secondary pigmentary deposition, and ocular melanoma.2 These conditions (besides ocular melanoma) are benign.
Although ocular melanoma is the most common primary intraocular malignancy in adults, and the second most likely location for primary melanoma after the skin, it is still exceedingly rare. In the Causasian population, it has an average annual incidence of 6 cases per million, with approximately 1200 cases diagnosed each year. Ocular melanoma occurs in the uvea much more commonly than in the conjunctiva, at a ratio of 35:1. Conjunctival melanomas have a propensity for regional spread to the lymph nodes analogous to cutaneous disease, with 10-year survival rates of more than 80%.3
In this case, the patient had this dark spot since childhood and had noted no growth or change. It was consistent with a conjunctival nevus and did not need biopsy.
Diagnostic tests: only for cases that do not respond
When viral conjunctivitis is suspected, no laboratory tests are routinely recommended. Bacterial and viral cultures may be helpful to establish the diagnosis in cases that do not resolve or when patients have recurrent episodes. Infections that do not respond to empiric treatment should be cultured for the suspected organisms (bacteria, chlamydia, or herpes simplex). When chlamydial conjunctivitis is suspected, the diagnosis should be confirmed by means of an immunodiagnostic test (direct fluorescent antibody [DFA]) or culture (level of evidence [LOE]=1a).4
A fluorescein exam is helpful in cases with a question of corneal involvement from foreign-body trauma, herpes simplex, or epidemic kerato-conjunctivitis. Herpes simplex infections have a dendritic pattern of ulceration, and epidemic keratoconjunctivitis infections cause multiple small areas of increased fluorescein uptake.
Management: conjunctivitis usually self-limiting
Typical viral conjunctivitis caused by the adenoviruses or other common viruses (not herpes) does not require medication. Warm compresses may be recommended to reduce discomfort. Infectious conjunctivitis caused by bacteria are also usually self-limiting; however, a recent meta-analysis indicates that treatment with antibiotics can shorten the clinical duration (LOE=1a).5
Appropriate medications for bacterial conjunctivitis include 0.3% tobramycin or gentamycin, 10% sodium sulfacetamide, or erythromycin ophthalmic ointment. If herpetic keratoconjuntivitis is suspected, prompt ophthalmologic referral is indicated.1
Patient’s treatment and outcome
This patient was managed with reassurance and symptomatic treatment of her viral respiratory illness. Her red eyes and upper respiratory infection both resolved spontaneously within 1 week.
As her nevus had not changed in many years, she was instructed to continue to watch the nevus and report any changes to a physician for evaluation. If the lesion changed in the future, she should be referred to an ophthalmologist.
- Erythromycin (ophthalmic) • Ilotycin
- Gentamycin (ophthalmic) • Garamycin, Genoptic Liquifilm, Genoptic SOP, Gentacidin, Gentafair, Gentak, Ocu-Mycin, Spectro-Genta
- Sulfacetamide (ophthalmic) • AK-Sulf, Bleph-10, Cetamide, Isopto Cetamide, Ocusulf-10, Sodium Sulamyd, Sulf-10
- Tobramycin (ophthalmic) • AKTob, Tobrex
Correspondence
Richard P. Usatine, Editor, Photo Rounds, University of Texas Health Sciences Center at San Antonio, Dept of Family and Community Medicine, MC 7794, 7703 Floyd Curl Drive, San Antonio, TX 78229-3900. E-mail: [email protected].
A 32-year-old woman came to the rescue mission clinic with her 2 sons because she had red eyes and a runny nose. Her sons both had symptoms highly suggestive of viral upper respiratory infection. They lived in a homeless shelter.
The patient stated she did not use contact lenses or have any eye trauma, itching, photophobia, loss or change of vision, eye pain, eye discharge, or previous episodes of pinkeye. She had no other medical problems or history of allergies.
On physical exam, her vital signs were normal. She had conjunctival injection, without purulent discharge or limbal blush (Figures 1 and 2). Eyelids were mildly erythematous with no cobble-stoning. Pupils were equal, round, and reactive to light. The anterior chamber by flashlight exam from the side did not show a narrow angle. Visual acuity was normal by Snellen exam. She had clear nasal discharge and bilateral preauricular lymphadenopathy.
In addition, she had a brown macule under the left iris on the conjunctiva. The patient said this had been present since childhood and it had not changed.
FIGURE 1
Red eyes
FIGURE 2
Brown macule
What is the differential iagnosis?
What about the brown macule?
Are any diagnostic tests Necessary for either condition?
Differential diagnosis
The differential diagnosis of a red eye includes:
- Conjunctivitis
- Uveitis
- Acute glaucoma
- Corneal disease or foreign body trauma
- Scleritis and episcleritis.1
For this patient, conjunctivitis is the most likely diagnosis. The absence of eye pain or loss of vision makes uveitis, acute glaucoma, or corneal disease (including foreign-body trauma) less likely. The round shape of the pupil and the absence of the limbal blush also make uveitis less likely. The pattern of injection does not match the wedge-shaped inflammation of episcleritis or the depth of scleritis.
Diagnosis: viral conjunctivitis
This patient has viral conjunctivitis. Conjunctivitis can be infectious, allergic, chemical/irritative, or autoimmune in origin. The most common infectious agents are viral—specifically, the adenoviruses. Other infectious agents include bacteria (Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria gonorrhoeae), chlamydia, and herpes simplex virus.
Both infectious and allergic conjunctivitis are common. In this patient, the presence of nasal discharge, preauricular lymphadenopathy, and the lack of pruritus make viral infection more likely than allergic. Conjunctivitis that is bilateral without purulent discharge is more likely to be viral than bacterial.
What about the brown macule?
This patient also had a brown macule on her conjunctiva. The differential diagnosis of pigmented areas on the conjunctiva includes nevus, racial melanosis, primary acquired melanosis, secondary pigmentary deposition, and ocular melanoma.2 These conditions (besides ocular melanoma) are benign.
Although ocular melanoma is the most common primary intraocular malignancy in adults, and the second most likely location for primary melanoma after the skin, it is still exceedingly rare. In the Causasian population, it has an average annual incidence of 6 cases per million, with approximately 1200 cases diagnosed each year. Ocular melanoma occurs in the uvea much more commonly than in the conjunctiva, at a ratio of 35:1. Conjunctival melanomas have a propensity for regional spread to the lymph nodes analogous to cutaneous disease, with 10-year survival rates of more than 80%.3
In this case, the patient had this dark spot since childhood and had noted no growth or change. It was consistent with a conjunctival nevus and did not need biopsy.
Diagnostic tests: only for cases that do not respond
When viral conjunctivitis is suspected, no laboratory tests are routinely recommended. Bacterial and viral cultures may be helpful to establish the diagnosis in cases that do not resolve or when patients have recurrent episodes. Infections that do not respond to empiric treatment should be cultured for the suspected organisms (bacteria, chlamydia, or herpes simplex). When chlamydial conjunctivitis is suspected, the diagnosis should be confirmed by means of an immunodiagnostic test (direct fluorescent antibody [DFA]) or culture (level of evidence [LOE]=1a).4
A fluorescein exam is helpful in cases with a question of corneal involvement from foreign-body trauma, herpes simplex, or epidemic kerato-conjunctivitis. Herpes simplex infections have a dendritic pattern of ulceration, and epidemic keratoconjunctivitis infections cause multiple small areas of increased fluorescein uptake.
Management: conjunctivitis usually self-limiting
Typical viral conjunctivitis caused by the adenoviruses or other common viruses (not herpes) does not require medication. Warm compresses may be recommended to reduce discomfort. Infectious conjunctivitis caused by bacteria are also usually self-limiting; however, a recent meta-analysis indicates that treatment with antibiotics can shorten the clinical duration (LOE=1a).5
Appropriate medications for bacterial conjunctivitis include 0.3% tobramycin or gentamycin, 10% sodium sulfacetamide, or erythromycin ophthalmic ointment. If herpetic keratoconjuntivitis is suspected, prompt ophthalmologic referral is indicated.1
Patient’s treatment and outcome
This patient was managed with reassurance and symptomatic treatment of her viral respiratory illness. Her red eyes and upper respiratory infection both resolved spontaneously within 1 week.
As her nevus had not changed in many years, she was instructed to continue to watch the nevus and report any changes to a physician for evaluation. If the lesion changed in the future, she should be referred to an ophthalmologist.
- Erythromycin (ophthalmic) • Ilotycin
- Gentamycin (ophthalmic) • Garamycin, Genoptic Liquifilm, Genoptic SOP, Gentacidin, Gentafair, Gentak, Ocu-Mycin, Spectro-Genta
- Sulfacetamide (ophthalmic) • AK-Sulf, Bleph-10, Cetamide, Isopto Cetamide, Ocusulf-10, Sodium Sulamyd, Sulf-10
- Tobramycin (ophthalmic) • AKTob, Tobrex
Correspondence
Richard P. Usatine, Editor, Photo Rounds, University of Texas Health Sciences Center at San Antonio, Dept of Family and Community Medicine, MC 7794, 7703 Floyd Curl Drive, San Antonio, TX 78229-3900. E-mail: [email protected].
1. Ricketson CW. Conjunctivitis in 5-minute clinical consult. Dambro, MR (ed). InfoRetriever [electronic database]. Charlottesville, Va: InfoPOEMs, Inc; 2004.
2. Shields CL, Shields JA. Tumors of the conjunctiva and cornea. Surv Ophthalmol 2004;49:3-24.
3. Hurst EA, Harbour JW, Cornelius LA. Ocular melanoma: a review and the relationship to cutaneous melanoma. Arch Dermatol 2003;139:1067-1073.
4. American Academy of Ophthalmology. Preferred Practice Patterns. Conjunctivitis. Available at: www.aao.org/aao/education/library/ppp/index.cfm. Accessed on February 3, 2004.
5. Sheikh A, Hurwitz B, Cave J. Antibiotics versus placebo for acute bacterial conjunctivitis (Cochrane Review). In: The Cochrane Library, Issue 4, 2003.
1. Ricketson CW. Conjunctivitis in 5-minute clinical consult. Dambro, MR (ed). InfoRetriever [electronic database]. Charlottesville, Va: InfoPOEMs, Inc; 2004.
2. Shields CL, Shields JA. Tumors of the conjunctiva and cornea. Surv Ophthalmol 2004;49:3-24.
3. Hurst EA, Harbour JW, Cornelius LA. Ocular melanoma: a review and the relationship to cutaneous melanoma. Arch Dermatol 2003;139:1067-1073.
4. American Academy of Ophthalmology. Preferred Practice Patterns. Conjunctivitis. Available at: www.aao.org/aao/education/library/ppp/index.cfm. Accessed on February 3, 2004.
5. Sheikh A, Hurwitz B, Cave J. Antibiotics versus placebo for acute bacterial conjunctivitis (Cochrane Review). In: The Cochrane Library, Issue 4, 2003.
Bald spots on a young girl
An 8-year-old Hispanic girl was brought to see her family physician by her mother, who noticed 2 bald spots on the back of her daughter’s scalp while brushing her hair. The child had no itching or pain. No obvious precipitating events preceded the hair loss.
The mother was more worried than the child: she didn’t want to see her beautiful girl become bald. The girl was pleased that the bald spots could be completely covered with her long hair, but she didn’t want anyone to see them. The child was otherwise healthy. She did not have any chronic medical problems and was not taking any medications. No one else in the family had a similar problem.
When the mother lifted the hair in the back, 2 round areas of hair loss were evident (Figure 1). On close inspection, there was no scaling or scarring. Her nails were normal. The child was afebrile, and the remainder of her exam was unremarkable.
FIGURE 1
Two round areas of hair loss
What is the diagnosis?
What are the management options?
Diagnosis: alopecia areata
This is the typical appearance of alopecia areata, a chronic inflammatory disease that affects the hair follicles, causing sudden hair loss. Sometimes it affects the nails as well.1 Alopecia areata occurs in both males and females of all ages and races.
Alopecia areata may be an autoimmune disease, though this is unproven. The affected skin may be slightly erythematous but otherwise appears normal. Short broken hairs (exclamation-mark hairs) may be seen around the margins of expanding patches of baldness. The nails are involved in about 10% of patients with severe enough alopecia to be referred to a specialist.1
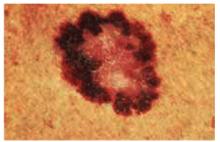
Many cases begin in childhood and can be psychologically devastating. Alopecia areata is part of a spectrum of diseases with mild to extensive hair loss (Figure 2), including alopecia totalis, in which all the hair on the scalp is lost, and alopecia universalis (Figure 3), in which all the hair on the body is lost. Extensive involvement, early age of onset, and Down syndrome are all poor prognostic factors for alopecia areata.
FIGURE 2
More extensive alopecia
FIGURE 3
Alopecia universalis
Differential diagnoses
The differential diagnosis for alopecia areata includes tinea capitis, trichotillomania, early scarring alopecia, telogen effluvium, anagen effluvium (drug-induced), systemic and discoid lupus erythematosus, and secondary syphilis. In most cases the history and physical exam are adequate to make the diagnosis.
This patient does not have the typical scalp scaling and inflammation seen with tinea capitis. Trichotillomania—hair loss caused by the purposeful pulling of hair by the patient—is likely to cause the most confusion because it coexists with alopecia areata in some cases. This child has shown no evidence of such behavior. She also has no evidence of scalp scarring as may be seen in lupus. Telogen effluvium and anagen effluvium cause a more even distribution of hair loss. The patient has no known risk factors for secondary syphilis.
Laboratory testing
No lab tests are needed in this case. If there were some scalp scaling or inflammation, a potassium hydroxide preparation of the involved area would be useful to look for fungal elements; a fungal culture might also be warranted. If needed, further investigations might include serological testing for lupus erythematosus and syphilis, and a skin biopsy if the diagnosis is still unknown.
Treatment: time, drug therapies, aromatherapy
Spontaneous remission occurs in up to 80% of patients with limited patchy hair loss of less than 1 year.1 Spontaneous remission rates are significantly lower with more extensive hair loss.
Treatments are potentially painful, expensive, or time-consuming, and few randomized controlled trials support their use. Often the best treatment is watching for spontaneous remission.
The only adverse health effect of alopecia areata is the psychological distress that it may cause. While this is not to be taken lightly, the lack of evidence for successful treatments needs to be weighed with the patient’s ability to cope with leaving the hair loss untreated over time. In cases of extensive hair loss, the best treatment may be a wig.
For patients that have more visible and extensive areas of hair loss, the psychological impact might prompt the patient to want any treatment available despite the lack of evidence. Alopecia totalis or universalis may cause considerable psychological and social disability. Patients can be referred to the National Alopecia Areata Foundation for support groups and additional information. Individual counseling may be needed for some patients.
National Alopecia Areata Foundation Web site: www.alopeciaareata.com. Patients can order a 7-minute video, This Weird Thing That Makes My Hair Fall Out: Alopecia Areata, which is available for any children who want a way to share their feelings about alopecia areata with friends, family, peers, schoolmates, principals, and teachers.
European Hair Research Society Web site: www.ehrs.org. Web site has links to several alopecia areata sites.
Steroid injections
Intralesional steroid injections may stimulate regrowth of hair at the site of injection (level of evidence [LOE]=5).1 The effect may last a few months, but there is no evidence that it improves the long-term outcome or increases the probability of a cure. New areas of alopecia can still develop.
Injections are typically performed with 5–10 mg/mL of triamcinolone acetonide using a small-gauge needle. Most children will not be able to tolerate the scalp injections and should not be forced to endure this type of therapy even if the parent is pushing for it.
Other medications
Topical diphenylcyclopropenone (DPCP) is a contact immunotherapy that has some proven benefit with extensive alopecia areata (LOE=2b).1,2 In 1 study, 56 patients with chronic, extensive alopecia areata (duration ranging from 1 to 10 years, involving 30% to 100% of the scalp) were treated with progressively higher concentrations of DPCP in a randomized crossover trial.2 Twenty-five of 56 patients had total hair regrowth at 6 months, and no relapse occurred in 60% of patients. Side effects included local inflammation, eczema, autosensitization reaction, and eyelid edema.
Unfortunately, contact immunotherapy involves multiple visits to the office over several months, and it stimulates cosmetically worthwhile hair regrowth in <50% of patients with extensive patchy hair loss.1 It is a reasonable alternative for patients who do not have spontaneous remission after 1 year.
While potent topical steroids and topical minoxidil are prescribed for limited patchy alopecia areata, no convincing evidence shows they are effective.1 Likewise, no evidence warrants the use systemic steroids or psoralen/ultraviolet light treatment (PUVA).1
Aromatherapy
The best evidence may be for aromatherapy. A single-blinded randomized controlled trial was performed with 86 patients.3 As Dr Ebell points out in his InfoPOEMs review of this study, aromatherapy involves rubbing scented essential oils into the skin to treat localized and systemic disease.4 Patients with alopecia areata were randomized to nightly aromatherapy—with Thymus vulgaris (thyme), Lavandula angustifolia (lavender), Rosmarinus officinalis (rosemary), and Cedrus atlantica (cedar)—or to a control consisting of carrier oils only.
Improvement was seen in 54% of the treatment group and 21% of the control group (P=.008; number needed to treat=3). Of the 19 patients in the active treatment group who reported improvement, 11 had “very good” or “excellent” improvement. The results show aromatherapy to be a safe and effective treatment for alopecia areata (LOE=1b).4
The main problem with this study is that the researchers did not describe the duration of the patients’ alopecia. However, in a reply to a letter, they described the patients as having had alopecia areata from less than 1 year to more than 9 years. This explains the low improvement rates in both groups but does not invalidate the statistically significant difference for those that received the essential oils.
Conclusion of visit, follow-up
For a mild case like this in which the hair loss can be hidden, the best treatment is reassurance and observation. The physician explained the natural history of the disease, including the fact that regrowth will take at least 3 months for any single patch. Therapeutic options were also discussed. The mother and child were reassured that the hair is likely to grow in on its own. Neither of them wanted intralesional injections or topical therapies.
One year later during a well-child check, it was noted that the girl’s hair had fully regrown.
1. MacDonald Hull SP, Wood ML, Hutchinson PE, Sladden M, Messenger AG. Guidelines for the management of alopecia areata. Br J Dermatol 2003;149:692-699.
2. Cotellessa C, Peris K, Caracciolo E, Mordenti C, Chimenti S. The use of topical diphenylcyclopropenone for the treatment of extensive alopecia areata. J Am Acad Dermatol 2001;44:73-76.
3. Hay IC, Jamieson M, Ormerod AD. Randomized trial of aromatherapy: successful treatment for alopecia areata. Arch Derm 1998;134:1349-1352.
4. Ebell M. Aromatherapy effective for alopecia areata. Review of Hay et al 1998. InfoPOEMs, Inc. March 1999.
An 8-year-old Hispanic girl was brought to see her family physician by her mother, who noticed 2 bald spots on the back of her daughter’s scalp while brushing her hair. The child had no itching or pain. No obvious precipitating events preceded the hair loss.
The mother was more worried than the child: she didn’t want to see her beautiful girl become bald. The girl was pleased that the bald spots could be completely covered with her long hair, but she didn’t want anyone to see them. The child was otherwise healthy. She did not have any chronic medical problems and was not taking any medications. No one else in the family had a similar problem.
When the mother lifted the hair in the back, 2 round areas of hair loss were evident (Figure 1). On close inspection, there was no scaling or scarring. Her nails were normal. The child was afebrile, and the remainder of her exam was unremarkable.
FIGURE 1
Two round areas of hair loss
What is the diagnosis?
What are the management options?
Diagnosis: alopecia areata
This is the typical appearance of alopecia areata, a chronic inflammatory disease that affects the hair follicles, causing sudden hair loss. Sometimes it affects the nails as well.1 Alopecia areata occurs in both males and females of all ages and races.
Alopecia areata may be an autoimmune disease, though this is unproven. The affected skin may be slightly erythematous but otherwise appears normal. Short broken hairs (exclamation-mark hairs) may be seen around the margins of expanding patches of baldness. The nails are involved in about 10% of patients with severe enough alopecia to be referred to a specialist.1
Many cases begin in childhood and can be psychologically devastating. Alopecia areata is part of a spectrum of diseases with mild to extensive hair loss (Figure 2), including alopecia totalis, in which all the hair on the scalp is lost, and alopecia universalis (Figure 3), in which all the hair on the body is lost. Extensive involvement, early age of onset, and Down syndrome are all poor prognostic factors for alopecia areata.
FIGURE 2
More extensive alopecia
FIGURE 3
Alopecia universalis
Differential diagnoses
The differential diagnosis for alopecia areata includes tinea capitis, trichotillomania, early scarring alopecia, telogen effluvium, anagen effluvium (drug-induced), systemic and discoid lupus erythematosus, and secondary syphilis. In most cases the history and physical exam are adequate to make the diagnosis.
This patient does not have the typical scalp scaling and inflammation seen with tinea capitis. Trichotillomania—hair loss caused by the purposeful pulling of hair by the patient—is likely to cause the most confusion because it coexists with alopecia areata in some cases. This child has shown no evidence of such behavior. She also has no evidence of scalp scarring as may be seen in lupus. Telogen effluvium and anagen effluvium cause a more even distribution of hair loss. The patient has no known risk factors for secondary syphilis.
Laboratory testing
No lab tests are needed in this case. If there were some scalp scaling or inflammation, a potassium hydroxide preparation of the involved area would be useful to look for fungal elements; a fungal culture might also be warranted. If needed, further investigations might include serological testing for lupus erythematosus and syphilis, and a skin biopsy if the diagnosis is still unknown.
Treatment: time, drug therapies, aromatherapy
Spontaneous remission occurs in up to 80% of patients with limited patchy hair loss of less than 1 year.1 Spontaneous remission rates are significantly lower with more extensive hair loss.
Treatments are potentially painful, expensive, or time-consuming, and few randomized controlled trials support their use. Often the best treatment is watching for spontaneous remission.
The only adverse health effect of alopecia areata is the psychological distress that it may cause. While this is not to be taken lightly, the lack of evidence for successful treatments needs to be weighed with the patient’s ability to cope with leaving the hair loss untreated over time. In cases of extensive hair loss, the best treatment may be a wig.
For patients that have more visible and extensive areas of hair loss, the psychological impact might prompt the patient to want any treatment available despite the lack of evidence. Alopecia totalis or universalis may cause considerable psychological and social disability. Patients can be referred to the National Alopecia Areata Foundation for support groups and additional information. Individual counseling may be needed for some patients.
National Alopecia Areata Foundation Web site: www.alopeciaareata.com. Patients can order a 7-minute video, This Weird Thing That Makes My Hair Fall Out: Alopecia Areata, which is available for any children who want a way to share their feelings about alopecia areata with friends, family, peers, schoolmates, principals, and teachers.
European Hair Research Society Web site: www.ehrs.org. Web site has links to several alopecia areata sites.
Steroid injections
Intralesional steroid injections may stimulate regrowth of hair at the site of injection (level of evidence [LOE]=5).1 The effect may last a few months, but there is no evidence that it improves the long-term outcome or increases the probability of a cure. New areas of alopecia can still develop.
Injections are typically performed with 5–10 mg/mL of triamcinolone acetonide using a small-gauge needle. Most children will not be able to tolerate the scalp injections and should not be forced to endure this type of therapy even if the parent is pushing for it.
Other medications
Topical diphenylcyclopropenone (DPCP) is a contact immunotherapy that has some proven benefit with extensive alopecia areata (LOE=2b).1,2 In 1 study, 56 patients with chronic, extensive alopecia areata (duration ranging from 1 to 10 years, involving 30% to 100% of the scalp) were treated with progressively higher concentrations of DPCP in a randomized crossover trial.2 Twenty-five of 56 patients had total hair regrowth at 6 months, and no relapse occurred in 60% of patients. Side effects included local inflammation, eczema, autosensitization reaction, and eyelid edema.
Unfortunately, contact immunotherapy involves multiple visits to the office over several months, and it stimulates cosmetically worthwhile hair regrowth in <50% of patients with extensive patchy hair loss.1 It is a reasonable alternative for patients who do not have spontaneous remission after 1 year.
While potent topical steroids and topical minoxidil are prescribed for limited patchy alopecia areata, no convincing evidence shows they are effective.1 Likewise, no evidence warrants the use systemic steroids or psoralen/ultraviolet light treatment (PUVA).1
Aromatherapy
The best evidence may be for aromatherapy. A single-blinded randomized controlled trial was performed with 86 patients.3 As Dr Ebell points out in his InfoPOEMs review of this study, aromatherapy involves rubbing scented essential oils into the skin to treat localized and systemic disease.4 Patients with alopecia areata were randomized to nightly aromatherapy—with Thymus vulgaris (thyme), Lavandula angustifolia (lavender), Rosmarinus officinalis (rosemary), and Cedrus atlantica (cedar)—or to a control consisting of carrier oils only.
Improvement was seen in 54% of the treatment group and 21% of the control group (P=.008; number needed to treat=3). Of the 19 patients in the active treatment group who reported improvement, 11 had “very good” or “excellent” improvement. The results show aromatherapy to be a safe and effective treatment for alopecia areata (LOE=1b).4
The main problem with this study is that the researchers did not describe the duration of the patients’ alopecia. However, in a reply to a letter, they described the patients as having had alopecia areata from less than 1 year to more than 9 years. This explains the low improvement rates in both groups but does not invalidate the statistically significant difference for those that received the essential oils.
Conclusion of visit, follow-up
For a mild case like this in which the hair loss can be hidden, the best treatment is reassurance and observation. The physician explained the natural history of the disease, including the fact that regrowth will take at least 3 months for any single patch. Therapeutic options were also discussed. The mother and child were reassured that the hair is likely to grow in on its own. Neither of them wanted intralesional injections or topical therapies.
One year later during a well-child check, it was noted that the girl’s hair had fully regrown.
An 8-year-old Hispanic girl was brought to see her family physician by her mother, who noticed 2 bald spots on the back of her daughter’s scalp while brushing her hair. The child had no itching or pain. No obvious precipitating events preceded the hair loss.
The mother was more worried than the child: she didn’t want to see her beautiful girl become bald. The girl was pleased that the bald spots could be completely covered with her long hair, but she didn’t want anyone to see them. The child was otherwise healthy. She did not have any chronic medical problems and was not taking any medications. No one else in the family had a similar problem.
When the mother lifted the hair in the back, 2 round areas of hair loss were evident (Figure 1). On close inspection, there was no scaling or scarring. Her nails were normal. The child was afebrile, and the remainder of her exam was unremarkable.
FIGURE 1
Two round areas of hair loss
What is the diagnosis?
What are the management options?
Diagnosis: alopecia areata
This is the typical appearance of alopecia areata, a chronic inflammatory disease that affects the hair follicles, causing sudden hair loss. Sometimes it affects the nails as well.1 Alopecia areata occurs in both males and females of all ages and races.
Alopecia areata may be an autoimmune disease, though this is unproven. The affected skin may be slightly erythematous but otherwise appears normal. Short broken hairs (exclamation-mark hairs) may be seen around the margins of expanding patches of baldness. The nails are involved in about 10% of patients with severe enough alopecia to be referred to a specialist.1
Many cases begin in childhood and can be psychologically devastating. Alopecia areata is part of a spectrum of diseases with mild to extensive hair loss (Figure 2), including alopecia totalis, in which all the hair on the scalp is lost, and alopecia universalis (Figure 3), in which all the hair on the body is lost. Extensive involvement, early age of onset, and Down syndrome are all poor prognostic factors for alopecia areata.
FIGURE 2
More extensive alopecia
FIGURE 3
Alopecia universalis
Differential diagnoses
The differential diagnosis for alopecia areata includes tinea capitis, trichotillomania, early scarring alopecia, telogen effluvium, anagen effluvium (drug-induced), systemic and discoid lupus erythematosus, and secondary syphilis. In most cases the history and physical exam are adequate to make the diagnosis.
This patient does not have the typical scalp scaling and inflammation seen with tinea capitis. Trichotillomania—hair loss caused by the purposeful pulling of hair by the patient—is likely to cause the most confusion because it coexists with alopecia areata in some cases. This child has shown no evidence of such behavior. She also has no evidence of scalp scarring as may be seen in lupus. Telogen effluvium and anagen effluvium cause a more even distribution of hair loss. The patient has no known risk factors for secondary syphilis.
Laboratory testing
No lab tests are needed in this case. If there were some scalp scaling or inflammation, a potassium hydroxide preparation of the involved area would be useful to look for fungal elements; a fungal culture might also be warranted. If needed, further investigations might include serological testing for lupus erythematosus and syphilis, and a skin biopsy if the diagnosis is still unknown.
Treatment: time, drug therapies, aromatherapy
Spontaneous remission occurs in up to 80% of patients with limited patchy hair loss of less than 1 year.1 Spontaneous remission rates are significantly lower with more extensive hair loss.
Treatments are potentially painful, expensive, or time-consuming, and few randomized controlled trials support their use. Often the best treatment is watching for spontaneous remission.
The only adverse health effect of alopecia areata is the psychological distress that it may cause. While this is not to be taken lightly, the lack of evidence for successful treatments needs to be weighed with the patient’s ability to cope with leaving the hair loss untreated over time. In cases of extensive hair loss, the best treatment may be a wig.
For patients that have more visible and extensive areas of hair loss, the psychological impact might prompt the patient to want any treatment available despite the lack of evidence. Alopecia totalis or universalis may cause considerable psychological and social disability. Patients can be referred to the National Alopecia Areata Foundation for support groups and additional information. Individual counseling may be needed for some patients.
National Alopecia Areata Foundation Web site: www.alopeciaareata.com. Patients can order a 7-minute video, This Weird Thing That Makes My Hair Fall Out: Alopecia Areata, which is available for any children who want a way to share their feelings about alopecia areata with friends, family, peers, schoolmates, principals, and teachers.
European Hair Research Society Web site: www.ehrs.org. Web site has links to several alopecia areata sites.
Steroid injections
Intralesional steroid injections may stimulate regrowth of hair at the site of injection (level of evidence [LOE]=5).1 The effect may last a few months, but there is no evidence that it improves the long-term outcome or increases the probability of a cure. New areas of alopecia can still develop.
Injections are typically performed with 5–10 mg/mL of triamcinolone acetonide using a small-gauge needle. Most children will not be able to tolerate the scalp injections and should not be forced to endure this type of therapy even if the parent is pushing for it.
Other medications
Topical diphenylcyclopropenone (DPCP) is a contact immunotherapy that has some proven benefit with extensive alopecia areata (LOE=2b).1,2 In 1 study, 56 patients with chronic, extensive alopecia areata (duration ranging from 1 to 10 years, involving 30% to 100% of the scalp) were treated with progressively higher concentrations of DPCP in a randomized crossover trial.2 Twenty-five of 56 patients had total hair regrowth at 6 months, and no relapse occurred in 60% of patients. Side effects included local inflammation, eczema, autosensitization reaction, and eyelid edema.
Unfortunately, contact immunotherapy involves multiple visits to the office over several months, and it stimulates cosmetically worthwhile hair regrowth in <50% of patients with extensive patchy hair loss.1 It is a reasonable alternative for patients who do not have spontaneous remission after 1 year.
While potent topical steroids and topical minoxidil are prescribed for limited patchy alopecia areata, no convincing evidence shows they are effective.1 Likewise, no evidence warrants the use systemic steroids or psoralen/ultraviolet light treatment (PUVA).1
Aromatherapy
The best evidence may be for aromatherapy. A single-blinded randomized controlled trial was performed with 86 patients.3 As Dr Ebell points out in his InfoPOEMs review of this study, aromatherapy involves rubbing scented essential oils into the skin to treat localized and systemic disease.4 Patients with alopecia areata were randomized to nightly aromatherapy—with Thymus vulgaris (thyme), Lavandula angustifolia (lavender), Rosmarinus officinalis (rosemary), and Cedrus atlantica (cedar)—or to a control consisting of carrier oils only.
Improvement was seen in 54% of the treatment group and 21% of the control group (P=.008; number needed to treat=3). Of the 19 patients in the active treatment group who reported improvement, 11 had “very good” or “excellent” improvement. The results show aromatherapy to be a safe and effective treatment for alopecia areata (LOE=1b).4
The main problem with this study is that the researchers did not describe the duration of the patients’ alopecia. However, in a reply to a letter, they described the patients as having had alopecia areata from less than 1 year to more than 9 years. This explains the low improvement rates in both groups but does not invalidate the statistically significant difference for those that received the essential oils.
Conclusion of visit, follow-up
For a mild case like this in which the hair loss can be hidden, the best treatment is reassurance and observation. The physician explained the natural history of the disease, including the fact that regrowth will take at least 3 months for any single patch. Therapeutic options were also discussed. The mother and child were reassured that the hair is likely to grow in on its own. Neither of them wanted intralesional injections or topical therapies.
One year later during a well-child check, it was noted that the girl’s hair had fully regrown.
1. MacDonald Hull SP, Wood ML, Hutchinson PE, Sladden M, Messenger AG. Guidelines for the management of alopecia areata. Br J Dermatol 2003;149:692-699.
2. Cotellessa C, Peris K, Caracciolo E, Mordenti C, Chimenti S. The use of topical diphenylcyclopropenone for the treatment of extensive alopecia areata. J Am Acad Dermatol 2001;44:73-76.
3. Hay IC, Jamieson M, Ormerod AD. Randomized trial of aromatherapy: successful treatment for alopecia areata. Arch Derm 1998;134:1349-1352.
4. Ebell M. Aromatherapy effective for alopecia areata. Review of Hay et al 1998. InfoPOEMs, Inc. March 1999.
1. MacDonald Hull SP, Wood ML, Hutchinson PE, Sladden M, Messenger AG. Guidelines for the management of alopecia areata. Br J Dermatol 2003;149:692-699.
2. Cotellessa C, Peris K, Caracciolo E, Mordenti C, Chimenti S. The use of topical diphenylcyclopropenone for the treatment of extensive alopecia areata. J Am Acad Dermatol 2001;44:73-76.
3. Hay IC, Jamieson M, Ormerod AD. Randomized trial of aromatherapy: successful treatment for alopecia areata. Arch Derm 1998;134:1349-1352.
4. Ebell M. Aromatherapy effective for alopecia areata. Review of Hay et al 1998. InfoPOEMs, Inc. March 1999.
Painful genital ulcers
A colleague came into the charting area and said he thought he had just seen his first case of chancroid. He asked me if I had a moment to see the patient, a 32-year-old African American man who noted the onset of painful sores on his penis 1 week ago. The patient consented to a second opinion. On further questioning, he remembered a tingling pain that started a few days prior to the sores. When asked about any previous outbreaks, he thought he may have had something like this 1 year ago. He did not remember seeing blisters before the sores appeared.
The last time the patient had sexual relations was 2 months ago, with someone he met at a party. He claimed he used a condom. He did not have any lesions at that time and had never had a sexually transmitted disease before.
He had recently fallen in love, and was concerned about these ulcers—he did not want to give her any diseases. They had only kissed so far and he wanted to know what he should tell her. He said he had never had sex with men or injected any drugs. He has had a number of serially monogamous relationships and reported no other human immunodeficiency virus (HIV) risk factors.
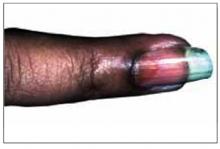
The patient was a healthy-looking young man. Examination of his penis (Figure 1) showed the ulcers clearly visible (Figure 2). He had only shotty inguinal adenopathy that was nontender.
FIGURE 1
Painful sores on the genitals
FIGURE 2
Close-up of ulcers on the penis
What is the diagnosis?
What is the treatment and prevention strategy?
Differential diagnosis
The most likely causes of painful genital ulcers in this case are herpes simplex, chancroid, and syphilis. Granuloma inguinale and lymphogranuloma venereum (LGV) are rare causes of genital ulceration in the United States. A zipper accident or other trauma can cause genital ulceration, but the patient should be able to give a clear history of such an event.
By epidemiology alone, the order of likelihood for the cause of any genital ulceration is herpes, syphilis, then chancroid.
This case points to herpes
Herpes simplex is by far the most common cause of painful genital ulcers in the United States; at least 50 million people have genital herpes simplex virus (HSV) infection1 The features of this case pointing to herpes are the appearance of multiple ulcers, the tingling pain that preceded the ulcers, and the history of a possible episode in the preceding year. While it would be helpful to have a history of blisters that preceded the ulcers, the evidence still points to herpes as the most likely diagnosis.
Could it be syphilis?
While the primary chancre of syphilis is classically described as painless, the patient with syphilis may experience pain. Syphilis tends to present as a single ulcer but may cause multiple ulcers.
Why not chancroid?
Chancroid may also cause multiple small painful ulcers. However, the ulcers of chancroid tend to be deeper than those of herpes and bleed more easily.
Other characteristics to look for
All of these sexually transmitted diseases can cause tender painful adenopathy, which is particularly characteristic of chancroid and LGV. Suppurative inguinal adenopathy with painful genital ulcers is almost pathognomonic of chancroid. With LGV, there may be a self-limited genital ulcer at the site of inoculation, which is often gone by the time a patient seeks care. Granuloma inguinale causes painless, progressive ulcerative lesions without regional lymphadenopathy. These lesions are highly vascular (with a characteristic beefy red appearance) and bleed easily on contact.1 While it would be helpful to have a history of blisters that preceded the ulcers, the evidence still points to herpes as the most likely diagnosis.
Laboratory examination
Herpes
All patients with genital ulcers thought to be from an STD should be tested for syphilis and HIV regardless of other risk factors.1 This patient should additionally be tested for herpes simplex. A bacteriologic test for chancroid is not necessary, but the clinician who first saw the patient asked that we conduct the test for chancroid—a culture for the Haemophilus ducreyi bacterium.
Isolation of HSV in cell culture is the preferred virologic test for patients with genital ulcers.1Unfortunately, the sensitivity of culture declines rapidly as lesions begin to heal, usually within a few days of onset. Direct fluorescent antibody tests are also available. Both herpes culture and the direct fluorescent antibody test distinguish HSV-1 from HSV-2. Polymerase chain reaction assays for HSV DNA are highly sensitive, but their role in the diagnosis of genital ulcer disease has not been well-defined.
Most cases of recurrent genital herpes are caused by HSV-2. Specific serologic testing can be expensive, and is not needed at the time of the initial virologic screening. However, consider ordering the test at a subsequent visit, because the distinction between HSV serotypes influences prognosis and counseling. Also, because false-negative HSV cultures are common—especially with recurrent infection or healing lesions—type-specific serologic tests are useful for confirming a diagnosis of genital herpes.1 Herpes serologies can also be used to help manage sexual partners of persons with genital herpes.
Syphilis
The Venereal Disease Research Laboratory (VDRL) test or rapid plasma reagin (RPR) test should be used to detect syphilis. Both tests are used for nonspecific screening only, because they measure anticardiolipin antibodies. A positive result should be confirmed with a specific treponemal test such as a fluorescent treponemal antibody absorption test (FTA-ABS).
The results of these laboratory tests are not available immediately during the patient’s visit. If there was a high suspicion for syphilis, a dark field examination from the ulcer exudate could be used to look for spirochetes while the patient was still in the office. In this case, the suspicion for syphilis was low.
Treatment: Antivirals
The major question is whether the patient should be treated empirically with medication. The most likely diagnosis is herpes simplex. Randomized trials indicate that 3 antiviral medications— acyclovir, famciclovir, and valacyclovir—provide clinical benefit for genital herpes (level of evidence [LOE]=1a).1
The Centers for Disease Control and Prevention (CDC) 2002 treatment guidelines for STDs recommend the following medications for the first clinical episode of genital herpes:
- Acyclovir 400 mg orally, 3 times daily for 7–10 days or until clinically resolved, OR
- Acyclovir 200 mg orally, 5 times daily for 7–10 days or until clinically resolved, OR
- Famciclovir 250 mg orally, 3 times daily for 7–10 days or until clinically resolved, OR
- Valacyclovir 1 g orally, twice daily for 7–10 days or until clinically resolved.
Topical acyclovir is less effective than the oral formulaton and its use is discouraged.
The suspicion for syphilis is too low to warrant an intramuscular shot of penicillin, which is painful and can cause anaphylaxis in some patients. The likelihood of chancroid is too low to prescribe an oral antibiotic such as erythromycin.
The patient wanted empirical treatment for herpes. He was given valacyclovir, 1 gm for 7 days, taken twice daily, with the option to call in for more if the ulcers did not resolve by day 7. He was told he might apply petrolatum and clean gauze to the ulcers to diminish the pain when open ulcers rub against underwear. Acetaminophen or other analgesics were recommended for pain, and he was advised to avoid sexual activity until the ulcers had fully healed.
Preventing transmission
The patient is appropriately concerned about the transmission of this condition to a new partner. Not having a firm diagnosis makes definitive counseling more difficult. However, general principles of safe sex and condom use were discussed. On the follow-up visit the patient was told that the result of his herpes test was positive for HSV-2. Results of his RPR, HIV antibody test, and H ducreyiculture were all negative.
Information about condom use was reinforced, and the patient was told there is definitive evidence that condom use does diminish the risk of transmission of herpes from a man to a woman (LOE=1b).2 That same study did not show that condom use prevents transmission from women to men. Also, changes in sexual behavior, correlated with counseling about avoiding sex when a partner has lesions, were associated with reduction in HSV-2 acquisition over time (LOE=1b).2
One study showed that the overall risk of genital HSV transmission in couples is low (10%/year). The risk may be significantly increased in women and in seronegative individuals.3 This speaks for serologic testing for the potential partner of this patient.
When recurrences are frequent, antiviral agents can decrease the frequency (LOE=1a).1 If this patient has frequent recurrences, antiviral agents would be appropriate and would decrease the times when the patient is shedding virus asymptomatically.
Herpes is transmitted between sexual partners during asymptomatic shedding.1 Acyclovir 400 mg twice daily can reduce asymptomatic viral shedding significantly among women with recurrent herpes simplex (LOE=1b).4 While it is likely this will decrease transmission from women to men, this has not been proven. Data on decreasing viral transmission from men to women by antiviral therapy is not available. At some point, the Glycoprotein-D-adjuvant vaccine may be an option to prevent genital herpes transmission to his partner.5
Note. The CDC 2002 sexually transmitted diseases treatment guidelines are available for download and use on a Palm handheld computer at www.cdcnpin.org/scripts/std/pda.asp.
1. Centers for Disease Control and Prevention. 2002 sexually transmitted diseases treatment guidelines. MMWR Recomm Rep 2002;51(RR-6).-Available online at: http://www.cdc.gov/std/treatment/. Accessed on November 4, 2003.
2. Wald A, Langenberg AG, Link K, et al. Effect of condoms on reducing the transmission of herpes simplex virus type 2 from men to women. JAMA 2001;285:31003106.
3. Bryson Y, Dillon M, Bernstein DI, Radolf J, Zakowski P, Garratty E. Risk of acquisition of genital herpes simplex virus type 2 in sex partners of persons with genital herpes: a prospective couple study. J Infect Dis 1993;167:942-946.
4. Wald A, Zeh J, Barnum G, et al. Suppression of subclinical shedding of herpes simplex virus type 2 with acyclovir. Ann Intern Med 1996;124:8-15.
5. Stanberry LR, Spruance SL, Cunningham AL, et al. GlaxoSmithKline Herpes Vaccine Efficacy Study Group. Glycoprotein-D-adjuvant vaccine to prevent genital herpes. N Engl J Med 2002;347:1652-1661.
A colleague came into the charting area and said he thought he had just seen his first case of chancroid. He asked me if I had a moment to see the patient, a 32-year-old African American man who noted the onset of painful sores on his penis 1 week ago. The patient consented to a second opinion. On further questioning, he remembered a tingling pain that started a few days prior to the sores. When asked about any previous outbreaks, he thought he may have had something like this 1 year ago. He did not remember seeing blisters before the sores appeared.
The last time the patient had sexual relations was 2 months ago, with someone he met at a party. He claimed he used a condom. He did not have any lesions at that time and had never had a sexually transmitted disease before.
He had recently fallen in love, and was concerned about these ulcers—he did not want to give her any diseases. They had only kissed so far and he wanted to know what he should tell her. He said he had never had sex with men or injected any drugs. He has had a number of serially monogamous relationships and reported no other human immunodeficiency virus (HIV) risk factors.
The patient was a healthy-looking young man. Examination of his penis (Figure 1) showed the ulcers clearly visible (Figure 2). He had only shotty inguinal adenopathy that was nontender.
FIGURE 1
Painful sores on the genitals
FIGURE 2
Close-up of ulcers on the penis
What is the diagnosis?
What is the treatment and prevention strategy?
Differential diagnosis
The most likely causes of painful genital ulcers in this case are herpes simplex, chancroid, and syphilis. Granuloma inguinale and lymphogranuloma venereum (LGV) are rare causes of genital ulceration in the United States. A zipper accident or other trauma can cause genital ulceration, but the patient should be able to give a clear history of such an event.
By epidemiology alone, the order of likelihood for the cause of any genital ulceration is herpes, syphilis, then chancroid.
This case points to herpes
Herpes simplex is by far the most common cause of painful genital ulcers in the United States; at least 50 million people have genital herpes simplex virus (HSV) infection1 The features of this case pointing to herpes are the appearance of multiple ulcers, the tingling pain that preceded the ulcers, and the history of a possible episode in the preceding year. While it would be helpful to have a history of blisters that preceded the ulcers, the evidence still points to herpes as the most likely diagnosis.
Could it be syphilis?
While the primary chancre of syphilis is classically described as painless, the patient with syphilis may experience pain. Syphilis tends to present as a single ulcer but may cause multiple ulcers.
Why not chancroid?
Chancroid may also cause multiple small painful ulcers. However, the ulcers of chancroid tend to be deeper than those of herpes and bleed more easily.
Other characteristics to look for
All of these sexually transmitted diseases can cause tender painful adenopathy, which is particularly characteristic of chancroid and LGV. Suppurative inguinal adenopathy with painful genital ulcers is almost pathognomonic of chancroid. With LGV, there may be a self-limited genital ulcer at the site of inoculation, which is often gone by the time a patient seeks care. Granuloma inguinale causes painless, progressive ulcerative lesions without regional lymphadenopathy. These lesions are highly vascular (with a characteristic beefy red appearance) and bleed easily on contact.1 While it would be helpful to have a history of blisters that preceded the ulcers, the evidence still points to herpes as the most likely diagnosis.
Laboratory examination
Herpes
All patients with genital ulcers thought to be from an STD should be tested for syphilis and HIV regardless of other risk factors.1 This patient should additionally be tested for herpes simplex. A bacteriologic test for chancroid is not necessary, but the clinician who first saw the patient asked that we conduct the test for chancroid—a culture for the Haemophilus ducreyi bacterium.
Isolation of HSV in cell culture is the preferred virologic test for patients with genital ulcers.1Unfortunately, the sensitivity of culture declines rapidly as lesions begin to heal, usually within a few days of onset. Direct fluorescent antibody tests are also available. Both herpes culture and the direct fluorescent antibody test distinguish HSV-1 from HSV-2. Polymerase chain reaction assays for HSV DNA are highly sensitive, but their role in the diagnosis of genital ulcer disease has not been well-defined.
Most cases of recurrent genital herpes are caused by HSV-2. Specific serologic testing can be expensive, and is not needed at the time of the initial virologic screening. However, consider ordering the test at a subsequent visit, because the distinction between HSV serotypes influences prognosis and counseling. Also, because false-negative HSV cultures are common—especially with recurrent infection or healing lesions—type-specific serologic tests are useful for confirming a diagnosis of genital herpes.1 Herpes serologies can also be used to help manage sexual partners of persons with genital herpes.
Syphilis
The Venereal Disease Research Laboratory (VDRL) test or rapid plasma reagin (RPR) test should be used to detect syphilis. Both tests are used for nonspecific screening only, because they measure anticardiolipin antibodies. A positive result should be confirmed with a specific treponemal test such as a fluorescent treponemal antibody absorption test (FTA-ABS).
The results of these laboratory tests are not available immediately during the patient’s visit. If there was a high suspicion for syphilis, a dark field examination from the ulcer exudate could be used to look for spirochetes while the patient was still in the office. In this case, the suspicion for syphilis was low.
Treatment: Antivirals
The major question is whether the patient should be treated empirically with medication. The most likely diagnosis is herpes simplex. Randomized trials indicate that 3 antiviral medications— acyclovir, famciclovir, and valacyclovir—provide clinical benefit for genital herpes (level of evidence [LOE]=1a).1
The Centers for Disease Control and Prevention (CDC) 2002 treatment guidelines for STDs recommend the following medications for the first clinical episode of genital herpes:
- Acyclovir 400 mg orally, 3 times daily for 7–10 days or until clinically resolved, OR
- Acyclovir 200 mg orally, 5 times daily for 7–10 days or until clinically resolved, OR
- Famciclovir 250 mg orally, 3 times daily for 7–10 days or until clinically resolved, OR
- Valacyclovir 1 g orally, twice daily for 7–10 days or until clinically resolved.
Topical acyclovir is less effective than the oral formulaton and its use is discouraged.
The suspicion for syphilis is too low to warrant an intramuscular shot of penicillin, which is painful and can cause anaphylaxis in some patients. The likelihood of chancroid is too low to prescribe an oral antibiotic such as erythromycin.
The patient wanted empirical treatment for herpes. He was given valacyclovir, 1 gm for 7 days, taken twice daily, with the option to call in for more if the ulcers did not resolve by day 7. He was told he might apply petrolatum and clean gauze to the ulcers to diminish the pain when open ulcers rub against underwear. Acetaminophen or other analgesics were recommended for pain, and he was advised to avoid sexual activity until the ulcers had fully healed.
Preventing transmission
The patient is appropriately concerned about the transmission of this condition to a new partner. Not having a firm diagnosis makes definitive counseling more difficult. However, general principles of safe sex and condom use were discussed. On the follow-up visit the patient was told that the result of his herpes test was positive for HSV-2. Results of his RPR, HIV antibody test, and H ducreyiculture were all negative.
Information about condom use was reinforced, and the patient was told there is definitive evidence that condom use does diminish the risk of transmission of herpes from a man to a woman (LOE=1b).2 That same study did not show that condom use prevents transmission from women to men. Also, changes in sexual behavior, correlated with counseling about avoiding sex when a partner has lesions, were associated with reduction in HSV-2 acquisition over time (LOE=1b).2
One study showed that the overall risk of genital HSV transmission in couples is low (10%/year). The risk may be significantly increased in women and in seronegative individuals.3 This speaks for serologic testing for the potential partner of this patient.
When recurrences are frequent, antiviral agents can decrease the frequency (LOE=1a).1 If this patient has frequent recurrences, antiviral agents would be appropriate and would decrease the times when the patient is shedding virus asymptomatically.
Herpes is transmitted between sexual partners during asymptomatic shedding.1 Acyclovir 400 mg twice daily can reduce asymptomatic viral shedding significantly among women with recurrent herpes simplex (LOE=1b).4 While it is likely this will decrease transmission from women to men, this has not been proven. Data on decreasing viral transmission from men to women by antiviral therapy is not available. At some point, the Glycoprotein-D-adjuvant vaccine may be an option to prevent genital herpes transmission to his partner.5
Note. The CDC 2002 sexually transmitted diseases treatment guidelines are available for download and use on a Palm handheld computer at www.cdcnpin.org/scripts/std/pda.asp.
A colleague came into the charting area and said he thought he had just seen his first case of chancroid. He asked me if I had a moment to see the patient, a 32-year-old African American man who noted the onset of painful sores on his penis 1 week ago. The patient consented to a second opinion. On further questioning, he remembered a tingling pain that started a few days prior to the sores. When asked about any previous outbreaks, he thought he may have had something like this 1 year ago. He did not remember seeing blisters before the sores appeared.
The last time the patient had sexual relations was 2 months ago, with someone he met at a party. He claimed he used a condom. He did not have any lesions at that time and had never had a sexually transmitted disease before.
He had recently fallen in love, and was concerned about these ulcers—he did not want to give her any diseases. They had only kissed so far and he wanted to know what he should tell her. He said he had never had sex with men or injected any drugs. He has had a number of serially monogamous relationships and reported no other human immunodeficiency virus (HIV) risk factors.
The patient was a healthy-looking young man. Examination of his penis (Figure 1) showed the ulcers clearly visible (Figure 2). He had only shotty inguinal adenopathy that was nontender.
FIGURE 1
Painful sores on the genitals
FIGURE 2
Close-up of ulcers on the penis
What is the diagnosis?
What is the treatment and prevention strategy?
Differential diagnosis
The most likely causes of painful genital ulcers in this case are herpes simplex, chancroid, and syphilis. Granuloma inguinale and lymphogranuloma venereum (LGV) are rare causes of genital ulceration in the United States. A zipper accident or other trauma can cause genital ulceration, but the patient should be able to give a clear history of such an event.
By epidemiology alone, the order of likelihood for the cause of any genital ulceration is herpes, syphilis, then chancroid.
This case points to herpes
Herpes simplex is by far the most common cause of painful genital ulcers in the United States; at least 50 million people have genital herpes simplex virus (HSV) infection1 The features of this case pointing to herpes are the appearance of multiple ulcers, the tingling pain that preceded the ulcers, and the history of a possible episode in the preceding year. While it would be helpful to have a history of blisters that preceded the ulcers, the evidence still points to herpes as the most likely diagnosis.
Could it be syphilis?
While the primary chancre of syphilis is classically described as painless, the patient with syphilis may experience pain. Syphilis tends to present as a single ulcer but may cause multiple ulcers.
Why not chancroid?
Chancroid may also cause multiple small painful ulcers. However, the ulcers of chancroid tend to be deeper than those of herpes and bleed more easily.
Other characteristics to look for
All of these sexually transmitted diseases can cause tender painful adenopathy, which is particularly characteristic of chancroid and LGV. Suppurative inguinal adenopathy with painful genital ulcers is almost pathognomonic of chancroid. With LGV, there may be a self-limited genital ulcer at the site of inoculation, which is often gone by the time a patient seeks care. Granuloma inguinale causes painless, progressive ulcerative lesions without regional lymphadenopathy. These lesions are highly vascular (with a characteristic beefy red appearance) and bleed easily on contact.1 While it would be helpful to have a history of blisters that preceded the ulcers, the evidence still points to herpes as the most likely diagnosis.
Laboratory examination
Herpes
All patients with genital ulcers thought to be from an STD should be tested for syphilis and HIV regardless of other risk factors.1 This patient should additionally be tested for herpes simplex. A bacteriologic test for chancroid is not necessary, but the clinician who first saw the patient asked that we conduct the test for chancroid—a culture for the Haemophilus ducreyi bacterium.
Isolation of HSV in cell culture is the preferred virologic test for patients with genital ulcers.1Unfortunately, the sensitivity of culture declines rapidly as lesions begin to heal, usually within a few days of onset. Direct fluorescent antibody tests are also available. Both herpes culture and the direct fluorescent antibody test distinguish HSV-1 from HSV-2. Polymerase chain reaction assays for HSV DNA are highly sensitive, but their role in the diagnosis of genital ulcer disease has not been well-defined.
Most cases of recurrent genital herpes are caused by HSV-2. Specific serologic testing can be expensive, and is not needed at the time of the initial virologic screening. However, consider ordering the test at a subsequent visit, because the distinction between HSV serotypes influences prognosis and counseling. Also, because false-negative HSV cultures are common—especially with recurrent infection or healing lesions—type-specific serologic tests are useful for confirming a diagnosis of genital herpes.1 Herpes serologies can also be used to help manage sexual partners of persons with genital herpes.
Syphilis
The Venereal Disease Research Laboratory (VDRL) test or rapid plasma reagin (RPR) test should be used to detect syphilis. Both tests are used for nonspecific screening only, because they measure anticardiolipin antibodies. A positive result should be confirmed with a specific treponemal test such as a fluorescent treponemal antibody absorption test (FTA-ABS).
The results of these laboratory tests are not available immediately during the patient’s visit. If there was a high suspicion for syphilis, a dark field examination from the ulcer exudate could be used to look for spirochetes while the patient was still in the office. In this case, the suspicion for syphilis was low.
Treatment: Antivirals
The major question is whether the patient should be treated empirically with medication. The most likely diagnosis is herpes simplex. Randomized trials indicate that 3 antiviral medications— acyclovir, famciclovir, and valacyclovir—provide clinical benefit for genital herpes (level of evidence [LOE]=1a).1
The Centers for Disease Control and Prevention (CDC) 2002 treatment guidelines for STDs recommend the following medications for the first clinical episode of genital herpes:
- Acyclovir 400 mg orally, 3 times daily for 7–10 days or until clinically resolved, OR
- Acyclovir 200 mg orally, 5 times daily for 7–10 days or until clinically resolved, OR
- Famciclovir 250 mg orally, 3 times daily for 7–10 days or until clinically resolved, OR
- Valacyclovir 1 g orally, twice daily for 7–10 days or until clinically resolved.
Topical acyclovir is less effective than the oral formulaton and its use is discouraged.
The suspicion for syphilis is too low to warrant an intramuscular shot of penicillin, which is painful and can cause anaphylaxis in some patients. The likelihood of chancroid is too low to prescribe an oral antibiotic such as erythromycin.
The patient wanted empirical treatment for herpes. He was given valacyclovir, 1 gm for 7 days, taken twice daily, with the option to call in for more if the ulcers did not resolve by day 7. He was told he might apply petrolatum and clean gauze to the ulcers to diminish the pain when open ulcers rub against underwear. Acetaminophen or other analgesics were recommended for pain, and he was advised to avoid sexual activity until the ulcers had fully healed.
Preventing transmission
The patient is appropriately concerned about the transmission of this condition to a new partner. Not having a firm diagnosis makes definitive counseling more difficult. However, general principles of safe sex and condom use were discussed. On the follow-up visit the patient was told that the result of his herpes test was positive for HSV-2. Results of his RPR, HIV antibody test, and H ducreyiculture were all negative.
Information about condom use was reinforced, and the patient was told there is definitive evidence that condom use does diminish the risk of transmission of herpes from a man to a woman (LOE=1b).2 That same study did not show that condom use prevents transmission from women to men. Also, changes in sexual behavior, correlated with counseling about avoiding sex when a partner has lesions, were associated with reduction in HSV-2 acquisition over time (LOE=1b).2
One study showed that the overall risk of genital HSV transmission in couples is low (10%/year). The risk may be significantly increased in women and in seronegative individuals.3 This speaks for serologic testing for the potential partner of this patient.
When recurrences are frequent, antiviral agents can decrease the frequency (LOE=1a).1 If this patient has frequent recurrences, antiviral agents would be appropriate and would decrease the times when the patient is shedding virus asymptomatically.
Herpes is transmitted between sexual partners during asymptomatic shedding.1 Acyclovir 400 mg twice daily can reduce asymptomatic viral shedding significantly among women with recurrent herpes simplex (LOE=1b).4 While it is likely this will decrease transmission from women to men, this has not been proven. Data on decreasing viral transmission from men to women by antiviral therapy is not available. At some point, the Glycoprotein-D-adjuvant vaccine may be an option to prevent genital herpes transmission to his partner.5
Note. The CDC 2002 sexually transmitted diseases treatment guidelines are available for download and use on a Palm handheld computer at www.cdcnpin.org/scripts/std/pda.asp.
1. Centers for Disease Control and Prevention. 2002 sexually transmitted diseases treatment guidelines. MMWR Recomm Rep 2002;51(RR-6).-Available online at: http://www.cdc.gov/std/treatment/. Accessed on November 4, 2003.
2. Wald A, Langenberg AG, Link K, et al. Effect of condoms on reducing the transmission of herpes simplex virus type 2 from men to women. JAMA 2001;285:31003106.
3. Bryson Y, Dillon M, Bernstein DI, Radolf J, Zakowski P, Garratty E. Risk of acquisition of genital herpes simplex virus type 2 in sex partners of persons with genital herpes: a prospective couple study. J Infect Dis 1993;167:942-946.
4. Wald A, Zeh J, Barnum G, et al. Suppression of subclinical shedding of herpes simplex virus type 2 with acyclovir. Ann Intern Med 1996;124:8-15.
5. Stanberry LR, Spruance SL, Cunningham AL, et al. GlaxoSmithKline Herpes Vaccine Efficacy Study Group. Glycoprotein-D-adjuvant vaccine to prevent genital herpes. N Engl J Med 2002;347:1652-1661.
1. Centers for Disease Control and Prevention. 2002 sexually transmitted diseases treatment guidelines. MMWR Recomm Rep 2002;51(RR-6).-Available online at: http://www.cdc.gov/std/treatment/. Accessed on November 4, 2003.
2. Wald A, Langenberg AG, Link K, et al. Effect of condoms on reducing the transmission of herpes simplex virus type 2 from men to women. JAMA 2001;285:31003106.
3. Bryson Y, Dillon M, Bernstein DI, Radolf J, Zakowski P, Garratty E. Risk of acquisition of genital herpes simplex virus type 2 in sex partners of persons with genital herpes: a prospective couple study. J Infect Dis 1993;167:942-946.
4. Wald A, Zeh J, Barnum G, et al. Suppression of subclinical shedding of herpes simplex virus type 2 with acyclovir. Ann Intern Med 1996;124:8-15.
5. Stanberry LR, Spruance SL, Cunningham AL, et al. GlaxoSmithKline Herpes Vaccine Efficacy Study Group. Glycoprotein-D-adjuvant vaccine to prevent genital herpes. N Engl J Med 2002;347:1652-1661.
New rash on the right hand and neck
A 43-year-old African-American woman was seen for a rash on her right hand and neck. The rash appeared 2 weeks earlier, and was itchy. The patient had been applying alcohol directly to the affected skin.
The patient said she had experienced rashes on and off during her adult life. She has not worn necklaces for years because they irritate the skin around her neck. She also cannot wear wool clothing or any shirts with bright colors. She had not discussed this with a physician before, and she did not know why her skin is so sensitive.
The patient was not taking any new medications, using new bath products, or wearing new clothing before the rash appeared. However, she did remember getting new perfume 2 weeks earlier. She did not have asthma, but did have a mild hay fever. She was adopted and therefore did not know her biologic family’s medical history.
On close inspection, prominent erythema was seen around her neck and on the dorsum of her right hand (Figures 1 and 2).
FIGURE 1
Itchy rash on the neck…
FIGURE 2
…and the right hand
What is the diagnosis?
What are the management options?
Diagnosis: contact dermatitis
The patient demonstrated how she applied perfume to her neck using the back of her right hand. She has acute contact dermatitis on top of previously undiagnosed eczema. Her history is positive for contact dermatitis in reaction to metal (probably nickel) in necklaces and to various fabrics.
Contact dermatitis is a common inflammatory skin condition in which erythematous and pruritic skin lesions result from contact with a foreign substance. The term describes 2 diagnostic categories—allergic contact dermatitis and irritant contact dermatitis. In this case, the chemicals in the perfume may have acted as irritants. The alcohol she used to treat the rash was probably an irritant as well.
A hypersensitivity reaction to irritants and allergens
The mechanism of allergic contact dermatitis is a delayed hypersensitivity reaction. A foreign substance comes into contact with skin and links to skin protein, forming an antigen complex recognized by the immune system. In the skin, the major antigen-presenting cell is the Langerhans cell. When the epidermis is re-exposed to the antigen, the sensitized T-cells initiate an inflammatory cascade leading to changes in the skin. The reaction generally occurs within 12 to 48 hours in a sensitized person. The differential diagnoses for this patient include atopic dermatitis, psoriasis, and fungal infection.
Cosmetics, perfumes, and chemicals in cleaning solutions are known to cause irritant contact dermatitis. The most typical locations are hands or feet, with the dorsum affected more often than the palm or the sole. The lesions are usually erythematous and not well demarcated. The lesions may be macular, papular, or vesicular.
Allergic contact dermatitis often occurs after contact with allergens such as nickel in jewelry, or resins in plants such as poison ivy or poison oak. Vesicles may appear, and the hands are most commonly affected. The lesions may form a linear pattern, as in the case of plant dermatitis.
Evaluation: tests usually not needed
A diagnosis of contact dermatitis usually requires nothing more than findings in the patient’s history and physical exam. If a fungal infection is suspected, use a potassium hydroxide (KOH) preparation to look for hyphae or spores (see page 854 in this issue). Patch testing—placing common antigens on the patient’s skin and observing for reactions—is used to confirm the diagnosis of contact dermatitis and to determine the offending agent.
In this case, neither test was necessary or warranted because the history and physical exam led to a clear diagnosis that was treatable without having to analyze the chemicals in the perfume.
Treatment: remove the irritant, stop the swelling
Whether this is irritant or allergic contact dermatitis, the first line of treatment is to stop further exposure to the offending substance. A mid- to high-potency topical corticosteroid is recommended to stopping the inflammatory process (level of evidence [LOE]=5). (For an explanation of evidence-based medicine ratings, see page 000.) Ointments are more potent and particularly useful when the affected skin is dry and scaly.
Oral steroids are often used for severe local dermatitis, such as that caused by poison ivy (LOE=5). Topical tacrolimus ointment 0.1% is a more expensive option for the treatment of allergic contact dermatitis induced by nickel (LOE=2b).1 Oral H1 blocking sedating anti-histamines (such as diphenhydramine and hydroxyzine) provide relief from itching and help with sleep. Sedating antihistamines may be more effective for itching, but are probably inadvisable for persons who must drive or operate machinery. Newer nonsedating anti-histamines are an option when sedating agents should be avoided.
Conclusion of visit
The patient was given 0.1% triamcinolone ointment (a generic mid-potency steroid) to apply 2 to 3 times a day to the affected areas. She did not want any oral medications for the itching, but understood that diphenhydramine is available without a prescription if needed. She planned to give the perfume away and understood it was now on her list of items to avoid. Her physician explained her underlying eczema and what could be done to prevent rashes.
1. Saripalli YV, Gadzia JE, Belsito DV. Tacrolimus ointment 0.1% in the treatment of nickel-induced allergic contact dermatitis. J Am Acad Dermatol 2003;49:477-482.
A 43-year-old African-American woman was seen for a rash on her right hand and neck. The rash appeared 2 weeks earlier, and was itchy. The patient had been applying alcohol directly to the affected skin.
The patient said she had experienced rashes on and off during her adult life. She has not worn necklaces for years because they irritate the skin around her neck. She also cannot wear wool clothing or any shirts with bright colors. She had not discussed this with a physician before, and she did not know why her skin is so sensitive.
The patient was not taking any new medications, using new bath products, or wearing new clothing before the rash appeared. However, she did remember getting new perfume 2 weeks earlier. She did not have asthma, but did have a mild hay fever. She was adopted and therefore did not know her biologic family’s medical history.
On close inspection, prominent erythema was seen around her neck and on the dorsum of her right hand (Figures 1 and 2).
FIGURE 1
Itchy rash on the neck…
FIGURE 2
…and the right hand
What is the diagnosis?
What are the management options?
Diagnosis: contact dermatitis
The patient demonstrated how she applied perfume to her neck using the back of her right hand. She has acute contact dermatitis on top of previously undiagnosed eczema. Her history is positive for contact dermatitis in reaction to metal (probably nickel) in necklaces and to various fabrics.
Contact dermatitis is a common inflammatory skin condition in which erythematous and pruritic skin lesions result from contact with a foreign substance. The term describes 2 diagnostic categories—allergic contact dermatitis and irritant contact dermatitis. In this case, the chemicals in the perfume may have acted as irritants. The alcohol she used to treat the rash was probably an irritant as well.
A hypersensitivity reaction to irritants and allergens
The mechanism of allergic contact dermatitis is a delayed hypersensitivity reaction. A foreign substance comes into contact with skin and links to skin protein, forming an antigen complex recognized by the immune system. In the skin, the major antigen-presenting cell is the Langerhans cell. When the epidermis is re-exposed to the antigen, the sensitized T-cells initiate an inflammatory cascade leading to changes in the skin. The reaction generally occurs within 12 to 48 hours in a sensitized person. The differential diagnoses for this patient include atopic dermatitis, psoriasis, and fungal infection.
Cosmetics, perfumes, and chemicals in cleaning solutions are known to cause irritant contact dermatitis. The most typical locations are hands or feet, with the dorsum affected more often than the palm or the sole. The lesions are usually erythematous and not well demarcated. The lesions may be macular, papular, or vesicular.
Allergic contact dermatitis often occurs after contact with allergens such as nickel in jewelry, or resins in plants such as poison ivy or poison oak. Vesicles may appear, and the hands are most commonly affected. The lesions may form a linear pattern, as in the case of plant dermatitis.
Evaluation: tests usually not needed
A diagnosis of contact dermatitis usually requires nothing more than findings in the patient’s history and physical exam. If a fungal infection is suspected, use a potassium hydroxide (KOH) preparation to look for hyphae or spores (see page 854 in this issue). Patch testing—placing common antigens on the patient’s skin and observing for reactions—is used to confirm the diagnosis of contact dermatitis and to determine the offending agent.
In this case, neither test was necessary or warranted because the history and physical exam led to a clear diagnosis that was treatable without having to analyze the chemicals in the perfume.
Treatment: remove the irritant, stop the swelling
Whether this is irritant or allergic contact dermatitis, the first line of treatment is to stop further exposure to the offending substance. A mid- to high-potency topical corticosteroid is recommended to stopping the inflammatory process (level of evidence [LOE]=5). (For an explanation of evidence-based medicine ratings, see page 000.) Ointments are more potent and particularly useful when the affected skin is dry and scaly.
Oral steroids are often used for severe local dermatitis, such as that caused by poison ivy (LOE=5). Topical tacrolimus ointment 0.1% is a more expensive option for the treatment of allergic contact dermatitis induced by nickel (LOE=2b).1 Oral H1 blocking sedating anti-histamines (such as diphenhydramine and hydroxyzine) provide relief from itching and help with sleep. Sedating antihistamines may be more effective for itching, but are probably inadvisable for persons who must drive or operate machinery. Newer nonsedating anti-histamines are an option when sedating agents should be avoided.
Conclusion of visit
The patient was given 0.1% triamcinolone ointment (a generic mid-potency steroid) to apply 2 to 3 times a day to the affected areas. She did not want any oral medications for the itching, but understood that diphenhydramine is available without a prescription if needed. She planned to give the perfume away and understood it was now on her list of items to avoid. Her physician explained her underlying eczema and what could be done to prevent rashes.
A 43-year-old African-American woman was seen for a rash on her right hand and neck. The rash appeared 2 weeks earlier, and was itchy. The patient had been applying alcohol directly to the affected skin.
The patient said she had experienced rashes on and off during her adult life. She has not worn necklaces for years because they irritate the skin around her neck. She also cannot wear wool clothing or any shirts with bright colors. She had not discussed this with a physician before, and she did not know why her skin is so sensitive.
The patient was not taking any new medications, using new bath products, or wearing new clothing before the rash appeared. However, she did remember getting new perfume 2 weeks earlier. She did not have asthma, but did have a mild hay fever. She was adopted and therefore did not know her biologic family’s medical history.
On close inspection, prominent erythema was seen around her neck and on the dorsum of her right hand (Figures 1 and 2).
FIGURE 1
Itchy rash on the neck…
FIGURE 2
…and the right hand
What is the diagnosis?
What are the management options?
Diagnosis: contact dermatitis
The patient demonstrated how she applied perfume to her neck using the back of her right hand. She has acute contact dermatitis on top of previously undiagnosed eczema. Her history is positive for contact dermatitis in reaction to metal (probably nickel) in necklaces and to various fabrics.
Contact dermatitis is a common inflammatory skin condition in which erythematous and pruritic skin lesions result from contact with a foreign substance. The term describes 2 diagnostic categories—allergic contact dermatitis and irritant contact dermatitis. In this case, the chemicals in the perfume may have acted as irritants. The alcohol she used to treat the rash was probably an irritant as well.
A hypersensitivity reaction to irritants and allergens
The mechanism of allergic contact dermatitis is a delayed hypersensitivity reaction. A foreign substance comes into contact with skin and links to skin protein, forming an antigen complex recognized by the immune system. In the skin, the major antigen-presenting cell is the Langerhans cell. When the epidermis is re-exposed to the antigen, the sensitized T-cells initiate an inflammatory cascade leading to changes in the skin. The reaction generally occurs within 12 to 48 hours in a sensitized person. The differential diagnoses for this patient include atopic dermatitis, psoriasis, and fungal infection.
Cosmetics, perfumes, and chemicals in cleaning solutions are known to cause irritant contact dermatitis. The most typical locations are hands or feet, with the dorsum affected more often than the palm or the sole. The lesions are usually erythematous and not well demarcated. The lesions may be macular, papular, or vesicular.
Allergic contact dermatitis often occurs after contact with allergens such as nickel in jewelry, or resins in plants such as poison ivy or poison oak. Vesicles may appear, and the hands are most commonly affected. The lesions may form a linear pattern, as in the case of plant dermatitis.
Evaluation: tests usually not needed
A diagnosis of contact dermatitis usually requires nothing more than findings in the patient’s history and physical exam. If a fungal infection is suspected, use a potassium hydroxide (KOH) preparation to look for hyphae or spores (see page 854 in this issue). Patch testing—placing common antigens on the patient’s skin and observing for reactions—is used to confirm the diagnosis of contact dermatitis and to determine the offending agent.
In this case, neither test was necessary or warranted because the history and physical exam led to a clear diagnosis that was treatable without having to analyze the chemicals in the perfume.
Treatment: remove the irritant, stop the swelling
Whether this is irritant or allergic contact dermatitis, the first line of treatment is to stop further exposure to the offending substance. A mid- to high-potency topical corticosteroid is recommended to stopping the inflammatory process (level of evidence [LOE]=5). (For an explanation of evidence-based medicine ratings, see page 000.) Ointments are more potent and particularly useful when the affected skin is dry and scaly.
Oral steroids are often used for severe local dermatitis, such as that caused by poison ivy (LOE=5). Topical tacrolimus ointment 0.1% is a more expensive option for the treatment of allergic contact dermatitis induced by nickel (LOE=2b).1 Oral H1 blocking sedating anti-histamines (such as diphenhydramine and hydroxyzine) provide relief from itching and help with sleep. Sedating antihistamines may be more effective for itching, but are probably inadvisable for persons who must drive or operate machinery. Newer nonsedating anti-histamines are an option when sedating agents should be avoided.
Conclusion of visit
The patient was given 0.1% triamcinolone ointment (a generic mid-potency steroid) to apply 2 to 3 times a day to the affected areas. She did not want any oral medications for the itching, but understood that diphenhydramine is available without a prescription if needed. She planned to give the perfume away and understood it was now on her list of items to avoid. Her physician explained her underlying eczema and what could be done to prevent rashes.
1. Saripalli YV, Gadzia JE, Belsito DV. Tacrolimus ointment 0.1% in the treatment of nickel-induced allergic contact dermatitis. J Am Acad Dermatol 2003;49:477-482.
1. Saripalli YV, Gadzia JE, Belsito DV. Tacrolimus ointment 0.1% in the treatment of nickel-induced allergic contact dermatitis. J Am Acad Dermatol 2003;49:477-482.
A red rash on the face
A 28-year-old man came to the office with a rash on his face. He reported he has had this rash on and off for 3 years. The rash sometimes itches around his moustache, and it gets worse with stress—he has been under increasing stress for the past 2 months. He is in good health and does not have any other symptoms, and he denies any risk factors for human immunodeficiency virus (HIV).
Physical examination reveals erythema and scale across his eyebrows, cheeks, and near his moustache. On close inspection, the scale is visible under his moustache and eyebrows as well.
FIGURE 1
Erythema on the face
FIGURE 2
Close-up of erythema
What is the diagnosis?
What are the management options?
DIAGNOSIS
This young man has seborrhea (seborrheic dermatitis), a superficial inflammatory dermatitis. It is a common condition characterized by patches of erythema and scaling, usually on the scalp (ie, dandruff), eyebrows, nasolabial creases, forehead, cheeks, around the nose, behind the ears, and under facial hair. Seborrhea can also occur over the sternum and in the axillae, submammary folds, umbilicus, groin, and gluteal creases. These areas are regions with a greater number of pilosebaceous units, which produce sebum.
Seborrhea is thought to be caused by an inflammatory hypersensitivity to epidermal, bacterial, or yeast antigens. Persons with seborrhea have a profusion of Pityrosporum yeast on the skin. This yeast can be a normal part of skin flora; seborrhea is an inflammatory reaction to its presence. Seborrhea is characterized by remissions and exacerbations. The most common precipitating factors are stress, immuno suppression, and cold weather. The treatment of seborrhea should be directed at the inflammation and the Pityrosporum.
Epidemiology
Seborrhea is most commonly seen in patients aged 20 and 50 years, and mostly in males. The prevalence of seborrhea is approximately 3% to 5% in young adults who are HIV-negative. The prevalence of seborrhea is as high as 36% in HIV-positive persons, although the vast majority of persons with seborrhea have a normal immune system. No lab tests are required to make the diagnosis.
Treatment: antifungals and topical steroids
Treat seborrhea with a 2-pronged plan: antifungal agents for the yeast and topical corticosteroids for the inflammation. The antifungals can also be used to prevent exacerbations; steroids should only be applied to active areas of inflammation.
Fortunately, seborrhea on the face responds well to low-potency topical corticosteroids, such as 1% hydrocortisone cream or lotion. Still, corticosteroids should not be used on the face for prolonged periods to avoid skin atrophy and other side effects. The lotion is better for hair-covered areas as it is less messy to apply than a cream.
Antifungal shampoos
Over-the-counter dandruff shampoos have been the mainstay of therapy for seborrhea of the scalp. These products often contain selenium (ie, Selsun Blue) or zinc (ie, Head and Shoulders), both of which are toxic to Pityrosporum. Often patients have both seborrhea on the scalp and the face, and using these shampoos can cut down the amount of Pityrosporumon both. Instruct patients with facial hair to lather their beards and moustache with shampoo as well.
Both ketoconazole (Nizoral) 2% shampoo and selenium sulfide 2.5% shampoo are effective in the treatment of moderate to severe dandruff (level of evidence [LOE]: 1b).1 Ketoconazole 2% shampoo is highly effective not only for clearing seborrheic dermatitis on the scalp but also for preventing relapse when used prophylactically once weekly (LOE: 1b).2 Ketoconazole has become available in a 1% over-the-counter dandruff shampoo, but the 2% shampoo still requires a prescription.
Treating severe cases
When seborrhea of the scalp becomes more severe, add a higher-potency steroid solution or lotion to the treatment until the exacerbation is under control. Ketoconazole cream is also a good treatment for seborrheic dermatitis in areas other than the scalp. Other antifungal creams such as miconazole can be used to treat seborrhea of the face.
One trial demonstrated the effectiveness of topical 1% metronidazole gel in seborrheic dermatitis (LOE: 1b). At the 8-week follow-up, 14 patients in the metronidazole group showed a marked to complete improvement compared with 2 in the placebo group (P<.001; number needed to treat=2).3 This is not an approved indication for metronidazole gel, but it may be considered when other topical medications fail. In a randomized controlled trial using crossover design, treatment with a low-dose homeopathic preparation provided significant improvement in seborrheic dermatitis and dandruff after 10 weeks of dosing (LOE: 2b).4
Most seborrheic dermatitis is fully treatable with topical agents. When topical medications are not providing adequate results, oral antifungal agents may be considered. In 1 study, oral terbinafine was found to be effective in the treatment of moderate to severe seborrheic dermatitis. Clinical improvement following 4 weeks treatment with terbinafine was maintained 8 weeks after completing treatment (LOE: 1b).5
Conclusion of visit
The patient was given a prescription for 1% hydrocortisone lotion and 2% ketoconazole cream, both to be applied twice daily to the affected areas. He also planned to investigate the homeopathy option for the future. It was explained to the patient that these treatments may not be curative, and seborrhea may come back when he is under stress.
1. Danby FW, Maddin WS, Margesson LJ, Rosenthal D. A randomized, double-blind, placebo-controlled trial of ketoconazole 2% shampoo versus selenium sulfide 2.5% shampoo in the treatment of moderate to severe dandruff. J Am Acad Dermatol 1993;29:1008-1012.
2. Peter RU, Richarz-Barthauer U. Successful treatment and prophylaxis of scalp seborrhoeic dermatitis and dandruff with 2% ketoconazole shampoo: results of a multicentre, double-blind, placebo-controlled trial. Br J Dermatol 1995;132:441-445.
3. Parsad D, Pandhi R, Negi KS, Kumar B. Topical metronidazole in seborrheic dermatitis—a double-blind study. Dermatology 2001;202:35-37.
4. Smith SA, Baker AE, Williams JH. Effective treatment of seborrheic dermatitis using a low dose, oral homeopathic medication consisting of potassium bromide, sodium bromide, nickel sulfate, and sodium chloride in a double-blind, placebo-controlled study. Altern Med Rev 2002;7:59-67.
5. Scaparro E, Quadri G, Virno G, Orifici C, Milani M. Evaluation of the efficacy and tolerability of oral terbinafine (Daskil) in patients with seborrhoeic dermatitis. A multicentre, randomized, investigator-blinded, placebo-controlled trial. Br J Dermatol 2001;144:854-857.
A 28-year-old man came to the office with a rash on his face. He reported he has had this rash on and off for 3 years. The rash sometimes itches around his moustache, and it gets worse with stress—he has been under increasing stress for the past 2 months. He is in good health and does not have any other symptoms, and he denies any risk factors for human immunodeficiency virus (HIV).
Physical examination reveals erythema and scale across his eyebrows, cheeks, and near his moustache. On close inspection, the scale is visible under his moustache and eyebrows as well.
FIGURE 1
Erythema on the face
FIGURE 2
Close-up of erythema
What is the diagnosis?
What are the management options?
DIAGNOSIS
This young man has seborrhea (seborrheic dermatitis), a superficial inflammatory dermatitis. It is a common condition characterized by patches of erythema and scaling, usually on the scalp (ie, dandruff), eyebrows, nasolabial creases, forehead, cheeks, around the nose, behind the ears, and under facial hair. Seborrhea can also occur over the sternum and in the axillae, submammary folds, umbilicus, groin, and gluteal creases. These areas are regions with a greater number of pilosebaceous units, which produce sebum.
Seborrhea is thought to be caused by an inflammatory hypersensitivity to epidermal, bacterial, or yeast antigens. Persons with seborrhea have a profusion of Pityrosporum yeast on the skin. This yeast can be a normal part of skin flora; seborrhea is an inflammatory reaction to its presence. Seborrhea is characterized by remissions and exacerbations. The most common precipitating factors are stress, immuno suppression, and cold weather. The treatment of seborrhea should be directed at the inflammation and the Pityrosporum.
Epidemiology
Seborrhea is most commonly seen in patients aged 20 and 50 years, and mostly in males. The prevalence of seborrhea is approximately 3% to 5% in young adults who are HIV-negative. The prevalence of seborrhea is as high as 36% in HIV-positive persons, although the vast majority of persons with seborrhea have a normal immune system. No lab tests are required to make the diagnosis.
Treatment: antifungals and topical steroids
Treat seborrhea with a 2-pronged plan: antifungal agents for the yeast and topical corticosteroids for the inflammation. The antifungals can also be used to prevent exacerbations; steroids should only be applied to active areas of inflammation.
Fortunately, seborrhea on the face responds well to low-potency topical corticosteroids, such as 1% hydrocortisone cream or lotion. Still, corticosteroids should not be used on the face for prolonged periods to avoid skin atrophy and other side effects. The lotion is better for hair-covered areas as it is less messy to apply than a cream.
Antifungal shampoos
Over-the-counter dandruff shampoos have been the mainstay of therapy for seborrhea of the scalp. These products often contain selenium (ie, Selsun Blue) or zinc (ie, Head and Shoulders), both of which are toxic to Pityrosporum. Often patients have both seborrhea on the scalp and the face, and using these shampoos can cut down the amount of Pityrosporumon both. Instruct patients with facial hair to lather their beards and moustache with shampoo as well.
Both ketoconazole (Nizoral) 2% shampoo and selenium sulfide 2.5% shampoo are effective in the treatment of moderate to severe dandruff (level of evidence [LOE]: 1b).1 Ketoconazole 2% shampoo is highly effective not only for clearing seborrheic dermatitis on the scalp but also for preventing relapse when used prophylactically once weekly (LOE: 1b).2 Ketoconazole has become available in a 1% over-the-counter dandruff shampoo, but the 2% shampoo still requires a prescription.
Treating severe cases
When seborrhea of the scalp becomes more severe, add a higher-potency steroid solution or lotion to the treatment until the exacerbation is under control. Ketoconazole cream is also a good treatment for seborrheic dermatitis in areas other than the scalp. Other antifungal creams such as miconazole can be used to treat seborrhea of the face.
One trial demonstrated the effectiveness of topical 1% metronidazole gel in seborrheic dermatitis (LOE: 1b). At the 8-week follow-up, 14 patients in the metronidazole group showed a marked to complete improvement compared with 2 in the placebo group (P<.001; number needed to treat=2).3 This is not an approved indication for metronidazole gel, but it may be considered when other topical medications fail. In a randomized controlled trial using crossover design, treatment with a low-dose homeopathic preparation provided significant improvement in seborrheic dermatitis and dandruff after 10 weeks of dosing (LOE: 2b).4
Most seborrheic dermatitis is fully treatable with topical agents. When topical medications are not providing adequate results, oral antifungal agents may be considered. In 1 study, oral terbinafine was found to be effective in the treatment of moderate to severe seborrheic dermatitis. Clinical improvement following 4 weeks treatment with terbinafine was maintained 8 weeks after completing treatment (LOE: 1b).5
Conclusion of visit
The patient was given a prescription for 1% hydrocortisone lotion and 2% ketoconazole cream, both to be applied twice daily to the affected areas. He also planned to investigate the homeopathy option for the future. It was explained to the patient that these treatments may not be curative, and seborrhea may come back when he is under stress.
A 28-year-old man came to the office with a rash on his face. He reported he has had this rash on and off for 3 years. The rash sometimes itches around his moustache, and it gets worse with stress—he has been under increasing stress for the past 2 months. He is in good health and does not have any other symptoms, and he denies any risk factors for human immunodeficiency virus (HIV).
Physical examination reveals erythema and scale across his eyebrows, cheeks, and near his moustache. On close inspection, the scale is visible under his moustache and eyebrows as well.
FIGURE 1
Erythema on the face
FIGURE 2
Close-up of erythema
What is the diagnosis?
What are the management options?
DIAGNOSIS
This young man has seborrhea (seborrheic dermatitis), a superficial inflammatory dermatitis. It is a common condition characterized by patches of erythema and scaling, usually on the scalp (ie, dandruff), eyebrows, nasolabial creases, forehead, cheeks, around the nose, behind the ears, and under facial hair. Seborrhea can also occur over the sternum and in the axillae, submammary folds, umbilicus, groin, and gluteal creases. These areas are regions with a greater number of pilosebaceous units, which produce sebum.
Seborrhea is thought to be caused by an inflammatory hypersensitivity to epidermal, bacterial, or yeast antigens. Persons with seborrhea have a profusion of Pityrosporum yeast on the skin. This yeast can be a normal part of skin flora; seborrhea is an inflammatory reaction to its presence. Seborrhea is characterized by remissions and exacerbations. The most common precipitating factors are stress, immuno suppression, and cold weather. The treatment of seborrhea should be directed at the inflammation and the Pityrosporum.
Epidemiology
Seborrhea is most commonly seen in patients aged 20 and 50 years, and mostly in males. The prevalence of seborrhea is approximately 3% to 5% in young adults who are HIV-negative. The prevalence of seborrhea is as high as 36% in HIV-positive persons, although the vast majority of persons with seborrhea have a normal immune system. No lab tests are required to make the diagnosis.
Treatment: antifungals and topical steroids
Treat seborrhea with a 2-pronged plan: antifungal agents for the yeast and topical corticosteroids for the inflammation. The antifungals can also be used to prevent exacerbations; steroids should only be applied to active areas of inflammation.
Fortunately, seborrhea on the face responds well to low-potency topical corticosteroids, such as 1% hydrocortisone cream or lotion. Still, corticosteroids should not be used on the face for prolonged periods to avoid skin atrophy and other side effects. The lotion is better for hair-covered areas as it is less messy to apply than a cream.
Antifungal shampoos
Over-the-counter dandruff shampoos have been the mainstay of therapy for seborrhea of the scalp. These products often contain selenium (ie, Selsun Blue) or zinc (ie, Head and Shoulders), both of which are toxic to Pityrosporum. Often patients have both seborrhea on the scalp and the face, and using these shampoos can cut down the amount of Pityrosporumon both. Instruct patients with facial hair to lather their beards and moustache with shampoo as well.
Both ketoconazole (Nizoral) 2% shampoo and selenium sulfide 2.5% shampoo are effective in the treatment of moderate to severe dandruff (level of evidence [LOE]: 1b).1 Ketoconazole 2% shampoo is highly effective not only for clearing seborrheic dermatitis on the scalp but also for preventing relapse when used prophylactically once weekly (LOE: 1b).2 Ketoconazole has become available in a 1% over-the-counter dandruff shampoo, but the 2% shampoo still requires a prescription.
Treating severe cases
When seborrhea of the scalp becomes more severe, add a higher-potency steroid solution or lotion to the treatment until the exacerbation is under control. Ketoconazole cream is also a good treatment for seborrheic dermatitis in areas other than the scalp. Other antifungal creams such as miconazole can be used to treat seborrhea of the face.
One trial demonstrated the effectiveness of topical 1% metronidazole gel in seborrheic dermatitis (LOE: 1b). At the 8-week follow-up, 14 patients in the metronidazole group showed a marked to complete improvement compared with 2 in the placebo group (P<.001; number needed to treat=2).3 This is not an approved indication for metronidazole gel, but it may be considered when other topical medications fail. In a randomized controlled trial using crossover design, treatment with a low-dose homeopathic preparation provided significant improvement in seborrheic dermatitis and dandruff after 10 weeks of dosing (LOE: 2b).4
Most seborrheic dermatitis is fully treatable with topical agents. When topical medications are not providing adequate results, oral antifungal agents may be considered. In 1 study, oral terbinafine was found to be effective in the treatment of moderate to severe seborrheic dermatitis. Clinical improvement following 4 weeks treatment with terbinafine was maintained 8 weeks after completing treatment (LOE: 1b).5
Conclusion of visit
The patient was given a prescription for 1% hydrocortisone lotion and 2% ketoconazole cream, both to be applied twice daily to the affected areas. He also planned to investigate the homeopathy option for the future. It was explained to the patient that these treatments may not be curative, and seborrhea may come back when he is under stress.
1. Danby FW, Maddin WS, Margesson LJ, Rosenthal D. A randomized, double-blind, placebo-controlled trial of ketoconazole 2% shampoo versus selenium sulfide 2.5% shampoo in the treatment of moderate to severe dandruff. J Am Acad Dermatol 1993;29:1008-1012.
2. Peter RU, Richarz-Barthauer U. Successful treatment and prophylaxis of scalp seborrhoeic dermatitis and dandruff with 2% ketoconazole shampoo: results of a multicentre, double-blind, placebo-controlled trial. Br J Dermatol 1995;132:441-445.
3. Parsad D, Pandhi R, Negi KS, Kumar B. Topical metronidazole in seborrheic dermatitis—a double-blind study. Dermatology 2001;202:35-37.
4. Smith SA, Baker AE, Williams JH. Effective treatment of seborrheic dermatitis using a low dose, oral homeopathic medication consisting of potassium bromide, sodium bromide, nickel sulfate, and sodium chloride in a double-blind, placebo-controlled study. Altern Med Rev 2002;7:59-67.
5. Scaparro E, Quadri G, Virno G, Orifici C, Milani M. Evaluation of the efficacy and tolerability of oral terbinafine (Daskil) in patients with seborrhoeic dermatitis. A multicentre, randomized, investigator-blinded, placebo-controlled trial. Br J Dermatol 2001;144:854-857.
1. Danby FW, Maddin WS, Margesson LJ, Rosenthal D. A randomized, double-blind, placebo-controlled trial of ketoconazole 2% shampoo versus selenium sulfide 2.5% shampoo in the treatment of moderate to severe dandruff. J Am Acad Dermatol 1993;29:1008-1012.
2. Peter RU, Richarz-Barthauer U. Successful treatment and prophylaxis of scalp seborrhoeic dermatitis and dandruff with 2% ketoconazole shampoo: results of a multicentre, double-blind, placebo-controlled trial. Br J Dermatol 1995;132:441-445.
3. Parsad D, Pandhi R, Negi KS, Kumar B. Topical metronidazole in seborrheic dermatitis—a double-blind study. Dermatology 2001;202:35-37.
4. Smith SA, Baker AE, Williams JH. Effective treatment of seborrheic dermatitis using a low dose, oral homeopathic medication consisting of potassium bromide, sodium bromide, nickel sulfate, and sodium chloride in a double-blind, placebo-controlled study. Altern Med Rev 2002;7:59-67.
5. Scaparro E, Quadri G, Virno G, Orifici C, Milani M. Evaluation of the efficacy and tolerability of oral terbinafine (Daskil) in patients with seborrhoeic dermatitis. A multicentre, randomized, investigator-blinded, placebo-controlled trial. Br J Dermatol 2001;144:854-857.
Back from the Peace Corps— with skin lesions from South America
A 25-year-old woman visited her family doctor for treatment of skin lesions on her left leg, which had developed over the previous 8 weeks. The patient had just returned to the US after working with the Peace Corps in the Amazon rain forest for 3 months. During that time, she slept outside in the jungle without any skin protection—no mosquito netting, no insect repellent, no protective clothing on her extremities. She reported no recent history of trauma, burns, or chemical exposure to the leg, and she had been healthy prior to this skin condition. She reported that she was taking no medications, and was not using alcohol or tobacco.
The lesions started with the development of small pustules on her left leg and ankle. Over the next 3 weeks, these grew into larger, ulcerated lesions. The ulcers persisted for 5 more weeks despite multiple attempts at local topical treatments in Ecuador. No pain or itching were associated with the lesions.
The physical examination revealed a generally healthy woman, remarkable only for the 2 skin ulcers on her left lower leg and ankle (Figure 1 and Figure 2). The patient was afebrile, and had no lymphadenopathy or hepatosplenomegaly.
FIGURE 1
Cutaneous ulceration with indurated border.
Two active ulcers with small healed satellite lesion near the medial malleolus (see arrow).
How would you treat this condition?
Differential diagnosis of tropical skin ulcers
The woman’s family physician used the Internet to determine that the differential diagnosis of tropical skin ulcers includes localized cutaneous leishmaniasis, foreign body reaction, impetigo, pyoderma gangrenosum, bacterial or deep fungal infection, atypical mycobacterial infection, sarcoidosis, squamous and basal cell carcinoma, and superinfected insect bites. The combination of the patient’s history of potential exposure, clinical presentation, and epidemiology of leishmaniasis within the region in which she was working supports a presumptive diagnosis of localized cutaneous leishmaniasis.
Leishmaniasis
Leishmaniasis is comprised of several diverse diseases with varying degrees of severity, ranging from spontaneously healing skin ulcers to a disfiguring mucocutaneous disease, and even to fatal visceral illness. Endemic worldwide except Australia, Oceania, and Antarctica, leishmaniasis is found in the tropics and subtropics.
Approximately 2 million new cases occur each year, with markedly increasing incidence in several parts of the world resulting from international travel, immigration, military deployment, and human immunodeficiency virus coinfection.1
An estimated 10% of the world’s population is at risk for contracting leishmaniasis. Most cases reported in the US are in travelers to countries where the disease is endemic, although sporadic cases have been reported in Texas and Oklahoma.2
Characteristics
Leishmaniasis is a vector-borne disease, caused by obligate intracellular protozoa of the genus Leishmaniaand transmitted by the bite of infected female sandflies. The disease may take several forms, including cutaneous, mucocutaneous, and visceral leishmaniasis, depending on the particular Leishmaniaspecies and host response.
Localized cutaneous leishmaniasis is characterized clinically by the appearance of skin lesions at the site of the sandfly bite, which typically present as inflammatory papules before progressing to nodules and ulcers. Local lymphadenopathy may occur. Sores may be painless or painful.
Both cutaneous and mucocutaneous forms generally yield normal laboratory values, although complete blood counts may show mild anemia, leukopenia, or thrombocytopenia.3 US travelers may consult numerous physicians before leishmaniasis is diagnosed. The median time from recognition of skin lesions to drug treatment is 112 days.4
Lab results
The patient’s complete blood count with differential, electrolytes, creatinine, liver function tests, and electrocardiogram were within normal limits. An infectious disease consultant suggested direct microscopic visualization of skin biopsies, dermal scrapings, and needle aspirates using Giemsa and Leishman stains, but these failed to reveal any parasitic organisms. It was thought these results were most likely false negatives.
In the best situation, the diagnosis of leishmaniasis is confirmed by isolating, visualizing, and culturing the parasite from infected tissue. Dermal scrapings or needle aspirates may reveal Leishmania amastigotes using a Giemsa stain. Early in the course of localized disease, Leishmania organisms may be numerous and found readily within the cytoplasm of macrophages. However, biopsy specimens from old lesions (>6 months), partially or incompletely treated, are frequently negative.
In vitro culture of the parasite from tissue samples using Nicolle-Noy-McNeal medium is often obtained to aid in diagnosis and to identify Leishmania species. With successful culture, the parasite can be sent to the Centers for Disease Control for speciation. New, rapid tests for leishmaniasis are being developed.
Treatment
Although 90% of skin lesions caused by cutaneous leishmaniasis heal spontaneously to form atrophic scars, the infectious disease consultant recommended treatment to prevent development of disfiguring mucocutaneous disease (level of evidence [LOE]=5)—otherwise, immunity may not be complete and skin ulcers can recur.
Experts believe it is important to treat cutaneous leishmaniasis if a species known or suspected of being capable of converting to the mucocutaneous disease form—eg, New World L braziliensis—is present. These lesions may appear months or even years after the initial exposure, and can be refractory to further treatment. However, surgical excision usually is not recommended because of the risk of relapse and further cosmetic disfigurement.3
Yearly follow-up to evaluate for recurrence or evolution of mucocutaneous leishmaniasis is crucial; early treatment of this form of the disease is more efficacious and can yield more favorable outcomes by limiting potential facial involvement (LOE=5).
Meglumine antimonate
The patient’s initial treatment included gluteal injections of meglumine antimonate at a dosage of 20 mg antimony/kg/d intramuscularly for a total course of 21 days (LOE=5). In addition, one tenth of each dose was injected directly into skin lesions under the peripheral margins, as shown in Figure 3 (LOE=5).
Side effects. The patient’s side effects from the meglumine antimonate therapy included insomnia, lightheadedness, increased fatigue, pain at the gluteal injection sites, bone aches, painful splenomegaly, and left leg myoclonic spasms. These signs and symptoms resolved shortly after completion of the course of therapy with no apparent sequelae. Monitoring cardiac, renal, and hepatic function before and during treatment is important, as meglumine antimonate has significant potential to cause renal and hepatic toxicity.
Outcome
The patient’s skin lesions began to show signs of healing after a few days of treatment. Healed lesions can be seen in Figure 4 Of course, we don’t know that these lesions would not have healed without treatment.
Follow-up diagnostic tests including electrocardiograms, liver function tests, and renal function showed normal values at the conclusion of the 21-day course of therapy.
Fluconazole studied
Since this patient was treated, a Saudi Arabian study was published on use of oral fluconazole 200 mg/d for 6 weeks in patients with cutaneous leishmaniasis (L major).5 At the 3-month followup, healing of lesions was complete for 79% of patients in the fluconazole group and 34% patients in the placebo group (LOE=2b).
The toxicity of this treatment is much lower than the antimonials; we should be looking for further evidence of its benefits in other countries with other species of Leishmania.
FIGURE 3
Perilesional infiltration of leishmaniasis lesion using meglumine antimonate.
FIGURE 4
Healed cutaneous leishmaniasis lesions on left leg.
Preventing sandfly bites
Leishmaniasis is preventable by avoiding contact with the vector—the sandfly—while living or traveling in endemic areas. Sandflies are most active from dusk to dawn. Though relatively poor fliers, they are small enough to fit through standard mosquito netting and make no audible noise. Effective prevention may be achieved by avoiding nighttime outdoor activities, using topical insecticides (eg, N, N diethyl-m-toluamide [DEET]) on exposed skin surfaces, using insecticide-impregnated clothing (permethrin stays in material for many washings), using fine-mesh mosquito netting, and sleeping with a fan.3
In this time of the globalization of infectious diseases, family doctors in the US should be aware of the tropical diseases that our patients may bring to their offices.
1. Roberts LJ, Handman E, Foote SJ. Science, medicine and the future: leishmaniasis. BMJ 2000;321:801-804.
2. Melby PC, Kreutzer RD, McMahon-Pratt D, Gam AA, Neva FA. Cutaneous leishmaniasis: review of 59 cases seen at the National Institutes of Health. Clin Infect Dis 1992;15:924-937.
3. Kenner JR, Kaugh YC. Leishmaniasis. eMedicine J. 2001 2(11). Available at http://www.emedicine.com/derm/topic219.htm Accessed on May 29, 2003.
4. Herwaldt BL, Stokes SL, Juranek DD. American cutaneous leishmaniasis in U.S. travelers. Ann Intern Med 1993;118:779-784.
5. Alrajhi AA, Ibrahim EA, De Vol EB, Khairat M, Faris RM, Maguire JH. Fluconazole for the treatment of cutaneous leishmaniasis caused by Leishmania major. N Engl J Med 2002;346:891-895.
A 25-year-old woman visited her family doctor for treatment of skin lesions on her left leg, which had developed over the previous 8 weeks. The patient had just returned to the US after working with the Peace Corps in the Amazon rain forest for 3 months. During that time, she slept outside in the jungle without any skin protection—no mosquito netting, no insect repellent, no protective clothing on her extremities. She reported no recent history of trauma, burns, or chemical exposure to the leg, and she had been healthy prior to this skin condition. She reported that she was taking no medications, and was not using alcohol or tobacco.
The lesions started with the development of small pustules on her left leg and ankle. Over the next 3 weeks, these grew into larger, ulcerated lesions. The ulcers persisted for 5 more weeks despite multiple attempts at local topical treatments in Ecuador. No pain or itching were associated with the lesions.
The physical examination revealed a generally healthy woman, remarkable only for the 2 skin ulcers on her left lower leg and ankle (Figure 1 and Figure 2). The patient was afebrile, and had no lymphadenopathy or hepatosplenomegaly.
FIGURE 1
Cutaneous ulceration with indurated border.
Two active ulcers with small healed satellite lesion near the medial malleolus (see arrow).
How would you treat this condition?
Differential diagnosis of tropical skin ulcers
The woman’s family physician used the Internet to determine that the differential diagnosis of tropical skin ulcers includes localized cutaneous leishmaniasis, foreign body reaction, impetigo, pyoderma gangrenosum, bacterial or deep fungal infection, atypical mycobacterial infection, sarcoidosis, squamous and basal cell carcinoma, and superinfected insect bites. The combination of the patient’s history of potential exposure, clinical presentation, and epidemiology of leishmaniasis within the region in which she was working supports a presumptive diagnosis of localized cutaneous leishmaniasis.
Leishmaniasis
Leishmaniasis is comprised of several diverse diseases with varying degrees of severity, ranging from spontaneously healing skin ulcers to a disfiguring mucocutaneous disease, and even to fatal visceral illness. Endemic worldwide except Australia, Oceania, and Antarctica, leishmaniasis is found in the tropics and subtropics.
Approximately 2 million new cases occur each year, with markedly increasing incidence in several parts of the world resulting from international travel, immigration, military deployment, and human immunodeficiency virus coinfection.1
An estimated 10% of the world’s population is at risk for contracting leishmaniasis. Most cases reported in the US are in travelers to countries where the disease is endemic, although sporadic cases have been reported in Texas and Oklahoma.2
Characteristics
Leishmaniasis is a vector-borne disease, caused by obligate intracellular protozoa of the genus Leishmaniaand transmitted by the bite of infected female sandflies. The disease may take several forms, including cutaneous, mucocutaneous, and visceral leishmaniasis, depending on the particular Leishmaniaspecies and host response.
Localized cutaneous leishmaniasis is characterized clinically by the appearance of skin lesions at the site of the sandfly bite, which typically present as inflammatory papules before progressing to nodules and ulcers. Local lymphadenopathy may occur. Sores may be painless or painful.
Both cutaneous and mucocutaneous forms generally yield normal laboratory values, although complete blood counts may show mild anemia, leukopenia, or thrombocytopenia.3 US travelers may consult numerous physicians before leishmaniasis is diagnosed. The median time from recognition of skin lesions to drug treatment is 112 days.4
Lab results
The patient’s complete blood count with differential, electrolytes, creatinine, liver function tests, and electrocardiogram were within normal limits. An infectious disease consultant suggested direct microscopic visualization of skin biopsies, dermal scrapings, and needle aspirates using Giemsa and Leishman stains, but these failed to reveal any parasitic organisms. It was thought these results were most likely false negatives.
In the best situation, the diagnosis of leishmaniasis is confirmed by isolating, visualizing, and culturing the parasite from infected tissue. Dermal scrapings or needle aspirates may reveal Leishmania amastigotes using a Giemsa stain. Early in the course of localized disease, Leishmania organisms may be numerous and found readily within the cytoplasm of macrophages. However, biopsy specimens from old lesions (>6 months), partially or incompletely treated, are frequently negative.
In vitro culture of the parasite from tissue samples using Nicolle-Noy-McNeal medium is often obtained to aid in diagnosis and to identify Leishmania species. With successful culture, the parasite can be sent to the Centers for Disease Control for speciation. New, rapid tests for leishmaniasis are being developed.
Treatment
Although 90% of skin lesions caused by cutaneous leishmaniasis heal spontaneously to form atrophic scars, the infectious disease consultant recommended treatment to prevent development of disfiguring mucocutaneous disease (level of evidence [LOE]=5)—otherwise, immunity may not be complete and skin ulcers can recur.
Experts believe it is important to treat cutaneous leishmaniasis if a species known or suspected of being capable of converting to the mucocutaneous disease form—eg, New World L braziliensis—is present. These lesions may appear months or even years after the initial exposure, and can be refractory to further treatment. However, surgical excision usually is not recommended because of the risk of relapse and further cosmetic disfigurement.3
Yearly follow-up to evaluate for recurrence or evolution of mucocutaneous leishmaniasis is crucial; early treatment of this form of the disease is more efficacious and can yield more favorable outcomes by limiting potential facial involvement (LOE=5).
Meglumine antimonate
The patient’s initial treatment included gluteal injections of meglumine antimonate at a dosage of 20 mg antimony/kg/d intramuscularly for a total course of 21 days (LOE=5). In addition, one tenth of each dose was injected directly into skin lesions under the peripheral margins, as shown in Figure 3 (LOE=5).
Side effects. The patient’s side effects from the meglumine antimonate therapy included insomnia, lightheadedness, increased fatigue, pain at the gluteal injection sites, bone aches, painful splenomegaly, and left leg myoclonic spasms. These signs and symptoms resolved shortly after completion of the course of therapy with no apparent sequelae. Monitoring cardiac, renal, and hepatic function before and during treatment is important, as meglumine antimonate has significant potential to cause renal and hepatic toxicity.
Outcome
The patient’s skin lesions began to show signs of healing after a few days of treatment. Healed lesions can be seen in Figure 4 Of course, we don’t know that these lesions would not have healed without treatment.
Follow-up diagnostic tests including electrocardiograms, liver function tests, and renal function showed normal values at the conclusion of the 21-day course of therapy.
Fluconazole studied
Since this patient was treated, a Saudi Arabian study was published on use of oral fluconazole 200 mg/d for 6 weeks in patients with cutaneous leishmaniasis (L major).5 At the 3-month followup, healing of lesions was complete for 79% of patients in the fluconazole group and 34% patients in the placebo group (LOE=2b).
The toxicity of this treatment is much lower than the antimonials; we should be looking for further evidence of its benefits in other countries with other species of Leishmania.
FIGURE 3
Perilesional infiltration of leishmaniasis lesion using meglumine antimonate.
FIGURE 4
Healed cutaneous leishmaniasis lesions on left leg.
Preventing sandfly bites
Leishmaniasis is preventable by avoiding contact with the vector—the sandfly—while living or traveling in endemic areas. Sandflies are most active from dusk to dawn. Though relatively poor fliers, they are small enough to fit through standard mosquito netting and make no audible noise. Effective prevention may be achieved by avoiding nighttime outdoor activities, using topical insecticides (eg, N, N diethyl-m-toluamide [DEET]) on exposed skin surfaces, using insecticide-impregnated clothing (permethrin stays in material for many washings), using fine-mesh mosquito netting, and sleeping with a fan.3
In this time of the globalization of infectious diseases, family doctors in the US should be aware of the tropical diseases that our patients may bring to their offices.
A 25-year-old woman visited her family doctor for treatment of skin lesions on her left leg, which had developed over the previous 8 weeks. The patient had just returned to the US after working with the Peace Corps in the Amazon rain forest for 3 months. During that time, she slept outside in the jungle without any skin protection—no mosquito netting, no insect repellent, no protective clothing on her extremities. She reported no recent history of trauma, burns, or chemical exposure to the leg, and she had been healthy prior to this skin condition. She reported that she was taking no medications, and was not using alcohol or tobacco.
The lesions started with the development of small pustules on her left leg and ankle. Over the next 3 weeks, these grew into larger, ulcerated lesions. The ulcers persisted for 5 more weeks despite multiple attempts at local topical treatments in Ecuador. No pain or itching were associated with the lesions.
The physical examination revealed a generally healthy woman, remarkable only for the 2 skin ulcers on her left lower leg and ankle (Figure 1 and Figure 2). The patient was afebrile, and had no lymphadenopathy or hepatosplenomegaly.
FIGURE 1
Cutaneous ulceration with indurated border.
Two active ulcers with small healed satellite lesion near the medial malleolus (see arrow).
How would you treat this condition?
Differential diagnosis of tropical skin ulcers
The woman’s family physician used the Internet to determine that the differential diagnosis of tropical skin ulcers includes localized cutaneous leishmaniasis, foreign body reaction, impetigo, pyoderma gangrenosum, bacterial or deep fungal infection, atypical mycobacterial infection, sarcoidosis, squamous and basal cell carcinoma, and superinfected insect bites. The combination of the patient’s history of potential exposure, clinical presentation, and epidemiology of leishmaniasis within the region in which she was working supports a presumptive diagnosis of localized cutaneous leishmaniasis.
Leishmaniasis
Leishmaniasis is comprised of several diverse diseases with varying degrees of severity, ranging from spontaneously healing skin ulcers to a disfiguring mucocutaneous disease, and even to fatal visceral illness. Endemic worldwide except Australia, Oceania, and Antarctica, leishmaniasis is found in the tropics and subtropics.
Approximately 2 million new cases occur each year, with markedly increasing incidence in several parts of the world resulting from international travel, immigration, military deployment, and human immunodeficiency virus coinfection.1
An estimated 10% of the world’s population is at risk for contracting leishmaniasis. Most cases reported in the US are in travelers to countries where the disease is endemic, although sporadic cases have been reported in Texas and Oklahoma.2
Characteristics
Leishmaniasis is a vector-borne disease, caused by obligate intracellular protozoa of the genus Leishmaniaand transmitted by the bite of infected female sandflies. The disease may take several forms, including cutaneous, mucocutaneous, and visceral leishmaniasis, depending on the particular Leishmaniaspecies and host response.
Localized cutaneous leishmaniasis is characterized clinically by the appearance of skin lesions at the site of the sandfly bite, which typically present as inflammatory papules before progressing to nodules and ulcers. Local lymphadenopathy may occur. Sores may be painless or painful.
Both cutaneous and mucocutaneous forms generally yield normal laboratory values, although complete blood counts may show mild anemia, leukopenia, or thrombocytopenia.3 US travelers may consult numerous physicians before leishmaniasis is diagnosed. The median time from recognition of skin lesions to drug treatment is 112 days.4
Lab results
The patient’s complete blood count with differential, electrolytes, creatinine, liver function tests, and electrocardiogram were within normal limits. An infectious disease consultant suggested direct microscopic visualization of skin biopsies, dermal scrapings, and needle aspirates using Giemsa and Leishman stains, but these failed to reveal any parasitic organisms. It was thought these results were most likely false negatives.
In the best situation, the diagnosis of leishmaniasis is confirmed by isolating, visualizing, and culturing the parasite from infected tissue. Dermal scrapings or needle aspirates may reveal Leishmania amastigotes using a Giemsa stain. Early in the course of localized disease, Leishmania organisms may be numerous and found readily within the cytoplasm of macrophages. However, biopsy specimens from old lesions (>6 months), partially or incompletely treated, are frequently negative.
In vitro culture of the parasite from tissue samples using Nicolle-Noy-McNeal medium is often obtained to aid in diagnosis and to identify Leishmania species. With successful culture, the parasite can be sent to the Centers for Disease Control for speciation. New, rapid tests for leishmaniasis are being developed.
Treatment
Although 90% of skin lesions caused by cutaneous leishmaniasis heal spontaneously to form atrophic scars, the infectious disease consultant recommended treatment to prevent development of disfiguring mucocutaneous disease (level of evidence [LOE]=5)—otherwise, immunity may not be complete and skin ulcers can recur.
Experts believe it is important to treat cutaneous leishmaniasis if a species known or suspected of being capable of converting to the mucocutaneous disease form—eg, New World L braziliensis—is present. These lesions may appear months or even years after the initial exposure, and can be refractory to further treatment. However, surgical excision usually is not recommended because of the risk of relapse and further cosmetic disfigurement.3
Yearly follow-up to evaluate for recurrence or evolution of mucocutaneous leishmaniasis is crucial; early treatment of this form of the disease is more efficacious and can yield more favorable outcomes by limiting potential facial involvement (LOE=5).
Meglumine antimonate
The patient’s initial treatment included gluteal injections of meglumine antimonate at a dosage of 20 mg antimony/kg/d intramuscularly for a total course of 21 days (LOE=5). In addition, one tenth of each dose was injected directly into skin lesions under the peripheral margins, as shown in Figure 3 (LOE=5).
Side effects. The patient’s side effects from the meglumine antimonate therapy included insomnia, lightheadedness, increased fatigue, pain at the gluteal injection sites, bone aches, painful splenomegaly, and left leg myoclonic spasms. These signs and symptoms resolved shortly after completion of the course of therapy with no apparent sequelae. Monitoring cardiac, renal, and hepatic function before and during treatment is important, as meglumine antimonate has significant potential to cause renal and hepatic toxicity.
Outcome
The patient’s skin lesions began to show signs of healing after a few days of treatment. Healed lesions can be seen in Figure 4 Of course, we don’t know that these lesions would not have healed without treatment.
Follow-up diagnostic tests including electrocardiograms, liver function tests, and renal function showed normal values at the conclusion of the 21-day course of therapy.
Fluconazole studied
Since this patient was treated, a Saudi Arabian study was published on use of oral fluconazole 200 mg/d for 6 weeks in patients with cutaneous leishmaniasis (L major).5 At the 3-month followup, healing of lesions was complete for 79% of patients in the fluconazole group and 34% patients in the placebo group (LOE=2b).
The toxicity of this treatment is much lower than the antimonials; we should be looking for further evidence of its benefits in other countries with other species of Leishmania.
FIGURE 3
Perilesional infiltration of leishmaniasis lesion using meglumine antimonate.
FIGURE 4
Healed cutaneous leishmaniasis lesions on left leg.
Preventing sandfly bites
Leishmaniasis is preventable by avoiding contact with the vector—the sandfly—while living or traveling in endemic areas. Sandflies are most active from dusk to dawn. Though relatively poor fliers, they are small enough to fit through standard mosquito netting and make no audible noise. Effective prevention may be achieved by avoiding nighttime outdoor activities, using topical insecticides (eg, N, N diethyl-m-toluamide [DEET]) on exposed skin surfaces, using insecticide-impregnated clothing (permethrin stays in material for many washings), using fine-mesh mosquito netting, and sleeping with a fan.3
In this time of the globalization of infectious diseases, family doctors in the US should be aware of the tropical diseases that our patients may bring to their offices.
1. Roberts LJ, Handman E, Foote SJ. Science, medicine and the future: leishmaniasis. BMJ 2000;321:801-804.
2. Melby PC, Kreutzer RD, McMahon-Pratt D, Gam AA, Neva FA. Cutaneous leishmaniasis: review of 59 cases seen at the National Institutes of Health. Clin Infect Dis 1992;15:924-937.
3. Kenner JR, Kaugh YC. Leishmaniasis. eMedicine J. 2001 2(11). Available at http://www.emedicine.com/derm/topic219.htm Accessed on May 29, 2003.
4. Herwaldt BL, Stokes SL, Juranek DD. American cutaneous leishmaniasis in U.S. travelers. Ann Intern Med 1993;118:779-784.
5. Alrajhi AA, Ibrahim EA, De Vol EB, Khairat M, Faris RM, Maguire JH. Fluconazole for the treatment of cutaneous leishmaniasis caused by Leishmania major. N Engl J Med 2002;346:891-895.
1. Roberts LJ, Handman E, Foote SJ. Science, medicine and the future: leishmaniasis. BMJ 2000;321:801-804.
2. Melby PC, Kreutzer RD, McMahon-Pratt D, Gam AA, Neva FA. Cutaneous leishmaniasis: review of 59 cases seen at the National Institutes of Health. Clin Infect Dis 1992;15:924-937.
3. Kenner JR, Kaugh YC. Leishmaniasis. eMedicine J. 2001 2(11). Available at http://www.emedicine.com/derm/topic219.htm Accessed on May 29, 2003.
4. Herwaldt BL, Stokes SL, Juranek DD. American cutaneous leishmaniasis in U.S. travelers. Ann Intern Med 1993;118:779-784.
5. Alrajhi AA, Ibrahim EA, De Vol EB, Khairat M, Faris RM, Maguire JH. Fluconazole for the treatment of cutaneous leishmaniasis caused by Leishmania major. N Engl J Med 2002;346:891-895.
A terrible itch
A 74-year-old Caucasian woman visited an outpatient clinic at a homeless shelter. Her chief concern was itching all over her body. Her chart revealed a history of chronic scabies and mental illness. She had been seen in the clinic on 4 separate occasions over a 2-year period for scabies. She claimed on this visit that she could not get rid of the scabies because people kept taking away her medication. She also stated she could see the creatures feed on her and move in and out of her skin.
The physical exam revealed that she was unwashed and disheveled. She had multiple excoriations on her extremities, hands, abdomen, back, and the nape of her neck (Figure 1).
FIGURE 1
Excoriations on the abdomen
FIGURE 2
Adult body lice and nymphs on clothing seams
Diagnosis
The woman’s appearance and mental status are consistent with schizophrenia; however, a diagnosis of scabies is not possible if she is really seeing the “bugs” on her body, as opposed to just imagining them. The scabies mite can only be seen with the aid of a microscope.
We looked for the bugs to confirm her story. While this could have been a case of delusions of parasitosis, on close inspection small “bugs” were indeed visible on her abdomen and along the seams of her pants. Multiple nits appeared attached to the hairs of her head, and a “bug” is noted to be feeding on the nape of her neck. This homeless woman has a massive infestation of body and head lice (Figure 2).
In the past she may have had a scabies infestation, but there was no documentation in the chart of any skin scrapings looked at under the microscope for diagnosis. It is more likely that she has been chronically infested with lice. Due to her mental illness, this patient may have been misdiagnosed with scabies based on the assumption that her claim to see the bugs was a hallucination. A close exam may not have been performed due to her mental illness and poor hygiene, along with the health care providers’ fears of catching scabies. Repeated documentation of scabies may have discouraged further investigation into another cause.
Pediculosis
Lice are bloodsucking obligate parasites. There are hundreds of millions of cases of pediculosis worldwide affecting men, women, and children from all socioeconomic classes.
Three types of lice infest humans: the head louse (Pediculus humanus capitis), the body louse (Pediculus humanus corporis), and the pubic louse (Phthirus pubis). Lice cling to hairs with their clawlike legs and pierce the skin, inject saliva, and then defecate while obtaining their blood meal. When exposed to lice, people clinically experience little irritation from the first bite, but after a short period they become sensitized. A hypersensitivity reaction—producing reddening of the skin, itching, and overall inflammation— subsequently develops.
Body lice are similar to head lice, except they are slightly larger. They are primarily seen in the homeless and indigent populations, with transmission occurring with direct body contact or sharing of contaminated clothes or bedding.
The body louse, contrary to popular belief, does not live on the body. It lives in the seams of clothing, clinging to the fibers. It will feed, remaining on the clothes, and only in massive infestations are they typically seen moving about the body. The axillae, groin, and truncal areas are the most severely affected. Patients have severe itching and tend to excoriate these regions. In chronically infested patients a postinflammatory hyperpigmentation can be observed.
Treatment
Persons infested with body lice need to discard or launder their clothing using hot water, and then bathe themselves. In cases of massive infestation—such as this case, in which head lice were also found—a pediculicide should be applied to the hair and entire body from head to toe. This can then be washed off in the shower (level of evidence [LOE]=1a, from Cochrane Review). This same Cochrane systematic review of the treatment of head lice found no evidence that any one pediculicide has greater effect than another (LOE=1a).1
In this case, the patient did not want to get rid of her green pants because she was able to find the “bugs” easily in its seams, which she thought helped keep them under control. When we explained that the full treatment of this condition required her to be given new clothes, she finally accepted this course of action.
Arrangements were made for her to shower at the shelter and obtain new clothes, and she was given permethrin shampoo to apply over her entire body from head to toe. She was scheduled to follow up in 1 week but unfortunately never returned to the clinic.
1. Dodd CS. Interventions for treating headlice (Cochrane Review). In: The Cochrane Library, Issue 2, 2002. Oxford.
A 74-year-old Caucasian woman visited an outpatient clinic at a homeless shelter. Her chief concern was itching all over her body. Her chart revealed a history of chronic scabies and mental illness. She had been seen in the clinic on 4 separate occasions over a 2-year period for scabies. She claimed on this visit that she could not get rid of the scabies because people kept taking away her medication. She also stated she could see the creatures feed on her and move in and out of her skin.
The physical exam revealed that she was unwashed and disheveled. She had multiple excoriations on her extremities, hands, abdomen, back, and the nape of her neck (Figure 1).
FIGURE 1
Excoriations on the abdomen
FIGURE 2
Adult body lice and nymphs on clothing seams
Diagnosis
The woman’s appearance and mental status are consistent with schizophrenia; however, a diagnosis of scabies is not possible if she is really seeing the “bugs” on her body, as opposed to just imagining them. The scabies mite can only be seen with the aid of a microscope.
We looked for the bugs to confirm her story. While this could have been a case of delusions of parasitosis, on close inspection small “bugs” were indeed visible on her abdomen and along the seams of her pants. Multiple nits appeared attached to the hairs of her head, and a “bug” is noted to be feeding on the nape of her neck. This homeless woman has a massive infestation of body and head lice (Figure 2).
In the past she may have had a scabies infestation, but there was no documentation in the chart of any skin scrapings looked at under the microscope for diagnosis. It is more likely that she has been chronically infested with lice. Due to her mental illness, this patient may have been misdiagnosed with scabies based on the assumption that her claim to see the bugs was a hallucination. A close exam may not have been performed due to her mental illness and poor hygiene, along with the health care providers’ fears of catching scabies. Repeated documentation of scabies may have discouraged further investigation into another cause.
Pediculosis
Lice are bloodsucking obligate parasites. There are hundreds of millions of cases of pediculosis worldwide affecting men, women, and children from all socioeconomic classes.
Three types of lice infest humans: the head louse (Pediculus humanus capitis), the body louse (Pediculus humanus corporis), and the pubic louse (Phthirus pubis). Lice cling to hairs with their clawlike legs and pierce the skin, inject saliva, and then defecate while obtaining their blood meal. When exposed to lice, people clinically experience little irritation from the first bite, but after a short period they become sensitized. A hypersensitivity reaction—producing reddening of the skin, itching, and overall inflammation— subsequently develops.
Body lice are similar to head lice, except they are slightly larger. They are primarily seen in the homeless and indigent populations, with transmission occurring with direct body contact or sharing of contaminated clothes or bedding.
The body louse, contrary to popular belief, does not live on the body. It lives in the seams of clothing, clinging to the fibers. It will feed, remaining on the clothes, and only in massive infestations are they typically seen moving about the body. The axillae, groin, and truncal areas are the most severely affected. Patients have severe itching and tend to excoriate these regions. In chronically infested patients a postinflammatory hyperpigmentation can be observed.
Treatment
Persons infested with body lice need to discard or launder their clothing using hot water, and then bathe themselves. In cases of massive infestation—such as this case, in which head lice were also found—a pediculicide should be applied to the hair and entire body from head to toe. This can then be washed off in the shower (level of evidence [LOE]=1a, from Cochrane Review). This same Cochrane systematic review of the treatment of head lice found no evidence that any one pediculicide has greater effect than another (LOE=1a).1
In this case, the patient did not want to get rid of her green pants because she was able to find the “bugs” easily in its seams, which she thought helped keep them under control. When we explained that the full treatment of this condition required her to be given new clothes, she finally accepted this course of action.
Arrangements were made for her to shower at the shelter and obtain new clothes, and she was given permethrin shampoo to apply over her entire body from head to toe. She was scheduled to follow up in 1 week but unfortunately never returned to the clinic.
A 74-year-old Caucasian woman visited an outpatient clinic at a homeless shelter. Her chief concern was itching all over her body. Her chart revealed a history of chronic scabies and mental illness. She had been seen in the clinic on 4 separate occasions over a 2-year period for scabies. She claimed on this visit that she could not get rid of the scabies because people kept taking away her medication. She also stated she could see the creatures feed on her and move in and out of her skin.
The physical exam revealed that she was unwashed and disheveled. She had multiple excoriations on her extremities, hands, abdomen, back, and the nape of her neck (Figure 1).
FIGURE 1
Excoriations on the abdomen
FIGURE 2
Adult body lice and nymphs on clothing seams
Diagnosis
The woman’s appearance and mental status are consistent with schizophrenia; however, a diagnosis of scabies is not possible if she is really seeing the “bugs” on her body, as opposed to just imagining them. The scabies mite can only be seen with the aid of a microscope.
We looked for the bugs to confirm her story. While this could have been a case of delusions of parasitosis, on close inspection small “bugs” were indeed visible on her abdomen and along the seams of her pants. Multiple nits appeared attached to the hairs of her head, and a “bug” is noted to be feeding on the nape of her neck. This homeless woman has a massive infestation of body and head lice (Figure 2).
In the past she may have had a scabies infestation, but there was no documentation in the chart of any skin scrapings looked at under the microscope for diagnosis. It is more likely that she has been chronically infested with lice. Due to her mental illness, this patient may have been misdiagnosed with scabies based on the assumption that her claim to see the bugs was a hallucination. A close exam may not have been performed due to her mental illness and poor hygiene, along with the health care providers’ fears of catching scabies. Repeated documentation of scabies may have discouraged further investigation into another cause.
Pediculosis
Lice are bloodsucking obligate parasites. There are hundreds of millions of cases of pediculosis worldwide affecting men, women, and children from all socioeconomic classes.
Three types of lice infest humans: the head louse (Pediculus humanus capitis), the body louse (Pediculus humanus corporis), and the pubic louse (Phthirus pubis). Lice cling to hairs with their clawlike legs and pierce the skin, inject saliva, and then defecate while obtaining their blood meal. When exposed to lice, people clinically experience little irritation from the first bite, but after a short period they become sensitized. A hypersensitivity reaction—producing reddening of the skin, itching, and overall inflammation— subsequently develops.
Body lice are similar to head lice, except they are slightly larger. They are primarily seen in the homeless and indigent populations, with transmission occurring with direct body contact or sharing of contaminated clothes or bedding.
The body louse, contrary to popular belief, does not live on the body. It lives in the seams of clothing, clinging to the fibers. It will feed, remaining on the clothes, and only in massive infestations are they typically seen moving about the body. The axillae, groin, and truncal areas are the most severely affected. Patients have severe itching and tend to excoriate these regions. In chronically infested patients a postinflammatory hyperpigmentation can be observed.
Treatment
Persons infested with body lice need to discard or launder their clothing using hot water, and then bathe themselves. In cases of massive infestation—such as this case, in which head lice were also found—a pediculicide should be applied to the hair and entire body from head to toe. This can then be washed off in the shower (level of evidence [LOE]=1a, from Cochrane Review). This same Cochrane systematic review of the treatment of head lice found no evidence that any one pediculicide has greater effect than another (LOE=1a).1
In this case, the patient did not want to get rid of her green pants because she was able to find the “bugs” easily in its seams, which she thought helped keep them under control. When we explained that the full treatment of this condition required her to be given new clothes, she finally accepted this course of action.
Arrangements were made for her to shower at the shelter and obtain new clothes, and she was given permethrin shampoo to apply over her entire body from head to toe. She was scheduled to follow up in 1 week but unfortunately never returned to the clinic.
1. Dodd CS. Interventions for treating headlice (Cochrane Review). In: The Cochrane Library, Issue 2, 2002. Oxford.
1. Dodd CS. Interventions for treating headlice (Cochrane Review). In: The Cochrane Library, Issue 2, 2002. Oxford.
Prostatitis and pruritus
A 47-year-old man had severe itching that started the previous day and kept him up all night. We examined his rash (Figure ) as we inquired about his history. He had no previous skin problems and no known allergies. He had no fever, pain, or malaise.
We discovered that a month ago he had started taking 1 trimethoprim-sulfamethoxazole double-strength tablet twice daily for chronic prostatitis. He was told he would need to take the medication for 3 months. Other than prostatitis, he had no other medical problems and was not taking any other medications.
FIGURE
What is the diagnosis?
What is the best course of management?
Diagnosis
This patient has urticaria (hives), presenting as variously shaped wheals on his chest and arms, resulting from a drug allergy.
These wheals are erythematous, nonpitting, edematous plaques that change size and shape by peripheral extension or regression. Urticaria is a dynamic process in which new wheals evolve as old ones resolve. Wheals result from localized capillary vasodilation, followed by transudation of protein-rich fluid into the surrounding skin. The wheals resolve when the fluid is slowly reabsorbed.
Urticaria symptoms and signs
Itching is the hallmark symptom of urticaria. Patients may also experience burning or stinging. Acute urticaria may exhibit a rapid or gradual onset. The onset and resolution of wheals vary with the cause, and vary even among persons who have the same underlying cause.
It is easier to determine the precipitating factor—a drug allergy in this case—with acute urticaria than chronic urticaria (lasting 6 or more weeks). Angioedema causes a deeper edematous area that involves transudation of fluid into the dermis and subcutaneous tissue.
Wheals vary in size from the small, 2-mm papules of cholinergic urticaria to giant hives that may cover an extremity or part of the abdomen in a single wheal. The wheal may be all red or white, or the border may be red with the remainder of the surface white. Wheals may be surrounded by a red halo. The larger lesions (over 5 mm in diameter) are called plaques. In patients with darker skin, the wheals may be skin-colored only, with no visible erythema.
Differential diagnosis
The full differential diagnosis of urticaria includes angioedema, insect bites, food allergies, erythema multiforme, bullous pemphigoid, dermatitis herpetiformis, urticarial contact dermatitis, pruritic urticarial papules and plaques of pregnancy (known as PUPPP), mast cell releasability syndromes, and urticarial vasculitis.
Food allergies and insect bites can sometimes cause urticarial reactions. Angioedema is seen more often on the face and is especially found around the mouth and eyes.
Management
First-generation antihistamines
H1 antihistamines, which compete with histamine for the H1 receptor sites, are the first-line therapy for urticaria. First-generation antihistamines—such as diphenhydramine, chlorpheniramine, and hydroxyzine—can be very effective, particularly in acute cases. Diphenhydramine and chlorpheniramine are available over-the-counter and are relatively inexpensive. Hydroxyzine still requires a prescription, and it is thought to be more potent than diphenhydramine and chlorpheniramine.
The sedation experienced with these agents may help reduce pruritus, but it may also be a danger when a patient is driving or operating machinery. Because people respond to these medicines differently, you must weigh the bene fits and risks for each person based on their response to the medicine.
The pathophysiology of urticaria and angioedema can be mediated by immunoglobulin E, complement, physical stimuli, or autoantibodies, or it may be idiopathic. These mechanisms lead to mast cell degranulation, resulting in the release of histamine. Histamine and other inflammatory mediators produce the wheals, edema, and pruritus.
Second-generation antihistamines
Second-generation H1 antihistamines—such as astemizole, loratadine, desloratadine, and cetirizine—cause less sedation and are better for long-term daytime use. While more expensive, they are valuable in the management of chronic urticaria.
In the most refractory cases, combinations of various antihistamines may be useful in suppressing symptomatology. A nonsedating H1 antihistamine in the daytime can be combined with a sedating H1antihistamine and doxepin at night. An H2antihistamine can be added to this regimen before starting oral prednisone (level of evidence=5 for all the treatment regimes cited, based on expert opinion without explicit critical appraisal and based on physiology).
This patient’s treatment
The patient understood that he must stop taking the trimethoprim-sulfamethoxazole tablets and was given a fluoroquinolone for his chronic prostatitis. He took 1 dose of diphenhydramine (Benadryl, in this case) in the office, and the itching and wheals began to subside.
He was also told the could purchase diphenhydramine over the counter to continue to relieve his itching and wheals. He was advised that if it made him sleepy, he could call the office for a prescription for a nonsedating antihistamine.
This patient’s outcome
The patient was significantly better the next day and never needed additional medications for urticaria. His chronic prostatitis did resolve with a 2-month course of fluoroquinolone.
A 47-year-old man had severe itching that started the previous day and kept him up all night. We examined his rash (Figure ) as we inquired about his history. He had no previous skin problems and no known allergies. He had no fever, pain, or malaise.
We discovered that a month ago he had started taking 1 trimethoprim-sulfamethoxazole double-strength tablet twice daily for chronic prostatitis. He was told he would need to take the medication for 3 months. Other than prostatitis, he had no other medical problems and was not taking any other medications.
FIGURE
What is the diagnosis?
What is the best course of management?
Diagnosis
This patient has urticaria (hives), presenting as variously shaped wheals on his chest and arms, resulting from a drug allergy.
These wheals are erythematous, nonpitting, edematous plaques that change size and shape by peripheral extension or regression. Urticaria is a dynamic process in which new wheals evolve as old ones resolve. Wheals result from localized capillary vasodilation, followed by transudation of protein-rich fluid into the surrounding skin. The wheals resolve when the fluid is slowly reabsorbed.
Urticaria symptoms and signs
Itching is the hallmark symptom of urticaria. Patients may also experience burning or stinging. Acute urticaria may exhibit a rapid or gradual onset. The onset and resolution of wheals vary with the cause, and vary even among persons who have the same underlying cause.
It is easier to determine the precipitating factor—a drug allergy in this case—with acute urticaria than chronic urticaria (lasting 6 or more weeks). Angioedema causes a deeper edematous area that involves transudation of fluid into the dermis and subcutaneous tissue.
Wheals vary in size from the small, 2-mm papules of cholinergic urticaria to giant hives that may cover an extremity or part of the abdomen in a single wheal. The wheal may be all red or white, or the border may be red with the remainder of the surface white. Wheals may be surrounded by a red halo. The larger lesions (over 5 mm in diameter) are called plaques. In patients with darker skin, the wheals may be skin-colored only, with no visible erythema.
Differential diagnosis
The full differential diagnosis of urticaria includes angioedema, insect bites, food allergies, erythema multiforme, bullous pemphigoid, dermatitis herpetiformis, urticarial contact dermatitis, pruritic urticarial papules and plaques of pregnancy (known as PUPPP), mast cell releasability syndromes, and urticarial vasculitis.
Food allergies and insect bites can sometimes cause urticarial reactions. Angioedema is seen more often on the face and is especially found around the mouth and eyes.
Management
First-generation antihistamines
H1 antihistamines, which compete with histamine for the H1 receptor sites, are the first-line therapy for urticaria. First-generation antihistamines—such as diphenhydramine, chlorpheniramine, and hydroxyzine—can be very effective, particularly in acute cases. Diphenhydramine and chlorpheniramine are available over-the-counter and are relatively inexpensive. Hydroxyzine still requires a prescription, and it is thought to be more potent than diphenhydramine and chlorpheniramine.
The sedation experienced with these agents may help reduce pruritus, but it may also be a danger when a patient is driving or operating machinery. Because people respond to these medicines differently, you must weigh the bene fits and risks for each person based on their response to the medicine.
The pathophysiology of urticaria and angioedema can be mediated by immunoglobulin E, complement, physical stimuli, or autoantibodies, or it may be idiopathic. These mechanisms lead to mast cell degranulation, resulting in the release of histamine. Histamine and other inflammatory mediators produce the wheals, edema, and pruritus.
Second-generation antihistamines
Second-generation H1 antihistamines—such as astemizole, loratadine, desloratadine, and cetirizine—cause less sedation and are better for long-term daytime use. While more expensive, they are valuable in the management of chronic urticaria.
In the most refractory cases, combinations of various antihistamines may be useful in suppressing symptomatology. A nonsedating H1 antihistamine in the daytime can be combined with a sedating H1antihistamine and doxepin at night. An H2antihistamine can be added to this regimen before starting oral prednisone (level of evidence=5 for all the treatment regimes cited, based on expert opinion without explicit critical appraisal and based on physiology).
This patient’s treatment
The patient understood that he must stop taking the trimethoprim-sulfamethoxazole tablets and was given a fluoroquinolone for his chronic prostatitis. He took 1 dose of diphenhydramine (Benadryl, in this case) in the office, and the itching and wheals began to subside.
He was also told the could purchase diphenhydramine over the counter to continue to relieve his itching and wheals. He was advised that if it made him sleepy, he could call the office for a prescription for a nonsedating antihistamine.
This patient’s outcome
The patient was significantly better the next day and never needed additional medications for urticaria. His chronic prostatitis did resolve with a 2-month course of fluoroquinolone.
A 47-year-old man had severe itching that started the previous day and kept him up all night. We examined his rash (Figure ) as we inquired about his history. He had no previous skin problems and no known allergies. He had no fever, pain, or malaise.
We discovered that a month ago he had started taking 1 trimethoprim-sulfamethoxazole double-strength tablet twice daily for chronic prostatitis. He was told he would need to take the medication for 3 months. Other than prostatitis, he had no other medical problems and was not taking any other medications.
FIGURE
What is the diagnosis?
What is the best course of management?
Diagnosis
This patient has urticaria (hives), presenting as variously shaped wheals on his chest and arms, resulting from a drug allergy.
These wheals are erythematous, nonpitting, edematous plaques that change size and shape by peripheral extension or regression. Urticaria is a dynamic process in which new wheals evolve as old ones resolve. Wheals result from localized capillary vasodilation, followed by transudation of protein-rich fluid into the surrounding skin. The wheals resolve when the fluid is slowly reabsorbed.
Urticaria symptoms and signs
Itching is the hallmark symptom of urticaria. Patients may also experience burning or stinging. Acute urticaria may exhibit a rapid or gradual onset. The onset and resolution of wheals vary with the cause, and vary even among persons who have the same underlying cause.
It is easier to determine the precipitating factor—a drug allergy in this case—with acute urticaria than chronic urticaria (lasting 6 or more weeks). Angioedema causes a deeper edematous area that involves transudation of fluid into the dermis and subcutaneous tissue.
Wheals vary in size from the small, 2-mm papules of cholinergic urticaria to giant hives that may cover an extremity or part of the abdomen in a single wheal. The wheal may be all red or white, or the border may be red with the remainder of the surface white. Wheals may be surrounded by a red halo. The larger lesions (over 5 mm in diameter) are called plaques. In patients with darker skin, the wheals may be skin-colored only, with no visible erythema.
Differential diagnosis
The full differential diagnosis of urticaria includes angioedema, insect bites, food allergies, erythema multiforme, bullous pemphigoid, dermatitis herpetiformis, urticarial contact dermatitis, pruritic urticarial papules and plaques of pregnancy (known as PUPPP), mast cell releasability syndromes, and urticarial vasculitis.
Food allergies and insect bites can sometimes cause urticarial reactions. Angioedema is seen more often on the face and is especially found around the mouth and eyes.
Management
First-generation antihistamines
H1 antihistamines, which compete with histamine for the H1 receptor sites, are the first-line therapy for urticaria. First-generation antihistamines—such as diphenhydramine, chlorpheniramine, and hydroxyzine—can be very effective, particularly in acute cases. Diphenhydramine and chlorpheniramine are available over-the-counter and are relatively inexpensive. Hydroxyzine still requires a prescription, and it is thought to be more potent than diphenhydramine and chlorpheniramine.
The sedation experienced with these agents may help reduce pruritus, but it may also be a danger when a patient is driving or operating machinery. Because people respond to these medicines differently, you must weigh the bene fits and risks for each person based on their response to the medicine.
The pathophysiology of urticaria and angioedema can be mediated by immunoglobulin E, complement, physical stimuli, or autoantibodies, or it may be idiopathic. These mechanisms lead to mast cell degranulation, resulting in the release of histamine. Histamine and other inflammatory mediators produce the wheals, edema, and pruritus.
Second-generation antihistamines
Second-generation H1 antihistamines—such as astemizole, loratadine, desloratadine, and cetirizine—cause less sedation and are better for long-term daytime use. While more expensive, they are valuable in the management of chronic urticaria.
In the most refractory cases, combinations of various antihistamines may be useful in suppressing symptomatology. A nonsedating H1 antihistamine in the daytime can be combined with a sedating H1antihistamine and doxepin at night. An H2antihistamine can be added to this regimen before starting oral prednisone (level of evidence=5 for all the treatment regimes cited, based on expert opinion without explicit critical appraisal and based on physiology).
This patient’s treatment
The patient understood that he must stop taking the trimethoprim-sulfamethoxazole tablets and was given a fluoroquinolone for his chronic prostatitis. He took 1 dose of diphenhydramine (Benadryl, in this case) in the office, and the itching and wheals began to subside.
He was also told the could purchase diphenhydramine over the counter to continue to relieve his itching and wheals. He was advised that if it made him sleepy, he could call the office for a prescription for a nonsedating antihistamine.
This patient’s outcome
The patient was significantly better the next day and never needed additional medications for urticaria. His chronic prostatitis did resolve with a 2-month course of fluoroquinolone.
Recognition of skin cancer patterns
This Photo Rounds aims to help you hone your visual diagnostic skills to recognize the 3 most common types of skin cancer (in order of prevalence): basal cell carcinoma, squamous cell carcinoma, and melanoma. (See also “Diagnosis of skin malignancy,”.)
Pattern recognition informs us about the initial differential diagnosis and the appropriate biopsy method.
Basal cell carcinoma
The most common basal cell carcinoma is nodular. Figure 1 shows nodular basal cell carcinoma with a raised pearly pink and white nodule with a smooth, shiny, translucent surface. The smooth surface reflects a loss of the normal pore pattern. Telangiectasias can be seen within the lesion, and the border may appear to be rolled.
Figure 2 shows a nodular basal cell carcinoma that is both pigmented and has some central ulceration. This figure demonstrates how difficult it is to distinguish a melanoma from a pigmented basal cell carcinoma.
Figure 3 shows the next most frequently seen basal cell carcinoma, the superficial basal cell carcinoma. These lesions are found most often on the trunk and extremities rather than the face, and may appear as a pink scaling plaque. Sometimes shallow crusts or erosions may be seen within the lesion. Note the thready border present around this scaling plaque. This slightly elevated border is the best tip-off to recognizing this scaling plaque as a skin cancer rather than a plaque of psoriasis or nummular eczema.
Figure 4 shows the least prevalent basal cell carcinoma, the sclerosing type. These lesions are often ivory-colored or colorless. The skin may be appear atrophic and feel indurated. A sclerosing basal cell carcinoma may resemble a scar and can be easily overlooked. These carcinomas are often called morpheaform because of the resemblance to localized scleroderma (morphea). They are also called infiltrating basal cell carcinoma because they infiltrate into the surrounding normal skin in a way not easily visible to the naked eye.
FIGURE 1
Squamous cell carcinoma
The next most common type of skin cancer is squamous cell carcinoma. These cancers are most often found on the lips, ears, and scalp. Figure 5 shows a squamous cell carcinoma on the lower lip. The lower lip catches more ultraviolet rays from the sun than the upper lip, and therefore is the more prevalent site for this carcinoma.
Figure 6 shows a squamous cell carcinoma on the face in an area of sun exposure. This carcinoma looks very much like the superficial basal cell carcinoma in Figure 3, except that the squamous cell carcinoma has one area of crusting. The only way to make a definitive diagnosis is to perform biopsy and get a pathologic reading.
FIGURE 5
There are many different types of melanomas. Figure 7 shows one version of the most common melanoma, the superficial spreading melanoma. The dark pigmentation around the outside of this melanoma is where the lesion is superficially spreading away from the center (which has lost its pigmentation). This lesion meets all of the ABCDE criteria for malignant melanoma.
Figure 8 shows a melanoma arising in a lentigo maligna on the face of an older patient. It is not necessary to know the type of melanoma before the biopsy, but you should recognize that the lesion may be melanoma and perform a full-thickness biopsy. What may have started off as a simple age spot in this patient has become a malignant melanoma (see page 214).
Figure 9 shows a very thick and deadly nodular melanoma. One can recognize a nodular melanoma by the increased thickness and its darker pigmentation.
Figure 10 shows an uncommon type of melanoma but one of the deadliest—the acrallentiginous melanoma. This melanoma is often not detected until it has metastasized. Any pigmented lesion on the hands, feet, or under the fingernails that looks like melanoma should be biopsied early before it gets to this deadly stage.
FIGURE 7
Choice of biopsy technique
Choice of biopsy technique depends on the type of skin lesion. Most basal cell and squamous cell carcinomas can be adequately biopsied by the shave technique because the pathology is superficial and the prognosis is not determined by thickness. Exceptions include sclerosing basal cell carcinomas and very flat superficial basal cell carcinomas, which are best biopsied with a full-thickness specimen in the form of a punch biopsy or excisional biopsy.
All lesions you suspect may be melanoma should be biopsied with a full-thickness specimen. Very small and very large lesions can initially be biopsied using a punch instrument. The excisional biopsy is preferred when the lesion can be removed with one surgical procedure. Depending upon the depth of the melanoma, you may need to perform a second surgery to get adequate margins.
This Photo Rounds aims to help you hone your visual diagnostic skills to recognize the 3 most common types of skin cancer (in order of prevalence): basal cell carcinoma, squamous cell carcinoma, and melanoma. (See also “Diagnosis of skin malignancy,”.)
Pattern recognition informs us about the initial differential diagnosis and the appropriate biopsy method.
Basal cell carcinoma
The most common basal cell carcinoma is nodular. Figure 1 shows nodular basal cell carcinoma with a raised pearly pink and white nodule with a smooth, shiny, translucent surface. The smooth surface reflects a loss of the normal pore pattern. Telangiectasias can be seen within the lesion, and the border may appear to be rolled.
Figure 2 shows a nodular basal cell carcinoma that is both pigmented and has some central ulceration. This figure demonstrates how difficult it is to distinguish a melanoma from a pigmented basal cell carcinoma.
Figure 3 shows the next most frequently seen basal cell carcinoma, the superficial basal cell carcinoma. These lesions are found most often on the trunk and extremities rather than the face, and may appear as a pink scaling plaque. Sometimes shallow crusts or erosions may be seen within the lesion. Note the thready border present around this scaling plaque. This slightly elevated border is the best tip-off to recognizing this scaling plaque as a skin cancer rather than a plaque of psoriasis or nummular eczema.
Figure 4 shows the least prevalent basal cell carcinoma, the sclerosing type. These lesions are often ivory-colored or colorless. The skin may be appear atrophic and feel indurated. A sclerosing basal cell carcinoma may resemble a scar and can be easily overlooked. These carcinomas are often called morpheaform because of the resemblance to localized scleroderma (morphea). They are also called infiltrating basal cell carcinoma because they infiltrate into the surrounding normal skin in a way not easily visible to the naked eye.
FIGURE 1
Squamous cell carcinoma
The next most common type of skin cancer is squamous cell carcinoma. These cancers are most often found on the lips, ears, and scalp. Figure 5 shows a squamous cell carcinoma on the lower lip. The lower lip catches more ultraviolet rays from the sun than the upper lip, and therefore is the more prevalent site for this carcinoma.
Figure 6 shows a squamous cell carcinoma on the face in an area of sun exposure. This carcinoma looks very much like the superficial basal cell carcinoma in Figure 3, except that the squamous cell carcinoma has one area of crusting. The only way to make a definitive diagnosis is to perform biopsy and get a pathologic reading.
FIGURE 5
There are many different types of melanomas. Figure 7 shows one version of the most common melanoma, the superficial spreading melanoma. The dark pigmentation around the outside of this melanoma is where the lesion is superficially spreading away from the center (which has lost its pigmentation). This lesion meets all of the ABCDE criteria for malignant melanoma.
Figure 8 shows a melanoma arising in a lentigo maligna on the face of an older patient. It is not necessary to know the type of melanoma before the biopsy, but you should recognize that the lesion may be melanoma and perform a full-thickness biopsy. What may have started off as a simple age spot in this patient has become a malignant melanoma (see page 214).
Figure 9 shows a very thick and deadly nodular melanoma. One can recognize a nodular melanoma by the increased thickness and its darker pigmentation.
Figure 10 shows an uncommon type of melanoma but one of the deadliest—the acrallentiginous melanoma. This melanoma is often not detected until it has metastasized. Any pigmented lesion on the hands, feet, or under the fingernails that looks like melanoma should be biopsied early before it gets to this deadly stage.
FIGURE 7
Choice of biopsy technique
Choice of biopsy technique depends on the type of skin lesion. Most basal cell and squamous cell carcinomas can be adequately biopsied by the shave technique because the pathology is superficial and the prognosis is not determined by thickness. Exceptions include sclerosing basal cell carcinomas and very flat superficial basal cell carcinomas, which are best biopsied with a full-thickness specimen in the form of a punch biopsy or excisional biopsy.
All lesions you suspect may be melanoma should be biopsied with a full-thickness specimen. Very small and very large lesions can initially be biopsied using a punch instrument. The excisional biopsy is preferred when the lesion can be removed with one surgical procedure. Depending upon the depth of the melanoma, you may need to perform a second surgery to get adequate margins.
This Photo Rounds aims to help you hone your visual diagnostic skills to recognize the 3 most common types of skin cancer (in order of prevalence): basal cell carcinoma, squamous cell carcinoma, and melanoma. (See also “Diagnosis of skin malignancy,”.)
Pattern recognition informs us about the initial differential diagnosis and the appropriate biopsy method.
Basal cell carcinoma
The most common basal cell carcinoma is nodular. Figure 1 shows nodular basal cell carcinoma with a raised pearly pink and white nodule with a smooth, shiny, translucent surface. The smooth surface reflects a loss of the normal pore pattern. Telangiectasias can be seen within the lesion, and the border may appear to be rolled.
Figure 2 shows a nodular basal cell carcinoma that is both pigmented and has some central ulceration. This figure demonstrates how difficult it is to distinguish a melanoma from a pigmented basal cell carcinoma.
Figure 3 shows the next most frequently seen basal cell carcinoma, the superficial basal cell carcinoma. These lesions are found most often on the trunk and extremities rather than the face, and may appear as a pink scaling plaque. Sometimes shallow crusts or erosions may be seen within the lesion. Note the thready border present around this scaling plaque. This slightly elevated border is the best tip-off to recognizing this scaling plaque as a skin cancer rather than a plaque of psoriasis or nummular eczema.
Figure 4 shows the least prevalent basal cell carcinoma, the sclerosing type. These lesions are often ivory-colored or colorless. The skin may be appear atrophic and feel indurated. A sclerosing basal cell carcinoma may resemble a scar and can be easily overlooked. These carcinomas are often called morpheaform because of the resemblance to localized scleroderma (morphea). They are also called infiltrating basal cell carcinoma because they infiltrate into the surrounding normal skin in a way not easily visible to the naked eye.
FIGURE 1
Squamous cell carcinoma
The next most common type of skin cancer is squamous cell carcinoma. These cancers are most often found on the lips, ears, and scalp. Figure 5 shows a squamous cell carcinoma on the lower lip. The lower lip catches more ultraviolet rays from the sun than the upper lip, and therefore is the more prevalent site for this carcinoma.
Figure 6 shows a squamous cell carcinoma on the face in an area of sun exposure. This carcinoma looks very much like the superficial basal cell carcinoma in Figure 3, except that the squamous cell carcinoma has one area of crusting. The only way to make a definitive diagnosis is to perform biopsy and get a pathologic reading.
FIGURE 5
There are many different types of melanomas. Figure 7 shows one version of the most common melanoma, the superficial spreading melanoma. The dark pigmentation around the outside of this melanoma is where the lesion is superficially spreading away from the center (which has lost its pigmentation). This lesion meets all of the ABCDE criteria for malignant melanoma.
Figure 8 shows a melanoma arising in a lentigo maligna on the face of an older patient. It is not necessary to know the type of melanoma before the biopsy, but you should recognize that the lesion may be melanoma and perform a full-thickness biopsy. What may have started off as a simple age spot in this patient has become a malignant melanoma (see page 214).
Figure 9 shows a very thick and deadly nodular melanoma. One can recognize a nodular melanoma by the increased thickness and its darker pigmentation.
Figure 10 shows an uncommon type of melanoma but one of the deadliest—the acrallentiginous melanoma. This melanoma is often not detected until it has metastasized. Any pigmented lesion on the hands, feet, or under the fingernails that looks like melanoma should be biopsied early before it gets to this deadly stage.
FIGURE 7
Choice of biopsy technique
Choice of biopsy technique depends on the type of skin lesion. Most basal cell and squamous cell carcinomas can be adequately biopsied by the shave technique because the pathology is superficial and the prognosis is not determined by thickness. Exceptions include sclerosing basal cell carcinomas and very flat superficial basal cell carcinomas, which are best biopsied with a full-thickness specimen in the form of a punch biopsy or excisional biopsy.
All lesions you suspect may be melanoma should be biopsied with a full-thickness specimen. Very small and very large lesions can initially be biopsied using a punch instrument. The excisional biopsy is preferred when the lesion can be removed with one surgical procedure. Depending upon the depth of the melanoma, you may need to perform a second surgery to get adequate margins.
Abnormal fingernails
A 48-year-old African American woman came to our office because the discoloration of one fingernail that began months earlier had spread to a second finger, and the first finger to become discolored had begun to hurt.
The patient had initially seen another physician, who prescribed itraconazole for presumptive onychomycosis. The patient received a pulse therapy course of itraconazole for 3 months and had no improvement. Therapy ended 4 months ago, and a month ago the end of her left index finger began to ache.
The patient works at a computer, and typing causes pain in the left index finger. A review of her chart reveals she is taking a diuretic for hypertension; there are no other health problems.
What is the diagnosis?
Before taking a more extensive history, it is appropriate to look at her fingers more closely to collect data that will inform questioning. By applying pattern recognition skills first, you can form hypotheses and use the remainder of the exam to test them.
How would you describe the abnormalities seen in Figure 1 and Figure 2 (pattern recognition), and what would be the differential diagnosis (hypotheses)?
What further history, physical exam, or laboratory tests should be completed (hypothesis testing)?
FIGURE 1
This patient’s fingernail had been discolored for months and the fingertip had recently begun to hurt.
A brown discoloration (oil spot) in the patient’s proximal nail.
Figure 1 shows a brownish discoloration of the fingernail, with small pits particularly prominent around the lunula (the semicircular light area adjacent to the proximal nail fold). There is also evidence of onycholysis (separation of the nail from the nail bed). The vertical ridging is not abnormal.
Figure 2 shows a well-circumscribed brown discoloration in the proximal nail called an oil spot. These nail findings are classic for psoriasis.1
Figure 1 also shows subtle swelling of the distal interphalangeal (DIP) joint. It is this area the patient said was painful, and she had joint tenderness to palpation over this DIP joint only.
Hypotheses
The 2 most likely diagnoses are:
- psoriasis causing nail changes while psoriatic arthritis is developing
- onychomycosis with incidental joint pain of the DIP joint.
Other causes of nail changes include lichen planus, chronic candida paronychia, and Reiter’s disease. Epidemiologically the most likely diagnosis is onychomycosis, which is far more prevalent than the other conditions. However, this patient has already failed a course of an oral antifungal agent, and her nail changes are more consistent with psoriasis.
Hypothesis testing
Questions and physical examination focus on collecting data to determine the more likely of the two diagnoses, psoriasis and fungal nail disease. The patient denied having any skin lesions and a history of psoriasis. She also said she had no athlete’s foot or problems with her toenails or other hand. Her knees ache from time to time, which she attributed to aging.
Physical exam revealed no evidence of psoriasis on the skin and no tinea pedis or onychomycosis of the toenails. She had no other skin findings suggestive of lichen planus or Reiter’s disease. Looking more closely at the fingernails, we saw no evidence of subungual keratoses, which are frequently found in onychomycosis.
A scraping and clipping of the fingernail was sent for fungal culture, and an x-ray film of that digit revealed no bony changes. The fungal culture results 2 weeks later were negative.
Patient follow-up
We made a presumptive diagnosis of psoriatic nail changes and psoriatic arthritis, and the patient was sent to a rheumatologist for consultation. The rheumatologist agreed with the diagnosis and placed the patient on nonsteroidal anti-inflammatory drugs to treat the early psoriatic arthritis.
The patient developed more areas of psoriatic arthritis involvement over the subsequent years and became less concerned about the appearance of her nails. Eventually the psoriatic arthritis progressed to the point where the patient was taking remititive agents for inflammatory arthropathy. She never did develop the skin lesions of psoriasis.
Nail changes of psoriasis
It has been reported that 30% of patients with psoriasis have nail changes, the most common being pitting. Onycholysis is the next most frequent change, and the oil spot is less frequent but not rare.
Not everyone with nail pitting has psoriasis; however, there is a high correlation between psoriatic arthritis and nail pitting.
Patients with psoriasis and psoriatic arthritis have a higher percentage of nail changes than patients with psoriasis of the skin only. In 1 study, nail changes were noted in 86.5% of patients affected by arthropathic psoriasis, and the most common fingernail change was pitting.2
This particular case shows it is possible to have psoriatic arthritis and psoriatic nail changes without psoriasis of the skin. Fortunately, the patient did not have an adverse reaction to the itraconazole prescribed for the incorrectly diagnosed onychomycosis.
It is debatable whether fungal cultures are needed before prescribing oral antifungal agents for onychomycosis. This was 1 case in which the nail findings may have steered the clinician toward getting a nail scraping for microscopic analysis using potassium hydroxide or a fungal culture. Negative findings would have spared the patient the treatment with an expensive agent with known liver toxicity.
The onset of pain, swelling, and tenderness of the DIP joint of the affected nail helped to make the diagnosis. It is the finger joint most commonly affected by psoriatic arthritis.
Treatment of psoriasis of the nails
There is no good treatment for psoriasis of the nails. Treatment regimens that have been studied include injection of steroids into the nail matrix and use of topical retinoids. Intralesional steroid injections are very painful, and the results are not adequate to recommend this treatment.
A study of topical retinoid tazorotene showed some promise.3 The study size was small, however, and the measured change was not great. But for patients desperately looking for help for psoriatic nail changes, the topical treatment may be worth a try.
Figure 3 shows a different patient with an interesting connection between involvement of psoriatic arthritis in the finger and accompanying nail changes. This man had psoriatic plaques over his fingers and a severely swollen DIP joint of the middle finger with significant accompanying nail changes. The inflammatory reaction in the DIP joint is accompanied by abnormal changes in the nail matrix, producing a psoriatic nail on the same finger.
FIGURE 3
Another patient’s hand, with psoriatic plaques and swollen distal interphalangeal joint.
1. Habif T. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 3rd ed. St. Louis, Mo: Mosby; 1996.
2. Lavaroni G, Kokelj F, Pauluzzi P, Trevisan G. The nails in psoriatic arthritis. Acta Derm Venereol Suppl (Stockh) 1994;186:113.-
3. Scher RK, Stiller M, Zhu YI. Tazarotene 0.1% gel in the treatment of fingernail psoriasis: a double-blind, randomized, vehicle-controlled study. Cutis 2001;68:355-8.
A 48-year-old African American woman came to our office because the discoloration of one fingernail that began months earlier had spread to a second finger, and the first finger to become discolored had begun to hurt.
The patient had initially seen another physician, who prescribed itraconazole for presumptive onychomycosis. The patient received a pulse therapy course of itraconazole for 3 months and had no improvement. Therapy ended 4 months ago, and a month ago the end of her left index finger began to ache.
The patient works at a computer, and typing causes pain in the left index finger. A review of her chart reveals she is taking a diuretic for hypertension; there are no other health problems.
What is the diagnosis?
Before taking a more extensive history, it is appropriate to look at her fingers more closely to collect data that will inform questioning. By applying pattern recognition skills first, you can form hypotheses and use the remainder of the exam to test them.
How would you describe the abnormalities seen in Figure 1 and Figure 2 (pattern recognition), and what would be the differential diagnosis (hypotheses)?
What further history, physical exam, or laboratory tests should be completed (hypothesis testing)?
FIGURE 1
This patient’s fingernail had been discolored for months and the fingertip had recently begun to hurt.
A brown discoloration (oil spot) in the patient’s proximal nail.
Figure 1 shows a brownish discoloration of the fingernail, with small pits particularly prominent around the lunula (the semicircular light area adjacent to the proximal nail fold). There is also evidence of onycholysis (separation of the nail from the nail bed). The vertical ridging is not abnormal.
Figure 2 shows a well-circumscribed brown discoloration in the proximal nail called an oil spot. These nail findings are classic for psoriasis.1
Figure 1 also shows subtle swelling of the distal interphalangeal (DIP) joint. It is this area the patient said was painful, and she had joint tenderness to palpation over this DIP joint only.
Hypotheses
The 2 most likely diagnoses are:
- psoriasis causing nail changes while psoriatic arthritis is developing
- onychomycosis with incidental joint pain of the DIP joint.
Other causes of nail changes include lichen planus, chronic candida paronychia, and Reiter’s disease. Epidemiologically the most likely diagnosis is onychomycosis, which is far more prevalent than the other conditions. However, this patient has already failed a course of an oral antifungal agent, and her nail changes are more consistent with psoriasis.
Hypothesis testing
Questions and physical examination focus on collecting data to determine the more likely of the two diagnoses, psoriasis and fungal nail disease. The patient denied having any skin lesions and a history of psoriasis. She also said she had no athlete’s foot or problems with her toenails or other hand. Her knees ache from time to time, which she attributed to aging.
Physical exam revealed no evidence of psoriasis on the skin and no tinea pedis or onychomycosis of the toenails. She had no other skin findings suggestive of lichen planus or Reiter’s disease. Looking more closely at the fingernails, we saw no evidence of subungual keratoses, which are frequently found in onychomycosis.
A scraping and clipping of the fingernail was sent for fungal culture, and an x-ray film of that digit revealed no bony changes. The fungal culture results 2 weeks later were negative.
Patient follow-up
We made a presumptive diagnosis of psoriatic nail changes and psoriatic arthritis, and the patient was sent to a rheumatologist for consultation. The rheumatologist agreed with the diagnosis and placed the patient on nonsteroidal anti-inflammatory drugs to treat the early psoriatic arthritis.
The patient developed more areas of psoriatic arthritis involvement over the subsequent years and became less concerned about the appearance of her nails. Eventually the psoriatic arthritis progressed to the point where the patient was taking remititive agents for inflammatory arthropathy. She never did develop the skin lesions of psoriasis.
Nail changes of psoriasis
It has been reported that 30% of patients with psoriasis have nail changes, the most common being pitting. Onycholysis is the next most frequent change, and the oil spot is less frequent but not rare.
Not everyone with nail pitting has psoriasis; however, there is a high correlation between psoriatic arthritis and nail pitting.
Patients with psoriasis and psoriatic arthritis have a higher percentage of nail changes than patients with psoriasis of the skin only. In 1 study, nail changes were noted in 86.5% of patients affected by arthropathic psoriasis, and the most common fingernail change was pitting.2
This particular case shows it is possible to have psoriatic arthritis and psoriatic nail changes without psoriasis of the skin. Fortunately, the patient did not have an adverse reaction to the itraconazole prescribed for the incorrectly diagnosed onychomycosis.
It is debatable whether fungal cultures are needed before prescribing oral antifungal agents for onychomycosis. This was 1 case in which the nail findings may have steered the clinician toward getting a nail scraping for microscopic analysis using potassium hydroxide or a fungal culture. Negative findings would have spared the patient the treatment with an expensive agent with known liver toxicity.
The onset of pain, swelling, and tenderness of the DIP joint of the affected nail helped to make the diagnosis. It is the finger joint most commonly affected by psoriatic arthritis.
Treatment of psoriasis of the nails
There is no good treatment for psoriasis of the nails. Treatment regimens that have been studied include injection of steroids into the nail matrix and use of topical retinoids. Intralesional steroid injections are very painful, and the results are not adequate to recommend this treatment.
A study of topical retinoid tazorotene showed some promise.3 The study size was small, however, and the measured change was not great. But for patients desperately looking for help for psoriatic nail changes, the topical treatment may be worth a try.
Figure 3 shows a different patient with an interesting connection between involvement of psoriatic arthritis in the finger and accompanying nail changes. This man had psoriatic plaques over his fingers and a severely swollen DIP joint of the middle finger with significant accompanying nail changes. The inflammatory reaction in the DIP joint is accompanied by abnormal changes in the nail matrix, producing a psoriatic nail on the same finger.
FIGURE 3
Another patient’s hand, with psoriatic plaques and swollen distal interphalangeal joint.
A 48-year-old African American woman came to our office because the discoloration of one fingernail that began months earlier had spread to a second finger, and the first finger to become discolored had begun to hurt.
The patient had initially seen another physician, who prescribed itraconazole for presumptive onychomycosis. The patient received a pulse therapy course of itraconazole for 3 months and had no improvement. Therapy ended 4 months ago, and a month ago the end of her left index finger began to ache.
The patient works at a computer, and typing causes pain in the left index finger. A review of her chart reveals she is taking a diuretic for hypertension; there are no other health problems.
What is the diagnosis?
Before taking a more extensive history, it is appropriate to look at her fingers more closely to collect data that will inform questioning. By applying pattern recognition skills first, you can form hypotheses and use the remainder of the exam to test them.
How would you describe the abnormalities seen in Figure 1 and Figure 2 (pattern recognition), and what would be the differential diagnosis (hypotheses)?
What further history, physical exam, or laboratory tests should be completed (hypothesis testing)?
FIGURE 1
This patient’s fingernail had been discolored for months and the fingertip had recently begun to hurt.
A brown discoloration (oil spot) in the patient’s proximal nail.
Figure 1 shows a brownish discoloration of the fingernail, with small pits particularly prominent around the lunula (the semicircular light area adjacent to the proximal nail fold). There is also evidence of onycholysis (separation of the nail from the nail bed). The vertical ridging is not abnormal.
Figure 2 shows a well-circumscribed brown discoloration in the proximal nail called an oil spot. These nail findings are classic for psoriasis.1
Figure 1 also shows subtle swelling of the distal interphalangeal (DIP) joint. It is this area the patient said was painful, and she had joint tenderness to palpation over this DIP joint only.
Hypotheses
The 2 most likely diagnoses are:
- psoriasis causing nail changes while psoriatic arthritis is developing
- onychomycosis with incidental joint pain of the DIP joint.
Other causes of nail changes include lichen planus, chronic candida paronychia, and Reiter’s disease. Epidemiologically the most likely diagnosis is onychomycosis, which is far more prevalent than the other conditions. However, this patient has already failed a course of an oral antifungal agent, and her nail changes are more consistent with psoriasis.
Hypothesis testing
Questions and physical examination focus on collecting data to determine the more likely of the two diagnoses, psoriasis and fungal nail disease. The patient denied having any skin lesions and a history of psoriasis. She also said she had no athlete’s foot or problems with her toenails or other hand. Her knees ache from time to time, which she attributed to aging.
Physical exam revealed no evidence of psoriasis on the skin and no tinea pedis or onychomycosis of the toenails. She had no other skin findings suggestive of lichen planus or Reiter’s disease. Looking more closely at the fingernails, we saw no evidence of subungual keratoses, which are frequently found in onychomycosis.
A scraping and clipping of the fingernail was sent for fungal culture, and an x-ray film of that digit revealed no bony changes. The fungal culture results 2 weeks later were negative.
Patient follow-up
We made a presumptive diagnosis of psoriatic nail changes and psoriatic arthritis, and the patient was sent to a rheumatologist for consultation. The rheumatologist agreed with the diagnosis and placed the patient on nonsteroidal anti-inflammatory drugs to treat the early psoriatic arthritis.
The patient developed more areas of psoriatic arthritis involvement over the subsequent years and became less concerned about the appearance of her nails. Eventually the psoriatic arthritis progressed to the point where the patient was taking remititive agents for inflammatory arthropathy. She never did develop the skin lesions of psoriasis.
Nail changes of psoriasis
It has been reported that 30% of patients with psoriasis have nail changes, the most common being pitting. Onycholysis is the next most frequent change, and the oil spot is less frequent but not rare.
Not everyone with nail pitting has psoriasis; however, there is a high correlation between psoriatic arthritis and nail pitting.
Patients with psoriasis and psoriatic arthritis have a higher percentage of nail changes than patients with psoriasis of the skin only. In 1 study, nail changes were noted in 86.5% of patients affected by arthropathic psoriasis, and the most common fingernail change was pitting.2
This particular case shows it is possible to have psoriatic arthritis and psoriatic nail changes without psoriasis of the skin. Fortunately, the patient did not have an adverse reaction to the itraconazole prescribed for the incorrectly diagnosed onychomycosis.
It is debatable whether fungal cultures are needed before prescribing oral antifungal agents for onychomycosis. This was 1 case in which the nail findings may have steered the clinician toward getting a nail scraping for microscopic analysis using potassium hydroxide or a fungal culture. Negative findings would have spared the patient the treatment with an expensive agent with known liver toxicity.
The onset of pain, swelling, and tenderness of the DIP joint of the affected nail helped to make the diagnosis. It is the finger joint most commonly affected by psoriatic arthritis.
Treatment of psoriasis of the nails
There is no good treatment for psoriasis of the nails. Treatment regimens that have been studied include injection of steroids into the nail matrix and use of topical retinoids. Intralesional steroid injections are very painful, and the results are not adequate to recommend this treatment.
A study of topical retinoid tazorotene showed some promise.3 The study size was small, however, and the measured change was not great. But for patients desperately looking for help for psoriatic nail changes, the topical treatment may be worth a try.
Figure 3 shows a different patient with an interesting connection between involvement of psoriatic arthritis in the finger and accompanying nail changes. This man had psoriatic plaques over his fingers and a severely swollen DIP joint of the middle finger with significant accompanying nail changes. The inflammatory reaction in the DIP joint is accompanied by abnormal changes in the nail matrix, producing a psoriatic nail on the same finger.
FIGURE 3
Another patient’s hand, with psoriatic plaques and swollen distal interphalangeal joint.
1. Habif T. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 3rd ed. St. Louis, Mo: Mosby; 1996.
2. Lavaroni G, Kokelj F, Pauluzzi P, Trevisan G. The nails in psoriatic arthritis. Acta Derm Venereol Suppl (Stockh) 1994;186:113.-
3. Scher RK, Stiller M, Zhu YI. Tazarotene 0.1% gel in the treatment of fingernail psoriasis: a double-blind, randomized, vehicle-controlled study. Cutis 2001;68:355-8.
1. Habif T. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 3rd ed. St. Louis, Mo: Mosby; 1996.
2. Lavaroni G, Kokelj F, Pauluzzi P, Trevisan G. The nails in psoriatic arthritis. Acta Derm Venereol Suppl (Stockh) 1994;186:113.-
3. Scher RK, Stiller M, Zhu YI. Tazarotene 0.1% gel in the treatment of fingernail psoriasis: a double-blind, randomized, vehicle-controlled study. Cutis 2001;68:355-8.