User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


A 4-point thrombocytopenia score was found able to rule out suspected HIT
The real strength of the 4T score for heparin-induced thrombocytopenia (HIT) is its negative predictive value, according to hematologist Adam Cuker, MD, of the department of medicine at the University of Pennsylvania, Philadelphia.
The score assigns patients points based on degree of thrombocytopenia, timing of platelet count fall in relation to heparin exposure, presence of thrombosis and other sequelae, and the likelihood of other causes of thrombocytopenia.
A low score – 3 points or less – has a negative predictive value of 99.8%, “so HIT is basically ruled out; you do not need to order lab testing for HIT or manage the patient empirically for HIT,” and should look for other causes of thrombocytopenia, said Dr. Cuker, lead author of the American Society of Hematology’s most recent HIT guidelines.
Intermediate scores of 4 or 5 points, and high scores of 6-8 points, are a different story. The positive predictive value of an intermediate score is only 14%, and of a high score, 64%, so although they don’t confirm the diagnosis, “you have to take the possibility of HIT seriously.” Discontinue heparin, start a nonheparin anticoagulant, and order a HIT immunoassay. If it’s positive, order a functional assay to confirm the diagnosis, he said.
Suspicion of HIT “is perhaps the most common consult that we get on the hematology service. These are tough consults because it is a high-stakes decision.” There is about a 6% risk of thromboembolism, amputation, and death for every day treatment is delayed. “On the other hand, the nonheparin anticoagulants are expensive, and they carry about a 1% daily risk of major bleeding,” Dr. Cuker explained during his presentation at the 2020 Update in Nonneoplastic Hematology virtual conference.
ELISA immunoassay detects antiplatelet factor 4 heparin antibodies but doesn’t tell whether or not they are able to activate platelets and cause HIT. Functional tests such as the serotonin-release assay detect only those antibodies able to do so, but the assays are difficult to perform, and often require samples to be sent out to a reference lab.
ASH did not specify a particular nonheparin anticoagulant in its 2018 guidelines because “the best choice for your patient” depends on which drugs you have available, your familiarity with them, and patient factors, Dr. Cuker said at the conference sponsored by MedscapeLive.
It makes sense, for instance, to use a short-acting agent such as argatroban or bivalirudin in patients who are critically ill, at high risk of bleeding, or likely to need an urgent unplanned procedure. Fondaparinux or direct oral anticoagulants (DOACs) make sense if patients are clinically stable with good organ function and no more than average bleeding risk, because they are easier to administer and facilitate transition to the outpatient setting.
DOACs are newcomers to ASH’s guidelines. Just 81 patients had been reported in the literature when they were being drafted, but only 2 patients had recurrence or progression of thromboembolic events, and there were no major bleeds. The results compared favorably with other options.
The studies were subject to selection and reporting biases, “but, nonetheless, the panel felt the results were positive enough that DOACs ought to be listed as an option,” Dr. Cuker said.
The guidelines note that parenteral options may be the best choice for life- or limb-threatening thrombosis “because few such patients have been treated with a DOAC.” Anticoagulation must continue until platelet counts recover.
Dr. Cuker is a consultant for Synergy and has institutional research support from Alexion, Bayer, Sanofi, and other companies. MedscapeLive and this news organization are owned by the same parent company.
The real strength of the 4T score for heparin-induced thrombocytopenia (HIT) is its negative predictive value, according to hematologist Adam Cuker, MD, of the department of medicine at the University of Pennsylvania, Philadelphia.
The score assigns patients points based on degree of thrombocytopenia, timing of platelet count fall in relation to heparin exposure, presence of thrombosis and other sequelae, and the likelihood of other causes of thrombocytopenia.
A low score – 3 points or less – has a negative predictive value of 99.8%, “so HIT is basically ruled out; you do not need to order lab testing for HIT or manage the patient empirically for HIT,” and should look for other causes of thrombocytopenia, said Dr. Cuker, lead author of the American Society of Hematology’s most recent HIT guidelines.
Intermediate scores of 4 or 5 points, and high scores of 6-8 points, are a different story. The positive predictive value of an intermediate score is only 14%, and of a high score, 64%, so although they don’t confirm the diagnosis, “you have to take the possibility of HIT seriously.” Discontinue heparin, start a nonheparin anticoagulant, and order a HIT immunoassay. If it’s positive, order a functional assay to confirm the diagnosis, he said.
Suspicion of HIT “is perhaps the most common consult that we get on the hematology service. These are tough consults because it is a high-stakes decision.” There is about a 6% risk of thromboembolism, amputation, and death for every day treatment is delayed. “On the other hand, the nonheparin anticoagulants are expensive, and they carry about a 1% daily risk of major bleeding,” Dr. Cuker explained during his presentation at the 2020 Update in Nonneoplastic Hematology virtual conference.
ELISA immunoassay detects antiplatelet factor 4 heparin antibodies but doesn’t tell whether or not they are able to activate platelets and cause HIT. Functional tests such as the serotonin-release assay detect only those antibodies able to do so, but the assays are difficult to perform, and often require samples to be sent out to a reference lab.
ASH did not specify a particular nonheparin anticoagulant in its 2018 guidelines because “the best choice for your patient” depends on which drugs you have available, your familiarity with them, and patient factors, Dr. Cuker said at the conference sponsored by MedscapeLive.
It makes sense, for instance, to use a short-acting agent such as argatroban or bivalirudin in patients who are critically ill, at high risk of bleeding, or likely to need an urgent unplanned procedure. Fondaparinux or direct oral anticoagulants (DOACs) make sense if patients are clinically stable with good organ function and no more than average bleeding risk, because they are easier to administer and facilitate transition to the outpatient setting.
DOACs are newcomers to ASH’s guidelines. Just 81 patients had been reported in the literature when they were being drafted, but only 2 patients had recurrence or progression of thromboembolic events, and there were no major bleeds. The results compared favorably with other options.
The studies were subject to selection and reporting biases, “but, nonetheless, the panel felt the results were positive enough that DOACs ought to be listed as an option,” Dr. Cuker said.
The guidelines note that parenteral options may be the best choice for life- or limb-threatening thrombosis “because few such patients have been treated with a DOAC.” Anticoagulation must continue until platelet counts recover.
Dr. Cuker is a consultant for Synergy and has institutional research support from Alexion, Bayer, Sanofi, and other companies. MedscapeLive and this news organization are owned by the same parent company.
The real strength of the 4T score for heparin-induced thrombocytopenia (HIT) is its negative predictive value, according to hematologist Adam Cuker, MD, of the department of medicine at the University of Pennsylvania, Philadelphia.
The score assigns patients points based on degree of thrombocytopenia, timing of platelet count fall in relation to heparin exposure, presence of thrombosis and other sequelae, and the likelihood of other causes of thrombocytopenia.
A low score – 3 points or less – has a negative predictive value of 99.8%, “so HIT is basically ruled out; you do not need to order lab testing for HIT or manage the patient empirically for HIT,” and should look for other causes of thrombocytopenia, said Dr. Cuker, lead author of the American Society of Hematology’s most recent HIT guidelines.
Intermediate scores of 4 or 5 points, and high scores of 6-8 points, are a different story. The positive predictive value of an intermediate score is only 14%, and of a high score, 64%, so although they don’t confirm the diagnosis, “you have to take the possibility of HIT seriously.” Discontinue heparin, start a nonheparin anticoagulant, and order a HIT immunoassay. If it’s positive, order a functional assay to confirm the diagnosis, he said.
Suspicion of HIT “is perhaps the most common consult that we get on the hematology service. These are tough consults because it is a high-stakes decision.” There is about a 6% risk of thromboembolism, amputation, and death for every day treatment is delayed. “On the other hand, the nonheparin anticoagulants are expensive, and they carry about a 1% daily risk of major bleeding,” Dr. Cuker explained during his presentation at the 2020 Update in Nonneoplastic Hematology virtual conference.
ELISA immunoassay detects antiplatelet factor 4 heparin antibodies but doesn’t tell whether or not they are able to activate platelets and cause HIT. Functional tests such as the serotonin-release assay detect only those antibodies able to do so, but the assays are difficult to perform, and often require samples to be sent out to a reference lab.
ASH did not specify a particular nonheparin anticoagulant in its 2018 guidelines because “the best choice for your patient” depends on which drugs you have available, your familiarity with them, and patient factors, Dr. Cuker said at the conference sponsored by MedscapeLive.
It makes sense, for instance, to use a short-acting agent such as argatroban or bivalirudin in patients who are critically ill, at high risk of bleeding, or likely to need an urgent unplanned procedure. Fondaparinux or direct oral anticoagulants (DOACs) make sense if patients are clinically stable with good organ function and no more than average bleeding risk, because they are easier to administer and facilitate transition to the outpatient setting.
DOACs are newcomers to ASH’s guidelines. Just 81 patients had been reported in the literature when they were being drafted, but only 2 patients had recurrence or progression of thromboembolic events, and there were no major bleeds. The results compared favorably with other options.
The studies were subject to selection and reporting biases, “but, nonetheless, the panel felt the results were positive enough that DOACs ought to be listed as an option,” Dr. Cuker said.
The guidelines note that parenteral options may be the best choice for life- or limb-threatening thrombosis “because few such patients have been treated with a DOAC.” Anticoagulation must continue until platelet counts recover.
Dr. Cuker is a consultant for Synergy and has institutional research support from Alexion, Bayer, Sanofi, and other companies. MedscapeLive and this news organization are owned by the same parent company.
FROM 2020 UNNH
Physicians react: Doctors worry about patients reading their clinical notes
Patients will soon be able to read the notes that physicians make during an episode of care, as well as information about diagnostic testing and imaging results, tests for STDs, fetal ultrasounds, and cancer biopsies. This open access is raising concerns among physicians.
As part of the 21st Century Cures Act, patients have the right to see their medical notes. Known as Open Notes, the policy will go into effect on April 5, 2021. The Department of Health & Human Services recently changed the original start date, which was to be Nov. 2, 2020.
The mandate has some physicians worrying about potential legal risks and possible violation of doctor-patient confidentiality. When asked to share their views on the new Open Notes mandate, many physicians expressed their concerns but also cited some of the positive effects that could come from this.
Potentially more legal woes for physicians?
A key concern raised by one physician commenter is that patients could misunderstand legitimate medical terminology or even put a physician in legal crosshairs. For example, a medical term such as “spontaneous abortion” could be misconstrued by patients. A physician might write notes with the idea that a patient is reading them and thus might alter those notes in a way that creates legal trouble.
“This layers another level of censorship and legal liability onto physicians, who in attempting to be [politically correct], may omit critical information or have to use euphemisms in order to avoid conflict,” one physician said.
She also questioned whether notes might now have to be run through legal counsel before being posted to avoid potential liability.
Another doctor questioned how physicians would be able to document patients suspected of faking injuries for pain medication, for example. Could such documentation lead to lawsuits for the doctor?
As one physician noted, some patients “are drug seekers. Some refuse to aid in their own care. Some are malingerers. Not documenting that is bad medicine.”
The possibility of violating doctor-patient confidentiality laws, particularly for teenagers, could be another negative effect of Open Notes, said one physician.
“Won’t this violate the statutes that teenagers have the right to confidential evaluations?” the commenter mused. “If charts are to be immediately available, then STDs and pregnancies they weren’t ready to talk about will now be suddenly known by their parents.”
One doctor has already faced this issue. “I already ran into this problem once,” he noted. “Now I warn those on their parents’ insurance before I start the visit. I have literally had a patient state, ‘well then we are done,’ and leave without being seen due to it.”
Another physician questioned the possibility of having to write notes differently than they do now, especially if the patients have lower reading comprehension abilities.
One physician who uses Open Notes said he receives patient requests for changes that have little to do with the actual diagnosis and relate to ancillary issues. He highlighted patients who “don’t want psych diagnosis in their chart or are concerned a diagnosis will raise their insurance premium, so they ask me to delete it.”
Will Open Notes erode patient communication?
One physician questioned whether it would lead to patients being less open and forthcoming about their medical concerns with doctors.
“The main problem I see is the patient not telling me the whole story, or worse, telling me the story, and then asking me not to document it (as many have done in the past) because they don’t want their spouse, family, etc. to read the notes and they have already given their permission for them to do so, for a variety of reasons,” he commented. “This includes topics of STDs, infidelity, depression, suicidal thoughts, and other symptoms the patient doesn’t want their family to read about.”
Some physicians envision positive developments
Many physicians are unconcerned by the new mandate. “I see some potential good in this, such as improving doctor-patient communication and more scrupulous charting,” one physician said.
A doctor working in the U.S. federal health care system noted that open access has been a part of that system for decades.
“Since health care providers work in this unveiled setting for their entire career, they usually know how to write appropriate clinical notes and what information needs to be included in them,” he wrote. “Now it’s time for the rest of the medical community to catch up to a reality that we have worked within for decades now.
“The world did not end, malpractice complaints did not increase, and physician/patient relationships were not damaged. Living in the information age, archaic practices like private notes were surely going to end at some point.”
One doctor who has been using Open Notes has had experiences in which the patient noted an error in the medical chart that needed correcting. “I have had one patient correct me on a timeline in the HPI which was helpful and I made the requested correction in that instance,” he said.
Another physician agreed. “I’ve had patients add or correct valuable information I’ve missed. Good probably outweighs the bad if we set limits on behaviors expressed by the personality disordered group. The majority of people don’t seem to care and still ask me ‘what would you do’ or ‘tell me what to do.’ It’s all about patient/physician trust.”
Another talked about how Open Notes should have little or no impact. “Here’s a novel concept – talking to our patients,” he commented. “There is nothing in every one of my chart notes that has not already been discussed with my patients and I dictate (speech to text) my findings and plan in front of them. So, if they are reviewing my office notes, it will only serve to reinforce what we have already discussed.”
“I don’t intend to change anything,” he added. “Chances are if they were to see a test result before I have a chance to discuss it with them, they will have already ‘Googled’ its meaning and we can have more meaningful interaction if they have a basic understanding of the test.”
“I understand that this is anxiety provoking, but in general I think it is appropriate for patients to have access to their notes,” said another physician. “If physicians write lousy notes that say they did things they didn’t do, that fail to actually state a diagnosis and a plan (and they often do), that is the doc’s problem, not the patient’s.”
A version of this article first appeared on Medscape.com.
Patients will soon be able to read the notes that physicians make during an episode of care, as well as information about diagnostic testing and imaging results, tests for STDs, fetal ultrasounds, and cancer biopsies. This open access is raising concerns among physicians.
As part of the 21st Century Cures Act, patients have the right to see their medical notes. Known as Open Notes, the policy will go into effect on April 5, 2021. The Department of Health & Human Services recently changed the original start date, which was to be Nov. 2, 2020.
The mandate has some physicians worrying about potential legal risks and possible violation of doctor-patient confidentiality. When asked to share their views on the new Open Notes mandate, many physicians expressed their concerns but also cited some of the positive effects that could come from this.
Potentially more legal woes for physicians?
A key concern raised by one physician commenter is that patients could misunderstand legitimate medical terminology or even put a physician in legal crosshairs. For example, a medical term such as “spontaneous abortion” could be misconstrued by patients. A physician might write notes with the idea that a patient is reading them and thus might alter those notes in a way that creates legal trouble.
“This layers another level of censorship and legal liability onto physicians, who in attempting to be [politically correct], may omit critical information or have to use euphemisms in order to avoid conflict,” one physician said.
She also questioned whether notes might now have to be run through legal counsel before being posted to avoid potential liability.
Another doctor questioned how physicians would be able to document patients suspected of faking injuries for pain medication, for example. Could such documentation lead to lawsuits for the doctor?
As one physician noted, some patients “are drug seekers. Some refuse to aid in their own care. Some are malingerers. Not documenting that is bad medicine.”
The possibility of violating doctor-patient confidentiality laws, particularly for teenagers, could be another negative effect of Open Notes, said one physician.
“Won’t this violate the statutes that teenagers have the right to confidential evaluations?” the commenter mused. “If charts are to be immediately available, then STDs and pregnancies they weren’t ready to talk about will now be suddenly known by their parents.”
One doctor has already faced this issue. “I already ran into this problem once,” he noted. “Now I warn those on their parents’ insurance before I start the visit. I have literally had a patient state, ‘well then we are done,’ and leave without being seen due to it.”
Another physician questioned the possibility of having to write notes differently than they do now, especially if the patients have lower reading comprehension abilities.
One physician who uses Open Notes said he receives patient requests for changes that have little to do with the actual diagnosis and relate to ancillary issues. He highlighted patients who “don’t want psych diagnosis in their chart or are concerned a diagnosis will raise their insurance premium, so they ask me to delete it.”
Will Open Notes erode patient communication?
One physician questioned whether it would lead to patients being less open and forthcoming about their medical concerns with doctors.
“The main problem I see is the patient not telling me the whole story, or worse, telling me the story, and then asking me not to document it (as many have done in the past) because they don’t want their spouse, family, etc. to read the notes and they have already given their permission for them to do so, for a variety of reasons,” he commented. “This includes topics of STDs, infidelity, depression, suicidal thoughts, and other symptoms the patient doesn’t want their family to read about.”
Some physicians envision positive developments
Many physicians are unconcerned by the new mandate. “I see some potential good in this, such as improving doctor-patient communication and more scrupulous charting,” one physician said.
A doctor working in the U.S. federal health care system noted that open access has been a part of that system for decades.
“Since health care providers work in this unveiled setting for their entire career, they usually know how to write appropriate clinical notes and what information needs to be included in them,” he wrote. “Now it’s time for the rest of the medical community to catch up to a reality that we have worked within for decades now.
“The world did not end, malpractice complaints did not increase, and physician/patient relationships were not damaged. Living in the information age, archaic practices like private notes were surely going to end at some point.”
One doctor who has been using Open Notes has had experiences in which the patient noted an error in the medical chart that needed correcting. “I have had one patient correct me on a timeline in the HPI which was helpful and I made the requested correction in that instance,” he said.
Another physician agreed. “I’ve had patients add or correct valuable information I’ve missed. Good probably outweighs the bad if we set limits on behaviors expressed by the personality disordered group. The majority of people don’t seem to care and still ask me ‘what would you do’ or ‘tell me what to do.’ It’s all about patient/physician trust.”
Another talked about how Open Notes should have little or no impact. “Here’s a novel concept – talking to our patients,” he commented. “There is nothing in every one of my chart notes that has not already been discussed with my patients and I dictate (speech to text) my findings and plan in front of them. So, if they are reviewing my office notes, it will only serve to reinforce what we have already discussed.”
“I don’t intend to change anything,” he added. “Chances are if they were to see a test result before I have a chance to discuss it with them, they will have already ‘Googled’ its meaning and we can have more meaningful interaction if they have a basic understanding of the test.”
“I understand that this is anxiety provoking, but in general I think it is appropriate for patients to have access to their notes,” said another physician. “If physicians write lousy notes that say they did things they didn’t do, that fail to actually state a diagnosis and a plan (and they often do), that is the doc’s problem, not the patient’s.”
A version of this article first appeared on Medscape.com.
Patients will soon be able to read the notes that physicians make during an episode of care, as well as information about diagnostic testing and imaging results, tests for STDs, fetal ultrasounds, and cancer biopsies. This open access is raising concerns among physicians.
As part of the 21st Century Cures Act, patients have the right to see their medical notes. Known as Open Notes, the policy will go into effect on April 5, 2021. The Department of Health & Human Services recently changed the original start date, which was to be Nov. 2, 2020.
The mandate has some physicians worrying about potential legal risks and possible violation of doctor-patient confidentiality. When asked to share their views on the new Open Notes mandate, many physicians expressed their concerns but also cited some of the positive effects that could come from this.
Potentially more legal woes for physicians?
A key concern raised by one physician commenter is that patients could misunderstand legitimate medical terminology or even put a physician in legal crosshairs. For example, a medical term such as “spontaneous abortion” could be misconstrued by patients. A physician might write notes with the idea that a patient is reading them and thus might alter those notes in a way that creates legal trouble.
“This layers another level of censorship and legal liability onto physicians, who in attempting to be [politically correct], may omit critical information or have to use euphemisms in order to avoid conflict,” one physician said.
She also questioned whether notes might now have to be run through legal counsel before being posted to avoid potential liability.
Another doctor questioned how physicians would be able to document patients suspected of faking injuries for pain medication, for example. Could such documentation lead to lawsuits for the doctor?
As one physician noted, some patients “are drug seekers. Some refuse to aid in their own care. Some are malingerers. Not documenting that is bad medicine.”
The possibility of violating doctor-patient confidentiality laws, particularly for teenagers, could be another negative effect of Open Notes, said one physician.
“Won’t this violate the statutes that teenagers have the right to confidential evaluations?” the commenter mused. “If charts are to be immediately available, then STDs and pregnancies they weren’t ready to talk about will now be suddenly known by their parents.”
One doctor has already faced this issue. “I already ran into this problem once,” he noted. “Now I warn those on their parents’ insurance before I start the visit. I have literally had a patient state, ‘well then we are done,’ and leave without being seen due to it.”
Another physician questioned the possibility of having to write notes differently than they do now, especially if the patients have lower reading comprehension abilities.
One physician who uses Open Notes said he receives patient requests for changes that have little to do with the actual diagnosis and relate to ancillary issues. He highlighted patients who “don’t want psych diagnosis in their chart or are concerned a diagnosis will raise their insurance premium, so they ask me to delete it.”
Will Open Notes erode patient communication?
One physician questioned whether it would lead to patients being less open and forthcoming about their medical concerns with doctors.
“The main problem I see is the patient not telling me the whole story, or worse, telling me the story, and then asking me not to document it (as many have done in the past) because they don’t want their spouse, family, etc. to read the notes and they have already given their permission for them to do so, for a variety of reasons,” he commented. “This includes topics of STDs, infidelity, depression, suicidal thoughts, and other symptoms the patient doesn’t want their family to read about.”
Some physicians envision positive developments
Many physicians are unconcerned by the new mandate. “I see some potential good in this, such as improving doctor-patient communication and more scrupulous charting,” one physician said.
A doctor working in the U.S. federal health care system noted that open access has been a part of that system for decades.
“Since health care providers work in this unveiled setting for their entire career, they usually know how to write appropriate clinical notes and what information needs to be included in them,” he wrote. “Now it’s time for the rest of the medical community to catch up to a reality that we have worked within for decades now.
“The world did not end, malpractice complaints did not increase, and physician/patient relationships were not damaged. Living in the information age, archaic practices like private notes were surely going to end at some point.”
One doctor who has been using Open Notes has had experiences in which the patient noted an error in the medical chart that needed correcting. “I have had one patient correct me on a timeline in the HPI which was helpful and I made the requested correction in that instance,” he said.
Another physician agreed. “I’ve had patients add or correct valuable information I’ve missed. Good probably outweighs the bad if we set limits on behaviors expressed by the personality disordered group. The majority of people don’t seem to care and still ask me ‘what would you do’ or ‘tell me what to do.’ It’s all about patient/physician trust.”
Another talked about how Open Notes should have little or no impact. “Here’s a novel concept – talking to our patients,” he commented. “There is nothing in every one of my chart notes that has not already been discussed with my patients and I dictate (speech to text) my findings and plan in front of them. So, if they are reviewing my office notes, it will only serve to reinforce what we have already discussed.”
“I don’t intend to change anything,” he added. “Chances are if they were to see a test result before I have a chance to discuss it with them, they will have already ‘Googled’ its meaning and we can have more meaningful interaction if they have a basic understanding of the test.”
“I understand that this is anxiety provoking, but in general I think it is appropriate for patients to have access to their notes,” said another physician. “If physicians write lousy notes that say they did things they didn’t do, that fail to actually state a diagnosis and a plan (and they often do), that is the doc’s problem, not the patient’s.”
A version of this article first appeared on Medscape.com.
Updated ACC decision pathway embraces new heart failure treatment strategies
A newly updated expert consensus from the American College of Cardiology for management of heart failure with reduced ejection fraction includes several new guideline-directed medical therapies among other substantial changes relative to its 2017 predecessor.
The advances in treatment of heart failure with reduced ejection fraction (HFrEF) have resulted in a substantial increase in complexity in reaching treatment goals, according to the authors of the new guidance. Structured similarly to the 2017 ACC Expert Consensus Decision Pathway, the update accommodates a series of practical tips to bring all patients on board with the newer as well as the established therapies with lifesaving potential.
The potential return from implementing these recommendations is not trivial. Relative to an ACE inhibitor and a beta-blocker alone, optimal implementation of the current guideline-directed medical therapies (GDMT) “can extend medical survival by more than 6 years,” according to Gregg C. Fonarow, MD, chief of cardiology at the University of California, Los Angeles.
A member of the writing committee for the 2021 update, Dr. Fonarow explained that the consensus pathway is more than a list of therapies and recommended doses. The detailed advice on how to overcome the barriers to GDMT is meant to close the substantial gap between current practice and unmet opportunities for inhibiting HFrEF progression.
“Optimal GDMT among HFrEF patients is distressingly low, due in part to the number and complexity of medications that now constitute GDMT,” said the chair of the writing committee, Thomas M. Maddox, MD, executive director, Healthcare Innovation Lab, BJC HealthCare/Washington University, St. Louis. Like Dr. Fonarow, Dr. Maddox emphasized that the importance of the update for the practical strategies it offers to place patients on optimal care.
In the 2017 guidance, 10 pivotal issues were tackled, ranging from advice of how to put HFrEF patients on the multiple drugs that now constitute optimal therapy to when to transition patients to hospice care. The 2021 update covers the same ground but incorporates new information that has changed the definition of optimal care.
Perhaps most importantly, sacubitril/valsartan, an angiotensin receptor neprilysin inhibitor (ARNi), and SGLT2 inhibitors represent major new additions in HFrEF GDMT. Dr. Maddox called the practical information about how these should be incorporated into HFrEF management represents one of the “major highlights” of the update.
Two algorithms outline the expert consensus recommendations of the order and the dose of the multiple drugs that now constitute the current GDMT. With the goal of explaining exactly how to place patients on all the HFrEF therapies associated with improved outcome, “I think these figures can really help us in guiding our patients to optimal medication regimens and dosages,” Dr. Maddox said. If successful, clinicians “can make a significant difference in these patients’ length and quality of life.”
Most cardiologists and others who treat HFrEF are likely aware of the major improvements in outcome documented in large trials when an ARNi and a SGLT2 inhibitor were added to previously established GDMT, but the update like the 2017 document is focused on the practical strategies of implementation, according to Larry A. Allen, MD, medical director of advanced heart failure at the University of Colorado at Denver, Aurora.
“The 2017 Expert Consensus Decision Pathway got a lot of attention because it takes a very practical approach to questions that clinicians and their patients have to tackle everyday but for which there was not always clean answers from the data,” said Dr. Allen, a member of the writing committee for both the 2017 expert consensus and the 2021 update. He noted that the earlier document was one of the most downloaded articles from the ACC’s journal in the year it appeared.
“There is excellent data on the benefits of beta-blockers, ARNi, mineralocorticoid antagonists, and SGLT2 inhibitors, but how does one decide what order to use them in?” Dr. Allen asked in outlining goals of the expert consensus.
While the new update “focuses on the newer drug classes, particularly SGLT2 inhibitors,” it traces care from first-line therapies to end-of-life management, according to Dr. Allen. This includes information on when to consider advanced therapies, such as left ventricular assist devices or transplant in order to get patients to these treatments before the opportunity for benefit is missed.
Both the 2017 version and the update offer a table to summarize triggers for referral. The complexity of individualizing care in a group of patients likely to have variable manifestations of disease and multiple comorbidities was a theme of the 2017 document that has been reprised in the 2021 update,
“Good communication and team-based care” is one of common management gaps that the update addresses, Dr. Allen said. He indicated that the checklists and algorithms in the update would help with complex decision-making and encourage the multidisciplinary care that ensures optimal management.
SOURCE: Maddox TM et al. J Am Coll Cardiol. 2021 Jan 11. doi: 10.1016/j.jacc.2020.11.022.
A newly updated expert consensus from the American College of Cardiology for management of heart failure with reduced ejection fraction includes several new guideline-directed medical therapies among other substantial changes relative to its 2017 predecessor.
The advances in treatment of heart failure with reduced ejection fraction (HFrEF) have resulted in a substantial increase in complexity in reaching treatment goals, according to the authors of the new guidance. Structured similarly to the 2017 ACC Expert Consensus Decision Pathway, the update accommodates a series of practical tips to bring all patients on board with the newer as well as the established therapies with lifesaving potential.
The potential return from implementing these recommendations is not trivial. Relative to an ACE inhibitor and a beta-blocker alone, optimal implementation of the current guideline-directed medical therapies (GDMT) “can extend medical survival by more than 6 years,” according to Gregg C. Fonarow, MD, chief of cardiology at the University of California, Los Angeles.
A member of the writing committee for the 2021 update, Dr. Fonarow explained that the consensus pathway is more than a list of therapies and recommended doses. The detailed advice on how to overcome the barriers to GDMT is meant to close the substantial gap between current practice and unmet opportunities for inhibiting HFrEF progression.
“Optimal GDMT among HFrEF patients is distressingly low, due in part to the number and complexity of medications that now constitute GDMT,” said the chair of the writing committee, Thomas M. Maddox, MD, executive director, Healthcare Innovation Lab, BJC HealthCare/Washington University, St. Louis. Like Dr. Fonarow, Dr. Maddox emphasized that the importance of the update for the practical strategies it offers to place patients on optimal care.
In the 2017 guidance, 10 pivotal issues were tackled, ranging from advice of how to put HFrEF patients on the multiple drugs that now constitute optimal therapy to when to transition patients to hospice care. The 2021 update covers the same ground but incorporates new information that has changed the definition of optimal care.
Perhaps most importantly, sacubitril/valsartan, an angiotensin receptor neprilysin inhibitor (ARNi), and SGLT2 inhibitors represent major new additions in HFrEF GDMT. Dr. Maddox called the practical information about how these should be incorporated into HFrEF management represents one of the “major highlights” of the update.
Two algorithms outline the expert consensus recommendations of the order and the dose of the multiple drugs that now constitute the current GDMT. With the goal of explaining exactly how to place patients on all the HFrEF therapies associated with improved outcome, “I think these figures can really help us in guiding our patients to optimal medication regimens and dosages,” Dr. Maddox said. If successful, clinicians “can make a significant difference in these patients’ length and quality of life.”
Most cardiologists and others who treat HFrEF are likely aware of the major improvements in outcome documented in large trials when an ARNi and a SGLT2 inhibitor were added to previously established GDMT, but the update like the 2017 document is focused on the practical strategies of implementation, according to Larry A. Allen, MD, medical director of advanced heart failure at the University of Colorado at Denver, Aurora.
“The 2017 Expert Consensus Decision Pathway got a lot of attention because it takes a very practical approach to questions that clinicians and their patients have to tackle everyday but for which there was not always clean answers from the data,” said Dr. Allen, a member of the writing committee for both the 2017 expert consensus and the 2021 update. He noted that the earlier document was one of the most downloaded articles from the ACC’s journal in the year it appeared.
“There is excellent data on the benefits of beta-blockers, ARNi, mineralocorticoid antagonists, and SGLT2 inhibitors, but how does one decide what order to use them in?” Dr. Allen asked in outlining goals of the expert consensus.
While the new update “focuses on the newer drug classes, particularly SGLT2 inhibitors,” it traces care from first-line therapies to end-of-life management, according to Dr. Allen. This includes information on when to consider advanced therapies, such as left ventricular assist devices or transplant in order to get patients to these treatments before the opportunity for benefit is missed.
Both the 2017 version and the update offer a table to summarize triggers for referral. The complexity of individualizing care in a group of patients likely to have variable manifestations of disease and multiple comorbidities was a theme of the 2017 document that has been reprised in the 2021 update,
“Good communication and team-based care” is one of common management gaps that the update addresses, Dr. Allen said. He indicated that the checklists and algorithms in the update would help with complex decision-making and encourage the multidisciplinary care that ensures optimal management.
SOURCE: Maddox TM et al. J Am Coll Cardiol. 2021 Jan 11. doi: 10.1016/j.jacc.2020.11.022.
A newly updated expert consensus from the American College of Cardiology for management of heart failure with reduced ejection fraction includes several new guideline-directed medical therapies among other substantial changes relative to its 2017 predecessor.
The advances in treatment of heart failure with reduced ejection fraction (HFrEF) have resulted in a substantial increase in complexity in reaching treatment goals, according to the authors of the new guidance. Structured similarly to the 2017 ACC Expert Consensus Decision Pathway, the update accommodates a series of practical tips to bring all patients on board with the newer as well as the established therapies with lifesaving potential.
The potential return from implementing these recommendations is not trivial. Relative to an ACE inhibitor and a beta-blocker alone, optimal implementation of the current guideline-directed medical therapies (GDMT) “can extend medical survival by more than 6 years,” according to Gregg C. Fonarow, MD, chief of cardiology at the University of California, Los Angeles.
A member of the writing committee for the 2021 update, Dr. Fonarow explained that the consensus pathway is more than a list of therapies and recommended doses. The detailed advice on how to overcome the barriers to GDMT is meant to close the substantial gap between current practice and unmet opportunities for inhibiting HFrEF progression.
“Optimal GDMT among HFrEF patients is distressingly low, due in part to the number and complexity of medications that now constitute GDMT,” said the chair of the writing committee, Thomas M. Maddox, MD, executive director, Healthcare Innovation Lab, BJC HealthCare/Washington University, St. Louis. Like Dr. Fonarow, Dr. Maddox emphasized that the importance of the update for the practical strategies it offers to place patients on optimal care.
In the 2017 guidance, 10 pivotal issues were tackled, ranging from advice of how to put HFrEF patients on the multiple drugs that now constitute optimal therapy to when to transition patients to hospice care. The 2021 update covers the same ground but incorporates new information that has changed the definition of optimal care.
Perhaps most importantly, sacubitril/valsartan, an angiotensin receptor neprilysin inhibitor (ARNi), and SGLT2 inhibitors represent major new additions in HFrEF GDMT. Dr. Maddox called the practical information about how these should be incorporated into HFrEF management represents one of the “major highlights” of the update.
Two algorithms outline the expert consensus recommendations of the order and the dose of the multiple drugs that now constitute the current GDMT. With the goal of explaining exactly how to place patients on all the HFrEF therapies associated with improved outcome, “I think these figures can really help us in guiding our patients to optimal medication regimens and dosages,” Dr. Maddox said. If successful, clinicians “can make a significant difference in these patients’ length and quality of life.”
Most cardiologists and others who treat HFrEF are likely aware of the major improvements in outcome documented in large trials when an ARNi and a SGLT2 inhibitor were added to previously established GDMT, but the update like the 2017 document is focused on the practical strategies of implementation, according to Larry A. Allen, MD, medical director of advanced heart failure at the University of Colorado at Denver, Aurora.
“The 2017 Expert Consensus Decision Pathway got a lot of attention because it takes a very practical approach to questions that clinicians and their patients have to tackle everyday but for which there was not always clean answers from the data,” said Dr. Allen, a member of the writing committee for both the 2017 expert consensus and the 2021 update. He noted that the earlier document was one of the most downloaded articles from the ACC’s journal in the year it appeared.
“There is excellent data on the benefits of beta-blockers, ARNi, mineralocorticoid antagonists, and SGLT2 inhibitors, but how does one decide what order to use them in?” Dr. Allen asked in outlining goals of the expert consensus.
While the new update “focuses on the newer drug classes, particularly SGLT2 inhibitors,” it traces care from first-line therapies to end-of-life management, according to Dr. Allen. This includes information on when to consider advanced therapies, such as left ventricular assist devices or transplant in order to get patients to these treatments before the opportunity for benefit is missed.
Both the 2017 version and the update offer a table to summarize triggers for referral. The complexity of individualizing care in a group of patients likely to have variable manifestations of disease and multiple comorbidities was a theme of the 2017 document that has been reprised in the 2021 update,
“Good communication and team-based care” is one of common management gaps that the update addresses, Dr. Allen said. He indicated that the checklists and algorithms in the update would help with complex decision-making and encourage the multidisciplinary care that ensures optimal management.
SOURCE: Maddox TM et al. J Am Coll Cardiol. 2021 Jan 11. doi: 10.1016/j.jacc.2020.11.022.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Complications and death within 30 days after noncardiac surgery
Background: There have been advances in perioperative care and technology for adults, but at the same time the patient population is increasingly medically complex. We do not know the current mortality risk of noncardiac surgery in adults.
Study design: Prospective cohort study.
Setting: Twenty-eight academic centers in 14 countries in North America, South America, Asia, Europe, Africa, and Australia. At least four academic centers represented each of these continents, except Africa, with one center reporting there.
Synopsis: The VISION study included 40,004 inpatients, aged 45 years and older, followed for 30-day mortality after noncardiac surgery. One-third of surgeries were considered low risk. A startling 99.1% of patients completed the study. Mortality rate was 1.8%, with 71% of patients dying during the index admission and 29% dying after discharge.
Nine events were independently associated with postoperative death, but the top three – major bleeding, myocardial injury after noncardiac surgery (MINS), and sepsis – accounted for 45% of the attributable fraction. These, on average, occurred within 1-6 days after surgery. The other events (infection, kidney injury with dialysis, stroke, venous thromboembolism, new atrial fibrillation, and congestive heart failure) constituted less than 3% of the attributable fraction. Findings suggest that closer monitoring in the hospital and post discharge might improve survival after noncardiac surgery.
Limitations for hospitalists include that patients were younger and less medically complex than our typically comanaged patients: More than half of patients were aged 45-64, less than 10% had chronic kidney disease stage 3b or greater, and only 20% had diabetes mellitus.
Bottom line: Postoperative and postdischarge bleeding, myocardial injury after noncardiac surgery, and sepsis are major risk factors for 30-day mortality in adults undergoing noncardiac surgery. Closer postoperative monitoring for these conditions should be explored.
Citation: The Vision Study Investigators (Spence J et al.) Association between complications and death within 30 days after noncardiac surgery. CMAJ. 2019 Jul 29;191(30):E830-7.
Dr. Brouillette is a med-peds hospitalist at Maine Medical Center in Portland.
Background: There have been advances in perioperative care and technology for adults, but at the same time the patient population is increasingly medically complex. We do not know the current mortality risk of noncardiac surgery in adults.
Study design: Prospective cohort study.
Setting: Twenty-eight academic centers in 14 countries in North America, South America, Asia, Europe, Africa, and Australia. At least four academic centers represented each of these continents, except Africa, with one center reporting there.
Synopsis: The VISION study included 40,004 inpatients, aged 45 years and older, followed for 30-day mortality after noncardiac surgery. One-third of surgeries were considered low risk. A startling 99.1% of patients completed the study. Mortality rate was 1.8%, with 71% of patients dying during the index admission and 29% dying after discharge.
Nine events were independently associated with postoperative death, but the top three – major bleeding, myocardial injury after noncardiac surgery (MINS), and sepsis – accounted for 45% of the attributable fraction. These, on average, occurred within 1-6 days after surgery. The other events (infection, kidney injury with dialysis, stroke, venous thromboembolism, new atrial fibrillation, and congestive heart failure) constituted less than 3% of the attributable fraction. Findings suggest that closer monitoring in the hospital and post discharge might improve survival after noncardiac surgery.
Limitations for hospitalists include that patients were younger and less medically complex than our typically comanaged patients: More than half of patients were aged 45-64, less than 10% had chronic kidney disease stage 3b or greater, and only 20% had diabetes mellitus.
Bottom line: Postoperative and postdischarge bleeding, myocardial injury after noncardiac surgery, and sepsis are major risk factors for 30-day mortality in adults undergoing noncardiac surgery. Closer postoperative monitoring for these conditions should be explored.
Citation: The Vision Study Investigators (Spence J et al.) Association between complications and death within 30 days after noncardiac surgery. CMAJ. 2019 Jul 29;191(30):E830-7.
Dr. Brouillette is a med-peds hospitalist at Maine Medical Center in Portland.
Background: There have been advances in perioperative care and technology for adults, but at the same time the patient population is increasingly medically complex. We do not know the current mortality risk of noncardiac surgery in adults.
Study design: Prospective cohort study.
Setting: Twenty-eight academic centers in 14 countries in North America, South America, Asia, Europe, Africa, and Australia. At least four academic centers represented each of these continents, except Africa, with one center reporting there.
Synopsis: The VISION study included 40,004 inpatients, aged 45 years and older, followed for 30-day mortality after noncardiac surgery. One-third of surgeries were considered low risk. A startling 99.1% of patients completed the study. Mortality rate was 1.8%, with 71% of patients dying during the index admission and 29% dying after discharge.
Nine events were independently associated with postoperative death, but the top three – major bleeding, myocardial injury after noncardiac surgery (MINS), and sepsis – accounted for 45% of the attributable fraction. These, on average, occurred within 1-6 days after surgery. The other events (infection, kidney injury with dialysis, stroke, venous thromboembolism, new atrial fibrillation, and congestive heart failure) constituted less than 3% of the attributable fraction. Findings suggest that closer monitoring in the hospital and post discharge might improve survival after noncardiac surgery.
Limitations for hospitalists include that patients were younger and less medically complex than our typically comanaged patients: More than half of patients were aged 45-64, less than 10% had chronic kidney disease stage 3b or greater, and only 20% had diabetes mellitus.
Bottom line: Postoperative and postdischarge bleeding, myocardial injury after noncardiac surgery, and sepsis are major risk factors for 30-day mortality in adults undergoing noncardiac surgery. Closer postoperative monitoring for these conditions should be explored.
Citation: The Vision Study Investigators (Spence J et al.) Association between complications and death within 30 days after noncardiac surgery. CMAJ. 2019 Jul 29;191(30):E830-7.
Dr. Brouillette is a med-peds hospitalist at Maine Medical Center in Portland.
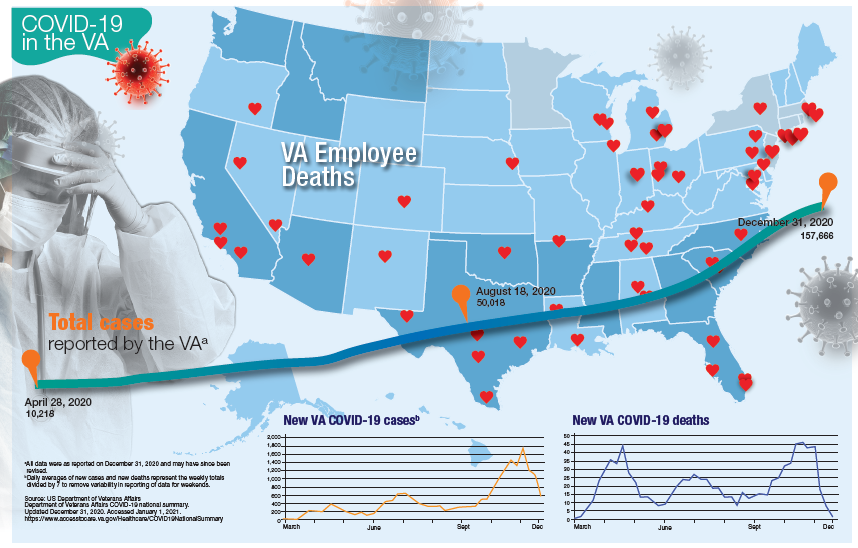
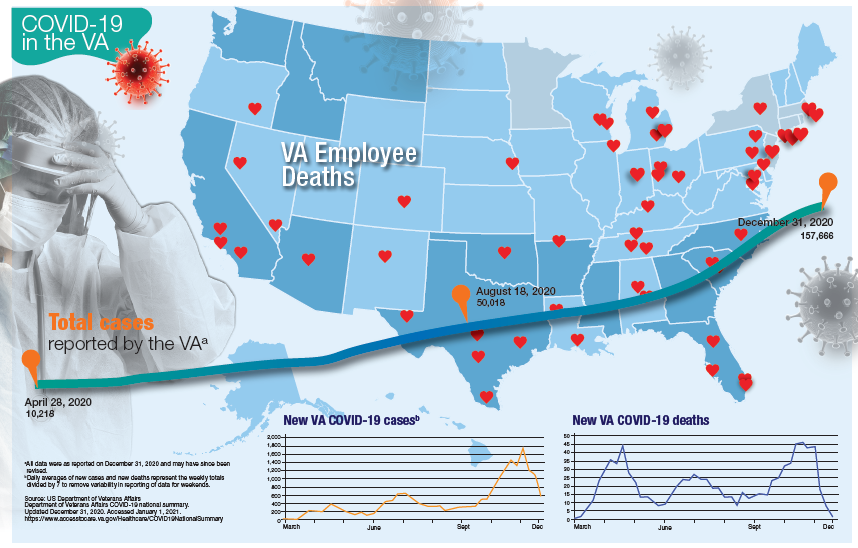
VA Ramps up Vaccinations as COVID-19 Cases Continue to Rise
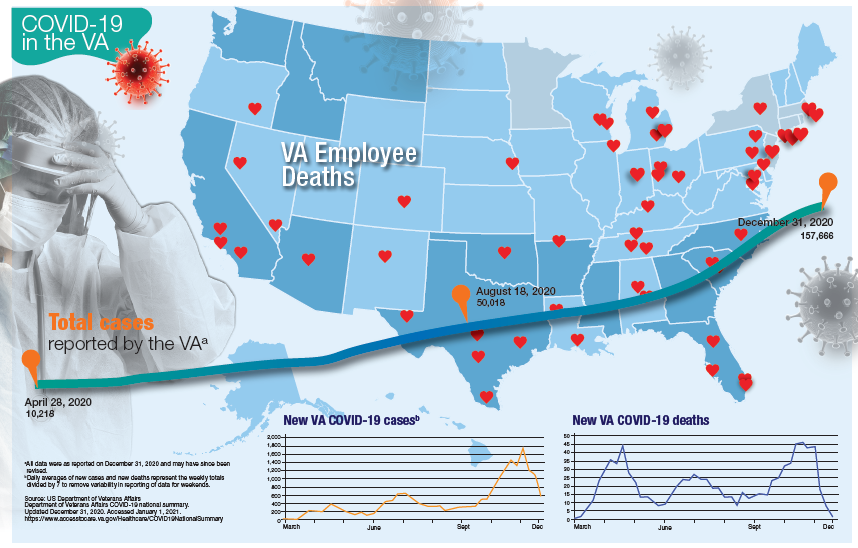
Updated January 12, 2020
More than 181,000 veterans have contracted the COVID-19 virus and 7,385 have died, according to data released by the US Department of Veterans Affairs (VA) on January 12, 2020. The number of cases and deaths have increased sharply since November 2020. The VA also reports that it has administered at least 1 dose of the 2 approved vaccines to 33,875 veterans and 174,724 employees as of January 6.
Currently, the VA reports nearly 19,000 active cases of COVID-19, including 1,270 among VA employees. One hundred five VA employees have died from COVID-19.
Although facilities across the country are facing increased pressure as the number of cases rise, those in Southern California and Texas are reporting significant infection rates. Thirteen facilities have at least 300 active cases, including facilities in Loma Linda (418), Long Beach (381), Greater Los Angeles (361), and San Diego (274), all in California. In Texas, San Antonio (394), Dallas (370), Temple (338), and Houston (328) have all seen large numbers of active cases. Facilities in Columbia, South Carolina (420); Phoenix (407); Atlanta, Georgia (359); Cleveland, Ohio (352); and Orlando, (341) and Gainesville, Florida (340) also have reported significant numbers of cases.
While early on in the pandemic facilities in New York and New Jersey had reported the largest number of deaths, now nearly every facility has reported at least 1 death. Fourteen facilities have reported at least 100 deaths and 53 have reported between 50 and 99 deaths. The 7,385 VA COVID-19 deaths represent 2.0% of the 375,300 deaths reported in the US by Johns Hopkins University. VA has reported 0.8% of the total number of COVID-19 cases.
The VA also reports the demographic breakdown of its COVID-19 cases. Among the active cases, 56.9% are White, 18.3% Black, 9.4% Hispanic, and 1.4% Native American, Alaska Native, or Pacific Islander.
Updated January 12, 2020
More than 181,000 veterans have contracted the COVID-19 virus and 7,385 have died, according to data released by the US Department of Veterans Affairs (VA) on January 12, 2020. The number of cases and deaths have increased sharply since November 2020. The VA also reports that it has administered at least 1 dose of the 2 approved vaccines to 33,875 veterans and 174,724 employees as of January 6.
Currently, the VA reports nearly 19,000 active cases of COVID-19, including 1,270 among VA employees. One hundred five VA employees have died from COVID-19.
Although facilities across the country are facing increased pressure as the number of cases rise, those in Southern California and Texas are reporting significant infection rates. Thirteen facilities have at least 300 active cases, including facilities in Loma Linda (418), Long Beach (381), Greater Los Angeles (361), and San Diego (274), all in California. In Texas, San Antonio (394), Dallas (370), Temple (338), and Houston (328) have all seen large numbers of active cases. Facilities in Columbia, South Carolina (420); Phoenix (407); Atlanta, Georgia (359); Cleveland, Ohio (352); and Orlando, (341) and Gainesville, Florida (340) also have reported significant numbers of cases.
While early on in the pandemic facilities in New York and New Jersey had reported the largest number of deaths, now nearly every facility has reported at least 1 death. Fourteen facilities have reported at least 100 deaths and 53 have reported between 50 and 99 deaths. The 7,385 VA COVID-19 deaths represent 2.0% of the 375,300 deaths reported in the US by Johns Hopkins University. VA has reported 0.8% of the total number of COVID-19 cases.
The VA also reports the demographic breakdown of its COVID-19 cases. Among the active cases, 56.9% are White, 18.3% Black, 9.4% Hispanic, and 1.4% Native American, Alaska Native, or Pacific Islander.
Updated January 12, 2020
More than 181,000 veterans have contracted the COVID-19 virus and 7,385 have died, according to data released by the US Department of Veterans Affairs (VA) on January 12, 2020. The number of cases and deaths have increased sharply since November 2020. The VA also reports that it has administered at least 1 dose of the 2 approved vaccines to 33,875 veterans and 174,724 employees as of January 6.
Currently, the VA reports nearly 19,000 active cases of COVID-19, including 1,270 among VA employees. One hundred five VA employees have died from COVID-19.
Although facilities across the country are facing increased pressure as the number of cases rise, those in Southern California and Texas are reporting significant infection rates. Thirteen facilities have at least 300 active cases, including facilities in Loma Linda (418), Long Beach (381), Greater Los Angeles (361), and San Diego (274), all in California. In Texas, San Antonio (394), Dallas (370), Temple (338), and Houston (328) have all seen large numbers of active cases. Facilities in Columbia, South Carolina (420); Phoenix (407); Atlanta, Georgia (359); Cleveland, Ohio (352); and Orlando, (341) and Gainesville, Florida (340) also have reported significant numbers of cases.
While early on in the pandemic facilities in New York and New Jersey had reported the largest number of deaths, now nearly every facility has reported at least 1 death. Fourteen facilities have reported at least 100 deaths and 53 have reported between 50 and 99 deaths. The 7,385 VA COVID-19 deaths represent 2.0% of the 375,300 deaths reported in the US by Johns Hopkins University. VA has reported 0.8% of the total number of COVID-19 cases.
The VA also reports the demographic breakdown of its COVID-19 cases. Among the active cases, 56.9% are White, 18.3% Black, 9.4% Hispanic, and 1.4% Native American, Alaska Native, or Pacific Islander.
Over half of COVID-19 transmission may occur via asymptomatic people
As COVID-19 cases surge and vaccinations lag, health authorities continue to seek additional ways to mitigate the spread of the novel coronavirus.
Now, a modeling study estimates that more than half of transmissions come from pre-, never-, and asymptomatic individuals, indicating that symptom-based screening will have little effect on spread.
The Centers for Disease Control and Prevention study, published online Jan. 7 in JAMA Network Open, concludes that for optimal control, protective measures such as masking and social distancing should be supplemented with strategic testing of potentially exposed but asymptomatic individuals .
“In the absence of effective and widespread use of therapeutics or vaccines that can shorten or eliminate infectivity, successful control of SARS-CoV-2 cannot rely solely on identifying and isolating symptomatic cases; even if implemented effectively, this strategy would be insufficient,” CDC biologist Michael J. Johansson, PhD, and colleagues warn. “Multiple measures that effectively address transmission risk in the absence of symptoms are imperative to control SARS-CoV-2.”
According to the authors, the effectiveness of some current transmission prevention efforts has been disputed and subject to mixed messaging. Therefore, they decided to model the proportion of COVID-19 infections that are likely the result of individuals who show no symptoms and may be unknowingly infecting others.
“Unfortunately, there continues to be some skepticism about the value of community-wide mitigation efforts for preventing transmission such as masking, distancing, and hand hygiene, particularly for people without symptoms,” corresponding author Jay C. Butler, MD, said in an interview. “So we wanted to have a base assumption about how much transmission occurs from asymptomatic people to underscore the importance of mitigation measures and of creating immunity through vaccine delivery.”
Such a yardstick is especially germane in the context of the new, more transmissible variant. “It really puts [things] in a bigger box and underscores, boldfaces, and italicizes the need to change people’s behaviors and the importance of mitigation,” Dr. Butler said. It also highlights the advisability of targeted strategic testing in congregate settings, schools, and universities, which is already underway.
The analysis
Based on data from several COVID-19 studies from last year, the CDC’s analytical model assumes at baseline that infectiousness peaks at the median point of symptom onset, and that 30% of infected individuals never develop symptoms but are nevertheless 75% as infectious as those who develop overt symptoms.
The investigators then model multiple scenarios of transmission based pre- and never-symptomatic individuals, assuming different incubation and infectious periods, and varying numbers of days from point of infection to symptom onset.
When combined, the models predicts that 59% of all transmission would come from asymptomatic transmission – 35% from presymptomatic individuals and 24% from never-symptomatic individuals.
The findings complement those of an earlier CDC analysis, according to the authors.
The overall proportion of transmission from presymptomatic and never-symptomatic individuals is key to identifying mitigation measures that may be able to control SARS-CoV-2, the authors stated.
For example, they explain, if the infection reproduction number (R) in a particular setting is 2.0, a reduction in transmission of at least 50% is needed in order to reduce R to below 1.0. “Given that in some settings R is likely much greater than 2 and more than half of transmissions may come from individuals who are asymptomatic at the time of transmission, effective control must mitigate transmission risk from people without symptoms,” they wrote.
The authors acknowledge that the study applies a simplistic model to a complex and evolving phenomenon, and that the exact proportions of presymptomatic and never-symptomatic transmission and the incubation periods are not known. They also note symptoms and transmissions appear to vary across different population groups, with older individuals more likely than younger persons to experience symptoms, according to previous studies.
“Assume that everyone is potentially infected”
Other experts agree that expanded testing of asymptomatic individuals is important. “Screening for fever and isolation of symptomatic individuals is a common-sense approach to help prevent spread, but these measures are by no means adequate since it’s been clearly documented that individuals who are either asymptomatic or presymptomatic can still spread the virus,” said Brett Williams, MD, an infectious disease specialist and assistant professor of medicine at Rush University in Chicago.
“As we saw with the White House Rose Garden superspreader outbreak, testing does not reliably exclude infection either because the tested individual has not yet become positive or the test is falsely negative,” Dr. Williams, who was not involved in the CDC study, said in an interview. He further noted that when prevalence is as high as it currently is in the United States, the rate of false negatives will be high because a large proportion of those screened will be unknowingly infected.
At his center, all visitors and staff are screened with a temperature probe on entry, and since the earliest days of the pandemic, universal masking has been required. “Nationally there have been many instances of hospital break room outbreaks because of staff eating lunch together, and these outbreaks also demonstrate the incompleteness of symptomatic isolation,” Dr. Williams said.
For his part, virologist Frank Esper, MD, a pediatric infectious disease specialist at the Cleveland Clinic, said that while it’s been understood for some time that many infected people will not exhibit symptoms, “the question that remains is just how infectious are they?”
Dr. Esper’s takeaway from the modeling study is not so much that we need more screening of possibly exposed but asymptomatic people, but rather testing symptomatic people and tracing their contacts is not enough.
“We need to continue to assume that everyone is potentially infected whether they know it or not. And even though we have ramped up our testing to a much greater capacity than in the first wave, we need to continue to wear masks and socially distance because just identifying people who are sick and isolating or quarantining them is not going to be enough to contain the pandemic.”
And although assumption-based modeling is helpful, it cannot tell us “how many asymptomatic people are actually infected,” said Dr. Esper, who was not involved in the CDC study.
Dr. Esper also pointed out that the study estimates are based on data from early Chinese studies, but the virus has since changed. The new, more transmissible strain in the United States and elsewhere may involve not only more infections but also a longer presymptomatic stage. “So the CDC study may actually undershoot asymptomatic infections,” he said.
He also agreed with the authors that when it comes to infection, not all humans are equal. “Older people tend to be more symptomatic and become symptomatic more quickly so the asymptomatic rate is not the same across board from young people age 20 to older people.”
The bottom line, said David. A. Hirschwerk, MD, an infectious disease specialist at Northwell Health in Manhasset, N.Y., is that these data support the maintenance of protective measures we’ve been taking over the past months. “They support the concept that asymptomatic people are a significant source of transmission and that we need to adhere to mask wearing and social distancing, particularly indoors,” Dr. Hirschwerk, who was not involved in the analysis, said in an interview. “More testing would be better but it has to be fast and it has to be efficient, and there are a lot of challenges to overcome.”
The study was done as part of the CDC’s coronavirus disease 2019 response and was supported solely by federal base and response funding. The authors and commentators have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
As COVID-19 cases surge and vaccinations lag, health authorities continue to seek additional ways to mitigate the spread of the novel coronavirus.
Now, a modeling study estimates that more than half of transmissions come from pre-, never-, and asymptomatic individuals, indicating that symptom-based screening will have little effect on spread.
The Centers for Disease Control and Prevention study, published online Jan. 7 in JAMA Network Open, concludes that for optimal control, protective measures such as masking and social distancing should be supplemented with strategic testing of potentially exposed but asymptomatic individuals .
“In the absence of effective and widespread use of therapeutics or vaccines that can shorten or eliminate infectivity, successful control of SARS-CoV-2 cannot rely solely on identifying and isolating symptomatic cases; even if implemented effectively, this strategy would be insufficient,” CDC biologist Michael J. Johansson, PhD, and colleagues warn. “Multiple measures that effectively address transmission risk in the absence of symptoms are imperative to control SARS-CoV-2.”
According to the authors, the effectiveness of some current transmission prevention efforts has been disputed and subject to mixed messaging. Therefore, they decided to model the proportion of COVID-19 infections that are likely the result of individuals who show no symptoms and may be unknowingly infecting others.
“Unfortunately, there continues to be some skepticism about the value of community-wide mitigation efforts for preventing transmission such as masking, distancing, and hand hygiene, particularly for people without symptoms,” corresponding author Jay C. Butler, MD, said in an interview. “So we wanted to have a base assumption about how much transmission occurs from asymptomatic people to underscore the importance of mitigation measures and of creating immunity through vaccine delivery.”
Such a yardstick is especially germane in the context of the new, more transmissible variant. “It really puts [things] in a bigger box and underscores, boldfaces, and italicizes the need to change people’s behaviors and the importance of mitigation,” Dr. Butler said. It also highlights the advisability of targeted strategic testing in congregate settings, schools, and universities, which is already underway.
The analysis
Based on data from several COVID-19 studies from last year, the CDC’s analytical model assumes at baseline that infectiousness peaks at the median point of symptom onset, and that 30% of infected individuals never develop symptoms but are nevertheless 75% as infectious as those who develop overt symptoms.
The investigators then model multiple scenarios of transmission based pre- and never-symptomatic individuals, assuming different incubation and infectious periods, and varying numbers of days from point of infection to symptom onset.
When combined, the models predicts that 59% of all transmission would come from asymptomatic transmission – 35% from presymptomatic individuals and 24% from never-symptomatic individuals.
The findings complement those of an earlier CDC analysis, according to the authors.
The overall proportion of transmission from presymptomatic and never-symptomatic individuals is key to identifying mitigation measures that may be able to control SARS-CoV-2, the authors stated.
For example, they explain, if the infection reproduction number (R) in a particular setting is 2.0, a reduction in transmission of at least 50% is needed in order to reduce R to below 1.0. “Given that in some settings R is likely much greater than 2 and more than half of transmissions may come from individuals who are asymptomatic at the time of transmission, effective control must mitigate transmission risk from people without symptoms,” they wrote.
The authors acknowledge that the study applies a simplistic model to a complex and evolving phenomenon, and that the exact proportions of presymptomatic and never-symptomatic transmission and the incubation periods are not known. They also note symptoms and transmissions appear to vary across different population groups, with older individuals more likely than younger persons to experience symptoms, according to previous studies.
“Assume that everyone is potentially infected”
Other experts agree that expanded testing of asymptomatic individuals is important. “Screening for fever and isolation of symptomatic individuals is a common-sense approach to help prevent spread, but these measures are by no means adequate since it’s been clearly documented that individuals who are either asymptomatic or presymptomatic can still spread the virus,” said Brett Williams, MD, an infectious disease specialist and assistant professor of medicine at Rush University in Chicago.
“As we saw with the White House Rose Garden superspreader outbreak, testing does not reliably exclude infection either because the tested individual has not yet become positive or the test is falsely negative,” Dr. Williams, who was not involved in the CDC study, said in an interview. He further noted that when prevalence is as high as it currently is in the United States, the rate of false negatives will be high because a large proportion of those screened will be unknowingly infected.
At his center, all visitors and staff are screened with a temperature probe on entry, and since the earliest days of the pandemic, universal masking has been required. “Nationally there have been many instances of hospital break room outbreaks because of staff eating lunch together, and these outbreaks also demonstrate the incompleteness of symptomatic isolation,” Dr. Williams said.
For his part, virologist Frank Esper, MD, a pediatric infectious disease specialist at the Cleveland Clinic, said that while it’s been understood for some time that many infected people will not exhibit symptoms, “the question that remains is just how infectious are they?”
Dr. Esper’s takeaway from the modeling study is not so much that we need more screening of possibly exposed but asymptomatic people, but rather testing symptomatic people and tracing their contacts is not enough.
“We need to continue to assume that everyone is potentially infected whether they know it or not. And even though we have ramped up our testing to a much greater capacity than in the first wave, we need to continue to wear masks and socially distance because just identifying people who are sick and isolating or quarantining them is not going to be enough to contain the pandemic.”
And although assumption-based modeling is helpful, it cannot tell us “how many asymptomatic people are actually infected,” said Dr. Esper, who was not involved in the CDC study.
Dr. Esper also pointed out that the study estimates are based on data from early Chinese studies, but the virus has since changed. The new, more transmissible strain in the United States and elsewhere may involve not only more infections but also a longer presymptomatic stage. “So the CDC study may actually undershoot asymptomatic infections,” he said.
He also agreed with the authors that when it comes to infection, not all humans are equal. “Older people tend to be more symptomatic and become symptomatic more quickly so the asymptomatic rate is not the same across board from young people age 20 to older people.”
The bottom line, said David. A. Hirschwerk, MD, an infectious disease specialist at Northwell Health in Manhasset, N.Y., is that these data support the maintenance of protective measures we’ve been taking over the past months. “They support the concept that asymptomatic people are a significant source of transmission and that we need to adhere to mask wearing and social distancing, particularly indoors,” Dr. Hirschwerk, who was not involved in the analysis, said in an interview. “More testing would be better but it has to be fast and it has to be efficient, and there are a lot of challenges to overcome.”
The study was done as part of the CDC’s coronavirus disease 2019 response and was supported solely by federal base and response funding. The authors and commentators have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
As COVID-19 cases surge and vaccinations lag, health authorities continue to seek additional ways to mitigate the spread of the novel coronavirus.
Now, a modeling study estimates that more than half of transmissions come from pre-, never-, and asymptomatic individuals, indicating that symptom-based screening will have little effect on spread.
The Centers for Disease Control and Prevention study, published online Jan. 7 in JAMA Network Open, concludes that for optimal control, protective measures such as masking and social distancing should be supplemented with strategic testing of potentially exposed but asymptomatic individuals .
“In the absence of effective and widespread use of therapeutics or vaccines that can shorten or eliminate infectivity, successful control of SARS-CoV-2 cannot rely solely on identifying and isolating symptomatic cases; even if implemented effectively, this strategy would be insufficient,” CDC biologist Michael J. Johansson, PhD, and colleagues warn. “Multiple measures that effectively address transmission risk in the absence of symptoms are imperative to control SARS-CoV-2.”
According to the authors, the effectiveness of some current transmission prevention efforts has been disputed and subject to mixed messaging. Therefore, they decided to model the proportion of COVID-19 infections that are likely the result of individuals who show no symptoms and may be unknowingly infecting others.
“Unfortunately, there continues to be some skepticism about the value of community-wide mitigation efforts for preventing transmission such as masking, distancing, and hand hygiene, particularly for people without symptoms,” corresponding author Jay C. Butler, MD, said in an interview. “So we wanted to have a base assumption about how much transmission occurs from asymptomatic people to underscore the importance of mitigation measures and of creating immunity through vaccine delivery.”
Such a yardstick is especially germane in the context of the new, more transmissible variant. “It really puts [things] in a bigger box and underscores, boldfaces, and italicizes the need to change people’s behaviors and the importance of mitigation,” Dr. Butler said. It also highlights the advisability of targeted strategic testing in congregate settings, schools, and universities, which is already underway.
The analysis
Based on data from several COVID-19 studies from last year, the CDC’s analytical model assumes at baseline that infectiousness peaks at the median point of symptom onset, and that 30% of infected individuals never develop symptoms but are nevertheless 75% as infectious as those who develop overt symptoms.
The investigators then model multiple scenarios of transmission based pre- and never-symptomatic individuals, assuming different incubation and infectious periods, and varying numbers of days from point of infection to symptom onset.
When combined, the models predicts that 59% of all transmission would come from asymptomatic transmission – 35% from presymptomatic individuals and 24% from never-symptomatic individuals.
The findings complement those of an earlier CDC analysis, according to the authors.
The overall proportion of transmission from presymptomatic and never-symptomatic individuals is key to identifying mitigation measures that may be able to control SARS-CoV-2, the authors stated.
For example, they explain, if the infection reproduction number (R) in a particular setting is 2.0, a reduction in transmission of at least 50% is needed in order to reduce R to below 1.0. “Given that in some settings R is likely much greater than 2 and more than half of transmissions may come from individuals who are asymptomatic at the time of transmission, effective control must mitigate transmission risk from people without symptoms,” they wrote.
The authors acknowledge that the study applies a simplistic model to a complex and evolving phenomenon, and that the exact proportions of presymptomatic and never-symptomatic transmission and the incubation periods are not known. They also note symptoms and transmissions appear to vary across different population groups, with older individuals more likely than younger persons to experience symptoms, according to previous studies.
“Assume that everyone is potentially infected”
Other experts agree that expanded testing of asymptomatic individuals is important. “Screening for fever and isolation of symptomatic individuals is a common-sense approach to help prevent spread, but these measures are by no means adequate since it’s been clearly documented that individuals who are either asymptomatic or presymptomatic can still spread the virus,” said Brett Williams, MD, an infectious disease specialist and assistant professor of medicine at Rush University in Chicago.
“As we saw with the White House Rose Garden superspreader outbreak, testing does not reliably exclude infection either because the tested individual has not yet become positive or the test is falsely negative,” Dr. Williams, who was not involved in the CDC study, said in an interview. He further noted that when prevalence is as high as it currently is in the United States, the rate of false negatives will be high because a large proportion of those screened will be unknowingly infected.
At his center, all visitors and staff are screened with a temperature probe on entry, and since the earliest days of the pandemic, universal masking has been required. “Nationally there have been many instances of hospital break room outbreaks because of staff eating lunch together, and these outbreaks also demonstrate the incompleteness of symptomatic isolation,” Dr. Williams said.
For his part, virologist Frank Esper, MD, a pediatric infectious disease specialist at the Cleveland Clinic, said that while it’s been understood for some time that many infected people will not exhibit symptoms, “the question that remains is just how infectious are they?”
Dr. Esper’s takeaway from the modeling study is not so much that we need more screening of possibly exposed but asymptomatic people, but rather testing symptomatic people and tracing their contacts is not enough.
“We need to continue to assume that everyone is potentially infected whether they know it or not. And even though we have ramped up our testing to a much greater capacity than in the first wave, we need to continue to wear masks and socially distance because just identifying people who are sick and isolating or quarantining them is not going to be enough to contain the pandemic.”
And although assumption-based modeling is helpful, it cannot tell us “how many asymptomatic people are actually infected,” said Dr. Esper, who was not involved in the CDC study.
Dr. Esper also pointed out that the study estimates are based on data from early Chinese studies, but the virus has since changed. The new, more transmissible strain in the United States and elsewhere may involve not only more infections but also a longer presymptomatic stage. “So the CDC study may actually undershoot asymptomatic infections,” he said.
He also agreed with the authors that when it comes to infection, not all humans are equal. “Older people tend to be more symptomatic and become symptomatic more quickly so the asymptomatic rate is not the same across board from young people age 20 to older people.”
The bottom line, said David. A. Hirschwerk, MD, an infectious disease specialist at Northwell Health in Manhasset, N.Y., is that these data support the maintenance of protective measures we’ve been taking over the past months. “They support the concept that asymptomatic people are a significant source of transmission and that we need to adhere to mask wearing and social distancing, particularly indoors,” Dr. Hirschwerk, who was not involved in the analysis, said in an interview. “More testing would be better but it has to be fast and it has to be efficient, and there are a lot of challenges to overcome.”
The study was done as part of the CDC’s coronavirus disease 2019 response and was supported solely by federal base and response funding. The authors and commentators have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The importance of community pediatric hospital medicine
According to data from the American Academy of Pediatrics, over 2,000 physicians – or approximately 70% of all physicians practicing pediatric hospital medicine – do so in a community hospital. Like all areas of hospital medicine, community pediatric hospital medicine (CPHM) strives to fulfill one of our field’s central tenets – providing high-quality, evidence-based care to our patients.
A phrase often used among CPHM practitioners is that, “if you’ve seen one CPHM program, you’ve seen one CPHM program.” Every CPHM program is different. While this phrase may seem rather simplistic, it quite accurately portrays a unique aspect of our place in the hospital medicine field. CPHM programs usually require their practitioners to perform a broader range of roles and responsibilities than our colleagues who practice in university or children’s hospitals. Typically, these roles are aligned with the unique needs of each hospital within which we practice and the communities we serve. Factors such as the distance to a tertiary care referral center, access to subspecialists, availability and expertise of ancillary services for children, and the particular needs of each community further shape the role that CPHM practitioners may be asked to play.
In 2014, the AAP section on hospital medicine’s subcommittee on community hospitalists surveyed all CPHM programs to understand the unique roles that practitioners play within their institutions. Under the leadership of Clota Snow, MD, and Jacques Corriveau, MD, the aim was to contact every hospital in the country using the American Hospital Directory to see if they had a PHM program and to identify what roles the program was responsible for within their hospital.
Of the 535 programs identified, the primary responsibilities included inpatient care (85%), ED consultations (76%) and newborn nursery care (73%). Other common roles not typically associated with a university-based hospitalist’s responsibilities included delivery room attendance/neonatal resuscitations (44%), neonatal ICU management (47%) and subspecialty or surgical comanagement (52%). In some communities, even pediatric ICU management, sedation, and patient transport are part of our role. Because of the large breadth of roles that a CPHM practitioner may cover, we have often been referred to as “pediatric hospital-based generalists.”
Ideally, the presence of a pediatric hospitalist in a community hospital allows children to obtain high-quality, evidence-based care within their home communities. Most hospitalized children do not require direct access to subspecialists or all the pediatric-specific resources only available within a university or children’s hospital. Thus, if these resources are not required for the child’s care, CPHM practitioners can provide the care that a child needs in a setting that is less disruptive to the family and typically more cost effective.
CPHM physicians are often drawn to a career in a community hospital because it allows them to use their entire skill set to care for children with a wide variety of conditions. As they are often the only physicians in an adult hospital with a full understanding of the unique aspects of care that children require, it is important that they be comfortable in their role of managing the majority of pediatric care independently. Yet they also need to understand the limitations of their own ability, as well as their institution’s level of expertise in pediatric-specific care. They must be confident and vocal advocates for pediatric-specific needs throughout their institution and its numerous committees, and form close working relationships with colleagues and administrators in the different fields with whom we share care of our patients (e.g., ED, obstetrics, radiology, trauma, and other medical and surgical subspecialties).
CPHM physicians are particularly well suited to partner with local outpatient providers as well as tertiary care physicians to provide coordinated transitions between the inpatient and outpatient management of a child’s illness. In addition, a CPHM physician can often bring a unique and valuable perspective of the particular ethnic, cultural, and socioeconomic diversity of their community, as well as its available resources, to facilitate a greater level of engagement with the child’s needs and ultimate success of their care.
The 2014 survey of CPHM programs identified several major challenges to recruitment and career satisfaction as a CPHM physician. These include a lack of access to subspecialists, a lack of pediatric-specific ancillary services and the perception that our importance as community hospital providers was not valued as much in the PHM community as PHM physicians working in a university/children’s hospital setting. With the recent recognition of PHM as an official subspecialty by the American Board of Pediatrics, the concern has intensified within our field that a two-tiered system will develop with some PHM physicians being board certified and others not.
While the development of board subspecialization was not meant to limit the pool of providers available to staff community hospital sites, there is nowhere near the number of fellowship trained physicians to provide an adequate workforce to staff CPHM programs. This means that many CPHM physicians will not be board certified in pediatric hospital medicine but does not mean that CPHM programs will be unable to provide high-quality local care that benefits children and their families, including safe care for children who require the skills that an immediately available CPHM physician can provide.
Many pediatric residency programs do not currently provide their trainees with exposure to community hospital medicine. Further, with increased sub-specialization throughout pediatrics, fewer residents are developing the necessary skill set to perform roles integral to a caring for children in community hospitals such as stabilization of a critically ill child prior to transport and complex neonatal resuscitation.
A career in CPHM provides physicians with the opportunity to work together with a close-knit group to provide exceptional care to children and to advocate for the medical needs of children in their hospital and their community. The AAP’s subcommittee has made it a priority to engage physicians during all parts of their pediatric training about why a career in CPHM is exciting, fulfilling and a great life, as well as continuing to educate training programs at every level – as well as the larger PHM community – about why CPHM is a valuable and important part of pediatric medicine.
Dr. Welsh is a clinical associate professor of pediatrics at the Stanford (Calif.) University in the division of pediatric hospital medicine. He has practiced community pediatric hospital medicine for over 27 years in Washington state and the San Francisco Bay Area. He is the chair of the working group of the Future of Community Pediatric Hospital Medicine for the AAP section on hospital medicine’s subcommittee on community hospitalists.
According to data from the American Academy of Pediatrics, over 2,000 physicians – or approximately 70% of all physicians practicing pediatric hospital medicine – do so in a community hospital. Like all areas of hospital medicine, community pediatric hospital medicine (CPHM) strives to fulfill one of our field’s central tenets – providing high-quality, evidence-based care to our patients.
A phrase often used among CPHM practitioners is that, “if you’ve seen one CPHM program, you’ve seen one CPHM program.” Every CPHM program is different. While this phrase may seem rather simplistic, it quite accurately portrays a unique aspect of our place in the hospital medicine field. CPHM programs usually require their practitioners to perform a broader range of roles and responsibilities than our colleagues who practice in university or children’s hospitals. Typically, these roles are aligned with the unique needs of each hospital within which we practice and the communities we serve. Factors such as the distance to a tertiary care referral center, access to subspecialists, availability and expertise of ancillary services for children, and the particular needs of each community further shape the role that CPHM practitioners may be asked to play.
In 2014, the AAP section on hospital medicine’s subcommittee on community hospitalists surveyed all CPHM programs to understand the unique roles that practitioners play within their institutions. Under the leadership of Clota Snow, MD, and Jacques Corriveau, MD, the aim was to contact every hospital in the country using the American Hospital Directory to see if they had a PHM program and to identify what roles the program was responsible for within their hospital.
Of the 535 programs identified, the primary responsibilities included inpatient care (85%), ED consultations (76%) and newborn nursery care (73%). Other common roles not typically associated with a university-based hospitalist’s responsibilities included delivery room attendance/neonatal resuscitations (44%), neonatal ICU management (47%) and subspecialty or surgical comanagement (52%). In some communities, even pediatric ICU management, sedation, and patient transport are part of our role. Because of the large breadth of roles that a CPHM practitioner may cover, we have often been referred to as “pediatric hospital-based generalists.”
Ideally, the presence of a pediatric hospitalist in a community hospital allows children to obtain high-quality, evidence-based care within their home communities. Most hospitalized children do not require direct access to subspecialists or all the pediatric-specific resources only available within a university or children’s hospital. Thus, if these resources are not required for the child’s care, CPHM practitioners can provide the care that a child needs in a setting that is less disruptive to the family and typically more cost effective.
CPHM physicians are often drawn to a career in a community hospital because it allows them to use their entire skill set to care for children with a wide variety of conditions. As they are often the only physicians in an adult hospital with a full understanding of the unique aspects of care that children require, it is important that they be comfortable in their role of managing the majority of pediatric care independently. Yet they also need to understand the limitations of their own ability, as well as their institution’s level of expertise in pediatric-specific care. They must be confident and vocal advocates for pediatric-specific needs throughout their institution and its numerous committees, and form close working relationships with colleagues and administrators in the different fields with whom we share care of our patients (e.g., ED, obstetrics, radiology, trauma, and other medical and surgical subspecialties).
CPHM physicians are particularly well suited to partner with local outpatient providers as well as tertiary care physicians to provide coordinated transitions between the inpatient and outpatient management of a child’s illness. In addition, a CPHM physician can often bring a unique and valuable perspective of the particular ethnic, cultural, and socioeconomic diversity of their community, as well as its available resources, to facilitate a greater level of engagement with the child’s needs and ultimate success of their care.
The 2014 survey of CPHM programs identified several major challenges to recruitment and career satisfaction as a CPHM physician. These include a lack of access to subspecialists, a lack of pediatric-specific ancillary services and the perception that our importance as community hospital providers was not valued as much in the PHM community as PHM physicians working in a university/children’s hospital setting. With the recent recognition of PHM as an official subspecialty by the American Board of Pediatrics, the concern has intensified within our field that a two-tiered system will develop with some PHM physicians being board certified and others not.
While the development of board subspecialization was not meant to limit the pool of providers available to staff community hospital sites, there is nowhere near the number of fellowship trained physicians to provide an adequate workforce to staff CPHM programs. This means that many CPHM physicians will not be board certified in pediatric hospital medicine but does not mean that CPHM programs will be unable to provide high-quality local care that benefits children and their families, including safe care for children who require the skills that an immediately available CPHM physician can provide.
Many pediatric residency programs do not currently provide their trainees with exposure to community hospital medicine. Further, with increased sub-specialization throughout pediatrics, fewer residents are developing the necessary skill set to perform roles integral to a caring for children in community hospitals such as stabilization of a critically ill child prior to transport and complex neonatal resuscitation.
A career in CPHM provides physicians with the opportunity to work together with a close-knit group to provide exceptional care to children and to advocate for the medical needs of children in their hospital and their community. The AAP’s subcommittee has made it a priority to engage physicians during all parts of their pediatric training about why a career in CPHM is exciting, fulfilling and a great life, as well as continuing to educate training programs at every level – as well as the larger PHM community – about why CPHM is a valuable and important part of pediatric medicine.
Dr. Welsh is a clinical associate professor of pediatrics at the Stanford (Calif.) University in the division of pediatric hospital medicine. He has practiced community pediatric hospital medicine for over 27 years in Washington state and the San Francisco Bay Area. He is the chair of the working group of the Future of Community Pediatric Hospital Medicine for the AAP section on hospital medicine’s subcommittee on community hospitalists.
According to data from the American Academy of Pediatrics, over 2,000 physicians – or approximately 70% of all physicians practicing pediatric hospital medicine – do so in a community hospital. Like all areas of hospital medicine, community pediatric hospital medicine (CPHM) strives to fulfill one of our field’s central tenets – providing high-quality, evidence-based care to our patients.
A phrase often used among CPHM practitioners is that, “if you’ve seen one CPHM program, you’ve seen one CPHM program.” Every CPHM program is different. While this phrase may seem rather simplistic, it quite accurately portrays a unique aspect of our place in the hospital medicine field. CPHM programs usually require their practitioners to perform a broader range of roles and responsibilities than our colleagues who practice in university or children’s hospitals. Typically, these roles are aligned with the unique needs of each hospital within which we practice and the communities we serve. Factors such as the distance to a tertiary care referral center, access to subspecialists, availability and expertise of ancillary services for children, and the particular needs of each community further shape the role that CPHM practitioners may be asked to play.
In 2014, the AAP section on hospital medicine’s subcommittee on community hospitalists surveyed all CPHM programs to understand the unique roles that practitioners play within their institutions. Under the leadership of Clota Snow, MD, and Jacques Corriveau, MD, the aim was to contact every hospital in the country using the American Hospital Directory to see if they had a PHM program and to identify what roles the program was responsible for within their hospital.
Of the 535 programs identified, the primary responsibilities included inpatient care (85%), ED consultations (76%) and newborn nursery care (73%). Other common roles not typically associated with a university-based hospitalist’s responsibilities included delivery room attendance/neonatal resuscitations (44%), neonatal ICU management (47%) and subspecialty or surgical comanagement (52%). In some communities, even pediatric ICU management, sedation, and patient transport are part of our role. Because of the large breadth of roles that a CPHM practitioner may cover, we have often been referred to as “pediatric hospital-based generalists.”
Ideally, the presence of a pediatric hospitalist in a community hospital allows children to obtain high-quality, evidence-based care within their home communities. Most hospitalized children do not require direct access to subspecialists or all the pediatric-specific resources only available within a university or children’s hospital. Thus, if these resources are not required for the child’s care, CPHM practitioners can provide the care that a child needs in a setting that is less disruptive to the family and typically more cost effective.
CPHM physicians are often drawn to a career in a community hospital because it allows them to use their entire skill set to care for children with a wide variety of conditions. As they are often the only physicians in an adult hospital with a full understanding of the unique aspects of care that children require, it is important that they be comfortable in their role of managing the majority of pediatric care independently. Yet they also need to understand the limitations of their own ability, as well as their institution’s level of expertise in pediatric-specific care. They must be confident and vocal advocates for pediatric-specific needs throughout their institution and its numerous committees, and form close working relationships with colleagues and administrators in the different fields with whom we share care of our patients (e.g., ED, obstetrics, radiology, trauma, and other medical and surgical subspecialties).
CPHM physicians are particularly well suited to partner with local outpatient providers as well as tertiary care physicians to provide coordinated transitions between the inpatient and outpatient management of a child’s illness. In addition, a CPHM physician can often bring a unique and valuable perspective of the particular ethnic, cultural, and socioeconomic diversity of their community, as well as its available resources, to facilitate a greater level of engagement with the child’s needs and ultimate success of their care.
The 2014 survey of CPHM programs identified several major challenges to recruitment and career satisfaction as a CPHM physician. These include a lack of access to subspecialists, a lack of pediatric-specific ancillary services and the perception that our importance as community hospital providers was not valued as much in the PHM community as PHM physicians working in a university/children’s hospital setting. With the recent recognition of PHM as an official subspecialty by the American Board of Pediatrics, the concern has intensified within our field that a two-tiered system will develop with some PHM physicians being board certified and others not.
While the development of board subspecialization was not meant to limit the pool of providers available to staff community hospital sites, there is nowhere near the number of fellowship trained physicians to provide an adequate workforce to staff CPHM programs. This means that many CPHM physicians will not be board certified in pediatric hospital medicine but does not mean that CPHM programs will be unable to provide high-quality local care that benefits children and their families, including safe care for children who require the skills that an immediately available CPHM physician can provide.
Many pediatric residency programs do not currently provide their trainees with exposure to community hospital medicine. Further, with increased sub-specialization throughout pediatrics, fewer residents are developing the necessary skill set to perform roles integral to a caring for children in community hospitals such as stabilization of a critically ill child prior to transport and complex neonatal resuscitation.
A career in CPHM provides physicians with the opportunity to work together with a close-knit group to provide exceptional care to children and to advocate for the medical needs of children in their hospital and their community. The AAP’s subcommittee has made it a priority to engage physicians during all parts of their pediatric training about why a career in CPHM is exciting, fulfilling and a great life, as well as continuing to educate training programs at every level – as well as the larger PHM community – about why CPHM is a valuable and important part of pediatric medicine.
Dr. Welsh is a clinical associate professor of pediatrics at the Stanford (Calif.) University in the division of pediatric hospital medicine. He has practiced community pediatric hospital medicine for over 27 years in Washington state and the San Francisco Bay Area. He is the chair of the working group of the Future of Community Pediatric Hospital Medicine for the AAP section on hospital medicine’s subcommittee on community hospitalists.
Anaphylaxis cases after COVID-19 vaccine rising but still rare: CDC
Health care providers should be ready to treat rare cases of anaphylaxis following administration of COVID-19 vaccines, federal medical officials have urged. The officials also stressed the importance of continuing vaccinations, despite reports of the rare side effect.
There have been 29 cases of anaphylaxis to date following administration of a COVID-19 vaccine, officials from the Centers for Disease Control and Prevention said in a call with reporters on Jan. 6.
The severe allergic reaction, which appears to be rare, can happen with either the Pfizer-BioNTech vaccine or the rival Moderna product. The Food and Drug Administration granted emergency use authorizations for these two vaccines in December.
Even with the cases seen to date, the COVID-19 vaccines remain a “good value proposition,” Nancy Messonnier, MD, director of the CDC’s National Center for Immunization, said in the call.
There have been about 11.1 cases of anaphylaxis per million doses with the Pfizer-BioNTech COVID-19 vaccine, which is higher than the estimated 1.3 cases per million doses with influenza vaccines, she said. But the low risk of anaphylaxis must be balanced against the threat of COVID-19, which currently claims about 2,000 lives a day in the United States, she said. In addition, many people are reporting long-term complications with COVID-19 even if they recover.
Kept in context, the data on anaphylaxis should not scare people away from getting a COVID-19 vaccine, she added.
“Their risk from COVID and poor outcomes is still more than the risk of a severe outcome from the vaccine,” Dr. Messonnier said. “And fortunately, we know how to treat anaphylaxis.”
Dr. Messonnier urged health care workers administering COVID-19 vaccines to be prepared.
“Anybody administering vaccines needs not just to have the EpiPen available, but frankly, to know how to use it,” Dr. Messonnier said.
MMWR details
The CDC on Jan. 6 also provided an update on anaphylaxis in Morbidity and Mortality Weekly Report (MMWR).
The information included in the report was based on cases reported with the Pfizer-BioNTech vaccine – the first to get emergency use authorization from the FDA. On the call with reporters, CDC officials confirmed there have been additional reports since then and anaphylaxis has been reported with both the Pfizer-BioNTech and Moderna vaccines. CDC officials said they could not give a breakdown of how many cases were linked to each of these products at this time.
Between Dec. 14 and 23, 2020, monitoring by the Vaccine Adverse Event Reporting System detected 21 cases of anaphylaxis after administration of a reported 1,893,360 first doses of the Pfizer-BioNTech COVID-19 vaccine. Most reactions – 71% – occurred within 15 minutes of vaccination.
A version of this article first appeared on Medscape.com.
Health care providers should be ready to treat rare cases of anaphylaxis following administration of COVID-19 vaccines, federal medical officials have urged. The officials also stressed the importance of continuing vaccinations, despite reports of the rare side effect.
There have been 29 cases of anaphylaxis to date following administration of a COVID-19 vaccine, officials from the Centers for Disease Control and Prevention said in a call with reporters on Jan. 6.
The severe allergic reaction, which appears to be rare, can happen with either the Pfizer-BioNTech vaccine or the rival Moderna product. The Food and Drug Administration granted emergency use authorizations for these two vaccines in December.
Even with the cases seen to date, the COVID-19 vaccines remain a “good value proposition,” Nancy Messonnier, MD, director of the CDC’s National Center for Immunization, said in the call.
There have been about 11.1 cases of anaphylaxis per million doses with the Pfizer-BioNTech COVID-19 vaccine, which is higher than the estimated 1.3 cases per million doses with influenza vaccines, she said. But the low risk of anaphylaxis must be balanced against the threat of COVID-19, which currently claims about 2,000 lives a day in the United States, she said. In addition, many people are reporting long-term complications with COVID-19 even if they recover.
Kept in context, the data on anaphylaxis should not scare people away from getting a COVID-19 vaccine, she added.
“Their risk from COVID and poor outcomes is still more than the risk of a severe outcome from the vaccine,” Dr. Messonnier said. “And fortunately, we know how to treat anaphylaxis.”
Dr. Messonnier urged health care workers administering COVID-19 vaccines to be prepared.
“Anybody administering vaccines needs not just to have the EpiPen available, but frankly, to know how to use it,” Dr. Messonnier said.
MMWR details
The CDC on Jan. 6 also provided an update on anaphylaxis in Morbidity and Mortality Weekly Report (MMWR).
The information included in the report was based on cases reported with the Pfizer-BioNTech vaccine – the first to get emergency use authorization from the FDA. On the call with reporters, CDC officials confirmed there have been additional reports since then and anaphylaxis has been reported with both the Pfizer-BioNTech and Moderna vaccines. CDC officials said they could not give a breakdown of how many cases were linked to each of these products at this time.
Between Dec. 14 and 23, 2020, monitoring by the Vaccine Adverse Event Reporting System detected 21 cases of anaphylaxis after administration of a reported 1,893,360 first doses of the Pfizer-BioNTech COVID-19 vaccine. Most reactions – 71% – occurred within 15 minutes of vaccination.
A version of this article first appeared on Medscape.com.
Health care providers should be ready to treat rare cases of anaphylaxis following administration of COVID-19 vaccines, federal medical officials have urged. The officials also stressed the importance of continuing vaccinations, despite reports of the rare side effect.
There have been 29 cases of anaphylaxis to date following administration of a COVID-19 vaccine, officials from the Centers for Disease Control and Prevention said in a call with reporters on Jan. 6.
The severe allergic reaction, which appears to be rare, can happen with either the Pfizer-BioNTech vaccine or the rival Moderna product. The Food and Drug Administration granted emergency use authorizations for these two vaccines in December.
Even with the cases seen to date, the COVID-19 vaccines remain a “good value proposition,” Nancy Messonnier, MD, director of the CDC’s National Center for Immunization, said in the call.
There have been about 11.1 cases of anaphylaxis per million doses with the Pfizer-BioNTech COVID-19 vaccine, which is higher than the estimated 1.3 cases per million doses with influenza vaccines, she said. But the low risk of anaphylaxis must be balanced against the threat of COVID-19, which currently claims about 2,000 lives a day in the United States, she said. In addition, many people are reporting long-term complications with COVID-19 even if they recover.
Kept in context, the data on anaphylaxis should not scare people away from getting a COVID-19 vaccine, she added.
“Their risk from COVID and poor outcomes is still more than the risk of a severe outcome from the vaccine,” Dr. Messonnier said. “And fortunately, we know how to treat anaphylaxis.”
Dr. Messonnier urged health care workers administering COVID-19 vaccines to be prepared.
“Anybody administering vaccines needs not just to have the EpiPen available, but frankly, to know how to use it,” Dr. Messonnier said.
MMWR details
The CDC on Jan. 6 also provided an update on anaphylaxis in Morbidity and Mortality Weekly Report (MMWR).
The information included in the report was based on cases reported with the Pfizer-BioNTech vaccine – the first to get emergency use authorization from the FDA. On the call with reporters, CDC officials confirmed there have been additional reports since then and anaphylaxis has been reported with both the Pfizer-BioNTech and Moderna vaccines. CDC officials said they could not give a breakdown of how many cases were linked to each of these products at this time.
Between Dec. 14 and 23, 2020, monitoring by the Vaccine Adverse Event Reporting System detected 21 cases of anaphylaxis after administration of a reported 1,893,360 first doses of the Pfizer-BioNTech COVID-19 vaccine. Most reactions – 71% – occurred within 15 minutes of vaccination.
A version of this article first appeared on Medscape.com.
Children’s hospitals grapple with wave of mental illness
Krissy Williams, 15, had attempted suicide before, but never with pills.
The teen was diagnosed with schizophrenia when she was 9. People with this chronic mental health condition perceive reality differently and often experience hallucinations and delusions. She learned to manage these symptoms with a variety of services offered at home and at school.
But the pandemic upended those lifelines. She lost much of the support offered at school. She also lost regular contact with her peers. Her mother lost access to respite care – which allowed her to take a break.
On a Thursday in October, the isolation and sadness came to a head. As Krissy’s mother, Patricia Williams, called a mental crisis hotline for help, she said, Krissy stood on the deck of their Maryland home with a bottle of pain medication in one hand and water in the other.
Before Patricia could react, Krissy placed the pills in her mouth and swallowed.
Efforts to contain the spread of the novel coronavirus in the United States have led to drastic changes in the way children and teens learn, play and socialize. Tens of millions of students are attending school through some form of distance learning. Many extracurricular activities have been canceled. Playgrounds, zoos, and other recreational spaces have closed. Kids like Krissy have struggled to cope and the toll is becoming evident.
Government figures show the proportion of children who arrived in EDs with mental health issues increased 24% from mid-March through mid-October, compared with the same period in 2019. Among preteens and adolescents, it rose by 31%. Anecdotally, some hospitals said they are seeing more cases of severe depression and suicidal thoughts among children, particularly attempts to overdose.
The increased demand for intensive mental health care that has accompanied the pandemic has worsened issues that have long plagued the system. In some hospitals, the number of children unable to immediately get a bed in the psychiatric unit rose. Others reduced the number of beds or closed psychiatric units altogether to reduce the spread of COVID-19.
“It’s only a matter of time before a tsunami sort of reaches the shore of our service system, and it’s going to be overwhelmed with the mental health needs of kids,” said Jason Williams, PsyD, a psychologist and director of operations of the Pediatric Mental Health Institute at Children’s Hospital Colorado, Aurora.
“I think we’re just starting to see the tip of the iceberg, to be honest with you.”
Before COVID, more than 8 million kids between ages 3 and 17 were diagnosed with a mental or behavioral health condition, according to the most recent National Survey of Children’s Health. A separate survey from the Centers for Disease Control and Prevention found one in three high school students in 2019 reported feeling persistently sad and hopeless – a 40% increase from 2009.
The coronavirus pandemic appears to be adding to these difficulties. A review of 80 studies found forced isolation and loneliness among children correlated with an increased risk of depression.
“We’re all social beings, but they’re [teenagers] at the point in their development where their peers are their reality,” said Terrie Andrews, PhD, a psychologist and administrator of behavioral health at Wolfson Children’s Hospital in Jacksonville, Fla. “Their peers are their grounding mechanism.”
Children’s hospitals in Colorado, Missouri, and New York all reported an uptick in the number of patients who thought about or attempted suicide. Clinicians also mentioned spikes in children with severe depression and those with autism who are acting out.
The number of overdose attempts among children has caught the attention of clinicians at two facilities. Dr. Andrews said the facility gives out lockboxes for weapons and medication to the public – including parents who come in after children attempted to take their life using medication.
Children’s National Hospital in Washington, D.C., also has experienced an uptick, said Colby Tyson, MD, associate director of inpatient psychiatry. She’s seen children’s mental health deteriorate because of a likely increase in family conflict – often a consequence of the chaos caused by the pandemic. Without school, connections with peers or employment, families don’t have the opportunity to spend time away from one another and regroup, which can add stress to an already tense situation.
“That break is gone,” she said.
The higher demand for child mental health services caused by the pandemic has made finding a bed at an inpatient unit more difficult.
Now, some hospitals report running at full capacity and having more children “boarding,” or sleeping in EDs before being admitted to the psychiatric unit. Among them is the Pediatric Mental Health Institute at Children’s Hospital Colorado. Williams said the inpatient unit has been full since March. Some children now wait nearly 2 days for a bed, up from the 8-10 hours common before the pandemic.
Cincinnati Children’s Hospital Medical Center in Ohio is also running at full capacity, said clinicians, and had several days in which the unit was above capacity and placed kids instead in the emergency department waiting to be admitted. In Florida, Dr. Andrews said, up to 25 children have been held on surgical floors at Wolfson Children’s while waiting for a spot to open in the inpatient psychiatric unit. Their wait could last as long as 5 days, she said.
Multiple hospitals said the usual summer slump in child psychiatric admissions was missing last year. “We never saw that during the pandemic,” said Andrews. “We stayed completely busy the entire time.”
Some facilities have decided to reduce the number of beds available to maintain physical distancing, further constricting supply. Children’s National in D.C. cut five beds from its unit to maintain single occupancy in every room, said Adelaide Robb, MD, division chief of psychiatry and behavioral sciences.
The measures taken to curb the spread of COVID have also affected the way hospitalized children receive mental health services. In addition to providers wearing protective equipment, some hospitals like Cincinnati Children’s rearranged furniture and placed cues on the floor as reminders to stay 6 feet apart. The University of Pittsburgh Medical Center’s Western Psychiatric Hospital and other facilities encourage children to keep their masks on by offering rewards like extra computer time. Patients at Children’s National now eat in their rooms, a change from when they ate together.
Despite the need for distance, social interaction still represents an important part of mental health care for children, clinicians said. Facilities have come up with various ways to do so safely, including creating smaller pods for group therapy. Children at Cincinnati Children’s Hospital can play with toys, but only with ones that can be wiped clean afterward. No cards or board games, said Suzanne Sampang, MD, clinical medical director for child and adolescent psychiatry at the hospital.
“I think what’s different about psychiatric treatment is that, really, interaction is the treatment,” she said, “just as much as a medication.”
The added infection-control precautions pose challenges to forging therapeutic connections. Masks can complicate the ability to read a person’s face. Online meetings make it difficult to build trust between a patient and a therapist.
“There’s something about the real relationship in person that the best technology can’t give to you,” said Dr. Robb.
For now, Krissy Williams is relying on virtual platforms to receive some of her mental health services. Despite being hospitalized and suffering brain damage due to the overdose, she is now at home and in good spirits. She enjoys geometry, dancing on TikTok, and trying to beat her mother at Super Mario Bros. on the Wii. But being away from her friends, she said, has been a hard adjustment.
“When you’re used to something,” she said, “it’s not easy to change everything.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of Kaiser Family Foundation, which is not affiliated with Kaiser Permanente.
Krissy Williams, 15, had attempted suicide before, but never with pills.
The teen was diagnosed with schizophrenia when she was 9. People with this chronic mental health condition perceive reality differently and often experience hallucinations and delusions. She learned to manage these symptoms with a variety of services offered at home and at school.
But the pandemic upended those lifelines. She lost much of the support offered at school. She also lost regular contact with her peers. Her mother lost access to respite care – which allowed her to take a break.
On a Thursday in October, the isolation and sadness came to a head. As Krissy’s mother, Patricia Williams, called a mental crisis hotline for help, she said, Krissy stood on the deck of their Maryland home with a bottle of pain medication in one hand and water in the other.
Before Patricia could react, Krissy placed the pills in her mouth and swallowed.
Efforts to contain the spread of the novel coronavirus in the United States have led to drastic changes in the way children and teens learn, play and socialize. Tens of millions of students are attending school through some form of distance learning. Many extracurricular activities have been canceled. Playgrounds, zoos, and other recreational spaces have closed. Kids like Krissy have struggled to cope and the toll is becoming evident.
Government figures show the proportion of children who arrived in EDs with mental health issues increased 24% from mid-March through mid-October, compared with the same period in 2019. Among preteens and adolescents, it rose by 31%. Anecdotally, some hospitals said they are seeing more cases of severe depression and suicidal thoughts among children, particularly attempts to overdose.
The increased demand for intensive mental health care that has accompanied the pandemic has worsened issues that have long plagued the system. In some hospitals, the number of children unable to immediately get a bed in the psychiatric unit rose. Others reduced the number of beds or closed psychiatric units altogether to reduce the spread of COVID-19.
“It’s only a matter of time before a tsunami sort of reaches the shore of our service system, and it’s going to be overwhelmed with the mental health needs of kids,” said Jason Williams, PsyD, a psychologist and director of operations of the Pediatric Mental Health Institute at Children’s Hospital Colorado, Aurora.
“I think we’re just starting to see the tip of the iceberg, to be honest with you.”
Before COVID, more than 8 million kids between ages 3 and 17 were diagnosed with a mental or behavioral health condition, according to the most recent National Survey of Children’s Health. A separate survey from the Centers for Disease Control and Prevention found one in three high school students in 2019 reported feeling persistently sad and hopeless – a 40% increase from 2009.
The coronavirus pandemic appears to be adding to these difficulties. A review of 80 studies found forced isolation and loneliness among children correlated with an increased risk of depression.
“We’re all social beings, but they’re [teenagers] at the point in their development where their peers are their reality,” said Terrie Andrews, PhD, a psychologist and administrator of behavioral health at Wolfson Children’s Hospital in Jacksonville, Fla. “Their peers are their grounding mechanism.”
Children’s hospitals in Colorado, Missouri, and New York all reported an uptick in the number of patients who thought about or attempted suicide. Clinicians also mentioned spikes in children with severe depression and those with autism who are acting out.
The number of overdose attempts among children has caught the attention of clinicians at two facilities. Dr. Andrews said the facility gives out lockboxes for weapons and medication to the public – including parents who come in after children attempted to take their life using medication.
Children’s National Hospital in Washington, D.C., also has experienced an uptick, said Colby Tyson, MD, associate director of inpatient psychiatry. She’s seen children’s mental health deteriorate because of a likely increase in family conflict – often a consequence of the chaos caused by the pandemic. Without school, connections with peers or employment, families don’t have the opportunity to spend time away from one another and regroup, which can add stress to an already tense situation.
“That break is gone,” she said.
The higher demand for child mental health services caused by the pandemic has made finding a bed at an inpatient unit more difficult.
Now, some hospitals report running at full capacity and having more children “boarding,” or sleeping in EDs before being admitted to the psychiatric unit. Among them is the Pediatric Mental Health Institute at Children’s Hospital Colorado. Williams said the inpatient unit has been full since March. Some children now wait nearly 2 days for a bed, up from the 8-10 hours common before the pandemic.
Cincinnati Children’s Hospital Medical Center in Ohio is also running at full capacity, said clinicians, and had several days in which the unit was above capacity and placed kids instead in the emergency department waiting to be admitted. In Florida, Dr. Andrews said, up to 25 children have been held on surgical floors at Wolfson Children’s while waiting for a spot to open in the inpatient psychiatric unit. Their wait could last as long as 5 days, she said.
Multiple hospitals said the usual summer slump in child psychiatric admissions was missing last year. “We never saw that during the pandemic,” said Andrews. “We stayed completely busy the entire time.”
Some facilities have decided to reduce the number of beds available to maintain physical distancing, further constricting supply. Children’s National in D.C. cut five beds from its unit to maintain single occupancy in every room, said Adelaide Robb, MD, division chief of psychiatry and behavioral sciences.
The measures taken to curb the spread of COVID have also affected the way hospitalized children receive mental health services. In addition to providers wearing protective equipment, some hospitals like Cincinnati Children’s rearranged furniture and placed cues on the floor as reminders to stay 6 feet apart. The University of Pittsburgh Medical Center’s Western Psychiatric Hospital and other facilities encourage children to keep their masks on by offering rewards like extra computer time. Patients at Children’s National now eat in their rooms, a change from when they ate together.
Despite the need for distance, social interaction still represents an important part of mental health care for children, clinicians said. Facilities have come up with various ways to do so safely, including creating smaller pods for group therapy. Children at Cincinnati Children’s Hospital can play with toys, but only with ones that can be wiped clean afterward. No cards or board games, said Suzanne Sampang, MD, clinical medical director for child and adolescent psychiatry at the hospital.
“I think what’s different about psychiatric treatment is that, really, interaction is the treatment,” she said, “just as much as a medication.”
The added infection-control precautions pose challenges to forging therapeutic connections. Masks can complicate the ability to read a person’s face. Online meetings make it difficult to build trust between a patient and a therapist.
“There’s something about the real relationship in person that the best technology can’t give to you,” said Dr. Robb.
For now, Krissy Williams is relying on virtual platforms to receive some of her mental health services. Despite being hospitalized and suffering brain damage due to the overdose, she is now at home and in good spirits. She enjoys geometry, dancing on TikTok, and trying to beat her mother at Super Mario Bros. on the Wii. But being away from her friends, she said, has been a hard adjustment.
“When you’re used to something,” she said, “it’s not easy to change everything.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of Kaiser Family Foundation, which is not affiliated with Kaiser Permanente.
Krissy Williams, 15, had attempted suicide before, but never with pills.
The teen was diagnosed with schizophrenia when she was 9. People with this chronic mental health condition perceive reality differently and often experience hallucinations and delusions. She learned to manage these symptoms with a variety of services offered at home and at school.
But the pandemic upended those lifelines. She lost much of the support offered at school. She also lost regular contact with her peers. Her mother lost access to respite care – which allowed her to take a break.
On a Thursday in October, the isolation and sadness came to a head. As Krissy’s mother, Patricia Williams, called a mental crisis hotline for help, she said, Krissy stood on the deck of their Maryland home with a bottle of pain medication in one hand and water in the other.
Before Patricia could react, Krissy placed the pills in her mouth and swallowed.
Efforts to contain the spread of the novel coronavirus in the United States have led to drastic changes in the way children and teens learn, play and socialize. Tens of millions of students are attending school through some form of distance learning. Many extracurricular activities have been canceled. Playgrounds, zoos, and other recreational spaces have closed. Kids like Krissy have struggled to cope and the toll is becoming evident.
Government figures show the proportion of children who arrived in EDs with mental health issues increased 24% from mid-March through mid-October, compared with the same period in 2019. Among preteens and adolescents, it rose by 31%. Anecdotally, some hospitals said they are seeing more cases of severe depression and suicidal thoughts among children, particularly attempts to overdose.
The increased demand for intensive mental health care that has accompanied the pandemic has worsened issues that have long plagued the system. In some hospitals, the number of children unable to immediately get a bed in the psychiatric unit rose. Others reduced the number of beds or closed psychiatric units altogether to reduce the spread of COVID-19.
“It’s only a matter of time before a tsunami sort of reaches the shore of our service system, and it’s going to be overwhelmed with the mental health needs of kids,” said Jason Williams, PsyD, a psychologist and director of operations of the Pediatric Mental Health Institute at Children’s Hospital Colorado, Aurora.
“I think we’re just starting to see the tip of the iceberg, to be honest with you.”
Before COVID, more than 8 million kids between ages 3 and 17 were diagnosed with a mental or behavioral health condition, according to the most recent National Survey of Children’s Health. A separate survey from the Centers for Disease Control and Prevention found one in three high school students in 2019 reported feeling persistently sad and hopeless – a 40% increase from 2009.
The coronavirus pandemic appears to be adding to these difficulties. A review of 80 studies found forced isolation and loneliness among children correlated with an increased risk of depression.
“We’re all social beings, but they’re [teenagers] at the point in their development where their peers are their reality,” said Terrie Andrews, PhD, a psychologist and administrator of behavioral health at Wolfson Children’s Hospital in Jacksonville, Fla. “Their peers are their grounding mechanism.”
Children’s hospitals in Colorado, Missouri, and New York all reported an uptick in the number of patients who thought about or attempted suicide. Clinicians also mentioned spikes in children with severe depression and those with autism who are acting out.
The number of overdose attempts among children has caught the attention of clinicians at two facilities. Dr. Andrews said the facility gives out lockboxes for weapons and medication to the public – including parents who come in after children attempted to take their life using medication.
Children’s National Hospital in Washington, D.C., also has experienced an uptick, said Colby Tyson, MD, associate director of inpatient psychiatry. She’s seen children’s mental health deteriorate because of a likely increase in family conflict – often a consequence of the chaos caused by the pandemic. Without school, connections with peers or employment, families don’t have the opportunity to spend time away from one another and regroup, which can add stress to an already tense situation.
“That break is gone,” she said.
The higher demand for child mental health services caused by the pandemic has made finding a bed at an inpatient unit more difficult.
Now, some hospitals report running at full capacity and having more children “boarding,” or sleeping in EDs before being admitted to the psychiatric unit. Among them is the Pediatric Mental Health Institute at Children’s Hospital Colorado. Williams said the inpatient unit has been full since March. Some children now wait nearly 2 days for a bed, up from the 8-10 hours common before the pandemic.
Cincinnati Children’s Hospital Medical Center in Ohio is also running at full capacity, said clinicians, and had several days in which the unit was above capacity and placed kids instead in the emergency department waiting to be admitted. In Florida, Dr. Andrews said, up to 25 children have been held on surgical floors at Wolfson Children’s while waiting for a spot to open in the inpatient psychiatric unit. Their wait could last as long as 5 days, she said.
Multiple hospitals said the usual summer slump in child psychiatric admissions was missing last year. “We never saw that during the pandemic,” said Andrews. “We stayed completely busy the entire time.”
Some facilities have decided to reduce the number of beds available to maintain physical distancing, further constricting supply. Children’s National in D.C. cut five beds from its unit to maintain single occupancy in every room, said Adelaide Robb, MD, division chief of psychiatry and behavioral sciences.
The measures taken to curb the spread of COVID have also affected the way hospitalized children receive mental health services. In addition to providers wearing protective equipment, some hospitals like Cincinnati Children’s rearranged furniture and placed cues on the floor as reminders to stay 6 feet apart. The University of Pittsburgh Medical Center’s Western Psychiatric Hospital and other facilities encourage children to keep their masks on by offering rewards like extra computer time. Patients at Children’s National now eat in their rooms, a change from when they ate together.
Despite the need for distance, social interaction still represents an important part of mental health care for children, clinicians said. Facilities have come up with various ways to do so safely, including creating smaller pods for group therapy. Children at Cincinnati Children’s Hospital can play with toys, but only with ones that can be wiped clean afterward. No cards or board games, said Suzanne Sampang, MD, clinical medical director for child and adolescent psychiatry at the hospital.
“I think what’s different about psychiatric treatment is that, really, interaction is the treatment,” she said, “just as much as a medication.”
The added infection-control precautions pose challenges to forging therapeutic connections. Masks can complicate the ability to read a person’s face. Online meetings make it difficult to build trust between a patient and a therapist.
“There’s something about the real relationship in person that the best technology can’t give to you,” said Dr. Robb.
For now, Krissy Williams is relying on virtual platforms to receive some of her mental health services. Despite being hospitalized and suffering brain damage due to the overdose, she is now at home and in good spirits. She enjoys geometry, dancing on TikTok, and trying to beat her mother at Super Mario Bros. on the Wii. But being away from her friends, she said, has been a hard adjustment.
“When you’re used to something,” she said, “it’s not easy to change everything.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of Kaiser Family Foundation, which is not affiliated with Kaiser Permanente.
Study confirms key COVID-19 risk factors in children
Children and adolescents who receive positive COVID-19 test results are not only more likely to have been in close contact with someone with a confirmed case of the virus but also are less likely to have reported consistent mask use among students and staff inside the school they attended, reported Charlotte V. Hobbs, MD, and colleagues at the University of Mississippi, Jackson.
In partnership with the Centers for Disease Control and Prevention’s COVID-19 Response Team, Dr. Hobbs and colleagues conducted a case-control study of 397 children and adolescents under 18 years of age to assess school, community, and close contact exposures associated with pediatric COVID-19. Patients tested for COVID-19 at outpatient health centers or emergency departments affiliated with the University of Mississippi Medical Center between Sept. 1 and Nov. 5, 2020, were included in the study.
Nearly two-thirds reported that exposure came from family members
Of the total study participants observed, 82 (21%) were under 4 years of age; 214 (54%) were female; 217 (55%) were non-Hispanic black, and 145 (37%) were non-Hispanic white. More than half (53%) sought testing because of COVID-19 symptoms. Of those who tested positive, 66% reported having come into close contact with a COVID-19 case, and 64% reported that those contacts were family members, compared with 15% of contacts who were schoolmates and 27% who were child care classmates.
All participants completed in-person school or child care attendance less than 14 days before testing positive for the virus, including 62% of patients testing positive and 68% of those testing negative. The authors noted that school attendance itself was not found to be associated with any positive test results. In fact, parents in 64% of positive cases and 76% of negative cases reported mask wearing among children and staff inside places of learning.
Of those study participants testing positive who did come into close contact with someone with COVID-19, the contacts were more likely to be family members than school or child care classmates. Specifically, they were more likely, in the 2-week period preceding testing, to have attended gatherings with individuals outside their immediate households, including social events and activities with other children. Parents of students testing positive were also less likely to report consistent indoor mask use among their children older than 2 years and school staff members.
School attendance was not found to increase likelihood of testing positive
Attending in-person school or child care during the 2 weeks before the SARS-CoV-2 test was not associated with greater likelihood of testing positive, the study authors noted, adding that the majority of study respondents reported universal mask use inside school and child care facilities, consistent with Mississippi State Department of Health recommended guidelines.
Dr. Hobbs and colleagues reported at least four limitations of the study. They noted that the study participants may not be representative of youth in other geographic regions of the country. They considered the possibility of unmeasured confounding of participant behaviors that may not have been factored into the study. No attempt was made to verify parent claims of mask use at schools and child care programs. Lastly, they acknowledged that “case or control status might be subject to misclassification because of imperfect sensitivity or specificity of PCR-based testing.
As of Dec. 14, 2020, the CDC reported that 10.2% of all COVID-19 cases in the United States were in children and adolescents under the age of 18.
“Continued efforts to prevent transmission at schools and child care programs are important, as are assessments of various types of activities and exposures to identify risk factors for COVID-19 as children engage in classroom and social interactions.” Promoting behaviors to reduce exposures to the virus among youth in the household, the community, schools, and child care programs is important to preventing outbreaks of the virus at schools, the authors cautioned.
In a separate interview with this news organization, Karalyn Kinsella, MD, general pediatrician in a small group private practice in Cheshire, Conn., said, “What this report tells me is that COVID cases are more common when mask use is inconsistent in schools and at home and in schools that don’t properly adhere to CDC guidelines. Overall, so long as social distancing guidelines are followed, schools are pretty safe places for kids during this pandemic.”
This finding is important, since many families are keeping their children out of school over fears of contracting the virus, she added. Some of the consequences these children are suffering include a lack of social connection and structure, which in some cases is leading to worsening anxiety and depression, and for those with disabilities, such as those who receive physical therapy, occupational therapy, speech or have IEPs, they’re not getting the full benefit of the services that they would otherwise receive in person, she observed.
“I don’t think families really understand the risks of getting together with family or friends “in their bubble” or the risk of continuing sports participation. This is where the majority of COVID cases are coming from,” she said, adding that it is important to discuss this risk with them at appointments. So, when families ask us what we think of in-person learning, I think we should feel fairly confident that the benefit may outweigh the risk.”
Dr. Hobbs and colleagues, and Dr. Kinsella, had no conflicts of interest to report.
SOURCE: MMWR Morb Mortal Wkly Rep. 2020;69:1925-9. doi: 10.15585/mmwr.mm6950e3.
Children and adolescents who receive positive COVID-19 test results are not only more likely to have been in close contact with someone with a confirmed case of the virus but also are less likely to have reported consistent mask use among students and staff inside the school they attended, reported Charlotte V. Hobbs, MD, and colleagues at the University of Mississippi, Jackson.
In partnership with the Centers for Disease Control and Prevention’s COVID-19 Response Team, Dr. Hobbs and colleagues conducted a case-control study of 397 children and adolescents under 18 years of age to assess school, community, and close contact exposures associated with pediatric COVID-19. Patients tested for COVID-19 at outpatient health centers or emergency departments affiliated with the University of Mississippi Medical Center between Sept. 1 and Nov. 5, 2020, were included in the study.
Nearly two-thirds reported that exposure came from family members
Of the total study participants observed, 82 (21%) were under 4 years of age; 214 (54%) were female; 217 (55%) were non-Hispanic black, and 145 (37%) were non-Hispanic white. More than half (53%) sought testing because of COVID-19 symptoms. Of those who tested positive, 66% reported having come into close contact with a COVID-19 case, and 64% reported that those contacts were family members, compared with 15% of contacts who were schoolmates and 27% who were child care classmates.
All participants completed in-person school or child care attendance less than 14 days before testing positive for the virus, including 62% of patients testing positive and 68% of those testing negative. The authors noted that school attendance itself was not found to be associated with any positive test results. In fact, parents in 64% of positive cases and 76% of negative cases reported mask wearing among children and staff inside places of learning.
Of those study participants testing positive who did come into close contact with someone with COVID-19, the contacts were more likely to be family members than school or child care classmates. Specifically, they were more likely, in the 2-week period preceding testing, to have attended gatherings with individuals outside their immediate households, including social events and activities with other children. Parents of students testing positive were also less likely to report consistent indoor mask use among their children older than 2 years and school staff members.
School attendance was not found to increase likelihood of testing positive
Attending in-person school or child care during the 2 weeks before the SARS-CoV-2 test was not associated with greater likelihood of testing positive, the study authors noted, adding that the majority of study respondents reported universal mask use inside school and child care facilities, consistent with Mississippi State Department of Health recommended guidelines.
Dr. Hobbs and colleagues reported at least four limitations of the study. They noted that the study participants may not be representative of youth in other geographic regions of the country. They considered the possibility of unmeasured confounding of participant behaviors that may not have been factored into the study. No attempt was made to verify parent claims of mask use at schools and child care programs. Lastly, they acknowledged that “case or control status might be subject to misclassification because of imperfect sensitivity or specificity of PCR-based testing.
As of Dec. 14, 2020, the CDC reported that 10.2% of all COVID-19 cases in the United States were in children and adolescents under the age of 18.
“Continued efforts to prevent transmission at schools and child care programs are important, as are assessments of various types of activities and exposures to identify risk factors for COVID-19 as children engage in classroom and social interactions.” Promoting behaviors to reduce exposures to the virus among youth in the household, the community, schools, and child care programs is important to preventing outbreaks of the virus at schools, the authors cautioned.
In a separate interview with this news organization, Karalyn Kinsella, MD, general pediatrician in a small group private practice in Cheshire, Conn., said, “What this report tells me is that COVID cases are more common when mask use is inconsistent in schools and at home and in schools that don’t properly adhere to CDC guidelines. Overall, so long as social distancing guidelines are followed, schools are pretty safe places for kids during this pandemic.”
This finding is important, since many families are keeping their children out of school over fears of contracting the virus, she added. Some of the consequences these children are suffering include a lack of social connection and structure, which in some cases is leading to worsening anxiety and depression, and for those with disabilities, such as those who receive physical therapy, occupational therapy, speech or have IEPs, they’re not getting the full benefit of the services that they would otherwise receive in person, she observed.
“I don’t think families really understand the risks of getting together with family or friends “in their bubble” or the risk of continuing sports participation. This is where the majority of COVID cases are coming from,” she said, adding that it is important to discuss this risk with them at appointments. So, when families ask us what we think of in-person learning, I think we should feel fairly confident that the benefit may outweigh the risk.”
Dr. Hobbs and colleagues, and Dr. Kinsella, had no conflicts of interest to report.
SOURCE: MMWR Morb Mortal Wkly Rep. 2020;69:1925-9. doi: 10.15585/mmwr.mm6950e3.
Children and adolescents who receive positive COVID-19 test results are not only more likely to have been in close contact with someone with a confirmed case of the virus but also are less likely to have reported consistent mask use among students and staff inside the school they attended, reported Charlotte V. Hobbs, MD, and colleagues at the University of Mississippi, Jackson.
In partnership with the Centers for Disease Control and Prevention’s COVID-19 Response Team, Dr. Hobbs and colleagues conducted a case-control study of 397 children and adolescents under 18 years of age to assess school, community, and close contact exposures associated with pediatric COVID-19. Patients tested for COVID-19 at outpatient health centers or emergency departments affiliated with the University of Mississippi Medical Center between Sept. 1 and Nov. 5, 2020, were included in the study.
Nearly two-thirds reported that exposure came from family members
Of the total study participants observed, 82 (21%) were under 4 years of age; 214 (54%) were female; 217 (55%) were non-Hispanic black, and 145 (37%) were non-Hispanic white. More than half (53%) sought testing because of COVID-19 symptoms. Of those who tested positive, 66% reported having come into close contact with a COVID-19 case, and 64% reported that those contacts were family members, compared with 15% of contacts who were schoolmates and 27% who were child care classmates.
All participants completed in-person school or child care attendance less than 14 days before testing positive for the virus, including 62% of patients testing positive and 68% of those testing negative. The authors noted that school attendance itself was not found to be associated with any positive test results. In fact, parents in 64% of positive cases and 76% of negative cases reported mask wearing among children and staff inside places of learning.
Of those study participants testing positive who did come into close contact with someone with COVID-19, the contacts were more likely to be family members than school or child care classmates. Specifically, they were more likely, in the 2-week period preceding testing, to have attended gatherings with individuals outside their immediate households, including social events and activities with other children. Parents of students testing positive were also less likely to report consistent indoor mask use among their children older than 2 years and school staff members.
School attendance was not found to increase likelihood of testing positive
Attending in-person school or child care during the 2 weeks before the SARS-CoV-2 test was not associated with greater likelihood of testing positive, the study authors noted, adding that the majority of study respondents reported universal mask use inside school and child care facilities, consistent with Mississippi State Department of Health recommended guidelines.
Dr. Hobbs and colleagues reported at least four limitations of the study. They noted that the study participants may not be representative of youth in other geographic regions of the country. They considered the possibility of unmeasured confounding of participant behaviors that may not have been factored into the study. No attempt was made to verify parent claims of mask use at schools and child care programs. Lastly, they acknowledged that “case or control status might be subject to misclassification because of imperfect sensitivity or specificity of PCR-based testing.
As of Dec. 14, 2020, the CDC reported that 10.2% of all COVID-19 cases in the United States were in children and adolescents under the age of 18.
“Continued efforts to prevent transmission at schools and child care programs are important, as are assessments of various types of activities and exposures to identify risk factors for COVID-19 as children engage in classroom and social interactions.” Promoting behaviors to reduce exposures to the virus among youth in the household, the community, schools, and child care programs is important to preventing outbreaks of the virus at schools, the authors cautioned.
In a separate interview with this news organization, Karalyn Kinsella, MD, general pediatrician in a small group private practice in Cheshire, Conn., said, “What this report tells me is that COVID cases are more common when mask use is inconsistent in schools and at home and in schools that don’t properly adhere to CDC guidelines. Overall, so long as social distancing guidelines are followed, schools are pretty safe places for kids during this pandemic.”
This finding is important, since many families are keeping their children out of school over fears of contracting the virus, she added. Some of the consequences these children are suffering include a lack of social connection and structure, which in some cases is leading to worsening anxiety and depression, and for those with disabilities, such as those who receive physical therapy, occupational therapy, speech or have IEPs, they’re not getting the full benefit of the services that they would otherwise receive in person, she observed.
“I don’t think families really understand the risks of getting together with family or friends “in their bubble” or the risk of continuing sports participation. This is where the majority of COVID cases are coming from,” she said, adding that it is important to discuss this risk with them at appointments. So, when families ask us what we think of in-person learning, I think we should feel fairly confident that the benefit may outweigh the risk.”
Dr. Hobbs and colleagues, and Dr. Kinsella, had no conflicts of interest to report.
SOURCE: MMWR Morb Mortal Wkly Rep. 2020;69:1925-9. doi: 10.15585/mmwr.mm6950e3.
FROM MORBIDITY AND MORTALITY WEEKLY REPORT