User login
Drug granted fast track designation for MF

mycosis fungoides
The US Food and Drug Administration (FDA) has granted fast track designation to Resimmune® (A-dmDT390-bisFv[UCHT1]) for the treatment of mycosis fungoides (MF).
Resimmune is an anti-CD3 immunotoxin that targets and transiently depletes a high percentage of malignant and normal T cells.
Researchers believe this high rate of T-cell depletion may “reset” a patient’s immune system, leading to immunomodulation. However, the safety and efficacy of Resimmune has not been established.
Resimmune is being developed by Angimmune LLC.
Resimmune research
The FDA’s fast track designation for Resimmune is based on results from a phase 1 trial, which were published in haematologica last year.
The trial included 25 patients with cutaneous T-cell lymphoma (CTCL)—17 with stage IB-IIB disease and 8 with stage III-IV disease. The patients received Resimmune at varying doses—between 2.5 µg/kg and 11.25 µg/kg.
Safety
Drug-related adverse events for the entire study cohort (n=30) included:
- Grade 2-3 AST/ALT elevations (n=6)
- Grade 2 chills (n=10)
- Grade 5 EBV infection (n=1)
- Grade 3 EBV/CMV infection (n=5)
- Grade 2 fever (n=6)
- Grade 5 heart failure (n=2)
- Grade 2-3 hypoalbuminemia (n=11)
- Grade 2 hypomagnesemia (n=1)
- Grade 3 hypophosphatemia (n=3)
- Grade 2-4 hypotension (n=3)
- Grade 4 hypoxia (n=1)
- Grade 4 liver failure (n=1)
- Grade 4 metabolic acidosis (n=1)
- Grade 3 supraventricular tachycardia (n=2)
- Grade 3-4 uremia (n=3)
- Grade 2-4 vascular leak syndrome (n=5).
Efficacy and phase 2
Nine of the CTCL patients (36%) responded to Resimmune, and 4 (16%) had complete responses (CRs). The duration of CR was more than 38 months for 1 patient, more than 60 months for another, and more than 72 months for 2 patients.
Of the 5 partial responses, 2 lasted 3 months, 1 lasted more than 3 months, 1 lasted more than 6 months, and the longest lasted 14 months.
The researchers said this trial revealed a subgroup of CTCL patients with a very high response rate.
When they excluded patients whose mSWAT scores never exceeded 50 and who never had lymph node involvement or stage III disease, the researchers were left with 9 patients. This subgroup had an overall response rate of 89% and a CR rate of 50% (at 6 months of follow-up).
“Results from our phase 1 trial demonstrated a particularly robust response among certain patients with early stage disease, and the randomized phase 2 trial is designed to further explore this potential therapeutic benefit,” said David Neville, MD, president and chief scientific officer of Angimmune.
The objective of this phase 2 trial is to document the incidence of CRs with Resimmune compared to oral vorinostat after a maximum of 12 months of treatment. The trial will enroll patients with stage IB/IIB MF with mSWAT < 50 who have never had lymphoid disease or a prior hematopoietic stem cell transplant.
About fast track designation
The FDA’s fast track program is designed to facilitate and expedite the development and review of new drugs intended to treat serious or life-threatening conditions and address unmet medical need.
Through the fast track program, a product may be eligible for priority review. In addition, the company developing the drug may be allowed to submit sections of the biologic license application or new drug application on a rolling basis as data become available.
Fast track designation also provides the company with opportunities for more frequent meetings with the FDA to discuss the drug’s development plan and ensure collection of the appropriate data needed to support drug approval. And the designation allows for more frequent written communication from the FDA about things such as the design of proposed clinical trials and the use of biomarkers. ![]()

mycosis fungoides
The US Food and Drug Administration (FDA) has granted fast track designation to Resimmune® (A-dmDT390-bisFv[UCHT1]) for the treatment of mycosis fungoides (MF).
Resimmune is an anti-CD3 immunotoxin that targets and transiently depletes a high percentage of malignant and normal T cells.
Researchers believe this high rate of T-cell depletion may “reset” a patient’s immune system, leading to immunomodulation. However, the safety and efficacy of Resimmune has not been established.
Resimmune is being developed by Angimmune LLC.
Resimmune research
The FDA’s fast track designation for Resimmune is based on results from a phase 1 trial, which were published in haematologica last year.
The trial included 25 patients with cutaneous T-cell lymphoma (CTCL)—17 with stage IB-IIB disease and 8 with stage III-IV disease. The patients received Resimmune at varying doses—between 2.5 µg/kg and 11.25 µg/kg.
Safety
Drug-related adverse events for the entire study cohort (n=30) included:
- Grade 2-3 AST/ALT elevations (n=6)
- Grade 2 chills (n=10)
- Grade 5 EBV infection (n=1)
- Grade 3 EBV/CMV infection (n=5)
- Grade 2 fever (n=6)
- Grade 5 heart failure (n=2)
- Grade 2-3 hypoalbuminemia (n=11)
- Grade 2 hypomagnesemia (n=1)
- Grade 3 hypophosphatemia (n=3)
- Grade 2-4 hypotension (n=3)
- Grade 4 hypoxia (n=1)
- Grade 4 liver failure (n=1)
- Grade 4 metabolic acidosis (n=1)
- Grade 3 supraventricular tachycardia (n=2)
- Grade 3-4 uremia (n=3)
- Grade 2-4 vascular leak syndrome (n=5).
Efficacy and phase 2
Nine of the CTCL patients (36%) responded to Resimmune, and 4 (16%) had complete responses (CRs). The duration of CR was more than 38 months for 1 patient, more than 60 months for another, and more than 72 months for 2 patients.
Of the 5 partial responses, 2 lasted 3 months, 1 lasted more than 3 months, 1 lasted more than 6 months, and the longest lasted 14 months.
The researchers said this trial revealed a subgroup of CTCL patients with a very high response rate.
When they excluded patients whose mSWAT scores never exceeded 50 and who never had lymph node involvement or stage III disease, the researchers were left with 9 patients. This subgroup had an overall response rate of 89% and a CR rate of 50% (at 6 months of follow-up).
“Results from our phase 1 trial demonstrated a particularly robust response among certain patients with early stage disease, and the randomized phase 2 trial is designed to further explore this potential therapeutic benefit,” said David Neville, MD, president and chief scientific officer of Angimmune.
The objective of this phase 2 trial is to document the incidence of CRs with Resimmune compared to oral vorinostat after a maximum of 12 months of treatment. The trial will enroll patients with stage IB/IIB MF with mSWAT < 50 who have never had lymphoid disease or a prior hematopoietic stem cell transplant.
About fast track designation
The FDA’s fast track program is designed to facilitate and expedite the development and review of new drugs intended to treat serious or life-threatening conditions and address unmet medical need.
Through the fast track program, a product may be eligible for priority review. In addition, the company developing the drug may be allowed to submit sections of the biologic license application or new drug application on a rolling basis as data become available.
Fast track designation also provides the company with opportunities for more frequent meetings with the FDA to discuss the drug’s development plan and ensure collection of the appropriate data needed to support drug approval. And the designation allows for more frequent written communication from the FDA about things such as the design of proposed clinical trials and the use of biomarkers. ![]()

mycosis fungoides
The US Food and Drug Administration (FDA) has granted fast track designation to Resimmune® (A-dmDT390-bisFv[UCHT1]) for the treatment of mycosis fungoides (MF).
Resimmune is an anti-CD3 immunotoxin that targets and transiently depletes a high percentage of malignant and normal T cells.
Researchers believe this high rate of T-cell depletion may “reset” a patient’s immune system, leading to immunomodulation. However, the safety and efficacy of Resimmune has not been established.
Resimmune is being developed by Angimmune LLC.
Resimmune research
The FDA’s fast track designation for Resimmune is based on results from a phase 1 trial, which were published in haematologica last year.
The trial included 25 patients with cutaneous T-cell lymphoma (CTCL)—17 with stage IB-IIB disease and 8 with stage III-IV disease. The patients received Resimmune at varying doses—between 2.5 µg/kg and 11.25 µg/kg.
Safety
Drug-related adverse events for the entire study cohort (n=30) included:
- Grade 2-3 AST/ALT elevations (n=6)
- Grade 2 chills (n=10)
- Grade 5 EBV infection (n=1)
- Grade 3 EBV/CMV infection (n=5)
- Grade 2 fever (n=6)
- Grade 5 heart failure (n=2)
- Grade 2-3 hypoalbuminemia (n=11)
- Grade 2 hypomagnesemia (n=1)
- Grade 3 hypophosphatemia (n=3)
- Grade 2-4 hypotension (n=3)
- Grade 4 hypoxia (n=1)
- Grade 4 liver failure (n=1)
- Grade 4 metabolic acidosis (n=1)
- Grade 3 supraventricular tachycardia (n=2)
- Grade 3-4 uremia (n=3)
- Grade 2-4 vascular leak syndrome (n=5).
Efficacy and phase 2
Nine of the CTCL patients (36%) responded to Resimmune, and 4 (16%) had complete responses (CRs). The duration of CR was more than 38 months for 1 patient, more than 60 months for another, and more than 72 months for 2 patients.
Of the 5 partial responses, 2 lasted 3 months, 1 lasted more than 3 months, 1 lasted more than 6 months, and the longest lasted 14 months.
The researchers said this trial revealed a subgroup of CTCL patients with a very high response rate.
When they excluded patients whose mSWAT scores never exceeded 50 and who never had lymph node involvement or stage III disease, the researchers were left with 9 patients. This subgroup had an overall response rate of 89% and a CR rate of 50% (at 6 months of follow-up).
“Results from our phase 1 trial demonstrated a particularly robust response among certain patients with early stage disease, and the randomized phase 2 trial is designed to further explore this potential therapeutic benefit,” said David Neville, MD, president and chief scientific officer of Angimmune.
The objective of this phase 2 trial is to document the incidence of CRs with Resimmune compared to oral vorinostat after a maximum of 12 months of treatment. The trial will enroll patients with stage IB/IIB MF with mSWAT < 50 who have never had lymphoid disease or a prior hematopoietic stem cell transplant.
About fast track designation
The FDA’s fast track program is designed to facilitate and expedite the development and review of new drugs intended to treat serious or life-threatening conditions and address unmet medical need.
Through the fast track program, a product may be eligible for priority review. In addition, the company developing the drug may be allowed to submit sections of the biologic license application or new drug application on a rolling basis as data become available.
Fast track designation also provides the company with opportunities for more frequent meetings with the FDA to discuss the drug’s development plan and ensure collection of the appropriate data needed to support drug approval. And the designation allows for more frequent written communication from the FDA about things such as the design of proposed clinical trials and the use of biomarkers. ![]()
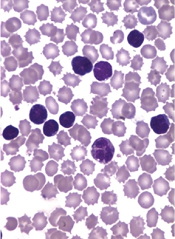
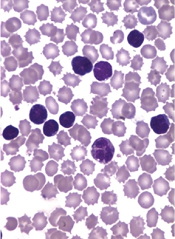
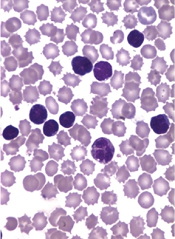
Studies reveal potential therapeutic targets for resistant AML

Image by NIGMS
A pair of studies suggest the DNA replication checkpoint pathway could be targeted to treat resistant acute myeloid leukemia (AML).
One study indicated that the kinase CHK1, which coordinates the DNA damage response and cell-cycle checkpoint response, might be targeted to overcome cytarabine resistance in AML.
The other study suggested that ATR, a kinase that activates CHK1, and ATM, a second upstream kinase in the DNA damage response, might be therapeutic targets in MLL-rearranged AML.
Both studies were published in Science Sigaling.
Laure David, of La Ligue Contre Le Cancer in Toulouse, France, and colleagues conducted this study.
The researchers integrated gene expression data with survival data from 198 AML patients who were previously treated with cytarabine-based chemotherapy.
The data showed that patients with high expression of CHEK1, the gene that encodes CHK1, had poor survival. And patient cells with high CHK1 abundance were resistant to cytarabine.
However, when the researchers exposed the cells with high CHK1 abundance to the CHK1 inhibitor SCH900776, they observed “reduced clonogenic ability and progression of DNA replication in the presence of cytarabine.”
The team therefore concluded that treatment with a CHK1 inhibitor might overcome resistance to cytarabine-based treatments in AML. They also said that monitoring CHEK1 expression in AML patients could potentially predict outcomes and reveal patients who might benefit from treatment with a CHK1 inhibitor.
The second study was conducted by Isabel Morgado-Palacin, of the Spanish National Cancer Research Center in Madrid, and colleagues.
The researchers investigated ATR, which is the primary sensor of DNA replication stress, and ATM, a kinase that senses DNA double-strand breaks, as possible therapeutic targets in MLL-rearranged AML.
The team found that inhibiting ATR induced chromosomal breakage and death in murine AML-MLL cells in vitro. And inhibiting ATR in vivo reduced the tumor burden and prevented tumors from growing.
The researchers also found that inhibiting ATM prolonged survival in the mouse model of AML-MLL, which suggests that both ATR and ATM might be therapeutic targets in MLL-rearranged AML. ![]()

Image by NIGMS
A pair of studies suggest the DNA replication checkpoint pathway could be targeted to treat resistant acute myeloid leukemia (AML).
One study indicated that the kinase CHK1, which coordinates the DNA damage response and cell-cycle checkpoint response, might be targeted to overcome cytarabine resistance in AML.
The other study suggested that ATR, a kinase that activates CHK1, and ATM, a second upstream kinase in the DNA damage response, might be therapeutic targets in MLL-rearranged AML.
Both studies were published in Science Sigaling.
Laure David, of La Ligue Contre Le Cancer in Toulouse, France, and colleagues conducted this study.
The researchers integrated gene expression data with survival data from 198 AML patients who were previously treated with cytarabine-based chemotherapy.
The data showed that patients with high expression of CHEK1, the gene that encodes CHK1, had poor survival. And patient cells with high CHK1 abundance were resistant to cytarabine.
However, when the researchers exposed the cells with high CHK1 abundance to the CHK1 inhibitor SCH900776, they observed “reduced clonogenic ability and progression of DNA replication in the presence of cytarabine.”
The team therefore concluded that treatment with a CHK1 inhibitor might overcome resistance to cytarabine-based treatments in AML. They also said that monitoring CHEK1 expression in AML patients could potentially predict outcomes and reveal patients who might benefit from treatment with a CHK1 inhibitor.
The second study was conducted by Isabel Morgado-Palacin, of the Spanish National Cancer Research Center in Madrid, and colleagues.
The researchers investigated ATR, which is the primary sensor of DNA replication stress, and ATM, a kinase that senses DNA double-strand breaks, as possible therapeutic targets in MLL-rearranged AML.
The team found that inhibiting ATR induced chromosomal breakage and death in murine AML-MLL cells in vitro. And inhibiting ATR in vivo reduced the tumor burden and prevented tumors from growing.
The researchers also found that inhibiting ATM prolonged survival in the mouse model of AML-MLL, which suggests that both ATR and ATM might be therapeutic targets in MLL-rearranged AML. ![]()

Image by NIGMS
A pair of studies suggest the DNA replication checkpoint pathway could be targeted to treat resistant acute myeloid leukemia (AML).
One study indicated that the kinase CHK1, which coordinates the DNA damage response and cell-cycle checkpoint response, might be targeted to overcome cytarabine resistance in AML.
The other study suggested that ATR, a kinase that activates CHK1, and ATM, a second upstream kinase in the DNA damage response, might be therapeutic targets in MLL-rearranged AML.
Both studies were published in Science Sigaling.
Laure David, of La Ligue Contre Le Cancer in Toulouse, France, and colleagues conducted this study.
The researchers integrated gene expression data with survival data from 198 AML patients who were previously treated with cytarabine-based chemotherapy.
The data showed that patients with high expression of CHEK1, the gene that encodes CHK1, had poor survival. And patient cells with high CHK1 abundance were resistant to cytarabine.
However, when the researchers exposed the cells with high CHK1 abundance to the CHK1 inhibitor SCH900776, they observed “reduced clonogenic ability and progression of DNA replication in the presence of cytarabine.”
The team therefore concluded that treatment with a CHK1 inhibitor might overcome resistance to cytarabine-based treatments in AML. They also said that monitoring CHEK1 expression in AML patients could potentially predict outcomes and reveal patients who might benefit from treatment with a CHK1 inhibitor.
The second study was conducted by Isabel Morgado-Palacin, of the Spanish National Cancer Research Center in Madrid, and colleagues.
The researchers investigated ATR, which is the primary sensor of DNA replication stress, and ATM, a kinase that senses DNA double-strand breaks, as possible therapeutic targets in MLL-rearranged AML.
The team found that inhibiting ATR induced chromosomal breakage and death in murine AML-MLL cells in vitro. And inhibiting ATR in vivo reduced the tumor burden and prevented tumors from growing.
The researchers also found that inhibiting ATM prolonged survival in the mouse model of AML-MLL, which suggests that both ATR and ATM might be therapeutic targets in MLL-rearranged AML. ![]()
Drug warrants further investigation in ATLL, team says
Researchers say lenalidomide exhibited clinically meaningful antitumor activity and an acceptable safety profile in a phase 2 study of patients with relapsed adult T-cell leukemia/lymphoma (ATLL).
Of the 26 patients enrolled in the trial, 42% responded to lenalidomide, and 35% experienced serious adverse events (AEs).
Results from this trial were published in the Journal of Clinical Oncology. Data were previously presented at the 8th Annual T-cell Lymphoma Forum. The study was sponsored by Celgene K.K.
Patients and treatment
All 26 patients had relapsed ATLL—15 with the acute subtype, 7 with the lymphoma subtype, and 4 with the unfavorable chronic subtype. The patients’ median age was 68.5 (range, 53-81), all were Japanese, and 54% were male.
The median number of prior treatment regimens was 2 (range, 1-4). Thirty-five percent of patients had prior mogamulizumab (n=9), 35% had received LSG15 (n=3) or modified LSG15 (n=6), and 27% had prior CHOP (n=7).
The patients received lenalidomide at 25 mg per day, given continuously until disease progression or intolerability.
Results
Five patients (19%) were still receiving lenalidomide at the data cutoff, which was November 20, 2014.
Thirteen patients (50%) stopped treatment due to progression, 6 (23%) because of AEs, 1 (4%) due to investigator decision, and 1 (4%) because of concerns about the increased possibility of disease recurrence.
The median follow-up was 3.9 months. Eleven patients (42%) responded to lenalidomide, including 4 complete responses and 1 unconfirmed complete response.
The median duration of response was not reached (range, 0.5 months to not reached), and the mean duration of response was 5.2 months (range, 0 to 16.6 months).
The median progression-free survival was 3.8 months (range, 1.9 months to not reached), and the median overall survival was 20.3 months (range, 9.1 months to not reached).
Nine patients (35%) experienced serious AEs. The only serious AE that occurred in more than 1 patient was thrombocytopenia, which occurred in 2 patients.
The most frequent AEs of any grade were thrombocytopenia (77%), neutropenia (73%), lymphopenia (69%), anemia (54%), and leukopenia (50%).
The most frequent grade 3 or higher AEs were neutropenia (65%), leukopenia (38%), lymphopenia (38%), and thrombocytopenia (23%). These events were all manageable and reversible, according to the researchers.
Based on these results, the team concluded that lenalidomide warrants further investigation as a treatment for ATLL. ![]()
Researchers say lenalidomide exhibited clinically meaningful antitumor activity and an acceptable safety profile in a phase 2 study of patients with relapsed adult T-cell leukemia/lymphoma (ATLL).
Of the 26 patients enrolled in the trial, 42% responded to lenalidomide, and 35% experienced serious adverse events (AEs).
Results from this trial were published in the Journal of Clinical Oncology. Data were previously presented at the 8th Annual T-cell Lymphoma Forum. The study was sponsored by Celgene K.K.
Patients and treatment
All 26 patients had relapsed ATLL—15 with the acute subtype, 7 with the lymphoma subtype, and 4 with the unfavorable chronic subtype. The patients’ median age was 68.5 (range, 53-81), all were Japanese, and 54% were male.
The median number of prior treatment regimens was 2 (range, 1-4). Thirty-five percent of patients had prior mogamulizumab (n=9), 35% had received LSG15 (n=3) or modified LSG15 (n=6), and 27% had prior CHOP (n=7).
The patients received lenalidomide at 25 mg per day, given continuously until disease progression or intolerability.
Results
Five patients (19%) were still receiving lenalidomide at the data cutoff, which was November 20, 2014.
Thirteen patients (50%) stopped treatment due to progression, 6 (23%) because of AEs, 1 (4%) due to investigator decision, and 1 (4%) because of concerns about the increased possibility of disease recurrence.
The median follow-up was 3.9 months. Eleven patients (42%) responded to lenalidomide, including 4 complete responses and 1 unconfirmed complete response.
The median duration of response was not reached (range, 0.5 months to not reached), and the mean duration of response was 5.2 months (range, 0 to 16.6 months).
The median progression-free survival was 3.8 months (range, 1.9 months to not reached), and the median overall survival was 20.3 months (range, 9.1 months to not reached).
Nine patients (35%) experienced serious AEs. The only serious AE that occurred in more than 1 patient was thrombocytopenia, which occurred in 2 patients.
The most frequent AEs of any grade were thrombocytopenia (77%), neutropenia (73%), lymphopenia (69%), anemia (54%), and leukopenia (50%).
The most frequent grade 3 or higher AEs were neutropenia (65%), leukopenia (38%), lymphopenia (38%), and thrombocytopenia (23%). These events were all manageable and reversible, according to the researchers.
Based on these results, the team concluded that lenalidomide warrants further investigation as a treatment for ATLL. ![]()
Researchers say lenalidomide exhibited clinically meaningful antitumor activity and an acceptable safety profile in a phase 2 study of patients with relapsed adult T-cell leukemia/lymphoma (ATLL).
Of the 26 patients enrolled in the trial, 42% responded to lenalidomide, and 35% experienced serious adverse events (AEs).
Results from this trial were published in the Journal of Clinical Oncology. Data were previously presented at the 8th Annual T-cell Lymphoma Forum. The study was sponsored by Celgene K.K.
Patients and treatment
All 26 patients had relapsed ATLL—15 with the acute subtype, 7 with the lymphoma subtype, and 4 with the unfavorable chronic subtype. The patients’ median age was 68.5 (range, 53-81), all were Japanese, and 54% were male.
The median number of prior treatment regimens was 2 (range, 1-4). Thirty-five percent of patients had prior mogamulizumab (n=9), 35% had received LSG15 (n=3) or modified LSG15 (n=6), and 27% had prior CHOP (n=7).
The patients received lenalidomide at 25 mg per day, given continuously until disease progression or intolerability.
Results
Five patients (19%) were still receiving lenalidomide at the data cutoff, which was November 20, 2014.
Thirteen patients (50%) stopped treatment due to progression, 6 (23%) because of AEs, 1 (4%) due to investigator decision, and 1 (4%) because of concerns about the increased possibility of disease recurrence.
The median follow-up was 3.9 months. Eleven patients (42%) responded to lenalidomide, including 4 complete responses and 1 unconfirmed complete response.
The median duration of response was not reached (range, 0.5 months to not reached), and the mean duration of response was 5.2 months (range, 0 to 16.6 months).
The median progression-free survival was 3.8 months (range, 1.9 months to not reached), and the median overall survival was 20.3 months (range, 9.1 months to not reached).
Nine patients (35%) experienced serious AEs. The only serious AE that occurred in more than 1 patient was thrombocytopenia, which occurred in 2 patients.
The most frequent AEs of any grade were thrombocytopenia (77%), neutropenia (73%), lymphopenia (69%), anemia (54%), and leukopenia (50%).
The most frequent grade 3 or higher AEs were neutropenia (65%), leukopenia (38%), lymphopenia (38%), and thrombocytopenia (23%). These events were all manageable and reversible, according to the researchers.
Based on these results, the team concluded that lenalidomide warrants further investigation as a treatment for ATLL. ![]()
SpHb monitoring may reduce use of RBC transfusion

Photo by Elisa Amendola
HONG KONG—Continuous and noninvasive hemoglobin monitoring may reduce the excessive use of intraoperative red blood cell (RBC) transfusion, according to researchers.
The team conducted a retrospective study of patients who received intraoperative RBC transfusions at a single institution, comparing patients who had noninvasive and continuous monitoring of hemoglobin concentrations by spectrophotometry (SpHb) to those who did not.
The results showed a significantly lower mean RBC transfusion volume per 1 g of blood loss in the SpHb group than in the control group.
The researchers presented these findings at the 16th World Congress of Anaesthesiologists (abstract PR607).
The study included 371 patients who received intraoperative RBC transfusions between 2012 and 2014 at Fukushima Medical University in Japan.
The researchers compared 94 patients who had SpHb with the Radical-7® Pulse CO-Oximeter (a product of Masimo) to 277 patients who did not.
The team noted that measured SpHb values are similar to the Hb concentration values obtained by blood sampling, and the procedure allows for continuous monitoring of changes in SpHb levels over time.
The median blood loss during surgery was 1160 g in the SpHb group and 900 g in the control group.
There was no significant difference in the average RBC transfusion volume between the SpHb group and the control group—815 ± 819 mL and 785 ± 773 mL, respectively (P=0.75).
Likewise, there was no significant difference in the preoperative hemoglobin concentration in the SpHb group and the control group—10.4 ± 1.9 g/dL and 10.2 ± 2.4 g/dL, respectively (P=0.27).
However, the researchers did find that patients in the SpHb group had a significantly lower mean RBC transfusion volume per 1 g of blood loss when compared to controls—0.9 ± 1.0 mL/g blood loss and 2.4 ± 5.9 mL/g blood loss, respectively (P<0.01).
“This is the third study, published by different researchers on 3 continents (US1, Egypt2, and now Japan) that has shown that, in addition to other clinical tools, SpHb may be used to help clinicians make informed transfusion decisions during different types of surgery,” said Steven Barker, MD, PhD, chief science officer of Masimo.
Though Masimo’s Radical-7® Pulse CO-Oximeter was used in this study, the researchers declared no conflicts of interest. ![]()

Photo by Elisa Amendola
HONG KONG—Continuous and noninvasive hemoglobin monitoring may reduce the excessive use of intraoperative red blood cell (RBC) transfusion, according to researchers.
The team conducted a retrospective study of patients who received intraoperative RBC transfusions at a single institution, comparing patients who had noninvasive and continuous monitoring of hemoglobin concentrations by spectrophotometry (SpHb) to those who did not.
The results showed a significantly lower mean RBC transfusion volume per 1 g of blood loss in the SpHb group than in the control group.
The researchers presented these findings at the 16th World Congress of Anaesthesiologists (abstract PR607).
The study included 371 patients who received intraoperative RBC transfusions between 2012 and 2014 at Fukushima Medical University in Japan.
The researchers compared 94 patients who had SpHb with the Radical-7® Pulse CO-Oximeter (a product of Masimo) to 277 patients who did not.
The team noted that measured SpHb values are similar to the Hb concentration values obtained by blood sampling, and the procedure allows for continuous monitoring of changes in SpHb levels over time.
The median blood loss during surgery was 1160 g in the SpHb group and 900 g in the control group.
There was no significant difference in the average RBC transfusion volume between the SpHb group and the control group—815 ± 819 mL and 785 ± 773 mL, respectively (P=0.75).
Likewise, there was no significant difference in the preoperative hemoglobin concentration in the SpHb group and the control group—10.4 ± 1.9 g/dL and 10.2 ± 2.4 g/dL, respectively (P=0.27).
However, the researchers did find that patients in the SpHb group had a significantly lower mean RBC transfusion volume per 1 g of blood loss when compared to controls—0.9 ± 1.0 mL/g blood loss and 2.4 ± 5.9 mL/g blood loss, respectively (P<0.01).
“This is the third study, published by different researchers on 3 continents (US1, Egypt2, and now Japan) that has shown that, in addition to other clinical tools, SpHb may be used to help clinicians make informed transfusion decisions during different types of surgery,” said Steven Barker, MD, PhD, chief science officer of Masimo.
Though Masimo’s Radical-7® Pulse CO-Oximeter was used in this study, the researchers declared no conflicts of interest. ![]()

Photo by Elisa Amendola
HONG KONG—Continuous and noninvasive hemoglobin monitoring may reduce the excessive use of intraoperative red blood cell (RBC) transfusion, according to researchers.
The team conducted a retrospective study of patients who received intraoperative RBC transfusions at a single institution, comparing patients who had noninvasive and continuous monitoring of hemoglobin concentrations by spectrophotometry (SpHb) to those who did not.
The results showed a significantly lower mean RBC transfusion volume per 1 g of blood loss in the SpHb group than in the control group.
The researchers presented these findings at the 16th World Congress of Anaesthesiologists (abstract PR607).
The study included 371 patients who received intraoperative RBC transfusions between 2012 and 2014 at Fukushima Medical University in Japan.
The researchers compared 94 patients who had SpHb with the Radical-7® Pulse CO-Oximeter (a product of Masimo) to 277 patients who did not.
The team noted that measured SpHb values are similar to the Hb concentration values obtained by blood sampling, and the procedure allows for continuous monitoring of changes in SpHb levels over time.
The median blood loss during surgery was 1160 g in the SpHb group and 900 g in the control group.
There was no significant difference in the average RBC transfusion volume between the SpHb group and the control group—815 ± 819 mL and 785 ± 773 mL, respectively (P=0.75).
Likewise, there was no significant difference in the preoperative hemoglobin concentration in the SpHb group and the control group—10.4 ± 1.9 g/dL and 10.2 ± 2.4 g/dL, respectively (P=0.27).
However, the researchers did find that patients in the SpHb group had a significantly lower mean RBC transfusion volume per 1 g of blood loss when compared to controls—0.9 ± 1.0 mL/g blood loss and 2.4 ± 5.9 mL/g blood loss, respectively (P<0.01).
“This is the third study, published by different researchers on 3 continents (US1, Egypt2, and now Japan) that has shown that, in addition to other clinical tools, SpHb may be used to help clinicians make informed transfusion decisions during different types of surgery,” said Steven Barker, MD, PhD, chief science officer of Masimo.
Though Masimo’s Radical-7® Pulse CO-Oximeter was used in this study, the researchers declared no conflicts of interest. ![]()
Therapy can provide clinical benefit in haplo-HSCT, data suggest

Photo by Chad McNeeley
BARCELONA—Results from 2 studies suggest an immunogene therapy can provide a clinical benefit in adults with high-risk hematologic malignancies undergoing haploidentical hematopoietic stem cell transplant (haplo-HSCT).
When compared to historical controls, patients who received the immunogene therapy, Zalmoxis, had lower rates of non-relapse mortality (NRM) and chronic graft-vs-host disease (GVHD), as well as improved overall survival (OS).
The only adverse event related to Zalmoxis was GVHD, which was resolved.
These data were presented at the EBMT International Transplant Course. The studies were funded by MolMed S.p.A., the company developing Zalmoxis.
About the therapy
Zalmoxis is a treatment consisting of allogeneic, genetically modified T cells. The cells are intended to be given to haplo-HSCT recipients to help fight off infection, enhance the success of the transplant, and support long-lasting anticancer effects.
Because the genetically modified T cells can also cause GVHD, they are equipped with a suicide gene, which makes them susceptible to treatment with ganciclovir or valganciclovir. So if a patient develops GVHD, he or she can receive ganciclovir/valganciclovir, which should kill the modified T cells and prevent further development of GVHD.
Trial data
The data presented at the EBMT International Transplant Course were from the phase 1/2 TK007 trial and the ongoing phase 3 TK008 trial.
The TK007 trial included haplo-HSCT recipients with various high-risk hematologic malignancies, while the TK008 trial is enrolling patients with high-risk acute leukemia who are undergoing haplo-HSCT.
Researchers have compared 37 Zalmoxis-treated patients from these trials to 140 contemporaneous control patients from the database of the EBMT registry.
Results of this pair-matched analysis showed an OS improvement in Zalmoxis-treated patients, which was driven by a reduction in NRM. The OS was 49% in the Zalmoxis group and 37% in controls (P=0.01), and the NRM was 22% and 43%, respectively (P=0.014).
Among controls dying from non-relapse causes, the majority (78%) died from either infection (56%) or GVHD (22%), while the only adverse event related to Zalmoxis treatment was GVHD. And this GVHD was fully resolved by activating the suicide-gene system with ganciclovir treatment, without any GVHD-related death.
Furthermore, the incidence of chronic GVHD was lower in Zalmoxis-treated patients than in controls—6% and 25%, respectively (P=0.04).
Therefore, the researchers concluded that the protective effects of Zalmoxis in controlling infection and GVHD mainly drove the decreased NRM in the Zalmoxis group.
These data supported the European Commission’s recent decision to grant conditional marketing authorization for Zalmoxis. ![]()

Photo by Chad McNeeley
BARCELONA—Results from 2 studies suggest an immunogene therapy can provide a clinical benefit in adults with high-risk hematologic malignancies undergoing haploidentical hematopoietic stem cell transplant (haplo-HSCT).
When compared to historical controls, patients who received the immunogene therapy, Zalmoxis, had lower rates of non-relapse mortality (NRM) and chronic graft-vs-host disease (GVHD), as well as improved overall survival (OS).
The only adverse event related to Zalmoxis was GVHD, which was resolved.
These data were presented at the EBMT International Transplant Course. The studies were funded by MolMed S.p.A., the company developing Zalmoxis.
About the therapy
Zalmoxis is a treatment consisting of allogeneic, genetically modified T cells. The cells are intended to be given to haplo-HSCT recipients to help fight off infection, enhance the success of the transplant, and support long-lasting anticancer effects.
Because the genetically modified T cells can also cause GVHD, they are equipped with a suicide gene, which makes them susceptible to treatment with ganciclovir or valganciclovir. So if a patient develops GVHD, he or she can receive ganciclovir/valganciclovir, which should kill the modified T cells and prevent further development of GVHD.
Trial data
The data presented at the EBMT International Transplant Course were from the phase 1/2 TK007 trial and the ongoing phase 3 TK008 trial.
The TK007 trial included haplo-HSCT recipients with various high-risk hematologic malignancies, while the TK008 trial is enrolling patients with high-risk acute leukemia who are undergoing haplo-HSCT.
Researchers have compared 37 Zalmoxis-treated patients from these trials to 140 contemporaneous control patients from the database of the EBMT registry.
Results of this pair-matched analysis showed an OS improvement in Zalmoxis-treated patients, which was driven by a reduction in NRM. The OS was 49% in the Zalmoxis group and 37% in controls (P=0.01), and the NRM was 22% and 43%, respectively (P=0.014).
Among controls dying from non-relapse causes, the majority (78%) died from either infection (56%) or GVHD (22%), while the only adverse event related to Zalmoxis treatment was GVHD. And this GVHD was fully resolved by activating the suicide-gene system with ganciclovir treatment, without any GVHD-related death.
Furthermore, the incidence of chronic GVHD was lower in Zalmoxis-treated patients than in controls—6% and 25%, respectively (P=0.04).
Therefore, the researchers concluded that the protective effects of Zalmoxis in controlling infection and GVHD mainly drove the decreased NRM in the Zalmoxis group.
These data supported the European Commission’s recent decision to grant conditional marketing authorization for Zalmoxis. ![]()

Photo by Chad McNeeley
BARCELONA—Results from 2 studies suggest an immunogene therapy can provide a clinical benefit in adults with high-risk hematologic malignancies undergoing haploidentical hematopoietic stem cell transplant (haplo-HSCT).
When compared to historical controls, patients who received the immunogene therapy, Zalmoxis, had lower rates of non-relapse mortality (NRM) and chronic graft-vs-host disease (GVHD), as well as improved overall survival (OS).
The only adverse event related to Zalmoxis was GVHD, which was resolved.
These data were presented at the EBMT International Transplant Course. The studies were funded by MolMed S.p.A., the company developing Zalmoxis.
About the therapy
Zalmoxis is a treatment consisting of allogeneic, genetically modified T cells. The cells are intended to be given to haplo-HSCT recipients to help fight off infection, enhance the success of the transplant, and support long-lasting anticancer effects.
Because the genetically modified T cells can also cause GVHD, they are equipped with a suicide gene, which makes them susceptible to treatment with ganciclovir or valganciclovir. So if a patient develops GVHD, he or she can receive ganciclovir/valganciclovir, which should kill the modified T cells and prevent further development of GVHD.
Trial data
The data presented at the EBMT International Transplant Course were from the phase 1/2 TK007 trial and the ongoing phase 3 TK008 trial.
The TK007 trial included haplo-HSCT recipients with various high-risk hematologic malignancies, while the TK008 trial is enrolling patients with high-risk acute leukemia who are undergoing haplo-HSCT.
Researchers have compared 37 Zalmoxis-treated patients from these trials to 140 contemporaneous control patients from the database of the EBMT registry.
Results of this pair-matched analysis showed an OS improvement in Zalmoxis-treated patients, which was driven by a reduction in NRM. The OS was 49% in the Zalmoxis group and 37% in controls (P=0.01), and the NRM was 22% and 43%, respectively (P=0.014).
Among controls dying from non-relapse causes, the majority (78%) died from either infection (56%) or GVHD (22%), while the only adverse event related to Zalmoxis treatment was GVHD. And this GVHD was fully resolved by activating the suicide-gene system with ganciclovir treatment, without any GVHD-related death.
Furthermore, the incidence of chronic GVHD was lower in Zalmoxis-treated patients than in controls—6% and 25%, respectively (P=0.04).
Therefore, the researchers concluded that the protective effects of Zalmoxis in controlling infection and GVHD mainly drove the decreased NRM in the Zalmoxis group.
These data supported the European Commission’s recent decision to grant conditional marketing authorization for Zalmoxis. ![]()
FDA grants drug orphan designation for PNH

The US Food and Drug Administration (FDA) has granted orphan drug designation to Coversin as a treatment for paroxysmal nocturnal hemoglobinuria (PNH).
Coversin is a recombinant small protein (16,740 Da) derived from a native protein found in the saliva of the Ornithodoros moubata tick.
The drug is a second-generation complement inhibitor that acts on complement component C5, preventing release of C5a and formation of C5b-9 (also known as the membrane attack complex).
Coversin is being developed by Akari Therapeutics.
In vitro experiments have shown that Coversin inhibits red blood cell lysis in PNH, and Coversin can achieve full complement inhibition in the blood of PNH patients who are resistant to eculizumab.
In a phase 1a trial of healthy volunteers, Coversin completely inhibited complement C5 activity within 12 hours of administration.
Akari Therapeutics is currently conducting a phase 1b study of Coversin in healthy volunteers and is enrolling patients with eculizumab-resistant PNH in a phase 2 trial.
The company has also been administering Coversin to a patient with eculizumab-resistant PNH. Thus far, Coversin has prevented hemolytic episodes and improved disease symptoms in this patient. The only drug-related adverse event has been occasional local and transient irritation at the injection site.
“We have continued to see complete complement inhibition and symptom control in a PNH patient with resistance to eculizumab, who has been self-administering subcutaneous Coversin for over 7 months,” said Gur Roshwalb, MD, CEO of Akari Therapeutics.
“We believe that Coversin, when approved, could provide important benefits for all patients with PNH.”
Coversin is also being studied in atypical hemolytic uremic syndrome and Guillain Barré syndrome.
About orphan designation
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()

The US Food and Drug Administration (FDA) has granted orphan drug designation to Coversin as a treatment for paroxysmal nocturnal hemoglobinuria (PNH).
Coversin is a recombinant small protein (16,740 Da) derived from a native protein found in the saliva of the Ornithodoros moubata tick.
The drug is a second-generation complement inhibitor that acts on complement component C5, preventing release of C5a and formation of C5b-9 (also known as the membrane attack complex).
Coversin is being developed by Akari Therapeutics.
In vitro experiments have shown that Coversin inhibits red blood cell lysis in PNH, and Coversin can achieve full complement inhibition in the blood of PNH patients who are resistant to eculizumab.
In a phase 1a trial of healthy volunteers, Coversin completely inhibited complement C5 activity within 12 hours of administration.
Akari Therapeutics is currently conducting a phase 1b study of Coversin in healthy volunteers and is enrolling patients with eculizumab-resistant PNH in a phase 2 trial.
The company has also been administering Coversin to a patient with eculizumab-resistant PNH. Thus far, Coversin has prevented hemolytic episodes and improved disease symptoms in this patient. The only drug-related adverse event has been occasional local and transient irritation at the injection site.
“We have continued to see complete complement inhibition and symptom control in a PNH patient with resistance to eculizumab, who has been self-administering subcutaneous Coversin for over 7 months,” said Gur Roshwalb, MD, CEO of Akari Therapeutics.
“We believe that Coversin, when approved, could provide important benefits for all patients with PNH.”
Coversin is also being studied in atypical hemolytic uremic syndrome and Guillain Barré syndrome.
About orphan designation
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()

The US Food and Drug Administration (FDA) has granted orphan drug designation to Coversin as a treatment for paroxysmal nocturnal hemoglobinuria (PNH).
Coversin is a recombinant small protein (16,740 Da) derived from a native protein found in the saliva of the Ornithodoros moubata tick.
The drug is a second-generation complement inhibitor that acts on complement component C5, preventing release of C5a and formation of C5b-9 (also known as the membrane attack complex).
Coversin is being developed by Akari Therapeutics.
In vitro experiments have shown that Coversin inhibits red blood cell lysis in PNH, and Coversin can achieve full complement inhibition in the blood of PNH patients who are resistant to eculizumab.
In a phase 1a trial of healthy volunteers, Coversin completely inhibited complement C5 activity within 12 hours of administration.
Akari Therapeutics is currently conducting a phase 1b study of Coversin in healthy volunteers and is enrolling patients with eculizumab-resistant PNH in a phase 2 trial.
The company has also been administering Coversin to a patient with eculizumab-resistant PNH. Thus far, Coversin has prevented hemolytic episodes and improved disease symptoms in this patient. The only drug-related adverse event has been occasional local and transient irritation at the injection site.
“We have continued to see complete complement inhibition and symptom control in a PNH patient with resistance to eculizumab, who has been self-administering subcutaneous Coversin for over 7 months,” said Gur Roshwalb, MD, CEO of Akari Therapeutics.
“We believe that Coversin, when approved, could provide important benefits for all patients with PNH.”
Coversin is also being studied in atypical hemolytic uremic syndrome and Guillain Barré syndrome.
About orphan designation
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
FDA approves cord blood product

The US Food and Drug Administration (FDA) has issued a biologics license to the Cleveland Cord Blood Center (CCBC) for Clevecord™ (HPC, Cord Blood), a hematopoietic progenitor cell product derived from umbilical cord blood.
Under this license, CCBC is authorized to manufacture Clevecord at its facility in Warrensville Heights, Ohio.
Clevecord is indicated for use in unrelated donor transplant procedures, in conjunction with an appropriate preparative regimen.
The product can be used for hematopoietic and immunologic reconstitution in patients with disorders that affect the hematopoietic system, whether they are inherited, acquired, or result from myeloablative treatment.
Each Clevecord unit contains a minimum of 5 x 108 total nucleated cells with at least 1.25 x 106 viable CD34+ cells at the time of cryopreservation. The recommended minimum dose is 2.5 x 107 nucleated cells/kg at cryopreservation.
Clevecord has been approved with a black box warning, which states that use of the product may result in fatal infusion reactions, graft-vs-host disease, engraftment syndrome, and graft failure.
For more details on Clevecord, see the package insert on the FDA website.
“Obtaining FDA licensure for Clevecord is reflective of the Cleveland Cord Blood Center’s dedication to meeting the highest quality standards in the industry for distribution of our cord blood products to transplant centers throughout the US and around the world,” said Wouter Van’t Hof, cord blood bank director at CCBC.
CCBC collects, processes, stores, and distributes umbilical cord blood units for use in transplants and advanced research in cellular therapy.
The organization says its cord blood collections represent a diverse cross-section of donor ethnicity to support transplant needs, particularly in the underserved African-American population.
“Up to 50% of parents giving birth in our partner hospitals donate their baby’s umbilical cord blood, a rate well above the national average,” said Marcie Finney, executive director of CCBC.
CCBC cord blood units can be searched and accessed through registries, including the National Bone Marrow Donor Program and Bone Marrow Donors Worldwide. ![]()

The US Food and Drug Administration (FDA) has issued a biologics license to the Cleveland Cord Blood Center (CCBC) for Clevecord™ (HPC, Cord Blood), a hematopoietic progenitor cell product derived from umbilical cord blood.
Under this license, CCBC is authorized to manufacture Clevecord at its facility in Warrensville Heights, Ohio.
Clevecord is indicated for use in unrelated donor transplant procedures, in conjunction with an appropriate preparative regimen.
The product can be used for hematopoietic and immunologic reconstitution in patients with disorders that affect the hematopoietic system, whether they are inherited, acquired, or result from myeloablative treatment.
Each Clevecord unit contains a minimum of 5 x 108 total nucleated cells with at least 1.25 x 106 viable CD34+ cells at the time of cryopreservation. The recommended minimum dose is 2.5 x 107 nucleated cells/kg at cryopreservation.
Clevecord has been approved with a black box warning, which states that use of the product may result in fatal infusion reactions, graft-vs-host disease, engraftment syndrome, and graft failure.
For more details on Clevecord, see the package insert on the FDA website.
“Obtaining FDA licensure for Clevecord is reflective of the Cleveland Cord Blood Center’s dedication to meeting the highest quality standards in the industry for distribution of our cord blood products to transplant centers throughout the US and around the world,” said Wouter Van’t Hof, cord blood bank director at CCBC.
CCBC collects, processes, stores, and distributes umbilical cord blood units for use in transplants and advanced research in cellular therapy.
The organization says its cord blood collections represent a diverse cross-section of donor ethnicity to support transplant needs, particularly in the underserved African-American population.
“Up to 50% of parents giving birth in our partner hospitals donate their baby’s umbilical cord blood, a rate well above the national average,” said Marcie Finney, executive director of CCBC.
CCBC cord blood units can be searched and accessed through registries, including the National Bone Marrow Donor Program and Bone Marrow Donors Worldwide. ![]()

The US Food and Drug Administration (FDA) has issued a biologics license to the Cleveland Cord Blood Center (CCBC) for Clevecord™ (HPC, Cord Blood), a hematopoietic progenitor cell product derived from umbilical cord blood.
Under this license, CCBC is authorized to manufacture Clevecord at its facility in Warrensville Heights, Ohio.
Clevecord is indicated for use in unrelated donor transplant procedures, in conjunction with an appropriate preparative regimen.
The product can be used for hematopoietic and immunologic reconstitution in patients with disorders that affect the hematopoietic system, whether they are inherited, acquired, or result from myeloablative treatment.
Each Clevecord unit contains a minimum of 5 x 108 total nucleated cells with at least 1.25 x 106 viable CD34+ cells at the time of cryopreservation. The recommended minimum dose is 2.5 x 107 nucleated cells/kg at cryopreservation.
Clevecord has been approved with a black box warning, which states that use of the product may result in fatal infusion reactions, graft-vs-host disease, engraftment syndrome, and graft failure.
For more details on Clevecord, see the package insert on the FDA website.
“Obtaining FDA licensure for Clevecord is reflective of the Cleveland Cord Blood Center’s dedication to meeting the highest quality standards in the industry for distribution of our cord blood products to transplant centers throughout the US and around the world,” said Wouter Van’t Hof, cord blood bank director at CCBC.
CCBC collects, processes, stores, and distributes umbilical cord blood units for use in transplants and advanced research in cellular therapy.
The organization says its cord blood collections represent a diverse cross-section of donor ethnicity to support transplant needs, particularly in the underserved African-American population.
“Up to 50% of parents giving birth in our partner hospitals donate their baby’s umbilical cord blood, a rate well above the national average,” said Marcie Finney, executive director of CCBC.
CCBC cord blood units can be searched and accessed through registries, including the National Bone Marrow Donor Program and Bone Marrow Donors Worldwide.
Effects of caring for advanced cancer patients
SAN FRANCISCO—Family caregivers of patients with high-mortality cancers may often experience high levels of depression and anxiety, results of a survey suggest.
The survey showed that caregivers can spend more than 8 hours a day providing care.
And as caregiving time increases, self-care behaviors such as sleep and exercise decline, which may confer poorer mental health.
These findings were presented at the 2016 Palliative Care in Oncology Symposium (abstract 239).
“Caregivers and patients are faced with an enormous physical and emotional toll when dealing with advanced cancer,” said study investigator J. Nicholas Dionne-Odom, PhD, RN, of the University of Alabama at Birmingham.
“When they put their own health and well-being on the back burner, it can affect their care to the patient.”
Dr Dionne-Odom and his colleagues conducted a cross-sectional survey of 294 family caregivers of Medicare beneficiaries diagnosed with pancreatic, lung, brain, ovarian, head and neck, hematologic, or stage IV cancers.
The survey was fielded across 8 cancer centers in Alabama, Florida, and Tennessee. Survey questions explored measures of self-care behaviors and quality of life.
The caregivers had an average age of 66. They were mostly female (72.8%), white (91.2%), retired (54.4%), and the patient’s spouse/partner (60.2%). Nearly half of the caregivers lived in rural areas (46.9%), and more than half had annual incomes less than $50,000 (53.8%).
Most of the caregivers said they provided care 6 to 7 days a week (71%) for more than 1 year (68%).
Twenty-three percent of caregivers reported a high level of depressive symptoms, and 34% reported borderline or high levels of anxiety symptoms, associated with significantly lower scores for self-care.
Lower self-care behavior scores were associated with a longer overall duration of caregiving, more hours in the day spent caregiving, more days of the week spent caregiving, and with fair or poor patient health.
“We hope our research rallies the oncology palliative care communities to develop assessment tools and services that support caregivers,” Dr Dionne-Odom said. “These efforts would help ensure that caregivers are supported and healthy when they take on the important role of caring for an individual with advanced cancer.”
SAN FRANCISCO—Family caregivers of patients with high-mortality cancers may often experience high levels of depression and anxiety, results of a survey suggest.
The survey showed that caregivers can spend more than 8 hours a day providing care.
And as caregiving time increases, self-care behaviors such as sleep and exercise decline, which may confer poorer mental health.
These findings were presented at the 2016 Palliative Care in Oncology Symposium (abstract 239).
“Caregivers and patients are faced with an enormous physical and emotional toll when dealing with advanced cancer,” said study investigator J. Nicholas Dionne-Odom, PhD, RN, of the University of Alabama at Birmingham.
“When they put their own health and well-being on the back burner, it can affect their care to the patient.”
Dr Dionne-Odom and his colleagues conducted a cross-sectional survey of 294 family caregivers of Medicare beneficiaries diagnosed with pancreatic, lung, brain, ovarian, head and neck, hematologic, or stage IV cancers.
The survey was fielded across 8 cancer centers in Alabama, Florida, and Tennessee. Survey questions explored measures of self-care behaviors and quality of life.
The caregivers had an average age of 66. They were mostly female (72.8%), white (91.2%), retired (54.4%), and the patient’s spouse/partner (60.2%). Nearly half of the caregivers lived in rural areas (46.9%), and more than half had annual incomes less than $50,000 (53.8%).
Most of the caregivers said they provided care 6 to 7 days a week (71%) for more than 1 year (68%).
Twenty-three percent of caregivers reported a high level of depressive symptoms, and 34% reported borderline or high levels of anxiety symptoms, associated with significantly lower scores for self-care.
Lower self-care behavior scores were associated with a longer overall duration of caregiving, more hours in the day spent caregiving, more days of the week spent caregiving, and with fair or poor patient health.
“We hope our research rallies the oncology palliative care communities to develop assessment tools and services that support caregivers,” Dr Dionne-Odom said. “These efforts would help ensure that caregivers are supported and healthy when they take on the important role of caring for an individual with advanced cancer.”
SAN FRANCISCO—Family caregivers of patients with high-mortality cancers may often experience high levels of depression and anxiety, results of a survey suggest.
The survey showed that caregivers can spend more than 8 hours a day providing care.
And as caregiving time increases, self-care behaviors such as sleep and exercise decline, which may confer poorer mental health.
These findings were presented at the 2016 Palliative Care in Oncology Symposium (abstract 239).
“Caregivers and patients are faced with an enormous physical and emotional toll when dealing with advanced cancer,” said study investigator J. Nicholas Dionne-Odom, PhD, RN, of the University of Alabama at Birmingham.
“When they put their own health and well-being on the back burner, it can affect their care to the patient.”
Dr Dionne-Odom and his colleagues conducted a cross-sectional survey of 294 family caregivers of Medicare beneficiaries diagnosed with pancreatic, lung, brain, ovarian, head and neck, hematologic, or stage IV cancers.
The survey was fielded across 8 cancer centers in Alabama, Florida, and Tennessee. Survey questions explored measures of self-care behaviors and quality of life.
The caregivers had an average age of 66. They were mostly female (72.8%), white (91.2%), retired (54.4%), and the patient’s spouse/partner (60.2%). Nearly half of the caregivers lived in rural areas (46.9%), and more than half had annual incomes less than $50,000 (53.8%).
Most of the caregivers said they provided care 6 to 7 days a week (71%) for more than 1 year (68%).
Twenty-three percent of caregivers reported a high level of depressive symptoms, and 34% reported borderline or high levels of anxiety symptoms, associated with significantly lower scores for self-care.
Lower self-care behavior scores were associated with a longer overall duration of caregiving, more hours in the day spent caregiving, more days of the week spent caregiving, and with fair or poor patient health.
“We hope our research rallies the oncology palliative care communities to develop assessment tools and services that support caregivers,” Dr Dionne-Odom said. “These efforts would help ensure that caregivers are supported and healthy when they take on the important role of caring for an individual with advanced cancer.”
Study reveals barriers to accessing palliative care services

©ASCO/Todd Buchanan 2016
SAN FRANCISCO—Patients may face challenges when trying to access palliative and supportive care services at cancer centers, a new study suggests.
Researchers took a “mystery shopper” approach and placed calls to cancer centers inquiring about palliative and supportive care services for a family member.
The callers sometimes had difficulty obtaining information about these services, even though all of the centers offer them.
“It’s sobering to hear that such services are not readily accessible at many centers,” said study investigator Kathryn Hutchins, a medical student at Duke University in Durham, North Carolina.
“However, it provides an opportunity for cancer centers to empower their front-line staff, as well as the oncology care team, through education and training so that the entire enterprise has a common understanding of palliative care and how to access it.”
Hutchins and her colleagues presented this research at the 2016 Palliative Care in Oncology Symposium (abstract 122).
The researchers placed 160 calls to 40 major cancer centers. The team chose to focus on National Cancer Institute-designated cancer centers because they all provide palliative care services along with other supportive care services.
The researchers used the same script for every call, asking about services for a 58-year-old female who was recently diagnosed with inoperable liver cancer. The team called each center 4 times on different days.
In 38.2% of the calls, the researchers were not able to receive complete information about supportive care services.
In 9.5% of calls, cancer center staff gave an answer other than “yes” regarding the availability of palliative care services, even though such services were available.
The answers varied and included responses such as:
- Palliative care was for end-of-life patients only (n=2)
- No physicians specialized in symptom management (n=3)
- A medical record review would be needed first (n=2).
In addition, 10 staff members said they were unsure about the availability of palliative care, and 2 were unfamiliar with the term.
Overall, 37.6% of the callers were told that all 7 supportive care services they inquired about were offered.
“As oncologists, we like to believe that, when we refer patients to our institution’s helpline, they will get connected to the services they need, but that doesn’t always happen,” said study investigator Arif Kamal, MD, of Duke Cancer Institute.
“It’s important for oncologists to be aware of these barriers and to work to eliminate them.”

©ASCO/Todd Buchanan 2016
SAN FRANCISCO—Patients may face challenges when trying to access palliative and supportive care services at cancer centers, a new study suggests.
Researchers took a “mystery shopper” approach and placed calls to cancer centers inquiring about palliative and supportive care services for a family member.
The callers sometimes had difficulty obtaining information about these services, even though all of the centers offer them.
“It’s sobering to hear that such services are not readily accessible at many centers,” said study investigator Kathryn Hutchins, a medical student at Duke University in Durham, North Carolina.
“However, it provides an opportunity for cancer centers to empower their front-line staff, as well as the oncology care team, through education and training so that the entire enterprise has a common understanding of palliative care and how to access it.”
Hutchins and her colleagues presented this research at the 2016 Palliative Care in Oncology Symposium (abstract 122).
The researchers placed 160 calls to 40 major cancer centers. The team chose to focus on National Cancer Institute-designated cancer centers because they all provide palliative care services along with other supportive care services.
The researchers used the same script for every call, asking about services for a 58-year-old female who was recently diagnosed with inoperable liver cancer. The team called each center 4 times on different days.
In 38.2% of the calls, the researchers were not able to receive complete information about supportive care services.
In 9.5% of calls, cancer center staff gave an answer other than “yes” regarding the availability of palliative care services, even though such services were available.
The answers varied and included responses such as:
- Palliative care was for end-of-life patients only (n=2)
- No physicians specialized in symptom management (n=3)
- A medical record review would be needed first (n=2).
In addition, 10 staff members said they were unsure about the availability of palliative care, and 2 were unfamiliar with the term.
Overall, 37.6% of the callers were told that all 7 supportive care services they inquired about were offered.
“As oncologists, we like to believe that, when we refer patients to our institution’s helpline, they will get connected to the services they need, but that doesn’t always happen,” said study investigator Arif Kamal, MD, of Duke Cancer Institute.
“It’s important for oncologists to be aware of these barriers and to work to eliminate them.”

©ASCO/Todd Buchanan 2016
SAN FRANCISCO—Patients may face challenges when trying to access palliative and supportive care services at cancer centers, a new study suggests.
Researchers took a “mystery shopper” approach and placed calls to cancer centers inquiring about palliative and supportive care services for a family member.
The callers sometimes had difficulty obtaining information about these services, even though all of the centers offer them.
“It’s sobering to hear that such services are not readily accessible at many centers,” said study investigator Kathryn Hutchins, a medical student at Duke University in Durham, North Carolina.
“However, it provides an opportunity for cancer centers to empower their front-line staff, as well as the oncology care team, through education and training so that the entire enterprise has a common understanding of palliative care and how to access it.”
Hutchins and her colleagues presented this research at the 2016 Palliative Care in Oncology Symposium (abstract 122).
The researchers placed 160 calls to 40 major cancer centers. The team chose to focus on National Cancer Institute-designated cancer centers because they all provide palliative care services along with other supportive care services.
The researchers used the same script for every call, asking about services for a 58-year-old female who was recently diagnosed with inoperable liver cancer. The team called each center 4 times on different days.
In 38.2% of the calls, the researchers were not able to receive complete information about supportive care services.
In 9.5% of calls, cancer center staff gave an answer other than “yes” regarding the availability of palliative care services, even though such services were available.
The answers varied and included responses such as:
- Palliative care was for end-of-life patients only (n=2)
- No physicians specialized in symptom management (n=3)
- A medical record review would be needed first (n=2).
In addition, 10 staff members said they were unsure about the availability of palliative care, and 2 were unfamiliar with the term.
Overall, 37.6% of the callers were told that all 7 supportive care services they inquired about were offered.
“As oncologists, we like to believe that, when we refer patients to our institution’s helpline, they will get connected to the services they need, but that doesn’t always happen,” said study investigator Arif Kamal, MD, of Duke Cancer Institute.
“It’s important for oncologists to be aware of these barriers and to work to eliminate them.”
Pregnancy screening lacking in girls with AML, ALL

patient and her father
Photo by Rhoda Baer
Many adolescent females are not being screened for pregnancy before beginning chemotherapy or undergoing computed tomography (CT) scans, according to research published in Cancer.
In this study, pregnancy screening was underused in adolescents with acute lymphoblastic leukemia (ALL), those with acute myeloid leukemia (AML), and those who received CT scans of the abdomen or pelvis during visits to the emergency room (ER).
“We found that adolescent girls are not adequately screened for pregnancy prior to receiving chemotherapy or CT scans that could harm a developing fetus,” said study author Pooja Rao, MD, of Penn State Health’s Milton S. Hershey Medical Center in Hershey, Pennsylvania.
“Adolescents with ALL, the most common childhood cancer, had the lowest rates of pregnancy screening of the patients we studied.”
Dr Rao and her colleagues examined pregnancy screening patterns among adolescent females newly diagnosed with ALL or AML, as well as adolescent females who visited the ER and received CT scans of the abdomen or pelvis. (In emergency medicine, pregnancy screening protocols exist for adolescents prior to receiving radiation due to the known teratogenic risks of radiation.)
The analysis included patients ages 10 to 18 who were admitted to hospitals across the US from 1999 to 2011. There were a total of 35,650 patient visits—127 for AML patients, 889 for ALL patients, and 34,634 ER admissions with CT scans of the abdomen/pelvis.
The proportion of visits with an appropriately timed pregnancy test was 35% for the ALL patients, 64% for the AML patients, and 58% in the ER group.
The researchers noted that ALL patients tended to be younger than the AML patients and the ER patients, and there was substantial variation in pregnancy screening patterns among the different hospitals.
However, in a generalized estimating equation (GEE) model adjusted for hospital clustering and patient age, patients with ALL were significantly less likely to have an appropriately timed pregnancy test when compared to patients in the ER cohort. The adjusted prevalence ratio was 0.71 (95% CI, 0.65-0.78).
And in a GEE model adjusted for hospital clustering, patients with AML were more likely to have an appropriately timed pregnancy test than patients in the ER cohort, but this difference was not statistically significant. The adjusted prevalence ratio was 1.12 (95% CI, 0.99-1.27).
The researchers also found that pregnancy screening continued to increase over time in the ALL cohort but remained “relatively stable” from 2008 onward in the AML and ER cohorts.
“Since nearly all chemotherapy agents used for childhood/adolescent acute leukemia can cause potential harm to a developing fetus, our findings indicate a need for standardized pregnancy screening practices for adolescent patients being treated for cancer,” Dr Rao said.
She also noted that the low rates of pregnancy screening observed in this study may indicate a reluctance on the part of pediatric oncologists to discuss sexual health practices with adolescent patients.
“While sexual health discussions and education may traditionally be thought to be the responsibility of the patient’s primary care provider, adolescents with cancer will often see their oncologist frequently over the course of their cancer treatment and afterwards,” Dr Rao said. “Oncologists therefore are well-positioned to initiate discussions about sexual health with their patients.”

patient and her father
Photo by Rhoda Baer
Many adolescent females are not being screened for pregnancy before beginning chemotherapy or undergoing computed tomography (CT) scans, according to research published in Cancer.
In this study, pregnancy screening was underused in adolescents with acute lymphoblastic leukemia (ALL), those with acute myeloid leukemia (AML), and those who received CT scans of the abdomen or pelvis during visits to the emergency room (ER).
“We found that adolescent girls are not adequately screened for pregnancy prior to receiving chemotherapy or CT scans that could harm a developing fetus,” said study author Pooja Rao, MD, of Penn State Health’s Milton S. Hershey Medical Center in Hershey, Pennsylvania.
“Adolescents with ALL, the most common childhood cancer, had the lowest rates of pregnancy screening of the patients we studied.”
Dr Rao and her colleagues examined pregnancy screening patterns among adolescent females newly diagnosed with ALL or AML, as well as adolescent females who visited the ER and received CT scans of the abdomen or pelvis. (In emergency medicine, pregnancy screening protocols exist for adolescents prior to receiving radiation due to the known teratogenic risks of radiation.)
The analysis included patients ages 10 to 18 who were admitted to hospitals across the US from 1999 to 2011. There were a total of 35,650 patient visits—127 for AML patients, 889 for ALL patients, and 34,634 ER admissions with CT scans of the abdomen/pelvis.
The proportion of visits with an appropriately timed pregnancy test was 35% for the ALL patients, 64% for the AML patients, and 58% in the ER group.
The researchers noted that ALL patients tended to be younger than the AML patients and the ER patients, and there was substantial variation in pregnancy screening patterns among the different hospitals.
However, in a generalized estimating equation (GEE) model adjusted for hospital clustering and patient age, patients with ALL were significantly less likely to have an appropriately timed pregnancy test when compared to patients in the ER cohort. The adjusted prevalence ratio was 0.71 (95% CI, 0.65-0.78).
And in a GEE model adjusted for hospital clustering, patients with AML were more likely to have an appropriately timed pregnancy test than patients in the ER cohort, but this difference was not statistically significant. The adjusted prevalence ratio was 1.12 (95% CI, 0.99-1.27).
The researchers also found that pregnancy screening continued to increase over time in the ALL cohort but remained “relatively stable” from 2008 onward in the AML and ER cohorts.
“Since nearly all chemotherapy agents used for childhood/adolescent acute leukemia can cause potential harm to a developing fetus, our findings indicate a need for standardized pregnancy screening practices for adolescent patients being treated for cancer,” Dr Rao said.
She also noted that the low rates of pregnancy screening observed in this study may indicate a reluctance on the part of pediatric oncologists to discuss sexual health practices with adolescent patients.
“While sexual health discussions and education may traditionally be thought to be the responsibility of the patient’s primary care provider, adolescents with cancer will often see their oncologist frequently over the course of their cancer treatment and afterwards,” Dr Rao said. “Oncologists therefore are well-positioned to initiate discussions about sexual health with their patients.”

patient and her father
Photo by Rhoda Baer
Many adolescent females are not being screened for pregnancy before beginning chemotherapy or undergoing computed tomography (CT) scans, according to research published in Cancer.
In this study, pregnancy screening was underused in adolescents with acute lymphoblastic leukemia (ALL), those with acute myeloid leukemia (AML), and those who received CT scans of the abdomen or pelvis during visits to the emergency room (ER).
“We found that adolescent girls are not adequately screened for pregnancy prior to receiving chemotherapy or CT scans that could harm a developing fetus,” said study author Pooja Rao, MD, of Penn State Health’s Milton S. Hershey Medical Center in Hershey, Pennsylvania.
“Adolescents with ALL, the most common childhood cancer, had the lowest rates of pregnancy screening of the patients we studied.”
Dr Rao and her colleagues examined pregnancy screening patterns among adolescent females newly diagnosed with ALL or AML, as well as adolescent females who visited the ER and received CT scans of the abdomen or pelvis. (In emergency medicine, pregnancy screening protocols exist for adolescents prior to receiving radiation due to the known teratogenic risks of radiation.)
The analysis included patients ages 10 to 18 who were admitted to hospitals across the US from 1999 to 2011. There were a total of 35,650 patient visits—127 for AML patients, 889 for ALL patients, and 34,634 ER admissions with CT scans of the abdomen/pelvis.
The proportion of visits with an appropriately timed pregnancy test was 35% for the ALL patients, 64% for the AML patients, and 58% in the ER group.
The researchers noted that ALL patients tended to be younger than the AML patients and the ER patients, and there was substantial variation in pregnancy screening patterns among the different hospitals.
However, in a generalized estimating equation (GEE) model adjusted for hospital clustering and patient age, patients with ALL were significantly less likely to have an appropriately timed pregnancy test when compared to patients in the ER cohort. The adjusted prevalence ratio was 0.71 (95% CI, 0.65-0.78).
And in a GEE model adjusted for hospital clustering, patients with AML were more likely to have an appropriately timed pregnancy test than patients in the ER cohort, but this difference was not statistically significant. The adjusted prevalence ratio was 1.12 (95% CI, 0.99-1.27).
The researchers also found that pregnancy screening continued to increase over time in the ALL cohort but remained “relatively stable” from 2008 onward in the AML and ER cohorts.
“Since nearly all chemotherapy agents used for childhood/adolescent acute leukemia can cause potential harm to a developing fetus, our findings indicate a need for standardized pregnancy screening practices for adolescent patients being treated for cancer,” Dr Rao said.
She also noted that the low rates of pregnancy screening observed in this study may indicate a reluctance on the part of pediatric oncologists to discuss sexual health practices with adolescent patients.
“While sexual health discussions and education may traditionally be thought to be the responsibility of the patient’s primary care provider, adolescents with cancer will often see their oncologist frequently over the course of their cancer treatment and afterwards,” Dr Rao said. “Oncologists therefore are well-positioned to initiate discussions about sexual health with their patients.”

